Beyond the Questionnaire: Advanced Strategies to Overcome Food Frequency Questionnaire Limitations in Clinical Research
Food Frequency Questionnaires (FFQs) are indispensable yet imperfect tools for assessing dietary intake in large-scale epidemiological studies and clinical trials.
Beyond the Questionnaire: Advanced Strategies to Overcome Food Frequency Questionnaire Limitations in Clinical Research
Abstract
Food Frequency Questionnaires (FFQs) are indispensable yet imperfect tools for assessing dietary intake in large-scale epidemiological studies and clinical trials. This article provides a comprehensive resource for researchers and drug development professionals seeking to navigate and mitigate the inherent limitations of FFQs. We explore the foundational sources of measurement error, detail advanced methodological adaptations for enhanced accuracy, present cutting-edge computational and machine learning techniques for optimization, and establish rigorous protocols for validation. By synthesizing current research and emerging methodologies, this guide aims to empower scientists to generate more reliable nutritional data, thereby strengthening the investigation of diet-disease relationships and the development of targeted nutritional interventions.
Understanding the Core Challenges: Why FFQs Fall Short and What It Means for Research
Frequently Asked Questions (FAQs)
Q1: What are the primary sources of measurement error in self-reported dietary data? The main sources are recall bias, portion size estimation errors, and day-to-day variation in diet. Recall bias occurs when participants inaccurately remember their past food consumption, a particular issue with Food Frequency Questionnaires (FFQs) that ask about intake over long periods [1]. Portion size estimation is a major cause of error, as individuals struggle to judge the quantities of food they consumed, with single-unit foods (e.g., a slice of bread) being reported more accurately than amorphous foods (e.g., pasta) or liquids [2]. Day-to-day variation is the natural fluctuation in a person's diet from one day to the next, which can introduce substantial random error if only a small number of days are assessed [3].
Q2: How does the error structure differ between a 24-Hour Recall (24HR) and an FFQ? Data from 24HRs typically contain larger within-person random error (due to day-to-day variation) but smaller systematic error [3]. In contrast, FFQs exhibit more systematic error, which is often driven by the cognitive challenge of recalling long-term intake and the instrument's design, such as its finite food list [3]. One study found that systematic error accounted for over 22% of measurement error variance for 24-hour recalls, but over 50% for the FFQ [4].
Q3: Can biomarkers help validate self-reported dietary intake? Yes, biomarkers are crucial for validation, but their utility depends on the type. Recovery biomarkers, like doubly labeled water for energy intake and urinary nitrogen for protein intake, are considered the strongest objective validators because they are not substantially affected by inter-individual differences in metabolism [3]. Concentration biomarkers, such as blood carotenoid levels for fruit and vegetable intake, are correlated with diet but are influenced by an individual's metabolism and other characteristics like smoking status or body size, making them less suitable as direct proxies for absolute intake [4] [1].
Q4: Which dietary assessment instrument provides less biased estimates of intake? Evidence from large biomarker-based validation studies suggests that 24-hour recalls provide less biased estimates of intake compared to FFQs and are thus the preferred tool for most purposes [3]. For example, one study reported the validity (correlation with true intake) of the instruments was 0.44 for 24-hour recalls and 0.39 for the FFQ [4].
Q5: How can portion size estimation errors be mitigated? Using Portion Size Estimation Aids (PSEAs) can help, though they do not eliminate error. Research compares text-based aids (using household measures and standard sizes) to image-based aids. One study found that although both methods introduced error, text-based descriptions (TB-PSE) showed better performance, with 50% of estimates falling within 25% of true intake, compared to 35% for image-based aids (IB-PSE) [2]. For 24-hour recalls, the use of pictorial recall aids has been shown to help participants remember omitted food items, significantly modifying dietary outcomes [5].
Troubleshooting Guides
Problem 1: High Recall Bias in FFQ Data
Background: Participants frequently misreport the frequency of food consumption when recalling intake over extended periods (e.g., the past year) [1]. This can be due to genuine memory limitations or social desirability bias, where individuals report what they believe the researcher wants to hear [6].
Solution: Implement a Machine Learning-Based Error Adjustment A novel method uses a supervised machine learning model to identify and correct for likely misreporting.
- Experimental Protocol:
- Data Collection: Gather data that includes FFQ responses and objective measures such as blood lipids (LDL, total cholesterol), blood glucose, body fat percentage, BMI, age, and sex [6].
- Define a "Healthy" Reference Group: Split your dataset. Use participants classified as "healthy" based on objective cut-offs for body fat, age, and sex to create a training set. This group is assumed to report their dietary intake more accurately [6].
- Train a Predictive Model: Use the healthy group's data to train a Random Forest (RF) classifier. The model learns to predict food frequency categories based on the objective variables (e.g., blood lipids, BMI) [6].
- Apply the Model and Adjust Data: Use the trained RF model to predict the expected food frequency categories for the remaining ("unhealthy") participants.
- For foods with a high likelihood of underreporting (e.g., high-fat foods like bacon), if the originally reported frequency is lower than the model's prediction, replace it with the predicted value [6].
- This method has demonstrated high model accuracies, ranging from 78% to 92%, in correcting underreported entries [6].
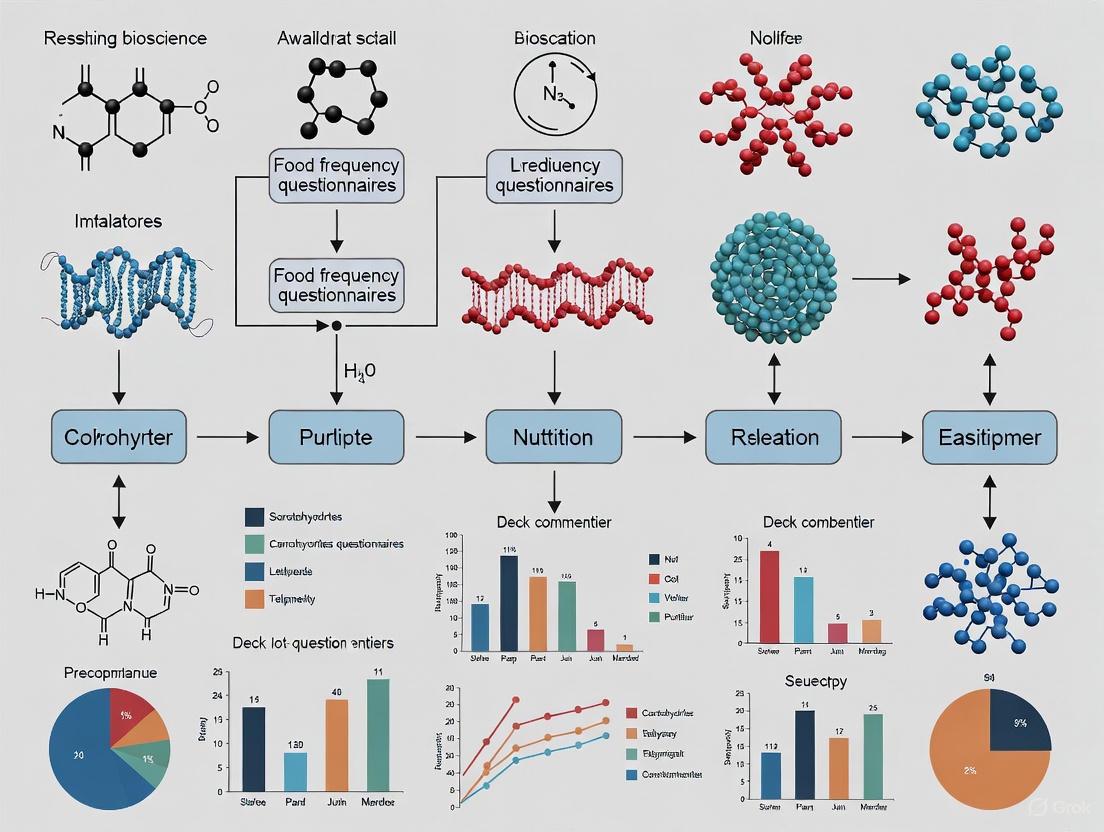
Workflow for Mitigating Recall Bias with Machine Learning:
Problem 2: Inaccurate Portion Size Estimation
Background: Individuals consistently struggle to estimate portion sizes, with a tendency to overestimate small portions and underestimate large ones (the "flat-slope phenomenon") [2]. The accuracy varies greatly by food type.
Solution: Optimize Portion Size Estimation Aids (PSEAs) Carefully select and design the aids used to help participants report quantities.
- Experimental Protocol for Comparing PSEAs:
- Control True Intake: In a study setting, provide participants with pre-weighed, ad libitum amounts of various food types (amorphous, liquids, single-units, spreads) [2].
- Measure Plate Waste: Weigh the leftovers to calculate the exact amount each participant consumed [2].
- Administer PSEAs: At set intervals (e.g., 2 and 24 hours after eating), have participants report their intake using different PSEAs in a randomized order. Key comparisons are:
- Analyze Accuracy: Compare reported portion sizes to true intake. Metrics include the median relative error, and the proportion of estimates within 10% and 25% of the true value [2].
Results to Inform Your Protocol: A study using this protocol found that text-based aids (TB-PSE) outperformed image-based aids (IB-PSE) [2].
Table 1. Accuracy of Portion Size Estimation Aids (PSEAs)
| Food Type | PSEA Method | Median Relative Error | Within 25% of True Intake |
|---|---|---|---|
| All Foods Combined | Text-Based (TB-PSE) | 0% | 50% |
| All Foods Combined | Image-Based (IB-PSE) | 6% | 35% |
| Single-unit foods | Both Methods | More Accurate | More Accurate |
| Amorphous foods & Liquids | Both Methods | Less Accurate | Less Accurate |
Recommendation: For web-based or paper tools, prioritize clear textual descriptions of portion sizes using standard household measures and predefined sizes. While image aids can be helpful, they should not be relied upon as the sole method [2].
Problem 3: Excessive Day-to-Day Variation Obscuring Usual Intake
Background: A single day of intake, as captured by one 24-hour recall, is a poor indicator of a person's habitual diet due to large daily fluctuations. Treating this as usual intake introduces significant random error (within-person variation) [3].
Solution: Administer Multiple Non-Consecutive 24-Hour Recalls The key is to spread assessments over time to capture this variation and statistically model the usual intake.
- Experimental Protocol:
- Plan Multiple Administrations: Do not collect recalls on consecutive days. Intakes on adjacent days are often correlated. Space them out over different seasons to account for seasonal variation [7].
- Include All Days of the Week: Ensure your recalls cover both weekdays and weekend days, as eating patterns often differ [7].
- Use Automated Tools: Leverage low-cost, automated self-administered 24HR tools (e.g., ASA24) to make multiple administrations feasible in large studies [3].
- Apply Statistical Modeling: Use specialized software (e.g., the National Cancer Institute's method) to estimate the distribution of usual intake in your population by separating within-person variation from between-person variation [3].
Evidence for Protocol Efficacy: Research comparing 3-day food records to 9-day records (as a reference) found that the 3-day records showed higher correlation and better agreement in quartile classification than an FFQ, demonstrating that multiple short-term records better capture habitual intake [7].
Workflow for Addressing Day-to-Day Variation:
The Scientist's Toolkit: Key Research Reagents & Materials
Table 2: Essential Materials for Dietary Validation and Error Mitigation Studies
| Item | Function in Research |
|---|---|
| Doubly Labeled Water (DLW) | A recovery biomarker used to measure total energy expenditure, providing an unbiased estimate of energy intake for validation studies [3]. |
| 24-Hour Urine Collection | Used to measure urinary nitrogen (a recovery biomarker for protein intake), potassium, and sodium, allowing for objective validation of self-reported intake of these nutrients [3]. |
| Blood Samples (Serum/Plasma) | Analyzed for concentration biomarkers, such as carotenoids (e.g., α-carotene, β-carotene, lutein), which serve as objective indicators of fruit and vegetable intake [4]. |
| High-Performance Liquid Chromatography (HPLC) | The laboratory method used to separate and quantify specific carotenoids and other nutrient biomarkers in blood plasma with high precision [4]. |
| Automated Self-Administered 24-HR (ASA24) | A web-based tool that automates the 24-hour recall process, eliminating the need for an interviewer and reducing coding errors, making multiple administrations feasible [3]. |
| Portion Size Image Sets (e.g., from ASA24) | Standardized photographic aids used in image-based portion size estimation (IB-PSE) to help participants visualize and select the amount of food they consumed [2]. |
| Random Forest Classifier | A machine learning algorithm that can be trained to identify and correct for misreporting in FFQ data based on relationships with objective health measures [6]. |
| JW 618 | JW 618, CAS:1416133-88-4, MF:C17H14F6N2O2, MW:392.29 g/mol |
| 1,7-Bis(4-hydroxyphenyl)hept-6-en-3-one | 1,7-Bis(4-hydroxyphenyl)hept-6-en-3-one |
Technical Support Center: Troubleshooting Food Frequency Questionnaire (FFQ) Research
This support center provides targeted guidance for researchers encountering common methodological challenges in dietary assessment, with a specific focus on the localization and adaptation of Food Frequency Questionnaires (FFQs).
Frequently Asked Questions (FAQs)
How can I correct for underreporting of specific food items in my FFQ data? A machine learning-based error adjustment method can be applied. This involves using a Random Forest classifier trained on objectively measured health biomarkers (e.g., blood lipids, body fat percentage) from a "healthy" participant subgroup to predict likely consumption of underreported foods (e.g., high-fat items) in the rest of the cohort. If the model's prediction for an unhealthy food is higher than the participant's reported intake, the value is corrected [6].
What is the most effective way to adapt portion sizes in an FFQ for a new region? Conduct a local utensil survey. Systematically measure the volume of commonly used serving utensils (e.g., bowls, glasses) from a representative sample of households. Classify these into small, medium, and large portion sizes based on the derived volumes. Using these local sizes, instead of national reference portions, can prevent underestimation of food consumption by over 50% and significantly improves correlation with 24-hour recall data [8].
Our FFQ significantly misestimates macronutrient intake. How can we validate and improve it? Validate your FFQ against multiple 24-hour dietary recalls or, ideally, controlled feeding studies. One study feeding subjects diets of known composition found that an FFQ significantly underestimated absolute fat and protein intake and overestimated carbohydrate intake on a high-fat diet. If such miscalibration is found, the relationship between FFQ-reported values and actual intake can be quantified and used to create calibration factors [9].
What is the step-by-step process for translating and adapting an international FFQ? Follow a structured adaptation and validation protocol:
- Forward Translation: Translate the original FFQ into the local language.
- Local Food Inclusion: Add culturally relevant food items identified via market surveys and literature reviews.
- Back Translation: Have a different translator convert the local version back to the original language to check for conceptual consistency.
- Portion Size Standardization: Define portion sizes using local household measures and/or photographs.
- Pilot Testing: Test the draft FFQ in a small sample to identify difficulties in comprehension.
- Validation: Assess the final FFQ's validity against multiple 24-hour recalls or food records [10].
Experimental Protocols for FFQ Localization and Validation
Protocol 1: Local Portion Size Derivation
Objective: To define context-specific portion sizes for a semi-quantitative FFQ to mitigate measurement error.
Materials:
- Measuring scale and standard measuring cup (e.g., 240 mL)
- Digital weighing scale (accuracy 0.1 g) for solid foods
- Standardized spoons for liquid ingredients
Methodology:
- Utensil Survey: Randomly select households in the target region. Inventory and measure the dimensions and volumes of all commonly used serving utensils (SUs).
- Data Pooling: Pool the volume data from all collected SUs. Classify them into categories (e.g., small, medium, large) based on statistical frequency.
- Recipe Standardization: In a food lab, prepare common local dishes using recipes and ingredients reported in the survey.
- Weight Conversion: Weigh the total cooked dish. Determine the weight of the cooked dish that fits into the classified portion sizes (e.g., a "small" local bowl). This converts local portion sizes into gram weights for nutrient calculation [8].
Protocol 2: Cross-Cultural Adaptation and Validation of an FFQ
Objective: To adapt an existing FFQ to a new cultural setting and test its reproducibility and validity.
Materials:
- Original FFQ to be adapted
- Local food composition tables and databases (e.g., FAO, USDA, or national tables)
- 24-hour dietary recall forms
Methodology:
- Adaptation: Add traditional and commonly consumed local food items to the original FFQ list. Retain non-relevant items from the original FFQ for international comparability.
- Translation: Perform forward and backward translation following WHO Standard Operational Procedures.
- Study Design: Administer the following to participants:
- The adapted FFQ at time zero (FFQ1).
- Three 24-hour dietary recalls (including a weekend day) spread over one month.
- The same adapted FFQ one month later (FFQ2).
- Data Analysis:
- Validity: Calculate Pearson correlation coefficients between nutrient intakes from FFQ1 and the average of the three 24-hour recalls. Apply de-attenuation to correct for within-person variation [10].
- Reproducibility: Calculate the Intra-class Correlation Coefficient (ICC) between nutrient intakes from FFQ1 and FFQ2 [10].
Summarized Quantitative Data from FFQ Validation Studies
Table 1: Correlation Coefficients from an FFQ Adaptation Study in Moroccan Adults [10]
| Nutrient | Validity (De-attenuated Correlation with 24-hr Recall) | Reproducibility (Intra-class Correlation) |
|---|---|---|
| Energy | 0.51 | 0.76 |
| Fat | 0.69 | 0.69 |
| Protein | 0.58 | 0.78 |
| Carbohydrates | 0.46 | 0.75 |
| Total MUFA | 0.93 | 0.83 |
| Fiber | 0.24 | 0.76 |
| Vitamin A | 0.67 | 0.84 |
Table 2: Impact of Local vs. Reference Portion Sizes on Food Estimation [8]
| Metric | Result from Indian Rural Study |
|---|---|
| Potential Underestimation using Reference Portions | 55-60% of actual food consumed |
| Correlation with 24-hr Recall | Better with locally derived portion sizes |
Workflow Diagrams for FFQ Adaptation
Diagram Title: FFQ Cross-Cultural Adaptation Process
Diagram Title: Machine Learning Workflow for Underreporting Correction
The Scientist's Toolkit: Essential Reagents & Materials
Table 3: Key Research Reagents and Materials for FFQ Studies
| Item | Function / Application in FFQ Research |
|---|---|
| Standardized Measuring Utensils | Critical for conducting local utensil surveys to derive accurate portion sizes for converting food frequencies into gram weights [8]. |
| Digital Food Scales | Required for weighing raw ingredients and cooked dishes in a lab setting to determine the weight of food corresponding to local portion sizes [8]. |
| Local & International Food Composition Tables | Databases (e.g., USDA, FAO, CIQUAL, national tables) used to assign nutrient values to the food items and portion sizes listed in the adapted FFQ [10]. |
| 24-Hour Dietary Recall Forms | The standard tool used as a reference method to validate the nutrient intake estimates generated by the new FFQ [10]. |
| Biomarker Assay Kits | Kits for analyzing objective measures like blood lipids (LDL, total cholesterol) and glucose. Used to identify reporting biases and train error-correction models [6]. |
| Block 2005 FFQ / GA2LEN FFQ | Examples of established, pre-defined FFQs that can serve as a starting framework for cultural adaptation and localization [6] [10]. |
| Exendin 3 | Exendin 3, CAS:130391-54-7, MF:C184H282N50O61S, MW:4203 g/mol |
| Desethyl Terbuthylazine-d9 | Desethyl Terbuthylazine-d9, CAS:1219798-52-3, MF:C7H12ClN5, MW:210.71 g/mol |
FAQs: Core Concepts and Methodological Challenges
Q1: Why is the traditional focus on single nutrients insufficient for modern nutritional research?
Traditional methods that analyze foods and nutrients in isolation overlook crucial food synergies, which can lead to an incomplete understanding of dietary patterns and their health implications. For example, a study found that garlic may counteract some of the detrimental effects associated with red meat consumption, a synergy that would be missed by examining nutrients alone [11]. Furthermore, studies focusing on individual nutrients like magnesium, potassium, calcium, and fiber have produced inconsistent results, potentially because nutrients from supplements may not benefit health as effectively as those obtained from whole foods due to synergistic interactions [11].
Q2: What are the primary limitations of traditional dietary pattern analysis methods like PCA or cluster analysis?
Methods like Principal Component Analysis (PCA) and cluster analysis share a significant limitation: they are often unable to fully capture the complex interactions and synergies between different dietary components [11]. By reducing dietary intake to composite scores or broad patterns, they disregard the multidimensional nature of diet and can hide crucial food synergies [11]. These methods often assume that dietary patterns are relatively static, ignoring potential changes in diet over time due to ageing, economic changes, or health conditions, which can result in obscured or false associations [11].
Q3: How can measurement error in Food Frequency Questionnaires (FFQs) be mitigated?
FFQs are susceptible to errors like underreporting, particularly for unhealthy foods. A novel approach uses a supervised machine learning method involving a Random Forest (RF) classifier to identify and correct for these errors [6]. The protocol involves:
- Splitting the dataset into groups (e.g., based on health status using objective measures like body fat percentage).
- Training the RF model on data from the "healthy" group to learn the relationship between objective biomarkers (e.g., LDL cholesterol, total cholesterol) and food consumption.
- Predicting and correcting values in the "unhealthy" group. If the originally reported value for an unhealthy food is lower than the model's prediction, it is considered underreported and replaced with the predicted value [6].
Q4: What is the evidence that overall dietary patterns are linked to long-term health outcomes?
Large prospective cohort studies provide strong evidence. Research from the Nurses' Health Study and the Health Professionals Follow-Up Study (following 105,015 participants for up to 30 years) found that greater adherence to healthy dietary patterns was consistently associated with higher odds of "healthy aging" [12]. Healthy aging was defined as surviving to 70 years free of major chronic diseases and maintaining intact cognitive, physical, and mental health. The study showed that for each dietary pattern, the highest adherence was associated with 1.45 to 1.86 times greater odds of healthy aging compared to the lowest adherence [12].
Troubleshooting Guides: Addressing Common Research Problems
Problem: Inability to Model Complex, Non-Linear Food Interactions
- Challenge: Traditional statistical models assume simple, linear relationships and fail to capture the complex, non-linear web of how foods interact and are consumed together.
- Solution: Employ Network Analysis, such as Gaussian Graphical Models (GGMs).
- Experimental Protocol:
- Data Preparation: Collect high-dimensional dietary intake data (e.g., from multiple 24-hour recalls or a validated FFQ).
- Model Selection: Apply a Gaussian Graphical Model (GGM). GGMs use partial correlations to identify conditional dependencies between foods, revealing how foods are directly connected after accounting for all other foods in the network [11].
- Regularization: Use regularization techniques like the graphical LASSO to handle high-dimensional data and produce a sparse, interpretable network [11].
- Validation & Interpretation: Visualize the network. Nodes represent foods, and edges represent conditional dependencies. Centrality metrics can identify key foods, but these must be interpreted with caution due to known limitations [11].
Problem: Balancing Multiple, Sometimes Conflicting, Research Objectives
- Challenge: Designing a diet that simultaneously optimizes for nutrient adequacy, environmental sustainability (e.g., low greenhouse gas emissions), and other dimensions like food biodiversity.
- Solution: Implement Multi-Objective Optimization (MOO).
- Experimental Protocol:
- Define Objectives: Clearly state the goals (e.g., maximize nutrient adequacy score, minimize dietary greenhouse gas emissions).
- Set Constraints: Define nutritional and practical constraints (e.g., meet recommended dietary allowances for all essential nutrients).
- Model Application: Use MOO algorithms to generate a spectrum of optimal diets that represent the best trade-offs between the chosen objectives. This approach was successfully applied in the EPIC cohort to show that diets adhering to the EAT-Lancet recommendations, with higher biodiversity and lower ultra-processed foods, can synergistically improve nutrient adequacy while reducing environmental impact [13] [14].
Problem: Validating FFQ Data Against Objective Measures
- Challenge: Self-reported FFQ data may not accurately reflect true biological intake, especially in specific disease populations.
- Solution: Biochemical validation using serum or urine biomarkers.
- Experimental Protocol:
- Cohort and Sample Collection: Recruit participants from your target population. Collect dietary data via FFQ and concurrently collect fasting blood or 24-hour urine samples [15] [16].
- Biomarker Analysis: Measure biomarkers relevant to the nutrients of interest (e.g., serum vitamins A, C, D, E, zinc, iron) [16].
- Statistical Comparison: Assess agreement between FFQ-derived intake and biomarker levels using correlation coefficients (e.g., Pearson or Spearman) and cross-classification into quartiles [15] [16]. Note that poor agreement may indicate issues with the FFQ or reflect altered nutrient metabolism in the study population [16].
Key Experimental Protocols in Detail
Protocol 1: Validating a Food Frequency Questionnaire (FFQ)
This protocol is based on the methodology used by the large PERSIAN Cohort validation study [15].
- Aim: To assess the validity and reproducibility of an FFQ for ranking individuals based on their nutrient intakes.
- Materials:
- Designed FFQ (e.g., 113-item, semi-quantitative)
- Standard portion size tools (food models, utensils, picture album)
- Biological sample collection kits (for serum and 24-hour urine)
- Procedure:
- Baseline Assessment (Day 0):
- Administer the first FFQ (FFQ1) via a trained interviewer.
- Collect baseline fasting blood and 24-hour urine samples.
- Longitudinal Data Collection (Months 1-12):
- Conduct two non-consecutive 24-hour dietary recalls (24HR) each month (total of 24 recalls) as a reference method.
- Collect fasting blood and 24-hour urine samples each season (total of 4 collections).
- Follow-up Assessment (Month 12):
- Administer the FFQ a second time (FFQ2) to assess reproducibility.
- Baseline Assessment (Day 0):
- Data Analysis:
- Validity: Calculate correlation coefficients (e.g., Pearson) between nutrient intakes from FFQ1 and the average of the 24HRs.
- Reproducibility: Calculate correlation coefficients between nutrient intakes from FFQ1 and FFQ2.
- Biomarker Comparison: Use the triad method to compare correlations between the FFQ, 24HR, and biomarker levels [15].
Protocol 2: Applying Network Analysis to Dietary Data
This protocol outlines the use of Gaussian Graphical Models to uncover dietary patterns [11].
- Aim: To map and analyze the complex web of conditional dependencies between different dietary components in a population.
- Materials:
- High-dimensional dietary intake dataset (e.g., food items or food groups).
- Statistical software capable of network estimation (e.g., R with
qgraphorhugepackages).
- Procedure:
- Data Preprocessing: Address non-normal data distribution through transformations (e.g., log-transformation) or by using non-parametric extensions of GGMs [11].
- Model Estimation: Apply the graphical LASSO to estimate the GGM. This technique uses an L1-penalty to shrink small partial correlations to zero, resulting in a sparse and interpretable network [11].
- Network Visualization: Create a network graph where nodes are foods and edges represent significant partial correlations. Visually inspect the network for clusters of strongly connected foods.
- Robustness Analysis: Check the stability of the network structure using methods like bootstrapping.
- Interpretation: Identify central food items that may play a key role in the dietary pattern. However, the review notes that 72% of studies employing centrality metrics did not acknowledge their limitations, so conclusions should be drawn cautiously [11].
Research Reagent Solutions: Essential Materials for Dietary Pattern Research
The following table details key tools and databases essential for conducting high-quality research in this field.
| Item Name | Function / Application | Key Features |
|---|---|---|
| Food and Nutrient Database for Dietary Studies (FNDDS) [17] | Provides the energy and nutrient values for foods and beverages reported in dietary surveys. | Contains data for energy and 64 nutrients for ~7,000 foods; essential for nutrient analysis in studies like What We Eat in America (WWEIA), NHANES [17]. |
| Food Pattern Equivalents Database (FPED) [17] | Converts foods and beverages into USDA Food Patterns components (e.g., cup equivalents of fruits, ounce equivalents of whole grains). | Used to examine food group intakes and assess adherence to Dietary Guidelines recommendations; crucial for dietary pattern analysis [17]. |
| 24-Hour Dietary Recalls (24HR) [15] [17] | A reference method for dietary assessment that captures detailed intake over the previous 24 hours. | Uses multiple-pass method to enhance accuracy; less prone to systematic error than FFQs; used for validation and in NHANES [15] [17]. |
| Biomarkers (Serum/Urine) [15] [16] | Objective biological measures used to validate self-reported dietary intake. | Examples: serum folate, fatty acids, urinary nitrogen and sodium. Provide an objective measure to triangulate with FFQ and 24HR data [15] [16]. |
| Multi-Objective Optimization (MOO) Algorithms [13] | Computational tools to simultaneously optimize multiple, competing objectives (e.g., nutrient adequacy and environmental sustainability). | Generates a spectrum of optimal trade-offs; identifies synergies between dietary dimensions without requiring a priori decisions on their relative importance [13]. |
Conceptual Diagrams
From Data to Dietary Patterns: An Analytical Workflow
This diagram visualizes the pathway from raw dietary data to the identification and interpretation of complex dietary patterns, integrating key methodologies discussed in the FAQs and protocols.
The Synergistic Relationship of Key Dietary Dimensions
This diagram illustrates the interconnected relationship between three critical dimensions of a sustainable and healthy diet, as identified by multi-objective optimization research.
FAQ: Understanding FFQ Limitations and Their Impact on Research
Q1: What are the primary types of measurement error introduced by FFQs?
Food Frequency Questionnaires (FFQs) are susceptible to several measurement errors that can distort diet-disease relationships. The main types of error include:
- Recall Bias: Participants inaccurately remember the type or frequency of foods consumed over a long period (e.g., the past year) [18] [19].
- Systematic Bias: This includes under-reporting of foods perceived as "unhealthy" (e.g., high-fat foods like bacon and fried chicken) and over-reporting of foods perceived as "healthy" [20] [6] [19]. This is also known as social desirability bias.
- Misclassification: The structure of FFQs, which often group foods and use fixed portion sizes, can lead to incorrect categorization of individuals' true usual intake. This is particularly problematic for ranking subjects in epidemiological studies [18] [19].
Q2: How do these errors ultimately affect the analysis of diet-disease relationships?
These errors do not just add noise; they introduce bias that can obscure or distort true relationships. The primary consequences are:
- Attenuation of Risk Estimates: Correlation coefficients and relative risks (e.g., Hazard Ratios) are biased towards the null value, making real associations between diet and disease appear weaker than they truly are [21] [22].
- Loss of Statistical Power: The increased variability from measurement error makes it more difficult to detect statistically significant associations, potentially causing important findings to be missed [19].
- Erroneous Conclusions: In severe cases, the combined effect of attenuation and misclassification can lead to completely false conclusions about the presence or absence of a relationship [18].
Q3: Aren't biomarkers the ultimate solution for validating FFQ data?
Biomarkers are a powerful tool but are not a perfect gold standard. Their utility varies greatly:
- High-Valued Correlations: Some biomarkers show strong correlations with intake. For example, adipose tissue levels of linoleic acid (18:2 ω-6) correlated at 0.72 with dietary intake, and urinary 1-methyl-histidine for meat consumption correlated at 0.69 [21].
- Moderate to Low-Valued Correlations: Many other biomarkers, such as those for certain vitamins and carotenoids, show only moderate (0.30-0.49) or poor correlations with FFQ-reported intake [21] [16].
- Inherent Limitations: Biomarkers are influenced by individual differences in absorption, metabolism, and homeostatic regulation, meaning their levels cannot always be directly translated into absolute dietary intake [18] [21]. A study on patients with Peripheral Arterial Disease (PAD) found poor agreement between FFQ-reported intake and serum levels of vitamins A, C, D, E, zinc, and iron, suggesting disease-specific physiology can further decouple intake from biomarker levels [16].
Troubleshooting Guide: Mitigating Specific FFQ Issues
Table 1: Common FFQ Issues and Direct Mitigation Strategies
| Problem | Impact on Data | Recommended Mitigation Strategy | Key Considerations |
|---|---|---|---|
| Under-Reporting of Unhealthy Foods | Attenuates positive associations with disease risk (e.g., saturated fat and heart disease). | Machine Learning Reclassification: Use objective measures (LDL, BMI, body fat %) to train a model (e.g., Random Forest) to identify and correct implausible responses [20] [6]. | Requires a subset of participants with objective biomarker and anthropometric data. Model accuracy demonstrated from 78% to 92% [6]. |
| Inability to Capture Usual Intake | High day-to-day variation obscures long-term exposure. | Combine Instruments: Use the FFQ to rank individuals, but calibrate using multiple 24-Hour Recalls (24HR) in a subset [18] [22]. | 24HRs are considered less biased but require multiple (non-consecutive) administrations to estimate usual intake [19] [22]. |
| Systematic Bias (Social Desirability) | Overall energy and nutrient intake is under-reported. | Biomarker-Guided Regression Calibration: Use recovery biomarkers (energy, protein) to correct for systematic bias in reported intake [21] [22]. | Recovery biomarkers exist only for energy, protein, potassium, and sodium. They are expensive to measure [19] [22]. |
| Use of Generic Food Composition Databases | Inaccurate nutrient assignment, especially across different cultures and food varieties. | Leverage Specialized Databases: Use targeted databases (e.g., FAO/INFOODS for regional, biodiversity, or pulses data) to improve nutrient estimation [23] [24]. | Nutrient content can vary up to 1000-fold among varieties of the same food, making database specificity critical [24]. |
Protocol 1: Machine Learning Workflow for Correcting Under-Reporting
This protocol is based on a published method that uses a Random Forest (RF) classifier to mitigate under-reporting of specific food items [20] [6].
1. Objective: To correct for under-reported entries of specific foods (e.g., high-fat items) in an FFQ dataset. 2. Materials and Input Data:
- FFQ Data: The complete dataset, including the specific food items to be corrected.
- Objective Covariates: Data with low measurement error, such as:
- Blood biomarkers (LDL cholesterol, total cholesterol, blood glucose)
- Anthropometric measures (Body Mass Index, body fat percentage from DXA)
- Demographics (age, sex) 3. Procedure:
- Step 1 - Data Segmentation: Split the dataset into a "Healthy" group and an "Unhealthy" group based on objective health risk cut-offs (e.g., body fat percentage, age, and sex) [6]. The underlying assumption is that the "Healthy" group is more likely to report their intake accurately.
- Step 2 - Model Training: Train a Random Forest classification model using the "Healthy" group data. The model learns the relationship between the objective covariates (e.g., LDL, BMI) and the FFQ responses for the target foods.
- Step 3 - Prediction and Adjustment: Apply the trained model to the "Unhealthy" group to predict their expected (and likely more accurate) food intake category.
- Adjustment Rule: For an unhealthy food item, if the originally reported FFQ value is lower than the model's predicted value, replace the original value with the predicted value. The reported value is kept unchanged if it is higher than the prediction [6].
The following diagram illustrates this workflow:
Protocol 2: Biomarker-Guided Regression Calibration
This statistical protocol uses biomarkers to correct measurement error in diet-disease risk models [21].
1. Objective: To correct the regression coefficient (β) for a dietary variable in a disease risk model, reducing attenuation caused by FFQ measurement error. 2. Materials:
- Primary Study Data: FFQ (Q) and disease outcome data for the entire cohort.
- Calibration Substudy Data: A representative sample from the cohort with data from:
- Two different dietary biomarkers (M1, M2) of the nutrient of interest.
- The FFQ (Q). 3. Key Assumptions: Errors in the two biomarkers are independent of each other and independent of errors in the FFQ. Using long half-life biomarkers (e.g., adipose tissue for fatty acids) helps meet these assumptions [21]. 4. Procedure:
- Step 1: In the calibration subsample, perform a regression of the first biomarker (M1) on the FFQ (Q) and the second biomarker (M2). The second biomarker acts as a surrogate for true intake to account for the error in M1.
- Step 2: Use the regression parameters from Step 1 to predict the expected value of the biomarker M1 (which is a proxy for true intake) for everyone in the main cohort.
- Step 3: In the disease risk model for the full cohort, replace the error-prone FFQ values (Q) with the predicted values from Step 2. The resulting regression coefficient for the dietary variable is the error-corrected estimate.
The logical relationship for selecting a calibration method is shown below:
| Category | Resource / Reagent | Function in Research | Specific Example / Note |
|---|---|---|---|
| Reference Dietary Instruments | 24-Hour Dietary Recall (24HR) | Serves as a less-biased reference method to validate or calibrate FFQ data. Can be interviewer-administered or automated (e.g., ASA-24) [18] [22]. | The Automated Multiple-Pass Method (AMPM) used in NHANES is a standardized approach [18]. |
| Objective Biomarkers | Recovery Biomarkers | Provide an unbiased estimate of true intake for a few specific nutrients. Used to quantify and correct for systematic bias in self-reports [19] [22]. | Only available for energy (doubly labeled water), protein (urinary nitrogen), potassium, and sodium (urinary excretion) [19]. |
| Concentration Biomarkers | Act as objective indicators of intake or exposure for a wider range of nutrients, though influenced by metabolism [21]. | Adipose tissue fatty acids, serum carotenoids, urinary isoflavones [21]. Correlations with intake can vary from poor to high. | |
| Food Composition Data | FAO/INFOODS Databases | Provide region-specific and food-specific nutrient data crucial for accurately converting food intake to nutrient values [23] [24]. | Examples include the Global Food Composition Database for Fish and Shellfish (uFiSh1.0) and the database for Biodiversity (BioFoodComp4.0) [23]. |
| Statistical & Computational Tools | Regression Calibration | A standard statistical method to correct attenuation bias in relative risks using data from a calibration study [21] [6]. | Can be implemented using standard statistical software (e.g., R, SAS). |
| Machine Learning Classifiers (Random Forest) | A modern computational approach to identify and correct for misreporting (under/over) in categorical FFQ data [20] [6]. | Demonstrated to operate independently of specific diet-disease models, reducing noise in the FFQ data itself [6]. |
Building Better Tools: Methodological Innovations for Robust FFQ Design
Technical Support Center: Food Frequency Questionnaire (FFQ) Troubleshooting
Frequently Asked Questions (FAQs)
FAQ 1: How do we create a food list that is representative of our specific study population?
Creating a representative food list is the most critical step in developing a culturally valid FFQ. The process must be systematic and evidence-based.
Recommended Protocol:
- Conduct a Preliminary Dietary Survey: Use open-ended methods like 24-hour dietary recalls or food records within your target population to identify commonly consumed foods [18].
- Review Existing Cultural Resources: Consult local cookbooks, market surveys, and previously published dietary studies in your region to compile a comprehensive list of traditional and popular dishes [25].
- Engage Local Experts: Form a panel of local nutrition professionals to review the draft food list for cultural relevance, religious dietary laws (e.g., Halal), and commonality of food items [25].
- Perform Market Research: Visit local supermarkets and community food stores to verify the availability of processed and branded food items, ensuring the list reflects what is actually consumed [25].
Troubleshooting Tip: If your population is multi-ethnic, ensure the food list captures the unique dietary habits of all major ethnic groups to avoid measurement error and misclassification.
FAQ 2: What is the best way to validate our newly developed or adapted FFQ?
Validation is essential to confirm that your FFQ accurately measures what it is intended to measure. The choice of a reference method is key.
Recommended Protocol: The standard approach involves comparing nutrient or food group intake estimates from your FFQ against a more precise reference method. The table below summarizes validation metrics from recent case studies.
Troubleshooting Tip: Always assess both validity (comparison against a reference method) and reliability (test-retest reproducibility) to ensure your FFQ is both accurate and consistent.
Table 1: Validation Metrics from Recent FFQ Adaptation Studies
| Country / Region | Reference Method Used | Key Statistical Results | Citation |
|---|---|---|---|
| Oman | Test-Retest Reliability | Weighted Kappa (frequency): 0.38 - 0.60; Intraclass Correlation Coefficients (ICCs): 0.57 - 0.80 | [25] |
| Italy (Adolescents) | 3-Day Food Diary | Adjusted Spearman Correlations: Legumes/Vegetables (>0.5), Meat/Fruits (>0.4), Fish/Bread (variable, improved with age stratification) | [26] |
| Trinidad & Tobago | 4x Food Records + Digital Images | Correlation Coefficients for Nutrients: Carbohydrates (r=0.83), Vitamin C (r=0.59); Cross-classification agreement for fiber/Vitamin A: 89% | [27] |
FAQ 3: Our FFQ data seems to have a high degree of under-reporting, particularly for unhealthy foods. How can we mitigate this?
Under-reporting of energy-dense or "unhealthy" foods is a common form of measurement error in self-reported dietary data [6].
- Recommended Protocol: A Machine Learning Adjustment Workflow A novel method to correct for this bias uses a supervised machine learning model, such as a Random Forest (RF) classifier, to identify and adjust likely under-reported entries [6]. The workflow is as follows:
- Troubleshooting Tip: This method requires a dataset that includes both FFQ responses and objective health biomarkers (e.g., blood lipids, body fat percentage) to function effectively [6].
FAQ 4: How can we effectively incorporate portion size estimation without over-burdening respondents?
The ability of respondents to accurately assess portion sizes is often limited. The choice between a qualitative and semi-quantitative FFQ must be deliberate.
Recommended Protocol:
- Use Visual Aids: Provide photographs of different portion sizes (small, medium, large) for common foods and dishes to help respondents estimate quantities [26] [28].
- Standardized Frequency Factors: For a semi-quantitative FFQ, use pre-defined standard portion sizes. For example, one serving of fruit could be defined as "one medium apple or a half-cup of chopped fruit" [29].
- Pilot Testing: Conduct a pilot study to test the clarity and usability of your portion size questions and visual aids with a small sample from your target population [30].
Troubleshooting Tip: For large epidemiological studies where ranking individuals by intake is the primary goal, a qualitative FFQ (without portion sizes) can be sufficient and significantly reduces participant burden [29].
The Scientist's Toolkit: Key Research Reagents & Materials
Table 2: Essential Reagents and Tools for FFQ Adaptation and Validation
| Item Name / Concept | Function / Application in FFQ Research |
|---|---|
| 24-Hour Dietary Recall (24HR) | An open-ended interview used as a reference method for validation studies. It collects detailed intake data over the previous 24 hours and is used to check the accuracy of the FFQ [18] [28]. |
| Food Composition Table/Database | A software or data table that links each food item on the FFQ to its nutrient content. It is essential for converting frequency data into estimates of nutrient intake [26] [31]. |
| Statistical Validation Metrics | A suite of statistical tests (Correlation Coefficients, Kappa statistics, Intraclass Correlation Coefficients - ICCs) used to quantitatively assess the agreement between the FFQ and the reference method [25] [26] [27]. |
| Digital Data Collection Platform | Tools like REDCap, Google Forms, or other web-based platforms used to administer the FFQ electronically. This reduces data entry errors, facilitates data collection from diverse locations, and can improve data quality [27] [31]. |
| Block 2005 / DHQ II / EPIC COS FFQ | Examples of well-established, pre-validated FFQs that are often used as a starting point or template for cultural adaptation, saving development time and resources [25] [26] [6]. |
| Octadeca-9,17-diene-12,14-diyne-1,11,16-triol | Octadeca-9,17-diene-12,14-diyne-1,11,16-triol, CAS:211238-60-7, MF:C18H26O3, MW:290.4 g/mol |
| Ribociclib D6 | Ribociclib D6, MF:C23H30N8O, MW:440.6 g/mol |
Detailed Experimental Protocols
Protocol 1: Comprehensive FFQ Validation Study Design
This protocol outlines the steps for a robust validation study, as implemented in the Italian and Caribbean case studies [26] [27].
- Participant Recruitment: Recruit a convenience sample of at least 100-200 participants from the target population. The sample should reflect the age, sex, and ethnic diversity of the larger study cohort [26] [30].
- FFQ Administration: Administer the new FFQ to all participants. The FFQ should be designed to assess habitual dietary intake over the previous year [26] [28].
- Reference Method Administration:
- Test-Retest Reliability: Re-administer the FFQ to the same participants after a suitable interval (e.g., 3-10 months) to assess its reproducibility over time [27] [30].
- Data Analysis: Calculate correlation coefficients, cross-classification tables, and measures of agreement (e.g., ICCs) to compare the intake of nutrients and food groups derived from the FFQ with those from the reference method.
Protocol 2: Cultural Adaptation of an Existing FFQ
This protocol is based on the successful development of the Omani FFQ (OFFQ) [25].
- Selection of a Base FFQ: Choose a well-validated, comprehensive FFQ from the literature (e.g., the Diet History Questionnaire II from the US National Cancer Institute) [25].
- Initial Item Review: Have nutrition experts independently review each food item on the base FFQ for cultural and religious relevance to the new population. Remove, modify, or add items as needed.
- Translation: Translate the modified FFQ into the target language. Perform a back-translation into the original language to ensure conceptual and linguistic accuracy [25] [32].
- Pilot Testing and Refinement: Administer the translated FFQ to a small sample from the target population. Use qualitative feedback to identify confusing items, portion size estimations, or missing foods. Refine the questionnaire accordingly.
- Formal Validation: Subject the final adapted FFQ to a formal validation study, as detailed in Protocol 1.
Technical Support Center: Troubleshooting Guides and FAQs
This section addresses common methodological challenges researchers face when developing and validating targeted Food Frequency Questionnaires (FFQs).
Frequently Asked Questions
Q1: How can I overcome the low accuracy of FFQs for sporadically consumed foods, such as many fermented products?
A: This is a recognized limitation when using generic FFQs. The solution is to develop a targeted FFQ that uses specific, culturally relevant examples and visual aids.
- Recommended Protocol: Develop a food-specific FFQ, like the Fermented Food Frequency Questionnaire (3FQ). The 3FQ stratifies foods into 16 major groups and uses validated food pictures (a "food atlas") to help participants identify and quantify their usual portions. For fermented foods, it further breaks down categories into specific, common examples (e.g., under "hard cheese," listing Parmigiano for Italy and Graviera for Greece) to trigger more accurate recall [33] [34].
Q2: What is the best way to classify ultra-processed foods (UPFs) when the NOVA system has known limitations?
A: A critical reassessment and modification of the NOVA system is recommended. One effective approach is to combine the level of processing with nutritional profile data.
- Recommended Protocol: Develop a modified NOVA (mNOVA) classification. In this system, processed foods (Group 3) and UPFs (Group 4) are subdivided based on thresholds for salt, sugar, and fat as recommended by the Food Standard Agency (FSA). This creates subgroups (e.g., 3a, 3b, 4a, 4b) and adds a nutritional dimension to the purely processing-based classification, leading to a more precise categorization of foods [30].
Q3: How can I correct for measurement errors, such as underreporting of unhealthy foods, in my FFQ data?
A: Supervised machine learning methods can be employed to identify and adjust for systematic reporting errors.
- Recommended Protocol: Use a Random Forest (RF) classifier. This method uses objectively measured variables (e.g., blood lipids, BMI, age, sex) from a subset of "healthy" participants to train a model that predicts food intake. This model is then applied to the wider dataset. If a participant's reported intake of an unhealthy food is lower than the model's prediction, the value is adjusted upward to correct for probable underreporting [6].
Q4: How do I validate a new targeted FFQ to ensure its reliability for population studies?
A: A robust validation study must assess both reproducibility (repeatability) and criterion validity (accuracy).
- Recommended Protocol:
- Reproducibility: Administer the FFQ twice to the same participants at a predefined interval (e.g., 6 weeks to 10 months). Calculate Intra-Class Correlation (ICC) coefficients to measure test-retest reliability [30] [33].
- Criterion Validity: Compare intake data from the FFQ against a reference method, such as multiple 24-hour dietary recalls or a weighed dietary record, collected from the same participants. Use Spearman's correlation coefficients and Bland-Altman plots to assess the level of agreement between the two methods [30] [7] [33].
Q5: What are the key considerations for designing an FFQ for multi-country or multi-ethnic cohorts?
A: Cross-cultural adaptability is paramount. The tool must capture region-specific foods and consumption habits without sacrificing data comparability.
- Recommended Protocol:
- Develop a Universal Core: Create a base FFQ in a common language (e.g., English) with broad food groups.
- Localize with Examples: Populate these groups with country-specific food examples (e.g., different types of fermented vegetables or cheeses).
- Standardize Translation: Use a back-translation method to ensure conceptual equivalence across different language versions.
- Use Visual Aids: Employ picture atlases with standardized portion sizes to overcome language and educational barriers [34] [35].
Summarized Quantitative Data from Validation Studies
The table below summarizes key metrics from recent validation studies for targeted FFQs, providing benchmarks for researchers.
Table 1: Validation Metrics for Targeted Food Frequency Questionnaires
| FFQ Focus & Study | Validation Measure | Results / Correlation Coefficients | Key Findings |
|---|---|---|---|
| General Food Groups [35] | Validity (FFQ vs. 24-hr Recall) | Weakest: Fresh Juice, Other Meats (0.23-0.32)Moderate: Red Meat, Chicken, Eggs (0.42-0.59)Strongest: Tea, Sugars, Grains, Fats/Oils (0.60-0.79) | The FFQ is appropriate for ranking individuals by intake of most food groups. |
| PERSIAN Cohort FFQ [35] | Reproducibility (FFQ1 vs. FFQ2) | Range: 0.42 (Legumes) to 0.72 (Sugar & Sweetened Drinks) | Showed moderate to strong reproducibility for all food groups over a 12-month interval. |
| Fermented Foods (3FQ) [33] | Repeatability (ICC) | Most Groups: 0.4 to 1.0Infrequent Items: Lower (e.g., Fermented Fish) | High repeatability for most fermented food groups, with challenges for rarely consumed items. |
| Fermented Foods (3FQ) [33] | Validity (vs. 24-hr Recall) | Agreement within Intervals: >90% for most groupsStrongest Agreement: >95% for Dairy, Coffee, Bread | Excellent agreement with 24-hour recalls for frequently consumed fermented foods. |
| 3-day Food Records [7] | Validity (vs. 9-day Records) | Pearson's Correlation Range: 0.14 to 0.56 | 3-day records showed higher correlations with reference method than the FFQ did. |
Experimental Protocols for Key Methodologies
Protocol 1: Validating a Targeted FFQ for Ultra-Processed Foods
This protocol is adapted from a study designed to develop and validate a UPF-focused FFQ for the Italian population [30].
1. Study Design:
- A two-phase, multicenter study.
- Phase 1 (Pilot): Investigate current food consumption via 24-hour dietary recalls and test the face validity of the draft FFQ (n=20-50).
- Phase 2 (Validation): Assess criterion validity and reproducibility in a larger sample (n≥436).
2. Population:
- Recruit healthy adults (≥18 years) from workplaces/universities.
- Exclude individuals with chronic diseases, restrictive diets, or who are pregnant/lactating.
3. Dietary Assessment:
- FFQ Administration: A self-administered, semi-quantitative FFQ designed to distinguish between industrial, artisanal, and home-made products.
- Reference Method: Participants complete a 7-day weighed dietary record (WDR) after each FFQ administration.
- Reproducibility: Administer the FFQ twice, with an interval of 3-10 months (test-retest).
4. Data Analysis:
- Criterion Validity: Compare nutrient and UPF intake data from the first FFQ against the two WDRs.
- Reproducibility: Compare UPF intake data from the first and second FFQ administrations.
Protocol 2: Machine Learning Adjustment for FFQ Underreporting
This protocol outlines the method for using a Random Forest classifier to correct measurement error [6].
1. Data Preparation:
- Obtain a dataset containing FFQ responses, demographic data (age, sex), and objective clinical biomarkers (LDL cholesterol, total cholesterol, blood glucose, body fat percentage, BMI).
2. Classifier Training:
- Split the dataset into "Healthy" and "Unhealthy" groups based on clinical cut-offs for biomarkers.
- Use the data from the "Healthy" group to train a Random Forest model. The model learns the relationship between the objective biomarkers (input features) and the FFQ responses (output labels).
3. Error Adjustment Algorithm:
- Apply the trained model to the "Unhealthy" group to predict their expected FFQ responses based on their biomarkers.
- Compare the model's prediction to the participant's actual self-reported intake.
- For unhealthy foods (e.g., bacon, fried chicken): If the self-reported value is lower than the predicted value, replace it with the predicted value to correct for underreporting.
Workflow and Pathway Diagrams
FFQ Development and Validation Workflow
Machine Learning Error Correction Process
The Scientist's Toolkit: Key Research Reagents & Materials
| Item / Resource | Function & Application in FFQ Research |
|---|---|
| Validated Food Atlas / Portion Size Pictures | Visual aids to improve the accuracy of portion size estimation by participants. Crucial for cross-cultural studies and for quantifying fermented foods and ready-to-eat UPFs [33] [35]. |
| Modified NOVA (mNOVA) Classification | A food classification system that combines processing level with nutritional thresholds (e.g., for fat, sugar, salt). Provides a more precise tool for categorizing and analyzing UPF intake than NOVA alone [30]. |
| 24-Hour Dietary Recalls (24-hr) | A short-term dietary assessment method used as a "gold standard" reference to validate the criterion validity of a new FFQ. Multiple recalls are needed to account for day-to-day variation [30] [7] [33]. |
| Weighed Dietary Record (WDR) | Another reference method where participants weigh and record all consumed foods and beverages. Provides highly detailed intake data for validation studies but is burdensome for participants [30]. |
| Random Forest Classifier | A supervised machine learning algorithm used to identify and correct for systematic reporting errors (e.g., underreporting of unhealthy foods) in existing FFQ datasets [6]. |
| Harvard FFQ & Nutrient Database | A well-established, extensively validated semi-quantitative FFQ and database. Serves as a strong methodological foundation and can be adapted for developing new targeted questionnaires [31]. |
| Clinical Biomarkers | Objective measures (e.g., blood lipids, blood glucose, BMI) used to train machine learning models for error correction or to provide ancillary validation of FFQ-derived dietary patterns [6]. |
| NOS1-IN-1 | NOS1-IN-1, CAS:357965-99-2, MF:C14H24F9N7O8, MW:589.37 g/mol |
| rac-2-Aminobutyric Acid-d3 | rac-2-Aminobutyric Acid-d3, CAS:1219373-19-9, MF:C4H9NO2, MW:106.14 g/mol |
Technical Support Center: Troubleshooting Guides and FAQs
This section addresses common technical and methodological challenges researchers face when implementing web-based and electronic Food Frequency Questionnaires (e-FFQs).
Frequently Asked Questions (FAQs)
Q1: Our study population has diverse dietary cultures. How can we ensure the e-FFQ accurately captures all relevant foods?
A: Implement a data-driven, culturally-specific development process. This involves:
- Preliminary Dietary Data Collection: Use 24-hour dietary recalls from your target population to identify commonly consumed foods [36] [37].
- Statistical Selection: Employ stepwise regression analysis on the recall data to identify the foods that contribute most significantly (>90%) to the variance in intake of key energy and nutrients [36].
- Include Local and Street Foods: Actively add culturally specific dishes and street foods to the food list, as demonstrated in the Trinidad and Tobago e-FFQ, which included 14 such items [37].
Q2: Participant compliance is low for our current dietary assessment tool. What features can improve user engagement?
A: Leverage the inherent advantages of e-FFQs and add user-centric features.
- Self-Administration & Automation: Web-based FFQs allow participants to complete surveys at their convenience, reducing the burden on research staff and minimizing data entry errors [36] [38].
- Visual Aids: Integrate graphical elements, such as multiple portion size pictures, to improve estimation accuracy and user-friendliness [38].
- Adaptive Design: Use complex skip patterns to show only relevant questions, shortening completion time and reducing fatigue [38].
Q3: We are concerned about measurement error, particularly underreporting of unhealthy foods. Can technology help mitigate this?
A: Yes, advanced computational methods can be applied to adjust for reporting biases.
- Machine Learning Correction: One proposed method uses a Random Forest classifier to identify potentially misreported entries. The model is trained on data from participants assumed to be accurate reporters (e.g., those classified as "healthy" based on objective biomarkers) and then predicts expected intake values for others. An error adjustment algorithm can then correct underreported entries for unhealthy foods [6].
Q4: How can we validate a newly developed or adapted e-FFQ for our specific study population?
A: Validation is critical and follows a standard protocol comparing the e-FFQ against a reference method.
- Reference Methods: Common reference methods include multiple 24-hour dietary recalls (24HDR) or food records (FR) [39] [37] [35].
- Assessment Metrics: Evaluate both validity (how well the e-FFQ measures what it should) and reproducibility (its consistency over time).
- Validity: Compare the e-FFQ against the reference method using correlation coefficients (e.g., Spearman) and cross-classification analysis (percentage of participants classified into the same or adjacent tertile/quintile) [39] [37] [35].
- Reproducibility (Reliability): Administer the same e-FFQ twice to participants with a time interval (e.g., 1 month). Assess agreement using intraclass correlation coefficients (ICCs) and weighted Kappa statistics [39].
Troubleshooting Common Technical Issues
| Problem | Possible Cause | Solution |
|---|---|---|
| Low completion rates | Long, tedious questionnaire; complex interface. | Shorten the food list using data-driven methods [36] [35]; use adaptive questioning and a mobile-friendly design. |
| Implausible energy intake values | Portion size misestimation; misunderstanding of questions. | Use validated portion size pictures and household measures [39] [35]; include clear instructions and tooltips. |
| Poor agreement with reference method for specific food groups | Food list is not representative; recall bias for certain foods. | Re-evaluate and refine the food list based on local consumption [37] [35]; consider using short, repeated recalls for better accuracy [40]. |
| Technical errors in data export | Software bugs; improper database linking. | Perform pilot testing of the entire data pipeline; ensure the e-FFQ platform is securely integrated with the food composition database. |
Experimental Protocols for e-FFQ Validation
The following table summarizes the core methodologies used in recent studies to validate e-FFQs, providing a template for researchers.
| Study (Population) | e-FFQ Items | Reference Method | Validation & Reliability Metrics |
|---|---|---|---|
| Swiss eFFQ [36] | 83 items | Two non-consecutive 24h dietary recalls | Validity: Food list created via stepwise regression to explain >90% variance in key nutrient intake. |
| Trinidad & Tobago [37] | 139 items | Four 1-day food records (using smartphone photos) | Validity: Energy-adjusted deattenuated correlations; cross-classification.Reliability: Test-retest correlation (3-month interval). |
| PERSIAN Cohort [35] | 113 core + local items | Two 24h recalls/month for 12 months | Validity: Correlation between FFQ and 24h recalls.Reliability: Correlation between two FFQs (12-month interval). |
| Fujian, China [39] | 78 items | Three-day 24h dietary recall | Validity: Spearman correlation, Bland-Altman plots, cross-classification into tertiles.Reliability: ICC and weighted Kappa for two FFQs (1-month interval). |
| Charité-14 Item FFQ [41] | 14 items | Weighted food records | Validity: Method agreement analysis (Bland-Altman) and correlation for specific food groups and habits. |
The Scientist's Toolkit: Essential Research Reagents & Materials
| Item | Function in e-FFQ Research | Example / Specification |
|---|---|---|
| 24-Hour Dietary Recalls (24HDR) | Serves as a reference method for validating the e-FFQ and for data-driven development of the food list. | Use multiple, non-consecutive recalls (e.g., two 24HDRs) [36]. Software like GloboDiet or Automated Multiple-Pass Method (AMPM) can standardize collection [18] [36]. |
| Food Composition Database | Converts food consumption data from the e-FFQ into estimated nutrient intakes. | Must be tailored to the study population's specific foods and recipes. Databases are often national (e.g., USDA, Swiss Food Composition Database). |
| Portion Size Estimation Aids | Improves the accuracy of self-reported food quantities in a semi-quantitative FFQ. | Picture albums with standardized portions [35], digital images, household measure descriptions (cups, spoons), or 3D food models [18]. |
| Biomarker Data | Provides an objective measure to help correct for reporting bias (e.g., under-reporting). | Biomarkers like LDL cholesterol, total cholesterol, and blood glucose can be used in machine learning models to identify misreporting of related foods [6]. |
| Professional Dietary Analysis Software | Used to code and analyze data from reference methods like food records. | Software such as PRODI is used to input and calculate nutrient intake from detailed food records [41]. |
| Alisol B 23-acetate | Alisol B 23-acetate, CAS:19865-76-0, MF:C32H50O5, MW:514.74 | Chemical Reagent |
| (-)-Catechol | 2-(3,4-Dihydroxyphenyl)chroman-3,5,7-triol|(±)-Catechin |
Experimental Workflow Diagram
The diagram below visualizes the end-to-end process for developing and validating a culture-specific e-FFQ.
Diagram Title: e-FFQ Development and Validation Workflow
Frequently Asked Questions (FAQs)
Q1: Why can't I just use an FFQ by itself in my research? While Food Frequency Questionnaires (FFQs) are excellent for ranking individuals based on their long-term dietary habits, they are known for containing measurement errors, including systematic underreporting. It has been demonstrated that all self-report tools involve some misreporting, with FFQs underestimating energy intake by 29–34% on average, a greater degree than other methods [42]. Integrating FFQs with more precise short-term methods, like 24-hour recalls, allows researchers to calibrate the FFQ data and improve the accuracy of habitual intake estimates [15] [6].
Q2: How many 24-hour recalls are needed to properly validate an FFQ? There is no one-size-fits-all number, but best practices suggest multiple recalls collected over different seasons to account for day-to-day and seasonal variations. One major validation study conducted twenty-four 24-hour recalls per participant over twelve months to serve as a robust reference method [15]. Another study used multiple 24-hour recalls and found they provided better estimates of absolute dietary intakes than FFQs alone [42]. The key is to collect enough recalls to reliably estimate a person's "usual intake."
Q3: What is the main type of error I should look for in FFQ data? Underreporting is the most common and significant error, particularly for energy-dense foods and certain nutrients. This is frequently observed in studies that compare self-reported data with recovery biomarkers [42] [6]. For instance, one study focusing on high-fat foods like bacon and fried chicken used a machine learning model to successfully identify and correct for this underreporting [6].
Q4: Can new technologies like AI help with the limitations of FFQs? Yes, Artificial Intelligence (AI) and Machine Learning (ML) present promising avenues for mitigating errors in dietary data. These methods can be used to create error adjustment algorithms. For example, a random forest classifier has been used to identify underreported entries in an FFQ with high accuracy (78% to 92%), demonstrating the potential to correct data without solely relying on additional resource-intensive calibration methods [6].
Troubleshooting Guides
Problem: Systematic underreporting of energy and nutrient intakes in FFQ data. Solution:
- Calibrate with Reference Methods: Use the data from multiple 24-hour recalls or food records to calibrate your FFQ data. This can involve statistical techniques like regression calibration, which uses the relationship between the FFQ and the more accurate reference method to correct the FFQ values [6].
- Leverage Biomarkers: Where possible, incorporate objective biomarkers. For example, use doubly labeled water for energy intake and 24-hour urinary nitrogen and potassium for their respective nutrient intakes. The "triad method" compares FFQs, reference dietary methods, and biomarkers to assess validity [15] [42].
- Implement Machine Learning: For large datasets, consider a supervised machine learning approach. The workflow involves training a model (e.g., a random forest classifier) on data from participants assumed to be accurate reporters. This model can then predict likely intake values for other participants based on objective health metrics (like cholesterol levels or BMI), and an algorithm can adjust underreported entries [6].
Problem: My FFQ and 24-hour recall data show poor correlation for specific nutrients. Solution:
- Investigate the Nutrient: Some nutrients are more challenging to measure than others. For example, one study found that vitamins B6 and B12 were poorly correlated between FFQs and 24-hour recalls, while correlations for many other micronutrients were moderate to high [15]. Consult existing validation literature for your specific FFQ to set realistic expectations.
- Check Your Food Composition Table: Inconsistencies can arise from using different nutrient databases for the FFQ and the reference method. A meta-analysis found that when mobile diet records and their reference method used the same food-composition table, heterogeneity in energy intake estimation dropped to 0%, and the mean difference was negligible [43]. Always strive for database consistency.
- Increase Number of Recalls: Poor correlation may simply be due to high within-person variation for that nutrient, which isn't fully captured by your number of recall days. Increasing the number of 24-hour recalls can improve the reliability of your reference method for that nutrient.
Problem: High participant burden leads to dropouts or incomplete food records. Solution:
- Use Technology: Employ user-friendly, automated self-administered 24-hour recall systems (ASA24s). Research shows that multiple ASA24s are a feasible means to collect high-quality dietary data and can provide better estimates of absolute intake than FFQs [42].
- Optimize Protocol: While ideal, completing 24 recalls over a year may not be feasible. A well-designed protocol with non-consecutive, seasonal 3-day food records (including one weekend day) can capture variation while being less burdensome [7]. Clear communication and training for participants are vital for compliance.
Quantitative Data from Validation Studies
Table 1: Correlation Coefficients between FFQs and Multiple 24-Hour Recalls [15]
| Nutrient | Correlation with FFQ1 | Correlation with FFQ2 |
|---|---|---|
| Energy | 0.57 | 0.63 |
| Protein | 0.56 | 0.62 |
| Lipids (Fats) | 0.51 | 0.55 |
| Carbohydrates | 0.42 | 0.51 |
This data shows that the PERSIAN Cohort FFQ has acceptable reproducibility (FFQ1 vs. FFQ2) and moderate correlation with the reference method for most macronutrients. [15]
Table 2: Average Underreporting of Energy Intake Compared to Biomarkers [42]
| Dietary Assessment Method | Average Underestimation of Energy |
|---|---|
| Automated 24-hour Recalls (ASA24) | 15–17% |
| 4-Day Food Records (4DFR) | 18–21% |
| Food Frequency Questionnaire (FFQ) | 29–34% |
This study highlights the systematic underreporting inherent in all self-report methods, with FFQs showing the greatest degree of underestimation when checked against the doubly labeled water method. [42]
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Key Tools for Integrating Dietary Assessment Methods
| Item | Function in Research |
|---|---|
| Validated FFQ | The core tool for assessing long-term, habitual dietary intake in large epidemiological studies. It must be validated for the specific population being studied [15] [42]. |
| 24-Hour Dietary Recall Protocol | A structured interview or automated system (e.g., ASA24) used as a reference method to collect detailed intake from the previous day, reducing long-term recall bias [15] [42]. |
| Food Record/Diary | A tool where participants prospectively record all foods and beverages consumed over a specific period (e.g., 3-4 days), providing detailed data without relying on memory [7]. |
| Recovery Biomarkers | Objective biological measurements used to validate reported intakes of specific nutrients. Examples include Doubly Labeled Water for energy, 24-Hour Urinary Nitrogen for protein, and 24-Hour Urinary Sodium & Potassium [15] [42]. |
| Food Composition Database | A standardized nutrient lookup table. Consistency in the database used for both the FFQ and the reference method is critical for accurate comparison and to reduce heterogeneity in results [43]. |
| Statistical Software (e.g., R, SAS) | Essential for performing complex analyses, including regression calibration, correlation analysis, de-attenuation for within-person variation, and machine learning algorithms for error adjustment [7] [6]. |
Experimental Protocol: Validating an FFQ Against 24-Hour Recalls
The following is a detailed methodology based on established validation studies [15] [7]:
Study Population & Sampling: Recruit a sub-sample (typically n=100-200) from your main cohort that is representative in terms of age, sex, and BMI. Ensure ethical approval and informed consent.
Baseline Data Collection:
- Administer the FFQ (FFQ1) at the start of the study, asking about dietary habits over the past year.
- Collect baseline biological samples (if biomarkers are part of the protocol).
Reference Method Data Collection:
- Schedule multiple 24-hour dietary recalls over a period of at least 6-12 months to account for seasonal variation.
- A typical protocol involves conducting two non-consecutive recalls per month for twelve months, totaling 24 recalls per participant.
- Recalls should be conducted by trained dietitians using a multiple-pass method (e.g., USDA protocol) to enhance completeness and accuracy. Interviews can be in-person or by phone.
Follow-up Data Collection:
- At the end of the study period (e.g., month 12), administer the FFQ again (FFQ2) to assess reproducibility.
Data Processing & Analysis:
- Nutrient Calculation: Process all dietary data (FFQs and 24HRs) using the same food composition database.
- Statistical Analysis:
- Validity: Calculate correlation coefficients (Pearson or Spearman) between the nutrient intakes from FFQ1 and the average intake from all 24-hour recalls.
- Reproducibility: Calculate correlation coefficients between nutrient intakes from FFQ1 and FFQ2.
- Classification Analysis: Perform cross-classification to determine the proportion of participants categorized into the same or adjacent quartile by both methods.
- Adjust for Within-Person Variation: Apply de-attenuation correction to the correlation coefficients to account for day-to-day variation in the 24-hour recalls [7].
Optimizing for Efficiency and Accuracy: Data-Driven and Computational Approaches
Food Frequency Questionnaires (FFQs) are essential tools in nutritional epidemiology for assessing habitual dietary intake and investigating diet-disease relationships. A fundamental challenge in FFQ design lies in creating a food list that is comprehensive enough to accurately capture all nutrients of interest, yet short enough to minimize respondent burden and maintain high completion rates. Traditional, expert-led methods for compiling these food lists can be time-consuming, non-standardized, and may yield unnecessarily long questionnaires.
This technical support guide explores how Mixed Integer Linear Programming (MILP), an operations research technique, provides a rigorous, mathematical framework to overcome this limitation. By optimizing the selection of food items, researchers can develop shorter, more efficient FFQs without compromising their nutritional coverage or ability to detect inter-individual variation in intake [44] [45] [46].
Core Concepts: How MILP Optimizes Food Lists
The Optimization Goal and Constraints
The primary goal of the MILP model in FFQ design is to minimize the number of food items on the list. This objective is subject to crucial nutritional constraints [44] [47] [46]:
- Nutrient Coverage Constraint: Ensures the selected food items account for a large proportion (e.g., ≥ a threshold
b) of the total population intake for each nutrient of interest. - Variance Coverage Constraint: Ensures the selected food items account for a large proportion of the interindividual variance in intake for each nutrient. This is critical for the FFQ's ability to rank individuals within a population [44] [46].
The model uses binary decision variables (xn) where a value of 1 indicates the food item n is included in the FFQ, and 0 indicates it is excluded [44].
The Food Tree: Managing Aggregation Levels
A key consideration is the level of food item aggregation. Foods are often organized in a hierarchical "food tree" [46]:
- High Aggregation (e.g., "Fresh Fruit"): Covers nutrient intake with fewer items but may poorly capture between-person variance.
- Low Aggregation (e.g., "Apples," "Oranges"): Better at capturing variance but requires more items to achieve nutrient coverage.
The MILP model can be applied at different levels of this tree to find the optimal balance [44] [46].
Diagram 1: MILP-based FFQ food list optimization workflow.
Troubleshooting Guides & FAQs
Frequently Asked Questions
Q1: My model fails to find a feasible solution that meets all nutrient constraints. What should I do? A: This often indicates that the constraints are too strict. Try the following:
- Gradually lower the coverage threshold (
b) for nutrient and variance constraints. Start with a lower value (e.g., 0.60) and incrementally increase it to find the point where the model becomes infeasible [44] [47]. - Check your input data for errors in nutrient composition or consumption amounts.
- Review the set of target nutrients. Highly correlated nutrients might be imposing conflicting constraints. Consider if all nutrients are essential for your specific study aim.
Q2: How do I decide the appropriate level of food aggregation for my model? A: The choice involves a trade-off.
- Use higher aggregation (e.g., food subgroups) for a generalized survey where the primary goal is efficient nutrient intake coverage [44].
- Use lower aggregation (e.g., individual foods) when your study aims to capture specific dietary behaviors or when foods within a group have highly variable nutrient profiles [46]. Running the model at different aggregation levels and comparing the performance indicators (length, coverage, R²) can help inform your decision.
Q3: The solver is taking too long to find an optimal solution. How can I speed up the process? A: MILP problems can be computationally complex (NP-hard) [48].
- Use a efficient solver like GLPK, CPLEX, or Gurobi within an optimization interface (e.g., the R
ROIpackage) [44] [47]. - Limit the number of food items in the initial candidate pool by pre-filtering out foods with negligible consumption.
- If working with a very large number of nutrients, consider solving the model for a subset of key nutrients first, then validating the resulting food list's performance for all other nutrients.
Q4: How does the MILP approach improve upon traditional stepwise regression methods for food list generation? A: Traditional stepwise methods add food items for one nutrient at a time, which can lead to unnecessarily long lists because the procedure never removes items and the final list depends on the order in which nutrients are considered [46]. The MILP model optimizes for all nutrients simultaneously, actively seeking the smallest set of items that collectively satisfy all constraints, resulting in a shorter and more efficient food list [45] [46].
Experimental Protocol: Implementing MILP for FFQ Optimization
The following protocol, based on published research, provides a step-by-step methodology for optimizing an FFQ food list using MILP [44] [47] [46].
Objective: To identify the minimal set of food items that meets pre-defined nutrient coverage and variance coverage thresholds.
Materials & Software:
- Statistical Software: R (version 4.3.0 or higher).
- R Packages:
ROI(with theROI.plugin.glpkplugin) or similar optimization interfaces. - Solver: GLPK (GNU Linear Programming Kit) or a commercial equivalent.
- Input Data: A dataset of dietary consumption (e.g., from 24-hour recalls or food records) at the individual level, linked to a food composition database.
Procedure:
- Data Preparation:
- Obtain dietary intake data from a representative sample of your target population (e.g., National Nutrition Survey data).
- Calculate the average daily intake for each food item and nutrient for every person.
- Aggregate food consumption data to the desired level (e.g., 184 food subgroups or 1908 individual foods) [44]. For any food not consumed by a person, assign a value of 0g to correctly compute variance.
Parameter Definition:
- Define the nutrient set (
J): List all nutrients of interest (e.g., start with energy, then add macros, then vitamins/minerals) [44]. - Set the coverage threshold (
b): Choose an initial threshold (e.g., 0.80, meaning 80% coverage). This will be varied later to analyze its impact on food list length. - Calculate Input Matrices:
- Nutrient Coverage (
Cj,n): For each food itemnand nutrientj, calculate its percentage contribution to the total population intake ofj[44] [47]. - Variance Coverage (
Sj,n): For each food itemnand nutrientj, calculate its percentage contribution to the sum of variances of the overall intake ofj[44] [47].
- Nutrient Coverage (
- Define the nutrient set (
Model Formulation:
- Objective Function: Minimize the sum of binary decision variables
xn(i.e., minimize the number of selected food items). - Constraints:
- Nutrient Coverage: For each nutrient
j, the sum ofCj,n * xnfor all selected items must be ≥b. - Variance Coverage: For each nutrient
j, the sum ofSj,n * xnfor all selected items must be ≥b.
- Nutrient Coverage: For each nutrient
- Implement the model in R using the
ROIpackage and the GLPK solver.
- Objective Function: Minimize the sum of binary decision variables
Model Execution and Validation:
- Run the optimization for your chosen threshold
b. - If the model is infeasible, lower
band rerun. - Once a solution is found, the items where
xn = 1constitute your optimized food list. - Validate the output by calculating the actual R² (explained variance) and coverage for the optimized list and comparing it to a manually compiled or existing FFQ food list [46].
- Run the optimization for your chosen threshold
Performance Data: MILP Optimization Results
The application of MILP has demonstrated significant improvements in FFQ design. The table below summarizes key quantitative findings from relevant studies.
Table 1: Performance comparison of MILP-optimized food lists versus traditional methods.
| Study & Aggregation Level | Number of Nutrients | Benchmark / Traditional FFQ Length | MILP-Optimized FFQ Length | Key Performance Findings |
|---|---|---|---|---|
| German Survey (BLS Subgroups) [44] | 40 (Energy, macros, vitamins, minerals) | 156 items (eNutri FFQ) | Shorter lists achieved (exact number varies with threshold b) |
Optimized lists were shorter than the validated eNutri FFQ while meeting coverage constraints. |
| Dutch Survey (Multi-level Food Tree) [46] | 10 (Energy, protein, fats, carbs, fiber, potassium) | Not specified (Benchmark from Molag et al. procedure) | 32-40% shorter than benchmark | The quality (R²) of the MILP-generated lists was similar to that of the longer benchmark list. |
| General MILP Application [45] | 10 (Energy + 9 nutrients) | Manual expert compilation | Shorter or more informative lists | The selection process was faster, more standardized, and transparent than manual procedure. |
Table 2: The Scientist's Toolkit - Essential reagents and resources for MILP-based FFQ optimization.
| Tool / Resource | Category | Function / Description | Example |
|---|---|---|---|
| Dietary Intake Data | Input Data | Provides the foundational consumption patterns of the target population for calculating nutrient coverage and variance. | 24-hour recalls, Food records (e.g., from a National Nutrition Survey) [44] [49]. |
| Food Composition Database | Input Data | Links consumed foods to their nutrient content, enabling the calculation of nutrient intakes. | USDA Food Data Bank, German Nutrient Database (BLS), Dutch NEVO table [44] [50] [46]. |
| Statistical Software | Software Platform | The environment for data preparation, calculation of input matrices, and model implementation. | R, Python [44]. |
| Optimization Package & Solver | Software Tool | Provides the algorithms to formulate and solve the MILP model. | R ROI package with GLPK solver [44] [47]. |
| Computational Proxy (pj,n) | Methodology | A linear substitute for R² used in the MILP constraints to select items that explain variance. | Based on a food item's contribution to population intake (MOM1) or to the sum of variances (MOM2) [46]. |
Diagram 2: Logical data flow and relationship between key components in the FFQ optimization process.
Frequently Asked Questions
FAQ 1: What is the core benefit of using Machine Learning for feature selection in FFQs? Machine Learning (ML) streamlines Food Frequency Questionnaires (FFQs) by identifying a minimal set of food items that most effectively predict overall dietary intake or quality. This process reduces participant burden, improves user experience on digital platforms, and maintains, or even enhances, the predictive accuracy for key nutrients [51] [52].
FAQ 2: My dataset has a high number of food items relative to my sample size. Which ML method is suitable? Penalized regression methods, like LASSO (Least Absolute Shrinkage and Selection Operator), are particularly well-suited for high-dimensional data. They perform automatic feature selection by shrinking the coefficients of non-informative food items to zero, helping to prevent overfitting [53].
FAQ 3: How can I personalize a short FFQ based on a user's specific dietary goals? A multi-target regression approach can be used. First, predict a user's scores for various nutritional goals (e.g., fruit/vegetables, sugar, protein). Then, calculate how far these predictions are from the ideal targets. Use these distances as weights to identify and ask only about the food items most critical for the user's specific underachieving goals, creating a dynamic and personalized questionnaire [51].
FAQ 4: I need to build a new, short FFQ from a large dataset of consumed foods. What is a proven method? Mixed Integer Linear Programming (MILP) is a powerful optimization technique for this task. You can define constraints, such as "the selected food items must cover 90% of the population's intake for energy and key nutrients," and the MILP algorithm will find the smallest set of food items that meets all your criteria [44].
FAQ 5: How can I correct for the common issue of under-reporting in FFQ data? A supervised ML method using a Random Forest classifier can be applied. The model is trained on data from a sub-population assumed to report more accurately (e.g., healthier participants) using objective biomarkers (e.g., blood lipids, BMI) and demographic data as features. This trained model can then predict likely consumption frequencies for other participants, and an adjustment algorithm can correct probable under-reports by replacing them with the model's predictions [6].
The Scientist's Toolkit: Key Research Reagents & Materials
Table 1: Essential components for building machine learning-powered FFQs.
| Item Name | Function & Application in FFQ Research |
|---|---|
| 24-Hour Dietary Recalls (24HR) | Serves as a high-quality reference method for validating FFQ predictions and for building optimization models, as they provide detailed, short-term intake data [6] [44]. |
| Food Composition Database | A critical lookup table used to convert reported food consumption frequencies and portions into estimated nutrient intakes (e.g., grams of sugar, fiber) [44]. |
| Biomarker Data (LDL, Glucose, BMI) | Provides objective, non-self-reported data used to train machine learning models for identifying and correcting misreporting in FFQ responses [6]. |
| Mixed Integer Linear Programming (MILP) Solver | Software tool used to execute the MILP optimization algorithm, which identifies the minimal set of food items needed for a new FFQ based on defined nutrient coverage and variance constraints [44]. |
| PROMETHEE Method | A multi-criteria decision-making algorithm used to compare and rank the performance of different machine learning models across various reduced food item subsets, helping to select the best overall model [52]. |
Experimental Protocols & Performance Data
Protocol 1: Personalizing FFQs via Multi-Target Regression
This protocol outlines a method to dynamically shorten an FFQ based on a user's previous answers and activated health goals [51].
- Data Collection: Collect complete FFQ responses (e.g., all 24 food items) and calculate quality scores for 11 nutritional goals (e.g., Fruits & Vegetables, Sweets, Proteins).
- Model Training: Train a multi-target regression model (e.g., Random Forest) to predict all 11 goal scores from the 24 food items.
- Prediction & Weighting: For a new user, use their initial answers to predict their 11 goal scores. Calculate the distance between each predicted score and its ideal target value. Transform these distances into weights, giving higher importance to goals where the user is furthest from the target.
- Feature Selection: Recalculate the importance of each food item, factoring in the goal-specific weights. Select the top N most important items (e.g., 6, 9, or 12) to form the user's personalized short FFQ.
- Validation: Evaluate performance by comparing the predictions of the short FFQ to the full FFQ using metrics like Mean Absolute Error (MAE).
Table 2: Performance of personalized vs. generic short FFQs. Adapted from [51].
| Question Selection Method | Number of Questions | Prediction Error (MAE) | Key Advantage |
|---|---|---|---|
| Random Selection | 6 | Baseline | Serves as a control; generally higher error. |
| Generic Feature Selection | 6 | Lower than Random | Static shortness; not tailored to individual needs. |
| Personalized (Goal-Weighted) | 6 | Lowest | Dynamically adapts to user's specific dietary gaps. |
Protocol 2: Developing a Short FFQ using Mixed Integer Linear Programming
This protocol uses MILP to design a static, short FFQ from scratch using population dietary data [44].
- Input Data Preparation: Use detailed dietary intake data from a representative population sample (e.g., two non-consecutive 24-hour recalls). Aggregate food consumption data into specific food items or groups.
- Define Constraints: For each nutrient of interest (e.g., energy, sugar, fiber, protein), set a constraint. For example, mandate that the selected food items must explain at least 90% of the total population intake and/or a certain percentage of the inter-individual variance for that nutrient.
- Run MILP Optimization: Define the objective function to minimize the total number of food items selected. The MILP solver will then identify the smallest set of items that satisfies all nutrient constraints.
- Formulate FFQ: Use the selected food items to construct the new short FFQ.
- Validation: Compare the nutrient intake estimates from the new short FFQ against the original 24-hour recalls or a validated, longer FFQ to assess agreement.
Table 3: Illustrative output of an MILP optimization for FFQ development. Data based on [44].
| Nutrient Coverage Constraint | Variance Explained Constraint | Optimal Number of Food Items | Comparison to eNutri FFQ (156 items) |
|---|---|---|---|
| 95% | 95% | ~120 items | 36 items shorter |
| 90% | 90% | ~80 items | 76 items shorter |
| 85% | 85% | ~50 items | 106 items shorter |
Protocol 3: Correcting for Under-Reporting with a Random Forest Classifier
This protocol uses ML to identify and adjust for under-reported food items in an existing FFQ dataset [6].
- Define Healthy Cohort: Split your dataset. Define a "healthy" group based on objective measures (e.g., body fat percentage, blood lipids, age) where dietary reporting is assumed to be more accurate.
- Train Random Forest Model: Using only the healthy cohort, train a Random Forest classifier for a specific under-reported food (e.g., bacon). Use objective variables (LDL cholesterol, BMI, age, sex) as features to predict the frequency category of that food.
- Predict for Main Cohort: Apply the trained model to the rest of the dataset (the "unhealthy" cohort). For each participant, the model outputs a probability for each consumption frequency category.
- Apply Error Adjustment Algorithm: For each participant's response on an unhealthy food item, compare their self-reported frequency to the model's predicted frequency. If the self-reported value is lower than the predicted one, replace it with the most probable category that is higher than the reported one. This corrects the under-reporting.
Frequently Asked Questions (FAQs)
FAQ 1: What is a Gaussian Graphical Model (GGM) and how does it improve upon traditional dietary pattern analysis? Gaussian Graphical Models (GGMs) are a statistical framework used to model conditional dependencies between multiple variables. In dietary pattern analysis, GGMs represent food groups as nodes in a network, and the edges (connections) between them represent partial correlations, indicating how two food groups are related after accounting for all other foods in the network [54]. This provides a more nuanced view than traditional methods like Principal Component Analysis (PCA), as it reveals the complex web of how foods are actually consumed together, moving beyond simple pairwise correlations [55].
FAQ 2: My dietary intake data from FFQs is not normally distributed. Can I still use GGMs? Yes. Non-normal data is a common challenge with FFQ data. To address this, you can use the Semiparametric Gaussian Copula Graphical Model (SGCGM), a nonparametric extension of GGM that does not require normally distributed data [56]. Alternatively, a common practice is to log-transform your intake data before estimating the network [55]. A 2025 scoping review recommends robust handling of non-normal data as a key guiding principle for reliable dietary network analysis [55].
FAQ 3: How do I interpret "centrality" in a food co-consumption network, and what are the pitfalls? Centrality metrics help identify the most influential food groups in your network [57].
- Degree Centrality: A food group with a high number of connections (high degree) is a "hub," meaning its consumption is strongly linked to many other foods. For example, one study found "sweet desserts" to be a hub [57].
- Betweenness Centrality: A food group with high betweenness acts as a bridge between different clusters of foods (e.g., "visceral meat" was found to connect healthy and unhealthy modules) [57].
A key pitfall, noted in a 2025 review, is that 72% of studies use centrality metrics without acknowledging their limitations [55]. Be cautious: centrality does not imply causation, and its value can be sensitive to the network estimation method.
FAQ 4: What are the best practices for visualizing my food co-consumption network? Effective visualization is crucial for interpreting and communicating results.
- Color for Clarity: Use color palettes that enhance contrast and differentiation between nodes and edges. Employ complementary colors for links (edges) to enhance the discriminability of node colors, and consider using shades of blue for quantitative encoding rather than yellow [58]. Ensure colors are accessible for colorblind readers [59].
- Give Color Room: Avoid coloring only small nodes, as it makes color hard to perceive. Coloring edges can help, but manage the drawing order to prevent one color from dominating due to arbitrary layering [60].
- Highlight Structure: Use hulls or other techniques to visually group clusters (modules) of foods identified by community detection algorithms [60].
Troubleshooting Guides
Problem 1: My estimated network is too dense and uninterpretable. This is often due to many spurious connections. The solution is regularization.
- Solution: Apply the graphical LASSO (Least Absolute Shrinkage and Selection Operator). This technique zeroes out weak, likely spurious, partial correlations, resulting in a sparse, more interpretable network. Most modern GGM applications (93%) pair the model with a regularization technique like LASSO [55].
- Protocol:
- Input your preprocessed food consumption data (e.g., log-transformed, energy-adjusted).
- Estimate the partial correlation matrix using the graphical LASSO. This can be done in R using packages like
hugeorqgraph. - The LASSO introduces a penalty parameter (λ). Use model selection criteria like the Extended Bayesian Information Criterion (EBIC) to select the optimal λ value, which controls the sparsity of the network.
Problem 2: I need to validate my network model, but I only have cross-sectional FFQ data. This is a fundamental limitation, as cross-sectional data cannot establish causality.
- Solution: Employ internal and external validation strategies.
- Stability Analysis: Use a nonparametric bootstrap procedure to assess the stability of edges and centrality indices. If edges frequently appear in bootstrap samples, they are more reliable.
- Sensitivity Analysis: Re-run your model with different correlation thresholds or penalty parameters to see if key network structures (hubs, modules) persist.
- Biological Plausibility: Validate your network findings by testing their association with health outcomes. For example, if you identify an "unhealthy cluster," check if participants with higher adherence to this pattern have significantly worse metabolic profiles [57] [61]. This connects your network back to biological reality.
Problem 3: I have identified dietary clusters, but how do I link them to health outcomes?
- Solution: Create cluster adherence scores and use them in regression models.
- Protocol:
- Identify Clusters: Use an algorithm like the Label Propagation Algorithm to partition your network into clusters (e.g., "healthy" and "unhealthy" modules) [57].
- Calculate Adherence Scores: For each participant and each cluster, calculate a score (e.g., the sum or average z-score of the food groups within that cluster).
- Statistical Modeling: Use these scores as independent variables in logistic or linear regression models with your health outcome (e.g., NAFLD, MetS components) as the dependent variable. Adjust for relevant confounders like age, sex, and energy intake.
- Example: One study found that an "unhealthy module" was associated with a significantly higher CAP score (a measure of liver fat) compared to a "healthy module" (253.7 ± 47.8 vs. 218.0 ± 46.4, p < 0.001) [57].
Table 1: Network Metrics and Health Associations in Dietary Pattern Studies
| Study & Population | Central Food Groups (Hubs) | Key Clusters/Modules Identified | Association with Health Outcomes |
|---|---|---|---|
| Iqbal et al. (German adults) [56] | Red and processed meat, chicken, certain vegetables [61] | Not specified in available abstract. | Adherence to Western-type patterns was linked to a higher risk of T2DM in women [61]. |
| Food Co-consumption in NAFLD (Iranian adults, n=1500) [57] | Sweet dessert (Degree: 11°). | Unhealthy Cluster (20 nodes, 57 edges): meats, sweets, industrial drinks. Healthy Cluster (18 nodes, 33 edges): vegetables, fruits, legumes. | Unhealthy module members had significantly higher CAP scores (liver fat): 253.7 ± 47.8 vs 218.0 ± 46.4 in the healthy module (p < 0.001) [57]. |
| GGM in Overweight/Obese (Iranian adults, n=647) [61] | Raw vegetables, grain, fresh fruit, snack, margarine, red meat were central to their respective networks. | Six dietary networks: vegetable, grain, fruit, snack, fish/dairy, and fat/oil. | Higher adherence to the vegetable network was associated with lower TC and higher HDL. The grain network was linked to lower SBP, DBP, TG, LDL and higher HDL [61]. |
Table 2: Essential Research Reagent Solutions for GGM Analysis
| Item / Reagent | Function / Explanation |
|---|---|
| Graphical LASSO | A regularization method that produces a sparse, interpretable network by penalizing small partial correlations, effectively setting them to zero [55]. |
| Semiparametric Gaussian Copula Graphical Model (SGCGM) | An extension of GGM used when dietary intake data violates the assumption of normality, providing more robust estimates [56]. |
| Label Propagation Algorithm | A community detection algorithm used to identify clusters (modules) of food groups that are more strongly connected to each other than to the rest of the network [57]. |
| EBIC Model Selection | The Extended Bayesian Information Criterion is used to select the optimal regularization parameter (λ) in graphical LASSO, balancing model fit and complexity [55]. |
| Stability Assessment | A bootstrap procedure to evaluate the reliability of estimated edges and centrality measures, crucial for validating findings from a single sample [55]. |
Detailed Experimental Protocol
Protocol: Conducting a Gaussian Graphical Model Analysis on FFQ Data
1. Data Preprocessing:
- Input: Raw data from a validated Food Frequency Questionnaire (FFQ). A typical example is a 168-item FFQ [61].
- Energy Adjustment: Adjust food intake values for total energy intake using the residual method.
- Handling Non-Normality: Log-transform the energy-adjusted food intake values for each food group to approximate a normal distribution [55]. Alternatively, use SGCGM.
- Standardization: Convert the data to z-scores.
2. Network Estimation:
- Model: Estimate a GGM using the graphical LASSO regularization.
- Software: Implement in R using the
hugeorqgraphpackages. - Parameter Tuning: Use EBIC to select the optimal tuning parameter (λ) for the graphical LASSO, which controls network sparsity.
3. Network Visualization and Analysis:
- Visualization: Plot the network where nodes represent food groups and edges represent regularized partial correlations. Use the
qgraphpackage in R. - Identify Communities: Apply the Label Propagation Algorithm to detect clusters of food groups [57].
- Calculate Centrality: Compute node centrality metrics (e.g., degree, betweenness).
4. Validation and Association with Health:
- Stability: Perform a nonparametric bootstrap (e.g., 1000 samples) to calculate correlation-stability coefficients for edges and centrality indices.
- Adherence Scores: For each identified dietary cluster, calculate an adherence score for every participant.
- Health Association: Use multivariate regression analysis to test the association between cluster adherence scores and health outcome variables (e.g., blood pressure, cholesterol levels, liver fat scores), adjusting for confounders like age, sex, and BMI [61].
Workflow and Signaling Pathways
GGM Analysis Workflow for FFQ Data
Example Food Co-consumption Network
Troubleshooting Common FFQ Development Challenges
FAQ: How can I reduce the length of my FFQ without losing critical information about nutrient intake?
The Problem: Extensive FFQs can overwhelm respondents, potentially reducing completion rates and data quality. However, arbitrarily removing questions risks losing information about key nutrients.
The Solution: Use computational optimization to identify the most informative food items.
- Methodology: Apply Mixed Integer Linear Programming (MILP) to select food items that maximize nutrient coverage and interindividual variability while minimizing the number of questions [62] [45].
- Workflow:
- Collect dietary intake data from your target population using 24-hour recalls or food records [62].
- Calculate each food item's contribution to total nutrient intake and its variance across the population [62].
- Set constraints defining the minimum proportion of nutrient coverage and variance you wish to retain (e.g., 90%) [62].
- Run the MILP algorithm to find the smallest set of food items that satisfies these constraints [62].
Experimental Protocol: A study using this method with German National Nutrition Survey data created optimized food lists shorter than the 156-item eNutri FFQ while maintaining comprehensive nutrient assessment [62].
FAQ: My FFQ data is prone to measurement error, such as underreporting of unhealthy foods. How can I correct for this bias?
The Problem: Self-reported dietary data is susceptible to systematic errors like underreporting of "unhealthy" items (e.g., high-fat foods) and overreporting of "healthy" ones, which can distort diet-disease relationships [20] [29].
The Solution: Implement a supervised machine learning model to identify and correct for misreported entries.
- Methodology: Use a Random Forest (RF) classifier trained on objectively measured biomarkers to predict true consumption categories [20].
- Workflow:
- Split Dataset: Divide data into a "healthy" group (based on objective biomarkers like blood lipids and body fat percentage) and an "unhealthy" group. The healthy group's data is assumed to be more accurately reported [20].
- Train Model: Train the RF classifier on the "healthy" group, using biomarkers (LDL cholesterol, total cholesterol, blood glucose, BMI, age, sex) to predict FFQ responses for specific foods [20].
- Apply Correction: For the "unhealthy" group, compare their original FFQ responses to the model's predictions. For unhealthy foods likely to be underreported, if the predicted frequency is higher than reported, replace the response with the predicted value [20].
Experimental Protocol: This approach achieved high model accuracies (78%-92%) in correcting underreported entries for foods like bacon and fried chicken [20]. The following diagram illustrates this workflow.
FAQ: How do I adapt an existing FFQ for a new cultural context or a specific sub-population?
The Problem: FFQs are population-specific. Using a questionnaire developed for one group on another can miss key local foods and lead to invalid intake estimates [25] [29].
The Solution: Conduct a structured adaptation and validation process.
- Methodology: A hybrid approach using qualitative methods (expert panels, focus groups) and quantitative data analysis (population surveys) [25] [63].
- Workflow for Cultural Adaptation [25]:
- Select Base FFQ: Choose a comprehensive, validated FFQ as a starting point.
- Expert Review: Have nutrition experts review all items for cultural and religious relevance, commonality of consumption, and local availability.
- Market Research: Verify the availability of processed and packaged foods in local markets and compare their nutritional composition to original items.
- Modify List: Add culturally important dishes and foods; remove irrelevant ones.
- Translation: Translate the FFQ into the local language and perform back-translation to ensure accuracy.
- Pilot Test: Administer the draft FFQ to a small sample from the target population and refine based on feedback.
Considerations for Specific Populations: For older adults, a population survey revealed they needed more questions to capture the same between-person variability for certain nutrients (zinc, magnesium) and consumed smaller portion sizes compared to younger adults [63]. Relying on standard FFQs without adaptation can therefore be misleading.
Essential Reagents & Computational Tools for FFQ Optimization
The table below summarizes key tools and their functions for developing and optimizing FFQs.
Table 1: Key Reagents and Tools for FFQ Research and Development
| Tool / Reagent | Function in FFQ Development | Example Use Case |
|---|---|---|
| Biomarkers (e.g., Urinary Nitrogen, Potassium) [64] | Serve as objective, gold-standard reference methods to validate nutrient intake and correct for measurement error. | Calibrating protein intake estimates from an FFQ against urinary nitrogen to derive a correction factor for diet-disease models [64]. |
| 24-Hour Dietary Recalls (24HR) [62] | Provide detailed quantitative intake data from the target population used for compiling and optimizing the food list. | Serving as the data source for calculating nutrient coverage and interindividual variance in a MILP optimization model [62]. |
| Mixed Integer Linear Programming (MILP) [62] [45] | A computational optimization technique to select the minimal set of food items that explain maximum nutrient variance. | Automating the creation of a short but comprehensive food list for a general population FFQ [62]. |
| Random Forest (RF) Classifier [20] | A machine learning algorithm used to identify and correct for systematic misreporting in FFQ responses. | Correcting for underreporting of high-fat foods by predicting the likely true intake based on biomarker data [20]. |
| Physical Activity Sensors [65] | Objectively measure physical activity and sedentary time to validate lifestyle-related components of a questionnaire. | Used as a reference method to validate the physical activity estimates of the digital DIGIKOST-FFQ [65]. |
Advanced Protocols: Workflow for a Comprehensive FFQ Optimization
This integrated protocol combines multiple techniques to develop a robust, population-specific FFQ.
Aim: To create a shortened, culturally adapted FFQ with a built-in method to mitigate measurement error.
Background: A valid dietary assessment tool must be population-specific, as short as possible, and account for inherent reporting biases [25] [62] [29]. The following workflow integrates solutions to these concurrent challenges.
Table 2: Quantitative Outcomes from Key FFQ Optimization Studies
| Optimization Technique | Key Metric | Reported Outcome | Reference |
|---|---|---|---|
| Machine Learning (RF) Error Correction | Model Accuracy | 78% - 92% in participant data; 88% in simulated data [20]. | [20] |
| MILP for Food List Reduction | Questionnaire Length | Generated food lists shorter than the validated 156-item eNutri FFQ [62]. | [62] |
| Cultural Adaptation & Reliability Testing | Test-Retest Reliability (Weighted Kappa) | Fair to moderate agreement (KW: 0.38 - 0.60) for frequency questions in the Omani FFQ [25]. | [25] |
| Biomarker Calibration | Impact on Diet-Disease Association | Corrected a true RR of 2.0 from an observed 1.4 (protein) and 1.5 (potassium) [64]. | [64] |
Step-by-Step Protocol:
Phase 1: Foundational Data Collection
Phase 2: Food List Compilation & Optimization
- Aggregate foods from the 24-hour recalls into conceptually similar groups [63].
- Use MILP to identify the minimal set of food items that explain a high percentage (e.g., ≥90%) of the population's intake and variance for your nutrients of interest [62].
- Validate the shortened list by comparing its nutrient estimates against the original, full dataset from the 24-hour recalls.
Phase 3: Cultural & Population Refinement
- Convene an expert panel (nutritionists, dietitians) to review the optimized food list for local relevance, add iconic dishes, and adjust portion size images [25].
- Conduct focus groups with the target population to ensure the questionnaire is understandable and comprehensive [66].
- Translate and back-translate the FFQ if needed [25].
Phase 4: Mitigating Measurement Error
- Program the FFQ for digital administration if possible, as this can incorporate clear instructions and portion images to reduce error [65].
- Implement a machine learning pipeline (e.g., Random Forest) to be applied after data collection. Train the model on a subset of your data with the best biomarker profiles to identify and correct for likely under/overreporting [20].
Phase 5: Validation
- Perform a test-retest reliability study (administer the FFQ twice, 1-2 weeks apart) and calculate reliability coefficients (e.g., Intraclass Correlation Coefficients, Weighted Kappa) [25].
- Conduct a validation study against a superior reference method (e.g., multiple 24-hour recalls, biomarkers like urinary nitrogen or potassium) in an independent sample to assess the relative validity of your optimized FFQ [65] [64]. The following diagram visualizes this multi-phase protocol.
By following these structured workflows and utilizing the provided toolkit, researchers can systematically overcome the major limitations inherent in FFQ research, leading to more valid, reliable, and practical dietary assessment instruments.
Ensuring Scientific Rigor: Protocols for Validating and Comparing Dietary Assessment Methods
Frequently Asked Questions (FAQs)
When should I use ICC versus Weighted Kappa for reliability analysis? The choice between Intraclass Correlation Coefficients (ICC) and Weighted Kappa depends on your data type and research design. Use ICC for continuous data (e.g., scores, measurements) and Weighted Kappa for ordinal categorical data (e.g., Likert scales, severity ratings) [67] [68]. ICC is preferred for test-retest, intra-rater, and inter-rater reliability of continuous measurements, while Weighted Kappa is specifically designed for ordered categories where some disagreements are more serious than others [69] [68].
How do I select the appropriate ICC model for my study? Selecting the correct ICC form depends on your experimental design and how you plan to generalize results. Answer these key questions to guide your selection [67]:
- Are the same raters used for all subjects? (Yes → Two-way model; No → One-way model)
- Were raters randomly selected from a larger population? (Yes → Random-effects; No → Mixed-effects)
- Do you need reliability for single or multiple raters?
- Is absolute agreement or consistency more important?
Table 1: ICC Model Selection Guide
| Model Type | When to Use | Generalizability |
|---|---|---|
| One-way random effects | Different random raters for each subject [67] | To any raters from the same population |
| Two-way random effects | Same random raters for all subjects [67] | To any raters with similar characteristics |
| Two-way mixed effects | Specific raters of interest only [67] | Only to the exact raters in your study |
What are the accepted interpretation guidelines for ICC and Kappa values? Both statistics have established interpretation frameworks, though context should influence final decisions [70] [67].
Table 2: Reliability Interpretation Guidelines
| Value Range | ICC Interpretation | Kappa Interpretation |
|---|---|---|
| <0.50 | Poor | Slight Agreement |
| 0.50-0.75 | Moderate | Fair Agreement |
| 0.75-0.90 | Good | Moderate Agreement |
| >0.90 | Excellent | Substantial Agreement |
Why does my weighted kappa give different results with linear versus quadratic weights? Linear and quadratic weighted kappa differ in how they penalize disagreements. Linear weighted kappa uses weights based on linear distance between categories, while quadratic weighted kappa uses squared distances, making larger disagreements more heavily penalized [68]. For example, a disagreement between categories 1 and 3 would receive a weight of 0.67 with linear weights but 0.33 with quadratic weights on a 5-point scale [68]. Report both when disagreements have varying importance [68].
How do I handle missing data in reliability studies? For missing data in reliability analysis, several approaches exist [71]:
- Predictive Mean Matching (PMM): A multiple imputation method that outperforms others in maintaining correlation structure
- Listwise Deletion: Removes cases with missing data, valid only when data is Missing Completely at Random (MCAR)
- Weighted Gwet's Kappa: Specifically designed for agreement studies with missing data PMM generally provides the best performance in terms of bias and root mean squared error [71].
Troubleshooting Common Experimental Issues
Low reliability values in test-retest analysis
Problem: You obtain low ICC or Kappa values despite careful experimental design.
Solution:
- Check for prevalence effects: Kappa is sensitive to imbalanced category distributions. If one category dominates, consider reporting percent agreement alongside kappa [70] [68].
- Verify measurement interval: For test-retest, too short interval may introduce memory effects, while too long may allow actual change. Typical intervals range from 2-4 weeks [69].
- Assess rater training: In one bone density study, intra-rater reliability ranged from 0.15 to 0.90, highlighting training impact [70].
- Examine category definitions: Poorly defined categories reduce reliability. Redefine categories or combine problematic ones [71].
Discrepancies between different reliability statistics
Problem: ICC, Kappa, and percent agreement give conflicting results.
Solution:
- Understand what each statistic measures: Percent agreement doesn't account for chance [70], Cohen's Kappa corrects for chance but is affected by prevalence [70] [68], and ICC measures both correlation and agreement [67].
- For continuous data, ICC is generally preferred over Pearson correlation, which only measures correlation but not agreement [67].
- Report multiple statistics to provide a complete picture, especially when using weighted kappa [68].
Inconsistent results across study sites or rater groups
Problem: Reliability varies significantly between different research sites or rater groups.
Solution:
- Standardize procedures: Use the same training protocols, measurement tools, and instructions across all sites [72].
- Consider one-way random effects models: If different raters assess different subjects, this model appropriately accounts for the design [67].
- Implement quality control: Regular calibration sessions and ongoing monitoring can maintain consistency [72].
Experimental Protocols
Protocol 1: Test-Retest Reliability Using ICC
Purpose: To assess the stability of measurements over time using ICC [69].
Materials:
- Validated measurement instrument
- Standardized administration protocol
- Data collection forms or electronic system
- Statistical software capable of ICC calculation (e.g., SPSS, R)
Procedure:
- Administer first assessment (T1) to all participants following standardized protocol
- Determine appropriate time interval based on construct stability (typically 2-4 weeks) [69]
- Administer second assessment (T2) under identical conditions
- Exclude participants with intervening changes that affect measurements (e.g., medical changes in clinical populations) [69]
- Calculate appropriate ICC form based on your experimental design [67]
- Interpret results using standard guidelines (Table 2) [67]
Workflow Diagram: Test-Retest Reliability Assessment
Protocol 2: Inter-Rater Reliability Using Weighted Kappa
Purpose: To assess agreement between two raters on ordinal categorical data [68].
Materials:
- Clearly defined rating manual with category definitions
- Training materials for raters
- Sample cases for training and calibration
- Data recording system
- Statistical software capable of weighted kappa calculation
Procedure:
- Develop comprehensive rating manual with explicit category criteria and examples
- Train raters using sample cases not included in the actual study
- Establish preliminary agreement through calibration sessions
- Have raters independently assess the same set of subjects or items
- Calculate both linear and quadratic weighted kappa to fully understand disagreement patterns [68]
- Analyze specific disagreements to identify problematic categories
- Report kappa values with confidence intervals and percent agreement
Workflow Diagram: Weighted Kappa Decision Process
Research Reagent Solutions
Table 3: Essential Materials for Reliability Studies
| Item | Function | Example Applications |
|---|---|---|
| Standardized Protocol Documents | Ensure consistent administration across raters and timepoints | Food frequency questionnaires [73] [72], clinical assessments [69] |
| Rater Training Materials | Calibrate raters to consistent standards | Rating manuals, example cases, training videos [71] |
| Quality Control Checklists | Monitor adherence to study protocols | Data collection audits, rater drift assessments [72] |
| Statistical Software Packages | Calculate reliability statistics | SPSS, R, SAS with appropriate reliability modules [67] |
| Reference Standard Methods | Validate new assessment tools | 24-hour dietary recalls [73] [72], clinical expert consensus [68] |
Application in Food Frequency Questionnaire Research
Within nutritional epidemiology, these reliability measures are crucial for validating dietary assessment tools. For example:
- In Malaysian preschool children, an FFQ showed good reliability with ICC values of 0.71-0.83 for food groups and 0.71-0.83 for nutrients between repeated administrations [73]
- A simplified FFQ in Chinese adults demonstrated moderate reliability with energy-adjusted ICC of 0.59 for food groups and 0.47 for nutrients [74]
- The PERSIAN Cohort FFQ validation showed moderate to strong reproducibility correlations (0.42-0.72) across food groups [72]
When implementing these protocols in FFQ research, ensure adequate sample size (typically 50-100 participants for validation studies), appropriate time intervals between administrations (2-4 weeks), and careful attention to portion size estimation methods, which often introduce significant measurement error [73] [72] [74].
Frequently Asked Questions
Q1: Why is it inappropriate to use a significance test for difference (e.g., a t-test) to prove my new method agrees with a gold standard? A1: A non-significant result from a test of difference (e.g., p > 0.05) does not prove agreement. This result can often occur due to low statistical power, especially with small sample sizes. Using it to claim agreement increases the risk of a Type II error (falsely concluding no difference exists) and can be misleading [75].
Q2: I have a near-perfect correlation (e.g., r = 0.99) between my new method and the gold standard. Can I conclude they are in agreement? A2: No. A high correlation indicates a strong linear relationship, not that the two methods produce the same values. It is possible for methods to be perfectly correlated yet have one consistently over- or under-estimate the other. Correlation alone is an inadequate test of agreement [75].
Q3: What is the key difference between assessing reliability and assessing agreement? A3: Reliability (often measured by ICC) assesses whether two methods can rank subjects in the same order. Agreement (assessed by Bland-Altman analysis) determines if the two methods produce interchangeable results by quantifying how much the measurements differ from each other [75] [76].
Q4: In my FFQ validation study, the Bland-Altman analysis shows a bias. What does this mean? A4: A bias in a Bland-Altman plot indicates a systematic difference between the two methods. For example, in a validation study, the FFQ might consistently report fat intake 13.8 grams lower than a diet diary, revealing a specific direction of measurement error that must be accounted for [77].
Q5: My FFQ validation showed good agreement with a diet history but poor agreement with serum biomarkers. What could explain this? A5: This discrepancy is not uncommon. It suggests that while your FFQ may accurately capture reported dietary intake, the relationship between intake and actual serum levels may be confounded by endogenous physiological processes, nutrient utilization, or the specific pathophysiology of the study population [16].
Troubleshooting Guides
Issue: Disagreement Between Statistical Tests of Agreement
Problem Statement: When validating a new dietary assessment method against a gold standard, different statistical tests (Pearson's correlation, t-test, Bland-Altman) provide seemingly conflicting results.
Symptoms & Error Indicators:
- High, significant correlation coefficient (e.g., r > 0.9, p < 0.05).
- Non-significant difference between methods via paired t-test (p > 0.05).
- However, Bland-Altman analysis reveals wide Limits of Agreement (LOA) and/or a significant systematic bias.
Root Cause: Relying solely on tests of relationship (correlation) or difference (t-test) to infer agreement. These methods answer different questions and are not suitable for quantifying the actual concordance between two measurement methods [75].
Step-by-Step Resolution Process:
- Run Correct Analyses: Perform both a correlation analysis (Spearman) and a Bland-Altman analysis.
- Interpret Spearman Correlation First: Use this to understand if your methods rank subjects similarly. A strong positive correlation (e.g., r = 0.51 for fruits) is a good initial sign but is not sufficient for proving agreement [77].
- Conduct Bland-Altman Analysis:
- Calculate the mean difference between the two methods (
d̄, the bias). - Calculate the standard deviation (SD) of the differences.
- Determine the 95% Limits of Agreement:
d̄ ± 1.96 * SD.
- Calculate the mean difference between the two methods (
- Make a Decision Based on LOA:
- Assess if the bias (
d̄) is clinically or scientifically acceptable. - Determine if the width of the LOA is acceptable for your research context. The new method is only a valid replacement if the differences between methods (bias and random error) are small enough to be insignificant in practice [75].
- Assess if the bias (
Validation Step: The methods are considered in agreement only if the bias is negligible and the 95% LOA represent an acceptable range of error for your specific field of research.
Issue: Poor Agreement with Biomarkers Despite Good Agreement with Dietary Recalls
Problem Statement: A Food Frequency Questionnaire (FFQ) shows reasonable agreement with a reference method like a 4-day diet diary (4DDD) or 24-hour recall, but demonstrates poor correlation with serum biomarker levels.
Symptoms & Error Indicators:
- Significant correlations and acceptable Bland-Altman results between FFQ and 24-hour recall for certain food groups or nutrients [77] [78].
- Non-significant, weak correlation coefficients and poor quartile agreements between nutrient intake from the FFQ and their respective serum biomarkers [16].
Root Cause: The disconnect may not be due to the FFQ's inaccuracy in capturing dietary intake, but rather due to factors affecting nutrient absorption, metabolism, and homeostasis within the body. In specific patient populations (e.g., Peripheral Arterial Disease), endogenous physiological processes can alter the relationship between dietary intake and serum concentrations [16].
Step-by-Step Resolution Process:
- Verify FFQ Design: Ensure the FFQ is context-specific, has been validated for the population being studied, and includes relevant food items [72] [78].
- Confirm Laboratory Methods: Verify the accuracy and precision of the biochemical assays used for biomarker quantification.
- Account for Covariates: Statistically control for known confounders that affect biomarker levels (e.g., age, BMI, inflammation status, kidney function, time of blood draw).
- Interpret Results in Context: Conclude that the FFQ is a valid tool for assessing habitual dietary intake based on its agreement with other dietary assessment methods. The poor agreement with biomarkers should be interpreted as a biological or physiological phenomenon worthy of further investigation, not solely as a failure of the FFQ [16].
Escalation Path: If the disagreement persists after these steps, consider using a more objective dietary biomarker (e.g., doubly labeled water for energy expenditure) or conducting a controlled feeding study to better understand the nutrient metabolism in your target population.
Experimental Protocols for Validation
Protocol 1: Validating an FFQ against a Gold Standard Dietary Record
This protocol outlines the steps to validate a new or adapted Food Frequency Questionnaire (FFQ) using a detailed dietary record as a reference method.
- Objective: To assess the relative validity of an FFQ for estimating habitual intake of foods and nutrients in a specific population.
- Materials:
- The target FFQ (e.g., a 48-item SFFQ for NAFLD patients) [77].
- Gold standard method: Multiple-day dietary records (e.g., 4-day diet diary) or multiple 24-hour dietary recalls [77] [72].
- Food composition database or analysis software (e.g., myfood24) [77].
- Statistical software (e.g., R, SPSS, Stata).
- Methodology:
- Participant Recruitment: Recruit a representative sample from the target population. A sample size of at least 50-100 participants is recommended, though larger samples are ideal [78].
- Data Collection:
- Administer the FFQ, typically in a short interview setting to ensure completeness.
- Instruct participants to complete the gold standard dietary record (e.g., 4DDD) over a specified period, with clear instructions on how to record portion sizes.
- Data Processing:
- Process both the FFQ and the dietary records using the same nutrient database to calculate daily intakes for energy, nutrients, and food groups.
- Statistical Analysis:
- Descriptive Statistics: Report medians, means, and percentiles for intakes from both methods.
- Spearman Rank-Order Correlation: Calculate correlation coefficients for nutrients and food groups to assess the ability to rank individuals. Correlations above 0.5 are generally considered good [77].
- Bland-Altman Analysis: Plot the difference between the two methods against their mean for key nutrients to visually inspect for bias and heteroscedasticity, and calculate the 95% Limits of Agreement [77].
- Interpretation: The FFQ is considered valid for assessing habitual diet if it shows moderate to strong rank-order correlations and the bias and Limits of Agreement from the Bland-Altman analysis are within an acceptable range for the intended application.
Protocol 2: Biochemical Validation of an FFQ
This protocol is used to determine if nutrient intake measured by an FFQ correlates with biological concentrations.
- Objective: To validate an FFQ by comparing dietary intake of specific nutrients against their corresponding biomarkers in serum or plasma.
- Materials:
- A validated FFQ.
- Equipment for phlebotomy and serum/plasma processing.
- Access to a clinical laboratory for biomarker analysis (e.g., for vitamins A, C, D, E, zinc, iron).
- Methodology:
- Participant Recruitment & Data Collection:
- Recruit participants and administer the FFQ.
- Collect fasting blood samples within a close timeframe to the FFQ administration.
- Process and store samples according to laboratory standards.
- Laboratory Analysis:
- Analyze serum/plasma for the specific nutrients using standardized, quality-controlled assays (e.g., HPLC for vitamins, ICP-MS for minerals).
- Statistical Analysis:
- Correlation Analysis: Use Spearman correlation to assess the relationship between dietary intake from the FFQ and serum biomarker levels.
- Cross-Classification: Analyze the agreement by categorizing participants into quartiles of intake (FFQ) and quartiles of biomarker levels. A high rate of correct classification (same or adjacent quartile) and a low rate of gross misclassification (extreme quartiles) supports validity.
- Participant Recruitment & Data Collection:
- Interpretation: Significant correlations and good quartile agreement suggest the FFQ is a reasonable proxy for biochemical status. Poor agreement, as seen in some studies, may indicate issues with the FFQ, the biomarker, or physiological factors affecting nutrient metabolism [16].
Data Presentation
Table 1: Example Validation Metrics from a Short FFQ for NAFLD Patients [77]
| Nutrient / Food Group | Spearman Correlation Coefficient (vs. 4DDD) | Bland-Altman Bias (FFQ - 4DDD) |
|---|---|---|
| Total Fat | 0.44 (P=0.001) | -13.8 g/day |
| Total Sugar | 0.408 (P=0.002) | +12.9 g/day |
| Fruits | 0.51 (P=0.0001) | Not Reported |
| Vegetables | 0.40 (P=0.0024) | Not Reported |
Table 2: Validity of Food Group Intake from an FFQ in an Ethiopian Population [78]
| Food Group | Validity Coefficient (vs. 24-h Recall) |
|---|---|
| Legumes | 0.9 |
| Vegetables | 0.8 |
| Roots/Tubers | 0.8 |
| Dairy Products | 0.75 |
| Meat/Poultry | 0.64 |
| Cereal | 0.5 |
The Scientist's Toolkit: Key Reagents & Materials
Table 3: Essential Research Reagents and Materials for FFQ Validation Studies
| Item | Function / Application |
|---|---|
| Standardized Food Composition Database | Provides the nutrient profile for thousands of foods, essential for converting food intake data from FFQs and diet records into nutrient values. Examples include the USDA FoodData Central or country-specific databases [77]. |
| Portion Size Aids | Visual aids like a picture album of standard portions, household measures (cups, spoons), and food models. These help participants and researchers estimate portion sizes more accurately during interviews and when completing diet records [72]. |
| Dietary Analysis Software | Software platforms (e.g., myfood24) that automate the calculation of nutrient intake from dietary data using linked food composition tables, reducing manual errors and processing time [77]. |
| Validated FFQ | The core tool under investigation. It should be a context-specific questionnaire, with a list of food items relevant to the dietary habits of the target population, to accurately capture habitual intake [72] [78]. |
| Biomarker Assay Kits | Commercially available or in-house developed kits for the quantitative analysis of specific nutrients in biological samples (serum, plasma, urine). Critical for biochemical validation. |
Method Comparison Workflow
Statistical Decision Pathway for Method Agreement
FAQs & Troubleshooting Guides
How can I handle class imbalance when evaluating classifier performance?
Problem: My dataset has a significant class imbalance (e.g., many more control subjects than cases). Standard accuracy metrics are misleading, as a model that always predicts the majority class appears highly accurate.
Solution:
- Use Robust Metrics: Prioritize Precision-Recall Area Under the Curve (PR-AUC) and F1-score over Receiver Operating Characteristic Area Under the Curve (ROC-AUC). PR-AUC remains informative with class imbalance as it focuses on the minority class and is not inflated by true negatives [79].
- Metric Selection Rationale: In a supernova classification study with a 3.19 imbalance ratio, researchers emphasized that PR-AUC and F1-score provide a more reliable performance picture than ROC-AUC [79]. The standard F1-score offers a balanced harmonic mean of precision and recall.
Experimental Protocol:
- Calculate Metrics: Compute ROC-AUC, PR-AUC, and F1-score on your test set.
- Compare Results: If ROC-AUC is high but PR-AUC is low, your model's performance on the minority class is likely poor.
- Report Transparently: Always report PR-AUC and F1-score alongside ROC-AUC for imbalanced datasets.
What is a statistically sound way to compare two models using cross-validation?
Problem: When I use different cross-validation (CV) setups to compare two models, the statistical significance of their performance difference changes, leading to inconsistent conclusions.
Solution:
- Avoid Flawed Practices: Do not directly apply a paired t-test to the
K x Maccuracy scores from a K-fold CV repeated M times. This violates the independence assumption of the test, as the data across folds are not independent, and can lead to artificially significant p-values [80]. - Awareness of Variability: Understand that the choice of
K(number of folds) andM(number of repetitions) can influence the perceived significance of the difference between two models, even when their intrinsic predictive power is identical [80].
Troubleshooting Steps:
- Check Your Method: Review your model comparison procedure for the misuse of repeated CV with standard t-tests.
- Seek Robust Tests: Investigate statistical tests designed for correlated samples, such as those accounting for data dependency in CV results [80].
How can I correct for systematic underreporting in my FFQ data?
Problem: Self-reported Food Frequency Questionnaire (FFQ) data is known to contain measurement errors, such as the underreporting of unhealthy foods, which introduces noise and bias into analyses.
Solution: Employ a supervised machine learning framework to identify and adjust for likely misreported entries [6].
Experimental Protocol:
- Define a "Healthy" Reference Group: Split your dataset. Identify a subgroup of participants considered "healthy" based on objective clinical biomarkers (e.g., body fat percentage, cholesterol levels) and demographic data [6].
- Train a Predictive Model: Use the data from the "healthy" group to train a Random Forest classifier. The model learns to predict food intake (e.g., frequency of bacon consumption) based on the objective biomarkers and demographics [6].
- Predict and Adjust: Apply the trained model to the remaining "unhealthy" group. For unhealthy food items, if a participant's self-reported value is lower than the model's prediction, replace it with the predicted value to correct for presumed underreporting [6].
Table: Key Biomarkers for FFQ Error Adjustment Models
| Biomarker / Variable | Role in Error Adjustment Model |
|---|---|
| LDL Cholesterol | Explanatory variable correlated with saturated fat intake [6]. |
| Total Cholesterol | Explanatory variable correlated with dietary habits [6]. |
| Blood Glucose | Explanatory variable related to dietary patterns [6]. |
| Body Fat Percentage | Objective anthropometric measure used for health status classification [6]. |
| Body Mass Index (BMI) | Anthropometric variable used as a predictor [6]. |
| Age & Sex | Demographic variables generally reported accurately, used to improve prediction [6]. |
How do I validate a new dietary assessment tool like a Fermented Foods FFQ?
Problem: I have developed a new specialized FFQ and need to assess its validity and reliability for use in research.
Solution: Validate your questionnaire against a gold-standard method and assess its repeatability over time.
Experimental Protocol:
- Relative Validity Assessment:
- Gold-Standard Comparison: Administer your new FFQ and multiple 24-hour dietary recalls (24HR) to the same participants [33].
- Statistical Analysis: Use Bland-Altman plots to assess the agreement between the two tools for estimating consumption quantities and frequencies. Successful validation is indicated by over 90% of data points falling within the limits of agreement for most food groups [33].
- Repeatability (Test-Retest Reliability) Assessment:
- Re-administer the FFQ: Have the same participants complete the FFQ a second time, approximately 6 weeks after the first administration [33].
- Statistical Analysis: Calculate Intra-Class Correlation Coefficients (ICC). High repeatability is generally indicated by ICC values ranging from 0.4 to 1.0 for most food groups, though less frequently consumed items (e.g., fermented fish) may yield lower values [33].
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Components for Cross-Classification and FFQ Validation Research
| Item / Reagent | Function / Application |
|---|---|
| The PANCAN Dataset (UCI) | A benchmark RNA-seq gene expression dataset for developing and testing cancer type classification models [81]. |
| SPCC Dataset | The Supernova Photometric Classification Challenge dataset, used for evaluating classification algorithms on imbalanced data [79]. |
| 24-Hour Dietary Recalls (24HR) | A gold-standard dietary assessment tool used to validate the relative validity of new FFQs [33]. |
| Fermented Food Frequency Questionnaire (3FQ) | A validated tool designed to assess the consumption of diverse fermented food groups across different populations [33]. |
| Random Forest Classifier | A robust machine learning algorithm used for both classification tasks and correcting measurement error in self-reported data [81] [6]. |
| Support Vector Machine (SVM) | A classifier often achieving high accuracy in genomic and clinical data classification, as demonstrated in cancer research [81] [82]. |
| Logistic Regression (LR) | A linear modeling technique useful as a baseline model and for investigating statistical variability in model comparisons [80]. |
| Lasso (L1) Regression | A feature selection method that identifies the most significant genes or variables by driving less important coefficients to zero [81]. |
Experimental Workflows
Diagram: Machine Learning Workflow for FFQ Error Adjustment
Diagram: Model Comparison Pitfalls in Cross-Validation
Frequently Asked Questions (FAQs)
1. How do FFQs fundamentally perform compared to more detailed dietary records? Multiple studies consistently show that Food Frequency Questionnaires (FFQs) have greater measurement error and higher rates of underreporting compared to multi-day food records (FRs) and 24-hour recalls. When evaluated against objective recovery biomarkers, FFQs systematically underestimate intakes more than other methods [42]. For instance, one major study found that compared to energy intake measured by doubly labeled water, intake was underestimated by 15-17% on automated 24-hour recalls (ASA24s), 18-21% on 4-day food records (4DFRs), and 29-34% on FFQs [42].
2. Can the performance of an FFQ be improved? Yes, statistical calibration can significantly improve the validity of dietary estimates from all self-report tools, including FFQs. By using regression calibration equations that incorporate factors like body mass index (BMI), age, and ethnicity, the proportion of explainable biomarker variation can be dramatically increased [83]. Furthermore, emerging machine learning techniques show promise in identifying and correcting for misreported data, such as underreporting of unhealthy foods, with model accuracies ranging from 78% to 92% in some studies [20].
3. Is it necessary to develop a new FFQ for my specific study population? For populations with unique dietary patterns, a culture-specific FFQ is highly recommended. A validated FFQ designed for one population may not be appropriate for another due to different food cultures. Research demonstrates that developing a culture-specific FFQ that includes local dishes and street foods results in a valid tool for assessing food group intake in that specific population [37] [84]. The process involves modifying existing questionnaires, including relevant food items, and testing the tool for validity and reproducibility within the target population.
4. Do FFQs perform poorly for all nutrients? No, the performance of FFQs varies by nutrient. Energy intake is particularly prone to misreporting on FFQs. However, for some nutrient densities (e.g., protein density—the fraction of energy from protein), the differences between assessment methods can be smaller and non-significant [83]. Some studies have found that energy adjustment can improve estimates from FFQs for certain nutrients, like protein and sodium, though this is not universally true for all nutrients, such as potassium [42].
5. Are there some contexts where FFQ data may be less reliable? Yes, FFQ validity can be lower in specific sub-populations or for certain nutrients. For example, one study that attempted biochemical validation in patients with Peripheral Arterial Disease (PAD) found poor agreement between FFQ-reported intake of immune-modulating nutrients and their corresponding serum biomarker levels [16]. This suggests that physiological states specific to a disease might affect nutrient metabolism or reporting, complicating the validation process.
Troubleshooting Common Experimental Challenges
Problem 1: Significant underreporting of energy and nutrient intake in FFQ data.
- Potential Cause: Underreporting, especially of unhealthy or socially undesirable foods, is a common form of measurement error in self-reported dietary data [20] [84]. This is more prevalent in individuals with obesity and can be influenced by social desirability bias [42].
- Solution:
- Statistical Calibration: Develop and apply calibration equations using recovery biomarkers (e.g., doubly labeled water for energy, urinary nitrogen for protein) from a subset of your study population. This can correct for systematic bias [83] [21].
- Machine Learning Correction: Consider using a predictive model, like a random forest classifier, to identify and correct for likely underreported entries. A model trained on objective health metrics (e.g., blood lipids, BMI) from a "healthy" subset of your cohort can predict plausible intake values for the rest of the population [20].
Problem 2: The existing FFQ is not suitable for the unique dietary patterns of your study population.
- Potential Cause: Using an FFQ developed for a different cultural or ethnic group can lead to misclassification of habitual intake, as it may miss key local foods or preparation methods [37].
- Solution:
- Develop a Culture-Specific FFQ: Follow a multi-stage adaptation and validation process [37] [84]:
- Adapt a Base FFQ: Modify an existing questionnaire by adding common local dishes, street foods, and removing irrelevant items.
- Conduct a Pilot Study: Test the face validity and comprehensibility of the new tool.
- Formal Validation: Administer the new FFQ alongside a reference method (e.g., multiple 24-hour recalls or food records) to a sample of your population.
- Assess Reproducibility: Re-administer the FFQ after a period of time (e.g., 3 months) to assess test-retest reliability.
- Develop a Culture-Specific FFQ: Follow a multi-stage adaptation and validation process [37] [84]:
Problem 3: Weak or non-significant correlations between FFQ estimates and biomarker measurements.
- Potential Cause: This is a known limitation of FFQs. The error structure of FFQs means they explain a much smaller portion of the true biological variation in intake compared to more detailed methods [83] [16].
- Solution:
- Use Multiple Dietary Assessments: If resources allow, use multiple 24-hour recalls or food records as your primary dietary assessment tool, as they have been shown to provide better estimates of absolute intake for several nutrients [83] [42].
- Focus on Energy-Adjusted Nutrients and Density: Analyze nutrient densities (e.g., percent of energy from fat) or use energy-adjusted models, as these can sometimes improve validity and reduce the impact of general underreporting [83] [42].
- Leverage Biomarker-Guided Regression Calibration: In your analysis, use biomarkers not just for validation but for calibration. This statistical technique uses the correlation between two biomarkers (or a biomarker and the FFQ) to correct for measurement error in diet-disease association studies [21].
Table 1: Comparison of Underreporting Against Recovery Biomarkers [42]
| Dietary Assessment Method | Average Underestimation of Energy Intake (vs. Doubly Labeled Water) |
|---|---|
| Automated 24-hour Recalls (ASA24s) | 15% - 17% |
| 4-day Food Records (4DFRs) | 18% - 21% |
| Food Frequency Questionnaires (FFQs) | 29% - 34% |
Table 2: Proportion of Biomarker Variation Explained by Different Dietary Tools (Before Calibration) [83]
| Nutrient | Food Frequency Questionnaire (FFQ) | 4-day Food Record | 24-hour Recalls (x3) |
|---|---|---|---|
| Energy | 3.8% | 7.8% | 2.8% |
| Protein | 8.4% | 22.6% | 16.2% |
| Protein Density | 6.5% | 11.0% | 7.0% |
Table 3: Validity Correlation Coefficients (FFQ vs. Food Records) [7]
| Nutrient | Correlation Coefficient Range (FFQ vs. 9-day FRs) |
|---|---|
| Various Nutrients | 0.07 to 0.41 |
| Interpretation: Correlation coefficients below 0.5 generally indicate moderate to weak agreement between the FFQ and the reference method. |
Detailed Experimental Protocols
Protocol 1: Validating an FFQ Using Recovery Biomarkers
This protocol is based on the methodology used in large cohort studies like the Women's Health Initiative (WHI) and the Adventist Health Study-2 (AHS-2) [83] [21].
- Study Population: Recruit a representative sub-sample (calibration study) from your main cohort. Aim for several hundred participants to ensure statistical power.
- Dietary Assessment: Administer the FFQ to all participants.
- Biomarker Measurement:
- Energy Intake: Measure total energy expenditure over a 1-2 week period using the doubly labeled water (DLW) technique. In weight-stable individuals, this is equivalent to energy intake [83].
- Protein Intake: Collect 24-hour urine samples. Analyze for urinary nitrogen. Calculate protein intake using the formula: Protein (g) = 6.25 × (24-h urinary nitrogen ÷ 0.81), where 0.81 represents the average recovery rate of dietary nitrogen in urine [83].
- Quality Control: Use a marker like para-aminobenzoic acid (PABA) to verify completeness of the 24-hour urine collection [83].
- Data Analysis:
- Calculate the correlation (de-attenuated for within-person variation) between the FFQ estimates and the biomarker measurements.
- Develop regression calibration equations where the biomarker is the outcome variable and the FFQ estimate, along with covariates like BMI, age, and sex, are the predictors.
Diagram 1: Biomarker validation workflow for an FFQ.
Protocol 2: A Machine Learning Approach to Correct for Underreporting
This protocol outlines the method described by [20] to correct for underreporting of specific foods.
- Data Collection: Gather a dataset that includes:
- FFQ Data: The specific food frequency and quantity variables you wish to correct (e.g., bacon, fried chicken).
- Objective Health Metrics: LDL cholesterol, total cholesterol, blood glucose, body fat percentage, and BMI.
- Demographics: Age and sex.
- Data Splitting: Split your dataset into two groups:
- Healthy Group: Participants classified as having low health risk based on predefined cut-offs for body fat, age, and sex. Their data is assumed to be more accurately reported.
- Unhealthy Group: The remaining participants, where underreporting is assumed to be more likely.
- Model Training: Using only the Healthy Group data, train a Random Forest (RF) classifier. The model learns to predict the FFQ food response based on the objective health metrics and demographics.
- Prediction and Correction:
- Use the trained RF model to predict the most probable food frequency category for each participant in the Unhealthy Group.
- For unhealthy foods (where underreporting is suspected), compare the model's prediction to the participant's original FFQ response. If the predicted value is higher than the reported value, replace the original response with the predicted value.
Diagram 2: Machine learning correction for underreporting.
The Scientist's Toolkit: Key Research Reagents & Materials
Table 4: Essential Materials for Dietary Validation Studies
| Item | Function in Research | Key Considerations |
|---|---|---|
| Doubly Labeled Water (DLW) | The gold-standard recovery biomarker for measuring total energy expenditure in free-living individuals over 1-2 weeks [83] [42]. | Expensive and requires specialized mass spectrometry for analysis. Best used in a calibration sub-study. |
| Para-aminobenzoic acid (PABA) | A tablet taken with meals to verify the completeness of a 24-hour urine collection. Recovery of 85-110% of the dose indicates a complete collection [83]. | Crucial for ensuring the accuracy of urinary nitrogen and other urinary biomarker measurements. |
| Semi-Quantitative FFQ | The tool being validated. It lists foods with portion size options and asks about frequency of consumption over a defined period (e.g., past year) [37] [84]. | Must be culture-specific. Should be adapted and piloted for the target population before the main study. |
| 24-Hour Dietary Recalls / Food Records | Used as a reference method against which the FFQ is validated when biomarkers are not available. Multiple non-consecutive days (including weekends) are needed to estimate usual intake [7] [84]. | Prone to some of the same self-report biases as FFQs, but less reliant on long-term memory. |
| Biomarker Specimen Collection Kits | Kits for the collection, preservation, and shipping of biological samples (e.g., blood, urine, adipose tissue) for biomarker analysis [21]. | Must include appropriate tubes, preservatives, and cold-chain shipping materials to maintain sample integrity. |
Conclusion
Overcoming the limitations of Food Frequency Questionnaires is not a singular task but a continuous process of refinement grounded in methodological rigor. By integrating cultural specificity, leveraging advanced computational optimization, and adhering to stringent validation protocols, researchers can significantly enhance the reliability and validity of dietary data. The future of nutritional epidemiology and clinical research hinges on these improved tools, which will enable more precise investigations into the role of diet in chronic diseases and more effective evaluation of nutritional interventions in drug development. Embracing these multifaceted strategies will transform the FFQ from a source of uncertainty into a powerful, validated instrument for generating actionable scientific insights.
References
- 1. Dietary assessment methods in epidemiological research [https://pmc.ncbi.nlm.nih.gov/articles/PMC5482335/]
- 2. The accuracy of portion size estimation using food images and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9291996/]
- 3. Evaluating the Measurement Error Structure of Self-Report ... [https://dietassessmentprimer.cancer.gov/concepts/error/error-affecting.html]
- 4. Validity and Systematic Error in Measuring Carotenoid ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5673110/]
- 5. The Use of Pictorial Recall Aids Modifies Dietary ... [https://www.sciencedirect.com/science/article/pii/S2475299124023862]
- 6. Mitigating underreported error in food frequency questionnaire ... [https://bmcmedinformdecismak.biomedcentral.com/articles/10.1186/s12911-023-02262-9]
- 7. Relative validities of 3- day and the food frequency... records food [https://pmc.ncbi.nlm.nih.gov/articles/PMC2867225/]
- 8. Adaptation of Locally Available Portion Sizes for Food ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4919938/]
- 9. Lack of efficacy of a food-frequency questionnaire in ... [https://www.sciencedirect.com/science/article/pii/S0002916523070661]
- 10. Adaptation and validation of a food frequency questionnaire ... [https://nutritionj.biomedcentral.com/articles/10.1186/s12937-018-0368-4]
- 11. Unveiling Dietary Complexity: A Scoping Review and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12567371/]
- 12. Optimal dietary patterns for healthy aging | Nature Medicine [https://www.nature.com/articles/s41591-025-03570-5]
- 13. SYNERGIES BETWEEN FOOD BIODIVERSITY ... [https://www.sciencedirect.com/science/article/abs/pii/S0002916525006744]
- 14. A MULTI-OBJECTIVE OPTIMIZATION USING THE EPIC ... [https://pubmed.ncbi.nlm.nih.gov/41260521/]
- 15. Comparisons to 24-Hour Dietary Recalls and Selected ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12569992/]
- 16. Biochemical validation of a food frequency questionnaire ... [https://www.sciencedirect.com/science/article/pii/S0939475325000882]
- 17. Data Analysis for the 2025 Guidelines Committee Report [https://www.dietaryguidelines.gov/2025-advisory-committee-report/data-analysis]
- 18. Dietary assessment methods in epidemiologic studies - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4154347/]
- 19. Overview of Dietary Assessment Methods for Measuring ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8338737/]
- 20. Mitigating underreported error in food frequency ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10492312/]
- 21. Biomarkers of Dietary Intake Are Correlated with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4763486/]
- 22. Principles Underlying Recommendations [https://dietassessmentprimer.cancer.gov/approach/principles.html]
- 23. FAO/INFOODS Food Composition Databases [https://www.fao.org/infoods/infoods/tables-and-databases/faoinfoods-databases/en/]
- 24. Food composition | Nutrition [https://www.fao.org/nutrition/food-composition/en/]
- 25. Development, Validity, and Reliability of a Food Frequency ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12251943/]
- 26. Relative Validity of an Italian EPIC Food Frequency ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8069881/]
- 27. Smartphone Validation of a Food Frequency Questionnaire ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12305569/]
- 28. A new self-administered semi-quantitative food frequency ... [https://www.sciencedirect.com/science/article/abs/pii/S0271531720304474]
- 29. Food frequency questionnaires [https://www.measurement-toolkit.org/diet/subjective-methods/food-frequency-questionnaire]
- 30. The Development of a Food Frequency Questionnaire for ... [https://www.mdpi.com/2072-6643/16/22/3896]
- 31. Nutrition Questionnaire Service Center | Department of Nutrition [https://hsph.harvard.edu/department/nutrition/nutrition-questionnaire-service-center/]
- 32. Updated-Food Choice Questionnaire: Cultural Adaptation ... [https://www.mdpi.com/2072-6643/16/21/3749]
- 33. Validation of the fermented food frequency questionnaire to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12608085/]
- 34. Fermented Food Consumption Across European Regions [https://pmc.ncbi.nlm.nih.gov/articles/PMC12455144/]
- 35. Validity and reproducibility of a food frequency ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2023.1059870/full]
- 36. Development of a Multilingual Web-Based Food Frequency ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10610353/]
- 37. Validity and Reproducibility of a Culture-Specific Electronic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11450712/]
- 38. Evaluation of Web-Based, Self-Administered, Graphical ... [https://www.sciencedirect.com/science/article/abs/pii/S2212267213017760]
- 39. Evaluation of the Reliability and Validity of a Food ... [https://www.mdpi.com/2072-6643/17/14/2270]
- 40. Protocol for a Mixed Methods Study [https://www.researchprotocols.org/2025/1/e70194]
- 41. Dietary assessment in intermittent fasting: validation of a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12336244/]
- 42. Comparison of self-reported dietary intakes from the ... [https://www.sciencedirect.com/science/article/pii/S0002916522027459]
- 43. A Systematic Review and Meta-Analysis of Validation ... [https://www.sciencedirect.com/science/article/pii/S2161831322005099]
- 44. A Proof of Concept Based on Data from the Second ... [https://www.mdpi.com/2072-6643/15/24/5098]
- 45. Use of OR to design food frequency questionnaires in ... [https://www.sciencedirect.com/science/article/abs/pii/S2211692312000082]
- 46. Optimising the selection of food items for FFQs using Mixed ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10271084/]
- 47. 2.3. Optimization and Comparison of FFQ Length [https://bio-protocol.org/exchange/minidetail?id=17024553&type=30]
- 48. A MILP-based decomposition algorithm and case studies [https://www.sciencedirect.com/science/article/abs/pii/S0098135419311147]
- 49. Evaluation of the Reliability and Validity of a Food Frequency ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12298913/]
- 50. Promoting and Updating Food Frequency Questionnaire ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8724669/]
- 51. Food Frequency Questionnaire Personalisation Using Multi ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9571126/]
- 52. Optimising an FFQ Using a Machine Learning Pipeline to ... [https://pubmed.ncbi.nlm.nih.gov/33321959/]
- 53. Are Machine Learning Algorithms More Accurate in ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2022.740898/full]
- 54. Gaussian graphical models with applications to omics analyses [https://pubmed.ncbi.nlm.nih.gov/36161666/]
- 55. Unveiling Dietary Complexity: A Scoping Review and ... [https://pubmed.ncbi.nlm.nih.gov/41156513/]
- 56. Gaussian Graphical Models Identify Networks of Dietary ... [https://www.sciencedirect.com/science/article/pii/S0022316623005539]
- 57. Food co-consumption network as a new approach to ... [https://www.nature.com/articles/s41598-023-47752-y]
- 58. Discriminability of node colors in node-link diagrams and ... [https://www.sciencedirect.com/science/article/pii/S2468502X25000713]
- 59. Make Your Network Maps Shine with 16 New Analyzer ... [https://visiblenetworklabs.com/2025/03/06/make-your-network-maps-shine-with-16-new-analyzer-color-palettes/]
- 60. How to render a network map, part 3: color - Reticular [https://reticular.hypotheses.org/7285]
- 61. Dietary patterns derived by Gaussian graphical models ... [https://www.nature.com/articles/s41598-025-92361-6]
- 62. Optimization of a Food List for Food Frequency ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10745589/]
- 63. Development of a Food Frequency Questionnaire (FFQ) for ... [https://www.sciencedirect.com/science/article/pii/S002231662216253X]
- 64. Comparison of approaches to correct intake–health ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10271542/]
- 65. Digital Food Frequency Questionnaire Assessing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11094607/]
- 66. Optimising an FFQ Using a Machine Learning Pipeline to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7764455/]
- 67. A Guideline of Selecting and Reporting Intraclass ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4913118/]
- 68. Kappa statistic considerations in evaluating inter-rater ... [https://bmccancer.biomedcentral.com/articles/10.1186/s12885-023-11325-z]
- 69. Test-Retest Reliability and Agreement of the Work Ability ... [https://www.sciencedirect.com/science/article/pii/S0003999324013509]
- 70. Interrater reliability: the kappa statistic - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3900052/]
- 71. Weighted Kappa for Interobserver Agreement and Missing ... [https://www.mdpi.com/2504-4990/7/1/18]
- 72. Validity and reproducibility of a food frequency questionnaire ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10436288/]
- 73. Validity and Reliability of a Food Frequency Questionnaire ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6926524/]
- 74. Validity and reliability of a simplified food frequency ... [https://nutritionj.biomedcentral.com/articles/10.1186/s12937-020-00630-z]
- 75. Testing agreement between a new method and the gold ... [https://www.sciencedirect.com/science/article/abs/pii/S0021929013004065]
- 76. ICC to compare against a gold standard [https://real-statistics.com/reliability/interrater-reliability/intraclass-correlation/icc-compare-against-gold-standard/]
- 77. Development and relative validation of a short food ... frequency [https://pubmed.ncbi.nlm.nih.gov/30805696/]
- 78. Validation of food frequency questionnaire for food intake ... [https://www.frontiersin.org/journals/public-health/articles/10.3389/fpubh.2024.1438008/full]
- 79. Optimizing Supernova Classification with Interpretable ... [https://arxiv.org/html/2510.13765v1]
- 80. Statistical variability in comparing accuracy of ... [https://www.nature.com/articles/s41598-025-12026-2]
- 81. Machine learning approach to identify significant genes ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12547461/]
- 82. A machine learning framework for cross-institute ... [https://www.sciencedirect.com/science/article/pii/S0010482525007450]
- 83. Evaluation and Comparison of Food Records, Recalls ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3202154/]
- 84. Development of an online food frequency questionnaire ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2022.949330/full]