Dietary Modulation of the Gut-Brain Axis: Mechanisms, Therapeutic Applications, and Drug Development
This article provides a comprehensive review for researchers and drug development professionals on the critical role of diet in gut-brain-axis communication.
Dietary Modulation of the Gut-Brain Axis: Mechanisms, Therapeutic Applications, and Drug Development
Abstract
This article provides a comprehensive review for researchers and drug development professionals on the critical role of diet in gut-brain-axis communication. It explores the foundational science of the microbiota-gut-brain axis (MGBA), detailing the neural, endocrine, and immune pathways through which dietary components influence brain function and mental health. The content covers methodological approaches for investigating these interactions, including dietary interventions like probiotics, prebiotics, and specific diets (e.g., Mediterranean, high-fiber). It further addresses current challenges in the field, such as individual microbiome variability and barriers to effective signaling, and evaluates the validation of therapeutic strategies through preclinical models and clinical trials. The synthesis aims to inform the development of novel, microbiota-targeted therapeutics and nutritional psychiatry approaches.
The Gut-Brain Dialogue: Unraveling the Core Pathways and Dietary Influences
Core Concepts and Components of the MGBA
The Microbiota-Gut-Brain Axis (MGBA) represents a complex, bidirectional communication network that integrates gastrointestinal tract activity with central nervous system (CNS) functions through neural, immune, endocrine, and metabolic pathways [1] [2]. This integrated system facilitates continuous crosstalk between the gut's resident microbiota and the brain, influencing everything from neurodevelopment to neurodegenerative processes [2] [3]. The conceptual framework of the MGBA has evolved beyond simple gut-brain communication to encompass a broader gut-immune-brain paradigm, recognizing the immune system as a critical intermediary [4].
Central to this axis is the gut microbiota—a diverse ecosystem of trillions of microorganisms including bacteria, viruses, archaea, and fungi that reside primarily in the colon [2]. The collective genome of these intestinal microorganisms contains over three million genes, far surpassing the approximately 23,000 protein-coding genes in the human genome, enabling production of metabolites vital for host functions including immune regulation and gut-brain signaling [1]. The gut microbiome can therefore be considered a functional "second genome" that significantly influences host physiology and brain health [5].
The major components of the MGBA include: (1) the gut microbiota; (2) the intestinal barrier and mucosal immune system; (3) circulating immune cells and cytokines; (4) the enteric nervous system (ENS) and vagus nerve; (5) central autonomic circuits and hypothalamic-pituitary-adrenal (HPA) stress pathways; and (6) CNS interfaces including the blood-brain barrier (BBB) and microglia [2]. Disruption of any single component can reverberate throughout this interconnected system, potentially contributing to neurological and psychiatric disorders [2] [4].
Table 1: Major Components of the Microbiota-Gut-Brain Axis
| Component | Description | Key Functions |
|---|---|---|
| Gut Microbiota | Diverse community of microorganisms in gastrointestinal tract | Produces metabolites (SCFAs, neurotransmitters), regulates immunity, maintains barrier integrity |
| Enteric Nervous System (ENS) | Extensive network of ~500 million neurons in gut wall | Regulates gut motility, secretion, blood flow; communicates with CNS via vagus nerve |
| Vagus Nerve | Primary neural pathway connecting gut and brain | Bidirectional communication; transmits sensory signals from gut to brainstem and efferent commands back to gut |
| Hypothalamic-Pituitary-Adrenal (HPA) Axis | Neuroendocrine stress response system | Releases cortisol in response to stress; modulates gut permeability and immune function |
| Blood-Brain Barrier (BBB) | Semi-permeable interface between blood and CNS | Regulates passage of substances; affected by gut-derived metabolites and inflammatory mediators |
| Immune System | Gut-associated lymphoid tissue (GALT) and systemic immunity | Produces cytokines and inflammatory mediators; shaped by microbial signals |
Key Communication Pathways
The MGBA utilizes multiple interdependent signaling routes to maintain bidirectional communication between gut and brain. These pathways can be categorized into four primary mechanisms: neural, immune, endocrine, and metabolic.
Neural Pathways
The vagus nerve serves as a direct neural highway between the gut and brainstem, with afferent fibers transmitting sensory information from intestinal receptors to the brain and efferent fibers carrying commands back to influence gut activity [2]. This pathway enables rapid communication, allowing gut microbes to influence brain function in real-time through production of neurotransmitters and neuromodulators including GABA, serotonin, and histamine that can activate vagal afferent endings [2]. The critical role of vagal signaling is highlighted by observations that individuals who underwent vagotomy have a lower subsequent risk of developing Parkinson's disease, supporting the hypothesis that α-synuclein pathology may originate in the gut and spread to the brain via this neural route [2].
Immune and Inflammatory Pathways
The gut microbiota profoundly shapes host immunity from development through adulthood [4]. Microbial-associated molecular patterns (MAMPs), such as lipopolysaccharide (LPS) from Gram-negative bacteria, can breach a compromised intestinal barrier and enter circulation, where they activate Toll-like receptors (TLRs) in peripheral tissues and the brain [2]. Even low-grade endotoxin leakage can trigger chronic neuroinflammation through microglial activation via TLR4/NF-κB signaling [2]. Additionally, gut-resident T cells conditioned by microbiota can traffic to the CNS, with specific bacteria driving expansion of pro-inflammatory Th17 cells or anti-inflammatory regulatory T cells (Tregs) that significantly impact neuroinflammation [2].
Endocrine Pathways
The HPA axis represents a key neuroendocrine component of the MGBA, translating stress signals into systemic hormone release that alters gut barrier integrity and immune function [2]. Stress-induced activation of this axis leads to cortisol release that can suppress immune function and shift microbial composition toward a more pro-inflammatory state [1]. Additionally, gut microbes influence the production of various gut hormones including peptide YY (PYY) and glucagon-like peptide-1 (GLP-1) that integrate metabolic and cognitive functions [6].
Metabolic Pathways
Gut microbes produce numerous metabolites through fermentation of dietary components that significantly impact brain function [1]. Short-chain fatty acids (SCFAs) including butyrate, propionate, and acetate are produced from dietary fiber fermentation and function as epigenetic regulators through histone deacetylase (HDAC) inhibition [6]. These metabolites can cross the BBB, influence microglial function, and promote neurotrophic factor expression [1]. Additionally, microbial transformation of primary bile acids into secondary bile acids activates nuclear receptors that modulate metabolic and inflammatory pathways systemically [6].
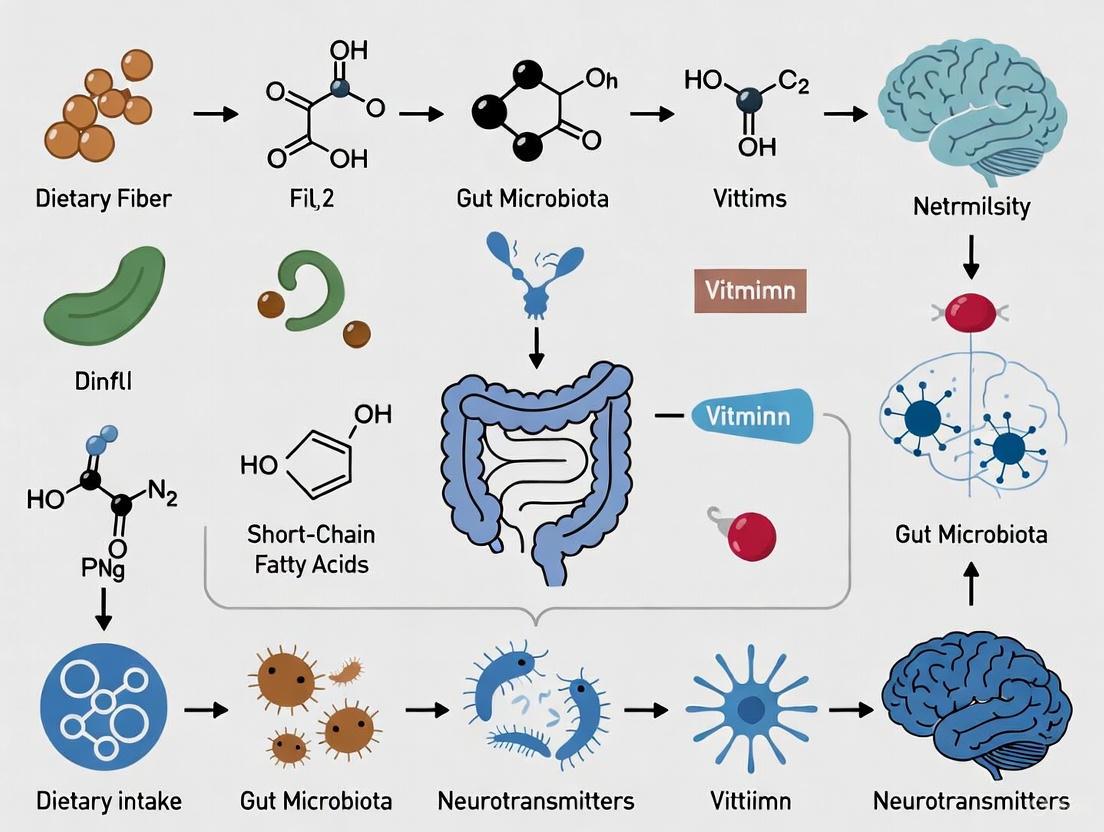
MGBA Communication Pathways Diagram
Microbial Metabolites and Signaling Molecules
The gut microbiota produces a diverse array of metabolites that serve as key signaling molecules along the MGBA. These microbial byproducts represent crucial mechanisms through which gut microbes influence brain function and behavior.
Table 2: Key Microbial Metabolites in MGBA Signaling
| Metabolite Class | Major Representatives | Production Process | Effects on Brain Function |
|---|---|---|---|
| Short-Chain Fatty Acids (SCFAs) | Butyrate, Acetate, Propionate | Fermentation of dietary fiber by gut bacteria | Cross BBB, restore microglial density and morphology, promote GDNF expression in astrocytes, support cognitive function [1] |
| Neurotransmitters | GABA, Serotonin, Dopamine, Glutamate | Synthesis by specific gut bacteria (e.g., Lactobacillus, Bifidobacterium) | Modulate neuronal activity; gut-derived serotonin (90% of body's total) influences mood, sleep, behavior; GABA affects vagus nerve and ENS activity [1] [7] |
| Bile Acids | Primary: cholic acid, chenodeoxycholic acid; Secondary: deoxycholic acid, lithocholic acid | Liver produces primary bile acids; gut bacteria transform to secondary bile acids | Activate nuclear receptors (FXR, TGR5) to modulate metabolic and inflammatory pathways systemically [1] [6] |
| Tryptophan Derivatives | Kynurenine, Indole derivatives | Microbial metabolism of dietary tryptophan | Regulate neuroinflammation; influence microglia immune cells and astrocyte activity in the brain [2] |
| Branch-Chain Amino Acids (BCAAs) | Leucine, Isoleucine, Valine | Microbial metabolism | Serve as precursors for neurotransmitters; influence CNS function [1] |
Short-chain fatty acids (SCFAs) are particularly crucial metabolites produced when undigested dietary fibers reach the colon and are fermented by specific gut bacteria [1]. These compounds include propionic acid (C3), butyric acid (C4), valeric acid (C5), acetic acid (C2), and formic acid (C1) [1]. Under stable conditions, monocarboxylate transporters facilitate the passage of SCFAs across the BBB, where they are detected in human cerebrospinal fluid [1]. Butyrate, specifically, promotes glial cell-derived neurotrophic factor (GDNF) expression in astrocytes, which are essential for regulating neuronal growth, survival, and synaptic differentiation [1].
The production of neurotransmitters by gut microbiota represents another significant pathway. Notably, approximately 90% of serotonin is generated in the gut under microbial influence, interfering with mood, sleep, and other brain functions [1] [7]. GABA, the main inhibitory neurotransmitter in the brain, is produced by human microbiota communities including Lactobacillus brevis and Bifidobacterium dentium [1]. While GABA produced in the gut cannot cross the BBB directly, it can indirectly affect brain activity by influencing vagus nerve or enteric nervous system activity [1].
Experimental Methodologies in MGBA Research
Research investigating the microbiota-gut-brain axis employs diverse methodologies ranging from preclinical animal models to human clinical trials and advanced omics technologies. Understanding these experimental approaches is essential for evaluating evidence in this rapidly evolving field.
Animal Models
Germ-free (GF) mouse models have been fundamental in establishing the importance of gut microbiota for normal brain development and function [4]. These studies revealed that the absence of gut microbiota leads to alterations in stress responses, neurotransmitter levels, and neurodevelopment [4]. Colonization of GF mice with specific microbiota restores normal levels of stress hormones and brain-derived neurotrophic factor (BDNF), highlighting microbial influence on neuronal function [4]. Importantly, recolonization later in life fails to fully restore typical brain function, indicating critical windows for microbiota-brain interactions during early development [3].
Fecal microbiota transplantation (FMT) studies in animals provide evidence for causal relationships between gut microbiota and behavior. For instance, transplantation of intestinal flora from patients with autism spectrum disorder (ASD) into germ-free mice induced ASD-like behaviors in recipient animals [5]. Similarly, transplants of feces from anxiety-like mice promoted anxiety-like behavior in sterile mice and vice versa [5].
Human Studies
Human research encompasses observational studies that compare gut microbiota composition between healthy individuals and those with neurological or psychiatric conditions, intervention studies investigating probiotics, prebiotics, and dietary modifications, and correlational studies examining relationships between microbial metabolites, imaging findings, and behavioral measures [8].
Large-scale epidemiological analyses, such as those leveraging the US National Health and Nutrition Examination Survey (NHANES) data, have established associations between dietary patterns, gut microbiota profiles, and disease risk [6]. Additionally, randomized controlled trials (RCTs) demonstrate that specific probiotic formulations can mitigate stress and inflammation in humans via gut microbiota modulation [6].
Analytical Techniques
Advanced omics technologies have revolutionized MGBA research. 16S ribosomal RNA and whole genome sequencing techniques enable characterization of gut microbiota diversity [5]. Metagenomics, metabolomics, and other omics analysis techniques combined with microbiome-wide association studies facilitate identification of intestinal flora types associated with disease and elucidate molecular mechanisms of specific interactions [5].
Integration of multi-omics data including metagenomics, metabolomics, and transcriptomics is increasingly essential to elucidate mechanistic links between diet, microbial metabolites, and host physiological outcomes [6]. These approaches are being enhanced by artificial intelligence and machine learning to analyze complex datasets and predict individual responses to dietary interventions [6].
MGBA Research Workflow Diagram
The Scientist's Toolkit: Research Reagent Solutions
MGBA research requires specialized reagents and tools to investigate the complex interactions between diet, gut microbiota, and brain function. The following table details essential research materials and their applications in experimental protocols.
Table 3: Essential Research Reagents and Materials for MGBA Investigations
| Research Tool Category | Specific Examples | Research Applications | Key Functions |
|---|---|---|---|
| Probiotic Strains | Lactobacillus brevis, Bifidobacterium dentium, Bifidobacterium adolescentis CCFM1447, Bifidobacterium longum subsp. infantis CCFM1426 | Intervention studies; mechanistic investigations | Produce neurotransmitters (GABA); modulate immune responses; enrich beneficial bacteria; mitigate osteoporosis; enhance anti-colitic effects [1] [6] |
| Prebiotics & Dietary Fibers | Human milk oligosaccharides (HMOs), granola with multiple prebiotics, high-fiber diets | Dietary intervention studies; microbial metabolism research | Serve as substrates for SCFA production; increase Bifidobacterium abundance; improve stress/sleepiness; shape microbial community structure [1] [6] |
| Germ-Free Animal Models | Germ-free (axenic) mice, Gnotobiotic animals | Causal mechanism studies; microbiota transfer experiments | Enable study of microbiota absence on neurodevelopment; permit colonization with specific microbial communities; establish causal relationships [5] [4] |
| Molecular Biology Reagents | 16S rRNA sequencing kits, Metagenomic sequencing reagents, Metabolomics platforms | Microbiome composition analysis; functional characterization | Enable taxonomic profiling; facilitate whole genome sequencing; identify microbial metabolic pathways; quantify microbial metabolites [5] [8] |
| Immunoassay Kits | Cytokine panels (TNF-α, IL-10), LPS detection assays, Cortisol/ Corticosterone ELISA | Inflammatory pathway analysis; HPA axis assessment | Quantify inflammatory mediators; measure endotoxin translocation; assess stress hormone levels; evaluate gut barrier integrity [1] [2] |
| Vegfr-2-IN-13 | Vegfr-2-IN-13, MF:C24H18N6O2S, MW:454.5 g/mol | Chemical Reagent | Bench Chemicals |
| Rifasutenizol | Rifasutenizol, CAS:1001314-13-1, MF:C48H61N7O13, MW:944.0 g/mol | Chemical Reagent | Bench Chemicals |
Dietary Modulation of the MGBA
Diet represents the most significant modifiable factor influencing the gut microbiota and consequently the MGBA. Nutritional neuroscience has emerged as a promising approach for managing gut-brain axis communication and mental health disorders through various pathways [9].
Dietary Patterns and Microbial Composition
Different dietary patterns exert distinct effects on gut microbial communities. High-fiber, plant-based diets including the Mediterranean diet enhance microbial diversity, decrease inflammation, and improve gut-brain communication [7]. These diets act as prebiotics that nourish beneficial bacteria like Bifidobacteria and Lactobacilli, which produce SCFAs essential for maintaining intestinal barrier integrity and regulating immune responses [7].
Conversely, Western dietary patterns high in refined sugars, animal fats, and low in fiber are associated with dysbiosis—a microbial imbalance marked by decreased diversity and increased populations of pathogenic bacteria like Bacteroides and Alistipes that promote systemic inflammation and increase gut permeability [7]. Such diets reduce beneficial bacterial populations, diminishing SCFA production and potentially exacerbating symptoms of mood disorders [7].
Specific Dietary Components
Polyphenols, found in plant-based foods like berries, tea, and olive oil, possess antioxidant and anti-inflammatory properties that benefit the gut microbiota by supporting growth of beneficial bacteria while inhibiting harmful species [7]. Similarly, plant-based proteins in legumes and nuts encourage growth of health-promoting microbes, whereas high intake of animal protein is associated with bile-tolerant bacteria such as Bilophila that are linked to inflammation and increased gut permeability [7].
Soluble fibers, abundant in foods like oats, apples, and citrus fruits, serve as food sources for gut bacteria while also reducing harmful bacterial adhesion to the gut lining, thus supporting the gut barrier and enhancing immune function [7]. In contrast, diets high in processed foods can lead to production of harmful metabolites like trimethylamine-N-oxide (TMAO), which is associated with cardiovascular disease risks [7].
Timing of Dietary Interventions
Emerging evidence suggests the existence of sensitive periods when microbiome-targeted interventions may exert maximal and long-lasting effects on neurodevelopment [3]. The prenatal period is particularly critical, with maternal microbial metabolites such as SCFAs crossing the placenta and influencing fetal immune and brain development [3]. During infancy (0-3 years), a highly dynamic microbiota coincides with rapid synaptogenesis, myelination, and immune system maturation [3]. Studies in germ-free animals indicate that outside this early-life window, successful restoration of normal brain function cannot be fully achieved [3].
Implications for Neurological and Neuropsychiatric Disorders
Dysregulation of the MGBA has been implicated in a wide spectrum of neurological and neuropsychiatric conditions, offering new perspectives on disease mechanisms and potential therapeutic approaches.
Neurodevelopmental Disorders
Pediatric neurodevelopmental disorders including autism spectrum disorder (ASD), attention deficit hyperactivity disorder (ADHD), Rett syndrome (RTT), and Tourette syndrome (TS) are associated with alterations in the MGBA [3]. Children with ASD often exhibit distinct gut microbiota profiles characterized by increased abundances of genera such as Clostridium, Ruminococcus, Sutterella, and Lactobacillus, alongside decreased levels of Bifidobacterium, Akkermansia, Blautia, and Prevotella [1]. Fecal microbiota transplantation from ASD patients to germ-free mice is sufficient to induce ASD-like behaviors in recipient animals, suggesting a causal role for gut microbes in these neurodevelopmental conditions [5].
Neurodegenerative Diseases
The MGBA plays significant roles in the onset and progression of neurodegenerative diseases including Alzheimer's disease (AD), Parkinson's disease (PD), and multiple sclerosis (MS) [2]. Associations between specific gut microbiota and neurodegenerative processes focus on the role of certain bacteria in amyloid aggregation and neuroinflammation [1]. In PD, misfolded α-synuclein protein aggregates may originate in the gut and spread to the brain via vagal nerve fibers [2]. Additionally, distinct gut microbiota profiles are observed in AD patients compared to healthy peers, with chronic constipation often preceding PD motor symptoms by up to 20 years [2].
Psychiatric Conditions
The gut microbiota significantly influences depression, anxiety, and other psychiatric conditions through multiple pathways [1] [8]. Probiotic supplementation has been shown to reduce anxiety and depression in both animal models and clinical trials [5]. The mechanisms underlying these effects involve microbial production of neurotransmitters, regulation of the HPA axis, modulation of systemic inflammation, and influence on neuroplasticity [8]. Psychobiotics—specific probiotics and prebiotics with mental health benefits—demonstrate potential in easing symptoms of anxiety, depression, and stress-related disorders by balancing gut microbiota, decreasing neuroinflammation, and modulating neurotransmitter activity [7].
The microbiota-gut-brain axis represents a transformative paradigm in neuroscience, microbiology, and nutrition research. This bidirectional communication network integrates signals from the gut microbiota, immune system, and brain through neural, endocrine, immune, and metabolic pathways, significantly influencing neurodevelopment, neurodegenerative processes, and psychiatric conditions [1] [2] [4].
Future research will likely focus on precision nutrition strategies that account for individual variability in microbiome composition, host genetics, and environmental factors [6]. Development of targeted interventions using specific dietary components—such as prebiotics, polyphenols, and fermented foods—aims to selectively modulate microbial taxa and metabolic pathways that influence extra-intestinal organs including the brain [6]. Advanced multi-omics integration will be essential to elucidate mechanistic links between diet, microbial metabolites, and host physiological outcomes [6].
Significant challenges remain in establishing causal relationships, accounting for inter-individual variability, and ensuring reproducibility in therapeutic outcomes [2]. Longitudinal human cohorts, mechanistic models, and large-scale clinical trials are needed to clarify the role of the MGBA in health and disease [2] [3]. Additionally, ethical and safety considerations must be addressed in implementing early-life microbiome-based interventions, particularly within pediatric populations [3].
Despite these challenges, understanding the MGBA provides unprecedented opportunities for developing innovative, personalized therapies tailored to individual microbiomes and immune profiles. As research continues to unravel the complexities of this intricate communication network, targeting the MGBA may ultimately redefine clinical approaches to neurological, neurodevelopmental, and psychiatric disorders.
The gut-brain axis represents one of the most dynamic frontiers in physiological research, constituting a complex, multidirectional communication network that integrates gastrointestinal function with cognitive and emotional centers in the brain. While historically conceptualized as primarily neural in nature, contemporary research has revealed that this axis operates through three principal signaling pathways: neural (vagus nerve), endocrine (HPA axis), and immune signaling. These pathways do not operate in isolation but rather form an integrated communication network that enables the gut to influence brain function and vice versa. Within the context of diet-gut-brain research, understanding these pathways is paramount, as nutritional interventions represent the most accessible modality for modulating this axis for therapeutic benefit. This whitepaper delineates the core mechanisms governing these communication pathways, provides experimental methodologies for their investigation, and contextualizes their function within the framework of dietary influence on gut-brain communication.
Core Communication Pathways of the Gut-Brain Axis
Neural Signaling: The Vagus Nerve
The vagus nerve (Cranial Nerve X) serves as the primary neural conduit for rapid communication between the gut and the brain. Accounting for approximately 80-90% of all afferent fibers in the autonomic nervous system, it functions as a critical information superhighway [10] [11].
Anatomical and Functional Basis: Vagal afferent fibers possess endings in the intestinal lamina propria that are in close proximity to the gut epithelium, enabling them to sample a wide array of signals from the gut lumen, including mechanical stretch, nutrients, and microbial metabolites [11]. This sensory information is relayed to the nucleus of the solitary tract (NTS) in the brainstem, which then projects to higher brain centers such as the hypothalamus and amygdala, influencing autonomic regulation, mood, and behavior [12].
The Inflammatory Reflex: A critical function of the vagus nerve is its role in the inflammatory reflex, a hardwired circuit that detects peripheral inflammation and relays this information to the brain, which in turn activates vagal efferent pathways to suppress pro-inflammatory cytokine production in the periphery [13] [11]. This cholinergic anti-inflammatory pathway primarily acts through the release of acetylcholine, which binds to α7 nicotinic acetylcholine receptors (α7 nAChR) on macrophages and other immune cells, inhibiting the release of TNF-α, IL-1β, and IL-6 [13].
Dietary Interactions: Dietary components directly influence vagal tone. For instance, short-chain fatty acids (SCFAs) like butyrate, produced by microbial fermentation of dietary fiber, can directly activate vagal afferents [4] [14]. Furthermore, gut microbes stimulated by a healthy diet can produce neurotransmitters (e.g., GABA) that are sensed by the vagus nerve [15].
Endocrine Signaling: The HPA Axis
The hypothalamic-pituitary-adrenal (HPA) axis is the body's central stress response system and a major endocrine pathway in gut-brain communication. Its activation culminates in the production of glucocorticoids (cortisol in humans), which exert widespread effects on metabolism, immunity, and brain function [16] [11].
Pathway Mechanism: In response to physical or psychological stressors, the hypothalamus releases corticotropin-releasing hormone (CRH). CRH stimulates the pituitary gland to secrete adrenocorticotropic hormone (ACTH), which in turn prompts the adrenal cortex to release glucocorticoids into the systemic circulation [16].
Gut Microbiota and HPA Development: The gut microbiota is essential for the normal developmental programming of the HPA axis. Studies in germ-free (GF) mice demonstrate an exaggerated HPA stress response, which can be normalized by reconstitution with specific microbiota early in life [4]. This highlights a critical window in early life where microbial colonization shapes long-term neuroendocrine resilience.
Dietary and Microbial Modulation: The gut microbiota can modulate HPA axis activity through multiple mechanisms. Microbial metabolites like SCFAs can regulate the activity of enteroendocrine cells, which release gut hormones (e.g., GLP-1, PYY) that indirectly influence the HPA axis [11]. Additionally, gut bacteria can metabolize dietary tryptophan into various indole derivatives and neuroactive substances that can influence systemic levels of serotonin, a key regulator of mood and stress [15] [11]. Dysbiosis, often driven by a Western-style diet, can lead to HPA axis dysregulation and increased susceptibility to stress-related disorders [14].
Immune Signaling
The immune system acts as a fundamental interface translating signals from the gut lumen, including those derived from the microbiota and diet, into systemic and neural messages that can impact brain function [4] [11].
Gut Mucosa as an Immune Interface: The gastrointestinal tract houses the largest collection of immune cells in the body, collectively known as the gut-associated lymphoid tissue (GALT). The gut microbiota plays a crucial role in the development and regulation of both innate and adaptive immunity [4]. For instance, segmented filamentous bacteria drive the differentiation of pro-inflammatory Th17 cells, while other commensals like Clostridium species promote the expansion of anti-inflammatory regulatory T cells (Tregs) [4].
Key Signaling Molecules:
- Microbial Metabolites: SCFAs (acetate, propionate, butyrate) are potent immunomodulators. They inhibit histone deacetylases (HDACs) and activate G-protein-coupled receptors (GPCRs) such as GPR43 and GPR109a on immune cells, leading to the suppression of NF-κB and the promotion of Treg differentiation, thereby exerting anti-inflammatory effects [4] [15].
- Microbial-Associated Molecular Patterns (MAMPs): Bacterial components such as lipopolysaccharide (LPS), peptidoglycan, and flagellin are recognized by pattern-recognition receptors (e.g., Toll-like receptors, TLRs) on host immune cells. This interaction is crucial for maintaining immune homeostasis but can trigger neuroinflammation if the intestinal barrier is compromised ("leaky gut"), allowing excessive MAMP translocation into circulation [4] [12].
Communication to the Brain: Peripheral immune activation leads to the production of pro-inflammatory cytokines (e.g., IL-1β, IL-6, TNF-α). These cytokines can signal the brain directly by crossing the blood-brain barrier via active transport, indirectly via vagal afferents, or by interacting with the brain's vasculature to induce local neuroinflammation, influencing synaptic plasticity and contributing to the pathophysiology of neuropsychiatric and neurodegenerative diseases [4] [15].
Table 1: Key Immune-Modulating Microbial Metabolites and Their Mechanisms
| Metabolite | Primary Microbial Producers | Immunological Mechanism | Impact on Brain Function |
|---|---|---|---|
| Short-Chain Fatty Acids (SCFAs) | Faecalibacterium prausnitzii, Roseburia spp., Lachnospiraceae family [14] [12] | HDAC inhibition; activation of GPCRs (GPR41, GPR43) [4] | Promote microglial homeostasis; strengthen BBB; reduce neuroinflammation [15] |
| Tryptophan Derivatives | Various species metabolizing dietary tryptophan [11] | Aryl hydrocarbon receptor (AhR) activation; regulation of T cell differentiation [4] | Influences production of serotonin and kynurenine pathways; regulates mood and behavior [11] |
| Secondary Bile Acids | Bacteria with bile salt hydrolase activity [15] | Modulation of Farnesoid X Receptor (FXR) and TGR5 signaling [15] | Can compromise gut barrier; systemic influx may trigger neuroinflammatory responses [11] |
Experimental Protocols for Investigating Gut-Brain Communication
To elucidate the mechanisms of the gut-brain axis, researchers employ a combination of animal models, biochemical assays, and neural manipulation techniques. Below are detailed protocols for key experiments.
Assessing Vagus Nerve Dependency
Objective: To determine if a specific dietary or microbial intervention (e.g., a probiotic or SCFA) exerts its effects on the brain via the vagus nerve.
Methodology:
- Animal Model: Utilize adult C57BL/6 mice or Sprague-Dawley rats.
- Surgical Intervention:
- Experimental Group: Perform subdiaphragmatic vagotomy, surgically severing the vagal trunks below the diaphragm.
- Control Group: Undergo a sham surgery, involving identical procedures except for the nerve transection.
- Treatment: Administer the intervention (e.g., oral gavage of a bacterial strain or intraperitoneal injection of a metabolite) post-recovery.
- Outcome Measures:
- Behavioral Tests: Assess anxiety-like behavior (elevated plus maze, open field test) and memory (fear conditioning, Morris water maze).
- Molecular Analysis: Quantify neuroinflammatory markers (IL-1β, TNF-α) and activation of microglia (Iba1 staining) in brain regions such as the hippocampus and hypothalamus.
- Interpretation: If the behavioral or neuroinflammatory benefits of the intervention are abolished in the vagotomy group but preserved in the sham group, the effect is considered vagus nerve-dependent [10] [11].
Evaluating HPA Axis Function
Objective: To measure the impact of gut microbiota manipulation on the neuroendocrine stress response.
Methodology:
- Models of Manipulation:
- Germ-Free (GF) Models: Compare HPA function in GF mice versus conventionally colonized controls.
- Probiotic/FMT Models: Administer a probiotic consortium or perform fecal microbiota transplantation (FMT) from donor mice and test HPA response.
- Dietary Models: Feed animals a defined diet (e.g., high-fat, high-fiber) and monitor subsequent HPA activity.
- Stress Challenge: Subject animals to an acute stressor, such as restraint stress for 15-30 minutes or a forced swim test.
- Sample Collection: Collect blood plasma via tail nick or cardiac puncture at baseline and at multiple time points post-stress (e.g., 0, 30, 60, 90 minutes).
- Biochemical Analysis: Measure circulating corticosterone (in rodents) or cortisol (in humans) levels using a standardized enzyme-linked immunosorbent assay (ELISA) kit.
- Interpretation: An exaggerated or prolonged corticosterone response in GF or dysbiotic animals indicates impaired HPA axis regulation, which can be corrected by microbial or dietary intervention [4] [16].
Profiling the Peripheral Immune Response
Objective: To characterize how dietary interventions alter systemic and mucosal immunity in relation to brain health.
Methodology:
- Intervention: Feed mice a control diet vs. an experimental diet (e.g., Mediterranean-style diet vs. Western-style diet) for 8-12 weeks.
- Sample Collection: At endpoint, collect blood (serum/plasma), mesenteric lymph nodes, and intestinal lamina propria.
- Immune Cell Isolation: Isolate immune cells from lamina propria and spleen using collagenase digestion and density gradient centrifugation.
- Flow Cytometry Analysis:
- Stain cells with fluorescently labeled antibodies against key surface markers.
- Key Cell Populations: Analyze frequencies of T helper (Th)1, Th17, and Regulatory T (Treg) cells (e.g., CD4+FoxP3+ for Tregs).
- Activation Status: Measure expression of activation markers like CD44 and CD69.
- Cytokine Measurement: Quantify levels of pro-inflammatory (IFN-γ, IL-17, IL-6) and anti-inflammatory (IL-10) cytokines in serum and cell culture supernatants using a multiplex cytokine array.
- Correlation with Neural Outcomes: Statistically correlate immune parameters with behavioral data and brain immunohistochemistry to establish functional links [4] [11].
Visualization of Signaling Pathways
The following diagrams, generated using Graphviz DOT language, illustrate the core communication pathways and an integrated experimental workflow.
Neural and Immune Signaling Pathway
Diagram 1: Gut-Brain Neural and Immune Signaling
Integrated Experimental Workflow
Diagram 2: Integrated Gut-Brain Axis Research Workflow
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Reagents and Models for Gut-Brain Axis Research
| Category | Reagent / Model | Specific Example | Primary Function in Research |
|---|---|---|---|
| Animal Models | Germ-Free (GF) Mice | C57BL/6 GF mice [4] | Establish causal role of microbiota by comparing physiology and behavior in absence vs. presence of microbes. |
| Gnotobiotic Models | Mice mono-colonized with specific bacteria (e.g., Bifidobacterium) [4] | Determine the specific function of a single microbial species in the host. | |
| Molecular Tools | ELISA Kits | Corticosterone/Cortisol ELISA, Multiplex Cytokine Panels [16] | Precisely quantify hormone and cytokine levels in plasma, serum, and tissue homogenates. |
| Antibodies for Flow Cytometry | Anti-CD4, Anti-FoxP3 (for Tregs), Anti-CD11b, Anti-Iba1 (for microglia) [4] [11] | Identify, characterize, and sort specific immune cell populations from tissues. | |
| Dietary Components | Defined Diets | High-Fiber Diet, High-Fat Diet (Western Diet) [14] | Systematically investigate the impact of specific macronutrients on the gut-brain axis. |
| Prebiotics | Fructooligosaccharides (FOS), Galactooligosaccharides (GOS) [14] | Selectively stimulate the growth of beneficial gut bacteria to study their downstream effects. | |
| Surgical & Neural Tools | Subdiaphragmatic Vagotomy | Surgical transection of vagal trunks [10] [11] | Critically test the necessity of the vagus nerve in mediating a gut-to-brain signal. |
| Vagus Nerve Stimulation (VNS) | Implantable or non-invasive VNS devices [13] [10] | Therapeutically modulate vagal activity to study impact on inflammation and behavior. | |
| Moclobemide-d4 | Moclobemide-d4, MF:C13H17ClN2O2, MW:272.76 g/mol | Chemical Reagent | Bench Chemicals |
| Cox-2-IN-23 | Cox-2-IN-23, MF:C24H25N5O3S2, MW:495.6 g/mol | Chemical Reagent | Bench Chemicals |
The intricate communication along the gut-brain axis through neural, endocrine, and immune pathways represents a fundamental biological system with profound implications for human health and disease. The vagus nerve provides a rapid, hardwired communication line, the HPA axis integrates stress and metabolic signals, and the immune system acts as a pervasive translator of microbial and dietary cues. These pathways are not merely parallel but are deeply intertwined, creating a robust and adaptive communication network. For researchers and drug development professionals, targeting these pathways—particularly through dietary interventions that modify the gut microbiota—offers a promising, multi-pronged strategy for addressing conditions ranging from neuropsychiatric disorders to neurodegenerative diseases. The future of this field lies in further dissecting the molecular mechanisms of these interactions and leveraging this knowledge to develop precise, microbiota-targeted therapeutics that can effectively modulate this critical axis for improved brain health.
The microbiota-gut-brain axis represents one of the most dynamic frontiers in neurobiology, serving as a critical communication network between gastrointestinal tract microbiota and the central nervous system. This review systematically examines the fundamental roles of microbial-derived metabolites as essential messengers within this axis, focusing on three principal classes: short-chain fatty acids (SCFAs), neurotransmitters, and tryptophan derivatives. We synthesize current understanding of their production, transport mechanisms, and molecular pathways through which they influence neuroimmunoendocrine regulation. Within the context of diet-gut-brain research, we highlight how nutritional interventions shape microbial metabolite production and subsequently impact brain health and disease pathogenesis. The comprehensive analysis presented herein provides a foundation for developing novel therapeutic strategies targeting microbial metabolite pathways for neurological and neuropsychiatric disorders.
The human gastrointestinal tract hosts an extraordinarily complex ecosystem of microorganisms collectively known as the gut microbiota, comprising trillions of bacteria, fungi, viruses, and archaea [17] [15]. This microbial community possesses a genetic potential approximately 150 times greater than the human genome, enabling extensive metabolic capabilities that significantly influence host physiology [15]. The concept of the microbiota-gut-brain axis has emerged as a fundamental framework for understanding the bidirectional communication between these gut microorganisms and the central nervous system (CNS) [17] [15] [18]. This multidirectional signaling network incorporates neuronal, endocrine, metabolic, and immune pathways that continuously mediate cross-talk between the gut and brain [15].
The gut microbiota influences CNS processes through multiple interconnected mechanisms: direct neural signaling via the vagus nerve [17]; modulation of the immune system and neuroinflammation [15] [18]; regulation of the hypothalamic-pituitary-adrenal (HPA) axis [17]; and through the production of myriad neuroactive metabolites [17] [19]. These microbial-derived metabolites, including SCFAs, neurotransmitters, and tryptophan derivatives, have emerged as crucial mediators of gut-brain communication, potentially influencing the development and progression of various neurodegenerative, neuropsychiatric, and neurodevelopmental disorders [17] [19] [15].
Diet represents a primary modulator of the gut-brain axis, serving as both a source of precursors for microbial metabolism and a determinant of microbiota composition [20]. Nutritional components shape the functional capacity of the gut microbiome, influencing the production of key metabolites that subsequently affect brain physiology [20] [21]. This review will explore the specific roles of SCFAs, neurotransmitters, and tryptophan derivatives within this complex network, emphasizing their mechanisms of action and potential therapeutic applications.
Short-Chain Fatty Acids: Microbial Fermentation Products with Systemic Effects
Production, Absorption, and Distribution
Short-chain fatty acids (SCFAs), primarily acetate (C2), propionate (C3), and butyrate (C4), are the main metabolites produced in the colon through bacterial fermentation of indigestible dietary fibers and resistant starch [17] [18]. The human gut produces approximately 500-600 mmol of SCFAs daily, with a typical molar ratio of 60:20:20 for acetate, propionate, and butyrate, respectively, though this ratio can vary significantly based on dietary composition [17] [18]. Following their production, SCFAs are absorbed by colonocytes via H+-dependent monocarboxylate transporters (MCTs) and sodium-coupled monocarboxylate transporters (SMCTs) [17]. While a substantial portion is metabolized locally by gut epithelial cells and hepatocytes, the remainder enters systemic circulation, with concentrations reflecting their production and metabolism rates [18].
Table 1: Primary SCFA-Producing Bacteria and Their Metabolic Pathways
| SCFA | Key Producing Bacteria | Major Metabolic Pathways | Relative Abundance |
|---|---|---|---|
| Acetate | Lactobacillus spp., Bifidobacterium spp., Akkermansia muciniphila, Bacteroides spp. | Glycolysis, Wood-Ljungdahl pathway | ~60% (Highest in circulation) |
| Propionate | Akkermansia muciniphila, Bacteroides spp. | Succinate, acrylate, propanediol pathways | ~20% |
| Butyrate | Faecalibacterium prausnitzii, Eubacterium rectale, Eubacterium hallii | Butyryl-CoA:acetate CoA-transferase, phosphate butyryltransferase, butyrate kinase | ~20% (Lowest in circulation) |
SCFAs readily cross the blood-brain barrier, with measured concentrations in cerebrospinal fluid ranging from 0-171 mM for acetate, 0-6 mM for propionate, and 0-2.8 mM for butyrate [18]. Their presence in the central nervous system enables direct effects on brain cells, particularly microglia, the resident immune cells of the CNS [18].
Molecular Mechanisms of Action
SCFAs exert their physiological effects through two primary molecular mechanisms: activation of G protein-coupled receptors (GPCRs) and inhibition of histone deacetylases (HDACs) [18]. The most extensively studied SCFA receptors are free fatty acid receptor 2 (FFAR2/GPR43) and free fatty acid receptor 3 (FFAR3/GPR41), which are expressed in various tissues including colonic epithelium, immune cells, and the peripheral nervous system [18]. Butyrate's potent inhibition of HDACs leads to epigenetic modifications that alter gene expression patterns in both peripheral tissues and CNS cells [17] [18].
The "SCFAs-microglia pathway" has recently been identified as a crucial communication link within the gut-brain network [18]. SCFAs, particularly butyrate, are essential for maintaining microglial homeostasis and function, influencing their maturation, immune activity, and phagocytic capacity [18]. During dysbiosis or SCFA deficiency, microglia develop dysfunctional characteristics, impairing their ability to perform essential CNS maintenance functions [18].
Experimental Approaches for SCFA Research
Table 2: Key Methodologies for SCFA Analysis in Gut-Brain Axis Research
| Methodology | Application | Key Considerations |
|---|---|---|
| Gas Chromatography-Mass Spectrometry (GC-MS) | Quantification of SCFA concentrations in feces, blood, CSF, and brain tissue | Requires derivatization for volatility; high sensitivity and specificity [18] |
| Liquid Chromatography-Mass Spectrometry (LC-MS) | SCFA quantification in biological samples | No derivatization needed; can detect multiple SCFAs simultaneously [18] |
| Germ-free (GF) animal models | Studying SCFA deficiency effects on microglia and brain function | Complete absence of microbiota; requires strict sterile conditions [18] |
| Gnotobiotic models | Investigating specific bacterial functions | Animals colonized with defined microbial communities [15] |
| SCFA supplementation studies | Therapeutic potential assessment | Direct administration of SCFAs or precursors; dose-dependent effects [17] |
| Receptor knockout models | Elucidating FFAR2/FFAR3 mechanisms | Tissue-specific knockouts reveal localized functions [18] |
Microbial Modulation of Neurotransmitters
Direct and Indirect Regulation of Neurotransmitter Pathways
The gut microbiota significantly influences neurotransmitter systems through both direct production of neuroactive molecules and indirect regulation of host synthesis pathways [19]. Numerous bacterial species can independently synthesize or modulate the synthesis of key neurotransmitters, including γ-aminobutyric acid (GABA), serotonin (5-HT), dopamine, and noradrenaline [17] [19]. Additionally, gut bacteria can signal enteroendocrine cells to regulate the synthesis and release of neurotransmitters, acting locally on the enteric nervous system or transmitting rapid signals to the brain via the vagus nerve [19].
Table 3: Microbial Regulation of Neurotransmitter Systems
| Neuro-transmitter | Key Microbial Genera | Synthesis Mechanism | Primary Functions in Gut-Brain Axis |
|---|---|---|---|
| GABA | Bifidobacterium, Bacteroides fragilis, Parabacteroides, Eubacterium | Direct synthesis from glutamate via gad gene | Modulates synaptic transmission in ENS; regulates feelings of fear and anxiety [19] [21] |
| Serotonin | Clostridial species, Staphylococcus | Induction of synthesis by enterochromaffin cells; precursor availability | Promotes intestinal motility; >90% of body's serotonin located in GI tract [19] [22] |
| Dopamine | Staphylococcus | Direct synthesis; precursor conversion | Affects gastric secretion, motility, and mucosal blood flow [19] |
| Acetylcholine | Lactobacillus plantarum, Bacillus subtilis | Direct synthesis via choline metabolism | Regulates intestinal motility, secretion, and enteric neurotransmission [19] |
| Glutamate | Lactobacillus plantarum, Bacteroides vulgatus | Direct synthesis; stimulation of enteroendocrine cells | Transfer intestinal sensory signals to brain via vagus nerve [19] |
Serotonin: A Prime Example of Gut-Brain Communication
The serotonergic system exemplifies the complex interplay between gut microbiota and neurotransmitter pathways. Over 90% of the body's serotonin is synthesized in the gastrointestinal tract, primarily by enterochromaffin cells (ECs) [22]. The gut microbiota regulates peripheral serotonin production through multiple mechanisms: direct modulation of ECs activity; provision of serotonin precursors; and metabolism of serotonin itself [19] [22]. Importantly, peripheral serotonin cannot cross the blood-brain barrier, highlighting the existence of distinct central and peripheral pools that are differentially regulated yet communicate through neural pathways [22].
Tryptophan serves as the exclusive precursor for serotonin synthesis, with its metabolism representing a critical juncture at which the gut microbiota exerts profound influence [22]. The availability of tryptophan for serotonin synthesis depends on competing metabolic pathways, particularly the kynurenine pathway, which is similarly subject to microbial regulation [22]. This metabolic competition establishes a delicate balance that significantly impacts both gastrointestinal and central nervous system function.
Tryptophan Metabolism: A Microbial-Driven Pathway
Host and Microbial Metabolic Pathways
Tryptophan, an essential amino acid obtained exclusively from dietary sources, serves as a crucial substrate for multiple metabolic pathways that collectively influence gut-brain communication [22] [23]. The host metabolizes tryptophan through three major pathways: the serotonin pathway (1-2% of tryptophan), the kynurenine pathway (>90%), and direct microbial metabolism (remaining tryptophan that reaches the large intestine) [22]. The complex interplay between these pathways determines the physiological consequences of tryptophan metabolism on brain function and behavior.
The kynurenine pathway represents the major route of tryptophan catabolism in the host, producing metabolites with diverse neurological effects [22]. This pathway is initiated by the rate-limiting enzymes indoleamine-2,3-dioxygenase (IDO) and tryptophan-2,3-dioxygenase (TDO), which are expressed in various tissues including the brain, gastrointestinal tract, and liver [22]. Kynurenine is subsequently metabolized through two distinct branches: the kynurenic acid (KYNA) pathway, which produces neuroprotective NMDA receptor antagonists, and the quinolinic acid (QUIN) pathway, which generates neurotoxic NMDA receptor agonists [22]. The balance between these neuroprotective and neurotoxic metabolites is crucial for maintaining CNS homeostasis.
Microbial Metabolites of Tryptophan
Gut microorganisms metabolize tryptophan into various bioactive compounds including indole, tryptamine, and indole derivatives such as indole-3-aldehyde (IAld), indole-3-acetic-acid (IAA), and indole-3-propionic acid (IPA) [22]. These microbial metabolites serve as important signaling molecules that influence host physiology through multiple mechanisms: activation of aryl hydrocarbon receptor (AhR) pathways; modulation of intestinal barrier function; and regulation of immune responses [22] [23].
Specific bacterial taxa demonstrate specialized capacity for tryptophan metabolism. For instance, Clostridium sporogenes and Ruminococcus gnavus convert tryptophan to tryptamine via tryptophan decarboxylases (TrpDs) [22]. Escherichia coli, Clostridium, and Bacteroides species produce indole through tryptophanase (TnaA) activity [22]. Additionally, Lactobacillus and Bifidobacterium species transform tryptophan into indole-3-lactic acid (ILA), which can be further converted to IPA by bacteria including Clostridium and Peptostreptococcus [22]. These microbial metabolites collectively influence gut-brain communication and potentially impact the development of neuropsychiatric conditions.
Methodological Approaches for Tryptophan Research
Investigation of tryptophan metabolism within the gut-brain axis requires integrated methodological approaches that capture the complexity of host-microbe interactions. High-performance liquid chromatography (HPLC) coupled with fluorescence or mass spectrometry detection enables simultaneous quantification of tryptophan and its metabolites in biological samples [22]. Targeted metabolomic approaches provide sensitive measurement of pathway-specific metabolites, while untargeted metabolomics offers discovery-based characterization of novel microbial derivatives [22].
Germ-free animal models demonstrate the essential role of gut microbiota in tryptophan metabolism, showing significantly reduced tryptamine levels and altered kynurenine pathway activity compared to conventionally colonized counterparts [22]. Microbial transplantation studies using defined bacterial communities further elucidate the specific contributions of individual bacterial species to tryptophan metabolic pathways [23]. Additionally, isotopic tracer techniques using stable isotope-labeled tryptophan enable precise tracking of metabolic flux through competing pathways in response to dietary interventions or microbial modulation [22].
The Scientist's Toolkit: Essential Research Reagents and Methodologies
Table 4: Essential Research Reagents and Platforms for Gut-Brain Axis Investigation
| Category | Specific Reagents/Platforms | Research Applications | Key Considerations |
|---|---|---|---|
| SCFA Analysis | GC-MS, LC-MS platforms; commercial SCFA standards; monocarboxylate transporter inhibitors | Quantifying SCFA production, transport, and tissue distribution | Butyrate has lowest systemic concentration due to colonocyte metabolism [18] |
| Neuro-transmitter Detection | HPLC with electrochemical detection; ELISA kits for serotonin/dopamine; receptor agonists/antagonists | Measuring neurotransmitter levels and receptor interactions | Peripheral vs. central neurotransmitter pools must be distinguished [19] |
| Tryptophan Pathway Tools | IDO/TDO inhibitors; kynurenine pathway metabolites; AhR agonists/antagonists | Manipulating tryptophan metabolic flux | Balance between neuroprotective KYNA and neurotoxic QUIN is critical [22] |
| Microbial Manipulation | Antibiotics cocktails; probiotic formulations; prebiotic fibers; gnotobiotic animal facilities | Establishing causal relationships between specific microbes and host physiology | Germ-free models show complete absence of microbial influence [22] [18] |
| Cell Culture Models | Primary microglial cultures; enteroendocrine cell lines; gut organoid systems | Mechanistic studies of host-microbe interactions | Co-culture systems required for cell-cell communication studies [19] |
| Zikv-IN-3 | Zikv-IN-3|Zika Virus Inhibitor|For Research | Zikv-IN-3 is a potent Zika virus inhibitor for research use only (RUO). It is not for human, veterinary, or household use. | Bench Chemicals |
| Phaeosphaone D | Phaeosphaone D, MF:C20H27N3O3S2, MW:421.6 g/mol | Chemical Reagent | Bench Chemicals |
The intricate communication network comprising the microbiota-gut-brain axis represents a paradigm shift in our understanding of how peripheral microbial communities influence central nervous system function and behavior. Microbial-derived metabolites, including SCFAs, neurotransmitters, and tryptophan derivatives, serve as essential messengers within this axis, mediating bidirectional communication through neural, endocrine, metabolic, and immune pathways. The evidence synthesized in this review underscores the fundamental role of diet as a primary modulator of this system, shaping microbial community structure and function with consequent effects on metabolite production.
Future research directions should prioritize elucidating the precise molecular mechanisms through which specific microbial metabolites influence brain physiology, particularly their effects on microglial function, neuroinflammation, and blood-brain barrier integrity. Advanced gnotobiotic models, multi-omics integration, and sophisticated imaging techniques will enable deeper exploration of the dynamic interplay between dietary factors, microbial metabolism, and neuronal signaling. From a therapeutic perspective, targeted interventions modulating microbial metabolite production—including precision probiotics, prebiotics, and postbiotics—hold significant promise for treating neurological and neuropsychiatric disorders. As our understanding of these complex relationships matures, dietary and microbial-based interventions may emerge as viable strategies for optimizing brain health across the lifespan.
The human gut microbiome, a complex ecosystem of bacteria, archaea, fungi, and viruses, plays a critical role in host physiology, influencing everything from digestion and metabolism to immune function and brain health [24] [25] [26]. Diet is one of the most potent modulators of this microbial community's composition and functional output. The intricate communication network between the gut and the brain, known as the gut-brain axis, involves neural, hormonal, immune, and microbial signaling pathways [24] [25]. Understanding how specific dietary components—fiber, polyphenols, fats, and proteins—influence the gut microbiome provides a scientific foundation for developing targeted nutritional strategies to support human health, a key pursuit in modern microbiota research.
Dietary Fiber and the Microbiome
Mechanisms of Microbial Fermentation
Dietary fibers (DFs) are complex, non-digestible carbohydrates that escape digestion in the upper gastrointestinal tract and reach the colon, where they serve as primary substrates for microbial fermentation [27]. This process is crucial for maintaining gut homeostasis. Fermentable fibers include a wide array of plant-derived polysaccharides such as pectin, arabinoxylan, beta-glucans, fructo-oligosaccharides (FOS), galacto-oligosaccharides (GOS), inulin, and resistant starches [27]. The fermentation of these fibers by gut bacteria primarily results in the production of short-chain fatty acids (SCFAs), which include acetate (C2), propionate (C3), and butyrate (C4) in an approximate ratio of 3:1:1 [27]. The ability to generate SCFAs is functionally redundant across different bacterial taxa, with acetate being produced by the majority of gut bacteria, while propionate and butyrate are synthesized by specific, functionally distinct groups [27].
Key SCFAs, Their Producers, and Host Functions
Table 1: Key Short-Chain Fatty Acids (SCFAs), Their Microbial Producers, and Host Functions
| SCFA | Producing Genera | Host-Relevant Functions |
|---|---|---|
| Acetate | Produced by a majority of gut bacteria; involved in cross-feeding. | Energy source; substrate for butyrate production; stimulates mucin 2 expression, mucus production and secretion [27]. |
| Propionate | Akkermansia, Bacteroides, Dialister, Phascolarctobacterium, Phocaeicola (succinate pathway); Anaerobutyricum, Blautia, Mediterraneibacter (propanediol pathway). | Substrate for gluconeogenesis; anti-inflammatory; reduces CD4+ T cell responses by inhibiting NF-κB and HDAC activity [27]. |
| Butyrate | Agathobacter, Anaerobutyricum, Anaerostipes, Butyricicoccus, Coprococcus, Faecalibacterium, Gemminger, Lachnospira, Oscillibacter, Roseburia, Ruminococcus. | Main energy source for colonocytes; enhances tight junction assembly and wound healing; increases mucin production; inhibits NF-κB; has anti-inflammatory immunoregulatory effects [27]. |
SCFAs exert their effects through multiple mechanisms. They serve as signaling molecules by binding to G-protein-coupled receptors (e.g., GPR41, GPR43) on epithelial, fat, and immune cells [27]. They also inhibit histone deacetylase (HDAC) activity, which can regulate T-cell differentiation and promote anti-inflammatory responses [27]. Butyrate is particularly vital for colonocyte health, providing up to 70% of their energy requirements and strengthening the gut barrier [27].
Experimental Insights
Protocol: Investigating SCFA Production from Fiber Fermentation
- In Vitro Fermentation Models: Systems like the in vitro Mucosal ARtificial COLon (M-ARCOL) simulate the human colon environment to study fiber fermentation and pathogen interactions [24].
- Intervention Design: Human trials often employ controlled diets supplemented with specific fibers (e.g., inulin, FOS, GOS, resistant starch). The Green-Mediterranean diet, rich in polyphenols and fiber, is an example of a whole-diet intervention [27].
- Sample Collection and Analysis: Fecal samples are collected pre-, during, and post-intervention. Microbiome profiling is performed via 16S rRNA gene sequencing or shotgun metagenomics. SCFA concentrations are quantified in fecal samples using techniques like gas chromatography-mass spectrometry (GC-MS) [27].
- Key Findings: Supplementation with fiber- and polyphenol-rich foods consistently enriches SCFA-producing bacteria such as Faecalibacterium, Eubacterium, Roseburia, and Blautia [27]. For instance, combining nuts with caloric restriction was shown to increase levels of propionic acid [27].
Bioactive Polyphenols and Microbial Modulation
Metabolism and Microbial Interactions
(Poly)phenols are a diverse group of bioactive compounds found in plant-based foods like fruits, vegetables, tea, coffee, and cereals [25] [28]. Their bioavailability is limited in the upper GI tract, and a significant portion reaches the colon, where they are metabolized by the gut microbiota [28]. This microbial metabolism transforms complex polyphenols into more bioavailable and often more active metabolites, such as phenolic acids and urolithins [27] [25]. Polyphenols selectively modulate the gut microbiome, typically promoting the growth of beneficial bacteria (e.g., Bifidobacterium, Lactobacillus, Akkermansia, Faecalibacterium) and inhibiting potential pathogens (e.g., Proteobacteria) [25] [28]. These shifts are associated with improved gut barrier function and anti-inflammatory effects.
Synergy with Dietary Fiber
Polyphenols and dietary fibers often coexist in plant cell walls, and their interaction creates a synergistic effect on gut health [28]. They can interact through covalent bonds (forming DF-polyphenol complexes) or non-covalent bonds (hydrogen bonding, hydrophobic interactions) [28]. This synergy enhances the production of health-promoting metabolites and supports microbial diversity more effectively than either component alone.
- Mechanisms of Synergy: DF acts as a delivery system, protecting polyphenols from early digestion and ensuring their arrival in the colon. The combined fermentation leads to increased SCFA production and greater enrichment of beneficial taxa compared to individual components [28].
- Health Implications: Diets rich in both DF and polyphenols, such as the Mediterranean diet, are linked to reduced risks of metabolic disorders, supported by enhanced SCFA production and gut barrier integrity [27] [28].
Diagram 1: Synergistic interaction between dietary polyphenols and fiber in shaping the gut microbiome and host health.
Dietary Proteins and Lipids: Complex Roles in Microbial Metabolism
Protein Fermentation: Dual Outcomes
Unlike carbohydrate fermentation, which primarily yields SCFAs, microbial fermentation of undigested dietary protein in the colon is a more complex process that generates a diverse range of metabolites with both beneficial and detrimental potential [29] [30].
Protocol: Assessing Protein Fermentation Products
- Model Systems: In vitro models (e.g., M-ARCOL) or animal models (e.g., gnotobiotic mice) are used to control protein sources and intake.
- Dietary Intervention: Participants consume defined diets varying in protein quantity and source (animal vs. plant). High-protein diets, especially from animal sources, are often tested [29] [30].
- Metabolite Profiling: Metabolites like branched-chain fatty acids (BCFAs), ammonia, hydrogen sulfide, p-Cresol, and indoles are measured in fecal samples using GC-MS and LC-MS. BCFAs are reliable markers of proteolytic fermentation [29].
- Microbiome Analysis: 16S rRNA sequencing tracks shifts in microbial composition. Bacteria from phyla Firmicutes, Bacteroidetes, and Proteobacteria are often implicated in proteolysis [29].
Protein fermentation products have been linked to increased inflammatory response, tissue permeability, and colitis severity in the gut, and are implicated in obesity, diabetes, and non-alcoholic fatty liver disease (NAFLD) [29]. Conversely, some tryptophan metabolites (e.g., indole derivatives) can activate the aryl hydrocarbon receptor, improving gut barrier function and providing anti-inflammatory benefits [29].
Lipid Metabolism and Microbial Influence
The gut microbiota can both transform and synthesize lipids, as well as break down dietary lipids to generate secondary metabolites with host modulatory properties [26] [31]. Bioactive lipids derived from microbial metabolism impact host physiology, particularly immunity and metabolism [31].
- Short-Chain Fatty Acids (SCFAs): As previously detailed, these fiber fermentation products also influence lipid metabolism by serving as signaling molecules and energy sources, affecting insulin sensitivity and fat storage [27] [26].
- Trimethylamine-N-Oxide (TMAO): Gut microbes metabolize dietary choline and L-carnitine (abundant in red meat) into trimethylamine (TMA), which is then oxidized in the liver to TMAO. Elevated TMAO levels are associated with an increased risk of cardiovascular disease [25] [26].
- Bile Acid Metabolism: The gut microbiota modifies primary bile acids into secondary bile acids through enzymatic activities like bile salt hydrolase (BSH). This process regulates host lipid metabolism, cholesterol homeostasis, and immune signaling [26].
- Lipopolysaccharide (LPS): LPS, a component of the cell wall of Gram-negative bacteria, can translocate into systemic circulation, particularly under high-fat diet conditions, triggering low-grade chronic inflammation ("metabolic endotoxemia") that is linked to insulin resistance and obesity [26].
Table 2: Impact of Dietary Components on Gut Microbiota and Host Physiology
| Dietary Component | Key Microbial Shifts | Major Microbial Metabolites | Potential Health Impacts |
|---|---|---|---|
| Dietary Fiber | ↑ Faecalibacterium, Roseburia, Blautia, Bifidobacterium | SCFAs (Acetate, Propionate, Butyrate) | Enhanced gut barrier integrity, anti-inflammation, improved metabolic health [27] [28]. |
| Polyphenols | ↑ Akkermansia, Bifidobacterium, Lactobacillus; ↓ Proteobacteria | Phenolic acids (e.g., Urolithins) | Antioxidant, anti-inflammatory, neuroprotective effects [27] [25] [28]. |
| Dietary Protein (High) | ↑ Bacteroides, Alistipes, Firmicutes; ↓ Bifidobacterium | BCFAs, Ammonia, H₂S, p-Cresol | Increased gut permeability, inflammation; potential risk for metabolic disease & CRC [29] [30]. |
| Dietary Lipids (High/Saturated) | ↑ LPS-producing bacteria; altered bile acid metabolism | TMAO, Secondary Bile Acids, LPS | Systemic inflammation, insulin resistance, increased CVD risk [26] [31]. |
The Gut-Brain Axis: A Translational Perspective
The gut-brain axis is a bidirectional communication system where the gut microbiota plays a central role, influencing emotional regulation, brain function, and even dietary behaviors [24] [25]. Microbial metabolites, including SCFAs, neurotransmitter precursors (e.g., serotonin, GABA), and immune modulators, are critical mediators of this communication [24] [25] [32].
- Neuroinflammation and Ageing: Low-grade chronic inflammation, or "inflammageing," is promoted by gut microbiota and is a risk factor for neurodegenerative diseases [25]. Dietary (poly)phenols can modulate the gut microbiota to reduce intestinal permeability and lower pro-inflammatory gut bacteria-derived mediators, thereby potentially attenuating neuroinflammation [25] [32].
- Experimental Evidence: Exploratory analyses have linked gut microbiota composition to conditions like ADHD and reactive aggression, with high-energy intake associated with higher aggression scores [24]. Furthermore, specific microbial-derived metabolites have been linked to depression and quality of life, leading to the identification of "gut-brain modules" for neuroactive compound production [32].
Diagram 2: Key pathways of the microbiota-gut-brain axis, highlighting the role of diet and microbial metabolites.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Models for Gut Microbiome Research
| Tool / Reagent | Function / Application | Examples / Notes |
|---|---|---|
| In Vitro Colon Models | Simulates human colon environment for studying fermentation, pathogen interactions, and metabolite production. | M-ARCOL (Mucosal ARtificial COLon); allows testing of life-threatening pathogens like EHEC [24]. |
| Gnotobiotic Mice | Germ-free animals colonized with specific microbes; essential for establishing causal relationships between microbes and host phenotype. | Used to demonstrate that gut microbiome from obese donors can increase fat mass in recipients [26]. |
| 16S rRNA Sequencing | Profiling microbial community composition and diversity based on the 16S ribosomal RNA gene. | Standard method; often performed on Illumina MiSeq or similar platforms [24] [33]. |
| Shotgun Metagenomics | Unbiased sequencing of all genetic material in a sample; allows for functional gene analysis and strain-level resolution. | Hi-seq-PacBio hybrid method for characterizing low-abundance species [26]. |
| GC-MS / LC-MS | Gas or Liquid Chromatography-Mass Spectrometry for identifying and quantifying metabolites (SCFAs, BCFAs, TMAO, etc.). | Crucial for measuring the metabolic output of the microbiome [27] [29]. |
| Prebiotics & Probiotics | Defined supplements to modulate the gut microbiome in intervention studies. | Prebiotics: Inulin, FOS, GOS. Probiotics: Bifidobacterium longum APC1472 (shown to have anti-obesity effects) [27] [32]. |
| D-Lyxose-13C-3 | D-Lyxose-13C-3, MF:C5H10O5, MW:151.12 g/mol | Chemical Reagent |
| Anti-ToCV agent 1 | Anti-ToCV agent 1, MF:C22H19FN2O5S, MW:442.5 g/mol | Chemical Reagent |
The evidence is unequivocal: diet profoundly shapes the gut microbiome, with specific components like fiber, polyphenols, proteins, and fats dictating microbial composition and metabolic output. These microbial changes, in turn, have far-reaching consequences for host health, including metabolic, immune, and neurological outcomes via the gut-brain axis. The synergistic effects of dietary components, particularly fiber and polyphenols, highlight the superiority of whole-diet approaches over isolated nutrients. Future research must focus on mechanistic, longitudinal human studies and account for individual microbiota variability to realize the full potential of personalized, microbiome-targeted dietary interventions for improving human health.
The microbiota-gut-brain axis (MGBA) represents a critical bidirectional communication network linking the gastrointestinal tract with the central nervous system (CNS). Growing evidence indicates that gut dysbiosis, an imbalance in the gut microbial community, and compromised intestinal barrier integrity are intimately involved in the pathogenesis of neuroinflammatory and neurodegenerative diseases. Dysbiosis can trigger a cascade of events including increased intestinal permeability, systemic inflammation, impaired blood-brain barrier function, and ultimately neuroinflammation through multiple pathways. This review synthesizes current knowledge on the mechanisms by which gut barrier dysfunction contributes to neuroinflammation, details experimental methodologies for investigating these relationships, and explores potential therapeutic interventions targeting the gut-brain axis. The content is framed within the context of how dietary patterns significantly influence MGBA communication, thereby modulating neurodegenerative disease risk and progression.
The human gastrointestinal tract hosts a complex ecosystem of microorganisms collectively known as the gut microbiota, which plays a fundamental role in host physiology, immune function, and nervous system homeostasis [34]. The concept of the microbiota-gut-brain axis (MGBA) has emerged as a pivotal framework for understanding how gut microbes communicate with the brain through neural, endocrine, immune, and metabolic pathways [15]. Recent research has illuminated how disruption of this delicate ecosystem—termed gut dysbiosis—can compromise intestinal barrier integrity, leading to systemic inflammation and neuroinflammation that potentially drives neurodegenerative pathologies including Alzheimer's disease (AD), Parkinson's disease (PD), and others [34] [15].
The intestinal barrier, comprised of a single layer of epithelial cells joined by tight junction proteins, serves as a critical interface regulating the passage of nutrients while restricting the translocation of harmful substances and microorganisms [35]. When this barrier becomes compromised, a condition often referred to as "leaky gut," bacterial products such as lipopolysaccharides (LPS) can enter systemic circulation, triggering immune responses that may ultimately affect brain function [36]. This review comprehensively examines the links between gut dysbiosis, barrier integrity, and neuroinflammation, with particular emphasis on mechanistic insights, experimental approaches, and the modulatory role of diet within this context.
Gut Dysbiosis and Pathological Mechanisms
Definition and Features of Gut Dysbiosis
Gut dysbiosis refers to an alteration in the composition and function of the gut microbiota, typically characterized by:
- Reduced microbial diversity
- Loss of beneficial microorganisms
- Overgrowth of potentially pathogenic species
- Shifts in metabolic capacity and functional output
In healthy adults, the gut microbiota is dominated by the phyla Bacteroidetes and Firmicutes, with specific beneficial genera including Bacteroides, Bifidobacterium, Lactobacillus, and Faecalibacterium [34] [37]. Dysbiotic states associated with neurodegenerative diseases often show:
- Increased Firmicutes/Bacteroidetes ratio [37]
- Reduced abundance of short-chain fatty acid (SCFA)-producing bacteria
- Increased abundance of pro-inflammatory microbes such as Escherichia and Clostridium species [34]
Table 1: Microbial Taxa Associated with Dysbiosis in Neurodegenerative Conditions
| Taxonomic Level | Associated Taxa | Change in Dysbiosis | Potential Impact |
|---|---|---|---|
| Phylum | Firmicutes | Increased | Potential pro-inflammatory effects |
| Phylum | Bacteroidetes | Decreased | Reduced SCFA production |
| Genus | Escherichia | Increased | LPS production, inflammation |
| Genus | Clostridium | Increased | Toxin production |
| Genus | Bacteroides | Decreased | Reduced immune regulation |
| Genus | Lactobacillus | Decreased | Reduced GABA production |
| Genus | Bifidobacterium | Decreased | Reduced anti-inflammatory mediators |
Mechanisms Linking Gut Dysbiosis to Neuroinflammation
Several interconnected mechanisms explain how gut dysbiosis contributes to neuroinflammation and neurodegeneration:
Bacterial Amyloids and LPS Production: Certain gut bacteria produce bacterial amyloids and lipopolysaccharides (LPS) that can trigger macrophage dysfunction, increase gut permeability, and promote systemic inflammation [34]. These bacterial products can cross the compromised intestinal barrier and travel to the brain, where they may activate microglia and promote the aggregation of pathological proteins like Aβ and α-synuclein [34] [15].
Immune System Activation: Dysbiosis can lead to hyperimmune activation and increased production of pro-inflammatory cytokines including IL-1β, IL-6, and IL-8, as well as activation of the NLRP3 inflammasome [34]. These inflammatory mediators can breach the blood-brain barrier, activating microglia and astrocytes, which subsequently produce additional neuroinflammatory molecules [34] [15].
Vagus Nerve Signaling: The vagus nerve serves as a direct communication pathway between the gut and brain. Gut microbes and their metabolites can stimulate vagal afferents, influencing brain function and behavior. Interestingly, the vagus nerve may also serve as a physical conduit for the transmission of protein aggregates in a prion-like manner [34].
Microbial Metabolite Production: Gut microbiota produce numerous neuroactive metabolites, including short-chain fatty acids (SCFAs), neurotransmitters (serotonin, GABA, dopamine), and bile acid metabolites that can directly or indirectly influence brain function [34] [7]. Dysbiosis alters the production of these metabolites, potentially disrupting neuro-immune homeostasis.
Intestinal Barrier Structure and Regulation
Anatomy of the Intestinal Barrier
The intestinal barrier consists of multiple components working in concert:
- Mucosal Layer: A glycoprotein layer secreted by goblet cells that forms the first physical and chemical barrier
- Epithelial Cell Layer: A single layer of specialized intestinal epithelial cells (IECs) including enterocytes, goblet cells, Paneth cells, and enteroendocrine cells
- Junctional Complexes: Multi-protein structures that seal the paracellular space between epithelial cells
- Immune Cells: Located in the lamina propria, including dendritic cells, T cells, B cells, and macrophages
Tight Junction Proteins and Regulation
Tight junctions are the most apical component of the junctional complexes and represent the primary determinant of paracellular permeability [35]. Key tight junction proteins include:
Table 2: Major Tight Junction Proteins and Their Functions
| Protein | Function | Role in Barrier Integrity |
|---|---|---|
| Occludin | First identified tight junction protein; provides structural integrity | Crucial for tight junction stability rather than assembly |
| Claudins | Large family of proteins with different isoforms; regulate paracellular transport | Different isoforms have opposing effects on permeability |
| Zonula Occludens (ZO-1, ZO-2, ZO-3) | Cytosolic scaffold proteins; link transmembrane proteins to actin cytoskeleton | Essential for tight junction formation and maintenance |
| Junctional Adhesion Molecules (JAMs) | Immunoglobulin-like transmembrane proteins | Contribute to barrier maintenance; JAM-A deficiency increases permeability |
The expression and function of tight junction proteins are regulated by multiple signaling pathways, including those involving small GTP-binding proteins, tyrosine kinases (c-Src, c-Yes), and protein kinase C (PKC) [35]. Inflammatory cytokines such as TNF-α and IFN-γ can disrupt tight junction integrity, increasing paracellular permeability.
Experimental Models and Methodologies
Assessing Intestinal Permeability In Vivo
FITC-Dextran Method: A well-established technique for measuring intestinal permeability in animal models [36].
Diagram 1: Intestinal Permeability Assessment Workflow
Procedure Details:
- Animals are fasted for 4 hours to ensure accurate measurement
- FITC-labeled dextran (4 kDa molecular weight) is administered by oral gavage at a dose of 40 mg per 100 g body weight
- After 3 hours, blood samples are collected
- Plasma fluorescence is measured using a fluorescence spectrophotometer (excitation: 490 nm, emission: 520 nm)
- FITC-dextran concentrations are calculated from standard curves generated by serial dilution of FITC-dextran [36]
Evaluating Intestinal Barrier Protectants
Experimental Design for Testing Barrier Protectants: The impact of potential barrier-protective compounds can be assessed using specific inhibitors and protectors:
Diagram 2: Experimental Design for Barrier Function Studies
Key Reagents:
- Intestinal Alkaline Phosphatase (IAP): A gut barrier protector administered in drinking water at 120 units/mL [36]
- L-phenylalanine (L-Phe): An intestinal homeostasis inhibitor administered by gavage at 150 mM in saline (200 μL) twice daily [36]
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Gut-Brain Axis Studies
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| Barrier Assessment | FITC-dextran (4 kDa) | Measures intestinal permeability in vivo |
| Ussing chambers | Ex vivo measurement of transepithelial electrical resistance | |
| Tight Junction Analysis | Anti-occludin antibodies | Immunofluorescence and Western blot detection of occludin |
| Anti-ZO-1 antibodies | Detection of zonula occludens-1 protein | |
| Anti-claudin antibodies | Isoform-specific detection of claudin family members | |
| Microbial Products | Lipopolysaccharide (LPS) | Tool to induce inflammation and barrier disruption |
| Bacterial amyloids | Investigate cross-seeding with host proteins | |
| Cytokine Measurement | ELISA kits for IL-1β, IL-6, TNF-α | Quantify inflammatory mediators in plasma and tissue |
| Multiplex immunoassays | Simultaneous measurement of multiple cytokines | |
| Microbiota Modulation | Antibiotics (e.g., penicillin) | Create microbiota-depleted models |
| Probiotics (e.g., Lactobacillus, Bifidobacterium) | Investigate beneficial microbial interventions | |
| Prebiotics (e.g., inulin, FOS) | Study effects of microbiota-directed dietary components | |
| Neuroinflammation Assessment | Anti-Iba1 antibodies | Detect microglial activation in brain tissue |
| Anti-CD68 antibodies | Identify phagocytic microglia | |
| GlcN-6-P Synthase-IN-1 | GlcN-6-P Synthase-IN-1, MF:C20H21N7S, MW:391.5 g/mol | Chemical Reagent |
| cis-Dihydro Tetrabenazine-d7 | cis-Dihydro Tetrabenazine-d7, MF:C19H29NO3, MW:326.5 g/mol | Chemical Reagent |
Signaling Pathways Linking Gut Barrier Dysfunction to Neuroinflammation
The mechanistic connection between impaired intestinal barrier function and neuroinflammation involves multiple interconnected signaling pathways:
Diagram 3: Gut-Brain Axis Signaling in Neuroinflammation
Key Pathway Components:
Toll-like Receptor 4 (TLR4) Signaling:
- LPS from gut bacteria binds to TLR4 on microglia
- Activates downstream NF-κB signaling pathway
- Promotes production of pro-inflammatory cytokines (IL-1β, IL-6, TNF-α)
- Sustains microglial activation in a chronic neuroinflammatory state [36]
Short-Chain Fatty Acid (SCFA) Signaling:
- SCFAs (butyrate, acetate, propionate) are produced by microbial fermentation of dietary fiber
- Butyrate reinforces intestinal barrier function by promoting expression of tight junction proteins
- SCFAs can cross the blood-brain barrier and influence microglial homeostasis and function [34] [7]
Vagal Pathway:
- Gut microbes and their metabolites can directly stimulate the vagus nerve
- Vagal afferents transmit signals to brainstem nuclei
- Anti-inflammatory cholinergic output can modulate peripheral and central inflammation [34]
Role of Diet in Modulating the Gut-Brain Axis
Dietary patterns significantly influence the composition and function of the gut microbiota, thereby affecting MGBA communication and potentially modifying neurodegenerative disease risk.
Dietary Patterns and Their Impacts
Table 4: Dietary Interventions for Gut-Brain Axis Modulation
| Dietary Pattern | Key Components | Impact on Gut Microbiota | Effects on Brain Health |
|---|---|---|---|
| Mediterranean Diet | High fruits, vegetables, whole grains, olive oil, fish | Increases microbial diversity, promotes SCFA production | Associated with reduced cognitive decline, lower neuroinflammation |
| High-Fiber/Plant-Based | Dietary fiber, polyphenols, plant proteins | Enhances beneficial bacteria (Bifidobacteria, Lactobacilli), increases SCFA | Supports cognitive function, reduces depression and anxiety symptoms |
| Western Diet | High refined sugars, saturated fats, processed foods | Reduces diversity, increases pro-inflammatory species | Promotes neuroinflammation, exacerbates neurodegenerative pathology |
| Fermented Foods | Yogurt, kefir, kimchi, kombucha | Provides probiotics, increases microbial diversity | Reduces inflammation, may improve stress resilience |
Molecular Mechanisms of Dietary Interventions
Fiber and SCFA Production: Dietary fibers resistant to host digestion are fermented by gut bacteria to produce SCFAs, particularly butyrate, acetate, and propionate. These metabolites:
- Strengthen intestinal barrier function by upregulating tight junction proteins
- Modulate systemic and neuroinflammation through immune cell regulation
- Directly influence microglial maturation and function [7] [38]
Polyphenols: Plant-derived polyphenols from berries, tea, olive oil, and other sources:
- Possess antioxidant and anti-inflammatory properties
- Support the growth of beneficial bacteria while inhibiting pathogenic species
- Reduce intestinal permeability and systemic inflammation [7]
Omega-3 Fatty Acids: Found in fatty fish, flaxseeds, and walnuts:
- Incorporated into cell membranes, influencing fluidity and signaling
- Metabolized to specialized pro-resolving mediators that actively resolve inflammation
- Modulate gut microbiota composition toward anti-inflammatory profiles [7]
Therapeutic Implications and Future Directions
Microbiota-Targeted Interventions
Several therapeutic approaches targeting the gut microbiota show promise for managing neuroinflammatory conditions:
Probiotics and Prebiotics:
- Specific probiotic strains (Lactobacillus, Bifidobacterium) can improve barrier function and reduce inflammation
- Prebiotics (inulin, FOS, GOS) selectively nourish beneficial gut bacteria
- "Psychobiotics" specifically target mental health outcomes through MGBA modulation [7]
Fecal Microbiota Transplantation (FMT):
- Transfer of entire microbial communities from healthy donors
- Has shown efficacy in recurrent C. difficile infection
- Emerging research exploring potential for neurodegenerative diseases [15]
Dietary Interventions:
- Personalized nutrition approaches based on individual microbiome composition
- Targeted dietary patterns to correct dysbiosis and reinforce barrier integrity
- Combination approaches using dietary interventions with other microbiota-targeted therapies [7] [32]
Drug-Microbiome Interactions
The gut microbiota significantly influences drug metabolism and efficacy through:
- Direct enzymatic transformation of drugs
- Alteration of host metabolic pathways
- Modulation of immune responses that affect drug action
- Influence on drug bioavailability through barrier function effects [39]
Understanding these interactions is crucial for developing effective therapeutics for neurodegenerative diseases, as individual variations in microbiome composition may significantly influence treatment responses.
The intricate relationship between gut dysbiosis, barrier integrity, and neuroinflammation represents a paradigm shift in our understanding of neurodegenerative disease pathogenesis. The evidence reviewed demonstrates that disruption of the gut microbial ecosystem can compromise intestinal barrier function, leading to systemic inflammation that ultimately affects brain homeostasis through multiple interconnected pathways. The MGBA serves as a critical communication network, with dietary patterns playing a fundamental role in modulating these interactions.
Future research should focus on elucidating the specific microbial taxa and metabolites most critically involved in neurodegenerative processes, developing standardized protocols for assessing gut barrier function in clinical settings, and designing targeted interventions that leverage dietary components to maintain MGBA homeostasis. The integration of gut-focused therapeutic approaches with conventional neurology treatments holds significant promise for addressing the growing burden of neurodegenerative diseases worldwide.
From Mechanism to Therapy: Dietary Interventions and Research Methodologies
The gut-brain axis (GBA) represents a paradigm-shifting frontier in neurogastroenterology, facilitating bidirectional communication between the gastrointestinal tract and the central nervous system. Emerging evidence positions dietary patterns as powerful modulators of this axis, primarily through structural and functional modifications of the gut microbiome. This whitepaper synthesizes current evidence on three promising dietary patterns—Mediterranean, plant-based, and high-fiber diets—examining their mechanistic influences on gut-brain communication pathways. We analyze specific microbial metabolites, host receptor interactions, and downstream neurological effects, providing researchers and drug development professionals with a technical foundation for developing microbiome-targeted therapeutic interventions. The synthesis reveals that these dietary patterns consistently enhance microbial diversity, strengthen intestinal barrier integrity, promote anti-inflammatory states, and facilitate neuroprotective signaling through multiple complementary biological pathways.
The gut-brain axis (GBA) constitutes a complex, bidirectional communication network integrating neural, endocrine, immune, and metabolic pathways between the gastrointestinal tract and central nervous system [7] [40]. This system has gained significant attention for its role in maintaining physiological and psychological homeostasis, with particular relevance for neuropsychiatric and neurodegenerative disorders. The gut microbiota—a diverse ecosystem of microorganisms residing in the gastrointestinal tract—serves as a critical mediator of GBA signaling, influencing brain function through multiple mechanisms including neurotransmitter production, immune modulation, and barrier integrity maintenance [7].
Diet represents the most potent environmental factor shaping gut microbiota composition and function, thereby directly influencing GBA communication [7] [9]. Nutritional neuroscience has emerged as a pivotal discipline for understanding how dietary components modulate neurological outcomes through microbial metabolism. The gut microbiota functions as a versatile metabolic organ, converting dietary components into bioactive molecules that directly or indirectly influence brain function [9]. These include short-chain fatty acids (SCFAs), neurotransmitter precursors, and various immunomodulatory metabolites that can cross the blood-brain barrier or initiate signaling cascades that ultimately affect central nervous system function [7].
This technical review examines three evidence-based dietary patterns with demonstrated efficacy in modulating the GBA: the Mediterranean diet, plant-based diets, and high-fiber diets. For each pattern, we analyze the mechanistic pathways, key microbial metabolites, and potential therapeutic applications relevant to drug development and clinical translation.
Mechanistic Pathways of Gut-Brain Communication
Dietary influences on the GBA operate through several well-characterized biological pathways that enable gut-derived signals to influence brain function and vice versa. Understanding these mechanisms is crucial for developing targeted nutritional interventions and microbiome-based therapeutics.
Neural Pathways
The vagus nerve serves as a direct neural communication highway between the gut and brain, transmitting sensory information from the gastrointestinal tract to the CNS [7] [40]. This cranial nerve provides bidirectional signaling capability, with gut microbes and their metabolites directly influencing vagal afferent firing patterns. Research demonstrates that vagus nerve signaling can be modulated by specific microbial metabolites, including serotonin and dopamine precursors, thereby affecting mood, motivation, and stress responses [40]. The enteric nervous system, sometimes termed the "second brain," contains over 100 million neurons that autonomously regulate gastrointestinal function while maintaining constant communication with the central nervous system via the vagus nerve [40].
Endocrine and Humoral Pathways
The hypothalamic-pituitary-adrenal (HPA) axis represents a key neuroendocrine pathway interfacing with the GBA. Gut microbiota significantly influence HPA axis regulation, particularly in stress response modulation [7]. Microbial metabolites including SCFAs and tryptophan derivatives function as endocrine signaling molecules that can enter systemic circulation and cross the blood-brain barrier [7] [4]. Notably, approximately 90% of the body's serotonin is synthesized in the gut under microbial influence, highlighting the profound endocrine capacity of the gastrointestinal system [7]. Other gut-derived neuroactive compounds include gamma-aminobutyric acid (GABA), dopamine, and norepinephrine precursors, all of which can influence central nervous system function [9].
Immune and Inflammatory Pathways
The gut microbiota plays a fundamental role in immune system development and regulation, with significant implications for brain function [4]. Dysbiosis can compromise intestinal barrier integrity, leading to a "leaky gut" condition that allows translocation of pro-inflammatory molecules into circulation [7]. These inflammatory mediators can cross the blood-brain barrier, triggering neuroinflammation that has been implicated in depression, anxiety, and neurodegenerative conditions [7] [4]. Gut microbes regulate systemic immunity through multiple mechanisms, including SCFA-mediated modulation of immune cell function, direct immune cell activation via microbial-associated molecular patterns (MAMPs), and regulation of inflammatory cytokine production [4]. The gut-immune-brain axis particularly emphasizes how microbiota-driven immune signaling can influence neurological outcomes [4].
Figure 1: Gut-Brain Axis Signaling Pathways. This diagram illustrates the primary communication pathways through which dietary patterns influence brain function, including neural, endocrine, and immune mechanisms mediated by gut microbiota and their metabolites.
Evidence-Based Dietary Patterns
Mediterranean Diet
The Mediterranean diet (MD) represents a plant-forward dietary pattern characterized by high consumption of fruits, vegetables, whole grains, legumes, nuts, and olive oil; moderate intake of fish and wine; and limited consumption of red meat and processed foods [41]. This dietary pattern has demonstrated significant promise for modulating the GBA and supporting cognitive health.
Mechanisms of Action
The MD influences the GBA through multiple complementary mechanisms. The diet enhances microbial diversity and increases fecal SCFA concentrations, particularly butyrate, acetate, and propionate [41]. The high polyphenol content from olive oil, berries, nuts, and wine provides antioxidant and anti-inflammatory properties that inhibit the proliferation of harmful bacteria while supporting beneficial microbial populations [7] [41]. Additionally, the MD's favorable fatty acid profile—rich in monounsaturated fats from olive oil and omega-3 polyunsaturated fats from fish—reduces neuroinflammation and supports neuronal membrane integrity [41]. The combination of prebiotic fibers from diverse plant sources and probiotic components from fermented foods further enhances the diet's impact on microbial ecosystems [7].
Cognitive and Mental Health Outcomes
Epidemiological studies consistently associate MD adherence with reduced risk of cognitive decline and neurodegenerative disorders. Research demonstrates that the MD delays progression of Alzheimer's disease and vascular dementia, with superior neuroprotective effects compared to single-nutrient interventions [41]. Clinical trials show that MD interventions, particularly when enhanced with high-polyphenol extra virgin olive oil, improve cognitive performance in elderly populations and slow age-related cognitive decline [41]. A longitudinal study across U.S., French, Spanish, and Greek cohorts found MD adherence associated with improved cognitive performance, with specific benefits for visuospatial/executive function [41]. The MD's multi-system effects on inflammation, oxidative stress, and neurogenesis position it as a compelling dietary pattern for GBA optimization.
Plant-Based Diets
Plant-based diets (PBDs), including vegetarian and vegan patterns, emphasize foods derived from plants while minimizing or excluding animal products. These diets are typically rich in fiber, polyphenols, and other bioactive compounds that selectively promote beneficial gut bacteria [42].
Microbial Modulation
PBDs significantly alter gut microbiota composition by increasing SCFA-producing bacteria including Roseburia, Eubacterium rectale, and Faecalibacterium prausnitzii [42]. The high fiber content acts as a prebiotic, stimulating bacterial growth necessary for SCFA production, which in turn reduces inflammation, enhances gut barrier integrity, and improves metabolic health [42]. The diverse phytobioactive compounds in plant foods—including polyphenols, carotenoids, and vitamins—selectively promote commensal bacteria while inhibiting pathogenic species [42]. However, research indicates that not all PBDs confer equal benefits, with poorly planned versions potentially leading to nutrient deficiencies that may contribute to gut microbiome dysbiosis [42].
Neurological Applications
PBDs are associated with reduced risk of cognitive decline and improved neurological outcomes. Studies indicate that plant-based dietary patterns during middle age are associated with lower risk of cognitive impairment later in life [41]. The neuroprotective effects are mediated through multiple pathways, including enhanced SCFA production, reduced systemic inflammation, and decreased oxidative stress [42] [41]. A plant-based diet intervention enriched with Raphanus sativus L. (radish seed) in perimenopausal women demonstrated beneficial effects on gut microbial composition and brain function, with participants showing improved visuospatial/executive function and altered intrinsic brain activity patterns [43]. This suggests specific plant-based interventions can modulate the GBA in clinically relevant populations.
High-Fiber Diets
High-fiber diets specifically emphasize dietary components resistant to host digestion but fermentable by gut microbiota. These diets directly fuel microbial production of beneficial metabolites, particularly SCFAs, that influence brain function through multiple pathways.
SCFA-Mediated Mechanisms
Short-chain fatty acids, including butyrate, acetate, and propionate, are the primary mediators of high-fiber diet effects on the GBA. Butyrate strengthens the intestinal barrier by enhancing tight junction protein expression and promoting colonocyte health [7]. Acetate and propionate modulate immune function through G protein-coupled receptor activation (GPR41 and GPR43) and histone deacetylase inhibition, reducing neuroinflammation [4]. SCFAs also influence neurotransmitter synthesis, with approximately 90% of body serotonin production occurring in the gut under microbial influence [7]. These microbial metabolites can cross the blood-brain barrier directly or activate vagal afferents, thereby influencing central nervous system function [7].
Therapeutic Evidence
Human studies demonstrate that high-fiber interventions significantly impact both gut microbiota composition and brain function. A randomized controlled trial using a plant-based, Raphanus sativus L.-rich diet (mean 5g/day) for 12 weeks in perimenopausal women resulted in improved Montreal Cognitive Assessment (MoCA) scores, particularly in visuospatial/executive function, and increased amplitude of low-frequency fluctuation (ALFF) values in brain regions associated with cognitive processing [43]. These changes correlated with increased abundances of Synergistetes and Verrucomicrobia phyla, suggesting a direct microbiota-brain functional relationship [43]. High-fiber diets also counter the detrimental effects of Western diets by increasing microbial diversity, reducing intestinal permeability, and decreasing systemic inflammation—all factors with significant implications for brain health [7].
Table 1: Comparative Analysis of Dietary Patterns and Their Gut-Brain Axis Effects
| Dietary Pattern | Key Components | Microbial Changes | Primary Metabolites | Demonstrated Neurological Outcomes |
|---|---|---|---|---|
| Mediterranean Diet | EVOO, vegetables, fruits, whole grains, legumes, nuts, fish, moderate wine | ↑ Microbial diversity, ↑ Bifidobacteria, ↑ Lactobacilli, ↓ Firmicutes/Bacteroidetes ratio | SCFAs (butyrate, acetate, propionate), polyphenols, omega-3s | Improved cognitive performance, delayed Alzheimer's progression, reduced age-related decline [41] |
| Plant-Based Diets | Vegetables, fruits, whole grains, legumes, nuts, seeds; exclusion/reduction of animal products | ↑ Roseburia, ↑ E. rectale, ↑ F. prausnitzii, ↑ SCFA producers | SCFAs, polyphenols, phytoestrogens | Reduced cognitive impairment risk, improved visuospatial/executive function, altered brain activity patterns [42] [43] |
| High-Fiber Diets | Whole grains, legumes, fruits, vegetables, nuts, seeds, resistant starch | ↑ Microbial diversity, ↑ SCFA-producing bacteria, ↑ Synergistetes, ↑ Verrucomicrobia | SCFAs (particularly butyrate), secondary bile acids | Enhanced cognitive function, improved brain connectivity, reduced neuroinflammation [7] [43] |
Experimental Models and Methodologies
Human Dietary Intervention Protocols
Well-designed human studies provide the most clinically relevant evidence for dietary impacts on the GBA. The following methodology from a recent clinical trial illustrates key considerations for intervention studies.
Raphanus Sativus L. Intervention Study
A 12-week longitudinal single-arm study investigated the effects of a plant-based RSL-rich diet on perimenopausal women [43]. The experimental protocol included:
Participant Selection: 24 perimenopausal women meeting specific eligibility criteria were initially enrolled, with 10 completing the study (58.3% attrition rate). The study employed a single-arm longitudinal exploratory design with post-hoc power analysis indicating the sample could detect large effects (d ≥ 1.0) [43].
Dietary Intervention: Participants adhered to a controlled, RSL-rich plant-based diet with mean RSL intake of 5g/day for 12 weeks. The diet emphasized whole plant foods while controlling for specific RSL supplementation [43].
Assessment Timepoints: Evaluations occurred at baseline (T0) and post-intervention (T1), with follow-up one month post-intervention to monitor adverse effects [43].
Outcome Measures:
- Gut Microbiota Composition: Fecal samples analyzed using 16S rRNA sequencing to assess microbial diversity and specific taxon abundance
- Cognitive Function: Montreal Cognitive Assessment (MoCA) evaluating visuospatial/executive function, naming, memory, attention, language, abstraction, delayed recall, and orientation
- Brain Activity: Resting-state functional MRI (rs-fMRI) measuring amplitude of low-frequency fluctuation (ALFF) to assess regional spontaneous brain activity
- Gastrointestinal Symptoms: Standardized questionnaires assessing GI comfort and function [43]
Key Findings: The intervention resulted in trending improvements in visuospatial/executive function and total MoCA scores (p=0.051 and p=0.089, respectively), elevated ALFF values in the left middle occipital gyrus, left precentral gyrus, and left middle cingulum gyrus, and significant correlations between Synergistetes and Verrucomicrobia abundance and ALFF values in these regions [43].
Figure 2: Experimental Workflow for Dietary Intervention Study. This diagram outlines the key methodological stages and assessment timepoints for a human dietary intervention study investigating gut-brain axis modulation, based on the Raphanus sativus L. clinical trial [43].
Animal Models and Translational Considerations
Animal studies, particularly rodent models, provide critical mechanistic insights into GBA pathways but present translational challenges.
Germ-Free (GF) Mouse Models: GF mice raised in sterile conditions lack gut microbiota entirely, allowing researchers to study the fundamental role of microbes in neurodevelopment and behavior. Studies show GF mice exhibit altered stress responses, neurotransmitter levels, and neurodevelopment that can be partially reversed through microbial colonization [4].
Fecal Microbiota Transplantation (FMT): Transfer of gut microbiota from human donors or treated animals to recipient mice enables investigation of causal relationships between specific microbial profiles and brain function. For example, FMT from exercising mice to sedentary recipients transferred exercise-induced cognitive benefits, demonstrating microbial mediation of exercise effects on brain function [44].
Limitations and Translation Challenges: Significant species differences in gut microbiota composition, diet metabolism, and neuroanatomy complicate extrapolation from rodent models to humans. The controlled laboratory environment and simplified diets used in animal studies often fail to replicate human dietary complexity [4].
Research Reagents and Methodological Tools
Table 2: Essential Research Reagents for Gut-Brain Axis Investigations
| Reagent/Category | Specific Examples | Research Application | Technical Considerations |
|---|---|---|---|
| DNA Sequencing Reagents | 16S rRNA primers (V3-V4), shotgun sequencing kits, DNA extraction kits (e.g., QIAamp PowerFecal) | Gut microbiota profiling, taxonomic classification, functional potential assessment | 16S for community structure, shotgun for functional genes; control for extraction efficiency bias |
| SCFA Analysis | GC-MS standards (acetate, propionate, butyrate), derivatization reagents, internal standards | Quantification of microbial fermentation products in fecal, serum, or brain samples | Requires proper sample preservation; rapid processing to prevent ex vivo fermentation |
| Neuroimaging | Resting-state fMRI protocols, ALFF analysis software, contrast agents | Measurement of spontaneous brain activity, functional connectivity | ALFF detects regional spontaneous activity; correlate with microbial measures |
| Cognitive Assessment | Montreal Cognitive Assessment (MoCA), visuospatial/executive function subitems | Standardized evaluation of multiple cognitive domains | Sensitive to subtle changes; appropriate for repeated measures designs |
| Cell Culture Models | Caco-2 intestinal barrier models, SH-SY5Y neuroblastoma cells, primary microglia | Investigation of barrier integrity, neuroinflammation, direct microbial metabolite effects | Limited complexity compared to in vivo systems but enable mechanistic studies |
| Immunoassays | ELISA kits for cytokines (TNF-α, IL-6, IL-1β), LPS-binding protein, zonulin | Quantification of inflammatory markers, intestinal permeability indicators | Multiplex approaches preferred for comprehensive immune profiling |
| Gnotobiotic Animals | Germ-free mice, defined microbial consortia (e.g., Altered Schaedler Flora) | Controlled colonization studies to establish causality | Technically challenging facilities required; enables reductionist approaches |
The evidence synthesized in this review substantiates Mediterranean, plant-based, and high-fiber diets as effective nutritional strategies for optimizing gut-brain axis communication. These dietary patterns operate through complementary mechanistic pathways—primarily via microbial production of SCFAs, reduction of systemic inflammation, and enhancement of intestinal barrier integrity—to exert beneficial effects on brain function and cognitive health.
Significant research gaps remain that merit investigation. The field requires long-term, large-scale, multicenter randomized controlled trials to establish durable effects of dietary interventions on neurological outcomes [41]. The substantial individual variability in microbiome composition and response to dietary interventions necessitates personalized nutrition approaches based on microbial biomarkers [7]. Future studies should explore synergistic combinations of dietary patterns with other GBA modulators, such as physical exercise, which has been shown to independently enhance microbial diversity and intestinal barrier function [44]. Advanced microbial therapeutics, including next-generation probiotics (psychobiotics) and targeted prebiotics, represent promising avenues for precise GBA modulation [7] [9].
For drug development professionals, these dietary patterns offer valuable insights for developing microbiome-targeted therapeutics. The microbial metabolites and signaling pathways identified in dietary studies provide novel targets for neurological drug development. Additionally, dietary interventions may serve as effective adjuncts to pharmacological treatments for neuropsychiatric and neurodegenerative conditions, potentially enhancing therapeutic efficacy through multi-system mechanisms. The growing understanding of the gut-immune-brain axis further expands potential intervention strategies for immune-mediated neurological conditions [4].
As research methodologies advance—particularly in multi-omics integration and neuroimaging—our capacity to decode the complex relationships between diet, gut microbiota, and brain function will continue to improve. This progress promises to yield more targeted, effective nutritional and therapeutic strategies for optimizing brain health through deliberate modulation of the gut-brain axis.
The gut-brain axis (GBA) represents a complex, bidirectional communication network linking the gastrointestinal tract with the central nervous system (CNS) through neural, endocrine, immune, and metabolic pathways [45] [9]. This communication system is profoundly influenced by the gut microbiota, the diverse community of microorganisms residing in the human gastrointestinal tract. Over the past decade, research has illuminated the critical role of dietary components in shaping the microbiota and subsequently modulating brain function and mental health [14] [9]. The emergence of nutritional psychiatry and microbial biotherapies has highlighted the potential of targeted nutritional interventions to manage gut-brain communication, offering novel approaches for preventing and treating neuropsychiatric and neurodegenerative disorders [9].
Within this framework, specific nutritional components—probiotics (particularly those with psychobiotic properties), prebiotics, and postbiotics—have garnered significant scientific interest for their ability to modulate the microbiota-gut-brain axis [46] [45]. These "biotics" represent increasingly precise tools for influencing gut-brain communication, with potential applications ranging from stress reduction to managing depression, anxiety, and cognitive decline [46] [47]. This technical review examines the mechanisms, experimental evidence, and practical applications of these targeted nutritional components within the context of diet-driven GBA research, providing researchers and drug development professionals with a comprehensive resource for developing novel microbiota-targeted therapeutic strategies.
Defining the Nutritional Components
Probiotics and Psychobiotics
Probiotics are defined as "live microorganisms which when administered in adequate amounts confer a health benefit on the host" [45] [48]. The most extensively studied probiotic genera include Lactobacillus and Bifidobacterium, with common species being Lacticaseibacillus casei, Lactiplantibacillus plantarum, Lactobacillus acidophilus, Lactobacillus helveticus, Lacticaseibacillus rhamnosus, Bifidobacterium longum, Bifidobacterium bifidum, and Bifidobacterium breve [45]. To be classified as a probiotic, a strain must be non-pathogenic, non-toxic, free from transferable antibiotic resistance genes, adequately characterized, and proven to confer health benefits [45].
The term "psychobiotic" was later coined to describe any exogenous intervention that leads to a bacterially mediated impact on the brain, primarily referring to probiotics with mental health benefits [47]. Psychobiotics are specifically defined as probiotics or prebiotics that, when consumed in adequate amounts, produce positive psychiatric effects in psychopathological conditions [46]. These specialized probiotics modulate the gut-brain axis through various mechanisms, including production of neuroactive compounds, immunomodulation, and enhancement of intestinal barrier function [45].
Prebiotics
Prebiotics are "compounds indigestible by the human gastrointestinal tract that travel through the intestine and reach the colon intact" [46]. In the colon, they serve as selective substrates for beneficial gut bacteria, stimulating their growth and activity. The most important prebiotics belong to the carbohydrate family, including galactooligosaccharides (GOS), fructooligosaccharides (FOS), and xylooligosaccharides [46]. Other compounds with prebiotic activity include inulin, resistant starch, and various dietary fibers [14].
Prebiotics exert their effects at relatively low doses. For instance, the effective amount of polydextrose is approximately 2-7.5 g per day, resistant starch 2.5-5 g per day, and inulin 1-6 g per day [46]. The concept of prebiotics has expanded beyond traditional carbohydrates to include human milk oligosaccharides, certain polyphenols, lactulose, and β-glucan, though more research is needed to fully characterize these emerging prebiotics [32].
Postbiotics
Postbiotics represent the newest category among biotics, defined as a "preparation of inanimate microorganisms and/or their components that confers a health benefit on the host" [48]. This category includes inactivated microbial cells, cell fragments, and metabolites produced by probiotic microorganisms during fermentation or in the gut environment [49]. Postbiotics encompass a wide range of bioactive compounds, including short-chain fatty acids (SCFAs), exopolysaccharides, lipoteichoic acid, peptidoglycans, and surface layer proteins [49].
The advantages of postbiotics over probiotics include enhanced safety profile (no risk of bacteremia), greater stability during storage, no requirement for viability, and avoidance of transmitting antibiotic resistance genes through horizontal gene transfer [48]. These characteristics make postbiotics particularly attractive for clinical applications in vulnerable populations and for pharmaceutical development.
Table 1: Comparative Analysis of Key Nutritional Components Targeting the Gut-Brain Axis
| Component | Definition | Key Examples | Typical Dosage | Primary Mechanisms |
|---|---|---|---|---|
| Probiotics | Live microorganisms conferring health benefits | Lactobacillus, Bifidobacterium species | ≥7 log CFU/day [46] | Neurotransmitter production, pathogen inhibition, barrier enhancement [45] |
| Psychobiotics | Probiotics with psychiatric benefits | Specific strains of Lactobacillus and Bifidobacterium | Strain-dependent | GABA, serotonin production; HPA axis modulation; inflammation reduction [47] |
| Prebiotics | Non-digestible compounds stimulating beneficial microbes | GOS, FOS, inulin, XOS | FOS: 10g/day; GOS: 7g/day [46] | SCFA production, selective growth stimulation, gut pH modulation [46] |
| Postbiotics | Inanimate microorganisms and/or their components | SCFAs, EPS, cell fragments, peptidoglycans | Preparation-dependent | Immunomodulation, receptor activation, barrier protection [49] [48] |
Mechanisms of Action in Gut-Brain Communication
Neural and Neuroendocrine Pathways
The gut-brain axis employs multiple communication channels, with the nervous system providing the most direct pathway. The enteric nervous system (ENS), often called the "second brain," contains 200-600 million neurons and is directly connected to the central nervous system via the vagus nerve [46]. While gut microbes do not have direct access to the ENS due to the mucous layer separating them, they communicate indirectly through bacterial secretions and metabolites that can cross the intestinal cell wall and affect the ENS [46]. These include short-chain fatty acids (SCFAs), exopolysaccharides (EPS), lipopolysaccharides (LPS), and glutamate, which can interact with specific receptors on nerve cells [46].
The hypothalamic-pituitary-adrenal (HPA) axis represents another critical pathway, with gut microbes influencing stress response and cortisol production. Psychobiotics have been shown to modulate this axis, potentially explaining their stress-reducing effects [47]. Additionally, gut bacteria can synthesize various neurotransmitters, including serotonin, gamma-aminobutyric acid (GABA), and dopamine, which can influence brain function and behavior [9].
Immunological Pathways
The immune system serves as a major conduit for gut-brain communication, with gut microbes and their products continuously interacting with intestinal immune cells. Pattern recognition receptors (PRRs), including Toll-like receptors (TLRs), nucleotide-binding oligomerization domain-like receptors (NLRs), C-type lectin-like receptors (CTLRs), and G-protein-coupled receptors (GPCRs), play crucial roles in detecting microbial components and initiating immune responses [49].
TLRs recognize different microbe-associated molecular patterns (MAMPs): TLR2 identifies lipoteichoic acid and peptidoglycan; TLR2/TLR4 identifies bacterial exopolysaccharides through RP105/MD1; and TLR9 responds to unmethylated CpG oligonucleotides [49]. NLRs such as NOD1 and NOD2 recognize specific peptidoglycan components from bacterial cell walls [49]. Activation of these receptors triggers signaling cascades that result in the release of cytokines, which can either promote inflammation or exert anti-inflammatory effects, depending on the specific microbial signals and receptors involved.
GPCRs, particularly GPR41, GPR43, and GPR109A, are primarily activated by SCFAs produced by gut bacteria [49]. These receptors are expressed by epithelial cells, adipocytes, enteroendocrine cells, and sympathetic nervous system cells. Butyrate and propionate interaction with GPR43, for instance, regulates the formation of Foxp3+ regulatory T cells, which play critical roles in controlling inflammation and maintaining immune homeostasis [49].
Metabolic and Endocrine Pathways
Gut microbes significantly influence host metabolism through the production of numerous bioactive metabolites. SCFAs (acetate, propionate, and butyrate) are among the most extensively studied microbial metabolites, produced through fermentation of dietary fibers and prebiotics [49]. Beyond their immunomodulatory effects via GPCRs, SCFAs influence lipid metabolism, glucose homeostasis, and insulin sensitivity [49].
Gut bacteria also participate in the metabolism of tryptophan, an essential amino acid and precursor to serotonin. Approximately 90% of the body's serotonin is produced in the gut, and microbial activities influence its synthesis and availability [9] [47]. Changes in urinary tryptophan metabolites have been observed following psychobiotic interventions, suggesting microbial involvement in this pathway [47].
Other microbial metabolites, including bile acid derivatives, branched-chain fatty acids, and various lipids, also contribute to gut-brain signaling. Recent studies have identified significant changes in specific fecal lipids and urinary tryptophan metabolites following psychobiotic dietary interventions, though the precise mechanisms by which these metabolites influence brain function require further investigation [47].
Experimental Evidence and Clinical Outcomes
Quantitative Analysis of Intervention Studies
Table 2: Summary of Clinical Outcomes from Probiotic and Prebiotic Interventions on Mental Health
| Study Focus | Population | Intervention | Key Outcomes | Effect Size/Statistics |
|---|---|---|---|---|
| Psychobiotic Effects [46] | Diverse populations from students to elderly (2,726 patients) | Pre- or probiotic vs. placebo | Significant decrease in Beck Depression Inventory (BDI) scores; Reduced depressive symptoms; Improved HAM-D scores | Overall effect: -0.87 (-1.66 - -0.099) |
| CNS Function [46] | Healthy adults and those with mental disorders (3,017 patients) | Viable and non-viable microorganisms | Reduction of depressive symptoms in both healthy and disordered groups | Effect size: -0.37 (-0.55, -0.20); Heterogeneity: 48% |
| Psychobiotic Diet [47] | Healthy adults with poor dietary habits (n=45) | High prebiotic/fermented food diet vs. control | Reduction in perceived stress | 32% reduction in diet group vs. 17% in control group |
| B. longum APC1472 [32] | Overweight/obese otherwise healthy individuals | Bifidobacterium longum APC1472 | Attenuated effects of early-life high-fat high-sugar diet; improved food intake regulation | Positive effects on hypothalamic molecular alterations |
Methodological Approaches in Psychobiotic Research
Psychobiotic Diet Intervention Study
A representative experimental protocol for investigating psychobiotic effects was described in a 2023 study examining the impact of a psychobiotic diet on stress in healthy adults [47]. The methodology can be summarized as follows:
Study Design: Single-blind, randomized, controlled trial with parallel groups. Participants: 45 healthy adults aged 18-59 years with poor dietary habits, block-randomized (block of 4, stratified by gender) to either intervention (psychobiotic diet, n=24) or control (n=21) group. Intervention Duration: 4 weeks. Psychobiotic Diet Composition:
- Prebiotic-rich fruits and vegetables: 6-8 servings per day (onions, leeks, cabbage, apples, bananas, oats)
- Grains: 5-8 servings per day
- Legumes: 3-4 servings per week
- Fermented foods: 2-3 servings per day (sauerkraut, kefir, kombucha)
- Calorie guidance: 2000-2200 kcal/day for females, 2400-2800 kcal/day for males
Control Diet: Minimal input focused mainly on standard food pyramid guidelines, matched for dietitian contact time. Dietary Adherence Monitoring: 7-day food records completed at baseline, week 2, and week 4; Food Frequency Questionnaire (FFQ) at pre- and post-intervention. Primary Outcome Measure: Perceived Stress Scale (PSS). Secondary Measures: Microbiota composition (shotgun sequencing), metabolic profiling (plasma, urine, feces), gastrointestinal symptoms (VAS), stool type (Bristol Stool Chart), sleep quality (PSQI). Sample Collection: Fecal samples collected in containers with AnaeroGen sachets, aliquoted and stored at -80°C; blood collected in lithium-heparin tubes for plasma separation.
This study found that while the dietary intervention elicited only subtle changes in microbial composition and function, it resulted in significant reductions in perceived stress, with higher adherence to the diet correlating with stronger stress reduction [47]. Additionally, significant changes were observed in the level of 40 specific fecal lipids and urinary tryptophan metabolites, suggesting potential metabolic pathways for the observed effects.
Probiotic vs. Postbiotic Comparative Study
A 2022 study directly compared the effects of probiotics and postbiotics in a dextran sulfate sodium (DSS)-induced colitis mouse model, providing important insights into their differential effects [48]:
Experimental Groups: Four groups of mice (n=7 per group):
- Control (water plus saline)
- DSS (DSS without intervention)
- Postbiotic (DSS plus postbiotic)
- Probiotic (DSS plus probiotic)
Intervention: Bifidobacterium adolescentis B8589 administered as either viable probiotics (probiotic group) or heat-inactivated cells (postbiotic group). Assessment Parameters:
- Body weight measurement daily
- Disease Activity Index (DAI) scores
- Colon length measurement
- Histological scoring of colon tissue
- Fecal microbiota analysis (whole-metagenome shotgun sequencing)
Key Findings: Both probiotic and postbiotic administration ameliorated colitis, reflected by decreased histology scores compared to the DSS group. However, postbiotic treatment showed stronger effects on modulating fecal microbiota beta diversity, composition, and metagenomic potential than probiotic treatment [48]. This suggests that while both interventions improved disease phenotype, they exerted distinct effects on the gut microbial ecosystem.
Research Reagent Solutions Toolkit
Table 3: Essential Research Materials and Methodologies for Gut-Brain Axis Studies
| Research Tool | Specific Examples | Application/Function | Technical Notes |
|---|---|---|---|
| Microbiota Analysis | Shotgun metagenomic sequencing | Comprehensive characterization of microbial composition and functional potential | Superior to 16S sequencing for functional inference [47] |
| Metabolomic Profiling | LC-MS, GC-MS for SCFAs, lipids, tryptophan metabolites | Identification of microbial-derived bioactive molecules | Fecal, plasma, and urine samples provide complementary data [47] |
| Cell Receptors | TLRs (TLR2, TLR4, TLR9), GPCRs (GPR41, GPR43), NLRs (NOD1, NOD2) | Study of host-microbe interaction mechanisms | Knockout models essential for establishing causal relationships [49] |
| Animal Models | DSS-induced colitis, germ-free models, maternal separation | Investigation of microbiota-GBA interactions in controlled settings | Allow for manipulation not possible in human studies [48] |
| Psychological Assessments | Cohen's Perceived Stress Scale (PSS), Beck Depression Inventory (BDI), HAM-D | Quantification of mental health outcomes | Essential for correlating microbial changes with psychological effects [46] [47] |
| Dietary Assessment | 7-day food records, Food Frequency Questionnaires (FFQ) | Monitoring dietary adherence and nutrient intake | Critical for interpreting microbiota changes in nutritional studies [47] |
| Epi Lovastatin-d3 | Epi Lovastatin-d3, MF:C24H36O5, MW:407.6 g/mol | Chemical Reagent | Bench Chemicals |
| Piroxicam-d4 | Piroxicam-d4, MF:C15H13N3O4S, MW:335.4 g/mol | Chemical Reagent | Bench Chemicals |
Future Directions and Research Applications
The investigation of probiotics, prebiotics, and postbiotics as modulators of the gut-brain axis represents a rapidly evolving field with significant implications for both nutritional science and neuropharmacology. Future research directions should prioritize several key areas:
Mechanistic Elucidation: While multiple pathways have been identified connecting gut microbes to brain function, the precise molecular mechanisms remain incompletely understood [45]. Future studies should employ multi-omics approaches (genomics, transcriptomics, proteomics, metabolomics) to develop more comprehensive models of gut-brain communication.
Clinical Translation: The promising results from animal studies have not always translated consistently to human populations [45]. Larger-scale, randomized controlled trials with standardized protocols, adequate sample sizes, and well-defined clinical endpoints are needed to establish definitive efficacy for specific conditions.
Personalized Approaches: Emerging evidence suggests that individual responses to microbiota-targeted interventions depend on baseline microbiota composition [14] [32]. Future research should explore biomarkers that predict treatment response, enabling more personalized nutritional and therapeutic approaches.
Novel Formulations: The development of next-generation probiotics, synbiotics (combinations of probiotics and prebiotics), and postbiotics with enhanced stability and targeted effects represents a promising avenue for clinical application [32]. These advanced formulations may offer more consistent and potent modulation of the gut-brain axis.
For drug development professionals, the targeted nutritional components reviewed here offer compelling opportunities for the development of novel therapeutic agents. Postbiotics particularly warrant attention due to their favorable safety profiles, stability, and potent modulatory effects on host physiology [49] [48]. As research continues to unravel the complexities of gut-brain communication, these nutritional components are likely to play increasingly important roles in the maintenance of brain health and the treatment of neurological and psychiatric disorders.
The microbiota-gut-brain axis represents one of the most dynamic interfaces in biomedical research, facilitating bidirectional communication between gastrointestinal microbiota and the central nervous system. Within this complex signaling network, diet emerges as a principal modifiable factor capable of shaping microbial composition and function, thereby influencing brain development, behavior, and susceptibility to neuropsychiatric disorders. Germ-free (GF) animal models, fecal microbiota transplantation (FMT), and the Simulator of the Human Intestinal Microbial Ecosystem (SHIME) constitute three foundational methodologies enabling mechanistic investigation into how dietary interventions translate into neurological outcomes. This whitepaper provides an in-depth technical analysis of these core investigative platforms, detailing their applications, methodologies, and synergistic integration within diet-focused gut-brain axis research.
Germ-Free (GF) Animal Models
Germ-free animals are raised in sterile isolators completely devoid of all microorganisms, providing a blank canvas for investigating microbial influences on host physiology. This model has been instrumental in establishing proof-of-principle for microbiota-gut-brain communication, demonstrating that the absence of microbiota induces permanent neurodevelopmental deficits affecting stress responsivity, anxiety-like behaviors, sociability, and cognition [50]. In dietary studies, GF models allow researchers to introduce defined bacterial consortia or humanized microbiota at specific developmental time points to investigate causal relationships between nutritional components, specific microbes, and brain function [50] [51].
Key findings from GF studies have revealed that the microbiota is essential for normal blood-brain barrier integrity, immune function, and neurotransmission systems [50]. These discoveries fundamentally underscore why dietary modulation of microbiota can profoundly influence brain health and disease susceptibility.
Technical Methodology for GF Animal Experiments
Core Protocol: Conventionalization Studies
The power of the GF model for diet research lies in "conventionalization" experiments, where GF animals are colonized with specific microbial communities to observe resulting physiological changes.
- Animal Housing: Maintain GF rodents in flexible-film or rigid isolators with sterile bedding, food, and water. Autoclave all incoming materials and chemically sterilize (e.g., with peracetic acid) any equipment entering the isolator [50].
- Dietary Control: Utilize sterilized, defined diets (e.g., high-fiber, high-fat, protein-specific) to eliminate confounding microbial exposure from food.
- Microbial Inoculation:
- Sample Collection and Analysis:
- Behavioral Testing: Assess anxiety (e.g., open field test), sociability, and cognition after dietary and microbial interventions [50].
- Tissue Collection: Analyze brain, blood, and intestinal tissues post-sacrifice.
- Molecular Analysis: Quantify neurochemicals, plasma metabolites, immune markers, and gene expression changes in relevant pathways [50].
Key Signaling Pathways Investigated
GF studies have been pivotal in identifying how microbiota, modulated by diet, influence the brain through multiple pathways:
- Immune Pathway: Microbiota regulate microglial function, maturation, and immune homeostasis. GF animals display altered microglia and impaired immune response, which can be normalized by microbial colonization [15].
- Neuroendocrine Pathway: The hypothalamic-pituitary-adrenal (HPA) axis stress response is hyperactive in GF animals, demonstrated by increased corticosterone levels after stress, which is reversible with bacterial supplementation [50].
- Neural Pathway: The vagus nerve is a critical conduit for gut-brain signaling. Certain microbial and dietary effects on behavior are abrogated by vagotomy [50].
- Metabolic Pathway: Gut bacteria produce neuroactive metabolites (e.g., SCFAs, neurotransmitters) from dietary components. GF animals have altered levels of these metabolites, directly linking diet to brain function via microbial metabolism [9] [15].
The following diagram illustrates these core gut-brain signaling pathways, which are central to investigations using GF models:
Simulator of the Human Intestinal Microbial Ecosystem (SHIME)
SHIME is a dynamic, multi-compartment in vitro simulator that replicates the entire human gastrointestinal tract, including the stomach, small intestine, and ascending, transverse, and descending colon regions [52]. This platform allows for controlled, reproducible investigation of dietary compounds without the ethical and practical constraints of human or animal studies. SHIME is particularly valuable for screening the effects of specific dietary components (e.g., prebiotics, fibers, polyphenols, food additives) on microbial composition, metabolic activity, and the production of gut-brain active metabolites (e.g., short-chain fatty acids, neurotransmitters) before moving to complex in vivo models [52].
Technical Methodology
A standard SHIME experiment runs through a series of controlled phases to establish a baseline, test an intervention, and observe its persistence.
- System Setup: The reactor consists of five double-jacketed, pH-controlled glass vessels simulating the stomach/small intestine, ascending colon (AC), transverse colon (TC), and descending colon (DC). The system is maintained at 37°C under anaerobic conditions [52].
- Inoculation: The colon compartments are inoculated with fecal material from healthy human donors or specific patient populations [52].
- Operational Phases:
- Stabilization (~2 weeks): The microbial community adapts to the SHIME environment.
- Basal Period (~2 weeks): Operations under standard conditions to establish a stable baseline for microbial composition and metabolic output [52].
- Treatment/Intervention Period (2-4 weeks): A defined dietary intervention (e.g., probiotic, prebiotic fiber, drug) is introduced to the system. The medium composition is modified to reflect the dietary intervention being tested [52].
- Wash-out Period (~2 weeks): The intervention is halted to monitor the resilience of the microbial community and the persistence of observed effects [52].
- Sample Analysis:
- Microbial Analysis: 16S rRNA sequencing and qPCR to monitor shifts in microbial diversity and abundance.
- Metabolite Analysis: HPLC, GC-MS to quantify SCFAs, bile acids, neurotransmitters (e.g., GABA, serotonin), and other microbial metabolites [52].
- pH and Redox Potential: Continuously monitored in each compartment.
The following workflow summarizes the standard experimental phases in a SHIME study:
SHIME Model Variations
The standard SHIME platform has been adapted into specialized models to address specific research questions [52]:
Table 1: Variations of the SHIME Model
| Model | Description | Primary Research Application |
|---|---|---|
| M-SHIME | Incorporates a mucosal compartment with mucin-coated surfaces. | Studies of host-microbe interactions and biofilm formation relevant to dietary interventions. |
| Twin-SHIME | Parallel systems operated simultaneously. | Comparative studies (e.g., different diets/donors) under identical conditions. |
| Triple-SHIME | Three parallel systems. | High-throughput screening of multiple interventions. |
| Toddle SHIME | Simulates the infant gastrointestinal tract. | Pediatric nutrition and early-life microbiome development. |
Fecal Microbiota Transplantation (FMT)
FMT involves the transfer of processed fecal material from a healthy, screened donor into the gastrointestinal tract of a recipient to restore a healthy microbial community. In research, FMT is a powerful tool to demonstrate causality between a donor's microbiota phenotype (often shaped by diet) and a recipient's physiological outcome [53]. For example, transplantation of microbiota from animals on a high-fiber diet can confer protective phenotypes (e.g., reduced liver injury) to recipient animals, directly proving the functional role of diet-shaped microbiota [54]. Conversely, FMT from donors on a Western-style diet can exacerbate disease susceptibility in recipients [54].
Technical Methodology
Core Protocol: Rodent FMT
- Donor Selection and Screening:
- Fecal Slurry Preparation:
- Fresh fecal pellets from donor animals or human stool are homogenized in sterile anaerobic saline or skim milk containing glycerol (as a cryoprotectant) [54].
- The slurry is filtered to remove large particulate matter.
- Recipient Preparation:
- Antibiotic Pre-treatment (optional but common): Recipient mice are often treated with a cocktail of broad-spectrum antibiotics (e.g., vancomycin, ampicillin, neomycin, metronidazole) in their drinking water for 1-2 weeks to deplete the indigenous microbiota and enhance engraftment of the donor microbiota [54].
- Transplantation:
- Recipients are gavaged with the donor slurry (e.g., 200 μL per mouse) repeatedly over several days [54].
- Control groups receive autologous FMT (their own stool) or FMT from control donors.
- Post-FMT Monitoring:
- Monitor engraftment success via fecal 16S rRNA sequencing.
- Conduct behavioral, biochemical, and molecular analyses to assess functional outcomes relevant to the gut-brain axis.
The Role of Diet in FMT Efficacy
While not yet standardized in clinical practice, diet is recognized as a critical factor influencing the long-term success of FMT. A survey of FMT clinicians and researchers found that 71% agreed that diet is an important consideration for both recipients and donors, though confidence in providing specific dietary advice remains low due to a lack of standardized evidence [53]. Pre-clinical studies show that combining FMT with dietary interventions (e.g., prebiotic fiber) can enhance and prolong the beneficial effects of the transplantation [53]. This highlights the synergistic potential of combining dietary management with microbial therapeutics for treating gut-brain axis disorders.
Research Reagent Solutions
The following table catalogues essential materials and reagents central to conducting experiments with these three investigative models.
Table 2: Essential Research Reagents and Materials
| Item | Function/Application | Example Use Case |
|---|---|---|
| Germ-Free Isolators | Provides a sterile environment for housing and manipulating GF animals. | Fundamental infrastructure for maintaining the GF status of mice and rats during dietary studies [50]. |
| Defined Microbial Consortia | A defined mixture of bacterial strains for colonizing GF or antibiotic-treated animals. | Used in "conventionalization" studies to investigate the specific role of a microbial community in mediating a diet's effect [50] [51]. |
| Sterilized Defined Diets | AIN-93G, high-fat diet (D12492), high-fiber diet, etc., that are irradiated or autoclaved. | Ensures that the dietary intervention is the only variable introduced to GF animals, excluding confounding microbes from food [50] [54]. |
| SHIME Growth Media | Nutritional medium simulating chyme, added to the stomach compartment. | Provides the substrate for microbial growth in the in vitro system; its composition can be modified to test different dietary components [52]. |
| Mucin-agar | A gel used to coat surfaces in the M-SHIME model. | Mimics the host mucosal layer, allowing for the study of mucosa-associated microbiota in response to dietary interventions [52]. |
| Anaerobic Workstation | Creates an oxygen-free environment for handling microbiota-sensitive samples. | Essential for preparing FMT slurries and SHIME inoculum without oxygen exposure, which can kill strict anaerobes [52] [53]. |
| Antibiotic Cocktail | A mixture of antibiotics (e.g., vancomycin, ampicillin, neomycin, metronidazole). | Depletes the native gut microbiota of recipient animals prior to FMT, creating a niche for donor microbiota engraftment [54]. |
| Cryoprotectants (Glycerol/Skim Milk) | Protects bacterial cells during freezing. | Used in the preparation of standardized, bankable FMT inoculum for consistent study replication [54] [53]. |
Integrated Application in Diet-Gut-Brain Research
The true power of these tools is realized when they are applied in a complementary, sequential manner. A typical research pipeline might begin with a SHIME screen to identify promising dietary components, followed by mechanistic studies in GF animals, and finally validation using FMT in rodent models.
For instance, a 2024 study on drug-induced liver injury (DILI) exemplified this integrated approach [54]:
- Dietary Modulation: Mice were fed a high-fiber diet (HFiD) or Western-style diet (WSD).
- FMT Validation: Microbiota from these donor mice were transplanted into antibiotic-treated recipients, which then exhibited the same DILI susceptibility as their donors, proving the microbial role.
- Mechanistic Insight: The study further identified Lactobacillus acidophilus and its metabolite, indole-3-lactic acid (ILA), as key mediators of the HFiD's protective effect, activating the AhR/Nrf2 antioxidant pathway in the liver [54]. Such detailed mechanistic insights are often followed up using GF models to confirm the causal role of specific bacteria.
This workflow demonstrates how these tools can deconstruct the complex interplay between diet, gut microbiota, and host physiology, ultimately sowing the seeds for targeted dietary interventions and microbiota-directed therapies to optimize brain health and treat neuropsychiatric disorders.
The gut-brain axis (GBA) represents a bidirectional communication network that intricately connects the gastrointestinal (GI) tract with the central nervous system (CNS) [7]. This complex system integrates neural, hormonal, and immune pathways to maintain physiological and psychological homeostasis [55] [7]. The gut microbiota, often termed the 'second brain,' plays a pivotal role in this communication, influencing brain function through multiple mechanisms including neurotransmitter production, immune modulation, and the synthesis of microbial metabolites [56] [7]. Emerging evidence demonstrates that dietary patterns significantly shape the composition and functionality of the gut microbiota, thereby exerting profound effects on emotional, cognitive, and neurological health [7] [57]. This whitepaper examines the mechanisms underlying nutritional interventions for anxiety, depression, and cognitive decline through the lens of GBA research, providing technical insights and methodological approaches for researchers and drug development professionals.
Imbalances in microbial communities (dysbiosis) can disrupt GBA signaling, potentially leading to neuroinflammation and neurotransmitter disturbances implicated in mood and cognitive disorders [7]. The vagus nerve serves as a primary neural pathway facilitating direct communication between the gut and brain, modulating brain activity and behaviors associated with anxiety and mood [7]. Furthermore, approximately 90% of serotonin is synthesized in the gut under microbial influence, underscoring the microbiota's critical role in mental health [7]. Understanding these mechanisms provides a scientific foundation for developing targeted nutritional interventions and novel therapeutic approaches for neuropsychiatric conditions.
Mechanisms of Gut-Brain Communication
Neural and Endocrine Pathways
The GBA utilizes multiple sophisticated communication pathways that enable continuous crosstalk between the gut and brain:
Vagus Nerve Signaling: As the primary neural pathway, the vagus nerve transmits gut-derived signals directly to the brainstem, modulating stress responses, mood, and behavior [7]. Research indicates that specific probiotic strains (Lactobacillus and Bifidobacterium) influence the body's stress response system via the vagus nerve and the hypothalamic-pituitary-adrenal (HPA) axis [7].
Neuroendocrine Signaling: Enteroendocrine cells in the gut epithelium produce over 20 hormones that regulate gut-brain communication [55]. These cells respond to nutritional cues by releasing hormones that influence neurotransmitter production, including serotonin, which plays a crucial role in regulating mood, sleep, and appetite [57].
Neurotransmitter Production: Gut microbiota actively synthesize various neurotransmitters, including gamma-aminobutyric acid (GABA), serotonin, dopamine, and norepinephrine [56] [7]. These microbial-derived neurotransmitters can influence brain function either directly or through vagal nerve stimulation.
Immune and Inflammatory Pathways
Immunological mechanisms represent a critical component of gut-brain communication:
Cytokine-Mediated Signaling: Dysbiosis can trigger the release of pro-inflammatory cytokines (e.g., IL-6, TNF-α) that circulate systemically, cross the blood-brain barrier (BBB), and induce neuroinflammation [55] [7]. Chronic neuroinflammation is associated with worsened symptoms of mood disorders and cognitive impairment [55].
Gut Barrier Integrity: The "leaky gut" phenomenon, characterized by increased intestinal permeability, allows pro-inflammatory molecules to enter circulation and potentially cross the BBB [7]. This disruption of gut integrity is strongly influenced by dietary patterns and microbial composition [7].
Short-Chain Fatty Acids (SCFAs): Gut bacteria produce SCFAs (butyrate, acetate, propionate) through fermentation of dietary fiber [56] [7]. These metabolites reinforce the gut barrier, support anti-inflammatory pathways, and regulate neurotransmitter production [56]. Butyrate, in particular, has demonstrated anti-inflammatory effects by inhibiting microglial activation and pro-inflammatory cytokine secretion [56].
Metabolic Pathways
Microbial metabolites serve as key signaling molecules in gut-brain communication:
Short-Chain Fatty Acid Signaling: SCFAs influence brain function by crossing the BBB, modulating microglial function, and affecting gene expression through epigenetic mechanisms [56]. Butyrate functions as a histone deacetylase inhibitor, potentially influencing neural plasticity and cognitive function [56].
Tryptophan Metabolism: Gut microbiota regulate the availability of tryptophan, a serotonin precursor, by controlling its metabolism along the kynurenine pathway [7]. Imbalances in this pathway have been implicated in depression and other neuropsychiatric conditions.
Bile Acid Signaling: Gut microbes modify primary bile acids into secondary bile acids that can function as signaling molecules, influencing systemic inflammation and potentially affecting brain function.
The following diagram illustrates the primary communication pathways of the Gut-Brain Axis:
Figure 1: Gut-Brain Axis Communication Pathways. This diagram illustrates the primary neural, immune, endocrine, and metabolic pathways facilitating bidirectional communication between the gastrointestinal tract and the central nervous system.
Dietary Interventions and Their Neurological Impacts
Evidence-Based Dietary Patterns
Research has identified several dietary patterns that significantly influence mental health outcomes through GBA modulation:
Table 1: Dietary Patterns and Their Impact on Mental Health
| Dietary Pattern | Key Components | GBA Mechanisms | Clinical Outcomes |
|---|---|---|---|
| Mediterranean Diet | High in fruits, vegetables, legumes, whole grains, fish, olive oil; modest lean meats and dairy [55] [57] | Enhances microbial diversity [7], increases SCFA production [7], boosts plasma BDNF levels [55], reduces neuroinflammation | 25-35% reduced depression risk [57], 42% reduced depression risk in cohort study [55], improved cognitive resilience [7] |
| Traditional Diets (Japanese, Norwegian) | Fermented foods, seafood, vegetables, unprocessed grains [57] | Provides natural probiotics [57], increases omega-3 fatty acids [55], supports beneficial gut bacteria | Lower depression prevalence compared to Western diets [57] |
| Western Diet | High in processed foods, refined sugars, unhealthy fats, low in fiber [55] [7] [57] | Reduces microbial diversity [7], increases gut permeability [7], promotes systemic inflammation [55] [7] [57] | Increased risk of depression [55], ADHD [55], and cognitive impairment [55] |
| Plant-Based/High-Fiber Diet | Fruits, vegetables, legumes, whole grains, nuts, seeds [7] | Promotes beneficial bacterial growth [7], enhances SCFA production [7], reduces inflammation [7] | Supports emotional regulation [7], enhances cognitive function [7] |
Key Nutritional Components and Their Mechanisms
Specific dietary components have been identified with direct impacts on neurological health through the GBA:
Table 2: Key Nutritional Components and Neurological Impacts
| Nutrient Category | Specific Components | GBA Mechanisms | Evidence & Outcomes |
|---|---|---|---|
| Omega-3 Fatty Acids | EPA, DHA (fatty fish, seafood, grass-fed beef) [55] | Reduce neuroinflammation [55], regulate neurotransmission [55], influence gene expression [55], support neuronal survival [55] | Effective for ADHD, major depression, bipolar depression, PTSD [55]; Optimal omega-6:omega-3 ratio crucial [55] |
| Probiotics & Psychobiotics | Lactobacillus, Bifidobacterium strains [7] | Produce neurotransmitters (GABA, serotonin) [7], strengthen gut barrier [57], reduce inflammation [57], modulate HPA axis [7] | Symptom reduction in anxiety, depression, stress-related disorders [7]; B. longum APC1472 shows anti-obesity effects [32] |
| Prebiotics & Dietary Fiber | Inulin, FOS, GOS, psyllium [32] | Stimulate beneficial bacteria growth [56] [7], increase SCFA production [56] [7], improve gut barrier function [7] | Improved gut health, constipation relief [32]; Psyllium delays colonic fermentation of inulin [32] |
| Polyphenols & Antioxidants | Berries, tea, olive oil, dark chocolate [7] | Antioxidant and anti-inflammatory properties [7], support beneficial bacteria [7], inhibit harmful species [7] | Reduced intestinal permeability in aging [32]; Lowered pro-inflammatory mediators [32] |
Experimental Models and Methodologies
Research Models for GBA Investigation
The following experimental models are employed in GBA research to elucidate mechanisms and test interventions:
Figure 2: Experimental Models in GBA Research. This diagram outlines the primary research methodologies used to investigate the Gut-Brain Axis, from in vitro systems to human clinical trials.
Standardized Experimental Protocols
Dietary Intervention Study Protocol
Objective: To evaluate the efficacy of a Mediterranean diet intervention on depressive symptoms and associated GBA biomarkers.
Methodology:
- Participant Selection: Recruit adults (18-65) with moderate depressive symptoms, excluding those with specific gastrointestinal disorders, antibiotic use, or severe psychiatric comorbidities [55].
- Study Design: Randomized controlled trial with parallel groups:
- Intervention Duration: Minimum 12 weeks with dietary counseling and monitoring [55].
- Primary Outcomes: Depression rating scales (HAM-D, MADRS) at baseline, 4, 8, and 12 weeks.
- GBA Biomarkers:
- Microbiome Analysis: Fecal samples for 16S rRNA sequencing at baseline and endpoint [7]
- SCFA Measurement: Fecal SCFA levels via gas chromatography [56]
- Inflammatory Markers: Plasma CRP, IL-6, TNF-α [55]
- Neurotrophic Factors: Serum BDNF levels [55]
- Metabolomic Profiling: LC-MS-based plasma metabolomics [32]
Psychobiotic Efficacy Protocol
Objective: To assess the impact of specific probiotic strains on stress response and anxiety symptoms.
Methodology:
- Strain Selection: Multi-strain probiotic containing Lactobacillus helveticus R0052 and Bifidobacterium longum R0175 or specific psychobiotic strains [7].
- Study Design: Randomized, double-blind, placebo-controlled trial.
- Participants: Otherwise healthy adults with moderate anxiety symptoms.
- Intervention Duration: 8-12 weeks with daily supplementation.
- Outcome Measures:
Research Reagent Solutions
Table 3: Essential Research Reagents for GBA Investigations
| Reagent Category | Specific Examples | Research Applications | Technical Considerations |
|---|---|---|---|
| Microbiome Analysis | 16S rRNA sequencing kits [7], shotgun metagenomics [32], GA-map Dysbiosis Test [32] | Microbial community profiling, diversity assessment, dysbiosis quantification | Control for confounders (transit time, regional changes) [32]; Consider unsupervised analysis for novel discoveries [32] |
| SCFA Measurement | Gas chromatography-mass spectrometry (GC-MS) systems [56], commercial SCFA assay kits | Quantification of acetate, propionate, butyrate in fecal samples | Standardize sample collection methods; Account for dietary influences on SCFA production |
| Immunoassays | ELISA kits for cytokines (IL-6, TNF-α, CRP) [55], BDNF assays [55] | Inflammation monitoring, neurotrophic factor quantification | Use validated assays; Consider diurnal variations in biomarkers |
| Cell Culture Models | Caco-2 cells (gut barrier model), SHIME systems [58], primary microglial cultures | Gut permeability assessment, microbial metabolism simulation, neuroinflammation studies | SHIME systems simulate human digestion for nutrient release and gut bacteria effects [58] |
| Omics Technologies | LC-MS metabolomics platforms [32], RNA sequencing, epigenomic tools | Multi-omics integration for pathway analysis | Bioinformatics expertise required for data integration; Use gut-brain modules for neuroactive potential [32] |
Biomarkers and Outcome Measures
Quantifiable biomarkers are essential for evaluating GBA-targeted interventions in clinical and preclinical research:
Microbiome Biomarkers
- Alpha Diversity: Measures microbial richness and evenness within individual samples; reduced diversity associated with Western diets and psychological stress [7].
- Firmicutes to Bacteroidetes Ratio: Altered ratio linked to obesity, depression, and cognitive impairment [56].
- Specific Bacterial Taxa: Faecalibacterium prausnitzii (butyrate producer) reduction associated with depression; Bifidobacterium and Lactobacillus abundances increased with probiotic interventions [56] [7].
Metabolic and Neurochemical Biomarkers
- SCFA Profiles: Butyrate, acetate, and propionate concentrations in fecal samples; butyrate particularly important for gut barrier integrity and anti-inflammatory effects [56] [7].
- BDNF Levels: Serum or plasma brain-derived neurotrophic factor; low levels associated with depression and cognitive decline; increased by Mediterranean diet with nuts [55].
- Tryptophan-Kynurenine Pathway Metabolites: Ratio of kynurenine to tryptophan indicates inflammatory activation; associated with depression pathogenesis [7].
Inflammatory Biomarkers
- C-Reactive Protein (CRP): Systemic inflammatory marker; elevated in depression and metabolic syndrome [55].
- Pro-inflammatory Cytokines: IL-6, TNF-α, IL-1β; elevated in neuroinflammatory states [55].
- Bacterial DNA in Blood: Emerging biomarker for intestinal barrier dysfunction; identifies vulnerable populations for targeted interventions [32].
Future Directions and Personalized Interventions
The field of nutritional neuroscience is advancing toward personalized interventions based on individual genetic and microbiome profiles. Research reveals that our gut microbiome is highly variable and unique to each individual, with twins sharing only 34% of their gut microbes and unrelated individuals sharing 30% [32]. This variability influences individual responses to dietary interventions. For instance, women with gut microbial communities capable of converting soy isoflavones to equol experience a 75% greater reduction in menopausal symptoms when supplemented with isoflavones compared to those lacking these specific microbial species [32].
Emerging research areas include:
- Microbiome-Based Personalized Nutrition: Tailoring dietary recommendations based on individual microbiome composition to optimize mental health outcomes [32].
- Next-Generation Psychobiotics: Developing targeted microbial interventions based on mechanistic understanding of strain-specific effects [32].
- Genetic Considerations: Accounting for host genetic factors that influence response to dietary interventions, such as sucrase-isomaltase (SI) gene variation in carbohydrate maldigestion [32].
- Multi-Omics Integration: Combining microbiome, metabolome, and transcriptome data to develop comprehensive biomarkers for GBA health [32].
The integration of nutraceuticals into GBA health management represents a promising approach for transforming malnutrition treatment and improving cognitive and metabolic health [56]. As research continues to uncover the complex interplay between diet, gut microbiota, and brain function, targeted nutritional interventions offer significant potential for addressing the global burden of mental health disorders through scientifically-validated, mechanism-based approaches.
The microbiota-gut-brain (MGB) axis represents a critical signaling pathway that integrates dietary patterns with brain health and neurodegenerative disease progression. This whitepaper synthesizes current evidence demonstrating how specific dietary interventions modulate gut microbiota composition and function to exert therapeutic effects in Parkinson's (PD) and Alzheimer's disease (AD). Through systematic analysis of clinical and preclinical studies, we identify ketogenic, Mediterranean, and vegetarian diets as promising adjunct strategies that target neuroinflammation, reduce protein aggregation, and support neuronal function via microbial-derived metabolites. Our analysis reveals that dietary modulation of the MGB axis offers a multi-target approach to complement conventional pharmacological treatments, with particular efficacy for non-motor symptoms in PD and early intervention in mild cognitive impairment preceding AD. This review provides researchers and drug development professionals with standardized experimental frameworks, mechanistic insights, and translational considerations for incorporating dietary strategies into comprehensive neurodegenerative disease therapeutic pipelines.
The recognition that gut microbiota significantly influences central nervous system function through bidirectional communication has fundamentally transformed neurodegenerative disease research. The MGB axis comprises complex pathways involving immune mechanisms, vagus nerve signaling, microbial metabolite production, and neuroendocrine system communication [59] [15]. Dietary patterns directly shape gut microbiota composition, diversity, and metabolic output, thereby influencing neuroinflammatory processes and neuronal homeostasis [14]. Emerging evidence positions nutritional intervention as a viable adjunct strategy to counter pathological hallmarks of PD and AD, including α-synuclein aggregation, amyloid-beta deposition, tau phosphorylation, and chronic neuroinflammation.
The therapeutic potential of dietary intervention lies in its capacity for multi-target modulation of disease-relevant pathways. Unlike single-target pharmacological approaches, dietary patterns simultaneously influence numerous biological systems, including gut barrier integrity, blood-brain barrier function, peripheral immune activation, and microbial production of neuroactive compounds [15]. This systems-level approach is particularly relevant for neurodegenerative diseases, which involve multifaceted pathological processes developing over decades. Within the broader thesis of MGB axis research, dietary strategies represent non-invasive, scalable interventions with potential for both prevention and disease modification across the AD and PD continuum.
Mechanistic Foundations: How Dietary Patterns Influence Neurodegenerative Pathology
Key Signaling Pathways in the Microbiota-Gut-Brain Axis
The MGB axis comprises several interconnected communication pathways that translate dietary influences into neurological outcomes. Microbial metabolites, particularly short-chain fatty acids (SCFAs) like butyrate, propionate, and acetate, mediate many dietary effects through immune modulation, epigenetic regulation, and barrier function enhancement [59] [14]. These metabolites directly influence microglial activation states, shifting them from pro-inflammatory to homeostatic phenotypes, and strengthen intestinal and blood-brain barriers, reducing systemic inflammation that drives neuroinflammation [15].
Neuroimmune pathways represent another crucial mechanism, with gut microbiota regulating peripheral immune cell function and cytokine production that can directly impact brain inflammation. The vagus nerve serves as a direct neural connection between the gut and brain, transmitting signals generated by microbial activity and gut hormone secretion [15]. Additionally, gut microbiota significantly influence the production and metabolism of neurotransmitters, including serotonin, dopamine, GABA, and norepinephrine, through direct synthesis or modulation of host synthesis pathways [14] [15]. These mechanisms collectively contribute to the impact of dietary interventions on neurodegenerative disease progression.
Glial Cell Modulation via Dietary Influences
Glial cells, particularly microglia and astrocytes, serve as crucial intermediaries between gut-derived signals and neuronal health. Microglia, the brain's resident immune cells, exist on a functional spectrum from homeostatic to disease-associated states [15]. Dietary patterns significantly influence microglial transition between these states through microbial metabolite production. The Mediterranean diet, rich in polyphenols and fiber, promotes homeostatic microglia via SCFA receptor signaling, while Western diets high in saturated fats and simple carbohydrates drive microglia toward pro-inflammatory phenotypes through LPS signaling and toll-like receptor activation [59] [15].
Astrocytes similarly respond to dietary-modulated gut signals, altering their support functions for neurons. SCFAs enhance astrocytic glutamate clearance and antioxidant production, while dysbiosis-induced inflammatory cytokines impair astrocytic support capacity [15]. The ketogenic diet demonstrates particular efficacy in modulating glial function, with studies showing reduced microglial activation and enhanced astrocytic ketone body production that provides alternative energy sources for neurons compromised in neurodegenerative diseases [59]. These glial modifications represent a primary mechanism through which dietary interventions exert neuroprotective effects in AD and PD.
Quantitative Analysis of Dietary Interventions in Neurodegenerative Diseases
Comparative Efficacy of Dietary Patterns in Alzheimer's Disease
Table 1: Dietary Intervention Effects in Alzheimer's Disease and Mild Cognitive Impairment
| Dietary Pattern | Study Model | Duration | Microbiota Changes | Key Biochemical Outcomes | Clinical/Cognitive Outcomes |
|---|---|---|---|---|---|
| Ketogenic Diet (Modified) | 11 MCI, 6 CN patients [59] | 6 weeks | Enterobacteriaceae↑, Akkermansia↑, Slackia↑, Christensenellaceae↑, Bifidobacterium↓ | Fecal lactate↓, acetate↓, propionate↑, butyrate↑ | Improved AD biomarkers in CSF |
| Ketogenic Diet | C57BL/6 male mice [59] | 16 weeks | Akkermansia muciniphila↑, Lactobacillus↑, Desulfovibrio↓ | Improved neurovascular function, BBB integrity | Lower AD risk, improved cerebral blood flow |
| Intermittent Fasting & High-Carbohydrate Diet | Male Sprague Dawley rats [59] | 8 weeks | Proteobacteria↑ (KD), Bacteroidetes↑ (HCD) | Reduced insulin resistance | Improved cognitive function in water maze test |
| Western Diet | Male C57BL/6 mice [59] | 2 weeks | Reduced microbial diversity | Increased systemic inflammation | Impaired cognitive flexibility, memory deficits |
Comparative Efficacy of Dietary Patterns in Parkinson's Disease
Table 2: Dietary Intervention Effects in Parkinson's Disease
| Dietary Pattern | Study Model | Duration | Microbiota Changes | Key Biochemical Outcomes | Clinical/Motor Outcomes |
|---|---|---|---|---|---|
| Mediterranean Diet | 8 PD patients [59] | 5 weeks | Proteobacteria↑, Desulfovibrionaceae↓, Bilophila↓, Roseburia↑ | No change in intestinal permeability | Constipation symptoms alleviated |
| Vegetarian Diet | 54 PD, 16 CN patients [59] | 14 days | No significant difference | Anti-inflammatory effects, SCFA production | Potential longer-term benefits on clinical course |
| Low-Protein High-Carbohydrate Diet | C57BL/6 mice [59] | 30 days | Bifidobacterium↑, Ileibacterium↑, Turicibacter↑, Blautia↑, Bilophila↓ | Increased FGF-21 in serum and midbrain | Dopaminergic neuron protection, improved motor function |
| Medicinal-Food Homology Approach | Preclinical models [60] | Variable | Not specified | Nrf2/ARE activation, NF-κB suppression, mitochondrial stabilization | Multi-target oxidative stress modulation |
Experimental Methodologies for Investigating Diet-MGB Axis Interactions
Standardized Protocols for Preclinical Dietary Interventions
Robust investigation of diet-MGB axis interactions in neurodegenerative diseases requires standardized methodologies. For preclinical studies, the ketogenic diet protocol typically consists of a 6:1 to 4:1 fat-to-carbohydrate plus protein ratio administered for 8-16 weeks in murine models [59]. The Mediterranean diet intervention employs a formulation rich in polyphenols (from extra virgin olive oil, berries), omega-3 fatty acids (from fish oil), and complex carbohydrates (from whole grains and legumes) for 5-30 days [59]. The low-protein, high-carbohydrate diet for PD models contains approximately 5% protein, 14.4% fat, and 77.2% carbohydrates administered for 30 days [59].
Essential outcome measures include behavioral assessments (Y-maze, water maze, pole test, traction test, rota-rod test), microbiota analysis (16S rRNA sequencing, metagenomics, metabolomics), biochemical assays (CSF Aβ42, Aβ40, total tau, tau-p181, serum FGF-21), and immunohistochemical analysis of brain and gut tissues [59]. For clinical trials, the modified Mediterranean ketogenic diet follows a 6-week intervention with <10% carbohydrates, 60-65% fat, and 30-35% protein, followed by washout and control diet phases [59]. Primary endpoints include MDS-UPDRS scores for PD studies and CSF biomarkers plus cognitive assessments for AD studies, with microbiota composition and SCFA measurements as secondary endpoints [59].
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Key Research Reagent Solutions for Diet-MGB Axis Investigations
| Category | Specific Reagents/Platforms | Research Application | Key References |
|---|---|---|---|
| Microbiota Analysis | 16S rRNA sequencing (V3-V4 region), Shotgun metagenomics, LC-MS metabolomics | Taxonomic profiling, functional potential assessment, metabolite quantification | [59] [14] |
| SCFA Measurement | Gas chromatography-mass spectrometry (GC-MS), Nuclear magnetic resonance (NMR) spectroscopy | Quantification of butyrate, propionate, acetate in fecal and serum samples | [59] [14] |
| Neurodegeneration Biomarkers | Aβ42, Aβ40, total tau, tau-p181 ELISA kits, α-synuclein ELISA, NfL assays | Quantification of pathological proteins in CSF, plasma, and tissue extracts | [59] [61] |
| Gut Barrier Integrity Assessment | FITC-dextran permeability assay, zonulin ELISA, occludin/claudin immunohistochemistry | Intestinal barrier function assessment | [59] [15] |
| Cell Culture Models | SH-SY5Y, PC12, Caco-2, primary microglial cultures, gut organoids | In vitro mechanistic studies of microbial metabolites | [15] [60] |
| Animal Models | MPTP/6-OHDA (PD), 5xFAD/APP-PS1 (AD), germ-free mice, fecal transplant models | Preclinical efficacy and mechanism studies | [59] [15] |
| Nos-IN-3 | Nos-IN-3|Potent nNOS Inhibitor|For Research Use | Nos-IN-3 is a selective neuronal nitric oxide synthase (nNOS) inhibitor. This product is For Research Use Only and is not intended for diagnostic or personal use. | Bench Chemicals |
Integration with Conventional Therapeutics and Clinical Translation
The strategic integration of dietary interventions with established and emerging pharmacological treatments represents a promising approach for comprehensive neurodegenerative disease management. In Alzheimer's disease, dietary approaches may complement anti-amyloid immunotherapies (lecanemab, donanemab) by addressing multiple pathological processes beyond amyloid deposition, including neuroinflammation, insulin resistance, and oxidative stress [61]. Similarly, in Parkinson's disease, dietary strategies may enhance the efficacy of levodopa and emerging non-dopaminergic therapies (e.g., solengepras) by improving gut motility, reducing systemic inflammation, and supporting mitochondrial function [62] [60].
Clinical translation requires careful consideration of intervention timing, patient stratification, and safety monitoring. The most compelling evidence supports dietary interventions in early disease stages—mild cognitive impairment for AD and early untreated PD—where microbial modulation may exert maximal impact on disease trajectory [59] [61]. Patient stratification based on baseline microbiota composition, genetic risk factors, and metabolic profile may enhance intervention efficacy, as individual microbial ecosystems respond differently to dietary modifications [14]. Safety monitoring should include assessment of nutritional status, gastrointestinal tolerability, and potential interactions with pharmacological treatments, particularly for ketogenic diets in cardiometabolic-compromised individuals and high-fiber interventions in patients with significant gastrointestinal dysfunction [59] [60].
Future research directions should prioritize randomized controlled trials with biomarker-driven endpoints, development of personalized nutrition algorithms based on microbial profiling, and investigation of synergistic timing between dietary interventions and pharmacological treatments. Additionally, mechanistic studies exploring how specific dietary components influence glial cell biology, protein aggregation clearance, and neuronal resilience will provide critical insights for optimizing therapeutic dietary strategies in neurodegenerative diseases.
Dietary intervention emerges as a scientifically grounded adjunct strategy for modulating neurodegenerative disease progression through the microbiota-gut-brain axis. Ketogenic, Mediterranean, and medicinal-food homology approaches demonstrate specific effects on gut microbiota composition, microbial metabolite production, and subsequent neuroinflammatory processes relevant to both Alzheimer's and Parkinson's disease pathology. The integration of these nutritional strategies with conventional and emerging pharmacological therapies represents a multifaceted approach to addressing the complex pathophysiology of neurodegenerative diseases. While further research is needed to refine personalized nutrition approaches and establish optimal integration with pharmacotherapies, current evidence strongly supports the inclusion of targeted dietary interventions in comprehensive neurodegenerative disease management paradigms.
Navigating Challenges and Personalizing Gut-Brain Axis Interventions
Within the rapidly advancing field of gut-brain-axis (GBA) research, diet has emerged as a central modulator of bidirectional communication pathways. The concept of psychobiotics—dietary interventions that positively influence mental health via the microbiota—highlights the therapeutic potential of nutritional strategies [14]. However, a significant challenge impedes clinical translation: the profound individual variability in response to dietary interventions. This variability is largely mediated by the subject's pre-existing, or baseline, gut microbiota composition [63]. The baseline gut microbiome acts as a critical biological filter, determining the metabolic fate of dietary components and ultimately influencing the magnitude and direction of host physiological and neurological responses [64]. Understanding and predicting this variability is therefore not merely an academic exercise but a prerequisite for developing effective, microbiota-targeted nutritional therapies for brain and mental health.
The Evidence: Baseline Microbiota as a Predictor of Dietary Response
A growing body of evidence from interventional studies demonstrates that an individual's baseline microbiota composition is a key determinant of their response to dietary changes, effectively creating responder and non-responder phenotypes.
Key Studies Demonstrating Microbiome-Dependent Responses
Table 1: Summary of Key Studies on Baseline Microbiome and Dietary Response
| Study Intervention | Baseline Microbiome Clusters / Features | Response in Cluster P (Prevotella-rich) | Response in Cluster B (Bacteroides-rich) | Primary Outcome Measured |
|---|---|---|---|---|
| RS-rich Unripe Banana Flour (UBF) [64] | Cluster P: Prevotella-rich, higher diversity.Cluster B: Bacteroides-rich, lower diversity. | Significant global microbiota shifts (PERMANOVA p=0.007) & major functional changes (533 KEGG orthologs). | No significant effects observed. | Microbiota composition & function. |
| Inulin [64] | Cluster P: Prevotella-rich.Cluster B: Bacteroides-rich. | Modest functional modulation (19 KOs). | No significant effects observed. | Microbiota composition & function. |
| Barley Kernel Bread [63] | High baseline Prevotella/Bacteroides ratio. | Improved glucose metabolism. | No improvement in glucose metabolism. | Host glucose metabolism. |
| Restricted Diet (Oats, Milk, Water) [65] | Individual-specific baseline compositions. | N/A (Study did not cluster by enterotype) | N/A (Study did not cluster by enterotype) | Microbiota composition (Effect Size: 3.4%, range 1.67–16.42%). |
The seminal study by et al. (2025) provides a clear example. In a double-blind, randomized, placebo-controlled trial, subjects consumed unripe banana flour (UBF, high in resistant starch), inulin, or a placebo. At baseline, subjects were stratified into two distinct clusters: a Prevotella-rich (P) cluster and a Bacteroides-rich (B) cluster [64]. The results were striking: only individuals in the P cluster who consumed UBF showed significant global shifts in their microbiota and major changes in its predicted metabolic function. Those in the B cluster showed no significant response to UBF, and inulin produced only modest effects in the P cluster [64]. This demonstrates that the efficacy of a specific fiber is contingent upon the baseline microbial community equipped to utilize it.
This phenomenon extends beyond microbiota composition to host physiology. Studies on high-fiber bread interventions have shown that improved glucose metabolism following consumption is predominantly observed in individuals with a high baseline Prevotella/Bacteroides ratio, designating them as "responders" [63]. Furthermore, a study restricting dietary options to oats, milk, and water found that while the intervention had an overall effect, the effect size varied dramatically between individuals, from 1.67% to 16.42%, underscoring the personalized nature of dietary modulation [65].
Methodological Framework for Research
To systematically study the role of the baseline microbiome, robust and standardized methodologies are required for dietary assessment, microbiota analysis, and experimental design.
Dietary Assessment and Indexing
Controlling for habitual diet is critical. Dietary indices that summarize complex dietary patterns into a single measure are valuable tools for covariate analysis in microbiota studies.
Table 2: Dietary Indices for Controlling for Habitual Diet in Microbiota Studies
| Dietary Index | Basis of Calculation | Key Findings in Microbiota Studies |
|---|---|---|
| Healthy Eating Index (HEI) [66] | Compliance with US Dietary Guidelines (0-100 scale). | Explains the greatest variance in microbiota composition; strongest associations with alpha diversity and specific microbial taxa in Western populations. |
| Mediterranean Diet Score (MDS) [66] | Adherence to Mediterranean dietary patterns (0-10 scale). | Significantly associated with microbiota measures, though explains less variance than the HEI. |
| Healthy Food Diversity (HFD) Index [66] | Diversity of food intake weighted by health value (0-1 scale). | Shows significant but weaker and fewer associations with microbiota composition compared to HEI and MDS. |
Experimental Design and Protocols
Recommended Workflow for a Diet-Microbiome Intervention Study:
Screening & Baseline Assessment:
- Recruit participants according to study criteria (e.g., healthy adults, specific age range, no recent antibiotic use).
- Collect baseline stool samples for 16S rRNA gene sequencing or shotgun metagenomics.
- Assess habitual diet using a validated Food Frequency Questionnaire (FFQ) or multiple 24-hour recalls to calculate a dietary index like the HEI [66].
- Measure baseline host phenotypes (e.g., blood biochemistry, anthropometrics).
Stratification & Randomization:
- Process baseline microbiota samples and perform clustering analysis (e.g., Jensen-Shannon Distance, Partitioning Around Medoids) to identify enterotypes or clusters (e.g., Prevotella-rich vs. Bacteroides-rich) [64].
- Stratify participants by their baseline microbiota cluster before randomizing them into intervention and control groups. This ensures balanced representation of different microbiome types across study arms.
Intervention Phase:
- Adminiate the dietary intervention (e.g., UBF, inulin) or placebo control for a sufficient duration. Animal studies suggest direct dietary effects on the microbiota can be seen in days, but microbiome-mediated effects on the host may require weeks or months [63].
- Provide dietary instructions to minimize changes in background diet.
Longitudinal Sampling & Endpoint Assessment:
- Collect multiple consecutive stool samples per study timepoint to account for intra-individual variation [63].
- At the end of the intervention, repeat all baseline host phenotype measurements and collect final stool samples.
Analysis:
- Primary: Test for interaction effects between baseline microbiota cluster and intervention group on outcome measures (e.g., microbial diversity, SCFA levels, host biomarkers).
- Secondary: Conduct within-cluster analyses to identify responders.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Materials for Diet-Microbiome Studies
| Item / Reagent | Function / Application | Example Use Case |
|---|---|---|
| DNA Extraction Kit (e.g., PowerMicrobiome) [65] | Isolation of high-quality microbial DNA from complex stool samples. | Essential preparatory step for all downstream sequencing analyses. |
| 16S rRNA Gene Primers (e.g., 515F/806R for V4 region) [65] | Amplification of a conserved bacterial gene region for taxonomic profiling. | Cost-effective analysis of microbial community composition and structure. |
| Shotgun Metagenomics Sequencing | Random sequencing of all genetic material in a sample. | Provides higher resolution (strain-level) and functional gene (KO) profiling [64]. |
| PICRUSt2 Software | Phylogenetic Investigation of Communities by Reconstruction of Unobserved States. | Predicts the functional potential of a microbiota based on 16S rRNA gene data [64]. |
| Flow Cytometry | Absolute cell counting in fecal samples. | Enables creation of Quantitative Microbiome Profiles (QMP), moving beyond relative abundance [65]. |
| Resistant Starch / Prebiotics (e.g., Unripe Banana Flour, Inulin) [64] | Defined dietary interventions to test specific hypotheses on fiber fermentation. | Used to elicit a microbiota response and study cluster-specific effects. |
| Short-Chain Fatty Acid (SCFA) Analysis (e.g., GC-MS) | Quantification of microbial metabolites (acetate, propionate, butyrate). | Connects microbial metabolic output to host health outcomes. |
Mechanistic Pathways and Conceptual Synthesis
The differential response based on baseline microbiota can be conceptualized through a mechanistic pathway where diet is metabolized by the existing microbial community, leading to distinct host outcomes.
The evidence is clear: the "one-size-fits-all" approach to nutritional intervention for GBA modulation is obsolete. The baseline gut microbiome is a decisive factor that can predict the success or failure of a dietary strategy. Future research must move beyond simply associating diet with microbiota changes and focus on elucidating the precise mechanisms—including the production of SCFAs, secondary bile acids, and other neuroactive metabolites—by which a pre-existing microbial community transforms dietary input into host signal [14]. The integration of deep phenotypic data, including brain-related biomarkers, with multi-omics microbiota profiling in longitudinal, well-designed dietary studies is the next frontier. This will accelerate the development of personalized, effective, and microbiota-targeted nutritional therapies to improve brain and mental health.
The gut-brain axis represents a complex, bidirectional communication network that integrates gastrointestinal function with cognitive and emotional centers in the brain. Within this system, two crucial signaling barriers—the intestinal barrier and the blood-brain barrier (BBB)—play pivotal roles in regulating homeostasis and information flow. Recent research has established that dysfunction in these barriers contributes significantly to the pathophysiology of various psychiatric and neurological disorders, creating a permissive environment for disease development and progression [67]. The integrity of these barriers is increasingly recognized as being modulated by dietary patterns, positioning nutrition as a critical factor in maintaining signaling fidelity within the gut-brain axis.
These biological barriers share remarkable anatomical and functional similarities, both relying on specialized cellular complexes to maintain selective permeability. The BBB serves as the brain's first line of defense, preventing unwanted substances from entering the central nervous system (CNS) while ensuring essential nutrients can cross [68]. Similarly, the intestinal barrier regulates the passage of dietary components and microorganisms while preventing the translocation of harmful substances into systemic circulation. Psychological stress and dietary factors can simultaneously compromise both barriers, creating a vicious cycle of exacerbated inflammation and neurological dysfunction [67]. Understanding the coordinated regulation of these barriers opens new avenues for therapeutic interventions targeting psychiatric and neurological disorders through dietary modification.
Physiological Architecture of Signaling Barriers
Blood-Brain Barrier Structure and Function
The BBB is a highly specialized, multi-cellular structure that forms a selective interface between the peripheral circulation and the CNS. Its core anatomical foundation consists of microvascular endothelial cells joined together by extensive tight junctions and adherens junctions, creating a physical barrier that limits paracellular diffusion [68]. Unlike peripheral endothelial, BBB endothelial cells exhibit minimal fenestrations and significantly reduced transcellular vesicular transport, resulting in high transendothelial electrical resistance that effectively restricts the passive movement of most molecules [68].
The BBB's functionality extends beyond this physical barrier through an ensemble of supporting cells that form the neurovascular unit:
- Astrocytes: These glial cells extend end-feet processes that envelop approximately 99% of the BBB surface area, contributing to barrier induction and maintenance through the release of regulatory factors [68]. They express specialized proteins including aquaporin IV and the dystroglycan-dystrophin complex that facilitate interaction with the basal lamina [68].
- Pericytes: Embedded within the capillary basement membrane, pericytes cover nearly 100% of CNS endothelial surfaces and play crucial roles in angiogenesis, BBB development, and regulation of endothelial tight junction integrity [68]. Pericyte-endothelial communication occurs through pathways such as PDGF-B/PDGFRβ signaling, with pericyte deficiency leading to increased barrier permeability [68].
- Neurons: Contributing to neurovascular coupling, neurons help coordinate BBB function with regional neural activity and metabolic demands.
Together, these cellular components create a dynamic interface that maintains CNS homeostasis through tight regulation of ion balance, nutrient transport, and exclusion of potential neurotoxins.
Intestinal Barrier Organization
The intestinal barrier represents the largest interface between the internal milieu and the external environment, with an estimated surface area of nearly 400 m² in humans. Its hierarchical organization includes:
- Epithelial cell layer: A single layer of specialized intestinal epithelial cells interconnected by tight junctions, including enterocytes, goblet cells, Paneth cells, and enteroendocrine cells.
- Mucus layers: Secreted by goblet cells, forming a physicochemical barrier that separates the epithelium from luminal contents.
- Gut-vascular barrier (GVB): A recently discovered structure that shares anatomical and functional similarities with the BBB, providing an additional regulatory interface before substances enter portal circulation [67].
- Immune components: Including gut-associated lymphoid tissue (GALT) and resident macrophages that sample luminal antigens.
Both the BBB and intestinal barrier utilize similar cellular adhesion molecules and tight junction proteins—including claudin-5, occludin, and zonula occludens-1—to maintain their selective permeability [67]. This architectural parallelism explains why these barriers often exhibit coordinated dysfunction in disease states.
Table 1: Cellular Components of Signaling Barriers
| Cell Type | Blood-Brain Barrier | Intestinal Barrier | Primary Functions |
|---|---|---|---|
| Endothelial/Epithelial Cells | Non-fenestrated endothelial cells | Enterocytes, colonocytes | Physical barrier formation; transport regulation |
| Tight Junction Components | Claudin-5, occludin, ZO-1 | Claudin-5, occludin, ZO-1 | Paracellular sealing; barrier selectivity |
| Support Cells | Astrocytes, pericytes | Enteric glial cells | Barrier induction/maintenance; immune regulation |
| Immune Sentinels | Microglia | Gut-associated lymphoid tissue | Pathogen surveillance; inflammatory mediation |
Molecular Signaling Pathways in Barrier Regulation
Key Developmental and Homeostatic Pathways
Several evolutionarily conserved signaling pathways coordinate the development and maintenance of both the BBB and intestinal barrier:
Wnt/β-catenin signaling serves as a master regulator of BBB development during embryogenesis. In endothelial cells, binding of Wnt ligands to Frizzled receptors prevents β-catenin degradation, allowing its translocation to the nucleus where it induces expression of barrier-specific genes including those encoding glucose transporter 1 (Glut1) and claudin-5 [67]. This pathway remains active in certain adult brain regions, contributing to barrier maintenance throughout life.
Vascular Endothelial Growth Factor (VEGF) signaling exhibits context-dependent effects on barrier function. Under physiological conditions, VEGF contributes to angiogenesis and vascular maintenance. However, during inflammation or injury, elevated VEGF levels disrupt tight junctions by downregulating occludin and claudin-5 expression, thereby increasing paracellular permeability at both the BBB and intestinal barrier [67].
Fibroblast Growth Factor-2 (FGF-2) influences barrier integrity through modulation of tight junction assembly and promotion of endothelial cell survival. FGF-2 signaling has been demonstrated to strengthen barrier function under stress conditions, potentially offering therapeutic applications [67].
Sonic Hedgehog (Shh) signaling contributes to barrier maturation and maintenance through regulation of tight junction protein expression and interaction with pericytes. Shh pathway activation enhances barrier resistance to inflammatory insults [67].
Stress-Induced Barrier Dysregulation
Psychological stress activates the hypothalamic-pituitary-adrenal (HPA) axis, culminating in glucocorticoid release that directly impacts both intestinal and BBB integrity. Chronic stress disrupts tight junction proteins through several mechanisms:
- Nuclear Factor Kappa B (NF-κB) activation: Stress and inflammatory cytokines activate this pathway, leading to increased production of matrix metalloproteinases (MMP-9) and pro-inflammatory cytokines (TNF-α, IL-6, IL-1β) that degrade tight junction components [67].
- Reactive Oxygen Species (ROS) generation: Oxidative stress directly damages endothelial and epithelial cells while activating inflammatory cascades that further compromise barrier function.
- Mitogen-Activated Protein Kinase (MAPK) signaling: Stress hormones can activate p38 and JNK pathways, leading to internalization of tight junction proteins and increased permeability.
These molecular events create a feed-forward cycle wherein barrier disruption permits increased translocation of immune mediators that further exacerbate barrier dysfunction, ultimately facilitating neuroinflammation associated with psychiatric disorders.
Diagram 1: Stress-Induced Barrier Disruption
Experimental Models and Assessment Methodologies
In Vitro Barrier Models
Reductionist in vitro systems enable controlled investigation of specific aspects of barrier function:
BBB models typically employ primary human brain microvascular endothelial cells (HBMECs) or immortalized cell lines (hCMEC/D3) cultured on semi-permeable transwell filters. These systems generate a polarized endothelial monolayer with measurable transendothelial electrical resistance (TEER). For enhanced physiological relevance, co-culture models incorporating astrocytes, pericytes, or neuronal cells more accurately recapitulate the neurovascular unit [68].
Intestinal barrier models utilize epithelial cell lines (Caco-2, T84, HT-29) that spontaneously differentiate into polarized monolayers with well-developed tight junctions when cultured on transwell inserts. Co-culture systems incorporating immune cells (macrophages, lymphocytes) or enteric glial cells provide more complex interactions relevant to gut-brain signaling.
Table 2: Quantitative Assessment Parameters for Barrier Function
| Assessment Method | Normal/Healthy Range | Dysfunctional Range | Applications |
|---|---|---|---|
| Transendothelial/Epithelial Electrical Resistance (TEER) | BBB: >150 Ω·cm²Intestinal: >300 Ω·cm² | BBB: <100 Ω·cm²Intestinal: <150 Ω·cm² | Real-time barrier integrity monitoring |
| Paracellular Tracer Flux | <0.5%/hour for 4kDa FITC-dextran | >2.0%/hour for 4kDa FITC-dextran | Macromolecule permeability assessment |
| Tight Junction Protein Expression | Western blot: >80% control levelsImmunofluorescence: Continuous membrane localization | Western blot: <50% control levelsImmunofluorescence: Disrupted/cytoplasmic localization | Molecular characterization of barrier defects |
| Serum Biomarkers | Lipopolysaccharide: <0.5 EU/mLS100β: <0.15 μg/LZO-1: <7.5 ng/mL | Lipopolysaccharide: >1.0 EU/mLS100β: >0.25 μg/LZO-1: >15 ng/mL | Clinical assessment of barrier integrity |
In Vivo Assessment Techniques
Preclinical models enable investigation of barrier function within intact physiological systems:
Chronic stress paradigms including chronic social defeat stress (CSDS) and chronic restraint stress reliably induce barrier disruption in rodents. These models reproduce key features of stress-related psychiatric disorders and permit investigation of gut-brain interactions [67].
Genetic models with targeted disruption of tight junction proteins or signaling pathway components (e.g., claudin-5 knockout, β-catenin deletion) provide mechanistic insights into barrier regulation.
Imaging approaches include dynamic contrast-enhanced magnetic resonance imaging (DCE-MRI) with gadolinium-based tracers for non-invasive BBB assessment, and intravital microscopy for real-time visualization of barrier function.
Functional permeability assays involve administration of molecular tracers of varying sizes (e.g., Evans Blue, sodium fluorescein, FITC-dextran conjugates) with subsequent quantification in target tissues or biological fluids.
Diagram 2: Experimental Assessment Workflow
Dietary Modulation of Barrier Function
Nutritional Interventions and Mechanisms
Dietary patterns significantly influence the integrity of both intestinal and blood-brain barriers through multiple interconnected mechanisms. Research presented at NeuroGASTRO 2025 highlighted that specific dietary components can enhance gut barrier function and subsequently improve brain health [32].
Mediterranean diets rich in polyphenols, omega-3 fatty acids, and fermentable fibers demonstrate particular efficacy in maintaining barrier integrity. These dietary components enhance microbial diversity, decrease systemic inflammation, and improve gut-brain communication [69] [32]. Polyphenol-rich dietary patterns specifically reduce intestinal permeability and lower pro-inflammatory gut bacteria-derived mediators, potentially slowing age-related barrier dysfunction [32].
Prebiotics and probiotics directly modulate barrier function through multiple mechanisms. Specific probiotic strains (e.g., Bifidobacterium longum APC1472) demonstrate barrier-strengthening effects, attenuating the enduring impact of early-life nutritional stress on hypothalamic regulation [32]. Prebiotic fibers (inulin-type fructans, psyllium) improve gut barrier function while delaying colonic fermentation that can exacerbate symptoms in gastrointestinal disorders [32].
Fermentable oligosaccharides, disaccharides, monosaccharides, and polyols (FODMAPs) present a complex relationship with barrier function. While some fermentable fibers can initially increase permeability in sensitive individuals, tolerance can be improved through utilization of modified fiber gels (methylcellulose and psyllium) that alter the rate of colon gas production [32].
Microbial Metabolites as Key Mediators
The gut microbiota processes dietary components into neuroactive metabolites that directly influence barrier function:
- Short-chain fatty acids (SCFAs): Produced from microbial fermentation of dietary fiber, SCFAs (butyrate, propionate, acetate) enhance intestinal barrier function by stimulating mucus production and tight junction protein expression. Butyrate additionally strengthens the BBB through anti-inflammatory effects and histone deacetylase inhibition [69].
- Secondary bile acids: Microbial metabolism of primary bile acids generates signaling molecules that activate membrane receptors (TGR5) and nuclear receptors (FXR), modulating barrier function and inflammatory responses [32].
- Tryptophan metabolites: Dietary tryptophan is metabolized by gut microbes into various indole derivatives and kynurenine pathway metabolites that regulate barrier function through aryl hydrocarbon receptor (AhR) activation and immunomodulatory effects [67].
Recent research has identified 56 different gut-brain modules (GBMs)—biochemical pathways corresponding to neuroactive compound production or degradation—that provide a framework for understanding how microbial metabolism of dietary components influences brain function [32].
Research Reagent Solutions
Table 3: Essential Research Reagents for Barrier Function Studies
| Reagent Category | Specific Examples | Research Applications | Key Functions |
|---|---|---|---|
| Cell Culture Models | hCMEC/D3 (BBB)Caco-2 (Intestinal)Primary cells | Barrier integrity assaysDrug transport studies | Physiologically relevant in vitro systems |
| Tight Junction Markers | Anti-claudin-5 antibodiesAnti-occludin antibodiesAnti-ZO-1 antibodies | ImmunofluorescenceWestern blottingFlow cytometry | Localization and quantification of junctional proteins |
| Permeability Tracers | Sodium fluorescein (376 Da)FITC-dextran (4-70 kDa)Evans Blue albumin | Paracellular flux assessmentIn vivo permeability measurements | Size-dependent permeability profiling |
| Cytokine Assays | TNF-α, IL-6, IL-1β ELISAMultiplex cytokine panels | Inflammatory challenge studiesTreatment efficacy assessment | Quantification of barrier-disrupting mediators |
| Microbiome Tools | 16S rRNA sequencingShotgun metagenomicsTargeted metabolomics | Dietary intervention studiesMicrobiome-barrier interactions | Microbial community analysis and functional assessment |
Therapeutic Implications and Future Directions
The recognition of signaling barrier dysfunction in psychiatric and neurological disorders opens new avenues for therapeutic intervention. Current pharmacological treatments for conditions like major depressive disorder (MDD) and bipolar disorder (BD) demonstrate limited efficacy, with treatment resistance estimated at 30-50% for MDD and 26-52% for BD [67]. Barrier-targeted approaches represent a paradigm shift from traditional monoamine-focused treatments.
Promising therapeutic strategies include:
- Barrier-stabilizing compounds: Drugs that enhance expression of tight junction proteins or modulate key signaling pathways (Wnt/β-catenin, FGF-2) could potentially restore barrier integrity in neuropsychiatric conditions [67].
- Microbiome-targeted interventions: Specific probiotics, prebiotics, and postbiotics that strengthen barrier function offer non-pharmacological approaches with potentially fewer side effects [32].
- Personalized nutrition: Genetic variations in carbohydrate-active enzyme genes (e.g., sucrase-isomaltase) may predispose to barrier dysfunction, supporting the development of genotype-based dietary interventions [32].
- Combined therapeutic approaches: Integrating barrier-stabilizing strategies with conventional treatments may enhance efficacy, particularly in treatment-resistant populations.
Future research priorities include developing more sophisticated human-relevant barrier models, validating non-invasive biomarkers for clinical barrier assessment, and conducting randomized controlled trials of barrier-targeted interventions in specific patient populations. The emerging recognition of bacterial DNA in blood as a potential biomarker for vulnerable individuals who could benefit most from protective dietary interventions represents a particularly promising direction for personalized medicine approaches [32].
The gut-brain axis represents one of the most promising yet challenging frontiers in translational research, particularly within the context of nutritional science. This complex bidirectional communication network connects the gastrointestinal tract with the central nervous system through multiple pathways including neural, endocrine, immune, and metabolic signaling routes [7] [4]. While preclinical models have generated compelling evidence that dietary interventions can modulate this axis to improve brain function and treat neurological disorders, translating these findings into robust clinical outcomes has proven exceptionally difficult. The field faces a fundamental translational gap between promising mechanistic insights from animal studies and effective, reproducible interventions in human populations [3] [70].
The complexity of the gut-brain axis necessitates sophisticated research approaches that can account for the multifactorial nature of diet-microbiome-host interactions. Traditional research models, particularly animal studies, have provided valuable foundational insights but often overlook intricate and human-specific interactions within this axis [70]. Consequently, the translation of findings from these models into clinical applications has been challenging. Recent analyses highlight that microbiome metrics and microbiota-targeted therapies, while promising, remain largely experimental and not yet ready for broad clinical application [32] [3]. This whitepaper examines the core challenges in gut-brain axis translational research and outlines emerging methodologies and frameworks to bridge the preclinical-clinical divide.
Fundamental Translational Challenges
Model System Limitations
Figure 1: Limitations of traditional animal models in predicting human physiology and the emerging role of New Approach Methodologies (NAMs).
Traditional animal models, particularly germ-free and gnotobiotic mice, have been instrumental in establishing causal relationships between gut microbiota and brain function [4]. However, these models present significant limitations when translating findings to human physiology. Germ-free animals exhibit marked abnormalities in stress regulation, social interaction, and synaptic signaling that do not fully recapitulate human neurodevelopment [3]. More critically, recolonization of these animals later in life fails to fully restore typical brain function, indicating the importance of timing in microbiota-brain interactions that may differ in humans [3].
The simplification of human microbial ecosystems into single-strain or limited-consortium representations in animal models ignores the complex interactions that characterize human gut microbiomes. Studies demonstrate that microbial diversity and functional redundancy in humans create resilience that simplified models cannot capture [24]. Additionally, fundamental physiological differences between species—including metabolism, blood-brain barrier characteristics, and immune function—complicate extrapolation from rodent data to human applications [70]. The failure to account for the "dietary dark matter"—including unquantified nutrients, food additives, preparation methods, and culturally-specific foods—further limits the translational validity of animal studies [71].
Methodological and Measurement Heterogeneity
The field suffers from significant inconsistencies in methodology and measurement approaches that impede comparison across studies and replication of findings. Research presented at the 2025 Gut Microbiota for Health Summit highlighted how available dietary assessment tools designed for research, such as food frequency questionnaires and 24-hour dietary recalls, ignore crucial dietary components that impact the microbiome, including phytochemicals, emulsifiers, probiotic content, and food preparation methods [71].
A critical challenge lies in the variability of microbiome assessment techniques. Aonghus Lavelle, PhD, from University College Cork, emphasized at NeuroGASTRO 2025 the importance of controlling for confounders including transit time, regional changes, and horizontal transmission of the microbiome to improve precision in the field [32]. While exploratory analysis helps understand disease mechanisms and illuminates targets to modify, microbiome metrics are not yet ready for clinical application [32]. The problem is compounded by inconsistencies in classification systems; a narrative review on ultra-processed foods and the gut microbiome identified considerable variability in UPF classification methods across studies, with only four studies directly assessing the impact of UPFs on the human gut microbiome [24].
Individual Variability and Personalized Responses
Perhaps the most significant translational challenge arises from the substantial inter-individual variability in microbiome composition and function. Research presented at NeuroGASTRO 2025 revealed that our gut microbiome is highly variable and unique to each individual, with twins sharing only 34% of their gut microbes and unrelated individuals sharing 30% [32]. This variability creates profound challenges for universal dietary recommendations and one-size-fits-all interventions.
The personalized nature of dietary responses was highlighted by research showing that if a woman has a gut microbial makeup that enables conversion of soy isoflavones to equol, she may experience a 75% greater reduction in some menopause symptoms when supplemented with isoflavones compared to someone lacking those specific microbial species [32]. Similarly, Benoit Chassaing, PhD, from Institut Pasteur presented findings that individual sensitivity to the dietary emulsifier carboxymethylcellulose can be predicted by specific metagenomic signatures, with bacteria including Adlercreutzia equolifaciens and Frisingicoccus caecimuris correlating positively with intestinal inflammation [71]. This high degree of individual variability necessitates personalized approaches that current research frameworks are poorly equipped to address.
Table 1: Key Sources of Variability in Gut-Brain Axis Research
| Variability Source | Impact on Translation | Potential Mitigation Approaches |
|---|---|---|
| Microbial composition individuality (30-34% shared between individuals) | One-size-fits-all interventions likely ineffective for substantial portions of population | Stratification by microbial enterotypes; personalized nutrition approaches |
| Dietary response heterogeneity | Similar dietary interventions produce divergent clinical outcomes | Predictive biomarkers for dietary responsiveness; precision nutrition |
| Methodological inconsistencies in microbiome assessment | Limited reproducibility and comparability across studies | Standardized protocols; reference materials; validated measurement frameworks |
| Life stage-specific effects | Interventions effective at one life stage may not translate to others | Life course approaches; critical window identification |
Promising Translational Frameworks
Advanced Human-Relevant Model Systems
The field is increasingly shifting toward human-centered New Approach Methodologies (NAMs) that better recapitulate human physiology. These include organoids, organs-on-chip, and advanced in vitro systems that offer more accurate models for investigating diet-gut-brain interactions [70]. The M-ARCOL (Mucosal ARtificial COLon) system represents one such advancement, enabling researchers to study human diet-microbiome-pathogen interactions in a controlled yet human-relevant environment [24].
These human-centered models allow for investigation of complex host-microbiome interactions that were previously inaccessible. For instance, researchers are now utilizing these systems to examine how microbial metabolites including short-chain fatty acids, bile acids, and neurotransmitter precursors mediate host-microbiome communication across the gut-brain axis [24]. The integration of NAMs with multi-omics technologies represents a particularly promising approach for deconvoluting the complexity of diet-gut-brain interactions and generating more translationally relevant data.
Systems Biology and Multi-Omics Integration
A systems biology approach that integrates multiple data layers is essential for advancing translational research in the diet-gut-brain axis. Karine Clément, MD, PhD, emphasized at the GMFH Summit the importance of adopting a systems approach focused on microbiome-host interactions in connected ecosystems to better understand microbiome impacts and leverage microbial functions [71]. New unpublished findings from the Nutriomics study demonstrated that predicting weight loss response with GLP1 analogues and physical exercise is possible when stratifying participants by microbiome gene richness, opening possibilities for incorporating gut microbiome information for disease stratification and personalized therapy [71].
Mireia Valles-Colomer, PhD, presented research at NeuroGASTRO 2025 that exemplifies this approach, using large population cohorts and state-of-the-art bioinformatics tools to strengthen the link between microbial disturbances, depression, and quality of life [32]. The research team mined existing literature to identify potential microbial-derived metabolites with neuroactive potential and biochemical pathways, which were subsequently clustered into 56 different gut-brain modules, each corresponding to a single neuroactive compound production or degradation process [32]. This systematic mapping of gut-brain modules provides a framework for more targeted and mechanistically grounded interventions.
Table 2: Multi-Omics Approaches in Gut-Brain Axis Research
| Omics Layer | Application in Gut-Brain Research | Translational Value |
|---|---|---|
| Metagenomics | Characterizing microbial community composition and functional potential | Identifying therapeutic targets; patient stratification |
| Metatranscriptomics | Assessing active microbial functions and responses to dietary interventions | Understanding dynamic microbial responses to diet |
| Metabolomics | Profiling microbial and host metabolites in biofluids | Identifying mechanistic links; biomarker discovery |
| Proteomics | Characterizing host and microbial protein expression | Understanding functional host-microbe interactions |
| Integrative multi-omics | Combining multiple data layers for systems-level understanding | Comprehensive mechanistic insights; personalized interventions |
Experimental Models and Methodologies
Pathway Mapping and Experimental Workflows
Figure 2: Key experimental pathways in diet-gut-brain axis research showing major communication routes.
Understanding the complex pathways linking dietary interventions to brain function outcomes requires sophisticated experimental designs that account for multiple communication routes. The gut-brain axis operates through neural, endocrine, immune, and metabolic pathways that can be systematically investigated using structured methodological approaches [4]. The vagus nerve serves as a direct neural connection, while microbial metabolites including short-chain fatty acids, tryptophan derivatives, and bile acids mediate humoral and immune signaling [7] [4].
Methodologically robust investigation requires simultaneous assessment of multiple pathway components. For neural pathways, vagal tone measurement and manipulation through subdiaphragmatic vagotomy or pharmacological approaches provide mechanistic insights. For immune pathways, cytokine profiling in blood and tissue, along with immune cell characterization, reveals inflammatory components. Metabolic pathway investigation requires metabolomic profiling of gut-derived metabolites in systemic circulation and assessment of blood-brain barrier transport. Finally, behavioral and cognitive assessments provide functional readouts of brain function modifications [3] [4]. This multi-level assessment enables researchers to deconvolve the complex mechanisms underlying diet-gut-brain communication.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents and Materials for Gut-Brain Axis Investigations
| Reagent/Material | Research Application | Key Considerations |
|---|---|---|
| Gnotobiotic animals | Establishing causal microbiome-brain relationships | Limited translational validity to complex human microbiomes |
| Synthetic fecal pellets (3D-printed) | Quantifying gut motility and neural function | Enables precise measurement of enteric nervous system function |
| Organ-on-chip systems (e.g., M-ARCOL) | Human-relevant investigation of microbiome interactions | Bridges gap between traditional in vitro and in vivo models |
| Targeted metabolomics panels | Quantifying microbial metabolites (SCFAs, tryptophan derivatives) | Essential for mechanistic pathway validation |
| Toll-like receptor agonists/antagonists | Investigating immune signaling pathways | Critical for dissecting microbiome-immune-brain axis |
| Vagus nerve stimulation/inhibition tools | Establishing neural communication mechanisms | Both invasive and non-invasive approaches available |
Clinical Translation Strategies
Biomarker Development and Validation
The development of validated biomarkers represents a critical bridge between preclinical discovery and clinical application. Several promising biomarker classes are emerging from gut-brain axis research. Bacterial DNA in blood has been identified as a potential microbiome biomarker that may identify vulnerable people who could benefit most from protective dietary interventions [32]. Similarly, microbiome gene richness shows promise for stratifying patients for weight loss interventions, potentially predicting response to GLP1 analogues and physical exercise [71].
Beyond microbial biomarkers, microbial metabolites offer another promising biomarker class. Research presented at NeuroGASTRO 2025 highlighted the potential of using a multi-omics approach in longitudinal cohort studies to identify metabolic signatures associated with clinical outcomes [32]. For instance, unpublished data from a longitudinal cohort study of infants with severe acute malnutrition in Zimbabwe and Zambia showed that a disturbed gut microbiota in early life may lead to increased cysteine/methionine loss and use, contributing to long-term clinical outcomes of malnutrition following treatment [32]. Such metabolic signatures could serve as valuable biomarkers for identifying at-risk individuals and monitoring intervention efficacy.
Targeted Dietary Intervention Strategies
Moving beyond generic dietary recommendations to targeted, evidence-based interventions is essential for improving translational success. Several promising approaches are emerging from recent research:
Prebiotic Fibers with Differential Effects: Research indicates that not all prebiotic fibers impact the gut microbiome and host similarly. Studies in mice show that the benefits of fiber-rich foods are not recapitulated by supplemental fiber, and different fibers have distinct effects—psyllium and wheat bran have shown benefits in restoring the colonic microbiota depleted by a low-fiber diet and reducing the severity of diet-induced obesity, respectively [71].
Low Emulsifier Interventions: The ADDapt trial presented at the GMFH Summit 2025 demonstrated that emulsifier dietary restriction is a safe and effective intervention for mild-to-moderately active Crohn's disease, reducing clinical symptoms and fecal calprotectin [71]. This represents a targeted dietary approach for specific patient populations.
Fermented Food Interventions: Human studies, mainly on fermented dairy, indicate that fermented foods can improve digestive health, with new findings showing that fermented cabbage can affect intestinal barrier function, with effects varying based on fermentation time, probiotic inoculant presence, and production methodology [71].
Precision Nutrition Based on Microbial Phenotypes: Research shows that genetic variation in sucrase-isomaltase (SI) and other human carbohydrate-active enzyme genes may predispose to carbohydrate maldigestion across a continuum of mild to severe bowel symptoms, supporting the development of genotype-based dietary interventions [32].
The translation of promising preclinical findings in diet-gut-brain research to robust clinical outcomes remains challenging but increasingly feasible with advanced methodologies. The field requires a paradigm shift from simplified model systems to human-relevant approaches that account for the complexity and individuality of human microbiome-host interactions. Future research priorities should include larger longitudinal studies with multi-omics integration, standardized methodological approaches to reduce variability, development of validated biomarkers for patient stratification, and personalized nutrition strategies that account for individual differences in microbiome composition and function.
The substantial progress in understanding basic mechanisms coupled with emerging methodological advances provides optimism that targeting the gut-brain axis through dietary interventions will eventually yield effective strategies for preventing and treating brain disorders. However, researchers must maintain scientific rigor and acknowledge the current limitations while working toward more robust translational frameworks. As the field matures, the integration of systems biology, human-relevant models, and precision nutrition approaches will likely accelerate the translation of promising preclinical findings into meaningful clinical applications for brain health and disorders.
The role of diet in modulating gut-brain-axis communication has emerged as a critical area of scientific inquiry, with probiotics representing a key therapeutic interface. Defined as "live microorganisms which confer a health benefit to the host when administered in adequate amounts" [72] [73], probiotics have demonstrated potential in managing conditions ranging from gastrointestinal disorders to neuropsychiatric diseases through their influence on the gut-brain axis [46] [74]. The complex bidirectional communication between the gastrointestinal tract and the central nervous system involves neural, endocrine, immune, and metabolic pathways [74] [75], with gut microbiota producing essential metabolites, neurotransmitters, and other neuroactive chemicals that significantly affect brain function and the development of central nervous system diseases [75]. However, the translation of this promise into validated clinical applications faces substantial challenges related to standardization, long-term efficacy, and safety profiling. This review systematically examines these limitations within the context of advancing gut-brain-axis research and therapeutic development, providing researchers with critical frameworks for navigating current constraints.
Major Limitations in Probiotic Research and Application
Standardization Challenges
The absence of standardized methodologies across probiotic research presents a fundamental barrier to reproducibility and clinical translation. Key standardization challenges are detailed in Table 1.
Table 1: Standardization Challenges in Probiotic Research
| Challenge Category | Specific Limitations | Impact on Research & Development |
|---|---|---|
| Strain Identification & Characterization | Inconsistent characterization beyond genus/species level; lack of strain-specific mechanism data [76] [74] | Unknown mode of action; strain-specific effects obscured; difficult to replicate studies |
| Dosage & Formulation | Variable viability (CFU) across production lots; inadequate encapsulation technologies [72] [73] | Uncertain delivery of viable organisms to intestinal target; compromised efficacy in clinical trials |
| Viability & Stability | Susceptibility to heat, oxygen, acidity during processing/storage [72] [73] | Poor shelf-life; inconsistent product quality between batches |
| Study Design & Reporting | Heterogeneous populations, small sample sizes, lack of standardized protocols [74] | Reduced generalizability; inconclusive clinical efficacy; limited meta-analyses |
The strain-specificity of probiotic effects presents particular challenges, as different strains within the same species may exhibit markedly different physiological effects [76]. For instance, effects demonstrated by one specific strain of Lactobacillus cannot be extrapolated to other Lactobacillus strains [76]. This variability is compounded by the lack of precise dosage requirements, with considerable uncertainty regarding the most appropriate doses for specific health outcomes [76]. Furthermore, the technical challenges of maintaining probiotic viability throughout manufacturing, storage, and gastrointestinal transit necessitate advanced encapsulation technologies [72] [73], yet standardized approaches to viability assessment remain elusive.
Long-Term Efficacy and Durability
The long-term efficacy and durability of probiotic interventions represent another significant limitation, with particular concerns regarding the transient nature of probiotic colonization and persistent changes to the native gut microbiome.
Table 2: Limitations in Long-Term Efficacy Assessment
| Aspect | Current Understanding | Research Gaps |
|---|---|---|
| Colonization Persistence | Most probiotics show transient colonization; minimal long-term integration with resident microbiota [74] | Duration of functional effects post-discontinuation unknown; ecological factors governing persistence uncharacterized |
| Microbiome Resilience | Host-native microbiome typically returns to pre-treatment state after probiotic cessation [74] | Limited understanding of how to overcome colonization resistance for lasting modification |
| Clinical Evidence | Short-term clinical trials show benefits; long-term follow-up studies rare [76] [74] | Durability of clinical effects beyond immediate intervention period remains unestablished |
| Personalization Gaps | "One-size-fits-all" approach ignores interindividual variability in host physiology and baseline microbiome [77] | Lack of biomarkers to predict long-term responders versus non-responders |
The strong beneficial effects observed in animal studies have not consistently translated to human applications [74], with randomized controlled trials reporting both positive effects and null results [74]. This translation gap highlights the complexity of human gut ecosystems and the need for more sophisticated study designs that account for long-term outcomes. The emerging field of personalized probiotic therapeutics, guided by genetic and microbiome profiling, offers promising avenues to address these limitations [77], though robust clinical validation remains pending.
Safety and Side Effects
While probiotics generally have a strong safety profile in healthy populations, specific risks warrant careful consideration, particularly in vulnerable patient groups and with long-term use.
Table 3: Safety Concerns and Side Effects of Probiotics
| Safety Concern | Affected Populations | Current Evidence & Recommendations |
|---|---|---|
| Systemic Infections | Immunocompromised, critically ill, premature infants, hospitalized patients [72] [76] | Rare cases of bacteremia/fungemia; FDA warning for preterm infants due to fatal infections [76] |
| Metabolic & Immunological Effects | General population with long-term use [72] | Theoretical risks of deleterious metabolic or immunological effects; limited long-term safety data |
| Antibiotic Resistance Gene Transfer | All populations, particularly with prolonged use [74] | Horizontal gene transfer to pathogens; stringent screening for transferable genes recommended [74] |
| Quality Control Issues | All consumer populations | Contamination with harmful bacteria, mycotoxins, heavy metals; inaccurate strain identification [72] [73] |
Government regulation of probiotics remains complex, with varying oversight depending on intended use [76]. Many probiotics are sold as dietary supplements, which do not require FDA approval before marketing [76], creating potential gaps in quality assurance. Furthermore, international guidelines emphasize that probiotics intended for human use must be free of transferable antibiotic resistance genes [74], though intrinsic, non-transferable resistance is generally acceptable.
Methodological Approaches and Experimental Protocols
Standardized Viability and Stability Assessment
To address viability challenges, researchers should implement comprehensive assessment protocols:
- Acid and Bile Tolerance Testing: Incubate probiotics in simulated gastric fluid (pH 2.0-3.0) for 3 hours followed by simulated intestinal fluid (0.3% bile salts) for 4 hours at 37°C [73]. Calculate survival rates via plate counts before and after exposure.
- Encapsulation Efficacy Evaluation: Utilize spray drying or coacervation with natural encapsulating materials (sodium alginate, calcium chloride, gel beads, polysaccharides) [72] [73]. Assess protective capacity during in vitro gastrointestinal transit models.
- Stability Monitoring: Conduct accelerated stability testing under various temperature (4°C, 25°C, 37°C) and humidity conditions over 6-12 months [72]. Determine viability loss kinetics using linear regression models.
- Flow Cytometry with Viability Staining: Implement propidium iodide (membrane integrity) and carboxyfluorescein diacetate (esterase activity) staining as complementary method to plate counts for accurate viability assessment [73].
Long-Term Colonization and Efficacy Monitoring
For evaluating long-term efficacy and persistence:
- Longitudinal Sampling Design: Collect fecal samples at baseline, during intervention (2-4 week intervals), and post-intervention (4-8 week follow-up) for at least 6 months total duration [74].
- Microbiome Sequencing: Perform shotgun metagenomic sequencing to track strain-level persistence and functional genomics, complemented by 16S rRNA gene sequencing for community structure analysis [74] [77].
- Metabolomic Profiling: Apply LC-MS/MS for quantification of microbially-derived metabolites (SCFAs, neurotransmitters, bile acids) in fecal and serum samples to assess functional persistence [74] [77].
- Host Response Biomarkers: Measure inflammatory markers (CRP, cytokines), intestinal permeability (LPS-binding protein), and neuroactive compounds (BDNF, serotonin) in blood samples [46] [75].
Gut-Brain-Axis Communication Pathways
The mechanistic basis for probiotic effects on brain function involves multiple interconnected pathways, illustrated in the following diagram:
Gut-Brain-Axis Communication Pathways
This diagram illustrates the complex bidirectional communication system through which probiotics influence brain function. Probiotics and prebiotics modulate the gut microbiota, which produces various bioactive metabolites including short-chain fatty acids (SCFAs) and neurotransmitters [46] [74]. These microbial products then stimulate the enteric nervous system (ENS) and modulate immune responses [46] [75]. Neural signals are relayed to the central nervous system (CNS) primarily via the vagus nerve, while the CNS can conversely influence gut function and microbiota composition through efferent pathways [74] [75].
The molecular mechanisms involved in gut-brain communication include:
- SCFA Signaling: Microbial-derived SCFAs (acetate, propionate, butyrate) stimulate GPCRs (GPR41, GPR43, GPR109A) on enteroendocrine and immune cells, influencing neuroinflammation and blood-brain barrier integrity [46].
- Neurotransmitter Production: Certain probiotic strains synthesize GABA, serotonin precursors, dopamine, and norepinephrine, potentially influencing central neurotransmitter balance [46] [74].
- Immune Modulation: Probiotics regulate cytokine production (IL-10, IL-6, TNF-α) and microglial activation through interactions with Toll-like receptors (TLRs) [46] [75].
- Endocrine Pathways: Gut microbes influence the HPA axis regulation, affecting cortisol release and stress responsiveness [46] [74].
The Scientist's Toolkit: Essential Research Reagents
Table 4: Essential Research Reagents for Probiotic-Gut-Brain-Axis Studies
| Reagent/Category | Specific Examples | Research Application |
|---|---|---|
| Probiotic Strains | Lactobacillus spp. (L. acidophilus, L. rhamnosus), Bifidobacterium spp. (B. longum, B. breve), Saccharomyces boulardii [78] [72] [73] | Core test articles for intervention studies; strain-specific effects investigation |
| Prebiotics | Galactooligosaccharides (GOS), Fructooligosaccharides (FOS), Xylooligosaccharides, Inulin [46] [74] | Synbiotic formulations; selective stimulation of beneficial microbes |
| Encapsulation Materials | Sodium alginate, Calcium chloride, Gel beads, Polysaccharide matrices [72] [73] | Viability protection during GI transit; targeted delivery to intestinal sites |
| Cell Culture Models | Caco-2, HT-29, SH-SY5Y, Primary glial cells [46] [75] | Barrier function assessment; neuroimmune axis mechanistic studies |
| Molecular Biology Tools | TLR agonists/antagonists, GPCR modulators, Cytokine ELISA kits, qPCR primers for tight junction proteins [46] [75] | Mechanism of action studies; pathway validation |
| Germ-Free Animals | GF mice, Gnotobiotic zebrafish [74] [75] | Causal relationship establishment; microbial requirement demonstration |
The field of probiotic research stands at a pivotal juncture, where acknowledging current limitations provides the foundation for meaningful advancement. The constraints of standardization, long-term efficacy, and safety profiling represent significant but addressable barriers to translating gut-brain-axis research into validated therapeutic applications. Future research priorities should include the development of universally accepted reference materials for key probiotic strains, establishment of standardized viability assessment protocols, implementation of long-term safety surveillance systems, and adoption of personalized approaches that account for interindividual variability in host genetics, microbiome composition, and dietary patterns [77]. The emergence of next-generation probiotics (NGPs) and live biotherapeutic products (LBPs) designed for enhanced specificity and function represents a promising direction [77], though these novel interventions will require even more rigorous safety and efficacy assessment. By systematically addressing these limitations through collaborative science and innovative methodologies, researchers can fully realize the potential of probiotics as therapeutic agents within the gut-brain-axis paradigm.
The gut-brain axis (GBA) represents one of the most compelling frontiers in neurogastroenterology and nutritional neuroscience. This complex bidirectional communication network integrates neural, endocrine, immune, and metabolic pathways between the gastrointestinal tract and central nervous system. Synbiotics—defined as mixtures comprising live microorganisms and substrate(s) selectively utilized by host microorganisms that confer a health benefit—and personalized nutrition represent promising interventions for modulating this axis [79]. This whitepaper provides a technical overview of the current evidence, mechanistic underpinnings, and methodological frameworks for developing targeted interventions that leverage the diet-microbiota-brain relationship. We synthesize contemporary research on synbiotic formulations, explore artificial intelligence (AI)-driven personalization approaches, and provide standardized experimental protocols for preclinical and clinical validation of GBA-targeted interventions for researchers and drug development professionals.
The gut-brain axis has emerged as a critical regulator of brain health, cognitive function, and emotional well-being. The human gut harbors a complex ecosystem of approximately 2000 bacterial species, dominated by five main phyla: Firmicutes (79.4%), Bacteroidetes (16.9%), Actinobacteria (2.5%), Proteobacteria (1%), and Verrucomicrobia (0.1%) [45]. This microbial community interacts with the host through multiple signaling pathways, including production of microbial metabolites, immune modulation, neuroendocrine signaling, and neural communication via the vagus nerve [7] [15].
Dysbiosis, or an imbalance in the gut microbiota, has been implicated in various neurological and psychiatric disorders, including Alzheimer's disease, Parkinson's disease, depression, and anxiety [45] [4] [15]. This dysbiosis can lead to increased intestinal permeability ("leaky gut"), allowing pro-inflammatory molecules to enter circulation and cross the blood-brain barrier, resulting in neuroinflammation that exacerbates symptoms of mood disorders and accelerates neurodegenerative processes [7] [15].
Diet represents a powerful modulator of the GBA, with nutritional interventions offering promising avenues for therapeutic intervention. The conceptual framework of "smart neuronutrition" has emerged at the intersection of nutritional science, neuroscience, and artificial intelligence, aiming to enhance cognitive resilience and mental well-being through precision dietary strategies [80].
Synbiotics: Rational Formulation and Mechanisms of Action
Definitions and Classification
The International Scientific Association for Probiotics and Prebiotics (ISAPP) consensus panel defines a synbiotic as "a mixture comprising live microorganisms and substrate(s) selectively utilized by host microorganisms that confers a health benefit on the host" [79]. This definition encompasses two distinct formulations:
- Complementary synbiotics: Combinations of proven probiotics and prebiotics, with each component acting independently but providing a combined health benefit [81] [79].
- Synergistic synbiotics: Formulations where the substrate is selectively utilized by the co-administered microorganisms, designed to function cooperatively [81] [79].
Table 1: Classification and Characteristics of Synbiotics
| Type | Components | Mechanism | Evidence Requirements |
|---|---|---|---|
| Complementary | Probiotic + Prebiotic | Independent action of components | Each component must meet probiotic/prebiotic criteria; combined health benefit must be demonstrated |
| Synergistic | Microorganism + Selectively utilized substrate | Cooperative function between components | Substrate must enhance persistence/activity of co-administered microorganism; health benefit greater than either component alone |
Mechanisms of Action on the Gut-Brain Axis
Synbiotics influence brain function and behavior through multiple interconnected mechanisms:
Microbial Metabolite Production: Synbiotics enhance production of short-chain fatty acids (SCFAs) including butyrate, acetate, and propionate through bacterial fermentation of prebiotic fibers. SCFAs reinforce intestinal barrier integrity, reduce systemic inflammation, and modulate neuroimmune function [7]. Butyrate, in particular, exerts histone deacetylase (HDAC) inhibitor activity, influencing gene expression in both peripheral and central tissues [4].
Neurotransmitter Modulation: Gut microbes produce and influence various neurotransmitters. Approximately 90% of serotonin is synthesized in the gut under microbial influence, with specific strains capable of producing gamma-aminobutyric acid (GABA), dopamine, and other neuroactive molecules [7] [15].
Immune System Regulation: Synbiotics modulate both mucosal and systemic immunity through interaction with toll-like receptors (TLRs) and regulation of inflammatory cytokines. They promote differentiation of regulatory T cells (Tregs) and their production of anti-inflammatory IL-10, while reducing pro-inflammatory pathways [4].
Barrier Function Enhancement: Synbiotics strengthen both intestinal and blood-brain barriers, reducing translocation of inflammatory molecules and potentially harmful substances into systemic circulation and the central nervous system [7] [15].
Figure 1: Mechanism of Action of Synbiotics on the Gut-Brain Axis
Personalized Nutrition in Gut-Brain Axis Modulation
AI-Driven Precision Nutrition
Artificial intelligence is revolutionizing the field of nutritional neuroscience by enabling truly personalized dietary recommendations. Machine learning (ML) models, wearable biosensors, and mobile dietary tracking platforms offer real-time insights into dietary behavior, nutrient intake, metabolic responses, and brain health outcomes [80].
Key technological advancements include:
- Image-Based Dietary Assessment: AI-powered tools such as goFOOD and DietGlance can estimate nutrient content from food images, enabling more accurate tracking of dietary intake [80].
- Multi-Omics Integration: Advanced ML models integrate genomic, metabolomic, and microbiome data to predict individual responses to dietary interventions [80].
- Cognitive Trajectory Prediction: AI systems analyze multimodal data to predict individual cognitive trajectories and identify at-risk populations for early intervention [80].
Biomarkers for Personalization
Several biomarker classes have emerged as critical for personalizing GBA-targeted interventions:
- Microbial Diversity Metrics: Alpha-diversity (within-individual diversity) and beta-diversity (between-individual diversity) serve as key indicators of gut ecosystem health [14].
- Microbial Metabolites: Quantification of SCFAs, bile acids, and tryptophan derivatives in blood and feces provides functional readouts of microbial activity [4] [7].
- Inflammatory Markers: Cytokine profiles (e.g., IL-6, TNF-α, IL-1β) and C-reactive protein (CRP) levels indicate systemic inflammatory status [4] [7].
- Intestinal Permeability Markers: Serum zonulin, lipopolysaccharide (LPS) levels, and Claudin-3 provide measures of gut barrier integrity [7].
Table 2: Response Biomarkers for Personalized Nutrition Interventions
| Biomarker Category | Specific Markers | Detection Method | Significance |
|---|---|---|---|
| Microbial Composition | 16S rRNA sequencing, metagenomics | Fecal samples | Determines baseline microbiota and diversity |
| Microbial Metabolites | SCFAs, bile acids, tryptophan derivatives | LC-MS/MS of feces/plasma | Functional output of microbiota |
| Barrier Integrity | Zonulin, LPS, I-FABP | ELISA of serum | Intestinal permeability assessment |
| Inflammatory Status | CRP, IL-6, TNF-α | Multiplex immunoassays | Systemic and neuroinflammation |
| Neuroactive Compounds | Serotonin, GABA, BDNF | HPLC, immunoassays | Direct neurochemical measures |
Experimental Protocols for GBA Research
In Vitro Screening of Synbiotic Combinations
Objective: To identify synergistic synbiotic pairs by screening probiotic strains with various prebiotic substrates.
Materials:
- Probiotic strains (e.g., Lactobacillus spp., Bifidobacterium spp.)
- Prebiotic substrates (FOS, GOS, XOS, inulin, resistant starch)
- Anaerobic chamber (85% Nâ‚‚, 10% Hâ‚‚, 5% COâ‚‚)
- MRS broth or other appropriate culture media
- Spectrophotometer for OD measurements
- HPLC system for SCFA analysis
Procedure:
- Inoculate probiotic strains individually in MRS broth and incubate anaerobically at 37°C for 24 hours.
- Prepare basal medium supplemented with 1% (w/v) of each prebiotic substrate.
- Inoculate each probiotic strain into each prebiotic-supplemented medium at 1% inoculum.
- Measure optical density (OD₆₀₀) at 0, 6, 12, 24, and 48 hours to generate growth curves.
- Quantify SCFA production (acetate, propionate, butyrate) using HPLC after 48 hours incubation.
- Identify synergistic pairs demonstrating enhanced growth and metabolite production compared to controls.
Validation: Strains showing ≥50% enhancement in growth parameters and SCFA production with specific prebiotics qualify for further in vivo testing [81] [82].
Animal Model Testing Protocol
Objective: To evaluate the effects of synbiotic interventions on behavior and neuroinflammation in rodent models.
Animals: C57BL/6J mice (8-10 weeks old, n=10-12/group)
Intervention Groups:
- Control (vehicle)
- Probiotic only
- Prebiotic only
- Complementary synbiotic
- Synergistic synbiotic
Administration: Interventions administered daily via oral gavage for 8 weeks.
Behavioral Assessments:
- Open Field Test: Locomotor activity and anxiety-like behavior (week 8)
- Forced Swim Test: Depressive-like behavior (week 8)
- Morris Water Maze: Spatial learning and memory (weeks 6-7)
Tissue Collection and Analysis:
- Collect fecal samples at baseline, 4 weeks, and 8 weeks for microbiome analysis (16S rRNA sequencing).
- At sacrifice, collect plasma, colon tissue, and brain tissue.
- Analyze inflammatory markers (IL-6, TNF-α, IL-1β) in plasma and brain homogenates.
- Perform immunohistochemistry for microglial activation (Iba1) and neurogenesis (DCX) in brain sections.
- Quantify SCFA levels in cecal content and plasma.
Statistical Analysis: Two-way ANOVA with post-hoc tests, p<0.05 considered significant [45] [15].
Clinical Trial Design for Synbiotic Interventions
Objective: To evaluate the efficacy of synbiotic interventions on cognitive function and mental health in human subjects.
Study Design: Randomized, double-blind, placebo-controlled trial with parallel groups.
Participants: Adults (40-65 years) with mild cognitive complaints or subjective cognitive decline.
Intervention:
- Group 1: Synergistic synbiotic (e.g., Bifidobacterium longum + GOS)
- Group 2: Complementary synbiotic
- Group 3: Placebo
- Treatment duration: 12 weeks
Primary Outcomes:
- Cognitive function (CANTAB battery, MMSE)
- Quality of life (SF-36)
- Inflammatory markers (CRP, IL-6)
Secondary Outcomes:
- Gut microbiota composition (shotgun metagenomics)
- Fecal SCFA levels
- Intestinal permeability (lactulose/mannitol test)
- Stress biomarkers (cortisol, alpha-amylase)
Assessment Timeline:
- Screening (week -2)
- Baseline (week 0)
- Mid-intervention (week 6)
- End-of-intervention (week 12)
- Follow-up (week 16)
Sample Size Calculation: Based on expected effect size of 0.4 on primary cognitive outcome, 80% power, α=0.05, requiring ~50 participants per group [45] [7].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for GBA Studies
| Reagent Category | Specific Products | Application | Key Considerations |
|---|---|---|---|
| Probiotic Strains | Lactobacillus spp., Bifidobacterium spp., B. longum APC1472 | Synbiotic formulation | Select strains with genomic sequencing; verify absence of transferable antibiotic resistance genes |
| Prebiotic Substrates | FOS, GOS, XOS, inulin, resistant starch, polyphenols | Synbiotic formulation | Purity and structural characterization essential; dose optimization required |
| Cell Culture Models | Caco-2, HT-29, SH-SY5Y, primary microglial cultures | Barrier function, neuroinflammation | Use appropriate co-culture systems for gut-brain axis modeling |
| Animal Models | Germ-free mice, GF mice colonized with human microbiota, stress models | Mechanistic studies | Consider sex, age, and genetic background; include appropriate controls |
| Microbiome Analysis | 16S rRNA sequencing, shotgun metagenomics, metabolomics | Composition and functional assessment | Standardize sample collection, storage, and processing protocols |
| SCFA Analysis | GC-MS, LC-MS/MS platforms | Microbial metabolite quantification | Standardize calibration curves; use internal standards for quantification |
Current Challenges and Future Directions
Despite promising advances, several challenges remain in the development of synbiotics and personalized nutrition for GBA modulation:
- Individual Variability: The highly personalized nature of gut microbiota composition and host response necessitates individualized approaches. A one-size-fits-all strategy is unlikely to be effective [14].
- Methodological Standardization: Lack of standardized protocols for synbiotic testing, outcome measures, and manufacturing consistency hampers comparability across studies [81].
- Regulatory Hurdles: Evolving regulatory frameworks for synbiotics and microbiome-based interventions create uncertainty for product development and claims [79].
- Technical Limitations: Current AI models often lack integration with multi-omics datasets and may demonstrate algorithmic bias when trained on homogenous populations [80].
Future research should prioritize:
- Large-scale, longitudinal clinical trials with multimodal assessment
- Development of explainable AI systems for personalized nutrition
- Standardization of synbiotic formulation and testing protocols
- Investigation of critical windows for intervention across the lifespan
- Exploration of combination therapies integrating synbiotics with other interventions
The convergence of nutritional science, microbiology, neuroscience, and artificial intelligence offers unprecedented opportunities to develop targeted, effective interventions for optimizing brain health through the gut-brain axis.
Evaluating Efficacy: Preclinical and Clinical Evidence for Dietary Strategies
The pursuit of effective therapeutics for neurodegenerative diseases relies heavily on preclinical research using animal models. However, the translation of findings from these models to clinical success in humans has been largely unsuccessful, in part because traditional models fail to fully capture disease complexity [83]. This whitepaper analyzes the major animal models used in neurodegeneration research, with a particular focus on their application within the emerging framework of the microbiota-gut-brain axis (MGBA). We examine how dietary interventions and gut microbiome modulation can influence stress responses, neurodegenerative pathology, and behavioral outcomes across different model systems. By integrating quantitative data comparisons, detailed experimental protocols, and mechanistic pathway visualizations, this review provides researchers with a critical evaluation of current methodologies and offers a strategic direction for future investigations that leverage the gut-brain connection.
Animal models have been indispensable for deciphering the underlying mechanisms of neurodegenerative diseases (NDDs) and evaluating new therapeutic strategies [84]. These models span multiple species, from rodents to Drosophila, each offering unique advantages for studying specific aspects of disease pathogenesis. The traditional neurocentric view of NDDs has focused primarily on protein misfolding, synaptic dysfunction, and central immune activation [2]. However, the growing recognition of the microbiota-gut-brain axis (MGBA) as a critical modulator of brain health has expanded the scope of preclinical research to include gastrointestinal and microbiome components [15] [2].
The MGBA represents a complex, bidirectional communication network linking the gut's resident microbiota with the central nervous system (CNS) through neural, immune, endocrine, and metabolic signaling pathways [2]. Within this framework, the gut microbiome influences brain physiology, while the brain can modulate gut microbial composition via stress hormones and autonomic innervation [2]. This axis comprises several integrated components: (1) the gut microbiota; (2) the intestinal barrier and mucosal immune system; (3) circulating immune cells and cytokines; (4) the enteric nervous system (ENS) and vagus nerve; (5) central autonomic circuits and hypothalamic-pituitary-adrenal (HPA) stress pathways; and (6) CNS interfaces including the blood-brain barrier (BBB) and microglia [2].
Disruption of any MGBA component can reverberate throughout the entire system. Patients with NDDs frequently exhibit gastrointestinal disturbances or microbiome alterations years before classic neurological symptoms emerge [2]. For example, chronic constipation can precede Parkinson's disease motor symptoms by up to 20 years, and many Alzheimer's disease patients show distinct gut microbiota profiles compared to healthy peers [2]. These observations suggest that perturbations in the MGBA may play a role in disease initiation or progression, making it a compelling target for therapeutic intervention.
Critical Analysis of Major Animal Models
Rodent Models
Rodent models represent the most widely used animal systems in neurodegeneration research. These models are primarily based on dominant hypotheses of disease mechanisms, including amyloid-β plaque accumulation, neurofibrillary tangle formation, neuroinflammation, and neuronal loss [83]. Transgenic mice harboring human mutations associated with familial neurodegenerative diseases have been particularly valuable for studying specific pathological processes.
However, significant concerns have emerged regarding how accurately these models represent human disease conditions. A critical analysis reveals that animal models based on these frameworks may not fully recapitulate the complexity of AD in people [83]. This limitation has substantially contributed to the poor historical translation of preclinical results to clinical success. The 5xFAD mouse model, which harbors five mutations associated with familial Alzheimer's disease, has been instrumental for studying amyloid pathology and microglial responses [15]. In this model, microglia transform from a homeostatic state to a "disease-associated microglia" (DAM) phenotype, clustering in close proximity to Aβ plaques and undergoing considerable morphological changes—transitioning from thin cell bodies with highly ramified extensions into ameba-like cells with fewer branches [15].
The strengths of rodent models include well-established behavioral paradigms for assessing cognitive and motor functions, extensive characterization of pathological markers, and the ability to perform intricate mechanistic studies through genetic manipulation. Their weaknesses encompass incomplete recapitulation of human disease pathology, limited representation of the human immune system, and substantial differences in gut microbiome composition and regulation compared to humans [83]. Additionally, rodent models often exhibit more rapid disease progression than the typically slow neurodegeneration in humans.
Drosophila Models
The fruit fly (Drosophila melanogaster) has positioned itself as a prominent model organism for neurodegenerative disease research since the beginning of the 20th century [84]. Compared to other animal models with sequenced genomes, Drosophila offers significant advantages in cost-effectiveness, shorter developmental time, and minimal genetic redundancy. Sophisticated genetic tools and the high degree of orthology between fly and mammalian genes make Drosophila a powerful system for studying human diseases [84].
While the Drosophila brain is simpler than mammalian brains, it contains well-organized centers for distinct functions such as olfactory, visual, gustatory, motor control, and learning and memory [84]. This moderate complexity makes it possible to decipher pathways responsible for phenotypes reminiscent of human symptoms, such as behavioral and learning deficits. The fly model has been particularly valuable for genetic screens and rapid assessment of therapeutic compounds.
The limitations of Drosophila models include substantial anatomical differences from mammalian systems, a less complex nervous system, and the absence of some mammalian-specific cell types and processes. However, for MGBA research, Drosophila offers a simplified yet relevant system for studying how dietary components and microbiome alterations influence neurodegeneration and behavior.
Comparative Analysis of Model Systems
Table 1: Quantitative Comparison of Animal Models in Neurodegeneration Research
| Model Characteristic | Rodent Models | Drosophila Models | Non-Human Primate Models |
|---|---|---|---|
| Genetic Manipulation Efficiency | Moderate | High | Low |
| Experimental Timeline | Months | Weeks | Years |
| Approximate Cost per Study | High | Low | Very High |
| Behavioral Paradigm Complexity | High | Moderate | High |
| Similarity to Human Neuroanatomy | Moderate | Low | High |
| Gut Microbiome Complexity | High | Moderate | High |
| Human Disease Gene Orthology | ~80% | ~75% | ~95% |
| MGBA Pathway Conservation | High | Moderate | High |
Table 2: Model-Specific Assessment of MGBA Research Applications
| Research Application | Rodent Models | Drosophila Models | Considerations for Model Selection |
|---|---|---|---|
| Microbiome-Diet-Brain Interactions | High | Moderate | Rodents preferred for complex microbiome studies; Drosophila for rapid screening |
| Neuroimmune Signaling | High | Low | Rodents essential for mammalian immune pathway validation |
| Vagal Nerve Communication | High | Not applicable | Rodents only for vertebrate-specific neural pathways |
| Blood-Brain Barrier Permeability | High | Low (has BBB analogs) | Rodents for comprehensive BBB transport studies |
| Therapeutic Compound Screening | Moderate | High | Drosophila superior for high-throughput initial screening |
| Gut-Derived Metabolite Effects | High | Moderate | Both useful; rodents for translation to mammalian systems |
The Gut-Brain Axis Framework in Preclinical Models
Key Communication Pathways
The MGBA comprises multiple interdependent signaling routes that mediate bidirectional communication between the gut and brain. These pathways can be categorized into four primary mechanisms [2]:
Neural Pathways: The vagus nerve serves as a direct neural highway between the gut and brainstem, with afferent fibers transmitting sensory signals from intestinal receptors to the brain and efferent fibers carrying brain commands to influence gut activity [2]. Certain gut bacteria can directly stimulate vagal pathways by producing neurotransmitters or neuromodulators, such as γ-aminobutyric acid (GABA), serotonin (5-HT), and histamine [2].
Immune and Inflammatory Pathways: Gut microbes profoundly shape the host immune system from development through adulthood. Microbial-associated molecular patterns (MAMPs), such as lipopolysaccharide (LPS) from Gram-negative bacteria, can breach a compromised gut barrier and enter circulation, where they activate innate immune sensors in peripheral tissues and the brain [2]. Even low-grade endotoxin leakage can trigger chronic neuroinflammation through microglial activation via TLR4/NF-κB signaling [2].
Metabolic Pathways: Gut microbiota produce a diverse range of metabolites that can directly or indirectly influence brain function. Short-chain fatty acids (SCFAs)—including acetate, propionate, and butyrate—are produced by bacterial fermentation of dietary fiber and can cross the blood-brain barrier to exert neuroactive effects [15] [2]. Bile acids transformed by gut microbes and microbiota-related neurotransmitters also contribute to metabolic signaling along the MGBA [15].
Neuroendocrine Pathways: Enteroendocrine cells in the gut lining detect luminal contents and release neuroactive hormones that can influence brain function. The HPA axis represents a crucial neuroendocrine arm of the MGBA, translating stress signals into systemic hormone release (e.g., cortisol) that can alter gut barrier integrity and immune function [2].
Glial Cell Interactions in the MGBA
The MGBA represents an important regulator of glial functions, making it an actionable target to ameliorate the development and progression of neurodegenerative diseases [15]. Microglia, the primary innate immune cells of the CNS, account for nearly 10% of CNS cells and possess diverse context-dependent functions central to CNS development, homeostasis, and diseases [15]. Under homeostatic conditions, microglia contribute to neurogenesis, angiogenesis, maintaining BBB integrity, synaptic pruning and remodeling, synaptic transmission, myelin health, and phagocytosis of cellular debris [15].
The importance of microglia in Alzheimer's disease has been clearly illustrated by spatiotemporal analyses showing that microglia are the primary responders to beta-amyloid plaques, accumulating in close vicinity to these pathological structures [15]. Genome-wide association studies have also implicated microglia as the primary cell type expressing Alzheimer's disease genes [15]. In Parkinson's disease, postmortem analysis revealed significantly increased numbers of microglia with an amoeboid shape, suggestive of an activated state, in the ventral midbrains of PD patients [15].
A core function of microglia is the efficient recognition and phagocytic clearance of protein aggregates and cellular debris without damaging surrounding tissue [15]. This phagocytic activity is crucial for the removal of Aβ, tau, and α-synuclein [15]. However, during aging and neurodegenerative diseases, microglial phagocytic activity becomes dysfunctional, resulting in the gradual accumulation of toxic compounds and cognitive decline [15]. Several regulators of microglial phagocytosis have been identified, including TYROBP, the TREM2-APOE pathway, spleen tyrosine kinase (SYK), the classical complement system, purinergic system, sialic acid binding immunoglobulin-like lectins, and the mechanosensor Piezo1 [15].
Experimental Methodologies and Protocols
Assessing Gut-Brain Axis Communication in Rodent Models
Protocol 1: Evaluating Microbiota-Dependent Neuroimmune Signaling
Objective: To investigate how gut microbiome alterations influence microglial activation states and neuroinflammatory responses in neurodegenerative models.
Materials:
- Transgenic neurodegenerative disease models (e.g., 5xFAD mice, APP/PS1 mice)
- Germ-free (GF) or gnotobiotic housing facilities
- Specific pathogen-free (SPF) control animals
- Antibiotic cocktail (e.g., ampicillin, vancomycin, neomycin, metronidazole)
- Fecal microbiota transplantation (FMT) equipment
- Immunohistochemistry reagents for microglial markers (Iba1, CD68, TREM2)
- Cytokine profiling arrays (TNF-α, IL-1β, IL-6)
- RNA sequencing supplies for transcriptomic analysis
Procedure:
- Microbiome Depletion: Administer broad-spectrum antibiotic cocktail in drinking water for 4-6 weeks to deplete gut microbiota. Verify depletion through 16S rRNA sequencing of fecal samples.
- Microbiota Reconstitution: Perform FMT from donor mice with specific microbial profiles (e.g., healthy controls, humanized microbiota) to antibiotic-treated mice.
- Behavioral Assessment: Conduct behavioral tests at 2, 4, and 8 weeks post-FMT using Morris water maze for spatial memory, open field test for anxiety-like behavior, and fear conditioning for associative memory.
- Tissue Collection: Euthanize animals and collect brain tissue for immunohistochemical analysis, colonic tissue for barrier integrity assessment, and blood plasma for cytokine measurement.
- Microglial Analysis: Quantify microglial density, morphology, and activation state using Iba1 immunohistochemistry in brain regions relevant to the specific neurodegenerative disease (e.g., hippocampus for AD, substantia nigra for PD).
- Molecular Profiling: Perform RNA sequencing on isolated microglia to characterize transcriptional profiles and identify differentially expressed genes in neuroinflammatory pathways.
Outcome Measures:
- Microglial transition from homeostatic state to disease-associated microglia (DAM) phenotype
- Changes in phagocytic activity toward Aβ or α-synuclein aggregates
- Alterations in pro-inflammatory cytokine levels in brain tissue and plasma
- Correlation between specific microbial taxa abundance and neuropathological markers
Dietary Intervention Studies in Drosophila Models
Protocol 2: Investigating Diet-Microbiome-Brain Interactions in Drosophila
Objective: To examine how specific dietary components modulate neurodegeneration and behavioral outcomes through microbiome-dependent mechanisms in fly models.
Materials:
- Drosophila strains expressing human neurodegenerative disease proteins (e.g., Aβ42, tau, α-synuclein)
- Axenic fly generation equipment (egg dechorionation, sterilization)
- Customizable fly diets (standard, high-sugar, high-fat, probiotic-supplemented)
- Behavioral tracking apparatus (locomotion, climbing ability, learning assays)
- Lifespan analysis setup
- Microbial sequencing supplies for fly microbiome analysis
- Metabolomic profiling equipment for microbial metabolites
Procedure:
- Gnotobiotic Fly Generation: Generate axenic (germ-free) flies by dechorionating embryos with bleach and raising them on sterile diet. Conventionalize with specific bacterial species (e.g., Lactobacillus plantarum) for monocolonization studies.
- Dietary Manipulation: Rear flies on isocaloric diets varying in specific components:
- High-polyphenol diet: Supplement with blueberry or pomegranate extract
- Prebiotic diet: Supplement with inulin or fructooligosaccharides (FOS)
- Probiotic diet: Supplement with specific bacterial strains (e.g., Bifidobacterium longum)
- Behavioral Phenotyping: Assess climbing ability using negative geotaxis assay at weekly intervals to monitor motor function decline. Evaluate learning and memory using olfactory conditioning paradigm.
- Neuropathological Analysis: Examine retinal degeneration in eye models or brain pathology using immunohistochemistry for human transgene expression and aggregation.
- Microbiome-Metabolome Correlation: Characterize microbial community structure through 16S rRNA sequencing and measure microbial metabolites (SCFAs, branched-chain amino acids) in fly homogenates.
Outcome Measures:
- Lifespan extension or reduction under different dietary conditions
- Rate of motor function decline measured by climbing index
- Learning and memory performance in associative conditioning paradigms
- Protein aggregation burden in brain tissue
- Correlation between specific microbial abundances and neurodegenerative phenotypes
Integrated Multi-Omics Approach for MGBA Analysis
Protocol 3: Systems Biology Analysis of Gut-Brain Signaling
Objective: To implement an integrated multi-omics approach for comprehensive characterization of MGBA components in preclinical models.
Materials:
- Tissue collection supplies for parallel sampling of brain, gut, and blood
- Metagenomic sequencing kits for microbiome analysis
- Metabolomic profiling platforms (LC-MS, GC-MS)
- Transcriptomic analysis supplies (RNA extraction, library preparation)
- Proteomic analysis equipment
- Bioinformatics pipelines for multi-omics integration
Procedure:
- Sample Collection: Collect matched samples from the same animals:
- Fecal samples for metagenomic sequencing
- Blood plasma for metabolomic and cytokine profiling
- Brain regions (cortex, hippocampus, striatum) for transcriptomic and proteomic analysis
- Colonic tissue for barrier function assessment and immune profiling
- Multi-Omics Data Generation:
- Perform shotgun metagenomics on fecal samples for taxonomic and functional profiling
- Conduct untargeted metabolomics on plasma and brain tissue
- Implement RNA sequencing on brain regions and colonic tissue
- Analyze proteomic profiles in brain tissue using mass spectrometry
- Data Integration: Use multivariate statistical methods and network analysis to identify correlations between microbial features, metabolite levels, gene expression, and pathological markers.
- Pathway Analysis: Apply enrichment analysis to identify biological pathways significantly associated with disease progression and dietary interventions.
Outcome Measures:
- Identification of microbial taxa and functions associated with neuroprotection or neurodegeneration
- Discovery of metabolite biomarkers that track with disease severity
- Integrated molecular networks highlighting key regulators of MGBA communication
- Validation of candidate mechanisms through targeted experiments
Table 3: Research Reagent Solutions for MGBA Studies
| Reagent Category | Specific Examples | Research Applications | Technical Considerations |
|---|---|---|---|
| Gnotobiotic Models | Germ-free rodents, Axenic Drosophila | Establishing causal microbiome roles | Requires specialized facilities, careful contamination monitoring |
| Microbial Consortia | Defined microbial communities, Humanized microbiota | Reduced complexity microbiome studies | Community stability, proper colonization verification |
| Fecal Microbiota Transplantation (FMT) | Donor screening protocols, FMT administration equipment | Microbiome transfer between hosts | Standardized processing, donor phenotype characterization |
| Bacterial Sequencing | 16S rRNA primers, Shotgun metagenomics kits | Microbiome composition and function | Choice of variable region, sequencing depth, contamination control |
| Metabolite Analysis | SCFA standards, Bile acid panels, Tryptophan metabolites | Functional microbiome output | Sample stability, internal standards, detection sensitivity |
| Microglial Markers | Iba1, TREM2, P2RY12, TMEM119 | Microglial activation state assessment | Antibody specificity, quantitative image analysis |
| Barrier Integrity Assays | FITC-dextran, ELISA for zonulin, Claudin antibodies | Intestinal and blood-brain barrier function | Timing after tracer administration, tissue processing methods |
Dietary Interventions and Microbiome-Targeted Therapies
Evidence from Preclinical Studies
Dietary interventions represent a powerful non-pharmacological approach to modulating the MGBA. Specific dietary patterns, including high-fiber, plant-based, and Mediterranean diets, have been shown to enhance microbial diversity, decrease inflammation, and improve gut-brain communication [69]. The mechanisms underlying these benefits involve multiple pathways, including microbial metabolite production, neuroendocrine signaling, and immune modulation.
Preclinical studies have demonstrated that the bacterial DNA in blood emerges as a potential microbiome biomarker that may identify vulnerable individuals who could benefit most from protective dietary interventions [32]. Additionally, host and microbial genetic factors influence responses to dietary interventions. Genetic variation in sucrase-isomaltase (SI) and other human carbohydrate-active enzyme genes may predispose to carbohydrate maldigestion across a continuum of mild to severe bowel symptoms and manifestations, supporting the development of genotype-based dietary interventions [32].
The influence of early-life nutrition on long-term brain health has been documented in several models. Findings from the COGNIS study showed that the short-term impact of infant formulas and complementary foods enriched with bioactive compounds and human milk-derived probiotics may shape the development of the microbiota-gut-brain axis [32]. Similarly, unpublished findings in mice showed that microbiota-targeted interventions with Bifidobacterium longum APC1472 or fructooligosaccharides and galactooligosaccharides can attenuate the enduring effects of early-life high-fat high-sugar diet, including food intake dysregulation and hypothalamic molecular alterations [32].
Therapeutic Targeting of the MGBA
Several microbiota-targeted therapeutic approaches have shown promise in preclinical models of neurodegeneration:
Probiotics: Specific bacterial strains have demonstrated neuroprotective effects in animal models. For example, Bifidobacterium longum APC1472 has shown anti-obesity effects in otherwise healthy individuals with overweight/obesity [32]. Multi-strain probiotic formulations have been more effective than single strains in many studies, potentially due to synergistic effects between different bacterial species.
Prebiotics: Dietary fibers that selectively promote the growth of beneficial gut bacteria have improved outcomes in neurodegeneration models. Prebiotics such as inulin-type fructans, psyllium, and human milk oligosaccharides have shown efficacy in maintaining gut barrier function and reducing neuroinflammation [32]. The European Food Safety Authority has authorized health claims for inulin for improving gut health (constipation, gut transit) and improving glycemic index for inulin/fructooligosaccharides [32].
Fecal Microbiota Transplantation (FMT): Transfer of whole microbial communities from healthy donors to diseased recipients has demonstrated therapeutic potential in several models. FMT from young wild-type mice to Alzheimer's model mice has been shown to reduce Aβ pathology and improve cognitive function, suggesting that restoring a healthy gut microbiome can ameliorate neurodegenerative processes.
Dietary Patterns: Specific dietary regimens, such as the Mediterranean diet, ketogenic diet, and time-restricted feeding, have shown beneficial effects on neurodegeneration in animal models. These effects are mediated through multiple mechanisms, including reduction of neuroinflammation, enhancement of autophagy, and improvement of mitochondrial function.
Table 4: Microbiome-Targeted Interventions in Neurodegeneration Models
| Intervention Type | Specific Formulations | Mechanisms of Action | Efficacy in Preclinical Models |
|---|---|---|---|
| Probiotics | Bifidobacterium longum APC1472, Lactobacillus plantarum, Multi-strain mixtures | Gut barrier reinforcement, SCFA production, anti-inflammatory effects | Moderate to strong evidence for cognitive and motor improvement |
| Prebiotics | Inulin, Fructooligosaccharides, Galactooligosaccharides, Resistant starch | Selective growth of beneficial taxa, increased SCFA production, enhanced gut barrier | Consistent improvements in gut health, variable effects on neurodegeneration |
| Synbiotics | Probiotic + prebiotic combinations | Enhanced probiotic survival and colonization, synergistic benefits | Generally superior to individual components in comprehensive outcomes |
| Fecal Microbiota Transplantation | Young donor microbiota, Healthy wild-type donor microbiota | Complete microbial community restoration, functional pathway recovery | Strong evidence for pathology reduction and behavioral improvement |
| Postbiotics | Bacterial lysates, SCFA supplements, Microbial metabolites | Direct bioactive compound delivery, bypassing need for live microbes | Promising for specific mechanisms, limited comprehensive testing |
| Dietary Patterns | Mediterranean diet, Ketogenic diet, High-polyphenol diet | Multi-targeted effects on microbiome composition and function | Strong evidence for disease modification, translation challenges |
The integration of the microbiota-gut-brain axis into preclinical research on neurodegeneration has provided transformative insights into disease mechanisms and therapeutic opportunities. Animal models, despite their limitations, remain essential tools for deciphering the complex interactions between diet, gut microbiota, and brain health. The strategic use of multiple model systems—each with complementary strengths—offers the most promising approach for advancing our understanding of these relationships.
Future research directions should prioritize several key areas:
- Development of More Human-Relevant Models: Creating animal models that better recapitulate human disease progression, including the slow time course of neurodegeneration and the complexity of human immune responses.
- Standardization of Methodologies: Establishing consistent protocols for microbiome manipulation, behavioral assessment, and molecular analysis across laboratories to improve reproducibility and comparability.
- Personalized Medicine Approaches: Identifying biomarkers that predict individual responses to dietary interventions and microbiome-targeted therapies, enabling more precise treatment strategies.
- Multi-Omics Integration: Implementing systems biology approaches to unravel the complex networks connecting specific microbial taxa, their metabolic outputs, and host neurobiological responses.
- Translation to Clinical Applications: Bridging the gap between promising preclinical findings and clinical applications through careful experimental design and validation in human cohorts.
The growing recognition that the gut microbiome provides essential cues to microglia, astrocytes, and oligodendrocytes underscores the importance of viewing neurodegenerative diseases not as isolated brain disorders, but as systemic conditions with significant gastrointestinal components [15]. This perspective opens new avenues for therapeutic intervention that extend beyond the central nervous system to target the gut microbiome and its metabolic outputs. As research in this field advances, the microbiota-gut-brain axis will likely play an increasingly prominent role in both understanding and treating neurodegenerative diseases.
The burgeoning field of gut-brain axis research has established a paradigm shift in our understanding of mental health, highlighting the gastrointestinal tract as a critical interface between diet, gut microbiota, and brain function. This in-depth technical review examines the efficacy of probiotics, prebiotics, and specific dietary interventions on mental health markers through the lens of human clinical trials. The microbiota-gut-brain axis constitutes a complex, bidirectional communication network involving neural, endocrine, immune, and metabolic pathways [85]. Within this framework, nutritional interventions offer promising avenues for modulating gut microbial composition and activity, thereby influencing neurological and psychological outcomes [86] [87]. This review synthesizes current evidence from randomized controlled trials (RCTs) and meta-analyses, providing researchers and drug development professionals with a critical assessment of experimental methodologies, quantitative outcomes, and mechanistic insights into gut-targeted therapies for mental health.
Quantitative Synthesis of Clinical Evidence
Recent meta-analyses of randomized controlled trials provide compelling evidence supporting the therapeutic potential of biotics for mood disorders. The following tables summarize the quantitative findings on the efficacy of probiotics, prebiotics, and synbiotics for depression and anxiety symptoms across diverse clinical populations.
Table 1: Meta-Analysis Results for Probiotic Interventions on Depression and Anxiety
| Population | Number of Studies & Participants | Intervention Duration | Effect Size on Depression (SMD, 95% CI) | Effect Size on Anxiety (SMD, 95% CI) | Heterogeneity (I²) | Citation |
|---|---|---|---|---|---|---|
| Clinically Diagnosed Samples | 18 RCTs (n=NR) | 4-10 weeks | -0.96 (-1.31, -0.61) | -0.59 (-0.98, -0.19) | High | [88] |
| Patients with Depression | 19 RCTs (n=1405) | Variable | -1.76 (-2.42, -1.10) | -1.60 (-2.83, -0.36) | 96.29% (Depression) | [85] |
| Mixed/General Populations | 4295 samples | Variable | 0.2894 (p=0.0139) | 0.2942 (p=0.0335) | 92.4% (Anxiety) | [89] |
Table 2: Effects of Prebiotics, Synbiotics, and Probiotics on Cognitive Function
| Intervention Type | Number of Studies & Participants | Cognitive Domain Assessed | Effect Size (SMD, 95% CI or p-value) | Primary Assessment Tools | Citation |
|---|---|---|---|---|---|
| Probiotics & Prebiotics | 915 samples | General Cognitive Function | 0.4819 (p=0.0027) | MMSE, PHES | [89] |
| Polysaccharide-Based Systems | Preclinical focus | Neuroprotection | N/A (Mechanistic) | Targeted delivery efficiency | [87] |
Table 3: Key Bacterial Strains and Intervention Formulations in Clinical Trials
| Bacterial Strain / Formulation | Typical Dosage (CFU/day) | Common Delivery Format | Reported Primary Effects | Notable Clinical Studies |
|---|---|---|---|---|
| Multi-strain Probiotics (e.g., Ecologic Barrier) | 2.5x10â¹ - 10x10â¹ | Freeze-dried powder in sachets | Reduced negative mood, improved depression scores | [90] |
| Bifidobacterium strains (e.g., B. longum APC1472) | Variable | Capsules, fermented foods | Attenuated obesity-related phenotypes, mood support | [32] |
| Lactobacillus strains | Variable | Capsules, dairy products | Gut barrier support, immune modulation | [85] |
| Fructooligosaccharides (FOS) & Galactooligosaccharides (GOS) | 5-15 g/day | Powder, fortified foods | Prebiotic for beneficial bacteria, anxiety reduction | [32] [88] |
Methodological Approaches in Clinical Trial Design
Participant Recruitment and Eligibility Criteria
Recent high-quality trials employ stringent eligibility criteria to minimize confounding variables. Common inclusion/exclusion parameters comprise: absence of antibiotic or probiotic use for at least 3 months prior to enrollment; body mass index maintained within 18-30 range; exclusion of individuals with diagnosed psychiatric, gastrointestinal, hepatic, or renal disorders; and restrictions on concomitant medication use beyond hormonal contraceptives [90]. Studies focusing on clinical populations specifically enroll participants with validated diagnoses of major depressive disorder or generalized anxiety disorder using standardized diagnostic criteria such as DSM-5 [88] [85].
Intervention Protocols and Control Conditions
Typical intervention protocols administer probiotics at doses ranging from 1×10⹠to 10×10¹Ⱐcolony-forming units (CFU) daily, with durations extending from 4 weeks to 12 weeks [88] [85]. Multi-strain formulations frequently incorporate Lactobacillus and Bifidobacterium species, such as the well-characterized Ecologic Barrier formulation containing nine bacterial strains including Bifidobacterium bifidum W23, B. lactis W51/W52, and various Lactobacillus species [90]. Prebiotic interventions commonly utilize fructooligosaccharides (FOS), galactooligosaccharides (GOS), or inulin-type fructans at doses of 5-15 g/day [32]. Control conditions employ meticulously matched placebos consisting of the carrier materials only (e.g., maize starch, maltodextrins) that are indistinguishable from active interventions in taste, appearance, and packaging [90].
Outcome Assessment and Monitoring Strategies
Outcome assessment incorporates both validated psychological instruments and emerging monitoring technologies:
- Depression Symptoms: Hamilton Depression Rating Scale (HDRS), Beck Depression Inventory (BDI), Center for Epidemiological Studies Depression Scale (CES-D) [88].
- Anxiety Symptoms: Beck Anxiety Inventory (BAI), State-Trait Anxiety Inventory (STAI), Penn State Worry Questionnaire (PSWQ) [90].
- Cognitive Function: Mini-Mental State Examination (MMSE), Psychometric Hepatic Encephalopathy Score (PHES) [89].
- Daily Monitoring: Emerging evidence suggests that daily self-reports using visual analog scales or ecological momentary assessment provide superior sensitivity for detecting mood changes compared to pre-post designs alone, particularly in healthy populations [90].
- Biomarker Analysis: Increasingly, trials incorporate inflammatory biomarkers (e.g., CRP, IL-6, TNF-α), cortisol measurements, and metabolomic profiling of gut-derived metabolites such as short-chain fatty acids [85] [87].
Mechanistic Pathways in the Gut-Brain Axis
The gut-brain axis represents a complex, multidirectional communication system that integrates neural, endocrine, immune, and metabolic signaling pathways between the gastrointestinal tract and the central nervous system.
The diagram above illustrates the primary communication pathways through which gut microbiota influence brain function and behavior. These pathways include:
- Neural Pathway: The vagus nerve serves as a direct communication channel, transmitting gut-derived signals to the brain. Probiotics such as Lactobacillus rhamnosus have been shown to modulate vagal afferent activity, influencing emotional behavior [90] [40].
- Endocrine Pathway: The hypothalamic-pituitary-adrenal (HPA) axis mediates stress responses, with gut microbiota influencing cortisol release. Probiotic and prebiotic interventions can attenuate HPA axis hyperactivity, reducing cortisol levels in humans [90] [85].
- Immune Pathway: Gut microbiota regulate systemic inflammatory responses, producing cytokines that can cross the blood-brain barrier and influence neuroinflammation. Probiotics reduce pro-inflammatory cytokines (e.g., TNF-α, IL-6) while promoting anti-inflammatory mediators like IL-10 [89] [85].
- Metabolic Pathway: Gut bacteria produce neuroactive metabolites including short-chain fatty acids (SCFAs; acetate, propionate, butyrate), neurotransmitters (GABA, serotonin precursors), and branched-chain amino acids that systemically influence brain function [32] [87].
The Scientist's Toolkit: Essential Research Reagents and Methodologies
Table 4: Key Research Reagent Solutions for Gut-Brain Axis Investigation
| Reagent/Technology | Primary Application | Key Function in Research | Representative Examples |
|---|---|---|---|
| Multi-Strain Probiotic Formulations | Clinical interventions | Live microorganisms providing health benefits when administered in adequate amounts | Ecologic Barrier (9 strains), Lactobacillus and Bifidobacterium combinations [90] [85] |
| Prebiotic Compounds | Clinical & preclinical studies | Non-digestible food ingredients that selectively stimulate growth of beneficial gut bacteria | Fructooligosaccharides (FOS), Galactooligosaccharides (GOS), Inulin-type fructans [32] [88] |
| Polysaccharide Encapsulation Systems | Bioavailability enhancement | Improve stability and targeted delivery of neuroprotective compounds; possess inherent prebiotic properties | Chitosan, Alginate, Pectin, β-Glucan-based delivery systems [87] |
| Gut Microbiota Analysis Tools | Microbiome assessment | Profiling of microbial composition and functional potential | 16S rRNA sequencing, Shotgun metagenomics, GA-map Dysbiosis Test [32] |
| Neuroactive Metabolite Profiling | Mechanistic studies | Quantification of gut-derived molecules with neuroactive potential | LC-MS/MS for SCFAs, GABA, serotonin; Gut-brain module analysis [32] [87] |
Experimental Workflow for Clinical Trials
The following diagram outlines a standardized workflow for conducting clinical trials investigating the effects of biotics on mental health markers, incorporating methodological insights from recent studies.
This workflow highlights critical methodological considerations, including the importance of daily monitoring to detect subtle mood changes that might be missed in pre-post assessments alone [90]. The incorporation of biomarker analysis and microbiome profiling strengthens mechanistic interpretations of clinical outcomes.
The cumulative evidence from human clinical trials substantiates the efficacy of specific probiotic strains and prebiotic compounds for improving mental health markers, particularly in clinically depressed populations. Future research should prioritize standardization of intervention protocols, including strain selection, dosage, and treatment duration. Additionally, personalized nutrition approaches that account for individual differences in baseline gut microbiota, host genetics, and dietary patterns represent a promising frontier for enhancing therapeutic efficacy [32] [87]. The integration of advanced technologies such as polysaccharide-based encapsulation systems for improved bioactive delivery [87] and multi-omics approaches for comprehensive mechanistic understanding will further advance the translation of gut-brain axis research into targeted clinical applications for mental health disorders.
The microbiota-gut-brain axis (MGBA) represents one of the most dynamic interfaces in physiological research, forming a complex, bidirectional communication network that integrates central nervous system functions with peripheral gastrointestinal processes. Dietary patterns serve as primary modulators of this axis, exerting profound influence on microbial composition, gut barrier integrity, neuroimmune signaling, and ultimately, brain health. Within the context of escalating neuropsychiatric and neurodegenerative disorders, understanding how specific dietary patterns—particularly the Western Diet (WD) versus plant-based (PBD) and Mediterranean diets (MD)—orchestrate MGBA communication has become a critical research frontier. This whitepaper provides a systematic analysis of the mechanistic pathways through which these diets influence MGBA physiology, synthesizing current evidence to inform future research and therapeutic development.
Impact of Dietary Patterns on Gut Microbiota Composition
The gut microbiota, comprising trillions of microorganisms, is fundamentally shaped by long-term and short-term dietary intake. Comparative analyses reveal distinct microbial signatures associated with WD, PBD, and MD.
Table 1: Microbial Signatures Associated with Different Dietary Patterns
| Dietary Pattern | Key Microbial Shifts (vs. Healthy Baseline) | Impact on Microbial Diversity |
|---|---|---|
| Western Diet (WD) | ↑ Firmicutes:Bacteroidetes ratio [14] [91]↑ Proteobacteria (e.g., Enterobacteriaceae) [91] [92]↑ Bilophila spp. [91]↓ Bifidobacterium [91]↓ Lactobacillus [91]↓ Akkermansia muciniphila [91] | Decreased diversity and richness; loss of beneficial symbionts [14] |
| Plant-Based Diet (PBD) | ↑ Prevotella [14]↑ Bifidobacterium [14]↑ Lactobacillus [14]↑ Roseburia, Faecalibacterium prausnitzii [14]↓ Clostridium sensu stricto [14] | Increased microbial richness and biodiversity [14] [93] |
| Mediterranean Diet (MD) | ↑ Faecalibacterium prausnitzii [14]↑ Roseburia [14]↑ Bifidobacterium adolescentis, B. longum [14]↑ Prevotella [14] | Increased microbial diversity and stability [14] [92] |
The WD, characterized by high saturated fat, refined sugars, and processed foods while being low in fiber, consistently promotes a state of dysbiosis. This includes a reduced abundance of SCFA-producing bacteria and an expansion of pro-inflammatory microbial taxa [14] [91]. In contrast, PBD and MD, rich in dietary fiber, polyphenols, and unsaturated fats, promote a symbiotic microbiota. These diets enhance the abundance of bacteria instrumental in fermenting indigestible fibers to produce short-chain fatty acids (SCFAs)—such as acetate, propionate, and butyrate—which are critical metabolites for gut-brain communication [14] [92].
Mechanistic Pathways in the Microbiota-Gut-Brain Axis
Diet-induced changes in the gut microbiota influence brain physiology and function through multiple interconnected pathways. The diagrams below delineate the primary mechanistic routes for Western versus plant-based/Mediterranean diets.
Western Diet-Induced Pathways
Figure 1: Western Diet MGBA Disruption Pathway. LPS: Lipopolysaccharide.
The WD promotes a pro-inflammatory cascade, initiating with microbial dysbiosis that compromises intestinal epithelial tight junctions, leading to a "leaky gut" [91]. This allows the translocation of bacterial endotoxins, such as lipopolysaccharide (LPS), into systemic circulation—a state known as metabolic endotoxemia. LPS triggers a chronic low-grade inflammatory response, which can disrupt the blood-brain barrier (BBB), promote neuroinflammation via activated microglia, and induce central insulin resistance [91]. These events collectively contribute to neuronal dysfunction and impairments in hippocampal-dependent memory and learning [91].
Plant-Based/Mediterranean Diet-Induced Pathways
Figure 2: Protective MGBA Pathway of Plant-Based/Mediterranean Diets. SCFA: Short-Chain Fatty Acid.
PBD and MD foster a symbiotic gut environment that supports MGBA health through several key mechanisms. The fermentation of dietary fiber produces SCFAs, with butyrate serving as a primary energy source for colonocytes and enhancing intestinal barrier function [14] [92]. SCFAs also possess potent anti-inflammatory properties, inhibiting histone deacetylases and modulating immune cell activity. Furthermore, gut microbes in this environment produce or influence a range of neuroactive metabolites, including serotonin and GABA, which can signal to the brain via the vagus nerve or systemic circulation [75] [9]. The anti-inflammatory and antioxidant compounds (e.g., polyphenols) in these diets further contribute to a systemic environment that supports neuroprotection and cognitive health [69] [41].
Experimental Models and Methodological Approaches
Investigating the MGBA requires sophisticated, multi-system experimental models. The following workflow outlines a standard protocol for delineating diet-microbiota-brain interactions.
Experimental Workflow for MGBA Research
Figure 3: Experimental Workflow for MGBA Diet Studies. L/M: Lactulose/Mannitol; NGF: Nerve Growth Factor.
This workflow initiates with a controlled dietary intervention in animal models or human cohorts. Subsequent steps involve comprehensive microbiota profiling via sequencing technologies and metabolomic analysis to quantify key microbial metabolites [14] [32]. Critical to the workflow is the assessment of gut and blood-brain barrier integrity using a combination of molecular probes, permeability tests, and biomarker assays. Neurophenotyping employs behavioral tests (e.g., for anxiety, memory) and neuroimaging to link dietary and microbial changes to brain function [91] [93]. The final, crucial step for establishing causality is the use of fecal microbiota transplantation (FMT) into germ-free or antibiotic-treated recipients to determine if the diet-induced phenotype is transferable via the microbiota alone [91].
Table 2: Key Analytical Methods in MGBA Research
| Method Category | Specific Technique | Primary Application in MGBA Research |
|---|---|---|
| Microbiome Analysis | 16S rRNA Gene Sequencing | Taxonomic profiling of bacterial communities [14] |
| Shotgun Metagenomics | Functional potential analysis of the entire microbiome [14] | |
| Metabolomics | Liquid Chromatography-Mass Spectrometry (LC-MS) | Quantification of SCFAs, neurotransmitters, bile acids [91] [75] |
| Gas Chromatography-Mass Spectrometry (GC-MS) | Targeted analysis of volatile fatty acids (SCFAs) [91] | |
| Barrier Function | Lactulose/Mannitol Test | Assessment of intestinal permeability in vivo [91] |
| ELISA for Zonulin/FABP2 | Measurement of plasma markers for gut barrier damage [91] | |
| Lipopolysaccharide (LPS) Assay | Quantification of systemic endotoxemia [91] | |
| Neurobiology | Behavioral Test Batteries (e.g., Morris Water Maze) | Assessment of cognitive function, anxiety, and memory [91] [93] |
| Magnetic Resonance Imaging (MRI) | Volumetric analysis of brain structures (e.g., hippocampus) [94] [41] | |
| Immunoassays (ELISA/MSD) | Measurement of inflammatory cytokines (e.g., IL-6, TNF-α) and neurotrophic factors (e.g., BDNF) [91] [9] |
Table 3: Essential Research Reagents for MGBA Investigations
| Reagent / Resource | Function / Application | Example Use Case |
|---|---|---|
| Gnotobiotic Mice | Germ-free animals for FMT studies to establish causal roles of specific microbiota. | Validating transferability of WD-induced cognitive deficits [91]. |
| 16S rRNA Sequencing Kits (e.g., Illumina) | Taxonomic classification and diversity analysis of bacterial communities. | Profiling dysbiosis in WD-fed models versus controls [14] [93]. |
| SCFA Standards (Acetate, Propionate, Butyrate) | Calibration standards for mass spectrometry-based quantification of SCFAs. | Measuring fecal/plasma SCFA levels as a functional readout of microbial activity [91] [92]. |
| Lipopolysaccharide (LPS) ELISA Kits | Quantification of bacterial endotoxin in plasma/serum. | Assessing the degree of metabolic endotoxemia and gut permeability [91]. |
| Probiotic Strains (e.g., Bifidobacterium longum, Lactobacillus spp.) | Live microbial supplements to modulate host microbiota. | Testing therapeutic potential for reversing WD-induced deficits [9] [32]. |
| Prebiotic Fibers (e.g., Inulin, Fructooligosaccharides - FOS) | Non-digestible food ingredients that stimulate growth of beneficial bacteria. | Investigating selective amplification of SCFA-producing taxa [92] [32]. |
| Anti-Zonulin Antibodies | Detection and measurement of zonulin, a regulator of intestinal tight junctions. | Evaluating gut barrier integrity in intervention studies [75]. |
The evidence unequivocally demonstrates that the Western Diet disrupts MGBA homeostasis through pro-inflammatory, barrier-disrupting pathways, while plant-based and Mediterranean diets promote a resilient, anti-inflammatory MGBA environment. The translation of this knowledge into clinical applications and public health policy represents a significant opportunity. Future research must prioritize long-term, large-scale randomized controlled trials in diverse populations to move beyond correlations and establish causality in humans [93] [41]. A critical frontier is the development of personalized nutritional interventions, informed by an individual's baseline microbiota, genetic makeup, and MGBA responsiveness [14] [32]. Furthermore, the exploration of microbiota-targeted therapeutics, including next-generation probiotics, prebiotics, and postbiotics, holds immense promise for harnessing the MGBA to combat neuropsychiatric and neurodegenerative disorders, offering novel avenues for drug development beyond conventional pharmacology.
The gut-brain axis (GBA) represents one of the most compelling frontiers in therapeutic science, forming a complex, bidirectional communication network that integrates neural, endocrine, immune, and metabolic pathways between the gastrointestinal tract and the central nervous system (CNS) [95] [7]. The gut microbiota plays a fundamental role in this communication, producing a vast repertoire of neuroactive substances including neurotransmitters, short-chain fatty acids (SCFAs), and secondary bile acids that profoundly influence brain function and behavior [15] [95]. Approximately 90% of the body's serotonin is synthesized in the gut under microbial influence, highlighting the microbiota's critical role in regulating neurochemistry [7]. Disruption of this intricate ecosystem, known as dysbiosis, has been implicated in a range of neurodegenerative and neuropsychiatric disorders, including Alzheimer's disease (AD), Parkinson's disease (PD), depression, and anxiety [15] [7] [4]. This mechanistic link establishes the GBA as a promising therapeutic target for innovative treatment strategies.
The role of diet in modulating this axis is foundational. Dietary patterns directly shape the composition and function of the gut microbiome, which in turn influences the production of microbial metabolites that communicate with the brain [9] [7]. Diets rich in fiber, polyphenols, and fermented foods promote microbial diversity and the production of beneficial metabolites like SCFAs, which enhance intestinal barrier integrity, reduce systemic inflammation, and support cognitive function [9] [7]. Conversely, Western diets high in processed foods and low in fiber can promote dysbiosis, increase intestinal permeability ("leaky gut"), and trigger neuroinflammation [7]. This establishes a critical rationale for developing interventions that can precisely modulate the gut environment to exert therapeutic effects on the brain.
Despite this compelling target, conventional drug delivery approaches face significant biological barriers, including digestive degradation, poor intestinal absorption, and the impermeable blood-brain barrier (BBB) [96]. Biomimetic and nanoparticle-based drug delivery systems (DDS) represent a paradigm shift in overcoming these challenges. These systems are engineered to mimic biological processes and leverage natural pathways of the GBA, enabling targeted, efficient, and sustained therapeutic action with minimized off-target effects [97] [96] [98]. This whitepaper provides an in-depth technical guide to the core principles, methodologies, and applications of these novel DDS for targeting the gut-brain axis.
Core Communication Pathways of the Gut-Brain Axis
Understanding the multifaceted communication pathways of the GBA is essential for rational drug delivery design. These pathways operate in concert, providing multiple entry points for therapeutic intervention. The table below summarizes the key mechanisms, their mediators, and the opportunities they present for targeted drug delivery.
Table 1: Key Communication Pathways in the Gut-Brain Axis
| Pathway | Key Mediators & Mechanisms | Implications for Drug Delivery |
|---|---|---|
| Neural Pathway | Vagus nerve activation by microbial metabolites (e.g., SCFAs, serotonin); Afferent signaling to CNS [95] [7]. | Target vagal nerve endings in the gut; Design for neuron-specific uptake. |
| Endocrine & Metabolic Pathway | Gut hormone secretion (GLP-1, PYY); Microbial production of neurotransmitters (GABA, serotonin, dopamine); Tryptophan metabolism [15] [9] [95]. | Mimic gut hormones; Engineer responsive release to microbial metabolites. |
| Immune Pathway | Cytokine release (IL-1β, IL-6, TNF-α); Microglial activation by microbial products (e.g., LPS, SCFAs); Systemic and neuroinflammation [15] [96] [4]. | Target immune cells (e.g., macrophages); Deliver anti-inflammatory agents to gut or brain. |
| Barrier Integrity Pathway | Microbial regulation of intestinal tight junctions; SCFA-mediated maintenance of blood-brain barrier (BBB) [95] [7]. | Co-deliver drugs with barrier-strengthening agents (e.g., butyrate). |
The following diagram synthesizes these pathways into an integrated view of the Gut-Brain Axis, illustrating the primary communication channels and their interconnections that drug delivery systems can exploit.
Diagram 1: The Gut-Brain Axis Communication Network. This diagram illustrates the primary neural, endocrine, and immune pathways facilitating bidirectional communication between the gut and the brain. Key targets for therapeutic intervention, including the vagus nerve, immune signaling cascades, and biological barriers, are highlighted.
Biomimetic and Nanoparticle Platforms for GBA Targeting
Rationale and Core Design Principles
Conventional oral therapeutics face immense challenges in traversing the GBA, including degradation in the harsh gastrointestinal environment, poor permeability across the gut epithelium, and an inability to cross the highly selective BBB [96]. Nanoparticle (NP) systems are engineered to overcome these barriers through tunable physicochemical properties—such as size, surface charge, and material composition—that protect therapeutic cargo and enhance bioavailability [96] [98]. The paradigm of biomimetics elevates this approach by explicitly designing NPs to mimic biological structures or exploit natural physiological pathways [97]. For instance, nanoparticles can be functionalized with microbial metabolites or designed to respond to specific gut environmental cues (e.g., pH, enzymes) to achieve targeted release and improved interaction with gut epithelial cells and nerve endings [97] [98].
Classification of Promising Nanocarrier Systems
Table 2: Nanocarrier Platforms for GBA-Targeted Drug Delivery
| Nanocarrier Type | Key Composition & Characteristics | Proposed Mechanism of GBA Targeting | Therapeutic Cargo Examples |
|---|---|---|---|
| Lipid-Based NPs | Liposomes, Solid-Lipid NPs (SLNs); Biocompatible lipid bilayers [98]. | Fuse with intestinal cell membranes; Enhance absorption of lipophilic drugs; Can be coated for mucoadhesion. | Anti-inflammatory drugs, Neuropeptides, SCFAs [98]. |
| Polymeric NPs | Poly(lactic-co-glycolic acid) (PLGA), Chitosan; Biodegradable and controllable release [96]. | Sustained drug release in gut lumen; Mucopenetration (Chitosan); Functionalized for receptor-mediated uptake. | Probiotics, Antibodies, Enzyme inhibitors [96] [99]. |
| Metabolite-Inspired Biomimetic NPs | NPs coated with or encapsulating microbial metabolites (e.g., SCFAs, bile acids) [97] [98]. | Exploit natural metabolite transport pathways; Modulate gut barrier and immune function; Signal via vagus nerve. | Butyrate, Tryptophan metabolites, Psychobiotics [97] [7]. |
A key advancement in this field is the development of nanocarriers designed for intracellular receptor targeting, as exemplified by recent work on the PAR2 receptor. The following diagram details the experimental workflow and mechanistic insight from a seminal study that used nanoparticles to inhibit PAR2 within endosomes, a strategy that could be adapted for various GBA targets.
Diagram 2: Workflow and Mechanism of Intracellular Receptor Targeting via Nanoparticles. This diagram outlines the key experimental steps and the mechanistic rationale for using nanoparticles to target intracellular compartments, based on a study targeting the PAR2 receptor in gut pain [99].
Experimental Protocols for GBA-Targeted DDS Development
Protocol: Formulation and Characterization of Metabolite-Loaded Polymeric NPs
This protocol details the synthesis of PLGA nanoparticles loaded with the microbial metabolite butyrate, a SCFA with demonstrated neuroprotective and anti-inflammatory properties [15] [7].
Materials:
- Polymer: PLGA (50:50, acid-terminated, MW 10-20 kDa).
- Organic Solvent: Dichloromethane (DCM), HPLC grade.
- Aqueous Phase: Polyvinyl alcohol (PVA, 1% w/v in Milli-Q water).
- Drug/Cargo: Sodium butyrate.
- Equipment: Probe sonicator, magnetic stirrer, centrifuge, dynamic light scattering (DLS) instrument.
Methodology:
- Formulation via Double Emulsion (W/O/W): Dissolve 100 mg PLGA and 10 mg sodium butyrate in 2 mL DCM. Sonicate this organic phase (5 sec, 30% amplitude) while adding 0.5 mL of a 0.5% PVA solution to form a primary water-in-oil (W/O) emulsion.
- Secondary Emulsion: Immediately pour this primary emulsion into 20 mL of a 2% w/v PVA solution under vigorous stirring (1000 rpm) to form the double emulsion (W/O/W). Stir for 3-4 hours to allow complete solvent evaporation and nanoparticle hardening.
- Purification & Storage: Collect nanoparticles by ultracentrifugation (20,000 rpm, 30 min at 4°C). Wash the pellet twice with Milli-Q water to remove excess PVA and unencapsulated butyrate. Resuspend the final nanoparticle pellet in PBS or lyophilize for long-term storage.
Characterization:
- Size and Zeta Potential: Determine hydrodynamic diameter and polydispersity index (PDI) via DLS. Measure zeta potential using electrophoretic light scattering. Target: 150-200 nm, PDI <0.2, zeta potential ~ -25 mV.
- Encapsulation Efficiency (EE): Lyse a known amount of NPs in DCM and PBS. Quantify unencapsulated butyrate in the aqueous phase using HPLC-UV. Calculate EE% = (Total butyrate - Free butyrate) / Total butyrate × 100.
- In Vitro Release Profile: Dialyze a known amount of butyrate-loaded NPs against PBS (pH 7.4 and 6.5 to simulate gut pH) at 37°C under gentle agitation. Collect release medium at predetermined time points and quantify butyrate via HPLC to generate a release profile over 48-72 hours.
Protocol: Evaluating Efficacy in Preclinical Models of Neuroinflammation
This protocol describes how to evaluate the therapeutic efficacy of the formulated NPs in a mouse model of neuroinflammation, which is a hallmark of neurodegenerative diseases [15] [96].
Induction of Neuroinflammation:
- Use 8-10 week old C57BL/6 mice.
- Induce systemic inflammation via intraperitoneal (i.p.) injections of low-dose LPS (0.5-1 mg/kg) daily for 7 days. This model induces gut-derived systemic inflammation that leads to microglial activation and neuroinflammation [96].
Treatment Groups and Dosing:
- Group 1 (Control): Healthy mice, oral gavage with empty NPs.
- Group 2 (Disease Control): LPS-treated mice, oral gavage with empty NPs.
- Group 3 (Treatment): LPS-treated mice, oral gavage with butyrate-loaded NPs.
- Group 4 (Free Drug Control): LPS-treated mice, oral gavage with free sodium butyrate solution (dose-matched to NP group).
- Administer treatments daily via oral gavage, commencing concurrently with LPS injections. Dose volume: 100-200 µL.
Endpoint Analyses:
- Behavioral Assessment: Conduct open field and elevated plus maze tests at the end of the treatment period to assess anxiety-like behavior and locomotor activity.
- Tissue Collection: Euthanize mice and collect blood, colon tissue, and brain regions of interest (e.g., hippocampus, cortex).
- Molecular Analysis:
- ELISA: Measure pro-inflammatory cytokines (TNF-α, IL-6, IL-1β) in plasma and brain homogenates.
- Immunohistochemistry: Stain brain sections for microglial marker Iba1 and astrocyte marker GFAP to quantify neuroinflammation.
- Gut Permeability: Assess in vivo using FITC-dextran assay; ex vivo via measurement of tight junction proteins (e.g., occludin, ZO-1) in colon tissue by western blot.
The Scientist's Toolkit: Key Reagents and Models
Table 3: Essential Research Tools for GBA-Targeted DDS Development
| Category / Reagent | Specifications & Selection Criteria | Primary Function in Research |
|---|---|---|
| Nanoparticle Polymers | PLGA (varied ratios, MW), Chitosan (low MW, >85% deacetylated), PVA (87-89% hydrolyzed). | Forms biodegradable, biocompatible nanoparticle matrix for controlled drug release. |
| Microbial Metabolites | Sodium Butyrate (SCFA), Secondary Bile Acids (e.g., DCA, LCA), Tryptophan metabolites (Indole). | Serves as therapeutic cargo or surface functionalizer to exploit natural GBA pathways [97] [98]. |
| Cell Lines | Caco-2 (human colorectal adenocarcinoma), SH-SY5Y (human neuroblastoma), HMC3 (human microglial). | In vitro models of intestinal epithelium, neurons, and CNS immune cells for permeability and toxicity studies. |
| Animal Models | LPS-induced neuroinflammation, Germ-Free (GF) mice, 5xFAD (Alzheimer's model), APP/PS1 mice. | Preclinical in vivo systems to study GBA pathophysiology and evaluate DDS efficacy [15] [96] [99]. |
| Key Assays | Dynamic Light Scattering (DLS), HPLC/LC-MS, Enzyme-Linked Immunosorbent Assay (ELISA), Immunohistochemistry. | Characterizes NP properties, quantifies drug/metabolite levels, and measures inflammatory biomarkers. |
The convergence of nanomedicine and gut-brain axis research is forging a new frontier in CNS therapeutics. Biomimetic and nanoparticle-based delivery systems offer a powerful strategy to overcome the formidable biological barriers that have traditionally impeded treatment of neurodegenerative and neuropsychiatric diseases. By leveraging the natural communication pathways of the GBA—particularly those influenced by diet and the gut microbiome—these platforms enable unprecedented precision in targeting the underlying mechanisms of disease, from peripheral inflammation to central neuroinflammation [97] [96] [98].
The future of this field lies in increasing sophistication and personalization. The integration of artificial intelligence and multi-omics data will be crucial for designing next-generation DDS, predicting individual patient responses, and identifying novel microbiome-derived targets [96]. Furthermore, the emerging concept of the exposome—the cumulative measure of environmental influences on an individual—underscores the need to consider diet, lifestyle, and environmental toxins when designing therapeutic interventions [96]. As we deepen our understanding of the intricate dialogue between the gut and the brain, the potential grows for developing truly transformative, personalized medicines that can effectively halt or reverse the progression of devastating neurological disorders.
The microbiota-gut-brain axis (MGBA) represents a transformative frontier in therapeutic development for neurological and neurodevelopmental disorders. This whitepaper assesses the current landscape of microbiome-targeted therapies, evaluating the status of clinical trials for probiotics, prebiotics, synbiotics, and fecal microbiota transplantation (FMT). Despite promising preclinical data, clinical translation reveals significant heterogeneity and variable efficacy, underscoring the need for robust biomarkers, personalized approaches, and standardized protocols. Framed within the critical context of dietary modulation of gut-brain communication, this analysis provides a technical guide for researchers and drug development professionals, highlighting future directions for precision microbiome medicine.
The microbiota-gut-brain axis (MGBA) is a complex, bidirectional communication network integrating the central nervous system (CNS), enteric nervous system (ENS), and gastrointestinal tract microbiota through neural, immune, endocrine, and metabolic pathways [2] [15]. The gut microbiome directly influences brain physiology, with emerging evidence demonstrating its role in neurodevelopment, neuroinflammation, and neurodegeneration [4] [3]. The metabolic activity of gut microbes generates a diverse array of neuroactive compounds, including short-chain fatty acids (SCFAs), neurotransmitters, and tryptophan derivatives, which can directly or indirectly modulate CNS function [2] [100].
Diet is a primary modulator of the gut microbiome's composition and functional output, thereby serving as a foundational element in MGBA research [32]. Dietary patterns and interventions, such as fiber-rich or Mediterranean diets, directly shape the microbial ecosystem, influencing the production of key metabolites like SCFAs and subsequently affecting neuroinflammation and brain health [32] [101]. This establishes diet as a critical, modifiable environmental factor in the development of microbiome-targeted therapeutic strategies.
Current therapeutic approaches aim to correct gut dysbiosis—an imbalance in the microbial community associated with various diseases—to restore healthy gut-brain communication. Major intervention categories include probiotics (live beneficial microbes), prebiotics (dietary fibers that foster beneficial microbes), synbiotics (combinations of pro- and prebiotics), and Fecal Microbiota Transplantation (FMT) [2] [101] [15]. While preclinical models show compelling results, the translation into consistent clinical benefits has proven challenging. This review assesses the current clinical trial status of these interventions and outlines the necessary future directions to advance the field.
Current Clinical Trial Landscape: Efficacy and Challenges
The clinical application of microbiome-targeted therapies is characterized by promising but heterogeneous results. The following table summarizes the current evidence and status for major intervention types across key neurological and neurodevelopmental conditions.
Table 1: Status of Microbiome-Targeted Therapies in Clinical Application
| Therapy Type | Key Findings & Efficacy | Associated Conditions | Major Challenges & Gaps |
|---|---|---|---|
| Probiotics | • Most extensive clinical data exists for newborns: Specific combinations (e.g., Lactobacillus & Bifidobacterium) reduce risk of severe necrotizing enterocolitis (NEC) and all-cause mortality in preterm infants [102].• Conditional recommendations from AGA, ESPGHAN, and WHO for preterm infants, but opposed by AAP due to safety and heterogeneity concerns [102].• Variable, often modest, effects in adult neurodegenerative diseases (AD, PD) and neurodevelopmental disorders (ASD) [101] [3]. | Necrotizing Enterocolitis, Alzheimer's Disease, Parkinson's Disease, Autism Spectrum Disorder (ASD), Major Depressive Disorder (MDD) [102] [101] [3]. | • Strain-specific effects: Efficacy is not uniform across probiotic strains.• Inter-individual variability: Host baseline microbiome, diet, and genetics influence outcomes [2] [32].• Lack of robust biomarkers: Few validated biomarkers to predict response or measure target engagement.• Safety in vulnerable populations: Risk of bacteremia in extremely preterm infants or immunocompromised individuals [102]. |
| Prebiotics | • European Food Safety Authority (EFSA) has authorized health claims for inulin-type fructans regarding gut health (constipation) and glycaemic control [32].• Evidence for improving chronic constipation symptoms (psyllium, inulin-type fructans) is stronger than for direct neurological benefits [32].• High-fiber diets boost SCFA production, demonstrating reduced CNS inflammation in animal models of MS [2]. | Chronic Constipation, General Gut Health, Metabolic Health [32]. | • Complexity of background diet: Diet confounds the efficacy of prebiotic interventions in trials [32].• Mechanistic understanding: Limited knowledge of how specific prebiotics translate into precise neurological benefits in humans. |
| Synbiotics | • A large RCT in rural India showed Lactiplantibacillus plantarum + fructooligosaccharide reduced sepsis and death in newborns [102].• Potential for enhanced efficacy compared to probiotics or prebiotics alone, though clinical evidence in neurology is nascent. | Neonatal Sepsis, Metabolic Health [102]. | • Optimal pairing: Identifying the most effective probiotic-prebiotic combinations for specific conditions is an ongoing challenge. |
| Fecal Microbiota Transplantation (FMT) | • Established efficacy for recurrent Clostridioides difficile infection; conditional AGA recommendation based on low-certainty evidence [102].• Investigated in ASD, PD, and MS, with early-phase trials showing potential for modulating symptoms [2] [3]. | Recurrent C. difficile Infection, Autism Spectrum Disorder (ASD), Parkinson's Disease (PD), Multiple Sclerosis (MS) [2] [102] [3]. | • Long-term safety: Risks of transferring pathogens or destabilizing the recipient's microbiota are not fully known.• Donor-recipient matching: Lack of standardization for donor selection and recipient matching.• Regulatory status: Classified as a drug in some regions, creating regulatory hurdles [102]. |
A significant challenge across all intervention types is the high variability in clinical trial results. This is driven by factors such as differences in product formulation, dosing, intervention duration, and patient selection criteria [2] [102]. Furthermore, the field is hampered by a reliance on low-certainty evidence for many indications outside of NEC and C. difficile infection, highlighting the need for larger, more rigorous, and reproducible clinical trials [102].
Detailed Experimental and Methodological Insights
Advancing the field requires standardized and mechanistic-driven experimental protocols. Below is a detailed workflow for a clinical trial investigating a microbiome-targeted intervention, incorporating state-of-the-art methodologies.
Table 2: The Scientist's Toolkit: Key Reagents and Technologies for MGBA Research
| Item / Technology | Function & Application in MGBA Research |
|---|---|
| Gnotobiotic Animals | Germ-free or defined-flora animal models (e.g., mice) are essential for establishing causality between specific microbes and host phenotypes [4] [3]. |
| Multi-omics Platforms | Integrative analysis of metagenomics (microbial community genes), metabolomics (microbial and host metabolites), and transcriptomics (host gene expression) to unravel mechanisms [2] [32]. |
| In Vivo Barrier Permeability Assays | Techniques like FITC-dextran assay for intestinal permeability and imaging to assess blood-brain barrier integrity in response to microbial changes [2] [15]. |
| Gas-Sensing Capsule | A novel technology to measure in vivo colonic gas production (e.g., Hâ‚‚, COâ‚‚), providing real-time data on microbial fermentation of dietary substrates [32]. |
| Cell-Based Reporter Assays | Using engineered cell lines (e.g., TLR-reporter cells) to screen for immunomodulatory effects of microbial metabolites [4]. |
| 16S rRNA & Shotgun Metagenomic Sequencing | 16S for profiling microbial community structure; shotgun sequencing for higher resolution, including functional gene analysis [2] [100]. |
| Gut-on-a-Chip / Organoids | Advanced in vitro models that mimic the human intestinal environment for studying host-microbe interactions in a controlled setting [15]. |
Experimental Workflow for a Clinical Trial of a Microbiome-Targeted Therapy:
Participant Stratification & Baseline Profiling: Recruit a well-characterized patient cohort (e.g., prodromal Alzheimer's disease). At baseline, collect:
- Microbiome Samples: Stool for 16S rRNA or shotgun metagenomic sequencing to define baseline microbial diversity and composition.
- Host Biological Samples: Blood for measuring inflammatory cytokines (e.g., IL-6, TNF-α), microbial metabolites (e.g., SCFAs, TMAO, PAGln), and biomarkers of blood-brain barrier integrity [2] [103].
- Clinical & Dietary Data: Comprehensive dietary records using validated food frequency questionnaires are critical to account for the confounding effects of background diet on the intervention's outcome [32].
Randomization & Intervention: Participants are randomized to receive the active intervention (e.g., a defined probiotic consortium, prebiotic, or FMT) or a matched placebo for a predefined period. The intervention should be paired with dietary guidance (e.g., controlled fiber intake) to minimize background noise [32].
Longitudinal Sampling & Monitoring: Repeat the collection of microbiome and host biological samples at predetermined intervals during and post-intervention to track dynamic changes and their relationship to clinical endpoints.
Endpoint Assessment:
- Primary Endpoints: Disease-specific clinical scores (e.g., ADAS-Cog for Alzheimer's, UPDRS for Parkinson's).
- Secondary/Mechanistic Endpoints: Changes from baseline in microbial diversity/SCFA levels, inflammatory markers, neuroimaging findings, and cognitive performance on specialized tasks.
Data Integration & Analysis: Employ bioinformatics and statistical modeling to integrate multi-omics data with clinical outcomes. The goal is to identify microbial taxa, metabolic pathways, and host biomarkers associated with clinical response, thereby uncovering potential mechanisms of action [2] [32].
To overcome current challenges and realize the therapeutic potential of the MGBA, the field must pivot towards more precise and mechanistic strategies.
Key Future Directions:
- Personalized and Precision Medicine: Future trials must move beyond a one-size-fits-all approach. Interventions should be tailored based on an individual's baseline microbiome, immune profile, diet, and genetic background [2]. This requires the development of predictive biomarkers to identify likely responders.
- Elucidation of Causal Mechanisms: Leveraging multi-omics integration and synthetic bacterial communities (manually defined consortia) will be crucial to move from correlation to causation and define the specific microbes and molecular pathways responsible for therapeutic effects [2] [102].
- Advanced Therapeutic Modalities: Research should expand into next-generation therapies, including:
- Synthetic Bacterial Consortia: Defined communities of bacteria designed to perform specific, robust functions [102].
- Phage Therapy: Using bacteriophages to precisely target and remove pathobionts without disrupting commensals [102].
- Postbiotics: Using inactivated microbial cells or their beneficial metabolic products, which may offer safer and more stable alternatives to live probiotics [32].
- Longitudinal Studies and Standardization: Large, long-term longitudinal cohorts are needed to understand the temporal dynamics of the MGBA in health and disease. Furthermore, the field urgently requires standardized protocols for intervention manufacturing, FMT donor screening, and outcome measurements [102] [3].
- Focus on Diet as a Fundamental Modulator: Dietary interventions should be integrated into clinical trial design not as a confounder to be controlled, but as a central therapeutic variable. Research must define how specific dietary patterns can be used to prime the microbiome for enhanced response to other biologic therapies [32] [101].
Conclusion Targeting the microbiota-gut-brain axis holds immense promise for preventing and treating a wide spectrum of neurological and neurodevelopmental conditions. While the current clinical landscape is marked by promising yet variable success, the path forward is clear. By embracing personalized medicine, deepening our mechanistic understanding, developing next-generation therapies, and fully integrating the role of diet, researchers and drug developers can unlock the transformative potential of the MGBA. This will pave the way for a new era of precision microbiome medicine, ultimately improving brain health across the lifespan.
Conclusion
The evidence unequivocally positions diet as a powerful, non-invasive modulator of the gut-brain axis with profound implications for mental health and neurological disease. Key takeaways confirm that dietary patterns directly influence microbial composition and the production of neuroactive metabolites, which in turn regulate brain function through well-defined neural, endocrine, and immune pathways. While dietary interventions such as the Mediterranean diet, psychobiotics, and prebiotics show significant therapeutic promise, their efficacy is moderated by individual microbiome profiles and signaling barrier integrity. Future research must prioritize long-term human studies, standardize intervention protocols, and leverage advanced technologies like personalized drug delivery systems and multi-omics approaches. For biomedical and clinical research, this field opens avenues for novel drug development targeting microbial metabolites and pathways, ultimately paving the way for personalized nutrition and microbial biotherapies as integral components of neurological and psychiatric treatment.
References
- 1. Bidirectional crosstalk between the gut microbiota and ... [https://www.nature.com/articles/s41398-025-03504-2]
- 2. Microbiota–gut–brain axis in neurodegenerative diseases [https://pmc.ncbi.nlm.nih.gov/articles/PMC12436269/]
- 3. Harnessing the microbiota-gut–brain axis to prevent and treat ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-07279-4]
- 4. decoding the gut–immune–brain axis in health and disease [https://www.nature.com/articles/s41423-025-01333-3]
- 5. Bibliometric Visualization Analysis of Microbiome-Gut-Brain ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9119018/]
- 6. Editorial: Dietary modulation of gut microbiota-X axis [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1693629/full]
- 7. The Gut-Brain Axis and Mental Health: How Diet Shapes Our ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12366197/]
- 8. Bibliometric and Visual Analysis of Research on the Links ... [https://www.frontiersin.org/journals/psychiatry/articles/10.3389/fpsyt.2020.587670/full]
- 9. Dietary Influences on the Gut-Brain Pathways: Mechanisms ... [https://www.sciencedirect.com/science/article/pii/S2666149725000532]
- 10. Vagus nerve and brain–gut communication in ... [https://www.sciencedirect.com/science/article/pii/S1043661825003998]
- 11. The gut microbiota-immune-brain axis: Therapeutic implications [https://pmc.ncbi.nlm.nih.gov/articles/PMC11970326/]
- 12. The brain-gut axis and chronic pain: mechanisms ... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2025.1545997/full]
- 13. Decoding the peripheral neuro-immune Axis: A new ... [https://www.sciencedirect.com/science/article/pii/S0969996125004000]
- 14. Diet and the Microbiota–Gut–Brain Axis: Sowing the Seeds of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8321864/]
- 15. Microbiota–gut–brain axis and its therapeutic applications ... [https://www.nature.com/articles/s41392-024-01743-1]
- 16. Neuroendocrine-Immune Circuits, Phenotypes, and Interactions [https://pmc.ncbi.nlm.nih.gov/articles/PMC5203943/]
- 17. The Role of Short-Chain Fatty Acids From Gut Microbiota in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7005631/]
- 18. Elucidating the specific mechanisms of the gut-brain axis [https://jneuroinflammation.biomedcentral.com/articles/10.1186/s12974-025-03454-y]
- 19. Regulation of Neurotransmitters by the Gut Microbiota and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8234057/]
- 20. and the Microbiota- Diet - Gut : Sowing the Seeds of Good... Brain Axis [https://pubmed.ncbi.nlm.nih.gov/33693453/]
- 21. The Gut-Brain Connection: How it Works and The Role of ... [https://www.healthline.com/nutrition/gut-brain-connection]
- 22. Tryptophan Metabolism: A Link Between the Gut Microbiota ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7231603/]
- 23. Tryptophan metabolism and the gut-brain axis [https://www.sciencedirect.com/science/article/pii/S2772566925000862]
- 24. Emerging Research on the Relationship Between Diet, Gut ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12389052/]
- 25. Dietary (Poly)phenols and the Gut–Brain Axis in Ageing - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11124177/]
- 26. The intestinal microbiome associated with lipid metabolism ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9804742/]
- 27. Gut microbiome-mediated health effects of fiber and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12425962/]
- 28. The mutual effect of dietary fiber and polyphenol on gut ... [https://www.sciencedirect.com/science/article/abs/pii/S0144861725003224]
- 29. Microbial Fermentation of Dietary Protein: An Important Factor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6352118/]
- 30. Review Dietary protein and the intestinal microbiota [https://www.sciencedirect.com/science/article/pii/S2589004222015851]
- 31. Gut microbiome lipid metabolism and its impact on host ... [https://www.sciencedirect.com/science/article/pii/S1931312823000343]
- 32. Nutrition & microbiome research highlights NeuroGASTRO ... [https://www.gutmicrobiotaforhealth.com/nutrition-and-microbiome-research-highlights-from-neurogastro-2025/]
- 33. Consumption of only wild foods induces large scale ... [https://www.nature.com/articles/s41598-025-00319-5]
- 34. Emerging role of gut microbiota dysbiosis in ... - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC10225576/]
- 35. Mechanisms regulating intestinal barrier integrity and its ... [https://www.nature.com/articles/s12276-018-0126-x]
- 36. Intestinal Barrier Dysfunction Exacerbates Neuroinflammation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8378453/]
- 37. Gut Microbiota Profiles of Treated Metabolic Syndrome ... [https://www.nature.com/articles/s41598-020-67078-3]
- 38. The Human Microbiome as a Therapeutic Target for Metabolic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11280041/]
- 39. Gut Microbiome Interactions with Drug Metabolism, Efficacy ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5718288/]
- 40. The gut-brain connection: What the science says [https://med.stanford.edu/news/insights/2025/03/gut-brain-connection-long-covid-anxiety-parkinsons.html]
- 41. The intricate interplay between dietary habits and cognitive ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1539355/full]
- 42. Plant-based diet as a precursor to human gut diversity [https://www.sciencedirect.com/science/article/abs/pii/S0022316625007175]
- 43. Effects of a healthy diet based on seed-rich vegetables ... [https://www.nature.com/articles/s41598-025-99406-w]
- 44. Exercise, Diet, and Brain Health: From the Perspective of ... [https://www.mdpi.com/2072-6643/17/10/1686]
- 45. A comprehensive overview of the effects of probiotics ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12575349/]
- 46. The role of probiotics and prebiotics in modulating of the gut ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10410452/]
- 47. Feed your microbes to deal with stress: a psychobiotic diet ... [https://www.nature.com/articles/s41380-022-01817-y]
- 48. Stronger gut microbiome modulatory effects by postbiotics ... [https://www.nature.com/articles/s41538-022-00169-9]
- 49. Postbiotics as the key mediators of the gut microbiota-host ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9177191/]
- 50. Growing up in a Bubble: Using Germ-Free Animals to Assess ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5006193/]
- 51. Food and drug design for gut microbiota-directed regulation [https://www.sciencedirect.com/science/article/pii/S1043661823002232]
- 52. Simulator of the Human Intestinal Microbial Ecosystem ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11677124/]
- 53. Dietary Management for Faecal Microbiota Transplant [https://pmc.ncbi.nlm.nih.gov/articles/PMC8572886/]
- 54. Dietary modulation of gut microbiota affects susceptibility to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11649229/]
- 55. Food, Mood, and Brain Health: Implications for the Modern ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6170050/]
- 56. Nutraceuticals for Gut–Brain Axis Health: A Novel Approach to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12073618/]
- 57. Nutritional psychiatry: Your brain on food [https://www.health.harvard.edu/blog/nutritional-psychiatry-your-brain-on-food-201511168626]
- 58. Gut-Brain Axis Research: How Food Affects Your Mind & ... [https://health.oregonstate.edu/moore-center/news/2025-10/gut-brain-axis-research-how-food-affects-your-mind-body]
- 59. Modulation of Gut Microbiota Through Dietary Intervention in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11133127/]
- 60. Medicine–food homology bioactives in Parkinson's disease [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1677749/full]
- 61. A 2025 update on treatment strategies for the Alzheimer's ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12637128/]
- 62. Treatment for Early-Stage Parkinson's Disease at AD/PD ... [https://www.cerevance.com/media/cerevance-presents-topline-results-from-phase-2-ascend-trial-of-solengepras-as-monotherapy-treatment-for-early-stage-parkinsons-disease-at-ad-pd-2025]
- 63. A Guide to Diet-Microbiome Study Design - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7303276/]
- 64. Baseline intestinal microbiota composition influences ... [https://www.nature.com/articles/s41522-025-00817-4]
- 65. Dietary convergence induces individual responses in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12182192/]
- 66. Use of dietary indices to control for diet in human gut ... [https://microbiomejournal.biomedcentral.com/articles/10.1186/s40168-018-0455-y]
- 67. Blood–Brain and Gut Barrier Signaling in Psychiatric Disorders [https://pmc.ncbi.nlm.nih.gov/articles/PMC12636271/]
- 68. The blood–brain barrier: Structure, regulation and drug ... [https://www.nature.com/articles/s41392-023-01481-w]
- 69. The Gut-Brain Axis and Mental Health: How Diet Shapes ... [https://pubmed.ncbi.nlm.nih.gov/40842787/]
- 70. Modernizing gut-brain axis research in nutritional Science [https://www.sciencedirect.com/science/article/pii/S0924224425001165]
- 71. takeaways from the 2025 GMFH Summit [https://www.gutmicrobiotaforhealth.com/clinical-translation-of-microbiome-research-takeaways-from-the-2025-gmfh-summit/]
- 72. A comprehensive review of probiotics and human health ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11743475/]
- 73. A comprehensive review of probiotics and human health ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2024.1487641/full]
- 74. A comprehensive overview of the effects of probiotics ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1651965/full]
- 75. The communication mechanism of the gut-brain axis and ... [https://www.sciencedirect.com/science/article/pii/S0753332224010916]
- 76. Probiotics: Usefulness and Safety | NCCIH [https://www.nccih.nih.gov/health/probiotics-usefulness-and-safety]
- 77. The role of probiotics in personalized therapeutics [https://www.sciencedirect.com/science/article/pii/S2950194625002651]
- 78. Unveiling The Therapeutic Potential of Probiotics: A Review [https://www.sciencedirect.com/science/article/pii/S2772566925002630]
- 79. The International Scientific Association for Probiotics and ... [https://www.nature.com/articles/s41575-020-0344-2]
- 80. Harnessing Artificial Intelligence and Precision Diets for ... [https://www.sciencedirect.com/science/article/abs/pii/S0022316625004857]
- 81. The Future of Synbiotics: Rational Formulation and Design [https://pmc.ncbi.nlm.nih.gov/articles/PMC9354465/]
- 82. Multifaceted role of synbiotics as nutraceuticals ... [https://www.sciencedirect.com/science/article/abs/pii/S0009279722004288]
- 83. Rodent models of Alzheimer's disease: Critical analysis ... [https://www.sciencedirect.com/science/article/pii/S0301008225001121]
- 84. Animal Models of Neurodegenerative Disease - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC9063566/]
- 85. The impact of probiotics, prebiotics, and synbiotics on ... [https://www.sciencedirect.com/science/article/abs/pii/S002239562500353X]
- 86. Current Evidence on Mental Health and the Microbiota-Gut ... [https://pubmed.ncbi.nlm.nih.gov/41026445/]
- 87. Prospective Strategies for Modulating the Gut-Brain Axis ... [https://www.sciencedirect.com/science/article/abs/pii/S0924224425005357]
- 88. Effects of Prebiotics and Probiotics on Symptoms ... [https://pubmed.ncbi.nlm.nih.gov/39731509/]
- 89. The Effect of Prebiotics and Probiotics on Levels of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11879892/]
- 90. Probiotics reduce negative mood over time: the value of ... [https://www.nature.com/articles/s44184-025-00123-z]
- 91. Gut to Brain Dysbiosis: Mechanisms Linking Western Diet ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5277010/]
- 92. How plant-based, Mediterranean, and Western diets affect ... [https://www.news-medical.net/news/20240920/How-plant-based-Mediterranean-and-Western-diets-affect-gut-microbiota-and-disease.aspx]
- 93. The effects of plant-based diets on the body and the brain [https://www.nature.com/articles/s41398-019-0552-0]
- 94. benefits, deficiencies, and research needs of plant-based ... [https://www.sciencedirect.com/science/article/abs/pii/S0306452225009194]
- 95. The Gut–Brain Axis and the Microbiome - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC6999848/]
- 96. Nanomedicine-Driven Modulation of the Gut–Brain Axis [https://pmc.ncbi.nlm.nih.gov/articles/PMC12470747/]
- 97. Harnessing Gut Microbiota for Biomimetic Innovations in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11852373/]
- 98. Biomimetic nanocarriers harnessing microbial metabolites ... [https://www.sciencedirect.com/science/article/pii/S2790676023000547]
- 99. Microbiome and Nanoparticle Discoveries Hold Promise ... [https://www.nyu.edu/about/news-publications/news/2025/october/gut-pain-microbiome-nanoparticles.html]
- 100. Gut–Brain Axis and Brain Microbiome Interactions from a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11853140/]
- 101. The microbiota–gut–brain axis in mental and ... [https://www.frontiersin.org/journals/aging-neuroscience/articles/10.3389/fnagi.2025.1667448/full]
- 102. Present and future of microbiome-targeting therapeutics [https://pmc.ncbi.nlm.nih.gov/articles/PMC12126222/]
- 103. Molecular Mechanisms of the Microbiota-Gut-Brain Axis in ... [https://pubmed.ncbi.nlm.nih.gov/41155363/]