Advanced Strategies for Bioavailability Enhancement of Bioactive Compounds: From Formulation Technologies to Clinical Translation
This article provides a comprehensive overview of contemporary strategies to overcome the critical challenge of low bioavailability in bioactive compounds and small-molecule drugs.
Advanced Strategies for Bioavailability Enhancement of Bioactive Compounds: From Formulation Technologies to Clinical Translation
Abstract
This article provides a comprehensive overview of contemporary strategies to overcome the critical challenge of low bioavailability in bioactive compounds and small-molecule drugs. Tailored for researchers, scientists, and drug development professionals, it synthesizes current scientific knowledge across four key areas: the fundamental physicochemical and biological barriers governing absorption; innovative formulation technologies like solid dispersions, lipid-based systems, and nanocarriers; practical troubleshooting and optimization approaches for development pipelines; and the essential regulatory frameworks and validation methods for proving bioequivalence and clinical efficacy. The content leverages the latest research and market trends to serve as a strategic guide for enhancing the therapeutic potential of promising molecules.
Understanding Bioavailability: The Foundation for Effective Drug Development
Frequently Asked Questions (FAQs)
1. What is the fundamental definition of bioavailability in a clinical pharmacology context? Bioavailability (denoted as F) is defined as the fraction of an administered dose of a drug that reaches the systemic circulation unaltered, and the rate at which this occurs [1] [2]. It is a core component of the pharmacokinetics paradigm (ABCD: Administration, Bioavailability, Clearance, Distribution) and is crucial for determining the correct dosage to achieve a therapeutic effect [1].
2. How is bioavailability quantitatively measured and calculated? The most reliable measure of a drug's bioavailability is the Area Under the plasma concentration-time Curve (AUC) [1] [2]. Bioavailability is typically calculated by comparing the AUC of a drug administered via a specific route (e.g., oral) to the AUC of the same drug dose administered intravenously (IV), which is assumed to have 100% bioavailability [1].
- Absolute Bioavailability is determined by the formula: F = AUC~oral~ / AUC~IV~ [1] [3].
- Relative Bioavailability compares the bioavailability of two different dosage forms of the same drug (e.g., tablet vs. syrup) [4].
3. What is the key difference between the "rate" and "extent" of bioavailability? These are two distinct but critical parameters:
- Extent: Refers to the total amount of the active drug that reaches systemic circulation. This is measured by the AUC [2] [3].
- Rate: Refers to how quickly the drug enters the systemic circulation. This is measured by the peak time (T~max~), which is the time taken to reach the maximum plasma concentration (C~max~) [4] [2]. A slower absorption results in a later T~max~.
4. Why does an intravenously administered drug have 100% bioavailability? Intravenous (IV) administration delivers the drug directly into the systemic circulation, completely bypassing absorption barriers and first-pass metabolism. Therefore, the entire dose is immediately and completely available to the body [1].
5. What are the most common physiological causes of low oral bioavailability? The primary causes are related to barriers encountered before a drug reaches systemic circulation:
- First-Pass Metabolism: After oral absorption, drugs pass through the liver via the portal system, where they can be extensively metabolized by enzymes (e.g., Cytochrome P450) before reaching the systemic circulation [1] [2].
- Poor Solubility and Permeability: A drug must dissolve in the gastrointestinal (GI) fluids and be able to penetrate the intestinal epithelial membrane. Poorly water-soluble or slowly absorbed drugs often have low bioavailability [5] [2].
- Insufficient Time for Absorption: If a drug does not dissolve readily or cannot penetrate the membrane quickly, it may pass through the GI tract without adequate absorption [2].
6. How can drug formulation strategies overcome poor bioavailability? Strategic formulation decisions can dramatically improve bioavailability, especially for poorly soluble drugs [6] [5]. Key techniques include:
- Particle Size Reduction: Micronization or nanonization to increase surface area and dissolution rate [6] [5].
- Salt Formation: Creating salt forms of ionizable compounds to enhance aqueous solubility [5].
- Amorphous Solid Dispersions: Dispersing the drug in an amorphous state within a polymer matrix to increase apparent solubility [5].
- Lipid-Based Delivery Systems: Using nanoemulsions or liposomes to improve solubility and absorption [6].
- Co-crystals: Combining the drug with non-toxic coformers to alter crystal packing and improve solubility [5].
Troubleshooting Guide: Common Bioavailability Experimental Issues
Issue 1: Irregular or Uninterpretable Melt Curves in Thermal Shift Assays (TSAs)
TSAs, like Differential Scanning Fluorimetry (DSF), are used to study drug-target binding by detecting shifts in a protein's melting temperature [7].
- Potential Causes and Solutions:
- Compound Interference: The test compound itself may be fluorescent or may interact with the fluorescent dye used in the assay (e.g., SyproOrange). This can cause irregular curve shapes [7].
- Solution: Run a control well with the compound and dye but no protein to identify intrinsic fluorescence or compound-dye interactions [7].
- Buffer Incompatibility: Certain buffer additives (e.g., detergents, viscosity enhancers) can increase background fluorescence or interfere with the dye [7].
- Solution: Optimize the buffer system and ensure compatibility with the fluorescent dye. Refer to dye-specific incompatibility guides [7].
- Protein Purity and Stability: The target protein must be stable, soluble, and not aggregated at ambient temperature in the chosen buffer for reliable melting curves [7].
- Solution: Characterize protein stability in different buffers and include appropriate controls.
- Compound Interference: The test compound itself may be fluorescent or may interact with the fluorescent dye used in the assay (e.g., SyproOrange). This can cause irregular curve shapes [7].
Issue 2: Low Oral Bioavailability in In Vivo Studies
When an orally dosed drug shows lower-than-expected systemic exposure in animal or human studies.
- Potential Causes and Solutions:
- First-Pass Metabolism: High metabolic extraction in the liver or intestinal wall [1] [2].
- Poor Solubility/Dissolution: The drug fails to dissolve in the GI tract, limiting absorption [5] [2].
- Efflux Transporters: Active transport of the drug back into the gut lumen by transporters like P-glycoprotein [1] [3].
- Solution: Investigate the use of pharmaceutical excipients that can inhibit these transporters or perform structural modification of the drug candidate to avoid recognition by the transporter [1].
Issue 3: No Observed Target Engagement in Cellular Assays (e.g., CETSA)
In a Cellular Thermal Shift Assay (CETSA), a test compound does not show a stabilization or destabilization effect on the target protein in whole cells [7].
- Potential Causes and Solutions:
- Poor Cell Membrane Permeability: The compound cannot efficiently cross the cell membrane to reach its intracellular target [7].
- Insufficient Compound Incubation Time: The incubation period may be too short for the compound to be taken up by the cells and bind its target [7].
- Solution: Optimize the incubation time to ensure adequate cellular uptake and binding, while avoiding phenotypic effects that could complicate the readout [7].
- Compound Instability in Cell Culture: The compound may be degraded in the culture medium before it can act [7].
- Solution: Assess the stability of the compound in the assay medium.
Quantitative Data for Bioavailability Assessment
Table 1: Key Pharmacokinetic Parameters for Assessing Bioavailability [1] [4] [2]
| Parameter | Description | Interpretation & Impact on Therapy |
|---|---|---|
| AUC (Area Under the Curve) | Total exposure of the body to the active drug over time. | Directly proportional to the extent of bioavailability. A larger AUC indicates greater total drug absorption. |
| C~max~ (Max Concentration) | The peak plasma concentration achieved after administration. | Impacts the intensity of both therapeutic and toxic effects. A high C~max~ may lead to toxicity. |
| T~max~ (Time to C~max~) | Time taken to reach the maximum plasma concentration. | Indicates the rate of absorption. A short T~max~ suggests rapid onset of action. |
| Absolute Bioavailability (F) | Fraction of drug reaching systemic circulation compared to an IV dose. | Determines the dosing requirements. A drug with low F requires a higher oral dose to match the IV effect. |
Table 2: Strategies to Enhance Bioavailability of Poorly Soluble Drugs [6] [5]
| Strategy | Mechanism of Action | Typical Use Case |
|---|---|---|
| Particle Size Reduction (Nanonization) | Increases surface area to enhance dissolution rate. | BCS Class II drugs (High Permeability, Low Solubility). |
| Amorphous Solid Dispersions | Creates a high-energy amorphous form with higher apparent solubility than the crystalline form. | Drugs with very low solubility and high crystallinity. |
| Lipid-Based Delivery Systems | Solubilizes the drug in lipid matrices, facilitating absorption via lymphatic transport. | Highly lipophilic drugs. |
| Salt Formation | Improves aqueous solubility for ionizable compounds. | Drugs with acidic or basic functional groups. |
| Cyclodextrin Complexation | Encapsulates the drug molecule to increase solubility and stability. | Molecules suitable for host-guest inclusion complexes. |
Experimental Protocols for Bioavailability Research
Protocol 1: In Vitro Dissolution Testing
Objective: To simulate and assess the release of a drug from its dosage form under standardized conditions, which is a critical indicator of potential in vivo performance [6].
Methodology:
- Apparatus: Use a USP-compliant dissolution apparatus (e.g., paddle or basket type).
- Dissolution Medium: Select a suitable medium (e.g., pH 1.2 HCl buffer for gastric fluid, pH 6.8 phosphate buffer for intestinal fluid) maintained at 37±0.5 °C [6].
- Procedure: Place the dosage form (tablet, capsule) in the vessel containing the medium. Operate the apparatus at a specified rotational speed (e.g., 50-75 rpm).
- Sampling: Withdraw aliquots of the medium at predetermined time intervals (e.g., 10, 20, 30, 45, 60 minutes).
- Analysis: Filter the samples and analyze the drug concentration using a validated analytical method (e.g., HPLC-UV). Calculate the percentage of drug dissolved at each time point.
- Data Interpretation: Plot the dissolution profile (% released vs. time). Compare the profile to a reference standard or specifications to evaluate performance.
Protocol 2: Determining Absolute Bioavailability in a Preclinical Model
Objective: To quantify the fraction of an orally administered dose that reaches the systemic circulation by comparing it to an intravenous dose [1] [2].
Methodology:
- Study Design: A crossover design is ideal, where the same animal receives both the oral (PO) and intravenous (IV) formulation after a suitable washout period.
- Dosing: Administer the drug at the same dose level via both PO and IV routes. The IV dose must be administered as a solution or suspension that ensures complete availability.
- Blood Sampling: Collect serial blood samples at multiple time points after both doses (e.g., pre-dose, 5, 15, 30 min, 1, 2, 4, 8, 12, 24 hours).
- Bioanalysis: Process plasma from blood samples and determine the drug concentration in each sample using a validated bioanalytical method (e.g., LC-MS/MS).
- Pharmacokinetic Analysis: For both routes, calculate the AUC from time zero to infinity (AUC~0-∞~).
- Calculation: Determine Absolute Bioavailability (F) using the formula: F (%) = (AUC~PO~ / AUC~IV~) × (Dose~IV~ / Dose~PO~) × 100 [1] [3].
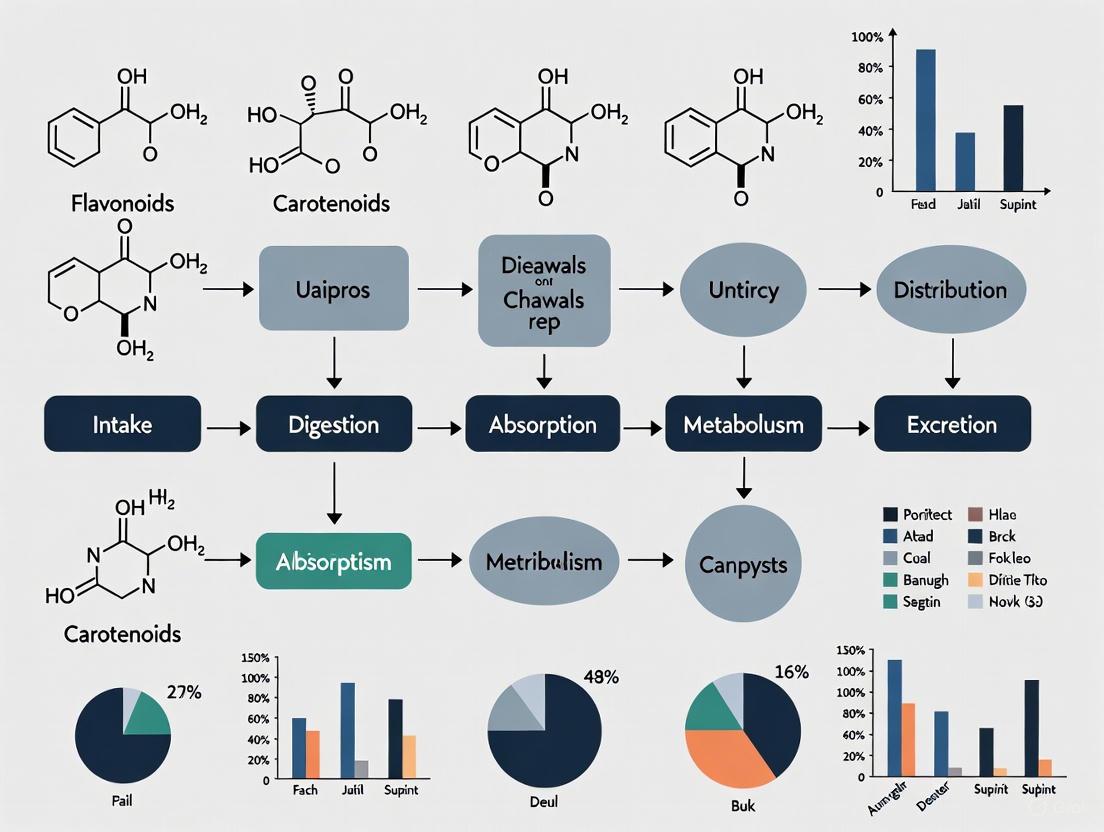
Visualization: The Journey of an Oral Drug and Key Bioavailability Barriers
The following diagram illustrates the pathway and major barriers an orally administered drug faces before reaching systemic circulation, which directly impact its bioavailability.
Diagram 1: Oral Drug Bioavailability Pathway. This workflow highlights key barriers like dissolution, enzymatic degradation, efflux transporters, and first-pass metabolism that reduce the amount of drug reaching systemic circulation. [1] [2] [3]
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Key Bioavailability Experiments
| Reagent / Material | Function / Application | Example in Context |
|---|---|---|
| Caco-2 Cell Line | An in vitro model of the human intestinal epithelium used to predict drug permeability and absorption [5]. | Studying passive diffusion and active transporter effects (e.g., P-gp efflux). |
| Polarity-Sensitive Dyes (e.g., SyproOrange) | Used in Differential Scanning Fluorimetry (DSF) to detect protein unfolding by binding to exposed hydrophobic residues [7]. | Identifying drug-target interactions through thermal stability shifts. |
| Simulated Gastrointestinal Fluids | Buffers mimicking the pH and composition of gastric and intestinal fluids for in vitro dissolution testing [6]. | Assessing drug release and stability in a physiologically relevant environment. |
| Cytochrome P450 Isoenzyme Assays | Enzyme systems used to study the metabolic stability of a drug and identify specific metabolic pathways [1] [5]. | Evaluating the potential for first-pass metabolism and drug-drug interactions. |
| Polymer Carriers (e.g., HPMC, PVPVA) | Used to create amorphous solid dispersions, maintaining the drug in a high-energy state to enhance solubility [6] [5]. | Formulation strategy for BCS Class II/IV drugs with poor aqueous solubility. |
| LC-MS/MS System | Gold-standard bioanalytical instrumentation for the sensitive and specific quantification of drug concentrations in complex biological matrices (e.g., plasma) [4]. | Generating pharmacokinetic data (AUC, C~max~, T~max~) from in vivo studies. |
Frequently Asked Questions
FAQ 1: What is the fundamental difference between logP and logD, and when should each be used?
- Answer:
logPdescribes the partition coefficient of a neutral (unionized) compound between octanol and water, representing its inherent lipophilicity. In contrast,logDis the distribution coefficient at a specific pH, accounting for all forms of the compound (ionized and unionized). You should uselogPfor neutral compounds andlogDfor ionizable compounds, aslogDprovides a more accurate picture of a compound's behavior under physiological pH conditions [8]. For compounds with ionizable sites,logDis essential for predicting solubility and membrane permeability accurately [8].
- Answer:
FAQ 2: During early-stage development, my compound shows poor aqueous solubility. What are the first parameters I should investigate and potentially optimize?
- Answer: The first parameters to investigate are
lipophilicity (logP/logD)andmolecular size/weight. High lipophilicity (logP > 5) often correlates with low aqueous solubility [9]. According to Lipinski's Rule of Five, a molecular weight exceeding 500 Da can also negatively impact solubility and permeability [8]. Your initial optimization efforts should focus on modifying the molecular structure to lower logP/logD, perhaps by introducing polar functional groups, while being mindful of the molecular size [9].
- Answer: The first parameters to investigate are
FAQ 3: How does the ionization state (pKa) of my compound influence its lipophilicity and solubility?
- Answer: The ionization state, determined by the compound's
pKaand the environmental pH, directly controls the balance betweensolubilityandlipophilicity[9] [8]. A charged species (ionized form) will have significantly higheraqueous solubilityand a lowerlogD(more hydrophilic). The unionized form has higherlipophilicity (logP)and bettermembrane permeability. ThelogDcurve, which plots logD against pH, visually represents this relationship and is critical for predicting behavior in different parts of the GI tract [8].
- Answer: The ionization state, determined by the compound's
Troubleshooting Guides
- Problem 1: Inconsistent or inaccurate determination of lipophilicity (logP/logD).
| Symptom | Possible Cause | Recommended Solution |
|---|---|---|
| Highly variable logD values across different pH levels. | Normal behavior for ionizable compounds; logD is pH-dependent [8]. | Characterize the full logD-pH profile instead of a single value. Use automated potentiometric titration for accuracy [9]. |
| Results do not align with in vitro permeability data. | logP was measured instead of physiologically relevant logD. | Switch to measuring logD at pH 6.5 for jejunal permeability prediction [8]. Ensure the assay buffers mimic physiological pH. |
| Low throughput is a bottleneck for screening. | Using traditional, manual shake-flask methods. | Implement automated instrumentation like the SiriusT3, which can perform up to 80 lipophilicity assays per day with sub-milligram quantities [9]. |
- Problem 2: Poor aqueous solubility leading to low bioavailability.
| Symptom | Possible Cause | Recommended Solution |
|---|---|---|
| Low kinetic and intrinsic solubility. | High molecular lipophilicity (excessively high logP) [9]. | Medify the chemical structure to reduce logP by adding ionizable or polar groups. Consider salt formation for ionizable compounds [9]. |
| Compound precipitates during dissolution. | Formation of unstable supersaturated states. | Use the CheqSol method to experimentally determine the extent and duration of supersaturation, which can guide formulation strategies [9]. |
| Poor solubility across various biological pH. | Unfavorable ionization profile (pKa). | Determine the pKa and model the solubility-pH profile. This can identify the optimal pH for solubility and guide salt or prodrug design [9]. |
- Problem 3: Inefficient isolation and characterization of bioactive compounds from natural extracts.
| Symptom | Possible Cause | Recommended Solution |
|---|---|---|
| Difficulty isolating the specific bioactive compound from a complex mixture. | Standard separation techniques are not target-directed. | Employ TLC bio-autography. This technique combines chromatographic separation with in situ activity determination to directly locate antimicrobial compounds on a TLC plate [10]. |
| Isolated compound loses activity upon purification. | The bioactive component may be a specific polymorphic form with higher solubility. | Perform solid-state characterization using techniques like X-ray Diffraction (XRD) or Differential Scanning Calorimetry (DSC) to identify and select the optimal polymorph [9]. |
| Low yield of the target bioactive compound. | Inefficient extraction method. | Utilize modern extraction techniques like Microwave-Assisted Extraction or Pressurized-Liquid Extraction, which can improve extraction efficiency and selectivity while reducing solvent use and degradation [10]. |
| Property | Target Range for Oral Drugs (Rule of 5) | Extended Range (Beyond Rule of 5) | Rationale & Impact |
|---|---|---|---|
| Molecular Weight | ≤ 500 Da | < 1000 Da | Affects transport across membranes; larger size can hinder diffusion [8]. |
| logP | < 5 | -2 to 10 | Governs membrane permeability and distribution; high values linked to toxicity and poor solubility [8]. |
| logD (at pH 7.4) | Not specified in Ro5 | Critical to assess | Determines actual lipophilicity at physiological pH; crucial for ionizable compounds [8]. |
| H-Bond Donors | ≤ 5 | ≤ 6 | Impacts permeability through H-bonding with water and membrane components [8]. |
| H-Bond Acceptors | ≤ 10 | ≤ 15 | Influences solubility and permeability [8]. |
- Table 2: Common Experimental Techniques for Property Determination
| Property | Common Experimental Techniques | Key Advantages | Throughput & Sample Need |
|---|---|---|---|
| Solubility | CheqSol, Shake-Flask, HPLC | CheqSol provides kinetic and intrinsic solubility and identifies supersaturation [9]. | Automated systems (e.g., SiriusT3) enable high-throughput with sub-milligram samples [9]. |
| Lipophilicity (logP/logD) | Shake-Flask, Potentiometric Titration (SiriusT3) | Potentiometric titration is automated and provides a full logD-pH profile [9]. | Up to 80 assays/day; < 2 hours for a logD profile; sub-milligram sample [9]. |
| pKa | Potentiometric Titration, Spectrophotometric | Determines ionization constant critical for understanding solubility and permeability [9]. | Automated titration takes <6 minutes per analysis [9]. |
| Identification/Isolation | TLC, HPLC, HPLC/MS, FTIR | TLC bioautography links chemical separation to biological activity for targeted isolation [10]. | Varies by method; HPLC/MS is robust and widely used for complex mixtures [10]. |
Experimental Protocols
Protocol 1: Determination of Intrinsic Solubility and Supersaturation Using the CheqSol Method
- Principle: This method rapidly determines intrinsic solubility by inducing a transition between supersaturated and undersaturated states through controlled addition of acid or base, while monitoring pH [9].
- Procedure:
- Preparation: Dissolve a small quantity (sub-milligram) of the compound in a water-miscible solvent like DMSO to create a stock solution.
- Initial Supersaturation: Add a known aliquot of the stock solution to a aqueous buffer, creating a supersaturated solution.
- Titration and Monitoring: Use an automated titrator (e.g., SiriusT3) to titrate with acid or base while continuously monitoring the pH. The software tracks the rate of pH change.
- Equilibrium Point: The titration continues until the solution reaches a state where the pH is stable, indicating equilibrium between the dissolved and solid drug (the intrinsic solubility).
- Data Analysis: The software calculates the intrinsic solubility and provides data on the kinetics of supersaturation, including the maximum supersaturation ratio and its persistence time [9].
Protocol 2: Measuring Lipophilicity (logD-pH Profile) via Automated Potentiometric Titration
- Principle: This technique measures the pKa of a compound in both water and water-octanol mixtures. The difference in pKa values between the two solvents is used to calculate the logP and subsequently the entire logD-pH profile [9].
- Procedure:
- Aqueous Titration: Dissolve the compound in a ionic strength-adjusted water solution. Perform a potentiometric titration from low to high pH (or vice-versa) to determine the aqueous pKa(s).
- Octanol-Water Titration: Add water-saturated octanol to the system and perform the titration again. The compound will partition into the octanol as it becomes neutral, shifting the apparent pKa.
- Data Processing: The instrument's software (e.g., SiriusT3 Refinement) analyzes the two titration curves. It calculates the logP from the pKa shift and then generates the full logD-pH profile [9].
- Output: The key deliverable is a graph of logD versus pH, which shows how the compound's lipophilicity changes across the physiological pH range [8].
Protocol 3: Bioassay-Guided Isolation Using TLC-Bioautography
- Principle: This method separates compounds via Thin-Layer Chromatography (TLC) and then uses an agar overlay inoculated with a test microorganism to visually locate antimicrobial compounds on the plate through zones of inhibition [10].
- Procedure:
- Separation: Spot the crude plant or natural extract on a TLC plate and develop it using an appropriate mobile phase.
- Drying: Ensure the plate is completely dry to remove all residual solvent, which could inhibit microbial growth.
- Inoculation: Overlay the TLC plate with a thin layer of molten nutrient agar that has been seeded with a log-phase culture of the target microorganism (e.g., S. aureus or E. coli).
- Incubation: Incub the plate in a humid chamber at the optimal temperature for the microorganism for a specified period (e.g., 24 hours).
- Visualization: After incubation, visualize the zones of inhibition (clear zones where microbial growth is prevented) against a background of confluent growth.
- Isolation: Correlate the inhibition zones with the Rf values from a reference TLC plate. The silica from the corresponding areas on a preparative TLC plate can be scraped off and eluted with a solvent like methanol to isolate the active compound for further characterization (e.g., by HPLC or LC-MS) [10].
The Scientist's Toolkit: Essential Research Reagents & Materials
- Table 3: Key Reagents and Instruments for Physicochemical Characterization
| Item | Function & Application |
|---|---|
| SiriusT3 Instrument | An automated platform for high-throughput determination of pKa, logP/logD, and solubility, using both potentiometric and spectrophotometric methods [9]. |
| n-Octanol & Aqueous Buffers | The two immiscible phases used in the shake-flask method and as reference systems in automated instruments for measuring partition/distribution coefficients [8]. |
| HPLC/MS Systems | Used for analyzing purity, stability, and for the identification and characterization of isolated bioactive compounds from complex mixtures [10]. |
| TLC Plates & Phytochemical Spray Reagents | Used for quick, low-cost separation of mixture components and for visualizing specific phytochemical classes (e.g., alkaloids, flavonoids) through color reactions [10]. |
| Differential Scanning Calorimetry (DSC) | Determines thermal stability and identifies polymorphic forms of a compound, which is critical for understanding solubility and bioavailability [9]. |
Relationships and Workflows
Diagram 1: Property Interplay in Bioavailability
Diagram 2: Bioactive Compound Discovery Workflow
For researchers focused on improving the bioavailability of bioactive compounds, biological barriers represent the most significant challenge to therapeutic efficacy. These barriers—comprising cellular interfaces, enzymatic systems, and efflux transporters—protect the body from xenobiotics but simultaneously limit the absorption and distribution of therapeutic agents [11]. The passage of a compound across biological barriers depends on its physico-chemical properties, formulation, degree of protein binding, and concentration gradient [11]. This technical resource addresses key experimental challenges in predicting and overcoming these barriers, with particular emphasis on practical methodologies for assessing and modulating permeability, metabolic stability, and efflux transporter activity.
Troubleshooting Common Experimental Challenges
FAQ: Addressing Variable Permeability Results
Q: Our Caco-2 permeability assays show high variability between replicates. What could be causing this inconsistency?
A: Caco-2 variability typically stems from three main sources: monolayer integrity, cell passage number, and assay conditions. First, always validate monolayer integrity by measuring transepithelial electrical resistance (TEER) before experiments; values should exceed 1000 Ω·cm², with optimal ranges between 2000-4000 Ω·cm² [12]. Second, control for passage number effects by using cells within consistent passages (e.g., P32-P72); extended passage can alter transporter expression and barrier function [12]. Third, ensure consistent culture duration—a standardized 10-day culture period improves differentiation and produces more reproducible results [12].
Q: How can we distinguish between passive diffusion and transporter-mediated flux in our absorption studies?
A: Implement selective inhibition protocols. For passive diffusion assessment, conduct experiments at 4°C to inhibit active transport processes or use specific transporter inhibitors. To identify specific transporter contributions, employ chemical inhibitors (e.g., zosuquidar for P-gp, Ko143 for BCRP, MK571 for MRP2) or genetic approaches using transporter-knockout cell lines [12]. Always include positive control substrates for each transporter (e.g., esitropram sulfate for BCRP, sulfasalazine for MRP2) to validate your inhibition approach [12].
FAQ: Managing Efflux Transporter Interference
Q: Our lead compound shows excellent solubility but poor oral bioavailability. Could efflux transporters be responsible?
A: Absolutely. ATP-dependent efflux transporters (P-gp, BCRP, MRP2) expressed on the apical membrane of intestinal epithelial cells significantly limit oral bioavailability for many compounds [13]. These transporters recognize structurally diverse compounds: P-gp prefers neutral and positively charged hydrophobic compounds; MRP2 transports hydrophilic conjugates; while BCRP recognizes relatively hydrophilic anticancer agents [13]. To assess this, compare bidirectional transport (A-B vs B-A) in Caco-2 or MDCK models. An efflux ratio (B-A/A-B) >2 suggests significant transporter involvement [13].
Q: What experimental approaches can identify efflux transporter inhibition without using probe substrates?
A: Recent advances enable detection of transporter inhibition through intracellular metabolomic signatures. Using targeted LC-MS, researchers have identified specific metabolite patterns associated with P-gp, BCRP, and MRP2 inhibition [12]. For P-gp inhibition, 11 intracellular metabolites show consistent changes; BCRP inhibition alters 4 metabolites; while MRP2 inhibition affects 9 metabolites [12]. This approach provides additional information on transporter inhibition in standard Caco-2 assays without compromising throughput.
FAQ: Overcoming Compound Degradation
Q: Our peptide compound is unstable in gastrointestinal fluids. What formulation strategies can protect it during transit?
A: Several advanced formulation approaches can address this challenge. Nano-delivery systems (niosomes, lipid nanoparticles) physically protect peptides from enzymatic degradation [14]. Chemical modification (e.g., Stapled Peptide technology) enhances stability against proteases [15]. Permeability enhancers (e.g., Intravail technology for transmucosal absorption) can significantly improve stability and absorption [15]. For oral delivery, consider enteric coatings that release compounds in the intestine rather than the stomach, or lipid-based systems that provide a protective environment [16] [17].
Experimental Protocols for Key Assays
Standardized Caco-2 Permeability and Efflux Assay
Purpose: To evaluate intestinal permeability and identify efflux transporter substrates.
Protocol:
- Cell Culture: Seed Caco-2 cells at 2×10⁴ cells/well on 96-well transwell plates (0.4 µM pore size). Culture for 10 days in DMEM with 10% FBS, 1% non-essential amino acids, and 1% penicillin-streptomycin, changing media every 2-3 days [12].
- TEER Validation: Measure TEER before experimentation using an epithelial voltohmmer. Accept only monolayers with TEER values >1000 Ω·cm² (optimal 2000-4000 Ω·cm²) [12].
- Bidirectional Transport:
- Prepare test compound in HBSS (pH 7.4) at relevant concentrations (typically 1-10 µM).
- For apical-to-basolateral (A-B) transport: Add compound to apical chamber, sample from basolateral chamber over 120 minutes.
- For basolateral-to-apical (B-A) transport: Add compound to basolateral chamber, sample from apical chamber over 120 minutes.
- Maintain at 37°C with gentle agitation [12] [13].
- Inhibition Studies: Co-incubate with selective inhibitors: 5 µM zosuquidar (P-gp), 10 µM Ko143 (BCRP), or 200 µM MK571 (MRP2) in both compartments [12].
- Sample Analysis: Quantify compound concentration in samples using LC-MS/MS. Calculate apparent permeability (Papp) and efflux ratio (B-A/A-B).
Troubleshooting Notes:
- Include positive controls for each transporter to validate system performance.
- For low-solubility compounds, use concentrations below solubility limits and verify stability throughout assay.
- Ensure pH stability throughout experiment as pH shifts can affect compound ionization and permeability.
Efflux Transporter Inhibition Screening via Metabolomics
Purpose: To identify potential efflux transporter inhibitors using intracellular metabolic signatures.
Protocol:
- Cell Treatment: Culture Caco-2 cells as described above. On day 10, treat with test compound (typically 1-10 µM) or vehicle control (1% DMSO in HBSS) for 60-120 minutes [12].
- Metabolite Extraction: Wash cells twice with cold PBS, then extract intracellular metabolites using 80% methanol containing internal standards. Scrape cells, vortex vigorously, and centrifuge at 14,000×g for 15 minutes at 4°C [12].
- LC-MS Analysis: Analyze supernatant using targeted LC-MS/MS with a focused panel of metabolites known to respond to transporter inhibition. Use a C18 column with gradient elution (water/acetonitrile with 0.1% formic acid) and multiple reaction monitoring (MRM) [12].
- Data Analysis: Normalize metabolite levels to protein content and internal standards. Compare patterns to established signatures for P-gp (11 metabolites), BCRP (4 metabolites), and MRP2 (9 metabolites) [12].
- Validation: Confirm findings with traditional probe substrate assays for positive hits.
Quantitative Data Tables
Table 1: Efflux Transporter Inhibitors and Experimental Concentrations
| Transporter | Inhibitor | Working Concentration | Positive Control Substrates |
|---|---|---|---|
| P-gp (MDR1) | Zosuquidar | 5 µM | Digoxin, Loperamide |
| Valspodar | 50 nM | ||
| Ritonavir | 10 µM | ||
| BCRP (ABCG2) | Ko143 | 10 µM | Esitropram sulfate, Methotrexate |
| Fumitremorgin C | 5 µM | ||
| Novobiocin | 30 µM | ||
| MRP2 (ABCC2) | MK571 | 200 µM | Sulfasalazine, Glutathione conjugates |
| Benzbromarone | 66.7 µM |
Data compiled from [12] and [13]
Table 2: Commercial Formulation Technologies for Bioavailability Enhancement
| Technology | Mechanism | Representative Products/Trade Names |
|---|---|---|
| Solid Dispersion | Maintains drug in amorphous state | ISOPTIN-SRE (Verapamil), GRIS-PEG (Griseofulvin) |
| Lipid-Based Systems | Enhances solubility & lymphatic transport | Fenoglide (Fenofibrate), Norvir (Ritonavir) |
| Nanoparticle Formulation | Increases surface area for dissolution | Invega Sustenna (Paliperidone), Rapamune (Sirolimus) |
| Cyclodextrin Complexation | Molecular encapsulation for solubility | Sporanox (Itraconazole), Geodon (Ziprasidone) |
| Polymer-Based Matrices | Controls release & enhances stability | INCIVEK (Telaprevir), ONMEL (Itraconazole) |
Data compiled from [16] and [15]
Visual Experimental Workflows
Transporter Inhibition Screening Workflow
Inhibition Screening Process
Intestinal Absorption Pathways
Compound Absorption Mechanisms
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Tools for Absorption Studies
| Reagent/System | Function | Application Notes |
|---|---|---|
| Caco-2 Cell Line | Model for intestinal permeability screening | Use passages 32-72; requires 10-day differentiation for optimal transporter expression [12] |
| Transwell Plates (0.4 µM) | Support for cell monolayer growth | Polycarbonate membranes preferred for compound compatibility [12] |
| TEER Measurement System | Monolayer integrity validation | Essential pre-experiment quality control; values >2000 Ω·cm² indicate tight junctions [12] |
| Selective Transporter Inhibitors | Mechanistic studies | Zosuquidar (P-gp), Ko143 (BCRP), MK571 (MRP2) at established concentrations [12] |
| LC-MS/MS Systems | Quantitative compound & metabolite analysis | Enables permeability calculations & metabolomic signature detection [12] |
| Transporter-Knockout Cells | Control for specific transporter effects | Available through commercial providers (e.g., SOLVO Biotechnology) [12] |
| HBSS Buffer (pH 7.4) | Physiological transport medium | Maintain pH stability throughout experiments [12] |
Advanced Technical Notes
Emerging Technologies in Bioavailability Enhancement
The field of bioavailability enhancement continues to evolve with several promising technologies. Lipid-based delivery systems enhance solubility and facilitate lymphatic transport, bypassing first-pass metabolism [15]. Amorphous solid dispersions stabilize drugs in high-energy states, significantly improving dissolution rates for BCS Class II compounds [16] [17]. Nanoparticle formulations (including nanocrystals and polymeric nanoparticles) increase surface area and enable targeted delivery [16] [18]. Additionally, advanced penetration enhancers for transdermal delivery—including fatty acid derivatives, terpenes, and physical methods like iontophoresis—are gaining traction for their ability to reversibly modify barrier function [19].
Regulatory Considerations
When developing formulations to overcome biological barriers, regulatory agencies provide specific guidance on bioavailability enhancement approaches. The FDA and EMA have established pathways for novel formulation technologies, particularly when bioequivalence studies demonstrate improved performance [15] [17]. For efflux transporter studies, regulatory guidelines emphasize evaluating potential drug-drug interactions during development, requiring assessment against key transporters (P-gp, BCRP) using established in vitro systems [12] [13].
BCS Framework FAQs: Core Principles and Regulatory Application
FAQ 1: What is the Biopharmaceutics Classification System (BCS) and what is its primary purpose in drug development?
The Biopharmaceutics Classification System (BCS) is an advanced, science-based framework that categorizes drug substances based on key biopharmaceutical properties: solubility, intestinal permeability, and dissolution [20]. Its primary objective is to evaluate the in vivo performance (bioavailability) of drug products based on in vitro data, thereby serving as a regulatory tool that can, under certain conditions, replace costly and time-consuming bioequivalence studies in humans (biowaiver) [20] [21]. For formulation scientists, the BCS provides a rational approach to designing novel dosage forms, moving away from empirical methods towards more predictive, modernistic strategies [20].
FAQ 2: How are drugs classified within the BCS framework?
The BCS classifies drugs into four main categories based on their aqueous solubility and intestinal permeability [20]. The following table summarizes the defining characteristics, key challenges, and examples for each class.
Table 1: The Four Classes of the Biopharmaceutics Classification System
| BCS Class | Solubility | Permeability | Rate-Limiting Step for Absorption | Key Challenge | Example Drugs |
|---|---|---|---|---|---|
| Class I | High | High | Gastric emptying | None (Ideal) | Acetaminophen, Verapamil [20] [22] |
| Class II | Low | High | Drug dissolution / Solubility | Low and variable bioavailability | Voriconazole, Griseofulvin, Lemborexant [20] [22] |
| Class III | High | Low | Permeability across the intestinal membrane | Limited absorption | Cimetidine, Metformin [20] |
| Class IV | Low | Low | A combination of solubility and permeability | Poor and variable absorption | Voxelotor, Fedratinib (in certain conditions) [21] [22] |
FAQ 3: What are the specific criteria for a drug to be considered "highly soluble" or "highly permeable"?
The regulatory definitions for the key BCS parameters are as follows [20]:
- High Solubility: A drug substance is considered highly soluble when the highest single therapeutic dose is completely soluble in 250 mL or less of aqueous media across a pH range of 1.0 to 6.8 (or up to 7.5 for some agencies) at 37°C.
- High Permeability: A drug substance is considered highly permeable when the extent of intestinal absorption in humans is determined to be 90% or more of the administered dose, based on mass balance studies or in comparison to an intravenous reference dose.
- Rapid Dissolution: A drug product is considered to have rapid dissolution when 85% or more of the labeled amount of drug substance dissolves within 30 minutes using standard USP apparatus (e.g., basket at 100 rpm or paddle at 50 rpm) in 900 mL of various buffer media.
FAQ 4: What is a BCS-based biowaiver and which drug classes are typically eligible?
A biowaiver is an official exemption from conducting in vivo bioequivalence studies. For immediate-release (IR) solid oral dosage forms, a biowaiver can be granted based on demonstrating that the product meets BCS-based criteria for solubility, permeability, and dissolution [21].
- BCS Class I: These drugs (high solubility, high permeability) with rapid dissolution are the strongest candidates for biowaivers [21].
- BCS Class III: Drugs with high solubility and low permeability are also considered for biowaivers by major regulatory agencies, provided they exhibit very rapid dissolution [21].
- BCS Class II & IV: Traditionally, these classes were not eligible for biowaivers due to absorption challenges. However, the World Health Organization has broadened its scope and now considers biowaivers for all BCS classes on a case-by-case basis, provided sufficient evidence is presented [21].
Troubleshooting Guide: Overcoming BCS Class II Drug Challenges
Challenge: The bioavailability of our BCS Class II drug candidate is unacceptably low and highly variable due to its poor solubility.
Solution Strategy: The primary goal is to enhance the apparent solubility and/or dissolution rate of the drug. This can be achieved through various physical and chemical modification techniques.
Table 2: Techniques to Enhance Solubility and Bioavailability of BCS Class II Drugs
| Technique Category | Specific Method | Brief Description & Mechanism | Research Reagent / Tool |
|---|---|---|---|
| Particle Size Reduction | Micronization | Reduces particle size to 1-10 microns, increasing surface area for dissolution [20]. | Jet Mill, Fluid Energy Mill |
| Nanoionization | Reduces drug particles to nanocrystals (200-600 nm), dramatically increasing saturation solubility [20]. | High-Pressure Homogenizer | |
| Solid-State Modification | Amorphous Solid Dispersions | Creates a high-energy, amorphous form of the drug dispersed in a polymer matrix, enhancing solubility [20]. | Povidone, Polyethylene Glycol |
| Polymorphs / Solvates | Utilizes metastable crystalline forms or anhydrates which have higher solubility than their stable counterparts [20]. | Solvents for Recrystallization | |
| Complexation | Cyclodextrin Inclusion | The drug molecule is entrapped in the hydrophobic cavity of cyclodextrin, improving aqueous solubility [20]. | Hydroxypropyl-β-Cyclodextrin |
| Novel Formulation Systems | Microemulsion / Nanoemulsion | Uses oil, surfactant, and co-surfactant to solubilize the drug in fine dispersions for improved absorption [20]. | Surfactants (Tween 80, Pluronic F-68) |
| Lipid-Based Systems | Incorporates the drug into lipids, surfactants, and co-solvents to keep the drug in a solubilized state in the GI tract [20]. | Medium-Chain Triglycerides |
Experimental Protocol: Preparation of a Solid Dispersion via the Hot-Melt Method
Objective: To create a solid dispersion of a BCS Class II drug in a hydrophilic polymer carrier to enhance its dissolution rate.
Materials:
- Active Pharmaceutical Ingredient (API): The BCS Class II drug.
- Carrier: Polyethylene Glycol (PEG) 6000 or Povidone (PVP K30).
- Equipment: Heating mantle with magnetic stirrer, aluminum dish, desiccator, mortar and pestle.
Methodology:
- Weighing: Accurately weigh the drug and the carrier in a predetermined ratio (e.g., 1:5).
- Melting: Transfer the physical mixture to an aluminum dish and heat directly on a heating mantle until both components melt, forming a clear, homogenous melt. Maintain constant, gentle stirring.
- Solidification: Rapidly cool the molten mixture by placing the dish on an ice bath while continuing to stir until the mass solidifies completely.
- Size Reduction: Break the solidified mass, crush it in a mortar, and pass it through a sieve to obtain a uniform powder.
- Storage: Store the final solid dispersion in a desiccator at room temperature until further use [20].
Validation: The success of the protocol can be validated by conducting an in vitro dissolution study comparing the solid dispersion against the pure API, expecting a significant increase in the dissolution rate for the solid dispersion.
The Scientist's Toolkit: Essential Reagents and Methods
Table 3: Key Research Reagent Solutions for BCS Characterization and Formulation
| Reagent / Material | Function in BCS Research |
|---|---|
| USP Dissolution Apparatus 1 & 2 | Standard equipment for determining drug dissolution profiles in 900 mL of various buffer media (e.g., 0.1 N HCl, pH 4.5, pH 6.8 buffers) [20]. |
| Caco-2 Cell Lines | In vitro model of the human intestinal epithelium used for predicting passive drug permeability [20]. |
| Povidone (PVP) | A common hydrophilic polymer used as a carrier in amorphous solid dispersions to inhibit crystallization and enhance solubility [20]. |
| Surfactants (e.g., Sodium Lauryl Sulfate) | Used in dissolution media to simulate sink conditions for poorly soluble drugs or as formulation components to improve wettability and solubility [20]. |
| High-Pressure Homogenizer | Key equipment for producing drug nanocrystals via top-down approaches like nanoionization [20]. |
| Cyclodextrins (e.g., HP-β-CD) | Oligosaccharides that form inclusion complexes with drug molecules, effectively increasing their apparent solubility and stability [20]. |
Decision Framework for Oral Drug Formulation
The following workflow outlines a strategic approach for formulating drug candidates based on their BCS classification, with a focus on overcoming absorption challenges. This process integrates BCS principles with the refined Developability Classification System (rDCS), which provides a more nuanced, animal-free risk assessment to guide formulation design [22].
Workflow Title: BCS-Driven Formulation Strategy
This diagram emphasizes that while BCS provides the initial classification, leveraging the refined Developability Classification System (rDCS) can offer a more detailed risk profile. For instance, some BCS Class II drugs may be reclassified as rDCS Class I, indicating a lower development risk and suitability for conventional formulations, while others may be stratified into higher-risk subclasses (IIa/IIb) requiring specific solubility-enhancement strategies [22].
FAQs: Core Principles and Regulatory Standards
What is the fundamental bioequivalence assumption and how does it link bioavailability to clinical outcomes?
The fundamental bioequivalence (BE) assumption states that if two drug products (e.g., a generic and a reference product) demonstrate comparable rate and extent of absorption (as measured by pharmacokinetic parameters AUC and Cmax), they will produce the same clinical effect (safety and efficacy) in patients [23]. This principle allows regulators to approve generic drugs without repeating extensive clinical trials, relying instead on demonstrated bioavailability equivalence.
What are the standard regulatory acceptance criteria for establishing bioequivalence?
For most drugs, average bioequivalence (ABE) requires that the 90% confidence interval for the ratio of geometric means (Test/Reference) for both AUC (extent of absorption) and Cmax (rate of absorption) falls entirely within the 80-125% range [23]. This is typically demonstrated through crossover studies in healthy volunteers.
How do bioequivalence requirements differ for highly variable drugs (HVDs)?
For highly variable drugs (within-subject variability >30%), the Reference-scaled Average Bioequivalence (RSABE) approach is employed [23]. This method widens the acceptance limits proportionally to the reference product's variability, making BE demonstration feasible without impractically large sample sizes. Key requirements include:
- Replicated crossover designs where subjects receive the reference product multiple times
- Minimum 24 subjects for FDA studies
- Point estimate of geometric mean ratio must remain within 80-125%
What recent international harmonization efforts affect bioequivalence testing?
The ICH M13 series represents a major global harmonization initiative. ICH M13A (effective January 2025) addresses BE for immediate-release solid oral dosage forms, while the draft M13B guidance describes criteria for waiving BE studies for additional strengths when one strength has demonstrated BE in vivo [24] [25]. These guidelines aim to standardize BE requirements across regulatory jurisdictions.
Troubleshooting Common Bioequivalence Study Issues
Problem: High within-subject variability causing failure to demonstrate bioequivalence
Solution: Implement Reference-scaled Average Bioequivalence (RSABE) approach [23]
- Protocol Modification: Employ replicated crossover designs (3-period: RRT, RTR, TRR or 4-period: RTRT, TRTR)
- Statistical Adjustment: Scale bioequivalence limits based on reference product variability (SWR)
- Regulatory Compliance: Pre-specify RSABE approach in protocol before study initiation
- Sample Size Consideration: Ensure adequate sample size (minimum 24 subjects for FDA)
Problem: Uncertain sample size for achieving sufficient statistical power
Solution: Utilize sample size calculation tools with appropriate parameters [26]
- Key Inputs: Within-subject CV%, expected Geometric Mean Ratio (GMR), BE limits (typically 80-125%)
- Study Design Selection: Choose between 2x2 crossover, replicated crossover, or parallel designs based on drug characteristics
- Power Target: Set statistical power at 80% or higher with alpha typically at 5%
- Online Resources: Use specialized calculators (e.g., powerTOST package) for reliable estimates
Problem: Determining when clinical endpoint BE studies are necessary
Solution: Follow FDA tiered approach for different product types [27]
- Tier 1: Blood level BE studies preferred when feasible
- Tier 2: Pharmacologic endpoint studies for drugs with directly measurable pharmacological effects
- Tier 3: Clinical endpoint studies when neither Tier 1 nor Tier 2 approaches are possible
- Biowaiver Eligibility: Certain products (IV solutions, oral solutions, topical solutions for local effect) may qualify for biowaivers based on Q1/Q2 sameness
Research Reagent Solutions for Bioequivalence Studies
Table: Essential Materials and Analytical Tools for Bioequivalence Research
| Item/Category | Function/Purpose | Key Specifications |
|---|---|---|
| Bioanalytical Method Validation [27] | Quantify drug concentrations in biological matrices | FDA Guidance #145 compliance; validation for precision, accuracy, selectivity |
| Phoenix WinNonlin [23] | Statistical analysis of BE data using RSABE | FDA/EMA-compliant templates for replicate designs; partial & full replicate support |
| Replicated Crossover Design [23] | Account for high within-subject variability | 3-period (TRR, RTR, RRT) or 4-period (TRTR, RTRT) designs |
| Sample Size Calculators [26] | Determine optimal subject numbers | powerTOST-based; parameters: CV%, GMR, BE limits, target power, alpha |
| Biowaiver Documentation [27] [25] | Justify in vivo BE study waivers | Q1/Q2 qualitative/quantitative sameness evidence; physicochemical comparison |
Experimental Protocols and Methodologies
Standard Two-Period Crossover Bioequivalence Study Protocol
- Study Design: Randomized, two-period, two-treatment, single-dose crossover with adequate washout period
- Subjects: Healthy volunteers (typically n=24-36) meeting inclusion/exclusion criteria
- Dosing: Administration of test and reference products under fasting/fed conditions as specified
- Blood Sampling: Serial blood collection over sufficient time span to characterize complete PK profile
- Bioanalysis: Validated method for drug quantification in plasma/serum
- PK Analysis: Non-compartmental analysis to determine AUC0-t, AUC0-∞, and Cmax
- Statistical Analysis: ANOVA on log-transformed parameters; calculation of 90% CI for T/R ratio
Replicated Crossover Design for Highly Variable Drugs [23]
- Design Selection: Choose 3-period or 4-period replicated design based on expected variability
- Reference Repetition: Ensure each subject receives reference product at least twice
- Within-Subject Variability Calculation: Determine SWR (within-subject standard deviation of reference)
- RSABE Application Criteria: Apply when SWR ≥ 0.294 (CV ≥ 30%)
- Statistical Analysis: Use scaling approach per FDA or EMA guidelines with point estimate constraint
Biowaiver Application Protocol for Additional Strengths [25]
- Reference Product: Identify Reference Listed Drug with demonstrated BE
- Strength proportionality: Demonstrate linear pharmacokinetics across strengths
- Formulation Similarity: Show same qualitative and quantitative composition (Q1/Q2)
- In Vitro Dissolution: Conduct comparative dissolution studies per regulatory requirements
- Documentation: Submit detailed justification with formulation comparison data
Bioequivalence Establishment Workflows
Regulatory Decision Pathways for Highly Variable Drugs
Regulatory Comparison Table: FDA vs. EMA Bioequivalence Approaches
Table: Comparative Bioequivalence Requirements for Highly Variable Drugs
| Parameter | Agency | Low Variability (SWR < 0.294) | High Variability (SWR ≥ 0.294) |
|---|---|---|---|
| AUC | FDA | Standard ABE (CI 80-125%) | RSABE permitted; CI can be widened; Point estimate within 80-125% |
| EMA | Standard ABE (CI 80-125%) | Standard ABE (CI 80-125%) only | |
| Cmax | FDA | Standard ABE (CI 80-125%) | RSABE permitted; CI can be widened; Point estimate within 80-125% |
| EMA | Standard ABE (CI 80-125%) | RSABE permitted; CI can be widened up to 70-143%; Point estimate within 80-125% | |
| Study Design | FDA | Standard 2x2 crossover or replicated | Replicated crossover required |
| EMA | Standard 2x2 crossover or replicated | Replicated crossover required | |
| Minimum Sample Size | FDA | Not specified | 24 subjects |
| EMA | Not specified | Not specified |
Table: RSABE Acceptance Range Widening at Different Variability Levels
| CVWR (%) | SWR | EMA RSABE Limits | FDA RSABE Limits |
|---|---|---|---|
| <30 | — | ABE method (80-125%) | ABE method (80-125%) |
| 30 | 0.294 | 80.00 – 125.00 | 76.94 – 129.97 |
| 35 | 0.340 | 77.23 – 129.48 | 73.82 – 135.47 |
| 40 | 0.385 | 74.62 – 134.02 | 70.89 – 141.06 |
| 45 | 0.429 | 72.15 – 138.59 | 68.15 – 146.74 |
| 50 | 0.472 | 69.84 – 143.19 | 65.58 – 152.48 |
| 60 | 0.555 | 69.84 – 143.19 (max widening) | 60.95 – 164.08 |
Cutting-Edge Formulation Technologies for Bioavailability Enhancement
In modern pharmaceutical development, a significant challenge is the poor aqueous solubility of new chemical entities (NCEs), which limits their bioavailability and therapeutic efficacy. It is estimated that 40% to 90% of drugs in development can be characterized as poorly water-soluble, falling into BCS Class II or IV [28] [29]. To address this, amorphous solid dispersions (ASDs) have emerged as a reliable strategy. Among the various production techniques, hot-melt extrusion (HME) and spray drying are two of the most prevalent and effective methods used to produce ASDs [30]. These technologies enhance the dissolution rate and oral bioavailability of active pharmaceutical ingredients (APIs) by stabilizing them in a high-energy, amorphous form within a polymer matrix [31]. This technical support center provides a foundational guide for researchers and scientists, offering troubleshooting advice and detailed methodologies for implementing these critical bioavailability enhancement technologies.
Hot-melt extrusion and spray drying are enabling technologies designed to transform poorly soluble crystalline APIs into amorphous solid dispersions.
Hot-Melt Extrusion (HME) is a continuous, solvent-free process that uses thermal and mechanical energy to mix and melt a blend of API and polymer, forming a homogeneous amorphous matrix [32] [28]. It is a mature technology known for its robust and scalable nature [33] [34].
Spray Drying is a continuous solvent evaporation process that transforms a liquid feed solution (containing API and polymer dissolved in a volatile solvent) into a dry, powdered ASD through atomization and rapid drying [35] [29]. It is particularly valued for its flexibility in polymer selection and applicability to heat-sensitive compounds [29].
The table below summarizes a direct comparison of these core technologies:
Table 1: Quantitative Comparison of Hot-Melt Extrusion and Spray Drying
| Feature | Hot-Melt Extrusion (HME) | Spray Drying |
|---|---|---|
| Process Nature | Continuous, solvent-free [32] [34] | Continuous, solvent-based [35] [29] |
| Key Mechanism | Melting and mixing via heat and shear [32] | Rapid solvent evaporation from atomized droplets [29] |
| Typical Polymer Selection | Thermoplastic polymers (e.g., PVP VA64) [36] | Broad range, including cellulose-based polymers [35] [29] |
| Drug Loading | Can be limited by API-polymer miscibility [35] | Can achieve higher drug loading [31] |
| Scalability | Readily scalable; equipment is compact [34] | Scalable, but equipment is larger and complex [34] |
| Relative Bioavailability Improvement | Demonstrated significant enhancement (e.g., Oleanolic acid) [36] | Typically 3 to 15-fold improvement [33] |
| Key Advantage | Superior stability against recrystallization [30] | Higher intrinsic dissolution rates (IDR) [30] |
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful formulation of ASDs requires careful selection of excipients and solvents. The following table details key materials and their functions in developing solid dispersions.
Table 2: Key Research Reagents and Materials for Solid Dispersions
| Item | Function / Role | Examples & Selection Criteria |
|---|---|---|
| Polymeric Carriers | Stabilize the amorphous API, inhibit recrystallization, and enhance dissolution [35] [31]. | PVP K30: Offers strong drug-polymer interactions, enhancing both dissolution rate and stability [30].HPMC E5: A commonly used cellulose derivative [30].Soluplus: A long-chain polymer with strong solubilizing capabilities [35].PVP/VA 64 (copovidone): Can stabilize formulations via H-bonding, inhibiting recrystallization [35]. |
| Solvents | Dissolve the API and polymer to create a homogeneous feed solution for spray drying [35]. | Acetone, Methanol, Ethanol: Volatile organic solvents with low boiling points, preferred for faster drying and smaller particle size [35] [29]. Selection is based on solvation power and safety. |
| Surfactants | Further improve wettability and bioavailability, can be added to the formulation blend [28]. | Often incorporated as additional components in HME formulations to aid in dispersion and dissolution [28]. |
| Model Compounds | Poorly soluble APIs used for proof-of-concept and method development. | Indomethacin: A widely used model compound for poorly soluble drugs [30].Oleanolic Acid: A BCS Class IV model compound whose bioavailability was enhanced via HME [36]. |
Experimental Protocols for Key Experiments
Protocol for Preparing ASDs via Hot-Melt Extrusion
This protocol outlines the methodology for enhancing the bioavailability of a poorly soluble compound, such as Oleanolic Acid, using Hot-Melt Extrusion [36].
1. Objective: To prepare an amorphous solid dispersion of a poorly soluble API (e.g., Oleanolic Acid) using HME to enhance its dissolution rate and oral bioavailability.
2. Materials:
- API (e.g., Oleanolic Acid) [36].
- Polymer (e.g., PVP VA64) [36].
- Twin-screw hot-melt extruder (co-rotating preferred for pharmaceuticals) [32].
3. Methodology:
- Step 1: Pre-blending. The API and the polymer (e.g., PVP VA64) are physically mixed in a predetermined ratio to ensure a homogeneous powder blend before feeding into the extruder [28] [36].
- Step 2: Extrusion. The powder blend is fed into the extruder. Critical process parameters (CPPs) to control include:
- Barrel Temperature Profile: Set above the glass transition temperature (Tg) of the polymer-API blend but below the degradation temperature of the components [32].
- Screw Speed (RPM): Controls the residence time and shear rate, typically ranging from 100 to 500 rpm [32].
- Feed Rate: Must be optimized to ensure consistent output and filling of the screw channels [32].
- Step 3: Cooling & Collection. The molten extrudate is forced through a die and cooled on a conveyor belt to form a solid ribbon or strand [32].
- Step 4: Downstream Processing. The cooled extrudate is milled or ground into granules or powders suitable for subsequent dosage form development, such as compression into tablets or filling into capsules [28].
4. Characterization: The final ASD should be characterized using Differential Scanning Calorimetry (DSC) and Powder X-Ray Diffraction (PXRD) to confirm the conversion to the amorphous state [36]. An in vitro dissolution test and in vivo pharmacokinetic study in animal models (e.g., rats) are conducted to validate the enhancement in dissolution rate and bioavailability [36].
Protocol for Preparing ASDs via Spray Drying
This protocol is adapted from general spray drying processes and tailored for small-scale development using limited API, as described in the literature [35] [29].
1. Objective: To produce an amorphous solid dispersion of a poorly soluble API using spray drying to improve its solubility and bioavailability.
2. Materials:
- API and suitable polymer (see Table 2).
- Volatile organic solvent (e.g., acetone, methanol, or mixture) [35] [29].
- Small-scale spray dryer (e.g., Büchi Nano Spray Dryer B-90 or ProCepT 4M8-TriX for milligram-scale studies) [29].
3. Methodology:
- Step 1: Feed Solution Preparation. The API and polymer are dissolved in a common volatile solvent to create a homogeneous feed solution. The total solid content is dictated by solubility and solution viscosity [35].
- Step 2: Atomization. The feed solution is pumped into a spray nozzle (e.g., piezoelectric, ultrasonic, or pressure nozzle) and atomized into a fine mist of droplets inside the drying chamber [35] [29].
- Step 3: Drying. The droplets are contacted with hot drying gas (e.g., nitrogen). The inlet air temperature (typically 50°C to 200°C) is controlled to rapidly evaporate the solvent [35] [31].
- Step 4: Collection. The dried solid particles are separated from the gas stream and collected using a cyclone or an electrostatic collector [35] [29]. The outlet temperature is a critical response parameter influenced by the inlet temperature and feed rate.
4. Characterization: The resulting spray-dried dispersion (SDD) powder is characterized for particle size and morphology, amorphization (using PXRD), residual solvent content, and in vitro dissolution performance [35] [31].
Troubleshooting Guides and FAQs
Hot-Melt Extrusion Troubleshooting
Q1: During HME, my API is degrading. What could be the cause and how can I prevent this?
- A: Thermal degradation is a primary concern. To mitigate this:
- Lower Processing Temperature: Optimize the barrel temperature profile to the minimum required to form a homogeneous melt. Using a polymer with a lower glass transition temperature (Tg) can facilitate this [28].
- Optimize Screw Speed and Residence Time: Reducing the screw speed can shorten the time the API is exposed to high temperatures [32].
- Formulation Screening: Conduct thorough pre-formulation screening to identify APIs with sufficient thermal stability for HME or consider alternative polymers that process at lower temperatures [28].
Q2: My HME extrudate shows signs of incomplete mixing or phase separation. What should I check?
- A: Inhomogeneity can compromise the stability and performance of the ASD.
- Screw Configuration: Ensure the screw design includes mixing elements (e.g., kneading blocks) to provide adequate distributive and dispersive mixing [32].
- Feed Rate Consistency: A fluctuating feed rate can lead to poor mixing. Verify that the powder feeder is calibrated and operating consistently [32].
- API-Polymer Miscibility: Re-evaluate the compatibility between the API and polymer. The drug should be miscible with the polymer at the processing temperature to form a single-phase system [35].
Spray Drying Troubleshooting
Q1: The yield of my spray-dried product is very low, especially at a small scale. How can I improve it?
- A: Low yield is a common challenge in lab-scale spray drying.
- Optimize Collector Type: For small-scale dryers like the Büchi B-90, the electrostatic collector is highly efficient for sub-5µm particles. Ensure it is functioning correctly [29].
- Adjust Process Parameters: High powder loss can occur due to wall adhesion. Optimizing the inlet/outlet temperature, spray rate, and the use of anti-static agents can reduce electrostatic adherence [35].
- Check Nozzle/Capillary: For small-scale units, ensure the spray mesh or nozzle is not clogged and is appropriate for the solution's viscosity and desired particle size [29].
Q2: My spray-dried powder is sticky, agglomerating, or has high residual solvent. What steps can I take?
- A: These issues are often linked to the drying efficiency and formulation.
- Increase Outlet Temperature: A higher outlet temperature indicates more efficient drying. This can be achieved by increasing the inlet temperature or reducing the feed rate [35]. However, balance is needed to avoid degrading the API.
- Implement Secondary Drying: A dedicated secondary drying step (e.g., using a fluid bed dryer or vacuum oven) is often necessary to reduce residual solvents to levels compliant with ICH guidelines [34] [31].
- Reformulate: Consider adjusting the polymer type or ratio in your formulation. Some polymers act as better moisture barriers or provide better drying characteristics [35].
General ASD Troubleshooting
Q1: My ASD is recrystallizing upon storage or during dissolution. How can I improve its physical stability?
- A: Recrystallization is a critical failure mode for ASDs.
- Polymer Selection: Choose a polymer that has strong molecular interactions with the API (e.g., hydrogen bonding). Studies show that PVP K30 can outperform other polymers like HPMC E5 in stabilizing indomethacin against recrystallization [30].
- Storage Conditions: Store the ASD in airtight containers with desiccants. Exposure to moisture and high temperature can plasticize the polymer and mobilize the API molecules, facilitating crystallization [30].
- Add Stabilizers: Incorporate small amounts of surfactants into the formulation to improve wettability and help maintain supersaturation during dissolution [28].
Q2: When scaling up from lab to pilot/commercial scale, the performance of my ASD changes. What is the key to successful scale-up?
- A:
- For HME: The continuous nature of HME makes it highly scalable. Successful scale-up relies on maintaining consistent key parameters such as specific mechanical energy (SME), melt temperature, and shear rate by adjusting screw configuration and speed [34].
- For Spray Drying: Scale-up is more complex due to changes in chamber geometry and gas flow dynamics. The key is to maintain consistent droplet size and drying kinetics (e.g., by keeping the outlet temperature constant across scales) rather than directly copying all parameters [31]. Using a Quality by Design (QbD) approach and Process Analytical Technology (PAT) is highly recommended for both techniques [32].
Lipid-based drug delivery systems have emerged as a cornerstone technology for enhancing the bioavailability of poorly water-soluble bioactive compounds and drugs [37]. These systems, which include self-emulsifying drug delivery systems (SEDDS) and liposomes, address fundamental challenges in pharmaceutical development by improving solubility, protecting active ingredients from degradation, and facilitating targeted delivery [38]. For researchers focused on improving bioactive compound bioavailability, understanding the formulation strategies, troubleshooting common issues, and implementing optimized protocols is essential for successful experimental outcomes.
The following technical support content provides practical guidance structured in a question-and-answer format, specifically addressing challenges researchers might encounter during experimentation with SEDDS and liposomal formulations. This resource integrates current methodologies, troubleshooting guides, and essential reagent information to support your research within the broader context of bioavailability enhancement.
Self-Emulsifying Drug Delivery Systems (SEDDS): Technical Guide
SEDDS Troubleshooting FAQs
Q1: My SEDDS formulation shows drug precipitation upon dilution in gastrointestinal fluids. What are the potential causes and solutions?
- Cause: Insufficient surfactant concentration or inappropriate surfactant-to-oil ratio.
- Solution: Increase surfactant concentration or incorporate polymeric precipitation inhibitors such as HPMC or PVP [37].
- Preventive Approach: Conduct in vitro lipolysis studies during formulation development to predict precipitation tendencies and optimize lipid composition [39].
Q2: What causes chemical instability of the drug in SEDDS, and how can it be mitigated?
- Cause: Interaction between drug and excipients, or susceptibility to enzymatic degradation.
- Solution: Use alternative lipid excipients with better compatibility, or incorporate antioxidants like butylated hydroxytoluene (BHT) [37].
- Advanced Strategy: Transition from liquid SEDDS (L-SEDDS) to solid SEDDS (S-SEDDS) via spray drying or adsorption to solid carriers to enhance stability [37].
Q3: How can I improve the poor emulsification efficiency of my SEDDS formulation?
- Cause: Suboptimal selection of surfactants or cosurfactants.
- Solution: Systematically screen surfactants (e.g., Tween 80, Labrasol) and cosurfactants (e.g., Transcutol HP) using phase diagram studies [37].
- Diagnostic Tool: Use droplet size analysis after emulsification; optimal SEDDS should form microemulsions with droplet size <300 nm [37].
Q4: My solid SEDDS formulation shows slow drug release. What could be the reason?
- Cause: Improper solidification technique or excessive carrier material.
- Solution: Optimize the spray drying parameters or reduce the adsorbent carrier ratio [37].
- Alternative Approach: Use hot-melt extrusion instead of adsorption for solidification to create more porous structures [37].
SEDDS Experimental Protocols
Protocol: Preparation and Characterization of Solid SEDDS
Objective: To formulate solid SEDDS (S-SEDDS) with enhanced stability and dissolution properties.
Materials:
- Drug compound
- Lipids: Medium-chain triglycerides (e.g., Captex 355), long-chain triglycerides (e.g., Soybean oil)
- Surfactants: Tween 80, Labrasol, Cremophor RH 40
- Cosurfactants: PEG 400, Transcutol HP
- Solid carriers: Neusilin US2, Aerosil 200, Syloid 244FP
Procedure:
- Liquid SEDDS Preparation:
- Dissolve drug in mixture of oil, surfactant, and cosurfactant
- Stir continuously at 40°C until clear solution forms
- Conduct preliminary emulsification studies in 0.1N HCl and phosphate buffer pH 6.8
Transition to Solid SEDDS:
- Adsorption Method: Mix liquid SEDDS with solid carriers in 1:1 to 1:2 ratio
- Spray Drying: Dissolve solid carriers in liquid SEDDS and spray dry at inlet temperature 100°C, outlet temperature 60°C
- Melt Extrusion: Incorporate lipids and drug into hot-melt extruder at temperature 10°C above lipid melting point
Characterization:
- Droplet size analysis using dynamic light scattering
- Dissolution studies in biorelevant media
- Solid-state characterization (DSC, PXRD) to confirm amorphous state
Critical Parameters:
- Maintain temperature below drug degradation point during processing
- Optimize carrier ratio to avoid poor flow properties or excessive moisture absorption
- Conduct stability studies at accelerated conditions (40°C/75% RH) for 3 months [37]
Quantitative Composition Data for SEDDS Formulations
Table 1: Typical Composition Ranges for SEDDS Formulations
| Component | Type | Concentration Range (% w/w) | Function | Examples |
|---|---|---|---|---|
| Oils/Lipids | Medium-chain triglycerides | 20-50% | Solubilize lipophilic drugs, promote lymphatic transport | Captex 355, Miglyol 812 |
| Long-chain triglycerides | 20-50% | Enhance drug solubilization, resist precipitation | Soybean oil, Peanut oil | |
| Surfactants | Non-ionic | 30-60% | Lower interfacial tension, facilitate emulsion formation | Tween 80, Cremophor RH 40 |
| Co-surfactants | Short-chain alcohols | 10-30% | Further reduce interfacial tension, increase emulsion stability | PEG 400, Ethanol, Transcutol HP |
| Drug Load | Active compound | 5-20% | Therapeutic agent | Varies by drug properties |
Table 2: Characterization Parameters for SEDDS Quality Control
| Parameter | Method | Acceptance Criteria | Significance |
|---|---|---|---|
| Droplet Size | Dynamic light scattering | <300 nm for SNEDDS, <5000 nm for SMEDDS | Determines absorption rate and bioavailability |
| Polydispersity Index | Dynamic light scattering | <0.3 | Indicates uniformity of emulsion droplets |
| Emulsification Time | Visual observation in USP dissolution apparatus | <2 minutes | Ensures rapid self-emulsification |
| Drug Content | HPLC analysis | 95-105% of labeled claim | Ensures dosage accuracy |
| Stability | Accelerated stability testing | No precipitation or phase separation | Predicts shelf life |
SEDDS Workflow Visualization
SEDDS Formulation Development Workflow
Liposomal Formulations: Technical Guide
Liposome Troubleshooting FAQs
Q1: My liposome formulation shows low encapsulation efficiency for hydrophilic drugs. How can I improve this?
- Cause: Leakage of drug during formation or inappropriate loading method.
- Solution: For hydrophilic drugs, use active loading techniques with gradient methods (e.g., pH gradient, ammonium sulfate) [40].
- Advanced Technique: Implement remote loading using calcium acetate gradient as demonstrated for dexamethasone hemisuccinate [40].
Q2: What causes liposome aggregation during storage, and how can it be prevented?
- Cause: Insufficient surface charge or inappropriate lipid composition.
- Solution: Incorporate charged lipids (e.g., dicetyl phosphate for negative charge) or optimize cholesterol content (typically 30-50 mol%) [41] [42].
- Storage Solution: Lyophilize with cryoprotectants (e.g., trehalose, sucrose) and store at 4°C [42].
Q3: My liposomes show rapid clearance in vivo. How can I extend circulation time?
- Cause: Recognition by mononuclear phagocyte system (MPS).
- Solution: Incorporate PEGylated lipids (5-10 mol%) to create "stealth" liposomes [42].
- Optimization Note: Balance PEG content as excessive PEG can hinder cellular uptake and cause ABC phenomenon with repeated dosing [42].
Q4: How can I achieve consistent liposome size with minimal batch-to-batch variation?
- Cause: Inefficient sizing methods or variable process parameters.
- Solution: Implement microfluidic techniques instead of traditional thin-film hydration [40].
- Validation Data: Microfluidics produces unilamellar vesicles with higher loading capacity and lower batch-to-batch differences compared to multilamellar vesicles from thin-film hydration [40].
Liposome Experimental Protocols
Protocol: Microfluidic Preparation of Liposomes
Objective: To prepare unilamellar liposomes with controlled size and high encapsulation efficiency using microfluidic technology.
Materials:
- Lipids: Phosphatidylcholine, cholesterol, PEGylated lipids (e.g., DSPE-PEG2000)
- Aqueous phase: Phosphate buffer saline (PBS), pH 7.4
- Organic phase: Ethanol or isopropanol
- Microfluidic device (staggered herringbone mixer or hydrodynamic flow focusing design)
Procedure:
- Lipid Solution Preparation:
- Dissolve lipid mixture in organic phase at 10-20 mg/mL concentration
- Maintain molar ratio based on desired composition (typical: 55:40:5 PC:Chol:PEG-lipid)
Microfluidic Process:
- Set aqueous to organic phase flow rate ratio between 3:1 to 5:1
- Maintain total flow rate at 10-15 mL/min
- Collect liposome suspension in PBS buffer
Purification and Characterization:
- Dialyze against buffer or use tangential flow filtration to remove organic solvent
- Characterize particle size, PDI, and zeta potential
- Determine encapsulation efficiency via mini-column centrifugation or dialysis
Critical Parameters:
- Optimize flow rate ratio to control liposome size
- Ensure complete solvent removal to maintain stability
- Sterilize by filtration through 0.22μm membrane for in vivo studies [40]
Quantitative Composition Data for Liposomal Formulations
Table 3: Lipid Composition for Different Liposome Types
| Lipid Component | Conventional Liposomes | Stealth Liposomes | Cationic Liposomes | Function |
|---|---|---|---|---|
| Phosphatidylcholine | 50-70 mol% | 50-65 mol% | 40-60 mol% | Main bilayer component |
| Cholesterol | 30-50 mol% | 30-45 mol% | 30-40 mol% | Membrane stability, reduce leakage |
| PEGylated Lipid | - | 5-10 mol% | 0-5 mol% | Prolong circulation time |
| Cationic Lipid | - | - | 20-50 mol% | Bind nucleic acids, enhance uptake |
| Charged Lipid | 0-10 mol% | 0-5 mol% | - | Provide surface charge |
Table 4: Liposome Characterization Specifications
| Parameter | Analytical Method | Target Specifications | Impact on Performance |
|---|---|---|---|
| Particle Size | Dynamic light scattering | 80-150 nm (for long circulation) | Affects clearance, EPR effect |
| Polydispersity Index | Dynamic light scattering | <0.2 (monodisperse) | Indicates homogeneity |
| Zeta Potential | Electrophoretic light scattering | ±10-30 mV (for stability) | Affects physical stability |
| Encapsulation Efficiency | Mini-column centrifugation/HPLC | >90% (optimal) | Determines drug loading |
| Lamellarity | Cryo-TEM or NMR | Unilamellar preferred | Affects release kinetics |
Liposome Preparation Workflow Visualization
Liposome Preparation Method Selection
Research Reagent Solutions
Table 5: Essential Materials for Lipid-Based Delivery System Research
| Reagent/Category | Specific Examples | Function in Formulation | Research Application |
|---|---|---|---|
| Lipid Materials | Phosphatidylcholine, Cholesterol, DSPE-PEG2000 | Form bilayer structure, enhance stability, prolong circulation | Liposome formation, membrane engineering |
| Medium-chain triglycerides, Long-chain triglycerides | Solubilize lipophilic drugs, promote lymphatic transport | SEDDS oil phase component | |
| Surfactants | Tween 80, Cremophor RH 40, Labrasol | Lower interfacial tension, facilitate self-emulsification | SEDDS emulsification component |
| Analytical Tools | Dynamic Light Scattering (DLS) instrument | Measure particle size and distribution | Quality control of nanoformulations |
| HPLC systems with appropriate detectors | Quantify drug content and encapsulation efficiency | Assay development and validation | |
| Specialty Equipment | Microfluidic devices | Produce uniform nanoparticles with high reproducibility | Liposome and LNP manufacturing |
| Spray dryer, Hot-melt extruder | Convert liquid to solid dosage forms | S-SEDDS production |
Advanced Technical Considerations
Computational Approaches in Formulation Development
The development of lipid-based delivery systems is increasingly supported by computational methods that can accelerate formulation optimization:
- Molecular Dynamics (MD) Simulations: Model molecular-level interactions between lipids and drugs to predict encapsulation efficiency and membrane behavior [43].
- Machine Learning Applications: Analyze complex formulation data to identify optimal component ratios and predict performance outcomes [43].
- Constant pH Molecular Dynamics (CpHMD): Particularly valuable for ionizable lipids in LNPs, accurately predicting environment-dependent protonation states that affect LNP charge and interactions [43].
These computational approaches can significantly reduce experimental time and costs while providing molecular insights difficult to obtain through traditional experimental methods alone.
Bioavailability Enhancement Mechanisms
Understanding how lipid-based systems enhance bioavailability is essential for rational formulation design:
- Solubilization Enhancement: Lipid systems maintain drugs in solubilized state throughout gastrointestinal transit, avoiding precipitation [37].
- Lymphatic Transport: Especially with long-chain lipids, facilitates bypass of first-pass metabolism [37].
- P-Glycoprotein Inhibition: Certain lipid excipients can inhibit efflux transporters, increasing intestinal absorption [37].
- Controlled Release Profiles: Liposomal systems can provide sustained release, extending therapeutic effect [42].
By systematically addressing the troubleshooting guides, implementing the detailed protocols, and utilizing the research reagent solutions provided, researchers can overcome common challenges in lipid-based delivery system development. These technical resources support the broader thesis objective of improving bioactive compound bioavailability through advanced formulation strategies, ultimately contributing to more effective therapeutic interventions.
Fundamental Principles and Impact on Bioavailability
How does particle size reduction improve the bioavailability of bioactive compounds?
Bioavailability is the rate and extent to which an active drug ingredient or therapeutic moiety is absorbed and becomes available at the site of action. For many bioactive compounds, particularly those classified under the Biopharmaceutics Classification System (BCS) as Class II (low solubility, high permeability) or Class IV (low solubility, low permeability), poor water solubility is the primary rate-limiting step for absorption [44] [45] [46]. Particle size reduction directly addresses this challenge through two main mechanisms:
- Increased Dissolution Rate: Reducing particle size increases the specific surface area (surface area-to-volume ratio) of the drug particles. A larger surface area allows for greater interaction with the gastrointestinal fluid, which directly enhances the dissolution rate, as described by the Noyes-Whitney equation [47] [45]. For instance, a study on esomeprazole showed that reducing the particle size (X50) from 648 µm to 494 µm decreased the median dissolution time (T50) from about 61 minutes to 38 minutes [45].
- Enhanced Membrane Absorption: In the intestine, the mucus layer has pores ranging from 10 nm to 200 nm. Drug particles with sizes below 200 nm can more easily traverse this bilayer mucus, enter epithelial cells, and be absorbed into the systemic circulation. Smaller particles are also subject to enhanced cellular uptake mechanisms like persorption [45] [48].
It is crucial to distinguish between the effects of micronization and nanonization. Micronization (particles between 1–1000 µm) primarily improves the dissolution rate without significantly altering the equilibrium solubility. In contrast, nanonization (particles in the submicron range, typically <1 µm) can enhance both the dissolution rate and the equilibrium solubility of a compound, as below a critical size limit (around 1 µm), the solubility becomes dependent on the particle size [44].
Technology Comparison and Selection
What are the key differences between nano-milling and microfluidization, and how do I choose?
The following table provides a structured comparison of nano-milling and microfluidization to aid in the selection of the appropriate technology.
Table 1: Comparison of Nano-milling and Microfluidization Technologies
| Feature | Nano-Milling (Media Milling) | Microfluidization |
|---|---|---|
| Principle | 'Top-down' approach using mechanical energy from milling media (beads) to shear and break down particles [47]. | 'Top-down' approach using high pressure to force a suspension through a narrow interaction chamber, generating shear forces and impact to reduce size [49]. |
| Typical Particle Size | 100s of nanometers [47]. | Can achieve nanoscale; particle size depends on pressure and cycles [50]. |
| Key Advantages | Universally applicable to most insoluble APIs; easy scale-up; highly reproducible; avoids harsh solvents [47] [46]. | No media contamination; efficient for emulsions and dispersions; scalable process [49]. |
| Key Challenges | Potential for metal contamination (ceramic media); heat generation; requires stabilizers to prevent aggregation/ripening [47] [45]. | Risk of chamber clogging; heat generation; potential for nozzle wear [49]. |
| Ideal Candidate | BCS Class II/IV APIs with solubility <200 µg/mL; high crystalline lattice energy compounds [47] [46]. | Formulations requiring narrow size distribution; lipid-based nanosystems; production of nanoemulsions and liposomes [49] [51]. |
Table 2: Overview of Common Particle Size Reduction Techniques
| Method | Typical Particle Size Limit | Key Advantages | Key Disadvantages |
|---|---|---|---|
| High-Pressure Homogenization | ~100 nm [45] | Avoids amorphization and polymorphic transformation [45]. | May require pre-micronization steps [45]. |
| Liquid Antisolvent Crystallization | ~100 nm [45] | Overcomes chemical and thermal degradation issues [45]. | Recovery and disposal of organic solvents [45]. |
| Spray Drying | ~1000 nm [45] | Adjustable parameters to control particle size distribution [45]. | May cause chemical and thermal degradation [45]. |
| Ball Milling | ~1000 nm [45] | Simple principle, wide application. | Wide particle size distribution; high energy consumption and low efficiency [45]. |
Technology Selection Workflow
Nano-Milling: Troubleshooting Common Issues
FAQ 1: Our nano-suspension is aggregating or showing particle growth over time. What could be the cause?
Particle aggregation and growth (often via Ostwald ripening) are common stability challenges in nanosuspensions due to the high surface energy of nanoparticles [47].
- Root Cause & Solution:
- Inadequate Stabilizer System: The primary cause is often an insufficient or suboptimal stabilizer. Stabilizers, typically polymers (e.g., PVA, PVP) and/or surfactants, function by providing steric hindrance or electrostatic repulsion to prevent particles from coming together [47].
- Action: Screen different stabilizers and their concentrations. Polymeric stabilizers like PVPK-25 have been shown to inhibit aggregation more effectively than PVA in some cases due to their molecular structure [44]. A secondary surfactant (e.g., Tween 80) can be added to improve wetting and lower surface tension [47] [52].
- Suboptimal Milling Parameters:
- Action: Optimize process parameters like milling time and agitator speed. While longer milling times may be needed to reach the target size, excessive milling can lead to surface activation and instability. Similarly, the agitator speed must balance efficient size reduction against excessive heat and energy input [47].
- Inadequate Stabilizer System: The primary cause is often an insufficient or suboptimal stabilizer. Stabilizers, typically polymers (e.g., PVA, PVP) and/or surfactants, function by providing steric hindrance or electrostatic repulsion to prevent particles from coming together [47].
FAQ 2: The milling process is taking too long to achieve the target particle size. How can we optimize it?
- Root Cause & Solution:
- Inefficient Media Load or Size:
- Action: Increase the media load in the milling chamber to raise the number of collisions. Furthermore, using smaller media beads (e.g., 0.2 µm vs. 1.0 µm) can be more effective for achieving very small particle sizes and can reduce processing time [47].
- Low Agitator Speed:
- Action: Increasing the agitator speed introduces more energy into the system, resulting in more frequent and violent collisions. However, this must be balanced against increased heat and potential impurity levels [47].
- API Properties: APIs with a high crystalline lattice energy are inherently more difficult to mill.
- Action: For such challenging compounds, extended milling times (potentially multiple days) may be unavoidable. Process parameter optimization becomes critical [47].
- Inefficient Media Load or Size:
Microfluidization: Troubleshooting Common Issues
FAQ 1: The reaction chamber in our microfluidizer is frequently plugging. How can we resolve and prevent this?
Chamber clogging is a frequent operational issue in microfluidization, often due to the presence of large, coarse particles in the initial suspension [49].
Immediate Resolution:
- Disassemble and Reverse Flush: Disassemble the reaction chamber. A key troubleshooting step is to reinsert the chamber in the reverse direction and run the machine for a few cycles to push the plug out. Then, reassemble it correctly and resume [49].
- Ultrasonic Cleaning: If reverse flushing fails, place the clogged chamber in an ultrasonic bath with a solvent (e.g., denatured alcohol) to break down the obstruction [49].
- Spare Parts Kit: To maintain production continuity, it is highly recommended to keep a spare reaction chamber on hand [49].
Prevention:
- Effective Pre-homogenization: Ensure the feed suspension is well pre-homogenized using a high-shear mixer or a rotor-stator homogenizer to break down large aggregates before microfluidization [49].
- Filtration: Pre-filter the suspension through a coarse filter to remove any oversized particulates.
FAQ 2: We are observing a leak from the fitting or the hydraulic cylinder. What should we do?
- Root Cause & Solution:
- Loose or Improperly Seated Fittings:
- Action: Tighten all high-pressure fittings. Ensure that the cone fittings are properly seated with about "two threads" visible, as misalignment can prevent a proper seal. Most high-pressure fittings have "weep holes" that will leak fluid if the fitting is not tight enough, providing a clear indicator [49].
- Worn Piston Seal:
- Action: If fluid is leaking from the pump's hydraulic cylinder port, it indicates a worn plunger seal. These seals are consumable parts under high pressure and need to be replaced periodically. The system is designed to allow for relatively quick seal changes [49].
- Loose or Improperly Seated Fittings:
Essential Experimental Protocols
Protocol 1: Preparing a Nanosuspension via Media Milling
This protocol is adapted from established nanomilling practices [47] [46].
Formulation:
- Prepare an aqueous dispersion containing 5-40% (w/w) of the poorly soluble API [47].
- Add stabilizers to the water phase. Common stabilizers include:
- The choice and ratio of stabilizer are API-dependent and require screening.
Milling Process:
- Load the milling chamber with appropriate milling media (e.g., crosslinked polystyrene or ceramic beads of 0.2-1.0 mm diameter) [47].
- Pump the pre-mixed API suspension from a holding tank through the milling chamber.
- Set the agitator speed to the required RPM (typically in the thousands) and begin recirculation.
- Use a coolant to maintain the temperature of the milling chamber (e.g., 10-25°C) to protect thermosensitive APIs [47] [45].
- Continue milling for a predetermined time (hours to days) until the target particle size is achieved, as confirmed by laser diffraction or dynamic light scattering.
Separation and Recovery:
- Once milling is complete, separate the nanosuspension from the milling media using an in-line screen.
- The resulting nanosuspension can be used directly for liquid dosage forms or further processed (e.g., spray-drying) into a powder for solid dosage forms [47].
Protocol 2: Particle Size Reduction via Microfluidization
This protocol is based on standard microfluidization operation and a recent application for bioactive compound delivery [49] [50].
Pre-emulsion/Pre-dispersion Formation:
- For a bioactive compound like curcumin, first create a coarse pre-emulsion. Dissolve the compound and a carrier (e.g., casein, PLGA) in a suitable organic solvent (e.g., dichloromethane, acetone) to form the organic phase [52] [50].
- Slowly add this organic phase into an aqueous solution containing a surfactant (e.g., PVA) under continuous stirring to form a coarse emulsion [52].
Microfluidization:
- Prime the microfluidizer with distilled water, then with the sample.
- Pass the coarse pre-emulsion through the microfluidizer interaction chamber at a defined pressure (e.g., 10,000 - 30,000 PSI) for multiple cycles.
- The number of cycles and the pressure will determine the final particle size and distribution. More cycles and higher pressure generally yield smaller particles [49] [50].
Solvent Evaporation & Recovery:
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Reagents and Materials for Particle Size Reduction Experiments
| Item | Function | Example Use Cases |
|---|---|---|
| Stabilizers: Polymers | Provide steric stabilization to prevent nanoparticle aggregation by coating the particles [47]. | PVA [44] [52], PVP/Kollidon [44], Poloxamers, Cellulose derivatives (HPMC). |
| Stabilizers: Surfactants | Lower interfacial tension, improve wetting of particles, and provide electrostatic stabilization [47]. | Polysorbate 80 (Tween 80) [52], Sodium lauryl sulfate (SLS), Lecithin [44]. |
| Milling Media | Beads that impart shear forces and collision energy to break down API particles in nano-milling [47]. | Cross-linked polystyrene (less dense, less contamination), Yttria-stabilized Zirconia (denser, for hard crystals) [47]. |
| Biorelevant Media | Simulate the pH and composition (bile salts, lecithin) of gastrointestinal fluids for predictive solubility/dissolution testing [44]. | FaSSIF (Fasted State Simulated Intestinal Fluid), FeSSIF (Fed State Simulated Intestinal Fluid) [44]. |
| PLGA | A biodegradable and FDA-approved copolymer used to form nanoparticles for controlled release of bioactives [52]. | Encapsulation of curcumin, quercetin, piperine to enhance bioavailability and provide sustained release [52]. |
| Casein | A milk protein used as a natural encapsulating material for hydrophobic bioactives in food and pharmaceutical applications [50]. | Formulation of casein-curcumin nanodispersions for improved stability and controlled release in functional foods [50]. |
Analytical Techniques for Particle Characterization
How do we accurately measure particle size and distribution after processing?
Accurate characterization is non-negotiable. The following table summarizes the most common techniques.
Table 4: Comparison of Mainstream Particle Size Analysis Techniques
| Technique | Principle | Size Range | Key Advantages | Key Limitations |
|---|---|---|---|---|
| Laser Diffraction (LD) | Measures the angular variation of light scattered by particles. | ~0.1 - 5000 µm [45] | Fast; provides volume-based distribution; high reproducibility [45]. | Assumes spherical particles; sample dilution required [45]. |
| Dynamic Light Scattering (DLS) | Measures Brownian motion to calculate hydrodynamic diameter. | ~1 nm - 5 µm [45] | Measures particles in suspension; fast analysis; high sensitivity for small nanoparticles [45]. | Assumes spherical particles; sensitive to dust/aggregates; intensity-weighted distribution can be skewed by a few large particles [45]. |
| Scanning Electron Microscopy (SEM) | Direct imaging using a focused electron beam. | ~1 nm - 100 µm [45] | Direct visual information on particle size, shape, and morphology [45]. | Sample must be vacuum-compatible; tedious sample preparation; limited field of view statistics [45]. |
Bioavailability Enhancement Pathway
In the critical field of bioactive compound research, improving bioavailability remains a fundamental challenge. A significant number of promising therapeutic compounds, both synthetic and natural, are hampered by poor aqueous solubility and low stability, which drastically limit their therapeutic potential [53]. Among the most effective strategies to overcome these limitations is the formation of inclusion complexes using cyclodextrins (CDs).
Cyclodextrins are cyclic oligosaccharides with a unique structure: a hydrophilic exterior and a hydrophobic internal cavity [54] [55]. This structure allows them to act as molecular "hosts," encapsulating hydrophobic "guest" molecules within their cavity. This encapsulation process, driven by non-covalent interactions, can profoundly alter the physicochemical properties of the guest molecule, leading to enhanced solubility, protection from degradation, and consequently, improved bioavailability [53] [56] [57]. This technical resource provides a practical guide for researchers utilizing this powerful technology.
Cyclodextrin Fundamentals: A Researcher's Reference
Types of Cyclodextrins and Their Properties
The three naturally occurring cyclodextrins are α-, β-, and γ-cyclodextrin, composed of six, seven, and eight glucopyranose units, respectively [54] [56]. Their structural differences translate into distinct functional properties, guiding the selection of the appropriate CD for a specific application. Beta-cyclodextrin (β-CD) is the most widely used due to its cavity size being suitable for a wide range of drug molecules, though its native form has relatively low water solubility [56].
To improve upon the properties of native CDs, various chemically modified derivatives have been developed. The table below summarizes the key cyclodextrin types and their characteristics relevant to pharmaceutical and nutraceutical applications.
Table 1: Key Characteristics of Native and Modified Cyclodextrins
| Cyclodextrin Type | Abbreviation | Glucose Units | Cavity Diameter (Å) | Key Characteristics & Solubility |
|---|---|---|---|---|
| Alpha-Cyclodextrin | α-CD | 6 | 4.7 - 5.3 [56] | Moderate solubility; suitable for small molecules [58] |
| Beta-Cyclodextrin | β-CD | 7 | 6.0 - 6.5 [56] | Lowest solubility (~18.5 g/L) among native CDs; most common and cost-effective [56] |
| Gamma-Cyclodextrin | γ-CD | 8 | 7.5 - 8.3 [56] | High solubility; suitable for larger molecules [58] |
| Hydroxypropyl-Beta-Cyclodextrin | HP-β-CD | 7 | ~6.5 | Very high solubility (>600 g/L); widely used, improved safety profile [56] |
| Sulfobutylether-Beta-Cyclodextrin | SBE-β-CD | 7 | ~6.5 | Very high solubility (>500 g/L); often used in parenteral formulations [56] |
| Randomly Methylated-Beta-Cyclodextrin | RM-β-CD | 7 | ~6.5 | Very high solubility (500-700 g/L); powerful solubilizing capacity [56] |
Mechanism of Action: How Complexation Enhances Bioavailability
The enhancement of a compound's bioavailability through CD complexation is a multi-faceted process. The following diagram illustrates the key mechanisms and their interrelationships, from complex formation to the final physiological outcome.
Core Experimental Protocols
This section details standard methodologies for preparing and analyzing cyclodextrin inclusion complexes.
Preparation Methods: Freeze-Drying (Lyophilization)
Freeze-drying is a highly effective method for producing solid inclusion complexes with high purity and good stability.
Detailed Workflow:
- Solution Preparation: Dissolve the guest molecule (e.g., drug) and the cyclodextrin (e.g., HP-β-CD) in a suitable solvent, most commonly water or a water/solvent mixture. A typical molar ratio for optimization is 1:1, but this should be determined experimentally for each pair [59].
- Complexation: Stir the mixture for a defined period (e.g., 24 hours) at a controlled temperature in the dark to prevent photodegradation [60].
- Filtration: Filter the resulting solution through a 0.45 μm or 0.22 μm membrane filter to remove any non-complexed, particulate matter.
- Lyophilization: Freeze the filtrate and place it in a freeze-dryer. Lyophilization typically runs for 24-48 hours until a dry, porous powder is obtained. This powder is the solid inclusion complex.
Preparation Methods: Kneading
The kneading method is a simple, solid-state-based technique that requires minimal equipment.
Detailed Workflow:
- Slurry Formation: Thoroughly mix the cyclodextrin with a small volume of solvent (e.g., water or ethanol) in a mortar to form a homogeneous paste.
- Incorporation of Guest: Gradually add the guest molecule to the paste while continuously kneading with a pestle.
- Kneading Process: Knead the mixture consistently for 30-60 minutes. The physical pressure and the presence of a small amount of solvent facilitate the complexation process.
- Drying: The resulting paste is dried in an oven at a moderate temperature (e.g., 40-50°C) until dry, then gently ground and sieved to obtain a uniform powder.
Phase Solubility Studies
Phase solubility studies are critical for determining the stability constant (K1:1) of the complex and its stoichiometry, providing a quantitative basis for formulation development.
Detailed Workflow:
- Excess Drug Preparation: Place an excess amount of the guest molecule (drug) into a series of vials.
- CD Solution Series: Add increasing concentrations of cyclodextrin solution (e.g., 0-15 mM) to each vial. Use a constant final volume in all vials.
- Equilibration: Seal the vials and agitate them in a water bath shaker at a constant temperature (e.g., 25°C or 37°C) for a sufficient time to reach equilibrium (often 24-72 hours).
- Analysis: After equilibration, filter or centrifuge the samples to remove any undissolved guest material. Analyze the concentration of the dissolved guest in each vial using a validated analytical method (e.g., HPLC, UV-Vis spectroscopy).
- Data Processing: Plot the concentration of dissolved guest versus the concentration of cyclodextrin. The stability constant K1:1 can be calculated from the slope of the linear phase of the curve using the following equation, where S0 is the intrinsic solubility of the guest: K1:1 = Slope / [S0 (1 - Slope)]
The diagram below illustrates the experimental workflow for these key preparation and characterization methods.
Quantitative Data: Demonstrating Efficacy
The primary goal of complexation is to achieve measurable improvements in key properties. The following table compiles quantitative data from recent research, demonstrating the significant enhancement in solubility achievable with cyclodextrins.
Table 2: Experimental Efficacy of Cyclodextrin Inclusion Complexes
| Active Substance | Native Solubility (mg/mL) | Cyclodextrin Used | Complex Solubility (mg/mL) | Fold-Increase & Key Outcome | Reference |
|---|---|---|---|---|---|
| Chlortetracycline HCl | 4.0 | HP-β-CD | 36.0 | ~9x increase; enhanced antimicrobial activity in vivo [59] | |
| Amphotericin B | 0.001 | SBE-β-CD | 0.15 | 150x increase; improved bioavailability [53] | |
| Itraconazole | 0.001 | HP-β-CD | 4.0 - 5.0 | >4000x increase [53] | |
| Diclofenac | 4.0 | HP-β-CD | 20.0 | 5x increase [53] | |
| Ibuprofen | 0.1 | Methyl-β-CD | 10.0 | 100x increase [53] | |
| ITH12674 (Melatonin Hybrid) | 0.31 | HP-β-CD | 10.7 | ~34.5x increase; improved stability at various pH and temperature [53] | |
| Limonium bellidifolium Extracts | N/A | β-CD | N/A | Significantly higher recovery of quercetin, catechin, and ferulic acid after simulated digestion; increased antioxidant activity [60] |
The Scientist's Toolkit: Essential Reagents & Materials
Table 3: Key Research Reagent Solutions for Cyclodextrin Research
| Reagent / Material | Function / Application in Research |
|---|---|
| Native Cyclodextrins (α-, β-, γ-CD) | Foundation for complexation studies; β-CD is the most common starting point for screening. |
| Hydroxypropyl-β-Cyclodextrin (HP-β-CD) | A versatile, highly soluble, and well-tolerated derivative; often the first choice for enhancing solubility and stability for parenteral and oral delivery [56] [57]. |
| Sulfobutylether-β-Cyclodextrin (SBE-β-CD) | A negatively charged, highly soluble derivative; particularly valuable for complexing cationic drugs and used in parenteral formulations [56]. |
| Randomly Methylated-β-CD (RM-β-CD) | A powerful, non-ionic solubilizer with very high solubility; useful for challenging compounds but requires careful toxicological evaluation [56]. |
| Dimethyl Sulfoxide (DMSO) | A common solvent for preparing stock solutions of poorly soluble guest molecules before dilution into aqueous CD solutions. |
| Simulated Gastric/Intestinal Fluids | Used in in vitro models to study the stability and release profile of inclusion complexes under biologically relevant conditions [60]. |
Troubleshooting Guide & FAQs
FAQ 1: My inclusion complex is not providing the expected increase in solubility. What could be wrong?
- Incorrect Stoichiometry: The molar ratio of CD to guest is critical. A 1:1 ratio is common, but some complexes require 1:2 or 2:1 ratios. Perform phase solubility studies to determine the optimal ratio [54].
- Cavity Size Mismatch: The guest molecule must fit into the CD cavity. If the guest is too large or too small, complexation will be weak or non-existent. Screen different CDs (α-, β-, γ-) to find the best fit [54] [56].
- Insufficient Complexation Time/Kinetics: The formation of the inclusion complex is an equilibrium process. Ensure the reaction mixture is stirred for a sufficient duration (often 24 hours or more) to reach equilibrium [60].
- Inefficient Preparation Method: The chosen method (e.g., kneading) might not be effective for your specific molecule. Try an alternative method like freeze-drying or solvent evaporation.
FAQ 2: How can I conclusively prove that a true inclusion complex has formed, and not just a simple mixture?
Characterization requires a combination of techniques. Key analytical methods include:
- Phase Solubility Analysis: A linear AL-type diagram is a classic indicator of complex formation and provides the stability constant [57].
- Differential Scanning Calorimetry (DSC): The disappearance, shift, or broadening of the melting endotherm of the guest molecule in the complex indicates interaction and loss of crystallinity [57].
- FTIR Spectroscopy: Shifts in the characteristic absorption bands of the guest molecule (or the CD) suggest molecular interactions within the cavity [60].
- X-ray Powder Diffraction (XRPD): A change in the crystalline pattern of the physical mixture towards a more amorphous pattern in the complex is a strong evidence of complex formation [57].
- NMR Spectroscopy: NMR, especially 2D ROESY, can provide definitive proof by showing spatial proximity between protons of the guest and the inner cavity of the CD [56].
FAQ 3: I am working with a large, complex molecule (e.g., a peptide or protein). Can cyclodextrins still be useful?
Yes. While full encapsulation may not be possible, cyclodextrins can interact with hydrophobic regions on large biomolecules. For example, HP-β-CD has been shown to improve the stability and particle properties of spray-dried IgG for inhalable formulations [58]. Furthermore, γ-CD complexation improved the chemical half-life and reduced aggregation of the peptide hormone glucagon by interacting with its hydrophobic amino acid residues [58].
FAQ 4: Are there safety concerns with using chemically modified cyclodextrins in formulations?
Cyclodextrins are generally considered safe and biocompatible. Native α- and γ-CDs are on the FDA's GRAS (Generally Recognized as Safe) list. The safety profile of modified CDs is also favorable; for instance, HP-β-CD and SBE-β-CD are approved for use in various pharmaceutical products [56] [58]. However, parent β-CD has limited oral use due to nephrotoxicity observed in parenteral administrations, which is why its modified derivatives are preferred for such routes [56]. Always consult regulatory guidelines and conduct appropriate toxicological studies for your specific application.
The efficacy of many therapeutic compounds, especially those with poor water solubility, is often limited by low bioavailability. Within the framework of the Biopharmaceutics Classification System (BCS), a significant number of drugs and bioactive compounds fall into Class II (low solubility, high permeability) or Class IV (low solubility, low permeability), where dissolution rate, permeability, and stability in the gastrointestinal (GI) tract are major barriers to absorption [61]. Advanced carrier systems, including Solid Lipid Nanoparticles (SLNs), Nanostructured Lipid Carriers (NLCs), and polymeric Micelles, have emerged as powerful nanotechnological strategies to overcome these challenges. These nanocarriers enhance bioavailability by improving solubility, protecting compounds from enzymatic degradation, enabling controlled release, and facilitating transport across intestinal membranes [62] [61] [63]. This technical support center provides targeted troubleshooting guides and detailed methodologies to assist researchers in the development and characterization of these advanced delivery systems.
Troubleshooting Guides for Common Experimental Challenges
Troubleshooting Lipid Nanoparticle Formulation (SLNs & NLCs)
Table 1: Common Issues in Lipid Nanoparticle Development and Solutions
| Problem Phenomenon | Potential Root Cause | Proposed Solution | Key References |
|---|---|---|---|
| Low Drug Entrapment Efficiency | Highly organized crystalline lipid core expelling drug; Drug-lipid incompatibility. | Use a blend of solid and liquid lipids to create a less ordered, imperfect crystal structure (NLC approach). | [64] |
| Particle Aggregation/Physical Instability | Inadequate surfactant type or concentration; High surface energy of nanoparticles. | Optimize surfactant blend (use combination surfactants); Consider high-pressure homogenization for uniform size. | [65] [64] |
| Rapid Burst Release or Incomplete Release | Drug localization on particle surface instead of core; Solid lipid matrix too dense for drug diffusion. | Optimize the solid-to-liquid lipid ratio; Use lipids that form less perfect crystals; Test different surfactant combinations. | [64] |
| Particle Size Too Large or Polydisperse | Insufficient energy input during size reduction; Cold homogenization temperature causing lipid recrystallization. | Increase homogenization pressure/cycles; Ensure lipid melt is fully molten before homogenization (Hot HPH). | [66] [64] |
| Drug Expulsion During Storage | Lipid matrix polymorphic transition from α/β' to more stable β form. | Formulate with lipids that are less prone to crystallization (e.g., hydroxyoctacosanyl hydroxystearate). | [64] |
Troubleshooting Polymeric Micelle Formulation
Table 2: Common Issues in Polymeric Micelle Development and Solutions
| Problem Phenomenon | Potential Root Cause | Proposed Solution | Key References |
|---|---|---|---|
| Low Drug Loading Capacity | Poor compatibility between drug and hydrophobic core of micelle; Core-forming block is too short. | Select a core-forming polymer with chemical structure similar to the drug (e.g., PCL for highly hydrophobic drugs). | [67] |
| Premature Drug Release (Low Stability in Biorelevant Media) | Critical Micelle Concentration (CMC) is too high, causing dissociation upon dilution. | Use polymers with lower CMC (e.g., higher molecular weight hydrophobic blocks); Consider cross-linking the core or shell. | [63] [67] |
| Difficulty in Reproducible Preparation | Method relies on manual, multi-step processes like dialysis or thin-film hydration. | Transition to more controlled methods like microfluidics or PEG-assisted assembly for better reproducibility. | [67] |
| Organic Solvent Residue | Use of organic solvents in dialysis or solvent evaporation methods. | Implement solvent-free methods or supercritical fluid technology to eliminate solvent residues. | [67] |
Frequently Asked Questions (FAQs) for Researchers
Q1: When should I choose NLCs over SLNs for my poorly soluble compound? A: NLCs are the second-generation lipid nanoparticles designed to overcome the key limitations of SLNs. If you are encountering low drug loading capacity or drug expulsion during storage with SLNs, switching to NLCs is recommended. The blend of solid and liquid lipids in NLCs creates a more disordered matrix, providing more space for drug accommodation and preventing the formation of a perfect crystal lattice that pushes the drug out [64].
Q2: How can I determine if my micellar formulation is stable upon oral administration and absorption? A: Stability is a common concern. Evaluate your micelles by determining the Critical Micelle Concentration (CMC). A lower CMC indicates a more stable micelle that is less likely to dissociate upon dilution in the GI tract [63] [67]. Furthermore, conduct in vitro release studies in simulated gastric and intestinal fluids to assess drug release kinetics and integrity under biorelevant conditions.
Q3: What are the key characterization parameters for these nanocarriers, and which techniques are essential? A: Comprehensive characterization is non-negotiable for quality control. The essential parameters and techniques are summarized in the table below.
Table 3: Essential Characterization Techniques for Advanced Carriers
| Parameter | Importance | Standard Techniques | ||
|---|---|---|---|---|
| Particle Size & Distribution (PDI) | Affects stability, drug release, and cellular uptake. | Dynamic Light Scattering (DLS), Laser Diffraction (LD) [65]. | ||
| Zeta Potential | Predicts colloidal stability; high value (> | ±25 | mV) indicates good stability. | Zeta Potential Analyzer [65]. |
| Entrapment Efficiency & Drug Loading | Critical for evaluating formulation success and dosage. | Indirect method (centrifugation/ultrafiltration) followed by drug assay via HPLC/UV-Vis [66]. | ||
| Surface Morphology | Visual confirmation of particle size, shape, and structure. | Transmission Electron Microscopy (TEM), Scanning Electron Microscopy (SEM), Atomic Force Microscopy (AFM) [66] [65]. | ||
| Crystallinity & Lipid Modification | Impacts drug release profile and long-term stability. | Differential Scanning Calorimetry (DSC), X-Ray Diffraction (XRD) [65]. | ||
| In Vitro Drug Release | Predicts in vivo performance and release mechanism. | Dialysis bag method in suitable dissolution media (e.g., PBS, simulated GI fluids) [66]. |
Q4: Can you provide a specific example of a successful bioactive compound delivered via these carriers? A: Yes. Ginger extracts, rich in bioactive but poorly soluble polyphenols like gingerols and shogaols, have been successfully encapsulated in NLCs and other lipid-based systems. These formulations demonstrated significant improvements in oral bioavailability, enhanced stability against degradation, and increased therapeutic efficacy in studies, including selective cytotoxicity against cancer cell lines and potent anti-inflammatory activity [68].
Detailed Experimental Protocols
Protocol: Preparation of NLCs via Hot High-Pressure Homogenization (HPH)
This is a widely used and scalable method for producing NLCs, as exemplified in the formulation of Tenofovir Disoproxil Fumarate NLCs [66].
1. Principle: A hot oil-in-water (o/w) microemulsion is formed by dispersing a melted lipid phase containing the drug into a hot aqueous surfactant phase. This pre-emulsion is then passed through a high-pressure homogenizer, where the intense shear forces and cavitation break down the droplets to the nanoscale. Upon cooling, the lipid core solidifies, forming solid nanoparticles [64].
2. Materials:
- Lipid Phase: Solid lipid (e.g., Glyceryl monostearate, Compritol 888 ATO), Liquid lipid (e.g., Oleic acid, Miglyol 812), Drug (e.g., Bioactive compound).
- Aqueous Phase: Surfactant(s) (e.g., Tween 80, Poloxamer 188, Lecithin), Water (purified).
- Equipment: Heated magnetic stirrer, High-pressure homogenizer (e.g., Panda or similar), Water bath.
3. Step-by-Step Workflow:
4. Critical Parameters for Success:
- Temperatures: Ensure both phases are heated at least 5-10°C above the melting point of the solid lipid throughout the process to prevent premature solidification.
- Homogenization Parameters: The number of cycles and applied pressure are directly correlated with final particle size and distribution. Optimization is required (e.g., 3-5 cycles at 500-1500 bar) [64].
- Surfactant Selection: Using a combination of surfactants often results in a more stable system with smaller particle size [64].
Protocol: Preparation of Polymeric Micelles via Solvent Evaporation/Dialysis
This is a common laboratory-scale method for encapsulating hydrophobic drugs in polymeric micelles [67].
1. Principle: Amphiphilic block copolymers and the hydrophobic drug are first dissolved in a water-miscible organic solvent (e.g., acetone, DMSO). This organic solution is then added slowly to an aqueous phase under vigorous stirring. As the organic solvent diffuses into the water, it reduces the solvent quality for the hydrophobic blocks, driving the self-assembly of micelles with the drug encapsulated in the core. The remaining solvent is removed by evaporation or dialysis.
2. Materials:
- Polymer: Amphiphilic block copolymer (e.g., PEG-PLA, PEG-PCL).
- Drug: Hydrophobic bioactive compound.
- Solvents: Organic solvent (e.g., Acetone, Acetonitrile), Water (purified).
- Equipment: Magnetic stirrer, Round-bottom flask, Dialysis tubing (appropriate MWCO).
3. Step-by-Step Workflow:
4. Critical Parameters for Success:
- Solvent Selection: The organic solvent must be miscible with water and a good solvent for both the polymer and the drug.
- Addition Rate: Slow, dropwise addition of the organic phase into the aqueous phase is crucial for controlled self-assembly and uniform micelle formation.
- Dialysis: Effective dialysis is required to completely remove the organic solvent, which is critical for in vivo applications.
The Scientist's Toolkit: Key Research Reagent Solutions
Table 4: Essential Materials for Formulating Advanced Carriers
| Category | Item / Reagent | Function / Application Note | Key References |
|---|---|---|---|
| Solid Lipids | Glyceryl monostearate, Compritol 888 ATO, Cetyl palmitate | Forms the solid matrix of SLNs and NLCs; provides controlled release. | [66] [64] |
| Liquid Lipids (Oils) | Oleic acid, Miglyol 812, Caprylic/Capric Triglycerides | Creates imperfections in NLC core to boost drug loading and prevent expulsion. | [66] [64] |
| Surfactants (Stabilizers) | Poloxamer 188, Tween 80, Soy Lecithin | Reduces interfacial tension during formation; prevents aggregation in storage. | [66] [65] [64] |
| Block Copolymers | PEG-PLA (Poly(ethylene glycol)-Poly(lactic acid)), PEG-PCL (Poly(ε-caprolactone)) | The building blocks of polymeric micelles; PEG is the hydrophilic shell, PLA/PCL the hydrophobic core. | [67] |
| Characterization Kits/Standards | Latex size standards (for DLS calibration), Zeta potential transfer standard | Ensures accuracy and reproducibility of particle size and zeta potential measurements. | [65] |
Emerging Green Extraction Technologies for Bioactive Compounds
Troubleshooting Guides for Green Extraction Techniques
Low Extraction Yield
Problem: The yield of target bioactive compounds from plant material is lower than expected.
Potential Causes and Solutions:
| Problem Cause | Diagnostic Steps | Proposed Solution | Preventive Measures |
|---|---|---|---|
| Inefficient Cell Disruption [69] | Analyze residual biomass with SEM/FTIR to see if cell walls remain intact. | Switch from UAE to MAE; microwaves better disrupt lignocellulosic structures like buckwheat husk [69]. | Pre-treat biomass with milling; use techniques like MAE known for effective cell wall breakdown [70] [69]. |
| Suboptimal Solvent System [71] | Test solubility of target compound; try different solvent mixtures on a small scale. | For polyphenols, use a mixture of 50% ethanol and 50% water [71]. For resveratrol, a 69% ethanol solution was optimal for MAE [72]. | Use green solvents like Natural Deep Eutectic Solvents (NADES) or aqueous ethanol, which are effective for a wide range of polyphenols [73] [70]. |
| Poor Method Selection [72] | Review literature on techniques (UAE, MAE, SFE) used for your specific compound and biomass. | For heat-stable compounds in a woody matrix, use MAE. For heat-labile compounds, use UAE or SFE [72] [74]. | Perform a literature review and preliminary tests to select the most effective technique for your specific biomass and target compound [70]. |
Compromised Bioactivity of Extract
Problem: The extracted compounds show degraded or reduced antioxidant/biological activity.
Potential Causes and Solutions:
| Problem Cause | Diagnostic Steps | Proposed Solution | Preventive Measures |
|---|---|---|---|
| Thermal Degradation [69] | Compare bioactivity (e.g., via ABTS/DPPH assays) of extracts from high-temp vs. low-temp methods. | Use milder techniques like Ultrasound-Assisted Extraction (UAE). For MAE, optimize temperature and time; in one study, 80°C for 4 minutes preserved phenolics well [72] [69]. | Optimize time/temperature parameters. Prefer non-thermal methods (UAE, SFE) for highly heat-labile compounds [70] [74]. |
| Inappropriate Solvent Polarity [71] | Analyze the extract's phenolic profile via HPLC; key compounds may be missing. | Target specific compounds: Use water for hydrophilic compounds; aqueous acetone (50%) for a broader polyphenol range [71]. | Match solvent polarity to the target bioactive compounds. Ethanol/water mixtures are often a safe and effective starting point [70] [75]. |
Challenges in Process Scale-Up
Problem: The extraction process that worked well in the lab is inefficient or too costly at a larger scale.
Potential Causes and Solutions:
| Problem Cause | Diagnostic Steps | Proposed Solution | Preventive Measures |
|---|---|---|---|
| High Solvent Consumption [74] | Calculate solvent-to-feed ratio and compare with industrial benchmarks. | Implement intensified techniques like MAE or Pressurized Liquid Extraction (PLE), which significantly reduce solvent volume and extraction time [73] [74]. | Design the process with scale-up in mind, prioritizing methods with low solvent and energy requirements from the start [75]. |
| High Energy Costs [75] | Perform an energy audit of the extraction process step-by-step. | Use energy-recovery systems. Employ technologies like MAE which transfer energy directly to the material, reducing overall consumption [75] [69]. | Integrate energy consumption as a key metric during initial method development and optimization [70]. |
| Viscosity of Green Solvents [73] | Measure viscosity and mass transfer rates of the solvent system. | For viscous solvents like certain DES, gently heat the system or add a small percentage of water to reduce viscosity and improve mass transfer [73]. | When developing Natural Deep Eutectic Solvents (NADES), consider viscosity and pumpability as critical factors [73] [70]. |
Frequently Asked Questions (FAQs)
FAQ 1: What makes an extraction technology "green"?
Green extraction technologies are defined by their adherence to the principles of green chemistry. The core objectives are to reduce energy consumption, allow for alternative solvents, and ensure a safe, high-quality extract [75]. This is achieved by:
- Using Green Solvents: Replacing petroleum-based solvents with water, ethanol, supercritical CO₂, or Deep Eutectic Solvents (DES) [73] [70] [75].
- Reducing Energy Consumption: Employing innovative technologies like microwave or ultrasound that are more energy-efficient than conventional heating [75] [74].
- Producing Co-products: Designing processes where waste streams are converted into valuable co-products, integrating with a circular bio-economy [73] [75].
FAQ 2: How do I choose between UAE, MAE, and SFE?
The choice depends on the properties of your target compound and your operational constraints.
- Ultrasound-Assisted Extraction (UAE) is excellent for heat-sensitive compounds as it operates at lower temperatures. It works via acoustic cavitation, which disrupts cell walls. It is generally easy to implement and scale up [72] [74].
- Microwave-Assisted Extraction (MAE) is very fast and efficient, especially for matrices with high moisture content. It uses microwave energy to heat the solvent and plant matrix internally, leading to rapid cell disruption. It is ideal for compounds that are not thermally labile [69] [74].
- Supercritical Fluid Extraction (SFE), typically with CO₂, is superb for extracting non-polar, heat-labile compounds. It produces a solvent-free extract and is highly tunable by adjusting pressure and temperature. However, the equipment cost is high, and it is less effective for polar compounds without modifiers [73] [74]. A summary is provided in the table below.
FAQ 3: Can green extraction techniques directly improve the bioavailability of my extracted compound?
While extraction itself does not directly enhance bioavailability, it is a critical first step. Green extraction can improve bioavailability research by:
- Preserving Bioactive Structure: By using milder conditions (e.g., low-temperature UAE), these methods can prevent the degradation of thermolabile compounds, ensuring the active molecule is intact for delivery [70] [72].
- Producing Cleaner Extracts: The use of non-toxic solvents like water, ethanol, or supercritical CO₂ means solvent residues are less of a concern in subsequent formulation steps, simplifying the development of delivery systems [76] [77].
- Enabling Co-extraction: Some methods may co-extract natural compounds that can act as absorption enhancers or stabilizers in a final formulation [73].
FAQ 4: Are there standardized protocols for green extraction?
Fully standardized protocols are limited due to the vast diversity of plant matrices and target compounds. However, the scientific community is moving towards establishing standardized principles rather than rigid protocols. The "six principles of Green Extraction" provide a framework for designing sustainable processes [75]. Researchers are encouraged to optimize key parameters such as solvent type, temperature, time, and power settings for their specific application using tools like response surface methodology [72] [69].
Comparison of Major Green Extraction Technologies
| Feature | Ultrasound-Assisted Extraction (UAE) | Microwave-Assisted Extraction (MAE) | Supercritical Fluid Extraction (SFE) |
|---|---|---|---|
| Working Principle | Acoustic cavitation disrupts cell walls [72] [69]. | Microwave energy causes internal heating and cell rupture [69] [74]. | Uses supercritical fluids (e.g., CO₂) as solvent with high diffusivity [73] [74]. |
| Best For | Heat-labile compounds; easy scale-up [72] [74]. | Rapid extraction; hard plant matrices [69] [74]. | Non-polar compounds; solvent-free extract requirement [73] [74]. |
| Typical Solvents | Water, ethanol, DES [72] [71]. | Water, ethanol [69]. | Supercritical CO₂ (often with ethanol modifier) [73] [74]. |
| Energy Consumption | Moderate [75]. | Low to Moderate (rapid heating) [75]. | High (due to pressure maintenance) [74]. |
| Relative Cost | Low to Moderate [74]. | Moderate [74]. | High (capital investment) [74]. |
| Key Limitation | May be less effective on woody matrices [69]. | Risk of degrading very heat-sensitive compounds [69]. | High cost; less efficient for polar molecules [73] [74]. |
Experimental Protocol: Microwave-Assisted Extraction (MAE) of Polyphenols from Buckwheat Husk
This protocol is adapted from a study that achieved a 43.6% increase in polyphenol yield compared to conventional solvent extraction [69].
Objective
To efficiently extract polyphenolic compounds from buckwheat husk using microwave energy.
Materials and Equipment
- Plant Material: Dried buckwheat husk.
- Solvent: Aqueous acetic acid solution (or alternatively, a 69% ethanol in water solution, which has been proven effective for similar extractions [72]).
- Equipment: Microwave-assisted extraction system, analytical balance, centrifuge, vacuum filtration setup, rotary evaporator, lyophilizer.
- Analysis: Spectrophotometer for Total Phenolic Content (TPC) assay (e.g., Folin-Ciocalteu method) and antioxidant activity assays (e.g., ABTS, DPPH).
Step-by-Step Procedure
- Sample Preparation: Mill the dried buckwheat husk into a fine powder to increase the surface area for extraction.
- Loading: Weigh a precise amount of the powder and place it in the MAE vessel. Add the selected solvent at a predetermined solvent-to-solid ratio (e.g., 20:1 mL/g).
- First Extraction (MAE1):
- Separation: After the cycle, allow the vessel to cool. Separate the liquid extract from the solid residue via vacuum filtration or centrifugation.
- Second Extraction (MAE2 - Recommended):
- Subject the solid residue from MAE1 to a second MAE cycle under the same or slightly modified conditions to maximize yield [69].
- Combine the extracts from MAE1 and MAE2.
- Extract Concentration: Concentrate the combined extract using a rotary evaporator at low temperature (e.g., <40°C) to remove the solvent. For a completely dry powder, follow with lyophilization (freeze-drying).
Analysis and Validation
- Yield: Determine the total extraction yield by weighing the dry extract obtained.
- Total Phenolic Content (TPC): Quantify the polyphenol content using the Folin-Ciocalteu method, expressing results as mg of Gallic Acid Equivalents (GAE) per gram of dry extract [69].
- Antioxidant Activity: Assess the bioactivity of the extract using standard assays like ABTS and DPPH radical scavenging assays [69].
- Bioavailability Assessment: For bioavailability studies, the extract can be incorporated into various drug delivery systems (e.g., nanoemulsions, liposomes) and tested in relevant in vitro or in vivo models [76] [77].
The Scientist's Toolkit: Essential Research Reagents & Materials
| Item | Function/Application in Green Extraction & Bioavailability |
|---|---|
| Deep Eutectic Solvents (DES) | Green solvents formed from a hydrogen bond donor and acceptor. They are biodegradable, low-toxicity, and can be tailored for specific compound classes, improving extraction yield and selectivity [73] [70]. |
| Agro-Solvents (e.g., Bioethanol) | Renewable solvents produced from biomass, such as ethanol from sugarcane or corn. They are a key green alternative to petroleum-based solvents for extracting a wide range of bioactives [70] [75]. |
| Supercritical CO₂ | A non-toxic, non-flammable solvent that is gaseous at room temperature, leaving no residue. Ideal for producing high-purity extracts of lipophilic compounds and is easily tunable with pressure and temperature [73] [74]. |
| Nanocarrier Systems (Liposomes, Nanoemulsions) | Delivery systems used post-extraction to encapsulate bioactive compounds. They enhance solubility, protect against degradation, and can improve absorption, thereby directly addressing low bioavailability issues [76] [77]. |
| Polysaccharide-Based Matrices | Biopolymers (e.g., from soy protein, starches) used to form nanocomplexes or microcapsules with hydrophobic compounds like octacosanol, enhancing their stability and bioaccessibility in the gut [77]. |
Workflow and Pathway Diagrams
Green Extraction to Bioavailability R&D
Bioavailability Enhancement Pathway
Navigating Development Challenges and Optimizing Formulation Strategy
Frequently Asked Questions
Q1: Why is preventing crystallization and particle growth critical for the bioavailability of bioactive compounds?
Physical instability, such as particle growth or unintended crystallization, directly compromises the therapeutic potential of a bioactive compound. For poorly water-soluble drugs (common in BCS Class II and IV), reduced surface area from particle growth slows dissolution, limiting the amount of drug available for absorption in the gastrointestinal tract [45] [16]. Furthermore, a deliberate, stable amorphous solid dispersion can inadvertently recrystallize during storage, negating the solubility advantages engineered into the formulation and leading to variable and reduced bioavailability [16] [78].
Q2: What are the primary mechanisms that cause particle growth in nanosuspensions?
The main mechanisms driving particle growth in nanosuspensions are Ostwald Ripening and Aggregation/Agglomeration. Ostwald Ripening occurs where smaller particles, having higher solubility, dissolve and re-deposit onto larger, less soluble particles, leading to an overall increase in median particle size over time [79]. Aggregation is the physical clumping of particles due to attractive surface forces, which can be mitigated by using appropriate stabilizers that provide electrostatic or steric repulsion [45] [79].
Q3: Which formulation strategies can improve stability and suppress crystallization for hygroscopic compounds?
For moisture-sensitive and hygroscopic compounds, several formulation strategies act as barriers against the environment [78]:
- Film Coating: Applying a thin polymeric film around a solid dosage form to act as a moisture barrier.
- Encapsulation: Enveloping the active ingredient within a polymer matrix using techniques like spray-drying.
- Co-crystallization: Altering the crystal structure by introducing a safe co-former, which can improve stability and reduce hygroscopicity [78].
Troubleshooting Guides
Problem: Rapid Crystal Growth and Particle Size Increase in Nanosuspensions
Potential Causes and Solutions:
- Cause: Inadequate Stabilizer System
- Solution: The type, concentration, and combination of stabilizers (surfactants and polymers) are critical. Screen various stabilizers like HPMC, PVP, and polysorbates. A combination of a polymer (for steric stabilization) and a surfactant (for electrostatic stabilization) often provides superior inhibition of particle growth and aggregation [79].
- Cause: Storage Conditions
- Solution: Temperature fluctuations and high humidity can accelerate particle growth. Store nanosuspensions in controlled, cool conditions. For solid products, consider packaging with desiccants to minimize moisture uptake [78].
- Cause: Polymorphic Transitions
Problem: Recrystallization of Amorphous Solid Dispersions
Potential Causes and Solutions:
- Cause: Moisture-Induced Plasticization
- Solution: Amorphous materials are often hygroscopic. Absorbed water acts as a plasticizer, lowering the glass transition temperature (Tg) and enabling molecular mobility that leads to recrystallization. Formulate using moisture-protective polymers like HPMCAS and employ packaging that provides a moisture barrier [16] [78].
- Cause: Inadequate Polymer Selection
- Solution: The polymer in a solid dispersion must effectively suppress crystal nucleation and growth. Use polymers that have specific molecular interactions with the API (e.g., hydrogen bonding). Advanced polymers like HPMCAS and PVP-VA are specifically designed to inhibit recrystallization [16].
Table 1: Impact of Particle Size on Pharmacokinetic Parameters [45]
| Compound | Particle Size | Model | Result (vs. Control) |
|---|---|---|---|
| Aprepitant | 0.12 µm | Beagle dogs | Cmax 4 times higher than 5.5 µm formulation |
| Rosuvastatin Calcium | Nanoparticles | Rabbits | Cmax 2 times higher; AUC 1.5 times higher |
| Candesartan cilexetil | 127 nm | Rats | AUC 2.5 times higher; Cmax 1.7 times higher; Tmax reduced |
Table 2: Comparison of Particle Size Reduction Techniques [45] [79]
| Method | Typical Particle Size Limit | Key Advantages | Key Disadvantages |
|---|---|---|---|
| High-Pressure Homogenization | ~100 nm | Avoids thermal/chemical degradation; scalable | May require pre-micronization; high energy input |
| Wet Bead Milling | ~100 nm | Well-established; effective for hard crystals | Risk of material contamination from beads; long process times |
| Spray Drying | ~1000 nm | Continuous process; good for thermostable compounds | Thermal degradation risk; organic solvent use |
| Liquid Antisolvent | ~100 nm | Overcomes thermal degradation | Organic solvent recovery and disposal |
| Supercritical Fluid | ~100 nm | Narrow particle distribution; mild conditions | High cost; not ideal for large-scale |
| Combinative (e.g., NANOEDGE) | <200 nm | Faster production; smaller final particle size | More complex two-step process |
Experimental Protocols
Protocol 1: Nanoparticle Production via Liquid Antisolvent Precipitation with Focused Ultrasonication
This protocol is effective for producing nanoparticles with a target size below 200 nm [45].
- Preparation: Select a water-miscible organic solvent in which the drug has high solubility (e.g., acetone, ethanol). Prepare an aqueous phase containing a stabilizer (e.g., 1% w/v Poloxamer 407 or HPMC).
- Precipitation: Rapidly inject the drug solution (organic phase) into the antisolvent (aqueous stabilizer solution) under magnetic stirring.
- Size Reduction (Focused Ultrasonication): Immediately process the pre-suspension using a focused ultrasonication device (e.g., Covaris).
- Key Parameters:
- Duration: 4500 seconds
- Bath Temperature: 10°C (controlled to prevent dissolution/recrystallization)
- Power Mode: Frequency sweeping
- Degassing Mode: Continuous [45]
- Key Parameters:
- Evaporation: Remove the organic solvent under reduced pressure with gentle stirring.
- Analysis: Characterize the final nanosuspension for particle size (e.g., by Dynamic Light Scattering), particle size distribution (e.g., by Laser Diffraction), and solid state (e.g., by pXRD).
Experimental Workflow for Nanoparticle Production
Protocol 2: Combinative Technology (NANOEDGE) for Enhanced Nanosizing
This two-step process uses a bottom-up pretreatment to create a friable material that is more easily nanosized in a subsequent top-down step [79].
- Microprecipitation (Bottom-Up):
- Dissolve the drug in a suitable organic solvent.
- Rapidly mix this solution with an antisolvent (typically water containing a stabilizer) under controlled stirring to form a microparticulate precipitate.
- High-Pressure Homogenization (Top-Down):
- Process the resulting suspension from step 1 using a high-pressure homogenizer.
- Key Parameters:
- Pressure: 20,000 psi (≈1380 bar)
- Cycles: 30 minutes (or number of passes required)
- This step efficiently breaks down the friable precipitate into a stable nanocrystalline suspension [79].
Combinative NANOEDGE Technology Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Stability and Particle Size Control
| Item | Function/Benefit | Example Applications |
|---|---|---|
| Stabilizer: HPMC | Polymer for steric stabilization; inhibits crystal growth and aggregation. | Wet bead milling; Nanosuspensions [16] [79] |
| Stabilizer: PVP/ PVP-VA | Polymer for steric stabilization and crystallization inhibition in solid dispersions. | Amorphous solid dispersions [16] |
| Stabilizer: Poloxamer 407 | Non-ionic surfactant for electrostatic and steric stabilization. | Homogenization; Antisolvent precipitation [45] |
| Stabilizer: Sodium Lauryl Sulfate | Ionic surfactant for electrostatic stabilization. | Nanocrystal formulations [79] |
| Polymer: HPMCAS | A pH-responsive polymer that enhances solubility and inhibits recrystallization in the GI tract. | Amorphous solid dispersions [16] |
| Solvent/Antisolvent System | Basis for precipitation methods. Solvent dissolves drug, antisolvent induces crystallization. | Liquid antisolvent precipitation [45] [79] |
| Milling Beads (ZrO₂) | Grinding media for particle size reduction via mechanical attrition. | Wet bead milling [79] |
Frequently Asked Questions
What is the most critical first step in addressing poor bioavailability? The first step is an early evaluation of the API's physicochemical properties according to the Developability Classification System (DCS) to identify the root cause of low bioavailability, which is most often poor solubility or low permeability [81].
My poorly soluble API is also highly permeable (DCS Class II). What are my primary formulation options? For DCS Class II APIs, the primary technological solutions aim to increase solubility and dissolution rate. The most common and effective strategies include creating amorphous solid dispersions (via spray drying or hot-melt extrusion), reducing particle size to increase surface area, and optimizing the crystal structure through salt or co-crystal formation [82] [81].
What are the key API characteristics to consider for a transdermal delivery system? For passive transdermal delivery, an ideal API should generally have a molecular weight < 400 D, a daily dose < 20 mg, a melting point < 200 °C, and a log P (O/W) between -1.0 and 4.0 [83]. Note that successful commercial products exist outside these ranges, but they serve as a useful feasibility guide.
When is Hot-Melt Extrusion (HME) a suitable choice? Hot-Melt Extrusion is a highly effective technique for formulating amorphous solid dispersions, which are used to enhance the solubility of poorly water-soluble APIs. It is a continuous process that can improve dissolution rates and bioavailability [82].
Troubleshooting Common Experimental Issues
Problem: Low yield of an isotopically labeled protein for NMR studies.
- Potential Cause: Poor expression of the recombinant protein in minimal media, which is required for introducing isotopic labels.
- Solution: Implement a protocol where cells are first grown in rich media to achieve high density. The cells are then pelleted and transferred to the labeled minimal media. After allowing one hour for the cells to clear unlabeled metabolites, protein expression is induced. This method uses labeled media efficiently while achieving high cell density [84].
Problem: No product band or weak bands in standard PCR.
- Potential Cause: Missing or non-optimized PCR reagents, poor sample quality, or a non-optimal PCR program.
- Solution:
- Check Reagents: Verify the concentrations and integrity of all reaction components, especially the DNA polymerase, dNTPs, and primers.
- Assess Sample: Check the quality and quantity of the template DNA.
- Optimize Program: Adjust the annealing temperature and extension time of the PCR cycle. Consider using touchdown or stepdown PCR methods to improve specificity [85].
Problem: Suspected proteolytic degradation of an Intrinsically Disordered Protein (IDP) during purification.
- Potential Cause: IDPs are often highly sensitive to proteolysis because their flexible regions are exposed and accessible to proteases.
- Solution: Perform all purification steps at low temperatures (4°C). Include a broad-spectrum protease inhibitor cocktail in all buffers. Use fast purification techniques and work quickly to minimize the time the protein spends in extract [84].
API Property-Based Technology Selection Guide
The table below summarizes key API properties and how they can guide the selection of appropriate formulation technologies to improve bioavailability.
Table 1: Technology Selection Based on API Properties
| API Property / Challenge | Developability Class | Recommended Technology | Brief Rationale |
|---|---|---|---|
| Low Solubility | DCS Class II (Low Solubility, High Permeability) [81] | Amorphous Solid Dispersions (ASD) [82] [81], Particle Size Reduction [81], Salt/Co-crystal Formation [81] | Increases apparent solubility and dissolution rate. ASDs create a high-energy amorphous form; size reduction increases surface area. |
| Low Solubility & Low Permeability | DCS Class IV (Low Solubility, Low Permeability) [81] | Lipid-Based Formulations, Nanoformulations [82], Permeation Enhancers | Addresses both solubility and permeability limitations simultaneously. |
| High First-Pass Metabolism | N/A | Transdermal Drug Delivery Systems [83] | Bypasses hepatic metabolism, allowing for lower doses and reducing side effects. |
| Molecular Weight > 400 Daltons | N/A | Re-evaluate feasibility for passive transdermal delivery. Consider active methods (e.g., iontophoresis) or alternative routes [83]. | Passive skin permeability drops significantly for larger molecules. |
| Need for Complex Drug Release Profiles | N/A | Gastro-retentive Drug Delivery Systems (GRDDS) [82], Coated or Multi-layer Formulations | Provides controlled release, extends drug exposure, and can improve absorption. |
Essential Research Reagent Solutions
Table 2: Key Reagents for Bioavailability Enhancement Experiments
| Reagent / Material | Function in Experiment |
|---|---|
| Hydroxypropyl Methylcellulose Acetate Succinate (HPMCAS) | A common polymer used in amorphous solid dispersions to inhibit crystallization and maintain the API in a soluble, amorphous state [82]. |
| Polyvinylpyrrolidone-vinyl acetate (PVP-VA) | Another commonly used copolymer for forming stable amorphous solid dispersions via hot-melt extrusion or spray drying [82]. |
| Poly(D,L-Lactide-Co-Glycolide) (PLGA) | A biodegradable polymer used in nanomedicine formulations and controlled-release systems to encapsulate APIs [82]. |
| Tocopheryl Polyethylene Glycol Succinate (TPGS) | A polymer that functions as both a solubilizer and a permeability enhancer in formulations [82]. |
| Polyethylene Glycol (PEG) | Used to improve solubility, as a plasticizer in solid dispersions, and to functionalize nanoparticles to reduce immune clearance [82]. |
| Protease Inhibitor Cocktail | Essential for purifying sensitive proteins, especially Intrinsically Disordered Proteins (IDPs), to prevent degradation during extraction and purification [84]. |
| Stable Isotopes (¹⁵N, ¹³C) | Required for labeling proteins for NMR spectroscopy studies to characterize the structure and dynamics of bioactive compounds and IDPs [84]. |
Experimental Workflow for Technology Selection
The following diagram outlines a logical, molecule-driven workflow for selecting the right technology based on API properties. This workflow integrates the concepts from the FAQs and troubleshooting guides above.
API Technology Selection Workflow
Troubleshooting Guides and FAQs
Frequently Asked Questions
FAQ 1: What are the main biological barriers that limit the bioavailability of bioactive compounds for intracellular and organ-specific targeting?
The primary hurdles include poor aqueous solubility of the compound, instability in biological environments, and inefficient cellular uptake or tissue penetration [51]. For intracellular delivery, the compound must not only cross the plasma membrane but also avoid endosomal degradation and potentially reach specific organelles [86]. For organ-specific targeting, the compound must evade clearance mechanisms and selectively accumulate in the desired tissue, which often requires overcoming endothelial barriers [86].
FAQ 2: My lead compound shows high in vitro efficacy but poor in vivo performance. What formulation strategies can I explore to improve its solubility and stability?
Several advanced formulation strategies can be employed:
- Lipid-Based Nanosystems: Liposomes, solid lipid nanoparticles (SLNs), and nanostructured lipid carriers (NCLs) can encapsulate both hydrophilic and lipophilic compounds, enhancing solubility and providing protection from degradation [51].
- Solid Dispersions: Dispensing the compound in a polymer matrix (e.g., using HPMC, PVP, or PVP-VA) can create amorphous solid dispersions that significantly enhance solubility and dissolution rates [16].
- Nanosizing: Reducing the particle size to the nanoscale (e.g., drug nanocrystals) increases the surface area, leading to a higher dissolution rate and improved bioavailability [16].
- Complexation: The formation of phenolate-based salts or metal-phenolic networks (MPNs) can boost drug solubility, stability, and bioavailability [87].
FAQ 3: How can I design an experiment to identify which constituent in a complex natural extract is responsible for the observed bioactivity?
A powerful approach is the ELINA (Eliciting Nature's Activities) workflow, which combines microfractionation with heterocovariance analysis (HetCA) [88].
- Microfractionation: Separate the crude extract using a standard method like reversed-phase flash chromatography. Deliberately pool fractions to ensure constituents are spread across multiple fractions in varying concentrations.
- Parallel Analysis: Acquire 1H NMR spectra and LC-HRMS data for all microfractions. In parallel, test each microfraction in your biological assay.
- Data Correlation: Use statistical heterocovariance analysis to correlate the 1H NMR spectral data with the bioactivity results. This generates "pseudo-spectra" that highlight "hot" signals (positively correlated with activity) and "cold" signals (negatively correlated with activity), identifying the bioactive constituents prior to isolation [88].
FAQ 4: What are some common pitfalls in developing lipid nanoparticle (LNP) formulations for targeted delivery, and how can I avoid them?
Common challenges include:
- Limited Targeting: Conventional LNPs often accumulate primarily in the liver. To target other tissues (e.g., brain, specific muscles), you need to pioneer new LNP formulations with different lipid compositions and potentially incorporate targeting moieties [89].
- Formulation Complexity: LNP performance is holistically affected by the design of the delivery vehicle, the chemistry of the components, particle size, and the ratio of all components. Formulation optimization must take all these parameters into account simultaneously [89].
- Stability and Storage: Many advanced formulations require careful control of storage conditions, including ultra-low temperatures, which necessitates specialized equipment and stability testing protocols [89].
Troubleshooting Common Experimental Issues
Problem: Low encapsulation efficiency of a hydrophilic bioactive compound in liposomes.
- Potential Cause: The compound is leaking out during the preparation process or the liposome composition is not optimal for retaining hydrophilic molecules.
- Solution: Consider using active loading techniques if applicable. Optimize the lipid composition, particularly the cholesterol content, to reduce membrane permeability. Alternative vesicular systems like ethosomes or transfersomes may also be explored [51].
Problem: Asynchronous release of multiple active compounds from a plant extract loaded into a delivery system.
- Potential Cause: The different physicochemical properties of the various metabolites lead to non-uniform release profiles, which can decrease the overall bioactivity.
- Solution: Design delivery systems that enable synchronized release. This aims to control the release of multiple metabolites in a specific time frame while maintaining their inter-component ratio. Lipid-based systems and certain polymeric nanoparticles have been investigated for this purpose [51].
Problem: High viscosity of a concentrated protein-based therapeutic, making subcutaneous injection difficult.
- Potential Cause: The required high protein concentration for subcutaneous dosing leads to viscous solutions that are hard to administer with acceptable needles.
- Solution: Explore the addition of excipients like hydrophobic salts, inorganic salts, lysine, or arginine to reduce viscosity. Another strategy is the co-injection of recombinant human hyaluronidase to degrade hyaluronic acid in the subcutaneous space, increasing diffusion and allowing for larger injection volumes [90].
Experimental Protocols & Data Presentation
Detailed Methodology: The ELINA Workflow for Bioactivity-Guided Isolation
This protocol is adapted from the ELINA approach for identifying steroid sulfatase (STS) inhibitors from a fungal extract [88].
1. Microfractionation of Crude Extract:
- Material: Bioactive crude extract (e.g., MeOH extract of Fomitopsis pinicola).
- Equipment: Reversed-phase flash chromatography system.
- Procedure:
- Separate the crude extract using a linear gradient (e.g., H2O/MeOH or H2O/CH3CN).
- Collect time-based fractions (e.g., 125 tubes).
- Pool these primary tubes into a smaller number of microfractions (e.g., 32) based on TLC patterns, ensuring that constituents are deliberately spread across several fractions to create concentration variations.
2. Parallel Chemical and Biological Analysis:
- 1H NMR Profiling:
- Prepare identical samples from each microfraction.
- Acquire 1H NMR spectra under the same, quantitative conditions (e.g., same number of scans, receiver gain, and relaxation delay).
- Process all spectra uniformly (careful phasing and baseline correction).
- LC-HRESIMS Analysis:
- Analyze aliquots of each microfraction by LC-HRESIMS to gather complementary data on molecular weight and tentative identities.
- Biological Testing:
- Test aliquots of each microfraction in the target bioassay (e.g., STS inhibition assay).
- Include appropriate positive (e.g., STX64) and vehicle controls (e.g., 0.1% DMSO).
- Express the effect as percentage of inhibition compared to controls.
3. Data Integration and Heterocovariance Analysis (HetCA):
- Use statistical software to perform heterocovariance analysis.
- Correlate the 1H NMR spectral data (binned or segmented) with the bioactivity data across the series of microfractions.
- Generate HetCA plots ("pseudo-spectra") that visually display "hot" features (positive correlation with activity) and "cold" features (negative correlation).
4. Targeted Isolation:
- Use the HetCA plots to pinpoint the specific 1H NMR signals of the bioactive constituents.
- Use semi-preparative HPLC to isolate ("cherry-pick") these prioritized compounds from the active microfractions for full structure elucidation.
Quantitative Data on Bioavailability Enhancement Strategies
Table 1: Commercially Available Solid Dispersion Products for Bioavailability Enhancement
| Trade Name | Drug | Therapeutic Use | Specialized Polymer (Excipient) | Manufacturing Technology |
|---|---|---|---|---|
| ISOPTIN-SRE [16] | Verapamil | Antihypertensive | HPC/HPMC | Melt Extrusion |
| Cesamet [16] | Nabilone | Anti-emetic, Analgesic | PVP | Melt Extrusion |
| GRIS-PEG [16] | Griseofulvin | Antifungal | PEG | Melt Extrusion |
| KALETRA [16] | Lopinavir, Ritonavir | HIV | PVP-VA | Melt Extrusion |
| INCIVEK [16] | Telaprevir | Antiviral (Hepatitis C) | HPMCAS | Spray Drying |
Table 2: Comparison of Lipid-Based Delivery Systems for Bioactive Compounds
| Delivery System | Typical Size Range | Key Advantages | Ideal for Compound Type | Common Preparation Methods |
|---|---|---|---|---|
| Liposomes [51] | ~50 nm - several µm | Encapsulates both hydrophilic & lipophilic drugs; biodegradable; high bioavailability. | Peptides, proteins, antibiotics, antioxidants. | Thin-film hydration, sonication, microemulsification. |
| Solid Lipid Nanoparticles (SLNs) [51] | ~50-1000 nm | Improved stability vs. liposomes; controlled release; avoids organic solvents. | Lipophilic small molecules. | High-pressure homogenization, microemulsion. |
| Nanoemulsions [51] | ~20-200 nm | Ease of preparation; high stability; enhances solubility and bioavailability. | Essential oils, hydrophobic drugs. | High-energy methods (ultrasonication, microfluidization). |
Visualizations
Diagram: ELINA Experimental Workflow
Diagram: Decision Guide for Delivery System Selection
The Scientist's Toolkit
Table 3: Key Research Reagent Solutions for Bioavailability Research
| Reagent / Material | Function / Application | Key Characteristics |
|---|---|---|
| Hydroxypropyl Methylcellulose (HPMC) [16] | Polymer for amorphous solid dispersions. Inhibits drug recrystallization, enhances solubility and dissolution. | Hydrophilic polymer, commonly used in controlled-release formulations. |
| Polyvinylpyrrolidone (PVP) [16] | Polymer for solid dispersions and nanoparticle stabilization. | Good wetting properties, helps maintain supersaturation. |
| Phospholipids (e.g., Lecithin) [51] | Primary building block for liposomes and other vesicular systems. | Amphiphilic nature allows self-assembly into bilayers in aqueous solution. |
| Poly(lactic-co-glycolic acid) (PLGA) [90] | Biodegradable polymer for controlled-release microparticles and nanoparticles. | Biocompatible, mechanically strong, degradation rate can be tuned by lactic/glycolic ratio. |
| Methanol (with/without CD₃OD or D₂O) [91] | Versatile solvent for metabolite extraction prior to NMR and LC-MS analysis. | Effectively extracts a broad range of metabolites; deuterated forms aid NMR locking. |
| Metal-Phenolic Networks (MPNs) [87] | Smart delivery system for phenolate-based compounds; can be used for theranostics. | Formed by complexing phenolic drugs with metals; offer pH-responsive release and bioimaging potential. |
Strategies for Potent Compounds and Pediatric Populations
Developing effective formulations for pediatric populations presents unique challenges that differ significantly from adult drug development. This technical support center addresses the specific issues researchers and scientists encounter when working to improve the bioavailability of bioactive compounds in children. The physiological differences in pediatric patients, regulatory requirements, and formulation complexities create a landscape that demands specialized troubleshooting approaches and tailored experimental strategies.
Foundational Knowledge for Pediatric Formulation
Pediatric Population Classifications
Table 1: Pediatric Age Classifications and Considerations [92]
| Age Group | Age Range | Key Physiological Considerations | Formulation Preferences |
|---|---|---|---|
| Neonate | Birth to 27 days | Higher gastric pH, immature hepatic function | Liquid forms, minimal excipients |
| Infant and Toddlers | 28 days to 23 months | Developing taste preferences, variable saliva flow | Palatable liquids, mini-tablets |
| Children | 2 to 11 years | Improving swallowing ability, distinct taste rejection | Chewables, small tablets, flavored liquids |
| Adolescent | 12 to 16-18 years | Nearly adult-like physiology | Similar to adults with dose adjustment |
Bioactive Compound Profiles
Table 2: Key Bioactive Compounds and Dosage Considerations [93]
| Compound Class | Examples | Key Health Benefits | Pediatric Dose Considerations | Bioavailability Challenges |
|---|---|---|---|---|
| Polyphenols | Quercetin, Catechins | Antioxidant, anti-inflammatory | 300-600 mg/day (dose-adjusted) | Rapid metabolism, poor solubility |
| Carotenoids | Beta-carotene, Lutein | Vision support, immune function | 2-7 mg/day (dose-adjusted) | Fat-soluble, requires emulsification |
| Omega-3 Fatty Acids | EPA, DHA | Cognitive development, anti-inflammatory | 0.8-1.2 g/day (dose-adjusted) | Oxidation sensitivity, formulation stability |
| Probiotics | Lactobacillus, Bifidobacterium | Gut health, immune modulation | Strain-specific CFU counts | Gastric acid sensitivity, viability maintenance |
Troubleshooting Guides and FAQs
Frequently Asked Questions
Q: What are the major physiological factors affecting bioavailability in pediatric populations versus adults?
A: Key differences include variable saliva flow rates (0.22-0.82 mL/min in children vs. 0.33-1.42 mL/min in adults), which impacts buccal absorption; higher gastric pH in neonates (>4) affecting drug solubility; and developing gastrointestinal transit times that influence absorption windows. Additionally, age-dependent metabolic enzyme activity significantly alters first-pass metabolism and clearance rates [92].
Q: How can we overcome the challenge of bitter-tasting bioactive compounds in pediatric formulations?
A: Implement taste-masking strategies such as lipid-based encapsulation, sweetener incorporation, or ion-exchange resin complexes. Consider delivery system selection - buccal films bypass taste buds more effectively than oral liquids. Flavor modulation using bitter blockers like adenosine monophosphate can improve palatability without compromising stability [92] [93].
Q: What regulatory considerations are critical for pediatric formulation development?
A: The Best Pharmaceuticals for Children Act (BPCA) and Pediatric Research Equity Act (PREA) mandate pediatric studies for relevant new drugs. Pediatric Investigation Plans (PIPs) in Europe and Pediatric Study Plans (PSPs) in the US require early strategy development. Formulations must address age-appropriate dosing, excipient safety profiles, and administration feasibility across developmental stages [92] [94].
Q: Which experimental approaches best predict in vivo performance of bioavailability enhancement systems?
A: Utilize biorelevant dissolution systems that simulate pediatric GI conditions (pH, enzymes, volume). Implement permeability assays using cell cultures representing pediatric intestinal epithelia. Consider in silico modeling incorporating age-dependent physiological parameters to predict absorption. Animal models should be carefully selected with developmental stage considerations [92] [93].
Q: How do we balance formulation complexity with practical administration in pediatric patients?
A: Focus on flexible dosage forms that allow accurate dose titration across age groups. Consider orodispersible systems for children unable to swallow solids. Develop concentrated formulations to minimize administration volume, especially for neonates. Incorporate compatibility with enteral feeding tubes for hospitalized patients. Always include dosing devices with clear markings for accurate home administration [92].
Common Experimental Challenges and Solutions
Problem: Inconsistent bioavailability results across pediatric age subgroups
Solution pathway:
- Stratify study populations according to physiological development rather than chronological age
- Implement population pharmacokinetic modeling to account for developmental changes
- Consider food effects specific to pediatric diets (milk-based vs. solid food)
- Validate biomarkers of exposure and response appropriate for each age group
Problem: Poor compound stability in liquid formulations
Solution pathway:
- Evaluate lyophilized powder for reconstitution with improved stability profiles
- Implement nanoencapsulation technologies to protect sensitive compounds
- Utilize antioxidant systems compatible with pediatric safety requirements
- Develop extemporaneous compounding guidelines for pharmacy preparation
Problem: Lack of predictive in vitro models for pediatric absorption
Solution pathway:
- Develop age-specific dissolution media reflecting changing GI physiology
- Create engineered tissue models representing developmental stages of intestinal epithelium
- Incorporate relevant fluid volumes and transit times into absorption models
- Validate models against emerging pediatric clinical data when available
Experimental Protocols
Protocol 1: Development of Pediatric Buccal Delivery Systems
Objective: Enhance bioavailability of bioactive compounds using buccal mucosal delivery to overcome first-pass metabolism and gastric degradation.
Materials:
- Mucoadhesive polymers (chitosan, carbopol, hydroxypropyl methylcellulose)
- Permeation enhancers (bile salts, fatty acids, cyclodextrins)
- Plasticizers (glycerol, polyethylene glycol)
- Taste-masking agents (sucralose, monoammonium glycyrrhizinate)
- In vitro buccal permeability model (TR146 cell line or porcine buccal mucosa)
Methodology:
- Film preparation: Dissolve mucoadhesive polymer (2-4% w/v) in appropriate solvent system
- Drug incorporation: Add bioactive compound (0.5-5% w/v) with continuous stirring
- Plasticizer addition: Incorporate glycerol (0.5-1.5% w/v) to improve flexibility
- Casting and drying: Pour solution onto Petri dishes, dry at 40°C for 12 hours
- Characterization: Evaluate thickness, folding endurance, mucoadhesion time, and drug content uniformity
- Permeability assessment: Using Franz diffusion cells with buccal mucosa, sample at 0.5, 1, 2, 4, 6, 8 hours
- Taste evaluation: Conduct electronic tongue analysis or human taste panel (age-appropriate volunteers)
Troubleshooting notes:
- If films are too brittle: Increase plasticizer concentration incrementally (0.2% steps)
- If drug crystallization occurs: Add crystallization inhibitors (PVP, PVA) or reduce drug loading
- If mucoadhesion insufficient: Increase polymer concentration or incorporate secondary bioadhesive polymer
- If permeation low: Incorporate safe permeation enhancers at minimum effective concentrations [92]
Protocol 2: Lipid-Based Delivery System for Lipophilic Bioactives
Objective: Improve solubility and absorption of lipophilic bioactive compounds using self-emulsifying drug delivery systems (SEDDS).
Materials:
- Lipids (medium-chain triglycerides, sesame oil, oleic acid)
- Surfactants (Tween 80, Cremophor EL, Labrasol)
- Co-surfactants (PEG-400, propylene glycol, Transcutol P)
- Antioxidants (ascorbyl palmitate, vitamin E TPGS)
- In vitro lipolysis model with pediatric-relevant conditions
Methodology:
- Solubility screening: Determine drug saturation solubility in various lipids, surfactants, and cosurfactants
- Pseudo-ternary phase diagram: Construct diagrams to identify self-emulsification regions
- Formulation optimization: Select ratios from emulsification zone with maximum drug loading capacity
- Emulsion characterization: Assess droplet size, zeta potential, emulsification time, and stability
- In vitro lipolysis: Simulate pediatric gastrointestinal conditions (varying pH, enzyme levels, bile salt concentrations)
- Bioavailability assessment: Conduct pharmacokinetic studies in appropriate animal models
Troubleshooting notes:
- If precipitation occurs during digestion: Modify lipid-surfactant ratio or include precipitation inhibitors
- If emulsion droplet size too large: Optimize surfactant-to-co-surfactant ratio or incorporate cosolvent
- If chemical instability: Include appropriate antioxidants compatible with pediatric use
- If poor reproducibility: Implement quality by design (QbD) approach with design of experiments [93]
Protocol 3: Age-Appropriate Palatability Assessment
Objective: Systematically evaluate and improve taste and acceptability of pediatric formulations.
Materials:
- Electronic taste sensing systems (Astree e-tongue, Insent Taste Sensing System)
- Age-appropriate taste panel (with ethical approval and parental consent)
- Visual analog scales with child-friendly imagery
- Reference standard solutions (sweet, salty, sour, bitter, umami)
Methodology:
- Initial screening: Use electronic taste sensing to identify major taste defects
- Formulation optimization: Iteratively adjust sweeteners, flavors, and taste maskers based on sensor output
- Small panel testing: Begin with adult trained panel to identify safety concerns
- Expanded panel testing: Progress to target age group with appropriate consent procedures
- Acceptability assessment: Use facial hedonic scales or preference ranking methods
- Data analysis: Apply appropriate statistical methods for ordinal data from pediatric panels
Troubleshooting notes:
- If children reject formulation despite good e-tongue results: Consider texture/mouthfeel issues
- If variability high between participants: Increase sample size or implement crossover design
- If ethical concerns with taste testing: Utilize in vitro models until formulation optimized
- If age-dependent preferences observed: Develop age-stratified formulations [92] [93]
Visualization of Experimental Workflows
Bioavailability Enhancement Strategy Map
Pediatric Formulation Development Workflow
Bioavailability Barrier Assessment
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Pediatric Bioavailability Research [92] [93]
| Category | Specific Reagents | Function | Pediatric-Specific Considerations |
|---|---|---|---|
| Permeation Enhancement | Sodium taurocholate, Caprylic acid, Chitosan | Improve mucosal absorption | Safety profiling critical; concentration limits for age groups |
| Taste Masking | Monoammonium glycyrrhizinate, Sucralose, Neotame | Improve palatability and compliance | Age-appropriate sweetness preferences; safety at developmental stages |
| Stability Enhancement | Ascorbyl palmitate, Vitamin E TPGS, Cyclodextrins | Prevent compound degradation | Excipient safety database review required for pediatric use |
| Mucoadhesive Polymers | Carbopol, Chitosan, Sodium alginate | Extend residence time at absorption site | Mucosal irritation potential assessment needed |
| Lipid-Based Carriers | Medium-chain triglycerides, Oleic acid, Labrasol | Enhance lipophilic compound solubility | Digestibility and nutritional impact consideration |
| Nanocarrier Systems | PLGA, PCL, Phospholipids | Control release and improve bioavailability | Rigorous size characterization and safety assessment |
Regulatory and Compliance Framework
Essential Documentation Requirements
Table 4: Regulatory Considerations for Pediatric Formulations [92] [94]
| Requirement | Agency/Guideline | Key Elements | Documentation Strategy |
|---|---|---|---|
| Pediatric Investigation Plan (PIP) | European Medicines Agency (EMA) | Formulation development strategy, age-appropriate dosing, safety studies | Early regulatory consultation; justified extrapolation plans |
| Pediatric Study Plan (PSP) | US Food and Drug Administration (FDA) | Pharmacokinetic studies, safety monitoring, efficacy assessment | Age de-escalation strategy; biomarker validation |
| Excipient Safety Assessment | FDA Guidance on Inactive Ingredients | Justification of excipients, literature-based safety data | Comprehensive literature review; tiered toxicity testing |
| Age-Appropriate Formulation | ICH E11 Guideline | Matching formulation to developmental stage, administration feasibility | User acceptability testing; dosing flexibility demonstration |
| Bioavailability/Bioequivalence | FDA Guidance for Industry | Pediatric-specific study designs, ethical considerations | Population PK approaches; sparse sampling strategies |
This technical support resource will be regularly updated as new research and regulatory guidance emerges in the field of pediatric bioavailability enhancement. Researchers are encouraged to consult with regulatory agencies early in their formulation development process to ensure compliance with current requirements.
The Role of AI and Predictive Modeling in Bioavailability Optimization
Frequently Asked Questions (FAQs)
1. How can AI models improve the prediction of a bioactive compound's bioavailability? AI models, particularly machine learning (ML) and deep learning (DL), can analyze large datasets to uncover complex relationships between a compound's chemical structure, its physicochemical properties, and its absorption in the body. Unlike traditional linear models, AI can integrate multi-omics data and predict key parameters like solubility and intestinal absorption efficiency, thereby providing a more accurate and rapid assessment of bioavailability before costly lab experiments are conducted [95] [96].
2. My AI model for predicting bioavailability is performing poorly. What could be wrong? Poor model performance can stem from several issues. First, examine the quality and quantity of your training data; models trained on incomplete, biased, or low-quality datasets often lead to overfitting and inaccurate predictions [97] [95]. Second, ensure you are using meaningful features (molecular descriptors) for the model. Employing advanced feature selection techniques, such as Ant Colony Optimization, can help identify the most relevant parameters and improve predictive accuracy [98].
3. What is the difference between a traditional compartmental model and an AI-enhanced model for drug delivery? Traditional compartmental models use a set of differential equations to represent drug distribution between predefined anatomical compartments. They are well-established but can be limited in capturing complex biological interactions. AI-enhanced models, such as those integrated with an AI Bio-Cyber Interface, can learn from real-time data, adapt to the dynamic tumor microenvironment, and enable precise, external control of drug concentration at the target site, thereby improving therapeutic efficacy and reducing side effects [99].
4. How can I validate an AI prediction for bioavailability in the laboratory? AI predictions should be validated through a combination of in vitro and in vivo studies. For solubility and permeability, established methods include:
- High-Throughput Screening (HTS): To rapidly test the solubility of AI-prioritized compounds [97].
- In vitro digestion models: To simulate gastrointestinal conditions and assess the absorption efficiency of bioactive compounds, such as peptides from food [95] [100].
- Ex vivo models: Using patient-derived tissue samples can provide more translatable data on a compound's efficacy and absorption [101].
5. Are there specific AI models recommended for different types of bioactive compounds (e.g., peptides vs. carbohydrates)? While many AI models are broadly applicable, some are better suited for specific tasks:
- Proteins/Peptides: Deep learning models combined with molecular docking simulations are highly effective for identifying bioactive peptides from protein hydrolysates and predicting their stability in the gastrointestinal tract [95] [100].
- Carbohydrates: Machine learning models like Random Forest can be used to establish structure-bioactivity relationships and optimize carbohydrate metabolism and delivery systems [95].
- Small Molecules: Neural Ordinary Differential Equations (Neural ODEs) and graph neural networks show strong performance in population pharmacokinetic modeling and predicting drug-target interactions [102] [98].
Troubleshooting Guides
Issue: Inconsistent Results Between AI Predictions and Experimental Bioavailability Data
Potential Causes and Solutions:
Cause 1: Data Quality and Bias The AI model was trained on a dataset that does not adequately represent the chemical space of your bioactive compounds or lacks critical experimental parameters.
Cause 2: Model Overfitting The model has learned the noise and specific patterns of the training data too closely and fails to generalize to new, unseen data.
Cause 3: Incorrect Feature Representation The molecular descriptors or features used to train the model do not sufficiently capture the properties that govern the bioavailability of your specific bioactive compound.
Issue: Handling the "Black Box" Nature of Complex AI Models for Regulatory Submissions
Potential Causes and Solutions:
- Cause: Lack of Model Interpretability
Regulatory bodies require understanding and validation of the models used in the drug development process. Complex DL models can be difficult to interpret.
- Solution:
- Use Explainable AI (XAI) Techniques: Apply methods like SHAP (SHapley Additive exPlanations) or LIME (Local Interpretable Model-agnostic Explanations) to explain individual predictions.
- Prioritize Interpretable Models: Where possible, use models that offer a balance between performance and explainability, such as Random Forests or Neural ODEs, which provide strong performance while maintaining some degree of interpretability [102].
- Document Rigorously: Maintain comprehensive documentation of the model's development, training data, validation protocols, and performance metrics to build a case for regulatory review [96].
- Solution:
Quantitative Data on AI Model Performance in Bioavailability and Drug Discovery
The table below summarizes performance metrics of various AI models as reported in recent studies, providing a benchmark for researchers.
| AI Model | Application | Key Performance Metrics | Reference / Context |
|---|---|---|---|
| Context-Aware Hybrid Ant Colony Optimized Logistic Forest (CA-HACO-LF) | Drug-target interaction prediction | Accuracy: 98.6%, Precision, Recall, F1-Score: High performance [98] | Tested on Kaggle dataset with 11,000 drug details [98] |
| AI/ML Models (Various) | Population Pharmacokinetics (PPK) | Often outperformed traditional NONMEM in RMSE, MAE, R² on real clinical data [102] | Comparison with NONMEM on data from 1,770 patients [102] |
| Neural ODEs | Population Pharmacokinetics (PPK) | Strong performance and explainability, especially with large datasets [102] | Comparative analysis on simulated and real clinical data [102] |
| Generative Adversarial Networks (GANs) | De novo molecular design | Accelerates design of compounds with desired potency, selectivity, and safety profiles [96] | Used for generating novel molecular structures [96] |
| FP-GNN (Fingerprints & Graph Neural Network) | Predicting drug inhibition | Effective representation of structural features for anticancer drug discovery [98] | Modeled inhibitory effects on targets and tumor cells [98] |
Detailed Experimental Protocol: AI-Guided Bioavailability Prediction for Bioactive Peptides
This protocol outlines a methodology for using AI to predict and validate the bioavailability of bioactive peptides derived from food proteins.
1. Hypothesis: Machine learning models can accurately predict the bioavailability and bioactivity of peptides from protein hydrolysates based on their amino acid sequence and physicochemical properties.
2. Data Curation and Pre-processing:
- Data Collection: Gather a dataset of known bioactive peptides from public databases (e.g., BIOPEP-UWM) and scientific literature. Include data on their amino acid sequences, molecular weight, hydrophobicity, charge, and experimentally measured bioavailability (e.g., Caco-2 cell permeability) or bioactivity (e.g., IC50 for ACE inhibition) [95] [100].
- Data Cleaning: Perform text normalization on peptide sources and activities. Handle missing values using appropriate imputation methods or by excluding the entry.
- Feature Extraction: Convert peptide sequences into numerical features using techniques like:
- N-Grams: To capture sequence patterns.
- Molecular Descriptors: Calculate using software like RDKit (e.g., logP, polar surface area, number of hydrogen bond donors/acceptors).
- Cosine Similarity: Can be used to compare peptide sequences based on their feature vectors [98].
3. Model Training and Validation:
- Model Selection: Train and compare multiple ML models, such as:
- Validation: Use a strict train-validation-test split (e.g., 70-15-15). Perform k-fold cross-validation on the training set. Finally, evaluate the final model on the held-out test set. Use metrics like Accuracy, Precision, Recall, F1-Score, and AUC-ROC [98] [96].
4. Experimental Validation:
- In Vitro Digestion: Subject the top-ranked AI-predicted peptides (and a control) to a simulated gastrointestinal digestion model to assess stability [95].
- Caco-2 Cell Permeability Assay: Measure the apparent permeability (Papp) of the peptides across a monolayer of Caco-2 cells to experimentally determine their absorption potential [95] [100].
- Bioactivity Assay: Perform a relevant bioactivity test (e.g., an ACE-inhibition assay for antihypertensive peptides) to confirm the predicted function [100].
AI-Driven Bioavailability Optimization Workflow
AI-Driven Bioavailability Optimization Workflow Diagram
AI Model Selection and Interpretation Pathway
AI Model Selection and Interpretation Pathway Diagram
Research Reagent Solutions for AI-Enhanced Bioavailability Studies
| Reagent / Tool | Function in Experiment | Application Context |
|---|---|---|
| DNA-encoded Library (DEL) | Generates massive, high-quality interaction data between compounds and protein targets for training AI models [97]. | Target identification and validation in early drug discovery. |
| Caco-2 Cell Line | A well-established in vitro model of the human intestinal mucosa used to experimentally measure permeability and absorption of compounds [95] [100]. | Validating AI predictions of intestinal absorption for bioactive compounds. |
| Simulated Gastrointestinal Fluids | Used in in vitro digestion models to study the stability and release of bioactive compounds under physiological conditions [95]. | Testing AI predictions of compound stability in the GI tract. |
| Alcalase & other Proteases | Enzymes used for the controlled hydrolysis of proteins to generate bioactive peptides for activity and bioavailability testing [100]. | Producing samples for validating AI models predicting peptide bioactivity. |
| Quadrant 2 Predictive Platform (Thermo Fisher) | An example of a commercial computational platform that uses AI to analyze molecular structure and recommend optimal formulation strategies for solubility and bioavailability enhancement [103]. | In silico formulation design and excipient selection. |
Proving Efficacy: Validation, Bioequivalence, and Regulatory Standards
Frequently Asked Questions (FAQs)
FAQ 1: What is the fundamental difference between single-dose and multiple-dose bioavailability studies, and when should each be used?
Single-dose studies are often the preferred initial approach due to their simplicity and reduced drug exposure for participants. They involve administering a single dose and collecting blood samples over an extended period to determine key parameters like terminal half-life and the total area under the plasma concentration-time curve (AUC) [104]. However, they do not reliably simulate steady-state conditions or account for the inter-individual variability observed in long-term drug use [104].
Multiple-dose studies, where the drug is administered over five to six elimination half-lives, are essential when the study objective is to achieve steady-state concentrations [104]. This design closely mimics clinical drug usage, provides reliable steady-state predictions, reduces inter-participant variability, and is valuable for detecting nonlinear pharmacokinetics [104]. The choice depends on the study objectives, drug properties, and the need to balance reliable data with resource and safety constraints [104].
FAQ 2: What are the key statistical parameters for assessing bioavailability and bioequivalence?
The assessment of bioavailability and bioequivalence is primarily based on pharmacokinetic parameters derived from the plasma concentration-time curve [105]. The key parameters include:
- AUC (Area Under the Curve): Represents the total systemic exposure to the drug over time [106].
- Cmax (Maximum Concentration): The peak plasma concentration, which provides information on the rate of absorption [106].
- Tmax (Time to Cmax): The time taken to reach the peak plasma concentration [106].
For bioequivalence, the calculated 90% confidence interval for the geometric mean ratio (test product/reference product) of AUC and Cmax should fall within the bioequivalence range, which is typically 80-125% [105]. Tmax is usually analyzed using non-parametric methods [105].
FAQ 3: What are the common pitfalls in bioanalytical method validation that can invalidate BA/BE study results?
A critical pitfall is the improper handling of Incurred Sample Reanalysis (ISR), which is required to assess the reliability of the bioanalytical method during study sample analysis [107]. ISR failure can occur due to various reasons, including:
- Execution errors: such as switched samples or instrument issues.
- Method-related issues: such as metabolite interferences or back conversion of metabolites.
- Sample handling problems: such as mislabelling or matrix effects [107].
A lack of ISR data requires a strong scientific justification, especially for pivotal studies. Justification may consider factors like the known metabolic profile of the drug, other ISR data from the same laboratory, and the overall reliability of the pharmacokinetic data obtained [107].
FAQ 4: How do study design considerations differ for nutraceuticals compared to pharmaceutical drugs?
Nutraceuticals present unique challenges that influence study design [106]. Key considerations include:
- Formulation Impact: The use of advanced delivery systems (e.g., liposomes, nanoparticles) to enhance solubility and absorption is common and must be evaluated [106].
- Food and Matrix Effects: The absorption of many nutraceuticals (e.g., fat-soluble compounds like curcumin) is highly sensitive to co-ingestion with food, particularly fats, requiring fed-state studies [106].
- Variable Composition: For botanical or multi-component formulations, measuring surrogate biomarkers or metabolites may be necessary instead of, or in addition to, the parent compound [106].
- Operational Challenges: Poor solubility and high inter-individual variability in absorption, often influenced by gut microbiota and diet, require careful control and standardization during the study [106].
Troubleshooting Common Experimental Issues
Problem: High Variability in Pharmacokinetic Parameters
| Potential Cause | Investigation & Verification | Corrective Action |
|---|---|---|
| Inadequate dietary control [106] | Review study records for standardized meal composition and timing relative to dosing. | Implement strict dietary controls, including provided meals and restrictions on caffeine, alcohol, and other supplements [106]. |
| Improper washout period in crossover design [104] | Check if the washout period was shorter than 5-6 elimination half-lives, leading to carryover effects [104]. | Ensure the washout period is sufficiently long (at least 5-7 half-lives) to eliminate carryover from the previous dose [104] [105]. |
| Uncontrolled subject factors (e.g., genetics, microbiome) [106] | Analyze demographic and health screening data for homogeneity. | Tighten participant inclusion/exclusion criteria and recruit a larger sample size to account for inherent variability [105] [106]. |
Problem: Failure to Demonstrate Bioequivalence
| Potential Cause | Investigation & Verification | Corrective Action |
|---|---|---|
| True formulation differences | Review formulation data (excipients, manufacturing process). Perform in vitro dissolution testing. | Reformulate the test product to better match the reference product's release profile. |
| Insufficient statistical power [105] | Check if the sample size was adequate to detect a 20% difference with 80% power. | Recalculate and increase the sample size in a subsequent study to ensure sufficient power. A minimum of 12 subjects is often required, but more may be needed [105]. |
| Inaccurate or imprecise bioanalytical method [107] | Audit the bioanalytical method validation data, particularly the results of Incurred Sample Reanalysis (ISR) [107]. | Re-validate the analytical method, address sources of inaccuracy (e.g., metabolite back-conversion), and re-analyze samples if possible [107]. |
Quantitative Data in Bioavailability Studies
Table 1: Key Pharmacokinetic Parameters and Statistical Criteria for Bioequivalence Assessment
| Parameter | Definition | Interpretation | Statistical Criteria for BE |
|---|---|---|---|
| AUC0-t | Area under the plasma concentration-time curve from zero to the last measurable time point | Represents the total exposure to the drug up to time t [106]. | The 90% confidence interval for the ratio (Test/Reference) should be within 80-125% [105]. |
| AUC0-∞ | Area under the curve from zero to infinity | Represents the total total drug exposure over infinite time, extrapolated from AUC0-t [104]. | The 90% confidence interval for the ratio (Test/Reference) should be within 80-125% [105]. |
| Cmax | Maximum observed plasma concentration | Indicates the peak systemic exposure and is related to the rate of absorption [106]. | The 90% confidence interval for the ratio (Test/Reference) should be within 80-125% [105]. |
| Tmax | Time to reach Cmax | Reflects the absorption rate [106]. | Analyzed using non-parametric methods; no confidence interval is required [105]. |
Table 2: Comparison of Single-Dose vs. Multiple-Dose Study Designs
| Characteristic | Single-Dose Study | Multiple-Dose Study |
|---|---|---|
| Primary Objective | Determine fundamental PK parameters (e.g., AUC, Cmax, half-life) after one administration [104]. | Simulate clinical use and assess PK parameters at steady-state [104]. |
| Key Advantages | Simplicity, shorter duration, reduced drug exposure, lower risk of adverse reactions [104]. | Reliable steady-state predictions, reduced inter-individual variability, detects nonlinear PK [104]. |
| Key Limitations | Does not simulate steady-state; may not predict variability in chronic use [104]. | Time-consuming, resource-intensive, higher cost, increased risk of adverse reactions [104]. |
| Typical Application | Initial BA assessment of a new chemical entity; BE studies for immediate-release products [104] [105]. | Assessment of modified-release formulations; drugs with long half-lives or nonlinear kinetics [104] [105]. |
Essential Experimental Workflows
Bioequivalence Study Workflow
Bioavailability Prediction Framework
The Scientist's Toolkit: Key Reagents & Materials
Table 3: Essential Research Reagent Solutions for Bioavailability Studies
| Reagent / Material | Function / Application |
|---|---|
| Stable Isotope-Labeled Compounds | Used as internal standards in Mass Spectrometry to ensure accurate and precise quantification of analytes, correcting for matrix effects and recovery losses [108]. |
| Blank Biological Matrix (e.g., drug-free human plasma) | Used for the preparation of calibration standards and quality control (QC) samples during bioanalytical method validation and sample analysis. |
| Protein Precipitation Reagents (e.g., Acetonitrile, Methanol) | Employed in sample preparation to precipitate proteins from biological samples (plasma, serum), thereby cleaning up the sample before chromatographic analysis. |
| Solid Phase Extraction (SPE) Cartridges | Provide a more selective sample clean-up than protein precipitation, used to isolate and concentrate the analyte from the biological matrix, reducing ion suppression in MS. |
| LC-MS/MS Mobile Phases & Buffers | Solvents and volatile buffers (e.g., ammonium formate, ammonium acetate) used in the liquid chromatography system to separate the analyte from matrix components prior to mass spectrometric detection. |
In the critical field of bioavailability research, reliable pharmacokinetic (PK) data is the cornerstone of understanding how the body utilizes bioactive food compounds and oral drugs. Bioavailability is a complex process involving several stages: liberation, absorption, distribution, metabolism, and elimination (LADME) [109]. Bioanalytical method validation provides the essential foundation for this research, ensuring that the analytical methods used to generate PK data produce accurate, precise, and reproducible results. For researchers investigating the bioavailability of bioactive compounds—from (poly)phenols in blueberries to fatty acids in fish oil—rigorously validated methods are not merely a regulatory hurdle but a scientific necessity to ensure that conclusions about health benefits and efficacy are built upon trustworthy data [109] [110].
FAQs on Bioanalytical Method Validation
What is bioanalytical method validation and why is it critical for PK studies?
Bioanalytical method validation is the documented process of ensuring that an analytical test method is suitable for its intended use, such as measuring drug or bioactive compound concentrations in biological matrices [111]. It involves a series of experiments on the procedure, materials, and equipment to demonstrate that the method consistently produces reliable results during routine sample analysis [111].
For PK studies, which measure the concentration of a compound over time to determine its absorption, distribution, metabolism, and excretion, validated methods are indispensable [112]. The pharmacological response is generally related to the drug concentration at the receptor site. Since these concentrations usually cannot be measured directly, PK studies rely on determining drug levels in biological fluids like blood or plasma, operating on the premise that the drug at the site of action is in equilibrium with the drug in the blood [112]. Without a validated method to accurately quantify these levels, the resulting PK parameters and any subsequent bioavailability conclusions would be fundamentally unreliable.
What are the key parameters assessed during method validation?
The validation of a bioanalytical method involves evaluating several key performance characteristics to establish its scientific validity [113]. The table below summarizes the core parameters:
| Validation Parameter | Description | Role in Ensuring Data Quality |
|---|---|---|
| Accuracy | Closeness of the measured value to the true value. | Ensures reported drug concentrations reflect actual levels in biological samples. |
| Precision | Degree of scatter between a series of measurements. | Confirms reproducible results across multiple runs, analysts, and days. |
| Specificity | Ability to measure the analyte unequivocically in the presence of other components. | Verifies that the signal measured is from the analyte and not from matrix interferences. |
| Linearity & Range | The ability to obtain results proportional to analyte concentration over a specified range. | Defines the concentrations (from LLOQ to ULOQ) over which the method is valid. |
| Lower Limit of Quantification (LLOQ) | The lowest concentration that can be measured with acceptable accuracy and precision. | Determines the sensitivity of the method for detecting low drug concentrations. |
| Stability | The integrity of the analyte under specific conditions and time periods. | Guarantees analyte concentration remains unchanged during sample handling and storage. |
What common challenges arise during method validation for bioavailability studies, and how can they be troubleshooted?
Bioanalysis often involves measuring very low analyte concentrations in complex and variable biological matrices, which presents several challenges [112].
Challenge: Matrix Effects
- Description: Matrix effects occur when co-eluting compounds from the biological sample suppress or enhance the ionization of the analyte in the mass spectrometer, leading to inaccurate quantification [112]. This is a common issue in LC-MS/MS methods.
- Troubleshooting: The USFDA guidance requires the assessment of matrix effects. One effective troubleshooting approach is post-column infusion of the analyte. Here, the analyte is infused into the MS detector post-column while a blank matrix sample is injected. Any deviation from the baseline in the resulting chromatogram indicates a region of ion suppression or enhancement, allowing for chromatographic conditions to be adjusted to move the analyte's retention time away from this problematic region [112].
Challenge: Inadequate Extraction Recovery
- Description: This refers to the incomplete extraction of the analyte from the biological matrix (e.g., plasma), reducing the method's sensitivity and potentially affecting accuracy.
- Troubleshooting: Recovery is determined by comparing the analytical response of an extracted sample with the response of a standard spiked into a blank matrix after extraction. Low recovery indicates a suboptimal extraction process. The extraction procedure (e.g., Liquid-Liquid Extraction, Solid-Phase Extraction, Protein Precipitation) should be selected and optimized based on the physicochemical properties of the drug, such as its molecular weight, solubility, and dissociation constant (pKa) [112].
How does validation differ for PK assays versus biomarker assays?
While both are critical in drug development, their validation approaches differ significantly due to the nature of the analyte.
- PK Assays measure the administered drug or its metabolites. A fully characterized reference standard identical to the analyte is typically available. This allows for a "spike-and-recover" approach to validation, as outlined in guidelines like ICH M10, where known amounts of the reference standard are added to a blank matrix to assess parameters like accuracy and precision [114].
- Biomarker Assays measure endogenous compounds (e.g., glucose, cytokines). A reference standard identical to the endogenous analyte is often unavailable. Therefore, validation relies more heavily on a "fit-for-purpose" approach. A key unique parameter is parallelism, which assesses the similarity between the behavior of the endogenous analyte and the calibrator (often a recombinant protein) used in the assay [114]. The focus shifts to demonstrating that the assay generates reliable data for its specific Context of Use (COU), such as understanding a drug's mechanism of action [114].
Experimental Protocols: Key Methodologies
Protocol 1: Determining the Lower Limit of Quantification (LLOQ)
The LLOQ is a fundamental parameter defining the sensitivity of a bioanalytical method.
- Preparation: Prepare a minimum of five samples independent of the calibration curve at the proposed LLOQ concentration.
- Analysis: Analyze these samples against a freshly prepared calibration curve.
- Calculation and Acceptance Criteria: The LLOQ is accepted if the samples have a precision (expressed as %CV) of ≤ 20% and an accuracy (expressed as % nominal concentration) of 80-120% [112]. The signal-to-noise ratio for the LLOQ should typically be greater than 5:1. The target LLOQ is often set at 1/20th of the expected maximum plasma concentration (Cmax) of the drug [112].
Protocol 2: Assessing Method Specificity and Selectivity
Specificity ensures that the measured response is from the analyte alone and not from interferences.
- Source of Blanks: Obtain and analyze a minimum of six individual sources of the blank biological matrix (e.g., plasma from six different donors).
- Analysis: Analyze these blank samples to check for any interfering peaks at the retention time of the analyte and the internal standard.
- Acceptance Criteria: The response of any interference at the retention time of the analyte should be less than 20% of the LLOQ response, and the response for any interference at the retention time of the internal standard should be less than 5% of the internal standard response [112].
Essential Workflow Diagrams
Bioanalytical Method Validation Workflow
Troubleshooting Matrix Effects in LC-MS/MS
The Scientist's Toolkit: Key Research Reagent Solutions
The following table details essential materials and reagents used in developing and validating a robust bioanalytical method.
| Reagent/Material | Function and Importance |
|---|---|
| Certified Reference Standard | High-purity analyte used to prepare calibration standards and quality control samples. Its integrity is paramount for establishing method accuracy and linearity [113]. |
| Stable Isotope-Labeled Internal Standard (IS) | An isotopically labeled version of the analyte (e.g., Deuterated) added to every sample. It corrects for variability in sample preparation and ionization efficiency in LC-MS/MS, improving precision and accuracy [112]. |
| Appropriate Biological Matrix | The blank biological fluid (e.g., plasma, serum) from multiple individual sources. Used to prepare calibration standards and assess method specificity and selectivity against endogenous interferences [112]. |
| Quality Control (QC) Samples | Samples with known concentrations of the analyte (Low, Mid, High) prepared in the biological matrix. QCs are analyzed alongside study samples to monitor the ongoing performance and reliability of the method during a study run. |
| Solid-Phase Extraction (SPE) Cartridges | Used for sample clean-up and pre-concentration of the analyte. Selecting the right sorbent (e.g., C18, mixed-mode) is crucial for achieving high recovery and reducing matrix effects [112]. |
Bioequivalence is a critical concept in pharmaceutical development, defined as the absence of a significant difference in the rate and extent to which the active ingredient becomes available at the site of drug action when administered at the same molar dose under similar conditions [115] [116]. For researchers working to improve the bioavailability of bioactive compounds, establishing bioequivalence provides a scientific foundation for claiming therapeutic equivalence between formulations without lengthy clinical trials [117].
The 80/125 rule serves as the primary statistical criterion for demonstrating average bioequivalence in most regulatory jurisdictions. This standard is particularly valuable when developing enhanced formulations of bioactive food compounds or generic pharmaceuticals, where it enables researchers to scientifically demonstrate that their new formulation performs equivalently to an established reference [109].
The Statistical Foundation of the 80/125 Rule
Understanding the Confidence Interval Requirement
A common misconception suggests that the 80/125 rule allows individual pharmacokinetic measurements to vary between 80% and 125% of the reference value. The reality is more statistically rigorous: for average bioequivalence to be established, the 90% confidence interval for the ratio of the geometric means of key pharmacokinetic parameters (AUC and Cmax) must fall entirely within the 80-125% range [115].
This distinction is crucial for researchers designing bioavailability studies. The requirement that the entire confidence interval must fall within the bounds means that the actual difference between formulations is typically much smaller than the apparent 45% range (80-125%) might suggest. FDA studies have demonstrated that the mean difference for AUC values between approved test and reference products is approximately 3.5%, with most differences falling within a 5% range [115].
Logarithmic Transformation of Pharmacokinetic Data
The 80-125% range originates from the log-normal distribution characteristic of pharmacokinetic parameters. Drug absorption and metabolism measures (AUC and Cmax) typically follow a log-normal distribution, requiring logarithmic transformation to achieve normality for valid statistical testing [118] [116].
After log transformation, a symmetrical ±20% clinical range translates to the asymmetric 80-125% range on the original scale. The natural logarithm of the ratio values demonstrates this symmetry: ln(0.8) = -0.223 and ln(1.25) = 0.223 [118].
Table 1: Transformation Between Original and Logarithmic Scales
| Test/Reference Ratio | Percentage | ln(Ratio) |
|---|---|---|
| 0.8 | 80% | -0.223 |
| 0.9 | 90% | -0.105 |
| 1.0 | 100% | 0 |
| 1.1 | 110% | 0.095 |
| 1.2 | 120% | 0.182 |
| 1.25 | 125% | 0.223 |
Experimental Design and Methodologies
Standard Bioequivalence Study Designs
For most small molecule drugs, regulatory agencies recommend specific study designs to establish bioequivalence:
- Two-period, two-sequence, two-treatment, single-dose crossover design: This is the most commonly used design, where each subject receives both the test and reference formulations in randomized sequence with an appropriate washout period [116]
- Single-dose parallel design: Used when a crossover design is not feasible due to long half-life or other considerations [116]
- Replicate design: Employed for drugs with high variability or for narrow therapeutic index drugs [116]
These studies are typically conducted in healthy volunteers (age ≥18 years), though patient populations may be more appropriate for certain drug classes [116].
Key Pharmacokinetic Parameters
Bioequivalence assessment focuses on primary pharmacokinetic parameters that reflect the rate and extent of absorption:
- AUC0-t: Area under the concentration-time curve from zero to the last measurable time point, indicating the extent of absorption [116]
- AUC0-∞: Area under the concentration-time curve from zero to infinity, representing total drug exposure [116]
- Cmax: Maximum observed concentration, reflecting the rate of absorption [116]
- Tmax: Time to reach Cmax, providing additional information on absorption rate [116]
Bioequivalence Study Workflow: This diagram illustrates the standard workflow for a crossover bioequivalence study, from subject recruitment through regulatory decision.
Troubleshooting Guides and FAQs
Common Experimental Challenges and Solutions
Problem: High intra-subject variability in pharmacokinetic parameters Solution: Consider using a replicate study design that allows precise estimation of within-subject variability for both test and reference formulations. For highly variable drugs (HV drugs), reference-scaled average bioequivalence approaches may be appropriate [116].
Problem: Failure to meet the 80-125% criterion for one parameter Solution: Examine potential causes such as food effects, analytical issues, or formulation differences. For certain drugs with established wide therapeutic windows, regulatory agencies may permit wider acceptance ranges based on justification [116].
Problem: Outliers affecting study results Solution: Pre-specified statistical methods for handling outliers should be included in the study protocol. Replicate designs provide additional data to assess whether outliers are formulation-dependent or random occurrences [116].
Frequently Asked Questions
Why was the 80-125% range originally selected? The range was established based on expert opinion that differences in systemic drug exposure up to 20% are not clinically significant for most drugs [119]. The symmetrical ±20% clinical judgment translates to the 80-125% range after log transformation of the typically log-normally distributed pharmacokinetic data [118].
Can the bioequivalence criteria be modified for special cases? Yes, different acceptance criteria may apply for:
- Narrow therapeutic index drugs: Stricter criteria (e.g., 90-111%) may be required [116]
- Highly variable drugs: Reference-scaled average bioequivalence approaches with widened limits may be permitted [116] [117]
- Specific drug classes: Biologics and complex products may have unique requirements
How does food affect bioequivalence assessment? Food can significantly impact drug bioavailability by altering gastric emptying, intestinal transit, and drug solubility. For compounds with known food effects, regulatory agencies often require both fasted and fed bioequivalence studies [109].
Advanced Applications in Bioactive Compound Research
Bioavailability Enhancement Technologies
For bioactive food compounds with inherently poor bioavailability, several technologies can improve absorption:
- Structural modifications: Enhancing solubility or stability through chemical modification [109]
- Nanotechnology: Using nanoemulsions or nanoparticles to improve absorption [109]
- Colloidal systems: Employing liposomes or micelles to enhance bioaccessibility [109]
These approaches are particularly valuable for polyphenols and other bioactive compounds with demonstrated health benefits but limited native bioavailability [109].
Special Considerations for Bioactive Food Compounds
Unlike pharmaceutical drugs, bioactive food compounds present unique challenges for bioavailability assessment:
- Complex food matrices: Release from the food matrix is a prerequisite for bioavailability [109]
- Gut microbiota interactions: Colonic metabolism can generate bioactive metabolites [109]
- Inter-individual variability: Gut microbiota composition significantly influences bioavailability [109]
Table 2: Bioequivalence Ranges for Different Clinical Scenarios
| Clinical Range | ± ln(Ratio) | Acceptable Range |
|---|---|---|
| ± 20% | ± 0.223 | 80 - 125% |
| ± 30% | ± 0.357 | 70 - 143% |
| ± 50% | ± 0.693 | 50 - 200% |
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions for Bioavailability Studies
| Reagent/Material | Function in Bioavailability Research |
|---|---|
| LC-MS/MS Systems | High-sensitivity quantification of drugs and metabolites in biological matrices |
| Validated Reference Standards | Accurate calibration and quality control for bioanalytical methods |
| In vitro Dissolution Apparatus | Preliminary assessment of drug release characteristics |
| Caco-2 Cell Lines | Prediction of intestinal permeability and absorption mechanisms |
| Simulated Gastrointestinal Fluids | Evaluation of bioaccessibility under physiological conditions |
| Stable Isotope-Labeled Compounds | Internal standards for precise bioanalytical quantification |
Statistical Decision Process for Bioequivalence: This flowchart outlines the statistical decision process for establishing average bioequivalence according to the 80/125 rule.
Regulatory Context and Global Harmonization
The 80/125 criterion has been adopted by major regulatory agencies worldwide, including the FDA (United States) and EMA (Europe) [120]. Recent efforts by the Global Bioequivalence Harmonization Initiative (GBHI) and International Council for Harmonisation (ICH) aim to further harmonize bioequivalence requirements across regions, potentially reducing the need for repetitive studies in different jurisdictions [116].
For researchers developing enhanced bioavailability formulations of bioactive compounds, understanding these global standards is essential for designing development programs that will meet regulatory requirements across multiple markets. The ICH M9 guideline on biopharmaceutics classification system-based biowaivers provides additional guidance for certain compounds [116].
When designing bioavailability enhancement studies, researchers should consider regional specificities in reference product selection, fasting/fed study requirements, and analytical method validation to ensure global regulatory compliance.
For researchers focused on improving the bioavailability of bioactive compounds, mastering advanced Pharmacokinetic/Pharmacodynamic (PK/PD) evaluation is crucial. Modern drug development has moved beyond simple static models to dynamic systems that can accurately predict human physiological responses. This technical support center provides essential guidance for navigating the experimental complexities of these advanced models, enabling more reliable assessment of novel formulations like biologics, antibody-drug conjugates, and innovative delivery systems such as plant-derived exosomes [121] [122]. The following FAQs and troubleshooting guides address common challenges in implementing these sophisticated evaluation methodologies.
Core Concepts FAQ
What is the fundamental shift in how PK/PD is applied in modern drug discovery?
Traditional approaches treated PK/PD modeling as a late-stage, data-driven exercise primarily used to support candidate selection and clinical trial design. The modern paradigm advocates for "PKPD thinking" to begin much earlier—during target selection and before lead optimization. This shift allows medicinal chemists to design molecules with optimal binding and residence time properties based on the specific target biology, rather than retrofitting PK properties to already-synthesized compounds [123].
Why are traditional static models insufficient for evaluating novel formulations?
Static models maintain constant drug concentrations, which fails to mimic the dynamic concentration-time profiles (absorption, distribution, metabolism, excretion) that occur in living systems. This limitation makes them poor predictors of how drug resistance emerges over time or how formulations perform under realistic physiological conditions. Dynamic models that precisely control drug concentration over time are necessary to bridge the gap between static assays and clinical outcomes [124].
How can we enhance the bioavailability of bioactive compounds in formulation development?
Beyond traditional approaches, plant-derived exosomes (PDEs) represent a promising natural nanocarrier system for bioactive compounds. These 30-200 nm vesicles exhibit high biocompatibility and structural stability, protecting encapsulated compounds from degradation in the gastrointestinal tract. Engineering strategies—including self-loading, physical modification (e.g., ultrasonic insertion), and covalent modification—can further enhance their loading efficiency and targeting capabilities for site-specific delivery [122].
Technical Troubleshooting Guides
Issue 1: Inconsistent PK/PD Relationships in Preclinical Models
Problem: Unable to establish a consistent relationship between systemic drug concentration and pharmacological response, leading to poor translatability to human trials.
Diagnosis Steps:
- Verify that the drug concentration at the target site mirrors the systemic circulation.
- Characterize the target engagement and downstream biology, including feedback mechanisms and pathway redundancy.
- Assess whether the disease model accurately reflects human pathophysiology.
Solutions:
- Implement a Two-Compartment Hollow Fiber Model: This system physically separates test organisms in the extracapillary space while allowing drugs to equilibrate rapidly through a semi-permeable membrane. It enables independent control of absorption and elimination kinetics, better mimicking human PK profiles [124].
- Apply Early Mechanism-Based Modeling: Before extensive in vivo studies, build preliminary PKPD models using literature-derived physiological data and targeted in vitro experiments to identify critical knowledge gaps [123].
Prevention: Incorporate tool compounds with known PKPD relationships to validate new disease models before testing novel formulations.
Issue 2: Poor Bioavailability of Bioactive Compounds
Problem: Bioactive compounds degrade in the gastrointestinal tract or fail to reach target tissues at therapeutic concentrations.
Diagnosis Steps:
- Analyze compound stability under simulated gastric and intestinal conditions.
- Evaluate cellular uptake efficiency using in vitro models.
- Assess whether the compound reaches the intended site of action.
Solutions:
- Utilize Plant-Derived Exosomes as Natural Carriers: Isolate exosomes from dietary plants (e.g., ginger, grape, lemon) using ultracentrifugation or precipitation-based methods. Load bioactive compounds via ultrasonic insertion, which creates temporary pores in the vesicle membrane for enhanced encapsulation [122].
- Implement Targeted Delivery Approaches: Functionalize exosome surfaces with targeting ligands (e.g., glycyrrhetinic acid for liver targeting) using covalent modification strategies to achieve site-specific delivery [122].
Prevention: Conduct thorough pre-formulation studies on compound solubility, permeability, and stability to guide carrier selection.
Issue 3: Modeling Complex Drug Mechanisms
Problem: Traditional PKPD models fail to adequately describe the behavior of complex modalities like PROTACs, covalent inhibitors, or biologics.
Diagnosis Steps:
- Identify the key pharmacological processes driving the drug's mechanism of action.
- Determine whether target engagement is irreversible or involves complex downstream pathways.
- Assess the time course of target engagement relative to plasma concentrations.
Solutions:
- Adopt a Model-Based Target Pharmacology Assessment (mTPA): Combine PBPK/PD modeling with machine learning to define the optimal combination of drug properties needed for targeted pharmacology early in discovery [123].
- Leverage Hollow Fiber Systems for Complex Dosing: Use systems capable of modeling combination therapies and drug-drug interactions by precisely controlling the kinetics of multiple drugs simultaneously [124].
Prevention: Invest in understanding the fundamental biology of novel targets before committing to extensive chemistry optimization.
Experimental Protocols & Data Presentation
Hollow Fiber Bioreactor Setup for PK/PD Studies
The following workflow details the establishment of a hollow fiber infection model for evaluating antimicrobial formulations. This diagram illustrates the key components and flow path:
Detailed Methodology:
- System Assembly: Use pre-sterilized hollow fiber cartridges with appropriate molecular weight cut-off (typically 20 kD) compatible with your drug's properties [124].
- Organism Inoculation: Inject test organisms into the extracapillary space (ECS) through sample ports. Bacterial loads can reach 10^8-10^9 cells depending on cartridge size [124].
- Drug Dosing: Add the novel formulation to the central reservoir where it circulates through fiber lumens and equilibrates with the ECS within minutes.
- PK Control: Mimic human elimination kinetics by adding diluent to the central reservoir at a controlled rate while maintaining constant volume.
- Sampling: Regularly sample both the central reservoir and ECS to measure drug concentrations and bacterial counts over time.
Quantitative Data from Recent Formulation Studies
Table 1: Performance Metrics of Novel Therapeutic Formulations in Late-Stage Development
| Drug Candidate | Mechanism/Type | Key PK/PD Improvement | Clinical Outcome | Reference |
|---|---|---|---|---|
| Lerodalcibep (LIB Therapeutics) | PCSK9-binding fusion protein | 56% LDL-C reduction over 52 weeks; monthly dosing (vs. biweekly for mAbs) | 90% patients achieved guideline LDL-C targets | [121] |
| Plant-Derived Exosomes (Various) | Natural nanocarrier | Enhanced gastrointestinal stability and cellular uptake of bioactive compounds | Effective intervention in dry eye and NAFLD models | [122] |
| Depemokimab (GSK) | Long-acting anti-IL-5 mAb | 48-54% reduction in asthma exacerbations with 6-month dosing interval | Dual indication in severe asthma and chronic rhinosinusitis | [121] |
Table 2: Critical Research Reagents for Advanced PK/PD Formulation Studies
| Reagent / System | Specifications | Research Application | Key Supplier |
|---|---|---|---|
| Hollow Fiber Bioreactor Cartridge | 4000 cm² surface area, 20 kD MWCO, 15 mL ECS volume | Mimicking human PK profiles for antibiotics, antivirals, and novel formulations | FiberCell Systems [124] |
| 5-Port Reservoir Cap | Precision fluid control, maintains constant reservoir volume | Enables accurate modeling of drug elimination kinetics | FiberCell Systems [124] |
| Plant-Derived Exosomes | 30-200 nm diameter, lipid bilayer structure | Natural carrier system for enhancing bioactive compound bioavailability | Laboratory isolation [122] |
Advanced PK/PD Modeling Approach
The relationship between drug exposure and response has evolved from simple correlations to sophisticated modeling that informs decision-making throughout drug discovery. This diagram outlines the integrated approach:
Implementation Framework:
- Model-Based Target Pharmacology Assessment: Combine PBPK/PD modeling with machine learning to define optimal drug properties before synthetic chemistry begins [123].
- Integrated Data Analysis: Use all available information—literature knowledge, in vitro data, and preliminary in vivo results—to build models that fill knowledge gaps strategically.
- Machine Learning Enhancement: Apply artificial neural networks and other ML approaches to identify complex PK/PD relationships that traditional models might miss [123].
This approach moves beyond the traditional view of PKPD as merely a data-fitting exercise to a strategic framework that guides compound optimization and improves decision-making throughout the discovery and development process.
Regulatory Pathways for Generic Drugs and Product Line Extensions
FAQs: Generic Drug Approval and Regulatory Pathways
Q: What is an Abbreviated New Drug Application (ANDA), and what data must it include? A: An ANDA is an application submitted to the FDA for the review and potential approval of a generic drug product. Its purpose is to provide a safe, effective, and lower-cost alternative to a brand-name drug. Unlike applications for new drugs, ANDAs are "abbreviated" because they are generally not required to include preclinical (animal) and clinical (human) data to establish safety and effectiveness. Instead, the generic applicant must scientifically demonstrate that their product is bioequivalent to the reference listed drug. This means demonstrating that the generic drug delivers the same amount of active ingredients into a patient's bloodstream in the same amount of time as the innovator drug [125].
Q: What are product-specific regulatory pathways for generic drugs? A: In recent years, the FDA has approved several generic drugs using product-specific testing to determine therapeutic equivalence. This approach is tailored to the unique features of a particular drug and is often used in two situations [126]:
- Cases where standard bioequivalence studies are not relevant.
- Cases involving complex molecules that require specially tailored pharmaceutical equivalence studies. Examples of drugs approved via such pathways include enoxaparin and venlafaxine extended-release. While these pathways are essential for making low-cost generic drugs available without duplicating lengthy clinical trials, they also highlight the need for strategies to monitor the safety and effectiveness of generics approved via these modified pathways [126].
Q: How do regulatory bodies approach the approval of biotechnology products? A: Various national and international regulatory bodies, including the FDA and the European Medicines Agency (EMA), regulate biotech products. These bodies use a risk-based approach to evaluate the safety, efficacy, and quality of biotechnology products. They assess data from preclinical and clinical trials to make an approval decision and continue to monitor products after approval to ensure ongoing safety and efficacy. Companies must maintain rigorous quality control systems and accurate documentation to ensure compliance [127].
Q: What is "evergreening," and how does it affect the generic drug market? A: "Evergreening" is a strategy used by brand-name drug manufacturers to extend their market exclusivity periods and delay generic competition. A common tactic is the strategic timing of a "line extension," such as introducing an extended-release (ER) formulation of a drug just before a generic version of the original immediate-release (IR) formulation is set to enter the market. This new formulation can be granted its own three-year exclusivity period, allowing the brand manufacturer to maintain market share. This practice can limit competition, thereby increasing costs for patients, insurers, and government payers [128].
Troubleshooting Guides for Bioavailability and Bioequivalence Experiments
Guide 1: Addressing Lack of Assay Window in TR-FRET-based Bioequivalence Studies
Problem: A complete lack of assay window during analysis.
Solution:
- Step 1: Check Instrument Setup. The most common reason for no assay window is an improperly configured instrument. Verify that the correct emission filters are installed, as the wrong filters can prevent signal detection. Consult your instrument's setup guide [129].
- Step 2: Test the Development Reaction. If the instrument is set up correctly, the issue may lie with the assay reagents. Perform a control development reaction [129]:
- For the 100% phosphopeptide control, do not expose it to any development reagent. This should yield the lowest ratio value.
- For the substrate (0% phosphopeptide), expose it to a 10-fold higher concentration of development reagent than recommended. This should yield the highest ratio value.
- A properly functioning assay should show a significant difference (e.g., a 10-fold ratio change) between these two controls. If not, the dilution of the development reagent may be incorrect [129].
Guide 2: Troubleshooting Inconsistent Oral Bioavailability in Preclinical Models
Problem: Inconsistent or low oral bioavailability (F) in animal models, which is critical for predicting human performance. Bioavailability is the product of the fraction absorbed (FAbs), the fraction escaping gut metabolism (FG), and the fraction escaping hepatic first-pass extraction (FH): F = FAbs · FG · FH [130].
Solution:
- Step 1: Identify the Limiting Barrier. Profile your compound to identify the primary cause of poor bioavailability [130]:
- Solubility/Dissolution: If dissolution is the rate-limiting step, the dosing vehicle or formulation is likely at fault.
- Permeability: Use in vitro models like Caco-2 or MDCK cell monolayers to assess passive diffusion and active transport.
- First-Pass Metabolism: Use liver microsomes or hepatocytes to determine metabolic stability.
- Step 2: Optimize the Dosing Formulation. For the initial PK study, using a solution formulation rather than a suspension maximizes the chance of achieving good absorption by eliminating dissolution as a variable. For poorly soluble compounds, use solubilizing vehicles like PEG 400, propylene glycol, or surfactants (e.g., polysorbate 80). However, test these for potential precipitation upon dilution in GI fluids [130].
- Step 3: Consider Structural Modifications. If formulation changes are insufficient, explore chemical approaches to improve key properties. This may include salt formation to enhance solubility or modifying the molecular structure to reduce metabolism by cytochrome P450 enzymes [130].
Experimental Protocols for Key Bioavailability Experiments
Protocol 1: Parallel Artificial Membrane Permeability Assay (PAMPA)
Objective: To rapidly assess the passive transcellular permeability of a compound.
Methodology:
- Membrane Preparation: Create an artificial lipid membrane by coating a filter with a mixture of lecithin in an organic solvent (e.g., dodecane) to simulate the intestinal epithelial barrier.
- Compound Incubation: Add a solution of the test compound to the donor plate. The acceptor plate contains a blank buffer solution.
- Incubation and Analysis: Stack the donor and acceptor plates and incubate for a set period (e.g., 2-16 hours) to allow for passive diffusion. The concentration of the compound that permeates into the acceptor compartment is quantified using UV spectroscopy or LC-MS/MS.
- Data Calculation: Permeability (
Papp) is calculated based on the rate of compound appearance in the acceptor compartment. This data helps categorize compounds as having high or low permeability, a key parameter in the Biopharmaceutics Classification System (BCS) [131] [130].
Protocol 2: Determination of Bioequivalence in Human Volunteers
Objective: To demonstrate that a generic drug product is bioequivalent to the reference (brand-name) drug.
Methodology:
- Study Design: A single-dose, crossover study is the standard. Healthy volunteers are randomly assigned to receive either the test (generic) or reference product first, followed by a "washout" period, after which they receive the alternative product.
- Blood Sampling: Serial blood samples are collected from each volunteer over a period sufficient to define the entire pharmacokinetic profile (typically up to 3-5 times the elimination half-life).
- Bioanalytical Analysis: Plasma samples are analyzed using a validated method (e.g., LC-MS/MS) to determine the concentration of the active drug over time.
- Pharmacokinetic and Statistical Analysis: Key parameters are calculated, including the area under the concentration-time curve (AUC) and the maximum concentration (Cmax). The 90% confidence intervals for the ratios of these parameters (test/reference) must fall within the range of 80.00% to 125.00% to conclude bioequivalence [125].
Visualization of Pathways and Workflows
Generic Drug Development and Approval Workflow
Bioavailability Optimization Strategy
The Scientist's Toolkit: Research Reagent Solutions
Table: Key Reagents for Bioavailability and Bioequivalence Research
| Reagent/Assay Type | Function | Example Application |
|---|---|---|
| Caco-2 Cell Line | An in vitro model of the human intestinal mucosa to predict drug absorption and permeability [130]. | Assessing a compound's passive diffusion and active transport across the intestinal barrier. |
| TR-FRET Assay Kits | Time-Resolved Förster Resonance Energy Transfer assays used for studying molecular interactions (e.g., kinase binding) with high sensitivity [129]. | Screening for compounds that may inhibit enzyme activity relevant to drug metabolism. |
| Liver Microsomes | Subcellular fractions containing drug-metabolizing enzymes (e.g., Cytochrome P450s) [130]. | Evaluating a compound's metabolic stability and identifying potential for first-pass metabolism. |
| PAMPA Plate | Parallel Artificial Membrane Permeability Assay plate for high-throughput assessment of passive permeability [130]. | Early-stage, rapid screening of permeability for large compound libraries. |
| Z'-LYTE Assay Kit | A fluorescence-based kinase assay that utilizes a coupled enzyme system for detection [129]. | Profiling the selectivity and potency of kinase inhibitors. |
Market Trends and the Growing Demand for Bioavailability Enhancement Services
The global bioavailability enhancement technologies and services market is experiencing significant growth, propelled by the critical need to improve the efficacy of poorly soluble drugs. This expansion is quantified in the table below.
Table 1: Bioavailability Enhancement Market Size and Projections
| Market Metric | Value in 2024/2025 | Projected Value in 2035 | Compound Annual Growth Rate (CAGR) | Source |
|---|---|---|---|---|
| Market Size (Projection 1) | USD 3.6 billion (2025) | USD 10.2 billion | 11.11% (2025-2035) | [132] |
| Market Size (Projection 2) | USD 3.2 billion (2025) | USD 10.22 billion | 11.11% (2025-2035) | [133] |
| Technology Market Size | ~USD 1.8 billion (2024) | ~USD 4.2 billion | 8.8% (2025-2033) | [134] |
This growth is driven by several key factors:
- High Prevalence of Poorly Soluble Drugs: A substantial 70-90% of New Chemical Entities (NCEs) in development pipelines and nearly 40% of marketed drugs face challenges related to low aqueous solubility and/or permeability, creating a persistent demand for enhancement solutions [133] [135] [134].
- Dominance of BCS Class II Compounds: The Biopharmaceutics Classification System (BCS) Class II (low solubility, high permeability) represents the largest segment, accounting for over 77% of the market share. Enhancing the bioavailability of these compounds is crucial for their therapeutic success [133] [132].
- Strategic Outsourcing: Pharmaceutical companies are increasingly outsourcing these complex formulation challenges to specialized contract research and manufacturing organizations (CROs/CMOs). Nearly 115 companies now offer specialized bioavailability enhancement services, with over 80% employing solid dispersion approaches to improve drug solubility [133] [132].
- Focus on Innovative Formulations: There is a growing emphasis on reformulating existing drugs to improve their performance and extend commercial life, often utilizing regulatory pathways like the 505(b)(2) for approval [132].
Frequently Asked Questions (FAQs) & Troubleshooting
This section addresses common technical and strategic challenges researchers face.
Q1: What are the primary physicochemical properties we should focus on to diagnose bioavailability issues early in development? The key properties are solubility, lipophilicity, and molecular size/weight. Poor aqueous solubility is a primary culprit, as a drug must dissolve to be absorbed. Lipophilicity (LogP/LogD) affects membrane permeability; an optimal range of 1-3 is generally favorable for oral bioavailability. Molecular weight also influences diffusion rates, with compounds under 500 Da being more likely to have good absorption, though this is not an absolute rule [131].
Q2: Why is the solid dispersion approach so prevalent, and what are its common failure points? Solid dispersion is dominant because it effectively increases the apparent solubility and dissolution rate of a drug by dispersing it in an amorphous state within a hydrophilic polymer matrix [133] [132]. Common failure points include:
- Drug Recrystallization: The amorphous drug can recrystallize over time during storage, losing its solubility advantage. This is often due to physical instability.
- Incompatibility with Carrier Polymer: Poor choice of polymer can lead to phase separation, inadequate dissolution, or chemical instability.
- Manufacturing Process Variability: Techniques like hot-melt extrusion and spray drying require precise control of parameters (e.g., temperature, feed rate) to ensure a homogeneous, stable product [16] [135].
Q3: How can we mitigate food-effect variability in our final formulation? Food effects can alter bioavailability by affecting solubility, gastric emptying, and bile secretion. To mitigate this:
- Utilize Lipid-Based Formulations: Self-emulsifying Drug Delivery Systems (SEDDS/SMEDDS) can enhance the solubility of lipophilic drugs and reduce variability by promoting solubilization in the gut, independent of dietary lipids [135].
- Create Acidic/Basic Microenvironments: Technologies like Diffucaps use organic acid or alkaline buffers within the formulation to control the local pH, stabilizing the dissolution profile of pH-dependent drugs regardless of gastric contents [135].
- Conduct Early In Vitro Testing: Use advanced biorelevant media that simulate fed and fasted states to predict and model food effects during development [136].
Q4: What emerging technologies show the most promise for enhancing the bioavailability of large molecule therapeutics? While many technologies focus on small molecules, promising approaches for large molecules like peptides and nucleic acids include:
- Permeation Enhancers: Compounds such as SNAC (N-[8-(2-hydroxybenzoyl) amino] caprylate) can temporarily improve the transport of poorly absorbed actives across biological barriers like the intestinal mucosa [135] [136].
- Lipid Nanoparticles (LNPs): Initially famous for mRNA vaccines, LNPs are now being explored for oral delivery of various macromolecules, protecting them from degradation and facilitating absorption [136].
- Cyclodextrin Complexation: Cyclodextrins can form inclusion complexes with hydrophobic portions of larger molecules, improving their aqueous solubility and stability [135].
Essential Experimental Protocols
Below are detailed methodologies for key experiments in bioavailability enhancement research.
Protocol: Preparation of Amorphous Solid Dispersions (ASD) via Hot-Melt Extrusion
Objective: To produce a stable amorphous solid dispersion of a poorly water-soluble API using hot-melt extrusion to enhance dissolution rate and apparent solubility.
Materials:
- API: Poorly water-soluble model drug (e.g., Itraconazole).
- Polymer Carrier: Hydrophilic polymer (e.g., HPMC (Hypromellose), HPMCAS, PVP-VA).
- Equipment: Twin-screw hot-melt extruder, analytical balance, vacuum oven, mortar and pestle, dissolution apparatus, HPLC.
Procedure:
- Pre-blending: Weigh the API and polymer accurately in a predetermined ratio (e.g., 20:80 w/w). Blend in a bag or mixer for 10-15 minutes to achieve a homogeneous physical mixture.
- Extrusion: Feed the pre-blended mixture into the hopper of the hot-melt extruder. Set the temperature profile along the extruder barrels to above the glass transition temperature (Tg) of the polymer but below the melting point of the API to ensure amorphization without degradation. Typical temperatures range from 100°C to 180°C, depending on the polymer.
- Screw Configuration: Use a high-shear screw configuration to ensure adequate mixing and dispersion of the API within the polymer melt.
- Extrudate Collection: As the molten mass exits the die, collect the transparent or translucent strand. Allow it to cool on a conveyor belt at room temperature.
- Size Reduction: Mill the cooled, brittle extrudate using a laboratory mill or mortar and pestle to form a fine powder with a consistent particle size distribution.
- Characterization:
- Solid-State Analysis: Use Differential Scanning Calorimetry (DSC) and X-Ray Powder Diffraction (XRPD) to confirm the conversion of the crystalline API to an amorphous state.
- In Vitro Dissolution: Perform a dissolution test (e.g., USP Apparatus II) in a biorelevant medium and compare the dissolution profile against the pure crystalline API.
Troubleshooting:
- Air Bubbles in Extrudate: Apply a vacuum venting system during extrusion to remove entrapped air and moisture.
- API Degradation: Lower the extrusion temperature or residence time; consider a more thermally stable polymer.
- Poor Miscibility: Screen different polymer carriers or incorporate a surfactant (e.g., SLS, TPGS) to improve compatibility [16] [135].
Protocol: Formulation of a Self-Nanoemulsifying Drug Delivery System (SNEDDS)
Objective: To develop a liquid SNEDDS preconcentrate that spontaneously forms an oil-in-water nanoemulsion upon aqueous dilution, thereby enhancing the solubility and absorption of a lipophilic drug.
Materials:
- API: Lipophilic model drug (e.g., Fenofibrate).
- Lipid Component: Medium-chain triglycerides (e.g., Miglyol 812), mixed mono/diglycerides.
- Surfactant: Non-ionic surfactants (e.g., Tween 80, Cremophor EL).
- Co-surfactant/Solvent: Ethanol, Propylene glycol, PEG 400.
- Equipment: Magnetic stirrer, vortex mixer, graduated pipettes, dynamic light scattering (DLS) instrument.
Procedure:
- Solubility Screening: Dissolve an excess of the API in each potential excipient (oil, surfactant, co-surfactant). Shake/vortex for 24-48 hours at 37°C. Centrifuge and analyze the supernatant by HPLC to identify the excipients with the highest solubilizing capacity for the drug.
- Pseudo-Ternary Phase Diagram: Construct phase diagrams by mixing the selected oil, surfactant, and co-surfactant at different weight ratios (e.g., 1:9, 2:8, ... 9:1). Slowly titrate each mixture with water under magnetic stirring at 37°C. Visually observe and note the points of transition from clear nanoemulsion to coarse emulsion or gel. The goal is to identify the region that provides the largest area of spontaneous nanoemulsion formation.
- Formulation of Preconcentrate: Based on the phase diagram, select an optimal composition from the nanoemulsion region. Dissolve the API into the blend of oil, surfactant, and co-surfactant under gentle heating and stirring until a clear, homogeneous solution is obtained.
- Self-Emulsification Assessment: Dilute 1 mL of the preconcentrate in 250 mL of distilled water and 0.1N HCl in a glass vessel at 37°C with gentle agitation. Observe the tendency to form an emulsion and the resulting appearance (should be clear or bluish).
- Characterization:
- Droplet Size and Zeta Potential: Analyze the diluted nanoemulsion using Dynamic Light Scattering (DLS). A successful SNEDDS will typically produce droplets < 200 nm. Zeta potential indicates the physical stability of the emulsion.
- Robustness to Dilution: Test the formulation against different dilution volumes and pH levels to ensure it does not precipitate the drug.
Troubleshooting:
- Precipitation upon Dilution: The formulation may be too rich in drug. Reduce the drug load or adjust the S/CoS ratio to improve solubilization capacity.
- Large Droplet Size: Optimize the surfactant-to-oil ratio; consider using a high-energy mixing step during preconcentrate preparation [16] [135].
Workflow and Pathway Visualizations
Bioavailability Enhancement Decision Pathway
This diagram outlines a logical workflow for selecting the appropriate bioavailability enhancement strategy based on the drug's properties.
Key ADME Processes Governing Bioavailability
This diagram visualizes the core ADME (Absorption, Distribution, Metabolism, Excretion) pathways that determine a drug's bioavailability after oral administration.
Research Reagent Solutions Toolkit
Table 2: Essential Materials and Technologies for Bioavailability Enhancement Research
| Category | Item / Technology | Primary Function & Rationale |
|---|---|---|
| Polymer Carriers (for ASDs) | HPMC, HPMCAS, PVP-VA | Inhibit drug recrystallization and maintain supersaturation in the gut by forming a stable amorphous solid dispersion. [16] [135] |
| Lipid-Based Excipients | Medium-Chain Triglycerides (MCT Oil), Tween 80, Cremophor EL | Formulate SEDDS/SMEDDS to keep lipophilic drugs in a solubilized state during gastrointestinal transit, enhancing absorption. [135] |
| Particle Engineering Tech | Wet Milling, High-Pressure Homogenization | Reduce API particle size to the nano/micro scale, dramatically increasing the surface area and dissolution rate (NanoSol). [16] [135] |
| Complexation Agents | Cyclodextrins (e.g., SBE-β-CD) | Form non-covalent inclusion complexes with hydrophobic drug molecules, improving their apparent aqueous solubility and stability. [135] |
| Permeation Enhancers | SNAC, Sodium Caprate | Temporarily and reversibly disrupt intestinal epithelial tight junctions to improve the absorption of poorly permeable drugs (e.g., peptides). [135] [136] |
| Analytical Tools | DSC, XRPD, Dynamic Light Scattering (DLS) | DSC/XRPD: Confirm amorphous state and physical stability of formulations.DLS: Characterize nanoparticle and nanoemulsion droplet size and stability. [16] |
Conclusion
Enhancing the bioavailability of bioactive compounds is a multidisciplinary endeavor crucial for unlocking the full therapeutic potential of a vast number of molecules, particularly as the drug development pipeline increasingly features lipophilic and poorly soluble compounds. Success hinges on a holistic strategy that integrates a deep understanding of fundamental bioavailability principles with the judicious selection and application of advanced formulation technologies. Furthermore, navigating the complexities of physical stability, scaling up processes, and adhering to rigorous regulatory validation standards is paramount for clinical translation. Future progress will be driven by the continued integration of innovative approaches such as artificial intelligence for predictive modeling, personalized medicine strategies, and the development of sophisticated active targeting mechanisms for site-specific delivery. By embracing these advanced strategies, researchers and drug developers can significantly improve patient outcomes through more effective, reliable, and accessible therapeutics.
References
- 1. Drug Bioavailability - StatPearls - NCBI Bookshelf - NIH [https://www.ncbi.nlm.nih.gov/books/NBK557852/]
- 2. Drug Bioavailability - Clinical Pharmacology [https://www.merckmanuals.com/professional/clinical-pharmacology/pharmacokinetics/drug-bioavailability]
- 3. Drug Bioavailability - an overview [https://www.sciencedirect.com/topics/medicine-and-dentistry/drug-bioavailability]
- 4. The Bioavailability of Drugs—The Current State ... [https://www.mdpi.com/1420-3049/28/24/8038]
- 5. Overcoming Challenges in Small-Molecule Drug ... [https://www.mdpi.com/1422-0067/25/23/13121]
- 6. Formulation Impact on Drug Stability & Bioavailability [https://www.pharmsky.com.au/formulation-impact-drug-stability-bioavailability/]
- 7. Thermal shift assays in drug discovery [https://www.sciencedirect.com/science/article/abs/pii/S1056871925008007]
- 8. vs LogD - What is the Difference? - ACD/Labs LogP [https://www.acdlabs.com/blog/partitioning-logp-or-logd-are-you-using-measuring-the-right-descriptor/]
- 9. SiriusT3: Physicochemical Property Analysis for Drug Development in... [https://www.aimil.com/blog/physicochemical-property-analysis-for-drug-development-in-india/]
- 10. Extraction, Isolation and Characterization of Bioactive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3218439/]
- 11. Transport of Drugs Through Biological Barriers—An Asset or ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12030761/]
- 12. Intracellular Metabolomics Identifies Efflux Transporter ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9601193/]
- 13. Expression and function of efflux drug transporters in the ... [https://www.sciencedirect.com/science/article/abs/pii/S0163725805001373]
- 14. Review Absorption of food-derived peptides: Mechanisms ... [https://www.sciencedirect.com/science/article/abs/pii/S0963996924012602]
- 15. Bioavailability Enhancement Strategies & Opportunities [https://drug-dev.com/bioavailability-enhancement-strategies-opportunities/]
- 16. Bioavailability Enhancement Techniques for Poorly Aqueous ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9495787/]
- 17. Innovative Pharmaceutical Formulation Strategies to ... [https://www.upm-inc.com/innovative-approaches-in-pharmaceutical-formulation-for-improving-drug-bioavailability]
- 18. Key trends and technologies in drug delivery for 2025 and ... [https://www.europeanpharmaceuticalreview.com/article/254459/key-trends-and-technologies-in-drug-delivery-for-2025-and-beyond/]
- 19. Topical Drug Delivery Trends 2025 [https://tiogaresearch.com/topical-drug-delivery-trends-2025-advanced-formulation-science-and-smart-delivery-systems/]
- 20. Emerging Role of Biopharmaceutical Classification and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9780568/]
- 21. Biowaiver based on biopharmaceutics classification system [https://www.sciencedirect.com/science/article/pii/S2773216923000181]
- 22. Using the refined Developability Classification System ... [https://www.sciencedirect.com/science/article/pii/S0022354924004313]
- 23. The Reference-scaled Average Bioequivalence (RSABE) ... [https://www.certara.com/blog/reference-scaled-average-bioequivalence-2/]
- 24. Investigation of bioequivalence - Scientific guideline [https://www.ema.europa.eu/en/investigation-bioequivalence-scientific-guideline]
- 25. M13B Bioequivalence for Immediate-Release Solid Oral ... [https://www.federalregister.gov/documents/2025/06/02/2025-09900/m13b-bioequivalence-for-immediate-release-solid-oral-dosage-forms-additional-strengths-biowaiver]
- 26. Online Bioequivalence Study Sample Size Calculator [https://www.biostatistics.ca/online-bioequivalence-study-sample-size-calculator/]
- 27. Bioequivalence [https://www.fda.gov/animal-veterinary/abbreviated-new-animal-drug-applications/bioequivalence]
- 28. What is hot melt extrusion and how can it benefit your drug ... [https://www.abbviecontractmfg.com/news-and-insights/what-is-hot-melt-extrusion-and-how-can-it-benefit-your-drug-product.html]
- 29. Solving solubility issues with amorphous solid dispersions [https://www.europeanpharmaceuticalreview.com/article/34476/spray-drying-solving-solubility-issues-with-amorphous-solid-dispersions/]
- 30. Stability and recrystallization of amorphous solid ... [https://www.sciencedirect.com/science/article/pii/S037851732500167X]
- 31. Spray Dried Dispersion (SDD) Services [https://www.altasciences.com/our-solutions/manufacturing-and-analytical-services/spray-dried-dispersions]
- 32. Hot-Melt Extrusion: from Theory to Application in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4766118/]
- 33. Bioavailability Enhancement [https://www.lonza.com/advanced-synthesis/small-molecules/particle-engineering-services/bioavailability-enhancement]
- 34. Operational advantages of using hot melt extrusion to ... [https://www.abbviecontractmfg.com/news-and-insights/Operational-advantages-of-using-hot-melt-extrusion-to-create-amorphous-solid-dispersions.html]
- 35. Tackling Challenging Molecules by Spray Drying [https://drug-dev.com/formulation-forum-tackling-challenging-molecules-by-spray-drying-making-the-impossible-possible/]
- 36. Application of hot melt extrusion to enhance the dissolution ... [https://www.sciencedirect.com/science/article/pii/S1818087616300630]
- 37. Self-Emulsifying Drug Delivery Systems (SEDDS) [https://www.mdpi.com/1999-4923/17/1/63]
- 38. The future of lipid-based drug delivery systems [https://www.cas.org/resources/cas-insights/future-lipid-drug-delivery]
- 39. A Step-by-Step Guide to SEDDS for Enhanced Oral ... [https://drug-dev.com/expert-content/from-concept-to-optimization-a-step-by-step-guide-to-sedds-for-enhanced-oral-bioavailability/]
- 40. Dexamethasone Loaded Liposomes by Thin-Film Hydration and... [https://pubmed.ncbi.nlm.nih.gov/32111100/]
- 41. Lipid-Based Drug Delivery Systems: Concepts and Recent ... [https://www.mdpi.com/2079-4991/15/17/1326]
- 42. Liposomal Formulations in Clinical Use Progress Challenges and... [https://www.preprints.org/manuscript/202503.1663/v1]
- 43. Challenges and opportunities in computational studies for ... [https://www.nature.com/articles/s44386-025-00024-3]
- 44. The Effect of the Particle Size Reduction on the Biorelevant ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9865396/]
- 45. Particle Size Analysis and Reduction Techniques to ... [https://dmpkservice.wuxiapptec.com/articles/457-particle-size-analysis-and-reduction-techniques-to-enhance-drug-bioavailability-in-preclinical-studies/]
- 46. Wet Nanomilling and Liquid Vial Filling [https://www.altasciences.com/manufacturing-and-analytical-services/wet-nanomilling-and-liquid-vial-filling]
- 47. Nanomilling: A Key Option For Formulating Water-Insoluble ... [https://agnopharma.com/blog/nanomilling-option-for-formulating-water-insoluble-apis/]
- 48. The effect of particle size on drug bioavailability in various ... [https://www.sciencedirect.com/science/article/pii/S2773216923000296]
- 49. Setting Up M110 Microfluidizer & Troubleshooting Plugged ... [https://newlifescientific.com/blogs/videos/m110-operation-and-troubleshooting-microfluidizers?srsltid=AfmBOoruNimuGunfLnVaFnwdUB3mGce-O_WNJmt1Ahr2Htzmjo9BKZgc]
- 50. Formulation of casein–curcumin nanodispersions using... [https://pubs.rsc.org/en/content/articlelanding/2025/fb/d5fb00558b]
- 51. Innovative Delivery Systems Loaded with Plant Bioactive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8234206/]
- 52. Synthesis and performance optimization of multi-bioactive ... [https://www.nature.com/articles/s41598-025-25043-y]
- 53. Cyclodextrins: Enhancing Drug Delivery, Solubility and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11945013/]
- 54. Cyclodextrins, Surfactants and Their Inclusion Complexes - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12525991/]
- 55. Cyclodextrins and Their Inclusion Complexes for ... [https://www.mdpi.com/journal/pharmaceutics/special_issues/cyclodextrin_pharm]
- 56. Cyclodextrins as Multifunctional Platforms in Drug Delivery ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12299055/]
- 57. Cyclodextrin Inclusion Complexes for Improved Drug ... [https://www.mdpi.com/1999-4923/15/9/2345]
- 58. Applications of Cyclodextrins to Improve the Stability, ... [https://www.biosynth.com/blog/blog-series-3-applications-of-cyclodextrins-to-improve-the-stability-bioavailability-and-solubility-of-bioactive-compounds]
- 59. Cyclodextrin inclusion complex enhances solubility and ... [https://www.sciencedirect.com/science/article/pii/S0039914025004679]
- 60. Enhancing bioactivity and bioavailability of Limonium ... [https://www.nature.com/articles/s41598-025-20905-x]
- 61. Advances in Nanotechnology for Enhancing the Solubility and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11070169/]
- 62. Polymeric micelles for oral drug delivery [https://pubmed.ncbi.nlm.nih.gov/41223952/]
- 63. Polymeric micelles for oral drug delivery [https://www.sciencedirect.com/science/article/abs/pii/S0378517325012104]
- 64. An Overview of Nanostructured and its Application in... Lipid Carriers [https://pmc.ncbi.nlm.nih.gov/articles/PMC10460807/]
- 65. Techniques in the characterization of lipid-based ... [https://link.springer.com/article/10.1007/s44395-025-00021-5]
- 66. Journal of Research in Pharmacy » Submission » Experimental ... [https://dergipark.org.tr/en/pub/jrespharm/issue/91588/1687174]
- 67. Recent Advances in Polymeric Micelle Preparation for Drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12566873/]
- 68. Recent advances in the improvement of the bioavailability ... [https://www.sciencedirect.com/science/article/abs/pii/S0308814625044139]
- 69. Setting Up a “Green” Extraction Protocol for Bioactive ... [https://www.mdpi.com/1422-0067/26/15/7407]
- 70. Green Extraction Techniques of Bioactive Compounds [https://www.mdpi.com/2227-9717/11/8/2255]
- 71. Green Extraction of Bioactive Compounds from Plant Biomass ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8466011/]
- 72. Emerging Trends in Green Extraction Techniques ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12189258/]
- 73. Green solvent extraction and eco-friendly novel techniques ... [https://www.sciencedirect.com/science/article/pii/S2772502225007395]
- 74. Emerging Trends in Green Extraction Techniques for ... [https://www.mdpi.com/2227-9717/11/12/3444]
- 75. Green Extraction of Natural Products: Concept and Principles [https://pmc.ncbi.nlm.nih.gov/articles/PMC3430255/]
- 76. Advancements in curcuminoid formulations: An update on ... [https://pubmed.ncbi.nlm.nih.gov/40688407/]
- 77. Octacosanol: Biological activities and bioavailability ... [https://www.sciencedirect.com/science/article/abs/pii/S0308814625041433]
- 78. Formulation Strategies to Improve the Stability and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9611293/]
- 79. Combinative Particle Size Reduction Technologies for the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4590828/]
- 80. Recent research progress on crystallization strategies for ... [https://www.sciencedirect.com/science/article/pii/S221171562300098X]
- 81. Bioavailability - SEQENS [https://www.seqens.com/service/bioavailability/]
- 82. Poorly water-soluble APIs in fixed-dose combinations [https://www.sciencedirect.com/science/article/pii/S177322472500615X]
- 83. for Transdermal API Systems characteristics Drug Delivery [https://amarintech.com/api-characteristics-for-transdermal-drug-delivery-systems/]
- 84. Frontiers | Troubleshooting to Expressing Intrinsically... Guide [https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2018.00118/full]
- 85. Understand and Troubleshoot PCR with The BitesizeBio Guide to PCR [https://bitesizebio.com/21840/understand-and-troubleshoot-pcr-with-the-bitesizebio-guide-to-pcr/]
- 86. Bioformulative concepts on intracellular organ specific bioavailability [https://pubmed.ncbi.nlm.nih.gov/30277133/]
- 87. Phenolate-based bioactive compounds: Design, delivery ... [https://www.sciencedirect.com/science/article/pii/S0010854525005119]
- 88. 1H NMR-MS-based heterocovariance as a drug discovery ... [https://www.nature.com/articles/s41598-019-47434-8]
- 89. Challenges to the Development of Emerging Therapies [https://www.biopharminternational.com/view/challenges-to-the-development-of-emerging-therapies]
- 90. Overcoming the challenges in administering biopharmaceuticals [https://pmc.ncbi.nlm.nih.gov/articles/PMC4455970/]
- 91. Optimization of Extraction Methods for NMR and LC-MS ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12388471/]
- 92. Formulation Challenges and Strategies to Develop Pediatric ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9027946/]
- 93. Functional Foods Enriched With Bioactive Compounds [https://pmc.ncbi.nlm.nih.gov/articles/PMC12501769/]
- 94. Paediatric Strategy for Drug Development [https://www.biopharma-excellence.com/solutions/establishing-a-strategy/paediatric-strategy/]
- 95. Artificial intelligence-enhanced bioavailability studies [https://www.sciencedirect.com/science/article/abs/pii/S0924224425003395]
- 96. Artificial Intelligence (AI) Applications in Drug Discovery and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11510778/]
- 97. Learn So You Can Optimize: What AI Drug Discovery ... - Logica [https://www.logica.ai/resources/learn-so-you-can-optimize-what-ai-drug-discovery-companies-need-to-know/]
- 98. AI-driven drug discovery using a context-aware hybrid ... [https://www.nature.com/articles/s41598-025-19593-4]
- 99. Intelligent deep learning model for targeted cancer drug ... [https://www.nature.com/articles/s41598-025-96149-6]
- 100. sciencedirect.com/topics/agricultural-and-biological-sciences/ bioactive ... [https://www.sciencedirect.com/topics/agricultural-and-biological-sciences/bioactive-compound]
- 101. Leading AI-Driven Drug Discovery Platforms [https://www.sciencedirect.com/science/article/abs/pii/S0031699725075118]
- 102. A Comparative Analysis of NONMEM and AI-based Models ... [https://pubmed.ncbi.nlm.nih.gov/41254220/]
- 103. Predictive modeling for solubility and bioavailability ... [https://www.patheon.com/us/en/insights-resources/blog/predictive-modeling-for-solubility-and-bioavailability-enhancement.html]
- 104. Video: Bioavailability : Single Versus Multiple Dose... Study Design [https://www.jove.com/science-education/v/17145/bioavailability-study-design-single-versus-multiple-dose-studies]
- 105. and bioequivalance Bioavailability | PPTX studies [https://www.slideshare.net/slideshow/bioavailability-and-bioequivalance-studies/23379315]
- 106. BA & BE Studies For Nutraceuticals: A Comprehensive Guide [https://credevo.com/articles/2025/02/05/ba_-be-studies-for-nutraceuticals/]
- 107. Clinical pharmacology and pharmacokinetics: questions and ... [https://www.ema.europa.eu/en/human-regulatory-overview/research-development/scientific-guidelines/clinical-pharmacology-pharmacokinetics/clinical-pharmacology-pharmacokinetics-questions-answers]
- 108. Framework for Developing Prediction Equations ... [https://pubmed.ncbi.nlm.nih.gov/40683371/]
- 109. Bioavailability of bioactive food compounds: a challenging ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3575927/]
- 110. Bioavailability and pharmacokinetics of (poly)phenols ... [https://www.sciencedirect.com/science/article/pii/S0002916525000644]
- 111. Frequently Asked Questions about Method Validation [https://www.ofnisystems.com/services/method-validation/frequently-asked-questions-about-method-validation/]
- 112. TROUBLE SHOOTING DURING BIOANALYTICAL ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3255387/]
- 113. Analytical Method Validation Questions and Answers [https://www.complianceonline.com/resources/analytical-method-validation-questions-and-answers.html]
- 114. Why is Biomarker Assay Validation Different from that of ... [https://link.springer.com/article/10.1208/s12248-025-01135-5]
- 115. The 80-125% Bioequivalence Rule [https://www.pharmacytimes.com/view/debunking-a-common-pharmacy-myth-the-80-125-bioequivalence-rule]
- 116. Bioequivalence Criteria & Requirements [https://www.biopharmaservices.com/services-support/bioequivalence-criteria-and-requirements-explained/]
- 117. Bioavailability and Bioequivalence in Drug Development [https://pmc.ncbi.nlm.nih.gov/articles/PMC4157693/]
- 118. Where Did the 80-125% Bioequivalence Criteria Come ... [https://www.certara.com/blog/where-did-the-80-125-bioequivalence-criteria-come-from/]
- 119. The-History-of-the-FDA-80-125-Rule-for-Bioequivalence-of ... [https://aesnet.org/abstractslisting/the-history-of-the-fda-80-125-rule-for-bioequivalence-of-generic-drugs-including-aeds]
- 120. Where did the 80-125% bioequivalence criteria come from? [https://www.linkedin.com/posts/praveen-nainaram-malviya-70016823a_where-did-the-80-125-bioequivalence-criteria-activity-7342073001862950913-7aHH]
- 121. Innovative Biologics - Expected Drug Approvals in 2025 [https://www.mabion.eu/science-hub/articles/innovative-biologics-expected-approvals-in-2025/]
- 122. Plant-derived exosomes as bioactive compounds carriers ... [https://www.sciencedirect.com/science/article/abs/pii/S092422442500384X]
- 123. PKPD In Drug Discovery: Guiding Decisions With Modeling [https://www.pharmaron.com/knowledge-center/dmpk-insights-15-pkpd-drug-discovery/]
- 124. Antibiotic PK/PD [https://www.fibercellsystems.com/applications/pk-pd/]
- 125. Abbreviated New Drug Application (ANDA) | FDA [https://www.fda.gov/drugs/types-applications/abbreviated-new-drug-application-anda]
- 126. -Specific Product to Approve Regulatory ... Pathways Generic Drugs [https://pubmed.ncbi.nlm.nih.gov/26105011/]
- 127. Regulatory Compliance Guide for Biotech Companies [https://www.arbourgroup.com/blog/2023/february/regulatory-compliance-guide-for-biotech-companies/]
- 128. Limiting Evergreening for Name-Brand Prescription Drugs -Mon... [https://www.crfb.org/papers/limiting-evergreening-name-brand-prescription-drugs]
- 129. Drug Discovery Assays Support—Troubleshooting [https://www.thermofisher.com/us/en/home/technical-resources/technical-reference-library/drug-discovery-development-support-center/drug-discovery-assays-support/drug-discovery-assays-support-troubleshooting.html]
- 130. Review Optimizing Oral Bioavailability in Drug Discovery [https://www.sciencedirect.com/science/article/abs/pii/S0022354916418915]
- 131. Overcoming Challenges in Small-Molecule Drug Bioavailability [https://pmc.ncbi.nlm.nih.gov/articles/PMC11642056/]
- 132. Drug Bioavailability Enhancement Market Size Overview [https://www.rootsanalysis.com/reports/bioavailability-enhancement-technologies-and-services/198.html]
- 133. Bioavailability Sector Set to Reach USD 10.22 Billion by ... [https://finance.yahoo.com/news/bioavailability-enhancement-technologies-services-market-082000400.html]
- 134. Global Bioavailability Enhancement Technology Market to ... [https://www.openpr.com/news/4264452/global-bioavailability-enhancement-technology-market-to-grow]
- 135. SPECIAL FEATURE - Improving Bioavailability & Solubility [https://drug-dev.com/special-feature-improving-bioavailability-solubility-the-never-ending-quest/]
- 136. Current challenges and future perspectives in oral ... [https://www.sciencedirect.com/science/article/pii/S0169409X21000351]