Controlled Feeding Trials for Dietary Biomarker Discovery: Methodology, Validation, and Clinical Applications
This article explores the critical role of controlled feeding trials in discovering and validating objective dietary biomarkers.
Controlled Feeding Trials for Dietary Biomarker Discovery: Methodology, Validation, and Clinical Applications
Abstract
This article explores the critical role of controlled feeding trials in discovering and validating objective dietary biomarkers. Aimed at researchers, scientists, and drug development professionals, it covers the foundational need for biomarkers beyond self-reported data, detailed methodological approaches for trial design and execution, strategies for troubleshooting common challenges, and rigorous multi-phase validation processes. The content synthesizes current consortium-led efforts and technological advances in metabolomics, providing a comprehensive guide for implementing these trials to enhance precision in nutritional science and clinical research.
The Critical Need for Objective Dietary Biomarkers in Nutrition Science
Limitations of Self-Reported Dietary Assessment Methods
Accurate dietary assessment is fundamental to nutritional epidemiology, enabling the investigation of links between diet and health outcomes. However, the field relies heavily on self-reported dietary instruments that introduce substantial measurement error, potentially compromising research validity and dietary recommendations. This document examines the limitations of these methods within the context of controlled feeding trials for dietary biomarker discovery, providing researchers with critical insights and methodological frameworks to advance nutritional science.
The subjective nature of self-reported intake data presents numerous challenges to obtaining accurate dietary exposure assessment. This limitation is increasingly being addressed through the development and validation of objective dietary biomarkers that can assess dietary consumption without the bias inherent in self-reported methods [1]. Controlled feeding studies represent a critical methodological bridge for identifying and validating these biomarkers, thereby strengthening the foundation of nutrition research.
Quantitative Limitations of Self-Reported Methods
Systematic Underreporting of Energy and Nutrients
Table 1: Documented Underreporting in Self-Reported Dietary Assessment
| Nutrient/Food Group | Degree of Underreporting | Factors Influencing Underreporting | Source Study |
|---|---|---|---|
| Energy Intake | 30-50% among overweight/obese individuals | Increases with BMI; weight concern | [2] |
| Protein Intake | 47% underestimation vs. urinary nitrogen biomarker | Weight loss context; less underreported than other macronutrients | [2] |
| Fruits & Vegetables | Moderate reliability (ICC*: 0.68) | Fair validity vs. objective measures (ICC: 0.53) | [3] |
| Grain Products | Fair reliability (ICC: 0.56) | Fair validity vs. objective measures (ICC: 0.41) | [3] |
| Meat & Alternatives | Fair reliability (ICC: 0.41) | Slight validity vs. objective measures (ICC: 0.34) | [3] |
*ICC: Intraclass Correlation Coefficient
Evidence consistently demonstrates systematic underreporting across various self-reported dietary instruments. The discrepancy between self-reported energy intake and energy expenditure measured by doubly labeled water is particularly well-documented, with underreporting increasing substantially with body mass index [2]. This systematic error is not uniform across nutrients; protein is typically less underreported compared to other macronutrients, suggesting selective reporting of perceived "healthy" foods [2].
Food Composition Variability Compounds Measurement Error
Table 2: Impact of Food Composition Variability on Intake Estimates
| Bioactive Compound | Variability in Food Content | Impact on Intake Estimation | Validation Method | |
|---|---|---|---|---|
| Flavan-3-ols | >2-fold variability in same foods | Large uncertainty in ranking high/low consumers | Biomarker calibration in EPIC-Norfolk study (n=18,684) | [4] |
| (-)-Epicatechin | >2-fold variability in same foods | Significant overlap in intake ranges between participants | Biomarker calibration in EPIC-Norfolk study | [4] |
| Nitrate | >2-fold variability in same foods | Difficulty identifying true consumption extremes | Biomarker calibration in EPIC-Norfolk study | [4] |
Food composition databases rely on single-point estimates (mean values) that mask the substantial natural variation in nutrient content between individual food items, even of the same type. This variability introduces considerable uncertainty when estimating actual nutrient intake, as demonstrated by research showing more than twofold differences in flavan-3-ols, (-)-epicatechin, and nitrate content between apparently identical foods [4]. When combined with self-reporting errors, this variability fundamentally challenges our ability to accurately assess dietary exposure.
Experimental Protocols for Biomarker Discovery
Controlled Feeding Study Design for Biomarker Development
Controlled Feeding Study Workflow
Participant Recruitment and Baseline Assessment
- Target Population: Recruit 150+ participants representing the study population of interest, with oversampling for demographic diversity when needed [5]. For the Women's Health Initiative Nutrition and Physical Activity Assessment Study Feeding Study (NPAAS-FS), participants were postmenopausal women aged 50-80 [6].
- Eligibility Criteria: Exclude conditions affecting metabolism or specimen collection (e.g., diabetes, kidney disease, routine oxygen use) [5].
- Baseline Dietary Assessment: Administer a 4-day food record to capture habitual dietary patterns, food preferences, and eating behaviors [5]. Conduct standardized interviews to clarify portion sizes, brand preferences, preparation methods, and meal timing.
Individualized Diet Formulation
- Menu Development: Create individualized menus using diet analysis software (e.g., Nutrition Data System for Research, ProNutra) to approximate each participant's habitual diet [5].
- Energy Adjustment: Adjust calories based on estimated energy requirements using standard equations and previous calibration data. In NPAAS-FS, 73% of participants required upward calorie adjustments (average +335±220 kcal/day) to meet energy needs [5].
- Food Sourcing: Select foods with well-characterized nutrient composition using standardized sourcing and preparation protocols in a metabolic kitchen [5].
Controlled Feeding and Biospecimen Collection
- Feeding Period: Implement a 2-week controlled feeding period with all meals prepared in a metabolic kitchen [5].
- Specimen Collection: Collect fasting blood samples and 24-hour urine collections at beginning and end of feeding period [6] [5].
- Objective Measures: Implement doubly labeled water protocol for total energy expenditure and 24-hour urinary nitrogen for protein intake validation [5].
Biomarker Analytical Methods
Metabolomic Profiling
- Platform Selection: Employ liquid chromatography-mass spectrometry (LC-MS) and nuclear magnetic resonance (NMR) spectroscopy for comprehensive metabolomic coverage [7].
- Targeted Analysis: Quantify specific nutrient biomarkers including:
- Carotenoids (α-carotene, β-carotene, lutein, zeaxanthin, lycopene)
- Tocopherols (α-tocopherol, γ-tocopherol)
- B vitamins (folate, B-12)
- Phospholipid fatty acids [5]
- Quality Control: Implement pooled quality control samples, standard reference materials, and batch correction algorithms.
Biomarker Validation Protocol
- Statistical Analysis: Perform linear regression of (ln-transformed) consumed nutrients on (ln-transformed) biomarker concentrations [5].
- Validation Criteria: Evaluate biomarkers using coefficient of determination (R²) values, with R² ≥0.36 considered acceptable for explaining intake variation [6].
- Performance Benchmarks: Compare novel biomarkers against established recovery biomarkers (doubly labeled water for energy: R²=0.53; urinary nitrogen for protein: R²=0.43) [5].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Materials for Dietary Biomarker Discovery
| Category | Specific Reagents/Assays | Research Application | Performance Characteristics |
|---|---|---|---|
| Energy Expenditure Biomarkers | Doubly labeled water (²H₂¹â¸O) | Objective measure of total energy expenditure | Accuracy: 1-2%; Precision: 7% for individuals [2] |
| Protein Intake Biomarkers | Urinary nitrogen analysis | Validation of protein intake assessment | Correlation with intake: R²=0.43 [5] |
| Vitamin Status Assays | Serum folate, vitamin B-12 | Biomarkers of vitamin intake | Explained variation: Folate R²=0.49; B-12 R²=0.51 [5] |
| Carotenoid Analysis | HPLC-based carotenoid profiling | Fruit and vegetable intake biomarkers | Explained variation: α-carotene R²=0.53; β-carotene R²=0.39 [5] |
| Fatty Acid Profiling | Phospholipid fatty acid analysis | Biomarkers of fatty acid intake | PUFA% energy: R²=0.27; weaker for SFA/MUFA [5] |
| Tetrahydrocurcumin | Tetrahydrocurcumin (CAS 36062-04-1) - For Research Use | High-purity Tetrahydrocurcumin, a key curcumin metabolite. Explore its research applications in oncology, metabolism, and more. For Research Use Only. | Bench Chemicals |
| Gingerdione | High-purity Gingerdione for research into ferroptosis, cancer mechanisms, and anti-inflammatory pathways. For Research Use Only. Not for human consumption. | Bench Chemicals |
Biomarker Application in Nutritional Epidemiology
Regression Calibration for Measurement Error Correction
Regression Calibration for Error Correction
Advanced statistical methods enable the use of biomarkers to correct systematic measurement error in self-reported data. Regression calibration employs biomarker measurements to develop calibration equations that adjust self-reported intake for systematic bias [8]. This approach has been successfully applied in major cohort studies like the Women's Health Initiative to correct measurements of energy, protein, and sodium/potassium ratio [8].
The calibration process involves:
- Model Development: Regressing biomarker measurements on self-reported intake in feeding studies or biomarker substudies
- Equation Application: Using derived coefficients to calibrate self-reported data in the full cohort
- Association Analysis: Employing calibrated values in diet-disease association models
This method has demonstrated particular value in examining associations between sodium/potassium ratio and cardiovascular disease risk, revealing positive relationships with coronary heart disease, myocardial infarction, and stroke that were obscured by measurement error in self-reported data [8].
Dietary Pattern Biomarkers
Beyond single nutrients, researchers have successfully developed biomarker signatures for overall dietary patterns. The NPAAS feeding study identified biomarker panels for Healthy Eating Index-2010 (HEI-2010) and alternative Mediterranean Diet (aMED) patterns that met prespecified criteria (cross-validated R² ≥36%) [6]. These pattern biomarkers provide objective measures of overall diet quality, overcoming limitations of pattern analysis based on error-prone self-reports.
Self-reported dietary assessment methods contain fundamental limitations that impede nutritional epidemiology and the development of evidence-based dietary guidance. Controlled feeding studies provide an essential platform for developing objective dietary biomarkers that overcome these limitations. The integration of metabolomic profiling, recovery biomarkers, and statistical calibration methods represents a paradigm shift toward more precise nutritional exposure assessment. Future research should focus on expanding the repertoire of validated biomarkers, particularly for whole dietary patterns, and implementing these tools in large-scale cohort studies to strengthen our understanding of diet-disease relationships.
Defining Dietary Biomarkers and Their Role in Precision Nutrition
Within nutritional science and the development of targeted therapies, the accurate assessment of dietary intake remains a formidable challenge. Current methodologies, including food frequency questionnaires and 24-hour recalls, are plagued by systematic and random measurement errors inherent to self-reported data [9]. Dietary biomarkers—objectively measurable indicators of food intake—present a transformative solution. These biomarkers, measured in biological specimens like blood and urine, reflect the true "bioavailable" dose of a dietary exposure, moving beyond mere consumption to biological impact [9]. Their discovery and validation are paramount for advancing Precision Nutrition, a framework that tailors dietary advice to individual characteristics such as genetics, metabolism, and microbiome composition [10]. This document details the application notes and experimental protocols for discovering dietary biomarkers within the context of controlled feeding trials, providing a roadmap for researchers and drug development professionals engaged in this cutting-edge field.
Dietary Biomarker Discovery Workflow
The discovery and validation of robust dietary biomarkers require a systematic, multi-phase approach. The following workflow, formalized by initiatives such as the Dietary Biomarkers Development Consortium (DBDC), outlines this rigorous process from initial discovery to real-world application [7] [9].
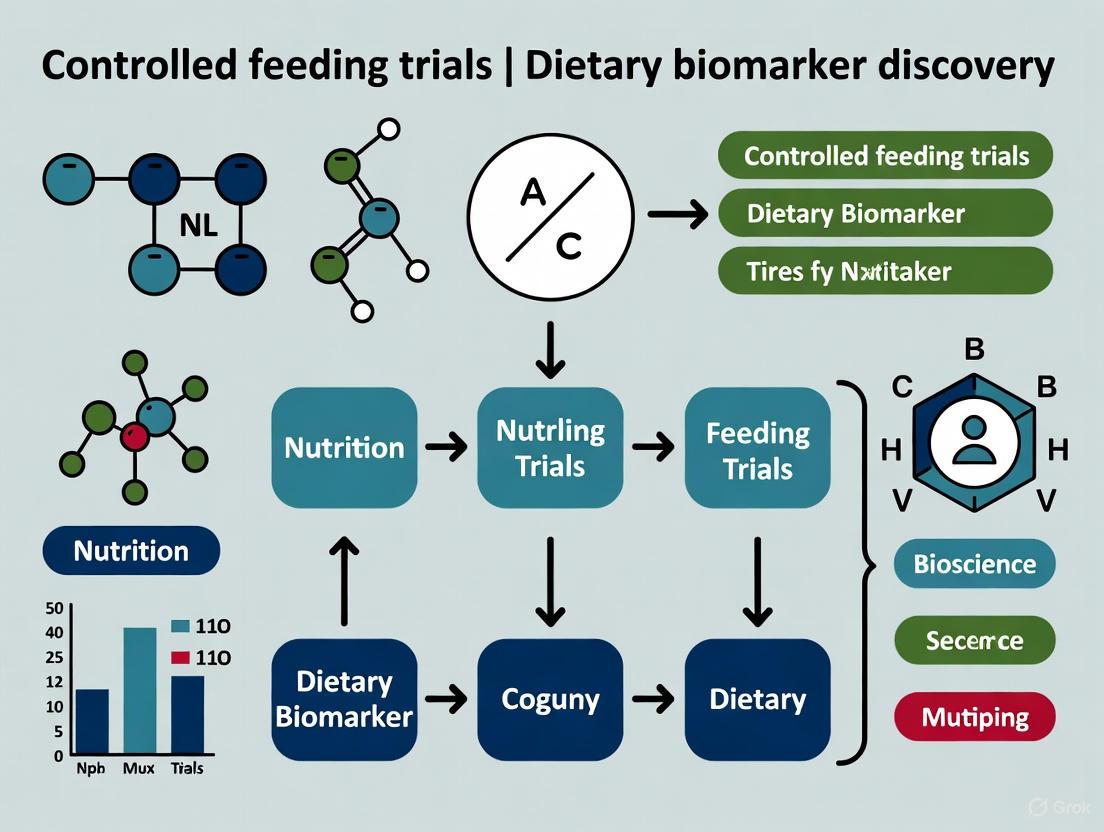
Diagram 1: Dietary biomarker discovery and validation workflow.
Core Principles for Validated Biomarkers
For a metabolite to be considered a valid dietary biomarker, it should fulfill several criteria beyond mere detectability. As proposed by Dragsted et al. and adopted by the DBDC, these principles include [9]:
- Plausibility: A biologically plausible connection must exist between the food component and the candidate biomarker.
- Dose-Response (DR) & Time-Response (Pharmacokinetics): A predictable relationship must be demonstrated between the amount of food consumed (dose) and the biomarker level, as well as its kinetics over time.
- Robustness, Reliability, and Analytical Performance: The biomarker must be stable, reliably measurable with high sensitivity and specificity using standard platforms like liquid chromatography-mass spectrometry (LC-MS), and perform consistently across diverse populations and complex dietary backgrounds [9].
Experimental Protocols for Controlled Feeding Trials
Protocol 1: Phase 1 Discovery and Pharmacokinetic Studies
Objective: To identify candidate biomarker compounds and characterize their pharmacokinetic (PK) parameters following the consumption of a specific test food.
Materials:
- Participants: Healthy adult volunteers, recruited based on predefined inclusion/exclusion criteria [9].
- Test Foods: Pre-specified, commonly consumed foods (e.g., selected based on USDA MyPlate Guidelines), prepared in standardized portions [9].
- Biospecimen Collection: Blood collection tubes (e.g., EDTA for plasma), urine collection containers, equipment for processing and aliquoting (e.g., centrifuges, pipettes, cryovials).
- Analytical Platform: Liquid Chromatography-Mass Spectrometry (LC-MS) systems, preferably using Hydrophilic-Interaction Liquid Chromatography (HILIC) for broad metabolite capture [9].
Methodology:
- Pre-Intervention Baseline: Following an overnight fast, collect baseline fasting blood and urine samples from participants.
- Controlled Administration: Administer a single, known dose of the test food to participants.
- Intensive Pharmacokinetic Sampling: Collect serial blood and urine specimens at predetermined time points post-consumption (e.g., 30min, 1h, 2h, 4h, 6h, 8h, 24h) to capture the absorption, peak, and elimination phases of potential biomarkers [9].
- Metabolomic Profiling: Perform untargeted metabolomic analysis on all biospecimens using LC-MS.
- Data Analysis: Use high-dimensional bioinformatics to compare pre- and post-consumption metabolomic profiles. Identify significantly elevated compounds as candidate biomarkers. Model the PK parameters (e.g., C~max~, T~max~, AUC) for each candidate [7] [9].
Protocol 2: Phase 2 Evaluation in Varied Dietary Patterns
Objective: To evaluate the specificity and sensitivity of candidate biomarkers for identifying consumption of the target food against the background of different complex dietary patterns.
Materials: As in Protocol 1, with the addition of full menus representing different dietary patterns (e.g., Western, Mediterranean, Vegetarian).
Methodology:
- Dietary Intervention Design: Implement controlled feeding studies where participants are randomized to follow different dietary patterns for a set period (e.g., 2-4 weeks). One group receives the target food, while control groups do not.
- Biospecimen Collection: Collect fasting or timed biospecimens at regular intervals throughout the intervention.
- Biomarker Measurement: Analyze samples using targeted or untargeted metabolomics to quantify the levels of the candidate biomarkers.
- Statistical Evaluation: Assess the biomarker's ability to correctly classify consumers vs. non-consumers of the test food. Calculate performance metrics such as sensitivity, specificity, and area under the receiver operating characteristic curve (AUC-ROC) [7].
Table 1: Key Quantitative Data from Biomarker Discovery Phases
| Study Phase | Primary Objective | Key Measured Parameters | Typical Sample Size (per group) | Data Output |
|---|---|---|---|---|
| Phase 1: Discovery & PK | Identify candidate biomarkers and their kinetics | C~max~ (peak concentration), T~max~ (time to peak), AUC (Area Under Curve), half-life | 10-20 healthy participants | List of candidate compounds with PK profiles |
| Phase 2: Evaluation | Test specificity in complex diets | Sensitivity, Specificity, AUC-ROC | 30-50 participants per dietary arm | Performance metrics for classifying food intake |
| Phase 3: Validation | Assess predictive power in free-living populations | Correlation coefficients with habitual intake, predictive accuracy | Hundreds of participants in observational cohorts | Validated biomarker for use in epidemiological studies [7] [9] |
The Scientist's Toolkit: Research Reagent Solutions
Successful dietary biomarker research relies on a suite of specialized reagents, technologies, and methodologies. The following table catalogs essential components of the research toolkit.
Table 2: Essential Research Reagents and Solutions for Dietary Biomarker Studies
| Item / Solution | Function / Application | Specifications & Examples |
|---|---|---|
| Liquid Chromatography-Mass Spectrometry (LC-MS) | High-throughput, untargeted and targeted analysis of metabolites in biospecimens. The primary platform for biomarker discovery. | Hydrophilic-interaction liquid chromatography (HILIC) for polar metabolites; reverse-phase LC for lipids [9]. |
| Stable Isotope-Labeled Standards | Internal standards for absolute quantification of metabolites; used to track specific nutrient metabolism. | Carbon-13 (^13^C) or Nitrogen-15 (^15^N) labeled compounds added to samples for calibration and recovery calculations. |
| Controlled Diets & Test Foods | Provide a precise and reproducible dietary exposure to eliminate confounding from self-reported intake. | Foods prepared in metabolic kitchens, with compositions verified by chemical analysis [7] [9]. |
| Biospecimen Collection Kits | Standardized collection, processing, and archiving of biological samples to preserve biomarker integrity. | EDTA tubes for plasma; cryovials for long-term storage in -80°C freezers; protocols for urine dilution and refractive index targeting [9]. |
| Bioinformatics Software | Process raw metabolomic data, perform statistical analyses, and identify significant metabolite patterns. | Packages for peak alignment, compound identification using MS/MS libraries, and multivariate statistics (e.g., PCA, OPLS-DA). |
| Multi-Omics Data Integration Platforms | Combine metabolomic data with genomic, proteomic, and microbiomic data for a systems-level view. | AI and machine learning algorithms to predict individual glycemic responses and integrate food-polygenic variant interactions [10]. |
| (Rac)-Atropine-d3 | (Rac)-Atropine-d3, CAS:51-55-8, MF:C17H23NO3, MW:289.4 g/mol | Chemical Reagent |
| Isorhoifolin | Isorhoifolin (CAS 552-57-8) - High-Purity RUO Flavonoid | Isorhoifolin, a high-purity flavonoid for Research Use Only. Explore its antioxidant and cardiac research applications. Not for diagnostic or therapeutic use. |
Application in Precision Nutrition and Therapeutic Development
The ultimate application of validated dietary biomarkers is in realizing the vision of precision nutrition, as illustrated by the following framework which integrates multi-omics data to deliver personalized dietary advice.
Diagram 2: Precision nutrition implementation framework.
Validated dietary biomarkers serve critical functions across research and clinical practice:
- Calibrating Self-Reported Data: Biomarkers provide an objective measure to correct for errors in dietary questionnaires, significantly improving the accuracy of nutritional epidemiology [9].
- Quantifying Compliance: In clinical trials for drug development, especially those where diet is a confounding factor (e.g., for metabolic diseases), biomarkers offer an unbiased method for monitoring participant adherence to dietary interventions [11].
- Understanding Interindividual Variability: Biomarkers are integral to multi-omics profiling that helps explain why individuals respond differently to the same foods. This is key for developing personalized dietary interventions for conditions like obesity and diabetes [10] [11].
- Identifying Novel Therapeutic Targets: Research into the neurobiological impact of diet, such as brain activity associated with "food preoccupation" under incretin-based therapies, can reveal new biomarker-driven targets for drug development [12].
The systematic discovery and validation of dietary biomarkers, as detailed in these application notes and protocols, are foundational to building a future where nutrition is a precise, personalized, and powerful component of health maintenance and disease therapy.
Diet is a complex exposure that significantly affects human health across the lifespan. The accurate assessment of dietary intake remains a fundamental challenge in nutritional epidemiology, largely due to the substantial measurement errors inherent in self-reported dietary data such as food frequency questionnaires and dietary recalls [6]. To address this limitation, the field has increasingly turned toward the discovery and validation of objective biomarkers that can reliably reflect intake of specific nutrients, foods, and overall dietary patterns [13] [7].
The Dietary Biomarkers Development Consortium (DBDC) represents the first major coordinated effort to systematically improve dietary assessment through the discovery and validation of biomarkers for foods commonly consumed in the United States diet [13]. This multi-center initiative connects experts in nutrition, data science, and statistics with the shared goal of identifying objective measures that can inform individual dietary patterns and advance nutritional science [14]. The consortium's work is particularly framed within the context of controlled feeding trials, which provide the rigorous experimental conditions necessary for biomarker discovery and validation.
The DBDC Organizational Infrastructure and Mission
The DBDC operates through a collaborative network of research centers employing standardized protocols and shared data resources. The consortium's central mission is to significantly expand the list of validated biomarkers of intake for foods consumed in the United States diet, thereby enabling more precise investigations of how diet influences human health and chronic disease risk [13] [7]. This expansion is crucial for advancing the field of precision nutrition, which aims to provide individualized dietary recommendations based on objective measures rather than self-reported data alone.
The organizational structure of the DBDC facilitates the integration of diverse expertise across multiple disciplines, including nutrition, metabolomics, bioinformatics, and statistics [14]. This cross-disciplinary approach is essential for addressing the complex challenges inherent in dietary biomarker development, from the initial discovery phase to eventual application in large-scale epidemiological studies.
The Three-Phase Biomarker Development Framework
The DBDC has implemented a systematic, three-phase approach to biomarker discovery and validation that leverages controlled feeding studies as its foundational element. This rigorous framework ensures that candidate biomarkers undergo comprehensive evaluation before being recommended for use in research settings.
Phase 1: Discovery and Pharmacokinetic Characterization
In Phase 1, controlled feeding trial designs are implemented by administering test foods in prespecified amounts to healthy participants [13] [7]. This initial discovery phase employs metabolomic profiling of blood and urine specimens collected during the feeding trials to identify candidate compounds that may serve as biomarkers [15]. The controlled feeding environment allows researchers to characterize the pharmacokinetic parameters of candidate biomarkers associated with specific foods, including their appearance, peak concentration, and clearance rates in biological fluids [13].
The DBDC's feeding studies are designed to investigate specific food groups. For example, the Fruit and Vegetable Biomarker Discovery study focuses on identifying biomarkers for bananas, peaches, strawberries, tomatoes, green beans, and carrots [16]. These studies typically involve multiple test days where participants consume prescribed combinations of target foods while providing repeated biological samples, enabling researchers to track the temporal patterns of potential biomarker compounds [16].
Phase 2: Evaluation in Varied Dietary Patterns
Phase 2 assesses the performance of candidate biomarkers identified in Phase 1 using controlled feeding studies of various dietary patterns [13] [7]. This critical evaluation phase tests whether candidate biomarkers retain their specificity and sensitivity when the target food is consumed as part of different dietary backgrounds, rather than in isolation. The ability of a biomarker to accurately identify consumption of its associated food across diverse dietary contexts is essential for its utility in free-living populations where people consume complex mixtures of foods.
Phase 3: Validation in Observational Settings
Phase 3 represents the final validation step, where the performance of candidate biomarkers is evaluated in independent observational settings [13] [7]. This phase tests whether biomarkers can predict recent and habitual consumption of specific test foods under free-living conditions [15]. Successful validation in observational cohorts provides the final evidence needed to recommend a biomarker for use in nutritional epidemiology studies.
Throughout all three phases, data generated by the DBDC are archived in a publicly accessible database, serving as a valuable resource for the broader research community [13] [7]. This commitment to data sharing accelerates the pace of biomarker discovery and validation beyond the consortium itself.
Application Notes: Experimental Protocols for Biomarker Discovery
Protocol 1: Fruit and Vegetable Biomarker Discovery
Objective: To identify biomarkers in blood and urine that provide specific information about intake of bananas, peaches, strawberries, tomatoes, green beans, and carrots [16].
Study Population: Healthy adults with BMI between 18.5-39.9, excluding those with gastrointestinal disorders, recent significant weight change, or use of certain medications that might interfere with metabolic responses [16].
Experimental Design:
- Screening: Initial telephone interview (15-20 minutes) followed by in-person screening visit (40-60 minutes) including body measurements, vital signs, and blood draw for eligibility assessment [16].
- Study Duration: Approximately 15 days conducted over 3 weeks, with 9 study visits including three extended test days lasting ~8 hours each [16].
- Test Meals: Participants consume three different combinations of fruits (strawberries, peaches, bananas) and three different combinations of vegetables (green beans, tomatoes, carrots) across three test days [16].
- Lead-in Diet: Participants receive two days' worth of food and beverages leading into each test day, with instructions to consume only the provided items during each test period [16].
- Sample Collection: On test days, participants provide 9 blood draws and multiple urine samples, with an additional blood draw and urine collection 24 hours post-test [16].
Compensation: Participants receive $250 upon completion of all study visits [16].
Protocol 2: Metabolomic Response to Ultra-Processed Dietary Patterns
Objective: To identify metabolomic markers that differentiate between dietary patterns high in versus void of ultra-processed foods according to NOVA classification [17] [18].
Study Design: Randomized, crossover, controlled feeding trial involving 20 healthy participants (mean age 31±7 years, BMI 22±11.6, 50% female) [17].
Dietary Interventions:
- UPF-DP: Dietary pattern containing 80% ultra-processed foods
- UN-DP: Unprocessed dietary pattern containing 0% ultra-processed foods
- Matching: Both diets matched for energy, macronutrients, total fiber, total sugar, and sodium
- Feeding Protocol: Diets presented at 200% of energy requirements and consumed ad libitum for two weeks per condition with no washout period [17]
Sample Collection and Analysis:
- Metabolite Profiling: Untargeted liquid chromatography with high resolution/tandem mass spectrometry
- Sample Types: EDTA plasma collected at end of each dietary period (week 2); 24-hour and spot urine collected at weeks 1 and 2
- Data Processing: Metabolites with <80% missing data and coefficients of variation <30% were assigned minimum detected values, scaled to median of 1, and log2-transformed [17]
- Statistical Analysis: Linear mixed models identified metabolites differing between UPF-DP and UN-DP, adjusted for trial, sequence, timepoint, and body weight changes, with Benjamini-Hochberg multiple comparison correction [17]
Quantitative Results from Metabolomic Studies
Table 1: Metabolomic Differences Between Ultra-Processed and Unprocessed Dietary Patterns
| Sample Type | Total Metabolites Measured | Differentially Abundant Metabolites | Consistently Different Metabolites |
|---|---|---|---|
| Plasma | 1,000 | 183 at week 2 | 20 across all sample types and timepoints |
| 24-hour Urine | 1,272 | 461 at weeks 1 and 2 | 20 across all sample types and timepoints |
| Spot Urine | 1,281 | 68 at weeks 1 and 2 | 20 across all sample types and timepoints |
Table 2: Metabolic Pathways Represented by Consistent Metabolomic Biomarkers
| Metabolic Pathway | Number of Metabolites | Examples |
|---|---|---|
| Glutamate metabolism | 1 | Not specified |
| Ascorbate and aldarate metabolism | 1 | Not specified |
| Benzoate metabolism | 2 | Not specified |
| Methionine, cysteine, SAM and taurine metabolism | 2 | Not specified |
| Secondary bile acid metabolism | 2 | Not specified |
| Fatty acid dicarboxylate | 1 | Not specified |
| Plant-food components | 2 | Not specified |
| Unannotated | 9 | Not specified |
Visualizing Experimental Workflows
DBDC Three-Phase Biomarker Development Pipeline
Fruit and Vegetable Biomarker Study Design
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents and Materials for Dietary Biomarker Studies
| Item | Specification | Function/Application |
|---|---|---|
| Liquid Chromatography with High Resolution/Tandem Mass Spectrometry | Untargeted metabolomics platform | Comprehensive profiling of metabolites in biological samples; enables detection of thousands of compounds simultaneously [17] |
| EDTA Plasma Collection Tubes | Standard blood collection tubes with EDTA anticoagulant | Preservation of blood samples for metabolomic analysis; prevents coagulation and maintains sample integrity [17] |
| 24-hour Urine Collection Containers | Sterile, large-volume containers | Quantitative collection of all urine produced over 24-hour period for comprehensive metabolomic profiling [6] |
| Metabolon Reference Library | Commercial metabolite database | Annotation and identification of detected metabolites using authentic standards [17] |
| Doubly Labeled Water (DLW) | Stable isotope-labeled water (²H₂¹â¸O) | Objective assessment of total energy expenditure as biomarker of energy intake in validation studies [6] |
| Controlled Feeding Study Materials | Standardized food preparation facility | Provision of precisely controlled test meals and diets; essential for biomarker discovery phase [16] |
| Liquid Handling Systems | Automated pipetting systems | Precise and reproducible processing of biological samples for high-throughput metabolomic analyses |
| Ibandronate | Ibandronate, CAS:114084-78-5, MF:C9H23NO7P2, MW:319.23 g/mol | Chemical Reagent |
| alpha-Estradiol | 17alpha-Estradiol Research Grade|RUO |
Analytical Framework and Statistical Approaches
The DBDC employs sophisticated statistical methods to handle the high-dimensional data generated by metabolomic platforms and to address the challenge of dietary measurement error in association studies.
Regression Calibration for Measurement Error Correction
A key application of dietary biomarkers is in regression calibration methods to correct for systematic measurement error in self-reported dietary data [19]. This approach is particularly important in association studies examining relationships between dietary intake and chronic disease risk, where measurement error can substantially attenuate or distort true associations.
The statistical framework involves using biomarkers developed through controlled feeding studies to calibrate self-reported intake measures, thereby providing more accurate estimates of diet-disease associations [19]. This method has been successfully applied to examine associations between sodium/potassium ratio and cardiovascular disease risk, revealing significant positive associations with coronary heart disease, nonfatal myocardial infarction, coronary death, ischemic stroke, and total cardiovascular disease incidence [19].
Biomarker Signature Development for Dietary Patterns
Beyond biomarkers for individual foods, the DBDC approach also supports the development of biomarker signatures for overall dietary patterns. Research has demonstrated that panels of nutritional biomarkers can identify signatures associated with established dietary patterns such as the Healthy Eating Index-2010 (HEI-2010) and alternative Mediterranean diet (aMED) [6].
This methodology typically involves two stages:
- Discovery: Biomarker identification using biospecimens from controlled feeding studies where dietary intake is known
- Calibration: Application of discovered biomarkers in regression models to correct measurement error in dietary self-reports from observational studies [6]
The successful application of this approach has been demonstrated in studies of postmenopausal women, where biomarker-calibrated measurements showed improved predictive validity for diet-disease associations compared to self-report data alone [6].
The Dietary Biomarkers Development Consortium represents a transformative initiative in nutritional science, addressing fundamental limitations in dietary assessment through rigorous biomarker discovery and validation. The consortium's systematic three-phase approach, grounded in controlled feeding trials and advanced metabolomic technologies, provides a robust framework for expanding the repertoire of validated dietary biomarkers.
As the DBDC continues to identify and validate biomarkers for an increasing number of foods and dietary patterns, its contributions will significantly advance precision nutrition and enhance our understanding of diet-health relationships. The consortium's commitment to data sharing through publicly accessible databases ensures that its findings will benefit the broader research community and ultimately support the development of more effective, evidence-based dietary recommendations for health promotion and disease prevention.
The Three-Phased Approach to Biomarker Discovery and Validation
The discovery and validation of robust biomarkers are fundamental to advancing nutritional science, particularly in the context of controlled feeding trials. Biomarkers serve as objective indicators of biological processes, pathogenic states, or pharmacological responses to therapeutic intervention, and in nutrition research, they provide crucial insights into dietary exposure, nutritional status, and physiological responses to dietary interventions [20] [21]. The development of these biomarkers follows a structured pathway designed to ensure that the final biomarkers are clinically relevant, reproducible, and actionable.
This pathway is typically described as being divided into three consecutive phases: the discovery phase, the verification phase, and the validation phase [20] [21]. The process is characterized by a funnel approach, where a large number of candidate biomarkers identified in the discovery phase are progressively narrowed down through rigorous, iterative testing to a few analytically validated biomarkers. Within nutrition research, this framework is especially valuable for linking specific dietary patterns, such as those high in ultra-processed foods, to measurable molecular changes, thereby moving beyond traditional self-reported dietary assessment methods [17]. This article details the experimental protocols and considerations for each phase within the specific context of controlled feeding trials for dietary biomarker discovery.
The Three Phases of Biomarker Development
Phase 1: Discovery
The discovery phase is the initial, hypothesis-generating stage focused on the untargeted identification of a large number of candidate biomarkers [20]. In controlled feeding trials, this involves in-depth molecular profiling to pinpoint metabolites or proteins that differ significantly between intervention groups, such as a diet high in ultra-processed foods (UPF-DP) versus an unprocessed diet (UN-DP) [17].
Experimental Protocol for Metabolomic Discovery
- Sample Collection: Biological samples (e.g., EDTA plasma, 24-hour urine, spot urine) are collected from participants at the end of each dietary intervention period in a randomized, crossover, controlled feeding trial [17].
- Sample Preparation: Proteins are precipitated, and samples are diluted appropriately with solvent for analysis.
- Data Acquisition: Profiling is performed using untargeted liquid chromatography coupled with high-resolution tandem mass spectrometry (LC-HRMS/MS). This platform provides accurate mass measurements for putative identification.
- Data Processing: Raw data are processed using software (e.g., Progenesis QI, XCMS) for peak picking, alignment, and normalization. Metabolites are annotated against reference libraries (e.g., Metabolon's library) and authentic standards.
- Statistical Analysis: Data are log2-transformed. Linear mixed models are used to identify metabolites that differ significantly between dietary groups, adjusting for covariates like trial sequence, timepoint, and body weight change. A false discovery rate (FDR) correction is applied.
Table 1: Representative Data from a Discovery Phase Feeding Study [17]
| Sample Type | Total Metabolites Measured | Metabolites Differing Between Diets | Key Differentiating Sub-pathways |
|---|---|---|---|
| Plasma | ~1,000 | 183 | Glutamate metabolism, ascorbate and aldarate metabolism, benzoate metabolism |
| 24-hour Urine | ~1,270 | 461 | Methionine, cysteine, SAM and taurine metabolism, secondary bile acid metabolism, plant-food components |
| Spot Urine | ~1,280 | 68 | Fatty acid dicarboxylate, benzoate metabolism |
Phase 2: Verification
The verification phase focuses on confirming that the abundances of the target candidate biomarkers are consistently and significantly different between the dietary groups using quantitative measurements [20]. This phase acts as a confirmatory step to eliminate false positives from the discovery phase.
Experimental Protocol for Targeted Verification
- Assay Development: Develop a targeted mass spectrometry-based assay, typically using multiple reaction monitoring (MRM) on a triple quadrupole mass spectrometer. This method offers high sensitivity, specificity, and quantitative accuracy for a predefined set of metabolites [20].
- Synthetic Standards: Source or synthesize stable-isotope-labeled internal standards for each candidate biomarker. These are spiked into every sample at a known concentration to correct for sample preparation losses and instrument variability.
- Sample Analysis: Re-analyze a subset of the original samples (or a similar, independent set from the same trial) using the targeted MRM assay. The confident detection is determined by the co-elution and similarity of the MS/MS fragment pattern compared to the synthetic standards [20].
- Data Analysis: Perform power analysis to determine the sample size sufficient to confirm the differential abundance of the candidates. The number of samples in this phase is larger than in discovery and is often in the dozens to hundreds [20].
Table 2: Key Parameters for Biomarker Phases in Feeding Trials
| Parameter | Discovery Phase | Verification/Validation Phase |
|---|---|---|
| Primary Goal | Hypothesis generation; identify candidates | Confirm and quantify candidates |
| Approach | Untargeted profiling | Targeted analysis |
| Typical Platform | LC-HRMS/MS | LC-MRM/MS |
| Number of Analytes | Thousands | Tens to a few hundred |
| Sample Number | Limited (e.g., 20-30 participants) | Dozens to hundreds |
| Statistical Emphasis | Fold-change, multivariate analysis | Power analysis, confidence intervals |
| Use of Internal Standards | Limited | Essential (stable isotope-labeled) |
Phase 3: Validation
The validation phase is the final stage, which confirms the utility and robustness of the biomarker assay by analyzing samples from an expanded or fully independent cohort [20] [21]. The goal is to demonstrate that the biomarker performs reliably in a broader population.
Experimental Protocol for Analytical Validation
- Cohort Selection: Secure a large, independent set of samples from a new controlled feeding trial or an observational study with detailed dietary records. This cohort should represent the target population and include relevant control groups [20].
- High-Throughput Analysis: Perform targeted MS analysis on the large sample set. The analytical method must be optimized for high throughput and robustness.
- Assay Validation: Determine key analytical performance parameters for the biomarker assay, including:
- Precision: Repeatability (within-day variability) and reproducibility (day-to-day variability).
- Accuracy: Recovery of spiked analytes.
- Sensitivity: Limit of detection (LOD) and limit of quantification (LOQ).
- Specificity: Ability to measure the analyte unequivocally in the presence of other components.
- Clinical/Biological Validation: Statistically evaluate the biomarker's performance in classifying the dietary exposure or nutritional status in the new, larger cohort.
The Scientist's Toolkit: Research Reagent Solutions
Successful execution of the three-phase approach relies on a suite of essential reagents and materials. The following table details key solutions for a metabolomics-based dietary biomarker study.
Table 3: Essential Research Reagents for Metabolomic Biomarker Studies
| Research Reagent / Material | Function & Application |
|---|---|
| Stable Isotope-Labeled Internal Standards (e.g., 13C, 15N) | Spiked into samples to correct for matrix effects and analytical variability; essential for accurate quantification in targeted MS (verification/validation) [20]. |
| Authentic Chemical Standards | Pure compounds used to confirm the identity of metabolites by matching retention time and fragmentation spectrum; crucial for annotation in discovery and verification [17]. |
| Quality Control (QC) Pools | A pooled sample created by combining a small aliquot of every sample in the study; analyzed repeatedly throughout the analytical batch to monitor instrument stability and data quality [20]. |
| Standard Operating Procedures (SOPs) | Predefined, step-by-step protocols for sample collection, processing, and analysis; ensures uniformity, quality, and reproducibility across the study [20]. |
| Reference Spectral Libraries (e.g., Metabolon, NIST, HMDB) | Databases of known mass spectra and retention indices used to putatively identify metabolites from untargeted MS data in the discovery phase [17]. |
| Dobutamine | Dobutamine |
| N,N-Dimethylarginine | N,N-Dimethylarginine|ADMA|NOS Inhibitor |
Critical Experimental Design Considerations
Cohort Selection and Statistical Power
Critical to making appropriate inference is the selection of samples representative of both the intervention group and the control population from which the cases are drawn [20]. In controlled feeding trials, proper randomization, crossover designs, and sample matching (e.g., for age, BMI, baseline health status) improve comparative analysis and reduce the number of samples required to achieve proper statistical power [20] [17]. Underpowered studies are a primary cause of failure in biomarker development [20]. A power analysis should be performed before the verification and validation phases to determine the minimum number of samples needed to detect a biologically meaningful fold-change, given the expected technical and biological variability [20].
Blinding, Randomization, and Quality Control
To reduce or eliminate biases due to expectations, both researchers and participants should be blinded to the dietary assignment where possible [20]. The order of sample analysis by MS should be randomized to avoid batch effects. Implementing rigorous quality control (QC) is non-negotiable. This includes using QC pools to monitor instrument performance and applying pre-defined criteria for data cleaning, such as removing metabolites with high rates of missing data or poor measurement precision (e.g., >30% coefficient of variation) [20] [17].
The three-phased approach to biomarker discovery and validation provides a rigorous, structured framework that is directly applicable to controlled feeding trials in nutritional science. By moving from untargeted discovery to targeted verification and final analytical validation, researchers can systematically identify and confirm molecular indicators of dietary intake. Adherence to best practices in experimental design—including careful cohort selection, blinding, randomization, and stringent quality control—is paramount to ensuring that the resulting biomarkers are robust, reproducible, and capable of providing meaningful insights into the relationships between diet and health.
Metabolomics and Bioinformatics as Foundational Technologies
Metabolomics has emerged as a powerful analytical technology for comprehensively characterizing small molecule metabolites in biological systems, providing a direct readout of cellular activity and physiological status. When coupled with bioinformatics, these foundational technologies enable unprecedented insights into metabolic pathways and biological mechanisms. Within nutritional science, metabolomics is particularly valuable for discovering dietary biomarkers that objectively reflect food intake, overcoming limitations of traditional self-reported dietary assessment methods. The integration of controlled feeding studies with advanced computational approaches creates a robust framework for identifying, validating, and implementing biomarkers that accurately track specific dietary patterns and nutritional interventions. This application note details experimental protocols and analytical workflows for applying metabolomics and bioinformatics technologies within controlled feeding trials for dietary biomarker discovery.
Experimental Design for Dietary Biomarker Discovery
Controlled Feeding Trial Framework
The Dietary Biomarkers Development Consortium (DBDC) has established a systematic 3-phase approach for dietary biomarker discovery and validation within controlled feeding studies [15]. This framework ensures rigorous evaluation of candidate biomarkers across varying conditions:
Phase 1: Biomarker Identification
- Administration of test foods in prespecified amounts to healthy participants under controlled conditions
- Metabolomic profiling of blood and urine specimens collected during feeding trials
- Characterization of pharmacokinetic parameters of candidate biomarkers
- Identification of compounds with appropriate sensitivity and specificity
Phase 2: Biomarker Evaluation
- Assessment of candidate biomarkers' ability to identify individuals consuming biomarker-associated foods
- Utilization of controlled feeding studies with various dietary patterns
- Determination of detection thresholds and inter-individual variability
Phase 3: Biomarker Validation
- Evaluation of candidate biomarkers' predictive validity for recent and habitual consumption
- Testing in independent observational settings
- Verification of performance in free-living populations
Sample Size Considerations
Table 1: Recommended Sample Sizes for Controlled Feeding Trials
| Study Phase | Participants | Duration | Control Group | Biological Replicates |
|---|---|---|---|---|
| Phase 1 | 15-30 | 1-3 days | Required | 3-5 collections per subject |
| Phase 2 | 30-50 | 1-2 weeks | Multiple arms | Weekly collections |
| Phase 3 | 100+ | 1-6 months | Required | Pre/post intervention |
Metabolomics Workflow: From Sample to Data
Sample Preparation Protocol
Based on established protocols for global metabolomics by LC-MS, the following procedures ensure high-quality samples for biomarker discovery [22]:
Plasma/Serum Processing:
- Collect blood samples in EDTA-containing tubes
- Centrifuge at 2,000 × g for 15 minutes at 4°C within 30 minutes of collection
- Aliquot plasma/serum into cryovials and store at -80°C
- Deproteinize using ice-cold acetonitrile (2:1 ratio) in 96-well plates
- Centrifuge at 15,000 × g for 15 minutes
- Transfer supernatant for LC-MS analysis
Urine Processing:
- Collect mid-stream urine in sterile containers
- Centrifuge at 10,000 × g for 10 minutes to remove debris
- Aliquot supernatant and store at -80°C
- Dilute 1:5 with ultrapure water prior to analysis
Quality Control Measures:
- Include pooled quality control (QC) samples from all study samples
- Process QC samples throughout analytical batch to monitor instrument performance
- Implement internal standards prior to extraction to account for procedural variability
LC-MS Analysis for Metabolite Profiling
The untargeted metabolomics protocol utilizes liquid chromatography coupled to high-resolution mass spectrometry for comprehensive metabolite coverage [23]:
Chromatographic Conditions: Table 2: LC-MS Parameters for Untargeted Metabolomics
| Parameter | Reverse Phase (C18) | HILIC |
|---|---|---|
| Column | Waters HSS T3 (100×2.1mm, 1.7µm) | BEH Amide (100×2.1mm, 1.7µm) |
| Mobile Phase A | 0.1% formic acid in water | 5mM NHâ‚„OAc, 0.05% FA in water |
| Mobile Phase B | 100% acetonitrile | 100% acetonitrile |
| Gradient | 1-99% B over 15 min | 99-1% B over 15 min |
| Flow Rate | 0.3 mL/min | 0.3 mL/min |
| Column Temperature | 40°C | 40°C |
| Injection Volume | 2-5 μL | 2-5 μL |
Mass Spectrometry Parameters:
- Instrument: High-resolution mass spectrometer (e.g., TripleTOF 5600+, Orbitrap)
- Polarity: Positive and negative ion modes
- Mass Range: 50-1200 m/z
- Source Temperature: 500°C
- Ion Spray Voltage: ±5500 V
- Collision Energy: 10-40 eV
- Data Acquisition: Full scan with information-dependent acquisition (IDA) of MS/MS spectra
Bioinformatics Data Processing Pipeline
Raw Data Processing Workflow
Metabolomics data processing converts raw instrumental data into meaningful biological information through a multi-step computational workflow [24]:
Data Preprocessing Steps:
- Format Conversion: Convert vendor-specific files to open formats (mzML, mzXML) using MSConvert [25]
- Peak Detection: Identify chromatographic peaks using algorithms such as XCMS or MZmine [24]
- Retention Time Correction: Align peaks across samples to correct for retention time shifts
- Peak Alignment: Group corresponding peaks across all samples
- Peak Integration: Quantify peak areas for each metabolite feature
- Compound Identification: Annotate metabolites using accurate mass, MS/MS fragmentation, and database matching
Metabolite Identification and Annotation
Metabolite identification follows the Metabolomics Standards Initiative (MSI) guidelines with four confidence levels [24]:
- Level 1: Identified metabolites (matched to authentic standard using retention time and MS/MS)
- Level 2: Putatively annotated compounds (characteristic fragmentation spectra without RT match)
- Level 3: Putatively characterized compound classes (based on physicochemical properties)
- Level 4: Unknown compounds (distinct m/z signal without annotation)
Key Databases for Metabolite Annotation:
- Human Metabolome Database (HMDB)
- METLIN
- MassBank
- LipidMaps (for lipidomics)
- KEGG (for pathway analysis)
Statistical Analysis and Biomarker Validation
Multivariate Statistical Methods
Statistical analysis identifies differentially abundant metabolites between dietary intervention groups:
Data Preprocessing:
- Normalization using probabilistic quotient normalization or internal standards
- Pareto or unit variance scaling
- Log transformation to approximate normal distribution
Multivariate Analysis:
- Principal Component Analysis (PCA) for unsupervised pattern recognition
- Orthogonal Partial Least Squares-Discriminant Analysis (OPLS-DA) for supervised classification
- Variable Importance in Projection (VIP) scores to identify significant metabolites
Validation Methods:
- Cross-validation (7-fold) to assess model robustness
- Permutation testing (n=200-1000) to prevent overfitting
- Random Forest analysis for feature selection
- Receiver Operating Characteristic (ROC) analysis for diagnostic performance
Biomarker Validation Framework
The statistical framework for biomarker validation in time-course metabolomic data includes [26]:
- Smoothing Splines Mixed Effects (SME) Model: Treats longitudinal measurements as smooth functions of time
- Functional Test Statistic: Detects between-group differences across time points
- Non-parametric Bootstrap: Assesses statistical significance while controlling false discovery rate
Table 3: Statistical Criteria for Biomarker Validation
| Parameter | Threshold | Interpretation |
|---|---|---|
| Fold Change | >1.5 or <0.67 | Biological relevance |
| VIP Score (OPLS-DA) | >1.0 | Contribution to group separation |
| p-value (Mann-Whitney) | <0.05 | Statistical significance |
| FDR | <0.05 | Multiple testing correction |
| AUC (ROC) | >0.8 | Diagnostic performance |
Metabolic Pathway Analysis
Pathway Mapping and Interpretation
Bioinformatics tools enable the interpretation of metabolite changes in the context of metabolic pathways:
Key Metabolic Pathways in Nutritional Studies:
- Tricarboxylic Acid (TCA) Cycle: Central energy metabolism, responsive to carbohydrate intake
- Amino Acid Metabolism: Reflects protein intake and nitrogen balance
- Fatty Acid Metabolism: Indicators of lipid consumption and processing
- Linoleic and α-Linolenic Acid Metabolism: Essential fatty acid status [25]
- Glycerophospholipid Metabolism: Membrane lipid composition
- Bile Acid Metabolism: Gut microbiome-host co-metabolism
The Scientist's Toolkit
Research Reagent Solutions
Table 4: Essential Materials for Metabolomics in Dietary Biomarker Discovery
| Reagent/Material | Function | Example Products |
|---|---|---|
| EDTA Blood Collection Tubes | Prevents coagulation and preserves metabolite stability | BD Vacutainer K2EDTA |
| Mass Spectrometry Grade Solvents | Low contamination mobile phases for LC-MS | Fisher Optima LC/MS, Honeywell LC-MS Grade |
| Stable Isotope Internal Standards | Quantification and quality control | Cambridge Isotopes, Sigma-Isotrace |
| 96-well Protein Precipitation Plates | High-throughput sample preparation | Waters 96-well Protein Precipitation Plates |
| C18 and HILIC Columns | Complementary chromatographic separations | Waters HSS T3, BEH Amide |
| Quality Control Materials | Instrument performance monitoring | NIST SRM 1950 (Metabolites in Plasma) |
| Database Subscriptions | Metabolite identification and pathway analysis | HMDB, METLIN, KEGG |
| Carnitine Chloride | Carnitine Chloride, CAS:461-05-2, MF:C7H16NO3.Cl, MW:197.66 g/mol | Chemical Reagent |
| Paracetamol-d4 | Paracetamol-d4, CAS:64315-36-2, MF:C8H9NO2, MW:155.19 g/mol | Chemical Reagent |
Bioinformatics Software Tools
MetaboAnalystR 4.0 provides a comprehensive pipeline for LC-MS/MS raw spectral processing to functional interpretation [27]. Key features include:
- Auto-optimized peak picking parameters based on regions of interest
- MS/MS spectral deconvolution for DDA and DIA data
- Compound annotation against ~1.5 million MS2 reference spectra
- Functional interpretation via mummichog algorithm for pathway analysis
- Integration with statistical analysis and visualization
Additional Bioinformatics Resources:
- XCMS Online (cloud-based metabolomics data processing)
- MZmine 3 (modular data processing platform)
- CyVerse (cyberinfrastructure for omics data analysis)
- GNPS (Global Natural Products Social Molecular Networking)
Application in Nutritional Research: Case Example
A recent study investigating Generalized Ligamentous Laxity (GLL) demonstrates the application of metabolomics for biomarker discovery [25]. The researchers employed:
- Sample Collection: 65 GLL patients and 35 healthy controls
- Analysis Platform: UPLC-HRMS with positive and negative ionization modes
- Data Processing: XCMS for peak detection and alignment
- Statistical Analysis: OPLS-DA, random forest, and binary logistic regression
- Biomarker Identification: Hexadecanamide (AUC=0.907) as a diagnostic biomarker
- Pathway Analysis: Altered α-linolenic acid and linoleic acid metabolism in GLL
This case study exemplifies the complete workflow from sample collection to biological interpretation, highlighting the power of integrated metabolomics and bioinformatics approaches.
Metabolomics and bioinformatics technologies provide an indispensable foundation for advancing nutritional science through dietary biomarker discovery. The controlled feeding trial framework establishes rigorous conditions for identifying and validating intake biomarkers, while advanced LC-MS platforms enable comprehensive metabolite profiling. Bioinformatics tools transform complex raw data into biologically meaningful information through sophisticated processing algorithms, statistical analysis, and pathway mapping. As these technologies continue to evolve, they will enhance our understanding of diet-health relationships and enable more precise nutritional recommendations and interventions. The integration of standardized protocols, quality control measures, and computational approaches outlined in this application note provides a roadmap for researchers pursuing dietary biomarker discovery.
Designing and Implementing Controlled Feeding Trials: A Methodological Deep Dive
In the field of dietary biomarker discovery, controlled feeding trials are essential for establishing a causal link between dietary intake and measurable biological compounds. The integrity of this research hinges on selecting an appropriate trial design, primarily choosing between parallel and crossover structures. This article details the application, statistical considerations, and practical protocols for these two fundamental designs within the context of nutritional biomarker studies.
Core Design Principles and Comparison
Definition and Rationale
- Parallel Group Design: Participants are randomly allocated to one of two or more treatment groups. Each group receives a different intervention (e.g., a specific diet), and outcomes are measured and compared between these distinct groups at the end of the study period [28] [29].
- Crossover Design: Each participant receives multiple interventions in a sequentially random order, separated by a "washout" period. This design allows for within-participant comparisons, as each individual acts as their own control [30].
The intuitive appeal of the crossover design lies in its increased efficiency, as treatment comparisons are made within patients rather than between different patients [30].
Quantitative Comparison of Design Characteristics
Table 1: Key characteristics of parallel versus crossover designs
| Characteristic | Parallel Design | Crossover Design |
|---|---|---|
| Participant Allocation | Each participant receives only one intervention. | Each participant receives all interventions in sequence. |
| Comparison Type | Between-group comparison. | Within-participant comparison. |
| Sample Size Requirement | Larger for equivalent statistical power. | Smaller; can require approximately half the participants of a parallel trial for the same power [30]. |
| Ethical & Economic Impact | More participants receive a potentially less efficacious treatment; higher cost [30]. | Fewer participants exposed to inferior treatments; lower cost per participant [30]. |
| Primary Concern | Inter-individual variability can obscure treatment effects. | Carryover effects between periods; requires an adequate washout [29]. |
| Risk of Attrition | Lower risk of data loss. | Higher risk; dropouts lead to loss of data for all intervention periods [29]. |
| Suitability for Biomarker Studies | Ideal for long-term interventions or when a washout is impractical (e.g., biomarkers with long half-lives). | Highly efficient for studying short-term metabolic responses to foods [31] [32]. |
Application in Dietary Biomarker Discovery
Empirical Evidence and Concordance
Evidence from meta-analyses shows that crossover designs contribute to evidence in approximately a fifth of systematic reviews. Furthermore, the results from crossover and parallel trials on the same clinical questions tend to agree well (effect sizes correlate at rho = 0.72), although there is a trend for more conservative treatment effect estimates in parallel arm trials [33]. This supports the validity of using the more efficient crossover design in nutritional research.
Design-Specific Considerations for Biomarker Research
- Washout Period Determination: In crossover studies, the washout period must be long enough for the biological effects and biomarkers from the previous dietary intervention to return to baseline. This duration depends on the pharmacokinetics of the target food metabolites [29]. For example, a study investigating urinary metabolite biomarkers may only require a few days between interventions [32], whereas a study examining longer-term adaptations of the gut microbiome may require a much longer washout.
- Minimizing Period Effects: Changes in participant behavior, seasonality, or laboratory procedures over time can introduce period effects. Randomizing the order of interventions helps mitigate this bias.
- Precision and Dietary Collinearity: In whole-diet interventions, changing one dietary component can lead to compensatory changes in others, a problem known as dietary collinearity. Feeding trials, whether parallel or crossover, allow for quantification and control of this collinearity by providing all food to participants [29]. The MAIN Study, which provided all meals to free-living participants, is an excellent example of a design that ensures high adherence and precision for biomarker discovery [32].
Experimental Protocols for Controlled Feeding Trials
Protocol for a Parallel Group Feeding Trial
The following protocol is adapted from the PREVENTOMICS trial, a double-blinded randomized intervention investigating biomarker-based nutrition plans for weight loss [28].
- Participant Recruitment and Screening: Recruit adults meeting specific inclusion criteria (e.g., age 18-65, BMI ≥27 but <40 kg/m²). Exclude individuals with conditions or medications that could interfere with biomarker metabolism, or with disordered eating patterns to ensure safety and compliance [29] [32].
- Baseline Assessment and Randomization:
- Collect baseline data: anthropometrics, blood for clinical chemistry, biospecimens for baseline biomarker levels.
- Assess habitual diet via a 4-day food record or 24-hour recalls.
- Randomize participants in a 1:1 ratio to intervention or control group using a computer-generated sequence.
- Diet Formulation and Delivery:
- Intervention Group: Develop personalized meals based on the participant's metabolic cluster. Meals are prepared and provided for 6 days a week.
- Control Group: Develop standardized meals following general dietary recommendations, matched for energy content.
- Deliver all meals and beverages to participants in a blinded fashion, using similar-looking packaging to maintain blinding.
- Intervention Period:
- The intervention lasts for 10 weeks.
- Provide concomitant behavioral support via electronic push notifications (personalized for the intervention group, generic for the control).
- Outcome Measurement:
- The primary outcome (e.g., change in fat mass) and secondary outcomes (e.g., weight, body composition, fasting blood glucose, lipid profile, inflammatory biomarkers) are measured at the end of the 10-week period.
- Collect biospecimens (blood, urine) for targeted biomarker analysis.
- Statistical Analysis:
- Analyze the effect of the intervention on the primary outcome using linear mixed models, adjusting for baseline values.
Protocol for a Crossover Feeding Trial
This protocol is modeled after the MAIN Study, which was designed to discover and validate urinary metabolite biomarkers of food intake in a real-world context [32].
- Participant Recruitment and Screening: Recruit healthy participants willing to consume provided diets. Exclude based on medical conditions, medications, or high-level athletic activity [32].
- Randomization and Menu Sequence:
- Randomly assign participants to a sequence of menu plans. For example, in a two-period crossover, randomize to sequence A-B or B-A.
- Design menu plans to emulate real-world eating patterns and include target foods for biomarker discovery.
- Intervention Periods and Washout:
- Each experimental period typically lasts 1-3 weeks. The MAIN Study used 3-day menu plans [32].
- Separate periods with an adequate washout (e.g., several days to weeks) to allow biomarker levels to return to baseline.
- Diet Delivery and Consumption:
- Provide participants with all foods and drinks for the duration of each experimental period.
- Participants prepare and consume meals in their own homes as free-living individuals, which increases the real-world applicability of the findings.
- Biospecimen Collection:
- Laboratory and Statistical Analysis:
- Analyze urine samples using mass spectrometry-based metabolomics to identify candidate biomarkers.
- Use linear mixed models for statistical analysis, with participant included as a random effect to account for the within-individual correlation inherent in the crossover design.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential materials and reagents for controlled feeding trials in biomarker discovery
| Item | Function/Application | Example from Literature |
|---|---|---|
| Controlled Diets | Precisely defined interventions to isolate the effect of specific foods or nutrients on biomarker levels. | The Women's Health Initiative Feeding Study provided individually tailored menus to mimic participants' habitual diets [5]. |
| Doubly Labeled Water (DLW) | The gold standard biomarker for total energy expenditure, used to validate energy intake and under-reporting. | Used as an objective recovery biomarker for energy in the WHI feeding study [5]. |
| 24-Hour Urine Collection | Allows for the measurement of urinary recovery biomarkers, such as nitrogen (for protein intake) or specific food metabolites. | Urinary nitrogen was used to calibrate self-reported protein intake [5]. The MAIN Study used spot urine for metabolite discovery [32]. |
| Mass Spectrometry | A core analytical platform for metabolomics, enabling the untargeted or targeted discovery and quantification of dietary biomarkers in biospecimens. | Used to profile urine specimens and identify candidate biomarkers in controlled feeding studies [31] [32]. |
| Validated Biomarker Assays | Commercially available or in-house developed kits for measuring specific nutritional biomarkers (e.g., carotenoids, vitamins, fatty acids). | Serum carotenoids, tocopherols, folate, and vitamin B-12 were evaluated as concentration biomarkers in the WHI cohort [5]. |
| Dietary Assessment Software | Tools for analyzing food records, designing nutritionally balanced menus, and ensuring dietary prescriptions are met. | The Nutrition Data System for Research (NDS-R) and ProNutra software were used in the WHI and MAIN studies [32] [5]. |
| Urethane-d5 | Urethane-d5, CAS:73962-07-9, MF:C3H7NO2, MW:94.12 g/mol | Chemical Reagent |
| Valproic acid-d6 | Valproic acid-d6, CAS:87745-18-4, MF:C8H16O2, MW:150.25 g/mol | Chemical Reagent |
The choice between parallel and crossover designs is a fundamental step in planning a controlled feeding trial for dietary biomarker discovery. While the crossover design offers superior statistical power and efficiency for studying short-term metabolic responses, the parallel design remains the pragmatic choice for long-term interventions or when a sufficient washout cannot be guaranteed. By adhering to the detailed protocols and considerations outlined in this article, researchers can optimize their trial design to robustly discover and validate objective biomarkers that advance the field of precision nutrition.
Domiciled, Partial-Domiciled, and Non-Domiciled Feeding Settings
Controlled feeding trials are a cornerstone of rigorous nutrition science, providing the high intervention accuracy necessary for dietary biomarker discovery [34]. These trials are classified by the degree of control over the participant's environment and food provision, primarily falling into three categories: fully domiciled, partial-domiciled, and nondomiciled settings [34]. The selection of an appropriate feeding setting is a critical methodological decision that directly impacts the precision of dietary exposure assessment, the validity of recovered biomarkers, and the practical execution of the study. This document outlines application notes and detailed protocols for implementing these settings within the specific context of controlled feeding trials for dietary biomarker research.
Comparative Analysis of Feeding Settings
The choice between fully domiciled, partial-domiciled, and nondomiciled settings involves balancing control, practicality, and the specific research objectives related to biomarker discovery. Each setting offers distinct advantages and limitations.
Table 1: Comparative Characteristics of Feeding Trial Settings for Biomarker Research
| Characteristic | Fully Domiciled | Partial-Domiciled | Non-Domiciled |
|---|---|---|---|
| Setting & Control | Participants reside at a research facility (e.g., metabolic chamber) [34]. | Participants consume some/all meals on-site but live at home [34]. | All meals are provided to participants for home consumption [34]. |
| Typical Duration | Short-term (days to a few months) [34]. | Short to medium-term (days to weeks) [34]. | Medium-term (weeks to months) [34]. |
| Intervention Precision | Very high: Direct control over diet, environment, and sample collection [34]. | High: Good control over dietary intake during on-site meals. | Moderate: Relies on participant compliance away from the research facility. |
| Adherence Monitoring | Direct observation and measurement [34]. | Combination of direct observation and self-reporting. | Indirect (e.g., food returns, dietary biomarkers) [34]. |
| Participant Burden | Very high [34]. | Moderate. | Low [34]. |
| Cost & Resources | Very high and logistically demanding [34]. | Moderate. | Lower cost compared to domiciled settings [34]. |
| Blinding Potential | Possible to double-blind [34]. | Possible to double-blind. | Possible to double-blind [34]. |
| Ideal Application in Biomarker Discovery | Proof-of-concept studies; characterizing acute metabolic responses; pharmacokinetic profiling of candidate biomarkers [15]. | Evaluating biomarker stability under semi-free-living conditions; time-restricted feeding studies [34]. | Assessing biomarker performance in near real-world conditions; validating biomarker utility in free-living populations [15]. |
Experimental Protocols for Biomarker Discovery
Protocol 1: Fully Domiciled Feeding for Biomarker Pharmacokinetics
Aim: To identify and characterize the pharmacokinetic parameters of novel dietary biomarkers under conditions of maximal dietary control and intensive monitoring.
Methods:
- Participant Domiciling: House participants in a metabolic research unit for the entire study duration. Provide all meals and beverages, ensuring no other food is consumed [34].
- Dietary Intervention: Administer a precisely controlled test food or diet in a prespecified amount. A crossover design, where participants later receive a control diet, is often advantageous for reducing intra-individual variability [34].
- Sample Collection: Collect longitudinal biospecimens (e.g., blood, urine) at fixed and frequent intervals (e.g., pre-dose, and at 1, 2, 4, 6, 8, 12, and 24 hours postprandially) [15].
- Metabolomic Profiling: Analyze serial blood and urine specimens using high-throughput metabolomics platforms to identify candidate compounds associated with the test food [15].
- Data Analysis: Model the appearance and clearance rates of candidate biomarkers to establish pharmacokinetic curves, including parameters such as T~max~, C~max~, and AUC.
Protocol 2: Partial-Domiciled Feeding for Biomarker Evaluation
Aim: To evaluate the ability of candidate biomarkers to detect consumption of specific foods within complex dietary patterns.
Methods:
- Meal Provision: Provide participants with all meals, requiring them to consume at least one main meal per day (e.g., breakfast and dinner) under supervision at the research facility [34].
- Dietary Patterns: Implement controlled feeding studies of various dietary patterns that either include or exclude the biomarker-associated foods [15].
- Biospecimen Collection: Collect non-fasting spot urine samples or first-morning voids daily at the research facility. Schedule periodic fasting blood draws.
- Adherence Monitoring: Use provided food checklists for off-site meals and verify adherence through returned food containers and objective biomarker levels where available [34].
- Biomarker Validation: Analyze biospecimens for candidate biomarkers to determine their sensitivity and specificity for identifying recent consumption of the target food within a mixed diet [15].
Protocol 3: Non-Domiciled Feeding for Biomarker Validation
Aim: To validate the utility of candidate biomarkers for predicting recent and habitual consumption of specific test foods in an independent, free-living observational setting [15].
Methods:
- Home-Delivered Diet: Prepare and deliver all meals and snacks to participants for consumption at home, following a standardized menu [34].
- Free-Living Observation: Allow participants to maintain their normal daily routines while adhering to the provided diet.
- Biospecimen Collection: Instruct participants to collect first-morning urine voids or 24-hour urine samples at home using provided kits. Schedule clinic visits for blood collection.
- Dietary Assessment: Employ a combination of provided food checklists and 24-hour dietary recalls to cross-verify self-reported adherence against biomarker levels [35].
- Predictive Modeling: Use statistical models to assess the validity of candidate biomarkers to predict the intake of the target foods, correcting for potential confounders such as BMI, age, and gut microbiota composition.
Visual Workflows for Experimental Execution
Feeding Trial Workflow
Biomarker Validation Pathway
The Scientist's Toolkit: Key Research Reagents & Materials
Table 2: Essential Materials for Controlled Feeding Trials in Biomarker Research
| Item Category | Specific Examples | Function & Application |
|---|---|---|
| Biospecimen Collection | EDTA tubes (blood), Urine collection cups (sterile), Salivettes, Home 24-hour urine collection kits | Standardized collection of biological samples for subsequent metabolomic analysis to identify and quantify dietary biomarkers [35]. |
| Sample Processing & Storage | Portable centrifuge, Cryogenic vials, Liquid nitrogen or -80°C freezer | Preparation and long-term preservation of biospecimens to maintain biomarker integrity before batch analysis [15]. |
| Metabolomic Analysis | LC-MS/MS systems, NMR spectroscopy platforms | High-throughput, untargeted, and targeted identification and quantification of small molecule metabolites (candidate biomarkers) in biospecimens [15]. |
| Diet Preparation | Metabolic kitchen, Precision scales, Standardized recipe software | Ensures exact replication of dietary interventions, precise portioning, and consistent nutrient composition across all participants, which is critical for linking intake to biomarker levels [34]. |
| Adherence Monitoring | Food checklists, Weighed food records, Returned food containers | Provides measures of participant compliance with the feeding protocol, essential for interpreting biomarker data and ensuring internal validity [34]. |
| Data Management | Laboratory Information Management System (LIMS), Electronic Data Capture (REDCap) software | Securely manages and organizes vast amounts of data generated from dietary intake, biomarker assays, and participant information [35]. |
| Piribedil D8 | Piribedil D8|Deuterated Dopamine Agonist | Piribedil D8 is a deuterium-labeled internal standard for Parkinson's disease research. This product is for Research Use Only and is not for diagnostic or therapeutic use. |
| Vasicinol | Vasicinol, CAS:5081-51-6, MF:C11H12N2O2, MW:204.22 g/mol | Chemical Reagent |
Menu Design and Nutritional Standardization with Linear Programming
In controlled feeding trials for dietary biomarker discovery, researchers provide participants with all meals for a prescribed period to precisely control nutrient intake and establish cause-effect relationships between diet and measurable metabolic outcomes [36]. A core challenge in this research is designing menus that simultaneously meet rigorous nutritional standards, ensure sufficient contrast in nutrients under investigation between intervention groups, and remain practical for daily implementation [36] [37]. *Linear programming (LP) and its extension, *mixed integer linear programming (MILP), have emerged as powerful computational tools to overcome this challenge, enabling the generation of nutritionally precise, cost-effective, and varied menus in a fast, objective, and reproducible manner [36] [38].
Key Applications in Nutritional Research
Designing Menus for Controlled Feeding Trials
LP methods support the design of individualized, isoenergetic menus for controlled feeding trials, ensuring all menus comply with strict trial standards [36]. This approach allows researchers to impose tight ranges on nutrient composition and manage complex design features, such as ensuring key nutrient levels differ sufficiently between intervention groups (e.g., high vs. low protein) while remaining similar for all energy levels within the same group [36]. The model excels at managing numerous energy levels and nutrients simultaneously, proposing alternative menus, and adapting to last-minute disruptions, thereby greatly facilitating the design procedure and lowering development costs [36].
Optimizing Institutional Menu Formulation
MILP has been successfully applied to develop nutritionally optimized menus for institutional foodservices, such as the Workers' Food Program in Brazil [38]. The model generates daily menus that meet specific nutritional recommendations while minimizing cost and maintaining quality aspects like variety, color combination, texture, and spacing of dish repetitions to avoid monotony [38]. This formulation considers typical eating habits and ensures the provision of healthy, nutritionally balanced meals over a full month, complying with national dietary guidelines that prioritize minimally processed foods [38].
Experimental Protocols and Methodologies
Core Mathematical Model Formulation
The foundation of menu optimization relies on establishing a mathematical model with clear objective functions and constraints. A typical MILP model for menu formulation uses binary variables to indicate whether each preparation is present on each day over the planning period [38].
Key Model Components:
- Objective Function: Minimize overall cost while respecting nutritional requirements and eating habits [38]
- Decision Variables: Binary variables representing the selection of specific food preparations or dishes
- Constraints: Nutritional requirements, cost limits, frequency of dish repetition, and sensory attributes
Implementation Workflow:
Diet Standardization and Validation Protocol
The DELTA program established a comprehensive protocol for diet standardization and validation in multicenter controlled feeding trials [37]:
Diet Standardization: Central procurement of fat-containing foods, use of standard ingredients, precision weighing of foods (especially sources of fat and cholesterol), and implementation of standardized written procedures across all centers [37]
Menu Validation: Pre-study chemical validation where duplicate sets of menus are prepared and chemically assayed to verify compliance with nutrient specifications [37]
Continuous Monitoring: Throughout the study, ongoing sampling and assay of diets to ensure nutrient target goals are met and maintained [37]
Statistical Analysis: Comparison of chemically analyzed nutrient compositions with target specifications using means and standard errors [37]
Nutritional Adequacy Assessment
The nutritional adequacy of generated menus should be verified against established standards:
Table 1: Nutritional Composition Targets for Optimized Menus
| Nutrient | Target Range | Application Context | Reference |
|---|---|---|---|
| Energy | 716.97 kcal/meal average | Workers' Food Program | [38] |
| Carbohydrates | 58.28% of energy/meal | Workers' Food Program | [38] |
| Proteins | 17.89% of energy/meal | Workers' Food Program | [38] |
| Total Fats | 24.88% of energy/meal | Workers' Food Program | [38] |
| Saturated Fatty Acids | 5-16% of energy | DELTA Program | [37] |
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials and Computational Tools for Menu Optimization Research
| Item | Function/Application | Implementation Context |
|---|---|---|
| Mixed Integer Linear Programming Framework | Core optimization engine for menu generation | Formulating daily menus that meet nutritional constraints [38] |
| Standardized Food Composition Database | Provides nutritional profiles of ingredients | Accurate calculation of nutrient content in menu plans [38] |
| Controlled Diet Software | Supports diet design and nutrient analysis | Implementing adjustable fortification protocols [39] |
| Chemical Assay Kits | Validates nutrient composition of prepared menus | Pre-study menu validation and continuous monitoring [37] |
| Precision Weighing Systems | Ensures accurate ingredient measurement | Standardized food preparation across multiple centers [37] |
| (+)-Eudesmin | (+)-Eudesmin, CAS:526-06-7, MF:C22H26O6, MW:386.4 g/mol | Chemical Reagent |
| Nyasol | Nyasol, CAS:96895-25-9, MF:C17H16O2, MW:252.31 g/mol | Chemical Reagent |
Advanced Implementation Framework
The relationship between model components, constraints, and outcomes in menu optimization can be visualized as an integrated system:
Application in Specialized Clinical Trials
The nutrIMM study exemplifies the application of controlled feeding trial methodologies in specialized populations, investigating immune function in obesity and type 2 diabetes [40]. This single-centre, non-randomized, four-arm, parallel-group, controlled feeding trial assigns participants to consume a standard North American-type diet for 4 weeks, with primary outcomes including plasma concentration of C-reactive protein and ex-vivo interleukin-2 secretion upon T-cell stimulation [40]. Such studies demonstrate how standardized menu design enables researchers to dissect the impact of specific physiological factors (e.g., excess body fat, dysglycemia) independent of dietary intake variations [40].
Linear programming and mixed integer linear programming provide robust methodological frameworks for addressing the complex challenge of menu design and nutritional standardization in controlled feeding trials. These computational approaches enable researchers to generate menus that simultaneously satisfy multiple nutritional, sensory, economic, and practical constraints while maintaining scientific rigor. The implementation of standardized protocols for diet validation and continuous monitoring ensures compliance with nutritional targets throughout study periods. As dietary biomarker discovery research advances, these optimization methodologies will play an increasingly vital role in ensuring the precision, reproducibility, and efficiency of controlled feeding studies across diverse populations and research contexts.
Accurate dietary assessment is fundamental to nutritional epidemiology, yet traditional self-reporting tools like food frequency questionnaires (FFQs) are prone to systematic measurement errors and participant biases [35] [41]. Metabolomic profiling of biospecimens, particularly blood and urine, provides an objective methodology for discovering dietary exposure biomarkers, thereby strengthening research on diet-disease relationships [15] [42]. The Dietary Biomarkers Development Consortium (DBDC) represents a major coordinated effort to discover and validate biomarkers for foods commonly consumed in the United States diet through a structured 3-phase approach involving controlled feeding trials [15] [7]. The quality of biospecimen collection, processing, and storage is paramount in these studies, as pre-analytical variations can significantly impact metabolomic profiles and compromise data integrity [43] [44]. This protocol outlines standardized procedures for blood and urine collection, processing, and storage optimized for metabolomic analyses in dietary biomarker discovery research.
Standardized Protocols for Biospecimen Collection
Pre-Collection Participant Management and Standardization
Controlling for inter- and intra-individual variability is critical for obtaining reliable metabolomic data. Key pre-collection protocols include:
- Standardized Evening Meal: Participants should consume a standardized "metabolically neutral" evening meal low in plant polyphenols 12-14 hours before biospecimen collection. This meal should be acceptable to a wide range of volunteers and easy to replicate across study periods [43] [45].
- Behavioral Restrictions: Participants should avoid alcohol consumption, strenuous physical activity, and use of medications or supplements for 24-48 hours prior to sample collection, depending on study requirements [43] [44].
- Fasting Period: A minimum 12-hour overnight fast (water permitted) should be observed prior to blood collection to establish a stable metabolic baseline [43].
Blood Collection and Processing Protocol
Table: Blood Collection and Processing Parameters for Metabolomic Analysis
| Parameter | Specification | Rationale |
|---|---|---|
| Collection Tube | EDTA plasma tubes (preferred) | Inhibits coagulation; preserves metabolite integrity [44] |
| Collection Time | Morning (after overnight fast) | Minimizes diurnal variation [43] |
| Processing Temperature | 4°C | Stabilizes thermolabile metabolites [44] |
| Centrifugation | 2,500-3,000 × g for 10-15 minutes | Efficient cell separation without cell lysis [44] |
| Aliquot Volume | 100-500 µL | Minimizes freeze-thaw cycles [44] |
| Storage | -80°C | Preserves long-term metabolite stability [44] |
Detailed Procedure:
- Perform venipuncture using appropriate gauge needle (typically 21G) and collect blood into pre-chilled EDTA tubes.
- Gently invert tubes 8-10 times to ensure proper mixing with anticoagulant.
- Place tubes immediately on wet ice and process within 30 minutes of collection.
- Centrifuge at 2,500-3,000 × g for 10-15 minutes at 4°C.
- Carefully transfer plasma supernatant to pre-labeled cryovials using sterile pipettes, avoiding disturbance of the buffy coat.
- Flash-freeze aliquots in dry ice or liquid nitrogen before transfer to -80°C freezer for long-term storage.
- Document all processing times and any deviations from protocol.
Urine Collection and Processing Protocol
Table: Urine Collection Schemes for Dietary Metabolomic Studies
| Collection Type | Timing | Advantages | Limitations |
|---|---|---|---|
| First-Void Morning | Upon waking | Concentrated; reflects overnight metabolism [42] | Influenced by previous evening's intake |
| Spot Collection | Fasted or postprandial (2-4h) | Convenient; captures acute dietary responses [43] | Requires normalization for dilution |
| Timed Pooled | Overnight (e.g., 8-12h) | Integrates over longer period; better for habitual intake [45] | Compliance challenges |
| 24-Hour Collection | Full day | Gold standard for quantitative measures [42] | Burdensome; potential collection errors |
Detailed Procedure:
- Provide participants with pre-labeled collection containers containing preservative if required (e.g., sodium azide for microbial inhibition).
- For timed collections, instruct participants to discard first morning void then collect all subsequent urines for specified period, including next first-morning void.
- For spot collections, collect mid-stream urine into sterile containers.
- Record total volume and collection duration for timed specimens.
- Aliquot 1-2 mL samples into cryovials after gentle mixing.
- Centrifuge at 2,000 × g for 10 minutes to remove particulates if needed.
- Flash-freeze aliquots and store at -80°C within 4 hours of collection completion.
- Document collection start/end times, total volume, and any protocol deviations.
Quality Control and Sample Integrity Assessment
Quality Control Samples
Incorporating quality control (QC) samples throughout the collection and analysis process is essential for data quality:
- Pooled QC: Create a pooled sample from aliquots of all study samples for monitoring instrument performance [44].
- Reference QC: Use commercial reference plasma/serum as external control [44].
- Blank Samples: Include phosphate-buffered saline or water blanks to monitor contamination.
- Technical Replicates: Process and analyze a subset of samples in duplicate to assess technical variability.
Assessment of Pre-Analytical Variables
Table: Quality Markers for Assessing Plasma Sample Integrity [44]
| Marker Category | Specific Metabolites | Direction of Change in Compromised Samples | Biological Interpretation |
|---|---|---|---|
| Energy Metabolism | Glucose, Succinic acid | Decreased | Glycolysis continues ex vivo |
| Cell Membrane Turnover | Lysophospholipids | Increased | Enzymatic degradation of phospholipids |
| Protein Degradation | Dipeptides | Increased | Proteolytic activity |
| Oxidative Stress | Fatty acids | Variable | Lipid peroxidation |
| Cell Lysis | Amino acids | Increased | Cellular breakdown |
Monitoring these quality markers allows researchers to evaluate sample quality and identify potentially compromised specimens before extensive metabolomic analysis.
Analytical Workflow and Data Processing
Metabolomic Analysis Platforms
The two primary analytical platforms for metabolomic analysis in dietary biomarker studies are:
Liquid Chromatography-Mass Spectrometry (LC-MS):
Nuclear Magnetic Resonance (NMR) Spectroscopy:
Data Preprocessing and Normalization
Urine Normalization Strategies:
- Creatinine Correction: Traditional approach but limited by intra-individual variation [42]
- Urine Volume: Effective for 24-hour collections [43]
- Specific Gravity: Accounts for urinary concentration [42]
- Probabilistic Quotient Normalization: Mathematical approach to account for dilution effects [44]
Plasma/Serum Normalization:
- Quality Control-Based Normalization: Using pooled QC samples to correct for instrumental drift [44]
- Internal Standard Normalization: Using added stable isotope-labeled compounds [44]
Experimental Workflow for Dietary Biomarker Discovery
The Scientist's Toolkit: Essential Research Reagents and Materials
Table: Essential Research Reagents and Materials for Biospecimen Metabolomics
| Category | Specific Items | Application/Function |
|---|---|---|
| Collection Materials | EDTA blood collection tubes, Sterile urine containers, Sodium azide, Cryovials with O-rings | Biospecimen collection and primary storage |
| Sample Processing | Methanol (LC-MS grade), Acetonitrile (LC-MS grade), Formic acid, Ammonium hydroxide, Deproteinization plates (e.g., Sirocco), 96-well plate formats | Sample preparation for metabolomic analysis |
| Internal Standards | Stable isotope-labeled compounds (e.g., amino acids, fatty acids, sugars), Instrument performance standards | Quality control and quantification |
| Analytical Consumables | UHPLC columns (C18, HILIC), Syringes, Vials, Liners, Mobile phase filters | LC-MS analysis |
| Quality Control | Commercial reference plasma (e.g., Human Sterile Plasma), Pooled quality control samples, Blank matrices | Monitoring analytical performance |
| Angiotensin Ii | Angiotensin Ii, CAS:11128-99-7, MF:C50H71N13O12, MW:1046.2 g/mol | Chemical Reagent |
Applications in Dietary Biomarker Discovery
The DBDC's phased approach to biomarker development provides a framework for utilizing these biospecimen collection protocols [15] [7]:
- Phase 1 (Discovery): Controlled feeding trials with prescribed test foods followed by metabolomic profiling of blood and urine to identify candidate biomarkers and characterize their pharmacokinetics [15].
- Phase 2 (Evaluation): Assessment of candidate biomarkers' ability to identify consumption of specific foods using controlled feeding studies with various dietary patterns [15].
- Phase 3 (Validation): Evaluation of candidate biomarkers' predictive validity for recent and habitual food consumption in independent observational settings [15].
Analytical Process from Sample to Biomarker
Standardized protocols for blood and urine collection are fundamental to generating high-quality metabolomic data for dietary biomarker discovery. Implementation of rigorous pre-collection participant management, careful attention to sample processing parameters, comprehensive quality control measures, and appropriate data normalization strategies significantly enhances the reliability and reproducibility of metabolomic studies. These standardized protocols support the discovery and validation of robust dietary biomarkers that can advance nutritional epidemiology and precision nutrition research by providing objective measures of dietary exposure complementary to traditional self-reported assessment methods.
Application Note: Operational Infrastructure for Controlled Feeding Trials
Controlled feeding trials are fundamental to advancing precision nutrition, particularly in the discovery and validation of dietary biomarkers. These trials require a sophisticated operational infrastructure that integrates consortium models for large-scale collaboration and specialized core facilities for technical execution. This framework ensures the methodological rigor, reproducibility, and high-dimensional data generation necessary to objectively measure dietary exposures and their physiological effects.
The Dietary Biomarkers Development Consortium (DBDC) exemplifies this approach, implementing a structured, multi-phase strategy to identify and validate biomarkers for foods commonly consumed in the United States diet [15]. This consortium model leverages shared protocols, resources, and data to overcome the traditional challenges of dietary assessment. The execution of its complex feeding trials is facilitated by specialized research cores, which provide centralized access to state-of-the-art instrumentation, expert personnel, and standardized services [47] [48]. These cores, which can include metabolomics, biomarker analysis, and clinical trials units, function as recharge centers, offering cost-efficient and consistent support to investigators [48]. This synergistic relationship between consortium models and specialized cores creates an optimized ecosystem for conducting domiciled and non-domiciled feeding trials, ultimately accelerating the discovery of biomarkers that can clarify the role of diet in health and disease [15] [49].
Experimental Protocols
Protocol 1: Three-Phase Biomarker Discovery and Validation (DBDC Framework)
This protocol outlines the core methodology employed by the Dietary Biomarkers Development Consortium for the systematic discovery and validation of dietary biomarkers using controlled feeding trials [15].
1. Purpose To identify, evaluate, and validate sensitive and specific biomarkers of intake for specific foods and dietary patterns through a phased, controlled feeding approach.
2. Experimental Workflow
Phase 1: Biomarker Identification
- Design: Controlled feeding trials where specific test foods are administered in prespecified amounts to healthy participants.
- Procedure: Collect blood and urine specimens at predetermined time points following food consumption.
- Analysis: Perform untargeted metabolomic profiling on biospecimens to identify candidate biomarker compounds. Characterize the pharmacokinetic parameters of these candidates [15].
Phase 2: Biomarker Evaluation
- Design: Controlled feeding studies utilizing various dietary patterns.
- Procedure: Evaluate the ability of candidate biomarkers (identified in Phase 1) to correctly classify individuals consuming the biomarker-associated foods against a background of different diets [15].
Phase 3: Biomarker Validation
- Design: Independent observational studies.
- Procedure: Assess the validity of candidate biomarkers for predicting recent and habitual consumption of specific test foods in free-living populations [15].
3. Data Management All data generated across all phases, including metabolomic profiles and associated metadata, are archived in a publicly accessible database to serve as a resource for the broader research community [15].
Protocol 2: Implementation of a Domiciled Controlled Feeding Trial
This protocol details the key steps for designing and conducting a domiciled feeding trial, which provides the highest level of dietary control for proof-of-concept and mechanistic studies [50] [49].
1. Purpose To precisely evaluate the effects of a known quantity of a food, nutrient, or dietary pattern on physiological outcomes by providing all meals to participants in a residential setting.
2. Experimental Workflow
Step 1: Menu Design and Development
Step 2: Participant Selection and Weight Maintenance
- Define a study population that maximizes retention, safety, and generalizability.
- Determine individual energy requirements for each participant. Throughout the study, adjust diet portions as required, most often for the purpose of weight maintenance [50].
Step 3: Diet Preparation and Delivery
Step 4: Biospecimen Collection and Analysis
Data Presentation
Table 1: Overview of the three-phase feeding trial design for dietary biomarker development as implemented by the DBDC [15].
| Phase | Primary Objective | Study Design | Key Deliverables |
|---|---|---|---|
| Phase 1: Discovery | Identify candidate biomarker compounds | Controlled feeding of test foods with metabolomic profiling | Candidate biomarkers with pharmacokinetic data |
| Phase 2: Evaluation | Assess specificity of candidates across diets | Controlled feeding of various dietary patterns | Evaluation of classification accuracy |
| Phase 3: Validation | Confirm predictive value in free-living populations | Independent observational studies | Validated biomarkers for recent and habitual intake |
Research Reagent Solutions for Feeding Trials and Metabolomics
Table 2: Essential materials and reagents used in controlled feeding trials and subsequent biomarker analysis.
| Item | Function/Application |
|---|---|
| Research Diets | Precisely formulated meals designed to test specific dietary interventions while controlling for confounding nutrients [50] [49]. |
| Standard Reference Materials | Certified materials used to validate the accuracy of menu chemical analysis and calibrate laboratory equipment [50]. |
| LC-MS/MS Metabolomics Platforms | High-resolution mass spectrometry systems for untargeted and targeted profiling of metabolite changes in blood and urine in response to dietary interventions [15]. |
| Stable Isotope Tracers | Labeled compounds (e.g., 13C) used to track the metabolic fate of specific nutrients or food components within the body. |
| Biospecimen Collection Kits | Standardized kits for the consistent collection, processing, and storage of blood (serum, plasma) and urine samples to preserve biomarker integrity. |
Workflow Visualization
Dietary Biomarker Discovery
Specialized Cores in Research
Overcoming Practical Challenges in Feeding Trial Execution
Optimizing Participant Adherence and Retention Strategies
High participant adherence and retention are fundamental to the scientific integrity of controlled feeding trials, especially in dietary biomarker discovery research. These trials, which involve providing most or all food to participants, are the gold standard for establishing proof-of-concept and understanding the physiological effects of specific dietary interventions [34]. Unlike dietary counseling trials, feeding studies offer high intervention precision and enable the design of blinded placebo controls, but they come with significant participant burden that can threaten adherence and retention if not carefully managed [34]. Successfully maintaining participant involvement ensures accurate assessment of biomarker-diet relationships and enhances the validity of findings that inform precision nutrition. This document provides detailed application notes and protocols to optimize these critical aspects in the context of controlled feeding trials for dietary biomarker research.
Protocol Design for Enhanced Adherence
The foundation of strong adherence and retention is laid during the initial planning and design phase of the trial. Strategic decisions about the study population, intervention structure, and participant communication significantly influence long-term engagement.
Study Population and Setting
- Inclusion and Exclusion Criteria: Develop criteria that are stringent enough to ensure the research question can be answered but general enough to maintain some real-world applicability. Key exclusion criteria should encompass eating disorders, inability to consume the diet provided, food allergies, and severe food intolerances [34].
- Trial Setting Selection: Choose a setting that balances control, participant burden, and cost:
- Fully Domiciled: Participants reside at a research facility. This offers the highest control over dietary intake and environmental factors but has the highest participant burden [34].
- Non-Domiciled: Participants collect provided meals for consumption at home. This is more practical and less burdensome, making longer study durations feasible, though it requires robust methods to monitor and support remote adherence [34].
Intervention and Control Design
- Dietary Intervention Design: The diet should be developed and validated by a qualified dietitian or clinical nutrition researcher. It is crucial to design menus that fit within the target population's typical energy requirements and cultural food preferences to enhance acceptability [34].
- Control Diet Design: When possible, design the control diet as a placebo. The double-blind nature of feeding trials makes this feasible and is a key advantage over counseling studies. A successful placebo control minimizes expectation bias [34].
- Informed Consent Process: Employ a transparent yet strategic consent process. Within ethical boundaries, consider limited disclosure of research aims to protect blinding. Always show prospective participants a sample menu to help them make an informed decision about participation and clearly state all restrictions, such as limitations on travel or consumption of non-study foods [34].
Monitoring and Measuring Adherence
Objective and subjective measures are required to accurately assess participant adherence, which is critical for interpreting the relationship between dietary exposure and biomarker levels.
Adherence Metrics
Establish and report adherence targets and measurement methods a priori. The following table summarizes primary methods for monitoring adherence in feeding trials.
Table 1: Methods for Monitoring Adherence in Controlled Feeding Trials
| Method | Description | Application Context | Key Considerations |
|---|---|---|---|
| Objective Dietary Biomarkers | Measurement of compounds in biological samples (e.g., blood, urine) that reflect intake of specific foods or nutrients [15]. | All feeding trials, but especially critical for biomarker discovery and validation research. | Provides objective, quantitative data. Metabolomic profiling is a key technology for discovering novel biomarkers [15]. |
| Weighed Food Records | Participants weigh and record any uneaten food items. | Most applicable to non-domiciled trials [34]. | Relies on participant compliance but provides quantitative data. |
| Direct Observation | Research staff directly observe and record food consumption. | Primarily used in fully or partial-domiciled settings [34]. | Provides the highest level of accuracy but is resource-intensive. |
| Food and Drink Checklists | Simplified forms for participants to quickly check off consumed items. | Non-domiciled trials to minimize participant burden [34]. | Easier for participants but less detailed than weighed records. |
| Returned Food Containers | Weighing or visual inspection of uneaten food returned by participants. | Non-domiciled trials. | A simple, practical measure of compliance. |
Adherence and Retention Strategies
Proactive and multi-faceted strategies are essential to prevent non-adherence and dropout. The following workflow outlines a comprehensive strategy from enrollment to study completion.
The strategies visualized above can be implemented as follows:
Pre-Trial Strategies:
- Careful Screening and Run-In Periods: Screen participants during enrollment to identify those most likely to complete the study. Using a run-in period where participants follow the study protocol before randomization can help exclude those who are unable or unwilling to adhere [51].
- Transparent Communication: Fully inform participants of the study burden, explain the randomization process, and determine their prior history with similar interventions. This manages expectations and builds trust [51].
In-Trial Support Systems:
- Reminders and Human Support: Reminders (e.g., for meal pick-ups) and human support (e.g., regular check-ins from staff) are evidence-based strategies that significantly reduce dropout rates, as demonstrated in digital health trials [52]. This principle is directly applicable to feeding studies.
- Flexibility and "Free Foods": Offer flexible meal pick-up times and provide a list of "free foods" (e.g., water, certain low-energy vegetables) that participants can consume ad libitum. This helps participants with higher energy needs feel satiated and reduces the sense of restriction [34].
- Participant Safeguards: Incorporate both physical safeguards (e.g., physician approval for high-risk patients, regular body weight monitoring) and mental safeguards (e.g., regular mental health monitoring) to ensure participant safety and well-being throughout the trial [34].
Post-Trial and Retention Activities:
- Long-Term Follow-up: For long-term studies, such as the 14-year follow-up of a maternal choline feeding trial, use flexible methods like remote cognitive testing to maximize retention when participants have relocated [53]. This study successfully retained 80% of its original cohort.
- Feedback and Results: Solicit participant feedback on diet tolerability and acceptability. Sharing aggregate study results with participants after the trial's conclusion acknowledges their valuable contribution.
Application to Dietary Biomarker Discovery
In the specific context of dietary biomarker discovery, participant adherence is not just a methodological concern but is central to the scientific objective. The Dietary Biomarkers Development Consortium (DBDC) employs a phased approach to discover and validate intake biomarkers, a process that fundamentally depends on precise dietary control in feeding trials [15].
- Phase 1 - Biomarker Identification: Controlled feeding trials administer test foods in prespecified amounts to healthy participants. Metabolomic profiling of blood and urine specimens collected during these trials is used to identify candidate biomarker compounds. High participant adherence in this phase is essential to ensure that the metabolomic signatures accurately reflect the intended dietary exposure and are not confounded by non-study foods [15].
- Phase 2 - Biomarker Evaluation: The ability of candidate biomarkers to identify individuals consuming the target foods is evaluated using controlled feeding studies of various dietary patterns. Consistent adherence allows researchers to assess the specificity and sensitivity of the biomarkers across different dietary backgrounds.
- Phase 3 - Biomarker Validation: The validity of candidate biomarkers is assessed in independent observational settings. Data on adherence from the earlier phases informs the interpretation of biomarker levels in free-living populations.
Without high adherence in the initial controlled trials, the discovered biomarkers may be imprecise or non-specific, leading to flawed tools for assessing dietary intake in future research and clinical practice.
The Scientist's Toolkit
The following table details key resources and methodologies essential for implementing the adherence and retention strategies outlined in this protocol.
Table 2: Research Reagent Solutions for Adherence and Retention
| Tool / Resource | Function in Protocol | Application Notes |
|---|---|---|
| Qualified Dietitian/ Nutrition Scientist | Designs nutritionally adequate, culturally appropriate, and palatable diets; validates menus. | Critical from the planning stage through to analysis. Ensures diets are acceptable and meet study targets [34]. |
| Metabolomics Platform | Enables high-throughput profiling of blood/urine to discover objective biomarkers of dietary adherence. | Used to identify candidate intake biomarkers and objectively verify participant compliance in a blinded manner [15]. |
| Electronic Participant Tracking System | Logs participant contact, meal pick-ups, adherence data, and schedule for follow-ups. | A systematic tracking system is a core strategy for enhancing adherence and managing longitudinal follow-up [51]. |
| Standardized Tolerability & Acceptability Questionnaires | Quantifies participant perception of the diet (e.g., palatability, gastrointestinal effects). | Provides critical data on real-world applicability and identifies potential causes of non-adherence [34]. |
| Remote Assessment Technologies (e.g., CANTAB Connect, Videoconferencing) | Facilitates cognitive testing and follow-up data collection from participants who cannot visit the site. | Proven to enable high (80%) long-term retention in multi-year follow-up studies [53]. |
| Blinded and Unblinded Research Staff | Separate staff handle diet preparation/delivery (unblinded) and participant interaction/assessment (blinded). | Maintains the integrity of double-blinding, a key advantage of feeding trials, to minimize bias [34]. |
Menu Design Complexities and Computational Optimization Solutions
The accurate discovery and validation of dietary biomarkers rely fundamentally on the precision of dietary exposure control in feeding trials. Menu design for these studies presents significant complexities, requiring meticulous nutritional composition management, individual adherence monitoring, and mitigation of confounding factors, all while accommodating diverse dietary patterns and participant preferences. Computational optimization approaches provide essential methodologies for addressing these challenges, enabling the rigorous dietary control necessary for advancing precision nutrition research. This document details the application notes and experimental protocols for implementing these solutions within the context of controlled feeding trials for dietary biomarker discovery.
Quantitative Landscape of Dietary Biomarker Research
Current research has identified numerous candidate urinary metabolites as potential biomarkers for various food groups. The following table synthesizes findings from a recent systematic review (2000-2022) quantifying the evidence base for these biomarkers [35].
Table 1: Urinary Metabolites as Biomarkers of Dietary Intake: Evidence from a Systematic Review
| Food Group / Item | Number of Identified Studies | Key Candidate Biomarker Classes | Distinguishing Capability |
|---|---|---|---|
| Fruits | 13 | Polyphenols, Organic Acids | Distinguishes broad groups (e.g., citrus) |
| Vegetables | 5 | Sulfurous Compounds (e.g., from cruciferous) | Distinguishes broad groups (e.g., cruciferous) |
| Soy | 10 | Isoflavones (e.g., Daidzein, Genistein) | Good for specific soy foods |
| Coffee/Cocoa/Tea | 9 | Alkaloids (e.g., Caffeine), Polyphenols | Good for specific items |
| Alcohol | 6 | Ethyl Glucuronide, Ethyl Sulfate | Good for specific items |
| Grains/Fiber | 5 | Dietary Fiber Metabolites (e.g., Arabinitol) | Distinguishes whole grains |
| Dairy | 3 | Galactose Derivatives, Calcium | Distinguishes dairy intake |
| Meat & Proteins | 6 | Amino Acid Metabolites (e.g., 1-Methylhistidine) | Potential for protein sources |
| Nuts/Seeds | 3 | Specific Fatty Acid Metabolites | Emerging evidence |
| Sugar & Sweeteners | 4 | Sucrose, Artificial Sweetener Excretion | Good for specific sweeteners |
| Aromatics | 5 | Volatile Compound Metabolites | Good for specific items (e.g., garlic) |
The data demonstrates that urinary biomarkers are particularly effective for discerning intake of plant-based foods, often through their characteristic polyphenol profiles, and for specific compounds like those in coffee and alcohol. The challenge remains in designing feeding trials that can isolate the metabolic signatures of individual foods within complex dietary patterns [35].
Experimental Protocols for Biomarker-Ready Feeding Trials
The following protocol outlines a comprehensive approach for designing and implementing controlled feeding trials aimed at dietary biomarker discovery, aligning with the framework established by the Dietary Biomarkers Development Consortium (DBDC) [15].
Protocol: Controlled Feeding Trial for Biomarker Discovery
Objective: To identify and validate candidate dietary biomarkers through rigorously controlled dietary interventions and subsequent metabolomic profiling.
Phase 1: Pre-Trial Planning and Menu Formulation
Dietary Pattern Definition:
- Define specific test foods and dietary patterns for investigation (e.g., high-cruciferous vegetable pattern vs. low-cruciferous control) [15].
- Utilize computational diet optimization models to create isocaloric menu variants that meet all nutritional guidelines while varying only the target food components.
Menu and Recipe Standardization:
- Develop precise, standardized recipes with exact weights for all ingredients.
- Use nutritional analysis software to calculate the complete nutrient composition of each meal and the daily diet.
Participant Screening and Randomization:
- Recruit healthy adult participants with no metabolic diseases [35].
- Obtain informed consent and randomly assign participants to intervention sequences using a crossover or parallel-group design, as appropriate.
Phase 2: Trial Execution and Monitoring
Food Preparation and Distribution:
- Establish a metabolic kitchen with strict protocols for food weighing, preparation, and storage.
- Provide participants with all meals and beverages for the duration of each feeding period.
Adherence Monitoring:
- Require participants to consume all meals under supervision or document any uneaten food.
- Use objective measures such as doubly labeled water for energy intake and urinary nitrogen for protein intake to validate compliance [35].
Biospecimen Collection:
- Collect longitudinal biospecimens according to a fixed schedule to characterize pharmacokinetic parameters [15].
- Primary Samples: Fasting blood samples and 24-hour urine collections.
- Processing: Centrifuge blood to obtain plasma/serum; aliquot and freeze all samples at -80°C immediately.
Phase 3: Metabolomic Analysis and Data Processing
Sample Analysis:
- Perform untargeted metabolomic profiling on blood and urine specimens using high-resolution mass spectrometry coupled with liquid or gas chromatography (LC-MS/GC-MS) [15].
Data Preprocessing:
- Process raw metabolomic data for peak picking, alignment, and annotation using high-dimensional bioinformatics pipelines [15].
- Normalize data to account for technical variation (e.g., using internal standards and quality control samples).
Phase 4: Biomarker Identification and Validation
Statistical Analysis:
- Employ multivariate statistical models (e.g., PLS-DA) to identify metabolites whose levels significantly differ between intervention and control diets.
- Establish dose-response relationships for candidate biomarkers.
Validation:
- Validate candidate biomarkers in independent observational cohorts (Phase 3 of the DBDC framework) to assess their predictive value for recent and habitual food intake [15].
Computational Optimization Frameworks for Menu Design
Computational optimization is critical for solving the high-dimensional problems inherent in menu design for feeding trials. The table below details key optimization approaches and their applications.
Table 2: Computational Optimization Models for Addressing Menu Design Complexities
| Optimization Challenge | Computational Approach | Application in Feeding Trial Menu Design |
|---|---|---|
| Multivariate Nutrient Balancing | Linear & Quadratic Programming | Formulate isocaloric menus that simultaneously meet dozens of nutrient constraints (e.g., protein, fat, vitamins, minerals) while minimizing deviation from a target pattern. |
| Individual Diet Customization | Stochastic & Integer Programming | Generate multiple, equivalent menu rotations to prevent participant fatigue and menu monotony, which is crucial for long-term adherence. |
| Constraint Satisfaction & Palatability | Genetic Algorithms & Heuristic Search | Optimize for participant acceptance and cost while adhering to all nutritional and dietary restrictions (e.g., allergies, cultural preferences). |
| Ingredient Portfolio Selection | Combinatorial Optimization | Select the optimal set of ingredients and portion sizes across an entire trial period to minimize waste and cost while maximizing nutritional targets. |
These algorithms, falling under the domain of large-scale and nondifferentiable optimization, are implemented in software environments to provide practical solutions for researchers [54]. Their application ensures that the diets are not only scientifically valid but also logistically feasible and palatable for participants.
Visualization of Workflows and Relationships
Dietary Biomarker Discovery Workflow
Optimization in Menu Design Logic
The Scientist's Toolkit: Research Reagent Solutions
The following table catalogs essential materials and computational tools required for implementing the described feeding trials and biomarker analyses.
Table 3: Essential Research Reagents and Tools for Biomarker Feeding Trials
| Item Name | Function / Application | Specific Usage Example |
|---|---|---|
| Standardized Food Ingredients | Provides consistent nutritional composition and minimizes variability in the dietary exposure. | Sourcing from certified suppliers; used in metabolic kitchen for precise recipe formulation. |
| Internal Standards for Metabolomics | Enables quantitative and semi-quantitative analysis of metabolites by correcting for instrument variability. | Added to blood and urine samples prior to LC-MS/GC-MS analysis for data normalization. |
| Doubly Labeled Water (²H₂¹â¸O) | Objective biomarker for total energy expenditure, used to validate participant adherence and energy intake. | Administered orally at trial start; urine samples collected to measure isotope elimination. [35] |
| LC-MS/GC-MS Grade Solvents | High-purity solvents for metabolomic sample preparation and analysis to prevent contamination and ion suppression. | Used for protein precipitation from plasma, metabolite extraction, and mobile phase preparation. |
| Optimization Software (e.g., GAMS, CPLEX) | Provides solvers for linear, quadratic, and integer programming problems for computational menu design. | Implemented to solve the multivariate optimization problem of creating isocaloric, nutrient-adequate menus. [54] |
| Bioinformatics Pipeline (e.g., XCMS Online, MetaboAnalyst) | Processes raw metabolomic data for peak detection, alignment, statistical analysis, and metabolite annotation. | Used in Phase 3 to identify spectral features significantly altered by the dietary intervention. [15] |
Managing Logistical and Resource-Intensive Demands
Controlled feeding trials are a cornerstone of rigorous nutritional science, providing the high-fidelity data essential for discovering and validating dietary biomarkers. Unlike dietary counseling trials, where adherence is variable, feeding trials involve the provision of all or most food to participants, ensuring precise control over nutrient intake [34]. This control is paramount for establishing clear dose-response relationships and identifying objective biomarkers of dietary exposure, which are critical for advancing the field of precision nutrition [15] [35]. However, this scientific precision comes with significant logistical and resource-intensive demands. The management of these trials requires meticulous planning in design, staffing, food procurement, and adherence monitoring. This document outlines detailed protocols and applications notes to navigate these complexities, framed within the broader context of dietary biomarker discovery research.
Logistical Framework for Feeding Trials
The design and execution of a feeding trial must balance scientific rigor with practical feasibility. Key logistical considerations include the trial's setting, design, duration, and the composition of the research team.
Trial Configurations and Their Applications
Feeding trials can be conducted in various settings, each offering distinct advantages and challenges that impact the level of control, participant burden, and cost. The choice of setting is often dictated by the specific research question and available resources.
Table 1: Configurations of Controlled Feeding Trials
| Trial Configuration | Setting | Key Advantages | Key Logistical Challenges | Ideal Application |
|---|---|---|---|---|
| Fully Domiciled [34] | Participants reside in a metabolic chamber or inpatient facility. | Extreme control over diet and environment; real-time biomarker monitoring. | Highest financial cost and participant burden; requires major resources. | Proof-of-concept studies; investigating acute metabolic mechanisms. |
| Partial-Domiciled [34] | Participants consume meals on-site but do not reside there. | Good balance of control and practicality; lower cost than fully domiciled. | Requires dedicated kitchen and dining facilities; multiple daily site visits from participants. | Evaluating the effect of specific dietary patterns (e.g., time-restricted eating) [34]. |
| Non-Domiciled [34] | Meals are provided for participants to consume at home. | Highest participant convenience; greater generalizability; lower cost. | Susceptible to lower adherence; requires robust food packaging and delivery systems. | Longer-term efficacy trials (e.g., DASH diet) [34]. |
Core Research Team and Roles
A multidisciplinary team is essential for successfully managing the demands of a feeding trial. The core team should include:
- Principal Investigator: Provides overall scientific direction and oversight.
- Project Manager: Coordinates all operational aspects, timelines, and personnel.
- Registered Dietitian/Nutritionist: Critical for diet design, menu creation, and nutritional assessment [34]. Their early involvement is crucial for planning.
- Study Coordinators: Manage participant recruitment, scheduling, and daily operations.
- Medical Specialist: Integral for studying clinical populations, ensuring participant safety, and managing health-related events [34].
- Biostatistician: Guides trial design (e.g., sample size, randomization) and data analysis plans.
- Laboratory Staff: Process and analyze biological samples (e.g., blood, urine) for biomarker assessment [35].
- Blinded and Unblinded Staff: A double-blinding procedure is recommended to minimize bias, requiring a clear plan for who is blinded and how blinding is maintained [34].
Experimental Design and Duration
The choice between a parallel-group and a crossover design is a key strategic decision. Crossover designs, where participants receive all treatments in a randomized sequence, are common in feeding trials because they reduce intra-individual variability, thereby requiring a smaller sample size [34]. A critical logistical consideration for this design is the duration of the washout period between interventions to prevent carryover effects [34].
Trial duration is typically shorter than in counseling trials, often ranging from several days to months. A minimum duration of 2–4 weeks is often implemented to allow for biomarker stabilization and assessment [34]. The DELTA program, for instance, successfully employed 8-week feeding periods in a crossover design [37].
Protocol for Dietary Biomarker Discovery in Controlled Feeding Trials
The following protocol integrates the rigorous control of feeding trials with a systematic framework for the discovery and validation of novel dietary biomarkers, as championed by initiatives like the Dietary Biomarkers Development Consortium (DBDC) [15].
Workflow for Biomarker Discovery and Validation
The process from a controlled feeding intervention to a validated dietary biomarker involves multiple, sequential stages. The diagram below outlines this core workflow.
The DBDC's Three-Phase Validation Protocol
The Dietary Biomarkers Development Consortium (DBDC) proposes a rigorous, multi-phase protocol to move from candidate compounds to validated biomarkers. This systematic approach is designed to ensure that biomarkers are both sensitive and specific to the dietary exposure of interest [15].
Phase 1: Discovery and Pharmacokinetics
- Objective: Identify candidate biomarker compounds and characterize their pharmacokinetic parameters.
- Protocol: Administer a single test food or nutrient in prespecified amounts to healthy participants in a controlled setting [15]. For example, a study might provide a specific dose of cruciferous vegetables.
- Methods: Collect serial blood and urine specimens at predetermined timepoints post-consumption. Perform untargeted metabolomic profiling using high-resolution mass spectrometry (e.g., LC-MS, GC-MS) to discover compounds that appear or increase in response to the test food [15] [35]. Data analysis characterizes the appearance, peak, and clearance rates of candidate biomarkers.
Phase 2: Evaluation of Specificity
- Objective: Test the ability of candidate biomarkers to distinguish individuals consuming the target food from those on different dietary patterns.
- Protocol: Conduct controlled feeding studies using various dietary patterns (e.g., a pattern rich in fruits vs. one rich in vegetables) [15].
- Methods: Measure candidate biomarker levels in biospecimens from these different groups. A robust biomarker should show significantly higher levels in the group consuming the target food, demonstrating specificity.
Phase 3: Validation in Observational Settings
- Objective: Evaluate the validity of candidate biomarkers for predicting recent and habitual consumption in free-living populations.
- Protocol: Measure biomarker levels in samples from independent observational cohort studies where dietary intake has been assessed using traditional tools like 24-hour recalls [15].
- Methods: Analyze the correlation between biomarker levels and reported intake. A strong, consistent association confirms the biomarker's utility for monitoring dietary exposure in real-world settings.
The Scientist's Toolkit: Key Reagents and Materials
The successful execution of a feeding trial for biomarker discovery relies on a suite of specialized reagents and materials.
Table 2: Essential Research Reagents and Materials for Feeding Trials and Biomarker Discovery
| Item | Function/Application | Specific Examples/Notes |
|---|---|---|
| Standardized Food Ingredients | To ensure dietary consistency and meet precise nutrient targets across the trial [37]. | Centralized procurement of fat-containing foods and other key ingredients is recommended to minimize variability [37]. |
| Biospecimen Collection Kits | For standardized, consistent collection, processing, and storage of biological samples. | Kits for plasma, serum, and urine, containing appropriate anticoagulants, preservatives, and cryovials for biobanking at -80°C. |
| Metabolomics Platforms | For the high-throughput, unbiased profiling of small molecules in biospecimens to discover candidate biomarkers [15] [35]. | Liquid Chromatography-Mass Spectrometry (LC-MS) and Gas Chromatography-Mass Spectrometry (GC-MS). |
| Stable Isotope Tracers | To definitively track the metabolic fate of specific nutrients or food compounds. | 13C-labeled compounds can be incorporated into foods or administered orally to trace metabolic pathways. |
| Dietary Assessment Software | For designing and analyzing research diets to ensure they meet nutritional targets and for comparing against self-reported intake. | Software needs a comprehensive, customizable nutrient database. |
| Food Preparation & Packaging Equipment | To maintain blinding, ensure food safety, and provide convenience for participants. | Industrial kitchen equipment, precision scales, and standardized, opaque containers for meal delivery. |
Application Note: Managing Adherence and Biomarker Verification
High participant adherence is the linchpin of a successful feeding trial. The following integrated strategies are critical for managing this demand.
Pre-Study Preparation: During the informed consent process, use sample menus to clearly illustrate the dietary restrictions and help participants self-assess their ability to comply [34]. Transparently state that all, most, or some food will be provided and outline any restrictions on travel or consumption of non-study foods.
Diet Tolerability and Flexibility: To improve long-term adherence, design diets with participant acceptability in mind. Measure and report diet tolerability and acceptability as secondary outcomes [34]. Offer a selection of "free foods" (e.g., low-energy vegetables, water, specific condiments) to provide choice without compromising the diet's nutritional integrity, particularly for participants with higher energy needs [34].
Multi-Modal Adherence Monitoring: Adherence should not rely on a single method. A robust strategy includes:
- Direct Observation: The gold standard for fully or partial-domiciled trials [34].
- Weighed Food Records: For non-domiciled trials, where participants weigh and record any uneaten food [34].
- Food Checklists: Low-burden tools for participants to quickly check off consumed foods and report any non-study food intake [34].
- Objective Biomarkers: The ultimate verification tool. As outlined in the protocol above, biomarkers in blood (e.g., plasma carotenoids for fruit/vegetable intake) or urine (e.g., urinary nitrogen for protein, sulfur compounds for cruciferous vegetables) provide an objective measure of compliance independent of self-report [15] [35]. The systematic review by Frontiers in Nutrition provides a comprehensive list of urinary metabolites associated with various food groups [35].
Managing the logistical and resource-intensive demands of controlled feeding trials is a complex but achievable endeavor. By adopting a structured framework for trial design, implementing a rigorous multi-phase protocol for biomarker discovery, and leveraging a dedicated toolkit and adherence strategies, researchers can successfully generate high-quality, reproducible data. These efforts are fundamental to expanding the list of validated dietary biomarkers, which will, in turn, refine our understanding of diet-health relationships and empower the development of personalized nutrition strategies. The integration of controlled feeding trials with advanced metabolomic technologies represents a powerful pathway toward more objective and precise dietary assessment.
Ensuring Blinding and Minimizing Bias in Diet Interventions
In controlled feeding trials for dietary biomarker discovery, the ability to establish a direct causal relationship between a dietary intervention and a quantifiable change in a biological marker is paramount. The integrity of this discovery process is heavily dependent on minimizing bias, with double-blinding being a cornerstone methodology. While placebo-controlled trials are routine in pharmaceutical research, they present significant, though not insurmountable, challenges in dietary intervention research. Properly implemented blinding protects the findings from expectation bias (from participants) and measurement bias (from researchers), ensuring that the identified biomarkers reflect true biological responses to the nutritional intervention rather than psychological or methodological artifacts. This document outlines application notes and detailed protocols to achieve this goal.
Application Notes: Principles for Bias Minimization
Comparison of Trial Designs for Biomarker Discovery
The choice of trial design fundamentally impacts the validity and generalizability of biomarker findings. The table below compares key design features.
Table 1: Comparison of Whole Diet Counseling vs. Feeding Trials in Biomarker Research
| Aspect | Whole Diet Counseling Trials | Whole Diet Feeding Trials |
|---|---|---|
| Setting | Free-living | Fully domiciled, partial-domiciled, or free-living [34] |
| Intervention Fidelity | Variable between participants; lower precision [34] | High adherence and precision; proof-of-concept evidence [34] |
| Blinding Potential | Impossible to double-blind; possible to single-blind [34] | Possible to double-blind [34] |
| Control Diet Design | Extremely challenging to design a placebo [34] | Possible to design and implement a placebo/control [34] |
| Biomarker Application | Real-world effectiveness [34] | Ideal for evaluating effect of known food/nutrient quantities on physiology; facilitates identification of objective biomarkers of adherence [34] |
Essential Criteria for Sham/Placebo Diets
For a dietary advice intervention, a credible sham (placebo) diet should be designed to act as an inert control. The following criteria are essential for its development [55]:
- Plausibility: The sham diet must be credible and convincing to participants as a potentially beneficial dietary intervention.
- Inertness: The dietary advice given must not alter the outcome of interest (e.g., it should not exclude foods suspected to be related to the target biomarker).
- Distinction: It must be distinctly different from the active intervention diet.
- Blinding: It should be possible to blind participants and researchers to the diet assignment.
- Ethicality: The sham diet must be nutritionally adequate and safe for the study duration.
- Cultural Acceptability: The diet should be acceptable within the cultural context of the study population.
- Equivalence of Support: The same amount of researcher-participant contact time and support should be given to both groups.
- Manual-Based: Both interventions should be delivered using a standardized manual to ensure consistency.
- Pilot Testing: The sham diet should be piloted to assess its credibility and blinding success.
Experimental Protocols
Protocol for Designing and Implementing a Blinded Controlled Feeding Trial
Objective: To provide a standardized methodology for conducting a double-blind, placebo-controlled feeding trial aimed at discovering dietary biomarkers with minimal bias.
Workflow Overview: The following workflow diagrams the key stages of a blinded feeding trial, from initial design to data analysis.
Detailed Procedures:
Step 1: Define Study Population and Exclusion Criteria
- Purpose: To maximize retention, safety, and generalizability while minimizing non-adherence.
- Action: Implement stringent inclusion/exclusion criteria. Typically, exclude individuals with eating disorders, food allergies or severe intolerances to study foods, or an inability to consume the diet provided [34]. The sample size calculation should be clearly reported, noting that calculations based on data from counseling trials may be overestimates for the more tightly controlled feeding trials [34].
Step 2: Design the Control Intervention (Sham Diet)
- Purpose: To create a credible control that does not alter the outcome of interest.
- Action: For a whole-diet intervention, design a control diet that is structurally similar but biologically inert regarding the hypothesized biomarker pathway. For example, if testing a low-fermentable carbohydrate diet, the control might be a diet similar in appearance and fiber content but with different types of carbohydrates that do not affect the gut microbiome in the same way. The rationale for diet targets and the foods provided should be thoroughly described [34] [55].
Step 3: Develop and Validate Menus
- Purpose: To ensure dietary interventions are delivered as intended and are acceptable to participants.
- Action: Develop cycle menus that meet the nutritional targets of both active and control diets. Conduct a validation phase to ensure meals are palatable, culturally appropriate, and achieve the desired nutrient composition. Consider showing a sample menu to potential participants during the informed consent process to aid their decision [34].
Step 4: Implement Randomization and Blinding
- Purpose: To eliminate selection bias and prevent expectation bias.
- Action:
- Randomization: Use a computer-generated randomization sequence, managed by an independent third party not involved in participant recruitment or outcome assessment.
- Double-Blinding: Ensure both participants and research staff involved in data collection, outcome assessment, and data analysis are blinded to group assignment. A plan for who is blinded and how blinding will be maintained must be developed a priori [34]. For domiciled trials, ensure that kitchen staff preparing meals are also blinded, typically by having a separate, unblinded team manage meal coding and distribution.
Step 5: Provide Meals and Monitor Adherence
- Purpose: To ensure high intervention fidelity.
- Action: Provide all or most food to participants. In domiciled settings, direct observation is possible. In non-domiciled settings, use precise methods like weighed food records and provide checklists to minimize participant burden [34]. Establish and report an adherence target and measurement method before the trial begins.
- Adherence Biomarkers: Where possible, use objective dietary biomarkers (e.g., plasma carotenoids, urinary metabolites, stable isotopes) to quantitatively verify compliance beyond self-report [34].
Step 6: Collect and Analyze Data with Blinding Maintained
- Purpose: To prevent measurement and analysis bias.
- Action: Blinded researchers should collect all clinical endpoint data and biological samples. The analysis of biomarkers (e.g., using metabolomics platforms) should be performed using blinded sample codes. Only after the final statistical analysis plan is locked should the blinding be broken.
Protocol for Assessing Blinding Success and Diet Tolerability
Objective: To empirically verify the integrity of the blinding and the real-world applicability of the intervention.
Procedure:
- Blinding Success Assessment: At the end of the intervention period, but before unblinding, ask participants and key blinded research staff to guess which intervention group they believe the participant was assigned to (active or control). Provide options "Active," "Control," or "Don't Know."
- Statistical Analysis: Calculate the blinding index (BI) for both groups. A BI close to 0.5 indicates successful blinding (random guessing), while values significantly different from 0.5 indicate that blinding may have been compromised.
- Tolerability and Acceptability Assessment: Use validated questionnaires or structured interviews to assess gastrointestinal tolerance, palatability, satisfaction, and overall ease of adhering to the diet.
- Interpretation: The results inform the interpretation of the primary findings. Successful blinding strengthens the validity of the results, while high tolerability supports the real-world applicability of the dietary intervention for future studies.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials and Tools for Blinded Feeding Trials
| Item / Reagent | Function & Application in Biomarker Trials |
|---|---|
| Standardized Meal Kits | Pre-portioned, nutritionally defined meals and snacks are the fundamental "reagent" for ensuring consistent delivery of the dietary intervention and control diets. |
| Placebo Food Items | Specially formulated food items that match the active intervention items in appearance, taste, and texture but lack the bioactive component of interest, crucial for maintaining blinding [55]. |
| Dietary Assessment Software | Used for precise menu design and nutrient analysis to ensure active and control diets meet specific nutritional targets while differing only in the components under investigation. |
| Adherence Biomarkers | Objective biochemical measures (e.g., plasma phospholipid fatty acids for fat intake, urinary nitrogen for protein) used to verify participant compliance beyond self-report [34]. |
| Blinded Sample Kits | Pre-labeled, coded kits for the collection, processing, and storage of biological samples (blood, urine, stool) to ensure laboratory analysts remain blinded to participant group assignment. |
| Automated Randomization System | A computer-based system, managed by an independent statistician or third party, to generate and conceal the allocation sequence, preventing selection bias. |
Adapting Protocols for Clinical Populations and Special Scenarios
Controlled feeding trials are the gold standard in nutritional science for establishing cause-and-effect relationships between diet and physiological outcomes [49] [56]. In dietary biomarker discovery research, these studies provide the precise intake data essential for validating candidate biomarkers against known consumption [15] [57]. However, standard feeding trial protocols often require significant adaptation when applied to clinical populations or complex real-world scenarios. The Dietary Biomarkers Development Consortium (DBDC) exemplifies the structured approach needed, implementing a 3-phase process for biomarker discovery and validation that spans from controlled feeding studies to observational settings [15]. This protocol outlines specific adaptations for implementing controlled feeding trials in clinical populations, ensuring methodological rigor while addressing unique practical and ethical considerations.
Specialized Methodological Considerations
Defining Clinical Population Adaptations
Clinical populations present unique challenges including altered metabolism, polypharmacy, reduced mobility, and comorbidities that necessitate protocol modifications. Unlike healthy populations, clinical participants often have specific nutritional requirements, medication schedules that interact with nutrients, and physical limitations affecting food consumption. The DBDC's approach involves administering test foods in prespecified amounts to healthy participants initially, but emphasizes that subsequent phases must evaluate biomarkers in various populations [15]. For clinical trials, defining the study population requires balancing safety concerns with the generalizability of findings, often requiring specialized screening protocols and safety monitoring [49].
Key Adaptation Framework
The following table summarizes core adaptations required for clinical feeding trials compared to standard protocols:
Table 1: Adaptation Framework for Clinical Feeding Trials
| Protocol Element | Standard Population Protocol | Clinical Population Adaptation | Rationale |
|---|---|---|---|
| Diet Design | Fixed macronutrient targets based on population averages [37] | Individualized prescriptions accounting for disease-specific metabolism, drug-nutrient interactions | Addresses altered nutrient requirements and prevents iatrogenic harm |
| Compliance Monitoring | Returned food weighing, periodic urinary biomarkers (e.g., nitrogen, sodium) [56] | Enhanced monitoring: daily PABA checks, supervised meals, medication reviews | Ensures data validity despite complex health status and polypharmacy |
| Energy Requirement Calculation | Predictive equations (e.g., Mifflin-St Jeor), indirect calorimetry [56] | Disease-specific equations, continuous glucose monitoring for diabetics, clinical biomarkers | Accounts for disease-related metabolic alterations and enhances safety |
| Menu Cycle Length | 3- to 7-day repeating cycles [56] | Shorter (1-3 day) cycles with greater variety | Reduces dietary fatigue in populations with likely anorexia of disease |
| Ethical Safeguards | Standard informed consent | Comprehensive consent processes, independent patient advocates, more frequent withdrawal options | Protects vulnerable populations with potentially impaired decision-making capacity |
Experimental Protocols for Clinical Scenarios
Protocol 1: Controlled Feeding in Cardiometabolic Populations
This protocol adapts standard procedures for individuals with obesity, metabolic syndrome, or cardiovascular disease, based on the mini-MED trial which included participants with overweight/obesity [57].
3.1.1 Participant Screening and Safety
- Implement a two-stage screening process: initial electronic health record review followed by in-person assessment with study physician
- Establish exclusion criteria:
- Unstable cardiac disease (recent MI, unstable angina)
- Severe renal impairment (eGFR <30 mL/min/1.73m²)
- Hepatic dysfunction (ALT/AST >3× upper limit of normal)
- Uncontrolled hypertension (SBP >160 or DBP >100 mmHg)
- Require primary care provider clearance for all participants with chronic conditions
- Conduct baseline electrocardiogram for participants >50 years or with cardiac history
3.1.2 Diet Design and Preparation
- Utilize the DELTA program methodology for precise diet standardization across multiple sites if applicable [37]
- Implement chemical validation of all menus prior to study initiation through commercial laboratory analysis
- Develop crisis menus for clinical events (e.g., hypoglycemia protocols for diabetic participants)
- Establish nutrient-drug interaction review process by clinical pharmacist for all menu cycles
3.1.3 Specialized Compliance Monitoring
- Employ multi-modal compliance assessment:
- Daily returned food inventories
- Twice-weekly 24-hour urine collections for sodium and nitrogen
- Daily para-aminobenzoic acid (PABA) checks in clinical populations [56]
- Weekly medication reconciliation to identify potential interactions
- Implement continuous glucose monitoring for diabetic participants with predefined intervention thresholds
Protocol 2: Mobility-Impaired and Assistive Technology Populations
This protocol addresses challenges for participants with physical disabilities affecting self-feeding, drawing insights from real-world trials of assistive feeding technology [58].
3.2.1 Environmental and Accessibility Adaptations
- Conduct pre-study home environment assessment for participants with severe mobility limitations
- Implement assistive feeding technology with standardized training protocols:
- Robotic feeding arms (e.g., ADA - Assistive Dexterous Arm) with web application control [58]
- Customized utensil options based on individual physical capabilities
- Specialized containers and stabilizing equipment
- Establish environmental control protocols addressing:
- Table stability and height adjustments
- Lighting conditions for vision-impaired participants
- Temperature maintenance for meal delivery
3.2.2 Social and Psychological Considerations
- Incorporate social dining experiences when possible to maintain normalcy and assess social facilitation of eating
- Provide training sessions for caregivers assisting with feeding during the study
- Implement quality of life measures specific to mealtime experience and independence
3.2.3 Data Collection Adaptations
- Utilize modified biological sampling protocols accommodating physical limitations:
- Alternative positions for blood draws
- Assisted urine collection devices
- Reduced frequency collections when full protocols are not feasible
- Document assistance levels required for each feeding session as potential covariates in analysis
Protocol 3: Multi-Center Clinical Feeding Trials
This protocol extends single-site methodologies to multi-center designs, essential for adequate recruitment of specialized clinical populations, based on the DELTA program experience [37].
3.3.1 Centralized Diet Standardization
- Establish centralized food procurement for key ingredients, particularly fat-containing foods [37]
- Implement cross-center validation through duplicate meal preparation and chemical analysis
- Develop standardized preparation manuals with photographic documentation of plate composition
- Conduct regular site audits using standardized checklists for protocol adherence
3.3.2 Quality Assurance Framework
- Implement continuous diet sampling with predefined sampling frequency (e.g., 8-day diet cycle sampled twice per feeding period) [37]
- Establish centralized laboratory analysis of all diet samples to minimize inter-laboratory variability
- Create rapid feedback mechanisms for diet composition deviations with predefined correction protocols
Visualization of Workflows
Clinical Participant Screening Pathway
The following diagram illustrates the specialized screening process required for clinical populations in controlled feeding trials:
Clinical Feeding Trial Compliance Monitoring
This workflow details the enhanced compliance monitoring necessary for clinical populations:
The Scientist's Toolkit
Table 2: Essential Research Reagents and Materials for Clinical Feeding Trials
| Tool/Reagent | Function/Application | Clinical Population Considerations |
|---|---|---|
| Para-aminobenzoic acid (PABA) | Compliance marker incorporated into study foods and measured in urine [56] | Particularly critical in clinical populations with potential cognitive impairment; verify no interactions with medications |
| Standardized Food Ingredients | Central procurement ensures consistency across study sites and participants [37] | May require specialized formulations (e.g., pureed, texture-modified) for participants with dysphagia or physical limitations |
| Assistive Feeding Technology | Robotic arms (e.g., ADA system) with web application control for participants with motor impairments [58] | Requires pre-study training and environmental adaptation; includes "kill button" for safety |
| Chemical Analysis Standards | For pre-study menu validation and continuous diet sampling assessment [37] | May require additional analysis for disease-specific nutrients (e.g., potassium in renal disease) |
| Portable Cooler Systems | Daily food provision to participants in free-living phases of semi-controlled trials | May require specialized containers for participants with physical limitations or temperature-sensitive medications |
| Electronic Diet Design Software | Research-quality software (e.g., NDS-R, ProNutra) for precise menu development [56] | Must accommodate disease-specific nutrient restrictions and special dietary requirements |
| Biospecimen Collection Supplies | Standardized kits for blood, urine, and other biospecimen collection for biomarker assessment [15] [57] | May require adaptive collection devices for participants with physical disabilities |
Data Collection and Biomarker Specifics
Quantitative Outcomes in Clinical Feeding Trials
Table 3: Data Collection Schedule and Biomarker Assessment
| Data Category | Specific Measures | Collection Frequency | Clinical Adaptations |
|---|---|---|---|
| Dietary Compliance | Returned food weight, urinary PABA, urinary nitrogen [56] | Daily (PABA, food weight); Weekly (24-h urine) | Increased frequency for cognitively impaired; simplified tracking methods |
| Cardiometabolic Biomarkers | Blood pressure, lipids, glucose, inflammatory markers [57] | Baseline and end of each intervention period | Additional safety monitoring (e.g., weekly BP in hypertensives) |
| Novel Food Intake Biomarkers | Food-specific compounds (FSCs) in blood/urine via metabolomics [15] [57] | Baseline and end of each intervention period | Account for disease-related alterations in metabolism and pharmacokinetics |
| Safety Parameters | Adverse events, weight changes, clinical labs | Continuous (AEs); Daily (weight); Periodic (labs) | Disease-specific safety parameters (e.g., INR for anticoagulated patients) |
| Gut Microbiome | Diversity and community composition via sequencing [57] | Baseline and end of intervention | Consider disease-mediated microbiome alterations in interpretation |
Adapting controlled feeding trials for clinical populations requires meticulous attention to safety, ethical considerations, and methodological rigor while maintaining the precision necessary for dietary biomarker discovery. The protocols outlined provide a framework for implementing these complex studies while generating high-quality data suitable for validating food intake biomarkers. As the field progresses toward precision nutrition, these adapted methodologies will enable researchers to establish robust biomarkers that can ultimately be deployed in clinical populations to assess dietary intake and guide nutritional interventions for disease management and health promotion.
From Discovery to Application: Validating and Comparing Biomarker Performance
The initial phase of dietary biomarker discovery serves as the critical foundation for establishing a direct, causal relationship between specific food intake and measurable biological compounds. Within the framework of the Dietary Biomarkers Development Consortium (DBDC), Phase 1 is explicitly designed to identify candidate compounds through highly controlled feeding trials followed by comprehensive metabolomic profiling [15] [7]. This phase addresses a fundamental challenge in nutritional epidemiology: the reliance on self-reported dietary data, which is often subject to significant measurement error and recall bias. By administering test foods in prespecified amounts to healthy participants under controlled conditions, researchers can characterize the pharmacokinetic parameters of candidate biomarkers associated with specific foods, thereby establishing a objective measure of intake that is not contingent on participant memory or perception [15].
The biological rationale for this approach stems from the understanding that consumed foods are broken down into various metabolites that enter systemic circulation and are eventually excreted. These metabolites represent objective indicators of food intake that can be detected in biological specimens such as blood and urine. The controlled feeding trial design allows researchers to distinguish true food-derived metabolites from background dietary noise and inter-individual metabolic variation, paving the way for discovering compounds that can serve as sensitive and specific biomarkers of dietary exposures [15] [7]. This systematic approach represents a significant advancement in the field of precision nutrition, as it enables the development of validated tools for assessing associations between diet and health outcomes with unprecedented accuracy.
Experimental Designs for Controlled Feeding Trials
Phase 1 biomarker discovery employs three primary controlled feeding trial designs, each with distinct applications and methodological considerations. The DBDC has implemented these designs to systematically identify candidate biomarkers for foods commonly consumed in the United States diet [15].
Table 1: Controlled Feeding Trial Designs for Phase 1 Biomarker Discovery
| Trial Design | Key Characteristics | Primary Applications | Data Outputs |
|---|---|---|---|
| Single-Dose, Acute Response | Administration of a single portion of test food; intensive biospecimen collection over short duration (typically 0-24 hours) | Characterize acute metabolic response; identify short-term biomarkers; establish initial pharmacokinetic profiles | Time-course concentration data; rapid appearance/disappearance kinetics; candidate biomarkers with short half-lives |
| Repeated-Dose, Steady-State | Multiple administrations of test food over several days; biospecimen collection at presumed steady-state | Identify biomarkers of habitual intake; detect cumulative metabolites; assess depot effects | Steady-state concentration levels; biomarkers with accumulation patterns; identification of medium-to-long term biomarkers |
| Crossover, Dose-Response | Administration of varying doses of test food in randomized order with washout periods; identical biospecimen collection protocol for each dose | Establish dose-response relationships; determine sensitivity of biomarkers to intake levels; identify linear and non-linear response patterns | Dose-response curves; quantification of biomarker sensitivity to intake levels; minimum detection thresholds |
The single-dose, acute response design involves administering a single portion of a test food to healthy participants after a period of dietary restriction, followed by intensive biospecimen collection over a short time frame (typically 0-24 hours) [15]. This design is particularly valuable for characterizing the initial metabolism of food components, identifying rapid appearance and disappearance kinetics of potential biomarkers, and capturing short-term metabolic profiles. For example, this approach might reveal metabolites that peak in plasma within 2-4 hours post-consumption, providing candidates for assessing recent intake.
The repeated-dose, steady-state design extends the intervention period to multiple days or weeks, with participants consuming the test food regularly until metabolic steady-state is presumed to be achieved [15]. This design is essential for identifying biomarkers that reflect habitual consumption rather than single exposures, detecting metabolites that may accumulate over time, and understanding how sustained intake influences metabolic profiles. This approach is particularly relevant for foods that are typically consumed regularly rather than occasionally.
The crossover, dose-response design represents the most sophisticated approach, wherein participants receive varying doses of the test food in randomized order, separated by appropriate washout periods [15]. This design enables researchers to establish quantitative relationships between intake levels and biomarker concentrations, determine the sensitivity of potential biomarkers to different consumption amounts, and identify both linear and non-linear response patterns that inform about the dynamic range of candidate biomarkers.
Core Methodological Protocols
Participant Selection and Preparation
The selection of appropriate participants forms the critical foundation for generating valid and generalizable biomarker data. Phase 1 trials typically enroll healthy adult volunteers who meet specific inclusion criteria designed to minimize confounding metabolic factors [59]. Key considerations include:
- Health Status: Participants should be free from metabolic diseases (e.g., diabetes, renal impairment, hepatic dysfunction) that might alter nutrient metabolism or metabolite clearance [59].
- Age and Sex Distribution: Balanced recruitment across age decades and both sexes to identify potential demographic variations in food metabolism [59].
- Genetic Background: Consideration of genetic polymorphisms that may affect nutrient metabolism (e.g., lactase persistence, bitter taste receptors) [59].
- Medication Usage: Exclusion of individuals taking medications known to interfere with metabolic pathways or nutrient absorption [59].
- Baseline Diet: Implementation of a standardized wash-in period (typically 3-7 days) where participants consume a controlled diet low in the food of interest and its potential metabolic precursors to establish a consistent metabolic baseline [15].
Prior to trial initiation, all study protocols must receive approval from an institutional review board (IRB) or equivalent ethics committee to ensure the protection of participant rights and welfare [59]. Informed consent must be obtained from all participants, with clear communication about study procedures, potential risks, and the extent of dietary control involved.
Biospecimen Collection and Processing
Standardized collection, processing, and storage of biological specimens are paramount for generating high-quality, reproducible biomarker data. The following protocols represent best practices for Phase 1 feeding trials:
Table 2: Biospecimen Collection Protocol for Phase 1 Feeding Trials
| Specimen Type | Collection Timeline | Processing Requirements | Storage Conditions | Primary Analytical Applications |
|---|---|---|---|---|
| Plasma | Fasting baseline, then at 30min, 1h, 2h, 4h, 6h, 8h, 12h, 24h post-dose | Centrifugation at 4°C within 30min of collection; aliquoting without repeated freeze-thaw cycles | -80°C in cryogenic vials | Untargeted metabolomics; quantification of circulating metabolites; pharmacokinetic modeling |
| Urine | Pre-dose (overnight), then cumulative collections: 0-4h, 4-8h, 8-12h, 12-24h | Volume measurement; aliquoting; acidification if necessary for stability | -80°C with minimal headspace | Metabolic profiling of excreted compounds; calculation of recovery rates; identification of elimination products |
| Serum | Fasting baseline, 2h, 4h, 8h, 24h post-dose | Clotting at room temperature (30min); centrifugation; aliquoting | -80°C in cryogenic vials | Complementary to plasma analysis; protein-bound metabolites |
| Optional Specimens | Saliva (timed with plasma); Feces (24h collection) | Species-specific processing | -80°C with appropriate preservatives | Complementary metabolic information; gut microbiota-related metabolites |
All biospecimen collections should follow a strict timeline relative to test food administration, with precise recording of collection times [15]. Implementation of standardized operating procedures (SOPs) for specimen processing is essential to minimize technical variability. Additionally, inclusion of quality control (QC) samples—such as pooled reference samples, process blanks, and calibration standards—throughout the collection and analysis workflow enables monitoring of analytical performance and data quality [59].
Metabolomic Profiling and Analysis
Metabolomic profiling represents the core analytical methodology for identifying candidate biomarkers in Phase 1 trials. The integrated workflow encompasses sample preparation, instrumental analysis, and data processing:
Sample Preparation Protocol:
- Protein Precipitation: Add 300μL of cold methanol (-20°C) to 100μL of plasma/urine, vortex for 30 seconds, incubate at -20°C for 1 hour, centrifuge at 14,000×g for 15 minutes [59].
- Supernatant Collection: Transfer 350μL of supernatant to a fresh tube, evaporate to dryness under nitrogen stream.
- Reconstitution: Reconstitute dried extract in 100μL of mobile phase initial condition, vortex for 30 seconds, centrifuge at 14,000×g for 10 minutes.
- Quality Control Pools: Create QC pools by combining equal aliquots (10μL) from all samples, process alongside experimental samples.
Liquid Chromatography-Mass Spectrometry (LC-MS) Analysis:
- Liquid Chromatography: Employ reversed-phase C18 column (2.1×100mm, 1.7μm) with mobile phase A (0.1% formic acid in water) and B (0.1% formic acid in acetonitrile) [59]. Use gradient elution from 5% to 95% B over 20 minutes, flow rate 0.3mL/min, column temperature 40°C.
- Mass Spectrometry: Operate in both positive and negative electrospray ionization modes with data-dependent acquisition [59]. Settings: source temperature 150°C, desolvation temperature 350°C, cone gas flow 50L/h, desolvation gas flow 800L/h, capillary voltage 3.0kV, mass range 50-1200m/z.
Data Processing and Metabolite Identification:
- Feature Detection: Use software (e.g., XCMS, Progenesis QI) for peak picking, alignment, and integration [15].
- Compound Identification: Match accurate mass and fragmentation spectra against databases (HMDB, MetLin, MassBank) with tiered confidence levels [15].
- Kinetic Analysis: Calculate pharmacokinetic parameters (C~max~, T~max~, AUC, half-life) for significantly changing metabolites using non-compartmental analysis.
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful execution of Phase 1 biomarker discovery requires carefully selected reagents, materials, and instrumentation. The following toolkit details essential components for conducting controlled feeding trials and subsequent metabolomic analyses:
Table 3: Research Reagent Solutions for Phase 1 Biomarker Discovery
| Category | Specific Items | Function & Application | Technical Specifications |
|---|---|---|---|
| Chromatography | C18 reversed-phase columns (2.1×100mm, 1.7μm); HILIC columns; LC vials and caps; Mobile phase solvents (HPLC-grade water, acetonitrile, methanol); Formic acid | Separation of complex metabolite mixtures prior to mass spectrometry analysis; provides orthogonal separation mechanisms | Column temperature stability: ±0.5°C; Flow rate precision: <0.5% RSD; Particle size: 1.6-1.8μm for improved resolution |
| Mass Spectrometry | Reference mass standards; Calibration solutions; Instrument quality control samples (QC); Ionization sources (ESI, APCI) | Accurate mass measurement; instrument calibration; monitoring analytical performance; ionization of metabolites for detection | Mass accuracy: <5ppm; Resolution: >20,000 FWHM; Dynamic range: 4-5 orders of magnitude |
| Sample Preparation | Protein precipitation reagents (methanol, acetonitrile); Solid-phase extraction (SPE) cartridges; Internal standards (stable isotope-labeled compounds); Derivatization reagents | Removal of interfering matrix components; metabolite extraction; normalization of analytical variation; enhancement of detection | Recovery efficiency: >85% for target analytes; Precision: <15% CV; Minimal matrix effects |
| Biospecimen Collection | EDTA/K2EDTA blood collection tubes; Urine collection containers (sterile); Cryogenic vials; Protein preservatives; Portable cooling equipment | Standardized specimen collection; prevention of analyte degradation; maintaining sample integrity during transport | Storage temperature: -80°C±10°C; Tube additives: appropriate for downstream analyses |
| Data Analysis | Metabolomic databases (HMDB, MetLin, MassBank); Processing software (XCMS, Progenesis QI, Compound Discoverer); Statistical packages (R, Python libraries) | Metabolite identification; data preprocessing; statistical analysis; biomarker candidate selection | Database comprehensiveness; Algorithm transparency; Compatibility with instrument raw data formats |
The selection of appropriate stable isotope-labeled internal standards is particularly critical for ensuring analytical quality [59]. These compounds, which are chemically identical to target analytes but contain heavier isotopes (e.g., ^13^C, ^15^N, ^2^H), enable correction for variations in sample preparation, matrix effects, and instrument performance. For untargeted discovery analyses, a combination of class-specific internal standards (e.g., labeled amino acids, fatty acids, carbohydrates) provides broad coverage across major metabolite classes.
Quality control materials should include both instrument QC samples (e.g., reference standards analyzed at regular intervals) and process QC samples (e.g., pooled biological reference materials extracted alongside study samples) [59]. These QC materials enable monitoring of instrument stability, batch effects, and overall process reproducibility, which is essential for generating high-quality data suitable for biomarker discovery.
Data Analysis and Candidate Selection
The transformation of raw metabolomic data into meaningful candidate biomarkers requires a sophisticated analytical pipeline that integrates kinetic analysis, statistical evaluation, and biological prioritization.
Kinetic Analysis of Metabolite Profiles
The temporal profiles of metabolite concentrations following test food consumption provide critical information for assessing their utility as biomarkers. Key pharmacokinetic parameters are calculated for each significantly changing metabolite:
- C~max~: The maximum observed concentration, indicating the potential strength of the biomarker signal.
- T~max~: The time to reach maximum concentration, informing about the temporal window for detecting intake.
- AUC~0-t~: The area under the concentration-time curve from zero to the last measurable timepoint, representing total exposure and potentially correlating with dose.
- Half-life (t~1/2~): The time required for concentration to decrease by half, indicating persistence in the body and utility for detecting recent versus habitual intake.
Statistical Approaches for Biomarker Selection
The selection of candidate biomarkers employs a multi-stage statistical approach designed to balance discovery sensitivity with confirmation of robustness:
Univariate Analysis: For each metabolite, conduct paired statistical tests (e.g., paired t-tests, Wilcoxon signed-rank tests) comparing post-dose concentrations to baseline levels, with application of false discovery rate (FDR) correction for multiple comparisons [59].
Multivariate Analysis: Employ projection methods such as Principal Component Analysis (PCA) and Orthogonal Projections to Latent Structures (OPLS) to identify metabolite patterns that distinguish post-dose from pre-dose samples, while accounting for correlated metabolite responses [15].
Time-Course Analysis: Implement linear mixed-effects models to analyze metabolite trajectories across all timepoints, accounting for within-subject correlation and identifying metabolites with consistent kinetic profiles across participants [15].
Dose-Response Assessment: For dose-response studies, apply regression models (linear or non-linear) to evaluate relationships between administered dose and metabolite response, prioritizing metabolites with strong, consistent dose-response relationships [15].
Candidate biomarkers are prioritized based on a composite score incorporating effect size (fold-change), statistical significance (FDR-adjusted p-value), consistency across participants (low inter-individual variation), kinetic properties (appropriate T~max~ and persistence), and dose-response characteristics [15]. This multi-dimensional prioritization strategy ensures the selection of candidates with the highest potential for success in subsequent validation phases.
Quality Assurance and Data Management
Rigor and reproducibility in Phase 1 biomarker discovery necessitate comprehensive quality assurance practices and systematic data management. The DBDC and similar consortia have implemented standardized frameworks to ensure data quality and accessibility [15] [59].
Quality Control Measures:
- Process Blinding: Implementation of sample blinding and randomization protocols to prevent analytical bias during metabolomic profiling [59].
- Batch Balancing: Strategic distribution of samples from different participants, timepoints, and doses across analytical batches to avoid confounding technical and biological variation [59].
- QC Sample Integration: Regular analysis of quality control samples (pooled reference samples, process blanks) throughout the analytical sequence to monitor instrument performance and process stability [59].
- Standard Operating Procedures: Development and strict adherence to SOPs for all experimental processes, from participant preparation through data analysis [15].
Data Management and Sharing: Data generated during Phase 1 studies should be archived in publicly accessible databases to serve as resources for the broader research community [15]. The DBDC specifically emphasizes creating a publicly accessible database containing all data generated during feeding trials, including raw and processed metabolomic data, food composition information, and associated clinical metadata [15]. This commitment to data sharing accelerates biomarker research by enabling secondary analyses, method development, and cross-validation of findings across different research groups and populations.
Comprehensive documentation should accompany all datasets, including detailed protocols, sample information, data processing parameters, and analytical performance metrics. Such thorough documentation ensures that data remain interpretable and usable by the scientific community, facilitating the translation of Phase 1 discoveries into validated biomarkers for precision nutrition.
Within the framework of controlled feeding trials for dietary biomarker discovery, Phase 2 represents a critical step in establishing the practical utility of candidate biomarkers identified in initial discovery studies (Phase 1) [15]. The primary objective of this phase is to evaluate whether candidate biomarkers can accurately distinguish consumption of a target food or food group across diverse dietary backgrounds. This assessment is vital for determining a biomarker's specificity and robustness, moving beyond the controlled conditions of a single test food administration to simulate real-world dietary complexity [15] [60]. A biomarker's performance in this phase dictates its potential for reliable application in large-scale observational studies.
Experimental Design and Dietary Patterns
This phase employs controlled feeding studies that incorporate various dietary patterns to challenge the specificity of candidate biomarkers. The fundamental question is whether a biomarker remains sensitive to its target food even when that food is consumed as part of different overall dietary regimes.
Table 1: Key Characteristics of Dietary Patterns for Specificity Testing
| Dietary Pattern | Core Composition | Purpose in Specificity Testing | Example Target Foods for Biomarker Evaluation |
|---|---|---|---|
| Western Pattern | High in refined grains, red meat, processed foods, and sugary beverages [60]. | Tests specificity against a background high in processed ingredients and fats. | Fruits, vegetables, whole grains, fish. |
| Mediterranean Pattern | High in fruits, vegetables, whole grains, legumes, nuts, and olive oil; moderate in fish and poultry [60]. | Tests specificity in a healthful, high-plant-food background with shared food groups. | Specific fruits (e.g., citrus), fish, olive oil, red meat. |
| DASH Pattern | Emphasizes fruits, vegetables, whole grains, and low-fat dairy; low in saturated fat and sodium [60]. | Evaluates performance in a pattern designed for health promotion. | Low-fat dairy, specific vegetables, nuts. |
| Vegetarian/Plant-Based Pattern | Excludes meat and sometimes other animal products; high in plant-based foods [60]. | Challenges specificity for animal-based foods in their absence and plant-based foods amid high background. | Meat, fish, dairy, eggs, specific legumes. |
Table 2: Core Experimental Design Matrix for Phase 2 Trials
| Design Element | Recommended Protocol | Rationale |
|---|---|---|
| Study Population | Healthy adults (n=30-50 per arm); may include at-risk groups based on biomarker target [60]. | Ensures generalizability and assesses biomarker performance in relevant physiological states. |
| Study Design | Randomized, controlled, crossover or parallel-arm feeding trials. | Minimizes confounding and allows for within-subject comparisons (crossover). |
| Dietary Interventions | 2-4 distinct dietary patterns, each incorporating the target food/food group in prespecified amounts. | Directly tests biomarker specificity across varying dietary backgrounds. |
| Duration of Intervention | Typically 2 to 6 weeks per dietary period. | Allows for biomarker levels to reach a new steady state and captures medium-term adaptation [61]. |
| Biospecimen Collection | Repeated blood (plasma/serum) and urine collections, typically at baseline and end of each feeding period. | Captures kinetic profiles and provides sufficient material for robust metabolomic analysis [62]. |
| Blinding | Participants and staff involved in outcome assessment should be blinded to the dietary assignment. | Reduces measurement bias and ensures objective evaluation of biomarker performance. |
Detailed Methodological Protocols
Controlled Feeding Study Protocol
Objective: To administer tightly controlled diets representing different dietary patterns and collect high-quality biospecimens for biomarker analysis.
Materials:
- Metabolic kitchen with standardized food procurement and preparation.
- Dietary analysis software for menu planning and nutrient calculation.
- Standardized portioning tools.
- Biological sample collection kits (e.g., vacutainers, urine collection jugs).
- Equipment for sample processing (centrifuge, -80°C freezer).
Procedure:
- Menu Development & Validation: Develop cycle menus for each dietary pattern that meet the target nutrient composition. Incorporate the test food(s) in fixed, pre-determined amounts. Analyze menus using dietary software to verify nutritional content.
- Food Preparation and Distribution: Prepare all meals and snacks in a dedicated metabolic kitchen. Weigh all ingredients to ensure accuracy. Provide participants with all food and beverages they are to consume, with clear instructions.
- Compliance Monitoring: Employ multiple strategies to enhance and monitor compliance, including:
- Daily check-ins with participants.
- Consumption of provided meals on-site where possible.
- Use of returned food containers to estimate uneaten food.
- Incorporation of a recovery biomarker (e.g., urinary nitrogen) if feasible [62].
- Biospecimen Collection: Standardize the timing and conditions of sample collection.
- Blood: Collect fasting blood samples into appropriate vacutainers (e.g., EDTA for plasma). Process samples promptly by centrifugation (e.g., 1500-2000 x g for 15 minutes at 4°C). Aliquot plasma/serum and store immediately at -80°C [62].
- Urine: Collect 24-hour urine samples. Participants should be provided with jugs containing a preservative if needed (e.g., boric acid). Assess completeness of collection using para-aminobenzoic acid (PABA) tablets [62]. Aliquot and store at -80°C.
Biomarker Specificity Analysis Protocol
Objective: To quantify candidate biomarker levels and statistically evaluate their specificity and predictive power across the different dietary patterns.
Materials:
- Targeted or untargeted metabolomics platforms (e.g., LC-MS, GC-MS).
- Internal standards for quantification.
- Statistical software (e.g., R, Python with appropriate packages).
Procedure:
- Biomarker Quantification: Analyze biospecimens using pre-specified metabolomic methods. For candidates from Phase 1, a targeted assay is preferred for precise quantification. Include quality control samples (pooled quality control, blanks) in each batch.
- Data Preprocessing: Perform peak integration, alignment, and normalization. Correct for batch effects using internal standards and statistical methods.
- Specificity Assessment:
- Use generalized linear mixed models to test the association between the candidate biomarker level and the consumption of the target food, adjusting for the underlying dietary pattern, participant (as a random effect), and other covariates (e.g., age, BMI).
- A significant interaction term between the target food and the dietary pattern indicates that the biomarker's performance is context-dependent, reducing its specificity.
- Predictive Modeling:
- Apply machine learning algorithms (e.g., Random Forest, Support Vector Machines) to evaluate the ability of a single biomarker or a panel to classify individuals according to their intake of the target food across all dietary patterns.
- Use cross-validation to assess model performance and prevent overfitting [61].
- Performance Metrics: Calculate key metrics to summarize biomarker performance:
- Area Under the Curve (AUC) from Receiver Operating Characteristic (ROC) analysis.
- Sensitivity and Specificity at optimal cut-points.
- Spearman's correlation coefficients between biomarker levels and actual intake within and across dietary patterns.
Diagram 1: Phase 2 Specificity Evaluation Workflow.
Computational Analysis and Integration
The complexity of data generated in Phase 2 requires robust computational tools for integration and visualization.
Integrated Biomarker Response (IBR) Analysis: For studies evaluating multiple biomarkers for a single food or pattern, the IBR index can be a useful tool to integrate the responses into a unified score. The IBRtools R package provides a standardized method for this calculation, allowing researchers to account for the direction and magnitude of change across all biomarkers simultaneously [63]. The analysis involves standardizing biomarker data, calculating the IBR index, and visualizing the integrated response via radar charts.
Data Integration and Visualization: The primary outcome of Phase 2 is a validated biomarker or biomarker panel with known specificity. The performance of different candidates can be visualized using ROC curves or bar charts of AUC values across dietary patterns. This allows for the direct comparison and selection of the most robust biomarkers for progression to Phase 3, where they will be validated in free-living populations [15].
Table 3: Key Reagent and Resource Solutions for Phase 2 Trials
| Category | Item | Specification/Function |
|---|---|---|
| Biospecimen Collection | EDTA Vacutainers | Prevents coagulation for plasma separation [62]. |
| Urine Collection Jugs with PABA | For 24-hour urine collection; PABA tablets verify completeness [62]. | |
| Cryogenic Vials | For long-term storage of aliquoted samples at -80°C [62]. | |
| Laboratory Analysis | Internal Standards (Isotope-Labeled) | Enables precise quantification of metabolites in mass spectrometry [15]. |
| Quality Control Materials (Pooled QC, NIST SRM) | Monitors analytical precision and accuracy across batches [15]. | |
| Data Analysis | IBRtools R Package | Calculates Integrated Biomarker Response (IBR) and IBRv2 indexes for multi-biomarker studies [63]. |
| Statistical Software (R, Python) | For data preprocessing, statistical modeling, and machine learning [61]. |
The validation of biomarkers in independent observational cohorts represents a critical final step in confirming their utility for objective dietary assessment. This phase moves beyond the controlled conditions of feeding trials to evaluate how candidate biomarkers perform in real-world, free-living populations. The primary purpose is to confirm that biomarkers can reliably predict recent and habitual consumption of specific foods or dietary patterns outside experimental settings [15]. This stage is essential for establishing that biomarkers discovered under controlled conditions maintain their sensitivity, specificity, and robustness when applied to broader populations with varying characteristics, behaviors, and genetic backgrounds.
Within the broader context of dietary biomarker discovery research, this phase addresses a crucial translational gap. While controlled feeding trials provide ideal conditions for initial biomarker discovery and characterization, they lack the environmental complexity and variability inherent to normal life. Validation in observational cohorts thus serves as the bridge between experimental discovery and practical application in nutritional epidemiology, clinical practice, and public health monitoring [15] [59]. Successful validation enables researchers to move from merely identifying compounds associated with food intake to deploying tools that can accurately measure dietary exposure in diverse populations.
Key Validation Parameters and Metrics
The validation of dietary biomarkers requires assessment against multiple analytical and performance parameters. The table below summarizes the core metrics that must be evaluated during Phase 3 validation studies.
Table 1: Key Parameters for Biomarker Validation
| Parameter | Description | Target Threshold/Considerations |
|---|---|---|
| Analytical Validity | Assessment of the assay's precision, accuracy, and reliability [64] [59] | Coefficient of variation <20-30% is often targeted for robust assays [64] [59]. |
| Sensitivity | The proportion of true consumers who test positive for the biomarker [65] | Should be maximized to correctly identify individuals consuming the target food. |
| Specificity | The proportion of non-consumers who test negative for the biomarker [65] | Should be maximized to correctly exclude individuals not consuming the target food. |
| Positive Predictive Value (PPV) | Proportion of biomarker-positive individuals who are true consumers [65] | Highly dependent on the prevalence of food consumption in the population. |
| Negative Predictive Value (NPV) | Proportion of biomarker-negative individuals who are true non-consumers [65] | Highly dependent on the prevalence of food consumption in the population. |
| Discrimination | Ability to distinguish consumers from non-consumers [65] | Often measured by the area under the Receiver Operating Characteristic (ROC) curve. |
| Calibration | How well biomarker levels estimate the amount or frequency of food intake [65] | Assesses the agreement between predicted and actual intake levels. |
Beyond these metrics, researchers must also evaluate clinical or epidemiological validity, which determines how well the biomarker correlates with the dietary exposure of interest in the target population, and clinical utility, which assesses whether the biomarker provides useful information for improving health outcomes or guiding dietary recommendations [64].
Experimental Design and Cohort Considerations
Cohort Selection and Recruitment
The fundamental requirement for Phase 3 validation is the use of an independent observational cohort that was not involved in the initial discovery and verification phases [15]. The study population must closely recapitulate the general population for which the biomarker is intended, both in terms of demographic characteristics and the prevalence of the dietary habits being assessed [64]. Key considerations for cohort selection include:
- Sample Size and Power: The cohort must be sufficiently large to provide adequate statistical power for validation. Power analysis should be conducted to determine the number of subjects required to detect clinically meaningful differences in biomarker performance [59].
- Representativeness: Participants should represent the spectrum of the target population in terms of age, sex, body mass index, ethnicity, and socio-economic status [59]. This ensures the biomarker's applicability across subpopulations.
- Confounding Factors: The study design must account for potential confounding factors that could influence biomarker levels, such as medications, comorbidities, lifestyle habits (e.g., smoking), and genetic variations [64] [59].
Study Design and Data Collection
Rigorous study design is paramount to avoid bias and ensure the validity of findings. Recommended approaches include:
- Prospective and Retrospective Designs: Validation can utilize both prospective cohort studies and retrospective studies using archived specimens from well-characterized cohorts [64] [59].
- Blinding and Randomization: To minimize bias, personnel conducting biomarker assays should be blinded to the participants' dietary exposure status. Randomization should be used in the processing and analysis of samples to control for technical variability and batch effects [65].
- Standardized Procedures: All samples should be collected, processed, and stored using predefined standard operating procedures (SOPs) to minimize pre-analytical variations [64]. This includes standardized protocols for blood draws, urine collection, processing timelines, and storage conditions.
Detailed Experimental Protocol
Pre-Validation Preparations
Step 1: Ethical Approval and Cohort Access
- Obtain approval from an Institutional Review Board (IRB) or equivalent ethics committee before study initiation [59].
- Secure access to the independent observational cohort, ensuring appropriate informed consent is in place for biomarker validation studies.
Step 2: Power Analysis and Sample Size Calculation
- Perform a power analysis based on effect sizes (e.g., expected fold-change in biomarker levels between consumers and non-consumers) and variability estimates from earlier phases [59].
- The number of samples is often large, potentially ranging from hundreds to thousands, to ensure robust statistical power [59].
Step 3: Finalize Analytical Assay
- Transition from discovery-phase platforms (e.g., untargeted metabolomics) to more precise, high-throughput quantitative assays for validation, such as targeted mass spectrometry or immunoassays (ELISA) [59].
- Complete analytical validation of the chosen assay, establishing its precision, accuracy, linear range, and limit of detection [64] [59].
Sample Processing and Analysis Workflow
Step 4: Sample Selection and Randomization
- Select samples from the cohort that represent the spectrum of the population, including cases (consumers) and controls (non-consumers), matched for key covariates where appropriate [59].
- Randomly assign samples to analytical batches to avoid systematic bias and batch effects [65].
Step 5: Biomarker Quantification
- Analyze samples using the validated quantitative assay.
- Incorporate quality control (QC) samples, including pooled reference samples and blanks, within each analytical batch to monitor instrument performance and reproducibility [59].
- Maintain blinding of the analytical team to the dietary exposure status of the samples.
Step 6: Dietary and Covariate Data Collection
- Collect reference dietary data from the cohort, which may include food frequency questionnaires, 24-hour dietary recalls, or dietary records. It is critical to acknowledge and account for the measurement error inherent in these self-reported tools [15].
- Gather comprehensive data on potential covariates, including demographic, clinical, and lifestyle information.
Data Analysis and Validation
Step 7: Statistical Analysis for Validation
- Assess the biomarker's performance against the key parameters listed in Table 1.
- Use regression models to evaluate the association between biomarker levels and reported dietary intake, adjusting for relevant covariates (e.g., age, sex, BMI) [65].
- Evaluate discrimination using ROC curves and calculate the area under the curve (AUC) to determine how well the biomarker separates consumers from non-consumers [65].
- If applicable, assess calibration to determine how well biomarker levels predict the amount or frequency of intake.
Step 8: Interpretation and Reporting
- Interpret the results in the context of the biomarker's intended use. Does it successfully predict recent and habitual consumption in a free-living population? [15]
- Report findings transparently, including all performance metrics and any limitations, such as the influence of confounding factors or the performance of the reference dietary assessment method.
The following workflow diagram illustrates the key stages of the Phase 3 validation process.
The Scientist's Toolkit: Research Reagent Solutions
Successful execution of a biomarker validation study requires specific reagents and materials. The following table details essential components of the research toolkit.
Table 2: Essential Research Reagents and Materials for Biomarker Validation
| Reagent/Material | Function/Description | Application Notes |
|---|---|---|
| Stable Isotope-Labeled Internal Standards | Synthetic peptides or metabolites with heavy isotopes (e.g., ^13C, ^15N) used for precise quantification in mass spectrometry [59]. | Spiked into samples prior to processing to correct for analyte loss and ion suppression; essential for achieving high precision. |
| Quality Control (QC) Materials | Pooled reference samples, blanks, and calibrators used to monitor assay performance across batches [59]. | Should be analyzed intermittently throughout the analytical batch to assess reproducibility and instrument drift. |
| Targeted Mass Spectrometry Kits | Pre-configured assay kits for quantitative analysis (e.g., SRM, PRM, MRM) on triple quadrupole or similar MS systems [59]. | Offer higher specificity, sensitivity, and throughput compared to untargeted discovery platforms. |
| Immunoassay Kits (e.g., ELISA) | Antibody-based kits for biomarker quantification if robust antibodies are available [64] [59]. | Useful for very high-throughput analysis in large cohorts; dependent on antibody specificity and affinity. |
| Standard Operating Procedures (SOPs) | Documented, step-by-step protocols for sample collection, processing, storage, and analysis [64]. | Critical for minimizing pre-analytical variability and ensuring consistency and reproducibility across the study. |
Troubleshooting and Common Pitfalls
Even well-designed validation studies can encounter challenges. The following table outlines common issues and recommended solutions.
Table 3: Common Troubleshooting Scenarios in Biomarker Validation
| Problem | Potential Cause | Recommended Solution |
|---|---|---|
| Poor Discrimination (Low AUC) | Biomarker is not specific to the target food; influenced by other dietary or physiological factors. | Return to discovery phase to identify more specific biomarkers; consider using a panel of biomarkers instead of a single marker [65] [59]. |
| High Analytical Variability | Unoptimized assay protocol; instrument instability; improper sample handling. | Re-optimize assay conditions; increase use of QC samples and internal standards; review and adhere to strict SOPs [64] [59]. |
| Inconsistent Performance Across Subgroups | Effect modification by age, sex, genetics, or health status. | Perform stratified analyses to identify modifying factors; consider developing subgroup-specific cutoff values if biologically justified. |
| Weak Correlation with Dietary Data | High measurement error in self-reported dietary reference method; biomarker reflects different time frame of intake. | Use multiple dietary assessment methods to reduce error; align the time frame of dietary assessment with the biomarker's pharmacokinetics [15]. |
The successful validation of dietary biomarkers in independent observational cohorts is a pivotal achievement that transforms a candidate compound from a research finding into a practical tool for nutritional science. This phase provides the critical evidence that a biomarker can perform reliably in free-living populations, thereby enabling its use in large-scale epidemiological studies, clinical trials, and ultimately, public health monitoring. By adhering to rigorous experimental design, robust statistical analysis, and transparent reporting, researchers can build a foundation of validated biomarkers that will significantly advance the field of precision nutrition and enhance our understanding of the complex relationships between diet and health.
Assessing Pharmacokinetic Parameters and Dose-Response Relationships
In the field of dietary biomarker discovery, the precise assessment of pharmacokinetic (PK) parameters and dose-response relationships is fundamental for establishing a causal link between food intake and biomarker presence. Controlled feeding trials provide the experimental framework necessary to characterize the absorption, distribution, metabolism, and excretion (ADME) of food-specific compounds, thereby validating their utility as objective biomarkers of intake [15] [66]. Unlike conventional drug development, nutritional research faces unique challenges due to the complexity of diet as an exposure, which encompasses interactions between numerous nutrients, food matrices, and individual metabolic variations [15]. The Dietary Biomarkers Development Consortium (DBDC) exemplifies a structured approach to this challenge, implementing controlled feeding studies to discover and validate intake biomarkers for foods commonly consumed in the United States diet [15]. This protocol details the application of PK and dose-response analyses within controlled feeding trials, providing a rigorous methodology to advance precision nutrition.
Key Pharmacokinetic Parameters in Dietary Biomarker Discovery
In controlled dietary studies, specific PK parameters are quantified to evaluate the kinetics of candidate biomarker appearance and clearance in biological fluids. The table below summarizes the core parameters and their significance in the context of dietary biomarker validation.
Table 1: Essential Pharmacokinetic Parameters for Dietary Biomarker Assessment
| Parameter | Definition | Significance in Dietary Biomarker Discovery |
|---|---|---|
Cₘâ‚â‚“ |
Maximum observed concentration of the biomarker in plasma or urine. | Indicates the extent of absorption and bioavailability from the food matrix. |
Tₘâ‚â‚“ |
Time to reach Cₘâ‚â‚“ after consumption of the test food. | Reflects the rate of absorption; can be influenced by food form (solid vs. liquid) [67]. |
| AUC | Area Under the concentration-time Curve. | Represents the total exposure to the biomarker over time; used for dose-response modeling. |
Tâ‚/â‚‚ |
Elimination Half-Life: time for biomarker concentration to reduce by half. | Determines the time window for detecting intake; critical for assessing suitability as a short-term vs. long-term intake marker [67]. |
| Apparent Clearance | The rate of biomarker removal from the body, normalized by bioavailability. | Describes the body's efficiency in eliminating the biomarker compound. |
The interpretation of these parameters directly informs the applicability of a candidate biomarker. For instance, a study investigating avenanthramides (AVAs) and avenacosides (AVEs) as biomarkers of oat intake found that Tₘâ‚â‚“ values were shorter for a liquid oat product (0.7–1.6 hours) compared to a solid form (1.1–2.3 hours), demonstrating a clear matrix effect on absorption rate [67]. Furthermore, the relatively short elimination half-lives of these compounds (e.g., 1.3-3.8 hours) suggested they are better suited as biomarkers for recent intake or compliance monitoring in intervention studies, rather than for assessing long-term habitual intake in nutritional epidemiology [67].
Experimental Protocol for a Controlled Feeding Trial with PK Analysis
The following protocol outlines a comprehensive procedure for a randomized crossover controlled feeding study designed to characterize the pharmacokinetics and dose-response relationship of a candidate dietary biomarker.
Study Design and Randomization
- Design: A non-blinded, randomized two-way crossover study is recommended to compare the PK of a candidate biomarker from different food matrices (e.g., solid vs. liquid) or at different doses [67].
- Participants: Recruit healthy participants. A sample size of 20-30 is typically a good compromise between feasibility and the ability to assess variation and estimate PK parameters [67].
- Randomization: A scientist not involved in the study should perform the randomization using validated software (e.g., RandomizeR package in R) to generate treatment sequence allocations [67].
Diet Preparation and Feeding
- Menu Development: A research dietitian develops cycle menus using nutrition software (e.g., NDS-R, ProNutra) to meet specific nutrient targets. Foods should be palatable, familiar to the study population, and consistently available [66].
- Energy Requirements: Determine each participant's total daily energy needs using prediction equations, indirect calorimetry, or doubly labeled water. To maintain weight stability, provide optional 250-300 kcal food modules that match the study diet's macronutrient profile [66].
- Diet Provision: Prepare and pack all foods and beverages into portable cooler bags for daily pick-up by participants. Staff involved in food preparation must have safe food handling training [66].
Specimen Collection and Data Recording
- Pharmacokinetic Phase (Single Dose): After an overnight fast, participants consume a single dose of the test food. Serial blood samples are collected at predetermined time points (e.g., 0, 0.25, 0.5, 0.75, 1, 1.5, 2, 3, 4, 5, 6, 7, 8, and 24 hours) [67]. Plasma is separated and stored at -80°C until analysis.
- Dose-Response Phase (Repeated Dose): Following a washout period, participants consume the test food at varying doses (e.g., low, medium, high) three times per day for four days. A fasting blood sample is collected on the fifth day to assess the relationship between repeated dosing and fasting biomarker levels [67].
- Compliance Monitoring: Verify adherence through daily body weight checks, return of uneaten food, and objective biomarkers (e.g., urinary nitrogen or para-aminobenzoic acid (PABA)) [66].
Bioanalysis and Pharmacokinetic Modeling
- Metabolomic Analysis: Analyze plasma samples using targeted or untargeted metabolomic platforms (e.g., LC-MS) to quantify the candidate biomarker and its metabolites.
- Compartmental Modeling: Fit the concentration-time data to PK models (e.g., one- or two-compartment models) using specialized software (e.g., NONMEM, Phoenix WinNonlin) to estimate primary PK parameters (
Cₘâ‚â‚“,Tₘâ‚â‚“, AUC,Tâ‚/â‚‚). - Dose-Response Modeling: Plot the dose of the test food against the corresponding AUC of the biomarker. Fit the data using a sigmoid Emax model or other non-linear regression to characterize the relationship [68].
Table 2: Key Research Reagents and Materials
| Category | Item | Function/Application |
|---|---|---|
| Software | NDS-R / ProNutra | Research-quality software for designing controlled diets and analyzing nutrient composition [66]. |
| NONMEM / Phoenix WinNonlin | Industry-standard software for pharmacokinetic and pharmacodynamic modeling and simulation. | |
| Laboratory Analysis | LC-MS/MS System | High-sensitivity instrumentation for quantifying candidate biomarkers and metabolites in biological samples. |
| Stable Isotope-Labeled Standards | Internal standards for mass spectrometry to ensure accurate quantification. | |
| Participant Compliance | Para-aminobenzoic acid (PABA) | A marker incorporated into study foods to objectively monitor dietary compliance via urinary excretion [66]. |
Workflow Visualization
The following diagram illustrates the logical workflow and signaling pathways involved in the discovery and validation of a dietary biomarker, from controlled intake to data analysis.
Data Analysis and Interpretation
Establishing Dose-Response Relationships
A fundamental objective is to model the relationship between the dose of the consumed food and the systemic exposure to the candidate biomarker, typically represented by the AUC. A sigmoid dose-response curve is often observed, which can be described by the Hill equation: E = (Eₘâ‚â‚“ × Dâ¿) / (EC₅₀⿠+ Dâ¿), where E is the effect (AUC of the biomarker), Eₘâ‚â‚“ is the maximum effect, D is the dose, ECâ‚…â‚€ is the dose that produces half of the maximal effect, and n is the Hill coefficient that describes the steepness of the curve [68]. The ECâ‚…â‚€ is a key parameter for estimating the potency of the food to elicit a biomarker response. For example, a quantitative systems pharmacology approach can be used to predict in vivo efficacy from in vitro data, linking pharmacokinetics with pharmacodynamic response [69].
Integration with the Dietary Biomarker Development Consortium (DBDC) Framework
The experimental protocol aligns with the multi-phase validation strategy employed by the DBDC [15]:
- Phase 1 (Discovery): This protocol's PK phase corresponds to DBDC's Phase 1, where controlled feeding trials are used to identify candidate compounds and characterize their pharmacokinetic parameters.
- Phase 2 (Evaluation): The dose-response phase of this protocol evaluates the candidate biomarker's ability to reflect intake across different dietary patterns, consistent with DBDC's Phase 2 goals.
- Phase 3 (Validation): Ultimately, the most promising biomarkers from this protocol would proceed to independent observational studies to validate their predictive power for habitual consumption.
The rigorous assessment of pharmacokinetic parameters and dose-response relationships through controlled feeding trials is an indispensable component of modern dietary biomarker discovery. The structured protocol outlined herein, which incorporates detailed experimental design, robust specimen collection, advanced metabolomic profiling, and comprehensive data modeling, provides a clear path for researchers to generate high-quality, reproducible data. By adhering to this framework, scientists can effectively transition from simply identifying candidate compounds in food to validating them as reliable, quantitative biomarkers. This process, as championed by initiatives like the DBDC, is critical for building the foundational evidence needed to advance precision nutrition and objectively understand the complex links between diet and human health.
{ document outline here }
Comparative Analysis with Traditional Dietary Assessment Tools
Accurate dietary assessment is a fundamental challenge in nutritional science, critical for investigating the links between diet and health. Traditional self-reported tools have been the cornerstone of dietary assessment for decades. However, a growing body of evidence indicates they are prone to significant inaccuracies, thereby limiting the validity of diet-disease association studies [2]. Within the context of controlled feeding trials for dietary biomarker discovery, the comparative analysis of these traditional methods against emerging biomarker-based approaches is not merely academic; it is a essential step towards achieving precision nutrition [70]. Controlled feeding studies, where participants consume known amounts of food, provide the critical benchmark for evaluating the performance of both self-reported instruments and novel nutritional biomarkers, paving the way for a more objective and reliable future in dietary assessment [5] [71] [6]. This document provides a structured comparative analysis and detailed protocols to guide researchers in this evolving field.
Traditional dietary assessment methods primarily rely on self-report and can be categorized into retrospective and prospective instruments. Each tool has distinct mechanisms, strengths, and inherent weaknesses that influence its application in research and clinical practice.
Table 1: Key Traditional Dietary Assessment Tools and Their Characteristics
| Assessment Tool | Methodology | Primary Use | Key Strengths | Inherent Limitations |
|---|---|---|---|---|
| Food Frequency Questionnaire (FFQ) | A finite list of foods and beverages where respondents indicate usual frequency of consumption over a long period (e.g., past month or year) [72]. | Estimating habitual intake of specific nutrients or total diet quality in large epidemiological studies [72] [73]. | Cost-effective for large populations; captures long-term dietary patterns [72]. | Relies on memory and general insights; must be validated for specific target populations; cognitively challenging [72] [73]. |
| 24-Hour Dietary Recall (24HR) | A structured interview (e.g., the 5-step Automated Multi-Pass Method (AMPM)) capturing detailed intake of all foods, beverages, and supplements consumed in the previous 24 hours [72]. | Capturing detailed recent intake for individuals or populations; multiple non-consecutive recalls can estimate usual intake [72]. | Reduces memory burden by focusing on a short, specific period; interviewer-administered version accessible to those with low literacy [72]. | Prone to day-to-day variation; underreporting is common; requires trained interviewers for traditional methods [72]. |
| Food Record / Diary | A prospective method where individuals record all foods and beverages, portion sizes, and preparation methods in real-time for 1 to 7 days [72] [73]. | Evaluating detailed dietary patterns and behaviors over a short term; useful for self-monitoring [72]. | Limits reliance on memory; provides detailed, real-time data [72]. | Labor-intensive; high participant burden; prone to underreporting and changes in habitual intake (reactivity) [72] [73]. |
A critical and well-documented limitation across all these self-reported instruments is systematic misreporting, particularly the underreporting of energy intake (EIn) [2]. This underreporting is not random; it increases with body mass index (BMI) and is influenced by an individual's concern about their body weight [2]. Furthermore, macronutrients are not underreported equally, with protein being less underreported compared to fats and carbohydrates [2]. This systematic error attenuates and distorts observed diet-disease relationships, posing a major challenge to nutritional epidemiology.
The Emergence of Biomarkers in Dietary Assessment
Dietary biomarkers are objectively measured indicators of food intake, nutritional status, or food-related metabolic processes. They offer a powerful means to overcome the limitations of self-reported data. The overarching goal of initiatives like the Dietary Biomarkers Development Consortium (DBDC) is to significantly expand the list of validated biomarkers for foods commonly consumed in the U.S. diet [15] [7].
Biomarkers are categorized based on their characteristics and applications:
- Recovery Biomarkers: Provide a quantitative estimate of total intake over a specific period, as a known and constant proportion of intake is excreted. Examples include urinary nitrogen for protein intake and doubly labeled water for total energy expenditure (a biomarker of habitual energy intake) [5] [71] [6].
- Concentration Biomarkers: Reflect the concentration of a nutrient or food compound in blood or urine. Their relationship with intake is more complex and influenced by individual metabolism. Examples include serum carotenoids (for fruit/vegetable intake) and phospholipid fatty acids (for fatty acid intake) [5] [71].
- Predictive Biomarkers: Often composed of a panel of metabolites, these biomarkers are discovered via metabolomics and are used to classify or predict consumption of specific foods or dietary patterns, even in the absence of a direct chemical relationship [70] [6].
The utility of a biomarker is ranked based on key validation criteria, including its plausibility (chemical relationship to the food), robustness (performance across different diets and populations), and reliability (agreement with other intake measurements) [70].
Table 2: Examples of Validated and Candidate Dietary Biomarkers
| Food or Food Group | Biomarker Matrix | Candidate Biomarkers | Utility & Validation Level |
|---|---|---|---|
| Citrus Fruits | Urine | Proline betaine | Validated (Level 1): Plausible, robust, and reliable for classifying and quantifying intake [70]. |
| Whole-Grain Wheat/Rye | Urine | Alkylresorcinols | Validated (Level 1): Well-established biomarkers for quantifying intake [70]. |
| Fatty Fish | Urine / Blood | TMAO, EPA/DHA in phospholipids | Validated (Level 1): TMAO in urine; fatty acid profiles in blood are reliable biomarkers [70]. |
| Total Meat / Chicken | Urine | 1-Methylhistidine, 3-Methylhistidine | Validated (Level 1): Useful for classifying intake, though specificity can be a challenge [70]. |
| General Fruit & Vegetable Intake | Blood | Carotenoids (α-carotene, β-carotene, lutein, zeaxanthin) | Candidate (Level 2): Good correlation with intake in feeding studies (e.g., R² 0.32-0.53) but influenced by absorption and metabolism [5] [71]. |
| Dietary Patterns (e.g., HEI-2010, aMED) | Blood / Urine | Panels of vitamins, carotenoids, and fatty acids | Emerging: Panels of biomarkers can discover and calibrate overall dietary pattern scores, mitigating measurement error [6]. |
Direct Comparative Analysis: Traditional Tools vs. Biomarkers
A direct comparison reveals fundamental differences in the nature of the data produced by traditional tools and biomarkers, highlighting the latter's role in correcting and enhancing the former.
Table 3: Quantitative Comparison of Method Performance in Controlled Studies
| Method | Performance Metric | Findings from Controlled Studies | Interpretation |
|---|---|---|---|
| Self-Reported Energy Intake | Underreporting vs. Doubly Labeled Water | Systematic underreporting, increasing with BMI; can reach 30-50% in overweight/obese individuals [5] [2]. | Self-reported EIn is not a valid measure for studies of energy balance and obesity. |
| Self-Reported Protein Intake | Underreporting vs. Urinary Nitrogen | Underreporting is less pronounced than for energy but still significant [5]. | Protein is less underreported than other macronutrients, but self-reports still require calibration. |
| Serum Concentration Biomarkers | Variance in Intake Explained (R²) | In a WHI feeding study: Serum folate (R²=0.49), Vitamin B-12 (R²=0.51), α-carotene (R²=0.53) performed similarly to urinary recovery biomarkers for energy (R²=0.53) and protein (R²=0.43) [5] [71]. | Several serum biomarkers can represent nutrient intake variation as effectively as established recovery biomarkers in a controlled setting. |
| Biomarker-Calibrated Self-Reports | Impact on Diet-Disease Hazard Ratios | Calibrating meat intake with biomarkers reduced the hazard ratio for type 2 diabetes from 37% to 8% per 40% increment in intake [70]. | Using biomarkers to correct self-reports can dramatically alter and likely clarify true diet-disease associations. |
Key Comparative Workflows
The following diagrams illustrate the fundamental differences in workflow and data output between traditional assessment methods and biomarker-based approaches, underscoring the objective nature of biomarkers.
Diagram 1: The subjective workflow of traditional dietary assessment introduces multiple points for measurement error, from memory reliance to biased reporting.
Diagram 2: The objective workflow of biomarker-based assessment, starting from controlled intake and leading to a quantitative biochemical measurement.
Detailed Experimental Protocols for Comparative Analysis in Feeding Trials
The following protocols are designed to be implemented within a controlled feeding study framework, which serves as the gold standard for validating dietary intake and is the cornerstone of rigorous biomarker discovery research [15] [5].
Protocol 1: Integrated Assessment for Biomarker Validation
Objective: To discover and validate novel dietary biomarkers by comparing self-reported intake against objective biomarker measurements in a controlled feeding setting that mimics habitual diet.
Background: This protocol, modeled on the Women's Health Initiative (WHI) feeding study and the DBDC framework, preserves individual variation in food consumption while controlling for all intake, minimizing the perturbation of biological measures [15] [5] [71].
Materials:
- Research Reagent Solutions: See Table 4.
- Dietary Assessment Instruments: 4-day food record (4DFR) booklet, FFQ, 24HR interview guide.
- Biospecimen Collection: Blood collection tubes (serum, EDTA), urine collection containers (24-hour), aliquoting tubes, freezer (-80°C).
Table 4: Research Reagent Solutions for Biomarker Discovery
| Reagent / Material | Function / Application |
|---|---|
| Doubly Labeled Water (DLW) ( [5] [6]) | Stable isotope-based method to measure total energy expenditure (TEE), serving as a recovery biomarker for habitual energy intake in weight-stable individuals. |
| 24-Hour Urinary Nitrogen ( [5] [6]) | A recovery biomarker for total protein intake. |
| LC-MS/MS & NMR Platforms ( [15] [70]) | High-throughput metabolomics platforms for the discovery and quantification of a wide range of candidate biomarker compounds in blood and urine. |
| Targeted Assay Kits (e.g., for carotenoids, folate, tocopherols) ( [5] [71]) | Validated immunoassays or HPLC assays for precise quantification of specific nutrient biomarkers. |
| ProNutra / Diet Planning Software ( [5]) | Software for creating individualized controlled feeding menus based on self-reported habitual intake and specific nutrient databases. |
Procedure:
- Participant Screening & Habitual Diet Assessment:
- Recruit participants meeting study criteria (e.g., postmenopausal women, specific age range, health status) [5].
- Obtain informed consent.
- Administer a 4DFR and conduct an in-depth diet history interview to capture usual food choices, patterns, and portion sizes.
Formulate Controlled Diet:
- Analyze the 4DFR using nutrition software (e.g., Nutrition Data System for Research - NDSR).
- Use diet formulation software (e.g., ProNutra) to design a 2-week controlled menu that closely approximates each participant's habitual diet, adjusted for estimated energy requirements [5].
- Source all foods and prepare all meals in a metabolic kitchen to ensure precise composition and portion control.
Baseline & Endpoint Biospecimen Collection:
- At the beginning (Day 0) and end (Day 14) of the feeding period, collect fasting blood samples.
- Perform a 24-hour urine collection at the end of the feeding period.
- Process, aliquot, and store all biospecimens at -80°C.
Administer Self-Reported Instruments:
- At the end of the feeding period, administer a 24HR (e.g., using the AMPM method) and/or an FFQ referring to the feeding period.
Laboratory Analysis:
Data Analysis & Biomarker Validation:
- Use linear regression to model the relationship between the consumed nutrient (ln-transformed) and the potential biomarker (ln-transformed), controlling for participant characteristics like BMI [5] [71].
- Calculate the R² value to determine the proportion of variance in intake explained by the biomarker. An R² > 0.36 is considered a strong performance, comparable to recovery biomarkers [5] [6].
- Statistically compare self-reported intake (from 24HR/FFQ) to the known controlled intake and to the biomarker levels to quantify misreporting and bias.
Protocol 2: Biomarker-Based Calibration of Self-Reports
Objective: To develop calibration equations that use biomarker data to correct for measurement error in self-reported dietary intake from FFQs or 24HRs in observational studies.
Background: This two-stage protocol, as implemented in WHI studies, uses biomarkers identified from a controlled feeding study (Stage 1) to calibrate self-reports collected in an independent observational cohort (Stage 2), thereby strengthening diet-disease analyses [19] [6].
Procedure:
- Stage 1: Biomarker Discovery (Feeding Study):
- Follow Protocol 1 to identify a panel of biomarkers that robustly predict intake of specific nutrients or dietary patterns (e.g., HEI-2010 score) [6].
- The outcome is a biomarker signature for a given dietary exposure.
- Stage 2: Calibration Model Development (Observational Study):
- In a large observational cohort, collect self-reported diet (FFQ, 24HR) and biospecimens from a subset of participants.
- Assay the pre-validated biomarker panel from Stage 1 in these biospecimens.
- Using stepwise regression or similar models, regress the biomarker panel values on the self-reported dietary pattern scores or nutrient intakes.
- The resulting calibration equations quantify the relationship between the objective biomarkers and the self-reported data, allowing for the correction of measurement error in the entire cohort when studying disease outcomes [19] [6].
The Scientist's Toolkit
This section details essential reagents, instruments, and software crucial for executing the comparative analyses and protocols described in this document.
Table 5: Essential Research Reagents and Materials
| Category | Item | Specific Example / Model | Critical Function |
|---|---|---|---|
| Biomarker Validation | Doubly Labeled Water (DLW) | ²H₂¹â¸O | Criterion method for validating self-reported energy intake via measurement of total energy expenditure [5] [6]. |
| Biomarker Validation | Urinary Nitrogen Assay | Chemiluminescence-based analyzer | Criterion method for validating self-reported protein intake [5] [6]. |
| Metabolomic Analysis | High-Resolution Mass Spectrometer | LC-MS/MS, Q-TOF platforms | Discovery and quantification of thousands of small molecule metabolites as candidate dietary biomarkers [15] [70]. |
| Targeted Assays | Immunoassays / HPLC Kits | Carotenoid, folate, vitamin B-12, tocopherol assays | Precise and accurate quantification of specific, pre-validated nutrient biomarkers in serum/plasma [5] [71]. |
| Diet Formulation | Diet Planning Software | ProNutra, NDSR | Software used to design and analyze controlled feeding study menus, ensuring nutritional targets are met [5]. |
| Data Analysis | Statistical Software | R, SAS, Python with appropriate packages (e.g., metabolomics) |
Performing regression calibration, metabolomic data analysis, and managing high-dimensional datasets [19] [6]. |
The comparative analysis unequivocally demonstrates that traditional self-reported dietary assessment tools are compromised by substantial and systematic measurement error. While they remain useful for capturing broad dietary patterns, they are inadequate for quantifying precise intake, especially in studies of energy balance and for many nutrients. Controlled feeding trials provide the indispensable framework for validating these tools and, more importantly, for discovering and validating objective dietary biomarkers. The integration of biomarker data—from single compounds to complex metabolomic panels—offers a path to correct self-reported data and significantly enhance the accuracy and reliability of nutritional science. The future of diet-disease research hinges on the continued development and routine application of these objective biomarkers, moving the field toward true precision nutrition.
Conclusion
Controlled feeding trials are indispensable for advancing dietary biomarker discovery, providing the rigorous evidence needed to move beyond error-prone self-reported data. The structured, multi-phase approach—from initial discovery in controlled settings to real-world validation—ensures that biomarkers are both specific and clinically applicable. Future directions include expanding the library of validated biomarkers, integrating these tools into large-scale epidemiological studies and clinical trials for more precise diet-disease relationship assessments, and ultimately enabling true precision nutrition. Consortium-led efforts, supported by advanced metabolomics and computational methods, are paving the way for a new era in nutritional science and therapeutic development.
References
- 1. biomarkers: advances, Dietary and future directions limitations [https://pubmed.ncbi.nlm.nih.gov/23237668/]
- 2. Frontiers | Traditional Self - Reported Instruments Are Prone to... Dietary [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2020.00090/full]
- 3. and Reliability of the weight status and validity intake... dietary [https://ijbnpa.biomedcentral.com/articles/10.1186/1479-5868-10-42]
- 4. Reliance on self - reports and estimated food composition data in... [https://elifesciences.org/articles/92941]
- 5. Dietary biomarker evaluation in a controlled feeding study in women from the Women’s Health Initiative cohort - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5267309/]
- 6. Novel Application of Nutritional Biomarkers From a Controlled Feeding Study and an Observational Study to Characterization of Dietary Patterns in Postmenopausal Women - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8799924/]
- 7. The Dietary Biomarkers Development Consortium: An Initiative for Discovery and Validation of Dietary Biomarkers for Precision Nutrition - ScienceDirect [https://www.sciencedirect.com/science/article/pii/S2475299125028951]
- 8. Using Controlled Feeding Study for Biomarker Development in Regression Calibration for Disease Association Estimation - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10270384/]
- 9. The Dietary Biomarkers Development Consortium [https://pmc.ncbi.nlm.nih.gov/articles/PMC12242990/]
- 10. Editorial: Precision nutrition and nutrients: making the ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1553149/full]
- 11. Precision Nutrition Forum and PREDIMED Omics Symposium ... [https://hsph.harvard.edu/nutrition/events/precision-nutrition-forum-and-predimed-omics-symposium/]
- 12. Brain activity associated with breakthrough food ... [https://www.nature.com/articles/s41591-025-04035-5]
- 13. The Dietary Development Consortium: An Initiative for... Biomarkers [https://escholarship.org/uc/item/7h68r2dp]
- 14. Dietary Biomarker Development Consortium [https://dietarybiomarkerconsortium.org/]
- 15. The Dietary : An Initiative for... Biomarkers Development Consortium [https://pubmed.ncbi.nlm.nih.gov/40641655/]
- 16. Fruit and Vegetable Biomarker Study: Dietary ... : USDA ARS [https://www.ars.usda.gov/pacific-west-area/davis-ca/whnrc/docs/fruit-and-vegetable-biomarker-study-dietary-biomarker-development-center-dbdc/]
- 17. Plasma and Urine Metabolomic Response to an Ultra-Processed... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9193526/]
- 18. Plasma and Urine Metabolomic Response to an Ultra-Processed Dietary Pattern: A Biomarker Discovery Analysis in a Domiciled Randomized Controlled Crossover Feeding Trial - ScienceDirect [https://www.sciencedirect.com/science/article/pii/S2475299123134020]
- 19. Using Controlled Feeding Study for Biomarker Development in Regression Calibration for Disease Association Estimation - PubMed [https://pubmed.ncbi.nlm.nih.gov/37324058/]
- 20. Tutorial: best practices and considerations for... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8830262/]
- 21. in Targeted Metabolomics Validating Biomarkers [https://www.news-medical.net/life-sciences/Validating-Biomarkers-in-Targeted-Metabolomics.aspx]
- 22. Establishment of Protocols for Global Metabolomics by LC-MS for Biomarker Discovery - PubMed [https://pubmed.ncbi.nlm.nih.gov/27579980/]
- 23. A Protocol for Untargeted Metabolomic Analysis: From Sample... [https://experiments.springernature.com/articles/10.1007/978-1-0716-1266-8_27?error=cookies_not_supported&code=6f07dda4-71d4-4788-b8f3-967189124540]
- 24. Guide to Metabolomics Analysis: A Bioinformatics Workflow - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9032224/]
- 25. Frontiers | Clinical metabolomics reveals potential diagnostic biomarkers in serum samples from patients with generalized ligamentous laxity [https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2025.1554936/full]
- 26. A statistical framework for biomarker discovery in metabolomic time course data - PubMed [https://pubmed.ncbi.nlm.nih.gov/21729866/]
- 27. MetaboAnalyst [https://www.metaboanalyst.ca/docs/RTutorial.xhtml]
- 28. Empowering consumers to PREVENT diet -related diseases through... [https://pubmed.ncbi.nlm.nih.gov/35351696/]
- 29. Optimal Design of Clinical Trials of Dietary Interventions in Disorders of Gut-Brain Interaction - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9169766/]
- 30. | 9 | Statistical Methodology in the Crossover Versus Parallel Designs [https://www.taylorfrancis.com/chapters/edit/10.1201/b16950-9/crossover-versus-parallel-designs-andrew-grieve]
- 31. Addressing the pitfalls when designing intervention studies to discover and validate biomarkers of habitual dietary intake - PubMed [https://pubmed.ncbi.nlm.nih.gov/31049735/]
- 32. Frontiers | Design and Characterisation of a Randomized Food Intervention That Mimics Exposure to a Typical UK Diet to Provide Urine Samples for Identification and Validation of Metabolite Biomarkers of Food Intake [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2020.561010/full]
- 33. Evidence from crossover trials: empirical evaluation and comparison ... [https://pubmed.ncbi.nlm.nih.gov/17301102/]
- 34. Recommendations for Designing, Conducting, and Reporting Feeding ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11480951/]
- 35. Frontiers | Urinary metabolites as biomarkers of dietary intake... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1596543/full]
- 36. A linear based method for programming for... designing menus [https://pubmed.ncbi.nlm.nih.gov/36863831/]
- 37. Diet design for a multicenter controlled : the DELTA... feeding trial [https://pubmed.ncbi.nlm.nih.gov/9664917/]
- 38. formulation to enhance nutritional goals: Optimized of... menu design [https://bmcnutr.biomedcentral.com/articles/10.1186/s40795-023-00705-0]
- 39. adequacy of a novel human milk fortifier from donkey milk... Nutritional [https://nutritionj.biomedcentral.com/articles/10.1186/s12937-017-0308-8]
- 40. Frontiers | The nutrition and immunity (nutrIMM) study: protocol for... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2023.1243359/full]
- 41. Intake Biomarkers for Nutrition and Health: Review and Discussion of Methodology Issues - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11123464/]
- 42. Identification and Reproducibility of Urinary Metabolomic Biomarkers of Habitual Food Intake in a Cross-Sectional Analysis of the Cancer Prevention Study-3 Diet Assessment Sub-Study - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8072637/]
- 43. Development and validation of a standardized protocol to monitor human dietary exposure by metabolite fingerprinting of urine samples - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3193537/]
- 44. Establishment of Protocols for Global Metabolomics by... | PLOS One [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0160555]
- 45. Dietary exposure biomarker-lead discovery based on metabolomics analysis of urine samples | Proceedings of the Nutrition Society | Cambridge Core [https://www.cambridge.org/core/journals/proceedings-of-the-nutrition-society/article/dietary-exposure-biomarkerlead-discovery-based-on-metabolomics-analysis-of-urine-samples/326015718EEC0499C49241594AA9001B]
- 46. Metabolomics: Analytical Insights into Disease Mechanisms and Biomarker Discovery | Medical Research Archives [https://esmed.org/MRA/mra/article/view/6549]
- 47. : Making science easier, more fruitful, and... | Yale News Research cores [https://news.yale.edu/2024/01/16/research-cores-making-science-easier-more-fruitful-and-more-efficient]
- 48. | Office of the Vice President for Research Cores Research [https://research.virginia.edu/resources/research-cores]
- 49. Recommendations for Designing, Conducting, and Reporting Feeding Trials in Nutrition Research - ScienceDirect [https://www.sciencedirect.com/science/article/pii/S2161831324001170]
- 50. An overview of methodologies, proficiencies, and training resources for controlled feeding studies - PubMed [https://pubmed.ncbi.nlm.nih.gov/12778045/]
- 51. Enhancing adherence in randomized controlled clinical trials - PubMed [https://pubmed.ncbi.nlm.nih.gov/11018580/]
- 52. Addressing Uptake, Adherence, and Attrition in Mental Health Apps | AJMC [https://www.ajmc.com/view/addressing-uptake-adherence-and-attrition-in-mental-health-apps]
- 53. JMIR Research Protocols - The Effect of Maternal Choline Intake on... [https://www.researchprotocols.org/2025/1/e73508]
- 54. and Applications Computational Optimization [https://www.scimagojr.com/journalsearch.php?q=28459&tip=sid]
- 55. cambridge.org/core/journals/proceedings-of-the-nutrition-society/article... [https://www.cambridge.org/core/journals/proceedings-of-the-nutrition-society/article/challenges-of-control-groups-placebos-and-blinding-in-clinical-trials-of-dietary-interventions/CD0D06FBF583C0E1DE908002A4133335]
- 56. Frontiers | Advances in Nutrition Science and Integrative Physiology: ... [https://www.frontiersin.org/articles/10.3389/fphys.2019.01341/full]
- 57. mini-MED: study protocol for a randomized, multi-intervention... [https://trialsjournal.biomedcentral.com/articles/10.1186/s13063-024-07939-8]
- 58. Real-World Trials: UW’s Assistive Feeding Robot Tested Beyond the [https://bioengineer.org/real-world-trials-uws-assistive-feeding-robot-tested-beyond-the-laboratory/]
- 59. Tutorial: best practices and considerations for... | Nature Protocols [https://www.nature.com/articles/s41596-021-00566-6?error=cookies_not_supported&code=8353164d-84b7-4aa5-9b4a-1119fe3814f8]
- 60. Biomarkers of dietary patterns: a systematic review of randomized controlled trials - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9263887/]
- 61. for Biomarker High in Ultra-processed Foods - NCI Diets [https://dceg.cancer.gov/news-events/news/2025/biomarker-ultra-processed-foods]
- 62. Measurement Toolkit - Nutritional biomarkers [https://www.measurement-toolkit.org/diet/objective-methods/biomarkers]
- 63. IBRtools: An R package for calculating integrated biomarker indexes... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10834099/]
- 64. sciencedirect.com/topics/biochemistry-genetics-and-molecular-biology... [https://www.sciencedirect.com/topics/biochemistry-genetics-and-molecular-biology/biomarker-validation]
- 65. Discovery and Biomarker : Statistical Considerations - PMC Validation [https://pmc.ncbi.nlm.nih.gov/articles/PMC8012218/]
- 66. Frontiers | Advances in Nutrition Science and Integrative Physiology... [https://www.frontiersin.org/journals/physiology/articles/10.3389/fphys.2019.01341/full]
- 67. Avenanthramides and avenacosides as biomarkers of oat intake... [https://nutritionj.biomedcentral.com/articles/10.1186/s12937-025-01204-7]
- 68. Quantitative modeling of dose–response and drug combination based on pathway network - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4476235/]
- 69. Predicting In Vivo Efficacy from In Vitro Data: Quantitative Systems Pharmacology Modeling for an Epigenetic Modifier Drug in Cancer - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7070804/]
- 70. Towards nutrition with precision: unlocking biomarkers as dietary ... [https://www.nature.com/articles/s42255-024-01067-y?error=cookies_not_supported&code=7e92f23e-3bd4-49a9-8a88-439d084ed937]
- 71. Dietary biomarker evaluation in a controlled feeding study in women from the Women's Health Initiative cohort - PubMed [https://pubmed.ncbi.nlm.nih.gov/28031191/]
- 72. An Overview of Traditional and Novel Tools to Assess - PMC Diet [https://pmc.ncbi.nlm.nih.gov/articles/PMC11384832/]
- 73. For the Athlete: Pros and Cons of... Dietary Assessment Methods [https://www.gssiweb.org/sports-science-exchange/article/sse-150-dietary-assessment-methods-for-the-athlete-pros-and-cons-of-different-methods]