Advanced Strategies for Enhancing the Bioavailability of Functional Food Components: From Molecular Mechanisms to Clinical Translation
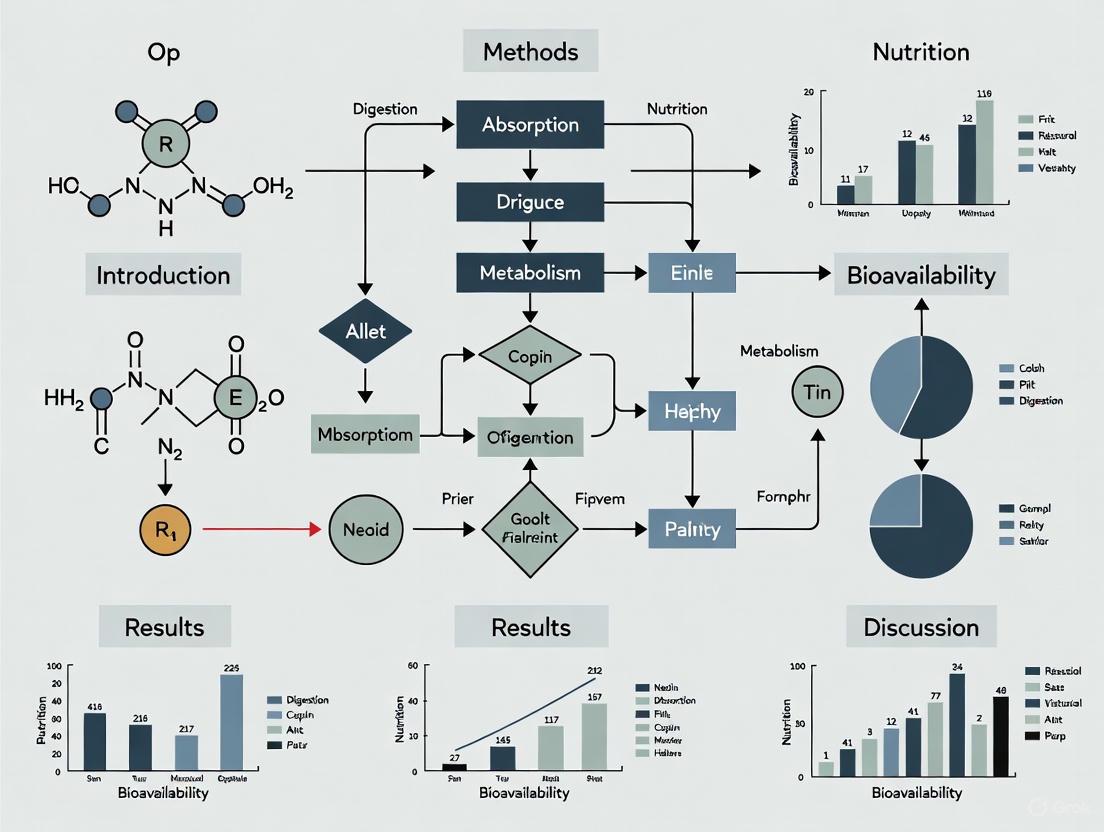
This article provides a comprehensive analysis of the scientific and technological advancements aimed at optimizing the bioavailability of functional food components.
Advanced Strategies for Enhancing the Bioavailability of Functional Food Components: From Molecular Mechanisms to Clinical Translation
Abstract
This article provides a comprehensive analysis of the scientific and technological advancements aimed at optimizing the bioavailability of functional food components. Tailored for researchers and drug development professionals, it explores the fundamental barriers limiting the efficacy of bioactive compounds—such as poor solubility, metabolic instability, and inefficient absorption. The scope encompasses a critical evaluation of innovative delivery systems, including nanoencapsulation, lipid-based carriers, and biotransformation approaches. Furthermore, it addresses troubleshooting for common formulation challenges, comparative analysis of validation methodologies, and the emerging role of AI and precision nutrition in designing next-generation functional foods with enhanced therapeutic potential for combating chronic diseases.
Understanding Bioavailability Barriers: The Science Behind Bioactive Compound Absorption
Core Concepts of Bioavailability and ADME
Bioavailability is a critical pharmacokinetic (PK) parameter defined as the fraction of an administered drug or active compound that reaches the systemic circulation unaltered [1] [2]. It is quantitatively expressed as a percentage, ranging from 0% (no active compound reaches circulation) to 100% [2]. For an intravenous (IV) dose, bioavailability is by definition 100% because the drug is injected directly into the bloodstream [1] [2].
The journey of a compound within the body is described by the ADME framework, which encompasses Absorption, Distribution, Metabolism, and Excretion [3] [4]. Bioavailability is an integral part of this paradigm, representing the combined result of absorption and first-pass metabolism [3] [1]. The extent and rate of these processes determine the concentration of the active compound at its target site, thereby influencing its therapeutic efficacy [3].
- Absolute vs. Relative Bioavailability: Absolute bioavailability compares the systemic availability of a drug from a non-IV formulation to that of an IV dose. Relative bioavailability compares the bioavailability of two different non-IV formulations (e.g., an oral solution versus a tablet) [2].
- First-Pass Effect: For orally administered compounds, a significant barrier to bioavailability is the first-pass effect. After ingestion, the compound must survive the gastrointestinal (GI) environment, cross the gut wall, and then travel via the portal vein to the liver, where it may be extensively metabolized before ever reaching the systemic circulation [3] [2]. This sequential reduction in the active compound's amount is a key reason why oral bioavailability is often less than 100% [2].
Table 1: Key Pharmacokinetic Parameters and Their Definitions
| Parameter | Definition | Formula/Description |
|---|---|---|
| Bioavailability (F) | The fraction of an administered dose that reaches systemic circulation [1] [2]. | ( F = \frac{AUC{PO}}{AUC{IV}} \times \frac{Dose{IV}}{Dose{PO}} ) (For absolute bioavailability) [1] |
| Volume of Distribution (Vd) | The apparent theoretical volume required to distribute the total amount of drug in the body to achieve the measured plasma concentration [3]. | ( Vd = \frac{Total\ Amount\ of\ Drug\ in\ Body}{Plasma\ Drug\ Concentration} ) [3] [1] |
| Clearance (CL) | The volume of plasma from which a drug is completely removed per unit of time [3]. | ( CL = \frac{Elimination\ Rate}{Plasma\ Drug\ Concentration} ) [3] [1] |
| Half-Life (t½) | The time required for the plasma drug concentration to reduce by 50% [3]. | ( t_{1/2} = \frac{0.693 \times Vd}{CL} ) [3] |
| Area Under the Curve (AUC) | A measure of the total drug exposure over time in the plasma, used to calculate bioavailability [3] [1]. | Integral of the plasma concentration-time curve [3] |
Troubleshooting Guide: Common Bioavailability Challenges and Solutions
Researchers often encounter specific, measurable problems when evaluating bioavailability. This section addresses these issues with targeted troubleshooting advice.
FAQ 1: How do I troubleshoot low oral bioavailability in a new chemical entity?
Low oral bioavailability can stem from poor absorption, high first-pass metabolism, or both. A systematic approach is required to isolate the root cause [5].
Table 2: Troubleshooting Low Oral Bioavailability
| Observed Issue | Potential Root Cause | Diagnostic Experiments & Solutions |
|---|---|---|
| Low Solubility & Dissolution Rate | The compound does not dissolve adequately in the GI fluids, limiting absorption [6]. | Diagnose: Determine solubility across physiological pH range (1.2-7.5). Perform dissolution testing [6].Solve: Implement salt formation, cocrystallization, particle size reduction (nanonization), or amorphous solid dispersions [6]. |
| Poor Permeability | The compound cannot efficiently cross the intestinal epithelial membrane [6]. | Diagnose: Use in vitro models like Caco-2 cell monolayers or PAMPA to assess permeability [6].Solve: Explore structural modifications to optimize lipophilicity (LogP/D), or formulate with permeability enhancers [6]. |
| High First-Pass Metabolism | The compound is extensively metabolized in the gut wall or liver before reaching systemic circulation [3] [2]. | Diagnose: Compare AUC after oral vs. intra-arterial administration. Use liver microsomes or hepatocytes to assess metabolic stability [4].Solve: Consider a prodrug strategy or alternative route of administration (e.g., sublingual) to bypass first-pass effects [6]. |
| Efflux by Transporters | The compound is a substrate for efflux transporters like P-glycoprotein (P-gp), which pumps it back into the gut lumen [1]. | Diagnose: Conduct transport assays in cell lines overexpressing specific efflux transporters (e.g., MDCK-MDR1) [1].Solve: Investigate structural analogs that are not P-gp substrates, or use pharmaceutical excipients that inhibit P-gp [1]. |
FAQ 2: Our in vitro data does not correlate with in vivo bioavailability results. What could be wrong?
This common problem often arises from oversimplified in vitro models that fail to capture the complexity of the in vivo environment.
- Solution: Adopt more physiologically relevant models and ensure experimental rigor.
- Change one variable at a time: When troubleshooting, only change one experimental parameter at a time to clearly identify its effect [5].
- Use higher-fidelity systems: Move from simple microsomal stability assays to plated hepatocytes or hepatocytes in suspension, which contain a fuller complement of Phase I and Phase II enzymes and can provide a better prediction of in vivo metabolism [4].
- Account for protein binding: In vitro systems often lack plasma proteins. The free, unbound drug concentration, not the total, more closely correlates with pharmacological effect and metabolism. Measure plasma protein binding and consider its impact [3].
- Plan experiments carefully: A failed experiment due to poor planning may not be repeated, causing the loss of a potentially good idea. Meticulous experimental design is crucial for generating reliable and reproducible data [5].
FAQ 3: How can we improve the predictive power of our early ADME studies?
Modern tools and strategies can significantly enhance the translation from early discovery to clinical outcomes.
- Solution: Integrate advanced in silico and analytical technologies.
- Leverage Artificial Intelligence (AI): Machine learning (ML) and deep learning (DL) models can predict complex structure-bioavailability relationships, forecast dissolution dynamics, and identify bioactive peptides, reducing reliance on costly and time-consuming in vivo trials in the early stages [7].
- Utilize Cassette Dosing: For compounds within a specific chemical template, "cassette" or "n-in-1" dosing (administering several compounds together to a single animal) can be a powerful high-throughput screening tool. This approach relies on highly selective analytical methods like LC-MS/MS for quantitative analysis [4].
- Apply Mass Spectrometry Imaging (MSI): Techniques like MALDI or DESI MSI allow for the direct visualization of drug and metabolite distribution within tissue slices, providing unparalleled insight into a compound's in vivo distribution profile [4].
Experimental Protocols for Key Bioavailability Studies
This section provides detailed methodologies for foundational experiments in bioavailability research.
Protocol: Determining Absolute Oral Bioavailability in a Rodent Model
Objective: To calculate the absolute bioavailability (F) of a test compound by comparing its systemic exposure after oral (PO) and intravenous (IV) administration.
Materials:
- Test compound (for PO and IV formulation)
- Vehicle/solvent for formulation (e.g., saline, PEG, DMSO)
- Laboratory rodents (e.g., rats or mice)
- IV catheterization supplies
- Oral gavage needles
- Microcentrifuge tubes (containing anticoagulant, e.g., Kâ‚‚EDTA)
- LC-MS/MS system with validated bioanalytical method
Methodology:
- Formulation: Prepare two formulations.
- IV Formulation: Ensure the compound is in a sterile, soluble form suitable for bolus injection (e.g., in saline).
- PO Formulation: Prepare a solution or suspension for oral gavage. The dose may be higher than the IV dose to account for expected lower bioavailability.
- Dosing and Sampling:
- Divide animals into two groups (IV and PO). A crossover design can be used but requires a sufficient washout period.
- Administer the IV dose via a tail or jugular vein catheter. Administer the PO dose via oral gavage.
- Collect serial blood samples (e.g., at 0.083, 0.25, 0.5, 1, 2, 4, 8, 12, and 24 hours post-dose) from each animal. The specific timepoints should be pilot-tested.
- Centrifuge blood samples immediately to obtain plasma and store at -80°C until analysis.
- Bioanalysis:
- Use a selective and sensitive LC-MS/MS method to determine the plasma concentration of the test compound in all samples.
- Generate standard curves and quality control (QC) samples in the same biological matrix to ensure accuracy and precision.
- Data Analysis:
- For each animal and each route, plot the plasma concentration versus time curve.
- Use a PK software package to calculate the Area Under the Curve (AUC) from zero to the last time point (AUC₀–t) and extrapolated to infinity (AUC₀–∞) for both routes.
- Calculate absolute bioavailability using the formula: ( F = \frac{AUC{PO} \times Dose{IV}}{AUC{IV} \times Dose{PO}} \times 100\% ) where ( AUC{PO} ) and ( AUC{IV} ) are the dose-normalized AUC values [1] [2].
Protocol: Assessing Metabolic Stability Using Liver Microsomes
Objective: To determine the in vitro half-life (t½) and intrinsic clearance (CLint) of a test compound using liver microsomes, predicting its metabolic stability.
Materials:
- Test compound
- Liver microsomes (from human or relevant animal species)
- NADPH-regenerating system (e.g., NADP+, glucose-6-phosphate, glucose-6-phosphate dehydrogenase)
- 100 mM Phosphate buffer, pH 7.4
- Methanol or Acetonitrile (HPLC grade)
- Heating block or water bath at 37°C
- LC-MS/MS system
Methodology:
- Incubation Preparation:
- Prepare an incubation mixture in microcentrifuge tubes containing:
- 0.1 mg/mL microsomal protein
- 1 µM test compound
- 100 mM Phosphate buffer, pH 7.4
- Pre-incubate the mixture for 5 minutes at 37°C.
- Prepare an incubation mixture in microcentrifuge tubes containing:
- Initiation and Quenching:
- Start the reaction by adding the NADPH-regenerating system.
- At predetermined time points (e.g., 0, 5, 10, 20, 30, 45, 60 minutes), remove an aliquot of the incubation mixture and quench it with a cold volume of methanol or acetonitrile (containing an internal standard) that is at least twice the volume of the aliquot.
- Vortex and centrifuge at high speed (e.g., 14,000 rpm) for 10 minutes to precipitate proteins.
- Bioanalysis:
- Inject the supernatant into the LC-MS/MS system to quantify the remaining parent compound at each time point.
- Data Analysis:
- Plot the natural logarithm (ln) of the parent compound's remaining percentage against time.
- The slope of the linear regression of this plot is the elimination rate constant (k).
- Calculate the in vitro half-life: ( t_{1/2} = \frac{0.693}{k} )
- Calculate the intrinsic clearance: ( CL{int} = \frac{0.693}{t{1/2}} \times \frac{Incubation\ Volume}{Microsomal\ Protein} ) [4].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions for Bioavailability Studies
| Reagent / Material | Function in Bioavailability Research |
|---|---|
| Caco-2 Cell Line | A human colon adenocarcinoma cell line that, upon differentiation, forms a monolayer with tight junctions and expresses transporters, mimicking the intestinal barrier. Used for in vitro permeability assessment [6]. |
| Liver Microsomes | Subcellular fractions containing membrane-bound cytochrome P450 (CYP450) enzymes. Used for high-throughput screening of metabolic stability and reaction phenotyping [4]. |
| Cryopreserved Hepatocytes | Intact liver cells containing a full suite of metabolizing enzymes (Phase I and Phase II). Provide a more physiologically relevant model for metabolism and toxicity studies than microsomes [4]. |
| NADPH Regenerating System | Supplies a constant source of NADPH, a crucial cofactor for CYP450-mediated oxidative metabolism. Essential for activity in microsomal and hepatocyte incubations [4]. |
| Mass Spectrometry-Grade Solvents | High-purity solvents (water, acetonitrile, methanol) with minimal alkali metal ion contamination. Critical for preventing adduct formation and maintaining sensitivity in LC-MS analysis, especially for oligonucleotides and polar molecules [5]. |
| Artificial Gastrointestinal Fluids | Simulated gastric and intestinal fluids (e.g., FaSSGF, FaSSIF) with defined pH, buffer capacity, and bile salt/phospholipid content. Used in dissolution testing to predict in vivo dissolution behavior [6]. |
| Glycidyl Palmitate-d5 | Glycidyl Palmitate-d5 Stable Isotope|CAS 1794941-80-2 |
| Mesalazine-D3 | Mesalazine-D3 Stable Isotope |
For researchers in functional food development, the therapeutic promise of a bioactive compound is often limited by its bioavailability—the proportion that reaches systemic circulation to exert its desired physiological effect [8]. This journey is governed by three major, interconnected factors: solubility, stability, and mucosal permeability [9] [6].
A compound must first dissolve in the gastrointestinal fluids (solubility), survive the harsh biochemical environment of the gut and during processing (stability), and then efficiently cross the mucosal barrier to be absorbed (permeability) [9]. The Biopharmaceutics Classification System (BCS) provides a framework for predicting a compound's absorption based on these properties, with BCS Class II (low solubility, high permeability) and Class IV (low solubility, low permeability) posing the most significant development challenges [9] [10]. Overcoming these hurdles is paramount for enhancing the efficacy of functional food components, from lipophilic vitamins and omega-3 fatty acids to various polyphenols and carotenoids [8] [11].
Troubleshooting Guides & FAQs
Solubility
Q: My bioactive compound shows poor aqueous solubility. What are my primary strategies to enhance it for a functional food formulation?
Poor aqueous solubility is a major hurdle, as a compound must be dissolved to be absorbed [10]. The following strategies are commonly employed, each with distinct advantages.
Table: Strategies for Enhancing Bioactive Compound Solubility
| Strategy | Brief Principle | Common Techniques/Examples |
|---|---|---|
| Physical Modification [9] [10] | Alters the physical state of the drug to increase surface area or energy. | Micronization, Nanosuspensions, Solid Dispersions (in carriers like polymers), Cryogenic Techniques, Supercritical Fluid Technology |
| Chemical Modification [9] [10] | Modifies the chemical form of the drug to improve dissolution. | Salt Formation, Prodrug Formation |
| Formulation-Based Approaches [9] [11] | Uses excipients or carrier systems to solubilize the compound. | Cosolvency (e.g., using ethanol, PEG), Hydrotropy, Surfactants, Lipid-Based Delivery Systems (e.g., SNEDDS, NLCs, Nanoemulsions) |
Q: How can I rapidly and accurately determine the kinetic solubility of new candidate compounds during early-stage screening?
A: Nephelometry is a high-throughput, non-destructive technique ideal for kinetic solubility screening [12] [13]. It measures the light scattered by insoluble particles in a solution, allowing you to identify the concentration at which a compound begins to precipitate.
Experimental Protocol: Kinetic Solubility Assay via Nephelometry
- Sample Preparation: Prepare a concentrated stock solution of your compound in DMSO. Perform serial dilutions in your target aqueous buffer (e.g., PBS) across a 96- or 384-well microplate, ensuring a final DMSO concentration that does not artificially enhance solubility (typically ≤1-5%) [12] [13].
- Incubation: Allow the plate to incubate for a standardized period (e.g., 15-60 minutes) at a controlled temperature (e.g., 37°C) to reach equilibrium.
- Nephelometry Measurement: Use a microplate nephelometer (e.g., NEPHELOstar Plus). The instrument directs a laser beam (e.g., 635 nm) through each well and a detector measures the intensity of light scattered at a 90-degree angle [12]. A higher signal indicates more insoluble particles.
- Data Analysis: Plot the nephelometric signal (scattered light intensity) against the compound concentration. The kinetic solubility is identified as the point where the scatter signal increases dramatically, indicating the onset of precipitation. This is often determined by the intersection of two linear regression lines fitted to the soluble and precipitate-dominated data points [13].
Figure 1: Experimental workflow for determining kinetic solubility using nephelometry.
Stability
Q: The lipophilic bioactive (e.g., carotenoid, omega-3) in my functional food product degrades during processing (heat, pH) and storage. How can I protect it?
A: Encapsulation within delivery systems is the primary strategy to shield sensitive compounds from environmental stresses like heat, oxygen, light, and pH fluctuations [11]. These systems create a physical barrier around the bioactive.
Table: Delivery Systems for Enhancing Bioactive Stability
| Delivery System Type | Key Components | Protective Mechanism & Advantages |
|---|---|---|
| Lipid-Based Nanocarriers [9] [11] | Lipids, Surfactants, Water | Encapsulates bioactives in oil droplets or lipid matrices, protecting from the aqueous environment and enabling high retention during processing. |
| Polymer-Based Nanocarriers [9] [11] | Proteins (e.g., whey, zein), Polysaccharides (e.g., alginate, chitosan) | Forms a dense polymer matrix or wall around the bioactive. Can be engineered for controlled release and offers protection against ionic strength and pH changes. |
Q: How do I experimentally evaluate the stability of an emulsion-based delivery system for my bioactive compound?
A: Stability is a multi-faceted parameter. You should assess it using a combination of the following techniques, which monitor different instability mechanisms like creaming, flocculation, and coalescence [14].
Experimental Protocol: Assessing Emulsion System Stability
- Visual Observation & Creaming Index: Fill a sealed, transparent vial or cylinder with a known volume of the emulsion. Store it under controlled conditions (e.g., 25°C or 40°C) and observe for phase separation over time. The Creaming Index can be calculated as:
(Height of Cream or Sediment Layer / Total Height of Emulsion) × 100%[14]. - Particle Size Analysis: Use dynamic light scattering (DLS) to measure the droplet size and particle size distribution (PSD) of the emulsion initially and at regular time points. An increase in mean droplet size or the appearance of a larger population indicates droplet aggregation (flocculation) or fusion (coalescence) [14].
- Zeta Potential Measurement: Using electrophoretic light scattering, determine the zeta potential—a key indicator of the electrostatic repulsion between droplets. A high absolute zeta potential (typically > ±30 mV) suggests good stability against aggregation [14].
- Microscopy: Use optical or confocal laser scanning microscopy (CLSM) to visually observe the microstructure of the emulsion, confirming droplet distribution, aggregation, or the presence of crystals that might destabilize the system [14].
Figure 2: Multi-technique approach for comprehensive emulsion stability assessment.
Mucosal Permeability
Q: What are the key anatomical and physiological factors limiting the permeability of my compound through the oral mucosa?
A: Permeability across the oral mucosa is primarily determined by the epithelium, which acts as the main barrier [15]. The key factors are:
- Epithelial Type: The oral cavity has regions with keratinized (e.g., hard palate) and non-keratinized epithelium (e.g., buccal, sublingual). Non-keratinized epithelium is generally thinner and more permeable, making the buccal and sublingual routes preferred for systemic delivery [15].
- Mucus Layer: A semipermeable barrier that can trap macromolecules and slow diffusion. Nanoparticles smaller than ~200 nm can diffuse through it more effectively [9].
- Enzymes and Efflux Transporters: Enterocytes contain metabolizing enzymes (e.g., CYP450) and efflux pumps like P-glycoprotein (P-gp), which can actively pump compounds back into the lumen, significantly reducing the absorbed fraction [9].
Q: Which ex vivo models are most suitable for studying drug permeability across the oral mucosa, and how do I ensure data reproducibility?
A: Ex vivo models using animal tissue are common, but reproducibility is a challenge due to variability in tissue thickness and viability [15] [16].
Experimental Protocol: Ex Vivo Permeability Study Using Franz Diffusion Cell
- Tissue Preparation: Obtain fresh porcine or rodent buccal mucosa. Carefully separate the epithelium from the underlying connective tissue. The thickness of the mucosa should be measured and recorded, as it is a critical variable [15] [16].
- Mounting: Mount the mucosal tissue between the donor and receptor compartments of a Franz diffusion cell, with the epithelial side facing the donor compartment. The receptor compartment should be filled with a suitable buffer (e.g., Krebs–Ringer bicarbonate solution) maintained at 37°C and continuously stirred [15].
- Sample Application: Apply the formulation containing your bioactive compound (e.g., solution, gel, patch) to the donor compartment.
- Sampling: At predetermined time intervals, withdraw samples from the receptor compartment and replace with fresh buffer to maintain sink conditions.
- Analysis: Quantify the amount of permeated compound in the samples using a sensitive analytical method (e.g., HPLC, LC-MS).
- Data Normalization & Viability: To ensure reproducibility, normalize permeation data to a standard mucosal thickness using mathematical models, especially if tissue thickness varies significantly [16]. Assess tissue viability before and after the experiment using an assay like MTT to confirm barrier integrity was maintained [15].
The Scientist's Toolkit: Essential Research Reagents & Materials
Table: Key Reagents and Materials for Bioavailability Enhancement Studies
| Category / Item | Specific Examples | Function / Application |
|---|---|---|
| Lipid-Based Carrier Components [9] [11] | Medium-chain triglycerides (MCTs), Lectihin, Polysorbates (Tweens) | Form the core and stabilize nanoemulsions, SNEDDS, and solid lipid nanoparticles (SLNs). |
| Polymer-Based Carrier Components [9] [11] | Chitosan, Alginate, Zein, Whey Protein Isolate, Cellulose derivatives (e.g., HPMC) | Form polymeric nanoparticles, hydrogels, and micelles; provide mucoadhesion and controlled release. |
| Solubility & Stability Assay Tools [12] [13] | DMSO, Phosphate Buffered Saline (PBS), NEPHELOstar Plus, Zetasizer | For preparing samples and conducting high-throughput solubility (nephelometry) and stability (zeta potential, DLS) screens. |
| Ex Vivo Permeability Model [15] | Porcine buccal mucosa, Franz diffusion cell, Krebs–Ringer bicarbonate buffer | Provides a biologically relevant model for studying and quantifying compound permeability. |
| Permeability Enhancers & Inhibitors [9] | P-gp inhibitors (e.g., Verapamil), Permeation enhancers (e.g., Chitosan) | Used in mechanistic studies to overcome efflux transport or temporarily increase mucosal permeability. |
| Diacetolol D7 | Diacetolol D7, MF:C16H24N2O4, MW:315.42 g/mol | Chemical Reagent |
| Monoisobutyl Phthalate-d4 | Monoisobutyl Phthalate-d4, CAS:1219802-26-2, MF:C12H14O4, MW:226.26 g/mol | Chemical Reagent |
The Impact of Food Matrix and Gastrointestinal Transformations on Bioaccessibility
For researchers and scientists focused on optimizing the bioavailability of functional food components, understanding the impact of the food matrix and gastrointestinal transformations on bioaccessibility is fundamental. Bioaccessibility, defined as the fraction of a compound released from the food matrix into the gastrointestinal tract and thus available for intestinal absorption, is the critical first step toward achieving biological efficacy [17] [18]. The complex interactions between bioactive compounds and other food components—such as proteins, dietary fibers, and lipids—can either enhance or inhibit this release, directly influencing the outcome of your experiments and the potential health benefits of the final product [19] [20]. This guide addresses specific experimental challenges and provides actionable methodologies to advance your research in functional food development.
Core Concepts: Food Matrix Effects
The food matrix is the complex assembly of nutrients and non-nutrients in a food structure that can physically entrap or chemically interact with bioactive compounds. Understanding these interactions is paramount for predicting and improving the bioaccessibility of your target compounds.
Key Mechanisms of Food Matrix Effects
| Mechanism | Impact on Bioaccessibility | Research Implications |
|---|---|---|
| Complexation with Nutrients [19] | Significantly affected, either enhanced or reduced. Effects are polyphenol- and nutrient-specific. | Requires individual investigational approaches for each food/nutrient and phenolic compound pair. |
| Interaction with Dietary Fiber [19] | May reduce bioaccessibility by trapping compounds; some fibers may promote stability. | Necessary to characterize the specific type of fiber (e.g., cellulose, pectin, inulin) used in the model. |
| Interaction with Proteins [19] | Casein shown to significantly affect hydroxytyrosol and tyrosol permeability. | Consider the role of the protein corona when studying inorganic ENMs [20]. |
| Changes in GI Tract Physiology [19] | Alters luminal pH, enzyme capacity, bile salt content, and GI motility. | Fed vs. fasted state models will yield different results; state must be standardized. |
| Binding to Soil/Sediment Matrices [21] | Reduces metal bioaccessibility via sorption to clays, organic matter, and oxides. | Critical for assessing risk from contaminated foods; pore water concentration is a key indicator. |
Standardized Experimental Protocols
Employing standardized and harmonized methods is crucial for generating reproducible and comparable data on bioaccessibility. The following protocol is widely recognized in the field.
The INFOGEST Static In Vitro Digestion Model
This harmonized method simulates the human gastrointestinal process and is particularly suited for initial screening of bioaccessibility in functional food ingredients [18].
1. Preparation of Simulated Digestive Fluids Prepare Simulated Salivary Fluid (SSF), Simulated Gastric Fluid (SGF), and Simulated Intestinal Fluid (SIF) as per the INFOGEST standardized recipe [19] [18]. For fed-state studies, use Fed State Simulated Gastric Fluid (FeSSGF) and Fed State Simulated Intestinal Fluid (FeSSIF) [19].
2. Digestion Phases
- Gastric Phase: Mix the food sample with SGF and pepsin (e.g., 268 units/mL). Adjust pH to 3.0 and incubate for 60 minutes with constant agitation [18]. Sample at t=0 (G0) and t=60 (G60) minutes.
- Intestinal Phase: Transfer the gastric chyme to a vessel containing SIF, pancreatin (e.g., 16 units/mL trypsin activity), and bile salts (e.g., 1.38 mM bovine bile). Adjust pH to 6.0-7.0 and incubate for up to 120 minutes [18]. Sample at t=30 (I30), t=60 (I60), and t=120 (I120) minutes.
3. Sampling and Analysis Stop the enzymatic reaction at each time point (e.g., by snap-freezing at -80°C or using enzyme inhibitors). Centrifuge samples (e.g., ~10,000 g) to separate the bioaccessible fraction (supernatant) from the non-bioaccessible residue. Analyze the supernatant for your target bioactive compounds using appropriate techniques (HPLC, LC-MS) [17] [18].
Calculation:
Bioaccessibility (%) = (Amount of compound in supernatant / Total amount in original sample) × 100
Experimental Workflow for In Vitro Bioaccessibility
Troubleshooting Common Experimental Issues
FAQ 1: Why is my measured bioaccessibility lower than expected based on the total compound content in the food?
Potential Cause & Solution: The most common cause is strong binding or entrapment of the bioactive compound within the food matrix.
- Confirm Nutrient Interactions: Systematically test the effect of individual macronutrients. For instance, research shows casein and specific dietary fibers can significantly reduce the bioaccessibility of hydroxytyrosol and tyrosol from olive pomace extract [19].
- Analyze the Solid Residue: After centrifugation, analyze the non-bioaccessible pellet to determine the fraction of the compound that was not released. This can confirm physical entrapment.
- Optimize the Matrix: Consider food processing techniques (e.g., heating, fermentation, high-pressure processing) that can break down the matrix structure and enhance compound release.
FAQ 2: How do I account for the effect of other meal components during digestion assays?
Potential Cause & Solution: The presence of a full meal drastically alters gastrointestinal conditions.
- Use Fed-State Simulated Fluids: Replace standard SGF and SIF with Fed State Simulated Fluids (FeSSGF and FeSSIF). These fluids have different pH, buffer capacity, and composition (e.g., containing lecithin and taurocholate) that more accurately mimic the fed state [19].
- Incorporate a Standardized Food Model: Use a well-defined food model like the Standardized Food Model (SFM) in your experiments. This model often includes components like sodium caseinate dissolved in a phosphate buffer to simulate a protein-rich food background [19].
FAQ 3: My bioactive compound is unstable under gastrointestinal conditions. How can I accurately assess its bioaccessibility?
Potential Cause & Solution: Many phenolic compounds and vitamins can degrade at low pH or in the presence of enzymes and oxygen.
- Track Compound Degradation: Monitor not only the parent compound but also its degradation products or metabolites throughout the digestion process. An apparent stability might be due to the degradation of secoiridoids into hydroxytyrosol and tyrosol [19].
- Use Advanced In Vitro Models: Consider moving from static to semi-dynamic or dynamic in vitro models that can continuously remove digestion products, providing a more accurate picture of stability and absorption [17].
- Employ Encapsulation Strategies: Test the efficacy of delivery systems like cyclodextrins or lipid-based nanoparticles. Studies have shown that cyclodextrins can partially neutralize the negative effects of the OPE matrix on hydroxytyrosol and tyrosol permeability [19].
Visualizing the Bioaccessibility & Bioavailability Pathway
To systematically approach bioavailability optimization, it is essential to understand the entire pathway from ingestion to physiological effect.
Pathway from Food to Physiological Effect
The Scientist's Toolkit: Essential Research Reagents
| Research Reagent | Function in Bioaccessibility Research | Application Example |
|---|---|---|
| Pepsin (porcine gastric mucosa) [19] [18] | Proteolytic enzyme for gastric digestion phase. | Simulates protein hydrolysis in the stomach in INFOGEST protocol. |
| Pancreatin (porcine pancreas) [19] [18] | Enzyme mixture containing trypsin, amylase, and lipase for intestinal digestion. | Simulates complex macronutrient digestion in the small intestine. |
| Bile Salts [19] [18] | Emulsify lipids, facilitating the solubilization of hydrophobic compounds. | Critical for the bioaccessibility of lipophilic bioactive compounds. |
| Caco-2 & HT29-MTX-E12 Cell Lines [19] [18] | Model the human intestinal epithelium for absorption studies. | Co-cultures mimic enterocytes and goblet cells for permeability assays. |
| Simulated Digestive Fluids (SSF, SGF, SIF) [19] [18] | Provide inorganic ions and electrolytes to mimic GI tract environment. | Essential for maintaining physiologically relevant pH and ionic strength. |
| Standardized Food Model (SFM) [19] | Provides a consistent background food matrix for fed-state studies. | Used to investigate nutrient interactions under standardized conditions. |
| Hydroxypropyl β-cyclodextrin (HPβCD) [19] | Molecular encapsulation agent to improve solubility and stability. | Shown to enhance the permeability of hydroxytyrosol and tyrosol [19]. |
| Pipecolic acid-d9 | Pipecolic acid-d9, CAS:790612-94-1, MF:C6H11NO2, MW:138.21 g/mol | Chemical Reagent |
| trans-Isoferulic acid-d3 | trans-Isoferulic acid-d3, CAS:1028203-97-5, MF:C10H10O4, MW:197.20 g/mol | Chemical Reagent |
Octacosanol is a long-chain fatty alcohol (C₂₈H₅₈O) found naturally in sugarcane wax, wheat germ oil, rice bran oil, and beeswax [22]. It exhibits a broad spectrum of documented biological activities, including anti-fatigue, anti-inflammatory, hypolipidemic, antioxidant, and antitumor properties [22]. Despite this significant therapeutic potential, its practical application in functional foods and pharmaceuticals is severely limited by one critical factor: extremely low oral bioavailability [22].
The high hydrophobicity of octacosanol results in poor water solubility, which subsequently leads to low bioaccessibility in the gastrointestinal tract, limited intestinal absorption, and inefficient systemic distribution [22]. Recent pharmacokinetic studies reveal that after gavage administration of octacosanol to Sprague-Dawley rats at a dose of 80 mg/kg body weight, the serum concentration reached only 417 ng/mL and liver levels were merely 445 ng/g [22]. This fundamental challenge of delivering sufficient concentrations to target sites necessitates advanced formulation strategies to unlock octacosanol's full clinical potential.
Quantitative Bioavailability Assessment
Table 1: Key Pharmacokinetic Parameters of Unformulated Octacosanol
| Parameter | Value | Experimental Conditions |
|---|---|---|
| Serum Concentration | 417 ng/mL | 80 mg/kg dose in Sprague-Dawley rats, measured at 1 hour [22] |
| Liver Concentration | 445 ng/g | 80 mg/kg dose in Sprague-Dawley rats, measured at 1 hour [22] |
| Plasma Concentration | ~30 ng/mL | 60 mg/kg dose in rats [23] |
| Fecal Excretion | 31-33% | Indicator of poor absorption [23] |
Table 2: Bioavailability Enhancement Using Delivery Systems
| Formulation Strategy | Key Performance Metrics | Bioavailability Improvement |
|---|---|---|
| O/W Nanoemulsion [23] | Particle size: 71.54 nm; PDI: 0.195; Zeta potential: -3.98 mV | Significant enhancement in solubility and intestinal absorption efficiency |
| Microencapsulation (GA-Malt-PPI) [24] | Encapsulation Efficiency: >90%; Sustained release profile in simulated GI tract | Improved efficacy in alleviating HFD-induced obesity symptoms in mice compared to octacosanol monomer |
Troubleshooting Guide: Common Experimental Challenges
FAQ 1: How can I improve the water dispersibility of octacosanol for in vitro assays?
Challenge: Octacosanol's high hydrophobicity causes precipitation in aqueous experimental systems, leading to inconsistent results and inaccurate bioactivity measurements.
Solutions:
- Microencapsulation: Use a composite shell system with gum Arabic (GA), maltose (Malt), and pea protein isolate (PPI) in a ratio of 2:1:2 with a core-to-shell ratio of 1:7.5 [24]. Emulsify at 70°C and pH 9.0 for optimal results.
- Nanoemulsion Formulation: Prepare oil-in-water (O/W) nanoemulsions using PEG-40 hydrogenated castor oil (PHCO) as surfactant and ethyl acetate as co-surfactant [23]. This green, low-energy method significantly enhances dispersibility.
- Protein Complexation: Form nanocomplexes with soy protein isolate (SPI), which has demonstrated improved stability of octacosanol in neutral conditions [22].
FAQ 2: What methods effectively enhance octacosanol absorption in pharmacokinetic studies?
Challenge: Despite promising in vitro activity, octacosanol shows poor in vivo performance due to limited intestinal absorption and extensive pre-systemic metabolism.
Solutions:
- Nanoemulsion Delivery: The O/W nanoemulsion system significantly improves intestinal absorption efficiency as demonstrated by both in vitro digestion models and in vivo distribution studies [23].
- Sustained-Release Microcapsules: The GA-Malt-PPI microcapsule system provides sustained release of octacosanol throughout the gastrointestinal tract, reducing premature metabolism and enhancing systemic exposure [24].
- Nanocrystal Technology: Previous research has developed modified octacosanol nanocrystals that improve dissolution rate and oral bioavailability through increased surface area [22].
FAQ 3: How can I stabilize octacosanol during storage and processing?
Challenge: Octacosanol formulations may face physical instability, degradation, or loss of activity during storage and processing.
Solutions:
- Optimized Nanoemulsion Parameters: Formulate nanoemulsions that maintain stability across varying temperatures (4-60°C), pH levels (4-9), NaCl concentrations (0-200 mM), and sucrose content (0-10%) [23].
- Composite Shell Systems: The GA-Malt-PPI microcapsule significantly improves storage stability compared to unencapsulated octacosanol, maintaining activity over extended periods [24].
- Antioxidant Protection: Incorporate appropriate antioxidants into formulations, as octacosanol's stability can be compromised by oxidative degradation under certain conditions [22].
Experimental Protocols
Protocol 1: Green Synthesis of O/W Nanoemulsion for Octacosanol
Objective: To prepare a stable oil-in-water nanoemulsion to enhance octacosanol solubility and bioavailability using a simple, low-energy method [23].
Materials:
- Octacosanol (purity ≥90%)
- PEG-40 hydrogenated castor oil (PHCO) as surfactant
- Ethyl acetate as co-surfactant
- Deionized water
Procedure:
- Solution Preparation: Dissolve octacosanol in ethyl acetate to form the oil phase.
- Surfactant Addition: Add PHCO to the oil phase at an optimized ratio (octacosanol:ethyl acetate:PHCO = 1:9:10).
- Emulsification: Slowly add the organic phase to deionized water with continuous stirring at room temperature.
- Homogenization: Process the mixture using a homogenizer at 10,000 rpm for 5 minutes to form a coarse emulsion.
- Particle Reduction: Sonicate the emulsion using a probe sonicator at 400W for 10 minutes (pulse mode: 5s on, 2s off) while maintaining temperature in an ice bath.
- Characterization: Determine particle size (target: ~70 nm), PDI (target: <0.2), and zeta potential using dynamic light scattering.
Validation:
- Confirm stability under various environmental conditions (temperature, pH, ionic strength)
- Evaluate in vitro digestibility using simulated gastrointestinal fluids
- Assess cellular uptake using Caco-2 cell models
Protocol 2: Microencapsulation of Octacosanol Using GA-Malt-PPI Complex
Objective: To develop sustained-release microcapsules that protect octacosanol from gastrointestinal metabolism and improve its efficacy [24].
Materials:
- Octacosanol (purity ≥90%)
- Gum Arabic (GA)
- Maltose (Malt)
- Pea protein isolate (PPI)
- pH adjustment solutions (HCl and NaOH)
Procedure:
- Shell Solution Preparation: Dissolve GA, Malt, and PPI in deionized water at 60°C with mass ratio GA:Malt:PPI = 2:1:2.
- Core Addition: Add octacosanol (core material) to the GA-Malt-PPI solution with continuous stirring to achieve core-to-shell ratio of 1:7.5.
- Emulsification: Homogenize the mixture twice using a high-speed homogenizer.
- pH Optimization: Adjust pH to 9.0 and maintain for 30 seconds to expose hydrophobic groups on PPI.
- Temperature Conditioning: Heat the emulsion to 70°C for 30 seconds with continuous mixing.
- Neutralization: Adjust pH back to neutral (7.0).
- Characterization: Determine encapsulation efficiency (>90% target), loading capacity, particle size, and zeta potential.
Quality Control:
- Monitor sustained release profile using in vitro simulated gastrointestinal tract model
- Evaluate storage stability at different temperatures and humidity conditions
- Confirm in vivo efficacy using HFD-induced obesity mouse model
Visualization of Key Concepts
Diagram 1: Octacosanol Absorption Pathway
Diagram 2: Nanoemulsion Development Workflow
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Octacosanol Bioavailability Research
| Reagent/Material | Specifications | Research Application |
|---|---|---|
| PEG-40 Hydrogenated Castor Oil (PHCO) | Pharmaceutical grade, high purity [23] | Non-ionic surfactant for nanoemulsion formation; provides high biosafety and stabilization |
| Gum Arabic-Maltose-Pea Protein Isolate (GA-Malt-PPI) | Food grade, optimized ratio 2:1:2 [24] | Composite shell material for microencapsulation; enables sustained release in GI tract |
| Ethyl Acetate | High purity, low toxicity solvent (LDâ‚…â‚€ > 5600 mg/kg in rats) [23] | Co-surfactant in nanoemulsion preparation; offers moderate polarity and biodegradability |
| In Vitro Digestion Model Components | Pepsin, pancreatin, bile salts, electrolytes [24] | Simulated gastrointestinal fluids for predicting release profiles and absorption potential |
| Analytical Standards | Octacosanol reference standard (≥90% purity) [24] | Quantification of octacosanol in biological samples and formulation quality control |
| Piperaquine D6 | Piperaquine D6 | Piperaquine D6 CAS 1261394-71-1 is a deuterium-labeled internal standard for antimalarial pharmacokinetics research. For Research Use Only. Not for human use. |
| L-5-Hydroxytryptophan-d4 | L-5-Hydroxytryptophan-d4, CAS:1246818-91-6, MF:C11H12N2O3, MW:224.25 g/mol | Chemical Reagent |
Emerging Technologies and Future Perspectives
The field of octacosanol bioavailability enhancement is rapidly evolving with several promising technological approaches emerging beyond the formulation strategies discussed above. Artificial intelligence (AI) and machine learning are now being applied to predict optimal formulation parameters, absorption pathways, and even individual metabolic responses to octacosanol supplementation [7]. These computational approaches can significantly accelerate the development of next-generation delivery systems by modeling complex structure-activity relationships and predicting in vivo performance based on in vitro data.
Additionally, innovative encapsulation technologies including solid lipid nanoparticles, nanostructured lipid carriers, and hybrid drug nanocrystals represent promising avenues for further improving octacosanol bioavailability [22]. The integration of precision nutrition concepts, which account for inter-individual variability in genetics, microbiome composition, and metabolic phenotypes, may enable the development of personalized octacosanol formulations optimized for specific population subgroups [7]. As these advanced technologies mature, they will undoubtedly contribute to overcoming the longstanding bioavailability challenges that have limited the clinical translation of octacosanol's promising biological activities.
Gut Microbiota's Role in the Biotransformation of Phenolics and Polysaccharides
Troubleshooting Guide: Common Experimental Challenges
Issue 1: Low Metabolite Yield in Biotransformation Assays
Problem: After incubating phenolic compounds or polysaccharides with gut microbiota, expected metabolite concentrations are low or undetectable.
| Possible Cause | Recommended Solution |
|---|---|
| Suboptimal microbial community | Use standardized, metabolically active fecal samples; verify donor health and avoid long-term antibiotic use [25]. |
| Incorrect substrate preparation | For polyphenols: use glycosylated forms; for polysaccharides: ensure proper solubility and molecular weight [25] [26]. |
| Oxygen contamination in anaerobic system | Strictly maintain anaerobic conditions (e.g., anaerobic chamber, nitrogen gas flushing) [25]. |
| Insufficient fermentation time | Extend incubation; polysaccharide fermentation to SCFAs may require 24-72 hours [27]. |
Issue 2: High Variability in Metabolite Profiles Between Replicates
Problem: Significant inconsistency in biotransformation products across technical or biological replicates.
| Possible Cause | Recommended Solution |
|---|---|
| Inconsistent microbiota source | Pool samples from multiple donors or use standardized, commercially available bacterial consortia [28]. |
| Uncontrolled pH during fermentation | Use pH-controlled bioreactors or include sufficient buffering capacity in media [27]. |
| Degradation of parent compounds | Verify substrate stability under experimental conditions; add protease inhibitors if necessary [29]. |
Issue 3: Poor Bacterial Survival or Activity
Problem: Microbiota viability decreases significantly during the biotransformation assay.
| Possible Cause | Recommended Solution |
|---|---|
| Toxic compound accumulation | Monitor and remove inhibitory metabolites (e.g., lactate) via medium exchange in continuous systems [29]. |
| Inadequate nutrient media | Use rich, complex media supporting diverse bacteria; consider adding mucin or other gut-specific factors [28]. |
| Incorrect temperature | Maintain 37°C, the optimal temperature for human gut microbiota [29]. |
Detailed Experimental Protocols
Protocol 1: In Vitro Biotransformation of Phenolic Compounds
Objective: To assess the conversion of dietary polyphenols into bioavailable metabolites by human gut microbiota.
Materials:
- Fecal inoculum: Fresh or frozen fecal samples from healthy donors, diluted in anaerobic phosphate-buffered saline [25]
- Substrate: Polyphenol compound (e.g., grape seed extract, chlorogenic acid) [25]
- Anaerobic medium: Such as YCFA or M2GSC, pre-reduced for 24 hours [25]
- Equipment: Anaerobic workstation, shaking incubator, centrifuge, UPLC-MS for analysis [25]
Methodology:
- Inoculum Preparation: Homogenize 10% (w/v) feces in anaerobic PBS, centrifuge to remove large particles [25].
- Reaction Setup: In anaerobic tubes, combine 10% inoculum, 80% anaerobic medium, and 10% polyphenol substrate (1-2 mg/mL). Include no-substrate controls [25].
- Incubation: Ferment at 37°C with constant shaking (150 rpm) for 24-48 hours under anaerobic conditions [25].
- Sampling: Collect samples at 0, 6, 12, 24, and 48 hours for metabolite and bacterial analysis [25].
- Analysis:
Protocol 2: Polysaccharide Fermentation and SCFA Analysis
Objective: To evaluate the prebiotic potential of polysaccharides and quantify short-chain fatty acid production.
Materials:
- Polysaccharide substrate: Purified polysaccharides (e.g., from mushrooms, marine organisms) [26]
- SCFA standards: Acetate, propionate, butyrate for calibration curves [27]
- Equipment: GC-FID system, anaerobic fermentation system, pH meter [26]
Methodology:
- Polysaccharide Purification: Extract using hot water or UPE, deproteinize, purify via column chromatography [26].
- Fermentation: Incolate 1% (w/v) polysaccharide with fecal inoculum in anaerobic medium for 48 hours [26].
- SCFA Quantification:
- Microbiota Analysis: Monitor enrichment of specific taxa (e.g., Bifidobacterium, Roseburia) via 16S rRNA sequencing [26].
Mechanisms and Pathways
The gut microbiota enhances the bioavailability of dietary compounds through four primary pathways. Pathway 1 involves direct biotransformation of parent compounds into beneficial metabolites. Pathway 2 occurs when non-parent components trigger microbial metabolism to produce additional beneficial molecules. In Pathway 3, gut microbiota modulation decreases the production of detrimental metabolites. Pathway 4 involves inhibiting specific bacteria that would otherwise transform parent drugs into inactive compounds [27].
Fig. 1: Four pathways of gut microbiota-mediated bioavailability. Pathway 1: Direct biotransformation; Pathway 2: Non-parent enhanced metabolism; Pathway 3: Reduced detrimental metabolites; Pathway 4: Prevented inactivation [27].
Polyphenol and polysaccharide metabolism follows distinct but complementary pathways. Polyphenols undergo extensive microbial modification including deglycosylation, ring fission, and conversion to aromatic acids, while polysaccharides are fermented to SCFAs which provide systemic health benefits [25] [27].
Fig. 2: Microbial biotransformation of phenolics and polysaccharides. Gut bacterial enzymes convert dietary compounds into bioactive metabolites with systemic health effects [25] [27].
Frequently Asked Questions (FAQs)
Q1: How does interindividual variability in gut microbiota affect biotransformation studies? Significant interpersonal differences in microbial composition dramatically impact metabolic outcomes. Studies show individuals with higher abundances of Enterobacteriaceae and Fusobacteria metabolize quercetin more efficiently, while Surreellaceae and Oscillospiraceae are negatively correlated with its metabolism. For robust experiments, use pooled samples from multiple donors or characterize donor microbiota to account for this variability [25].
Q2: What are the key bacterial species involved in polyphenol and polysaccharide metabolism? Critical taxa include:
- Polyphenol metabolism: Eubacterium ramulus (ring fission), Enterobacteria spp. (quercetin conversion), Lactobacillus plantarum (increases 3-HPPA production) [25]
- Polysaccharide metabolism: Bifidobacterium spp. (fiber degradation), Ruminococcus spp., Eubacterium spp. (butyrate production) [25] [26]
- SCFA production: Faecalibacterium prausnitzii, Roseburia spp. (butyrate), Bacteroides spp. (acetate, propionate) [27]
Q3: How can I improve the detection of microbial metabolites in complex samples?
- Sample preparation: Use solid-phase extraction or protein precipitation before analysis [25]
- Analytical methods: Employ UPLC-MS/MS with multiple reaction monitoring for sensitive quantification [25]
- Derivatization: For SCFAs, consider derivatization for improved GC separation and detection [27]
- Internal standards: Use stable isotope-labeled analogs of target metabolites for accurate quantification [25]
Q4: What controls are essential for interpreting biotransformation experiments?
- No-substrate controls: Account for metabolites from endogenous sources [25]
- No-inoculum controls: Assess non-enzymatic degradation of substrates [25]
- Heat-killed inoculum: Confirm microbial activity is required for biotransformation [25]
- Reference compounds: Use known metabolites to verify identification and quantify recovery [27]
The Scientist's Toolkit: Research Reagent Solutions
| Essential Material | Function & Application | Key Considerations |
|---|---|---|
| Standardized Gut Microbiota | Provides consistent metabolic capacity for screening; from companies like ATCC | Verify metabolic competence for specific substrates; check viability after thawing [25] |
| Anaerobic Culture Systems | Maintains obligate anaerobes; essential for representative fermentation | Use anaerobic chambers or sealed systems with oxygen indicators; pre-reduce media [25] |
| Reference Metabolites | Quantification standards for microbial metabolites (e.g., SCFAs, phenolic acids) | Source certified standards; prepare fresh stock solutions; include internal standards [25] [27] |
| Polysaccharide Purification Kits | Isolate high-purity polysaccharides from natural sources | Confirm structural integrity after purification; check for protein contamination [26] |
| 16S rRNA Sequencing Kits | Monitor microbial community changes during biotransformation | Select appropriate variable region; include positive controls; plan bioinformatics pipeline [25] |
| UPLC-MS/MS Systems | Sensitive detection and quantification of diverse microbial metabolites | Optimize MRM transitions for target analytes; use HILIC and reverse-phase methods [25] |
| Amlodipine-d4 | Amlodipine-d4 Deuterated Standard|1 | Amlodipine-d4 is a deuterium-labeled internal standard for precise MS quantification in ADME studies. For Research Use Only. Not for diagnostic or therapeutic use. |
| Crystal Violet-d6 | Crystal Violet-d6, CAS:1266676-01-0, MF:C25H30ClN3, MW:414.0 g/mol | Chemical Reagent |
Table 1: Key Microbial Metabolites from Phenolic and Polysaccharide Biotransformation
| Parent Compound | Key Microbial Metabolites | Concentration Range | Biological Significance |
|---|---|---|---|
| Grape Seed Polyphenols | 3-HBA, 3-HPP | Detected in brain tissue | Promotes resilience against cognitive decline [25] |
| Green Tea Catechins | Polyhydroxyphenyl-γ-valerolactones | 10x higher than other conjugates in urine | Potential protection against oxidative damage in adipocytes [25] |
| Mulberry Anthocyanins | Protocatechuic, vanillic, p-coumeric acids | Varies with microbiota composition | Dependent on specific gut bacteria for conversion [25] |
| Dietary Polysaccharides | Acetate, propionate, butyrate (SCFAs) | mM range in gut lumen | Immune modulation, energy metabolism, gut barrier function [27] |
Table 2: Optimized Experimental Conditions for Biotransformation Assays
| Parameter | Polyphenol Studies | Polysaccharide Studies | Critical Factors |
|---|---|---|---|
| Incubation Time | 24-48 hours | 48-72 hours | SCFA production increases with longer fermentation [25] [27] |
| Substrate Concentration | 1-2 mg/mL | 1% (w/v) | Higher concentrations may inhibit microbial growth [25] [26] |
| Inoculum Density | 10% (v/v) | 10% (v/v) | Standardized across experiments for reproducibility [25] |
| Key Analytical Methods | UPLC-MS/MS for phenolic acids | GC-FID for SCFAs | Method validation essential for accurate quantification [25] [27] |
Innovative Formulation Technologies: Engineering Enhanced Delivery Systems
Frequently Asked Questions (FAQs)
Q1: What are the primary advantages of using nanoencapsulation for functional food ingredients? Nanoencapsulation enhances the stability, solubility, and bioavailability of functional food ingredients, many of which are hydrophobic and unstable in harsh processing or digestive conditions [30]. It protects bioactive compounds from environmental degradation (e.g., light, oxygen, pH fluctuations) and enables controlled or targeted release at the desired site in the gastrointestinal tract, thereby improving their therapeutic efficacy [31].
Q2: How do I select the most suitable nanocarrier for my bioactive compound? The selection depends on the physicochemical properties of your bioactive compound (hydrophilic vs. hydrophobic) and your application goals [32] [31]:
- Liposomes are ideal for encapsulating both hydrophilic (in the aqueous core) and hydrophobic (in the lipid bilayer) compounds [32] [33].
- Solid Lipid Nanoparticles (SLNs) and Nanostructured Lipid Carriers (NLCs) offer high biocompatibility and are particularly suitable for lipophilic compounds, with NLCs providing improved drug loading capacity over SLNs by using a blend of solid and liquid lipids [32].
- Polymeric Nanoparticles (e.g., those made from PLGA, chitosan) offer high structural precision, tunable release profiles, and protection against enzymatic degradation [34].
Q3: What are the most critical parameters to characterize for nanocarrier formulations? Key parameters include [35]:
- Size and Size Distribution: Affects stability, cellular uptake, and biodistribution.
- Surface Charge (Zeta Potential): Indicates colloidal stability and influences interaction with biological membranes.
- Encapsulation Efficiency: Measures the fraction of successfully encapsulated bioactive.
- Physical Stability: Assesses aggregation or degradation under storage conditions.
- Sterility and Endotoxin Levels: Critical for in vivo applications to avoid immunogenic reactions [35].
Q4: A common problem is the instability of nanoemulsions. How can this be addressed? Nanoemulsion instability can be mitigated by optimizing the emulsifier type and concentration, controlling processing conditions (e.g., homogenization pressure, energy input), and formulating with stabilizers like weighting or ripening inhibitors [32]. High-pressure homogenization and ultrasonication are common methods to produce stable nanoemulsions with small droplet sizes (≤100 nm) [32].
Q5: What are the major challenges in scaling up nanoencapsulation processes for industrial production? Challenges include ensuring batch-to-batch consistency, achieving cost-effective production at large scale, maintaining the physicochemical properties (size, PDI, encapsulation efficiency) during scale-up, and meeting stringent regulatory and safety requirements for food or pharmaceutical applications [35] [34]. Techniques like high-pressure homogenization are easier to scale than methods like ionic gelation [32] [34].
Troubleshooting Guides
Common Synthesis and Purification Issues
The table below summarizes frequent issues encountered during the preparation of nanocarriers, their potential causes, and recommended solutions.
Table 1: Troubleshooting Guide for Nanocarrier Synthesis and Purification
| Problem | Potential Causes | Recommended Solutions |
|---|---|---|
| Large Particle Size & High Polydispersity [35] | Inefficient emulsification or homogenization; Aggregation during synthesis; Incorrect lipid:polymer ratio. | Increase homogenization pressure/cycles; Use a more efficient surfactant; Optimize solvent displacement parameters; Filter through a sterile membrane (e.g., 0.45 or 0.22 µm). |
| Low Encapsulation Efficiency [32] | Rapid precipitation of bioactive; Leakage during synthesis; Mismatch between bioactive lipophilicity and core material. | Modify the core composition (e.g., use NLCs over SLNs); Add the bioactive at a specific stage in the process; Increase the concentration of the wall material. |
| Endotoxin Contamination [35] | Use of non-sterile reagents/equipment; Contaminated water (not LAL-grade/pyrogen-free); Synthesis in a non-aseptic environment. | Work under a biological safety cabinet; Use depyrogenated glassware and sterile filters; Test all reagents, especially water and commercial starting materials, for endotoxin. |
| Physical Instability (Aggregation/Ostwald Ripening) [32] | Low zeta potential (inadequate surface charge); Inadequate stabilizer; Storage at high temperatures. | Optimize pH and ionic strength of the dispersion medium; Incorporate steric stabilizers (e.g., PEG); Store formulations at 4°C. |
Characterization and Analytical Challenges
Accurate characterization under biologically relevant conditions is essential for meaningful data.
Table 2: Troubleshooting Guide for Nanocarrier Characterization
| Problem | Potential Causes | Recommended Solutions |
|---|---|---|
| Inconsistent Sizing Results [35] | Technique-specific artifacts (e.g., DLS overweighs large aggregates); Nanoparticle interference in assays; Analysis in non-physiological buffers. | Use multiple techniques (e.g., DLS, TEM, AFM) for cross-verification; Characterize in physiologically relevant media (e.g., plasma, PBS); Perform appropriate controls for assay interference. |
| Interference in LAL Endotoxin Assay [35] | Colored formulations interfere with chromogenic assays; Turbid samples interfere with turbidity assays; Cellulose-based filters introduce beta-glucans. | Switch LAL assay format (e.g., from chromogenic to gel-clot); Use Glucashield buffer to negate beta-glucan interference; Employ a recombinant Factor C assay. |
| Poor In Vitro-In Vivo Correlation | In vitro assays not mimicking in vivo conditions (e.g., protein corona formation); Premature release in simulated GI fluids. | Include biomolecule-containing media (e.g., serum) in stability studies; Use more complex in vitro digestion models (e.g., TIM-1) to better predict bioavailability [30]. |
Experimental Protocols
This is a standard method for producing multi-lamellar vesicles (MLVs) that can be downsized to small unilamellar vesicles (SUVs).
Objective: To prepare nanoliposomes for the encapsulation of hydrophilic or hydrophobic bioactive compounds.
Materials:
- Phospholipid (e.g., Soy phosphatidylcholine)
- Cholesterol (to enhance membrane stability)
- Chloroform or other organic solvent
- Rotary Evaporator with a round-bottom flask
- Water Bath Sonicator or High-Pressure Homogenizer
- Buffer Solution (e.g., Phosphate Buffered Saline, PBS, for hydration)
Method:
- Dissolution: Dissolve the phospholipid and cholesterol (e.g., in a 7:3 molar ratio) in chloroform in a round-bottom flask.
- Thin Film Formation: Attach the flask to a rotary evaporator. Evaporate the solvent under reduced pressure at a temperature above the lipid transition temperature (e.g., 40-45°C for soy PC) to form a thin, uniform lipid film on the inner wall of the flask.
- Hydration: Continue rotation under vacuum for at least 30 minutes to remove any trace of solvent. Hydrate the dry lipid film with an aqueous buffer (pre-heated to above the lipid transition temperature) containing the hydrophilic bioactive to be encapsulated. Rotate gently for 1 hour to hydrate and form multilamellar vesicles (MLVs).
- Size Reduction: Sonicate the MLV dispersion using a probe sonicator in an ice bath (to prevent overheating) for 10-30 minutes until the solution becomes translucent. Alternatively, extrude the suspension through polycarbonate membranes (e.g., 100 nm pore size) using a high-pressure extruder to obtain a uniform population of SUVs.
- Purification: Separate the non-encapsulated material using dialysis, size exclusion chromatography, or centrifugation.
Visualization: Liposome Preparation Workflow
This is a robust and scalable method for producing SLNs.
Objective: To produce solid lipid nanoparticles for the encapsulation of lipophilic bioactives.
Materials:
- Solid Lipid (e.g., Glyceryl monostearate, Compritol)
- Surfactant (e.g., Poloxamer 188, Tween 80)
- High-Pressure Homogenizer
- Heating Mantles
Method:
- Melt Dispersion: Melt the solid lipid at approximately 5-10°C above its melting point.
- Aqueous Phase: Heat the aqueous surfactant solution to the same temperature as the lipid melt.
- Pre-Emulsification: Add the hot aqueous phase to the molten lipid under high-speed stirring to form a coarse pre-emulsion.
- High-Pressure Homogenization: Pass the hot pre-emulsion through a high-pressure homogenizer for 3-5 cycles at a pressure of 500-1500 bar while maintaining the temperature.
- Cooling and Crystallization: Allow the resulting nanoemulsion to cool down to room temperature (or 4°C) under mild stirring. The lipid droplets solidify, forming SLNs.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Nanoencapsulation Research
| Reagent/Material | Function/Application | Key Considerations |
|---|---|---|
| Phospholipids (e.g., Phosphatidylcholine) | Primary building block for liposomes and nanoliposomes [33]. | Source (soy, egg) and purity affect consistency and stability. Use hydrogenated phospholipids for higher oxidative stability. |
| Solid Lipids (e.g., Compritol, Precirol) | Form the solid matrix of SLNs and NLCs [32]. | The crystalline structure of the lipid impacts drug loading and release kinetics. |
| Biodegradable Polymers (e.g., PLGA, Chitosan) | Form the core of polymeric nanoparticles [34]. | Molecular weight, copolymer ratio (for PLGA), and degree of deacetylation (for chitosan) determine degradation and release profiles. |
| Surfactants (e.g., Poloxamer 188, Tween 80) | Stabilize nanoemulsions and prevent aggregation of nanoparticles during and after formation [32]. | Must be non-toxic and approved for the intended application (food/pharma). HLB value determines suitability for O/W or W/O systems. |
| Cholesterol | Incorporated into lipid bilayers (liposomes) to modify membrane fluidity and enhance physical stability [33]. | Typically used at a molar ratio of 0.1:1 to 0.5:1 (Cholesterol:Phospholipid). |
| Cross-linkers (e.g., Tripolyphosphate - TPP) | Used in ionic gelation to cross-link polymers like chitosan, forming stable nanoparticles [36]. | Concentration and addition rate control particle size and uniformity. |
| Salicyluric acid-13C2,15N | 2-Hydroxy Hippuric Acid-13C2,15N Isotope | 2-Hydroxy Hippuric Acid-13C2,15N, a stable isotope-labeled tracer for metabolic and proteomic research. For Research Use Only. Not for diagnostic or human use. |
| Trimethylammonium chloride-d9 | Trimethylammonium chloride-d9, CAS:18856-86-5, MF:C3H10ClN, MW:104.63 g/mol | Chemical Reagent |
Decision Pathway for Nanocarrier Selection
The following diagram outlines a logical workflow for selecting the most appropriate nanocarrier system based on the properties of the bioactive compound and the desired release profile, all within the context of optimizing bioavailability.
Visualization: Nanocarrier Selection Pathway
Micellar Solubilization and Emulsion-Based Delivery for Lipophilic Compounds
Troubleshooting Guides and FAQs
Frequently Asked Questions
Q1: Why is my micellar formulation precipitating, and how can I improve its stability?
A: Precipitation often occurs due to drug loading exceeding the solubilization capacity of the micelles or instability upon dilution. To address this:
- Check Drug Loading: Ensure the drug concentration does not surpass the capacity of the micellar core. The solubilized amount should be determined experimentally in the specific surfactant system [37].
- Optimize Surfactant Combination: Use mixed surfactant systems. Combining ionic and non-ionic surfactants can improve micellar stability and drug loading capacity [38].
- Consider Hydrophilic Corona: Incorporate polymers like polyethylene glycol (PEG) in the shell. A PEG corona provides steric stabilization, reducing micelle aggregation and disassembly upon dilution, which is a common cause of precipitation [39].
Q2: My emulsion-based delivery system has a low drug encapsulation efficiency. What factors should I investigate?
A: Low encapsulation efficiency for lipophilic compounds typically stems from suboptimal formulation or process parameters.
- Match Drug and Oil Phase: Select an oil in which the drug has high solubility. Pre-formulation solubility studies in various oils are crucial [40] [41].
- Optimize Emulsifier Type and Concentration: The emulsifier must sufficiently reduce interfacial tension. Non-ionic surfactants like Tweens (polysorbates) are often used. Ensure the concentration is well above the Critical Micelle Concentration (CMC) for effective nanoemulsion formation [37] [42].
- Control Processing Conditions: Use high-energy methods like high-pressure homogenization to achieve smaller droplet sizes (r < 100 nm), which can enhance encapsulation and prevent drug crystallization [40].
Q3: How can I experimentally determine the Critical Micelle Concentration (CMC) of a surfactant, and why is it important?
A: The CMC is a critical parameter as it indicates the minimum surfactant concentration required for spontaneous micelle formation, which directly impacts drug solubilization.
- Standard Techniques: Two common methods are:
- Surface Tension Measurement: Plot surface tension against surfactant concentration. The CMC is identified at the point where the surface tension stops decreasing and forms a plateau [38].
- Conductivity Measurement: For ionic surfactants, plot specific conductivity against concentration. A distinct change in the slope of the plot indicates the CMC [38].
- Importance: Formulations should operate at concentrations above the CMC to ensure micelles are present to solubilize the drug. A low CMC is generally preferred for in vivo stability, as it prevents micellar disassembly upon dilution in the biological system [39].
Troubleshooting Common Experimental Issues
The table below summarizes specific problems, their potential causes, and evidence-based solutions.
| Problem | Potential Causes | Recommended Solutions |
|---|---|---|
| Low Drug Solubilization | Poor compatibility between drug and micelle core; Surfactant below CMC; Incorrect surfactant type. | Conduct drug solubility screening in different oils/surfactants [41]; Increase surfactant concentration above CMC [37]; Use surfactants with longer hydrophobic chains for larger micellar cores [37]. |
| Micelle / Nanoemulsion Instability (Aggregation) | Inadequate steric or electrostatic stabilization; High polydispersity; Dilution in physiological fluids. | Incorporate a PEG corona for steric hindrance [39]; Use charged surfactants (e.g., SDS) for electrostatic repulsion [38]; Employ precise homogenization techniques for uniform droplet size [40]. |
| Poor Bioavailability Despite High Drug Loading | Rapid drug precipitation in GI tract; Instability in pH gradients; Poor permeability. | Integrate polymers to increase kinetic stability; Use lipid-based systems (e.g., SNEDDS) that maintain drug in a solubilized state [9] [41]; Add permeability enhancers (e.g., bio-surfactants) [42]. |
| Drug Crystallization in Emulsion | Drug concentration exceeds solubility in carrier oil at storage/body temperature; Insufficient emulsifier. | Select an oil with higher drug solubility capacity [40]; Add co-solvents (e.g., ethanol, PEG) to the oil phase to enhance drug loading [40] [41]. |
Experimental Protocols for Formulation and Characterization
Protocol: Determination of Critical Micelle Concentration (CMC)
Objective: To determine the CMC of a surfactant using the surface tension method [38].
Materials:
- Surfactant solution of varying concentrations
- Surface tensiometer (e.g., Du Noüy ring or Wilhelmy plate)
- Thermostatted water bath
- Glassware
Methodology:
- Prepare a series of surfactant solutions with concentrations spanning a wide range (e.g., 0.1 mM to 10 mM).
- Equilibrate all solutions at a constant temperature (e.g., 25°C or 37°C) using a water bath.
- Measure the surface tension of each solution, starting from the most dilute to the most concentrated.
- Plot the surface tension (y-axis) against the logarithm of surfactant concentration (x-axis).
- Identify the CMC as the concentration at the intersection of the two linear segments of the plot—the point where the surface tension ceases its sharp decline.
Diagram: CMC Determination Workflow
Protocol: Preparation and Characterization of a Self-Nanoemulsifying Drug Delivery System (SNEDDS)
Objective: To formulate a SNEDDS to enhance the solubility and dissolution of a poorly water-soluble drug like Felodipine [41].
Materials:
- Lipophilic drug (e.g., Felodipine)
- Oils (e.g., cinnamon oil, oleic acid, isopropyl myristate)
- Surfactants (e.g., Tween 80, Tween 20)
- Co-surfactants/Co-solvents (e.g., PEG 400, ethanol, propylene glycol)
Methodology:
- Solubility Screening: Use the shake-flask method to determine the drug's equilibrium solubility in various oils, surfactants, and co-surfactants. Select the components that yield the highest drug solubility.
- Construction of Pseudo-Ternary Phase Diagram:
- Prepare mixtures of oil, surfactant, and co-surfactant (S~mix~) at different weight ratios (e.g., 1:1, 2:1, 3:1).
- Titrate these mixtures with aqueous phase (water) under gentle vortexing.
- After each addition, note the visual appearance (clear, transparent, or turbid) to identify the self-nanoemulsifying region.
- Plot the diagram using software to visualize the stable nanoemulsion zone.
- Formulation of SNEDDS: From the nanoemulsion region on the phase diagram, select a specific composition. Dissolve the drug in the isotropic mixture of oil, surfactant, and co-surfactant.
- Characterization of SNEDDS:
- Droplet Size Analysis: Use Dynamic Light Scattering (DLS) to confirm the formation of nano-sized droplets (typically < 100 nm).
- In Vitro Dissolution Study: Compare the drug release profile of the SNEDDS formulation against the pure drug using a dissolution apparatus. A successful SNEDDS should release over 95% of the drug within a short time (e.g., 20 minutes) [41].
Diagram: SNEDDS Development Workflow
The Scientist's Toolkit: Key Research Reagent Solutions
The table below lists essential materials and their functions for developing micellar and emulsion-based delivery systems.
| Category | Reagent / Material | Function / Rationale |
|---|---|---|
| Surfactants | Polysorbates (Tween 20, Tween 80) | Non-ionic surfactants; commonly used for forming micelles and stabilizing nanoemulsions. They provide a good safety profile and effective reduction of interfacial tension [37] [41]. |
| Sodium Lauryl Sulfate (SLS) | Anionic surfactant; useful for imparting a negative charge to droplets, preventing aggregation via electrostatic repulsion. Also used in solubility studies [37] [42]. | |
| Block Co-polymers (e.g., PEG-PLA, PEG-PCL) | Form polymeric micelles with a hydrophobic core (e.g., PLA, PCL) and a hydrophilic PEG corona. They offer low CMC, high stability, and prolonged circulation time [39]. | |
| Oils / Lipid Phases | Medium-Chain Triglycerides (MCT) | Commonly used as the oil phase in SNEDDS and nanoemulsions due to their good solubilizing capacity and ability to form fine dispersions [40] [41]. |
| Oleic Acid | A long-chain fatty acid; acts as an oil phase and can also serve as a permeability enhancer [41]. | |
| Co-Solvents / Co-Surfactants | Polyethylene Glycol (PEG 400) | A water-soluble co-solvent that enhances drug solubility in the pre-concentrate and can modify the viscosity of the system, aiding emulsification [41]. |
| Ethanol / Propylene Glycol | Short-chain co-solvents that increase the solvent capacity of the formulation and facilitate the formation of a microemulsion by penetrating the surfactant film [42] [41]. | |
| Characterization Tools | Dynamic Light Scattering (DLS) | Instrumental technique for determining the particle size, size distribution (PDI), and zeta potential of micelles and nanoemulsions [39] [42]. |
| Surface Tensiometer | Key instrument for determining the CMC of surfactants and assessing the effectiveness of emulsifiers [38]. | |
| Valorphin | Valorphin, CAS:144313-54-2, MF:C44H60N8O12, MW:893.0 g/mol | Chemical Reagent |
| Intedanib-d3 | Intedanib-d3 | Intedanib-d3 is a deuterated internal standard for LC-MS quantification of nintedanib in pharmacokinetic studies. For Research Use Only. Not for human use. |
Cyclodextrin Complexation and Hydrophilic Carrier Systems
Within research aimed at optimizing the bioavailability of functional food components, cyclodextrin (CD) complexation stands as a pivotal technology. These cyclic oligosaccharides possess a unique structure—a hydrophilic exterior and a hydrophobic interior cavity—that enables them to form inclusion complexes with a wide range of hydrophobic bioactive compounds [43] [44]. This interaction is fundamental to overcoming the primary challenge of poor water solubility, which severely limits the absorption and efficacy of many nutraceuticals [43] [45]. By enhancing solubility, stability, and bioavailability, cyclodextrin-based carrier systems directly contribute to developing more effective and reliable functional food ingredients [43] [44].
This technical support guide provides researchers with practical methodologies, troubleshooting advice, and essential data to facilitate the successful implementation of cyclodextrin complexation in experimental protocols.
Core Experimental Protocols
Phase Solubility Studies
Purpose: To determine the efficiency of complex formation between a bioactive compound and a cyclodextrin, and to calculate the stability constant (K1:1) of the resulting complex [46].
Detailed Methodology:
- Solution Preparation: Prepare a series of aqueous solutions containing increasing concentrations of the selected cyclodextrin (e.g., 0-200 mM for hydroxypropyl derivatives) [46]. Use deionized water or an appropriate buffer (e.g., phosphate buffer, pH 7.4) as the solvent.
- Saturation: Add an excess amount of the bioactive compound (the "guest" molecule) to each cyclodextrin solution. Include a control with no cyclodextrin to determine the intrinsic solubility (S0) of the compound.
- Equilibration: Seal the suspensions and agitate them continuously for a period of 7 days at a constant ambient temperature (e.g., 22-24°C) to ensure equilibrium is reached [46].
- Separation: After equilibration, allow the suspensions to settle and then filter through a 0.45 μm membrane filter to remove any undissolved excess compound.
- Analysis: Analyze the filtered solutions to determine the concentration of dissolved guest molecule. Techniques like High-Performance Liquid Chromatography (HPLC) with UV detection are commonly employed. The specific conditions (mobile phase, column, flow rate) will depend on the analyte [46].
Data Analysis: Construct a phase-solubility diagram by plotting the concentration of dissolved guest molecule against the concentration of cyclodextrin. The stability constant (K1:1) for a 1:1 complex can be calculated from the slope of the linear region of the plot and the intrinsic solubility (S0) using the following equation [46]:
K1:1 = Slope / [S0 (1 - Slope)]
The Complexation Efficiency (CE) can also be calculated as CE = Slope / (1 - Slope) and may provide a more precise evaluation for compounds with very low intrinsic solubility [46].
Preparation of Inclusion Complexes
Several methods can be used to prepare solid inclusion complexes for subsequent use in formulations.
- Kneading Method: The bioactive compound and cyclodextrin are mixed in a mortar with a small volume of solvent (e.g., water or ethanol) to form a paste. This paste is then kneaded for a specified time (e.g., 45-60 minutes) before being dried and sieved [43].
- Co-precipitation Method: The guest molecule is dissolved in a suitable organic solvent and added to an aqueous solution of cyclodextrin. The mixture is stirred vigorously for several hours (e.g., 24 hours) at a controlled temperature. The resulting precipitate (the inclusion complex) is then filtered, washed, and dried [43].
- Lyophilization (Freeze-Drying): A solution or suspension containing the complex is frozen and then subjected to a high vacuum to remove water by sublimation. This method is particularly suitable for heat-sensitive compounds and produces an amorphous powder that is easily reconstituted [46].
Confirmation of Complex Formation
Differential Scanning Calorimetry (DSC) is a widely used technique to confirm the formation of an inclusion complex [46]. In a DSC thermogram, the melting endotherm of the pure bioactive compound will diminish or disappear in the physical mixture and will be absent in the lyophilized complex, indicating that the guest molecule is no longer in its crystalline form but is incorporated into the cyclodextrin cavity [46].
Workflow Diagram: Cyclodextrin Inclusion Complexation
The following diagram illustrates the logical workflow for developing and analyzing a cyclodextrin-based delivery system.
Troubleshooting Guide & FAQs
FAQ 1: Why is the observed increase in my compound's solubility lower than expected?
- A1: Several factors can lead to suboptimal solubility enhancement.
- Incorrect Cyclodextrin Fit: The size and geometry of your bioactive molecule may not be compatible with the cavity size of the selected cyclodextrin. β-CD is often suitable for drug-sized molecules, but α- and γ-CD may be better for very small or large guests, respectively [43]. Consider screening different native and modified cyclodextrins.
- Weak Complexation: The stability constant (K1:1) may be too low, indicating a weak interaction. Using a modified cyclodextrin (e.g., HP-β-CD, SBE-β-CD) can often enhance complexation efficiency and solubility compared to native CDs [45] [46].
- Insufficient Equilibration Time: The system may not have reached equilibrium. Ensure adequate stirring time (up to 7 days as per protocol) [46].
FAQ 2: How can I improve the stability of a compound sensitive to oxidation or light?
- A2: The cyclodextrin cavity can act as a molecular barrier, shielding encapsulated compounds from external factors [43] [44]. For example, complexation with β-CD protected vitamin A palmitate from degradation caused by temperature, oxygen, and UV light [43] [44]. If stability remains an issue, ensure the sensitive part of the molecule is fully encapsulated within the hydrophobic cavity and consider using an antioxidant in the formulation.
FAQ 3: My complex is precipitating out of solution. What could be the cause?
- A3: Precipitation often indicates the formation of insoluble complexes, particularly with native β-cyclodextrin at higher concentrations, which displays a type B phase-solubility profile [46]. This can also occur if non-inclusion aggregates form. Switching to a more soluble cyclodextrin derivative, such as HP-β-CD or SBE-β-CD, which maintain high solubility across a wide concentration range, typically resolves this issue [45] [46].
FAQ 4: Are there computational methods to predict complexation performance before lab experiments?
- A4: Yes, modern computational approaches are increasingly valuable. Machine Learning models, such as Light Gradient Boosting Machine (LightGBM), can predict complexation free energy with high accuracy using molecular descriptors, saving experimental time [47]. Additionally, Molecular Dynamics Simulations (MDS) can provide insights into the geometry, thermodynamics, and stability of the complex by modeling the docking of the drug into the cyclodextrin cavity [46] [47]. The integration of both methods offers a powerful synergistic approach for formulation design [47].
Quantitative Solubility Enhancement Data
The table below summarizes experimental data demonstrating the solubility enhancement of various bioactive compounds achieved through cyclodextrin complexation, as reported in the literature.
Table 1: Experimentally Observed Solubility Enhancement via Cyclodextrin Complexation
| Active Substance | Water Solubility (mg/mL) | Solubility with Cyclodextrin (mg/mL) | Cyclodextrin Used | Fold Increase | Reference |
|---|---|---|---|---|---|
| Amphotericin B | 0.001 | 0.15 | SBE-β-CD | 150 | [43] |
| Itraconazole | 0.001 | 4-5 | HP-β-CD | ~4500 | [43] |
| Paclitaxel | 0.003 | 2.0 | HP-β-CD | ~667 | [43] |
| Ceftiofur | 0.03 | 2.18 | HP-β-CD | ~73 | [43] [45] |
| Dexamethasone | 0.1 | 2.5 | β-CD | 25 | [43] |
| Valsartan | Data not specified | Data not specified | HP-β-CD | 18 | [45] |
| Diclofenac | 4.0 | 20.0 | HP-β-CD | 5 | [43] |
| Chloramphenicol | Data not specified | Data not specified | SBE-β-CD | ~2-3 | [45] |
The Scientist's Toolkit: Key Research Reagents
This table lists essential materials and their functions for developing cyclodextrin-based delivery systems.
Table 2: Essential Reagents for Cyclodextrin Complexation Research
| Reagent / Material | Function / Explanation |
|---|---|
| Native Cyclodextrins (α-, β-, γ-CD) | Core host molecules for initial complexation screening. β-CD is most common for drug-sized molecules [43] [46]. |
| 2-Hydroxypropyl-β-CD (HP-β-CD) | A widely used, water-soluble derivative that improves complexation efficiency and reduces the renal toxicity risk associated with native β-CD [43] [45] [46]. |
| Sulfobutyl Ether-β-CD (SBE-β-CD) | An anionic, highly soluble derivative often used to enhance solubility and stability for a wide range of drugs, including antifungal and antibiotic compounds [43] [45]. |
| Randomly Methylated-β-CD (M-β-CD) | A methylated derivative with enhanced hydrophobic character and ability to solubilize compounds like ibuprofen; also used to disrupt cellular membranes [43] [45]. |
| Polymer Additives (e.g., Poloxamers) | Used as a third component to improve complex stability, control release, or aid in the formation of nanocarriers [43] [45]. |
| Amphiphilic Cyclodextrins | Chemically modified CDs with hydrophobic chains that can self-assemble into nanoparticles (nanospheres, nanocapsules), enabling advanced targeting and delivery [45]. |
| Polyrotaxanes | Supramolecular structures where CD rings are threaded onto a polymer chain. They show promise for high-efficiency cellular cholesterol removal and as advanced biomaterials [45]. |
| Cyclazodone-d5 | Cyclazodone-d5, MF:C12H12N2O2, MW:221.27 g/mol |
| Monoethyl phthalate-d4 | Monoethyl phthalate-d4, CAS:1219806-03-7, MF:C10H10O4, MW:198.21 g/mol |
3D/4D Printing for Precision Fabrication of Functional Food Matrices
Troubleshooting Guides & FAQs
Frequently Asked Questions
Q1: Why does my 3D printed structure lack detail and collapse after printing?
- A: This is typically a rheology and recovery issue. The food ink likely has an insufficient yield stress (should be between 500–1500 Pa) or poor thixotropic recovery, meaning it cannot quickly regain its gel-like structure after the shear force of extrusion ceases. To correct this, optimize your hydrocolloid content (e.g., starch, κ-carrageenan, gelatin) and ensure the formulation exhibits strong shear-thinning behavior [48] [49].
Q2: How can I protect heat-sensitive antioxidants (e.g., vitamins, polyphenols) during the extrusion printing process?
- A: The primary strategy is microencapsulation or using lipid-based delivery systems. Encapsulating sensitive compounds in a protective matrix (e.g., using proteins, polysaccharides, or liposomes) shields them from the thermal and mechanical shear stress of extrusion. Alternatively, consider using printing technologies with lower thermal impact, such as binder jetting or cold extrusion setups [50] [51].
Q3: My multi-material print with acidic and anthocyanin-rich components shows slow or incomplete color change. What is wrong?
- A: In 4D printing, the kinetics of pH-driven changes depend on ion mobility. Slow color change can result from high gel strength or low water mobility in the stimulating (acidic/alkaline) component, which hinders the diffusion of H+ or OH- ions. Reduce the starch or gelling agent concentration in the stimulating component to enhance water mobility and ion diffusion for a faster response [52].
Q4: How can I ensure the bioaccessibility of the encapsulated nutrients in the final 3D printed food?
- A: Bioaccessibility is maximized when the delivery system is designed for targeted release in the gastrointestinal tract. Use enteric coatings or materials that are resistant to gastric pH but degrade in the intestinal environment. Research indicates that mucus-penetrating or mucoadhesive delivery systems can significantly enhance the bioavailability of compounds like quercetin by improving their interaction with the intestinal wall [53] [51].
Q5: Why is there a consistency issue between different batches of the same food ink?
- A: Food materials are inherently variable. Batch inconsistency often stems from slight differences in the rheological properties of raw ingredients. Implement strict quality control of incoming materials and use precise, standardized preparation protocols. Characterizing each batch's rheology (yield stress, viscoelastic moduli) before printing is recommended for high-precision research [49].
Quantitative Data for Formulation Design
Table 1: Critical Rheological Parameters for Printability
This table summarizes the target rheological properties for successful extrusion-based 3D printing, crucial for structural integrity and precision [49].
| Printing Phase | Rheological Property | Target Value / Behavior | Function in Printing Process |
|---|---|---|---|
| Extrusion | Viscosity (under shear) | Shear-thinning behavior | Ensures easy flow through the nozzle under pressure. |
| Extrusion | Yield Stress (Ï„) | 500 - 1500 Pa | Material must overcome this stress to begin flowing from the nozzle. |
| Recovery | Thixotropy | High recovery rate | Measures how quickly the material regains its structure after extrusion. |
| Self-Supporting | Storage Modulus (G') | G' > Loss Modulus (G") | Indicates solid-like, elastic behavior to support subsequent layers. |
Table 2: Impact of Printing Technology on Bioactive Stability
The choice of printing technology directly influences the retention and stability of functional compounds [50].
| Printing Technology | Typical Process Conditions | Impact on Bioactives (e.g., Antioxidants) | Recommended Applications |
|---|---|---|---|
| Extrusion-Based | Moderate temp (40-80°C), High shear | Can degrade heat- and shear-sensitive compounds. | Robust bioactives, post-print infusion of sensitives. |
| Inkjet Printing | Low mechanical stress, Possible heat bursts | Minimal shear degradation; thermal risk depends on actuation. | Surface decoration, 2D patterns with water-soluble nutrients. |
| Binder Jetting | Room temperature, Low shear | Low thermal degradation; potential pH/solvent risks from binder. | Powder-based matrices (e.g., vitamins, probiotics in starch/sugar). |
| Selective Laser Sintering | Intense, localized heat | High risk of thermal degradation of most bioactives. | Primarily for thermostable materials like sugars and fats. |
Experimental Protocols for Bioavailability Optimization
Protocol 1: Microencapsulation of Curcumin for Enhanced Stability and Bioaccessibility
This protocol details the creation of a stable curcumin emulsion for incorporation into 3D printed foods, protecting the compound during processing and enhancing its bioavailability [52].
- Objective: To produce a curcumin-in-water emulsion that protects the bioactive from degradation during printing and enables controlled release.
- Materials:
- Curcumin powder (≥95% purity)
- Medium-chain triglycerides (MCTs)
- Tween 80
- Deionized water
- High-speed homogenizer (e.g., JHG-54-P100)
- High-pressure homogenizer
- Ultrasonic bath with ice
- Methodology:
- Water Phase Preparation: Dissolve Tween 80 in deionized water at a 2% (w/v) concentration. Hydrate for 4 hours.
- Oil Phase Preparation: Dissolve 1.5g of curcumin powder in MCT oil. Sonicate the mixture in an ice bath at 390 W for 30 minutes to ensure complete dissolution. Centrifuge at 3000 rpm for 2 minutes to remove any undissolved particles.
- Pre-Emulsification: Mix the water and oil phases in a 3:1 (w/w) ratio. Homogenize using a high-speed homogenizer for 6 minutes to create a coarse emulsion.
- High-Pressure Homogenization: Process the coarse emulsion through a high-pressure homogenizer for 4 cycles at 60 MPa to form a fine, stable nanoemulsion.
- Quality Control: Test the encapsulation efficacy by adding a 5% sodium bicarbonate solution to the emulsion. A rapid and homogeneous color change to red indicates successful encapsulation and protection of curcumin, which is pH-sensitive [52].
- Integration with 3D Printing: This emulsion can be directly mixed with food-grade hydrocolloids (e.g., potato starch, gelatin) to create a functional food ink for 3D printing. The emulsion protects curcumin during the printing process, and its release can be triggered by the alkaline environment in the intestine.
Protocol 2: Fabricating a pH-Responsive 4D Food System with Anthocyanins
This protocol describes the creation of a dual-component 3D printed structure that undergoes a rapid, microwave-triggered color change, demonstrating the principle of 4D printing for dynamic food presentation [52].
- Objective: To construct a 3D printed food that changes color automatically upon microwave heating, driven by pH diffusion.
- Materials:
- Potato flakes
- Blueberry anthocyanin (25% content)
- K-carrageenan gum (KG) and Xanthan gum (XG)
- Concentrated lemon juice
- Potato starch
- Dual-nozzle 3D printer (e.g., SHINNOVE-D1)
- Methodology:
- Stimuli-Responsive Ink (Upper Part): Prepare mashed potatoes (MPs) with a 4:1 water-to-potato-flake ratio. Add 1% (w/w) of a mixed hydrocolloid (KG:XG = 3:2). After heating and cooling the MPs, incorporate 0.1% (w/w) blueberry anthocyanin and mix thoroughly.
- Stimulating Ink (Lower Part): Prepare Lemon Juice-Starch Gel (LJSG) by adding 25-30g of potato starch to 100g of concentrated lemon juice. Cook the mixture at 97°C for 20 minutes to gelatinize the starch, then cool to room temperature. The starch concentration can be adjusted to control gel strength and H+ diffusion speed.
- 3D Printing & Triggering: Using a dual-nozzle printer, design a stacked structure (e.g., a 32x32x3 mm³ rectangle of anthocyanin-MP on top of an identical rectangle of LJSG). Print the structure. Post-process the printed object in a household microwave oven. The heat will accelerate the diffusion of H+ ions from the LJSG into the anthocyanin-MP, triggering a rapid color change from purple to red/pink.
- Key Parameters: The speed of color change is negatively correlated with the gel strength of the LJSG and positively correlated with anthocyanin concentration [52].
Workflow & Pathway Visualizations
Diagram 1: Bioactive Integration Workflow
Diagram 2: Bioactive Protection Strategies
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Functional Food Ink Development
This table catalogs key reagents and their specific functions in formulating advanced 3D/4D printable food inks for bioavailability research [48] [50] [52].
| Material Category | Example Reagents | Primary Function in Formulation | Key Considerations for Bioavailability |
|---|---|---|---|
| Gelling & Thickening Agents | κ-Carrageenan, Starch, Sodium Alginate, Gelatin, Xanthan Gum | Provides yield stress and viscoelasticity for shape fidelity; controls texture. | Alginate-Gelatin blends can form biocompatible hydrogels for cell-based foods or probiotic protection [54]. |
| pH-Responsive Pigments | Anthocyanins (from blueberry), Curcumin | Acts as a natural colorant and visual marker for pH changes in 4D printing. | Enables non-invasive monitoring of pH-driven release mechanisms in the GI tract [52]. |
| Lipid-Based Delivery Systems | Medium-Chain Triglycerides (MCTs), Tween 80, Phospholipids | Forms emulsions (O/W) or liposomes to solubilize and protect hydrophobic bioactives (e.g., curcumin, vitamins). | Mimics body's fat absorption pathways; significantly improves bioavailability of lipid-soluble compounds [52] [51]. |
| Protein & Cell-Based Bioinks | Whey Protein Isolate, Soy Protein, Microalgae (Chlorella, Spirulina), Animal Myoblasts (C2C12) | Provides nutritional fortification, scaffolds for cell culture, and structural matrix. | Microalgae and cultured cells are used to create hybrid foods with tailored, high-density nutrient profiles [54]. |
| Stimuli Agents | Lemon Juice (Citric Acid), Baking Soda (NaHCO3) | Provides the ionic (H+ or OH-) stimulus for triggering dynamic changes in 4D prints (color, shape). | The diffusion rate of ions can be engineered to control the site and rate of nutrient release [52]. |
| Cyclopropylmethyl bromide-d3 | (Bromomethyl-d2)cyclopropane-1-d1|Isotopic Labeled Reagent | High-quality deuterated reagent, (Bromomethyl-d2)cyclopropane-1-d1, for advanced research in medicinal chemistry and pharmacology. For Research Use Only. Not for human or veterinary use. | Bench Chemicals |
Green Extraction and Processing Techniques to Preserve Bioactivity
Troubleshooting Guide: Common Experimental Issues and Solutions
Green Extraction Techniques
Problem: Low extraction yield of bioactive compounds (e.g., resveratrol, polyphenols) using green techniques.
- Possible Cause 1: Incorrect solvent selection for the target compound.
- Possible Cause 2: Suboptimal parameters for ultrasound-assisted extraction (UAE).
- Solution: For resveratrol from vine shoots, optimal conditions were 62% amplitude, 6 min, 59% ethanol, 55°C, yielding 1.05 mg/g trans-resveratrol. Systematically optimize amplitude, time, and temperature using response surface methodology [55].
- Possible Cause 3: Inefficient microwave-assisted extraction (MAE) setup.
- Solution: For higher phenolic content including 1.32 mg/g trans-resveratrol, use 80°C, 4 min, 69% ethanol. Higher temperatures (155°C) increase yield but significantly raise energy consumption [55].
Problem: Poor selectivity of green extraction, co-extracting interfering compounds.
- Possible Cause: Green solvent insufficiently selective.
- Solution: Implement ultrasound-assisted aqueous two-phase extraction (UAATPE). For resveratrol from Polygonum cuspidatum, an ethanol-ammonium sulfate system achieved 99.1% recovery while minimizing sugar co-extraction [55].
Problem: Degradation of thermolabile bioactives during extraction.
- Possible Cause: Excessive thermal or mechanical stress.
Bioavailability Enhancement
Problem: Poor bioavailability of encapsulated bioactive compounds.
- Possible Cause 1: Inefficient nanoencapsulation system.
- Solution: Chitosan nanoparticles (CNPs) synthesized via ionic gelation provide excellent biocompatibility for targeted delivery. Optimize the cross-linking density to control release kinetics [57].
- Possible Cause 2: Insufficient predictive modeling of bioavailability.
- Solution: Implement AI-driven models including machine learning (Random Forest) and deep learning (graph neural networks) to predict absorption, metabolism, and bioactive peptide stability in the gastrointestinal tract [7].
Problem: Inconsistent results in bioavailability assessment.
- Possible Cause: Limitations of traditional in vitro digestion models.
- Solution: Complement in vitro models with AI techniques that integrate food composition, host physiology, and metabolic data to account for inter-individual variability [7].
Processing and Preservation
Problem: Loss of bioactivity during food processing and storage.
- Possible Cause: Thermal degradation of bioactive compounds.
- Solution: Utilize non-thermal technologies like Pulsed Electric Fields (PEF) and High-Voltage Electric Field Discharge (HVED) which modify protein structures while preserving bioactivity better than thermal processing [58].
- Possible Cause: Oxidative degradation.
- Solution: Incorporate plant-based bio-preservatives like essential oils (thymol, cinnamaldehyde) and polyphenols in edible coatings. For marine fish, basil essential oil extended shelf life from 6 to 12.8 days at 4°C [59].
Frequently Asked Questions (FAQs)
Q1: What are the most promising green solvents for bioactive compound extraction?
- A: The most promising green solvents include:
- Deep Eutectic Solvents (DES): Tunable solvents with high extraction efficiency for polyphenols [56]
- Supercritical COâ‚‚: Ideal for non-polar compounds, with ethanol as co-solvent for increased polarity [56]
- Ionic Liquids: High thermal stability and adjustable properties, though toxicity concerns require careful selection [56]
- Water: The greenest solvent, particularly effective when used with switchable polarity systems [56]
Q2: How can I quickly optimize extraction parameters for a new plant material?
- A: Implement Response Surface Methodology (RSM) with a central composite design to efficiently explore multiple parameters (solvent concentration, time, temperature, power) with minimal experimental runs. This approach was successfully used to optimize resveratrol extraction from vine shoots [55].
Q3: What nanotechnology approaches are most effective for enhancing bioavailability?
- A: Chitosan nanoparticles (CNPs) are particularly effective due to their GRAS status, mucoadhesive properties, and ability to be functionalized for targeted delivery. Synthesis methods include ionic gelation, polyelectrolyte complexation, and microemulsion techniques [57].
Q4: How can AI enhance traditional bioavailability studies?
- A: AI technologies provide significant advantages:
- Machine Learning: Predicts structure-bioavailability relationships and nutrient transport efficiency [7]
- Deep Learning: Models complex drug-target interactions and dissolution dynamics [7]
- Natural Language Processing: Mines scientific literature to identify novel bioactive compounds and interactions [7]
- Computer Vision: Analyzes cellular responses and compound distribution in tissues [7]
Experimental Protocols
Protocol 1: Ultrasound-Assisted Extraction of Resveratrol from Plant Materials
Principle: Ultrasound induces acoustic cavitation, disrupting cell walls and enhancing mass transfer of bioactive compounds into the solvent [55].
Materials:
- Plant material (e.g., grape shoots, Polygonum cuspidatum)
- Food-grade ethanol
- Ultrasonic probe system with temperature control
- Deep Eutectic Solvent (e.g., choline chloride:urea)
- Centrifuge and filtration equipment
Procedure:
- Sample Preparation: Dry and grind plant material to 0.5-1mm particle size.
- Solvent System: Prepare ethanol-water (59%) or DES solvent system.
- Extraction Parameters: Set ultrasonic processor to 62% amplitude, 55°C.
- Extraction: Process sample for 6 minutes with pulsed sonication (5s on, 2s off).
- Separation: Centrifuge at 5000xg for 10 minutes, collect supernatant.
- Concentration: Evaporate solvent under reduced pressure at 40°C.
- Analysis: Quantify resveratrol content via HPLC [55].
Protocol 2: Bioavailability Assessment Using AI-Enhanced Prediction
Principle: Machine learning models predict bioavailability by analyzing compound structure, food matrix interactions, and physiological factors [7].
Materials:
- Chemical structure data (SMILES notation)
- Molecular descriptors software
- Machine learning platform (Python/R with scikit-learn)
- Training datasets (ChEMBL, DrugBank)
- In vitro permeability assay validation system
Procedure:
- Data Collection: Compile structural descriptors and known bioavailability data for similar compounds.
- Feature Selection: Identify critical molecular descriptors (logP, polar surface area, H-bond donors/acceptors).
- Model Training: Implement Random Forest or Graph Neural Network using 80% of data for training.
- Validation: Test model performance with remaining 20% of data.
- Prediction: Input candidate compound structures to predict bioavailability.
- Experimental Validation: Confirm predictions with Caco-2 cell monolayer assays [7].
Table 1: Comparison of Green Extraction Techniques for Bioactive Compounds
| Extraction Method | Target Compound | Optimal Conditions | Yield/Recovery | Key Advantages |
|---|---|---|---|---|
| Ultrasound-Assisted Extraction (UAE) | trans-Resveratrol | 62% amplitude, 6 min, 59% ethanol, 55°C [55] | 1.05 mg/g [55] | Lower temperature, shorter time |
| Microwave-Assisted Extraction (MAE) | trans-Resveratrol | 80°C, 4 min, 69% ethanol [55] | 1.32 mg/g [55] | Higher phenolic content |
| Ultrasound-Assisted Aqueous Two-Phase Extraction (UAATPE) | Resveratrol | Ethanol-ammonium sulfate system [55] | 99.1% recovery [55] | High selectivity, minimal sugar co-extraction |
| Surfactant-Assisted UAE | Resveratrol from peanut skin | 3% surfactant, 25:1 mL/g, 250W, 30°C [55] | Enhanced yield | Integrates extraction and bioconversion |
Table 2: Bioavailability Enhancement Strategies
| Strategy | Mechanism | Efficacy/Outcome | Considerations |
|---|---|---|---|
| Nanoencapsulation in Chitosan Nanoparticles | Enhanced solubility, targeted delivery, mucoadhesion [57] | Improved stability and controlled release [57] | GRAS status, tunable release kinetics |
| AI-Predictive Modeling | Structure-bioactivity relationship prediction [7] | Accurate peptide stability forecasting in GI tract [7] | Reduces need for in vivo trials |
| Polyphenol Nanoencapsulation | Protection from degradation, enhanced absorption [60] | Improved therapeutic effectiveness [60] | Maintains antioxidant activity |
| Essential Oil Bio-preservation | Antimicrobial and antioxidant activity [59] | Extended shelf life of fish by 113% [59] | Natural alternative to chemical preservatives |
Workflow Diagrams
Green Extraction and Bioavailability Workflow
Bioavailability Pathway and Enhancement
Research Reagent Solutions
Table 3: Essential Research Reagents for Green Extraction and Bioavailability Studies
| Reagent/Material | Function/Application | Key Features | References |
|---|---|---|---|
| Deep Eutectic Solvents (DES) | Green solvent for polyphenol extraction | Tunable polarity, biodegradable, high extraction efficiency | [55] [56] |
| Chitosan Nanoparticles | Nanoencapsulation for bioavailability enhancement | GRAS status, mucoadhesive, functionalizable surface | [57] |
| Essential Oils (Thymol, Oregano) | Natural bio-preservatives | Antimicrobial, antioxidant, extends shelf life | [59] |
| Ionic Liquids | Green extraction solvents | Thermal stability, adjustable properties | [56] |
| Supercritical COâ‚‚ | Non-polar compound extraction | Non-toxic, tunable with co-solvents | [56] |
| AI/ML Platforms | Bioavailability prediction | Predictive modeling of absorption and metabolism | [7] |
Overcoming Development Challenges: From Laboratory to Commercial Formulation
Addressing Chemical Instability and Rapid Metabolism of Bioactives
This technical support center provides troubleshooting guides and FAQs to help researchers overcome key challenges in optimizing the bioavailability of functional food components.
Troubleshooting Guides
Guide 1: Addressing Poor Water Solubility of Bioactives
Problem: Low aqueous solubility of bioactive compounds leading to poor dissolution and limited absorption in the gastrointestinal tract.
Symptoms: Low systemic concentration despite high oral dosing, inconsistent experimental results, poor correlation between in vitro and in vivo data.
Solution: Implement nano-formulation strategies to enhance solubility and dissolution rates.
Experimental Protocol: Green O/W Nanoemulsion Synthesis for Octacosanol [61]
- Preparation: Dissolve 1g octacosanol in 10mL medium-chain triglyceride (MCTG) oil as the oil phase.
- Emulsification: Heat the oil phase to 65°C. Separately, heat an aqueous solution containing 1.5g Tween 80 and 0.5g soy lecithin to the same temperature.
- Homogenization: Slowly add the aqueous phase to the oil phase with high-speed stirring at 10,000 rpm for 5 minutes using a digital disperser.
- Microfluidization: Process the coarse emulsion using a microfluidizer at 15,000 psi for three cycles to form a fine nanoemulsion.
- Characterization: Determine droplet size and distribution via dynamic light scattering (DLS). Measure zeta potential using electrophoretic light scattering. Analyze stability by storing at 4°C, 25°C, and 40°C for 30 days with periodic size measurements.
Expected Outcomes: Nanoemulsions can achieve droplet sizes <200 nm, significantly enhancing bioaccessibility. For octacosanol, this method increased serum concentration to 417 ng/mL at 1 hour post-administration in rat models, compared to negligible levels for unformulated compound [61].
Guide 2: Overcoming Rapid Metabolism and Elimination
Problem: Bioactive compounds undergo extensive first-pass metabolism and rapid systemic clearance, reducing their therapeutic window.
Symptoms: Short plasma half-life, low oral bioavailability, presence of multiple metabolites in plasma, reduced efficacy.
Solution: Utilize colloidal delivery systems to protect compounds from metabolic degradation.
Experimental Protocol: Liposome Formulation for Phenolic Compounds [62]
- Lipid Film Formation: Dissolve phosphatidylcholine (PC) and cholesterol (70:30 molar ratio) in chloroform in a round-bottom flask. Remove organic solvent under reduced pressure using a rotary evaporator (40°C) to form a thin lipid film.
- Hydration: Hydrate the lipid film with a phosphate buffer saline (PBS, pH 7.4) containing 5mg/mL of the target phenolic compound (e.g., curcumin). Rotate the flask for 1 hour at 60°C above the transition temperature of the lipids.
- Size Reduction: Sonicate the multilamellar vesicle suspension using a probe sonicator on ice (10 cycles of 30 seconds pulse, 30 seconds rest) or extrude through polycarbonate membranes (100-400 nm) using a liposome extruder.
- Purification: Separate unencapsulated compound using gel filtration chromatography (Sephadex G-50) or dialysis against PBS for 4 hours.
- Characterization: Determine encapsulation efficiency via HPLC after disruption of liposomes with methanol. Measure particle size and PDI by DLS. Confirm membrane integrity using microscopy.
Expected Outcomes: Liposomal encapsulation can improve bioavailability 5-10 fold compared to native compounds. For curcuminoids, liposomes typically achieve 70-80% encapsulation efficiency and significantly enhance stability in simulated intestinal fluids [63].
Frequently Asked Questions (FAQs)
FAQ 1: What are the most effective formulation strategies for compounds with both low solubility and chemical instability?
Answer: Combined matrix systems offer the best protection. Solid Lipid Nanoparticles (SLNs) are particularly effective as they provide a solid matrix at body temperature that protects against degradation while enhancing solubility [61]. For example, soy protein isolate/octacosanol nanocomplexes demonstrated enhanced physical stability in neutral conditions by forming hydrogen bonds and hydrophobic interactions, protecting the core material from environmental stress [61].
FAQ 2: How can I validate whether my bioavailability enhancement strategy is working in vitro before moving to animal studies?
Answer: Implement a sequential in vitro testing protocol:
- Solubility/Dissolution Test: Use shake-flask method or USP dissolution apparatus II to measure concentration in simulated gastric and intestinal fluids.
- Bioaccessibility Assay: Subject the formulation to simulated gastrointestinal digestion (INFOGEST protocol) and measure the fraction present in the digestible fraction after ultracentrifugation.
- Permeability Assessment: Use Caco-2 cell monolayers in Transwell plates to determine apparent permeability coefficient (Papp). A significant increase in Papp compared to unformulated compound indicates successful absorption enhancement.
- Metabolic Stability: Incubate with liver microsomes or hepatocytes and measure parent compound disappearance over time.
FAQ 3: What are the key differences between enhancing bioavailability for polar versus non-polar bioactive compounds?
Answer: The optimization strategy differs significantly based on compound polarity:
Table: Bioavailability Enhancement Strategies by Compound Polarity
| Characteristic | Non-Polar Compounds (e.g., Octacosanol, Curcumin) | Polar Compounds (e.g., Polyphenols, Bioactive Peptides) |
|---|---|---|
| Primary Limitation | Poor water solubility, crystallization in GI tract | Poor membrane permeability, enzymatic degradation |
| Optimal Formulation | Nanoemulsions, SLNs, self-emulsifying systems | Liposomes, nanoencapsulation, permeation enhancers |
| Key Excipients | Medium-chain triglycerides, surfactants (Tweens, lecithins) | Phospholipids, chitosan, cyclodextrins |
| Stability Concern | Oxidation, precipitation | Hydrolysis, enzymatic degradation |
| Absorption Pathway | Primarily lymphatic transport | Paracellular/transcellular transport |
FAQ 4: How do I determine whether to focus on solubility enhancement or metabolism inhibition for a specific compound?
Answer: Conduct preliminary pharmacokinetic studies to identify the primary limiting factor. After administering the pure compound in animal models:
- If you observe high parent compound concentration in the GI tract but low plasma levels → Focus on solubility and permeability enhancement
- If the compound disappears rapidly from the GI tract but has high metabolite-to-parent ratio in plasma → Focus on metabolism inhibition using nanoencapsulation or enzyme inhibitors
- If both issues are present → Implement a combined strategy like lipid-based nanoemulsions with polymeric coatings [61] [63]
Experimental Protocols & Data Analysis
Quantitative Analysis of Bioavailability Enhancement
Table: Efficacy Comparison of Bioavailability Enhancement Strategies [61] [62] [63]
| Strategy | Model Compound | Technical Approach | Bioavailability Improvement | Key Measurement Parameters |
|---|---|---|---|---|
| Nanoemulsions | Octacosanol | Green O/W nanoemulsion with Tween 80/lecithin | Serum concentration: 417 ng/mL vs. negligible (1h post-dose) | Droplet size: 150-200 nm; PDI <0.2; Zeta potential: > -30mV |
| Liposomal Encapsulation | Curcuminoids | Thin-film hydration with PC/cholesterol | 5-10x increase in AUC compared to native compound | Encapsulation efficiency: 70-80%; Size: 100-400 nm; Sustained release over 24h |
| Solid Lipid Nanoparticles | Octacosanol | Soy protein isolate nanocomplex | Enhanced stability in neutral conditions; retained bioactivity | Hydrogen bonding confirmation (FTIR); Controlled release profile |
| Nanosuspensions | Poorly soluble bioactives | Anti-solvent precipitation followed by homogenization | 3-5x increase in dissolution rate | Crystalline state (PXRD); Particle size: 200-500 nm; Enhanced saturation solubility |
Advanced Workflow for Systematic Bioavailability Optimization
The following diagram illustrates a comprehensive experimental workflow for addressing bioavailability challenges, integrating multiple strategies from the troubleshooting guides:
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Materials for Bioavailability Enhancement Research
| Research Reagent | Function & Application | Example Use Cases |
|---|---|---|
| Tween 80 & Lecithin | Non-ionic surfactant and natural emulsifier for nanoemulsions | Stabilizing oil-in-water nanoemulsions for lipophilic compounds like octacosanol [61] |
| Phosphatidylcholine (PC) | Primary phospholipid for liposomal formulations | Creating lipid bilayers for encapsulating both hydrophilic and hydrophobic compounds [62] |
| Medium-Chain Triglycerides (MCTG) | Lipid phase for lipid-based delivery systems | Enhancing lymphatic transport of poorly soluble compounds [61] |
| Chitosan | Mucoadhesive polymer for enhancing GI retention | Improving permeability of polar compounds through tight junction modulation [62] |
| Soy Protein Isolate | Natural polymer for nanocomplex formation | Creating stable delivery systems through hydrogen bonding and hydrophobic interactions [61] |
| Cyclodextrins | Molecular encapsulation hosts for solubility enhancement | Forming inclusion complexes with poorly soluble compounds [63] |
| PLGA Nanoparticles | Biodegradable polymer for controlled release | Sustained release delivery systems protecting compounds from metabolism [62] |
Optimizing Tissue Distribution and Targeting for Specific Health Benefits
Core Concepts in Bioavailability Optimization
What are the key differences between bioaccessibility, bioavailability, and bioactivity?
- Bioaccessibility: The fraction of a compound released from its food matrix during digestion that becomes available for intestinal absorption. This represents the maximum amount available for potential absorption. [64]
- Bioavailability: The proportion of an ingested nutrient or bioactive compound that reaches systemic circulation and is delivered to target tissues for physiological activity. It encompasses absorption, metabolism, distribution, and excretion. [64] [65]
- Bioactivity: The specific physiological effect exerted by the absorbed compound on target tissues or organs, such as antioxidant, anti-inflammatory, or immunomodulatory actions. [64]
How does the Biopharmaceutics Classification System (BCS) guide formulation strategy?
The BCS categorizes compounds based on their solubility and permeability characteristics, which directly informs the selection of appropriate bioavailability enhancement technologies. [66]
Table: Biopharmaceutics Classification System (BCS) and Corresponding Strategies
| BCS Class | Solubility | Permeability | Key Challenges | Recommended Enhancement Technologies |
|---|---|---|---|---|
| Class I | High | High | Limited need for enhancement | Conventional formulations often sufficient |
| Class II | Low | High | Dissolution rate-limited absorption | Solid dispersions, nano-sizing, lipid-based systems, crystal engineering [66] |
| Class III | High | Low | Permeability-limited absorption | Permeation enhancers, efflux transporter inhibitors [67] |
| Class IV | Low | Low | Both solubility and permeability challenges | Combined approaches (e.g., solid dispersions with permeation enhancers) [67] [66] |
Experimental Approaches & Methodologies
Protocol: Development of Amorphous Solid Dispersions for Bioavailability Enhancement
The following protocol details the development of amorphous solid dispersions (ASDs), a prominent technique for improving solubility and dissolution rates of poorly soluble bioactive compounds. [67]
Materials: Active compound, polymer carriers (e.g., Co-povidone VA 64, HPMCAS, Soluplus), surfactant (e.g., Vitamin E TPGS), organic solvent (e.g., methanol, ethanol, acetonitrile). [67]
Equipment: HPLC system with UV detector, spray dryer or rotary evaporator, differential scanning calorimetry (DSC), X-ray powder diffractometry (XRPD), dissolution apparatus, biorelevant dissolution media (FaSSGF, FaSSIF). [67]
Procedure:
- Pre-formulation Analysis:
- Determine solubility of the active compound in various organic solvents and aqueous media with different pH values.
- Characterize solid-state properties (melting point, crystallinity, polymorphism) using DSC and XRPD.
Polymer Screening:
- Prepare small-scale binary mixtures of the active compound with various polymers (typically in 1:1 to 1:3 drug:polymer ratios).
- Use solvent evaporation method to create solid dispersions.
- Evaluate miscibility and potential interactions using DSC and FTIR.
Preparation of Solid Dispersions:
- Dissolve calculated amounts of active compound and selected polymer in appropriate organic solvent.
- Remove solvent using spray drying or rotary evaporation under optimized conditions.
- Collect the resulting solid dispersion and dry under vacuum to remove residual solvent.
Characterization:
- Assess solid state (amorphous/crystalline) by XRPD.
- Determine glass transition temperature (Tg) by DSC.
- Evaluate dissolution performance in biorelevant media compared to unformulated active compound.
Formulation Optimization:
- Incorporate surfactants (e.g., 5-10% Vitamin E TPGS) to further enhance wettability and permeability.
- Optimize drug-to-polymer ratio based on dissolution performance and physical stability.
Quantitative Comparison of Bioavailability Enhancement Technologies
Table: Efficacy Comparison of Bioavailability Enhancement Technologies
| Technology | Mechanism of Action | Typical Bioavailability Improvement | Key Advantages | Limitations |
|---|---|---|---|---|
| Amorphous Solid Dispersions | Creates high-energy amorphous form with increased solubility | 30-50% for BCS Class II/IV drugs [67] | Significant dissolution enhancement, commercial feasibility | Physical stability concerns, potential for crystallization |
| Lipid-Based Systems (SMEDDS/SNEDDS) | Pre-dissolves compound in lipid vehicles, enhances lymphatic transport | 2-5 fold increase for lipophilic compounds [66] | Bypasses hepatic first-pass metabolism, improves permeability | Limited drug loading, stability challenges |
| Nano-sizing Technologies | Increases surface area for dissolution via particle size reduction | 40-70% for poorly soluble compounds [66] | Applicable to wide compound range, established technology | Potential for Ostwald ripening, physical instability |
| Cyclodextrin Complexation | Forms inclusion complexes improving aqueous solubility | 2-3 fold increase for appropriate compounds [66] | Well-characterized, protects against degradation | Limited to appropriately sized molecules, potential toxicity at high doses |
| Polymeric Micelles | Encapsulates compounds in hydrophobic core, enhances solubility and permeability | 3-4 fold increase for targeted delivery [68] | Dual functionality (solubility + targeting), controlled release | Critical micelle concentration limitations, stability issues |
Protocol: In Vivo Pharmacokinetic Study for Bioavailability Assessment
Objective: To evaluate the bioavailability enhancement of a formulated bioactive compound compared to its conventional form. [67]
Materials: Test formulation, reference standard, animal model (e.g., Wistar rats), appropriate anesthetic, heparinized blood collection tubes, HPLC-MS/MS system for analysis. [67]
Procedure:
- Study Design:
- Use a crossover design with appropriate washout period between administrations.
- Divide animals into two groups: Test formulation and reference formulation.
- Administer formulations at equivalent doses via oral gavage.
Sample Collection:
- Collect blood samples (0.2-0.5 mL) at predetermined time points: pre-dose, 0.25, 0.5, 1, 2, 4, 8, 12, and 24 hours post-administration.
- Centrifuge blood samples immediately to separate plasma.
- Store plasma at -80°C until analysis.
Bioanalytical Method:
- Develop and validate HPLC-MS/MS method for quantification of the bioactive compound and its major metabolites.
- Use protein precipitation or liquid-liquid extraction for sample preparation.
- Ensure linearity, accuracy, and precision meet acceptance criteria.
Pharmacokinetic Analysis:
- Calculate AUC0-t (area under the curve from zero to last measurable time point) using the trapezoidal rule.
- Determine Cmax (maximum concentration) and Tmax (time to reach Cmax) directly from concentration-time data.
- Calculate absolute bioavailability using the formula: F = (AUCoral × DoseIV) / (AUCIV × Doseoral) × 100 [65]
Statistical Analysis:
- Use ANOVA to compare pharmacokinetic parameters between test and reference formulations.
- Consider results statistically significant when p < 0.05.
Troubleshooting Common Experimental Challenges
Problem: Recrystallization of Amorphous Formulations During Storage
Possible Causes:
- Inadequate polymer selection with insufficient crystallization inhibition properties
- High residual solvent content acting as plasticizer
- Storage conditions at high humidity or temperature variations
- Drug loading exceeding polymer's ability to maintain amorphous state
Solutions:
- Optimize polymer selection based on crystallization driving force (CDF) and glass transition temperature (Tg) [67]
- Implement secondary polymers (e.g., 5-10% Vitamin E TPGS) to enhance physical stability [67]
- Ensure thorough drying to minimize residual solvent (typically <2%)
- Use appropriate packaging with desiccants and moisture barrier properties
- Consider adding crystallization inhibitors like PVP-VA or HPMCAS [66]
Problem: In Vitro-In Vivo Correlation (IVIVC) Failure
Possible Causes:
- Non-discriminatory dissolution method not reflecting gastrointestinal conditions
- Failure to account for supersaturation and precipitation in GI tract
- Permeability limitations not addressed in formulation design
- Species differences in physiology and metabolism
Solutions:
- Implement biorelevant dissolution media (FaSSGF, FaSSIF) to simulate gastrointestinal environment [67]
- Include precipitation inhibitors in formulation (e.g., polymers like HPMCAS)
- Conduct permeability studies using Caco-2 models or parallel artificial membrane permeability assay
- Consider species-specific differences when extrapolating animal data to humans
Problem: Poor Chemical Stability in Formulated Product
Possible Causes:
- Chemical degradation accelerated by amorphous state
- Incompatibility between active compound and excipients
- Moisture-induced degradation
- Oxidation of labile functional groups
Solutions:
- Conduct pre-formulation compatibility studies using DSC and FTIR
- Incorporate antioxidants (e.g., ascorbic acid, BHT) for oxidation-prone compounds
- Use oxygen-impermeable packaging and nitrogen purging
- Optimize pH of microenvironment in solid dispersions
Visualization of Key Pathways and Workflows
Bioavailability Enhancement Decision Pathway
Bioactive Compound Absorption and Targeting Pathway
The Scientist's Toolkit: Essential Research Reagents & Materials
Table: Key Research Reagents for Bioavailability Enhancement Studies
| Reagent Category | Specific Examples | Primary Function | Application Notes |
|---|---|---|---|
| Polymer Carriers | Co-povidone VA 64, HPMCAS, Soluplus, HPMC, PVP-VA | Stabilize amorphous state, inhibit crystallization, enhance dissolution | Selection based on drug-polymer miscibility, Tg, and crystallization inhibition capacity [67] [66] |
| Surfactants & Permeation Enhancers | Vitamin E TPGS, Polysorbate 80, Labrafac Lipophile WL 1349 | Improve wettability, inhibit efflux transporters (P-gp), enhance membrane permeability | Vitamin E TPGS particularly effective for P-gp inhibition; typically used at 5-10% w/w [67] |
| Lipid Excipients | Medium-chain triglycerides, Transcutol HP, Labrafac lipophile WL 1349 | Enhance lymphatic transport, improve solubility of lipophilic compounds | Critical for lipid-based drug delivery systems (SMEDDS/SNEDDS) [67] [66] |
| Biorelevant Media | FaSSGF, FaSSIF, FeSSIF | Simulate gastrointestinal conditions for predictive dissolution testing | Essential for establishing in vitro-in vivo correlations [67] |
| Analytical Standards | HPLC-grade solvents, ammonium acetate, reference standards | Quantification of drug and metabolites in biological matrices | Method validation required for accuracy, precision, and sensitivity [67] |
Frequently Asked Questions
What are the most critical parameters to monitor when scaling up amorphous solid dispersions?
Critical parameters include maintaining consistent particle size distribution, ensuring residual solvent levels remain within specifications, monitoring polymorphic stability during processing, and confirming that the glass transition temperature (Tg) remains sufficiently high to prevent crystallization during storage. Process parameters such as inlet temperature, feed rate, and atomization pressure must be carefully controlled during spray drying. [67] [69]
How can I determine whether poor solubility or poor permeability is the primary limitation for my compound?
Conduct a bidirectional permeability assay using Caco-2 cells or similar model. If the compound shows high permeability but low absorption in vivo, solubility is likely the limiting factor. Conversely, if the compound has good solubility but poor permeability, then permeability is the primary issue. For BCS Class IV compounds, both limitations exist and require combined strategies. [67] [66]
What is the typical timeframe for observing bioavailability improvement in animal studies?
Pharmacokinetic studies in animal models typically span 24-48 hours for single-dose administration, with blood sampling at multiple time points. For chronic studies assessing tissue distribution and accumulation, study durations of 1-4 weeks are common, depending on the compound's elimination half-life and target tissue accumulation kinetics. [67]
How do functional food matrices differ from pharmaceutical formulations in bioavailability optimization?
Functional foods face additional challenges including potential interactions with food components, sensitivity to processing conditions, and regulatory constraints on excipient use. Food matrices may also provide natural enhancement through inherent lipids, emulsifiers, or other components that can improve bioaccessibility. However, they also present stability challenges during shelf life and variable effects under different dietary conditions. [60] [64] [70]
Strategies for Masking Off-Flavors and Improving Sensory Properties
FAQs on Bitterness and Off-Flavor Management
What are the primary causes of off-flors in functional food components? Many bioactive compounds and drugs are inherently bitter due to their chemical structure. Humans possess approximately 25 different bitter taste receptors (TAS2Rs) designed to detect a wide range of potentially toxic compounds [71]. Ingredients like alkaloids, polyphenols, flavonoids, amino acids, and minerals are common culprits that activate these receptors, resulting in unpleasant, sharp, or lingering bitterness [71] [72].
How can I selectively mask bitterness without affecting the active ingredient's potency? Bitterness can be suppressed without compromising potency through several targeted approaches:
- Bitter Blockers: Compounds like homoeriodictyol or derivatives from allspice act as antagonists at TAS2R receptors, physically blocking the bitter signal before it is transmitted [72].
- Physical Encapsulation: Technologies like microencapsulation, liposomes, or hydrogel matrices physically separate the bitter compound from taste receptors in the mouth. The encapsulation breaks down after swallowing, allowing for release and absorption later in the digestive system [71] [51].
- Strategic Flavor Pairing: Using complementary tastes, such as combining natural sweeteners (e.g., stevia) with acids (e.g., citric acid) or incorporating umami notes, can create a harmonious flavor profile that distracts from or balances bitterness [72].
Why is sensory evaluation critical, and what are common pitfalls? Sensory evaluation is essential because it provides the data linking a product's sensory properties to consumer acceptance [73]. Common challenges include:
- Subjectivity and Panelist Selection: Individual taste preferences and sensitivities vary greatly. Using untrained panelists or those who are not frequent users of the product category can introduce significant variability and risk [74] [73].
- Environmental Factors: Factors like lighting, noise, and temperature can influence perception. Tests should be conducted in a controlled environment [74].
- Panelist Fatigue: Mentally exhausting evaluations can reduce accuracy. Sessions should be kept short with adequate breaks [74].
Troubleshooting Guides
Problem: Encapsulated Ingredient is Still Perceived as Bitter
Potential Cause and Solution
| Potential Cause | Recommended Action | Key Considerations |
|---|---|---|
| Premature Release in Mouth | Reformulate the encapsulant material to improve its stability in saliva. Consider polymers, lipids, or soy protein isolate-based nanocomplexes that are more resistant to the oral environment [71] [61]. | Conduct a descriptive analysis test with a trained panel to pinpoint the specific sensory attribute causing the issue (e.g., "late-breaking bitterness") [73]. |
| Insufficient Encapsulation Coverage | Optimize the core-to-wall ratio in your microencapsulation process. Explore nano-encapsulation techniques for a more complete and uniform barrier [51]. | The required loading capacity of the active ingredient must be balanced against the level of taste masking needed. |
| Inefficient Binding | For lipid-based encapsulates, ensure the bitter compound is sufficiently hydrophobic to be effectively bound. For systems using cyclodextrins or polymers, verify molecular compatibility for inclusion complex formation [71]. | Binding efficacy is concentration-dependent; confirm that the ratio of masking agent to bitterant is adequate [71]. |
Problem: Formulation Has Unacceptable Mouthfeel
Potential Cause and Solution
| Potential Cause | Recommended Action | Key Considerations |
|---|---|---|
| Astringency or Grittiness | Incorporate texturizing agents like pectin, xanthan gum, or modified starches. These can create a smoother, creamier texture that coats the palate and mitigates harsh sensations [72]. | A discrimination test (e.g., duo-trio test) can determine if the mouthfeel modification creates a significant sensory difference from a control sample [75]. |
| Low Viscosity Leading to Rapid Bitterant Release | Increase the viscosity of liquid formulations. This can delay the release of bitter compounds, allowing sweet or favorable flavor notes to be perceived first [72]. | Use a descriptive analysis panel to quantify attributes like "thickness," "smoothness," and "coating" [75]. |
Problem: New "Clean-Label" Formula is Less Palatable
Potential Cause and Solution
| Potential Cause | Recommended Action | Key Considerations |
|---|---|---|
| Removal of Effective Artificial Maskers | Replace synthetic sweeteners and masking agents with natural alternatives. Explore plant-based hydrogel technologies (e.g., FenuMat from fenugreek fiber) or natural bitter blockers [72] [51]. | Consumer hedonic testing is crucial to verify that the new, naturally masked product is as liked as the original [75] [73]. |
| Incompatible Flavor System | Re-engineer the flavor system using strategic pairing. Consider globally inspired, bold flavors like yuzu, hibiscus, or tamarind that can align with clean-label values while effectively masking [72]. | Flavor preferences are regional; ensure the new profile is tested with the target demographic [72]. |
Experimental Protocols for Key Evaluations
Protocol 1: Discrimination Testing for Formulation Changes
Objective: To determine if a change in processing or an ingredient (e.g., a new encapsulant) results in a perceivable sensory difference.
Methodology:
- Panel Recruitment: Use a minimum of 20-30 untrained panelists who are above-average users of the product category [73].
- Sample Presentation: In a controlled sensory booth, present each panelist with three coded samples. Two samples are identical (the control, A), and one is the test product (B). The presentation order (AAB, ABA, BAA, etc.) must be randomized and balanced across all panelists [75] [73].
- Task: Instruct the panelist to identify the odd sample.
- Replication: Have each panelist perform the test multiple times (replication) to increase the reliability of the data [73].
- Data Analysis: Use a binomial distribution to analyze the number of correct responses. A statistically significant number of correct identifications (p < 0.05) indicates a perceivable difference between the control and the test product [75].
Protocol 2: Descriptive Analysis for Profiling Off-Flavors
Objective: To identify and quantify the specific sensory attributes (e.g., type of bitterness, aroma, mouthfeel) that differentiate products.
Methodology:
- Panel Training: Recruit and extensively train 10-12 panelists over multiple sessions. Training involves term generation and consensus on a standardized vocabulary (lexicon) to describe the products, and practice in scoring attribute intensity [73].
- Sample Evaluation: In replicated sessions (typically 3-4 replicates), trained panelists evaluate the products in a balanced presentation order. They score the intensity of each attribute in the lexicon using a structured scale (e.g., 0-15 points) [73].
- Data Collection and Analysis: Collect data using computerized systems. Perform Analysis of Variance (ANOVA) for each attribute to identify which sensory properties differ significantly between products. Results are often visualized via sensory maps (e.g., spider plots) [75] [73].
The Scientist's Toolkit: Key Research Reagent Solutions
The following table details essential materials and technologies used in developing taste-masked, bioavailable functional foods.
| Reagent/Technology | Function & Mechanism | Example Applications |
|---|---|---|
| Bitter Blockers | Antagonists that bind to human bitter taste receptors (TAS2Rs), blocking signal transduction [72]. | Masking caffeine, green tea extracts, minerals (e.g., Mg salts), and branched-chain amino acids [72]. |
| Liposomes | Spherical vesicles with a phospholipid bilayer that encapsulates hydrophilic and hydrophobic compounds, protecting them from degradation and delaying taste release [51]. | Delivery of herbal phytonutrients, curcumin, CoQ10, and fish oils [51]. |
| Micelles | Microscopic, water-compatible structures formed by surfactants that encapsulate lipid-soluble actives, enhancing solubility and bioavailability by mimicking fat absorption [51]. | Formulating curcumin, vitamins, and CoQ10 in clear, stable beverages and shots [51]. |
| Hydrogel Technology | A plant-based, self-emulsifying matrix that creates a protective barrier around bioactives, improving stability and enabling sustained release [51]. | Effective for berberine, resveratrol, and curcumin; suitable for powders, gummies, and capsules [51]. |
| Cyclodextrins | Oligosaccharides with a hydrophobic cavity that forms inclusion complexes with bitter molecules, physically shielding them from taste receptors [71] [63]. | Complexation with compounds like curcuminoids to improve both solubility and mask bitterness [63]. |
| Soy Protein Isolate (SPI) | Used to form nanocomplexes with hydrophobic compounds, enhancing physical stability in neutral conditions and potentially masking taste [61]. | Documented use in forming stable nanocomplexes with octacosanol [61]. |
Leveraging AI for Predictive Modeling of Structure-Activity Relationships
In the field of functional food research, optimizing the bioavailability of bioactive compounds is a fundamental challenge. Bioavailability—the proportion of an active component that enters circulation and reaches the target site—determines the efficacy of functional ingredients. Artificial Intelligence (AI) has emerged as a transformative tool for predicting complex Structure-Activity Relationships (SAR) that govern the absorption, distribution, metabolism, and excretion (ADME) of these compounds. This technical support center provides researchers with practical guidance for implementing AI-driven approaches to overcome common experimental challenges in bioavailability optimization.
Frequently Asked Questions (FAQs)
Q1: What are the most effective AI modeling approaches for predicting the bioavailability of food bioactive compounds?
Multiple machine learning (ML) approaches have demonstrated strong performance in predicting bioavailability. Research indicates that ensemble methods consistently outperform other models for this application.
Table 1: Performance Comparison of AI Models for Bioavailability Prediction
| Model Type | Reported Accuracy/Prediction Power | Key Strengths | Best Applications |
|---|---|---|---|
| Random Forest | R² = 0.87, RMSE = 0.08 [76] | Handles high-dimensional data, robust to outliers | General bioavailability prediction, feature importance analysis |
| Gradient Boosting | High predictive accuracy [76] | Sequential error correction, high precision | Complex non-linear relationships in absorption |
| Neural Networks | Variable performance [76] | Captures complex patterns in large datasets | Large-scale multi-omics data integration |
| Quantum Mechanics/Molecular Dynamics (QM/MD) | >90% accuracy for technology selection [77] | Precise molecular-level interaction modeling | Solubility enhancement, ligand binding prediction |
Q2: Which molecular features have the greatest impact on bioavailability predictions?
Feature importance analysis consistently identifies several key molecular descriptors as most influential for bioavailability prediction:
- Topological Polar Surface Area (TPSA): A critical predictor of intestinal absorption and blood-brain barrier permeability [76]
- Solubility parameters: Particularly dose number at specific pH levels and dissolution characteristics [78]
- Permeability measures: Especially effective permeability, which influences transport across intestinal epithelium [78]
- Acid dissociation constant (pKa): Affects ionization state and absorption potential at different gastrointestinal pH levels [78]
Q3: How can we address the challenge of limited bioavailability data for novel food compounds?
Several strategies can mitigate data scarcity issues:
- Transfer Learning: Leverage models pre-trained on pharmaceutical compounds with similar structural properties [7]
- Data Augmentation: Generate simulated data through in silico methods to expand training datasets [76]
- Multi-omics Integration: Combine genomic, proteomic, and metabolomic data to create richer feature sets [79]
- Semi-supervised Learning: Utilize both labeled and unlabeled data to improve prediction reliability [80]
Troubleshooting Guides
Problem: Poor Model Performance Despite High-Quality Structural Data
Symptoms: Low R² values, high root mean square error (RMSE), inaccurate predictions on validation set
Solution Checklist:
- Verify Feature Selection: Ensure inclusion of top predictive features identified in research: TPSA, solubility, permeability [76] [78]
- Check Data Balance: Address class imbalance through techniques like SMOTE or weighted loss functions
- Validate Data Splitting: Implement stratified splitting to maintain distribution of key features across training and test sets
- Consider Ensemble Methods: Shift from single models to ensemble approaches like Random Forest, which demonstrate superior performance for bioavailability prediction [76]
Problem: Discrepancy Between Predicted Bioavailability and Observed Bioactivity
Symptoms: Compounds with favorable predicted bioavailability show limited efficacy in vitro/in vivo
Solution Checklist:
- Incorporate Protein-Polyphenol Interactions: Model binding interactions that affect compound release and activity [79]
- Integrate Gut Microbiome Metabolism: Account for bacterial transformation of compounds using microbiome data [7] [60]
- Implement Multi-omics Approaches: Combine proteomic and metabolomic profiling to capture system-level effects [79]
- Validate with Advanced In Vitro Models: Use complex gut models (e.g., gut-on-a-chip) that better simulate human physiology [7]
Experimental Protocols
Protocol 1: Developing a Machine Learning Workflow for Bioavailability Prediction
This protocol outlines the KNIME-based computational workflow validated in recent research for predicting bioactive compound bioavailability [76].
Materials and Reagents:
- Dataset of 475+ drug-like compounds with known bioavailability values
- Molecular descriptor calculation software (e.g., RDKit, PaDEL)
- KNIME Analytics Platform with machine learning extensions
- Cross-validation framework (5-fold recommended)
Procedure:
- Data Collection and Curation
- Compile dataset of compounds with experimentally determined bioavailability
- Calculate key molecular descriptors: TPSA, molecular weight, logP, H-bond donors/acceptors, rotatable bonds
- Apply FAIR (Findable, Accessible, Interoperable, and Reusable) data principles [76]
Feature Selection
Model Training and Validation
- Implement multiple algorithms: Random Forest, Gradient Boosting, Neural Networks
- Apply 5-fold cross-validation to assess performance
- Select best-performing model based on R² and RMSE metrics
Model Interpretation
- Analyze feature importance to identify key bioavailability drivers
- Validate predictions with external test set
- Deploy model for novel compound screening
Protocol 2: Multi-omics Integration for Bioavailability-Bioactivity Correlation
This protocol leverages integrated multi-omics approaches to bridge the gap between predicted bioavailability and observed biological activity [79].
Materials and Reagents:
- UHPLC-QTOF-MS system for metabolomic profiling
- Proteomics equipment for protein binding studies
- Microbiome sequencing platform (16S rRNA or shotgun metagenomics)
- Data integration software (e.g., MOFA, mixOmics)
Procedure:
- Compound Characterization
- Perform comprehensive structural profiling using LC-MS
- Identify potential protein-binding sites through limited proteolysis-mass spectrometry (LP-MS) [79]
- Characterize interaction partners using affinity chromatography
In Vitro Digestion Simulation
- Subject compounds to simulated gastrointestinal digestion
- Monitor degradation products and transformation metabolites
- Assess bioaccessibility at different digestion phases
Microbiome Interaction Mapping
- Incubate compounds with human gut microbiota cultures
- Sequence microbiome to identify transforming organisms
- Track microbial metabolites using metabolomic approaches
Data Integration and Modeling
- Integrate genomic, proteomic, and metabolomic datasets
- Build predictive models linking structural features to absorption and metabolism
- Validate predictions with in vivo data when available
Research Reagent Solutions
Table 2: Essential Research Reagents and Computational Tools for AI-Driven Bioavailability Research
| Reagent/Tool | Function | Application Notes |
|---|---|---|
| KNIME Analytics Platform | Workflow-based data analytics | Enables creation of reproducible ML workflows without extensive coding [76] |
| Quadrant 2 Platform | AI/ML-based formulation prediction | Uses QM/MD and QSAR models; >90% accuracy for technology selection [77] |
| Random Forest Algorithm | Ensemble machine learning | Demonstrates highest predictive performance (R² = 0.87) for bioavailability [76] |
| SWATH-MS Proteomics | Comprehensive protein quantification | Identifies protein-polyphenol interactions affecting bioavailability [79] |
| UHPLC-QTOF-MS | High-resolution metabolomics | Profiles bioactive compounds and their metabolites in complex samples [79] |
| MOFA (Multi-Omics Factor Analysis) | Multi-omics data integration | Uncover hidden structures in heterogeneous omics data [79] |
Workflow Diagrams
AI-Driven Bioavailability Prediction Workflow
Multi-Omics Data Integration for Bioavailability
Frequently Asked Questions (FAQs) for Researchers
FAQ 1: What are the primary sources of inter-individual variability that complicate the prediction of bioactive compound bioavailability?
Inter-individual variability is a significant challenge in precision nutrition. The key factors influencing bioavailability are summarized in the table below.
Table 1: Key Factors Causing Inter-Individual Variability in Bioavailability
| Factor Category | Specific Examples | Impact on Bioavailability |
|---|---|---|
| Gut Microbiome | Composition & metabolic capacity [81] [82] | Determines production of bioactive metabolites (e.g., SCFAs); affects metabolism of compounds like l-carnitine [81]. |
| Host Genetics | LCT (lactase) gene variants [81] | Influences persistence of lactase enzyme, affecting digestion of lactose and correlating with Bifidobacterium abundance [81]. |
| FUT2 (fucosyltransferase) gene variants [81] | Affects mucus composition, correlating with abundance of specific bacteria like Ruminococcus torques [81]. | |
| Long-Term Diet | High-fiber vs. Western diet (high fat, processed) [81] | Strongly shapes microbiome composition and diversity, thereby influencing its metabolic output [81]. |
| Medication Use | Proton pump inhibitors, laxatives, metformin [81] | Can directly or indirectly (e.g., by altering gut transit time) cause significant shifts in bacterial species [81]. |
| Geographical Location | Regional differences [81] | A major confounding factor, explaining ~5x more variation in microbiomes than the next largest factor (e.g., occupation) [81]. |
FAQ 2: How can we model and predict personalized bioavailability given this high variability?
Traditional in vivo and in vitro models are limited in cost and ability to simulate complex, individualized physiological environments [7]. Artificial Intelligence (AI) and machine learning models now offer a powerful alternative by predicting complex relationships between nutrient structure, host physiology, and absorption.
Table 2: AI/ML Approaches for Bioavailability Prediction
| AI Technology | Application in Bioavailability Research |
|---|---|
| Machine Learning (ML) | Establishes structure-bioavailability connections by integrating molecular features with pharmacokinetic descriptors [7]. |
| Deep Learning (DL) | Models complex, non-linear drug-target interactions and dissolution dynamics, overcoming limitations of linear regression [7]. |
| Natural Language Processing (NLP) | Mines vast scientific literature to identify novel ingredient interactions and health correlations [60] [7]. |
| Computer Vision (CV) | Used with spectroscopic data (e.g., Raman, FTIR) to predict drug release from delivery systems and detect contaminants [7]. |
Experimental Protocol: Predicting Peptide Bioavailability with AI
Objective: To utilize a machine learning model to identify and predict the bioavailability of bioactive peptides from a protein hydrolysate.
Materials:
- Data Source: Broad bean protein hydrolysate.
- Software/Tools: Machine learning software (e.g., Python with scikit-learn, TensorFlow, or PyTorch).
- Validation Method: In vivo trials to confirm model predictions [7].
Methodology:
- Data Collection & Featurization: Generate a library of peptides from broad bean hydrolysates. Define molecular features (descriptors) for each peptide, such as:
- Molecular weight
- Amino acid sequence
- Hydrophobicity
- Charge
- Model Training: Train a deep learning model using a dataset of known bioactive peptides. The model will learn to correlate the molecular features of the peptides with their known bioavailability and bioactivity.
- Prediction & Screening: Input the features of the broad bean-derived peptides into the trained model. The model will output a prediction of their bioavailability and potential bioactivity.
- Validation: Synthesize the top-ranking peptides identified by the AI model and validate their bioavailability and efficacy using in vivo trials [7].
FAQ 3: Our clinical trials show inconsistent responses to a probiotic intervention. How can we stratify responders from non-responders?
Differential responses to interventions like probiotics are common and can often be traced to baseline host characteristics [81]. The following workflow outlines a systematic approach to investigate this.
Experimental Protocol: Stratifying Intervention Responders via Baseline Microbiome
Objective: To identify baseline host features (microbiome, genetics) that predict responsiveness to a specific nutritional intervention.
Materials:
- Cohort: >100 participants with varying metabolic health statuses.
- Standardized Meal: Contains precise macronutrients (carbs, fats, proteins).
- Sampling Kits: For blood collection (e.g., dried blood spot (DBS) kits for home use) [83].
- Analysis Platforms: Next-generation sequencer for 16S rRNA or shotgun metagenomics [82], LC-MS/MS for metabolomics.
Methodology:
- Baseline Characterization: Prior to intervention, collect:
- Microbiome Profile: Fecal sample for 16S rRNA or shotgun metagenomic sequencing to assess baseline composition and metabolic gene abundance [82].
- Host Genetics: DNA from blood or saliva for genotyping (e.g., LCT, FUT2 SNPs) [81].
- Dynamic Metabolic Phenotyping: After an overnight fast, administer a standardized meal. Collect blood samples at fasting and at multiple postprandial intervals (e.g., 5 time points). Analyze for glucose, lipids, amino acids, and other metabolites [83].
- Intervention: Administer the nutritional intervention (e.g., probiotic strain) for a predefined period.
- Endpoint Measurement: Measure primary outcome(s) (e.g., change in LDL cholesterol, improvement in insulin sensitivity).
- Data Integration & Analysis: Cluster participants into responders and non-responders based on endpoint measurement. Use multivariate statistical models and machine learning to identify which baseline features (from Step 1) are most predictive of responsiveness.
The Scientist's Toolkit: Key Research Reagents & Materials
Table 3: Essential Reagents and Materials for Precision Nutrition Research
| Item Name | Function/Application |
|---|---|
| Dried Blood Spot (DBS) Cards | Enables simple, at-home collection of blood samples for cost-effective, high-throughput analysis of >40 nutritional markers (vitamins, fatty acids, amino acids) without cold chain [83]. |
| Standardized Meal Test Kit | A formulated meal with precise macronutrient composition used for dynamic metabolic phenotyping to capture individual postprandial responses beyond static fasting measures [83]. |
| DNA/RNA Shield Kit | Stabilizes microbial DNA/RNA in fecal samples during storage and transport, preserving an accurate snapshot of microbiome composition for subsequent sequencing [82]. |
| 16S rRNA Sequencing Kit | Targets and sequences hypervariable regions of the 16S rRNA gene for cost-effective, culture-independent identification and relative quantification of bacterial taxa in a sample [82]. |
| Shotgun Metagenomics Kit | Sequences all DNA in a sample, enabling not only taxonomic profiling at the species level but also functional analysis of microbial communities (e.g., metabolic pathways) [82]. |
| AI/ML Modeling Software | Software platforms (e.g., Python with scikit-learn, TensorFlow) used to build predictive models of nutrient bioavailability and intervention response based on complex, multi-modal data [60] [7]. |
| Encapsulation Matrices | Materials (e.g., liposomes, polysaccharides) used to create delivery systems that protect bioactive compounds from degradation and enhance their stability and targeted release in the gut [60] [84]. |
Assessing Efficacy and Clinical Relevance: Validation Models and Comparative Analysis
In Vitro and In Vivo Models for Bioavailability and Bioactivity Assessment
Frequently Asked Questions (FAQs)
FAQ 1: What are the primary causes of poor correlation between in vitro dissolution data and in vivo bioavailability results? Poor correlation, often referred to as the in vitro-in vivo (IVIVC) gap, can stem from several factors [85]:
- Physiological Discrepancies: In vitro systems often fail to fully replicate the complex inner-environment of a living subject, including dynamic pH changes, gastrointestinal motility, and the presence of bile salts or microbial flora [85].
- Formulation-Related Factors: Interactions between the active pharmaceutical ingredient (API) and excipients, or changes in drug release kinetics due to physiological conditions not modeled in vitro (e.g., hydrodynamic forces in the GI tract).
- API Properties: Inadequate simulation of the dissolution, precipitation, and permeation processes of the API across the gut wall in the in vitro setup [86].
FAQ 2: How can I use computational tools to improve the predictive power of my in vitro models? Computational tools can significantly enhance IVIVC by creating mechanistic models that bridge the gap [87] [85]:
- IVIVC Toolkits: Software like the Phoenix IVIVC Toolkit uses numerical deconvolution and correlation models (Level A, B, C) to establish a quantitative relationship between in vitro dissolution and in vivo pharmacokinetic response, which can support biowaivers [87].
- Toxicogenomics (TGx) and Factorization Methods: Advanced bioinformatic strategies, such as post-modified non-negative matrix factorization (NMF), can analyze gene expression data. They help estimate and correct for the inner-environmental factors present in in vivo data, thereby improving the simulation of in vivo outcomes from in vitro TGx data [85].
- Physiologically-Based Pharmacokinetic (PBPK) Modeling: Tools like GastroPlus can be integrated with dissolution software (e.g., DDDPlus) to build a PBPK model that incorporates in vitro dissolution data to predict in vivo absorption and exposure, aiding in formulation optimization and quality-by-design (QbD) implementation [86].
FAQ 3: What are the key considerations when selecting an in vivo model for assessing the bioactivity of functional food components? Selecting an appropriate in vivo model requires careful consideration of the research objectives and the component's mechanism of action [88] [8]:
- Genetic and Physiological Relevance: The model organism should have relevant biological pathways (e.g., similar metabolic, immune, or neurological pathways) to humans for the target bioactivity. Genomic comparisons can identify conserved pathways [88].
- Disease Induction Method: For disease-prevention studies (e.g., cancer, neurological diseases), the method of inducing the disease state in the model (genetic, dietary, chemical) should accurately reflect the human condition being studied [8].
- Longitudinal Study Design: Many chronic diseases develop over time. Longitudinal studies that track the development of disease symptoms in relation to the administration of the functional food component are crucial for establishing causality and understanding long-term effects [88].
Troubleshooting Guides
Issue 1: Low Predictive Power of In Vitro Toxicogenomics (TGx) Assays
Problem: Gene expression data from in vitro assays (e.g., using cell lines like HepG2) shows poor similarity and correlation with data from in vivo animal models, limiting its utility for predicting in vivo toxicity [85].
Solution: Implement a bioinformatic strategy to correct for systemic differences.
- Recommended Approach: Utilize a post-modified Non-negative Matrix Factorization (NMF) method [85].
- Step-by-Step Protocol:
- Data Collection: Obtain gene expression profiles from both your in vitro system (e.g., cultured cells treated with the compound) and a corresponding in vivo system (e.g., liver tissue from treated animals).
- Factorize In Vivo Data: Apply the NMF algorithm to the in vivo TGx data. The goal is to factorize the data into two main components: one representing the "drug effect" and the other representing the "inner-environmental factor" (encompassing systemic physiological responses) [85].
- Estimate Environmental Factor: Isolate the gene expression profile associated with the inner-environmental factor from the in vivo data.
- Simulate In Vivo Data: Use the drug-effect profile from your in vitro data and combine it with the estimated inner-environmental factor profile from the in vivo data to generate a "simulated in vivo" gene expression profile.
- Validation: Compare the simulated in vivo data to the real in vivo data. Studies have shown this method can increase the similarity metric from 0.56 (direct comparison) to 0.72 for single-dose studies [85].
Table: Quantitative Improvement in Similarity Using NMF Strategy
| Data Comparison | Similarity (Single-Dose) | Similarity (Repeat-Doses) |
|---|---|---|
| In Vitro vs. In Vivo (Direct) | 0.56 | 0.70 |
| Simulated vs. In Vivo (Post-NMF) | 0.72 | 0.75 |
Issue 2: Developing a Predictive In Vitro-In Vivo Correlation (IVIVC) for Solid Dosage Forms
Problem: Formulation scientists struggle to establish a validated Level A IVIVC, which is critical for obtaining biowaivers from regulatory agencies (e.g., FDA, EMA) for formulation changes [87].
Solution: Adopt a standardized workflow using specialized IVIVC software to streamline model development and validation.
- Recommended Approach: Use a validated IVIVC software toolkit, such as the Phoenix IVIVC Toolkit [87].
- Step-by-Step Protocol:
- Input Data Preparation: Gather pharmacokinetic (PK) data from human or animal studies for at least two formulations with different release rates (e.g., rapid-release and slow-release). Collect corresponding in vitro dissolution profiles for these formulations [87].
- Numerical Deconvolution: Use the software's numerical deconvolution function to determine the in vivo drug absorption or dissolution time course from the PK plasma concentration data. This method is known for its stability and accuracy [87].
- Model Fitting (Level A Correlation):
- The software will guide you through fitting a correlation model that relates the in vitro dissolution profile to the in vivo dissolution profile.
- This typically involves comparing the mean in vivo dissolution time course to the mean in vitro dissolution time course.
- Predictive Model Validation:
- Use the established correlation to predict the in vivo performance of a third formulation, whose in vivo data was not used to build the model.
- Compare the predicted PK profile (e.g., Cmax, AUC) to the observed profile. The prediction error for these parameters should generally be less than 10% to demonstrate a successful IVIVC [87].
- Regulatory Submission: The validated model can be used to support biowaivers for post-approval changes (SUPAC), waive in vivo bioequivalence studies for lower strengths, and set clinically relevant dissolution specifications [87].
Issue 3: Assessing Bioactivity of Functional Food Components in Clinical Trials
Problem: Clinical trials for functional foods face significant confounding variables (e.g., diet, lifestyle) and often yield small or non-significant treatment effects, making it difficult to substantiate health claims [8].
Solution: Implement rigorous clinical trial designs and leverage bioinformatic analysis of high-throughput data to elucidate mechanisms.
- Recommended Approach: Enhance trial design sophistication and integrate multi-omics data analysis [88] [8].
- Step-by-Step Protocol:
- Trial Design:
- Endpoint Measurement:
- Biomarker Analysis: Move beyond subjective reports and include objective biomarkers. For example, in probiotic studies, measure inflammatory cytokines (e.g., IL-6, IL-8, TNF-α, IL-10) and analyze gut microbiota composition through 16S rRNA sequencing to provide mechanistic insights [8].
- Bioinformatic Interrogation:
- High-Throughput Data: Collect genomic, transcriptomic, or proteomic data from blood or tissue samples pre- and post-intervention [88] [89].
- Target Identification: Use bioinformatic tools to compare molecular profiles between groups. This can connect the consumption of the functional food component to changes in genetic mutations, epigenetic modifications, or gene expression patterns, thereby identifying potential molecular targets and pathways (e.g., growth factors, inflammatory pathways) through which the bioactivity is mediated [88].
- Data Interpretation: The consistent and compelling results from well-designed trials, backed by mechanistic data, form the foundational knowledge required for healthcare practitioners and regulatory bodies [8].
Experimental Protocols & Workflows
Protocol 1: Molecular Docking for Predicting Bioactive Compound-Target Interactions
This protocol is used in silico to predict the binding mode and affinity of a functional food bioactive compound (e.g., a polyphenol) to a target protein (e.g., a receptor or enzyme) [89].
- Step 1: Structure Preparation
- Target Macromolecule: Obtain the 3D structure of the target protein from a protein databank (e.g., PDB). Remove water molecules and co-crystallized ligands. Add hydrogen atoms and assign correct protonation states.
- Ligand (Bioactive Compound): Obtain or draw the 3D structure of the bioactive compound. Energy-minimize the structure and assign appropriate charges [89].
- Step 2: Binding Site Identification
- Define the binding site on the target protein using computational tools that analyze the protein's surface, or based on known experimental data from the crystal structure of the protein with a native ligand [89].
- Step 3: Docking Simulation
- Run the docking algorithm. The software will generate multiple poses (orientations and conformations) of the ligand within the binding site [89].
- Step 4: Pose Scoring and Selection
- The scoring function of the docking software will rank the generated poses based on predicted binding affinity. Select the highest-scoring binding modes for further analysis [89].
- Step 5: Validation and Analysis
- Visually inspect the top poses for key interactions (hydrogen bonds, hydrophobic interactions). Validate the docking protocol by re-docking a known native ligand and checking if the software can reproduce the experimental binding mode [89].
Protocol 2: Establishing a Mechanistic IVIVC for an Extended-Release Formulation
This protocol outlines the key experimental steps for building a Level A IVIVC [87] [86].
- Step 1: Formulation Development
- Develop at least three formulations with different in vitro release rates (e.g., slow, medium, fast).
- Step 2: In Vitro Dissolution Testing
- Perform dissolution testing on all formulations using an appropriate apparatus (e.g., USP Apparatus I or II) and a physiologically relevant dissolution medium. Generate a detailed dissolution profile for each.
- Step 3: In Vivo Pharmacokinetic Study
- Conduct a human or animal bioavailability/bioequivalence study using a cross-over design. Administer each formulation and collect plasma samples at predetermined time points to determine the PK profile (e.g., concentration vs. time).
- Step 4: Data Analysis and Model Development
- Use IVIVC software (e.g., Phoenix IVIVC Toolkit) to perform numerical deconvolution on the in vivo PK data to obtain the in vivo absorption/time profile.
- Correlate the fraction of drug dissolved in vitro with the fraction of drug absorbed in vivo for each time point to establish the Level A correlation [87].
- Step 5: Internal Validation
- Use the correlation to predict the in vivo performance of one formulation (the "validation" formulation) based on its in vitro profile. Compare the predicted Cmax and AUC to the observed values. The model is considered predictive if the percent prediction error is ≤10% for each parameter and ≤15% overall [87].
The Scientist's Toolkit
Table: Essential Research Reagent Solutions and Materials
| Item | Function/Application |
|---|---|
| Caco-2 Cell Line | A human colon adenocarcinoma cell line used as an in vitro model of the human intestinal mucosa to predict drug absorption and permeability. |
| HepG2 Cell Line | A human liver cancer cell line commonly used in toxicogenomics (TGx) and hepatotoxicity studies to assess the metabolic and toxic effects of compounds [85]. |
| Phoenix IVIVC Toolkit | Software that provides advanced tools for in vitro-in vivo correlation studies, helping scientists improve bioequivalence study success and obtain biowaivers [87]. |
| DDDPlus | Mechanistic dissolution software that models and simulates the in vitro dissolution of active pharmaceutical ingredients under various experimental conditions, aiding formulation design [86]. |
| Probiotic Strains (e.g., Bifidobacterium, Lactobacillus) | Live microorganisms used in clinical trials to investigate health benefits on gastrointestinal disorders, immune modulation, and gut microbiota composition [8]. |
| Prebiotics (e.g., Inulin) | Non-digestible food ingredients that are selectively fermented by beneficial gut bacteria, used in studies to modulate the composition and/or activity of the gut microbiota [8]. |
| Position Weight Matrix (PWM) | A bioinformatic tool used to scan genomic sequences for known regulatory motifs (e.g., transcription factor binding sites), which can aid in understanding the genetic regulation of a drug target [88]. |
| Non-negative Matrix Factorization (NMF) Algorithm | A computational strategy used to factorize gene expression data, helping to extract specific factors (like drug effects) from complex in vivo TGx data and improve in vitro to in vivo extrapolation [85]. |
Experimental Workflows and Pathways
Diagram 1: IVIVC Development Workflow
Title: Steps to Build a Level A IVIVC
Diagram 2: In Vitro to In Vivo Extrapolation Strategy
Title: TGx Data Correction with NMF
Diagram 3: Functional Food Bioactivity Assessment
Title: From Trial to Mechanism
Fundamental Concepts and Importance in Bioavailability
What is the operational difference between 'Free' and 'Total' compound quantification? The distinction lies in what form of the compound is being measured. The 'Total' concentration refers to the overall amount of the compound in a sample, including both the unbound (free) fraction and the portion that is bound to other molecules, such as plasma proteins or specific target ligands [90]. In contrast, the 'Free' concentration measures only the unbound, pharmacologically active fraction that is immediately available to interact with its site of action, such as a cellular receptor or enzyme [91]. For monoclonal antibody therapeutics, the 'free' fraction is pragmatically defined as forms exerting equivalent biological activity to the unbound form, which includes both completely unbound and partially bound (e.g., monovalently bound) antibodies [90].
Why is measuring both 'Free' and 'Total' concentrations critical for optimizing bioavailability of functional food components? For functional food components and drugs, the free concentration is often more directly correlated with the biological effect or bioavailability, as it represents the fraction capable of crossing membranes and reaching target tissues [91]. However, the total concentration provides crucial information about the overall exposure and the dynamic equilibrium between bound and unbound states [90]. Understanding this relationship is essential because:
- Bioavailability Prediction: The free fraction is the driver of absorption, distribution, and initial pharmacological activity.
- Dose-Response Relationship: PK/PD (Pharmacokinetics/Pharmacodynamics) modeling relies on understanding the relationship between free drug concentrations and the observed effect [90] [91].
- Individual Variability: The ratio of free to total drug can vary between individuals due to differences in protein levels (e.g., albumin, SHBG) or health status, making free concentration a more accurate predictor of efficacy and safety in personalized nutrition and therapy [91].
Methodological Approaches and Protocols
Several bioanalytical techniques are employed to differentiate and quantify free and total compounds. The choice of method depends on the compound's nature, the required sensitivity, and the specific research question.
Ligand-Binding Assays (LBA) for Macromolecules
LBA are widely used for the analysis of protein biotherapeutics and their target ligands [90]. The assay format and reagent design determine whether a free, total, or bound form is measured.
Table 1: Ligand-Binding Assay Configurations for Free vs. Total Analysis
| Target Analyte | Assay Type | Typical Assay Format | Measures | Key Consideration |
|---|---|---|---|---|
| Total Monoclonal Antibody (mAb) | Non-inhibitory | Capture: Target LigandDetection: Anti-mAb Ab | All forms of the mAb (free, partially bound, fully bound) [90] | Ensures dissociation of complexes during assay. |
| Free Monoclonal Antibody (mAb) | Inhibitory | Capture: Anti-mAb AbDetection: Labeled Target Ligand | Pharmacologically active mAb (unbound and monovalently bound) [90] | Susceptible to perturbation of the in vivo equilibrium. |
| Total Target Ligand (L) | Non-inhibitory | Capture: mAb or Anti-Ligand AbDetection: Anti-Ligand Ab | All forms of the ligand (free and bound) [90] | Requires a capture reagent that does not compete with the mAb binding. |
| Free Target Ligand (L) | Inhibitory | Capture: Anti-Ligand AbDetection: Labeled mAb | Unbound ligand available for binding [90] | The assay environment must preserve the in vivo free fraction. |
Experimental Protocol: Bridging Immunoassay for Free Drug Analysis This protocol is typical for measuring the concentration of a free biotherapeutic (like a mAb) in plasma [90].
- Coating: Coat a microtiter plate with the target ligand (soluble receptor or antigen).
- Blocking: Block the plate with a protein-based buffer (e.g., BSA in PBS) to prevent non-specific binding.
- Sample Incubation: Incubate standards, quality controls, and study samples on the plate. The free drug in the sample will bind to the immobilized target.
- Washing: Wash the plate to remove unbound proteins, matrix components, and drug-target complexes.
- Detection: Add a detection antibody (specific for the drug) that is conjugated to a label (e.g., horseradish peroxidase or biotin).
- Signal Development: Add a substrate solution to produce a measurable signal (e.g., colorimetric, chemiluminescent).
- Data Analysis: Calculate free drug concentrations in samples by interpolating from the standard curve.
Separation-Based Techniques for Small Molecules
For small molecules like nutraceuticals (e.g., polyphenols, vitamins) or drugs, separation techniques are often coupled with sensitive detection.
A. Microextraction-Based Methods Methods like Solid-Phase Microextraction (SPME) use a coated fiber that exclusively extracts the free fraction of an analyte from a sample based on its affinity for the coating [91].
Experimental Protocol: Determining Free Concentration (Cf), Total Concentration (Ct), and Plasma Binding Capacity (PBC) using Microextraction and Isotopic Labeling [91] This comprehensive approach provides multiple parameters from a single sample.
- Calibration: Determine the extraction constant (ec) for the analyte by extracting it from a standard solution without binding proteins. The free concentration is calculated as Cf = me / ec, where me is the amount extracted.
- Sample Processing: To the plasma sample, add a known quantity of an isotopically labeled version of the analyte (e.g., deuterated or 13C-labeled).
- Equilibration: Allow the labeled and unlabeled analytes to equilibrate with plasma binding proteins.
- Microextraction: Perform microextraction to isolate the free fraction of both the natural and labeled analytes.
- Analysis: Analyze the extracted sample using LC-MS/MS to quantify the amounts of both the natural and labeled analytes.
- Calculation:
- Cf is calculated from the amount of natural analyte extracted and the pre-determined ec.
- Ct is determined by comparing the MS response of the natural analyte to the known amount of the labeled standard, accounting for the free fraction.
- PBC (Plasma Binding Capacity) is derived using the formula: Cf / Ct = 1 / (1 + PBC). PBC reflects the product of the association constant (K) and the concentration of binding proteins [91].
B. Ultrafiltration This method is commonly used in clinical labs for its simplicity [91].
Experimental Protocol: Free Concentration via Ultrafiltration
- Equilibration: Incubate the plasma or serum sample to ensure binding equilibrium.
- Separation: Transfer the sample into an ultrafiltration device equipped with a semi-permeable membrane (e.g., 10-30 kDa molecular weight cut-off).
- Centrifugation: Centrifuge the device at a controlled speed, temperature, and time. The hydrostatic pressure forces the free (unbound) analyte through the membrane into the filtrate, while protein-bound complexes are retained.
- Analysis: Quantify the analyte concentration in the filtrate (which represents the free concentration) using a suitable analytical technique like LC-MS/MS or immunoassay. The total concentration is typically measured from the initial, untreated sample.
Workflow for Free Analyte Quantification via Ultrafiltration
Troubleshooting Common Experimental Issues (FAQs)
FAQ 1: Our free drug measurements show high variability between replicates. What could be the cause? High variability in free concentration assays often stems from perturbations of the binding equilibrium during sample handling and analysis [90].
- Cause: Factors such as temperature fluctuations, pH changes, dilution of the sample, or prolonged processing times can shift the equilibrium between free and bound forms.
- Solution: Standardize and strictly control pre-analytical conditions. Maintain samples at a constant temperature (e.g., 37°C for equilibrium dialysis), minimize sample dilution, and ensure processing times are consistent and as short as possible. For LBAs, validate that the assay reagents and conditions do not themselves cause dissociation of complexes.
FAQ 2: Why might the measured 'free' concentration not correlate with the observed biological effect in my functional food study? A disconnect between measured free concentration and effect can occur due to several factors related to bioavailability.
- Cause 1: * *Non-Specific Binding: The analyte may be adhering to labware (tubes, pipette tips), which artificially lowers the measured free concentration.
- Solution: Use low-binding plasticware and add inert proteins or detergents to the buffer to minimize adsorption.
- Cause 2: * *Inadequate Method Selectivity: The analytical method might be measuring a metabolite or a structurally similar compound that is not the active form.
- Solution: Employ more specific detection methods, such as LC-MS/MS, to confirm the identity of the analyte being quantified.
- Cause 3: * *Cellular Uptake/Efflux: The compound might be subject to active transport (influx or efflux) at the cellular level, meaning the plasma free concentration does not directly reflect the intracellular concentration.
- Solution: Consider developing cellular assays or measuring concentrations in the target tissue if feasible.
FAQ 3: When developing a functional food, should I prioritize data on 'free' or 'total' bioactive compound concentrations? The choice depends on the stage of development and the intended use of the data [90].
- Preclinical/Early Development: Data on both free and total concentrations are valuable. Total concentration helps understand overall exposure and PK behavior. The dynamic relationship between free and total compound, and the modulation of the free target (e.g., a serum biomarker), provides proof-of-concept and helps select a biologically active dose [90].
- Clinical/Late-Stage Development: For correlating exposure with PD or efficacy endpoints, the free concentration is often more relevant as it represents the bioavailable fraction [91]. However, measuring total concentration is often simpler and may be sufficient if the free fraction is constant across the target population. The decision should be risk-based, considering inter-individual variability in protein binding [91].
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Reagents and Materials for Free and Total Assays
| Reagent / Material | Function | Application Notes |
|---|---|---|
| Recombinant Target Ligand / Antigen | Serves as the capture or detection agent in LBAs to specifically bind the therapeutic or endogenous compound. | Critical for the specificity of free drug assays. Must have high purity and maintained activity [90]. |
| Anti-Analyte Antibodies | Used as capture or detection reagents in immunoassays. Monoclonal antibodies are preferred for specificity. | Key for total assays. For free assays, the epitope should not compete with the target ligand binding [90]. |
| Isotopically Labeled Standards | (e.g., deuterated, 13C) Internal standards for MS-based assays to correct for recovery and matrix effects. | Essential for the accuracy and precision of microextraction and ultrafiltration methods [91]. |
| Ultrafiltration Devices | Centrifugal units with semi-permeable membranes to physically separate free from protein-bound analytes. | Choose the appropriate molecular weight cut-off to retain binding proteins while allowing the free analyte to pass through [91]. |
| SPME Fibers / Microextraction Probes | Coated fibers that extract the free fraction of an analyte directly from a complex sample. | Minimizes perturbation of the binding equilibrium. The coating chemistry must be optimized for the analyte [91]. |
| Binding Matrix (e.g., Pooled Plasma) | Used for preparing calibration standards and quality controls that mimic the protein binding in study samples. | The quality and consistency of the plasma are crucial for generating reliable standard curves [90] [91]. |
Clinical Trial Evidence for Cardioprotective, Cognitive, and Immune Benefits
Troubleshooting Guide: Common Experimental Challenges in Functional Food Research
This guide addresses frequent methodological issues encountered during clinical trials investigating the health benefits of functional foods, with a specific focus on overcoming barriers to optimizing bioavailability.
FAQ 1: How can we control for high variability and confounding factors in functional food trials?
The Problem: Clinical trials for functional foods are highly susceptible to confounding variables such as participants' varying dietary habits, lifestyles, and baseline gut microbiota, which can obscure the true treatment effect [8]. Data from these trials often show small effect sizes or no significant effects due to these complexities [8].
The Solution: Implement robust study designs and statistical plans.
- Solution 1: Strengthen Study Design. Utilize randomized, controlled, and ideally double-blind designs to minimize bias [8] [92]. Allocation concealment and pre-specified analysis plans are critical.
- Solution 2: Employ Adaptive Features. Consider group-sequential designs that allow for early stopping for efficacy or futility, or sample-size re-estimation to adjust for incorrect assumptions about variability [93].
- Solution 3: Stratify Randomization. Base randomization on key confounding factors known to influence the outcome, such as baseline BMI, age, or microbiome composition, to ensure balance between treatment groups [8].
Preventive Action: Conduct a thorough root cause analysis during the planning phase. Use the "5-Whys" method to anticipate potential sources of variability and confounders, and design the protocol to mitigate them from the start [94].
FAQ 2: What are the best practices for assessing the bioavailability of functional ingredients in human trials?
The Problem: Traditional methods for assessing bioavailability, such as in vivo trials and in vitro digestion models, can be costly, methodologically rigid, and may not fully simulate the human physiological environment [7]. The bioavailability of active components is influenced by a complex interplay of food matrix components, gastrointestinal dynamics, and host-specific factors like genetics and gut microbiota [7].
The Solution: Integrate advanced technologies and a multi-method approach.
- Solution 1: Leverage AI-Enhanced Modeling. Use Artificial Intelligence (AI), including machine learning (ML) and deep learning (DL), to predict complex relationships between nutrient structure, host physiology, and absorption. AI models can forecast the transport efficiency of bioactive compounds across physiological barriers, reducing the sole reliance on traditional methods [7] [84].
- Solution 2: Utilize Encapsulation Technologies. Improve the stability and targeted delivery of bioactives by employing encapsulation (e.g., microencapsulation, nano-delivery systems) to protect ingredients through the gastrointestinal tract and enhance their absorption [84].
- Solution 3: Incorporate Direct and Indirect Biomarkers. Measure both direct compounds in blood/plasma and their downstream effects. For gut-health ingredients like prebiotics, quantify microbial metabolites such as short-chain fatty acids (SCFAs) as indirect markers of bioavailability and activity [84].
Preventive Action: Plan for the collection and analysis of multi-faceted data, including food composition, host genetics (e.g., salivary amylase gene copy number), and gut microbiota profiles, to build robust AI models and better interpret inter-individual variability in response [7] [84].
FAQ 3: How should we handle inconsistent results between preclinical models and human clinical trials?
The Problem: Promising results from animal studies often fail to translate into significant health benefits in human trials. This can be due to differences in physiology, metabolism, or dose translation between species.
The Solution: Bridge the translational gap with more predictive models and careful trial design.
- Solution 1: Use AI to Improve Preclinical Predictions. Apply AI techniques to integrate preclinical data with human pharmacokinetic descriptors, creating models that better predict human bioavailability and physiological response from the outset [7].
- Solution 2: Conduct Phase 2 Proof-of-Concept Trials. Before embarking on large, costly Phase 3 trials, design Phase 2 studies to confirm the bioavailability of the bioactive compound and its mechanism of action in the target human population [92].
- Solution 3: Re-evaluate the Dose and Formulation. The lack of effect in humans may be due to insufficient bioavailability at the chosen dose. Return to bioavailability studies to optimize the delivery system or dosage, potentially using encapsulation or other formulation technologies to improve efficacy [84].
Preventive Action: From the beginning, incorporate human-relevant AI models and in vitro systems that more closely mimic human gastrointestinal conditions to de-risk the transition from lab to human trials [7].
Table 1: Clinical Evidence for Cardioprotective, Cognitive, and Immune Benefits of Functional Food Components
| Bioactive Component | Target Health Benefit | Key Clinical Evidence & Quantitative Outcomes | Reported Bioavailability Challenges |
|---|---|---|---|
| GLP-1 Agonists / Functional Ingredients | Cardioprotective | - Significant reduction in Major Adverse Cardiovascular Events (MACE) [95].- Liraglutide lowered systolic BP by 1.2 mmHg (LEADER trial) [95].- Semaglutide reduced LDL-C by 5-10% [95]. | - Susceptible to enzymatic degradation; requires specialized delivery (e.g., fatty acid conjugation) [7]. |
| Omega-3 Polyunsaturated Fatty Acids (PUFAs) | Cardioprotective, Cognitive | - Associated with reduced risk of cardiovascular and neurodegenerative diseases [84].- Specific quantitative outcomes from clinical trials are needed. | - Oxidation susceptibility; bioavailability influenced by food matrix and molecular form [84]. |
| Dietary Fiber & Prebiotics (e.g., Inulin) | Cardioprotective, Immune (Gut-Mediated) | - Modulates blood glucose and lipid levels [84].- 2-10g of inulin shown to influence gut microbiota (e.g., Bifidobacterium, Faecalibacterium) in healthy subjects [8]. | - Fermentation by gut microbiota; individual baseline microbiota affects response [8] [84]. |
| Probiotics (e.g., Lactobacillus, Bifidobacterium) | Immune, Gastrointestinal | - Demonstrated benefits for gastrointestinal (GI) disorder symptoms in adults and children [8].- Shown to reduce pro-inflammatory cytokines (IL-6, IL-8, TNF-α) and upregulate anti-inflammatory IL-10 [8]. | - Low viability under simulated GI conditions; requires encapsulation (e.g., transglutaminase capsules) for protection [8]. |
| Polyphenols | Cardioprotective, Cognitive, Antioxidant | - Associated with reduced risk of chronic diseases; wide-ranging biological activities [8] [84].- Specific quantitative outcomes from clinical trials are needed. | - Generally low bioavailability; extensive metabolism; stability during processing [84]. |
| Bioactive Peptides | Cardioprotective, Immune | - Identified for attenuating muscle atrophy; predicted to maintain bioavailability during GI digestion via AI models [7] [84]. | - Susceptibility to hydrolysis by digestive enzymes; requires identification of stable sequences [7]. |
Detailed Experimental Protocols
Protocol 1: Assessing the Impact of a Prebiotic Functional Food on Gut Microbiota and SCFA Production
Objective: To evaluate the efficacy and bioavailability of a prebiotic (e.g., inulin) by measuring its impact on gut microbiota composition and the production of microbial metabolites (SCFAs) in human subjects.
Methodology:
- Study Design: A randomized, double-blind, placebo-controlled, parallel-group trial.
- Participants: Healthy adults, stratified by baseline bifidobacteria counts if possible, as initial counts influence response [8].
- Intervention:
- Treatment Group: Receives a specific dose (e.g., 2g, 6g, or 10g per day) of the prebiotic (inulin) incorporated into a food vehicle (e.g., a yogurt) [8].
- Control Group: Receives a matched placebo without the prebiotic.
- Duration: A minimum of 4 weeks, with baseline, midpoint, and end-point assessments.
- Key Measurements:
- Microbiota Analysis: Collect fecal samples at baseline and post-intervention. Use 16S rRNA sequencing to quantify changes in specific bacterial taxa (e.g., Bifidobacterium adolescentis, Faecalibacterium prausnitzii) [8].
- Bioavailability Marker (SCFAs): Analyze fecal samples for concentrations of acetate, propionate, and butyrate using gas chromatography-mass spectrometry (GC-MS) as an indicator of prebiotic fermentation [84].
- Secondary Endpoints: Gastrointestinal symptom questionnaires, immune markers (e.g., cytokines in blood), or systemic metabolic markers.
Protocol 2: Evaluating the Bioavailability of Bioactive Peptides Using AI-Enhanced Modeling
Objective: To identify and predict the gastrointestinal stability and bioavailability of bioactive peptides from a protein hydrolysate (e.g., broad bean, goat milk) using in silico models and in vitro validation.
Methodology:
- AI-Driven Prediction:
- Data Preparation: Compile a dataset of known peptide sequences, their structures, and in vivo/in vitro bioavailability data.
- Model Training: Employ a deep learning (DL) model or machine learning (ML) algorithms (e.g., Random Forest) to establish structure-bioavailability relationships. The model learns to predict the stability of peptides during gastrointestinal digestion and their potential for absorption [7].
- Screening: Input the sequences of peptides from your novel protein hydrolysate into the trained model to identify those with the highest predicted bioavailability [7].
- In Vitro Validation:
- Simulated GI Digestion: Subject the selected protein hydrolysate to a simulated gastrointestinal digestion model that replicates gastric and intestinal phases [7].
- Analysis: Use techniques like mass spectrometry to track the degradation of peptides and the persistence of the AI-identified stable peptides throughout the digestion process [7].
- Cellular Uptake Assays: Further validate the absorption potential of the stable peptides using human intestinal cell lines (e.g., Caco-2 model).
Signaling Pathways and Workflows
Bioactive Compound Bioavailability Optimization
GLP-1 Agonist Cardioprotective Pathways
Research Reagent Solutions
Table 2: Essential Materials for Functional Food Bioavailability Research
| Reagent / Material | Function in Experiment | Specific Application Example |
|---|---|---|
| AI/Machine Learning Models | Predicts complex structure-bioavailability relationships and nutrient absorption. | Forecasting stable bioactive peptide sequences from protein hydrolysates that survive GI digestion [7]. |
| Encapsulation Systems (e.g., liposomes, microgels) | Protects bioactive compounds from degradation in the GI tract and enables targeted release. | Enhancing the viability of probiotics under simulated gastric conditions [8] [84]. |
| In Vitro Digestion Models (e.g., dynamic GI models) | Simulates human gastrointestinal conditions (pH, enzymes, transit time) to study bioaccessibility. | Screening the release and stability of polyphenols from a food matrix during digestion [7]. |
| Transglutaminase-based Capsules | Encapsulates live microbes (probiotics) to improve their resistance to gastric acid and bile salts. | Preserving the viability of Lactobacillus strains for delivery to the colon [8]. |
| Caco-2 Cell Line | A human colon adenocarcinoma cell line used as a model of the intestinal epithelium for absorption studies. | Measuring the transport efficiency and permeability of absorbed bioactive peptides [7]. |
| Gas Chromatography-Mass Spectrometry (GC-MS) | Identifies and quantifies volatile metabolites, such as gut microbiota-derived Short-Chain Fatty Acids (SCFAs). | Quantifying acetate, propionate, and butyrate in fecal samples as a marker of prebiotic fermentation [84]. |
Troubleshooting Guide: Common Experimental Challenges
Problem: Inconsistent Bioactivity Results in Cellular Assays
- Potential Cause: Rapid metabolism and degradation of the core bioactive compound (e.g., curcumin) before it reaches the target cells.
- Solution: Utilize nano-encapsulation to protect the compound. For instance, curcumin encapsulated in polymeric micelles or liposomes has shown significantly enhanced stability and sustained release profiles, leading to more reproducible anti-cancer and anti-inflammatory outcomes in vitro [96] [97]. Pre-test the stability of your formulation in the cell culture media.
Problem: Low Encapsulation Efficiency
- Potential Cause: Mismatch between the hydrophobicity of the core compound and the selected wall material, or suboptimal formulation parameters.
- Solution: For highly hydrophobic compounds like curcumin and many polyphenols, select lipid-based carriers (e.g., liposomes, bilosomes) or biopolymers with hydrophobic domains. Optimize process variables such as the core-to-wall material ratio, solvent type, and homogenization speed [98] [99]. Techniques like solvent evaporation and emulsification are often effective.
Problem: Poor Solubility in Aqueous Biological Buffers
- Potential Cause: The inherent hydrophobicity of polyphenolic compounds limits their dispersion in aqueous environments, affecting dosing accuracy.
- Solution: Employ nanocarriers like dendrimers, micelles, or nanoemulsions. These systems create a hydrophobic core to house the compound and a hydrophilic shell, improving dispersion. For example, a PAMAM G4 dendrimer-based carrier successfully enhanced the solubility and delivery of curcumin [100].
Problem: Lack of Targeted Delivery to Specific Tissues or Cells
- Potential Cause: The delivery system is non-specific, leading to widespread distribution and potential off-target effects.
- Solution: Functionalize the surface of nanocarriers with targeting ligands. A mitochondria-targeted curcumin nanocarrier modified with triphenylphosphonium (TPP) demonstrated significantly higher accumulation in hepatocellular carcinoma cells and induced stronger apoptosis compared to free curcumin [100].
Frequently Asked Questions (FAQs)
Q1: What are the primary factors limiting the bioavailability of curcumin and polyphenols, and which delivery systems best address them? The main limitations are poor aqueous solubility, instability in physiological pH, rapid metabolism, and swift systemic elimination [96] [97]. Advanced delivery systems address these as follows:
- For Solubility & Stability: Nanoencapsulation techniques (spray drying, emulsification) using biopolymers, lipids, and synthetic polymers create a protective barrier [98].
- For Metabolism & Bioavailability: Lipid-based systems (liposomes, bilosomes) and polymeric nanoparticles (e.g., PLGA) can facilitate lymphatic transport, bypassing first-pass metabolism [99] [97].
Q2: How do I select the most appropriate delivery system for my specific research application? The choice depends on the compound's properties and the desired therapeutic goal:
- For Enhanced Oral Bioavailability: Lipid-based carriers (e.g., bilosomes, nanoemulsions) and polymeric nanoparticles (e.g., Meriva) are well-documented for improving gastrointestinal absorption [99] [97].
- For Targeted Cancer Therapy: Actively targeted systems like TPP-conjugated dendrimers for mitochondrial delivery or nanoparticles functionalized with specific antibodies show great promise in preclinical models [100].
- For Wound Healing: Topical applications like hydrogels, nanofibrous membranes, and films provide controlled release and maintain a localized therapeutic concentration [97].
Q3: Are there any standardized protocols for evaluating the efficacy of these delivery systems in preclinical models? While specific protocols vary, a general workflow includes:
- In Vitro Characterization: Size, zeta potential, encapsulation efficiency, drug release profile.
- Cellular Studies: Cytotoxicity (MTT assay), cellular uptake (confocal microscopy), and mechanism-of-action studies (e.g., apoptosis, ROS generation) [100].
- In Vivo Evaluation: Pharmacokinetic studies (measuring AUC, C~max~, half-life), biodistribution analysis, and efficacy assessment in disease models (e.g., tumor volume reduction in HCC models) [99] [100].
Q4: What are the critical quality attributes to characterize a newly developed nanoparticle-based delivery system? Key attributes include:
- Particle Size & Polydispersity Index (PDI): Affects circulation time and tissue penetration. Typically measured by Dynamic Light Scattering (DLS).
- Zeta Potential: Indicates colloidal stability.
- Encapsulation Efficiency (EE) & Drug Loading (DL): Critical for assessing formulation success and determining dosage.
- Morphology: Visualized by Transmission Electron Microscopy (TEM) or Scanning Electron Microscopy (SEM).
- In Vitro Drug Release Profile: Evaluates release kinetics in simulated physiological conditions [100].
Table 1: Bioavailability Enhancement of Commercial Curcumin Formulations [97]
| Formulation Name | Key Technology | Reported Bioavailability Enhancement (vs. Standard Curcumin) |
|---|---|---|
| NovaSol | Micellar formulation | 185-fold |
| CurcuWin | Advanced dispersion technology | 136-fold |
| Longvida | Solid lipid particle | 100-fold |
| Meriva | Phytosome (complexed with phospholipids) | Not specified in search, but widely cited for improved absorption |
Table 2: Efficacy of Curcumin Nanoformulations in Preclinical HCC Models [99] [100]
| Nanoformulation Type | Key Findings | Model Used |
|---|---|---|
| Mitochondria-targeted Dendrimer (TDC) | Increased apoptosis 40-50%; 3.5x increase in sub-G1 cell population; upregulation of Bax, p53; downregulation of Bcl-2. | HCC-bearing mice |
| Liposomes, Micelles, Bilosomes | Improved bioavailability and tumor-targeting; enhanced apoptosis; suppression of PI3K/AKT/mTOR and JAK2/STAT3 pathways. | In vitro & In vivo |
| Hemoglobin-curcumin NPs | Reversal of drug resistance; promotion of ferroptosis via ACSL4 upregulation. | In vitro |
Detailed Experimental Protocols
Protocol 1: Synthesis of a Mitochondria-Targeted Curcumin Nanocarrier (TDC) [100]
Objective: To synthesize a PAMAM G4 dendrimer-based carrier conjugated with TPP for targeted delivery of curcumin to mitochondria.
Materials:
- PAMAM G4 dendrimer
- Carboxybutyl triphenylphosphonium bromide (TPP)
- Curcumin (95% purity)
- N,N'-Dicyclohexylcarbodiimide (DCC) and N-Hydroxysuccinimide (NHS) for activation
- 4-Nitrophenyl chloroformate (NPC)
- Anhydrous solvents: Methanol, Dichloromethane, Dimethyl Sulfoxide (DMSO)
Methodology:
- TPP Activation: Dissolve TPP in methanol. Add a mixture of DCC and NHS in methanol to the TPP solution. Stir the reaction for 3 days at room temperature (RT), protected from light and under a nitrogen atmosphere. Remove solvent using a rotary evaporator.
- Dendrimer Conjugation: Conjugate the activated TPP to the surface amine groups of the PAMAM G4 dendrimer.
- Curcumin Activation: Activate the hydroxyl group of curcumin using NPC in dichloromethane and triethylamine. Stir for 3 days at RT in the dark under nitrogen.
- Final Conjugation: Slowly add the activated curcumin to a solution of the TPP-PAMAM conjugate in DMSO. Stir the mixture for 5 days at RT in the dark.
- Purification: Dilute the final product with Milli-Q water and dialyze (using a membrane with a 3 kDa molecular weight cut-off) to remove unreacted compounds.
Protocol 2: Evaluating Anti-Cancer Efficacy in an HCC Mouse Model [99] [100]
Objective: To assess the therapeutic effects of a curcumin nanoformulation in a hepatocellular carcinoma model.
Materials:
- HCC-bearing BALB/c mice
- Test formulation (e.g., TDC) and free curcumin control
- Equipment for intra-tumoral or systemic administration
- Kits for ELISA, ROS, ATP, glutathione, etc.
- Flow cytometer, RT-PCR system
Methodology:
- Treatment: Administer the nanoformulation and controls to tumor-bearing mice via a predetermined route and dosing schedule.
- Cytokine Analysis: Isolate splenocytes and stimulate with tumor lysate. Measure secreted levels of cytokines like IFN-γ and IL-4 using ELISA.
- Cell Cycle Analysis: Analyze tumor cells by flow cytometry (e.g., PI staining) to determine the population in sub-G1 phase (indicative of apoptosis).
- Gene Expression: Extract RNA from liver tumor tissue. Perform RT-PCR to analyze the expression of pro-apoptotic (e.g., bax, p53) and anti-apoptotic (e.g., bcl2, xiap) genes.
- Mitochondrial Function: Isolate mitochondria from liver tissue. Measure key parameters including ATP levels, reactive oxygen species (ROS), malonaldehyde (MDA), and reduced glutathione (GSH).
- Biodistribution: Track the accumulation of the formulated vs. free curcumin in tumors and key organs to confirm targeted delivery.
Signaling Pathway Diagrams
Diagram 1: Curcumin's molecular targets in Hepatocellular Carcinoma (HCC). Curcumin inhibits key pro-survival and inflammatory pathways (red arrows) while promoting pro-apoptotic signals (green arrows), leading to reduced cancer cell viability [96] [99].
Diagram 2: Workflow for developing and testing a mitochondria-targeted nanocarrier. The process involves chemical synthesis and conjugation, followed by purification and characterization, leading to a mechanism of action centered on inducing mitochondrial dysfunction in cancer cells [100].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Advanced Delivery System Research
| Reagent / Material | Function / Application | Key Examples from Literature |
|---|---|---|
| PAMAM Dendrimers | Highly branched, monodisperse polymers used as nanocarriers. Internal cavities encapsulate hydrophobic drugs; surface groups allow conjugation. | PAMAM G4 used as a core for constructing mitochondria-targeted curcumin carriers [100]. |
| Triphenylphosphonium (TPP) | A lipophilic cation used as a targeting ligand. Exploits the high mitochondrial membrane potential for selective accumulation. | Conjugated to PAMAM dendrimers to create mitochondria-targeted curcumin (TDC) [100]. |
| Phospholipids | Primary components of liposomes and phytosomes. Enhance the bioavailability of polyphenols by facilitating absorption and mimicking cellular membranes. | Used in commercial formulations like Meriva; also in bilosomes for oral delivery of curcumin [99] [97]. |
| Poly(lactic-co-glycolic acid) (PLGA) | A biodegradable and biocompatible polymer used for controlled-release nanoparticle formulations. | Commonly used for sustained and targeted delivery of various polyphenolic compounds [96]. |
| N-Hydroxysuccinimide (NHS) / DCC | Crosslinking agents used in carbodiimide chemistry to activate carboxylic acid groups for conjugation with amines. | Used to activate TPP for conjugation to the amine groups on the PAMAM dendrimer surface [100]. |
For researchers and drug development professionals, establishing a robust evidence base for the health benefits of functional food components is a multi-stage process. It requires a rigorous journey from initial observational studies to post-market monitoring, with each phase presenting distinct methodological challenges and opportunities. In the specific context of optimizing bioavailability—the proportion of a nutrient that enters circulation and exerts an active effect—this pathway becomes particularly complex. Bioavailability is not a single property but a dynamic process influenced by food matrix interactions, host metabolism, and the gut microbiome [64] [101]. This technical support center is designed to provide actionable troubleshooting guidance for the common experimental and analytical hurdles encountered at each stage of evidence generation, directly supporting the broader thesis of advancing functional food component research.
The Evidence Hierarchy: Study Types and Data Interpretation
FAQ: What are the key types of evidence I need to build a compelling case for my functional food component?
Answer: A comprehensive evidence portfolio leverages multiple study designs, each with a specific role in establishing efficacy and safety. The table below summarizes the core study types, their primary functions, and key quantitative outputs.
Table 1: Hierarchy of Evidence in Functional Food Research
| Study Type | Primary Function & Role in Evidence Building | Key Quantitative Data Generated | Common Statistical Measures |
|---|---|---|---|
| In Vitro Studies | Initial screening of bioactivity and mechanism of action. Identifies potential therapeutic targets. | IC50 values, antioxidant capacity (ORAC, TEAC), cellular uptake rates, gene/protein expression changes. | Dose-response curves, p-values. |
| Animal Models | Assesses bioactivity and safety in a whole organism. Provides preliminary data on bioavailability and metabolism. | Bioavailability (% absorption), tissue concentration levels, biomarker changes (e.g., blood lipids, glucose). | Mean differences, standard deviation, t-tests. |
| Epidemiological Studies | Identifies correlations between dietary intake and health outcomes in free-living populations. Generates hypotheses. | Hazard Ratios (HR), Relative Risks (RR), Odds Ratios (OR) for disease incidence. | Confidence Intervals (CI), p-values. |
| Randomized Controlled Trials (RCTs) | The gold standard for establishing causal efficacy and dose-response relationships in humans. | Absolute and relative risk reduction, mean change in clinical endpoints (e.g., LDL-C reduction in mmol/L). | Effect size, confidence intervals, intention-to-treat analysis. |
| Post-Market Surveillance | Monitors long-term safety, effectiveness, and real-world usage patterns after commercial launch. | Incidence rates of adverse events, compliance data, consumer-reported outcomes. | Trend analysis, signal-to-noise ratios. |
Troubleshooting Guide: Interpreting Epidemiological Data
Problem: My analysis of nutritional epidemiology data shows a statistically significant association, but I am unsure how to describe the core findings of the distribution of health events. Solution: Descriptive epidemiology provides a systematic framework for summarizing and interpreting population health data. It answers the fundamental questions of what (the health condition), how much (the frequency), and the patterns of when, where, and among whom [102].
- Root Cause Analysis: A lack of a structured approach to data characterization can lead to missing key patterns or drawing incorrect inferences.
- Step-by-Step Resolution:
- Organize Data into a Line-Listing: Create a table with each row representing a single case and columns for key characteristics (e.g., patient demographics, exposure details, clinical findings). This facilitates sorting and pattern recognition [102].
- Calculate Correct Measures of Frequency:
- Use counts for the absolute number of cases.
- Use rates (e.g., incidence, prevalence) to correct for different population sizes or study periods, enabling valid comparisons. Never mix incident (new) and prevalent (existing) cases [102].
- Characterize by Time, Place, and Person:
- Time: Examine trends (secular), seasonal patterns, or sharp outbreaks.
- Place: Compare geographic distributions, from international down to specific neighborhoods.
- Person: Analyze by age, sex, ethnicity, occupation, and other relevant demographics.
- Compare with Expected Values: Compare observed case counts or rates with historical data or data from a control population to determine if the observed pattern is unusual [102].
Problem: I am preparing a table for a publication, but the data presentation is cluttered and difficult to interpret. Solution: Adhere to established guidelines for arranging statistical data to ensure clarity and coherence [102].
- Root Cause: Poor table structure, including excessive precision, inappropriate organization, and visual clutter.
- Step-by-Step Resolution:
- Round Data: Round data to two statistically significant or effective numbers to avoid interference with comparison and comprehension [102].
- Organize for Comparison: Place the most crucial data for comparison in columns, as numbers are more easily compared down a column than across a row. Organize data by magnitude (sort) across rows and down columns [102].
- Provide Marginal Summaries: Include averages, rates, or totals for rows and columns where possible.
- Guide the Eye Visually: Align columns of numbers on the decimal point, place numbers close together, and avoid dividing lines and grids within the data space. Use alternating light shading of rows to assist readers [102].
Experimental Protocols for Bioavailability Optimization
A central challenge in functional food science is that many bioactive compounds have poor inherent bioavailability due to low solubility, stability, or extensive metabolism [101]. The following protocols address this core issue.
Detailed Protocol: Nanoencapsulation of Phenolic Compounds
Aim: To enhance the stability and bioavailability of phenolic compounds by encapsulating them in a biopolymer-based nano-delivery system for application in food fortification [101].
Materials:
- Core Material: Target phenolic compound/extract (e.g., curcumin, quercetin, green tea polyphenols).
- Coating Material: Food-grade biopolymers (e.g., whey protein, soy phosphatidylcholine, chitosan, starch, maltodextrin).
- Equipment: High-pressure homogenizer or probe sonicator, magnetic stirrer, freeze-dryer, analytical balance, pH meter, dynamic light scattering (DLS) instrument.
Methodology:
- Solution Preparation: Prepare separate aqueous solutions of the coating biopolymer (e.g., 2-5% w/v) and the phenolic compound (in a suitable solvent if poorly water-soluble).
- Primary Emulsion/Loading: Slowly add the phenolic solution to the biopolymer solution under constant mechanical stirring (e.g., 1000 rpm for 15 min) to form a coarse emulsion or mixture.
- Nanoemulsion/Nanoparticle Formation:
- High-Pressure Homogenization: Pass the coarse emulsion through a high-pressure homogenizer for 3-5 cycles at a pressure of 50-150 MPa.
- Sonication: Alternatively, subject the mixture to probe sonication on ice (e.g., 100-400 W, 5-10 min, pulse mode 5s on/5s off) to reduce particle size.
- Lyophilization (Optional): Freeze the resulting nanosuspension at -80°C for 12 hours and then lyophilize for 48 hours to obtain a dry, stable powder for incorporation into solid food matrices.
- Characterization:
- Particle Size & Zeta Potential: Measure using DLS. Target a particle size < 1.0 µm and a zeta potential with an absolute value > ±30 mV for good physical stability [101].
- Encapsulation Efficiency (EE): Centrifuge the nanosuspension. Quantify the amount of free, unencapsulated phenolic in the supernatant using UV-Vis or HPLC. Calculate EE% = (Total phenolics - Free phenolics) / Total phenolics × 100.
- In Vitro Bioaccessibility: Subject the nanocapsules to a simulated gastrointestinal digestion model (INFOGEST protocol). Measure the fraction of the compound released from the capsule into the digest.
Troubleshooting:
- Problem: Low Encapsulation Efficiency.
- Potential Causes & Solutions:
- Incompatibility between core and wall material: Switch the biopolymer type (e.g., from polysaccharide to protein-based).
- Leakage during processing: Optimize homogenization pressure/sonication time to avoid damaging the capsule wall.
- Potential Causes & Solutions:
- Problem: Rapid Particle Aggregation.
- Potential Causes & Solutions:
- Low Zeta Potential: Adjust the pH of the solution away from the isoelectric point of the biopolymer or use a stabilizer.
- High Particle Concentration: Dilute the suspension before storage.
- Potential Causes & Solutions:
Experimental Workflow: From Ingredient to Evidence
The following diagram visualizes the integrated experimental workflow for developing and validating a bioavailability-enhanced functional ingredient.
Diagram 1: Bioavailability R&D Workflow
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Reagents and Materials for Bioavailability Research
| Research Reagent / Material | Primary Function in Experiments | Example Application in Protocol |
|---|---|---|
| Food-Grade Biopolymers (e.g., Whey Protein, Chitosan, Maltodextrin) | Act as encapsulation wall materials to protect and deliver bioactive compounds. | Forming the nanostructured matrix around phenolic compounds in nanoencapsulation [101]. |
| Simulated Gastrointestinal Fluids (e.g., SGF, SIF per INFOGEST model) | To mimic human digestion in vitro and assess the stability and release (bioaccessibility) of bioactives. | In vitro bioaccessibility assessment post-encapsulation [101]. |
| Cell Culture Models (e.g., Caco-2 cell line) | A human colon adenocarcinoma cell line that differentiates into enterocyte-like cells, used to model intestinal absorption. | Studying cellular uptake and transport of bioactives across the intestinal barrier. |
| Stable Isotopes (e.g., ¹³C-labeled compounds) | Tracers that allow for precise tracking of the metabolic fate and distribution of a nutrient within a biological system. | Quantifying the absorption, distribution, and metabolism of a functional ingredient in human trials. |
| Specific Biomarker Assay Kits (e.g., for Oxidative Stress, Inflammation) | To quantitatively measure the physiological response to a functional food intervention. | Evaluating the effect of an encapsulated antioxidant on reducing a specific inflammatory cytokine (e.g., IL-6) in a clinical trial [8]. |
| Prebiotics (e.g., Inulin, FOS) | Non-digestible food ingredients that selectively stimulate the growth of beneficial gut bacteria. | Used in studies to modulate the gut microbiome and assess its impact on the metabolism of bioactives [8] [84]. |
Troubleshooting Clinical Trials and Post-Market Evidence
FAQ: What are the major design challenges specific to clinical trials for functional foods?
Answer: Functional food trials share similarities with pharmaceutical trials but face unique methodological hurdles that can obscure true treatment effects [8].
- High Confounding Variables: Unlike drugs, food intake is part of a complex diet and lifestyle. Differences in background diet, physical activity, and genetic makeup between participants can confound results. Solution: Use a controlled feeding study design where possible, or meticulously collect and adjust for dietary data as a covariate.
- Small Effect Sizes: The mean treatment effects for most functional foods are often modest. Solution: Conduct power calculations a priori to ensure a sufficiently large sample size to detect a small, but biologically relevant, effect.
- Placebo Formulation: Creating a truly inert placebo that is indistinguishable in taste, texture, and appearance from the functional food is extremely challenging. Solution: Invest in food science expertise to develop a matched control product that lacks only the active ingredient(s) of interest.
- Compliance Monitoring: Solution: Use biomarkers of intake where available (e.g., specific fatty acid levels in blood for omega-3 trials) to objectively verify compliance, rather than relying solely on self-reporting [8].
Protocol: Designing a Post-Market Surveillance Plan for a Functional Food
Aim: To proactively and systematically monitor the continued safety and consumer experience of a functional food product after its launch into the market.
Background: While stringent for medical devices under MDR [103], the principles of post-market surveillance (PMS) can be adapted for high-end functional foods to build trust and gather real-world evidence.
Methodology:
- Data Collection:
- Passive Surveillance: Establish channels for collecting spontaneous reports from consumers and healthcare professionals on adverse events, product quality complaints, and lack of effect.
- Active Surveillance: Deploy targeted methods such as consumer usage surveys, follow-up studies with clinical trial participants, and analysis of data from consumer loyalty programs to gather more structured feedback.
- Literature Monitoring: Implement a systematic process to review newly published scientific literature related to the product's bioactive ingredients.
- Data Analysis:
- Trend Analysis: Regularly analyze complaint and adverse event data for any increasing trends or unexpected patterns.
- Benefit-Risk Assessment: Periodically re-evaluate the overall benefit-risk balance of the product based on the accumulated post-market data and the most current scientific evidence.
- Reporting and Action:
- Internal Reporting: Generate periodic summary reports for the quality and R&D teams.
- Corrective Actions: If a potential safety or quality issue is identified, initiate a root cause investigation and implement corrective and preventive actions (CAPA), which may include product recall or label updates.
Troubleshooting:
- Problem: Low rates of adverse event reporting from consumers.
- Solution: Make the reporting process clear and easily accessible (e.g., a dedicated section on the company website, clear instructions on packaging). Consider offering small incentives for participation in focused follow-up surveys.
- Problem: Differentiating product-related effects from background health events.
- Solution: Carefully define and document expected events related to the ingredient. Calculate the expected background rate of common events (e.g., headache, GI discomfort) in the general population and compare the reported rate to this baseline.
Conclusion
Optimizing the bioavailability of functional food components is a critical, multi-faceted challenge that requires an interdisciplinary approach integrating food science, nanotechnology, and nutritional biochemistry. The convergence of advanced delivery systems, AI-driven discovery, and precision nutrition paradigms marks a significant leap forward. Future success hinges on validating these strategies through robust clinical trials, establishing clear regulatory frameworks for health claims, and translating laboratory innovations into safe, effective, and commercially viable products. For biomedical research, this progression opens new avenues for developing food-based interventions that can act as powerful adjuvants in preventing and managing chronic diseases, ultimately bridging the gap between nutrition and pharmacology.
References
- 1. Drug Bioavailability - StatPearls - NCBI Bookshelf - NIH [https://www.ncbi.nlm.nih.gov/books/NBK557852/]
- 2. Understanding Bioavailability in Pharmacokinetics [https://www.certara.com/blog/bioavailability/]
- 3. Pharmacokinetics - StatPearls - NCBI Bookshelf - NIH [https://www.ncbi.nlm.nih.gov/books/NBK557744/]
- 4. Absorption Distribution Metabolism Excretion - an overview [https://www.sciencedirect.com/topics/medicine-and-dentistry/absorption-distribution-metabolism-excretion]
- 5. Troubleshooting Everywhere! An Assortment of Topics from ... [https://www.chromatographyonline.com/view/troubleshooting-everywhere-an-assortment-of-topics-from-pittcon-2025]
- 6. Overcoming Challenges in Small-Molecule Drug ... [https://www.mdpi.com/1422-0067/25/23/13121]
- 7. Artificial intelligence-enhanced bioavailability studies [https://www.sciencedirect.com/science/article/abs/pii/S0924224425003395]
- 8. Functional Foods in Clinical Trials and Future Research ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12346611/]
- 9. Advanced Drug Delivery Strategies to Overcome Solubility ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12444610/]
- 10. Drug Solubility: Importance and Enhancement Techniques [https://pmc.ncbi.nlm.nih.gov/articles/PMC3399483/]
- 11. Delivery systems designed to enhance stability and ... [https://www.sciencedirect.com/science/article/abs/pii/S0308814623025281]
- 12. How to measure the solubility of pharma compounds? [https://rheolution.com/application-notes/measuring-the-solubility-of-pharmaceutical-compounds/]
- 13. Drug solubility: why testing early matters in drug discovery [https://www.bmglabtech.com/en/blog/drug-solubility-why-testing-early-matters-in-drug-discovery/]
- 14. Techniques and methods to study functional characteristics ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9333426/]
- 15. Oral Mucosa Models to Evaluate Drug Permeability - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10220859/]
- 16. Evaluation of drug permeability across Ex vivo nasal mucosa [https://www.sciencedirect.com/science/article/pii/S1773224725003624]
- 17. Gastrointestinal digestion assays for evaluating the ... [https://www.sciencedirect.com/science/article/abs/pii/S0963996923004659]
- 18. In vitro Bioaccessibility and Intestinal Absorption of ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2021.818195/full]
- 19. Food (Matrix) Effects on Bioaccessibility and Intestinal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7764665/]
- 20. The Role of the Food Matrix and Gastrointestinal Tract in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5860850/]
- 21. Underlying issues in bioaccessibility and bioavailability [https://www.sciencedirect.com/science/article/abs/pii/S0147651303000502]
- 22. Octacosanol: Biological activities and bioavailability ... [https://www.sciencedirect.com/science/article/pii/S0308814625041433]
- 23. Enhancing solubility and bioavailability of octacosanol [https://www.sciencedirect.com/science/article/abs/pii/S0378517323011481]
- 24. Preparation of Gum Arabic–Maltose–Pea Protein Isolate ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9818909/]
- 25. The Role of the Gut Microbiota in the Metabolism of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6021178/]
- 26. Effects of Natural Polysaccharides on the Gut Microbiota ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12128006/]
- 27. Bioavailability Based on the Gut Microbiota [https://pmc.ncbi.nlm.nih.gov/articles/PMC7194497/]
- 28. FAQ: Human Microbiome - NCBI Bookshelf - NIH [https://www.ncbi.nlm.nih.gov/books/NBK562894/]
- 29. Bacterial Transformation Troubleshooting Guide [https://www.thermofisher.com/us/en/home/life-science/cloning/cloning-learning-center/invitrogen-school-of-molecular-biology/molecular-cloning/transformation/bacterial-transformation-troubleshooting-guide.html]
- 30. Nanotechnology for encapsulation of bioactive components [https://link.springer.com/article/10.1007/s44187-025-00386-7]
- 31. Recent overview of nanotechnology based approaches for ... [https://pubs.rsc.org/en/content/articlehtml/2025/fb/d5fb00122f]
- 32. A Review on Polymer and Lipid-Based Nanocarriers and Its ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8671830/]
- 33. An overview of liposomal nano-encapsulation techniques ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7447741/]
- 34. Hybrid nanoencapsulation systems: integrating natural ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12598503/]
- 35. Common Pitfalls in Nanotechnology: Lessons Learned ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3499664/]
- 36. Nanoencapsulation - an overview [https://www.sciencedirect.com/topics/biochemistry-genetics-and-molecular-biology/nanoencapsulation]
- 37. Micellar Solubilization - an overview [https://www.sciencedirect.com/topics/pharmacology-toxicology-and-pharmaceutical-science/micellar-solubilization]
- 38. Micelles transforming modern medicine [https://link.springer.com/article/10.1007/s44371-025-00292-y]
- 39. Recent Advances in Polymeric Micelle Preparation for Drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12566873/]
- 40. Nanoemulsion-based delivery systems for poorly water ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3367464/]
- 41. Enhancing solubility and dissolution of felodipine using self ... [https://www.nature.com/articles/s41598-025-90962-9]
- 42. Unlocking the Synergy: Exploring the Solubility ... [https://www.intechopen.com/chapters/1175603]
- 43. Cyclodextrins: Enhancing Drug Delivery, Solubility and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11945013/]
- 44. Cyclodextrins: Enhancing Drug Delivery, Solubility and ... [https://www.mdpi.com/1999-4923/17/3/288]
- 45. Carrier Systems for Advanced Drug Delivery - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC11279846/]
- 46. Experimental and Computational Studies of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4113631/]
- 47. Predicting complexation performance between ... [https://www.sciencedirect.com/science/article/pii/S2211383519300231]
- 48. Three-Dimensional Printing of Foods: A Critical Review ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10487194/]
- 49. Personalized, digitally designed 3D printed food towards ... [https://www.nature.com/articles/s41538-024-00296-5]
- 50. 3D food printing technologies for functional foods [https://www.sciencedirect.com/science/article/abs/pii/S2949824425001983]
- 51. Innovative delivery technologies that enhance ... [https://www.nutritionaloutlook.com/view/innovative-delivery-technologies-that-enhance-bioavailability-and-stability]
- 52. Microwave-Triggered 4D Automatic Color Change in 3D ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10217553/]
- 53. Recent advances and application challenges of quercetin- ... [https://www.sciencedirect.com/science/article/pii/S2772566925002046]
- 54. 3D bioprinting of plant and animal cell-based hybrid food [https://www.nature.com/articles/s41467-025-61996-4]
- 55. Emerging Trends in Green Extraction Techniques ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12189258/]
- 56. Green Extraction Techniques of Bioactive Compounds [https://www.mdpi.com/2227-9717/11/8/2255]
- 57. Chitosan nanoparticles: Green synthesis, biological ... [https://www.sciencedirect.com/science/article/pii/S2590006425009299]
- 58. Food Proteins: Processing, Interactions, Functionality and ... [https://www.mdpi.com/2304-8158/14/5/857]
- 59. New advances in biological preservation technology for ... [https://www.nature.com/articles/s41538-025-00372-4]
- 60. Functional Foods Enriched With Bioactive Compounds [https://pmc.ncbi.nlm.nih.gov/articles/PMC12501769/]
- 61. Octacosanol: Biological activities and bioavailability ... [https://www.sciencedirect.com/science/article/abs/pii/S0308814625041433]
- 62. Natural sources of bioactive compounds: recent advances ... [https://www.sciencedirect.com/science/article/abs/pii/S096399692502191X]
- 63. Advancements in curcuminoid formulations: An update on ... [https://pubmed.ncbi.nlm.nih.gov/40688407/]
- 64. Functionality of Food Components and Emerging Technologies [https://pmc.ncbi.nlm.nih.gov/articles/PMC7826514/]
- 65. How To Calculate Bioavailability (With Formula And Optimization Tips) [https://sportstechnologylabs.com/how-to-calculate-bioavailability/]
- 66. Bioavailability Enhancement Techniques for Poorly Aqueous ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9495787/]
- 67. Enhancement and Polymorphic Stabilization of One... Bioavailability [https://turkjps.org/articles/bioavailability-enhancement-and-polymorphic-stabilization-of-one-bcs-class-iv-metastable-drug-through-novel-formulation-approach/tjps.galenos.2025.89956]
- 68. Frontiers | From bench to bedside, boswellic acids in anti-inflammatory... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1692443/full]
- 69. Bioavailability Enhancement: A Seamless Path to Clinical ... [https://www.almacgroup.com/knowledge/library/bioavailability-enhancement-a-seamless-path-to-clinical-success/]
- 70. Food scientists detail the challenges of functional foods [https://www.supplysidefbj.com/food-development/8-rules-for-creating-fortified-functional-products-that-work]
- 71. Physical Approaches to Masking Bitter Taste - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC4898047/]
- 72. The Art and Science of Flavor Masking in Supplements [https://niemagazine.com/from-bitter-to-better-the-art-and-science-of-flavor-masking-in-supplements/]
- 73. Example food: What are its sensory properties and why is ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6550172/]
- 74. The challenges of sensory evaluation of food [https://www.foodresearchlab.com/blog/new-product-development/challenges-faced-while-carrying-out-the-sensory-evaluation-of-food/]
- 75. Sensory Evaluation Methods for Troubleshooting Quality ... [https://www.linkedin.com/advice/1/what-best-sensory-evaluation-methods-troubleshooting-ko0bc]
- 76. Machine learning-driven bioavailability prediction in early ... [https://pubmed.ncbi.nlm.nih.gov/40391875/]
- 77. AI-driven Drug Development for Poor Solubility and ... [https://www.patheon.com/us/en/insights-resources/blog/ai-driven-drug-development-for-poor-soubility-and-bioavailability.html]
- 78. Machine learning driven bioequivalence risk assessment ... [https://www.sciencedirect.com/science/article/pii/S0939641124003795]
- 79. Next-Generation Foodomics: Integrated Multi-omics ... [https://www.sciencedirect.com/science/article/pii/S0889157525014504]
- 80. Progress of AI-Driven Drug–Target Interaction Prediction and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12563295/]
- 81. Gut Microbiota–Informed Precision Nutrition in the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8421235/]
- 82. Unraveling the Gut Microbiota: Implications for Precision ... [https://www.mdpi.com/2072-6643/16/22/3806]
- 83. Advancing precision nutrition for better health [https://www.nature.com/articles/d42473-025-00199-3]
- 84. Functional Ingredients: From Molecule to Market—AI ... [https://www.mdpi.com/2304-8158/14/17/3141]
- 85. Narrowing the Gap Between In Vitro and In Vivo Genetic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6964707/]
- 86. DDDPlusâ„¢ - Simulations Plus Pharmaceutical Dosage ... [https://www.simulations-plus.com/software/dddplus/]
- 87. Phoenix IVIVC Toolkit [https://www.certara.com/software/phoenix-ivivc-toolkit/]
- 88. Bioinformatics and Drug Discovery - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC5421137/]
- 89. The role and application of bioinformatics techniques and ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1547131/full]
- 90. Bioanalytical Approaches to Quantify “Total†and “Free†... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3032085/]
- 91. Method for Simultaneous Determination of Free ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7938943/]
- 92. FAQs About Clinical Studies [https://www.cc.nih.gov/participate/faq-about-clinical-studies]
- 93. Common Questions in Clinical Trial Design [https://www.quanticate.com/blog/common-questions-in-clinical-trial-design]
- 94. Resolving and Preventing Repetitive Problems in Clinical ... [https://www.socra.org/blog/corrective-and-preventative-action/]
- 95. GLP-1 Agonists in Cardiovascular Diseases: Mechanisms, ... [https://www.mdpi.com/2077-0383/14/19/6758]
- 96. Curcumin: biochemistry, pharmacology, advanced drug ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1695200/full]
- 97. Curcumin-Loaded Drug Delivery Systems for Acute and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12383930/]
- 98. Recent progress in improving delivery, bioavailability and ... [https://www.sciencedirect.com/science/article/abs/pii/S0308814625023386]
- 99. Molecular targets and therapeutic implications of curcumin ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12495814/]
- 100. Novel curcumin nanocarrier for targeting drug delivery of ... [https://www.nature.com/articles/s41598-025-19147-8]
- 101. Improving functionality, bioavailability, nutraceutical and ... [https://www.sciencedirect.com/science/article/abs/pii/S0963996920305809]
- 102. Describing Epidemiologic Data | Field Epi Manual [https://www.cdc.gov/field-epi-manual/php/chapters/describing-epi-data.html]
- 103. MDR Requirements for Post-Market Surveillance [https://vantagemedtech.com/mdr-requirements-for-post-market-surveillance-best-practices-and-compliance-strategies/]