Designing Robust Nutritional RCT Protocols: A Comprehensive Guide from SPIRIT 2025 to Implementation
This comprehensive guide addresses the unique challenges in designing randomized controlled trial (RCT) protocols for nutritional interventions, providing researchers and clinical trial professionals with evidence-based methodologies to enhance study validity...
Designing Robust Nutritional RCT Protocols: A Comprehensive Guide from SPIRIT 2025 to Implementation
Abstract
This comprehensive guide addresses the unique challenges in designing randomized controlled trial (RCT) protocols for nutritional interventions, providing researchers and clinical trial professionals with evidence-based methodologies to enhance study validity and impact. Covering foundational principles from the updated SPIRIT 2025 guidelines to complex intervention design, the article explores practical implementation strategies for dietary clinical trials (DCTs), addresses common methodological challenges including blinding difficulties and adherence issues, and examines validation frameworks through systematic reviews and regulatory considerations. With special emphasis on digital health tools and behavioral interventions, this resource aims to improve the quality of nutritional evidence supporting clinical guidelines and public health policies.
Understanding the Landscape: Core Principles and Updated Guidelines for Nutritional RCTs
A high-quality clinical trial protocol serves as the fundamental blueprint for ensuring the scientific integrity, ethical compliance, and methodological rigor of an investigation. The Standard Protocol Items: Recommendations for Interventional Trials (SPIRIT) statement, first published in 2013, has become the internationally recognized benchmark for developing clinical trial protocols [1]. To address the evolving landscape of clinical research, including developing trends in open science and patient-centered principles, the SPIRIT working group undertook a comprehensive update, resulting in the SPIRIT 2025 statement [1] [2].
This update reflects a significant advancement in trial protocol methodology, incorporating a decade of accumulated empirical evidence and methodological refinements. The SPIRIT 2025 guideline emerges from a rigorous consensus process involving hundreds of international experts, including statisticians, trial investigators, clinicians, journal editors, and patient representatives [2] [3]. For researchers specializing in nutritional interventions, these updated guidelines provide a critical framework for enhancing the quality, transparency, and reproducibility of clinical trials in our field, where methodological challenges such as blinding difficulties, adherence monitoring, and intervention complexity have historically complicated trial design and interpretation [4] [5].
Core Updates in SPIRIT 2025 Statement
The SPIRIT 2025 statement introduces substantive changes from its 2013 predecessor, refining the checklist to address gaps in previous guidance and incorporating emerging best practices. The systematic update process, which included a scoping review of literature from 2013-2022 and an international three-round Delphi survey with 317 participants, led to several fundamental modifications [2] [3].
Structural and Content Changes
The updated guideline features significant structural reorganization and content refinement. The executive group added two new protocol items, revised five existing items, and deleted or merged several others to reduce redundancy and improve clarity [2]. A notable structural improvement is the creation of a dedicated open science section that consolidates items critical to promoting transparency and accessibility of trial methods and results [3]. This section encompasses trial registration, sharing of full protocols and statistical analysis plans, data sharing policies, and disclosure of funding sources and conflicts of interest [2].
Table 1: Key Structural Changes in SPIRIT 2025
| Change Type | Number of Items | Key Examples |
|---|---|---|
| New Items | 2 | Patient and public involvement (Item 11); Expanded open science section |
| Revised Items | 5 | Intervention description; Outcomes; Harms; Sample size; Consent materials |
| Deleted/Merged Items | 5 | Merger of related administrative items |
| Total Checklist Items | 34 | (Reduced from 33 items in SPIRIT 2013 with restructuring) |
Enhanced Focus on Patient-Centered Research
A groundbreaking addition to SPIRIT 2025 is Item 11, which requires researchers to describe how patients and the public will be involved in trial design, conduct, and reporting [2] [3]. This formalizes the expectation for meaningful patient engagement throughout the research process, moving beyond tokenistic representation to genuine partnership. For nutritional intervention research, this might involve collaborating with patients to design culturally appropriate dietary interventions, developing patient-friendly outcome measures, or creating accessible result summaries for participant communities [5].
Strengthened Reporting of Methodological Elements
The updated statement places additional emphasis on several methodological aspects critical to trial validity. There is enhanced guidance on the assessment of harms (integrating recommendations from CONSORT Harms 2022), more detailed description of interventions and comparators (informed by TIDieR), and clearer specification of outcome measures (incorporating SPIRIT-Outcomes 2022) [2] [3]. These refinements address common weaknesses identified in nutritional intervention trials, where inadequate description of comparator diets, insufficient documentation of adverse events, and ambiguous outcome measurement have hampered evidence synthesis and clinical application [4].
Application to Nutritional Intervention Research
Nutritional intervention trials present unique methodological challenges that distinguish them from conventional pharmaceutical trials. These include the complexity of dietary interventions, difficulties with blinding participants and personnel, challenges in standardizing control group conditions, and the multifaceted nature of adherence monitoring in free-living populations [4] [5]. The SPIRIT 2025 framework provides specific guidance to address these challenges while maintaining the flexibility needed for diverse nutritional study designs.
Implementing the Open Science Framework
The new open science module in SPIRIT 2025 has particular significance for nutritional research, where heterogeneous methodologies and variable reporting have historically limited evidence synthesis. Item 6 specifically addresses data sharing, requiring protocols to specify where and how de-identified participant data, data dictionaries, and statistical code will be accessible [2]. For nutritional researchers, this might include sharing detailed dietary assessment data, recipe formulations, nutrient composition databases, or behavioral intervention materials that enable replication and secondary analysis.
The following workflow illustrates the implementation of SPIRIT 2025's open science requirements within the context of a nutritional intervention trial:
Methodological Considerations for Nutritional Trials
SPIRIT 2025 provides a framework for addressing persistent methodological challenges in nutritional research. The updated intervention description item (Item 15) requires sufficient detail to enable replication, which for nutritional trials might include documenting food sourcing, meal preparation methods, nutrient composition analysis, and quality control procedures [2] [4]. Similarly, the enhanced guidance on adherence monitoring (Item 15) encourages researchers to move beyond simplistic measures like pill counts or session attendance toward more robust methodologies such as biomarker verification, digital monitoring technologies, or dietary assessment tools with demonstrated validity [4] [6].
Table 2: Essential Methodological Components for Nutritional Intervention Protocols
| SPIRIT 2025 Item | Nutritional Research Application | Recommended Methodology |
|---|---|---|
| Item 11: Patient Involvement | Engage participants in designing culturally appropriate interventions and acceptable outcome measures | Patient advisory boards; Co-design workshops; Preference assessment surveys |
| Item 15: Intervention Description | Detailed nutritional intervention specification with sufficient detail for replication | Standardized recipes; Nutrient composition analysis; Food procurement protocols; Preparation methods |
| Item 18: Outcomes | Selection of clinically meaningful endpoints with appropriate measurement methods | Primary outcome justification; Validated dietary assessment tools; Biomarker measurement protocols |
| Item 29: Trial Monitoring | Processes to ensure intervention fidelity and adherence assessment | Kitchen center audits; Digital photography of meals; Biomarker verification; Smart packaging for supplements |
Implementation Protocols for Nutritional Research
Translating SPIRIT 2025 recommendations into practical protocols requires careful consideration of the unique aspects of nutritional science. The following section provides detailed methodologies for implementing key updates within nutritional intervention trials.
Protocol for Patient and Public Involvement (Item 11)
Objective: To meaningfully involve patients and the public in the design, conduct, and reporting of a nutritional intervention trial.
Background: Patient involvement enhances trial relevance, acceptability, and impact, particularly for nutritional interventions where dietary behaviors are deeply embedded in cultural and personal preferences [2].
Procedures:
- Establish a Patient Advisory Group: Recruit 6-8 individuals representing the target population, ensuring diversity in age, gender, socioeconomic status, and dietary patterns.
- Design Consultation Phase: Conduct structured workshops to review and refine:
- Intervention components (dietary prescriptions, supplement formulations)
- Outcome measurement tools and schedules
- Participant-facing materials (consent forms, dietary instructions)
- Retention strategies and burden minimization
- Ongoing Involvement: Include patient representatives on trial steering committees with appropriate compensation and support.
- Reporting Integration: Document the influence of patient input on protocol development and disseminate results in formats accessible to lay audiences.
Deliverables: Modified protocol reflecting patient input; Plain language summary; Documentation of involvement impact.
Protocol for Nutritional Intervention Description (Item 15)
Objective: To provide comprehensive details of the nutritional intervention and comparator enabling replication and critical appraisal.
Background: Inadequate description of nutritional interventions remains a major limitation in evidence synthesis and clinical application [4] [5].
Procedures:
- Intervention Specification:
- Document specific foods, nutrients, or dietary patterns with quantitative targets
- Describe food sources, procurement methods, and quality control procedures
- Provide nutritional composition analysis using standardized methods
- Detail supplement formulations, manufacturing, and quality assurance
- Delivery Protocol:
- Define intervention setting (clinic, free-living, controlled environment)
- Specify staff qualifications, training procedures, and monitoring
- Describe intervention intensity, duration, and follow-up schedule
- Document behavior change strategies and educational materials
- Comparator Description: Apply the same detailed specification to control conditions, including attention control elements.
- Adherence Monitoring: Implement multi-modal assessment including:
- Biomarker verification (e.g., plasma nutrients, metabolites)
- Dietary intake assessment (validated tools appropriate to population)
- Digital monitoring (photographic food records, smart packaging)
- Process measures (session attendance, interventionist fidelity)
Deliverables: Comprehensive intervention manual; Standard operating procedures; Quality assurance protocols.
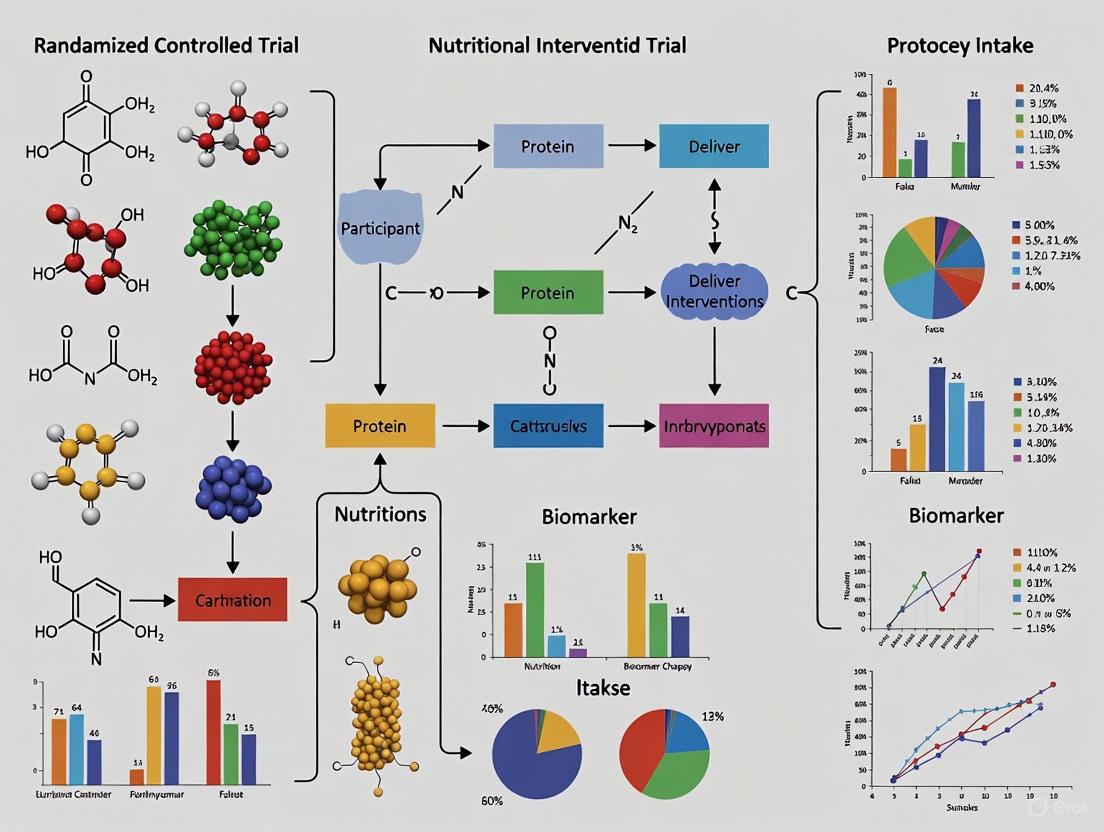
The following diagram illustrates the key methodological workflow for designing a nutritional intervention trial according to SPIRIT 2025 guidelines:
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Essential Research Reagents and Materials for Nutritional Intervention Trials
| Item Category | Specific Examples | Function/Application |
|---|---|---|
| Dietary Assessment Tools | 24-hour recall protocols; Food frequency questionnaires; Diet history interviews; Digital food photography apps | Quantify dietary intake and compliance with intervention targets |
| Biological Sample Collection | EDTA tubes for plasma; Serum separator tubes; Urine collection containers; DNA/RNA stabilization kits | Biomarker analysis for compliance verification and mechanism exploration |
| Nutritional Biomarkers | Plasma carotenoids; Omega-3 indices; Vitamin D [25(OH)D]; Magnesium (RBC); Fatty acid profiles | Objective verification of intervention adherence and nutrient status |
| Body Composition Tools | Bioelectrical impedance analyzers; DEXA scanners; Anthropometric kits (stadiometers, scales) | Assessment of body composition changes in response to intervention |
| Intervention Materials | Standardized food products; Nutrient supplements; Meal replacement formulations; Recipe manuals | Consistent delivery of nutritional intervention components |
| Data Management Systems | Electronic data capture platforms; Dietary analysis software; Randomization modules | Protocol implementation, data integrity, and allocation concealment |
| rac Darifenacin-d4 | rac Darifenacin-d4, CAS:1189701-43-6, MF:C28H30N2O2, MW:430.6 g/mol | Chemical Reagent |
| Protein Kinase C (530-558) | Protein Kinase C (530-558), CAS:122613-29-0, MF:C148H221N35O50S2, MW:3354.711 | Chemical Reagent |
Critical Analysis and Future Directions
While SPIRIT 2025 represents a significant advancement in trial protocol guidance, its implementation in nutritional research requires careful consideration of several methodological challenges. The updated statement has been critiqued for potentially insufficient emphasis on robust adherence monitoring methodologies, particularly concerning the removal of specific reference to laboratory tests for verifying medication exposure in favor of more general guidance [6]. For nutritional interventions, this underscores the importance of going beyond minimum standards to incorporate objective biomarkers of adherence, such as circulating nutrient levels or metabolic profiles, which provide verification beyond self-reported dietary intake or supplement container returns [4] [6].
Nutritional researchers should view SPIRIT 2025 as a foundational framework rather than a comprehensive solution. The field would benefit from developing a SPIRIT extension specifically tailored to the unique methodological considerations of nutritional science, addressing aspects such as dietary compliance biomarkers, control group design for complex dietary interventions, and standardized reporting of food composition and dietary assessment methodologies. Such specialized guidance would build upon the robust foundation of SPIRIT 2025 while addressing the particular evidence needs of nutrition science and policy.
Widespread adoption of SPIRIT 2025 within the nutritional research community has the potential to significantly enhance the quality, transparency, and clinical utility of trial evidence, ultimately strengthening the foundation of evidence-based nutritional recommendations and public health policy [1] [2] [3]. By embracing both the letter and spirit of these updated guidelines, nutritional researchers can address historical methodological limitations and produce more reliable, replicable, and impactful science.
Nutritional intervention research is fundamental to establishing causal links between diet and health, informing public health guidelines, and shaping dietary recommendations for populations [7]. Unlike pharmaceutical trials, nutritional research encompasses a broad spectrum of interventions, from isolated single nutrients to comprehensive dietary patterns, each presenting unique methodological challenges and considerations [7]. These interventions play a pivotal role in determining dietary requirements and understanding the role of supplementation for specific health outcomes.
The complexity of these interventions is amplified by factors such as the baseline nutritional status of participants, the difficulty of creating appropriate control groups, and the practical challenges of blinding participants to dietary changes [7]. This document outlines the core frameworks and protocols for designing rigorous randomized controlled trials (RCTs) across the spectrum of nutritional interventions, providing researchers with a structured approach to this critical area of clinical investigation.
Classifying Nutritional Interventions
Nutritional interventions in clinical research can be categorized along a continuum of complexity. The table below summarizes the primary categories, their key characteristics, and associated research challenges.
Table 1: Classification of Nutritional Interventions in Clinical Research
| Intervention Category | Description | Common Study Designs | Key Challenges |
|---|---|---|---|
| Single Nutrient/Compound | Investigation of an isolated micronutrient (e.g., Vitamin D, Selenium) or bioactive compound (e.g., coenzyme Q10) [7] [8]. | Double-blind RCTs, Depletion-repletion studies [7]. | Bioavailability influenced by form and matrix; baseline nutrient status of participants confounds outcomes [7]. |
| Dietary Supplement | Use of nutritional supplements, often combining multiple vitamins, minerals, or amino acids [9]. | RCTs, often as adjunct therapy to standard treatment [9]. | Standardizing "standard of care" for control groups; ensuring blinding; accounting for polypharmacy [7] [9]. |
| Whole Food/Food Group | Addition or subtraction of specific whole foods (e.g., walnuts, almonds) or food groups [8]. | RCTs, Controlled feeding studies, Parallel-group trials [10] [8]. | Difficult to isolate active compound; ensuring dietary compliance without full control of diet. |
| Macronutrient Modification | Alteration of the proportion of protein, fat, or carbohydrate in the diet [7]. | RCTs, Metabolic balance studies, Cross-over trials. | Inevitable displacement of other macronutrients; confounding by simultaneous caloric intake changes [7]. |
| Complex Dietary Pattern | Implementation of a holistic dietary regimen (e.g., Mediterranean Diet, DASH Diet) [7] [8]. | RCTs, Cluster-randomized trials, Community-based participatory research. | Extreme difficulty with participant blinding; high logistical burden; ensuring cultural appropriateness and compliance [7] [10]. |
The choice of intervention type directly influences the study design, logistical planning, and interpretation of results. For instance, while single-nutrient studies more easily facilitate blinding and mechanistic insights, complex dietary pattern studies often have greater direct applicability to public health messaging [7].
Methodological Framework and Experimental Protocols
Core Experimental Workflow
The following diagram illustrates the high-level workflow for developing and implementing a nutritional intervention trial, from conceptualization through to analysis.
Figure 1. High-level workflow for nutritional intervention trials.
Detailed Protocol for a Complex Dietary Pattern Intervention
This protocol is adapted from methodologies used in studies like the Dietary Approaches for Stopping Hypertension (DASH) trial [7].
1. Background & Objectives: Complex dietary patterns, such as the Mediterranean or DASH diet, are associated with improved health outcomes. This protocol aims to evaluate the effect of a specific dietary pattern on a primary health endpoint (e.g., blood pressure, telomere length) compared to a control diet [7] [8].
2. Study Design:
- Design: Randomized Controlled Trial, parallel-group design.
- Duration: Typically a minimum of 12 weeks to observe meaningful changes in many physiological endpoints, though longer durations (6 months or more) are often necessary for outcomes like telomere length [9] [8].
- Setting: The study can be conducted as a controlled feeding study or as a behavioral intervention with intensive dietary counseling, depending on resources and the need for dietary control [7].
3. Participants:
- Inclusion Criteria: Defined based on the study population of interest (e.g., adults with pre-hypertension, healthy elderly for aging studies). Age, gender, and health status criteria should be explicitly stated [10] [8].
- Exclusion Criteria: Often include conditions that significantly alter nutrient metabolism (e.g., renal disease, malabsorption disorders), use of medications interfering with the primary outcome, or pre-existing dietary practices that align too closely with the intervention diet [9].
- Sample Size: Calculated based on the primary outcome, expected effect size, power (typically 80-90%), and significance level (α = 0.05). A power calculation is mandatory for publication in leading journals [11] [12].
4. Intervention & Control:
- Intervention Group: Receives the defined complex dietary pattern (e.g., high in fruits, vegetables, whole grains, and low-fat dairy; reduced saturated fat). In a feeding study, all meals are provided. In a behavioral intervention, participants receive detailed meal plans, recipes, and intensive counseling [7] [10].
- Control Group: Receives a control diet, typically representative of a typical local diet or a alternative dietary pattern for comparison. The control diet must be designed to be distinct from the intervention diet in the key components of interest [7].
- Blinding: While true blinding of participants is nearly impossible in whole-diet studies, outcome assessors and data analysts should be blinded to group assignment [7].
5. Outcome Measures:
- Primary Outcomes: Align directly with the main research objective (e.g., change in systolic blood pressure, change in telomere length measured using standardized assays like qPCR) [9] [8].
- Secondary Outcomes: Can include biomarkers of compliance (e.g., urinary sodium for a low-sodium diet, plasma carotenoids for fruit/vegetable intake), quality of life measures, and other relevant health parameters [10] [9].
6. Data Collection & Management:
- Baseline & Follow-up: Collect demographic, anthropometric, clinical, and biochemical data at baseline and specified intervals during the study.
- Dietary Compliance: In feeding studies, compliance is monitored by requiring participants to consume all provided food. In behavioral interventions, use 24-hour dietary recalls, food frequency questionnaires, or food diaries, combined with biomarker analysis [7].
- Statistical Analysis: Specify methods a priori. Report p-values to two decimal places (e.g., P = .04), with values close to .05 reported to three places (e.g., P = .053). P values less than .001 should be reported as P < .001 [12].
The Scientist's Toolkit: Key Research Reagent Solutions
The following table details essential materials and tools required for conducting high-quality nutritional intervention research.
Table 2: Essential Research Reagents and Materials for Nutritional Interventions
| Item Category | Specific Examples | Function & Application |
|---|---|---|
| Biochemical Assay Kits | ELISA kits for vitamins (e.g., 25-hydroxy Vitamin D), hormones, inflammatory cytokines (e.g., IL-6, TNF-α). | Quantifying nutrient status and measuring secondary biochemical endpoints related to inflammation and oxidative stress [9] [8]. |
| Telomere Length Assay Kits | Quantitative PCR (qPCR) kits for relative telomere length measurement. | Assessing a biomarker of biological aging as a primary or secondary outcome in long-term nutritional studies [8]. |
| Validated Questionnaires | Food Frequency Questionnaires (FFQ), Sports Nutrition Knowledge (SNK) questionnaires, Quality of Life surveys (e.g., SF-36). | Assessing baseline dietary intake, monitoring compliance, and evaluating knowledge or patient-reported outcomes [10] [9]. |
| Dietary Supplement Formulations | Pharmaceutical-grade nutrient supplements (e.g., folic acid, vitamin D3, coenzyme Q10). | Serving as the active intervention in single-nutrient or dietary supplement trials; requires careful characterization of form and dosage [7] [9]. |
| Placebo Formulations | Microcrystalline cellulose pills, matched liquid placebos. | Creating a blinded control for supplement trials; must be identical in appearance, taste, and packaging to the active supplement [7]. |
| Sodium new houttuyfonate | Sodium New Houttuyfonate for Research | Research-grade Sodium New Houttuyfonate for studying antifungal, antibacterial, and anti-inflammatory mechanisms. This product is for Research Use Only (RUO), not for human use. |
| 4-Aminohippuric-d4 Acid | 4-Aminohippuric-d4 Acid, MF:C9H10N2O3, MW:198.21 g/mol | Chemical Reagent |
Special Considerations and Reporting Standards
Ethical and Logistical Challenges
Nutritional research faces several unique hurdles. A central ethical consideration is the definition of an appropriate control, especially when a nutrient is essential or a dietary pattern is believed to be beneficial. Withholding a potentially beneficial intervention from a control group known to be deficient poses an ethical dilemma for Institutional Review Boards (IRBs) [7]. Furthermore, baseline nutritional status can greatly influence the response to an intervention, as nutrients often have threshold effects beyond which no further benefit is observed. This necessitates careful screening and assessment of participants at baseline [7].
Logistically, providing entire diets or specific whole foods requires significant infrastructure for food procurement, preparation, and storage. Participant compliance is a higher bar than in drug trials, as the intervention must be appealing and culturally acceptable to be sustained [7] [10].
Pathway of Intervention Effect and Outcome Measurement
The mechanistic path from a nutritional intervention to a measured health outcome involves multiple biological systems, especially in complex interventions.
Figure 2. Pathway from nutritional intervention to health outcome.
Mandatory Reporting Guidelines
To ensure transparency, reproducibility, and quality, nutritional intervention research must adhere to international reporting standards. The following table outlines the critical guidelines.
Table 3: Essential Reporting Guidelines for Nutritional Intervention Research
| Study Type | Reporting Guideline | Primary Purpose | Key Reporting Elements |
|---|---|---|---|
| Randomized Controlled Trial (Completed) | CONSORT | To provide a checklist for transparent reporting of trial methods, results, and conclusions. | Flow diagram, randomization method, blinding, participant flow, baseline data, outcome estimates. |
| Randomized Controlled Trial (Protocol) | SPIRIT | To define standard protocol items for clinical trials to ensure completeness. | Background, rationale, objectives, trial design, methods, ethics, dissemination plans [11]. |
| Systematic Review | PRISMA | To ensure the transparent and complete reporting of systematic reviews and meta-analyses. | Search strategy, study selection process, risk of bias assessment, synthesis methods [9]. |
Furthermore, clinical trials must be registered in a publicly accessible registry such as ClinicalTrials.gov or a WHO-approved primary registry before participant enrollment begins [11] [12]. Authors should also follow the SAGER guidelines to promote appropriate sex and gender equity in their research [12].
Designing rigorous nutritional interventions requires careful consideration of the intervention type, from single nutrients to complex diets, and a thorough understanding of the associated methodological challenges. By adhering to established experimental protocols, utilizing appropriate tools and reagents, and complying with international reporting standards, researchers can generate high-quality, reliable evidence. This evidence is crucial for advancing the field of clinical nutrition and translating research findings into effective public health guidance and clinical practice. Future research will benefit from larger-scale, longer-term trials that address the current limitations of high heterogeneity and risk of bias, particularly in emerging areas like nutritional psychiatry and nutrigerontology [9] [8].
Nutrition research, particularly in the design and implementation of Randomized Controlled Trials (RCTs), faces a distinct set of complexities not typically encountered in pharmaceutical research. These challenges stem from the inherent nature of dietary interventions, which involve complex matrices of interacting components, are influenced by the pre-existing dietary status of participants, and are deeply embedded within socio-cultural contexts that shape food behaviors [13]. The physiological effects of a food are not solely determined by its gross chemical composition but are significantly modified by its physical structure, the combination of foods consumed, and an individual's cultural background and nutritional starting point [14] [13]. This Application Note details these unique challenges and provides structured protocols to enhance the rigor, reproducibility, and translatability of nutritional RCTs.
The Food Matrix Effect
Concept and Significance
The food matrix is defined as the intricate micro- and macro-structural organization of food components within a whole food. This structure can significantly alter the bioavailability, absorption, and metabolic fate of nutrients compared to when the same nutrients are consumed in an isolated, purified form [14]. For example, the same load of fats, sugars, or proteins can elicit different metabolic responses depending on the food's physical form (solid vs. liquid), texture (hard vs. soft), and cellular integrity [14]. A key illustration is the difference between consuming whole almonds (with an intact cell wall structure) and almond oil; the matrix of the whole nut reduces the bioaccessibility of lipids, thereby lowering the effective energy absorbed [14]. Ignoring the matrix effect can lead to misinterpretations of a food's health impact and flawed public health recommendations.
Experimental Protocol for Investigating the Matrix Effect
Objective: To compare the metabolic response (e.g., postprandial glycemia, insulinemia, or satiety hormones) to a nutrient delivered in two different physical forms: a whole food and an isolated/matched formulation.
Methodology:
- Selection of Test Foods: Choose a whole food of interest (e.g., an apple) and create a matched liquid formulation (e.g., apple juice) with an equivalent macronutrient and fiber profile based on chemical analysis.
- Study Population: Recruit healthy participants (e.g., n=20-25) to achieve adequate power. Participants should be randomized and act as their own controls in a crossover design.
- Intervention: After an overnight fast, participants consume the test meals on two separate visits:
- Visit 1: Whole food meal.
- Visit 2: Matched formulation meal.
- A washout period of at least 3 days should separate the visits.
- Data Collection:
- Blood Samples: Collect at baseline (fasting), 15, 30, 60, 90, and 120 minutes postprandially. Analyze for relevant metabolites (glucose, insulin, GLP-1, etc.).
- Satiety Assessment: Use Visual Analog Scales (VAS) to measure hunger, fullness, and prospective food consumption at the same time points.
- Oral Processing: Record eating rate (g/min) and number of chews for the solid meal.
Data Analysis: Compare the area under the curve (AUC) for blood metabolites and satiety scores between the two test conditions using paired t-tests. Correlate oral processing parameters with metabolic outcomes.
Figure 1: Experimental workflow for a crossover study designed to isolate and measure the food matrix effect on metabolic responses.
Research Reagent Solutions for Matrix Studies
Table 1: Key Materials and Reagents for Food Matrix Research
| Item | Function/Description | Application Example |
|---|---|---|
| Controlled Diets | Meals with precisely defined composition and form (liquid, solid, semi-solid). | Isolating the effect of food form on satiety and energy intake [14]. |
| In Vitro Digestion Models | (e.g., INFOGEST) Simulated gastrointestinal environments. | Predicting nutrient bioaccessibility from different food structures [14]. |
| Standard Reference Materials | (e.g., from NIST) Certified food materials with known composition. | Validating analytical methods for nutrient analysis in complex foods. |
| Textural Profile Analyzer | Instrument to quantitatively measure hardness, cohesiveness, springiness. | Objectively characterizing food texture to correlate with oral processing [14]. |
Baseline Nutritional Status
Concept and Significance
The baseline nutritional status of a study participant refers to their body's existing reserves and circulating levels of the nutrient under investigation prior to the intervention. This status is a critical moderator of the intervention's effect [13]. A supplementation trial may show a significant effect in a deficient population but no effect—or even a negative effect—in a replete population. This is a fundamental difference from most drug trials, where the drug is a novel exogenous compound. Factors such as subclinical deficiencies, genetic polymorphisms affecting nutrient metabolism, and habitual dietary intake can create high inter-individual variability in response, obscuring the true efficacy of an intervention [13].
Protocol for Assessing and Stratifying by Baseline Status
Objective: To determine if the efficacy of a nutritional intervention depends on the participants' baseline status of the nutrient of interest.
Methodology:
- Screening and Recruitment: Screen potential participants using a biomarker of status for the nutrient of interest (e.g., plasma 25-hydroxyvitamin D for vitamin D, serum ferritin for iron).
- Pre-Defined Stratification: Pre-define cutoff points for "low," "normal," and "high" status based on established clinical guidelines.
- Randomization: Within each stratification group, randomly assign participants to the intervention or control group. This ensures balanced groups for analysis.
- Intervention: Administer the nutrient supplement or placebo for the predefined study period.
- Outcome Measurement: Assess the primary outcome (e.g., change in a functional endpoint like insulin sensitivity or a disease biomarker) at the end of the study.
Data Analysis: Use an analysis of covariance (ANCOVA) model with the final outcome as the dependent variable, treatment group as a fixed factor, and baseline nutrient status as a covariate. Test for a significant interaction term between treatment group and baseline status.
Table 2: Impact of Baseline Status on Intervention Outcomes: A Hypothetical Example
| Nutrient | Population with Deficient Baseline | Population with Adequate Baseline | Implication for Trial Design |
|---|---|---|---|
| Vitamin D | Significant improvement in insulin sensitivity after supplementation. | No significant change or minimal improvement. | Failure to stratify may lead to conclusion of "no overall effect" [13]. |
| Iron | Marked increase in hemoglobin and reduction in fatigue. | No change in hemoglobin; risk of iron overload. | Safety and efficacy are contingent on baseline status. |
| Omega-3 Fatty Acids | Greater reduction in inflammatory markers (e.g., CRP). | Muted anti-inflammatory response. | Baseline dietary intake (e.g., fish consumption) must be assessed. |
Figure 2: A protocol for a randomized controlled trial incorporating pre-stratification of participants based on baseline nutritional status to account for its modulating effect.
Socio-Cultural Influences on Dietary Behavior
Concept and Significance
Dietary practices are not merely biological but are deeply rooted in socio-cultural norms, traditions, and gender roles. These factors profoundly influence food choices, meal patterns, and the acceptability of dietary interventions [15] [16]. A one-size-fits-all approach in nutrition research is likely to fail if it does not account for these influences. For instance, a study in rural Bangladesh found that gendered norms limited adolescent girls' participation in physical activity and shaped their access to certain foods, while taste preferences and the popularity of street foods heavily influenced adolescent diets [15]. Overlooking these factors can lead to poor adherence in trials and render effective interventions unimplementable in real-world settings.
Protocol for Integrating Socio-Cultural Context into RCTs
Objective: To design a dietary intervention that is culturally appropriate and acceptable, thereby maximizing adherence and real-world applicability.
Methodology (Mixed-Methods Approach):
- Formative Qualitative Research (Pre-Trial):
- Conduct Focus Group Discussions (FGDs) and semi-structured interviews with members of the target community (including different genders, ages, and socio-economic groups) [15].
- Themes to Explore: Common foods and meals, perceptions of "healthy" food, barriers and facilitators to dietary change, typical eating patterns, and gender roles in food procurement and preparation.
- Intervention Co-Development: Use the qualitative findings to adapt the intervention. This may involve:
- Modifying recommended foods to align with local availability and preferences.
- Tailoring educational materials to align with local health beliefs and language.
- Scheduling intervention activities around culturally important events or daily routines.
- Quantitative RCT with Embedded Process Evaluation:
- Implement the co-developed RCT.
- Monitor Adherence: Use culturally appropriate tools (e.g., locally validated food frequency questionnaires, photographic food records).
- Process Evaluation: Conduct follow-up interviews or surveys to understand participants' experiences, perceived barriers, and facilitators.
Data Analysis: Integrate qualitative and quantitative data. Thematic analysis for qualitative data; standard statistical methods for quantitative outcomes. Compare adherence and outcomes with historical controls or less tailored interventions.
Research Toolkit for Socio-Cultural Investigations
Table 3: Key Methodologies for Socio-Cultural Research in Nutrition
| Methodology | Function | Application in Nutrition Research |
|---|---|---|
| Focus Group Discussions | To explore group norms, shared beliefs, and common practices. | Understanding collective perceptions of healthy body image or barriers to buying fruits and vegetables [15]. |
| Semi-Structured Interviews | To gain in-depth, individual-level insights and personal experiences. | Exploring an individual's journey with weight management or specific dietary restrictions. |
| Dietary Acculturation Scales | To measure the adoption of dietary patterns from a new culture. | Studying how immigration affects diet-related disease risk. |
| Participatory Mapping | To visually document food sources and food environments within a community. | Identifying "food deserts" and barriers to accessing healthy foods. |
| Cetrimonium bromide-d42 | Hexadecyltrimethylammonium Bromide-d42 | Research-grade Hexadecyltrimethylammonium Bromide-d42 for advanced studies. Applications include NMR, mechanism analysis, and nanoparticle synthesis. For Research Use Only. |
| Swietemahalactone | Swietemahalactone, MF:C27H30O10, MW:514.5 g/mol | Chemical Reagent |
For researchers designing randomized controlled trials (RCTs) for nutritional interventions, navigating the U.S. Food and Drug Administration (FDA) regulatory landscape is crucial. The foundational principle governing this space is the distinction between a dietary supplement and a drug, which is determined primarily by intended use as established in the Food, Drug, and Cosmetic Act [17]. A substance is regulated as a drug if it is intended for use in the "diagnosis, cure, mitigation, treatment, or prevention of disease" [17]. Conversely, dietary supplements are intended to supplement the diet and must not be represented for disease treatment or prevention.
This distinction becomes critically important when designing clinical trials. Any clinical investigation designed to evaluate a product's effect on the structure or function of the body for disease treatment transforms the product into an investigational drug in the eyes of the FDA, requiring an Investigational New Drug (IND) application [17]. This regulatory framework ensures patient safety and scientific validity while presenting researchers with specific compliance requirements.
IND Requirements for Dietary Intervention Studies
When an IND is Required
The necessity for an IND application hinges entirely on the study's intent and endpoints. Research involving dietary ingredients or supplements may require an IND if it investigates disease outcomes, even if the product is lawfully marketed as a supplement outside the research context.
Case Study: Relaxium Sleep: A recent FDA warning letter illustrates this critical distinction. A sponsor conducted "Protocol ABRI-002 on Relaxium Sleep in insomnia subjects without an IND" [17]. The sponsor argued that the product was "marketed as a supplement, not a drug," and that "studying effects on sleep doesn't make it a drug" [17]. The FDA explicitly disagreed, stating that "measuring treatment endpoints constitutes intended use as drug" [17]. The outcome was a warning letter demanding "immediate corrective actions, including IND submission" [17]. This case underscores that investigating a dietary supplement for effects on a disease condition (insomnia) without an IND constitutes a violation of FDA regulations.
Table: Determining IND Requirement for Dietary Intervention Studies
| Study Characteristic | IND Likely Required? | Regulatory Rationale |
|---|---|---|
| Endpoint: Diagnosis, mitigation, treatment, or prevention of a disease | Yes | Meets statutory definition of "drug" [17] |
| Endpoint: Effect on structure/function without disease reference | No | Consistent with dietary supplement claims |
| Intent: To establish therapeutic effect | Yes | Creates a new drug indication |
| Intent: To characterize nutritional effects | No | Consistent with supplement labeling |
| Population: Patients with specific disease | Yes | Implies disease treatment intent |
| Population: Healthy volunteers | No (but context-dependent) | More consistent with supplement research |
Consequences of Non-Compliance
Failure to submit a required IND application can result in serious regulatory consequences:
- FDA Warning Letters: Official agency communication demanding immediate corrective action [17]
- Clinical Hold: Order to delay or suspend the proposed clinical investigation [17]
- Data Invalidation: Collected study data may be deemed unusable for regulatory submissions [17]
- Resource Depletion: Wasted financial and temporal investments in non-compliant research [17]
FDA Guidance Agenda for Human Foods and Dietary Supplements
2025 Human Foods Program Guidance
The FDA's Human Foods Program has published its proposed 2025 guidance agenda, highlighting priority topics for the agency. While this list represents planned guidance and does not carry legally enforceable requirements, it signals critical areas for researcher awareness [18].
Key topics relevant to dietary intervention researchers include:
- Action Level for Opiate Alkaloids on Poppy Seeds: Draft Guidance for Industry
- Food Colors Derived from Natural Sources: Fruit Juice and Vegetable Juice as Color Additives in Food; Draft Guidance for Industry
- New Dietary Ingredient Notifications and Related Issues: Identity and Safety Information About the NDI: Guidance for Industry [18]
The FDA acknowledges this list is not exhaustive and may issue additional guidance not currently identified. The agency welcomes public comments on these topics through Regulations.gov using Docket FDA-2022-D-2088 [18].
New Dietary Ingredient (NDI) Notification Framework
The FDA is continuing its "piecemeal approach" to finalizing the NDI guidance, with significant developments expected in 2025 [19]. The NDI notification process requires manufacturers to submit safety data to the FDA for any dietary ingredient not marketed in the U.S. before October 15, 1994 [19].
Recent developments include:
- March 2024: FDA released final guidance "Dietary Supplements: New Dietary Ingredient Notification Procedures and Timeframes: Guidance for Industry" [19]
- April 2024: FDA issued draft guidance "New Dietary Ingredient Notification Master Files for Dietary Supplements" [19]
- June 2025: FDA released educational videos and a supplemental fact sheet to boost awareness of the NDIN review process [19]
Outstanding issues that may be addressed in upcoming guidance include "synthetic botanicals, toxicology testing and so on and so forth" [19]. For researchers studying new dietary ingredients, compliance with NDI notification requirements is essential, particularly when the research involves ingredients not previously marketed in the U.S.
Specific Ingredient Considerations
N-Acetyl Cysteine (NAC)
The FDA is working toward "rulemaking to provide by regulation that an ingredient is not excluded from the dietary supplement definition," which is widely expected to address NAC [19]. Despite being used in supplements since the early 1990s, the FDA previously declared NAC not a legal dietary ingredient due to prior approval as a drug in 1963 [19]. The agency currently exercises enforcement discretion, allowing NAC supplement sales provided they do not make "non-compliant disease claims" [19]. Formal rulemaking is anticipated to provide more stable regulatory footing.
Nicotinamide Mononucleotide (NMN)
For NMN, the FDA has stated it "does not intend to prioritize enforcement action" related to NMN-containing dietary supplements, pending resolution of a Citizen Petition filed by the Natural Products Association and the Alliance for Natural Health [19]. This enforcement discretion is contingent upon the absence of new safety concerns [19].
Application Notes for RCT Protocol Development
Regulatory Assessment Protocol
Researchers should implement a systematic approach to determining IND requirements during trial design. The following workflow outlines key decision points:
RCT Design Considerations for Dietary Interventions
Randomized controlled trials represent the "gold standard for effectiveness research" because "randomization reduces bias and provides a rigorous tool to examine cause-effect relationships between an intervention and outcome" [20]. For nutritional interventions, several design considerations are particularly important:
- Blinding: "RCTs are often blinded so that participants and doctors, nurses or researchers do not know what treatment each participant is receiving, further minimizing bias" [20]. Effective blinding can be challenging with dietary interventions but is crucial for validity.
- Population Selection: "Participants who enroll in RCTs differ from one another in known and unknown ways that can influence study outcomes" [21]. Careful inclusion/exclusion criteria are essential.
- Control Group Design: Selection of appropriate control (placebo, active comparator, or standard care) must be scientifically and ethically justified [21].
Table: RCT Design Configurations for Dietary Interventions
| Design Type | Description | Applications in Nutrition Research |
|---|---|---|
| Parallel-group | Each participant randomly assigned to one group; all group members receive same intervention [21] | Most common design; suitable for most supplement efficacy studies |
| Crossover | Participants receive multiple interventions in random sequence [21] | Useful for studying short-term metabolic effects; requires washout periods |
| Cluster | Pre-existing groups (communities, schools) randomly selected [21] | Ideal for population-level dietary interventions or educational programs |
| Factorial | Participants assigned to groups receiving different intervention combinations [21] | Efficient for studying multiple nutrient interactions |
| Stepped-wedge | Sequential crossover of clusters from control to intervention [21] | Appropriate for phased implementation of dietary programs |
Compliance Documentation Framework
Researchers should maintain comprehensive documentation to demonstrate regulatory compliance:
- Protocol Intent Documentation: Clear statements of research objectives consistent with supplement research parameters
- Endpoint Justification: Scientific rationale for selected endpoints avoiding disease claims
- Labeling and Informed Consent Review: Ensure all participant-facing materials avoid therapeutic claims
- Substantiation Records: For any "healthy" content claims, manufacturers "must make and keep written records substantiating the 'healthy' claims" under new FDA requirements [22]
Experimental Protocols for Complimentary Dietary Intervention Research
Dietary Supplement Safety and Bioavailability Study Protocol
This protocol outlines a compliant approach for studying dietary supplements without triggering IND requirements.
Objective: To evaluate the safety, tolerability, and bioavailability of [DIETARY INGREDIENT] in healthy adult volunteers.
Primary Endpoints:
- Plasma/serum concentrations of [ACTIVE COMPONENTS] over 24 hours
- Incidence and severity of adverse events
- Vital sign measurements (blood pressure, heart rate)
Secondary Endpoints:
- Participant-reported quality of life measures
- Compliance with supplementation regimen
Methodology:
- Design: Randomized, double-blind, placebo-controlled, parallel-group
- Participants: 50 healthy adults, aged 18-65 years
- Intervention: [DIETARY INGREDIENT] or matching placebo for 30 days
- Assessments: Blood sampling at baseline, 2, 4, 8, 12, and 24 hours post-dose on day 1 and day 30; daily symptom diaries; vital signs at each study visit
Regulatory Status: This study does not require an IND as it investigates safety and bioavailability in healthy volunteers, not disease treatment or prevention.
Research Reagent Solutions for Dietary Intervention Studies
Table: Essential Materials for Dietary Intervention RCTs
| Reagent/Material | Function | Application in Nutrition Research |
|---|---|---|
| Standardized Investigational Product | Consistent formulation and dosage across study period | Ensures product quality and reliability of results |
| Placebo Matching Investigational Product | Participant and investigator blinding | Minimizes bias in outcome assessment |
| Dietary Assessment Tools (e.g., 24-hour recall, FFQ) | Measures background dietary intake | Controls for confounding from habitual diet |
| Biological Sample Collection Kits | Standardized specimen processing | Ensures sample integrity for biomarker analysis |
| Compliance Measures (e.g., pill counts, biomarkers) | Verifies participant adherence to protocol | Critical for validity of intention-to-treat analysis |
| Adverse Event Documentation Forms | Systematic safety monitoring | Meets ethical and regulatory requirements for participant protection |
CONSORT Guidelines Implementation
Proper reporting of RCTs is essential for research validity and translation. The CONSORT (Consolidated Standards of Reporting Trials) guidelines provide an evidence-based framework for transparent reporting [23]. Key elements for dietary intervention studies include:
- Participant Flow Diagram: "Documentation of the flow of the trial participants using a diagram" is recommended by Item 13 of CONSORT guidelines [23]. This should include:
- Number of participants assessed for eligibility
- Randomly allocated to each group
- Receiving intended intervention
- Completing study protocol
- Included in primary analysis
- Loss to Follow-up Documentation: "Reasons for loss to follow-up and exclusions from the RCT analysis were poorly reported" in many trials [23]. Comprehensive reporting of attrition reasons is methodologically crucial.
- Trial Registration: All RCTs "should be registered with a clinical trials database" [20] such as ClinicalTrials.gov prior to participant enrollment.
Navigating the FDA regulatory framework for dietary intervention research requires careful attention to the distinction between dietary supplement and drug research. The fundamental determinant is intended use, with studies designed to investigate disease diagnosis, treatment, or prevention requiring IND applications [17]. Researchers should implement systematic regulatory assessments during trial design, maintain comprehensive documentation, and adhere to methodological standards including CONSORT guidelines for reporting [23]. With the FDA's 2025 guidance agenda highlighting continued focus on human foods and dietary supplements [18], researchers must remain current with evolving regulatory expectations to ensure compliant and scientifically valid research protocols.
Ethical Considerations and Documentation Standards in Nutrition Research
Core Ethical Principles in Human Nutrition Research
Respect for participant autonomy, transparency, and accountability form the foundational ethical pillars for conducting rigorous and trustworthy nutrition research [24].
Participant Rights and Autonomy
- Informed Consent: Researchers must provide clear, concise information about the study's purpose, methods, potential risks, benefits, and participant responsibilities. Participants must understand their right to refuse or withdraw from the study without penalty [24].
- Protection of Confidential Information: Researchers have a duty to protect participant data through secure storage, transmission methods, limited access to authorized personnel, and anonymization where possible, complying with regulations like GDPR [24].
- Withdrawal Mechanisms: Clear, accessible processes must allow participants to withdraw from the study at any time, without affecting their care or treatment. Withdrawn data should be anonymized per protocol [24].
Transparency and Accountability
- Clear Disclosure: Research methods, outcomes, and limitations must be presented clearly, avoiding technical jargon to ensure findings are accessible [24].
- Accurate Representation: Researchers must avoid selective reporting or data manipulation, acknowledge potential biases or errors, and discuss findings' implications and limitations honestly [24].
- Complaint Mechanisms: Establish clear, timely processes for participants to report concerns or complaints, with transparent resolution and corrective actions [24].
Artificial Intelligence and Emerging Technologies
The application of AI in nutrition and behavior change introduces unique ethical challenges, requiring domain-specific frameworks to ensure trustworthy systems [25]. Key issues include:
- Algorithmic Bias: AI systems trained on unrepresentative datasets (e.g., non-Western dietary patterns, historical under-representation of women in trials) risk perpetuating biases and widening health inequalities [25].
- Black Box Problem: Lack of transparency and explainability in AI systems can erode trust. Expert scrutiny and validation are essential [25].
Table 1.1: Key Ethical Challenges and Mitigation Strategies in Nutrition Research
| Ethical Challenge | Potential Consequences | Recommended Mitigation Strategies |
|---|---|---|
| Coercion & Undue Influence | Compromised autonomy, invalid consent | Clear consent processes emphasizing voluntary participation; no penalty for refusal/withdrawal [24]. |
| Data Privacy Breaches | Loss of confidentiality, participant harm | Data anonymization; secure storage; compliance with data protection regulations (e.g., GDPR) [24]. |
| Unrepresentative Datasets | Biased algorithms, skewed results, widening health inequalities | Ensure diverse participant recruitment; include varied dietary patterns and nutritional needs [25]. |
| Lack of AI Transparency | Unexplainable recommendations, eroded trust | Implement explainable AI (XAI) principles; external validation of AI systems [25]. |
Figure 1.1: Comprehensive Ethics Framework for Nutrition Research
Documentation and Reporting Standards for Nutritional RCTs
Adherence to standardized documentation and reporting protocols is critical for ensuring scientific rigor, reproducibility, and transparency in nutritional intervention research.
Protocol Development and Registration
Ahead of trial commencement, researchers should develop and register a detailed protocol, as demonstrated by a systematic review on nutritional supplementation for Obsessive-Compulsive Disorder (OCD) [9] [26]. Key protocol elements include:
- Background and Rationale: Justify the research question and its significance within current evidence gaps. For example, the OCD review notes standard treatments often provide incomplete symptom relief, warranting investigation into nutritional adjuncts [9].
- Pre-defined Methodology:
- Eligibility Criteria: Define study designs, participant characteristics (e.g., adults ≥18 years with DSM-5 diagnosed OCD), interventions, comparators, and outcomes using frameworks like PICO [9].
- Primary and Secondary Outcomes: Specify primary outcomes (e.g., cognition, quality of life, psychiatric symptoms) and secondary outcomes (e.g., comorbidities) with identified measurement tools (e.g., Stroop Test, SF-36) [9].
- Search Strategy: Detail electronic databases (e.g., MEDLINE, Embase, CENTRAL), search terms, and timelines without date or language restrictions [9].
- Registration: Publicly register the protocol in repositories like Open Science Framework (OSF) to enhance transparency and reduce reporting bias [9] [26].
Systematic Review Methodology
The Nutrition Evidence Systematic Review (NESR) methodology, used by the 2025 Dietary Guidelines Advisory Committee, provides a gold-standard framework [27]:
- Protocol-driven Approach: Develop a pre-specified protocol for all review stages [27].
- Comprehensive Search and Screening: Systematic searches across multiple databases, with duplicate independent screening of citations and full-text articles [9] [27].
- Data Extraction and Risk of Bias: Standardized data extraction from included studies, with independent assessment of methodological quality and risk of bias using validated tools [9] [27].
- Evidence Synthesis and Grading: Synthesize evidence, develop conclusion statements, and grade the strength of evidence [27].
- Peer Review: The 2025 Dietary Guidelines Advisory Committee's systematic reviews underwent external peer review coordinated by the National Institutes of Health (NIH) [27].
Table 2.1: Essential Documentation Elements for Nutritional RCT Protocols
| Protocol Section | Key Components | Reporting Standards & Examples |
|---|---|---|
| Study Objectives | Primary & secondary research questions | PICO framework; clearly defined hypotheses [9]. |
| Intervention | Supplement details (type, dose, frequency); administration method; quality control (e.g., DSID) [28] | Use Dietary Supplement Ingredient Database (DSID) for predicted ingredient levels [28]. |
| Comparator | Placebo or active control; co-interventions allowed in both groups | Ensure comparators are clearly defined and justified [9]. |
| Outcomes | Primary & secondary outcomes; specific measurement tools & timepoints | Validated instruments (e.g., Yale-Brown Obsessive Compulsive Scale) [9]. |
| Sample Size | Justification via power calculation; enrollment targets | Detail statistical power, alpha, effect size, and expected attrition [9]. |
| Randomization & Blinding | Randomization procedure; allocation concealment; blinding methods | Specify who is blinded (participants, intervenors, outcome assessors) [9]. |
| Data Management | Data collection methods; confidentiality measures; statistical analysis plan | Secure storage; pre-specified analysis plan for primary outcomes [24]. |
| Ethical Compliance | Ethics approval; informed consent process; data safety monitoring board | IRB approval number; consent documentation process [24]. |
Figure 2.1: Systematic Review Workflow per NESR Methodology
Quantitative Data Presentation in Nutrition Research
Effective presentation of quantitative data is essential for clear communication of research findings. The choice of graphical representation depends on the type of data and the research question [29] [30].
Data Tabulation and Frequency Distributions
Tabulation is the foundational step before data analysis, requiring design principles for clarity [31]:
- Frequency Tables: For quantitative data, create class intervals of equal size to group data. The number of classes should typically be 5-16 for optimal presentation. Calculate the range (highest-lowest value) and divide into subranges [29] [31].
- Table Design Principles:
Graphical Data Representation
- Histograms: Used for displaying frequency distributions of continuous quantitative data. The horizontal axis is a numerical scale with contiguous, touching bars where area represents frequency [29] [31].
- Frequency Polygons: Created by joining the midpoints of the tops of the bars in a histogram, useful for comparing multiple distributions on the same diagram [29] [31].
- Line Diagrams: Illustrate time trends of an event (e.g., birth rates, disease incidence) with time on the horizontal axis [31].
- Scatter Diagrams: Display correlation between two quantitative variables, with points indicating values for each subject [31] [30].
- Bar Charts: Suitable for categorical data (nominal or ordinal) where bars do not touch. For continuous data, use histograms with touching bars [29] [30].
Table 3.1: Selection Guide for Quantitative Data Visualizations
| Data Type | Research Question | Recommended Visualization | Key Considerations |
|---|---|---|---|
| Continuous (e.g., weight, blood levels) | Distribution of values | Histogram | Bars must be touching; area represents frequency [29]. |
| Continuous (multiple groups) | Compare distributions | Frequency Polygon | Plot multiple lines on same axes for comparison [29] [31]. |
| Continuous over Time | Trend analysis | Line Diagram | Time on X-axis; connect data points with straight lines [31]. |
| Two Continuous Variables | Relationship/Correlation | Scatter Diagram | X and Y axes for the two variables; pattern shows correlation [31] [30]. |
| Categorical (e.g., supplement type) | Compare values between categories | Bar Chart | Bars should not touch; space between categories [29] [30]. |
Experimental Protocols for Nutritional Intervention Research
Defining Study Parameters
The OCD systematic review protocol exemplifies rigorous methodology for nutritional intervention research [9]:
- Participant Eligibility: Apply strict inclusion/exclusion criteria. For example: adults ≥18 years with DSM-5 diagnosed OCD; exclude organic OCD causes, schizophrenia, bipolar disorder, or significant comorbid conditions [9].
- Intervention and Comparator Specification:
- Outcome Measurement:
- Primary: Changes in cognitive performance (validated instruments: Stroop Test, Trail-Making Test), quality of life (SF-36, Functional Assessment Short Test), and psychiatric symptoms (depression, anxiety, obsession/compulsion scales) [9].
- Secondary: Presence of comorbidities (e.g., metabolic syndrome) measured using standardized indices (Charlson Comorbidity Index) [9].
- Trial Duration and Follow-up: Minimum 12-week intervention with at least 6-month follow-up to assess sustained effects [9].
Data Collection and Analysis Protocols
- Search Methodology: Comprehensive searches across multiple databases (MEDLINE, Embase, CENTRAL, ClinicalTrials.gov) from inception, without language or date restrictions. Include keywords for nutritional supplements, cognition, quality of life, psychiatric symptoms, and randomized studies [9].
- Study Selection Process: Dual independent screening of titles/abstracts, followed by full-text review. Document reasons for exclusion at full-text stage [9].
- Data Extraction and Synthesis: Independent extraction of study characteristics, methods, outcomes, and results. Calculate association measures with 95% confidence intervals. Analyze potential heterogeneity sources [9].
- Risk of Bias Assessment: Use validated tools (e.g., Cochrane Risk of Bias tool) to evaluate study quality. This is a critical component of NESR's gold-standard methodology [9] [27].
The Scientist's Toolkit: Research Reagent Solutions
Table 5.1: Essential Resources for Nutritional Intervention Research
| Resource Category | Specific Resource | Function and Application |
|---|---|---|
| Protocol Registries | Open Science Framework (OSF) | Publicly register study protocols to enhance transparency, reduce reporting bias, and establish precedence [9] [26]. |
| Reporting Guidelines | PRISMA-P (Preferred Reporting Items for Systematic Reviews and Meta-Analyses Protocols) | Standardized framework for reporting systematic review protocols, ensuring comprehensive methodology documentation [9]. |
| Data Sources | Dietary Supplement Ingredient Database (DSID) | Provides statistically predicted estimates of ingredient levels in dietary supplements, which may differ from labeled amounts; essential for quality control and intervention standardization [28]. |
| Statistical Tools | Dietary Index Analysis (R package) | Streamlines compilation of dietary intake data into index-based patterns, enabling assessment of adherence to dietary patterns in epidemiologic and clinical studies for precision nutrition [28]. |
| Large-Scale Studies | National Health and Nutrition Examination Survey (NHANES) | Provides comprehensive health and nutritional status data for US population; useful for baseline comparisons, power calculations, and epidemiological context [28]. |
| Ethical Framework | 7-Pillar Framework for AI in Nutrition | Domain-specific ethical guidelines for developing AI solutions in nutrition and behavior change, addressing transparency, bias prevention, and explainability [25]. |
| Apremilast-d5 | Apremilast-d5, MF:C22H24N2O7S, MW:465.5 g/mol | Chemical Reagent |
| 1-Linoleoyl Glycerol | 3-Linoleoyl-sn-glycerol|High-Purity Reference Standard |
Implementation Strategies: Designing and Executing Robust Nutritional Trials
Selecting Appropriate Control Groups and Comparators for Dietary Interventions
Within the framework of randomized controlled trial (RCT) protocols for nutritional interventions research, the selection of an appropriate control group is a fundamental methodological decision that directly impacts the validity, interpretability, and ethical integrity of a study. RCTs are considered the gold standard for evaluating the efficacy or safety of an intervention because their design—which involves the random allocation of participants to one or more comparison groups—minimizes selection bias and the influence of known and unknown confounding factors [21]. The control group provides the essential baseline against which the effects of the dietary intervention are measured [32]. Without a well-chosen control, it is impossible to determine whether observed changes are truly due to the intervention itself or to other external variables such as the passage of time, participant expectations, or concurrent changes in lifestyle or environment.
The choice of control group is particularly complex in dietary intervention studies. Unlike pharmaceutical trials, where a placebo pill can often be visually identical to the active drug, creating a truly blinded design for a dietary pattern, whole food, or nutrient-based intervention is frequently challenging, and sometimes impossible. This protocol document provides a detailed framework for selecting, designing, and implementing control groups and comparators for dietary interventions, ensuring that researchers can make informed decisions that strengthen the scientific rigor and practical applicability of their findings.
Theoretical Foundations: Types of Control Groups
The primary function of a control group is to answer the question: "Compared to what?" The optimal control condition depends on the specific research question, the stage of investigation (e.g., efficacy vs. effectiveness), and ethical considerations. The following table summarizes the common types of control groups used in dietary intervention trials, their applications, and key considerations.
Table 1: Types of Control Groups for Dietary Intervention Trials
| Control Type | Description | Best Use Cases | Advantages | Disadvantages & Considerations |
|---|---|---|---|---|
| Placebo Control | Participants receive an inert intervention designed to be indistinguishable from the active intervention. | Testing a specific supplement, fortified food, or dietary component where a believable placebo can be manufactured. | Maximizes blinding; provides a strong measure of the specific physiological effect vs. the placebo effect. | Difficult or unethical to create for whole-diet or food-based interventions; requires validation that blinding was successful. |
| Usual Diet / No Intervention | Participants are asked to continue their habitual dietary intake without any changes. | Pragmatic trials aiming to measure the real-world effect of adding an intervention to typical behavior. | High external validity and practicality; avoids co-intervention. | Lack of blinding leads to high risk of performance and detection bias; cannot isolate placebo effects. |
| Attention Control | Participants receive a similar level of researcher interaction, education, or monitoring on a topic unrelated to the primary intervention. | Trials where the "dose" of attention or the behavioral support package is a key confounding variable. | Controls for the non-specific effects of participant engagement and regular monitoring. | Requires careful design of a credible alternative protocol; can be resource-intensive. |
| Active Comparator / Alternative Diet | Participants are assigned to a different, active dietary pattern for comparison (e.g., Standard American Diet vs. Mediterranean Diet). | Comparing the efficacy of two distinct dietary patterns or to test for non-inferiority. | Provides direct, clinically relevant comparative effectiveness data; can be more ethical if both diets are potentially beneficial. | Does not provide information on efficacy vs. no intervention; may require a larger sample size to detect differences between two active groups. |
| Wait-List Control | Participants in the control group are offered the intervention after a designated delay period, serving as their own control during the initial phase. | Studies where it is ethically permissible to delay a potentially beneficial intervention. | All participants eventually receive the intervention, which can aid recruitment and is often perceived as fair. | Contamination can occur if control participants seek out the intervention early; not suitable for long-term outcomes. |
The following diagram illustrates the decision-making pathway for selecting the most appropriate type of control group based on the research context.
Experimental Protocols for Control Group Implementation
Protocol: Designing and Validating a Placebo for a Nutritional Supplement
Objective: To create an inert substance that is sensorially identical to the active nutritional supplement to ensure participant and personnel blinding.
Materials:
- Active supplement (e.g., omega-3 capsule, probiotic sachet, protein powder).
- Placebo base materials (e.g., microcrystalline cellulose for capsules, maltodextrin for powders, olive oil for oil-based supplements).
- Food-grade colorants and flavorings.
- Encapsulation machine or powder packaging equipment.
- Standardized sensory evaluation forms.
Methodology:
- Formulation: Develop the placebo using the base material. Match the color, size, and shape of capsules/tablets. For powders, match the texture, color, solubility, and taste using inert ingredients and minimal, matched flavorings.
- Pilot Testing: Conduct a blinding validation study with a small panel of healthy volunteers (n=20-30). Present them with both active and placebo products in a randomized order and ask them to identify which is the active product.
- Success Criterion: Blinding is considered successful if the correct identification rate is not statistically different from 50% (chance) using a binomial test (p > 0.05).
- Packaging and Labeling: Package active and placebo products in identical, coded containers. A third party not involved in participant interaction or outcome assessment should hold the randomization code.
Protocol: Implementing an Attention Control Group
Objective: To control for the non-specific effects of participant contact time, education, and monitoring received by the intervention group.
Materials:
- Standardized educational materials on a neutral health topic (e.g., sleep hygiene, foot care, general health screenings).
- Identical session logs and monitoring tools as used in the intervention group.
- Trained personnel to deliver the control protocol.
Methodology:
- Session Structure: Match the number, duration, and format of counseling sessions between the intervention and attention control groups. For example, if the intervention group has eight sessions on Mediterranean diet cooking, the attention control group should have eight sessions on a matched, but neutrally-themed, topic.
- Participant Interaction: Maintain the same frequency of phone calls, text messages, or other forms of follow-up for both groups. The content should differ, but the level of attention and support should be perceived as equivalent by participants.
- Outcome Assessment: Use the same primary and secondary outcome measures for both groups, assessed at identical time points by personnel blinded to group assignment.
Protocol: Ensuring Compliance and Minimizing Contamination
Objective: To monitor and enhance adherence to the assigned diet in both the intervention and control groups, while minimizing cross-over (contamination) between groups.
Materials:
- Food diaries and digital food photography apps.
- Biomarker assay kits (e.g., for specific fatty acids, vitamins, or urinary metabolites).
- Standardized questionnaires to assess self-reported compliance and intake of non-study foods.
- Participant incentive structure.
Methodology:
- Compliance Monitoring:
- Self-Report: Collect detailed 3-day or 7-day food records at baseline, mid-intervention, and end-of-study.
- Biomarkers: Collect and analyze biological samples (blood, urine, adipose tissue) for nutrients or metabolites specific to the intervention (e.g., plasma alpha-linolenic acid for a flaxseed intervention, urinary nitrogen for protein).
- Pill Counts: For supplement studies, weigh returned bottles or count returned pills.
- Minimizing Contamination:
- Education: Clearly explain to participants the importance of adhering only to their assigned group.
- Separate Sessions: Hold group sessions for intervention and control participants at different times to prevent informal sharing of information or strategies.
- Statistical Analysis: Plan to conduct both Intention-To-Treat (ITT) and Per-Protocol (PP) analyses. The ITT analysis includes all randomized participants and preserves the value of randomization, providing an estimate of the "real-world" effectiveness. The PP analysis includes only participants who adhered to the protocol, providing an estimate of the efficacy under ideal conditions.
The Scientist's Toolkit: Research Reagent Solutions
The following table details essential materials and tools required for the rigorous implementation of control groups and compliance monitoring in dietary intervention trials.
Table 2: Essential Research Reagents and Materials for Dietary RCTs
| Item | Function / Application | Specification Notes |
|---|---|---|
| Placebo Base Materials | Creation of inert comparators for supplements and fortified foods. | Microcrystalline cellulose (capsules), maltodextrin (powders), olive/sunflower oil (liquid supplements). Must be devoid of the active compound and generally recognized as safe (GRAS). |
| Blinded Supplement Kits | Packaging for active and placebo supplements to maintain allocation concealment. | Identical in weight, appearance, and packaging. Should use a randomized, unique alphanumeric code generated by a third-party statistician. |
| Biomarker Assay Kits | Objective verification of dietary compliance and biological effect. | Examples: ELISA kits for specific nutrients, HPLC kits for fatty acid profiles, mass spectrometry for metabolomic profiling. Must be validated for the specific matrix (serum, plasma, urine). |
| Digital Dietary Assessment Tools | Tracking habitual intake and adherence to the prescribed diet. | Includes 24-hour dietary recall software, digital food frequency questionnaires, or image-based food logging apps with integrated nutrient analysis databases. |
| Standardized Participant Education Materials | Ensuring consistent delivery of dietary instructions across all participants and study staff. | Should include lesson plans, visual aids, recipe books, and FAQ sheets. Materials for attention control must be equally professional and engaging. |
| Data Management System | Securely housing randomization lists, compliance data, and outcome measures. | REDCap (Research Electronic Data Capture) or similar clinical data management platform that provides audit trails and controlled access to protect blinding. |
| Adipic acid-13C6 | Adipic Acid-13C6|(1,2,3,4,5,6-13C6)hexanedioic acid | Get high-purity Adipic Acid-13C6, the 13C-labeled tracer for metabolic and pharmacokinetic research. This product, (1,2,3,4,5,6-13C6)hexanedioic acid, is for Research Use Only. Not for human or veterinary diagnostic or therapeutic use. |
| Suberic acid-d12 | 1,8-Octanedioic-D12 Acid|Isotopic Labeled Standard | High-purity 1,8-Octanedioic-D12 Acid (Suberic-d12 acid), a deuterated internal standard for metabolic research. For Research Use Only. Not for human or animal use. |
The strategic selection and meticulous implementation of control groups are cornerstones of high-quality dietary intervention research. The choice between a placebo, usual care, attention, or active comparator control must be driven by the specific research hypothesis, the nature of the intervention, and ethical principles. By adhering to the protocols outlined in this document—including blinding validation, compliance monitoring, and the use of objective biomarkers—researchers can significantly strengthen the internal validity of their trials. This rigorous approach ensures that the conclusions drawn about the efficacy and effectiveness of nutritional interventions are reliable, interpretable, and capable of informing evidence-based dietary guidelines and clinical practice.
Randomized controlled trials (RCTs) represent the highest level of evidence in clinical research due to their ability to minimize bias through random allocation of participants to intervention groups [33]. The fundamental principle of randomization ensures that both known and unknown baseline characteristics are balanced across treatment arms, thereby reducing confounding factors and improving the internal validity of the results [33]. In the specific context of nutritional interventions, where participant characteristics and baseline nutritional status can significantly influence outcomes, appropriate randomization strategies are crucial for generating valid, interpretable results.
The importance of randomization is particularly evident in nutritional science, where heterogeneous populations and complex covariate interactions are common. Proper randomization strategies not only address chance imbalances in baseline covariates but also increase the precision of treatment effect estimates [34]. This document provides a comprehensive framework for randomization strategies, with specific application to nutritional intervention trials, addressing both theoretical foundations and practical implementation considerations for researchers, scientists, and drug development professionals.
Fundamental Randomization Techniques
Basic Randomization Methods
Simple Randomization: Similar to flipping a coin, each participant has an equal chance of assignment to any study group. While conceptually straightforward and easy to implement, simple randomization can lead to chance imbalances in sample sizes, particularly in smaller trials common in early-phase nutritional research.
Block Randomization: This method ensures balanced group sizes by randomizing participants in small blocks (e.g., blocks of 4, 6, or 8). For example, in a block of size 4 for two groups (A and B), there would be exactly two As and two Bs in random order. This approach maintains roughly equal group sizes throughout the recruitment period but may introduce predictability if block sizes are not concealed from investigators.
Stratified Randomization: For nutritional trials where certain baseline covariates (e.g., BMI category, diabetes status, age groups) are known to strongly influence outcomes, stratified randomization ensures balance within these important subgroups. Participants are first grouped into strata based on key prognostic factors, then randomized within each stratum using block randomization.
Adaptive Randomization Methods
Covariate-Adaptive Randomization: This technique dynamically adjusts assignment probabilities based on previously recruited participants' characteristics to maintain balance across multiple covariates simultaneously. Minimization is the most common covariate-adaptive method, particularly useful when balancing numerous prognostic factors in complex nutritional studies.
Response-Adaptive Randomization: Less common in nutritional trials, this method adjusts assignment probabilities based on interim outcome data, potentially allocating more participants to the better-performing treatment arm while the trial is ongoing.
Table 1: Comparison of Fundamental Randomization Techniques
| Method | Key Principle | Advantages | Limitations | Best Suited For |
|---|---|---|---|---|
| Simple Randomization | Equal probability for all assignments | Simple implementation; perfect randomness | Risk of imbalance in small samples | Large trials >200 participants |
| Block Randomization | Randomization within fixed-size blocks | Balanced group sizes throughout trial | Potential predictability if block size known | Most nutritional trials |
| Stratified Randomization | Block randomization within predefined strata | Controls for important prognostic factors | Limited to few key strata; complexity increases with more strata | Trials with strong known prognostic factors |
| Covariate-Adaptive | Dynamic adjustment based on accrued covariates | Balances multiple covariates simultaneously | Complex implementation; requires specialized software | Complex nutritional studies with multiple prognostic factors |
Covariate Adjustment in Randomized Trials
The Role of Covariate Adjustment
Despite proper randomization, chance imbalances in baseline covariates can occur, particularly in smaller trials or those with heterogeneous populations [34]. Covariate adjustment accounts for these imbalances in baseline characteristics that are predictive of the outcome (prognostic factors), thereby increasing the precision of treatment effect estimates and improving face validity [34]. In nutritional research, where factors such as baseline nutritional status, age, sex, genetic markers, and metabolic parameters can strongly influence outcomes, appropriate covariate adjustment is essential for accurate effect estimation.
The two primary classes of covariate adjustment methods in randomized trials are outcome regression (analysis of covariance - ANCOVA) and propensity score weighting [34]. In outcome regression, the outcome is regressed on the treatment and covariates, with the treatment effect estimated by the coefficient of the treatment variable [34]. Propensity score weighting, particularly overlap weighting, has emerged as an attractive alternative with conceptual and practical advantages, though the two methods are asymptotically equivalent [34].
Handling Missing Covariate Data
A significant practical challenge in nutritional trials is missing covariate data, which complicates adjustment. Several approaches exist for handling missing covariates:
- Complete-case analysis: Using only participants with fully observed covariates (generally not recommended due to potential bias) [34]
- Missing-indicator method: Including a dummy variable for missingness while setting missing values to a constant [34]
- Imputation methods: Filling in missing values based on observed data (multiple imputation is preferred) [34]
Recent methodological developments show that a modified missing-indicator method, where missing covariates are imputed with zeros and the analysis includes interaction terms between missing indicators and covariates, provides valid estimates regardless of the missing data mechanism [34].
Table 2: Covariate Adjustment Methods with Missing Data
| Method | Approach | Assumptions | Implementation | Considerations for Nutritional Trials |
|---|---|---|---|---|
| Complete-case Analysis | Excludes participants with missing covariates | Missing completely at random (MCAR) | Simple but reduces sample size | Not recommended; may bias results if missingness related to outcomes |
| Missing-indicator Method | Includes missingness indicators in model | Missingness may depend on observed data | Straightforward implementation | Valid for randomized trials; includes interaction terms with treatment |
| Multiple Imputation | Generates multiple complete datasets | Missing at random (MAR) | Requires specialized software | Preferred when missingness mechanism understood |
| Complete-covariate Analysis | Uses only fully observed covariates | MCAR for partially observed covariates | Simple but may omit important prognostic factors | Suboptimal if partially observed covariates are strong predictors |
Special Population Considerations
Challenges in Special Populations
Nutritional interventions often target specific populations with unique characteristics, including elderly individuals, pediatric groups, pregnant women, ethnic minorities, and those with specific metabolic disorders or comorbidities. These special populations present distinct challenges for randomization and analysis, including limited sample sizes, ethical constraints, heterogeneous responses to interventions, and practical recruitment difficulties.
Special populations often exhibit greater variability in baseline characteristics, increased susceptibility to comorbidities, and different adherence patterns to nutritional interventions. These factors must be carefully considered in both randomization strategies and statistical analysis plans to ensure valid and generalizable results.
Stratification and Subgroup Analysis
For special populations, stratified randomization becomes particularly important to ensure balance within demographic or clinical subgroups. Key considerations include:
- Identifying truly prognostic factors versus general demographic variables
- Limiting stratification factors to avoid over-stratification
- Pre-specifying subgroup analyses in the statistical analysis plan
- Accounting for multiple comparisons in subgroup analyses
In nutritional research, common stratification factors for special populations include age categories, disease severity stages, genetic polymorphisms affecting nutrient metabolism, baseline nutritional status, and comorbidities. These factors should be selected based on strong biological rationale and previous evidence of their prognostic value.
Sample Size Considerations
Special populations often present challenges in recruitment, potentially leading to underpowered studies. Sample size planning should account for:
- Expected higher dropout rates in certain populations (e.g., elderly with comorbidities)
- Greater variability in response measures
- Potential need for oversampling to ensure adequate representation of subgroups
- Adaptive designs that allow sample size re-estimation
Realistic timeline planning with contingency for slower recruitment is essential, as premature trial discontinuation due to poor recruitment represents a significant waste of research resources [35].
Experimental Protocols and Implementation
Protocol Development for Nutritional Trials
Comprehensive protocol development is fundamental to successful randomized trials. The study protocol should contain detailed background, objectives, rationale, design, methodology, Institutional Review Board approval processes, informed consent procedures, and statistical considerations [33]. For complex nutritional trials, a procedures manual should supplement the main protocol, containing study definitions, descriptions, and instructions for each procedure and data collection item [33].
The Standard Protocol Items: Recommendations for Interventional Trials (SPIRIT) guidelines provide evidence-based recommendations for minimum protocol content [35]. Adherence to SPIRIT guidelines improves protocol completeness and facilitates thorough critical appraisal of trial methodology. Key elements specific to nutritional trials include:
- Detailed description of intervention and control products
- Nutritional composition analysis documentation
- Compliance assessment methods (e.g., food diaries, biomarkers)
- Contamination prevention strategies
- Standardization procedures for concomitant dietary influences
Randomization Implementation Protocol
Materials and Equipment:
- Secure computer system with randomization software
- Access-controlled database for allocation concealment
- Communication system for treatment assignment notification
- Audit trail documentation system
Step-by-Step Procedure:
- Eligibility Assessment: Verify all inclusion/exclusion criteria documented
- Baseline Data Collection: Record all stratification variables and prognostic factors
- Randomization Initiation: Authorized personnel access the randomization system
- Stratification Application: System applies stratification rules if used
- Treatment Allocation: System generates assignment based on chosen method
- Assignment Communication: Secure notification to appropriate staff
- Documentation: Complete record of randomization process and timing
Quality Control Measures:
- Regular audit of allocation concealment
- Verification of stratification factor balance
- Monitoring of implementation errors
- Documentation of any protocol deviations
Covariate Adjustment Analysis Protocol
Pre-analysis Steps:
- Examine balance in baseline characteristics across groups
- Identify prognostic factors strongly associated with outcome
- Assess missing data patterns for covariates and outcomes
- Select appropriate adjustment method based on missing data mechanism
Analysis Implementation:
- For complete covariates: Implement ANCOVA or propensity score weighting
- For missing covariates: Apply appropriate missing data method
- For missing outcomes: Consider inverse probability weighting
- For both missing covariates and outcomes: Implement combined weighting approaches
Sensitivity Analyses:
- Compare adjusted and unadjusted estimates
- Vary assumptions about missing data mechanisms
- Examine model assumptions and fit
- Assess robustness to different covariate selections
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Methodological Tools for Randomization and Covariate Adjustment
| Tool Category | Specific Solutions | Function | Application Context |
|---|---|---|---|
| Randomization Software | SAS PROC PLAN, R randomizeR, Web-based systems | Implements randomization algorithms | All trial phases; ensures reproducible randomization |
| Stratification Management | Minimization software, Dynamic allocation systems | Maintains balance across multiple factors | Complex nutritional studies with multiple prognostic factors |
| Covariate Adjustment Statistical Packages | R (covaadjust package), SAS PROC GLM, Stata teffects | Implements ANCOVA, propensity score methods | Analysis phase for precision improvement |
| Missing Data Handling Tools | R mice package, SAS PROC MI, Multiple imputation software | Addresses missing covariate and outcome data | When missing data is anticipated or encountered |
| Sample Size Calculation Software | nQuery, PASS, R pwr package | Determines optimal sample size | Trial design phase for adequate power |
| Data Collection Systems | REDCap, Electronic data capture systems | Standardized collection of baseline covariates | Ensures complete covariate information |
| Protocol Development Tools | SPIRIT checklist, Protocol templates | Ensures comprehensive protocol documentation | Protocol development phase |
| 3,4-Dimethoxyphenylacetic acid-d2 | 3,4-Dimethoxyphenylacetic acid-d2, MF:C10H12O4, MW:198.21 g/mol | Chemical Reagent | Bench Chemicals |
| Trimethyl-D9 phosphate | Trimethyl-D9 phosphate, CAS:32176-12-8, MF:C3H9O4P, MW:149.13 g/mol | Chemical Reagent | Bench Chemicals |
Diagram: Randomization Strategy Selection Algorithm
Effective randomization strategies in nutritional intervention research require careful consideration of covariate adjustment methods and special population needs. Based on current methodological evidence and practical experience, the following best practices are recommended:
First, always pre-specify randomization and covariate adjustment strategies in the trial protocol and statistical analysis plan, including detailed handling of missing data. This prevents data-driven decisions that may introduce bias. The SPIRIT guidelines provide a comprehensive framework for protocol development [35] [36].
Second, select randomization methods based on trial size, number of important prognostic factors, and special population considerations. While stratified randomization balances known prognostic factors, it should be limited to few key strata to avoid over-stratification.
Third, implement covariate adjustment for precision gains, regardless of whether significant baseline imbalances exist. Recent methodological developments demonstrate that even simple imputation methods for missing covariates (like the modified missing-indicator method) can provide valid estimates while improving precision [34].
Finally, for special populations, consider adaptive designs or enrichment strategies that address recruitment challenges while maintaining scientific validity. Always account for potential increased variability and specific ethical considerations in these populations.
Proper implementation of these randomization strategies will enhance the validity, precision, and interpretability of nutritional intervention trials, ultimately contributing to higher-quality evidence for nutritional recommendations and policies.
Blinding is a cornerstone methodology in randomized controlled trials (RCTs) to minimize performance and detection bias [37]. In nutrition research, where interventions range from whole foods to dietary supplements, effective blinding presents unique practical challenges not typically encountered in pharmaceutical trials [38] [39]. Empirical evidence demonstrates that lack of blinding can exaggerate treatment effects by 27% to 68% in some cases, highlighting its critical importance for internal validity [37]. This application note synthesizes current evidence and practical strategies for implementing robust blinding methodologies within the context of nutritional intervention trials, addressing both their application and inherent limitations.
Core Concepts and Definitions
Distinguishing Blinding from Allocation Concealment
A fundamental principle in trial methodology is understanding that allocation concealment and blinding serve distinct purposes [37] [40]. Allocation concealment occurs before randomization and prevents foreknowledge of upcoming treatment assignments, thereby defending against selection bias [41] [40]. In contrast, blinding occurs after randomization and involves withholding information about assigned interventions from various parties involved in the trial to prevent performance and detection bias during the trial's conduct and outcome assessment [37]. While allocation concealment is universally recommended and always possible, blinding presents greater feasibility challenges in certain nutrition intervention contexts [40].
Levels of Blinding in Practice
Blinding operates on a continuum, with varying levels applicable to different trial stakeholders [37]. The terminology used describes who remains unaware of treatment assignments.
Table: Levels of Blinding in Clinical Trials
| Blinding Level | Parties Kept Unaware | Common Applications in Nutrition Research |
|---|---|---|
| Single-blind | Participants only OR researchers only | Device trials where participants are unaware, or trials where outcome assessors are blinded but participants are not [40]. |
| Double-blind | Both participants and the researchers/clinicians administering the intervention | Placebo-controlled supplement trials where identical capsules/tablets are feasible [40]. |
| Triple-blind | Participants, researchers, and outcome assessors | Trials requiring centralized assessment of paraclinical or imaging outcomes to prevent assessor bias [42] [39]. |
Beyond these core groups, up to 11 distinct parties may be blinded, including data managers, trial managers, pharmacists, laboratory technicians, outcome adjudicators, statisticians, and manuscript writers [37]. The principle of partial blinding—where blinding some study groups is feasible even when maximal blinding is not—can still tangibly improve trial validity [37].
Practical Blinding Strategies for Nutritional Interventions
Blinding Participants and Intervention Administrators
Pharmaceutical-Based Approaches
For nutritional supplements, standard pharmaceutical blinding techniques are often applicable. These include using identical capsules or tablets containing the active compound versus placebo, centralized preparation of similar-looking bottles and syringes, and flavor-masking for oral liquids to conceal distinctive tastes of active treatments [37]. The double-dummy technique is valuable when comparing interventions with different modes of administration (e.g., tablet vs. drink), where each group receives one active treatment and one placebo designed to mimic the other administration form [37].
Food-Based Intervention Strategies
Blinding becomes particularly challenging when the intervention involves whole foods or food-derived powders with distinctive sensory properties. Innovative approaches include:
- Sham Procedures and Placebo Diets: Developing control foods that mimic the appearance, taste, and texture of the active intervention food without containing the bioactive components of interest [39]. For example, in a blueberry intervention trial, researchers formulated control products without blueberries that resembled the active products in appearance and taste [38].
- Attention-Control Interventions: Providing control groups with an intervention that matches the contact time and procedural involvement of the active group without delivering the specific nutritional component under investigation [39].
- Blinding to Study Hypothesis: In some cases where the intervention cannot be fully concealed, blinding participants to the specific study hypothesis can reduce expectation bias [39].
A specific case study illustrates these challenges: in an NIH-funded trial of freeze-dried blueberry powder on bone health, researchers incorporated the powder into three product forms (a drink, spread, and granola bar) for a self-selected diet [38]. While double-blinding was attempted through coding of products by kitchen staff, the distinctive color and taste of blueberries presented inherent blinding difficulties [38].
Blinding Outcome Assessors and Data Analysts
Centralized Assessment Methods
Blinding of outcome assessors is crucial, particularly for trials with subjective endpoints. Effective strategies include:
- Centralized assessment of paraclinical examinations (e.g., laboratory values, imaging studies) by evaluators unaware of treatment allocation [37] [39].
- Use of video, audio, or photographic records of clinical examinations for later assessment by blinded evaluators [39].
- Adjudication committees for clinical events who review predefined criteria without knowledge of treatment assignment [37].
Empirical evidence from nutrition RCTs suggests that lack of blinding in outcome assessment may lead to exaggerated treatment effects, particularly for subjective outcomes [43].
Statistical Analysis Blinding
Blinding of statisticians presents unique methodological considerations. While guidelines recommend blinding statisticians until after database lock, practical implementation varies [44]. Different working models exist:
- Fully blinded statistician until final analysis specification
- Coded allocation groups where statisticians analyze data without knowing which group received active intervention
- Independent statisticians for interim and final analyses
A qualitative study found that blinding statisticians is considered most important in fully blinded trials (e.g., placebo-controlled), while in open-label trials, the insight from an unblinded statistician is often deemed more valuable than the potential bias risk [44]. Practical constraints often necessitate a risk-proportionate approach rather than universal blinding of statisticians [44].
Experimental Protocol: Implementing Blinding in a Feeding Trial
Protocol for a Double-Blind, Placebo-Controlled Bioactive Supplement Trial
Background and Objectives
This protocol outlines methodology for a 12-week RCT investigating the effects of a plant-derived bioactive compound on cardiometabolic biomarkers in adults with elevated cardiovascular risk. The primary outcome is the change in LDL-cholesterol from baseline to 12 weeks.
Intervention and Control
- Active Intervention: Capsule containing 500mg of standardized plant extract
- Placebo Control: Identical capsule containing microcrystalline cellulose matched for appearance, weight, and taste
- Administration: One capsule daily with breakfast
Blinding Procedures
Manufacturing and Packaging
- Capsules are manufactured and packaged by an independent compounding pharmacy not involved in trial conduct.
- All bottles are identical in appearance, labeled with unique randomization codes according to a computer-generated sequence.
- The randomization list is held securely by the pharmacy and independent data monitoring committee.
Participant and Researcher Blinding
- Participants receive standardized instructions not to break open capsules or discuss sensory characteristics with study staff.
- Clinical staff administering interventions and collecting outcome data have no access to the randomization code.
- Bottles are dispensed by a designated unblinded pharmacist not involved in outcome assessment.
Outcome Assessment Blinding
- Blood samples are processed by laboratory technicians unaware of group assignment.
- Laboratory assays are conducted using automated systems with minimal subjective interpretation.
- Clinical examinations are recorded electronically for potential adjudication by blinded external experts.
Statistical Analysis Blinding
- The lead statistician remains blinded to group allocation until the statistical analysis plan is finalized and database is locked.
- Analysis is conducted using group codes (A/B) rather than actual treatment labels.
- The independent data monitoring committee maintains unblinded status for safety monitoring.
Blinding Maintenance and Success Assessment
- Participants and researchers are questioned about perceived group assignment at trial completion to assess blinding success.
- Any accidental unblinding incidents are documented with rationale and impact assessment.
- Centralized dosage adjustment is performed if needed by the unblinded pharmacist to maintain blinding.
Decision Framework for Blinding Methodology
The following workflow outlines a systematic approach for selecting appropriate blinding strategies based on intervention type and outcome characteristics:
The Researcher's Toolkit: Essential Materials for Blinding
Table: Key Research Reagent Solutions for Blinding Methodologies
| Material/Reagent | Function in Blinding | Application Notes |
|---|---|---|
| Microcrystalline Cellulose | Placebo filler for capsules and tablets | Inert, tasteless, and compatible with most encapsulation processes; allows matching of weight and appearance [37]. |
| Food-Grade Colorants & Flavors | Sensory matching of active and control foods | Must be inert and not interfere with the intervention; requires stability testing throughout the trial duration [38]. |
| Double-Dummy Placebos | Enables blinding when comparing different administration forms | Requires manufacturing two placebos; increases complexity but enables valid comparisons [37]. |
| Coded Blinding Kits | Maintains allocation concealment during dispensing | Sequential numbering with tamper-evident seals; often managed by independent pharmacy [40]. |
| Active Placebo | Mimics side effects of active treatment | Contains inert substance plus agents that reproduce expected side effects; reduces unblinding from perceived effects [37]. |
| Triethyl-D15-phosphate | Triethyl-D15-phosphate, CAS:135942-11-9, MF:C6H15O4P, MW:197.25 g/mol | Chemical Reagent |
| 4-Chlorobenzen-2,3,5,6-d4-amine | 4-Chlorobenzen-2,3,5,6-d4-amine, CAS:191656-33-4, MF:C6H6ClN, MW:131.59 g/mol | Chemical Reagent |
Limitations and Barriers to Effective Blinding
Intervention-Specific Challenges
Nutritional interventions present distinctive blinding obstacles that differ from pharmaceutical trials. Whole foods and complex dietary patterns often cannot be fully blinded due to distinctive sensory properties (e.g., color, taste, texture) [38]. In such cases, complete blinding may be impossible, necessitating alternative methodological approaches. Dietary supplements with strong flavors or colors (e.g., turmeric, spirulina) present similar challenges even in encapsulated forms if the capsules are opened or have distinctive odors [38]. Additionally, background nutritional status of participants, such as deficiency or sufficiency in specific nutrients, may influence both treatment response and potential for unblinding through perceived effects [38].
Practical and Ethical Constraints
Practical implementation barriers include the high cost and expertise required for developing adequate placebos for complex nutritional interventions, particularly whole foods [39]. For some bioactive compounds, creating truly inert placebos that do not interact with biological systems is challenging, especially when the compounds are ubiquitous in foods [38]. Ethical considerations emerge when testing essential nutrients in deficient populations, where placebo control may raise concerns, necessitating active control or other modified designs [41].
Empirical Evidence from Nutrition Research
A recent meta-epidemiological study of nutrition RCTs found that while most methodological characteristics did not consistently exaggerate intervention effect estimates, lack of blinding in outcome assessment was associated with exaggerated effect estimates (RRR 0.81, 95% CI 0.70 to 0.94), particularly for subjective outcomes [43]. This underscores the critical importance of blinding outcome assessors even when participant blinding presents challenges.
Effective blinding methodologies are essential for generating valid evidence in nutrition research, yet they present distinct challenges that require innovative solutions. While complete blinding is not always feasible, particularly for whole-food interventions, partial blinding strategies and focus on blinding outcome assessors can significantly reduce bias risk. The methodological approaches outlined in this application note provide a framework for designing nutrition RCTs that maximize internal validity while acknowledging the practical constraints inherent to dietary interventions. As the field evolves, continued development and validation of blinding techniques specific to nutritional sciences will strengthen the evidence base for dietary recommendations and policies.
Digital Health Tools and Mobile Applications in Modern Nutritional RCTs
Application Notes: Current Evidence and Efficacy
Digital health tools are revolutionizing the delivery and monitoring of nutritional interventions within randomized controlled trials (RCTs), enabling more personalized and scalable research methodologies. The following table summarizes key quantitative findings from recent systematic reviews and meta-analyses in this domain.
Table 1: Impact of Digital Health Technology-Based Nutritional Interventions on Key Outcomes
| Population | Number of Studies & Participants | Key Outcome Measures Showing Significant Improvement | Intervention Formats | Sources |
|---|---|---|---|---|
| Hemodialysis Patients | 23 studies (n=2,762) [45] | Modified Quantitative Subjective Global Assessment (MQSGA), hemoglobin, albumin, prealbumin, phosphorus, potassium, BMI, mid-arm muscle circumference, triceps skinfold thickness, body weight (%) [45] | Applications, mobile platforms [45] | |
| People with Cancer | 13 interventions (n=783) [46] | Body weight/composition, dietary compliance, nutritional status, quality of life [46] | Commercial or cancer-specific mobile apps [46] |
The evidence indicates that digital nutritional interventions are effective across diverse clinical populations. A major systematic review and meta-analysis focusing on hemodialysis patients demonstrated that digital health technology (DHT)-based interventions improved 13 different nutritional and biochemical parameters, addressing the critical challenge of malnutrition in this group [45]. Similarly, for populations with cancer, mobile app interventions have shown significant improvements in body composition, dietary compliance, and overall quality of life, though the evidence for long-term efficacy remains an area for further research [46].
These tools extend beyond simple tracking. Modern nutrition apps incorporate features for personalized dietary planning, nutrient analysis, behavioral and motivational support (e.g., through gamification), integration with wearables, and support for special diets and conditions [47]. This functionality allows researchers to implement complex, adaptive nutritional interventions directly in participants' daily lives.
Experimental Protocols for RCT Implementation
Integrating digital health tools into nutritional RCTs requires meticulous planning across all trial phases. The protocol below outlines a comprehensive methodology.
Pre-Trial Planning and Tool Selection
- Define a Clear Hypothesis and Outcomes: Formulate a single, simple, and clear primary hypothesis, accompanied by a limited number of secondary ones [33]. Select clinically relevant, patient-centered outcome measures (e.g., MQSGA, biomarkers, quality of life) that can be practically verified through the digital tool [45] [33].
- Develop a Detailed Study Protocol and Manual of Operations: The protocol must detail the background, objective, rationale, design, methodology, and statistical considerations [33]. A companion manual of operations is crucial for complex RCTs, containing detailed definitions, descriptions, and instructions for every procedure and data point [33].
- Select and Configure the Digital Tool: Choose a digital application or platform that aligns with the intervention's goals (e.g., food logging, personalized feedback, educational content) [45] [47]. Ensure the tool can seamlessly integrate with other devices (e.g., wearables, smart scales) via APIs and has robust data security and privacy measures, complying with regulations like HIPAA [47].
- Determine Sample Size and Recruitment Strategy: Conduct a power analysis to determine a sufficient sample size, factoring in potential challenges like under-recruitment and loss to follow-up [33]. Establish selection criteria that balance the need for a standardized patient group with the generalizability of the results to a broader population [33].
RCT Execution and Monitoring
- Randomization and Blinding: Implement a robust random allocation method to assign participants to intervention and control groups. While full blinding may not always be feasible, outcome evaluation should, at a minimum, be performed by assessors blinded to group allocation [33].
- Intervention Delivery:
- Intervention Group: Receives access to the digital health tool (e.g., a mobile app). The intervention may include features such as:
- Control Group: Typically receives standard care, an alternative intervention, or a low-intensity version of the digital support (e.g., static educational materials) without active monitoring or personalization [10].
- Data Collection:
- Primary Outcome: e.g., change in sports nutrition knowledge score, MQSGA score, or body weight [45] [10].
- Secondary Outcomes: e.g., anthropometric measures (BMI, mid-arm muscle circumference), biochemical parameters (albumin, hemoglobin), dietary intake, and quality of life [45] [10] [46].
- Process Data: Collect data on user engagement with the app (e.g., log-in frequency, feature usage) [46].
- Follow-up Schedule: Schedule follow-up assessments at predetermined intervals (e.g., 4, 8, and 16 weeks) to evaluate short-term and sustained effects of the intervention [10].
Diagram 1: Nutritional RCT Digital Tool Workflow
Data Analysis and Reporting
- Check Randomization and Balance: Use descriptive statistics to compare baseline characteristics of the treatment and control groups, ensuring the randomization process was successful. Avoid hypothesis testing for baseline comparisons, as any differences are, by definition, random if the randomization was not flawed [48].
- Choose the Appropriate Analysis Method: Select statistical models (e.g., linear regression for continuous outcomes, logistic regression for binary outcomes) based on the type of outcome variable. Account for any clustering, stratification, or repeated measures in the data [48].
- Integrate Quantitative and Qualitative Data: To generate deeper insights, use integration techniques such as joint displays. These tables or figures can juxtapose quantitative outcomes with qualitative interview data to explore reasons for variation in treatment response, adherence, and outcomes [49]. This can help explain how the intervention works and for whom.
- Report Results and Assess Robustness: Report effect sizes, confidence intervals, and p-values clearly. Conduct sensitivity analyses to assess the robustness of the findings and discuss potential sources of bias, such as attrition or measurement error [48].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Digital and Methodological "Reagents" for Nutritional RCTs
| Item / Solution | Function / Rationale | Example Use-Case / Note |
|---|---|---|
| Mobile Application Platform | Core delivery mechanism for the nutritional intervention; enables logging, feedback, and personalization. | Can be a commercial app (e.g., MyFitnessPal, Yazio) or a custom-built, study-specific application [46] [47]. |
| Application Programming Interfaces (APIs) | Enable seamless integration with wearables, electronic health records (EHRs), and other digital health tools for automated data collection. | Critical for creating a layered tech stack and ensuring data accuracy from devices like smart scales and fitness trackers [47]. |
| Validated Nutritional Assessment Tool | Provides a standardized, reliable measure of nutritional status as a primary or secondary endpoint. | Tools like the Modified Quantitative Subjective Global Assessment (MQSGA) have been validated in digital intervention studies [45]. |
| Behavioral Change Theory Framework | Informs the design of app features (e.g., prompts, rewards) to enhance user engagement and long-term adherence. | Found in apps like Noom, which combines coaching with behavioral science [47]. |
| Mixed Methods Research Framework | Provides a structured approach for integrating quantitative trial data with qualitative process data. | Generates insights into intervention mechanisms, user experience, and outcome variation [49]. |
| 3-Bromopropan-1-ol-d6 | 3-Bromopropan-1-ol-d6, CAS:284474-43-7, MF:C3H7BrO, MW:145.03 g/mol | Chemical Reagent |
| Glucosamine-15N hydrochloride | Glucosamine-15N hydrochloride, CAS:42927-60-6, MF:C6H14ClNO5, MW:216.623 | Chemical Reagent |
Data Integration and Analysis Pathway
A major advantage of using digital tools is the rich, mixed-methods dataset they can generate. The following diagram outlines a pathway for integrating these diverse data types to derive comprehensive conclusions.
Diagram 2: Mixed-Methods Data Integration Pathway
Within the framework of randomized controlled trial (RCT) protocols for nutritional interventions research, the selection and implementation of rigorous data collection methodologies are paramount. The accurate assessment of dietary intake serves as a cornerstone for generating reliable and valid research outcomes, directly influencing the interpretation of an intervention's efficacy [50]. This field primarily utilizes two complementary approaches: highly precise controlled feeding studies and more ecologically valid free-living assessments. Controlled feeding studies, often conducted in metabolic research units, provide the highest level of internal validity by ensuring complete control over the nutrient composition and quantity of food consumed. In contrast, free-living assessments, which employ tools like 24-hour dietary recalls and food records, capture habitual intake in real-world settings, thereby offering greater external validity. This document outlines detailed application notes and experimental protocols for both methodologies, providing researchers, scientists, and drug development professionals with a structured guide for their nutritional RCTs.
The choice between controlled feeding and free-living assessment methods involves a fundamental trade-off between precision and practicality. The following table summarizes the core characteristics, advantages, and limitations of each approach, guiding researchers in selecting the most appropriate method for their specific research objectives.
Table 1: Key Characteristics of Controlled Feeding vs. Free-Living Assessment Methods
| Characteristic | Controlled Feeding Studies | Free-Living Assessments |
|---|---|---|
| Primary Objective | To determine the precise metabolic effects of a diet with known composition; to validate dietary assessment tools. | To estimate habitual dietary intake in a natural environment. |
| Internal Validity | Very High. Eliminates self-reporting bias and ensures dietary adherence. | Variable. Subject to memory bias, measurement error, and misreporting. |
| External Validity | Lower. Artificial setting may not reflect real-world eating behaviors. | Higher. Reflects intake in a participant's normal environment. |
| Data Collection Context | Fully controlled research setting (e.g., clinical research unit) [50]. | Participant's home or community. |
| Common Tools | Provision of pre-weighed, compositionally defined meals. | Automated web-based 24-hour recalls (e.g., R24W), food diaries, food frequency questionnaires (FFQs) [50]. |
| Major Source of Error | Reactivity bias (participants may change behavior because they are being observed) [50]. | Memory bias (forgetting items), portion size estimation error, and social desirability bias [50]. |
| Cost & Resources | Very high (food preparation, facility costs, high participant burden). | Relatively low to moderate, especially for automated systems. |
| Ideal Application | Phase I/II trials, mechanistic studies, validation of free-living tools. | Large-scale cohort studies, Phase III/IV trials, long-term effectiveness studies. |
Experimental Protocol for Controlled Feeding Studies
Controlled feeding studies represent the gold standard for measuring dietary intake without the bias of self-reporting. The following protocol details the methodology for conducting such a study, which can serve either as a primary intervention or as a validation ground for other dietary assessment tools.
Application Notes
This protocol is designed to test the specific metabolic effects of a dietary intervention with maximal internal validity. By providing all food and beverages to participants, researchers can be confident that the nutrient intake is known and adhered to, thereby isolating the effects of the nutritional intervention itself. This design is also critical for the validation of self-reported dietary assessment tools, as the "true" intake is known and can be compared against participant-reported data [50].
Detailed Methodology
Objective: To administer a tightly controlled dietary intervention and measure subsequent physiological outcomes, or to validate a self-reported dietary assessment tool against known intake.
Participant Selection and Inclusion Criteria:
- Population: Recruit non-smoking men and women aged between 18 and 75 years.
- Health Status: Participants must have stable weight and be free from cardiovascular, endocrine, or other metabolic diseases that could interfere with the study outcomes. They must have no known food allergies or aversions to the food items used in the protocol.
- Ethical Considerations: The study must receive approval from an Institutional Review Board (IRB) or Ethics Committee. All participants must provide written informed consent prior to enrollment. For validation components, consent must explicitly cover the use of dietary recall tools [50].
Dietary Intervention Protocol:
- Menu Design: Develop a cyclic menu (e.g., 7-day cycle) based on the research objectives, using typical food items relevant to the study population.
- Individualization: Calculate individual energy requirements using established equations (e.g., Mifflin-St Jeor) and adjust portion sizes to ensure energy balance and stable body weight throughout the study. All other nutrient compositions remain constant across the experimental conditions.
- Food Provision: Provide all meals and snacks to participants. Meals should be prepared in a dedicated metabolic kitchen, with each food item precisely weighed.
- Consumption Monitoring: Instruct participants to consume all and only the food items provided. Monitor body weight regularly (e.g., twice weekly) and adjust energy provision in increments of 250 kcal/day if a participant gains or loses more than a pre-specified amount (e.g., >1 kg) to maintain isoenergetic conditions [50].
Data Collection and Outcome Measures:
- Actual Intake Data: Record the precise weight and composition of all food items provided to each participant.
- Physiological Biomarkers: Collect biospecimens (blood, urine) for analysis of relevant biomarkers (e.g., lipids, glucose, hormones, nutrients).
- Anthropometrics: Measure body weight, height, and other relevant metrics (waist circumference, body composition) at baseline and regularly throughout the intervention.
- Validation-Specific Data: If validating a tool like the R24W, participants complete the recall for the previous day's intake. The tool-reported items and portion sizes are then compared to the actual known intake [50].
Experimental Protocol for Free-Living Assessments
For large-scale trials or studies prioritizing ecological validity, free-living assessment methods are essential. This protocol focuses on the use of automated, web-based 24-hour dietary recalls (24HR), which are becoming the tool of choice over traditional food frequency questionnaires due to their superior precision and reduced bias [50].
Application Notes
The R24W is an example of a French-language, web-based, self-administered, and fully automated 24-hour recall [50]. Such tools are cost-effective, convenient, and reduce several biases associated with traditional methods. Because recalls are completed on unannounced, random days, they limit reactivity bias. As self-administered tools, they reduce social desirability bias compared to interviewer-administered recalls. The inclusion of memory cues and portion size images further mitigates memory and estimation errors [50].
Detailed Methodology
Objective: To accurately assess the dietary intake of participants in their free-living environment over a series of non-consecutive days.
Tool Setup and Administration:
- Platform: Utilize a web-based application (e.g., R24W) that is accessible via computer or mobile device.
- Database: Ensure the tool's food database is comprehensive and linked to an appropriate nutrient composition database (e.g., the Canadian Nutrient File or USDA Database) [50].
- Recall Scheduling: Program the application to send automated prompts (e.g., via email) to participants on randomly selected days, including a proportion of weekdays and weekend days to capture habitual intake variation.
- Meal-Based Approach: The recall should guide the participant through the previous day in a chronological, meal-based sequence, allowing for an unlimited number of eating occasions.
Data Collection Workflow: The participant journey through an automated 24-hour recall can be visualized as a sequential process designed to maximize accuracy and completeness.
Diagram 1: Automated 24HR Workflow
Key Features to Minimize Bias:
- Memory Cues: The tool should ask about the context of meals (e.g., time, location, with whom) to help trigger memory [50].
- Systematic Review: The application should include a step that systematically prompts the participant about commonly forgotten food items (e.g., condiments, sugary drinks, snacks) [50].
- Portion Size Estimation: Use of up to eight images of predetermined portion sizes in a neutral setup, with options to select fractions or multiples of the displayed portion. This method can improve estimation accuracy by up to 60% [50].
Quantitative Data and Validation
Validation is a critical step before deploying any new dietary assessment tool in a cohort study. Controlled feeding studies provide the ideal setting for this validation, allowing for direct comparison between reported and actual intake.
Performance Metrics from a Validation Study
The following table summarizes quantitative results from a validation study of the R24W tool conducted within a controlled feeding context, demonstrating its performance against known intake [50].
Table 2: Validation Metrics for the R24W Web-Based 24-Hour Recall Tool
| Validation Metric | Performance Result | Context and Details |
|---|---|---|
| Item Reporting Accuracy | 89.3% of received items were reported. | Participants received an average of 16 food items per day. The most frequently omitted categories were vegetables in recipes (40%) and side vegetables (20%). |
| Portion Size Correlation | Strong correlation (r = 0.80, P < 0.001). | Correlation between offered and self-reported portion sizes for all items. |
| Portion Size Agreement | Strong agreement (Kappa score = 0.62). | Statistical measure of agreement between offered and reported portions beyond chance. |
| Overall Portion Bias | Average overestimation of 3.2 g per item. | Non-significant trend across all food items. |
| Large Portions (≥100 g) | Underestimated by 2.4% on average. | Correlation: r = 0.68; Agreement: Kappa = 0.50. |
| Small Portions (<100 g) | Overestimated by 17.1% on average. | Correlation: r = 0.46; Agreement: Kappa = 0.43. |
| Energy Intake Bias | Non-significant underestimation of -13.9 kcal (±646.3 kcal). | No systematic bias in total energy intake reporting was detected (P = 0.83). |
The Researcher's Toolkit: Essential Reagents and Materials
Successful implementation of the protocols above requires a set of standardized tools and resources. The following table details key research reagent solutions for dietary assessment research.
Table 3: Essential Research Reagents and Materials for Dietary Intake Assessment
| Item / Solution | Function / Application Notes |
|---|---|
| Metabolic Kitchen | A dedicated facility for the precise preparation, weighing, and portioning of all meals and snacks provided in a controlled feeding study. Essential for ensuring dietary protocol adherence. |
| Web-Based 24HR Platform (e.g., R24W) | A self-administered, automated software platform for collecting dietary data in free-living individuals. It reduces interviewer burden, automates coding, and incorporates memory aids and portion size images [50]. |
| Standardized Food Composition Database | A comprehensive nutrient database (e.g., Canadian Nutrient File, USDA FoodData Central) linked to the 24HR platform. It is used to convert reported food consumption into estimated nutrient intakes [50]. |
| Portion Size Image Atlas | A standardized set of food photographs depicting multiple portion sizes. Shown to participants during a 24HR to improve the accuracy of portion size estimation, potentially reducing error by up to 60% [50]. |
| Biospecimen Collection Kits | Standardized kits for the collection, processing, and storage of biological samples (e.g., blood, urine) used to measure objective biomarkers of nutritional status or compliance. |
| Energy Requirement Prediction Equations | Equations (e.g., Mifflin-St Jeor) used at the study outset to estimate participants' daily energy needs for the purpose of individualizing diets in controlled feeding studies or interpreting energy intake data from free-living assessments [50]. |
| Pentanedioic-d6 acid | Pentanedioic-d6 acid, MF:C5H8O4, MW:138.15 g/mol |
Integrated Workflow for Protocol Selection
Choosing and implementing the correct dietary assessment method is a strategic decision. The following diagram outlines a logical decision pathway to guide researchers through the selection process based on their primary research goal, available resources, and required level of precision.
Diagram 2: Dietary Assessment Selection Pathway
Overcoming Methodological Challenges in Dietary Clinical Trials
Within the framework of randomized controlled trial (RCT) protocols for nutritional interventions, participant adherence (the degree to which participants follow the prescribed intervention) and attrition (the loss of participants before study completion) present formidable challenges to scientific validity and statistical power [51] [52]. High attrition rates and poor adherence can compromise the integrity of trial findings, leading to Type II errors (false negatives) and reducing the generalizability of results [51]. In lifestyle interventions, which include dietary components, attrition rates of 25-50% are common, with adherence rates averaging around 66% [53]. This document outlines detailed application notes and experimental protocols designed to address these critical issues, with a specific focus on nutritional intervention research.
Theoretical Foundations and Quantitative Evidence
Understanding the factors that influence adherence and attrition is the first step in mitigating them. Evidence indicates that interventions designed to accommodate participants' schedules and initial fitness levels can improve retention. For instance, intermittent exercise protocols (multiple short bouts) have been shown to yield comparable adherence and attrition rates to sustained protocols (single long bouts), offering a flexible alternative that may reduce perceived barriers [53]. The following table synthesizes key evidence from comparative intervention studies.
Table 1: Summary of Evidence on Adherence and Attrition in Behavioral Interventions
| Study/Context | Participant Profile | Intervention Comparison | Key Findings on Adherence/Attrition |
|---|---|---|---|
| Sustained vs. Intermittent Exercise Review [53] | 783 adults (76% female); mean age 42.3 ± 6.6 years | Sustained (e.g., 1x20+ min/day) vs. Intermittent (e.g., 3x10 min/day) aerobic exercise | No consistent differences in attrition or adherence were found between protocol types. Highlights the universality of adherence challenges. |
| IDEA-P Trial (Prostate Cancer on ADT) [54] | Men with prostate cancer undergoing androgen deprivation therapy | Group-Mediated Cognitive Behavioral (GMCB) lifestyle intervention vs. Standard Care | Previous similar trials cited high attrition (32-44%). Proposed GMCB approach aims to provide self-regulatory skills to improve adherence and maintenance. |
| BOT & JITAI for Dietary Lapses [55] | Adults with overweight/obesity and CVD risk factors | Behavioral Obesity Treatment (BOT) + Just-in-Time Adaptive Intervention (JITAI) | Dietary lapses occur 3-4 times/week and stymie weight loss. JITAI proactively delivers support in moments of high lapse risk to improve adherence. |
A critical analysis of the evidence reveals that a one-size-fits-all approach is insufficient. Successful strategies are often multifactorial, addressing behavioral, psychological, and contextual barriers. The relationship between these core concepts and the strategies to address them can be visualized as a strategic framework.
Detailed Experimental Protocols
This section provides granular methodological details for implementing two promising strategies to combat attrition and poor adherence.
Protocol 1: Group-Mediated Cognitive Behavioral (GMCB) Intervention
This protocol is based on the Individualized Diet and Exercise Adherence Pilot Trial (IDEA-P), which targeted men with prostate cancer undergoing androgen deprivation therapy [54]. Its principles are highly applicable to nutritional RCTs.
- Objective: To examine the feasibility and preliminary efficacy of a GMCB lifestyle intervention, designed to promote independent self-management of exercise and dietary behavior, compared to standard care.
- Study Design: Two-arm, single-blind, randomized controlled pilot trial.
- Participants:
- Sample Size: 40 participants.
- Inclusion Criteria:
- Histologically confirmed prostate cancer.
- Currently undergoing ADT with a planned course of ≥3 months.
- Sedentary lifestyle (<60 min of structured exercise/week).
- Free of serious medical conditions precluding safe exercise.
- Physician consent and willingness to be randomized.
- Randomization & Blinding:
- Computer-generated 1:1 allocation sequence concealed in opaque envelopes.
- Outcome assessors are blinded to group assignment.
- Intervention Arm (GMCB):
- Structure: Initial supervised, center-based sessions incorporating resistance and aerobic exercise, coupled with dietary counseling.
- Core Behavioral Component: Integrates self-regulatory skills counseling (e.g., goal setting, self-monitoring, problem-solving) to foster independence. The group dynamic is used to model and reinforce skills, with a phased reduction in supervision to promote self-management.
- Control Arm (Standard Care):
- Receives usual medical care and general disease management education without the structured behavioral component.
- Outcome Assessments:
- Timing: Baseline, 2-month, and 3-month follow-ups.
- Key Metrics:
- Objectively Assessed Physical Function: 400-meter walk, stair climb, lift-and-carry task [54].
- Self-Reported Function: Abbreviated Late-Life Function and Disability Inventory.
- Body Composition: Measured via DEXA or similar.
- Muscular Strength: e.g., 1-repetition maximum.
- Quality of Life: Validated questionnaires (e.g., EORTC QLQ-C30).
- Adherence Measures: Self-reported exercise/physical activity logs, dietary recalls, and objective measures (e.g., accelerometry) where feasible.
Protocol 2: Just-in-Time Adaptive Intervention (JITAI) for Dietary Lapses
This protocol is adapted from an MRT designed to optimize a JITAI for preventing dietary lapses during behavioral obesity treatment [55].
- Objective: To optimize a smartphone-based JITAI that uses ecological momentary assessment (EMA) and a machine learning algorithm to deliver theory-driven interventions at moments of high dietary lapse risk.
- Study Design: Microrandomized trial (MRT) embedded within a 6-month behavioral obesity treatment (BOT) program.
- Participants:
- Sample Size: 159 adults with overweight or obesity and at least one cardiovascular disease risk factor.
- Intervention Workflow:
- Risk Assessment: Participants receive 6 EMA prompts per day via smartphone. Surveys assess behavioral, psychological, and environmental triggers for dietary lapse (e.g., location, mood, cravings).
- Algorithmic Risk Calculation: A machine learning algorithm analyzes EMA responses in real-time to calculate a lapse risk score.
- Microrandomization: Each time a participant is identified as high-risk, they are randomly assigned to one of six conditions:
- No Intervention
- Generic Risk Alert
- One of Four Theory-Driven Interventions:
- Enhanced Education: Information on dietary goals.
- Building Self-Efficacy: Skills to build confidence in resisting temptation.
- Fostering Motivation: Messages to enhance intrinsic motivation.
- Improving Self-Regulation: Strategies like cognitive restructuring.
- Primary Proximal Outcome:
- Occurrence of a dietary lapse, reported via EMA, in the 2.5 hours following randomization.
- Data Analysis & JITAI Optimization:
- The massive number of randomization events per participant provides data to determine which intervention is most effective for which context (e.g., time of day, location).
- Results inform an optimized decision-making algorithm for a future RCT where the JITAI is evaluated for its effect on distal outcomes like weight loss.
The workflow for this sophisticated protocol is complex and involves multiple, real-time decision points, as illustrated below.
The Scientist's Toolkit: Reagents and Materials
The following table details key resources and methodologies essential for implementing the adherence and attrition strategies discussed in this protocol.
Table 2: Essential Research Reagent Solutions for Adherence and Attrition Research
| Item Name | Function/Application | Specific Examples/Context |
|---|---|---|
| Ecological Momentary Assessment (EMA) | A data collection method that repeatedly samples participants' behaviors and experiences in real-time and in their natural environment. | Used in the JITAI protocol to assess lapse triggers (e.g., mood, location, cravings) multiple times per day via smartphone [55]. |
| Microrandomized Trial (MRT) Design | An experimental design for optimizing adaptive interventions where participants are randomized dozens or hundreds of times throughout the study. | Used to test the momentary effect of different JITAI intervention options on the immediate outcome of a dietary lapse [55]. |
| Group-Mediated Cognitive Behavioral (GMCB) Framework | A counseling framework that uses group dynamics to teach self-regulatory skills, with the goal of fostering independent maintenance of behavior change. | Core component of the IDEA-P trial, designed to improve long-term adherence to diet and exercise prescriptions [54]. |
| Validated Functional Batteries | A set of objective performance tests used to quantify physical function and frailty, which are key secondary outcomes in lifestyle interventions. | The IDEA-P protocol uses a 400-meter walk, a timed stair climb, and a lift-and-carry task [54]. |
| Machine Learning Algorithm for Risk Prediction | A computational model that processes real-time data (e.g., from EMA) to predict the probability of an imminent event (e.g., dietary lapse). | The core "brain" of the JITAI that determines when a participant is at high enough risk to trigger an intervention [55]. |
| Blinded Outcome Assessment Protocol | A standardized procedure where researchers collecting primary outcome data are unaware of the participants' group assignment to reduce bias. | A critical feature of high-quality RCTs like the IDEA-P trial, ensuring the integrity of physical function and QoL measurements [54]. |
Managing Nutrient Collinearity and Multi-Target Effects of Interventions
Well-conducted Randomized Controlled Trials (RCTs) represent the gold standard for establishing causal evidence in clinical research [52]. However, dietary clinical trials (DCTs) present unique methodological challenges that distinguish them from conventional pharmaceutical trials. Unlike pharmaceutical interventions that typically investigate isolated chemical compounds with specific molecular targets, nutrition interventions involve complex mixtures of nutrients and bioactive components that exhibit multi-target effects and high collinearity between dietary components [56]. This complexity is further compounded by diverse food matrices, varied food processing methods, and diverse dietary behaviors and cultural practices across populations [56]. Understanding and managing these challenges is essential for designing robust RCT protocols that can generate reliable, translatable evidence in nutritional research.
Core Methodological Challenges in Nutritional RCTs
Nutrient Collinearity: Interdependence in Dietary Exposure
Nutrient collinearity refers to the statistical interdependence between different nutrients within foods and dietary patterns. This phenomenon creates significant challenges for isolating the specific effects of individual nutrients or food components.
Key manifestations of collinearity include:
- Synergistic or antagonistic relationships between nutrients that obscure individual effects
- High correlation between dietary components in habitual diets
- Food matrix effects where the chemical and physical structure of food modifies nutrient bioavailability
- Background dietary patterns that confound specific intervention effects [56]
Multi-Target Effects: Systemic Nature of Nutritional Interventions
Nutritional interventions typically exert effects through multiple simultaneous biological pathways rather than discrete molecular targets, creating challenges in attribution of causality.
Characteristics of multi-target effects include:
- Pleiotropic actions of individual nutrients across multiple physiological systems
- Simultaneous modulation of metabolic, inflammatory, and microbial pathways
- Systemic downstream effects that emerge from primary interventions
- Ubiquitous nature of nutrition interventions throughout the body [56]
Methodological Framework and Solutions
Statistical Approaches to Manage Collinearity
Table 1: Statistical Methods for Addressing Nutrient Collinearity
| Method | Application | Limitations |
|---|---|---|
| Principal Component Analysis | Identifies patterns of intercorrelated nutrients to create composite dietary exposure scores | Results may be population-specific and difficult to translate to interventions |
| Reduced Rank Regression | Derives dietary patterns that explain variation in response biomarkers | Requires valid nutritional biomarkers |
| Residual Method | Creates adjusted nutrient variables to assess effects independent of energy intake | May not fully eliminate confounding from overall diet pattern |
| Stratified Analysis | Examins nutrient effects within strata of other dietary components | Reduces statistical power and increases complexity |
| Nutrient Density Models | Evaluates nutrients proportionally within total energy context | May not reflect biological reality of nutrient interactions |
Study Design Strategies for Multi-Target Effects
Table 2: RCT Designs for Complex Nutrition Interventions
| Design Approach | Key Features | Suitable For |
|---|---|---|
| Factorial Designs | Tests multiple intervention components simultaneously; can evaluate interactions | Isolating effects of individual nutrients within complex mixtures |
| Crossover Designs | Participants receive multiple interventions in sequence with washout periods | Acute metabolic studies with transient effects |
| Cluster Randomization | Randomizes groups rather than individuals | Community-based interventions where individual randomization is contaminated |
| N-of-1 Trials | Intensive repeated measures within individuals | Personalizing nutrition approaches; understanding individual variability |
| Multiphase Optimization Strategy (MOST) | Systematic approach to optimizing multicomponent interventions | Developing effective behavioral nutrition interventions with multiple components |
Detailed Experimental Protocols
Protocol for Isolating Nutrient Effects in Collinear Systems
Title: Controlled Feeding Study with Systematic Nutrient Variation
Objective: To isolate specific nutrient effects while controlling for collinear nutrients through dietary control.
Methodology:
- Domiciled Feeding Control: Participants receive all meals from a metabolic kitchen for precise dietary control [57]
- Background Diet Standardization: Implement a standardized base diet with known composition
- Nutrient Titration: Systematically vary the target nutrient while holding collinear nutrients constant using mathematical diet optimization
- Washout Periods: Include adequate washout between phases with monitoring of nutrient status biomarkers
- Blinding Procedures: Implement appropriate blinding using placebos or matched formulations where feasible
Key Measurements:
- Primary Outcomes: Specific metabolic or functional endpoints relevant to the nutrient
- Compliance Biomarkers: Biochemical verification of nutrient exposure and adherence
- Collinearity Monitoring: Regular assessment of non-target nutrients to confirm isolation of intervention
- Nutrient Status Assessment: Baseline and endpoint status of target and collinear nutrients [56]
Protocol for Evaluating Multi-Target Effects
Title: Multi-Omic Assessment of Systemic Nutrition Intervention Effects
Objective: To comprehensively capture the multi-target nature of nutritional interventions using systems biology approaches.
Methodology:
- Pre-intervention Phenotyping: Comprehensive baseline assessment including clinical, metabolic, microbial, and genetic markers
- Multi-level Response Monitoring:
- Transcriptomic profiling of relevant tissues
- Metabolomic profiling of serum/urine
- Microbiome sequencing
- Inflammatory and metabolic biomarkers
- Pathway Analysis: Integrative bioinformatics to identify affected biological pathways
- Network Modeling: Construct interaction networks to visualize multi-target effects
Implementation Considerations:
- Temporal Sampling: Multiple sampling timepoints to capture dynamic responses
- Dose-Response Elements: Include multiple intervention doses where feasible
- Integration Framework: Develop analytical plan for data integration across omics platforms [56]
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents and Materials for Nutritional RCTs
| Reagent/Material | Function | Application Notes |
|---|---|---|
| Stable Isotope Tracers | Metabolic pathway tracing; nutrient absorption and kinetics studies | Enables precise tracking of specific nutrients despite background diet |
| Placebo Formulations | Blinding for nutrient supplements; control for non-specific effects | Must match sensory properties while being inert for target nutrient |
| Food Composition Databases | Assessment of collinear nutrients in background diets | Requires comprehensive, up-to-date, culturally appropriate data |
| Nutrient Biomarkers | Objective verification of nutrient exposure and status | Critical for compliance monitoring and addressing measurement error |
| Standard Reference Materials | Analytical quality control for nutrient assays | Ensures accuracy across multiple analytical batches |
| DNA/RNA Preservation Kits | Stabilization of biological samples for omics analyses | Enables molecular assessment of multi-target effects |
| Dietary Assessment Platforms | Quantification of background dietary intake | Digital tools can improve accuracy of collinearity assessment |
Visualization of Methodological Approaches
Nutrient Collinearity Management Workflow
Multi-Target Effects Assessment Framework
Implementation Considerations for Nutritional RCT Protocols
Individualization and Generalizability Balance
Nutritional interventions must balance the need for standardized protocols with recognition of individual variability in response. Key considerations include:
- Baseline Nutritional Status: Account for deficiency, adequacy, or excess states that modify intervention effects [56]
- Genetic Polymorphisms: Consider genotyping for nutrient-relevant polymorphisms (e.g., MTHFR, APOE)
- Microbiome Composition: Baseline microbiome assessment may explain heterogeneous responses
- Life Stage Considerations: Adapt protocols for pregnancy, aging, or other physiological states [57]
Practical Implementation Framework
Successful implementation requires addressing practical challenges unique to nutrition research:
- Adherence Monitoring: Combine self-report, biomarkers, and digital monitoring where possible
- Control Diet Design: Carefully matched control conditions that isolate the specific intervention component
- Blinding Challenges: Develop credible placebos for food-based interventions where feasible
- Dietary Assessment: Select appropriate methods (24-hour recalls, FFQs, biomarkers) based on research question
- Covariate Adjustment: Pre-specify adjustment for key potential confounders in analysis plan [56]
Effectively managing nutrient collinearity and multi-target effects requires sophisticated methodological approaches that acknowledge the inherent complexity of nutritional interventions. By implementing controlled feeding designs where feasible, applying appropriate statistical methods for addressing collinearity, employing comprehensive assessment strategies to capture system-wide effects, and clearly acknowledging limitations, nutritional RCTs can generate robust evidence to advance the field. The protocols and frameworks outlined here provide a foundation for designing nutrition research that accounts for these unique challenges while maintaining scientific rigor.
Standardizing Interventions Across Diverse Food Cultures and Habits
Application Note: Framework for Culturally Standardized Nutritional RCTs
Core Challenge in Nutritional Research
Randomized Clinical Trials (RCTs) constitute a fundamental pillar of evidence-based medicine, yet nutritional intervention trials present unique methodological challenges not commonly encountered in pharmaceutical research [4]. The inherent heterogeneity of food cultures, traditional eating patterns, and diverse dietary habits across global populations creates significant obstacles for standardizing interventions while maintaining ecological validity and cultural appropriateness. This application note addresses the critical need for methodological frameworks that balance scientific rigor with cultural responsiveness in nutritional RCTs.
Nutritional interventions range from behavioral modifications and fortification to supplementation and regulatory approaches, each requiring distinct methodological considerations [4]. Unlike pharmaceutical trials where the active compound can be precisely standardized, dietary interventions must account for cultural food wisdom, traditional preparation methods, and deeply ingrained eating patterns that vary significantly across populations [58]. The standardization challenge is further compounded by the fact that most clinical recommendations in nutrition are currently classified as level II and III evidence, with only 26% representing level I evidence, highlighting the urgent need for improved methodological quality in nutritional RCTs [4].
Quantitative Framework for Cultural Standardization
Table 1: Core Domains for Standardizing Interventions Across Food Cultures
| Domain | Standardization Parameters | Measurement Approach | Cultural Adaptation Flexibility |
|---|---|---|---|
| Nutrient Composition | Macronutrient ratios, Micronutrient density, Phytochemical profiles | Standardized laboratory analysis, Food composition databases | ±15% acceptable variance for traditional ingredient substitutions |
| Dietary Patterns | Meal frequency, Timing, Food combinations | 24-hour dietary recall, Food frequency questionnaires | Alternative culturally-equivalent food group substitutions permitted |
| Food Preparation | Cooking methods, Processing techniques, Traditional practices | Standardized operating procedures with visual guides | Traditional methods allowed with documented thermal profiles |
| Sensory Properties | Flavor profiles, Texture, Palatability | Sensory evaluation scales, Hedonic testing | Region-specific spice blends within defined antioxidant capacity ranges |
| Contextual Factors | Social eating patterns, Religious dietary laws, Seasonal variations | Cultural practice assessment questionnaires | Accommodations for religious observances and traditional dining customs |
Experimental Protocol: Cross-Cultural Nutritional Intervention
This protocol provides a standardized framework for implementing nutritional interventions across diverse cultural contexts while maintaining methodological rigor required for high-quality RCTs. The approach integrates four key CONSORT extensions relevant to nutritional research: Non-Pharmacologic Treatment Interventions, Controlled Trials of Herbal Interventions, Non-Inferiority and Equivalence Trials, and Cluster Trials [4]. The primary objective is to establish methodological consistency while allowing appropriate cultural adaptations that respect diverse food traditions and eating patterns.
The protocol emphasizes the importance of transparent reporting and rigorous methodology to enhance the evidence quality of nutritional recommendations. Proper implementation requires careful consideration of randomization procedures, blinding techniques, control group design, and culturally-relevant outcome measures that acknowledge the health benefits of diverse traditional foods and spices [58].
Pre-Intervention Phase
Cultural Food Assessment and Adaptation
- Community Engagement: Establish a Cultural Food Advisory Board comprising cultural knowledge keepers, traditional food practitioners, registered dietitians, and community representatives from target populations.
- Traditional Food Documentation: Conduct systematic documentation of traditional food patterns, including staple foods, preparation methods, seasonal variations, and culturally-significant eating occasions using structured interviews and focus groups.
- Nutrient Analysis: Perform standardized nutrient analysis of core traditional foods using certified laboratory methods to establish baseline nutritional composition data.
- Cultural Adaptation Mapping: Identify culturally-equivalent food substitutions that maintain nutritional integrity while respecting cultural preferences, documenting potential variations in a cultural adaptation guide.
Study Population and Randomization
- Participant Selection: Define inclusion criteria that account for cultural dietary practices, food security status, and traditional food access. Employ stratified randomization based on key cultural and demographic variables to ensure balanced group allocation.
- Randomization Procedure: Implement block randomization with varying block sizes to maintain allocation concealment, using central web-based randomization systems to prevent selection bias. For small sample sizes or when studying populations with significant cultural heterogeneity, stratified randomization ensures balanced distribution of cultural factors across study arms [4].
- Sample Size Calculation: Calculate sample size accounting for anticipated cultural diversity within populations, with appropriate inflation factors to maintain statistical power despite potential within-group cultural variations.
Intervention Implementation Phase
Dietary Intervention Delivery
- Culturally Standardized Meal Provision: Provide study meals through centralized facilities using standardized recipes with documented nutrient composition, while offering culturally-appropriate alternatives within defined nutritional parameters.
- Behavioral and Educational Components: Implement culturally-tailored nutrition education that acknowledges traditional food wisdom and incorporates evidence-based nutritional principles without cultural disparagement.
- Traditional Food Incorporation: Design intervention protocols that allow for incorporation of traditional foods and preparation methods while maintaining nutritional standardization through portion control and recipe modification.
Blinding Procedures
- Investigator Blinding: Ensure outcome assessors, data analysts, and laboratory personnel are blinded to group allocation through separate team structures and coded sample identification.
- Partial Participant Blinding: Implement active control conditions with similar appearance, taste profiles, and engagement requirements to reduce participant expectation bias, acknowledging the difficulty of complete blinding in dietary interventions.
- Cultural Consistency Maintenance: Regular monitoring of cultural adherence through food diaries, biomarker analysis, and cultural compliance checks to ensure interventions remain both culturally appropriate and scientifically standardized.
Data Collection and Monitoring
Primary Outcome Measures
- Biomarker Collection: Standardized collection of biological samples (blood, urine, stool) for nutrient status, inflammatory markers, metabolomic profiling, and gut microbiome analysis with appropriate stabilization for batch analysis.
- Clinical Measurements: Anthropometric measurements (weight, BMI, waist circumference), vital signs (blood pressure, heart rate), and physical function assessments using calibrated instruments with standardized protocols.
- Dietary Adherence Monitoring: Combined approach using food diaries, 24-hour dietary recalls, photograph-based food records, and culturally-appropriate food frequency questionnaires to assess intervention adherence.
Cultural and Behavioral Measures
- Cultural Food Connectedness Scale: Validated instrument assessing participants' connection to traditional foodways and perception of cultural preservation within the intervention.
- Dietary Satisfaction Measures: Assessment of intervention acceptability, palatability, and cultural congruence using Likert scales and qualitative interviews.
- Social and Environmental Factors: Documentation of social support for dietary changes, food environment characteristics, and potential barriers to adherence specific to cultural context.
Table 2: Standardized Cultural Adaptation Metrics for Nutritional Interventions
| Metric Category | Specific Measures | Target Range | Assessment Frequency |
|---|---|---|---|
| Cultural Congruence | Cultural Food Connectedness Score, Traditional Food Frequency Index | ≥70% of maximum score | Baseline, Mid-point, Endpoint |
| Nutritional Equivalence | Macronutrient distribution, Micronutrient density, Energy content | ≤15% deviation from target | Weekly meal analysis |
| Biomarker Consistency | Nutrient biomarkers, Inflammatory markers, Metabolic profiles | Within pre-defined equivalence margins | Baseline, Endpoint |
| Intervention Fidelity | Protocol adherence, Recipe modification frequency, Staff cultural competency | ≥85% adherence to protocol | Monthly audit |
| Participant Engagement | Session attendance, Drop-out rates, Satisfaction scores | ≤20% attrition, ≥80% satisfaction | Continuous monitoring |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Materials for Cross-Cultural Nutritional Trials
| Item Category | Specific Examples | Function in Research | Cultural Considerations |
|---|---|---|---|
| Cultural Food Assessment Tools | Cultural Food Frequency Questionnaire, Traditional Food Inventory, Cultural Identity and Food Scale | Quantifies consumption of traditional foods, measures cultural connection to diet, identifies culturally-significant foods | Must be validated in specific cultural context, available in appropriate languages |
| Standardized Recipe Database | Cultural Recipe Modification Guide, Nutrient Analysis Database, Traditional Food Composition Tables | Ensures nutritional consistency while allowing cultural variations, provides framework for culturally-appropriate substitutions | Includes traditional preparation methods, accounts for regional ingredient variations |
| Biological Sample Collection | Stabilization tubes for metabolomics, DNA/RNA preservation kits, Portable centrifuge, Dried blood spot cards | Enables biomarker analysis for intervention efficacy, provides objective adherence measures, allows for nutrigenomic studies | Accommodates cultural concerns regarding blood sampling when necessary |
| Dietary Intake Validation | Digital food photography equipment, Mobile dietary assessment apps, Standardized portion size visuals, Multiple-pass 24-hour recall forms | Objectively documents dietary intake, standardizes portion size estimation, validates self-reported data | Includes culturally-familiar portion references, incorporates traditional eating occasions |
| Cultural Competency Resources | Cultural humility training modules, Traditional food safety protocols, Multilingual consent materials, Community engagement toolkit | Builds researcher capacity for culturally-responsive trial implementation, ensures ethical community partnerships | Developed in collaboration with cultural knowledge holders, regularly updated |
Methodological Considerations and Signaling Pathways
Cultural Adaptation Framework
Statistical Analysis Plan
The analysis plan for cross-cultural nutritional RCTs must account for both the hierarchical structure of data (participants nested within cultural groups) and potential effect modification by cultural factors. Primary analyses should follow intention-to-treat principles using mixed-effects models that include cultural group as a random effect. Pre-specified subgroup analyses should examine intervention effects across different cultural contexts, with appropriate statistical correction for multiple comparisons. Sensitivity analyses should assess the impact of varying levels of cultural adherence on observed outcomes.
Mediation analyses can elucidate whether intervention effects operate through intended biological pathways or through cultural mechanisms such as enhanced connectedness to traditional foodways. Equivalence testing may be appropriate when comparing culturally-adapted versions of interventions to establish whether they produce biologically similar effects despite cultural variations in implementation.
Ethical and Community Considerations
Successful implementation of cross-cultural nutritional RCTs requires ongoing community engagement and ethical practices that respect cultural knowledge and food sovereignty. Research partnerships should be established with cultural communities early in the research design process, with fair compensation for cultural knowledge holders. Data ownership agreements should respect community rights to cultural knowledge while enabling scientific advancement. Dissemination plans must include culturally-appropriate reporting of results to participant communities in accessible formats and languages.
The protocol should address potential conflicts between scientific standardization requirements and cultural food practices, establishing clear processes for resolving such conflicts through community consultation while maintaining scientific integrity. This approach aligns with the broader healthcare aims of promoting diversity, equity, inclusion, and belonging while advancing nutritional science [58].
Optimizing Recruitment and Retention in Long-Term Nutrition Studies
Application Notes: Strategic Frameworks for Participant Engagement
Successful execution of long-term nutrition studies hinges on effective participant recruitment and retention. These phases present distinct challenges, requiring tailored, evidence-based strategies to ensure study validity, power, and timely completion.
Recruitment aims to identify, screen, and enroll a representative sample of participants that meets predefined sample size goals. Inefficient recruitment can lead to underpowered studies, prolonged timelines, and increased costs, ultimately threatening the study's internal and external validity [59]. Retention focuses on maintaining participant involvement for the entire study duration. Poor retention rates can similarly compromise statistical power and introduce bias, particularly if dropout is differential between intervention and control groups [59].
Young adults (aged approximately 17-35 years), a common target for nutrition research, present specific challenges due to age-normative life transitions, competing time demands, and changing contact information [59] [60]. However, strategic use of modern communication channels and flexible scheduling can effectively overcome these barriers.
Protocols for Recruitment and Retention
This protocol provides a systematic approach to participant management in long-term nutritional intervention studies.
Pre-Recruitment Phase
- Ethical Approval: Secure approval from the relevant Institutional Review Board (IRB) or ethics committee.
- Sample Size Calculation: Determine the target sample size through a formal power analysis.
- Define Eligibility Criteria: Establish clear, justified inclusion and exclusion criteria.
- Develop Materials: Prepare all participant-facing materials, including informed consent documents, recruitment advertisements, and data collection forms.
Core Recruitment Protocol
- Multi-Channel Recruitment Strategy: Implement a diverse recruitment plan. Primary channels should include:
- Social Media Advertising: Utilize platforms like Facebook and Twitter. These have been demonstrated to be highly successful, enabling rapid recruitment by directly reaching the target demographic in their digital environments [60].
- Institutional Channels: Use university campus noticeboards, email lists to staff and students, and promotion in relevant lectures or classes [60].
- Community Outreach: Place flyers in community centers, gyms, and daycare centers. Engage with existing research volunteer registries [60].
- Screening and Enrollment:
- Eligibility Screening: Conduct a standardized screening process (e.g., via online survey or phone call) to assess potential participants against the predefined criteria.
- Informed Consent Process: Conduct the informed consent process, ensuring participants fully understand the study's purpose, procedures, risks, and benefits.
- Baseline Data Collection: Schedule and conduct the first baseline assessment.
Core Retention Protocol
- Communication and Reminders:
- Regular Contact: Maintain regular, non-intrusive contact with participants throughout the study period.
- Reminder Systems: Use a combination of email, SMS text messages, and phone calls to send reminders for upcoming appointments, data collection timepoints, or intervention activities. This multi-modal approach has been shown to assist in achieving low attrition rates [60].
- Participant Convenience and Support:
- Flexible Scheduling: Offer flexible testing times, including outside standard business hours, to accommodate work, study, and family commitments [60].
- Easy Communication Channels: Provide a dedicated phone number and email address for participants to contact the research team with questions or concerns.
- Incentives and Feedback:
- Compensation: Provide appropriate compensation for time and travel, which can be tiered to incentivize completion of all study phases.
- Personalized Feedback: Where ethically and scientifically permissible, offer participants personalized feedback on their results (e.g., basic blood test parameters) to maintain engagement and demonstrate the value of their contribution [60].
The following workflow diagram summarizes the key stages and decision points in managing participants throughout a long-term study.
Monitoring and Evaluation
- Track Metrics: Systematically document key performance indicators for both recruitment (e.g., number invited, screened, eligible, enrolled) and retention (number completing each follow-up) [59].
- Assess Reasons for Ineligibility/Withdrawal: Record reasons for ineligibility during screening and for withdrawal among enrolled participants. This information is critical for refining future protocols [60].
Data Presentation: Strategy Effectiveness and Outcomes
Structured evaluation of strategy effectiveness is paramount. The following tables summarize evidence on the performance of various recruitment and retention techniques.
Table 1: Effectiveness of Common Recruitment Strategies in Nutrition Research
| Recruitment Strategy | Reported Effectiveness | Key Considerations and Context |
|---|---|---|
| Social Media (Facebook, Twitter) | High; most successful for rapid recruitment [60]. | Reached 751 eligible participants for an online survey within one month [60]. Ideal for targeting younger demographics. |
| University Email Lists | Moderate to High | Effective for reaching a captive audience of students and staff; success depends on list reach and email engagement. |
| University Noticeboards & Lectures | Moderate | Recruited 57% of target sample in first 12 months in one RCT; useful but slower than digital methods [60]. |
| Community Flyers (Gyms, Daycares) | Moderate | Extends reach beyond university setting; contributed to final 23% of sample in a prolonged recruitment phase [60]. |
| Research Volunteer Registries | Low to Moderate | Mailed questionnaires to 250 individuals yielded 10 participants (4% response rate) [60]. Can be inefficient. |
Table 2: Effectiveness of Common Retention Strategies in Nutrition Research
| Retention Strategy | Reported Effectiveness / Outcome | Key Considerations and Context |
|---|---|---|
| SMS Text Message Reminders | High; associated with low attrition [60]. | A key component of a protocol that achieved 93% completion in an RCT [60]. |
| Email Reminders | High; assists in maintaining contact [60]. | Used in conjunction with phone and SMS for a multi-modal approach. |
| Phone Call Reminders | High; provides personal touch [60]. | Effective for resolving issues and confirming attendance at key visits. |
| Flexible Testing Times | Recommended as best practice [60]. | Accommodates participants' work and study schedules, a major barrier to retention. |
| Providing Personal Results Feedback | Anecdotally effective [60]. | Offers a direct benefit to participants, increasing perceived value of continued involvement. |
The Scientist's Toolkit: Essential Research Reagent Solutions
This section details key materials and tools beyond biological reagents that are essential for executing the recruitment and retention protocols described above.
Table 3: Essential Research Reagent Solutions for Participant Management
| Item / Solution | Function in Research Protocol |
|---|---|
| Social Media Management Tool | Used to schedule and deploy targeted recruitment advertisements on platforms like Facebook and Twitter, enabling efficient reach to the desired demographic. |
| Email Broadcasting Service | Facilitates the sending of bulk, personalized email invitations and reminders to potential participants on distribution lists while maintaining professional communication. |
| SMS/Text Messaging Platform | A critical tool for sending timely appointment reminders and brief check-ins, which is a proven strategy for maintaining high retention rates [60]. |
| Online Survey Software | Enables the creation and distribution of digital eligibility screening surveys and follow-up questionnaires, streamlining data collection and management. |
| Electronic Participant Management System | A database for tracking participant contact information, study milestones, and communication logs. This is vital for organizing follow-ups and monitoring retention. |
| Customer Relationship Management (CRM) Software | An advanced organizational tool that can automate reminder sequences, track participant engagement, and flag individuals who may be at risk of dropping out. |
Randomized Controlled Trials (RCTs) represent the gold standard for establishing causal relationships in nutritional intervention research [61]. However, the inherent complexity of human nutrition introduces significant confounding challenges that can compromise study validity if not adequately addressed. Confounding occurs when a factor is associated with both the exposure (or intervention) and the outcome, without being part of the causal pathway [62]. In nutritional epidemiology, dietary and nutritional factors often correlate strongly with socioeconomic, lifestyle, genetic, and physiological variables, many of which are inaccurately measured or entirely unmeasured [61]. While randomization theoretically distributes such factors equally between intervention groups, practical constraints often result in residual confounding, particularly when sample sizes are limited or subgroup analyses are performed.
This protocol addresses three critical confounding domains that require specialized methodological approaches: ethnicity, genotype, and physiological status. Each domain presents unique challenges for causal inference in nutritional RCTs and demands specific mitigation strategies throughout study design, execution, and analysis phases. By implementing these evidence-based protocols, researchers can enhance the internal validity of their findings and generate more reliable evidence for nutritional guidelines and personalized nutrition approaches.
Quantitative Data Synthesis: Evidence Base for Confounding Mitigation
Table 1: Documented Impacts of Ethnicity, Genotype and Physiological Status on Nutritional Responses
| Confounding Domain | Specific Factor | Documented Impact on Nutritional Response | Key Supporting Evidence |
|---|---|---|---|
| Genotype | APOE ε4 haplotype | Altered lipid metabolism; Modified Alzheimer's disease risk from Mediterranean diet and PUFA | ε4 carriers: 7x increased AD risk with high saturated fat [63] |
| Genotype | FADS1 rs174546 (TT) | Enhanced erythrocyte DHA incorporation with supplementation | Stronger response to ALA for ischemic stroke reduction [63] |
| Genotype | MTHFR rs1801133 (TT) | Reduced stroke risk with folic acid supplementation; Responsive to vitamin B2 for blood pressure | Gene-nutrient interaction for homocysteine reduction [63] |
| Genotype | TCF7L2 rs7903146 (TT) | Exaggerated plasma glucose and free fatty acid response to OGTT | Increased diabetes risk with certain dietary patterns [63] |
| Ethnicity/Race | Population stratification | Differential bioavailability and metabolism of nutrients | Genomic diversity affects nutrient bioavailability across ethnic groups [64] |
| Physiological Status | Microbiome composition | Variable nutrient absorption and metabolite production | Affects nutrient bioavailability and metabolic outcomes [65] |
| Physiological Status | Inflammatory status | Modifies response to anti-inflammatory dietary components | Alters metabolic pathways and nutrient requirements [65] |
Table 2: Federal Reporting Requirements for RCT Subgroup Analyses (NIH-Funded Trials)
| Subgroup Category | Reporting Requirement | Historical Compliance (2004-2015) | Recent Compliance (2021) |
|---|---|---|---|
| Sex/Sex | Analysis/reporting of outcomes by sex | Low, with no improvement over time | 43.0% (significant increase, p<0.01) [66] |
| Race/Ethnicity | Analysis/reporting of outcomes by race/ethnicity | Consistently low across previous waves | 26.9% (significant increase, p<0.01) [66] |
| Enrollment | Representative participant recruitment | Median female participation: ~43% | No significant increase in enrollment diversity [66] |
Experimental Protocols for Confounding Mitigation
Protocol 1: Genotype-Stratified Randomization and Analysis
Purpose: To control for confounding by genetic variants with known nutrient-gene interactions.
Methodology:
- Pre-Screening and Stratification:
- Identify candidate genes with documented nutrient-gene interactions relevant to the intervention (e.g., APOE for lipid studies, MTHFR for folate interventions) [63] [64].
- Genotype participants during screening phase using established methods (TaqMan assays, genome-wide arrays, or next-generation sequencing).
- Create randomization blocks within each relevant genotype group (e.g., APOE ε4 carriers vs. non-carriers) to ensure balanced allocation across intervention arms.
Intervention Delivery:
- Implement controlled feeding protocols when possible to ensure precise dietary exposure [67].
- Maintain isocaloric conditions while varying nutrient composition of interest.
- Provide all foods and beverages to participants with precise gram-weight measurements.
Compliance Monitoring:
Statistical Analysis:
- Include genotype × intervention interaction terms in primary statistical models.
- Pre-specify genotype-stratified analyses in statistical analysis plan.
- Adjust for multiple testing using appropriate methods (e.g., Bonferroni, False Discovery Rate).
Applications: Nutrigenetic trials investigating differential responses to dietary components based on genetic variants in metabolic pathways.
Protocol 2: Ethnicity-Robust Study Design and Analysis
Purpose: To address confounding arising from population stratification and ethnic differences in nutrient metabolism.
Methodology:
- Study Design Phase:
- Implement stratified recruitment to ensure adequate representation of ethnic subgroups relevant to research questions.
- Collect detailed data on socioeconomic status, education, income, food environment, and cultural dietary patterns that may covary with ethnicity [62].
- Use geographic information systems to document neighborhood-level food access and environmental factors.
Dietary Exposure Assessment:
- Employ culturally appropriate dietary assessment tools validated for specific ethnic subgroups.
- Incorporate traditional foods and eating patterns into intervention designs when relevant.
- Use multiple dietary assessment methods (24-hour recalls, food frequency questionnaires, and food records) to enhance validity [62].
Statistical Analysis:
- Include ethnicity × intervention interaction terms in primary models.
- Conduct sensitivity analyses adjusting for socioeconomic and cultural covariates.
- Use directed acyclic graphs (DAGs) to identify potential confounding paths specific to ethnic subgroups.
- Apply multilevel modeling to account for neighborhood-level and individual-level factors.
Applications: Multi-ethnic trials investigating dietary patterns, community-based interventions, and studies of traditional diets.
Protocol 3: Physiological Status Monitoring and Control
Purpose: To control for confounding by dynamic physiological variables that modify nutritional responses.
Methodology:
- Baseline Characterization:
- Conduct comprehensive phenotyping including body composition (DXA), resting metabolic rate (indirect calorimetry), and cardiometabolic biomarkers.
- Assess microbiome composition through 16S rRNA sequencing or metagenomics [65].
- Quantify inflammatory status via high-sensitivity C-reactive protein, IL-6, and TNF-α.
Intervention Period Monitoring:
- Implement daily weight checks with protocol-defined thresholds for energy intake adjustment [67].
- Collect serial biospecimens for biomarker monitoring at predetermined intervals.
- Use digital health technologies (continuous glucose monitors, activity trackers) to capture real-time physiological data.
Statistical Control:
- Include relevant physiological variables as covariates in primary analysis models.
- Implement mediation analysis to distinguish direct nutritional effects from effects mediated through physiological changes [61].
- Use latent class analysis to identify subgroups with distinct physiological response patterns.
Applications: Trials investigating dietary interventions for metabolic diseases, weight management, and microbiome-targeted nutrition.
Signaling Pathways and Workflow Visualization
Diagram 1: Integrated Workflow for Confounding Mitigation in Nutritional RCTs. This diagram outlines the sequential process for designing and implementing confounding control strategies throughout a nutritional intervention trial.
Diagram 2: Nutrigenetic Pathways and Potential Confounding. This diagram illustrates how genetic variants (SNPs) can modify responses to nutrients through multiple molecular pathways, creating genotype-specific effects that can confound nutritional RCTs if unaccounted for.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents and Platforms for Confounding Mitigation
| Reagent/Platform | Primary Function | Application in Confounding Control |
|---|---|---|
| Genotyping Arrays (Infinium Global Screening Array, TaqMan assays) | Genetic variant detection | Identification of nutrigenetic variants for stratification; ancestry informative markers for ethnicity control [63] [64] |
| Targeted Metabolomics Panels (Biocrates, Nightingale) | Metabolic phenotyping | Objective biomarkers of dietary compliance; monitoring physiological status changes [67] [64] |
| Microbiome Sequencing Kits (16S rRNA, Shotgun Metagenomics) | Gut microbiota characterization | Assessment of microbiome as potential effect modifier; covariate in statistical models [65] |
| Multiplex Immunoassays (Mesoscale Discovery, Luminex) | Inflammatory biomarker quantification | Monitoring physiological status; inflammatory markers as covariates or outcomes [65] |
| Controlled Feeding Software (NDS-R, ProNutra) | Diet design and nutrient analysis | Precise dietary intervention delivery; reduces exposure misclassification [67] |
| Digital Diet Assessment (ASA24, Metabolomize) | Dietary intake assessment | Reduced measurement error compared to traditional FFQs; digital biomarkers of intake [62] [65] |
| Bioinformatics Platforms (PLINK, METASOFT, GCTA) | Genetic data analysis | Population stratification control; genotype × intervention interaction testing [63] [64] |
Evaluating Evidence and Ensuring Trial Quality and Impact
Application Note: Interpreting Heterogeneity in Nutritional RCT Outcomes
Quantitative Synthesis of Nutritional Intervention Effects
Table 1: Efficacy of Nutritional Interventions Across Health Conditions
| Health Condition | Intervention Type | Primary Outcomes | Effect Size & Key Findings | Population Context |
|---|---|---|---|---|
| Type 2 Diabetes [68] | Low-Carbohydrate Diets (LCD) | HbA1c, Fasting Glucose, Weight | - HbA1c: -0.29% (short-term)- Fasting Glucose: -7.12 mg/dL- Weight loss: Greatest at 3 months, attenuates thereafter | Cultural differences noted between Eastern vs. Western populations; benefits diminish over time |
| Obsessive-Compulsive Disorder (OCD) [9] | Nutritional Supplements (e.g., Vitamin D, B12, Glycine) | Cognition, Quality of Life, Psychiatric Symptoms | - Potential benefits for OCD symptoms- Acts as adjunctive therapy to standard treatments | Adults (≥18) meeting DSM-5 criteria; excludes major comorbid psychiatric disorders |
| Telomere Length & Aging [8] | Micronutrients (e.g., Selenium, CoQ10, Vitamin D), Walnuts, Fish Oil | Telomere Length (TL) | - Most consistent evidence: Selenium, CoQ10, Vitamin D- Promising but weaker evidence: Walnuts, fish oil- No effect: Almonds, pistachios, zinc, caloric restriction | Healthy elderly populations; evidence limited by small samples and short duration |
| Mild Cognitive Impairment (MCI) & Alzheimer's Disease (AD) [69] | Mediterranean Diet, Ketogenic Diet, Fatty Acids, Antioxidants, Vitamins | Cognitive Function (MMSE, ADAS-Cog) | - Investigated for potential to delay or prevent cognitive decline- Synergistic effects of nutrition on health | Participants >50 years with MCI or AD; intervention duration >12 weeks |
Methodological Framework for Cross-Population Analysis
The systematic review on low-carbohydrate diets for type 2 diabetes exemplifies a robust framework for analyzing intervention efficacy across diverse populations. The analysis included 27 RCTs (n=2,870) with explicit stratification into 7 Eastern and 20 Western trials [68]. This approach successfully identified that while LCDs provided modest short-term metabolic benefits, these advantages diminished over time and were influenced by cultural context. No study arm sustained carbohydrate intake below 10% of total energy, indicating findings generalize to low-to-moderate carbohydrate intake rather than very-low-carbohydrate regimens [68]. This highlights the critical importance of defining intervention intensity consistently across studies and accounting for adherence patterns that may differ culturally.
Experimental Protocols for Nutritional RCTs
Protocol I: Assessing Nutritional Interventions for Cognitive Health
Objective: To assess the effectiveness of nutritional interventions in preventing cognitive decline among patients with MCI or AD [69].
Study Design:
- Trial Type: Randomized Controlled Trial (RCT)
- Blinding: Double-blind (participants and outcome assessors)
- Follow-up Duration: Minimum 12 weeks intervention, with outcomes assessed at least 6 months post-initiation
Population:
- Inclusion Criteria: Adults >50 years with diagnosis of MCI or AD according to NINCDS-ADRDA or DSM criteria [69]
- Exclusion Criteria: Vascular dementia, Parkinson's disease-related dementia, delirium, major depressive disorder, other psychiatric comorbidities [69]
- Sample Size Calculation: Power analysis required to detect clinically significant differences in cognitive scores
Intervention Groups:
- Experimental: Specific nutritional intervention (e.g., Mediterranean diet, omega-3 supplementation, vitamin E)
- Control: Placebo or standard care with matched contact time
Outcome Measures:
- Primary Outcomes: Cognitive function measured by Mini-Mental State Examination (MMSE) and Alzheimer's Disease Assessment Scale cognitive subscale (ADAS-Cog) [69]
- Secondary Outcomes: Clinical Dementia Rating Scale (CDR), Wechsler Adult Intelligence Scale-Revised (WAIS-R), quality of life measures [69]
Analysis Plan:
- Intention-to-treat analysis
- Network meta-analysis to compare multiple interventions
- Subgroup analysis based on baseline cognitive status, age, and genetic factors
Protocol II: Evaluating Adjunctive Nutritional Supplementation for OCD
Objective: To evaluate the efficacy of nutritional supplements as adjunctive therapy for reducing obsessive-compulsive symptoms [9].
Study Design:
- Trial Type: RCT with parallel groups
- Blinding: Triple-blind (participants, care providers, outcome assessors)
- Duration: Minimum 12 weeks intervention with at least 6 months follow-up [9]
Population:
- Inclusion Criteria: Adults ≥18 years with OCD diagnosed per DSM-5 criteria [9]
- Exclusion Criteria: Organic causes of OCD, comorbid schizophrenia, bipolar disorder, depressive disorder, eating disorders, suicidal behavior [9]
- Sample Size: Adequately powered to detect clinically meaningful differences in Yale-Brown Obsessive Compulsive Scale scores
Intervention Groups:
- Experimental: Standard treatment + nutritional supplement (e.g., Vitamin D, Vitamin B12, glycine)
- Control: Standard treatment + matched placebo
Outcome Measures:
- Primary Outcomes:
- Secondary Outcomes: Morbidity/comorbidity indices (e.g., Charlson Comorbidity Index) [9]
Analysis Plan:
- Mixed-effects models to account for repeated measures
- Adjustment for potential confounders (e.g., baseline severity, concomitant medications)
- Safety analysis of adverse events
Visualizing Systematic Review Workflows and Biological Pathways
Systematic Review Workflow for Nutritional RCTs
Biological Pathways of Nutritional Interventions
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents and Materials for Nutritional RCTs
| Item Category | Specific Examples | Function/Application | Protocol Considerations |
|---|---|---|---|
| Validated Assessment Tools | MMSE, ADAS-Cog, Y-BOCS, Stroop Test, Trail-Making Test | Quantifying cognitive outcomes, psychiatric symptoms, and executive function [9] [69] | Require trained administrators; consider cultural validation and language adaptations |
| Biomarker Assays | HbA1c, fasting glucose, inflammatory markers (CRP, cytokines), telomere length assays | Objective measures of metabolic health, inflammation, and biological aging [68] [8] | Standardize collection timing and methods; consider stability during storage |
| Dietary Compliance Tools | Food diaries, 24-hour recalls, food frequency questionnaires, biomarker validation (e.g., plasma fatty acids) | Monitoring adherence to nutritional interventions [68] | Combine subjective and objective measures; frequency depends on intervention duration |
| Nutritional Supplements | Pharmaceutical-grade vitamins, minerals, amino acids, purified omega-3 fatty acids | Ensuring intervention purity, consistency, and precise dosing [9] [8] | Use matched placebos for blinding; verify composition through third-party testing |
| Data Management Systems | Electronic data capture (EDC) systems, REDCap, clinical trial management systems | Maintaining data integrity, supporting randomization, and facilitating monitoring [70] | Must comply with regulatory standards (e.g., 21 CFR Part 11); include audit trails |
The synthesis of current evidence highlights both opportunities and challenges in nutritional intervention research. While nutritional approaches show promise across multiple health domains, the modest effect sizes, heterogeneity of responses, and attenuation of benefits over time underscore the need for more sophisticated trial designs [68] [8] [69]. Future protocols should prioritize adequate sample sizes, longer follow-up periods, standardized outcome measures, and careful consideration of cultural and individual factors that may influence intervention efficacy. The integration of objective biomarkers alongside clinical outcomes will strengthen the evidence base for nutritional interventions in diverse populations.
The Consolidated Standards of Reporting Trials (CONSORT) statement establishes a minimum set of evidence-based recommendations for reporting randomized controlled trials (RCTs), aimed at reducing the risk of biased, incomplete, or uninterpretable reports [71]. While the standard CONSORT checklist is applicable to all RCTs, the unique methodological complexities inherent in non-pharmacological and herbal interventions necessitate the use of specialized extensions to ensure complete and transparent reporting [72] [4]. Inadequate reporting of these complex trials hinders critical appraisal, evidence synthesis, and the development of reliable clinical guidelines, ultimately impeding the translation of research into practice [4].
For researchers in nutritional and herbal sciences, applying the appropriate extensions is crucial for producing methodologically sound and scientifically valuable research. These extensions address specific challenges not fully covered by the main CONSORT guideline, such as detailing complex interventions, standardizing control groups, implementing blinding where possible, and describing the expertise of personnel involved [72] [4]. This article provides detailed application notes and protocols for utilizing these specialized CONSORT extensions within the context of RCT protocols for nutritional and related intervention research.
Essential CONSORT Extensions and Their Applications
Several CONSORT extensions provide critical, tailored guidance for trials beyond conventional drug studies. The most relevant for nutritional and herbal intervention research are summarized in the table below.
Table 1: Key CONSORT Extensions for Non-Pharmacological and Herbal Trials
| Extension Name | Primary Focus & Rationale | Specific Reporting Considerations | Example Use Case in Nutrition/Herbal Research |
|---|---|---|---|
| CONSORT for Non-Pharmacologic Treatment (NPT) [72] | Addresses unique aspects of non-drug trials (e.g., surgery, rehabilitation, dietary interventions, behavioral therapies). | Description of intervention customization. Qualifications of those delivering the intervention. Details of how the control group was managed. Implementation of blinding (participants, interveners, outcome assessors). | A trial comparing a structured Mediterranean diet program to general dietary advice for cardiovascular health. |
| CONSORT for Herbal Interventions [72] | Provides standards for trials using herbal medicines, which have complex, often variable compositions. | Standardized botanical nomenclature and plant part used. Method of extraction and solvent used. Chemical characterization of the product (e.g., chromatographic fingerprint). Quality control methods during production. Dosage and dosage regimen. | A trial investigating the efficacy of a specific extract of Ginkgo biloba for cognitive function. |
| CONSORT for Non-Inferiority and Equivalence Trials [4] | For trials aiming to show a new intervention is not worse than, or equivalent to, an existing one. | Justification for the non-inferiority/equivalence hypothesis. Pre-specified non-inferiority/equivalence margin with rationale. Statistical methods for testing non-inferiority/equivalence. | A trial testing whether a plant-based protein blend is equivalent to whey protein for muscle synthesis post-exercise. |
| CONSORT for Cluster Trials [4] | For trials where groups of individuals (e.g., clinics, communities) are randomized, not individuals. | Justification for the cluster design. How clustering was accounted for in sample size calculation. Statistical methods adjusting for cluster effects. Number of clusters and average cluster size. | A community-based nutrition education program where entire towns are randomized to intervention or control. |
The Emerging CONSORT-Nut Extension
Recognizing the specific challenges in nutritional RCTs, a dedicated extension, CONSORT-Nut, is currently under development [73]. A recent Delphi survey achieved a 100% consensus on a proposed 29-item checklist, indicating strong expert agreement on the need for specialized reporting standards in the field [73]. This forthcoming extension aims to consolidate and enhance guidance for nutritional interventions, which often face issues such as poor description of the control group, inadequate blinding, and a lack of detail on the composition and delivery of the intervention [4]. Researchers planning nutritional trials should proactively consult the developing CONSORT-Nut guidelines to align their protocols with these emerging best practices.
Detailed Application Notes and Experimental Protocols
Workflow for Selecting and Applying CONSORT Extensions
The following diagram outlines a systematic protocol for determining and implementing the correct CONSORT extensions during the trial design and reporting phases.
Protocol for Describing Complex Interventions using TIDieR
A common weakness in trial reporting is the inadequate description of the intervention and control conditions. The Template for Intervention Description and Replication (TIDieR) checklist is a complementary tool designed to work alongside CONSORT to rectify this [72]. The following protocol provides a step-by-step guide for its application.
Table 2: TIDieR-Based Protocol for Intervention Description
| Step | TIDieR Item | Application Notes for Nutritional/Herbal Trials | Research Reagent & Documentation Solutions |
|---|---|---|---|
| 1. Why | Rationale, theory or goal. | Briefly explain the biological or behavioral mechanism (e.g., "The high-polyphenol intervention aims to reduce oxidative stress..."). | - Literature Reference Manager (e.g., Zotero, EndNote): To systematically manage foundational studies supporting the rationale. |
| 2. What | Physical or informational materials. | For nutritional supplements: provide manufacturer, batch number, certificate of analysis. For diets: provide sample menus, recipes. | - Certified Reference Materials: Use certified standards from organizations like NIST for quantitative analysis of active compounds. |
| 3. Who | Provider expertise and background. | Detail qualifications (e.g., "Dietary advice was delivered by registered dietitians with >5 years' experience"). | - Personnel CV/Portfolio: Document staff qualifications as part of the trial master file. |
| 4. How | Modes of delivery (face-to-face, web-based). | Describe the setting (e.g., "Cooking sessions were conducted in a community kitchen equipped with..."). | - Standard Operating Procedures (SOPs): Document all delivery protocols to ensure consistency across interveners and sites. |
| 5. Where | Location of delivery (home, clinic). | Critical for contextualizing the intervention's real-world applicability. | - Site Characterization Log: Document relevant features of all intervention locations. |
| 6. When & How Much | Dosage, intensity, duration. | Specify dosage form (e.g., capsule, powder), timing, and total duration. For diets, specify energy/macronutrient targets. | - Dosing Log/Diary: A tool for participants or interveners to record adherence, which is a key outcome. |
| 7. Tailoring | Intervention customization. | Describe if/why the intervention was personalized (e.g., "Protein intake was tailored to baseline lean body mass"). | - Customization Algorithm: A predefined, documented rule set for any personalization to avoid ad-hoc modifications. |
| 8. Modifications | Changes during the trial. | Document any protocol changes with rationale (e.g., "Supplement flavor was changed mid-trial to improve adherence"). | - Protocol Amendment Tracker: A system to formally log, approve, and communicate any changes. |
| 9. Fidelity | How well the intervention was delivered as planned. | Plan and report adherence assessments (e.g., pill counts, diet diaries, biomarker analysis). | - Adherence Biomarkers: Use objective measures like alkylresorcinols for whole-grain intake or doubly labeled water for total energy expenditure. |
Protocol for Randomization and Blinding in Nutritional Trials
A 2017 meta-analysis found that a quarter of nutrition education interventions failed to perform or report the randomization process adequately [4]. The protocol below outlines key methodological considerations.
Table 3: Reagent and Methodology Solutions for Randomization & Blinding
| Methodological Aspect | Common Challenges in Nutrition Trials | Recommended Protocols & Reagent Solutions |
|---|---|---|
| Randomization | Imbalance: Small sample sizes can lead to unequal groups for key prognostic factors. | - Block Randomization: Ensures balanced group numbers over time, ideal for slow recruitment [4].- Stratified Randomization: Use for small trials or when factors like age, sex, or BMI are strong effect modifiers. An independent statistician should generate the allocation sequence. |
| Allocation Concealment | Selection Bias: Researchers may consciously or unconsciously influence which group a participant enters. | - Central Web-Based System: The gold standard. Prevents foreknowledge of assignment.- Sequentially Numbered, Opaque, Sealed (SNOSE) Envelopes: A practical, low-tech solution. Must be strictly controlled. |
| Blinding (Participants & Personnel) | Inherent Difficulties: It is often impossible to blind participants to a dietary intervention (e.g., vegan vs. omnivorous diet). | - Active Placebo Control: For supplements, use matched placebos (e.g., identical-tasting/ looking pills/milk shakes).- "Sham" Interventions: In behavioral trials, control groups can receive a similar-but-inert intervention (e.g., general health advice vs. specific dietary advice). |
| Blinding (Outcome Assessors) | Ascertainment Bias: Knowledge of group assignment can influence outcome measurement, especially for subjective outcomes. | - Centralized Endpoint Adjudication: Use a committee blinded to group assignment.- Objective Biomarkers: Prioritize blinded laboratory analyses (e.g., HbA1c, inflammatory markers) over subjective self-reports where possible. |
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful implementation of CONSORT extensions requires meticulous planning and the use of specific tools and materials to ensure methodological rigor and transparent reporting.
Table 4: Essential Research Reagents and Materials for High-Quality Trials
| Category / Item | Function & Purpose in Trial Protocol | Application Notes |
|---|---|---|
| Standardized Herbal Extract | To ensure consistent and reproducible dosing of the active intervention. | Must be chemically characterized (e.g., HPLC fingerprint) and standardized to marker compounds. Requires a Certificate of Analysis (CoA) from the supplier detailing composition and contaminants [72]. |
| Matched Placebo | To enable participant and personnel blinding, reducing performance bias. | Must be indistinguishable from the active intervention in taste, appearance, smell, and texture. Requires collaboration with a specialized manufacturer. |
| Dietary Assessment Tool | To quantify dietary intake and monitor adherence to the intervention protocol. | Options include Food Frequency Questionnaires (FFQs), 24-hour recalls, or weighed food records. The choice depends on the required precision and resources. |
| Adherence Biomarkers | To provide an objective measure of compliance, supplementing self-reported data. | Examples: plasma alkylresorcinols (whole grains), plasma carotenoids (fruit/vegetable intake), urinary nitrogen (protein intake). |
| Allocation Concealment System | To prevent foreknowledge of the next treatment assignment, protecting the random sequence. | A central, 24-hour web-based randomization service is the gold standard. Alternatives include a pharmacy-controlled system or sequentially numbered, opaque, sealed envelopes. |
| Data Management System | To ensure accurate, secure, and reliable data collection, storage, and audit trails. | Electronic Data Capture (EDC) systems are preferred for multi-center trials. Must have role-based access and an audit trail function. |
| Statistical Analysis Plan (SAP) | A pre-defined, detailed plan for the final analysis to prevent data dredging and selective reporting. | Must be finalized before database lock and unblinding. It should detail how all CONSORT items related to analysis (e.g., handling missing data, subgroup analyses) will be addressed. |
The rigorous application of CONSORT extensions for non-pharmacological and herbal interventions is not merely a bureaucratic exercise for journal submission; it is a fundamental component of methodological rigor in nutritional sciences research. By systematically employing the CONSORT-NPT, CONSORT-Herbal, and other relevant extensions, alongside complementary tools like TIDieR, researchers can design protocols that proactively address the unique challenges of their field. This structured approach ensures that the resulting trial reports are transparent, complete, and reproducible, thereby maximizing the validity, utility, and impact of their research. This, in turn, strengthens the evidence base necessary to inform public health policy and clinical practice in nutrition.
Core Feasibility Indicators for Nutritional Intervention Trials
Feasibility and pilot studies are a necessary first step to assess the feasibility of methods and procedures to be used in a larger-scale study [74]. They test logistical aspects of the future study to incorporate them into the final study design, increasing the likelihood of success in the future definitive trial [74] [75]. The table below outlines primary feasibility indicators to be evaluated.
Table 1: Key Feasibility Indicators and Assessment Methods for Nutritional Intervention Trials
| Feasibility Domain | Specific Indicator | Quantitative Assessment Method | Qualitative Assessment Method | Progression Criteria for Main Trial |
|---|---|---|---|---|
| Recruitment Feasibility | Recruitment rate; Screen-to-randomization ratio [74] | Number of participants approached, eligible, and consented per month; Reasons for ineligibility [74] | Interviews with potential participants on barriers/facilitators to participation | >80% of target recruitment rate met; <50% of screened participants found ineligible |
| Retention & Adherence | Drop-out rate; Intervention adherence rate [74] | Percentage of completed follow-up assessments; Percentage of prescribed nutritional sessions/dosages consumed [74] [4] | Exit interviews with drop-outs; Focus groups on adherence challenges | <20% attrition rate; >70% protocol adherence |
| Intervention Fidelity | Provider competence; Protocol deviation rate [74] | Structured observer ratings using checklists; Number of major protocol deviations [74] | Semi-structured interviews with interventionists | >90% of key intervention components delivered correctly |
| Acceptability | Participant satisfaction; Perceived burden [74] | Structured surveys (e.g., 5-point Likert scales); Completion times for data collection [74] | Open-ended interviews regarding program components and burden | >80% of participants rate intervention as "acceptable" or "highly acceptable" |
| Data Collection Procedures | Completion rates; Data quality [74] | Percentage of missing data for key outcomes; Evidence of reliability/validity in target population (e.g., floor/ceiling effects) [74] | Cognitive interviews to ensure understanding of questions and measures | <5% missing data for primary outcome measures |
Experimental Protocols for Feasibility Assessment
Protocol for Testing Participant Recruitment and Retention Strategies
Objective: To determine the feasibility of recruitment strategies and the acceptability of retention procedures for a full-scale nutritional RCT.
Materials:
- Research Reagent Solutions: Screening logs (electronic or paper-based), standardized eligibility checklist, informed consent forms, participant tracking system (e.g., REDCap database), reminder system (e.g., SMS, email).
Methodology:
- Screening: Maintain a detailed screening log documenting the number of individuals approached, assessed for eligibility, and the specific reasons for exclusion [74]. This log is essential for calculating the screen-to-randomization ratio.
- Consenting: Pilot the informed consent process. Document the time taken for participants to understand the information and note any frequently asked questions.
- Randomization: Test the randomization procedure. For nutritional interventions, consider the most appropriate type (e.g., block randomization to ensure equal group sizes if recruitment is slow or stratified randomization if age or disease stage is a major factor influencing the outcome) [4].
- Retention: Implement and test a multi-modal retention strategy, which may include regular check-ins, flexible scheduling of assessments, and low-burden data collection methods. Track adherence to the nutritional protocol and follow-up assessment completion rates [74].
- Assessment: At the end of the study, conduct brief exit interviews or surveys with a sub-sample of participants to assess the perceived burden of the intervention and data collection procedures, and reasons for continued participation or dropout.
Protocol for Assessing Intervention Fidelity and Acceptability
Objective: To ensure the nutritional intervention can be delivered as intended and is acceptable to the target population.
Materials:
- Research Reagent Solutions: Standardized Intervention Manual, Participant Program Manual, Fidelity Checklists, Adherence Measures (e.g., food diaries, biomarker assays, returned supplement containers), Acceptability Surveys.
Methodology:
- Interventionist Training: Recruit and train interventionists using a standardized protocol and training manual. Record the number of interventionists starting and completing training [74].
- Competence Assessment: Assess interventionist competence post-training through knowledge tests and role-playing exercises observed with a structured checklist [74].
- Delivery Fidelity: During the pilot study, directly observe or audio-record a random sample (e.g., 20%) of intervention sessions. Use a fidelity checklist to score the adherence to the manualized protocol.
- Participant Adherence: Monitor participant adherence to the nutritional intervention. This is critical in nutrition research and can be measured via self-report (e.g., daily food records, 24-hour dietary recalls) [4], objective measures (e.g., biomarkers in blood or urine), or returned product counts for supplementation studies.
- Acceptability Evaluation: Administer a structured acceptability survey to all participants post-intervention. Supplement this with qualitative semi-structured interviews to explore in-depth perceptions of the intervention's benefits, drawbacks, and suggested improvements [74].
Visualization of Feasibility Study Workflow
The following diagram outlines the key stages and decision points in a feasibility or pilot study for a nutritional intervention trial.
Essential Research Reagents and Materials for Nutritional Feasibility Studies
Table 2: Research Reagent Solutions for Nutritional Intervention Trials
| Item | Function/Application in Feasibility Context |
|---|---|
| Standardized Intervention Manual | Ensizes consistent delivery of the nutritional intervention across providers and sessions, which is critical for testing fidelity [74]. |
| Participant Program Manual | Provides participants with clear guidelines on intervention adherence; its clarity and usability can be tested for acceptability during the pilot [74]. |
| Dietary Assessment Tools (e.g., Food Frequency Questionnaires, 24-hr recall protocols, food diaries) | Used to test the feasibility and burden of data collection methods and to preliminarily assess participant adherence to dietary protocols [4]. |
| Biospecimen Collection Kits (e.g., for blood, urine, saliva) | Tests the feasibility of complex, intrusive, or logistically challenging collection protocols (e.g., fasting bloods, 24-hour urine) and sample stability [74]. |
| Validated Acceptability Surveys | Quantitative tools to systematically assess participant and provider satisfaction with the intervention and study procedures [74]. |
| Adherence Biomarkers (e.g., plasma nutrients, urinary metabolites) | Provides an objective measure of compliance with the nutritional intervention, complementing self-reported data [4]. |
| Electronic Data Capture (EDC) System (e.g., REDCap) | Tests the feasibility of data management workflows, including data entry, quality checks, and security, before the main trial [74]. |
Randomized controlled trials (RCTs) represent the gold standard for evaluating interventions in clinical research [76]. While pharmaceutical trials have established, rigorous methodologies governed by international regulatory standards, nutritional intervention trials present unique and complex challenges that necessitate distinct methodological approaches [4] [77]. The fundamental differences stem from the nature of the interventions: pharmaceutical drugs typically consist of single, purified chemical compounds, while nutritional interventions involve complex mixtures of food components with synergistic and antagonistic effects [77]. This analysis details the key methodological differences between nutritional and pharmaceutical trial paradigms and provides structured protocols for designing rigorous nutritional interventions within the broader context of randomized controlled trial protocols for nutritional research.
Comparative Analysis of Trial Methodologies
The design, implementation, and interpretation of clinical trials differ substantially between nutritional and pharmaceutical domains. The table below summarizes the core methodological distinctions researchers must consider when designing trials.
Table 1: Fundamental Methodological Distinctions Between Nutritional and Pharmaceutical Trials
| Methodological Aspect | Pharmaceutical Trials | Nutritional Trials |
|---|---|---|
| Intervention Nature | Single, purified chemical compound with precise dosage [77] | Complex mixture of components (food) with variable composition [77] |
| Primary Regulatory Pathway | Investigational New Drug (IND) application leading to formal drug approval [78] | Often classified as dietary supplements or foods; no pre-market efficacy approval required [79] |
| Preclinical Requirements | Extensive animal studies for toxicity and pharmacokinetics mandatory before human trials [78] | Not routinely required, varying by claim and jurisdiction [79] |
| Control Group Design | Placebo-controlled with identical inert substance; double-blinding is standard [77] | Placebo design is complex; often impossible to blind due to taste/smell; "usual care" or active comparisons are common [4] [77] |
| Dosing Precision | High precision with known concentration and pharmacokinetics [77] | Lower precision; dose and composition can be variable; affected by dietary collinearity [77] |
| Key Methodological Challenge | Managing pharmacological side effects and drug interactions | Managing dietary compliance, background diet, and pre-existing food beliefs [77] |
Essential Protocols for Nutritional Intervention Trials
Protocol for Defining and Delivering the Nutritional Intervention
A clearly defined intervention is critical for reproducibility and validity.
- Step 1: Classify the Intervention Type. Determine whether the intervention is a nutrient supplementation (e.g., specific vitamin capsule), food supplementation (e.g., kiwifruit), or whole-diet intervention (e.g., Mediterranean diet) [77] [80]. This determines the level of control and precision possible.
- Step 2: Select the Mode of Delivery. Choose based on the research question, budget, and desired applicability:
- Feeding Trials: Provide all food to participants. This offers the highest control and adherence but is costly and less representative of real-world conditions [77].
- Dietary Counseling: Participants are counseled on what to eat, often by a dietitian. This is highly applicable to clinical practice but introduces variability in the actual intervention delivered and lower precision [77].
- Hybrid or Pragmatic Designs: Combine elements of both, such as providing some meals while counseling on others, or using a preference-adaptive design where participants choose their intervention arm to better reflect real-world decision-making [81] [77].
- Step 3: Standardize and Document the Intervention. Provide detailed documentation of the nutritional composition, including any specific brands, recipes, or nutrient profiles. For nutraceuticals, verify the composition through independent assay if possible [80].
Protocol for Comparator Selection and Blinding
The choice of an appropriate comparator is paramount for attributing any observed effect to the intervention.
- Step 1: Select a Control Group. Options include:
- Placebo Control: An inert substance designed to be indistinguishable from the active intervention. This is the ideal for nutrient supplementation trials (e.g., identical-looking capsule) [77].
- Attention Control: The control group receives a similar amount of contact and education from researchers, but on a neutral topic unrelated to the intervention, to control for the Hawthorne effect (behavior modification due to observation) [77].
- Active Comparator: The intervention is compared against an existing, standard-of-care diet or another active intervention (e.g., comparing oral nutritional supplements to dietary education) [81].
- Usual Care/Waitlist Control: The control group continues with their typical diet and receives the intervention after the trial period.
- Step 2: Maximize Blinding. While full blinding is often unattainable in whole-diet studies, partial blinding can be implemented.
- Single-Blind: The participant is unaware of their group assignment. This can sometimes be achieved in feeding trials where the specific intervention is masked within the provided food.
- Assessor-Blind: The personnel collecting outcome data are kept unaware of the group assignment. This is a critical and feasible step to reduce measurement bias in all nutritional trials [4].
Protocol for Participant Selection and Retention
- Step 1: Define Eligibility with Nutrition in Mind. Beyond standard medical criteria, assess and document baseline dietary habits, food allergies, intolerances, and strong pre-existing dietary beliefs or disordered eating patterns, as these can significantly impact compliance and response [77].
- Step 2: Implement a Run-In Period (Optional). A run-in period can be used to habituate participants to key aspects of the study diet (e.g., high-fiber) or to assess initial compliance. However, this should not be used solely to select highly adherent participants, as it reduces generalizability [77].
- Step 3: Monitor Adherence Rigorously. Use multiple methods: food diaries, 24-hour dietary recalls, biomarkers (e.g., blood levels of specific nutrients), or returned product/package counts for supplements [77] [80].
Protocol for Outcome Assessment and Biostatistics
- Step 1: Select Validated, Clinically Relevant Endpoints. Use patient-centered outcomes relevant to the condition. In nutritional psychiatry, for example, this could include validated scales for depression, anxiety, or quality of life [80]. For gut-brain interaction disorders, symptom severity scores are key [77].
- Step 2: Pre-Specify the Statistical Analysis Plan (SAP). Define all primary and secondary outcomes, the statistical methods for analyzing them, and how missing data and confounding factors (like baseline dietary intake) will be handled [76] [82]. Collaboration with a statistician from the design stage is essential.
The following workflow diagram illustrates the key decision points and processes in designing a nutritional intervention trial.
The Researcher's Toolkit for Nutritional Trials
Successful implementation of nutritional trials requires specialized materials and expertise beyond those needed for standard pharmaceutical research.
Table 2: Essential Research Reagent Solutions for Nutritional Intervention Trials
| Item / Solution | Function & Application | Considerations |
|---|---|---|
| Placebo Matching | To create a credible inert control for blinding, especially in supplementation trials. | Must match the active intervention in taste, appearance, and texture. For foods, this can be extremely challenging and costly [77]. |
| Standardized Dietary Assessment Tools (e.g., FFQs, 24-hr recalls) | To quantify baseline diet, monitor adherence, and assess dietary collinearity during the trial [77]. | Choose validated tools appropriate for the target nutrients and population. |
| Biomarker Assay Kits | To objectively measure nutrient levels (e.g., vitamins, fatty acids) and validate compliance or biological effect [80]. | Adds cost but significantly strengthens the evidence by providing an objective measure of adherence. |
| Specialized Personnel (Dietitians, Nutrition Scientists) | To design a nutritionally adequate, culturally appropriate intervention and deliver dietary counseling [77] [80]. | Essential for ensuring the intervention is safe, palatable, and feasible for participants to follow. |
| Pre-specified Statistical Analysis Plan (SAP) | A detailed plan outlining how data will be analyzed, including how to handle confounding from background diet [76] [82]. | Critical for maintaining statistical rigor and reducing bias in data analysis. |
Navigating the methodological landscape of nutritional intervention trials requires a nuanced understanding of their inherent complexities, including intervention complexity, blinding difficulties, and compliance dynamics. By implementing the detailed protocols outlined for intervention delivery, control group design, and participant management, researchers can significantly enhance the internal validity and clinical relevance of their studies. Adherence to these specialized methodological standards, supported by a multidisciplinary team, is fundamental to generating high-quality evidence that can effectively inform public health guidelines and clinical practice in the field of nutrition.
Quality Assessment Tools and Risk of Bias Evaluation for Nutritional RCTs
Randomized controlled trials (RCTs) constitute a fundamental pillar of evidence-based nutrition research, yet they present unique methodological challenges that distinguish them from pharmaceutical trials. The complex nature of dietary interventions, which often involve behavioral components, educational strategies, and environmental modifications, introduces specific considerations for quality assessment and risk of bias evaluation [4]. Nutritional interventions range from single-nutrient supplementation to comprehensive dietary pattern changes, each carrying distinct implementation challenges that can influence trial outcomes. Without rigorous quality assessment, nutrition research may yield biased results that misinform clinical practice and public health policy.
The current evidence base for nutritional guidelines suffers from significant limitations. Only approximately 26% of clinical recommendations from nutrition professionals are classified as level I evidence, with the remaining 74% relying on lower-quality evidence [4]. This concerning statistic underscores the critical importance of proper quality assessment methodologies in nutritional RCTs. Furthermore, a recent meta-epidemiological study examining nutrition RCTs found that 70% of trials were rated as having "some concerns" regarding risk of bias, while 11.7% were rated as "high risk" of bias [83]. These findings highlight the pervasive nature of methodological challenges in nutrition research and the need for standardized assessment approaches.
Risk of Bias Assessment Tools for Nutritional RCTs
Cochrane Risk of Bias Tools
The Cochrane Risk of Bias (RoB) tools represent the most widely accepted methodology for assessing methodological quality in clinical trials. For nutritional RCTs, both the RoB 2.0 tool for randomized trials and the ROBINS-I tool for non-randomized studies provide structured approaches to evaluate potential biases [83] [84].
The Cochrane RoB 2.0 tool assesses five critical domains: (1) bias arising from the randomization process; (2) bias due to deviations from intended interventions; (3) bias due to missing outcome data; (4) bias in measurement of the outcome; and (5) bias in selection of the reported result [83]. Each domain is evaluated with a series of signaling questions, leading to an overall judgment of "low risk," "some concerns," or "high risk" of bias. A recent meta-epidemiological study applying this tool to nutrition RCTs found that most methodological characteristics did not significantly exaggerate effect estimates, except for biases related to deviations from intended interventions (RRR 1.29, 95% CI 1.13 to 1.48) [83].
For nutritional epidemiologic studies, which often employ observational designs due to the practical challenges of randomizing dietary exposures, the ROBINS-I tool provides a structured evaluation of bias risk across seven domains: confounding, participant selection, exposure classification, departures from intended exposures, missing data, outcome measurement, and selective reporting [85]. However, a methodological review found that 87.3% of systematic reviews of nutritional epidemiologic studies attempted risk of bias assessment, but commonly used tools frequently neglected important sources of bias and included constructs unrelated to risk of bias [85].
Table 1: Cochrane Risk of Bias 2.0 (RoB 2.0) Domains and Nutritional Research Considerations
| Domain | Key Considerations for Nutritional RCTs | Common Challenges |
|---|---|---|
| Randomization Process | Adequate sequence generation and allocation concealment | Difficulty blinding participants to dietary interventions |
| Deviations from Intended Interventions | Adherence to dietary protocol, contamination between groups | Cross-over between intervention and control diets |
| Missing Outcome Data | Incomplete outcome data, loss to follow-up | Differential dropout related to dietary intervention burden |
| Outcome Measurement | Blinding of outcome assessors, objective vs. subjective measures | Self-reported dietary intake and outcomes |
| Selection of Reported Results | Pre-specified analysis plan, selective reporting | Multiple testing across numerous nutritional biomarkers |
Additional Quality Assessment Instruments
Beyond the Cochrane tools, several other instruments are commonly employed to assess study quality in nutrition research. The Newcastle-Ottawa Scale is frequently used for observational studies, evaluating selection, comparability, and outcome assessment [86]. For systematic reviews of nutritional interventions, the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines provide a structured framework for ensuring comprehensive reporting [9] [86].
A methodological review of systematic reviews in nutritional epidemiology revealed important limitations in how risk of bias assessments are conducted and applied. Most reviews (65.3%) did not adequately incorporate risk of bias assessments in their synthesis of evidence, and while more than half considered biases due to confounding and exposure misclassification, other biases such as selective reporting were rarely considered (0.7%) [85]. This highlights a significant gap in the application of quality assessment tools in nutrition research synthesis.
Methodological Protocols for Risk of Bias Assessment
Standardized Assessment Workflow
Implementing a standardized protocol for risk of bias assessment ensures consistency and comprehensiveness across evaluations. The following workflow provides a structured approach for assessing nutritional RCTs:
Step 1: Pre-assessment Preparation
- Register the assessment protocol a priori using platforms such as OSF (Open Science Framework) or PROSPERO [9] [86]
- Define specific assessment criteria tailored to nutritional interventions
- Train multiple reviewers and establish calibration exercises to ensure consistent application of assessment tools [85]
Step 2: Domain-Specific Evaluation
- Systematically evaluate each domain of the selected risk of bias tool
- Document supporting information and justifications for each judgment
- Pay particular attention to nutritional-specific challenges including adherence measurement, blinding difficulties, and dietary assessment methods [4]
Step 3: Synthesis and Application
- Summarize risk of bias judgments across studies
- Incorporate assessments into evidence synthesis through sensitivity or subgroup analyses
- Consider the potential impact of identified biases on overall conclusions [85]
The following workflow diagram illustrates the standardized risk of bias assessment process for nutritional RCTs:
Domain-Specific Assessment Criteria for Nutritional RCTs
Each domain in risk of bias assessment requires specific considerations for nutritional interventions:
Bias arising from the randomization process: Assess whether the allocation sequence was random and adequately concealed. For nutritional RCTs, consider whether baseline nutritional status or dietary patterns were balanced between groups, as these can be important prognostic factors [4] [87]. In trials with small sample sizes, check whether stratified randomization was used to balance key nutritional covariates.
Bias due to deviations from intended interventions: Evaluate adherence to the nutritional intervention and whether appropriate analysis methods (such as intention-to-treat) were used. This domain is particularly challenging in nutrition research, as deviations from dietary protocols are common and often poorly reported [83] [4]. A recent meta-epidemiological study found this domain was particularly problematic in nutrition RCTs, with biases in this area leading to potential underestimation of intervention effects [83].
Bias due to missing outcome data: Assess whether missingness is related to the true value of the outcome, which may occur if participants finding dietary interventions burdensome are more likely to drop out. Statistical methods such as multiple imputation or pattern-mixture models should be considered when substantial missing data exists [87].
Bias in measurement of outcomes: Evaluate whether outcome assessors were blinded to intervention groups, which is particularly important for subjective outcomes such as patient-reported symptoms. For objective nutritional biomarkers, consider the reliability and validity of the assessment methods [86].
Bias in selection of the reported result: Determine whether the published analyses are consistent with pre-specified statistical plans, and whether multiple outcome measurements or analyses create selective reporting issues. This is especially relevant in nutritional research where numerous biomarkers and secondary outcomes are often measured [85].
Application in Evidence Synthesis
Incorporating Risk of Bias Assessments in Systematic Reviews
Risk of bias assessments should directly inform the synthesis and interpretation of evidence in systematic reviews of nutritional interventions. The following approaches ensure appropriate incorporation:
Stratified Analysis and Meta-Regression
- Group studies by overall risk of bias or specific domain judgments
- Use meta-regression to explore the association between methodological features and effect sizes [85] [83]
- Consider excluding studies with high risk of bias from primary analyses, but include them in sensitivity analyses
Sensitivity Analysis
- Conduct analyses with and without studies at high risk of bias
- Explore the impact of specific methodological limitations on pooled effect estimates [86]
- For nutrition RCTs, pay particular attention to how deviations from intended interventions and missing data are handled
A recent meta-epidemiological study of nutrition RCTs demonstrated the value of this approach, finding that most methodological characteristics did not significantly affect intervention effect estimates, except for biases related to deviations from intended interventions [83]. This underscores the importance of domain-specific rather than overall quality assessments.
Table 2: Interpreting Nutrition RCT Results: Effect Measures and Applications
| Effect Measure | Calculation | Interpretation in Nutrition Context |
|---|---|---|
| Risk Difference (RD) | Riskcontrol - Riskintervention | Absolute difference in outcomes; easily interpretable for clinical decisions |
| Relative Risk (RR) | Riskintervention / Riskcontrol | Ratio of outcomes between groups; consistent across populations |
| Odds Ratio (OR) | Oddsintervention / Oddscontrol | Approximates RR for rare outcomes; commonly used in nutritional epidemiology |
| Hazard Ratio (HR) | Derived from time-to-event analysis | Incorporates timing of events; useful for long-term nutrition trials |
| Number Needed to Treat (NNT) | 1 / RD | Number of patients needing nutritional intervention to prevent one adverse outcome |
Reporting and Interpretation Guidelines
Transparent reporting of risk of bias assessments is essential for interpreting systematic review conclusions. The following practices enhance transparency:
- Include risk of bias tables or figures in publications (such as the robvis visualization tool output) [84]
- Clearly describe how assessments informed inclusion criteria, data synthesis, and conclusions
- Acknowledge limitations of assessment tools when applied to nutritional studies
When interpreting nutrition RCT results, consider both statistical significance and clinical importance. For example, a statistically significant reduction in a nutritional biomarker may not translate to meaningful health outcomes for patients [87]. Additionally, consider the precision of effect estimates through confidence intervals and the applicability of findings to specific populations or settings.
Table 3: Research Reagent Solutions for Nutritional RCT Quality Assessment
| Tool/Resource | Primary Function | Application Context |
|---|---|---|
| Cochrane RoB 2.0 Tool | Domain-based bias assessment for RCTs | Primary evaluation of randomized nutrition trials |
| ROBINS-I Tool | Bias assessment for non-randomized studies | Observational nutritional epidemiologic studies |
| Newcastle-Ottawa Scale (NOS) | Quality assessment for observational studies | Cohort and case-control studies in nutrition |
| PRISMA Guidelines | Reporting standards for systematic reviews | Protocol development and reporting of nutrition meta-analyses |
| CONSORT Statement | Reporting standards for randomized trials | Protocol development and reporting of nutrition RCTs |
| robvis Visualization Tool | Risk of bias visualization | Creating summary plots for publications |
| GRADE System | Certainty of evidence assessment | Translating risk of bias assessments into evidence certainty |
Quality assessment and risk of bias evaluation are essential components of rigorous nutritional research. The unique methodological challenges of dietary interventions—including difficulties with blinding, adherence measurement, and dietary assessment—require tailored approaches to quality assessment. While standard tools like the Cochrane RoB 2.0 provide a foundation for evaluation, their application to nutrition research requires careful consideration of domain-specific issues, particularly those related to deviations from intended interventions and outcome measurement.
Recent evidence suggests that methodological characteristics in nutrition RCTs generally do not exaggerate effect estimates, though biases in implementation and analysis may lead to underestimation of intervention effects [83]. This nuanced understanding highlights the importance of comprehensive quality assessment rather than simplistic quality scoring systems. By implementing standardized assessment protocols, incorporating risk of bias judgments into evidence synthesis, and transparently reporting methodological limitations, nutrition researchers can enhance the validity and utility of clinical trials in informing practice and policy.
Future development of nutritional-specific extensions to existing guidelines and validation of assessment tools across diverse nutritional interventions will further strengthen the evidence base for dietary recommendations. As the field evolves, continued attention to methodological rigor and quality assessment will be essential for advancing nutritional science and translating research findings into effective interventions.
Conclusion
Developing methodologically sound protocols for nutritional RCTs requires careful attention to the unique complexities of dietary interventions, from accounting for food matrix effects and cultural dietary patterns to implementing appropriate blinding and control strategies. The integration of updated SPIRIT 2025 guidelines with nutrition-specific methodological considerations provides a robust framework for enhancing trial quality and translational potential. Future directions should focus on adapting decentralized trial models for nutrition research, developing standardized outcomes for complex dietary patterns, strengthening regulatory pathways for food-based interventions, and increasing patient and public involvement in trial design. By addressing these challenges systematically, researchers can generate higher-quality evidence to inform clinical guidelines and public health policies for nutritional interventions.
References
- 1. [Interpretation and Examples: Key in Updates Statement] SPIRIT 2025 [https://pubmed.ncbi.nlm.nih.gov/40964111/]
- 2. statement: updated SPIRIT for protocols of randomised... 2025 guideline [https://pmc.ncbi.nlm.nih.gov/articles/PMC12035670/]
- 3. statement: SPIRIT guideline for 2025 of... updated protocols [https://www.nature.com/articles/s41591-025-03668-w?error=cookies_not_supported&code=2ccc10b7-f9bc-4e7d-84de-3240eb675a2f]
- 4. Methodological Aspects in Randomized Clinical Trials of Nutritional Interventions - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9227614/]
- 5. Designing and Conducting Randomized Controlled Trials: Basic Concepts for Educating Early Researchers in the Field of Clinical Nutrition - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8425776/]
- 6. : SPIRIT & Adherence Gaps - AARDEX 2025 Trial Protocols [https://aardexgroup.com/revisiting-adherence-in-spirit-2025-guidelines/]
- 7. Challenges in conducting clinical nutrition research - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5654371/]
- 8. and telomere length in humans: a systematic... Nutritional interventions [https://ejim.springeropen.com/articles/10.1186/s43162-025-00569-9]
- 9. JMIR Research Protocols - Nutritional Supplementation for... [https://www.researchprotocols.org/2025/1/e80240]
- 10. The effects of a nutritional on the sports intervention ... nutrition [https://pubmed.ncbi.nlm.nih.gov/39980058/]
- 11. Study protocol | Nutrition Journal [https://nutritionj.biomedcentral.com/submission-guidelines/preparing-your-manuscript/study-protocol]
- 12. Author Guidelines | Clinical Science of Nutrition [https://clinscinutr.org/authorGuidelines]
- 13. Common Limitations and Challenges of Dietary Clinical Trials for... [https://brieflands.com/articles/ijem-108170]
- 14. Interrelations Between Food Form, Texture, and Matrix Influence... [https://link.springer.com/article/10.1007/s13668-022-00413-4]
- 15. Sociocultural Influences on Dietary Practices and Physical Activity Behaviors of Rural Adolescents—A Qualitative Exploration - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6950241/]
- 16. Frontiers | Exploring Socio-Cultural Factors in Human Nutrition: The Importance of Multidimensional Approaches. [https://www.frontiersin.org/research-topics/68861/exploring-socio-cultural-factors-in-human-nutrition-the-importance-of-multidimensional-approaches]
- 17. Avoid FDA Letters: When Supplement Studies Require an IND [https://www.linkedin.com/pulse/drug-vs-dietary-supplement-research-legal-traps-sponsors-db04e]
- 18. Releases FDA Human 2025 Program Foods Agenda | Guidance FDA [https://www.fda.gov/food/hfp-constituent-updates/fda-releases-2025-human-foods-program-guidance-agenda]
- 19. NPA updates on dietary supplement issues, from the NDI guidance to... [https://www.nutraingredients.com/Article/2025/07/07/npa-updates-on-dietary-supplement-issues-from-the-ndi-guidance-to-nac-and-nmn/]
- 20. Randomised controlled trials—the gold standard for effectiveness research - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6235704/]
- 21. Randomized controlled trial - Wikipedia [https://en.wikipedia.org/wiki/Randomized_controlled_trial]
- 22. Make Food “Healthy†Again: FDA ’s Resolution for a Healthier 2025 [https://www.foley.com/insights/publications/2025/02/make-food-healthy-again-fda-resolution-healthier-2025/]
- 23. Reporting of flow diagrams in randomised controlled trials published in periodontology and implantology: a survey | BMC Medical Research Methodology | Full Text [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-023-01923-7]
- 24. in Ethical Studies Considerations Nutrition [https://www.numberanalytics.com/blog/ethical-considerations-nutrition-studies]
- 25. Frontiers | Perspective on the ethics of AI at the intersection of... [https://www.frontiersin.org/journals/aging/articles/10.3389/fragi.2025.1423759/full]
- 26. Supplementation for Obsessive-Compulsive Disorder... Nutritional [https://pubmed.ncbi.nlm.nih.gov/41252714/]
- 27. 2025 Dietary Guidelines Advisory Committee Systematic Reviews | Nutrition Evidence Systematic Review [https://nesr.usda.gov/2025-dietary-guidelines-advisory-committee-systematic-reviews]
- 28. Statistics and Data on Nutrition - Nutrition and Dietetic Resources - Levy Library Guides at Icahn School of Medicine at Mount Sinai [https://libguides.mssm.edu/nutrition-dietetic-resources/statistics-data]
- 29. Presenting Quantitative Data Graphically | Mathematics for the Liberal Arts [https://courses.lumenlearning.com/waymakermath4libarts/chapter/presenting-quantitative-data-graphically/]
- 30. Presentation of Quantitative Data: Graphical | StudySmarter [https://www.studysmarter.co.uk/explanations/psychology/data-handling-and-analysis/presentation-of-quantitative-data/]
- 31. Presentation of Quantitative Data | PSM Made Easy [https://ihatepsm.com/blog/presentation-quantitative-data]
- 32. What is Randomized ( Controlled ) Trial ? RCT Methodology [https://insights.swayable.com/rct-methodology-overview]
- 33. How to design a randomized clinical trial: tips and tricks for conduct a successful study in thoracic disease domain - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5594116/]
- 34. in Covariate Clinical Trials with Missing... Adjustment Randomized [https://pmc.ncbi.nlm.nih.gov/articles/PMC12094063/]
- 35. Rationale and design of repeated cross-sectional studies to evaluate... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7594472/]
- 36. Guidelines for randomized clinical trial protocol content: a systematic review | Systematic Reviews | Full Text [https://systematicreviewsjournal.biomedcentral.com/articles/10.1186/2046-4053-1-43]
- 37. Blinding in Clinical Trials: Seeing the Big Picture - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8308085/]
- 38. Frontiers | Designing, Conducting, and Documenting Human Nutrition ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2021.782703/full]
- 39. Reporting Methods of Blinding in Randomized Trials Assessing Nonpharmacological Treatments - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC1800311/]
- 40. Sealed Envelope | Blinding and allocation concealment [https://www.sealedenvelope.com/randomisation/blinding/]
- 41. Selection of Control, Randomization , Blinding , and Allocation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6743387/]
- 42. Unlocking the Power of RCTs in Community Nutrition Research [https://www.numberanalytics.com/blog/unlocking-power-rcts-community-nutrition-research]
- 43. Empirical evidence of study design biases in nutrition ... randomised [https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-022-02540-9]
- 44. Blinding of study statisticians in clinical trials: a qualitative study in UK clinical trials units | Trials | Full Text [https://trialsjournal.biomedcentral.com/articles/10.1186/s13063-022-06481-9]
- 45. Impact of digital technology-based health interventions on... nutritional [https://pubmed.ncbi.nlm.nih.gov/41235312/]
- 46. JMIR Cancer - The Effect of Nutritional on Populations... Mobile Apps [https://cancer.jmir.org/2025/1/e50662]
- 47. in the Real World: 5 Uses You'll Actually See ( Nutrition ) Apps 2025 [https://www.linkedin.com/pulse/nutrition-apps-real-world-5-uses-youll-actually-see-2025-vkhoc]
- 48. What are some methods to analyze and report the results of RCTs using statistical software? [https://www.linkedin.com/advice/1/what-some-methods-analyze-report-results]
- 49. Integrating quantitative and qualitative data and findings when undertaking randomised controlled trials - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6886933/]
- 50. Validation of a newly automated web-based 24-hour dietary recall using... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7050885/]
- 51. guides.himmelfarb.gwu.edu/studydesign101/ randomized - controlled ... [https://guides.himmelfarb.gwu.edu/studydesign101/randomized-controlled-trial]
- 52. Randomized Controlled Trials [https://pubmed.ncbi.nlm.nih.gov/32658656/]
- 53. and Attrition Rates of Sustained vs. Intermittent Exercise... Adherence [https://pmc.ncbi.nlm.nih.gov/articles/PMC3181282/]
- 54. The Individualized Diet and Exercise Adherence Pilot Trial (IDEA-P) in... [https://trialsjournal.biomedcentral.com/articles/10.1186/1745-6215-15-354]
- 55. JMIR Research Protocols - Optimizing a Just-in-Time Adaptive... [https://www.researchprotocols.org/2021/12/e33568/]
- 56. Common Limitations and Challenges of Dietary Clinical Trials for... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8453651/]
- 57. Nature of the evidence base and approaches to guide nutrition interventions for individuals: a position paper from the Academy of Nutrition Sciences - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11074602/]
- 58. Frontiers | From plate to planet: culturally responsive culinary practices for health system innovation [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2024.1476503/full]
- 59. and retaining young adults: what can we learn from... Recruiting [https://pmc.ncbi.nlm.nih.gov/articles/PMC10195641/]
- 60. and Recruitment of young women into retention research... nutrition [https://trialsjournal.biomedcentral.com/articles/10.1186/1745-6215-15-23]
- 61. Causal Inference in Diet, Nutrition and Health Outcomes [https://www.frontiersin.org/research-topics/37849/causal-inference-in-diet-nutrition-and-health-outcomes/magazine]
- 62. Nutritional epidemiology: abolition vs defending the status quo - Peter Attia [https://peterattiamd.com/nutritional-epidemiology-abolition-vs-defending-the-status-quo/]
- 63. Personalized nutrition : A review of genotype -based nutritional ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9500586/]
- 64. Polymorphisms, diet and nutrigenomics - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9710387/]
- 65. A Need for a Paradigm Shift in Healthy Nutrition Research - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9062514/]
- 66. Federally Funded Randomized Increase Analysis... Controlled Trials [https://pubmed.ncbi.nlm.nih.gov/37930690/]
- 67. Frontiers | Advances in Nutrition Science and Integrative Physiology: Insights From Controlled Feeding Studies [https://www.frontiersin.org/journals/physiology/articles/10.3389/fphys.2019.01341/full]
- 68. of low-carbohydrate diets on type 2 diabetes... Effectiveness [https://pubmed.ncbi.nlm.nih.gov/40930317/]
- 69. JMIR Research Protocols - Nutritional for the... Interventions [https://www.researchprotocols.org/2024/1/e47196]
- 70. Interactive Visual Displays for Interpreting the Results of Clinical Trials: Formative Evaluation With Case Vignettes - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6037946/]
- 71. Guidelines Simplified for Trial Reporting CONSORT [https://editverse.com/consort-guidelines-simplified-for-trial-reporting/]
- 72. 2025 Statement: updated CONSORT for guideline ... reporting [https://www.equator-network.org/reporting-guidelines/consort/]
- 73. Delphi survey to gather feedback on a CONSORT extension proposal for nutrition intervention trials - PubMed [https://pubmed.ncbi.nlm.nih.gov/39891676/]
- 74. Guidelines for Designing and Evaluating Feasibility - PMC Pilot Studies [https://pmc.ncbi.nlm.nih.gov/articles/PMC8849521/]
- 75. Guidance for conducting feasibility and pilot for... studies [https://pilotfeasibilitystudies.biomedcentral.com/articles/10.1186/s40814-020-00634-w]
- 76. Clinical Trial Design - an overview | ScienceDirect Topics [https://www.sciencedirect.com/topics/pharmacology-toxicology-and-pharmaceutical-science/clinical-trial-design]
- 77. Optimal Design of Clinical Trials of Dietary Interventions in Disorders of Gut-Brain Interaction - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9169766/]
- 78. Step 3: Clinical Research | FDA [https://www.fda.gov/patients/drug-development-process/step-3-clinical-research]
- 79. Nutraceutical- Difference, Trends & Opportunities Pharmaceutical vs [https://www.wbcil.com/blog/pharma-vs-nutraceutical-apis-what-brands-should-understand-in-2025/]
- 80. Methodological and reporting recommendations for clinical trials in Nutritional Psychiatry: Guidelines from the International Society for Nutritional Psychiatry Research | British Journal of Nutrition | Cambridge Core [https://www.cambridge.org/core/journals/british-journal-of-nutrition/article/methodological-and-reporting-recommendations-for-clinical-trials-in-nutritional-psychiatry-guidelines-from-the-international-society-for-nutritional-psychiatry-research/3122BD9864B2333D3FFF967C33F71C64]
- 81. Frontiers | Comparative effects of oral nutritional supplementation vs .... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1606008/full]
- 82. Clinical Trials Methodology [https://www.ejprarediseases.org/clinical-trials-methodology/]
- 83. Most methodological characteristics do not exaggerate effect estimates... [https://pubmed.ncbi.nlm.nih.gov/41177372/]
- 84. Risk of Bias in Randomized Controlled Trials of Nutrition Interventions for Frailty in Older Adults | medRxiv [https://www.medrxiv.org/content/10.1101/2025.08.28.25334686v2.full]
- 85. Assessments of risk of bias in systematic reviews of observational nutritional epidemiologic studies are often not appropriate or comprehensive: a methodological study - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8718856/]
- 86. Background [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1667389/xml]
- 87. Nutrition Users’ Guides: RCTs Part 2 – structured guide for interpreting and applying study results from randomised controlled trials on therapy or prevention questions - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11773662/]