Biomarker Validation Against Controlled Feeding Studies: A Roadmap from Discovery to Clinical Application
This article provides a comprehensive guide for researchers and drug development professionals on validating biomarkers using controlled feeding studies.
Biomarker Validation Against Controlled Feeding Studies: A Roadmap from Discovery to Clinical Application
Abstract
This article provides a comprehensive guide for researchers and drug development professionals on validating biomarkers using controlled feeding studies. It covers the foundational role of these studies in establishing causal intake-biomarker relationships, details the multi-phase methodological frameworks for biomarker development, addresses common analytical and translational challenges, and outlines the rigorous validation and qualification criteria required for clinical and regulatory acceptance. By synthesizing current methodologies and future trends, this resource aims to bridge the gap between preclinical discovery and the application of robust, validated dietary biomarkers in clinical research and precision medicine.
The Foundational Role of Controlled Feeding Studies in Biomarker Discovery
In the complex field of nutrition science, establishing definitive cause-and-effect relationships between diet and health outcomes represents a significant methodological challenge. While observational studies can identify associations, they often struggle to disentangle true causal effects from confounding factors such as lifestyle, genetics, and environmental influences [1] [2]. Causal inference—the process of determining whether one variable actually causes changes in another—provides the philosophical and statistical framework to move beyond mere correlation to establish true cause-and-effect relationships [1] [3].
Within this framework, controlled feeding studies emerge as the undisputed gold standard for establishing causality in diet-health relationships. These studies, where researchers provide all or most foods consumed by participants under strictly monitored conditions, offer the experimental precision necessary to isolate the specific effects of dietary interventions [2] [4]. For researchers and drug development professionals focused on biomarker validation, controlled feeding studies provide the essential foundational evidence that links potential biomarkers directly to dietary intake, creating a critical bridge between dietary exposure and physiological response [5] [6].
This guide objectively compares controlled feeding studies against alternative methodological approaches, examining their respective roles in establishing causal inference and validating biomarkers for precision nutrition and drug development.
Causal Inference Frameworks: From Observation to Experimentation
The Foundations of Causal Inference
The statistical foundation for modern causal inference rests heavily on the Potential Outcomes Framework (also known as the Rubin Causal Model). This framework conceptualizes each individual as having two potential outcomes: one under treatment (Yâ‚) and one under control (Yâ‚€) [1] [3]. The fundamental challenge in causal inference—the "missing data problem"—arises because we can only observe one of these outcomes for each individual [3]. The Average Treatment Effect is defined as E[Yâ‚ - Yâ‚€], representing the expected difference in outcomes between the treatment and control conditions [1] [3].
Directed Acyclic Graphs provide visual tools to represent causal assumptions and identify confounding variables that might create misleading associations [1]. These conceptual diagrams help researchers structure their causal reasoning and select appropriate statistical methods to account for potential confounders.
Methodological Spectrum in Nutrition Research
Nutritional research employs a spectrum of methodological approaches with varying strengths for causal inference, as compared in the table below.
Table 1: Comparison of Research Methods for Causal Inference in Nutrition
| Method Type | Key Characteristics | Causal Inference Strength | Primary Limitations | Role in Biomarker Research |
|---|---|---|---|---|
| Observational Studies | Analyzes existing data without intervention; uses statistical adjustments | Limited for causal claims; identifies associations | Confounding; recall bias; reverse causality | Initial discovery of candidate biomarkers [5] |
| Randomized Behavioral Interventions | Participants randomly assigned to dietary advice or counseling | Moderate; random assignment reduces confounding | Variable intervention fidelity; self-reported intake | Limited utility for biomarker validation |
| Controlled Feeding Studies | Researchers provide all food under controlled conditions | High; maximum control over independent variable | Resource-intensive; limited generalizability | Gold standard for biomarker validation [5] [2] |
Controlled Feeding Studies: The Experimental Gold Standard
Fundamental Principles and Design
Controlled feeding studies are specifically designed to determine cause-and-effect relationships between dietary intake and physiological or health outcomes by eliminating the confounding effects of differences in dietary intake [2]. These studies provide the most rigorous approach for controlling the independent variable (diet) in nutrition research, creating experimental conditions that mirror the precision achieved in pharmaceutical trials [2] [4].
The basic elements of controlled feeding studies include:
- Menu Development: Research dietitians use specialized software to develop menus meeting specific nutrient targets, typically using 3- to 7-day repeating cycles to minimize food variety requirements while maintaining participant compliance [2].
- Food Provision: All foods are prepared and provided to participants, with precise documentation of gram weights and nutrient composition [2].
- Energy Adjustment: Individual energy needs are determined through prediction equations, indirect calorimetry, or doubly labeled water, with adjustments made to maintain weight stability [2].
Experimental Protocols and Compliance Monitoring
Compliance monitoring represents a critical component of high-quality controlled feeding studies. Both in-patient and out-patient approaches employ multiple strategies to verify adherence to study protocols:
- Objective Biomarkers: Urinary sodium, nitrogen, or para-aminobenzoic acid excretion provide quantitative measures of compliance with study diets [2].
- Direct Observation: Some protocols require participants to consume at least one daily meal under staff supervision [2].
- Returned Food Weights: Uneaten foods are returned, weighed, and documented to calculate actual intake [2].
- Rapport Building: Establishing strong researcher-participant relationships encourages honest self-reporting of dietary deviations [2].
Table 2: Key Methodological Considerations in Controlled Feeding Trials
| Design Element | Options | Considerations | Impact on Causal Inference |
|---|---|---|---|
| Study Design | Parallel vs. Crossover | Crossover designs increase statistical power but require washout periods | Stronger internal validity with participant-as-own-control [5] |
| Participant Selection | Various populations based on research question | Homogeneous groups reduce variability; diverse groups enhance generalizability | Balance between statistical power and external validity |
| Dietary Control Level | Complete provision vs. partial provision | Degree of control over confounding foods | Greater control strengthens causal claims |
| Intervention Duration | Acute vs. chronic effects | Must align with expected biological response time | Must be sufficient to detect hypothesized effects |
| Blinding | Single, double, or open-label | Maximized when using matched control diets | Reduces performance and detection bias |
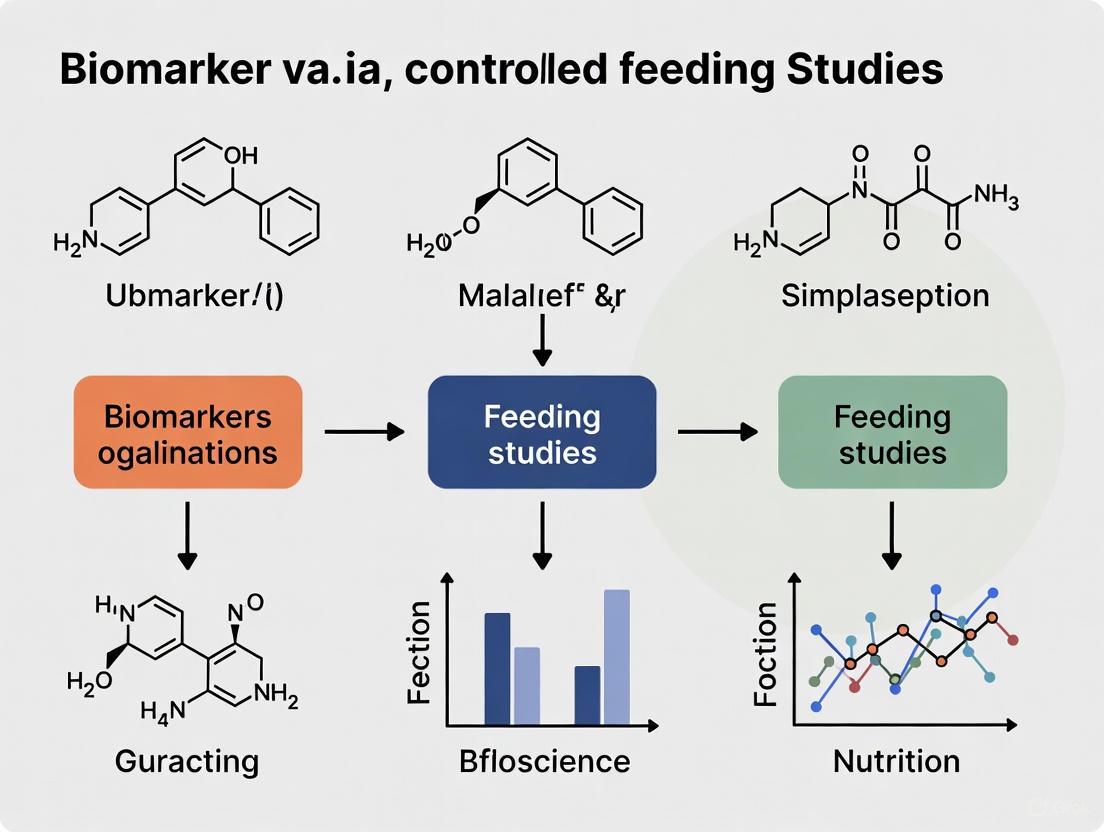
The following diagram illustrates the typical workflow and causal logic of a controlled feeding study:
Case Study: Validating Ultra-Processed Food Biomarkers
Experimental Evidence from Complementary Study Designs
A compelling example of controlled feeding's critical role in causal inference comes from recent research on ultra-processed food biomarkers [5]. This research program employed a sophisticated multi-stage approach that combined observational and experimental methodologies:
- Observational Discovery Phase: The IDATA study analyzed 718 free-living adults with diverse dietary intakes, using metabolomic profiling to identify hundreds of serum and urine metabolites correlated with UPF intake [5].
- Controlled Validation Phase: A randomized, controlled, crossover-feeding trial of 20 subjects admitted to the NIH Clinical Center compared diets containing 80% versus 0% energy from UPF [5].
Quantitative Results and Causal Interpretation
The experimental data from this research provides compelling evidence for the causal relationship between UPF intake and specific metabolic signatures:
Table 3: Experimental Data from UPF Biomarker Validation Study
| Metabolite | Specimen | Correlation with UPF (rs) | Controlled Feeding Result | Biological Interpretation |
|---|---|---|---|---|
| S-Methylcysteine sulfoxide | Serum & Urine | -0.23 (serum), -0.19 (urine) | Significant difference between diets | Potential marker of vegetable intake |
| N2,N5-diacetylornithine | Serum & Urine | -0.27 (serum), -0.26 (urine) | Significant difference between diets | Microbial-host co-metabolite |
| Pentoic acid | Serum & Urine | -0.30 (serum), -0.32 (urine) | Significant difference between diets | Carbohydrate metabolism intermediate |
| N6-carboxymethyllysine | Serum & Urine | +0.15 (serum), +0.20 (urine) | Significant difference between diets | Advanced glycation end product |
The poly-metabolite scores developed from the observational study successfully differentiated, within individuals, between the 80% and 0% UPF diet phases in the controlled feeding trial (P-value for paired t-test < 0.001) [5]. This cross-validation across study designs provides particularly strong evidence for a causal relationship between UPF consumption and specific metabolic profiles.
The following diagram illustrates the complementary strengths of this hybrid study design approach:
Research Reagent Solutions for Controlled Feeding Studies
Table 4: Essential Materials and Methods for Controlled Feeding Research
| Tool Category | Specific Examples | Research Function | Application in Causal Inference |
|---|---|---|---|
| Diet Design Software | NDS-R, ProNutra [2] | Menu development and nutrient analysis | Precisely defines and controls the independent variable |
| Metabolomic Platforms | UPLC-MS/MS [5] | High-throughput metabolite profiling | Objective measurement of biochemical responses to diet |
| Compliance Biomarkers | Urinary nitrogen, PABA, sodium [2] | Verification of dietary adherence | Ensures intervention fidelity and reduces misclassification |
| Energy Assessment Tools | Indirect calorimetry, doubly labeled water [2] | Determination of individual energy requirements | Maintains energy balance and weight stability |
| Biospecimen Collection | Serial blood, 24-hour urine [5] | Biological sampling for biomarker analysis | Enables temporal analysis of diet-metabolite relationships |
Methodological Considerations for Implementation
Successful implementation of controlled feeding studies requires attention to several methodological complexities:
- Resource Intensity: Controlled feeding studies typically cost $25-30 per participant daily for food and supplies alone, requiring significant staffing and infrastructure [2].
- Weight Stability Management: Participants are weighed daily, with energy adjustments made to maintain stable body weight—a critical consideration since weight changes themselves can confound physiological outcomes [2].
- Palatability and Compliance: Foods must be palatable and familiar to the target population to maximize long-term compliance, particularly in studies of extended duration [2].
Controlled feeding studies represent an indispensable methodology for establishing causal inference in nutrition science and validating dietary biomarkers. While observational studies and behavioral interventions play important roles in the broader research ecosystem, neither can match the experimental control afforded by providing all study foods under monitored conditions.
For drug development professionals and researchers pursuing biomarker qualification, controlled feeding studies provide the causal evidence necessary to advance biomarkers from exploratory status to probable or known valid biomarkers [6]. The integration of controlled feeding data with observational evidence creates a powerful evidence base for regulatory submissions and clinical implementation.
As precision nutrition advances, the continued development and refinement of controlled feeding methodologies will be essential for translating population-level associations into individualized dietary recommendations and targeted therapies. Their role as the gold standard for causal inference in nutrition science remains unchallenged, providing the foundational evidence upon which effective nutritional interventions and validated biomarkers are built.
In the field of precision nutrition, the discovery and validation of robust dietary biomarkers represents a critical scientific frontier. Unlike pharmaceutical research where controlled dosing is straightforward, nutrition science faces the unique challenge of quantifying intake of complex food matrices and their biological effects. The Dietary Biomarkers Development Consortium (DBDC) is leading a major effort to address this challenge through systematic discovery and validation of biomarkers for commonly consumed foods [7] [8]. Establishing precise dose-response relationships and comprehensive pharmacokinetic parameters for dietary biomarkers requires specialized experimental approaches that account for the complexity of food as an "exposure." These parameters form the foundation for understanding how specific foods and nutrients are absorbed, distributed, metabolized, and excreted by the human body, ultimately enabling the development of objective measures that can complement or replace traditional self-reported dietary assessment methods [7].
The validation of dietary biomarkers against controlled feeding studies represents a paradigm shift in nutritional science. Whereas drug assay validation can utilize spiked reference standards against target nominal levels, biomarker measurement presents a fundamentally different challenge because researchers must demonstrate accuracy and precision by measuring endogenous molecules with varying native analyte levels [9]. This complexity necessitates sophisticated experimental designs that can isolate the effects of specific dietary components amid background noise from habitual diets and individual metabolic variations.
Experimental Protocols for Establishing Pharmacokinetic Parameters
Controlled Feeding Trial Designs
The gold standard for establishing pharmacokinetic parameters for dietary biomarkers involves controlled feeding trials with precise dietary manipulation. The DBDC implements a structured 3-phase approach for biomarker discovery and validation [7] [8]. In Phase 1, researchers administer test foods in prespecified amounts to healthy participants under highly controlled conditions. This is followed by comprehensive metabolomic profiling of blood and urine specimens collected at strategic time points to identify candidate biomarker compounds and characterize their kinetic profiles. These initial feeding studies are specifically designed to characterize the pharmacokinetic parameters of candidate biomarkers, including absorption rates, distribution patterns, metabolic conversion, and elimination half-lives [7].
The execution of controlled feeding studies requires meticulous attention to methodological details. Research dietitians utilize specialized software such as Nutrition Data System for Research (NDS-R) and ProNutra to design menus that meet specific nutrient targets while accommodating individual energy requirements [10] [2]. Foods are carefully selected based on consistent availability through reliable vendors, with some studies incorporating a combination of fresh, frozen, ready-to-eat, canned, dried, cured, and manufactured foods to represent realistic market supply [11]. Menu cycles typically span 3-7 days to minimize the variety of study foods needed while maintaining participant acceptability [2].
Protocol Implementation and Compliance Monitoring
Successful implementation of controlled feeding studies requires rigorous protocols for diet preparation and compliance monitoring. In the Women's Health Initiative Feeding Study (NPAAS-FS), researchers designed individual menu plans for each of 153 postmenopausal women that approximated their habitual food intake as estimated from 4-day food records, adjusted for energy requirements [10]. This innovative approach preserved normal variation in nutrient and food consumption while maintaining controlled conditions—a critical consideration for subsequent biomarker validation.
Compliance monitoring employs both objective and subjective measures. Objective indicators include urinary nitrogen excretion compared to dietary nitrogen intake, doubly labeled water for energy intake validation, and in some cases, incorporation of para-aminobenzoic acid (PABA) into study foods with subsequent assessment of urinary excretion [2]. Daily weight checks ensure energy balance is maintained throughout the study, with adjustments made to calorie levels if unintended weight changes occur [2]. Additional compliance measures include daily food checklists, weigh-backs of uneaten food containers, and supervised meal consumption when feasible [11] [2].
Table 1: Key Pharmacokinetic Parameters Measured in Dietary Biomarker Studies
| Parameter | Description | Significance in Dietary Biomarkers | Common Measurement Methods |
|---|---|---|---|
| AUC (Area Under Curve) | Total exposure to biomarker over time | Reflects overall bioavailability of food components | Serial blood/urine measurements over 24-72 hours |
| C~max~ | Maximum concentration observed | Indicates peak absorption potential | Peak value from serial measurements |
| T~max~ | Time to reach maximum concentration | Reveals absorption kinetics | Time of C~max~ occurrence |
| Elimination Half-life | Time for concentration to reduce by half | Informs on suitable sampling windows & biomarker persistence | Calculation from elimination phase slope |
| Urinary Recovery | Percentage of ingested compound excreted in urine | Provides quantitative recovery assessment | 24-hour urine collection analysis |
Methodologies for Determining Dose-Response Relationships
Dose-Fractionation and Exposure-Response Studies
The establishment of dose-response relationships for dietary biomarkers requires specialized study designs that systematically vary the amount of test food or nutrient administered. Drawing from methodologies established in tuberculosis drug development, nutritional research adapts dose-fractionation approaches where the same total exposure is divided into different dosing regimens to identify the optimal pattern of intake [12]. These studies are complemented by exposure-effect investigations that correlate varying doses of food components with corresponding biomarker concentrations in biological fluids [12].
In practice, these studies involve administering predetermined amounts of test foods to participants according to carefully designed protocols. For example, the DBDC implements three distinct controlled feeding trial designs in its initial discovery phase, administering test foods in prespecified amounts to healthy participants to identify candidate compounds that exhibit dose-dependent responses [7]. The resulting data enable researchers to establish quantitative relationships between dietary intake levels and subsequent biomarker concentrations, creating mathematical models that can predict intake based on biomarker measurements.
Statistical Considerations and Biomarker Performance Metrics
The evaluation of dose-response relationships requires appropriate statistical approaches and performance metrics. As highlighted in biomarker validation literature, the analytical plan should be predefined before data collection to avoid bias from data-driven analyses [13]. When assessing biomarker performance, key metrics include sensitivity (the proportion of cases with high intake that test positive), specificity (the proportion of cases with low intake that test negative), and receiver operating characteristic (ROC) curves that plot sensitivity versus 1-specificity across all possible biomarker thresholds [13].
Statistical modeling of dose-response data often employs linear regression of log-transformed consumed nutrients on log-transformed biomarker concentrations. In the Women's Health Initiative feeding study, this approach yielded R² values ranging from 0.32 for lycopene to 0.53 for α-carotene, indicating the proportion of variance in intake explained by the biomarker [10]. For biomarkers with potential clinical applications, positive predictive value (proportion of test-positive participants who actually have high intake) and negative predictive value (proportion of test-negative participants who truly have low intake) provide additional important performance characteristics, though these metrics are influenced by the prevalence of consumption patterns in the study population [13].
Table 2: Performance Metrics for Dietary Biomarkers from Controlled Feeding Studies
| Biomarker Category | Example Biomarkers | R² Values from WHI Study | Performance Classification | Key Influencing Factors |
|---|---|---|---|---|
| Vitamins | Serum folate, Vitamin B-12 | 0.49–0.51 | Strong | Supplement use, metabolic status |
| Carotenoids | α-carotene, β-carotene, lutein + zeaxanthin | 0.39–0.53 | Moderate to Strong | Fat intake, genetic variation |
| Tocopherols | α-tocopherol | 0.47 | Moderate | Supplement use, fat intake |
| Fatty Acids | Phospholipid polyunsaturated fatty acids | 0.27 | Weak to Moderate | Background diet, metabolism |
| Reference Biomarkers | Urinary nitrogen, Doubly labeled water | 0.43–0.53 | Established benchmark | Protein turnover, metabolic efficiency |
Comparative Analysis of Biomarker Validation Approaches
Nutritional vs. Pharmaceutical Biomarker Validation
The validation of dietary biomarkers differs significantly from pharmaceutical biomarker validation in several key aspects. While drug assays can measure recovery of spiked reference standards against target nominal levels, dietary biomarker validation must demonstrate accuracy and precision for endogenous molecules with varying native analyte levels [9]. This fundamental distinction necessitates different scientific approaches for accuracy assessment, though precision evaluation still relies on repeated measurements of the same samples to evaluate measurement variability.
Another critical difference lies in the complexity of the exposure. Pharmaceutical studies typically involve administration of a single chemical entity, whereas nutritional research must account for complex food matrices that contain numerous interacting compounds that may influence bioavailability and metabolism [7] [11]. Additionally, dietary biomarkers must function against the background of habitual diet, requiring them to be sufficiently specific to detect the signal of interest amid considerable metabolic noise.
Assessment of Biomarker Accuracy and Precision
For dietary biomarkers, accuracy assessment presents particular challenges because reference materials with known endogenous analyte concentrations are generally unavailable [9]. Scientifically sound approaches include method comparison with established reference methods when available, and spike-and-recovery experiments at varying concentration levels across the assay range. Parallelism testing using serially diluted patient samples helps demonstrate that the assay maintains linearity across the measuring range for actual patient samples rather than just spiked standards [9].
Precision evaluation follows more conventional approaches, involving repeated measurements of the same samples to evaluate measurement variability [9]. This includes within-run precision (repeatability), between-run precision, and total precision assessed across multiple days, operators, and instrument calibrations. However, the key distinction from drug assays lies in the sample type—dietary biomarker precision must be demonstrated using actual biological samples with inherent analyte variability rather than controls spiked with reference material [9].
Research Reagent Solutions for Biomarker Studies
The successful execution of controlled feeding studies for establishing dose-response and pharmacokinetic parameters requires specialized research reagents and resources. The following table summarizes essential materials and their applications in dietary biomarker research.
Table 3: Essential Research Reagents and Resources for Dietary Biomarker Studies
| Resource Category | Specific Examples | Application in Biomarker Research | Technical Considerations |
|---|---|---|---|
| Nutrition Software | NDS-R, ProNutra | Menu development, nutrient analysis, production sheets | Database completeness critical for accurate nutrient targeting |
| Biospecimen Collection Systems | EDTA tubes, serum separator tubes, urine collection containers | Biological sample preservation for metabolomic analysis | Strict protocols for handling, processing, and storage stability |
| Analytical Instrumentation | LC-MS, GC-MS, NMR spectrometers | Metabolomic profiling and biomarker quantification | Sensitivity requirements dependent on expected biomarker concentrations |
| Reference Biomarkers | Doubly labeled water, para-aminobenzoic acid (PABA) | Objective compliance monitoring and energy expenditure measurement | Cost considerations for stable isotopes |
| Food Composition Resources | USDA FoodData Central, branded food databases | Recipe development and nutrient calculation | Regular updates needed to reflect changing food supply |
| Quality Control Materials | Pooled plasma, in-house quality control samples, NIST reference materials | Assay performance monitoring and inter-laboratory standardization | Stability monitoring essential for long-term studies |
The establishment of dose-response relationships and pharmacokinetic parameters for dietary biomarkers represents a methodological cornerstone in the advancement of precision nutrition. Controlled feeding studies provide the experimental foundation for characterizing how food components are processed by the human body and identifying objective biomarkers that can reliably reflect dietary intake. The systematic approach implemented by initiatives such as the Dietary Biomarkers Development Consortium—progressing from initial discovery under highly controlled conditions to validation in free-living populations—offers a robust framework for expanding the limited repertoire of validated dietary biomarkers [7].
As this field advances, the integration of sophisticated metabolomic technologies with rigorous controlled feeding designs will enable researchers to develop increasingly sensitive and specific biomarkers for a wider range of foods and dietary patterns. These tools hold tremendous promise for strengthening diet-disease association studies, improving dietary assessment in clinical practice, and ultimately advancing our understanding of how diet influences human health across the lifespan. The methodological considerations outlined in this guide provide a foundation for researchers seeking to contribute to this rapidly evolving field at the intersection of nutrition, metabolomics, and precision health.
Controlled feeding studies are the gold standard in nutritional research for discovering and validating dietary biomarkers, which are objective biological measurements that accurately reflect dietary intake. These biomarkers are crucial for moving beyond error-prone self-reported diet data in understanding diet-disease relationships. The fundamental challenge in nutritional science lies in designing studies that balance rigorous experimental control with real-world applicability. Research designs span a spectrum from highly standardized meals, where all participants consume identical foods, to mimicked habitual diets, where study meals are personalized to approximate each participant's usual intake [10]. Each approach offers distinct advantages and limitations in biomarker development, influencing the types of biomarkers that can be discovered, the feasibility of study execution, and the eventual applicability of findings to free-living populations. This guide compares these key study designs, detailing their experimental protocols, applications, and roles in building robust evidence for dietary biomarkers.
Comparison of Key Study Design Approaches
The table below summarizes the core characteristics, advantages, and limitations of the major controlled feeding study designs used in dietary biomarker research.
Table 1: Comparison of Controlled Feeding Study Designs for Dietary Biomarker Research
| Study Design Approach | Core Characteristics | Primary Applications in Biomarker Research | Key Advantages | Inherent Limitations |
|---|---|---|---|---|
| Standardized Meals(e.g., DBDC Phase 1 [7] [8]) | All participants receive the same fixed menus, often with specific test foods administered in prespecified amounts. | - Discovery of candidate biomarkers [7] [8].- Characterization of pharmacokinetic parameters (e.g., appearance, peak, clearance in blood/urine) [7] [8].- Testing biomarker specificity. | - Controls for dietary variance.- Simplifies food preparation and logistics.- Ideal for establishing causal links between a specific food and a metabolite. | - Low ecological validity; does not reflect habitual diets.- Limited ability to test biomarker performance with different food matrices or background diets. |
| Mimicked Habitual Diets(e.g., WHI Feeding Study [10]) | Individualized menu plans are created for each participant based on their self-reported habitual intake (e.g., from food records). | - Validation of candidate biomarkers in a context that preserves usual dietary variation [10].- Evaluating how well biomarkers reflect intake variation in a cohort. | - Preserves normal inter-individual variation in food consumption [10].- Higher participant compliance due to food familiarity.- More realistic for evaluating biomarker performance for epidemiological use. | - Extremely resource-intensive (diet formulation, food procurement, preparation).- Relies on accuracy of self-reported habitual diet for personalization. |
| Semi-Controlled / Hybrid(e.g., mini-MED Trial [14]) | Study provides specific, set intervention foods or diet patterns, but participants prepare and consume meals in their own homes. | - Evaluating biomarker response to incremental dietary changes.- Testing biomarker robustness in real-world settings. | - Good balance between control and real-world applicability.- Allows assessment of compliance in free-living conditions.- Can test biomarker generalizability across food preparations. | - Less control over exact food preparation and timing.- Requires careful monitoring to ensure protocol adherence. |
| Free-Living with Provided Food(e.g., MAIN Study [15]) | All foods and drinks are provided to participants, who prepare and consume them in their own homes while following specific menu plans. | - Discovery and validation of biomarkers in a real-world context [15].- Testing urine sampling strategies for optimal biomarker detection [15]. | - High ecological validity while maintaining known dietary exposure.- Assesses impact of home cooking methods on biomarkers [15].- Well-suited for large-scale epidemiological study protocols. | - Logistically complex to package and distribute all food.- Dependent on participant compliance without direct supervision. |
Detailed Experimental Protocols
Standardized Meal Design: The Dietary Biomarkers Development Consortium (DBDC) Protocol
The Dietary Biomarkers Development Consortium (DBDC) employs a highly structured, multi-phase protocol for biomarker discovery and validation [7] [8]. In Phase 1, the focus is on discovery through controlled feeding trials.
- Participant Recruitment: Healthy participants are recruited, often with specific exclusion criteria (e.g., high-level athletes, individuals with certain medical conditions or medications) to minimize metabolic confounding [15].
- Dietary Intervention: Test foods are administered in prespecified amounts. For example, a study might involve a run-in period followed by a day where a single test food or a simple diet with the test food is consumed [7].
- Biospecimen Collection: Blood and urine specimens are collected at multiple timed intervals (e.g., fasted, and then at 2, 4, 6, and 8 hours post-prandially) to characterize the pharmacokinetic profile of candidate biomarkers [7] [8].
- Metabolomic Profiling: Collected specimens are analyzed using high-throughput metabolomics platforms, typically mass spectrometry coupled with liquid or gas chromatography, to generate comprehensive metabolic profiles [7] [15].
- Data Analysis: Bioinformatic analyses compare pre- and post-consumption metabolomic profiles to identify compounds that significantly increase after ingestion of the test food. These are considered candidate biomarkers [7].
Mimicked Habitual Diet Design: The Women's Health Initiative (WHI) Protocol
The WHI Feeding Study protocol is designed to validate biomarkers under conditions that mirror a cohort's natural eating patterns [10].
- Baseline Dietary Assessment: Participants first complete a 4-day food record (4DFR) and an in-depth interview with a study dietitian to assess usual food choices, brands, recipes, and meal patterns [10].
- Individualized Diet Formulation: Each participant's study menu is designed to approximate her habitual food intake. Food record data is entered into nutritional analysis software (e.g., Nutrition Data System for Research, NDS-R), and menus are created using specialized diet formulation software (e.g., ProNutra) [10].
- Energy Intake Calibration: To prevent under-reporting bias and ensure energy needs are met, the prescribed energy intake is often calibrated using equations that incorporate BMI, age, and previously developed calibration factors from the larger cohort [10].
- Controlled Feeding Period: Participants consume their personalized diets for a set period (e.g., 2 weeks). All meals are prepared in a metabolic kitchen [10].
- Biomarker Assessment: Biospecimens (serum, urine) are collected at the beginning and end of the feeding period. The relationship between the consumed nutrients and the concentration of potential biomarkers is analyzed using linear regression, with the explained variation (R²) used to evaluate biomarker performance [10].
Real-World Validation Design: The MAIN Study Protocol
The MAIN (Metabolomics at Aberystwyth, Imperial and Newcastle) Study protocol validates biomarker methodology in a free-living context [15].
- Menu Plan Design: Six daily menu plans are designed to emulate real-world UK eating patterns, delivering a wide range of foods within conventional meals [15].
- Food Provision and Home Consumption: Free-living participants are provided with all foods and drinks but prepare and consume them in their own homes, following protocols for meal timing [15].
- Urine Sampling Strategy: Participants collect spot urine samples at home at multiple specified time points post-meals. This tests a minimally invasive sampling protocol and identifies the optimal time for biomarker detection in free-living individuals [15].
- Compliance Monitoring: Adherence to menu plans and urine collection protocols is monitored, for example, through self-report and returned food packaging [15].
- Metabolome Analysis: Urine samples are analyzed using mass spectrometry, and data mining techniques are used to confirm known biomarkers and discover novel putative biomarkers for an extended range of foods [15].
Logical Workflow for Biomarker Validation
The following diagram illustrates the multi-stage, iterative pathway from initial biomarker discovery to final validation for use in epidemiological studies.
The Scientist's Toolkit: Essential Reagents and Materials
Successful execution of controlled feeding studies for biomarker development relies on a suite of specialized reagents, software, and laboratory materials.
Table 2: Essential Research Reagent Solutions for Dietary Biomarker Studies
| Tool Category | Specific Examples | Critical Function in Research |
|---|---|---|
| Diet Formulation Software | ProNutra [10], Nutrition Data System for Research (NDS-R) [10] | Creates menus, recipes, and production sheets; tracks planned vs. consumed nutrient intake to ensure dietary control. |
| Metabolomics Platforms | Liquid Chromatography-Mass Spectrometry (LC-MS), Gas Chromatography-MS (GC-MS) [15] [14] | Provides high-throughput, sensitive detection and quantification of thousands of metabolites in biospecimens for biomarker discovery. |
| Biospecimen Collection Kits | Urine collection containers (e.g., 30mL cups), blood collection tubes (e.g., EDTA, serum separator) [15] [10] | Ensures standardized, stable, and contamination-free sample collection from participants at multiple time points. |
| Reference Databases | FoodB (University of Alberta), Phenol-Explorer (INRA) [15], MassBank [16] | Aids in identifying detected metabolites by providing reference mass spectra and compound concentrations in foods. |
| Calibration Biomarkers | Doubly Labeled Water (DLW), 24-hour Urinary Nitrogen [10] | Provides objective, recovery biomarkers for total energy and protein intake to validate dietary intake data and self-report. |
| Procyanidin | Procyanidin | |
| Atorvastatin-d5 Lactone | Atorvastatin-d5 Lactone, MF:C33H33FN2O4, MW:545.7 g/mol | Chemical Reagent |
The journey from standardized meals to mimicked habitual diets represents a critical pathway for strengthening dietary biomarker research. Standardized designs are unparalleled for initial discovery and establishing causal intake-biomarker relationships under highly controlled conditions. In contrast, mimicked habitual diet designs are essential for subsequent validation, demonstrating that candidate biomarkers perform reliably amidst the complex variation of real-world diets. The emerging paradigm, exemplified by the DBDC framework and hybrid trials like mini-MED, is a sequential, multi-phase strategy that leverages the strengths of both approaches [7] [14]. This integrated methodology ensures that the biomarkers of the future are not only chemically identifiable but also robust, specific, and meaningful tools for accurately assessing dietary exposure in large-scale epidemiological studies and clinical trials, thereby advancing the field of precision nutrition.
The accurate measurement of dietary intake and early disease states represents a fundamental challenge in medical research and public health. Traditional reliance on self-reported data, such as food frequency questionnaires, introduces substantial measurement error that can obscure true diet-disease associations [17]. Similarly, in clinical diagnostics, traditional metabolic screening approaches often provide limited diagnostic yield, potentially missing treatable conditions [18]. Metabolomic profiling has emerged as a powerful solution to these challenges, offering a comprehensive analysis of small molecules in biological systems that reflects both genetic predisposition and environmental exposures, including diet.
This objective data is particularly crucial for validating findings from nutritional epidemiology and improving diagnostic precision. Controlled feeding studies, where participants consume precisely measured diets, serve as the gold standard for discovering and validating dietary biomarkers because they provide known intake against which metabolomic changes can be calibrated [19] [17]. The transition from traditional targeted biochemical analyses to untargeted metabolomic profiling represents a paradigm shift in biomarker science, enabling the simultaneous assessment of hundreds to thousands of metabolites from minimal biological samples [18] [20].
This guide compares the performance of traditional metabolic assessment methods against modern metabolomic approaches, providing researchers with experimental data and protocols to inform study design and biomarker selection. We objectively evaluate these technologies within the critical context of biomarker validation, with a special emphasis on insights gained from controlled feeding studies.
Performance Comparison: Traditional Screening vs. Modern Metabolomic Profiling
Diagnostic Yield and Applications
Different metabolic profiling approaches offer varying capabilities depending on the research or clinical context. The table below compares the performance characteristics of traditional metabolic screening versus contemporary metabolomic profiling.
Table 1: Performance comparison of traditional metabolic screening versus untargeted metabolomic profiling
| Feature | Traditional Metabolic Screening | Untargeted Metabolomic Profiling |
|---|---|---|
| Typical Analytes | Plasma amino acids, acylcarnitines, urine organic acids [18] | Hundreds to thousands of small molecule metabolites simultaneously [18] [20] |
| Diagnostic Rate | 1.3% (19/1483 families) [18] | 7.1% (128/1807 families) [18] |
| Conditions Identified | 14 IEMs, including 3 not on RUSP [18] | 70 different metabolic conditions, including 49 not on RUSP [18] |
| Dietary Prediction (CV-R²) | Not applicable for direct dietary assessment | 36.3% for protein intake; 37.1% for carbohydrate intake [19] |
| Key Strengths | Standardized protocols, established clinical interpretation | ~6-fold higher diagnostic yield, broader condition detection, objective dietary assessment [18] |
Biomarker Prediction Accuracy for Dietary Intake
Metabolomic biomarkers show varying predictive performance for different macronutrients. The following table summarizes the prediction accuracy of metabolomic-based biomarkers for macronutrient intake, with and without incorporation of established recovery biomarkers.
Table 2: Prediction accuracy (cross-validated R²) of metabolomic biomarkers for macronutrient intake
| Dietary Component | Metabolites Only | With Established Biomarkers |
|---|---|---|
| Energy (kcal/day) | Information not available | 55.5% [19] |
| Protein (g/day) | Information not available | 52.0% [19] |
| Protein (% energy) | 36.3% [19] | 45.0% [19] |
| Carbohydrate (g/day) | Information not available | 55.9% [19] |
| Carbohydrate (% energy) | 37.1% [19] | 37.0% [19] |
Experimental Protocols and Methodologies
Controlled Feeding Study Design for Biomarker Discovery
The most robust metabolomic biomarkers originate from controlled feeding studies, which minimize the measurement error inherent to self-reported dietary data [17]. The Women's Health Initiative Nutrition and Physical Activity Assessment Study Feeding Study (NPAAS-FS) provides a exemplary protocol:
- Participant Profile: 153 postmenopausal women from the Women's Health Initiative (WHI) [19] [17]
- Study Duration: 2-week controlled feeding period [19]
- Dietary Design: Individualized menus created to mimic each participant's habitual diet based on pre-study 4-day food records, preserving natural intake variation while controlling for exact composition [17]
- Sample Collection: Fasting blood samples, 24-hour urine collections, and spot urine samples [19]
- Control Measures: All foods prepared under controlled conditions at a dedicated nutrition laboratory [17]
This design creates the necessary conditions for discovering reliable biomarkers by establishing known intake levels against which metabolomic changes can be correlated.
Metabolomic Analysis Workflows
Sample Processing and Data Acquisition
Comprehensive metabolomic profiling employs multiple analytical platforms to capture diverse biochemical classes:
- Serum Metabolomics: Fasting serum samples are typically analyzed using targeted liquid chromatography-tandem mass spectrometry (LC-MS/MS) for aqueous metabolites combined with direct-injection quantitative lipidomics platforms [19]
- Urinary Metabolomics: 24-hour urine and spot urine samples can be analyzed using ¹H nuclear magnetic resonance (NMR) spectroscopy at 800 MHz and untargeted gas chromatography-mass spectrometry (GC-MS) [19]
- Data Preprocessing: Raw data undergoes noise filtering, peak detection and deconvolution, metabolite identification, peak alignment, and creation of a final data matrix for statistical analysis [21]
Data Analysis and Interpretation
- Statistical Analysis: Variable selection methods build prediction models for each dietary variable, with performance evaluated through cross-validated multiple correlation coefficients (CV-R²) [19]
- Pathway Analysis: Metabolites identified as significant are mapped to biochemical pathways to interpret biological relevance [20]
- Validation: Biomarker panels discovered in feeding studies are moved forward to create calibration equations for dietary self-reports in observational studies [17]
Figure 1: Comprehensive workflow for metabolomic biomarker discovery and validation, spanning from controlled study design to clinical application.
Biomarker Validation Through Regression Calibration
Once candidate biomarkers are identified through controlled feeding studies, they can be applied to correct measurement error in self-reported dietary data from observational studies:
- Calibration Equations: Biomarker panels meeting prespecified criteria (e.g., cross-validated R² ≥ 36%) are used to create calibration equations for dietary self-reports [17]
- Disease Association Estimation: The calibrated intake values are then used in diet-disease association analyses, substantially reducing bias from measurement error [22]
- Application Example: This method has been successfully applied to examine associations between sodium/potassium intake ratio and cardiovascular disease incidence in the Women's Health Initiative cohort [22]
Metabolic Pathways in Health and Disease
Pathway Dysregulation in Disease States
Metabolomic profiling reveals consistent alterations in key biochemical pathways across various disease states:
- Cancer Metabolism: Breast cancer subtypes show distinct metabolic signatures, with HER2-enriched and basal-like subtypes demonstrating increased glycolytic activity, glutamine metabolism, and lipid biosynthesis [20]
- Energy Metabolism: Luminal A breast tumors typically rely more on oxidative phosphorylation, while Luminal B tumors show higher glycolytic activity, contributing to differences in aggressiveness [20]
- Amino Acid Metabolism: Proline catabolism via proline dehydrogenase (PRODH) supports growth and spread of metastatic breast cancer cells, with elevated activity observed in metastatic versus primary tumors [20]
- Redox Homeostasis: Cancer cells upregulate antioxidant pathways to maintain redox balance amidst increased oxidative stress and mitochondrial dysfunction [20]
Dynamic Visualization of Metabolic Networks
Advanced visualization techniques now enable researchers to observe metabolic changes over time:
- GEM-Vis Method: This approach creates animated visualizations of time-course metabolomic data within metabolic network maps, allowing observation of metabolic state changes throughout experiments or disease processes [23]
- Visual Representation: Nodes (metabolites) are represented with fill levels corresponding to their concentrations, enabling intuitive interpretation of quantitative changes across pathways [23]
- Application Examples: This method has been applied to human platelet and erythrocyte metabolism under cold storage conditions, revealing nicotinamide accumulation patterns that mirror hypoxanthine changes [23]
Figure 2: Key metabolic pathways in health and disease, showing how nutrient processing through core biochemical modules supports cellular functions and contributes to disease signatures detectable by metabolomics.
Essential Research Reagent Solutions
Successful metabolomic biomarker studies require specific research reagents and platforms. The following table details essential solutions for conducting comprehensive metabolomic analyses.
Table 3: Essential research reagents and platforms for metabolomic biomarker studies
| Reagent/Platform | Primary Function | Application Examples |
|---|---|---|
| LC-MS/MS Systems | Targeted analysis of aqueous metabolites with high sensitivity and specificity | Quantification of amino acids, carbohydrates, organic acids in serum [19] |
| Quantitative Lipidomics Platforms | Direct-injection mass spectrometry for comprehensive lipid profiling | Analysis of phospholipids, sphingolipids, and other lipid classes [17] [20] |
| ¹H NMR Spectroscopy | Structural analysis of metabolites without extensive sample preparation | Profiling of urinary metabolites at 800 MHz frequency [19] |
| GC-MS Systems | Untargeted analysis of volatile and derivatized metabolites | Discovery of novel metabolic patterns in urine samples [19] |
| Stable Isotope Tracers | Tracking metabolic flux through pathways | Dynamic assessment of nutrient utilization [20] |
| Quality Control Materials | Monitoring analytical performance across batches | Pooled quality control samples for data normalization [21] |
| Metabolomic Databases | Metabolite identification and pathway mapping | HMDB, KEGG, BioModels for data interpretation [21] [23] |
Metabolomic profiling represents a transformative approach for identifying candidate biomarkers that outperform traditional metabolic screening methods in both nutritional assessment and clinical diagnostics. The ~6-fold higher diagnostic yield for inborn errors of metabolism and the ability to objectively quantify dietary intake through calibrated biomarker panels demonstrate the superior performance of comprehensive metabolomic approaches.
The power of metabolomic profiling is maximally realized when biomarkers are discovered through well-controlled feeding studies that provide known intake data for validation. These rigorously validated biomarkers can then correct measurement error in self-reported data from large observational studies, leading to more accurate diet-disease association estimates.
As metabolomic technologies continue to advance, with improved sensitivity, computational visualization tools, and dynamic pathway mapping, researchers and drug development professionals can leverage these approaches to develop more precise biomarkers for early disease detection, prognosis assessment, and therapeutic monitoring across a broad spectrum of metabolic conditions.
The Dietary Biomarkers Development Consortium (DBDC) as a Case Study
Accurately measuring what people eat is a fundamental challenge in nutritional science and epidemiology. Traditional methods, such as food frequency questionnaires and dietary recalls, are hampered by significant limitations, including recall bias and an individual's inability to accurately report their own intake [7]. These subjective methods have impeded progress in understanding the precise links between diet and health outcomes. Objective biomarkers of dietary intake, which are measurable biological indicators of food consumption, are widely recognized as a critical tool for advancing the field of precision nutrition [7] [13]. The Dietary Biomarkers Development Consortium (DBDC) represents a coordinated, large-scale scientific initiative designed to address this challenge by systematically discovering and validating robust biomarkers for foods commonly consumed in the United States diet [7] [24]. This article uses the DBDC as a case study to explore the rigorous experimental protocols and validation frameworks required to translate biomarker discovery from controlled research settings into clinically and epidemiologically useful tools.
The DBDC's Systematic Three-Phase Validation Framework
The DBDC employs a structured, three-phase approach to biomarker development, moving from initial discovery to real-world evaluation. This framework ensures that candidate biomarkers are rigorously tested for their sensitivity, specificity, and reliability. The overarching workflow of the consortium's strategy is illustrated below.
DBDC Validation Workflow
Phase 1: Biomarker Discovery and Pharmacokinetic Profiling
The initial discovery phase focuses on identifying candidate compounds and understanding their behavior in the body. This phase employs controlled feeding trials where specific test foods are administered to healthy participants in predetermined amounts [7]. For instance, the "Fruit and Vegetable Biomarker Study" (Aim 2) investigates biomarkers for bananas, peaches, strawberries, tomatoes, green beans, and carrots [25]. Key methodological steps include:
- Controlled Diets: Participants are provided with all foods and beverages and are required to consume only what is provided, ensuring exact knowledge of intake [25].
- Specimen Collection: Serial blood and urine specimens are collected at precise time points following test food consumption [7] [25].
- Metabolomic Profiling: Advanced metabolomic techniques are used to analyze the specimens, generating comprehensive profiles of small molecules to identify compounds that change in response to food intake [7].
- Pharmacokinetics: The data are used to characterize the pharmacokinetic parameters—such as the rise time, peak concentration, and clearance rate—of candidate biomarkers [7].
Phase 2: Biomarker Evaluation in Diverse Dietary Patterns
In Phase 2, the ability of the candidate biomarkers to accurately classify individuals who have consumed the target food is evaluated. This phase also uses controlled feeding studies, but the test foods are incorporated into various complex dietary patterns to assess the biomarker's specificity and performance in a more realistic, mixed-diet context [7]. This step is crucial for determining whether a biomarker remains valid when the background diet changes.
Phase 3: Validation in Observational Settings
The final validation phase tests the performance of the most promising biomarkers in independent, free-living populations. This assesses the biomarker's utility for predicting both recent and habitual consumption of specific foods without the constraints of a controlled feeding study [7]. Success in this phase demonstrates that a biomarker is ready for deployment in large-scale epidemiological research.
Comparative Analysis: DBDC Versus General Biomarker Validation
The DBDC's methodology aligns with established best practices for biomarker validation but is specially tailored to the unique challenges of dietary exposure. The table below contrasts the DBDC's approach with general biomarker validation principles.
Table 1: Comparison of Validation Frameworks
| Validation Component | General Biomarker Best Practices [13] [26] | DBDC Application & Protocol [7] [25] |
|---|---|---|
| Intended Use Definition | Define the biomarker's purpose (e.g., diagnostic, prognostic) early. | Purpose: Objective measurement of specific food intake for nutritional epidemiology. |
| Study Population | Patients and specimens must reflect the target population. | Healthy adults (BMI 18.5-39.9); controlled diet to define true exposure. |
| Specimen Collection | Proper handling and storage protocols are essential. | Strict protocols for serial blood, urine, and optional stool collection. |
| Analytical Techniques | Use of high-throughput technologies (e.g., mass spectrometry, NGS). | Primary use of metabolomics for high-throughput profiling of small molecules. |
| Blinding & Randomization | Critical to avoid bias during data generation and patient evaluation. | Random assignment to dietary intervention groups (e.g., high vs. low fruit/vegetable arms). |
| Statistical & Analytical Methods | Pre-planned analysis; control for multiple comparisons; use of ROC curves, sensitivity/specificity. | High-dimensional bioinformatics; public database archiving for broad research access. |
| Context of Use | Validation should be fit-for-purpose [26]. | Tailored for precision nutrition and association studies in public health. |
Core Experimental Protocols in Controlled Feeding Studies
The DBDC's work relies on meticulously designed controlled feeding studies, which serve as the gold standard for establishing a causal link between dietary intake and biomarker presence.
Study Design and Participant Selection
The protocol for the Fruit and Vegetable Biomarker Study exemplifies a robust design:
- Design: Randomized, controlled dietary intervention with three distinct arms: a diet high in test fruits and vegetables, a diet low in them, and a diet devoid of them [25].
- Duration: Approximately 10 days of controlled feeding [25].
- Participants: Relatively healthy adults screened for specific criteria to minimize confounding variables. Exclusion criteria include allergies to test foods, pregnancy, gastrointestinal disorders, unstable cardiovascular disease, and recent cancer treatment [25].
Dietary Intervention and Sample Collection
- Dietary Control: Participants are provided with all food and beverages for the entire study period and are instructed to consume only these items [25]. This eliminates dietary misreporting and ensures precise knowledge of exposure.
- Biospecimen Collection: Multiple biological samples are collected to capture a comprehensive metabolic picture. This typically includes:
- 2-3 blood samples
- 2-3 overnight urine samples
- 2 optional stool collections [25]
The Researcher's Toolkit: Essential Reagents and Materials
Successful execution of dietary biomarker studies requires a suite of specialized reagents and analytical platforms. The following table details key components of the research toolkit as employed in the DBDC and related biomarker discovery efforts.
Table 2: Essential Research Reagent Solutions for Dietary Biomarker Discovery
| Item / Solution | Function / Application | Specific Examples from Literature |
|---|---|---|
| Mass Spectrometry Platforms | Identification and quantification of metabolites in biospecimens; central to metabolomic profiling. | Used for proteomic [27] and metabolomic analysis in DBDC [7]. |
| Bioinformatic Analysis Software | Processing and interpreting high-dimensional data from omics platforms; statistical analysis. | Used for high-dimensional bioinformatics in DBDC [7]; machine learning for pattern recognition [28] [29]. |
| Stable Isotope Standards | Internal standards for mass spectrometry to enable precise quantification of analyte concentrations. | Implied in precise metabolomic quantification; standard in mass spectrometry-based assays [27]. |
| Protein & Gene Expression Arrays | High-throughput screening of protein or gene expression patterns for candidate biomarker discovery. | Protein arrays for detecting proteins in complex samples [27]; DNA microarrays for gene expression [27]. |
| Next-Generation Sequencing (NGS) | Genomic analysis to understand host-genome interactions with diet and for microbial profiling. | Used to identify genetic mutations in cancer biomarker research [27]. |
| Chromatography Columns | Separation of complex biological mixtures prior to mass spectrometry analysis. | Essential for liquid chromatography-mass spectrometry (LC-MS), a core metabolomics technology. |
| 4-Bromobenzoic-d4 Acid | 4-Bromobenzoic-d4 Acid, MF:C7H5BrO2, MW:205.04 g/mol | Chemical Reagent |
| 3-Phenoxybenzoic acid-13C6 | 3-Phenoxybenzoic acid-13C6, CAS:1793055-05-6, MF:C13H10O3, MW:219.18 g/mol | Chemical Reagent |
Integrating Multi-Omics and AI in Biomarker Discovery
The DBDC and the broader field are increasingly leveraging integrated technologies to manage the complexity of diet as a biological exposure. The relationship between these technologies is shown below.
Multi-Omics & AI Integration
- Multi-Omics Approaches: The DBDC primarily utilizes metabolomics, but the wider field is moving toward integrating genomics, proteomics, and metabolomics to achieve a holistic view of biological responses to diet [28] [27]. This systems biology approach is crucial for identifying comprehensive biomarker signatures that reflect the complexity of food as an exposure.
- Artificial Intelligence and Machine Learning: AI and ML are revolutionizing biomarker discovery by enabling the analysis of these vast, complex datasets. Key applications include:
- Predictive Analytics: Building models to forecast individual metabolic responses to specific foods [28].
- Automated Data Interpretation: ML algorithms significantly reduce the time required for biomarker discovery and validation by automating the analysis of complex datasets [28].
- Pattern Recognition: These tools are essential for uncovering subtle patterns in omics data that distinguish between dietary exposures [29].
The Dietary Biomarkers Development Consortium serves as a paradigm for rigorous biomarker validation within a fit-for-purpose framework. Its structured three-phase approach, reliance on controlled feeding studies as a foundational benchmark, and adoption of advanced metabolomic and bioinformatic technologies create a robust model for translating complex dietary exposures into reliable, objective measures. The biomarkers emerging from this and similar consortia are poised to dramatically improve the precision of nutritional epidemiology, enabling stronger evidence-based linkages between diet and health. This progress, in turn, will empower the development of more effective, personalized dietary recommendations and public health strategies.
Methodological Frameworks and Analytical Applications
In nutritional science and drug development, the journey from biomarker discovery to clinical application presents a significant challenge. Biomarkers—objective biological indicators of exposure, response, or susceptibility—require rigorous validation to transition from promising discoveries to trusted tools for research and clinical decision-making. This process is particularly complex for dietary biomarkers, where the multifaceted nature of food intake, metabolic variability, and confounding factors necessitate a structured, multi-phase approach. Controlled feeding studies serve as the cornerstone of this validation pathway, providing the scientific community with high-quality evidence for biomarker utility.
The validation pathway for dietary biomarkers has evolved substantially with advances in metabolomics and analytical technologies. This guide examines the current methodologies, benchmarks performance across alternative approaches, and provides the experimental protocols essential for implementing a robust biomarker validation strategy.
A Three-Phase Framework for Biomarker Validation
The biomarker validation pathway is systematically structured into consecutive phases, each with distinct objectives and evaluation criteria. The Dietary Biomarkers Development Consortium (DBDC) has pioneered a comprehensive 3-phase approach specifically for dietary biomarkers that represents the current gold standard in the field [7] [8].
Table 1: Core Phases in the Biomarker Validation Pathway
| Phase | Primary Objective | Study Designs | Key Outcomes |
|---|---|---|---|
| Phase 1: Discovery & Identification | Identify candidate compounds associated with specific dietary exposures | Controlled feeding trials with predefined test foods; metabolomic profiling of blood/urine [7] | Candidate biomarkers with characterized pharmacokinetic parameters [7] |
| Phase 2: Evaluation & Qualification | Assess ability of candidates to identify consumers of target foods | Controlled feeding studies of various dietary patterns; dose-response and time-response analyses [30] | Biomarkers with demonstrated specificity, sensitivity, and performance across patterns [7] |
| Phase 3: Real-World Prediction | Validate predictive value in independent observational settings [7] | Large-scale cohort studies; free-living populations [30] | Biomarkers validated for predicting habitual consumption in diverse, real-world settings [7] |
This phased approach ensures rigorous evaluation before biomarkers are deployed in research or clinical settings. The transition between phases depends on achieving predefined performance benchmarks, creating a gated pathway that prioritizes biomarker quality.
Experimental Protocols for Validation Studies
Controlled Feeding Study Design
Controlled feeding studies represent the foundation of Phase 1 biomarker validation. The Women's Health Initiative feeding study implemented a robust protocol where 153 postmenopausal women were provided with a 2-week controlled diet specifically designed to approximate each participant's habitual food intake based on 4-day food records [10]. This innovative approach preserved normal variation in nutrient consumption while maintaining controlled conditions—a critical balance for meaningful biomarker validation.
Key methodological considerations:
- Diet Formulation: Individualized menus created using professional nutrition software (e.g., ProNutra) with selective sourcing of foods with complete nutrient database values [10]
- Energy Adjustment: Food prescriptions adjusted based on calibrated energy estimates using standard energy equations and previous calibration data [10]
- Sample Collection: Blood and urine specimens collected at baseline and post-intervention under standardized conditions [10]
- Biomarker Analysis: Serum biomarkers including carotenoids, tocopherols, folate, vitamin B-12, and phospholipid fatty acids analyzed with established analytical methods [10]
Metabolomic Profiling Techniques
Metabolomic profiling serves as the primary technological platform for biomarker discovery in Phase 1. The choice of analytical platform depends on the specific research questions and required sensitivity [30].
Table 2: Metabolomic Platforms for Biomarker Discovery
| Platform | Principle | Sensitivity | Sample Requirements | Key Applications |
|---|---|---|---|---|
| NMR Spectroscopy | Measures nuclear spin transitions in magnetic fields | Lower sensitivity, high abundance metabolites | Larger sample volumes (non-destructive) | Broad-based metabolic profiling, quantitative analysis [30] |
| LC/GC-MS | Separates compounds by chromatography with mass detection | High sensitivity | Small sample volumes (non-recoverable) | Targeted and untargeted analysis of diverse metabolites [30] |
| Tandem MS (MS/MS) | Fragments ions for structural identification | Very high sensitivity | Minimal sample volume | Structural elucidation, confirmation of biomarker identity [31] |
Liquid-chromatography-mass-spectrometry (LC-MS) has emerged as particularly valuable for protein and metabolite biomarker discovery due to its sensitivity and specificity. Best practices include rigorous sample randomization, blinding, and quality control throughout the analytical process [31].
Performance Comparison: Validation Criteria and Biomarker Classes
The validation of food intake biomarkers requires demonstration of performance across multiple criteria. Different classes of biomarkers exhibit distinct performance characteristics across these validation criteria.
Table 3: Biomarker Performance Against Validation Criteria
| Validation Criterion | Definition | Exemplary Biomarkers | Performance Assessment |
|---|---|---|---|
| Plausibility | Biological plausibility and food specificity | Proline betaine (citrus), Tartaric acid (grape) [30] | Compound confirmed in food source and biological samples [30] |
| Dose-Response | Relationship between intake amount and biomarker level | Urinary sucrose/fructose (dietary sugars) [30] | Linear regression of consumed nutrients on potential biomarkers (R²: 0.32-0.53 for various vitamins) [10] |
| Time-Response | Kinetic profile including half-life and excretion timeline | Guanidoacetate (chicken intake) [30] | Characterization of pharmacokinetic parameters in controlled studies [7] |
| Robustness | Performance across diverse populations and conditions | Urinary nitrogen (protein intake) [30] | Validation in multiple free-living populations with different habitual diets [30] |
| Reliability | Consistency of measurement across repeated exposures | Serum carotenoids, tocopherols [10] | Demonstration of consistent performance in repeated feeding studies [10] |
The regression analysis approach used in the WHI feeding study provides a quantitative framework for biomarker evaluation, where linear regression of consumed nutrients on potential biomarkers yielded R² values ranging from 0.32 for lycopene to 0.53 for α-carotene, performing similarly to established energy and protein urinary recovery biomarkers [10].
The Scientist's Toolkit: Essential Research Reagents and Platforms
Successful implementation of biomarker validation studies requires specific reagents, platforms, and methodologies. The following toolkit summarizes essential components for establishing a biomarker validation pipeline.
Table 4: Essential Research Reagents and Platforms for Biomarker Validation
| Category | Specific Tools/Platforms | Function in Validation Pipeline |
|---|---|---|
| Analytical Platforms | NMR spectrometers, LC-MS/MS systems, GC-MS systems | Metabolite profiling and quantification in biological samples [30] |
| Nutrition Software | ProNutra, Nutrition Data System for Research (NDS-R) | Diet formulation, menu creation, and nutrient analysis [10] |
| Reference Standards | Certified metabolite standards, stable isotope-labeled internal standards | Compound identification and quantification accuracy [31] |
| Sample Collection | Standardized blood collection tubes, urine containers, temperature-controlled storage | Biological specimen integrity and pre-analytical consistency [31] |
| Data Analysis | Cross-validation algorithms, feature selection methods, statistical packages | Robust classification and performance evaluation [32] |
| Pathway Databases | KEGG, Reactome, HMDB | Biological context and pathway analysis for candidate biomarkers [33] |
| Dihydrocapsaicin-d3 | Dihydro Capsaicin-d3 | Dihydro Capsaicin-d3, a deuterated capsaicinoid. For research applications only. Not for human consumption. For Research Use Only. |
| Mefenamic Acid D4 | Mefenamic Acid D4, MF:C15H15NO2, MW:245.31 g/mol | Chemical Reagent |
Advanced Methodologies: Multi-Omics Integration and Pathway Analysis
The integration of multi-omics data represents a cutting-edge approach to enhance biomarker validation. Methods such as integrative Directed Random Walk (iDRW) incorporate pathway information to improve the biological relevance and predictive performance of biomarker panels [33]. This approach constructs directed gene-gene interaction graphs that reflect the impact of genomic variants on gene expression, creating more robust models for survival prediction in cancer studies [33].
The MultiP (Multi-Platform Precision Pathway) framework further extends this concept by developing clinical precision pathways that mimic real-world diagnostic processes. This framework introduces an "uncertain" class in classification models, allowing for multi-stage decision processes where individuals receive additional testing only when initial biomarkers provide inconclusive results [32]. This approach mirrors clinical reality and optimizes resource allocation in diagnostic pathways.
The multi-phase validation pathway from identification to real-world prediction represents a rigorous framework for establishing credible dietary biomarkers. Through controlled feeding studies, metabolomic profiling, and progressive validation in increasingly complex environments, researchers can develop biomarker panels with demonstrated utility for both research and clinical applications.
The future of biomarker validation lies in the intelligent integration of multi-omics data, the application of sophisticated computational methods, and the development of phase-appropriate validation strategies that balance scientific rigor with practical feasibility. As the field advances, this structured approach will continue to yield biomarkers that transform our understanding of diet-health relationships and enable more precise nutritional interventions.
Measurement error, though ubiquitous in biomedical research, is often unacknowledged in epidemiologic studies, leading to biased parameter estimates, loss of statistical power, and distorted relationships between variables [34]. In the specific context of biomarker development and validation, these errors present particular challenges for establishing accurate diet-disease associations and treatment effect estimates [35] [13]. Controlled feeding studies represent a crucial methodological approach for addressing these challenges by providing robust biomarker development and validation frameworks [35] [36]. This guide compares advanced statistical models designed to correct for measurement error and bias, evaluating their performance characteristics, implementation requirements, and applicability within biomarker research.
Comparative Analysis of Statistical Correction Methods
The table below summarizes five prominent statistical approaches for correcting measurement error and bias, highlighting their key applications and methodological requirements.
| Method | Primary Application | Data Requirements | Key Advantages | Key Limitations |
|---|---|---|---|---|
| Regression Calibration [35] [34] | Correcting systematic error in self-reported dietary data | Gold-standard biomarker for a subset of dietary components | Simple implementation; useful for continuous covariates | Biomarkers only available for limited dietary components |
| Corrected LASSO [37] | Variable selection with high-dimensional biomarker data | Validation subset re-measured with precise method | Reduces false positives; handles high-dimensional data | Requires validation data; computationally intensive |
| Bootstrap Bias Correction [38] [39] | Correcting bias after data-driven biomarker cutoff selection | Internal bootstrap samples from original data | Reduces over-optimism from selection; general applicability | Computationally intensive; may not eliminate all bias |
| Approximate Bayesian Computation (ABC) [38] [39] | Bias correction in treatment effect estimates | Dataset from a randomized clinical trial | Does not rely on asymptotic theory; provides full posterior | Requires careful selection of summary statistics and tolerance |
| Two-Stage Error Correction [40] [41] | Multilevel modeling; data streams with improved instruments | Initial error-prone data followed by precise measurements | Practical for complex models; handles sequentially improving data | Requires precise measurements at a known point in the data stream |
Experimental Protocols for Key Methodologies
Regression Calibration in Controlled Feeding Studies
Controlled feeding studies provide a robust foundation for biomarker development and calibration. The typical protocol involves:
- Study Design: Participants are provided with a controlled diet that approximates their habitual food intake, as estimated from preliminary dietary assessments like food records or recalls [36]. For example, the Women's Health Initiative (WHI) feeding study provided 153 postmenopausal women with a 2-week controlled diet tailored to their usual intake [36].
- Biomarker Measurement: Throughout the feeding period, biological samples (e.g., blood, urine) are collected to measure potential nutritional biomarkers. Established recovery biomarkers, such as urinary nitrogen for protein intake and doubly labeled water for energy intake, serve as benchmarks for evaluation [35] [36].
- Calibration Model Development: Statistical models are developed to associate the objectively measured biomarker levels with the actual dietary intake from the controlled diet. This establishes a calibration equation that corrects for the systematic measurement error present in self-reported dietary data [35].
- Application in Association Studies: In the main cohort study (e.g., WHI), this calibration equation is applied to the self-reported data to obtain biomarker-calibrated intake estimates. These calibrated estimates are then used in disease association models, such as Cox proportional hazards models for cardiovascular disease risk, leading to more accurate hazard ratio estimations [35].
Corrected LASSO with Internal Validation Data
For high-dimensional biomarker data from multiplex assays, which are prone to high variability, a corrected LASSO procedure can be implemented using an internal validation subset:
- Data Structure Setup: The full study sample (n) has biomarkers measured by an error-prone multiplex assay ((Wi)). A randomly selected internal validation subset ((ξi = 1)) has biomarkers re-measured using a more precise "gold standard" method ((X_i)) [37].
- Bias Correction Term Estimation: Using the internal validation set, estimate the covariance matrix of the measurement error ((Σ{uu})) by comparing the error-prone measurements (Wi) to the precise measurements (X_i) [37].
- Corrected Loss Function Minimization: The corrected LASSO estimator is obtained by minimizing a penalized least squares function that incorporates the bias correction term. The function is: [ \frac{1}{2} \cdot \sum{i=1}^n [Yi - \beta0 - (\xii Xi^T \beta + \bar{\xii} Wi^T \beta)]^2 - \frac{n}{2} \cdot \beta^T \hat{\Sigma}{uu} \beta + n \cdot \lambda \cdot \sum{j=1}^p |\betaj| ] Here, the bias correction term (\beta^T \hat{\Sigma}{uu} \beta) is subtracted only for subjects not in the validation set ((\bar{\xii} = 1)) [37].
- Model Fitting via Coordinate Descent: A modified coordinate descent algorithm is used to fit the model, updating one parameter at a time while keeping others fixed, which accounts for the bias correction term in the estimation process [37].
Bootstrap Bias Correction for Biomarker Cutoff Selection
When an optimal cutoff for a continuous predictive biomarker is selected through a data-driven process, treatment effect estimates become biased. Bootstrap Bias Correction addresses this:
- Cutoff Selection on Original Data: From a set of K candidate cutoffs (c1, ..., cK), select the optimal cutoff (c{select}) based on a pre-defined rule (e.g., largest treatment effect difference) using the original dataset. Record the estimated treatment effect (\hat{\theta}{select}^{MLE}) in the subgroup defined by (c_{select}) [38].
- Bootstrap Resampling: Generate B bootstrap samples by resampling with replacement from the original dataset.
- Bootstrap Replication: For each bootstrap sample b (where b = 1 to B):
- Repeat the identical data-driven cutoff selection procedure to find (c_{select}^b).
- Estimate the treatment effect (\hat{\theta}{select}^{b}) within the subgroup defined by (c{select}^b).
- Bias Calculation and Adjustment: Calculate the bootstrap-estimated bias as the difference between the average of the bootstrap estimates and the original estimate: (\text{Bias} = \frac{1}{B} \sum{b=1}^B \hat{\theta}{select}^{b} - \hat{\theta}{select}^{MLE}). The bias-corrected estimate is then: (\hat{\theta}{corrected} = \hat{\theta}_{select}^{MLE} - \text{Bias}) [38].
Workflow and Method Relationships
The following diagram illustrates the logical workflow for selecting and applying these advanced statistical corrections, highlighting the relationship between different methodological approaches.
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful implementation of these advanced statistical methods requires specific data and computational resources, as detailed in the table below.
| Tool/Resource | Function in Research | Application Context |
|---|---|---|
| Controlled Feeding Study | Provides ground-truth data for developing calibrated intake estimates [35] [36]. | Foundation for regression calibration methods in nutritional epidemiology. |
| Internal Validation Subset | A random subset of participants with measures from both error-prone and gold-standard assays [37]. | Enables estimation of measurement error covariance for Corrected LASSO. |
| Gold-Standard Biomarker | An objectively measured biomarker used to correct self-reported intake [35] [34]. | Serves as the calibration reference in regression calibration (e.g., urinary sodium for sodium intake). |
| High-Performance Computing | Computational resources for resampling-based methods (bootstrap) and high-dimensional algorithms [37] [38]. | Essential for Bootstrap Bias Correction and Corrected LASSO with large datasets. |
| Multiplex Assay Platform | Technology to measure multiple serum biomarkers simultaneously, though with potential for higher variability [37]. | Primary source of high-dimensional biomarker data requiring error correction. |
| (R)-Norfluoxetine-d5 | (R)-Norfluoxetine-d5, CAS:1185132-92-6, MF:C16H17ClF3NO, MW:336.79 g/mol | Chemical Reagent |
| 4-Hydroxypropranolol-d7 | 4-Hydroxypropranolol-d7, CAS:1219908-86-7, MF:C16H21NO3, MW:282.39 g/mol | Chemical Reagent |
The selection of an appropriate method for correcting measurement error and bias depends critically on the research question, data structure, and available validation resources. Regression calibration provides a foundational approach when gold-standard biomarkers exist, particularly in nutritional epidemiology leveraging controlled feeding studies. For high-dimensional biomarker data, the corrected LASSO method with internal validation offers a powerful approach for variable selection. When data-driven biomarker cutoff selection is unavoidable, bootstrap methods provide a practical bias correction. By integrating these advanced statistical corrections with robust study designs like controlled feeding studies, researchers can significantly improve the validity and reliability of biomarker-disease associations and treatment effect estimates in drug development and precision medicine.
Developing Calibration Equations for Self-Reported Dietary Data
Accurate dietary assessment is fundamental for nutritional epidemiology, yet traditional self-report methods are plagued by systematic measurement error that obscures true diet-disease relationships. This guide compares the performance of biomarker-based calibration approaches against conventional dietary assessment methods, with supporting experimental data from controlled feeding studies. We objectively evaluate how regression calibration techniques using recovery biomarkers correct for measurement inaccuracies in self-reported data, enabling researchers to obtain nearly unbiased estimates of diet-disease associations. The methodology presented is framed within the broader context of biomarker validation against controlled feeding studies, providing drug development professionals and researchers with practical frameworks for implementing these approaches in nutritional research and clinical trials.
For decades, nutritional epidemiology has relied primarily on self-reported dietary assessment instruments including food frequency questionnaires (FFQs), 24-hour dietary recalls (24HRs), and food records [42]. Substantial evidence demonstrates these traditional methods contain systematic measurement errors that significantly attenuate diet-disease associations and reduce statistical power in observational studies [43]. The pervasive issue of energy intake underreporting has been particularly well-documented, with studies consistently showing underreporting increases with body mass index (BMI) and affects macronutrient reporting unevenly [43].
The biomarker calibration approach has emerged as a robust methodological framework for correcting systematic measurement error in self-reported dietary data. This methodology utilizes objective biological measurements that adhere to classical measurement model assumptions, serving as criterion measures against which self-report instruments can be calibrated [42]. By applying regression calibration equations derived from biomarker sub-studies to larger cohort data, researchers can obtain calibrated consumption estimates that substantially reduce measurement error bias and enhance the reliability of nutritional epidemiology findings [42] [44].
Theoretical Foundation of Regression Calibration
Statistical Framework and Assumptions
Regression calibration operates through a well-defined statistical framework that relates biomarker measurements to self-reported values and other relevant participant characteristics. The foundational model assumes biomarker assessments (W) adhere to a classical measurement model:
W = Z + u
where Z represents the true (log-transformed) dietary consumption over a specified time period, and u is random error independent of Z and all relevant study subject characteristics V [42]. The corresponding self-report (Q) is allowed to have a biased target (Z*) according to:
Z* = aâ‚€ + aâ‚Z + aâ‚‚Váµ€
Q = Z* + e
where the error term e is independent of Z and u, given V [42]. Under joint normality assumptions for (Z, e, V), the expected value of true consumption given the self-report and other characteristics becomes:
E(Z|Q,V) = bâ‚€ + bâ‚Q + bâ‚‚Váµ€
This formulation enables development of calibration equations that correct systematic biases related to V in the self-report Q while recovering a substantial fraction of the variation in Z within the study population [42].
Biomarker Classification and Validation Criteria
Dietary biomarkers are categorized based on their physiological basis and application in nutritional research. Recovery biomarkers represent the gold standard, demonstrating near-complete recovery in biological samples over a specific time period [30]. These include doubly labeled water (DLW) for energy expenditure and 24-hour urinary nitrogen for protein intake. Concentration biomarkers reflect circulating nutrient levels but don't necessarily correlate directly with intake amounts, while predictive biomarkers utilize metabolomic profiling to identify metabolite patterns associated with specific food intake [30].
For robust biomarker validation, researchers have established eight essential criteria: plausibility, dose-response, time-response, robustness, reliability, stability, analytical performance, and reproducibility [30]. These validation parameters ensure identified biomarkers perform consistently across diverse populations and experimental conditions, making them suitable for application in regression calibration frameworks.
Table 1: Biomarker Classification in Nutritional Research
| Biomarker Type | Physiological Basis | Examples | Key Applications |
|---|---|---|---|
| Recovery | Near-complete recovery in biological samples over specified period | Doubly labeled water (energy), 24-hour urinary nitrogen (protein) | Gold standard for calibration equations |
| Concentration | Circulating levels in blood or other tissues | Serum carotenoids, phospholipid fatty acids | Reflect status but not necessarily intake |
| Predictive | Metabolomic patterns associated with food intake | Proline betaine (citrus), tartaric acid (grape) | Specific food intake assessment |
Methodological Approaches: Controlled Feeding Studies and Biomarker Development
Controlled Feeding Study Designs
Controlled feeding studies represent the methodological gold standard for dietary biomarker development and validation. These studies involve providing participants with all foods and beverages in known quantities, enabling precise characterization of the relationship between consumed nutrients and their corresponding biomarker measurements [10]. The Women's Health Initiative (WHI) Nutrition and Physical Activity Assessment Study Feeding Study (NPAAS-FS) implemented an innovative design where 153 postmenopausal women received individualized menus approximating their habitual food intake over a two-week period [10]. This approach preserved the normal variation in nutrient consumption present in the study population while maintaining controlled conditions essential for biomarker evaluation.
The WHI feeding study collected extensive biological samples including fasting blood specimens and 24-hour urine collections at both beginning and end of the feeding period [10]. These samples were analyzed for an extensive panel of potential nutritional biomarkers including carotenoids, tocopherols, folate, vitamin B-12, and phospholipid fatty acids, alongside established recovery biomarkers (DLW for energy, urinary nitrogen for protein) which served as benchmarks for evaluation [10]. This comprehensive approach enabled simultaneous evaluation of multiple candidate biomarkers under highly controlled conditions, providing robust data for developing calibration equations.
Biomarker Discovery and Validation Pipeline
The Dietary Biomarkers Development Consortium (DBDC) has established a systematic three-phase approach to biomarker discovery and validation. Phase 1 involves controlled feeding trials where test foods are administered in prespecified amounts to healthy participants, followed by metabolomic profiling of blood and urine specimens to identify candidate compounds [8]. Phase 2 evaluates the ability of candidate biomarkers to identify individuals consuming biomarker-associated foods using controlled feeding studies of various dietary patterns [8]. Phase 3 assesses the validity of candidate biomarkers for predicting recent and habitual consumption of specific test foods in independent observational settings [8]. This rigorous pipeline ensures identified biomarkers meet the validation criteria necessary for implementation in regression calibration models.
Biomarker Development and Calibration Workflow
Comparative Performance: Biomarker vs. Self-Report Assessment
Energy and Protein Intake Assessment
Direct performance comparisons between biomarker measurements and self-reported assessments reveal substantial discrepancies in accuracy. In the WHI Nutrient Biomarker Study (NBS), which included 544 women, the doubly labeled water method demonstrated superior accuracy for energy assessment compared to FFQs, with the latter showing systematic underreporting that increased with BMI [42]. Similarly, the urinary nitrogen biomarker provided more objective protein intake assessment, with self-reports showing similar but less pronounced underreporting compared to energy [42].
The WHI Nutrition and Physical Activity Assessment Study (NPAAS), conducted among 450 women in the WHI Observational Study, provided direct comparative data on the performance of multiple self-report instruments against biomarker measures [42]. This study incorporated concurrent FFQs, 4-day food records (4DFRs), and three 24-hour dietary recalls alongside DLW and urinary nitrogen biomarkers, enabling comprehensive evaluation of measurement error properties across different self-report modalities [42]. Results demonstrated that without calibration, disease associations for energy and protein were mostly absent, whereas bias-corrected calibrated estimates showed positive relationships with chronic disease risk [10].
Micronutrient and Food Compound Biomarkers
The NPAAS Feeding Study evaluated serum concentration biomarkers for several vitamins and carotenoids, comparing their performance to established recovery biomarkers. Linear regression of (ln-transformed) consumed nutrients on (ln-transformed) potential biomarkers yielded the following coefficients of determination (R²): folate (0.49), vitamin B-12 (0.51), α-carotene (0.53), β-carotene (0.39), lutein + zeaxanthin (0.46), lycopene (0.32), and α-tocopherol (0.47) [10]. These values were comparable to established recovery biomarkers for energy and protein intake (R² = 0.53 and 0.43, respectively), suggesting several serum concentration biomarkers perform similarly to recovery biomarkers for representing nutrient intake variation [10].
Table 2: Performance Comparison of Dietary Assessment Methods in WHI Studies
| Assessment Method | Nutrients/Foods Assessed | Key Performance Metrics | Major Limitations |
|---|---|---|---|
| Food Frequency Questionnaire (FFQ) | Comprehensive nutrient profile | Practical for large cohorts; machine-readable | Systematic underreporting (30-50% for energy); BMI-dependent bias |
| 24-Hour Dietary Recall | Short-term nutrient intake | Multiple administrations improve precision | Within-person variability; relies on memory |
| Food Records | Short-term nutrient intake | Does not rely on memory | Participant burden; may alter eating behavior |
| Recovery Biomarkers | Energy, protein, sodium, potassium | Objective measurement; R² = 0.43-0.53 in feeding studies | Limited to specific nutrients; expensive methods |
| Concentration Biomarkers | Vitamins, carotenoids, fatty acids | Objective measurement; R² = 0.32-0.53 in feeding studies | Reflect status rather than direct intake |
In contrast, phospholipid saturated fatty acids, monounsaturated fatty acids, and serum γ-tocopherol showed only weak associations with intake (R² < 0.25), indicating limited utility as intake biomarkers without further development [10]. These findings highlight the importance of rigorous biomarker validation before implementation in calibration equations, as performance varies substantially across different nutrients and food compounds.
Experimental Protocols for Biomarker Calibration
Biomarker Sub-Study Implementation
The successful application of regression calibration requires careful implementation of biomarker sub-studies within larger cohort investigations. The WHI NPAAS-OS protocol provides an exemplary model, incorporating DLW for total energy expenditure assessment, 24-hour urine collection for urinary nitrogen measurement, indirect calorimetry, fasting blood draws, anthropometry, and multiple dietary assessment instruments (FFQ, 4DFR, and three 24HRs) [17]. This comprehensive approach enables characterization of measurement error properties across different self-report modalities while providing objective biomarker measures for calibration development.
Critical methodological considerations include the timing of assessments to ensure biomarker measurements correspond appropriately with self-report periods, incorporation of reliability subsamples (typically 20%) to account for within-person variability, and standardized protocols for specimen collection, processing, and analysis [42] [17]. In the WHI NPAAS, most procedures were conducted during two clinic visits over a two-week period, with 24-hour recalls completed subsequently, and a 20% reliability subsample repeated the entire protocol approximately six months later [17]. This design enabled estimation of both within-person variability and temporal stability of biomarker measurements.
Development of Calibration Equations
The statistical development of calibration equations follows a systematic process beginning with linear regression of (log-transformed) biomarker values on corresponding self-report values and pertinent participant characteristics. For example, in the Hispanic Community Health Study/Study of Latinos, calibration equations for sodium and potassium intake were developed by regressing objective 24-hour urinary excretion measures on self-report data from two interviewer-administered 24-hour dietary recalls and participant characteristics including BMI and supplement use [45].
The initial R² values were 19.7% and 25.0% for the sodium and potassium calibration models, respectively, but increased to 59.5% and 61.7% after adjusting for within-person variability in each biomarker [45]. This substantial improvement highlights the importance of accounting for measurement error structure in calibration development. The resulting equations take the form:
Ạ= bÌ‚â‚€ + bÌ‚â‚Q + bÌ‚â‚‚Váµ€
where Ạrepresents the calibrated consumption estimate, Q is the self-reported intake, and V comprises participant characteristics that influence reporting error (e.g., BMI, age, ethnicity) [42]. These equations are subsequently applied to the entire cohort to generate calibrated consumption estimates for disease association analyses.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents for Dietary Biomarker Studies
| Research Reagent | Specification | Application in Biomarker Studies | Validation Requirements |
|---|---|---|---|
| Doubly Labeled Water | Enriched doses of stable isotopes ¹â¸O and ²H | Gold standard measurement of total energy expenditure over 10-14 days | Weight stability during measurement period |
| 24-Hour Urine Collection Kits | Standardized containers with preservatives | Measurement of urinary nitrogen (protein), sodium, potassium, and other analytes | Completeness of collection verification (e.g., para-aminobenzoic acid) |
| Liquid Chromatography-Mass Spectrometry | High-resolution platforms with electrospray ionization | Metabolomic profiling for biomarker discovery and validation | Standard operating procedures for sample preparation and analysis |
| Stable Isotope Standards | ¹³C, ¹âµN-labeled compounds | Quantification of specific nutrients and metabolites | Isotopic purity certification |
| Dietary Assessment Software | Nutrition Data System for Research (NDS-R) or equivalent | Standardized analysis of food records and recalls | Regular database updates for food composition |
| Biospecimen Storage Systems | -80°C freezers with inventory management | Long-term preservation of blood, urine, and other specimens | Temperature monitoring and backup systems |
| rac Tenofovir-d6 | rac Tenofovir-d6, CAS:1020719-94-1, MF:C9H14N5O4P, MW:293.25 g/mol | Chemical Reagent | Bench Chemicals |
| Endoxifen-d5 | Endoxifen-d5, CAS:1584173-54-5, MF:C25H22NO2D5, MW:378.53 | Chemical Reagent | Bench Chemicals |
Application to Dietary Patterns and Disease Association Analyses
Biomarker Signatures for Dietary Patterns
Recent research has extended the biomarker calibration approach from single nutrients to overall dietary patterns, recognizing that dietary guidance increasingly emphasizes holistic eating patterns rather than isolated nutrients. The WHI NPAAS-FS investigated whether biomarker panels could identify signatures for four established dietary patterns: Healthy Eating Index 2010 (HEI-2010), Alternative Healthy Eating Index 2010 (AHEI-2010), alternative Mediterranean diet (aMED), and Dietary Approaches to Stop Hypertension (DASH) [17].
Using a cross-validated model R² ≥ 36% criterion, HEI-2010 and aMED analyses met the discovery threshold, while AHEI-2010 and DASH did not [17]. The R² values for HEI-2010 calibration equations in stage 2 were 63.5% for FFQ, 83.1% for 4-day food record, and 77.8% for 24-hour recall [17]. For aMED, stage 2 R² values ranged from 34.9% to 46.8% across different self-report instruments [17]. These findings demonstrate the potential for dietary pattern biomarkers to calibrate self-reports and enhance studies of diet-disease associations, though performance varies across different patterns.
Impact on Disease Association Analyses
The application of biomarker-calibrated dietary estimates has demonstrated substantial impact on observed diet-disease associations in large cohort studies. In the Women's Health Initiative, analyses using self-reported energy and protein intake typically showed null or weak associations with chronic disease outcomes [10]. In contrast, analyses employing biomarker-calibrated consumption estimates revealed positive associations between energy and protein intake and cancer risk among postmenopausal women [10]. Similarly, biomarker-calibrated energy and protein consumption showed significant associations with diabetes risk in this population [45].
Similar improvements have been observed for other nutrients. Application of regression calibration to examine associations between sodium/potassium ratio and cardiovascular disease in the WHI revealed positive associations with coronary heart disease, nonfatal myocardial infarction, coronary death, ischemic stroke, and total cardiovascular disease incidence [22]. These findings demonstrate how correction of systematic measurement error through biomarker calibration can uncover important diet-disease relationships obscured by conventional analytical approaches.
Regression Calibration Data Integration
Comparative Analysis: Traditional vs. Biomarker-Calibrated Approaches
The fundamental differences between traditional self-report assessments and biomarker-calibrated approaches yield distinct advantages and limitations for nutritional epidemiology research. Traditional FFQs offer practical advantages for large-scale studies due to low cost, ease of administration, and ability to assess habitual diet over extended periods [42]. However, they suffer from systematic measurement error that varies by participant characteristics including BMI, age, and ethnicity [43] [45]. This systematic error not only attenuates effect estimates but may also introduce bias in diet-disease associations if measurement error correlates with other study factors.
Biomarker-calibrated approaches address these limitations by providing objective measures of dietary intake that adhere to classical measurement error assumptions [42]. The regression calibration framework enables correction of systematic bias in self-reports while maintaining the practical advantages of self-report instruments for large-scale data collection. Limitations include the current scarcity of validated recovery biomarkers, which exist for only a handful of nutrients (energy, protein, sodium, potassium), and the substantial costs associated with biomarker measurement in sufficiently large subsamples [22] [30].
Emerging approaches seek to expand the biomarker toolbox through metabolomic profiling and controlled feeding studies designed specifically for biomarker discovery [8] [30]. The Dietary Biomarkers Development Consortium represents a major coordinated effort to identify and validate biomarkers for foods commonly consumed in the United States diet, which would significantly enhance the scope and precision of calibrated dietary assessment [8]. As this field advances, biomarker-calibrated approaches are poised to become the methodological standard for nutritional epidemiology and diet-disease association studies.
Biomarker-based calibration equations represent a methodological advancement in nutritional epidemiology, effectively addressing the persistent challenge of measurement error in self-reported dietary data. Controlled feeding studies provide the foundational evidence for biomarker validation, enabling development of calibration equations that correct systematic biases in conventional assessment methods. The comparative data presented in this guide demonstrates the superior performance of biomarker-calibrated approaches for quantifying diet-disease associations with reduced bias and enhanced statistical power.
As the field progresses toward a expanded biomarker toolbox encompassing specific foods and dietary patterns, researchers and drug development professionals should prioritize incorporation of biomarker sub-studies within larger cohort investigations. The experimental protocols and methodological frameworks outlined provide practical guidance for implementing these approaches, while the comparative performance data facilitates informed selection of dietary assessment methods appropriate to specific research contexts and objectives. Through continued refinement and application of biomarker calibration methodologies, nutritional epidemiology will achieve enhanced precision in characterizing the complex relationships between diet and human health.
Accurate dietary assessment is a fundamental challenge in nutritional science and epidemiology. Traditional reliance on self-reported data from questionnaires, diaries, or interviews introduces substantial measurement error due to their subjective nature, potentially obscuring true diet-disease associations [46]. Biomarkers of food intake (BFIs) offer a promising solution by providing objective, biological measures of dietary exposure. The strategic choice between single biomarkers and multi-biomarker panels significantly impacts the comprehensiveness and accuracy of dietary assessment.
The validation of these biomarkers against controlled feeding studies represents a cornerstone of nutritional research, providing the rigorous evidence base needed to translate candidate biomarkers into validated tools for scientific and clinical application [10]. This comparison guide examines the performance characteristics of single biomarkers versus biomarker panels, providing researchers with experimental data and methodological frameworks to inform study design and biomarker selection within the context of a broader thesis on biomarker validation.
Theoretical Foundations: Single Biomarkers vs. Multi-Biomarker Panels
The Case for Single Biomarkers
Single biomarkers are individual, measurable substances in biological samples (e.g., blood, urine) that indicate intake of a specific food or nutrient. Their primary strength lies in specificity—a well-validated single biomarker can provide unambiguous evidence of consumption of its target food. Examples include alkylresorcinols for whole-grain wheat and rye intake, or proline betaine for citrus consumption [46]. From a practical standpoint, single biomarkers offer simplicity in analytical method development, lower cost per analyte, and straightforward interpretation. They are particularly valuable in targeted interventions or studies focusing on specific dietary components.
The Rationale for Multi-Biomarker Panels
Multi-biomarker panels consist of several biomarkers measured simultaneously to provide a more comprehensive assessment of dietary intake. Their development is driven by the recognition that single biomarkers often lack sufficient sensitivity or specificity to characterize complex dietary patterns, meals, or overall diet quality. Panels address this limitation by capturing multiple dimensions of intake through different metabolic pathways or food-specific signatures. The statistical advantage is profound: by combining multiple imperfect biomarkers, panels can achieve superior classification accuracy and predictive power compared to any single biomarker alone [47].
Performance Comparison: Quantitative Evidence from Meta-Analyses and Controlled Studies
Evidence from large-scale analyses consistently demonstrates the superior performance of biomarker panels across multiple domains, particularly in complex disease detection where the principles directly apply to dietary assessment.
Table 1: Diagnostic Performance of Single Biomarkers vs. Multi-Biomarker Panels in Disease Detection
| Biomarker Strategy | Condition | Pooled AUC | 95% Confidence Interval | Performance Comparison |
|---|---|---|---|---|
| Single Biomarkers | Pancreatic Ductal Adenocarcinoma | 0.803 | 0.78 - 0.83 | Reference |
| Multi-Biomarker Panels | Pancreatic Ductal Adenocarcinoma | 0.898 | 0.88 - 0.91 | Significantly higher (P < 0.0001) |
| CA 19-9 Alone | Pancreatic Ductal Adenocarcinoma | Lower than panels | - | Significantly lower vs. panels containing CA 19-9 (P < 0.0001) |
| Novel Single Biomarkers | Pancreatic Ductal Adenocarcinoma | Lower than panels | - | Significantly lower vs. novel multi-biomarker panels (P < 0.0001) |
This meta-analysis of blood-based biomarkers for pancreatic cancer revealed that multi-biomarker panels demonstrated significantly superior diagnostic accuracy compared to single biomarkers, establishing an important principle that likely extends to nutritional biomarker applications [47].
Similar advantages are evident in other medical fields. In Alzheimer's disease research, a combined plasma panel (pTau217, pTau181, GFAP, NFL, Aβ42/40, and total tau) achieved >92% accuracy in identifying amyloid positivity, with performance increasing to 93.4% at early clinical stages [48]. Notably, while pTau217 alone achieved comparable accuracy (>90%), the panel approach provided robust performance across diverse clinical scenarios and patient populations.
Table 2: Performance of a Novel Autoantibody Biomarker Panel for Pancreatic Ductal Adenocarcinoma Detection
| Biomarker Panel Composition | Comparison Group | AUC | Sensitivity | Specificity |
|---|---|---|---|---|
| CEACAM1, DPPA2, DPPA3, MAGEA4, SRC, TPBG, XAGE3 | Training Cohort | 85.0% | 0.828 | 0.684 |
| 11-Biomarker Panel (including above) | PDAC vs. Other Pancreatic Cancers | 70.3% | - | - |
| 11-Biomarker Panel (including above) | PDAC vs. Colorectal Cancer | 84.3% | - | - |
| 11-Biomarker Panel (including above) | PDAC vs. Prostate Cancer | 80.2% | - | - |
| 11-Biomarker Panel (including above) | PDAC vs. Healthy Controls | 80.9% | - | - |
This seven-autoantibody signature for pancreatic ductal adenocarcinoma demonstrates how carefully constructed panels can maintain diagnostic sensitivity while achieving specificity across multiple comparison groups, effectively addressing the limited specificity of single biomarkers [49].
Validation Frameworks: Methodological Standards for Biomarker Evaluation
The Controlled Feeding Study Paradigm
Controlled feeding studies represent the gold standard for biomarker validation, providing rigorous evidence of the relationship between dietary intake and biomarker response [10]. In one exemplar study, 153 postmenopausal women from the Women's Health Initiative were provided with a 2-week controlled diet in which each individual's menu approximated her habitual food intake as estimated from her 4-day food record [10]. This design preserved normal variation in nutrient and food consumption while controlling actual intake, enabling robust evaluation of candidate biomarkers.
The key strength of this approach is its ability to simultaneously associate dietary intake with a range of potential nutritional biomarkers under controlled conditions. Researchers used doubly labeled water and urinary nitrogen as recovery biomarkers to validate energy and protein intake, then evaluated serum concentration biomarkers of vitamins and carotenoids against these established standards [10].
Comprehensive Validation Criteria for Biomarkers of Food Intake
A consensus-based procedure has established eight essential criteria for systematic validation of BFIs [46]:
- Plausibility: The biological relationship between biomarker and food intake is credible
- Dose-response: Biomarker response changes proportionally with intake amount
- Time-response: Kinetics of appearance and elimination are characterized
- Robustness: Performance is consistent across different populations and settings
- Reliability: Repeated measurements yield consistent results
- Stability: Biomarker remains intact during sample storage and processing
- Analytical performance: Measurement methods are precise, accurate, and sensitive
- Inter-laboratory reproducibility: Consistent results across different laboratories
This comprehensive framework ensures that validated biomarkers meet both analytical and biological standards, with specific validation pathways depending on the intended application [46].
Advanced Analytical Strategies for Panel Development
Modern approaches to panel development employ sophisticated analytical strategies. One validated method enables simultaneous quantification of 62 food biomarkers in urine using liquid chromatography-mass spectrometry, demonstrating how comprehensive biomarker panels can discriminate between different dietary patterns [50]. This methodology successfully showed quantitative relationships between four biomarker concentrations in urine and dietary intake, providing proof-of-principle for complex panel-based assessment.
The strategic workflow for developing and validating biomarker panels involves multiple stages from discovery to full validation, with controlled feeding studies playing an essential role in establishing dose-response relationships and kinetic parameters.
Biomarker Development and Validation Workflow
Experimental Protocols: Key Methodologies for Biomarker Validation
Controlled Feeding Study Design
The WHI Feeding Study implemented a sophisticated protocol where each participant (n=153) received an individualized diet for two weeks designed to approximate her habitual intake based on 4-day food records [10]. Key methodological elements included:
- Menu Formulation: Food records were entered into Nutrition Data System for Research software for nutrient analysis and menu planning
- Energy Adjustment: Food prescriptions were increased proportionally (average 335±220 kcal/d) for women whose recorded energy intake fell below correction values based on calibrated equations
- Food Preparation: All meals were prepared in a dedicated Human Nutrition Laboratory using ProNutra software for menu creation, recipes, production sheets, and labels
- Biomarker Assessment: Serum biomarkers (carotenoids, tocopherols, folate, vitamin B-12, phospholipid fatty acids) were measured at beginning and end of feeding period
- Reference Biomarkers: Doubly labeled water and 24-hour urinary nitrogen provided objective measures of energy and protein intake
This design preserved the normal variation in nutrient consumption while controlling actual intake, creating an ideal setting for biomarker validation [10].
Cancer Antigen Microarray for Autoantibody Detection
The pancreatic cancer autoantibody panel was developed using a high-throughput, custom cancer antigen microarray platform [49]:
- Array Fabrication: CT100+ microarrays comprising 113 cancer-testis or tumor-associated antigens were printed in a 4-plex format on streptavidin-coated hydrogel substrates with technical triplicates
- Sample Analysis: Serum samples from 94 patients (PDAC, chronic pancreatitis, other cancers, dyspepsia, healthy controls) were profiled
- Data Analysis: Combinatorial ROC curve analysis identified optimal biomarker combinations
- Validation: The panel was validated in an independent cohort of 223 samples using a custom protein microarray and in silico analysis of public immunohistochemistry datasets
This rigorous methodology enabled identification of a 7-marker panel (CEACAM1-DPPA2-DPPA3-MAGEA4-SRC-TPBG-XAGE3) with 85.0% AUC, 0.828 sensitivity, and 0.684 specificity [49].
Multiplex Biomarker Quantification Platform
A standardized strategy for simultaneous quantification of 62 food biomarkers in urine demonstrates the analytical framework for panel-based assessment [50]:
- Analytical Platform: Triple quadrupole mass spectrometry with extensive validation of chromatographic and ionization behavior
- Validation Studies: Application in both controlled inpatient studies (n=19) and free-living studies with provided menu plans (n=15)
- Performance Verification: Demonstration that the biomarker panel could discriminate between different menu plans by detecting distinctive urinary metabolite patterns
- Quantitative Relationships: Establishment of correlation between four biomarker concentrations and dietary intake levels
This approach enables management of structurally diverse metabolites present at wide concentration ranges, essential for comprehensive dietary assessment [50].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents for Biomarker Validation Studies
| Reagent/Material | Function/Application | Example Use Case |
|---|---|---|
| Cancer-Testis Antigen Microarrays | High-throughput autoantibody profiling | Identification of cancer-specific autoantibody signatures [49] |
| Triple Quadrupole Mass Spectrometers | Simultaneous quantification of multiple metabolites | Targeted analysis of 62 food biomarkers in urine [50] |
| Doubly Labeled Water (²H₂¹â¸O) | Objective measure of total energy expenditure | Validation of energy intake in feeding studies [10] |
| 24-Hour Urine Collection Kits | Complete urinary nitrogen measurement | Protein intake validation via urinary nitrogen [10] |
| Nutrition Data System for Research (NDS-R) | Nutrient analysis and menu planning | Analysis of food records and formulation of controlled diets [10] |
| ProNutra Software | Diet design and production management | Creation of individualized menus in feeding studies [10] |
| Multiplex Immunoassay Platforms | Simultaneous measurement of multiple protein biomarkers | Analysis of sepsis biomarker panels [51] |
| Stable Isotope-Labeled Standards | Internal standards for mass spectrometry | Quantitative accuracy in metabolite profiling [50] |
| Hydroxy Tolbutamide-d9 | Hydroxy Tolbutamide-d9, CAS:1185112-19-9, MF:C12H18N2O4S, MW:295.40 g/mol | Chemical Reagent |
| PF-06751979 | PF-06751979|Potent, Selective BACE1 Inhibitor | PF-06751979 is a potent, brain-penetrant BACE1 inhibitor for Alzheimer's disease research. This product is For Research Use Only. Not for human or veterinary diagnostic or therapeutic use. |
The evidence consistently demonstrates that multi-biomarker panels outperform single biomarkers for comprehensive dietary assessment, particularly for complex conditions and dietary patterns. While single biomarkers remain valuable for targeted applications with well-defined single nutrients or foods, panels offer superior classification accuracy, robustness, and comprehensive coverage.
The strategic integration of controlled feeding studies within the validation pipeline is essential for establishing dose-response relationships, understanding kinetic parameters, and verifying biomarker performance under standardized conditions. As biomarker science advances, the development of standardized, validated panels for complex dietary patterns will increasingly enable objective assessment of diet-disease relationships in both research and clinical settings.
Researchers should prioritize panel-based approaches when seeking comprehensive dietary assessment, while maintaining single biomarker strategies for targeted applications where specific foods or nutrients are of primary interest. The continuing refinement of analytical platforms, statistical methods, and validation frameworks will further enhance our ability to objectively measure dietary exposure, ultimately strengthening the scientific foundation for nutritional recommendations and public health policy.
The integration of biomarkers into chronic disease risk assessment represents a paradigm shift in epidemiological research, moving from traditional self-reported data to objective molecular measurements. Biomarkers, defined as measurable characteristics indicating normal or pathological biological processes, provide critical tools for understanding the complex relationship between exposures, such as diet, and chronic disease development [52] [6]. The validation of these biomarkers against controlled feeding studies establishes a necessary foundation for their reliable application in large-scale cohort studies, enabling researchers to move beyond associative relationships toward causal inference in chronic disease etiology.
The challenge in chronic disease research lies in establishing biomarkers that accurately reflect long-term exposure or disease trajectory, particularly for conditions like cancer, cardiovascular disease, and diabetes that develop over decades. Unlike acute conditions, where biomarker responses may be immediate and pronounced, chronic disease biomarkers must demonstrate stability over time, specificity to underlying processes, and sensitivity to subtle changes that precede clinical manifestation [53] [54]. The validation pathway for these biomarkers requires a rigorous, multi-stage process that bridges controlled experimental settings and free-living populations, ensuring that measurements obtained in cohort studies accurately reflect biological reality rather than methodological artifacts.
Methodological Approaches for Biomarker Validation
Validation Frameworks and Study Designs
The journey from biomarker discovery to clinical application follows a structured pathway emphasizing rigorous validation at each stage. This process typically encompasses analytical validation (assessing assay performance), clinical validation (establishing association with clinical endpoints), and utilization validation (demonstrating value in specific contexts) [55] [6]. For chronic disease applications, this pathway must account for the extended temporal relationship between biomarker measurement and disease onset, requiring longitudinal study designs with sufficient follow-up duration to capture meaningful endpoints.
The U.S. Food and Drug Administration's Biomarker Qualification Program outlines a formal, three-stage submission process for biomarker development that emphasizes context of use and fit-for-purpose validation [52]. This regulatory framework encourages a collaborative approach where multiple stakeholders work through consortia to develop biomarkers, sharing resources and reducing individual burden. The process begins with a Letter of Intent outlining the proposed biomarker and its intended application, progresses to a detailed Qualification Plan describing the development strategy, and culminates in a Full Qualification Package containing comprehensive evidence to support regulatory decision-making [52].
Table 1: Key Validation Study Designs for Chronic Disease Biomarkers
| Study Design | Primary Purpose | Typical Sample Size | Advantages | Limitations |
|---|---|---|---|---|
| Controlled Feeding Studies | Establish causal relationship between exposure and biomarker | Small (20-100 participants) | Controlled conditions, known exposures, pharmacokinetic data | Artificial setting, short duration, expensive |
| Prospective Cohort Studies | Validate biomarker-disease association in free-living populations | Large (>10,000 participants) | Real-world relevance, pre-disease biospecimens, multiple endpoints | Confounding factors, long follow-up, expensive |
| Nested Case-Control Studies | Efficient evaluation within existing cohorts | Moderate (hundreds to thousands) | Cost-effective, pre-disease biospecimens, efficient for rare outcomes | Sampling framework complexity, limited to archived samples |
| Cross-Sectional Studies | Initial feasibility and association assessment | Variable | Rapid implementation, low cost | Temporal ambiguity, prevalent bias |
| Method Comparison Studies | Analytical validation against gold standards | Small to moderate | Technical performance assessment, interoperability | Limited clinical relevance |
Statistical Considerations and Performance Metrics
Robust statistical approaches are essential for proper biomarker validation, with methods tailored to the intended application. For prognostic biomarkers (which provide information about overall disease outcomes), statistical significance is typically evaluated through main effect tests in multivariable models adjusting for clinical covariates [13]. For predictive biomarkers (which inform treatment response), validation requires testing a treatment-by-biomarker interaction in randomized clinical trials to demonstrate that treatment effects differ across biomarker-defined subgroups [13].
Key performance metrics for biomarker validation vary based on the specific application. Diagnostic biomarkers require high sensitivity and specificity, while risk stratification biomarkers prioritize positive and negative predictive values [13]. For continuous biomarkers, the area under the receiver operating characteristic curve (AUC-ROC) provides a measure of discrimination ability, while calibration assesses how well predicted risks match observed outcomes [13]. In chronic disease applications, where biomarkers often aim to predict long-term outcomes, time-dependent ROC curves and C-index for survival models offer more appropriate performance measures that account for censoring in time-to-event data.
Biomarker Validation Pathway from Discovery to Implementation
Practical Applications in Chronic Disease Research
Case Study: Multi-Cancer Risk Prediction Model
A recent large-scale prospective study demonstrates the practical application of biomarker validation in chronic disease risk assessment. The FuSion study recruited 42,666 participants from Taizhou, China, with a discovery cohort (n=16,340) and an independent validation cohort (n=26,308) [56]. Researchers integrated multi-scale data from 54 blood-derived biomarkers and 26 epidemiological exposures to develop a risk prediction model for five common cancers: lung, esophageal, liver, gastric, and colorectal cancer [56].
The study employed five supervised machine learning approaches with LASSO-based feature selection to identify the most informative predictors. The final model comprised four key biomarkers along with age, sex, and smoking intensity, achieving an AUROC of 0.767 (95% CI: 0.723-0.814) for five-year risk prediction [56]. High-risk individuals (17.19% of the cohort) accounted for 50.42% of incident cancer cases, with a 15.19-fold increased risk compared to the low-risk group [56]. During prospective follow-up of 2,863 high-risk subjects, 9.64% were newly diagnosed with cancer or precancerous lesions, demonstrating the model's utility in identifying candidates for advanced screening [56].
Table 2: Performance Metrics for Multi-Cancer Risk Prediction Model
| Performance Measure | Discovery Cohort | Validation Cohort | Prospective Follow-up |
|---|---|---|---|
| AUROC (5-year risk) | 0.792 (0.751-0.833) | 0.767 (0.723-0.814) | N/A |
| High-Risk Proportion | 16.83% | 17.19% | 100% |
| Sensitivity | 52.34% | 50.42% | N/A |
| Cases in High-Risk Group | 51.87% | 50.42% | 9.64% detection rate |
| Risk Ratio (High vs. Low) | 16.45 | 15.19 | 5.02 |
Dietary Biomarkers in Chronic Disease Research
The Dietary Biomarkers Development Consortium (DBDC) represents a systematic approach to address the significant limitation of self-reported dietary data in chronic disease research. The DBDC implements a 3-phase validation approach to identify and verify food intake biomarkers [7]. In phase 1, controlled feeding trials administer test foods in prespecified amounts to healthy participants, followed by metabolomic profiling of blood and urine specimens to identify candidate compounds and characterize their pharmacokinetic parameters [7].
Phase 2 evaluates the ability of candidate biomarkers to identify individuals consuming biomarker-associated foods using controlled feeding studies of various dietary patterns [7]. Finally, phase 3 assesses the validity of candidate biomarkers to predict recent and habitual consumption of specific test foods in independent observational settings [7]. This systematic approach significantly expands the list of validated biomarkers of intake for foods consumed in the United States diet, enabling more precise assessment of diet-chronic disease relationships [7].
Experimental Protocols and Methodologies
Sample Collection and Processing Protocols
Standardized sample collection and processing protocols are fundamental to biomarker validity in chronic disease cohort studies. The FuSion study implemented rigorous sample handling procedures: peripheral blood samples (8 to 10 mL) were collected in K2 EDTA vacutainers and stored at 4°C until processing at the end of the day [56]. After centrifugation, plasma was separated and aliquoted into barcoded cryovials, then stored at -80°C or lower until analysis [56]. Such standardized protocols minimize pre-analytical variability that could compromise biomarker measurements and subsequent risk predictions.
For tissue-based biomarkers in cancer research, standardization of staining and imaging procedures is equally critical. In the immunohistochemistry biomarker study, slides were randomly assigned to pathology cyto-technicians and processed in batches to control for technical variability [57]. The use of a single reagent lot and manual staining according to manufacturer instructions helped maintain consistency across samples [57]. These methodological details, though often overlooked, significantly impact biomarker reproducibility and validity when applied to chronic disease classification and risk assessment.
Data Analysis and Computational Approaches
Modern biomarker validation for chronic disease applications increasingly relies on advanced computational approaches. The FuSion study employed multiple supervised machine learning methods including LASSO regularization for feature selection to identify the most predictive biomarkers from the initial panel of 54 candidates [56]. For data preprocessing, they used the K-nearest neighbors algorithm to impute missing values for continuous variables, locating the 50 closest individuals based on Euclidean distances and using their median values for imputation [56]. All continuous biomarkers were standardized using Z-score transformation to facilitate model fitting and interpretation.
In cancer biomarker research, deep learning approaches have demonstrated remarkable success in automated biomarker quantification. The WI-Net architecture, a fully convolutional network, can automatically localize and quantify regions expressing biomarkers in immunohistochemistry images [57]. This approach eliminates the need for manual feature engineering by automatically learning relevant feature descriptors in convolution kernels during network training [57]. Such computational advances enable more reproducible and scalable biomarker analysis across large cohort studies, though they require substantial computational resources and large training datasets.
Computational Workflow for Biomarker-Based Risk Model Development
Analytical Platforms and Reagent Solutions
Table 3: Essential Research Resources for Biomarker Discovery and Validation
| Resource Category | Specific Tools/Platforms | Primary Application | Key Considerations |
|---|---|---|---|
| Molecular Profiling Platforms | Next-generation sequencing, Mass spectrometry, Microarrays | Biomarker discovery and quantification | Throughput, sensitivity, dynamic range, cost |
| Immunoassay Reagents | CINtec PLUS kit, Antibody panels, Detection systems | Protein biomarker detection and localization | Specificity, sensitivity, reproducibility |
| Bioinformatics Tools | SurvExpress, R/Bioconductor, Python scikit-learn | Data analysis and model development | Statistical methods, visualization, interoperability |
| Biospecimen Collection Materials | K2 EDTA tubes, PAXgene RNA tubes, Cryovials | Sample integrity preservation | Stability, compatibility, storage conditions |
| Cell Culture Models | Primary cells, Cell lines, Organoids | Mechanistic studies and functional validation | Physiological relevance, reproducibility, scalability |
| Imaging Systems | Whole slide scanners, Confocal microscopes | Spatial biomarker analysis and quantification | Resolution, throughput, multiplexing capability |
Several specialized computational resources support biomarker validation in chronic disease research. SurvExpress provides a cancer-wide gene expression database with clinical outcomes and a web-based tool for survival analysis and risk assessment [58]. This platform enables researchers to validate multi-gene biomarkers for clinical outcomes using a database of over 20,000 samples and 130 datasets covering tumors from more than 20 tissues [58]. The tool performs multivariate survival analysis in approximately one minute, significantly accelerating the biomarker validation process [58].
Additional computational resources include The Cancer Genome Atlas for genomic data, Gene Expression Omnibus for public data repository, and various R/Bioconductor packages for specialized analytical needs. These resources enable researchers to validate findings across multiple independent datasets, addressing the critical need for replication in biomarker development. For dietary biomarkers, the DBDC is developing a publicly accessible database to archive data generated during all study phases as a resource for the research community [7].
The integration of validated biomarkers into chronic disease research represents a transformative approach to understanding disease etiology and improving risk stratification. The systematic validation of biomarkers against controlled feeding studies and their subsequent application in large prospective cohorts provides a robust framework for moving beyond association to causation. As demonstrated by the multi-cancer risk prediction model, strategically selected biomarker panels can significantly enhance our ability to identify high-risk individuals up to five years before diagnosis, creating opportunities for targeted prevention and early intervention [56].
Future directions in biomarker research will likely focus on several key areas: First, the integration of multi-omics data (genomics, proteomics, metabolomics) to capture the complexity of chronic disease processes. Second, the development of dynamic biomarkers that can track changes in risk over time, enabling personalized screening intervals and prevention strategies. Third, the standardization of analytical methods and reporting standards to facilitate comparability across studies and populations. Finally, the translation of validated biomarkers into clinical practice through regulatory qualification and the development of clinical guidelines for their appropriate use. As these efforts advance, biomarker-based risk assessment will play an increasingly central role in precision prevention strategies for chronic diseases.
Navigating Analytical and Translational Challenges
Accurate measurement of dietary intake is fundamental to nutritional science, yet it remains a significant challenge due to the limitations of self-reported data such as food frequency questionnaires and diet diaries, which are prone to misreporting and bias [59]. Biomarkers of food intake (BFIs) offer an objective alternative, providing measurable indicators of food consumption in biological samples like blood or urine [27]. However, a major hurdle in their development is the issue of specificity – the ideal biomarker is highly specific for one food item or food group, not detected when the food is not consumed, and shows a distinct dose- and time-dependent response after consumption [59]. In practice, many potential biomarkers are not unique to a single food, complicating their interpretation and validation. This article explores the experimental designs and methodologies being used to overcome these specificity hurdles within the critical context of controlled feeding studies.
The Fundamental Challenge: Why Biomarkers Lack Specificity
A biomarker's lack of specificity for a single food can stem from several biological and dietary realities:
- Ubiquitous Metabolites: Many characteristic metabolites are present in a range of related foods. For example, certain carotenoids are found in many orange and green vegetables, and specific polyphenols might be shared among various berries [15].
- Complex Metabolic Pathways: After consumption, food components are metabolized by host enzymes and gut microbiota. These transformations can produce metabolites that are common to several different parent compounds or foods [15].
- Complex Meal Matrices: In real-world settings, foods are rarely consumed in isolation. When eaten as part of complex meals, the bioavailability and metabolism of food components can be altered, and the resulting biomarker profile may reflect the combined meal rather than a single ingredient [59].
Overcoming these challenges requires moving beyond study designs that test single foods in isolation and adopting more sophisticated, holistic approaches that better emulate habitual eating patterns.
Advanced Experimental Designs to Tackle Specificity
Innovative controlled feeding studies are addressing specificity by designing protocols that test biomarkers in realistic, multi-food environments. The table below summarizes the key features of two such advanced study designs.
Table 1: Comparison of Controlled Feeding Study Designs for Biomarker Validation
| Study Feature | NPAAS-FS (Women's Health Initiative) [10] | MAIN Study (Newcastle) [59] [15] |
|---|---|---|
| Primary Objective | Evaluate serum concentration biomarkers for vitamins and carotenoids against established recovery biomarkers. | Discover and validate BFIs for a wide range of foods within conventional eating patterns. |
| Study Population | 153 postmenopausal women. | 51 healthy participants (mixed age and sex). |
| Diet Design | 2-week controlled diet mimicking each participant's habitual intake based on their food record. | Two 3-day randomized menu plans emulating typical UK diets, providing structured exposure to many common foods. |
| Key Strength | Preserved normal variation in individual nutrient intake for biomarker evaluation. | Tests biomarker performance in real-world conditions with free-living participants preparing meals at home. |
| Approach to Specificity | Linear regression of consumed nutrients on potential biomarkers to quantify explained variation (R²). | Comprehensiveness of menu design allows testing of biomarker specificity within a biobank of urine samples from multi-food diets. |
These studies highlight a paradigm shift. The NPAAS-FS focused on preserving individual variation to see how well biomarkers reflected usual intake, while the MAIN Study prioritized comprehensive menu design to challenge and test biomarker specificity across a full diet.
Detailed Experimental Protocol from the MAIN Study
The MAIN Study provides a robust protocol for free-living biomarker validation [59] [15]:
- Participant Recruitment: Recruit free-living participants willing to consume all provided foods and collect urine samples at home. Exclusion criteria typically include conditions or medications that could alter normal metabolism.
- Menu Plan Design: Develop 3-day menu plans that reflect the whole diet of the target population (e.g., typical UK diet). Menus should include many commonly-consumed foods, delivered in the context of conventional meals (breakfast, lunch, dinner).
- Food Provision and Consumption: Provide all foods and drinks to participants in appropriate portion sizes. Participants prepare and consume meals in their own homes, following prescribed meal timings to mimic real-life conditions.
- Urine Sample Collection: Participants collect spot urine samples at multiple predetermined times (e.g., post-dinner, first morning void, fasting, post-breakfast, post-lunch). They record volume, date, and time, and store aliquots at -80°C after transport to the lab.
- Sample Normalization and Analysis: Normalize urine samples using refractive index to account for differences in fluid intake. Analyze using mass spectrometry-based metabolomics for high-throughput, non-targeted metabolite fingerprinting.
- Data Mining and Biomarker Identification: Use statistical and bioinformatics tools to identify metabolite patterns that distinguish consumption of specific foods, even within the complex background of a whole diet.
Quantitative Biomarker Performance in Feeding Studies
The performance of a biomarker is quantitatively assessed by how well its concentration in a biological fluid explains the variation in intake of its target nutrient or food. The following table summarizes the performance of several serum biomarkers from the NPAAS-FS controlled feeding study, using established urinary recovery biomarkers as a benchmark [10].
Table 2: Performance of Serum Biomarkers in Explaining Nutrient Intake Variation in a Controlled Feeding Study (n=153) [10]
| Biomarker | Regression R² Value | Performance Interpretation |
|---|---|---|
| Urinary Nitrogen (Protein Intake) | 0.43 | Established recovery biomarker benchmark |
| Doubly Labeled Water (Energy Intake) | 0.53 | Established recovery biomarker benchmark |
| Serum Vitamin B-12 | 0.51 | Similar to established benchmarks |
| Serum α-Carotene | 0.53 | Similar to established benchmarks |
| Serum Folate | 0.49 | Similar to established benchmarks |
| Serum Lutein + Zeaxanthin | 0.46 | Good performance |
| Serum β-Carotene | 0.39 | Moderate performance |
| Serum Lycopene | 0.32 | Moderate performance |
| % Energy from Polyunsaturated Fatty Acids | 0.27 | Weaker association with intake |
| Serum γ-Tocopherol | <0.25 | Weak association with intake |
The data shows that several serum concentration biomarkers performed similarly to established urinary recovery biomarkers, suggesting they are suitable for objective intake assessment in this population. In contrast, other markers like γ-tocopherol and certain fatty acids were only weakly associated with intake, highlighting the ongoing need for further biomarker development in these areas [10].
The Scientist's Toolkit: Essential Reagents and Technologies
The discovery and validation of dietary biomarkers with robust specificity rely on a suite of specialized reagents, technologies, and methodologies.
Table 3: Essential Research Toolkit for Dietary Biomarker Validation
| Tool / Reagent | Function / Application | Specific Example / Note |
|---|---|---|
| Controlled Feeding Study | Provides ground-truth data on dietary intake for biomarker calibration [10] [22]. | The NPAAS-FS used individual menu plans to approximate habitual diet. |
| Doubly Labeled Water (DLW) | Objective biomarker of total energy expenditure; used to validate energy intake assessments [10]. | Serves as a recovery biomarker to calibrate self-reported energy intake. |
| Urinary Nitrogen | Objective biomarker of total protein intake; another established recovery biomarker [10] [15]. | Used to calibrate self-reported protein intake and as a benchmark for new biomarkers. |
| Mass Spectrometry | High-throughput, sensitive analysis of metabolites in biofluids for discovery and quantification [59] [15]. | Central to both non-targeted discovery and targeted validation in proteomic and metabolomic approaches. |
| Bioinformatics & Statistical Tools | Process and interpret complex omics data to identify promising biomarker candidates [27] [60]. | Includes tools for multivariate analysis to identify biosignatures (collections of features). |
| Biobanks | Repositories of high-quality clinical samples essential for large-scale validation studies [61] [62]. | International collaborations help alleviate the bottleneck of sample availability for validation. |
| Standardized Urine Collection Protocol | Ensures sample integrity and minimizes pre-analytical variability in free-living participants [59]. | The MAIN Study used home collection with immediate refrigeration and later aliquoting. |
| BMS-986158 | BMS-986158|Potent BET Inhibitor for Research | BMS-986158 is a potent BET bromodomain inhibitor for cancer and HIV latency research. This product is for Research Use Only (RUO). Not for human use. |
| BP-1-108 | BP-1-108, MF:C32H38N2O6S, MW:578.7 g/mol | Chemical Reagent |
Visualizing the Pathways: From Specificity Challenge to Validated Biomarker
The following diagram illustrates the logical workflow and key decision points in overcoming specificity hurdles to arrive at a validated, specific biomarker or biosignature.
Figure 1: A workflow for validating specific dietary biomarkers, demonstrating pathways to overcome lack of uniqueness.
Overcoming the specificity hurdles in dietary biomarker development is a complex but surmountable challenge. The path forward relies on moving beyond simplified study designs and embracing controlled feeding studies that reflect the complexity of real-world diets. As demonstrated by research initiatives like the MAIN Study and NPAAS-FS, the key lies in using comprehensive menu plans, recruiting free-living participants, applying high-throughput metabolomics, and leveraging sophisticated data analysis to identify robust biosignatures. By adopting these advanced methodologies, researchers can develop the specific, objective tools needed to accurately monitor dietary exposure, ultimately strengthening public health guidelines and our understanding of the diet-health relationship.
In the field of nutritional epidemiology and clinical research, accurate measurement of dietary intake is fundamental to understanding diet-disease relationships. Self-reported dietary data, however, are prone to substantial measurement error, necessitating objective biological measurements for validation [10]. Biomarkers serve as critical molecular signposts that illuminate intricate pathways of health and disease, bridging the gap between benchside discovery and bedside application [27]. Controlled feeding studies, where types and quantities of specific foods and beverages are known, provide the optimal setting for biomarker discovery and validation [22] [17]. The choice between blood and urine as primary biofluids, along with strategic sampling protocols, significantly impacts the quality, reliability, and practical applicability of biomarker data in both research and clinical settings. This guide objectively compares urine and blood collection methodologies within the context of biomarker validation against controlled feeding studies, providing evidence-based recommendations for researchers and drug development professionals.
Fundamental Comparison: Urine vs. Blood for Biomarker Research
Biological and Practical Characteristics
Biofluid selection fundamentally shapes research design, logistical complexity, and participant burden. The table below summarizes core characteristics of urine and blood relevant to biomarker studies.
Table 1: Fundamental Characteristics of Blood and Urine in Research Contexts
| Characteristic | Blood | Urine |
|---|---|---|
| Invasiveness of Collection | Invasive (venipuncture or fingerstick) | Non-invasive |
| Participant Burden & Acceptance | Moderate to high; requires clinical setting or trained phlebotomist | Low; suitable for self-collection in free-living settings |
| Inherent Composition | Reflects real-time systemic physiology; homeostatically regulated | Reflects renal filtration and concentration of metabolic by-products; not homeostatically regulated [63] |
| Sample Volume Typically Available | Limited (mL range) | More readily available in larger volumes (tens to hundreds of mL) |
| Primary Analytical Strengths | Direct measurement of circulating biomarkers; comprehensive metabolic snapshot | Measurement of excreted metabolites; insights into kidney function and metabolic waste |
| Key Pre-analytical Challenges | Requires rapid processing to separate plasma/serum; complex EV isolation | Requires normalization for concentration variations; stability of some analytes |
Diagnostic and Biomarker Potential
Both biofluids offer rich information content, albeit reflecting different physiological processes.
Blood Analysis: Blood tests measure biomarkers directly circulating in the body, reflecting real-time physiological status. They provide a comprehensive overview of organ functions and metabolic processes through a systemic approach [64]. Blood is particularly valuable for measuring nutrients, hormones, and other circulating factors.
Urine Analysis: Urine serves as a sensitive and non-invasive biological matrix with considerable potential for yielding diagnostic information. It reflects the body's metabolic status, offering a rich source of diagnostic and prognostic information [64]. While every compound found in urine can also be found in blood, urine contains additional compounds not typically present in blood, likely arising from the kidneys' role in filtering blood and concentrating certain metabolites for excretion [64].
Analytical Performance in Controlled Studies
Stability and Storage Considerations
Analyte stability directly impacts protocol feasibility, especially in large-scale or remote studies.
Table 2: Stability Profiles of Blood and Urine Analytes Under Different Storage Conditions
| Biofluid / Sample Type | Short-Term Stability (Room Temperature) | Long-Term Stability (-20°C) | Key Evidence from Studies |
|---|---|---|---|
| Dried Blood Spots (DBS) | Stable up to 4 weeks | Stable for 1 year | Metabolites in DBS showed good stability when stored at -20°C for 1 year [65] |
| Dried Urine Spots (DUS) | Stable up to 4 weeks | Stable for 1 year | Similar stability profile to DBS; not stable over 1 year at +21°C [65] |
| Plasma/Serum | Requires rapid processing and freezing | Generally stable for extended periods | Traditional liquid samples require consistent frozen storage |
| Liquid Urine | Variable depending on analyte; EVs stable at RT for up to 6 months [63] | Generally stable with proper preservation | Urine EV RNAs showed long-term stability upon urine storage at room temperature [63] |
Biomarker Recovery and Analytical Performance
Controlled studies demonstrate distinct performance characteristics for different biofluid processing methods.
Table 3: Biomarker Recovery and Correlation with Intake in Controlled Feeding Studies
| Biomarker Type | Biofluid | Performance in Controlled Studies | Correlation with Intake (R² values) |
|---|---|---|---|
| Carotenoids (α-carotene) | Serum | Strong performance similar to established biomarkers | 0.53 [10] |
| Folate | Serum | Strong performance in representing nutrient intake | 0.49 [10] |
| Vitamin B-12 | Serum | Strong performance in representing nutrient intake | 0.51 [10] |
| Phospholipid Fatty Acids | Serum | Weaker association with intake | <0.25 [10] |
| Urinary Nitrogen | Urine | Established recovery biomarker for protein intake | 0.43 [10] |
| Urinary Potassium | Urine | Used in dietary pattern validation | Applied in HEI-2010 and aMED validation [17] |
| Urinary Sodium | Urine | Used in dietary pattern validation | Applied in HEI-2010 and aMED validation [17] |
| Small Extracellular Vesicles (sEVs) | Urine | Recoverable from 10mL urine with high purity | Successful isolation from small volumes for downstream applications [66] |
Sampling Timing and Protocol Strategies
Strategic Timing for Dietary Biomarker Capture
Temporal collection patterns should align with biomarker pharmacokinetics and research objectives.
24-hour Urine Collections: Considered the "gold standard" for many nutritional biomarkers as they provide a total daily excretion rate, overcoming diurnal variation [67]. However, they impose significant participant burden and are logistically challenging.
Spot Urine Samples: First morning void, post-prandial spot, or random urines can be collected depending on study purpose [67]. Research shows spot fasting samples can adequately discriminate exposure class for several dietary components, potentially substituting for 24-hour collections [67].
Postprandial Sampling: In acute food intervention studies, 3-hour postprandial urines provided strong classification models, with relatively stable urine composition over a 2–4 hour window after eating [67].
Longitudinal Spot Sampling: Multiple spot samples over days can capture habitual intake while reducing participant burden compared to 24-hour collections.
Integrated Sampling Protocols for Controlled Feeding Studies
Successful biomarker validation requires carefully designed sampling protocols that balance scientific rigor with practical feasibility.
The MAIN Study Protocol:
- Provided all food to free-living participants for three consecutive days with menu plans representing a typical annual diet [67]
- Collected multiple spot urine samples stored at home by participants
- Demonstrated acceptability for volunteers and delivered samples suitable for biomarker quantification [67]
Women's Health Initiative (WHI) Feeding Study Protocol:
- Implemented a 2-week controlled feeding study where each participant's menu approximated her habitual food intake [10] [17]
- Used 4-day food records as a guide for menu creation to minimize perturbations in blood and urine measurements
- Preserved intake variation while maintaining controlled conditions [10]
Experimental Protocols for Biofluid Processing
Urine Processing for Metabolomic Analysis
Proper urine handling is essential for reliable biomarker data.
Collection and Storage:
- Collect mid-stream urine into sterile containers
- Process within 1-2 hours or freeze at -80°C
- For extracellular vesicle (EV) studies, urine can be stored at room temperature for extended periods without significant RNA degradation [63]
Normalization Strategies:
- Creatinine normalization: Most common but can mask disease-correlated variations [63]
- Total urine protein: Shows excellent correlation with EV content [63]
- Specific RNA normalizers: RNY4 and specific miRNA panels well reflect inter-sample EV variation [63]
- Avoid relying solely on creatinine, particularly for EV studies or when renal function may be compromised
Blood Collection and Processing Protocols
Plasma Preparation:
- Collect peripheral blood in EDTA-treated tubes
- Centrifuge at 1,500-2,000 × g for 10 minutes at 4°C
- Carefully pipette plasma layer without disturbing buffy coat
- Aliquot and store at -80°C [66]
Dried Blood Spot (DBS) and Dried Urine Spot (DUS) Methods:
- Spot whole blood or urine onto specialized filter paper
- Dry at room temperature
- Store with desiccant
- Transport at room temperature within 28 days
- For long-term storage, keep at -20°C or below [65]
Small Extracellular Vesicle (sEV) Isolation Protocol
A streamlined method for isolating sEVs from multiple biofluids:
Differential Ultracentrifugation Protocol:
- Pre-clearing: Centrifuge urine (10,000 × g, 15 min, 4°C) to remove cell fragments and organelles [66]
- Filtration: Pass supernatant through 0.22 μm PES membrane syringe filters [66]
- Ultracentrifugation: Transfer filtrate to ultracentrifuge tubes and spin at high speed (typically 100,000 × g) for 70-120 minutes [66]
- Washing: Resuspend pellet in PBS and repeat ultracentrifugation
- Characterization: Validate sEVs using Nanoparticle Tracking Analysis (NTA), Transmission Electron Microscopy (TEM), and Western blotting for markers (CD9, CD63, Flotillin-1, TSG101) [66]
Visualizing Biomarker Validation Workflows
Integrated Biofluid Biomarker Validation Pipeline
Biomarker Validation Workflow: This diagram illustrates the integrated pipeline from controlled feeding studies to clinical application, highlighting parallel processing of blood and urine samples.
Biofluid Selection Decision Framework
Biofluid Selection Framework: This decision diagram provides guidance for researchers selecting between blood and urine based on study objectives and constraints.
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 4: Key Reagents and Materials for Biofluid Biomarker Research
| Reagent/Material | Primary Application | Function in Workflow | Considerations for Selection |
|---|---|---|---|
| EDTA-treated Blood Collection Tubes | Plasma isolation | Prevents coagulation; preserves protein integrity | Standard for plasma metabolomics; different additives needed for specific applications |
| Sterile Urine Containers | Urine collection | Maintain sample integrity; prevent contamination | Screw-cap preferred; sufficient volume (30-50mL) for multiple analyses |
| PES Membrane Syringe Filters (0.22μm) | EV isolation | Removes debris and larger particles prior to ultracentrifugation | Low protein binding crucial for high biomarker recovery |
| Protease Inhibitor Cocktails | Biofluid storage | Prevents proteolysis during processing and storage | Essential for preserving protein biomarkers and EV membrane proteins |
| CD9/CD63/TSG101 Antibodies | EV characterization | Western blot validation of exosome markers | Confirm specificity for target species; quality critical for reliable characterization |
| Doubly Labeled Water (DLW) | Energy expenditure biomarker | Gold standard for total energy expenditure measurement | Expensive but essential for validating energy intake in feeding studies |
| C18 and HILIC UHPLC Columns | Untargeted metabolomics | Complementary separation mechanisms for broad metabolite coverage | Essential for comprehensive metabolite profiling in both blood and urine |
The choice between urine and blood for biomarker studies involves trade-offs between analytical richness, practical feasibility, and biological relevance. Blood provides a direct window into circulating biomarkers and systemic physiology, with specific nutritional biomarkers like carotenoids and folate showing strong correlation with intake in controlled feeding studies [10]. Urine offers unparalleled advantages for non-invasive, frequent sampling in free-living populations, with demonstrated stability for many analytes and practical protocols for EV isolation [66] [63].
For comprehensive dietary biomarker validation, an integrated approach utilizing both biofluids provides complementary insights. Blood biomarkers effectively capture circulating nutrients and intake of specific food components, while urine biomarkers excel at measuring excretion metabolites and capturing overall dietary patterns when multiple biomarkers are combined [17]. The development of dried spot techniques for both blood and urine has further enhanced feasibility for large-scale studies and remote sampling [65].
Strategic timing of sample collection should align with study objectives—24-hour collections for total daily excretion, targeted postprandial sampling for acute intake response, or longitudinal spot sampling for habitual intake assessment. By matching biofluid selection and sampling protocols to specific research questions within the framework of controlled feeding studies, researchers can optimize biomarker discovery and validation efforts, ultimately strengthening diet-disease association studies through improved measurement accuracy.
Addressing Technological Barriers in Analyzing Structurally Diverse Metabolites
The precise analysis of structurally diverse metabolites is a foundational challenge in modern nutritional science and drug development. This process is critical for biomarker validation, where objective biochemical indicators are used to confirm dietary intake and understand metabolic responses. The Dietary Biomarkers Development Consortium (DBDC) exemplifies the scale of this challenge, leading a systematic effort to discover and validate biomarkers for foods commonly consumed in the United States diet through controlled feeding trials and metabolomic profiling [7]. Without advanced technological solutions for separating, identifying, and quantifying thousands of distinct metabolic species simultaneously, researchers cannot reliably correlate specific dietary exposures with health outcomes. The complexity of biological matrices, the vast structural diversity of metabolites, and the wide dynamic range of concentrations present interconnected technological barriers that this comparison guide addresses through objective evaluation of current analytical platforms and methodologies.
Comparative Analysis of Metabolomic Technologies
The technological landscape for metabolite analysis comprises complementary platforms, each with distinct strengths and limitations for specific analytical scenarios. The selection of an appropriate platform depends heavily on research objectives, whether targeting known metabolite classes or conducting untargeted discovery of novel compounds.
Table 1: Comparison of Major Analytical Technologies for Metabolite Analysis
| Technology | Optimal Use Cases | Metabolite Coverage | Sensitivity | Throughput | Structural Resolution |
|---|---|---|---|---|---|
| LC-MS (QTOF) | Untargeted profiling, Secondary metabolites, Lipids | Broad (~1000s features) | High (pM-nM) | Moderate | High (RMS < 5 ppm) |
| GC-MS (TOF) | Primary metabolism, Volatiles, Polar metabolites | Targeted (~100-200 compounds) | High (pM-nM) | High | Moderate |
| MALDI Imaging | Spatial distribution, Tissue localization | Limited by ionization | Moderate | Low | High with MS/MS |
| NMR Spectroscopy | Structural elucidation, Absolute quantification | Narrow (~10s-100s) | Low (μM-mM) | Low | Excellent (atomic level) |
Liquid Chromatography-Mass Spectrometry (LC-MS) utilizing quadrupole time-of-flight (QTOF) detectors, such as the Bruker Maxis 2 QTOF-MS system, provides exceptional coverage for semi-polar compounds including secondary metabolites, phytosterols, vitamins, hormones, and hydrophobic analytes like lipids [68]. This platform generates thousands of non-redundant chromatographic features that can be partially annotated using accurate mass, isotopic pattern, and MS/MS fragment spectra against databases like KNApSAcK and KEGG [68]. The key advantage of LC-HRMS lies in its untargeted capabilities and high resolution (R = 85,000, mass accuracy ≈ 0.6 ppm), enabling detection of novel metabolites without prior knowledge of their existence [68] [69].
Gas Chromatography-Mass Spectrometry (GC-MS) systems, such as the LECO HT time-of-flight MS coupled with an AGILENT 7890A gas chromatograph, excel at quantifying polar plant metabolites, typically covering 60-100 known metabolites including amino acids, organic acids, polyamines, sugars, and sugar phosphates, along with twice as many unknown compounds [68]. The platform utilizes in-line derivatization to improve measurement quality for large sample numbers, offering highly reproducible quantification ideal for primary metabolism studies [68]. While covering a narrower metabolic space than LC-MS, GC-TOF-MS provides superior sensitivity and quantification precision for core metabolic pathways.
Computational Metabolite Annotation Tools
The computational annotation of mass spectrometry data represents perhaps the most significant bottleneck in metabolomic analysis, with only approximately 10% of detected molecules typically annotated in untargeted studies [69]. This limitation severely hampers biological interpretation and cross-study comparison. Several computational strategies have emerged to address this challenge, each employing different algorithmic approaches to structural elucidation.
Table 2: Comparison of Computational Metabolite Annotation Approaches
| Tool Category | Representative Tools | Methodology | Annotation Level | Strengths | Limitations |
|---|---|---|---|---|---|
| Spectral Library Matching | GNPS, MS-DIAL | Experimental spectrum matching | MSI Level 2 (confident) | High confidence with references | Limited to known compounds in libraries |
| In-Silico Fragmentation | CFM-ID, CSI:FingerID | Machine learning prediction | MSI Level 3 (putative) | Can annotate novel compounds | Computational intensive, higher error rates |
| Molecular Networking | GNPS, FBMN | Spectral similarity networks | MSI Level 2-3 | Contextual annotation propagation | Dependent on spectral quality |
| Hybrid Approaches | MS2LDA, MolNetEnhancer | Combinatorial meta-strategies | MSI Level 2-3 | Increased annotation rates | Complex computational workflows |
Molecular networking approaches, particularly as implemented in the Global Natural Products Social Molecular Networking (GNPS) platform, have revolutionized metabolite annotation by grouping molecules of likely high chemical similarity based on their MS/MS spectra [69]. This enables Network Annotation Propagation, where identified molecules allow propagation of chemical identity to improve annotation of other unidentified members within the same molecular family [69]. The strength of this approach lies in its ability to visualize structural relationships across complex datasets, though it remains dependent on spectral quality and reference databases.
Machine learning-based tools represent the cutting edge of computational metabolomics, using deep learning models to predict structural properties from MS/MS spectra. These methods can learn fragmentation patterns and chemical properties from large spectral databases, enabling annotation of novel compounds not present in existing libraries [69]. However, these tools typically report lower accuracy than library matching and often rank the correct annotation within the top 5-10 hits rather than as the top prediction [69]. This necessitates careful validation and consideration of multiple candidates rather than automatic acceptance of the top hit.
Experimental Protocols for Enhanced Metabolite Detection
Controlled Feeding Studies for Biomarker Validation
The Dietary Biomarkers Development Consortium (DBDC) has established a rigorous 3-phase protocol for biomarker discovery and validation that serves as a gold standard in the field [7]. This methodology directly addresses the technological barrier of linking metabolic signatures to specific dietary exposures through controlled experimental design:
Phase 1: Candidate Identification - Controlled feeding trials administer test foods in prespecified amounts to healthy participants, followed by metabolomic profiling of blood and urine specimens to identify candidate compounds. These studies characterize pharmacokinetic parameters of candidate biomarkers associated with specific foods [7].
Phase 2: Evaluation - The ability of candidate biomarkers to identify individuals consuming biomarker-associated foods is evaluated using controlled feeding studies of various dietary patterns, testing specificity across different dietary backgrounds [7].
Phase 3: Validation - The validity of candidate biomarkers to predict recent and habitual consumption of specific test foods is evaluated in independent observational settings, establishing real-world applicability [7].
This systematic approach generates data archived in publicly accessible databases as resources for the broader research community, significantly expanding the list of validated biomarkers for foods consumed in the United States diet [7].
OSMAC (One Strain Many Compounds) Approach
For maximizing the structural diversity of detectable metabolites, particularly from microbial sources, the OSMAC protocol provides a simple yet powerful strategy to activate silent biogenetic gene clusters [70]. This approach recognizes that a large portion of microbial gene clusters remain silenced under standard fermentation conditions, drastically limiting metabolite detection [70]. The protocol involves systematic variation of cultivation parameters to stimulate alternative metabolic pathways:
Medium Composition Variation - Adjusting carbon and nitrogen sources, C/N ratio, salinity, and metal ion composition to trigger different metabolic responses. For example, a marine-derived strain Asteromyces cruciatus 763 produced a new pentapeptide when cultivated with arginine as the sole nitrogen source instead of NaNO₃ [70].
Co-cultivation - Growing the target strain with other microorganisms to simulate ecological interactions and induce defensive metabolite production.
Enzyme Inhibition - Adding epigenetic modifiers like DNA methyltransferase and histone deacetylase inhibitors to alter gene expression patterns.
Precursor Supplementation - Providing biosynthetic precursors to bypass metabolic bottlenecks and enhance production of specific metabolite classes.
The OSMAC approach has demonstrated remarkable success in activating silent gene clusters, with one study showing that Streptomyces sp. C34 produced different ansamycin-type polyketides when grown on ISP2 medium with glucose versus modified ISP2 containing glycerol [70].
Metabolic Pathway Analysis and Similarity Assessment
Understanding the metabolic fate of compounds is essential for interpreting their biological activity and potential toxicological effects. The Metabolic Forest approach represents an advanced computational framework that overcomes limitations of traditional "sites of metabolism" predictions by generating exact metabolite structures through systematic biotransformation simulations [71]. This system accurately predicts diverse metabolite structures with performance reaching 79.42% for direct substrate-product pathway linking, improving to 88.77% with depth-three breadth-first search [71]. The methodology includes specialized algorithms for accurate quinone structure prediction, the most common type of reactive metabolite, achieving 91.84% accuracy on a validation set of 576 quinone reactions [71].
For quantitative assessment of metabolic relationships between compounds, the OASIS metabolic similarity functionality provides critical metrics for read-across predictions in toxicological assessments [72]. This approach compares documented or simulated metabolic maps between target and source compounds, quantifying similarity based on common transformations, metabolic pathways, and transformants [72]. The methodology has proven particularly valuable in explaining cases where structurally similar chemicals demonstrate dissimilar toxicological effects due to divergent metabolic pathways generating different reactivity patterns [72].
Metabolomics Analysis Workflow
Essential Research Reagent Solutions
Successful metabolomic analysis requires carefully selected reagents and materials optimized for different stages of the analytical workflow. The selection below represents key solutions validated through experimental protocols cited in this review.
Table 3: Essential Research Reagents for Metabolite Analysis
| Reagent/Material | Application | Function | Technical Considerations |
|---|---|---|---|
| Czapek-Dox Broth | Microbial cultivation | Defined medium for metabolite induction | Arginine as nitrogen source triggers different metabolites vs. NaNO₃ [70] |
| PDB (Potato Dextrose Broth) | Fungal fermentation | Rich medium for secondary metabolism | Metabolite production sensitive to potato source [70] |
| Methanol & Chloroform | Metabolite extraction | Biphasic solvent system | Comprehensive polar/non-polar metabolite coverage, 2:1 ratio |
| Derivatization Reagents | GC-MS sample prep | Chemical modification of metabolites | MSTFA, BSTFA improve volatility & thermal stability |
| Solid Phase Extraction | Sample cleanup | Fractionation & concentration | C18 for non-polar, HILIC for polar metabolites |
| Isotope-Labeled Internal Standards | Quantitation | Mass spectrometry calibration | ^13^C, ^15^N labeled compounds essential for absolute quantitation |
| CRISPR-Cas9 System | Metabolic engineering | Gene editing for pathway manipulation | Activates silent biosynthetic gene clusters [73] |
Integrated Workflows for Enhanced Metabolite Detection
Addressing the technological barriers in analyzing structurally diverse metabolites requires integrating complementary approaches across the entire analytical pipeline. No single technology or methodology suffices for comprehensive metabolic coverage; instead, strategically combined workflows provide synergistic advantages.
The most promising integrated workflow begins with OSMAC-inspired cultivation to maximize metabolic diversity at the production stage, followed by dual LC-MS and GC-MS analysis to cover broad chemical space, then computational integration of molecular networking with in-silico fragmentation prediction for comprehensive annotation, and finally targeted validation through controlled feeding studies for biomarker verification [70] [68] [69]. This pipeline directly addresses the critical bottleneck in metabolomics—the annotation gap—while ensuring biological relevance through rigorous validation.
Metabolic Fate of Dietary Compounds
For researchers focusing on specific metabolite classes, specialized workflows offer advantages. Marine endophyte studies benefit from incorporating host tissue mimics in cultivation media to simulate natural symbiotic environments, triggering production of specialized metabolites through ecological interaction cues [73]. Drug metabolism applications require the Metabolic Forest approach for predicting sequential biotransformations and reactive metabolite formation, essential for toxicological risk assessment [71]. Nutritional biomarker discovery demands the DBDC validation framework with controlled feeding studies to establish causal relationships between dietary intake and metabolic signatures [7].
The continued development of computational approaches, particularly machine learning-based annotation tools and metabolic similarity algorithms, promises to further overcome current technological barriers. However, these in-silico methods must be benchmarked using standardized datasets and validated against experimental results to establish reliability [69] [72]. Integration of multiple annotation strategies consistently outperforms reliance on any single method, providing orthogonal validation and increased confidence in metabolite identifications essential for both drug development and nutritional science applications.
The journey from promising preclinical discoveries to clinically applicable tools represents one of the most significant challenges in modern biomedical research. This translational gap is particularly pronounced in the field of biomarker development, where fewer than 1% of published biomarkers ultimately achieve clinical utility [74]. The disconnect between controlled laboratory environments and heterogeneous human populations leads to substantial failures in biomarker validation, resulting in delayed treatments for patients and wasted research investments [74]. This guide examines the critical roadblocks in translational science and provides objective comparisons of approaches aimed at bridging this divide, with special emphasis on biomarker validation against the gold standard of controlled feeding studies.
The fundamental challenge stems from multiple sources: over-reliance on traditional animal models with poor human correlation, lack of robust validation frameworks, inadequate reproducibility across cohorts, and failure to account for disease heterogeneity in human populations versus the uniformity in preclinical testing [74]. While preclinical studies rely on controlled conditions to ensure clear and reproducible results, human diseases manifest with remarkable diversity, varying not just between patients but even within individual disease sites over time [74]. This complexity demands more sophisticated approaches to translational research that maintain scientific rigor while acknowledging clinical reality.
The Translational Roadblock: A Quantitative Analysis of Failure Points
Root Causes of Translational Failure
Table 1: Primary Causes of Translational Failure in Biomarker Development
| Failure Category | Specific Issues | Impact Magnitude |
|---|---|---|
| Model Systems | Over-reliance on traditional animal models with poor human correlation; Use of syngeneic mouse models that don't match human disease | 25-40% failure attribution |
| Validation Frameworks | Lack of robust validation methodologies; Proliferation of exploratory studies with dissimilar strategies; Variable evidence benchmarks | 30-45% failure attribution |
| Population Complexity | Disease heterogeneity in humans vs. preclinical uniformity; Genetic diversity; Varying treatment histories; Comorbidities | 35-50% failure attribution |
| Technical Variability | Assay performance drift between experiments; Absence of certified standards; Reagent changes | 15-25% failure attribution |
The statistics reveal a troubling landscape: the overwhelming majority of biomarker discoveries fail to progress beyond initial publication. This translational chasm persists despite remarkable advances in our understanding of disease mechanisms and technological capabilities [74]. The failure points cluster around several key areas, with model system limitations representing the most significant contributor to translational failure.
The problem extends beyond technical considerations to fundamental methodological flaws. Unlike the well-established phases of drug discovery, the process of biomarker validation lacks standardized methodology and is characterized by a proliferation of myriad exploratory studies using dissimilar strategies [74]. Without agreed-upon protocols to control variables or sample sizes, results vary between tests and laboratories, failing to translate to wider patient populations. This methodological inconsistency undermines confidence in potentially valuable biomarkers and delays their implementation in clinical practice.
Comparative Performance of Model Systems
Table 2: Model System Performance in Translational Research
| Model Type | Advantages | Limitations | Clinical Predictive Value |
|---|---|---|---|
| Traditional Animal Models | Controlled environment; Clear endpoints; Reproducible conditions | Poor human disease correlation; Limited genetic diversity; Simplified biology | Low (10-20%) |
| Patient-Derived Xenografts (PDX) | Retain tumor heterogeneity; Better clinical mimicry; Recapitulate progression | Time-consuming; Expensive; Requires immunodeficient hosts | Moderate-High (40-60%) |
| Organoids (3D Structures) | Retain biomarker expression; Personalization potential; Human-relevant biology | Limited microenvironment; No systemic influences | Moderate (50-70%) |
| 3D Co-culture Systems | Comprehensive microenvironment; Physiological cellular interactions; Multiple cell types | Technical complexity; Standardization challenges | Moderate-High (50-75%) |
Advanced model systems demonstrate significantly improved clinical predictive value compared to traditional approaches. Patient-derived xenografts (PDX) have proven particularly valuable, producing what researchers describe as "the most convincing" preclinical results by effectively recapitulating cancer characteristics, tumor progression, and evolution in human patients [74]. The superior performance of PDX models is evidenced by their crucial role in investigating key biomarkers including HER2, BRAF, and KRAS mutations.
Three-dimensional co-culture systems that incorporate multiple cell types (including immune, stromal, and endothelial cells) provide comprehensive models of the human tissue microenvironment [74]. These systems have become essential for replicating in vivo environments and more physiologically accurate cellular interactions, enabling the identification of complex biomarker signatures such as chromatin biomarkers that identify treatment-resistant cancer cell populations.
Controlled Feeding Studies: The Gold Standard for Biomarker Validation
Methodological Framework for Nutritional Biomarker Development
Controlled feeding studies represent the methodological gold standard for dietary biomarker validation, providing rigorous assessment of potential biomarkers under precisely monitored conditions. The Women's Health Initiative (WHI) Nutrition and Physical Activity Assessment Study Feeding Study (NPAAS-FS) exemplifies this approach, implementing a sophisticated protocol where 153 postmenopausal women were provided with a 2-week controlled diet in which each individual's menu approximated her habitual food intake [10] [17]. This innovative design preserved normal variation in nutrient consumption while maintaining controlled conditions essential for biomarker validation.
The study incorporated multiple objective measures including doubly labeled water for total energy expenditure assessment, 24-hour urine collection for urinary nitrogen measurement (biomarker of protein intake), and fasting blood draws for analysis of vitamins, carotenoids, and phospholipid fatty acids [10]. The dietary intake records were used to calculate validated dietary pattern scores including Healthy Eating Index 2010 (HEI-2010), Alternative Healthy Eating Index 2010 (AHEI-2010), alternative Mediterranean diet (aMED), and Dietary Approaches to Stop Hypertension (DASH) scores [17]. This comprehensive approach enabled researchers to establish robust correlations between controlled nutrient intake and biomarker levels.
Figure 1: Controlled Feeding Study Workflow for Biomarker Validation
Biomarker Performance in Controlled Feeding Studies
The NPAAS-FS yielded crucial data on biomarker performance for various nutrients. Linear regression of consumed nutrients on potential biomarkers and participant characteristics revealed the following coefficients of determination (R²) for serum concentration biomarkers: folate (0.49), vitamin B-12 (0.51), α-carotene (0.53), β-carotene (0.39), lutein + zeaxanthin (0.46), lycopene (0.32), and α-tocopherol (0.47) [10]. These values demonstrated that serum concentration biomarkers of several vitamins and carotenoids performed similarly to established energy and protein urinary recovery biomarkers in representing nutrient intake variation.
The study further identified that phospholipid saturated fatty acids and monounsaturated fatty acids, along with serum γ-tocopherol, were weakly associated with intake (R² < 0.25), highlighting limitations for certain biomarker classes [10]. This rigorous validation approach allowed researchers to distinguish between robust and marginal biomarkers, providing crucial guidance for their application in nutritional epidemiology. The successful biomarkers identified through this process were subsequently used to develop calibration equations for correcting measurement error in self-reported dietary data from observational studies.
Strategic Solutions for Bridging the Translational Gap
Advanced Model Systems and Multi-Omics Integration
The integration of human-relevant models with multi-omics technologies represents a powerful strategy for enhancing translational success. Unlike conventional preclinical models, advanced platforms like organoids, patient-derived xenografts (PDX), and 3D co-culture systems can better simulate the host-tumor ecosystem and forecast real-life responses, which is essential if biomarkers are to translate from preclinical to clinical settings [74]. Organoids particularly excel in retaining characteristic biomarker expression, making them valuable for predicting therapeutic responses and guiding personalized treatment selection.
Multi-omics approaches substantially enhance the value of these advanced models by providing comprehensive biological insights. Rather than focusing on single targets, multi-omic strategies make use of multiple technologies (including genomics, transcriptomics, and proteomics) to identify context-specific, clinically actionable biomarkers that may be missed with single approaches [74]. The depth of information obtained through these integrated methods enables identification of potential biomarkers for early detection, prognosis, and treatment response, ultimately contributing to more effective clinical decision-making. Recent studies demonstrate that multi-omic approaches have helped identify circulating diagnostic biomarkers in gastric cancer and discover prognostic biomarkers across multiple cancers [74].
Longitudinal and Functional Validation Strategies
Traditional biomarker analysis relying on single time-point measurements provides limited insights compared to longitudinal assessment strategies. Repeatedly measuring biomarkers over time offers a more dynamic view, revealing subtle changes that may indicate disease development or recurrence even before symptoms appear [74]. By capturing temporal biomarker dynamics through approaches like longitudinal plasma sampling, researchers can identify patterns and trends that offer a more complete and robust picture than static measurements.
Functional validation represents another critical enhancement to traditional biomarker assessment. While conventional approaches focus primarily on the presence or quantity of specific biomarkers, they often fail to confirm whether these biomarkers play direct, biologically relevant roles in disease processes or treatment responses [74]. Functional assays complement traditional approaches by revealing more about a biomarker's activity and function, shifting from correlative to functional evidence that strengthens the case for real-world utility. This approach is particularly valuable given that many functional tests are already displaying significant predictive capacities that surpass conventional biomarker measurements.
Figure 2: Enhanced Biomarker Validation Workflow
The Scientist's Toolkit: Essential Research Reagent Solutions
Critical Reagents for Robust Biomarker Development
Table 3: Essential Research Reagents for Biomarker Validation
| Reagent Category | Specific Examples | Function in Validation | Performance Requirements |
|---|---|---|---|
| Recombinant Antibodies | Anti-PD-L1; Anti-HER2; Anti-estrogen receptor | Core reagents for IHC, ELISA; Target specificity for protein biomarkers | High specificity; Batch-to-batch consistency; Renewable production |
| Multi-omics Platforms | Genomic sequencing; Transcriptomic arrays; Proteomic mass spectrometry | Identify context-specific biomarkers; Comprehensive profiling | Platform stability; Reproducibility; Quantitative accuracy |
| Cell Culture Systems | Organoid media; 3D matrix materials; Differentiation factors | Human-relevant model systems; Personalized therapeutic testing | Defined composition; Lot consistency; Physiological relevance |
| Immunoassays | ELISA kits; Multiplex bead arrays; Lateral flow devices | Biomarker quantification; High-throughput screening | Sensitivity; Dynamic range; Minimal cross-reactivity |
Recombinant antibodies have emerged as particularly transformative reagents in biomarker development workflows. Using recombinant platforms, scientists can identify, clone, and express specific antibody sequences to help ensure precise epitope targeting and minimize variability [75]. These antibodies are produced in a controlled and standardized manner, ensuring batch-to-batch consistency that reduces variability and improves reproducibility—a crucial consideration for translational success.
The application of rigorous antibody validation standards is equally essential to avoid misleading results and address reproducibility concerns in biomarker discovery and analysis [75]. Validation strategies should include genetic experiments for target specificity, quantitative affinity measurements, target recognition in biological samples, and independent recognition with multiple epitopes to assess cross-reactivity and specificity. Manufacturers that prioritize standardized antibody validation and performance transparency save researchers valuable time and resources during planning and execution.
Data Analytics and Decision Support Tools
Artificial intelligence and machine learning technologies are revolutionizing biomarker discovery by identifying patterns in large datasets that could not be found using traditional, manual means [74]. These computational approaches are increasingly integrated into biomarker workflows, with AI-driven genomic profiling already demonstrating improved responses to targeted therapies and immune checkpoint inhibitors, resulting in better response rates and survival outcomes for patients with various cancer types [74].
Maximizing the potential of these advanced analytical technologies requires access to large, high-quality datasets that include comprehensive data and characterization from multiple sources [74]. This can only be achieved through collaborative efforts among all stakeholders, giving research teams access to larger sample sizes and more diverse patient populations. Strategic partnerships between research teams and organizations with validated preclinical tools, standardized protocols, and expert insights play a crucial role in accelerating biomarker translation [74].
Bridging the translational gap between preclinical findings and clinical utility requires multifaceted strategies addressing model systems, validation methodologies, and analytical frameworks. The integration of human-relevant models like PDX and organoids with multi-omics technologies provides a more physiologically relevant foundation for biomarker development. Longitudinal and functional validation approaches offer enhanced rigor beyond traditional correlative studies. Most importantly, controlled feeding studies establish the methodological gold standard for biomarker validation, creating an essential bridge between laboratory discovery and clinical application.
The path forward demands increased collaboration across institutions, standardization of validation protocols, and commitment to sharing comprehensive datasets. By adopting these approaches, researchers can systematically address the historical failure points in translation, ultimately accelerating the development of robust biomarkers that improve patient care and treatment outcomes. As the field continues to evolve, the principles of rigorous validation against controlled standards will remain fundamental to transforming promising preclinical discoveries into clinically valuable tools.
The validation of robust biomarkers against the controlled conditions of feeding studies is a cornerstone of modern nutritional science and therapeutic development. This field is undergoing a rapid transformation, driven by technological advances that are future-proofing research methodologies—making them more resilient, predictive, and adaptable. Three approaches are at the forefront of this shift: Artificial Intelligence (AI) for predictive model building, Multi-Omics Integration for a holistic biological view, and Single-Cell Analysis for resolving cellular heterogeneity. This guide objectively compares the performance, protocols, and applications of these methodologies, providing a structured overview for researchers and drug development professionals focused on precise biomarker validation.
Methodological Comparison and Performance Data
The table below summarizes the core characteristics and performance metrics of the three future-proofing methods, based on current literature and meta-analyses.
Table 1: Performance Comparison of Future-Proofing Methodologies in Biomarker Research
| Methodology | Primary Function | Key Performance Metrics | Typical Data Output | Advantages | Limitations |
|---|---|---|---|---|---|
| AI & Machine Learning | Pattern recognition and predictive modeling from complex datasets. | Pooled Sensitivity: 85% (83%-87%)Pooled Specificity: 91% (90%-92%)AUC: 0.95 (0.92-0.96) for diagnostic tasks [76]. | Predictive scores, classification models, feature importance rankings. | High accuracy; automates data interpretation; identifies non-linear relationships. | "Black box" nature requires Explainable AI (XAI); high risk of bias without external validation [76] [77]. |
| Multi-Omics Approaches | Integrative analysis of biological layers (genome, proteome, metabolome, etc.). | Enhances diagnostic accuracy by providing comprehensive biomarker signatures rather than single-marker data [28]. | Integrated models of interacting biological pathways and networks. | Provides a holistic, systems biology view; reveals complex interactions between biological layers [78] [79]. | Computationally intensive; requires sophisticated bioinformatic tools for data integration and interpretation [79]. |
| Single-Cell Analysis | Resolution of cellular heterogeneity within tissues or populations. | Identifies rare cell populations (e.g., <0.1% abundance) that drive disease processes, masked in bulk analyses [78] [28]. | Cell-type-specific expression profiles, clusters of novel cell states, trajectory mappings. | Reveals hidden cellular diversity and rare cell types; defines cell-specific responses to interventions [78] [79]. | High cost; technical artifacts from low-input amplification; complex data analysis with batch effect challenges [78] [79]. |
Detailed Experimental Protocols
To ensure reproducibility and provide a clear framework for implementation, this section details the core experimental workflows for each methodology.
AI-Driven Biomarker Discovery Workflow
The validation of AI models, especially for digital biomarkers, requires a shift from traditional deterministic software testing to a probabilistic framework [77].
- Problem Formulation & Data Sourcing: Define the clinical or biological question (e.g., predicting response to a specific diet). Acquire high-dimensional datasets, which can include genomic, proteomic, clinical, or real-world data from wearables [28] [80].
- Data Preprocessing & Feature Engineering: Clean the data to handle missing values and normalize distributions. Identify and select the most relevant features (biomarkers) for model training.
- Model Training & Selection: Split data into training and validation sets. Train multiple AI algorithms (e.g., Random Forest, Support Vector Machines, Deep Neural Networks). A meta-analysis showed machine learning models achieved higher sensitivity (85%) and specificity (92%) compared to deep learning (77% and 85%, respectively) in certain diagnostic tasks, though this is context-dependent [76].
- Model Validation & Explainability (XAI): Perform external validation on a completely independent dataset; this significantly increases model specificity (94% with validation vs. 89% without) [76]. Implement Explainable AI (XAI) tools like SHAP (Shapley Additive exPlanations) or LIME (Local Interpretable Model-agnostic Explanations) to interpret model decisions and identify which biomarkers most influenced the output, which is crucial for regulatory approval and clinical adoption [77].
- Deployment & Continuous Monitoring: Deploy the validated model in a clinical or research setting. Continuously monitor for "model drift," where performance degrades over time due to changes in underlying data, requiring periodic retraining [77].
Single-Cell Multi-Omics Integration Workflow
This protocol outlines the steps for generating a multi-omic profile from individual cells, a method that is transforming our understanding of cellular responses in heterogeneous tissues [78] [79].
- Single-Cell Isolation and Barcoding: Create a single-cell suspension from tissue using enzymatic or mechanical dissociation. Isolate individual cells using microfluidic technologies (e.g., 10X Genomics), fluorescence-activated cell sorting (FACS), or microwell-based platforms. Each cell is labeled with a unique molecular barcode during this step to preserve cellular identity throughout the process [78].
- Library Preparation: For multi-omics, perform simultaneous library preparations from the same cell. For example, techniques like CITE-seq (Cellular Indexing of Transcriptomes and Epitopes by Sequencing) allow for concurrent measurement of transcriptome (RNA) and surface proteome (antibody-derived tags) from single cells [79]. Other methods can combine genome, epigenome (e.g., scATAC-seq), and transcriptome data.
- High-Throughput Sequencing: Sequence the generated libraries using next-generation sequencing (NGS) platforms.
- Bioinformatic Data Integration and Analysis:
- Quality Control & Preprocessing: Filter out low-quality cells, doublets, and cells with high mitochondrial content.
- Normalization and Dimensionality Reduction: Normalize the data and use techniques like Principal Component Analysis (PCA) to reduce dimensions.
- Clustering and Annotation: Cluster cells based on their integrated molecular profiles and annotate cell types using known marker genes and proteins.
- Advanced Analysis: Perform trajectory inference (pseudotime analysis) to model cellular differentiation pathways, or analyze cell-cell communication networks [79].
The following diagram illustrates the core workflow and data integration process for a single-cell multi-omics experiment.
Validation Against Controlled Feeding Studies
Integrating these methods with controlled feeding studies provides a powerful framework for validating nutritional biomarkers.
- Pre-Intervention Baseline Profiling: Before the dietary intervention, collect biospecimens (blood, tissue biopsies) from participants. Perform baseline multi-omics profiling (e.g., metabolomics, proteomics) and single-cell analysis if feasible.
- Controlled Intervention: Administer a tightly controlled diet to the cohort, ensuring precise monitoring of nutrient intake.
- Longitudinal Sampling and Analysis: Collect biospecimens at multiple time points during and after the intervention.
- Data Integration and Biomarker Discovery:
- Use AI/ML models to identify complex patterns and predictive signatures that correlate with specific nutrient exposures or physiological changes.
- Integrate multi-omics data from bulk or single-cell analyses to understand the mechanistic pathways through which the diet exerts its effects. For instance, single-cell RNA sequencing can reveal how a specific nutrient alters gene expression in a rare but critical immune cell population [78] [79].
- Validate discovered biomarkers by triangulating findings across different omics layers and against clinical health outcomes measured in the study.
The Scientist's Toolkit: Research Reagent Solutions
Successful implementation of these advanced methodologies relies on a suite of specialized reagents and platforms.
Table 2: Essential Research Reagents and Platforms for Future-Proofed Biomarker Research
| Item | Function | Application Examples |
|---|---|---|
| Microfluidic Single-Cell Kits | High-throughput isolation, barcoding, and library preparation for thousands of single cells. | 10X Genomics Chromium, Drop-seq [78]. |
| Cell Barcoding Oligonucleotides | Unique molecular identifiers (UMIs) and cell barcodes that tag molecules from each cell, enabling sample multiplexing and noise reduction. | CITE-seq antibodies, CellPlex kits, MULTI-seq barcodes [78] [79]. |
| Multi-Omic Assay Kits | Integrated reagent systems for simultaneous co-assay of different molecular layers from the same cell. | 10X Multiome ATAC + Gene Expression, TEA-seq, DOGMA-seq [79]. |
| AI/ML Software Frameworks | Open-source programming environments for building, training, and validating predictive models. | Python (Scanpy, Scikit-learn), R (Seurat, SingleCellExperiment) [79]. |
| Explainable AI (XAI) Tools | Software libraries to interpret AI model decisions and identify feature importance. | SHAP (SHapley Additive exPlanations), LIME (Local Interpretable Model-agnostic Explanations) [77]. |
Signaling Pathways in Biomarker Validation
A key application of multi-omics and single-cell data is elucidating how nutritional interventions influence core signaling pathways, which in turn serve as validated biomarker sources. The following diagram maps the interaction of four key biochemical biomarkers with central aging and inflammation pathways, highly relevant to longevity and interventional studies.
Validation, Qualification, and Regulatory Standards
In the rigorous world of pharmaceutical development and biomedical research, the terms "validation" and "qualification" are foundational to ensuring product quality and data integrity. While often used interchangeably, they represent distinct, critical processes. Qualification confirms that equipment or systems are installed correctly and operate as intended, whereas Validation provides documented evidence that a process—such as a manufacturing method or an analytical procedure—consistently produces results meeting pre-determined standards [81] [82] [83].
This distinction is paramount in advanced research fields, such as developing biomarkers against controlled feeding studies. Here, qualification might verify that a mass spectrometer is functioning to specification, while validation would prove that the entire biomarker assay consistently and accurately measures nutritional intake in a diverse population.
Core Concepts: Qualification and Validation Defined
The following table summarizes the fundamental differences between these two key concepts.
| Aspect | Qualification | Validation |
|---|---|---|
| Primary Focus | Equipment, instruments, utilities, facilities, and computerized systems [81] [82] | Processes (e.g., manufacturing, cleaning, analytical methods) [81] [84] [82] |
| Fundamental Question | "Is this tool installed correctly and does it work as designed?" [81] | "Does this entire procedure consistently produce a result that meets its quality attributes?" [81] [84] |
| Objective | To provide documented evidence that a system is fit and ready for its intended use [85] [83] | To provide a high degree of assurance that a specific process will consistently meet its predetermined specifications [84] [85] |
| Key Documentation | Installation/Operational/Performance Qualification (IQ/OQ/PQ) protocols [81] [82] | Validation Master Plan (VMP), Process Validation protocols (Stages 1-3) [81] [84] |
| Relationship | A prerequisite that must be completed before process validation can begin [81] [82] | Builds upon successful qualification to prove consistent performance of the entire process [81] [83] |
The Qualification Foundation: IQ, OQ, PQ
Qualification is a structured, sequential process that verifies every aspect of a system's functionality. It is typically broken down into three primary stages [81] [82]:
Installation Qualification (IQ): This is the documented verification that a piece of equipment or a system has been delivered, installed, and configured according to its approved design specifications and manufacturer's recommendations. It confirms that the correct components are present and properly installed [81] [85].
Operational Qualification (OQ): Following a successful IQ, OQ is the documented testing to confirm that the equipment or system will perform as intended throughout its specified operating ranges, including worst-case conditions. This stage challenges alarms, interlocks, and software functions to ensure operational robustness [81] [82].
Performance Qualification (PQ): This is the final stage, providing documented evidence that the equipment or system can consistently perform its intended functions under real-world production conditions, using actual or simulated materials. Successful PQ demonstrates that the system is ready for use in the validated process [81] [85].
The logical progression and key objectives of this qualification lifecycle can be visualized as follows:
The Validation Lifecycle: A Stage-Gate Process
Validation is not a single event but a lifecycle approach applied to processes and methods. For process validation, regulatory guidance like the FDA's outlines a three-stage model [81] [84]:
Stage 1: Process Design: In this initial stage, the process is developed and defined based on knowledge gained through research and development. The critical process parameters (CPPs) and their impact on critical quality attributes (CQAs) are established, forming the foundation for the control strategy [84].
Stage 2: Process Performance Qualification (PPQ): This stage combines the qualified facilities, utilities, and equipment with the designed process to demonstrate commercial manufacturing consistency. It involves executing the process at a commercial scale according to a predefined protocol to prove it is capable of reproducible, reliable operation [81] [84].
Stage 3: Continued Process Verification (CPV): After successful PPQ, ongoing monitoring and control are instituted to ensure the process remains in a state of control during routine production. This involves collecting and analyzing data from every batch to provide continuous assurance of the validated state [81] [84].
Application in Biomarker Research: A Case Study
The principles of qualification and validation directly translate to the development of biomarkers for nutritional research. A study by the National Institutes of Health (NIH) on developing a biomarker score for predicting diets high in ultra-processed foods serves as an excellent case study [86].
Experimental Protocol
The research employed a multi-faceted approach to ensure the biomarker score was both accurate and reliable:
Observational Study: Researchers used data from 718 older adults who provided biospecimens (blood and urine) and detailed dietary information over a 12-month period. This long-term observational data helped identify natural variations in metabolites correlated with self-reported intake of ultra-processed foods [86].
Randomized Controlled Crossover Feeding Trial: To establish causal links, a controlled experiment was conducted with 20 adults at the NIH Clinical Center. Participants consumed two distinct diets in random order, each for two weeks:
- Diet A: A diet high in ultra-processed foods (80% of energy intake).
- Diet B: A diet containing no ultra-processed foods (0% of energy intake) [86]. This rigorous design allowed researchers to isolate the metabolic changes directly attributable to the consumption of ultra-processed foods, independent of other lifestyle factors.
Metabolomic Analysis and Machine Learning: Using biospecimens from both study arms, researchers identified hundreds of metabolites whose levels correlated with the percentage of energy from ultra-processed foods. Machine learning techniques were then applied to these data to discern complex metabolic patterns and calculate a poly-metabolite score for both blood and urine [86].
Validation of the Score: The poly-metabolite scores were tested and validated by demonstrating their ability to accurately differentiate, within the same trial subject, between the phase consuming the highly processed diet and the phase consuming the unprocessed diet [86].
This workflow, from initial study design to the final validated biomarker score, is illustrated below:
The Scientist's Toolkit: Key Reagents and Materials
The following table details essential research reagent solutions and their functions in the context of such a biomarker validation study.
| Item / Solution | Function in Experiment |
|---|---|
| Biospecimen Collection Kits | Standardized tools for consistent collection, preservation, and initial processing of blood and urine samples from study participants. |
| Metabolomics Standards | Certified reference materials and internal standards used to calibrate analytical instruments (e.g., Mass Spectrometers) and ensure accurate quantification of metabolites. |
| Controlled Diets | Precisely formulated diets (e.g., 80% vs. 0% ultra-processed food) that serve as the controlled experimental variable to establish a causal metabolic response. |
| Analytical Instrumentation (e.g., LC-MS/MS) | Highly sensitive equipment used to identify and measure the concentration of hundreds to thousands of metabolites in the collected biospecimens. |
| Data Analysis & Machine Learning Platforms | Software solutions for processing complex metabolomic data, identifying patterns, and building predictive models (poly-metabolite scores). |
The roadmap from qualification to validation is a journey from proving technical functionality to demonstrating consistent, reliable performance. In the context of biomarker research against controlled feeding studies, this means moving beyond simply having a qualified mass spectrometer to having a fully validated metabolic biomarker score. This score must be proven to accurately reflect dietary intake consistently across different populations and over time.
Adhering to this rigorous evidentiary roadmap is what separates preliminary research findings from robust, clinically applicable tools. It builds the foundation of trust necessary for biomarkers to inform drug development, shape public health policies, and ultimately, improve patient outcomes.
In the field of precision nutrition, the discovery of dietary biomarkers represents merely the initial phase of a comprehensive research pipeline. The true value of these biomarkers is unlocked only through rigorous validation, a process that demonstrates their accuracy, reliability, and fitness for specific applications. Within the context of controlled feeding studies—where researchers administer precise amounts of test foods to participants under controlled conditions—validation becomes the critical bridge between preliminary discovery and clinically meaningful application. The Dietary Biomarkers Development Consortium (DBDC) exemplifies this systematic approach, implementing a structured framework to identify, evaluate, and validate biomarkers for commonly consumed foods [7]. This article examines the three cornerstone validation criteria—sensitivity, specificity, and reproducibility—within this research paradigm, providing methodological guidance and comparative analysis of validation approaches for researchers and drug development professionals.
Defining the Key Validation Criteria
The validation of dietary biomarkers relies on a triad of fundamental performance parameters that collectively determine their utility in both research and clinical settings. These criteria establish the minimum standards for biomarker acceptance and provide the quantitative foundation for assessing analytical performance.
Sensitivity: Also referred to as analytical sensitivity, this parameter encompasses two complementary concepts: the limit of detection (LOD), which represents the lowest concentration of an analyte that can be reliably distinguished from background noise, and the limit of quantification (LOQ), the lowest concentration that can be measured with acceptable precision and accuracy [87]. In practical terms, sensitivity determines a biomarker's ability to detect true positive results, particularly at physiologically relevant concentrations following controlled dietary interventions.
Specificity: This criterion evaluates a biomarker's ability to exclusively measure the intended analyte without interference from structurally similar compounds, matrix effects, or unrelated metabolic byproducts [87]. For dietary biomarkers, this is particularly challenging given the complex composition of foods and individual variations in metabolism. High specificity ensures that the measured signal genuinely reflects consumption of the target food or nutrient rather than confounding factors.
Reproducibility: Encompassing both repeatability (within-lab precision under identical conditions over a short timeframe) and reproducibility (between-lab precision under varying conditions), this parameter measures the precision and reliability of biomarker measurements across different instruments, operators, and testing environments [87]. Reproducibility establishes the confidence limits for biomarker applications across multiple research sites and over extended longitudinal studies.
Experimental Protocols for Validation
The validation of dietary biomarkers requires carefully controlled experimental designs that systematically evaluate each criterion against established standards. The following methodologies represent best practices derived from current biomarker research frameworks.
Protocol for Sensitivity Assessment
- Sample Preparation: Prepare a dilution series of the purified biomarker standard in the appropriate biological matrix (e.g., plasma, urine) across a concentration range expected in human samples post-consumption. Include blank matrix samples for background correction [87].
- Experimental Analysis: Analyze each sample across multiple replicates (typically n≥5) using the designated analytical platform (e.g., LC-MS, GC-MS). Repeat analyses across different days to account for inter-day variability.
- Data Analysis and Interpretation: Calculate the LOD typically as 3.3 × σ/S, where σ is the standard deviation of the response and S is the slope of the calibration curve. Determine the LOQ as 10 × σ/S. For dietary biomarkers, the LOQ should fall below the anticipated concentration in samples from controlled feeding studies with known dietary intakes [87].
Protocol for Specificity Assessment
- Sample Preparation: Spike the biomarker of interest into relevant biological matrices at physiologically relevant concentrations. Additionally, prepare samples containing structurally similar compounds or known metabolites that could potentially interfere with detection and quantification [87].
- Chromatographic and Mass Spectrometric Analysis: Employ chromatographic methods that achieve baseline separation of the target biomarker from potential interferents. Use high-resolution mass spectrometry to confirm the identity of the biomarker through accurate mass measurement and fragmentation pattern matching [7].
- Data Analysis and Interpretation: Assess chromatographic peak purity and the absence of co-eluting compounds. Verify that the measured biomarker concentration remains unchanged in the presence of potential interferents. A specificity of ≥90% is generally considered acceptable for dietary biomarker applications [87].
Protocol for Reproducibility Assessment
- Sample Preparation: Prepare quality control (QC) samples at low, medium, and high concentrations of the biomarker within the quantitative range. Aliquot and store these samples appropriately to ensure stability throughout the testing period [87].
- Multi-Site Experimental Design: Distribute identical QC samples and standardized protocols to multiple participating laboratories. Ensure each site analyzes the samples over multiple independent runs (typically n≥5) by different analysts using different instrument configurations [7].
- Data Analysis and Interpretation: Calculate the intra- and inter-laboratory coefficients of variation (CV). For dietary biomarkers, a CV of ≤15% is generally acceptable, with ≤20% at the LOD. Statistical analysis using ANOVA can help partition variance components between and within laboratories [87].
The experimental workflow for biomarker validation progresses through these critical phases, each addressing specific validation criteria:
Comparative Analysis of Biomarker Validation Approaches
The validation of dietary biomarkers employs different methodological approaches, each with distinct advantages and limitations. The following table summarizes these key methodological considerations:
Table 1: Comparison of Biomarker Validation Methodological Approaches
| Validation Aspect | Targeted Analysis | Untargeted Metabolomics | Multi-Omics Integration |
|---|---|---|---|
| Sensitivity | High sensitivity for known compounds through optimized detection methods | Moderate sensitivity, limited by detection of low-abundance metabolites | Variable, depends on integrated platforms and data normalization |
| Specificity | Excellent specificity through compound-specific parameters and separation | Lower specificity, requires confirmation of compound identity | Enhanced specificity through orthogonal verification across platforms |
| Reproducibility | High reproducibility with standardized protocols and stable isotope standards | Moderate reproducibility, affected by platform drift and batch effects | Challenging, requires standardization across multiple analytical domains |
| Throughput | Moderate to high throughput for focused analyte panels | High throughput for comprehensive metabolite profiling | Low to moderate throughput due to data integration complexity |
| Best Applications | Validation of candidate biomarkers in controlled feeding studies [7] | Discovery of novel biomarker candidates in exploratory phases | Understanding biochemical pathways and mechanism of action |
The DBDC's validation framework implements a phased approach that systematically progresses from discovery to confirmation, addressing each validation criterion at appropriate stages. In Phase 1, controlled feeding trials administer test foods in prespecified amounts to healthy participants, followed by metabolomic profiling to identify candidate compounds and characterize their pharmacokinetic parameters [7]. This initial phase emphasizes sensitivity and specificity in detecting intake-responsive compounds. Phase 2 evaluates the ability of candidate biomarkers to identify individuals consuming biomarker-associated foods using controlled feeding studies of various dietary patterns, thus testing specificity across different dietary backgrounds [7]. Phase 3 assesses the validity of candidate biomarkers to predict recent and habitual consumption in independent observational settings, essentially a real-world test of reproducibility and generalizability [7].
The Scientist's Toolkit: Essential Research Reagents and Materials
The successful validation of dietary biomarkers relies on a carefully selected suite of laboratory reagents and materials that ensure analytical rigor and reproducibility. The following table catalogues these essential components:
Table 2: Essential Research Reagents and Materials for Biomarker Validation
| Reagent/Material | Function in Validation | Key Considerations |
|---|---|---|
| Stable Isotope-Labeled Standards | Internal standards for quantification; tracking analyte recovery | Essential for controlling matrix effects and calculating precise concentrations [87] |
| Certified Reference Materials | Calibration and method verification | Provides traceability to reference measurements and ensures accuracy [87] |
| Quality Control Materials | Monitoring assay performance over time | Should mirror study samples in matrix composition; used at multiple concentrations [87] |
| Chromatography Columns | Separation of biomarkers from matrix components | Column chemistry should be optimized for compound class; multiple columns may be needed |
| Mass Spectrometry Solvents | Mobile phase for LC-MS; sample preparation | High-purity, LC-MS grade solvents minimize background interference and ion suppression |
| Sample Preparation Kits | Extraction, purification, and concentration of biomarkers | Standardized protocols enhance reproducibility across laboratories [87] |
| Biological Matrix Lots | Validation of matrix effects | Multiple lots of plasma, urine, etc., assess variability in different sample backgrounds |
Data Presentation and Visualization in Validation Studies
Effective presentation of quantitative data from validation studies requires careful consideration of graphical representation principles. Histograms provide an optimal format for displaying frequency distributions of quantitative validation data, such as reproducibility measurements across multiple laboratories [88] [89]. Unlike bar charts with arbitrary spacing, histograms treat the horizontal axis as a true number line, making them particularly suitable for representing continuous data such as biomarker concentrations, CV values, or sensitivity measurements [88].
For comparative analyses—such as method comparison studies or inter-laboratory results—frequency polygons offer distinct advantages by allowing multiple distributions to be overlaid on the same axes, facilitating direct visual comparison [88]. When designing data visualizations for validation studies, researchers should implement class intervals of equal size throughout the distribution and maintain between 5-20 intervals to optimize clarity without sacrificing detail [88].
The analytical process for biomarker validation involves multiple steps from sample preparation to data interpretation, with careful attention to quality control at each stage:
The validation of dietary biomarkers against controlled feeding studies demands a systematic, multi-stage approach that rigorously assesses sensitivity, specificity, and reproducibility. These criteria are not independent measures but interconnected components of a comprehensive validation framework. The phased strategy employed by the DBDC—progressing from initial discovery in controlled settings to real-world observational validation—provides a robust model for establishing biomarker reliability [7]. As precision nutrition advances, the integration of these validated biomarkers into nutritional epidemiology and clinical practice will enable more objective assessment of dietary exposures, ultimately strengthening our understanding of diet-health relationships. Future directions will likely focus on standardized reporting of validation parameters, creating publicly accessible databases of validation studies, and establishing consensus guidelines for biomarker qualification across different applications.
In the development of new anticancer drugs and other therapeutics, successful clinical introduction is often hampered by a lack of qualified biomarkers [90]. Fit-for-purpose validation has emerged as a strategic framework that aligns biomarker method validation with the specific intended use of the data generated, ensuring appropriate resource allocation and technical rigor [91] [92]. This approach recognizes that the validation requirements for an exploratory pharmacodynamic biomarker in early research differ substantially from those for a diagnostic biomarker intended for patient selection in late-phase trials [91]. The fundamental principle is that assays should be validated as appropriate for the intended use of the data and associated regulatory requirements, with the understanding that additional validation may be conducted iteratively if the intended use changes [92].
The position of a biomarker on the spectrum between research tool and clinical endpoint dictates the stringency of experimental proof required to achieve method validation [91]. This paradigm has been widely adopted by the pharmaceutical community and regulatory agencies, appearing in the 2018 FDA Guidance for Industry as a recognized standard for biomarker method validation [92]. For researchers conducting controlled feeding studies, implementing fit-for-purpose validation principles ensures that biomarker measurements accurately reflect nutritional interventions rather than analytical variability or pre-analytical artifacts.
Biomarker Categories and Their Validation Requirements
Classification of Biomarker Assays
The American Association of Pharmaceutical Scientists (AAPS) and US Clinical Ligand Society have identified five general classes of biomarker assays, each with distinct validation requirements [91]. Understanding these categories is essential for selecting appropriate validation approaches.
Definitive quantitative assays utilize fully characterized reference standards representative of the biomarker and employ calibration curves to calculate absolute quantitative values for unknowns [91]. Relative quantitative assays also use response-concentration calibration but with reference standards that are not fully representative of the biomarker [91]. Quasi-quantitative assays do not employ calibration standards but produce continuous responses expressed in terms of sample characteristics [91]. Qualitative categorical assays include ordinal types relying on discrete scoring scales (e.g., immunohistochemistry) and nominal types pertaining to yes/no situations such as presence or absence of a gene product [91].
Validation Parameters by Assay Category
The validation parameters requiring investigation vary significantly across these assay categories. The following table summarizes the core validation elements for each assay type based on established scientific consensus.
Table 1: Essential Validation Parameters by Biomarker Assay Category
| Validation Parameter | Definitive Quantitative | Relative Quantitative | Quasi-Quantitative | Qualitative Categorical |
|---|---|---|---|---|
| Accuracy | Required | Recommended | Not applicable | Not applicable |
| Precision | Required | Required | Required | Required |
| Sensitivity | Required | Recommended | Recommended | Recommended |
| Specificity | Required | Required | Required | Required |
| Reference Standard | Fully characterized | Partially characterized | Not applicable | Not applicable |
| Calibration Curve | Required | Required | Not applicable | Not applicable |
| Stability | Required | Required | Recommended | Recommended |
| Range | Required | Required | Not applicable | Not applicable |
For definitive quantitative methods, the objective is to determine unknown biomarker concentrations in patient samples as accurately as possible, with analytical accuracy dependent on the total error encompassing both systematic and random error components [91]. In contrast, relative quantitative methods such as ligand-binding assays for endogenous protein biomarkers face additional challenges due to the difficulty of obtaining analyte-free matrices and fully characterized calibration standards [91].
Experimental Design and Methodologies
Fit-for-Purpose Validation Framework
The fit-for-purpose validation process proceeds through discrete stages, beginning with definition of purpose and candidate assay selection [91]. This initial stage is arguably the most critical, as it establishes the foundation for all subsequent validation activities. During stage 2, researchers assemble appropriate reagents and components, write the method validation plan, and finalize assay classification [91]. Stage 3 constitutes the experimental phase of performance verification, leading to evaluation of fitness-for-purpose and development of standard operating procedures [91].
The subsequent stages address in-study validation (stage 4), which allows assessment of fitness-for-purpose in the clinical context and identification of patient sampling issues, and routine use (stage 5), where quality control monitoring, proficiency testing, and batch-to-batch quality control issues are comprehensively explored [91]. This framework drives continual improvement through iterative cycles that may necessitate returning to earlier stages as new information emerges or requirements evolve.
Experimental Protocols for Key Biomarker Platforms
Ligand Binding Assay Protocol: For protein biomarkers such as soluble CD73 (sCD73), hybrid immunocapture-liquid chromatography-tandem-mass spectrometry (IC-LC-MS/MS) platforms provide robust quantification methods [93]. The protocol typically involves: (1) Sample preparation using a non-competing antibody to isolate and enrich the target protein from biological matrix; (2) Enzymatic digestion of the enriched sample after immunocapture; (3) Quantification through monitoring of a surrogate peptide via LC-MS/MS [93]. This approach has demonstrated good accuracy, precision, specificity, and sensitivity with LLOQ of 1.00 ng/mL for sCD73, successfully applied in clinical studies to measure total sCD73 as a potential pharmacodynamic marker [93].
Mass Spectrometry-Based Proteomics: For protein biomarker discovery and validation, both bottom-up and top-down proteomic approaches are employed [94] [27]. Bottom-up proteomics, the basis for most protein research in mass spectrometry laboratories, involves proteolytic digestion of proteins (typically with trypsin), separation of resulting peptides using multidimensional liquid chromatography, and analysis via electrospray ionization mass spectrometry [94]. Top-down proteomics analyzes intact proteins without prior digestion, preserving information about degradation products, sequence variants, and combinations of post-translational modifications [94].
Genomic Biomarker Validation: Next-generation sequencing (NGS) technologies enable comprehensive genetic biomarker discovery and validation. A typical protocol involves: (1) DNA/RNA extraction from appropriate specimens; (2) Library preparation and sequencing; (3) Bioinformatic analysis for variant calling; (4) Statistical validation using appropriate cohorts [27]. For example, in colorectal cancer, NGS analysis of 526 patients identified that wild-type profiles across 22 cancer-related genes correlated with longer progression-free survival with cetuximab treatment [27].
Comparative Performance Data
Validation Metrics Across Technologies
The performance of biomarker assays varies significantly across technological platforms and intended applications. The following table summarizes key validation metrics for different biomarker methods based on published studies and validation reports.
Table 2: Performance Comparison of Biomarker Assay Platforms
| Platform/Assay | Precision (% CV) | Sensitivity | Dynamic Range | Sample Throughput | Key Applications |
|---|---|---|---|---|---|
| ELISA | 4.5-17.6% [90] | ng-pg/mL | 3-4 logs | Medium | Protein quantification, clinical trials |
| Multiplex ELISA | 5.0-16.5% [90] | ng-pg/mL | 2-3 logs | High | Multi-analyte profiling, biomarker panels |
| LC-MS/MS | 10-15% [93] | pg-fg/mL | 3-5 logs | Low-medium | Targeted quantification, structural confirmation |
| Next-Generation Sequencing | NA | Single molecule | 5-6 logs | Low | Genomic alterations, expression profiling |
| Flow Cytometry | 5-20% [92] | 100-1000 cells | 3-4 logs | Medium | Cellular biomarkers, immunophenotyping |
For ELISA platforms, precision performance varies by specific analyte, with coefficients of variation (CV) ranging from 2.25% for Angiopoietin-1 to 17.6% for Keratinocyte Growth Factor (KGF) in quality control samples [90]. During fit-for-purpose validation of 17 different ELISAs representing potential biomarkers of antivascular drugs, 15 of 17 assays demonstrated precision within acceptable limits, while KGF and VEGF-C failed to meet pre-established criteria [90].
Impact of Sample Handling on Biomarker Measurements
Pre-analytical variables significantly impact biomarker measurement accuracy and reproducibility. Studies of angiogenesis biomarkers highlight that for measurement of extracellular circulating analytes, platelet depletion should be conducted before freezing of plasma to prevent release of PDGF-BB, FGFb, and VEGF-A from platelets during sample processing [90]. Researchers developed a protocol to remove >90% of platelets from plasma requiring centrifugation at 2000 g for 25 minutes [90].
Stability studies performed using recombinant proteins in surrogate matrices and endogenous analytes in healthy volunteer and cancer patient plasma revealed that stability at -80°C was maintained for 3 months with all recombinant proteins in surrogate matrices, whereas instability was observed with KGF in platelet-rich and platelet-depleted plasma, and with PDGF-BB in platelet-depleted plasma from cancer patients under the same conditions [90]. These findings underscore the importance of matrix-specific stability assessments in fit-for-purpose validation.
Research Reagent Solutions
The following table outlines essential research reagents and materials commonly employed in fit-for-purpose biomarker validation studies, along with their specific functions in the experimental workflow.
Table 3: Essential Research Reagents for Biomarker Validation
| Reagent/Material | Function | Application Examples |
|---|---|---|
| Quantikine ELISA Kits | Protein biomarker quantification | Validation of angiogenesis biomarkers (VEGF-A, PlGF, VEGFR-1/2) [90] |
| SearchLight Multiplex ELISA | Simultaneous measurement of multiple analytes | Validation of biomarker panels (VEGFR1, VEGFR2, IL8, KGF, PIGF) [90] |
| Immunocapture Antibodies | Target enrichment and purification | Isolation of soluble CD73 for LC-MS/MS analysis [93] |
| Surrogate Peptide Standards | Quantitative reference for LC-MS/MS | Absolute quantification of protein biomarkers [93] |
| Quality Control Materials | Assay performance monitoring | Recombinant proteins and endogenous QCs for precision assessment [90] [92] |
| Stabilization Cocktails | Sample integrity preservation | Prevention of analyte degradation during processing/storage [90] |
| Platelet Depletion Reagents | Sample preprocessing | Removal of platelets to prevent analyte release [90] |
The selection of appropriate reagent solutions is critical for successful biomarker validation. Notably, the use of endogenous quality controls instead of recombinant material for stability determination and assay performance monitoring is recommended, as recombinant protein calibrators may behave differently from endogenous biomarkers [92]. Understanding the limitations of validated assays is crucial when deploying assays and interpreting data in controlled feeding studies and clinical trials.
Visualization of Validation Workflows
Fit-for-Purpose Validation Process
Biomarker Assay Categorization Framework
Fit-for-purpose biomarker validation represents a pragmatic framework that aligns analytical rigor with intended application, ensuring efficient resource utilization while generating data of sufficient quality for specific decision-making contexts [91] [92]. The approach emphasizes that biomarker method validation constitutes an indispensable component of successful biomarker qualification and acknowledges that biomarkers often fail in clinical applications not because of flawed scientific rationale but due to poor assay choice and inadequate validation [90] [91]. For researchers designing controlled feeding studies, implementing these principles ensures that biomarker measurements accurately reflect biological responses rather than analytical artifacts.
The dynamic nature of fit-for-purpose validation supports iterative development, allowing assay validation to evolve alongside changing research needs and regulatory requirements [92]. As biomarker applications continue to expand across therapeutic areas including oncology, neurodegenerative disorders, endocrinology, and nutrition research, robust fit-for-purpose validation strategies will remain essential for translating promising biomarker candidates into clinically useful tools [94] [27].
The successful regulatory acceptance of a biomarker is a pivotal achievement in modern drug development and nutritional science. It signifies that a regulatory body endorses the use of that biomarker for a specific context within drug development or therapeutic decision-making. The European Medicines Agency (EMA) defines a biomarker as "a defined characteristic that is measured as an indicator of normal biological processes, pathogenic processes, or responses to an exposure or intervention" [95]. Similarly, the U.S. Food and Drug Administration (FDA) emphasizes their role in advancing public health by encouraging efficiencies and innovation in drug development [96]. For biomarkers intended to reflect dietary intake—a critical exposure in chronic disease etiology—the path to regulatory acceptance is particularly rigorous. It necessitates robust validation against gold-standard methods, with controlled feeding studies serving as the foundational pillar for establishing a causal link between intake and biomarker measurement [22] [10]. This guide objectively compares the regulatory pathways of the FDA and EMA, framing the discussion within the essential context of validation against controlled feeding research.
Comparative Analysis of FDA and EMA Biomarker Guidelines
While the FDA and EMA share the common goal of ensuring that biomarkers are reliable tools for decision-making, their procedural frameworks and focal points exhibit distinct characteristics. The following table provides a structured, high-level comparison of the two agencies' approaches.
Table 1: Key Characteristics of FDA and EMA Biomarker Qualification Programs
| Aspect | FDA (U.S. Food and Drug Administration) | EMA (European Medicines Agency) |
|---|---|---|
| Core Program | Biomarker Qualification Program (BQP) [96] | Qualification of Novel Methodologies (QoNM) [95] |
| Primary Goal | Qualify biomarkers as drug development tools for specific Contexts of Use (CoU) [96] | Qualify innovative methodologies for a specific intended use in pharmaceutical R&D [95] |
| Defining Guidance | 2025 Bioanalytical Method Validation (BMV) for Biomarkers [97] [98] | Based on ICH definitions and best practices; detailed in various scientific publications [99] [95] |
| Key Guidance Principles | Method validation should address accuracy, precision, sensitivity, etc. ICH M10 is a starting point, but differences for endogenous biomarkers are acknowledged [97] [98]. | Evidence generation is tailored to the proposed CoU. A thorough validation strategy is critical, covering biomarker properties and assay performance [99] [95]. |
| Typical Applicant | Increasingly consortia and public-private partnerships | Primarily consortia (shift from single companies) [95] |
| Common Challenges | Applying bioanalytical methods validated for xenobiotics to endogenous biomarkers; lack of explicit CoU in guidance [98] | Issues frequently raised on biomarker properties and assay validation (in >75% of procedures) [95] |
| Success Rate & Output | Not specified in search results | 13 qualified biomarkers from 86 procedures (2008-2020) [95] |
A critical insight from recent analyses is that consortia-led applications are becoming the norm, especially within the EMA framework, as they help pool resources and data to build the substantial evidence required for qualification [95] [100]. Furthermore, the regulatory landscape is dynamic. The FDA's recent 2025 BMV guidance has sparked discussion within the scientific community for directing applicants to ICH M10—a guidance for drug bioanalysis that explicitly excludes biomarkers—as a starting point [97] [98]. This highlights a persistent tension in the field: the need to adapt frameworks designed for xenobiotic drugs to the unique challenges of measuring endogenous biomarkers.
The Critical Role of Context of Use (CoU)
Both agencies' qualification processes are fundamentally driven by the Context of Use (CoU), which is a precise description of how the biomarker is to be used in drug development and the decisions it will inform [99]. The CoU dictates the necessary level of evidence. For instance, a biomarker intended for early research to understand disease mechanisms will face less stringent evidence requirements than one used to select patients for a multi-million dollar Phase III clinical trial or to support a drug label claim. The European Bioanalysis Forum (EBF) has strongly emphasized that biomarker validation must be CoU-driven rather than following a standard operating procedure designed for pharmacokinetic assays [97] [98].
Experimental Validation Against Controlled Feeding Studies
For dietary biomarkers, the most conclusive evidence for a causal relationship between intake and biomarker levels comes from controlled feeding studies. These studies, where participants consume diets prepared by a research kitchen, provide known and verifiable intakes of nutrients, thereby serving as a gold standard for biomarker validation [22] [10].
Key Experimental Protocol: The Women's Health Initiative (WHI) Model
A seminal example of this approach is the controlled feeding study conducted within the Women's Health Initiative (WHI) cohort, which offers a robust methodological blueprint [10].
Objective: To evaluate the performance of serum nutrients as potential biomarkers by providing a controlled diet that mimicked each participant's habitual intake and measuring the correlation between consumed nutrients and biomarker concentrations.
Participant Recruitment: The study enrolled 153 postmenopausal women from the WHI extension study who were ≤80 years of age and free of conditions like diabetes or kidney disease that could confound results [10].
Diet Formulation & Feeding Protocol:
- Habitual Diet Assessment: Each participant completed a 4-day food record (4DFR) and attended an in-depth interview with a study dietitian to assess usual food choices, brands, and meal patterns.
- Menu Planning: Individualized 2-week menu plans were created to approximate each woman's habitual diet. Food records were analyzed using the Nutrition Data System for Research (NDS-R) software.
- Energy Intake Calibration: To mitigate the common issue of under-reporting, energy prescriptions were adjusted based on the 4DFR, standard energy equations, and previously developed WHI calibration equations. On average, an additional 335 ± 220 kcal/day were added for 73% of the participants [10].
- Meal Preparation: All meals were prepared in the dedicated Human Nutrition Laboratory using sourced foods with complete nutrient database information. The ProNutra software system was used for menu and recipe management.
Biomarker Measurement:
- Blood and urine samples were collected at the beginning and end of the 2-week feeding period.
- Serum was analyzed for carotenoids, tocopherols, folate, vitamin B-12, and phospholipid fatty acids.
- Objective measures of energy and protein intake were obtained using the doubly labeled water method and 24-hour urinary nitrogen, respectively, which served as benchmark recovery biomarkers [10].
Data Analysis: Linear regression of ln-transformed consumed nutrients on ln-transformed potential biomarkers was performed. The coefficient of determination (R²) was used to quantify the proportion of variation in intake explained by the biomarker. The study established that serum biomarkers for several vitamins and carotenoids (e.g., folate R²=0.49, vitamin B-12 R²=0.51, α-carotene R²=0.53) performed similarly to established energy and protein recovery biomarkers, deeming them suitable for use in this population [10].
The workflow below visualizes the logical progression of a biomarker validation study against a controlled feeding regime.
Biomarker Validation Workflow
Quantitative Performance of Dietary Biomarkers
The following table summarizes the performance metrics (R² values) for selected biomarkers from the WHI feeding study, demonstrating how controlled studies generate the quantitative evidence required for regulatory submissions.
Table 2: Performance of Candidate Biomarkers from the WHI Controlled Feeding Study [10]
| Biomarker | Matrix | Regression R² Value | Performance Interpretation |
|---|---|---|---|
| α-Carotene | Serum | 0.53 | Good representation of intake variation |
| Folate | Serum | 0.49 | Good representation of intake variation |
| Vitamin B-12 | Serum | 0.51 | Good representation of intake variation |
| Lutein + Zeaxanthin | Serum | 0.46 | Moderate representation of intake variation |
| β-Carotene | Serum | 0.39 | Moderate representation of intake variation |
| α-Tocopherol | Serum | 0.47 | Good representation of intake variation |
| Lycopene | Serum | 0.32 | Moderate representation of intake variation |
| Energy Intake | Urine (Doubly Labeled Water) | 0.53 | Benchmark recovery biomarker |
| Protein Intake | Urine (Urinary Nitrogen) | 0.43 | Benchmark recovery biomarker |
| Polyunsaturated Fatty Acids | Serum (PLFA) | 0.27 | Weaker association with intake |
The Scientist's Toolkit: Essential Reagents and Materials
Successfully executing a controlled feeding study for biomarker validation requires a suite of specialized tools and reagents. The table below details key solutions used in the featured WHI study and contemporary metabolomic studies.
Table 3: Research Reagent Solutions for Biomarker Validation Studies
| Item / Solution | Function in Experiment | Example from Research |
|---|---|---|
| Doubly Labeled Water (DLW) | Gold-standard, objective measure of total energy expenditure to validate energy intake [10]. | Used as a benchmark to validate self-reported energy intake and calibrate dietary prescriptions [10]. |
| Nutrition Data System for Research (NDS-R) | Software for the comprehensive analysis of nutrient intake from food records and for designing controlled menus [10]. | Used to analyze 4-day food records and plan individualized diets with precise nutrient composition [10]. |
| ProNutra Software | A specialized system for creating controlled menus, generating recipes, production sheets, and tracking planned vs. consumed intake [10]. | Utilized to manage the entire food preparation process in the research kitchen, ensuring dietary adherence [10]. |
| Ultra-High-Performance Liquid Chromatography-Tandem Mass Spectrometry (UHPLC-MS/MS) | Platform for untargeted metabolomic profiling to discover and quantify a wide range of candidate biomarker compounds in biofluids [101]. | Used in modern trials to identify panels of discriminatory metabolites that reflect adherence to specific dietary patterns [101]. |
| Stable Isotope-Labeled Internal Standards | Added to biological samples during mass spectrometry analysis to correct for matrix effects and ensure accurate quantification of metabolites. | Essential for the precise measurement of endogenous biomarkers in complex biological matrices like plasma and urine [98]. |
| 24-Hour Urinary Nitrogen | Objective, recovery biomarker for protein intake, as virtually all ingested nitrogen is excreted in urine [10]. | Served as a benchmark to validate protein intake and assess the performance of other candidate biomarkers [10]. |
Navigating the regulatory landscapes of the FDA and EMA for biomarker acceptance demands a strategic and evidence-based approach. The core differentiators between the agencies are procedural, with the EMA's QoNM process being highly documented and the FDA's BQP emphasizing ICH M10 as a starting point amidst ongoing scientific debate. The universal cornerstone for dietary biomarker acceptance, however, remains the controlled feeding study. As demonstrated by the WHI and other trials, these studies provide the irrefutable, quantitative evidence (e.g., R² values) needed to prove that a biomarker reliably reflects intake. For researchers, early engagement with regulators, a clear definition of the CoU, and a robust validation strategy grounded in high-quality feeding experiments are non-negotiable steps on the path to successful biomarker qualification.
In the rigorous world of clinical research and drug development, precise terminology is not merely academic—it is a fundamental requirement for clear communication, robust trial design, and valid regulatory submissions. Within this framework, biomarkers and clinical endpoints represent distinct but often interconnected concepts. A biomarker is defined as a biological measure that can indicate a normal or pathological process, or a response to a therapeutic intervention. In contrast, a clinical endpoint is a characteristic or variable that reflects how a patient feels, functions, or survives. Clinical endpoints are the ultimate measures of treatment value from a patient's perspective [102]. The process of establishing a biomarker's validity, particularly its ability to predict a clinical endpoint, is a complex, multi-stage endeavor. This guide provides a comparative analysis of these two pivotal elements, with a specific focus on the role of controlled feeding studies as a gold standard for biomarker validation in nutritional research.
Fundamental Concepts and Definitions
Biomarkers: The Objective Biological Signals
Biomarkers are objective measures of biological processes. They can be classified based on their application:
- Diagnostic Biomarkers: Identify the presence of a disease.
- Prognostic Biomarkers: Predict the likely course of a disease.
- Predictive Biomarkers: Identify individuals more likely to respond to a specific treatment.
- Pharmacodynamic Biomarkers: Show that a biological response has occurred in a patient who has received a therapeutic intervention.
A surrogate endpoint is a specific type of biomarker that is intended to substitute for a clinical endpoint. A surrogate endpoint is expected to predict clinical benefit, harm, or lack of benefit/harm based on epidemiologic, therapeutic, pathophysiologic, or other scientific evidence [103]. A classic example is the use of LDL cholesterol levels as a surrogate endpoint for the clinical endpoint of myocardial infarction in the development of statin drugs [103].
Clinical Endpoints: The Patient-Centric Outcomes
Clinical endpoints are direct measures of patient experience. The FDA often requires direct evidence of a drug's effect on how patients feel, function, or survive [102]. These endpoints can include:
- Overall survival (OS)
- Patient-Reported Outcomes (PROs) such as pain scores
- Objective measures of function like the results of a six-minute walk test
The critical distinction is that a clinical endpoint is a measure of the patient's health and experience, whereas a biomarker is a measure of a biological state.
Methodological Frameworks for Biomarker Validation
The Controlled Feeding Study: A Gold Standard
Controlled feeding studies are a powerful methodological tool for discovering and validating dietary biomarkers. In these studies, participants are provided with all their meals, allowing researchers to know the exact composition and quantity of the diet. This controlled environment eliminates the substantial measurement errors inherent in self-reported dietary data [10] [22].
A prominent example is the Nutrition and Physical Activity Assessment Study Feeding Study (NPAAS-FS), which was conducted within the Women's Health Initiative (WHI) cohort. In this study, 153 postmenopausal women were provided with a 2-week controlled diet that was individually designed to approximate each participant's habitual food intake based on 4-day food records [10]. This design preserved the normal variation in nutrient consumption across the study population while providing researchers with known intake levels, creating an ideal setting for biomarker evaluation.
Multi-Phase Validation Consortia
Large-scale consortia have been established to systematize the biomarker validation process. The Dietary Biomarkers Development Consortium (DBDC), for example, employs a structured 3-phase approach [7] [8]:
- Phase 1: Discovery. Controlled feeding trials administer test foods in prespecified amounts to healthy participants, followed by metabolomic profiling of blood and urine to identify candidate biomarker compounds. This phase also characterizes the pharmacokinetic parameters of these candidates.
- Phase 2: Evaluation. The ability of candidate biomarkers to identify individuals consuming the associated foods is tested using controlled feeding studies of various dietary patterns.
- Phase 3: Validation. The validity of candidate biomarkers for predicting recent and habitual consumption is evaluated in independent observational settings.
This phased approach ensures that only the most robust and reliable biomarkers are advanced for use in broader research contexts.
Quantitative Comparison of Biomarker Performance
The performance of a biomarker is quantitatively assessed by its ability to explain variation in actual intake. The table below summarizes the performance of various serum biomarkers from the NPAAS-FS controlled feeding study, using the established urinary recovery biomarkers of energy and protein as benchmarks [10].
Table 1: Performance of Serum Biomarkers vs. Established Recovery Biomarkers in a Controlled Feeding Study
| Biomarker | Regression R² Value | Performance Interpretation |
|---|---|---|
| Urinary Nitrogen (Protein) | 0.43 | Established recovery biomarker benchmark |
| Doubly Labeled Water (Energy) | 0.53 | Established recovery biomarker benchmark |
| Serum Vitamin B-12 | 0.51 | Similar to established benchmarks |
| Serum Folate | 0.49 | Similar to established benchmarks |
| Serum α-Carotene | 0.53 | Similar to established benchmarks |
| Serum β-Carotene | 0.39 | Moderate performance |
| Serum Lutein + Zeaxanthin | 0.46 | Similar to established benchmarks |
| Serum Lycopene | 0.32 | Moderate performance |
| Serum α-Tocopherol | 0.47 | Similar to established benchmarks |
| PLFA % Energy from Polyunsaturated | 0.27 | Weaker performance |
R² values represent the proportion of variance in nutrient intake explained by the biomarker in linear regression models. Biomarkers with R² values close to or exceeding those of the established benchmarks (Urinary Nitrogen and Doubly Labeled Water) are considered suitable for application in the study population [10].
Statistical Frameworks for Biomarker-Endpoint Relationships
Beyond simple correlation, advanced statistical models are employed to formalize the relationship between biomarkers and clinical endpoints. A Bayesian meta-analytic approach can build a prediction model for a clinical endpoint using trial-level summary data from historical trials [104]. This model uses link functions (e.g., logit, odds, cloglog) to describe the relationship between the biomarker and clinical endpoint response proportions in treatment and control groups. The predictive ability of such models is often evaluated using metrics like Positive Predictive Value (PPV) and Negative Predictive Value (NPV), with a proposed condition of PPV/NPV ≥ 0.5 for reliable prediction [104].
Furthermore, the statistical approach must account for the specific characteristics of the biomarker. In Alzheimer's disease, for example, biomarkers are classified as either early accelerating (e.g., amyloid PET, plasma p-tau) or late accelerating (e.g., tau PET, volumetric MRI), depending on their temporal window of change relative to clinical symptom manifestation [105]. This classification is critical for selecting the appropriate analytical method.
Experimental Protocols and Workflows
Protocol for a Controlled Feeding Study in Biomarker Evaluation
The following workflow outlines the key steps in implementing a controlled feeding study for biomarker validation, based on the NPAAS-FS and DBDC protocols [7] [10].
Analytical Workflow for Biomarker-Endpoint Relationship Assessment
After biomarker and clinical endpoint data are collected, a structured analytical workflow is applied to assess their relationship. This involves distinct subject-level and group-level analyses [105].
The Scientist's Toolkit: Essential Research Reagents and Solutions
The following table details key reagents, technologies, and methodologies essential for conducting research in biomarker discovery and validation.
Table 2: Essential Research Reagents and Solutions for Biomarker Validation Studies
| Tool / Reagent | Function / Application | Example Use Case |
|---|---|---|
| Controlled Feeding Diets | Provides known dietary exposure for precise intake measurement. | Formulating individualized menus in the NPAAS-FS to mimic habitual intake [10]. |
| Doubly Labeled Water (DLW) | Objective recovery biomarker for total energy expenditure. | Serving as a benchmark for validating self-reported energy intake and other biomarkers [10]. |
| 24-Hour Urinary Nitrogen | Objective recovery biomarker for total protein intake. | Calibrating self-reported protein intake and evaluating other serum biomarkers [10]. |
| Metabolomics Platforms | High-throughput profiling of small molecules in biospecimens. | Discovering novel candidate food intake biomarkers in blood and urine in the DBDC [7]. |
| Liquid Chromatography-Mass Spectrometry (LC-MS) | Sensitive identification and quantification of chemical compounds. | Measuring serum concentrations of carotenoids, tocopherols, and other candidate biomarkers [10]. |
| Bayesian Statistical Models | Quantifying the predictive relationship between a biomarker and a clinical endpoint. | Predicting clinical outcome rate ratios from dichotomous biomarker data using historical trial data [104]. |
| Standard Reference Materials (SRMs) | Calibrating laboratory equipment to ensure analytical validity. | Ensuring accuracy and cross-laboratory reproducibility in biomarker concentration measurements. |
The comparative analysis of biomarkers and clinical endpoints reveals a nuanced landscape where each has a distinct and vital role in advancing biomedical science. Biomarkers offer objective, early, and often mechanistic insights into biological processes and responses to intervention. Clinical endpoints remain the indisputable benchmark for evaluating how a patient truly benefits from a therapy. The rigorous validation of biomarkers, particularly through gold-standard methodologies like controlled feeding studies, is paramount for establishing their utility. As frameworks for statistical and clinical validation continue to mature, the successful integration of robust biomarkers with patient-centric clinical endpoints will accelerate the development of effective therapeutics and deepen our understanding of human health and disease.
Conclusion
Controlled feeding studies are an indispensable component of a rigorous, multi-phase framework for biomarker validation, moving candidates from initial discovery to clinically useful tools. Success hinges on a thorough understanding of foundational principles, the application of robust methodological and statistical techniques, proactive troubleshooting of analytical challenges, and adherence to stringent validation and regulatory standards. The future of dietary biomarker research will be shaped by the integration of advanced technologies like AI and multi-omics, a stronger focus on patient-centric approaches, and collaborative efforts to standardize data sharing and validation protocols. By following this comprehensive roadmap, researchers can develop validated biomarkers that reliably translate dietary intake into objective data, ultimately accelerating the development of targeted therapies and advancing the field of precision nutrition.
References
- 1. Methods: Understanding Causal and Effect... Inference Cause [https://www.netguru.com/blog/causal-inference]
- 2. Frontiers | Advances in Nutrition Science and Integrative Physiology: Insights From Controlled Feeding Studies [https://www.frontiersin.org/journals/physiology/articles/10.3389/fphys.2019.01341/full]
- 3. in Practice: Strategies for Empirical Research Success Causal Inference [https://www.numberanalytics.com/blog/causal-inference-in-practice-strategies]
- 4. Recommendations for Designing, Conducting, and Reporting Feeding Trials in Nutrition Research - ScienceDirect [https://www.sciencedirect.com/science/article/pii/S2161831324001170]
- 5. Identification and validation of poly-metabolite scores... | PLOS Medicine [https://journals.plos.org/plosmedicine/article?id=10.1371/journal.pmed.1004560]
- 6. Validation of Analytical Methods for Biomarkers Employed in Drug Development - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2744124/]
- 7. The Dietary Biomarkers Development Consortium: An Initiative for... [https://pubmed.ncbi.nlm.nih.gov/40641655/]
- 8. The Dietary Biomarkers Development Consortium: An Initiative for Discovery and Validation of Dietary Biomarkers for Precision Nutrition - ScienceDirect [https://www.sciencedirect.com/science/article/pii/S2475299125028951]
- 9. Understanding Biomarker : Method & Precision... Validation Accuracy [https://www.linkedin.com/pulse/understanding-biomarker-method-validation-xyhhe]
- 10. Dietary biomarker evaluation in a controlled feeding study in women from the Women’s Health Initiative cohort - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5267309/]
- 11. Challenges in Designing and Delivering Diets and Assessing Adherence: A Randomized Controlled Trial Evaluating the 2010 Dietary Guidelines for Americans - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7066378/]
- 12. Pharmacokinetic-pharmacodynamic and dose-response relationships of antituberculosis drugs: recommendations and standards for industry and academia - PubMed [https://pubmed.ncbi.nlm.nih.gov/26009618/]
- 13. Discovery and Biomarker : Statistical Considerations - PMC Validation [https://pmc.ncbi.nlm.nih.gov/articles/PMC8012218/]
- 14. mini-MED: study protocol for a randomized, multi-intervention... [https://trialsjournal.biomedcentral.com/articles/10.1186/s13063-024-07939-8]
- 15. Design and Characterisation of a Randomized Food Intervention That... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7609501/]
- 16. (PDF) Addressing the pitfalls when designing intervention studies to... [https://www.academia.edu/129785547/Addressing_the_pitfalls_when_designing_intervention_studies_to_discover_and_validate_biomarkers_of_habitual_dietary_intake]
- 17. Novel Application of Nutritional Biomarkers From a Controlled Feeding Study and an Observational Study to Characterization of Dietary Patterns in Postmenopausal Women - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8799924/]
- 18. Comparison of Untargeted Metabolomic ... Profiling vs Traditional [https://pmc.ncbi.nlm.nih.gov/articles/PMC8276086/]
- 19. Evaluation of potential metabolomic -based biomarkers of protein... [https://pubmed.ncbi.nlm.nih.gov/33991228/]
- 20. Lipidomics and metabolomics as potential biomarkers for breast... [https://www.nature.com/articles/s44324-024-00027-0?error=cookies_not_supported&code=dbfdb526-1474-41d5-a097-04bedbdabb93]
- 21. Metabolomics Data Analysis, Visualization, and Integration | SpringerLink [https://link.springer.com/protocol/10.1007/978-1-59745-535-0_20]
- 22. Using Controlled Feeding Study for Biomarker Development in Regression Calibration for Disease Association Estimation - PubMed [https://pubmed.ncbi.nlm.nih.gov/37324058/]
- 23. Visualizing metabolic network dynamics through time-series metabolomic data | BMC Bioinformatics | Full Text [https://bmcbioinformatics.biomedcentral.com/articles/10.1186/s12859-020-3415-z]
- 24. Dietary Biomarker Development Consortium [https://dietarybiomarkerconsortium.org/]
- 25. Fruit and Vegetable Biomarker : Study ... : USDA ARS Dietary [https://www.ars.usda.gov/pacific-west-area/davis-ca/whnrc/docs/fruit-and-vegetable-biomarker-study-dietary-biomarker-development-center-dbdc-aim-2/]
- 26. A biomarker assay validation approach tailored to the context of use and bioanalytical platform - PubMed [https://pubmed.ncbi.nlm.nih.gov/37526064/]
- 27. Biomarker discovery and validation: Bridging research and clinical application | Abcam [https://www.abcam.com/en-us/knowledge-center/immunology-and-infectious-disease/biomarker-discovery-and-validation]
- 28. Challenges and Future Trends in Biomarker Analysis for Clinical Research: What’s Ahead in 2025 [https://blog.crownbio.com/challenges-and-future-trends-in-biomarker-analysis-for-clinical-research-whats-ahead-in-2025]
- 29. Machine Learning Strategies for Biomarker Discovery: A Senescence Case Study [https://kilthub.cmu.edu/articles/thesis/Machine_Learning_Strategies_for_Biomarker_Discovery_A_Senescence_Case_Study/29304683]
- 30. Potential of food intake biomarkers in nutrition research | Proceedings of the Nutrition Society | Cambridge Core [https://www.cambridge.org/core/journals/proceedings-of-the-nutrition-society/article/potential-of-food-intake-biomarkers-in-nutrition-research/B55C010EE170A3E799978FA9404BC9BD]
- 31. Tutorial: best practices and considerations for... | Nature Protocols [https://www.nature.com/articles/s41596-021-00566-6?error=cookies_not_supported&code=8353164d-84b7-4aa5-9b4a-1119fe3814f8]
- 32. Construction and optimization of multi-platform precision pathways for precision medicine | Scientific Reports [https://www.nature.com/articles/s41598-024-54517-8]
- 33. Robust pathway-based multi-omics data integration using directed random walks for survival prediction in multiple cancer studies - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6489180/]
- 34. The Measurement Error Elephant in the Room: Challenges and Solutions to Measurement Error in Epidemiology - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9005058/]
- 35. Using Controlled for Feeding Development in... Study Biomarker [https://link.springer.com/article/10.1007/s12561-022-09349-3]
- 36. (PDF) Dietary biomarker evaluation in a controlled in... feeding study [https://www.academia.edu/53032472/Dietary_biomarker_evaluation_in_a_controlled_feeding_study_in_women_from_the_Womens_Health_Initiative_cohort]
- 37. the least absolute shrinkage and... Measurement error correction in [https://pmc.ncbi.nlm.nih.gov/articles/PMC7449511/]
- 38. Bias correction in treatment effect estimates following data-driven biomarker cutoff selection [https://arxiv.org/html/2504.19776]
- 39. [2504.19776] Bias correction in treatment effect estimates following data-driven biomarker cutoff selection [https://arxiv.org/abs/2504.19776]
- 40. Measurement bias and error correction in a two-stage estimation for multilevel IRT models - PubMed [https://pubmed.ncbi.nlm.nih.gov/33550594/]
- 41. Online updating method to correct for measurement error in big data streams - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/S0167947320300670]
- 42. Of Calibration - Self Measures Using Biomarkers: An... Reported Dietary [https://pmc.ncbi.nlm.nih.gov/articles/PMC3832356/]
- 43. Frontiers | Traditional Self - Reported Instruments Are Prone to... Dietary [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2020.00090/full]
- 44. Using regression calibration that combine equations - self ... reported [https://asu.elsevierpure.com/en/publications/using-regression-calibration-equations-that-combine-self-reported]
- 45. Applying recovery biomarkers to calibrate - self measures of... report [https://www.nature.com/articles/jhh201698?error=cookies_not_supported]
- 46. Validation of biomarkers of food intake—critical assessment of candidate biomarkers | Genes & Nutrition | Full Text [https://genesandnutrition.biomedcentral.com/articles/10.1186/s12263-018-0603-9]
- 47. Diagnostic Accuracy of Blood-based Biomarkers for Pancreatic... [https://pubmed.ncbi.nlm.nih.gov/36969742/]
- 48. Optimizing timing and cost-effective use of plasma biomarkers in... [https://alzres.biomedcentral.com/articles/10.1186/s13195-025-01851-2]
- 49. Frontiers | Identification and validation of a novel autoantibody... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1494446/full]
- 50. A Standardized Strategy for Simultaneous Quantification of Urine Metabolites to Validate Development of a Biomarker Panel Allowing Comprehensive Assessment of Dietary Exposure - PubMed [https://pubmed.ncbi.nlm.nih.gov/32926540/]
- 51. Multiplex Sepsis Biomarker Market Panels [https://www.futuremarketinsights.com/reports/multiplex-sepsis-biomarker-panels-market]
- 52. About Biomarkers and Qualification | FDA [https://www.fda.gov/drugs/biomarker-qualification-program/about-biomarkers-and-qualification]
- 53. Discovery and validation of biomarkers to aid the development of safe and effective pain therapeutics: challenges and opportunities | Nature Reviews Neurology [https://www.nature.com/articles/s41582-020-0362-2]
- 54. of Validation of aging biomarkers [https://pubmed.ncbi.nlm.nih.gov/38355974/]
- 55. Knowledge Graphs in Biomarker Discovery & Validation – Wisecube... [https://www.wisecube.ai/blog/knowledge-graphs-in-biomarker-discovery-validation/]
- 56. Development and validation of an integrative 54 biomarker -based risk... [https://biomarkerres.biomedcentral.com/articles/10.1186/s40364-025-00812-z]
- 57. Automatic labeling of molecular biomarkers of... | PLOS One [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0190783]
- 58. SurvExpress: An Online Biomarker Tool and... | PLOS One Validation [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0074250]
- 59. Addressing the pitfalls when designing intervention studies to discover... [https://link.springer.com/article/10.1007/s11306-019-1532-3]
- 60. Challenges in Biomarker Discovery: Combining Expert Insights with Statistical Analysis of Complex Omics Data - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3548234/]
- 61. sciencedirect.com/topics/biochemistry-genetics-and-molecular-biology... [https://www.sciencedirect.com/topics/biochemistry-genetics-and-molecular-biology/biomarker-validation]
- 62. Challenges and prospects for biomarker research: A current perspective from the developing world - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/S1570963914000028]
- 63. stabilization and normalization Urine favor unbiased... strategies [https://www.nature.com/articles/s41598-022-22577-3?error=cookies_not_supported&code=639e2612-be4f-4f07-9d1d-b150fe3bfbf4]
- 64. . Urine Analysis: Comparative Insights for Wellness Apps vs Blood [https://www.vivoo.io/blogs/vivoo/urine-vs-blood-analysis]
- 65. Investigation of the 12-Month Stability of Dried Blood and Urine Spots... [https://pubmed.ncbi.nlm.nih.gov/31618007/]
- 66. A streamlined method for isolating and characterizing small... [https://bmcmethods.biomedcentral.com/articles/10.1186/s44330-025-00040-9]
- 67. Developing a Food Exposure and Urine for Dietary... Sampling Strategy [https://pmc.ncbi.nlm.nih.gov/articles/PMC8629115/]
- 68. Metabolic Diversity | Leibniz-Institut (IPK) [https://www.ipk-gatersleben.de/en/research/molecular-genetics/metabolic-diversity]
- 69. Good practices and recommendations for using and benchmarking computational metabolomics metabolite annotation tools - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9722809/]
- 70. Exploring Structural of Microbe Secondary Diversity ... Metabolites [https://pmc.ncbi.nlm.nih.gov/articles/PMC6399155/]
- 71. Metabolic Forest: Predicting the Diverse Structures of Drug Metabolites - PubMed [https://pubmed.ncbi.nlm.nih.gov/32881497/]
- 72. Criteria for quantitative assessment of metabolic similarity between chemicals. II. Application to human health endpoints - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/S2468111321000219]
- 73. Frontiers | Marine endophytes: biosynthetic engines for novel bioactive... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1684777/full]
- 74. Bridging the Gap: Translating Preclinical Biomarkers to Clinical Success [https://blog.crownbio.com/bridging-the-gap-translating-preclinical-biomarkers-to-clinical-success]
- 75. Traversing the Path from Bench to Cancer Biomarker Validation [https://www.the-scientist.com/traversing-the-path-from-bench-to-cancer-biomarker-validation-73484]
- 76. Journal of Medical Internet Research - AI -Derived Blood Biomarkers ... [https://www.jmir.org/2025/1/e67922]
- 77. -driven digital Validating | Digital Health | Waracle AI biomarkers [https://waracle.com/insights/digital-health/validating-ai-driven-digital-biomarkers/]
- 78. Advances in single-cell omics and multiomics for high-resolution molecular profiling | Experimental & Molecular Medicine [https://www.nature.com/articles/s12276-024-01186-2]
- 79. Single-cell sequencing to multi-omics: technologies and applications | Biomarker Research | Full Text [https://biomarkerres.biomedcentral.com/articles/10.1186/s40364-024-00643-4]
- 80. Frontiers | Biomarker integration and biosensor technologies enabling... [https://www.frontiersin.org/journals/aging/articles/10.3389/fragi.2025.1703698/full]
- 81. : Understand The Key Differences Qualification Vs Validation [https://gmpinsiders.com/qualification-vs-validation-key-differences/]
- 82. Demystified: What You Must Know Qualification vs Validation [https://pharmuni.com/2025/07/11/qualification-vs-validation-demystified-what-you-must-know/]
- 83. . Qualification : Key Differences & When to Use vs Validation [https://www.linkedin.com/pulse/qualification-vs-validation-key-differences-when-use-saket-yeotikar-er0hf]
- 84. : A Guide to Ensuring Quality and Compliance Process Validation [https://trainual.com/manual/process-validation]
- 85. | PPTX Validation qualification [https://www.slideshare.net/slideshow/validation-qualification-234521466/234521466]
- 86. NIH researchers develop biomarker score for predicting diets high in... [https://www.nih.gov/news-events/news-releases/nih-researchers-develop-biomarker-score-predicting-diets-high-ultra-processed-foods]
- 87. How to Validate PCR Assays for Clinical or Diagnostic Use [https://www.linkedin.com/advice/0/how-can-you-validate-pcr-assays-clinical-nq7ce]
- 88. Presenting Quantitative Data Graphically | Mathematics for the Liberal Arts [https://courses.lumenlearning.com/waymakermath4libarts/chapter/presenting-quantitative-data-graphically/]
- 89. Presentation of Quantitative Data | PSM Made Easy [https://ihatepsm.com/blog/presentation-quantitative-data]
- 90. Issues on fit - for - purpose of a panel of ELISAs for... validation [https://pmc.ncbi.nlm.nih.gov/articles/PMC2869162/]
- 91. - Fit - for method purpose for application in... biomarker validation [https://www.nature.com/articles/6605910?error=cookies_not_supported&code=82a1db8c-9017-4561-b03b-b2076a3f78d9]
- 92. Best practices for the development and fit - for - purpose of... validation [https://aapsopen.springeropen.com/articles/10.1186/s41120-021-00050-1]
- 93. - Fit - for protein purpose assay biomarker strategies using... validation [https://pubmed.ncbi.nlm.nih.gov/32736718/]
- 94. Protein Biomarker Discovery & Validation | Thermo Fisher Scientific - US [https://www.thermofisher.com/us/en/home/clinical/clinical-translational-research/protein-analysis/protein-biomarker-discovery-validation.html]
- 95. Biomarker Qualification at the European Medicines Agency: A Review of Biomarker Qualification Procedures From 2008 to 2020 - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9313861/]
- 96. Qualification Program | Biomarker FDA [https://www.fda.gov/drugs/drug-development-tool-ddt-qualification-programs/biomarker-qualification-program]
- 97. The 2025 FDA Biomarker Guidance: Understanding ... [https://www.linkedin.com/pulse/2025-fda-biomarker-guidance-understanding-lxoke]
- 98. FDA Guidance for Industry on Bioanalytical Method Validation (BMV) for Biomarkers [https://labs.iqvia.com/blog/fda-guidance-bioanalytical-method-validation-biomarkers]
- 99. Requirements for regulatory acceptance of biomarkers [https://link.springer.com/article/10.1007/s40629-024-00312-w]
- 100. Biomarkers in Medicines Development—From Discovery to Regulatory Qualification and Beyond - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9086587/]
- 101. Metabolomic Profiling and Diet Quality Scoring in a Randomized Crossover Trial of Healthy and Typical Dietary Patterns - PubMed [https://pubmed.ncbi.nlm.nih.gov/41031481/]
- 102. . Biomarkers Outcome Assessments (COA) vs . Clinical vs Endpoints [https://www.vivosense.com/biomarkers-vs-clinical-outcome-assessments-coa-vs-endpoints]
- 103. Slow Aging, Extend Healthy Life | Federation of American Scientists [https://fas.org/publication/validation-biomarkers-endpoints/]
- 104. A Bayesian prediction model between a biomarker and the clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4307375/]
- 105. A Statistical Framework for Assessing the Relationship between... [https://link.springer.com/article/10.14283/jpad.2024.126]