Applying the Theoretical Domains Framework (TDF) to Advance Dietary Behavior Change in Clinical Research and Drug Development
This article provides a comprehensive resource for researchers, scientists, and drug development professionals on applying the Theoretical Domains Framework (TDF) and Behavior Change Wheel (BCW) to dietary behavior change interventions. It covers the foundational theory and history of the TDF, offers a step-by-step methodological guide for implementation, addresses common challenges and optimization strategies in real-world application, and reviews the framework's validation and comparative effectiveness against other models. By synthesizing current evidence and practical guidance, this article aims to bridge the gap between behavioral science and clinical practice, enhancing the design and evaluation of interventions from early-phase trials to clinical implementation.
Applying the Theoretical Domains Framework (TDF) to Advance Dietary Behavior Change in Clinical Research and Drug Development
Abstract
This article provides a comprehensive resource for researchers, scientists, and drug development professionals on applying the Theoretical Domains Framework (TDF) and Behavior Change Wheel (BCW) to dietary behavior change interventions. It covers the foundational theory and history of the TDF, offers a step-by-step methodological guide for implementation, addresses common challenges and optimization strategies in real-world application, and reviews the framework's validation and comparative effectiveness against other models. By synthesizing current evidence and practical guidance, this article aims to bridge the gap between behavioral science and clinical practice, enhancing the design and evaluation of interventions from early-phase trials to clinical implementation.
Understanding the TDF and COM-B Model: A Theoretical Foundation for Dietary Change
The Behavior Change Wheel (BCW) is a comprehensive, evidence-based framework for characterizing and designing behavior change interventions. Developed through a synthesis of 19 existing frameworks of behavior change, it was created to overcome limitations of prior models by being comprehensive, coherent, and clearly linked to an overarching model of behavior [1] [2]. At the heart of the BCW lies the COM-B model, a behavioral system that posits three essential conditions for any behavior to occur: Capability, Opportunity, and Motivation (forming the COM acronym) that interact to produce Behavior (the B in the model) [1] [3] [2]. This integrated system provides researchers and intervention designers with a systematic method for diagnosing behavioral barriers and developing targeted interventions.
The COM-B model represents a significant advancement in the field because it provides a "behavior system" at the hub of the BCW, encircled by intervention functions and policy categories [1]. This structure offers a coherent framework that links an understanding of the target behavior to specific intervention types and policy-level implementations. The model has been reliably applied across diverse domains including tobacco control, obesity prevention, chronic disease management, and dietary behavior change [1] [4] [5]. For researchers focusing on dietary behavior change, the BCW and COM-B provide a robust methodological approach for designing, implementing, and evaluating interventions with precision and theoretical grounding.
Theoretical Foundations and Model Architecture
The COM-B Behavioral System
The COM-B model provides a foundational framework for understanding the components necessary for behavior to occur. The model conceptualizes behavior as an interactive system within which capability, opportunity, and motivation influence each other in dynamic feedback loops [6]. The components are defined as follows:
Capability (C): An individual's psychological and physical capacity to engage in the activity concerned. Psychological capability includes having the necessary knowledge, mental skills, attention, memory, and decision-making processes. Physical capability encompasses bodily functions, strength, stamina, and dexterity required to perform the behavior [7] [3] [6].
Opportunity (O): All factors that lie outside the individual that make the behavior possible or prompt it. Physical opportunity includes environmental factors, resources, time, and triggers. Social opportunity encompasses the cultural milieu, social norms, and influences from others that define how others behave around the subject [7] [3] [6].
Motivation (M): All brain processes that energize and direct behavior, including both reflective and automatic mechanisms. Reflective motivation involves conscious decision-making, plans, evaluations, and beliefs. Automatic motivation includes emotional reactions, desires, impulses, and habituated responses that occur without conscious awareness [7] [3] [6].
These components interact within a dynamic system where changes in one component can directly affect behavior and indirectly influence other components through feedback loops [6]. For example, enhancing capability may increase motivation, while expanding opportunities may make individuals feel more capable.
The Behavior Change Wheel Structure
The Behavior Change Wheel builds upon the COM-B foundation with two additional layers:
Intervention Functions: The middle layer of the wheel consists of nine categories of interventions aimed at addressing deficits in one or more of the COM components [1] [8] [3]. These include education, persuasion, incentivization, coercion, training, restriction, environmental restructuring, modeling, and enablement.
Policy Categories: The outer layer identifies seven types of policies that can support the delivery of these interventions: communication/marketing, guidelines, fiscal measures, regulation, legislation, environmental/social planning, and service provision [1] [8].
The relationship between these layers forms a coherent structure where policies enable interventions that target specific COM-B components to bring about behavior change. This comprehensive architecture allows researchers and policymakers to systematically develop and evaluate behavior change initiatives.
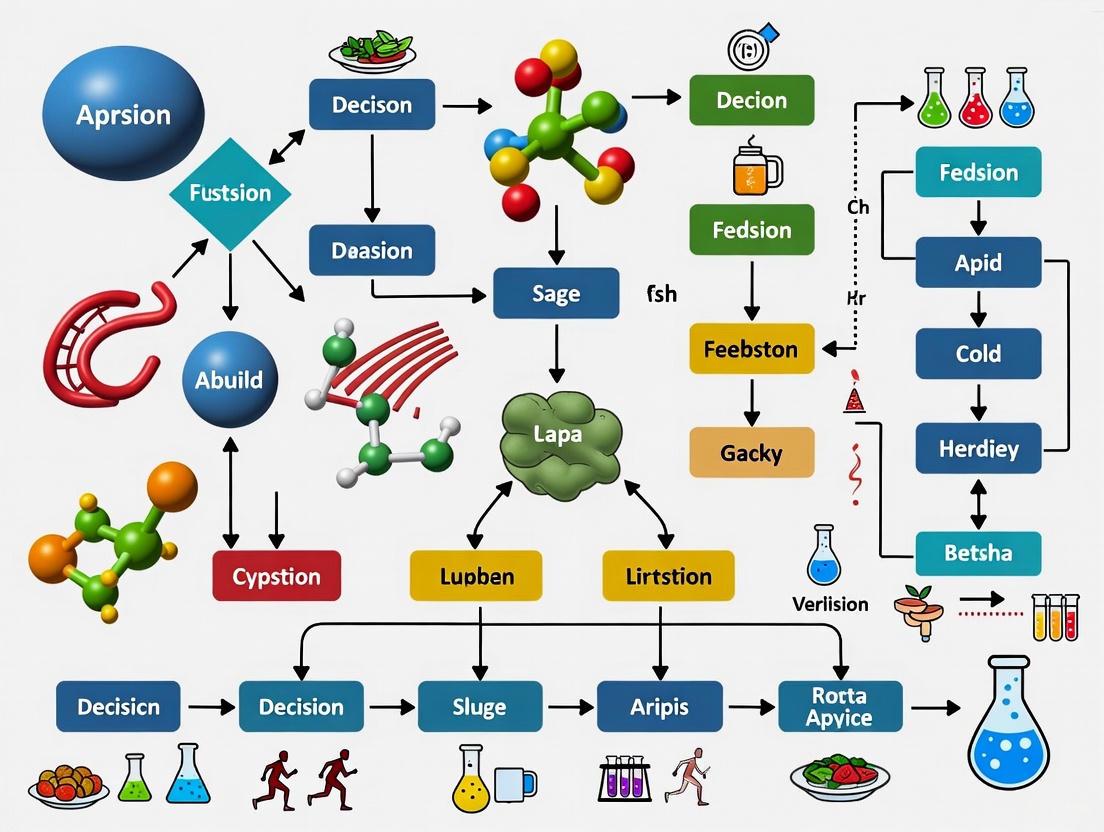
Figure 1: The Behavior Change Wheel Architecture showing the relationship between COM-B core components, intervention functions, and policy categories.
Methodological Framework for Intervention Design
The BCW Development Process
The development of the Behavior Change Wheel followed a rigorous methodological approach. Michie et al. conducted a systematic search of electronic databases and consulted with behavior change experts to identify existing frameworks of behavior change interventions [1] [2]. These frameworks were evaluated according to three criteria:
- Comprehensiveness: The framework should apply to every intervention that has been or could be developed
- Coherence: The categories should be all exemplars of the same type of entity and have similar specificity
- Linkage to a model of behavior: The framework should be linked to an overarching model of behavior [1]
The resulting BCW incorporated all identified intervention functions and policy categories from the 19 frameworks reviewed, organized around the COM-B behavior system [1] [2]. The reliability of this new framework was tested by applying it to characterize interventions within the English Department of Health's 2010 tobacco control strategy and the National Institute of Health and Clinical Excellence's guidance on reducing obesity, demonstrating its practical utility [1].
Step-by-Step Application Protocol
Implementing the BCW framework involves a structured process for designing behavior change interventions:
Table 1: BCW Intervention Design Protocol
| Step | Description | Key Activities |
|---|---|---|
| 1. Define Outcome Behavior | Identify the target behavior in precise terms | - Define the problem in behavioral terms- Establish clear, measurable behavioral outcomes |
| 2. Select Target Behavior | Choose specific behaviors to change | - Apply criteria: likely impact, ease of implementation, spillover effects, measurement feasibility |
| 3. Specify Target Behavior | Detail behavioral parameters | - Specify what, where, when, how, with whom, and in what context the behavior occurs |
| 4. Diagnose Barriers | Identify what needs to change using COM-B | - Assess Capability, Opportunity, and Motivation barriers- Use COM-B model or Theoretical Domains Framework for granular analysis |
| 5. Identify Intervention Functions | Select appropriate intervention types | - Match interventions to COM-B barriers using BCW mapping- Apply APEASE criteria (Affordability, Practicality, Effectiveness, Acceptability, Safety, Equity) |
| 6. Identify Policy Categories | Determine enabling policies | - Select policy categories that support chosen intervention functions |
| 7. Identify Behavior Change Techniques | Specify intervention content | - Select specific Behavior Change Techniques (BCTs) from taxonomy |
This protocol provides researchers with a systematic approach to intervention design, ensuring that all relevant factors are considered and that interventions are theoretically grounded and practically feasible [8] [9]. The process emphasizes beginning with a thorough understanding of the behavior in context before selecting intervention strategies, moving from behavioral diagnosis to implementation planning.
COM-B Component Analysis and Assessment Framework
Detailed COM-B Component Specification
For effective diagnosis of behavioral barriers, each COM-B component can be further analyzed through subcomponents and linked to the Theoretical Domains Framework (TDF), which provides 14 detailed domains essential for behavior change [6] [9]:
Table 2: COM-B Component Specification with Associated Assessment Questions
| COM-B Component | Sub-components | Associated TDF Domains | Diagnostic Assessment Questions |
|---|---|---|---|
| Capability | Physical: skills, strength, stamina | Physical skills | Do individuals have the physical capacity, strength, or stamina to perform the behavior? |
| Psychological: knowledge, cognitive skills | Knowledge; Cognitive & interpersonal skills; Memory & decision processes; Behavioral regulation | Do individuals have the necessary knowledge, understanding, cognitive skills, and attention to perform the behavior? | |
| Opportunity | Physical: environment, resources, time | Environmental context & resources | Do individuals have the necessary resources, time, environmental triggers, and physical space to perform the behavior? |
| Social: norms, cultural expectations | Social influences | Is the behavior socially acceptable? Do social norms, peers, or authority figures influence the behavior? | |
| Motivation | Reflective: plans, evaluations, beliefs | Professional/social identity; Beliefs about capabilities; Optimism; Beliefs about consequences; Intentions; Goals | Do individuals have the conscious motivation, intentions, plans, and positive outcome expectations to perform the behavior? |
| Automatic: emotions, impulses, habits | Reinforcement; Emotion | Do individuals have automatic emotional responses, desires, impulses, or established habits related to the behavior? |
This detailed specification enables researchers to conduct granular analyses of behavioral determinants and identify precise targets for intervention. The linkage to TDF domains is particularly valuable for comprehensive behavioral diagnosis in complex research contexts [6].
Intervention Function Mapping
The BCW provides explicit mapping between COM-B components and intervention functions, guiding researchers in selecting appropriate strategies based on identified barriers:
Table 3: Intervention Functions Mapped to COM-B Components
| Intervention Function | Definition | Primary COM-B Targets | Example Applications |
|---|---|---|---|
| Education | Increasing knowledge or understanding | Psychological Capability, Reflective Motivation | Providing information on health consequences of dietary choices [10] |
| Persuasion | Using communication to induce feelings or stimulate action | Reflective & Automatic Motivation | Using imagery to motivate healthy eating [10] |
| Incentivization | Creating expectation of reward | Reflective & Automatic Motivation | Offering rewards for achieving dietary goals |
| Coercion | Creating expectation of punishment or cost | Reflective & Automatic Motivation | Implementing consequences for non-adherence |
| Training | Imparting skills | Physical & Psychological Capability, Automatic Motivation | Teaching food preparation skills [10] |
| Restriction | Using rules to reduce opportunity to engage in target behavior | Physical & Social Opportunity | Limiting access to unhealthy foods |
| Environmental Restructuring | Changing physical or social context | Physical & Social Opportunity, Automatic Motivation | Providing healthy foods in workplace [10] |
| Modelling | Providing an example for imitation | Social Opportunity, Reflective & Automatic Motivation | Demonstrating healthy eating by peers |
| Enablement | Increasing means/reducing barriers to increase capability or opportunity | All COM-B components | Providing resources to overcome barriers [10] |
This mapping enables precision in intervention design by directly linking identified behavioral barriers to evidence-based intervention strategies. Researchers can use this table to select intervention functions that specifically target the COM-B components identified as problematic in their behavioral analysis.
Experimental Applications in Dietary Behavior Change Research
Dietary Intervention for Gestational Diabetes Prevention
A 2024 study exemplifies the application of the BCW and COM-B in dietary behavior change research for preventing gestational diabetes mellitus (GDM) [10]. The "Healthy Gut Diet" study was a complex behavior change intervention co-designed with women who had lived experience of GDM. The research followed the BCW process for designing interventions:
Methodology: The study involved six researchers and twelve women with lived experience of GDM participating in online workshops to co-design the intervention [10]. Content analysis of workshop transcripts and activities was undertaken, underpinned by the COM-B model and TDF. The target behaviors were: (1) eating more plant foods and (2) eating less ultra-processed/saturated fat containing foods.
Barriers Identification: Through COM-B analysis, researchers identified barriers and enablers across all six COM-B components and ten TDF domains [10]. This comprehensive diagnostic process revealed the multifaceted nature of dietary behavior in the context of pregnancy.
Intervention Design: Based on this analysis, the intervention functions selected were education, enablement, environmental restructuring, persuasion, and incentivization [10]. The researchers integrated forty behavior change techniques into five modes of delivery for the intervention.
Implementation: The feasibility, acceptability, and effectiveness of the Healthy Gut Diet is being tested within a randomized controlled trial, demonstrating the rigorous experimental validation of BCW-informed interventions [10].
Nutritional Intervention for Female Recreational Footballers
Another recent study applied the COM-B model to enhance nutritional knowledge and intake in female recreational football players, demonstrating the framework's application in sports nutrition [4]:
Study Design: The study assessed players pre-intervention (n=54) and post-intervention (n=20) to evaluate changes in knowledge, dietary intakes, and risk of low energy availability following a COM-B behavior change intervention [4].
Intervention Development: The researchers followed a systematic process using COM-B guidelines to develop and implement the intervention with clear goals and implementation strategies [4]. The step-by-step intervention components were identified using COM-B principles and the BCW.
Target Behaviors: The study focused on increasing energy intake and carbohydrate intake in line with calculated targets and recommendations [4]. Specific target behaviors included increasing knowledge of players about health and performance benefits of adequate nutrition, providing regular email support over six months, and offering game-day nutritional support.
Results: While the results did not reach statistical significance, moderate effect sizes were observed for sports nutrition knowledge (d=.469), energy availability (d=.432), and carbohydrate intake (d=.419), suggesting practical relevance of the COM-B intervention [4]. This highlights the importance of considering both statistical and practical significance in behavior change research.
Table 4: Essential Research Reagents and Methodological Tools for BCW Research
| Tool/Resource | Function/Purpose | Application in Dietary Behavior Research |
|---|---|---|
| Theoretical Domains Framework (TDF) | Extends COM-B with 14 detailed domains for granular barrier analysis | Provides detailed assessment of behavioral determinants in complex dietary interventions [10] |
| Behavior Change Technique Taxonomy (BCT Taxonomy v1) | Standardized taxonomy of 93 hierarchically clustered BCTs | Enables precise specification of active intervention components for replication [10] [4] |
| Template for Intervention Description and Replication (TIDieR) | 12-item checklist for comprehensive intervention description | Ensures complete reporting of dietary interventions for research replication [4] |
| APEASE Criteria | Evaluation framework: Affordability, Practicality, Effectiveness, Acceptability, Safety, Equity | Assesses intervention feasibility in real-world settings [4] |
| COM-B Self-Evaluation Questions | Structured diagnostic questions for barrier assessment | Systematically identifies capability, opportunity, and motivation barriers [6] |
These methodological tools provide researchers with standardized approaches for designing, implementing, and reporting behavior change interventions, enhancing scientific rigor and reproducibility.
Digital Implementation and Technological Integration
Recent advances have integrated the BCW and COM-B model into digital health platforms for scalable behavior change interventions. A 2025 study developed a multidomain behavioral change digital coaching system for chronic disease management in patients with type 2 diabetes using the BCW and COM-B as theoretical foundations [5].
Framework Development: The system employed a multiagent reasoning system that selected optimal digital coaching techniques based on individual assessments [5]. The BCW was used to design the program based on unique behavioral, population, and setting characteristics, linking evidence-based intervention functions to the COM-B behavioral model.
Implementation: The COM-B model served as the basis for user assessment, translating raw data into behavioral constructs [5]. In the experimental phase, the COM-B model was used to measure real-time changes in behavioral determinants, while the BCW guided the selection and prioritization of behavior change techniques.
Results: In a study of 9 patients with type 2 diabetes, the approach demonstrated notable results including reduced fasting glucose (-17.3 mg/dL), weight (-2.89 kg), and BMI (-1.05 kg/m²), with large effect sizes (Cohen d ≈ 1.05) and statistical significance (P=.01) [5]. This demonstrates the efficacy of BCW-informed digital implementations.
The technological implementation workflow can be visualized as follows:
Figure 2: Digital Implementation Workflow showing the integration of BCW/COM-B into digital health platforms for adaptive behavior change interventions.
The Behavior Change Wheel and COM-B model provide a robust, evidence-based framework for diagnosing behavioral barriers and designing targeted interventions in dietary behavior change research. Its systematic approach - moving from behavioral diagnosis through intervention selection to implementation and policy development - offers researchers a comprehensive methodology for developing theoretically grounded and practically feasible interventions.
The framework's strength lies in its integration of multiple behavioral theories into a coherent structure, its flexibility across diverse populations and settings, and its utility for both individual-level and population-level interventions. For researchers in dietary behavior change, the BCW and COM-B provide essential tools for addressing the complex interplay of biological, psychological, social, and environmental factors that influence eating behaviors.
As the field advances, integration of the BCW with digital health technologies and adaptive intervention platforms presents promising avenues for scalable, personalized behavior change interventions. The continued refinement and application of this framework will contribute significantly to developing more effective, sustainable dietary interventions that improve health outcomes across diverse populations.
The field of clinical nutrition faces a profound paradox: despite robust evidence demonstrating the critical role of nutrition in preventing and managing disease, the implementation of this evidence into routine practice remains inconsistent and fragmented. Research indicates that only approximately 20% of nutritional research findings ever translate into clinical practice, leaving patients without access to proven, effective nutritional care [11]. This evidence-practice gap represents a significant challenge to healthcare systems worldwide, potentially compromising patient outcomes, increasing healthcare costs, and diminishing the return on investment in nutrition research. The translation of evidence into practice is particularly complex in nutrition support, which requires agreement and coordination across entire multidisciplinary healthcare teams [11]. The challenge is further compounded by the individualized nature of nutritional requirements, which are deeply influenced by factors such as life stage, health status, and the presence of disease, all of which can affect the processes of consuming, digesting, absorbing, metabolizing, or excreting nutrients [12].
The conscientious, explicit, and judicious use of current best evidence in making decisions about the care of individual patients represents the core of evidence-based practice [12]. In nutrition, this has been formalized as evidence-based nutrition practice, which integrates the best available nutrition evidence with clinical experience to help patients prevent, resolve, or cope with problems related to their physical, mental, and social health [12]. However, the journey from research evidence to positive patient outcomes is neither straightforward nor automatic. It requires a systematic approach to implementation that acknowledges and addresses the complex interplay of biological, behavioral, environmental, and organizational factors that influence how evidence is adopted, implemented, and sustained in real-world settings. This whitepaper explores how theoretical frameworks, particularly the Theoretical Domains Framework (TDF) and Behavior Change Wheel (BCW), provide essential methodological tools for addressing the evidence-practice gap in nutrition support and dietary interventions.
Theoretical Foundations: A Framework for Change
The science of implementing evidence into practice has evolved substantially since its early beginnings in the 1940s, culminating in the development of sophisticated theoretical frameworks specifically designed to promote evidence-based clinical change [11]. Among these, the Theoretical Domains Framework (TDF) and Behavior Change Wheel (BCW) provide a comprehensive, systematic approach to mapping effective implementation strategies to address barriers and enablers to behavior change [11]. The TDF was developed through a process that merged multiple behavior theories, consensus processes, piloting, and validation to produce a final framework containing 14 key domains and 84 theoretical constructs that help researchers and clinicians identify potential barriers and enablers to behavior change [11].
The TDF is intrinsically linked to the Capability, Opportunity, Motivation-Behavior (COM-B) model, which forms the hub of the BCW [11]. This model posits that for any behavior to occur, an individual must have the capability (physical and psychological), opportunity (physical and social), and motivation (reflective and automatic) to perform the behavior. The TDF domains can be systematically mapped to the COM-B components to guide the selection of intervention types and strategies that are most likely to prompt behavior modification [11]. The relationship between these frameworks creates a powerful methodology for addressing implementation challenges in nutrition support.
Table 1: Theoretical Domains Framework (TDF) and COM-B Mapping
| TDF Domain | COM-B Component | Description |
|---|---|---|
| Knowledge | Psychological Capability | Understanding of nutrition guidelines and evidence base |
| Skills | Physical Capability | Proficiency in performing nutritional assessment and support |
| Social/Professional Role | Reflective Motivation | Perceived responsibility for nutritional care within professional identity |
| Beliefs about Capabilities | Reflective Motivation | Confidence in ability to provide effective nutrition support |
| Optimism | Reflective Motivation | Belief that nutritional interventions will achieve desired outcomes |
| Beliefs about Consequences | Reflective Motivation | Anticipation of outcomes of providing or not providing nutrition support |
| Reinforcement | Automatic Motivation | Previous positive or negative experiences with nutrition support |
| Intentions | Reflective Motivation | Conscious decision to engage in evidence-based nutrition practice |
| Goals | Reflective Motivation | Mental representations of aims or desired outcomes |
| Memory, Attention, Decision Processes | Psychological Capability | Ability to remember and prioritize nutrition support during care |
| Environmental Context/Resources | Physical Opportunity | Availability of resources, equipment, protocols, and time |
| Social Influences | Social Opportunity | Perceived social pressures from colleagues, patients, or organization |
| Emotion | Automatic Motivation | Emotional responses to providing nutrition support |
| Behavioral Regulation | Psychological Capability | Ability to plan, monitor, and adjust nutrition support behaviors |
The Implementation Process Using TDF and BCW
The process of using the TDF and BCW to address evidence-practice gaps involves three systematic steps [11]:
- Identify barriers and enablers using the TDF: The first step involves conducting qualitative interviews with key stakeholders to explore potential barriers and enablers across all 14 domains of the TDF. This ensures a comprehensive investigation without researcher bias or preconceived assumptions.
- Map domains to the COM-B: Once key domains are identified, they are mapped to the relevant components of the COM-B system to determine whether the intervention needs to address capability, opportunity, motivation, or a combination of these.
- Identify intervention categories and specific strategies: Based on the COM-B analysis, appropriate intervention types are selected from the BCW, followed by specific implementation strategies within each intervention type.
This systematic approach represents a significant advancement over traditional implementation efforts, which often employed generic, one-size-fits-all strategies without adequately addressing the specific barriers and enablers in a given context.
Quantifying the Evidence-Practice Gap in Nutrition
The evidence-practice gap in nutrition support is not merely a theoretical concern but a measurable phenomenon with significant implications for patient care and resource utilization. Research has demonstrated alarming discrepancies between evidence-based recommendations and actual clinical practice. For instance, one study found that only 37% of dietitian recommendations were actioned within the hospital setting, often due to non-evidence-based beliefs of physicians [11]. This implementation failure means many patients are denied optimal nutrition care, potentially leading to worse clinical outcomes, prolonged recovery times, and increased healthcare costs.
Case Example: Malnutrition Screening
Malnutrition screening within the inpatient setting provides a compelling example of an evidence-practice gap. International agreement supports the implementation of nutrition screening to identify those at risk of malnutrition to provide early interventions to prevent further decline and commence early nutrition support where needed [11]. However, numerous cross-sectional studies have shown that the practice of nutrition screening is not universal across healthcare settings in multiple countries [11]. Documented barriers include lack of resourcing, knowledge deficits, unclear ownership, and competing clinical priorities [11].
Case Example: Preoperative Prehabilitation
An emerging evidence-practice gap exists in the implementation of preoperative prehabilitation, which represents a multidisciplinary approach to physical, nutritional, and psychological optimization before surgery [11]. Evidence supports significant benefits including improved functional capacity, enhanced surgical recovery, reduced complication rates, and improved healthcare costs [11]. Nutrition is a fundamental component of prehabilitation, with strong positive clinical, patient-reported, and economic evidence supporting its implementation as standard care, particularly for high-risk groups such as malnourished and frail populations [11]. Despite this evidence base, the majority of hospitals across developed countries have not implemented prehabilitation programs [11]. Studies exploring impediments to implementation have identified multiple barriers, including limited resources, complex clinical pathways, declining medical condition of patients, and individual motivation challenges [11].
Table 2: Evidence-Practice Gaps in Nutrition Support
| Area of Practice | Evidence Base | Current Implementation Status | Key Barriers |
|---|---|---|---|
| Malnutrition Screening | Strong international consensus supporting routine screening [11] | Not universal across healthcare settings [11] | Lack of resourcing, knowledge, ownership, competing priorities [11] |
| Preoperative Prehabilitation | Strong evidence for clinical, patient-reported, and economic benefits [11] | Majority of hospitals not implemented [11] | Resource limitations, complex pathways, patient motivation [11] |
| Community-Based Stunting Interventions | Effective components identified: screening, education, supplementation, follow-up [13] | Limited implementation in resource-poor settings [13] | Socioeconomic factors, healthcare access, resource constraints [13] |
| Dietitian Recommendations | Evidence-based nutrition care plans [11] | Only 37% actioned [11] | Non-evidence-based beliefs of physicians [11] |
Experimental Methodology and Analytical Approaches
Qualitative Investigation of Implementation Barriers
The initial phase of addressing evidence-practice gaps involves rigorous qualitative investigation to identify barriers and enablers. This process should include [11]:
- Stakeholder Identification: Engage all key decision-makers involved in clinical, administrative, and financial aspects of the targeted nutrition practice. This typically includes a range of clinicians from junior to senior levels across medical, surgical, nursing, and allied health professions.
- Interview Protocol Development: Create semi-structured interview questions designed to explore all 14 domains of the TDF to ensure comprehensive coverage without researcher bias.
- Qualitative Rigor: Ensure methodological rigor through established criteria of credibility, transferability, dependability/consistency, and confirmability to minimize research bias.
- Thematic Analysis: Analyze interview transcripts to identify prominent themes related to specific TDF domains that function as either barriers or enablers.
This qualitative approach provides rich, contextual understanding of the specific challenges in implementing evidence-based nutrition practices within particular healthcare settings.
Quantitative Evaluation of Intervention Effectiveness
Quantitative methods are essential for evaluating both the implementation process and the effectiveness of nutrition interventions. Key quantitative data analysis methods include [14]:
- Descriptive Statistics: Summarize and describe the characteristics of datasets using measures of central tendency (mean, median, mode) and dispersion (range, variance, standard deviation) to provide a clear snapshot of implementation outcomes.
- Inferential Statistics: Use sample data to make generalizations about larger populations through techniques such as hypothesis testing, t-tests, ANOVA, regression analysis, and correlation analysis.
- Cross-Tabulation: Analyze relationships between categorical variables, such as comparing implementation success across different clinical departments or professional groups.
- Gap Analysis: Compare actual performance against established benchmarks or goals to identify specific areas for improvement in the implementation process.
These quantitative approaches provide objective measures of implementation success and can help identify factors associated with better or worse adoption of evidence-based practices.
Diagram 1: TDF/BCW Implementation Framework for Nutrition Support
Research Reagent Solutions: Essential Methodological Tools
Table 3: Research Reagent Solutions for Implementation Science in Nutrition
| Research Tool | Function | Application in Nutrition Implementation Research |
|---|---|---|
| Theoretical Domains Framework (TDF) | Identifies barriers and enablers across 14 behavioral domains [11] | Systematic diagnosis of implementation challenges in nutrition support |
| Behavior Change Wheel (BCW) | Links identified barriers to evidence-based intervention strategies [11] | Selection of targeted implementation strategies for nutrition programs |
| COM-B System | Analyzes capability, opportunity, and motivation components of behavior [11] | Understanding fundamental drivers of healthcare professional behavior |
| Qualitative Interview Guides | Structured protocols for exploring stakeholder perspectives [11] | Eliciting rich, contextual data on nutrition implementation barriers |
| Cross-Tabulation Analysis | Examines relationships between categorical variables [14] | Analyzing associations between provider characteristics and implementation success |
| Gap Analysis Methodology | Compares actual performance against desired benchmarks [14] | Quantifying evidence-practice gaps in nutrition care |
| Implementation Outcome Measures | Assesses adoption, fidelity, penetration, sustainability [11] | Evaluating success of nutrition implementation strategies |
Case Study: Multi-faceted Interventions for Childhood Stunting
The application of theoretical frameworks to address evidence-practice gaps is particularly relevant in global nutrition challenges, such as childhood stunting in low- and middle-income countries. A comprehensive review of multi-faceted nutritional interventions for stunting reduction identified critical components of effective programs, yet also highlighted significant implementation challenges [13]. The review screened 1,636 studies and ultimately included 9 research studies from China, Colombia, Guatemala, Haiti, India, Mexico, Peru, and Vietnam for final analysis [13]. These studies evaluated clinical outcomes such as anthropometrics and dietary intake, with most including caregiver nutrition education (7 of 9 studies), but none implementing routine and frequent nutrition screening [13].
Based on this comprehensive review, effective stunting interventions should include four key components: (i) routine screening of every child for nutritional risk based on WHO and UNICEF guidance; (ii) caregiver-targeted nutrition education; (iii) supplementation with macro- and micronutrients as needed; and (iv) regular follow-up to monitor growth and nutritional status [13]. The limited number of studies meeting inclusion criteria highlights the need for expanded implementation research, particularly in under-resourced regions [13]. This case demonstrates how theoretical frameworks could help address the implementation challenges in delivering these comprehensive, multi-level strategies essential to addressing the long-term health risks of pediatric undernutrition.
Table 4: Effectiveness of Stunting Intervention Components in Low- and Middle-Income Countries
| Intervention Component | Frequency in Reviewed Studies (n=9) | Effectiveness Assessment |
|---|---|---|
| Caregiver Nutrition Education | 7 studies [13] | Foundational component for sustainable behavior change |
| Macronutrient and Micronutrient Supplementation | 4 studies [13] | Essential for addressing nutrient deficiencies |
| Frequent Follow-up (at least monthly) | 4 studies [13] | Critical for monitoring progress and adherence |
| Breastfeeding Assessment | 3 studies [13] | Important for infant and young child feeding |
| Routine Nutrition Screening | 0 studies [13] | Identified as missing but essential component |
The evidence-practice gap in nutrition support represents a significant challenge to optimizing patient outcomes and healthcare system efficiency. Theoretical frameworks, particularly the Theoretical Domains Framework and Behavior Change Wheel, provide essential methodological tools for systematically addressing this gap by identifying context-specific barriers and enablers, mapping these to behavioral determinants, and selecting evidence-based implementation strategies. The application of these frameworks moves the field beyond generic implementation approaches to targeted, theory-informed strategies that address the specific capability, opportunity, and motivation challenges in a given healthcare setting. As the case examples in malnutrition screening, preoperative prehabilitation, and childhood stunting demonstrate, the complexity of implementing evidence-based nutrition practice requires multifaceted approaches that acknowledge the individual, organizational, and system-level factors influencing healthcare professional behavior. Future research should prioritize the application of these theoretical frameworks across diverse nutrition support contexts, with rigorous evaluation of their impact on both implementation success and patient outcomes. Only through such systematic, theory-informed approaches can the field of nutrition support fully bridge the evidence-practice gap and realize the potential of nutritional interventions to improve health outcomes.
In dietary behavior change research, precisely defining the problem represents the critical foundation upon which all subsequent intervention success depends. The identification of key dietary behaviors for change constitutes a complex process that extends beyond merely recognizing poor nutritional habits. Within the context of the Theoretical Domains Framework (TDF), this process requires a systematic investigation of the multifaceted determinants influencing dietary behaviors across cognitive, affective, social, and environmental domains [15]. The TDF provides a comprehensive, theory-informed approach to identify determinants of behavior, synthesizing 128 theoretical constructs from 33 theories of behaviour and behaviour change into an accessible framework [15]. This guide presents a rigorous methodology for researchers seeking to define dietary behavior problems with the precision necessary to develop effective, theory-driven interventions, thereby bridging the gap between nutritional epidemiology and implementation science.
Theoretical Foundation: The Theoretical Domains Framework in Dietary Research
The Theoretical Domains Framework offers a systematic structure for investigating barriers and enablers to implementing evidence-based practices, including dietary behaviors. The TDF was developed through a consensus process involving behavioural scientists and implementation researchers who identified, evaluated, and synthesized theoretical constructs most relevant to implementation questions [15]. The framework's evolution has resulted in a validated version comprising 14 domains encompassing 84 theoretical constructs, providing comprehensive coverage of potential influences on behavior [15].
In dietary research, the TDF enables investigators to move beyond simplistic explanations for dietary non-adherence and instead conduct a multidimensional analysis of the problem space. When applied to dietary behaviors, the framework facilitates exploration of capabilities (physical and psychological), opportunities (social and physical), and motivations (reflective and automatic) that constitute the COM-B system—a central component of the Behavior Change Wheel [11] [16]. This theoretical grounding ensures that problem identification is not based on assumptions but rather on a structured investigation of the theoretical constructs that may influence the target dietary behavior.
Table 1: Theoretical Domains Framework (v2) Domains and Applications to Dietary Behavior
| Domain Number | Domain Name | Application to Dietary Behavior Research |
|---|---|---|
| 1 | Knowledge | Understanding nutritional principles, dietary guidelines, food composition |
| 2 | Physical skills | Food preparation techniques, portion control measurement |
| 3 | Social/professional role and identity | Perception of personal responsibility for health, family food provider roles |
| 4 | Beliefs about capabilities | Confidence in ability to change dietary habits (self-efficacy) |
| 5 | Optimism | Belief that dietary changes will lead to desired health outcomes |
| 6 | Beliefs about consequences | Beliefs about benefits and costs of dietary change |
| 7 | Reinforcement | Internal and external rewards for maintaining dietary changes |
| 8 | Intentions | Conscious decision to engage in specific dietary behaviors |
| 9 | Goals | Setting specific, measurable dietary targets |
| 10 | Memory, attention and decision processes | Cognitive processes in food choice and consumption |
| 11 | Environmental context and resources | Food availability, accessibility, affordability |
| 12 | Social influences | Family, peer, cultural influences on eating behaviors |
| 13 | Emotion | Stress eating, emotional connections to certain foods |
| 14 | Behavioral regulation | Self-monitoring, planning, habit formation |
Methodological Approach: A Systematic Process for Problem Identification
Defining the Target Behavior with Precision
The initial step in identifying key dietary behaviors requires precise specification of the target behavior. Vague characterizations such as "eat healthier" or "improve diet" lack the specificity necessary for effective intervention design. Instead, researchers should define behaviors using explicit criteria that specify the action, context, target, time, and actors involved [15]. For example, rather than targeting "increased fruit and vegetable consumption," a precisely defined behavior would be "parents serving two different vegetables with weekday evening meals for family members." This precision enables accurate measurement and facilitates identification of specific barriers and enablers.
The process of specifying target behaviors should incorporate multiple stakeholder perspectives, including patients, food service providers, healthcare professionals, and policy makers where relevant. This collaborative approach ensures the identified behaviors have clinical relevance, practical significance, and align with the lived experiences of the target population [16]. In transdisciplinary research, such as the SWITCH project focusing on adolescent dietary behaviors, expert panels from both academia and practice provide critical insights into which determinants are most relevant, urgent, and changeable [17].
Dietary Assessment Methodologies for Behavior Identification
Accurate identification of problematic dietary behaviors requires robust assessment methodologies that capture both the quantitative and qualitative dimensions of dietary intake. The selection of assessment tools must align with the research question, study design, sample characteristics, and available resources [18].
Table 2: Dietary Assessment Methods for Identifying Target Behaviors
| Method | Primary Use | Strengths | Limitations | Alignment with TDF Domains |
|---|---|---|---|---|
| 24-Hour Dietary Recall | Captures recent detailed intake | High specificity for recent foods consumed; does not require literacy | Relies on memory; subject to day-to-day variation; trained interviewers often needed | Memory, attention and decision processes |
| Food Frequency Questionnaire | Assesses habitual intake over time | Cost-effective for large samples; captures patterns rather than daily variation | Limited food list; reliance on generic memory; less precise for absolute intakes | Knowledge, Goals, Behavioral regulation |
| Food Records | Detailed recording of current intake | Does not rely on memory; provides detailed quantitative data | Reactivity (participants may change behavior); high participant burden; requires literacy | Behavioral regulation, Environmental context and resources |
| Screening Tools | Rapid assessment of specific dietary components | Low participant burden; targeted to specific behaviors | Limited scope; must be validated for specific populations | Knowledge, Beliefs about consequences, Intentions |
Emerging technologies including digital photography of meals, mobile applications for real-time tracking, and automated dietary assessment tools are expanding methodological options for capturing dietary behaviors with reduced participant burden and enhanced objectivity [18]. Regardless of the methodology selected, researchers must acknowledge and account for measurement error inherent in all self-reported dietary assessment methods [18].
Applying the TDF to Identify Behavioral Determinants
Once target behaviors are specified, the TDF provides a structured approach to identify determinants through qualitative, quantitative, or mixed methods. Semi-structured interviews based on the TDF domains represent the most comprehensive approach for exploring the full range of potential influences on dietary behaviors [15].
Interview guides should include open-ended questions designed to elicit information about each of the 14 TDF domains without introducing researcher bias. For example, to explore the "Environmental Context and Resources" domain regarding vegetable consumption, researchers might ask: "Tell me about the situations or environments that make it easier or more difficult for you to eat vegetables?" [15]. Similarly, to investigate "Social Influences," appropriate questions might include: "How do people who are important to you affect your food choices?" [17].
Focus groups can provide valuable insights into shared experiences and social norms, particularly for dietary behaviors that have strong cultural or familial components [17]. Questionnaire-based approaches using validated instruments for specific TDF domains, such as self-efficacy scales or knowledge assessments, can complement qualitative methods and enable larger sample sizes [19].
The research team should include members with expertise in behavioral theory and qualitative methods to ensure appropriate application of the TDF throughout data collection and analysis. Transcription and coding of qualitative data using the TDF as a framework allows for systematic identification of salient domains influencing the target dietary behavior [16] [15].
Data Analysis and Interpretation
Analytical Framework for TDF-Based Qualitative Data
Analysis of TDF-based qualitative data involves a multi-stage process designed to identify key domains influencing the target dietary behavior. The process typically begins with familiarization with the entire dataset, followed by coding of specific belief statements to relevant TDF domains [15]. Researchers should establish coding protocols that specify how to handle data that fits multiple domains or does not clearly align with any domain.
Thematic analysis within each domain identifies specific beliefs that may operate as barriers or enablers. For example, when examining barriers to healthy eating among adolescents, analysis might reveal that within the "Social Influences" domain, peer pressure emerges as a significant barrier, while within "Environmental Context and Resources," limited access to affordable healthy options near schools is identified as a structural barrier [17]. Similarly, research in hospital foodservices identified "Environmental Context and Resources" as a dominant domain, with subthemes including lack of labor, time constraints, and inadequate equipment [16].
Determining the importance of each domain requires consideration of both the frequency of beliefs expressed and their perceived influence on the target behavior. Some beliefs may be mentioned infrequently yet represent critical barriers for specific subgroups, highlighting the importance of contextual factors in dietary behaviors [15].
Identifying Key Dietary Behaviors for Intervention
Synthesis of analytical findings leads to the identification of key dietary behaviors meriting intervention focus. Prioritization should consider the modifiability of the behavior, its likely impact on health outcomes, and the practical feasibility of addressing it within resource constraints [17]. The TDF-based analysis enables researchers to move beyond superficial characterizations of dietary problems to understand the underlying mechanisms maintaining suboptimal behaviors.
Research demonstrates that dietary interventions based on thorough behavioral analysis yield more significant improvements in clinical outcomes. For instance, in type 2 diabetes management, specific behavior change techniques including 'instruction on how to perform a behavior,' 'behavioral practice/rehearsal,' 'demonstration of the behavior,' and 'action planning' were associated with clinically significant reductions in HbA1c (>0.3%) [20]. These techniques directly address identified barriers in domains such as Knowledge, Skills, and Beliefs about capabilities.
Table 3: Research Reagent Solutions for Dietary Behavior Assessment
| Tool Category | Specific Instrument | Primary Application | Key Features | Validation |
|---|---|---|---|---|
| Dietary Assessment Platforms | Automated Self-Administered 24-hour Recall (ASA24) | 24-hour dietary recall data collection | Self-administered; reduces interviewer burden; free for researchers | Developed by National Cancer Institute [18] |
| Behavioral Assessment Frameworks | Theoretical Domains Framework Interview Guide | Identifying barriers and enablers to dietary change | Semi-structured format covering 14 theoretical domains | Validated in multiple implementation studies [15] |
| Stage of Change Algorithm | Stages of Change for Healthy Eating | Assessing readiness to change dietary behaviors | Classifies participants into pre-contemplation, contemplation, decision, action, maintenance | Validated with adolescent and young adult populations [19] |
| Self-Efficacy Scales | Self-Efficacy for Healthy Eating Scale | Measuring confidence in adopting healthy eating practices | 19-item Likert scale assessing intention to adopt healthy behaviors | Validated for Brazilian adolescents [19] |
| Food Environment Assessment | Nutrition Environment Measures Survey (NEMS) | Assessing food availability, quality, and price in various settings | Adaptable for schools, workplaces, healthcare facilities | Widely used in food environment research [17] |
The systematic identification of key dietary behaviors for change represents a foundational step in developing effective nutritional interventions. By applying the Theoretical Domains Framework through rigorous methodological approaches, researchers can move beyond superficial characterizations of dietary problems to understand the complex interplay of cognitive, affective, social, and environmental factors influencing food-related behaviors. This process enables precisely targeted interventions that address the most salient and modifiable determinants, ultimately enhancing the efficacy and impact of efforts to improve dietary behaviors and health outcomes across diverse populations. The integration of robust dietary assessment methods with theoretically grounded behavioral analysis provides a powerful approach for advancing nutritional science and translating evidence into practice.
A Step-by-Step Guide to Applying the TDF and BCW in Dietary Intervention Design
The Theoretical Domains Framework (TDF) is an integrative framework developed to simplify and synthesize theories of behavior change, making them more accessible for implementation research [21]. It consolidates 33 theories and 128 theoretical constructs into a coherent structure for analyzing behavioral determinants [21]. Within dietary behavior change research, the TDF provides a systematic methodology for identifying barriers and enablers that influence the adoption of evidence-based nutrition practices, from clinical settings to public health interventions [11] [22].
The TDF is particularly valuable for addressing the evidence-practice gaps commonly found in nutrition support. For instance, studies demonstrate that only about 37% of dietitian recommendations are actioned in hospital settings, often due to non-evidence-based beliefs of physicians [11]. The framework offers a structured approach to diagnose implementation problems and design theoretically-grounded interventions [21].
The TDF Domain Structure and Definitions
The validated TDF comprises 14 domains, each representing a grouping of related theoretical constructs that influence behavior [21]. These domains provide comprehensive coverage of individual, social, and environmental factors affecting behavior change implementation.
Table 1: The 14 Domains of the Theoretical Domains Framework with Definitions
| Domain Number | Domain Name | Description |
|---|---|---|
| 1 | Knowledge | An awareness of the existence of something, including procedural knowledge of how to perform behaviors [23] |
| 2 | Skills | Proficiency or dexterity acquired through practice and experience [23] |
| 3 | Social/Professional Role and Identity | A coherent set of behaviors and displayed personal qualities of an individual in a social or work setting [23] |
| 4 | Beliefs about Capabilities | Acceptance of the truth, reality, or validity about an ability, talent, or facility that a person can put to constructive use [23] |
| 5 | Optimism | The confidence that things will happen for the best or that desired goals will be attained [23] |
| 6 | Beliefs about Consequences | Acceptance of the truth, reality, or validity about outcomes of a behavior in a given situation [23] |
| 7 | Reinforcement | Increasing the probability of a response by arranging a dependent relationship, or contingency, between the response and a given stimulus [23] |
| 8 | Intentions | A conscious decision to perform a behavior or a resolve to act in a certain way [23] |
| 9 | Goals | Mental representations of outcomes or end states that an individual wants to achieve [23] |
| 10 | Memory, Attention and Decision Processes | The ability to retain information, focus selectively on aspects of the environment, and choose between two or more alternatives [23] |
| 11 | Environmental Context and Resources | Any circumstance of a person's situation or environment that discourages or encourages the development of skills and abilities, independence, social competence, and adaptive behavior [23] |
| 12 | Social Influences | Those interpersonal processes that can cause individuals to change their thoughts, feelings, or behaviors [23] |
| 13 | Emotion | A complex reaction pattern, involving experiential, behavioral, and physiological elements, by which an individual attempts to deal with a personally significant matter or event [23] |
| 14 | Behavioral Regulation | Anything aimed at managing or changing objectively observed or measured actions [23] |
Methodological Protocol for TDF-Based Qualitative Research
Study Design and Stakeholder Identification
The first step involves identifying all key stakeholders relevant to the dietary behavior being studied. In clinical nutrition research, this typically includes:
- Clinical stakeholders: Junior to senior-level medical and surgical staff, nursing professionals, dietitians, and allied health professionals [11]
- Administrative and financial decision-makers: Individuals responsible for resource allocation and system-level implementation [11]
- End-users: Patients, families, or community members whose behaviors are targeted for change [22]
Qualitative interviews with these stakeholders represent the primary methodology for exploring barriers and enablers [11]. Interviews should continue until theoretical saturation is reached, typically with 25-30 participants, as demonstrated in a recent study on family vegetable feeding practices that conducted 25 semi-structured interviews [22].
Interview Guide Development
Creating qualitative questions designed to explore all 14 domains of the TDF ensures comprehensive coverage without researcher bias or preconceived assumptions [11]. The interview guide should include:
- Grand tour questions: Broad opening questions about participants' experiences with the target behavior
- Domain-specific probes: Questions tailored to each TDF domain to elicit relevant barriers and enablers
- Scenario-based questions: Concrete situations to help participants articulate influences on their behavior
Example questions for dietary behavior change research might include:
- Knowledge: "What training have you received about nutrition screening protocols?"
- Environmental Context and Resources: "What resources are available to you for providing nutrition support?"
- Beliefs about Consequences: "What do you believe would happen if you consistently implemented these nutrition practices?"
Ensuring Methodological Rigor
Qualitative interviews must ensure rigor through four key criteria [11]:
Table 2: Criteria for Ensuring Qualitative Research Rigor in TDF Studies
| Criterion | Definition | Application in TDF Studies |
|---|---|---|
| Credibility | Confidence in the truth of the data and interpretations | Use of multiple coders, member checking, and triangulation of data sources |
| Transferability | Extent to which findings can be applied to other contexts | Thick description of context, participants, and implementation setting |
| Dependability/Consistency | Whether findings would be consistent if replicated with similar participants | Audit trails, detailed documentation of analytical decisions |
| Neutrality | Freedom from bias in the research process and findings | Reflexivity, bracketing of preconceptions, transparent reporting |
Analytical Framework for TDF Data
Data Coding and Analysis Process
Analysis of qualitative interviews follows a structured framework approach [23]:
- Familiarization: Reading and re-reading transcripts to become immersed in the data
- Coding against TDF domains: Identifying segments of text relevant to each TDF domain
- Content analysis within domains: Further analyzing content within each domain to identify specific barriers and enablers
- Synthesis: Generating themes that represent the key influences on behavior
This process was successfully applied in a study on self-care for minor ailments, where framework synthesis using the TDF enabled systematic analysis of both interview and survey data across multiple reviews [23].
Mapping to the COM-B Model
Once key domains are identified using the TDF, they can be mapped to the Capability, Opportunity, Motivation-Behavior (COM-B) model, which forms the hub of the Behavior Change Wheel [11] [23]. This mapping helps determine which component of the behavior system requires intervention:
- Capability: The individual's psychological and physical capacity to engage in the activity concerned
- Opportunity: All the factors that lie outside the individual that make the behavior possible or prompt it
- Motivation: All the brain processes that energize and direct behavior
TDF to COM-B Mapping Framework
Research Toolkit for TDF-Based Dietary Behavior Studies
Table 3: Essential Research Reagents and Tools for TDF Qualitative Studies
| Tool Category | Specific Tool/Technique | Function in TDF Research |
|---|---|---|
| Theoretical Framework | 14-domain TDF [21] | Provides comprehensive coding framework for identifying behavioral determinants |
| Behavior Model | COM-B System [23] | Serves as hub for mapping TDF findings to intervention design |
| Qualitative Methodology | Semi-structured interviews [11] | Primary data collection method for exploring barriers and enablers |
| Analysis Method | Framework synthesis [23] | Systematic approach for coding data against TDF domains |
| Quality Assessment | Rigor criteria (credibility, transferability, dependability, neutrality) [11] | Ensures trustworthiness of qualitative findings |
| Triangulation Method | Multiple stakeholder perspectives [11] [23] | Enhances comprehensiveness of identified barriers and enablers |
| Mirodenafil dihydrochloride | Mirodenafil dihydrochloride, CAS:862189-96-6, MF:C26H39Cl2N5O5S, MW:604.6 g/mol | Chemical Reagent |
| ML327 | ML327, MF:C19H18N4O4, MW:366.4 g/mol | Chemical Reagent |
Application in Dietary Behavior Change Research
The TDF has been successfully applied in various nutrition-related behavior change contexts. For example, in a study on family vegetable feeding practices, researchers used the TDF and COM-B model to explore barriers and enablers to repeatedly reoffering vegetables, role-modeling consumption, and offering non-food rewards [22]. The analysis identified eleven core themes mapped to 11 of the 14 TDF domains, including 'Child factors,' 'Eating beliefs,' 'Effectiveness beliefs,' and 'Practical issues' [22].
Another application addressed the evidence-practice gap in malnutrition screening within inpatient settings, where TDF-based interviews identified barriers such as lack of resourcing, knowledge gaps, competing priorities, and ownership issues [11]. Similarly, in implementing preoperative prehabilitation programs, TDF analysis revealed barriers including resource limitations, complex clinical pathways, declining patient medical conditions, and individual motivation challenges [11].
The systematic identification of barriers and enablers using TDF-based qualitative methods represents a critical first step in developing effective, theory-informed interventions for dietary behavior change. This approach ensures that implementation strategies address the actual determinants of behavior rather than presumed barriers, increasing the likelihood of successful adoption and maintenance of evidence-based nutrition practices.
The Capability, Opportunity, Motivation-Behaviour (COM-B) model and the Theoretical Domains Framework (TDF) provide a systematic approach for understanding and implementing behaviour change in healthcare and research settings. The COM-B model posits that for any behaviour (B) to occur, an individual must have the physical and psychological capability (C), the physical and social opportunity (O), and the reflective and automatic motivation (M) to perform the behaviour [7]. These components interact within a system where behaviour also influences these components, creating a feedback loop [24].
The TDF offers a more detailed theoretical lens through which to view behavioural determinants. Originally developed through a synthesis of 33 theories of behaviour and behaviour change, it comprises 14 domains that capture the spectrum of cognitive, affective, social, and environmental influences on behaviour [15]. The TDF was specifically designed to help identify barriers and enablers to implementing evidence-based practices [11] [15].
When used together, these frameworks provide a comprehensive methodology: the TDF allows researchers to conduct a detailed diagnostic assessment of implementation problems, and the COM-B model provides a structure for categorizing these determinants to inform intervention design [25] [11]. This mapping is a crucial step within the broader Behaviour Change Wheel (BCW) framework for developing theory-informed interventions [11] [26].
Theoretical Foundations of Domain Mapping
The Structural Relationship Between TDF and COM-B
The TDF and COM-B model share a foundational relationship, with the 14 domains of the TDF being systematically mappable to the six components of the COM-B model. This mapping is not arbitrary but reflects the theoretical coherence between the constructs [15]. The COM-B model serves as the central hub of the Behaviour Change Wheel, with the TDF providing the granular theoretical constructs that elaborate each component [27] [28].
This integrated approach allows researchers to progress from a broad understanding of behavioural determinants to specific intervention design. The mapping process creates a theoretically-grounded pathway from identifying barriers and enablers (via TDF) to categorizing them according to the COM-B system, which then directly links to intervention types through the BCW [11]. The relationship is structured such that TDF domains aligned with Capability address the individual's capacity to engage in the behaviour, those aligned with Opportunity address factors external to the individual that make the behaviour possible, and those aligned with Motivation address brain processes that energize and direct behaviour [15] [24].
The Mapping Methodology
The mapping between TDF domains and COM-B components follows a systematic process established through consensus methods and validation exercises [15]. Each of the 14 TDF domains corresponds to one of the six COM-B components based on theoretical alignment and empirical evidence [15] [24]. For instance, TDF domains related to knowledge and cognitive processes map to Psychological Capability, while domains related to environmental factors map to Physical Opportunity.
This mapping has been validated across multiple healthcare contexts and behaviours, including implementation of evidence-based nutrition practices [11] [26], dietary behaviour change [27] [29], and healthcare professional behaviour [15] [28]. The methodology ensures comprehensive coverage of potential behavioural determinants while maintaining theoretical integrity.
Table 1: Comprehensive Mapping of TDF Domains to COM-B Components
| COM-B Component | COM-B Subcomponent | TDF Domain | Domain Description and Constructs |
|---|---|---|---|
| Capability | Psychological Capability | Knowledge | Awareness of existence, knowledge about condition, scientific rationale, procedural knowledge |
| Cognitive and Interpersonal Skills | Memory, attention, decision processes, cognitive overload, behavioural regulation | ||
| Behavioural Regulation | Self-monitoring, breaking habit, action planning | ||
| Physical Capability | Skills | Physical skills, competence, ability, practical knowledge, assessment of complexity | |
| Opportunity | Physical Opportunity | Environmental Context and Resources | Barriers and facilitators, environmental stressors, resources, time, triggers |
| Social Opportunity | Social Influences | Social norms, group conformity, social support, power, conflict | |
| Motivation | Reflective Motivation | Social/Professional Role and Identity | Professional identity, professional boundaries, group identity |
| Beliefs about Capabilities | Self-confidence, self-efficacy, perceived competence, empowerment | ||
| Optimism | Optimism, pessimism, unrealistic optimism, identity | ||
| Beliefs about Consequences | Outcome expectancies, characteristics of outcome expectancies, anticipated regret | ||
| Intentions | Stability of intentions, certainty, readiness to change | ||
| Goals | Goal targeting, goal priority, goal conflict | ||
| Automatic Motivation | Emotion | Fear, anxiety, affect, stress, positive/negative consequences | |
| Reinforcement | Rewards, incentives, punishment, contingencies |
Experimental Protocols for Mapping TDF to COM-B
Qualitative Assessment Methodology
The most common approach for mapping TDF domains to COM-B components involves qualitative methods, particularly semi-structured interviews and focus groups [15]. The protocol begins with developing an interview schedule based on the 14 TDF domains, with questions designed to elicit barriers and enablers for each domain [15] [27]. For example, in a study on implementing the MIND diet, researchers developed questions targeting each TDF domain to understand barriers and facilitators to dietary adoption [27].
The recommended sample size for such qualitative investigations typically ranges from 25-50 participants, depending on the complexity of the behaviour and diversity of the population [15] [27]. Data collection continues until thematic saturation is achieved. Transcripts are then coded using a two-stage process: first, data are categorized into the 14 TDF domains; second, these domains are mapped to the relevant COM-B components based on the established theoretical relationships [15] [28]. This process requires multiple independent coders and consensus meetings to ensure reliability.
Quantitative Assessment Methodology
Quantitative approaches to mapping TDF to COM-B employ cross-sectional survey designs with validated measures for each construct [24] [29]. For instance, a study examining young adults' eating and physical activity behaviours sourced pre-validated measures appropriate for capturing the latency of COM-B constructs, with surveys administered to 455-582 participants [24].
The analytical approach typically uses structural equation modeling (SEM) to test the hypothesized relationships between COM-B components and their influence on behaviour [24]. Model fit indices (CFI, TLI, RMSEA) are used to assess how well the mapping aligns with observed data. This method allows for testing both direct and mediated pathways, such as how capability and opportunity influence behaviour through motivation as a mediator [24].
Mixed-Methods Approaches
Mixed-methods designs combine qualitative and quantitative approaches to provide a more comprehensive mapping [27] [28]. For example, in a study with midwifery leaders, researchers conducted focus groups and interviews (qualitative) alongside survey measures (quantitative) to map barriers and facilitators to COM-B components [28]. The qualitative data provided rich contextual understanding, while the quantitative data enabled assessment of the relative importance of different domains.
This approach is particularly valuable for complex implementation challenges where both the depth of understanding (qualitative) and generalizability (quantitative) are important. The integration of findings typically occurs during the interpretation phase, where qualitative themes and quantitative relationships are synthesized into a coherent mapping [27] [28].
Application in Dietary Behaviour Change Research
Case Study: MIND Diet Adoption
Research on adoption of the MIND diet provides a compelling case study for TDF to COM-B mapping in dietary behaviour change. A qualitative study with 40-55-year-olds in Northern Ireland used TDF-based interviews to identify barriers and facilitators, which were then mapped to COM-B components [27]. The mapping revealed that time constraints, work environment, taste preferences, and convenience were primary barriers mapping to Physical Opportunity, while improved health, memory benefits, planning skills, and food access were key facilitators mapping to both Physical Opportunity and Reflective Motivation [27].
A cross-sectional survey with female caregivers of people with Alzheimer's disease further demonstrated this application, showing how budget constraints (Physical Opportunity), cooking skills (Physical Capability), and social support (Social Opportunity) influenced MIND diet adoption through motivational pathways [30]. These findings highlight how TDF to COM-B mapping can identify specific, targetable factors for interventions.
Streamlined Approaches for Dietary Research
Recent research has explored streamlined versions of the COM-B model for dietary behaviour contexts to reduce measurement burden while maintaining predictive validity [29]. One study with Australian young adults tested a simplified model focusing on seven core constructs rather than the full complement of TDF domains, finding that automatic motivation, physical environment, and physical capability were particularly critical for healthy eating behaviours [29].
This streamlined approach maintains the theoretical integrity of the TDF to COM-B mapping while increasing practical utility for researchers and practitioners. The simplification involves selecting key TDF domains most relevant to dietary behaviours based on prior evidence, then mapping these to the corresponding COM-B components [29].
Table 2: Dietary Behaviour Change Studies Using TDF to COM-B Mapping
| Study Population | Research Design | Key TDF Domains Identified | Mapped COM-B Components | Primary Findings |
|---|---|---|---|---|
| Middle-aged adults (40-55 years) adopting MIND diet [27] | Qualitative (focus groups & interviews) | Environmental Context & Resources; Goals; Beliefs about Consequences | Physical Opportunity; Reflective Motivation | Barriers: time, work environment, taste preference. Facilitators: improved health, planning/organization |
| Female caregivers of people with ADRD [30] | Cross-sectional survey (n=299) | Environmental Context & Resources; Skills; Social Influences | Physical Opportunity; Physical Capability; Social Opportunity | Main barriers: budget, time, transportation. Main facilitators: budget planning, cooking skills, family support |
| Young adults' eating behaviours [24] | Cross-sectional survey (n=455) | Goals; Reinforcement; Environmental Context & Resources | Reflective Motivation; Automatic Motivation; Physical Opportunity | COM-B model explained 23% of variance in eating behaviour |
| Young adults' physical activity [24] | Cross-sectional survey (n=582) | Goals; Reinforcement; Environmental Context & Resources | Reflective Motivation; Automatic Motivation; Physical Opportunity | COM-B model explained 31% of variance in physical activity |
| Australian young adults' healthy eating [29] | Cross-sectional survey (n=347) | Environmental Context & Resources; Reinforcement; Skills | Physical Opportunity; Automatic Motivation; Physical Capability | Streamlined COM-B highlighted automatic motivation, physical environment, physical capability |
The Researcher's Toolkit: Essential Materials and Methods
Table 3: Key Research Reagent Solutions for TDF to COM-B Mapping Studies
| Research Tool | Function/Application | Implementation Example |
|---|---|---|
| TDF-Based Interview Schedule | Elicit barriers and enablers across all 14 theoretical domains | Semi-structured guide with questions for each TDF domain [15] |
| COM-B Coding Framework | Systematically map TDF-derived data to COM-B components | Codebook with decision rules for assigning TDF domains to COM-B [28] |
| Thematic Analysis Guide | Analyze qualitative data using a theory-informed approach | Iterative coding process from transcripts to TDF domains to COM-B [27] |
| Structural Equation Modeling (SEM) | Test hypothesized relationships in COM-B model quantitatively | Analysis of direct and mediated pathways between COM-B components [24] |
| Behaviour Change Wheel Framework | Design interventions based on COM-B diagnosis | Linking identified COM-B components to intervention functions [11] |
| ML349 | ML349, MF:C23H22N2O4S2, MW:454.6 g/mol | Chemical Reagent |
| ML390 | ML390 DHODH Inhibitor|Research Use Only | ML390 is a potent human DHODH inhibitor for leukemia and antiviral research. This product is For Research Use Only. Not for diagnostic or personal use. |
Figure 1: Theoretical Mapping of TDF Domains to COM-B System
Selecting appropriate intervention functions and policy categories constitutes a critical step in the Behavior Change Wheel (BCW) framework, serving as the crucial bridge between behavioral analysis and actionable intervention strategies. This step transforms the theoretical understanding of barriers and enablers, identified through the Theoretical Domains Framework (TDF) and categorized via the COM-B model, into practical methods for changing behavior [11]. For researchers in dietary behavior change, this systematic selection process ensures that interventions target the specific mechanisms influencing dietary practices, thereby increasing the likelihood of successful implementation and lasting effect [31]. The BCW offers a comprehensive synthesis of 19 behavior change frameworks, providing a coherent structure for designing interventions that are theoretically grounded, evidence-based, and contextually appropriate [32].
This section provides an in-depth technical guide for researchers and scientists on executing this pivotal step, with particular emphasis on applications within dietary behavior change research. The process demands careful judgment to identify the most promising, feasible, and culturally appropriate intervention functions and policy categories based on the specific behavioral diagnosis and context [32]. By following a structured approach, researchers can enhance the methodological rigor of their intervention development and contribute to more effective strategies for promoting healthy dietary behaviors in diverse populations.
Conceptual Foundation: From COM-B to Intervention Options
The BCW is structured in layers, with the COM-B model (Capability, Opportunity, Motivation-Behavior) at its core. The process of selecting intervention functions is fundamentally about identifying which of the nine broad categories of intervention can effectively address the deficits or leverage the strengths identified in the COM-B analysis [32]. Intervention functions are defined as broad categories of means by which an intervention can change behavior [11]. The nine intervention functions within the BCW are: Education, Persuasion, Incentivization, Coercion, Training, Restriction, Environmental restructuring, Modelling, and Enablement [11] [32].
Surrounding the intervention functions in the BCW framework are seven policy categories that represent the types of decisions made by authorities at a higher level to support the implementation of interventions [32]. These include: Communication/Marketing, Guidelines, Fiscal measures, Regulation, Legislation, Environmental/social planning, and Service provision [11] [32]. The relationship between COM-B components and these intervention functions is not arbitrary; rather, it follows a systematic mapping based on which functions are most likely to effect change in specific COM-B components [11]. For instance, a deficit in psychological capability (e.g., knowledge about nutritional requirements) might effectively be addressed through Education, whereas a problem with physical opportunity (e.g., lack of access to healthy foods) would likely require Environmental restructuring [31].
Table 1: Mapping COM-B Components to Intervention Functions
| COM-B Component | Most Relevant Intervention Functions |
|---|---|
| Capability - Physical | Training, Restriction, Environmental restructuring |
| Capability - Psychological | Education, Training, Enablement |
| Opportunity - Physical | Environmental restructuring, Restriction |
| Opportunity - Social | Environmental restructuring, Modelling, Enablement |
| Motivation - Reflective | Education, Persuasion, Incentivization, Coercion |
| Motivation - Automatic | Incentivization, Coercion, Training, Restriction |
The selection process requires a systematic approach to ensure that the chosen intervention functions align with the behavioral diagnosis. Research in dietary interventions during pregnancy, for example, has revealed that most interventions predominantly target psychological capability and reflective motivation, while often overlooking social opportunity and environmental restructuring [31]. This narrow focus may limit the effectiveness and sustainability of dietary behavior change efforts, highlighting the importance of a comprehensive approach that addresses all relevant COM-B components.
Methodological Protocol for Selection
Systematic Selection of Intervention Functions
The selection of intervention functions should follow a structured protocol to ensure methodological rigor. Based on the COM-B analysis conducted in the previous step, researchers should systematically evaluate which intervention functions can address the identified barriers and enhance the enablers [11]. The process involves:
- Matrix-Based Mapping: Refer to the established mapping between COM-B components and intervention functions, as partially illustrated in Table 1. For each barrier and enabler identified in the COM-B analysis, identify the corresponding intervention functions that have evidence of effectiveness for that specific component [11] [32].
- Stakeholder Engagement: Incorporate perspectives from key stakeholders, including the target population (e.g., patients, healthcare providers) and implementation partners. This can be achieved through co-production workshops, advisory groups, or structured surveys [33]. In dietary research, this might involve engaging pregnant women, dietitians, and obstetricians to ensure the selected functions are acceptable and feasible.
- Evidence Integration: Review existing literature and evidence for the effectiveness of different intervention functions for similar behavioral targets and populations. For instance, a systematic review of pregnancy dietary interventions found that commonly employed techniques included goal setting (linked to Enablement), action planning (Enablement), knowledge shaping (Education), and feedback (Enablement) [31].
Application of the APEASE Criteria
After generating a list of potential intervention functions, evaluate each one against the APEASE criteria (Affordability, Practicability, Effectiveness, Acceptability, Side-effects, Equity) to determine their feasibility in the specific context [33]. This evaluation can be quantified to support decision-making.
Table 2: Quantitative Evaluation of Intervention Functions Using APEASE Criteria
| Intervention Function | Affordability (0-10) | Practicability (0-10) | Effectiveness (0-10) | Acceptability (0-10) | Side-effects (0-10) | Equity (0-10) | Total Score (0-60) |
|---|---|---|---|---|---|---|---|
| Education | 10 | 10 | 4.9 | 2.9 | 7 | 10 | 44.8 |
| Persuasion | 10 | 10 | 7.3 | 7.1 | 10 | 10 | 54.4 |
| Training | 10 | 8 | 5.9 | 8.6 | 10 | 10 | 52.5 |
| Modelling | 10 | 8 | 5.9 | 5.7 | 5 | 10 | 44.6 |
Note: Scores are hypothetical examples from a co-development process [33]. The side-effects score is inverted here (higher = fewer side effects) for consistent scoring.
The APEASE evaluation forces explicit consideration of practical implementation constraints. For example, while Restriction might be highly effective for certain dietary behaviors, it may score low on Acceptability among a target population, necessitating consideration of alternative or complementary functions [33].
Selection of Policy Categories
The selection of policy categories follows a similar logic, supporting the delivery of the chosen intervention functions. Each intervention function can be achieved through several policy categories [11] [32].
Table 3: Linking Intervention Functions to Policy Categories
| Intervention Function | Compatible Policy Categories |
|---|---|
| Education | Communication/Marketing, Guidelines, Regulation, Legislation |
| Persuasion | Communication/Marketing, Guidelines, Regulation, Legislation |
| Incentivization | Fiscal measures, Regulation, Legislation |
| Coercion | Regulation, Legislation |
| Training | Guidelines, Regulation, Legislation, Service provision |
| Restriction | Regulation, Legislation, Environmental/social planning |
| Environmental Restructuring | Guidelines, Regulation, Legislation, Environmental/social planning, Service provision |
| Modelling | Communication/Marketing, Guidelines |
| Enablement | Guidelines, Regulation, Legislation, Environmental/social planning, Service provision |
The choice of policy category depends heavily on the context and level of implementation (e.g., organizational, regional, national). For instance, a hospital-based dietary intervention might leverage Service Provision and Guidelines, while a public health campaign might use Communication/Marketing and Environmental/Social Planning [11].
Experimental Workflow and Visualization
The following diagram illustrates the complete logical workflow for selecting intervention functions and policy categories, from the initial COM-B analysis through to the final implementation components.
This workflow demonstrates the systematic progression from behavioral diagnosis (COM-B and TDF) to intervention planning. The process is iterative, as findings from later stages may necessitate re-evaluation of earlier decisions. For example, if a chosen policy category is deemed impracticable after further investigation, researchers may need to revisit the selection of intervention functions [32].
Research Reagents and Essential Materials
Implementing this phase of the BCW framework requires specific "research reagents" and methodological tools to ensure rigorous application.
Table 4: Essential Methodological Reagents for BCW Intervention Design
| Research Reagent / Tool | Function in the Selection Process |
|---|---|
| COM-B Behavioral Diagnosis Matrix | A structured template to document and map identified barriers and enablers to Capability, Opportunity, and Motivation components. |
| Intervention Function Mapping Chart | A visual aid or checklist showing the theoretical links between COM-B components and the nine intervention functions. |
| APEASE Evaluation Scale | A standardized scoring system (e.g., 0-10 scales) for systematically assessing each intervention function against the six APEASE criteria. |
| Stakeholder Co-production Workshop Protocol | A structured guide for facilitating workshops with stakeholders to inform the selection and refinement of intervention functions and policies. |
| Policy Category Linkage Framework | A reference table (like Table 3 in this guide) that identifies which policy categories can deliver each intervention function. |
These methodological reagents provide the necessary tools for operationalizing the theoretical framework. For instance, the Stakeholder Co-production Workshop Protocol was used successfully to develop a mental health intervention for students, where tasks were directly informed by the BCW steps, and language was adapted to be more accessible to non-experts [33]. Similarly, the APEASE Evaluation Scale allows for quantitative comparison of different intervention options, bringing objectivity to the selection process [33].
Application in Dietary Behavior Change Research
In the context of dietary behavior change research, the selection of intervention functions must account for the complex interplay of biological, psychological, social, and environmental factors influencing food choices. A recent systematic review of pregnancy dietary interventions through the lens of the COM-B model revealed that most interventions predominantly targeted psychological capability (via knowledge shaping, information provision) and reflective motivation (via goal setting, action planning) [31]. Far fewer interventions addressed social opportunity (e.g., through social support or modelling) or physical opportunity (e.g., through environmental restructuring to improve food access) [31].
This finding indicates a significant gap and opportunity for researchers. When selecting intervention functions for dietary research, a more comprehensive approach that incorporates functions like Environmental Restructuring (to make healthy foods more accessible) and Modelling (to demonstrate healthy eating behaviors through peers or mentors) could enhance the effectiveness and sustainability of interventions. Furthermore, the policy categories selected must align with the intervention setting. For clinical nutrition support, relevant policy categories might include Guidelines (protocols for malnutrition screening) and Service Provision (structuring prehabilitation clinics) [11]. For community-based dietary interventions, Environmental/Social Planning (food environment policies) and Communication/Marketing (public health campaigns) may be more appropriate [31].
The BCW's structured approach ensures that interventions are not based on intuition alone but are systematically designed to address the specific barriers and enablers identified through rigorous behavioral analysis. This methodology enhances the potential for developing dietary interventions that are not only effective but also feasible and acceptable to the target population, thereby bridging the critical evidence-practice gap in nutrition support [11] [31].
Specifying evidence-based Behavior Change Techniques (BCTs) is a critical step in translating theoretical understanding into practical, effective interventions for dietary behavior change. BCTs are defined as the "smallest observable and replicable 'active ingredients' for designing interventions" [34]. Within the context of the Theoretical Domains Framework (TDF) for dietary behavior change research, this step ensures that identified barriers and enablers are addressed through targeted, measurable, and theoretically-grounded active components. This guide provides researchers and drug development professionals with a structured approach to selecting, specifying, and implementing BCTs, complete with quantitative data summaries, experimental protocols, and visualization tools to enhance intervention design, reproducibility, and efficacy.
Core BCT Taxonomy and Linkage to Theoretical Domains
The most widely adopted framework for classifying BCTs is the 93-item BCT Taxonomy v1 [34]. For dietary interventions, BCTs from the 'Goals and planning' and 'Feedback and monitoring' categories are particularly recommended [34]. The table below summarizes the most frequently used and effective BCTs in dietary interventions, mapping them to their corresponding TDF domains and COM-B model components to illustrate the theoretical pathway to behavior change.
Table 1: Evidence-Based BCTs for Dietary Behavior Change, Mapped to TDF and COM-B
| BCT Number & Label | TDF Domain(s) | COM-B Component | Definition & Application in Dietary Research |
|---|---|---|---|
| 1.1 Goal setting (behavior) [35] | Goals, Intentions | Motivation (Reflective) | Setting a defined target related to dietary behavior (e.g., "Eat 5 servings of vegetables daily"). Informs outcome measures. |
| 1.4 Action planning [35] | Goals, Behavioral regulation | Motivation (Reflective) | Detaling the plan of when, where, and how to perform a dietary behavior (e.g., "Prepare a healthy lunch every Sunday"). |
| 2.2 Feedback on behavior [35] | Knowledge of results, Beliefs about consequences | Motivation (Reflective) | Providing data about the person's performance of the dietary behavior (e.g., "You met your fruit & vegetable goal on 5 of 7 days this week"). |
| 2.3 Self-monitoring of behavior [34] [35] | Memory/attention, Behavioral regulation | Capability (Psychological) | Instructing the person to record and monitor their own dietary behavior (e.g., using a food diary or app to log all meals). |
| 3.1 Social support (unspecified) [34] | Social influences | Opportunity (Social) | Advising on how to arrange practical or emotional support from others for the dietary change (e.g., cooking healthy meals with family). |
| 4.1 Instruction on how to perform the behavior [35] | Skills, Knowledge | Capability (Psychological) | Providing information on how to execute the dietary behavior (e.g., giving recipes or guidance on reading nutrition labels). |
Quantitative Data on BCT Effectiveness and Usage
The selection of BCTs must be informed by empirical evidence of their effectiveness and frequency of use in successful interventions. The following tables consolidate quantitative data from recent systematic reviews and meta-analyses to guide this selection.
Table 2: Frequency and Effectiveness of Key BCTs in Digital Dietary Interventions
| BCT | Frequency in Apps (n=29 RCTs) [35] | Effectiveness Evidence | Target Population Context |
|---|---|---|---|
| Self-monitoring of behavior | 25 (86.2%) | Significant weight loss association [34]; enhances engagement in adolescents [36] | Adults with overweight/obesity; Adolescents |
| Instruction on how to perform | 24 (82.8%) | Foundational for building capability | Adults with overweight/obesity |
| Feedback on behavior | 20 (69.0%) | Promotes adherence in adolescent interventions [36] | Adults with overweight/obesity; Adolescents |
| Goal setting (behavior) | 19 (65.5%) | One of the most effective for adolescent adherence [36] | Adults with overweight/obesity; Adolescents |
| Action planning | 15 (51.7%) | Improves intervention effectiveness [35] | Adults with overweight/obesity |
Table 3: Impact of Mobile App-Based Interventions on Health Outcomes (Meta-Analysis of 29 RCTs) [35]
| Outcome | Mean Difference (MD) | 95% Confidence Interval (CI) | P-value |
|---|---|---|---|
| Weight | -1.45 kg | -2.01 to -0.89 | < .001 |
| Body Mass Index (BMI) | -0.35 kg/m² | -0.57 to -0.13 | .002 |
| Waist Circumference (WC) | -1.98 cm | -3.42 to -0.55 | .007 |
| Diastolic Blood Pressure (DBP) | -1.76 mm Hg | -3.47 to -0.04 | .04 |
| Hemoglobin A1c (HbA1c) | -0.13% | -0.22 to -0.04 | .005 |
Subgroup analyses from the same meta-analysis indicate that interventions are more effective when they combine diet and physical activity, have a medium-term duration, and employ 8 or more BCTs [35].
Experimental Protocol for BCT Identification and Specification
To ensure a systematic and reproducible approach to BCT specification, follow this detailed experimental protocol, adapted from methodologies used in recent high-quality research.
Protocol: Content Analysis of Interventions for Behavior Change Techniques (BCTs)
1. Objective: To identify, code, and report the BCTs present within a dietary behavior change intervention (e.g., app, manual, protocol).
2. Materials and Equipment:
- Intervention Material: The complete intervention to be analyzed (e.g., access to mobile app, intervention manual, transcripts).
- Coding Framework: The BCT Taxonomy v1 [34].
- Data Recording Tool: Microsoft Excel or similar software with a pre-designed checklist.
- Training Materials: BCT Taxonomy training modules to ensure coder competency.
3. Step-by-Step Procedure: Step 1: Coder Training. All raters must complete formal BCT taxonomy training and achieve a minimum of >80% inter-rater reliability in coding exercises to ensure consistency and accuracy [34]. Step 2: Independent Coding. Each coder works through the intervention material independently. For a BCT to be coded as present, it must: * Be directly related to the target dietary behavior. * Explicitly match the BCT label and definition in the taxonomy (inference is not permitted). * Be contained within the core intervention environment (external links are not coded). * Be counted only once, even if it appears multiple times [34]. Step 3: Data Recording. For each BCT identified, coders record it in the Excel checklist and take a screenshot to provide an audit trail, which is essential for verifying coding accuracy during discussion. Step 4: Reconciliation of Coding. Coders meet to discuss their independent coding. Disagreements are resolved through consensus, referring to the taxonomy definitions and the collected audit trail (screenshots). Step 5: Reliability Assessment. A minimum inter-rater agreement of 70% is required for the coding to be considered reliable. If this threshold is not met, the process is repeated for the discrepant sections of the intervention [34].
Visualizing the Causal-Structural Chain of BCTs
The relationship between BCTs, their targets, and the intended behavior change can be complex. Acyclic Behavior Change Diagrams (ABCDs) are a tool designed to make the implicit assumptions of an intervention explicit [37]. An ABCD visually represents the causal-structural chain linking the BCPs to the target behavior via determinants and sub-determinants.
The diagram below illustrates the structural-causal pathway through which a BCT operates to change dietary behavior, from the application of the technique to the ultimate target behavior.
Diagram 1: The Causal-Structural Chain of a BCT
The Scientist's Toolkit: Research Reagent Solutions
In the context of behavior change research, "research reagents" refer to the standardized tools, frameworks, and methods required to develop, specify, and evaluate BCTs. The following table details the essential components of this methodological toolkit.
Table 4: Key Research Reagents for BCT Specification and Evaluation
| Reagent / Tool | Function & Application in BCT Research | Example / Source |
|---|---|---|
| BCT Taxonomy v1 | The core classification system for identifying and labeling 93 distinct BCTs. Ensures standardized reporting and replication. | Michie et al. (2013) [34] |
| Theoretical Domains Framework (TDF) | Used to identify barriers and enablers to behavior change, which are then mapped to relevant BCTs for intervention design. | Cane et al. (2012) [11] |
| Behavior Change Wheel (BCW) | A comprehensive system that incorporates the COM-B model and TDF to guide the selection of intervention functions and BCTs. | Michie et al. (2011) [11] |
| Mobile App Rating Scale (MARS) | A validated tool to assess the quality of mobile health interventions, including engagement, functionality, and information quality. Correlates with BCT number. | Stoyanov et al. (2015) [34] |
| Acyclic Behavior Change Diagrams (ABCDs) | A visual tool for mapping and reporting the hypothesized causal-structural chains linking BCTs to behavior change, enhancing transparency. | Crutzen et al. (2022) [37] |
| BCT Coding Protocol | A standardized experimental procedure (as detailed in Section 4) to ensure reliable and systematic identification of BCTs within interventions. | Content Analysis Method [34] |
| MM-401 | MM-401, CAS:1442106-10-6, MF:C29H46N8O5, MW:586.73 | Chemical Reagent |
| m-PEG5-Boc | m-PEG5-Boc, CAS:874208-93-2, MF:C16H32O7, MW:336.42 g/mol | Chemical Reagent |
The translation of evidence-based nutrition practices into consistent clinical care remains a significant challenge. Research indicates that only a fraction of research findings, approximately 20%, ever achieve successful implementation in clinical settings [11]. The Theoretical Domains Framework (TDF) and Behavior Change Wheel (BCW) provide a systematic methodology for addressing this evidence-practice gap by analyzing and influencing the behaviors of healthcare professionals [11]. This technical guide examines the application of these frameworks to two critical clinical nutrition areas: malnutrition screening in hospitalized patients and preoperative prehabilitation for advanced heart failure and colorectal cancer patients. By dissecting the behavioral components of these implementation challenges, researchers and clinical innovators can develop more effective, theoretically-grounded interventions to improve patient outcomes and standardize care processes across diverse healthcare environments.
Theoretical Foundation: TDF and BCW Framework Architecture
The TDF and BCW constitute complementary frameworks for diagnosing implementation barriers and designing targeted interventions. The TDF synthesizes 33 theories of behavior change into 14 domains encompassing 84 theoretical constructs, providing a comprehensive taxonomy for identifying barriers and enablers to behavior change [11] [16]. These domains map directly to the Capability, Opportunity, Motivation-Behavior (COM-B) model, which forms the hub of the BCW [11].
The systematic implementation process involves three critical phases: (1) identifying barriers and enablers using the TDF; (2) mapping these factors to COM-B components; and (3) selecting intervention functions and policy categories from the BCW to address identified barriers [11]. This structured approach moves beyond single-component interventions, recognizing that complex healthcare behaviors typically require multifaceted strategies targeting multiple behavioral determinants simultaneously [11].
Core Framework Components
Table: Theoretical Domains Framework (TDF) Domains and COM-B Mapping
| TDF Domain | COM-B Component | Description |
|---|---|---|
| Knowledge | Psychological Capability | Awareness of existence of something |
| Skills | Physical Capability | Ability or proficiency acquired through practice |
| Social/Professional Role & Identity | Reflective Motivation | Coherent set of behaviors and displayed personal qualities |
| Beliefs about Capabilities | Reflective Motivation | Acceptance of the truth, reality, or validity about an ability, talent, or facility |
| Optimism | Reflective Motivation | Confidence that things will happen for the best |
| Beliefs about Consequences | Reflective Motivation | Acceptance of the truth, reality, or validity about outcomes of a behavior |
| Reinforcement | Automatic Motivation | Increasing the probability of a response by arranging a dependent relationship |
| Intentions | Reflective Motivation | A conscious decision to perform a behavior |
| Goals | Reflective Motivation | Mental representations of outcomes or end states |
| Memory, Attention & Decision Processes | Psychological Capability | Ability to retain information, focus selectively, and choose between alternatives |
| Environmental Context & Resources | Physical Opportunity | Circumstances that facilitate or hinder behavior |
| Social Influences | Social Opportunity | Interpersonal processes that can change thoughts, feelings, or behaviors |
| Emotion | Automatic Motivation | A complex reaction pattern involving experiential, behavioral, and physiological elements |
| Behavioral Regulation | Psychological Capability | Managing and changing actions to achieve goals |
Table: Behavior Change Wheel Intervention Functions
| Intervention Function | Definition | COM-B Targets |
|---|---|---|
| Education | Increasing knowledge or understanding | Psychological Capability |
| Persuasion | Using communication to induce feelings | Automatic Motivation |
| Incentivization | Creating expectation of reward | Automatic Motivation |
| Coercion | Creating expectation of punishment | Automatic Motivation |
| Training | Imparting skills | Physical Capability, Psychological Capability |
| Restriction | Using rules to reduce opportunity | Physical Opportunity, Social Opportunity |
| Environmental Restructuring | Changing physical/social context | Physical Opportunity, Social Opportunity |
| Modeling | Providing an example for imitation | Social Opportunity |
| Enablement | Increasing means/reducing barriers | All COM-B components |
Figure 1: TDF and BCW Implementation Workflow
Case Study 1: Implementing Malnutrition Screening in Hospital Settings
Clinical Context and Evidence Gap
Malnutrition affects 20-50% of hospitalized patients, contributing to increased morbidity, mortality, length of stay, and healthcare costs [38]. Despite international consensus supporting systematic malnutrition screening, implementation remains inconsistent, with only approximately 52% of European hospitals routinely conducting nutritional risk screening [38]. This evidence-practice gap represents a significant quality and safety concern amenable to behavior change approaches.
TDF-Based Barrier Analysis
Application of the TDF to identify barriers to malnutrition screening reveals multiple influencing factors across COM-B components:
- Psychological Capability: Lack of knowledge about screening tools and protocols among clinical staff [38]
- Physical Opportunity: Insufficient resources, time constraints, and competing clinical priorities [11] [38]
- Social Opportunity: Absence of organizational ownership and leadership support [38]
- Reflective Motivation: Beliefs that nutrition is less critical than other medical priorities [11]
Evidence-Based Screening Tools
Table: Standardized Malnutrition Screening Tools for Clinical Use
| Tool Name | Target Population | Components Assessed | Scoring & Interpretation | ESPEN Recommendation |
|---|---|---|---|---|
| MNA-SF (Mini Nutritional Assessment Short-Form) | Older adults (65+) | Food intake, weight loss, mobility, acute disease, neuropsychological stress, BMI | 0-14 points; ≤11 indicates risk/malnutrition | First-line for elderly [38] |
| MUST (Malnutrition Universal Screening Tool) | Community/outpatient settings | BMI, unintentional weight loss, acute disease effect | 0=low risk, 1=medium risk, ≥2=high risk | Community level [38] |
| NRS-2002 (Nutritional Risk Screening) | Hospital inpatients | BMI, weight loss, food intake, disease severity | Score ≥3 indicates nutritional risk | Hospitalized patients [38] |
BCW-Informed Implementation Strategy
Mapping identified barriers to the BCW yields targeted intervention functions:
- Education: Training sessions on screening tool administration and clinical importance [11]
- Training: Hands-on practice with screening tools and documentation [11]
- Environmental Restructuring: Embedding screening tools into electronic health records and admission protocols [11] [38]
- Enablement: Designating clinical nutrition champions and providing administrative support [11]
Case Study 2: Implementing Preoperative Prehabilitation Protocols
Clinical Context and Evidence Base
Preoperative prehabilitation aims to optimize patients' functional capacity before major surgery to enhance resilience and improve postoperative outcomes. For patients with advanced heart failure awaiting mechanical circulatory support (MCS) or colorectal cancer patients undergoing resection, prehabilitation has demonstrated significant benefits including reduced complications, shorter hospital stays, and improved functional recovery [39] [40]. The International Society for Heart and Lung Transplantation now strongly recommends prehabilitation before durable left ventricular assist device (LVAD) implantation [39].
TDF-Based Analysis of Prehabilitation Implementation
Analysis of prehabilitation implementation barriers using the TDF reveals several challenges:
- Physical Opportunity: Limited resources, complex clinical pathways, and declining medical condition of patients [11]
- Psychological Capability: Lack of knowledge and skills among staff regarding prehabilitation protocols [39]
- Reflective Motivation: Individual patient motivation and beliefs about capabilities [11]
- Environmental Context & Resources: Infrastructure requirements for multidisciplinary coordination [39] [11]
UCSF Prehabilitation Protocol Specification
The UCSF MCS program developed a structured 4-step prehabilitation protocol led by an acute care nurse practitioner (ACNP) [39]:
- Initial Frailty Assessment: Comprehensive baseline evaluation using standardized measures
- Patient Education: Provision of information about prehabilitation to enhance motivation
- Multidisciplinary Team Intervention: Coordinated optimization of physical, cognitive, and nutritional function
- Reassessment: Preoperative and postoperative (3-month) evaluation of outcomes
Quantitative Outcomes from UCSF Implementation
Table: Prehabilitation Outcome Metrics from UCSF MCS Program [39]
| Outcome Measure | Baseline Assessment | 3-Month Postoperative | Clinical Significance |
|---|---|---|---|
| 6-Minute Walk Test | 240 feet | 1,045 feet | 4-fold improvement in functional capacity |
| Hospital Discharge | N/A | Postoperative day 14 | Reduced acute care utilization |
| Cognitive Function | Impaired | Measurable improvement | Reversal of frailty components |
| Quality of Life | Poor | Significant improvement | Enhanced patient-reported outcomes |
Uniform Prehabilitation Protocol for Colorectal Cancer
A nationwide multicenter study in the Netherlands has developed uniform prehabilitation protocols based on the multimodal program from the PREHAB randomized controlled trial [40]. This implementation study will compare 535 patients undergoing prehabilitation with 535 matched controls, with primary outcomes including 90-day postoperative complications, length of stay, and readmission rates [40].
Figure 2: Prehabilitation Clinical Workflow
Integrated Implementation Strategy Using BCW
Matching Interventions to Behavioral Domains
The BCW provides a systematic method for selecting intervention functions based on COM-B diagnoses:
- Capability Barriers (Psychological): Address through Education and Training interventions [11] [16]
- Opportunity Barriers (Physical): Address through Environmental Restructuring and Enablement [11] [16]
- Motivation Barriers (Reflective): Address through Persuasion, Modeling, and Incentivization [11]
Multifaceted Implementation Approach
Successful implementation requires addressing multiple barriers simultaneously through coordinated strategies:
- Staff Education: Structured training on protocols and clinical rationale [39] [11]
- Audit & Feedback: Regular monitoring of screening and prehabilitation completion rates [38]
- Clinical Champions: Identification of opinion leaders to model desired behaviors [39] [16]
- Workflow Integration: Embedding protocols into standard clinical pathways [39] [40]
- Resource Allocation: Ensuring adequate staffing and equipment for implementation [39] [11]
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Resources for TDF/BCW Implementation Research
| Research Tool | Function/Application | Implementation Context |
|---|---|---|
| TDF Interview Guide | Semi-structured questions exploring 14 domains to identify barriers/enablers | Qualitative data collection with healthcare professionals [11] [16] |
| COM-B Mapping Matrix | Worksheet for linking identified TDF domains to COM-B components | Systematic analysis of qualitative data [11] |
| BCW Intervention Selector | Guide for matching COM-B diagnoses to intervention functions | Evidence-based selection of implementation strategies [11] |
| Standardized Screening Tools (MNA-SF, MUST, NRS-2002) | Validated instruments for nutritional risk identification | Malnutrition screening implementation [38] |
| Prehabilitation Protocol Templates | Structured programs for functional optimization | Prehabilitation implementation for surgical candidates [39] [40] |
| Implementation Outcome Measures | Fidelity, adoption, and sustainability metrics | Evaluating implementation success [39] [40] |
| MRTX-1257 | MRTX-1257, CAS:2206736-04-9, MF:C33H39N7O2, MW:565.722 | Chemical Reagent |
The systematic application of the Theoretical Domains Framework and Behavior Change Wheel provides a robust methodology for addressing the persistent evidence-practice gaps in clinical nutrition. The case examples of malnutrition screening and preoperative prehabilitation demonstrate how structured behavioral analysis can inform targeted implementation strategies that address the specific barriers in each clinical context. For researchers and clinical innovators, these frameworks offer a replicable approach for moving beyond simple dissemination of guidelines to creating sustainable practice change through theoretically-grounded interventions. Future implementation efforts should prioritize multidimensional strategies that address capability, opportunity, and motivation barriers simultaneously while measuring both clinical and implementation outcomes to refine approaches and advance the science of healthcare behavior change.
Addressing Real-World Challenges: Optimizing TDF-Based Dietary Interventions
Within digital behavioral weight loss interventions, self-monitoring stands as a cornerstone strategy, consistently correlated with successful outcomes [41] [42]. However, a critical challenge persists: participant engagement in self-monitoring tasks often declines over time due to the perceived burden and effort required [41] [42]. This creates a tension between intervention efficacy and participant burden. The Theoretical Domains Framework (TDF) provides a valuable lens for understanding this challenge, as self-monitoring intersects multiple theoretical domains, including Knowledge (understanding one's dietary habits), Skills (in tracking behaviors), Goals (setting and pursuing targets), and Environmental Context and Resources (the tools and time available) [41].
Traditional intervention designs often bundle multiple self-monitoring strategies—such as tracking dietary intake, physical activity, and body weight—into a single package [41]. While this comprehensive approach can be effective, it fails to identify which components are the "active ingredients" and which are "inactive", unnecessarily adding to participant burden [41]. This whitepaper examines the application of the Multiphase Optimization Strategy (MOST) to isolate the effects of individual self-monitoring components, with the goal of designing optimized interventions that maximize weight loss while minimizing demands on participants [41].
Core Self-Monitoring Components and Methodological Considerations
Key Self-Monitoring Domains and Assessment Methods
Digital weight loss interventions commonly focus on three primary self-monitoring domains, each with its own methodological approaches for assessment [41] [18].
Table 1: Core Self-Monitoring Domains and Assessment Methodologies
| Self-Monitoring Domain | Primary Assessment Methods | Key Characteristics & Considerations |
|---|---|---|
| Dietary Intake | - Food Records- 24-Hour Dietary Recalls (24HR)- Food Frequency Questionnaires (FFQ)- Dietary Screening Tools | - Reactivity (changing diet for ease of recording) is a concern with food records [18].- Multiple 24HRs on non-consecutive days are needed to account for day-to-day variation [18].- FFQs are cost-effective for large samples but less precise for absolute nutrient intake [18]. |
| Physical Activity | - Steps tracked via wearable activity trackers [41] | - Provides an objective, easily quantifiable metric.- Reduces participant burden compared to manual activity logging. |
| Body Weight | - Smart scales [41] | - Provides objective, reliable data with minimal participant effort.- Allows for frequent monitoring without manual entry. |
Statistical Methods for Dietary Pattern Analysis
Analyzing dietary data to derive meaningful patterns requires robust statistical methods. These can be broadly categorized as follows [43]:
- Investigator-Driven Methods (A Priori): Utilize predefined dietary scores or indexes (e.g., Healthy Eating Index, Mediterranean Diet Score) based on existing nutritional knowledge and guidelines. These are useful for assessing adherence to recommended dietary patterns [43].
- Data-Driven Methods (A Posteriori): Use statistical techniques like Principal Component Analysis (PCA) or Cluster Analysis to derive dietary patterns directly from the collected consumption data without predefined hypotheses, identifying common eating habits within a population [43].
- Hybrid Methods: Approaches like Reduced Rank Regression (RRR) incorporate both dietary intake data and health outcomes to identify patterns that explain variation in the outcome [43].
Experimental Framework for Optimization: The Spark Trial
The Spark trial serves as a prime example of applying the MOST framework to optimize self-monitoring components in a fully digital, 6-month weight loss intervention for adults with overweight or obesity [41].
Experimental Design and Protocol
- Design: A 2 × 2 × 2 full factorial randomized clinical trial, creating 8 distinct experimental conditions [41].
- Participants: US adults (N=176) with overweight or obesity [41].
- Randomization: Participants were randomized to receive 0, 1, 2, or all 3 of the core self-monitoring strategies (dietary intake, steps, weight) [41].
- Intervention Core Components:
- Self-Monitoring Strategies: Participants used commercially available digital tools (mobile apps, wearables, smart scales) for their assigned tracking tasks [41].
- Goals and Feedback: Each self-monitoring strategy was paired with a corresponding goal (e.g., daily calorie goal) and participants received weekly automated, personalized feedback [41].
- Theoretical Foundation: All participants received core educational content, including weekly lessons and action plans informed by Social Cognitive Theory and Control Theory, which posit that behavior change occurs through a cyclical process of goal setting, self-monitoring, feedback, and behavioral adjustment [41].
- Data Collection: Assessments occurred at baseline, 1, 3, and 6 months. The primary outcome was objectively measured weight change via a smart scale at 6 months [41].
Diagram 1: Spark Trial Factorial Design (Total Width: 760px)
Cognitive and Behavioral Dynamics of Adherence
Understanding how and why participants engage with self-monitoring is crucial. Research leveraging the Adaptive Control of Thought-Rational (ACT-R) cognitive architecture has modeled the dynamics of dietary self-monitoring adherence over a 21-day intervention [42] [44]. The ACT-R model distinguishes between two key cognitive mechanisms [42]:
- Goal Pursuit: A conscious, effortful process where individuals use self-monitoring to achieve a specific, desired outcome (e.g., weight loss). This mechanism is driven by utility calculations and requires cognitive resources.
- Habit Formation: An automatic process that develops through repeated execution of the self-monitoring behavior in a consistent context, gradually reducing the cognitive effort required.
Findings indicate that the goal pursuit mechanism remains dominant throughout the intervention, whereas the influence of habit formation tends to diminish in the later stages [42]. This suggests that sustained adherence relies heavily on continuous motivation and goal relevance rather than becoming an automated habit within the timeframe of typical interventions.
Table 2: Impact of Intervention Strategies on Adherence Mechanisms (ACT-R Model Findings)
| Intervention Group | Sample Size | Model RMSE | Impact on Goal Pursuit | Impact on Habit Formation |
|---|---|---|---|---|
| Self-Management | 49 | 0.099 | Baseline level | Diminished in later stages |
| Tailored Feedback | 23 | 0.084 | Increased and sustained | Diminished in later stages |
| Intensive Support | 25 | 0.091 | Increased and sustained | Diminished in later stages |
The data shows that interventions providing tailored feedback and intensive support were associated with stronger and more sustained goal pursuit compared to self-management alone [42]. This aligns with Social Cognitive Theory, which emphasizes the importance of feedback in successful behavior change by allowing participants to compare their behaviors with goals and gain self-relevant information [42].
Diagram 2: Adherence Dynamics Model (Total Width: 760px)
The Researcher's Toolkit: Key Reagents and Materials
Table 3: Essential Research Reagents and Digital Solutions for Self-Monitoring Trials
| Item / Solution | Function / Rationale | Example Application in Research |
|---|---|---|
| Commercial Wearable Activity Tracker | To objectively and automatically monitor physical activity (steps), reducing participant burden and recall bias. | Provided to participants in the Spark trial assigned to step tracking for continuous, passive data collection [41]. |
| Smart Scale with Wireless Connectivity | To objectively measure body weight and automatically transmit data to a research platform, ensuring data fidelity and minimizing manual entry. | Used in the Spark trial for the primary outcome (weight change) and for participants assigned to weight self-monitoring [41]. |
| Mobile Application for Dietary Tracking | To facilitate the self-monitoring of dietary intake in real-time, often using digital food databases to simplify logging. | Provided to participants in the Spark trial assigned to dietary tracking, paired with a daily calorie goal [41]. |
| Automated Feedback System | To provide weekly, personalized feedback based on self-monitored data, reinforcing goal pursuit as per Social Cognitive Theory. | Implemented in the Spark trial to give participants insights on their progress relative to their goals for each assigned tracking domain [41]. |
| ACT-R Computational Modeling Framework | To simulate and analyze the cognitive dynamics (goal pursuit vs. habit formation) of participant adherence over time. | Used to model dietary self-monitoring adherence over 21 days, revealing the dominant role of goal pursuit [42] [44]. |
Optimizing self-monitoring components requires a shift from bundling strategies to strategically isolating their effects. The MOST framework, as exemplified by the Spark trial, provides a rigorous methodology for identifying the active ingredients of digital weight loss interventions [41]. The evidence suggests that a "one-size-fits-all" approach is suboptimal. Instead, efficacy and burden must be balanced by determining the necessary and sufficient self-monitoring components for a given context or subgroup.
Future research should prioritize several key areas:
- Extended Intervention Duration: Longer studies are needed to explore if and when habit formation can overtake goal pursuit as the primary driver of long-term adherence [42].
- Personalization: Investigations into which subgroups of individuals benefit most from specific self-monitoring strategies (e.g., based on baseline motivation, cognitive style, or environmental resources) are crucial for building tailored interventions [41].
- Just-in-Time Adaptive Interventions (JITAIs): Dynamic computational models, like ACT-R, can inform the development of JITAIs that deliver support (e.g., tailored feedback) at moments when a participant's adherence is predicted to wane, thereby optimizing engagement with minimal intrusion [42].
By continuing to dissect the cognitive and behavioral mechanisms underlying self-monitoring and applying systematic optimization frameworks, researchers can develop the next generation of highly efficient, effective, and scalable digital health interventions.
Adapting Interventions for Socioeconomically Disadvantaged and Hard-to-Reach Groups
The persistent socioeconomic gradient in diet quality underscores a critical challenge in public health nutrition. Individuals with a lower socioeconomic position (SEP) consistently demonstrate unhealthier diets, characterized by higher intakes of sugar, salt, and saturated fats alongside reduced consumption of vegetables, fruits, and nuts [45]. This disparity contributes significantly to the unequal burden of non-communicable diseases among disadvantaged populations. While behavioral interventions offer promise for improving dietary habits, traditional approaches often fail to adequately reach and engage socioeconomically disadvantaged groups, who are less likely to perceive the need for dietary advice, participate in interventions, and maintain engagement over time [45]. The Theoretical Domains Framework (TDF) provides a systematic methodology for understanding and addressing these implementation challenges by identifying specific barriers and enablers to behavior change across multiple theoretical domains [11]. This technical guide examines evidence-based strategies for adapting dietary behavior change interventions for socioeconomically disadvantaged and hard-to-reach groups within the context of the TDF, offering researchers and practitioners a structured approach to developing culturally relevant, effective, and equitable nutrition interventions.
Theoretical Foundations: The TDF and COM-B Model
The Theoretical Domains Framework (TDF) and its associated Behavior Change Wheel (BCW) offer comprehensive frameworks for systematically developing and evaluating behavior change interventions. The TDF was developed through a consensus process merging multiple behavior theories, resulting in 14 key domains and 84 theoretical constructs that help identify barriers and enablers for behavior change in healthcare settings [11]. These domains can be mapped directly to the Capability, Opportunity, Motivation-Behavior (COM-B) component of the BCW, which provides a model for understanding the sources of behavior and guiding intervention development [11].
Table 1: TDF Domains and Corresponding COM-B Components
| TDF Domain | COM-B Component | Description |
|---|---|---|
| Knowledge | Psychological Capability | Understanding of nutrition guidelines and health consequences |
| Skills | Physical Capability | Food preparation, budgeting, and planning abilities |
| Social and Professional Role and Identity | Reflective Motivation | Perception of social roles related to food provision |
| Beliefs about Capabilities | Reflective Motivation | Confidence in ability to change dietary habits (self-efficacy) |
| Optimism | Reflective Motivation | Belief that changes will lead to desired outcomes |
| Beliefs about Consequences | Reflective Motivation | Understanding of potential benefits of dietary change |
| Reinforcement | Automatic Motivation | Rewards and incentives for healthy eating behaviors |
| Intentions | Reflective Motivation | Commitment to changing dietary behaviors |
| Goals | Reflective Motivation | Target outcomes for dietary improvement |
| Memory, Attention, and Decision Processes | Psychological Capability | Cognitive resources for food-related decisions |
| Environmental Context and Resources | Physical Opportunity | Access to affordable healthy foods and cooking facilities |
| Social Influences | Social Opportunity | Family, peer, and cultural norms around food |
| Emotion | Automatic Motivation | Emotional responses to food and eating |
| Behavioral Regulation | Psychological Capability | Planning and monitoring of dietary intake |
The TDF and COM-B system provides a structured approach to addressing evidence-practice gaps in nutrition support by first identifying barriers and enablers using the TDF, mapping these to COM-B components, and then selecting appropriate intervention strategies [11]. This method is particularly valuable when working with hard-to-reach populations, as it forces explicit consideration of the specific contextual factors that influence behavior within these groups.
Methodological Approaches for Engagement and Research
Community-Engaged Recruitment Strategies
Engaging hard-to-reach populations requires moving beyond traditional recruitment methods to approaches that build trust and reduce barriers to participation. Successful strategies include:
Community Partnerships: Establishing collaborations with community leaders and organizations serving target populations builds essential trust and provides a platform for sustainable engagement [46]. These partnerships should be established early in the research process and maintained throughout all study phases.
Culturally Appropriate Venues: Conducting recruitment in spaces where the population naturally gathers, such as places of worship, community centers, clinics, and grocery stores in specific neighborhoods, increases accessibility and comfort [46].
Linguistic and Cultural Competence: Employing bilingual research staff from the population of interest or cultural brokers who can bridge cultural gaps is essential for effective communication and trust-building [46]. All materials should be available in the preferred languages of the target population, with attention to literacy levels through use of plain language and visual aids.
Non-Probability Sampling: Methods such as respondent-driven sampling (starting with initial "seeds" who then refer others from their social networks) and purposive sampling are often more effective than random sampling for reaching hidden or marginalized populations [46].
Qualitative Assessment Methodologies
Qualitative methods are essential for identifying the specific barriers and enablers to dietary change within the TDF framework:
Focus Group Discussions: Conducting structured discussions with 7-12 participants per group allows researchers to explore shared perspectives and collective experiences related to dietary practices [47]. Focus group guides should be developed using theoretical frameworks like Social Cognitive Theory and culturally relevant intervention development frameworks [47].
Trauma-Informed Approaches: Creating safe, supportive research environments is particularly important when working with populations who may have experienced historical trauma or marginalization in healthcare settings [46]. This involves being aware of potential trauma triggers and prioritizing participants' emotional safety.
Iterative Protocol Refinement: Pilot testing interview protocols and refining them based on cultural nuances ensures that assessment methods are appropriate and relevant to the specific population [46].
Table 2: Effective Engagement Strategies for Different Hard-to-Reach Populations
| Population | Key Barriers | Effective Engagement Strategies | Research Considerations |
|---|---|---|---|
| African American Communities | Historical mistrust of research, cultural mismatches in dietary guidelines [47] | Community-based participatory research, involvement of cultural insiders in intervention delivery [47] | Focus groups to explore cultural acceptability of dietary patterns [47] |
| Rural Populations | Geographic isolation, limited access to resources [46] | Mobile technologies, partnerships with local community centers | Adaptation to local food environments and traditions |
| Immigrant Communities | Language barriers, fear of disclosing immigration status, cultural norms [46] | Bilingual staff, cultural brokers, trust-building through community leaders [46] | Understanding traditional dietary practices and acculturation effects |
| Low SEP Groups | Time constraints, financial limitations, health literacy challenges [45] | Plain language materials, reading assistance, flexible timing for interventions [45] | Addressing structural barriers in intervention design |
Intervention Adaptation Frameworks
Cultural Adaptation of Dietary Interventions
Cultural adaptation involves modifying evidence-based interventions to align with the cultural values, preferences, and experiences of specific population groups. Research with African American adults participating in dietary interventions based on U.S. Dietary Guidelines revealed several key considerations for cultural adaptation [47]:
Cultural Food Traditions: Interventions must acknowledge and incorporate traditional foods and preparation methods rather than simply replacing them with unfamiliar alternatives. Participants in the DG3D study expressed the need for adaptations to USDG dietary patterns to ensure cultural relevance for African American adults [47].
Family and Social Context: Dietary interventions should account for the social dynamics of food within families and communities, recognizing that individuals often make food decisions within complex social networks rather than in isolation.
Visual Representation: Intervention materials should depict people from the target population in familiar environments, using food imagery that reflects culturally familiar items and presentation styles [47].
Digital Intervention Adaptations for Low SEP Groups
Digital health interventions offer promising avenues for reaching socioeconomically disadvantaged populations at scale, but require specific adaptations:
Design for Lower Health Literacy: Present information in bite-sized portions using plain language, accompanied by reading functions, appealing visuals, animations, and speech recognition to accommodate varying literacy levels [45].
Platform Accessibility: Ensure interventions are compatible with older mobile devices and function well with limited bandwidth, acknowledging that disadvantaged individuals may have less access to latest technologies and high-speed internet [45].
Behavior Change Technique Selection: Evidence suggests that digital dietary interventions for low SEP groups most frequently employ BCTs from the 'Goals and planning' cluster (25 applications across studies), followed by 'Shaping knowledge' (18 applications) and 'Natural consequences' (18 applications) [45]. Other frequently applied clusters include 'Feedback and monitoring' (15 applications) and 'Comparison of behavior' (13 applications) [45].
Effective Behavior Change Techniques for Dietary Interventions
Systematic reviews of dietary interventions reveal specific Behavior Change Techniques (BCTs) with demonstrated effectiveness across various populations. The BCT Taxonomy v1 provides a standardized classification system with 93 techniques organized into 16 clusters [48].
Table 3: Effective Behavior Change Techniques for Dietary Interventions with Disadvantaged Groups
| Behavior Change Technique | Effectiveness Evidence | Application in Digital Interventions | Considerations for Low SEP Groups |
|---|---|---|---|
| Goal Setting (behavior) | Most common BCT in effective digital interventions [36] [49] | 14 of 16 digital interventions included this technique [36] | Ensure goals are realistic given resource constraints |
| Feedback on Behavior | Present in 56% of digital dietary interventions [50] | 14 of 16 digital interventions included this technique [36] | Provide specific, actionable feedback |
| Social Support | Effective for adolescent adherence [36] | Used in 14 of 16 digital interventions [36] | Leverage existing community support structures |
| Prompts/Cues | Most common BCT in JITAIs (n=29) [49] | 13 of 16 digital interventions included prompts [36] | Consider timing and frequency to avoid overwhelm |
| Self-Monitoring | Associated with improved dietary outcomes [36] | 12 of 16 digital interventions included self-monitoring [36] | Simplify tracking to reduce participant burden |
| Habit Formation | 100% effectiveness ratio in young adults [48] | Less commonly implemented in digital formats | Focus on creating affordable healthy habits |
| Salience of Consequences | 83% effectiveness ratio [48] | Can be delivered through videos or testimonials | Emphasize immediate, tangible benefits |
| Adding Objects to Environment | 70% effectiveness ratio [48] | Challenging in digital-only interventions | Consider providing practical resources |
For young adults, specific BCTs including habit formation (showing 100% effectiveness ratio), salience of consequences (83%), and adding objects to the environment (70%) have demonstrated particularly high effectiveness [48]. Meta-analyses show that interventions incorporating appropriate BCTs can significantly increase fruit and vegetable consumption by +68.6 g/day after three months and maintain improvements of +65.8 g/day for longer interventions [48].
Digital interventions for adolescents have shown that combinations of BCTs—particularly goal setting, feedback on behavior, social support, prompts/cues, and self-monitoring—are most effective for promoting adherence and engagement [36]. Personalized feedback and gamification elements have demonstrated adherence rates between 63% and 85.5% in this population [36].
Implementation and Evaluation Framework
Implementation Strategies
Successful implementation of adapted interventions requires attention to several key factors:
Multicomponent Approaches: Single-strategy interventions are generally less effective than those employing multiple complementary BCTs. Research indicates that digital dietary interventions include an average of 6.9 BCTs (ranging from 3-15 across different interventions) [45].
Stakeholder Involvement: Engaging end-users in the design process enhances satisfaction and engagement by ensuring interventions address their unique needs and preferences [50]. However, only 59% of digital dietary interventions report stakeholder involvement in design, with just 5% utilizing co-design methodologies [50].
Long-term Maintenance: Interventions should plan for sustained engagement beyond initial implementation, as many digital interventions show reduced effects after several weeks [36]. Building habits and creating supportive environments are crucial for maintaining changes.
Evaluation Methods
Comprehensive evaluation of adapted interventions should include:
Process Measures: Assess reach, engagement, usability, and perceived cultural appropriateness across different socioeconomic groups [45]. Mixed-methods approaches combining quantitative engagement metrics with qualitative feedback are particularly valuable.
Equity-Focused Outcomes: Explicitly examine intervention effects across socioeconomic strata to identify potential intervention-generated inequalities [45]. Disaggregate data by SEP indicators to ensure interventions benefit disadvantaged groups.
Long-term Follow-up: Evaluate maintenance of behavior change beyond immediate post-intervention assessments, as limited long-term follow-up represents a significant gap in current literature [51].
Research Reagent Solutions Toolkit
Table 4: Essential Research Tools for Dietary Intervention Adaptation
| Research Tool | Function | Application Example |
|---|---|---|
| Theoretical Domains Framework (TDF) | Identifies barriers/enablers across 14 behavioral domains [11] | Mapping specific challenges to dietary change in low-SEP populations |
| Behavior Change Technique Taxonomy v1 | Standardized classification of 93 active intervention components [48] | Specifying active ingredients in adapted interventions |
| COM-B System Diagnostic | Links identified barriers to Capability, Opportunity, and Motivation components [11] | Selecting appropriate intervention types based on barrier analysis |
| Cultural Relevance Assessment Framework | Evaluates intervention alignment with cultural values and practices [47] | Adapting dietary guidelines for African American populations |
| Digital Engagement Metrics | Tracks usage patterns, feature utilization, and adherence rates [50] | Evaluating engagement with digital intervention components |
| Equity-Focused Evaluation Framework | Assesses differential intervention effects across socioeconomic groups [45] | Identifying potential intervention-generated inequalities |
Adapting dietary interventions for socioeconomically disadvantaged and hard-to-reach groups requires a systematic approach that addresses the specific barriers and enablers relevant to these populations. The Theoretical Domains Framework provides a comprehensive structure for identifying implementation challenges and developing targeted strategies. Evidence suggests that successful adaptations incorporate cultural relevance, appropriate behavior change techniques, and consideration of the practical constraints facing disadvantaged groups. Digital platforms offer promising delivery channels but require careful design to ensure accessibility and engagement across socioeconomic strata. Future research should prioritize co-design methodologies, long-term follow-up, and explicit attention to evaluating equity impacts to advance the field of tailored dietary interventions for populations most in need.
Integrating TDF with Experimental Medicine Models for Early-Phase Drug Development
The integration of established antiretroviral drugs like tenofovir disoproxil fumarate (TDF) with experimental medicine models represents a transformative approach in early-phase HIV drug development. This whitepaper examines how model-informed drug development (MIDD) strategies, particularly physiologically-based pharmacokinetic (PBPK) modeling and simulation, can optimize tenofovir-based regimens while framing these advancements within the Theoretical Domains Framework (TDF) for understanding medication adherence behavior. By leveraging quantitative systems pharmacology models that incorporate drug transport, cellular phosphorylation, and mucosal tissue distribution, researchers can better predict clinical outcomes from variable adherence patterns and design more effective prevention strategies for at-risk populations.
Tenofovir disoproxil fumarate (TDF) is a nucleotide reverse transcriptase inhibitor approved for both HIV treatment and prevention [52]. As a prodrug, TDF is rapidly converted by plasma esterases to tenofovir (TFV), which undergoes intracellular phosphorylation to its active metabolite tenofovir diphosphate (TFV-DP) [53]. This anabolite competes with endogenous deoxyadenosine triphosphate for incorporation into viral DNA by HIV-1 reverse transcriptase, thereby terminating DNA chain elongation and inhibiting viral replication [53].
The pharmacokinetic profile of TDF is characterized by its conversion to tenofovir in plasma, while the newer prodrug tenofovir alafenamide (TAF) is metabolized predominantly intracellularly, resulting in lower circulating plasma tenofovir levels and an improved renal and bone safety profile [52]. Understanding these pharmacokinetic differences is crucial for designing appropriate experimental medicine models that can accurately predict drug behavior across different tissue compartments and patient populations.
Experimental Medicine Models for TDF Development
Mechanism-Based Pharmacokinetic-Pharmacodynamic (PK-PD) Modeling
Mechanistic PK-PD models for TDF incorporate mass transport principles and enzyme kinetics to examine uptake and phosphorylation mechanisms. These models typically include:
- Passive diffusion and saturable channel-mediated uptake of tenofovir into target cells
- MRP4 channel-based efflux of tenofovir from peripheral blood mononuclear cells (PBMCs)
- Intracellular phosphorylation through kinases to form the active TFV-DP metabolite
- Competitive inhibition of HIV reverse transcription through molecular mechanisms of action (MMOA) models [53]
These models have demonstrated that diffusion plays a minimal role in TFV uptake due to its negative charge at physiological pH (pKa1 = 3.8 and pKa2 = 6.7), explaining the saturable uptake observed clinically and the need for prodrug development to improve bioavailability [53].
Multicompartment Population PK Modeling
Advanced semi-physiological population PK models enable simultaneous prediction of TFV, FTC, and their active metabolites across multiple anatomical compartments. A recently developed 16-compartment model incorporates:
- Plasma compartments for parent drugs and metabolites
- Intracellular compartments for active phosphorylated metabolites
- Mucosal tissue compartments (cervical, vaginal, rectal) as viral exposure sites
- Gut transit delay components to describe drug distribution to rectal tissue [54]
This modeling approach allows researchers to predict drug exposure under varying adherence scenarios and alternative pre-exposure prophylaxis dosing strategies before conducting clinical trials [54].
Table 1: Key Parameters from Multicompartment PK Model for TDF/FTC
| Parameter | TDF/TFV Estimate | FTC Estimate | Biological Significance |
|---|---|---|---|
| Kâ‚ (1/h) | 0.863 | 0.649 | Absorption rate constant |
| V꜀ (L) | 331 | 72.3 | Central volume of distribution |
| Vâ‚š (L) | 843 | 122 | Peripheral volume of distribution |
| CL (L/h) | 58.7 | 18.9 | Clearance |
| Fáµ¥ (fraction, ×10â»âµ) | 7.90 | 131 | Vaginal tissue distribution |
| Fâ‚‘ (fraction, ×10â»âµ) | 1.50 | 6.90 | Cervical tissue distribution |
| Fáµ£ (fraction, ×10â»âµ) | 7.00 | 401 | Rectal tissue distribution |
Adherence-Protection Relationship Modeling
Model-based analysis of clinical PrEP trials has established critical adherence-efficacy relationships for TDF-based regimens in different populations. By dichotomizing trial participants based on detectable plasma tenofovir levels, researchers have demonstrated that:
- Individuals with undetectable plasma TFV (taking PrEP at most once weekly) derive negligible protection [55]
- Studies with adequate adherence (HPTN 084 and Partners-PrEP) show 90-100% efficacy in women with detectable drug [55]
- With 14% adherence (approximately once weekly), median efficacy is 65% (IQR = 35-90%) [55]
These models have challenged hypotheses about biological differences in PrEP efficacy between men and women, suggesting instead that adherence behavior explains most outcome variations [55].
Experimental Protocols for TDF Model Development
Protocol for Population PK Model Building
Objective: To develop a population PK model for TFV and TFV-DP in plasma and mucosal tissues.
Methods:
- Study Design: Phase I, open-label, dose-ranging study with single oral doses of TDF (150, 300, or 600 mg) in healthy female volunteers [54]
- Sample Collection: Intensive blood sampling over 48 hours for plasma drug concentration quantification
- Tissue Sampling: Single cervical, vaginal, and rectal tissue samples at 6, 12, 24, or 48 hours post-dose
- Bioanalytical Methods: LC-MS/MS quantification of TFV, FTC, TFV-DP, and FTC-TP concentrations
- Model Building: Nonlinear mixed-effects modeling with NONMEM 7.3 using FOCE-I on Linux computing clusters with parallel processing [54]
Key Parameters Fixed:
- Rectal tissue volume: 0.17 L (based on physiological estimates)
- Cervical tissue volume: 0.01 L
- Vaginal tissue volume: 0.09 L
- Tissue density assumption: 1 g/mL [54]
Protocol for Mechanism-Based PK-PD Modeling
Objective: To develop an integrated PK model accounting for TFV transport and phosphorylation.
Methods:
- Model Structure: Two-compartment PK model with dosing compartment for plasma TFV combined with PBMC submodel for TFV-DP [53]
- Transport Mechanisms: Passive diffusion, saturable channel-mediated uptake, MRP4-based efflux
- Metabolism: Enzyme kinetics for phosphorylation steps (TFV→TFV-MP→TFV-DP)
- Model Validation: Visual predictive check against clinical data from MTN-001 study with simulation of 100 subjects [53]
- Sensitivity Analysis: Calculation of sensitivity indices for key parameters (efflux rate, enzyme concentration, turnover number, Km values)
Implementation:
- Initial testing with single and multiple-dose simulations (75, 150, 300, and 600 mg TDF)
- Time spans: 240 hours (single dose) and 480 hours (multiple dose)
- Between-subject variability incorporated from literature values [53]
Visualization of TDF Pharmacokinetic-Pharmacodynamic Relationships
Diagram 1: TDF Pharmacokinetic-Pharmacodynamic Pathway
Diagram 2: Adherence-Protection Relationship Modeling Framework
Research Reagent Solutions for TDF Experimental Models
Table 2: Essential Research Reagents for TDF Experimental Medicine Studies
| Reagent/Assay | Function | Application in TDF Models |
|---|---|---|
| LC-MS/MS Systems | Quantification of drug concentrations | Measurement of TFV, FTC, TFV-DP, and FTC-TP in plasma, PBMCs, and tissue homogenates [54] |
| Peripheral Blood Mononuclear Cells (PBMCs) | Primary target cells for HIV | In vitro assessment of TFV uptake, phosphorylation, and intracellular metabolite kinetics [53] |
| Mucosal Tissue Explants (cervical, vaginal, rectal) | Simulation of viral exposure sites | Ex vivo evaluation of tissue penetration and local metabolite formation [54] |
| Population PK Modeling Software (NONMEM) | Nonlinear mixed-effects modeling | Development of mechanistic PK-PD models and simulation of adherence scenarios [54] |
| Cathepsin A Enzyme Assays | TAF activation monitoring | Comparison of prodrug metabolism pathways between TDF and TAF [52] |
| MRP4 Transporter Assays | Efflux transport evaluation | Assessment of cellular TFV efflux mechanisms [53] |
Integration with Theoretical Domains Framework for Adherence Behavior
The Theoretical Domains Framework (TDF) provides a structured approach to understanding medication adherence behavior, with direct relevance to TDF-based regimen development. Several TDF domains intersect with experimental medicine models:
Knowledge and Beliefs About Consequences
Model-based predictions demonstrate that even partial adherence (2-3 doses per week) provides substantial protection [55], information that can reshape patient beliefs about consequences of non-perfect adherence. Clinical trial simulations show that individuals with detectable drug levels achieve 90-100% protection, creating powerful educational messages about the consequences of taking some versus no medication [55].
The development of long-acting formulations addresses environmental barriers to daily adherence. Research shows that long-acting slow effective release antiretroviral therapies can overcome limitations of life-long daily regimen adherence [56], directly modifying the environmental context of medication taking.
Behavioral Regulation
Pharmacokinetic-pharmacodynamic models that establish adherence-efficacy relationships enable precisely timed dosing strategies. For instance, models predict that taking 4 doses per week provides 90% protection [55], creating clear behavioral targets for patients struggling with daily adherence.
The integration of TDF with experimental medicine models represents a powerful paradigm for early-phase HIV drug development. Mechanism-based PK-PD modeling, multicompartment population PK approaches, and adherence-protection relationship analyses provide quantitative frameworks to optimize dosing strategies and predict clinical outcomes. When viewed through the lens of the Theoretical Domains Framework, these models offer insights not only into pharmacological behavior but also the psychological and environmental determinants of medication adherence.
Future directions include the development of ultra-long-acting tenofovir formulations, integration of pharmacogenomics into adherence-efficacy models, and the application of artificial intelligence to personalize PrEP regimens based on individual adherence patterns. By continuing to bridge experimental pharmacology with behavioral science frameworks, researchers can accelerate the development of more effective and adherence-resilient HIV prevention strategies.
Evaluating Impact: Evidence for TDF Efficacy and Comparative Framework Analysis
The evaluation of behavioral treatments for conditions like obesity has not traditionally been subject to the same rigorous standards as pharmaceutical interventions, despite their widespread use and potential risks [57]. These treatments, including dietary interventions, require patients' time and investment and may carry unintended psychological or physiological consequences. The Food and Drug Administration (FDA) has developed a systematic procedure for evaluating drugs that balances safety against the dangerousness of the target condition, then establishes efficacy across increasingly broad populations [57]. Applying this established framework to behavioral treatments offers a powerful methodology for identifying critical research gaps and strengthening the evidence base for dietary behavior change interventions. This approach aligns with the core mission of the Theoretical Domains Framework (TDF) by providing a structured mechanism to evaluate the implementation and effectiveness of behavior change strategies, thereby addressing the significant evidence-practice gaps common in nutrition support [11].
The need for such rigor is underscored by the complex challenge of diet-related diseases. Poor nutrition is a key player in chronic but preventable diseases, which are leading causes of death and disability in the U.S. and disproportionately affect underserved communities [58]. While the FDA's nutrition initiatives aim to empower consumers and promote a healthier food supply, the interventions designed to change dietary behavior must themselves be held to a high standard of evidence [58]. This whitepaper outlines a structured, FDA-like framework for researchers to apply when developing and evaluating behavioral treatments, ensuring that the strategies deployed to improve public health are both safe and effective.
The FDA Evaluation Framework: A Model for Behavioral Science
The FDA's drug evaluation process is a phased model that answers sequential questions about a treatment's viability. This process can be directly adapted to evaluate behavioral interventions for dietary change [57].
- Phase 1: Safety and Need. This initial phase addresses two critical questions: First, "Is the treatment safe?" For a behavioral treatment like caloric restriction, potential "side effects" must be systematically evaluated, which could include eating disorder pathology, binge eating, psychological distress, or weight cycling [57]. Second, "How dangerous is the condition being treated?" The risks of a treatment must be balanced against the severity of the problem. For obesity, this requires a nuanced understanding of the mortality and disability risks associated with different Body Mass Index (BMI) categories, as the risks of being overweight are not consistent across all populations [57].
- Phase 2: Efficacy. This phase asks, "Is the treatment effective?" The primary endpoint for evaluation must be clearly defined. While weight loss is often the default metric for dietary interventions, a strong argument can be made that improved health outcomes (e.g., reduced hypertension, improved metabolic markers) should be the true measure of success [57]. Establishing efficacy requires evidence from randomized controlled trials (RCTs), which are the gold standard for establishing causal inference [57].
- Phase 3: Effectiveness. The final pre-approval phase expands the scope to ask, "Is the treatment safe and effective for large numbers of people?" This involves larger trials that gather information on the diverse populations and real-world contexts in which the intervention is effective, and may include comparisons to current standard treatments [57].
Table 1: Applying the FDA's Phased Evaluation Model to a Behavioral Treatment for Obesity
| FDA Phase | Core Question | Application to Behavioral Treatment (e.g., Caloric Restriction) |
|---|---|---|
| Phase 1 | Is the treatment safe? | Identify and quantify side effects: binge eating, psychological distress, nutritional deficiencies, weight cycling. |
| Phase 1 | How dangerous is the condition? | Evaluate the mortality and disability risks associated with the target condition (e.g., obesity) across BMI categories and populations. |
| Phase 2 | Is the treatment effective? | Conduct RCTs to determine if the intervention causes weight loss and/or improvements in health outcomes (e.g., blood pressure, cholesterol). |
| Phase 3 | Is it effective for large populations? | Conduct large-scale trials to test generalizability across diverse populations and compare effectiveness to other available treatments. |
Integrating the FDA Framework with the Theoretical Domains Framework (TDF) and COM-B Model
The FDA framework establishes what to evaluate (safety, efficacy), while implementation frameworks like the Theoretical Domains Framework (TDF) and the Capability, Opportunity, Motivation-Behaviour (COM-B) model provide the structure for understanding how to implement and measure change, particularly in complex clinical settings [11]. Integrating these models creates a comprehensive approach for developing and evaluating robust dietary behavior change research.
The TDF includes 14 key domains that help identify barriers and enablers to behavior change, such as Knowledge, Environmental context and resources, Skills, and Beliefs about consequences [11]. These domains can be mapped directly to the components of the COM-B system, which posits that successful behavior change (B) requires the target population or individual to have the Capability (physical and psychological), Opportunity (physical and social), and Motivation (reflective and automatic) to perform the behavior [11]. This integrated model is especially relevant for addressing evidence-practice gaps in nutrition, such as improving malnutrition screening in hospitals or implementing preoperative prehabilitation clinics [11].
Table 2: Linking TDF Domains to an FDA-Phase Evaluation for a Dietary Intervention
| TDF Domain (Barrier/Enabler) | Relevant COM-B Component | Application in FDA-Like Evaluation |
|---|---|---|
| Knowledge | Psychological Capability | Phase 2: Measure if participants understand dietary guidelines. Phase 3: Assess if knowledge translates to behavior change in large populations. |
| Environmental Context & Resources | Physical Opportunity | Phase 1/3: Evaluate if access to healthy food affects intervention safety or effectiveness across different communities. |
| Skills | Physical Capability | Phase 2: Test if participants can execute food preparation skills required by the intervention. |
| Beliefs about Consequences | Reflective Motivation | Phase 1: Gauge perceived risks/side effects. Phase 2: Measure how outcome expectations influence adherence and efficacy. |
| Social Influences | Social Opportunity | Phase 3: Determine how family, culture, and social norms impact widespread effectiveness. |
For example, a hospital aiming to improve clinician adherence to malnutrition screening (a policy-driven behavior) would first use the TDF to identify barriers, such as lack of knowledge, competing priorities, or insufficient resources [11]. These barriers would be mapped to COM-B components to identify the types of interventions needed—such as education to improve psychological capability, or environmental restructuring to improve physical opportunity [11]. The FDA-like framework would then provide the structure for rigorously evaluating the safety, feasibility, and effectiveness of this implementation strategy itself.
Workflow Diagram: Integrated Evaluation Framework
The following diagram visualizes the integrated workflow for applying an FDA-like framework alongside the TDF and COM-B model to the development and evaluation of a dietary behavior change intervention.
Quantitative Evaluation and Measurement in Implementation Research
For an evaluation to meet FDA-like rigor, it must incorporate quantitative measures of key implementation outcomes. The Implementation Outcomes Framework (IOF) includes critical metrics such as acceptability, adoption, feasibility, fidelity, and sustainability [59] [60]. Measuring these outcomes is essential for moving beyond the question of whether an intervention works in a controlled setting, to understanding how it can be successfully implemented in practice.
A systematic review of mental health policy implementation found that the most frequently assessed implementation determinants were readiness for implementation (including training and other resources), actor relationships/networks, and organizational culture and climate [59]. The most prevalent implementation outcome measured was fidelity (the degree to which the intervention was implemented as intended), followed by penetration (the integration of the intervention within a service setting) and acceptability (the perception among stakeholders that the intervention is agreeable) [59]. However, the review noted that many existing measurement tools lack information on their psychometric properties, highlighting a need for more valid, reliable, and pragmatic measures in the field [59].
In the context of a dietary intervention, this means researchers should not only measure primary health endpoints (e.g., weight loss, biomarker changes) but also implementation outcomes such as:
- Fidelity: Were the dietary protocols followed as designed by participants?
- Adoption: What percentage of the eligible target population enrolled and engaged with the program?
- Acceptability: Did participants and providers find the dietary changes acceptable and manageable?
- Cost: What were the resources required to implement the intervention effectively? [60]
These quantitative evaluations can be conducted using a variety of data sources, including electronic health records, administrative data, patient-reported outcomes, and structured audits [60].
Experimental Protocols and the Scientist's Toolkit
To conduct evaluations that meet this rigorous standard, researchers require a clear experimental protocol and a suite of reliable "research reagents" – the standardized tools and methods used to generate evidence.
Sample Experimental Protocol: Evaluating a Novel Dietary Intervention
This protocol outlines a phased approach that integrates FDA-like principles with implementation science frameworks.
- Phase 1a (Safety & TDF Identification): Conduct a small-scale pilot (n=20-30) to monitor for adverse effects (e.g., emergence of disordered eating behaviors, significant nutrient deficiencies, psychological distress). Concurrently, use qualitative interviews guided by the TDF domains with key stakeholders (participants, clinicians, dietitians) to identify barriers and enablers to the intervention [11].
- Phase 1b (COM-B Analysis & Refinement): Map the identified TDF barriers and enablers to the COM-B model. For example, a barrier in the "Skills" domain maps to "Physical Capability," suggesting the intervention may need a skills-training component. Use these insights to refine the intervention protocol [11].
- Phase 2 (Efficacy & Mechanism): Conduct a randomized controlled trial (RCT) (n=100-200) comparing the refined intervention to an appropriate control (e.g., standard care, an alternative diet). The primary endpoint should be pre-specified (e.g., ≥5% weight loss, improvement in HbA1c). The study must be powered to detect a clinically significant difference. Crucially, measure proposed mechanisms of action (e.g., changes in automatic motivation, improvements in psychological capability) using validated quantitative tools [29].
- Phase 3 (Effectiveness & Implementation): Execute a large-scale (n>500), pragmatic trial or a series of smaller, coordinated studies across diverse settings and populations. The goal is to assess effectiveness in real-world conditions and collect robust data on implementation outcomes like fidelity, cost, and sustainability [60]. This phase should also seek to confirm the mechanisms of action identified in Phase 2.
- Phase 4 (Post-Market Surveillance): Plan for ongoing monitoring after the intervention is deployed. This involves collecting real-world evidence (RWE) to preserve efficacy, detect unexpected safety signals, and understand the long-term impact on health and behavior [61]. This mirrors the FDA's emphasis on post-market evidence gathering for therapies approved under novel pathways [61].
The Scientist's Toolkit: Key Research Reagents
Table 3: Essential Reagents for Evaluating Dietary Behavior Change Interventions
| Research Reagent | Function/Purpose | Example in Dietary Research |
|---|---|---|
| Validated TDF Interview Guide | To systematically identify barriers and enablers to behavior change across 14 theoretical domains. | A semi-structured interview guide with questions targeting each TDF domain (e.g., "What knowledge is needed to follow this diet?" - Knowledge domain) [11]. |
| COM-B Mapping Matrix | A structured tool to link identified TDF barriers to Capability, Opportunity, and Motivation components, guiding intervention design. | A table that helps researchers decide that a "Skills" barrier requires a "Training" intervention, and an "Environmental Context" barrier requires "Environmental Restructuring" [11]. |
| Standardized Implementation Outcome Measures | Quantitative tools to assess the success of the implementation process itself (e.g., fidelity, acceptability). | The Implementation Outcomes Framework (IOF) surveys to rate participant acceptability or objective checklists to measure provider fidelity to the protocol [59] [60]. |
| Mechanism of Action Probes | Validated questionnaires or biological assays to test hypothesized psychological or physiological mechanisms. | Surveys measuring automatic motivation (e.g., food cravings) or physical capability (e.g., cooking confidence), or biomarkers like ghrelin/leptin levels [29]. |
| Randomized Controlled Trial (RCT) Protocol | The experimental gold standard for establishing causal efficacy of an intervention. | A pre-registered, protocol detailing participant randomization, intervention and control conditions, primary/secondary endpoints, and statistical analysis plan [57]. |
Diagram: Logic Model for a Dietary Intervention Trial
The following logic model maps the theoretical connections between a dietary intervention's resources, activities, and intended outcomes, providing a structured blueprint for evaluation.
Applying an FDA-like framework, integrated with the structured approach of the Theoretical Domains Framework and COM-B model, provides a transformative pathway for elevating the rigor and impact of dietary behavior change research. This methodology ensures that behavioral treatments are held to a high standard of evidence regarding their safety, efficacy, and effectiveness, much like their pharmaceutical counterparts. By systematically identifying implementation barriers, targeting specific behavioral mechanisms, and employing phased experimental protocols with quantitative outcome measures, researchers can generate more robust, generalizable, and clinically meaningful evidence. This rigorous approach is essential for closing the pervasive evidence-practice gap in nutrition and delivering behavior change interventions that reliably improve public health.
The complex interplay between nutrition and behavior represents a critical frontier in public health, yet significant evidence-practice gaps impede progress. The Theoretical Domains Framework (TDF) and Behavior Change Wheel (BCW) provide systematic methodologies for identifying and addressing these gaps, offering a structured approach to understanding and modifying the behaviors of both healthcare providers and patients [11]. These frameworks are particularly valuable in nutrition, where implementing evidence-based practice remains challenging despite recognized benefits in areas such as malnutrition screening and preoperative prehabilitation [11]. This technical guide examines priority research areas through the lens of the TDF, proposing rigorous methodological approaches to advance the science of dietary behavior change.
Theoretical Foundation: TDF and BCW in Nutrition Research
Historical Development and Validation
The TDF was developed through a consensus process involving psychological theorists and health service researchers to simplify and integrate numerous behavior change theories. The framework has evolved from its original 12 domains to a validated structure comprising 14 domains of theoretical constructs [21]. This refinement was validated through rigorous methodologies including Discriminant Content Validation and Fuzzy Cluster Analysis, with the current framework demonstrating strong empirical support (average silhouette value 0.29) [21].
The TDF interconnects with the BCW, which encompasses the COM-B system (Capability, Opportunity, Motivation-Behavior) [11]. This integrated approach allows researchers to systematically map barriers and enablers to behavior change, then identify appropriate intervention strategies and policy categories [16]. The COM-B model posits that successful behavior change requires interaction between three components: physical and psychological capability, physical and social opportunity, and automatic and reflective motivation [11].
Current Applications in Nutrition Research
Application of these frameworks in nutrition research has revealed significant gaps in implementation. For instance, studies show only approximately 37% of dietitian recommendations are actioned in hospital settings, often due to non-evidence-based beliefs of physicians [11]. Similarly, despite international agreement supporting nutrition screening to identify malnutrition risk, practice is not universal across healthcare settings, with documented barriers including lack of resourcing, knowledge, ownership, and competing priorities [11].
Table 1: TDF Domains and Corresponding COM-B Components
| TDF Domain | COM-B Component |
|---|---|
| Knowledge | Psychological Capability |
| Skills | Physical Capability |
| Social/Professional Role and Identity | Reflective Motivation |
| Beliefs about Capabilities | Reflective Motivation |
| Optimism | Reflective Motivation |
| Beliefs about Consequences | Reflective Motivation |
| Reinforcement | Automatic Motivation |
| Intentions | Reflective Motivation |
| Goals | Reflective Motivation |
| Memory, Attention and Decision Processes | Psychological Capability |
| Environmental Context and Resources | Physical Opportunity |
| Social Influences | Social Opportunity |
| Emotions | Automatic Motivation |
| Behavioral Regulation | Reflective Motivation |
Critical Evidence Gaps in Nutrition and Behavior
Implementation Gaps in Clinical Nutrition
Research using the TDF has identified significant disparities between evidence and practice in clinical settings:
Malnutrition Screening: Despite recognition of major benefits for patient care, malnutrition screening is not consistently implemented in hospitals [11]. Cross-sectional studies demonstrate this implementation gap persists across multiple countries, with identified barriers spanning multiple TDF domains including environmental context and resources (e.g., lack of equipment), knowledge (e.g., insufficient training), and social influences (e.g., lack of organizational priority) [11].
Preoperative Prehabilitation: Emerging evidence supports this multidisciplinary approach to physical, nutrition, and psychological optimization before surgery, with benefits including improved functional capacity, enhanced surgical recovery, reduced complication rates, and improved healthcare costs [11]. Despite being considered best evidence-based care, most hospitals across developed countries have not implemented prehabilitation, with barriers including resources, complex clinical pathways, declining medical condition of patients, and individual motivation [11].
Methodological Gaps in Dietary Assessment
Accurate dietary assessment remains challenging, with significant methodological limitations:
Measurement Error: Self-reported dietary data are subject to both random and systematic measurement error [18]. Traditional assessment methods include food records, food frequency questionnaires (FFQs), 24-hour recalls, and screening tools, each with distinct limitations in scope, time frame, and type of measurement error [18].
Limited Biomarkers: The accuracy of self-reported data can only be assessed for a limited number of dietary components using recovery biomarkers, which currently exist for just energy, protein, sodium, and potassium [18]. This constraint significantly limits validation capabilities for most nutrients and dietary components.
Table 2: Dietary Assessment Methods and Their Characteristics
| Method | Scope of Interest | Time Frame | Primary Measurement Error | Participant Burden |
|---|---|---|---|---|
| 24-Hour Recall | Total diet | Short term | Random | High |
| Food Record | Total diet | Short term | Systematic | High |
| Food Frequency Questionnaire | Total diet or specific components | Long term | Systematic | Medium |
| Screening Tools | Limited components | Variable | Systematic | Low |
Research Gaps Identified Through TDF Applications
Recent studies applying the TDF and BCW to nutrition behavior have revealed specific theoretical domains requiring further investigation:
Food Waste Auditing in Hospital Foodservices: Research identified dominant COM-B constructs affecting audit completion included psychological capability (knowledge, skills), physical opportunity (environmental context and resources), and reflective motivation (social/professional role and identity, beliefs about capabilities) [16]. These were driven by staff's lack of knowledge, labor, time, and hospitals avoiding responsibility for audit completion.
Health Equity in Dietary Guidelines: The 2025 Dietary Guidelines Advisory Committee incorporated a health equity lens, focusing on social determinants of health and socioeconomic position, recognizing increased dietary risk for communities unable to afford or access healthy food options [62]. This represents a significant shift in addressing systemic barriers to healthy eating.
Experimental Protocols and Methodologies
Protocol for Identifying Barriers Using TDF
Objective: To systematically identify barriers and enablers to evidence-based nutrition practices using the TDF.
Methodology:
- Stakeholder Recruitment: Use purposive sampling to recruit key stakeholders including clinicians, administrators, and financial decision-makers [11]. Sample size determination should follow estimates for sort and cluster analysis tasks (6-36 participants) [21].
- Data Collection: Conduct semi-structured interviews using questions designed to explore the 14 domains of the TDF [11]. Ensure methodological rigor through credibility, transferability, dependability, and neutrality [11].
- Analysis: Employ deductive analysis using the TDF and COM-B model to identify dominant drivers of behavior [16]. Code transcripts according to TDF domains, with multiple coders to ensure reliability.
- Intervention Mapping: Map identified TDF domains to corresponding intervention functions using the Behavior Change Wheel [16]. Determine policy categories that could enable intervention implementation.
Validation Measures: Conduct Discriminant Content Validation and Fuzzy Cluster Analysis to confirm domain structure and construct allocation [21].
Protocol for Dietary Assessment Validation
Objective: To validate self-reported dietary assessment methods using recovery biomarkers.
Methodology:
- Participant Recruitment: Recite participants representing diverse socioeconomic, racial/ethnic, and health status backgrounds to ensure generalizability [18].
- Data Collection:
- Collect multiple 24-hour dietary recalls (minimum 2, preferably 3-4 non-consecutive days) using automated self-administered systems to reduce interviewer burden [18].
- Obtain biological samples for recovery biomarkers (doubly labeled water for energy, urinary nitrogen for protein, urinary sodium and potassium) [18].
- Administer FFQs and food records for comparison.
- Statistical Analysis:
- Calculate correlation coefficients between self-reported intakes and biomarker measurements.
- Use measurement error models to correct for within-person variation [18].
- Assess differential bias by participant characteristics (e.g., BMI, age, socioeconomic status).
Quality Control: Implement standardized protocols for biomarker analysis, train staff in dietary assessment administration, and use multiple quality checks during data processing.
Visualization Frameworks
TDF-COM-B Integration Framework
Behavior Change Intervention Development Pathway
Research Reagent Solutions
Table 3: Essential Research Tools for Nutrition and Behavior Studies
| Research Tool | Function | Application Example |
|---|---|---|
| Theoretical Domains Framework (TDF) | Identifies barriers and enablers across 14 behavioral domains | Diagnosing implementation problems in clinical nutrition practices [11] [21] |
| Behavior Change Wheel (BCW) | Maps barriers to intervention functions and policy categories | Developing theory-informed interventions for dietary behavior change [11] [16] |
| COM-B System | Provides behavioral diagnosis through Capability, Opportunity, Motivation assessment | Understanding drivers of food waste auditing behavior in hospital foodservices [16] |
| 24-Hour Dietary Recall | Captures detailed recent dietary intake | Assessing short-term dietary exposures in diverse populations [18] |
| Food Frequency Questionnaire (FFQ) | Assesses usual intake over extended periods | Ranking individuals by nutrient exposure in large epidemiological studies [18] |
| Recovery Biomarkers | Objectively measures energy and nutrient intake | Validating self-reported dietary data for energy, protein, sodium, potassium [18] |
| National Food and Nutrition Databases | Provides food composition and consumption data | Supporting analysis of dietary patterns and their health outcomes [63] |
Future Research Directions
Priority Research Areas
Based on evidence gaps identified through the TDF and BCW frameworks, priority research areas include:
Multilevel Interventions: Develop and test interventions addressing multiple TDF domains simultaneously, particularly focusing on the interaction between individual-level factors (e.g., knowledge, skills) and system-level factors (e.g., environmental context, resources) [11] [16].
Health Equity in Nutrition: Investigate how social determinants of health moderate the effectiveness of nutrition interventions, with particular attention to socioeconomic position and its impact on dietary risk [62].
Digital Dietary Assessment: Validate novel technologies (mobile apps, sensors, image-based intake assessment) against recovery biomarkers to reduce measurement error in self-reported data [18].
Implementation Strategies: Identify the most effective intervention functions from the BCW for specific nutrition behaviors, particularly in clinical settings with documented evidence-practice gaps [11] [16].
Methodological Innovations
Future research should incorporate several methodological advances:
Integrated Knowledge Translation: Engage stakeholders throughout the research process using integrated knowledge translation approaches to ensure findings are relevant and applicable [16].
Advanced Measurement Methods: Develop and validate new recovery biomarkers for additional nutrients beyond the current limited set [18].
Longitudinal Behavior Tracking: Employ intensive longitudinal methods to capture dynamic relationships between TDF domains and behavior change over time.
Adaptive Intervention Designs: Utilize sequential multiple assignment randomized trial (SMART) designs to develop adaptive interventions that respond to individual and contextual factors.
Conclusion
The Theoretical Domains Framework provides a robust, systematic methodology for developing, implementing, and evaluating dietary behavior change interventions. By moving from a theoretical understanding of behavioral determinants to practical application and rigorous validation, the TDF and BCW offer a powerful toolkit for addressing the complex challenge of evidence-based nutrition practice. For biomedical and clinical research, this translates to more effective interventions, better patient outcomes, and a deeper understanding of the mechanisms driving dietary change. Future directions should focus on optimizing framework application for digital health technologies, integrating TDF with experimental medicine models for early-phase proof-of-concept studies, and expanding its use in diverse and underserved populations to ensure equitable health benefits. The continued refinement and judicious application of this framework hold significant promise for advancing the field of nutritional science and clinical practice.
References
- 1. The behaviour change wheel: A new method for ... [https://implementationscience.biomedcentral.com/articles/10.1186/1748-5908-6-42]
- 2. The behaviour change wheel: a new method for ... [https://pubmed.ncbi.nlm.nih.gov/21513547/]
- 3. Behavior Change Wheel [https://paloaltou.edu/resources/business-of-practice-blog/behavior-change-wheel]
- 4. The impact of a COM - B ... | Behaviour Square Change Research [https://www.researchsquare.com/article/rs-6989358/v1]
- 5. JMIR Formative Research - Multidomain Behavioral Digital... Change [https://formative.jmir.org/2025/1/e73807]
- 6. The COM-B Model [https://www.habitweekly.com/models-frameworks/the-com-b-model]
- 7. The COM-B Model for Behavior Change [https://thedecisionlab.com/reference-guide/organizational-behavior/the-com-b-model-for-behavior-change]
- 8. The Behavior Change Wheel: A Simple Introduction [https://people-shift.com/articles/the-behavior-change-wheel/]
- 9. COM-B & Behaviour Change Wheel [https://modelthinkers.com/mental-model/com-b-behaviour-change-wheel]
- 10. Designing a behaviour intervention using change - COM and the... B [https://pubmed.ncbi.nlm.nih.gov/39054768/]
- 11. Using the Theoretical Domains Framework and Behavior ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12590314/]
- 12. Nature of the evidence base and approaches to guide nutrition interventions for individuals: a position paper from the Academy of Nutrition Sciences - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11074602/]
- 13. Frontiers | Multi-faceted nutritional interventions are imperative to reduction of stunting among children in low- and middle-income countries [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1479850/full]
- 14. Top 6 Visualizations for Quantitative Data Analysis Methods [https://chartexpo.com/blog/quantitative-data-analysis-methods]
- 15. A guide to using the Theoretical Domains Framework of ... [https://implementationscience.biomedcentral.com/articles/10.1186/s13012-017-0605-9]
- 16. Applying the theoretical domains framework and behavior ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2023.1204980/full]
- 17. Experts' perceptions on motivators and barriers of healthy ... [https://www.sciencedirect.com/science/article/pii/S0195666323026582]
- 18. Overview of Dietary Assessment Methods for Measuring ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8338737/]
- 19. Stages of change and self-efficacy are related to ... [https://www.frontiersin.org/journals/public-health/articles/10.3389/fpubh.2022.1006898/full]
- 20. Behaviour change techniques targeting both diet and physical ... [https://ijbnpa.biomedcentral.com/articles/10.1186/s12966-016-0436-0]
- 21. Validation of the theoretical domains framework for use in ... [https://implementationscience.biomedcentral.com/articles/10.1186/1748-5908-7-37]
- 22. Role-model, reoffer, reward: A thematic analysis and TDF ... [https://www.sciencedirect.com/science/article/pii/S0195666323017440]
- 23. Using the theoretical domains framework and the behavioural ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6596985/]
- 24. Capability, opportunity, and motivation: an across contexts ... [https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-021-11019-w]
- 25. COM-B + TDF [https://thecenterforimplementation.com/toolbox/com-b-tdf]
- 26. Using the Theoretical Domains Framework and Behavior ... [https://pubmed.ncbi.nlm.nih.gov/40878445/]
- 27. Using the COM-B model to identify barriers and facilitators ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8094434/]
- 28. Exploring the usability of the COM-B model and Theoretical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7805209/]
- 29. Streamlining COM-B model: Insights from the Healthy ... [https://www.sciencedirect.com/science/article/pii/S0195666324004963]
- 30. The COM-B model: a cross-sectional survey assessing ... [https://www.frontiersin.org/journals/dementia/articles/10.3389/frdem.2024.1451310/full]
- 31. Behavior change techniques in pregnancy dietary interventions [https://bmcpregnancychildbirth.biomedcentral.com/articles/10.1186/s12884-025-07876-7]
- 32. Behavior change wheel as a tool to promote physical ... [https://www.frontiersin.org/journals/psychology/articles/10.3389/fpsyg.2025.1498351/full]
- 33. Coâ€Development of the CoMUni Intervention: A Social†... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12374232/]
- 34. Behaviour change techniques, intervention features and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12127858/]
- 35. Behavior Change Resources Used in Mobile App–Based ... [https://mhealth.jmir.org/2025/1/e63313]
- 36. Digital dietary interventions for healthy adolescents: A ... [https://www.sciencedirect.com/science/article/pii/S0261561425000135]
- 37. Acyclic behavior change diagrams: a tool to report and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9744208/]
- 38. Malnutrition Screening and Assessment - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9228435/]
- 39. Prehabilitation Protocol Shows Promise [https://www.aacn.org/newsroom/prehabilitation-protocol-shows-promise]
- 40. Multimodal Prehabilitation for Colorectal Cancer Patients [https://pubmed.ncbi.nlm.nih.gov/40175315/]
- 41. Optimizing Self-Monitoring in a Digital Weight Loss ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12504904/]
- 42. Exploring the Dynamics of Dietary Self-Monitoring ... [https://www.jmir.org/2025/1/e65431]
- 43. A review of statistical methods for dietary pattern analysis [https://nutritionj.biomedcentral.com/articles/10.1186/s12937-021-00692-7]
- 44. Exploring the Dynamics of Dietary Self-Monitoring ... [https://pubmed.ncbi.nlm.nih.gov/40279647/]
- 45. Digital health interventions to improve eating behaviour of ... [https://bmcnutr.biomedcentral.com/articles/10.1186/s40795-022-00635-3]
- 46. overcoming challenges in health research with hard-to-reach ... [https://equityhealthj.biomedcentral.com/articles/10.1186/s12939-024-02145-z]
- 47. Perceptions of the Three Dietary Patterns of the 2020– ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12608769/]
- 48. Effectiveness of Interventions and Behaviour Change ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6520715/]
- 49. Implementation of Behavior Change Theories and ... [https://www.mdpi.com/1660-4601/22/7/1133]
- 50. Digital behavioral dietary interventions to promote a healthy ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11610228/]
- 51. Systematic Review of Easy-to-Learn Behavioral ... [https://www.sciencedirect.com/science/article/pii/S1499404623000908]
- 52. A Review and Clinical Understanding of Tenofovir [https://pmc.ncbi.nlm.nih.gov/articles/PMC7163232/]
- 53. Linking the Population Pharmacokinetics of Tenofovir and Its ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4260001/]
- 54. A multicompartment population PK model to predict ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10725258/]
- 55. Model-based predictions of protective HIV pre-exposure ... [https://www.nature.com/articles/s41591-023-02615-x]
- 56. Advances in long-acting slow effective release ... [https://www.sciencedirect.com/science/article/pii/S0169409X23003241]
- 57. Evaluating eating behavior treatments by FDA standards [https://pmc.ncbi.nlm.nih.gov/articles/PMC3879478/]
- 58. FDA's Nutrition Initiatives [https://www.fda.gov/food/nutrition-food-labeling-and-critical-foods/fdas-nutrition-initiatives]
- 59. Quantitative measures used in empirical evaluations of mental ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9924289/]
- 60. Quantitative approaches for the evaluation of ... [https://www.sciencedirect.com/science/article/pii/S0165178119307024]
- 61. FDA's New “Plausible Mechanism Pathway†and Other ... [https://www.arnoldporter.com/en/perspectives/advisories/2025/11/fda-plausible-mechanism-pathway-and-other-initiatives-drugs-for-ultra-rare-conditions]
- 62. Hoelscher Provides Nutritional Expertise on Newly ... [https://sph.uth.edu/news/story/hoelscher-provides-nutritional-expertise-on-newly-released-scientific-report-of-the-2025-dietary-guidelines-advisory-committee]
- 63. Food Assistance Data & Collaborative Research Programs [http://www.ers.usda.gov/topics/food-nutrition-assistance/food-assistance-data-collaborative-research-programs/national-data-sets]