Dietary Patterns and Chronic Disease Prevention: From Mechanistic Insights to Clinical and Public Health Translation
This article synthesizes the latest epidemiological and clinical evidence on the role of dietary patterns in chronic disease prevention, tailored for researchers, scientists, and drug development professionals.
Dietary Patterns and Chronic Disease Prevention: From Mechanistic Insights to Clinical and Public Health Translation
Abstract
This article synthesizes the latest epidemiological and clinical evidence on the role of dietary patterns in chronic disease prevention, tailored for researchers, scientists, and drug development professionals. It explores the foundational associations between diets like the Mediterranean, DASH, and plant-based patterns with outcomes spanning cardiovascular disease, diabetes, cancer, and healthy aging. The content delves into methodological approaches for dietary assessment and pattern analysis, examines challenges in implementation and optimization for diverse populations, and provides a comparative validation of various diets through network meta-analyses and biomarker studies. The review aims to bridge nutritional science with biomedical research, highlighting implications for future therapeutic strategies and public health guidelines.
Epidemiological Evidence: Linking Dietary Patterns to Chronic Disease Risk and Healthy Aging
Dietary patterns represent the combination of foods and beverages consumed over time, providing a holistic view of dietary habits that accounts for complex interactions between nutrients. Within nutritional epidemiology, the analysis of dietary patterns has emerged as a superior approach to studying the relationship between diet and chronic diseases, moving beyond the limitations of single-food or single-nutrient studies. This technical guide examines five predominant dietary patterns—AHEI, Mediterranean, DASH, MIND, and Plant-Based Diets—within the context of chronic disease research, providing researchers and drug development professionals with a comprehensive analysis of their defining components, associated health outcomes, biological mechanisms, and research methodologies.
The global burden of diet-related chronic diseases continues to escalate, with poor nutrition responsible for 11 million deaths and 255 million disability-adjusted life-years globally [1]. Chronic diseases account for more than half of all premature deaths and over 90% of yearly healthcare spending in the United States alone [1]. Understanding how dietary patterns influence disease pathways provides critical insights for preventive strategies and therapeutic development.
Dietary Pattern Definitions and Component Analysis
The five dietary patterns examined in this guide share common elements but differ in their specific emphasis and scoring approaches. The Alternative Healthy Eating Index (AHEI) was developed by Harvard nutritionists as a scoring system to predict chronic disease risk, with higher scores indicating lower risk [2]. The Mediterranean diet is inspired by traditional eating patterns in countries bordering the Mediterranean Sea, emphasizing plant-based foods, healthy fats, and moderate fish and poultry consumption [3]. The Dietary Approaches to Stop Hypertension (DASH) was specifically designed to prevent and treat hypertension through sodium reduction and increased consumption of potassium-rich foods [3]. The Mediterranean-DASH Intervention for Neurodegenerative Delay (MIND) diet hybridizes the Mediterranean and DASH diets with specific emphasis on neuroprotective foods [4]. Plant-Based Diets encompass a spectrum from vegetarian to vegan patterns, with the healthful plant-based diet index (hPDI) distinguishing between healthful and unhealthful plant foods [5].
Comparative Component Analysis
Table 1: Core Food Components of Major Dietary Patterns
| Food Component | AHEI | Mediterranean | DASH | MIND | Healthful Plant-Based |
|---|---|---|---|---|---|
| Vegetables | 5+ servings/day | High variety | 4-5 servings/day | 6+ servings leafy greens/week | Unlimited |
| Fruits | 4+ servings/day | Moderate | 4-5 servings/day | Berries emphasized (2+ servings/week) | Unlimited |
| Whole Grains | 5-6 servings/day | Moderate | 6-8 servings/day | 3+ servings/day | Emphasized |
| Nuts & Legumes | Daily | Daily | 4-5 servings/week | Nuts: 5+ servings/week; Legumes: 4+ servings/week | Emphasized |
| Fish/Poultry | Fish limited | Fish: 2+ servings/week; Poultry: moderate | Lean proteins emphasized | Fish: 1+ serving/week; Poultry: 2+ servings/week | Excluded or limited |
| Dairy | Limited | Moderate cheese/yogurt | Low-fat emphasized | Limited | Excluded (vegan) or limited |
| Fats | Unsaturated oils | Olive oil primary | Moderate total fat | Olive oil primary | Plant oils |
| Sodium | Limited | Not restricted | <1,500 mg/day | Not explicitly restricted | Not restricted |
| Red/Processed Meats | Limited | Limited | Limited | <4 servings/week | Excluded |
| Sweets | Limited | Limited | Limited | <5 servings/week | Limited |
Table 2: Scoring Systems and Health Outcomes for Dietary Patterns
| Dietary Pattern | Scoring Method | Primary Chronic Disease Association | Key Health Outcomes |
|---|---|---|---|
| AHEI | 0-110 scale based on adherence to food targets | Multifactorial chronic disease reduction | 86% higher odds of healthy aging [6]; 1.86 OR for healthy aging (highest vs. lowest quintile) [7] |
| Mediterranean | 0-9 scale based on median consumption of beneficial foods | Cardiovascular disease, diabetes | Improved lipid profiles, reduced CVD mortality [3] |
| DASH | 1-5 scale based on quintiles of food group intake | Hypertension, metabolic syndrome | Blood pressure reduction, diabetes risk reduction [3] |
| MIND | 0-15 score based on 10 brain-healthy and 5 unhealthy food groups | Neurodegenerative conditions, dementia | 53% lower Alzheimer's risk [4]; Reduced dementia (HR=0.87), depression (HR=0.77) [8] |
| Healthful Plant-Based | hPDI index scoring plant foods positively, with distinction between healthful/unhealthful | Cognitive impairment, cardiovascular disease | 45% higher odds of healthy aging [7]; 0.68 OR for cognitive impairment (highest vs. lowest hPDI) [5] |
Methodological Approaches in Dietary Pattern Research
Cohort Studies and Longitudinal Designs
Large-scale prospective cohort studies form the foundation of dietary pattern research. The Nurses' Health Study (NHS), Health Professionals Follow-Up Study (HPFS), and UK Biobank represent gold standard methodologies with extended follow-up periods. The NHS and HPFS collectively followed 205,852 healthcare professionals for up to 32 years, with dietary assessments every 2-4 years using validated food frequency questionnaires (FFQs) [1]. The UK Biobank study analyzed 166,916 participants over a median follow-up of 10.5 years, examining associations between ten dietary patterns and five major brain disorders [8].
Dietary assessment typically employs semi-quantitative FFQs that capture usual intake of 100-150 food items. The data processing workflow includes: (1) nutrient calculation using composition databases; (2) derivation of dietary pattern scores based on predefined algorithms; (3) energy adjustment using residual or density methods; (4) categorization into quintiles or quartiles of adherence; and (5) statistical modeling with multivariate adjustment for confounding factors including age, BMI, physical activity, smoking status, and total energy intake.
Statistical Analysis Protocols
Cox proportional hazards models serve as the primary analytical framework for time-to-event data, calculating hazard ratios (HRs) and 95% confidence intervals (CIs) for disease incidence across adherence levels to dietary patterns. For cross-sectional analyses of healthy aging outcomes, logistic regression models compute odds ratios (ORs) comparing extreme quintiles of dietary pattern adherence [7]. Meta-analyses employ fixed-effects or random-effects models to pool estimates across multiple studies, with statistical heterogeneity quantified using I² statistics [5].
Recent methodological advances incorporate mediation analyses to elucidate biological pathways. For example, the UK Biobank study used four-way decomposition models with multi-omics data (metabolomics, genomics, proteomics) to quantify proportion mediated through specific biological pathways [8]. This approach identified that a favorable metabolic signature mediated 60.63% of the MIND diet's protective effect against stroke, 38.97% for depression, and 26.06% for anxiety [8].
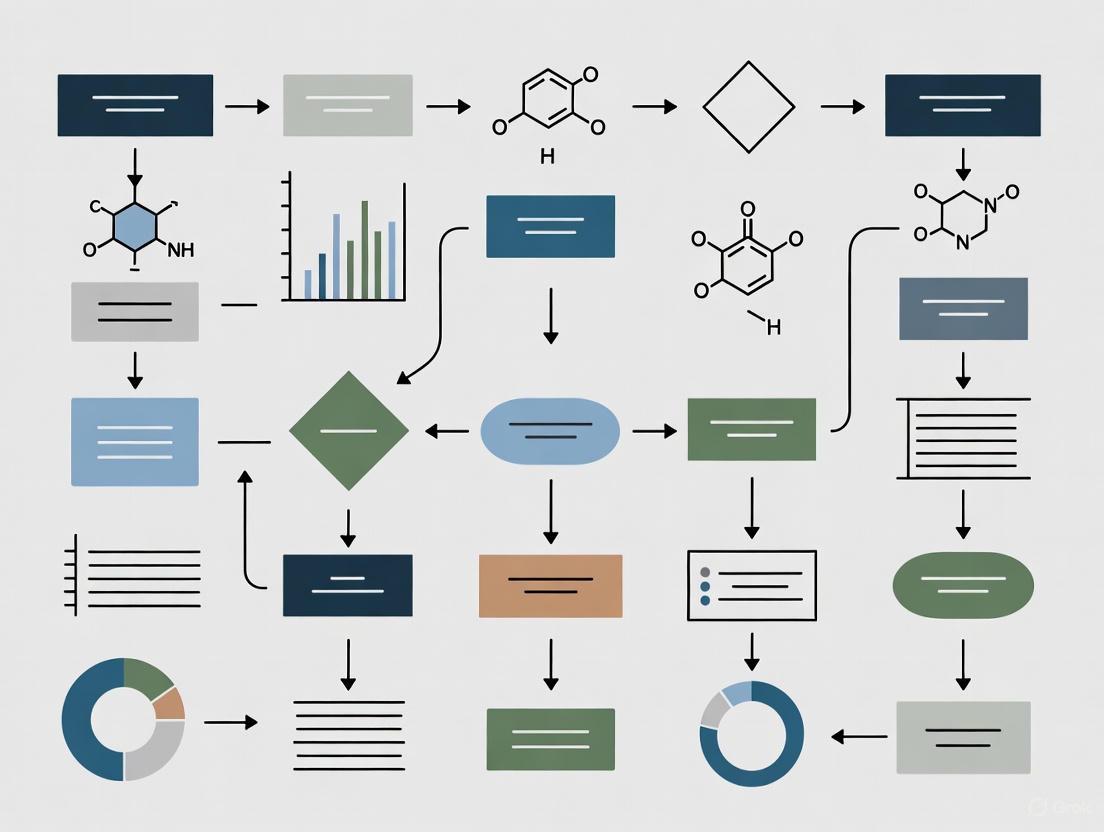
Diagram 1: Research workflow for dietary pattern studies
Research Reagent Solutions and Methodological Tools
Table 3: Essential Methodological Tools for Dietary Pattern Research
| Research Tool | Function/Application | Implementation Example |
|---|---|---|
| Food Frequency Questionnaire (FFQ) | Assess habitual dietary intake over extended periods | Harvard FFQ (131 food items, semiquantitative) used in NHS/HPFS cohorts [1] [7] |
| Dietary Pattern Scoring Algorithms | Quantify adherence to specific dietary patterns | AHEI (0-110), Mediterranean (0-9), MIND (0-15) scores based on food group intake [7] [4] |
| Multi-omics Platforms | Identify biological mediators between diet and health outcomes | Metabolomic profiling to quantify proportion mediated for depression (38.97%), anxiety (26.06%) [8] |
| Cox Proportional Hazards Models | Analyze time-to-event data for disease incidence | HRs for dementia, stroke, depression across dietary pattern adherence levels [8] |
| Bayesian Age-Period-Cohort Models | Project future disease burden attributable to dietary factors | Projected ASMR for diet-related chronic diseases through 2030 using GBD data [9] |
Health Outcomes and Mechanistic Pathways
Chronic Disease Risk Reduction
Systematic reviews and meta-analyses demonstrate consistent associations between dietary patterns and chronic disease risk. For cognitive outcomes, higher adherence to healthful plant-based diets is associated with significantly lower odds of cognitive impairment (OR=0.68 for hPDI, highest vs. lowest quartile) and reduced dementia risk (HR=0.85 for hPDI) [5]. The MIND diet shows particularly broad neuroprotective effects, with risk reduction for dementia (HR=0.87), stroke (HR=0.89), depression (HR=0.77), and anxiety (HR=0.82) [8].
For cardiometabolic diseases, comparative effectiveness research demonstrates that dietary patterns emphasizing insulinemic and inflammatory mechanisms show superior risk reduction. The reversed empirical dietary index for hyperinsulinemia (rEDIH) and reversed empirical dietary inflammatory pattern (rEDIP) show the strongest associations with major chronic disease risk reduction (HR=0.58 and HR=0.61, respectively, comparing 90th to 10th percentile) [1]. These patterns outperform even established dietary recommendations for CVD, diabetes, and cancer risk reduction in composite outcomes.
Biological Mechanisms Linking Diet to Chronic Diseases
The protective effects of healthful dietary patterns operate through multiple interconnected biological pathways. Oxidative stress reduction occurs through antioxidant compounds (flavonoids, carotenoids, vitamins C and E) that neutralize reactive oxygen and nitrogen species [10]. Anti-inflammatory effects manifest through reduced inflammatory biomarkers (CRP, IL-6) and modulation of the empirical dietary inflammatory pattern (EDIP) [1] [7].
Metabolic regulation pathways include improved insulin sensitivity, reduced hyperinsulinemia, and favorable lipid profiles [1]. Gut microbiome modulation occurs through prebiotic effects of dietary fiber and polyphenols, which influence microbial community structure and metabolite production [10]. Slower biological aging mediates a significant proportion of dementia risk reduction (19.40%) associated with the MIND diet [8].
Diagram 2: Biological mechanisms linking dietary patterns to health outcomes
Healthy Aging Outcomes
Beyond disease-specific outcomes, dietary patterns significantly influence multidimensional healthy aging. In a 30-year study of 105,015 participants, higher adherence to all dietary patterns was associated with greater odds of healthy aging—defined as reaching age 70 free of major chronic diseases while maintaining intact cognitive, physical, and mental health [7]. The AHEI demonstrated the strongest association (OR=1.86, highest vs. lowest quintile), followed by rEDIH, while hPDI showed the most modest association (OR=1.45) [7].
When examining specific aging domains, dietary patterns showed varying protective effects. For intact cognitive function, the Planetary Health Diet Index showed the strongest association (OR=1.65), while for intact physical function, AHEI demonstrated the strongest association (OR=2.30) [7]. These findings suggest that while all healthful dietary patterns promote healthy aging, specific patterns may offer domain-specific advantages.
The evidence reviewed in this technical guide demonstrates that dietary patterns emphasizing plant-based foods, healthy fats, whole grains, and lean proteins while limiting red and processed meats, sodium, and ultra-processed foods consistently associate with reduced chronic disease risk and promoted healthy aging. The AHEI, Mediterranean, DASH, MIND, and healthful plant-based diets share common elements but offer distinct advantages for specific health outcomes.
From a research perspective, the field requires more randomized controlled trials to establish causality, greater diversity in study populations to enhance generalizability, and deeper investigation into the molecular mechanisms mediating dietary effects. For drug development professionals, understanding these dietary patterns provides insights into modifiable risk factors that could complement pharmacological interventions. Future research should prioritize personalized nutrition approaches that identify which dietary patterns provide optimal benefit for specific genetic, metabolic, or microbiome profiles.
For nearly five decades, the Nurses' Health Study (NHS) and the Health Professionals Follow-Up Study (HPFS) have generated critical evidence illuminating the relationship between dietary patterns and chronic disease risk. Established as large-scale prospective investigations, these cohorts were designed to evaluate long-term hypotheses about how nutritional factors impact serious illnesses including cancer, cardiovascular disease, and diabetes [11] [12]. The NHS, initiated in 1976 under Dr. Frank Speizer, originally sought to investigate the long-term consequences of oral contraceptives, while the HPFS was established in 1986 by Dr. Walter Willett and colleagues to complement the NHS with an all-male cohort [11] [12]. Together, these studies have followed hundreds of thousands of healthcare professionals, leveraging their expertise to collect precise health information over decades through detailed biennial and dietary-specific questionnaires.
This whitepaper synthesizes key methodological approaches and foundational findings from these cohorts, with particular focus on their contributions to understanding how dietary patterns influence chronic disease pathogenesis. The unparalleled longitudinal data from these studies provides an evidence base that continues to inform both public health guidelines and targeted therapeutic development.
Cohort Methodologies: Design and Data Collection Protocols
Population Recruitment and Characteristics
The NHS and HPFS employed distinct but methodologically complementary recruitment strategies to establish their cohorts:
- NHS Original Cohort: In 1976, the study enrolled 121,700 married female registered nurses aged 30-55 from 11 populous U.S. states. Nurses were selected for their ability to provide accurate health information and maintain long-term participation [12].
- NHS II: Established in 1989 with 116,430 female nurses aged 25-42 to study diet, lifestyle, and oral contraceptive use in a younger population [12].
- HPFS: Launched in 1986 with 51,529 male health professionals aged 40-75 from various disciplines including dentistry, pharmacy, optometry, and veterinary medicine [11].
Longitudinal Data Collection Framework
Both studies implement rigorous, standardized protocols for ongoing data collection:
- Core Follow-up Questionnaires: Biennial surveys tracking disease incidence, weight, smoking status, physical activity, medication use, and menopausal status [11] [12].
- Dietary Assessments: Comprehensive food-frequency questionnaires (FFQs) administered every four years to quantify nutritional intake, including detailed questions on over 130 food items, portion sizes, and preparation methods [12].
- Biological Specimens: Systematic collection of blood, urine, toenail, and DNA samples from subsets of participants to analyze biomarkers, genetic factors, and their interactions with dietary exposures [12].
Table: Cohort Characteristics and Design Elements
| Characteristic | NHS (Original) | NHS II | HPFS |
|---|---|---|---|
| Launch Year | 1976 | 1989 | 1986 |
| Initial Cohort Size | 121,700 | 116,430 | 51,529 |
| Baseline Age Range | 30-55 | 25-42 | 40-75 |
| Sex | Female | Female | Male |
| Diet Assessment Interval | Every 4 years | Every 4 years | Every 4 years |
| Health Update Interval | Every 2 years | Every 2 years | Every 2 years |
| Biospecimen Collection | Blood, urine, toenails, DNA | Blood, urine, DNA | Blood, urine, DNA |
Dietary Pattern Operationalization
Researchers have developed and validated numerous dietary indices to quantify adherence to various eating patterns:
- Alternative Healthy Eating Index (AHEI): Scores intake of foods and nutrients predictive of chronic disease risk [13].
- Alternative Mediterranean Diet Score (aMED): Measures adherence to traditional Mediterranean dietary patterns [7].
- Dietary Approaches to Stop Hypertension (DASH): Assesses concordance with the DASH diet, emphasizing fruits, vegetables, and low-fat dairy [1].
- Healthful Plant-Based Diet Index (hPDI): Scores emphasizing healthy plant foods while distinguishing from less healthy plant foods [7].
- Empirical Dietary Inflammatory Pattern (EDIP): Derived from inflammatory biomarkers to assess diet's inflammatory potential [1].
Key Findings: Dietary Patterns and Chronic Disease Risk
Healthy Aging and Multidimensional Health Outcomes
A 2025 analysis published in Nature Medicine followed 105,015 participants from NHS and HPFS for up to 30 years to examine associations between dietary patterns and healthy aging, defined as surviving to age 70 years free of major chronic diseases and maintaining intact cognitive, physical, and mental health [7]. The findings demonstrated that:
- Higher adherence to all eight dietary patterns studied was associated with significantly greater odds of healthy aging, with multivariable-adjusted odds ratios comparing highest to lowest quintiles ranging from 1.45 for hPDI to 1.86 for AHEI [7].
- When the healthy aging threshold was raised to age 75 years, the AHEI showed the strongest association with an odds ratio of 2.24 [7].
- Higher intakes of fruits, vegetables, whole grains, unsaturated fats, nuts, legumes, and low-fat dairy were consistently associated with greater odds of healthy aging across all domains [7].
Table: Dietary Patterns and Healthy Aging Outcomes in NHS and HPFS
| Dietary Pattern | Odds Ratio (Highest vs. Lowest Quintile) | Strongest Health Domain Association |
|---|---|---|
| AHEI | 1.86 (95% CI: 1.71-2.01) | Mental Health (OR: 2.03) |
| aMED | 1.72 (95% CI: 1.58-1.87) | Physical Function (OR: 1.95) |
| DASH | 1.73 (95% CI: 1.59-1.88) | Physical Function (OR: 1.92) |
| MIND | 1.65 (95% CI: 1.52-1.79) | Mental Health (OR: 1.81) |
| hPDI | 1.45 (95% CI: 1.35-1.57) | Survival to Age 70 (OR: 1.33) |
| PHDI | 1.68 (95% CI: 1.55-1.82) | Cognitive Health (OR: 1.65) |
Major Chronic Disease Prevention
Research across these cohorts has consistently demonstrated that healthy dietary patterns significantly reduce the risk of major chronic diseases in composite:
- A study following 205,852 participants from NHS, NHS II, and HPFS for up to 32 years found that adherence to healthy dietary patterns was associated with hazard ratios of 0.58-0.80 for major chronic disease (composite of cardiovascular disease, type 2 diabetes, and cancer) when comparing the 90th to 10th percentile of dietary pattern scores [1].
- Diets characterized by low insulinemic potential (HR: 0.58), low inflammatory potential (HR: 0.61), or diabetes risk-reducing patterns (HR: 0.70) showed the strongest inverse associations [1].
- The AHEI demonstrated particularly strong protective effects against cardiovascular disease, with multivariate relative risks of 0.61 in men and 0.72 in women when comparing highest to lowest quintiles [13].
Disease-Specific Risk Reductions
Recent analyses have quantified associations between dietary patterns and individual chronic diseases:
- The Alternative Mediterranean Diet score demonstrated the broadest protection, associated with significantly lower risk of 32 individual chronic diseases across cardiometabolic, cancer, psychological/neurological, digestive, and other disease categories [14].
- Higher AMED scores were specifically associated with reduced risk of lung cancer (HR: 0.93), dementia (HR: 0.92), Parkinson's disease (HR: 0.92), and chronic obstructive pulmonary disease (HR: 0.88) per quintile increment in scores [14].
- All dietary patterns studied showed significant inverse associations with digestive disorders including dyspepsia, diverticular disease, irritable bowel syndrome, and chronic liver disease [14].
Mechanistic Insights: Biomarkers and Biological Pathways
Inflammation and Immune Function
Dietary patterns significantly influence inflammatory biomarkers that mediate chronic disease risk:
- The Mediterranean diet demonstrated the most potent anti-inflammatory effects among dietary patterns, with meta-analyses showing significant reductions in IL-6 (mean difference: -1.07 pg/mL), IL-1β (mean difference: -0.46 pg/mL), and C-reactive protein [15].
- The Empirical Dietary Inflammatory Pattern (EDIP), developed and validated in these cohorts, provides a food-based index for estimating the inflammatory potential of diet, with higher scores associated with elevated inflammatory biomarkers and increased chronic disease risk [1].
Metabolic Pathways
Dietary patterns influence chronic disease risk through multiple metabolic mechanisms:
- The Empirical Dietary Index for Hyperinsulinemia (EDIH) identifies diets associated with plasma C-peptide concentrations, providing a biomarker-based approach to assessing diets that modulate insulin response [1].
- Diets high in fruits, vegetables, whole grains, and legumes improve glycemic control and insulin sensitivity, thereby reducing diabetes risk and related complications [1].
- Specific dietary components including trans fats, sodium, and red/processed meats demonstrate adverse effects on metabolic health, while unsaturated fats, nuts, and low-fat dairy show beneficial effects [7].
Research Reagents and Methodological Tools
Table: Essential Research Reagents and Methodological Assets
| Resource Type | Specific Examples | Research Application |
|---|---|---|
| Validated Dietary Assessment Tools | Semi-quantitative Food Frequency Questionnaires (FFQs), Diet History Questionnaires | Standardized quantification of nutritional intake and dietary patterns |
| Biological Specimen Repositories | Plasma/serum, urine, DNA, toenail samples (63,000 in NHS) | Biomarker analysis, genetic studies, nutrient biomarker calibration |
| Dietary Pattern Indices | AHEI, aMED, DASH, hPDI, EDIP, EDIH | Standardized quantification of adherence to specific dietary patterns |
| Disease Validation Instruments | Medical record review protocols, supplemental disease-specific questionnaires | Endpoint adjudication and validation for specific disease outcomes |
| Genetic Data | Genome-wide association data, candidate gene polymorphisms | Gene-diet interaction studies, Mendelian randomization analyses |
Visualizing Cohort Research Workflows
Cohort Study Design and Analytical Approach
Cohort Research Workflow
Dietary Pattern Influence on Chronic Disease Pathways
Diet-Chronic Disease Pathways
Implications for Research and Therapeutic Development
The longitudinal evidence from NHS and HPFS provides critical insights for researchers and drug development professionals:
- Biomarker Validation: These cohorts have identified and validated numerous biomarkers (inflammatory, metabolic, nutritional) that can serve as intermediate endpoints in clinical trials, potentially reducing study duration and costs [15].
- Precision Nutrition Applications: Findings that dietary effects may be modified by factors such as sex, BMI, and smoking status highlight opportunities for targeted nutritional interventions [7].
- Combination Therapy Development: Understanding dietary mechanisms can inform development of pharmaceuticals that complement or enhance dietary interventions, particularly for metabolic and inflammatory conditions.
- Preventive Medicine Strategies: The robust association between dietary patterns and multimorbidity reduction supports integrative approaches that combine nutritional interventions with conventional therapeutics.
The continued follow-up of these cohorts, alongside emerging molecular data and advanced analytical methods, promises to further elucidate the complex relationships between diet, biological mechanisms, and chronic disease risk, offering valuable insights for the development of targeted interventions and therapeutic strategies.
Within the broader thesis investigating the link between dietary patterns and chronic disease, the role of nutrition in modulating multidimensional healthy aging represents a critical frontier. As the global population ages, the imperative to extend healthspan—the years lived in good physical, cognitive, and mental health—has intensified, shifting focus from merely delaying mortality to preserving functional capacity [16]. Diet stands as a first-line behavioral risk factor for non-communicable diseases and mortality burden, second only to tobacco use in older U.S. adults [7]. This whitepaper synthesizes evidence from large-scale prospective cohorts, randomized controlled trials, and emerging molecular studies to delineate the association between long-term dietary patterns and multidimensional health outcomes in aging populations. The findings herein are intended to guide future research, inform public health policy, and identify potential targets for therapeutic and drug development aimed at chronic disease prevention and healthspan extension.
Key Dietary Patterns and Their Associations with Multidimensional Health
Research has consistently identified several dietary patterns associated with healthy aging. A landmark 30-year prospective study published in Nature Medicine (2025), utilizing data from the Nurses’ Health Study and the Health Professionals Follow-Up Study (n=105,015), provides the most comprehensive evidence to date [7] [17]. The study defined healthy aging as surviving to age 70 years or older with intact cognitive, physical, and mental health, and freedom from major chronic diseases. Only 9.3% of the cohort achieved this multidomain outcome, underscoring its stringency [7] [17].
The study evaluated eight dietary patterns, all of which emphasized high intake of fruits, vegetables, whole grains, unsaturated fats, nuts, and legumes, with variations in the inclusion of animal-based foods. The association between higher adherence to these patterns and the likelihood of healthy aging was robust and statistically significant (p<0.0001) [7]. The table below summarizes the key associations for the highest versus lowest quintiles of adherence.
Table 1: Association of Dietary Pattern Adherence with Odds of Healthy Aging and Its Domains
| Dietary Pattern | Full Name | Odds Ratio for Healthy Aging (Highest vs. Lowest Quintile) | Key Associations with Aging Domains |
|---|---|---|---|
| AHEI | Alternative Healthy Eating Index | 1.86 (95% CI: 1.71–2.01) [7] | Strongest association with intact physical and mental health [7]. |
| rEDIH | reverse Empirical Dietary Index for Hyperinsulinemia | 1.83 (95% CI: Not specified in source) [7] | Strongest association with freedom from chronic diseases [7]. |
| DASH | Dietary Approaches to Stop Hypertension | 1.84 (95% CI: Not specified in source) [7] | Consistently associated with all healthy aging domains [7]. |
| aMED | Alternative Mediterranean Index | 1.81 (95% CI: Not specified in source) [7] | Associated with reduced inflammation and improved cognitive function [7] [16]. |
| PHDI | Planetary Health Diet Index | 1.71 (95% CI: Not specified in source) [7] | Strongest association with surviving to age 70 and intact cognitive health [7]. |
| MIND | Mediterranean-DASH Intervention for Neurodegenerative Delay | 1.59 (95% CI: Not specified in source) [7] | Specifically designed for brain health; associated with slower cognitive decline [18] [19]. |
| rEDIP | reverse Empirical Inflammatory Dietary Pattern | 1.52 (95% CI: Not specified in source) [7] | Weaker association with intact physical function [7]. |
| hPDI | healthful Plant-Based Diet Index | 1.45 (95% CI: 1.35–1.57) [7] | Weakest association with all healthy aging domains, including cognitive health [7]. |
The AHEI diet, rich in fruits, vegetables, whole grains, nuts, legumes, and healthy fats while low in red/processed meats, sugary beverages, sodium, and refined grains, demonstrated the most potent association, nearly doubling the odds of healthy aging [7] [17]. When the healthy age threshold was raised to 75 years, this association strengthened further (OR=2.24, 95% CI: 2.01–2.50) [7]. The MIND diet, a hybrid of the Mediterranean and DASH diets, has shown significant promise for cognitive health, with numerous observational studies linking it to slower global cognitive decline and reduced risk of dementia [18] [19].
Table 2: Association of Specific Food Groups with Odds of Healthy Aging
| Food/Nutrient | Direction of Association with Healthy Aging | Key Notes |
|---|---|---|
| Fruits, Vegetables, Whole Grains | Positive [7] | Foundation of all beneficial dietary patterns. |
| Nuts, Legumes | Positive [7] | Key components of plant-based patterns. |
| Unsaturated Fats | Positive [7] | Particularly associated with surviving to age 70 and intact physical/cognitive function [7]. |
| Low-Fat Dairy | Positive [7] | Provides high-quality protein and bone-supporting nutrients [20]. |
| Red and Processed Meats | Negative [7] | Associated with lower odds of healthy aging. |
| Sugary Beverages | Negative [7] | Associated with lower odds of healthy aging. |
| Sodium | Negative [7] | Associated with lower odds of healthy aging. |
| Trans Fats | Negative [7] | Associated with lower odds of healthy aging. |
| Ultra-Processed Foods | Negative [17] | Especially processed meats and sugary beverages. |
| Artificial Sweeteners | Negative (Cognitive) [21] | Associated with faster global cognitive decline (equivalent to 1.6 years of brain aging) [21]. |
Experimental Protocols and Key Methodologies
Large-Scale Prospective Cohort Studies
The primary evidence linking diet to multidimensional health originates from large, long-term prospective cohorts.
- Study Population: The 2025 Nature Medicine analysis pooled data from 70,091 women in the Nurses’ Health Study (NHS) and 34,924 men in the Health Professionals Follow-Up Study (HPFS) [7]. Participants were aged 39-69 at baseline and free of major chronic diseases.
- Dietary Assessment: Dietary intake was assessed every 2 to 4 years using validated semi-quantitative food frequency questionnaires (FFQs). Adherence to the eight dietary patterns was calculated using cumulative average scores from all available FFQs to represent long-term dietary intake [7] [17].
- Outcome Assessment: Healthy aging was assessed at the end of the 30-year follow-up (2016) and defined multidimensionally. Specific criteria included:
- Freedom from 11 major chronic diseases (e.g., cancer, diabetes, myocardial infarction).
- Intact cognitive function,
- Intact physical function,
- Intact mental health [7].
- Statistical Analysis: Multivariable-adjusted odds ratios (ORs) and 95% confidence intervals (CIs) for healthy aging were calculated comparing quintiles of dietary pattern scores using logistic regression models. Models were adjusted for age, sex, ethnicity, socioeconomic status, lifestyle factors (smoking, physical activity), body mass index, and multivitamin use [7].
Randomized Controlled Trials: The POINTER Study
The POINTER study (U.S. Study to Protect Brain Health Through Lifestyle Intervention to Reduce Risk) is a key RCT providing Level I evidence for lifestyle intervention [22].
- Population: 2,100 sedentary individuals aged 60-79 who had normal cognition but elevated risk for cognitive decline (due to suboptimal diet and sedentary lifestyle) [22].
- Intervention Protocol: A two-year, intensive, highly structured program:
- Aerobic Exercise: At least four times per week.
- Diet: Adherence to a heart-healthy Mediterranean-style diet.
- Cognitive Training: Online brain exercises.
- Social Activities: Mandatory participation.
- Health Monitoring: Regular tracking of blood pressure and blood sugar [22].
- Control Group: Participants were asked to develop their own plan for improving diet and exercise.
- Outcomes: The intensive intervention group showed significantly greater improvement in memory and thinking tests compared to the control group, effectively reducing their "brain age" by 1-2 years [22].
Molecular Mechanisms and Signaling Pathways
Dietary patterns influence aging trajectories through complex molecular mechanisms. The following diagram synthesizes key pathways described in the research.
Figure 1: Dietary Modulation of Aging Pathways
Key Mechanistic Insights
- Gut-Brain Axis and Microbiome: The gut microbiome evolves with age and diet. A diverse microbiome, supported by a variety of plant-based and fermented foods, enhances immune resilience, reduces inflammation, and is linked to better cognitive function. Conversely, ultra-processed foods disrupt microbial balance [16] [20]. Yogurt consumption has been associated with a reduced risk of dementia in observational studies [20].
- Inflammation and Oxidative Stress: Pro-inflammatory diets (high in red meat, refined carbs, saturated fats) elevate systemic inflammation, accelerating cellular aging. Anti-inflammatory patterns (rich in polyphenols, omega-3s) counteract this. For instance, increased consumption of dairy may boost brain glutathione, an antioxidant that reduces oxidative stress [16] [20].
- Nutrient-Sensing Pathways: Bioactive compounds from food modulate key aging pathways. For example, plant-based compounds can inhibit the mTOR pathway, while nutrients like polyphenols can activate sirtuins, both of which are involved in cellular repair and longevity [16].
- Epigenetic Regulation: Diet can influence biological aging as measured by epigenetic clocks. Nutrients like vitamin D3 act as immunomodulators and can impact DNA methylation patterns, potentially slowing the epigenetic aging process [16].
This section details key reagents, datasets, and tools for investigating diet and healthy aging.
Table 3: Key Research Resources for Diet-Aging Studies
| Resource/Tool | Function/Application | Example from Search Results |
|---|---|---|
| Food Frequency Questionnaire (FFQ) | Assesses long-term dietary intake and adherence to dietary patterns. | Used in NHS/HPFS to calculate scores for AHEI, MIND, etc. [7] [17]. |
| Validated Cognitive Batteries | Quantifies cognitive domains (memory, executive function, verbal fluency). | Montreal Cognitive Assessment, CERAD tests used in MIND diet studies [19] [21]. |
| Epigenetic Clocks | Measures biological age from DNA methylation patterns. | GrimAge (predicts mortality), PhenoAge (assesses disease risk) [16]. |
| Biobanks with Dietary Data | Links biological samples (blood, DNA) with dietary and health data for multi-omics research. | All of Us Research Program, Brazilian Longitudinal Study of Adult Health [23] [21]. |
| Precision Nutrition Algorithms | Predicts individual responses to food using AI and microbiome data. | Developed in the All of Us program to personalize dietary recommendations [23]. |
Discussion and Future Research Directions
The evidence demonstrates that dietary patterns, particularly the AHEI, DASH, and MIND diets, are robustly associated with multidomain healthy aging. These associations are biologically plausible, supported by mechanistic studies on inflammation, gut microbiome, and epigenetic regulation.
Future research must address critical gaps. First, findings from cohorts of health professionals need replication in more diverse socioeconomic and ancestral populations [7] [17]. Disparities exist, as evidenced by a study on SNAP benefits, where the protective effect on cognitive decline was stronger for non-Hispanic White participants compared to Black and Hispanic participants [24]. Second, while observational data is compelling, more large-scale, long-term RCTs like POINTER are needed to establish causality [22]. Third, the field of precision nutrition is nascent. Initiatives like the All of Us Research Program are building datasets to develop algorithms that predict individual responses to food, moving beyond a one-size-fits-all approach [23]. Finally, exploring Nutrition Dark Matter—the vast array of food-derived small molecules with unknown biological functions—represents a frontier for discovering novel bioactive compounds that modulate aging [16].
For researchers and drug development professionals, this body of evidence highlights that dietary interventions are a powerful, multi-mechanistic tool for preventing chronic disease and preserving functional capacity. Nutritional biochemistry provides a rich source of molecular targets for promoting healthspan, underscoring the need to integrate nutritional science into the broader framework of chronic disease research.
The escalating global burden of chronic diseases—including cardiovascular diseases (CVD), type 2 diabetes (T2DM), cancer, and neurodegenerative disorders—is inextricably linked to evolutionary shifts in dietary patterns. Modern diets have diverged significantly from ancestral patterns, characterized by increased consumption of saturated fats, ultra-processed foods (UPFs), and refined carbohydrates, alongside decreased intake of whole plant foods and unsaturated fats. This whitepaper synthesizes current evidence from clinical, epidemiological, and mechanistic studies to elucidate the specific roles of protective dietary components—namely, plant-derived bioactive compounds and unsaturated fatty acids—and the distinct dangers posed by ultra-processing. The analysis is framed within the context of dietary pattern research for chronic disease prevention, providing a scientific foundation for therapeutic development and public health guidance.
Protective Effects of Plant-Derived Bioactive Compounds
Classification and Molecular Diversity
Phytochemicals are bioactive compounds synthesized by plants, which play crucial roles in their defense systems and impart significant health benefits when consumed by humans. These compounds are broadly categorized based on their chemical structures and biological functions [25]. The major classes, their common representatives, and dietary sources are detailed in Table 1.
Table 1: Major Classes of Dietary Phytochemicals, Sources, and Primary Bioactivities
| Phytochemical Category | Common Phytochemicals | Primary Dietary Sources | Documented Bioactivities |
|---|---|---|---|
| Carotenoids | Beta-carotene, Lycopene, Lutein | Carrots, tomatoes, watermelon, kale, spinach, corn [25] | Antioxidant, vision health, immune support, prostate & cardiovascular health [25] |
| Flavonoids | Quercetin, Catechins, Anthocyanins | Apples, onions, green tea, cocoa, blueberries, blackberries [25] | Antioxidant, anti-inflammatory, anti-carcinogenic, cardiovascular health, weight management [25] [26] |
| Phenolic Acids | Caffeic acid, Ferulic acid | Coffee, berries, whole grains, oats, rice, citrus fruits [25] | Antioxidant, anti-inflammatory, cardiovascular health, skin health [25] |
| Glucosinolates | Sulforaphane, Indole-3-carbinol | Broccoli, Brussels sprouts, cabbage, kale [25] | Detoxification, anti-carcinogenic, hormone regulation, antioxidant [25] |
Mechanisms of Action: Molecular Pathways and Signaling Networks
The protective effects of phytochemicals are mediated through the modulation of key cellular signaling pathways involved in inflammation, oxidative stress, and carcinogenesis [25] [26].
- Modulation of Inflammatory Pathways: Chronic inflammation, driven by the overproduction of pro-inflammatory cytokines (e.g., IL-1β, IL-6, TNF-α) and sustained activation of inflammatory signaling pathways, is a cornerstone of many chronic diseases [26]. Phytochemicals such as curcumin, resveratrol, and quercetin exert anti-inflammatory effects primarily by inhibiting the Nuclear Factor-Kappa B (NF-κB) and Mitogen-Activated Protein Kinase (MAPK) pathways [26]. This inhibition suppresses the expression of cytokines, cyclooxygenase-2 (COX-2), and inducible nitric oxide synthase (iNOS).
- Alleviation of Oxidative Stress: Phytochemicals combat oxidative stress through direct free radical scavenging and by upregulating endogenous antioxidant defense systems. Key mechanisms include the activation of the Nrf2 (Nuclear factor erythroid 2-related factor 2) pathway, which promotes the transcription of antioxidant enzymes like catalase, superoxide dismutase (SOD), and glutathione peroxidase [26]. For instance, resveratrol and quercetin have been shown to enhance catalase activity via Nrf2 activation [26].
- Anti-Carcinogenic Actions: Beyond antioxidant and anti-inflammatory effects, phytochemicals like sulforaphane from cruciferous vegetables can modulate phase I and II detoxification enzymes, promote apoptosis in cancerous cells, and arrest cell cycle progression [25].
- Interaction with Gut Microbiota: Many phytochemicals are metabolized by the gut microbiota into more bioactive forms. This interaction can modulate the microbial composition, leading to increased production of short-chain fatty acids (SCFAs) like butyrate, which exert systemic anti-inflammatory and immunomodulatory effects [26].
The following diagram illustrates the core molecular mechanisms through which plant-derived compounds like curcumin and resveratrol exert their protective effects.
Experimental Protocols for Assessing Bioactivity
Protocol 1: Evaluating Anti-Inflammatory Activity In Vitro
- Objective: To quantify the inhibition of pro-inflammatory cytokine release in a macrophage cell model (e.g., RAW 264.7 cells) [26].
- Methodology:
- Cell Treatment: Pre-treat cells with varying concentrations of the phytochemical extract (e.g., quercetin) or vehicle control for 2 hours.
- Inflammation Induction: Stimulate inflammation by adding lipopolysaccharide (LPS) (e.g., 100 ng/mL) to the culture medium for 18-24 hours.
- Sample Collection: Collect cell culture supernatant by centrifugation.
- Cytokine Measurement: Quantify levels of TNF-α, IL-6, and IL-1β in the supernatant using enzyme-linked immunosorbent assay (ELISA) kits according to manufacturer protocols.
- Viability Assay: Perform a parallel MTT assay to ensure observed effects are not due to cytotoxicity.
- Data Analysis: Express cytokine levels as mean ± SEM. Use one-way ANOVA with post-hoc tests to compare treatment groups against the LPS-only control.
Protocol 2: Analyzing Antioxidant Pathway Activation
- Objective: To measure the nuclear translocation of Nrf2 and subsequent upregulation of target genes [26].
- Methodology:
- Cell Treatment and Fractionation: Treat HepG2 or similar cells with the test compound. Harvest cells and separate nuclear and cytosolic fractions using a commercial kit.
- Western Blotting: Resolve proteins from each fraction by SDS-PAGE. Transfer to a membrane and probe with primary antibodies against Nrf2 and a loading control (e.g., Lamin B1 for nuclear, β-actin for cytosolic fractions).
- qRT-PCR: Extract total RNA from treated cells. Synthesize cDNA and perform quantitative real-time PCR (qRT-PCR) using primers for Nrf2 target genes (e.g., HMOX1, NQO1, Catalase).
- Data Analysis: Quantify band density from Western blots to calculate nuclear-to-cytosolic Nrf2 ratio. Analyze qRT-PCR data using the 2^–ΔΔCt method to determine fold changes in gene expression.
The Scientist's Toolkit: Key Research Reagents
Table 2: Essential Reagents for Phytochemical Research
| Research Reagent | Function/Application in Experimental Protocols |
|---|---|
| Lipopolysaccharide (LPS) | A potent inflammatory agent used to induce a robust inflammatory response in cell models (e.g., macrophages) for screening anti-inflammatory compounds [26]. |
| ELISA Kits (TNF-α, IL-6, IL-1β) | Used for the specific, sensitive, and quantitative measurement of cytokine levels in cell culture supernatants, serum, or other biological fluids [26]. |
| Nrf2 Antibodies | Essential for detecting Nrf2 protein levels and tracking its translocation from the cytoplasm to the nucleus via Western blotting or immunofluorescence [26]. |
| qRT-PCR Primers (HMOX1, NQO1) | Used to measure the mRNA expression levels of key antioxidant genes that are downstream targets of the Nrf2 pathway, confirming pathway activation [26]. |
| Deep Eutectic Solvents (DES) | Green, efficient, and tunable solvents used in modern extraction techniques to isolate phytochemicals from plant matrices with high yield and minimal degradation [25]. |
| Harpagide | Harpagide, CAS:6926-08-5, MF:C15H24O10, MW:364.34 g/mol |
| 5-Hydroxyflavone | 5-Hydroxyflavone (CAS 491-78-1) For Research |
Unsaturated Fats and Seed Oils: Evidence-Based Analysis
Composition and Nutritional Profile
Seed oils, also termed vegetable oils, are extracted from plant seeds and are characterized by a high content of unsaturated fatty acids (UFAs) and relatively low levels of saturated fatty acids (SFAs) [27] [28]. They are primary dietary sources of the essential polyunsaturated fatty acid (PUFA) linoleic acid (LA), an omega-6 fatty acid, and some, like canola oil, also provide significant omega-3 alpha-linolenic acid (ALA) [29] [27]. The fatty acid composition of common oils is detailed in Table 3.
Table 3: Fatty Acid Composition of Common Plant Oils (g/100g) [27]
| Oil | Total Polyunsaturated | Linoleic Acid (LA) | Alpha-Linolenic Acid (ALA) | Monounsaturated | Saturated |
|---|---|---|---|---|---|
| Grapeseed | 69.9 | 69.6 | 0.1 | 16.1 | 9.6 |
| Soybean | 57.7 | 51.0 | 6.8 | 22.8 | 15.6 |
| Corn | 54.7 | 53.5 | 1.2 | 27.6 | 12.9 |
| Sunflower (Mid-oleic) | 29.0 | 28.9 | <0.1 | 57.3 | 9.0 |
| Canola | 28.1 | 19.0 | 9.1 | 63.3 | 7.4 |
| Olive | 10.5 | 9.8 | 0.9 | 73.0 | 13.8 |
Cardiovascular and Metabolic Benefits: Clinical Evidence
Decades of epidemiological and clinical research consistently demonstrate the cardioprotective effects of replacing SFAs with PUFAs.
- Lipid Profile Improvement: A robust body of evidence from randomized controlled trials (RCTs) shows that replacing saturated fats (e.g., butter, lard) with unsaturated fats from seed oils significantly lowers low-density lipoprotein cholesterol (LDL-C), a primary atherogenic risk factor [29] [27] [30]. This is one of the most well-established relationships in nutritional science.
- Reduction in Cardiovascular Disease Risk: Large-scale meta-analyses of prospective cohort studies show that higher LA intake and higher circulating levels of LA are associated with a lower risk of CVD, heart attack, and stroke [29] [27]. A 2019 study measuring LA in blood and adipose tissue of over 68,000 participants found that those with the highest levels had the lowest risk of cardiovascular diseases and mortality [29].
- Type 2 Diabetes Risk Reduction: Research indicates that LA can improve glucose metabolism and insulin sensitivity. In the same large cohort study, participants with the highest levels of LA had a 35% lower risk of developing T2DM compared to those with the lowest levels [29].
Addressing Controversies: Inflammation and Oxidation
Despite the evidence, misconceptions persist regarding the role of seed oils and omega-6 fats in promoting inflammation and oxidative stress.
- The Inflammation Misconception: A common claim is that omega-6 LA is pro-inflammatory. However, systematic reviews of RCTs have consistently demonstrated that higher intake of LA does not increase biomarkers of inflammation such as C-reactive protein (CRP) [27] [28] [30]. While omega-3s may have stronger anti-inflammatory effects, omega-6s do not promote inflammation in typical dietary amounts [29] [30].
- The Omega-6 to Omega-3 Ratio: The focus on achieving a specific dietary ratio (e.g., 1:1) is misguided [29]. Evidence indicates that the beneficial association between LA and cardiovascular risk is independent of omega-3 levels. Recommendations should focus on increasing omega-3 intake (e.g., from fatty fish, walnuts, canola oil) rather than reducing beneficial omega-6 intake [29].
- Oxidative Stability: Concerns that PUFAs are prone to oxidation and promote oxidative stress in vivo are not supported by clinical evidence. RCTs show that high-PUFA diets do not adversely affect markers of oxidative stress [27].
The following diagram summarizes the evidence-based health impacts of replacing saturated fats with unsaturated seed oils.
Experimental Protocol: Randomized Controlled Trial on Lipid Outcomes
Protocol: RCT on Replacing SFA with UFA and Lipid Profile Changes
- Objective: To determine the effects of replacing dietary saturated fats with unsaturated seed oils on the lipid profiles of adults with elevated LDL-C.
- Study Design: Parallel-group, randomized, controlled feeding trial.
- Participants: ~100 adults, 30-65 years, with LDL-C > 130 mg/dL.
- Intervention:
- Run-in Period: 2-week standardized diet (typical American fat composition).
- Randomization: Participants randomly assigned to one of two isoenergetic diets for 8 weeks:
- SFA Diet: ~14% of total calories from SFA (using butter, cream, palm oil).
- UFA Diet: ~14% of total calories from UFA, primarily LA (using soybean and corn oil).
- Data Collection:
- Blood Sampling: Fasting blood draws at baseline, 4 weeks, and 8 weeks.
- Primary Outcome: Change in LDL-C concentration.
- Secondary Outcomes: Changes in HDL-C, triglycerides, total cholesterol, and oxidized LDL.
- Compliance Monitoring: Provided meals, diet diaries, and biomarker tracking (e.g., plasma fatty acid composition).
- Statistical Analysis: Intention-to-treat analysis using linear mixed-models to compare changes in outcomes between groups over time, adjusting for baseline values.
The Dangers of Ultra-Processed Foods
Defining Ultra-Processed Foods and Consumption Trends
Ultra-processed foods (UPFs) are formulations of industrial ingredients, often containing little or no whole food. They are typically created through a series of industrial processes and frequently include additives like emulsifiers, sweeteners, artificial colors, and flavors not found in home kitchens [31] [32]. According to the NOVA classification system, this category includes soft drinks, packaged snacks, sweetened cereals, mass-produced breads, and reconstituted meat products [31]. UPFs are rapidly displacing fresh foods in diets globally; in the UK and US, they comprise over half of the average calorie intake, and this proportion is even higher among younger, poorer, or disadvantaged populations [31].
Epidemiological Evidence Linking UPFs to Harm
The world's largest scientific review, encompassing 104 long-term studies, has found that UPFs are linked to harm in every major organ system of the human body and are associated with an increased risk of a dozen health conditions [31]. Key findings from recent studies are consolidated in Table 4.
Table 4: Documented Health Risks Associated with High Consumption of Ultra-Processed Foods
| Health Outcome | Key Findings from Epidemiological Studies |
|---|---|
| All-Cause Mortality | Diets high in UPFs are associated with a higher risk of early death from all causes [31]. |
| Cardiometabolic Health | High UPF consumption is linked to significantly higher BMI, waist circumference, blood pressure, insulin levels, and blood triglyceride levels [33]. It is associated with increased risk of CVD and T2DM [31]. |
| Mental & Brain Health | A positive association has been found between UPF intake and depression [31]. |
| Systemic Inflammation | A strong link exists between UPF consumption and elevated C-reactive protein (CRP), a key marker of systemic inflammation [33]. |
Proposed Mechanisms of Harm
The detrimental health effects of UPFs are attributed to a combination of factors:
- Poor Nutritional Profile: UPFs are often high in added sugars, sodium, and unhealthy fats while being low in fiber, vitamins, and minerals [33] [31].
- Hyperpalatability and Overconsumption: Their engineered texture and flavor profile make it difficult to practice dietary moderation, leading to passive overconsumption of calories [32].
- Structural and Formulation Issues: The physical structure (e.g., lack of matrix) and specific industrial ingredients may affect satiety signaling, gut microbiota composition, and metabolic health in ways not fully explained by nutrient content alone [31].
- Displacement of Whole Foods: A primary danger is that UPFs displace fresh, minimally processed foods and traditional meals, reducing the intake of protective phytochemicals and nutrients [29] [31].
The Critical Distinction: Seed Oils vs. Ultra-Processed Foods
A critical point of confusion in public discourse is the conflation of seed oils themselves with the UPFs they are often contained within. The evidence indicates that the harm stems from the ultra-processed food matrix, not the seed oil per se [29] [30].
- Seed Oils as an Ingredient: Seed oils are used in UPFs because they are affordable, shelf-stable, and have a neutral flavor. Their presence is correlated with, but not the cause of, the poor health outcomes linked to UPFs [29].
- Attributing Harm Correctly: As stated by researchers, the harms of ultra-processed foods "have more to do with their calories and their high amounts of added sugar, sodium, and saturated fat than with seed oil" [30]. The public health recommendation is to "consider eating less ultraprocessed food and more whole foods, fruit, and vegetables—and then use seed oils together with those" [29].
The evidence is clear: dietary patterns rich in whole plant foods (with their diverse portfolio of bioactive phytochemicals) and unsaturated fats (from seed oils and other plant sources) are protective against chronic diseases. Conversely, diets high in ultra-processed foods pose a significant threat to global health. The mechanisms—ranging from molecular pathway modulation by phytochemicals to lipid profile improvement by unsaturated fats and the multifactorial harm from UPFs—provide a robust scientific basis for drug discovery and public health policy.
Future research should focus on:
- Elucidating UPF Mechanisms: Conducting controlled trials to disentangle the specific mechanisms by which UPFs cause harm, beyond their nutrient composition [31] [32].
- Personalized Nutrition: Exploring how genetic variation and individual gut microbiota profiles influence responses to specific phytochemicals and dietary fats [25].
- Technological Innovation: Developing advanced delivery systems (e.g., nanoparticles, liposomes) to overcome the bioavailability challenges of many beneficial phytochemicals [25] [34].
- Policy-Relevant Studies: Generating more data on the impact of UPFs on children and US populations specifically, to inform targeted dietary guidelines and regulatory actions, such as front-of-pack labeling and marketing restrictions [32].
Bridging the gap between this compelling scientific evidence and the development of effective clinical interventions and public health policies remains a paramount challenge and opportunity for researchers, clinicians, and drug development professionals.
Dietary Patterns as a Systems Approach to Understanding Chronic Disease Etiology
The escalating global burden of chronic diseases necessitates a paradigm shift from a reductionist focus on single nutrients to a holistic systems approach centered on dietary patterns. This whitepaper elucidates how dietary pattern analysis provides a comprehensive framework for understanding the complex, multifactorial etiology of chronic diseases. We detail the methodological underpinnings for deriving and evaluating dietary patterns, present robust epidemiological evidence linking these patterns to diverse health outcomes, and provide standardized experimental protocols for implementation in research settings. By synthesizing current evidence and methodologies, this guide aims to equip researchers and drug development professionals with the tools necessary to advance the field of nutritional systems biology and develop effective, evidence-based dietary interventions for chronic disease prevention and management.
Over the past century, chronic diseases have superseded infectious diseases as the leading causes of mortality and morbidity in the United States and globally [35]. The etiology of chronic diseases is profoundly complex and multifactorial, involving interactions between age, genetic predisposition, lifestyle factors, and diet [35]. While traditional nutritional epidemiology often focused on individual nutrients or foods, a growing consensus recognizes that this reductionist approach is insufficient for capturing the intricate synergies, antagonisms, and cumulative effects of the diet as a whole [36]. Isolating single components is difficult because typical diets consist of complex mixtures of foods where increased consumption of some items leads to decreased consumption of others, creating substitution effects and multicollinearity that complicate statistical inference [36].
Dietary pattern analysis has emerged as a powerful complementary methodology that addresses these limitations by examining the entire dietary landscape. Dietary patterns are defined as "the quantities, proportions, variety or combination of different foods, drinks, and nutrients in diets and the frequency with which they are consumed" [35]. This systems approach offers several distinct advantages: it reflects actual dietary habits, accounts for complex interactions among food components, provides more stable exposure measures over time than individual nutrients, and offers more practical guidance for public health interventions [36]. The transition toward dietary patterns represents an evolution in nutritional science, aligning with the understanding that health outcomes result from the integrated effects of countless dietary constituents consumed in combination over a lifetime.
Methodological Framework for Dietary Pattern Analysis
Dietary Assessment Methods
Accurate assessment of dietary intake is foundational to dietary pattern research. The choice of assessment tool depends on the research question, study design, sample characteristics, and required precision [37]. The most common methods are compared in Table 1 below.
Table 1: Comparison of Dietary Assessment Methods
| Method | Scope of Interest | Time Frame | Key Strengths | Key Limitations |
|---|---|---|---|---|
| 24-Hour Dietary Recall | Total diet | Short-term (previous 24 hours) | Does not require literacy; reduces reactivity; captures wide variety of foods | Relies on memory; expensive; requires multiple administrations to estimate usual intake |
| Food Frequency Questionnaire | Total diet or specific components | Long-term (months to years) | Cost-effective for large samples; assesses habitual intake | Limited food list; imprecise portion size estimation; requires literacy |
| Food Record | Total diet | Short-term (typically 3-4 days) | Does not rely on memory; detailed quantitative data | High participant burden; reactivity; requires literate, motivated participants |
| Screening Tools | Specific components (e.g., fruits/vegetables) | Variable (often prior month/year) | Rapid; low participant burden; cost-effective | Limited scope; must be validated for specific populations |
All self-reported dietary assessment methods are subject to both random and systematic measurement error [37]. Recovery biomarkers (e.g., doubly labeled water for energy intake, urinary nitrogen for protein) provide objective validation, though they exist for only a limited number of dietary components [37]. Emerging technologies including digital and mobile assessment tools are helping to reduce some limitations of traditional methods.
Analytical Approaches for Deriving Dietary Patterns
Statistical methods for deriving dietary patterns fall into three primary categories: investigator-driven (a priori), data-driven (a posteriori), and hybrid methods [36]. The selection of an appropriate method depends on the research question, with each approach offering distinct advantages and limitations.
Diagram 1: Dietary Pattern Analysis Workflow
Investigator-Driven (A Priori) Methods
Investigator-driven methods evaluate adherence to pre-defined dietary patterns based on existing nutritional knowledge or dietary guidelines [36]. These methods use scoring systems where points are awarded for consumption of recommended foods (e.g., fruits, vegetables, whole grains) and deducted for less healthful options (e.g., foods high in saturated fat, sodium, or added sugars) [35]. Commonly used indices include:
- Healthy Eating Index (HEI): Measures alignment with the U.S. Dietary Guidelines for Americans [35]
- Dietary Approaches to Stop Hypertension (DASH): Based on the diet used in the DASH clinical trials [35]
- Alternate Mediterranean Diet (AMED) Score: Assesses adherence to the traditional Mediterranean dietary pattern [14]
- Plant-based Diet Indices: Include the Healthful Plant-based Diet Index (hPDI) and Unhealthful Plant-based Diet Index (uPDI), which distinguish between quality of plant foods [36]
The primary advantage of a priori methods is their foundation in scientific evidence and dietary recommendations, facilitating comparisons across studies and direct links to policy [35]. Limitations include potential subjectivity in score construction and their focus on selected dietary aspects rather than the overall diet [36].
Data-Driven (A Posteriori) Methods
Data-driven methods derive dietary patterns empirically from consumption data without pre-defined hypotheses [36]. Principal techniques include:
- Principal Component Analysis (PCA) and Factor Analysis (FA): These correlated data reduction techniques identify common underlying factors (dietary patterns) based on the correlations between food groups [36]. PCA transforms correlated variables into a smaller set of uncorrelated principal components that explain maximum variance, while FA decomposes food groups into common and unique factors [36].
- Cluster Analysis: Classifies individuals into mutually exclusive groups with similar dietary habits [36]. Traditional cluster analysis uses algorithms like k-means clustering, while finite mixture models provide a model-based probabilistic approach [36].
These methods capture actual eating habits in a population but may yield patterns that are population-specific and not easily comparable across studies [35].
Hybrid Methods
Hybrid methods incorporate elements of both a priori and a posteriori approaches by using health outcome data to inform pattern derivation [36]. Key methods include:
- Reduced Rank Regression (RRR): Identifies dietary patterns that explain the maximum variation in predetermined response variables (often nutritional biomarkers or disease intermediates) [36]
- Least Absolute Shrinkage and Selection Operator (LASSO): A penalized regression approach that performs variable selection to identify foods most predictive of a health outcome [36]
These methods offer a direct pathway to understanding diet-disease relationships but may overlook patterns relevant to other health outcomes [36].
Evidence Linking Dietary Patterns to Chronic Disease Risk
Prospective cohort studies provide the strongest evidence for associations between dietary patterns and chronic disease incidence, as they assess diet at baseline in healthy participants and follow them over time for disease development, establishing temporality [35]. Table 2 summarizes key findings from large-scale epidemiological studies.
Table 2: Dietary Patterns and Chronic Disease Risk: Evidence from Prospective Studies
| Dietary Pattern | Cardiometabolic Disorders | Cancers | Psychological/ Neurological Disorders | Digestive Disorders | Other Chronic Diseases |
|---|---|---|---|---|---|
| Alternate Mediterranean Diet | Reduced risk of all 8 CMDs studied [14] | Reduced risk of lung, esophageal, and other cancers [14] | Reduced risk of dementia, Parkinson's, depression, anxiety, epilepsy [14] | Reduced risk of dyspepsia, constipation, diverticular disease, IBS, chronic liver disease [14] | Reduced risk of COPD, CKD, asthma, bronchiectasis, cataract [14] |
| AHEI-2010 | Reduced risk of CVD, hypertension; association with diabetes attenuated by BMI adjustment [14] | Reduced risk of non-melanoma skin, lung, breast, and other cancers [14] | Reduced risk of dementia, depression, epilepsy; strongest protective effect for substance abuse [14] | Reduced risk of all digestive disorders studied [14] | Reduced risk of COPD, CKD, prostate disorders [14] |
| Healthful Plant-based Diet Index | Reduced risk of 5 CMDs [14] | Reduced risk of colon, ovarian, and other cancers [14] | Reduced risk of depression and epilepsy [14] | Reduced risk of all digestive disorders studied [14] | Reduced risk of COPD, CKD, prostate disorders [14] |
| DASH Diet | Lower risk of cardiovascular disease, diabetes [35] | Evidence for some cancer risk reduction [35] | Emerging evidence for neurological benefits | Limited evidence | Limited evidence |
The preponderance of evidence indicates that healthy dietary patterns—generally characterized by higher intake of fruits, vegetables, whole grains, low and non-fat dairy, and lean protein, and lower in saturated fat, trans fat, sodium, and added sugars—reduce the risk of major chronic diseases [35]. A comprehensive study of 121,513 UK Biobank participants found the Alternate Mediterranean Diet score was inversely associated with 32 of 48 individual chronic diseases studied, spanning cardiometabolic, cancer, neurological, digestive, and other conditions [14].
The mechanisms underlying these protective effects are multifactorial and likely involve synergistic interactions between dietary components that reduce inflammation, oxidative stress, and metabolic dysregulation while promoting healthy gut microbiota and cellular function [14]. This systems-level impact explains why dietary patterns demonstrate broader health benefits than individual dietary components.
Experimental Protocols and Research Toolkit
Standardized Protocol for Dietary Pattern Analysis in Cohort Studies
Objective: To investigate associations between dietary patterns and chronic disease incidence in a prospective cohort design.
Study Design: Prospective cohort study with baseline dietary assessment and follow-up for disease endpoints.
Participants: Community-dwelling adults free of the chronic disease outcomes of interest at baseline.
Duration: Minimum 5-year follow-up (varies by outcome incidence).
Procedure:
- Dietary Assessment: Administer validated food frequency questionnaire (FFQ) at baseline. The FFQ should assess usual frequency and portion size of 100-150 food items over the previous year.
- Covariate Assessment: Collect comprehensive data on potential confounders including age, sex, BMI, physical activity, smoking status, alcohol consumption, education level, socioeconomic status, and medical history.
- Follow-up and Endpoint Ascertainment: Follow participants for disease outcomes via linkage to health records, registries, or repeated assessments. Use standardized diagnostic criteria for endpoint verification.
- Data Analysis:
- Derive dietary patterns using pre-defined scoring systems (e.g., AMED, AHEI-2010) or data-driven methods (e.g., PCA)
- Use Cox proportional hazards regression to calculate hazard ratios (HR) and 95% confidence intervals (CI) for associations between dietary patterns (analyzed as quintiles or per-quintile increment) and disease outcomes
- Adjust models for potential confounders identified in step 2
- Conduct sensitivity analyses to test robustness of findings
Quality Control:
- Validate FFQ against multiple 24-hour recalls or recovery biomarkers in a subset
- Implement blinding of outcome assessors where possible
- Account for multiple testing using false discovery rate methods [14]
Diagram 2: Cohort Study Design for Dietary Pattern Research
Research Reagent Solutions
Table 3: Essential Research Tools for Dietary Pattern Studies
| Tool Category | Specific Examples | Function/Application |
|---|---|---|
| Dietary Assessment Platforms | Automated Self-Administered 24-hour Recall (ASA-24); Food Frequency Questionnaires | Standardized collection of dietary intake data with nutrient calculation capabilities |
| Biomarker Assays | Doubly labeled water (energy expenditure); Urinary nitrogen (protein intake); Plasma carotenoids (fruit/vegetable intake); Serum fatty acids (dietary fat quality) | Objective validation of dietary intake and pattern adherence; measures not reliant on self-report |
| Statistical Software Packages | SAS (PROC FACTOR, PROC PHREG); R (psych, FactoMineR, survival, glmnet); STATA (factor, scoreplot) | Implementation of dietary pattern derivation and association analyses with appropriate statistical methods |
| Dietary Pattern Scoring Algorithms | HEI-2020 Scoring Algorithm; AHEI Scoring System; MEDAS (Mediterranean Diet Adherence Screener) | Standardized calculation of a priori dietary pattern scores for consistent application across studies |
| Data Linkage Systems | Cancer registries; Hospitalization databases; Mortality registries; Pharmacy claims | Objective endpoint ascertainment for prospective studies with long follow-up periods |
| Icariside Ii | Icariside Ii, CAS:113558-15-9, MF:C27H30O10, MW:514.5 g/mol | Chemical Reagent |
| Isorhamnetin 3-O-glucoside | Isorhamnetin-3-O-glucoside |
Dietary pattern analysis represents a fundamental systems approach that aligns with the complex, multifactorial nature of chronic disease etiology. By examining the cumulative and interactive effects of overall diet, this methodology provides insights that cannot be captured by studying isolated nutrients or foods. The consistent inverse associations between healthy dietary patterns—particularly the Mediterranean-style, healthy plant-based, and DASH-style patterns—and a wide spectrum of chronic diseases underscore the translational potential of this approach for public health and clinical practice.
Future research should prioritize the standardization of dietary assessment and pattern derivation methods, investigation of molecular mechanisms underlying observed associations, and development of personalized dietary recommendations based on individual characteristics and genetic predispositions. As the field evolves, dietary pattern analysis will continue to be an indispensable tool for unraveling the complex relationships between diet and health, ultimately informing more effective strategies for chronic disease prevention and management.
From Data to Diets: Analytical Frameworks, Biomarker Discovery, and Guideline Translation
Accurately assessing dietary adherence is a cornerstone of nutritional epidemiology, providing the critical link between dietary patterns and chronic disease risk in research. The shift from analyzing single nutrients to evaluating whole diets reflects the understanding that foods and nutrients are consumed in complex combinations, exerting synergistic effects on health [36] [38]. Dietary patterns are more consistent over time and often have a greater impact on health outcomes than individual nutrients [36]. This technical guide details the core methodologies—dietary indices, Food Frequency Questionnaires (FFQs), and scoring systems—used to quantify adherence to defined dietary patterns, providing researchers and drug development professionals with the protocols and tools necessary for rigorous investigation.
Methodological Approaches to Dietary Pattern Analysis
Dietary pattern analysis methodologies are broadly categorized into three approaches, each with distinct rationales and applications in chronic disease research [36] [38].
- Hypothesis-Driven (A Priori) Methods: These approaches test adherence to pre-defined dietary patterns based on existing scientific knowledge and dietary guidelines. They utilize dietary indices and scores, such as the Healthy Eating Index (HEI) or the Mediterranean Diet Score (MED), to assess diet quality [36] [38].
- Exploratory (A Posteriori) Methods: These data-driven approaches, including Principal Component Analysis (PCA) and Cluster Analysis, derive dietary patterns solely from the ingested dietary data without relying on prior hypotheses. They are useful for identifying prevailing eating habits within study populations [36] [38].
- Hybrid Methods: Techniques like Reduced Rank Regression (RRR) combine aspects of both a priori and a posteriori methods. They use prior knowledge about the diet-disease pathway (e.g., through biomarkers) to guide the derivation of dietary patterns from consumption data [36] [38].
The following workflow outlines the strategic selection and application of these core methodologies for assessing dietary adherence in research.
Hypothesis-Driven Methods: Dietary Indices and Scores
Hypothesis-driven methods use dietary indices to score individuals based on their adherence to a predefined dietary pattern aligned with nutritional knowledge or guidelines linked to health outcomes [36] [38]. These scores measure the extent to which an individual's diet aligns with dietary recommendations.
Common Dietary Indices and Their Composition
The table below summarizes the rationale, components, and scoring systems of major dietary indices used in chronic disease research.
Table 1: Key Dietary Indices for Assessing Adherence to Health-Promoting Dietary Patterns
| Index Name | Rationale & Hypothesis | Core Dietary Components & Scoring System | Scoring Range |
|---|---|---|---|
| Healthy Eating Index (HEI) [36] [38] | Adherence to the Dietary Guidelines for Americans. | Scores adequacy of total fruits, whole fruits, total vegetables, greens & beans, whole grains, dairy, total protein, seafood & plant proteins, and fatty acids ratio. Scores moderation for refined grains, sodium, added sugars, and saturated fats. | 0 - 100 |
| Mediterranean (MED) Diet Score [36] [38] | Adherence to the traditional Mediterranean diet, associated with reduced chronic disease risk. | Awards points for high consumption of non-refined grains, vegetables, potatoes, fruits, legumes, nuts, fish, and olive oil. Awards points for moderate consumption of alcohol and low consumption of red meat, poultry, and full-fat dairy. | 0 - 55 |
| Dietary Approaches to Stop Hypertension (DASH) [36] [38] | Diet to prevent and treat high blood pressure. | Awards points for meeting recommended servings of total grains, vegetables, fruits, dairy, nuts/seeds/legumes. Awards points for limiting meat/poultry/fish, total fat, saturated fat, sweets, and sodium. | 0 - 10 |
| EAT-Lancet Consumption Frequency Index (ELFI) [39] | Adherence to the EAT-Lancet planetary health diet, promoting health and environmental sustainability. | Uses a brief food propensity questionnaire (FPQ) of 14 food groups. Yields two factors: "foods to encourage" and "foods to balance and to limit." | N/A (Relative Adherence) |
Experimental Protocol: Implementing a Dietary Index
Aim: To assess participant adherence to the Mediterranean diet and analyze its association with cardiovascular event incidence in a prospective cohort.
Materials & Methods:
- Study Population: Recruit from a well-characterized cohort (e.g., n > 5,000) with baseline health data and biobank samples.
- Dietary Assessment: Administer a validated, quantitative FFQ. The FFQ should include food items relevant to the Mediterranean diet (e.g., olive oil, fish, legumes, red meat) and capture portion sizes [40] [37].
- Scoring Calculation:
- For each dietary component in the MED Score (e.g., fruits, vegetables, red meat), calculate the participant's median daily intake from the FFQ data.
- Assign points for each component based on predefined sex-specific population cut-offs or recommended servings. For example, assign 0-5 points for beneficial components, where a higher intake yields a higher score, and reverse-score for harmful components (e.g., red meat) [36] [38].
- Sum all component scores to create a total MED diet score for each participant.
- Outcome Ascertainment: Follow participants via linkage to electronic health records and disease registries to identify incident cases of myocardial infarction and stroke.
- Statistical Analysis: Use Cox proportional hazards models to calculate hazard ratios (HR) and 95% confidence intervals (CI) for the association between MED diet score (categorized in quartiles) and cardiovascular event risk, adjusting for confounders like age, sex, BMI, and physical activity.
The Food Frequency Questionnaire (FFQ)
The FFQ is a cornerstone instrument for assessing long-term, habitual dietary intake in large-scale epidemiological studies, making it the primary tool for calculating hypothesis-driven dietary indices [37].
FFQ Workflow and Considerations
The process of deploying an FFQ and processing its data involves several key stages, from study design to statistical analysis.
Key Considerations for Reliable Dietary Intake Estimation
Determining the optimal number of days for dietary assessment is critical for balancing reliability and participant burden. Recent research using digital tools provides refined guidance.
Table 2: Minimum Days Required for Reliable Estimation of Usual Intake for Selected Dietary Components [41]
| Dietary Component | Minimum Days for Reliability (r > 0.8) | Notes |
|---|---|---|
| Water, Coffee, Total Food Quantity | 1-2 days | Lowest day-to-day variability. |
| Macronutrients (Carbohydrates, Protein, Fat) | 2-3 days | Show good reliability with short-term assessment. |
| Micronutrients (Vitamins & Minerals) | 3-4 days | Generally require more days due to variability. |
| Food Groups (Meat, Vegetables) | 3-4 days | Intake is often episodic. |
| General Recommendation | 3-4 non-consecutive days, including one weekend day | Accounts for day-of-week effects (e.g., higher energy intake on weekends). |
Table 3: Essential Reagents and Resources for Dietary Adherence Research
| Item / Resource | Function & Application in Research |
|---|---|
| Validated Food Frequency Questionnaire (FFQ) | The primary research tool for estimating habitual long-term dietary intake in large cohorts. It consists of a predefined food list with frequency response options and portion size estimates [40] [37]. |
| Food Composition Database | A software or reference database (e.g., USDA FoodData Central, national databases) used to convert FFQ-reported food consumption into estimated nutrient intakes. Critical for calculating dietary index scores. |
| Dietary Index Algorithm | The predefined scoring system (e.g., HEI-2015, MED Score) that translates nutrient or food group intake data from the FFQ into a quantitative measure of dietary adherence [36] [38]. |
| 24-Hour Dietary Recall (24HR) | A short-term dietary assessment method often used for validation studies. It involves a detailed interview about all foods and beverages consumed in the previous 24 hours. Multiple non-consecutive 24HRs can be used to estimate usual intake and validate FFQ findings [37] [41]. |
| Recovery Biomarkers (e.g., Doubly Labeled Water, Urinary Nitrogen) | Objective, non-self-report measures used to validate the accuracy of energy and protein intake reported by FFQs or 24HRs. They are considered the gold standard for assessing dietary measurement error [37]. |
Dietary adherence assessment through rigorously implemented dietary indices, FFQs, and scoring systems provides a powerful approach for elucidating the role of diet in the etiology and prevention of chronic diseases. The choice of method must be aligned with the specific research question, study design, and available resources. As the field evolves, integrating novel technologies for dietary assessment, along with biomarkers and omics data, will further refine our ability to precisely measure adherence and deepen our understanding of the complex interplay between diet and health.
Within the broader thesis on the link between dietary patterns and chronic disease research, the accurate assessment of nutrient intake emerges as a foundational challenge. Establishing causal relationships between diet and health outcomes is hampered by the limitations of self-reported dietary data, including recall bias and measurement error. Objective biomarkers of intake are therefore critical for advancing nutritional science, particularly for complex dietary components like fiber. Dietary fiber represents a paradigmatic example of this challenge; it is not a single chemical entity but a category of non-digestible carbohydrates with diverse structures and physiological effects, all characterized by resistance to digestion and absorption in the human small intestine [42]. The complexity of fiber—encompassing its chemical diversity, its interaction with the gut microbiota, and its subsequent generation of microbial metabolites—makes the identification of robust, validated intake biomarkers particularly difficult. This whitepaper provides an in-depth technical guide to the current state, challenges, and methodologies involved in developing and validating biomarkers for dietary fiber intake, framed for an audience of researchers, scientists, and drug development professionals.
Candidate Biomarkers and Validation Frameworks
Putative Biomarkers of Fiber Intake
The identification of fiber biomarkers leverages the compound's common properties, particularly its fermentation by the gut microbiota. The following table summarizes the primary candidate biomarkers and the current assessment of their validity.
Table 1: Candidate Biomarkers for Total Dietary Fiber Intake
| Biomarker Category | Specific Biomarkers | Rationale & Mechanism | Validation Status & Key Challenges |
|---|---|---|---|
| Microbiota Metabolites | Fecal/Plasma Short-Chain Fatty Acids (SCFAs): Acetate, Propionate, Butyrate | Fiber fermentation by gut bacteria produces SCFAs, which can be measured in circulation and feces [42] [43]. | Putative; highly variable between individuals due to unique microbiome composition [42] [43]. |
| Plasma Odd-Chain Fatty Acids | Potential markers of fiber intake, though also influenced by other factors. | Putative; evidence is limited and fragmented [42]. | |
| Microbiota Composition | Fecal Microbiome Profile | Fiber intake shapes microbial community structure and diversity [42]. | One of the most promising candidates; yet, a specific "fiber intake" signature is elusive [42]. |
| Direct Measures & Byproducts | Fecal Fiber Components | Direct measurement of undigested fiber in stool [42]. | Challenging due to chemical diversity of fiber and extensive fermentation. |
| Stool Weight | Increased fecal bulk is a well-known physiological effect of fiber [42]. | Influenced by many non-dietary factors (e.g., gut motility, water intake). | |
| Functional Assays | Breath Hydrogen and Methane | Gases produced as byproducts of microbial fermentation [42]. | Breath hydrogen is a promising candidate; results can be confounded by small intestinal bacterial overgrowth (SIBO) [42]. |
| Inflammatory Biomarkers | Cytokines (e.g., IL-6, TNF-α-R2) & Composite Indices (SII, SIRI) | Fiber intake is inversely associated with systemic inflammation [44] [45]. | Reflect physiological effect rather than direct intake; useful for validating health impacts but not as specific intake biomarkers. |
Applying a Validation Framework
To move from a list of candidates to validated biomarkers, a structured validation framework is essential. The Food Biomarker Alliance (FoodBAll) Consortium has developed criteria for this purpose [42]. Key validation criteria include:
- Dose-Response Relationship: The biomarker should show a predictable change in concentration or level in response to varying doses of fiber intake.
- Time-Response Relationship: The kinetics of the biomarker's appearance and disappearance after consumption should be characterized.
- Robustness: The biomarker should perform reliably across different populations, genders, age groups, and health statuses.
- Specificity: The biomarker should be uniquely or predominantly associated with fiber intake and not confounded by other dietary components or physiological states.
- Analytical Reliability: The methods for measuring the biomarker must be reproducible, accurate, and sensitive.
A recent narrative review applying these criteria concluded that no single candidate biomarker for total fiber intake currently fulfills all validation criteria [42]. Among the candidates, microbiota composition and breath hydrogen were identified as the most promising, though significant work remains [42].
Methodologies and Experimental Protocols
Protocol for High-Resolution Biomarker Discovery
A pilot study by Myota exemplifies an advanced methodological approach for characterizing postprandial responses to fiber, highlighting the level of detail required for robust biomarker discovery [43].
- Study Design: A tightly controlled, repeated-measures crossover trial.
- Participants: Three healthy male participants (aged 21-36) were recruited.
- Interventions: Participants consumed three different 1200 kcal test meals over three weeks, with a six-day washout between conditions:
- Meal A: Mediterranean-style meal.
- Meal B: High-saturated-fat meal.
- Meal C: Identical to Meal B but supplemented with a 20 g personalized fiber supplement.
- Personalization: The fiber supplement was personalized based on pre-study stool analysis to determine the top two butyrate-producing fibers for each individual, mixed in a 1:1 ratio [43].
- Data Collection:
- Blood Sampling: Continuous blood collection over a 30-hour postprandial period for each meal condition.
- Biomarker Analysis: Measurement of a panel of inflammatory cytokines and plasma SCFA concentrations from the serial blood samples [43].
- Key Findings: The study revealed highly individualized inflammatory and SCFA profiles. It identified 26 meal-responsive biomarkers, but only three (CST5, FGF-19, ST1A1) responded consistently across all individuals and meal types. This underscores the profound inter-individual variability that complicates biomarker validation [43].
Protocol for Large-Scale Epidemiological Validation
Large-scale cross-sectional studies, such as those using NHANES data, are crucial for testing the association between fiber intake and systemic immune-inflammatory biomarkers in diverse populations [45].
- Data Source: National Health and Nutrition Examination Survey (NHANES) cycles (e.g., 2015-2020).
- Study Population: 14,392 participants aged 20 and older after applying exclusion criteria (e.g., lack of data on key variables) [45].
- Fiber Intake Assessment: The average daily intake was calculated from two 24-hour dietary recall interviews [45].
- Biomarker Measurement: A range of systemic immune and inflammatory biomarkers were measured from blood samples, including:
- Novel Composite Indices: Systemic Immune-Inflammation Index (SII), Systemic Inflammation Response Index (SIRI), Neutrophil-to-Lymphocyte Ratio (NLR), Platelet-to-Lymphocyte Ratio (PLR), Red blood cell distribution width-to-Albumin ratio (RA).
- Classical Biomarkers: Ferritin, high-sensitivity C-reactive protein (hs-CRP), total White Blood Cell (WBC) count, and neutrophil count [45].
- Statistical Analysis: Multiple linear regression models were used, adjusting for a comprehensive set of covariates including age, gender, race, BMI, smoking status, physical activity, and energy intake [45].
- Key Findings: Dietary fiber intake was significantly and inversely associated with a wide array of inflammatory markers, including SII, SIRI, NLR, RA, ferritin, hs-CRP, and WBC, reinforcing the anti-inflammatory role of fiber and the utility of these biomarkers in capturing its physiological effects [45].
Pathways, Workflows, and Research Tools
Pathway of Fiber-Induced Immunomodulation
The following diagram illustrates the primary mechanistic pathway through which dietary fiber intake is believed to modulate host inflammation and immunity, a core concept in linking fiber to chronic disease risk.
High-Resolution Biomarker Discovery Workflow
The experimental protocol for high-frequency, postprandial biomarker discovery, as implemented in recent pilot studies, can be visualized as follows.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Research Reagent Solutions for Fiber Biomarker Studies
| Reagent / Material | Function & Application | Example from Literature |
|---|---|---|
| Personalized Prebiotic Fiber Supplements | Tailored mixtures of specific fibers (e.g., inulin, resistant starch) designed to maximize SCFA production based on an individual's baseline microbiota. | 20 g supplement created from a 1:1 ratio of an individual's top two butyrate-producing fibers [43]. |
| Multiplex Cytokine Panels | Simultaneous measurement of a broad spectrum of inflammatory biomarkers (e.g., IL-6, TNF-α, CST5, FGF-19) from plasma/serum samples. | Used to characterize high-resolution, postprandial inflammatory dynamics [43]. |
| Gas Chromatography-Mass Spectrometry (GC-MS) | Gold-standard method for the identification and quantification of SCFAs (acetate, propionate, butyrate) in biological samples like plasma and feces. | Employed for pharmacokinetic analysis of plasma SCFAs over extended postprandial periods [43]. |
| 16S rRNA Sequencing Reagents | Profiling the composition and relative abundance of bacterial taxa in stool samples to assess microbiome changes associated with fiber intake. | Used for baseline characterization and to link microbial composition to biomarker production [42] [43]. |
| Standardized Meal Kits | Pre-formulated, calorie-controlled meals with defined macronutrient and fiber composition for controlled intervention studies. | Mediterranean diet meal (A) and high-saturated-fat meal (B) used in crossover trials [43]. |
| Food Frequency Questionnaires (FFQ) / 24-hr Recalls | Tools for estimating habitual dietary intake, including fiber, in large-scale observational studies. | WHI FFQ and two 24-hour recalls in NHANES used to correlate fiber intake with inflammatory biomarkers [44] [45]. |
| Tiliroside | Tiliroside, CAS:20316-62-5, MF:C30H26O13, MW:594.5 g/mol | Chemical Reagent |
| Galuteolin | Galuteolin, CAS:20344-46-1, MF:C21H20O11, MW:448.4 g/mol | Chemical Reagent |
The quest to validate robust biomarkers for dietary fiber intake remains a formidable challenge in nutritional epidemiology and chronic disease research. Current evidence, synthesized herein, indicates that while several putative biomarkers exist—from SCFAs and breath gases to inflammatory indices and microbiota profiles—none singularly meets all criteria for a validated intake marker. The complexity of fiber as a nutrient class and the profound inter-individual variation in host response, dictated largely by the gut microbiome, are the central obstacles [42] [43]. The future of this field lies in several promising directions. First, the move towards "smart" fibermaxxing or personalized nutrition, which involves consuming a diverse array of fibers tailored to an individual's gut microbiome, may yield more consistent metabolic responses and, consequently, more reliable biomarkers [43]. Second, methodological advances in high-frequency, multi-omics data collection will be critical to capture the dynamic and complex physiological changes post-consumption that traditional sampling misses [43]. Finally, there is a growing consensus that a combination or panel of biomarkers, rather than a single silver bullet, will be necessary to accurately reflect the intake of complex nutrients like fiber [42]. As technology evolves, the integration of continuous biomarker tracking with artificial intelligence could eventually provide real-time dietary guidance, solidifying the critical link between dietary patterns, validated intake biomarkers, and chronic disease risk [43].
Circulating biomarkers serve as critical quantitative indicators of biological processes, pathogenic states, or pharmacologic responses to therapeutic interventions. In nutritional epidemiology and chronic disease research, these biomarkers provide objective measures of the physiological pathways linking dietary patterns to disease risk. The investigation of inflammatory, insulinemic, and neurodegenerative biomarkers has proven particularly valuable for understanding the mechanistic connections between diet and chronic diseases. Research demonstrates that dietary components influence disease risk not only through caloric content but also through specific metabolic effects that modulate these biomarker profiles [46].
The growing recognition that circulating biomarkers mediate the relationship between dietary intake and chronic disease pathogenesis has transformed nutritional science. This whitepaper provides a comprehensive technical guide to the major biomarker classes that function as mediators along inflammatory, insulinemic, and neurodegenerative pathways, with specific application to dietary pattern research. We synthesize current evidence on biomarker responses to dietary interventions, detail methodological protocols for their assessment, and visualize the biological pathways through which they operate, providing researchers and drug development professionals with an integrated resource for investigating diet-disease relationships.
Biomarker Pathways and Dietary Influences
Inflammatory Biomarkers
Chronic low-grade inflammation represents a fundamental pathway connecting dietary patterns to various disease states. Inflammatory biomarkers provide quantifiable measures of this relationship, with circulating levels responsive to dietary intake.
Table 1: Key Inflammatory Biomarkers and Their Responses to Dietary Patterns
| Biomarker | Function | Pro-Inflammatory Diet Response | Anti-Inflammatory Diet Response | Key Dietary Influences |
|---|---|---|---|---|
| C-Reactive Protein (CRP) | Acute-phase protein produced in liver, general marker of inflammation | Increased concentrations [47] | Significant reduction, particularly with Mediterranean diet [48] | Mediterranean diet high in fruits, vegetables, whole grains, olive oil |
| Interleukin-6 (IL-6) | Pro-inflammatory cytokine, stimulates CRP production | Elevated levels [48] | Prominent reduction (-1.07 pg/mL) [48] | High intake of fruits, vegetables, omega-3 fatty acids |
| Tumor Necrosis Factor-Alpha (TNF-α) | Pro-inflammatory cytokine, regulates immune cells | Elevated levels [49] | Reduction associated with higher diet quality [49] | Diets rich in saturated fats, refined carbohydrates |
| Interleukin-1 Beta (IL-1β) | Pro-inflammatory cytokine, involved in immune response | Elevated levels | Significant reduction with Mediterranean diet (-0.46 pg/mL) [48] | Mediterranean dietary patterns |
Systematic reviews and meta-analyses of randomized controlled trials demonstrate that the Mediterranean diet produces the most consistent anti-inflammatory effects, with significant reductions in IL-6, IL-1β, and CRP compared to other dietary patterns [48]. The Dietary Inflammatory Index (DII) provides a standardized method for quantifying the inflammatory potential of overall diet, with higher scores predicting elevated inflammatory biomarker levels and increased chronic disease risk [50] [47].
Insulinemic Biomarkers
Dietary patterns influence glucose metabolism and insulin response, with certain food combinations promoting hyperinsulinemia—a pathological state of excessive insulin secretion that promotes chronic disease development.
Table 2: Insulinemic Biomarkers and Dietary Modulation
| Biomarker | Function | Hyperinsulinemic Diet Response | Beneficial Diet Response | Key Dietary Influences |
|---|---|---|---|---|
| Fasting Insulin | Baseline insulin secretion, indicates pancreatic β-cell function | Increased concentrations [47] | Reduction with high-quality diets [49] | High glycemic load foods, sugar-sweetened beverages |
| C-Peptide | Marker of insulin secretion, more stable than insulin | Elevated levels [47] | Reduction with diets low in processed foods | Processed meats, sugar-sweetened beverages |
| HOMA-IR | Measures insulin resistance from fasting glucose and insulin | Significant increase (+8%) [47] | Improvement with high-fiber, low-glycemic diets [49] | High saturated fat, low fiber diets |
| Leptin | Adipokine regulating appetite and metabolism | Increased levels [49] | Favorable reduction with diet quality improvement [49] | High-energy density diets |
| Adiponectin | Anti-inflammatory adipokine, improves insulin sensitivity | Reduced concentrations (-2.4%) [47] | Increased with Mediterranean and plant-based diets | Monounsaturated and omega-3 fatty acids |
The Empirical Dietary Index for Hyperinsulinemia (EDIH) score, derived from plasma C-peptide levels, provides a validated measure of a diet's potential to promote hyperinsulinemia [47]. Diets high in red meat, processed meat, and sugar-sweetened beverages consistently demonstrate hyperinsulinemic effects, while those rich in whole fruits, coffee, and green leafy vegetables show inverse associations [47].
Neurodegenerative Biomarkers
Circulating biomarkers reflecting neurodegenerative processes provide critical insights into the relationship between diet and brain health, with several demonstrating responsiveness to dietary patterns.
Table 3: Neurodegenerative Blood-Based Biomarkers and Dietary Connections
| Biomarker | Function | Association with Brain Disorders | Dietary Influences | Pathological Significance |
|---|---|---|---|---|
| Phosphorylated Tau (p-tau) | Microtubule-associated protein, hyperphosphorylation in AD | Core biomarker for Alzheimer's pathology | MIND diet associated with reduced levels through metabolic mediation [51] | Neuronal injury and neurofibrillary tangle formation |
| Amyloid-β (Aβ42/40 ratio) | Peptide forming plaques in AD brain | Altered ratio in Alzheimer's disease | Mediterranean and MIND diets associated with favorable ratios [52] | Amyloid plaque formation |
| Neurofilament Light Chain (NfL) | Structural protein released with axonal damage | Marker of neuronal injury | Anti-inflammatory diets associated with lower levels [52] | Non-specific neuronal damage |
| Glial Fibrillary Acidic Protein (GFAP) | Astrocytic protein, marker of neuroinflammation | Elevated in Alzheimer's and neuroinflammation | Inflammatory diets associated with increased levels [52] | Astrocyte activation and neuroinflammation |
The MIND diet (Mediterranean-DASH Intervention for Neurodegenerative Delay) demonstrates particularly promising neuroprotective effects, with adherence associated with reduced risk of dementia, stroke, depression, and anxiety [51]. Mechanistic studies suggest these benefits are mediated through favorable metabolic signatures and attenuated biological aging [51].
Experimental Protocols and Methodologies
Dietary Assessment and Pattern Analysis
Food Frequency Questionnaires (FFQ): Validated FFQs (e.g., Block 98.2, WHI FFQ) capture habitual dietary intake over extended periods (typically 3-12 months). These self-administered instruments include 69-122 food items with frequency categories and portion size options [53] [47]. Processing involves nutrient calculation using standardized databases (e.g., USDA Nutrient Database, NDSR) and subsequent derivation of dietary pattern scores.
Dietary Pattern Indices Calculation:
- Healthy Eating Index (HEI): Assesses adherence to Dietary Guidelines for Americans through 13 components (total fruits, whole fruits, total vegetables, greens and beans, whole grains, dairy, total protein foods, seafood and plant proteins, fatty acids, refined grains, sodium, added sugars, saturated fats) [53] [49].
- Mediterranean Diet Score (aMED): Nine-point scale evaluating intake of fruits, vegetables, whole grains, legumes, nuts, fish, monounsaturated-to-saturated fat ratio, red/processed meats, and alcohol [49].
- Dietary Inflammatory Index (DII): Literature-derived algorithm incorporating 28-45 food parameters, with higher scores indicating pro-inflammatory potential [50] [47].
- Empirical Dietary Index for Hyperinsulinemia (EDIH): Weighted score based on 18 food groups predictive of plasma C-peptide [47].
Biomarker Assessment Protocols
Sample Collection and Processing:
- Blood Collection: Fasting venipuncture (10-12 hour fast) using standardized tubes (EDTA, heparin, or serum separator tubes). Immediate processing (within 2 hours) with centrifugation at 1300-2000 × g for 15 minutes at 4°C [49] [47].
- Storage: Aliquotting into cryovials and storage at -80°C until analysis to maintain biomarker stability.
Analytical Techniques:
- Inflammatory Biomarkers: High-sensitivity CRP measured via immunoturbidimetric assays on automated analyzers (e.g., Roche COBAS Integra); cytokines (IL-6, TNF-α) quantified using Luminex multiplex assays or ELISA [49] [47].
- Insulinemic Biomarkers: Insulin measured by immuno-enzymometric assays (e.g., Tosoh 600 auto-analyzer); C-peptide via chemiluminescent immunoassays; glucose through enzymatic methods (e.g., hexokinase) on automated platforms [53] [47].
- Lipid Biomarkers: Enzymatic colorimetric methods for total cholesterol, HDL-C, and triglycerides on automated analyzers (e.g., Roche COBAS); LDL-C typically calculated via Friedewald equation [49].
- Neurodegenerative Biomarkers: Ultrasensitive immunoassays (e.g., Simoa, ELISA) for Aβ, p-tau, NfL; mass spectrometry for Aβ42/40 ratio quantification [52].
Quality Control: Inclusion of internal standards, blinded duplicate samples, and inter-laboratory validation with coefficients of variation <10-15% for acceptable precision [49] [47].
Statistical Analysis Approaches
Primary Analysis:
- Multivariable-adjusted linear regression models to examine diet-biomarker associations, typically expressing results as percent difference in biomarker concentrations per 1-standard deviation increment in dietary pattern score [47].
- Logistic regression for dichotomous outcomes (e.g., disease prevalence), with odds ratios and 95% confidence intervals calculated across dietary pattern quartiles [50].
Covariate Adjustment: Standard adjustment for age, sex, ethnicity, BMI, smoking status, physical activity, total energy intake, and socioeconomic factors [49] [50]. Additional consideration of genetic factors (e.g., APOE ε4 status for neurodegenerative biomarkers) [52].
Advanced Analytical Methods:
- Mediation analysis to quantify proportion of diet-disease relationships explained by specific biomarkers [51].
- Multi-omics integration (metabolomics, proteomics) to identify novel pathways linking diet to health outcomes [51] [54].
- Elastic net regression for high-dimensional data (e.g., microbiome data) to identify most predictive features [53].
Pathway Visualization and Biological Mechanisms
Dietary Influence on Inflammatory and Insulinemic Pathways
Neurodegenerative Pathway and Dietary Modulation
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 4: Essential Research Reagents and Methodologies for Circulating Biomarker Analysis
| Category | Specific Tools/Assays | Application | Key Features |
|---|---|---|---|
| Dietary Assessment | Block FFQ, WHI FFQ, 24-hour dietary recalls | Dietary pattern quantification | Validated, population-specific food lists, nutrient database integration |
| Biomarker Analysis Platforms | Roche COBAS Integra, Luminex, ELISA, Simoa | Multiplex biomarker quantification | High sensitivity, automation, simultaneous multi-analyte detection |
| Specialized Reagents | High-sensitivity CRP reagents, cytokine panels, metabolic arrays | Specific biomarker measurement | Low detection limits, standardized across batches |
| Omics Technologies | LC-MS metabolomics, proteomic arrays, 16S rRNA sequencing | Pathway analysis, mechanism discovery | Unbiased discovery, high-dimensional data generation |
| Data Analysis Tools | R packages (survey, meta), SAS, PICRUSt2, mediation analysis | Statistical modeling, pathway analysis | Accommodates complex designs, mediation testing, microbiome function prediction |
| Grisabutine | Berbamunine | High-purity Berbamunine for research. A natural bisbenzylisoquinoline alkaloid for biochemical studies. For Research Use Only. Not for human or veterinary use. | Bench Chemicals |
| Makisterone A | Makisterone A|28-Carbon Ecdysteroid|RUO | Makisterone A is a C28 ecdysteroid and molting hormone for research. This product is for Research Use Only and not for human or veterinary use. | Bench Chemicals |
Circulating biomarkers provide crucial mechanistic insights into the relationship between dietary patterns and chronic disease risk, serving as both mediators of dietary effects and quantitative indicators of physiological state. The integration of standardized dietary assessment with sophisticated biomarker measurement creates a powerful framework for understanding how diet influences health through inflammatory, insulinemic, and neurodegenerative pathways.
Future research directions should prioritize the application of multi-omics technologies to identify novel biomarker signatures, the development of personalized nutrition approaches based on individual biomarker profiles, and the implementation of standardized protocols to enhance cross-study comparability. As biomarker science advances, circulating biomarkers will play an increasingly important role in validating dietary interventions, identifying at-risk populations, and developing targeted nutritional strategies for chronic disease prevention and management.
Chronic diseases are the leading causes of death and disability in the United States, accounting for more than half of all premature deaths and over 90% of yearly healthcare spending [1]. Recent data from the Behavioral Risk Factor Surveillance System indicates that 76.4% of U.S. adults (approximately 194 million people) reported having at least one chronic condition in 2023, with 51.4% (130 million) reporting multiple chronic conditions [55]. The prevalence of chronic conditions is increasing most rapidly among young adults (ages 18-34), with a 7.0 percentage point increase from 2013 to 2023 [55].
Diet represents a modifiable risk factor for chronic disease development and progression. Poor nutrition accounts for an estimated 11 million deaths and 255 million disability-adjusted life-years globally [1]. The Dietary Guidelines for Americans (DGA) provide science-based recommendations for healthy dietary patterns to promote health and reduce the risk of chronic disease, with the 2020-2025 edition marking the first to provide guidance for healthy dietary patterns by life stage, from birth through older adulthood [56]. This technical review examines the evidence linking dietary patterns to chronic disease prevention and the translation of this evidence into public policy through the DGA and global recommendations.
Evidence Base: Dietary Patterns and Chronic Disease Risk
Major Studies on Dietary Patterns and Chronic Disease
Long-term prospective cohort studies provide the primary evidence base linking dietary patterns to chronic disease risk.
Table 1: Key Cohort Studies on Dietary Patterns and Chronic Disease
| Study Name | Population | Follow-up Duration | Primary Chronic Disease Outcomes |
|---|---|---|---|
| Nurses' Health Study (NHS) | 162,667 female nurses | Up to 32 years | Major CVD, type 2 diabetes, cancer [1] |
| Health Professionals Follow-up Study (HPFS) | 43,185 male health professionals | Up to 32 years | Major CVD, type 2 diabetes, cancer [1] |
| UK Biobank | 121,513 community-dwelling adults | Mean 8.4-8.6 years | 48 individual chronic diseases [14] |
| NHS & HPFS Healthy Aging | 105,015 participants | Up to 30 years | Multidimensional healthy aging [7] |
Dietary Patterns and Chronic Disease Risk Reduction
Research has examined multiple dietary patterns in relation to chronic disease risk, with consistent findings across diverse populations.
Table 2: Dietary Patterns and Associated Risk Reduction for Major Chronic Diseases
| Dietary Pattern | Risk Reduction (Highest vs. Lowest Adherence) | Strongest Evidence For |
|---|---|---|
| Alternative Healthy Eating Index (AHEI) | 14-40% lower risk across various chronic diseases [14] | Healthy aging (OR: 1.86); mental health; physical function [7] |
| Alternative Mediterranean Diet (AMED) | 8-44% lower risk across various chronic diseases [14] | 32 individual chronic diseases; cognitive health; chronic liver disease [14] [7] |
| Healthful Plant-based Diet Index (hPDI) | 5-42% lower risk across various chronic diseases [14] | Cardiometabolic disorders; epilepsy [14] |
| Planetary Health Diet (PHD) | 15 million annual premature deaths preventable with global adoption [57] | Environmental sustainability; cancer; neurodegenerative diseases [57] |
| Diabetes Risk Reduction Diet (DRRD) | 30% lower risk of major chronic disease [1] | Type 2 diabetes; major cardiovascular disease [1] |
A 2023 study examining associations with 48 individual chronic diseases found the Alternative Mediterranean Diet score was associated with a lower risk of 32 conditions, including cardiometabolic disorders, digestive disorders, and psychological/neurological disorders [14]. Similarly, the Alternative Healthy Eating Index-2010 and Healthful Plant-based Diet Index were inversely associated with 29 and 23 individual chronic diseases, respectively [14].
Methodological Approaches in Dietary Pattern Research
Dietary Assessment Methodologies
The evidence base for dietary guidelines relies on rigorous methodological approaches for dietary assessment and data analysis:
- 24-Hour Dietary Recalls: The "What We Eat in America" component of the National Health and Nutrition Examination Survey (NHANES) uses multiple-pass 24-hour dietary recalls, considered the gold standard for dietary assessment in large population studies [58].
- Food Frequency Questionnaires (FFQs): Validated semi-quantitative FFQs are used in large prospective cohorts (NHS, HPFS) to assess long-term dietary patterns [1] [7].
- Food Pattern Equivalents Database (FPED): Converts foods and beverages into 37 USDA Food Patterns components to examine adherence to dietary recommendations [58].
- Statistical Modeling: Uses multivariable-adjusted models controlling for age, sex, BMI, physical activity, smoking, alcohol intake, and other non-dietary factors [1] [14] [7].
Healthy Aging Outcome Assessment
Recent research has expanded beyond disease-specific outcomes to examine multidimensional healthy aging. A 2025 study defined healthy aging through four domains [7]:
- Survival to age 70 years
- Absence of 11 major chronic diseases
- Intact cognitive health (assessed by standardized instruments)
- Intact mental health (no depression or cognitive limitations)
- Intact physical function (no limitations in activities of daily living)
After up to 30 years of follow-up, only 9.3% of participants achieved healthy aging, highlighting the critical need for effective preventive strategies [7].
Diagram 1: Research workflow for dietary pattern and chronic disease studies showing sequential phases from data collection to policy translation.
Biological Mechanisms Linking Diet to Chronic Diseases
Key Pathways in Diet-Chronic Disease Relationships
Research has identified several biological mechanisms through which dietary patterns influence chronic disease risk:
- Inflammatory Pathways: The Empirical Dietary Inflammatory Pattern (EDIP) score quantifies the inflammatory potential of diet, with pro-inflammatory diets associated with elevated inflammatory biomarkers (IL-6, CRP, TNFαR2) and increased chronic disease risk [1] [7].
- Insulinemic Pathways: The Empirical Dietary Index for Hyperinsulinemia (EDIH) reflects diets that stimulate higher insulin responses, independently of glycemic load, and is associated with increased risk of type 2 diabetes, cardiovascular disease, and other conditions [1] [7].
- Oxidative Stress: Diets rich in fruits, vegetables, and other plant foods provide antioxidants that mitigate oxidative damage to cells and tissues.
- Gut Microbiome Modulation: Dietary fiber and plant compounds influence gut microbiota composition and production of metabolites like short-chain fatty acids.
Diagram 2: Biological mechanisms through which dietary patterns influence chronic disease risk, highlighting inflammatory, insulinemic, oxidative stress, and gut microbiome pathways.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Methodological Tools for Dietary Pattern and Chronic Disease Research
| Research Tool | Function | Application Example |
|---|---|---|
| Alternative Healthy Eating Index (AHEI) | Quantifies adherence to dietary guidelines based on foods and nutrients predictive of chronic disease risk | Strongest association with healthy aging (OR: 1.86) [7] |
| Alternative Mediterranean Diet (AMED) Score | Measures adherence to Mediterranean-style dietary pattern | Associated with lower risk of 32 individual chronic diseases [14] |
| Healthful Plant-based Diet Index (hPDI) | Assesses adherence to healthful plant-based foods while distinguishing from less healthful plant foods | Inverse association with 23 chronic diseases [14] |
| Empirical Dietary Inflammatory Pattern (EDIP) | Calculates inflammatory potential of diet based on biomarker studies | Higher adherence associated with 39% lower odds of healthy aging [7] |
| Empirical Dietary Index for Hyperinsulinemia (EDIH) | Estimates insulinemic potential of diet based on biomarker responses | Higher adherence associated with 42% lower odds of healthy aging [7] |
| Planetary Health Diet Index (PHDI) | Assesses alignment with diet that supports human and planetary health | Associated with 15 million preventable annual deaths globally [57] |
| Melicopidine | Melicopidine|CAS 475-91-2|Research Chemical | Melicopidine is a natural acridone alkaloid for research use. Studies indicate potential antimalarial and cytotoxic activities. This product is for Research Use Only (RUO). |
| Moniliformin sodium salt | Moniliformin sodium salt, CAS:71376-34-6, MF:C4HNaO3, MW:120.04 g/mol | Chemical Reagent |
Translation of Evidence into Dietary Guidelines
The Dietary Guidelines for Americans Development Process
The DGA development follows a rigorous scientific process:
- Systematic Reviews: The Nutrition Evidence Systematic Review (NESR) team conducts systematic reviews on specific dietary questions.
- Data Analysis: Federal data analysis teams analyze national datasets (NHANES, BRFSS) to describe current dietary intakes and health status [58].
- Advisory Committee: An appointed committee of scientific experts reviews evidence and provides recommendations.
- Implementation Materials: Development of consumer-friendly tools (MyPlate, "Start Simple" resources) to translate recommendations [59].
Challenges in Guideline Implementation
Despite strong evidence, implementation of dietary guidelines faces challenges:
- Consumer Adoption: Average Healthy Eating Index scores in the U.S. population increased only from 56 to 59 (out of 100) from 2005 to 2016 [59].
- Communication Barriers: Complex nutrition concepts like "nutrient density" are difficult for consumers to understand [59].
- Economic and Time Constraints: Cost and preparation time for healthy foods present implementation barriers [59].
- Food Environment: Limited access to healthy foods in many communities impedes adherence to recommendations.
Global Recommendations and the Planetary Health Diet
The EAT-Lancet Commission's Planetary Health Diet represents a global approach linking human and planetary health. This dietary pattern emphasizes:
- Minimally processed plant foods including fruits, vegetables, nuts, legumes, and whole grains
- Moderate amounts of meat and dairy (limiting red meat to approximately once weekly)
- Very little added sugar, saturated fat, and salt [57]
Widespread adoption of this pattern could prevent approximately 15 million premature deaths annually globally and reduce greenhouse gas emissions from agriculture by more than half [57]. The flexibility of this pattern allows for cultural adaptations while maintaining core health and sustainability principles.
Substantial evidence from large prospective cohorts demonstrates that dietary patterns emphasizing plant-based foods, healthy fats, whole grains, and limited processed foods significantly reduce the risk of multiple chronic diseases and promote healthy aging. The translation of this evidence into public policy through the Dietary Guidelines for Americans provides science-based recommendations, though effective implementation remains challenging.
Future directions include:
- Life-stage specific recommendations as introduced in the 2020-2025 DGA
- Integration of sustainability considerations into dietary guidance
- Personalized nutrition approaches based on individual biomarkers and genetics
- Enhanced communication strategies to improve consumer understanding and adoption
- Food system innovations to increase accessibility and affordability of healthy foods
The convergence of evidence from multiple large studies provides a robust foundation for dietary recommendations that can substantially reduce the global burden of chronic disease when effectively translated into public policy and practice.
Incorporating Dietary Patterns into Clinical Practice and Chronic Disease Management Protocols
The management and prevention of chronic diseases represent a formidable challenge for global healthcare systems. In recent decades, nutritional science has undergone a fundamental paradigm shift from a reductionist focus on individual nutrients to a holistic approach that examines dietary patterns—the combinations, quantities, and variety of foods and beverages consumed over time—and their synergistic effects on health [60]. This transition is driven by the recognition that individuals consume complex mixtures of foods with interacting components that act synergistically to influence physiological pathways and health outcomes [36] [60]. The 2020-2025 Dietary Guidelines for Americans formally acknowledges this approach, emphasizing that dietary patterns are the cornerstone of evidence-based dietary guidance [60].
This technical guide examines the incorporation of dietary patterns into clinical practice and chronic disease management protocols, framed within the broader thesis that specific dietary patterns significantly influence the development, progression, and management of major chronic diseases. For researchers, scientists, and drug development professionals, understanding these relationships is crucial for developing targeted nutritional interventions and understanding diet-drug interactions in therapeutic development.
Evidence Base: Dietary Patterns and Chronic Disease Outcomes
Major Dietary Patterns and Their Health Impacts
Longitudinal cohort studies provide compelling evidence linking dietary patterns with chronic disease risk and healthy aging outcomes. The evidence stems from both investigator-driven (a priori) patterns, based on dietary guidelines, and data-driven (a posteriori) patterns, derived from population data using statistical methods like principal component analysis and clustering [36].
Table 1: Major Dietary Patterns and Associations with Chronic Disease Outcomes
| Dietary Pattern | Core Components | Associated Health Outcomes | Strength of Evidence |
|---|---|---|---|
| Alternative Healthy Eating Index (AHEI) | High fruits, vegetables, whole grains, nuts, legumes; Low red/processed meats, sugar-sweetened beverages | Strongest association with healthy aging (OR: 1.86); Reduced major chronic disease risk [7] [1] | Multiple large prospective cohorts (NHS, HPFS) |
| Mediterranean-style (aMED) | High fruits, vegetables, whole grains, olive oil, fish; Moderate red wine | Reduced cardiovascular disease, cancer, and all-cause mortality [1] [36] | Systematic reviews and randomized trials |
| DASH (Dietary Approaches to Stop Hypertension) | High fruits, vegetables, low-fat dairy; Low sodium, saturated fat | Hypertension reduction, improved cardiovascular outcomes [1] [61] | Clinical trials and cohort studies |
| Healthful Plant-Based (hPDI) | Emphasis on whole plant foods; Limited animal products | Reduced coronary heart disease, type 2 diabetes, and all-cause mortality [7] [36] | Prospective cohort studies |
| Low-Inflammatory/ Low-Insulinemic | Foods modulating inflammation (e.g., leafy greens, nuts) and insulin response | Reduced risk for major CVD, type 2 diabetes, and cancer (HR: 0.58-0.61) [1] | Mechanistic and prospective studies |
Quantitative Evidence from Longitudinal Studies
Large-scale prospective cohorts provide the most compelling evidence for integrating dietary patterns into clinical practice. The Nurses' Health Study and Health Professionals Follow-Up Study, with over 30 years of follow-up data, demonstrate that higher adherence to healthy dietary patterns significantly increases the likelihood of healthy aging, defined as maintaining intact cognitive, physical, and mental health beyond age 70 free of chronic diseases [7].
After up to 30 years of follow-up, participants in the highest quintile of adherence to healthy dietary patterns had 46-86% greater odds of healthy aging compared to those in the lowest quintile [7]. The AHEI demonstrated the strongest association (OR: 1.86, 95% CI: 1.71-2.01), followed by empirically-based patterns targeting hyperinsulinemia and inflammation [7]. When the healthy aging threshold was raised to age 75, the association with AHEI strengthened further (OR: 2.24, 95% CI: 2.01-2.50), underscoring the cumulative benefit of long-term adherence [7].
Table 2: Dietary Components and Their Association with Healthy Aging Domains
| Dietary Component | Healthy Aging OR (95% CI) | Cognitive Function | Physical Function | Mental Health | Chronic Disease-Free |
|---|---|---|---|---|---|
| Fruits | 1.15 (1.10-1.20) | 1.10 (1.06-1.14) | 1.22 (1.17-1.27) | 1.16 (1.11-1.21) | 1.12 (1.08-1.17) |
| Vegetables | 1.20 (1.15-1.25) | 1.13 (1.09-1.17) | 1.28 (1.23-1.33) | 1.22 (1.17-1.27) | 1.18 (1.13-1.23) |
| Whole Grains | 1.25 (1.20-1.30) | 1.17 (1.13-1.21) | 1.35 (1.30-1.41) | 1.27 (1.22-1.32) | 1.23 (1.18-1.28) |
| Nuts & Legumes | 1.22 (1.17-1.27) | 1.14 (1.10-1.18) | 1.32 (1.27-1.38) | 1.25 (1.20-1.30) | 1.20 (1.15-1.25) |
| Red/Processed Meats | 0.80 (0.76-0.84) | 0.86 (0.83-0.89) | 0.74 (0.70-0.78) | 0.79 (0.75-0.83) | 0.83 (0.79-0.87) |
| Sugary Beverages | 0.82 (0.78-0.86) | 0.88 (0.85-0.91) | 0.76 (0.72-0.80) | 0.81 (0.77-0.85) | 0.85 (0.81-0.89) |
Methodological Framework: Assessing Dietary Patterns in Research and Practice
Dietary Assessment Methodologies
Accurate measurement of dietary intake is fundamental for both research and clinical applications. The choice of assessment method depends on the research question, study design, sample characteristics, and required precision [37].
Table 3: Dietary Assessment Methods in Research and Clinical Practice
| Method | Time Frame | Strengths | Limitations | Best Applications |
|---|---|---|---|---|
| 24-Hour Recall | Short-term (previous 24 hours) | High detail for recent intake; Low participant burden; Does not require literacy [37] | Relies on memory; High day-to-day variability; Multiple collections needed | Clinical assessment; National surveys; Cross-sectional studies |
| Food Frequency Questionnaire (FFQ) | Long-term (months to years) | Captures habitual intake; Cost-effective for large samples; Ranks individuals by intake [37] | Limited food list; Portion size estimation errors; Memory dependent | Large cohort studies; Epidemiological research |
| Food Records | Short-term (typically 3-7 days) | High detail without memory reliance; Weighed records most accurate [37] | High participant burden; Reactivity (changing diet for recording) | Metabolic studies; Intervention trials with high compliance |
| Screening Tools | Variable (often past month) | Rapid administration; Low burden; Target specific nutrients/foods [37] | Narrow focus; Population-specific validation required | Clinical screening; Brief interventions |
Statistical Approaches for Dietary Pattern Analysis
Advanced statistical methods enable researchers to derive meaningful dietary patterns from complex consumption data. These methods fall into three primary categories [36]:
- Investigator-driven methods: Based on prior knowledge or dietary guidelines (e.g., AHEI, DASH scores)
- Data-driven methods: Derived from population data using dimensionality reduction techniques (e.g., PCA, factor analysis, clustering)
- Hybrid methods: Incorporate health outcomes in pattern identification (e.g., reduced rank regression)
Emerging methodologies include finite mixture models, treelet transforms, and compositional data analysis (CODA), which accounts for the relative nature of dietary intake [36]. Each method has distinct advantages and limitations, and selection should align with research questions and analytical resources.
Food Pattern Modeling for Dietary Guidance
Food pattern modeling is a methodology used by the Dietary Guidelines Advisory Committee to illustrate how changes to the amounts or types of foods in existing dietary patterns affect nutrient adequacy [62]. This approach answers critical questions about:
- Implications of modifying food group quantities (e.g., Dairy, Fruits, Vegetables, Grains, Protein Foods)
- Nutrient impacts when emphasizing specific staple foods
- Accommodation levels for foods lower in nutrient density
- Meeting nutrient needs with variations like vegetarian or low-carbohydrate patterns [62]
This systematic modeling informs evidence-based dietary recommendations that form the foundation of clinical nutrition guidance.
Implementation Framework: Integrating Dietary Patterns into Clinical Practice
Table 4: Essential Resources for Dietary Pattern Research and Clinical Implementation
| Tool/Resource | Function | Application Context |
|---|---|---|
| ASA-24 (Automated Self-Administered 24-hour Recall) | Automated 24-hour dietary assessment without interviewer burden | Clinical research; Population monitoring; Efficient data collection [37] |
| FFQ Data Analysis Software | Analyzes food frequency questionnaire data to derive dietary patterns | Large epidemiological studies; Cohort analyses; Habitual intake assessment [37] |
| Food Pattern Modeling Algorithms | Tests how dietary modifications affect nutrient adequacy | Dietary guideline development; Clinical nutrition planning [62] |
| Recovery Biomarkers (Doubly Labeled Water, Urinary Nitrogen) | Objectively validates energy and protein intake against self-report | Methodological studies; Validation research; Calibration [37] |
| Dietary Pattern Scoring Algorithms | Quantifies adherence to specific dietary patterns (AHEI, DASH, MIND) | Clinical assessment; Intervention studies; Epidemiology [36] |
| NESR (Nutrition Evidence Systematic Review) | Systematic review methodology for nutrition evidence | Guideline development; Evidence synthesis; Policy formulation [63] |
Protocol for Dietary Pattern Assessment in Clinical Research
Clinical Translation: From Evidence to Practice
Translating dietary pattern research into clinical practice requires addressing several implementation considerations:
Personalization: Dietary patterns should be tailored to cultural preferences, health status, socioeconomic factors, and food access [64] [61]. The Healthy U.S.-Style Pattern, Healthy Mediterranean-Style Pattern, and Healthy Vegetarian Pattern described in the Dietary Guidelines provide flexible frameworks for customization [60] [61].
Addressing Social Determinants: Access to foods supporting healthy dietary patterns is influenced by neighborhood resources, transportation, food affordability, and availability of retail outlets [64]. Disparities in food access disproportionately affect racial/ethnic minority communities, low-income populations, and rural residents [64].
Life Stage Appropriateness: Dietary recommendations should consider unique nutritional needs across the lifespan, from infancy through older adulthood [60] [61]. The 2020-2025 Dietary Guidelines provides specific guidance for pregnancy, lactation, infancy, toddlerhood, and older adulthood.
Practical Implementation Tools: Resources like the MyPlate platform (https://www.myplate.gov) and the Start Simple with MyPlate app provide accessible translation of dietary pattern recommendations for clinical and public use [61].
The integration of dietary patterns into clinical practice and chronic disease management represents an evidence-based approach to addressing the global burden of noncommunicable diseases. Substantial research demonstrates that dietary patterns rich in plant-based foods, with moderate inclusion of healthy animal-based foods, significantly enhance healthy aging and reduce chronic disease risk [7] [1]. The Alternative Healthy Eating Index, Mediterranean-style, and DASH patterns show particularly strong associations with beneficial health outcomes.
For researchers and clinicians, implementing standardized assessment methodologies, understanding statistical approaches for dietary pattern analysis, and addressing practical implementation barriers are essential for translating this evidence into effective clinical practice and public health interventions. Future directions include refining statistical methodologies for pattern analysis, understanding biological mechanisms, and developing personalized nutrition approaches based on individual responses to dietary patterns.
As the scientific evidence continues to evolve, dietary pattern science will play an increasingly important role in chronic disease prevention and management, offering a powerful, cost-effective complement to pharmaceutical interventions in promoting population health and healthy aging.
Overcoming Implementation Barriers: Cultural Adaptation, Personalization, and Emerging Challenges
The relationship between dietary patterns and chronic disease risk represents a cornerstone of modern nutritional epidemiology. Chronic diseases, including heart disease, cancer, cerebrovascular disease, and diabetes mellitus, constitute the leading causes of death in the United States and place tremendous stress on healthcare systems [35]. The preponderance of evidence demonstrates that healthy dietary patterns are associated with beneficial outcomes for all-cause mortality, cardiovascular disease, overweight and obesity, type 2 diabetes, and certain cancers [64]. However, significant disparities exist in diet quality and chronic disease prevalence across racial and ethnic groups. For instance, the age-adjusted prevalence of obesity and diabetes is substantially higher among adult Hispanics and Black/African-Americans compared to non-Hispanic whites [35]. Understanding and addressing the factors underlying these disparities, particularly the role of cultural acceptability in dietary guidance, is imperative for improving population health and advancing chronic disease research.
This technical guide examines the critical need for cultural tailoring of dietary guidelines within the context of chronic disease prevention and management. It explores methodological approaches for assessing cultural acceptability, provides evidence-based frameworks for intervention, and outlines essential tools and protocols for researchers and drug development professionals working to reduce nutrition-related health disparities.
The Evidence Base: Cultural Relevance in Dietary Interventions
Limitations of Standardized Dietary Guidelines
The United States Dietary Guidelines (USDG) form the basis of federal nutrition programs and policies, recommending three primary dietary patterns: the Healthy U.S.-Style Eating Pattern (H-US), Healthy Mediterranean-Style Eating Pattern (Med), and Healthy Vegetarian Eating Pattern (Veg) [65]. However, these guidelines have been developed with limited consideration for the cultural foodways of diverse population groups. Research using the Healthy Eating Index (HEI) reveals that African American adults exhibit greater disparities in diet quality and adherence to dietary guidelines compared to White and Hispanic adults [65]. Similar disparities persist among individuals with hypertension, type 2 diabetes, and obesity [65].
Social and economic determinants—including income, education, access to healthy foods, and inequitable healthcare access—contribute significantly to these disparities [65] [64]. For populations facing these structural barriers, standardized dietary recommendations that do not account for cultural food preferences, traditional preparation methods, and community-specific barriers to access are unlikely to be effective. The food environment itself presents significant challenges; predominantly Black and Hispanic neighborhoods have fewer large chain supermarkets than predominantly White and non-Hispanic neighborhoods, and residents of low-income communities often face greater distances to grocery stores with limited transportation options [64].
Efficacy of Culturally Tailored Interventions
Emerging evidence demonstrates that culturally tailored interventions can significantly improve health outcomes in diverse populations. For African American individuals, such interventions have proven effective in promoting weight loss, dietary changes, and improving type 2 diabetes outcomes [65]. Specific examples include:
- Culturally Tailored Workplace Interventions: African American women who received culturally tailored workplace dietary interventions showed significant improvements in weight, waist circumference, and weight-related quality of life compared to those receiving standard counseling [65].
- Adapted DASH Diet: A nutrition intervention tailoring the Dietary Approaches to Stop Hypertension (DASH) diet for African American adults led to increased fruit and vegetable consumption and enhanced self-efficacy for healthier eating compared to a control group [65].
- USDG-Based Interventions: The Dietary Guidelines: 3 Diets (DG3D) study, a 12-week randomized controlled feeding trial implementing unmodified USDG dietary patterns with African American adults, achieved significant within-group improvements in weight (-2.4 to -2.6 kg) and diet quality, though it also identified needs for cultural adaptation to enhance long-term adherence [65].
Table 1: Key Findings from the DG3D Intervention Study
| Metric | Baseline Findings | Post-Intervention Results | Cultural Considerations Identified |
|---|---|---|---|
| Diet Quality (HEI) | Baseline mean HEI: 55-58 across groups | Significant within-group improvement; greater improvement in Mediterranean vs. Vegetarian (p=0.02) | Need for adaptations to enhance cultural relevance |
| Weight Outcomes | Mean BMI: 35.9 ± 0.8 kg/m² | Significant within-group weight loss (-2.4 to -2.6 kg, p=0.97) | Social and cultural barriers affect long-term maintenance |
| Participant Engagement | 83% female; mean age 48.0 ± 10.6 y | 42 participants completed qualitative follow-up | Cultural relevance crucial for program adherence |
Methodological Framework: Assessing Cultural Acceptability
Research Design and Participant Recruitment
The DG3D study provides a robust methodological template for investigating cultural acceptability in dietary interventions. This research employed a qualitative descriptive study embedded within a randomized controlled feeding trial—a design that allows for both quantitative outcome assessment and qualitative exploration of participant experiences [65].
Participant Criteria:
- Self-identification as African American adult
- BMI between 25 and 49.9 kg/m²
- Presence of ≥3 risk factors for type 2 diabetes
- Residence in the study area (Columbia, SC, or nearby) [65]
Recruitment Strategy: Conducted in summer 2021, with announcements during classes and instructions for signing up provided through multiple channels (email, phone calls) [65].
Data Collection Protocols
Focus Group Methodology:
- Six in-person focus group discussions (two per assigned dietary pattern)
- Conducted upon completion of the 12-week intervention (December 2021)
- Private rooms in the same building used for orientation and weekly food sample pickup
- $20 gift card incentive for participation [65]
Focus Group Guide Development: The focus group guide was developed using two theoretical frameworks:
- Social Cognitive Theory: Guided questions related to self-efficacy, acceptability of diets, and facilitators/barriers to diet adoption.
- Designing Culturally Relevant Intervention Development Framework: Examined factors including developmental considerations (age), cultural considerations (visual appeal/packaging), and intervention delivery channels (preferred communication means) [65].
Moderator Characteristics: Focus groups were facilitated by two trained African American female moderators who were staff members for the DG3D study, leveraging existing relationships with participants to enhance rapport and disclosure [65].
Analytical Approaches
Transcripts from focus group discussions were analyzed using an iterative constant comparative method. Verbatim transcripts were coded thematically and analyzed in Nvivo12, allowing for systematic identification of emergent themes regarding cultural acceptability, barriers, and facilitators to dietary change [65].
Table 2: Dietary Assessment Methods in Cultural Research
| Method | Time Frame | Strengths | Limitations | Cultural Application |
|---|---|---|---|---|
| 24-Hour Dietary Recall | Short-term (previous 24 hours) | Does not require literacy; reduces reactivity | Relies on memory; expensive to implement | Can be adapted with culturally specific food probes |
| Food Frequency Questionnaire (FFQ) | Long-term (months to year) | Cost-effective for large samples; ranks nutrient exposure | Limited food list; may miss cultural foods | Requires inclusion of culturally relevant food items |
| Food Records | Short-term (typically 3-4 days) | Detailed quantitative data | High participant burden; reactivity | Must account for culturally specific preparation methods |
| Screening Tools | Variable (often prior month/year) | Rapid, cost-effective for specific components | Narrow focus; must be validated for population | Can target specific cultural dietary components |
Statistical Approaches for Dietary Pattern Analysis in Diverse Populations
Understanding dietary patterns is fundamental to chronic disease research, as these patterns represent the complex combinations of foods and beverages consumed habitually and their synergistic effects on health [35] [36]. Dietary pattern analysis moves beyond single-nutrient approaches to capture the totality of dietary exposure, making it particularly valuable for understanding culturally influenced eating behaviors.
Methodological Categories for Dietary Pattern Analysis
Table 3: Statistical Methods for Dietary Pattern Analysis
| Method Category | Examples | Key Characteristics | Application in Cultural Research |
|---|---|---|---|
| Investigator-Driven (A Priori) | Healthy Eating Index (HEI), DASH Score | Based on existing nutritional knowledge or guidelines | Allows cross-population comparisons but may lack cultural specificity |
| Data-Driven (A Posteriori) | Principal Component Analysis (PCA), Factor Analysis, Cluster Analysis | Derived from population dietary data | Identifies culturally specific eating patterns within population subgroups |
| Hybrid Methods | Reduced Rank Regression (RRR), Data Mining | Combines dietary data with health outcome or biomarker data | Links culturally specific patterns to health outcomes |
| Compositional Data Analysis | Principal Component Coordinates, Balance Coordinates | Accounts for relative nature of dietary data (nutrients sum to total intake) | Appropriate for substitution effects in cultural food patterns |
Emerging Methodological Approaches
Several emerging statistical methods show particular promise for analyzing dietary patterns in diverse cultural contexts:
- Finite Mixture Model (FMM): A model-based clustering method that can identify latent subpopulations with distinct dietary patterns, potentially reflecting cultural subgroups within larger samples [36].
- Treelet Transform (TT): Combines principal component analysis and clustering algorithms in a one-step process, potentially identifying culturally influenced food combinations that traditional methods might miss [36].
- Compositional Data Analysis (CODA): Transforms dietary intake into log-ratios, effectively handling the substitution effects common in cultural diets where increases in some foods lead to decreases in others [36].
- Least Absolute Shrinkage and Selection Operator (LASSO): A variable selection method that can identify the most culturally relevant food items predictive of health outcomes [36].
Implementation Framework: Designing Culturally Relevant Interventions
Key Considerations for Cultural Tailoring
Based on qualitative findings from the DG3D study and related research, successful cultural tailoring of dietary guidelines should address several dimensions:
Developmental Considerations:
- Account for age-related food preferences and traditions
- Consider generational differences in food preparation knowledge
- Address life stage nutritional needs within cultural contexts [65]
Cultural and Traditional Considerations:
- Incorporate traditional foods and preparation methods
- Acknowledge cultural significance of certain foods and eating occasions
- Respect religious and ethical food restrictions (e.g., vegetarian patterns for specific cultural groups) [65]
Intervention Delivery Channels:
- Utilize preferred communication methods within communities
- Engage cultural influencers (e.g., chefs, community leaders)
- Provide materials with culturally appropriate visual appeal and packaging [65]
Addressing Structural Barriers
Beyond cultural preferences, effective interventions must address structural barriers to healthy eating:
Geographic Access:
- 23.5 million people in the U.S. live in low-income areas further than 1 mile from a large grocery store
- Predominantly Black neighborhoods have fewer large chain supermarkets than White neighborhoods
- Detroit study found Black low-income neighborhoods travel 1.1 miles farther to closest supermarket [64]
Economic Interventions:
- The Gus Schumacher Nutrition Incentive Program incentivizes fruit and vegetable purchases in low-income communities
- Financial incentives at farmers markets increase SNAP benefit usage for healthy foods
- Price reductions for healthier foods increase their purchasing [64]
Dietary Assessment Instruments
24-Hour Dietary Recall:
- Multiple non-consecutive recalls needed to account for day-to-day variation
- Automated Self-Administered (ASA-24) system reduces interviewer burden
- Requires specific probing for culturally relevant food details [37]
Food Frequency Questionnaires:
- Must be adapted to include culturally relevant food items
- Can be quantitative, semi-quantitative, or qualitative
- Population-specific FFQs necessary for accurate assessment [37]
Biomarker Validation:
- Recovery biomarkers (doubly labeled water for energy, urinary nitrogen for protein) address systematic error in self-report
- Metabolomics approaches emerging for dietary pattern validation [37] [36]
Analytical Implementation
Software and Packages:
- R: Multiple packages for PCA, factor analysis, clustering, FMM, LASSO, and CODA
- SAS: Procedures for factor analysis, cluster analysis, and specialized dietary pattern analysis
- STATA: Modules for dietary pattern estimation and analysis [36]
Validation Protocols:
- Reproducibility assessments through test-retest protocols
- Validity testing against recovery biomarkers where feasible
- Predictive validity for chronic disease outcomes [36]
Conceptual Framework for Cultural Tailoring of Dietary Guidelines
The following diagram illustrates the integrated mixed-methods approach for developing and evaluating culturally tailored dietary guidelines:
The evidence base consistently demonstrates that cultural tailoring of dietary guidelines is essential for reducing disparities in chronic disease prevalence and improving health outcomes across diverse populations. Future research should prioritize:
- Methodological Advancement: Developing and validating standardized protocols for cultural adaptation of dietary assessment tools and interventions.
- Implementation Science: Studying scale-up of successful culturally tailored programs in real-world settings.
- Biomarker Integration: Incorporating objective nutritional biomarkers to validate self-reported dietary data across cultural groups.
- Cross-Cultural Comparisons: Systematically comparing dietary patterns and their health effects across diverse racial, ethnic, and cultural groups.
- Policy Translation: Translating research findings into policy recommendations that support culturally appropriate federal nutrition programs.
As the field progresses, researchers must continue to engage community stakeholders in the design and implementation of dietary interventions, ensuring that cultural acceptability remains central to efforts aimed at reducing the burden of chronic diseases through improved nutrition.
Personalized nutrition represents a paradigm shift from generic dietary advice to targeted nutritional interventions based on individual biological characteristics. This whitepaper examines the three foundational pillars of personalized nutrition—genetics, gut microbiome, and metabolic phenotyping—and their integration into a comprehensive framework for chronic disease prevention and management. We synthesize current scientific evidence, detailing methodologies for assessing individual variability and providing practical protocols for researchers and clinicians. The convergence of these fields enables unprecedented precision in dietary recommendations, offering significant potential for addressing the global burden of nutrition-related chronic diseases through mechanisms that modulate gene expression, microbial ecology, and metabolic pathways.
Chronic degenerative diseases such as obesity, type 2 diabetes, cardiovascular diseases, and cancer represent a leading global health challenge. Their etiology is complex, arising from intricate interactions between genetic susceptibility and environmental factors, with diet being a principal modifiable component [66]. Traditional nutritional science has largely operated on a one-size-fits-all model, generating population-wide recommendations that fail to account for significant inter-individual variation in response to dietary interventions [67]. The new paradigm of personalized nutrition (PN) dismantles this approach by leveraging insights from genomics, microbiomics, and metabolomics to tailor dietary strategies to the individual [68].
The conceptual foundation of PN is encapsulated by the formula: Genotype + Environment + (Genotype × Environment) = Metabolic Phenotype [66]. This equation highlights that an individual's phenotypic transition from health to disease is a slow process influenced by changes in gene and/or protein expression, which can be modulated by dietary components. PN is thus a core element of P4 medicine—an approach that is predictive, preventive, personalized, and participatory [66]. By understanding an individual's unique genetic makeup, gut microbiota composition, and real-time metabolic responses, researchers and clinicians can develop nutritional strategies that more effectively maintain health and prevent or manage chronic diseases.
The Genetic Foundation: Nutrigenetics and Nutrigenomics
Core Concepts and Definitions
The genetic pillar of personalized nutrition is divided into two complementary fields: nutrigenetics and nutrigenomics.
Nutrigenetics examines how an individual's genetic variations affect their response to dietary components and nutrient metabolism [69]. It focuses on the influence of hereditary genetic variants, such as single nucleotide polymorphisms (SNPs), on the uptake and metabolism of micronutrients and macronutrients [69].
Nutrigenomics investigates how bioactive food components and nutrients influence gene expression, protein synthesis, and metabolic processes [66] [69]. It studies the effects of nutrients on the genome and the subsequent transcriptional, translational, and metabolic changes.
Nutrigenomics operates on three fundamental tenets: (1) Genomic diversity among ethnic groups affects nutrient bioavailability and metabolism; (2) Food choices and availability are influenced by cultural, geographical, and socio-economic factors; and (3) Malnutrition threatens genome stability by causing mutations or chromosomal instability [69].
Key Genetic Variants and Dietary Implications
Research has identified numerous genetic polymorphisms that modify an individual's response to dietary intake and influence disease risk. The following table summarizes well-characterized gene-diet interactions with significant implications for chronic disease risk.
Table 1: Key Genetic Variants Influencing Response to Dietary Components
| Gene | Polymorphism | Nutrient Interaction | Physiological Effect | Chronic Disease Association |
|---|---|---|---|---|
| FTO | rs9939609 | High-fat diet | Modulates hypothalamic expression of FTO, affecting energy homeostasis [66] | Increased risk of obesity; influences weight loss response to dietary intervention [66] [67] |
| TCF7L2 | rs7903146 | Dietary carbohydrate | Impairs glucose metabolism; carriers show improved glycemic control with low-glycemic diets [67] | Strongly associated with type 2 diabetes risk [67] |
| PPARG | rs1801282 | Dietary fatty acids | Carriers of the Ala12 allele benefit more from diets high in monounsaturated fats [67] | Modulates risk for obesity, insulin resistance, and cardiovascular disease [67] |
| APOA2 | rs5082 | Saturated fat intake | CC genotype associated with higher BMI and obesity risk with high saturated fat intake [67] | Obesity and metabolic syndrome [67] |
| MTHFR | rs1801133 | Folate metabolism | Altered folate metabolism affects DNA methylation and nucleotide synthesis [66] | Associated with cardiovascular disease and neural tube defects [66] |
| MC4R | Various | Energy intake | Receptor involved in leptin pathway; deficiency causes intense hunger and hyperphagia [66] | Monogenic form of obesity (0.5-4% of obese children) [66] |
Experimental Protocols for Gene-Nutrient Interaction Studies
Protocol 1: Genome-Wide Association Study (GWAS) for Nutritional Traits
- Subject Recruitment: Recruit large cohorts (typically thousands of participants) with detailed dietary assessment data (e.g., food frequency questionnaires, 24-hour recalls).
- Genotyping: Perform high-density genome-wide genotyping using microarray platforms.
- Phenotyping: Precisely measure nutritional traits of interest (e.g., nutrient levels in blood, postprandial responses, body composition changes in response to diet).
- Statistical Analysis: Conduct association testing between genetic variants and nutritional phenotypes, adjusting for multiple comparisons.
- Replication: Validate significant associations in independent populations to confirm findings.
- Functional Follow-up: Use molecular techniques (e.g., cell culture models, animal studies) to characterize the biological mechanism of identified gene-nutrient interactions [66].
Protocol 2: Nutrigenetic Intervention Study
- Genotype Screening: Pre-screen participants for specific genetic variants of interest (e.g., FTO, TCF7L2).
- Stratified Randomization: Randomize participants within genotype groups to different dietary interventions (e.g., low-fat vs. low-carbohydrate diets).
- Intervention Phase: Implement controlled feeding studies or intensive behavioral counseling for dietary change over a defined period (typically weeks to months).
- Outcome Assessment: Measure primary outcomes (e.g., weight change, glycemic improvement, lipid profiles) at baseline and follow-up.
- Gene-Diet Interaction Analysis: Test whether the effect of dietary assignment on outcomes differs by genotype [67] [70].
The Gut Microbiome: A Microbial Ecosystem Shaping Nutritional Response
Gut Microbiome Composition and Metabolic Function
The human gut microbiome comprises trillions of microorganisms, with the two dominant phyla being Firmicutes and Bacteroidetes, representing 90% of gut microbiota [71]. The gut microbiome encodes approximately 3.3 million genes, outnumbering human protein-coded genes by 150-fold, which significantly expands the metabolic capabilities of the host [71]. Key functions of the gut microbiome include:
- Fermentation: Conversion of indigestible dietary fibers into short-chain fatty acids (SCFAs) like acetate, propionate, and butyrate, which serve as energy sources for colonocytes and regulate immune function [71].
- Biosynthesis: Production of essential vitamins (e.g., vitamin K, B vitamins) and amino acids [72].
- Xenobiotic Metabolism: Transformation of drugs, toxins, and food components [71].
- Bile Acid Metabolism: Transformation of primary bile acids into secondary bile acids, influencing lipid absorption and signaling [72].
Diet is a primary driver of gut microbiome composition and function. A rapid shift in microbial community structure can occur within 24 hours of dietary change [71]. The relationship between diet, gut microbiota, and health outcomes is mediated through multiple mechanisms, including maintenance of intestinal barrier integrity, modulation of the immune system, and production of metabolites that regulate host metabolism.
Microbiome-Based Personalized Nutrition
Specific bacterial species and their metabolic outputs have been identified as key mediators of individual responses to diet:
- Akkermansia muciniphila: Higher abundance is associated with improved insulin sensitivity. Individuals with elevated A. muciniphila benefit more from high-fiber intake due to enhanced SCFA production [67].
- Bacteroidetes/Firmicutes Ratio: Shifts in this ratio are associated with obesity status and may influence energy harvest from diet [71].
- SCFA Producers: Bacteria such as Faecalibacterium prausnitzii (butyrate producer) respond to dietary fiber intake and contribute to maintaining gut barrier function and anti-inflammatory responses [71].
The following diagram illustrates the relationship between dietary components, gut microbiome metabolism, and host physiological effects:
Figure 1: Diet-Gut Microbiome-Host Interaction Pathway
Advanced Tools and Methodologies for Microbiome Research
coralME: A Novel Tool for Modeling Microbiome Metabolism
A groundbreaking tool called coralME, developed by researchers at UC San Diego, rapidly creates detailed genome-scale computer models of metabolism, gene, and protein expression from large amounts of data [73]. These "ME-models" link a microbe's genome to its phenotype and can predict how microbes respond to specific nutrients.
Key Applications of coralME:
- Simulates how different diets affect gut bacteria composition and function
- Identifies nutrients that promote beneficial microbes or harmful pathogens
- Predicts nutrient requirements for specific microbes and interspecies dependencies
- Models patient-specific microbial activities using real-time expression data [73]
Protocol 3: Microbiome-Based Personalized Nutrition Intervention
- Baseline Microbiome Profiling: Collect stool samples for 16S rRNA sequencing or shotgun metagenomics to characterize microbial community structure.
- Functional Assessment: Measure microbial metabolites in stool or blood (SCFAs, bile acids, tryptophan metabolites).
- Dietary Intervention Design: Formulate personalized dietary recommendations based on individual's microbial profile:
- For low microbial diversity: Increase variety of plant-based foods
- For low SCFA producers: Increase resistant starch and dietary fiber
- For high inflammatory potential: Reduce saturated fats and animal proteins
- Monitoring: Repeat microbiome and metabolite profiling after intervention to assess response.
- Iteration: Adjust dietary recommendations based on observed microbial changes and clinical outcomes [67] [71].
Table 2: Research Reagent Solutions for Gut Microbiome Studies
| Reagent/Technology | Function/Application | Key Features |
|---|---|---|
| 16S rRNA Sequencing | Profiling microbial community composition | Targets hypervariable regions of bacterial 16S gene; cost-effective for large cohorts |
| Shotgun Metagenomics | Comprehensive analysis of all genetic material in sample | Provides species-level resolution and functional gene annotation |
| Metatranscriptomics | Analysis of gene expression in microbial community | Identifies actively expressed metabolic pathways |
| coralME Platform | Genome-scale metabolic modeling | Generates ME-models linking genome to phenotype; predicts response to nutrients [73] |
| Gnotobiotic Mouse Models | Study host-microbe interactions | Germ-free animals colonized with defined microbial communities |
| SCFA Analysis (GC-MS/LC-MS) | Quantification of short-chain fatty acids | Measures butyrate, acetate, propionate in stool, blood, or culture supernatants |
Metabolic Phenotyping: The Functional Readout of Gene-Microbe-Environment Interactions
Defining Metabolic Phenotypes
Metabolic phenotypes represent the comprehensive characterization of an individual's metabolites at a specific point in time, reflecting the complex interactions among genetic background, environmental factors, lifestyle, and gut microbiome [72]. They serve as key molecular bridges between healthy homeostasis and disease-related metabolic disruption. The metabolic phenotype is dynamic and can be described as:
- Static Biomarkers: Traditional clinical indicators (fasting glucose, triglycerides) and novel molecular markers (branched-chain amino acids, specific lipids).
- Dynamic Balance: The capacity to restore metabolic homeostasis after challenges like a meal or exercise, influenced by physical activity, gut microbiota, and circadian rhythms [72].
High-throughput metabolomics strategies enable systematic analysis of small molecule metabolites in physiological and pathological processes. These metabolites serve as biomarkers for disease diagnosis, prognosis assessment, and treatment response prediction, while also elucidating novel mechanistic pathways in disease progression [72].
Technologies for Metabolic Phenotyping
The major analytical platforms for metabolomics include:
Mass Spectrometry (MS)
- Liquid Chromatography-MS (LC-MS): Preferred for broad, untargeted metabolomics
- Gas Chromatography-MS (GC-MS): Excellent for volatile compounds and after chemical derivatization
- Tandem MS (MS/MS): Provides structural information for compound identification
Nuclear Magnetic Resonance (NMR) Spectroscopy
- Advantages: Non-destructive, highly reproducible, quantitative
- Applications: In vivo metabolic profiling (e.g., via MRI), high-throughput screening
Emerging Technologies
- Spatial Metabolomics: Resolves spatial distribution of metabolites in tissues
- In Vivo Monitoring: Real-time metabolite tracking using biosensors
- Metabolic Flux Analysis: Tracks flow of isotopes through metabolic pathways [72]
Metabolic Signatures of Health and Disease
Table 3: Characteristic Metabolic Phenotypes in Health and Chronic Disease
| Condition | Key Metabolic Features | Potential Biomarkers | Nutritional Implications |
|---|---|---|---|
| Healthy Homeostasis | Robust circadian metabolic rhythms; balanced glucose and lipid metabolism; diverse bile acid pool; balanced SCFA profile | Normal branched-chain amino acids; balanced primary/secondary bile acid ratio; adequate adiponectin | Dietary patterns supporting metabolic flexibility and circadian alignment |
| Obesity | Impaired mitochondrial oxidation; elevated branched-chain amino acids; altered bile acid metabolism; reduced SCFA diversity | Increased glutamate, isoleucine, leucine, valine; reduced glycine; altered microbial metabolites | Energy-restricted diets; personalized macronutrient composition based on genotype; high-fiber for SCFA production |
| Type 2 Diabetes | Insulin resistance; elevated fasting branched-chain amino acids; altered lipid partitioning; mitochondrial dysfunction | N1-acetylspermidine (T lymphoblastic leukemia); succinate, uridine, lactate (gastric cancer) [72] | Low-glycemic diets; personalized carbohydrate restriction based on genetic and microbiome profile |
| Cardiovascular Disease | Dyslipidemia; altered cholesterol metabolism; increased oxidative stress markers; inflammation | Specific phospholipids, acylcarnitines; trimethylamine N-oxide (TMAO) | Reduced saturated fat for APOE4 carriers; increased omega-3 based on genetic variants |
| IBD | Gut inflammation; impaired barrier function; reduced SCFA production; altered microbial metabolism | Reduced butyrate; increased secondary bile acids; pH shifts [73] | Exclusive enteral nutrition; specific carbohydrate diet; low FODMAP based on individual tolerance |
Protocol 4: Comprehensive Metabolic Phenotyping for Nutrition Research
- Sample Collection: Collect multiple biofluids (fasting plasma, serum, urine) following standardized protocols.
- Sample Preparation:
- Protein precipitation for plasma/serum (e.g., methanol precipitation)
- Metabolite extraction from tissues (e.g., methyl-tert-butyl ether/methanol/water)
- Data Acquisition:
- Perform untargeted metabolomics using LC-MS in both positive and negative ionization modes
- Include quality control samples (pooled reference samples, solvent blanks)
- Data Processing:
- Use software (e.g., XCMS, MS-DIAL) for peak detection, alignment, and integration
- Annotate metabolites using databases (HMDB, METLIN, LipidMaps)
- Statistical Analysis:
- Multivariate analysis (PCA, PLS-DA) to identify differentiating metabolites
- Univariate analysis to test significance of individual metabolites
- Pathway analysis to identify affected metabolic pathways [72]
Integrating Multi-Omics for Personalized Nutrition
The true power of personalized nutrition emerges from the integration of genetic, microbiome, and metabolic data. This integrated approach provides a systems-level understanding of how individuals respond to dietary interventions.
A Framework for Integration
The following diagram illustrates the workflow for integrating multi-omics data to develop personalized nutrition recommendations:
Figure 2: Multi-Omics Integration for Personalized Nutrition
Digital Health Technologies in Personalized Nutrition
The integration of digital health technologies with personalized nutrition offers a transformative approach for managing chronic diseases [67]. Key technologies include:
- Continuous Glucose Monitors (CGMs): Provide real-time feedback on individual glycemic responses to different foods, enabling dynamic dietary adjustments [67].
- Artificial Intelligence (AI)-Driven Meal Planning: Algorithms integrate genetic, microbiome, and metabolic data to generate personalized meal recommendations [67].
- Mobile Health Applications: Enable tracking of food intake, symptoms, and behaviors while delivering personalized recommendations and behavioral nudges [67].
- Wearable Sensors: Monitor physical activity, sleep, and other physiological parameters that influence nutritional requirements [67].
Personalized nutrition represents the frontier of nutritional science, transforming our approach from population-based recommendations to individualized strategies that account for genetic makeup, gut microbiome composition, and metabolic phenotype. The integration of these three pillars enables unprecedented precision in dietary interventions for preventing and managing chronic diseases.
Future developments in the field will likely focus on:
- Advanced Multi-Omics Integration: Combining genomics, microbiomics, metabolomics, proteomics, and transcriptomics into unified models that better predict individual responses to diet.
- AI and Machine Learning: Developing sophisticated algorithms that can process complex multi-omics data and generate actionable, personalized nutritional recommendations [67] [72].
- Dynamic Monitoring: Moving from static assessments to continuous monitoring of metabolic responses using wearable sensors and digital technologies [67].
- Nutritional Epigenetics: Deepening our understanding of how nutrients influence gene expression through epigenetic mechanisms and how these changes can be modulated through dietary interventions [69].
- Microbiome Engineering: Developing targeted interventions, including prebiotics, probiotics, and postbiotics, to shape the gut microbiome toward health-promoting configurations [73] [71].
The implementation of personalized nutrition in clinical practice and public health requires addressing challenges related to cost, accessibility, data privacy, and the need for robust clinical validation. However, the potential benefits for preventing and managing chronic diseases are substantial. As research continues to unravel the complex interactions between genes, diet, microbiome, and metabolism, personalized nutrition will play an increasingly important role in the precision medicine landscape, ultimately contributing to improved healthspan and reduced burden of chronic diseases worldwide.
The advent of Glucagon-like peptide-1 receptor agonists (GLP-1 RAs) represents a paradigm shift in the therapeutic management of obesity and type 2 diabetes, with emerging benefits for cardiovascular, neurological, and hepatic health. These medications achieve substantial weight loss—ranging from 5% to over 20% of body weight in clinical trials—primarily through appetite suppression, slowed gastric emptying, and reduced food cravings. However, this potent efficacy presents a unique set of nutritional challenges. Rapid weight loss induced by GLP-1 RAs is associated with significant risks, including the loss of lean body mass, micronutrient deficiencies, and gastrointestinal side effects. This whitepaper examines these nutritional considerations within the critical context of chronic disease prevention, arguing that integrating evidence-based dietary patterns is not merely supportive but foundational to achieving long-term therapeutic success and overall health. The physiological consequences of GLP-1 RA therapy share remarkable similarities with those observed post-bariatric surgery, highlighting an urgent need to translate established nutritional frameworks from surgical care to pharmacotherapy.
The Intersection of GLP-1 RA Therapy and Chronic Disease Burden
Diet is a leading modifiable risk factor for non-communicable diseases (NCDs). The Global Burden of Disease Study 2021 identifies dietary risks as major contributors to mortality and disability-adjusted life years (DALYs) from cardiovascular diseases, neoplasms, and diabetes. From 1990 to 2021, despite a global decrease in age-standardized mortality rates, diet-related factors such as high red meat intake, low whole grain consumption, and high sodium intake remained pivotal drivers of chronic disease burden [9].
GLP-1 RAs offer a powerful tool to mitigate this burden. Beyond weight loss and glycemic control, their benefits extend to cardiorenal protection and reduced major adverse cardiovascular events (MACE), as demonstrated in outcomes trials [74]. The protective effects are partly mediated through weight-independent pathways, including direct impacts on metabolic signatures and biological aging [51]. This positions GLP-1 RAs not simply as weight-loss drugs but as agents capable of modulating fundamental pathways linking diet to chronic disease. Therefore, optimizing nutrition during GLP-1 RA therapy is essential to amplify these benefits and counteract the medication's potential to inadvertently exacerbate nutritional deficits that fuel chronic diseases.
Key Nutritional Risks and Challenges with GLP-1 RA Therapy
Loss of Lean Mass and Inadequate Protein Intake
While GLP-1 RAs facilitate significant fat mass reduction, a concerning 30–40% of the weight lost can derive from fat-free mass [75]. This loss of skeletal muscle can impair metabolic health, diminish physical function, and compromise long-term weight maintenance [75]. The risk is particularly acute for older adults and individuals with sarcopenic obesity.
Current evidence indicates that protein intake among GLP-1 RA users is often suboptimal. A 2025 cross-sectional study found that while the percentage of calories from protein was within acceptable ranges, when calculated as grams per kilogram per day, intake was significantly below daily needs for weight loss [76]. Furthermore, nutrient timing is poor, with approximately 40% of total daily protein intake consumed at dinner, a pattern that fails to optimally stimulate muscle protein synthesis throughout the day [77].
Table 1: Preserving Lean Mass: Protein Recommendations Derived from Bariatric Protocols
| Parameter | Recommendation | Rationale & Evidence Base |
|---|---|---|
| Daily Protein Intake | 0.8–1.6 g/kg/day or 80–120 g absolute [75] | Higher than RDA to maintain positive protein balance during hypocaloric diet [76]. |
| Protein Quality | High-quality (complete) proteins | Provides all essential amino acids crucial for muscle protein synthesis. |
| Protein Distribution | Evenly distributed across meals [77] | Superior for stimulating muscle protein synthesis compared to skewed intake. |
| Complementary Therapy | Progressive resistance training [75] | Anabolic stimulus that works synergistically with protein intake to preserve lean mass. |
Micronutrient Deficiencies and Suboptimal Diet Quality
Reduced energy intake, early satiety, and dietary changes during GLP-1 RA therapy can lead to insufficient intake of essential nutrients. Unlike bariatric surgery, where preoperative nutritional screening is standard, no formal consensus exists for patients commencing GLP-1 RAs [75].
Recent research confirms these concerns. A 2025 analysis using the Healthy Eating Index (HEI) revealed that the total HEI score of GLP-1 RA users was 54 ± 12, significantly below the target and indicating suboptimal diet quality [77]. This was reflected in low intakes of fruits, vegetables, whole grains, seafood, and plant proteins. Another 2025 cross-sectional study comparing nutrient intakes to Dietary Reference Intakes (DRI) found significant deficiencies in fiber, calcium, iron, magnesium, potassium, choline, and vitamins A, C, D, and E, while fat and saturated fat were overconsumed [76].
Table 2: Identified Micronutrient Deficiencies and Dietary Shortfalls in GLP-1 RA Users
| Nutrient/Food Group | Finding in GLP-1 RA Users | Recommended Daily Intake (DRI) |
|---|---|---|
| Fiber | 14.5 g [76] | 25-38 g |
| Calcium | 863 mg [76] | 1,000-1,200 mg |
| Vitamin D | 4 mcg [76] | 15-20 mcg |
| Iron | 12.1 mg [76] | 8-18 mg |
| Fruits & Vegetables | Did not meet MyPlate servings [76] | 4-6 cups (varies) |
| Whole Grains | Did not meet MyPlate servings [76] | 3-5 oz eq (varies) |
Gastrointestinal Symptoms and Altered Eating Behaviors
Nausea, vomiting, and constipation are commonly encountered side effects, particularly during dose titration [75]. These symptoms can interfere with treatment adherence and dietary quality.
Simultaneously, patients experience beneficial changes in eating behavior, including reduced hunger, fewer food cravings, and a decrease in "food noise" [75]. However, these shifts can also lead to unintended consequences, such as a reduced dietary variety or the development of aversions to certain nutrient-dense foods. Therefore, behavioral nutrition support is critical to help patients navigate these changes, manage side effects, and build sustainable, healthy dietary patterns.
Dietary Patterns for Therapeutic Synergy and Chronic Disease Prevention
The choice of an overall dietary pattern is critical for aligning GLP-1 RA therapy with long-term goals of chronic disease prevention and healthy aging. Large-scale cohort studies consistently demonstrate that high-quality dietary patterns are associated with a significantly greater likelihood of healthy aging—encompassing intact cognitive, physical, and mental health, and freedom from chronic diseases [7].
Evidence-Based Dietary Patterns
- Mediterranean-DASH Intervention for Neurodegenerative Delay (MIND) Diet: This pattern has demonstrated the broadest neuroprotective effects in large observational studies. Adherence to the MIND diet is significantly associated with a reduced risk of dementia, stroke, depression, and anxiety [51]. Its protective effects are mediated through favorable metabolic signatures and slower biological aging [51].
- Alternative Healthy Eating Index (AHEI): In the Nurses' Health Study and Health Professionals Follow-Up Study, the AHEI showed the strongest association with healthy aging. Participants in the highest quintile of AHEI adherence had 1.86 times greater odds of healthy aging compared to the lowest [7].
- Planetary Health Diet Index (PHDI) and Healthful Plant-based Diet (hPDI): These patterns also show strong associations with positive health outcomes, including better cognitive function and survival [7]. They emphasize plant-based foods while allowing for moderate, healthful inclusion of animal-based foods.
Conversely, high intake of ultra-processed foods (UPF) is consistently associated with an increased risk for dementia, Parkinson's disease, depression, and anxiety [51]. This underscores the importance of guiding GLP-1 RA patients toward whole-food, minimally processed dietary patterns.
Synergistic Mechanisms
These recommended dietary patterns share common denominators: they are rich in fruits, vegetables, whole grains, nuts, legumes, and unsaturated fats, while limiting processed foods, red meats, and sugary beverages. These components work synergistically with GLP-1 RA therapy by:
- Providing a high nutrient density to prevent deficiencies despite lower calorie intake.
- Supplying adequate dietary fiber to mitigate constipation, a common GLP-1 RA side effect, and support the gut microbiome.
- Offering anti-inflammatory benefits and promoting a healthy metabolic profile, which may enhance the cardiometabolic and neuroprotective effects of the medication.
Experimental Protocols and Research Methodologies
To advance the field, standardized methodologies are required to assess nutritional status and body composition in the context of GLP-1 RA therapy.
Protocol for Dietary Intake Assessment in GLP-1 RA Research
Objective: To accurately quantify dietary intake, diet quality, and nutrient timing in individuals using GLP-1 RAs. Methodology: Cross-sectional or longitudinal assessment using 3-day food records. Key Tools and Procedures:
- Tool: Automated Self-Administered 24-Hour Dietary Assessment Tool (ASA24) [77].
- Duration: Three consecutive days of food recording, ideally starting on the day of the weekly injection to standardize assessment [77].
- Participant Training: Provide a protocol covering system navigation, food selection, portion size estimation, and how to record complex meals [77].
- Data Analysis:
- Diet Quality: Calculate the Healthy Eating Index (HEI) total and component scores. The HEI is a validated measure of dietary quality independent of quantity [77].
- Nutrient Intake: Analyze average intakes of macro- and micronutrients and compare to Dietary Reference Intakes (DRI) using confidence intervals with appropriate statistical correction (e.g., Bonferroni) [76].
- Nutrient Timing: Analyze the distribution of calories, protein, and other nutrients across breakfast, lunch, dinner, and snacks [77].
Protocol for Body Composition and Functional Assessment
Objective: To evaluate changes in lean mass and physical function during GLP-1 RA-induced weight loss. Key Tools and Procedures:
- Body Composition: Direct measurement with Dual-Energy X-ray Absorptiometry (DXA) is preferred for its accuracy and accessibility. For studies focusing specifically on muscle mass preservation, Magnetic Resonance Imaging (MRI) should be prioritized [75].
- Functional Assessment: Measures like handgrip strength provide a practical and informative correlate of overall muscle strength and function [75].
- Biochemical Monitoring: Baseline and periodic assessment of key micronutrients (e.g., iron, Vitamin B12, Vitamin D, calcium) is recommended, especially for high-risk groups [75].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Tools for Nutritional Studies in GLP-1 RA Therapy
| Tool / Reagent | Function & Application | Example Use Case |
|---|---|---|
| Automated Self-Administered 24-Hour Dietary Assessment Tool (ASA24) | Electronic, self-administered 24-hour dietary recall or food record system. Improves validity of dietary intake data. | Collecting detailed 3-day food records from GLP-1 RA users in an observational study [77]. |
| Healthy Eating Index (HEI) | A validated score indicating overall diet quality, independent of quantity. Comprises 13 adequacy and moderation components. | Quantifying and comparing the diet quality of a cohort using GLP-1 RAs against national benchmarks [77]. |
| Dual-Energy X-ray Absorptiometry (DXA) | Imaging technology that provides precise measurement of body composition (fat mass, lean mass, bone density). | Tracking changes in lean body mass in a clinical trial of GLP-1 RA combined with a high-protein diet [75]. |
| Handgrip Dynamometer | Portable device for measuring isometric handgrip strength, a validated proxy for overall muscle strength and functional status. | Assessing functional correlates of muscle mass in sarcopenic obesity patients on GLP-1 RAs [75]. |
| Validated Food Noise Questionnaire | A recently developed tool to quantitatively assess the reduction in intrusive food-related thoughts [75]. | Evaluating the behavioral and psychological effects of GLP-1 RAs on eating behaviors in conjunction with dietary interventions. |
| Oxypeucedanin | Oxypeucedanin | High-purity Oxypeucedanin, a furanocoumarin from Angelica dahurica. Explore its research applications in cardiology and oncology. For Research Use Only. Not for human consumption. |
Signaling Pathways and Conceptual Workflow
The following diagram illustrates the conceptual framework linking GLP-1 RA therapy, nutritional interventions, and their combined impact on body composition and chronic disease risk, integrating the core concepts discussed in this whitepaper.
Diagram 1: GLP-1 RA and Nutrition Interaction Framework
GLP-1 RAs have irrevocably altered the therapeutic landscape for obesity and related chronic diseases. However, their long-term success is contingent upon integrating comprehensive nutritional strategies that address the inherent risks of rapid weight loss and leverage the synergy between diet and pharmacology. The research community must now prioritize the development of international, GLP-1 RA-specific nutritional consensus guidelines to bridge the current guidance gap [75]. Critical areas for future investigation include determining optimal protein dosing and timing, validating the efficacy of specific dietary patterns like the MIND diet in conjunction with therapy, and exploring the role of structured behavioral support to improve dietary adherence and psychological well-being. By adopting a multidisciplinary approach that places nutrition at the core of GLP-1 RA treatment protocols, researchers and clinicians can ensure that these powerful therapeutics realize their full potential in promoting not only weight loss but also lasting health and healthy aging.
Sustainable nutrition represents an critical frontier in public health, demanding dietary patterns that simultaneously reduce chronic disease risk and environmental impact. This review synthesizes evidence from large-scale prospective cohort studies and global burden of disease analyses to establish the dual-benefit potential of specific dietary frameworks. Findings demonstrate that dietary patterns emphasizing plant-based foods, with moderate inclusion of healthy animal-based foods, are associated with significantly lower risks of major chronic diseases and promote healthy aging, while concurrently reducing agricultural greenhouse gas emissions and environmental resource demand. The Planetary Health Diet emerges as a unifying framework capable of guiding future dietary recommendations that align human and planetary health objectives.
The global burden of chronic diseases and environmental degradation share a common driver: contemporary food systems. Chronic diseases account for more than half of all premature deaths and over 90% of yearly healthcare spending in the United States [1]. Simultaneously, food systems contribute significantly to environmental challenges, including greenhouse gas emissions, water scarcity, and land use change [78]. This intersection creates an urgent need for sustainable nutrition frameworks that simultaneously address human health and planetary boundaries.
Research has historically focused on either the health impacts of diet or environmental consequences in isolation. However, emerging evidence supports the integration of these dimensions. The 2025 EAT-Lancet Commission reports that adopting healthier, planet-friendly diets could prevent approximately 40,000 early deaths daily worldwide and cut agricultural greenhouse gas emissions by more than half [57]. This whitepaper examines the scientific evidence linking dietary patterns to chronic disease prevention within the context of sustainable nutrition, providing researchers and drug development professionals with methodological frameworks and quantitative data to inform future interventions and recommendations.
Dietary Patterns and Chronic Disease Outcomes
Evidence from Prospective Cohort Studies
Large-scale prospective cohorts provide robust evidence linking dietary patterns with chronic disease incidence and healthy aging outcomes. Analysis of 205,852 healthcare professionals from three U.S. cohorts followed for up to 32 years demonstrated that adherence to healthy dietary patterns was generally associated with a 20-42% lower risk of major chronic diseases—a composite outcome of incident major cardiovascular disease (CVD), type 2 diabetes, and cancer [1]. The hazard ratios (HRs) comparing the 90th to 10th percentile of dietary pattern scores ranged from 0.58 to 0.80, with the most significant risk reduction observed for diets with low insulinemic (HR 0.58, 95% CI 0.57-0.60) and low inflammatory (HR 0.61, 95% CI 0.60-0.63) potential [1].
Table 1: Association between Dietary Patterns and Major Chronic Disease Risk
| Dietary Pattern | Hazard Ratio (90th vs 10th percentile) | 95% Confidence Interval | Strongest Associated Risk Reduction |
|---|---|---|---|
| Low Insulinemic Diet | 0.58 | 0.57, 0.60 | Major CVD, Diabetes, Cancer |
| Low Inflammatory Diet | 0.61 | 0.60, 0.63 | Major CVD, Diabetes, Cancer |
| Diabetes Risk-Reducing Diet | 0.70 | 0.69, 0.72 | Diabetes |
| Alternative Healthy Eating Index | 0.76 | 0.74, 0.77 | Major CVD |
| Planetary Health Diet | 0.79 | 0.77, 0.81 | Major CVD, Cancer |
| Healthful Plant-Based Diet | 0.80 | 0.78, 0.82 | Diabetes |
Long-term studies examining healthy aging outcomes further support these associations. Research from the Nurses' Health Study and Health Professionals Follow-Up Study with up to 30 years of follow-up revealed that higher adherence to healthy dietary patterns was consistently associated with greater odds of healthy aging—defined according to measures of cognitive, physical, and mental health, plus living to 70 years free of chronic diseases [7]. Among 105,015 participants, 9.3% achieved healthy aging, with those adhering to optimal dietary patterns showing 45-86% greater odds of healthy aging compared to those with the lowest adherence [7].
Food and Nutrient Components of Healthy Dietary Patterns
Analysis of individual dietary components reveals consistent patterns across various healthy dietary frameworks. Higher intakes of fruits, vegetables, whole grains, unsaturated fats, nuts, legumes, and low-fat dairy products are consistently linked to reduced chronic disease risk and greater odds of healthy aging [7]. Conversely, higher intakes of trans fats, sodium, sugary beverages, and red or processed meats are inversely associated with healthy aging outcomes [7].
Table 2: Association of Specific Food Groups with Healthy Aging Domains
| Dietary Component | Healthy Aging OR (95% CI) | Chronic Disease-Free OR (95% CI) | Intact Cognitive Function OR (95% CI) | Intact Physical Function OR (95% CI) |
|---|---|---|---|---|
| Fruits | 1.12 (1.08-1.16) | 1.10 (1.06-1.14) | 1.08 (1.04-1.12) | 1.14 (1.10-1.18) |
| Vegetables | 1.10 (1.06-1.14) | 1.08 (1.04-1.12) | 1.09 (1.05-1.13) | 1.11 (1.07-1.15) |
| Whole Grains | 1.15 (1.11-1.19) | 1.12 (1.08-1.16) | 1.11 (1.07-1.15) | 1.17 (1.13-1.21) |
| Nuts | 1.18 (1.14-1.22) | 1.15 (1.11-1.19) | 1.14 (1.10-1.18) | 1.20 (1.16-1.24) |
| Legumes | 1.09 (1.05-1.13) | 1.07 (1.03-1.11) | 1.06 (1.02-1.10) | 1.11 (1.07-1.15) |
| Red/Processed Meats | 0.85 (0.81-0.89) | 0.87 (0.83-0.91) | 0.88 (0.84-0.92) | 0.83 (0.79-0.87) |
The comparative risk assessment framework from the Global Burden of Disease Study 2021 identifies specific dietary risk factors contributing significantly to chronic disease burden globally. Diets low in whole grains, fruits, and vegetables, and high in sodium, red meat, and processed meats represent the most substantial contributors to diet-related chronic disease burden [9].
Methodological Considerations in Dietary Patterns Research
Dietary Assessment Methods
Accurate dietary assessment presents methodological challenges with significant implications for research validity. Traditional methods include food records, food frequency questionnaires (FFQs), and 24-hour recalls, each with distinct strengths and limitations [37].
Food records involve comprehensive recording of all foods, beverages, and supplements consumed during a designated period, typically 3-4 days. While potentially detailed, this method requires literate, motivated participants and is susceptible to reactivity—where participants change their usual diet for ease of recording or social desirability bias [37]. The 24-hour dietary recall (24HR) assesses intake over the previous 24 hours through interviewer administration or automated self-administered systems. This method reduces literacy barriers and potential reactivity but relies heavily on memory and requires multiple administrations to account for day-to-day variation [37]. Food frequency questionnaires (FFQs) assess usual intake over extended periods (months to years) by querying consumption frequency of specific food items. FFQs offer cost-effective population-level assessment but lack precision for absolute intake measurement and require literacy and cognitive effort to complete [37].
Short dietary screening instruments provide rapid assessment of specific dietary components when comprehensive assessment isn't feasible. These tools are particularly useful for characterizing population median intakes, discriminating between individuals with higher versus lower intakes, and examining diet-disease relationships in large studies with limited dietary assessment capacity [79].
Dietary Assessment Method Selection
Dietary Pattern Assessment Methods
Dietary pattern assessment methods broadly fall into index-based (a priori) and data-driven (a posteriori) approaches. Index-based methods measure adherence to predefined dietary patterns based on existing knowledge of diet-health relationships [80]. Common indices include the Alternative Healthy Eating Index (AHEI), Alternative Mediterranean Diet Score (aMED), Dietary Approaches to Stop Hypertension (DASH), and Planetary Health Diet Index (PHDI) [7] [80].
Data-driven methods use multivariate statistical techniques to derive dietary patterns from consumption data. Principal component analysis and factor analysis identify common patterns of food consumption, while reduced rank regression derives patterns based on their relationship with specific biomarkers or health outcomes [80]. Cluster analysis groups individuals with similar dietary patterns [80].
Standardization in application and reporting of dietary pattern methods remains challenging. A systematic review of 410 studies found considerable variation in how methods are applied and reported, with important methodological details often omitted [80]. This heterogeneity complicates evidence synthesis and translation into dietary guidelines.
The Planetary Health Diet Framework
Conceptual Foundation and Health Impacts
The Planetary Health Diet (PHD) represents a science-based dietary pattern designed to promote human health while protecting planetary systems. Formulated by the EAT-Lancet Commission, the PHD emphasizes minimally processed plant foods: whole grains, fruits, vegetables, nuts, and legumes comprise a large proportion of foods consumed, with only moderate amounts of fish, dairy, and meat [78]. The diet allows for cultural diversity and individual preferences while operating within clear guidelines to achieve optimal health and sustainability outcomes worldwide [57].
The PHD is associated with significant chronic disease risk reduction. Higher adherence to the Planetary Health Diet Index demonstrates a 21% lower risk of major chronic diseases compared to lower adherence [1]. The diet shows particular strength in promoting survival, with the strongest association observed for surviving to age 70 years among healthy aging domains [7]. Recent analyses from the 2025 EAT-Lancet Commission suggest even greater population health benefits than initially estimated, with annual preventable deaths revised upward from 11.6 million to 15 million globally [57].
Environmental Impact and Implementation Considerations
The environmental case for dietary pattern transformation is compelling. Widespread adoption of the Planetary Health Diet could reduce greenhouse gas emissions from agriculture by more than half [57]. This reduction is critical since food systems currently contribute significantly to transgression of planetary boundaries, including climate change, biodiversity loss, and nitrogen cycle disruption [78].
Implementation requires consideration of regional variations in dietary transitions. The Global Burden of Disease Study 2021 reveals distinct dietary risk profiles across sociodemographic index (SDI) regions [9]. In high-SDI regions, neoplasm-related deaths show stronger correlation with diets high in red meat, while in low-SDI regions, diets low in vegetables show the strongest association with neoplasm-related mortality, and diets low in fruits significantly link to CVD and diabetes burden [9]. This regional variation underscores the need for context-specific implementation strategies within the overarching Planetary Health Diet framework.
Planetary Health Diet Dual Benefits
Research Toolkit for Sustainable Nutrition
Dietary Assessment Instruments
Validated dietary assessment instruments provide essential tools for researching sustainable nutrition. The National Cancer Institute developed several short instruments assessing intake of fruits and vegetables, percentage energy from fat, fiber, added sugars, whole grains, calcium, dairy products, and red and processed meats [79]. These tools have been evaluated in cross-sectional general population studies and large surveys including the National Health Interview Survey and California Health Interview Survey [79].
For comprehensive dietary assessment, 24-hour recalls using automated self-administered systems like ASA24 provide quantitative dietary data with reduced interviewer burden [37]. Food frequency questionnaires tailored to specific populations enable assessment of habitual dietary intake over extended periods, though they require validation for the target population [37].
Biomarkers and Outcome Measures
Objective biomarkers strengthen dietary assessment by complementing self-reported data. Recovery biomarkers exist for energy (doubly labeled water), protein (urinary nitrogen), sodium (urinary sodium), and potassium (urinary potassium) [37]. Concentration biomarkers, such as plasma fatty acids or carotenoids, provide additional validation for specific dietary components.
Health outcome assessment should encompass multiple dimensions. Beyond traditional chronic disease endpoints, healthy aging measures capture cognitive, physical, and mental health preservation alongside disease avoidance [7]. Environmental impact metrics include greenhouse gas emissions, water use, land use, and nitrogen application, enabling comprehensive sustainability assessment [81].
Table 3: Research Reagent Solutions for Sustainable Nutrition Studies
| Research Tool | Primary Application | Key Features | Validation Considerations |
|---|---|---|---|
| ASA24 (Automated Self-Administered 24-hour Recall) | Quantitative dietary assessment | Multiple recalls possible, reduced interviewer burden | Comparison with recovery biomarkers |
| NCI Dietary Screener Questionnaire | Population screening | Assesses key dietary components, low participant burden | Calibration against 24HR in subgroup |
| Planetary Health Diet Index | Adherence to PHD | 16 components scoring based on EAT-Lancet reference | Associated with chronic disease risk |
| Recovery Biomarkers (Doubly Labeled Water, Urinary Nitrogen) | Validation of self-report | Objective measures of energy & protein intake | High cost limits large-scale use |
| Plasma Carotenoids | Fruit & vegetable intake validation | Objective biomarker for plant food consumption | Influenced by individual absorption |
Integrated Assessment Methodologies
Combining health and environmental assessment requires methodological innovation. Three principal approaches have emerged: parallel assessment (health and environmental impacts assessed separately), scaled assessment (impacts normalized to comparable scales), and integrated assessment (combined impact evaluation) [81]. Health metrics commonly used in combined assessments include avoided deaths or cases, disability-adjusted life years (DALYs), and quality-adjusted life years (QALYs) [81].
Systematic review methodology provides a rigorous framework for synthesizing evidence on sustainable nutrition. Key steps include developing analytic frameworks, refining research questions, defining eligibility criteria, assessing methodological quality, and synthesizing results [82]. Unique nutrition-related considerations include baseline nutrient exposure, nutrient status, bioequivalence of bioactive compounds, bioavailability, and multiple biological functions [82].
Sustainable nutrition represents a critical convergence of human health and environmental stewardship. Evidence from prospective cohort studies demonstrates that dietary patterns emphasizing plant-based foods with moderate animal-based foods significantly reduce chronic disease risk and promote healthy aging. Simultaneously, these dietary patterns reduce environmental impacts, particularly greenhouse gas emissions, land use, and water resource demand.
The Planetary Health Diet provides a scientifically-grounded framework for aligning human health with planetary health. Its implementation requires contextual adaptation across different populations and regions while maintaining core principles. Future research should prioritize standardized dietary assessment methodologies, combined health and environmental impact evaluation, and implementation science to translate evidence into effective policies and interventions.
For researchers and drug development professionals, sustainable nutrition offers a compelling paradigm for chronic disease prevention that simultaneously addresses pressing environmental challenges. Integrating these principles into research agendas and product development represents an unprecedented opportunity to advance both human and planetary health.
The rising global prevalence of metabolic syndrome (MetS) presents a critical challenge for biomedical research and therapeutic development. MetS represents a cluster of interrelated metabolic abnormalities—including abdominal obesity, hypertension, dyslipidemia, and impaired fasting glucose—that collectively double the risk of type 2 diabetes and quintuple the risk of major cardiovascular events [83]. With adult prevalence exceeding 20% globally and continuing to increase over time, effective management strategies have become a paramount public health concern [83] [84].
Traditional nutritional epidemiology often focused on individual nutrients or specific foods, an approach that fails to capture the complex interactions within whole dietary patterns. In recent years, research has shifted toward evaluating comprehensive dietary patterns that reflect the synergistic effects of multiple food components consumed together [83] [85]. This paradigm recognizes that diets constitute complex interventions where the whole often differs from the sum of its parts.
Network meta-analysis represents a methodological advancement that enables direct and indirect comparisons of multiple interventions simultaneously, providing a hierarchical ranking of their efficacy. This approach is particularly valuable for comparing dietary patterns where head-to-head trials are limited. This technical review synthesizes evidence from recent network meta-analyses to guide researchers and clinical developers in understanding the comparative effectiveness of major dietary patterns for MetS management.
Methodological Framework: Network Meta-Analysis in Nutritional Science
Search Strategy and Study Selection
The foundational network meta-analysis examined herein employed a comprehensive search strategy across nine electronic databases including EMBASE, Cochrane Library, PubMed, Web of Science, Scopus, and Chinese databases from their inception through April 1, 2025 [83] [84]. The search integrated MeSH subject terms and free terms related to metabolic syndrome and dietary patterns, with the PubMed strategy detailed in Table 1.
Table 1: Search Strategy for Network Meta-Analysis
| Step | Search Query Components |
|---|---|
| #1 | (metabolic syndrome[Title/Abstract]) OR (Metabolic Syndrome[MeSH Terms]) |
| #2 | Dietary pattern terms: (diet) OR (dietary pattern) OR (Ketogenic diet) OR (DASH diet) OR (Vegetarian diet) OR (Vegan diet) OR (Mediterranean diet) OR (Low-fat diet) OR (Low-carbohydrate diet*) |
| #3 | #1 AND #2 |
| #4 | Limit to randomized controlled trials |
Inclusion and Exclusion Criteria
The analysis employed strict PICOS criteria for study selection:
- Population (P): Adults ≥18 years with diagnosed MetS [83]
- Intervention (I): One of six dietary patterns: DASH, vegan, low-carbohydrate, Mediterranean, low-fat, or ketogenic diet [83]
- Comparison (C): Control diet (usual diet or typical national diet) [83]
- Outcomes (O): Waist circumference, systolic/diastolic blood pressure, fasting blood glucose, triglycerides, HDL cholesterol [83]
- Study Design (S): Randomized controlled trials [83]
Exclusion criteria removed studies involving children, pregnant or lactating women, non-Chinese/English publications, and duplicate publications [83].
Statistical Analysis and Quality Assessment
The network meta-analysis was conducted using Stata 16.0 software, employing frequentist approaches with mean differences (MD) and 95% confidence intervals. The analysis integrated both direct and indirect evidence to compare the six dietary patterns against control diets and against each other. Methodological quality was assessed using the Cochrane risk of bias tool, and the certainty of evidence was evaluated using GRADE criteria where applicable [83] [84].
Comparative Efficacy of Dietary Patterns for Metabolic Syndrome Components
Network Meta-Analysis Results
The analysis included 26 randomized controlled trials encompassing 2,255 patients with MetS. The results demonstrated significant differences in the efficacy of various dietary patterns for specific MetS components, with ranking probabilities indicating the optimal patterns for each parameter [83] [86].
Table 2: Effects of Dietary Patterns on Metabolic Syndrome Components
| MetS Component | Most Effective Diet | Mean Difference (95% CI) | Secondary Effective Diet | Mean Difference (95% CI) |
|---|---|---|---|---|
| Waist Circumference | Vegan | MD = -12.00 (-18.96, -5.04) | DASH | MD = -5.72 (-9.74, -1.71) |
| Systolic Blood Pressure | Ketogenic | MD = -11.00 (-17.56, -4.44) | DASH | MD = -5.99 (-10.32, -1.65) |
| Diastolic Blood Pressure | Ketogenic | MD = -9.40 (-13.98, -4.82) | - | - |
| Fasting Blood Glucose | Mediterranean | Ranking probability: 84.5% | - | - |
| Triglycerides | Ketogenic | Ranking probability: 79.8% | - | - |
| HDL Cholesterol | Vegan | Ranking probability: 87.9% | - | - |
Hierarchical Ranking of Dietary Patterns
Based on surface under the cumulative ranking curve (SUCRA) probabilities, the network meta-analysis generated hierarchy of effectiveness for overall MetS management:
- Vegan diet: Most effective for reducing waist circumference and increasing HDL cholesterol levels [83]
- Ketogenic diet: Most effective for lowering blood pressure and triglyceride levels [83]
- Mediterranean diet: Most effective for regulating fasting blood glucose [83]
- DASH diet: Effective for reducing waist circumference and systolic blood pressure [83]
The current evidence indicates that the vegan, ketogenic, and Mediterranean diets have more pronounced effects on ameliorating MetS compared to low-fat, low-carbohydrate, and control diets [83] [86].
Experimental Protocols for Dietary Pattern Research
Defining Dietary Intervention Protocols
The network meta-analysis established specific nutritional compositions for each dietary pattern based on established guidelines:
- DASH Diet: High intake of fruits, vegetables, low-fat dairy products, and whole grains; limited red meat and sugar. Macronutrient distribution: 55% carbohydrate, 18% protein, 27% fat (6% saturated) [83]
- Vegan Diet: Whole grains, legumes, vegetables, fruits, nuts, mushrooms, and algae as core components; flexible carbohydrate-to-protein ratio with unsaturated fatty acids as primary fat [83]
- Mediterranean Diet: Vegetables, fruits, nuts, legumes, whole grains, olive oil; moderate fish, dairy, red wine; limited red meat. Macronutrient distribution: 35-45% fat (mainly monounsaturated), 40-45% carbohydrate, 15-18% protein [83]
- Ketogenic Diet: Severe carbohydrate restriction (5-10% of total energy), replaced with dietary fat and adequate protein [83]
- Low-Carbohydrate Diet: Carbohydrate intake strictly limited to <25% of total energy [83]
- Low-Fat Diet: Emphasis on high grain and cereal intake; fat <30% of total energy, 50-60% carbohydrate, 10-15% protein [83]
Outcome Measurement Protocols
Standardized measurement protocols were essential for ensuring comparability across studies:
- Waist Circumference: Measured at the midpoint between the lower rib and the iliac crest [87]
- Blood Pressure: Measured after 5 minutes rest, twice on the right arm, averaged [88]
- Biochemical Parameters: Fasting blood samples (12-hour fast) analyzed for glucose, triglycerides, HDL cholesterol using standardized enzymatic methods [85] [87]
- Dietary Adherence: Assessed using validated food frequency questionnaires, 24-hour recalls, or dietary records [85] [87]
Visualization of Dietary Pattern Efficacy
Network Relationships of Dietary Patterns and Metabolic Outcomes
The diagram below illustrates the conceptual network of relationships between dietary patterns and their primary metabolic outcomes based on the network meta-analysis results.
Research Workflow for Network Meta-Analysis of Dietary Patterns
This diagram outlines the methodological workflow for conducting network meta-analyses of dietary patterns, from literature search to evidence synthesis.
The Scientist's Toolkit: Research Reagent Solutions for Nutritional Epidemiology
Table 3: Essential Methodological Tools for Dietary Pattern Research
| Research Tool | Function | Application Example |
|---|---|---|
| Stata 16.0 with Network Package | Statistical software for network meta-analysis | Performing mixed-treatment comparisons of multiple dietary patterns [83] |
| Validated FFQ (Food Frequency Questionnaire) | Assess habitual dietary intake over specified period | Measuring adherence to dietary interventions in RCTs [85] [87] |
| Gaussian Graphical Models (GGM) | Identify dietary networks and conditional dependencies between food groups | Analyzing complex dietary pattern structures in observational studies [85] |
| Cochrane Risk of Bias Tool (RoB 2.0) | Assess methodological quality of randomized trials | Evaluating internal validity of included studies in systematic reviews [83] |
| GRADE (Grading of Recommendations, Assessment, Development, and Evaluations) | Rate certainty of evidence across studies | Translating network meta-analysis findings to clinical recommendations [83] |
| Dietary Diversity Score (DDS) | Quantitative measure of variety across food groups | Assessing dietary quality in relation to MetS risk [87] |
This synthesis of evidence from network meta-analyses demonstrates a stratified approach to dietary pattern recommendations for MetS, with vegan, ketogenic, and Mediterranean diets showing superior efficacy for specific metabolic parameters. Rather than a one-size-fits-all approach, these findings support precision nutrition strategies that match dietary patterns to individual metabolic presentations.
For the pharmaceutical and healthcare industries, these findings highlight the importance of considering dietary interventions as foundational components of comprehensive metabolic syndrome management. Future research should focus on long-term sustainability of these dietary patterns, their molecular mechanisms of action, and potential synergies with pharmacological interventions in the prevention and management of metabolic diseases.
The application of advanced methodological approaches like network meta-analysis and Gaussian graphical models represents a maturation of nutritional epidemiology, providing more robust evidence for clinical and public health decision-making. As dietary pattern research continues to evolve, these methodologies will be essential for translating complex nutritional data into actionable therapeutic strategies.
Head-to-Head Comparisons: Network Meta-Analyses, Biomarker Validation, and Diet Efficacy Rankings
Metabolic Syndrome (MetS) represents a cluster of interconnected metabolic abnormalities—including abdominal obesity, hypertension, dyslipidemia, and impaired fasting glucose—that collectively elevate the risk for cardiovascular disease, type 2 diabetes, and all-cause mortality [83]. With a global prevalence exceeding 20% in adults and continuing to rise, MetS has emerged as a critical public health challenge worldwide [83]. Dietary modification serves as a cornerstone of MetS management, yet with multiple dietary patterns advocated in clinical guidelines, determining their comparative efficacy remains challenging for researchers and clinicians.
Traditional pairwise meta-analyses face limitations in comparing multiple interventions simultaneously, particularly when direct head-to-head trials are scarce or unavailable [89]. Network meta-analysis (NMA) addresses this methodological gap by integrating both direct evidence (from trials comparing interventions directly) and indirect evidence (derived through a common comparator) within a unified analytical framework [89]. This approach enables quantitative ranking of multiple dietary interventions and provides more precise effect estimates, even for comparisons lacking direct trial evidence [90].
This technical guide examines the application of NMA to evaluate dietary interventions for MetS parameters, contextualizing findings within broader chronic disease research. We present comprehensive quantitative results, detailed methodological protocols, and specialized research tools to support evidence-based decision-making in nutritional science and chronic disease prevention.
Methodological Framework of Network Meta-Analysis
Core Principles and Assumptions
Network meta-analysis extends conventional pairwise meta-analysis by synthesizing evidence across a network of interventions [89]. The fundamental structure comprises nodes (representing interventions) connected by edges (representing direct comparisons from clinical trials) [89]. For dietary pattern comparisons, a typical network might include nodes for the ketogenic diet, Mediterranean diet, DASH diet, vegan diet, and a control group, with edges formed by randomized controlled trials (RCTs) comparing any two of these interventions.
The validity of NMA rests upon two critical assumptions: transitivity and consistency [89]. Transitivity implies that indirect comparisons are biologically and methodologically plausible—for example, that participants receiving different dietary interventions in separate trials are sufficiently similar in baseline characteristics to permit meaningful comparison. Statistical consistency requires agreement between direct and indirect evidence sources; significant inconsistency suggests effect modifiers may be unevenly distributed across comparisons [90].
Statistical Foundations
The NMA model estimates relative treatment effects for all pairwise comparisons, including those not directly studied in head-to-head trials [89]. For continuous outcomes common in MetS research (e.g., blood pressure, lipid levels), the effect size is typically expressed as a mean difference (MD) with 95% confidence intervals (CI).
The basic statistical model for an NMA can be represented as follows [89]:
- Direct evidence: Effect estimate θAB from trials directly comparing intervention A vs. B
- Indirect evidence: Effect estimate θAC derived through a common comparator B: θAC = θAB - θCB
- Network estimate: Combined direct and indirect evidence using multivariate meta-analysis
The variance of indirect comparisons incorporates uncertainties from both direct comparisons: Var(θAC) = Var(θAB) + Var(θCB) [89]. This typically results in wider confidence intervals for indirect estimates compared to direct evidence.
Diagram 1: NMA evidence synthesis from direct and indirect comparisons.
Comparative Efficacy of Dietary Patterns for Metabolic Syndrome
Network Meta-Analysis of Dietary Interventions
A recent network meta-analysis specifically addressed the comparative efficacy of six dietary patterns for MetS management, analyzing 26 randomized controlled trials with 2,255 patients [83] [84]. The investigated dietary patterns included the ketogenic diet, Dietary Approaches to Stop Hypertension (DASH) diet, vegan diet, Mediterranean diet, low-fat diet, and low-carbohydrate diet, all compared against control diets representing usual intake patterns [83].
The analysis employed frequentist NMA methods using Stata 16.0 software, with random-effects models to account for between-study heterogeneity [83]. Effect sizes were expressed as mean differences for continuous outcomes across all six MetS diagnostic components, enabling comprehensive assessment of each diet's metabolic impact.
Quantitative Efficacy Rankings Across Metabolic Parameters
Table 1: Efficacy of dietary patterns on waist circumference and blood pressure parameters in metabolic syndrome
| Dietary Pattern | Waist Circumference MD [95% CI] | Systolic BP MD [95% CI] | Diastolic BP MD [95% CI] |
|---|---|---|---|
| Vegan | -12.00 [-18.96, -5.04] | — | — |
| DASH | -5.72 [-9.74, -1.71] | -5.99 [-10.32, -1.65] | — |
| Ketogenic | — | -11.00 [-17.56, -4.44] | -9.40 [-13.98, -4.82] |
| Mediterranean | — | — | — |
| Low-carbohydrate | — | — | — |
| Low-fat | — | — | — |
MD: Mean Difference from control diet; BP: Blood Pressure; CI: Confidence Interval [83] [84]
Table 2: Efficacy of dietary patterns on glycemic and lipid parameters in metabolic syndrome
| Dietary Pattern | Fasting Blood Glucose MD [95% CI] | Triglycerides MD [95% CI] | HDL-C MD [95% CI] |
|---|---|---|---|
| Mediterranean | Most effective | — | — |
| Ketogenic | — | Most effective | — |
| Vegan | — | — | Most effective |
| DASH | — | — | — |
| Low-carbohydrate | — | — | — |
| Low-fat | — | — | — |
HDL-C: High-Density Lipoprotein Cholesterol [83] [84]
The NMA results demonstrated distinct specialization among dietary patterns for different MetS components [83] [84]. The vegan diet produced the most substantial reduction in waist circumference (MD -12.00 cm) and was most effective for increasing HDL-C levels. The ketogenic diet showed superior efficacy for blood pressure reduction (SBP MD -11.00 mmHg; DBP MD -9.40 mmHg) and triglyceride management. The Mediterranean diet excelled specifically in regulating fasting blood glucose, while the DASH diet provided significant benefits for both waist circumference (MD -5.72 cm) and systolic blood pressure (MD -5.99 mmHg) [83].
Based on cumulative ranking probabilities (SUCRA values), the vegan, ketogenic, and Mediterranean diets demonstrated the most pronounced overall effects for ameliorating MetS [84]. These findings highlight the potential for personalized dietary recommendations based on an individual's predominant metabolic abnormalities.
Methodological Protocols for Dietary NMA
Search Strategy and Study Selection
Comprehensive literature searches should encompass multiple electronic databases including EMBASE, Cochrane Library, PubMed, Web of Science, Scopus, and region-specific databases where relevant [83]. Search strategies must integrate Medical Subject Headings (MeSH) and free-text terms related to both metabolic syndrome and dietary patterns.
Sample PubMed Search Strategy [83]:
(metabolic syndrome[Title/Abstract]) OR (Metabolic Syndrome[MeSH Terms])((((diet*[Title/Abstract]) OR (dietary pattern*[Title/Abstract])) OR (Diet, Ketogenic[MeSH Terms])) OR (Ketogenic diet*[Title/Abstract])) OR (DASH diet*[Title/Abstract])(randomized controlled trial[Publication Type]) OR (randomized[Title/Abstract])#1 AND #2 AND #3
Study selection should follow the PRISMA-NMA guidelines, with independent duplicate screening and reconciliation processes [83]. Predefined inclusion criteria typically encompass: (1) Population: Adults ≥18 years with diagnosed MetS; (2) Intervention: One of the specified dietary patterns; (3) Comparison: Control diet or alternative dietary pattern; (4) Outcomes: Core MetS parameters; (5) Study design: Randomized controlled trials [83].
Data Extraction and Quality Assessment
Standardized data extraction should capture: study characteristics (author, year, country, design), participant demographics (sample size, age, gender distribution), intervention details (dietary composition, duration, adherence measures), and outcome data (means, standard deviations, sample sizes for all timepoints) [83].
Critical appraisal should utilize the Cochrane Risk of Bias tool, assessing domains of sequence generation, allocation concealment, blinding of participants and outcome assessors, incomplete outcome data, selective reporting, and other potential biases [83]. For dietary interventions, special attention should be paid to the methodological challenges of blinding and the robustness of adherence assessment methods.
Statistical Analysis and Model Implementation
Analysis typically employs frequentist or Bayesian NMA frameworks implemented in specialized software (Stata, R with netmeta package, or WinBUGS) [83] [89]. The core analytical sequence includes:
- Network geometry mapping to visualize available direct comparisons
- Pairwise meta-analyses for each direct comparison using random-effects models
- Global heterogeneity assessment using I² statistics and τ² estimates
- Network meta-analysis synthesizing direct and indirect evidence
- Consistency assessment using node-splitting or design-by-treatment interaction models
- Treatment ranking using surface under the cumulative ranking curve (SUCRA) values
- Sensitivity analyses and assessment of publication bias
Diagram 2: Workflow for dietary pattern network meta-analysis.
Integration with Broader Chronic Disease Research
The comparative efficacy of dietary patterns for MetS management aligns with their established roles in chronic disease prevention more broadly. Large prospective cohort studies with up to 32 years of follow-up have demonstrated that multiple healthy dietary patterns—including the Alternative Healthy Eating Index (AHEI), Mediterranean diet, DASH, and plant-based diets—are associated with significantly lower risks of major cardiovascular disease, type 2 diabetes, and cancer [1].
Mechanistically, dietary patterns associated with lower chronic disease risk typically share common features: emphasis on plant-based foods, unsaturated fats, high fiber, and limited processed foods, red meats, and added sugars [1] [7]. These patterns consistently correlate with favorable biomarkers including reduced inflammation, improved insulin sensitivity, and healthier lipid profiles—the same physiological pathways targeted for MetS management [1].
Recent research has specifically examined dietary patterns in relation to healthy aging, defined as survival to 70 years free of major chronic diseases with intact cognitive, physical, and mental health [7]. Higher adherence to healthy dietary patterns was associated with 45-86% greater odds of healthy aging, with the AHEI showing the strongest association (OR 1.86, 95% CI 1.71-2.01) [7]. This multidimensional outcome reinforces the importance of dietary pattern research beyond disease-specific endpoints to encompass overall healthspan and functional status.
Table 3: Essential methodological resources for dietary network meta-analysis
| Resource Category | Specific Tools/Software | Application in Dietary NMA |
|---|---|---|
| Statistical Software | Stata (network package) | Frequentist NMA implementation with various modeling options |
| R (netmeta, gemtc packages) | Comprehensive NMA platform supporting both frequentist and Bayesian approaches | |
| WinBUGS/OpenBUGS | Bayesian NMA implementation with flexible random-effects models | |
| Quality Assessment | Cochrane Risk of Bias tool | Standardized assessment of methodological quality in RCTs |
| CINeMA framework | Confidence in Network Meta-Analysis tool for certainty assessment | |
| Data Visualization | Network graphs | Visual representation of evidence structure and treatment comparisons |
| Contribution plots | Illustration of direct and indirect evidence proportions for estimates | |
| Rankograms | Display of treatment ranking probabilities across outcome measures | |
| Reporting Guidelines | PRISMA-NMA checklist | Standardized reporting framework for network meta-analyses |
Component network meta-analysis (CNMA) represents an advanced extension that disentangles the effects of individual dietary components within complex interventions [91]. This approach is particularly relevant for dietary research where interventions often share common elements (e.g., multiple plant-based diets emphasizing fruits and vegetables) while differing in other aspects. CNMA models can estimate component-specific effects and their potential interactions, providing insights into the active ingredients of complex dietary prescriptions [91].
Specialized visualization approaches have been developed to represent CNMA evidence structures, including CNMA-UpSet plots for arm-level data, CNMA heat maps for component co-occurrence patterns, and CNMA-circle plots for component combinations [91]. These visualization tools help researchers understand complex evidence networks and communicate findings effectively.
Network meta-analysis provides a powerful methodological framework for comparing the efficacy of multiple dietary patterns across the core parameters of metabolic syndrome. Current evidence indicates specialized efficacy profiles: vegan diets for weight management and HDL-C improvement, ketogenic diets for blood pressure and triglyceride reduction, and Mediterranean diets for glycemic control [83] [84]. These findings align with broader chronic disease research demonstrating consistent benefits of plant-emphasizing dietary patterns rich in fruits, vegetables, whole grains, and unsaturated fats [1] [7].
Methodological rigor in dietary NMA requires careful attention to transitivity assumptions, consistency assessments, and appropriate statistical modeling of direct and indirect evidence [89] [90]. Future research priorities include longer-term trials comparing optimized dietary patterns, exploration of individual response variability, and integration of multi-omics biomarkers to elucidate mechanistic pathways. As dietary pattern research evolves, NMA will continue to provide essential quantitative synthesis to inform evidence-based nutritional recommendations for metabolic syndrome management and chronic disease prevention.
Dietary patterns significantly influence systemic biomarkers, modulating risk for chronic diseases. This whitepaper provides a comparative analysis of four prominent dietary patterns—Vegan, Ketogenic, Mediterranean, and DASH—evaluating their efficacy based on specific biomarkers of inflammation, metabolic health, and cardiovascular risk. Current evidence from randomized controlled trials and longitudinal studies indicates that the quality and composition of a diet are as critical as its classification. The Mediterranean diet consistently demonstrates robust improvements in inflammatory biomarkers, including IL-6 and hs-CRP. Plant-based diets like Vegan and DASH show significant benefits for metabolic and cardiovascular biomarkers, though their effectiveness is highly dependent on food quality. The ketogenic diet, while effective for rapid weight loss and certain inflammatory conditions, presents a more complex biomarker profile. This analysis provides researchers and drug development professionals with a detailed overview of experimental protocols, biomarker outcomes, and mechanistic pathways to inform future research and therapeutic development.
The global burden of chronic diseases is inextricably linked to modifiable lifestyle factors, with diet being a principal component. Research has progressively shifted from examining single nutrients to evaluating comprehensive dietary patterns and their impact on health outcomes. This whitepaper frames its analysis within the broader thesis that understanding the effect of dietary patterns on specific biomarkers is crucial for advancing chronic disease research, informing public health policy, and developing targeted nutritional interventions.
The four dietary patterns reviewed here represent distinct philosophical and macronutrient approaches. Mediterranean and DASH diets are widely endorsed by health organizations for their cardiovascular benefits. Vegan diets eliminate all animal products, while Ketogenic diets are high-fat, very low-carbohydrate regimens. Evaluating their performance through the lens of specific biomarkers—such as inflammatory cytokines, lipid profiles, and insulin resistance indices—provides an objective framework for comparison and elucidates potential mechanistic pathways through which these diets exert their effects.
Methodological Framework for Diet Comparison
Literature Search and Study Selection
The evidence synthesis for this review is based on a systematic approach to identifying relevant scientific literature. The primary research question guiding the selection was: What is the effect of Vegan, Ketogenic, Mediterranean, and DASH dietary patterns on specific biomarkers in adults?
A comprehensive search strategy was employed across major electronic databases, including PubMed, Scopus, Web of Science, and Cochrane Library. Search terms combined dietary patterns ("vegan diet," "ketogenic diet," "Mediterranean diet," "DASH diet") with outcome categories ("biomarkers," "inflammation," "lipid profile," "insulin resistance," "chronic disease"). The search was limited to studies published between 2013 and 2025 to ensure the inclusion of recent evidence, with a focus on randomized controlled trials (RCTs), longitudinal studies, and systematic reviews/meta-analyses. Study selection followed a structured process of title/abstract screening, full-text review, and data extraction using standardized forms to collect information on study design, population, intervention, outcomes, and key findings [92].
Biomarker Assessment Protocols
The biomarkers discussed in this review were measured using standardized, high-fidelity protocols in controlled settings. The following details the core methodologies for key biomarkers:
- Inflammatory Biomarkers (hs-CRP, IL-6, TNF-α): Blood samples are collected after an overnight fast. High-sensitivity C-reactive protein (hs-CRP) is typically quantified using immunoturbidimetric or ELISA assays. Cytokines including Interleukin-6 (IL-6) and Tumor Necrosis Factor-alpha (TNF-α) are measured using multiplex bead-based immunoassays (e.g., Luminex) or ELISA kits, providing precision in the pg/mL range [93] [94] [95].
- Lipid Profile (LDL-C, HDL-C, Triglycerides): Plasma or serum is isolated from fasting blood samples. Low-density lipoprotein cholesterol (LDL-C), high-density lipoprotein cholesterol (HDL-C), and triglycerides are analyzed using automated enzymatic methods on clinical chemistry analyzers. LDL-C is often calculated using the Friedewald equation or measured directly [96].
- Glycemic Control Markers (Fasting Glucose, Insulin, HbA1c): Fasting glucose is measured via enzymatic methods (e.g., hexokinase). Insulin is quantified using chemiluminescent immunoassays. The Homeostatic Model Assessment for Insulin Resistance (HOMA-IR) is calculated as: [Fasting Glucose (mg/dL) × Fasting Insulin (mU/L)] / 405 [93] [95]. Glycated hemoglobin (HbA1c) is assessed using high-performance liquid chromatography (HPLC) [92].
- Cardiovascular Risk Scores: The Systematic COronary Risk Evaluation 2 (SCORE2) index is calculated using algorithms incorporating age, sex, systolic blood pressure, smoking status, and total and HDL-cholesterol levels. This score estimates the 10-year risk of fatal and non-fatal cardiovascular events [95].
Comparative Performance on Biomarkers
Inflammatory Biomarkers
Chronic low-grade inflammation is a key pathogenic driver of numerous chronic diseases. The modulation of inflammatory biomarkers is a critical metric for evaluating dietary patterns.
Table 1: Impact of Dietary Patterns on Inflammatory Biomarkers
| Dietary Pattern | hs-CRP | IL-6 | TNF-α | Key Evidence |
|---|---|---|---|---|
| Mediterranean | ↓↓ | ↓↓ | Meta-analysis (33 RCTs): Significant reduction in hs-CRP and IL-6. No significant effect on TNF-α [97] [15]. | |
| DASH | ↓ | ↓ | RCTs: Shows consistent reduction in hs-CRP and IL-6, though effects can be influenced by intervention duration and population [96]. | |
| Vegan/Vegetarian | ↓ | ↓ | Cohort Study (Vegans vs. Omnivores): Vegans had substantially lower hs-CRP and IL-6. Effect is strongest with high-quality, whole-food plant-based diets [94]. | |
| Ketogenic (VLCKD) | ↓ | ↓ | ↓ | Proof-of-Concept Study (PsA): Significant reductions in hs-CRP and improvements in disease activity scores (DAPSA). IL-1β, IL-17 also reduced [93] [95]. |
Summary: The Mediterranean diet demonstrates the most consistent and robust anti-inflammatory effects across populations. The Ketogenic diet shows promise in specific clinical contexts, such as psoriatic arthritis, by downregulating a broader range of pro-inflammatory cytokines. The anti-inflammatory benefits of Vegan and DASH diets are significant but highly dependent on the consumption of healthful, minimally processed plant foods [94] [15].
Metabolic and Cardiovascular Biomarkers
These biomarkers are central to assessing the risk and progression of metabolic syndrome, type 2 diabetes, and cardiovascular disease.
Table 2: Impact of Dietary Patterns on Metabolic and Cardiovascular Biomarkers
| Dietary Pattern | LDL-C | HDL-C | HbA1c / Fasting Glucose | Blood Pressure | Key Evidence |
|---|---|---|---|---|---|
| Mediterranean | ↓ | ↑/ | ↓ | ↓ | Longitudinal Cohorts & RCTs: Associated with improved lipid profile, insulin sensitivity, and reduced cardiovascular risk [7] [15]. |
| DASH | ↓ | ↓ | ↓↓ | RCTs & Reviews: Originally designed for hypertension; significantly reduces SBP/DBP. Also improves insulin resistance and lipid profiles [96]. | |
| Vegan/Vegetarian | ↓↓ | ↓ | ↓ | Systematic Review: Associated with lower BMI, improved insulin sensitivity, and up to 34% reduced risk of type 2 diabetes. Significant LDL-C reduction [92] [94]. | |
| Ketogenic (VLCKD) | /↑ | ↑ | ↓↓ | ↓ | Clinical Studies: Leads to rapid improvements in HOMA-IR and fasting glucose. Variable effects on LDL-C (can increase). Promotes weight loss and TG reduction [93] [95]. |
Summary: The Vegan diet is particularly effective for reducing LDL-C and preventing diabetes. The DASH diet excels in blood pressure control. The Ketogenic diet produces rapid and significant improvements in glycemic control and triglycerides, though its long-term impact on LDL-C requires careful monitoring. The Mediterranean diet offers a balanced, comprehensive improvement across multiple metabolic and cardiovascular parameters [92] [96] [7].
Mechanistic Pathways
The biomarker changes induced by these dietary patterns are mediated through distinct yet sometimes overlapping biological pathways. The following diagrams, generated with Graphviz, illustrate the primary mechanistic routes for the Mediterranean and Ketogenic diets.
Mediterranean Diet: Anti-Inflammatory and Metabolic Pathways
The Mediterranean diet's benefits are largely mediated through its high content of anti-inflammatory compounds and healthy fats.
Diagram 1: Mediterranean diet mechanistic pathways.
Ketogenic Diet: Metabolic and Immunomodulatory Pathways
The ketogenic diet's effects are driven by a fundamental shift in energy substrate from glucose to ketone bodies.
Diagram 2: Ketogenic diet mechanistic pathways.
The Scientist's Toolkit: Research Reagent Solutions
To experimentally investigate the effects of these dietary patterns, researchers require a suite of reliable reagents and tools for biomarker quantification and pathway analysis.
Table 3: Essential Research Reagents and Materials
| Reagent/Tool | Primary Function | Example Application in Diet Research |
|---|---|---|
| Multiplex Bead-Based Immunoassay Kits | Simultaneous quantification of multiple cytokines (e.g., IL-6, TNF-α, IL-1β) from a single small-volume serum/plasma sample. | Ideal for profiling inflammatory status in RCTs comparing dietary patterns, maximizing data yield from limited biospecimens [93] [95]. |
| ELISA Kits for Metabolic Hormones | Quantitative measurement of hormones like insulin, leptin, and adiponectin. | Essential for calculating HOMA-IR and understanding the impact of diets like Ketogenic and Vegan on metabolic regulation [93] [95]. |
| Automated Clinical Chemistry Analyzers | High-throughput, precise measurement of lipids (LDL-C, HDL-C, TG), HbA1c, and glucose. | The workhorse for generating core metabolic panel data in large-scale nutritional cohort studies and interventions [92] [96]. |
| PCR Arrays / RNA-Seq Kits | Profiling expression of genes related to inflammation, metabolism, and oxidative stress. | Used to uncover molecular mechanisms, e.g., how the Mediterranean diet downregulates NF-κB pathway genes in peripheral blood mononuclear cells. |
| 16S rRNA Sequencing Kits | Comprehensive analysis of gut microbiome composition and diversity. | Critical for investigating the diet-gut-health axis, such as the effect of high-fiber DASH and Vegan diets on microbial SCFA production [92]. |
| Validated Food Frequency Questionnaires (FFQs) | Standardized assessment of habitual dietary intake to calculate adherence scores (e.g., aMED, PDI). | Fundamental for classifying participants' diets in observational studies like the Nurses' Health Study [7] [94]. |
Discussion and Research Gaps
The ranking of these dietary patterns is context-dependent, varying by the biomarker of interest and the target population. The Mediterranean diet emerges as the most consistently beneficial for overall inflammatory and metabolic health. The DASH diet is unparalleled for hypertension management. A well-constructed Vegan diet is powerful for improving cardiometabolic risk factors, while the Ketogenic diet is a potent intervention for rapid glycemic control and shows unique immunomodulatory potential.
Critical research gaps remain. Long-term, head-to-head RCTs are needed to directly compare these patterns. Future studies must deeper explore mechanistic pathways, including the role of the gut microbiome and epigenetic modifications [92]. Furthermore, the critical role of diet quality—emphasized by the distinction between healthful and unhealthful plant-based indices (hPDI vs. uPDI)—requires integration into all dietary pattern research [7] [94]. Finally, there is a pressing need for greater inclusivity of diverse populations in nutritional research to ensure that dietary guidelines are culturally relevant and equitable [92] [65].
This biomarker-based ranking provides a scientific foundation for researchers and clinicians. The choice of an optimal dietary pattern should be guided by specific health outcomes, individual patient factors, and the quality of food choices within any dietary framework. Future research focused on personalized nutrition, molecular mechanisms, and direct comparisons will further refine our understanding, enabling more precise dietary recommendations for chronic disease prevention and management.
Within the context of chronic disease research, a paradigm shift is occurring from studying isolated nutrients to investigating comprehensive dietary patterns and their underlying biological mechanisms. This whitepaper details the methodology for mechanistically validating dietary patterns through their insulinemic and inflammatory potential, providing researchers and drug development professionals with a framework for linking diet to chronic disease pathophysiology. Diets can modulate inflammation and insulin response, which in turn impacts the development of chronic diseases and cellular aging markers such as telomere length [98]. The progression from traditional dietary assessment to mechanism-based validation represents a critical advancement in nutritional epidemiology and preventive medicine, enabling more targeted interventions and therapeutic development.
Core Dietary Indices: Composition and Calculation
Empirical Dietary Indices for Insulinemia and Inflammation
Mechanism-based dietary indices move beyond simple nutrient composition to predict specific physiological responses. These empirical indices are derived using statistical methods that identify food combinations predictive of biomarker levels.
Table 1: Mechanism-Based Dietary Indices and Their Components
| Index Name | Abbreviation | Target Mechanism | Validation Biomarkers | Key Food Components (Pro-) | Key Food Components (Anti-) |
|---|---|---|---|---|---|
| Empirical Dietary Inflammatory Pattern | EDIP | Inflammation | CRP, Leukocyte count [98] | High-fat dairy, margarine, carbonated drinks [98] | Leafy green vegetables, whole grains, dark meat fish [98] |
| Empirical Dietary Index for Hyperinsulinemia | EDIH | Hyperinsulinemia | Fasting insulin, C-peptide [98] | Potatoes, processed meat, low-energy carbonated drinks [98] | Coffee, nuts, fruit juice [98] |
| Empirical Dietary Index for Insulin Resistance | EDIR | Insulin Resistance | HOMA-IR [98] | Potatoes, red meat, processed meat [98] | Leafy green vegetables, coffee, dark yellow vegetables [98] |
| Dietary Inflammatory Index | DII | Inflammation | IL-1β, IL-4, IL-6, IL-10, TNF-α, CRP [99] | Energy, carbohydrates, protein, fiber, vitamin A, C, D [99] | Multiple anti-inflammatory nutrients [99] |
Dietary Pattern Calculation Methodology
The empirical dietary indices (EDIP, EDIH, EDIR) are derived through a standardized statistical process:
- Food Group Definition: Thirty-nine commonly consumed food groups are defined consistent with previous methodologies [98].
- Pattern Derivation: Reduced rank regression (RRR) techniques derive dietary patterns using inflammation or hyperinsulinemia biomarkers as response variables and the 39 food groups as predictors [98].
- Component Selection: Stepwise linear regression identifies key component food groups from the 39 predefined groups.
- Weight Assignment: Regression coefficients from the final stepwise model assign weights to each food component.
- Score Calculation: Weighted food group components are summed to generate individual dietary index scores, where higher scores indicate increased pro-inflammatory or insulinemic potential [98].
For the Dietary Inflammatory Index (DII), calculation involves:
- Assigning inflammatory effect scores to 45 food parameters based on their impact on six specific inflammatory markers [99]
- Summing scores across all parameters to obtain an individual's DII
- Interpreting scores where values > 0 indicate pro-inflammatory diets and values < 0 indicate anti-inflammatory diets [99]
Validation Studies and Quantitative Outcomes
Epidemiological Validation in Major Cohorts
Large-scale prospective cohort studies have validated the association between mechanism-based dietary patterns and chronic disease incidence.
Table 2: Chronic Disease Risk Reduction Across Dietary Patterns
| Dietary Pattern | Study Cohort | Follow-up Duration | Outcome Measure | Risk Reduction (Highest vs. Lowest Adherence) | References |
|---|---|---|---|---|---|
| Low Insulinemic | NHS, NHS II, HPFS | 32 years | Major Chronic Disease* | HR: 0.58 (95% CI: 0.57, 0.60) | [1] |
| Low Inflammatory | NHS, NHS II, HPFS | 32 years | Major Chronic Disease* | HR: 0.61 (95% CI: 0.60, 0.63) | [1] |
| Diabetes Risk Reduction Diet | NHS, NHS II, HPFS | 32 years | Major Chronic Disease* | HR: 0.70 (95% CI: 0.69, 0.72) | [1] |
| Alternative Healthy Eating Index | NHS, HPFS | 30 years | Healthy Aging | OR: 1.86 (95% CI: 1.71, 2.01) | [7] |
| Reverse EDIH | NHS, HPFS | 30 years | Healthy Aging | OR: 1.77 (95% CI: 1.64, 1.92) | [7] |
Major chronic disease defined as composite of incident major cardiovascular disease, type 2 diabetes, and cancer [1] *Healthy aging defined as survival to 70 years free of chronic diseases with intact cognitive, physical, and mental health [7]
Biomarker Validation Studies
Cross-sectional studies using NHANES data have demonstrated direct associations between dietary patterns and biomarkers of aging and inflammation:
- Telomere Length: EDIR (per 1-SD increase: percentage change = -0.99%, 95% CI: -1.83%, -0.15%) and EDIH (percentage change = -1.03%, 95% CI: -1.94%, -0.11%) were significantly associated with shorter relative telomere length [98].
- Inflammatory Markers: HEI-2015 shows significant inverse associations with white blood cell count, neutrophils, neutrophil-to-lymphocyte ratio, and systemic immune-inflammation index, while DII exhibits significant positive associations with these markers [99].
- Component Analysis: Weighted quantile sum regression revealed that adequacy components in HEI-2015 such as seafood, plant proteins, and whole grains contributed most to reduced inflammation, while fiber, alcohol, and energy intake were primary contributors to inflammatory markers in DII [99].
Experimental Protocols and Methodologies
Cohort Study Implementation Protocol
Study Population Recruitment and Assessment
- Source Populations: Utilize established cohorts (e.g., Nurses' Health Study, Health Professionals Follow-up Study, NHANES) with detailed longitudinal data [98] [7] [1].
- Inclusion Criteria: Adults aged 20+ years with complete dietary assessment data [98].
- Exclusion Criteria: Participants with missing dietary records, implausible energy intakes (<600 kcal/day for women, <800 kcal/day for men or >3,500 kcal/day for women, >4,200 kcal/day for men), and missing biomarker data [98] [99].
Dietary Assessment Methodology
- Data Collection: Implement 24-hour dietary recalls using standardized instruments (e.g., Automated Multiple Pass Method) [98].
- Assessment Timing: Conduct multiple recalls (at least two) including in-person and telephone interviews to account for day-to-day variation [99].
- Quality Control: Employ trained interviewers, standardized protocols, and validated assessment tools [98].
Biomarker Measurement Protocols
- Inflammatory Markers: Collect venous blood samples for analysis of CRP, leukocyte count using standardized laboratory methods (e.g., Beckman Coulter DxH-800 instrument) [98] [99].
- Insulinemic Markers: Measure fasting insulin, C-peptide, and plasma glucose for HOMA-IR calculation (HOMA-IR = Fasting Insulin (μU/mL) × Fasting Plasma Glucose (mmol/L)/22.5) [98].
- Cellular Aging Markers: Isolate DNA from whole blood for relative telomere length measurement via quantitative polymerase chain reaction [98].
Statistical Analysis Plan
- Primary Analysis: Employ multivariable-adjusted linear and logistic regression models to assess diet-biomarker associations.
- Covariate Adjustment: Include age, gender, race, physical activity, BMI, smoking status, education, and socioeconomic factors in models [98] [99].
- Joint Effect Analysis: Conduct stratified analyses to examine interactive effects of multiple dietary patterns [99].
- Sensitivity Analyses: Perform subgroup analyses by age, gender, BMI status, and physical activity levels to identify potential effect modifiers [98] [7].
Dietary Intervention Protocol for Mechanism Validation
Study Design Considerations
- Randomization: Use stratified random assignment based on age, gender, and baseline biomarker levels.
- Blinding: Implement single or double-blind designs where feasible, particularly for supplemented interventions.
- Duration: Minimum 12-week interventions to detect changes in chronic inflammation and insulin resistance markers.
Dietary Intervention Arms
- Active Intervention: Provide specific foods, meals, or detailed meal plans targeting reduced EDIH/EDIP scores.
- Control Group: Maintain usual diet or follow a standard healthy eating pattern without specific mechanistic targeting.
- Compliance Monitoring: Implement 24-hour dietary recalls, food diaries, and biomarker validation (e.g., plasma fatty acid profiles).
Endpoint Assessment
- Primary Endpoints: Changes in validated biomarkers (CRP, insulin, C-peptide, HOMA-IR).
- Secondary Endpoints: Changes in clinical outcomes (blood pressure, lipid profiles, body composition).
- Exploratory Endpoints: Multi-omics analyses (transcriptomics, metabolomics) for pathway validation.
Biological Mechanisms and Pathway Analysis
Inflammatory Pathways Modulated by Diet
Pro-inflammatory dietary components activate multiple inflammatory pathways through pattern recognition receptors, leading to increased production of cytokines including IL-1β, IL-6, and TNF-α [99]. These cytokines stimulate hepatic production of acute-phase reactants such as CRP, creating a chronic low-grade inflammatory state that promotes endothelial dysfunction, insulin resistance, and cellular aging [98] [99]. Anti-inflammatory dietary components, including omega-3 polyunsaturated fatty acids, polyphenols, and fiber, can inhibit activation of NF-κB and NLRP3 inflammasome pathways, thereby reducing systemic inflammation [99].
Insulinemic Pathways Modulated by Diet
Dietary patterns with high insulinemic potential promote postprandial hyperinsulinemia through multiple mechanisms, including rapid digestion of refined carbohydrates, specific amino acid profiles from processed meats, and saturated fatty acids that promote adipose tissue inflammation and ceramide accumulation [98]. These factors contribute to insulin resistance through impaired insulin signaling at receptor and post-receptor levels, ultimately leading to pancreatic β-cell exhaustion and dysglycemia [1]. Conversely, diets rich in coffee, nuts, and leafy green vegetables may improve insulin sensitivity through effects on gut hormones, hepatic glucose production, and peripheral glucose uptake [98].
Research Reagent Solutions and Methodological Tools
Table 3: Essential Research Materials and Analytical Tools
| Category | Specific Tool/Reagent | Application in Research | Key Features/Benefits |
|---|---|---|---|
| Dietary Assessment Platforms | Automated Multiple Pass Method (AMPM) | 24-hour dietary recall administration | Standardized data collection, reduced interviewer bias [98] |
| Dietary Index Calculation Packages (R "Dietaryindex") | Standardized calculation of HEI, DII, other indices | Reproducible scoring, validation across populations [99] | |
| Biomarker Assays | Beckman Coulter DxH-800 Instrument | Complete blood count with differential | Standardized leukocyte, neutrophil counts for inflammation assessment [99] |
| High-sensitivity CRP assays | Quantification of inflammatory status | Detection of low-grade chronic inflammation | |
| ELISA kits for insulin, C-peptide | Assessment of insulinemic status | Specific measurement of beta-cell function and insulin resistance [98] | |
| qPCR telomere length assays | Cellular aging measurement | Quantitative relative telomere length assessment [98] | |
| Statistical Analysis Tools | R Statistical Programming | Multivariable regression, WQS analysis | Open-source, reproducible analytical workflows [99] |
| Reduced Rank Regression | Dietary pattern derivation | Identifies patterns predictive of specific biomarkers [98] | |
| Weighted Quantile Sum (WQS) Regression | Identification of component effects | Determines relative contribution of individual dietary elements [99] |
Mechanism-based validation of dietary patterns through their insulinemic and inflammatory potential represents a robust approach for linking nutrition to chronic disease pathogenesis. The empirical dietary indices outlined in this whitepaper provide validated tools for researchers to quantify these mechanistic pathways in both observational and intervention studies. For drug development professionals, these approaches offer opportunities for identifying novel targets, designing dietary adjuncts to pharmacological therapies, and stratifying patient populations based on their dietary-induced physiological states. Future research should focus on further refinement of these indices across diverse populations, integration with multi-omics technologies for deeper mechanistic insights, and application in clinical trial settings to establish causality and dose-response relationships.
Alzheimer's disease (AD) represents one of the most significant public health challenges of the 21st century, with projections indicating a tripling of cases by 2050 due to increasing global life expectancy [100]. While traditional research has focused predominantly on amyloid-beta (Aβ) and tau pathology, recent controversies regarding the validity of foundational studies and the limited clinical success of Aβ-targeting therapies have challenged their centrality in AD pathogenesis [100]. This paradigm shift has accelerated interest in modifiable risk factors, particularly diet, and their influence on disease progression through measurable biological indicators.
The emergence of blood-based biomarkers (BBBM) has revolutionized Alzheimer's research by providing minimally invasive tools for detecting pathological processes years before clinical symptoms manifest [101]. These biomarkers include both AD-specific proteins (phosphorylated tau, Aβ42/40 ratio) and non-specific indicators of neural damage (neurofilament light chain - NfL, glial fibrillary acidic protein - GFAP) that correlate strongly with cerebrospinal fluid and neuroimaging findings [102] [103]. Understanding how dietary patterns influence these biomarkers provides critical insights for developing precision nutrition strategies to combat neurodegeneration within the broader context of chronic disease prevention.
This technical review synthesizes current evidence on the interface between dietary patterns, blood-based biomarker expression, and Alzheimer's pathology, with particular emphasis on underlying biological mechanisms, standardized methodological approaches for investigation, and implications for therapeutic development.
Dietary Patterns and Blood-Based Biomarkers: Quantitative Relationships
Epidemiological and clinical studies have consistently demonstrated that specific dietary patterns significantly influence concentrations of blood-based AD biomarkers. The Mediterranean (MeDi) and MIND (Mediterranean-DASH Intervention for Neurodegenerative Delay) diets exhibit particularly strong neuroprotective associations, while pro-inflammatory dietary patterns correlate with accelerated pathological processes.
Table 1: Association Between Dietary Patterns and Blood-Based AD Biomarkers
| Dietary Pattern | Biomarker Associations | Effect Size | Study Details |
|---|---|---|---|
| Mediterranean Diet | ↓ p-tau181 | β = -0.036 (-0.072, -0.001) at 75th percentile [102] | Cross-sectional study of 1,907 dementia-free older adults [103] |
| ↓ GFAP | Stronger association in participants ≥78 years [102] | ||
| MIND Diet | ↓ Amyloid-beta, tau, NfL | p < 0.0001 [104] | 5-year prospective cohort of 1,500 participants [104] |
| ↓ Inflammatory markers (CRP, IL-6, TNF-α) | p < 0.0001 [104] | ||
| Pro-Inflammatory Diet | ↑ NfL | β = 0.031 (0.008, 0.053) per 1-SD increment [102] | Swedish SNAC-K study [103] |
| ↑ Brain age gap | +0.5 years advancement vs. anti-inflammatory diet [105] | UK Biobank (n=21,473) [105] | |
| High Saturated Fat Diet | ↑ Neuroinflammation | Independent of obesity/insulin resistance [100] | Preclinical models [100] |
| ↑ Synaptic loss | TLR4 activation & complement-mediated pruning [100] | ||
| Plant-Based Diets | ↑ Aβ42/40 ratio | PV: +0.011, LOV: +0.011, SV: +0.015 vs. RME [106] | Australian study (n=237) [106] |
| ↑ p-tau181, NFL, GFAP (in some patterns) | Mixed results across vegetarian types [106] |
Table 2: Effects of Specific Dietary Components on AD Biomarkers and Pathways
| Dietary Component | Effect on Biomarkers/Pathology | Proposed Mechanism |
|---|---|---|
| Saturated Fatty Acids | ↑ Neuroinflammation, synaptic loss [100] | TLR4 activation, complement system overactivation [100] |
| Polyphenols | ↓ Amyloid-beta, tau, improved cognition [104] | Antioxidant, anti-inflammatory effects [104] |
| Omega-3 Fatty Acids | ↓ Amyloid-beta, tau, improved cognition [104] | Anti-inflammatory, membrane fluidity enhancement [104] |
| B Vitamins | ↓ Amyloid-beta, tau, improved cognition [104] | Reduction of homocysteine, role in neurotransmitter synthesis [104] |
| Fiber & Plant Foods | ↓ CRP, IL-6, TNF-α [104] | Gut microbiome modulation, SCFA production [106] |
The association between diet and biomarker expression is further modified by genetic predisposition. Research demonstrates that the inverse relationship between Mediterranean diet adherence and p-tau181 levels is significantly stronger in APOE-ε4 carriers compared to non-carriers [102] [103]. Similarly, the neuroprotective effects of the MIND diet show variability based on APOE-ε4 status [104], highlighting the importance of personalized nutritional approaches based on genetic risk profiles.
Methodological Approaches for Investigating Diet-Biomarker Relationships
Dietary Assessment and Biomarker Measurement Protocols
Robust assessment of dietary intake represents a critical methodological foundation for establishing valid diet-biomarker relationships. The Swedish SNAC-K study employed a validated 98-item food frequency questionnaire (FFQ) with a nine-point frequency scale ranging from 'never or less than once a year' to 'more than 4 times a day' [103]. Portion sizes were estimated using color photographs, and food composition tables from the Swedish National Food Agency facilitated nutrient intake calculations [103]. Dietary patterns were quantified using:
Mediterranean Diet Score (MDS): A 0-9 point scale based on sex-specific median consumption of beneficial components (vegetables, legumes, fruits, nuts, cereals, fish, monounsaturated-to-saturated fat ratio) and detrimental components (meat, dairy), with alcohol intake scored moderately [103].
Empirical Dietary Inflammatory Index (EDII): Calculated by weighting consumption of 17 food groups by their inflammatory effect scores (range: -1175 to +252), with higher scores indicating more pro-inflammatory diets [103].
Blood-based biomarker measurement protocols have been standardized across major studies. The SNAC-K study measured serum concentrations of t-tau, p-tau181, Aβ42/40, NfL, and GFAP using advanced immunoassays [103]. Similarly, the 5-year prospective neuroprotection study conducted by Huadu District People's Hospital employed Enzyme-Linked Immunosorbent Assay (ELISA) kits for quantification of amyloid-beta (Thermo Fisher Scientific, KHB3481), tau protein (R&D Systems, DTA00), neurofilament light chain (Peninsula Laboratories, 42-1001), and inflammatory markers (CRP, IL-6, TNF-α) [104]. All samples were collected following standardized fasting venipuncture procedures, processed through centrifugation, and stored at -80°C until analysis to maintain biomarker integrity [104] [106].
Statistical Analysis and Machine Learning Approaches
Complex statistical approaches are required to elucidate relationships between dietary patterns and biomarker concentrations. The SNAC-K study utilized quantile regression models at the 25th, 50th, and 75th percentiles of biomarker distributions to capture potential differential effects across the spectrum of biomarker levels [103]. All analyses adjusted for key confounders including age, sex, education, physical activity, smoking status, and comorbidities, with stratification by APOE-ε4 genotype to examine effect modification [103].
Machine learning techniques have emerged as powerful tools for analyzing complex diet-biomarker-cognition relationships. The 5-year prospective study on Mediterranean and MIND diets employed machine learning algorithms to identify dietary patterns, predict cognitive trajectories, and support personalized dietary recommendations [104]. These approaches can integrate multidimensional data from dietary assessments, biomarker profiles, neuroimaging parameters, and genetic information to develop predictive models of dietary response.
Biological Mechanisms Linking Diet to Alzheimer's Pathology
Diagram 1: Biological Pathways Linking Diet to Alzheimer's Biomarkers
Neuroinflammatory Pathways
Neuroinflammation serves as a central mechanism through which diet influences Alzheimer's pathology. High saturated fat diets (HFD) activate toll-like receptor 4 (TLR4) on microglia, the resident immune cells of the brain, triggering the release of proinflammatory cytokines including interleukin (IL)-1β and tumor necrosis factor alpha (TNF-α) [100]. This activation initiates a cascade of microglial priming, shifting these cells from a homeostatic surveillance state to a hyperreactive state characterized by exaggerated and protracted inflammatory responses to subsequent challenges [100].
Complement system activation represents a particularly consequential neuroinflammatory pathway. Under physiological conditions, the complement system refines neural circuitry by tagging damaged or redundant synapses for elimination. However, diet-induced neuroinflammation promotes complement overactivation, leading to indiscriminate synaptic tagging and excessive synaptic loss [100]. This process is mediated through increased expression of complement proteins C1q and C3, which facilitate microglial engulfment of synapses [100]. The critical finding that short-term HFD exposure can rapidly induce neuroinflammation and impair memory, independently of Aβ burden and metabolic dysfunction, underscores the direct nature of this relationship [100].
Metabolic and Nutrient-Specific Pathways
Beyond inflammation, dietary patterns influence Alzheimer's pathology through multiple complementary biological pathways. The integrated framework of bidirectional crosstalk between neuroinflammation, brain insulin resistance, and micronutrient deficiencies creates a self-perpetuating cycle of neurodegeneration [101]. Diets high in saturated fats and simple carbohydrates promote brain insulin resistance, which in turn accelerates amyloid-beta production and tau hyperphosphorylation through disrupted kinase/phosphatase activities [101].
Micronutrient deficiencies common in pro-inflammatory diets further exacerbate pathological processes. Inadequate levels of vitamins E, D, B12, and antioxidants compromise neuronal defense mechanisms against oxidative stress, indirectly promoting neuroinflammation and cellular damage [101]. Conversely, the Mediterranean and MIND diets provide abundant polyphenols, omega-3 fatty acids, and B vitamins that counteract these processes through antioxidant activities, enhancement of mitochondrial function, and support of synaptic integrity [104].
The gut-brain axis has emerged as another critical pathway, with plant-based and Mediterranean dietary patterns promoting beneficial gut microbiota composition that increases production of neuroprotective short-chain fatty acids (SCFAs) while reducing systemic inflammation [106].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents and Materials for Diet-AD Biomarker Investigations
| Reagent/Material | Specific Examples | Research Application | Technical Notes |
|---|---|---|---|
| Blood Collection & Processing | EDTA tubes, centrifuges (Heraeus Biofuge Stratos), -80°C freezers [106] | Plasma isolation for biomarker analysis | Standardized processing protocols essential for reproducibility |
| ELISA Kits | Thermo Fisher Scientific (Aβ42/40: KHB3481), R&D Systems (Tau: DTA00), Peninsula Laboratories (NfL: 42-1001) [104] | Quantification of specific AD biomarkers in blood | Verify cross-reactivity with human antigens; establish lab-specific reference ranges |
| Single Molecule Array (SIMOA) | Quanterix HD-X Analyzer [106] | Ultra-sensitive detection of low-abundance biomarkers | Critical for blood-based measurements where concentrations are lower than CSF |
| Dietary Assessment Tools | Validated FFQs, Mediterranean Diet Adherence Screener (MEDAS), MIND Diet Score [104] | Standardized quantification of dietary intake | Include portion size estimation aids (photographs, household measures) |
| Genetic Analysis | PCR kits for APOE-ε4 genotyping [104] | Stratification by genetic risk | Essential for personalized response analysis |
| Inflammatory Marker Panels | Commercial kits for CRP, IL-6, TNF-α (eBioscience/Thermo Fisher) [104] | Assessment of systemic inflammation | Multiplex platforms increase efficiency for multiple analytes |
The accumulating evidence unequivocally demonstrates that dietary patterns significantly influence blood-based biomarkers of Alzheimer's disease through multiple interconnected biological pathways. The consistency of findings across diverse populations and methodological approaches strengthens the validity of these relationships and underscores the importance of integrating nutritional strategies into comprehensive Alzheimer's prevention and management frameworks.
Several critical research priorities emerge from this synthesis. First, the field requires longer-term prospective studies with repeated biomarker measurements to establish causal relationships between dietary changes and biomarker trajectories. Second, greater attention to nutrient-biomarker interactions across diverse populations is needed to address current disparities in representation. Third, the integration of multi-omics approaches (including genomics, proteomics, and metabolomics) with dietary assessment will enable more precise mechanistic understanding of individual response variations.
For drug development professionals, these findings highlight the importance of accounting for dietary patterns as potential effect modifiers in clinical trials of Alzheimer's therapeutics. Similarly, the establishment of dietary biomarkers as secondary endpoints in trial designs could provide valuable insights into mechanism of action and participant responsiveness. The demonstrated association between dietary factors and blood-based biomarkers reinforces the potential of targeted nutritional interventions as complementary approaches to pharmaceutical strategies in addressing the growing global burden of Alzheimer's disease.
Within the field of nutritional epidemiology, establishing a robust link between dietary patterns and chronic disease presents a unique set of methodological challenges. The shift from examining single nutrients to analyzing complex dietary patterns reflects the growing understanding that diet affects health through the cumulative and interactive effects of numerous foods and nutrients consumed over a lifetime [35] [36]. This guide provides a framework for researchers and drug development professionals to critically evaluate the strength of evidence linking dietary patterns to chronic diseases, focusing on the comparability of findings across diverse study designs and populations. The very high prevalence of chronic diseases, which account for more than half of all premature deaths and over 90% of yearly healthcare spending in the United States, underscores the critical public health importance of this endeavor [35] [1]. This document is structured to provide an in-depth technical guide on core concepts, methodological considerations, and analytical frameworks for assessing this evidence.
Dietary Patterns and Chronic Disease: Core Concepts and Definitions
Defining Dietary Patterns
A dietary pattern represents the quantities, proportions, variety, and combination of different foods, drinks, and nutrients in diets, and the frequency with which they are consumed [35]. This holistic approach considers the whole diet over extended periods, moving beyond a reductionist focus on individual nutrients from a single day [35]. This is crucial because the relationship between diet and chronic disease risk involves long-term exposure [35].
Healthy dietary patterns are generally characterized as being high in fruits, vegetables, whole grains, low and non-fat dairy, and lean protein, while being low in saturated fat, trans fat, sodium, and added sugars [35]. The preponderance of evidence suggests that such patterns reduce the risk of major diet-related chronic diseases, including diabetes, cardiovascular disease, and some cancers [35].
Major Dietary Patterns in Chronic Disease Research
Several dietary patterns have been consistently associated with a lower risk of chronic diseases. The table below summarizes key patterns and their associations with health outcomes.
Table 1: Major Dietary Patterns and Their Associations with Chronic Disease
| Dietary Pattern | Core Components | Primary Health Outcomes | Key Evidence Strength |
|---|---|---|---|
| Alternative Healthy Eating Index (AHEI) | High in fruits, vegetables, whole grains, nuts, legumes; low in red/processed meats, sugar-sweetened beverages [7] [36]. | Strongest association with healthy aging (OR 1.86); reduced risk of CVD, cancer, diabetes [7]. | Consistently strong across multiple cohorts and outcomes [1] [7]. |
| Mediterranean-style (aMED) | High in fruits, vegetables, whole grains, olive oil, nuts; moderate fish/poultry [1]. | Reduced risk of major chronic disease, improved healthy aging [1] [7]. | Robust evidence from long-term prospective cohorts [1]. |
| DASH (Dietary Approaches to Stop Hypertension) | Emphasizes fruits, vegetables, whole grains, low-fat dairy; reduces saturated fat, sodium [35] [36]. | Lower risk of CVD, hypertension; associated with healthy aging [7]. | Recommended in Dietary Guidelines for Americans; supported by clinical trials and cohorts [35] [36]. |
| Healthful Plant-Based (hPDI) | High-quality plant foods (whole grains, fruits, vegetables, nuts, legumes); low in animal foods [36]. | Lower risk of coronary heart disease, type 2 diabetes, all-cause mortality [36]. | Distinguishes between healthy and unhealthy plant-based foods [36]. |
| Diabetes Risk Reduction Diet (DRRD) | Higher coffee, cereal fiber; low in trans fat, glycemic load; moderate alcohol [1]. | Lower risk of type 2 diabetes and major chronic disease [1]. | Mechanism-based (hyperinsulinemia); strong predictive value [1]. |
| Low Inflammatory/Empirical (rEDIP/rEDIH) | Pattern derived from inflammatory biomarkers [1] or hyperinsulinemia [7]. | Lower risk of major chronic disease, associated with healthy aging [1] [7]. | Directly linked to biological pathways; strong predictive value for disease [1]. |
Methodological Frameworks for Dietary Pattern Analysis
Statistical Approaches to Deriving Dietary Patterns
Dietary patterns are characterized using various statistical methods, each with distinct advantages and limitations. These can be broadly categorized into investigator-driven, data-driven, and hybrid methods [36].
Table 2: Statistical Methods for Dietary Pattern Analysis
| Method Category | Description | Common Examples | Advantages | Disadvantages |
|---|---|---|---|---|
| Investigator-Driven (A Priori) | Based on pre-defined scoring systems aligned with dietary guidelines or nutritional knowledge [35] [36]. | Healthy Eating Index (HEI), AHEI, DASH Score [35] [36]. | Consistent metric for cross-study comparison; direct link to policy [35]. | Components and scores can be subjective; may not capture overall diet correlations [36]. |
| Data-Driven (A Posteriori) | Patterns derived from population data using dimensionality reduction techniques [36]. | Principal Component Analysis (PCA), Factor Analysis, Cluster Analysis [36]. | Reflects actual eating habits in the population; no prior hypotheses needed [36]. | Patterns may not be consistent across different populations [35]. |
| Hybrid Methods | Incorporate biological pathways or disease outcomes into pattern derivation [36]. | Reduced Rank Regression (RRR), Empirical Dietary Index for Hyperinsulinemia (EDIH) [1] [36]. | Stronger predictive power for specific diseases; connects diet to mechanism [1]. | Complex interpretation; may be less generalizable to other health outcomes [36]. |
Dietary Assessment Methods
Accurate measurement of dietary exposure is foundational. The choice of assessment tool depends on the research question, study design, and sample size [37].
Table 3: Dietary Assessment Methods in Research
| Method | Time Frame | Primary Use | Strengths | Limitations |
|---|---|---|---|---|
| Food Frequency Questionnaire (FFQ) | Long-term (months to years) [37]. | Large epidemiological studies; ranks individuals by intake [37]. | Cost-effective for large samples; assesses habitual diet [37]. | Limited food list; imprecise for absolute intake; relies on memory [37]. |
| 24-Hour Dietary Recall (24HR) | Short-term (previous 24 hours) [37]. | Detailed intake data; national surveys [37]. | Does not require literacy; captures wide variety of foods [37]. | Relies on memory; within-person variation requires multiple recalls [37]. |
| Food Record | Short-term (typically 3-4 days) [37]. | Detailed quantitative data; intervention studies [37]. | Does not rely on memory; high detail if weighed/measured [37]. | High participant burden; reactivity (changing diet for recording) [37]. |
| Biomarkers | Varies (objective measure) [35]. | Validation of self-report; measuring specific nutrients [35]. | Objective; not subject to systematic self-report error [35]. | Limited to specific nutrients (e.g., energy, protein via doubly labeled water) [35]. |
Evaluating Strength of Evidence: Key Considerations
Study Design Hierarchy and Temporal Sequence
The strength of evidence is heavily influenced by study design. Prospective cohort studies are particularly well-suited for investigating diet-chronic disease relationships because participants are free of the disease endpoint at enrollment, and disease outcomes are accrued over follow-up, establishing a clearer temporal sequence between diet and disease [35]. These studies also allow for the collection of detailed data on potential confounders (e.g., physical activity, smoking, socioeconomic status), leading to more reliable analytical models [35]. While randomized controlled trials (RCTs) provide the strongest evidence for causality, they are often expensive, of short duration, and may not be feasible for studying long-term dietary patterns and chronic disease endpoints.
Consistency and Reproducibility Across Populations
Robust associations are reproducible across different populations and study settings. Recent large-scale studies have demonstrated that the benefits of healthy dietary patterns are generally consistent across sexes and diverse ethnic groups [1]. For example, adherence to healthy dietary patterns was associated with a lower risk of major chronic disease in a pooled analysis of over 200,000 U.S. healthcare professionals, with hazard ratios comparing the 90th to 10th percentile of dietary pattern scores ranging from 0.58 to 0.80 [1]. This consistency across three large cohorts (NHS, NHS II, and HPFS) strengthens the evidence base.
Quantitative Data from Large-Scale Studies
The following table synthesizes key quantitative findings from major cohort studies, highlighting the magnitude of risk reduction associated with adherence to various healthy dietary patterns.
Table 4: Quantitative Associations Between Dietary Patterns and Health Outcomes in Large Cohort Studies
| Dietary Pattern | Population (Study) | Health Outcome | Risk Estimate (High vs. Low Adherence) | Notes |
|---|---|---|---|---|
| Multiple Patterns [1] | 205,852 (HPFS, NHS, NHS II) | Major Chronic Disease (Composite) | HR: 0.58 - 0.80 | Comparison of 90th vs. 10th percentile of scores. Lowest HR for low insulinemic diet. |
| AHEI [7] | 105,015 (NHS, HPFS) | Healthy Aging | OR: 1.86 (95% CI: 1.71-2.01) | Healthy aging defined by cognitive, physical, and mental health, and freedom from chronic disease at age 70. |
| hPDI [7] | 105,015 (NHS, HPFS) | Healthy Aging | OR: 1.45 (95% CI: 1.35-1.57) | Weakest association among the eight patterns studied. |
| Low Inflammatory (rEDIP) [1] | 205,852 (HPFS, NHS, NHS II) | Major CVD | HR: 0.61 (95% CI: 0.60-0.63) | Strong association with cardiovascular disease risk reduction. |
| Diabetes Risk Reduction (DRRD) [1] | 205,852 (HPFS, NHS, NHS II) | Type 2 Diabetes | HR: 0.70 (95% CI: 0.69-0.72) | Specifically designed to predict diabetes risk. |
Accounting for Measurement Error and Confounding
All self-reported dietary assessment methods are subject to measurement error, which is often systematic (e.g., under-reporting of energy intake) [37]. The use of objective recovery biomarkers (e.g., doubly labeled water for energy intake, urinary nitrogen for protein) provides a means to validate self-report data and correct for measurement error, though such biomarkers exist for only a limited number of nutrients [37]. Failure to adequately measure and control for confounders such as physical activity, BMI, and socioeconomic status can lead to spurious associations or mask true effects [35].
The Scientist's Toolkit: Key Reagents and Materials
Table 5: Essential Research Reagents and Tools for Dietary Pattern and Chronic Disease Research
| Tool/Reagent | Function/Application | Examples/Specifications |
|---|---|---|
| Validated Food Frequency Questionnaire (FFQ) | Assesses habitual dietary intake over a long reference period (e.g., past year) in large epidemiological studies [37]. | Semi-quantitative FFQs (e.g., 130+ items); must be validated in the target population [37]. |
| 24-Hour Recall Interview Platform | Collects detailed dietary data for the previous 24 hours; used for more precise intake estimation or to calibrate FFQs [37]. | Automated Self-Administered 24-hour Recall (ASA-24); interviewer-administered recalls using multi-pass method [37]. |
| Dietary Analysis Software & Food Composition Database | Converts reported food consumption into nutrient intake estimates; calculates dietary pattern scores [35]. | USDA Food and Nutrient Database for Dietary Studies (FNDDS); software compatible with output from FFQs and 24HRs. |
| Nutritional Biomarkers | Objectively measures nutrient intake or status, validating self-report data and providing insights into biological mechanisms [35]. | Recovery biomarkers (doubly labeled water for energy, urinary nitrogen for protein); concentration biomarkers (serum carotenoids, fatty acids) [35] [37]. |
| Biospecimen Collection Kits | Standardized collection and storage of biological samples for biomarker analysis and -omics technologies [35]. | Kits for blood (serum, plasma), urine, and DNA collection; requires protocols for processing, aliquoting, and long-term storage at -80°C. |
| Metabolomics & Genotyping Platforms | High-throughput analysis for discovering novel dietary biomarkers and understanding gene-diet interactions in disease [35]. | LC-MS/MS for metabolomics; genome-wide SNP arrays for genotyping. |
Evaluating the strength of evidence linking dietary patterns to chronic disease requires a multifaceted approach that critically assesses study designs, methodological rigor, consistency of findings across diverse populations, and the magnitude and biological plausibility of associations. The evidence to date, synthesized from large, long-term prospective cohorts, strongly indicates that dietary patterns characterized by high intakes of fruits, vegetables, whole grains, unsaturated fats, nuts, and legumes, and low intakes of red and processed meats, sugary beverages, and refined grains, are consistently associated with a reduced risk of major chronic diseases and greater likelihood of healthy aging [35] [1] [7]. For researchers and drug development professionals, this evidence base provides a robust foundation for developing preventive health strategies and underscores the importance of diet as a modifiable risk factor in public health. Future research leveraging emerging technologies like metabolomics and novel statistical methods will further refine our understanding of the optimal diet for chronic disease prevention across the lifespan.
Conclusion
The synthesis of current evidence firmly establishes that overall dietary patterns—particularly those emphasizing plant-based foods, unsaturated fats, and whole grains while limiting processed items—are powerfully associated with reduced risk of major chronic diseases and promotion of healthy aging. The Mediterranean, DASH, and other healthful patterns consistently demonstrate benefits, with comparative analyses suggesting specific diets may be optimal for particular conditions, such as vegan diets for metabolic syndrome and Mediterranean diets for cognitive health. Key biological mechanisms involve modulation of chronic inflammation, insulin response, and specific disease pathologies. Future directions for biomedical research must include the development of more precise dietary biomarkers, deeper exploration of diet-gene-therapeutic interactions (e.g., with GLP-1 drugs), and the design of culturally adapted, personalized nutrition strategies. For clinical and translational science, integrating these evidence-based dietary patterns into preventive medicine and chronic disease management protocols represents a critical, cost-effective strategy for improving population health outcomes.
References
- 1. Optimal dietary patterns for prevention of chronic disease - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10294543/]
- 2. This Is the Best Diet for Healthy Aging, According to Science [https://www.prevention.com/food-nutrition/healthy-eating/a64297964/healthy-aging-diet-study/]
- 3. Integrative Nutrition for Chronic Disease [https://www.indwes.edu/articles/2025/11/integrative-nutrition-chronic-disease-what-research-really-says.html]
- 4. The MIND Diet: 2025 Guide for Alzheimer's and Brain Health [https://health.usnews.com/best-diet/mind-diet]
- 5. Plant-Based Diets and Cognitive Outcomes: A Systematic ... [https://www.sciencedirect.com/science/article/pii/S2161831325001759]
- 6. Which dietary patterns are best for healthy aging? [https://www.medicalnewstoday.com/articles/scientists-compare-8-dietary-patterns-to-see-how-they-affect-healthy-aging]
- 7. Optimal dietary patterns for healthy aging | Nature Medicine [https://www.nature.com/articles/s41591-025-03570-5]
- 8. Association between different dietary patterns and the risk ... [https://www.sciencedirect.com/science/article/pii/S2589537025005504]
- 9. Trends in the burden of chronic diseases attributable to diet ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1570321/full]
- 10. Associations of the MIND Diet with Human Health Outcomes [https://pmc.ncbi.nlm.nih.gov/articles/PMC12389411/]
- 11. Health Professionals Follow-Up Study [https://hsph.harvard.edu/research/health-professionals/]
- 12. History | Nurses' Health Study [https://nurseshealthstudy.org/about-nhs/history]
- 13. Diet quality and major chronic disease risk in men ... [https://www.sciencedirect.com/science/article/pii/S0002916523060574]
- 14. Healthy dietary patterns and the risk of individual chronic ... [https://www.nature.com/articles/s41467-023-42523-9]
- 15. Effects of Dietary Patterns on Biomarkers of Inflammation ... [https://www.sciencedirect.com/science/article/pii/S2161831322005312]
- 16. Modulating biological aging with food-derived signals [https://pmc.ncbi.nlm.nih.gov/articles/PMC12368197/]
- 17. Healthy eating in midlife linked to overall healthy aging [https://hsph.harvard.edu/news/healthy-eating-in-midlife-linked-to-overall-healthy-aging/]
- 18. The association between the MIND diet and cognitive ... [https://pubmed.ncbi.nlm.nih.gov/40644764/]
- 19. Effects of the MIND Diet on the Cognitive Function of Older ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12629411/]
- 20. The Healthy Eating TABLE Summer 2025 [https://dairycouncilofca.org/learning-resources/research-insights/detail/the-healthy-eating-table-june-2025]
- 21. Artificial sweeteners aged the brain by over 1.5 years ... [https://www.cnn.com/2025/09/03/health/artificial-sweetener-cognition-wellness]
- 22. Big study finds lifestyle changes after age 60 can enhance ... [https://www.npr.org/2025/07/28/nx-s1-5477556/aging-brain-health-lifestyle-diet-exercise-social-alzheimers]
- 23. All of Us Research Program Ready to Address Chronic ... [https://nihrecord.nih.gov/2025/04/25/all-us-research-program-ready-address-chronic-disease-nutrition]
- 24. SNAP Benefits Linked to Slower Cognitive Decline [https://aaic.alz.org/releases-2025/snap-nutrition-program-linked-slower-cognitive-decline.asp]
- 25. Dietary Phytochemicals in Health and Disease: Mechanisms ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11922683/]
- 26. Anti-Inflammatory Actions of Plant-Derived Compounds ... [https://www.mdpi.com/1422-0067/26/11/5206]
- 27. Perspective on the health effects of unsaturated fatty acids and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11600290/]
- 28. Nutrition Fact Check: Seed Oils [https://www.eatrightpro.org/news-center/practice-trends/nutrition-fact-check-seed-oils]
- 29. The Evidence Behind Seed Oils' Health Effects | Johns Hopkins [https://publichealth.jhu.edu/2025/the-evidence-behind-seed-oils-health-effects]
- 30. Five things to know about seed oils and your health [https://med.stanford.edu/news/insights/2025/03/5-things-to-know-about-the-effects-of-seed-oils-on-health.html]
- 31. Ultra-processed food linked to harm in every major human ... [https://www.theguardian.com/society/2025/nov/18/ultra-processed-food-linked-to-harm-in-every-major-human-organ-study-finds]
- 32. Ultra-Processed Foods: 4 Things to Know [https://nam.edu/news-and-insights/4-things-to-know-ultra-processed-food/]
- 33. Ultra-processed foods linked to poor health outcomes [https://www.health.harvard.edu/nutrition/ultra-processed-foods-linked-to-poor-health-outcomes]
- 34. Medicinal plants and human health: a comprehensive ... [https://link.springer.com/article/10.1007/s11101-025-10194-7]
- 35. The Importance of Healthy Dietary Patterns in Chronic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6328339/]
- 36. A review of statistical methods for dietary pattern analysis [https://nutritionj.biomedcentral.com/articles/10.1186/s12937-021-00692-7]
- 37. Overview of Dietary Assessment Methods for Measuring ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8338737/]
- 38. Advances in dietary pattern analysis in nutritional ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8572214/]
- 39. Assessing Sustainable and Healthy Diets in Large-Scale ... [https://www.sciencedirect.com/science/article/pii/S0022316625004031]
- 40. Food Frequency Questionnaire to Estimate Dietary Adherence ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12526287/]
- 41. Minimum days estimation for reliable dietary intake ... [https://www.nature.com/articles/s41430-025-01644-8]
- 42. Biomarkers of Total Dietary Fiber Intake: A Challenge to Meet [https://pubmed.ncbi.nlm.nih.gov/40587381/]
- 43. Why variety matters when fibermaxxing [https://www.nutraingredients.com/Article/2025/07/09/why-variety-matters-when-fibermaxxing/]
- 44. Association between dietary fiber and markers of systemic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2603616/]
- 45. The associations between dietary fibers intake and ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2023.1242115/full]
- 46. Pathways and mechanisms linking dietary components to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6530989/]
- 47. Proinflammatory and Hyperinsulinemic Dietary Patterns ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2021.690428/full]
- 48. Effects of Dietary Patterns on Biomarkers of Inflammation and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8803482/]
- 49. Diet Quality and Biomarker Profiles Related to Chronic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6952587/]
- 50. Relationship between dietary inflammatory index and chronic ... [https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-025-22544-3]
- 51. Association between different dietary patterns and the risk of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12615346/]
- 52. Biological determinants of blood-based biomarker levels in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12631643/]
- 53. Role of insulinemic and inflammatory dietary patterns on gut ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12045561/]
- 54. Identifying biomarkers of dietary patterns by using ... [https://www.sciencedirect.com/science/article/pii/S0002916522047773]
- 55. Trends in Multiple Chronic Conditions Among US Adults ... [https://www.cdc.gov/pcd/issues/2025/24_0539.htm]
- 56. 2020-2025 Dietary Guidelines and Online Materials [https://www.dietaryguidelines.gov/resources/2020-2025-dietary-guidelines-online-materials]
- 57. This dietary pattern could save lives and the planet [https://hsph.harvard.edu/news/this-dietary-pattern-could-save-lives-and-the-planet/]
- 58. Data Analysis for the 2025 Guidelines Committee Report [https://www.dietaryguidelines.gov/2025-advisory-committee-report/data-analysis]
- 59. Implementing the 2020–2025 Dietary Guidelines for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8662785/]
- 60. Dietary Guidelines for Americans, 2020–2025 [https://pmc.ncbi.nlm.nih.gov/articles/PMC8713704/]
- 61. Translating the 2020–2025 U.S. Dietary Guidelines into ... [https://www.aafp.org/pubs/afp/issues/2021/1100/p448.html]
- 62. Food Pattern Modeling for the 2025 Advisory Committee ... [https://www.dietaryguidelines.gov/2025-advisory-committee-report/food-pattern-modeling]
- 63. Dietary Patterns and Health: Insights From NESR ... [https://www.sciencedirect.com/science/article/pii/S1499404623005237]
- 64. Access to Foods That Support Healthy Dietary Patterns [https://odphp.health.gov/healthypeople/priority-areas/social-determinants-health/literature-summaries/access-foods-support-healthy-dietary-patterns]
- 65. Perceptions of the Three Dietary Patterns of the 2020– ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12608769/]
- 66. Role of Personalized Nutrition in Chronic-Degenerative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6723746/]
- 67. Personalized Nutrition in the Era of Digital Health [https://pmc.ncbi.nlm.nih.gov/articles/PMC12474561/]
- 68. Addressing the Nutritional Phenotype Through ... [https://www.sciencedirect.com/science/article/abs/pii/S0033062018302470]
- 69. Polymorphisms, diet and nutrigenomics - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9710387/]
- 70. Nutrients | Special Issue : Gene Polymorphism and Nutrition [https://www.mdpi.com/journal/nutrients/special_issues/gene_polymorphism_nutrition]
- 71. Influence of Foods and Nutrition on the Gut Microbiome and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9455721/]
- 72. Metabolic phenotypes: Molecular bridges between health ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12615335/]
- 73. Innovative new tool helps understand how gut microbes ... [https://www.news-medical.net/news/20251120/Innovative-new-tool-helps-understand-how-gut-microbes-interact-to-influence-health.aspx]
- 74. The expanding role of GLP-1 receptor agonists [https://pmc.ncbi.nlm.nih.gov/articles/PMC12303005/]
- 75. Bridging the nutrition guidance gap for GLP-1 receptor ... [https://www.nature.com/articles/s41366-025-01952-w]
- 76. Investigating nutrient intake during use of glucagon-like ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1566498/full]
- 77. Diet quality and nutrient distribution while using glucagon ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12369429/]
- 78. The Planetary Health Diet - EAT Forum [https://eatforum.org/eat-lancet/the-planetary-health-diet/]
- 79. Short Dietary Assessment Instruments | EGRP/DCCPS/NCI/NIH [https://epi.grants.cancer.gov/diet/screeners/]
- 80. A Systematic Review of the Methods Used to Assess and ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2022.892351/full]
- 81. Choice of health metrics for combined health and ... [https://www.sciencedirect.com/science/article/pii/S0959652622022211]
- 82. Application of Systematic Review Methodology to the ... - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK44076/]
- 83. Network meta-analysis of the effects of different dietary ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1634545/full]
- 84. Network meta-analysis of the effects of different dietary ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12585985/]
- 85. Dietary patterns derived by Gaussian graphical models ... [https://www.nature.com/articles/s41598-025-92361-6]
- 86. Network meta-analysis of the effects of different dietary ... [https://pubmed.ncbi.nlm.nih.gov/41200142/]
- 87. Relationship between metabolic syndrome and dietary ... [https://www.nature.com/articles/s41598-025-90086-0]
- 88. Network study of the nutritional patterns, the metabolic and ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1666688/full]
- 89. Chapter 12 Network Meta-Analysis [https://bookdown.org/MathiasHarrer/Doing_Meta_Analysis_in_R/netwma.html]
- 90. Network meta-analysis: a powerful tool for clinicians ... [https://www.sciencedirect.com/science/article/pii/S0895435624002932]
- 91. Data visualisation approaches for component network ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10502971/]
- 92. Plant-Based Diets and Their Role in Preventive Medicine [https://pmc.ncbi.nlm.nih.gov/articles/PMC11890674/]
- 93. Ketogenic diet improves disease activity and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12013891/]
- 94. Not All Plants Are Equal: Diet Quality and Inflammation in ... [https://www.mdpi.com/2072-6643/17/21/3361]
- 95. Ketogenic diet improves disease activity and cardiovascular ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0321140]
- 96. Frontiers | The DASH in diabetes related complications or... diet [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1689467/full]
- 97. Mediterranean Diet Reduces Inflammation in Adults [https://pubmed.ncbi.nlm.nih.gov/41211687/]
- 98. Diets with higher inflammatory and insulinemic potential ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12340096/]
- 99. Association of dietary quality and dietary inflammatory ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1596806/full]
- 100. Neuroinflammatory mechanisms linking highâ€fat diets to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12627239/]
- 101. Biological determinants of blood-based biomarker levels in ... [https://www.frontiersin.org/journals/aging-neuroscience/articles/10.3389/fnagi.2025.1614962/full]
- 102. Dietary patterns and blood-based biomarkers of ... [https://pubmed.ncbi.nlm.nih.gov/40089420/]
- 103. Dietary patterns and blood-based biomarkers of Alzheimer's ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12434269/]
- 104. The long-term neuroprotective effect of MIND and ... [https://www.nature.com/articles/s41598-025-17055-5]
- 105. Pro-inflammatory diets linked to accelerated brain aging in ... [https://www.psypost.org/pro-inflammatory-diets-linked-to-accelerated-brain-aging-in-older-adults/]
- 106. Blood biomarkers of Alzheimer's disease in Australians ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12284332/]