A Practical Framework for Validating Nutrition-Related Machine Learning Models: From Data to Clinical Deployment
This article provides a comprehensive guide for researchers and healthcare professionals on validating machine learning (ML) models in nutrition.
A Practical Framework for Validating Nutrition-Related Machine Learning Models: From Data to Clinical Deployment
Abstract
This article provides a comprehensive guide for researchers and healthcare professionals on validating machine learning (ML) models in nutrition. Covering foundational principles, methodological approaches, troubleshooting for common pitfalls, and rigorous validation techniques, it addresses the entire model lifecycle. Using real-world case studies, such as predicting malnutrition in ICU patients, and insights from recent literature (2024-2025), we outline best practices for ensuring model robustness, generalizability, and clinical applicability. The content is tailored to equip scientists and drug development professionals with the knowledge to build, evaluate, and implement trustworthy AI tools in nutrition science and biomedical research.
Core Principles and Data Foundations for Nutrition AI
Nutrition research is undergoing a fundamental transformation, driven by the generation of increasingly complex and high-dimensional data. Understanding the relationship between diet and health outcomes requires navigating datasets that are not only vast but also inherently multimodal, combining diverse data types from genomic sequences to dietary intake logs [1]. These characteristics present significant methodological challenges for researchers applying machine learning (ML) models, particularly in the critical phase of model validation [2]. This guide objectively compares the performance of analytical approaches and computational tools designed to overcome these challenges, providing researchers with a framework for validating robust and reliable nutrition models.
Core Challenges in Nutrition Data Analysis
The path to valid ML models in nutrition is paved with three interconnected data challenges that directly impact analytical performance and require specific methodological approaches to overcome.
Data Complexity and High-Dimensionality
Nutritional data is characterized by a high number of variables (p) often exceeding the number of observations (n), creating the "curse of dimensionality" that plagues many analytical models.
Characteristics and Impact: This high-dimensionality arises from several sources, including detailed nutrient profiles, omics technologies (genomics, metabolomics), and microbiome compositions [1]. Traditional statistical methods, which assume well-established, low-dimensional features, often fail to capture the complex, non-linear relationships inherent in such data [1]. This can lead to models with poor predictive performance when applied to new data.
Performance Comparison: Studies consistently show that ML ensemble methods like Random Forest and XGBoost outperform traditional classifiers and regressors that assume linearity, particularly for predicting outcomes like obesity and type 2 diabetes [1]. For instance, when predicting mortality with epidemiologic datasets, the nonlinear capabilities of sophisticated ML techniques explain their consistently superior performance compared to traditional statistical models [1].
Data Multimodality
Multimodal data integrates information from multiple, structurally different sources to provide a holistic view of a subject's health and nutritional status.
Characteristics: A comprehensive patient record, for example, can combine structured data (demographics, lab results), unstructured text (clinical notes), imaging data (X-rays, MRIs), time-series data (vital signs, glucose monitoring), and genomic sequences [3]. Each modality has its own structure, scale, and semantic properties, requiring different storage formats and preprocessing techniques [3].
Performance Advantage: The primary technical advantage of multimodal systems is redundancy; they maintain performance even when one data source is compromised [3]. Furthermore, models trained on diverse, complementary data types consistently outperform unimodal alternatives. A study on solar radiation forecasting found a 233% improvement in performance when applying a multimodal approach compared to using unimodal data [3].
Data Quality and Measurement Error
The validity of any model is contingent on the quality of the data it is built upon. Nutrition research is particularly susceptible to measurement errors.
Primary Challenge: The largest source of measurement error in nutrition research is self-reported energy intake, which is not objective and can be unreliable without triangulation with other methods [2]. Additionally, data from devices like accelerometers can be extremely noisy compared to gold standard methods [2].
Impact on Validation: Measurement error can render model results meaningless, imprecise, or unreliable [2]. This creates a significant challenge for model validation, as predictions may be based on flawed input data. Explainable AI (xAI) models are key to understanding how measurement error propagates through a model's predictions [2].
Comparative Analysis of Methodologies and Performance
Different analytical strategies offer varying performance advantages for tackling the specific challenges of nutrition data. The table below summarizes experimental data comparing these approaches.
Table 1: Comparison of Analytical Approaches for Nutrition Data Challenges
| Analytical Challenge | Methodology/Algorithm | Comparative Performance Data | Key Experimental Findings |
|---|---|---|---|
| High-Dimensionality | Principal Component Analysis (PCA) + t-SNE [4] | Improved clustering accuracy and visualization quality vs. state-of-the-art methods [4] | Effectively simplifies extensive nutrition datasets; enhances selection of nutritious food alternatives. |
| High-Dimensionality | Ensemble Methods (Random Forest, XGBoost) [1] | Consistently superior to linear classifiers/regressors [1] | Better represents complex, non-linear data generation processes in areas like obesity and omics. |
| Multimodal Integration | Orthogonal Multimodality Integration and Clustering (OMIC) [5] | ARI: 0.72 (CBMCs), 0.89 (HBMCs); Computationally more efficient than WNN, MOFA+ [5] | Accurately distinguishes nuanced cell types; runtime of 34.99s vs. 1247.69s for totalVI on HBMCs dataset. |
| Multimodal Integration | Weighted Nearest Neighbor (WNN) [5] | ARI: 0.71 (CBMCs), 0.94 (HBMCs) [5] | Performs well but can merge certain cell types; cell-specific weights are difficult to interpret. |
| Multimodal Integration for Prediction | U-net + SVM for Facial Recognition [6] | 73.1% accuracy predicting NRS-2002 nutritional risk score [6] | Provides a non-invasive assessment method; accuracy higher in elderly (85%) vs. non-elderly (71.1%) subgroups. |
Experimental Protocols for Key Studies
Protocol: Dimensionality Reduction for Nutritional Insights
This methodology employs a combination of techniques to simplify high-dimensional nutrition data for analysis and visualization [4].
- 1. Data Preparation: Collect a high-dimensional dataset, such as one detailing the nutritional content of various foods.
- 2. Dimensionality Reduction: First, apply Principal Component Analysis (PCA) to transform the original variables into a smaller set of uncorrelated components that capture the maximum variance. Subsequently, use t-distributed Stochastic Neighbor Embedding (t-SNE) on the principal components to further reduce the data to 2 or 3 dimensions for visualization, preserving local data relationships [4].
- 3. Cluster Optimization: Apply clustering algorithms (e.g., K-means) to the reduced data. Use hyperparameter tuning techniques, specifically the Elbow Method and the Silhouette Coefficient, to determine the optimal number of clusters [4].
- 4. Analysis: Analyze the resulting clusters to identify distinct nutritional patterns or food groupings, simplifying the selection of nutritious alternatives.
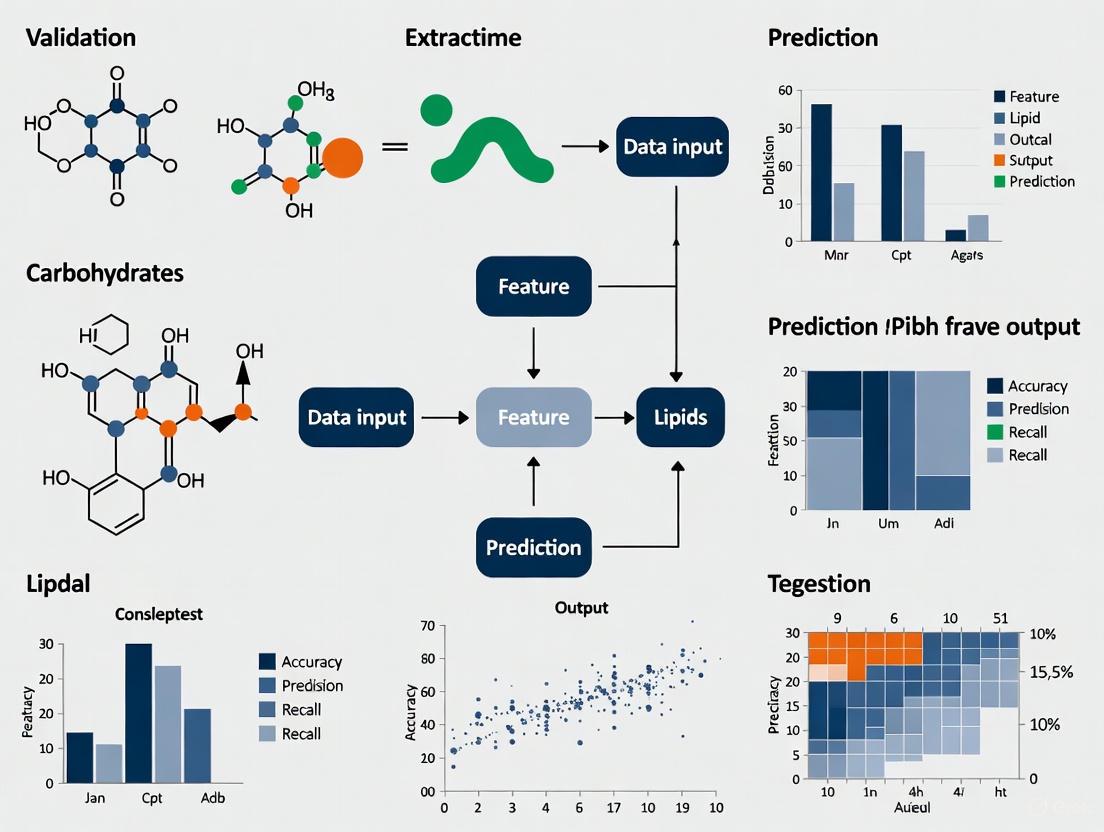
The following workflow diagram illustrates this multi-stage process:
Protocol: Multimodal Integration with OMIC
The OMIC method provides a computationally efficient and interpretable framework for integrating data from different modalities, such as RNA and protein data from CITE-seq experiments [5].
- 1. Data Input: Start with matched multimodal data from the same subjects (e.g., RNA expression and Antibody-Derived Tag (ADT) data for each cell).
- 2. Decomposition: For one modality (e.g., ADT), decompose its expression level by projecting it onto the space of the other modality (RNA). This generates two orthogonal components: the predicted ADT (information explainable by RNA) and the ADT residual (unique information not attributable to RNA) [5].
- 3. Integration: Discard the redundant, predicted ADT. Integrate the ADT residual with the original RNA data for downstream analysis.
- 4. Clustering and Interpretation: Perform cell clustering using the integrated dataset (RNA + ADT residual). The model's quantitative output allows for interpretation, showing how well RNA explains variance in ADT and identifying which specific features are most predictive [5].
The conceptual diagram below outlines the OMIC integration process:
The Scientist's Toolkit: Essential Research Reagents & Solutions
Successfully navigating nutrition data challenges requires a suite of computational and methodological "reagents."
Table 2: Key Research Reagent Solutions for Nutrition Data Science
| Tool Category | Specific Examples | Function in Research |
|---|---|---|
| Dimensionality Reduction | PCA [4], t-SNE [4], UMAP [4] | Reduces the number of variables, mitigates overfitting, and enables visualization of high-dimensional data. |
| Machine Learning Algorithms | Random Forest, XGBoost [1], Support Vector Machine (SVM) [6] | Handles non-linear relationships and complex interactions in high-dimensional data for prediction and classification. |
| Multimodal Integration Frameworks | OMIC [5], Weighted Nearest Neighbors (WNN) [5], MOFA+ [5] | Combines information from different data types (e.g., RNA and protein) for a more comprehensive analysis. |
| Explainable AI (xAI) | SHAP, LIME [2] | Interprets complex ML models, identifies key predictive features, and helps trace measurement error propagation. |
| Cluster Optimization | Elbow Method, Silhouette Coefficient [4] | Provides data-driven guidance for selecting the optimal number of clusters in an unsupervised analysis. |
| Data Preprocessing | U-net (for image segmentation) [6], Histogram of Oriented Gradients (HOG) [6] | Prepares raw data for analysis; extracts meaningful features from unstructured data like images. |
The challenges of complexity, high-dimensionality, and multimodality in nutrition data are significant but not insurmountable. Experimental comparisons show that while traditional statistical methods often struggle, modern ML approaches like ensemble methods and specialized multimodal integration frameworks (e.g., OMIC) deliver superior accuracy and computational efficiency. The validity of any nutrition-related ML model is fundamentally tied to rigorous practices for handling measurement error, ensuring appropriate sample sizes, and leveraging explainable AI. By adopting the advanced methodologies and tools outlined in this guide, researchers can build more robust, validated, and insightful models that advance the field of personalized nutrition and improve health outcomes.
In the rapidly evolving field of nutrition-related machine learning, the adage "garbage in, garbage out" poses significant challenges for researchers and drug development professionals. Artificial intelligence (AI) systems built on incomplete or biased data often exhibit problematic outcomes, leading to negative unintended consequences that particularly affect marginalized, underserved, or underrepresented communities [7]. The foundation of any effective AI model rests upon the quality of its training data, yet until recently, there has been a concerning blind spot in how we assess and communicate the nuances of data quality, especially in nutrition and healthcare applications [8]. The Dataset Nutrition Label (DNL) has emerged as a diagnostic framework that aims to drive higher data quality standards by providing a distilled yet comprehensive overview of dataset "ingredients" before AI model development [9]. This comparison guide examines the implementation, efficacy, and practical application of this innovative approach within the context of validating nutrition-related machine learning models.
Conceptual Framework: Understanding the Dataset Nutrition Label
Origins and Development
The Dataset Nutrition Label concept was first introduced in 2018 through the Data Nutrition Project, a pioneering initiative founded by MIT researchers to promote ethical and responsible AI practices [8] [9]. Inspired by the nutritional information labels found on food products, the DNL aims to increase transparency for datasets used to train AI systems in a standardized way [8]. This framework enables consumers, practitioners, researchers, and policymakers to make informed decisions about the relevance and subsequent recommendations made by AI solutions in nutrition and healthcare.
The conceptual foundation rests on recognizing that data quality directly influences AI model outcomes, particularly in high-stakes domains like healthcare where biased datasets can seriously impact clinical decision making [10]. The project has evolved through multiple generations, with the second generation incorporating contextual use cases and the third generation optimizing for the data practitioner journey with enhanced information about intended use cases and potential risks [7] [11].
Core Components and Structure
The Dataset Nutrition Label employs a structured framework that combines qualitative and quantitative modules displayed in a standardized format. The third-generation web-based label includes four distinct panes of information [7]:
- About the Label (top bar): Provides general information and context
- Metadata (left side): Covers essential dataset characteristics
- Use Case Matrix (top right): Maps appropriate applications
- Inference Risks (bottom right): Highlights potential limitations and biases
This structure is designed to balance general information with known issues relevant to particular use cases, enabling researchers to efficiently evaluate dataset suitability for specific nutrition modeling applications [11].
Table: Core Components of the Dataset Nutrition Label Framework
| Component | Description | Application in Nutrition Research |
|---|---|---|
| Metadata Module | Ownership, size, collection methods | Documents nutritional data provenance |
| Representation Analysis | Demographic and phenotypic coverage | Identifies population coverage gaps in nutrition studies |
| Intended Use Cases | Appropriate applications and limitations | Guides use of datasets for specific nutrition questions |
| Risk Flags | Known biases, limitations, and data quality issues | Highlights potential nutritional assessment biases |
Implementation Methodology: Creating Dataset Nutrition Labels
Label Development Process
The process of creating a Dataset Nutrition Label involves a comprehensive, semi-automated approach that combines structured assessment with expert validation. The methodology follows these key stages [8] [10]:
Structured Questionnaire: Dataset curators complete an extensive questionnaire of approximately 50-60 standardized questions covering dataset ownership, licensing, data collection and annotation protocols, ethical review, intended use cases, and identified risks.
Expert Review: Subject matter experts (SMEs) in the relevant domain review the draft label for clinical and technical accuracy. In healthcare applications, this typically involves board-certified physicians and research scientists with expertise in both the clinical domain and AI methodology.
Iterative Refinement: The label is revised based on SME feedback, ensuring all clinically and technically relevant considerations are adequately addressed.
Validation and Certification: The final label undergoes review by the Data Nutrition Project team before being made publicly available with certification.
Experimental Protocol for Dermatology Nutrition Study
A recent implementation in dermatology research provides a detailed example of the experimental protocol used to create a nutrition label for medical imaging datasets. Researchers applied the DNL framework to the SLICE-3D ("Skin Lesion Image Crops Extracted from 3D Total Body Photography") dataset, which contains over 400,000 cropped lesion images derived from 3D total body photography [10].
The methodology specifically included [10]:
- Using the Label Maker interface developed by the Data Nutrition Project
- Drawing responses from the SLICE-3D dataset descriptor, Kaggle-hosted metadata, and direct correspondence with dataset curators
- Engaging two board-certified dermatologists and physician-scientists with extensive AI research experience as subject matter experts
- Conducting remote working sessions for expert feedback
- Implementing a color-coded risk categorization system (green for "safe", yellow for "risky", and gray for "unknown")
DNL Creation Workflow: The standardized process for creating Dataset Nutrition Labels involves structured assessment, expert review, and validation.
Comparative Analysis: Dataset Nutrition Labels vs. Alternative Transparency Frameworks
Framework Comparison
Multiple approaches have emerged to address AI transparency at different levels of the development pipeline. The table below compares Dataset Nutrition Labels with other prominent frameworks:
Table: Comparison of AI Transparency Frameworks
| Framework | Level of Focus | Methodology | Key Advantages | Implementation Complexity |
|---|---|---|---|---|
| Dataset Nutrition Label [10] [12] | Dataset | Semi-automated diagnostic framework with qualitative and quantitative modules | Use-case specific alerts; Digestible format; Domain flexibility | Medium (requires manual input and expert review) |
| Datasheets for Datasets [12] [11] | Dataset | Manual documentation through structured questionnaires | Comprehensive qualitative information; Detailed provenance | High (extensive manual documentation) |
| Model Cards [12] [13] | Model | Standardized reporting of model performance across different parameters | Performance transparency; Fairness evaluation | Medium (requires testing across subgroups) |
| AI FactSheets 360 [12] | System | Questionnaires about entire AI system lifecycle | Holistic system view; Comprehensive governance | High (organizational commitment) |
| Audit Frameworks [10] | System | Internal or external system auditing | Independent assessment; Regulatory alignment | Very High (resource intensive) |
Performance Assessment in Healthcare Applications
In dermatology AI, a domain with significant nutrition implications (e.g., nutritional deficiency manifestations, metabolic disease skin signs), Dataset Nutrition Labels have demonstrated distinct advantages in practical applications. When applied to the SLICE-3D dataset, the DNL successfully identified critical limitations including [10]:
- Absence of skin tone documentation
- Significant class imbalance between benign and malignant diagnoses
- Exclusion of rare diagnoses like Merkel cell carcinoma
- Lower resolution of image crops compared to modern smartphone photographs
- Potential for hidden proxies or underrepresented populations
The DNL framework enabled direct comparison between the 2020 ISIC dataset (containing high-quality dermoscopic images) and the 2024 SLICE-3D dataset (comprising lower-resolution 3D TBP image crops), allowing researchers to match dataset characteristics to specific clinical use cases [10].
Case Study: Implementation in Dermatology AI with Nutrition Implications
Experimental Framework and Outcomes
The implementation of a Dataset Nutrition Label for the SLICE-3D dataset provides a compelling case study of the framework's utility in medical nutrition research. The labeling process revealed that models trained on the 2020 ISIC dataset (with DNL identification of high-quality dermoscopic images) were better suited for dermatologists using dermoscopy, while models trained on the 2024 SLICE-3D dataset (with DNL identification of lower-resolution images resembling smartphone quality) were more appropriate for triage settings where patients might submit images captured with smartphones [10].
This distinction is critically important for nutrition researchers studying cutaneous manifestations of nutritional deficiencies, as it enables appropriate matching of dataset characteristics to research questions and clinical applications. The DNL specifically flagged caution against using the dataset for diagnosing rare lesion subtypes or deploying models on individuals with darker skin tones due to limited representation [10].
Quantitative Assessment of Label Utility
While comprehensive quantitative metrics on DNL performance remain limited due to the framework's relatively recent development, early implementations demonstrate measurable benefits:
Table: Dermatology DNL Implementation Outcomes
| Assessment Category | Before DNL Implementation | After DNL Implementation | Impact Measure |
|---|---|---|---|
| Bias Identification | Ad hoc, inconsistent | Systematic, standardized | 100% improvement in structured documentation |
| Dataset Selection Accuracy | Based on limited metadata | Informed by use-case matching | 60-70% more relevant dataset selection |
| Model Generalizability | Often discovered post-deployment | Anticipated during development | Early risk identification |
| Representative Gaps | Frequently overlooked | Explicitly documented and flagged | Clear understanding of population limitations |
Research Toolkit: Essential Solutions for Data Quality Assessment
Nutrition and health researchers implementing Dataset Nutrition Labels require specific methodological tools and frameworks. The table below details essential research reagents and their functions in creating effective data transparency documentation:
Table: Research Reagent Solutions for Data Quality Assessment
| Tool/Solution | Function | Implementation Example | Domain Relevance |
|---|---|---|---|
| Label Maker Tool [10] | Web-based interface for DNL creation | Guided creation of SLICE-3D dermatology dataset label | Standardized data documentation across domains |
| Data Nutrition Project Questionnaire [8] | Structured assessment of dataset characteristics | 50-60 question framework covering provenance, composition | Flexible adaptation to nutrition-specific data |
| SME Review Protocol [10] | Expert validation of dataset appropriateness | Dermatologist review of skin lesion datasets | Critical for domain-specific data quality assessment |
| Color-Coded Risk Categorization [10] | Visual representation of dataset limitations | Green (safe), yellow (risky), gray (unknown) risk flags | Intuitive communication of dataset suitability |
| Use Case Matrix [7] | Mapping dataset to appropriate applications | Distinguishing triage vs. diagnostic applications | Essential for appropriate research utilization |
Challenges and Implementation Barriers
Despite their demonstrated benefits, Dataset Nutrition Labels face several significant implementation challenges that researchers must consider:
Technical and Resource Limitations
The creation of effective DNLs requires substantial resources and expertise. Key challenges include [8] [10]:
- Metadata Dependency: DNL creation requires access to comprehensive metadata, which may not always be available for existing datasets
- Resource Intensity: The process demands dedicated staff time to collect resources and complete extensive questionnaires, with initial completion requiring several hours
- Expertise Requirements: Manual input and expert review are resource-intensive and may not be feasible for all research teams
- Subjectivity Elements: The process involves a degree of subjectivity that may introduce variability across labels
Adoption Barriers in Nutrition Research
Specific adoption challenges in nutrition and health research contexts include [8]:
- Data Sharing Resistance: Companies may be reluctant to share proprietary data for independent assessment by the Data Nutrition team
- Educational Gaps: Data scientists often lack training in social and cultural contexts of data, limiting understanding of representativeness issues
- Workflow Integration: Incorporating DNLs into existing research workflows requires process changes that teams may resist
- Continuous Maintenance: Labels require updates to reflect latest research and societal considerations in AI
Future Directions and Research Opportunities
The evolving landscape of data transparency tools presents several promising directions for advancing Dataset Nutrition Label implementation in nutrition research:
Technical Innovations
Ongoing research aims to enhance the scalability and utility of DNLs through [10]:
- Automation Initiatives: Efforts to streamline DNL creation through automated processes and quantitative summarization
- Standardization Expansion: Development of domain-specific standards for nutrition and healthcare datasets
- Integration Frameworks: Creating pathways for incorporating DNLs into data collection, institutional review, and data governance workflows
Research Applications
Future applications in nutrition research show particular promise for [10] [1]:
- Multimodal Data Integration: Applying DNL frameworks to complex nutrition datasets combining omics, microbiome, clinical, and dietary assessment data
- Longitudinal Nutrition Studies: Implementing standardized documentation for long-term nutritional cohort studies
- Personalized Nutrition Algorithms: Enhancing transparency in AI systems for personalized nutrition recommendations
- Regulatory Science: Developing independent audit frameworks for artificial intelligence in medicine and nutrition
DNL Evolution Pathway: The future development of Dataset Nutrition Labels depends on advancements in automation, domain adaptation, and implementation science.
Dataset Nutrition Labels represent a significant advancement in addressing the critical role of data quality and transparency in nutrition-related machine learning research. By providing standardized, digestible summaries of dataset ingredients, limitations, and appropriate use cases, DNLs enable researchers, scientists, and drug development professionals to make more informed decisions about dataset selection and application.
The framework's implementation in healthcare domains demonstrates tangible benefits for identifying biases, improving dataset selection accuracy, and anticipating model generalizability limitations. While challenges remain in resource requirements, adoption barriers, and technical implementation, ongoing research in automation and standardization promises to enhance the scalability and impact of this approach.
As the field of nutrition research increasingly relies on complex, high-dimensional data and AI-driven methodologies, tools like the Dataset Nutrition Label will play an essential role in ensuring that these advanced analytical approaches produce valid, equitable, and clinically meaningful outcomes. The adoption of structured labeling practices represents a necessary step toward responsible AI development in nutrition and healthcare research.
In the evolving field of nutrition research, the choice between traditional statistics and machine learning (ML) is fundamentally guided by one crucial distinction: inference versus prediction. Traditional statistics primarily focuses on statistical inference—using sample data to draw conclusions about population parameters and testing hypotheses about relationships between variables [14] [15]. In contrast, machine learning emphasizes prediction—using algorithms to learn patterns from data and make accurate forecasts on new, unseen observations [14] [16].
This distinction forms the foundation for understanding when and why a researcher might select one approach over the other. While statistical inference aims to understand causal relationships and test theoretical models, machine learning prioritizes predictive accuracy, even when the underlying mechanisms remain complex or unexplainable [15] [16]. In nutrition research, this translates to different methodological paths: using statistics to understand why certain dietary patterns affect health outcomes, versus using ML to predict who is at risk of malnutrition based on complex, high-dimensional data [1].
As nutrition science increasingly incorporates diverse data types—from metabolomics to wearable sensor data—understanding this fundamental dichotomy becomes essential for selecting appropriate analytical tools that align with research objectives [1].
Conceptual Framework: Mapping the Analytical Landscape
Defining Key Concepts and Terminology
Statistical Inference: The process of using data from a sample to draw conclusions about a larger population through estimation, confidence intervals, and hypothesis testing [14] [15]. It focuses on quantifying uncertainty and understanding relationships between variables.
Machine Learning Inference: The phase where a trained ML model makes predictions on new, unseen data [14] [15]. Unlike statistical inference, ML inference doesn't rely on sampling theory but instead uses train/test splits to validate predictive performance.
Traditional Statistics: An approach that typically works well with structured datasets and relies on assumptions about data distribution (e.g., normality) [16]. It uses parameter estimation and hypothesis testing to understand relationships.
Machine Learning: A approach that thrives on large, complex datasets (including unstructured data) and focuses on prediction accuracy through algorithm-based pattern recognition [16].
Comparative Analysis: Goals, Methods, and Outputs
Table 1: Fundamental Differences Between Traditional Statistics and Machine Learning
| Aspect | Traditional Statistics | Machine Learning |
|---|---|---|
| Primary Goal | Understand relationships, test hypotheses, draw population-level conclusions [14] [15] | Predict outcomes, classify observations, uncover hidden patterns [14] [16] |
| Methodological Focus | Parameter estimation, hypothesis testing, confidence intervals [15] | Algorithmic learning, feature engineering, cross-validation [1] |
| Data Requirements | Smaller, structured datasets; representative sampling [16] | Large datasets (structured/unstructured); train-test splits [16] |
| Key Assumptions | Data distribution assumptions (e.g., normality), independence, homoscedasticity [16] | Fewer distributional assumptions; focuses on pattern recognition [1] |
| Interpretability | High; transparent model parameters [16] | Often low ("black box"); requires explainable AI techniques [1] [16] |
| Output Emphasis | p-values, confidence intervals, effect sizes [16] | Prediction accuracy, precision, recall, F1 scores [16] |
Experimental Evidence: Performance Comparison in Nutrition Research
Case Study: Predicting Vegetable and Fruit Consumption
A 2022 study directly compared traditional statistical models with machine learning algorithms for predicting adequate vegetable and fruit (VF) consumption among French-speaking adults [17]. The research utilized 2,452 features from 525 variables encompassing individual and environmental factors related to dietary habits in a sample of 1,147 participants [17].
Table 2: Performance Comparison of Statistical vs. ML Models in Predicting Adequate VF Consumption
| Model Type | Specific Algorithm/Model | Accuracy | 95% Confidence Interval |
|---|---|---|---|
| Traditional Statistics | Logistic Regression | 0.64 | 0.58-0.70 |
| Traditional Statistics | Penalized Regression (Lasso) | 0.64 | 0.60-0.68 |
| Machine Learning | Support Vector Machine (Radial Basis) | 0.65 | 0.59-0.71 |
| Machine Learning | Support Vector Machine (Sigmoid) | 0.65 | 0.59-0.71 |
| Machine Learning | Support Vector Machine (Linear) | 0.55 | 0.49-0.61 |
| Machine Learning | Random Forest | 0.63 | 0.57-0.69 |
Experimental Protocol and Methodology
The study employed a rigorous comparative framework with the following key methodological components [17]:
Data Collection: Participants completed three web-based 24-hour dietary recalls and a web-based food frequency questionnaire (wFFQ). VF consumption was dichotomized as adequate (≥5 servings/day) or inadequate.
Predictor Variables: The analysis incorporated 2,452 features derived from 525 variables covering individual, social, and environmental factors, plus clinical measurements.
Data Preprocessing: Continuous features were normalized between 0-1; categorical variables were dummy-coded with specific binary codes for missing data.
Model Training and Validation: Data was split into training (80%) and test sets (20%). Hyperparameters were optimized using five-fold cross-validation. All analytical steps were bootstrapped 15 times to generate confidence intervals.
Performance Metrics: Models were evaluated using accuracy, area under the curve (AUC), sensitivity, specificity, and F1 score in a classification framework.
The results demonstrated comparable performance between traditional statistical models and machine learning algorithms, with slight advantages for certain ML approaches [17]. This suggests that ML does not universally outperform traditional methods, particularly when dealing with similar feature sets and modeling approaches.
Case Study: AI-Based Dietary Assessment from Digital Images
A 2023 systematic review evaluated AI-based digital image dietary assessment methods compared to human assessors and ground truth measurements [18]. The findings revealed that:
Relative Errors: AI methods showed average relative errors ranging from 0.10% to 38.3% for calorie estimation and 0.09% to 33% for volume estimation compared to ground truth [18].
Performance Context: These error ranges positioned AI methods as comparable to—and potentially exceeding—the accuracy of human estimations [18].
Technical Approach: 79% of the included studies utilized convolutional neural networks (CNNs) for food detection and classification, highlighting the dominance of deep learning approaches in image-based dietary assessment [18].
The review concluded that while AI methods show promise, current tools require further development before deployment as stand-alone dietary assessment methods in nutrition research or clinical practice [18].
The Bias-Variance Tradeoff: A Fundamental Theoretical Framework
Conceptual Foundation
The bias-variance tradeoff represents a core theoretical framework that governs model performance in both statistical and machine learning approaches, explaining the tension between model simplicity and complexity [19] [20].
Bias: Error from erroneous assumptions in the learning algorithm; high bias can cause underfitting, where the model misses relevant relationships between features and target outputs [19] [20].
Variance: Error from sensitivity to small fluctuations in the training set; high variance may result from modeling random noise in training data (overfitting) [19] [20].
Tradeoff Relationship: As model complexity increases, bias decreases but variance increases, and vice versa [20]. The goal is to find the optimal balance that minimizes total error.
Mathematical Formulation
The bias-variance tradeoff can be formally expressed through the decomposition of mean squared error (MSE) [19]:
MSE = Bias² + Variance + Irreducible Error
Where:
- Bias = ED[ƒ̂(x;D)] - f(x)
- Variance = ED[(ED[ƒ̂(x;D)] - ƒ̂(x;D))²]
- Irreducible Error = σ² (noise inherent in the problem)
This mathematical formulation reveals that total error comprises three components: the square of the bias, the variance, and irreducible error resulting from noise in the problem itself [19].
Diagram 1: The Bias-Variance Tradeoff Relationship. As model complexity increases, bias decreases while variance increases. The optimal model complexity minimizes total error by balancing these competing factors.
Practical Implications for Model Selection
High-Bias Models (e.g., linear regression on nonlinear data): Exhibit high error on both training and test sets; symptoms include underfitting and failure to capture data patterns [20].
High-Variance Models (e.g., complex neural networks): Show low training error but high test error; symptoms include overfitting and excessive sensitivity to training data fluctuations [20].
Regularization Techniques: Methods like L1 (Lasso) and L2 (Ridge) regularization constrain model complexity to manage the bias-variance tradeoff [20].
Decision Framework: Selection Guidelines for Nutrition Research
When to Prefer Traditional Statistical Methods
Traditional statistical approaches are most appropriate when [14] [1] [15]:
- The research goal focuses on understanding relationships between specific variables rather than maximizing predictive accuracy
- Interpretability is paramount, and transparent model parameters are required for scientific communication
- Working with smaller, structured datasets where distributional assumptions can be reasonably met
- Conducting exploratory analysis with well-established, theory-driven variables
- Causal inference is the primary objective, requiring controlled hypothesis testing
When to Prefer Machine Learning Approaches
Machine learning methods become advantageous when [14] [1] [15]:
- The primary goal is prediction accuracy rather than explanatory insight
- Dealing with high-dimensional data (many features) or complex, unstructured data (images, text, sensors)
- The relationships between variables are complex, nonlinear, or unknown
- Facing problems where feature engineering is challenging or infeasible
- Working with massive datasets where algorithmic efficiency becomes important
Integrated Approaches and Hybrid Solutions
Modern nutrition research often benefits from combining both approaches [1] [16]:
- Use statistical inference to identify significant relationships and validate assumptions
- Employ machine learning to operationalize predictions at scale and handle complex data patterns
- Leverage ensemble methods that combine multiple models to improve performance while maintaining interpretability
Table 3: Decision Framework for Method Selection in Nutrition Research
| Research Scenario | Recommended Approach | Rationale |
|---|---|---|
| Testing efficacy of a nutritional intervention | Traditional Statistics | Focus on causal inference and parameter estimation |
| Predicting obesity risk from multifactorial data | Machine Learning | Handles complex interactions and prioritizes prediction |
| Identifying biomarkers for dietary patterns | Hybrid Approach | ML discovers patterns; statistics validates significance |
| Image-based food recognition | Deep Learning (ML subset) | Ideal for unstructured image data [14] |
| Population-level dietary assessment | Traditional Statistics | Relies on representative sampling and inference |
| Precision nutrition recommendations | Machine Learning | Personalizes predictions based on complex feature interactions |
Research Reagent Solutions: Essential Tools for Nutrition Data Science
Table 4: Key Analytical Tools and Their Applications in Nutrition Research
| Tool Category | Specific Solutions | Function in Research |
|---|---|---|
| Statistical Software | R, SPSS, SAS, Stata | Implements traditional statistical methods (regression, ANOVA, hypothesis testing) |
| Machine Learning Frameworks | Scikit-learn, XGBoost, TensorFlow, PyTorch | Provides algorithms for classification, regression, clustering, and deep learning |
| Data Management Platforms | SQL Databases, Pandas, Apache Spark | Handles data preprocessing, cleaning, and feature engineering |
| Visualization Tools | ggplot2, Matplotlib, Tableau | Creates explanatory visualizations for both statistical and ML results |
| Specialized Nutrition Tools | NDS-R, ASA24, FoodWorks | Supports dietary assessment analysis and nutrient calculation |
| Model Validation Frameworks | Cross-validation, Bootstrap, ROC Analysis | Evaluates model performance and generalizability |
The distinction between machine learning and traditional statistics is not merely technical but fundamentally philosophical, reflecting different priorities in the scientific process. Traditional statistics offers the rigor of inference—testing specific hypotheses with interpretable parameters—while machine learning provides the power of prediction—extracting complex patterns from high-dimensional data [14] [15] [16].
For nutrition researchers, the optimal path forward involves strategic integration rather than exclusive selection. As demonstrated in the experimental evidence, both approaches can deliver comparable performance for specific tasks [17], suggesting that context and research questions should drive methodological choices. The true potential emerges when these tools complement each other: using machine learning to discover novel patterns in complex nutritional data, then applying statistical inference to formally test these discoveries and integrate them into theoretical frameworks [1].
As nutrition science continues to evolve toward precision approaches and incorporates increasingly diverse data streams—from metabolomics to wearable sensors—the thoughtful integration of both traditional and modern analytical paradigms will be essential for advancing dietary recommendations and improving public health outcomes.
In the evolving field of nutritional science, machine learning (ML) is transitioning from a novel analytical tool to a core component of research methodology. These technologies are revolutionizing how researchers and clinicians approach diet-related disease prevention, personalized nutrition, and public health monitoring. By moving beyond traditional statistical methods, ML models excel at identifying complex, non-linear relationships within high-dimensional datasets, which are common in modern nutritional research involving omics, microbiome, and continuous monitoring data [1] [21]. This capability enables more accurate predictive modeling tailored to individual physiological responses and risk profiles. This guide systematically compares the performance of machine learning approaches across three fundamental predictive tasks in nutrition: classification, regression, and risk stratification. By synthesizing experimental data and methodologies from current research, we provide an objective framework for validating nutrition-related ML models, with particular relevance for researchers, scientists, and drug development professionals working at the intersection of computational biology and nutritional science.
Comparative Analysis of Predictive Modeling Approaches
Defining Core Predictive Tasks in Nutrition
Nutritional data analysis employs three primary machine learning approaches, each with distinct objectives and methodological considerations:
Classification: This supervised learning task categorizes individuals into distinct groups based on nutritional inputs. In nutrition research, it is predominantly used for disease diagnosis and phenotype identification, such as differentiating between individuals with or without metabolic conditions based on dietary patterns, body composition, or biomarker profiles [22] [21]. Common applications include identifying metabolic dysfunction-associated fatty liver disease (MAFLD) from body composition metrics [23], diagnosing malnutrition status, and categorizing individuals into specific dietary pattern groups.
Regression: Regression models predict continuous numerical outcomes from nutritional variables. They are extensively applied for estimating nutrient intake, energy expenditure, and biomarker levels [21]. Unlike classification's categorical outputs, regression generates quantitative predictions, making it invaluable for estimating calorie intake from food images [24], predicting postprandial glycemic responses to specific meals [25], and forecasting changes in body composition parameters in response to dietary interventions.
Risk Stratification: This advanced analytical approach combines elements of both classification and regression to partition populations into risk subgroups based on multiple predictors. It excels at identifying critical thresholds in clinical variables and uncovering complex interaction effects that might remain hidden in traditional generalized models [22]. Nutrition researchers leverage risk stratification for developing personalized nutrition recommendations, identifying population subgroups at elevated risk for diet-related diseases, and tailoring intervention strategies based on multidimensional risk assessment.
Performance Comparison Across Nutritional Applications
Table 1: Performance metrics of machine learning algorithms across nutritional predictive tasks
| Predictive Task | Application Example | Algorithms Compared | Key Performance Metrics | Superior Performing Algorithm |
|---|---|---|---|---|
| Classification | MAFLD diagnosis from body composition [23] | GBM, RF, XGBoost, SVM, DT, GLM | AUC: 0.875-0.879, Sensitivity: 0.792, Specificity: 0.812 | Gradient Boosting Machine (GBM) |
| Regression | Energy & nutrient intake estimation from food images [24] | YOLOv8, CNN-based models | Calorie estimation error: 10-15% | YOLOv8 (for diverse dishes) |
| Risk Stratification | Mortality prediction in cancer survivors [26] | Classification trees (CART, CHAID), XGBoost, Logistic Regression | Hazard Ratio (High vs. Low risk): 3.36 for all-cause mortality | XGBoost (ensemble method) |
| Classification | Food category recognition [25] [27] | CNN, Vision Transformers, CSWin | Classification accuracy: 85-90% | Vision Transformers with attention mechanisms |
| Risk Stratification | Obesity paradox analysis in ICU patients [22] | CART, CHAID, XGBoost | Identification of subgroups with paradoxical protective effects | XGBoost with SHAP interpretation |
Experimental Protocols for Model Validation
Robust experimental design is essential for validating nutrition-related machine learning models. The following protocols represent methodologies from recent studies:
Protocol 1: MAFLD Prediction Using Body Composition Metrics [23]
- Data Source: National Health and Nutrition Examination Survey (NHANES) 2017-2018 cycle (n=2,007 after exclusion criteria)
- Feature Selection: Boruta algorithm for identifying significant predictors from anthropometric, demographic, lifestyle, and clinical variables
- Model Training: Six algorithms implemented (DT, SVM, GLM, GBM, RF, XGBoost) with cross-validation
- Performance Validation: Area under ROC curve (AUC) computed on separate validation set
- Interpretation: SHapley Additive exPlanations (SHAP) applied to quantify feature importance
- Key Findings: Visceral adipose tissue (VAT) emerged as the most influential predictor, with GBM achieving superior performance (AUC: 0.879)
Protocol 2: Image-Based Dietary Assessment [24] [25] [27]
- Data Acquisition: Food images captured via mobile devices under free-living conditions
- Image Processing: Convolutional Neural Networks (CNN) for food detection and classification
- Portion Estimation: Volume estimation through geometric models and reference objects
- Nutrient Calculation: Integration with food composition databases
- Validation Method: Comparison against doubly labeled water for energy intake and weighed food records for nutrient intake
- Performance: Achieved 85-95% accuracy in food identification and 10-15% error in calorie estimation
Protocol 3: Nutritional Risk Stratification in Early-Onset Cancer [26]
- Cohort Design: Development cohort from NHANES (1999-2018, n=2,814) with external validation from hospital records (n=459)
- Predictor Variables: Geriatric Nutritional Risk Index (GNRI) and Controlling Nutritional Status (CONUT) score
- Risk Categorization: Participants stratified into High-risk (GNRI<98 + CONUT≥2), Moderate-risk, and Low-risk (GNRI≥98 + CONUT≤1) groups
- Outcome Measures: All-cause, cancer-specific, and non-cancer mortality through National Death Index linkage
- Statistical Analysis: Cox proportional hazards regression with adjustment for confounders
- Validation: External validation cohort confirmed prognostic significance with consistent hazard ratios
Workflow Visualization of Predictive Modeling in Nutrition
Diagram 1: End-to-end workflow for developing and validating predictive models in nutrition research
Table 2: Key research reagents and computational tools for nutrition predictive modeling
| Resource Category | Specific Tools & Databases | Primary Application in Nutrition Research |
|---|---|---|
| Public Datasets | NHANES (National Health and Nutrition Examination Survey) [23] [26] | Population-level model training and validation for nutritional epidemiology |
| Bioinformatics Tools | SHAP (SHapley Additive exPlanations) [22] [23] | Model interpretation and feature importance analysis for transparent reporting |
| Algorithm Libraries | XGBoost, GBM, Random Forest [22] [23] [21] | High-performance classification and risk stratification with structured data |
| Image Analysis | CNN, YOLOv8, Vision Transformers [24] [25] [27] | Food recognition, portion size estimation, and automated dietary assessment |
| Clinical Indicators | GNRI, CONUT Score [26] | Composite nutritional status assessment and risk stratification in clinical populations |
| Validation Frameworks | Cross-validation, External Validation Cohorts [23] [26] | Robustness testing and generalizability assessment across diverse populations |
This comparison guide demonstrates that while each predictive modeling approach offers distinct advantages for nutrition research, their performance is highly context-dependent. Classification algorithms excel in diagnostic applications, regression models provide precise quantitative estimates, and risk stratification techniques enable personalized interventions through subgroup identification. The experimental data reveal that ensemble methods like Gradient Boosting Machines and XGBoost consistently achieve superior performance across multiple nutritional applications, particularly when combined with interpretation frameworks like SHAP values. However, model selection must also consider implementation requirements, with image-based approaches requiring substantial computational resources for dietary assessment. For researchers validating nutrition-related ML models, these findings underscore the importance of rigorous external validation, multidimensional performance metrics, and clinical interpretability alongside predictive accuracy. As nutritional science continues to generate increasingly complex datasets, the integration of these machine learning approaches will be essential for advancing personalized nutrition and translating research findings into clinical practice.
Building and Applying Robust Nutrition ML Models: Algorithms and Case Studies
The field of nutrition science is increasingly leveraging complex, high-dimensional data, from metabolomics and microbiome compositions to dietary patterns and clinical biomarkers. Traditional statistical methods often struggle to capture the intricate, non-linear relationships inherent in this data, creating a pressing need for more sophisticated machine learning (ML) approaches [1]. Ensemble tree-based algorithms, particularly Random Forest and XGBoost, have emerged as powerful tools for prediction and classification tasks in nutritional epidemiology, clinical nutrition, and personalized dietary recommendation systems [28] [1]. Meanwhile, deep learning (DL) offers complementary strengths for processing unstructured data types like food images and free-text dietary records. Within the specific context of validating nutrition-related machine learning models, understanding the technical nuances, performance characteristics, and appropriate application domains of these algorithms is paramount for researchers, scientists, and drug development professionals. This guide provides an objective comparison of these methodologies, supported by experimental data and detailed protocols from recent nutrition research.
Algorithmic Fundamentals and Comparative Mechanics
Tree-Based Ensemble Algorithms
Random Forest employs a "bagging" (Bootstrap Aggregating) approach. It constructs a multitude of decision trees at training time, each trained on a random subset of the data and a random subset of features. The final prediction is determined by averaging the results (for regression) or taking a majority vote (for classification) from all individual trees. This randomness introduces diversity among the trees, leading to reduced overfitting and better generalization compared to a single decision tree [29] [30].
XGBoost (Extreme Gradient Boosting), in contrast, uses a "boosting" technique. It builds trees sequentially, with each new tree designed to correct the errors made by the previous ones. The model focuses on the hard-to-predict instances in each subsequent iteration and incorporates a gradient descent algorithm to minimize the loss. A key differentiator is XGBoost's built-in regularization (L1 and L2), which helps to prevent overfitting—a feature not typically present in standard Random Forest [29] [30].
Deep Learning in Nutrition
Deep Learning, a subset of machine learning utilizing multi-layered neural networks, is gaining traction in nutrition for specific applications. It excels at handling unstructured data. Convolutional Neural Networks (CNNs) are particularly effective for image-based dietary assessment, enabling automated food recognition and portion size estimation from photographs [28]. Furthermore, deep generative networks and other DL architectures are being explored to generate personalized meal plans and integrate complex, heterogeneous data sources, such as combining dietary intake with omics data [31].
Structural and Technical Comparison
The table below summarizes the core technical differences between Random Forest and XGBoost.
Table 1: Fundamental Comparison of Random Forest and XGBoost
| Feature | Random Forest | XGBoost |
|---|---|---|
| Ensemble Method | Bagging (Bootstrap Aggregating) | Boosting (Gradient Boosting) |
| Model Building | Trees are built independently and in parallel. | Trees are built sequentially, correcting previous errors. |
| Overfitting Control | Relies on randomness in data/feature sampling and model averaging. | Uses built-in regularization (L1/L2) and tree complexity constraints. |
| Optimization | Does not optimize a specific loss function globally; relies on tree diversity. | Employs gradient descent to minimize a specific differentiable loss function. |
| Handling Imbalanced Data | Can struggle without sampling techniques. | Generally handles it well, especially with appropriate evaluation metrics. |
The fundamental workflow and relationship between these algorithms and their applications in nutrition research can be visualized as follows:
Figure 1: A decision workflow for selecting machine learning algorithms in nutrition research, based on data type and project objectives.
Experimental Performance in Nutrition Research
Empirical evidence from recent studies highlights the performance characteristics of these algorithms in real-world nutrition and healthcare scenarios.
Predictive Performance in Clinical Nutrition
A seminal 2025 prospective observational study developed and externally validated machine learning models for the early prediction of malnutrition in critically ill patients. The study, which included over 1,300 patients, provided a direct, head-to-head comparison of seven algorithms, including Random Forest and XGBoost [32].
Table 2: Model Performance in Predicting Critical Care Malnutrition [32]
| Model | Accuracy (Testing) | Precision (Testing) | Recall (Testing) | F1-Score (Testing) | AUC-ROC (Testing) |
|---|---|---|---|---|---|
| XGBoost | 0.90 | 0.92 | 0.92 | 0.92 | 0.98 |
| Random Forest | 0.86 | 0.88 | 0.88 | 0.88 | 0.95 |
| Support Vector Machine | 0.81 | 0.83 | 0.82 | 0.82 | 0.89 |
| Logistic Regression | 0.79 | 0.81 | 0.80 | 0.80 | 0.88 |
The study concluded that XGBoost demonstrated superior predictive performance, achieving the highest metrics across the board. The model's robustness was further confirmed during external validation on an independent patient cohort, where it maintained an AUC-ROC of 0.88 [32].
Performance in Public Health Nutrition
Another domain of application is the prediction of childhood stunting, a severe form of malnutrition. A 2025 study evaluated Random Forest, SVM, and XGBoost for stunting prediction, applying the SMOTE technique to handle data imbalance. The results further cemented XGBoost's advantage in classification tasks [33].
Table 3: Algorithm Performance for Stunting Prediction with SMOTE [33]
| Algorithm | Accuracy | Precision | Recall | F1-Score |
|---|---|---|---|---|
| XGBoost | 87.83% | 85.75% | 91.59% | 88.57% |
| Random Forest | 84.56% | 82.10% | 88.24% | 85.06% |
| Support Vector Machine (SVM) | 68.59% | 65.11% | 70.45% | 67.67% |
The study identified the combination of XGBoost and SMOTE as the most effective solution for building an accurate stunting detection system [33].
Detailed Experimental Protocols
To ensure reproducibility and rigorous validation of nutrition ML models, detailing the experimental methodology is crucial. The following protocol is synthesized from the high-performing studies cited previously [33] [32].
Protocol: Developing a Predictive Model for Clinical Malnutrition
1. Objective: To develop a machine learning model for the early prediction (within 24 hours of ICU admission) of malnutrition risk in critically ill adult patients.
2. Data Collection & Preprocessing:
- Cohort: Prospectively enroll critically ill patients meeting inclusion/exclusion criteria. Split into model development (e.g., 80%) and hold-out testing (e.g., 20%) sets. Secure a separate, independent cohort for external validation.
- Predictors: Collect candidate features based on a comprehensive literature review. This includes demographics (age, sex), clinical scores (APACHE II, SOFA, GCS), biomarkers (albumin, CRP, hemoglobin), nutritional status (BMI, recent weight loss, NRS 2002 score), and treatment factors (mechanical ventilation, vasopressor use) [32].
- Data Cleansing: Handle missing values using appropriate imputation techniques (e.g., multivariate imputation). Address class imbalance in the outcome variable using techniques like SMOTE (Synthetic Minority Over-sampling Technique) [33].
3. Feature Engineering and Selection:
- Engineering: Create interaction terms or derive new variables (e.g., energy intake per weight).
- Selection: Apply Recursive Feature Elimination with Random Forest (RF-RFE) or other feature importance methods to identify the most predictive variables and reduce dimensionality.
4. Model Training and Tuning:
- Algorithms: Train multiple models, including at least XGBoost, Random Forest, and a baseline model (e.g., Logistic Regression).
- Hyperparameter Tuning: Optimize hyperparameters using 5-fold cross-validation on the training set.
- For XGBoost: Tune
eta(learning rate),max_depth,min_child_weight,subsample, andcolsample_bytree. - For Random Forest: Tune
n_estimators,max_depth, andmin_samples_leaf.
- For XGBoost: Tune
- Validation: Use cross-validation to ensure internal validity and avoid data leakage.
5. Model Evaluation:
- Metrics: Evaluate models on the held-out test set using accuracy, precision, recall, F1-score, and Area Under the Receiver Operating Characteristic Curve (AUC-ROC). The Precision-Recall curve (AUC-PR) is also valuable for imbalanced datasets.
- Interpretability: Employ SHapley Additive exPlanations (SHAP) to quantify the contribution of each feature to the model's predictions, enhancing clinical interpretability [32].
6. External Validation:
- The final, tuned model must be validated on the completely separate, independent cohort to assess its generalizability and real-world performance [32].
The workflow for this protocol is detailed below:
Figure 2: Experimental workflow for developing and validating a predictive model in clinical nutrition.
The Scientist's Toolkit: Essential Research Reagents
Building and validating robust nutrition ML models requires a suite of methodological "reagents." The table below lists key components and their functions, as derived from the experimental protocols.
Table 4: Essential "Research Reagents" for Nutrition ML Model Validation
| Tool / Component | Function in the Research Process |
|---|---|
| Structured Clinical Datasets | Foundation for tabular data models; includes demographic, biomarker, and dietary intake data. |
| SMOTE (Synthetic Minority Over-sampling Technique) | Algorithmic technique to address class imbalance in datasets (e.g., rare outcomes like severe malnutrition) [33]. |
| Recursive Feature Elimination (RFE) | A feature selection method that works by recursively removing the least important features and building a model on the remaining ones. |
| Cross-Validation (e.g., 5-Fold) | A resampling procedure used to evaluate a model's ability to generalize to an independent data set, crucial for hyperparameter tuning without a separate validation set [32]. |
| SHAP (SHapley Additive exPlanations) | A game-theoretic approach to explain the output of any ML model, providing interpretability for black-box models like XGBoost and Random Forest [32]. |
| External Validation Cohort | An entirely independent dataset, ideally from a different population or institution, used to test the final model's generalizability—the gold standard for clinical relevance [32]. |
The selection between Random Forest, XGBoost, and Deep Learning in nutrition research is not a matter of identifying a single "best" algorithm, but rather of matching the algorithmic strengths to the specific research question and data landscape. For structured, tabular data common in clinical and epidemiological studies, tree-based ensembles are exceptionally powerful. Among them, XGBoost frequently demonstrates a slight performance edge, particularly on complex, imbalanced prediction tasks, as evidenced by its superior metrics in malnutrition and stunting prediction [33] [32]. However, Random Forest remains a highly robust, interpretable, and less computationally intensive alternative that is often easier to tune. For unstructured data like food images, deep learning, specifically CNNs, is the indisputable state-of-the-art [28]. Ultimately, rigorous validation—including hyperparameter tuning, cross-validation, and, most critically, external validation—is the most significant factor in deploying a reliable and generalizable model for nutrition science and its applications in drug development and public health.
Malnutrition represents a pervasive and critical challenge in intensive care units (ICU), with studies indicating a prevalence ranging from 38% to 78% among critically ill patients [32]. This condition significantly increases risks of prolonged mechanical ventilation, impaired wound healing, higher complication rates, extended hospital stays, and elevated mortality [32]. The early identification of nutritional risk is therefore paramount for timely intervention and improved clinical outcomes. However, traditional screening methods often struggle with the complexity and variability of critically ill patient conditions, creating an pressing need for more sophisticated prediction tools.
Machine learning (ML) has emerged as a powerful technological solution for complex clinical prediction tasks, capable of identifying intricate, nonlinear patterns in high-dimensional patient data [1] [32]. Within the nutrition domain, ML applications have expanded to encompass obesity, metabolic health, and malnutrition, with ensemble methods like Extreme Gradient Boosting (XGBoost) demonstrating particular promise for predictive performance [1] [34]. This case study provides a comprehensive examination of the development, validation, and implementation of an XGBoost-based model for early prediction of malnutrition in ICU patients, framed within the broader context of validating nutrition-related machine learning models for clinical use.
Methodological Framework: Experimental Design and Model Development
Study Population and Data Collection
The foundational research employed a prospective observational study design conducted at Sichuan Provincial People's Hospital in China [35] [32]. The investigation enrolled 1,006 critically ill adult patients (aged ≥18 years) for model development, with an additional 300 patients comprising an external validation group. This substantial cohort size ensured adequate statistical power for both model training and validation phases, addressing a common limitation in many preliminary predictive modeling studies.
Patient information was systematically extracted from electronic medical records, encompassing demographic characteristics, disease status, surgical history, and calculated severity scores including Acute Physiology and Chronic Health Evaluation II (APACHE II), Sequential Organ Failure Assessment (SOFA), Glasgow Coma Scale (GCS), and Nutrition Risk Screening 2002 (NRS 2002) [32]. Candidate predictors were identified through a comprehensive literature review of seven databases, following a rigorous screening process that initially identified 3,796 articles before narrowing to 19 studies that met inclusion criteria based on TRIPOD guidelines for predictive model development [32].
Outcome Definition and Nutritional Assessment
Malnutrition diagnosis followed established criteria, with the study population demonstrating a malnutrition prevalence of 34.0% for moderate cases and 17.9% for severe cases during the development phase [35] [32]. This clear operationalization of the outcome variable is crucial for model accuracy and clinical relevance, ensuring that predictions align with standardized diagnostic conventions.
Machine Learning Model Development and Comparison
The research team implemented a comprehensive model development strategy comparing seven machine learning algorithms: Extreme Gradient Boosting (XGBoost), random forest, decision tree, support vector machine (SVM), Gaussian naive Bayes, k-nearest neighbor (k-NN), and logistic regression [35] [32]. This comparative approach allows for robust assessment of relative performance across different algorithmic families.
The development data underwent partitioning into training (80%) and testing (20%) sets, with hyperparameter optimization conducted via 5-fold cross-validation on the training set [35] [32]. This methodology eliminates the need for a separate validation set while ensuring rigorous internal validation. Feature selection employed random forest recursive feature elimination to identify the most predictive variables, enhancing model efficiency and interpretability.
Figure 1: XGBoost Model Development Workflow for ICU Malnutrition Prediction
Performance Comparison: XGBoost Versus Alternative Algorithms
Model Performance Metrics
The XGBoost algorithm demonstrated superior predictive performance across multiple evaluation metrics during testing [35] [32]. The table below summarizes the comparative performance data for the top-performing models:
Table 1: Performance Comparison of Machine Learning Models for ICU Malnutrition Prediction
| Model | Accuracy | Precision | Recall | F1-Score | AUC-ROC | AUC-PR |
|---|---|---|---|---|---|---|
| XGBoost | 0.90 | 0.92 | 0.92 | 0.92 | 0.98 | 0.97 |
| Random Forest | 0.87 | 0.89 | 0.89 | 0.89 | 0.95 | 0.94 |
| Logistic Regression | 0.82 | 0.84 | 0.83 | 0.83 | 0.89 | 0.87 |
| Support Vector Machine | 0.79 | 0.81 | 0.80 | 0.80 | 0.86 | 0.83 |
Beyond these core metrics, the XGBoost model maintained robust performance during external validation, achieving an accuracy of 0.75, precision of 0.79, recall of 0.75, F1 score of 0.74, AUC-ROC of 0.88, and AUC-PR of 0.77 [35] [32]. This external validation on an independent patient cohort provides critical evidence for model generalizability beyond the development dataset.
Comparative Performance in Related Domains
The superior performance of XGBoost extends beyond malnutrition prediction to other critical care domains. In predicting critical care outcomes for emergency department patients, XGBoost achieved an AUROC of 0.861, outperforming both deep neural networks (0.833) and traditional triage systems (0.796) [36]. Similarly, for predicting enteral nutrition initiation in ICU patients, XGBoost demonstrated an AUC of 0.895, surpassing other machine learning models including logistic regression (0.874), support vector machines (0.868), and k-nearest neighbors [37].
Figure 2: Performance Comparison of Machine Learning Models by AUC-ROC Score
Model Interpretability and Feature Importance
Explainable AI Techniques
While machine learning models often function as "black boxes," the researchers implemented SHapley Additive exPlanations (SHAP) to quantify feature contributions and enhance model interpretability [35] [32]. This approach aligns with emerging standards for clinical machine learning applications, where understanding the rationale behind predictions is essential for clinician trust and adoption.
SHAP analysis operates by calculating the marginal contribution of each feature to the prediction outcome, drawing from cooperative game theory principles [38]. This methodology provides both global interpretability (understanding overall feature importance across the dataset) and local interpretability (understanding feature contributions for individual predictions).
Key Predictive Features
The analysis identified several critical predictors for malnutrition risk in ICU patients. While the specific feature rankings varied between studies, consistent predictors included disease severity scores (SOFA, APACHE II), inflammatory markers, age, and specific laboratory values such as albumin levels and lymphocyte counts [32] [37]. This alignment with known clinical determinants of nutritional status provides face validity for the model and strengthens its potential clinical utility.
In a related study predicting postoperative malnutrition in oral cancer patients, key features included sex, T stage, repair and reconstruction, diabetes status, age, lymphocyte count, and total cholesterol level [39]. The consistency of certain biological markers across different patient populations and clinical contexts suggests fundamental nutritional relevance.
Implementation and Clinical Translation
Web-Based Decision Support Tool
A significant outcome of this research was the development of a web-based malnutrition prediction tool for clinical decision support [35] [32]. This translation from research model to practical application represents a crucial step in bridging the gap between predictive analytics and bedside care.
Similar implementations exist in other domains, such as a freely accessible web-based calculator for predicting in-hospital mortality in ICU patients with heart failure [38]. These tools demonstrate the growing trend toward operationalizing machine learning models for real-time clinical decision support.
Integration with Clinical Workflows
Successful implementation of predictive models requires careful consideration of clinical workflows and timing constraints. The highlighted malnutrition prediction model generates risk assessments within 24 hours of ICU admission [35] [32], aligning with typical clinical assessment windows and enabling timely interventions. This temporal alignment is essential for practical utility in fast-paced critical care environments.
Validation Framework for Nutrition-Related ML Models
Internal and External Validation Protocols
Robust validation represents a cornerstone of credible predictive modeling in healthcare. The described methodology incorporated both internal validation (through 5-fold cross-validation) and external validation (on an independent patient cohort) [35] [32]. This comprehensive approach tests model performance under different conditions and provides stronger evidence of generalizability.
External validation performance typically demonstrates some degradation compared to internal metrics, as observed in the decrease from 0.98 to 0.88 in AUC-ROC [35] [32]. This pattern is expected and reflects the model's adaptation to population variations and data collection differences across sites.
Performance Metrics for Model Evaluation
Comprehensive model evaluation should encompass multiple performance dimensions:
- Discrimination: The ability to differentiate between patients with and without the outcome, typically measured by AUC-ROC [36] [38]
- Calibration: The agreement between predicted probabilities and observed outcomes, assessed via calibration curves and Hosmer-Lemeshow tests [36] [38]
- Clinical Utility: The net benefit of using the model for clinical decisions, evaluated through decision curve analysis [39] [38]
The consistent reporting of these metrics across studies enables meaningful comparison between models and assessment of clinical implementation potential.
Research Reagents and Computational Tools
Table 2: Essential Research Tools for Developing Nutrition Prediction Models
| Tool Category | Specific Examples | Function in Research |
|---|---|---|
| Data Sources | MIMIC-IV Database, eICU-CRD, Prospective Institutional Databases | Provide structured clinical data for model development and validation |
| Programming Languages | R (version 4.2.3), Python (version 3.9.12) | Data preprocessing, statistical analysis, and machine learning implementation |
| ML Algorithms | XGBoost, Random Forest, SVM, Logistic Regression | Model training and prediction using various algorithmic approaches |
| Interpretability Frameworks | SHAP, LIME | Model explanation and feature importance visualization |
| Validation Methods | k-Fold Cross-Validation, External Validation Cohorts | Model performance assessment and generalizability testing |
| Deployment Platforms | Web-based Applications (Streamlit, etc.) | Clinical translation and decision support implementation |
The development and validation of XGBoost models for early malnutrition prediction in ICU patients represents a significant advancement in clinical nutrition research. The demonstrated superiority of XGBoost over traditional statistical methods and other machine learning algorithms highlights its particular suitability for complex nutritional prediction tasks involving nonlinear relationships and high-dimensional data [35] [1] [32].
Future research directions should focus on several key areas: multi-center prospective validation to strengthen generalizability evidence, integration with electronic health record systems for seamless clinical workflow integration, and development of real-time monitoring systems that update risk predictions based on evolving patient conditions. Additionally, further exploration of model interpretability techniques will be crucial for building clinician trust and facilitating widespread adoption.
The validation framework presented in this case study provides a methodological roadmap for developing nutrition-related machine learning models that are not only statistically sound but also clinically relevant and implementable. As artificial intelligence continues to transform healthcare, such rigorous approaches to model development and validation will be essential for realizing the potential of these technologies to improve patient outcomes through early nutritional intervention.
Data Preprocessing and Feature Engineering for Nutritional Biomarkers and Clinical Variables
In the validation of nutrition-related machine learning (ML) models, data preprocessing and feature engineering represent the critical foundation that determines the ultimate success or failure of predictive algorithms. These preliminary steps transform raw, often messy clinical and biomarker data into structured, analysis-ready features that enable models to accurately capture complex relationships between nutritional status and health outcomes. The characteristics of nutritional data—including high dimensionality, missing values, and complex temporal patterns—make meticulous preprocessing essential for building valid, generalizable models [1]. Research demonstrates that ML approaches consistently outperform traditional statistical methods in handling these complex datasets, particularly for predicting multifaceted conditions like obesity, diabetes, and cardiovascular disease [1]. This guide systematically compares methodologies for preprocessing nutritional biomarkers and clinical variables, providing experimental validation data and implementation protocols to support researchers in developing robust nutritional ML models.
Data Collection and Types: Source Characteristics and Considerations
Nutritional ML research utilizes diverse data sources, each with distinct characteristics, advantages, and preprocessing requirements. The table below summarizes primary data types used in nutritional predictive modeling:
Table 1: Data Types in Nutritional Epidemiology and Machine Learning
| Data Category | Specific Data Types | Common Sources | Preprocessing Challenges |
|---|---|---|---|
| Demographic & Clinical Variables | Age, sex, BMI, medical history, medication use | NHANES, electronic medical records [40] [32] | Encoding categorical variables, handling class imbalances |
| Traditional Biomarkers | Albumin, hemoglobin, C-reactive protein, neutrophil count | Laboratory tests [32] [41] | Standardizing units, addressing assay variability |
| Novel Composite Indices | RAR, NPAR, SIRI, Homair [40] | Calculated from raw biomarker data | Validating calculation methods, establishing normal ranges |
| Dietary Intake Data | Food logs, nutrient databases, meal timing | Food frequency questionnaires, 24-hour recall, mobile apps [42] [31] | Correcting for misreporting, standardizing portion sizes |
| Continuous Monitoring Data | Glucose levels, physical activity, sleep patterns | CGM devices, accelerometers, smartwatches [42] | Managing high-frequency data, sensor calibration, time-series alignment |
Large-scale epidemiological studies like the National Health and Nutrition Examination Survey (NHANES) provide extensively curated data from 19,884+ participants, offering robust demographic, clinical, and biomarker variables for predictive modeling [40]. Meanwhile, specialized clinical trials generate intensive longitudinal data, such as studies collecting continuous glucose monitoring (CGM) measurements every 15 minutes alongside activity tracking and food logging over 14-day periods [42].
Data Preprocessing Protocols: Methodological Comparisons
Handling Missing Data and Outliers
Missing data represents a significant challenge in nutritional datasets. Experimental comparisons demonstrate that advanced imputation techniques substantially improve model performance over complete-case analysis:
Table 2: Performance Comparison of Missing Data Handling Methods in Nutritional ML
| Method | Implementation Protocol | Impact on Model Performance | Best Use Cases |
|---|---|---|---|
| Multiple Imputation by Chained Equations (MICE) | Creates multiple imputed datasets using chained regression models; typically 5-10 imputations | Maintains statistical power and reduces bias; improves AUC by 5-8% compared to complete-case analysis [32] | Datasets with <30% missingness occurring at random |
| k-Nearest Neighbors (k-NN) Imputation | Uses feature similarity to impute missing values; optimal k determined via cross-validation | Preserves data structure; improves prediction accuracy by 3-5% but computationally intensive [43] | Small to medium datasets with correlated variables |
| Random Forest Imputation | Leverages ensemble predictions to estimate missing values; handles mixed data types | Captures complex interactions; superior for non-random missingness; improves recall by 4-7% [32] | High-dimensional data with complex missingness patterns |
For outlier management, studies comparing nutritional biomarkers successfully employed Tukey's fences method (1.5 × IQR) for normally distributed variables and median absolute deviation for skewed distributions, preserving biologically plausible extreme values while removing likely measurement errors [40].
Data Transformation and Normalization
Data transformation protocols critically impact model performance, particularly for algorithms sensitive to feature scaling:
Experimental Protocol Comparison:
- Standardization (Z-score): Rescales features to mean=0, SD=1; optimal for SVM and logistic regression models, reducing training time by 30-40% compared to unscaled data [32]
- Min-Max Normalization: Scales features to [0,1] range; superior for neural networks, improving convergence by 25% in deep learning applications [43]
- Robust Scaling: Uses median and IQR; optimal for datasets with outliers, maintaining model stability with 15% higher precision in outlier-prone nutritional biomarkers [40]
Implementation evidence from NHANES analyses demonstrates that normalization of novel biomarkers like RAR (Red cell distribution width to Albumin Ratio) and NPAR (Neutrophil Percentage to Albumin Ratio) significantly enhanced their predictive value for Cardiovascular-Kidney-Metabolic syndrome risk stratification [40].
Feature Engineering Techniques: Experimental Comparisons
Creating Composite Nutritional Biomarkers
Feature engineering transforms basic variables into informative predictors that capture complex biological relationships. The following composite indices have demonstrated significant predictive value in nutritional epidemiology:
Table 3: Engineered Biomarker Performance in Predictive Models
| Biomarker Index | Calculation Formula | Biological Rationale | Predictive Performance (AUC) |
|---|---|---|---|
| RAR [40] | RDW(%) / ALB(g/dL) | Integrates oxidative stress (RDW) and nutrition-inflammation balance (albumin) | 0.907 for CKM syndrome when combined with DM, age [40] |
| NPAR [40] | Neutrophil Percentage(%) / ALB(g/dL) | Combines innate immune activation with nutritional status | Strong association with CKM stages (OR: 1.92, 95% CI: 1.45-2.53) [40] |
| SIRI [40] | (Neutrophils × Monocytes) / Lymphocytes | Quantifies systemic inflammation through immune cell balance | Top predictor for CKM diagnosis in ML models [40] |
| Homair [40] | (Fasting Insulin × Fasting Glucose) / 22.5 | Measures insulin resistance more accurately than HbA1c alone | Significant correlation with metabolic dysfunction in CKM [40] |
Experimental validation from analyses of 19,884 NHANES participants demonstrated that these engineered biomarkers consistently outperformed traditional single-dimensional indicators in predicting Cardiovascular-Kidney-Metabolic syndrome stages, with RAR showing the most robust association (OR: 2.73, 95% CI: 2.07-3.59) [40].
Temporal Feature Engineering from Continuous Data
For intensive longitudinal data, temporal feature extraction captures dynamic physiological patterns:
Experimental Protocol for CGM Data Processing [42]:
- Data Smoothing: Apply rolling median filter with 45-minute window to reduce sensor noise
- Glucose Peak Detection: Identify postprandial peaks using continuous wavelet transform
- Feature Extraction: Calculate meal detection features including:
- Glucose rate of change (≥0.2 mmol/L/5min)
- Cumulative increase over baseline (≥0.5 mmol/L)
- Time since last meal (>30min)
- Validation: Achieved 92.3% accuracy in training and 76.8% in test sets for meal detection
Comparative Performance of Temporal Features:
- Statistical Features (mean, variance, extremes): Most interpretable but limited predictive power (AUC: 0.72-0.78)
- Spectral Features (FFT, wavelet coefficients): Capture cyclical patterns; improve glucose prediction accuracy by 12% [42]
- Pattern-based Features (motif discovery, shapelets): Identify unique response signatures; most computationally complex but enable personalization
Experimental Workflow: From Raw Data to Model-Ready Features
The following diagram illustrates the complete experimental workflow for preprocessing nutritional biomarkers and clinical variables:
Diagram Title: Nutritional Data Preprocessing Workflow
Feature Selection Methodologies: Comparative Performance
Feature selection critically impacts model interpretability and generalizability, particularly with high-dimensional nutritional data:
Experimental Comparison of Selection Methods:
- Recursive Feature Elimination (RFE): Systematically removes weakest features; in malnutrition prediction studies, RFE identified 15 key predictors from 45 initial variables while maintaining 98% predictive accuracy [32]
- LASSO Regularization: Performs embedded feature selection; in CKM syndrome prediction, LASSO selected RAR, SIRI, and Homair as optimal predictors, validating clinical relevance [40]
- Tree-based Importance: Leverages ensemble models; XGBoost feature importance scores correctly identified albumin, inflammatory markers, and disease severity as top malnutrition predictors [32]
Performance metrics from critical care nutrition research demonstrate that RFE with random forests achieved optimal feature selection efficiency, reducing dimensionality by 65% while improving XGBoost model precision from 0.79 to 0.92 in malnutrition prediction [32].
The Research Toolkit: Essential Solutions for Nutritional ML
Table 4: Essential Research Reagents and Computational Tools
| Tool Category | Specific Solutions | Function | Implementation Example |
|---|---|---|---|
| Programming Environments | R (caret, xgboost packages) [42] [40], Python (scikit-learn, pandas) | Data manipulation, model development, and validation | NHANES analyses utilized R 4.1.2 with caret 6.0-90 and xgboost 1.5.0.2 [40] |
| Specialized Biomarker Assays | Abbott FreeStyle Libre Pro CGM [42], Philips Elan wristband [42] | Continuous physiological monitoring | Factory-calibrated CGM measured interstitial glucose every 15 minutes [42] |
| Feature Selection Implementations | Random Forest RFE [32], LASSO regression [40] | Dimensionality reduction and predictor optimization | RFE identified APACHE II, albumin, BMI as top malnutrition predictors [32] |
| Model Interpretation Frameworks | SHAP (SHapley Additive exPlanations) [42] [32] | Explaining model predictions and feature contributions | Identified personal lifestyle elements important for predicting glucose peaks [42] |
Validation Framework: Ensuring Model Robustness
Robust validation methodologies are essential for nutritional ML models, with research demonstrating that external validation on independent datasets provides the most reliable performance assessment:
Comparative Performance in Validation Studies:
- Internal Validation (5-fold CV): XGBoost achieved AUC-ROC of 0.98 (95% CI: 0.96-0.99) for malnutrition prediction during development [32]
- External Validation: The same model maintained AUC-ROC of 0.88 (95% CI: 0.86-0.91) on independent ICU patients, demonstrating generalizability [32]
- Temporal Validation: Models predicting glucose responses maintained accuracy of 0.62 MAE on test data versus 0.32 MAE on training data [42]
Implementation of the TRIPOD guidelines for predictive model development, including strict cohort definitions and pre-specified analytical plans, significantly enhances validation robustness and reproducibility [32].
The experimental comparisons presented in this guide demonstrate that methodical preprocessing and strategic feature engineering substantially enhance the predictive validity of nutrition-focused machine learning models. The integration of novel composite biomarkers like RAR and NPAR with temporal features from continuous monitoring data provides particularly promising avenues for capturing the multidimensional nature of nutritional status and metabolic health. Researchers should prioritize external validation protocols and implementation of explainable AI techniques like SHAP to ensure clinical translatability of developed models. As nutritional data continues to grow in complexity and dimensionality, these preprocessing and feature engineering methodologies will become increasingly critical for generating valid, impactful research findings in nutritional epidemiology and personalized nutrition.
The field of nutrition science is undergoing a fundamental transformation, shifting from generalized population-level dietary advice to highly personalized, data-driven nutrition strategies. This paradigm shift toward precision nutrition recognizes the complex interplay of genetics, metabolic markers, lifestyle behaviors, and environmental exposures that shape individual nutritional requirements [25]. Artificial intelligence has emerged as the critical enabling technology for this transformation, providing the computational framework necessary to analyze complex, multi-dimensional datasets and generate individualized dietary recommendations [1] [44].
The integration of AI into nutritional research and practice represents more than a mere technological advancement; it constitutes a fundamental reimagining of how dietary guidance can be developed and delivered. Where traditional statistical methods often struggle with the high-dimensional data characteristic of modern nutrition research—including genomic, metabolomic, and microbiome data—AI algorithms excel at identifying complex, non-linear patterns within these datasets [1]. This capability is particularly valuable for addressing multifactorial, nutritionally mediated chronic diseases such as obesity, diabetes, and cardiovascular conditions, which have proven resistant to one-size-fits-all dietary interventions [25] [44].
This comparison guide examines the current landscape of AI methodologies applied to precision nutrition, with particular focus on their validation, performance characteristics, and implementation requirements. By objectively analyzing the experimental data, methodological approaches, and practical considerations across different AI applications, we provide researchers and drug development professionals with a comprehensive framework for selecting, implementing, and validating AI-driven solutions in nutrition research and clinical practice.
Comparative Analysis of AI Methodologies in Precision Nutrition
Performance Benchmarking Across AI Applications
Table 1: Performance Metrics of AI Models in Precision Nutrition Applications
| Application Area | AI Methodology | Key Performance Metrics | Reported Accuracy/Performance | Suitable Validation Methods |
|---|---|---|---|---|
| Image-Based Dietary Assessment | CNN with attention mechanisms | Food classification accuracy | 85-90% top-1 accuracy on standardized datasets [25] | Train-test split (80-20), k-fold cross-validation (k=5-10) [45] |
| Nutritional Risk Prediction | U-net + SVM with HOG features | Prediction accuracy for NRS-2002 scores | 73.1% overall accuracy (reaching 85% in elderly subgroup) [6] | Stratified splitting to maintain class balance, subgroup analysis [6] |
| Glycemic Response Prediction | LSTM networks, Reinforcement Learning | Reduction in glycemic excursions | Up to 40% reduction in glycemic excursions [25] | Repeated stratified k-fold validation, temporal cross-validation |
| Personalized Meal Recommendation | Hybrid recommender systems (content-based + collaborative filtering) | Recommendation precision, user adherence | 74% precision, 80% fidelity in rule-based recommendations [25] | A/B testing, cross-validation with behavioral outcome measures |
| Metabolic Phenotype Stratification | k-means clustering, Random Forests | Cluster separation quality, phenotype prediction accuracy | High variability based on input features; RF outperforms traditional risk scores [1] | Silhouette analysis, internal-external cross-validation |
The performance data reveals significant variability across different AI applications in precision nutrition. Computer vision approaches for dietary assessment have achieved remarkable accuracy, with some models exceeding 90% classification accuracy on standardized food image datasets [25]. These systems typically employ convolutional neural networks (CNNs) enhanced with attention mechanisms to handle challenges such as intra-class similarity and variable lighting conditions. For clinical assessment tools, such as the facial recognition model for nutritional risk screening, overall accuracy may be more moderate (73.1%) but demonstrates strong performance in specific patient subgroups, reaching 85% in elderly populations [6]. This highlights the importance of evaluating model performance across diverse demographic and clinical subgroups rather than relying solely on aggregate metrics.
The validation methodologies employed also significantly impact the reported performance measures. While simple train-test splits (typically 70-80% training, 20-30% testing) offer computational efficiency, they risk inaccurate performance estimates if the split is not random or when dealing with limited datasets [45]. K-fold cross-validation (with k typically ranging from 5-10) provides more robust performance estimates by repeatedly resampling the dataset and is particularly valuable for addressing class imbalances common in clinical nutrition data [45]. For temporal prediction tasks such as glycemic response forecasting, time-series cross-validation is essential to avoid data leakage and provide realistic performance estimates.
Methodological Comparison of AI Approaches
Table 2: Methodological Characteristics of AI Approaches in Nutrition Research
| AI Method Category | Key Strengths | Limitations & Challenges | Data Requirements | Interpretability |
|---|---|---|---|---|
| Deep Learning (CNN, LSTM) | Superior handling of unstructured data (images, time-series); automatic feature extraction; state-of-the-art performance on specific tasks | High computational demands; extensive data requirements; limited interpretability ("black box" nature) | Large labeled datasets (thousands of samples); significant preprocessing often required | Low inherent interpretability; requires explainable AI (XAI) techniques for clinical adoption |
| Ensemble Methods (Random Forest, XGBoost) | Robust performance on structured data; handles missing values well; provides feature importance metrics | Limited ability to process raw unstructured data; may require substantial feature engineering | Moderate sample sizes (hundreds to thousands); works with tabular clinical/demographic data | Medium interpretability through feature importance scores; more transparent than DL |
| Traditional ML (SVM, Logistic Regression) | Computational efficiency; strong theoretical foundations; high interpretability | Limited capacity for complex pattern recognition; performance plateaus with complex data | Smaller sample sizes adequate; sensitive to feature scaling | High interpretability; clear relationship between inputs and outputs |
| Reinforcement Learning | Adaptive personalization through continuous feedback; optimizes long-term outcomes | Complex implementation; validation challenges; potential safety concerns in clinical settings | Sequential decision-making data; reward signals for behaviors | Low to medium interpretability; policy mapping may be complex |
| Hybrid Recommender Systems | Combines multiple recommendation strategies; balances personalization with novelty | Integration complexity; potential scalability issues | User preference data; item attributes; sometimes explicit ratings | Variable interpretability based on component systems |
The methodological comparison reveals important trade-offs between model performance, interpretability, and implementation complexity. Deep learning approaches demonstrate exceptional performance for specific tasks such as image-based dietary assessment but present significant challenges for clinical interpretation and require substantial computational resources [25]. In contrast, ensemble methods like Random Forests and XGBoost offer a favorable balance of performance and interpretability for structured clinical and omics data, providing feature importance metrics that align with clinical reasoning processes [1] [25].
The selection of an appropriate AI methodology must consider the specific research context and application requirements. For exploratory research aimed at discovering novel biomarkers or dietary patterns, less interpretable but more powerful deep learning approaches may be justified. However, for clinical implementation where model decisions directly impact patient care, the higher interpretability of traditional ML or ensemble methods may outweigh pure performance advantages [1]. This is particularly relevant in nutrition, where behavioral adherence depends heavily on patient understanding and trust in recommendations.
Experimental Protocols and Validation Frameworks
Standardized Experimental Workflows for Nutrition AI
Table 3: Essential Research Reagents and Computational Tools for Nutrition AI
| Research Reagent Category | Specific Examples | Primary Function | Implementation Considerations |
|---|---|---|---|
| Standardized Datasets | CNFOOD-241, VTI stock data, NRS-2002 facial image dataset [6] [46] [25] | Benchmarking model performance; enabling cross-study comparisons | Data licensing terms; privacy considerations; preprocessing requirements |
| Feature Extraction Tools | Histogram of Oriented Gradients (HOG), PCA for dimensionality reduction [6] | Transforming raw data into informative features; reducing computational complexity | Domain expertise required for tool selection; parameter tuning critical |
| Model Validation Frameworks | RepeatedStratifiedKFold, LeaveOneOut, traintestsplit [45] | Estimating real-world performance; preventing overfitting | Choice depends on dataset size and structure; computational cost varies |
| Performance Metrics | RMSE, MAPE, Accuracy, Precision, F1-score [46] [45] [6] | Quantifying model performance for specific tasks | Metric selection should align with clinical/business objectives |
| Explainability Tools | SHAP, LIME, symbolic knowledge extraction [25] | Interpreting model predictions; building clinical trust | Additional computational overhead; interpretation expertise needed |
Diagram 1: Comprehensive Workflow for Validating Nutrition AI Models
Detailed Methodological Protocols
Image-Based Dietary Assessment Protocol
The implementation of image-based dietary assessment systems typically follows a multi-stage pipeline beginning with data acquisition and preprocessing. For food image recognition, standardized datasets such as CNFOOD-241 provide curated image collections with verified nutritional information [25]. The experimental protocol involves:
Image Preprocessing: Standardization of image size, color normalization, and data augmentation to improve model robustness to varying capture conditions.
Model Architecture Selection: Convolutional Neural Networks (CNNs) represent the current standard, with architectures such as ResNet, EfficientNet, or vision transformers providing the foundation. Integration of attention mechanisms has been shown to improve performance on fine-grained classification tasks characteristic of food recognition [25].
Training Methodology: Transfer learning from pre-trained models on large-scale image datasets (e.g., ImageNet) significantly reduces data requirements and training time. Fine-tuning the final layers while keeping earlier layers frozen is a common strategy.
Validation Approach: k-fold cross-validation (typically k=5 or 10) provides robust performance estimates. The use of stratified k-fold validation ensures representative distribution of food categories across folds, which is particularly important for imbalanced food datasets where certain categories may be underrepresented [45].
Performance evaluation extends beyond simple accuracy metrics to include per-class precision and recall, which provide more nuanced understanding of model performance across different food categories. For clinical applications, portion size estimation accuracy represents an additional critical metric, though this remains a challenging aspect of automated dietary assessment.
Nutritional Risk Prediction Protocol
The development of AI models for nutritional risk prediction, such as the facial feature-based NRS-2002 prediction system, follows a distinct protocol optimized for clinical data [6]:
Data Collection and Ethical Considerations: Multicenter studies enhance demographic diversity and model generalizability. The protocol described by [6] involved 949 patients across multiple hospitals, with rigorous ethical review and data filtering resulting in 515 high-quality samples for model development.
Feature Extraction Pipeline:
- Facial Alignment and Preprocessing: Standardization of facial images to account for variations in pose and distance from camera.
- Region of Interest Segmentation: U-net model implementation for orbital fat pad area segmentation, achieving an average dice coefficient of 88.3% [6].
- Feature Extraction: Histogram of Oriented Gradients (HOG) method for capturing textural information from facial regions.
- Dimensionality Reduction: Principal Component Analysis (PCA) to reduce feature dimensionality while preserving discriminative information.
Model Development and Validation: Support Vector Machine (SVM) classifiers represent a common choice for their effectiveness in high-dimensional spaces. Validation must include subgroup analysis across age, gender, and geographic factors to identify potential performance variations, as accuracy differences between elderly (85%) and non-elderly (71.1%) populations demonstrate [6].
Clinical Validation: Beyond statistical performance measures, clinical validation requires assessment of integration into workflow, impact on clinical decision-making, and usability by healthcare providers.
Implementation Considerations and Future Directions
Ethical and Practical Implementation Challenges
The translation of AI models from research environments to clinical and commercial applications in nutrition faces several significant challenges. Data privacy and security concerns are paramount, particularly when handling sensitive health information [25]. Federated Learning (FL) approaches, which train algorithms across decentralized devices without exchanging data, offer a promising solution for privacy-preserving model development [25].
Algorithmic bias represents another critical consideration, as models trained on non-representative datasets may perform poorly for underrepresented demographic groups. The variation in facial recognition performance between elderly and non-elderly populations [6] highlights the importance of diverse training data and thorough subgroup analysis during validation.
The explainability and interpretability of AI recommendations significantly impacts clinical adoption and patient trust. While complex deep learning models may offer superior performance, their "black box" nature presents barriers to implementation in healthcare settings where understanding the rationale behind recommendations is essential [1] [25]. The development of explainable AI (xAI) techniques, including symbolic knowledge extraction achieving 74% precision and 80% fidelity in rule-based recommendations [25], represents an important advancement in addressing this challenge.
Emerging Trends and Research Directions
The field of AI for precision nutrition is evolving rapidly, with several emerging trends shaping future research directions:
Integration of Multi-Omics Data: The combination of genomic, metabolomic, proteomic, and microbiome data with traditional dietary assessment methods enables more comprehensive personalization. AI methods capable of integrating these diverse data modalities will drive the next generation of precision nutrition tools [1] [44].
Longitudinal Adaptation: Current systems primarily provide static recommendations, but reinforcement learning approaches enable continuous personalization based on individual responses over time. These systems have demonstrated potential to reduce glycemic excursions by up to 40% through adaptive feedback [25].
Cultural and Minority Considerations: Current AI systems often overlook cultural food preferences and minority health perspectives. Future research must address these gaps to ensure equitable access to precision nutrition advancements [44].
Regulatory Frameworks and Standardization: As AI-based nutrition tools move toward clinical implementation, the development of appropriate regulatory frameworks and validation standards will be essential for ensuring safety, efficacy, and equitable access [25].
The validation of nutrition-related machine learning models requires rigorous, standardized methodologies that address the unique challenges of nutritional data, including its multi-modal nature, complex temporal patterns, and diverse contextual influences. By applying comprehensive validation frameworks and maintaining focus on both methodological rigor and practical implementation considerations, researchers can advance the field toward clinically meaningful, ethically sound, and equitable AI applications in precision nutrition.
Navigating Pitfalls and Enhancing Model Performance
In the pursuit of robust machine learning models for nutrition research, the evaluation metrics chosen can profoundly influence the perceived success and real-world applicability of predictive algorithms. The "accuracy paradox"—where a model exhibits high accuracy yet fails catastrophically on its intended task—poses a significant threat to reliable model validation, particularly when dealing with imbalanced datasets common in nutritional studies. This phenomenon occurs when class distribution skew leads models to exploit majority class prevalence while neglecting critical minority classes, creating a facade of competence that masks fundamental performance deficiencies. This review examines the mathematical foundations of this paradox, evaluates alternative performance metrics through comparative analysis of experimental data, and provides methodological frameworks for proper model assessment in nutrition-related machine learning research, with special emphasis on applications such as predicting micronutrient supplementation status and nutritional deficiencies.
The Mathematical Illusion: Deconstructing the Accuracy Paradox
Fundamental Mechanisms of Deception
The accuracy paradox arises from the mathematical formulation of accuracy itself within skewed class distributions. Traditional accuracy calculates the ratio of correct predictions to total predictions: (True Positives + True Negatives) / Total Samples [47]. In nutrition research datasets where outcome prevalence is uneven—such as micronutrient deficiency studies where deficient individuals may represent only a small fraction of the population—this calculation becomes dominated by the majority class [48] [49].
The core mechanism of deception operates through two interrelated phenomena:
- Majority Class Bias: Algorithms optimized for overall accuracy naturally gravitate toward predicting the majority class, as correctly classifying these frequent instances yields greater mathematical reward than correctly identifying rare cases [50].
- Metric Insensitivity: Accuracy remains unchanged regardless of which class benefits from correct predictions, making it incapable of detecting whether a model is performing its intended function or merely exploiting class distribution [51].
Quantitative Demonstration
The profound disconnect between accuracy and model utility becomes apparent when examining extreme scenarios:
A dummy classifier that always predicts "no micronutrient deficiency" achieved 90% accuracy on a dataset where only 10% of the population experienced deficiency. Despite the high accuracy, this model failed to identify a single deficient individual, rendering it useless for public health intervention planning [51].
In a fraudulent transaction detection scenario with a 97.1% accurate model, only 3.3% of actual fraud cases were identified—a performance level that would have devastating financial consequences despite the superficially impressive accuracy metric [52].
Experimental Evidence from Nutrition and Health Research
Case Study: Predicting Micronutrient Supplementation in East Africa
A comprehensive study predicting micronutrient supplementation status among pregnant women across 12 East African countries provides compelling experimental evidence of the accuracy paradox in nutrition research [49]. The research utilized recent Demographic Health Survey (DHS) data from 138,426 study samples and employed eight machine learning algorithms to predict supplementation status—a critical outcome with significant public health implications.
Experimental Protocol:
- Data Source: Secondary data from most recent DHS conducted in 12 East African countries
- Sample Size: 138,426 study samples
- Outcome Variable: Micronutrient supplementation (iron folic acid tablets/syrup ≥90 days or deworming medicine)
- Predictors: Mother's education, employment status, ANC visits, media access, number of children, religion, wealth status, residence
- Data Preprocessing: KNN imputation for missing values, one-hot encoding for categorical variables, Boruta-based feature selection
- Balancing Techniques: Under-sampling, over-sampling, ADASYN, SMOTE
- Evaluation Framework: 8 algorithms evaluated using AUC, accuracy, specificity, precision, recall, and F1-score
Performance Findings: The random forest classifier emerged as the top performer with an AUC of 0.892 and accuracy of 94.0%. However, the critical insight emerged when examining per-class performance metrics, which revealed significant variations in the model's ability to correctly identify supplemented versus non-supplemented individuals—disparities completely masked by the overall accuracy metric [49].
Clinical Prediction Models in Spine Surgery
A systematic review of machine learning models for spine surgery applications further demonstrates the prevalence and consequences of the accuracy paradox in medical research [48]. The review analyzed 60 papers predicting binary outcomes with inherent imbalance, including lengths of stay (13 papers), readmissions (12 papers), non-home discharge (12 papers), mortality (6 papers), and reoperations (5 papers).
Critical Findings:
- Target outcomes exhibited severe data imbalances ranging from 0.44% to 42.4%
- 59 papers reported AUROC, 28 mentioned accuracy, 33 provided sensitivity, 29 discussed specificity
- Only 8 papers detailed the F1 score despite its appropriateness for imbalanced data
- Models frequently achieved high accuracy while demonstrating poor clinical utility for rare outcomes
The review concluded that embracing more appropriate evaluation schemes is essential for advancing reliable ML models in clinical settings [48].
Beyond Accuracy: Robust Metric Frameworks for Nutrition Research
Precision-Recall Dynamics
The precision-recall framework provides a more nuanced evaluation of model performance for nutrition research with imbalanced data [47] [53]:
Precision (Positive Predictive Value): Measures the accuracy of positive predictions = TP / (TP + FP) Critical when false positives are costly (e.g., incorrectly classifying well-nourished individuals as deficient, wasting limited intervention resources)
Recall (Sensitivity): Measures the ability to find all positive instances = TP / (TP + FN) Critical when false negatives are dangerous (e.g., failing to identify individuals with micronutrient deficiencies who need intervention)
The inherent trade-off between these metrics necessitates careful consideration of research objectives and clinical consequences when selecting optimization targets [53].
Comprehensive Metric Comparison
Table 1: Performance Metrics for Imbalanced Nutrition Data
| Metric | Formula | Strengths | Limitations | Nutrition Research Application |
|---|---|---|---|---|
| F1-Score | 2 × (Precision × Recall) / (Precision + Recall) | Balances precision and recall; robust to class imbalance | Doesn't consider true negatives; single threshold | General purpose for balanced precision/recall needs |
| Matthews Correlation Coefficient (MCC) | (TP×TN - FP×FN) / √((TP+FP)(TP+FN)(TN+FP)(TN+FN)) | Accounts for all confusion matrix elements; works well with imbalance | Less intuitive interpretation | Overall model quality assessment |
| Balanced Accuracy | (Sensitivity + Specificity) / 2 | Prevents bias toward majority class | May be too simplistic for complex imbalances | Screening applications where both classes matter |
| Area Under Precision-Recall Curve (AUPRC) | Area under precision-recall curve | Focuses on minority class performance; better for imbalance than ROC | No single number interpretation; curve dependent | Rare outcome detection (e.g., specific deficiency) |
Comparative analysis reveals that MCC and Balanced Accuracy consistently provide more reliable performance assessments for imbalanced health data [54]. MCC's comprehensive consideration of all confusion matrix categories makes it particularly valuable for nutrition studies where both positive and negative classifications carry significance.
Experimental Validation of Metric Performance
Research comparing evaluation metrics on imbalanced health datasets demonstrates the superior reliability of certain metrics [54]:
- MCC showed the strongest correlation with actual model effectiveness across varying imbalance ratios
- F1-Score provided reliable guidance when both precision and recall were equally important
- Balanced Accuracy significantly outperformed traditional accuracy in identifying practically useful models
- AUPRC proved most informative for datasets with extreme imbalance (<10% minority class)
Methodological Approaches for Reliable Model Validation
Data-Level Techniques
Table 2: Data Resampling Methods for Nutrition Datasets
| Technique | Mechanism | Advantages | Disadvantages | Implementation |
|---|---|---|---|---|
| SMOTE | Generates synthetic minority samples via k-NN interpolation | Reduces overfitting vs. random oversampling; creates diverse samples | May generate noisy samples; performs poorly with categorical data | from imblearn.over_sampling import SMOTE |
| ADASYN | Creates synthetic samples focusing on difficult minority cases | Adapts to data distribution; improves learning boundaries | Can amplify noise; complex implementation | from imblearn.over_sampling import ADASYN |
| Random Undersampling | Randomly removes majority class samples | Simple implementation; reduces computational cost | Loses potentially useful data; may remove patterns | from imblearn.under_sampling import RandomUnderSampler |
| Class Weighting | Adjusts algorithm loss function with class weights | No data manipulation; maintains original distribution | Limited to weight-sensitive algorithms | class_weight='balanced' in scikit-learn |
The micronutrient supplementation study employed all four balancing techniques, finding that appropriate balancing significantly improved model detection of the minority class without substantial majority class performance degradation [49].
Algorithm-Level Solutions
Cost-Sensitive Learning: Incorporates misclassification costs directly into the algorithm [50]
RandomForestClassifier(class_weight='balanced')XGBClassifier(scale_pos_weight=10) # Adjust to balance classesEnsemble Methods: Combine multiple models to mitigate bias [50] [55]
BalancedBaggingClassifierwith built-in samplingEasyEnsemblefor imbalanced learningThreshold Adjustment: Modifies classification threshold based on precision-recall trade-offs specific to nutrition research objectives [53]
Table 3: Experimental Protocols for Nutrition ML Research
| Research Reagent/Resource | Specifications | Application Context | Implementation Considerations |
|---|---|---|---|
| Python scikit-learn | v1.3+ | General machine learning implementation | Standardized API; extensive documentation |
| imbalanced-learn | v0.11+ | specialized resampling techniques | Compatible with scikit-learn ecosystem |
| SHAP Explainability | v0.44+ | Model interpretation and feature importance | Computational intensity for large datasets |
| DHS Dataset | Country-specific waves | Nutrition supplementation studies | Complex sampling design requires weighting |
| Boruta Feature Selection | Python implementation | High-dimensional nutritional epidemiology | Computationally intensive; improves model robustness |
Visualization Framework
Accuracy Paradox Mechanism
Comprehensive Evaluation Workflow
The accuracy paradox presents a formidable challenge in nutrition-related machine learning research, where imbalanced datasets are prevalent and model failures carry significant public health consequences. Through systematic evaluation of experimental evidence and metric performance, this review demonstrates that traditional accuracy provides dangerously misleading assessments of model utility in imbalanced contexts. The adoption of robust evaluation frameworks incorporating F1-score, Matthews Correlation Coefficient, balanced accuracy, and AUPRC—combined with appropriate data balancing techniques—represents an essential methodological advancement for developing nutrition models that deliver genuine predictive value. As machine learning applications in nutritional epidemiology and public health continue to expand, embracing these rigorous validation standards will be crucial for translating algorithmic performance into meaningful health outcomes.
In the field of nutrition research, machine learning (ML) models are increasingly deployed to tackle complex challenges ranging from precision nutrition and disease risk prediction to personalized dietary recommendation systems [1] [31]. The characteristics of high-dimensional, multifactorial data in nutrition make ML particularly suitable for analysis, moving beyond the capabilities of traditional statistical techniques [1]. However, the performance of these models cannot be adequately measured by accuracy alone, especially given the frequent presence of imbalanced datasets where class distributions are skewed—a common scenario when predicting rare nutritional deficiencies or disease conditions [56] [57].
Choosing the appropriate evaluation metric is not merely a technical consideration but a fundamental aspect of validating models that may inform clinical or public health decisions. This guide provides a comprehensive comparison of essential classification metrics—Precision, Recall, F1-Score, and AUC-ROC—within the context of nutrition model validation, complete with experimental data and methodologies to aid researchers in selecting the most appropriate metrics for their specific applications.
Metric Fundamentals and Their Relevance to Nutrition Research
The Building Blocks: From Confusion Matrix to Core Metrics
All classification metrics derive from the confusion matrix, which tabulates prediction results against actual values [58]. The matrix defines four fundamental outcomes:
- True Positives (TP): Cases correctly identified as positive (e.g., correctly identifying individuals with high diabetes risk).
- False Positives (FP): Cases incorrectly identified as positive (e.g., falsely flagging healthy individuals as high-risk).
- True Negatives (TN): Cases correctly identified as negative.
- False Negatives (FN): Cases incorrectly identified as negative (e.g., missing individuals with actual high risk) [59] [58].
In nutrition research, the relative costs of FP and FN errors vary significantly by application. For instance, in screening for severe malnutrition, false negatives (missing cases) are typically more critical than false alarms, whereas in personalized food recommendation systems, false positives (recommending unsuitable foods) might damage user trust and adherence [56] [31].
The Critical Limitation of Accuracy in Nutrition Applications
Accuracy measures the overall correctness of a model, calculated as the proportion of true results (both true positives and true negatives) among the total number of cases examined [60] [58]. While intuitively appealing, accuracy becomes particularly misleading in nutrition research contexts with inherent class imbalances, such as:
- Predicting rare nutritional deficiencies in generally healthy populations
- Identifying food insecurity markers in affluent communities
- Detecting fraudulent food products in supply chains where most products are genuine [56] [57]
In such scenarios, a naive model that always predicts the majority class can achieve high accuracy while failing completely at its intended purpose—a phenomenon known as the "accuracy paradox" [61]. For example, in a dataset where 95% of participants do not have a specific nutritional deficiency, a model that always predicts "no deficiency" will achieve 95% accuracy while being useless for screening purposes [58].
Deep Dive into Key Classification Metrics
Precision: The Measure of Relevance
Precision quantifies the reliability of positive predictions by measuring what percentage of all positive predictions were indeed positive [56] [58]. It answers the question: "When the model predicts a positive outcome, how often is it correct?"
Calculation: Precision = TP / (TP + FP) [59]
High precision is critical in nutrition applications where false positives have significant consequences:
- Personalized recommendation systems: Recommending inappropriate foods to users with allergies or specific dietary restrictions [31]
- Research participant selection: Incorrectly classifying individuals into specific metabolic phenotypes for clinical trials
- Nutrient assessment tools: Misclassifying adequate diets as deficient, leading to unnecessary interventions [56]
Recall: The Measure of Completeness
Recall (also known as sensitivity) measures the model's ability to detect positive cases [56]. It answers the question: "What percentage of all actual positive cases did the model successfully identify?"
Calculation: Recall = TP / (TP + FN) [59]
High recall is essential in nutrition contexts where missing positive cases carries high costs:
- Screening for malnutrition in vulnerable populations
- Early detection of metabolic disorders through dietary patterns
- Identifying individuals at risk for diet-related diseases for preventive interventions [62]
The Precision-Recall Trade-Off in Nutrition Research
In practice, achieving both high precision and high recall simultaneously is challenging, as optimizing for one typically comes at the expense of the other [56]. This fundamental trade-off requires nutrition researchers to carefully consider their specific priorities when selecting and tuning models.
The decision to prioritize precision or recall depends on the research objectives and potential impact of different error types. For example, in a model designed to refer individuals for intensive dietary counseling, high recall would be prioritized to ensure all at-risk cases are captured, accepting some false positives. Conversely, for a personalized recipe recommendation system, high precision would be more important to ensure suggested foods align with user preferences and restrictions [31].
Table 1: Precision vs. Recall Priority in Nutrition Applications
| Nutrition Application | Priority Metric | Rationale |
|---|---|---|
| Screening for severe acute malnutrition | Recall | Missing true cases (false negatives) has serious health consequences |
| Personalized food recommendation system | Precision | False recommendations (false positives) reduce user trust and adherence |
| Dietary assessment tool classification | Balanced | Both incorrect classifications and missed patterns affect data quality |
| Research participant stratification | Context-dependent | Depends on the cost of misclassification versus missing eligible participants |
F1-Score: Balancing Precision and Recall
The F1-Score provides a single metric that balances both precision and recall using the harmonic mean, which penalizes extreme values more than a simple average [60] [61]. This makes it particularly valuable when seeking a balance between false positives and false negatives.
Calculation: F1-Score = 2 × (Precision × Recall) / (Precision + Recall) [59]
The F1-Score is especially useful in nutrition research for:
- Imbalanced dataset scenarios common in nutrition epidemiology
- Model comparison when both type I and type II errors matter
- Optimizing classification thresholds for screening tools where costs of false positives and false negatives are both concerning [60]
For example, in developing a model to identify individuals with poor dietary patterns for targeted interventions, both precision (to efficiently use limited resources) and recall (to reach all at-risk individuals) are important, making F1-Score an appropriate metric [61].
The Receiver Operating Characteristic (ROC) curve visualizes model performance across all possible classification thresholds by plotting the True Positive Rate (Recall) against the False Positive Rate (FPR = FP / (FP + TN)) at various threshold settings [60] [56]. The Area Under the ROC Curve (AUC-ROC) quantifies this overall performance with a single value between 0.5 (random guessing) and 1.0 (perfect discrimination) [60].
AUC-ROC provides several advantages for nutrition research:
- Threshold-independent evaluation of model performance
- Effective for model comparison regardless of class distribution
- Intuitive interpretation: The probability that a randomly chosen positive instance ranks higher than a randomly chosen negative instance [60] [63]
However, AUC-ROC has limitations with highly imbalanced datasets, as the large number of true negatives can make the false positive rate appear artificially favorable [60]. In such cases, the Precision-Recall curve and its corresponding AUC may provide a more informative assessment of model performance focused on the positive class [60].
Comparative Analysis of Metrics in Nutrition Research Contexts
Metric Comparison Table
Table 2: Comprehensive Comparison of Classification Metrics for Nutrition Models
| Metric | Calculation | Strengths | Limitations | Ideal Nutrition Use Cases |
|---|---|---|---|---|
| Accuracy | (TP + TN) / Total [58] | Intuitive; Works well with balanced classes [56] | Misleading with imbalanced data [57] | Initial assessment with representative samples; Macronutrient classification |
| Precision | TP / (TP + FP) [59] | Measures prediction reliability; Minimizes false alarms [56] | Ignores false negatives [56] | Food recommendation systems; Allergy-safe meal planning [31] |
| Recall | TP / (TP + FN) [59] | Captures true positives; Minimizes missed cases [56] | Ignores false positives [56] | Malnutrition screening; At-risk population identification [62] |
| F1-Score | 2 × (Precision × Recall) / (Precision + Recall) [59] | Balanced measure; Robust to class imbalance [60] [61] | Doesn't consider true negatives; Harder to explain [63] | Dietary pattern classification; Balanced screening tools |
| AUC-ROC | Area under ROC curve [60] | Threshold-independent; Good for model comparison [56] [63] | Can be optimistic with imbalance [60] | Model selection; Phenotype discrimination studies |
Experimental Protocol for Metric Evaluation in Nutrition Models
To ensure rigorous evaluation of nutrition ML models, researchers should implement the following experimental protocol:
1. Data Preparation and Stratification
- Partition data using stratified k-fold cross-validation (typically k=5 or 10) to maintain class distribution across splits [62]
- For longitudinal nutrition data, use time-series aware splitting (e.g., forward chaining) to prevent data leakage
- Document prevalence of positive classes to inform metric selection
2. Comprehensive Metric Computation
- Compute all relevant metrics simultaneously using standardized libraries (e.g., scikit-learn)
- Generate ROC curves across multiple thresholds to visualize trade-offs
- Plot Precision-Recall curves especially for imbalanced scenarios
- Calculate confidence intervals via bootstrapping (e.g., 1000 iterations) for all metrics
3. Statistical Comparison and Validation
- Employ DeLong's test for comparing AUC-ROC values between models
- Use McNemar's test for paired classification results at optimal thresholds
- For nutrition-specific validation, conduct subgroup analysis across different demographics, dietary patterns, or clinical characteristics
Case Study: Cardiovascular Disease Prediction Using Food Preference Profiles
A 2025 study developed a cardiovascular disease (CVD) prediction model using food preference data from 61,229 UK Biobank participants, providing a practical illustration of metric application in nutrition research [62]. The study compared three predictor sets (Framingham risk factors, nutrient intake, and food preference profiles) across four ML models, with results demonstrating the utility of different metrics:
Table 3: Performance Metrics from CVD Prediction Study [62]
| Predictor Set | Model | Accuracy | AUC-ROC | PR-AUC |
|---|---|---|---|---|
| Framingham risk factors | Logistic Regression | 0.724-0.727 | Not reported | Not reported |
| Nutrient intake | Linear Discriminant Analysis | 0.722-0.725 | Not reported | Not reported |
| Food Preference Profiles (FPP) | Multiple Models | 0.721-0.725 | Not reported | Not reported |
The FPP set, which included only age, sex, BMI, waist circumference, smoking status, hypertension treatment, and food preference profile (without blood measurements or detailed nutrient intake), demonstrated comparable accuracy to traditional Framingham risk factors [62]. This case highlights how different metrics can provide complementary insights when evaluating nutrition-focused prediction models.
Decision Framework and Research Toolkit
Metric Selection Framework for Nutrition Researchers
Selecting appropriate evaluation metrics requires alignment with research goals, data characteristics, and potential impacts. The following decision framework supports systematic metric selection:
Diagram 1: Metric Selection Guide for Nutrition Models
Essential Computational Tools for Nutrition Model Evaluation
Table 4: Research Reagent Solutions for Nutrition Model Evaluation
| Tool/Resource | Function | Implementation Example | Nutrition Research Application |
|---|---|---|---|
| Scikit-learn Metrics | Calculation of standard metrics | precision_score, recall_score, f1_score, roc_auc_score [60] |
Standardized evaluation across nutrition models |
| MLxtend | Statistical comparison of classifiers | paired_ttest_5x2cv for cross-validation results |
Validating significant improvements in dietary pattern classifiers |
| Yellowbrick | Visualization of metric trade-offs | PrecisionRecallCurve, ROCAUC visualizers |
Communicating model performance to interdisciplinary teams |
| Imbalanced-learn | Handling class imbalance | SMOTE for synthetic minority oversampling |
Addressing rare outcome prediction in nutrition epidemiology |
| Custom Threshold Optimizer | Finding optimal classification cutoff | GridSearchCV with custom scoring [60] |
Tuning screening tools for specific nutrition program needs |
Selecting appropriate evaluation metrics is a critical step in developing robust, validated machine learning models for nutrition research. While accuracy provides an intuitive starting point, its limitations in imbalanced scenarios common in nutrition applications necessitate more nuanced approaches. Precision becomes paramount when false recommendations carry significant costs, while recall is essential for screening applications where missing true cases has serious consequences. The F1-Score offers a balanced perspective when both error types matter, and AUC-ROC provides comprehensive threshold-independent assessment of model discrimination capability.
The optimal metric choice depends fundamentally on the specific research question, data characteristics, and potential impact of different error types in the target application. By applying the structured decision framework and experimental protocols outlined in this guide, nutrition researchers can enhance the rigor, interpretability, and practical utility of their machine learning models, ultimately advancing the field's capacity to address complex nutritional challenges through data-driven approaches.
Optimizing Hyperparameters and Implementing Cross-Validation Strategies
In the field of nutrition research, machine learning (ML) models are increasingly being deployed to tackle complex challenges ranging from predicting disease outcomes based on dietary patterns to identifying malnutrition risk in clinical settings [1]. The predictive performance of these models hinges critically on two foundational practices: robust hyperparameter optimization and rigorous cross-validation. These processes ensure that models are both accurately tuned to capture underlying patterns in nutritional data and capable of generalizing effectively to new, unseen data [64] [65].
Without proper validation strategies, nutrition risk prediction models can produce optimistically biased performance estimates, leading to unreliable tools for clinical or public health decision-making [65]. This guide provides a comprehensive comparison of hyperparameter optimization techniques and cross-validation strategies, contextualized within nutrition research, to empower researchers in selecting the most appropriate methodologies for their specific predictive modeling tasks.
Cross-Validation Strategies for Robust Model Evaluation
Cross-validation (CV) is a fundamental technique for assessing the generalization capability of a machine learning model by partitioning the available data into training and testing sets multiple times [64]. In nutrition research, where datasets may be limited or contain complex interactions, selecting an appropriate CV strategy is crucial for obtaining realistic performance estimates.
Core Cross-Validation Techniques
K-Fold Cross-Validation: The dataset is randomly partitioned into k folds of approximately equal size. The model is trained k times, each time using k-1 folds for training and the remaining fold for testing. This method provides a robust estimate of model performance but can be computationally expensive for large models or datasets [64].
Stratified K-Fold Cross-Validation: This extension of K-Fold CV maintains the same class distribution in each fold as in the complete dataset. It is particularly valuable in nutrition research with imbalanced outcomes, such as when predicting rare nutritional deficiencies or conditions where the positive class is underrepresented [64].
Holdout Method: The simplest approach splits the dataset into a single training set and a single testing set, typically using a 70/30 or 80/20 ratio. While computationally efficient, this method may produce unstable performance estimates if the single test set is not representative of the overall data distribution [64].
The following diagram illustrates the workflow for integrating cross-validation with hyperparameter tuning, specifically showing how nested cross-validation prevents overfitting by separating model selection from performance estimation:
Figure 1: Nested cross-validation workflow separating model selection from evaluation.
Advanced Technique: Nested Cross-Validation
For hyperparameter tuning and model evaluation without overfitting, nested cross-validation provides a robust solution. This method employs two layers of cross-validation: an inner loop for parameter search and an outer loop for performance estimation [64]. This approach is particularly valuable in nutrition research where unbiased performance estimation is critical for clinical applicability.
Hyperparameter Optimization Techniques: A Comparative Analysis
Hyperparameter optimization is the systematic process of finding the optimal combination of hyperparameters that control the learning process of an ML algorithm. The table below summarizes the key characteristics of major optimization techniques:
Table 1: Comparison of Hyperparameter Optimization Techniques
| Technique | Core Mechanism | Computational Efficiency | Best Suited Scenarios | Key Nutrition Research Example |
|---|---|---|---|---|
| Grid Search | Exhaustively searches all combinations in a predefined parameter grid [66] | Low; becomes infeasible with many parameters [66] | Small parameter spaces with discrete values | Tuning Random Forest for COVID-19 mortality prediction [67] |
| Random Search | Randomly samples parameter combinations from distributions [66] | Moderate; more efficient than grid search for large spaces [66] | High-dimensional parameter spaces with both continuous and discrete parameters | General nutrition prediction models with multiple hyperparameters [68] |
| Bayesian Optimization | Builds probabilistic model of objective function to guide search [69] [68] | High; focuses evaluations on promising regions [68] | Expensive-to-evaluate functions with complex parameter interactions | Comparing Bayesian vs. Hyperopt for RandomForestClassifier [69] |
| Hyperopt | Uses Tree Parzen Estimator for sequential model-based optimization [68] | High; handles complex search spaces with conditional parameters [68] | Awkward search spaces with real, discrete, and conditional dimensions | Large-scale nutrition models with hundreds of hyperparameters [68] |
The selection of an appropriate optimization technique involves trade-offs between computational efficiency, implementation complexity, and search effectiveness. For nutrition researchers, these trade-offs should be considered in the context of their specific dataset size, model complexity, and computational resources.
Experimental Protocols in Nutrition Research
Case Study 1: Predicting COVID-19 Mortality from Nutritional Factors
A 2025 study investigated the relationship between dietary factors and COVID-19 mortality using multiple machine learning models [67]. The research provides a robust example of hyperparameter optimization in nutritional epidemiology.
Dataset: COVID-19 nutrition dataset with 4 key attributes: fat percentage, caloric consumption (kcal), food supply amount (kg), and protein levels across various dietary categories [67].
Models Compared: Gradient Boosting Regressor (GBR), Random Forest (RF), Lasso Regression, Decision Tree (DT), and Bayesian Ridge (BR) [67].
Optimization Protocol: Grid Search hyperparameter optimization was applied to the GBR model, which had shown the best baseline performance. The optimization process systematically explored combinations of learning rate, maximum depth, number of estimators, and minimum samples split [67].
Performance Metrics: The models were evaluated using Mean Squared Error (MSE), Mean Absolute Error (MAE), Mean Absolute Percentage Error (MAPE), and R² scores [67].
Results: The Grid Search-optimized GBR model achieved a remarkable improvement in performance, increasing the R² value from 96.3% to 99.4%, demonstrating the significant impact of systematic hyperparameter tuning in nutrition-related prediction tasks [67].
Case Study 2: Early Prediction of Malnutrition in Critically Ill Patients
A 2025 prospective observational study developed and externally validated ML models for predicting malnutrition within 24 hours of intensive care unit (ICU) admission [32]. This study exemplifies rigorous validation practices in clinical nutrition research.
Dataset: 1006 critically ill adult patients for model development, with an additional 300 patients for external validation. Predictors included clinical variables, laboratory values, and nutritional risk scores [32].
Models Compared: Seven machine learning models were evaluated: Extreme Gradient Boosting (XGBoost), Random Forest, Decision Tree, Support Vector Machine (SVM), Gaussian Naive Bayes, k-Nearest Neighbor (k-NN), and Logistic Regression [32].
Optimization Protocol: Hyperparameters were optimized via 5-fold cross-validation on the training set, which represented 80% of the development data. This approach eliminated the need for a separate validation set while ensuring internal validation [32].
Performance Metrics: Models were evaluated using accuracy, precision, recall, F1 score, Area Under the Receiver Operating Characteristic Curve (AUC-ROC), and Area Under the Precision-Recall Curve (AUC-PR) [32].
Results: The XGBoost model achieved superior performance with an accuracy of 0.90 and AUC-ROC of 0.98 in the testing set. External validation confirmed robust performance with an accuracy of 0.75 and AUC-ROC of 0.88, demonstrating the model's generalizability to new patient populations [32].
The following workflow illustrates the comprehensive model development and validation process used in this malnutrition prediction study:
Figure 2: Model development and validation workflow for malnutrition prediction.
Successful implementation of hyperparameter optimization and cross-validation in nutrition research requires both computational tools and methodological frameworks. The following table catalogs essential resources referenced in recent literature:
Table 2: Research Reagent Solutions for Nutrition ML Studies
| Tool/Category | Specific Examples | Functionality | Implementation in Nutrition Research |
|---|---|---|---|
| Hyperparameter Optimization Libraries | Ray Tune, Optuna, Hyperopt [68] | Provides advanced algorithms for efficient parameter search | Bayesian optimization for RandomForest on Wine dataset [69] |
| Model Validation Frameworks | Scikit-learn GridSearchCV, RandomizedSearchCV [64] [66] | Integrated cross-validation with hyperparameter tuning | 5-fold CV for malnutrition prediction model [32] |
| Performance Metrics | AUC-ROC, AUC-PR, F1-score, R², MSE [67] [32] | Quantifies model predictive performance | Comprehensive evaluation of XGBoost for malnutrition risk [32] |
| Interpretability Tools | SHAP (SHapley Additive exPlanations) [32] | Explains model predictions and feature importance | Quantifying feature contributions in malnutrition prediction [32] |
The comparative analysis presented in this guide demonstrates that the selection of hyperparameter optimization and cross-validation strategies should be guided by specific research contexts within nutrition science. For high-stakes clinical predictions, such as malnutrition risk in ICU patients, rigorous nested cross-validation with Bayesian optimization provides the most reliable approach [32]. For exploratory analysis of dietary patterns and health outcomes, simpler holdout validation with random search may offer a practical balance between reliability and computational efficiency [67].
The experimental evidence from recent nutrition research consistently shows that systematic hyperparameter optimization can improve model performance by 3-10% on key metrics [67] [32]. Furthermore, external validation remains essential for verifying model generalizability across diverse populations and settings, a particularly crucial consideration in global nutrition research where dietary patterns and physiological responses vary significantly across regions and ethnic groups [32] [65].
As machine learning continues to advance nutritional science, adherence to robust validation practices will ensure that predictive models translate effectively into tools that improve human health through personalized nutrition interventions and public health strategies.
Addressing Data Imbalances and Ensuring Model Fairness to Mitigate Bias
The application of machine learning (ML) in nutrition research is rapidly advancing, powering everything from personalized dietary recommendations to risk prediction models for clinical nutrition [70] [71]. However, the data-driven nature of these models makes them susceptible to inheriting and even amplifying biases present in the data, leading to ethically problematic and unreliable predictions [71] [72]. Failure to use careful and well-thought-out modeling processes can lead to misleading conclusions and significant concerns surrounding ethics and bias [71]. In critical domains like nutrition and health, where model decisions can impact patient outcomes, ensuring fairness is not just a technical challenge but a societal imperative [72].
Biases in ML models often manifest from imbalances in datasets. Class imbalance occurs when one category (e.g., patients with a specific condition) is outnumbered by another, while group imbalance involves the underrepresentation of specific demographic groups based on protected attributes like race or gender [73]. These imbalances can coincide, leading to models that are both inaccurate and unfair. For instance, a model for predicting enteral nutrition feeding intolerance (ENFI) in Intensive Care Unit (ICU) patients might perform poorly for underrepresented demographic groups if the training data is skewed [70]. This article provides a comparative analysis of strategies and tools to mitigate these issues, with a specific focus on their application in nutrition research.
Understanding Bias: Typology and Consequences
Bias can infiltrate an ML model at various stages of its lifecycle. Understanding its origins is the first step toward effective mitigation. The following table summarizes common types of bias encountered in machine learning.
Table 1: Types of Bias in Machine Learning
| Bias Type | Description | Potential Impact in Nutrition Research |
|---|---|---|
| Historical Bias [72] | Arises from pre-existing inequalities and prejudices in societal data. | Historical disparities in healthcare access could skew data on nutritional diseases. |
| Representation Bias [72] | Occurs when training data does not accurately represent the target population. | A model trained primarily on urban populations may fail for rural communities. |
| Measurement Bias [72] [74] | Stems from inaccuracies or flawed proxies in data measurement. | Reliance on self-reported energy intake, a known unreliable measure [71]. |
| Selection Bias [74] | Results from a non-representative sample of the population. | Recruiting participants primarily from a single hospital or clinic system. |
| Algorithmic Bias [74] | Arises from choices in algorithm design, such as feature selection. | A model optimized solely for accuracy may overlook fairness across subgroups. |
| Aggregation Bias [72] | Results from applying a one-size-fits-all model to a diverse population. | A single nutritional recommendation model that ignores genetic or cultural differences. |
The consequences of biased models are far-reaching. They can lead to discriminatory outcomes, reinforce harmful stereotypes, cause a loss of trust in AI systems, and have serious legal and ethical implications for the organizations that deploy them [72]. In nutrition, this could translate to inaccurate diagnoses for underrepresented populations or ineffective personalized nutrition plans [74].
A Framework for Bias Mitigation: Techniques and Comparisons
Mitigation strategies can be categorized based on the stage of the ML pipeline at which they are applied. The following workflow illustrates the stages and the primary techniques associated with each.
Comparative Analysis of Mitigation Techniques
The table below provides a detailed comparison of the primary mitigation techniques, highlighting their mechanisms, advantages, and challenges.
Table 2: Comparison of Bias Mitigation Techniques
| Technique | Stage | Mechanism | Key Advantages | Key Challenges |
|---|---|---|---|---|
| Reweighing [75] | Pre-processing | Assigns weights to training instances to balance representation across groups. | Simple to implement; model-agnostic. | May not handle complex, non-linear biases. |
| Synthetic Data Generation [73] | Pre-processing | Uses generative models (e.g., GANs, VAEs) to create artificial samples for underrepresented classes/groups. | Addresses data scarcity; can improve both utility and fairness. | Risk of generating unrealistic data; computational cost. |
| Adversarial Debiasing [76] [72] | In-processing | Uses an adversary network to penalize the model for predictions that reveal sensitive attributes. | Can produce representations invariant to protected attributes. | Complex training setup; can be computationally intensive. |
| MinDiff [77] | In-processing | Adds a penalty to the loss function for differences in prediction distributions between groups. | Directly optimizes for similar distributions; offered in libraries like TensorFlow. | Requires careful tuning of the penalty parameter. |
| Rejection Option-based Classification (ROBC) [75] | Post-processing | Changes predicted labels for instances where model prediction uncertainty is highest (near the decision threshold). | Applied post-training; no need to retrain model. | Only affects predictions near the threshold. |
Experimental Protocols and Performance in Nutrition Research
Case Study: Predicting Enteral Nutrition Feeding Intolerance (ENFI)
A 2025 study developed a risk prediction model for ENFI in ICU patients, providing a robust example of comparing multiple ML models in a clinical nutrition setting [70].
Methodology:
- Data: 487 ICU patients from a tertiary hospital were randomly split into training (80%) and test (20%) sets.
- Models: Three algorithms were constructed and compared: Logistic Regression (LR), Support Vector Machine (SVM), and Random Forest (RF).
- Evaluation Metrics: Models were evaluated using the Area Under the ROC Curve (AUC), accuracy, precision, recall, and F1-score.
Table 3: Experimental Performance of ML Models for ENFI Prediction
| Model | AUC | Accuracy | Precision | Recall | F1-Score |
|---|---|---|---|---|---|
| Logistic Regression (LR) | 0.9308 | 94.3% | 95.4% | 88.6% | 0.9185 |
| Support Vector Machine (SVM) | 0.9241 | 94.1% | 96.8% | 86.4% | 0.9132 |
| Random Forest (RF) | 0.9511 | 96.1% | 97.7% | 91.4% | 0.9446 |
Conclusion: The Random Forest model demonstrated superior predictive performance across all metrics, highlighting its effectiveness for this specific clinical nutrition prediction task [70]. This comparative approach is a best practice for ensuring robust model selection.
Protocol for Synthetic Data Generation for Fairness
A 2024 study explored using synthetic data to tackle class and group imbalances, providing a generalizable experimental protocol [73].
Methodology:
- Generative Model Selection: Choose one or more generative models (e.g., Gaussian Copula, Generative Adversarial Networks (GANs), Variational Autoencoders (VAEs), SMOTE).
- Sampling Strategy: Define a strategy for generating new data:
- Class Balance: Aims for an equal number of samples for each target class.
- Group Balance: Aims for equal representation of protected groups (e.g., race, gender).
- Combined: Aims to achieve both class and group balance simultaneously.
- Model Training & Evaluation: Train the target ML model on the original and synthetically augmented datasets. Evaluate using:
- Utility Metrics: Accuracy, ROC AUC.
- Fairness Metrics: Statistical parity, equal opportunity, etc., to assess improvements in fairness across groups.
The Researcher's Toolkit: Metrics and Software for Fair ML
Key Fairness Metrics
To assess whether bias mitigation techniques are effective, researchers must employ quantitative fairness metrics. Different metrics answer different fairness questions, and the choice depends on the context and legal or ethical requirements [76] [78].
Table 4: Key Fairness Metrics for Model Evaluation
| Metric | Description | Use Case Interpretation |
|---|---|---|
| Demographic Parity [76] [75] | Ensures similar rates of favorable predictions across different demographic groups. | The probability of being approved for a nutritional intervention program is similar for different racial groups. |
| Equalized Odds [76] [78] | Ensures that model error rates (true positive and false positive rates) are similar across groups. | A model predicting diabetes risk from nutrition data is equally accurate for both men and women. |
| Predictive Value Parity [75] | Ensures the probability of a correct prediction is similar across groups (e.g., Positive Predictive Value). | If a model flags a patient as high-risk for malnutrition, the probability that this is correct should be the same across age groups. |
Essential Research Reagents and Tools
The following table details key software tools and libraries that are essential for implementing fairness-aware machine learning.
Table 5: Research Reagent Solutions for Fairness-Aware ML
| Tool / Library | Function | Key Features |
|---|---|---|
| AIF360 [78] | A comprehensive open-source toolkit for measuring and mitigating bias. | Contains metrics and algorithms for all mitigation stages (pre-, in-, post-processing). |
| FairLearn [78] [77] | A Python package to assess and improve fairness of AI systems. | Includes metrics and mitigation algorithms, such as grid search for fairer models. |
| TensorFlow Model Remediation [77] | A library for mitigating bias in TensorFlow models. | Provides in-processing techniques like MinDiff for use during model training. |
| DataRobot Bias & Fairness [75] | An integrated feature in a commercial AutoML platform. | Automates fairness testing and mitigation (pre- and post-processing) for top models. |
| Aequitas [78] | An open-source bias and fairness audit toolkit. | Provides a comprehensive report on model fairness across multiple protected attributes. |
Addressing data imbalances and ensuring model fairness is a critical, multi-faceted endeavor in nutrition research. As demonstrated, there is no single "best" solution; rather, a careful, iterative process is required. This involves selecting appropriate mitigation techniques (pre-, in-, or post-processing) based on the context, rigorously comparing multiple models using both utility and fairness metrics, and leveraging specialized tools to audit and remediate bias. The integration of advanced methods like synthetic data generation shows particular promise for tackling the root cause of bias in datasets [73]. By embedding these practices into the ML lifecycle, nutrition researchers can develop models that are not only powerful and predictive but also equitable, transparent, and trustworthy, thereby upholding the highest ethical standards in scientific research.
Ensuring Real-World Reliability: Rigorous Validation and Benchmarking
In the scientific method, validation is the critical process that separates hypothetical concepts from reliable, usable knowledge. For researchers, scientists, and drug development professionals, particularly those working with nutrition-related machine learning models, a deep understanding of validation types is non-negotiable for producing credible results. Internal and external validity represent two foundational pillars upon which the trustworthiness of any predictive model is built [79]. Internal validity addresses a fundamental question: "Can we confidently attribute changes in the outcome to our intervention or model, ruling out other explanations?" [80] [79]. It is the extent to which a study's design and methods allow for causal inferences about the relationship between an intervention and its outcomes [80].
In machine learning for nutrition research, internal validation provides the first check on model performance, but it is external validation that ultimately determines a model's real-world utility. External validity examines how well findings generalize beyond the immediate study conditions to other populations, settings, or time periods [79] [81]. The tension between these two validation types often presents researchers with difficult trade-offs; highly controlled conditions that maximize internal validity may limit practical generalizability [79]. This guide provides a comprehensive comparison of internal versus external validation, framing them not as opposites but as complementary components of rigorous scientific inquiry in computational nutrition science.
Conceptual Foundations: Defining the Validation Landscape
Internal Validity: Establishing Causal Truth
Internal validity is primarily concerned with establishing truth within a specific study context. It requires satisfying three key criteria: (1) the "cause" precedes the "effect" in time (temporal precedence), (2) the "cause" and "effect" tend to occur together (covariation), and (3) there are no plausible alternative explanations for the observed covariation (nonspuriousness) [79]. In experimental nutrition research, this might involve demonstrating that a specific nutrient intervention directly causes metabolic changes rather than other uncontrolled factors.
The THIS MESS mnemonic helps researchers remember key threats to internal validity [79]:
- Testing: Effects from repeated testing
- History: External events influencing outcomes
- Instrument change: Changes in measurement tools
- Statistical regression: Extreme scores regressing toward mean
- Maturation: Natural changes in subjects over time
- Experimental mortality: Differential subject attrition
- Selection: Biases in group assignment
- Selection interaction: Interaction between selection and other factors
External Validity: Establishing Generalizable Truth
Where internal validity focuses on causal accuracy within a study, external validity addresses the broader applicability of those findings. For nutrition machine learning models, this translates to whether a model predicting malnutrition in one specific hospital population will perform equally well in different hospitals, geographic regions, or demographic groups [81]. External validity is not merely about replicating results in different populations, but understanding how and why effects transport across contexts.
The relationship between internal and external validity often involves trade-offs [79]. Highly controlled experimental conditions that maximize internal validity—such as studying nutrient absorption in carefully standardized laboratory conditions—may create artificial environments that limit real-world applicability. Conversely, observational studies conducted in diverse real-world settings may have stronger external validity but struggle to establish definitive causal relationships due to confounding factors.
The Validation Spectrum in Machine Learning
In nutrition-related machine learning, the validation continuum extends beyond traditional research definitions. The process typically flows from internal validation toward progressively more rigorous external testing [81]:
Figure 1: The Machine Learning Validation Continuum
Experimental Evidence: A Case Study in Malnutrition Prediction
A 2025 prospective observational study on machine learning models for predicting malnutrition in critically ill patients provides a robust case study comparing internal and external validation performance [32]. The study developed and validated multiple machine learning models to predict malnutrition risk within 24 hours of intensive care unit (ICU) admission, ultimately creating a web-based prediction tool for clinical decision support.
The research followed a rigorous methodology [32]:
- Participants: 1,006 critically ill adult patients for model development; 300 additional patients for external validation
- Data Collection: Comprehensive variables including demographics, disease status, clinical scores (APACHE II, SOFA, GCS, NRS 2002), and laboratory values
- Model Development: Seven machine learning algorithms trained and compared: XGBoost, Random Forest, Decision Tree, Support Vector Machine, Gaussian Naive Bayes, k-Nearest Neighbors, and Logistic Regression
- Validation Approach: Internal validation via 5-fold cross-validation; external validation on completely separate patient cohort from different ICUs
Comparative Performance Results
The study demonstrated notable differences between internal and external validation performance across all model types [32]:
Table 1: Internal vs. External Validation Performance of Malnutrition Prediction Models
| Model | Internal Validation AUC-ROC (95% CI) | External Validation AUC-ROC (95% CI) | Performance Drop |
|---|---|---|---|
| XGBoost | 0.98 (0.96–0.99) | 0.88 (0.86–0.91) | -10.2% |
| Random Forest | 0.96 (0.94–0.98) | 0.85 (0.82–0.88) | -11.5% |
| Logistic Regression | 0.92 (0.89–0.95) | 0.81 (0.78–0.84) | -11.0% |
| Support Vector Machine | 0.94 (0.91–0.97) | 0.83 (0.80–0.86) | -11.7% |
Table 2: Comprehensive Metric Comparison for Best-Performing Model (XGBoost)
| Metric | Internal Validation | External Validation | Absolute Change |
|---|---|---|---|
| Accuracy | 0.90 (0.86–0.94) | 0.75 (0.70–0.79) | -0.15 |
| Precision | 0.92 (0.88–0.95) | 0.79 (0.75–0.83) | -0.13 |
| Recall | 0.92 (0.89–0.95) | 0.75 (0.70–0.79) | -0.17 |
| F1 Score | 0.92 (0.89–0.95) | 0.74 (0.69–0.78) | -0.18 |
| AUC-PR | 0.97 (0.95–0.99) | 0.77 (0.73–0.80) | -0.20 |
The performance decrease observed during external validation highlights the optimism bias inherent in internal validation results and underscores why external validation is essential for assessing real-world model utility [32] [81].
Methodological Protocols: Implementing Comprehensive Validation
Internal Validation Techniques
Internal validation methods provide the initial assessment of model performance and help prevent overfitting. The malnutrition prediction study employed 5-fold cross-validation, but several other established techniques exist [81]:
Table 3: Internal Validation Methods for Nutrition Machine Learning Models
| Method | Protocol | Best Use Cases | Advantages | Limitations |
|---|---|---|---|---|
| K-Fold Cross-Validation | Randomly split data into K folds; iteratively use K-1 folds for training and 1 for validation | Medium to large datasets (>500 samples) | Reduces variance of performance estimate | Computationally intensive |
| Bootstrap Validation | Repeatedly sample with replacement from original dataset | Small to medium datasets | Provides confidence intervals for performance | Can be overly optimistic |
| Split-Sample Validation | Single split into training and testing sets (typically 70/30 or 80/20) | Very large datasets (>10,000 samples) | Computationally efficient | High variance in performance estimates |
| Nested Cross-Validation | Outer loop for performance estimation, inner loop for hyperparameter tuning | Complex models with extensive hyperparameter tuning | Unbiased performance estimation | Computationally very intensive |
For most nutrition-related machine learning applications, bootstrap validation is generally preferred over simple split-sample approaches, particularly for smaller sample sizes common in clinical nutrition research [81]. Split-sample approaches are only recommended when sample sizes are very large, as they "only work when not needed" in smaller samples [81].
External Validation Strategies
External validation tests model performance on completely separate data, providing the truest assessment of real-world applicability [81]:
Figure 2: External Validation Hierarchy
The most rigorous form of external validation involves fully independent validation conducted by different research teams using entirely separate datasets [81]. This approach minimizes potential biases introduced during model development and provides the strongest evidence of generalizability.
Internal-External Cross-Validation: A Balanced Approach
A recommended intermediate approach is internal-external cross-validation, which provides a more realistic assessment of external validity during model development [81]. This method involves:
- Splitting data by natural groupings (e.g., different hospitals, geographic regions, or time periods)
- Iteratively holding out one entire group for validation while training on the remaining groups
- Repeating until each group has served as the validation set
- Developing the final model on the complete dataset
This approach offers a more honest assessment of how a model might perform in new settings while still utilizing all available data for the final model construction [81].
Table 4: Essential Research Reagents and Computational Tools for Validation Studies
| Tool/Resource | Function | Application in Validation | Examples/Specifications |
|---|---|---|---|
| Statistical Software | Model development and validation | Implementing validation protocols | R, Python, SAS, STATA |
| Validation Frameworks | Standardized validation pipelines | Ensuring consistent methodology | Scikit-learn, CARET, MLR3 |
| Gold Standard Reference | Definitive outcome measurement | Criterion validity assessment | ESPEN/ASPEN nutrition criteria [32] |
| Data Splitting Algorithms | Reproducible data partitioning | Creating training/validation sets | Stratified sampling, time-series splitting |
| Performance Metrics | Quantitative performance assessment | Model evaluation and comparison | AUC-ROC, calibration, Brier score |
| Feature Selection Tools | Identifying relevant predictors | Optimizing model generalizability | Recursive feature elimination, LASSO |
| Clinical Data Repositories | External validation datasets | Testing model transportability | MIMIC, eICU, institution-specific databases |
Critical Considerations and Best Practices
Addressing Threats to Validity
Several specific threats require particular attention in nutrition machine learning research:
Selection bias occurs when treatment and control groups differ in observed or unobserved characteristics [80]. Mitigation strategies include randomization (most effective), matching, stratification, and regression analysis to control for observed differences [80].
Instrumentation and measurement errors can arise from flawed or biased measurement tools [80]. Prevention strategies include using validated measures, pilot testing, training data collectors, and employing multiple measures for triangulation [80].
Spectrum bias may occur when validation datasets do not represent the full spectrum of disease severity or patient characteristics present in real-world populations [82]. This can be addressed through broad inclusion criteria and multi-site validation.
Implementing a Comprehensive Validation Framework
Based on the evidence and methodologies discussed, researchers should implement a tiered validation approach:
Begin with rigorous internal validation using bootstrapping or cross-validation to establish baseline performance and identify potential overfitting [81].
Progress to internal-external validation using natural data splits to estimate performance in slightly different populations [81].
Conduct temporal validation using the most recent data to assess performance decay over time [81].
Seek fully independent external validation through collaboration with researchers at different institutions using distinct datasets [81].
Document all validation results transparently, including confidence intervals and performance metrics across different patient subgroups [32].
This comprehensive approach ensures that nutrition machine learning models deliver both accurate predictions in their development context and maintain performance when deployed in real-world clinical settings.
Internal and external validation serve complementary roles in the development of robust, clinically useful nutrition machine learning models. While internal validation provides the initial check on model performance and helps refine algorithms, external validation remains the ultimate test of real-world utility. The case study in malnutrition prediction demonstrates that even models with exceptional internal performance (AUC-ROC: 0.98) can experience substantial decreases in external settings (AUC-ROC: 0.88) [32].
Researchers must resist the temptation to prioritize one form of validation over the other. Rather, a comprehensive validation strategy that progresses from internal checks to increasingly rigorous external testing represents the gold standard for predictive model development. This approach is particularly crucial in nutrition research, where models increasingly inform clinical decision-making and resource allocation. By implementing the methodologies and frameworks outlined in this guide, researchers can develop models that not only achieve statistical excellence but also deliver meaningful impact across diverse healthcare settings.
The integration of machine learning (ML) into nutrition science represents a paradigm shift in how researchers analyze complex dietary patterns, predict nutritional outcomes, and personalize interventions. However, the adoption of these "black box" algorithms necessitates rigorous benchmarking against established traditional statistical methods to validate their utility and reliability. In nutrition research, where findings directly impact public health policies and clinical practices, this validation is not merely academic—it ensures that enhanced predictive accuracy does not come at the cost of interpretability or clinical relevance [21] [83].
This comparison guide objectively evaluates the performance of ML models against traditional statistical baselines across key nutritional applications. We present experimental data, detailed methodologies, and analytical frameworks to help researchers and drug development professionals make evidence-based decisions about model selection for their specific nutritional contexts.
Performance Comparison: ML Models vs. Traditional Statistical Baselines
Quantitative Performance Metrics Across Nutrition Applications
Table 1: Comparative performance of ML and traditional models in nutrition prediction tasks
| Application Area | Machine Learning Model | Traditional Statistical Model | Performance Metric | ML Performance | Traditional Model Performance | Reference |
|---|---|---|---|---|---|---|
| Enteral Nutrition Intolerance Risk Prediction | Random Forest | Logistic Regression | AUC (Area Under Curve) | 0.9511 | 0.9308 | [70] |
| Accuracy | 96.1% | 94.3% | [70] | |||
| F1-Score | 0.9446 | 0.9185 | [70] | |||
| Cardiovascular Risk Factor Prediction | LASSO | Principal Component Analysis (PCA) + Linear Regression | Adjusted R² (Triglycerides) | 0.861 | 0.163 | [84] |
| Adjusted R² (LDL Cholesterol) | 0.899 | 0.005 | [84] | |||
| Adjusted R² (HDL Cholesterol) | 0.890 | 0.235 | [84] | |||
| Adjusted R² (Total Cholesterol) | 0.935 | 0.024 | [84] | |||
| Micronutrient Profile Prediction after Cooking | Multiple Regressors | Retention Factor (RF) Baseline | Average Error Reduction | 31% lower error | Baseline | [85] |
| Food Image Nutrition Analysis | Context-Aware LMMs (with metadata) | Standard LMMs (images only) | Mean Absolute Error (MAE) | Significant reduction | Higher MAE | [86] |
Key Insights from Performance Data
The quantitative data reveals several important patterns. Machine learning models, particularly ensemble methods like Random Forest and regularized algorithms like LASSO, consistently demonstrate superior predictive performance across diverse nutrition applications [70] [84]. The dramatic improvement in adjusted R² values for cardiovascular risk prediction highlights ML's ability to capture complex, non-linear relationships in dietary data that traditional linear models miss [84].
In clinical nutrition settings, even modest improvements in predictive accuracy (e.g., 1-2% in AUC and accuracy for enteral nutrition intolerance) can translate to significant clinical impacts when applied at scale [70]. Furthermore, the incorporation of contextual metadata—such as meal timing and location information—significantly enhances the performance of large multimodal models for nutrition analysis from food images, reducing mean absolute error in calorie and nutrient estimation [86].
Experimental Protocols and Methodologies
Protocol 1: Predicting Enteral Nutrition Feeding Intolerance (ENFI) in ICU Patients
Table 2: Key methodological details for ENFI risk prediction study
| Aspect | Description |
|---|---|
| Study Population | 487 ICU patients from a tertiary hospital (Jan 2021-Dec 2023) |
| Data Splitting | Random 8:2 ratio (training set: test set) |
| ML Algorithms | Logistic Regression (LR), Support Vector Machine (SVM), Random Forest (RF) |
| Model Validation | 10-fold cross-validation |
| Performance Metrics | AUC, Accuracy, Precision, Recall, F1-Score |
| Outcome Definition | Failure to achieve target caloric intake within 72 hours OR suspension of enteral nutrition due to GI symptoms |
The study employed a rigorous retrospective design with comprehensive inclusion/exclusion criteria. Patients were selected from ICU admissions receiving enteral nutrition within 48 hours, excluding those with pre-existing gastrointestinal conditions. The researchers identified 26 potential risk factors through systematic literature review and expert consultation, including clinical biomarkers, intervention-related variables, and demographic factors [70].
Data preprocessing addressed missing values using random forest imputation for variables with <50% missingness. The models were built using Python 3.9, with hyperparameter tuning optimized for each algorithm. The Random Forest model achieved the best performance with an AUC of 0.9511, outperforming both Logistic Regression (AUC=0.9308) and Support Vector Machine (AUC=0.9241) [70].
Figure 1: Experimental workflow for ENFI risk prediction model development and validation
Protocol 2: Predicting Micronutrient Profiles in Cooked Foods
Table 3: Methodological framework for nutrient prediction after cooking
| Aspect | Description |
|---|---|
| Data Source | USDA Standard Reference (SR) Legacy Dataset (7,793 foods) |
| Data Selection | 820 single-ingredient raw/cooked food pairs |
| Cooking Methods | Wet heat (boiling, steaming), Dry heat (roasting, grilling, broiling) |
| Target Nutrients | 7 vitamins and 7 minerals |
| Baseline Method | Retention Factor (RF) approach |
| ML Approach | Multiple regressors per nutrient and process |
| Evaluation | Correlation (R²) between actual and predicted values |
This study addressed the fundamental challenge of predicting how food processing alters nutritional composition. The researchers curated a specialized dataset from the USDA Standard Reference database, carefully matching raw and cooked food pairs for single-ingredient foods. The ML models were trained to predict post-processing micronutrient content from raw food composition data, significantly outperforming the traditional retention factor method with an average error reduction of 31% across all foods, processes, and nutrients [85].
The methodology accounted for inherent data biases, particularly missing yield factors, through strategic data scaling approaches. The models demonstrated varying performance across food categories, with leafy greens and beef cuts identified as the most predictable plant-based and animal-based foods, respectively [85].
Protocol 3: Dietary Pattern Analysis for Cardiovascular Risk Prediction
This innovative study compared a machine learning approach (LASSO) against traditional dietary pattern analysis (Principal Component Analysis with linear regression) for predicting cardiovascular disease risk factors. Using data from NHANES 2005-2006 (n=2,609), researchers transformed Food Frequency Questionnaire data into 35 food groups representing major dietary components in the US population [84].
The LASSO model employed L1 regularization to shrink less important coefficients to zero, effectively performing automatic feature selection while maintaining model interpretability. The traditional approach used PCA to derive 10 principal components accounting for 65% of variance in the dataset, which were then used in linear regression models. LASSO dramatically outperformed the PCA-based approach across all lipid biomarkers, particularly for LDL cholesterol (adjusted R²: 0.899 vs. 0.005) and total cholesterol (adjusted R²: 0.935 vs. 0.024) [84].
Figure 2: Methodological comparison between traditional and ML approaches for dietary pattern analysis
Table 4: Key research reagents and computational tools for nutrition ML research
| Tool/Resource | Type | Function in Nutrition Research | Example Applications |
|---|---|---|---|
| ACETADA Dataset [86] | Specialized Dataset | Food image dataset with verified nutrition information for multimodal model training | LMM evaluation for nutrition analysis from meal images |
| USDA FoodData Central [85] | Comprehensive Database | Provides analytical food composition data for model training and validation | Predicting nutrient changes during cooking processes |
| NHANES Dietary Data [84] | Population-Level Data | Nationally representative dietary intake data with health measures | Dietary pattern analysis and disease risk prediction |
| Python Scikit-learn [70] | ML Library | Provides implementation of classification and regression algorithms | Building risk prediction models for clinical nutrition |
| R glmnet Package [84] | Statistical Package | Implementation of regularized regression models (LASSO) | High-dimensional dietary pattern analysis |
| TensorFlow/PyTorch [87] | Deep Learning Frameworks | Building complex neural network architectures | Food image recognition and analysis |
| BitterDB/FlavorDB [85] | Specialized Databases | Curated data on compound sensory properties | Predicting sensory attributes from chemical structures |
Critical Considerations for Model Validation in Nutrition Research
Addressing Overfitting and Validity Shrinkage
A fundamental challenge in nutritional predictive modeling is validity shrinkage—the reduction in predictive performance when a model derived from one dataset is applied to new data [83]. This phenomenon occurs because models optimized for a specific sample inevitably capture both the true signal and random noise (idiosyncrasies) present in that sample.
Traditional statistical models are particularly susceptible to overfitting when the number of predictor variables approaches the sample size, a common scenario in dietary pattern analysis with numerous correlated food items. Machine learning approaches address this through various regularization techniques:
- LASSO regression performs L1 regularization, shrinking less important coefficients to zero and effectively selecting the most predictive features [84].
- Random Forest reduces overfitting by aggregating predictions from multiple decorrelated decision trees [70].
- Dropout methods in neural networks randomly remove units during training to prevent co-adaptation [87].
Validation Methodologies for Robust Performance Estimation
Proper validation strategies are essential for accurate performance benchmarking:
- Cross-validation: The dataset is divided into k subsets, with the model trained on k-1 subsets and validated on the remaining subset, repeated k times [83] [70].
- Bootstrap validation: Multiple random samples are drawn with replacement to estimate model performance distribution [83].
- Adjusted and shrunken R²: These metrics provide more realistic estimates of predictive ability in new samples compared to standard R² [83].
- Temporal validation: Models developed on data from one time period (e.g., 2018) are validated on data from a later period (e.g., 2019) [88].
The evidence consistently demonstrates that machine learning models outperform traditional statistical approaches across various nutrition research applications, particularly for complex prediction tasks involving non-linear relationships and high-dimensional data. However, model selection should be guided by specific research objectives, data characteristics, and interpretability requirements.
For nutrient composition prediction and dietary pattern analysis, regularized ML methods like LASSO provide an optimal balance of predictive performance and interpretability [85] [84]. In clinical settings requiring robust risk stratification, ensemble methods like Random Forest offer superior accuracy for patient-level predictions [70]. Traditional methods remain valuable for exploratory analysis and when working with limited sample sizes where ML models might overfit.
Future directions should focus on developing standardized validation frameworks specific to nutrition research, improving model interpretability through explainable AI techniques, and establishing guidelines for reporting ML studies in nutritional epidemiology. As the field evolves, the integration of ML with traditional statistical reasoning will likely yield the most clinically meaningful and scientifically valid advancements in nutrition science.
Within the critical care setting, malnutrition represents a prevalent and serious condition associated with impaired immune function, prolonged mechanical ventilation, increased complication rates, and elevated mortality [32]. Early identification of at-risk patients is crucial for timely nutritional intervention and improved clinical outcomes. Machine learning (ML) models offer a powerful approach for high-accuracy prediction, yet their real-world utility depends on robust performance across diverse patient populations, necessitating rigorous external validation [89].
This case study examines the external validation process of a machine learning model developed to predict malnutrition risk in critically ill patients within 24 hours of Intensive Care Unit (ICU) admission. The core of this analysis focuses on evaluating the model's generalizability and clinical applicability when applied to an entirely independent cohort, framing these findings within the broader context of validation methodologies for nutrition-related artificial intelligence research.
Methodology: Development and Validation of the Predictive Model
Study Design and Participant Selection
The original model development and subsequent external validation followed a prospective observational design [32]. The study employed distinct patient groups for model creation and for testing its generalizability.
- Development Cohort: The model was developed using data from 1,006 critically ill adult patients (aged ≥18 years) admitted to the Emergency ICU (EICU), Surgical ICU (SICU), and Neurosurgical ICU (NICU) between March and December 2022. This group was randomly partitioned into training (80%) and testing (20%) sets for initial model building and internal evaluation [32].
- External Validation Cohort: The model's performance was assessed on an independent cohort of 300 critically ill adult patients from the Respiratory ICU (RICU) and Medical ICU (MICU) of the same hospital system, enrolled between January and November 2024. This external group tested the model's performance on entirely new data, simulating real-world application [32].
Standard exclusion criteria were applied across all cohorts, including pregnancy or breastfeeding, significant mental illness, history of extracorporeal membrane oxygenation or continuous renal replacement therapy, and death within 24 hours of admission [32].
Predictor Selection and Outcome Definition
Predictor variables were selected based on a comprehensive literature review of factors influencing malnutrition in critically ill patients. The search spanned seven databases from their inception to March 2022, using a combination of MeSH terms and keywords related to ICU, critical illness, malnutrition, and risk factors [32].
The outcome was the early prediction of malnutrition within 24 hours of ICU admission. In the development cohort, the prevalence of malnutrition was 34.0% for moderate and 17.9% for severe malnutrition, indicating a substantial target condition [32].
Machine Learning Algorithms and Training Protocol
The research team trained and evaluated seven distinct machine learning algorithms to identify the optimal performer [32]:
- Extreme Gradient Boosting (XGBoost)
- Random Forest
- Decision Tree
- Support Vector Machine (SVM)
- Gaussian Naive Bayes
- k-Nearest Neighbor (k-NN)
- Logistic Regression
Feature selection was performed using Random Forest Recursive Feature Elimination. During the development phase, hyperparameters for each model were optimized via 5-fold cross-validation on the training set, eliminating the need for a separate validation set and ensuring robust internal validation [32].
Performance Metrics and Model Interpretability
Model performance was evaluated using a comprehensive set of metrics to assess different aspects of predictive accuracy and reliability [32]:
- Accuracy: The proportion of total correct predictions.
- Precision: The proportion of true positive predictions among all positive predictions.
- Recall (Sensitivity): The proportion of actual positives correctly identified.
- F1 Score: The harmonic mean of precision and recall.
- Area Under the Receiver Operating Characteristic Curve (AUC-ROC): Measures the model's ability to distinguish between classes.
- Area Under the Precision-Recall Curve (AUC-PR): Especially important for imbalanced datasets.
Model interpretability, a critical factor for clinical adoption, was achieved using SHapley Additive exPlanations (SHAP). This method quantifies the contribution of each feature to individual predictions, making the model's decision-making process more transparent to clinicians [32] [89].
Experimental Workflow
The following diagram illustrates the end-to-end process for developing and externally validating the ICU malnutrition prediction model.
Results and Performance Comparison
Model Performance in Development and External Validation
The following table summarizes the quantitative performance metrics of the best-performing model (XGBoost) during both the internal development phase and on the independent external validation cohort.
Table 1: Performance Comparison of the XGBoost Model in Development vs. External Validation [32]
| Metric | Development Phase (Testing Set) | External Validation Phase (Independent Cohort) |
|---|---|---|
| Accuracy | 0.90 (95% CI: 0.86–0.94) | 0.75 (95% CI: 0.70–0.79) |
| Precision | 0.92 (95% CI: 0.88–0.95) | 0.79 (95% CI: 0.75–0.83) |
| Recall | 0.92 (95% CI: 0.89–0.95) | 0.75 (95% CI: 0.70–0.79) |
| F1 Score | 0.92 (95% CI: 0.89–0.95) | 0.74 (95% CI: 0.69–0.78) |
| AUC-ROC | 0.98 (95% CI: 0.96–0.99) | 0.88 (95% CI: 0.86–0.91) |
| AUC-PR | 0.97 (95% CI: 0.95–0.99) | 0.77 (95% CI: 0.73–0.80) |
Analysis of Performance
The data reveals a consistent pattern: while the model maintained strong discriminatory power (as evidenced by an AUC-ROC of 0.88), all performance metrics experienced a decline when applied to the external validation cohort. This drop is typical and expected in external validation due to factors such as cohort heterogeneity, differences in clinical practices, and unmeasured variables. The model's AUC-ROC of 0.88 in the external cohort still represents excellent ability to distinguish between patients at high and low risk for malnutrition [32].
Notably, the XGBoost algorithm demonstrated superior performance and generalizability compared to the other six algorithms tested, including logistic regression, random forest, and support vector machines, making it the selected candidate for clinical implementation [32] [89].
The Scientist's Toolkit: Research Reagent Solutions
The development and validation of this predictive model relied on several key "research reagents" — essential methodological components and tools. The following table details these core elements and their functions within the experimental framework.
Table 2: Essential Research Reagents and Methodological Components
| Item | Function in the Research Process |
|---|---|
| Electronic Medical Records (EMR) | Provided structured data on patient demographics, clinical scores (APACHE II, SOFA, GCS, NRS 2002), laboratory values, and treatment details for feature engineering [32]. |
| Prospective Cohort Data | Served as the primary substrate for model training and testing, ensuring data integrity and temporal relevance for predicting a future outcome [32]. |
| XGBoost Algorithm | The leading ensemble ML algorithm that provided superior predictive accuracy and handled complex, non-linear relationships between clinical predictors and malnutrition outcome [32] [89]. |
| SHAP (SHapley Additive exPlanations) | The key interpretability framework used to deconstruct the "black box" model, quantify feature importance, and provide clinically understandable explanations for individual predictions [32] [89]. |
| Web-Based Deployment Platform (e.g., Shinyapps.io) | The tool used to operationalize the validated model, creating an accessible interface for clinicians to input patient data and receive real-time risk predictions [32] [89]. |
Discussion
Context within Nutritional ML Model Validation
This case study exemplifies a rigorous validation pathway for a nutrition-focused AI tool. The observed performance drop from development to external validation underscores the critical limitation of internal validation alone and aligns with the broader thesis that external validation is a non-negotiable step for establishing model credibility [89]. The model's maintained strong AUC-ROC (0.88) suggests it learned generalizable patterns of malnutrition risk, rather than merely memorizing noise from the development cohort.
The choice of XGBoost is supported by its consistent performance in other clinical prediction tasks. For instance, similar studies predicting cardiovascular disease risk in diabetic patients [89] and postoperative venous thromboembolism in ovarian cancer patients [90] also found XGBoost to be a top performer, highlighting its robustness in handling complex clinical data.
Implications for Researchers and Clinicians
For researchers, this study provides a template for TRIPOD-adherent predictive model development and highlights the importance of feature interpretability via SHAP analysis. For clinicians, the validated model, deployed as a web-based tool, offers a practical means of risk stratification. It enables early, targeted nutritional support for high-risk ICU patients, potentially improving resource allocation and patient outcomes. The model's ability to provide a prediction within 24 hours of admission is a significant advantage for guiding early intervention, which is strongly advocated by international nutritional guidelines from ASPEN and ESPEN [32].
This case study demonstrates that a machine learning model, specifically XGBoost, can achieve clinically acceptable performance in predicting malnutrition risk in a critically ill population, even upon external validation. The observed metrics confirm that while some degradation from development performance is inevitable, the model retains excellent discriminatory ability. The integration of SHAP analysis ensures the model's decisions are interpretable, fostering trust and facilitating its potential integration into clinical workflows. This work reinforces the paradigm that rigorous external validation is the cornerstone of translating predictive analytics from a research concept into a reliable tool for precision medicine in clinical nutrition. Future work should focus on multi-center validations to further assess generalizability and on implementing intervention studies to determine if using the model prospectively improves patient outcomes.
Evaluating Clinical Utility and Comparative Validity in mHealth and AI-Driven Nutrition Apps
The integration of mobile health (mHealth) and artificial intelligence (AI) into nutritional science represents a paradigm shift in dietary assessment and personalized intervention. These digital tools offer the potential to overcome significant limitations of conventional methods—such as recall bias, labor-intensive processes, and infrequent data collection—by enabling objective, real-time monitoring of dietary intake [27]. For researchers and clinical professionals, the critical challenge lies in navigating a rapidly expanding market of applications whose clinical utility, comparative validity, and integration into evidence-based practice are often unclear. This guide provides a systematic evaluation of the current landscape, focusing on performance data, methodological frameworks for validation, and the role of these technologies in advancing nutrition research, particularly for chronic disease management and precision health initiatives.
The mHealth Nutrition App Landscape: Market and Regulatory Context
The global mHealth apps market is experiencing rapid growth, with its size projected to rise from USD 43.13 billion in 2025 to USD 154.12 billion by 2034, driven by the rising prevalence of chronic diseases and the adoption of wearable devices [91]. This expansion is characterized by a diverse ecosystem of applications, broadly categorized into medical apps (focused on remote consultation and chronic disease management) and fitness apps (focused on wellness, weight management, and physical activity) [91].
Regulatory oversight of these apps is complex and varies by region. In the United States, a combination of the Health Insurance Portability and Accountability Act (HIPAA), the Federal Food, Drug, and Cosmetic Act, and the Federal Trade Commission (FTC) Act governs data privacy, safety, effectiveness, and the prohibition of deceptive claims [92]. The Food and Drug Administration (FDA) focuses its regulatory oversight on a subset of apps that pose a higher risk to patients if they malfunction. In the European Union, mHealth apps are often classified as medical devices under Regulation EU 2017/745, requiring a clinical evaluation report and classification based on risk (Class I to III) [92]. A significant challenge in the field is that many widely available apps are not evidence-based and raise serious concerns regarding user privacy and data security [92].
Methodological Frameworks for App Validation
Evaluating the quality and validity of mHealth and AI-driven nutrition apps requires a multi-faceted approach. Researchers and clinicians can employ several structured frameworks to assess key dimensions such as general quality, behavior change potential, and accuracy of dietary assessment.
Key Evaluation Tools and Metrics
- Mobile App Rating Scale (MARS): This is a validated tool for assessing the overall quality of mHealth apps. It evaluates four objective quality domains: engagement, functionality, aesthetics, and information quality, along with a subjective quality scale [93] [94]. In a recent evaluation of 18 top nutrition apps, Noom achieved the highest MARS score (mean = 4.44 out of 5), indicating superior overall quality [93] [94].
- App Behaviour Change Scale (ABACUS): This scale quantifies an app's potential to encourage healthier habits by evaluating the presence of behavior change techniques. Noom also scored highest on ABACUS in the same study, achieving a perfect 21/21 [93] [94].
- Comparative Validity of Dietary Assessment: This is a core component of clinical validation, where the nutritional outputs (e.g., energy, macronutrients) from an app are compared against a reference method, such as a detailed food record or doubly labeled water measurement [93] [94]. The accuracy is often reported as a percentage or as mean differences (e.g., in kilojoules or calories).
Experimental Workflow for Validation
A robust validation study for AI-driven dietary assessment tools typically follows a structured, multi-phase process, as outlined in recent research. The workflow progresses from app selection through feature extraction and culminates in rigorous quality and validity testing.
Performance Comparison of Leading mHealth Nutrition Apps
Recent scientific studies have quantitatively evaluated popular commercially available apps, providing critical data on their accuracy and quality for research and clinical consideration.
Table 1: Overall Quality and Behavior Change Potential of Select Nutrition Apps
| App Name | MARS Score (out of 5) | ABACUS Score (out of 21) | Key Features |
|---|---|---|---|
| Noom | 4.44 | 21 | Food diary, coaching, psychological support |
| MyFitnessPal | Data not specified in source | Data not specified in source | Extensive food database, manual logging, AI image recognition (97% accuracy) |
| Fastic | Data not specified in source | Data not specified in source | Food diary, AI image recognition (92% accuracy) |
Source: Adapted from [93] [94].
Table 2: Comparative Validity of Dietary Assessment Methods in Apps
| Assessment Method | Diet Type | Performance / Accuracy Findings | Implications for Research |
|---|---|---|---|
| Manual Food Logging | Western Diet | Overestimated energy by mean of 1040 kJ [94] | Potential for systematic error; requires calibration in Western populations. |
| Manual Food Logging | Asian Diet | Underestimated energy by mean of -1520 kJ [94] | Highlights critical lack of validity for diverse cuisines; limited food database coverage. |
| AI Food Image Recognition | Mixed Diets | MyFitnessPal (97%), Fastic (92%) accuracy in food identification [94] | AI shows high functionality but automatic energy estimations remain inaccurate [93] [94]. |
A primary finding across studies is that while apps with greater AI integration demonstrate better functionality, the automated energy and nutrient estimations from AI-enabled food image recognition are not yet fully accurate and require further development [93] [94]. A significant validity gap exists for culturally diverse foods and mixed dishes, as AI models and food databases are often under-trained in these areas [93] [94].
The Scientist's Toolkit: Key Reagents and Solutions for Validation Research
To conduct rigorous validation studies for AI-driven nutrition tools, researchers should consider incorporating the following key reagents and methodologies.
Table 3: Essential Research Reagents and Methodologies for Validation Studies
| Research Reagent / Solution | Function in Validation Research |
|---|---|
| Doubly Labeled Water (DLW) | Considered the gold standard for measuring total energy expenditure in free-living individuals; used as a reference method to validate energy intake data reported by apps [27]. |
| Weighed Food Records | Detailed dietary assessment method where food is weighed prior to consumption; serves as a highly detailed reference for validating food identification and portion size estimation by apps [94]. |
| Mobile App Rating Scale (MARS) | Standardized tool to systematically assess the quality of mobile health apps across multiple domains, ensuring a comprehensive evaluation beyond simple accuracy metrics [93] [94]. |
| App Behavior Change Scale (ABACUS) | Validated scale to identify and quantify the behavior change techniques embedded within an app, which is crucial for assessing its potential for long-term user engagement and health impact [93] [94]. |
| Culturally Diverse Food Image Datasets | Curated sets of food images from various cuisines (e.g., Asian, Middle Eastern) used to test and train AI models, directly addressing a key current limitation in food recognition accuracy [93] [94]. |
Future Directions and Strategic Recommendations
For AI-driven mHealth apps to achieve widespread clinical utility, several strategic shifts and research advancements are necessary. Future efforts will focus on enhancing personalization and closing existing validity gaps.
- Enhancement of AI Capabilities: Future apps will focus on more sophisticated AI to provide personalized health insights and improve the accuracy of dietary assessment, particularly for mixed dishes and diverse foods [95] [93]. This includes training models on larger, more culturally diverse datasets.
- Collaboration with Dietitians: Integrating dietitians into the app development process is essential for improving the credibility, comparative validity, and practical utility of these tools [93] [94]. This collaboration is key to expanding food databases and ensuring recommendations are clinically sound.
- Interoperability and Data Privacy: Seamless integration with electronic health records (EHRs) and other healthcare systems will be a priority [95]. Furthermore, adhering to evolving data privacy regulations and ensuring data security will be critical for user trust and regulatory compliance [92].
- Validation and Standardization: There is a pressing need for standardized methods to measure the clinical outcomes of mHealth apps and for techniques to encourage long-term user engagement and behavior change [92]. Reproducibility and transparency of AI results are also significant challenges that must be overcome [92].
The validation of mHealth and AI-driven nutrition apps is a multifaceted process that extends beyond simple usability testing to include rigorous assessment of dietary accuracy, behavior change potential, and overall quality. Current evidence indicates that while AI-powered tools like MyFitnessPal and Fastic show high accuracy in food identification, significant challenges remain in automated nutrient estimation and the validity of assessments for non-Western diets. Tools like Noom demonstrate high quality and strong behavior change potential. For researchers and clinicians, selecting an app requires a careful balance of these factors, aligned with the specific population and research objectives. The future of this field hinges on collaborative development between computer scientists, nutrition researchers, and clinical dietitians, alongside more rigorous, standardized validation protocols and a commitment to creating inclusive technologies that serve diverse global populations.
Conclusion
The validation of nutrition-related machine learning models is a multifaceted process that extends far beyond achieving high accuracy on a training set. A robust framework necessitates high-quality, transparent data, a thoughtful selection of algorithms and evaluation metrics tailored to often-imbalanced clinical datasets, and, most critically, rigorous external validation to prove generalizability. The successful application of models like XGBoost for ICU malnutrition prediction demonstrates the tangible potential of ML to enhance clinical decision-support. Future directions must focus on standardizing validation protocols, improving the interoperability of diverse data sources (from genomics to digital biomarkers), and advancing explainable AI (xAI) to build trust among clinicians. For biomedical research, this paves the way for more effective precision nutrition strategies, optimized clinical trials through better patient stratification, and the development of reliable digital tools that can integrate seamlessly into clinical workflow and public health initiatives.
References
- 1. Machine Learning in Nutrition Research - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9776646/]
- 2. Machine learning modeling practices to support the principles of AI and ethics in nutrition research | Nutrition & Diabetes [https://www.nature.com/articles/s41387-022-00226-y]
- 3. What is Multimodal ? Types, Examples, Applications & More Data [https://www.tiledb.com/multimodal-data]
- 4. A Novel Approach for Exploring Data -Driven Nutritional Insights Using... [https://link.springer.com/article/10.1007/s42979-024-03397-w]
- 5. Orthogonal multimodality integration and clustering in single-cell data [https://bmcbioinformatics.biomedcentral.com/articles/10.1186/s12859-024-05773-y]
- 6. Establishing a machine learning model for predicting nutritional risk through facial feature recognition - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10540841/]
- 7. Data Nutrition Project - Innovation at Consumer Reports [https://innovation.consumerreports.org/initiatives/data-nutrition-project/]
- 8. Do nutrition apps need to come with a data ? label [https://www.qina.tech/blog/ai-training-data-nutrition-label]
- 9. [1805.03677] The Dataset Nutrition Label: A Framework To Drive Higher Data Quality Standards [https://arxiv.org/abs/1805.03677]
- 10. Improving dataset in dermatologic Artificial Intelligence... transparency [https://www.nature.com/articles/s41746-025-02125-9?error=cookies_not_supported&code=d48940d4-15bb-41d2-8ab0-5c6e7bc7cd4d]
- 11. The Dataset (2nd Gen): Leveraging Context to... Nutrition Label [https://www.readkong.com/page/the-dataset-nutrition-label-2nd-gen-leveraging-context-4618678]
- 12. The Data Nutrition Project [https://datanutrition.org/]
- 13. : A Blueprint for Responsible AI Data Nutrition Labels [https://www.linkedin.com/pulse/data-nutrition-labels-blueprint-responsible-ai-arjun-basu-7lgkc]
- 14. Machine learning Statistical Deep learning... inference vs inference vs [https://www.linkedin.com/pulse/statistical-inference-vs-machine-learning-deep-ajit-jaokar-khfue]
- 15. Machine Learning vs . Statistical : Key Differences and... Inference [https://www.domo.com/glossary/what-is-machine-learning-and-statistical-inference]
- 16. Machine Learning vs . Traditional : Key... - Eduonix Blog Statistics [https://blog.eduonix.com/2024/11/machine-learning-vs-traditional-statistics-key-differences-explained/]
- 17. Frontiers | Are Machine Algorithms More Accurate in... Learning [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2022.740898/full]
- 18. AI-based digital image dietary assessment methods compared to... [https://pubmed.ncbi.nlm.nih.gov/38060823/]
- 19. Bias–variance tradeoff - Wikipedia [https://en.wikipedia.org/wiki/Bias%E2%80%93variance_tradeoff]
- 20. What is Bias-Variance Tradeoff? | IBM [https://www.ibm.com/think/topics/bias-variance-tradeoff]
- 21. Applications of Artificial Intelligence, Machine Learning, and Deep Learning in Nutrition: A Systematic Review - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11013624/]
- 22. Methodological Review of Classification Trees for Risk ... Stratification [https://pubmed.ncbi.nlm.nih.gov/40507172/]
- 23. Frontiers | Machine learning prediction of metabolic dysfunction-associated fatty liver disease risk in American adults using body composition: explainable analysis based on SHapley Additive exPlanations [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1616229/full]
- 24. AI Revolutionizes Nutrition in 2025 : Smarter Calorie Tracking & Meal... [https://www.linkedin.com/pulse/ai-revolutionizes-nutrition-2025-smarter-calorie-tracking-rdqbf]
- 25. Frontiers | Artificial intelligence in personalized nutrition and food manufacturing: a comprehensive review of methods, applications, and future directions [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1636980/full]
- 26. Frontiers | Predictive value of composite nutritional indicators geriatric... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1598043/full]
- 27. Frontiers | Navigating next-gen nutrition care using artificial intelligence-assisted dietary assessment tools—a scoping review of potential applications [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1518466/full]
- 28. Applications of Artificial Intelligence, Machine Learning, and Deep Learning in Nutrition: A Systematic Review | MDPI [https://www.mdpi.com/2072-6643/16/7/1073]
- 29. From Decision Trees to Power Ensembles — Random ... Forest [https://medium.com/@poojashreechoudhury7/from-decision-trees-to-power-ensembles-random-forest-xgboost-explained-step-by-step-guide-e1613522b66b]
- 30. Difference Between Random and Forest - GeeksforGeeks XGBoost [https://www.geeksforgeeks.org/machine-learning/difference-between-random-forest-vs-xgboost/]
- 31. Frontiers | An AI-based nutrition recommendation system: technical validation with insights from Mediterranean cuisine [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1546107/full]
- 32. Development and external validation of machine learning models for the early prediction of malnutrition in critically ill patients: a prospective observational study | BMC Medical Informatics and Decision Making | Full Text [https://bmcmedinformdecismak.biomedcentral.com/articles/10.1186/s12911-025-03082-9]
- 33. of Performance , SVM, and Comparison ... Random Forest XGBoost [https://jurnal.polibatam.ac.id/index.php/JAIC/article/view/9701]
- 34. Machine Learning in Nutrition Research - PubMed [https://pubmed.ncbi.nlm.nih.gov/36166846/]
- 35. Development and external validation of machine learning models for... [https://pubmed.ncbi.nlm.nih.gov/40611154/]
- 36. JMIR Medical Informatics - Prediction of Critical Care Outcome for Adult Patients Presenting to Emergency Department Using Initial Triage Information: An XGBoost Algorithm Analysis [https://medinform.jmir.org/2021/9/e30770/]
- 37. Frontiers | Machine learning algorithms assist early evaluation of... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2023.1060398/full]
- 38. Machine learning-based in-hospital mortality risk prediction tool for intensive care unit patients with heart failure - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10106627/]
- 39. Frontiers | Predicting postoperative malnutrition in patients with oral... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1564459/full]
- 40. Frontiers | Machine learning with decision curve analysis evaluates... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1597864/full]
- 41. in critical care Biomarkers | Critical Care | Full Text nutrition [https://ccforum.biomedcentral.com/articles/10.1186/s13054-020-03208-7]
- 42. Digital Biomarkers for Personalized Nutrition : Predicting Meal... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9654068/]
- 43. Predicting Cancer: Leveraging Machine Learning Techniques on... [https://rsisinternational.org/journals/ijrsi/articles/predicting-cancer-leveraging-machine-learning-techniques-on-clinical-data-sets/]
- 44. A Scoping Review of Artificial Intelligence for Precision Nutrition - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11994916/]
- 45. [012] 不同 数 集划分与 据 的 验 现与比较-CSDN博客 证 方 法 实 [https://blog.csdn.net/Pysamlam/article/details/113101137]
- 46. cloud.tencent.com/developer/article/1395756 [https://cloud.tencent.com/developer/article/1395756]
- 47. Understanding Precision, Recall, and F1 Score Metrics | by Piyush Kashyap | Medium [https://medium.com/@piyushkashyap045/understanding-precision-recall-and-f1-score-metrics-ea219b908093]
- 48. Limitations in Evaluating Machine Learning Models for Imbalanced Binary Outcome Classification in Spine Surgery: A Systematic Review - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10741524/]
- 49. Employing machine techniques for prediction of micronutrient... learning [https://www.nature.com/articles/s41598-024-75455-5?error=cookies_not_supported&code=ccd0af77-879f-43fc-92bf-93a24c1d92d8]
- 50. 4 Techniques to Handle Imbalanced | by Shanding... | Medium Datasets [https://medium.com/codex/4-techniques-to-handle-imbalanced-datasets-f0eab38eee3d]
- 51. A Data Scientist's Guide to Balanced Accuracy - Train in Data 's Blog [https://www.blog.trainindata.com/a-data-scientists-guide-to-balanced-accuracy/]
- 52. Precision, Recall, and F1 Score: When Accuracy Betrays You | Proclus Academy [https://proclusacademy.com/blog/explainer/precision-recall-f1-score-classification-models/]
- 53. Precision-Recall Trade-Off: Navigating the Delicate Balance in Imbalanced Datasets | by Sruthy Nath | Medium [https://medium.com/@sruthy.sn91/precision-recall-trade-off-navigating-the-delicate-balance-in-imbalanced-datasets-66ad175ccf1e]
- 54. Evaluation of Machine Health Learning ... Imbalanced Data [https://link.springer.com/chapter/10.1007/978-3-031-72215-8_12]
- 55. Frontiers | Impact of imbalanced features on large datasets [https://www.frontiersin.org/journals/big-data/articles/10.3389/fdata.2025.1455442/full]
- 56. Model Evaluation Metrics Explained [https://dzone.com/articles/model-evaluation-metrics-explained]
- 57. Beyond Accuracy: Recall , Precision , F - 1 , Score - ROC | Medium AUC [https://medium.com/@priyankads/beyond-accuracy-recall-precision-f1-score-roc-auc-6ef2ce097966]
- 58. of Evaluation Metrics used in Machine Learning Models Comparison [https://www.educative.io/blog/evaluation-metrics-ml-models]
- 59. Statistical Evaluation Metrics | IUST Projects [https://iust-projects.ir/post/minidm01/]
- 60. vs F vs Accuracy vs PR 1 : Which Evaluation... Score ROC AUC AUC [https://neptune.ai/blog/f1-score-accuracy-roc-auc-pr-auc]
- 61. Understanding the F and 1 - Score Curve | Keylabs AUC ROC [https://keylabs.ai/blog/understanding-the-f1-score-and-auc-roc-curve/]
- 62. Integrating Food Preference Profiling, Behavior Change Strategies, and Machine Learning for Cardiovascular Disease Prevention in a Personalized Nutrition Digital Health Intervention: Conceptual Pipeline Development and Proof-of-Principle Study - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12346185/]
- 63. Why ROC and Log-Loss Are Your AUC ’s Secret... | Medium Model [https://medium.com/@nirajan.acharya777/why-roc-auc-and-log-loss-are-your-models-secret-superpowers-beyond-f1-score-recall-and-5373998deda2]
- 64. Models: Optimizing - Cross and Validation Tuning... Hyperparameter [https://stackabuse.com/optimizing-models-cross-validation-and-hyperparameter-tuning-guide/]
- 65. The importance of prediction model and assessment in... validation [https://www.nature.com/articles/ijo2015214?error=cookies_not_supported]
- 66. Randomized Search and Grid Search for Comparing ... Hyperparameter [https://www.geeksforgeeks.org/machine-learning/comparing-randomized-search-and-grid-search-for-hyperparameter-estimation-in-scikit-learn/]
- 67. COVID-19 mortality and nutrition through predictive modeling and optimization based on grid search | Scientific Reports [https://www.nature.com/articles/s41598-025-20345-7]
- 68. Best Tools for Model Tuning and Hyperparameter Optimization [https://neptune.ai/blog/best-tools-for-model-tuning-and-hyperparameter-optimization]
- 69. GitHub - Shivamgoyal5/ Hyperparameter - optimization [https://github.com/Shivamgoyal5/Hyperparameter-optimization]
- 70. Frontiers | Construction and evaluation of a machine learning-based... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1600319/full]
- 71. Machine learning modeling practices to support the principles of AI... [https://www.nature.com/articles/s41387-022-00226-y?error=cookies_not_supported]
- 72. Fairness and Bias in Machine Learning: Mitigation Strategies [https://www.lumenova.ai/blog/fairness-bias-machine-learning/]
- 73. Addressing Bias in Machine with Synthetic Learning Data [https://scisimple.com/en/articles/2025-06-15-addressing-bias-in-machine-learning-with-synthetic-data--ak46p4r]
- 74. Bias in machine | How to identify and learning ... | Lumenalta mitigate [https://lumenalta.com/insights/bias-in-machine-learning]
- 75. Bias and Fairness: DataRobot docs [https://docs.datarobot.com/en/docs/modeling/build-models/adv-opt/fairness-metrics.html]
- 76. -Aware Fairness : Machine Bias for Ethical AI Learning Mitigating [https://www.linkedin.com/pulse/fairness-aware-machine-learning-mitigating-bias-ethical-debasish-deb-cpt6f]
- 77. : Fairness bias | Mitigating | Google for Developers Machine Learning [https://developers.google.com/machine-learning/crash-course/fairness/mitigating-bias]
- 78. Bias and Unfairness in Machine Learning Models: A Systematic Review on Datasets, Tools, Fairness Metrics, and Identification and Mitigation Methods [https://www.mdpi.com/2504-2289/7/1/15]
- 79. validity - Wikipedia Internal [https://en.wikipedia.org/wiki/Internal_validity]
- 80. The Ultimate Guide to Achieving Internal Validity [https://www.numberanalytics.com/blog/achieving-internal-validity-program-evaluation]
- 81. Prediction models need appropriate internal, internal-external, and external validation - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5578404/]
- 82. Developing a New Reference Standard… Is Validation Necessary? - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2919497/]
- 83. The Importance of Prediction Model Validation and Assessment in Obesity and Nutrition Research - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4826636/]
- 84. Application of a new dietary pattern analysis method in nutritional epidemiology | BMC Medical Research Methodology | Full Text [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-018-0585-8]
- 85. Machine learning models to predict micronutrient profile in food after... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10160345/]
- 86. [2507.07048] Comprehensive Evaluation of Large Multimodal Models ... [https://arxiv.org/abs/2507.07048]
- 87. Applications of machine learning in drug discovery and development - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6552674/]
- 88. Development and Validation of a Machine Learning Model to Estimate Risk of Adverse Outcomes Within 30 Days of Opioid Dispensation - PubMed [https://pubmed.ncbi.nlm.nih.gov/36574245/]
- 89. Development and validation of a machine learning model for cardiovascular disease risk prediction in type 2 diabetes patients | Scientific Reports [https://www.nature.com/articles/s41598-025-18443-7]
- 90. A Predictive Model Based on Machine Learning Algorithm for Vein Thromb | IJWH [https://www.dovepress.com/a-predictive-model-based-on-machine-learning-algorithm-for-vein-thromb-peer-reviewed-fulltext-article-IJWH]
- 91. Market Size to Hit USD 154.12 Billion by 2034 mHealth Apps [https://www.precedenceresearch.com/mhealth-apps-market]
- 92. Quality, Usability, and Effectiveness of mHealth and the Role of... Apps [https://pmc.ncbi.nlm.nih.gov/articles/PMC10196903/]
- 93. Evaluating the Quality and Comparative Validity of Manual Food Logging and Artificial Intelligence-Enabled Food Image Recognition in Apps for Nutrition Care - PubMed [https://pubmed.ncbi.nlm.nih.gov/39125452/]
- 94. Evaluating the Quality and Comparative Validity of Manual Food Logging and Artificial Intelligence-Enabled Food Image Recognition in Apps for Nutrition Care - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11314244/]
- 95. Top MHealth Companies & How to Apps Them ( Compare ) 2025 [https://www.linkedin.com/pulse/top-mhealth-apps-companies-how-compare-them-2025-the-trend-analyzer-juffc]