Machine Learning for Glycemic Response Prediction: From Algorithms to Clinical Applications in Diabetes Management
This comprehensive review explores the rapidly evolving field of machine learning (ML) for predicting glycemic responses, a critical capability for personalized diabetes care.
Machine Learning for Glycemic Response Prediction: From Algorithms to Clinical Applications in Diabetes Management
Abstract
This comprehensive review explores the rapidly evolving field of machine learning (ML) for predicting glycemic responses, a critical capability for personalized diabetes care. We examine foundational concepts including key glycemic metrics like Time in Range (TIR), postprandial glycemic response (PPGR), and hypoglycemia/hyperglycemia prediction. The article details diverse methodological approaches, from ensemble methods like XGBoost to advanced deep learning architectures and multi-task learning frameworks, highlighting their applications in clinical scenarios such as hemodialysis management and automated insulin delivery. We address crucial optimization challenges including data limitations, model interpretability through SHAP and XAI, and generalization strategies like Sim2Real transfer. Finally, we evaluate validation frameworks, performance metrics, and comparative algorithm analyses, providing researchers and drug development professionals with a rigorous assessment of current capabilities and future directions for integrating ML into diabetes therapeutics and management systems.
Foundations of Glycemic Response Prediction: Key Metrics and Clinical Significance
In the era of data-driven medicine, the management of diabetes has been transformed by continuous glucose monitoring (CGM), which provides a dynamic, high-resolution view of glucose fluctuations that traditional metrics like HbA1c cannot capture [1]. These advanced measurements form the critical foundation for developing machine learning (ML) algorithms aimed at predicting glycemic response and personalizing therapy. Where HbA1c offers a static, long-term average, CGM-derived metrics reveal the complex glycemic patterns throughout the day and night, exposing variability, hypoglycemic risk, and postprandial excursions [2]. For researchers and drug development professionals, understanding these core parameters—Time in Range (TIR), Time Above Range (TAR), Time Below Range (TBR), Coefficient of Variation (CV), and Postprandial Glucose Response (PPGR)—is essential for designing clinical trials, evaluating therapeutic interventions, and building robust predictive models [1] [3].
The international consensus on CGM metrics has standardized these parameters, enabling consistent application across clinical practice and research [1]. This standardization is particularly crucial for ML applications, as it ensures the generation of reliable, labeled datasets for model training. This document provides a detailed exploration of these metrics, their quantitative relationships, and their central role in modern glycemic research, with a specific focus on their application in machine learning algorithms for predicting glycemic responses.
Defining the Key Metrics and Their Interrelationships
Metric Definitions and Clinical Targets
The following table summarizes the definitions, targets, and clinical significance of the five core glycemic metrics, providing a concise reference for researchers.
Table 1: Core Glycemic Metrics: Definitions, Targets, and Clinical Relevance
| Metric | Definition | Primary Target | Clinical Relevance & Association with Complications |
|---|---|---|---|
| Time in Range (TIR) | Percentage of time glucose is between 70–180 mg/dL [1]. | ≥ 70% for most adults [1]. | Strongly associated with reduced risk of microvascular complications [1] [2]. |
| Time Above Range (TAR) | Percentage of time glucose is >180 mg/dL, with a subset >250 mg/dL [1]. | < 25% (>180 mg/dL), < 5% (>250 mg/dL) [1]. | Reflects hyperglycemia burden and long-term complication risk [1]. |
| Time Below Range (TBR) | Percentage of time glucose is <70 mg/dL, with a subset <54 mg/dL [1]. | < 4% (<70 mg/dL), < 1% (<54 mg/dL) [1]. | Key safety metric; measures hypoglycemia risk [1]. |
| Coefficient of Variation (CV) | Measure of glycemic variability: (Standard Deviation / Mean Glucose) × 100 [1]. | ≤ 36% [1]. | Predictor of hypoglycemia risk; higher CV indicates greater glucose instability [1] [4]. |
| Postprandial Glucose Response (PPGR) | Increase in blood glucose after meal consumption, often calculated as the incremental Area Under the Curve (AUC) in the 2-hour period after eating [3]. | N/A (Highly individualized) | Major driver of overall glycemic control and TAR; marked interindividual variability exists [3] [5]. |
Statistical and Mechanistic Relationships Between Metrics
The core glycemic metrics are not independent; they exist in a tightly coupled, and often inverse, relationship. Understanding these interrelationships is critical for both clinical interpretation and feature engineering in ML models.
- TIR, TAR, and TBR as a Closed System: By definition, TIR + TAR + TBR = 100% of a 24-hour period [1]. Consequently, an intervention that increases TIR will necessarily decrease TAR, TBR, or both. This inverse relationship is a fundamental constraint in any predictive system.
- The Critical Role of Glycemic Variability (CV): The CV is a powerful predictor of hypoglycemia. Research demonstrates a strong positive correlation between CV and TBR (r=0.708, p<0.0001), and specifically with time below 54 mg/dL (r=0.664, p<0.0001) [4]. A higher CV indicates greater glucose instability, which exponentially increases the risk of hypoglycemic events, even when mean glucose or HbA1c appears acceptable [6]. Conversely, CV shows a weak negative correlation with TIR (r=-0.398, p=0.003) and no significant correlation with TAR [4].
- PPGR as a Determinant of TAR: Elevated PPGR is a primary contributor to TAR. The postprandial state is a period of significant metabolic challenge, and the magnitude of the glucose excursion directly influences the number of hours spent above the 180 mg/dL threshold. Managing PPGR is therefore a key strategy for reducing TAR and increasing TIR [3].
Application in Machine Learning for Glycemic Response Prediction
The Role of Metrics in Model Development
In ML research for diabetes, glycemic metrics serve two primary functions: as model outputs/targets for prediction and as input features for personalized recommendations.
- TIR, TAR, and TBR as Prediction Targets: A key application of ML is forecasting future glycemic events. Studies have developed dual-prediction frameworks that simultaneously forecast postprandial hypoglycemia and hyperglycemia within a 4-hour window, using these metrics to define the prediction target [7]. The model's performance is then evaluated based on its ability to correctly classify these future events, with high AUC scores reported (0.84 for hypoglycemia and 0.93 for hyperglycemia) [7].
- CV and PPGR as Features for Personalization: The CV is a critical input feature for models assessing hypoglycemia risk due to its strong correlation with TBR [4] [6]. PPGR, given its significant interindividual variability, is a central outcome for personalized nutrition models. Research shows that predicting an individual's PPGR is feasible using machine learning that incorporates meal data, demographics, and other factors, achieving accuracy comparable to methods that rely on invasive data like microbiome analysis [5] [8].
A Protocol for Generating Machine Learning-Ready PPGR Data
The following protocol outlines a methodology for collecting high-quality, multi-modal data suitable for training ML models to predict PPGR, based on a contemporary research study [3].
Aim: To characterize interindividual variability in PPGR and identify factors associated with these differences for the creation of machine learning models. Population: Adults with Type 2 Diabetes (HbA1c ≥7%), treated with oral hypoglycemic agents. Duration: 14-day observational period. Primary Outcome: PPGR, calculated as the incremental AUC (iAUC) for the 2-hour period following each logged meal.
Table 2: Data Collection Protocol for PPGR Machine Learning Studies
| Data Domain | Specific Measures & Equipment | Collection Frequency & Protocol | Function in ML Model |
|---|---|---|---|
| Glucose Metrics | CGM (e.g., Abbott Freestyle Libre) [3]. | Worn continuously for 14 days; minimum 70% data capture required [1] [3]. | Target Variable (PPGR); features for TIR, TAR, TBR, CV. |
| Dietary Intake | Detailed food diary (via study app or logbook); standardized test meals [3]. | All meals, snacks, beverages logged in real-time. Standardized meals consumed on specific days. | Primary Input Features (food categories, macronutrients). |
| Physical Activity | Heart rate monitor (e.g., Xiaomi Mi Band) [3]. | Worn continuously, including during sleep. | Input Feature (for energy expenditure estimation). |
| Medication | Oral hypoglycemic agent use [3]. | Logged with timing and dosage for each dose. | Input Feature (confounding variable adjustment). |
| Biometrics & Labs | Blood pressure, weight, height, HbA1c, blood lipids, etc. [3]. | Collected at in-person baseline visit. | Static Input Features (for personalization). |
| Patient-Reported Outcomes | WHO-5 Well-Being Index, Diabetes Distress Scale, Pittsburgh Sleep Quality Index [3]. | Completed at baseline. | Input Features (for psychological and sleep context). |
The Scientist's Toolkit: Key Reagents and Solutions
Table 3: Essential Research Reagents and Platforms for Glycemic Response Studies
| Item | Specific Example | Function in Research |
|---|---|---|
| Continuous Glucose Monitor (CGM) | Abbott Freestyle Libre [3]. | Provides continuous interstitial glucose measurements, the primary data source for calculating TIR, TAR, TBR, CV, and PPGR. |
| Activity & Physiological Monitor | Xiaomi Mi Band (or equivalent smart wristband) [3]. | Captures heart rate and physical activity data, used as features for ML models to account for exercise-induced glycemic changes. |
| Data Integration & Logging Platform | Custom study app on participant smartphone [3]. | Synchronizes CGM, activity data, and meal/medication logs into a unified dataset; critical for ensuring data completeness and temporal alignment. |
| Standardized Test Meals | Protocol-defined vegetarian meals [3]. | Used to elicit a controlled PPGR, reducing dietary noise and enabling direct comparison of metabolic responses across participants. |
| Glucose Simulator | Customized simulator based on the Dalla Man model [7]. | Enables in silico testing and validation of ML models and insulin adjustment algorithms in a controlled, risk-free virtual environment. |
| BIBU1361 | BIBU1361, CAS:793726-84-8, MF:C22H29Cl3FN7, MW:516.9 g/mol | Chemical Reagent |
| Kisspeptin-10, rat | Kisspeptin-10, rat, MF:C63H83N17O15, MW:1318.4 g/mol | Chemical Reagent |
The standardized glycemic metrics of TIR, TAR, TBR, CV, and PPGR provide an indispensable framework for moving beyond the limitations of HbA1c. For the research community, and particularly for scientists developing machine learning algorithms, these metrics offer quantifiable, physiologically meaningful targets for prediction and optimization. The strong statistical relationships between them, especially the role of CV in predicting hypoglycemia risk, must be baked into the structure of predictive models. The ongoing integration of explainable ML with high-resolution CGM data, detailed dietary information, and other contextual factors promises to unlock a new era of personalized diabetes management, enabling dynamic interventions that maximize TIR while minimizing the risks of hypo- and hyperglycemia.
Clinical Importance of Predicting Hypoglycemia and Hyperglycemia Events
The predictive capacity of machine learning (ML) for hypoglycemia and hyperglycemia events represents a transformative advancement in diabetes management. For the millions of individuals living with diabetes worldwide, the threat of glycemic decompensation—blood glucose levels that fall too low (hypoglycemia) or rise too high (hyperglycemia)—presents a constant challenge with potentially severe health consequences [9] [10]. Both conditions have been associated with increased morbidity, mortality, and healthcare expenditures in hospital settings [10]. The integration of artificial intelligence and machine learning technologies enables a paradigm shift from reactive to proactive diabetes care, allowing for interventions before glucose levels reach dangerous thresholds [9] [11]. This application note details the clinical significance of glycemic event prediction and provides structured protocols for implementing ML approaches within glycemic response research.
Clinical Rationale and Impact
The Clinical Burden of Dysglycemia
Glycemic decompensations constitute a frequent and significant risk for inpatients and outpatients with diabetes, adversely affecting patient outcomes and safety [9]. Hypoglycemia can induce symptoms ranging from shakiness and confusion to seizures, loss of consciousness, and even death if untreated [12]. Hyperglycemia can cause fatigue, excessive urination, and thirst, progressing to more severe complications including diabetic ketoacidosis or hyperglycemic hyperosmolar state [9] [12]. In hospitalized patients, both conditions have been linked to increased length of stay, higher risk of infection, admission to intensive care units, and increased mortality [9] [10].
The management of dysglycemia poses substantial demands on healthcare systems. The increasing need for blood glucose management in inpatients places high demands on clinical staff and healthcare resources [9]. Furthermore, fear of exercise-induced hypoglycemia and hyperglycemia presents a significant barrier to regular physical activity in adults with type 1 diabetes (T1D), potentially compromising their overall cardiovascular health and quality of life [13].
The Predictive Approach: From Reaction to Prevention
Traditional diabetes management often involves reacting to glucose measurements after they have occurred. Predictive models shift this paradigm toward prevention by identifying at-risk periods before glucose levels become derailed. Research demonstrates that electronic health records and continuous glucose monitor (CGM) data can reliably predict blood glucose decompensation events with clinically relevant prediction horizons—7 hours for hypoglycemia and 4 hours for hyperglycemia in one inpatient study [9]. This advance warning system enables proactive interventions, such as carbohydrate consumption to prevent hypoglycemia or insulin adjustment to mitigate hyperglycemia, potentially reducing the detrimental health effects of both conditions [9].
Table 1: Clinical Consequences of Glycemic Dysregulation
| Condition | Definition | Short-term Consequences | Long-term Risks |
|---|---|---|---|
| Hypoglycemia | Blood glucose <70 mg/dL (<3.9 mmol/L) [9] | Shakiness, confusion, tachycardia, seizures, unconsciousness [12] | Increased mortality, reduced awareness of symptoms [10] |
| Hyperglycemia | Blood glucose >180 mg/dL (>10 mmol/L) [9] | Fatigue, excessive thirst, frequent urination [12] | Diabetic ketoacidosis, hyperosmolar state, increased infection risk [9] [10] |
Machine Learning Approaches and Performance
Algorithm Diversity and Performance Metrics
Multiple machine learning architectures have been successfully applied to glycemic event prediction, ranging from traditional regression techniques to sophisticated deep learning frameworks. The selection of an appropriate model depends on the specific clinical context, available data types, and prediction horizon requirements.
For glucose forecasting and hypoglycemia detection, a domain-agnostic continual multi-task learning (DA-CMTL) framework has demonstrated robust performance, achieving a root mean squared error (RMSE) of 14.01 mg/dL, mean absolute error (MAE) of 10.03 mg/dL, and sensitivity/specificity of 92.13%/94.28% for 30-minute predictions [11]. This unified approach simultaneously performs glucose level forecasting and hypoglycemia event classification within a single architecture, enhancing coordination for real-time insulin delivery systems.
In exercise-specific contexts, models incorporating continuous glucose monitoring data alone have shown excellent predictive performance for glycemic events, with cross-validated area under the receiver operating curves (AUROCs) ranging from 0.880 to 0.992 for different glycemic thresholds [13]. This remarkable performance using a single data modality highlights the richness of information embedded in CGM temporal patterns.
For inpatient settings, a multiclass prediction model for blood glucose decompensation events achieved specificities of 93.7-98.9% and sensitivities of 59-67.1% for nondecompensated cases, hypoglycemia, and hyperglycemia categories [9]. The high specificity is particularly valuable for minimizing false alarms that could lead to alert fatigue among clinical staff.
Table 2: Performance Metrics of Selected Machine Learning Models for Glycemic Event Prediction
| Model Type | Population | Prediction Horizon | Key Performance Metrics | Reference |
|---|---|---|---|---|
| Domain-Agnostic Continual Multi-Task Learning | Mixed T1D | 30 minutes | RMSE: 14.01 mg/dL; MAE: 10.03 mg/dL; Sensitivity/Specificity: 92.13%/94.28% | [11] |
| CGM-Based Exercise Event Prediction | T1D (during & post-exercise) | During and 1-hour post-exercise | AUROC: 0.880-0.992 (depending on glycemic threshold) | [13] |
| Gradient-Boosted Multiclass Prediction | Inpatients with diabetes | Median 7h (hypo), 4h (hyper) | Hypoglycemia: 67.1% sensitivity, 93.7% specificity; Hyperglycemia: 63.6% sensitivity, 93.9% specificity | [9] |
| Binary Decision Tree | General diabetes | Short-term prediction | 92.58% classification accuracy for glucose level categories | [12] |
Data Modalities and Feature Engineering
The predictive capacity of machine learning models for glycemic events depends heavily on the data modalities incorporated during training. Research indicates varying levels of contribution from different data types:
- Continuous Glucose Monitoring: CGM data provides the most powerful predictive signals for glycemic events, particularly for near-term predictions [13]. In exercise settings, models based solely on CGM data demonstrated statistically indistinguishable performance compared to models incorporating additional demographic, clinical, and exercise characteristics [13].
- Electronic Health Records: For inpatient populations, EHR data including laboratory results, medication administration, and diagnosis codes enables effective prediction of decompensation events [9] [10]. Derived variables from EHRs (mean, standard deviation, trends, and extreme values of laboratory analytes) effectively capture patient status for prediction.
- Food and Nutrition Data: Emerging evidence suggests that food category information may surpass macronutrient composition alone for predicting postprandial glycemic responses [5] [8]. Food categories potentially serve as proxies for micronutrients, processing levels, or physical properties that influence digestion and absorption.
- Contextual Factors: Menstrual cycle phases and time of day introduce significant variability in individual glycemic responses [5] [8]. Incorporating these temporal factors improves prediction accuracy by accounting for systematic patterns in insulin sensitivity fluctuations.
Experimental Protocols
Protocol for Predicting Postprandial Glycemic Responses in Type 2 Diabetes
Study Design: Prospective cohort study evaluating interindividual variability in postprandial glucose response (PPGR) among adults with Type 2 Diabetes (T2D) and suboptimal control (HbA1c ≥7%) [3].
Setting: 14 outpatient clinics across India with specialized diabetes care expertise [3].
Participant Criteria:
- Inclusion: Adults (18-75 years) with physician-diagnosed T2D treated with ≥1 oral hypoglycemic agents; HbA1c ≥7.0% within past 30 days; mobile phone capability with functional English literacy [3].
- Exclusion: Current prandial insulin use; pregnancy; estimated life expectancy ≤12 months; active cancer; myocardial infarction or stroke in previous 6 months; contraindications to CGM use [3].
Methodology:
- Baseline Assessment: Collect sociodemographic and medical information; administer standardized surveys (WHO STEPS, WHO-5 Well-Being Index, Diabetes Distress Scale, Wilson Adherence Scale, Pittsburgh Sleep Quality Index); perform biometric measurements; obtain blood and urine samples for laboratory analysis [3].
- Monitoring Phase: Participants wear Abbott Freestyle Libre CGM sensor and Xiaomi Mi Band smart wristband for 14 days [3].
- Data Logging: Participants record all dietary intake (using study app or paper logbook), exercise activities, and medication use throughout the 14-day period [3].
- Standardized Meal Protocol: Participants consume protocol-specified vegetarian breakfast meals with variations in carbohydrate, fiber, protein, and fat composition on designated days [3].
- Primary Outcome: PPGR calculated as incremental area under the curve 2 hours after each logged meal [3].
Analytical Approach: Machine learning models will be created to predict individual PPGR responses and facilitate personalized diet prescriptions [3].
Protocol for Exercise-Induced Glycemic Event Prediction in Type 1 Diabetes
Study Design: Analysis of free-living data from the Type 1 Diabetes Exercise Initiative (T1DEXI) study, incorporating at-home exercise with detailed concurrent phenotyping [13].
Participant Profile: 329 adults with T1D; median age 34 years (IQR 26-48); 74.8% female; 94.5% White; 55.3% using closed-loop insulin delivery systems [13].
Intervention: Participants completed 6 structured exercise sessions (aerobic, interval, or resistance) over 4 weeks, each approximately 30 minutes with warm-up and cool-down periods, while maintaining typical daily physical activities [13].
Data Collection:
- CGM Data: Dexcom G6 sensors collecting glucose measurements every 5 minutes [13].
- Carbohydrate Intake: Collected through T1DEXI mobile application [13].
- Insulin Dosing: Extracted from insulin pumps [13].
- Exercise Characteristics: Type, duration, intensity, and time of day recorded [13].
- Demographic and Clinical Data: Self-reported via portal including diabetes history and most recent HbA1c [13].
Analysis Framework:
- Decision Points: Two critical prediction timepoints—(1) pre-exercise to assess risk during exercise; (2) post-exercise to assess risk 1-hour post-exercise [13].
- Prediction Targets: Four glycemic events—severe hypoglycemia (≤54 mg/dL), hypoglycemia (≤70 mg/dL), hyperglycemia (≥200 mg/dL), severe hyperglycemia (≥250 mg/dL)—assessed separately during and post-exercise [13].
- Model Evaluation: Repeated stratified nested cross-validation for model selection and performance estimation; assessment of input modality contributions; evaluation of model calibration and noise resilience [13].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Materials and Technologies for Glycemic Prediction Studies
| Tool Category | Specific Examples | Research Function | Protocol Applications |
|---|---|---|---|
| Continuous Glucose Monitors | Abbott Freestyle Libre [3], Dexcom G6 [13] | Continuous measurement of interstitial glucose levels; primary data source for temporal glucose patterns | Used in both T1D and T2D protocols for real-world glucose monitoring [3] [13] |
| Activity Monitors | Xiaomi Mi Band Smart Wristband [3] | Heart rate monitoring and activity tracking; correlates physical exertion with glycemic variability | Protocol for assessing impact of exercise on glycemic responses [3] |
| Data Logging Platforms | Study-specific smartphone applications, Paper logbooks [3], T1DEXI app [13] | Capture participant-reported data on diet, medication, exercise; enables temporal alignment with CGM data | Dietary intake logging in free-living conditions [3] [13] |
| Standardized Meal Kits | Protocol-specified vegetarian breakfast meals with varying macronutrient composition [3] | Controls for nutritional input to assess interindividual variability in postprandial responses | Testing PPGR to standardized nutritional challenges [3] |
| Laboratory Analysis | HbA1c, complete blood count, blood electrolytes, creatinine, cholesterol, urinalysis [3] | Provides baseline metabolic status and inclusion criterion verification | Characterizing study population and ensuring eligibility [3] |
| Simulated Datasets | Physiologically validated diabetes simulators [11] | Generates synthetic patient data for initial model training; reduces reliance on real-world data collection | Sim2Real transfer learning in multi-task frameworks [11] |
| Epiequisetin | Epiequisetin, MF:C22H31NO4, MW:373.5 g/mol | Chemical Reagent | Bench Chemicals |
| Ivermectin monosaccharide | Ivermectin monosaccharide, MF:C41H62O11, MW:730.9 g/mol | Chemical Reagent | Bench Chemicals |
Regulatory and Implementation Considerations
The development of ML-based technologies for glycemic prediction must align with established regulatory frameworks to ensure safety and efficacy. The U.S. Food and Drug Administration, Health Canada, and the United Kingdom's Medicines and Healthcare products Regulatory Agency have identified ten guiding principles for Good Machine Learning Practice (GMLP) in medical device development [14]. These principles emphasize multi-disciplinary expertise throughout the product life cycle, representative training datasets, model design tailored to available data and intended use, and performance monitoring during clinically relevant conditions [14].
For clinical trial design incorporating AI and digital health technologies, the FDA emphasizes the importance of ensuring that decentralized clinical trials and digital health technologies are "fit for purpose" while considering the total context of the clinical trial, the intervention type, and the patient population involved [15]. Digital health technologies, including continuous glucose monitors and activity trackers, enable continuous or frequent measurements of clinical features that might not be captured during traditional study visits, thus providing more comprehensive data collection [15].
Ethical implementation of glycemic prediction algorithms requires attention to potential biases in training data, transparency in model performance limitations, and careful consideration of the clinical workflow integration to prevent alert fatigue. As these technologies evolve toward automated insulin delivery systems, robust safety frameworks and fail-safes become increasingly critical to prevent harm from prediction errors [11].
CONTINUOUS GLUCOSE MONITORING (CGM) AS A PRIMARY DATA SOURCE
Continuous Glucose Monitoring (CGM) provides a rich, high-frequency temporal data stream of subcutaneous interstitial glucose measurements, typically every 5 minutes, offering an unprecedented view into glycemic physiology [16]. For researchers developing machine learning (ML) algorithms to predict glycemic response, CGM data moves beyond the snapshot provided by HbA1c or self-monitored blood glucose to capture dynamic patterns, including glycemic variability, postprandial excursions, and nocturnal trends [17]. This data density and temporal resolution make CGM a foundational primary data source for training sophisticated models aimed at forecasting glucose levels, classifying hypoglycemic risk, and ultimately enabling personalized, proactive diabetes interventions [18] [16].
Data Sourcing and Selection Protocols
The selection of appropriate CGM datasets is a critical first step in building generalizable and robust predictive models. Research-grade and real-world CGM data each offer distinct advantages.
2.1 Research-Grade CGM Data Collection Protocol A standardized protocol for collecting research-grade CGM data ensures consistency and reliability for model training [18].
- Device and Placement: Use FDA-approved CGM systems (e.g., Medtronic Enlite Sensor with iPro2 recorder). Sensors are placed subcutaneously, typically in the abdominal region.
- Calibration: Per manufacturer guidelines, calibrate sensors against fingerstick blood glucose (BG) measurements using a Contour Next meter. Require a minimum of four calibrations per day. Exclude the first 24 hours of data from analysis due to initial sensor instability [18].
- Participant Cohort: Recruit a population that reflects the model's intended use case. For generalizable models, include individuals with normal glucose metabolism (NGM), prediabetes, and type 2 diabetes (T2D). A sample protocol from The Maastricht Study specifies >48 hours of CGM data per participant, with a target sample size of ~850 individuals [18].
- Data Inclusion/Exclusion: Include data from the full sensor wear period (e.g., 6 days) after the initial 24-hour warm-up. Apply quality checks to remove periods of sensor signal drop-out or artifact.
2.2 Utilizing Real-World and Public Datasets Leveraging existing datasets can accelerate research and provide benchmarks.
- Public Datasets: The OhioT1DM Dataset is a key resource for validating models on type 1 diabetes (T1D) data, containing CGM, insulin, and meal data for 6 individuals [18].
- Real-World Evidence (RWE): Data from commercial CGM use (e.g., Dexcom G6) collected over 90 days from 112 patients, encompassing over 1.6 million CGM values, provides insights into glycemic patterns under free-living conditions [19]. This data is essential for testing model robustness.
Table 1: Key CGM Datasets for ML Research
| Dataset Name | Population | Sample Size (n) | Key Variables | Primary Research Use |
|---|---|---|---|---|
| The Maastricht Study [18] | NGM, Prediabetes, T2D | 851 | CGM, Accelerometry | Generalizable glucose prediction model development |
| OhioT1DM Dataset [18] | Type 1 Diabetes | 6 | CGM, Insulin, Meals | Proof-of-concept translation to T1D |
| Dexcom G6 Real-World [19] | Type 1 Diabetes (Youth) | 112 | CGM, Insulin Pump Data | Hypoglycemia prediction and feature engineering |
Data Preprocessing & Feature Engineering Workflow
Raw CGM signals require extensive preprocessing and thoughtful feature engineering to be optimally useful for machine learning algorithms.
3.1 Data Preprocessing Protocol A standardized preprocessing workflow is essential for data quality [20].
- Handling Missing Data: For short gaps (<15-20 minutes), use linear interpolation to impute missing CGM values. For longer gaps, consider more advanced imputation methods (e.g., K-Nearest Neighbors) or exclude the data segment [20].
- Normalization: Scale CGM values to a standard range (e.g., 0 to 1) to ensure features contribute equally to model training and prevent dominance by features with larger native ranges [20].
- Synchronization: When integrating multimodal data (e.g., CGM and 15-second accelerometry), synchronize timestamps and interpolate CGM data to match the higher-frequency signal [18].
3.2 Feature Engineering for Glycemic Prediction Feature engineering transforms raw CGM time series into predictive variables. The following protocol, derived from hypoglycemia prediction research, categorizes features by their temporal relevance [19].
Table 2: Feature Engineering Protocol for Hypoglycemia Prediction
| Feature Category | Time Horizon | Example Features | Physiological Rationale |
|---|---|---|---|
| Short-Term | < 1 hour | glucose, diff_10, diff_20, diff_30, slope_1hr |
Captures immediate rate of change and current state [19] |
| Medium-Term | 1 - 4 hours | sd_2hr, sd_4hr, slope_2hr |
Reflects recent glycemic variability and trends [19] |
| Long-Term | > 4 hours | time_below70, time_above200, rebound_high, rebound_low |
Encodes patient-specific control patterns and historical events [19] |
| Snowball Effect | 2 hours | pos (sum of increments), neg (sum of decrements), max_neg |
Quantifies the accumulating effect of consecutive glucose changes [19] |
| Interaction/Non-Linear | N/A | glucose * diff_10, glucose_sq |
Models the non-linear risk of hypoglycemia (a fall is more critical at low baseline glucose) [19] |
Figure 1: CGM Data Preprocessing and Feature Engineering Workflow
Machine Learning Model Development & Experimental Protocols
With curated features, researchers can design and train ML models for specific predictive tasks.
4.1 Experimental Design for Glucose Prediction A standard experiment involves training models to predict glucose levels at a future time horizon (PH) [18].
- Input: A sliding window of prior CGM data (e.g., 30 minutes, equivalent to 6 data points).
- Output: Predicted glucose value at a specified prediction horizon (e.g., 15 or 60 minutes).
- Data Splitting: Split the dataset by participant (not by time) to prevent data leakage. A standard split is 70% for training, 10% for hyperparameter tuning, and 20% for held-out evaluation [18].
- Model Architectures: Compare a range of models, including:
- Recurrent Neural Networks (RNNs): Long Short-Term Memory (LSTM) and Gated Recurrent Unit (GRU) networks to capture temporal dependencies [18].
- Gradient-Boosting Machines: For feature-based approaches, models like XGBoost can effectively leverage engineered features [19].
- Foundation Models: For large-scale data, transformer-based models like GluFormer can be pre-trained on millions of CGM measurements and fine-tuned for specific tasks [21].
4.2 Model Evaluation Protocol Rigorous evaluation requires multiple metrics to assess both accuracy and clinical safety [18] [17].
- Root-Mean-Square Error (RMSE): Measures the absolute accuracy of predictions (in mmol/L or mg/dL).
- Spearman's Correlation Coefficient (rho): Assesses the monotonic relationship between predicted and actual glucose values.
- Surveillance Error Grid (SEG) Analysis: A critical clinical safety metric that categorizes prediction errors based on their perceived clinical risk (e.g., "no effect," "self-treatment," "dangerous"). Report the percentage of predictions in "clinically safe" zones (>99% for 15-minute, >98% for 60-minute horizons is achievable) [18].
- Sensitivity and Specificity: For hypoglycemia classification tasks (e.g., predicting <70 mg/dL), report sensitivity (>91% achievable) and specificity (>90% achievable) [19].
Table 3: Performance Benchmarks for Glucose Prediction Models
| Model / Study | Prediction Horizon | RMSE | Sensitivity/Specificity | Clinical Safety (SEG) |
|---|---|---|---|---|
| CGM-Based Model (Maastricht) [18] | 15 minutes | 0.19 mmol/L | N/A | >99% |
| CGM-Based Model (Maastricht) [18] | 60 minutes | 0.59 mmol/L | N/A | >98% |
| Feature-Based Hypoglycemia Prediction [19] | 60 minutes | N/A | >91% / >90% | N/A |
| Translated to T1D (OhioT1DM) [18] | 60 minutes | 1.73 mmol/L | N/A | >91% |
Figure 2: RNN-based Glucose Prediction Model Architecture
The Scientist's Toolkit: Research Reagent Solutions
This table details essential tools, datasets, and software for building ML models with CGM data.
Table 4: Essential Research Tools for CGM-based ML
| Tool / Resource | Type | Function in Research | Example / Source |
|---|---|---|---|
| CGM Devices | Hardware | Generate primary glucose time-series data. | Medtronic iPro2, Dexcom G6, Abbott FreeStyle Libre [18] [19] |
| Public CGM Datasets | Data | Provide benchmark data for model training and validation. | OhioT1DM Dataset, The Maastricht Study (upon request) [18] |
| Glycemic Variability Analysis Tool | Software | Calculate standard CGM metrics (Mean, SD, CV). | Glycemic Variability Research Tool (GlyVaRT) [18] |
| Python ML Stack | Software | Core programming environment for data preprocessing, model building, and evaluation. | Libraries: Pandas, NumPy, Scikit-learn, TensorFlow/PyTorch [20] |
| Consensus Error Grid | Analytical Tool | Evaluate the clinical safety of glucose predictions. | Available as a standardized Python script or library [17] |
| Tauroursodeoxycholate-d5 | Tauroursodeoxycholate-d5, MF:C26H45NO6S, MW:504.7 g/mol | Chemical Reagent | Bench Chemicals |
| Duloxetine-d7 | Duloxetine-d7, MF:C18H19NOS, MW:304.5 g/mol | Chemical Reagent | Bench Chemicals |
CGM data, when processed through the rigorous protocols outlined, provides a powerful foundation for predictive glycemic models. Current research demonstrates that ML models can achieve high accuracy and clinical safety for near-term prediction horizons [18] [19]. The future of this field lies in several key areas: the development of large, generalizable foundation models like GluFormer [21]; the effective integration of contextual data (e.g., insulin, meals, accelerometry) to improve longer-horizon predictions [18] [19]; and the translation of these algorithms into commercially viable, regulatory-approved closed-loop systems and decision-support tools that can improve the lives of people with diabetes. Adherence to emerging consensus standards for CGM evaluation will be crucial for validating these models for clinical use [17].
Patients with diabetes undergoing maintenance hemodialysis (HD) represent a distinct and challenging special population within glycemic management research. These individuals experience markedly reduced survival rates of approximately 3.7 years—nearly half that of HD patients without diabetes—underscoring the critical need for optimized treatment strategies [22]. The hemodialysis procedure itself induces significant glycemic variability, creating a paradoxical environment where patients face heightened risks of both hypoglycemia and hyperglycemia within a 24-hour cycle [22]. These challenges are compounded by the limitations of conventional glycemic markers like HbA1c, which can be biased by anemia, iron therapy, erythropoiesis-stimulating agents, and the uremic environment [23].
The integration of continuous glucose monitoring (CGM) and machine learning (ML) technologies offers promising avenues to address these complex challenges. By enabling detailed analysis of glycemic patterns and predicting adverse events, these approaches facilitate proactive interventions tailored to the unique physiological dynamics of HD patients [22]. This application note examines the specific challenges in this population and details advanced protocols for researching and implementing ML-driven glycemic management systems within the broader context of predicting glycemic response.
Key Challenges in Diabetes Management for Hemodialysis Patients
Physiological and Clinical Challenges
Managing diabetes in HD patients involves navigating a complex interplay of physiological alterations and clinical constraints, summarized in the table below.
Table 1: Key Challenges in Glycemic Management for Hemodialysis Patients with Diabetes
| Challenge Category | Specific Issue | Impact on Glycemic Control |
|---|---|---|
| Glycemic Variability | HD-induced fluctuations; increased glucose excursions | Significant differences between dialysis vs. non-dialysis days; highest hypoglycemia risk 24h post-dialysis start [22] |
| Hypoglycemia Risk | Reduced renal gluconeogenesis; insulin/glucose removal during HD | Increased morbidity/mortality; heightened risk of asymptomatic hypoglycemia during/after dialysis [22] [23] |
| Assessment Limitations | HbA1c inaccuracy due to anemia, ESA use, uremia | Unreliable glycemic assessment; necessitates alternative metrics like CGM-derived TIR, TBR, TAR [23] |
| Therapeutic Limitations | "Burnt-out diabetes" phenomenon; altered drug pharmacokinetics | Requires medication review/dose adjustment; increased hypoglycemia risk with certain agents [23] |
| Comorbidity Burden | Diabetic foot; cardiovascular disease; high mortality | Requires intensive multidisciplinary care approach [24] |
Limitations of Conventional Glycemic Metrics
In HD populations, traditional glycemic biomarkers present significant limitations that affect treatment decisions. HbA1c can be biased by factors affecting erythrocyte turnover, including iron deficiency, erythropoietin-stimulating agents, and frequent blood transfusions [23]. Alternative markers like glycated albumin (GA) and fructosamine are influenced by abnormal protein metabolism, hypoproteinemia, and the uremic environment, potentially leading to misleading values [23]. These limitations have accelerated the adoption of CGM-derived metrics—particularly Time in Range (TIR)—as more reliable indicators of glycemic control in this population [23].
Machine Learning for Glycemic Prediction in Hemodialysis
Research Foundation and Rationale
Machine learning offers a powerful approach to address glycemic variability in HD patients by identifying complex, non-linear patterns in CGM data that may not be apparent through conventional analysis. Recent research demonstrates that predicting substantial hypo- and hyperglycemia in HD patients with diabetes is feasible using ML models, enabling proactive interventions to prevent adverse events [22].
The international consensus from the Advanced Technologies & Treatments for Diabetes (ATTD) Congress recommends specific glycemic targets for high-risk populations, including those with renal disease: ≤1% Time Below Range (TBR <70 mg/dL), ≤10% Time Above Range (TAR >250 mg/dL), and ≥50% Time in Range (TIR 70–180 mg/dL) [22]. These metrics provide standardized endpoints for ML model development and validation.
Exemplary ML Implementation Protocol
Table 2: Machine Learning Protocol for Predicting Glycemic Events on Hemodialysis Days
| Protocol Component | Implementation Details |
|---|---|
| Study Objective | Develop ML models to predict substantial hypo- (TBR≥1%) and hyperglycemia (TAR≥10%) during the 24 hours following HD initiation [22] |
| Patient Population | 21 adults with type 1 or type 2 diabetes receiving chronic HD/hemodiafiltration and insulin therapy [22] |
| Data Collection | CGM data (Dexcom G6), HbA1c levels, pre-dialysis insulin dosages; 555 dialysis days analyzed [22] |
| Model Development | Three classification models trained/tested: Logistic Regression, XGBoost, and TabPFN [22] |
| Feature Engineering | CGM-derived metrics; feature selection via Recursive Feature Elimination with Cross-Validation (RFECV) [22] |
| Performance Results | - Hyperglycemia prediction: Logistic Regression (F1: 0.85; ROC-AUC: 0.87)- Hypoglycemia prediction: TabPFN (F1: 0.48; ROC-AUC: 0.88) [22] |
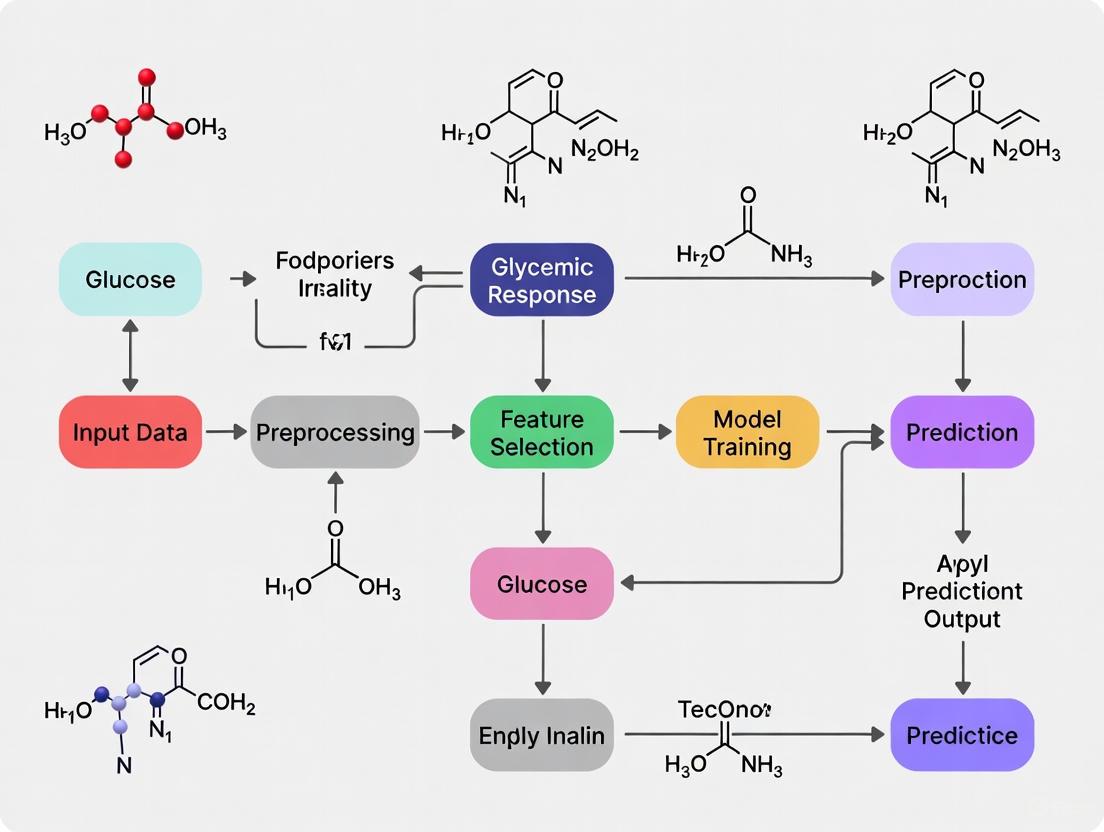
Figure 1: Machine learning workflow for predicting glycemic events in hemodialysis patients. The process begins with data collection from diabetic patients on HD, progresses through feature engineering and model training, and culminates in predictive outputs for clinical intervention.
Advanced CGM Application Protocol in Hemodialysis Research
CGM Deployment and Data Processing
The following protocol details the methodology for employing CGM in HD populations, based on validated research approaches:
Sensor Deployment: Apply CGM sensors (e.g., FreeStyle Libre Pro, Dexcom G6) to the upper arm contralateral to vascular access. Ensure continuous wear for 10-14 consecutive days, maintaining at least 70% sensor activity for data validity [25]. For HD sessions, document precise dialysis timing, dialysate glucose concentration, and any procedural interruptions.
Data Collection Parameters: Capture comprehensive glucose metrics including mean sensor glucose level, standard deviation (SD), coefficient of variation (%CV), and international consensus parameters: Time in Range (TIR: 70-180 mg/dL), Time Below Range (TBR: <70 mg/dL and <54 mg/dL), and Time Above Range (TAR: >180 mg/dL) [25].
Glycemic Event Definition: Define hypoglycemia as sensor glucose <70 mg/dL for >30 minutes. Categorize by timing: daytime (06:00-24:00) vs. nocturnal (00:00-06:00). Specifically identify HD-induced hypoglycemia as episodes occurring during or after dialysis until the next meal [25].
Data Processing: Calculate the incremental area under the curve (iAUC) over a 2-hour postprandial window for meal response analysis. Align CGM data with HD sessions, differentiating between dialysis and non-dialysis days. For ML applications, segment data into 24-hour pre-dialysis (feature segment) and 24-hour post-dialysis initiation (prediction segment) [22].
CGM-Derived Glycemic Metrics
Table 3: CGM-Derived Glycemic Metrics Following Semaglutide Intervention in HD Patients
| Glycemic Parameter | Baseline | 6-Month Follow-up | P-value |
|---|---|---|---|
| HbA1c (%) | 7.8 ± 1.2 | 6.9 ± 1.1 | 0.0318 |
| Glycated Albumin (%) | 23.6 ± 5.2 | 19.6 ± 4.3 | 0.0062 |
| Mean Sensor Glucose (mg/dL) | 172.0 ± 36.2 | 138.1 ± 25.4 | 0.0177 |
| Glucose Variability (SD) | 56.8 ± 24.4 | 42.1 ± 12.8 | 0.0264 |
| Time in Range (%) | 57.0 (34.0-86.0) | 78.0 (51.4-97.0) | 0.0420 |
Data presented as mean ± standard deviation or median (range). Source: Adapted from semaglutide study in HD patients [25].
Therapeutic Management Protocol
Pharmacologic Intervention Protocol
GLP-1 Receptor Agonists: For patients with T2D and obesity on HD, semaglutide demonstrates significant efficacy. Initiate at 0.25 mg subcutaneously once weekly. If tolerated, increase to 0.5 mg after 4 weeks, with potential escalation to 1.0 mg weekly after an additional 4 weeks [25]. For patients experiencing gastrointestinal intolerance, maintain the current dose without escalation if glycemic markers are adequately controlled.
Insulin Regimen De-intensification: The IDEAL trial protocol provides a framework for simplifying complex insulin regimens. For patients on multiple daily injection (MDI) insulin therapy, transition to fixed-ratio combinations like iGlarLixi (containing insulin glargine and lixisenatide), administered once daily [26]. This approach maintains glycemic control while reducing hypoglycemia risk and treatment burden.
Insulin Dose Adjustment: For HD patients initiating GLP-1RA therapy, closely monitor for hypoglycemia. Implement proactive insulin reduction when clinical hypoglycemia or CGM-detected glucose <70 mg/dL occurs. In the referenced semaglutide study, total daily insulin doses significantly decreased from 48.5 to 43.5 units/day while maintaining glycemic control [25].
Figure 2: Clinical decision pathway for glycemic management in hemodialysis patients. The flowchart outlines therapeutic choices based on patient presentation, including GLP-1RA initiation, insulin de-intensification, and dose adjustment guided by CGM monitoring.
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Research Materials and Technologies for HD Glycemia Studies
| Research Tool | Specification/Model | Research Application |
|---|---|---|
| Continuous Glucose Monitor | FreeStyle Libre Pro (Abbott); Dexcom G6 | Retrospective/prospective glucose monitoring; captures glycemic variability during/inter-dialysis [25] |
| Machine Learning Algorithms | Logistic Regression, XGBoost, TabPFN | Prediction of hypo-/hyper-glycemia events; pattern recognition in CGM data [22] |
| Glycemic Analysis Software | Custom Python/R pipelines with iAUC calculation | Processing CGM data; calculating TIR, TBR, TAR; feature extraction for ML models [22] |
| GLP-1 Receptor Agonist | Semaglutide (Ozempic/Wegovy) | Investigational intervention for glycemic/weight control in HD patients [25] |
| Fixed-Ratio Combination | iGlarLixi (Suliqua) | Insulin de-intensification strategy; reduces regimen complexity while maintaining control [26] |
| rac Felodipine-d3 | rac Felodipine-d3 Calcium Channel Blocker | rac Felodipine-d3is a deuterated calcium channel blocker for hypertension research. For Research Use Only. Not for human consumption. |
| Lopinavir-d8 | Lopinavir-d8, MF:C37H48N4O5, MW:636.8 g/mol | Chemical Reagent |
The integration of continuous glucose monitoring and machine learning prediction models represents a transformative approach to diabetes management in hemodialysis patients. These technologies address fundamental challenges in this population by enabling precise glycemic assessment and proactive intervention for the marked glycemic fluctuations induced by dialysis therapy. Current evidence supports the feasibility of predicting substantial hypo- and hyperglycemia on dialysis days using ML models, while novel therapeutic protocols using GLP-1RAs and insulin de-intensification strategies offer promising avenues for improved patient outcomes.
Future research should prioritize multicenter validation of ML algorithms in larger HD populations, development of real-time clinical decision support systems integrating CGM data with electronic health records, and randomized controlled trials evaluating the impact of these advanced technologies on hard clinical endpoints including mortality, hospitalization rates, and dialysis-related complications.
Interindividual and Intraindividual Variability in Glycemic Responses
Glycemic variability—differences in blood glucose responses to food—is a critical factor in diabetes management and metabolic health research. Interindividual variability (differences between people) and intraindividual variability (differences within the same person over time) complicate glycemic predictions. Machine learning (ML) algorithms can address this complexity by integrating multi-omics data, continuous glucose monitoring (CGM), and clinical variables to personalize forecasts. This document outlines experimental protocols, data sources, and reagent solutions for studying glycemic variability within ML-driven research.
Quantitative Data on Glycemic Variability
Table 1: Interindividual Variability in Postprandial Glycemic Responses (PPGRs) to Carbohydrate Meals
| Carbohydrate Source | Mean Delta Glucose Peak (mg/dL) | Correlation with Metabolic Phenotypes | Key Demographic Associations |
|---|---|---|---|
| Rice | Highest among starchy meals | Insulin resistance, beta cell dysfunction | More common in Asian individuals |
| Potatoes | High | Insulin resistance, lower disposition index | None reported |
| Grapes | High (early peak) | Insulin sensitivity | None reported |
| Beans | Lowest | None reported | None reported |
| Pasta | Low | None reported | None reported |
| Mixed Berries | Low | None reported | None reported |
Source: Adapted from [27]. Meals contained 50 g carbohydrates. PPGRs measured via CGM.
Table 2: Intraindividual Variability and Reproducibility of Glycemic Responses
| Variability Type | Cause/Source | Impact on PPGR | Statistical Evidence |
|---|---|---|---|
| Meal Replication | Same meal consumed on different days | Moderate reproducibility (ICC: 0.26–0.73) | ICC highest for pasta (0.73) |
| Time of Day | Lunch vs. dinner | Significant PPGR differences | P < 0.05 (lunch), P < 0.001 (dinner) [28] |
| Menstrual Cycle | Perimenstrual phase | Elevated Glumax | P < 0.05 [28] |
| Meal Composition | Fiber, protein, fat preloads | Reduced PPGR in insulin-sensitive individuals | Mitigators less effective in insulin-resistant individuals [27] |
ICC: Intraclass Correlation Coefficient; Glumax: Peak postprandial glucose rise.
Table 3: Machine Learning Performance in Glycemic Prediction
| Prediction Task | ML Model | Performance Metrics | Data Sources |
|---|---|---|---|
| BG Level Prediction (15 min) | Neural Network Model (NNM) | RMSE: 0.19 mmol/L; Correlation: 0.96 [29] | CGM |
| BG Level Prediction (60 min) | Neural Network Model (NNM) | RMSE: 0.59 mmol/L; Correlation: 0.72 [29] | CGM + Accelerometry |
| Hypoglycemia Prediction | Gradient Boosting | Sensitivity: 0.76; Specificity: 0.91 [29] | EHR, CGM, Medication data |
| PPGR Prediction | XGBoost | R = 0.61 (T1D), R = 0.72 (T2D) [28] | Demographics, Meal timing, Food categories |
RMSE: Root Mean Square Error; EHR: Electronic Health Records.
Experimental Protocols for Glycemic Variability Research
Protocol 1: Assessing PPGRs to Standardized Carbohydrate Meals
Objective: Quantify interindividual and intraindividual variability in PPGRs to carbohydrate-rich meals. Materials:
- CGM devices (e.g., Dexcom G6, FreeStyle Libre) [28] [30].
- Standardized meals (50 g available carbohydrates): rice, bread, potatoes, pasta, beans, grapes, mixed berries [27].
- Nutrient composition database (e.g., Food and Nutrient Database for Dietary Studies).
Procedure:
- Participant Preparation:
- Meal Administration:
- Administer each meal in duplicate on separate days in a randomized order.
- Ensure ≥8-hour fasting before meals.
- CGM Data Collection:
- Record glucose every 5–15 minutes for 2–3 hours postprandially [30].
- Extract PPGR features: AUC(>baseline), delta glucose peak, time to peak.
- Data Analysis:
- Calculate intraclass correlation coefficients (ICCs) for replicate meals.
- Cluster participants into "spikers" and "non-spikers" based on delta glucose peak [27].
Protocol 2: Evaluating Mitigators of PPGRs
Objective: Test the effect of fiber, protein, and fat preloads on PPGRs. Materials:
- Preloads: pea fiber (fiber), egg white (protein), cream (fat) [27].
- Standardized rice meal (50 g carbohydrates).
Procedure:
- Preload participants with one mitigator 10 minutes before the rice meal.
- Measure PPGRs using CGM as in Protocol 1.
- Compare AUC(>baseline) and delta glucose peak with/without preloads.
- Stratify analysis by insulin sensitivity (e.g., SSPG < 120 mg/dL vs. ≥120 mg/dL) [27].
Protocol 3: ML Model Development for Glycemic Prediction
Objective: Train ML models to predict PPGRs or hypoglycemia. Materials:
- Dataset: CGM data, accelerometry, EHR (e.g., insulin doses, meal timings) [31] [10].
- Software: Python (scikit-learn, TensorFlow).
Procedure:
- Data Preprocessing:
- Feature Engineering:
- Model Training:
- Validation:
Signaling Pathways and Workflow Diagrams
Diagram 1: Metabolic Pathways Influencing Glycemic Variability
Title: Metabolic Factors in Glycemic Responses
Diagram 2: Workflow for ML-Based Glycemic Prediction
Title: ML Pipeline for Glucose Forecasting
The Scientist’s Toolkit: Research Reagent Solutions
Table 4: Essential Materials for Glycemic Variability Studies
| Reagent/Equipment | Function | Example Use Case |
|---|---|---|
| Continuous Glucose Monitor (CGM) | Tracks interstitial glucose levels in real-time (e.g., every 5 minutes) | PPGR measurement post-meal [27] [30] |
| Standardized Meals | Provides consistent carbohydrate loads (50 g) for PPGR comparisons | Testing rice, bread, or potato responses [27] |
| Accelerometers | Measures physical activity’s impact on glucose metabolism | Improving 60-minute glucose predictions [31] |
| Electronic Health Records (EHR) | Source of clinical variables (insulin doses, medications) for ML models | Predicting hypoglycemia in ICU patients [10] |
| Multi-omics Datasets | Includes microbiome, metabolomics, and genomic data for personalized insights | Identifying PPGR-associated microbial pathways [27] |
| Gradient Boosting Algorithms (XGBoost) | Predicts PPGRs or hypoglycemia risks from complex datasets | Achieving R = 0.72 for T2D PPGR prediction [28] |
| Ferulic Acid-d3 | Ferulic Acid-d3, CAS:860605-59-0, MF:C10H10O4, MW:197.204 | Chemical Reagent |
| Voriconazole-d3 | Voriconazole-d3, MF:C16H14F3N5O, MW:352.33 g/mol | Chemical Reagent |
Interindividual and intraindividual glycemic variability is influenced by food composition, metabolic phenotypes, and temporal factors. ML models—especially neural networks and gradient boosting—can mitigate this variability by integrating CGM, EHR, and meal data. Standardized protocols for meal tests and mitigator interventions enable reproducible research. Future work should focus on real-time ML integration into clinical decision support systems.
Methodological Approaches and Clinical Applications of ML Algorithms
Within research aimed at predicting glycemic response, the selection of an appropriate machine learning model is paramount. Such predictions are critical for developing personalized treatment strategies, optimizing drug efficacy, and preventing adverse events like hypoglycemia in patients with diabetes. This document provides detailed application notes and experimental protocols for three foundational machine learning models—Logistic Regression, Random Forest, and XGBoost—tailored for researchers and scientists in the field of drug development and metabolic disease.
The following table summarizes the typical performance characteristics of these three models as applied to tasks like hypoglycemia prediction, based on recent research.
Table 1: Model Performance Comparison for Hypoglycemia Prediction [32]
| Model | Predictive Accuracy | Kappa Coefficient | Macro-average AUC | Key Strengths |
|---|---|---|---|---|
| Random Forest (RF) | 93.3% | 0.873 | 0.960 | High accuracy, robust to overfitting, good interpretability via feature importance |
| XGBoost | 92.6% | 0.860 | 0.955 | Superior handling of imbalanced data, high precision on structured/tabular data |
| Logistic Regression | 83.8% | 0.685 | 0.788 | High model interpretability, establishes baseline performance, efficient to train |
Experimental Protocols
Protocol 1: Building a Multinomial Logistic Regression Model
Application Note: Use this model for multi-class classification of hypoglycemia severity (e.g., normal, mild, moderate-to-severe) when interpretability of risk factors is a primary research objective [32] [33].
Workflow:
Data Preparation and Variable Coding
- Outcome Variable: Define hypoglycemia severity groups based on venous plasma glucose levels. Example categories:
- Normal glycemia: >3.9 mmol/L
- Mild hypoglycemia: 3.0 – 3.9 mmol/L
- Moderate-to-severe hypoglycemia: <3.0 mmol/L [32]
- Covariates: Include clinically relevant features such as age, HbA1c, mean blood glucose, serum creatinine, C-peptide, and medication usage [32].
- Reference Category: Designate one outcome category as the reference (e.g., "Normal glycemia"). The model will compute log odds for all other categories against this baseline [33].
- Outcome Variable: Define hypoglycemia severity groups based on venous plasma glucose levels. Example categories:
Model Estimation
- Use maximum likelihood estimation to fit the model.
- The logit functions for a 3-class outcome (with
0as reference) are:- ( g1(\mathbf{x}) = \ln\frac{P(Y=1|\mathbf{x})}{P(Y=0|\mathbf{x})} = \alpha1 + \beta{11}x1 + \cdots + \beta{1p}xp ) (Mild vs. Normal)
- ( g2(\mathbf{x}) = \ln\frac{P(Y=2|\mathbf{x})}{P(Y=0|\mathbf{x})} = \alpha2 + \beta{21}x1 + \cdots + \beta{2p}xp ) (Moderate-to-severe vs. Normal) [33]
Output Interpretation
- Interpret the results in terms of relative risk ratios by exponentiating the coefficients (( e^\beta )).
- A relative risk ratio greater than 1 for a given variable indicates an increased likelihood of being in the comparison group versus the reference group as the variable increases [33].
Diagram: Multinomial Logistic Regression Workflow
Protocol 2: Tuning a Random Forest Classifier
Application Note: Apply Random Forest for robust, high-accuracy prediction of hypoglycemic events. Its ensemble nature reduces overfitting and provides insights into feature importance [32] [34].
Workflow:
Data Preprocessing
- Handle missing values (RF can handle them, but imputation is often recommended).
- No need for feature scaling. RF is robust to the scale of features [34].
Hyperparameter Optimization
- Use RandomizedSearchCV or GridSearchCV for hyperparameter tuning [35].
- Key hyperparameters to optimize [35] [36]:
n_estimators: Number of trees in the forest (more trees increase stability but slow training).max_depth: Maximum depth of the trees (controls overfitting).min_samples_split: Minimum samples required to split an internal node.min_samples_leaf: Minimum samples required at a leaf node.max_features: Number of features to consider for the best split ("sqrt" is a common default).
Model Training & Validation
Feature Importance Analysis
- Extract feature importance scores from the trained model, which indicate the contribution of each variable to the model's predictions [32].
Diagram: Random Forest Hyperparameter Tuning Logic
Protocol 3: Optimizing XGBoost with Genetic Algorithms
Application Note: For maximum predictive performance on structured glycemic data, especially with class imbalances, XGBoost is often superior. Its performance can be further enhanced using advanced optimization techniques like Genetic Algorithms (GA) [37] [34].
Workflow:
Data Balancing
- Address class imbalance (e.g., few hypoglycemic events) using techniques like SMOTEENN (Synthetic Minority Oversampling Technique edited with Nearest Neighbors), which has shown efficiency in diabetes prediction tasks [37].
Hyperparameter Optimization with Genetic Algorithm
- Implement a GA to find the global optimum of XGBoost's complex parameter space [37].
- Key XGBoost parameters for GA to optimize:
learning_rate(eta): Shrinks feature weights to make boosting more robust.max_depth: Maximum depth of a tree.subsample: Fraction of samples used for training each tree.colsample_bytree: Fraction of features used for training each tree.reg_alpha(L1) andreg_lambda(L2): Regularization terms to prevent overfitting [34].
Model Training and Interpretation
- Train the final model with the GA-optimized parameters. XGBoost builds trees sequentially, with each new tree correcting the errors of the previous ones [34].
- Use SHAP (SHapley Additive exPlanations) values for model interpretation. SHAP provides consistent and theoretically robust feature importance values, showing both the magnitude and direction (increase or decrease) of a feature's impact on the prediction [37] [38].
Diagram: GA-XGBoost Optimization Pipeline
The Scientist's Toolkit: Key Research Reagents & Solutions
Table 2: Essential Materials for Glycemic Prediction Research [32] [31] [38]
| Item / Solution | Function / Application Note |
|---|---|
| Electronic Medical Record (EMR) Data | Source for retrospective clinical variables (e.g., HbA1c, creatinine, medication history). Crucial for training models on clinical outcomes like hypoglycemia severity [32]. |
| Continuous Glucose Monitor (CGM) | Provides high-frequency interstitial glucose measurements. The primary data stream for building time-series prediction models of future glucose levels [31] [38]. |
| Triaxial Accelerometer | Quantifies physical activity and energy expenditure. Used as an exogenous input variable to improve the accuracy of glucose prediction models by accounting for metabolic fluctuations [31]. |
| SHAP (SHapley Additive exPlanations) | A unified framework for interpreting model output. Critical for explaining "black-box" models like XGBoost and ensuring learned relationships (e.g., between insulin and glucose) are physiologically sound [38]. |
| Genetic Algorithm (GA) Library | An optimization technique for hyperparameter tuning. Used to efficiently navigate the complex parameter space of models like XGBoost to maximize predictive performance [37]. |
| Solifenacin-d5 Hydrochloride | Solifenacin-d5 Hydrochloride, MF:C23H27ClN2O2, MW:398.9 g/mol |
| rac Ramelteon-d3 | rac Ramelteon-d3, MF:C16H21NO2, MW:262.36 g/mol |
The management of diabetes, a chronic condition affecting hundreds of millions globally, hinges on effective glycemic control. Traditional approaches to predicting blood glucose levels and glycemic responses often rely on generic models that fail to account for significant interindividual variability. Recent advances in deep learning offer transformative potential for creating highly accurate, personalized predictive models. This article explores the application of three advanced deep learning architectures—Long Short-Term Memory (LSTM) networks, Gated Recurrent Units (GRUs), and Transformer networks—within glycemic response research. We provide a detailed comparative analysis, structured protocols for implementation, and practical toolkits to empower researchers and drug development professionals in harnessing these technologies.
Comparative Analysis of Deep Learning Architectures
Selecting an appropriate neural network architecture is foundational to building effective predictive models for glycemic response. The table below summarizes the key characteristics of LSTM, GRU, and Transformer models.
Table 1: Architectural Comparison of LSTM, GRU, and Transformer Networks
| Parameter | LSTM (Long Short-Term Memory) | GRU (Gated Recurrent Unit) | Transformers |
|---|---|---|---|
| Core Architecture | Memory cells with input, forget, and output gates [39] [40] | Combines input and forget gates into an update gate; fewer parameters [39] [40] | Attention-based mechanism without recurrence; uses self-attention [39] [40] |
| Handling Long-Term Dependencies | Excels in capturing long-term dependencies [39] | Better than RNNs but slightly less effective than LSTMs [39] | Excellent; uses self-attention to weigh importance of all elements in a sequence [39] [40] |
| Training Time & Parallelization | Slower due to complex gates; limited parallelism due to sequential processing [39] | Faster than LSTMs but slower than RNNs; same sequential processing limitations [39] | Requires heavy computation but allows full parallelization during training [39] |
| Key Advantages | Mitigates vanishing gradient problem; effective memory retention [39] [40] | Simplified structure; faster training; computationally efficient [39] [40] | Captures long-range dependencies effectively; highly scalable [39] [40] |
| Primary Limitations | Computationally intensive; high memory consumption [39] | Might not capture long-term dependencies as effectively as LSTM in some tasks [40] | High memory and data requirements; computationally expensive [39] [40] |
Performance in Glycemic Prediction
Empirical evidence from recent studies demonstrates the relative performance of these architectures in glucose forecasting. A 2024 comprehensive analysis evaluating deep learning models across diverse datasets found that LSTM demonstrated superior performance with the lowest Root Mean Square Error (RMSE) and the highest generalization capability, closely followed by the Self-Attention Network (SAN), a type of Transformer [41]. The study attributed this to the ability of LSTM and SAN to capture long-term dependencies in blood glucose data and their correlations with various influencing factors [41].
Conversely, research into novel methods like Neural Architecture Search combined with Deep Reinforcement Learning has shown that GRU-based models can be optimized to achieve performance comparable to LSTMs, with one study reporting a 12.6% improvement in RMSE for a specific patient after optimization, highlighting their efficiency [42]. In a direct comparison for stock price prediction (a similar time-series task), an LSTM model achieved 94% accuracy, outperforming GRU and Transformer models [43]. This suggests that for many glycemic prediction tasks, LSTMs may offer a favorable balance of performance and complexity, while GRUs present a compelling option when computational resources are a primary constraint.
Experimental Protocols for Glycemic Response Prediction
This section outlines a detailed protocol for a study designed to characterize interindividual variability in postprandial glycemic response (PPGR) and develop personalized prediction models, adapting methodologies from recent research [44].
Study Design and Participant Recruitment
Objective: To characterize PPGR variability among individuals with Type 2 Diabetes (T2D) and identify factors associated with these differences using machine learning. Design: Prospective cohort study. Duration: 14-day active monitoring period per participant. Participants:
- Cohort Size: 800+ participants (adaptable based on resources) [44] [45].
- Inclusion Criteria: Adults (age 18-75) with physician-diagnosed T2D, hemoglobin A1c (HbA1c) ≥7%, treated with ≥1 oral hypoglycemic agent, and mobile phone capable of running study applications [44].
- Exclusion Criteria: Use of prandial insulin, pregnancy, life expectancy ≤12 months, active cancer, contraindication to continuous glucose monitors (CGM) [44]. Setting: Multi-site recruitment from specialized diabetes clinics to ensure a diverse cohort [44].
Data Collection and Preprocessing Workflow
The following diagram illustrates the sequential workflow for data collection and preprocessing in a glycemic response study.
Title: Glycemic Response Study Workflow
Protocol Steps:
Baseline Assessment:
- Collect sociodemographic information, medical history, and current medications.
- Perform biometric measurements: weight, height, waist circumference, blood pressure.
- Administer baseline surveys (e.g., WHO-5 Well-Being Index, Diabetes Distress Scale) [44].
- Collect blood samples for HbA1c, complete blood count, lipids, and other relevant biomarkers [44].
Device Fitting and Training:
- Fit participants with a CGM sensor (e.g., Abbott Freestyle Libre) on the upper arm.
- Provide and synchronize a smart wristband (e.g., Xiaomi Mi Band) for heart rate and activity monitoring.
- Install and train participants on a study-specific smartphone application for dietary and activity logging. Provide a paper logbook as a backup [44].
14-Day Active Monitoring:
- CGM Data: Collect interstitial glucose readings at 5-15 minute intervals continuously.
- Dietary Logging: Participants log all meal intake. The protocol includes consumption of standardized test meals (e.g., varying carbohydrate, fiber, protein, and fat content) and free-living foods. Meals are logged with details including nutritional composition and timing [44].
- Physical Activity: Data is collected via the smart wristband (METs, step counts) and participant logs [44].
- Medication & Sleep: Participants log medication intake and sleep patterns.
Data Preprocessing:
- Synchronization: Align all temporal data streams (CGM, meals, activity) to a common timeline.
- Handling Missing Data: Apply techniques such as interpolation or masking for short gaps in CGM data. Exclude periods with significant data loss.
- Feature Engineering: Calculate key features from raw data, such as incremental Area Under the Curve (AUC) for PPGR 2 hours after each meal [44], glycemic variability metrics, and rolling averages.
Model Development and Training Protocol
Primary Outcome: Postprandial Glycemic Response (PPGR), calculated as the incremental AUC 2 hours after each logged meal [44].
- Input Features: Historical glucose sequences, meal nutrient profiles (carbs, fat, protein, fiber, sugar), timing, physical activity metrics, and baseline patient characteristics (e.g., HbA1c, BMI) [44] [46].
- Data Splitting: Partition data into training (70%), validation (15%), and test (15%) sets, ensuring data from a single participant is contained within one set to prevent data leakage.
- Model Architectures:
- LSTM/GRU Models: Implement using a many-to-one architecture. Tune hyperparameters like number of layers, hidden units, and learning rate.
- Transformer Models: Adapt for time-series by using positional encoding. Tune hyperparameters like number of attention heads, layers, and feed-forward dimension.
- Training with Imbalanced Data: Employ techniques to handle the rarity of hypo-/hyperglycemic events:
- Evaluation Metrics:
The Scientist's Toolkit: Research Reagent Solutions
The following table details essential materials, datasets, and software required for conducting research in deep learning-based glycemic prediction.
Table 2: Essential Research Reagents and Resources
| Item Name | Function/Application | Example Specifications / Notes |
|---|---|---|
| Continuous Glucose Monitor (CGM) | Measures interstitial glucose levels at high frequency (e.g., every 5-15 mins) for model training and validation [44] [46]. | Abbott Freestyle Libre, Dexcom G7; typically worn on the upper arm [44] [46]. |
| Smart Wristband / Activity Tracker | Captures physiological data related to energy expenditure and metabolic state [44]. | Xiaomi Mi Band; records heart rate, step counts, and calculates METs [44]. |
| Standardized Test Meals | Used to elicit and measure controlled postprandial glycemic responses, reducing dietary noise [44]. | Vegetarian meals with varying macronutrient proportions (carbohydrate, fiber, protein, fat) [44]. |
| Data Logging Application | Digital platform for participants to log dietary intake, activity, and medication in real-time. | A custom or commercially available app capable of timestamped logging and synchronization with other devices [44]. |
| Public Datasets (for Benchmarking) | Provide standardized data for model development, comparison, and reproducibility. | OhioT1DM [41] [47] (Type 1 Diabetes), other proprietary or public T2D datasets. |
| Clofibric-d4 Acid | Clofibric-d4 Acid, CAS:1184991-14-7, MF:C10H11ClO3, MW:218.67 g/mol | Chemical Reagent |
| Benzocaine-d4 | Benzocaine-d4 Deuterated Local Anesthetic | Benzocaine-d4 is a deuterated local anesthetic for research use only. It is used as an internal standard in bioanalytical studies and for investigating sodium channel block. Not for human or veterinary use. |
The integration of advanced deep learning architectures like LSTM, GRU, and Transformers into glycemic research marks a significant shift toward personalized diabetes management. LSTM networks currently offer a robust and well-validated approach for glucose prediction, consistently demonstrating strong performance. GRUs provide a compelling, computationally efficient alternative, especially in resource-constrained settings. While Transformers show immense promise due to their superior ability to capture long-range dependencies, their deployment may be gated by data and computational requirements. The future of this field lies in the continued refinement of these models through techniques like transfer learning and data augmentation, their application to diverse populations, and their ultimate integration into closed-loop systems and digital therapeutics that can deliver personalized dietary and therapeutic recommendations in real time.
Multi-Task Learning Frameworks for Simultaneous Glucose Forecasting and Hypoglycemia Detection
The management of diabetes mellitus requires continuous monitoring of glycemic states to prevent acute complications, such as hypoglycemia, and long-term sequelae. Traditional machine learning models have often approached glucose forecasting and hypoglycemia detection as separate tasks, potentially overlooking shared physiological patterns and leading to operational inefficiencies in clinical decision support systems [48]. Multi-task learning (MTL) frameworks address this limitation by learning these related tasks in parallel using a shared representation, which can improve generalization and performance, especially when data for individual tasks is scarce [49]. This document details the application of advanced MTL frameworks, namely GlucoNet-MM and a Domain-Agnostic Continual MTL (DA-CMTL) model, for the integrated and personalized prediction of blood glucose levels and hypoglycemic events. These protocols are situated within a broader research thrust aimed at developing machine learning algorithms that can predict individualized glycemic responses to improve diabetes care [44] [8].
Featured Multi-Task Learning Frameworks
GlucoNet-MM: A Multimodal Attention-Based Framework
GlucoNet-MM is a novel deep learning framework that combines an attention-based multi-task learning backbone with a Decision Transformer (DT) to generate personalized and explainable blood glucose forecasts [50].
- Architecture Overview: The model integrates heterogeneous, multimodal data streams, including continuous glucose monitoring (CGM), insulin dosage, carbohydrate intake, and physical activity. Its MTL backbone learns shared representations across multiple prediction horizons. The integrated DT module frames policy learning as a sequence modeling problem, conditioning future glucose predictions on desired glycemic outcomes [50].
- Interpretability and Uncertainty: The framework incorporates temporal attention visualizations and integrated gradient-based attribution methods to provide explainability for its predictions. Furthermore, it employs Monte Carlo dropout for uncertainty quantification, a critical feature for clinical trust and application [50].
DA-CMTL: A Domain-Agnostic Continual Learning Framework
The Domain-Agnostic Continual Multi-Task Learning (DA-CMTL) model is designed to perform generalized glucose level prediction and hypoglycemia event detection within a unified framework that adapts over time and across different patient populations [48].
- Architecture Overview: This model is trained on large-scale simulated datasets (Sim2Real transfer) and uses elastic weight consolidation to maintain performance on previously learned tasks when new data or tasks are introduced. This approach enhances the model's robustness and scalability for deployment in automated insulin delivery (AID) systems [48].
- Generalization Capability: Its domain-agnostic design supports generalization across different domains and patient cohorts, making it suitable for widespread clinical application [48].
Performance Comparison of MTL Frameworks
The following tables summarize the quantitative performance of the featured MTL frameworks as reported in validation studies on public datasets.
Table 1: Blood Glucose Forecasting Performance
| Framework | Dataset(s) | Root Mean Squared Error (mg/dL) | Mean Absolute Error (mg/dL) | R² Score |
|---|---|---|---|---|
| GlucoNet-MM [50] | BrisT1D, OhioT1DM | Not Specified | 0.031 (Normalized) | 0.94, 0.96 |
| DA-CMTL [48] | DiaTrend, OhioT1DM, ShanghaiT1DM | 14.19 | 10.09 | Not Specified |
Table 2: Hypoglycemia Detection Performance
| Framework | Dataset(s) | Sensitivity (%) | Specificity (%) | Time Below Range Reduction |
|---|---|---|---|---|
| DA-CMTL [48] | DiaTrend, OhioT1DM, ShanghaiT1DM (Real-world rat model) | 89.28 | 94.09 | 3.01% to 2.58% |
Experimental Protocols
Data Acquisition and Preprocessing Protocol
This protocol outlines the steps for gathering and preparing data suitable for training MTL models in glycemic response research, based on standardized methodologies [44].
- Objective: To collect high-temporal-resolution physiological and behavioral data from individuals with diabetes for model development.
- Participant Enrollment: Enroll adult participants (e.g., aged 18-75) with type 1 or type 2 diabetes. Key inclusion criteria comprise a diagnosis of diabetes and suboptimal glycemic control (e.g., HbA1c ≥7%). Exclude users of prandial insulin, pregnant individuals, and those with certain comorbid conditions to control for confounding variables [44].
- Equipment and Data Streams:
- Continuous Glucose Monitor (CGM): Fit participants with a CGM sensor (e.g., Abbott Freestyle Libre) on the upper arm to measure interstitial glucose levels at 5-15 minute intervals for a minimum of 14 days [44].
- Activity Monitoring: Provide a wearable smart wristband (e.g., Xiaomi Mi Band) to continuously monitor physical activity and heart rate.
- Digital Logging: Use smartphone applications or paper logbooks for participants to record dietary intake (including standardized test meals), medication (especially insulin dosage), and exercise.
- Biometric and Survey Data: Collect baseline biometrics (weight, height, blood pressure) and blood samples for HbA1c, lipid profile, and other relevant biomarkers. Administer well-being and lifestyle surveys (e.g., WHO-5 Well-Being Index, Pittsburgh Sleep Quality Index) [44].
- Data Preprocessing: Synchronize all data streams using timestamps. Clean CGM data to address signal dropouts and sensor noise. Normalize numerical features and encode categorical variables (e.g., food types).
Model Training and Validation Protocol
This protocol describes the procedure for training and evaluating an MTL framework like GlucoNet-MM or DA-CMTL.
- Objective: To train a single model that simultaneously performs glucose forecasting and hypoglycemia detection, and to rigorously evaluate its performance.
- Data Partitioning: Split the preprocessed dataset into training, validation, and testing sets, ensuring data from individual participants is contained within a single set to prevent data leakage and ensure realistic generalization assessment.
- Model Configuration:
- For GlucoNet-MM: Implement the multimodal architecture with attention mechanisms. Configure the multi-task learning heads for different prediction horizons (e.g., 30, 60, 120-minute forecasts) and a hypoglycemia classification head. Initialize the Decision Transformer to condition predictions on past glucose trajectories and actions [50].
- For DA-CMTL: Implement the continual learning framework with elastic weight consolidation. Set up the twin tasks of glucose level regression and hypoglycemia event classification.
- Training Procedure: Train the model using the training set. Use the validation set for hyperparameter tuning and to determine early stopping criteria. Employ mini-batch gradient descent with a suitable optimizer (e.g., Adam).
- Evaluation Metrics: On the held-out test set, calculate the primary outcomes for each task:
- Glucose Forecasting: Root Mean Squared Error (RMSE), Mean Absolute Error (MAE), and R² score.
- Hypoglycemia Detection: Sensitivity, Specificity, and Area Under the Receiver Operating Characteristic Curve (AUC-ROC).
- Explainability Analysis: For interpretable models like GlucoNet-MM, generate attention maps and integrated gradients to identify which input features (e.g., recent carbohydrate intake, insulin) most influenced key predictions [50].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Reagents for MTL Glycemic Research
| Item | Function/Application in Research |
|---|---|
| Continuous Glucose Monitor (CGM) [44] | Provides high-frequency, real-time measurements of interstitial glucose levels, forming the primary outcome variable for model training and validation. |
| Standardized Test Meals [44] | Used to elicit controlled postprandial glycemic responses (PPGR); essential for characterizing inter-individual variation and validating model predictions under controlled conditions. |
| Wearable Activity Monitor [44] | Captures objective data on physical activity and heart rate, which are critical behavioral covariates affecting glucose metabolism. |
| Digital Food Logging Platform [44] [8] | Enables detailed recording of dietary intake (including meal timing and composition), which is a major input variable for predicting postprandial glucose responses. |
| Simulated Datasets (e.g., from Simulators) [48] | Provides large-scale, synthetic patient data for initial model training (Sim2Real transfer), mitigating the challenges of data scarcity and privacy in the early stages of development. |
| rac Mephenytoin-d3 | rac Mephenytoin-d3, CAS:1185101-86-3, MF:C12H14N2O2, MW:221.27 g/mol |
Framework Architecture and Workflow Diagrams
GlucoNet-MM Multimodal Framework
DA-CMTL Continual Learning Workflow
Continuous Glucose Monitoring (CGM) systems generate dynamic, high-frequency data that provide a comprehensive view of glycemic physiology beyond static measures like HbA1c. For machine learning algorithms aimed at predicting glycemic response, appropriate feature engineering from CGM data is paramount. CGM-derived metrics capture essential aspects of glycemic control including average glucose, variability, and temporal patterns [51]. When combined with demographic and clinical variables, these features enable the development of robust prediction models that can account for the complex, multi-factorial nature of glucose regulation. This framework is essential for applications in personalized treatment optimization, clinical decision support systems, and artificial pancreas development [31] [10].
The standardization of CGM metrics through international consensus has established a foundational feature set for research applications [1]. These metrics quantify distinct physiological phenomena, from sustained hyperglycemia to acute hypoglycemic events and glycemic variability. For researchers developing predictive algorithms, understanding the clinical relevance, computational derivation, and appropriate application of these features is critical for creating models that are both accurate and clinically meaningful.
Core CGM-Derived Metrics for Predictive Modeling
Standardized Glucose Metrics
International consensus guidelines have established a core set of CGM metrics that serve as essential features for predictive modeling. These metrics capture complementary aspects of glycemic control and should be calculated from data spanning at least 10-14 days with ≥70% wear time to ensure reliability [51] [1].
Table 1: Core CGM-Derived Metrics for Predictive Modeling
| Metric | Definition | Clinical Significance | Target Range |
|---|---|---|---|
| Time in Range (TIR) | Percentage of glucose values between 70-180 mg/dL | Primary efficacy outcome; associated with complication risk | >70% for most adults [1] |
| Time Below Range (TBR) | Percentage of values <70 mg/dL (Level 1) and <54 mg/dL (Level 2) | Safety measure; hypoglycemia risk | <4% (<70 mg/dL); <1% (<54 mg/dL) [1] |
| Time Above Range (TAR) | Percentage of values >180 mg/dL (Level 1) and >250 mg/dL (Level 2) | Hyperglycemia exposure; correlates with long-term complications | <25% (>180 mg/dL); <5% (>250 mg/dL) [1] |
| Mean Glucose | Arithmetic average of all glucose values | Overall glycemic exposure | Individualized based on targets |
| Glucose Management Indicator (GMI) | Estimated HbA1c derived from mean CGM glucose | Facilitates comparison with standard care | Individualized based on targets [51] [1] |
| Coefficient of Variation (CV) | Standard deviation divided by mean glucose (expressed as percentage) | Measure of glycemic variability; predictor of hypoglycemia risk | ≤36% [51] [1] |
Advanced Glycemic Variability Metrics
Beyond the core metrics, research-focused measures of Glycemic Variability (GV) provide additional features for capturing dysglycemia, particularly in early stages of glucose intolerance:
- Mean Amplitude of Glycemic Excursions (MAGE): Calculates the arithmetic mean of glucose excursions exceeding one standard deviation of the average glucose. This metric is emerging as a sensitive identifier of early dysglycemia in prediabetes [52].
- Glycemic Variability Indices: Including standard deviation (SD), interquartile range (IQR), and mean absolute glucose (MAG) [51]. These measures capture different aspects of glucose fluctuations, with SD being highly correlated with mean glucose, while CV provides a more standardized measure of variability independent of the mean glucose level.
For prediabetes research, MAGE and other GV indices may be particularly valuable as they can identify early dysglycemia before changes in traditional metrics become apparent [52].
Data Acquisition and Preprocessing Protocols
CGM Data Collection and Sufficiency Standards
High-quality feature engineering begins with rigorous data collection. The following protocol ensures research-grade CGM data:
- Device Selection: Use FDA-cleared/CE-marked professional or personal CGM systems with documented accuracy (e.g., MARD <10%). Common research devices include Dexcom G6, Medtronic Guardian, FreeStyle Libre [53].
- Wear Time Requirements: Collect at least 14 days of CGM data to ensure representation of typical glycemic patterns. Studies have shown 14 days correlate well with 3-month patterns for key metrics [51].
- Data Sufficiency Threshold: Require ≥70% of possible CGM readings over the monitoring period for inclusion in analysis. This equates to approximately 10 days of a 14-day monitoring period [51] [1].
- Calibration Protocol: For devices requiring calibration, follow manufacturer instructions using capillary blood glucose measurements from validated meters. Document all calibrations.
Data Cleaning and Processing Algorithms
Raw CGM data often contains artifacts and errors that must be addressed before feature extraction:
Figure 1: CGM Data Processing Workflow
- Duplication Detection: Implement algorithms to identify and resolve duplicate or time-shifted CGM uploads from the same patient. A stepwise processing algorithm that considers glucose values, timestamps, Device IDs, and Observation IDs can effectively address this issue [54].
- Gap Imputation: For short gaps (<20-30 minutes), use linear interpolation. For longer gaps, consider model-based imputation or exclude the monitoring period if gaps exceed predefined thresholds.
- Metric Calculation: Use validated open-source tools like the
igluR package orcgmanalysisto ensure standardized computation of CGM metrics [54] [53]. These tools have demonstrated equivalence to proprietary software in calculating summary measures.
Integration of Demographic and Clinical Variables
Essential Non-Glucose Predictive Features
CGM metrics alone provide an incomplete picture for glycemic prediction. Incorporating demographic and clinical variables significantly enhances model performance:
Table 2: Demographic and Clinical Variables for Glycemic Prediction Models
| Variable Category | Specific Variables | Rationale for Inclusion | Data Collection Method |
|---|---|---|---|
| Basic Demographics | Age, sex, race/ethnicity, socioeconomic status | Affects glucose metabolism, healthcare access, and diabetes risk | Structured interview/questionnaire |
| Diabetes Status | Diabetes type, duration, medication (insulin, oral agents) | Direct impact on glycemic variability and treatment response | Medical record abstraction |
| Body Composition | BMI, waist circumference, weight history | Correlates with insulin resistance | Direct measurement |
| Comorbidities | Renal function (eGFR), cardiovascular disease, hypertension, cystic fibrosis | Affects glucose metabolism and medication clearance | Medical record abstraction |
| Lifestyle Factors | Physical activity (accelerometry), dietary patterns, sleep quality | Direct impact on glucose regulation | Accelerometers, dietary logs, questionnaires |
| Laboratory Values | HbA1c, fasting glucose, lipid profile, liver function | Provides additional glycemic and metabolic context | Blood sampling |
In specific populations, additional variables are particularly relevant. For cystic fibrosis-related diabetes screening, CGM metrics such as time above 140 mg/dL for >20% of wear time and time above 180 mg/dL for >6% of wear time have shown high specificity and sensitivity, respectively [55].
Integrating CGM with other data streams requires careful temporal alignment:
- CGM and Physical Activity: Synchronize CGM (5-minute intervals) with accelerometry (15-second intervals) through linear interpolation to create aligned time series [31].
- Meal and Medication Data: Time-stamp all meal intake and medication administration, accounting for expected onset of action (e.g., 15-30 minutes for rapid-acting insulin).
- Laboratory Values: Record timing of blood draws relative to CGM data acquisition, noting that HbA1c reflects approximately 3-month average glucose while CGM captures current status.
Experimental Protocols for Feature Validation
Protocol 1: Assessing Predictive Value of CGM Features
Objective: To evaluate the predictive performance of CGM-derived features for future glycemic events.
Materials:
- CGM data from target population (≥14 days with ≥70% wear time)
- Computational environment (R, Python) with CGM analysis packages (iglu, cgmanalysis)
- Statistical software for machine learning implementation
Procedure:
- Extract core CGM metrics (TIR, TBR, TAR, mean glucose, GMI, CV) using validated algorithms
- Calculate advanced GV metrics (MAGE, CONGA, J-index) using specialized packages
- Partition data into training (70%), tuning (10%), and testing (20%) sets, ensuring all data from individual participants resides in only one set
- Train multiple machine learning architectures (e.g., autoregressive models, neural networks, gradient boosting) using CGM features
- Evaluate prediction accuracy for targets (15-, 30-, 60-minute glucose prediction) using root-mean-square error (RMSE) and clinical accuracy metrics (Clarke Error Grid)
- Compare model performance with and without GV metrics to assess added value
Validation: Use k-fold cross-validation and external validation cohorts to assess generalizability.
Protocol 2: Multimodal Feature Integration Study
Objective: To determine whether integrating demographic/clinical variables with CGM metrics improves prediction accuracy.
Materials:
- Multimodal dataset (CGM, clinical variables, demographics)
- Data integration platform capable of handling heterogeneous data types
- Feature selection algorithms
Procedure:
- Collect and preprocess CGM data per Protocol 1
- Extract relevant clinical and demographic variables from electronic health records or study databases
- Create aligned multimodal dataset with consistent time indexing
- Perform feature scaling and normalization appropriate for each data type
- Apply feature selection techniques (recursive feature elimination, LASSO) to identify most predictive features
- Train models with increasing feature complexity:
- Model A: CGM metrics only
- Model B: CGM + demographic features
- Model C: CGM + demographic + clinical features
- Compare model performance using RMSE, AUC (for classification tasks), and clinical accuracy metrics
Analysis: Calculate variable importance scores to determine relative contribution of different feature types.
Implementation Tools and Research Reagents
Computational Tools for CGM Feature Engineering
Table 3: Essential Research Tools for CGM Feature Engineering
| Tool/Software | Primary Function | Application in Research | Access |
|---|---|---|---|
| iglu R Package | CGM metric calculation and visualization | Standardized computation of consensus CGM metrics | Open-source [54] |
| cgmanalysis | CGM data management and descriptive analysis | Processing raw CGM data from multiple manufacturers | Open-source [53] |
| Grammatical Evolution Framework | Symbolic regression for personalized model development | Generating customized prediction models using physiological inputs | Custom implementation [56] |
| Glycemic Variability Research Tool (GlyVaRT) | Advanced GV metric calculation | Research-specific variability indices not in consensus metrics | Commercial (Medtronic) [31] |
Data Quality Assessment Protocol
Before feature extraction, implement comprehensive data quality checks:
- Completeness Assessment: Verify ≥70% wear time over analysis period
- Plausibility Filters: Remove physiologically implausible values (e.g., <40 mg/dL or >400 mg/dL without confirmation)
- Stability Analysis: Check for sensor drift using modal day visualization
- Duplicate Resolution: Apply algorithms to detect and resolve duplicate CGM observations, which can affect metrics in approximately 25% of profiles [54]
Figure 2: Comprehensive Feature Engineering Pipeline
Effective feature engineering from CGM, demographic, and clinical sources is fundamental to advancing glycemic prediction research. The standardized metrics established by international consensus provide a foundational feature set, while emerging glycemic variability indices offer promise for detecting more subtle dysglycemia. Implementation of rigorous data processing protocols ensures feature quality, and appropriate integration of multimodal data sources enhances predictive capability. The experimental frameworks presented herein provide validated methodologies for developing and testing glycemic prediction models that can advance both clinical research and therapeutic applications. As machine learning approaches continue to evolve in diabetes research, systematic feature engineering will remain essential for creating clinically relevant, robust prediction tools.
The application of machine learning (ML) in healthcare is revolutionizing the management of complex metabolic conditions. By leveraging large-scale physiological data, ML algorithms can identify subtle patterns that precede adverse clinical events, enabling a shift from reactive to proactive care. This document details applied protocols and notes for three key scenarios: predicting complications during hemodialysis, forecasting individual postprandial metabolic responses, and automating insulin delivery for diabetes management. Together, these applications underscore the transformative potential of data-driven models within the broader research thesis of predicting human glycemic and metabolic response, offering new avenues for personalized treatment and improved patient outcomes.
Hemodialysis Complication Prediction
Application Notes
Hemodialysis complications, such as hypotension and arteriovenous (AV) fistula obstruction, critically threaten patient safety and treatment efficacy, often leading to session termination [57]. ML models address this by integrating high-dimensional data from the Internet of Medical Things (IoMT)—such as real-time vital signs from dialysis machines—and Electronic Medical Records (EMRs) to provide early warnings [57] [58]. Research demonstrates that ensemble methods like Random Forest and Gradient Boosting are particularly effective, achieving high predictive performance while allowing for model simplification through feature selection [58]. For instance, one study achieved 98% accuracy in predicting complications using only 12 selected features, which is vital for practical, low-burden clinical implementation [58].
Structured Data from Research
Table 1: Performance of Machine Learning Models in Predicting Hemodialysis Complications
| Complication | Best-Performing Model | Key Performance Metrics | Number of Key Features |
|---|---|---|---|
| Multiclass Complications | Random Forest [58] | Accuracy: 98% [58] | 12 [58] |
| Hypotension | Gradient Boosting [58] | F1-Score: 94% [58] | Not Specified |
| Hypertension | Gradient Boosting [58] | F1-Score: 92% [58] | Not Specified |
| Dyspnea | Gradient Boosting [58] | F1-Score: 78% [58] | Not Specified |
| AV Fistula Obstruction | XGBoost [57] | Precision: ~71-90%, Recall: ~71-90% [57] | Not Specified |
Experimental Protocol for Predicting Hemodialysis Complications
Objective: To develop an ML model for the early prediction of intra-dialytic hypotension and AV fistula obstruction.
Materials:
- Data Source: IoMT devices on dialysis machines and patient EMRs [57].
- Variables: Collect ~50-60 initial variables, including demographics, pre-dialysis blood pressure, heart rate, ultrafiltration rate, dialysate temperature, and past laboratory results (e.g., creatinine, hemoglobin) [57] [58].
- Software: Python with scikit-learn, XGBoost libraries.
Methodology:
- Data Collection & Labeling: Conduct over 6,000 hemodialysis sessions, with medical staff meticulously labeling the occurrence and type of complications [58].
- Feature Selection: Apply a filter technique (e.g., Pearson’s Correlation Coefficient) to identify and select the most relevant 6-12 predictive features from the initial dataset to reduce model complexity [57] [58].
- Model Training & Comparison:
- Implement individual classifiers: Support Vector Classifier (SVC), Multi-layer Perceptron (MLP), k-Nearest Neighbors (KNN), and Decision Tree (DT) [58].
- Implement ensemble techniques: Random Forest (Bagging), Gradient Boosting (Boosting), and a Voting classifier [58].
- Split data into training (e.g., 75%) and testing (e.g., 25%) sets [57].
- Model Evaluation: Evaluate models on the testing set using accuracy, F1-score, precision, and recall. Prioritize models that offer an optimal balance of high performance and low complexity [58].
Workflow Visualization
Postprandial Response Forecasting
Application Notes
Postprandial (post-meal) metabolic responses are highly individual and are independent risk factors for cardiometabolic diseases [59]. Large-scale studies like PREDICT 1 have demonstrated vast inter-individual variability in responses to identical meals, with population coefficients of variation of 103% for triglycerides, 68% for glucose, and 59% for insulin [60] [59]. This variability is influenced more by person-specific factors like the gut microbiome (explaining 7.1% of variance in lipemia) than by meal macronutrients alone, while genetic factors play a relatively modest role [60] [59]. Machine learning models that integrate these multi-faceted data—including meal context, physical activity, and sleep—can predict personalized glycemic responses with significantly higher accuracy (r = 0.77) than models based solely on carbohydrate content (r = 0.40) [61] [59].
Structured Data from Research
Table 2: Factors Influencing Postprandial Metabolic Responses and Model Performance
| Factor Category | Specific Example | Impact on Postprandial Response (Variance Explained) | Source |
|---|---|---|---|
| Inter-individual Variation | Response to Identical Meals | Triglyceride: 103% CV; Glucose: 68% CV; Insulin: 59% CV | [60] [59] |
| Person-Specific Factors | Gut Microbiome | 7.1% of variance in postprandial lipemia | [60] [59] |
| Meal Composition | Macronutrient Content | 15.4% of variance in postprandial glycemia | [60] [59] |
| Genetic Factors | SNP-based heritability | ~9.5% of variance in glucose response | [59] |
| Predictive Model | ML vs. Carbohydrate Counting | ML: r=0.77; Carbs-only: r=0.40 | [61] [59] |
Experimental Protocol for Predicting Postprandial Glycemic Responses
Objective: To build a personalized machine learning model for predicting an individual's postprandial glycemic response to food.
Materials:
- Participants: Recruit a large cohort (n>1,000) of healthy individuals and those with pre-diabetes [60] [59].
- Data Acquisition:
- Continuous Glucose Monitors (CGM): To collect blood glucose readings every 5 minutes [59].
- Dried Blood Spot (DBS) Kits: For at-home collection of postprandial triglyceride and C-peptide data [59].
- Stool Collection Kits: For 16S rRNA sequencing of the gut microbiome [59].
- Activity/Sleep Trackers and Food Frequency Questionnaires [59].
- Software: R or Python for data analysis and machine learning.
Methodology:
- Clinic Visit: After an initial fast, participants consume standardized test meals. Collect serial blood samples over 6 hours to measure triglyceride, glucose, and insulin responses [59].
- At-Home Phase: Over 13 subsequent days, participants consume standardized and ad libitum meals. Data is collected via CGM, DBS, and activity trackers. Meals are replicated to assess intra-individual variability [59].
- Data Integration: Compile a feature set encompassing:
- Model Building & Validation: Train a multivariable linear regression or more complex ML model (e.g., Random Forest) on the integrated dataset to predict glycemic responses (e.g., glucose iAUC). Validate the model in an independent cohort [59].
Workflow Visualization
Automated Insulin Delivery
Application Notes
Automated insulin delivery (AID) systems, or the artificial pancreas, represent the forefront of type 1 diabetes (T1D) management. Current systems are "hybrid" because they still require users to manually announce meals and estimate carbohydrates—a known source of error [62]. Fully closing the loop requires artificial intelligence to automatically detect meals and estimate carbohydrate content using data from Continuous Glucose Monitors (CGM) and insulin pumps [62]. A clinical trial of a Robust Artificial Pancreas (RAP) system utilizing a neural network for this purpose demonstrated a significant 10.8% reduction in postprandial time above range (glucose >180 mg/dL) compared to a control algorithm, without increasing hypoglycemia [62]. Meanwhile, systematic reviews confirm that Neural Network Models (NNM) show the highest relative performance for predicting blood glucose levels themselves [63].
Structured Data from Research
Table 3: Performance of Automated Insulin Delivery and Blood Glucose Prediction Systems
| System / Model | Key Feature | Performance Metric | Value / Outcome | Source |
|---|---|---|---|---|
| RAP System | Automated Meal Detection | Sensitivity / False Discovery Rate | 83.3% / 16.6% | [62] |
| RAP System | Postprandial Control | Reduction in Time Above Range (>180 mg/dL) | -10.8% (vs. control) | [62] |
| RAP System | Postprandial Control | Change in Time in Range (70-180 mg/dL) | +9.1% (vs. control, NS) | [62] |
| Neural Network Models (NNM) | BG Level Prediction | Relative Performance Ranking | Highest across prediction horizons | [63] |
| Various ML Models | BG Prediction (PH=30 min) | Mean Absolute RMSE | 21.40 mg/dL (SD 12.56) | [63] |
Experimental Protocol for an AI-Driven Insulin Delivery System
Objective: To develop and test a closed-loop insulin delivery system that uses AI for automated meal detection and insulin dosing.
Materials:
- Hardware: Commercial Continuous Glucose Monitor (CGM), insulin pump [62].
- Software Platform: A control system (e.g., running on a smartphone or dedicated device) integrating a Neural Network model for meal detection and a Model Predictive Control (MPC) algorithm for insulin dosing [62].
- Participants: Adults with type 1 diabetes [62].
Methodology:
- Algorithm Development:
- Meal Detection NN: Train a neural network on historical CGM and insulin delivery data to detect meal consumption patterns. The model outputs a probability of a meal occurring and estimates its size [62].
- Controller Integration: Integrate the meal detection model with an MPC algorithm. Upon meal detection, the system triggers a recommended insulin bolus.
- Clinical Validation (Crossover Trial):
- Data Collection & Outcome Measures:
- Primary: Postprandial Time in Range (TIR: 70-180 mg/dL) and Time Above Range (TAR: >180 mg/dL) in the 4 hours following the meal [62].
- Secondary: Meal detection sensitivity, false discovery rate, and mean detection time [62].
- Safety: Monitor Time Below Range (TBR: <70 mg/dL) and any hypoglycemic events [62].
Workflow Visualization
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 4: Key Reagents and Technologies for Glycemic Response Research
| Item | Function / Application | Example Use Case |
|---|---|---|
| Continuous Glucose Monitor (CGM) | Provides near real-time, high-frequency interstitial glucose measurements. Foundational for dynamic response tracking. | Core device for postprandial forecasting studies [59] and automated insulin delivery [62]. |
| IoMT-Enabled Hemodialysis Machine | Sources real-time physiological data (e.g., blood pressure, ultrafiltration rate) during dialysis sessions. | Data stream for predicting hemodialysis complications like hypotension [57]. |
| Dried Blood Spot (DBS) Kit | Allows for simplified at-home collection of capillary blood for later lab analysis of lipids (triglycerides) and C-peptide. | Enables scalable collection of postprandial metabolic data outside the clinic [59]. |
| 16S rRNA Sequencing Kit | Profiles the composition of the gut microbiome from stool samples. | Used to incorporate microbiome features as predictors in personalized nutrition models [59]. |
| Insulin Pump | Delivers subcutaneous insulin, capable of being controlled by an external algorithm. | Actuator in a closed-loop automated insulin delivery system [62]. |
| Activity/Sleep Tracker | Quantifies physical activity and sleep patterns, which are known modifiers of metabolic responses. | Captures "meal context" variables for improved postprandial prediction models [59]. |
Integrated Perspective and Future Directions
The convergence of data from IoMT, EMRs, and multi-omics is creating unprecedented opportunities for ML-driven personalized healthcare. The applications detailed herein—hemodialysis prediction, postprandial forecasting, and automated insulin delivery—share a common foundation: they transform continuous, high-dimensional physiological data into actionable clinical insights. Future progress will hinge on improving the interoperability of medical devices and data platforms, validating models in larger and more diverse populations, and navigating the regulatory landscape for AI-based clinical decision support tools. As these technologies mature, they will collectively advance the core thesis of glycemic response research, moving beyond one-size-fits-all approaches to deliver truly personalized metabolic management.
Optimization Strategies and Implementation Challenges in Real-World Settings
Simulation-to-Reality (Sim2Real) transfer learning has emerged as a pivotal strategy for developing robust machine learning models in glycemic response research, effectively addressing the critical challenge of data scarcity. This approach involves training models on large, physiologically realistic simulated datasets before adapting them for deployment on real-world data. The technique is particularly valuable in domains like diabetes management, where collecting extensive real-patient data is often prohibitively expensive, time-consuming, and fraught with privacy concerns [11]. By leveraging Sim2Real, researchers can generate diverse and comprehensive training scenarios, including rare but clinically critical events like severe hypoglycemia, thereby building more generalizable and safer models for predicting glycemic responses and optimizing therapies [11].
Core Principles and Relevance to Glycemic Research
The fundamental principle of Sim2Real is to first train a model within a simulated environment that encapsulates known domain knowledge and physiology. The model is then transferred and adapted to operate on real-world data. This process often incorporates continual learning (CL) techniques to prevent "catastrophic forgetting" of previously learned domains when adapting to new data [11].
In the context of glycemic research, simulators like the University of Virginia (UVa)/Padova T1DM Simulator provide a validated, in-silico population of virtual subjects with type 1 diabetes [64]. These platforms use mathematical models of glucose-insulin dynamics to generate synthetic patient data. However, a known limitation of such simulators is their inability to fully capture the behavioral and unmodeled physiological factors (e.g., stress, hormonal fluctuations) that influence blood glucose in real-life [64]. Sim2Real methods bridge this gap by using real-world data to estimate and account for these unmodeled residuals, creating a more personalized and accurate simulation framework.
Applications in Glycemic Response Prediction and Management
Sim2Real transfer learning is being applied across various frontiers of diabetes research, from forecasting glucose levels to optimizing insulin dosing and personalizing nutrition.
Glucose Forecasting and Hypoglycemia Prevention
A key application is the development of unified models for glucose prediction and hypoglycemia event classification. For instance, the Domain-Agnostic Continual Multi-Task Learning (DA-CMTL) framework leverages Sim2Real transfer to simultaneously perform both tasks [11].
- The framework is trained on diverse simulated datasets and uses elastic weight consolidation (EWC) for continual learning, enabling adaptation across different patient populations and real-world datasets without forgetting previous knowledge.
- When evaluated on real-world data, this approach demonstrated a root mean squared error (RMSE) of 14.01 mg/dL for 30-minute glucose prediction and a sensitivity/specificity of 92.13%/94.28% for hypoglycemia detection [11].
- In a real-world validation with diabetes-induced rats, the system reduced time below range from 3.01% to 2.58%, highlighting its potential as a safety layer in automated insulin delivery (AID) systems [11].
Optimizing Insulin Titration
Reinforcement Learning (RL) provides another powerful use case. A model-based RL framework for Dynamic Insulin Titration Regimen (RL-DITR) was developed for personalized type 2 diabetes management [65].
- The system learns optimal insulin dosing policies through trial-and-error interactions with a patient model (the environment) built from electronic health records (EHR).
- It was validated through a stepwise process from simulation to a prospective clinical trial. In a proof-of-concept trial with 16 patients, mean daily capillary blood glucose decreased from 11.1 (±3.6) to 8.6 (±2.4) mmol/L, meeting the pre-specified endpoint without severe hypoglycemic events [65].
Table 1: Performance Metrics of Selected Sim2Real Applications in Diabetes Management
| Application | Model/Method | Key Performance Metrics | Validation Context |
|---|---|---|---|
| Glucose Forecasting & Hypoglycemia Detection | Domain-Agnostic Continual Multi-Task Learning (DA-CMTL) [11] | RMSE: 14.01 mg/dL (30-min prediction); Hypo. Sensitivity/Specificity: 92.13%/94.28% | Real-world datasets (DiaTrend, OhioT1DM); Animal study |
| Insulin Titration for T2D | Model-based Reinforcement Learning (RL-DITR) [65] | Mean Absolute Error: 1.10 ± 0.03 U (vs. physician); Mean Daily Glucose: Reduction from 11.1 to 8.6 mmol/L | In-patient simulation; Proof-of-concept clinical trial (N=16) |
| Virtual Glucose Monitoring | Deep Learning (Bidirectional LSTM) [66] | RMSE: 19.49 ± 5.42 mg/dL; Correlation: 0.43 ± 0.2 | Healthy adults (N=171) using life-log data |
Replay Simulations for Personalized Treatment Design
Replay simulation is a specific Sim2Real technique for designing and evaluating individualized treatments for Type 1 Diabetes. This method uses data collected from a person's real life to create a subject-specific simulation model [64].
- The process involves personalizing a physiological model (like the Subcutaneous Oral Glucose Minimal Model) to an individual's insulin sensitivity and meal-absorption parameters.
- A residual signal is estimated to account for unmodeled factors and measurement noise. This allows researchers to run "what-if" scenarios by altering inputs (e.g., insulin doses, meal sizes) in the personalized model to replay the data under different therapeutic conditions.
- This method has shown high accuracy in silico, with a Mean Absolute Relative Difference (MARD) of <10% and over 95% of readings falling in clinically acceptable zones of error grid analysis [64].
Experimental Protocols
Protocol: Implementing a Sim2Real Pipeline for Glucose Forecasting
This protocol outlines the steps for developing a multi-task glucose forecasting model using a Sim2Real approach, based on the DA-CMTL framework [11].
1. Data Simulation and Preprocessing
- Simulated Training Data Generation: Use a accepted simulator like the UVa/Padova T1DM Simulator to generate a large, diverse dataset of glucose dynamics. Scenarios should include variations in meal intake, insulin administration, and physical activity, with an emphasis on incorporating challenging but clinically relevant edge cases (e.g., postprandial hyperglycemia, nocturnal hypoglycemia).
- Real-World Data Collection for Transfer: Collect real-world data for model adaptation and testing. This should ideally include continuous glucose monitoring (CGM) traces, records of insulin delivery (basal and bolus), logged meal carbohydrate content, and other life-log data like physical activity [66] [11].
2. Model Architecture and Training
- Model Design: Implement a multi-task neural network architecture with a shared encoder and separate task-specific heads for glucose level regression (forecasting) and hypoglycemia event classification.
- Simulated Phase Training: Train the model on the large, labeled simulated dataset. Use a combination of loss functions, such as Mean Squared Error (MSE) for glucose forecasting and Binary Cross-Entropy for hypoglycemia classification.
- Sim2Real Transfer with Continual Learning:
- Use the trained model as the initializer for adaptation on the real-world dataset.
- Apply a continual learning strategy like Elastic Weight Consolidation (EWC) during this fine-tuning phase. EWC adds a regularization term to the loss function that penalizes changes to model weights that were important for performance on the previous (simulated) task, thus mitigating catastrophic forgetting [11].
- The loss function during fine-tuning can be:
L(θ) = L_new(θ) + λ * Σ_i [F_i * (θ_i - θ_{0,i})^2], whereL_newis the loss on real data,θ_0are the weights from the simulated model, andF_iis the Fisher information matrix estimating the importance of each parameterθ_i.
3. Model Validation and Deployment
- Quantitative Evaluation: Validate the model on held-out real-world test sets. Report standard metrics including Root Mean Squared Error (RMSE), Mean Absolute Error (MAE), and for classification, Sensitivity and Specificity for hypoglycemia/alerts [11].
- Clinical Safety Validation: Perform analysis using Clarke Error Grid (CEG) or similar clinical consensus grids to assess the clinical accuracy of glucose predictions [64].
- Prospective Testing: Before full deployment, conduct controlled pilot studies or animal trials to assess the model's performance and safety in a live setting [11].
Protocol: Replay Simulations for Treatment Optimization
This protocol details the use of replay simulations to evaluate and optimize insulin therapy for an individual with diabetes, based on the methodology of Vettoretti et al. [64].
1. Data Collection and Model Personalization
- Input Data: Collect a period of real-life data from the target individual, including:
- CGM measurements.
- Timestamps and doses of insulin administration (basal and bolus).
- Timestamps and estimated carbohydrate content of meals.
- Model Selection: Select a base physiological model, such as the Subcutaneous Oral Glucose Minimal Model (SOGMM).
- Parameter Identification: Personalize the model to the individual by estimating key subject-specific parameters (e.g., insulin sensitivity
S_I, glucose effectivenessS_g, meal absorption rates) by fitting the model's predictions to the collected CGM data.
2. Residual Signal Estimation and Reconstruction
- Residual Calculation: Using the personalized model and the recorded input data (insulin, meals), perform a regularized deconvolution to estimate an additive residual signal
ω(t). This signal represents the discrepancy between the model's prediction and the actual CGM data, capturing unmodeled disturbances. - Signal Reconstruction: Feed the known inputs (insulin, meals) and the estimated residual signal
ω(t)back into the personalized model to accurately reconstruct the original CGM trace. This validates that the personalized model + residual can replicate reality.
3. 'What-if' Scenario Execution and Analysis
- Scenario Design: Define alternative therapeutic strategies to test. Examples include: modifying basal insulin rates, adjusting meal bolus timing or size, or virtually removing a meal to assess its impact.
- Replay Simulation: Run the personalized model forward in time using the modified inputs (e.g., the new insulin regimen) while keeping the estimated residual signal
ω(t)constant. This core assumption—that the residual is input-independent—defines the domain of validity. - Output Analysis: Analyze the resulting simulated CGM trace. Compare outcomes such as Time-in-Range (TIR), time in hypoglycemia, and glucose variability under the different simulated scenarios to inform the optimal treatment choice for that individual.
Table 2: Key Resources for Sim2Real Research in Glycemic Response
| Resource / Tool | Type | Primary Function in Research | Example Use Case |
|---|---|---|---|
| UVa/Padova T1DM Simulator [64] | Software Simulator | Provides a population of 300 in-silico virtual subjects with T1DM for generating synthetic training data and pre-clinical testing. | Generating large-scale datasets for initial model training; Testing safety of insulin delivery algorithms. |
| Continuous Glucose Monitor (CGM) [11] [44] | Hardware / Data Source | Measures interstitial glucose levels at regular intervals (e.g., every 5 mins), providing the core real-world time-series data. | Collecting real-world glycemic data for model fine-tuning and validation; Serving as input for real-time prediction models. |
| Elastic Weight Consolidation (EWC) [11] | Algorithm | A continual learning method that prevents catastrophic forgetting during Sim2Real transfer by regularizing important weights. | Fine-tuning a model pre-trained on simulated data onto a real-world dataset without losing simulated knowledge. |
| Clarke Error Grid Analysis (CEGA) [64] | Analytical Method | Assesses the clinical accuracy of glucose predictions by categorizing point-pairs into risk zones (A-E). | Validating the clinical acceptability of a glucose forecasting model's predictions before deployment. |
| Electronic Health Records (EHR) [65] [67] | Data Source | Provides large-scale, longitudinal data on patient demographics, treatments, and outcomes for model development and validation. | Training reinforcement learning agents for treatment optimization; Building patient models for in-silico trials. |
The adoption of artificial intelligence (AI) in glycemic response research is transforming the management of diabetes, enabling advanced prediction of glycemic events and personalized insulin therapy. However, the "black-box" nature of complex machine learning (ML) models remains a significant barrier to their clinical acceptance [68]. Explainable AI (XAI) has emerged as a critical subfield aimed at making AI systems transparent, interpretable, and accountable [69]. In high-stakes healthcare domains, clinicians require clear rationales behind model predictions to verify recommendations, ensure patient safety, and build trust [70] [68]. For researchers and drug development professionals working on machine learning algorithms for glycemic response, XAI methods are indispensable tools that provide insights into model behavior, help identify key physiological and lifestyle features influencing predictions, and facilitate the development of safer, more reliable, and clinically actionable models.
Core XAI Methods: SHAP and LIME
SHAP (SHapley Additive exPlanations) and LIME (Local Interpretable Model-agnostic Explanations) are two of the most prominent model-agnostic XAI methods used in the healthcare domain [70] [69]. Their core characteristics and comparative analysis are summarized in the table below.
Table 1: Comparative Analysis of SHAP and LIME
| Feature | SHAP (SHapley Additive exPlanations) | LIME (Local Interpretable Model-agnostic Explanations) |
|---|---|---|
| Theoretical Foundation | Game theory, specifically Shapley values, which fairly distribute the "payout" (prediction) among the "players" (features) [70]. | Local surrogate models; approximates a complex model locally with an interpretable one (e.g., linear regression) [70]. |
| Explanation Scope | Provides both global (model-level) and local (instance-level) explanations [70] [71]. | Primarily provides local explanations for a specific prediction [70] [71]. |
| Explanation Output | Assigns each feature an importance value (Shapley value) for a given prediction, indicating its contribution to the output [70] [69]. | Highlights the importance of features for a specific instance by fitting a local, interpretable model [70]. |
| Handling of Non-Linearity | Capable of capturing non-linear relationships, depending on the underlying model used [70]. | Incapable of capturing non-linear decisions directly, as it relies on local linear approximations [70]. |
| Computational Cost | Generally higher, especially with a large number of features, though approximations like KernelSHAP exist [70] [71]. | Lower and faster than SHAP [70]. |
| Key Strengths | Solid theoretical foundation, consistent explanations, comprehensive global view [70] [71]. | Intuitive local explanations, fast computation, simple to implement [70]. |
| Key Limitations | Computationally intensive; can be affected by feature collinearity [70]. | Explanations can be unstable due to random sampling; lacks a global perspective [70] [71]. |
Methodological Considerations and Pitfalls
When applying SHAP and LIME in glycemic research, understanding their limitations is crucial for robust interpretation. A primary concern is model-dependency: the explanations generated are highly dependent on the underlying ML model. For example, the top features identified by SHAP can differ significantly when applied to a Decision Tree versus a Logistic Regression model trained on the same myocardial infarction classification task [70]. Furthermore, both methods are sensitive to feature collinearity. SHAP may create unrealistic data instances when features are correlated by sampling from marginal distributions, which assumes feature independence [70]. LIME also typically treats features as independent, which can lead to misleading explanations if strong correlations exist in the data, such as between time-in-range metrics and HbA1c [70]. Researchers must therefore perform thorough feature analysis and consider model selection as an integral part of the interpretability pipeline.
Application in Glycemic Response Research: A Case Study
The practical application of SHAP and LIME is exemplified by a recent study developing an explainable, dual-prediction framework for postprandial glycemic events in Type 1 Diabetes (T1D) [7].
Experimental Protocol for Predicting Postprandial Glycemic Events
Objective: To simultaneously forecast postprandial hypoglycemia and hyperglycemia within a 4-hour window and provide interpretable insights for insulin dose optimization [7].
1. Data Acquisition and Preprocessing:
- Datasets: Use real-world data (e.g., from clinical trials like REPLACE-BG) or generate in-silico data using a validated simulator (e.g., based on the Dalla Man model) [7].
- Data Cleansing: Exclude participants or records with excessive missing data (e.g., >50%). For simulated data, incorporate real-world variability such as meal-time variation (±20 minutes), meal content uncertainty (±20%), and carbohydrate misestimation [7].
- Key Variables: Extract Continuous Glucose Monitoring (CGM) data, timestamps, estimated meal carbohydrates, and meal insulin bolus (MIB) data [7].
2. Feature Engineering:
- From the raw data, extract a set of informative, time-domain features. The referenced study started with 27 candidate features and refined them to 13 most informative ones using statistical methods like ANOVA F-measure ranking [7].
- Example Features: These typically include glucose levels at meal time, total insulin bolus, carbohydrate intake, and various metrics derived from CGM trend data [7].
3. Glycemic Profiling and Model Training:
- Unsupervised Clustering: Apply a hybrid unsupervised learning approach (e.g., combining Self-Organizing Maps and k-means clustering) to the dataset to identify distinct postprandial glycemic profiles [7].
- Personalized Ensemble Models: Train specialized prediction models (e.g., Random Forest classifiers) for each identified glycemic profile, creating a cluster-personalized ensemble system [7].
4. Model Interpretation and Explainability:
- Global Explanations: Use SHAP to understand the overall behavior of the trained Random Forest models. Generate summary plots to identify which features (e.g., carbohydrate intake, pre-meal insulin bolus) are most globally important for predicting hypo- and hyperglycemia across the entire dataset [7].
- Local Explanations: Use LIME to explain individual predictions. For a specific meal event, LIME can illustrate which factors locally contributed most to the risk classification, providing actionable insights for clinicians and patients [7].
- Interaction Analysis: Leverage SHAP's capability to reveal non-linear effects and interaction between key variables, such as the combined impact of carbohydrate intake and insulin bolus on postprandial glucose excursion [7].
5. Insulin Dose Optimization Module:
- Develop an algorithm that uses the model's prediction and the accompanying explanations to refine pre-meal bolus insulin recommendations. If the model predicts a high risk of hypoglycemia with high confidence, the adjustment module can suggest a reduced bolus dose [7].
Key Quantitative Outcomes
The application of this explainable framework yielded significant performance improvements, as detailed below.
Table 2: Performance Metrics of the Explainable Prediction Framework [7]
| Prediction Task | Area Under the Curve (AUC) | Matthews Correlation Coefficient (MCC) |
|---|---|---|
| Hypoglycemia | 0.84 | 0.47 |
| Hyperglycemia | 0.93 | 0.73 |
The high AUC values demonstrate the model's strong ability to discriminate between events and non-events, while the MCC scores, which are more informative for imbalanced datasets, indicate a good quality of predictions [7]. Simulated evaluations confirmed that this approach improved postprandial time-in-range and reduced hypoglycemia without causing excessive hyperglycemia [7].
Figure 1: Workflow for Explainable Prediction of Glycemic Events
For researchers aiming to replicate or build upon this work, the following table details essential "research reagents" – key datasets, algorithms, and software tools.
Table 3: Essential Research Resources for Glycemic ML Research
| Resource Name | Type | Function/Brief Explanation | Example/Reference |
|---|---|---|---|
| REPLACE-BG Dataset | Real-World Clinical Data | Provides real-world CGM, meal, and insulin data from individuals with T1D for model training and validation [7]. | [7] |
| Dalla Man Model Simulator | In-Silico Data Generator | A physiologically-based simulator for generating synthetic, customizable T1D patient data for initial algorithm testing [7]. | [7] |
| SHAP Python Library | Software Library | Calculates SHapley values for any ML model, providing global and local feature importance scores [70]. | [70] |
| LIME Python Library | Software Library | Generates local surrogate models to explain individual predictions of any black-box classifier/regressor [70]. | [70] |
| Self-Organizing Maps (SOM) | Algorithm | An unsupervised neural network for clustering and dimensionality reduction, used for glycemic profiling [7]. | [7] |
| Random Forest Classifier | Algorithm | An ensemble ML model robust to overfitting, suitable for tabular medical data like CGM features [7]. | [7] |
| ANOVA F-measure | Statistical Tool | Used for feature selection by ranking and filtering the most informative features from an initial candidate set [7]. | [7] |
Integrated Analysis and Best Practices
Combining SHAP and LIME offers a more comprehensive explainability strategy than relying on a single method. SHAP provides a consistent, global overview of model behavior, identifying the dominant features driving predictions across an entire population or sub-population (cluster). Conversely, LIME offers a granular, local view essential for understanding a specific prediction for a single patient at a specific meal event. This dual approach was successfully implemented in the case study, where SHAP revealed global interactions between carbohydrate intake and insulin bolus, while LIME provided patient-specific reasoning for clinical decision support [7]. This synergy is critical for developing personalized diabetes management tools.
To ensure effective usage, researchers should adopt several best practices. For LIME, employ selectivity in perturbation to ensure generated samples are realistic and relevant to the local data manifold [71]. For SHAP, carefully interpret feature importance values in the context of potential feature collinearity and remember that results are model-dependent [70] [71]. Furthermore, robust model validation is paramount. This includes validating XAI results against clinical ground truth where feasible and being mindful of potential biases in both the underlying model and the explanation methods [71] [68]. All explanations must be communicated transparently in scientific reports and publications, using standard visualizations like SHAP summary plots and LIME's local prediction plots to convey findings clearly [71].
Figure 2: Synergy of SHAP and LIME in Clinical Decision-Making
Handling Dataset Imbalance and Generalization Across Populations
The development of machine learning (ML) models for predicting personalized glycemic responses represents a frontier in diabetes management and precision nutrition. However, this research domain consistently grapples with the dual challenges of dataset imbalance and ensuring generalization across diverse populations. In glycemic prediction, imbalance manifests not only in unequal class distributions for outcomes like hypoglycemic events but also in the underrepresentation of certain demographic groups in research datasets. The core challenge is that standard ML algorithms tend to favor the majority class, leading to models that may achieve high overall accuracy but fail to detect clinically critical hypoglycemic events or perform equitably across patient subgroups [10] [72].
The clinical implications of these technical challenges are substantial. For glycemic prediction, poor performance on minority classes translates directly to failure to predict dangerous hypoglycemic events, while demographic disparities can lead to inequitable healthcare outcomes. Research has demonstrated high variability in postprandial glycemic responses to identical meals, suggesting that universal dietary recommendations have limited utility and emphasizing the need for personalized approaches that work reliably across populations [45]. This application note establishes structured protocols for addressing these interconnected challenges through data-centric ML approaches.
Quantitative Landscape of Imbalance in Diabetes Datasets
Publicly available diabetes datasets exhibit significant variability in sample sizes, demographic composition, and inherent class distributions. Understanding these characteristics is essential for selecting appropriate imbalance mitigation strategies.
Table 1: Characteristics of Publicly Available Diabetes Datasets
| Dataset Name | Diabetes Type | Sample Size | Demographic Focus | Key Features | Notable Imbalances |
|---|---|---|---|---|---|
| OhioT1DM [73] | Type 1 | 12 patients | U.S. population | CGM, insulin, meals, exercise, physiological sensors | Hypoglycemic events, meal types, exercise frequency |
| ShanghaiT1DM/T2DM [74] | Type 1 & 2 | 12 T1DM, 100 T2DM | Chinese population | Clinical characteristics, CGM, dietary information, medications | T1DM vs T2DM representation, dietary patterns |
| Dataset from Indian PPGR Study [44] | Type 2 | Multi-site recruitment | Indian population | CGM, standardized meals, physical activity, medication | Regional dietary practices, socioeconomic factors |
The time in range (TIR) metric, defined as the percentage of time spent in the target glucose range of 70-180 mg/dL, reveals significant variability across populations and diabetes types. The Advanced Technologies & Treatments for Diabetes (ATTD) consensus recommends targets of ≥70% for TIR, ≤25% for time above range (TAR), and ≤4% for time below range (TBR) [74]. These targets highlight the inherent imbalance in glucose measurements, where values within the target range naturally dominate, while clinically critical hypoglycemic events (TBR) represent the small minority class that is most important to predict accurately.
Table 2: Class Distribution in Glycemic Prediction Problems
| Prediction Task | Majority Class | Minority Class | Typical Imbalance Ratio | Clinical Impact of Missed Minority Class |
|---|---|---|---|---|
| Hypoglycemia prediction | Glucose in normal range | Glucose < 70 mg/dL | Varies; ~4% TBR target [74] | Severe: unconsciousness, seizures, death |
| Hyperglycemia prediction | Glucose in normal range | Glucose > 180 mg/dL | Varies; ~25% TAR target [74] | Long-term complications: retinopathy, nephropathy |
| Meal response prediction | Common food items | Rare food items | Depends on dietary habits | Reduced personalization accuracy |
| Demographic generalization | Well-represented populations | Underrepresented groups | Highly variable across studies [72] | Healthcare disparities, inequitable outcomes |
Technical Framework for Addressing Class Imbalance
Data-Level Approaches: Resampling Techniques
Data-level methods directly adjust the training dataset composition to create a more balanced distribution before model training:
Random undersampling: Reduces majority class examples by randomly removing instances. While computationally efficient, this approach risks discarding potentially useful information from the majority class [75]. Recommended when dealing with very large datasets where discarding some majority samples is acceptable.
Random oversampling: Increases minority class representation by randomly duplicating existing instances. This approach preserves information but may lead to overfitting, particularly if the duplicates do not add meaningful diversity [75] [76].
SMOTE (Synthetic Minority Over-sampling Technique): Generates synthetic minority class examples by interpolating between existing minority instances in feature space. This approach creates new examples rather than simply duplicating existing ones, potentially reducing overfitting [75]. SMOTE is particularly effective when combined with undersampling of the majority class [77].
ADASYN (Adaptive Synthetic Sampling): An extension of SMOTE that focuses on generating synthetic examples for minority class instances that are harder to learn, adaptively shifting the classification decision boundary toward difficult cases [75].
Algorithm-Level Approaches: Model-Centric Solutions
Algorithm-level methods modify the learning process to increase sensitivity to minority classes without changing the data distribution:
Class weighting: Assigns higher misclassification costs to minority class examples during model training. Many algorithms, including logistic regression, SVM, and tree-based methods, support class weight parameters that inversely proportional to class frequencies [75]. This approach is computationally efficient and conceptually straightforward.
Cost-sensitive learning: Extends class weighting by incorporating domain-specific misclassification costs that reflect the clinical severity of different error types (e.g., missing a hypoglycemic event vs. false alarm) [75].
Ensemble methods: Combine multiple models specifically designed for imbalanced data. Balanced Random Forests perform undersampling within each bootstrap sample, while EasyEnsemble creates multiple balanced subsets by undersampling the majority class and ensembles the resulting models [75] [78]. These approaches have demonstrated superior performance for certain imbalance scenarios.
Anomaly detection frameworks: Reformulate the problem by treating the minority class as "anomalies" and using specialized detection algorithms that are inherently designed to identify rare events [75].
Evaluation Metrics for Imbalanced Glycemic Data
Traditional accuracy metrics are misleading for imbalanced problems, as a model that always predicts the majority class can achieve high accuracy while being clinically useless. The following metrics provide more meaningful performance assessment:
Precision and Recall: Precision measures what proportion of positive identifications were actually correct, while recall measures what proportion of actual positives were identified correctly [77]. For hypoglycemia prediction, recall is particularly important due to the high cost of missed events.
F1-score and Fβ-score: The F1-score represents the harmonic mean of precision and recall, while the Fβ-score allows weighting recall β times more important than precision [77]. This is valuable when the clinical costs of false negatives and false positives are asymmetric.
ROC-AUC and Precision-Recall AUC: The Area Under the Receiver Operating Characteristic curve (ROC-AUC) plots true positive rate against false positive rate, while the Precision-Recall AUC (PR-AUC) is more informative for imbalanced data as it focuses on performance on the positive class [75] [10].
Threshold optimization: Instead of using the default 0.5 probability threshold for classification, optimize the decision threshold based on the clinical trade-offs between false positives and false negatives [78]. This simple but powerful approach can significantly improve model utility without changing the underlying algorithm.
Table 3: Evaluation Metric Selection Guide for Glycemic Prediction
| Clinical Scenario | Primary Metric | Secondary Metrics | Rationale |
|---|---|---|---|
| Hypoglycemia prediction | Recall (Sensitivity) | F2-score, PR-AUC | Missing true hypoglycemic events has severe consequences |
| Hyperglycemia prediction | Precision | F1-score, ROC-AUC | False alarms may reduce patient trust and adherence |
| Population screening | F1-score | ROC-AUC, Balanced Accuracy | Balanced consideration of both error types |
| Clinical decision support | Specificity | Precision, F0.5-score | Minimizing false alarms in treatment recommendations |
Protocol for Addressing Demographic Disparities in Multi-Cohort Studies
Demographic disparities occur when models perform differently across population subgroups, potentially exacerbating healthcare inequities. The Trans-Balance framework addresses this challenge by integrating transfer learning, imbalance handling, and privacy-preserving methodologies [72].
Trans-Balance Framework Protocol
Objective: To improve predictive performance for underrepresented demographic groups in the presence of class imbalance without sharing individual-level data across sites.
Materials and Setup:
- Data from multiple cohorts or sites with varying demographic compositions
- Local computational resources at each site
- Secure aggregation mechanism for model parameters (not raw data)
Procedure:
Site Preparation and Data Characterization:
- At each participating site, identify demographic subgroups and assess class balance within each subgroup
- Designate underrepresented demographic groups as target populations
- Establish secure computational environments and protocols for federated learning
Local Model Pre-training:
- At each source site, train a base model using all available data
- Apply appropriate class imbalance techniques (e.g., SMOTE, class weighting) based on local data characteristics
- Extract model parameters and performance metrics for aggregation
Knowledge Transfer Phase:
- Transfer learned representations from source populations to target populations using privacy-preserving methods
- Adjust for covariate shift between populations while maintaining individual data privacy
- Incorporate class imbalance correction during the transfer process
Iterative Refinement and Validation:
- Validate model performance on local test sets from each demographic group
- Focus evaluation on metrics relevant to imbalanced data (AUPRC, F1-score) within each demographic subgroup
- Assess relative disparity as R1/R2, where R1 is the highest and R2 is the lowest performance across groups [72]
Implementation Considerations for Multi-Cohort Studies
Successful implementation requires addressing several practical considerations:
Data Heterogeneity: Different cohorts may collect different variables, use varying measurement protocols, or have different data quality standards. Establish common data models and harmonization procedures before analysis.
Privacy Preservation: Utilize federated learning approaches that share only model parameters or aggregated statistics rather than individual patient data [72]. Implement appropriate de-identification techniques following standards such as HIPAA Safe Harbor method [73].
Regulatory Compliance: Ensure all participating sites have appropriate institutional review board approvals and data use agreements in place. Document informed consent processes that allow for data sharing in de-identified form.
Experimental Protocol for Glycemic Prediction with Imbalanced Data
Standardized Testing Protocol for Imbalance Methods
Objective: To systematically evaluate different imbalance handling techniques for predicting hypoglycemic events using continuous glucose monitoring (CGM) data.
Materials:
- CGM data with frequent measurements (e.g., every 5 minutes) [73]
- Annotated hypoglycemic events (self-reported or clinically validated)
- Additional patient data: insulin administration, meal information, physical activity [73]
- Computational environment with standard ML libraries (scikit-learn, imbalanced-learn)
Procedure:
Data Preprocessing and Feature Engineering:
- Extract CGM time series and calculate derived features: rate of change, moving averages, variability metrics
- Align temporal data (meals, insulin, exercise) with CGM readings
- Define prediction horizon based on clinical relevance (e.g., 30-60 minutes for hypoglycemia prediction)
- Label timepoints as positive class if hypoglycemia occurs within prediction horizon
Baseline Model Establishment:
- Train standard classification algorithms (logistic regression, random forest) without imbalance correction
- Evaluate using comprehensive metrics: accuracy, precision, recall, F1-score, ROC-AUC, PR-AUC
- Establish performance baseline for comparison
Imbalance Technique Implementation:
- Apply multiple imbalance handling strategies in parallel:
- Random undersampling and oversampling
- SMOTE and variant techniques (e.g., Borderline-SMOTE, SVM-SMOTE)
- Class weighting in algorithm implementations
- Ensemble methods (Balanced Random Forest, EasyEnsemble)
- Use consistent evaluation framework across all approaches
- Apply multiple imbalance handling strategies in parallel:
Threshold Optimization:
- For each trained model, vary the classification threshold from 0 to 1
- Calculate precision and recall at each threshold
- Select optimal threshold based on clinical requirements (e.g., maximize recall while maintaining precision above minimum acceptable value)
Cross-Validation and Statistical Comparison:
- Implement stratified cross-validation that preserves class distribution in splits
- Perform statistical testing to identify significant performance differences between methods
- Document computational requirements and training time for each approach
Validation Across Demographic Subgroups
Objective: To assess model performance consistency across different demographic groups and identify potential disparities.
Procedure:
- Stratify test data by demographic characteristics: age, gender, ethnicity, diabetes duration
- Calculate performance metrics separately for each subgroup
- Quantify disparity as relative performance ratio between best-performing and worst-performing subgroups
- Iteratively refine models to minimize performance gaps while maintaining overall performance
Table 4: Research Reagent Solutions for Imbalanced Glycemic Prediction
| Tool/Category | Specific Examples | Function/Purpose | Implementation Considerations |
|---|---|---|---|
| Software Libraries | Imbalanced-learn [78] | Provides implemented resampling algorithms | Integration with scikit-learn pipeline; consider computational efficiency for large datasets |
| XGBoost, CatBoost | Native handling of class imbalance | Strong performance without extensive resampling; built-in scaleposweight parameter | |
| Diabetes Datasets | OhioT1DM [73] | Real-world CGM, insulin, lifestyle data | Data Use Agreement required; 12 patients with 8 weeks of data each |
| ShanghaiT1DM/T2DM [74] | Chinese population data with dietary information | Includes clinical characteristics, lab measurements, medications | |
| Evaluation Metrics | Precision-Recall AUC | Better for imbalanced data than ROC-AUC | Focuses on performance for positive class |
| Fβ-score | Balances precision and recall with clinical weighting | β > 1 emphasizes recall (critical for hypoglycemia) | |
| Specialized Algorithms | Trans-Balance Framework [72] | Addresses demographic disparity with class imbalance | Requires multi-site collaboration; privacy-preserving |
| Balanced Random Forest | Ensemble method with built-in balancing | Performs undersampling within each bootstrap sample |
Addressing dataset imbalance and ensuring generalization across populations represents a critical challenge in the development of robust, equitable glycemic prediction models. The protocols outlined in this application note provide a systematic approach to these interconnected problems, emphasizing appropriate evaluation metrics, method selection based on dataset characteristics, and rigorous validation across demographic subgroups.
Emerging research directions include the development of more sophisticated transfer learning approaches that can adapt to local population characteristics while preserving privacy, automated imbalance detection and method selection pipelines, and standardized benchmarking frameworks for fair comparison across studies. As the field progresses, maintaining focus on both technical performance and equitable outcomes will be essential for realizing the promise of personalized glycemic management for all populations.
In the field of machine learning for predicting glycemic responses, the quality and relevance of input features directly determine model performance and clinical utility. Feature selection represents a critical preprocessing step that enhances model interpretability, reduces computational complexity, and mitigates the risk of overfitting, particularly when dealing with high-dimensional multimodal data. Recursive Feature Elimination (RFE) has emerged as a powerful wrapper-based feature selection technique that recursively removes the least important features based on model-derived importance metrics [79] [80]. When integrated with domain-specific knowledge from nutrition, metabolism, and diabetology, RFE transforms from a purely mathematical technique into a clinically relevant tool for identifying biologically plausible predictors of glycemic excursions [81] [82].
The integration of domain knowledge with algorithmic feature selection addresses fundamental challenges in glycemic prediction, including multicollinearity among physiological parameters, individual variability in glucose metabolism, and the complex temporal relationships between inputs and glycemic outcomes [83] [84]. This hybrid approach ensures that selected features not only optimize statistical performance but also align with established physiological principles, thereby increasing the translational potential of developed models for clinical decision support and personalized nutrition interventions [85] [45].
Theoretical Foundations of Recursive Feature Elimination
Algorithmic Principles and Mechanics
Recursive Feature Elimination operates through an iterative backward selection process that ranks features based on their importance to a predictive model and systematically eliminates the weakest performers [79]. The algorithm begins by training a designated estimator on the complete set of features, after which it computes importance scores for each feature typically derived from model-specific attributes such as coefficients for linear models or featureimportances for tree-based methods [79] [80]. The algorithm then prunes a predetermined number of least important features (controlled by the step parameter) and recursively repeats this process on the reduced feature subset until the target number of features is attained [79].
The core mathematical principle underlying RFE involves generating a feature ranking where selected features receive rank 1, while eliminated features are assigned higher ranks based on their removal order [79]. This ranking mechanism allows researchers to not only identify the optimal feature subset but also understand the relative importance hierarchy among features, which provides valuable biological insights beyond mere prediction accuracy [80] [83]. The RFE algorithm accommodates both classification and regression tasks, making it suitable for both categorical glycemic event prediction (e.g., hypoglycemia alerts) and continuous glucose level forecasting [84].
Comparative Analysis with Alternative Feature Selection Methods
Table 1: Comparison of Feature Selection Techniques in Glycemic Prediction Research
| Method Type | Representative Techniques | Key Advantages | Limitations | Suitability for Glycemic Prediction |
|---|---|---|---|---|
| Filter Methods | Correlation coefficients, Mutual information, Statistical tests | Computational efficiency, Model independence, Scalability | Ignores feature interactions, May select redundant features | Moderate - Useful for initial screening of large feature sets |
| Wrapper Methods | RFE, Sequential selection algorithms | Considers feature interactions, Model-specific selection, Optimizes performance | Computationally intensive, Risk of overfitting | High - Ideal for curated feature sets with known biological relevance |
| Embedded Methods | Lasso regression, Decision trees, Random forests | Built-in feature selection, Computational efficiency, Model-specific | Limited model flexibility, Algorithm-dependent results | High - Effective for high-dimensional biomarker data |
| Hybrid Methods | RFE with domain knowledge, Multi-agent reinforcement learning | Balances performance and interpretability, Incorporates expert knowledge | Implementation complexity, Domain knowledge requirement | Very High - Optimal for clinical translation |
When compared to alternative approaches, RFE's distinctive advantage lies in its ability to evaluate feature importance within the context of the complete feature set, thereby accounting for complex interactions and dependencies [86]. Filter methods, which assess features individually using statistical measures like correlation coefficients or mutual information, offer computational efficiency but fail to capture feature interdependencies that are particularly relevant in physiological systems [83] [86]. Embedded methods such as Lasso regularization or tree-based importance automatically perform feature selection during model training but provide less explicit control over the final feature subset [84].
Recent advancements have introduced sophisticated hybrid approaches like multi-agent reinforcement learning for feature selection, which individually evaluates variable contributions to determine optimal combinations for adverse glycemic event prediction [84]. However, RFE remains widely adopted due to its conceptual simplicity, interpretable output, and proven effectiveness across diverse glycemic prediction tasks [80] [87].
Integration of Domain Knowledge in Feature Selection for Glycemic Prediction
Domain-Specific Feature Categories in Glycemic Response Research
The prediction of glycemic responses requires the integration of diverse data modalities that capture different aspects of glucose metabolism and its determinants [85]. Domain knowledge guides both the generation of relevant features and their appropriate processing prior to application of algorithmic selection techniques like RFE [82]. These features can be categorized into several biologically meaningful domains:
Continuous Glucose Monitoring (CGM) Derivatives: Beyond raw glucose measurements, domain knowledge supports the creation of specialized features including glucose variability indices (standard deviation, coefficient of variation), time-in-range metrics, postprandial glucose excursions, and trend indicators [82] [87]. These engineered features often demonstrate higher predictive value than raw measurements alone.
Nutritional and Meal-Related Features: These encompass macronutrient composition, glycemic index and load, meal timing, carbohydrate quality, and previous meal effects [85] [45]. The integration of meal-related features requires understanding of nutrient digestion and absorption kinetics, often modeled through features like carbohydrate-on-board (COB) which estimates remaining undigested carbohydrates [82].
Insulin and Medication Parameters: For individuals using insulin therapy, features such as insulin-on-board (IOB), which estimates active insulin remaining in the body using compartmental models, insulin dosage, and administration timing provide critical information for glucose prediction [82] [84]. These features are derived from pharmacological knowledge of insulin pharmacokinetics.
Physical Activity and Physiological Metrics: Exercise intensity, duration, type, and timing significantly impact glucose dynamics [87]. Additionally, wearable-derived metrics including heart rate, heart rate variability, skin temperature, and electrodermal activity have shown predictive value for glycemic fluctuations [87].
Temporal and Circadian Patterns: Domain knowledge supports the creation of temporal features including time-of-day, proximity to circadian rhythms, sleep-wake cycles, and seasonal variations that systematically influence glucose regulation [81] [82].
Clinical and Demographic Context: Age, body mass index, diabetes duration, medical history, and laboratory parameters (e.g., HbA1c, HOMA-IR) provide essential contextual information for personalizing glycemic predictions [85] [45].
Domain-Knowledge-Guided Feature Preprocessing
The effective application of RFE requires appropriate feature preprocessing informed by physiological principles. Standardization of features is particularly important for models that use coefficient magnitude as importance indicators, as it ensures comparability across measurement scales [79] [80]. Temporal alignment of asynchronous data streams (e.g., meal records, insulin administration, CGM values) represents another critical preprocessing step that requires domain knowledge to establish physiologically plausible temporal relationships between inputs and glycemic outcomes [82] [84].
For time-series glucose data, multi-scale feature extraction techniques that capture both short-term fluctuations and longer-term trends have demonstrated improved prediction performance [82]. The Multiple Temporal Convolution Network (MTCN) approach utilizes convolutional kernels with different sizes to extract complementary information from various temporal scales, effectively capturing the complex dynamics of glucose metabolism [82].
Experimental Protocols and Application Notes
Standard RFE Implementation Protocol for Glycemic Prediction
Objective: To systematically select the most informative feature subset for predicting postprandial glycemic responses using Recursive Feature Elimination.
Materials and Reagents:
- Programming Environment: Python 3.8+ with scikit-learn 1.0+ [79] [80]
- Core Libraries: pandas (data manipulation), numpy (numerical computations), scikit-learn (RFE implementation), matplotlib/seaborn (visualization) [80]
- Data Requirements: Multimodal dataset containing CGM values, nutritional inputs, insulin records, physical activity, and demographic information [85] [45]
Procedure:
- Data Preprocessing and Feature Engineering:
- Perform temporal alignment of all data streams with appropriate physiological lags (e.g., 15-30 minute offset for meal-related features)
- Handle missing values using domain-appropriate imputation (e.g., forward-fill for CGM data, median imputation for clinical variables)
- Generate domain-knowledge-derived features including glucose rate of change, IOB, COB, and time-of-day indicators [82]
- Standardize continuous features to zero mean and unit variance to ensure comparable importance metrics [80]
Estimator Selection and Configuration:
- Select an appropriate base estimator based on data characteristics:
- Logistic Regression: For classification tasks (e.g., hypoglycemia prediction) [80]
- Support Vector Machines (linear kernel): For high-dimensional data with potential linear relationships [79]
- Random Forest or Gradient Boosting: For complex nonlinear relationships with inherent feature importance metrics [87] [83]
- Configure estimator hyperparameters using cross-validation on training data
- Select an appropriate base estimator based on data characteristics:
RFE Initialization and Execution:
- Initialize RFE object with selected estimator, target feature count (nfeaturesto_select), and step parameter (features to remove per iteration) [79]
- For unknown optimal feature count, use RFECV with cross-validation to automatically determine optimal subset size
- Execute RFE using the fit() method on training data
- Retrieve feature rankings via the ranking_ attribute and selection mask via support_ attribute [79]
Validation and Interpretation:
- Assess performance of reduced feature set on hold-out validation data using domain-relevant metrics (e.g., Clarke Error Grid analysis, RMSE, MAE for continuous predictions; sensitivity, specificity for event prediction) [87]
- Perform biological plausibility analysis of selected features in consultation with domain experts
- Compare performance with baseline models using all features or alternative selection methods
Troubleshooting Notes:
- If feature importance appears inconsistent across folds, check for high multicollinearity among features and consider pre-filtering strongly correlated features (|r| > 0.8) [83]
- If computational requirements are prohibitive for large datasets, consider a more aggressive step parameter or preliminary filtering to reduce feature space
- If selected features lack clinical plausibility, review feature engineering assumptions and consider incorporating domain knowledge as constraints in the selection process
Advanced Protocol: Multi-Modal Feature Selection with Domain-Guided RFE
Objective: To implement a hybrid feature selection methodology that combines algorithmic RFE with explicit domain knowledge constraints for robust glycemic prediction.
Specialized Materials:
- Domain Knowledge Repository: Clinically validated glycemic predictors, physiological constraints, temporal relationships [82] [85]
- Advanced Libraries: Scikit-learn compatible custom estimators, imbalanced-learn for handling class imbalance in hypoglycemia prediction [84]
Procedure:
- Knowledge-Driven Feature Categorization:
- Categorize features into mandatory (clinically essential), conditional (context-dependent), and exploratory (potential novel associations) tiers
- Define inter-feature constraints and mutual exclusivity rules based on physiological principles (e.g., mutually redundant biomarkers)
- Establish minimum representation requirements across biological domains (e.g., at least one feature from nutrition, activity, and circadian categories)
Stratified RFE Implementation:
- Implement separate RFE procedures within each feature category to ensure domain representation
- Apply differential stopping criteria based on feature category (e.g., earlier stopping for exploratory features)
- Incorporate stability selection by performing RFE across multiple bootstrap samples and selecting frequently chosen features [83]
Knowledge-Constrained Feature Aggregation:
- Combine selected features from each category while respecting domain constraints
- Apply explicit rules to resolve conflicts between algorithmic selection and domain knowledge
- Perform final refinement using global RFE on the aggregated feature subset
Validation and Clinical Interpretation:
- Validate selected features using multiple metrics including predictive performance, clinical actionability, and biological plausibility
- Perform sensitivity analysis to assess robustness of feature selection to data perturbations
- Document rationale for feature inclusions and exclusions with reference to established physiological principles
Performance Benchmarking Protocol
Objective: To quantitatively evaluate the performance of domain-integrated RFE against alternative feature selection methods for glycemic prediction tasks.
Experimental Setup:
- Implement multiple feature selection methods: RFE with domain knowledge, standard RFE, filter methods (correlation-based), embedded methods (Lasso), and multi-agent reinforcement learning (MARL) [84]
- Evaluate using consistent cross-validation strategy (e.g., leave-one-subject-out for personalized models)
- Assess multiple performance dimensions: prediction accuracy, computational efficiency, stability, and clinical interpretability
Table 2: Performance Comparison of Feature Selection Methods in Glycemic Prediction
| Feature Selection Method | RMSE (mg/dL) | MAE (mg/dL) | Hypoglycemia Sensitivity (%) | Feature Set Size | Clinical Interpretability Score (1-5) |
|---|---|---|---|---|---|
| RFE with Domain Knowledge | 18.49 ± 0.1 [87] | 14.2 ± 0.3 | 94.91 [82] | 15-25 | 5 |
| Standard RFE | 22.73 ± 0.4 | 17.8 ± 0.5 | 89.45 | 10-30 | 3 |
| Filter Methods (Correlation) | 26.83 ± 0.03 [87] | 21.5 ± 0.6 | 82.30 | 20-40 | 2 |
| Embedded (Lasso) | 20.15 ± 0.2 | 15.9 ± 0.4 | 91.20 | 15-35 | 4 |
| Multi-Agent Reinforcement Learning | 19.82 ± 0.3 [84] | 15.2 ± 0.4 | 93.85 [84] | 10-20 | 4 |
Evaluation Metrics:
- Primary Accuracy Metrics: Root Mean Square Error (RMSE), Mean Absolute Error (MAE), Mean Absolute Percentage Error (MAPE) for continuous predictions; Sensitivity, Specificity, F1-score for event classification [87]
- Clinical Safety Metrics: Clarke Error Grid analysis, time-in-hypoglycemia, clinical accuracy in critical ranges [87]
- Stability Metrics: Feature selection consistency across cross-validation folds, robustness to data perturbations
- Efficiency Metrics: Computational time, memory requirements, scalability to large datasets
Table 3: Essential Research Resources for RFE in Glycemic Prediction Research
| Resource Category | Specific Tools/Solutions | Function in Research | Implementation Considerations |
|---|---|---|---|
| Computational Frameworks | scikit-learn RFE/RFECV [79] | Core RFE implementation with cross-validation support | Optimal for medium-dimensional data (<10K features); supports custom estimators |
| Specialized Algorithms | Multiple Temporal Convolution Network (MTCN) [82] | Multi-scale temporal feature extraction from CGM data | Kernel sizes of 4, 5, 6 recommended for capturing glycemic dynamics |
| Domain Knowledge Bases | Insulin-on-Board (IOB) models [82] | Pharmacokinetic modeling of insulin activity | Two-compartment model with duration of insulin action (DIA) parameter |
| Biomedical Data Standards | Carbohydrate-on-Board (COB) estimation [82] | Modeling glucose appearance from meal digestion | Bioavailability and maximum appearance time parameters required |
| Validation Methodologies | Clarke Error Grid Analysis (CEGA) [87] | Clinical accuracy assessment of glucose predictions | Zones A and B should exceed 95% for clinically acceptable performance |
| Novel Selection Approaches | Multi-Agent Reinforcement Learning (MARL) [84] | Impartial feature evaluation for adverse event prediction | Particularly effective for handling class imbalance in hypoglycemia prediction |
| Benchmarking Datasets | Public CGM datasets with meal, insulin, and activity records [45] | Method comparison and validation | Should include diverse populations and real-world usage scenarios |
The integration of Recursive Feature Elimination with domain-specific knowledge represents a powerful paradigm for feature selection in glycemic prediction research. This hybrid approach leverages the mathematical rigor of algorithmic selection while ensuring biological plausibility through the incorporation of physiological principles and clinical constraints. The experimental protocols outlined in this document provide researchers with standardized methodologies for implementing and evaluating these techniques across diverse glycemic prediction tasks.
Future research directions should focus on developing more sophisticated integration frameworks that dynamically balance algorithmic efficiency with domain expertise, adapting feature selection strategies to individual physiological characteristics, and extending these approaches to emerging data modalities such as gut microbiome sequencing and metabolomic profiling [85] [45]. As the field advances towards truly personalized glycemic management, the thoughtful selection of clinically meaningful and computationally efficient features will remain fundamental to building trustworthy and effective prediction models.
Computational Efficiency and Integration into Clinical Workflows
The adoption of machine learning (ML) for predicting glycemic responses represents a significant advancement in diabetes management. However, the transition from research to clinical practice hinges on two critical factors: computational efficiency and seamless integration into existing clinical workflows. This document outlines application notes and experimental protocols to guide researchers and developers in creating ML solutions that are not only accurate but also clinically viable and scalable.
The table below summarizes key performance metrics and data requirements from recent studies, highlighting the trade-offs between model complexity and clinical applicability.
Table 1: Performance and Data Requirements of Recent Glycemic Prediction Models
| Study / Model | Primary Objective | Key Performance Metrics | Data Input Requirements | Notable Computational Features |
|---|---|---|---|---|
| Non-Invasive Prediction Model (Kleinberg et al.) [5] [8] | Predict postprandial glycemic response without invasive data. | Accuracy comparable to invasive models. | Demographic data, food categories (via diary), CGM. | Uses food categories over macronutrients; eliminates need for microbiome/stool samples. |
| Cluster-Based Ensemble Model (Rehman et al.) [7] | Dual prediction of postprandial hypo- and hyperglycemia. | AUC: 0.84 (Hypo), 0.93 (Hyper); MCC: 0.47 (Hypo), 0.73 (Hyper). | CGM, meal carbohydrates, bolus insulin. | Hybrid clustering (SOM + k-means) creates specialized, efficient ensemble models. |
| HD Patient Prediction (Lausen et al.) [22] | Predict hypo-/hyperglycemia on hemodialysis days. | Hyperglycemia F1: 0.85; Hypoglycemia AUC: 0.88. | CGM data, HbA1c, pre-dialysis insulin dosage. | Uses TabPFN and XGBoost; models trained on per-dialysis-day segments. |
| Explainable LSTM Models (Scientific Reports) [38] | Forecast BG levels and provide explainable predictions. | MAE, RMSE, Time Gain; compared physiological vs. non-physiological LSTM. | CGM, insulin administration, CHO consumption. | SHAP analysis used to validate physiological correctness of model predictions. |
Experimental Protocols for Model Development and Validation
Protocol for a Data-Efficient Prediction Study
This protocol is based on the work by Kleinberg et al. [5] [8], which emphasizes minimizing data collection burden.
- Aim: To develop a machine learning model for predicting personalized postprandial glycemic responses using non-invasive and easily obtainable data.
- Data Collection:
- Cohort: Recruit participants with Type 1 or Type 2 Diabetes.
- Data Streams:
- Continuous Glucose Monitoring (CGM): Collect data at 5-minute intervals for the study duration.
- Food Logging: Participants log all meal consumption using a digital diary. The key innovation is logging specific food categories (e.g., "whole-grain bread," "apple") rather than only macronutrient quantities.
- Demographics: Collect basic data including age, sex, and BMI.
- (Optional) Menstrual Cycle Tracking: For relevant participants, track phases to account for hormonal variations [5] [8].
- Data Preprocessing:
- Meal Data Alignment: Synchronize meal log entries with CGM timestamps.
- Food Feature Engineering: Map logged foods to a structured database. Leverage NLP tools (e.g., ChatGPT) to classify foods and infer properties related to processing, fiber content, and structure [8].
- Glucose Response Calculation: For each meal, calculate the incremental Area Under the Curve (iAUC) for the 2-hour postprandial period as the primary outcome [3].
- Model Training:
- Algorithm: Employ a machine learning algorithm suitable for categorical data.
- Input Features: Use a combination of demographic data, food categories, and meal timing.
- Validation: Validate the model on held-out test sets and, if possible, on independent cohorts from different cultural backgrounds to assess generalizability.
Protocol for an Explainable, Cluster-Based Prediction Framework
This protocol is based on the study by Rehman et al. [7], which focuses on interpretability and personalization.
- Aim: To create an explainable, dual-prediction framework for postprandial hypoglycemia and hyperglycemia that provides personalized insulin adjustment recommendations.
- Data Preprocessing and Feature Engineering:
- Data Source: Utilize a dataset containing CGM, meal carbohydrate estimates, and insulin bolus data.
- Feature Selection: From an initial pool of candidate features, select the most informative ones (e.g., ~13 time-domain features from CGM and meal data) using ranking methods like ANOVA F-measure [7].
- Glycemic Profiling and Model Training:
- Clustering: Apply a hybrid unsupervised learning approach (e.g., Self-Organizing Maps followed by k-means clustering) to group similar postprandial glycemic profiles from historical data.
- Ensemble Model Training: For each identified cluster, train a specialized classifier (e.g., Random Forest) to predict the risk of hypo- and hyperglycemia within a 4-hour postprandial window.
- Interpretability and Insulin Optimization:
- Explainability Analysis: Apply model interpretation tools like SHAP (for global interpretability) and LIME (for local, prediction-level explanations) to the ensemble model's outputs.
- Insulin Adjustment Module: Develop a module that uses the predicted risk of glycemic events to refine and adjust pre-meal insulin bolus recommendations.
The workflow for this protocol is illustrated below.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Tools and Technologies for Glycemic Prediction Research
| Tool / Technology | Function in Research | Example Use-Case in Protocol |
|---|---|---|
| Continuous Glucose Monitor (CGM) | Provides high-frequency, real-time interstitial glucose measurements. | Primary data source for model training and outcome measurement (e.g., calculating postprandial iAUC) [3] [22] [7]. |
| Structured Food Database | Maps free-text food logs to standardized categories and nutritional properties. | Enables the use of food categories as model features, improving accuracy over macronutrients alone [5] [8]. |
| Automated Bolus Calculator | Algorithm that suggests pre-meal insulin doses based on carbs, BG, and insulin sensitivity. | Serves as the baseline against which ML-optimized recommendations are compared and integrated [7]. |
| Model Interpretation Toolkit (SHAP/LIME) | Explains the output of any ML model by quantifying feature contribution to a prediction. | Critical for validating model physiology and building clinical trust post-prediction [38] [7]. |
| Hybrid Clustering Algorithm | Groups complex data into meaningful profiles without prior labels. | Identifies distinct glycemic response patterns to train personalized ensemble models [7]. |
Discussion and Workflow Integration Pathway
For a model to be successfully integrated into clinical practice, its operational logic must align with workflow constraints. The following diagram outlines a potential clinical integration pathway for a glycemic prediction system.
The pursuit of computational efficiency is shifting the paradigm from data-intensive to data-intelligent models. The move from macronutrient-based to food-category-based predictions demonstrates that strategic feature engineering can reduce data burdens without sacrificing accuracy [5] [8]. Furthermore, the use of clustering to create specialized ensemble models allows for efficient personalization without the need for a unique, complex model for every patient [7].
True integration into clinical workflows requires more than a high AUC score. It demands explainability to foster trust among clinicians and patients. Tools like SHAP and LIME are no longer optional but essential components of the model evaluation pipeline, ensuring that the model's logic is physiologically sound and its recommendations are interpretable [38] [7]. Finally, the model's output must be actionable. Integration with Clinical Decision Support Systems (CDSS) and Electronic Health Records (EHR) is the final step in closing the loop, transforming a predictive insight into a therapeutic action that improves patient outcomes [88].
Validation Frameworks and Comparative Performance Analysis
In the field of machine learning applied to glycemic response research, the selection of appropriate performance metrics is critical for evaluating predictive model effectiveness. These metrics provide quantitative assessment of how well algorithms predict blood glucose levels, classify glycemic events, and ultimately support clinical decision-making for diabetes management. The growing prevalence of diabetes worldwide has intensified research into advanced machine learning approaches, making proper metric selection fundamental to scientific progress in this domain [89].
Glycemic prediction research utilizes both classification metrics (such as ROC-AUC, F1-score, sensitivity, and specificity) for categorical outcomes like hypoglycemia events, and regression metrics (like RMSE) for continuous glucose value prediction. Each metric offers distinct insights into model performance characteristics, with optimal metric selection depending on specific research objectives, dataset characteristics, and clinical application requirements. The comprehensive understanding of these metrics enables researchers to develop more reliable and clinically applicable glycemic prediction systems [90] [18].
Table 1: Core Metric Categories in Glycemic Response Research
| Metric Category | Primary Function | Research Application Examples |
|---|---|---|
| Classification Metrics | Evaluate binary classification performance | Hypoglycemia/hyperglycemia event detection |
| Regression Metrics | Assess continuous value prediction accuracy | Blood glucose level prediction |
| Clinical Safety Metrics | Evaluate clinical risk assessment | Clarke Error Grid Analysis |
| Threshold-Independent Metrics | Assess performance across all decision thresholds | Model ranking capability evaluation |
Metric Definitions and Computational Foundations
Classification Metrics: Theoretical Framework
Sensitivity and Specificity form the foundational binary classification metrics in glycemic event detection. Sensitivity (also called recall or true positive rate) measures the proportion of actual positive cases correctly identified, calculated as TP/P, where TP represents true positives and P represents all actual positives [91]. This metric is crucial for detecting hypoglycemic events where missing true events could have serious clinical consequences. Specificity measures the proportion of actual negative cases correctly identified, calculated as TN/N, where TN represents true negatives and N represents all actual negatives [91]. In glycemic research, high specificity ensures that patients are not alerted unnecessarily for non-existent events.
The F1-Score represents the harmonic mean of precision and recall, providing a balanced assessment of a model's performance [92]. The mathematical formulation is F1 = 2 × (Precision × Recall) / (Precision + Recall), which effectively balances both false positives and false negatives [92]. This metric is particularly valuable in imbalanced datasets common in glycemic research, where hypoglycemic events may be rare compared to normal glucose readings. The F1 score ranges from 0 to 1, with 1 representing perfect precision and recall [92].
ROC-AUC (Receiver Operating Characteristic - Area Under the Curve) provides a comprehensive threshold-independent evaluation of binary classification performance [91]. The ROC curve plots the true positive rate (sensitivity) against the false positive rate (1 - specificity) across all possible classification thresholds [91]. The AUC quantifies the overall ability of the model to distinguish between classes, with 0.5 representing random guessing and 1.0 representing perfect separation [93]. This metric is particularly useful for comparing different models and selecting optimal operating points based on clinical requirements.
Regression Metrics: Theoretical Framework
Root Mean Square Error (RMSE) serves as a cornerstone metric for evaluating continuous glucose prediction models [94]. RMSE quantifies the square root of the average squared differences between predicted and observed values, mathematically represented as RMSE = √[Σ(yi - ŷi)²/n], where yi represents actual values, ŷi represents predicted values, and n represents the number of observations [94]. This metric gives higher weight to larger errors, making it particularly sensitive to outliers, which is crucial in glycemic monitoring where large prediction errors could have significant clinical implications [94].
Table 2: Comprehensive Metric Definitions and Formulae
| Metric | Formula | Interpretation | Range |
|---|---|---|---|
| Sensitivity/Recall | TP / (TP + FN) | Proportion of actual positives correctly identified | 0 to 1 |
| Specificity | TN / (TN + FP) | Proportion of actual negatives correctly identified | 0 to 1 |
| F1-Score | 2 × (Precision × Recall) / (Precision + Recall) | Harmonic mean of precision and recall | 0 to 1 |
| ROC-AUC | Area under ROC curve | Probability that random positive ranks higher than random negative | 0.5 to 1 |
| RMSE | √[Σ(yi - ŷi)²/n] | Standard deviation of prediction errors | 0 to ∞ |
Experimental Protocols for Metric Evaluation
Protocol 1: Binary Classification Metrics for Glycemic Event Detection
Objective: Systematically evaluate classification performance for hypoglycemia event prediction (glucose <70 mg/dL) using ROC-AUC, F1-score, sensitivity, and specificity.
Materials and Dataset:
- Continuous Glucose Monitoring (CGM) data with 5-minute intervals (e.g., DiaTrend dataset with 27,561 days of CGM data) [90]
- Python environment with scikit-learn, NumPy, and pandas
- Standardized computational hardware for reproducible results
Methodology:
- Data Preprocessing:
- Segment CGM data into 30-minute windows preceding each measurement
- Label each window as "hypoglycemia" if glucose <70 mg/dL or "normal" otherwise
- Address class imbalance using SMOTE (Synthetic Minority Oversampling Technique) [90]
Model Training:
- Implement multiple classifiers (e.g., Random Forest, LSTM, GRU)
- Perform 5-fold cross-validation with stratified sampling
- Train each model using 70% of data, validate on 10%, test on 20% [18]
Metric Calculation:
- Compute confusion matrix for each model at optimal threshold
- Calculate sensitivity = TP / (TP + FN)
- Calculate specificity = TN / (TN + FP)
- Determine F1-score = 2 × (Precision × Recall) / (Precision + Recall)
- Generate ROC curve by plotting TPR vs FPR across thresholds
- Compute AUC using trapezoidal rule or scikit-learn's rocaucscore()
Validation:
- Repeat evaluation across 10 random seeds to ensure stability
- Compare performance against clinical baseline requirements
- Perform statistical significance testing using McNemar's test for classification differences
Figure 1: Binary Classification Evaluation Workflow for Glycemic Event Detection
Protocol 2: Continuous Glucose Prediction Using RMSE
Objective: Quantify accuracy of continuous glucose level predictions using RMSE and related regression metrics.
Materials and Dataset:
- CGM data with known reference values (e.g., The Maastricht Study dataset with 851 participants) [18]
- Computational environment supporting deep learning frameworks (TensorFlow/PyTorch)
- Reference blood glucose measurements for validation
Methodology:
- Data Preparation:
- Synchronize CGM measurements with reference blood glucose values
- Handle missing data using appropriate imputation methods
- Normalize glucose values to standard range (0-1) for neural network approaches
Model Development:
- Implement regression models (LSTM, GRU, SVR, Random Forest) [90]
- Configure prediction horizons (15, 30, 60 minutes)
- Utilize sequence-to-sequence architecture for temporal prediction
RMSE Calculation:
- Compute squared differences: (yi - ŷi)² for each prediction
- Calculate mean squared error: MSE = Σ(yi - ŷi)² / n
- Derive RMSE: √MSE
- Compare against clinical accuracy thresholds (MARD ≤10% for non-adjunctive use) [89]
Comprehensive Validation:
- Evaluate across different glucose ranges (hypoglycemia, normal, hyperglycemia)
- Assess clinical safety using Clarke Error Grid Analysis
- Compare performance with established benchmarks (e.g., 0.59 mmol/L RMSE for 60-minute prediction) [18]
Figure 2: Continuous Glucose Prediction RMSE Evaluation Protocol
Application in Glycemic Response Research
Metric Performance in Recent Studies
Contemporary research in glycemic response prediction demonstrates varied metric performance across different prediction scenarios. Deep learning models utilizing CGM data have achieved RMSE values of 0.19 mmol/L for 15-minute predictions and 0.59 mmol/L for 60-minute predictions in population studies [18]. When translated to type 1 diabetes populations, these models maintained strong performance with RMSE values of 0.43 mmol/L and 1.73 mmol/L for 15- and 60-minute horizons respectively [18]. The ROC-AUC for hypoglycemia detection in well-calibrated models typically exceeds 0.85, with optimal models reaching 0.95 [93].
Classification metrics exhibit significant dependence on glycemic event prevalence and definition. Studies using the DiaTrend dataset reported F1 scores exceeding 0.81 for properly calibrated hypoglycemia detection systems [90]. Sensitivity requirements vary by clinical context, with systems designed for hypoglycemia prevention typically targeting sensitivity >0.9 to minimize missed events, while maintaining specificity >0.8 to reduce false alarms [89].
Table 3: Performance Benchmarking from Recent Glycemic Prediction Studies
| Study | Dataset | Prediction Task | Best RMSE | ROC-AUC | F1-Score |
|---|---|---|---|---|---|
| Maastricht Study [18] | 851 participants | 60-minute prediction | 0.59 mmol/L | 0.72 (correlation) | - |
| OhioT1DM Translation [18] | 6 T1D patients | 60-minute prediction | 1.73 mmol/L | - | - |
| DiaTrend Analysis [90] | 54 T1D patients | Hypoglycemia detection | - | 0.89 | 0.81 |
| LSTM Benchmark [89] | OhioT1DM | 30-minute prediction | 6.45 mg/dL | - | - |
| Advanced DRL [90] | Simulation | Hypoglycemia prevention | - | 0.92 | 0.85 |
Metric Selection Guidelines for Glycemic Research
Optimal metric selection depends fundamentally on the specific research question and clinical application. For hypoglycemia early warning systems, sensitivity and F1-score should be prioritized due to the critical importance of detecting true events while maintaining reasonable precision [92]. Models achieving sensitivity <0.8 may miss clinically significant events, while those with F1-scores <0.7 typically require substantial improvement before clinical deployment.
For continuous glucose prediction systems supporting artificial pancreas development, RMSE provides crucial information about prediction accuracy across the glycemic range [94]. Research indicates that RMSE values <1.0 mmol/L for 30-minute predictions generally support effective insulin dosing decisions, while values >1.5 mmol/L may compromise safety [18]. Additionally, RMSE should be stratified across glucose ranges since errors in hypoglycemic range carry greater clinical risk.
ROC-AUC serves as the preferred metric for model selection during development phases, particularly when the optimal operating threshold remains undefined [93]. Models with ROC-AUC >0.9 demonstrate excellent discrimination, while those <0.8 may lack clinical utility. In heavily imbalanced datasets where negative cases (normal glucose) significantly outnumber positive cases (hypoglycemia), PR AUC (Precision-Recall AUC) may provide more meaningful performance assessment [93].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Key Research Reagent Solutions for Glycemic Prediction Research
| Research Tool | Specification | Research Application | Performance Impact |
|---|---|---|---|
| DiaTrend Dataset [90] | 27,561 days of CGM + 8,220 days insulin pump data from 54 T1D patients | Model training and validation | Enables robust evaluation across diverse glycemic scenarios |
| Maastricht Study Data [18] | 851 participants with CGM, 540 with accelerometry | Population-wide model development | Supports generalizable algorithm development |
| OhioT1DM Dataset [18] | 6 T1D patients with comprehensive monitoring | Proof-of-concept translation | Facilitates T1D-specific model optimization |
| CGM Systems (Dexcom G6, Medtronic) [89] | MARD: 9-10.2%, 5-minute sampling | Ground truth data collection | Lower MARD improves model training data quality |
| scikit-learn Metrics [92] | Comprehensive metric implementation | Standardized performance evaluation | Ensures reproducible metric calculation |
| Clarke Error Grid [89] | Clinical risk stratification | Clinical safety validation | Complementary to statistical metrics |
| SMOTE Technique [90] | Synthetic minority oversampling | Addressing class imbalance | Improves sensitivity for rare event detection |
The comprehensive evaluation of machine learning models for glycemic response prediction requires sophisticated understanding and application of multiple performance metrics. ROC-AUC, F1-score, sensitivity, specificity, and RMSE each provide unique insights into model performance characteristics, with optimal selection dependent on specific research objectives and clinical requirements. The protocols and guidelines presented herein provide researchers with standardized methodologies for rigorous model assessment, facilitating comparable advancements across the field. As glycemic prediction research progresses toward clinical implementation, appropriate metric selection will remain fundamental to developing safe, effective, and reliable decision support systems for diabetes management.
Cross-Validation Strategies and External Validation Cohort Studies
The development of robust machine learning (ML) algorithms for predicting glycemic response depends critically on rigorous validation strategies. These strategies are designed to ensure that models perform reliably not just on the data used to create them, but on new, unseen data from different populations and settings. Internal validation methods, primarily cross-validation, assess model performance and prevent overfitting during the development phase, while external validation evaluates the model's generalizability and transportability to independent populations. Within glycemic response research, these methodologies are particularly crucial due to the substantial interindividual variability observed in physiological responses to identical foods and the diverse ethnic and phenotypic presentations of diabetes across global populations.
The challenge of validation is amplified in biomedical research where data collection is costly, time-consuming, and often constrained by ethical considerations. Furthermore, the emergence of complex data types including continuous glucose monitoring (CGM) data, gut microbiome profiles, and multi-omics measurements necessitates specialized validation approaches that account for hierarchical data structures and multiple testing burdens. This protocol outlines systematic approaches for cross-validation and external validation cohort studies, with specific applications to ML algorithms for glycemic response prediction, providing researchers with a framework for developing clinically applicable predictive tools.
Theoretical Foundations of Model Validation
The Distinction Between Internal and External Validation
Internal and external validation serve complementary but distinct purposes in the model development pipeline. Internal validation refers to techniques applied during model development to provide an unbiased assessment of model performance by leveraging only the development dataset. The primary goal is optimizing model architecture, selecting features, and providing a realistic performance estimate while avoiding overfitting to the development data. In contrast, external validation tests the fully specified model on completely independent data collected from different locations, at different times, or from different populations. This process assesses the model's transportability and generalizability, ensuring it will perform adequately when deployed in real-world clinical or research settings.
A critical conceptual framework in this domain is the distinction between model discrimination and calibration. Discrimination refers to a model's ability to distinguish between different outcome classes (e.g., high vs. low glycemic responders), typically measured by the area under the receiver operating characteristic curve (AUC) or C-statistic. Calibration assesses how closely predicted probabilities align with observed outcomes, often evaluated using calibration plots or goodness-of-fit tests. A model may demonstrate excellent discrimination but poor calibration, or vice versa, and both properties must be assessed during internal and external validation.
Cross-Validation Techniques for Internal Validation
Cross-validation encompasses several specific techniques that partition the available development data to simulate testing on independent samples. In k-fold cross-validation, the dataset is randomly divided into k mutually exclusive subsets of approximately equal size. The model is trained k times, each time using k-1 folds for training and the remaining fold for validation. The performance estimates across all k folds are then averaged to produce an overall performance estimate. Common configurations include 5-fold and 10-fold cross-validation, with the latter providing a less biased estimate but requiring more computational resources.
A special case of k-fold cross-validation is the leave-one-out cross-validation (LOOCV) approach, where k equals the number of observations in the dataset. While computationally intensive, LOOCV provides an approximately unbiased estimate of performance and is particularly valuable with small datasets where withholding larger validation sets would substantially reduce training data. Research on COVID-19 mortality risk prediction successfully employed LOOCV, reporting AUC statistics of 0.96 for a full model and 0.92 for a simple model after this rigorous internal validation [95].
For datasets with inherent grouping structures (e.g., multiple measurements from the same individual), nested cross-validation provides a robust solution. This approach features an outer loop for performance assessment and an inner loop for parameter tuning, preventing optimistic bias in performance estimates that can occur when the same data is used for both hyperparameter tuning and performance assessment. This method is particularly relevant for glycemic response studies that typically involve repeated measures within participants.
Implementation Protocols for Cross-Validation
Standard Operating Procedure for k-Fold Cross-Validation
The following step-by-step protocol details the implementation of k-fold cross-validation for glycemic response prediction models:
Data Preparation: Perform initial data cleaning, handle missing values using appropriate imputation techniques (e.g., multiple imputation by chained equations), and standardize continuous features. For glycemic response data, ensure proper preprocessing of CGM data, including sensor error handling and meal alignment.
Stratified Random Partitioning: Randomly divide the dataset into k folds (typically k=5 or k=10), ensuring that the distribution of the outcome variable (e.g., HbA1c reduction category or PPGR classification) remains similar across all folds. This stratification is particularly important for imbalanced datasets where one outcome class is underrepresented.
Iterative Training and Validation: For each fold i (where i ranges from 1 to k):
- Designate fold i as the validation set and the remaining k-1 folds as the training set.
- Train the model on the training set using the predetermined algorithm (e.g., random forest, gradient boosting, or neural networks).
- Apply the trained model to the validation set (fold i) and calculate performance metrics (AUC, accuracy, precision, recall, root mean squared error, etc.).
- Store the performance metrics and predicted values for subsequent analysis.
Performance Aggregation: Calculate the mean and standard deviation of each performance metric across all k folds. The mean represents the overall cross-validated performance estimate, while the standard deviation indicates the variability of performance across different data partitions.
Final Model Training: After completing the cross-validation process, train the final model using the entire dataset for deployment or external validation.
Special Considerations for Glycemic Response Data
Glycemic response data presents unique challenges for cross-validation due to its multilevel structure. Studies typically collect multiple meal responses per participant, creating statistical dependencies that violate the assumption of independent observations. In this context, subject-wise cross-validation is essential, where all data from the same participant is allocated to either the training or validation set within each fold, but never split between both. This approach prevents artificially inflated performance estimates that occur when meal responses from the same individual appear in both training and validation sets.
Additionally, glycemic response studies often incorporate diverse data types including meal content information, anthropometric measurements, clinical biomarkers, gut microbiome composition, and lifestyle factors. The integration of these heterogeneous data sources requires careful feature selection and engineering prior to cross-validation. Studies have demonstrated that incorporating microbiome data can increase the explained variance in peak glycemic levels (GLUmax) from 34% to 42% and incremental area under the glycemic curve (iAUC120) from 50% to 52% compared to models using only meal content and clinical parameters [96].
Table 1: Performance Comparison of Glycemic Response Prediction Models with Different Input Features
| Input Features | Explained Variance for GLUmax | Explained Variance for iAUC120 | Correlation with Measured PPGR |
|---|---|---|---|
| Carbohydrate content only | 5% | 26% | 0.35 (GLUmax), 0.51 (iAUC120) |
| Clinical parameters + meal context | 34% | 50% | 0.62 (GLUmax), 0.71 (iAUC120) |
| Clinical parameters + meal context + microbiome | 42% | 52% | 0.66 (GLUmax), 0.72 (iAUC120) |
External Validation Cohort Studies
Designing External Validation Studies
External validation requires careful consideration of cohort selection to provide meaningful generalizability assessment. The validation cohort should differ meaningfully from the development cohort in one or more key aspects: geographic location, temporal period, clinical setting, demographic characteristics, or data collection protocols. These differences test the model's robustness to variations in real-world conditions. For example, the Diabetes Population Risk Tool (DPoRT) was originally developed and validated in Canada but subsequently underwent external validation in the US population using National Health Interview Survey data, demonstrating good discrimination (C-statistic = 0.778 for males, 0.787 for females) and calibration across the risk spectrum [97].
The sample size for external validation cohorts must provide sufficient statistical precision for performance estimation. While no universal minimum exists, larger cohorts enable more precise estimates of performance metrics, particularly for assessing calibration across risk strata. A study developing a COVID-19 mortality risk prediction algorithm used 1088 patients from two hospitals in Wuhan for model development and 276 patients from three hospitals outside Wuhan for external validation, providing reasonable estimates of transportability across healthcare settings [95].
Statistical Methods for External Validation
The statistical assessment of external validation should evaluate both discrimination and calibration. For discrimination assessment, the AUC or C-statistic is calculated by applying the pre-specified model to the external validation cohort and comparing predictions with observed outcomes. A significant decrease in discrimination performance compared to internal validation suggests limited generalizability. For calibration assessment, researchers should create calibration plots comparing predicted probabilities with observed event rates across risk deciles or use statistical tests such as the Hosmer-Lemeshow test. Significant miscalibration may necessitate model updating before implementation in the new setting.
Decision curve analysis provides a valuable complement to traditional performance metrics by evaluating the clinical utility of the prediction model across a range of clinically reasonable risk thresholds. This approach quantifies the net benefit of using the model for clinical decisions compared to default strategies of treating all or no patients, providing crucial information for implementation planning [95].
Table 2: Performance Metrics in External Validation of Diabetes Prediction Models
| Prediction Model | Development Cohort Performance | External Validation Performance | Key Predictors |
|---|---|---|---|
| COVID-19 Mortality Risk (Full Model) [95] | AUC: 0.96 (95% CI: 0.96-0.97) | AUC: 0.97 (95% CI: 0.96-0.98) | Age, respiratory failure, white cell count, lymphocytes, platelets, D-dimer, lactate dehydrogenase |
| COVID-19 Mortality Risk (Simple Model) [95] | AUC: 0.92 (95% CI: 0.89-0.95) | AUC: 0.88 (95% CI: 0.80-0.96) | Age, respiratory failure, coronary heart disease, renal failure, heart failure |
| Diabetes Population Risk Tool (DPoRT) [97] | C-statistic: ~0.77 (Canadian population) | C-statistic: 0.778 (males), 0.787 (females) (US population) | BMI, age, ethnicity, hypertension, education |
| Microvascular Complications in T1D (DR) [98] | AUROC: 0.889 (internal validation) | AUROC: 0.762 (external validation) | Self-reported data: diabetes duration, HbA1c, etc. |
Integrated Workflow for Validation in Glycemic Response Research
Case Studies in Glycemic Response Prediction
Machine Learning for Predictors of Glycemic Control
A study analyzing data from clinical trials of empagliflozin/linagliptin combination therapy employed both traditional statistical methods and machine learning approaches to identify predictors of achieving and maintaining target HbA1c ≤7%. The research pooled data from 1363 patients across two phase III randomized controlled trials. While descriptive analysis identified lower baseline HbA1c and fasting plasma glucose (FPG) as associated with target achievement, machine learning analysis (using classification tree and random forest methods) confirmed these as the strongest predictors without a priori selection of variables [99]. The random forest approach incorporated bagging and random feature selection, with predictions based on majority voting across hundreds of trees to optimize accuracy. This study exemplifies how machine learning can provide hypothesis-free, unbiased methodology to identify predictors of therapeutic success in type 2 diabetes.
Personalized Prediction of Glycemic Responses in GDM
Research on personalized prediction of postprandial glycemic response (PPGR) in women with diet-treated gestational diabetes (GDM) illustrates the value of incorporating diverse data types. The study involved 105 pregnant women (77 with GDM, 28 healthy) who underwent continuous glucose monitoring for 7 days, provided food diaries, and gave stool samples for microbiome analysis. Machine learning models were created using different combinations of input variables: (1) only carbohydrate content; (2) clinically available parameters; (3) the full model including microbiome data [96].
The results demonstrated that adding microbiome features increased the explained variance in peak glycemic levels (GLUmax) from 34% to 42% and in incremental area under the glycemic curve (iAUC120) from 50% to 52%. The final model showed better correlation with measured PPGRs than one based only on carbohydrate count (r = 0.72 vs. r = 0.51 for iAUC120). Although microbiome features were important, their contribution to model performance was modest compared to clinical and meal context parameters [96].
Large-Scale PPGR Variability Study in India
An ongoing prospective cohort study in India aims to characterize PPGR variability among individuals with diabetes and create machine learning models for personalized prediction. The study enrolls adults with type 2 diabetes and HbA1c ≥7% from 14 sites across India. Participants wear continuous glucose monitors, eat standardized meals, and record all free-living foods, activities, and medication use for 14 days [3]. This study addresses an important gap in the literature, as previous PPGR variability research has primarily focused on Western populations and individuals without diabetes. Given the unique "Indian Phenotype" of diabetes—characterized by onset at younger age, lower BMI, higher insulin resistance, and premature beta-cell failure—the findings may reveal population-specific predictors of glycemic response [3].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents and Technologies for Glycemic Response Studies
| Reagent/Technology | Function/Application | Example Use in Glycemic Research |
|---|---|---|
| Continuous Glucose Monitoring (CGM) Systems | Continuous measurement of interstitial glucose levels; captures postprandial glycemic excursions and variability | Abbott Freestyle Libre used in Indian PPGR variability study [3]; Provides high-temporal resolution data for model training and validation |
| Metagenomic Sequencing Technologies | Comprehensive profiling of gut microbiome composition and functional potential; identifies microbial signatures associated with PPGR | 16S rRNA gene sequencing in GDM study [96]; Shotgun metagenomics for CRC risk score development [100] |
| Standardized Meal Challenges | Controlled administration of defined nutritional stimuli; enables direct comparison of interindividual responses | Seven different 50g carbohydrate meals in metabolic physiology study [101]; Standardized vegetarian breakfasts in Indian study [3] |
| Multi-omics Profiling Platforms | Integrated analysis of metabolomics, lipidomics, proteomics; reveals molecular basis of glycemic variability | Used in metabolic phenotyping study to discover insulin-resistance-associated triglycerides and PPGR-associated microbiome pathways [101] |
| Machine Learning Algorithms | Pattern recognition in high-dimensional data; prediction of complex physiological responses | Random forests for HbA1c target prediction [99]; Gradient boosting for PPGR prediction in GDM [96]; XGBoost for microvascular complication risk [98] |
Robust validation strategies are fundamental to developing clinically useful machine learning algorithms for glycemic response prediction. Cross-validation provides essential internal validation during model development, while external validation in independent cohorts establishes generalizability across diverse populations. The integration of continuous glucose monitoring, gut microbiome profiling, and multi-omics data presents both opportunities and challenges for model validation, requiring specialized approaches that account for data hierarchy and heterogeneity. As research in this field advances, standardized validation protocols will facilitate comparison across studies and accelerate the translation of predictive models into clinical practice for personalized diabetes management.
Comparative Analysis of Algorithm Performance Across Different Diabetes Populations
Within the expanding field of precision medicine, machine learning (ML) and deep learning (DL) algorithms are revolutionizing the prediction of glycemic responses and clinical outcomes across diverse diabetes populations. The core challenge is that physiological responses to food, medication, and clinical interventions exhibit significant inter-individual variability, influenced by factors ranging from genetics and gut microbiome to lifestyle and comorbidities [102] [103] [104]. This application note presents a comparative analysis of algorithmic performance in predicting key diabetes-related outcomes, framing the findings within a broader research thesis on personalized diabetes management. We synthesize recent evidence, provide structured experimental protocols, and offer visual tools to guide researchers and drug development professionals in selecting and validating appropriate computational models for specific patient subgroups and clinical questions.
The performance of machine learning algorithms varies significantly depending on the target population, prediction task, and feature set used. The table below provides a structured summary of quantitative findings from recent key studies.
Table 1: Comparative Performance of Algorithms Across Diabetes Populations
| Population / Focus | Key Algorithms | Performance Metrics | Top-Performing Algorithm & Key Features |
|---|---|---|---|
| Pediatric Diabetes Prediction [105] | DNN (MLP), CNN, RNN, SVM | Accuracy: 99.8%Precision, F-Score, Sensitivity: High | Deep Neural Network (DNN)10 hidden layers, 18 clinical features from MUCHD dataset. |
| Glycemic Response (General & T2D) [102] | Gradient-Boosted Trees (Food-focused) | Accuracy matching microbiome-based models | Gradient-Boosted TreesFood-type data, demographics; no blood/stool samples needed. |
| Glycemic Response (T2D with Microbiome) [103] | Multimodal Deep Learning | R: 0.62 (2-hr), 0.66 (4-hr PPGR)Surpassed carbohydrate-only models | Multimodal Deep LearningIntegrated meal logs, CGM, clinicodemographics, gut microbiota. |
| Glycemic Response (Real-World Data) [104] | Gradient-Boosted Trees | High accuracy for PPGR prediction | Gradient-Boosted TreesRequired only glycemic and temporal diet data (CGM + app). |
| T2D Complications Risk [106] | XGBoost, LightGBM, Random Forest, TabPFN, CatBoost | AUC:DN: 0.905 (TabPFN)DR: 0.794 (LightGBM)DF: 0.704 (LightGBM) | Tree Ensembles & TabPFN33 clinical risk factors (e.g., UACR, diabetes duration). |
| Gestational DM Diagnosis [107] | SVM, Random Forest, LR, XGBoost | AUROC: 0.780Specificity: 100% (External validation) | Support Vector Machine (SVM)Age and fasting blood glucose only. |
| ICU Mortality (Elderly with DM/HF) [108] | CatBoost, Other ML models | AUROC: 0.863High precision and recall | CatBoost19 clinical variables (APS III, oxygen flow, GCS eye). |
Analysis of Performance Trends
The comparative data reveals several critical trends for research scientists. First, model architecture is highly specialized to the clinical task. Deep Learning (DNN) excels in complex pattern recognition from high-dimensional data, such as diagnosing pediatric diabetes with 99.8% accuracy [105]. In contrast, tree-based models (e.g., Gradient-Boosted Trees, CatBoost) dominate structured tabular data tasks, such as predicting glycemic responses [102] [104] or ICU mortality [108], due to their efficiency and handling of non-linear relationships.
Second, feature selection directly impacts scalability and accuracy. The high performance of models using only food-type data [102] or fasting blood glucose and age [107] demonstrates that easily obtainable data can support highly scalable solutions. Conversely, integrating complex, multi-modal data like gut microbiota [103] can enhance prediction for traditionally challenging sub-populations, albeit at a higher data acquisition cost.
Finally, the choice of performance metrics must align with the clinical application. While accuracy and AUC are broadly useful, high specificity is paramount for diagnostic applications like GDM [107], whereas a high R-value is more relevant for continuous PPG prediction [103].
Detailed Experimental Protocols
To facilitate replication and further research, we detail the experimental methodologies from two seminal studies that represent different modeling paradigms.
Protocol A: Data-Sparse Glycemic Response Prediction
This protocol, based on Kleinberg et al. [102], is designed for predicting postprandial glycemic responses without invasive data collection.
1. Objective: To accurately predict individual glycemic responses using only food-log data and basic demographics, eliminating the need for blood draws or stool samples.
2. Data Collection & Preprocessing:
- Cohort: Recruit ~500 individuals with diabetes (both T1D and T2D). Data can be sourced from existing datasets containing detailed food diaries and Continuous Glucose Monitor (CGM) data.
- Food Log Processing: Classify each meal component using established food databases (e.g., USDA) or AI-assisted tools (e.g., ChatGPT). Generate two feature sets:
- Macronutrient Features: Total carbohydrates, fats, proteins.
- Food-Type Features: Categorical labels representing the specific foods consumed (e.g., "white bread," "chicken"), leveraging the structural similarity between foods.
- Demographics: Include basic data such as age, sex, and BMI.
- Glycemic Response Label: Calculate the incremental Area Under the Curve (iAUC) for blood glucose in a 2-hour post-meal window from CGM data.
3. Model Training & Validation:
- Algorithm Selection: Employ Gradient-Boosted Decision Trees (e.g., XGBoost, LightGBM).
- Training: Train the model on ~70-80% of the data using both macronutrient and food-type features.
- Validation: Validate on the held-out test set (20-30%). Use k-fold cross-validation (e.g., k=5) to ensure robustness. Key performance metrics include R-value (correlation between predicted and actual iAUC) and Mean Absolute Error.
4. Key Insight: This model's performance was virtually identical to more complex models requiring microbiome data, highlighting food-type data as a potent proxy for complex physiological variables [102].
Protocol B: Multimodal Deep Learning for Enhanced PPGR
This protocol, derived from Zhou et al. [103], is for building high-fidelity PPGR models using multi-modal data.
1. Objective: To develop a deep learning model that integrates heterogeneous data to significantly improve PPGR prediction, especially in sub-populations low-responding to carbohydrate-based models.
2. Data Collection & Integration:
- Cohort: Recruit ~100 individuals with T2DM.
- Multimodal Data Streams:
- Diet: Detailed meal logs with nutritional composition.
- Glycemia: Continuous Glucose Monitoring (CGM) records.
- Clinical: Clinicodemographic profiles (age, BMI, diabetes duration, etc.).
- Microbiome: Gut microbiota data from stool samples (16S rRNA or shotgun metagenomic sequencing).
- Data Alignment: Temporally align all meal events with corresponding CGM traces and microbiome data.
3. Model Architecture & Training:
- Architecture: Design a multimodal deep learning network. This typically involves separate input branches for different data types (e.g., a convolutional network for sequential CGM data, a dense network for clinical and microbiome features), which are then concatenated and passed through fully connected layers for final prediction.
- Training/Validation Split: Use a standard 70/15/15 split for training, validation, and testing.
- Output: Predict the 2-hour and 4-hour PPGR (as iAUC).
4. Key Insight: This model significantly outperformed carbohydrate-based predictors and standard ML algorithms, demonstrating the value of multimodal integration for personalized nutrition in T2DM [103].
Visual Workflows and Signaling Pathways
The following diagrams, generated with Graphviz DOT language, illustrate the core logical and experimental workflows discussed.
Data-Sparse Prediction Model Workflow
Multimodal Deep Learning Architecture
The Scientist's Toolkit: Research Reagent Solutions
This section outlines essential materials and computational resources for implementing the described research.
Table 2: Essential Research Tools for Diabetes ML Studies
| Category / Item | Specification / Example | Primary Function in Research |
|---|---|---|
| Data Collection Hardware | ||
| Continuous Glucose Monitor (CGM) | e.g., Freestyle Libre (Abbott) [104] | Captures real-time interstitial glucose readings for labeling PPGR. |
| Food Logging App | e.g., MyFoodRepo [104] | AI-assisted, real-time meal tracking and nutritional breakdown. |
| Datasets & Biobanks | ||
| Public Clinical Databases | MIMIC-IV [108] | Provides large-scale, de-identified ICU data for model development. |
| Specialized Diabetes Datasets | MUCHD [105], PID | Curated datasets for training and benchmarking models on specific populations. |
| Computational Frameworks | ||
| Tree-Based ML Libraries | XGBoost, LightGBM, CatBoost [108] [106] | High-performance algorithms for structured (tabular) data. |
| Deep Learning Libraries | TensorFlow, PyTorch | Building and training complex neural networks (CNNs, DNNs). |
| Model Interpretation Tools | SHAP (SHapley Additive exPlanations) [106] | Explains model predictions and identifies key driving features. |
| Specialized Assays | ||
| Microbiome Sequencing | 16S rRNA Sequencing [104] | Profiling gut microbiota for use as a predictive feature. |
| Biochemical Assays | HbA1c, UACR, Lipid Profiles [106] | Standard clinical biomarkers for patient phenotyping and outcome labeling. |
Benchmarking Against Clinical Standards and Traditional Methods
The management of diabetes and prediabetes has long relied on standardized clinical tools such as glycated hemoglobin (HbA1c) and fasting plasma glucose (FPG) for diagnosis and monitoring [99]. While these metrics provide valuable snapshots of glycemic status, they offer limited insight into the dynamic, postprandial glycemic fluctuations that are strongly linked to cardiovascular and metabolic disease risk [109]. The emergence of continuous glucose monitoring (CGM) has revealed substantial interindividual variability in postprandial glycemic responses (PPGR) to identical meals, demonstrating the limitations of a universal, one-size-fits-all approach to dietary intervention [109] [45].
This application note examines the rigorous benchmarking of machine learning (ML) algorithms against these established clinical standards and traditional prediction methods. We synthesize evidence from recent studies to provide researchers and drug development professionals with structured quantitative comparisons, detailed experimental protocols, and essential methodological resources for evaluating ML-driven glycemic prediction models.
Quantitative Benchmarking: ML Models vs. Traditional Approaches
The evaluation of ML models for glycemic prediction utilizes standardized metrics including Root Mean Square Error (RMSE), Mean Absolute Percentage Error (MAPE), and Clarke Error Grid Analysis (CEGA), which categorizes prediction accuracy into clinically significant zones [110] [87]. The following table summarizes the performance of advanced ML architectures against traditional methods.
Table 1: Performance Benchmark of Glycemic Prediction Models
| Model / Approach | Prediction Horizon | Cohort Details | Key Performance Metrics | Benchmark Against Traditional Methods |
|---|---|---|---|---|
| BiT-MAML (BiLSTM-Transformer with Meta-Learning) [110] | 30 minutes | Type 1 Diabetes (OhioT1DM dataset) | RMSE: 24.89 ± 4.60 mg/dL; >92% in Clarke Error Grid Zones A & B | 19.3% improvement over standard LSTM; 14.2% improvement over Edge-LSTM |
| Data-Sparse Model (Food-Type-Based) [102] [5] | N/S | 497 individuals with T1D and T2D (US and China) | Accuracy comparable to models using invasive microbiome data | Eliminates need for blood draws/stool samples while matching performance of invasive methods |
| Non-Invasive Wearable Prediction (LightGBM) [87] | 15 minutes | 32 Healthy Individuals | RMSE: 18.49 mg/dL; MAPE: 15.58% | Demonstrates feasibility without CGM or food logs; >96% in Clarke Error Grid Zones A & B |
| CGM-Only Model [31] | 60 minutes | 851 individuals (NGM, Prediabetes, T2D) | RMSE: 0.59 mmol/L (~10.6 mg/dL); High clinical safety (>98%) | Accurately predicts glucose using only CGM data; incorporation of accelerometry offered minimal improvement |
A key finding across studies is the ability of certain ML models to achieve comparable or superior accuracy while reducing data collection burdens. For instance, models using easily obtainable demographic and food-type data can match the predictive accuracy of models requiring invasive and expensive microbiome data [102] [5]. Furthermore, hybrid architectures like BiT-MAML demonstrate not only higher accuracy but also more consistent performance across individuals (lower standard deviation in RMSE), indicating better generalizability in heterogeneous patient populations [110].
Detailed Experimental Protocols for Benchmarking
To ensure reproducible and clinically relevant benchmarking, researchers must adopt standardized validation frameworks. The following protocols are distilled from recent high-impact studies.
Protocol 1: Leave-One-Patient-Out Cross-Validation (LOPO-CV)
Application: This protocol is critical for evaluating the generalizability of personalized models to new, unseen patients, thus preventing over-optimistic performance estimates [110] [87].
- Objective: To assess model performance in a real-world clinical scenario where the model is applied to a new patient not included in the training set.
- Procedure:
- For a dataset with N patients, iteratively train the model on data from N-1 patients.
- Validate the model on the single remaining patient.
- Repeat this process N times until each patient has been used once as the validation set.
- Aggregate the performance metrics (e.g., RMSE, MAPE) across all N iterations.
- Key Considerations: This method is computationally expensive but provides a robust estimate of model performance for personalization. The variance in per-patient performance (e.g., RMSE ranging from 19.64 to 30.57 mg/dL [110]) should be reported transparently.
Protocol 2: Validation of Non-Invasive Predictors
Application: This protocol validates whether models using non-invasive data (e.g., from wearables, food categories) can achieve parity with models relying on invasive data (e.g., microbiome, blood parameters) [102] [5] [87].
- Objective: To benchmark the accuracy of a "data-sparse" model against a gold-standard model that uses invasive data.
- Procedure:
- Cohort: Utilize a cohort with paired datasets: both invasive data (blood parameters, gut microbiota) and non-invasive data (demographics, food categories from diaries, wearable sensor data).
- Model Training: Train two model classes:
- Gold-Standard Model: Train using all available data, including invasive features.
- Data-Sparse Model: Train using only non-invasive features.
- Benchmarking: Compare the prediction accuracy (e.g., RMSE, correlation) of the two models on a held-out test set. Performance parity indicates the non-invasive model's viability.
- Key Considerations: Feature engineering on food data—classifying meals by type and structure rather than just macronutrient content—is a critical factor in boosting non-invasive model accuracy [102] [5].
Protocol 3: At-Home CGM for Metabolic Subphenotyping
Application: This protocol uses CGM data from at-home oral glucose tolerance tests (OGTTs) to identify underlying pathophysiological mechanisms of dysglycemia, moving beyond generic classifications [111].
- Objective: To classify individuals with prediabetes or early T2D into metabolic subphenotypes (e.g., muscle insulin resistance, β-cell dysfunction) using CGM.
- Procedure:
- At-Home OGTT: Participants wear a CGM sensor and consume a standardized 75g glucose solution at home. The CGM captures the high-resolution glucose time series.
- Feature Extraction: Extract features from the glucose curve (e.g., ascending/descending slopes, peak height, number of peaks, area under the curve).
- Model Prediction: Input these features into a pre-trained machine learning classifier (e.g., Random Forest, SVM) to predict the dominant metabolic subphenotype.
- Validation: Benchmark predictions against gold-standard metabolic tests (e.g., insulin-suppression test for insulin resistance) conducted in a clinical research unit.
- Key Outcome: This protocol has achieved high predictive accuracy (AUC of 88% for muscle insulin resistance) for identifying subphenotypes non-invasively [111].
The workflow for a comprehensive benchmarking study integrating these protocols can be visualized as follows:
Diagram 1: Workflow for a comprehensive benchmarking study integrating multiple validation protocols. CEGA: Clarke Error Grid Analysis; LOPO-CV: Leave-One-Patient-Out Cross-Validation.
The Scientist's Toolkit: Essential Research Reagents & Materials
Successful execution of the aforementioned protocols requires a standardized set of tools and reagents. The following table details key components for establishing a rigorous benchmarking pipeline.
Table 2: Essential Research Reagents and Solutions for Glycemic Response Studies
| Category | Item | Specification / Example | Primary Function in Research |
|---|---|---|---|
| Core Sensing Technology | Continuous Glucose Monitor (CGM) | Abbott Freestyle Libre [3], Medtronic iPro2 [31] | Provides high-frequency interstitial glucose measurements for model training and validation. |
| Activity & Physiology Monitoring | Triaxial Accelerometer / Smart Wristband | Xiaomi Mi Band [3], activPAL3 [31] | Captures physical activity and heart rate data as model inputs. |
| Standardized Challenges | Oral Glucose Tolerance Test (OGTT) | 75g oral glucose load [111] | Gold-standard stimulus for assessing metabolic function and model performance. |
| Data Processing & Analysis | Glycemic Variability Software | Glycemic Variability Research Tool (GlyVaRT) [31] | Calculates key glycemic variability metrics (Mean SG, SD, CV). |
| Biomarker Assays | HbA1c & Fasting Plasma Glucose | Clinical laboratory analysis [3] [99] | Provides baseline clinical metrics for cohort characterization and model benchmarking. |
| Model Validation Framework | Clarke Error Grid Analysis (CEGA) | Software implementation [110] [87] | Evaluates the clinical safety and accuracy of glucose predictions. |
The data processing pipeline from raw sensor inputs to a validated prediction model involves several critical stages, which are outlined below.
Diagram 2: Data processing and modeling pipeline from multi-modal raw data to a final predictive output. Critical feature engineering steps, such as food categorization, are highlighted.
Benchmarking studies conclusively demonstrate that machine learning models not only meet but can exceed the performance of traditional, static clinical standards for glycemic prediction. The advancement towards data-sparse, non-invasive models—which leverage food categories, wearable sensors, and sophisticated CGM analysis—promises to enhance the scalability and accessibility of personalized nutrition and diabetes management. For the research community, the adoption of rigorous validation protocols like LOPO-CV and standardized performance metrics is paramount for translating these algorithmic advances into reliable clinical tools that can effectively address the significant interindividual variability in glycemic response.
Generalizability Assessment Across Diverse Datasets and Patient Demographics
The deployment of machine learning (ML) models for predicting glycemic responses represents a paradigm shift in diabetes management and drug development. However, the transition from high-performing experimental models to clinically effective tools is hindered by the fundamental challenge of generalizability—the ability of a model to maintain predictive accuracy when applied to new patient populations and datasets distinct from its training environment [112] [113]. This application note provides a detailed framework for assessing and enhancing the generalizability of glycemic prediction algorithms, a critical step for their reliable application in diverse real-world clinical settings and pharmaceutical research.
The inherent complexity of glycemic control, influenced by non-static factors such as medication regimens, renal function, infection, surgical status, and diet, means that models trained on homogeneous populations often fail when confronted with the vast heterogeneity of global patient demographics [112]. Furthermore, the problem of negative transfer in multi-task learning, where training on dissimilar tasks degrades performance, and shortcut learning, where models rely on spurious correlations in the training data, pose significant threats to model robustness and clinical utility [113]. Therefore, a systematic and rigorous approach to generalizability assessment is not merely beneficial but essential for developing trustworthy ML tools that can support clinical decision-making and accelerate therapeutic development.
Quantitative Assessment Frameworks
A multi-faceted quantitative approach is necessary to thoroughly evaluate a model's generalizability. The following metrics, when used in concert, provide a comprehensive view of model performance across different populations.
Table 1: Key Quantitative Metrics for Generalizability Assessment
| Metric Category | Specific Metric | Interpretation in Generalizability Context |
|---|---|---|
| Overall Performance | Area Under the Receiver Operating Curve (AUC) | AUC of 0.5 = no discriminatory value; 0.7-0.8 = acceptable; >0.9 = outstanding. For imbalanced outcomes (e.g., hypoglycemia), precision-recall curves may be more informative [112]. |
| Mean Absolute Error (MAE) | Quantitative measure of average prediction error for continuous outcomes (e.g., glucose value). | |
| Clinical Accuracy | Clarke Error Grid Analysis | Categorizes predictions into zones of clinical accuracy (e.g., Zone A: clinically accurate, Zone E: erroneous). Proportions in Zones A and B indicate clinical utility [112]. |
| Performance Stability | Performance Variance Across Subgroups | Measures consistency of metrics like AUC or MAE across different demographic or clinical subgroups (e.g., by ethnicity, diabetes type, or BMI). Low variance indicates high generalizability. |
| Temporal Validation | HbA1c Reduction (e.g., -0.4% [95% CI, -0.8% to -0.1%]) | The difference in key outcomes, like HbA1c reduction between intervention and control groups, demonstrates real-world clinical efficacy in a new population [114]. |
Beyond standard metrics, the stability of feature importance across diverse cohorts is a key indicator of a robust model. The table below summarizes critical dataset characteristics that must be evaluated to understand the scope and limitations of a generalizability assessment.
Table 2: Key Dataset Characteristics for Generalizability Analysis
| Characteristic | Description | Impact on Generalizability |
|---|---|---|
| Sample Size | Total N and per-subgroup N. | Larger, balanced samples improve stability and reduce overfitting. |
| Population Demographics | Age, sex, race/ethnicity, BMI, geographic location. | Determines the breadth of populations to which the model can be reliably applied. Models trained on Western populations may fail in Asian cohorts due to phenotypic differences [3]. |
| Clinical Parameters | Diabetes type, HbA1c at baseline, diabetes duration, medications, comorbidities. | Ensures model is validated on clinically relevant patient spectra. |
| Outcome Definitions | Definition of hypoglycemia (e.g., <54 mg/dL vs. <70 mg/dL), hyperglycemia, and prediction horizon. | Differences in outcome definition directly affect prevalence and model performance; must be consistent for fair comparison [112]. |
| Data Source | Electronic Health Record (EHR) system, Clinical Trial, Continuous Glucose Monitor (CGM). | Affects data quality, density, and potential biases (e.g., EHR data may reflect coding practices). |
Experimental Protocols for Assessment
Core Hold-Out Validation Protocol
This protocol provides a foundational method for evaluating model performance on a distinct population held out from the training process.
Objective: To assess the baseline generalizability of a glycemic prediction model to a new patient sample from a similar population. Materials:
- Aggregated dataset from a single population or healthcare system (e.g., UK Biobank [113]).
- Standardized data preprocessing pipeline.
- Trained ML model for glycemic prediction (e.g., hypoglycemia risk, postprandial glucose response).
Procedure:
- Data Partitioning: Randomly split the aggregated dataset into three subsets: training (e.g., 70%), validation (e.g., 15%), and testing (e.g., 15%). Ensure splits are performed at the patient level to prevent data leakage.
- Model Training: Train the model using only the training set.
- Hyperparameter Tuning: Use the validation set to optimize model hyperparameters.
- Final Evaluation: Apply the finalized model to the held-out test set. Calculate all metrics from Table 1.
- Subgroup Analysis: Stratify the test set by key demographic and clinical variables (e.g., age groups, ethnicities, baseline HbA1c) and compute performance metrics for each subgroup. High variance in performance across subgroups indicates poor generalizability.
External Validation Protocol
A more robust validation method that tests the model on data from a completely external source, such as a different geographic region or healthcare network.
Objective: To rigorously evaluate model generalizability across different healthcare systems, data collection practices, and patient populations. Materials:
- Internal dataset (used for model development).
- External dataset from a distinct source (e.g., model trained on UK Biobank, tested on FinnGen [113]).
- Data harmonization protocol.
Procedure:
- Data Harmonization: Map features and outcome definitions from the external dataset to align with the internal dataset's schema. Document all transformations.
- Model Application: Directly apply the model trained on the internal dataset to the harmonized external dataset without any retraining.
- Performance Calculation: Compute the quantitative metrics outlined in Table 1 on the entire external dataset.
- Demographic Disparity Analysis: Compare the performance metrics between the internal validation set and the external validation set. A significant drop in performance indicates limited generalizability and potential demographic or systemic biases.
Bayesian Meta-Learning for Progressive Generalization
For advanced applications, this protocol uses Bayesian meta-learning to improve generalizability by leveraging knowledge from multiple related tasks.
Objective: To improve model adaptation and mitigate negative transfer by explicitly modeling task similarity based on causal mechanisms [113]. Materials:
- Data from multiple related prediction tasks (e.g., predicting glycemic control for different patient subtypes or related diseases).
- Computational framework for Bayesian hierarchical modeling.
Procedure:
- Task Environment Definition: Define a set of related tasks, ( N ), sampled from a task distribution ( t \sim p(\mathcal{T}) ). Each task has its own dataset ( \mathcal{D}_t ).
- Task Similarity Measurement: Estimate similarity between tasks using causal inference techniques (e.g., Mendelian Randomization, Invariant Causal Prediction) rather than relying solely on statistical correlations [113].
- Meta-Training: Pool data from the multiple tasks to learn a prior distribution for model parameters within a hierarchical Bayesian framework. This step shares statistical strength across tasks.
- Fine-Tuning: For a new target task (e.g., a new patient population), derive a task-specific model using the meta-learned priors and a small amount of data from the target task. The similarity measures guide the fine-tuning process to pool information from the most relevant tasks.
- Evaluation: Assess the fine-tuned model's performance on held-out data from the target task and compare it against models trained with standard meta-learning or single-task learning.
Methodological Considerations
Data Preprocessing and Harmonization
The foundation of any generalizable model is consistent and well-processed data. Raw data extracted from Electronic Health Records (EHRs) must undergo meticulous "data tidying" to structure the dataset according to the prediction problem's specific requirements, such as the index unit of observation and prediction horizon [112]. A critical step is ensuring the temporal integrity of the data; all exposure variables used for prediction must occur prior to the outcome. When dealing with medications like insulin or glucocorticoids, it is essential to account for their pharmacokinetic profiles to estimate the active "dose on board" at the time of prediction [112]. Failure to do so can introduce significant data leakage and invalidate the model.
Mitigating Negative Transfer and Shortcut Learning
In multi-task and meta-learning setups, negative transfer occurs when incorporating data from a task that is not sufficiently related to the target task, ultimately degrading performance [113]. To mitigate this, similarity between tasks should be measured not just by superficial statistical correlations but by the similarity of their underlying causal mechanisms. This approach helps the model learn invariant biological patterns rather than spurious associations. Furthermore, ML models are prone to shortcut learning, where they exploit coincidental patterns in the training data (e.g., a specific brand of test strips used predominantly in one hospital) that do not hold in broader contexts [113]. Techniques from causal inference, such as invariant causal prediction, can help the model focus on robust features that are causally linked to glycemic outcomes across diverse environments.
The Scientist's Toolkit
Successfully implementing the aforementioned protocols requires a suite of specific reagents, technologies, and methodologies. The following table details essential components for a generalizability research pipeline.
Table 3: Research Reagent Solutions for Generalizability Assessment
| Tool Category | Specific Tool / Solution | Function in Generalizability Research |
|---|---|---|
| Data Collection | Continuous Glucose Monitor (CGM) e.g., Abbott Freestyle Libre [3] | Provides high-frequency, real-world glycemic data (e.g., PPGR, time-in-range) as a robust outcome measure across diverse settings. |
| Electronic Health Record (EHR) System Data [112] | Source of large-scale, longitudinal clinical and demographic data for model training and validation. | |
| Biomarkers | Blood Parameters (HbA1c, Fasting Plasma Glucose) [99] [115] | Gold-standard measures of glycemic control used for model outcome definition and calibration. |
| Gut Microbiome Profiling [115] [116] | Provides features that enhance personalization and may capture causal mechanisms of glycemic response. | |
| Computational Methods | Machine Learning Algorithm (e.g., Gradient Boosting, Random Forest) [99] [116] | Core predictive engine. Random Forests, for example, are effective for identifying predictors from complex clinical data [99]. |
| Bayesian Meta-Learning Framework [113] | Advanced statistical framework for pooling information across tasks to improve adaptation and generalizability. | |
| Validation Tools | Clarke Error Grid Analysis [112] | Standard method for evaluating the clinical accuracy of glucose predictions. |
Conclusion
Machine learning algorithms demonstrate significant potential for transforming glycemic response prediction, with ensemble methods like XGBoost and advanced deep learning architectures achieving clinically relevant performance in forecasting hypoglycemia, hyperglycemia, and postprandial responses. Current research shows robust capabilities in specific clinical scenarios, such as predicting glycemic events on hemodialysis days and enabling safety layers in automated insulin delivery systems. However, key challenges remain in ensuring model interpretability, generalizability across diverse populations, and seamless integration into clinical workflows. Future directions should focus on developing standardized validation frameworks, addressing data scarcity through innovative transfer learning approaches, and conducting large-scale real-world trials to establish clinical efficacy. The convergence of explainable AI, multi-task learning, and continuous physiological monitoring presents a promising pathway toward truly personalized, predictive diabetes management systems that can adapt to individual patient dynamics and ultimately improve long-term health outcomes.
References
- 1. Core Glycemic Explained. Metrics , TIR , TBR , GMI, TAR , and... CV [https://www.adces.org/education/danatech/glucose-monitoring/continuous-glucose-monitors-(cgm)/glycemic-metrics--an-overview]
- 2. Time in range: a new parameter to evaluate blood glucose control in... [https://dmsjournal.biomedcentral.com/articles/10.1186/s13098-020-00529-z]
- 3. JMIR Research Protocols - Use of Machine to Learning ... Predict [https://www.researchprotocols.org/2025/1/e59308]
- 4. Association between the coefficient of glycemic variation and time in range, below and above range in continuous monitoring glucose systems in type 1 diabetes | ECE2022 | European Congress of Endocrinology 2022 | Endocrine Abstracts [https://www.endocrine-abstracts.org/ea/0081/ea0081p325]
- 5. Using Noninvasive Data Predicting Glycemic Responses [https://www.medscape.com/viewarticle/predicting-glycemic-responses-using-noninvasive-data-2025a1000au4]
- 6. Glucose Time In Range, Time Above Range, and Time Below Range... [https://pubmed.ncbi.nlm.nih.gov/31886733/]
- 7. Explainable cluster-based learning for prediction of postprandial... [https://journals.plos.org/digitalhealth/article?id=10.1371/journal.pdig.0000996]
- 8. put Researchers modeling on... | ScienceDaily glycemic response [https://www.sciencedaily.com/releases/2025/04/250410160702.htm]
- 9. Machine Learning Prediction of Hypoglycemia and Hyperglycemia ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9345028/]
- 10. Machine Learning Models for Inpatient Glucose Prediction - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9244155/]
- 11. Generalized multi task learning framework for glucose forecasting and hypoglycemia detection using simulation to reality | npj Digital Medicine [https://www.nature.com/articles/s41746-025-01994-4]
- 12. Evaluation of machine learning-based regression techniques for prediction of diabetes levels fluctuations - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11720924/]
- 13. JMIR Diabetes - Managing Exercise-Related Glycemic in Type... Events [https://diabetes.jmir.org/2025/1/e68948]
- 14. Good Machine Learning Practice for Medical Device Development: Guiding Principles | FDA [https://www.fda.gov/medical-devices/software-medical-device-samd/good-machine-learning-practice-medical-device-development-guiding-principles]
- 15. The Role of Artificial Intelligence in Clinical Trial Design and Research with Dr. ElZarrad | FDA [https://www.fda.gov/drugs/news-events-human-drugs/role-artificial-intelligence-clinical-trial-design-and-research-dr-elzarrad]
- 16. for artificial intelligence-based... Continuous glucose monitoring data [https://link.springer.com/article/10.1007/s13410-024-01349-x]
- 17. Consensus statement on standardizing CGM evaluation metrics in... [https://dmsjournal.biomedcentral.com/articles/10.1186/s13098-025-01851-0]
- 18. -based Machine with use of learning ... glucose prediction continuous [https://pmc.ncbi.nlm.nih.gov/articles/PMC8224858/]
- 19. Feature-Based Machine Learning Model for Real-Time Hypoglycemia Prediction - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8258517/]
- 20. Data Preprocessing and Feature Engineering in Machine Learning - Magnimind Academy [https://magnimindacademy.com/blog/data-preprocessing-and-feature-engineering-in-machine-learning/]
- 21. [2408.11876] From Glucose Patterns to Health Outcomes... [https://arxiv.org/abs/2408.11876]
- 22. Development of Machine Learning Models to Predict Hypoglycemia and Hyperglycemia on Days of Hemodialysis in Patients with Diabetes based on Continuous Glucose Monitoring | medRxiv [https://www.medrxiv.org/content/10.1101/2025.10.24.25338707v1.full]
- 23. Frontiers | Use of Continuous Glucose Monitoring in the Assessment and Management of Patients With Diabetes and Chronic Kidney Disease [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2022.869899/full]
- 24. [ Challenges in managing diabetes in chronic hemodialysis ] [https://pubmed.ncbi.nlm.nih.gov/31148425/]
- 25. Semaglutide in people with obesity and type 2 diabetes on... [https://rrtjournal.biomedcentral.com/articles/10.1186/s41100-025-00628-5]
- 26. The IDEAL ( Insulin DE-intensificAtion with iglarLixi)... therapy [https://link.springer.com/article/10.1007/s13300-024-01582-x]
- 27. Individual variations in glycemic to... | Nature Medicine responses [https://www.nature.com/articles/s41591-025-03719-2?error=cookies_not_supported]
- 28. Predicting Postprandial Glycemic With Limited Data in... Responses [https://pmc.ncbi.nlm.nih.gov/articles/PMC11883769/]
- 29. JMIR Medical Informatics - Machine Learning Models for Blood Glucose Level Prediction in Patients With Diabetes Mellitus: Systematic Review and Network Meta-Analysis [https://medinform.jmir.org/2023/1/e47833]
- 30. Individual Postprandial Glycemic Responses to Meal Types by Different Carbohydrate Levels and Their Associations with Glycemic Variability Using Continuous Glucose Monitoring - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10459284/]
- 31. Machine learning-based glucose prediction with use of continuous glucose and physical activity monitoring data: The Maastricht Study - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8224858/]
- 32. Frontiers | Machine learning-based prediction of hypoglycemia... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2025.1634358/full]
- 33. Chapter 9 Multinomial Logistic | Regression Analysis in... Data [https://bookdown.org/drki_musa/dataanalysis/multinomial-logistic-regression.html]
- 34. Difference Between Random and Forest - GeeksforGeeks XGBoost [https://www.geeksforgeeks.org/machine-learning/difference-between-random-forest-vs-xgboost/]
- 35. Hyperparameter Optimization on Random Forest Classifier | by Prabowo Yoga Wicaksana | Medium [https://medium.com/@prabowoyogawicaksana/hyperparameter-optimization-random-forest-classifier-550fd5ed8e14]
- 36. Tuning Random Forest Hyperparameters - KDnuggets [https://www.kdnuggets.com/2022/08/tuning-random-forest-hyperparameters.html]
- 37. Diabetes prediction model based on GA-XGBoost and stacking ensemble algorithm | PLOS One [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0311222]
- 38. The importance of interpreting machine learning models for blood glucose prediction in diabetes: an analysis using SHAP | Scientific Reports [https://www.nature.com/articles/s41598-023-44155-x]
- 39. RNN vs LSTM vs GRU vs Transformers - GeeksforGeeks [https://www.geeksforgeeks.org/deep-learning/rnn-vs-lstm-vs-gru-vs-transformers/]
- 40. Sequence Models Compared : RNNs, LSTMs, GRUs , and Transformers [https://aiml.com/compare-the-different-sequence-models-rnn-lstm-gru-and-transformers/]
- 41. Deep learning for blood glucose level prediction: How well do models generalize across different data sets? - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11423977/]
- 42. Advancing blood glucose prediction with neural architecture search and deep reinforcement learning for type 1 diabetics - ScienceDirect [https://www.sciencedirect.com/science/article/pii/S0208521624000536]
- 43. [2411.05790] Comparative Analysis of LSTM , GRU , and Transformer ... [https://arxiv.org/abs/2411.05790]
- 44. JMIR Research - Use of Protocols to Predict... Machine Learning [https://www.researchprotocols.org/2025/1/e59308/]
- 45. Personalized Nutrition by Prediction of Glycemic Responses [https://pubmed.ncbi.nlm.nih.gov/26590418/]
- 46. A deep learning framework for virtual continuous glucose monitoring and glucose prediction based on life-log data | Scientific Reports [https://www.nature.com/articles/s41598-025-01367-7]
- 47. Deep transfer learning and data augmentation improve glucose levels prediction in type 2 diabetes patients | npj Digital Medicine [https://www.nature.com/articles/s41746-021-00480-x]
- 48. A domain-agnostic continual multi - task ... | Research Square learning [https://www.researchsquare.com/article/rs-6576039/v1]
- 49. Multi-task learning with a natural metric for quantitative structure activity relationship learning - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6852942/]
- 50. GlucoNet-MM: A multimodal attention-based multi - task ... learning [https://pubmed.ncbi.nlm.nih.gov/40977343/]
- 51. Understanding Continuous Glucose Monitoring Data - Role of Continuous Glucose Monitoring in Diabetes Treatment - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK538967/]
- 52. for Prediabetes: What Are the Best... Continuous Glucose Monitoring [https://pmc.ncbi.nlm.nih.gov/articles/PMC11307227/]
- 53. Comparison of Cgmanalysis, a Free Open-Source Continuous Glucose Monitoring Data Management and Analysis Software, with Commercially Available CGM Platforms: Data Standardization for Diabetes Technology Research - PubMed [https://pubmed.ncbi.nlm.nih.gov/34524001/]
- 54. A Processing to Address Real-World Algorithm Quality Issues... Data [https://pmc.ncbi.nlm.nih.gov/articles/PMC11843558/]
- 55. May Aid Cystic Fibrosis-Related Diabetes Screening CGM [https://www.medscape.com/viewarticle/cgm-may-aid-cystic-fibrosis-related-diabetes-screening-2025a1000tdo]
- 56. Personalized blood glucose prediction: A hybrid approach using grammatical evolution and physiological models | PLOS One [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0187754]
- 57. Model for Predicting Complications of Hemodialysis Patients Using Data From the Internet of Medical Things and Electronic Medical Records - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10332468/]
- 58. Early prediction of hemodialysis complications employing ensemble... [https://link.springer.com/article/10.1186/s12938-022-01044-0]
- 59. Human Postprandial Responses to Food and Potential for Precision Nutrition - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8265154/]
- 60. Human postprandial responses to food and potential for precision nutrition - PubMed [https://pubmed.ncbi.nlm.nih.gov/32528151/]
- 61. Assessment of a Personalized Approach to Predicting Postprandial ... [https://pubmed.ncbi.nlm.nih.gov/30735238/]
- 62. Enabling fully automated insulin delivery through meal detection and size estimation using Artificial Intelligence | npj Digital Medicine [https://www.nature.com/articles/s41746-023-00783-1]
- 63. Machine Learning Models for Blood Glucose Level Prediction in Patients With Diabetes Mellitus: Systematic Review and Network Meta-Analysis - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10696506/]
- 64. Replay Simulations with Personalized Metabolic Model for Treatment Design and Evaluation in Type 1 Diabetes - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8655285/]
- 65. Optimized glycemic control of type 2 diabetes with reinforcement learning: a proof-of-concept trial | Nature Medicine [https://www.nature.com/articles/s41591-023-02552-9]
- 66. A deep learning framework for virtual continuous glucose monitoring and glucose prediction based on life-log data - PubMed [https://pubmed.ncbi.nlm.nih.gov/40348812/]
- 67. A drug mix and dose decision algorithm for individualized type 2 diabetes management | npj Digital Medicine [https://www.nature.com/articles/s41746-024-01230-5]
- 68. Explainable AI in Clinical Decision Support Systems: A Meta-Analysis of Methods, Applications, and Usability Challenges - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12427955/]
- 69. The role of explainable artificial intelligence in disease prediction ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11877768/]
- 70. A Perspective on Explainable Artificial Intelligence Methods: SHAP and LIME [https://arxiv.org/html/2305.02012v3]
- 71. LIME vs SHAP: A Comparative Analysis of Interpretability Tools [https://www.markovml.com/blog/lime-vs-shap]
- 72. Trans-Balance: Reducing Demographic Disparity for Prediction Models in the Presence of Class Imbalance - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10850917/]
- 73. The OhioT1DM Dataset for Blood Glucose Level Prediction: Update 2020 - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7881904/]
- 74. Chinese diabetes datasets for data-driven machine learning | Scientific Data [https://www.nature.com/articles/s41597-023-01940-7]
- 75. How do you handle imbalanced datasets ? | by Backlink 2025 | Medium [https://medium.com/@backlinking2025/how-do-you-handle-imbalanced-datasets-99152dc0fea5]
- 76. GitHub... [https://github.com/ojayballer/HANDLING-IMBALANCED-DATASET-IN-MACHINE-LEARNING-A-TUTORIAL-]
- 77. Class Imbalance, Outliers, and Distribution Shift · Introduction to Data-Centric AI [https://dcai.csail.mit.edu/2024/imbalance-outliers-shift/]
- 78. Should You Use Imbalanced-Learn in 2025 ? - Train in Data 's Blog [https://www.blog.trainindata.com/should-you-use-imbalanced-learn-in-2025/]
- 79. Gallery examples: Recursive feature elimination [https://scikit-learn.org/stable/modules/generated/sklearn.feature_selection.RFE.html]
- 80. - GeeksforGeeks Recursive Feature Elimination [https://www.geeksforgeeks.org/machine-learning/recursive-feature-elimination/]
- 81. Machine learning glucose forecasting models for septic patients | Scientific Reports [https://www.nature.com/articles/s41598-025-23057-0]
- 82. A prior-knowledge-guided dynamic attention mechanism to predict nocturnal hypoglycemic events in type 1 diabetes | BMC Medical Informatics and Decision Making | Full Text [https://bmcmedinformdecismak.biomedcentral.com/articles/10.1186/s12911-024-02761-3]
- 83. 11.3 Recursive | Feature Engineering and... Elimination Feature [https://bookdown.org/max/FES/recursive-feature-elimination.html]
- 84. Impartial feature selection using multi-agent reinforcement learning for adverse glycemic event prediction - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/S001048252400341X]
- 85. Dynamic Prediction of Postprandial Glycemic Response and Personalized Dietary Interventions Based on Machine Learning - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/S002231662500567X]
- 86. What Is Recursive (RFE) in Feature ? Elimination Machine Learning [https://fonzi.ai/blog/recursive-feature-elimination]
- 87. Digital biomarkers for interstitial glucose prediction in healthy individuals using wearables and machine learning | Scientific Reports [https://www.nature.com/articles/s41598-025-14172-z]
- 88. How To Improve Clinical Operations Efficiency In 2025 [https://murphi.ai/improve-clinical-operations-efficiency/]
- 89. Improving the Accuracy of Continuous Blood Glucose Measurement Using Personalized Calibration and Machine Learning - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10416969/]
- 90. Blood Glucose Level Prediction in Type 1 Diabetes Using Machine Learning [https://arxiv.org/html/2502.00065v1]
- 91. Receiver operating characteristic - Wikipedia [https://en.wikipedia.org/wiki/Receiver_operating_characteristic]
- 92. Understanding the F1 Score and AUC-ROC Curve | Keylabs [https://keylabs.ai/blog/understanding-the-f1-score-and-auc-roc-curve/]
- 93. F1 Score vs ROC AUC vs Accuracy vs PR AUC: Which Evaluation Metric Should You Choose? [https://neptune.ai/blog/f1-score-accuracy-roc-auc-pr-auc]
- 94. A Practical Guide to Root ( Mean ) | Coralogix Square Error RMSE [https://coralogix.com/ai-blog/root-mean-square-error-rmse-the-cornerstone-for-evaluating-regression-models/]
- 95. Development and external of a COVID-19 mortality risk... validation [https://pmc.ncbi.nlm.nih.gov/articles/PMC7768618/]
- 96. Personalized prediction of glycemic responses to food in women with diet-treated gestational diabetes: the role of the gut microbiota | npj Biofilms and Microbiomes [https://www.nature.com/articles/s41522-025-00650-9]
- 97. External validation and application of the Diabetes Population Risk Tool (DPoRT) for prediction of type 2 diabetes onset in the US population - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10921488/]
- 98. Development and external validation of an algorithm for self-identification of risk for microvascular complications in patients with type 1 diabetes - PubMed [https://pubmed.ncbi.nlm.nih.gov/39582347/]
- 99. to Identify Machine of Learning Control in Type... Predictors Glycemic [https://link.springer.com/article/10.1007/s40290-019-00281-4]
- 100. - Cross analysis identifies shared gut microbial signatures and... cohort [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06676-z]
- 101. Individual variations in glycemic responses to carbohydrates and underlying metabolic physiology | Nature Medicine [https://www.nature.com/articles/s41591-025-03719-2]
- 102. New data-sparse model accurately predicts individual glycemic ... [https://www.news-medical.net/news/20250410/New-data-sparse-model-accurately-predicts-individual-glycemic-responses.aspx]
- 103. Enhanced Post-Prandial Glycemic in Type... Response Prediction [https://pubmed.ncbi.nlm.nih.gov/40864582/]
- 104. Frontiers | Personalized glucose prediction using in situ data only [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1539118/full]
- 105. Pediatric diabetes prediction using deep learning | Scientific Reports [https://www.nature.com/articles/s41598-024-51438-4]
- 106. Frontiers | Characterizing clinical risk profiles of major complications in... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2025.1657366/full]
- 107. An Innovative Artificial Intelligence-Based App for the Diagnosis of Gestational Diabetes Mellitus (GDM-AI): Development Study - PubMed [https://pubmed.ncbi.nlm.nih.gov/32930674/]
- 108. Predicting Short-Term Mortality in Elderly ICU Patients with Diabetes ... [https://arxiv.org/html/2506.15058v1]
- 109. Dynamic Prediction of Postprandial Glycemic and... Response [https://pubmed.ncbi.nlm.nih.gov/40998126/]
- 110. Personalized blood glucose prediction in type 1 diabetes using meta-learning with bidirectional long short term memory-transformer hybrid model | Scientific Reports [https://www.nature.com/articles/s41598-025-13491-5]
- 111. Prediction of metabolic subphenotypes of type 2 diabetes via continuous glucose monitoring and machine learning | Nature Biomedical Engineering [https://www.nature.com/articles/s41551-024-01311-6]
- 112. Models for Inpatient Glucose Prediction - PMC Machine Learning [https://pmc.ncbi.nlm.nih.gov/articles/PMC9244155/]
- 113. Bayesian Meta- Learning for Improving Generalizability of Health... [https://arxiv.org/html/2310.12595v3]
- 114. Effect of Continuous Glucose Monitoring on Glycemic Control in Patients With Type 2 Diabetes Treated With Basal Insulin: A Randomized Clinical Trial - PubMed [https://pubmed.ncbi.nlm.nih.gov/34077499/]
- 115. Effects of personalized diets by prediction of glycemic responses on glycemic control and metabolic health in newly diagnosed T2DM: a randomized dietary intervention pilot trial | BMC Medicine | Full Text [https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-022-02254-y]
- 116. (PDF) Personalized Nutrition by Prediction of Glycemic Responses [https://www.academia.edu/40505388/Personalized_Nutrition_by_Prediction_of_Glycemic_Responses]