Beyond Self-Report: A Comprehensive Comparison of Traditional vs. Objective Dietary Assessment Methods for Clinical Research
Accurate dietary assessment is critical for understanding diet-disease relationships, informing public health policy, and monitoring intervention efficacy in clinical trials.
Beyond Self-Report: A Comprehensive Comparison of Traditional vs. Objective Dietary Assessment Methods for Clinical Research
Abstract
Accurate dietary assessment is critical for understanding diet-disease relationships, informing public health policy, and monitoring intervention efficacy in clinical trials. However, traditional self-report methods like food frequency questionnaires, 24-hour recalls, and food diaries are notoriously prone to systematic errors, including recall bias, social desirability bias, and significant underreporting, particularly for energy intake. This article provides a systematic review of both established and emerging dietary assessment methodologies, contrasting the limitations of traditional tools with the promise of novel objective technologies. We explore foundational principles, methodological applications, strategies for troubleshooting systematic errors, and validation techniques using recovery biomarkers. Aimed at researchers, scientists, and drug development professionals, this review synthesizes current evidence to guide the selection and optimization of dietary assessment methods, enhancing data quality and reliability in biomedical research.
The Dietary Assessment Landscape: Core Principles and the Critical Shift from Subjective to Objective Measures
Dietary assessment provides the fundamental data necessary to understand the complex relationships between diet and health. In both research and clinical settings, accurately capturing what individuals consume is crucial for investigating diet-disease associations, developing nutritional guidelines, and creating personalized intervention strategies [1] [2]. The field is currently undergoing a significant transformation, moving from traditional subjective recall methods toward more objective, technology-enhanced approaches that minimize inherent biases and participant burden [3] [4]. This evolution is particularly relevant for researchers and drug development professionals who require precise dietary metrics to evaluate nutritional interventions, understand nutrient-biomarker relationships, and assess lifestyle factors in clinical trials. This article compares the performance of traditional versus emerging dietary assessment methodologies, examining their experimental validation, relative accuracy, and appropriate applications in scientific research.
Traditional Dietary Assessment Methods: Foundations and Limitations
Traditional dietary assessment tools have formed the backbone of nutritional epidemiology for decades, though they come with well-documented methodological challenges.
- Methodologies and Applications: The most established methods include 24-hour dietary recalls (multiple-pass interviewer-administered or automated self-administered versions), food frequency questionnaires (FFQs), and food records (both estimated and weighed) [5] [2]. These tools are particularly valuable for capturing habitual intake (FFQs) or detailed recent consumption (24-hour recalls and food records) in large population studies.
- Inherent Limitations and Biases: These methods share significant limitations, including recall bias, portion size estimation errors, social desirability bias, and substantial participant burden [3] [4] [2]. Validation studies using doubly labeled water have revealed energy intake reporting errors ranging from 20% to 50%, with considerable inter-individual variability [4]. These measurement errors can substantially obscure true diet-disease relationships in research settings.
Table 1: Key Characteristics of Major Dietary Assessment Approaches
| Method Category | Specific Tools | Primary Use Cases | Key Strengths | Documented Limitations |
|---|---|---|---|---|
| Traditional Self-Report | 24-hour Recalls (ASA24) [2] | Population surveillance, intake quantification | Detailed nutrient data, multiple days capture memory dependence | Memory dependence, participant burden [3] |
| Food Frequency Questionnaire (FFQ) [2] | Habitual intake ranking, epidemiology | Captures long-term patterns, low participant burden | Portion size inaccuracy, memory bias [2] | |
| Food Records [2] | Clinical metabolic studies, validation | Prospective collection reduces memory bias | High participant burden, reactivity alters intake [4] | |
| Digital & Image-Based | Diet ID (DQPN) [6] [2] | Clinical screening, rapid diet quality assessment | <1 minute completion, high scalability, visual approach | Less granular nutrient data vs. recalls [2] |
| VISIDA Image-Voice System [7] | Low-literacy populations, field studies | Combines image/audio, low literacy requirement | Lower absolute intake estimates vs. recalls [7] | |
| Traqq (Repeated Short Recalls) [3] | Real-time monitoring, adolescent studies | Reduces memory bias via short intervals | Requires multiple daily engagements | |
| AI-Driven Analysis | Multimodal LLMs (ChatGPT-4o, Claude) [4] | Automated analysis, food image estimation | No user burden post-image capture, automated | Systematic underestimation (up to 37% error), portion size challenges [4] |
Emerging Methodologies: Technological Innovations and Objective Measures
Innovative approaches are addressing the limitations of traditional methods through pattern recognition, digital technology, and artificial intelligence.
Pattern Recognition and Digital Platforms
Diet Quality Photo Navigation (DQPN), implemented in the Diet ID platform, represents a paradigm shift from recall-based to pattern-recognition-based assessment. This method allows users to identify their dietary pattern from a series of images representing various cuisines and quality levels, generating almost instantaneous diet quality scores aligned with the Healthy Eating Index (HEI) [6] [2]. The platform completes comprehensive dietary assessments in approximately one minute while achieving 90% accuracy compared to traditional methods [6].
Another significant innovation is the Fixed-Quality Variable-Type (FQVT) dietary intervention approach. This methodology standardizes diet quality using validated tools like the HEI-2020 while accommodating diverse cultural preferences and dietary patterns [6] [8]. This approach is particularly valuable for multicultural nutrition research and personalized clinical interventions, as it enhances adherence and satisfaction while maintaining scientific rigor [8].
Artificial Intelligence and Image Analysis
Recent advances in artificial intelligence, particularly multimodal large language models (LLMs), offer promising solutions for automated dietary assessment. A 2025 validation study evaluated three leading LLMs—ChatGPT-4o, Claude 3.5 Sonnet, and Gemini 1.5 Pro—for estimating nutritional content from standardized food photographs [4].
- Performance Metrics: ChatGPT and Claude demonstrated similar accuracy with Mean Absolute Percentage Error (MAPE) values of 36.3% and 37.3% for weight estimation, and 35.8% for energy estimation—accuracy levels comparable with traditional self-reported methods but without associated user burden. Gemini showed substantially higher errors across all nutrients (MAPE 64.2%-109.9%) [4].
- Systematic Biases: All models exhibited systematic underestimation that increased with portion size, with bias slopes ranging from -0.23 to -0.50, indicating significant challenges in accurately assessing larger portions [4].
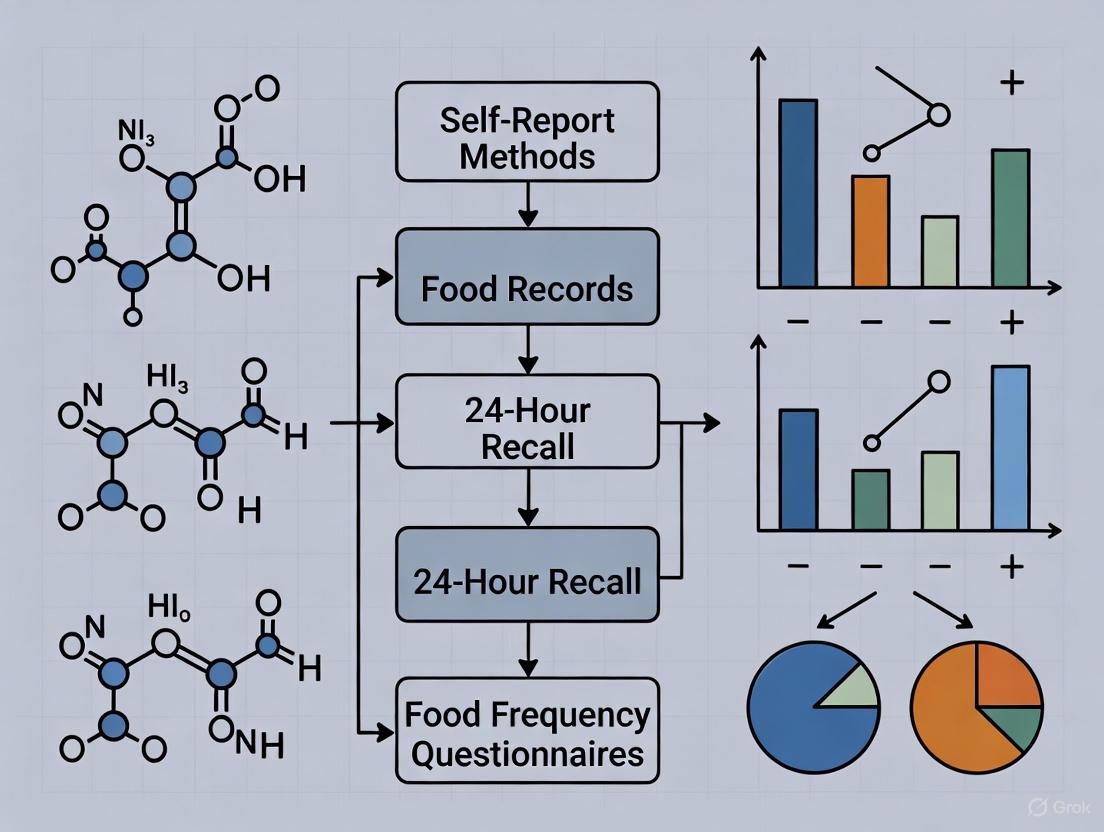
Figure 1: AI Dietary Analysis Workflow - This diagram illustrates the standardized process for AI-based dietary assessment from image capture to nutrient estimation, highlighting the systematic underestimation identified as a key limitation in current models [4].
Comparative Performance: Experimental Data and Validation Studies
Rigorous validation studies provide critical data for evaluating the relative performance of different dietary assessment methodologies.
Diet ID (DQPN) Validation Protocol
A 2023 study directly compared DQPN against traditional methods in a sample of 90 participants, with 58 completing all assessments [2].
- Experimental Protocol: Participants completed three assessment methods: DQPN, a 3-day food record via ASA24, and a Food Frequency Questionnaire (DHQ III). The study evaluated correlations for diet quality (HEI-2015), food groups, and nutrient intake [2].
- Key Findings: DQPN demonstrated strong correlation with traditional methods for overall diet quality measurement (r=0.58 vs. FFQ, r=0.56 vs. FR), with test-retest reliability of r=0.70 [2]. While DQPN performed excellently for diet quality assessment, traditional methods provided more granular nutrient-level data.
VISIDA Image-Voice System Evaluation
A 2025 study evaluated the Voice-Image Solution for Individual Dietary Assessment (VISIDA) in Cambodian women and children [7].
- Methodology: The study collected dietary data using VISIDA for two 3-day periods separated by interviewer-administered 24-hour recalls, comparing estimated nutrient intakes across methods [7].
- Results: VISIDA produced lower nutrient intake estimates compared to 24-hour recalls, with statistically significant differences for 80% of nutrients in mothers and 32% in children. However, the two VISIDA recordings showed no statistically significant differences, demonstrating high test-retest reliability [7].
Table 2: Quantitative Performance Metrics Across Dietary Assessment Methods
| Validation Metric | Diet ID (DQPN) [2] | Traditional FFQ [2] | Traditional Food Record [2] | AI (ChatGPT-4o) [4] |
|---|---|---|---|---|
| Completion Time | ~1 minute [6] | 30-60 minutes [2] | 15-30 minutes/day [2] | Near-instant after image capture |
| Diet Quality Correlation (HEI) | 0.56-0.58 [2] | Reference | 0.56 vs. DQPN [2] | Not tested |
| Test-Retest Reliability | 0.70 [2] | 0.40-0.70 (literature) [2] | Varies | Not established |
| Energy Intake MAPE | Not specified | Not specified | Not specified | 35.8% [4] |
| Weight Estimation MAPE | Not applicable | Not applicable | Not applicable | 36.3% [4] |
| Key Advantage | Speed, scalability | Habitual intake capture | Detailed nutrient data | No participant burden |
Researchers conducting dietary assessment studies require specific tools and resources to ensure methodological rigor. The following table details key solutions used in the validation studies discussed in this article.
Table 3: Research Reagent Solutions for Dietary Assessment Studies
| Tool/Resource | Primary Function | Research Application | Example Use in Validation Studies |
|---|---|---|---|
| ASA24 (Automated Self-Administered 24-hour Recall) [2] | Self-administered 24-hour dietary recall | Food record collection in validation studies | Used as reference method in DQPN validation [2] |
| Healthy Eating Index (HEI) [6] [8] | Diet quality scoring metric | Standardized assessment of overall diet quality | Primary outcome in FQVT and DQPN studies [6] [2] |
| DHQ III (Dietary History Questionnaire) [2] | Food frequency questionnaire | Assessment of habitual dietary intake | Comparison method in DQPN validation [2] |
| USDA Food and Nutrient Database for Dietary Studies (FNDDS) [5] [2] | Nutrient composition database | Conversion of foods to nutrient values | Underlying database for ASA24 and DHQ III [2] |
| Dietist NET [4] | Nutrient calculation software | Reference method nutrient analysis | Used for reference values in AI validation study [4] |
The evolving landscape of dietary assessment presents researchers and clinicians with multiple methodological options, each with distinct advantages and limitations. Traditional methods (24-hour recalls, FFQs, food records) continue to provide valuable, granular nutrient data but suffer from significant participant burden and measurement error [4] [2]. Emerging digital tools like Diet ID offer rapid, scalable diet quality assessment with minimal participant burden, making them particularly suitable for clinical screening and large-scale public health monitoring [6] [2]. AI-based approaches demonstrate promising automation capabilities but currently lack the precision required for clinical applications where accurate quantification is critical [4].
The choice of assessment method should be guided by the specific research question, population characteristics, and precision requirements. For drug development professionals and researchers, hybrid approaches that combine the scalability of digital tools with the precision of traditional methods for validation may offer the most robust strategy. The ongoing development of standardized quality assessment frameworks, such as the FNS-Cloud data quality assessment tool, will further support researchers in selecting appropriate methodologies and ensuring the scientific integrity of nutrition research [9].
Accurate dietary assessment is a cornerstone of nutritional epidemiology, essential for understanding the links between diet and health outcomes such as obesity, cardiovascular disease, and cancer [10] [11]. However, diet represents a complex, dynamic exposure prone to variation across days, seasons, and the lifecycle, making its precise measurement notoriously challenging [12] [13]. Among the most established tools for capturing dietary intake in research are three traditional self-report instruments: Food Frequency Questionnaires (FFQs), 24-Hour Dietary Recalls (24HRs), and Food Records (FRs). Each method possesses distinct strengths, limitations, and applications, and all introduce measurement error that must be considered in data analysis and interpretation [12] [14] [11]. This guide provides a comparative overview of these instruments, framing them within the broader context of dietary assessment research that increasingly seeks to validate self-reported data against objective biomarkers.
Instrument Profiles and Comparative Analysis
The following section details the design, application, and relative performance of each dietary assessment method.
Food Frequency Questionnaires (FFQs)
FFQs are designed to retrospectively measure habitual long-term dietary intake, typically over the past month or year [12] [11]. Participants report their consumption frequency for a predefined list of food items, often with semi-quantitative portion size estimates. The FFQ is a cost-effective and practical tool for large-scale epidemiological studies, enabling the ranking of individuals by their intake levels [12] [15]. However, because it limits the scope of foods that can be queried and relies on generic memory, it is less precise for measuring absolute intakes of specific nutrients [11].
- Relative Validity: A validation study of a web-based FFQ (WebFFQ) against repeated 24-hour recalls found Spearman's correlation coefficients ranging from 0.19 for iodine to 0.71 for juice, demonstrating reasonable ranking abilities for most nutrients and foods [12] [13].
- Measurement Error: FFQs are subject to systematic bias. Studies comparing FFQ-derived energy and protein intake against recovery biomarkers (doubly labeled water and urinary nitrogen) have found that FFQs explain only a small percentage of the variation in true intake (e.g., 3.8% for energy, 8.4% for protein) without calibration [10].
24-Hour Dietary Recalls (24HRs)
The 24HR involves a detailed account of all foods and beverages consumed by an individual over the previous 24 hours [11]. Traditionally administered by a trained interviewer using structured probes, automated self-administered versions are now available [11]. Multiple non-consecutive 24HRs are required to account for day-to-day variation and estimate usual intake.
- Relative Validity: While also prone to error, data from 24HRs are generally considered less biased than FFQs and are often used as a reference method in validation studies [12] [13].
- Measurement Error: Compared to FFQs, 24HRs have been shown to be a less biased estimator of energy intake. Biomarker studies indicate that 24HRs perform better than FFQs for estimating energy and protein, but still incorporate significant error, explaining 2.8% and 16.2% of biomarker variation for energy and protein, respectively, before calibration [10].
Food Records (FRs)
In this method, participants record all foods, beverages, and supplements consumed as they are consumed, typically for 3-4 days [11]. Foods are often weighed or measured, requiring a highly literate and motivated participant population. A key limitation is reactivity—the tendency for participants to alter their usual diet because they are recording it [11].
- Relative Performance: When compared against recovery biomarkers, food records provide a stronger estimate of energy and protein intake than FFQs, with 24HRs being intermediate. One study showed food records could explain 7.8% and 22.6% of biomarker variation for energy and protein, respectively, outperforming FFQs [10].
The table below summarizes the core characteristics and comparative performance of these three instruments.
Table 1: Comparative Overview of Traditional Dietary Assessment Instruments
| Feature | Food Frequency Questionnaire (FFQ) | 24-Hour Dietary Recall (24HR) | Food Record (FR) |
|---|---|---|---|
| Primary Purpose | Assess habitual, long-term intake | Capture recent or short-term intake | Capture current, detailed intake |
| Time Frame | Months to a year | Previous 24 hours | Real-time recording over multiple days |
| Data Collection | Self-administered; retrospective | Interviewer-administered or automated; retrospective | Self-administered; prospective |
| Key Strengths | Cost-effective for large studies; ranks individuals by intake | Does not require literacy; less reactivity than FRs | High detail for specific days; does not rely on memory |
| Key Limitations | Systematic bias; limited food list; less precise for absolute intake | Relies on memory; high day-to-day variability; multiple recalls needed | High participant burden; reactivity can alter intake |
| Correlation with Biomarkers | Lower for energy (r² = 3.8%) [10] | Intermediate for energy (r² = 2.8%) [10] | Higher for energy (r² = 7.8%) [10] |
| Participant Burden | Moderate | Low per recall, but higher for multiple | High |
| Ideal Use Case | Large epidemiological studies to rank exposure | Estimating population mean intake or usual intake with multiple recalls | Small studies requiring precise, short-term intake data |
Table 2: Key Experimental Findings from Validation Studies
| Study Context | Comparison | Key Metric | Finding |
|---|---|---|---|
| Hordaland Health Study [12] [13] | WebFFQ vs. three 24HRs | Spearman's Correlation (rs) | Range: 0.19 (Iodine) to 0.71 (Juice); >72% of participants classified in same/adjacent quartile. |
| Women's Health Initiative (NPAAS) [10] | FFQ, 24HR, FR vs. Biomarkers (Energy) | % of Biomarker Variation Explained (before calibration) | FFQ: 3.8%; 24HR: 2.8%; FR: 7.8% |
| Women's Health Initiative (NPAAS) [10] | FFQ, 24HR, FR vs. Biomarkers (Protein) | % of Biomarker Variation Explained (before calibration) | FFQ: 8.4%; 24HR: 16.2%; FR: 22.6% |
| Nutrition Journal Study [15] | FFQ vs. two 24HRs (Environmental Impact) | Attenuation Coefficient (λ) | FFQ attenuation coefficient for diet-related environmental impact was 0.56. |
Experimental Protocols for Validation
A critical component of dietary assessment research involves validating self-report instruments against more objective measures. The following workflows are central to this process.
Relative Validation: FFQ versus 24-Hour Recalls
This protocol evaluates the relative validity of an FFQ by using repeated 24-hour recalls as a reference method [12] [13].
Table 3: Key Reagents and Tools for Dietary Validation Studies
| Reagent/Tool | Function in Research |
|---|---|
| Web-based FFQ | The test instrument; assesses habitual diet over a reference period (e.g., 279 food items with portion size images) [12]. |
| 24-Hour Dietary Recalls (24HRs) | The reference instrument; multiple non-consecutive recalls capture day-to-day variation to estimate usual intake [12] [11]. |
| Food Composition Database | Converts reported food consumption into nutrient intakes (e.g., KostBeregningsSystemet, Dutch food composition table) [12] [15]. |
| Statistical Packages | Perform correlation analyses (Spearman's), cross-classification, and compute attenuation coefficients to quantify measurement error [12] [15]. |
Methodology:
- Participant Recruitment: A subsample representative of the main study population is recruited (e.g., n=67 in HUSK3) [12].
- Data Collection: Participants complete the FFQ and multiple (e.g., three) non-consecutive 24HRs, which can be conducted in-person or via telephone [12].
- Data Processing: Nutrient and food intakes from both methods are calculated by linking consumed items to a food composition database [12] [15].
- Statistical Analysis:
- Rank Correlation: Spearman's correlation coefficients are calculated between intake estimates from the two instruments.
- Cross-Classification: The proportion of participants classified into the same or adjacent quartile by both methods is determined.
- Bland-Altman Plots: Visualize the agreement between the two methods and identify any systematic bias.
- Calibration Coefficients: Linear regression models are used to compute coefficients (ranging from 0 to 1) that indicate how well the FFQ predicts intake measured by the 24HRs [12] [13].
Diagram 1: Workflow for FFQ vs. 24HR Validation Study
Biomarker Validation: Doubly Labeled Water and Urinary Nitrogen
The most rigorous assessment of dietary self-report accuracy involves recovery biomarkers, which objectively measure intake of specific nutrients [10] [14].
Methodology:
- Objective Intake Measurement:
- Energy: Total Energy Expenditure (TEE) is measured over a 1-2 week period using the Doubly Labeled Water (DLW) method. In weight-stable individuals, TEE equals habitual Energy Intake [10] [14].
- Protein: Protein intake is measured from 24-hour urinary nitrogen excretion, using the formula: Protein (g) = 6.25 × Urinary Nitrogen ÷ 0.81, where 0.81 represents the average recovery rate [10].
- Self-Report Data Collection: Participants concurrently complete the self-report instruments (FFQ, 24HR, FR).
- Comparison and Calibration: Reported intakes are compared to biomarker values. Regression calibration is used to develop equations that adjust self-reported data for systematic error related to factors like body mass index (BMI), age, and ethnicity [10].
Diagram 2: Biomarker Validation Study Design
The Challenge of Measurement Error
A consistent finding across nutritional research is that all self-report instruments are prone to measurement errors, which can be random or systematic [14] [11].
- Systematic Under-Reporting: A major issue is the systematic under-reporting of energy intake, which increases with BMI. This is thought to be related to concerns about body weight and social desirability bias [14].
- Differential Misreporting: Not all foods are under-reported equally. Protein intake tends to be less under-reported compared to other macronutrients, and the specific foods commonly under-reported may vary [14].
- Impact on Research: This systematic measurement error attenuates (weakens) observed diet-disease relationships, potentially obscuring real associations [10] [14]. For instance, in the Women's Health Initiative, associations between calibrated energy intake and cancer incidence became apparent only after correcting for measurement error in the FFQ [10].
FFQs, 24HRs, and Food Records each occupy a critical niche in dietary assessment. FFQs are unparalleled for ranking individuals by habitual intake in large-scale studies, while 24HRs provide valuable estimates of group-level mean intake and food records offer high detail for short-term studies. The fundamental challenge common to all is measurement error, predominantly systematic under-reporting. Consequently, the choice of instrument must be guided by the research question, study design, and target population. Modern research increasingly relies on multi-faceted approaches, using 24HRs as a reference standard and recovery biomarkers for objective validation, to better understand and correct for these errors, thereby strengthening the evidence base for diet and health relationships.
In nutritional epidemiology and clinical research, self-report instruments such as food frequency questionnaires (FFQs), 24-hour recalls, and food records serve as fundamental tools for capturing dietary intake data. While these methods are widely used due to their practicality and low cost, they are susceptible to significant measurement errors that can compromise data validity and subsequent research conclusions. These errors stem from the complex interaction between respondents and assessment methodologies, leading to three primary limitations: recall bias, social desirability bias, and reactivity. Understanding the mechanisms, magnitude, and impact of these biases is crucial for interpreting dietary data accurately and advancing nutritional science. This analysis examines the inherent limitations of self-reported dietary assessment methods within the broader context of moving toward more objective measurement approaches.
Defining the Biases: Mechanisms and Impacts
Recall Bias
Recall bias occurs when participants inaccurately remember or report past dietary consumption. This bias is particularly problematic for methods that rely on specific memory (like 24-hour recalls) or generic memory (like FFQs that ask about usual intake over months or years) [16] [17]. The cognitive process of reporting dietary intake is complex, involving multiple stages where memory lapses can occur [17].
Common manifestations of recall bias include:
- Omissions: Forgetting to report entire eating occasions, specific foods, or additions like condiments and salad dressings [17]. Research comparing 24-hour recalls to directly observed intake found that foods like tomatoes, mustard, and cheese were frequently omitted [17].
- Intrusions: Incorrectly reporting foods that were not actually consumed during the reference period [17].
- Inaccurate Details: Misremembering portion sizes, food preparation methods, or additions to foods [17].
The retention interval (time between consumption and recall) significantly impacts accuracy, with shorter intervals generally producing more reliable data [17]. Automated multiple-pass methods like the Automated Self-Administered 24-Hour Dietary Assessment Tool (ASA24) and the Automated Multiple-Pass Method (AMPM) incorporate probing questions and memory aids to mitigate recall bias by systematically prompting respondents to remember forgotten items [17].
Social Desirability Bias
Social desirability bias arises when respondents alter their reported intake to align with perceived social norms or research expectations. This bias disproportionately affects foods considered "healthy" or "unhealthy," leading to systematic misreporting rather than random error [18] [16].
Key findings on social desirability bias:
- Directional Under-reporting: A seminal study found social desirability scores were negatively correlated with reported energy intake, producing a downward bias of approximately 450 kcal over the interquartile range of social desirability scores [18]. This under-reporting was approximately twice as large for women as for men [18].
- Susceptibility Across Methods: Both FFQs and 24-hour recalls demonstrate susceptibility. A randomized controlled trial testing social approval bias found that participants who received materials emphasizing fruit and vegetable consumption reported significantly higher intakes than controls (5.2 vs. 3.7 servings per day on FFQ) [16].
- Differential Effects by Food Type: Social desirability bias more strongly affects reporting of foods with clear health perceptions (like fruits, vegetables, and high-fat foods) compared to neutral foods [16].
This bias poses particular challenges in nutritional intervention studies where participants may be aware of the study goals and modify their reports to demonstrate compliance [16].
Reactivity
Reactivity occurs when the process of measurement itself alters participants' normal dietary behavior. Also termed "reactivity bias," this phenomenon is especially prominent with food records, as participants may simplify their diets, choose different foods, or reduce intake to make recording easier [11] [19].
Characteristics of reactivity:
- Method-Specific Vulnerability: Food records have high potential for reactivity as participants know their intake is being recorded in real-time, whereas 24-hour recalls and FFQs have lower reactivity as intake is reported after consumption [11].
- Behavioral Change Mechanism: The awareness of being monitored can lead to conscious or unconscious modifications in eating patterns, potentially reducing consumption of foods perceived as undesirable or complex to record [11].
- Digital Method Considerations: Emerging image-based dietary assessment methods may also be susceptible to reactivity, as knowing one must photograph foods may influence food choices [19].
Comparative Quantitative Analysis of Bias Magnitude
Table 1: Comparative Magnitude of Self-Report Biases Across Assessment Methods
| Bias Type | Assessment Method | Reported Effect Size | Population Characteristics | Key Findings |
|---|---|---|---|---|
| Social Desirability | 7-day diet recall (similar to FFQ) | ~50 kcal/point on social desirability scale [18] | Adults (n=163) | Large downward bias, twice as large in women |
| Social Desirability | 7-day diet recall vs. 24-hour recall | ~450 kcal over interquartile range [18] | Free-living adults | Individuals with highest fat/energy intake showed largest downward bias |
| Social Approval | Food Frequency Questionnaire | 5.2 vs. 3.7 fruit/vegetable servings (intervention vs. control) [16] | Women aged 35-65 (n=163) | 41% higher reporting in prompted group |
| Social Approval | Limited 24-hour recall | 61% vs. 32% reported ≥3 eating occasions (intervention vs. control) [16] | Women aged 35-65 (n=163) | Near doubling of positive responses in intervention group |
| Recall Bias | 24-hour recall (omissions) | 42% tomatoes, 17% mustard, 16% peppers not reported [17] | Adults vs. observed intake | Condiments and vegetable additions most frequently omitted |
Table 2: Methodological Vulnerabilities to Different Bias Types
| Assessment Method | Recall Bias | Social Desirability Bias | Reactivity | Primary Error Type |
|---|---|---|---|---|
| Food Records | Low (real-time recording) | Moderate | High [11] | Systematic (reactivity) |
| 24-Hour Recalls | High [17] | Moderate [16] | Low [11] | Random (memory) |
| Food Frequency Questionnaires | High (generic memory) [16] | High [18] [16] | Low [11] | Systematic (social desirability) |
| Screening Tools | Moderate | Moderate | Low | Both random and systematic |
Experimental Protocols for Bias Quantification
Protocol 1: Social Desirability Bias Assessment
Hebert et al. developed a rigorous protocol to quantify social desirability bias in dietary self-report [18]:
Design: Comparative validation study with randomized administration of different dietary assessment methods.
Participants: Free-living adults representative of the general population.
Methodology:
- Administered social desirability scale to all participants to establish baseline tendency
- Collected dietary data using multiple 24-hour recalls on seven randomly assigned days as reference method
- Administered two 7-day diet recalls (cognitively similar to FFQs) - one at beginning (pre) and one at end (post) of test period
- Compared nutrient scores between methods using correlation and multiple linear regression analysis
Key Metrics: Difference in energy and nutrient estimates between 7-day diet recalls and 24-hour recalls, correlated with social desirability scores.
Statistical Analysis: Multiple linear regression to isolate effect of social desirability score on nutrient estimation while controlling for other variables.
Protocol 2: Social Approval Bias Randomized Trial
A randomized controlled trial specifically tested social approval bias using a blinded design [16]:
Design: Single-blind randomized controlled trial.
Participants: 163 women aged 35-65 years, randomly selected from commercial database.
Intervention:
- Intervention group received letter describing study as focused on fruit/vegetable intake, including health benefits statement, 5-A-Day sticker, and refrigerator magnet
- Control group received neutral letter describing study as general nutrition survey without specific fruit/vegetable messaging
Assessment:
- 8-item FFQ from Behavioral Risk Factor Surveillance System (BRFSS)
- Limited 24-hour recall specific to fruits and vegetables
- All interviewers blinded to treatment assignment
- Interviews conducted within 10 days of sending letters
Outcomes: Reported fruit/vegetable servings by FFQ; proportion reporting fruits/vegetables on ≥3 occasions via 24-hour recall.
Visualizing Cognitive Processes and Bias Pathways
Cognitive Processes and Bias Pathways in Dietary Self-Report
Table 3: Essential Research Reagents and Tools for Dietary Assessment Validation
| Tool/Resource | Function/Purpose | Application Context | Key Features |
|---|---|---|---|
| Doubly Labeled Water (DLW) | Reference method for measuring total energy expenditure [19] | Validation of energy intake reporting | Objective, non-invasive; considered gold standard for energy validation |
| Automated Self-Administered 24-Hour Dietary Assessment Tool (ASA24) | Self-administered 24-hour recall system [11] [1] | Large-scale dietary data collection | Automated multiple-pass method; reduces interviewer burden and cost |
| Automated Multiple-Pass Method (AMPM) | Interviewer-administered 24-hour recall [17] | National surveys (NHANES) | Standardized probing questions to enhance recall completeness |
| Food and Nutrient Database for Dietary Studies (FNDDS) | Provides nutrient values for foods [5] | Nutrient analysis of reported foods | Contains energy and 64 nutrients for ~7,000 foods |
| Social Desirability Scales | Quantifies tendency toward socially desirable responding [18] | Measurement of social desirability bias | Allows statistical control for this bias in analyses |
| Recovery Biomarkers | Objective measures of specific nutrient intake (protein, potassium, sodium) [11] | Validation of specific nutrient reporting | Limited to specific nutrients but highly accurate |
Implications for Research and Clinical Practice
The pervasive nature of self-report biases has significant implications across research contexts. In epidemiological studies, measurement error distorts observed associations between diet and disease, reducing statistical power to detect true relationships [17]. For public health monitoring, these biases can lead to erroneous estimates of population nutrient adequacy and inaccurate assessments of compliance with dietary guidelines [5] [17]. In intervention research, measurement error can mask true intervention effects, particularly if error differs between intervention and control groups [16] [17].
Mitigation strategies include:
- Using multiple assessment methods to triangulate findings
- Incorporating recovery biomarkers where possible for validation [11] [19]
- Applying statistical adjustment techniques to correct for measured biases [18]
- Developing technology-based methods that reduce cognitive burden [11] [19]
- Implementing standardized protocols with trained interviewers to minimize systematic error [20]
Recall bias, social desirability bias, and reactivity represent fundamental limitations of self-reported dietary assessment methods that significantly impact data validity across research and clinical contexts. The magnitude of these biases can be substantial, with social desirability alone capable of introducing under-reporting of approximately 450 kcal in vulnerable individuals. While methodological improvements like automated multiple-pass recalls and statistical adjustments can mitigate some error, these biases remain inherent to self-report methodologies. This understanding underscores the importance of continued development and validation of objective assessment methods, including recovery biomarkers and technology-enhanced tools, to advance nutritional epidemiology and inform evidence-based dietary recommendations. Researchers must carefully consider these limitations when designing studies, interpreting findings, and translating results into clinical practice and public health policy.
For decades, nutritional science has relied predominantly on self-reported dietary assessment methods including Food Frequency Questionnaires (FFQs), 24-hour recalls, and food diaries [11] [21]. While these tools have contributed valuable epidemiological data, they are notoriously subject to both random and systematic measurement error that fundamentally limits their reliability and accuracy [19] [22]. The emerging recognition of these limitations has catalyzed a paradigm shift toward objective biochemical measures that can complement or potentially replace traditional approaches.
Key limitations of self-reported methods include significant under-reporting of energy intake, particularly among females and overweight or obese individuals [19] [22]. Additional challenges include portion size estimation errors, memory reliance, social desirability bias, and reactivity where participants change their eating habits during assessment periods [21] [22]. A systematic review comparing self-reported energy intake to the gold standard doubly labeled water method found significant under-reporting across most studies, with particularly pronounced effects within recall-based methods [19].
The Emergence of Objective Biomarkers
Objective biomarkers of dietary intake provide independent measures that bypass the cognitive limitations and biases of self-report. These biomarkers are typically biological specimens that indicate intake of specific foods or nutrients through direct measurement of their metabolic products or related physiological compounds [22].
Classification of Dietary Biomarkers
Table 1: Classification of Dietary Biomarkers with Examples
| Biomarker Category | Definition | Research Applications | Examples |
|---|---|---|---|
| Recovery Biomarkers | Measures where intake is quantitatively recovered in biological samples | Validation of self-reported data; considered reference standards | Urinary nitrogen for protein intake; Doubly Labeled Water for energy expenditure [11] [19] |
| Concentration Biomarkers | Reflect circulating or tissue levels of dietary compounds | Assessing status and relative intake of specific nutrients | Serum carotenoids for fruit/vegetable intake; Omega-3 fatty acids for fish consumption [22] |
| Predictive Metabolite Patterns | Multiple metabolites combined using machine learning | Objective classification of dietary patterns and food intake | Poly-metabolite scores for ultra-processed food consumption [23] [24] |
Novel Biomarker Approaches
Recent technological advances have enabled the development of multi-metabolite panels that collectively provide a more comprehensive objective assessment of dietary intake. In a landmark study published in May 2025, NIH researchers identified hundreds of metabolites in blood and urine that correlated with ultra-processed food consumption [23] [24]. Using machine learning, they developed poly-metabolite scores that could accurately differentiate between highly processed and unprocessed diet phases in a controlled feeding trial [23]. This approach represents a significant advancement beyond single nutrient biomarkers toward comprehensive dietary pattern assessment.
Simultaneously, research initiatives like the Dietary Biomarkers Study are systematically investigating the body's absorption, digestion, and uptake responses to common foods to identify novel intake biomarkers [25]. These studies aim to establish objective measures for specific foods including chicken, beef, salmon, whole wheat bread, oats, potatoes, corn, cheese, soybeans, and yogurt [25].
Comparative Analysis: Traditional vs. Objective Methods
Table 2: Methodological Comparison of Dietary Assessment Approaches
| Characteristic | Traditional Self-Report Methods | Objective Biomarker Methods |
|---|---|---|
| Primary Data Source | Participant memory and recording | Biological samples (blood, urine, etc.) |
| Measurement Basis | Estimated consumption | Metabolic products or physiological responses |
| Susceptibility to Bias | High (memory, social desirability, reactivity) | Low (analytical variability only) |
| Time Frame Assessed | Variable (single day to years) | Typically recent intake (hours to weeks) |
| Nutrient/Food Specificity | Can assess entire diet | Often limited to specific nutrients/foods |
| Analytical Requirements | Low to moderate | High (specialized laboratory equipment) |
| Participant Burden | High (time and cognitive effort) | Low (sample collection only) |
| Cost Considerations | Lower per participant | Higher per participant |
The integration of traditional and objective methods represents a promising approach. As noted by Dr. Miriam Sonntag of the PAN Academy, "New methods are unlikely to replace traditional methods such as food diaries. But we can combine them to get a better picture of what and how much people consume" [22]. This integrated approach leverages the comprehensive dietary pattern data from self-report with the objective validation provided by biomarkers.
Experimental Protocols for Biomarker Development
Protocol 1: Poly-Metabolite Score Development for Ultra-Processed Foods
A recent NIH study exemplifies the rigorous methodology required for biomarker development [23] [24]:
Study Design: Combined observational and experimental data. Observational data came from 718 older adults in the Interactive Diet and Activity Tracking in AARP (IDATA) Study who provided biospecimens and detailed dietary information over 12 months. Experimental data came from a domiciled feeding study with 20 subjects admitted to the NIH Clinical Center [23].
Intervention Protocol: Participants were randomized to either a diet high in ultra-processed foods (80% of calories) or a diet with zero ultra-processed foods (0% energy) for two weeks, immediately followed by the alternate diet for two weeks in a crossover design [23] [24].
Biospecimen Collection: Blood and urine samples were collected throughout both study phases for comprehensive metabolomic analysis [24].
Analytical Approach: Machine learning algorithms identified patterns of metabolites predictive of high ultra-processed food intake, and poly-metabolite scores were calculated based on these signatures [23].
Validation: The biomarker scores were tested for their ability to accurately differentiate between the highly processed and unprocessed diet phases within the same individuals [24].
Protocol 2: Doubly Labeled Water Validation for Energy Intake
The doubly labeled water (DLW) method remains the gold standard for validating energy intake assessment:
Principle: Measures carbon dioxide production by assessing the difference in elimination rates of deuterium (²H) and oxygen-18 (¹â¸O) from labeled water [19].
Administration: Participants consume a dose of water containing both isotopes, with the initial dose determined by standardized equations according to body weight [19].
Sample Collection: Urine samples are collected over 7-14 days to account for short-term day-to-day variation in physical activity [19].
Analysis: Isotope elimination rates are used to calculate total energy expenditure, which in weight-stable individuals should equal energy intake [19].
This method has been used extensively to demonstrate the systematic under-reporting inherent in self-reported dietary assessment methods [19].
Visualizing Biomarker Development Workflows
Biomarker Development Workflow: This diagram illustrates the comprehensive process from initial study design through validation required for developing robust dietary biomarkers.
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Essential Research Reagents for Dietary Biomarker Studies
| Reagent/Category | Specific Examples | Research Application |
|---|---|---|
| Stable Isotopes | Doubly Labeled Water (²H₂¹â¸O) | Gold standard validation of energy intake assessment [19] |
| Metabolomics Kits | LC-MS/MS metabolite panels | Comprehensive profiling of hundreds to thousands of metabolites in biospecimens [23] |
| Biospecimen Collection | Urine collection kits, Blood collection tubes | Standardized sample acquisition for biomarker analysis [23] [25] |
| Reference Standards | Certified nutrient biomarkers | Analytical validation and quality control (e.g., urinary nitrogen, serum carotenoids) [11] [22] |
| Dietary Assessment Platforms | ASA24, Automated Multi-Pass Method | Collection of self-reported dietary data for correlation with biomarkers [11] [21] |
| Algorithm Development Tools | Machine learning libraries | Development of poly-metabolite scores and predictive models [23] [24] |
| Ononitol, (+)- | D-Pinitol | High-purity D-Pinitol for research. Explore its insulin-like, anti-diabetic, and anti-osteoporotic applications. For Research Use Only. Not for human consumption. |
| PTP1B-IN-4 | PTP1B Inhibitor | Explore our potent PTP1B inhibitor for diabetes, obesity, and cancer signaling research. For Research Use Only. Not for human consumption. |
Future Directions and Research Applications
The field of objective dietary assessment is rapidly evolving with several promising directions:
Fixed-Quality Variable-Type (FQVT) Dietary Interventions
A novel approach called Fixed-Quality Variable-Type dietary intervention standardizes diet quality using objective measures while allowing for a range of diet types that cater to individual preferences, ethnicities, and cultures [8] [26]. This method uses validated tools like the Healthy Eating Index (HEI) 2020 to fix diet quality within a prespecified range while accommodating diverse dietary patterns [26]. Biomarkers play a crucial role in objectively verifying that different diet types meet the same nutritional quality standards.
Integrated Assessment Approaches
Future dietary assessment will likely combine traditional methods, technological innovations, and biomarkers in complementary approaches:
- Image-assisted methods using smartphones to improve portion size estimation [21] [22]
- Wearable sensors that automatically capture dietary intake data [21] [22]
- Multi-metabolite panels for objective verification of specific dietary patterns [23] [22]
Integrated Assessment Approach: Combining multiple methodologies provides more robust dietary assessment than any single approach.
The paradigm shift from subjective to objective dietary assessment represents a fundamental transformation in nutritional science. While traditional self-reported methods will continue to have utility for capturing comprehensive dietary patterns, objective biomarkers provide essential validation and complementary data that bypass cognitive limitations and reporting biases. The integration of metabolomic profiles, recovery biomarkers, and technology-assisted methods with traditional approaches offers the most promising path forward for obtaining accurate, reliable dietary data.
For researchers and drug development professionals, these advances enable more precise quantification of dietary exposures in clinical trials, enhanced understanding of diet-disease relationships, and ultimately, more effective nutritional interventions and therapeutics. As the field continues to evolve, objective biomarkers will play an increasingly central role in advancing nutritional science from estimation to precise measurement.
Dietary assessment is a fundamental component of nutrition research, enabling the understanding of diet's role in human health and disease, and informing nutrition policy and dietary recommendations [11]. However, accurately measuring dietary exposures through self-report is notoriously challenging, subject to both random and systematic measurement error that can compromise data quality and subsequent conclusions [11] [14]. The selection of an appropriate dietary assessment method is therefore critical, as it must align with specific research questions, study designs, and population characteristics to yield meaningful results.
Traditional dietary assessment methods include food records, food frequency questionnaires (FFQs), and 24-hour recalls, each with distinct strengths and limitations [11]. In recent years, digital and mobile technologies have transformed these traditional methods, offering new opportunities to enhance accuracy, reduce burden, and improve efficiency in data collection and processing [21] [27]. Despite these advancements, methodological challenges persist, particularly concerning systematic misreporting that varies across population subgroups [14].
This comparison guide provides researchers, scientists, and drug development professionals with an evidence-based framework for selecting dietary assessment methods aligned with specific research objectives and population characteristics. By synthesizing current scientific evidence on method performance, validation protocols, and practical implementation considerations, we aim to support methodological decisions that optimize validity, reliability, and feasibility in nutrition research.
Comprehensive Comparison of Dietary Assessment Methods
Dietary assessment methods can be broadly categorized based on their temporal framework (short-term vs. long-term), scope (total diet vs. specific components), and administration approach (investigator-driven vs. participant-driven) [11]. Table 1 summarizes the primary methods, their applications, and key characteristics.
Table 1: Comparison of Primary Dietary Assessment Methods
| Method | Primary Use | Time Frame | Data Collection Approach | Key Outputs |
|---|---|---|---|---|
| 24-Hour Dietary Recall (24HR) | Individual intake assessment | Short-term (previous 24 hours) | Interviewer-administered or self-administered; multiple non-consecutive days | Quantitative nutrient intake; food group consumption |
| Food Record/Food Diary | Detailed intake documentation | Short-term (typically 3-7 days) | Prospective recording by participant | Comprehensive food, beverage, and supplement consumption with timing |
| Food Frequency Questionnaire (FFQ) | Habitual dietary patterns | Long-term (months to year) | Self-administered or interviewer-administered | Frequency of food category consumption; nutrient pattern rankings |
| Dietary Screeners | Specific nutrients/food groups | Variable (typically past month/year) | Brief self-administered questionnaires | Targeted data on specific dietary components |
| Technology-Assisted Methods | Various assessment purposes | Adaptable to different time frames | Mobile apps, sensors, web-based platforms | Multiple output formats with potential real-time feedback |
Quantitative Performance Comparison
The accuracy and precision of dietary assessment methods vary considerably, influenced by factors including population characteristics, study duration, and implementation quality. Table 2 presents comparative data on method performance based on validation studies against recovery biomarkers.
Table 2: Method Performance Characteristics Based on Biomarker Validation
| Method | Energy Underreporting Range | Most Accurately Measured Nutrients | Population Factors Affecting Accuracy | Biomarker Correlation Strength |
|---|---|---|---|---|
| 24-Hour Recall | 10-25% (varies by BMI) [14] | Macronutrients, protein [11] | BMI (increased underreporting with higher BMI) [14] | Moderate to strong for protein, potassium [11] |
| Food Records | 15-34% (higher in obese populations) [14] | Macronutrients, sodium [11] | Literacy, motivation, BMI [11] [21] | Moderate for protein, variable for other nutrients [14] |
| FFQ | 20-30% (systematic bias) [14] | Pattern ranking, select micronutrients [11] | Cognitive ability, memory, cultural appropriateness [11] | Weaker for energy, moderate for protein [14] |
| Technology-Assisted | Emerging evidence (potentially reduced) [21] | Dependent on implementation | Technological access, digital literacy [21] | Limited biomarker validation data available [27] |
Key Selection Criteria
Alignment with Research Objectives
The research question fundamentally dictates the most appropriate dietary assessment method. Studies investigating acute nutrient exposures or day-to-day variability in intake typically require short-term methods like 24-hour recalls or food records, which provide detailed snapshots of recent consumption [11]. For research examining long-term dietary patterns or habitual intake in relation to chronic disease outcomes, FFQs or repeated short-term measures are more appropriate, as they aim to capture usual consumption over extended periods [11] [28].
The scale of dietary assessment represents another critical consideration. Studies focusing on specific nutrients or food groups may utilize targeted screeners or modified FFQs, while comprehensive dietary assessment requires more extensive methods like multiple 24-hour recalls or detailed food records [11]. The level of detail needed also varies – while some research questions require precise quantification of absolute nutrient intakes, others may only need relative ranking of individuals within a population [11] [29].
Studies incorporating dietary supplements require additional assessment components, as traditional methods often fail to capture these exposures adequately. Approximately half of U.S. adults and one-third of children use dietary supplements, necessitating specific assessment strategies to comprehensively evaluate total nutrient exposure [30].
Population Considerations
Population characteristics significantly influence the suitability and performance of dietary assessment methods. Literacy and educational level affect the feasibility of self-administered methods like FFQs and food records, with low literacy populations often requiring interviewer-administered approaches [11] [21]. Age and cognitive ability impact memory recall and attention span, making shorter assessments or methods with external memory aids more appropriate for children, older adults, or cognitively impaired individuals [21] [31].
Body mass index (BMI) consistently correlates with underreporting, particularly for energy-dense foods, with higher BMI associated with greater underreporting across all self-report methods [14]. This systematic bias has profound implications for obesity research, suggesting caution when using self-reported energy intake in studies of energy balance [14].
Cultural and linguistic factors necessitate method adaptation, including food list modification for FFQs, use of culturally appropriate portion size estimation aids, and availability of bilingual materials or interpreters [11] [28]. Technological access and digital literacy increasingly influence method selection as technology-based tools become more prevalent, potentially excluding populations with limited resources or technology experience [21] [27].
Practical Implementation Factors
Participant burden varies substantially across methods, from brief screeners requiring <15 minutes to complete, to detailed food records or multiple 24-hour recalls demanding >20 minutes per assessment [11]. Higher burden methods typically experience reduced compliance and data quality over time, necessitating careful consideration of assessment duration and frequency [11] [29].
Resource requirements encompass personnel time, training needs, equipment, and data processing costs. Interviewer-administered 24-hour recalls require substantial trained personnel investment, while self-administered FFQs offer cost-efficiency for large samples [11]. Technology-based methods may reduce long-term costs but require significant initial development investment and technical support [21] [27].
Data processing and analysis considerations include the availability of appropriate nutrient databases, coding requirements, and analytical expertise. Methods producing quantitative output (24-hour recalls, food records) enable more detailed nutrient analysis, while FFQs primarily support pattern analysis and ranking [11] [28].
Experimental Validation Protocols
Biomarker Validation Approaches
The gold standard for validating self-reported dietary intake involves comparison with recovery biomarkers, which provide objective measures of nutrient consumption. The doubly labeled water (DLW) method measures total energy expenditure through the differential elimination kinetics of two stable isotopes (deuterium and 18O), providing a biomarker of habitual energy intake under weight-stable conditions [14]. Validation protocols typically involve administering the dietary assessment method concurrently with DLW measurement over 1-2 weeks, enabling direct comparison of reported energy intake against measured energy expenditure [14].
Urinary nitrogen measurement serves as a recovery biomarker for protein intake, based on the relatively constant proportion of dietary nitrogen excreted in urine [14]. Validation studies collect 24-hour urine samples alongside dietary reporting, with comparisons adjusted for known routes of nitrogen loss. Similarly, 24-hour urinary sodium and potassium provide recovery biomarkers for assessing sodium and potassium intake [11] [14].
These biomarker comparisons have consistently revealed significant underreporting of energy intake across self-assessment methods, with systematic biases related to BMI and macronutrient composition [14]. Protein is typically the least underreported nutrient, while energy and carbohydrates show greater reporting errors [14].
Method Comparison Protocols
When recovery biomarkers are unavailable or impractical, researchers often employ method comparison approaches, where the assessment method of interest is compared against a more detailed reference method. Common protocols include:
- Comparing FFQ results against multiple 24-hour recalls or food records collected over a representative period [11] [28]
- Evaluating short screeners against comprehensive FFQs or multiple recalls for specific nutrients or food groups [11]
- Testing technology-assisted methods against traditional pen-and-paper versions or interviewer-administered assessments [21] [27]
These comparisons typically evaluate correlation coefficients, agreement in classification into intake quartiles or quintiles, and mean differences between methods [11] [28]. While less definitive than biomarker validation, these approaches provide practical information about relative method performance and suitability for specific research contexts.
Visual Decision Framework
Diagram 1: Decision Framework for Dietary Assessment Method Selection. This flowchart illustrates key decision points when selecting dietary assessment methods based on population size, time frame of interest, and required level of detail.
Research Reagent Solutions
Table 3: Essential Research Reagents and Tools for Dietary Assessment Validation
| Reagent/Tool | Primary Function | Application Context | Key Considerations |
|---|---|---|---|
| Doubly Labeled Water (DLW) | Gold standard measurement of total energy expenditure | Validation of energy intake reporting; requires mass spectrometry analysis | High cost limits sample size; excellent accuracy for habitual intake |
| 24-Hour Urinary Nitrogen | Objective biomarker of protein intake | Validation of protein reporting; requires complete urine collection | Affected by non-dietary factors; requires participant compliance |
| Digital Photography Systems | Objective food documentation and quantification | Technology-assisted food records; portion size estimation | Standardization needed for lighting, angles; requires image analysis |
| Standardized Food Models | Visual aids for portion size estimation | Interviewer-administered 24HR; portion size training | Must be culturally appropriate; regular updates for new products |
| Brand-Specific Food Databases | Enhanced food identification and nutrient matching | Technology-based assessment tools; processed food documentation | Requires continuous updating; potential for participant overload |
| Integrated Nutrient Analysis Software | Automated nutrient calculation from food intake data | All assessment methods requiring nutrient output | Database quality determines accuracy; regular updates essential |
Selecting appropriate dietary assessment methods requires careful consideration of research objectives, population characteristics, and practical constraints. The 24-hour recall currently represents the most accurate method for assessing absolute food and nutrient intakes, while FFQs offer cost-efficient approaches for ranking individuals by habitual intake in large studies [11] [30]. Food records provide detailed intake documentation but are susceptible to reactivity and participant burden [11] [21].
Technology-based methods present promising opportunities to enhance dietary assessment through reduced burden, improved efficiency, and potentially enhanced accuracy [21] [27]. However, these approaches require validation against traditional methods and biomarkers, and may introduce new challenges related to technology access and digital literacy [21] [31].
Regardless of the method selected, researchers should acknowledge and address the systematic measurement errors inherent in all self-reported dietary assessment tools [14]. Methodological transparency, including detailed reporting of assessment protocols, validation studies, and potential limitations, remains essential for interpreting results and advancing the field of nutritional epidemiology [28]. By aligning method selection with specific research needs and implementing rigorous validation protocols, researchers can optimize the quality and utility of dietary assessment in nutrition research.
A Deep Dive into Methodologies: From Established Protocols to AI-Driven Innovations
Within nutritional epidemiology and clinical research, the accurate assessment of dietary intake is fundamental to understanding the links between diet and health. For decades, two methodologies have served as traditional workhorses in the field: the Automated Multiple-Pass Method (AMPM), a detailed 24-hour recall system, and the Diet History Questionnaire (DHQ), a type of Food Frequency Questionnaire (FFQ) designed to capture habitual intake. Framed within the broader thesis of traditional versus objective dietary assessment research, this guide provides an objective comparison of these tools' performance, supported by experimental data and detailed methodologies.
The AMPM and DHQ are built on fundamentally different approaches to capturing dietary data.
- The Automated Multiple-Pass Method (AMPM) is a computerized, interviewer-administered 24-hour dietary recall method. Its core strength lies in its structured, five-pass approach designed to enhance memory and reduce omission of foods [21] [32]. This method provides a detailed snapshot of all foods, beverages, and supplements consumed in the previous 24 hours and is the method used for the dietary interview component of the U.S. National Health and Nutrition Examination Survey (NHANES) [32].
- Diet History Questionnaires (DHQs) are typically self-administered forms that ask respondents to report their usual frequency of consumption and, in some cases, portion sizes, from a finite list of foods and beverages over a specified period, such as the past month or year [21]. The DHQ developed by the National Cancer Institute (NCI) is a prominent example intended to estimate an individual's habitual diet.
Table 1: Core Methodological Characteristics of AMPM and Diet History (DHQ)
| Feature | AMPM (24-Hour Recall) | Diet History (Food Frequency Questionnaire) |
|---|---|---|
| Primary Objective | Capture detailed intake for a specific day (absolute intake) | Capture habitual intake over a long period (rank individuals) |
| Time Frame | Previous 24 hours | Usually past month or year |
| Administration | Interviewer-administered (computer-assisted) | Primarily self-administered |
| Data Output | Detailed list of foods, portions, timing, and context | Frequency of consumption for a pre-defined food list |
| Cognitive Demand | Relies on short-term memory | Relies on long-term memory and generalization |
| Key Strength | Detailed, quantitative day-specific data | Efficient for assessing usual diet in large cohorts |
| Key Weakness | High day-to-day variation (requires multiple recalls) | Limited detail; prone to systematic bias and measurement error |
Performance Evaluation Against Objective Biomarkers
The most rigorous evaluations of dietary assessment tools involve comparison against objective recovery biomarkers, which are not subject to the same self-reporting biases. Data from such studies reveal critical differences in the performance of AMPM and FFQs like the DHQ.
Validation Against Doubly Labeled Water and Urinary Biomarkers
A key study compared the performance of the USDA AMPM and two FFQs—the Block FFQ and the NCI's DHQ—using doubly labeled water (DLW) total energy expenditure as the criterion measure for energy intake [33]. The study involved 20 highly motivated, premenopausal women.
Table 2: Comparison of Mean Reported Energy Intake vs. Doubly Labeled Water (DLW) Criterion
| Assessment Method | Mean Reported Energy Intake (kJ) | % Difference from DLW TEE | Pearson Correlation (r) with DLW TEE |
|---|---|---|---|
| DLW TEE (Criterion) | 8905 ± 1881 | - | - |
| AMPM Recall | 8982 ± 2625 | +0.9% | 0.53 (P=0.02) |
| Food Record (FR) | 8416 ± 2217 | -5.5% | 0.41 (P=0.07) |
| Block FFQ | 6365 ± 2193 | -28.5% | 0.25 (P=0.29) |
| NCI DHQ | 6215 ± 1976 | -30.2% | 0.15 (P=0.53) |
The findings were clear: the AMPM and food record estimates of total energy intake did not differ significantly from the DLW measurement, while both the Block and DHQ questionnaires underestimated energy intake by approximately 28% [33]. Furthermore, the AMPM showed a stronger linear relationship with the objective biomarker (r=0.53) than either FFQ.
A larger study of men and women aged 50-74 confirmed this pattern, finding that compared to energy expenditure biomarkers, energy intake was underestimated by 15-17% on multiple ASA24 recalls (a self-administered tool based on the AMPM), 18-21% on 4-day food records, and 29-34% on FFQs [34].
Experimental Protocol for Biomarker Validation
The methodology for the study cited in Table 2 is as follows [33]:
- Participants: 20 free-living, normal-weight, premenopausal women.
- Criterion Measure: Total energy expenditure (TEE) measured by the doubly labeled water (DLW) technique over a 14-day period.
- Dietary Assessment Methods:
- AMPM: Two unannounced, interviewer-administered 24-hour recalls were collected using the USDA AMPM.
- FFQs: Participants completed both the Block FFQ and the National Cancer Institute's Diet History Questionnaire (DHQ).
- Food Record (FR): Participants completed a 14-day estimated food record to serve as an additional comparison.
- Data Analysis: Mean reported energy intakes from each dietary tool were compared statistically to the DLW TEE. Pearson correlation coefficients were calculated to assess the strength of the linear relationship between each method and the biomarker.
Workflow and Research Reagents
The AMPM 5-Pass Workflow
The accuracy of the AMPM is attributed to its structured, multi-stage interview process, which is designed to systematically prompt memory and minimize omissions. The following diagram illustrates this workflow.
Essential Research Reagent Solutions
Conducting validated dietary assessment research requires a suite of reliable tools and databases. The following table details key resources used in studies featuring the AMPM and DHQ.
Table 3: Key Research Reagents for Dietary Assessment Validation
| Reagent / Solution | Function in Dietary Assessment | Example / Source |
|---|---|---|
| Doubly Labeled Water (DLW) | Objective biomarker for total energy expenditure; serves as a criterion to validate reported energy intake [33]. | Isotopes: ^2H (Deuterium) and ^18O (Oxygen-18) |
| 24-Hour Urinary Nitrogen | Objective biomarker for protein intake; used to validate reported protein consumption [34]. | Collection of all urine over a 24-hour period. |
| 24-Hour Urinary Potassium/Sodium | Objective biomarkers for potassium and sodium intake [34]. | Collection of all urine over a 24-hour period. |
| Standardized Nutrient Database | Provides the nutrient composition for foods and supplements reported by participants; essential for converting intake data into nutrient values. | USDA Food and Nutrient Database for Dietary Studies (FNDDS) [35], NHANES Dietary Supplement Database (DSD) [36] [37] |
| Standardized Assessment Tool | The software or questionnaire platform used to collect dietary data in a consistent manner. | USDA AMPM [32], NCI's ASA24 [38], NCI's Diet History Questionnaire (DHQ) |
The experimental data lead to a clear conclusion regarding the performance of these traditional workhorses. When the research objective requires accurate estimation of absolute energy and nutrient intake for a group or population, the AMPM is demonstrably superior, providing intake measures that are not significantly different from those obtained by objective biomarkers [33] [34]. Its detailed, multi-pass structure effectively mitigates memory-related underreporting. In contrast, Diet History Questionnaires like the DHQ show substantial underestimation of absolute energy intake (around 28-34%) and weaker correlations with biomarker data [33] [34]. This makes them less suitable for measuring absolute intake but, due to their lower cost and burden, they remain a practical tool for ranking individuals by their habitual intake in large epidemiological studies. The choice between them must be driven by the specific research question and an understanding of their inherent measurement characteristics.
The shift from traditional, memory-dependent dietary assessment methods toward technology-assisted, objective tools represents a significant advancement in nutritional science. Traditional tools like interviewer-administered 24-hour recalls and paper food diaries have long been plagued by limitations including recall bias, measurement error, and high participant burden [39] [40]. In response, researchers have developed innovative technological solutions that enhance accuracy, reduce administrative costs, and improve user compliance. Two major categories of these solutions have emerged: comprehensive, structured recall systems like the Automated Self-Administered 24-Hour Recall (ASA24), and a diverse ecosystem of mobile applications employing various methodologies from text entry to artificial intelligence (AI)-powered image recognition [41] [42]. This guide provides an objective comparison of these technology-assisted tools, supported by experimental data, to inform researchers, scientists, and drug development professionals in selecting appropriate dietary assessment methods for their work.
Technology-assisted dietary assessment tools can be broadly classified by their primary methodology and operational paradigm. The table below summarizes the key characteristics of major tools discussed in the scientific literature.
Table 1: Overview of Technology-Assisted Dietary Assessment Tools
| Tool Name | Primary Methodology | Developer/Context | Key Features | Nutrient Database & Outputs |
|---|---|---|---|---|
| ASA24 | Automated Self-Administered 24-Hour Recall | National Cancer Institute (NCI) [38] | Web-based, adapts USDA's Automated Multiple-Pass Method (AMPM), self-administered [38] [43] | Food and Nutrient Database for Dietary Studies (FNDDS); provides nutrient and food group data [38] [5] |
| DietAI24 | Multimodal LLM + Retrieval-Augmented Generation (RAG) | Research Framework (Yan et al.) [39] | Food image analysis, zero-shot nutrient estimation, combines MLLMs with FNDDS database [39] | FNDDS; estimates 65 distinct nutrients and food components [39] |
| NutriDiary | Smartphone-based Weighed Dietary Record | Research App (Germany) [44] | Text search, barcode scanning, free text entry; recipe editor; designed for epidemiological studies [44] | Custom database (LEBTAB) with 82 nutrients; includes branded products [44] |
| Traqq | Repeated Short Recalls (Ecological Momentary Assessment) | Research App (Netherlands) [3] | 2-hour and 4-hour recall windows to reduce memory bias; initially designed for adults [3] | Not specified in protocol; assesses energy, nutrient, and food group intake [3] |
| Bitesnap | Text + Image Entry | Commercial App [41] | Flexible food timing functionality; suitable for research and clinical settings [41] | Not specified; provides caloric and macronutrient estimates [41] |
| Voice-based Recall (DataBoard) | Voice Input/Speech Recognition | Research Tool (Pilot Study) [40] | Speech input for dietary recall; targets older adults and those with digital literacy challenges [40] | Not specified; focuses on meal composition and timing [40] |
Comparative Performance and Experimental Data
Accuracy Metrics in Controlled and Real-World Settings
Controlled studies and validation trials provide crucial data on the relative accuracy of different dietary assessment tools. The following table synthesizes key performance metrics reported in recent scientific literature.
Table 2: Comparative Accuracy and Performance Metrics of Dietary Assessment Tools
| Tool Name | Study Design | Key Performance Metrics | Reported Strengths | Reported Limitations |
|---|---|---|---|---|
| ASA24 | Extensive use in national surveillance (NHANES component via WWEIA) [38] [5] | Comparable error to interviewer-administered recalls when validated with recovery biomarkers [43] | High scalability, automated coding, free for researchers, extensive database [38] [43] | Usability issues for some populations, time-consuming, requires computer literacy [40] |
| DietAI24 | Evaluation on ASA24 and Nutrition5k datasets [39] | 63% reduction in MAE for food weight vs. existing methods; accurate estimation of 65 nutrients [39] | Handles real-world mixed dishes, no food-specific training required, high nutrient coverage [39] | Research framework, not yet a commercial product |
| Image-Based Tools (mFR, FoodView) | Controlled feeding studies & validation trials [43] [42] | More accurate than methods without images; better portion size estimation [43] | Reduces memory bias, provides visual documentation, user-friendly [43] [42] | Image quality dependency, limited adoption in research, potential user reactivity |
| Voice-based Recall (DataBoard) | Pilot study with older adults (n=20) [40] | Feasibility: 7.95/10; Acceptability: 7.6/10; Easier to use than ASA24 (6.7/10) [40] | Reduces digital literacy barriers, preferred by older adults [40] | Early development stage, limited validation, may struggle with complex food names |
Usability and Participant Burden
Usability is a critical factor influencing participant compliance and data quality, particularly in long-term studies.
Table 3: Usability and Practical Implementation Factors
| Tool | Target Population | Usability Metrics | Completion Time | Participant Preferences |
|---|---|---|---|---|
| ASA24 | Ages 12+ with 5th-grade reading level [38] | Challenging for some older adults [40] | Not explicitly reported, but considered time-consuming [40] | Less preferred compared to voice-based methods in older adults [40] |
| NutriDiary | German adults (evaluation study) [44] | SUS Score: 75 (IQR 63-88) - indicates "good" usability [44] | Median 35 min (IQR 19-52) for one-day record [44] | Preferred over paper-based method by most participants [44] |
| Voice-based Recall | Older adults (65+) [40] | Rated easier than ASA24 (6.7/10) [40] | Not explicitly reported | Preferred for frequent use over ASA24 (7.2/10) [40] |
| Mobile Apps (General) | Adolescents [3] | Varied; influenced by design features like autofill and gamification [3] | Shorter recalls (2-4 hours) reduce burden [3] | Preference for apps over web-based tools [3] |
Detailed Experimental Protocols
Understanding the methodological details of key validation studies is essential for researchers to evaluate evidence quality and design their own trials.
Protocol 1: DietAI24 Validation Study
Objective: To evaluate the accuracy of the DietAI24 framework in food recognition, portion size estimation, and nutrient content estimation from food images [39].
Methodology:
- Dataset: Used ASA24 and Nutrition5k datasets for evaluation [39].
- Indexing Phase: FNDDS database was segmented into concise, MLLM-readable food descriptions [39].
- Retrieval Phase: Implemented Retrieval-Augmented Generation (RAG) to ground MLLM responses in FNDDS database [39].
- Estimation Phase: Employed GPT Vision model for image-to-text reasoning and nutrient estimation [39].
- Analysis: Calculated mean absolute error (MAE) for food weight estimation and four key nutrients compared to existing methods and commercial platforms [39].
Workflow Diagram:
Protocol 2: Controlled Feeding Study for Technology-Assisted 24HR Methods
Objective: To compare accuracy, acceptability, and cost-effectiveness of three technology-assisted 24-hour dietary recall methods (ASA24, Intake24, and Image-Assisted mFR24) against observed intake [43].
Methodology:
- Design: Randomized, controlled feeding study with crossover design [43].
- Participants: 150 healthy adults (18-70 years) [43].
- Feeding Protocol: Participants consumed breakfast, lunch, and dinner at a university study center on three separate days with unobtrusive documentation of foods and amounts consumed [43].
- Recall Methods: Following each feeding day, participants completed a 24HR using one of the three methods in randomized order [43].
- Measures:
- Statistical Analysis: Linear mixed models to assess differences in 24HR methods; calculation of omission and intrusion rates; assessment of psychosocial and cognitive factors associated with misreporting [43].
Workflow Diagram:
Implementing technology-assisted dietary assessment requires access to specialized databases and tools. The following table outlines key resources referenced in the literature.
Table 4: Essential Research Resources for Dietary Assessment Studies
| Resource Name | Type | Developer/Maintainer | Key Applications in Research |
|---|---|---|---|
| Food and Nutrient Database for Dietary Studies (FNDDS) | Nutrient Database | USDA Agricultural Research Service [5] | Provides energy and 64 nutrient values for ~7,000 foods; used in ASA24 and NHANES [39] [5] |
| Healthy Eating Index (HEI) | Diet Quality Metric | USDA Food and Nutrition Service [8] | Measures adherence to Dietary Guidelines; used to standardize diet quality in interventions [8] |
| National Health and Nutrition Examination Survey (NHANES) | Population Survey Data | CDC National Center for Health Statistics [5] | Provides nationally representative dietary intake data; uses 24-hour recall method [5] |
| What We Eat in America (WWEIA) | Dietary Data Component | USDA Agricultural Research Service [5] | Dietary intake component of NHANES; uses automated multiple-pass 24-hour recall [5] |
| Food Pattern Equivalents Database (FPED) | Food Group Database | USDA Agricultural Research Service [5] | Converts FNDDS foods into 37 USDA Food Pattern components; assesses adherence to food group recommendations [5] |
| System Usability Scale (SUS) | Usability Assessment | Standardized Questionnaire | Validated tool for assessing perceived usability of systems and tools [44] |
The evidence compiled in this guide demonstrates that technology-assisted dietary assessment tools offer diverse approaches with distinct advantages and limitations. ASA24 provides a standardized, extensively validated system suitable for large-scale epidemiological research, with performance comparable to interviewer-administered methods [38] [43]. Emerging AI-powered frameworks like DietAI24 show remarkable potential for automating dietary assessment from images with accuracy surpassing existing methods [39]. Mobile applications offer advantages in specific populations: voice-based tools for older adults [40], repeated short recalls for adolescents [3], and image-based methods for real-time intake tracking [42].
When selecting appropriate tools, researchers should consider multiple factors: target population characteristics, required nutrient detail, available budget, and technological infrastructure. No single tool excels across all domains, but the expanding toolkit enables more precise, less burdensome dietary assessment across diverse research contexts. Future developments will likely focus on integrating multimodal approaches (e.g., combining images, voice, and text), enhancing AI capabilities for complex mixed dishes, and improving accessibility for vulnerable populations.
Accurate dietary assessment is crucial for nutrition research, clinical practice, and public health initiatives, yet traditional methods like food frequency questionnaires, 24-hour recalls, and food diaries are plagued by significant limitations including memory bias, estimation errors, and high participant burden [3]. These self-reported methods are particularly challenging for assessing portion sizes and specific nutrient content, creating a critical gap in nutrition science and evidence-based practice. In response to these challenges, Image-Based Dietary Assessment (IBDA) has emerged as a promising technological solution that leverages artificial intelligence (AI) and computer vision to objectively analyze food intake from digital images [45] [46].
IBDA represents a fundamental shift from subjective recall to objective measurement in dietary assessment. By combining smartphone cameras with sophisticated algorithms, these systems aim to automatically identify foods, estimate portion sizes, and calculate nutrient content with minimal human intervention [47]. This comparative guide examines the current state of IBDA technologies, their performance against traditional methods and ground truth standards, and their practical application within research and clinical contexts, particularly focusing on the validation and implementation of these rapidly evolving tools.
Core Technological Components of IBDA Systems
Image-based dietary assessment systems typically operate through a sequential computational pipeline that transforms food images into estimated nutrient data. Understanding these core components is essential for evaluating different system capabilities and limitations.
Technical Workflow and Architecture
The operational workflow of automated IBDA systems follows a structured sequence of computer vision tasks, each with distinct technical requirements and methodological approaches. The diagram below illustrates this multi-stage computational pipeline.
Food Image Segmentation involves isolating food items from the background and from each other within an image. Deep learning approaches, particularly convolutional neural networks (CNNs), have demonstrated superior performance in this initial phase by precisely delineating multiple food items on a plate [46]. Food Item Classification follows, where segmented food regions are identified using trained models. CNNs outperform traditional machine learning approaches, especially when trained on large-scale food databases, with performance directly correlated to dataset diversity and quality [46].
The most technically challenging component is Volume Estimation, which aims to convert two-dimensional food images into three-dimensional volume approximations. Despite various approaches including reference objects and shape templates, this phase remains a significant obstacle in IBDA systems, with few commercial platforms capable of reliable automated volume estimation [48]. Finally, Nutrient Analysis combines classification and volume data with nutritional databases to calculate calorie and nutrient content. This stage depends heavily on accurate volume estimation and comprehensive food composition databases [49].
Research Reagents and Computational Tools
Table 1: Essential Research Components for IBDA System Development
| Component Type | Specific Examples | Function/Role in IBDA |
|---|---|---|
| Public Food Image Datasets | Food-101, UEC-Food256, Pittsburgh Fast-food Image Dataset (PFID) | Training and benchmarking food recognition algorithms; varying in food categories, image quantity, and acquisition environments [46]. |
| Deep Learning Architectures | Convolutional Neural Networks (CNNs) | Primary method for food segmentation and classification; outperforms traditional machine learning on large datasets [46] [50]. |
| Nutrient Databases | USDA Food Composition Databases, Healthy Eating Index (HEI) | Converting identified foods and volumes into nutrient estimates; provides standardized nutritional profiling [8] [49]. |
| Validation Methodologies | Weighed food records, Doubly Labeled Water, Standardized photographic sets | Establishing ground truth for evaluating IBDA system accuracy against reference measures [50]. |
Comparative Performance Analysis of IBDA Approaches
The evolving landscape of IBDA technologies encompasses various approaches with distinct capabilities and performance characteristics. The table below summarizes quantitative performance data across key functional domains.
Table 2: Performance Comparison of IBDA Methods and Traditional Assessment Tools
| Assessment Method | Food Recognition Accuracy | Volume/Portion Estimation | Relative Error for Calories | Key Limitations |
|---|---|---|---|---|
| Commercial Image Recognition Platforms | Variable: 9% (Google Vision) to 63% (Calorie Mama) top-1 accuracy [48] | Limited: None of tested platforms provided automatic estimates [48] | Not reported | Inconsistent performance; inadequate volume estimation [48] |
| Research IBDA Systems | High: CNN-based approaches outperform other methods on large datasets [46] | Promising but challenging: Relative errors 0.09% to 33% vs. ground truth [50] | 0.10% to 38.3% vs. ground truth [50] | Methodological heterogeneity; limited standardization [50] |
| Traditional 24-Hour Recalls | Dependent on respondent knowledge and memory | Subjective estimation; prone to systematic bias [3] | Significant under-reporting, especially in specific populations [3] | Memory bias, social desirability bias, portion size estimation errors [3] |
| Digital Food Records | Dependent on user identification skills | Improved with photo assistance but still requires user input | Reduced but not eliminated under-reporting [3] | High participant burden, still reliant on self-report elements |
Analysis of Comparative Performance Data
The performance data reveals distinct patterns across IBDA approaches. For food recognition, deep learning-based research systems generally outperform commercial platforms, with CNN architectures achieving superior classification accuracy when trained on diverse, large-scale datasets [46]. The wide variation in commercial platform performance (9-63% accuracy) highlights significant differences in their underlying algorithms and training data [48].
For volume estimation and calorie calculation, research systems demonstrate promising accuracy with relative errors ranging from 0.09% to 38.3% compared to ground truth, suggesting potential alignment with or even superiority over human estimations [50]. However, this accuracy varies considerably based on food complexity, with simpler, single-item foods yielding better results than mixed dishes. A critical finding is that fully automated volume estimation remains a substantial challenge, with no commercial platforms currently providing reliable automated portion size estimates [48].
When compared to traditional methods, IBDA systems offer distinct advantages in objective measurement, reduced participant burden, and minimized memory-related biases. However, they have not yet fully replaced traditional methods in research settings due to persistent technical challenges and validation needs [50].
Experimental Protocols and Validation Methodologies
Standardized Testing Protocols for IBDA Systems
Rigorous validation of IBDA systems requires standardized experimental approaches that enable direct comparison against reference methods. The following diagram outlines a comprehensive mixed-methods validation protocol adapted from contemporary research methodologies.
Phase 1: Quantitative Evaluation involves comparative assessment where participants use the IBDA system concurrently with established reference methods such as interviewer-administered 24-hour recalls (24hR) and food frequency questionnaires (FFQ) [3]. Standardized food scenarios or actual consumption events are documented using both approaches, with statistical comparisons focusing on energy, macronutrient, and food group intake estimates. Key metrics include relative error calculations (|actual - estimated|/actual)*100) for portion sizes and nutrient estimates compared to ground truth measures like weighed food records [50].
Phase 2: Qualitative Assessment employs semi-structured interviews and experience questionnaires to evaluate usability factors including ease of use, time requirements, and perceived accuracy [3]. Standardized instruments like the System Usability Scale provide quantitative usability metrics, while open-ended interviews identify specific usability barriers and contextual challenges.
Phase 3: Co-Creation Sessions engage end-users in participatory design activities to refine IBDA tools based on real-world feedback and preferences [3]. This phase is particularly valuable for adapting systems to specific populations such as adolescents or culturally diverse groups whose needs may differ from the general population.
Ground Truth Establishment
A critical aspect of IBDA validation is establishing reliable ground truth measurements for comparison. Common approaches include:
- Weighed Food Records: Pre-consumption and post-consumption weights of food items provide precise consumption data but require substantial participant cooperation [50].
- Doubly Labeled Water: Considered the gold standard for energy expenditure measurement, providing indirect validation of energy intake assessment [50].
- Standardized Food Scenarios: Controlled laboratory settings with predetermined food items and portions enable precise accuracy measurement without participant variability [48].
Emerging Applications and Future Directions
Fixed-Quality Variable-Type (FQVT) Dietary Intervention
A significant paradigm shift in nutrition research methodology is the emergence of the Fixed-Quality Variable-Type (FQVT) approach, which leverages advances in dietary assessment technology [8] [6]. This innovative framework standardizes diet quality using objective measures like the Healthy Eating Index (HEI) 2020 while accommodating diverse dietary patterns tailored to individual preferences, cultural backgrounds, and health needs [8].
The FQVT methodology addresses critical limitations of traditional "one-size-fits-all" dietary interventions by enhancing cultural relevance, participant adherence, and real-world applicability [6]. This approach has particular significance for IBDA systems, as it relies on rapid, accurate diet quality assessment that digital tools can provide. Implementation of FQVT has been operationalized through platforms like Diet ID, which uses image-based assessment to measure diet quality in approximately one minute with reported 90% accuracy compared to traditional methods [6].
Specialized Population Applications
IBDA systems show particular promise for managing chronic conditions requiring precise dietary monitoring, such as diabetes. Automated carbohydrate counting and calorie estimation from food images can support diabetes self-management by providing real-time feedback on food choices [47]. Research indicates these systems can estimate carbohydrate content and caloric intake with accuracy levels potentially sufficient for clinical application, though further validation is needed [47] [50].
Beyond clinical applications, IBDA technologies are being adapted for specific populations including adolescents, who present unique assessment challenges due to irregular eating patterns and different technology engagement preferences [3]. Studies evaluating apps like Traqq with adolescent populations employ repeated short recalls (2-hour and 4-hour intervals) to reduce memory burden and improve accuracy compared to traditional 24-hour recalls [3].
Image-Based Dietary Assessment represents a promising technological advancement in nutritional science, offering objective, scalable alternatives to traditional self-reported methods. Current evidence indicates that while IBDA systems show significant potential, particularly in food recognition, they still face challenges in fully automated volume estimation and require further validation across diverse foods and populations.
For researchers and practitioners considering implementation, the following key points should guide decision-making:
- Technology Selection: Choose IBDA platforms based on specific assessment needs; while general food recognition is reasonably advanced, specialized applications may require custom solutions.
- Validation Requirements: Conduct pilot validation studies against appropriate reference methods specific to the target population and food types of interest.
- Integration Approach: Consider blended assessment strategies that combine IBDA strengths with complementary traditional methods to address current technological limitations.
- Future Development: Monitor emerging advancements in deep learning architectures, sensor technologies, and standardized food databases that continue to enhance IBDA capabilities.
As the field evolves toward greater standardization and validation, IBDA systems are poised to transform dietary assessment methodologies, enabling more precise, personalized nutrition interventions and advancing public health research through more accurate dietary intake measurement.
Accurately capturing dietary intake is fundamental to understanding its role in chronic disease development, yet traditional self-reporting tools like 24-hour recalls and food frequency questionnaires are plagued by significant limitations, including participant burden, recall bias, and systematic under-reporting [51] [19]. This measurement inaccuracy presents a major challenge for research and clinical practice. The emergence of sensor-based wearable technologies represents a paradigm shift, offering a passive, objective, and minimally burdensome method for detecting eating occasions [51] [52]. These technologies primarily leverage data on motion (via accelerometers) and sound (via acoustic sensors) to identify eating events based on proxies such as chewing, swallowing, and hand-to-mouth gestures. This guide provides a comparative analysis of the leading sensor-based technologies designed to capture eating occasions, detailing their operational principles, performance data, and experimental protocols to inform researchers and drug development professionals.
Comparative Performance Analysis of Sensor-Based Technologies
The following tables synthesize quantitative data from validation studies, offering a direct comparison of the performance and characteristics of different technological approaches.
Table 1: Performance Metrics of Eating Detection Technologies
| Technology Category | Primary Sensor(s) | Reported Sensitivity | Reported Precision | F1-Score | Key Strengths | Key Limitations |
|---|---|---|---|---|---|---|
| Integrated Sensor + Image System (AIM-2) [53] | Accelerometer, Camera | 94.59% | 70.47% | 80.77% | High sensitivity; reduces false positives via multi-modal data | Privacy concerns; data processed offline |
| Sensor-Only System (AIM) [54] | Acoustic, Accelerometer | Not Specified | Not Specified | Kappa: 0.77-0.78* | High agreement with video observation; reliable for bout detection | Performance can be confounded by non-eating activities |
| Wearable Camera (Autographer) [55] | Camera (Image) | N/A (Objective ground truth) | N/A (Objective ground truth) | N/A | Provides objective, first-person view of intake | High participant burden; major privacy concerns |
| Neck-Worn Acoustic Sensor [52] | Microphone (Acoustic) | >80% (in some studies) | Variable | Variable | Directly captures chewing and swallowing sounds | Sensitive to ambient noise; socially obtrusive |
Note: The Kappa statistic represents agreement with video observation, where 0.77-0.78 indicates substantial agreement [54].
Table 2: Feasibility Assessment for Research Settings (based on a scoping review of 53 devices) [52]
| Feasibility Criterion | Definition / Threshold | Percentage of Devices Meeting Criterion |
|---|---|---|
| Accuracy | Performance metric (e.g., F1-score, Accuracy) ≥80% | Limited reporting; many devices under development |
| Free-Living Testing | Evaluated in settings with free food and activity choice | 37% |
| Social Acceptability | Device is discrete and comfortable for long-term wear | 54% |
| Battery Life | Sufficient to cover waking hours without recharging | 9% (Most studies did not report this) |
| Rapid Detection | Ability to detect an eating episode in near real-time | Varied by device type |
Experimental Protocols for Key Validation Studies
A critical step in evaluating these technologies is understanding the rigour of their validation. Below are the detailed methodologies from two pivotal studies.
Protocol 1: Validation of the Automatic Ingestion Monitor (AIM) by Video Observation
- Objective: To validate the accuracy of a multi-sensor wearable system (AIM) for detecting food intake in a relatively unconstrained environment [54].
- Study Population: 40 participants.
- Environment: A 4-bedroom apartment where participants could move freely; monitoring occurred over three days.
- Sensor System: Participants wore the AIM, a device that uses a combination of sensors (including an accelerometer) to detect ingestion events at 30-second resolutions via a neural network classifier.
- Ground Truth: Established using a multi-camera video system (six cameras). Three trained human raters annotated the video footage for major activities of daily living (eating, drinking, etc.) and specific food intake bouts (individual bites and chewing).
- Validation Metrics: Inter-rater reliability was calculated using kappa statistics. The AIM's food intake detection was then compared against the video annotation ground truth using kappa agreement and one-way ANOVA to compare estimated eating durations.
Protocol 2: Integrated Image and Sensor-Based Detection in Free-Living
- Objective: To reduce false positives in eating episode detection by integrating image-based and accelerometer-based data from the AIM-2 device [53].
- Study Population: 30 participants (20 M, 10 F; mean age 23.5 ± 4.9 years).
- Environment: Two days per participant—one "pseudo-free-living" day (meals in lab, otherwise unrestricted) and one full free-living day.
- Sensor System: Participants wore the AIM-2, a device mounted on eyeglasses containing a camera (capturing an egocentric image every 15 seconds) and a 3-axis accelerometer (sampled at 128 Hz) to capture head movement and jaw motion.
- Ground Truth:
- Pseudo-free-living day: A foot pedal was used by participants to manually mark the start and end of each bite and swallow.
- Free-living day: Continuous images were manually reviewed to annotate the start and end times of all eating episodes.
- Data Integration: A hierarchical classification model was developed to combine confidence scores from two separate classifiers: one for recognizing solid foods and beverages in the images (using a deep learning-based object detector), and another for detecting chewing from the accelerometer signal.
- Validation Method: Leave-one-subject-out cross-validation was used to evaluate the integrated method against the image-annotated ground truth for the free-living day.
Visualizing the Workflow for Integrated Eating Detection
The following diagram illustrates the logical workflow and data fusion process for a multi-sensor system, as described in Protocol 2.
The Scientist's Toolkit: Key Research Reagents and Materials
For researchers aiming to develop or validate similar technologies, the following table details essential components and their functions in a typical sensor-based eating detection system.
Table 3: Essential Research Reagents and Materials for Eating Detection Studies
| Item Name / Category | Function / Description | Example in Cited Research |
|---|---|---|
| Multi-Sensor Wearable Device | Platform for data acquisition; often includes motion, sound, and image sensors. | Automatic Ingestion Monitor (AIM, AIM-2) [54] [53] |
| Inertial Measurement Unit (IMU) | A specific sensor type that captures motion data (acceleration, orientation). | 3D Accelerometer within AIM-2 for detecting jaw motion [53] |
| Microphone / Acoustic Sensor | Captures audio signals for detecting chewing and swallowing sounds. | Acoustic sensor in the AIM system [54] |
| Wearable Camera | Provides first-person view (egocentric) images for ground truth or image-based detection. | Autographer camera; AIM-2 camera [55] [53] |
| Ground Truth Annotation Tool | Software and hardware for establishing the reference standard for validation. | Multi-camera video system with annotation software [54] |
| Data Logger / Foot Pedal | Allows participants or researchers to manually mark events for ground truthing. | USB data logger with foot pedal for marking bites [53] |
| Neural Network Classifier | Machine learning algorithm for pattern recognition in sensor and image data. | Neural network for classifying AIM sensor data [54] |
| Object Detection Network | A deep learning model for identifying and localizing objects (e.g., food) in images. | Deep neural network for food/beverage detection in AIM-2 images [53] |
| L 731734 | L 731734, CAS:149786-89-0, MF:C19H38N4O3S, MW:402.6 g/mol | Chemical Reagent |
| LDC1267 | LDC1267, CAS:1361030-48-9, MF:C30H26F2N4O5, MW:560.5 g/mol | Chemical Reagent |
Discussion and Future Directions
Sensor-based technologies have firmly established their potential to overcome the systematic biases of traditional self-report dietary assessment methods. The current generation of devices demonstrates strong performance in detecting the timing and duration of eating occasions [51] [52]. However, as the data shows, key challenges remain. No single device currently meets all feasibility criteria for widespread clinical or research use, with issues around social acceptability, battery life, and robustness in fully free-living conditions being the most significant hurdles [52]. Furthermore, while technologies like the integrated AIM-2 system show improved accuracy by fusing motion and image data, this approach introduces privacy concerns that must be addressed [55] [53].
The future of this field lies in the development of more inconspicuous, multi-modal devices that can not only detect eating but also identify food types and estimate nutrient content. Emerging areas include the use of miniaturized sensors and the application of more sophisticated hierarchical machine learning models to further reduce false positives. As these technologies evolve and validation in large, diverse free-living populations continues, they are poised to become an indispensable tool for generating high-quality, objective dietary data in scientific research and clinical trials [51] [52].
Traditional dietary assessment in clinical and research settings has predominantly relied on tools like 24-hour dietary recalls, Food Frequency Questionnaires (FFQs), and diet histories [56]. These methods require participants to retrospectively summarize their eating habits over periods ranging from a single day to several months or even a year. However, a substantial body of evidence indicates that retrospective self-reporting is inherently vulnerable to numerous cognitive biases, including recall decay, telescoping, and estimation errors, which challenge the reliability and validity of the collected data [57]. The cumbersome nature of these traditional methods can also lead to participant burden and reduced engagement.
In contrast, Experience Sampling Methodology (ESM) represents a paradigm shift towards real-time, in-the-moment data capture. Also known as Ecological Momentary Assessment (EMA), ESM is a structured diary technique designed to appraise subjective experiences and behaviors as they occur in daily life [58]. By collecting data points multiple times per day within a participant's natural environment, ESM effectively circumvents the limitations of retrospective recall and provides a more dynamic, ecologically valid picture of dietary behavior [57] [59]. This guide objectively compares the performance of ESM against traditional dietary assessment methods, providing researchers with the experimental data and protocols needed to inform their study designs.
Understanding the Methodologies
Traditional Dietary Assessment Methods
Traditional methods are characterized by their retrospective nature and are typically administered at a single time point or infrequently.
- 24-Hour Dietary Recall: A structured interview where a participant is asked to recall all food and beverages consumed in the preceding 24 hours. While detailed, it is susceptible to under-reporting and misestimation of portion sizes [56] [5].
- Food Frequency Questionnaire (FFQ): A fixed-list questionnaire that asks respondents to report their usual frequency of consumption for each food item over a specified period (e.g., the past year). Its reliance on long-term memory makes it highly vulnerable to recall bias and heuristic processing [57].
- Diet History: A comprehensive, interviewer-led method that seeks to derive a detailed profile of an individual's habitual diet. Despite its depth, its validity can be compromised by the same cognitive burdens as other retrospective methods [56].
Experience Sampling Methodology (ESM)
ESM is an idiographic approach that focuses on rich, longitudinal data collection from individuals in their natural habitats [57]. Its core principles are:
- Collection in Real-World Environments: Data is gathered as participants go about their daily lives, increasing ecological validity [59].
- Focus on Current or Very Recent States: Assessments target the immediate moment, minimizing the cognitive burden of complex recall operations [57].
- Multiple Assessments Over Time: Data is collected intensively (e.g., several times per day) over a period of days or weeks, capturing variability and patterns [58] [60].
- Flexible Sampling Schedules: Prompts can be signal-contingent (random), interval-contingent (fixed intervals), or event-contingent (triggered by a specific event like eating or drinking) [60].
The following workflow illustrates a typical ESM study design, from protocol configuration to data analysis.
Head-to-Head Comparison: ESM vs. Traditional Methods
Quantitative Comparison of Key Metrics
The superiority of ESM is demonstrated across several key performance metrics, as summarized in the table below.
Table 1: Performance comparison of ESM against traditional dietary assessment methods.
| Metric | Traditional Methods (e.g., 24-hr Recall, FFQ) | Experience Sampling (ESM) | Supporting Experimental Data & Context |
|---|---|---|---|
| Recall Bias | High. Relies on long-term memory, leading to significant under-/over-reporting [57]. | Low. Captures experiences in the moment, drastically reducing memory reliance [59]. | Studies show marked discrepancies between retrospective reports and real-time data on mood, symptoms, and behavior [57]. |
| Ecological Validity | Limited. Abstracted from the context in which behavior occurs [57]. | High. Data is collected in the participant's natural environment as events unfold [58] [59]. | ESM assesses behavior embedded in normal daily life, capturing the influence of real-world contexts [58]. |
| Measurement Consistency | Single or sparse time points, providing a static snapshot [56]. | High. Repeated measures over time control for day-to-day variability [59]. | One ESM protocol (10 assessments/day for 6 days) yields 60 data points per variable, enabling robust within-person analysis [58]. |
| Participant Compliance & Data Accuracy | Variable; paper diaries are vulnerable to back-filling [57]. | High with electronic tools. Time-stamping prevents back-filling. Compliance often >85% [57]. | A 21-day ESM study found signal-contingent random sampling achieved a 76.4% response rate, with high accuracy verified against objective ground truth [60]. |
| Ability to Capture Context | Poor. Rarely inquires about the situational context of consumption [57]. | Excellent. Can sample environment (location, time, social context) alongside behavior [57] [58]. | ESM can link dietary intake to contextual factors like stress, location, or social setting, revealing triggers and patterns [57]. |
Experimental Protocols in ESM Research
To ensure the collection of high-quality, reliable data, ESM studies require carefully designed protocols. Below is a detailed methodology for a typical ESM study investigating dietary behaviors.
A Typical ESM/EMA Protocol for Dietary Assessment
1. Study Design and Sampling Schedule:
- Design Type: Prospective, longitudinal observational study.
- Sampling Method: A signal-contingent (random) schedule is often preferred to avoid anticipation and obtain a representative sample of the day. Notifications are typically sent 5-10 times per day at random intervals within the participant's waking hours [58] [60].
- Study Duration: Commonly ranges from 5 to 14 days to capture both weekday and weekend variations [58].
2. Questionnaire Design:
- The questionnaire must be brief, requiring less than 2 minutes to complete to ensure high compliance and minimize participant burden [58].
- Core Items:
- Current Activity: "What are you doing?" (e.g., working, eating, commuting).
- Social Context: "Who are you with?" (e.g., alone, friends, family).
- Food/Drink Consumption: "Since the last prompt, have you consumed any food or drinks?" If yes, "What did you consume?" (open-ended or checklist).
- Contextual Factors: Location, perceived stress level, or mood states can be included using Likert scales [58].
3. Technology and Data Collection:
- Device: Use electronic diaries (e-diaries) or dedicated smartphone applications (e.g., ExpiWell, PsyMate) [57] [59]. These devices time-stamp each entry, preventing back-filling and ensuring data integrity.
- Procedure: Upon receiving a prompt, the participant opens the app and completes the short questionnaire. Data is transmitted securely to a server in real-time or stored on the device until a connection is available.
4. Participant Training and Engagement:
- Participants receive comprehensive training on the device and protocol.
- Researchers emphasize the importance of responding promptly to prompts and provide a contact for technical support.
Experimental Data on Scheduling Contingencies
The choice of sampling schedule can significantly impact response rates and data accuracy. A rigorous 21-day field study with 20 participants compared three ESM contingency strategies using mobile instrumentation [60].
Table 2: Impact of ESM scheduling contingency on response rate and accuracy [60].
| Contingency Type | Description | Average Response Rate | Key Findings on Accuracy & Perception |
|---|---|---|---|
| Signal-Contingent (Random) | Notifications randomized throughout the day. | 76.4% | High recall accuracy. Perceived as moderately interruptive. |
| Interval-Contingent (Fixed) | Notifications at fixed, predictable intervals. | 68.5% | Lower accuracy due to potential "hoarding" of responses. Perceived as less interruptive. |
| Event-Contingent (Smartphone Unlock) | Notification triggered by a specific event (phone unlock). | 91.7% | Highest absolute number of correct responses due to high response rate. Lower participant strain. |
The study concluded that while event-contingent sampling (using smartphone unlocks as a trigger) yielded the highest response rate and was perceived as less burdensome, the choice of schedule should align with the research question [60]. The logical relationship and outcomes of these different scheduling strategies are visualized below.
The Researcher's Toolkit for ESM
Implementing a robust ESM study requires a suite of technological and methodological "reagents." The following table details essential components and their functions.
Table 3: Essential "Research Reagent Solutions" for ESM studies.
| Tool Category | Specific Solution / Platform | Primary Function |
|---|---|---|
| Data Collection Platforms | ExpiWell, PsyMate, LifeData, invivodata | Provides the software infrastructure for designing questionnaires, deploying prompts to participants' smartphones, and collecting time-stamped data [58] [59]. |
| Sampling Schedules | Signal-contingent, Interval-contingent, Event-contingent algorithms | Defines the timing and logic of prompts, crucial for capturing representative data and managing participant burden [60]. |
| Statistical Analysis Software | R, Python, Mplus, HLM | Specialized software capable of handling multilevel modeling (MLM) to account for nested data (repeated measures within individuals) [61]. |
| Compliance Monitoring | Automated time-stamping, response rate dashboards | Tracks participant adherence to the protocol in real-time, allowing for proactive support and ensuring data quality [57] [60]. |
| Lornoxicam | Lornoxicam | High-purity Lornoxicam, a potent NSAID for research. Explore its COX inhibition mechanism. For Research Use Only. Not for human or veterinary use. |
| MK-8876 | MK-8876, CAS:1426960-33-9, MF:C32H24F2N4O5S, MW:614.6 g/mol | Chemical Reagent |
The evidence clearly demonstrates that Experience Sampling Methodology offers a superior approach to capturing dynamic behaviors like dietary intake compared to traditional retrospective methods. Its key advantages—reduced recall bias, high ecological validity, and the ability to model within-person processes and contextual influences—make it an indispensable tool for modern clinical and translational research [57] [58] [59].
While ESM introduces complexities in study design and data analysis, particularly with multilevel modeling, technological platforms and statistical packages have made it increasingly accessible [61]. For researchers and drug development professionals seeking to understand the real-world, moment-to-day dynamics of dietary behavior and its links to health outcomes, ESM provides the rigorous, real-time data capture necessary to advance the field beyond the limitations of the past.
Addressing Systematic Error: Strategies to Mitigate Bias and Optimize Data Collection
Accurate dietary assessment is a cornerstone of nutritional epidemiology, essential for understanding the links between diet and chronic diseases. However, the pervasive challenge of energy intake (EI) misestimation systematically undermines data integrity, potentially obscuring true diet-disease relationships and compromising public health recommendations. Underreporting—where individuals report consuming less food than they actually do—represents the most frequent and significant form of this measurement error [19]. A comprehensive systematic review reveals that the majority of validation studies report significant underreporting when comparing self-reported EI to total energy expenditure (TEE) measured by the doubly labeled water (DLW) method, considered the gold standard for validation [19]. The scale of this problem is substantial; recent data from the UK National Diet and Nutrition Survey (2008-2015) indicates that EI from self-reported dietary data was underestimated by 27% on average when compared against DLW measurements [62]. This systematic error varies across populations but presents a fundamental validity crisis for self-report dietary methods, necessitating a critical comparison of traditional subjective tools against emerging objective methodologies.
Comparative Analysis of Dietary Assessment Methods
Dietary assessment methods span a spectrum from traditional subjective recalls to objective biomarker-based measures, each with distinct mechanisms, strengths, and vulnerability to underreporting.
Traditional Subjective Methods
24-Hour Dietary Recalls (24HR): This interviewer-administered method collects detailed information about all foods and beverages consumed in the preceding 24 hours. While it provides rich dietary detail and reduces participant burden compared to records, it relies heavily on participant memory and interviewer skill, making it susceptible to recall bias [63]. Validation studies show 24HRs typically demonstrate less variation and degree of underreporting compared to Food Frequency Questionnaires (FFQs), though significant under-reporting remains common [19].
Food Frequency Questionnaires (FFQs): These self-administered tools assess habitual intake over extended periods (typically months or a year) using a predefined food list with frequency response categories. FFQs are cost-effective for large-scale epidemiology but suffer from closed-ended format limitations, requiring careful population-specific adaptation [63]. They demonstrate substantial vulnerability to underreporting due to their dependence on long-term memory and conceptualization of usual intake.
Food Records/Diaries: Participants record all foods and beverages as consumed over multiple days, typically with detailed portion size information. This prospective method minimizes recall bias but introduces high participant burden, which can lead to reactivity (altered eating behavior) and non-compliance [63]. The significant effort required makes sustained underreporting a particular concern with this method.
Objective Reference Methods
Doubly Labeled Water (DLW): This biomarker method measures carbon dioxide production to calculate TEE in free-living individuals over 1-2 weeks. With accuracy to 1% and precision of 5-8%, DLW provides an objective measure against which self-reported EI can be validated, assuming weight stability [19] [64]. Its independence from self-report error makes it the criterion standard for EI validation studies, though high cost and technical requirements limit widespread use [19].
Energy Intake from Energy Balance Principle: A novel approach calculates measured EI (mEI) by combining DLW-measured TEE with changes in body energy stores (ΔES) derived from precise body composition measurements [65]. This method accounts for periods of weight change rather than assuming energy balance, potentially offering a more direct and accurate comparison for self-reported EI validation.
Table 1: Characteristics and Underreporting Vulnerabilities of Major Dietary Assessment Methods
| Assessment Method | Data Collection Approach | Time Frame | Primary Strengths | Vulnerability to Underreporting |
|---|---|---|---|---|
| 24-Hour Recall | Interviewer-administered retrospective recall | Previous 24 hours | Detailed intake data; relatively low participant burden | Moderate; relies on memory and portion size estimation |
| Food Frequency Questionnaire | Self-administered frequency responses | Months to 1 year | Cost-effective for large studies; captures habitual intake | High; depends on long-term memory and food list completeness |
| Food Record/Diary | Prospective self-recording | Multiple days (typically 3-7) | Minimizes recall bias; detailed portion data | High; significant participant burden leads to reactivity and non-compliance |
| Doubly Labeled Water | Biological sample (urine) analysis | 7-14 days | Gold standard objective measure; minimal participant burden | Not applicable (reference method) |
| Energy Balance Method | Combines DLW with body composition | 7-14 days | Accounts for weight change; direct EI comparison | Not applicable (reference method) |
Quantitative Evidence of Underreporting Magnitude
Systematic validation studies reveal consistent and substantial underreporting across populations and methodologies. The recent analysis of UK NDNS data demonstrated not only significant average underreporting (27%) but also identified key demographic predictors: higher BMI was associated with increased underreporting (-0.02 ratio units per kg/m²), as were female sex (mean difference: -173 kcal) and older age (-8.4 kcal/year) [62]. This demographic patterning indicates that underreporting is not random measurement error but a systematic bias that disproportionately affects specific population subgroups.
A 2025 methodological comparison study further quantified misreporting prevalence using different identification methods. When applying the traditional ratio of reported EI to measured EI (rEI:mEE), 50% of recalls were categorized as under-reported, 40.3% as plausible, and 10.2% as over-reported. However, a novel method using the ratio of reported EI to measured EI (rEI:mEI) that accounts for energy balance changes identified a different distribution: 50% under-reported, 26.3% plausible, and 23.7% over-reported [65]. This discrepancy highlights how methodological choices in identifying misreporting can significantly impact prevalence estimates and subsequent data interpretation.
Table 2: Underreporting Magnitude Across Different Populations and Methods
| Study/Data Source | Population | Assessment Method | Reference Method | Underreporting Magnitude |
|---|---|---|---|---|
| UK NDNS (2008-2015) [62] | 770 UK adults | Diet diaries (≥3 days) | Doubly labeled water | Average 27% underestimation |
| Systematic Review [19] | 6,298 adults across 59 studies | Various self-report methods | Doubly labeled water | Widespread significant underreporting (P < 0.05); highly variable |
| NY-TREAT Study [65] | Adults aged 50-75 with overweight/obesity | 3-6 non-consecutive day recalls | Energy balance method | 50% of participants under-reported |
Experimental Protocols for Underreporting Detection
Doubly Labeled Water Validation Protocol
The DLW method provides the foundational protocol for objective EI validation [19]:
Dose Administration: Participants consume an oral dose of water enriched with stable isotopes deuterium (²H) and oxygen-18 (¹â¸O), with the dose determined by body weight using standardized equations.
Urine Sample Collection: Baseline urine samples are collected pre-dose, followed by post-dose samples at 3-4 hours and again at the end of the measurement period (typically 12 days using the two-point protocol).
Isotope Analysis: Urine samples are analyzed using isotope ratio mass spectrometry to measure isotope elimination rates.
Energy Expenditure Calculation: The difference in elimination rates between ¹â¸O and ²H is used to calculate carbon dioxide production rate, which is then converted to TEE using the Weir equation [65].
Comparison with Self-Report: Self-reported EI is collected during the same period using the method under investigation (e.g., 24HR, food records) and compared to TEE assuming weight stability.
Energy Balance Method Protocol
A novel approach addresses the energy balance assumption limitation [65]:
Anthropometric Measurements: Body weight is measured to the nearest 0.1 kg using calibrated scales at the beginning and end of the assessment period.
Body Composition Analysis: Quantitative magnetic resonance (QMR) or other precise methods measure fat mass (FM) and fat-free mass (FFM) at baseline and follow-up, with participants fasting for 12 hours before each measurement.
Energy Expenditure Measurement: TEE is measured using the standard DLW protocol as described above.
Energy Store Change Calculation: ΔES is calculated from changes in FM and FFM using established energy equivalence constants (9,450 kcal/kg for fat, 1,860 kcal/kg for fat-free tissue).
Measured EI Calculation: mEI = TEE + ΔES, providing a biomarker-based EI estimate that accounts for weight change.
Plausibility Assessment: Reported EI (rEI) is compared to mEI using ratio methods, with cut-offs determined by within-subject errors in both measures.
Diagram 1: Experimental workflow for dietary underreporting detection (Width: 760px)
Factors Influencing Underreporting and Methodological Considerations
Demographic and Anthropometric Determinants
Research consistently identifies specific factors that predispose to underreporting. In the UK NDNS analysis, body mass index showed a significant inverse relationship with reporting accuracy (-0.02 ratio units per kg/m²), indicating that individuals with higher BMI tend to underreport more substantially [62]. This finding aligns with broader evidence patterns and suggests both psychological (social desirability) and practical (greater difficulty estimating larger portions) mechanisms. Sex differences are equally robust, with females underreporting more than males (mean difference: -173 kcal), while increasing age also correlates with greater underreporting (-8.4 kcal/year) [62]. These demographic patterns highlight that underreporting is not uniform across populations but represents a systematic bias that must be accounted for in study design and analysis.
Methodological and Behavioral Factors
The number of assessment days significantly impacts reliability. Recent research using AI-assisted dietary tracking indicates that most macronutrients can be reliably estimated (r = 0.8) with 2-3 days of data, while micronutrients and specific food groups generally require 3-4 days [66]. Importantly, day-of-week effects significantly influence intake patterns, with higher energy, carbohydrate, and alcohol consumption on weekends, particularly among younger participants and those with higher BMI [66]. This supports recommendations to include both weekdays and weekends in assessment protocols. Furthermore, assessment reactivity bias—where the act of recording influences dietary behavior—represents an additional methodological challenge, though its magnitude relative to underreporting is less well quantified [3].
Diagram 2: Key determinants of dietary underreporting (Width: 760px)
Emerging Approaches and Research Reagent Solutions
Technological Innovations
Novel digital tools are emerging to address traditional methodological limitations. The Traqq app utilizes repeated short recalls (2-hour and 4-hour recalls) rather than traditional 24-hour recalls to reduce memory burden and potentially enhance accuracy [3]. This approach leverages ecological momentary assessment principles to capture intake closer to consumption time. Similarly, AI-assisted tools like the MyFoodRepo app incorporate image recognition, barcode scanning, and machine learning classification to automate food identification and portion size estimation, potentially reducing user burden and assessment reactivity [66]. These technological solutions aim to maintain the detailed consumption data of traditional methods while minimizing the cognitive demands that contribute to underreporting.
Methodological Paradigms
The Fixed-Quality Variable-Type (FQVT) dietary intervention represents a conceptual shift that standardizes diet quality using objective measures like the Healthy Eating Index while allowing flexibility in diet types to accommodate cultural and individual preferences [8]. By focusing on diet quality rather than prescribed patterns, this approach may reduce social desirability bias and improve adherence and reporting accuracy in intervention studies. Additionally, statistical approaches that account for within- and between-subject variability continue to evolve, with methods like the coefficient of variation and intraclass correlation coefficient analysis helping determine optimal assessment days for different nutrients and food groups [66].
The Researcher's Toolkit: Essential Reagent Solutions
Table 3: Key Research Reagents and Methodological Solutions for Dietary Assessment Validation
| Tool/Solution | Category | Primary Function | Key Features/Applications |
|---|---|---|---|
| Doubly Labeled Water (DLW) | Biomarker | Measures total energy expenditure in free-living individuals | Gold standard validation; requires isotope ratio mass spectrometry |
| Quantitative Magnetic Resonance (QMR) | Body Composition | Precisely measures fat and fat-free mass changes | High precision (<0.5% CV for fat mass); used in energy balance method |
| Healthy Eating Index (HEI) | Diet Quality Metric | Standardized measure of overall diet quality | Objective quality benchmark for FQVT interventions; enables cross-diet pattern comparisons |
| Automated Multiple Pass Method (AMPM) | Interview Protocol | Standardized 24-hour recall administration | Reduces interviewer bias; used in NHANES |
| MyFoodRepo/Open FoodRepo | Digital Food Database | Comprehensive nutritional database for digitally logged foods | Integrates with AI-assisted tracking; enables automated nutrient calculation |
| Statistical Methods for Usual Intake | Analytical Approach | Estimates long-term intake from short-term measurements | Accounts for within-/between-person variation; essential for population estimates |
| MMG-0358 | 4-Chloro-2-(1H-1,2,3-triazol-4-yl)phenol|RUO | High-purity 4-chloro-2-(1H-1,2,3-triazol-4-yl)phenol for research. Explore its potential as a versatile bi-functional building block in medicinal chemistry. For Research Use Only. Not for human or veterinary use. | Bench Chemicals |
| Edelinontrine | Bench Chemicals |
Confronting the pervasive challenge of energy intake misestimation requires acknowledging the fundamental limitations of traditional self-report methods while strategically employing objective biomarkers for validation and calibration. The evidence consistently demonstrates that underreporting is not random error but systematic bias influenced by demographic, anthropometric, and methodological factors. Researchers must carefully select assessment methods based on study objectives, recognizing that each approach involves trade-offs between precision, participant burden, cost, and potential biases.
Moving forward, the integration of objective biomarker validation with traditional methods remains essential for quantifying and correcting systematic reporting errors. Emerging technologies offering reduced participant burden and enhanced objectivity present promising avenues, though they require further validation against criterion standards like DLW. Ultimately, advancing the field requires greater methodological transparency, standardized reporting of validation metrics, and thoughtful application of statistical corrections that account for the systematic nature of dietary misreporting across diverse populations.
Accurate dietary assessment is fundamental to public health surveillance, nutritional epidemiology, and clinical research, yet obtaining precise measurements presents a persistent scientific challenge [67]. Self-reported dietary data, collected through methods such as 24-hour recalls, food frequency questionnaires (FFQs), and food records, are subject to significant measurement errors that can compromise the validity of diet-health relationship studies and nutritional guidelines [68] [69]. These errors are not random; they are systematically influenced by participant characteristics including body mass index (BMI), age, and health status. Understanding these influences is crucial for interpreting nutritional science and developing improved assessment methodologies that bridge the gap between traditional self-reported measures and emerging objective biomarkers [67].
The fundamental issue lies in the phenomenon of misreporting, predominantly under-reporting of energy intake, which distorts the true picture of dietary consumption [69]. As research reveals, "BMI was the only consistent determinant of misreporting" across multiple dietary assessment methods [69]. This article provides a comprehensive comparison of how key participant factors—BMI, age, and health status—systematically influence the accuracy of dietary reporting, with implications for research design and data interpretation in nutritional science and drug development.
Quantitative Comparison of Participant Factors Across Assessment Methods
The following tables synthesize empirical findings from multiple validation studies that utilized objective biomarkers to quantify reporting accuracy across different participant factors and assessment methodologies.
Table 1: Impact of BMI on Energy Intake Misreporting Across Dietary Assessment Methods
| Assessment Method | Population | BMI Effect on Energy Reporting | Magnitude of Under-Reporting | Study Reference |
|---|---|---|---|---|
| Diet History Questionnaire (DHQ) | Japanese with Type 2 Diabetes (n=59) | Significant negative association with reporting accuracy | 12.5% lower in men, 14.6% lower in women vs. DR | [68] |
| Image-Based Mobile Food Record | Adults with BMI 25-40 kg/m² (n=155) | Higher BMI associated with lower plausible intake likelihood (OR=0.81) | Mean EI was 72% of estimated energy expenditure | [70] |
| Combined Methods Analysis | Dutch Adults (n=197) | Consistent association with under-reporting across DP, 24hR, and FFQ | Significant for energy and protein across all methods | [69] |
Table 2: Impact of Age and Sex on Nutrient Reporting Accuracy
| Factor | Assessment Method | Effect on Reporting Accuracy | Nutrients Affected | Study Reference |
|---|---|---|---|---|
| Older Age (Women) | Diet History Questionnaire | Significant positive association with energy reporting | Energy intake | [68] |
| Older Age | 24hR and FFQ | Associated with under-reporting | Potassium intake | [69] |
| Male Sex | Duplicate Portion Method | Tendency for under-reporting | Protein intake | [69] |
| Social Approval Need | Image-Based Food Record | Lower likelihood of plausible reports (OR=0.31) | Energy intake | [70] |
Table 3: Impact of Health Status on Dietary Misreporting
| Health Status | Assessment Method | Reporting Accuracy Findings | Comparative Context | Study Reference |
|---|---|---|---|---|
| Type 2 Diabetes | Diet History Questionnaire vs. Dietary Record | Under-reporting associated with obesity and younger age in women | Similar under-reporting patterns to general population | [68] |
| Eating Disorders | Diet History vs. Biomarkers | Moderate-good agreement for specific nutrients (e.g., iron) | Supplement use significantly affects accuracy | [71] |
| History of Weight Loss | Image-Based Food Record | Associated with reactive reporting (OR=3.4) | Behavioral response to measurement | [70] |
Experimental Protocols for Dietary Assessment Validation
Biomarker-Validated Methodology for Misreporting Assessment
The most robust studies investigating dietary misreporting employ recovery biomarkers as objective reference measures to quantify the accuracy of self-reported intake [69]. These biomarkers provide unbiased estimates that are not subject to the same reporting biases as traditional dietary assessment tools.
Key Experimental Protocol Components:
Doubly Labeled Water (DLW) Method: Considered the gold standard for validating energy intake assessment, the DLW method measures total energy expenditure through the differential elimination of stable isotopes (²Hâ‚‚O and H₂¹â¸O) administered orally [69]. Participants provide urine samples before and after isotope administration (typically at 4-6 timepoints over 11-14 days). Energy intake is assumed to equal total energy expenditure when participants are in energy balance.
24-Hour Urinary Biomarkers: Multiple 24-hour urine collections are used to validate specific nutrient intakes:
- Protein: Assessed using urinary nitrogen excretion via the Kjeldahl technique, with protein intake calculated using the Maroni formula: daily urea nitrogen excretion (g) + 0.031 (g/kg) × body weight (kg) × 6.25 + urinary protein [68] [69].
- Potassium: Measured using ion-selective electrodes in urine, with intake calculated assuming 77% of potassium intake is excreted renally [68] [69].
- Sodium: Similarly measured in urine, assuming 86% of sodium intake is excreted [68].
- Compliance Check: Participants ingest para-aminobenzoic acid (PABA) tablets to verify completeness of urine collections [69].
Dietary Assessment Methods: Participants concurrently complete one or more self-reported dietary assessment methods:
- 24-Hour Dietary Recalls (24hR): Conducted by trained dietitians using standardized multiple-pass protocols [69] [5].
- Food Frequency Questionnaires (FFQ): Self-administered surveys assessing habitual intake over extended periods [69].
- Food Records/Diaries: Participants record all foods and beverages consumed over multiple days, often with weighed portions [68].
- Image-Based Food Records: Participants capture before-and-after images of eating occasions using mobile applications [70].
Statistical Analysis: Misreporting is quantified by comparing self-reported intakes to biomarker values, typically using ratios (self-report/biomarker) and linear regression models to identify determinants of misreporting [68] [69].
Diagram 1: Biomarker Validation Workflow for Dietary Assessment Studies. This flowchart illustrates the experimental protocol for validating self-reported dietary intake against objective biomarkers.
Protocol for Assessing Reactivity Bias in Dietary Reporting
Reactivity bias represents a distinct methodological challenge wherein the act of measurement itself alters participants' normal dietary behaviors [70]. The following protocol specializes in detecting this phenomenon:
Experimental Approach:
Extended Recording Period: Participants maintain dietary records for multiple consecutive days (typically 4-7 days) to observe temporal trends in reported intake [70].
Objective Energy Expenditure Estimation: Researchers estimate energy expenditure using accelerometer data (≥4 days of hip-worn accelerometer data) or other objective measures to establish an energy reference value independent of self-report [70].
Statistical Detection of Reactivity:
- Individual regression slopes are calculated for each participant's energy intake across recording days.
- Negative slopes indicate decreasing intake over time, signifying reactive reporting.
- Participants are categorized as "Reactive Reporters" based on predetermined thresholds (e.g., those showing ≥10% decrease in reported energy intake across the recording period) [70].
Correlate Analysis: Demographic and psychosocial factors associated with reactivity are identified through multivariate regression models [70].
The Scientist's Toolkit: Research Reagents and Materials
Table 4: Essential Research Materials for Dietary Assessment Validation Studies
| Research Tool | Specific Function | Application in Validation Studies |
|---|---|---|
| Doubly Labeled Water (²Hâ‚‚O, H₂¹â¸O) | Gold standard measurement of total energy expenditure in free-living individuals | Objective validation of self-reported energy intake [69] |
| Para-aminobenzoic acid (PABA) Tablets | Compliance marker for complete 24-hour urine collections | Verification of sample validity in urinary biomarker studies [69] |
| Accelerometers (Hip-Worn) | Objective estimation of physical activity energy expenditure | Component of total energy expenditure calculation; reactivity bias detection [70] |
| Three-Factor Eating Questionnaire | Assessment of cognitive restraint, disinhibition, and hunger | Evaluation of psychological determinants of misreporting [70] |
| Social Desirability Scale | Measures tendency to provide socially acceptable responses | Identification of systematic bias in self-reported intake [70] |
| Image-Based Dietary Assessment Apps | Digital capture of food consumption via smartphone images | Reduced participant burden for portion size estimation; reactivity studies [70] |
| 24-Hour Dietary Recall Software | Standardized collection of self-reported intake via multiple-pass method | Traditional dietary assessment compared to biomarkers [69] [5] |
The evidence consistently demonstrates that participant characteristics—particularly elevated BMI—systematically influence the accuracy of self-reported dietary data across multiple assessment methods [68] [69] [70]. This has profound implications for nutritional epidemiology, clinical research, and public health policy.
Critical considerations for researchers and drug development professionals include:
BMI Adjustment: Given that "BMI should always be taken into account when assessing and correcting dietary intake" [69], statistical models should incorporate BMI as a covariate when analyzing self-reported dietary data.
Method Selection: Image-based records and biomarker approaches may reduce but do not eliminate reporting biases associated with participant factors [70].
Study Design: Protocols should anticipate reactivity effects, particularly in studies involving repeated measurements or participants with weight loss histories [70].
Population-Specific Considerations: Researchers must account for how health conditions like diabetes or eating disorders may introduce unique reporting patterns that affect data validity [68] [71].
The ongoing development of novel technologies and biomarkers represents the future of dietary assessment, potentially mitigating the systematic biases associated with traditional self-report methods [67] [72]. Until these methods mature, however, critical interpretation of dietary data must acknowledge and adjust for the substantial influences of BMI, age, and health status on reporting accuracy.
Accurate dietary assessment is fundamental for understanding diet-health relationships, informing public health policies, and developing effective nutritional interventions [66] [11]. However, researchers face a fundamental trade-off: collecting sufficient data to capture habitual intake while minimizing participant burden and associated costs [66] [14]. The inherent day-to-day variability in individual food consumption means that single-day snapshots often poorly represent usual intake, potentially obscuring true diet-disease relationships [66] [73]. This challenge is compounded by systematic measurement errors, including under-reporting—particularly prevalent among individuals with higher BMI and in studies using self-reported methods like food frequency questionnaires (FFQs) and 24-hour recalls [14] [19].
Determining the minimum number of days required for reliable estimation addresses this core challenge directly. Traditional methods like food records typically require 3-4 days to balance comprehensiveness with practical constraints, as longer recording periods often see declining data quality due to participant fatigue [11]. Meanwhile, technological advancements like AI-assisted food tracking apps and wearable sensors offer new opportunities to collect more extensive data with reduced burden, enabling more precise determinations of optimal assessment durations [66] [73]. This analysis compares methodological approaches and provides evidence-based recommendations for designing efficient dietary assessment protocols across research contexts.
Quantitative Analysis: Minimum Days Across Food and Nutrient Types
Evidence from Digital Cohort Studies
Recent large-scale studies leveraging digital technology provide nuanced insights into minimum day requirements. Research analyzing data from 958 participants who tracked meals for 2-4 weeks using the AI-assisted MyFoodRepo app found substantial variation in measurement reliability requirements across different dietary components [66]. The study employed multiple analytical approaches, including Linear Mixed Models (LMM), Intraclass Correlation Coefficient (ICC), and Coefficient of Variation (CV) methods to determine optimal assessment durations [66] [74].
Table 1: Minimum Days Required for Reliable Estimation of Dietary Components (ICC > 0.8)
| Dietary Component | Minimum Days Required | Reliability Level | Special Considerations |
|---|---|---|---|
| Water, Coffee | 1-2 days | High (ICC > 0.9) | Least variable components |
| Total Food Quantity | 1-2 days | High (ICC > 0.9) | By weight |
| Carbohydrates | 2-3 days | Good | Weekend effects significant |
| Protein | 2-3 days | Good | Less variable than fat |
| Fat | 3-4 days | Good | More day-to-day variability |
| Most Micronutrients | 3-4 days | Moderate to Good | Varies by specific nutrient |
| Meat, Vegetables | 3-4 days | Moderate to Good | Food group specific |
| Alcohol | 4+ days | Variable | Highly episodic consumption |
The analysis revealed that including both weekdays and weekends significantly enhanced reliability for most nutrients, with specific day combinations outperforming others [66]. Linear mixed models identified substantial day-of-week effects, with increased energy, carbohydrate, and alcohol consumption on weekends—particularly pronounced among younger participants and those with higher BMI [66]. These findings underscore how demographic factors influence variability and, consequently, measurement requirements.
Comparison with Traditional Method Recommendations
Table 2: Method-Specific Minimum Day Recommendations
| Assessment Method | Recommended Minimum Days | Key Strengths | Primary Limitations |
|---|---|---|---|
| Food Records | 3-4 days [11] | Detailed, prospective data collection | High participant burden; Reactivity bias |
| 24-Hour Recalls | Multiple non-consecutive days [11] | Reduced memory bias; Multiple days feasible | Under-reporting persistent; Interviewer cost |
| Food Frequency Questionnaires (FFQs) | N/A (assesses patterns) | Cost-effective for large samples; Habitual intake | Portion size inaccuracy; Memory dependent |
| Digital Photography Methods | 3-4 days [73] | Reduced burden; Objective record | Food identification challenges; Limited adoption |
| Wearable Camera Systems | Potential for longer assessment [73] | Passive data collection; Comprehensive capture | Privacy concerns; Data processing complexity |
Traditional dietary assessment methods each present distinct advantages and limitations in balancing data precision with practical constraints. Food records, while providing detailed prospective data, typically maintain quality for only 3-4 days before participant burden affects compliance [11]. Twenty-four-hour recalls mitigate some memory issues through interviewer assistance but require multiple administrations (often 2-3 non-consecutive days) to account for daily variation, with costs increasing accordingly [11]. FFQs assess habitual intake patterns over extended periods but suffer from systematic under-reporting and portion size estimation errors [11] [14].
Technological innovations show promise in transforming this balance. Image-based methods like the Remote Food Photography Method (RFPM) have demonstrated accuracy comparable to traditional methods when validated against doubly labeled water, with one study reporting only 3.7% underestimation of energy expenditure [73]. Similarly, data from the "Food & You" digital cohort study indicates that 3-4 days of assessment—ideally non-consecutive and including at least one weekend day—generally suffices for reliable estimation of most nutrients, refining earlier FAO recommendations with more nutrient-specific guidance [66] [74].
Methodological Approaches and Experimental Protocols
Statistical Frameworks for Determining Minimum Days
Researchers employ several statistical approaches to determine optimal assessment durations, each with distinct strengths and applications:
The Coefficient of Variation (CV) Method calculates within- and between-subject variability to estimate the number of days needed to achieve a specified precision level [66]. This approach directly addresses how day-to-day fluctuations impact measurement stability.
Intraclass Correlation Coefficient (ICC) Analysis evaluates the proportion of total variance attributable to between-person differences, with higher values indicating better reliability [66] [75]. The ICC framework facilitates direct comparison of reliability across different dietary components.
Linear Mixed Models (LMM) account for both fixed effects (age, BMI, sex, day of week) and random effects (individual participants), making them particularly suited for analyzing repeated measures data with multiple covariates [66]. These models effectively identify systematic patterns like weekend effects.
Spearman-Brown Prophecy Formula projects how aggregating multiple days of data enhances reliability, though recent evidence suggests it may overestimate actual reliability when compared to long-term test-retest assessments [75].
Determining Minimum Days: Methodological Framework
Experimental Protocol: Digital Dietary Assessment Validation
The "Food & You" study exemplifies a comprehensive approach to validating minimum day requirements using digital methodology [66] [74]:
Participant Recruitment and Characteristics:
- 958 adults from Switzerland with complete data sequences
- Age range: 18-65 years (46% below 35, 18% above 50)
- Balanced sex distribution (55% female, 45% male)
- BMI categories: 68% normal weight (18-25), 29% overweight/obese (≥25)
Data Collection Protocol:
- Tracking period: 2-4 weeks using MyFoodRepo mobile application
- Meal logging methods: 76.1% photographs, 13.3% barcode scanning, 10.6% manual entry
- Food composition mapping to comprehensive nutritional database (2,129 items)
- Standardized portion estimation using WHO MONICA study references
- Rigorous verification by trained annotators with participant clarification
Analytical Framework:
- Focus on longest sequence of ≥7 consecutive days per participant
- Exclusion of days with total energy intake <1,000 kcal
- Assessment of day-of-week patterns using linear mixed models
- Minimum days estimation via ICC and CV methods across all possible day combinations
- Subgroup analyses by age, BMI, sex, and season
This protocol yielded over 315,000 logged meals across 23,335 participant days, providing sufficient statistical power for precise reliability estimates across numerous nutrient and food group categories [66].
Table 3: Research Reagent Solutions for Dietary Assessment Studies
| Tool Category | Specific Examples | Primary Function | Implementation Considerations |
|---|---|---|---|
| Mobile Assessment Platforms | MyFoodRepo app [66] | Digital food logging via image, barcode, manual entry | Requires verification system; Integration with nutrient databases |
| Nutrient Databases | Swiss Food Composition Database, Open Food Facts [66] | Food item to nutrient conversion | Standardization across data sources; Regular updates |
| Statistical Analysis Packages | R, SAS, STATA [76] | Implementation of LMM, ICC, CV methods | Custom programming for dietary specific analyses |
| Biomarker Validation Tools | Doubly Labeled Water (DLW) [19] | Objective energy expenditure measurement | High cost; Specialized laboratory requirements |
| Wearable Sensors | Fitbit Flex, e-Button camera [75] [73] | Passive activity and eating behavior monitoring | Privacy considerations; Data processing challenges |
Integrating Traditional and Objective Methods: A Strategic Framework
Integrating Dietary Assessment Approaches
The convergence of traditional and objective methods represents the most promising path forward for dietary assessment research. Each approach brings complementary strengths: traditional methods offer established protocols and cost-effectiveness for large samples, while objective methods reduce systematic biases and enable longer assessment periods [73] [19]. Strategic integration might include:
- Using short-term digital assessments (3-4 days with smartphone apps or wearable cameras) to quantify within-person variability and correct for systematic errors in FFQ data [66] [73].
- Employing objective biomarkers like doubly labeled water in validation subsamples to calibrate self-reported energy and nutrient intakes, particularly for studies examining energy balance [14] [19].
- Implementing hybrid protocols where participants complete brief digital assessments multiple times throughout a study period, capturing seasonal variations while minimizing burden [77].
This integrated approach acknowledges that no single method perfectly balances precision, burden, and feasibility, but strategically combining methods can optimize this balance for specific research contexts and questions.
Determining minimum days for reliable dietary assessment requires careful consideration of research objectives, target nutrients, and participant characteristics. Based on current evidence:
- For macronutrient assessment, 3-4 non-consecutive days including weekend days typically provides sufficient reliability for most research contexts [66] [74].
- For episodically consumed foods and nutrients (e.g., alcohol, specific vitamins), longer assessment periods or more sophisticated statistical adjustment methods are necessary [11].
- Digital assessment methods can reduce participant burden while maintaining data quality, potentially enabling longer assessment periods than traditional paper-based methods [66] [73].
- Demographic and seasonal factors significantly influence variability patterns, necessitating tailored protocols for specific population subgroups [66].
Future research should prioritize developing standardized protocols for emerging technologies, validating minimum day requirements across diverse populations, and establishing best practices for integrating traditional and objective assessment methods. As technological innovations continue transforming dietary assessment, opportunities will grow to enhance measurement precision while simultaneously reducing participant burden—ultimately strengthening our understanding of diet-health relationships.
Accurate dietary assessment is fundamental to nutrition research, yet self-report methods are notoriously prone to error. A critical, and often overlooked, factor contributing to this measurement error is the temporal pattern of dietary intake. A robust dietary assessment protocol must systematically include both weekdays and weekend days to capture this intra-individual variation and provide a valid estimate of habitual intake.
The Scientific Basis for Weekend and Weekday Sampling
Dietary habits are not static; they fluctuate in predictable patterns throughout the week. Research consistently shows that energy intake, food choices, and meal timing differ significantly between weekdays and weekends [78]. These variations can be attributed to differences in daily routines, work schedules, social activities, and food accessibility.
Failing to account for these patterns introduces substantial measurement error and misclassification of an individual's usual intake. For instance, a protocol that only collects data from Monday to Friday would systematically miss the typically higher energy intake and different food choices often observed on weekends [78]. This can lead to biased results in studies examining the relationship between diet and health outcomes. The principle that behaviors—including dietary intake—are context-dependent is a cornerstone of the Experience Sampling Methodology (ESM), which emphasizes real-time data capture in natural settings to minimize recall bias [78].
Furthermore, the strategic timing of reporting is recognized in other fields. A study on corporate financial disclosures found that managers systematically time their announcements, preferring weekdays for positive news and weekends for negative news, to capitalize on patterns of investor attention [79]. This parallels how dietary reporting can be unconsciously influenced by social desirability and routine, underscoring the need for protocols that capture a complete and representative picture.
Comparative Analysis of Dietary Assessment Methods
The ability of a dietary assessment method to accurately capture weekly variation, including weekday-weekend differences, is a key metric of its robustness. The table below summarizes how major traditional and emerging methods handle this critical aspect.
Table 1: Comparison of Dietary Assessment Methods and Their Capture of Weekly Variation
| Assessment Method | Inherent Protocol Design for Weekday/Weekend Capture | Key Strengths | Key Limitations | Recommendation for Temporal Sampling |
|---|---|---|---|---|
| 24-Hour Dietary Recall (24HR) [63] [11] | High potential. Requires researcher to administer multiple recalls on random, non-consecutive days, explicitly including both weekdays and weekends. | • Open-ended, captures unexpected foods.• Does not alter behavior in advance (if unannounced).• Low literacy requirement when interviewer-administered. | • Relies on memory.• Multiple administrations needed for usual intake.• High cost and interviewer burden for traditional methods. | Optimal: At least 2 recalls, with one scheduled on a weekday and one on a weekend. |
| Food Frequency Questionnaire (FFQ) [63] [11] | Low. Designed to assess "usual" intake over a long period (e.g., months or a year) by its structure, it inherently blends weekday and weekend intake. | • Captures habitual intake.• Cost-effective for large studies.• Low participant burden for the data obtained. | • Uses a closed-ended food list, limiting scope.• Relies on generic memory.• Less precise for absolute intake; better for ranking. | Inherently blended. Not suitable for measuring weekly variation. |
| Food Record / Diary [63] [11] | High potential. Requires participant to record all foods and beverages consumed as they are eaten over a specific period. | • Minimal reliance on memory.• Provides detailed intake data. | • High participant burden can lead to reactivity (changing diet to simplify recording).• Requires high literacy and motivation.• Multiple days are needed. | Optimal: A minimum of 3-4 days, including at least one weekend day. A common protocol is 2 weekdays + 2 weekend days. |
| Experience Sampling Method (ESM) / Ecological Momentary Assessment (EMA) [3] [78] | Very High. Protocol is intentionally designed with intensive, repeated sampling over consecutive days, naturally spanning weekdays and weekends. | • Minimal recall bias through real-time reporting.• Captures context of eating.• High feasibility with mobile technology. | • Can be burdensome due to high frequency.• Requires careful protocol design to optimize compliance. | Inherently covered. Typical protocols involve 7 consecutive days of sampling, providing a complete weekly cycle. |
Experimental Protocols for Valid Dietary Intake Estimation
To ensure that study results reflect true habitual intake rather than artifacts of sampling design, researchers should adopt the following evidence-based protocols.
Protocol for 24-Hour Dietary Recalls (24HR)
The 24HR is a structured method where a participant details all food and beverages consumed in the previous 24 hours.
- Objective: To obtain detailed dietary data for specific days, enabling the calculation of usual intake distributions when multiple recalls are collected.
- Materials & Reagents:
- Automated Self-Administered 24HR (ASA24): A freely available web-based tool developed by the National Cancer Institute that automates the recall process, using the USDA's Automated Multiple-Pass Method to enhance accuracy [80].
- Interviewer Scripts and Probes: Standardized protocols for trained interviewers to help participants accurately remember and describe foods, portions, and preparation methods [63] [11].
- Portion Size Aids: Two-dimensional aids (e.g., photographs, shapes) or digital interfaces that help participants estimate the volume or weight of consumed foods [63].
- Procedure:
- Recruitment & Training: Recruit participants and obtain informed consent. For interviewer-administered recalls, train staff on probing techniques.
- Recall Scheduling: Schedule recalls to be collected on random, non-consecutive days. The schedule must explicitly include at least one weekday and one weekend day per participant.
- Data Collection: Conduct the recall via telephone, in person, or using a self-administered platform like ASA24. The Automated Multiple-Pass Method includes five steps: a quick list, forgotten foods list, time and occasion, detail cycle, and final review [11].
- Data Processing: Convert the reported foods into nutrient intakes using a linked food composition database. For population-level analysis, use statistical methods like the National Cancer Institute method to estimate usual intake and adjust for within-person variation [11].
Protocol for Experience Sampling Methodology (ESM)
ESM for dietary assessment involves prompting participants multiple times per day to report recent intake in near real-time.
- Objective: To assess dietary intake quantitatively or qualitatively with minimal memory-related bias by capturing data close in time to the eating event.
- Materials & Reagents:
- Smartphone Application: A dedicated app (e.g.,
Traqq,m-Path) configured to send prompts (signals) according to a fixed or semi-random schedule [3] [78]. - Customized ESM Questionnaire: A brief questionnaire embedded in the app, using multiple-choice questions adapted from food frequency lists or 24HR items to reduce participant burden [78].
- Smartphone Application: A dedicated app (e.g.,
- Procedure:
- App Configuration: Set the ESM sampling schedule. A common and effective protocol is fixed or semi-random sampling during waking hours (e.g., 8 AM–10 PM) for 7 consecutive days [78].
- Participant Briefing: Instruct participants to download the app and respond to prompts shortly after they are received. Explain the importance of reporting even if they are not 100% certain.
- Data Collection: The app sends prompts throughout the day. Upon receiving a signal, the participant completes the brief questionnaire, which typically uses a 2-hour to 4-hour recall period to report foods and beverages consumed since the last prompt [3] [78].
- Data Integration: Aggregate all data from the multiple daily prompts and consecutive days to reconstruct total daily and weekly intake, automatically capturing weekday and weekend patterns.
The workflow for designing a dietary assessment protocol that adequately accounts for temporal variation, from method selection to data analysis, is summarized below.
Diagram 1: Workflow for a temporally optimized dietary assessment protocol. Methods in green (e.g., FFQ) are less suitable for measuring variation, while red methods require explicit protocol design to capture weekday/weekend differences.
The Researcher's Toolkit: Essential Reagents and Materials
Table 2: Key Research Reagent Solutions for Dietary Assessment
| Tool / Reagent | Function | Example in Practice |
|---|---|---|
| ASA24 (Automated Self-Administered 24HR) | A free, web-based tool that automates the 24-hour recall process for researchers and participants, reducing cost and interviewer burden [80]. | Used in large-scale studies like the NIH-AARP Diet and Health Study to collect multiple 24HRs efficiently. |
| HEI-2020 (Healthy Eating Index) | A validated measure of diet quality that assesses compliance to the Dietary Guidelines for Americans. It can be used to "fix" diet quality in intervention studies across different diet types [26]. | Applied in the Fixed-Quality Variable-Type (FQVT) intervention model to standardize diet quality while allowing for cultural and personal food preferences [26]. |
| ESM Digital Platform (e.g., m-Path, PsyMate) | A configurable software platform to design and deploy Experience Sampling Method studies, including scheduling prompts and designing digital questionnaires [78]. | Used to implement a 7-day dietary ESM study with 5 semi-random prompts per day to assess real-time food intake and context [78]. |
| Standardized Food Composition Database | A comprehensive nutrient database used to convert reported food consumption into energy and nutrient intakes. | The Food and Nutrient Database for Dietary Studies (FNDDS) is used with ASA24; other examples include the USDA National Nutrient Database. |
| Portion Size Estimation Aids | Visual tools to improve the accuracy of reported amounts of food consumed. | Two-dimensional aids (e.g., printed images of plates, glasses, and rulers) or digital interfaces within apps that help users select portion sizes [63]. |
In conclusion, the strategic inclusion of both weekdays and weekend days is not a minor detail but a fundamental requirement for optimizing dietary assessment protocols. Whether employing traditional methods like 24-hour recalls or innovative digital tools like ESM, a sampling frame that encompasses the full weekly cycle is essential for generating accurate, reliable, and meaningful data in nutrition research.
Improving Compliance and Accuracy through User-Friendly Digital Interfaces and Training
Accurate dietary assessment is fundamental for public health surveillance, epidemiology, and nutritional intervention research. However, traditional methods are often plagued by significant limitations, including high participant burden, memory reliance, and measurement errors, which compromise data quality and compliance. This guide objectively compares the performance of emerging digital dietary assessment tools against traditional methods, examining how user-friendly digital interfaces and structured training protocols can enhance data accuracy and participant engagement.
Comparative Performance of Dietary Assessment Methods
The table below summarizes key performance metrics for various dietary assessment methods based on recent validation studies, highlighting the trade-offs between traditional, digital, and objective approaches.
TABLE: Comparative Performance of Dietary Assessment Methods
| Method Category | Specific Tool/Platform | Key Performance Metrics | Compliance & Usability Findings | Primary Limitations |
|---|---|---|---|---|
| Novel Digital (Pattern Recognition) | Diet ID (DQPN) | HEI-2015 correlation with FFQ: r=0.58; with 3-day FR: r=0.56; Test-retest reliability: r=0.70 [2] | Completion time: 1-4 minutes; Ease-of-use and scalability for clinical integration [2] | Relies on pattern matching rather than precise food item recall; Limited granular nutrient data [2] |
| Novel Digital (Repeated Short Recall) | Traqq App (2-hour & 4-hour recalls) | More accurate than traditional 24-hour recalls in adults; Evaluation in adolescents ongoing [3] | Reduced memory reliance via short intervals/reminders; 96% provided dietary data in adolescent study [3] | May be disruptive; Requires multiple daily engagements; App design may not appeal to all demographics [3] |
| AI-Assisted (Image-Based) | MyFoodRepo App | Enabled analysis of >315,000 meals; Data quality comparable to national surveys [66] | High adherence in "Food & You" cohort; 76.1% of entries via photographs [66] | Requires verification by trained annotators; Portion size estimation challenges persist [66] |
| Traditional (Food Frequency Questionnaire) | DHQ III | Often used as a validation benchmark; Captures habitual intake over a long period (e.g., 12 months) [2] [67] | Completion time: 30-60 minutes; High participant burden; Prone to memory and estimation errors [2] [42] | Significant recall bias; Struggles with infrequently consumed foods and portion size accuracy [67] [42] |
| Traditional (Food Record) | ASA24 (Automated 24-h Recall) | Used as a validation benchmark in multiple studies; Provides detailed nutrient intake using FNDDS [2] [1] | Completion time: 15-30 minutes per day; Self-administered but can be burdensome for multiple days [2] | Reactivity bias (participants may change diet); Under-reporting, especially for snacks/unhealthy foods [42] |
Detailed Experimental Protocols
To ensure the validity and reliability of new dietary assessment tools, researchers employ rigorous comparative study designs. The following protocols detail the methodologies used in key cited experiments.
Protocol 1: Validation of a Pattern Recognition Tool (Diet ID)
This study aimed to validate the Diet ID tool (using Diet Quality Photo Navigation - DQPN) against traditional methods [2].
- Study Population & Design: A cohort of 90 US adults was recruited online. The study employed a cross-over design where participants completed multiple assessment tools in a set sequence to minimize attrition and order effects [2].
- Intervention & Comparators: Each participant completed three different dietary assessments:
- DQPN (Test Method): A digital, image-based pattern recognition tool completed in ~1-4 minutes [2].
- Food Record (FR): A 3-day food record (2 weekdays, 1 weekend day) using the ASA24 (Automated Self-Administered 24-hour Dietary Assessment Tool), a web-based tool from the National Cancer Institute [2].
- Food Frequency Questionnaire (FFQ): The Dietary History Questionnaire III (DHQ III), a 135-item web-based questionnaire assessing habitual intake over the past year [2].
- Outcome Measures & Analysis: The primary outcome was overall diet quality, measured by the Healthy Eating Index (HEI)-2015 score. Pearson correlations were generated between the HEI scores from DQPN and the other two instruments. Nutrient and food group intake were also compared. Test-retest reliability for DQPN was assessed with a repeat administration [2].
Protocol 2: Evaluating a Smartphone App for Adolescents (Traqq)
This mixed-methods study holistically evaluated the Traqq app's use of repeated short recalls in a challenging demographic: adolescents [3].
- Study Population: 102 Dutch adolescents aged 12-18 years [3].
- Intervention & Comparators: The study was conducted in three phases:
- Phase 1 (Quantitative): Participants used the Traqq app on 4 random school days over 4 weeks, completing two 2-hour recalls and two 4-hour recalls. The reference methods were two interviewer-administered 24-hour recalls and a food frequency questionnaire [3].
- Phase 2 (Qualitative): A sub-sample of 24 participants participated in semi-structured interviews to explore user experiences in depth [3].
- Phase 3 (Co-creation): Planned sessions with 10-12 adolescents to use insights from phases 1 and 2 to inform app customization [3].
- Outcome Measures: Key metrics included the accuracy of energy, nutrient, and food group intake compared to reference methods, assessed via statistical correlation. Usability was quantitatively evaluated using the System Usability Scale (SUS) and an experience questionnaire [3].
Visualizing Methodological Workflows
The following diagram illustrates the logical pathway and key decision points for selecting a dietary assessment methodology, based on common research goals and constraints identified in the literature.
This table details key tools, databases, and platforms that form the foundation of modern dietary assessment research, as cited in the current literature.
TABLE: Key Research Reagent Solutions for Dietary Assessment
| Resource Name | Type/Function | Research Application |
|---|---|---|
| ASA24 (Automated Self-Administered 24-h Dietary Assessment Tool) | Web-based, self-administered 24-hour dietary recall system [2] [1]. | Freely available to researchers for collecting detailed dietary data; used as a benchmark in validation studies (e.g., Diet ID, Traqq evaluations) [2] [3]. |
| NHANES/WWEIA (National Health and Nutrition Examination Survey/What We Eat in America) | Nationally representative survey of food and beverage consumption in the United States [5]. | Provides gold-standard, population-level dietary intake data; essential for public health surveillance and modeling usual intakes [5]. |
| FNDDS (Food and Nutrient Database for Dietary Studies) | Comprehensive database of energy and nutrient values for ~7,000 foods and beverages [5]. | Used to process food intake data from WWEIA, NHANES, and ASA24 to estimate nutrient intakes; links reported foods to nutritional composition [5] [2]. |
| FPED (Food Pattern Equivalents Database) | Converts food and beverage data from FNDDS into 37 USDA Food Pattern components (e.g., fruit, vegetables, added sugars) [5]. | Used to assess adherence to Dietary Guidelines food group recommendations; analyzes diet quality in relation to federal guidance [5]. |
| Healthy Eating Index (HEI) | A scoring metric that measures diet quality by assessing conformity to the Dietary Guidelines for Americans [2] [1]. | A primary outcome in validation studies (e.g., Diet ID) to evaluate a tool's ability to capture overall diet quality rather than just specific nutrients [2]. |
| MyFoodRepo / Open Food Facts | Open-access databases of branded food products with barcode-linked nutritional information [66]. | Used in AI-assisted apps (e.g., MyFoodRepo) for automatic retrieval of nutrient data when users scan product barcodes [66]. |
The evidence demonstrates a clear trajectory in dietary assessment research toward digital tools that enhance compliance through reduced burden and improve accuracy via innovative data capture. Pattern recognition tools like Diet ID offer rapid, reliable diet quality screening, while apps using repeated short recalls and AI-assisted image analysis show promise for capturing more precise intake data with higher user engagement. The choice between traditional and emerging methods ultimately depends on the specific research question, required data granularity, and target population. However, the integration of user-centered design and training protocols is universally critical for maximizing the value of dietary data in both research and clinical practice.
Benchmarking Accuracy: Validation Frameworks and Comparative Analysis of Dietary Tools
In nutritional epidemiology and health research, accurately quantifying what people eat is a fundamental yet persistent challenge. Self-reported dietary data from tools like food frequency questionnaires (FFQs) and 24-hour recalls are plagued by systematic measurement errors, including recall bias, misestimation of portion sizes, and social desirability bias [81]. These inaccuracies have profound consequences, potentially leading to spurious diet-disease associations and flawed public health recommendations. For decades, the reliance on self-reported data created a paradigm where individuals with obesity appeared to have low energy intakes, erroneously suggesting their weight gain stemmed from low energy expenditure rather than misreporting [81].
The limitations of self-report have spurred the development and use of objective biomarkers to validate dietary assessment methods. Among these, recovery biomarkers represent the highest standard for validation. Unlike concentration biomarkers, which can be influenced by an individual's metabolism and health status, recovery biomarkers are based on the principle of the complete recovery of a nutrient or its metabolite in excreta over a specific time frame, providing a direct, objective measure of intake [82]. This guide focuses on the two most prominent recovery biomarkers: doubly labeled water (DLW) for energy intake and urinary nitrogen for protein intake.
What Are Recovery Biomarkers?
Recovery biomarkers are a specific category of nutritional biomarkers. They are characterized by a known, predictable relationship between dietary intake of a specific nutrient and its appearance in a biological compartment, typically urine. Under controlled conditions, a near-constant and high proportion of the ingested nutrient is recovered, allowing for a quantitative back-calculation of intake. This makes them unparalleled for the objective validation of self-reported dietary data.
Head-to-Head Comparison of the Gold Standards
The following table summarizes the key characteristics, applications, and protocols for DLW and urinary nitrogen.
Table 1: Comprehensive Comparison of Doubly Labeled Water and Urinary Nitrogen as Recovery Biomarkers
| Feature | Doubly Labeled Water (DLW) | Urinary Nitrogen |
|---|---|---|
| Biomarker Category | Recovery Biomarker | Recovery Biomarker |
| Measures | Total Energy Expenditure (TEE) | Total Protein Intake |
| Primary Use | Validation of reported energy intake; calculation of energy requirements | Validation of reported protein intake |
| Key Principle | Difference in elimination rates of hydrogen (²H) and oxygen (¹â¸O) isotopes from body water reflects carbon dioxide production, from which TEE is calculated [83]. | Over 90% of ingested nitrogen is excreted in urine as urea and other metabolites over 24-48 hours. Measured urinary nitrogen is used to calculate protein intake [84]. |
| Biological Sample | Urine, saliva, or blood | Urine |
| Collection Protocol | Baseline sample, oral dose of DLW, then post-dose samples over 1-2 weeks (e.g., days 1, 2, 3, 4, 7, and 14) [83]. | Multiple 24-hour urine collections, ideally over at least 2 non-consecutive days. Completeness of collection must be verified (e.g., using para-aminobenzoic acid - PABA) [84]. |
| Analysis Method | Isotope Ratio Mass Spectrometry | Kjeldahl method or Dumas combustion |
| Major Advantage | Considered the gold standard for measuring TEE in free-living individuals; non-invasive and does not alter routine behavior. | Provides an objective, quantitative measure of protein intake, independent of memory or portion size estimation. |
| Major Limitation | Extremely high cost of isotopes and analysis; requires specialized expertise; does not provide information on diet composition. | Requires highly compliant participants for complete 24-hour urine collections; affected by certain metabolic states (e.g., starvation, burns). |
| Validation Context | Used as reference to detect misreporting in dietary assessment tools. A new predictive equation derived from 6,497 DLW measurements can screen for erroneous self-reported energy intake [81]. | Serves as a reference method in validation studies, such as the ESDAM protocol, which compares self-reported protein intake against urinary nitrogen-derived values [83]. |
Experimental Protocols in Action
To understand how these biomarkers are applied in contemporary research, examining specific study protocols is invaluable. The following diagram illustrates the workflow of a comprehensive validation study that integrates both biomarkers.
Diagram 1: Workflow of a comprehensive dietary assessment validation study, integrating self-reported methods and objective biomarkers like DLW and urinary nitrogen [83] [85].
Detailed Methodology from a Recent Validation Protocol
A 2025 study protocol for validating an Experience Sampling-based Dietary Assessment Method (ESDAM) provides a clear blueprint for using these biomarkers in a research setting [83] [86] [85].
- Study Design: A 4-week prospective observational study. The first two weeks establish baseline data, including three 24-hour dietary recalls (24-HDRs). The final two weeks are the intervention period where the novel method (ESDAM) is tested against biomarkers.
- Biomarker Integration:
- Doubly Labeled Water: Participants ingest a dose of water containing stable isotopes ²Hâ‚‚ and H₂¹â¸O. Urine samples are collected at specified timepoints (e.g., post-dose days 1, 2, 3, 4, 7, and 14). Isotope enrichment in the samples is analyzed by mass spectrometry to calculate Total Energy Expenditure (TEE), which is equated to Energy Intake (EI) under conditions of energy balance [83].
- Urinary Nitrogen: Participants provide 24-hour urine collections. The total nitrogen content is measured, and protein intake is calculated using the formula: Protein (g/day) = (Urinary Nitrogen (g/day) + Fecal Losses + Integumental Losses) × 6.25. Fecal and integumental losses are often estimated as a fixed additional amount (e.g., 2 grams) [84].
- Compliance Monitoring: The ESDAM protocol uses blinded continuous glucose monitoring (CGM) as an objective measure of eating episodes to assess participant compliance with the app-based prompts [83].
- Statistical Validation: Validity is assessed by comparing self-reported intake from ESDAM and 24-HDRs to biomarker values using:
Applications and Limitations in Research & Regulation
Detecting and Correcting for Misreporting
The primary application of DLW and urinary nitrogen is to quantify the extent of misreporting in dietary studies. A landmark 2025 study applied a new DLW-derived predictive equation to two large national surveys (NDNS and NHANES), finding a misreporting rate of 27.4% [81]. The study further revealed that the macronutrient composition of dietary reports was systematically biased as misreporting increased. For instance, as under-reporting worsened, the reported percentage of energy from fat decreased, while the percentage from protein increased, leading to potentially false conclusions about diet-body weight relationships [81].
The Regulatory and Clinical Context
In drug development, biomarkers must undergo a "fit-for-purpose" validation process for regulatory acceptance by bodies like the U.S. Food and Drug Administration (FDA) [87]. This involves defining a Context of Use (COU) and providing analytical and clinical validation. While DLW and urinary nitrogen are established in research, their high cost and complexity limit widespread regulatory use. The FDA's Biomarker Qualification Program (BQP) has qualified only eight biomarkers since 2016, highlighting the high bar for formal acceptance [88].
In clinical practice, DLW remains a research tool. Predictive equations derived from large DLW datasets, like those from the National Academies of Sciences, Engineering, and Medicine (NASEM), are used to estimate energy requirements, though they must be applied with caution at the individual level [89].
Limitations and Complementary Biomarkers
While gold standards, DLW and urinary nitrogen have constraints. They are costly, technically demanding, and do not provide information on food patterns or specific nutrient intakes beyond energy and protein. Researchers often complement them with other biomarkers to build a more complete picture:
- Concentration Biomarkers: Serum carotenoids (for fruit/vegetable intake) and erythrocyte membrane fatty acids (for fatty acid composition) are used as secondary, albeit less direct, validation tools [83] [85].
- Emerging Urinary Metabolites: Systematic reviews are identifying urinary metabolites for broader food groups (e.g., citrus fruits, cruciferous vegetables, whole grains, soy), offering promise for future objective assessment of dietary patterns [82].
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 2: Key Reagents and Materials for Recovery Biomarker Analysis
| Item | Function / Application |
|---|---|
| Doubly Labeled Water (²H₂¹â¸O) | The core reagent for DLW studies. A precisely weighed oral dose is administered to the participant to label the body water pool. |
| Isotope Ratio Mass Spectrometer (IRMS) | The analytical instrument required to measure the minute differences in the ratio of ²H/H and ¹â¸O/¹â¶O in biological samples (urine, saliva) with high precision. |
| Para-Aminobenzoic Acid (PABA) Tablets | Used as a recovery biomarker in itself. Participants take PABA with meals during 24-hour urine collections; urinary PABA levels are measured to verify the completeness of the collection [84]. |
| Laboratory for Urinary Nitrogen Analysis | Facilities equipped to perform high-throughput, accurate nitrogen analysis via the Kjeldahl method or Dumas combustion. |
| Stable Quality Control Samples | Certified reference materials with known isotope ratios or nitrogen content are essential for calibrating equipment and ensuring analytical validity across batches. |
| Healthy Eating Index (HEI) 2020 | A validated metric used in dietary intervention research (like the Fixed-Quality Variable-Type approach) to standardize and objectively measure diet quality, complementing intake data from biomarkers [8]. |
Accurate measurement of dietary intake is a cornerstone of nutritional epidemiology, yet the field has long grappled with a fundamental validity problem. Traditional methods that rely on self-reporting—including 24-hour recalls, food frequency questionnaires (FFQs), and food diaries—are subject to systematic measurement errors that undermine their accuracy [14]. The emergence of objective biomarker-based methods represents a paradigm shift, allowing researchers to quantify this measurement gap and move toward more reliable exposure assessment in diet-health research.
Biomarkers utilize biological measurements to objectively capture nutrient consumption, bypassing the cognitive challenges and biases inherent in self-reporting [90]. This comparative analysis examines the quantitative evidence demonstrating the superiority of biomarker-measured intake over traditional self-reported methods, providing researchers with a framework for selecting appropriate assessment tools based on their specific research objectives.
Quantitative Comparison of Assessment Methods
Magnitude of Misreporting Across Self-Report Instruments
Multiple validation studies against recovery biomarkers have consistently revealed substantial underreporting across all major self-reported dietary assessment methods. The systematic bias varies significantly by instrument type, nutrient, and participant characteristics.
Table 1: Underreporting of Energy and Nutrient Intakes Across Dietary Assessment Methods
| Assessment Method | Energy Underreporting | Protein Underreporting | Population Studied | Reference Biomarker |
|---|---|---|---|---|
| Food Frequency Questionnaire (FFQ) | 29-34% | Not specified | Adults 50-74 years | Doubly Labeled Water [34] |
| 4-Day Food Record (4DFR) | 18-21% | Not specified | Adults 50-74 years | Doubly Labeled Water [34] |
| Automated 24-Hour Recall (ASA24) | 15-17% | Not specified | Adults 50-74 years | Doubly Labeled Water [34] |
| Food Records | 35±20% | More underreported than protein | Overweight adolescents | Doubly Labeled Water [91] |
The data demonstrates that FFQs exhibit the greatest systematic underreporting, likely due to their reliance on long-term memory and portion size estimation over extended periods [34]. More detailed methods like 24-hour recalls and food records perform better but still show significant underreporting, indicating that increased detail alone cannot overcome fundamental reporting biases.
Differential Misreporting by Nutrient Type
The macronutrient composition of foods significantly influences reporting accuracy. Research consistently demonstrates that not all nutrients are underreported equally, with protein showing the least underreporting compared to carbohydrates and fats [14]. This differential misreporting alters the apparent nutritional composition of diets.
Table 2: Nutrient-Specific Reporting Accuracy Compared to Recovery Biomarkers
| Nutrient | Reporting Pattern | Method(s) | Implications |
|---|---|---|---|
| Energy | Systematic underreporting (15-35%) | All self-report methods | Fundamental validity problem for energy balance studies [34] [91] |
| Protein | Least underreported nutrient | Urinary nitrogen biomarker | Possibly related to more equal distribution across meals [14] |
| Potassium | Variable reporting on FFQs | 24-hour urinary excretion | FFQs overestimate potassium density by 26-40% [34] |
| Sodium | Similar density to biomarkers | 24-hour urinary excretion | Absolute intake underreported, but density accurate [34] |
The finding that protein is the least underreported nutrient suggests that protein-containing foods may be more consistently reported, possibly because they often constitute main meal components rather than snacks [14]. This differential reporting macronutrients can substantially distort apparent diet-disease relationships.
Key Experimental Protocols in Biomarker Validation
Doubly Labeled Water Protocol for Energy Intake Validation
The doubly labeled water (DLW) method represents the gold standard for validating self-reported energy intake under conditions of weight stability [14]. The protocol involves administering water containing stable isotopes of hydrogen (²H) and oxygen (¹â¸O) and tracking their elimination kinetics.
Experimental Workflow:
- Baseline sample collection: Urine, blood, or saliva samples before isotope administration
- Isotope administration: Oral dose of ²H₂¹â¸O with precise dosing documentation
- Equilibration period: 4-6 hours for isotope distribution in body water
- Post-dose sampling: Regular biological sample collection over 7-14 days
- Isotope ratio analysis: Mass spectrometry measurement of ²H and ¹â¸O enrichment
- Calculation: Carbon dioxide production rate from difference in elimination kinetics
- Energy expenditure derivation: Using respiratory quotient assumptions [14]
This method provides an objective measure of total energy expenditure with 98-99% accuracy and 7% individual precision, making it an ideal reference for energy intake validation under weight-stable conditions [14].
Recovery Biomarkers for Nutrient Validation
Recovery biomarkers provide objective quantification of specific nutrient intakes through complete collection of biological excretions or using stable isotope tracers.
24-Hour Urinary Collections:
- Nitrogen excretion: Validated biomarker for protein intake assessment [34] [14]
- Sodium excretion: Direct measure of sodium intake [34]
- Potassium excretion: Validated biomarker for potassium intake [34]
Protocol Requirements:
- Complete 24-hour urine collections with volume measurement
- Aliquoting and preservation using acid or refrigeration
- Quality control checks using para-aminobenzoic acid (PABA) tablets to verify completeness
- Laboratory analysis for specific analytes of interest [34]
These recovery biomarkers typically capture 70-90% of actual nutrient intake over the collection period, providing a substantially more objective measure than self-report instruments [14].
Metabolomic Signatures for Dietary Pattern Assessment
Advanced metabolomic approaches now enable the development of poly-metabolite scores for complex dietary exposures like ultra-processed food consumption [23] [24].
Experimental Protocol:
- Study designs: Combine observational and experimental data
- Biospecimen collection: Plasma and urine samples under controlled conditions
- Metabolite profiling: Liquid chromatography-mass spectrometry (LC-MS)
- Machine learning analysis: Identify metabolite patterns predictive of specific dietary exposures
- Score validation: Test in controlled feeding studies and independent populations [23]
This approach has successfully identified hundreds of metabolites correlated with ultra-processed food intake and developed scores that accurately differentiate between highly processed and unprocessed diet phases in controlled trials [24].
Diagram Title: Biomarker Validation Experimental Workflows
The Researcher's Toolkit: Essential Reagents and Materials
Table 3: Key Research Reagents for Biomarker-Based Dietary Validation
| Reagent/Material | Application | Function in Research | Example Use Cases |
|---|---|---|---|
| Doubly Labeled Water (²H₂¹â¸O) | Energy intake validation | Gold standard for measuring total energy expenditure | Obesity research, energy balance studies [14] |
| Para-aminobenzoic acid (PABA) | Urinary recovery validation | Verifies completeness of 24-hour urine collections | Protein, sodium, potassium intake studies [34] |
| Stable isotope tracers | Nutrient metabolism studies | Tracing metabolic fate of specific nutrients | Mineral absorption, protein turnover studies |
| LC-MS instrumentation | Metabolomic biomarker discovery | High-throughput metabolite profiling | Dietary pattern validation, food compound bioactivity [23] [90] |
| Bomb calorimetry | Direct energy measurement | Quantifies gross energy in foods and excreta | Metabolizable energy determination [91] |
| Urinary nitrogen analysis | Protein intake validation | Direct measure of protein intake via nitrogen excretion | Protein requirement studies [14] |
Implications for Research and Clinical Applications
Impact on Diet-Disease Relationship Studies
The systematic measurement error inherent in self-reported dietary data has profound implications for nutritional epidemiology. Underreporting is not random but increases with body mass index (BMI), introducing bias that attenuates diet-disease relationships [14]. This systematic variation means that self-reported energy intake should not be used for studying energy balance in obesity research [14].
The development of objective biomarker-based measures for complex dietary exposures like ultra-processed foods represents a promising advancement for future studies of diet and chronic disease risk [23] [24]. These approaches can reduce reliance on self-report and provide novel insights into biological mechanisms linking diet to health outcomes.
Methodological Recommendations for Researchers
Based on the comparative validity evidence, researchers should consider the following recommendations:
Biomarkers should be incorporated whenever possible for validating self-report instruments or as primary exposure measures in high-precision studies [90]
Multiple automated 24-hour recalls (ASA24) provide the best estimates of absolute dietary intakes when biomarkers are not feasible [34]
Energy adjustment improves estimates for some nutrients (protein, sodium) but not others (potassium) in FFQs [34]
Recognize that all self-reported data contain systematic bias that varies by population subgroup, with greater underreporting among individuals with obesity [14] [91]
Emerging technologies like pattern recognition dietary assessment show promise for rapid diet quality measurement with reasonable correlation with traditional methods (r=0.56-0.58) [2]
The field continues to evolve with innovations like the Fixed-Quality Variable-Type approach that accommodates cultural diversity while maintaining diet quality standards [92], and the ongoing development of additional nutritional biomarkers that will further enhance our ability to objectively assess dietary exposures in research populations.
The accurate assessment of nutrient intake is a cornerstone of nutritional science, epidemiology, and the development of effective dietary interventions. However, the reliability of these assessments varies significantly between macronutrients and micronutrients, and is profoundly influenced by the methodology employed. This guide objectively compares the performance of traditional and novel objective dietary assessment methods, providing researchers with a critical analysis of their reliability for specific nutrient classes. As dietary assessment evolves from memory-dependent recalls to technologically advanced pattern recognition, understanding these nutrient-specific variations in reliability becomes paramount for research design and data interpretation in both academic and clinical settings.
Comparative Reliability of Dietary Assessment Methods
The reliability of nutrient intake data is not uniform across different assessment tools or nutrient types. Performance varies substantially, with method selection significantly influencing the resulting dietary data quality and its applicability for different research objectives.
Correlation Strength by Nutrient Type
A 2023 validation study compared the novel Diet Quality Photo Navigation (DQPN) method against traditional tools like Food Frequency Questionnaires (FFQs) and Food Records (FRs), revealing distinct patterns of correlation strength across nutrient categories [2].
Table 1: Correlation Coefficients (r) for Nutrient Intake Estimates Between DQPN and Traditional Methods
| Nutrient Category | Specific Nutrient/Food Group | DQPN vs. FFQ (r) | DQPN vs. FR (r) |
|---|---|---|---|
| Overall Diet Quality | Healthy Eating Index (HEI) | 0.58* | 0.56* |
| Macronutrients | Total Fat | 0.42* | 0.33 |
| Total Protein | 0.39* | 0.25 | |
| Micronutrients | Dietary Fiber | 0.49* | 0.40* |
| Sodium | 0.37 | 0.29 | |
| Calcium | 0.46* | 0.29 |
*Statistically significant (P < 0.001) [2]
Key findings demonstrate that overall diet quality, as measured by the Healthy Eating Index, can be assessed with moderate to strong reliability (r=0.56-0.58) using the novel DQPN method [2]. For macronutrients, correlations were generally moderate, with total fat showing stronger agreement (r=0.42 vs. FFQ) than total protein [2]. The reliability for micronutrients was more variable, with dietary fiber showing the strongest correlation (r=0.49 vs. FFQ), while sodium estimates correlated poorly between methods [2].
Methodological Comparison and Workflow
Traditional and modern assessment methods differ fundamentally in their approach, implementation, and underlying data processing, leading to variations in their suitability for different nutrient types.
Table 2: Methodological Comparison of Dietary Assessment Tools
| Characteristic | Traditional Food Record (FR) | Food Frequency Questionnaire (FFQ) | Novel DQPN (Pattern Recognition) |
|---|---|---|---|
| Primary Basis | Prospective recording of all foods/beverages consumed | Memory-based recall of past dietary frequency | Pattern recognition of habitual dietary intake |
| Completion Time | 15-30 min per day for multiple days [2] | 30-60 minutes for a full assessment [2] | 1-4 minutes for a single assessment [2] |
| Reference Period | Short-term (typically 3-7 days) | Long-term (typically past year) | Current, habitual diet |
| Key Databases | USDA FNDDS for nutrient conversion [5] [2] | FNDDS & NDSR Food and Nutrient Database [2] | NDSR Food and Nutrient Database [2] |
| Strengths | High detail for short-term intake, useful for macronutrient analysis | Efficient for large-scale epidemiology, captures seasonal variation | Rapid, low participant burden, scalable for clinical screening |
| Limitations | High participant burden, may alter eating behavior | Memory recall bias, portion size estimation error | Less granular nutrient data for some micronutrients |
The following workflow diagram illustrates the fundamental differences in operational approach between these methodological paradigms.
Foundational Concepts and Challenges in Nutrient Assessment
Macronutrients vs. Micronutrients: Fundamental Differences
The core distinction between these nutrient classes directly impacts the reliability of their assessment:
- Macronutrients (Proteins, Carbohydrates, Lipids): Provide energy and structural components, required in large amounts. They serve as sources of energy (carbohydrates and lipids at 4 kcal/g and 9 kcal/g, respectively) or primarily supply amino acids for structural and functional molecules (proteins) [93].
- Micronutrients (Vitamins and Minerals): Required in smaller amounts (mg or μg) for catalytic (enzymes) and regulatory functions. They do not provide energy but are critical for metabolic processes [93].
The Critical Role of Bioavailability
A paramount challenge in micronutrient assessment, largely absent for macronutrients, is bioavailability—the proportion of an ingested nutrient that is absorbed, transported to tissues, and utilized in normal physiological processes [94]. A nutrient's presence in food does not guarantee its systemic availability. Bioavailability is influenced by:
- Food Matrix Effects: Micronutrients may be entrapped in plant cellular structures or bound by antagonists like phytate and fiber, reducing their absorbability [94].
- Nutrient-Nutrient Interactions: Fat enhances absorption of fat-soluble vitamins (A, D, E, K), while vitamin C can improve non-heme iron absorption [94] [93].
- Host Factors: Gut health (e.g., microbiota, mucosal integrity), life stage (e.g., pregnancy), age, and genetic variability significantly impact an individual's ability to absorb and utilize micronutrients [94] [95].
This complexity means that two individuals consuming identical micronutrient amounts may have vastly different nutritional statuses, a critical limitation that simple intake assessment cannot overcome.
Experimental Protocols for Method Validation
Protocol 1: Comparative Validation of Dietary Assessment Tools
This protocol is adapted from a study validating the DQPN method against established tools [2].
Objective: To assess the validity of a novel dietary assessment tool (DQPN) in measuring diet quality, food group, and nutrient intake against traditional methods (FFQ and FR).
Design: Cross-sectional comparative study.
Participants: 90 adult participants recruited via an online research platform, with 58 completing all three assessment methods.
Intervention and Sequence:
- Week 1: Participants complete the DQPN assessment and a 3-day Food Record (FR) using the Automated Self-Administered 24-hour Dietary Assessment Tool (ASA24), capturing 2 weekdays and 1 weekend day.
- Week 2: Participants complete the Dietary History Questionnaire (DHQ) III, a web-based FFQ with 135 food and beverage line items.
- Week 3: Participants repeat the DQPN assessment to evaluate test-retest reliability.
Data Analysis:
- Descriptive statistics generated for diet quality (HEI-2015), food groups, and nutrients from all methods.
- Pearson correlation coefficients calculated between methods for diet quality scores, macro-, and micronutrients.
- Test-retest reliability for DQPN assessed via Pearson correlation between week 1 and week 3 administrations.
Key Validation Metrics: The primary outcome is the correlation coefficient for overall diet quality (HEI-2015). Secondary outcomes include correlation coefficients for specific nutrients and food groups.
Protocol 2: Controlled Feeding and Biomarker Validation
While not directly from the results, this protocol represents the gold-standard approach for validating assessment methods, particularly for micronutrients with available biomarkers.
Objective: To validate self-reported intake of specific nutrients against objective biological markers (biomarkers) in blood or urine.
Design: Controlled feeding study with biomarker analysis.
Participants: A smaller cohort (e.g., n=20-30) in a metabolic ward or highly controlled setting.
Intervention:
- Controlled Diet Period: Participants consume a defined diet for a set period (e.g., 2-4 weeks), with all food prepared and provided by the research facility. The nutrient composition of the diet is precisely known.
- Biosample Collection: Blood and/or urine samples are collected at baseline and the end of the controlled diet period for analysis of specific nutrient biomarkers (e.g., serum 25(OH)D for vitamin D, erythrocyte folate for folate, doubly labeled water for energy expenditure).
- Self-Reported Assessment: At the end of the controlled period, participants complete the dietary assessment method(s) being validated (e.g., FFQ, 24-hour recall).
Data Analysis:
- Compare self-reported nutrient intakes with the known intake values from the controlled diet.
- Correlate self-reported intakes with the corresponding biomarker concentrations in biosamples.
- Calculate recovery biomarkers (e.g., for energy, protein) where possible to quantify reporting error.
Successful dietary assessment research relies on standardized reagents, databases, and platforms. The following table details key resources used in the field.
Table 3: Essential Research Reagent Solutions for Dietary Assessment
| Resource Name | Type | Primary Function | Application Context |
|---|---|---|---|
| ASA24 (Automated Self-Administered 24-h Dietary Assessment Tool) [2] | Software System | Enables automated, self-administered 24-hour dietary recalls and food records. | Traditional, memory-based assessment for detailed short-term intake data. |
| USDA FNDDS (Food and Nutrient Database for Dietary Studies) [5] [2] | Nutrient Database | Provides energy and nutrient values for ~7,000 foods/beverages reported in WWEIA, NHANES. | Converts food intake data into nutrient estimates; used by ASA24 and DHQ III. |
| USDA FPED (Food Pattern Equivalents Database) [5] | Food Pattern Database | Converts FNDDS foods into 37 USDA Food Pattern components (e.g., whole fruit, refined grains). | Assesses adherence to food-based dietary guidelines (e.g., Dietary Guidelines for Americans). |
| DHQ III (Dietary History Questionnaire III) [2] | Assessment Tool | A 135-item food frequency questionnaire to characterize habitual intake over the past year. | Epidemiological research linking long-term diet to health outcomes. |
| NDSR (Nutrition Data System for Research) | Nutrient Database | A comprehensive dietary analysis software and database used for nutrient calculation. | Serves as the nutrient database for DQPN and DHQ III [2]. |
| Healthy Eating Index (HEI) [2] [96] | Diet Quality Metric | A scoring metric that measures alignment with the Dietary Guidelines for Americans. | Provides a standardized measure of overall diet quality for method comparison. |
Analysis of Reliability Challenges and Technological Advances
Conceptual Framework of Nutrient-Specific Reliability
The reliability of nutrient intake data is governed by a complex interaction between the nutrient's properties, the dietary source, and the assessment methodology. The following diagram maps this relationship and its impact on the final data quality.
Emerging Innovations: The Fixed-Quality Variable-Type (FQVT) Approach
A significant paradigm shift is emerging with approaches like the Fixed-Quality Variable-Type (FQVT) dietary intervention. This methodology standardizes diet quality (e.g., using the Healthy Eating Index) while allowing for variation in diet type (e.g., Mediterranean, Vegetarian, Asian) [96]. This is operationally enabled by digital tools like Diet ID, which use pattern recognition to rapidly assess and categorize diet quality. This advancement helps disentangle the effect of overall dietary patterns from specific nutrient composition, potentially offering a more reliable and culturally inclusive framework for linking diet to health outcomes than focusing solely on individual nutrient intake [96].
The reliability of nutrient intake data is inherently nutrient-specific and method-dependent. Macronutrients generally demonstrate higher inter-method reliability, while micronutrient assessment is complicated by bioavailability and database limitations. Traditional methods like FRs and FFQs provide valuable, detailed data but are constrained by participant burden, recall bias, and scalability. Novel pattern recognition tools offer a rapid, scalable alternative for assessing overall diet quality and major food groups, though with potentially less granularity for specific micronutrients.
The choice of assessment method must be aligned with the research question, the nutrients of interest, and the study's logistical constraints. Future directions point toward integrating objective biomarkers, improving food composition databases, and leveraging pattern-based approaches that prioritize diet quality within diverse cultural and personal dietary contexts.
The validation of dietary assessment methods in special populations represents a fundamental challenge in nutrition science, particularly when investigating the complex interplay between eating disorders, obesity, and diabetes. Traditional dietary assessment methods, including food frequency questionnaires (FFQs) and 24-hour recalls (24hRs), face significant limitations in these populations due to factors such as memory-related bias, social desirability bias, and the unique psychological relationships individuals have with food [3]. The co-occurrence of these conditions creates a clinical imperative for more objective assessment approaches. Research demonstrates that eating disorders and disordered eating behaviors are prevalent in diabetes populations, with one study finding that 35% of individuals with diabetes (25% with T1D, 55% with T2D) were at risk for disordered eating behaviors [97]. Similarly, in adults seeking obesity treatment, the pooled prevalence of binge-eating disorder is approximately 14% when assessed by clinical interview [98]. This article provides a comparative analysis of traditional versus emerging objective dietary assessment methodologies within these special populations, examining their respective protocols, applications, and empirical performance data to guide researchers and clinical professionals.
Comparative Performance of Dietary Assessment Methods
Table 1: Comparison of Dietary Assessment Method Performance Across Special Populations
| Assessment Method | Target Population | Key Performance Metrics | Major Limitations | Advantages |
|---|---|---|---|---|
| Traditional 24-hour Recall | Adolescents, T2DM, Obesity | High participant burden; prone to memory-related and social desirability bias [3] | Relies on memory, irregular eating patterns challenge accuracy [3] | Established protocol; allows for detailed nutrient analysis |
| Food Frequency Questionnaire (FFQ) | Adults with obesity, Diabetes | Captures long-term patterns but limited by portion size estimation errors [3] | Fixed food list may not capture disorder-specific behaviors | Efficient for large-scale studies; assesses habitual intake |
| Ecological Momentary Assessment (EMA) / Repeated Short Recalls | Adolescents, Adults with obesity | Potentially more accurate than 24hRs due to reduced memory reliance [3] | Requires technology access; multiple prompts may be intrusive | Near real-time data; reduces memory bias; captures contextual factors |
| Diabetes Eating Problem Survey-Revised (DEPS-R) | T1DM, T2DM on insulin therapy | Identifies DEB risk (35% overall diabetes population) [97] | Condition-specific; not a comprehensive dietary assessment | Validated screening tool; good internal consistency; diabetes-specific |
| Binge Eating Scale (BES) | Obesity, Binge Eating Disorder | Moderate severity: 26%; Severe: 12% in obesity treatment [98] | Self-report only; focuses on specific behavior pattern | Specifically targets binge eating pathology |
Experimental Protocols for Method Validation
Protocol for Digital Dietary Assessment Validation (Traqq App)
A recent mixed-methods study established a comprehensive protocol for validating a smartphone-based dietary assessment application in adolescents, a population with relevance to eating disorder research. The methodology employed a multi-phase approach to evaluate accuracy, usability, and user experience [3].
Phase 1: Quantitative Evaluation
- Participants downloaded the Traqq app and completed a demographic questionnaire
- Dietary intake was assessed via the app on 4 random non-consecutive days over 4 weeks
- Protocol included two 2-hour recall days and two 4-hour recall days
- Reference methods included two interviewer-administered 24hRs and an extensive FFQ
- Usability was evaluated using the System Usability Scale and an experience questionnaire
- Sample: 102 adolescents (mean age 15±2 years; 63% girls; mean BMI 19.9±3 kg/m²) [3]
Phase 2: Qualitative Evaluation
- Semistructured interviews were conducted with a subsample of 24 adolescents
- Explored user experiences and perceptions of the digital assessment tool
- Provided insights for technology refinement [3]
Phase 3: Co-creation Sessions
- Planned with 10-12 adolescents to inform app customization
- Aims to establish requirements for dietary assessment apps specifically tailored to adolescent needs [3]
This validation protocol addresses multiple dimensions of method performance, including accuracy compared to traditional methods, usability metrics, and qualitative user experience data, providing a comprehensive framework for evaluating digital dietary assessment tools.
Protocol for Eating Disorder Screening in Diabetes Populations
A cross-sectional study designed to assess diabetes-specific eating disorder risk employed the following methodology [97]:
- Participants: 120 individuals (80 with T1D, 40 with T2D) on intensive insulin therapy aged 18-65 years
- Assessment Tool: Diabetes Eating Problem Survey-Revised (DEPS-R) electronically delivered to participants
- Risk Threshold: DEPS-R score ≥20 indicated disordered eating behavior risk
- Clinical Data Collection: HbA1c, BMI, diabetes duration, insulin regimen, hypoglycemia frequency
- Statistical Analysis: Comparisons between risk and non-risk groups; correlations between DEBS risk and clinical parameters
This protocol demonstrates a standardized approach for identifying eating disorder risk in diabetes populations, with particular relevance for individuals requiring insulin therapy who may engage in maladaptive behaviors such as insulin restriction for weight control.
Signaling Pathways and Methodological Workflows
Dietary Assessment Validation Workflow
Eating Disorder-Diabetes Comorbidity Assessment
Research Reagent Solutions for Dietary Assessment and Eating Disorder Research
Table 2: Essential Research Tools and Assessment Methods
| Tool/Instrument | Primary Application | Key Features | Validation Status |
|---|---|---|---|
| Diabetes Eating Problem Survey-Revised (DEPS-R) | Eating disorder screening in diabetes | 16-item scale; score ≥20 indicates DEB risk; assesses insulin misuse, weight control behaviors | Validated in T1D and T2D; good internal consistency; available in multiple languages [97] |
| Eating Disorder Examination Questionnaire (EDE-Q) | General eating disorder pathology | 28-item self-report; assesses restraint, eating concern, weight concern, shape concern | Gold standard self-report measure; used in weight loss intervention studies [99] [100] |
| Binge Eating Scale (BES) | Binge eating severity in obesity | 16-item self-report; identifies moderate (26%) and severe (12%) binge eating in treatment-seeking adults | Widely used in obesity research; correlates with clinical interviews [98] |
| Traqq Mobile Application | Digital dietary assessment | Repeated short recalls (2-hour and 4-hour); reduces memory bias through ecological momentary assessment | Validated against 24hRs in adults; undergoing validation in adolescents [3] |
| Healthy Eating Index (HEI-2020) | Diet quality measurement | 100-point scale; assesses compliance with Dietary Guidelines; used in Fixed-Quality Variable-Type interventions | Validated objective diet quality measure; adaptable for multicultural applications [26] |
| Fixed-Quality Variable-Type (FQVT) | Multicultural nutrition research | Standardizes diet quality while accommodating diverse dietary patterns; uses HEI-2020 for quantification | Novel methodology addressing cultural diversity in dietary interventions [26] |
Discussion: Implications for Research and Clinical Practice
The comparative analysis of dietary assessment methods reveals significant methodological advancements in addressing the unique challenges presented by special populations with eating disorders, obesity, and diabetes. Traditional methods like 24-hour recalls and FFQs remain limited by their susceptibility to memory-related biases and social desirability effects, particularly problematic in populations where disordered eating behaviors may be concealed [3]. Emerging approaches such as ecological momentary assessment through digital platforms offer promising alternatives by reducing recall periods and capturing data in near real-time, potentially yielding more accurate dietary intake data in these challenging contexts.
The development of condition-specific validated tools like the DEPS-R for diabetes populations addresses a critical gap in eating disorder screening, with studies demonstrating that 35% of individuals with diabetes are at risk for disordered eating behaviors [97]. The higher prevalence in type 2 diabetes (55%) compared to type 1 diabetes (25%) highlights the need for increased clinical awareness and standardized screening protocols across diabetes subtypes. Furthermore, research on weight management interventions demonstrates that structured programs do not necessarily exacerbate eating disorder symptoms and may in fact improve them, with one randomized controlled trial showing a between-group difference of -0.8 points in EDE-Q global score favoring a total diet replacement intervention [99].
Future research directions should focus on refining objective assessment methodologies, expanding validation studies in diverse populations, and developing integrated approaches that address both physical and psychological aspects of these complex comorbid conditions. The emergence of concepts such as "food noise" – persistent, unwanted thoughts about food – as a measurable construct further highlights the evolving understanding of cognitive processes in eating behavior and the need for validated assessment tools in this domain [101].
Accurate dietary assessment is fundamental to nutritional epidemiology, clinical nutrition, and the development of evidence-based dietary guidelines. These methods enable researchers and clinicians to understand the complex relationships between diet and health outcomes, formulates nutrition policy, and provide personalized dietary recommendations [11]. Dietary assessment tools can be broadly categorized into traditional self-reported methods and emerging technology-enhanced objective methods. Traditional methods include food records, 24-hour dietary recalls (24HR), and food frequency questionnaires (FFQs), which have been the cornerstone of nutritional research for decades [11] [29]. Meanwhile, advances in technology have introduced artificial intelligence (AI)-assisted methods that leverage image recognition, wearable sensors, and machine learning algorithms to reduce reliance on memory and subjective reporting [102] [42]. The choice of assessment method depends on multiple factors including the research question, study design, sample characteristics, sample size, and available resources [11]. This synthesis provides a comprehensive comparison of these methods, their strengths, limitations, ideal use cases, and experimental protocols to guide researchers in selecting the most appropriate dietary assessment tool for their specific needs.
Traditional Dietary Assessment Methods
Traditional dietary assessment methods rely on participants' self-reporting of food consumption through various recording and recall mechanisms. These methods have been extensively validated and refined over decades of use in nutritional research and clinical practice.
Comparative Analysis of Traditional Methods
Table 1: Strengths, Limitations, and Applications of Traditional Dietary Assessment Methods
| Method | Key Strengths | Primary Limitations | Ideal Use Cases | Data Output |
|---|---|---|---|---|
| Food Record/Diet Diary | High detail for specific days; Does not rely on memory; Allows capture of cooking methods & portions | High participant burden; Reactivity (changes behavior); Requires literate/motivated population; Under-reporting common | Small cohort studies; Motivated populations; Research requiring precise nutrient data for specific days; Athlete monitoring [29] | Quantitative nutrient analysis; Food patterns; Meal timing data |
| 24-Hour Dietary Recall (24HR) | Does not require literacy; Low participant burden per recall; Captures unexpected foods; Less reactivity than records | Relies on memory; Requires multiple days to estimate usual intake; Interviewer administration can be costly; Within-person variation | Large population studies (e.g., NHANES); Cross-cultural comparisons; Populations with low literacy [11] [5] | Population mean intakes; Group-level dietary patterns; Snapshot of daily intake |
| Food Frequency Questionnaire (FFQ) | Captures long-term habitual diet; Cost-effective for large samples; Low administrative burden; Can rank individuals by intake | Limited food list; Portion size estimation challenging; Memory dependent; Less precise for absolute intakes | Large epidemiological studies; Diet-disease association research; Ranking individuals by nutrient intake [11] [28] | Habitual intake patterns; Nutrient intake rankings; Dietary pattern adherence |
| Dietary Screeners | Rapid administration; Focused on specific nutrients/foods; Low participant burden | Limited scope; Population-specific validation required; Not comprehensive | Clinical screening; Rapid assessment of specific dietary components; Large surveillance studies [11] | Targeted nutrient/food group intake; Risk categorization |
Methodological Protocols for Traditional Methods
Food Record Protocol
The weighed food record represents the most precise traditional method. Participants are trained to weigh all foods and beverages consumed using digital scales before and after consumption, recording detailed descriptions including cooking methods and brand names [29]. Standard protocol includes:
- Training Session: Participants receive hands-on training with portion size estimation aids, measurement devices, and recording procedures.
- Recording Period: Typically 3-7 days, including both weekdays and weekends to account for day-to-day variation.
- Data Processing: Trained nutritionists code foods using standardized databases (e.g., FNDDS, USDA) with appropriate software.
- Quality Control: Researchers review records for completeness and clarity, with follow-up queries to participants.
Studies indicate 14-30 days of records are needed to estimate an individual's true long-term intake of stable nutrients within 10%, though 3-4 days often suffices for group-level analyses [29].
24-Hour Dietary Recall Protocol
The multiple-pass 24-hour recall method employs a structured interview technique to enhance completeness and accuracy [11]:
- Quick List: Participant freely recalls all foods/beverages consumed in previous 24 hours.
- Forgotten Foods: Prompted recall of commonly omitted items (e.g., snacks, beverages, condiments).
- Time and Occasion: Clarification of eating occasions and times.
- Detail Cycle: Thorough probing for food descriptions, preparation methods, portions.
- Final Review: Participant confirms completeness of the recall.
The USDA's Automated Multiple-Pass Method (AMPM) used in What We Eat in America (WWEIA) NHANES represents the gold standard implementation, requiring extensive interviewer training and standardization [5].
Food Frequency Questionnaire Protocol
FFQ administration follows a standardized process [11]:
- Food List Selection: Population-specific food items (typically 100-150) accounting for major nutrient sources.
- Frequency Response: Participants indicate consumption frequency (per day, week, month, year).
- Portion Size Assessment: Typically uses standardized portions (small, medium, large) with visual aids.
- Data Processing: Algorithms convert frequency and portion data to nutrient estimates using composition databases.
Validation studies compare FFQ results against food records or biomarkers, with correlation coefficients of 0.5-0.7 generally considered acceptable for nutrients [11].
Emerging Objective and Technology-Enhanced Methods
Technological advances have introduced objective dietary assessment methods that reduce reliance on memory and subjective reporting.
AI-Assisted Dietary Assessment Methods
Table 2: Emerging Technology-Enhanced Dietary Assessment Methods
| Method Type | Technology Basis | Key Features | Reported Accuracy | Applications |
|---|---|---|---|---|
| Image-Based (IBDA) | Computer vision, Deep Learning (CNN) | Food recognition, volume estimation, nutrient calculation | Correlation >0.7 for energy, macronutrients [102] | Clinical monitoring; Free-living intake assessment; Pediatric populations [42] |
| Wearable Sensors | Accelerometers, Microphones, Motion sensors | Passive monitoring of eating behaviors, chewing, swallowing | Detects eating episodes with >80% accuracy [42] | Continuous monitoring; Dementia patients; Behavioral studies |
| AI-Enhanced 24HR | Natural Language Processing (NLP) | Automated interview administration, food coding | Reduces administrative costs; maintains accuracy [11] | Large-scale studies; Self-administered recalls |
Methodological Protocols for AI-Assisted Methods
Image-Based Dietary Assessment Protocol
The Food Image Recognition and Analysis protocol involves multiple processing stages [102] [42]:
- Image Capture: Participants capture images of food pre- and post-consumption using mobile devices.
- Image Pre-processing: Standardization of lighting, angle, and removal of background artifacts.
- Food Segmentation and Recognition: Convolutional Neural Networks (CNN) identify food items and separate them from background.
- Volume Estimation: 3D reconstruction or reference object comparison estimates food volume.
- Nutrient Calculation: Databases (e.g., FNDDS) convert food identification and volume to nutrient data.
Validation studies typically compare AI-derived estimates with weighed food records, with correlation coefficients exceeding 0.7 for energy and macronutrients considered acceptable [102].
Sensor-Based Monitoring Protocol
Wearable Sensor methodologies employ various detection approaches [42]:
- Device Placement: Sensors positioned on wrist (motion), neck (swallowing), or head (jaw motion).
- Data Collection: Continuous monitoring of movement patterns and eating-related sounds.
- Event Detection: Machine learning algorithms identify eating episodes from sensor data.
- Meal Characterization: Pattern recognition classifies intake type and estimates quantity.
These methods require individual calibration and validation against objective measures like doubly labeled water for energy intake [42].
Dietary Pattern Assessment Methods
Beyond individual nutrients, dietary pattern analysis examines overall eating patterns and their relationship to health outcomes.
Methodological Approaches to Dietary Patterns
Table 3: Dietary Pattern Assessment Methods in Nutritional Epidemiology
| Method Type | Approach | Key Strengths | Limitations | Common Applications |
|---|---|---|---|---|
| Index-Based (A Priori) | Predefined scoring based on dietary guidelines | Based on prior knowledge; Comparable across studies; Direct policy relevance | Assumes scoring reflects biological reality; May miss culturally specific patterns | Diet quality indices (HEI, AHEI); Mediterranean diet scores; DASH diet scores [28] |
| Data-Driven (A Posteriori) | Statistical derivation from dietary data (PCA, Factor Analysis, Cluster Analysis) | Reflects actual population eating patterns; Identifies novel patterns | Population-specific; Naming/interpretation subjective; Methodological decisions affect results | Identifying "Western" vs. "Prudent" patterns; Cultural dietary assessments [28] |
| Hybrid Methods (RRR) | Combines biological pathways with dietary data | Incorporates intermediate biomarkers; Potentially stronger disease associations | Complex interpretation; Requires biomarker data | Disease-specific pattern identification [28] |
Dietary Pattern Analysis Protocol
The standardized dietary pattern analysis protocol involves [28]:
- Food Grouping: Individual foods aggregated into meaningful groups (e.g., whole fruits, refined grains).
- Pattern Derivation:
- A Priori: Apply predefined scoring algorithms based on dietary guidelines.
- A Posteriori: Use factor analysis/principal component analysis to derive patterns.
- Validation: Internal consistency checks and comparison with biomarkers when available.
- Outcome Analysis: Statistical models (typically multivariate regression) examine pattern-health relationships.
The Dietary Patterns Methods Project demonstrated successful standardization across multiple cohorts using consistent food grouping and scoring protocols [28].
Decision Framework for Method Selection
Selecting the appropriate dietary assessment method requires consideration of multiple research dimensions. The following framework visualizes the decision pathway:
Research Reagents and Tools
Table 4: Essential Research Reagents and Tools for Dietary Assessment Research
| Tool/Resource | Function | Application Context | Key Features |
|---|---|---|---|
| USDA FNDDS | Food composition database | Nutrient analysis from dietary data | 64 nutrients for ~7,000 foods; Updated regularly [5] |
| USDA FPED | Converts foods to food pattern equivalents | Dietary pattern analysis | 37 food pattern components; Aligns with Dietary Guidelines [5] |
| ASA24 | Automated self-administered 24HR | Large-scale recall administration | Reduced interviewer burden; Free for researchers [11] |
| Doubly Labeled Water | Energy expenditure biomarker | Validation of energy intake | Gold standard for energy assessment [42] |
| Recovery Biomarkers (e.g., urinary nitrogen, potassium) | Objective intake measures | Validation of protein, sodium, potassium intake | Not reliant on self-report [11] |
| Food Photography Atlas | Portion size estimation | Food records, 24HR, FFQ | Standardized visual aids for quantification |
The selection of dietary assessment methods represents a critical decision point in nutrition research design, with significant implications for data quality, validity, and practical feasibility. Traditional methods including food records, 24-hour recalls, and FFQs each offer distinct advantages for specific research scenarios, with known limitations related to measurement error, participant burden, and systematic biases [11] [29]. Emerging technologies leveraging artificial intelligence, image recognition, and wearable sensors show considerable promise in addressing these limitations, particularly through reduced reliance on memory and subjective reporting [102] [42]. Dietary pattern analysis has evolved as an essential approach for capturing the complexity of whole diets, with both index-based and data-driven methods contributing valuable evidence for dietary guidelines [28]. The optimal method selection depends on careful consideration of research objectives, population characteristics, available resources, and required precision, with the decision framework provided offering guidance for researchers navigating these complex choices. As the field advances, integration of traditional methodological rigor with technological innovation will likely enhance the accuracy and applicability of dietary assessment in both research and clinical practice.
Conclusion
The evolution of dietary assessment is marked by a critical transition from error-prone self-report methods toward more objective, technology-enhanced tools. While traditional methods like FFQs and 24-hour recalls remain valuable for estimating habitual intake and ranking individuals within groups, their susceptibility to systematic underreporting, which is correlated with factors like BMI, necessitates cautious interpretation, especially for absolute energy intake. Emerging technologies—including AI-assisted image analysis, wearable sensors, and experience sampling—offer promising avenues to reduce recall bias, lessen participant burden, and provide more objective data. A hybrid, pragmatic approach is recommended for researchers: select the method based on the specific research question, target population, and available resources, and always incorporate validation strategies where possible. Future directions should focus on standardizing and validating these novel tools across diverse populations, integrating them seamlessly into clinical trial protocols, and advancing the development of cost-effective, robust biomarkers to further close the accuracy gap in dietary exposure measurement.
References
- 1. Dietary Assessment | EGRP/DCCPS/NCI/NIH [https://epi.grants.cancer.gov/dietary-assessment/]
- 2. Dietary Assessment by Pattern Recognition: a Comparative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10550800/]
- 3. Protocol for a Mixed Methods Study [https://www.researchprotocols.org/2025/1/e70194]
- 4. Performance Evaluation of 3 Large Language Models for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12513282/]
- 5. Data Analysis for the 2025 Guidelines Committee Report [https://www.dietaryguidelines.gov/2025-advisory-committee-report/data-analysis]
- 6. Advance in Dietary Assessment Powers New Approach to ... [https://fox40.com/business/press-releases/ein-presswire/865289591/advance-in-dietary-assessment-powers-new-approach-to-nutrition-research-programming]
- 7. An Image-Voice Dietary Assessment System for Estimating ... [https://www.jmir.org/2025/1/e65939]
- 8. the Fixed-Quality Variable-Type Dietary Intervention [https://pmc.ncbi.nlm.nih.gov/articles/PMC12592233/]
- 9. The development and evaluation of a quality assessment ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1519401/full]
- 10. Evaluation and Comparison of Food Records, Recalls ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3202154/]
- 11. Overview of Dietary Assessment Methods for Measuring ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8338737/]
- 12. Comparison of dietary intake measured by a web-based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9641502/]
- 13. Comparison of dietary intake measured by a web-based ... [https://www.cambridge.org/core/journals/journal-of-nutritional-science/article/comparison-of-dietary-intake-measured-by-a-webbased-ffq-and-repeated-24hour-dietary-recalls-the-hordaland-health-study/B59CD406183936B1AAD9ED54F48A875F]
- 14. Traditional Self-Reported Dietary Instruments Are Prone to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7350526/]
- 15. FFQ versus repeated 24-h recalls for estimating diet-related ... [https://nutritionj.biomedcentral.com/articles/10.1186/s12937-018-0425-z]
- 16. Effects of social approval bias on self-reported fruit and ... [https://nutritionj.biomedcentral.com/articles/10.1186/1475-2891-7-18]
- 17. Measurement Error in Dietary assessment [https://nutritionalassessment.org/errors/]
- 18. Social desirability bias in dietary self-report may ... [https://pubmed.ncbi.nlm.nih.gov/7635601/]
- 19. Validity of Dietary Assessment Methods When Compared ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2019.00850/full]
- 20. a pilot comparative validation study exploring the diet history ... [https://jeatdisord.biomedcentral.com/articles/10.1186/s40337-025-01392-x]
- 21. An Overview of Traditional and Novel Tools to Assess Diet [https://pmc.ncbi.nlm.nih.gov/articles/PMC11384832/]
- 22. Uncovering the Truth About Your Diet: Objective Strategies ... [https://pan-int.org/knowledge-hub/uncovering-the-truth-about-your-diet-objective-strategies-for-dietary-assessment]
- 23. Diets high in ultra-processed foods, which are ... [https://www.nih.gov/news-events/news-releases/nih-researchers-develop-biomarker-score-predicting-diets-high-ultra-processed-foods]
- 24. Biomarker for Diets High in Ultra-processed Foods - NCI [https://dceg.cancer.gov/news-events/news/2025/biomarker-ultra-processed-foods]
- 25. Dietary Biomarkers Study [https://hsph.harvard.edu/research/eat-biomarkers/]
- 26. The Fixed-Quality Variable-Type (FQVT) Dietary Intervention [https://pmc.ncbi.nlm.nih.gov/articles/PMC12592231/]
- 27. dilemmas for dietary assessment in large-scale nutrition ... [https://www.cambridge.org/core/journals/journal-of-nutritional-science/article/traditional-methods-v-new-technologies-dilemmas-for-dietary-assessment-in-largescale-nutrition-surveys-and-studies-a-report-following-an-international-panel-discussion-at-the-9th-international-conference-on-diet-and-activity-methods-icdam9-brisbane-3-september-2015/27A052A270BEC5F9A3B6D1BBB5676098]
- 28. A Systematic Review of the Methods Used to Assess and ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2022.892351/full]
- 29. Dietary Assessment Methods For the Athlete: Pros and ... [https://www.gssiweb.org/sports-science-exchange/article/sse-150-dietary-assessment-methods-for-the-athlete-pros-and-cons-of-different-methods]
- 30. Overview of dietary assessment methods for measuring ... [https://www.sciencedirect.com/science/article/abs/pii/S0958166921000422]
- 31. Traditional dietary assessment tools verses technology-based ... [https://www.mattioli1885journals.com/index.php/progressinnutrition/article/view/11107]
- 32. AMPM - USDA Automated Multiple-Pass Method [https://www.ars.usda.gov/northeast-area/beltsville-md-bhnrc/beltsville-human-nutrition-research-center/food-surveys-research-group/docs/ampm-usda-automated-multiple-pass-method/]
- 33. The USDA Automated Multiple-Pass Method Accurately ... [https://www.sciencedirect.com/science/article/pii/S002231662208484X]
- 34. Comparison of self-reported dietary intakes from the ... [https://www.sciencedirect.com/science/article/pii/S0002916522027459]
- 35. DietAI24 as a framework for comprehensive nutrition ... [https://www.nature.com/articles/s43856-025-01159-0]
- 36. Comparing reported dietary supplement intakes between ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6594012/]
- 37. Comparing Reported Dietary Supplement Intakes between ... [https://divisionofresearch.kaiserpermanente.org/publications/comparing-reported-dietary-supplement-intakes-between-two-24-hour-recall-methods-the-automated-self-administered-24-hour-dietary-assessment-tool-and-the-interview-administered-automated-multiple-pass/]
- 38. ASA24® Dietary Assessment Tool | EGRP/DCCPS/NCI/NIH [https://epi.grants.cancer.gov/asa24/]
- 39. DietAI24 as a framework for comprehensive nutrition ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12589391/]
- 40. Feasibility and usability of a voice-based dietary recall tool ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12612543/]
- 41. Mobile Apps for Dietary and Food Timing Assessment [https://formative.jmir.org/2023/1/e35858]
- 42. Navigating next-gen nutrition care using artificial ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1518466/full]
- 43. Accuracy and Cost-effectiveness of Technology-Assisted ... [https://www.researchprotocols.org/2021/12/e32891/]
- 44. NutriDiary, a Smartphone-Based Dietary Record App [https://pmc.ncbi.nlm.nih.gov/articles/PMC11833184/]
- 45. A Review of Image-Based Food Recognition and Volume ... [https://pubmed.ncbi.nlm.nih.gov/37276096/]
- 46. Applying Image-Based Food-Recognition Systems on ... [https://www.sciencedirect.com/science/article/pii/S2161831323000935]
- 47. Image-based food monitoring and dietary management for ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1501946/full]
- 48. Use of Different Food Image Recognition Platforms in ... [https://pubmed.ncbi.nlm.nih.gov/33284118/]
- 49. USDA Approved Nutrient Analysis Software [https://www.fns.usda.gov/tn/usda-approved-nutrient-analysis-software]
- 50. AI-based digital image dietary assessment methods compared ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10836267/]
- 51. Automatic, wearable-based, in-field eating detection ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7069988/]
- 52. Enhancing Nutrition Care Through Real-Time, Sensor ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2022.852984/full]
- 53. Integrated image and sensor-based food intake detection ... [https://www.nature.com/articles/s41598-024-51687-3]
- 54. Validation of Sensor-Based Food Intake Detection ... - PubMed [https://pubmed.ncbi.nlm.nih.gov/30871173/]
- 55. Using Wearable Cameras to Assess Foods and Beverages ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8228902/]
- 56. Dietary assessment methodologies in eating disorders [https://pubmed.ncbi.nlm.nih.gov/41024312/]
- 57. Using Experience Sampling Methods/Ecological Momentary ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4255457/]
- 58. Use of the experience sampling method in the context of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5040762/]
- 59. A Guide to the Experience Sampling Method [https://www.expiwell.com/post/what-is-the-experience-sampling-method]
- 60. Effect of experience sampling schedules on response rate ... [https://www.sciencedirect.com/science/article/abs/pii/S1071581918306797]
- 61. Mastering ESM Data Analysis: Advanced Methodological ... [https://web.fibion.com/articles/analyzing-esm-data-guide/]
- 62. Measurement error in total energy intake in the United ... [https://www.sciencedirect.com/science/article/pii/S000291652500588X]
- 63. Dietary assessment methods in epidemiologic studies - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4154347/]
- 64. Methodology - NCS Dietary Assessment Literature Review [https://epi.grants.cancer.gov/past-initiatives/assess_wc/review/about/methodology.html]
- 65. Dietary misreporting: a comparative study of recalls vs ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12034172/]
- 66. Minimum days estimation for reliable dietary intake ... [https://www.nature.com/articles/s41430-025-01644-8]
- 67. A Decade of Dietary Assessment Methodology Research at ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10196585/]
- 68. Impact of body mass index and age on the relative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7538486/]
- 69. BMI was found to be a consistent determinant related to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10261408/]
- 70. Demographic and psychosocial correlates of measurement ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9899562/]
- 71. Dietary assessment methodologies in eating disorders [https://pmc.ncbi.nlm.nih.gov/articles/PMC12482415/]
- 72. FDA and NIH Announce Innovative Joint Nutrition ... [https://www.fda.gov/news-events/press-announcements/fda-and-nih-announce-innovative-joint-nutrition-regulatory-science-program]
- 73. Future Directions for Integrative Objective Assessment of ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2020.00080/full]
- 74. Minimum Days Estimation for Reliable Dietary Intake ... [https://www.medrxiv.org/content/10.1101/2024.08.29.24312779v1]
- 75. How many days are needed? Measurement reliability of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9956594/]
- 76. A review of statistical methods for dietary pattern analysis [https://nutritionj.biomedcentral.com/articles/10.1186/s12937-021-00692-7]
- 77. Development and User Experience Evaluation of an ... [https://www.sciencedirect.com/science/article/pii/S2475299124024132]
- 78. Experience Sampling as a dietary assessment method [https://ijbnpa.biomedcentral.com/articles/10.1186/s12966-024-01643-1]
- 79. Weekdays vs. weekends: How reporting timing influences ... [https://www.sciencedirect.com/science/article/pii/S2214845025000857]
- 80. A Decade of Dietary Assessment Methodology Research at ... [https://www.sciencedirect.com/science/article/pii/S0022316623257211]
- 81. Predictive equation derived from 6497 doubly labelled ... [https://www.nature.com/articles/s43016-024-01089-5]
- 82. Urinary metabolites as biomarkers of dietary intake [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1596543/full]
- 83. Protocol of the validation of the experience sampling-based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12587619/]
- 84. Urine Nitrogen as a Biomarker for the Validation of Dietary ... [https://www.sciencedirect.com/science/article/pii/S0022316622157068]
- 85. Protocol of the validation of the experience sampling-based ... [https://nutritionj.biomedcentral.com/articles/10.1186/s12937-025-01232-3]
- 86. Protocol of the validation of the experience sampling ... [https://pubmed.ncbi.nlm.nih.gov/41194100/]
- 87. Use of Biomarkers in Drug Development for Regulatory ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12489174/]
- 88. New Study Shows Future Biomarker Development Needs ... [https://friendsofcancerresearch.org/news/new-study-shows-future-biomarker-development-needs-enhancements/]
- 89. Evaluation of new predictive equations for energy ... [https://www.sciencedirect.com/science/article/pii/S0261561425001682]
- 90. Reliance on self-reports and estimated food composition ... [https://elifesciences.org/articles/92941]
- 91. Comparison of self-reported and measured metabolizable ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2682993/]
- 92. Advance in Dietary Assessment Powers New Approach to ... [https://www.fox21news.com/business/press-releases/ein-presswire/865289591/advance-in-dietary-assessment-powers-new-approach-to-nutrition-research-programming]
- 93. Nutrition: Macronutrient Intake, Imbalances, and Interventions [https://www.ncbi.nlm.nih.gov/books/NBK594226/]
- 94. Micronutrient bioavailability: concepts, influencing factors, ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1646750/full]
- 95. Micronutrients vs. macronutrients, and where to find them [https://health.osu.edu/wellness/exercise-and-nutrition/micronutrients-vs-macronutrients]
- 96. Advance in Dietary Assessment Powers New Approach to ... [https://www.nbc4i.com/business/press-releases/ein-presswire/865289591/advance-in-dietary-assessment-powers-new-approach-to-nutrition-research-programming]
- 97. Assessment of diabetes-specific eating disorder risk in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11752928/]
- 98. The Prevalence of Eating Disorders and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12423590/]
- 99. An intensive weight loss programme with behavioural ... [https://www.sciencedirect.com/science/article/pii/S2215036625001269]
- 100. The impact of weight loss interventions on disordered ... [https://www.sciencedirect.com/science/article/pii/S258953702400628X]
- 101. Food noise: definition, measurement, and future research ... [https://www.nature.com/articles/s41387-025-00382-x]
- 102. Validity and accuracy of artificial intelligence-based dietary ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12229984/]