Decoding Dietary Complexity: From Molecular Interactions to Clinical Outcomes in Biomedical Research
This comprehensive review addresses the intricate correlations between dietary components and their profound implications for drug development and clinical outcomes.
Decoding Dietary Complexity: From Molecular Interactions to Clinical Outcomes in Biomedical Research
Abstract
This comprehensive review addresses the intricate correlations between dietary components and their profound implications for drug development and clinical outcomes. Targeting researchers, scientists, and drug development professionals, we explore foundational mechanisms of food-drug and food-component interactions, methodological approaches for assessment and prediction, troubleshooting strategies for analytical challenges, and validation frameworks for translating findings into clinical practice. The article synthesizes current scientific evidence to provide a robust framework for understanding how dietary complexity influences drug efficacy, safety, and nutritional status, while highlighting emerging technologies and standardized methodologies that are advancing this critical field of study.
Unraveling Core Mechanisms: How Dietary Components Interact with Drugs and Each Other
FAQ: Core Mechanisms and Clinical Significance
Q1: What are the fundamental pharmacokinetic mechanisms behind food-drug interactions?
Food-drug interactions primarily alter a drug's Absorption, Distribution, Metabolism, and Excretion (ADME) [1] [2].
- Absorption: Food can influence gastric acidity, stomach emptying rate, and gastrointestinal motility. It can also form complexes with drugs or modulate the activity of transport proteins like P-glycoprotein (P-gp) in the intestinal wall, thereby inhibiting or enhancing drug absorption [2] [3].
- Metabolism: This is a primary site of interaction. Food components can inhibit or induce key drug-metabolizing enzymes, most notably the Cytochrome P450 (CYP) enzyme family [2] [4]. For example, grapefruit juice is a potent inhibitor of the intestinal CYP3A4 enzyme, leading to dangerously increased absorption and systemic concentrations of certain drugs [3].
- Excretion: Interactions can affect the renal excretion of drugs or lead to drug-induced nutrient deficiencies by altering their distribution and excretion in the body [5] [3].
Q2: Which food components are most clinically significant in drug metabolism interactions?
The table below summarizes high-risk food components and their mechanisms [4] [3].
| Food Component | Key Mechanistic Action | Example Clinical Outcome |
|---|---|---|
| Grapefruit Juice | Inhibits CYP3A4 and P-glycoprotein in the intestine [3]. | Increased bioavailability of Calcium Channel Blockers, Statins, and some antivirals, raising the risk of toxicity [3]. |
| Tyramine-rich Foods | Metabolized by Monoamine Oxidase (MAO); concurrent use with MAO Inhibitors (MAOIs) prevents its breakdown [3]. | Prevents tyramine metabolism, causing a "cheese reaction"—a sudden, dangerous rise in blood pressure [3]. |
| High-Vitamin K Foods | Acts as a cofactor for clotting factors, antagonizing the drug's mechanism [3]. | Reduced anticoagulant effect of Warfarin, increasing risk of thrombosis [3]. |
| St. John's Wort | A potent inducer of CYP3A4 and P-glycoprotein [4]. | Increased metabolism and reduced plasma levels of drugs like oral contraceptives, cyclosporine, and some antidepressants, leading to therapeutic failure [4]. |
| Dietary Fiber | Can bind to drug molecules in the GI tract [3]. | Reduced absorption and efficacy of drugs like digoxin and certain antidepressants [3]. |
Q3: How do genetic polymorphisms in enzymes like CYP450 complicate food-drug interactions?
Genetic variations in enzymes such as CYP2C9, CYP2C19, and CYP2D6 result in populations of "poor metabolizers" or "ultrarapid metabolizers" [1]. The prevalence of these phenotypes varies significantly among different biogeographical groups. When a food component inhibits or induces one of these enzymes, the clinical impact will be dramatically different depending on an individual's innate metabolic phenotype, making personalized dosing strategies essential [1].
Table: Phenotype Frequencies of Key CYP Enzymes across Populations [1]
| Enzyme / Population | Ultrarapid Metabolizer | Normal Metabolizer | Intermediate Metabolizer | Poor Metabolizer |
|---|---|---|---|---|
| CYP2D6 (European) | 2% | 49% | 38% | 7% |
| CYP2D6 (East Asian) | 1% | 53% | 38% | 1% |
| CYP2C9 (European) | - | 63% | 35% | 3% |
| CYP2C9 (East Asian) | - | 84% | 15% | 1% |
| CYP2C19 (European) | 5% | 40% | 26% | 2% |
| CYP2C19 (East Asian) | 0% | 38% | 46% | 13% |
Troubleshooting Guide: Common Experimental Challenges
Q4: We are observing unexpected variability in our in vitro CYP inhibition screening results. What are potential sources of contamination?
Unexpected results, such as a loss of signal or strange peaks, can often be traced to contaminated solvents or reagents, even those from reputable suppliers [6].
- Problem: A sudden, unexplained drop in detection sensitivity (e.g., in LC-MS).
- Solution:
- Benchmark Reagents: Always retain a small portion of "old" reagents known to perform well. If issues arise with a new batch, switch back to the old one to confirm if the reagent is the source [6].
- System Flushing: Flush the entire LC system extensively with a new lot of solvent from a different batch or vendor [6].
- Quality Control: Establish baseline performance data for critical reagents, characterizing them for contaminants and their effect on detection sensitivity for your specific analytes [6].
- Problem: Strange chromatographic peaks or a shifting baseline in UV detection.
- Solution: Consider that different manufacturing lots of solvent may have significant variability in the levels of UV-absorbing contaminants. Testing multiple lots during method validation can help identify and avoid this issue [6].
Q5: In our HILIC separations, we are seeing a complete loss of analyte retention. Is the stationary phase faulty?
Before assuming column failure, investigate the sample solvent composition and injection volume [6].
- Problem: Analytes co-elute with the solvent front, showing no retention.
- Solution:
- Adjust Sample Solvent: In HILIC, the water content of the sample solvent is critical. A sample solvent with too high a water content can destroy retention. Prepare your sample in a solvent with a high percentage of organic phase (e.g., acetonitrile) to match the HILIC initial conditions [6].
- Reduce Injection Volume: A large injection volume of a strong solvent (high water content) can overwhelm the column, creating a localized zone where the stationary phase is ineffective. Significantly reducing the injection volume can often restore proper retention and separation [6].
Experimental Protocols & Methodologies
Protocol 1: Green HPLC Analysis of Multiple CYP Substrates using Temperature-Responsive Chromatography
This protocol enables the simultaneous analysis of cytochrome P450 (CYP) probe substrates and their metabolites using an aqueous, isocratic mobile phase, eliminating the need for organic solvents [7].
1. Principle: A silica column is grafted with a temperature-responsive polymer, Poly(N-isopropylacrylamide) (PNIPAAm). The polymer's hydrophobicity changes reversibly with temperature, allowing for control over separation selectivity without altering the mobile phase composition [7].
2. Materials:
- HPLC System: Standard HPLC system with a column oven capable of precise temperature control and a UV or DAD detector [7].
- Column: P(NIPAAm-co-BMA)-grafied silica column [7].
- Mobile Phase: 0.1 M Ammonium acetate buffer, pH 4.8. No organic solvent is used [7].
- Standards: CYP probe substrates (e.g., Phenacetin for CYP1A2, Coumarin for CYP2A6, Tolbutamide for CYP2C9, S-Mephenytoin for CYP2C19, Chlorzoxazone for CYP2E1, Testosterone for CYP3A4) [7].
3. Procedure: 1. Equilibrate the column with the ammonium acetate mobile phase at a constant flow rate (e.g., 1.0 mL/min). 2. Set the column oven temperature to 40°C for optimal separation of the six CYP substrates [7]. 3. Perform an isocratic elution. The entire separation is achieved without a solvent gradient. 4. For analyzing substrates and their metabolites (e.g., Testosterone and 6β-Hydroxytestosterone), investigate different temperatures (e.g., 10°C and 40°C) to achieve resolution, as the elution order follows analyte hydrophobicity at higher temperatures [7]. 5. For column cleaning, flush with cold water instead of organic solvents [7].
Experimental Workflow for Green HPLC Analysis
Protocol 2: Simultaneous Analysis of Food Additives and Caffeine in Powdered Drinks using HPLC-DAD
This method is useful for researchers studying excipients or formulating drug-food products, ensuring surveillance of common additives [8].
1. Principle: High-Performance Liquid Chromatography with Diode Array Detection (HPLC-DAD) separates and quantifies multiple analytes based on their interaction with a reversed-phase C18 column and a gradient mobile phase [8].
2. Materials:
- HPLC-DAD System: Binary pump, auto-sampler, DAD detector [8].
- Column: Reverse-phase C18 column (e.g., 150 mm x 4.6 mm, 5 µm) [8].
- Mobile Phase: Phase A: Phosphate Buffer (pH 6.7), Phase B: Methanol [8].
- Gradient Program:
- Initial: 8.5% B
- End: 90% B (linear gradient over 16 minutes) [8].
- Standards: Acesulfame potassium, benzoic acid, sorbic acid, sodium saccharin, tartrazine, caffeine, sunset yellow, aspartame [8].
3. Procedure: 1. Prepare standard stock and working solutions in a water-methanol (50:50 v/v) mixture [8]. 2. Weigh 0.5 g of powdered drink sample and dilute to 100 mL with water. Filter through a 0.45 µm nylon filter [8]. 3. Set the DAD detector to 210 nm for method optimization and monitoring all peaks. For quantification, use specific wavelengths: 200 nm (saccharin, tartrazine, caffeine, aspartame) and 225 nm (acesulfame, benzoate, sorbate) [8]. 4. Inject 20 µL of the sample. The method achieves complete separation of all eight compounds in under 16 minutes [8].
The Scientist's Toolkit: Essential Research Reagents & Materials
| Item | Function / Application | Key Consideration |
|---|---|---|
| CYP Probe Substrates (e.g., Phenacetin, Testosterone) | Selective substrates used in "cocktail" experiments to evaluate the inhibitory or inductive potential of a food component on specific CYP enzymes [7]. | Choose probes recommended by regulatory bodies (e.g., FDA) [7]. |
| Temperature-Responsive HPLC Column (P(NIPAAm-co-BMA)) | Allows for green chromatographic separation of compounds with diverse properties using only aqueous mobile phases by modulating column temperature [7]. | The Lower Critical Solution Temperature (LCST) of the polymer dictates the operational temperature range [7]. |
| PBPK Modeling Software | (Physiologically Based Pharmacokinetic) software platforms simulate ADME processes. They can incorporate genetic, life-stage, and disease-state variables to predict food-drug interaction outcomes in specific populations [1]. | Useful for in vitro to in vivo extrapolation and clinical trial optimization [1]. |
| Box-Behnken Design (BBD) | A response surface methodology for efficiently optimizing complex analytical methods (e.g., HPLC) with multiple variables (e.g., mobile phase composition, pH) with fewer experimental runs [8]. | Ideal for multi-response optimization using a desirability function [8]. |
| Lsd1-IN-26 | LSD1-IN-26|Potent LSD1 Inhibitor for Cancer Research | LSD1-IN-26 is a high-potency LSD1/KDM1A inhibitor for epigenetic and oncology research. For Research Use Only. Not for human use. |
| Encephalitic alphavirus-IN-1 | Encephalitic alphavirus-IN-1, MF:C27H25FN6O2, MW:484.5 g/mol | Chemical Reagent |
FAQs: Mechanisms and Clinical Significance
How do GLP-1 receptor agonists modulate taste perception and what is the clinical evidence?
GLP-1 receptor agonists (e.g., semaglutide, tirzepatide) influence taste perception through peripheral and central mechanisms. A 2025 cross-sectional study of 411 adults with obesity found that over 20% of participants reported increased perception of sweet and salty tastes during treatment. These subjective changes were statistically associated with beneficial appetite outcomes: increased sweet perception was linked with increased satiety (AOR=2.02), decreased appetite (AOR=1.67), and decreased food cravings (AOR=1.85) [9] [10]. The proposed mechanism involves GLP-1 receptor expression on taste bud cells and in brain regions processing taste and reward, subtly changing how strong flavours are perceived [10] [11].
What are the primary pathways through which medications cause nutrient depletion?
Medications can reduce nutrient bioavailability through several mechanisms: reduced dietary intake (e.g., via appetite suppression), impaired nutrient absorption in the gastrointestinal tract, altered metabolism, and increased excretion. For instance, GLP-1 agonists promote satiety, leading to reduced caloric and nutrient intake, which raises deficiency risks unless diet quality is improved [12]. Other medications may directly antagonize nutrient absorption or transform nutrients into biologically unavailable forms [13].
Which populations are most vulnerable to medication-induced nutritional deficiencies?
Populations at elevated risk include: (1) individuals on long-term GLP-1 therapy due to reduced food intake, (2) elderly patients with inherently reduced nutrient absorption capabilities, (3) those with pre-existing malnutrition or gastrointestinal disorders, and (4) people taking multiple medications that interact synergistically to deplete nutrients [13] [12]. Chronic drug users also represent a high-risk population, often presenting with multiple micronutrient deficiencies due to chaotic lifestyles and poor dietary choices [14].
Troubleshooting Common Research Challenges
Challenge: Disentangling direct taste modulation from central appetite regulation in study outcomes.
Solution: Implement a tiered experimental approach:
- Psychophysical Taste Testing: Use validated tools like the WETT test battery to obtain objective measures of taste threshold, intensity, and identification [10].
- Neuroimaging: Employ fMRI to measure neural activation in response to taste stimuli in brain regions like the angular gyrus, insula, and orbitofrontal cortex [10].
- Subjective Appetite Metrics: Collect self-reported data on satiety, appetite, and cravings using visual analog scales (VAS) or validated questionnaires to correlate with objective measures [9] [10].
Challenge: Controlling for confounding factors in nutrient bioavailability studies.
Solution: The following protocol outlines key control measures for nutrient bioavailability experiments.
Experimental Protocol: Controlling for Confounders in Bioavailability Studies
| Factor | Control Method | Rationale |
|---|---|---|
| Dietary Intake | Standardized diet (e.g., homogenized meals, nutrient-defined formulas) for 3-5 days prior to and during sample collection. | Eliminates variability from dietary antagonists (e.g., phytate) or enhancers (e.g., vitamin C for iron) [13]. |
| Host Physiology | Stratify participants by age, sex, and health status. Record medication use and health history. | Accounts for host factors known to alter absorption (e.g., age-related decline, gut dysbiosis) [13]. |
| Biomarker Selection | Use the most direct biomarker possible (e.g., 24h urinary excretion for water-soluble vitamins, stable isotopes for mineral absorption). | Avoids artifacts from post-absorptive metabolism; provides a more accurate measure of absorption [13]. |
| Sample Timing | Conduct serial blood/urine sampling to establish AUC (Area Under the Curve) for the nutrient or its biomarkers. | Captures the full kinetic profile of absorption and clearance, superior to single time-point measurements [13]. |
Challenge: Differentiating between malnutrition types in high-risk populations.
Solution: Combine anthropometric and biochemical assessments. Move beyond BMI by using bioelectrical impedance analysis (BIA) to identify "hidden obesity" (normal BMI with high body fat percentage) and low protein mass [15]. Simultaneously, measure plasma levels of key micronutrients (e.g., vitamins A, C, D, E, iron, zinc) to identify "hidden" deficiencies that are not apparent from dietary intake data alone [14].
Quantitative Data Synthesis
Table 1: Appetite and Taste Perception Changes in Patients Using GLP-1 RAs (N=411) [9] [10]
| Parameter | Wegovy (n=217) | Ozempic (n=148) | Mounjaro (n=46) | Overall |
|---|---|---|---|---|
| Median BMI Reduction | 17.6% | 17.4% | 15.5% | - |
| Reported Reduced Appetite | 54.4% | 62.1% | 56.5% | 58.4% |
| Reported Increased Satiety | 66.8% | 58.8% | 63.1% | 63.5% |
| Increased Sweet Perception | 19.4% | 21.6% | 21.7% | 21.3% |
| Increased Salty Perception | 26.7% | 16.2% | 15.2% | 22.6% |
| Reported Reduced Craving | 34.1% | 29.7% | 41.3% | - |
Table 2: Common Medication-Induced Nutrient Depletions and Research Assessment Methods
| Medication / Substance Category | At-Risk Nutrients | Recommended Biomarkers for Assessment |
|---|---|---|
| GLP-1 Receptor Agonists | Protein, Fiber, Omega-3, Iron, Calcium, Vitamin D [12] | Serum ferritin, 25-hydroxyvitamin D, BIA for lean mass, dietary intake logs. |
| Chronic Illicit Drug Use | Vitamins A, C, D, E; Iron, Selenium, Potassium [14] | Plasma vitamin levels, serum ferritin, complete blood count (CBC), electrolytes. |
| Opioid Substitution Therapy | Multiple vitamins and minerals; diet high in sugary foods [14] | Fasting glucose (for metabolic risk), plasma micronutrient panel, FFQ. |
Experimental Pathways and Workflows
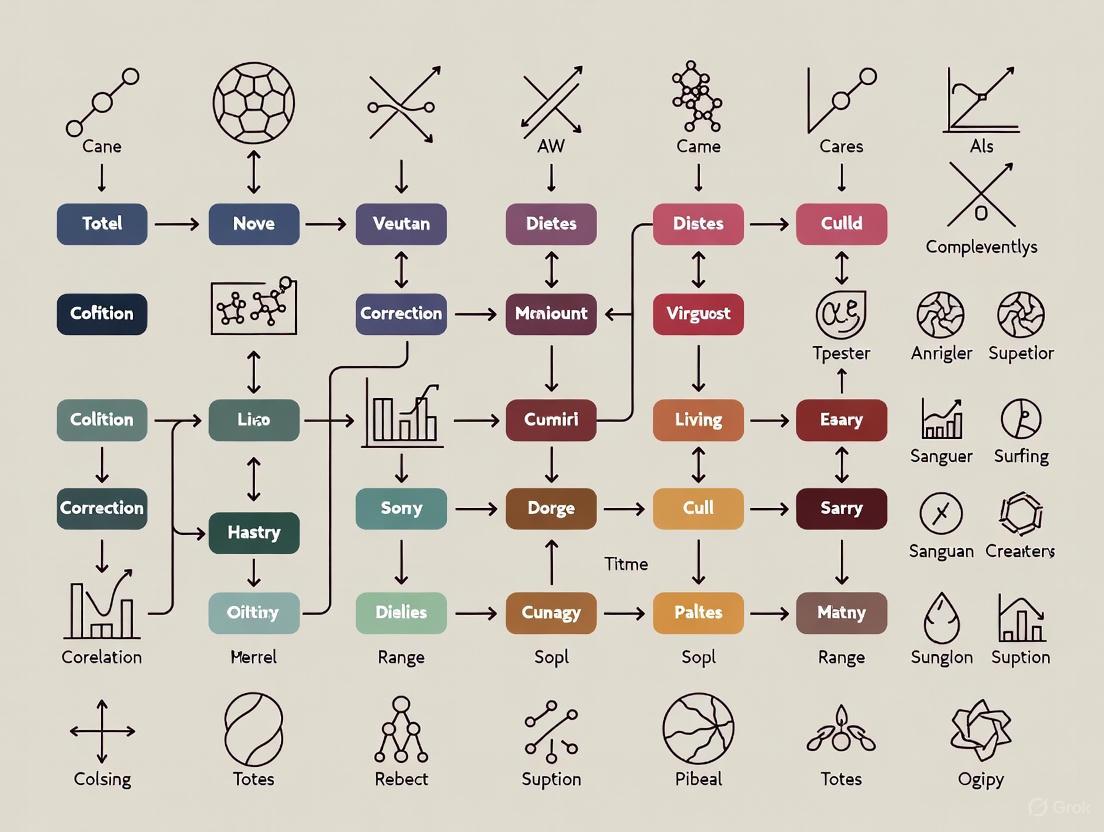
Diagram 1: GLP-1 RA Taste & Appetite Modulation Pathway.
Diagram 2: Research Workflow for Medication-Nutrition Studies.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Tools for Investigating Medication-Nutrition Interactions
| Tool / Reagent | Function / Application | Example Use Case |
|---|---|---|
| Bioelectrical Impedance Analyzer (BIA) | Measures body composition (fat mass, protein mass, water). | Identifying hidden obesity and low protein mass in patients on appetite-suppressing drugs [15]. |
| Validated Food Frequency Questionnaire (FFQ) | Assesses habitual dietary intake and patterns. | Evaluating shifts in food group consumption and nutrient density in GLP-1 RA users [15]. |
| WETT Test Battery | Objectively quantifies taste function (threshold, intensity, identification). | Differentiating true taste modulation from subjective reports in clinical trials [10]. |
| Stable Isotope Tracers | Tracks absorption and metabolism of specific nutrients. | Precisely measuring mineral (e.g., iron, zinc) bioavailability in the presence of a drug [13]. |
| Enzyme-Linked Immunosorbent Assay (ELISA) Kits | Quantifies specific nutrient biomarkers in plasma/serum (e.g., 25-hydroxyvitamin D, ferritin). | Monitoring micronutrient status to detect deficiencies in study populations [14] [13]. |
| Ret-IN-12 | Ret-IN-12, MF:C30H30F3N5O4, MW:581.6 g/mol | Chemical Reagent |
| Protriptyline-d3 | Protriptyline-d3, MF:C19H21N, MW:266.4 g/mol | Chemical Reagent |
Troubleshooting Common Experimental Challenges
FAQ 1: Why is my protein-polyphenol complex precipitating, and how can I improve its solubility?
- Problem: Precipitation often occurs due to overly strong non-covalent interactions or improper complexation conditions, leading to large, insoluble aggregates.
- Solution:
- Adjust pH: Operate away from the protein's isoelectric point (pI) where solubility is lowest. Alkaline conditions (e.g., pH 9.0) can promote covalent binding between polyphenol quinones and proteins, often yielding more soluble complexes than non-covalent complexes formed near the pI [16].
- Optimize Ratios: Use a lower molar ratio of polyphenol to protein. An excess of polyphenols can lead to over-saturation and "bridging" between multiple protein molecules, causing precipitation [17] [18].
- Apply Ultrasonication: Ultrasound treatment can unfold protein structures, increase solubility, and accelerate covalent complexation through cavitation-generated radicals, improving the stability of the final complex [16].
FAQ 2: The bioactivity (e.g., antioxidant capacity) of my polyphenol is lower after complexation. What went wrong?
- Problem: A decrease in measured antioxidant activity can result from the polyphenol's phenolic hydroxyl groups being involved in binding, making them less available for antioxidant assays.
- Solution:
- Confirm Complex Formation: This may not be a failure but an expected outcome. Use characterization techniques like fluorescence quenching or isothermal titration calorimetry to verify successful binding [17] [18].
- Re-evaluate the Application: The complex may offer controlled release, protecting the polyphenol during storage and gastrointestinal transit, with bioactivity manifesting later during colonic fermentation [18] [19]. Assess bioavailability and long-term stability instead of just initial antioxidant capacity.
- Check for Pro-oxidant Conditions: Under specific conditions (e.g., certain pH, presence of metal ions), some polyphenols can act as pro-oxidants and oxidize proteins, degrading the system. Control oxygen levels and avoid metal contaminants [18].
FAQ 3: My results are inconsistent between experimental replicates. What key factors should I control more strictly?
- Problem: Inconsistency is frequently caused by variations in the complexation process or the source/purity of materials.
- Solution:
- Standardize Polyphenol Source: The chemical structure (number of phenolic rings and OH groups) drastically affects binding affinity. Use high-purity, well-characterized polyphenols from a reliable supplier [17] [19].
- Control Temperature Precisely: Heat treatment can induce both polyphenol autoxidation and protein unfolding, strongly influencing covalent complex yield. Maintain a stable, documented temperature during mixing and reaction [17] [16].
- Account for Enzymatic Activity: If using plant extracts, the presence of endogenous Polyphenol Oxidase (PPO) can catalyze oxidation and covalent bonding during sample preparation, leading to variability. Inactivate PPO with heat or inhibitors if consistent non-covalent binding is desired [19].
FAQ 4: How can I distinguish between covalent and non-covalent complexes in my sample?
- Problem: It is methodologically challenging to separate and conclusively identify the type of interaction.
- Solution: Employ a multi-method verification approach:
- SDS-PAGE: Covalent complexes typically show a higher molecular weight band, which is resistant to SDS denaturation, while non-covalent complexes often dissociate [18] [16].
- Fourier-Transform Infrared Spectroscopy (FTIR): Look for the appearance of new characteristic peaks (e.g., C-N stretch at ~1100 cmâ»Â¹ for an amine-quinone adduct) that indicate covalent bond formation [16].
- Dialyze the Sample: Non-covalent complexes may partially or fully dissociate during extensive dialysis against a dissociating agent (e.g., urea), while covalent complexes will remain stable [17].
Table 1: Key Factors Influencing Complex Formation and Stability
| Factor | Effect on Complexation | Recommended Range for Stability | Key References |
|---|---|---|---|
| pH | Affects protein charge, polyphenol oxidation, and interaction mechanism. Alkaline pH favors covalent bonding. | Varies by protein (pI); Often pH 7.0-9.0 for covalent complexes. | [17] [16] |
| Temperature | Increases reaction kinetics; induces protein denaturation and polyphenol oxidation. | Controlled heating (e.g., 60-90°C) can enhance covalent complex yield. | [17] [16] |
| Polyphenol:Protein Ratio | Determines complex size and solubility. High ratios cause precipitation. | Typically 1:1 to 1:20 (w/w); requires empirical optimization. | [17] [18] |
| Ionic Strength | High salt concentration can screen electrostatic interactions, weakening non-covalent complexes. | Low to moderate (< 0.2 M NaCl) for electrostatic-driven complexes. | [17] [20] |
Table 2: Common Characterization Techniques for Molecular Complexes
| Technique | Information Provided | Utility for Troubleshooting |
|---|---|---|
| Fluorescence Spectroscopy | Quenching of protein intrinsic fluorescence indicates binding and can estimate binding constants. | Confirm interaction is occurring; compare affinity under different conditions. |
| Isothermal Titration Calorimetry (ITC) | Provides full thermodynamic profile: binding constant (K), enthalpy (ΔH), and entropy (ΔS). | Distinguish between binding modes (e.g., electrostatic vs. hydrophobic). |
| Dynamic Light Scattering (DLS) | Measures hydrodynamic diameter and polydispersity of particles in solution. | Identify aggregation or precipitation; check complex size stability. |
| Confocal Laser Scanning Microscopy (CLSM) | Visualizes spatial distribution and microstructure of components in a solid or gel matrix. | Directly observe phase separation, network formation, and component localization [21]. |
Standardized Experimental Protocols
Protocol 1: Preparing a Covalent Protein-Polyphenol Complex via Alkaline pH Method
This method leverages polyphenol autoxidation at high pH to form quinones that react covalently with nucleophilic amino acid residues (e.g., lysine, cysteine) in proteins [16].
- Preparation: Dissolve the protein (e.g., bovine serum albumin, β-lactoglobulin) in a phosphate or borate buffer (e.g., 0.01 M, pH 7.0) to a concentration of 1-5 mg/mL. Separately, dissolve the polyphenol (e.g., catechin, EGCG) in the same buffer or a compatible solvent.
- pH Adjustment: Adjust the protein solution to the desired alkaline pH (e.g., pH 9.0) using 1 M NaOH under constant stirring.
- Mixing: Add the polyphenol solution dropwise to the protein solution while stirring vigorously. Maintain a defined molar ratio (e.g., 1:1 to 1:10 protein:polyphenol).
- Reaction: Allow the reaction mixture to stir continuously in the dark for a set period (e.g., 1-24 hours) at a controlled temperature (e.g., 25°C or 37°C).
- Purification: Dialyze the final reaction mixture extensively against a suitable buffer (e.g., pH 7.4 phosphate buffer) using a membrane with an appropriate molecular weight cutoff to remove unreacted polyphenols and salts. Alternatively, use size-exclusion chromatography.
- Characterization: Lyophilize the purified complex and characterize using SDS-PAGE, FTIR, and UV-Vis spectroscopy.
Protocol 2: Forming a Non-Covalent Polysaccharide-Polyphenol Complex
This protocol relies on spontaneous self-assembly through hydrogen bonding, hydrophobic, and electrostatic interactions [17] [19].
- Preparation: Dissolve the polysaccharide (e.g., pectin, chitosan) in a suitable buffer or water to a concentration of 1 mg/mL. This may require mild heating and stirring for several hours. Separately, prepare a polyphenol solution in water or a water-miscible solvent.
- Mixing: Add the polyphenol solution dropwise to the polysaccharide solution under constant magnetic stirring.
- Equilibration: Continue stirring the mixture for a defined period (e.g., 1-4 hours) at room temperature to allow complexation to reach equilibrium.
- Purification (Optional): If necessary, remove unbound polyphenols via dialysis or ultrafiltration.
- Characterization: Analyze the complex using DLS for particle size, UV-Vis spectroscopy for binding assessment via spectral shift, and ITC for thermodynamic parameters.
Experimental Workflow and Interaction Mechanisms
Diagram 1: Experimental pathway for complex formation.
Research Reagent Solutions
Table 3: Essential Reagents and Materials for Complexation Studies
| Reagent/Material | Function/Application | Example Items |
|---|---|---|
| Model Proteins | Well-characterized biopolymers for mechanistic studies. | Bovine Serum Albumin (BSA), β-Lactoglobulin (β-LG), Lysozyme, Soy Protein Isolate (SPI), Zein [17] [18]. |
| Model Polysaccharides | Represent different structural features (charge, branching). | Pectin, Chitosan, Cellulose derivatives, Starch, Arabinoxylan [17] [20] [19]. |
| Model Polyphenols | Represent different classes and binding affinities. | Catechin, Epigallocatechin Gallate (EGCG), Tannic Acid, Quercetin, Anthocyanins [17] [16] [19]. |
| Buffers & Chemicals | Control pH and ionic strength; induce specific reactions. | Phosphate Buffered Saline (PBS), Borate Buffer, Urea, Polyphenol Oxidase (PPO), Sodium Hydroxide (NaOH) [16]. |
Frequently Asked Questions (FAQs)
FAQ 1: What is the core difference between the BCS and BDDCS?
While both the Biopharmaceutics Classification System (BCS) and the Biopharmaceutics Drug Disposition Classification System (BDDCS) classify drugs into four categories using the same solubility criteria, they differ in their purpose and the second classification parameter [22].
- BCS is used to determine if a drug product is eligible for a biowaiver of in vivo bioequivalence studies. Its second criterion is the extent of intestinal absorption (permeability) [22].
- BDDCS is used to predict a drug's disposition, including potential for drug-drug interactions in the intestine and liver. Its second criterion is the extent of drug metabolism, which was found to correlate with the rate of intestinal permeability [22].
FAQ 2: How can BCS/BDDCS classification predict food effects?
Food can change gastrointestinal conditions (e.g., pH, bile salt concentration, stomach emptying), which primarily affect drug solubility and dissolution. The BCS/BDDCS framework provides a initial, qualitative prediction of how these changes might impact drug absorption [23]:
- BCS/BDDCS Class 1 (High Solubility, High Permeability/Extensive Metabolism): These drugs typically show no significant food effects on the extent of absorption, though the rate of absorption may be delayed [23].
- BCS/BDDCS Class 2 (Low Solubility, High Permeability/Extensive Metabolism): These drugs are most likely to exhibit a positive food effect (increased absorption) because food-induced increases in solubility and dissolution can significantly enhance bioavailability [23].
- BCS/BDDCS Class 3 (High Solubility, Low Permeability/Low Metabolism): The absorption of these drugs is largely unaffected by solubility changes from food. Effects are less predictable and may be influenced by other factors like transporter interactions [22] [23].
- BCS/BDDCS Class 4 (Low Solubility, Low Permeability/Low Metabolism): These drugs generally have poor oral bioavailability. Predicting food effects is complex due to the interplay of multiple limiting factors [23].
FAQ 3: My compound is highly soluble but has low cellular permeability in Caco-2 assays. Yet, human data shows it is completely absorbed. Why does this happen, and how should I classify it?
This discordance occurs because high permeability in cellular systems like Caco-2 correlates with a high rate of jejunal permeability, whereas the BCS guidance for biowaivers is based on the extent of intestinal absorption [22]. For some non-metabolized drugs, low cellular permeability rates can still result in complete absorption if the drug has sufficient time in the gastrointestinal tract. To resolve this:
- For BCS classification, the FDA recommends using human data (mass balance, absolute bioavailability) to demonstrate high absorption [22].
- For BDDCS classification, you would use the extent of metabolism. A drug with low permeability but complete absorption is likely to be eliminated largely unchanged, suggesting BDDCS Class 3 or 4 [22].
FAQ 4: When is a drug eligible for a biowaiver?
According to the FDA, BCS Class 1 drugs (high solubility, high permeability) with rapid dissolution are eligible for a biowaiver of in vivo bioequivalence studies for immediate-release solid oral dosage forms [22]. The European Medicines Agency (EMA) may also grant biowaivers for some BCS Class 3 drugs [22].
Troubleshooting Guides
Issue: Inaccurate Food Effect Prediction Based on Solubility
Problem: A BCS/BDDCS Class 2 drug was predicted to have a positive food effect due to its low solubility. However, clinical data showed no significant change in exposure (AUC) under fed conditions.
| Potential Cause | Explanation | Solution |
|---|---|---|
| Formulation Optimization | The drug product (e.g., a solid dispersion or nanocrystal) may have already optimized the dissolution rate, effectively converting it to Class 1 behavior in the fasted state and minimizing the relative impact of food [23]. | Review the formulation's properties. Use biorelevant dissolution testing to compare fasted and fed state performance. |
| Solubility-Permeability Interplay | Food increases the concentration of bile micelles, which can solubilize the drug. However, for drugs whose absorption is limited by epithelial membrane permeation (SL-E cases), the increase in total solubility is counterbalanced by a decrease in the free fraction of the drug available for permeation, resulting in a negligible net effect on absorption [24]. | Determine the rate-limiting step for absorption. Use tools like the μFLUX system to measure the dissolution-permeation flux in FaSSIF and FeSSIF media [24]. |
| Incorrect Initial Classification | The drug's solubility may have been misclassified. The FDA solubility criteria require complete dissolution of the highest dose strength in 250 mL aqueous media across pH 1.0–7.5 [22]. | Re-evaluate solubility using biorelevant media (FaSSIF/FeSSIF) that simulate fasted and fed state intestinal conditions [25] [23]. |
Issue: Discrepancy Between Preclinical and Clinical Food Effect Data
Problem: A significant food effect was observed in a dog study, but the effect was much smaller or absent in human trials.
| Potential Cause | Explanation | Solution |
|---|---|---|
| Species Differences | Dogs and humans have physiological differences in GI anatomy, bile composition, and transit times. The extent of food effect observed in dogs does not always translate directly to humans [23]. | Do not rely solely on animal data. Use preclinical data to inform and parameterize a physiologically based absorption model (e.g., GastroPlus, Simcyp) for quantitative human prediction [23]. |
| Dose Number Discrepancy | The dose number (ratio of dose to solubility capacity) may be different between animal and human studies due to different doses or gut volumes, leading to different solubility-limited absorption profiles [23]. | Calculate the dose number for both preclinical species and humans to ensure the same biopharmaceutical challenges are being studied. |
Experimental Protocols
Protocol: Determining BCS/BDDCS Class and Predicting Food Effects
Purpose: To experimentally determine a compound's BCS/BDDCS class and qualitatively assess its potential for food effects in humans.
Methodology Summary: This protocol integrates in silico, in vitro, and in vivo preclinical data to establish a classification and predict food effects [23].
Materials:
- Test compound
- Biorelevant media: Fasted State Simulated Gastric Fluid (FaSSGF), Fasted State Simulated Intestinal Fluid (FaSSIF), Fed State Simulated Intestinal Fluid (FeSSIF) [25] [24]
- pH adjustment tools
- Shaking water bath (37°C)
- HPLC or UV-Vis spectrophotometer
- Caco-2 cell line or similar for permeability assessment
- Preclinical species (e.g., rat) for in vivo PK and metabolism studies
Procedure:
Preliminary In Silico/In Vitro Classification (pBCS/pBDDCS):
- Solubility: Determine the equilibrium solubility in aqueous buffers across pH 1.0–7.5. A drug is highly soluble if the highest dose strength dissolves in 250 mL of buffer [22].
- Permeability: Measure apparent permeability (
Papp) using a Caco-2 assay or similar. Use reference compounds for comparison [22]. - Metabolism (for BDDCS): Use in silico tools to predict
LogPand the probability of extensive metabolism. HighLogPoften correlates with extensive metabolism [23]. - Assign a preliminary class based on the table below.
Preclinical In Vivo Confirmation (rBCS/rBDDCS):
- Conduct radiolabeled mass balance and excretion studies in rats.
- Determine the fraction absorbed (Fa) and the route of elimination (percent excreted unchanged in urine and bile vs. metabolized) [23].
- A drug with high Fa and extensively metabolized aligns with Class 1 or 2. A drug with low Fa and primarily excreted unchanged aligns with Class 3 or 4.
Qualitative Food Effect Prediction:
- Consolidate the pBCS/pBDDCS and rBCS/rBDDCS to estimate the human class (hBCS/hBDDCS).
- Refer to the table in Section 4.1 to predict the likely direction of the food effect.
Protocol: Using Biorelevant Media and μFLUX for Mechanistic Food Effect Studies
Purpose: To quantitatively assess the mechanism of food effects, particularly for solubility-permeation limited (SL-E) drugs, by measuring dissolution-permeation flux under simulated fasted and fed conditions [24].
Materials:
- μFLUX system or similar dissolution-permeation apparatus
- Caco-2 cell monolayers or artificial membranes
- Biorelevant media: FaSSIF and FeSSIF
- Test compounds (e.g., Bosentan, Pranlukast for SL-E; Danazol for SL-U)
Procedure:
- Preparation: Prepare FaSSIF and FeSSIF donor solutions according to established recipes [24]. Set up the acceptor compartment with a suitable buffer.
- Experiment: Place the drug in the donor compartment (FaSSIF or FeSSIF) and initiate the experiment. The drug dissolves and permeates across the membrane into the acceptor compartment.
- Measurement: Sample from the acceptor compartment over time to determine the flux (JμFLUX), which represents the combined dissolution and permeation process.
- Analysis:
- For SL-E drugs, you may observe that while the total drug concentration (
CD) in FeSSIF is much higher than in FaSSIF, the resultingJμFLUXis only marginally increased. This is because the increased solubilization by bile micelles reduces the free fraction of drug available for permeation [24]. - For SL-U drugs, the increase in
CDin FeSSIF should directly translate to a proportional increase inJμFLUX.
- For SL-E drugs, you may observe that while the total drug concentration (
Data Presentation
BCS/BDDCS Classification and Food Effect Predictions
Table 1: Characteristics and typical food effects for each BCS/BDDCS class.
| Class | Solubility | Permeability/Metabolism | Key Characteristics | Typical Food Effect on Absorption |
|---|---|---|---|---|
| Class 1 | High | High / Extensive | Permeability is rate-limiting; transporter effects on absorption are minimal [26]. | Minimal effect on extent (AUC); possible delayed Cmax [23]. |
| Class 2 | Low | High / Extensive | Solubility/Dissolution is rate-limiting; efflux transporters can significantly impact absorption [26]. | Positive food effect likely (increased AUC and Cmax) due to enhanced solubility and dissolution [23]. |
| Class 3 | High | Low / Low | Permeability is rate-limiting; uptake transporters are critical for absorption [26]. | Unpredictable; minimal effect from solubility changes, but may be influenced by food-transporter interactions [22] [23]. |
| Class 4 | Low | Low / Low | Both solubility and permeability are poor; both uptake and efflux transporters are important [26]. | Unpredictable and often low bioavailability; positive food effect is possible but not guaranteed [23]. |
Research Reagent Solutions
Table 2: Key reagents and materials for BCS/BDDCS classification and food effect studies.
| Reagent/Material | Function | Example Use Case |
|---|---|---|
| FaSSIF/FeSSIF | Biorelevant media simulating the fasted and fed state intestinal environment, containing bile salts and phospholipids [25] [24]. | Measuring solubility and dissolution to predict food effects more accurately than in simple aqueous buffers [23] [24]. |
| Caco-2 Cell Line | A human colon adenocarcinoma cell line that differentiates to form a monolayer with enterocyte-like properties. | Assessing apparent permeability (Papp) as a surrogate for human intestinal permeability [22]. |
| Physiologically Based Absorption Software | Software platforms (e.g., GastroPlus, Simcyp) that implement ACAT or ADAM models. | Integrating in vitro data to build mechanistic models and quantitatively simulate human PK profiles and food effects [23]. |
| μFLUX System | An in vitro apparatus that simultaneously measures drug dissolution and permeation flux. | Investigating the mechanism of food effects, especially for distinguishing between SL-E and SL-U cases [24]. |
System Workflows and Diagrams
BDDCS-Based Food Effect Prediction Workflow
Bile Micelle Impact on Drug Absorption
Troubleshooting Guides
Guide 1: Investigating Therapeutic Failure in Clinical Studies
Problem: A drug candidate shows promising efficacy in preclinical models but fails to elicit the expected therapeutic response in a clinical trial population.
| Potential Cause | Investigation Methodology | Corrective & Preventive Actions |
|---|---|---|
| Unaccounted Patient Subgroups | Conduct subgroup analysis of clinical data; genotype patients for polymorphisms in drug-metabolizing enzymes (e.g., CYP450 family) or transport proteins [27]. | Implement personalized medicine strategies; develop companion diagnostic tests to identify likely responders [27]. |
| Drug-Diet Interactions | Use Food Frequency Questionnaires (FFQ) or 24-hour recalls to analyze patient dietary patterns. Assess for specific nutrient deficiencies (e.g., Iron, Vitamins) that may alter drug metabolism [28] [29]. | Include nutritional status as a covariate in trial analysis; provide standardized dietary guidance to participants. |
| Polypharmacy | Perform detailed medication reconciliation for trial participants. Review concomitant medications for known drug-drug interactions [30]. | Refine trial exclusion criteria; design studies to specifically investigate common pharmacological associations. |
| Inadequate Dosing Regimen | Perform therapeutic drug monitoring (TDM) to measure plasma drug concentrations in non-responders [30]. | Initiate pharmacokinetic/pharmacodynamic (PK/PD) modeling to optimize dosing schedules and formulations. |
Experimental Protocol: Analyzing the Impact of Nutritional Status on Drug Efficacy
- Objective: To determine if specific nutritional deficiencies correlate with reduced drug plasma levels or therapeutic failure.
- Materials: Patient serum/plasma samples, drug assay kits, nutritional biomarker assay kits (e.g., for ferritin, vitamin B12, vitamin D, zinc).
- Procedure:
- Collect blood samples from trial participants at baseline and at designated intervals post-drug administration.
- Use validated methods (e.g., HPLC, ELISA) to quantify plasma levels of the investigational drug.
- Assay the same samples for established nutritional biomarkers [28].
- Correlate nutritional biomarker levels with drug plasma concentrations and clinical outcome measures using statistical models (e.g., multivariate regression).
- Interpretation: A significant positive correlation between a nutrient level and drug concentration suggests that deficiency may impair drug absorption or metabolism.
Guide 2: Managing Toxicity Risks in Drug Development
Problem: A compound shows unexpected organ toxicity during animal studies or early-phase clinical trials.
| Potential Cause | Investigation Methodology | Corrective & Preventive Actions |
|---|---|---|
| Off-Target Activity | Conduct in vitro binding/functional assays against a panel of unrelated receptors and enzymes (e.g., hERG channel for cardiac risk) [31]. | Employ medicinal chemistry strategies to improve compound specificity; use structure-based drug design. |
| Reactive Metabolites | Perform in vitro metabolite identification studies using liver microsomes or hepatocytes. Screen for glutathione adducts or other markers of bioactivation [32]. | Redesign lead compound to block or divert metabolic pathways leading to reactive species. |
| Non-Linear Pharmacokinetics | Conduct detailed dose-ranging toxicology studies in two species. Analyze exposure (AUC, Cmax) versus dose to identify non-proportional increases [31] [33]. | Establish a safe therapeutic window (TI); adjust clinical dosing regimen to stay within linear PK range. |
| Dose-Dependent Effects | Re-evaluate all study data through the lens of dose-response. Determine the No Observed Adverse Effect Level (NOAEL) [31] [33]. | Apply a safety factor to the NOAEL to establish a safe starting dose for human trials. |
Experimental Protocol: Determining the No Observed Adverse Effect Level (NOAEL)
- Objective: To identify the highest dose of a test compound that does not produce a significant increase in adverse effects compared to a control group.
- Materials: Test compound, vehicle control, animal model (e.g., rodent), equipment for clinical pathology (clinical chemistry analyzer, hematology analyzer), histopathology.
- Procedure:
- Administer the test compound at three or more graded doses (low, mid, high) and a vehicle control to groups of animals for a specified duration (e.g., 28 days).
- Monitor animals daily for clinical signs of toxicity (mortality, morbidity, behavior).
- Collect blood samples at study termination for hematology and clinical chemistry analysis.
- Perform necropsy and histopathological examination on all major organs.
- Statistically compare all findings from dosed groups to the control group.
- Interpretation: The NOAEL is the highest dose level at which no statistically or biologically significant adverse effects are observed. This is a cornerstone for calculating safe human doses [31].
Frequently Asked Questions (FAQs)
Q1: How can we better account for patient variability in drug response to reduce therapeutic failure? A1: Moving beyond a "one-size-fits-all" approach is key. Strategies include:
- Pharmacogenomics: Identify genetic markers that predict drug metabolism (e.g., CYP polymorphisms) or target sensitivity [27].
- Precision Dosing: Use therapeutic drug monitoring (TDM) and PK/PD modeling to tailor doses to individual patients, especially for drugs with a narrow therapeutic index [30].
- Holistic Patient Profiling: Incorporate data on comorbidities, concomitant medications (polypharmacy), and nutritional status into clinical trial analysis and treatment plans [29] [30].
Q2: What are the key principles for assessing the risk of a toxic substance in a new chemical entity? A2: Risk is a function of both hazard and exposure [31] [32].
- Hazard Identification: What type of toxic effect does the substance cause? (e.g., liver damage, neurotoxicity).
- Dose-Response Assessment: What is the relationship between the dose and the incidence/severity of the effect? Establish a threshold like the NOAEL [31].
- Exposure Assessment: What is the dose, duration, and route of exposure (ingestion, inhalation, dermal) for the intended use? [32] [33].
- Risk Characterization: Integrate the above to describe the nature and likelihood of adverse effects under conditions of exposure.
Q3: How can nutritional deficiencies be accurately assessed in a research or clinical population? A3: Assessment requires a combination of methods, as no single tool is perfect [28] [29].
- Dietary Surveys: Use 24-hour recalls or Food Frequency Questionnaires (FFQ) to estimate habitual intake of nutrients.
- Biochemical Biomarkers: Measure serum/plasma levels of nutrients (e.g., vitamin D, ferritin for iron) or functional markers (e.g., erythrocyte transketolase for thiamine). Be aware that levels can be influenced by inflammation [28].
- Clinical Signs: Look for classic deficiency syndromes (e.g., glossitis, dermatitis, neuropathy) [34].
- Combined Approach: Using biomarkers in conjunction with dietary surveys provides the most robust estimate of nutritional status [29].
Research Reagent Solutions
| Reagent / Material | Function in Research |
|---|---|
| Food Frequency Questionnaire (FFQ) | A subjective dietary assessment tool to estimate the frequency and quantity of food consumption over a specific period, used to derive dietary patterns [29]. |
| Nutritional Biomarker Assay Kits | Kits (e.g., for folate, vitamin B12, zinc) used for the objective measurement of nutrient levels in biological samples like serum or plasma to assess nutritional status [28]. |
| Liver Microsomes | Subcellular fractions used in vitro to simulate Phase I drug metabolism (via cytochrome P450 enzymes), helping to identify potential toxic metabolites [31]. |
| Graphical LASSO | A regularisation technique used with Gaussian Graphical Models (GGMs) to create clear, interpretable networks of food co-consumption from complex dietary data [35]. |
| Human Epidermal Growth Factor Receptor 2 (HER2) Assay | A predictive test used in oncology to identify patients with HER2-positive breast cancer who are likely to respond to targeted therapy like trastuzumab, reducing therapeutic failure [27]. |
Visualizing Complex Relationships
Dietary Impact on Drug Response
Toxicology Risk Assessment
Nutritional Status Assessment
Advanced Assessment Techniques: From Computational Modeling to Analytical Frameworks
Quantitative Performance Data of PBPK in Food Effect Prediction
The predictive performance of PBPK modeling for food effects has been extensively evaluated across multiple studies. The table below summarizes key quantitative findings from large-scale analyses.
Table 1: Predictive Performance of PBPK Modeling for Food Effects
| Study Scope | Number of Compounds/Cases | Performance within 1.25-fold | Performance within 2-fold | Low Confidence (>2-fold) | Primary Citation |
|---|---|---|---|---|---|
| Literature & FDA Review | 48 food effect predictions | ~50% | 75% | Not specified | [36] |
| Industry Consortium (de novo models) | 30 compounds | 15 compounds (High confidence) | 23 compounds (High + Moderate) | 7 compounds | [37] [38] |
The performance of PBPK models is closely tied to the underlying mechanism of the food effect. Predictions are most reliable when the food effect is primarily driven by changes in gastrointestinal physiology and luminal fluids, such as:
- Altered solubility due to changes in bile salt and phospholipid concentrations [37] [38]
- Micellar entrapment [38]
- Changes in gastrointestinal pH [36] [39]
- Variations in gastric emptying time and intestinal fluid volumes [36] [39]
Conversely, models face greater challenges when food effects involve complex processes like enterohepatic recirculation or are significantly influenced by transporter-mediated absorption [40] [38].
Experimental Protocols & Workflows
Established PBPK Workflow for Food Effect Prediction
A generalized, robust workflow for developing and qualifying PBPK models for food effect prediction is outlined below. This "middle-out" approach leverages existing clinical data to build confidence before prospective application [39].
Step 1: Gather Drug-Specific Input Parameters
The foundation of a reliable PBPK model is accurate, high-quality input data [38].
- Physicochemical Properties: Determine pKa, logP, and molecular weight using standardized assays [41] [38].
- Permeability: Measure effective human permeability (Peff,man). A common method uses Madin-Darby canine kidney (MDCK-WT) cell monolayers in a Transwell system, with 10 µM cyclosporin A added to inhibit P-gp. Apparent permeability (Papp) is scaled to Peff,man using the software's built-in calibration curve [38].
- Solubility: Measure equilibrium solubility in:
- Aqueous buffers across a physiologically relevant pH range (e.g., pH 2, 4, 7).
- Biorelevant media: Fasted State Simulated Gastric Fluid (FaSSGF), Fasted State Simulated Intestinal Fluid (FaSSIF-V2), and Fed State Simulated Intestinal Fluid (FeSSIF-V2). Prepare these media according to established instructions (e.g., from Biorelevant.com Ltd.). Equilibrate excess drug substance at 37°C with stirring (200 rpm) and measure concentration after a plateau is reached (up to 24 hours) [38].
- Dissolution: Obtain in vitro dissolution profiles for the formulation in both fasted and fed state biorelevant media [39].
- Disposition Parameters: Incorporate clearance (CL) and volume of distribution (Vd) derived from clinical intravenous data or population PK analysis where possible to isolate absorption-related mechanisms [38].
Step 2: Define System-Specific Inputs
Leverage the physiological database within your PBPK platform (e.g., Simcyp, GastroPlus). For food effect studies, ensure the model accounts for fed-state physiological changes, including increased gastric emptying time, higher intestinal fluid volumes, altered GI pH, and elevated bile salt concentrations [36] [39].
Step 3: Verify the Base PBPK Model
Before predicting food effect, the model must be verified against observed clinical pharmacokinetic data, typically from the fasted state [36] [39]. A model is considered verified when predicted AUC and Cmax for an oral dose fall within 1.25–2.0 fold of observed values, and the shape of the concentration-time profile is captured adequately [36] [38].
Step 4: Apply Fed-State Physiology
Switch the system parameters in the verified model to the fed-state condition. Input fed-state specific drug parameters, particularly solubility and dissolution data measured in FeSSIF-V2 [39] [38].
Step 5: Simulate and Predict Food Effect
Run the simulation under fed-state conditions. Calculate the predicted food effect as the ratio of population geometric means (fed/fasted) for AUC and Cmax [36] [39].
Step 6: Quality Control and Potential Optimization
Compare the predicted AUC and Cmax ratios (AUCR, CmaxR) against observed clinical food effect data, if available.
- High Confidence: Prediction within 0.8- to 1.25-fold of observed [38].
- Moderate Confidence: Prediction within 0.5- to 2-fold of observed [38].
- Low Confidence: Prediction outside 2-fold of observed [38].
If the prediction has low confidence, investigate and optimize key parameters. Commonly optimized parameters to capture the food effect include dissolution rate and precipitation time [36]. A structured decision tree should guide this process to maintain consistency and rigor [38].
Decision Tree for Model Verification and Optimization
The following diagram details the decision-making process for model verification and optimization, a critical component of the workflow above.
Troubleshooting Guides and FAQs
Frequently Asked Questions
Q1: My PBPK model accurately predicts fasted-state PK but fails to capture the fed-state profile. What are the most common parameters to investigate?
A: The most frequently optimized parameters when a model fails to predict food effect are dissolution rate and precipitation time [36]. First, ensure that the solubility data input for the fed state accurately reflects the supersaturation and precipitation behavior of your compound in fed intestinal conditions. The use of kinetically-measured solubility and precipitation data from biorelevant media (FeSSIF) often improves predictions [39].
Q2: For which types of compounds and mechanisms is PBPK food effect prediction most reliable?
A: Predictive performance is highest when the food effect is primarily driven by changes in GI luminal fluids and physiology [37] [38]. This includes mechanisms like:
- Enhanced solubility of lipophilic, low-solubility (BCS II) compounds due to bile micelles [39] [38].
- Changes in absorption due to altered GI pH, fluid volume, or motility [36] [37]. PBPK models face greater challenges with compounds whose absorption is limited by intestinal uptake transporters or those involving complex enterohepatic recirculation [40] [38].
Q3: Can a qualified PBPK model replace a clinical food effect study for regulatory submission?
A: While regulatory acceptance is evolving, a robustly qualified PBPK model can potentially support or replace a clinical study in certain contexts. The model must be developed and verified according to a rigorous workflow, often using a "middle-out" approach with existing clinical data [39]. The FDA and EMA have begun to consider PBPK analyses in submissions, but this requires demonstrated predictive performance and transparency. It is crucial to follow emerging regulatory guidelines on model credibility [42] [43].
Q4: We are in early development and have no clinical data. Can we use a purely "bottom-up" PBPK model to predict food effect risk?
A: Yes. A bottom-up model built entirely on in vitro and in silico parameters can be used for early risk assessment to prioritize compounds or formulations [44]. However, the absolute predictive accuracy will be lower than for a model verified against clinical PK data. The predictions should be used internally to guide development strategy rather than for definitive regulatory decisions at this stage [45].
Troubleshooting Common Issues
Table 2: Troubleshooting Guide for PBPK Food Effect Modeling
| Problem | Potential Causes | Recommended Solutions |
|---|---|---|
| Under-prediction of positive food effect | Model underestimates solubility increase in fed state; Does not capture supersaturation; Incorrect precipitation kinetics. | Re-measure solubility and kinetic precipitation in FeSSIF-V2; Optimize precipitation time parameter in the model [36] [39]. |
| Failure to capture multiple peaks in PK profile | Model does not account for enterohepatic recirculation (EHR). | Incorporate a mechanistic EHR process into the model, for example by triggering a gallbladder emptying event at meal time [40]. |
| Poor prediction of Cmax but accurate AUC | Inaccurate representation of gastric emptying or dissolution rate in the fed state. | Perform sensitivity analysis on gastric emptying time and dissolution rate; Ensure fed-state dissolution profile is correctly input [39]. |
| Model fails verification in fasted state | Incorrect CL or Vd estimates; Poor in vitro-in vivo correlation for permeability or solubility. | Fit/optimize disposition parameters using IV data if available; Re-check experimental methods for permeability/solubility [38]. |
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagents and Software for PBPK Food Effect Modeling
| Item Name | Function/Application | Key Details & Examples |
|---|---|---|
| Biorelevant Media | Simulates fasted (FaSSGF, FaSSIF-V2) and fed (FeSSIF-V2) intestinal conditions for in vitro solubility and dissolution testing. | Critical for measuring physiologically relevant solubility. Prepared according to standardized instructions (e.g., from Biorelevant.com Ltd.) [38]. |
| MDCK Cell Line | Used in vitro to determine apparent permeability (Papp) of a compound, which is scaled to effective human permeability (Peff,man). | Often modified to knockdown endogenous canine P-gp. Experiments include a P-gp inhibitor like cyclosporin A for relevant baseline permeability [38]. |
| PBPK Software Platforms | Provides the technical infrastructure, physiological databases, and algorithms to build, simulate, and qualify PBPK models. | Industry standards include GastroPlus (Simulation Plus), Simcyp Simulator (Certara), and PK-Sim (Open Systems Pharmacology) [41] [42]. |
| Clinical IV PK Data | Used to accurately parameterize the disposition (CL, Vd) of the PBPK model, isolating uncertainty to the absorption process. | Sourced from literature or clinical studies. Not always mandatory, but highly recommended to simplify model development and increase confidence for food effect prediction [38]. |
| KRAS G12C inhibitor 43 | KRAS G12C Inhibitor 43|Potent Research Compound | Explore KRAS G12C inhibitor 43, a potent small molecule for cancer research. This product is for Research Use Only and is not intended for diagnostic or therapeutic use. |
| Trk-IN-8 | Trk-IN-8|Potent TRK Inhibitor|For Research Use | Trk-IN-8 is a potent TRK inhibitor for cancer research. This product is For Research Use Only and not intended for diagnostic or therapeutic use. |
A fundamental challenge in nutritional epidemiology is analyzing the effect of overall diet, rather than single nutrients, on health outcomes. Dietary components are highly correlated and interact in complex ways, making it difficult to isolate their individual effects [46]. Dietary pattern analysis addresses this by examining combinations of foods and beverages people consume [29]. This technical guide explores the two predominant methodological approaches for dietary pattern analysis—index-based (a priori) and data-driven (a posteriori) methods—within the context of research handling complex dietary correlations. You will find troubleshooting guidance, methodological protocols, and FAQs to support your research implementation.
Section 1: Core Methodological Approaches & Comparison
Understanding the Two Main Paradigms
Researchers generally classify dietary pattern assessment methods into two categories [47] [29] [48]:
- Index-Based Methods (A Priori): These investigator-driven approaches measure adherence to predefined dietary patterns based on existing nutritional knowledge and dietary guidelines. Examples include the Healthy Eating Index (HEI), Alternate Mediterranean Diet Score (aMED), and Dietary Approaches to Stop Hypertension (DASH) score [47] [48].
- Data-Driven Methods (A Posteriori): These approaches use multivariate statistical techniques to derive dietary patterns directly from population dietary intake data. Principal component analysis (PCA), factor analysis, cluster analysis, and reduced rank regression (RRR) are prominent examples [47] [49] [50].
Comparative Analysis of Methods
Table 1: Comparison of Index-Based and Data-Driven Dietary Pattern Analysis Methods
| Feature | Index-Based (A Priori) Methods | Data-Driven (A Posteriori) Methods |
|---|---|---|
| Core Principle | Measures adherence to predefined patterns based on dietary guidelines [29] [48] | Derives patterns empirically from dietary intake data [47] [48] |
| Basis for Pattern | Prior knowledge/hypothesis about diet-health relationships [47] | Correlations and variances in consumed food groups [47] [49] |
| Output | A score representing overall diet quality [48] | Patterns (factors/clusters) specific to the study population [47] |
| Comparability | High; allows direct comparison across different studies [47] [48] | Limited; patterns are population-specific [47] |
| Key Advantage | Objective, based on established evidence; easy to interpret [48] | Identifies real-world dietary combinations without preconceptions [48] |
| Key Limitation | Subjective choices in component selection and scoring [48] | Solutions depend on researcher's analytical choices [47] [50] |
| Common Techniques | HEI, AHEI, aMED, DASH score [47] [48] | PCA/Factor Analysis, Cluster Analysis (K-means), RRR [47] [50] [51] |
Section 2: Technical Guide & Troubleshooting FAQs
Frequently Asked Questions (FAQs)
FAQ 1: How do I choose the optimal number of factors in Principal Component Analysis (PCA)?
The number of factors to retain is typically determined by a combination of three criteria [49] [48]:
- Eigenvalue greater than one (Kaiser's rule)
- Scree plot visual inspection: Looking for the "elbow" point where the slope of the line levels off
- Interpretability: The retained factors should be meaningful and explain a reasonable proportion of the variance (often >5-10% per factor)
Troubleshooting Tip: If the derived patterns are not interpretable, even with a statistically justified number of factors, re-examine your initial food group aggregation. Overly broad or narrow food groups can obscure meaningful patterns.
FAQ 2: My cluster analysis solution is unstable. How can I validate it?
Cluster stability is a common challenge. To objectively select the most appropriate clustering method and number of clusters, use stability-based validation [50].
- Method: Randomly split your dataset into training and test sets multiple times (e.g., 20 iterations).
- Validation: Apply the clustering algorithm to both sets and compare the solutions using stability indices like the adjusted Rand index or misclassification rate.
- Output: The solution with the highest average stability (lowest misclassification rate) across iterations is considered the most robust and representative of the underlying population structure [50].
FAQ 3: Why is the diagnostic accuracy of my diet quality index lower than expected?
The predictive ability of a composite index is influenced by its components [46]:
- Number of Components: Diagnostic accuracy generally increases with the number of components, but only when the components have low or no intercorrelation.
- Intracorrelation: Ensure that the components included in your index are strongly associated with the health outcome of interest.
- Recommendation: For optimal accuracy, construct your index using multiple, low-intercorrelated components that are each independently associated with the target outcome [46].
FAQ 4: How should I handle highly correlated food items in my dataset before analysis?
This is a classic problem arising from the complex correlations in dietary data.
- Standard Practice: The initial step is to pre-aggregate individual food items into logically similar food groups [49] [50]. For example, combine various types of leafy greens, or different kinds of red meat.
- Rationale: This reduces multicollinearity, simplifies the model, and facilitates the interpretation of derived patterns by focusing on broader dietary behaviors.
Experimental Protocols for Key Methods
Protocol 1: Implementing Principal Component Analysis (PCA) for Dietary Patterns
This protocol is based on a cross-sectional analysis of Iranian adults [49].
- Data Preparation: Collect dietary intake data via a validated FFQ, 24-hour recall, or food diary. Pre-aggregate all consumed food items into 40-50 meaningful food groups (e.g., "citrus fruits," "hydrogenated fats," "non-leafy vegetables") based on nutritional similarity and culinary use [49].
- Input Variable Preparation: Use grams consumed per day per food group as input variables. Adjust for total energy intake using the residual method [50].
- Execution: Perform PCA with varimax rotation on the food group variables to derive principal components.
- Factor Retention & Naming: Retain factors with an eigenvalue >1.5 (or using scree plot interpretation). Name the resulting dietary patterns based on the food groups that load most strongly (e.g., absolute factor loading >0.20) on each component [49].
- Output: Generate standardized dietary pattern scores for each participant for use in subsequent analyses with health outcomes.
Protocol 2: Conducting K-Means Cluster Analysis for Dietary Patterns
This protocol is derived from a study on NAFLD in Hispanic patients [51] and a stability-based validation study [50].
- Data Preparation & Standardization: Prepare food group intake data as in the PCA protocol. Crucially, standardize the intake of each food group to a common scale (e.g., mean=0, standard deviation=1) to prevent variables with larger scales from dominating the cluster solution [50].
- Preliminary Analysis: Run the FASTCLUS (K-means) procedure for a range of pre-specified cluster numbers (e.g., 2 to 4) to assess interpretability [51].
- Stability Validation (Recommended): Use a stability-based validation procedure with multiple random splits of your dataset to objectively select the optimal number of clusters and clustering method [50].
- Final Clustering: Execute the K-means algorithm with the validated number of clusters. The algorithm will assign each participant to a single, mutually exclusive cluster based on the Euclidean distance between their diet and the cluster center [51].
- Output & Description: Characterize each cluster by comparing the mean intake of food groups between clusters. Name the clusters based on their predominant dietary features (e.g., "Plant-food/Prudent" vs. "Fast-food/Meats" pattern) [51].
Section 3: Visual Workflows & Research Toolkit
Decision Pathway for Method Selection
The following diagram outlines the logical process for selecting an appropriate dietary pattern analysis method based on your research objective.
The Researcher's Toolkit: Essential Reagents & Software
Table 2: Key Research Reagent Solutions for Dietary Pattern Analysis
| Item / Reagent | Function / Application in Analysis |
|---|---|
| Food Frequency Questionnaire (FFQ) | Primary tool for collecting habitual dietary intake data; assesses frequency and quantity of food consumption over a specified period [29]. |
| 24-Hour Dietary Recall | A detailed, interviewer-led method to capture all foods and beverages consumed in the previous 24 hours; often used for population-level estimates [49] [29]. |
| Food Composition Database | Converts reported food consumption into nutrient intake data; essential for calculating index scores and profiling the nutrient content of derived patterns [49]. |
| Statistical Software (SAS, R, Stata) | Platforms for implementing all data-driven methods (PCA, Cluster Analysis, RRR) and calculating most index-based scores [48]. |
| Stability Validation Script (R/Python) | Custom or packaged code to perform stability-based validation for cluster analysis, ensuring robust and reproducible results [50]. |
| Diet Quality Index (DQI) Framework | A predefined scoring structure (e.g., HEI, AHEI) used to calculate an individual's adherence to a specific dietary pattern [29] [48]. |
| Grb2 SH2 domain inhibitor 1 | Grb2 SH2 domain inhibitor 1, MF:C68H95N20O15P, MW:1463.6 g/mol |
| Cox-2-IN-30 | Cox-2-IN-30, MF:C17H16N6O3S, MW:384.4 g/mol |
Biorelevant solubility and precipitation testing uses laboratory test solutions that simulate the chemical and physical conditions of the human gastrointestinal (GI) tract to predict how drugs will behave in the body. Unlike conventional dissolution media, these media contain physiological components like bile salts and lipids to replicate actual GI fluids in both fasted and fed states. This approach provides more accurate prediction of in vivo drug performance before clinical trials, helping researchers screen formulations more effectively [52] [53].
The transition of a drug from the stomach to the intestine represents a critical phase where precipitation often occurs, particularly for poorly soluble compounds. Two-stage biorelevant dissolution testing, also known as a "biorelevant transfer test," is specifically designed to simulate this physiological process, where drug products initially in contact with simulated gastric fluid (FaSSGF) are subsequently converted to simulated intestinal fluid (FaSSIF) [54]. This method is particularly valuable for drug development of water-insoluble bases where drug solubility is higher in gastric fluid than intestinal fluid [54].
Frequently Asked Questions (FAQs)
FAQ 1: When should I use two-stage biorelevant dissolution testing instead of single-stage methods?
Two-stage dissolution is particularly crucial for immediate-release formulations of basic drugs with low water solubility, especially when the drug exhibits higher solubility in gastric fluid than intestinal fluid [54] [55]. This method provides critical insights into precipitation or supersaturation behavior as pH shifts from stomach to intestinal pH.
Key indicators for choosing two-stage testing:
- Poorly soluble basic drugs that may precipitate at intestinal pH
- Formulations where supersaturation maintenance is critical for absorption
- Compounds with significant food effects
- Amorphous solid dispersions (ASDs) where precipitation kinetics affect performance [55]
FAQ 2: Why does my drug show good solubility in gastric conditions but poor oral bioavailability?
This common issue often results from drug precipitation during the transition from stomach to small intestine. The solubility of many drugs is highly pH-dependent, particularly for weak bases that are highly soluble in acidic gastric environments but may precipitate rapidly at neutral intestinal pH [55]. Two-stage testing can identify this "precipitation risk" that single-stage methods in consistent pH media would miss.
The cinnarizine case study demonstrates how a drug can maintain supersaturation without precipitation during this transition, highlighting the importance of testing the entire GI journey [56].
FAQ 3: What are the critical differences between fasted and fed state simulated media?
Table 1: Comparison of Key Biorelevant Media Types
| Medium | Prandial State | Fluid Simulated | pH | Key Components |
|---|---|---|---|---|
| FaSSGF | Fasted | Gastric | 1.6 | Pepsin, low bile salts [52] |
| FaSSIF | Fasted | Small Intestinal | 6.5 | Bile salts, phospholipids [52] |
| FeSSIF | Fed | Small Intestinal | 5.0 | Higher bile salt/phospholipid concentration [52] |
| FaSSIF-V2 | Fasted | Small Intestinal | 6.5 | Updated formula [52] |
| FeSSIF-V2 | Fed | Small Intestinal | 5.8 | Updated formula [52] |
FAQ 4: How do I properly execute a two-stage dissolution experiment?
Standardized Two-Stage Protocol:
- Apparatus: USP Apparatus 2 (paddle) [54]
- Stage 1 (Gastric):
- Volume: 450 mL FaSSGF
- Duration: 1-2 hours
- Parameters: 37°C, 75 rpm [56]
- Stage 2 (Intestinal):
- Add 450 mL FaSSIF Converter to existing medium
- Duration: 2+ hours
- Parameters: 37°C, 75 rpm [56]
- Sampling: Use appropriate filtration (e.g., 13mm Glass Microfibre Syringe Filters) at predetermined timepoints [56]
Critical Consideration: Before conducting two-stage testing, researchers are strongly recommended to first test dissolution in FaSSIF alone to establish how the drug product releases prior to gastric exposure [54].
Troubleshooting Guides
Problem: Unexpected Precipitation During pH Transition
Symptoms: Rapid decrease in dissolved drug concentration after FaSSIF converter addition.
Possible Causes and Solutions:
Table 2: Precipitation Troubleshooting Guide
| Cause | Identification | Resolution Strategies |
|---|---|---|
| Poor supersaturation maintenance | Concentration drops >20% within 30 minutes of pH shift | Formulate with precipitation inhibitors (polymers like HPMC, HPMCAS) [55] |
| Inadequate bile salt concentration | Precipitation occurs faster than in vivo data suggests | Adjust bile salt/phospholipid ratios; consider fed state media for lipophilic drugs [53] |
| Too rapid pH transition | Sharp precipitation curve | Modify addition rate of FaSSIF converter; consider gradual pH shift methods |
| Drug-specific crystallization tendency | Variable results across similar compounds | Pre-classify drugs by crystallization tendency (slow/moderate/fast) [55] |
Problem: Poor Discrimination Between Formulations
Symptoms: Inability to distinguish performance differences between formulation prototypes.
Solutions:
- Ensure non-sink conditions to properly evaluate supersaturation maintenance [55]
- Extend sampling frequency during critical transition periods
- Consider incorporating additional analytical techniques (e.g., particle size analysis)
- Verify media composition freshness and preparation accuracy
Problem: Lack of In Vitro-In Vivo Correlation (IVIVC)
Symptoms: Dissolution data doesn't correlate with observed pharmacokinetic profiles.
Solutions:
- Review media selection appropriateness for your drug's properties
- Consider using more sophisticated systems like the Gastrointestinal Simulator (GIS) for complex formulations [55]
- Evaluate whether absorption limitations (rather than dissolution) may be controlling bioavailability
- Verify biorelevant media composition matches current physiological understanding
The Scientist's Toolkit
Essential Research Reagents
Table 3: Key Reagents for Biorelevant Testing
| Reagent/Kit | Function | Application Notes |
|---|---|---|
| 3F Powder | Base powder for preparing various biorelevant media | Enables preparation of FaSSGF, FaSSIF, FeSSIF [52] |
| FaSSIF Converter Buffer Concentrate | Converts FaSSGF to FaSSIF during two-stage testing | Critical for simulating gastric-to-intestinal transition [54] |
| FaSSGF Buffer Concentrate | Preparation of fasted state gastric fluid | Maintains physiological surface tension [52] |
| FaSSIF/FeSSIF-V2 Powders | Updated intestinal fluid simulations | Improved predictability for contemporary formulations [52] |
| AChE-IN-9 | AChE-IN-9, MF:C30H35N5O9, MW:609.6 g/mol | Chemical Reagent |
| Mat2A-IN-4 | Mat2A-IN-4|Potent MAT2A Inhibitor for Cancer Research | Mat2A-IN-4 is a potent MAT2A inhibitor for oncology research. It disrupts SAM production, targeting MTAP-deleted cancers. For Research Use Only. Not for human use. |
Experimental Workflow Visualization
Method Selection Algorithm
Standard Operating Procedure: Two-Stage Dissolution Testing
Materials and Equipment
- USP Apparatus 2 (paddle)
- FaSSGF media (prepared from 3F Powder and FaSSGF Buffer Concentrate)
- FaSSIF Converter (prepared from 3F Powder and FaSSIF Converter Buffer Concentrate)
- Temperature-controlled water bath (37°C ± 0.5°C)
- Appropriate filtration system (e.g., 13mm Glass Microfibre Syringe Filters)
- Validated HPLC method for analysis [56]
Step-by-Step Protocol
Media Preparation:
- Prepare FaSSGF according to manufacturer instructions using FaSSGF Buffer Concentrate
- Prepare FaSSIF Converter solution according to manufacturer specifications
- Degas media prior to use
Stage 1 (Gastric Phase):
- Add 450 mL FaSSGF to each dissolution vessel
- Equilibrate to 37°C
- Add dosage form (typically n=6 vessels)
- Operate at 75 rpm for 1-2 hours
- Sample at predetermined timepoints (e.g., 15, 30, 45, 60 minutes)
Stage 2 (Intestinal Phase):
- Add 450 mL pre-warmed FaSSIF Converter to each vessel
- Continue operation at 75 rpm for additional 2+ hours
- Sample at frequent intervals initially (5, 10, 15, 30, 45, 60 minutes), then less frequently
Sample Analysis:
- Filter samples immediately using appropriate filtration
- Analyze using validated HPLC method
- Compare concentration profiles to identify supersaturation and precipitation behavior
Context Within Dietary Components Research
Understanding complex correlations between dietary components represents a parallel challenge in nutritional science, where network analysis approaches have emerged to capture the intricate relationships between multiple dietary elements that traditional methods might overlook [57]. Similarly, biorelevant testing acknowledges the complex, multi-factorial nature of gastrointestinal physiology rather than examining drug solubility in isolation.
This holistic approach aligns with the recognition in nutritional research that focusing on individual nutrients provides an incomplete picture, and that synergistic interactions between components are crucial for understanding biological effects [57] [29]. The methodological rigor in biorelevant testing—carefully simulating the dynamic, multi-parameter environment of the GI tract—provides a template for how complex biological systems can be meaningfully modeled in vitro.
The same way that dietary pattern analysis has evolved from examining single nutrients to evaluating comprehensive dietary patterns [58], dissolution testing has advanced from simple aqueous buffers to sophisticated biorelevant media that capture the essential complexities of gastrointestinal fluids.
FAQs: Addressing Common Analytical Challenges
What are the most frequent causes of inaccurate results in MIDS analysis?
Inaccurate results often stem from matrix interferences, where components within the supplement co-elute or suppress/enhance the signal of your target analyte [59]. Other common issues include ingredient degradation during sample preparation or storage, and a lack of standardized, matrix-specific testing protocols for such complex mixtures [60].
How can I mitigate matrix effects and signal suppression in LC-MS analysis?
To mitigate matrix effects, consider these strategies:
- Sample Cleanup: Implement robust sample preparation techniques like Solid-Phase Extraction (SPE) to remove interfering compounds [59].
- Internal Standards: Use stable isotopically labeled internal standards (e.g., 13C or 15N labeled). These co-elute with the analyte and experience the same ionization effects, allowing for accurate correction. Note that deuterated standards can sometimes exhibit a deuterium isotope effect, leading to slightly different retention times [59].
- Dilution: A simple sample dilution can sometimes reduce matrix effects, though this may also reduce sensitivity [61].
My sample has low analyte recovery. What should I check?
Low recovery can be due to several factors in the sample preparation process. The following table outlines common causes and solutions.
| Problem Area | Specific Issue | Recommended Solution |
|---|---|---|
| Extraction | Inefficient or incomplete extraction of the analyte from the complex matrix [60]. | Optimize extraction solvents, temperature, and use techniques like accelerated solvent extraction (ASE) [62]. |
| Sample Pretreatment | Loss of trace components or degradation during pretreatment [60]. | Develop matrix-specific pretreatment protocols; shorten processing time; use inert atmospheres [60]. |
| Chemical Interactions | Analyte binding to other ingredients (e.g., proteins, carbohydrates) or the container [59]. | Modify extraction pH; add competing agents; use protein precipitation [59]. |
When is suitability testing required for microbiological methods?
Suitability testing (preparatory testing) is required when testing a product for the first time using USP methods (e.g., <61>, <62>, <2021>, <2022>). This ensures the product matrix does not cause false negatives by inhibiting the growth of microorganisms. It should also be repeated when there are changes in manufacturing, suppliers, or product formulation [63].
What should I do if my method lacks sensitivity and precision?
For poor sensitivity and precision, consider these steps:
- Check Sample Preparation: Confirm the accuracy of all dilutions and reconstitutions. Ensure reagents are freshly prepared and equilibrated to room temperature [61].
- Review Instrument Calibration: Regularly calibrate your instruments. For techniques like Luminex, running verification on the day of the assay is a best practice [61].
- Optimize Method Parameters: For LC-MS, optimize MRM transitions and instrument settings. For ICP-MS, parameters like carrier gas flow and laser energy (for LA-ICP-MS) must be fine-tuned [59] [64].
Troubleshooting Guides
Guide 1: Poor Chromatographic Separation
Observation: Poorly resolved peaks, peak tailing, or shoulder peaks.
| Possible Cause | Investigation & Resolution |
|---|---|
| Column Overload/Inappropriate Column | The complex sample matrix may be overwhelming the column. Investigate: Check peak shape at different dilutions. Resolve: Use a column with different selectivity (e.g., C18, phenyl, HILIC) or a longer column; dilute the sample [62]. |
| Mobile Phase Issue | The pH or solvent strength may not be optimal for separating all components. Investigate: Perform a mobile phase scouting gradient. Resolve: Adjust pH, buffer concentration, or organic solvent gradient; use mobile phase additives [59]. |
| Co-eluting Interferences | Other ingredients are eluting at the same time as your analyte. Investigate: Use a diode-array or mass spectrometric detector to check for peak purity. Resolve: Improve sample cleanup (e.g., SPE) or further optimize the chromatographic method [59]. |
Guide 2: High Background or Noise in Spectroscopic Detection
Observation: High baseline, noisy signal, or elevated blanks.
| Possible Cause | Investigation & Resolution |
|---|---|
| Contaminated Reagents or Solvents | Investigate: Run a blank with fresh, high-purity solvents. Resolve: Use higher purity (HPLC/MS-grade) solvents and reagents; filter mobile phases [61]. |
| Carryover from Previous Samples | Investigate: Closely inspect the blank injection following a high-concentration sample. Resolve: Increase wash volume and duration in the autosampler method; implement a more effective needle wash solvent [61]. |
| Dirty Flow Cell or Detector Lamp | Investigate: Check baseline noise and drift over time. Resolve: Follow manufacturer's instructions for flushing the flow cell; replace the UV lamp if it is near the end of its life [61]. |
The Scientist's Toolkit: Key Research Reagent Solutions
The following table lists essential materials and tools for ensuring accurate and reproducible analysis of Multi-Ingredient Dietary Supplements.
| Tool/Reagent | Function & Importance |
|---|---|
| Certified Reference Materials (CRMs) | Provides a metrologically traceable standard with certified values for specific analytes. Critical for method validation, calibration, and ensuring accuracy. A dedicated database (RMST) is available from NIH ODS to help find fit-for-purpose RMs [65]. |
| Stable Isotope-Labeled Internal Standards | Added to the sample at the beginning of preparation, they correct for analyte loss during cleanup and matrix effects during ionization in mass spectrometry, significantly improving data quality [59]. |
| Specialized Sorbents for SPE | Used in sample preparation to selectively retain target analytes or remove interfering matrix components (e.g., fats, pigments, proteins), thereby cleaning up the sample and reducing matrix effects [59]. |
| Matrix-Matched Calibrators | Calibration standards prepared in a solution that mimics the sample's blank matrix. This helps compensate for matrix effects that can otherwise suppress or enhance the analyte signal [64]. |
| Validated Methods (e.g., USP) | Scientifically valid methods, such as those from the United States Pharmacopeia (USP), are designed for complex matrices like dietary supplements and help avoid interferences, false positives, and false negatives [63]. |
| Ulonivirine | Ulonivirine (MK-8507)|Investigational HIV-1 NNRTI |
Experimental Workflow for MIDS Analysis
The diagram below outlines a generalized, robust workflow for the analysis of multi-ingredient dietary supplements, incorporating steps to address common challenges.
Frequently Asked Questions
What is the primary purpose of a standardized dietary assessment framework? These frameworks are designed to collect accurate and consistent dietary data across different studies and populations. The primary goal is to minimize measurement errors and biases, thereby ensuring that data on nutrient intake and health outcomes can be reliably compared and pooled, which is essential for establishing valid correlations between diet and disease [66] [67].
My data shows high intra-individual variation in nutrient intake. How can I account for this in my study design? High intra-individual variation is a common challenge. To account for this, you must increase the number of replicate observations (days) per individual. The required number of days can be calculated using established formulas that consider the ratio of within-person to between-person variation (σw/σb) and your desired correlation level between observed and usual intake [66]. For example, one method is: d = [r²/(1 - r²)] σw/σb, where 'd' is the number of days needed, and 'r' is the expected correlation. Nutrients with high day-to-day variability, like vitamin A or cholesterol, may require dozens of records to estimate usual intake reliably, whereas energy intake requires fewer days [66].
What are the main types of measurement error I need to consider in dietary assessment? The two main types are random error and systematic error (bias). It is crucial to distinguish between them, as they require different handling methods [66] [68].
- Random Error: Originates from day-to-day variations in an individual's food intake and from inherent limitations of the measurement tool. It can be reduced by increasing the number of observations and handled through statistical modeling [66].
- Systematic Error (Bias): A non-random error that consistently skews data in one direction. Examples include the under-reporting of calorie intake by obese individuals or differences in reporting between cases and controls in a case-control study (recall bias). Bias is more difficult to correct and requires careful study design and sampling to control [66].
Are digital dietary assessment tools more accurate than traditional methods? Digital tools, such as smartphone-based food records, offer advantages in automatic data handling, reduced researcher burden, and improved feasibility and acceptability among participants [67]. However, they do not fully resolve inherent issues like misreporting, recall bias, or the Hawthorne effect (where participants change their behavior because they are being observed) [67]. The accuracy depends more on the underlying methodology (e.g., using image recognition with authoritative databases) than the digital format itself [69].
How can I correct for measurement error in my dietary data analysis? Statistical modeling can attenuate the effects of random error. Several methods exist to adjust data and estimate "usual intake". The table below summarizes key features of common statistical models [66]:
| Model Name | Key Characteristics | Best Applied To |
|---|---|---|
| NCR/IOM | Uses power or log transformation to approximate normal distribution. | General intake data adjustment [66]. |
| ISU Method | Adjusts for individual bias (season, day of week); uses a two-stage transformation [66]. | Data requiring bias correction before transformation [66]. |
| MSM | Estimates probability of consumption; useful for sporadic foods and Food Frequency Questionnaires (FFQ) [66]. | Data with many zero-intake days [66]. |
| SPADE | Models intake as a direct correlation with age [66]. | Populations with strong age-intake relationships (e.g., children) [66]. |
What is an emerging technological solution for improving dietary assessment? The DietAI24 framework is a recent innovation that combines Multimodal Large Language Models (MLLMs) for food recognition with Retrieval-Augmented Generation (RAG) technology. Instead of relying on the model's internal knowledge, RAG grounds the recognition in authoritative nutrition databases like the Food and Nutrient Database for Dietary Studies (FNDDS). This approach has been shown to reduce mean absolute error for food weight and nutrient estimation by 63% compared to existing methods and can estimate 65 distinct nutrients [69].
Troubleshooting Guides
Problem: Inconsistent Food Identification and Classification Across Studies
Issue: Different studies use different food item classifications and ontologies, making data aggregation and comparison difficult.
Solution:
- Adopt a Standardized Food Ontology: Utilize a common, authoritative food code system, such as the Food and Nutrient Database for Dietary Studies (FNDDS) used in the United States. The FNDDS provides unique, 8-digit codes for thousands of foods and beverages, along with standardized portion sizes and comprehensive nutrient profiles [69].
- Implement a Unified Recognition Framework: Leverage advanced AI frameworks like DietAI24. This system addresses variability by:
- Food Recognition: Using an MLLM (e.g., GPT Vision) to identify food items in an image and map them to specific FNDDS food codes [69].
- Knowledge Grounding: Employing RAG technology to query the FNDDS database directly, ensuring the nutrient estimation is based on the authoritative source rather than the AI's general knowledge, thus reducing "hallucination" [69].
- Standardize Portion Size Estimation: Frame portion size estimation as a multiclass classification problem, selecting from FNDDS-standardized qualitative descriptors (e.g., "1 cup," "2 slices") rather than relying on open-ended regression, which introduces more error [69].
Problem: High Intra-individual Variation Obscures Usual Intake
Issue: A single day of dietary data does not represent an individual's "usual intake," leading to misclassification and loss of statistical power.
Solution:
- Determine the Required Number of Replicate Days: Before starting your study, calculate the number of dietary assessment days needed per individual. Use the formula:
d = (Zα * CVw / D₀)²
- d: Number of days required per individual.
- Zα: The Z-value for the desired confidence level (e.g., 1.96 for 95% confidence).
- CVw: The coefficient of intra-individual variation (intra-individual standard deviation divided by mean food intake).
- Dâ‚€: The specified level of error (e.g., 0.1 for 10%) [66].
- Apply Statistical Modeling: Collect multiple 24-hour recalls or food records and use a statistical model to estimate the distribution of usual intake. The workflow below generalizes the process used by several models (e.g., MSM, SPADE) [66].
Problem: Systematic Bias in Self-Reported Data
Issue: Data is skewed by factors like systematic under-reporting (common in obese individuals) or recall bias (in case-control studies).
Solution:
- Study Design is Key: Use prospective data collection where possible to reduce recall bias. For case-control studies, be aware that cases may report dietary intake differently from controls [66].
- Incorporate Biomarkers: Where feasible, use objective biomarkers (e.g., doubly labeled water for energy expenditure, nitrogen urine for protein intake) to calibrate self-reported intake data [68].
- Conduct Internal Validation Studies: Within your main study, perform a validation sub-study on a group of participants. In this sub-study, collect both the error-prone self-reported data (e.g., FFQ) and a more accurate reference measure (e.g., multiple 24-hour recalls or biomarker data). This allows you to quantify and correct for the specific systematic bias present in your study population using measurement error models [68].
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function in Dietary Assessment |
|---|---|
| Food and Nutrient Database for Dietary Studies (FNDDS) | An authoritative database providing standardized food codes, portion sizes, and values for 65+ nutrients for thousands of foods. Serves as the foundational source for nutrient calculation [69]. |
| Multimodal Large Language Model (MLLM) | An artificial intelligence model capable of understanding both images and text. In frameworks like DietAI24, it is used for the initial visual recognition of food items from photographs [69]. |
| Retrieval-Augmented Generation (RAG) | A technology that grounds an AI's responses in external, authoritative databases (like FNDDS). It prevents "hallucination" by retrieving actual data instead of generating nutrient values from internal knowledge [69]. |
| 24-Hour Dietary Recall (24HR) | A retrospective method where participants recall all foods and beverages consumed in the preceding 24 hours. It is often used as a standard in validation studies [69] [66]. |
| Statistical Modeling Software (e.g., for SPADE, MSM) | Software packages that implement statistical models to adjust for intra-individual variation and estimate the distribution of usual intake from short-term dietary data [66]. |
Solving Real-World Challenges: Analytical Interferences and Clinical Translation Barriers
Troubleshooting Guides
Guide 1: Diagnosing and Resolving LC-MS Matrix Effects
Problem: Inconsistent or inaccurate quantification of target analytes during LC-MS analysis, suspected to be due to matrix effects.
Matrix effects occur when components in a complex sample alter the ionization efficiency of your target analyte, leading to signal suppression or enhancement. This is a common challenge when analyzing complex formulations, where excipients, multiple active ingredients, or dietary components can co-elute and interfere [59] [70].
Step-by-Step Resolution:
Confirm the Presence of Matrix Effects: Use the post-column infusion method to identify regions of ion suppression or enhancement in your chromatogram [70].
- Procedure: Inject a blank, extracted sample matrix into the LC system. Use a T-piece to continuously infuse a standard solution of your analyte into the post-column eluent flowing into the MS.
- Diagnosis: A stable signal indicates no matrix effects. A depression or elevation in the baseline at specific retention times indicates ion suppression or enhancement, respectively [70].
Evaluate the Extent of Matrix Effects: Use the post-extraction spike method to quantify the effect [70].
- Procedure: Compare the MS response of your analyte in a pure standard solution to the response of the same amount of analyte spiked into a blank, extracted sample matrix.
- Calculation: Calculate the Matrix Effect (ME) as:
ME (%) = (B / A - 1) × 100, where A is the peak area of the neat standard and B is the peak area of the post-extracted spiked standard. An ME of 0% indicates no effect, negative values indicate suppression, and positive values indicate enhancement.
Implement Mitigation Strategies:
- Improve Sample Clean-up: If ME is significant, enhance your sample preparation. Solid-phase extraction (SPE) with a selective sorbent can effectively remove phospholipids and other common interferences found in complex matrices [59].
- Optimize Chromatography: Adjust the LC method to increase the separation between the analyte and the interfering compounds. This can be achieved by modifying the gradient, using a different stationary phase, or increasing the column length to improve resolution [70].
- Use Stable Isotope-Labeled Internal Standards (SIL-IS): This is the most effective way to compensate for matrix effects. The SIL-IS experiences nearly identical ionization suppression/enhancement as the analyte, correcting for the loss of accuracy [59] [70]. Nitrogen-15 (15N) or carbon-13 (13C) labeled standards are often preferred over deuterated ones to avoid chromatographic isotope effects [59].
- Adjust MS Instrumentation: For some applications, switching from an electrospray ionization (ESI) source, which is more prone to matrix effects in the liquid phase, to an atmospheric pressure chemical ionization (APCI) source can reduce interference [70].
Guide 2: Handling Multi-Ingredient Dietary Supplement (MIDS) Formulation Challenges
Problem: Analytical difficulties in MIDS due to ingredient interactions, formulation variability, and a lack of standardized testing protocols.
The combination of multiple functional ingredients, excipients, and specific dosage forms (like soft capsules or jellies) in MIDS can lead to unique challenges, including ingredient degradation, interferences, and poor recovery during analysis [71].
Step-by-Step Resolution:
Identify Ingredient Interactions: Review the formulation for known problematic interactions. For example, analytical difficulties have been reported between vitamin B12 and copper sulfate, or between saw palmetto fruit extract and Ginkgo leaf extract [71].
- Procedure: Perform a compatibility study by analyzing individual ingredients and then in combination to observe signal changes or the appearance of new peaks.
Address Formulation-Specific Issues:
- Soft Capsules/Jellies: These often require specialized sample preparation. For soft capsules, a solvent extraction may be needed to dissolve the gelatin shell and liberate the active ingredients. For jellies, a digestion or dissolution step might be necessary to break down the gelling agents [71].
- Liquid Formulations: These may contain stabilizers or emulsifiers that can cause interference or foul the LC column. A simple protein precipitation or filtration may be insufficient, requiring SPE or liquid-liquid extraction for cleaner extracts [71].
Develop a Matrix-Specific Pretreatment Protocol: There is no one-size-fits-all method. Based on expert recommendations, a systematic approach is required [71]:
- Modify Extraction Strategies: Optimize solvent type, pH, and extraction time for your specific formulation. For protein-bound analytes, enzymatic digestion might be necessary.
- Substitute Problematic Raw Materials: If certain raw materials cause persistent interference, work with formulators to find suitable alternatives that are more analytically amenable.
- Implement Internal Quality Controls: Use in-house reference materials and spike-and-recovery experiments to continuously monitor the performance of your analytical method.
Frequently Asked Questions (FAQs)
Q1: What are the most common sources of matrix effects in the analysis of dietary components? Matrix effects primarily arise from co-eluting compounds that alter ionization efficiency in the mass spectrometer. Common interferents include phospholipids from biological samples, salts, residual proteins, and other formulation components such as excipients (e.g., polyethylene glycol, polysorbates) or other active ingredients in multi-component supplements [70] [72] [71]. In complex dietary formulations, the interaction between different functional ingredients (e.g., vitamins, plant extracts, minerals) is a major source of analytical interference [71].
Q2: How can I choose between minimizing matrix effects versus compensating for them? The choice depends on the required sensitivity of your assay [70].
- Minimize ME when sensitivity is crucial: This involves reducing the source of the interference by improving sample clean-up (e.g., SPE, liquid-liquid extraction), optimizing chromatographic separation, or adjusting MS parameters. The goal is to remove or separate the interferent before it reaches the detector.
- Compensate for ME when a blank matrix is available: This is often a more practical approach. Use calibration standards prepared in a blank matrix (matrix-matched calibration) and employ stable isotope-labeled internal standards. The internal standard corrects for fluctuations in ionization efficiency, providing accurate quantification even if some matrix effect remains [70].
Q3: Are certain analytical techniques less prone to matrix effects? Yes, the susceptibility to matrix effects varies by technique. For instance, Atmospheric Pressure Chemical Ionization (APCI) is often less prone to matrix effects than Electrospray Ionization (ESI) because ionization occurs in the gas phase rather than in the liquid droplets [70]. In ICP-MS, techniques using collision/reaction cells can effectively mitigate polyatomic interferences [73] [74]. Furthermore, ligand-binding assays like ELISA are particularly susceptible to matrix endogenous interferences, whereas LC-MS/MS methods generally offer superior specificity and reliability in complex matrices [72].
Q4: What is the best internal standard to use for compensating for matrix effects? Stable isotope-labeled internal standards (SIL-IS) are considered the gold standard. They have nearly identical physicochemical properties to the analyte, ensuring they co-elute and experience the same matrix effects. While deuterated standards are common, nitrogen-15 (15N) or carbon-13 (13C) labeled internal standards are often preferred because they minimize the potential for deuterium isotope effects, which can cause slight retention time shifts in reversed-phase LC [59].
Experimental Protocols
Protocol 1: Evaluating Matrix Effects via Post-Extraction Spike Method
This protocol provides a quantitative measure of matrix effects for a specific analyte-matrix combination [70].
1. Materials and Reagents:
- Analytic standard
- Blank matrix (e.g., placebo formulation, control plasma)
- All solvents and reagents for sample preparation
- LC-MS/MS system
2. Procedure: a. Prepare a neat standard solution of the analyte at a known concentration in mobile phase (Solution A). b. Prepare a blank sample using the blank matrix and subject it to the entire sample preparation and extraction procedure. c. Spike the same known concentration of analyte into the prepared blank matrix extract (Solution B). d. Analyze both Solution A and Solution B using the LC-MS/MS method.
3. Data Analysis:
Calculate the matrix effect (ME) using the formula:
ME (%) = (Peak Area of Solution B / Peak Area of Solution A - 1) × 100
An ME value of -20% indicates 20% ion suppression, while a value of +15% indicates 15% ion enhancement.
Protocol 2: Solid-Phase Extraction (SPE) for Sample Clean-up
SPE is a highly effective sample preparation technique for preconcentrating analytes and removing matrix interferences from complex samples [59].
1. Materials and Reagents:
- SPE cartridges (select sorbent chemistry based on analyte, e.g., C18 for reversed-phase, SCX for cation exchange)
- Conditioning solvents (e.g., methanol, acetonitrile)
- Equilibration solvent (often water or a buffer)
- Wash solvents (e.g., water, 5% methanol in water)
- Elution solvent (e.g., methanol, acetonitrile, with a modifier if needed)
- Vacuum manifold or positive pressure system
2. Procedure: a. Conditioning: Pass 2-3 column volumes of methanol through the sorbent bed, followed by 2-3 column volumes of water or equilibration buffer. Do not let the bed dry out. b. Loading: Load the prepared sample onto the cartridge. Use a slow, drop-wise flow rate to maximize analyte retention. c. Washing: Pass 2-3 column volumes of a weak wash solvent to remove weakly retained matrix interferences without eluting the analyte. d. Elution: Pass 2-3 column volumes of a strong elution solvent to collect the analyte in a clean tube. e. Reconstitution: Evaporate the eluent to dryness under a gentle stream of nitrogen and reconstitute the residue in the initial mobile phase for LC-MS analysis.
Workflow and Pathway Visualizations
Matrix Effect Mitigation Workflow
The following diagram outlines a systematic decision-making process for diagnosing and mitigating analytical interferences in complex formulations.
Research Reagent Solutions
The following table details key reagents and materials essential for developing robust analytical methods resistant to matrix interference.
| Reagent/Material | Primary Function in Mitigating Interferences |
|---|---|
| Stable Isotope-Labeled Internal Standard (SIL-IS) | Compensates for analyte ionization suppression/enhancement by co-eluting with the analyte and experiencing identical matrix effects; considered the most effective compensation strategy [59] [70]. |
| Selective SPE Sorbents | Removes specific matrix interferences (e.g., phospholipids, salts, proteins) during sample preparation, leading to a cleaner extract and reduced ion suppression [59]. |
| LC Columns (C18, Phenyl, HILIC, etc.) | Provides chromatographic resolution to physically separate the target analyte from co-eluting interferents; different chemistries are selected based on analyte properties [70]. |
| Collision/Reaction Gases | Used in ICP-MS and some MS systems to eliminate polyatomic spectral interferences through chemical reactions or kinetic energy discrimination [73] [74]. |
Frequently Asked Questions (FAQs)
FAQ 1: What are the primary mechanisms behind nutrient-drug interactions? Nutrient-drug interactions occur through several key mechanisms:
- Absorption Alterations: Food can enhance, delay, or decrease drug absorption. For instance, many antibiotics have impaired absorption when taken with food. Minerals like calcium, iron, and magnesium can form complexes with drugs such as bisphosphonates, reducing the absorption of both the drug and the nutrient [75] [76].
- Enzyme Modulation: Dietary components can inhibit or induce drug-metabolizing enzymes. A well-documented example is grapefruit juice, which inhibits the cytochrome P-450 3A4 enzyme system, thereby slowing the metabolism of drugs like amiodarone, carbamazepine, and some statins, increasing their bioavailability and risk of toxicity [77] [75] [76].
- Transport Competition: Drugs and nutrients may compete for transport proteins or binding sites. For example, the drug levodopa competes with certain amino acids for absorption sites, which can interfere with its efficacy [77].
- Nutrient Depletion: Certain medications can deplete specific nutrients. Diuretics may cause excessive urinary excretion of minerals like potassium and magnesium, while drugs like colchicine can lead to malabsorption of fat, β-carotene, sodium, potassium, and vitamin B12 [77] [75].
FAQ 2: My cell-based PPI assay shows high background signal. How can I troubleshoot this? High background in cell-based protein-protein interaction (PPI) assays, such as BRET or FRET, can arise from several sources. The following troubleshooting guide outlines common causes and solutions:
| Potential Cause | Diagnostic Experiment | Corrective Action |
|---|---|---|
| Non-specific protein aggregation | Express each fusion protein (donor and acceptor) individually and measure signal. | Optimize fusion protein expression levels; use stable transfection over transient to ensure reproducible expression [78]. |
| Overexpression of fusion proteins | Titrate the expression of fusion proteins using an inducible system (e.g., Dox-on). | Use the minimal amount of inducer/fusion protein required to generate a sufficient signal-to-noise ratio [78]. |
| Incorrect fusion orientation | Test all possible fusion protein orientations (N- vs C-terminal). | Re-clone constructs to use the fusion orientation that yields the highest specific signal and lowest background [78]. |
| Insufficient assay reversibility | Treat cells with a known inhibitor and measure signal decay time. | For dynamic studies, use reversible assay formats like BRET or Bimolecular Luminescence Complementation (BiLC) [78]. |
FAQ 3: How can I experimentally validate that a dietary component is an enzyme modulator? Validating an enzyme modulator involves a combination of in vitro and cell-based assays. Below is a detailed protocol for a cell-based screening assay.
Experimental Protocol: Cell-Based Screening for Enzyme Modulators
Objective: To identify and characterize compounds from dietary components that modulate the activity of a specific enzyme, such as a deubiquitinase (DUB).
Materials:
- Plasmids: Plasmids encoding for the target enzyme (e.g., a DUB) and its substrate, tagged with appropriate reporters (e.g., Luciferase, GFP) [79].
- Cell Line: A mammalian cell line relevant to the enzyme's biology (e.g., HEK293T) [78].
- Test Compounds: Purified dietary components (e.g., flavonoids from grapefruit, polyphenols from tea).
- Controls: Known enzyme activators/inhibitors and vehicle control (e.g., DMSO).
Methodology:
- Cell Culture and Transfection:
- Culture cells in appropriate medium. For consistency, use a stable transfection system to express the enzyme and substrate reporter constructs. If stable lines are not available, perform transient transfection, ensuring transfection efficiency is consistent across experiments [78].
- Seed cells into 96-well or 384-well assay plates at a density optimized for confluence at the time of reading.
Compound Treatment:
- Pre-incubate cells with a range of concentrations of the dietary test compounds. Include positive (known inhibitor/activator) and negative (vehicle) controls on each plate.
- For enzymes involved in irreversible interactions, a pre-incubation step with the compound before inducing the expression of the interacting partners is recommended [78].
Signal Detection:
- Depending on the reporter system, measure the signal after an appropriate incubation period.
- For luciferase-based complementation assays (e.g., BiLC), add the substrate and measure luminescence using a multimodal plate reader [78].
- For FRET/BRET-based assays, measure energy transfer using a suitable plate reader or imaging system [78].
Data Analysis:
- Calculate the Z'-factor to validate the assay's robustness for each plate using the positive and negative controls. A Z'-factor between 0.5 and 1 is considered excellent for HTS [78].
- Normalize the signal from test wells to the vehicle control (0% inhibition/activation) and positive control (100% inhibition/activation).
- Generate dose-response curves to determine the IC50 (for inhibitors) or EC50 (for activators) values for the hit compounds.
FAQ 4: What computational tools can help predict allosteric modulation by nutrient metabolites? Computational methods are powerful for identifying potential allosteric sites and predicting modulator binding. The table below summarizes key tools and their applications:
| Computational Tool/Method | Primary Function | Application Example |
|---|---|---|
| Molecular Dynamics (MD) Simulations | Models physical movements of atoms over time to explore conformational changes and allosteric pathways. | Simulating the dynamics of Sirtuin 6 (SIRT6) to identify potential allosteric pockets [80]. |
| Normal Mode Analysis (NMA) | Predicts collective motions of proteins that are relevant to function and allosteric regulation. | Analyzing the MAPK/ERK kinase (MEK) to understand its allosteric landscape [80]. |
| Machine Learning (ML) Approaches | Uses algorithms to predict allosteric sites and the binding propensity of small molecules based on structural and evolutionary data. | High-throughput prediction of allosteric sites across diverse enzyme families [80]. |
| PASSer & AlloReverse | Specific platforms for predicting allosteric sites and designing allosteric modulators. | De novo identification of allosteric sites and design of selective modulators [80]. |
Research Reagent Solutions
The following table details essential reagents and tools for studying nutrient-drug competition and enzyme modulation.
| Reagent/Tool | Function in Research |
|---|---|
| Ubiquitin Variant Libraries | Massively diverse combinatorial libraries used to develop selective inhibitors or activators for enzymes in the ubiquitin system, such as deubiquitinases (DUBs) and ligases (E3s) [79]. |
| Stable Cell Lines | Cell lines with stably integrated genes for PPI or enzyme reporters ensure run-to-run reproducibility in high-throughput screens, which is critical for reliable data [78]. |
| FRET/BRET Pair Plasmids | Plasmids encoding for donor and acceptor proteins (e.g., GFP/RFP for FRET, Luciferase/GFP for BRET) fused to proteins of interest, enabling the study of PPIs in live cells [78]. |
| Inducible Expression Systems | Systems like Dox-on allow graded expression of target proteins, helping to determine minimal expression levels for optimal assay performance and reducing background signal [78]. |
| Consumer-Resource Models | Computational models that incorporate nutrient competition to quantitatively predict how drug perturbations will restructure complex microbial or cellular communities [81]. |
Experimental Workflow and Signaling Pathways
High-Throughput Screening Workflow for PPI Inhibitors
This diagram illustrates a generalized cell-based workflow for identifying inhibitors of protein-protein interactions.
Nutrient Competition in Gut Microbiome Restructuring
This diagram outlines the conceptual process by which drug-induced nutrient competition alters gut microbiome composition, as predicted by consumer-resource models.
Enzyme Modulation Pathways
This diagram shows the mechanistic pathways by which small molecules, such as dietary components, can modulate enzyme activity.
For researchers in drug development, understanding the complex interplay between food intake and pharmaceutical performance is paramount. The simultaneous intake of food and drugs can significantly alter drug release, absorption, distribution, metabolism, and elimination, thereby impacting the safety and efficacy of pharmacotherapy [82]. This guide addresses key technical challenges and provides foundational methodologies for managing these critical food-drug interactions in a research setting.
Core Mechanisms of Food-Drug Interactions
FAQ: What are the primary physiological mechanisms behind food-drug interactions?
The presence of food in the gastrointestinal tract creates a dynamic physiological environment that can alter a drug's fate. The main mechanisms include:
- Altered Gastric Emptying: Food can delay gastric emptying, which in turn delays the delivery of the drug to its primary absorption site in the small intestine [83].
- Changes in Gastric pH: Food intake stimulates acid secretion, which can change the solubility and dissolution rate of drugs, particularly those with pH-dependent solubility [83].
- Bile Flow and Secretion: Food, especially fatty meals, stimulates the secretion of bile. Bile salts can enhance the solubility and absorption of poorly water-soluble drugs [83].
- Splanchnic Blood Flow: Food intake increases blood flow to the gut and liver, which can influence the rate and extent of drug absorption and first-pass metabolism [83].
- Physical Interactions: Food components can physically or chemically interact with drug molecules (e.g., chelation), reducing their availability for absorption [83] [82].
FAQ: Why is this research critical for regulatory approval?
Regulatory agencies now frequently require data on food-induced dissolution and absorption profiles for new drug applications [83]. A food-effect bioavailability study is a standard expectation to determine the impact of food on the drug's pharmacokinetics and to inform appropriate labeling and dosing instructions.
Quantitative Food-Effect Profiles of Common Drugs
Table 1: Impact of Food on Drug Bioavailability: Representative Examples
| Drug Molecule | Observed Change with Food | Primary Postulated Mechanism |
|---|---|---|
| Propranolol | Improved Absorption [83] | Increased Splanchnic Blood Flow [83] |
| Ketoconazole | Improved Absorption [83] | Enhanced Solubility due to Lower Gastric pH [83] |
| Levothyroxine | 40-50% Reduction in Bioavailability [83] | Physical Adsorption or Chelation with Food Components [83] |
| Ciprofloxacin | 40-50% Reduction in Bioavailability [83] | Chelation with Divalent Cations (e.g., Ca²âº) in Food [83] |
Experimental Protocol: Assessing Food Effects in Preclinical Models
FAQ: What is a robust method for controlled oral dosing in rodent studies?
Traditional methods like drug-infused chow offer limited dosing control, while gavage can induce stress. A diet gel-based system provides a minimally invasive alternative for water-insoluble small molecules, allowing for precise dose adjustment and consumption monitoring [84].
Title: Controlled Oral Dosing in Mice Using a Diet Gel-Based System
Objective: To evaluate the efficacy of a small molecule (e.g., PLX5622) using a gel diet for controlled oral delivery.
Reagents:
- ClearH2O DietGel 93M (or similar complete gel-based maintenance diet)
- Small molecule drug (e.g., PLX5622)
- Vehicle (e.g., DMSO)
- Experimental mice (e.g., Cx3cr1gfp/+ reporter mice)
Methodology:
- Fasting: Fast mice for 16 hours prior to experimental start to facilitate transition to the gel diet and establish a baseline body weight [84].
- Drug Formulation:
- Weigh the required amount of DietGel 93M.
- Dissolve the drug in a minimal volume of a suitable vehicle (e.g., DMSO) and mix thoroughly into the gel diet to achieve the target concentration (e.g., 0.8 mg/g or 2.0 mg/g of gel) [84].
- Dosing Regimen:
- House mice individually.
- Provide a pre-determined daily portion of drug-infused gel (e.g., 8 g/day) in a Petri dish [84].
- Refresh the gel daily to ensure stability and accurate dosing.
- Data Collection:
- Consumption Monitoring: Weigh uneaten gel daily to calculate exact drug intake [84].
- Body Weight: Track body weight daily to monitor animal health and detect any treatment-related weight loss [84].
- Efficacy Endpoint: Use appropriate methods (e.g., longitudinal SLO imaging, endpoint histology) to assess the pharmacological outcome (e.g., microglia depletion) [84].
Troubleshooting Tip: If consumption is inconsistent, ensure the drug-vehicle mixture does not adversely affect the palatability of the gel. A pilot study to determine optimal consumption rates is recommended [84].
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Investigating Food-Drug Interactions
| Research Reagent / Technology | Primary Function in Research |
|---|---|
| DietGel 93M | A gel-based rodent diet used as a vehicle for controlled oral delivery of water-insoluble small molecules, allowing precise dosage adjustment [84]. |
| Food-Derived Natural Carriers (e.g., protein-, polysaccharide-based) | Serve as biocompatible delivery systems to enhance the stability and bioavailability of bioactive compounds, offering improved functionality and targeting to the intestine [85]. |
| Self-Emulsifying Drug Delivery Systems (SEDDS) | Formulation approach used to overcome low solubility and food-effects by improving drug dissolution and absorption [83]. |
| In Situ Gelling Systems | Formulations that gel upon contact with GI fluids, potentially modifying drug release profiles and mitigating variable food effects [83]. |
Troubleshooting Common Experimental Challenges
FAQ: How can I address high variability in drug response during fed-state studies?
- Standardize the Meal: Use a consistent, well-defined meal composition (e.g., high-fat vs. low-fat) for all subjects in a study group. The FDA often recommends a high-fat, high-calorie meal for food-effect bioavailability studies.
- Control Timing: Strictly control the time interval between food administration and drug dosing.
- Monitor Consumption: In preclinical models, always measure the exact amount of drug-infused food consumed, as done with the gel-based system, rather than assuming ad libitum intake [84].
FAQ: A drug candidate shows poor bioavailability in a fasted state. What formulation strategies can help?
- Lipid-Based Systems: Utilize SEDDS or SMEDDS (Self-Microemulsifying Drug Delivery Systems) to enhance the solubility and absorption of lipophilic drugs, mimicking the solubilizing effect of food [83].
- Nano-Formulations: Develop nanoemulsions or nanoparticles to increase the surface area and improve dissolution rates [83].
- Bioenhancers: Investigate the use of natural carriers or absorption enhancers that can strengthen the targeting capability and permeability of the drug without the need for food [85] [86].
The management of food-drug interactions is a sophisticated and essential component of modern drug development. Beyond traditional formulation approaches, emerging fields like precision nutrition and food-derived delivery systems offer promising avenues for creating more robust and patient-centric therapies [85] [87]. A deep understanding of the mechanisms outlined in this guide, combined with rigorous experimental practices, empowers researchers to anticipate, investigate, and overcome the challenges posed by the complex correlations between diet and drug delivery.
Frequently Asked Questions (FAQs)
Q1: Why are patient-specific factors like obesity considered confounding variables in nutritional research? Confounding variables are extraneous factors that can distort the apparent relationship between a dietary exposure and a health outcome. Patient-specific factors like obesity, age, and comorbidities are classic confounders because they are often associated with both dietary intake and disease risk, creating spurious associations if not properly accounted for [88]. For example, obesity is not only a health outcome but also a risk factor for numerous diseases and is associated with distinct dietary patterns [89] [90].
Q2: How does obesity biologically confound the relationship between diet and metabolic outcomes? Obesity is not a mere demographic trait but an active metabolic state. It acts as a mediator on the causal pathway between diet and many clinical endpoints, such as cardiovascular disease risk factors [91]. Statistical models show that dietary patterns have significant indirect effects on metabolic risk factors like HDL-cholesterol, triglycerides, and CRP, which are mediated through obesity [91]. Failing to model this relationship correctly can lead to an over- or under-estimation of a diet's direct effects.
Q3: What is the difference between confounding and mediation in this context? Confounding is a source of bias that must be controlled for, whereas mediation is a part of the causal pathway that you may wish to quantify.
- Confounding: An unmeasured common cause (e.g., socioeconomic status) that influences both a person's diet and their disease risk, creating a false association.
- Mediation: A variable (e.g., obesity) that lies on the path from an exposure (e.g., a high-fat diet) to an outcome (e.g., hypertension). The diet causes obesity, which in turn causes hypertension [91]. Advanced methods like Structural Equation Modeling (SEM) can partition these direct and indirect effects.
Q4: Can a healthy lifestyle eliminate the confounding effect of obesity? No. While a healthy lifestyle can significantly reduce the risk of obesity-related diseases, it does not entirely offset the risks associated with a high BMI [90]. This means that obesity remains an independent risk factor. In statistical terms, even after adjusting for lifestyle factors like physical activity and diet quality, the association between obesity and diseases such as diabetes and hypertension, though attenuated, persists [90]. Therefore, both lifestyle and BMI must be independently accounted for in analyses.
Troubleshooting Guides
Problem 1: Inconsistent or Counterintuitive Associations
- Scenario: Your analysis finds a protective effect for a dietary component (e.g., alcohol) on an outcome (e.g., type 2 diabetes), but the result contradicts physiological knowledge or other studies [88].
- Potential Cause: Residual confounding by overall dietary patterns. Individual dietary components are consumed as part of a broader diet. Failure to adjust for this larger pattern can leave residual confounding, as the observed effect might be due to other healthy foods consumed alongside the component of interest [88].
- Solution:
- Move beyond single-nutrient adjustments: Do not just adjust for a few selected nutrients (e.g., saturated fat, fiber).
- Use dietary pattern analysis: Employ data-driven methods like Factor Analysis (FA) or Partial Least Squares (PLS) to derive overall dietary patterns from your food consumption data [88] [48].
- Include pattern scores as covariates: Adjust for these pattern scores in your multivariate model to determine if the association with the single dietary component holds independent of the person's overall diet [88].
Problem 2: Isolating the Direct Effect of a Dietary Pattern
- Scenario: You want to understand how a specific dietary pattern directly influences a metabolic risk factor (e.g., HDL-cholesterol), separate from its effect via causing obesity.
- Potential Cause: Obesity as a mediator. The dietary pattern influences obesity, which in turn influences the metabolic risk factor. Standard regression adjusting for BMI would answer a different question (the direct effect only).
- Solution: Use Mediation Analysis, for instance, via Structural Equation Modeling (SEM) [91].
- Specify your model: Define the dietary pattern as the exposure, obesity (e.g., BMI) as the mediator, and the metabolic factor as the outcome.
- Fit an SEM: This model will estimate and provide P-values for:
- The direct effect of the diet on the outcome.
- The indirect effect of the diet on the outcome, mediated through obesity.
- The total effect (sum of direct and indirect effects) [91].
Problem 3: Handling Highly Correlated Dietary and Lifestyle Data
- Scenario: Multicollinearity makes model estimates unstable when including multiple dietary and lifestyle factors.
- Potential Cause: Lifestyle factors (diet, exercise, smoking) are often correlated, and dietary nutrients are consumed in complex mixtures [48] [90].
- Solution:
- Create a composite healthy lifestyle score: As done in large cohort studies, create a score (e.g., 0 to 4) where points are assigned for meeting criteria for non-smoking, adequate physical activity, moderate alcohol consumption, and a healthy diet [90]. This reduces dimensionality and handles collinearity.
- Use dimensionality reduction techniques: Apply Principal Component Analysis (PCA) or Exploratory Factor Analysis (EFA) to dietary data to derive a few, uncorrelated dietary patterns that represent the major variations in diet for your population [48] [91].
The following tables summarize core data on the epidemiology of obesity and its role as a risk factor, essential for power calculations and interpreting effect sizes.
Table 1: Global Obesity Prevalence and Projections (Adults) [92] [93]
| Year | Population with Obesity | Prevalence (%) | Notes |
|---|---|---|---|
| 1990 | -- | -- | Baseline (rates more than doubled since 1990) |
| 2022 | 890 million | 16% | 1 in 8 people globally were living with obesity |
| 2030 | ~1.13 billion | -- | Projected |
| 2035 | ~1.9 billion | ~25% | Projected |
| 2050 | ~3.80 billion | >50% | Projected (includes overweight and obesity) |
Table 2: Obesity as a Risk Factor for Comorbidities [89] [90]
| Comorbidity | Relative Risk / Hazard Ratio (HR) Increase with Obesity | Key Notes |
|---|---|---|
| Diabetes | HR = 7.16 (for obesity with 4 healthy lifestyle factors) [90] | Strongest association among outcomes studied. |
| Heart Failure | HR = 2.65 (for obesity with 4 healthy lifestyle factors) [90] | Associated with Heart Failure with preserved Ejection Fraction (HFpEF). |
| Hypertension | HR = 1.80 (for obesity with 4 healthy lifestyle factors) [90] | Linked to increased sympathetic activity and RAAS activation. |
| Coronary Artery Disease | 30% increased risk per 5-unit BMI increment [89] | Often comorbid with diabetes, dyslipidemia, and sleep apnea. |
| Atrial Fibrillation | 5% increased risk per 1-unit BMI increment (for BMI >30) [89] | Framingham Heart Study data. |
Detailed Experimental Protocols
Protocol 1: Adjusting for Confounding by Dietary Patterns using Factor Analysis
This protocol is based on the methodology used to isolate the effect of alcohol from the overall diet in the Framingham Offspring Study [88].
Application: To test whether an association between a single food/nutrient and a health outcome is independent of the individual's overall dietary pattern.
Workflow:
- Dietary Assessment: Collect dietary data using a validated, semi-quantitative food frequency questionnaire (FFQ) with ~100 items [88].
- Data Preprocessing: Group individual food items into logical food groups (e.g., whole grains, red meat, vegetables). Exclude participants with implausible energy intake (<600 or >4200 kcal/day) [88].
- Derive Dietary Patterns:
- Perform Factor Analysis (FA) or Principal Component Analysis (PCA) using the food group intake data.
- Use orthogonal rotation (e.g., Varimax) to create uncorrelated patterns.
- Determine the number of factors to retain based on scree plots, eigenvalues >1, and interpretability.
- Name the factors based on foods with high factor loadings (e.g., "Western," "Prudent") [88] [48].
- Statistical Modeling:
- Use a Cox proportional hazards model (for time-to-event data) or logistic regression (for binary outcomes).
- Model 1: Adjust for standard non-dietary confounders (age, sex, BMI, physical activity, smoking, etc.).
- Model 2: Add the single nutrient/food of interest.
- Model 3: Add the dietary pattern scores derived from FA/PCA to Model 2.
- Interpretation: A significant change in the effect estimate for the nutrient/food of interest between Model 2 and Model 3 indicates confounding by the overall dietary pattern [88].
Protocol 2: Quantifying Direct and Indirect Effects via Structural Equation Modeling
This protocol is adapted from a study analyzing the effects of dietary patterns on metabolic risk factors with obesity as a mediator [91].
Application: To partition the total effect of an exposure (e.g., diet) into its direct effect on an outcome and its indirect effect operating through a mediator (e.g., obesity).
Workflow:
- Variable Preparation:
- Exposure: Derive dietary patterns as in Protocol 1, or use predefined dietary scores.
- Mediator: Measure obesity using Body Mass Index (BMI) and/or waist circumference.
- Outcomes: Define metabolic risk factors (e.g., HDL-cholesterol, triglycerides, HbA1c, CRP, blood pressure).
- Confounders: Identify and measure variables like age, sex, education, physical activity, and alcohol consumption [91].
- Model Specification:
- Use an Exploratory Structural Equation Model (ESEM) which combines factor analysis for deriving dietary patterns with the structural regression model in a single step [91].
- Specify paths from the latent dietary patterns to the mediator (obesity).
- Specify paths from the dietary patterns and the mediator to each metabolic outcome.
- Include confounders as covariates in all relevant regression equations.
- Model Fitting and Interpretation:
- Fit the model using statistical software (e.g., Mplus, R's
lavaanpackage). - Extract and report the standardized estimates for:
- Direct effect: The path from diet -> outcome.
- Indirect effect: The path from diet -> mediator -> outcome.
- Total effect: The sum of direct and indirect effects [91].
- Fit the model using statistical software (e.g., Mplus, R's
Visualizing Relationships and Workflows
Diagram 1: Obesity as Confounder and Mediator
This diagram illustrates the fundamental conceptual difference between confounding and mediation, which require different statistical approaches.
Diagram 2: Statistical Workflow for Mediation Analysis
This diagram outlines the step-by-step analytical process for conducting a mediation analysis using Structural Equation Modeling (SEM).
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Methods for Managing Confounding
| Item / Method | Function / Application in Research | Example from Literature |
|---|---|---|
| Validated FFQ | To comprehensively assess habitual dietary intake and enable dietary pattern analysis. | 126-item FFQ used in the Framingham Offspring Study [88]. |
| Body Composition Measures | To quantify obesity beyond BMI, providing data on fat distribution. | Waist circumference used alongside BMI in the Tromsø Study [91]. |
| Dietary Pattern Analysis (PCA/FA) | Data-driven method to derive uncorrelated dietary patterns from FFQ data for use as adjustment variables. | Used to control for residual confounding by overall diet in alcohol-diabetes association [88] [48]. |
| Structural Equation Modeling (SEM) | A statistical framework to model complex pathways, including direct and indirect (mediated) effects. | Used to quantify obesity-mediated effects of diet on metabolic risk [91]. |
| Healthy Lifestyle Score | A composite index to adjust for the collective effect of multiple healthy behaviors in a single variable. | 4-factor score (smoking, diet, exercise, alcohol) used in UK Biobank analysis [90]. |
Frequently Asked Questions
Q1: What are the primary formulation approaches for a poorly soluble, crystalline API? For a poorly soluble crystalline Active Pharmaceutical Ingredient (API), the main technological pathways are Particle Size Reduction (e.g., nanomilling) and Amorphous Solid Dispersions (ASDs). Particle size reduction increases the surface area available for dissolution, while ASDs transform the API into a higher-energy amorphous form, which can lead to faster dissolution rates and increased solubility. The choice depends on the API's physicochemical properties, required drug load, and thermal stability [94].
Q2: What minimal API quantity is needed for an initial HME feasibility study? Using API-sparing techniques like Vacuum Compression Moulding (VCM) with prior cryomilling, it is possible to evaluate up to 12 different experimental conditions (e.g., various polymers and drug loadings) with less than 100 mg of API. This is a significant reduction compared to using an 11mm extruder, which could require at least 20g of API for a comparable number of experiments [94].
Q3: Which analytical techniques are critical during pre-formulation development for HME? A comprehensive pre-formulation assessment utilizes several tools to understand the material properties [94]:
- Differential Scanning Calorimetry (DSC): Determines melting temperature (Tm), glass transition temperature (Tg).
- Thermogravimetric Analysis (TGA): Assesses thermal degradation temperature (Tdeg).
- Hot Stage Microscopy (HSM): Visually observes thermal behavior.
- X-ray Powder Diffraction (XRPD): Confirms crystallinity or amorphicity.
Q4: How is a robust and scalable Hot Melt Extrusion (HME) process developed? Process development involves conducting a Design of Experiments (DOE) to establish a design space. This includes evaluating Critical Process Parameters (CPPs) like screw design, processing temperature profile, feed rate, and screw speed, and measuring their effect on dependent variables such as melt temperature and specific mechanical energy. This is typically done using a larger-scale extruder (e.g., 18mm) with batch sizes of 5-25 kg to ensure consistent product quality and define scale-up factors [94].
Troubleshooting Guides
Problem 1: Low Bioavailability Due to Poor Solubility
Potential Causes and Solutions:
| Cause | Proposed Solution | Key Considerations |
|---|---|---|
| Low Aqueous Solubility | Amorphous Solid Dispersions (ASD): Embed the API in a polymer carrier via Hot Melt Extrusion (HME) or spray drying. | HME is a continuous, solvent-free process suitable for APIs with adequate thermal stability [94]. |
| Particle Size Reduction: Use nanomilling to reduce crystalline API particle size. | Requires specialized equipment and careful control to achieve uniform particle size [94]. | |
| Lipid-Based Drug Delivery Systems (LBDDS): Dissolve or suspend the API in lipidic vehicles. | Effective for lipophilic compounds; requires evaluation of lipid compatibility [94]. | |
| Low Permeability | Incorporate permeation enhancers or use lipid-based formulations like nanoemulsions. | Requires safety and efficacy testing of the enhancers [95]. |
Experimental Protocol: API-Sparing HME Feasibility Screening
- Objective: To assess the viability of HME for a given API with minimal material usage.
- Method: Use Vacuum Compression Moulding (VCM) combined with cryomilling.
- Procedure:
- Screen 2-3 polymers with 3 different drug load (DL) values each.
- Cryomill physical mixtures of API and polymer.
- Process the mixtures using VCM to simulate extrusion.
- Characterize the resulting dispersions using PLM, DSC, and XRPD to confirm amorphicity.
- Materials Required: ~100 mg of API; selected polymers (e.g., HPMCAS, PVP-VA).
- Expected Outcome: Identification of promising polymer and DL combinations for further prototyping [94].
Problem 2: Recrystallization of the Amorphous Phase Upon Storage
Potential Causes and Solutions:
| Cause | Proposed Solution | Key Considerations |
|---|---|---|
| Insufficient API-Polymer Miscibility | Conduct a thermodynamic assessment during pre-formulation to select a polymer with better miscibility. | Perform miscibility studies using DSC to construct a phase diagram [94]. |
| High Drug Loading | Reduce the drug load to a level below the recrystallization curve identified in the phase diagram. | A phase diagram helps visualize the impact of DL on stability [94]. |
| Unoptimized Formulation | Add stabilizing additives like surfactants or plasticizers. | These additives can impact the glass transition temperature (Tg) and processability [94]. |
Experimental Protocol: Thermodynamic Miscibility Assessment
- Objective: To select the optimal carrier polymer and evaluate appropriate drug loadings for a stable ASD.
- Method: Use DSC and other tools to study API-polymer interactions.
- Procedure:
- Prepare physical mixtures of the API with 4-5 candidate polymers at 2-4 different drug loadings (requires ~1g API total).
- Analyze mixtures using DSC to evaluate melting point depression and the Tg of the mixture.
- Construct a phase diagram to understand the solubility of the API in the polymer melt and the recrystallization tendency.
- Materials Required: API candidate, polymer carriers, DSC instrument.
- Expected Outcome: A phase diagram identifying stable and unstable drug load ranges for each polymer [94].
Table 1: API and Excipient Requirements for Different HME Development Stages
| Development Stage | Primary Objective | Typical Batch Size | Approximate API Requirement | Key Analytical Tools |
|---|---|---|---|---|
| Pre-formulation | Physicochemical & thermodynamic API characterization | ~100 mg (for characterization) | 100 mg - 1 g | DSC, TGA, HSM, XRPD [94] |
| HME Feasibility | Screen polymers & drug loads (API-sparing) | 100-200 mg (formulation) | < 100 mg (with VCM) | VCM, PLM, DSC, XRPD [94] |
| Prototyping | Establish viable formulation & process parameters | 20-50 g | 50 - 100 g | 11mm extruder, DSC, XRPD, Dissolution testing [94] |
| Process Development | Establish robust, scalable process | 5-25 kg | 0.5 - 2 kg | 18mm extruder, DOE analysis [94] |
Table 2: Key Research Reagent Solutions for Formulation Optimization
| Reagent / Material | Function in Formulation | Brief Explanation |
|---|---|---|
| Carrier Polymers (e.g., HPMCAS, PVP-VA) | Form the matrix for ASDs, inhibiting API recrystallization. | Polymers maintain the API in its amorphous state, enhancing apparent solubility and dissolution [94]. |
| Surfactants (e.g., SLS, Vitamin E TPGS) | Improve wettability and dissolution rate. | Reduce interfacial tension, helping the dissolution medium to better wet and penetrate the formulation [94]. |
| Plasticizers (e.g., PEG, Triethyl Citrate) | Lower processing temperature in HME. | Reduce the Tg of the polymer, enabling extrusion at lower temperatures, which is crucial for thermolabile APIs [94]. |
| Lipidic Excipients (e.g., Medium Chain Triglycerides) | Solubilize lipophilic drugs in LBDDS. | Act as a solubilizing vehicle for the API, forming emulsified droplets upon dispersion in the GI tract [95]. |
| Permeation Enhancers | Increase intestinal membrane permeability. | Temporarily and reversibly alter the membrane integrity to facilitate API absorption [95]. |
Experimental Workflow and Pathway Diagrams
Diagram 1: Formulation Optimization Decision Workflow
Diagram 2: Hot Melt Extrusion Process and Critical Parameters
Evidence Synthesis and Clinical Correlation: From Bench to Bedside Translation
Frequently Asked Questions & Troubleshooting Guides
Q1: My computational model shows high accuracy on training data but fails to predict clinical outcomes. What could be wrong? A1: This common issue, known as overfitting, often arises from inadequate feature selection or insufficient data preprocessing. Troubleshoot by:
- Validate Feature Selection: Ensure biological relevance of input variables to dietary response pathways.
- Incorplement Cross-Validation: Use k-fold cross-validation during training to assess model generalizability.
- Clinical Data Alignment: Audit translational gaps between silico parameters and real-world patient variables like metabolism or comorbidities.
Q2: How can I handle missing clinical data points when validating my model? A2: Missing data requires careful handling to avoid validation bias:
- Use Multiple Imputation: Create several complete datasets using algorithms like MICE (Multiple Imputation by Chained Equations).
- Implement Sensitivity Analysis: Test how different missing-data assumptions affect your model's predictive performance.
- Document Exclusions: Clearly report any excluded data points and the rationale in your methodology.
Q3: What metrics are most appropriate for comparing model projections to clinical observations? A3: Select metrics that capture different aspects of predictive performance:
Table: Key Validation Metrics
| Metric | Best For | Interpretation | Threshold |
|---|---|---|---|
| Concordance Index (C-index) | Time-to-event data | Model discrimination ability | >0.7 acceptable; >0.8 good |
| Mean Absolute Error (MAE) | Continuous outcomes | Average prediction error | Lower values better |
| Calibration Slope | Probability estimates | Agreement between predicted and observed risks | Close to 1.0 ideal |
Q4: My model captures average responses well but fails for subpopulations. How can I improve this? A4: This suggests insufficient capture of dietary component interactions:
- Stratified Analysis: Validate models separately for different demographic or genetic subgroups.
- Interaction Terms: Explicitly model nutrient-gene interactions in your algorithms.
- Ensemble Methods: Combine multiple specialized models to better capture population heterogeneity.
Experimental Protocols for Key Validation Experiments
Protocol 1: Prospective Clinical Validation Study Objective: Compare model-predicted treatment responses with actual patient outcomes.
Participant Recruitment:
- Enroll 150-200 participants representing target population
- Stratify by key covariates: age (±5 years), BMI (±2 kg/m²), genetic markers
Dietary Intervention:
- Implement controlled dietary regimen for 12 weeks
- Collect biometric data weekly: glucose, lipids, inflammatory markers
- Monitor adherence via food diaries and biomarker analysis
Model Testing:
- Input baseline patient data into predictive model
- Generate individual outcome projections
- Compare predictions with observed outcomes at study endpoint
Statistical Analysis:
- Calculate C-index for time-to-event outcomes
- Compute calibration metrics (calibration-in-the-large, calibration slope)
- Perform subgroup analysis to identify population-specific performance
Protocol 2: Retrospective Validation Using Electronic Health Records Objective: Validate model using existing clinical data.
Data Curation:
- Extract structured data from EHR systems (5,000+ patient records)
- Harmonize variables across different healthcare systems
- Address missing data using multiple imputation techniques
Model Deployment:
- Execute batch predictions for all eligible patient records
- Compare predictions with documented clinical outcomes
Validation Framework:
- Temporal validation: Train on older data, test on recent data
- Geographical validation: Test on patients from different healthcare systems
- Calculate performance metrics with 95% confidence intervals
Research Reagent Solutions
Table: Essential Materials for Predictive Model Validation
| Reagent/Material | Function | Application Example |
|---|---|---|
| Luminex xMAP Assays | Multiplex biomarker quantification | Simultaneous measurement of 50+ inflammatory cytokines in serum samples |
| Mass Spectrometry Kits | Metabolite profiling | Comprehensive analysis of dietary metabolites in plasma |
| Electronic Health Record APIs | Structured data extraction | Automated retrieval of clinical variables for model input |
| Bioinformatics Suites (e.g., Galaxy, CLC) | Genomic data integration | Incorporation of genetic variants into predictive algorithms |
| Statistical Software (R, Python libraries) | Model development and validation | Implementation of machine learning algorithms and performance metrics |
Visualization of Experimental Workflows
Diagram Color Contrast Guidelines
All diagrams follow WCAG 2.2 Level AA contrast requirements [96] [97]:
- Text Contrast: Text colors provide minimum 4.5:1 contrast ratio against background colors [98] [99]
- Non-Text Elements: Arrows and symbols maintain 3:1 contrast ratio against background [97]
- Color Selection: Palette limited to specified colors with verified contrast relationships
- Dynamic Adjustment: For programmatically generated diagrams, use luminance calculation (Y = 0.2126(R/255)^2.2 + 0.7151(G/255)^2.2 + 0.0721*(B/255)^2.2) to select black (Y>0.18) or white (Y≤0.18) text [100]
FAQs: Unraveling Diet-Health Correlations
Q1: What are the primary mechanistic pathways through which a Western diet promotes chronic inflammation? A1: The Western diet, characterized by high levels of ultra-processed foods, unhealthy fats, and refined sugars, triggers chronic inflammation through several interconnected pathways. It induces immune dysregulation and promotes a pro-inflammatory state, as observed in a randomized controlled trial where a switch to a Western diet increased pro-inflammatory proteins in the blood [101]. It also causes microbial dysbiosis, reducing beneficial gut bacteria and the production of anti-inflammatory short-chain fatty acids (SCFAs) like butyrate, while increasing harmful metabolites that impair the intestinal barrier, leading to "leaky gut" and systemic inflammation [102]. Furthermore, it can directly alter arterial transcriptomes, upregulating genes associated with endothelial dysfunction, smooth muscle proliferation, and abnormal extracellular matrix dynamics, as seen in non-human primate studies [103] [104].
Q2: Beyond fiber intake, how do plant-based diets like the Mediterranean diet confer protective benefits against conditions like chronic constipation? A2: A long-term study of over 96,000 adults found that the benefits of healthy diets like the Mediterranean diet on preventing chronic constipation were independent of fiber intake. The research suggests that the overall quality of the diet, rich in vegetables, nuts, and healthy fats, plays a crucial role in gut health, pointing to synergistic effects from a complex mix of nutrients and compounds beyond just fiber [105].
Q3: In experimental models, how does social stress interact with dietary patterns to affect health outcomes? A3: Research in non-human primates demonstrates that social subordination (a model for chronic psychosocial stress) and Western diet have adverse, yet distinct, impacts on vascular health. The effects are tissue-specific: Western diet primarily increased atherosclerosis in coronary and iliac arteries, while social status significantly altered the transcriptome related to vascular tone and smooth muscle contractility in carotid arteries. This highlights the complex interplay between environmental stressors and diet composition [103] [104].
Q4: What is the evidence for the sustained metabolic impact of short-term dietary changes? A4: A randomized controlled trial in Tanzania found that switching from a heritage diet to a Western diet for just two weeks was sufficient to induce a pro-inflammatory state and affect metabolic pathways linked to non-communicable diseases. Notably, some of these negative changes in immune and metabolic profiles persisted four weeks after the intervention ended, indicating that even short-term dietary shifts can have a lasting physiological impact [101] [106].
Technical Guides & Experimental Protocols
Protocol for a Randomized Controlled Feeding Trial
Objective: To compare the effects of Mediterranean Diet (MD) vs. Western Diet (WD) on fatigue in patients with Autoimmune Hepatitis (AIH) using a randomized, blinded, crossover design [107].
- Study Population: 48 adult patients with AIH.
- Design: A two-phase crossover trial. Participants are randomized to either MD-first or WD-first sequence, with a 6-week washout period between phases.
- Dietary Interventions:
- MD: Characterized by high intake of fruits, vegetables, whole grains, legumes, nuts, and olive oil; moderate in fish and poultry; low in red meat and processed foods.
- WD: Characterized by high intake of red meat, saturated and trans fats, refined carbohydrates, and a low omega-3 to omega-6 fatty acid ratio.
- Intervention Duration: Each dietary phase lasts 5 weeks.
- Blinding: The study team (PI and coordinator) and patients are blinded to the dietary assignment. Only the nutritional team is unblinded for meal preparation.
- Primary Outcome: Change in the fatigue score of the PROMIS-29 survey.
- Secondary Outcomes: Changes in inflammatory markers (e.g., C-reactive protein), liver biomarkers (ALT, IgG), stool microbiome (16S sequencing and SCFAs), and liver stiffness (FibroScan).
- Compliance Monitoring: Utilizes weekly 3-day food logs and weekly check-ins with a dietary research coordinator.
Protocol for a Multi-omics Analysis in a Dietary Intervention Trial
Objective: To investigate the immune and metabolic effects of switching between heritage and Western diets using a multi-omics approach [101].
- Study Population: Healthy volunteers, assigned male at birth, from both urban and rural areas.
- Design: Three-arm, open-label randomized controlled trial.
- Arm 1: Rural residents habitually consuming a heritage diet switch to a WD for 2 weeks.
- Arm 2: Urban residents habitually consuming a WD switch to a heritage diet for 2 weeks.
- Arm 3: WD consumers add a traditional fermented beverage for 1 week.
- Sample Collection: Blood samples collected at baseline, post-intervention, and at a 4-week follow-up.
- Primary Outcomes (Multi-omics Profiling):
- Plasma Proteome: Analyzed using 92-plex Olink panels (inflammatory and cardiometabolic) to identify differentially abundant proteins.
- Immune Function: Whole-blood cytokine responses to microbial stimulation.
- Metabolome: Plasma metabolomic profiling.
- Transcriptome: Whole-blood RNA sequencing.
- Data Integration: Variance partition analysis is used to determine the proportion of variance in omics datasets explained by the intervention, adjusting for age, BMI, and physical activity.
Data Synthesis: Quantitative Outcomes
Table 1: Summary of Key Health Outcomes from Comparative Studies
| Health Outcome | Mediterranean / Heritage Diet Effect | Western Diet Effect | Study Details |
|---|---|---|---|
| Coronary Atherosclerosis | ↓ Intimal area (LAD artery) [103] | ↑ Intimal area (LAD artery) (F=5.25, p=0.03) [103] | 30-month RCT in non-human primates [103] [104] |
| Cognitive Health (Risk Reduction) | HR = 0.82 for cognitive impairment; HR = 0.70 for Alzheimer's Disease [108] | Not Reported | Meta-analysis of 23 studies [108] |
| Chronic Constipation Incidence | Lower incidence [105] | Higher incidence [105] | Cohort study (n=96,000) [105] |
| Systemic Inflammation | Anti-inflammatory effect; reduction in inflammatory proteins (e.g., CXCL1, IL-6) [101] | Pro-inflammatory effect; increase in inflammatory proteins (e.g., TWEAK, TRAIL) [101] | 2-week RCT in humans [101] [106] |
| Body Composition (in Chronic Disease) | Improved BMI, lean mass, and visceral adipose tissue, especially when combined with exercise [109] | Not Reported | Meta-analysis of 17 clinical trials [109] |
| Metabolic Syndrome Parameters | Significant improvements in BMI, waist circumference, triglycerides, and HOMA-IR [110] | Not Reported | Meta-analysis of 12 studies [110] |
Pathway Diagrams
Western Diet-Induced Inflammation in IBD
Western Diet Triggers Inflammatory Bowel Disease Pathways
Multi-omics Workflow in Dietary Intervention
Multi-omics Workflow for Diet Studies
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents and Kits for Dietary Intervention Studies
| Reagent / Kit | Function / Application | Example Use Case |
|---|---|---|
| Olink Proximity Extension Assay Panels (e.g., Inflammation, Cardiometabolic) | Multiplex immunoassay for high-sensitivity quantification of 92 proteins from low sample volumes. | Quantifying changes in inflammatory (e.g., IL-6) and cardiometabolic (e.g., ANGPTL3) plasma proteins in response to diet [101]. |
| 16S rRNA Sequencing Reagents | Profiling the composition and relative abundance of gut microbiota. | Assessing diet-induced dysbiosis and changes in microbial diversity (e.g., reduction in Faecalibacterium prausnitzii) [102] [107]. |
| Short-Chain Fatty Acid (SCFA) Assay Kits (e.g., GC-MS) | Quantitative measurement of SCFAs (butyrate, acetate, propionate) in stool or serum. | Evaluating the functional output of the microbiome and links to intestinal barrier integrity [102]. |
| RNA Sequencing Kits | Whole transcriptome analysis to identify differentially expressed genes. | Profiling gene expression changes in blood or tissue (e.g., arterial transcriptome) following dietary interventions [103] [101]. |
| Metabolomic Profiling Platforms (e.g., LC-MS) | Global, untargeted profiling of small molecule metabolites in biofluids. | Discovering diet-induced shifts in metabolic pathways and identifying potential nutritional biomarkers [101]. |
Troubleshooting Guide: Resolving Common Challenges in Dietary Intervention Research
Q1: What should I do if my dietary intake data contains a large number of zero values (non-consumption episodes), making analysis difficult?
A: This is a common issue known as semicontinuous data, where data has many zeros (non-intake) and a right-skewed distribution of positive values (intake amounts) [111]. Using standard linear models on this data can lead to incorrect conclusions.
- Recommended Solution: Employ a multilevel two-part model [111]. This method separately analyzes the two processes behind your data:
- The Occurrence of Eating: Use a multilevel logistic regression to model the probability that consumption occurs in a given time interval.
- The Amount Eaten: Use a multilevel gamma regression (suitable for skewed positive values) to model the amount consumed, given that eating occurred.
- Example Workflow: This approach can reveal, for instance, that a factor like stress influences whether a person eats but not how much they eat, or vice versa [111].
Q2: My study participants are inaccurately reporting their dietary intake. How can I improve data quality and account for these errors?
A: Inaccurate reporting is a major methodological challenge. Mitigation involves selecting the right tool and understanding its inherent errors [112].
- Strategies for Improvement:
- Method Selection: Choose an assessment method (e.g., 24-hour recall, food frequency questionnaire, food record) based on whether you need group averages or individual habitual intake [112].
- Combine Methods: Using a combination of dietary survey methods can improve accuracy [112].
- Control for Errors: Be aware of and document common errors:
- Reporting Bias: Participants may misreport foods they believe are socially undesirable [112].
- Day-to-Day Variability: A single 24-hour recall is not representative of habitual intake; multiple days of data are often needed [112].
- Instrument Error: Nutrient data from food composition tables are averages and may not reflect the specific food consumed [112].
Q3: When measuring Health-Related Quality of Life (HRQoL), how do I choose between a general or a disease-specific questionnaire?
A: The choice depends on your research goals and population [113].
- Use a General HRQoL Instrument (e.g., SF-36, EQ-5D) to capture a broad profile of physical and mental health and to allow for comparisons with the general population or across different disease states [113].
- Use a Disease-Specific HRQoL Instrument (e.g., EORTC-QLQ for cancer) to focus on aspects of health most relevant to a specific condition. These are often more sensitive to changes from an intervention [113].
- Best Practice: Consider using both a general and a disease-specific instrument together to gain a comprehensive understanding of the intervention's impact [113].
Q4: In a randomized controlled trial (RCT), a diet-plus-exercise intervention improved HRQoL, but the exercise-only intervention did not. What could explain this?
A: This result suggests that the improvements in HRQoL are likely mediated by different factors.
- Investigation Steps: Analyze whether changes in HRQoL are driven primarily by weight loss, improvements in aerobic fitness, or changes in psychosocial factors.
- Evidence from Research: One RCT in postmenopausal women found that a combined diet and exercise intervention improved multiple HRQoL aspects (physical functioning, vitality, mental health). Analysis showed that weight loss was a key predictor of improved HRQoL across several domains, while improved fitness was specifically linked to better physical functioning. Positive changes in depression and stress were also independently associated with better HRQoL [114].
Q5: I am collecting HRQoL and dietary data online. How could my recruitment method (open vs. rewarded survey) impact my findings?
A: Recruitment method can significantly influence the characteristics of your sample and the data you collect [115].
- Reported Differences: One large study found significant differences in sociodemographic, lifestyle, health, and HRQoL data between participants recruited via an open survey (OS) and a rewarded survey (RS) [115].
- Sample Bias: The OS sample was characterized as a healthier population with superior lifestyle habits compared to the RS participants [115].
- Actionable Advice: Always report your recruitment method and consider it as a potential confounding variable when analyzing and interpreting your results.
HRQoL Measurement Instruments: A Researcher's Guide
The table below summarizes the most commonly used HRQoL questionnaires in nutritional intervention research, as identified in a systematic review [113].
| Questionnaire Name | Type | Key Domains Measured | Example Use Case in Nutrition |
|---|---|---|---|
| SF-36 / SF-12 [113] [115] | General | Physical functioning, role limitations, pain, general health, vitality, social functioning, mental health [115] | Measuring broad impact of a weight loss intervention on physical and mental well-being [114] |
| EQ-5D [113] | General | Mobility, self-care, usual activities, pain/discomfort, anxiety/depression | Cost-effectiveness analysis of a dietary public health program |
| EORTC QLQ [113] | Disease-Specific | Cancer-related symptoms (e.g., fatigue, pain, nausea) and functional scales | Assessing nutritional support for cancer patients to manage treatment side effects |
| DRCQ | Disease-Specific | Diabetes-related symptoms, and impact on daily life | Evaluating a medical nutrition therapy program for diabetes management [113] |
| OBSQOR | Disease-Specific | Obesity-specific psychosocial burden and well-being | Measuring psychosocial outcomes in weight management studies [113] |
Experimental Protocols & Analytical Workflows
Protocol 1: Analyzing Semicontinuous Dietary Intake Data from EMA Studies
Ecological Momentary Assessment (EMA) involves collecting dietary data multiple times per day in a natural environment. The resulting data is often semicontinuous, requiring specialized analysis [111].
- Primary Objective: To identify factors that predict a) the occurrence of eating and b) the amount consumed.
- Materials & Software:
- Methodology:
- Data Structure: Ensure data is in a long format with repeated assessments (Level 1) nested within individuals (Level 2).
- Model Specification: Implement a multilevel two-part model using the
brmspackage. - Model Components:
- Part 1 (The Occurrence): A multilevel logistic regression predicting the probability of any consumption (a binary outcome: 0 for no intake, 1 for intake).
- Part 2 (The Amount): A multilevel gamma regression (with a log link) predicting the amount consumed, conditional on intake having occurred (i.e., using only positive intake values).
- Interpretation: Examine the results for each part separately. A predictor variable can be significant for the occurrence process, the amount process, both, or neither [111].
The following diagram illustrates the logical workflow and model structure for this analysis.
Protocol 2: Designing an RCT to Evaluate a Combined Diet and Exercise Intervention on HRQoL
This protocol is based on a randomized controlled trial conducted with overweight/obese postmenopausal women [114].
- Primary Aim: To examine the individual and combined effects of dietary weight loss and exercise on HRQoL and psychosocial factors.
- Study Design: Four-arm randomized controlled trial.
- Participant Allocation:
- Group 1: Dietary Weight Loss (n=118)
- Group 2: Aerobic Exercise (225 min/week; n=117)
- Group 3: Combined Diet + Exercise (n=117)
- Group 4: Control (n=87)
- Key Materials & Assessments:
- Statistical Analysis:
- Compare 12-month changes between groups using analysis of covariance (ANCOVA), adjusting for baseline scores.
- Use multiple regression to assess if changes in weight, fitness, and psychosocial factors mediate the change in HRQoL.
The workflow for this experimental design is summarized below.
This table details key materials and instruments used in the featured research.
| Item Name | Function/Application | Relevant Citation |
|---|---|---|
| SF-36 / SF-12 Health Survey | A validated, self-reported questionnaire measuring eight domains of health to generate physical and mental health summary scores. | [113] [114] [115] |
| MEDAS-14 (14-item Mediterranean Diet Adherence Screener) | A brief, validated dietary screening tool to assess adherence to the Mediterranean diet pattern. | [115] |
| International Physical Activity Questionnaire (IPAQ) | A validated survey for estimating levels of physical activity and sitting time in adults. | [115] |
Multilevel Two-Part Model (R package brms) |
A statistical modelling approach for analyzing semicontinuous data (e.g., EMA dietary intake) by separately modeling occurrence and amount. | [111] |
| Online Survey Platforms (e.g., QuestionPro) | Web-based tools for scalable, efficient data collection on demographics, lifestyle, and HRQoL; choice of platform (open vs. rewarded) can influence sample characteristics. | [115] |
Troubleshooting Guide: Common Methodological Issues
| Problem Area | Specific Challenge | Potential Solution | Key Considerations |
|---|---|---|---|
| Study Design & Complexity | High collinearity between dietary components obscures relationships with health outcomes [116]. | Treat nutrition interventions as "complex interventions" and adopt appropriate methods [116]. | Food is a heterogeneous mixture with multi-target effects, unlike single-compound drugs [116]. |
| Defining an appropriate control group is challenging [116]. | Carefully consider the nature of the control (e.g., placebo, usual diet, active comparator) [116]. | The choice of control impacts the contrast between study groups and the interpretability of findings [116]. | |
| Data Collection & Quality | Reliance on retrospective methods like Food Frequency Questionnaires (FFQs) prone to recall bias [117] [118]. | Use prospective methods like food diaries for more objective data, but be aware they can alter usual intake [118]. | For FFQs, use models or pictures to improve portion size estimation [118]. For diaries, monitor for under-reporting [118]. |
| Inaccurate data due to poor participant memory or estimation skills [117] [118]. | For food diaries, select a recording period that balances representativeness and participant burden (e.g., 3-7 days) [118]. | A 3-4 day diary is poor for estimating individual intake of variable nutrients; more days are needed [118]. | |
| Data Analysis & Reporting | Subjectivity in deriving and naming data-driven dietary patterns (e.g., PCA, Cluster Analysis) [47] [48]. | Pre-specify decisions on food grouping, number of patterns to retain, and naming conventions [47]. | Patterns like "Western" can have different compositions across studies, hindering comparability [47]. |
| Inconsistent application and reporting of index-based methods (e.g., HEI, MED scores) [47]. | Standardize the components, scoring criteria, and cut-off points used for the index [47]. | Use frameworks like the Dietary Patterns Methods Project to ensure consistent application across cohorts [47]. | |
| Result Interpretation | Limited translatability of findings due to high heterogeneity in population responses [116]. | Account for effect modifiers like ethnicity, genotype, and baseline nutritional status in the analysis [116]. | The effect size of a dietary intervention can be small and vary significantly between individuals [116]. |
| Difficulty synthesizing evidence from different studies for dietary guidelines [47]. | Report identified dietary patterns with detailed food and nutrient profiles, not just pattern names or scores [47]. | Quantitative descriptions of patterns are essential for evidence synthesis and translation into policy [47]. |
Frequently Asked Questions (FAQs)
On Study Design and Implementation
Q1: Our dietary clinical trial (DCT) showed a much smaller effect size than a similar pharmaceutical trial. Is this a failure of the intervention? A: Not necessarily. This is a common characteristic of DCTs. The complex nature of food, interactions between dietary components, and diverse individual responses (influenced by genetics, baseline diet, etc.) often lead to smaller, more heterogeneous effect sizes compared to single-drug interventions. The key is to design your trial with sufficient power to detect these smaller, yet still clinically relevant, effects [116].
Q2: How can we improve participant adherence in a long-term dietary intervention study? A: Poor adherence is a major challenge. Strategies include:
- Reducing Burden: Use less burdensome dietary assessment methods where possible (e.g., repeated 24-hour recalls instead of long food records) [119].
- Enhancing Engagement: Provide regular feedback to participants to maintain motivation [118].
- Practical Intervention: Design the dietary intervention to be as practical and adaptable to real-life as possible, considering different food cultures and habits [116].
On Data Collection and Assessment Methods
Q3: What is the best dietary intake assessment method for my research? A: There is no single "best" method; the choice depends on your research goal, resources, and target population [118]. The table below summarizes the pros and cons of common methods based on a study comparing them in older adults [119] and expert reviews [118].
| Method | Description | Best For | Limitations |
|---|---|---|---|
| Food Frequency Questionnaire (FFQ) | Retrospective; assesses habitual intake over a long period (e.g., past year) [118]. | Ranking individuals by intake of specific nutrients/foods; large epidemiological studies [118]. | Relies on memory; can over/under-estimate intake; less accurate for absolute intake values [117] [118]. |
| 24-Hour Recall | Retrospective; detailed interview about intake over the previous 24 hours [118]. | Estimating average intake of a group; less burdensome on participants [119]. | Depends on memory; single day is not representative of usual intake; requires multiple recalls [118] [119]. |
| Food Diary/Record | Prospective; participant records all foods/drinks consumed in real-time over a period (e.g., 3-7 days) [118]. | Often considered a more accurate "gold standard" for short-term intake; quantifiable data [118] [119]. | The act of recording can alter habitual intake; high participant burden; risk of under-reporting [118]. |
Q4: Why is there so much criticism of Food Frequency Questionnaires (FFQs)? A: FFQs are criticized primarily for their reliance on human memory and simplification of complex diets. Key issues include:
- Memory Dependency: Participants must recall their intake over the past year, which is highly unreliable [117].
- Forced Estimation: Questionnaires often force choices without "I don't know" options, creating artificial data [117].
- Limited Food List: They typically include only 100-150 items, missing the full complexity of modern diets and many processed food ingredients [117].
- Portion Size Ambiguity: Serving sizes are often vague (e.g., "small glass"), leading to estimation errors [117] [118].
On Analysis and Harmonization
Q5: What are the main statistical approaches for deriving dietary patterns, and how do I choose? A: The main approaches are [47] [48]:
- Investigator-Driven (A Priori): Uses pre-defined scores (e.g., HEI, Mediterranean Diet Score) based on dietary guidelines. Use this to test adherence to specific dietary recommendations.
- Data-Driven (A Posteriori): Uses statistical methods like Principal Component Analysis (PCA) or Cluster Analysis to derive patterns from your dataset. Use this to explore predominant eating habits in your population.
- Hybrid Methods: Methods like Reduced Rank Regression (RRR) incorporate health outcomes to derive patterns. Use this to identify patterns that explain variation in a specific biological outcome.
Q6: Our team derived dietary patterns using PCA, but our results are difficult to compare to another study that also used PCA. Why? A: This is a core issue that harmonization seeks to solve. Inconsistencies arise from subjective decisions made during analysis, including [47] [48]:
- Food Grouping: How individual foods are aggregated into food groups.
- Number of Patterns: The criteria used to decide how many patterns to retain.
- Naming and Interpretation: The subjective process of naming patterns based on high-loading foods. Standardizing these decisions and reporting them in detail is crucial for comparability [47].
Experimental Protocols for Standardized Assessment
Protocol 1: Applying an Index-Based Score (e.g., HEI)
Objective: To assess adherence to predefined dietary guidelines in a cohort study. Materials: Dietary intake data (e.g., from multiple 24-hour recalls or a validated FFQ), HEI scoring standards. Procedure:
- Data Preparation: Process raw dietary data to align with the food groups and nutrients required for the HEI.
- Component Scoring: For each HEI component (e.g., total fruits, whole grains, refined grains), calculate the participant's intake density (amount per 1000 calories). Assign a score from 0 to a set maximum based on pre-established adequacy or moderation standards.
- Total Score Calculation: Sum all component scores to obtain the total HEI score for each participant.
- Statistical Analysis: Use the total or component scores in statistical models to examine associations with health outcomes. Standardization Note: Follow a publicly available, standardized scoring system like the one developed by the Dietary Patterns Methods Project to ensure comparability across studies [47].
Protocol 2: Deriving Dietary Patterns via Principal Component Analysis (PCA)
Objective: To identify predominant dietary patterns from FFQ data in a population. Materials: FFQ data aggregated into meaningful food groups. Procedure:
- Food Grouping: Group individual FFQ items into ~30-50 food groups based on nutrient profile and culinary use. Report the grouping scheme in full.
- Input Matrix: Prepare a matrix of consumption values (e.g., g/day) for each food group for all participants.
- Analysis: Perform PCA on the correlation matrix of the food groups.
- Factor Retention: Decide on the number of patterns (components) to retain based on a combination of: a) Eigenvalue >1 rule, b) Scree plot interpretation, and c) Interpretability.
- Rotation: Apply an orthogonal rotation (e.g., Varimax) to simplify the factor structure and improve interpretability.
- Labeling: Label each retained pattern based on the food groups with the highest positive and negative factor loadings (e.g., |loading| > 0.2). Crucially, report the factor loadings table.
- Pattern Scores: Calculate each participant's score for each dietary pattern.
Diagram 1: PCA Dietary Pattern Workflow
The Scientist's Toolkit: Research Reagent Solutions
| Essential Material / Tool | Function in Dietary Pattern Research |
|---|---|
| Validated Food Frequency Questionnaire (FFQ) | A tool to assess habitual dietary intake over a long period. Critical for large-scale epidemiological studies of dietary patterns [47] [118]. |
| 24-Hour Recall Protocol | A structured interview method to collect detailed dietary data from the previous 24 hours. Useful for validating other methods or for cross-cultural adaptation [119]. |
| Nutrition Analysis Software (e.g., NDS-R, Diet*Calc) | Software used to convert reported food consumption into estimated nutrient intakes. Essential for calculating nutrient-based scores and profiling patterns [119]. |
| Dietary Pattern Indices (e.g., HEI, aMED, DASH) | Pre-defined algorithms and scoring systems to quantify adherence to a specific dietary pattern or set of guidelines [47] [48]. |
| Statistical Software Packages (e.g., R, SAS, STATA, SPSS) | Platforms for performing complex statistical analyses, including PCA, Factor Analysis, Cluster Analysis, and RRR, to derive and analyze dietary patterns [48]. |
| Global Dietary Database (e.g., FAO/WHO GIFT) | Platforms providing access to harmonized individual food consumption data from surveys worldwide, enabling comparative research [120]. |
Diagram 2: Core Pathways in Dietary Pattern Analysis
FAQs: Navigating Complexities in Dietary Components Research
FAQ 1: What are the fundamental methodological differences between Dietary Clinical Trials (DCTs) and pharmaceutical trials that impact their results?
Dietary Clinical Trials (DCTs) face unique complexities compared to pharmaceutical trials. Unlike drugs, which are single molecular compounds with specific targets, dietary interventions involve complex mixtures of nutrients and bioactive components with multi-target effects [116]. This complexity introduces several research challenges:
- Food Matrix Interactions: Nutrients within foods interact synergistically or antagonistically, creating effects that isolated supplements cannot replicate [116] [35]
- Baseline Nutritional Status: Participants' pre-existing nutrient levels significantly influence intervention effectiveness, unlike drug trials where baseline exposure is typically minimal [116]
- Dietary Background Variability: Habitual diets and food cultures vary widely, creating high inter-individual response variability [116]
- Blinding Difficulties: Creating appropriate placebos for food-based interventions is exceptionally challenging, potentially introducing performance bias [116]
These fundamental differences mean DCTs often show smaller effect sizes and require careful interpretation when comparing results to pharmaceutical interventions [116].
FAQ 2: How can researchers effectively analyze complex correlations between multiple dietary components?
Traditional methods like principal component analysis (PCA) and factor analysis have limitations in capturing food synergies. Network analysis approaches offer promising alternatives for mapping complex dietary relationships [35]:
- Gaussian Graphical Models (GGMs): Use partial correlations to identify conditional independence between dietary variables, revealing how nutrients interact within broader dietary contexts [35]
- Mutual Information Networks: Capture both linear and nonlinear associations between dietary components, identifying subtle dependencies and threshold effects [35]
- Mixed Graphical Models (MGMs): Accommodate both continuous (nutrient intake) and categorical variables (demographics) simultaneously [35]
These methods explicitly map webs of interactions and conditional dependencies between individual foods, moving beyond composite scores that may obscure crucial food synergies [35]. However, researchers must address methodological challenges including non-normal data distribution and careful interpretation of centrality metrics [35].
FAQ 3: What standardized reporting guidelines should researchers follow for dietary pattern studies?
Inconsistent methodology and reporting limit the translatability of dietary pattern research. To enhance reliability, implement these guiding principles:
- Adopt Standardized Checklists: Use the Minimal Reporting Standard for Dietary Networks (MRS-DN), a CONSORT-style checklist specifically for dietary network analysis [35]
- Transparent Method Documentation: Clearly report all subjective decisions in dietary pattern assessment, including food grouping criteria, cut-off points for scoring, and rationale for retaining factors [121]
- Comprehensive Pattern Description: Provide quantitative food and nutrient profiles of identified dietary patterns, not just pattern names [121]
- Model Justification: Explain why specific analytical methods were chosen and how they align with research questions [35]
The Dietary Patterns Methods Project demonstrated that standardized application of methods like the Healthy Eating Index and Mediterranean Diet Score across cohorts yields consistent, comparable evidence for guideline development [121].
Experimental Protocols for Comparative Effectiveness Research
Protocol 1: Head-to-Head Comparison of Dietary vs. Pharmacological Interventions
Objective: Directly compare the effectiveness of evidence-based dietary patterns against first-line pharmacological therapy for specific chronic conditions.
Methodology:
- Study Design: Pragmatic randomized controlled trial with three parallel arms:
- Arm A: Active pharmacological intervention (condition-specific)
- Arm B: Structured dietary intervention (Mediterranean, DASH, or other evidence-based pattern)
- Arm C: Usual care control
Participant Selection: Recruit adults with early-stage chronic conditions (hypertension, prediabetes, or mild dyslipidemia) who are naïve to pharmacological treatment.
Intervention Specifications:
- Dietary Arm: Implement supervised dietary modification with:
- Twice-weekly group education sessions for first month
- Weekly individual counseling with Registered Dietitian Nutritionists
- Food provision for initial 2 weeks to facilitate pattern adoption
- Monitoring through 3-day food records and biomarkers
- Pharmacological Arm: Standard medication titration protocol per clinical guidelines
- Control Arm: General healthy lifestyle advice without structured intervention
- Dietary Arm: Implement supervised dietary modification with:
Outcome Measures:
- Primary: Condition-specific clinical endpoints (blood pressure, HbA1c, LDL cholesterol)
- Secondary: Quality of life measures, cost-effectiveness, adherence rates, side effects
Statistical Analysis: Intention-to-treat analysis with multiple imputation for missing data. Non-inferiority margins pre-specified for dietary vs. pharmacological comparison [122].
Protocol 2: Mechanistic Study of Nutrient-Drug Interactions
Objective: Investigate how specific dietary patterns influence drug metabolism and efficacy through metabolic pathway modulation.
Methodology:
- Study Design: Randomized cross-over trial with repeated measures.
Participants: Patients stable on chronic medications (e.g., statins, antihypertensives, metformin).
Interventions: Three 4-week dietary periods with washout:
- High-phytonutrient plant-based diet
- Mediterranean diet
- Western-style diet (control)
Data Collection:
- Pharmacokinetics: Serial blood sampling for drug concentration analysis
- Metabolomics: LC-MS profiling of plasma metabolites
- Microbiome: 16S rRNA sequencing of fecal samples
- Transcriptomics: RNA sequencing from peripheral blood mononuclear cells
Integration Analysis: Apply multivariate methods to identify diet-microbiome-metabolite-drug concentration relationships [123].
Comparative Effectiveness Data Tables
Table 1: Documented Effect Sizes of Dietary vs. Pharmacological Interventions for Select Conditions
| Condition | Dietary Intervention | Dietary Effect Size | Pharmacological Intervention | Drug Effect Size | Comparative Notes |
|---|---|---|---|---|---|
| Hypertension | DASH Diet | SBP: -3.2 to -11.4 mm Hg [124] | First-line antihypertensives | SBP: -10 to -15 mm Hg | Dietary effects more pronounced in hypertensives; often combined |
| Type 2 Diabetes | Low-glycemic, carbohydrate-controlled diets | HbA1c: -0.3% to -1.0% [124] | Metformin | HbA1c: -1.0% to -1.5% | Diet often sufficient for prediabetes; drugs needed for established disease |
| Hyperlipidemia | Portfolio Diet (plant-based, high-fiber) | LDL-C: -13% to -29% [124] | Moderate-dose statins | LDL-C: -30% to -50% | Dietary portfolio can achieve ~50% of drug effect |
| Heart Failure | Mediterranean Diet | CVD risk: 10-67% reduction [124] | Standard medical therapy | Variable by drug class | Diet provides additional mortality benefit to pharmacotherapy |
Table 2: Methodological Challenges in Dietary vs. Pharmaceutical Clinical Trials
| Research Dimension | Dietary Clinical Trials | Pharmaceutical Trials | Impact on Evidence Generation |
|---|---|---|---|
| Intervention Complexity | Multi-component foods/nutrients [116] | Single molecular entities [116] | Dietary mechanisms harder to isolate |
| Blinding Possibility | Very difficult or impossible [116] | Standard practice with placebos [116] | Higher risk of performance bias in DCTs |
| Dose Standardization | Highly variable between subjects [116] | Precisely controlled [116] | More measurement error in DCTs |
| Adherence Monitoring | Self-report with inherent error [116] | Pill counts, blood levels [116] | Dietary adherence often overestimated |
| Time to Effect | Often slow (weeks-months) [124] | Relatively rapid (days-weeks) | DCTs require longer follow-up |
| Effect Size Magnitude | Typically small to moderate [116] | Often large [116] | DCTs require larger sample sizes |
Research Reagent Solutions for Dietary-Pharmacological Studies
| Research Need | Essential Materials/Tools | Function & Application Notes |
|---|---|---|
| Dietary Assessment | Multiple 24-hour recalls or 3-7 day food records | Captures usual intake with less bias than FFQs for intervention studies [121] |
| Adherence Biomarkers | Plasma carotenoids, omega-3 fatty acids, urinary sodium | Objective verification of dietary compliance independent of self-report |
| Drug Level Monitoring | LC-MS/MS systems with stable isotope standards | Quantifies drug and metabolite concentrations for pharmacokinetic analysis |
| Metabolic Profiling | Targeted metabolomics panels for nutrient-related metabolites | Measures intermediate endpoints linking diet to physiological effects [123] |
| Microbiome Analysis | 16S rRNA sequencing kits with standardized DNA extraction | Assesses gut microbiota as potential mediator of diet-drug interactions [123] |
| Statistical Analysis | R packages for network analysis (e.g., qgraph, bootnet) | Implements GGMs, MI networks for complex dietary data [35] |
Visualizing Research Approaches
Diagram 1: Comparative Effectiveness Research Framework for Dietary Interventions
Diagram 2: Dietary Pattern Analysis Workflow for Complex Correlations
Conclusion
The complex correlations between dietary components represent a critical frontier in biomedical research and drug development. By integrating foundational knowledge of interaction mechanisms with advanced methodological approaches, researchers can more accurately predict and mitigate adverse food-drug interactions while leveraging beneficial synergies. The field is moving toward standardized assessment frameworks, validated predictive models, and personalized nutrition strategies that account for individual variability. Future directions should focus on developing unified analytical protocols, incorporating emerging technologies like artificial intelligence and nutrigenomics, and conducting large-scale longitudinal studies to establish causal relationships between dietary patterns and clinical outcomes. Ultimately, a comprehensive understanding of dietary complexity will enable more precise drug dosing, optimized formulation strategies, and improved patient care through integrated dietary and pharmacological interventions.
References
- 1. Applications of PBPK Modeling to Estimate Drug Metabolism ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12473325/]
- 2. Food–drug interactions risk management: An emergent ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11239764/]
- 3. Knowledge of Food–Drug Interactions among Medical ... [https://www.mdpi.com/2072-6643/16/15/2425]
- 4. FDA's Examples of Drugs that Interact with CYP Enzymes ... [https://www.fda.gov/drugs/drug-interactions-labeling/healthcare-professionals-fdas-examples-drugs-interact-cyp-enzymes-and-transporter-systems]
- 5. Drug-food Interactions in the Era of Molecular Big Data ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10258917/]
- 6. What is Trending in LC Troubleshooting? [https://www.chromatographyonline.com/view/what-s-trending-lc-troubleshooting]
- 7. Green analytical method for the simultaneous analysis of ... [https://www.nature.com/articles/s41598-020-65270-z]
- 8. Development and Validation of HPLC-DAD Method for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7466259/]
- 9. -based obesity treatment: Medication perception could... altered taste [https://www.meduniwien.ac.at/web/en/ueber-uns/news/2025/news-in-october-2025/medication-based-obesity-treatment-altered-taste-perception-could-influence-appetite-regulation/]
- 10. Associations between changes in taste perception and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12326916/]
- 11. GLP-1s don't just suppress appetite — they change how ... [https://www.advisory.com/daily-briefing/2025/10/08/glp-1-taste]
- 12. Ten Key Health and Nutrition Trends for 2025 - KHNI [https://khni.kerry.com/trends-and-insights/ten-key-health-and-nutrition-trends-of-this-year/]
- 13. Micronutrient bioavailability: concepts, influencing factors, ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1646750/full]
- 14. and eating habits of people who use drugs and/or... Nutritional status [https://pmc.ncbi.nlm.nih.gov/articles/PMC8114851/]
- 15. Eating habits, nutritional status, and lifestyle correlates of ... [https://www.frontiersin.org/journals/public-health/articles/10.3389/fpubh.2025.1668307/full]
- 16. Covalent polyphenols-proteins interactions in food ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10951110/]
- 17. Interactions between polyphenols and polysaccharides ... [https://www.sciencedirect.com/science/article/abs/pii/S0141813025033458]
- 18. Dietary polyphenol-protein interactions: A literature review ... [https://www.sciencedirect.com/science/article/abs/pii/S0963996925020599]
- 19. Polyphenol-polysaccharide interactions - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC12397182/]
- 20. Protein-polysaccharide complexes and conjugates [https://www.sciencedirect.com/science/article/pii/S2666154324005477]
- 21. Assessment of food component distribution and structure ... [https://www.sciencedirect.com/science/article/pii/S0733521025001559]
- 22. The Role of BCS (Biopharmaceutics Classification System ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3684558/]
- 23. Case Studies for Practical Food Effect Assessments across ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3535115/]
- 24. Predicting Food Effect On Oral Drug Absorption For ... [https://link.springer.com/article/10.1007/s11095-025-03947-8]
- 25. Predicting pharmacokinetic food effects using biorelevant ... [https://pubmed.ncbi.nlm.nih.gov/17112297/]
- 26. Biopharmaceutical Drug Disposition Classification System [https://www.solvobiotech.com/knowledge-center/bddcs]
- 27. The Invisible Effects of Therapeutic Failure - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3227915/]
- 28. Main nutritional deficiencies - PMC - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC9710417/]
- 29. The relationship between lifestyle components and dietary ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7663317/]
- 30. Drug therapeutic failures in emergency department ... [https://pubmed.ncbi.nlm.nih.gov/14597157/]
- 31. Risks, risk assessment and risk competence in toxicology [https://pmc.ncbi.nlm.nih.gov/articles/PMC4507061/]
- 32. What You Know Can Help You - An Introduction to Toxic ... [https://www.health.ny.gov/environmental/chemicals/toxic_substances.htm]
- 33. Key Principles of Toxicology and Exposure - CHEMM [https://chemm.hhs.gov/toxprinciples.htm]
- 34. Vitamin Deficiency Types, Symptoms, Diagnosis [https://my.clevelandclinic.org/health/diseases/vitamin-deficiency]
- 35. Unveiling Dietary Complexity: A Scoping Review and ... [https://www.mdpi.com/2072-6643/17/20/3261]
- 36. Predictive Performance of Physiologically Based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5824104/]
- 37. Use of Physiologically Based Pharmacokinetic (PBPK) ... [https://pubmed.ncbi.nlm.nih.gov/32981010/]
- 38. Use of Physiologically Based Pharmacokinetic (PBPK) ... [https://link.springer.com/article/10.1208/s12248-020-00508-2]
- 39. Food Effect Projections via Physiologically Based ... [https://www.sciencedirect.com/science/article/abs/pii/S0022354918303320]
- 40. Physiologically based pharmacokinetic modeling to ... [https://www.sciencedirect.com/science/article/pii/S0928098723002063]
- 41. Application of Physiologically-Based Pharmacokinetic (PBPK ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12334468/]
- 42. Quality Assurance of PBPK Modeling Platforms and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9314283/]
- 43. Modelling and simulation: questions and answers [https://www.ema.europa.eu/en/human-regulatory-overview/research-and-development/scientific-guidelines/clinical-pharmacology-pharmacokinetics/modelling-simulation-questions-answers]
- 44. 6 Common Myths About PBPK Modeling [https://www.allucent.com/resources/blog/common-misconceptions-about-pbpk-modeling]
- 45. Real-world application of physiologically based ... [https://www.sciencedirect.com/science/article/abs/pii/S0090955624148556]
- 46. The Role of Intracorrelation and Intercorrelation Structure ... [https://www.sciencedirect.com/science/article/abs/pii/S1047279709001069]
- 47. A Systematic Review of the Methods Used to Assess and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9175067/]
- 48. A review of statistical methods for dietary pattern analysis [https://nutritionj.biomedcentral.com/articles/10.1186/s12937-021-00692-7]
- 49. Dietary patterns derived using principal component ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2023.1091555/full]
- 50. Stability-based validation of dietary patterns obtained by ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5237531/]
- 51. A Study of Dietary Patterns Derived by Cluster Analysis and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11001785/]
- 52. How Biorelevant Testing Can Help Oral Drug Development [https://biorelevant.com/]
- 53. The Use of Biorelevant Dissolution Media to Forecast the In ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2895438/]
- 54. Two stage biorelevant dissolution test [https://biorelevant.com/learning_center/two-stage-biorelevant-dissolution/]
- 55. Biorelevant Dissolution Method Considerations for the ... [https://www.sciencedirect.com/science/article/abs/pii/S0022354922005755]
- 56. Two-Stage Biorelevant Dissolution of Cinnarizine [https://biorelevant.com/learning_center/two-stage-biorelevant-dissolution-of-cinnarizine/]
- 57. Unveiling Dietary Complexity: A Scoping Review and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12567371/]
- 58. Optimal dietary patterns for healthy aging | Nature Medicine [https://www.nature.com/articles/s41591-025-03570-5]
- 59. Overview of Methods and Considerations for Handling ... [https://www.chromatographyonline.com/view/overview-methods-and-considerations-handling-complex-samples]
- 60. Expert Perspectives on Enhancing Analytical Methods for ... [https://www.mdpi.com/2304-8158/14/21/3598]
- 61. Luminex Troubleshooting Guide [https://www.rndsystems.com/resources/protocols/troubleshooting-guide-luminex]
- 62. Dietary Supplements Testing Information [https://www.thermofisher.com/us/en/home/industrial/food-beverage/food-beverage-learning-center/food-analytical-testing-information/dietary-supplements-testing-information.html]
- 63. USP Testing | Frequently Asked Questions [https://www.eurofinsus.com/food-testing/resources/usp-microbiology-services-frequently-asked-questions/]
- 64. Method Optimization for the Analysis of Food, Dietary ... [https://www.fda.gov/science-research/fda-science-forum/method-optimization-analysis-food-dietary-supplements-and-cosmetics-la-icp-ms]
- 65. A new database to guide reference material selection for ... [https://link.springer.com/article/10.1007/s00216-024-05664-4]
- 66. Handling random errors and biases in methods used for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4211566/]
- 67. Improving dietary data collection tools for better nutritional ... [https://www.sciencedirect.com/science/article/pii/S2666990022000180]
- 68. Impact on Nutrition Research and Adjustment for its Effects [https://prevention.cancer.gov/tools-resources/measurement-error-impact-nutrition-research-and-adjustment-its-effects]
- 69. DietAI24 as a framework for comprehensive nutrition ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12589391/]
- 70. Compensate for or Minimize Matrix Effects? Strategies ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7412464/]
- 71. Expert Perspectives on Enhancing Analytical Methods for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12607475/]
- 72. Peptide Bioanalysis: Mitigating Matrix Interference in ... [https://www.sannova.net/peptide-bioanalysis-mitigating-matrix-interference-in-preclinical-and-clinical-trials/]
- 73. How to Mitigate Matrix Effects in ICP-MS for Complex ... [https://www.drawellanalytical.com/how-to-mitigate-matrix-effects-in-icp-ms-for-complex-sample-analysis/]
- 74. Sample Matrix Effects in ICP-MS: Mitigation Techniques [https://eureka.patsnap.com/report-sample-matrix-effects-in-icp-ms-mitigation-techniques]
- 75. Nutrient-Drug Interactions - Nutritional Disorders [https://www.merckmanuals.com/professional/nutritional-disorders/nutrition-general-considerations/nutrient-drug-interactions]
- 76. Drug-Nutrient Interactions | Linus Pauling Institute [https://lpi.oregonstate.edu/mic/drug-nutrient-interactions]
- 77. interaction | PPTX Nutrient drug [https://www.slideshare.net/slideshow/nutrient-drug-interaction/21034336]
- 78. Inhibition of Protein-Protein Interactions: Cell-Based Assays [https://www.ncbi.nlm.nih.gov/books/NBK464632/]
- 79. A Strategy for Modulation of Enzymes in the Ubiquitin System [https://pubmed.ncbi.nlm.nih.gov/23287719/]
- 80. computational methodologies for enzyme modulation and ... [https://pubs.rsc.org/en/content/articlelanding/2025/cb/d4cb00282b]
- 81. predicts gut microbiome restructuring under... Nutrient competition [https://pubmed.ncbi.nlm.nih.gov/39211277/]
- 82. The mechanisms of pharmacokinetic food-drug interactions [https://www.sciencedirect.com/science/article/pii/S0928098719301411]
- 83. An overview on developing the formulation to keep away ... [https://www.sciencedirect.com/science/article/pii/S2949829525000555]
- 84. Diet gel-based oral drug delivery system for controlled ... [https://www.nature.com/articles/s41684-025-01617-1]
- 85. Precision nutrition based on food-derived delivery systems ... [https://www.sciencedirect.com/science/article/pii/S2590157525008405]
- 86. Advancements in delivery systems for dietary polyphenols ... [https://www.nature.com/articles/s41538-025-00419-6]
- 87. Advances in Food-As-Medicine Interventions and Their Impact ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12148425/]
- 88. Confounding by Dietary Patterns of the Inverse Association ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2733040/]
- 89. Obesity and Comorbid Conditions - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK574535/]
- 90. Association of Healthy Lifestyle Factors and Obesity-Related ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10220514/]
- 91. Analysis of dietary pattern effects on metabolic risk factors ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1540919/full]
- 92. Obesity: Prevalence, causes, consequences, management ... [https://www.sciencedirect.com/science/article/pii/S2589936825000313]
- 93. Obesity and overweight [https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight]
- 94. Improving Bioavailability & Solubility in OSDs [https://drug-dev.com/drug-development-improving-bioavailability-solubility-in-osds/]
- 95. Unlocking Bioavailability: Strategies for Formulation ... [https://www.hilarispublisher.com/open-access/unlocking-bioavailability-strategies-for-formulation-optimization-105057.html]
- 96. Contrast requirements for WCAG 2.2 Level AA [https://www.makethingsaccessible.com/guides/contrast-requirements-for-wcag-2-2-level-aa/]
- 97. Understanding Success Criterion 1.4.11: Non-text Contrast [https://www.w3.org/WAI/WCAG21/Understanding/non-text-contrast.html]
- 98. Text has enhanced contrast | ACT Rule | WAI [https://www.w3.org/WAI/standards-guidelines/act/rules/09o5cg/]
- 99. Text color must provide high contrast with its background [https://docs.acquia.com/web-governance/text-color-must-provide-high-contrast-its-background]
- 100. Choosing high contrast text color (in relation to background ... [https://ux.stackexchange.com/questions/8297/choosing-high-contrast-text-color-in-relation-to-background-color-dynamically]
- 101. Immune and metabolic effects of African heritage diets ... [https://www.nature.com/articles/s41591-025-03602-0]
- 102. Systems biology to unravel Western diet-associated triggers in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12549303/]
- 103. Differential effects of Mediterranean vs. Western diets on ... [https://pubmed.ncbi.nlm.nih.gov/40709334/]
- 104. Differential effects of Mediterranean vs. Western diets on ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1564741/full]
- 105. What 96000 adults taught scientists about preventing ... [https://www.sciencedaily.com/releases/2025/11/251123115437.htm]
- 106. Western diet causes inflammation, traditional African food ... [https://www.radboudumc.nl/en/news-items/2025/western-diet-causes-inflammation,-traditional-african-food-protects]
- 107. Protocol for a randomized crossover diet intervention trial [https://www.sciencedirect.com/science/article/pii/S1551714425001454]
- 108. The role of the Mediterranean diet in reducing the risk ... [https://pubmed.ncbi.nlm.nih.gov/39797935/]
- 109. The effects of Mediterranean diet with and without exercise ... [https://www.sciencedirect.com/science/article/pii/S0261561425001736]
- 110. Comparison of the Mediterranean Diet and Other ... [https://www.mdpi.com/1422-0067/26/12/5887]
- 111. Studying dietary intake in daily life through multilevel two-part ... [https://ijbnpa.biomedcentral.com/articles/10.1186/s12966-021-01187-8]
- 112. Methodological Considerations in Evaluating the Evidence [https://www.ncbi.nlm.nih.gov/books/NBK218763/]
- 113. How quality of life is measured in studies of nutritional ... [https://pubmed.ncbi.nlm.nih.gov/38267976/]
- 114. weight loss and exercise Dietary effects on interventions ... quality of [https://pubmed.ncbi.nlm.nih.gov/22026966/]
- 115. HRQoL and nutritional well-being dissimilarities between ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9706066/]
- 116. Common Limitations and Challenges of Dietary Clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8453651/]
- 117. The Problem with Epidemiological Studies [https://www.diagnosisdiet.com/full-article/epidemiological-studies]
- 118. Dietary Assessment Methods For the Athlete: Pros and ... [https://www.gssiweb.org/sports-science-exchange/article/sse-150-dietary-assessment-methods-for-the-athlete-pros-and-cons-of-different-methods]
- 119. The Correlation Among Three Different Dietary Intake ... [https://www.sciencedirect.com/science/article/pii/S2475299123091746]
- 120. FAO/WHO GIFT | Global Individual Food consumption data ... [https://www.fao.org/gift-individual-food-consumption/data/en]
- 121. A Systematic Review of the Methods Used to Assess and ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2022.892351/full]
- 122. Comparative Effectiveness Research: A Roadmap for Physical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5705253/]
- 123. Effects of dietary intervention on human diseases [https://www.nature.com/articles/s41392-024-01771-x]
- 124. The Role of Dietary Lifestyle Modification in Chronic Disease ... [https://www.ncbi.nlm.nih.gov/books/NBK587401/]