Bioaccessibility vs Bioavailability: Defining the Key Concepts for Drug and Nutrient Development
This article provides a comprehensive analysis of bioaccessibility and bioavailability, two fundamental yet distinct concepts in pharmaceutical and nutritional sciences.
Bioaccessibility vs Bioavailability: Defining the Key Concepts for Drug and Nutrient Development
Abstract
This article provides a comprehensive analysis of bioaccessibility and bioavailability, two fundamental yet distinct concepts in pharmaceutical and nutritional sciences. Tailored for researchers and drug development professionals, it clarifies definitions, explores established and emerging assessment methodologies, and addresses key challenges in enhancing compound efficacy. The scope spans from foundational principles and in vitro/in vivo models to optimization strategies and regulatory validation, offering a holistic guide for application in research and development.
Core Concepts: Defining Bioaccessibility and Bioavailability in Research and Development
In the development of functional foods and pharmaceuticals, two parameters are pivotal for predicting the efficacy of a bioactive compound: bioaccessibility and bioavailability. While often used interchangeably, they represent distinct phases in the journey of a compound from ingestion to systemic action. Bioaccessibility describes the fraction of a compound that is released from its food matrix and becomes available for intestinal absorption; it is the process of liberation into a form suitable for uptake. Bioavailability, however, refers to the proportion of the ingested compound that reaches the systemic circulation and is thus delivered to the site of physiological action [1]. This distinction is not merely semantic but is the critical path that determines the success or failure of a nutraceutical or therapeutic agent. For researchers and drug development professionals, a precise understanding of this continuum is essential for rational engineering of delivery systems that can navigate the harsh environment of the gastrointestinal tract and ensure optimal biological activity.
Quantitative Distinctions: A Data-Driven Perspective
The practical impact of this distinction is quantifiable. Recent studies on encapsulated vitamins and polyphenols provide clear data on the differential performance between these two parameters, highlighting the significant attrition that can occur even after a compound is liberated.
Table 1: Comparative Bioaccessibility and Bioavailability of Encapsulated Bioactives
| Bioactive Compound | Delivery System | Bioaccessibility (%) | Bioavailability (%) | Key Finding | Citation |
|---|---|---|---|---|---|
| Vitamins (General) | Nano-delivery Systems | 75 - 88 | Varies (2-8 fold increase) | Nano systems significantly enhance cellular transport. | [2] |
| Vitamin D | Nano-delivery Systems | - | Up to 5-fold enhancement | Enhanced cellular transport was observed. | [2] |
| Polyphenols | Purified Polyphenolic Extract (IPE) | - | 3-11 times higher | IPE showed higher indices vs. Fruit Matrix Extract (FME). | [3] |
| Curcumin | Og/W and W1/Og/W2 Emulsions | - | ~20% | 2.5x greater than literature values for free curcumin. | [1] |
| Curcumin | Oleogel | - | 41.8% of bioaccessible fraction | High efficiency post-release, but low overall bioaccessibility. | [1] |
Table 2: Stability Enhancements via Encapsulation
| Compound | Encapsulation System | Stability Provided | Citation | |
|---|---|---|---|---|
| Vitamin C | Liposomes, Oleogels | > 80% | [2] | |
| Vitamin A | Emulsion-based Systems | > 70% | [2] | |
| Vitamin B12 | Spray-dried Microcapsules | - | Bioavailability enhanced up to 1.5-fold. | [2] |
The Scientist's Toolkit: Key Reagents for Bioaccessibility and Bioavailability Studies
The accurate assessment of these parameters relies on well-established in vitro simulated digestion models. These protocols require a specific set of reagents to mimic the biochemical conditions of the human gastrointestinal tract.
Table 3: Essential Reagents for Simulated Gastrointestinal Protocols
| Reagent / Material | Function in Experimental Protocol | Simulated Phase |
|---|---|---|
| α-amylase (from human saliva) | Catalyzes the breakdown of starch, initiating oral digestion. | Oral (2 min) |
| Pepsin (from porcine gastric mucosa) | Proteolytic enzyme that degrades proteins in the acidic stomach environment. | Gastric (30 min) |
| Pancreatin (from porcine pancreas) | A mixture of digestive enzymes (e.g., proteases, lipase, amylase) for intestinal digestion. | Intestinal (180 min) |
| Lipase (from porcine pancreas) | Specifically catalyzes the hydrolysis of fats (lipolysis). | Intestinal |
| Bile Salts | Biological surfactants that emulsify lipids, facilitating the formation of mixed micelles for absorption. | Intestinal |
| Simulated Gastric Fluid (SGF) | Low-pH solution (with HCl, NaCl, etc.) replicating the chemical environment of the stomach. | Gastric |
| Simulated Intestinal Fluid (SIF) | Neutral-pH solution (with NaHCO₃, KH₂PO₄, etc.) replicating the chemical environment of the intestine. | Intestinal |
| Dialysis Membranes or Filters | Used to separate the bioaccessible fraction (micellar phase) from the non-absorbable residue in static models. | Absorption Phase |
| Dynamic in vitro systems (e.g., SimuGIT) | Advanced equipment that dynamically adjusts pH, introduces secretions gradually, and mimics peristalsis and gastric emptying. | Full GIT Transit |
Experimental Protocols: Methodologies for Assessment
StaticIn VitroDigestion Protocol
A widely adopted method for assessing bioaccessibility is the static in vitro simulation, often based on the INFOGEST protocol. The following diagram outlines the core workflow.
Assessing Bioavailability Using Cell Models
To move beyond bioaccessibility and estimate true bioavailability, the bioaccessible fraction is often applied to intestinal cell models, such as Caco-2 monolayers, to simulate transport and metabolism.
Engineering Enhanced Delivery: From Concept to Application
The core challenge in formulation science is to design delivery systems that bridge the gap between high bioaccessibility and meaningful bioavailability. Advanced encapsulation technologies are at the forefront of this endeavor. For instance, lipid-based nanoemulsions can enhance the bioaccessibility of lipophilic vitamins by solubilizing them within mixed micelles during the intestinal phase [2]. Furthermore, protein-based carriers, such as whey or soybean protein isolates, provide a protective barrier against harsh pH changes and enzymatic degradation throughout the gastrointestinal tract, thereby stabilizing the bioactive until it reaches the site of absorption [2].
The choice of delivery system can be rationalized based on the target release profile. For example, a study on curcumin delivery systems found that while a W1/Og/W2 multiple emulsion was suitable for rapid delivery, a simpler Og/W single emulsion was more appropriate for longer-term release applications [1]. This demonstrates that the critical distinction between bioaccessibility and bioavailability is not just a scientific concept but a fundamental design principle for creating effective nutraceuticals and pharmaceuticals. By first ensuring efficient liberation (bioaccessibility) and then focusing on promoting absorption and transport (bioavailability), researchers can systematically engineer solutions that maximize the therapeutic potential of bioactive compounds.
The LADME framework is a fundamental pharmacokinetic model that systematically describes the journey of any bioactive compound through a biological system. This acronym represents the sequential processes of Liberation, Absorption, Distribution, Metabolism, and Excretion that collectively determine the ultimate bioavailability and efficacy of compounds ranging from pharmaceutical drugs to nutritional bioactives [4] [5]. While these processes are presented as a sequence, they are not discrete events; rather, they often occur simultaneously, particularly with modified-release formulations where liberation may continue while previously absorbed compound is being distributed, metabolized, and eliminated [4].
In the broader context of bioaccessibility versus bioavailability research, LADME provides a critical structural framework for differentiating these related concepts. Bioaccessibility refers specifically to the fraction of a compound that is released from its matrix in the gastrointestinal tract and becomes available for intestinal absorption, representing the initial L (Liberation) phase [5]. In contrast, bioavailability encompasses the entire LADME sequence, describing the rate and extent to which the bioactive component is absorbed from the gastrointestinal tract and becomes available at the site of action [5] [6]. This distinction is particularly crucial in nutritional sciences, where bioactive food components must first be released from the food matrix (bioaccessible) before they can undergo the subsequent ADME processes that determine their systemic bioavailability [5].
Detailed Breakdown of LADME Processes
Liberation: The Critical First Step
Liberation represents the initial release of a bioactive compound from its delivery form, whether a pharmaceutical formulation or food matrix [4]. For orally administered compounds, this process begins with disintegration and dissolution in the gastrointestinal fluids. The liberation phase is particularly critical for compounds with poor solubility or those encapsulated in protective delivery systems designed to enhance stability. The rate and extent of liberation directly influence subsequent processes, as only dissolved molecules can permeate biological membranes [4] [6].
Advanced delivery systems have been developed to precisely control the liberation process. For sensitive compounds like vitamins, encapsulation techniques using liposomes, oleogels, or emulsion-based systems can provide over 80% stability for vitamin C and over 70% stability for vitamin A during processing and storage [2]. These protective barriers are designed to withstand harsh environmental conditions and gradually release their payload under specific physiological conditions, demonstrating how liberation can be engineered to optimize overall bioavailability.
Absorption: Gateway to Systemic Circulation
Absorption encompasses the movement of the liberated compound from the site of administration into the systemic circulation [4]. For oral administration, this primarily occurs across the intestinal epithelium through various mechanisms including passive diffusion, carrier-mediated transport, and paracellular pathways. The efficiency of absorption depends on multiple factors including the compound's molecular size, lipophilicity, ionization state, and stability in the gastrointestinal environment [6].
The critical distinction between bioaccessibility and bioavailability becomes most apparent at the absorption stage. A compound may be fully bioaccessible (released from its matrix) yet poorly bioavailable if absorption barriers prevent its transit into systemic circulation [5]. This is particularly relevant for compounds that are substrates for efflux transporters or those that undergo extensive gut metabolism. Research on zinc absorption illustrates how nutritional factors influence this process, with phytates negatively affecting absorption while proteins, peptides, and amino acids enhance bioavailability through complex formation and utilization of alternative transport pathways [7].
Distribution: Tissue Penetration and Target Engagement
Following absorption, distribution describes the reversible transfer of a compound from systemic circulation to various tissues and organs [4]. The extent of distribution determines the compound's access to its target site of action and is influenced by physiological factors including blood flow, membrane permeability, tissue composition, and binding to plasma proteins and tissue components [4] [8].
Distribution patterns vary significantly between compounds and are quantified using parameters such as volume of distribution (Vd). The distribution phase is crucial for therapeutic efficacy, as the compound must reach its target site in sufficient concentrations to exert the desired pharmacological effect. For instance, zinc distribution following absorption demonstrates the dynamic nature of this process, with over 95% of zinc located intracellularly and the highest concentrations found in muscles, bones, skin, and liver [7].
Metabolism: Biochemical Transformation
Metabolism encompasses the chemical conversion or transformation of compounds into metabolites, typically facilitating easier elimination [4]. Hepatic enzymes, particularly cytochrome P450 systems, play a major role in drug metabolism, but extrahepatic metabolism in the gut wall, kidneys, and other tissues also contributes significantly. Metabolism can produce inactive metabolites, active metabolites with similar or different pharmacological profiles, or occasionally toxic metabolites [4] [8].
Metabolic processes can be influenced by numerous factors including genetic polymorphisms, environmental factors, and interactions with other compounds. The gut microbiota plays a particularly important role in the metabolism of certain nutritional bioactives, as illustrated by the conversion of soy isoflavones into equol, which varies between individuals based on their gut microbiome composition [5]. This interindividual variability in metabolism contributes significantly to differences in compound bioavailability and efficacy across populations.
Excretion: Elimination from the Body
Excretion represents the final elimination of the parent compound and its metabolites from the body, primarily through renal (urinary) and biliary (fecal) routes, with minor contributions from pulmonary, sweat, and other pathways [4]. The rate and route of excretion determine the compound's elimination half-life and significantly influence dosing regimens [8].
For many compounds, excretion is not merely a passive elimination process but involves active transport systems. Zinc homeostasis, for example, is maintained through a balance of absorption in the duodenum and proximal jejunum and excretion primarily in feces, with urinary excretion playing a minor role [7]. When dietary zinc intake is low, fecal and urinary excretion decreases while intestinal absorption increases, demonstrating the dynamic regulation of excretion processes to maintain physiological homeostasis [7].
Table 1: LADME Processes and Their Determining Factors
| LADME Process | Key Determinants | Primary Influencing Factors |
|---|---|---|
| Liberation | Formulation characteristics, solubility, dissolution rate | Food matrix, particle size, encapsulation, digestive fluids |
| Absorption | Membrane permeability, transport mechanisms, stability | Molecular size, lipophilicity, pH, transporters, gut microbiota |
| Distribution | Blood flow, tissue permeability, protein binding | Plasma protein levels, tissue composition, blood-brain barrier |
| Metabolism | Enzyme activity, metabolic pathways | Genetic polymorphisms, drug interactions, nutritional status |
| Excretion | Renal function, biliary secretion, transporter activity | Kidney function, liver function, urine pH, enterohepatic recycling |
Contemporary Research Applications of LADME
Pharmaceutical Drug Development
In pharmaceutical research, the LADME framework forms the cornerstone of drug discovery and development, with significant resources dedicated to optimizing these properties during lead compound selection [9] [10]. The high attrition rate in drug development, previously dominated by poor pharmacokinetic properties, has substantially decreased due to early screening of LADME parameters [9]. Modern approaches incorporate both in silico predictions and high-throughput in vitro assays to assess critical parameters including solubility, permeability, metabolic stability, and drug-drug interaction potential before compounds advance to costly clinical trials [9].
Quantitative Systems Pharmacology (QSP) represents an advanced application of LADME principles, integrating complex mathematical models that account for detailed physiology, environmental factors, and individual patient characteristics [11]. These models evolve from simple pharmacokinetic descriptions to comprehensive frameworks that capture drug liberation, absorption, disposition, metabolism, and excretion alongside pharmacodynamic responses, enabling more accurate predictions of human responses from preclinical data [11].
Nutritional Science and Bioactive Compounds
The LADME framework has been increasingly applied in nutritional sciences to understand the bioavailability of bioactive food components and micronutrients [2] [5] [6]. Research on vitamin encapsulation technologies demonstrates how strategic intervention at the liberation stage can enhance overall bioavailability. Nano-delivery systems for vitamin D have been shown to offer 75-88% bioaccessibility and enhance cellular transport up to five-fold, while spray-dried microcapsules can increase vitamin B12 bioavailability by up to 1.5-fold [2].
Similar approaches have been applied to mineral bioavailability, with research on zinc demonstrating how dietary factors significantly influence absorption [7]. Organic forms of zinc complexed with amino acids demonstrate superior bioavailability compared to inorganic salts, attributed to their ability to utilize amino acid transporters during absorption [7]. These findings highlight how understanding specific LADME processes enables the design of more bioavailable nutritional supplements.
Interindividual Variability and Personalized Approaches
Recent research has increasingly focused on understanding the factors underlying interindividual variability in LADME processes, moving toward personalized nutrition and medicine approaches [5]. Genetic polymorphisms, gut microbiota composition, age, sex, and physiological status all contribute to significant differences in how individuals process bioactive compounds [5]. The well-documented example of soy isoflavone metabolism illustrates this principle, where only certain individuals (equol producers) possess gut microbiota capable of converting daidzein to the more bioactive equol, resulting in enhanced health benefits [5].
This understanding of interindividual variability has led to the identification of responder and non-responder subpopulations for various bioactive compounds, explaining why significant health benefits may be observed only in subgroups within clinical trials [5]. These findings underscore the importance of considering individual LADME characteristics when evaluating compound efficacy and designing personalized intervention strategies.
Table 2: Quantified Bioavailability Enhancement Through Advanced Delivery Systems
| Bioactive Compound | Delivery System | Bioavailability Enhancement | Key Mechanisms |
|---|---|---|---|
| Vitamin C | Liposomes, Oleogels | >80% stability | Protection from degradation, controlled release |
| Vitamin A | Emulsion-based systems | >70% stability | Enhanced solubility, gastrointestinal protection |
| Vitamin D | Nano-delivery systems | 75-88% bioaccessibility, 5-fold cellular transport | Improved solubility, enhanced mucosal permeability |
| Vitamin B12 | Spray-dried microcapsules | 1.5-fold bioavailability | Protection from gastric degradation, enhanced absorption |
| Zinc | Amino acid complexes | Superior to inorganic salts | Utilization of amino acid transporters, reduced antagonism |
Experimental Methodologies for LADME Assessment
In Silico Prediction Methods
Computational approaches for predicting LADME properties have become indispensable tools in early research phases, enabling virtual screening of compound libraries before synthetic or testing efforts [9]. These in silico methods range from quantitative structure-activity relationship (QSAR) models that correlate molecular descriptors with specific pharmacokinetic parameters to more complex physiologically based pharmacokinetic (PBPK) models that integrate compound properties with physiological system data [9] [11]. The number of computational models for various LADME processes has considerably increased in recent years, providing valuable insights for lead compound optimization despite their inability to fully replace experimental verification [9].
These computational approaches are particularly valuable for predicting difficult-to-measure parameters such as tissue distribution and for extrapolating between species during preclinical development [11]. The continued refinement of these models, particularly through the integration of artificial intelligence and machine learning approaches, represents an active area of research with significant potential to accelerate compound development while reducing resource requirements [9].
In Vitro Assays and Models
In vitro methodologies provide controlled systems for evaluating specific LADME processes without the complexity and ethical considerations of whole organisms [6]. These include dissolution testing for liberation assessment, cell monolayer models (particularly Caco-2 cells) for absorption prediction, metabolic stability assays using liver microsomes or hepatocytes, and plasma protein binding studies for distribution estimation [9] [6].
The combination of sequential in vitro systems to simulate gastrointestinal passage has become particularly valuable for bioaccessibility assessment. As highlighted in zinc bioavailability research, methods combining dialysis with Caco-2 cell models provide robust correlation with human absorption data while enabling high-throughput screening [7]. Similarly, research on luteolin glucosides utilized digestive stability assessments combined with Caco-2 cell models to demonstrate how glycosylation type influences both bioaccessibility and intracellular antioxidant effects [12].
In Vivo Methodologies
Despite advances in alternative methods, in vivo studies remain essential for comprehensive LADME characterization, providing integrated data on all processes within a complete physiological system [7]. These studies typically involve administering the compound to animal models or human volunteers and collecting serial biological samples (blood, urine, tissues) to quantify the parent compound and metabolites over time [7] [8].
The sophisticated application of in vivo methodologies is illustrated by compartmental modeling approaches used to describe the kinetics of β-carotene and its conversion to retinol in healthy older adults [2]. Similarly, advanced techniques for measuring vitamin B12 bioavailability using [13C]-cyanocobalamin in humans provide precise quantification of absorption and distribution processes [2]. These in vivo data remain the gold standard for validating in silico predictions and in vitro models, particularly for regulatory submissions [8].
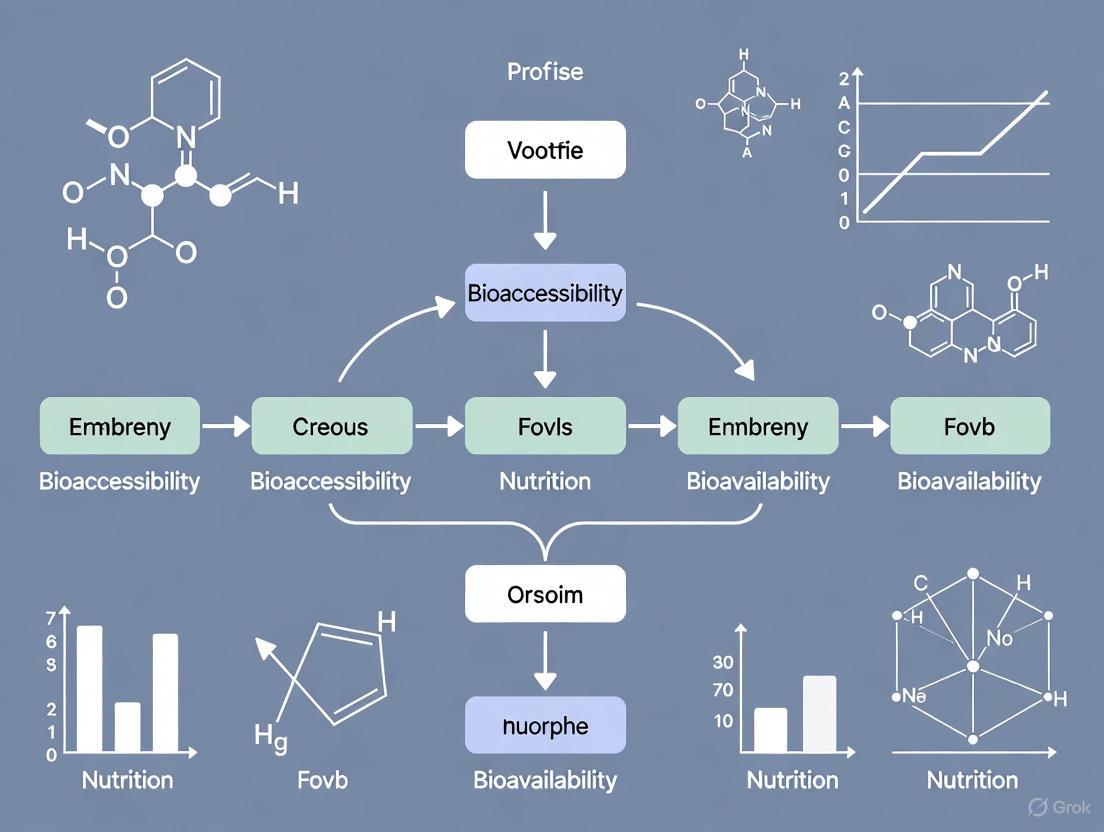
Diagram 1: The LADME Framework and Bioavailability Relationship. This workflow illustrates the sequential nature of LADME processes while highlighting how absorption, distribution, and metabolism directly influence overall bioavailability.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents for LADME and Bioavailability Studies
| Reagent/Material | Primary Application | Function in Research |
|---|---|---|
| Caco-2 cells | Absorption prediction | Human colorectal adenocarcinoma cell line that differentiates to form intestinal epithelium-like monolayers for permeability assessment |
| Liver microsomes | Metabolism studies | Subcellular fractions containing cytochrome P450 enzymes for metabolic stability and metabolite identification |
| Artificial digestive fluids | Bioaccessibility assessment | Simulated salivary, gastric, and intestinal fluids for in vitro digestion models to evaluate compound liberation |
| Dialysis membranes | Bioaccessibility measurement | Semi-permeable membranes with specific molecular weight cutoffs to separate bioaccessible fractions |
| LC-MS/MS systems | Compound quantification | High-performance liquid chromatography coupled with tandem mass spectrometry for sensitive detection and quantification of compounds and metabolites |
| Specific transporter substrates/inhibitors | Transport mechanism elucidation | Pharmacological tools to identify involvement of specific uptake or efflux transporters in absorption and distribution |
| Stable isotopically labeled compounds | Tracing studies | Compounds labeled with non-radioactive heavy isotopes for precise tracking of absorption, distribution, and elimination in complex biological matrices |
The LADME framework continues to provide an indispensable foundation for understanding and optimizing the bioavailability of bioactive compounds across pharmaceutical and nutritional domains. Its systematic approach enables researchers to identify specific rate-limiting steps in compound bioavailability and develop targeted strategies to overcome these barriers. The integration of advanced delivery systems, particularly nanoencapsulation technologies, demonstrates how strategic intervention at the liberation stage can dramatically enhance stability, bioaccessibility, and ultimate bioavailability of sensitive compounds [2].
Future applications of the LADME framework will increasingly focus on personalization approaches that account for interindividual variability in LADME processes due to genetic, microbiological, and physiological factors [5]. The continued refinement of integrated in silico, in vitro, and in vivo methodologies will enable more accurate predictions of human bioavailability while reducing development timelines and resource requirements [9] [11]. As these approaches mature, the LADME framework will remain central to the rational design and development of bioactive compounds with optimized bioavailability profiles tailored to specific population needs.
Diagram 2: Integrated Bioavailability Assessment Workflow. This methodology illustrates the complementary use of in silico, in vitro, and in vivo approaches to develop a comprehensive bioavailability profile, with PBPK modeling integrating data across all levels.
This whitepaper examines the distinct yet interconnected concepts of nutritional efficacy and pharmacological action through the critical lens of bioaccessibility and bioavailability. For researchers and drug development professionals, precise understanding of these terms is paramount, as they define fundamental processes from compound liberation to physiological effect. Despite their importance, inconsistent terminology persists in scientific literature, complicating cross-study comparisons and hampering development efforts. This paper provides standardized definitions, detailed experimental methodologies for in vitro and in vivo assessment, and visual workflows to clarify the pathways from ingestion to physiological impact. By framing these concepts within a rigorous technical context, we aim to establish a unified framework for evaluating compound efficacy across nutritional and pharmacological domains.
The efficacy of any ingested compound—whether a nutrient or an active pharmaceutical ingredient (API)—is governed by a series of sequential processes that determine its ultimate biological fate and physiological impact. Within this cascade, bioaccessibility and bioavailability represent critical, distinct phases. Bioaccessibility refers to the fraction of a compound that is released from its food or drug matrix and becomes soluble in the gastrointestinal tract, thereby available for intestinal absorption [13] [14]. It is primarily concerned with digestion-mediated release and solubilization. In contrast, bioavailability describes the proportion of an administered substance that reaches systemic circulation intact, from where it can be distributed to sites of action and exert its physiological effects [15] [14].
The distinction is crucial for both nutritional science and pharmacology. In nutrition, efficacy is often evaluated as the ability of a nutrient to perform its normal physiological functions, which is inherently dependent on its bioavailability. In pharmacology, therapeutic action is measured by the drug's capacity to bind to specific molecular targets at effective concentrations, which is a function of its pharmacokinetic profile, with bioavailability (F) being a fundamental parameter [15]. Understanding the relationship between these concepts is essential for developing effective nutraceuticals, functional foods, and pharmaceutical formulations.
Core Concepts and Terminological Framework
Standardized Definitions and Comparative Analysis
The following table provides standardized definitions for the core concepts governing compound efficacy, unifying terminology across nutritional and pharmacological contexts.
Table 1: Core Terminology in Bioaccessibility and Bioavailability
| Term | Technical Definition | Nutritional Context | Pharmacological Context |
|---|---|---|---|
| Bioaccessibility | The fraction of a compound released from its matrix into the gut lumen during digestion, making it potentially available for absorption [13] [14]. | Liberation of nutrients (e.g., Zn, Se) from food; measured via in vitro digestion models [7] [14]. | Dissolution and solubilization of an API from its dosage form in the GI tract. |
| Bioavailability | The proportion of an ingested compound that reaches systemic circulation and is available for tissue uptake and physiological action [15] [14]. | Fraction of ingested nutrient that is absorbed and utilized (e.g., for selenoprotein synthesis) [14]. | Fraction of administered drug dose (F) that reaches systemic circulation unchanged; key PK parameter [15]. |
| Absolute Bioavailability | The systemic availability of a compound after extravascular administration compared to intravenous administration [15]. | Rarely measured for nutrients, as intravenous reference is seldom used. | Standard pharmacokinetic measure (F) calculated as AUCev/AUCiv × Doseiv/Doseev [15]. |
| Relative Bioavailability | The bioavailability of a test formulation compared to a standard formulation administered via the same route [15]. | Used to compare different food formats or supplements (e.g., organic vs. inorganic Zn) [7]. | Used in bioequivalence studies to compare generic vs. innovator drug products. |
| Nutritional Efficacy | The demonstrated ability of a nutrient to perform its normal physiological roles (e.g., as cofactor, structural element) [7]. | Improvement in health status (e.g., Zn's role in immune function, endocrine health) [7]. | Not directly applicable. |
| Pharmacological Action | The specific biochemical interaction through which a drug substance produces its therapeutic effect [15]. | Not directly applicable. | Drug-receptor binding, enzyme inhibition, or other target modulation leading to a therapeutic outcome. |
The Sequential Pathway: From Liberation to Action
The journey from ingestion to effect follows a defined sequence. The following diagram illustrates this pathway, highlighting the distinct stages of bioaccessibility and bioavailability for both nutrients and drugs.
Methodologies for Assessment
In Vitro Experimental Protocols
In vitro models are indispensable for initial, high-throughput assessment of bioaccessibility, providing controlled, reproducible, and ethical alternatives to animal studies.
3.1.1 Standardized In Vitro Digestion Protocol This protocol simulates human gastrointestinal digestion to measure the bioaccessibility of compounds from food or oral dosage forms [13] [7] [14].
- Oral Phase: The sample is mixed with simulated salivary fluid (SSF) containing electrolytes and α-amylase. The pH is adjusted to 7.0, and the mixture is incubated for 2 minutes at 37°C with constant agitation.
- Gastric Phase: Simulated gastric fluid (SGF) containing pepsin is added. The pH is reduced to 3.0, and the mixture is incubated for 1-2 hours at 37°C.
- Intestinal Phase: The gastric chyme is mixed with simulated intestinal fluid (SIF) containing pancreatin and bile salts. The pH is raised to 7.0, and the mixture is incubated for 2 hours at 37°C.
- Bioaccessibility Analysis: The digested sample is centrifuged. The supernatant (bioaccessible fraction) is collected and filtered. The concentration of the target compound (e.g., nutrient, API) in this fraction is quantified via HPLC, MS, or ICP-MS. Bioaccessibility (%) is calculated as (Amount in supernatant / Total amount in sample) × 100.
3.1.2 Caco-2 Cell Absorption Model This model uses human colon adenocarcinoma cells (Caco-2) that spontaneously differentiate into enterocyte-like monolayers, providing a predictive tool for intestinal absorption and bioavailability [7] [14].
- Cell Culture: Caco-2 cells are cultured and seeded on porous Transwell filters. They are allowed to differentiate for 21-28 days to form a tight polarized monolayer. Transepithelial electrical resistance (TEER) is regularly monitored to confirm monolayer integrity.
- Sample Application: The bioaccessible fraction obtained from the in vitro digestion is applied to the apical (upper) compartment, simulating the intestinal lumen.
- Incubation and Sampling: The system is incubated at 37°C for a set period (e.g., 2-4 hours). Samples are taken from the basolateral (lower) compartment at timed intervals.
- Transport Analysis: The concentration of the compound that has traversed the monolayer into the basolateral compartment is quantified. Apparent permeability (Papp) is calculated, providing a measure of absorption potential.
In Vivo Experimental Protocols
In vivo studies in animals or humans provide the definitive assessment of absolute bioavailability and physiological efficacy.
3.2.1 Absolute Bioavailability Study Design (Pharmacology) This clinical trial design is the gold standard for determining a drug's absolute bioavailability (F) by using an intravenous (IV) reference [15].
- Study Population: Healthy volunteers or patients (n=12-24) are enrolled following ethical approval and informed consent.
- Study Design: A randomized, two-period, crossover design is typically used.
- Period 1: Administration of a single IV dose.
- Washout Period.
- Period 2: Administration of a single oral dose.
- Blood Sampling: Serial blood samples are collected over a period covering at least 5 elimination half-lives post-dose for both routes.
- Bioanalysis: Plasma/serum concentrations of the API are determined using a validated analytical method (e.g., LC-MS/MS).
- Pharmacokinetic Analysis: The Area Under the Curve (AUC) from zero to infinity (AUC0-∞) is calculated for both IV and oral administration. Absolute bioavailability (F) is determined as: F (%) = (AUCoral / AUCIV) × (DoseIV / Doseoral) × 100.
3.2.2 Post-Absorptive Efficacy Endpoints (Nutrition) For nutrients, bioavailability is often inferred through functional efficacy measures after oral administration, as an IV reference is typically unavailable [7] [14].
- Dosing and Sampling: Subjects consume a test meal or supplement containing the nutrient of interest. Blood samples are collected over time.
- Kinetic Analysis: The plasma concentration-time curve is analyzed for the nutrient or its functional biomarkers (e.g., specific selenoproteins for Se [14], activity of Zn-dependent enzymes [7]).
- Efficacy Outcome Measures: Longer-term studies measure changes in validated physiological or functional endpoints. For example:
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Reagents and Materials for Bioaccessibility and Bioavailability Research
| Reagent/Material | Function/Application | Example Use Cases |
|---|---|---|
| Simulated Gastrointestinal Fluids (SSF, SGF, SIF) | Provide a chemically defined environment mimicking the ionic composition and pH of human digestive secretions. | Standardized in vitro digestion models (INFOGEST protocol) [13]. |
| Digestive Enzymes (Pepsin, Pancreatin, α-Amylase) | Catalyze the breakdown of complex macronutrients (proteins, fats, carbohydrates) to liberate encapsulated compounds. | Simulating proteolysis in the stomach (pepsin) and small intestine (pancreatin) [13] [14]. |
| Bile Salts (e.g., Taurocholate) | Emulsify lipids and form micelles, facilitating the solubilization of hydrophobic compounds for absorption. | Critical for studying bioavailability of lipophilic drugs and nutrients (e.g., fat-soluble vitamins) [13]. |
| Caco-2 Cell Line | A well-established in vitro model of the human intestinal epithelium for predicting compound absorption and transport mechanisms. | Transport studies to determine apparent permeability (Papp) and identify active/passive transport pathways [7] [14]. |
| Transwell Permeable Supports | Porous filters that support the growth of polarized cell monolayers, allowing separate access to apical and basolateral compartments. | Essential for conducting Caco-2 cell transport assays [7]. |
| Analytical Standards | Highly pure reference compounds for accurate identification and quantification of analytes in complex biological matrices. | LC-MS/MS and HPLC quantification of drugs, nutrients, and their metabolites in plasma, urine, and digested samples [15] [14]. |
Signaling Pathways and Metabolic Interplay
The efficacy of bioactive compounds is often mediated through complex signaling pathways. Furthermore, the gut microbiota has emerged as a critical player in modulating bioavailability. The following diagram integrates the host's metabolic pathways with the emerging role of the gut microbiome in determining bioavailability and efficacy.
The precise distinction between bioaccessibility and bioavailability provides a foundational framework for evaluating compound efficacy across the nutritional and pharmacological spectra. While bioaccessibility is a prerequisite for absorption, it does not guarantee bioavailability, which is itself a necessary but insufficient condition for nutritional efficacy or pharmacological action. The experimental methodologies outlined—from standardized in vitro digestion and Caco-2 models to rigorous in vivo pharmacokinetic and functional studies—provide a robust toolkit for deconstructing this efficacy cascade. Future research must continue to integrate emerging factors, such as the role of the gut microbiome and host genetics, into these models. A consistent and nuanced application of this terminological and methodological framework is essential for advancing the development of more effective, targeted, and personalized interventions in both food and pharmaceutical sciences.
For any orally ingested compound—be it a drug or a bioactive food component—the journey from ingestion to systemic circulation is fraught with physiological challenges. Understanding this journey is critical for researchers and drug development professionals aiming to enhance the efficacy of their compounds. This process is formally captured by the concepts of bioaccessibility and bioavailability.
Bioaccessibility refers to the fraction of a compound that is released from its food or product matrix into the gastrointestinal lumen and thus becomes accessible for intestinal absorption [16] [17]. It is the first and prerequisite step, encompassing digestive transformations. In contrast, Bioavailability is a broader, more complex term. From a nutritional and pharmacological perspective, it describes the fraction of an ingested compound that reaches the systemic circulation and is utilized for physiological functions or delivered to the site of action [18] [19] [20]. Bioavailability therefore includes the processes of bioaccessibility, absorption, metabolism, tissue distribution, and bioactivity.
The path to bioavailability is systematically described by the LADME framework: Liberation, Absorption, Distribution, Metabolism, and Elimination [20]. This review will focus on the key physiological hurdles within the initial phases of this framework: digestive stability (liberation), absorption, and pre-systemic metabolism.
The Physiological Hurdle of Digestive Stability and Bioaccessibility
Before a compound can be absorbed, it must first be liberated from its product matrix and survive the harsh environment of the gastrointestinal (GI) tract. This stage, known as bioaccessibility, is the first major physiological hurdle.
The Digestive Process and Bioaccessibility
The process of bioaccessibility begins with mastication in the mouth and continues as the compound encounters various digestive fluids and enzymes throughout the stomach and intestines [20]. These digestive aids are crucial for breaking down the food or product matrix to release the compound. For lipid-soluble bioactive compounds and drugs, such as some vitamins, carotenoids, and polyunsaturated fatty acids (PUFAs), the sequential steps of lipid digestion—partial gastric hydrolysis, emulsification by bile, and further lipolysis by pancreatic lipases—are obligatory for their release into the GI lumen [20].
Factors Affecting Digestive Stability
Several factors determine whether a compound remains stable and is successfully released during digestion:
- Food Matrix Effect: The composition of the ingested matrix can have profound effects. Components like fat and protein can enhance the bioaccessibility of certain compounds. For instance, the bioavailability of isoflavonoids from foods containing fat and protein exceeds that from supplements consumed without food [20]. Similarly, fat in a salad dressing significantly improves the absorption of carotenoids from the salad [20].
- Impact of Processing: For plant-based compounds, processing can influence bioaccessibility by altering the plant cell wall structure. Ferulic acid in whole grain wheat, for example, has limited bioavailability due to its binding to polysaccharides. However, fermentation prior to baking can break these ester links, releasing the ferulic acid and improving its bioavailability [20].
- GI Tract Physiology: The caloric content and volume of the ingested material can cause physiological changes in the GI tract, such as altered pH, gastric emptying, and bile secretion, which in turn affect the release of the compound [20].
Table 1: Key Factors Influencing the Bioaccessibility of Oral Compounds
| Factor | Impact on Bioaccessibility | Example |
|---|---|---|
| Food Matrix | Can enhance or reduce release from the matrix. | Fat improves carotenoid and quercetin bioaccessibility [18] [20]. |
| Processing | Can break down physical barriers within the matrix. | Fermentation of wheat releases bound ferulic acid [20]. |
| GI Physiology | Alters the digestive environment (pH, enzymes, bile). | Caloric content affects bile secretion and emulsification [20]. |
| Compound Stability | Determines resilience to pH and enzymatic degradation. | Peptide drugs like insulin are degraded in the GI tract [21]. |
The Physiological Hurdle of Intestinal Absorption
Once a compound is bioaccessible, it must cross the intestinal epithelium to enter the systemic circulation or lymphatic system. The mechanisms of absorption and the factors influencing them constitute the second major hurdle.
Mechanisms of Absorption
Drugs and bioactive compounds cross the semipermeable cell membranes of the intestinal epithelium through several distinct mechanisms [19] [21]:
- Passive Diffusion: This is the most common mechanism for drug absorption. Molecules move from a region of high concentration (GI lumen) to one of low concentration (bloodstream) without energy expenditure. The rate is proportional to the concentration gradient and depends on the molecule's lipid solubility, size, and degree of ionization [19] [21]. The lipoid nature of the cell membrane means lipid-soluble (lipophilic) drugs diffuse most rapidly.
- Carrier-Mediated Membrane Transport:
- Active Transport: This process is selective, requires energy, and can transport compounds against a concentration gradient. It is typically limited to drugs structurally similar to endogenous substances (e.g., ions, sugars, amino acids) [19] [21].
- Facilitated Passive Diffusion: A carrier molecule assists the substrate across the membrane without energy expenditure. It is faster than passive diffusion for specific, low-lipid-solubility molecules but cannot transport against a concentration gradient [21].
- Pinocytosis: A process where the cell membrane engulfs fluid or particles, forming a vesicle that moves into the cell interior. It requires energy and plays a role in the transport of larger molecules, such as protein drugs [21].
The Critical Role of Solubility and Ionization
A compound must be in solution to be absorbed [21]. Its solubility and ionization state, governed by the pH of the GI environment and the compound's acid dissociation constant (pKa), are critical determinants of absorption.
Most drugs are weak acids or bases, existing in both un-ionized and ionized forms. The un-ionized form is typically lipid-soluble and diffuses readily across cell membranes, while the ionized form has low lipid solubility and high electrical resistance, preventing easy membrane penetration [19] [21]. The proportion of each form is determined by the Henderson-Hasselbalch equation:
- For a weak acid: When the environmental pH is lower than its pKa, the un-ionized form predominates.
- For a weak base: When the environmental pH is lower than its pKa, the ionized form predominates.
While theoretically a weak acidic drug (e.g., aspirin) would be best absorbed in the acidic stomach, and a weak basic drug in the more alkaline intestine, the reality is more nuanced. The small intestine is the primary site of absorption for most drugs due to its immense surface area, created by villi and microvilli, and highly permeable membranes [19] [21]. Therefore, the drug's ability to dissolve and remain in an absorbable form as it transits to the intestine is often the limiting factor.
Table 2: Key Patient-Specific and Drug-Specific Factors Affecting Absorption
| Category | Factor | Impact on Absorption |
|---|---|---|
| Patient-Specific (Physiological) | Age | Gastric pH, intestinal surface area, and blood flow can change with age, reducing absorption [19]. |
| Gastric Emptying & Intestinal Transit Time | Faster emptying speeds drug delivery to the intestine; transit time affects exposure to absorptive surfaces [19] [21]. | |
| Blood Flow | Reduced perfusion (e.g., in shock) lowers the concentration gradient and passive diffusion [21]. | |
| Disease Status | GI and systemic diseases (e.g., Crohn's, cystic fibrosis, diabetes) can alter GI tract anatomy and physiology [22]. | |
| GI Content (Food) | Can slow gastric emptying, bind to drugs, or enhance dissolution of poorly soluble drugs [19] [21]. | |
| Drug-Specific (Physicochemical) | Dissolution Rate | For solid forms, dissolution is the rate-limiting step before absorption can occur [19] [21]. |
| Particle Size & Surface Area | Smaller particle size increases surface area and dissolution rate [19]. | |
| Polymorphism | Different crystalline forms of the same drug can have different solubilities and bioavailability [19]. | |
| Dosage Form | Solutions are absorbed faster than solid dosage forms like tablets and capsules [19]. |
Diagram 1: The journey of an oral compound from ingestion to systemic circulation, highlighting key hurdles of digestive stability and absorption mechanisms.
The Physiological Hurdle of Metabolism
A compound that successfully navigates absorption then faces the third major hurdle: metabolism. This process can significantly reduce the amount of intact compound that reaches the systemic circulation.
First-Pass Metabolism
A pivotal challenge for orally administered compounds is first-pass metabolism (or pre-systemic metabolism) [19]. Before a drug or bioactive compound reaches the systemic circulation, it can be extensively metabolized in the gut wall and the liver. This phenomenon is a primary reason for the low oral bioavailability of many compounds.
- Gut Wall Metabolism: The enterocytes of the intestinal epithelium contain various metabolizing enzymes, most notably cytochrome P450 (CYP) enzymes, such as CYP3A4, which can metabolize compounds during the absorption process [20].
- Hepatic Metabolism: After absorption into the portal vein, the compound travels directly to the liver, where it is subjected to a battery of hepatic enzymes before it can enter the systemic circulation.
The Role of the Gut Microbiota
The human colon harbors a vast and diverse community of microorganisms that possess immense metabolic capability. The gut microbiota can metabolize compounds that are otherwise poorly absorbed in the upper GI tract [20]. For instance, many polyphenols are relatively poorly absorbed in the small intestine but are extensively metabolized by colonic bacteria into a range of metabolites that may be absorbed and contribute to the biological activity of the parent compound [20]. These microbial metabolites could be considered the missing link between the consumption of certain dietary compounds and their health effects.
The Scientist's Toolkit: Experimental Models and Reagents
To study and overcome these physiological hurdles, scientists employ a range of in vitro, in silico, and in vivo models. The choice of model is critical, as each offers a different balance of physiological relevance, throughput, cost, and ethical considerations [16].
In Vitro Digestion and Absorption Models
In vitro models are widely used to predict bioaccessibility and bioavailability, offering an ethical and high-throughput alternative to in vivo studies [16] [23].
- In Vitro Digestion Models: These simulate the physiological conditions of the human GI tract, including pH, digestive enzymes (e.g., pepsin, pancreatin), and bile salts, to study the release of compounds from their matrix (bioaccessibility) [16]. They can be static, semi-dynamic, or dynamic (computer-controlled to simulate peristalsis and secretion rates).
- Intestinal Absorption Models: To study the absorption phase, several cell-based models are used:
- Caco-2 Cell Model: This is a well-established model of the human intestinal epithelium. When cultured on permeable filters, these cells differentiate into a monolayer that exhibits microvilli and expresses brush-border enzymes and transporters, making it a standard for predicting passive and carrier-mediated intestinal drug absorption [23] [17].
- HT-29 Cell Lines: Other intestinal cell lines, such as HT-29, can be used to study specific aspects of intestinal function and immune response [23].
- Multi-Organs-on-a-Chip: Emerging microphysiological systems (MPS) can simulate the systemic distribution and interactions between different organs, such as the gut, liver, and kidney, on a microfluidic chip. This provides a more integrated view of the LADME process [16].
Table 3: Key Research Reagent Solutions for Studying Bioavailability Hurdles
| Research Tool | Function in Experiment | Key Reagents/Components |
|---|---|---|
| Static In Vitro Digestion Model | Simulates gastric and intestinal phases to assess bioaccessibility. | Pepsin (gastric phase), Pancreatin (intestinal phase), Bile salts, pH-adjusted buffers [16] [23]. |
| Caco-2 Intestinal Absorption Model | Models human intestinal epithelium for transepithelial transport studies. | Caco-2 cell line, DMEM culture medium, Transwell permeable supports, Transport buffer (e.g., HBSS) [23]. |
| CYP Enzyme Inhibition Assay | Evaluates potential for first-pass metabolism by key liver enzymes. | Human CYP enzymes (e.g., CYP3A4), CYP-specific substrates (e.g., Testosterone), NADPH regeneration system, LC-MS/MS for analysis. |
| P-glycoprotein (P-gp) Assay | Assesses if a compound is a substrate or inhibitor of this key efflux transporter. | Cell lines overexpressing P-gp (e.g., MDCK-MDR1), Reference substrates (e.g., Digoxin), Inhibitors (e.g., Verapamil) [19]. |
Diagram 2: A multi-stage experimental workflow for predicting bioavailability, integrating in vitro digestion, cellular absorption models, and advanced microphysiological systems.
The path to achieving effective oral delivery of drugs and bioactive compounds is governed by a series of defined yet interlinked physiological hurdles: digestive stability (bioaccessibility), intestinal absorption, and pre-systemic metabolism. A deep understanding of these processes—the LADME framework—is non-negotiable for rational drug and nutraceutical development.
The factors influencing these hurdles are multifaceted, stemming from both the physicochemical properties of the compound itself and the variable physiology of the patient. Overcoming these challenges requires a sophisticated toolkit. The continued refinement of in vitro models, particularly the development of more complex and physiologically relevant systems like multi-organs-on-a-chip, promises to enhance our predictive capabilities. By systematically investigating and addressing these key physiological hurdles, researchers can design better formulations, optimize dosing regimens, and ultimately develop safer and more effective therapeutic and functional food products.
Assessment Techniques: From In Vitro Models to Clinical Bioequivalence
Within nutritional sciences and drug development, understanding the journey of dietary compounds through the human body is paramount. Two critical concepts—bioaccessibility and bioavailability—form the foundation of this understanding, yet they represent distinct phases of nutrient release and absorption [24]. Bioaccessibility refers to the proportion of a compound that is released from its food matrix during digestion and becomes accessible for intestinal absorption. It is the fraction made available for potential uptake by the intestinal epithelium [24]. In contrast, bioavailability encompasses the complete pathway, referring to the proportion of an ingested compound that is absorbed, metabolized, reaches systemic circulation, and becomes available for physiological functions or storage in target tissues [24]. This distinction is crucial for researchers and drug development professionals when evaluating the efficacy of nutraceuticals, pharmaceuticals, and functional foods. The INFOGEST standardized static in vitro digestion model provides a robust, harmonized methodology to simulate the gastrointestinal processes that govern bioaccessibility, serving as a critical predictive tool before undertaking more complex and costly in vivo studies [25] [26].
The INFOGEST Protocol: A Standardized Framework
The INFOGEST protocol was developed through an international consensus by the COST Action INFOGEST network to address the critical lack of standardization in in vitro digestion methodologies [25] [26]. Prior to its introduction, research teams employed a wide range of non-physiological conditions, including varying pH levels, enzyme sources and activities, and digestion times, which impeded meaningful comparison of results across studies [26]. The INFOGEST framework provides a standardized, physiologically relevant static digestion method that simulates the successive phases of the upper gastrointestinal tract: oral, gastric, and intestinal [25]. This protocol is designed for use with standard laboratory equipment, making it highly accessible while ensuring reproducibility and comparability of data across the global scientific community [25] [27].
Detailed Methodological Workflow
The following diagram illustrates the sequential workflow of the INFOGEST static in vitro digestion protocol:
Phase-by-Phase Protocol Specifications
Oral Phase: Solid foods are typically minced to simulate chewing, then mixed with Simulated Salivary Fluid (SSF) containing electrolytes and α-amylase from human saliva (150 units per mL of SSF) at a 1:1 (v/w) ratio [26]. The mixture is incubated for 2 minutes at pH 7.0 and 37°C with constant agitation [25] [27]. For liquid samples or studies where starch digestion is irrelevant, this phase may be simplified or omitted [26].
Gastric Phase: The oral bolus is combined with Simulated Gastric Fluid (SGF) and porcine pepsin (2,000 U/mL of gastric contents) [26]. The pH is adjusted to 3.0 using HCl, and the mixture is incubated for 2 hours at 37°C with agitation [25] [27]. The recommended pH represents a mean fasting-state value, though some applications may adjust to pH 2.0 for an additional 30 minutes to model postprandial acidification [27].
Intestinal Phase: The gastric chyme is mixed with Simulated Intestinal Fluid (SIF) and porcine pancreatin (providing trypsin, chymotrypsin, amylase, and lipase activities) along with bile salts (10 mM final concentration) [28]. The pH is raised to 7.0, and the mixture is incubated for 2 hours at 37°C with agitation [25] [27]. Following digestion, the resulting chyme can be analyzed for nutrient hydrolysis products, bioaccessibility, or subjected to further absorption models.
Research Reagent Solutions Toolkit
The following table details the essential reagents and materials required for implementing the INFOGEST protocol, based on the standardized recommendations [25] [26] [28].
Table 1: Essential Research Reagents for INFOGEST Protocol Implementation
| Reagent/Equipment | Specifications & Sources | Physiological Function in Digestion |
|---|---|---|
| α-Amylase | Human salivary (e.g., Sigma A1031); 150 U/mL in SSF [26] | Initiates starch hydrolysis in the oral cavity |
| Pepsin | Porcine gastric mucosa (e.g., Sigma P7545); 2,000 U/mL in SGF [26] [28] | Primary proteolytic enzyme in the stomach, breaks down proteins |
| Pancreatin | Porcine pancreas (e.g., Sigma P7545); contains enzyme mix [28] | Provides key intestinal enzymes (proteases, amylase, lipase) for macronutrient digestion |
| Bile Salts | Porcine bile extract (e.g., Sigma B8631); 10 mM final concentration [28] | Emulsifies lipids, forming mixed micelles to solubilize hydrophobic compounds |
| Simulated Fluids | SSF, SGF, SIF with specific electrolyte compositions [25] [26] | Maintains physiologically relevant ionic strength and pH for optimal enzyme activity |
| Calcium Chloride (CaCl₂) | 0.3 M solution added incrementally [26] [28] | Cofactor for several digestive enzymes, including gastric lipase and pancreatic lipase |
Applications in Food and Nutritional Research
The INFOGEST model has been extensively applied to study the digestive fate of diverse foods and bioactive compounds, providing critical insights into bioaccessibility and informing product development.
Investigating Lipid Bioaccessibility
A prominent application of the INFOGEST protocol involves assessing the bioaccessibility of polyunsaturated fatty acids (PUFAs) from enriched oil supplements. A 2023 study investigated omega-3 (EPA and DHA), conjugated linoleic acid (CLA), and conjugated linolenic acid (CLNA) from various oil sources and soft-gel capsules [29]. The findings revealed several critical factors:
- Significant Lipid Degradation: The intestinal phase caused substantial degradation of the lipid fraction, with recovery indices for major bioactive PUFAs being remarkably low across all matrixes [29].
- Impact of Oxygen and Concentration: The presence of oxygen during digestion and higher initial PUFA concentrations were correlated with increased oxidation, reducing the recovery of these sensitive compounds [29].
- Variable Antioxidant Potential: The digestion process differentially affected the antioxidant potential of the oils, negatively impacting pomegranate oil, CLNA, and omega-3 capsules, while fish oil and CLA capsules showed improved antioxidant potential post-digestion [29].
Table 2: Bioaccessibility of Polyunsaturated Fatty Acids After INFOGEST Digestion [29]
| Oil Matrix | Major Bioactive PUFAs | Recovery Index (%) | Key Findings |
|---|---|---|---|
| Pomegranate Oil | Punicic Acid (CLNA) | ~2% | Strong degradation; negative impact on antioxidant potential |
| Fish Oil | EPA & DHA (Omega-3) | 11-13% | Highest recovery among tested oils; improved antioxidant potential |
| CLNA Capsules | Conjugated Linolenic Acid | ~17% | Highest recovery but suffered from oxidation |
| CLA Capsules | Conjugated Linoleic Acid | ~6% | Low recovery but improved antioxidant potential post-digestion |
| Omega-3 Capsules | EPA & DHA | ~3% | Very low recovery; negatively impacted antioxidant potential |
Broader Food Matrix Applications
Beyond lipids, the INFOGEST protocol has been validated across a wide spectrum of food matrices. A comprehensive review highlights its use for dairy, egg, meat, seafood, fruit, vegetable, cereal, and emulsified products [30]. The method is particularly valuable for studying the digestibility of next-generation plant-based foods, such as meat, seafood, dairy, and egg analogs, allowing researchers to optimize processing techniques that maximize nutrient release [30]. The protocol's standardized nature enables direct comparison between traditional and novel food products, providing crucial data for the food industry and regulatory bodies.
Technological Advancements and Automation
While the basic INFOGEST protocol is designed for manual execution with standard lab equipment, technological advancements are enhancing its reproducibility and throughput. Automated digestion systems, such as the BioXplorer 100, can be programmed to execute the INFOGEST protocol with minimal human intervention [28]. A comparative study digesting Ensure Plus Vanilla found no significant differences in protein or lipid hydrolysis between the manual tube method and the automated BioXplorer system [28]. This automation reduces human error and ensures superior control and monitoring of critical parameters like temperature and pH, thereby enhancing data robustness and reproducibility [28].
From Bioaccessibility to Bioavailability: Intestinal Absorption Models
The INFOGEST protocol concludes with the intestinal phase, providing data on bioaccessibility. To predict bioavailability, the digesta must be applied to intestinal absorption models. The most widely used cellular model employs human intestinal cell lines, particularly Caco-2 (human col adenocarcinoma) monolayers, often co-cultured with mucus-secreting cells like HT29-MTX [29] [24]. These cells spontaneously differentiate into enterocyte-like cells and form tight junctions, creating a model intestinal barrier for transport studies.
The diagram below illustrates the pathway from food consumption to systemic bioavailability, integrating in vitro digestion and absorption models:
In the fatty acid study, despite low bioaccessibility, researchers detected significant incorporation of bioactive PUFAs into Caco-2/HT29-MTX intestinal cells, highlighting that the fraction that does get absorbed may still exert local biological effects or influence cellular metabolism [29]. This underscores the importance of combining digestion models with intestinal absorption studies to gain a more complete picture of a compound's physiological potential.
The INFOGEST static in vitro digestion protocol represents a cornerstone methodological advancement for food scientists, nutrition researchers, and drug development professionals. By providing a standardized, physiologically relevant framework for simulating upper gastrointestinal digestion, it enables reliable and comparable assessment of the bioaccessibility of nutrients and bioactive compounds from diverse matrices. As research progresses, the integration of this harmonized digestion method with advanced intestinal absorption models and automated systems will continue to refine our predictive capacity for human bioavailability, ultimately guiding the development of more effective functional foods, nutraceuticals, and pharmaceutical formulations.
In nutritional sciences and drug development, understanding the journey of a compound from ingestion to physiological utilization is paramount. This journey is conceptualized through the terms bioaccessibility and bioavailability. Bioavailability is a broader concept defined as the proportion of an ingested nutrient or compound that is absorbed, becomes available for physiological functions, and is utilized by the body [31]. It encompasses the entire process of digestion, absorption, metabolism, and tissue distribution. In contrast, bioaccessibility is a subset of bioavailability. It refers specifically to the fraction of a compound that is released from its food or supplement matrix during digestion and becomes soluble in the gastrointestinal tract, thereby making it potentially available for absorption by the intestinal epithelium [31] [32] [33]. It is the "maximum or upper limit of bioavailability" [34], dependent solely on digestion and release from the food matrix, while excluding absorption, metabolism, and systemic distribution [33].
The measurement of bioaccessibility is a critical preliminary step in evaluating the efficacy of dietary supplements, functional foods, and pharmaceuticals. In vitro methods, primarily dialyzability and solubility assays, have been developed as efficient, cost-effective, and high-throughput screening tools to estimate this parameter before undertaking more complex and expensive in vivo studies [33]. This guide provides an in-depth technical examination of these two core assays, detailing their methodologies, applications, and relevance for researchers and drug development professionals.
Core In Vitro Methods for Assessing Bioaccessibility
The Principle of Solubility Assays
The solubility assay is a fundamental method for determining bioaccessibility. Its core principle is straightforward: a compound must be dissolved in the gastrointestinal fluids to be absorbable. The assay measures the fraction of a nutrient or compound that transitions into the soluble portion of the digestive chyme after the in vitro digestion process is complete [33].
Experimental Protocol for the Solubility Assay:
In Vitro Digestion: The sample first undergoes a simulated gastrointestinal digestion. This typically involves a two-step process:
- Gastric Phase: The sample is incubated with a simulated gastric fluid, usually containing pepsin (from porcine stomach) and adjusted to a low pH (e.g., pH 2.0 for adults, pH 4.0 for infants) to mimic stomach conditions [33].
- Intestinal Phase: The gastric digest is then neutralized to a pH between 5.5 and 7.0. A simulated intestinal fluid, containing pancreatin (a mixture of pancreatic enzymes such as trypsin and amylase) and bile salts, is added to mimic the environment of the small intestine [33].
Separation: Following the intestinal digestion, the entire digest is centrifuged at high speed (e.g., 10,000 × g) for a defined period. This separation yields a soluble supernatant and an insoluble precipitate [33].
Quantification: The nutrient or compound of interest is quantitatively analyzed in the supernatant. Analytical techniques such as Atomic Absorption Spectrophotometry (AAS), Inductively Coupled Plasma Mass Spectrometry (ICP-MS) for elements, or High-Performance Liquid Chromatography (HPLC) for organic compounds are commonly employed [33].
Calculation: The bioaccessibility is calculated as the percentage of the total compound present in the soluble supernatant.
% Bioaccessibility = (Amount in Supernatant / Total Amount in Test Sample) × 100[33].
The Principle of Dialyzability Assays
The dialyzability assay, introduced by Miller et al. in 1981 to estimate iron bioaccessibility, provides a more refined estimate [33]. It is based on equilibrium dialysis and aims to measure only the soluble compounds of low molecular weight that are capable of passing through a semi-permeable membrane, simulating passage across the intestinal mucosa [33].
Experimental Protocol for the Dialyzability Assay:
Gastric Digestion: The sample undergoes an initial gastric digestion phase with pepsin at low pH, similar to the solubility assay.
Dialysis Setup: Following gastric digestion, a dialysis tube or bag with a specific molecular weight cut-off (MWCO) is introduced into the mixture. This bag is filled with a buffer solution, such as NaHCO₃.
Intestinal Digestion and Dialysis: The system is incubated, allowing the bicarbonate buffer to slowly diffuse out of the bag and neutralize the gastric digest. Subsequently, a pancreatin/bile mixture is added to the solution outside the dialysis bag (the dialysate) to initiate the intestinal phase. During this incubation, low molecular weight, soluble compounds diffuse from the dialysate across the membrane into the buffer inside the bag.
Sample Collection: After incubation, the solution inside the dialysis bag is collected. This represents the fraction of the compound that is not only soluble but also of a size suitable for passive absorption.
Quantification and Calculation: The amount of the target compound in the dialysate (the bag's content) is quantified. The dialyzability is then calculated as:
% Dialyzability = (Amount in Dialysate / Total Amount in Test Sample) × 100[33].
An advanced variation of this method is the continuous-flow dialysis system, which uses a hollow-fibre system. This method offers a potential better estimate of in vivo bioavailability by continuously removing dialyzable components, preventing equilibrium and more closely mimicking the dynamic absorption process in the intestine [33].
The following diagram illustrates the workflow for both the solubility and dialyzability assays, highlighting their key differences:
Comparative Data and Applications
The application of solubility and dialyzability assays reveals significant variations in the bioaccessibility of different elements and compounds, heavily influenced by the food matrix and chemical speciation.
Table 1: Element Bioaccessibility in Different Matrices Measured via Solubility/Dialyzability Assays
| Element/Compound | Food Matrix | Assay Type | Bioaccessibility (%) | Key Findings & Reference |
|---|---|---|---|---|
| Selenium (Se) | Brazil Nut Flour | Not Specified | ~85% | High bioaccessibility attributed to organic speciation as selenomethionine. [35] |
| Barium (Ba) | Brazil Nut Flour | Not Specified | ~2% | Low bioaccessibility likely due to formation of insoluble salts like BaSO₄. [35] |
| Radium (Ra) | Brazil Nut Flour | Not Specified | ~2% | Very low bioaccessibility for radioactive elements. [35] |
| Iron (Fe) | Edible Herbs | BARGE (Solubility) | <30% (GI) | Bioaccessibility reduced from stomach (34-57%) to gastrointestinal phase. [36] |
| Zinc (Zn) | Edible Herbs | BARGE (Solubility) | <30% (GI) | Bioaccessibility reduced from stomach (28-80%) to gastrointestinal phase. [36] |
| Copper (Cu) | Edible Herbs | BARGE (Solubility) | 38-60% (GI) | More bioaccessible during gastrointestinal digestion than gastric. [36] |
| Magnesium (Mg) | Edible Herbs | BARGE (Solubility) | 79-95% (G), <30% (GI) | Highly soluble in gastric fluid, but precipitates in intestinal tract. [36] |
These assays are crucial for screening the impact of food matrices and processing. For instance, in vitro studies have shown that phytates negatively affect zinc absorption, while proteins, peptides, and amino acids increase its bioavailability [37] [7]. Similarly, the health benefits of polyphenols and carotenoids are not solely determined by their total content in food, but by their bioaccessible fraction, which can be significantly altered by processing techniques and interactions with other nutrients like lipids [32].
The Scientist's Toolkit: Essential Research Reagents
The following table details key reagents and materials required to perform standardized in vitro bioaccessibility assays, such as the unified BARGE method (UBM) or INFOGEST protocol.
Table 2: Key Reagent Solutions for In Vitro Bioaccessibility Assays
| Reagent / Material | Function / Physiological Role | Typical Composition / Example |
|---|---|---|
| Simulated Saliva Fluid | Mimics oral processing; initiates enzymatic (carbohydrate) digestion. | Contains electrolytes (KCl, KH₂PO₄, NaHCO₃, etc.), and often α-amylase. [34] [36] |
| Simulated Gastric Fluid | Mimics stomach environment; denatures proteins and initiates proteolysis. | Pepsin (from porcine stomach), HCl to adjust pH to 2.0 (adult) or 4.0 (infant). [33] [36] |
| Simulated Intestinal/Duodenal Fluid | Mimics small intestine environment; continues digestion of macronutrients. | Pancreatin (mixture of amylase, lipase, proteases), bile salts as emulsifiers, pH adjusted to 6.5-7.0. [33] [36] |
| Bile Salts | Emulsifies lipids, facilitating lipolysis and formation of mixed micelles for absorption of hydrophobic compounds. | Often porcine bile extract. [33] |
| Dialysis Tubing | For dialyzability assays; simulates the selective absorption barrier of the intestinal mucosa. | Semi-permeable membrane with a defined Molecular Weight Cut-Off (MWCO). [33] |
| Centrifuge | For solubility assays; separates the soluble (bioaccessible) fraction from the insoluble residue. | Capable of high-speed runs (e.g., 10,000 × g). [33] |
Advanced Models and Methodological Considerations
While solubility and dialyzability are foundational, more sophisticated models exist. The TNO Intestinal Model (TIM) is a dynamic, computer-controlled system that more accurately simulates physiological parameters like body temperature, peristalsis, gradual pH changes, and transit times [33]. It consists of multiple compartments representing the stomach, duodenum, jejunum, and ileum (TIM1), and can even include a colon simulation (TIM2) for fermentation studies [33].
To assess bioavailability (specifically, intestinal uptake and transport), the Caco-2 cell model is widely used. This human colon adenocarcinoma cell line differentiates into enterocyte-like cells when cultured on Transwell inserts, allowing researchers to measure the uptake of compounds from the apical side and their transport to the basolateral side, providing insight into absorption mechanisms [33] [38]. A co-culture of Caco-2 cells with mucus-producing HT29-MTX cells offers an even more physiologically relevant model by incorporating the protective intestinal mucus layer [33].
A critical methodological consideration is the need to protect these cell lines from the digestive enzymes used in the in vitro digestion prior to the absorption assay. This can be achieved by using a dialysis membrane placed over the cells, heat-inactivating the enzymes (which may denature other compounds), or utilizing the more physiologically relevant Caco-2/HT29-MTX co-culture where the mucus layer acts as a natural barrier [33].
The relationship between different models in the study of compound absorption is summarized below:
Dialyzability and solubility assays are indispensable tools in the scientist's arsenal for the initial assessment of bioaccessibility. They provide a critical, high-throughput link between the total content of a compound in a matrix and its potential for absorption. While these methods are powerful for screening and ranking, and for studying the effects of inhibitors, promoters, and processing, they represent a simplification of a complex in vivo reality. Therefore, data from these in vitro assays should be interpreted as an estimate of the maximum potential bioavailability. For a comprehensive understanding, these methods are best used as part of a tiered strategy, informing the design of more complex cell-based models and, ultimately, validating clinical trials to fully elucidate the bioavailability and health impacts of dietary bioactives, nutrients, and pharmaceutical compounds.
In the development of new drugs and functional foods, accurately predicting how a substance is absorbed by the human intestine is a critical challenge. Within this context, two distinct but related concepts—bioaccessibility and bioavailability—form the cornerstone of absorption research. Bioaccessibility refers to the fraction of a compound that is released from its food or dosage matrix and becomes soluble in the gastrointestinal tract, making it available for intestinal absorption. In contrast, bioavailability describes the proportion of the ingested substance that reaches the systemic circulation and is delivered to the site of action, thereby exerting a physiological effect. The difference between these two parameters is significant; a compound may be fully bioaccessible yet exhibit poor bioavailability due to extensive metabolism or active efflux during intestinal transit.
To bridge the gap between simple chemical tests and complex human studies, researchers have developed sophisticated in vitro models that simulate human intestinal absorption. Among these, the Caco-2 (human colorectal adenocarcinoma) cell line has emerged as the gold standard for predicting intestinal permeability. When cultured under specific conditions, these cells spontaneously differentiate to form a polarized monolayer that morphologically and functionally resembles the small intestinal epithelium, complete with tight junctions and brush border enzymes. This technical guide explores the pivotal role of Caco-2 cell cultures in simulating absorption, providing researchers with detailed methodologies, applications, and emerging advancements in the field.
The Caco-2 Model: Fundamentals and Validation
Biological and Functional Basis
The Caco-2 cell model is prized for its ability to mimic the human intestinal barrier without the ethical and practical complexities of human or animal studies. Upon reaching confluency, Caco-2 cells undergo a differentiation process over 14-21 days, developing critical characteristics of absorptive enterocytes:
- Formation of tight junctions that create a physiologically relevant barrier, allowing for the measurement of paracellular transport.
- Expression of a well-defined brush border with associated microvilli and digestive enzymes, such as alkaline phosphatase and sucrase-isomaltase [39].
- Presence of a comprehensive array of membrane transporters, including P-glycoprotein (P-gp), amino acid transporters, and others that mediate active and efflux transport processes [40] [41].
A key validation of the model's predictive power comes from a seminal study on iron bioavailability. The research demonstrated that ferritin formation in Caco-2 cells served as a reliable indicator of iron absorption. The model showed a strong correlation (R = 0.968, P < 0.001) with human absorption data for meals containing varying levels of ascorbic acid (an enhancer) and tannic acid (an inhibitor), establishing its ability to accurately predict the human response to dietary modifiers [42].
Addressing Limitations: Engineered and Enhanced Models
A recognized limitation of conventional Caco-2 cells is their low expression of cytochrome P450 (CYP) enzymes, particularly CYP3A4, which is the dominant drug-metabolizing enzyme in the human small intestine and accounts for approximately 80% of total intestinal CYP content [40]. This gap can lead to an overestimation of the bioavailability of compounds that are CYP3A4 substrates.
To address this, researchers have developed engineered cell lines. Using the piggyBac transposon system, scientists have successfully generated tetracycline-controllable CYP3A4-expressing Caco-2 cells (CYP3A4-Caco-2). These cells, when induced with doxycycline, exhibit CYP3A4 expression levels and metabolic activity (measured by metabolism of midazolam) comparable to or higher than those found in the adult human small intestine, without negatively impacting cell proliferation or barrier function [40]. This advanced model enables the simultaneous evaluation of a compound's absorption and first-pass metabolism, providing a more comprehensive prediction of its bioavailability.
Table 1: Key Characteristics of Standard and Engineered Caco-2 Models
| Feature | Standard Caco-2 Model | Engineered CYP3A4-Caco-2 Model |
|---|---|---|
| Differentiation Time | 14-21 days | 14-21 days |
| Barrier Integrity (TEER) | >300 Ω·cm² (often >1000 Ω·cm²) | Similar to standard, sufficient for monolayer formation |
| Key Transporters | P-gp, amino acid transporters, etc. | Retains transporter expression |
| CYP3A4 Expression | Very low or negligible | Tunable to in vivo levels or higher via doxycycline induction |
| Metabolic Capability | Lacks significant Phase I metabolism | Can metabolize CYP3A4 substrates (e.g., midazolam) |
| Primary Application | Predicting passive & transporter-mediated absorption | Simultaneous prediction of absorption and intestinal metabolism |
Experimental Protocols: Core Methodologies
Cell Culture and Monolayer Preparation
Protocol 1: Standard Monolayer Culture for Permeability Assays
- Culture Conditions: Maintain Caco-2 cells in high-glucose Dulbecco's Modified Eagle Medium (DMEM), supplemented with 10% fetal bovine serum (FBS), 1% non-essential amino acids (NEAA), and 1% penicillin-streptomycin in a humidified incubator at 37°C with 5% CO₂.
- Seeding for Assays: Seed cells onto collagen-coated polyester or polycarbonate membrane inserts (e.g., Transwell) at a density of 60,000-100,000 cells per cm².
- Differentiation and Maintenance: Culture the cells for 18-21 days, replacing the medium in both the apical (top) and basolateral (bottom) compartments every 48 hours. The monolayer is considered fully differentiated and ready for experiments when the transepithelial electrical resistance (TEER) stabilizes, typically reaching values above 300 Ω·cm², though higher values (e.g., >1000 Ω·cm²) are common and indicate robust barrier formation [40].
- Quality Control: Before each experiment, confirm monolayer integrity by measuring TEER and by performing a paracellular flux assay using a marker like Lucifer Yellow. An apparent permeability coefficient (Papp) for Lucifer Yellow of ≤ 1.0 × 10⁻⁶ cm/s indicates an intact monolayer suitable for absorption studies [40].
Permeability and Transport Assays
Protocol 2: Apparent Permeability (Papp) Assessment
- Dosing: Dissolve the test compound in an appropriate buffer (e.g., HBSS or PBS, pH 7.4). Add this solution to the donor compartment (typically apical for A→B transport). The receiver compartment (basolateral) contains blank buffer.
- Incubation: Place the plate in an incubator (37°C, 5% CO₂) on an orbital shaker (e.g., 50 rpm) to minimize the unstirred water layer effect.
- Sampling: At predetermined time points (e.g., 30, 60, 90, 120 minutes), sample an aliquot (e.g., 100-200 µL) from the receiver compartment and replace it with an equal volume of fresh pre-warmed buffer.
- Analysis: Quantify the concentration of the test compound in the samples using a validated analytical method such as HPLC or LC-MS/MS.
- Calculation: Calculate the Papp (cm/s) using the formula: Papp = (dQ/dt) / (A × C₀) where dQ/dt is the steady-state flux (mol/s), A is the surface area of the membrane (cm²), and C₀ is the initial concentration in the donor compartment (mol/mL).
Protocol 3: Assessing the Impact of Efflux Transporters To determine if a compound is a substrate for efflux transporters like P-glycoprotein (P-gp):
- Perform bidirectional transport assays: A→B (apical-to-basolateral) and B→A (basolateral-to-apical).
- Include a set of monolayers treated with a specific inhibitor (e.g., 10-20 µM verapamil or zosuquidar for P-gp) added to both compartments 30 minutes prior to and during the experiment.
- Calculate the Efflux Ratio (ER): ER = Papp (B→A) / Papp (A→B).
- An ER >> 1 (e.g., >2) that is significantly reduced in the presence of an inhibitor suggests active efflux.
In Vitro Bioaccessibility and Bioavailability Assessment
Caco-2 assays are often integrated into a more complex workflow that first simulates gastrointestinal digestion. This is particularly valuable in food and nutraceutical science.
Protocol 4: Coupled In Vitro Digestion/Caco-2 Model [42] [12]
- In Vitro Digestion: Subject the food or supplement to a simulated gastric and intestinal digestion using standardized protocols (e.g., INFOGEST). This step determines the bioaccessible fraction—the compound solubilized and available for absorption.
- Centrifugation: Centrifuge the intestinal digest to obtain a soluble fraction.
- Caco-2 Exposure: Apply this soluble fraction to the apical side of the Caco-2 monolayer. The fraction that is transported across the monolayer and detected in the basolateral compartment represents the bioavailable fraction.
- Cellular Uptake: Alternatively, lysing the cells and measuring the compound accumulated inside them can serve as an indicator of absorption, as demonstrated with ferritin formation for iron [42] or intracellular concentrations for antioxidants [12].
Applications in Drug Development and Food Science
Drug Discovery and Development
In pharmaceutical sciences, Caco-2 data are a critical component of the ADMET (Absorption, Distribution, Metabolism, Excretion, and Toxicity) profile for candidate drugs. The model is extensively used for:
- Rank-Ordering Compounds: Screening chemical series to select leads with optimal permeability characteristics.
- Mechanistic Studies: Investigating transport pathways (passive transcellular/paracellular, carrier-mediated) and identifying substrates of efflux transporters to anticipate drug-drug interactions [41].
- Formulation Optimization: Evaluating the impact of different formulations (e.g., nanoparticles, liposomes) on the absorption of poorly soluble drugs [2].
The permeability data generated is increasingly used to build in silico models, including Quantitative Structure-Activity Relationship (QSAR) models and sophisticated AI-powered Physiologically Based Pharmacokinetic (AI-PBPK) models. These models predict human intestinal absorption and pharmacokinetics directly from a compound's molecular structure, accelerating early-stage drug discovery [43] [44].
Food and Nutraceutical Research
The Caco-2 model is indispensable for evaluating the bioavailability of nutrients and bioactive food components, which is heavily influenced by the food matrix and processing.
- Mineral Bioavailability: The model accurately predicts the effects of enhancers (e.g., ascorbic acid for iron) and inhibitors (e.g., phytates for zinc and iron) on mineral absorption [42] [7].
- Vitamin and Phytochemical Bioavailability: Studies investigate how encapsulation in delivery systems (e.g., liposomes, emulsions, nanoparticles) can protect sensitive vitamins like C, D, and B12 from degradation during digestion and enhance their uptake by intestinal cells. For instance, nano-delivery systems can enhance the cellular transport of vitamin D up to five-fold [2]. Similarly, the model can reveal how the glycosylation type of flavonoids (e.g., alpha- vs. beta-glucosides of luteolin) affects their absorption and intracellular antioxidant activity [12].
Table 2: Key Reagent Solutions for Caco-2 Experiments
| Research Reagent / Material | Function and Role in Caco-2 Experiments |
|---|---|
| Transwell Inserts | Permeable supports that allow for the separation of apical and basolateral compartments, enabling the study of polarized transport. |
| Collagen (Type I) | A common extracellular matrix protein used to coat permeable inserts, improving cell attachment and monolayer formation. |
| Dulbecco's Modified Eagle Medium (DMEM) | The standard culture medium, typically supplemented with FBS, NEAA, and antibiotics to support cell growth and differentiation. |
| Hanks' Balanced Salt Solution (HBSS) | A physiological buffer used as the transport medium during permeability assays to maintain cell viability and ionic balance. |
| Lucifer Yellow | A fluorescent, membrane-impermeable paracellular marker used to validate the integrity of the monolayer before and after experiments. |
| Rhodamine 123 / Verapamil | A classic P-gp substrate (Rhodamine 123) and its inhibitor (Verapamil), used in combination to assess the activity of the efflux transporter P-gp. |
| Doxycycline | An inducer molecule used in engineered tet-on CYP3A4-Caco-2 cells to control the expression level of the CYP3A4 enzyme for metabolism studies [40]. |
Advanced Techniques and Future Directions
Co-culture and 3D Biomimetic Models
To more faithfully recapitulate the complex cellular environment of the human gut, researchers are developing advanced co-culture systems. A common approach involves culturing Caco-2 cells with mucus-producing HT29-MTX goblet cells. This results in a monolayer with a protective mucus layer, which is critical for studying host-microbe interactions and the absorption of compounds affected by mucoadhesion [39].
Furthermore, the field is moving beyond flat monolayers toward three-dimensional (3D) biomimetic cultures. By growing intestinal cells on specially engineered substrates that replicate the villus-crypt architecture, scientists can create in vitro tissues that more closely mirror the native intestinal structure. These 3D models promote faster and more robust cell differentiation and exhibit enhanced digestive functionality, such as higher production of brush border enzymes (e.g., sucrase and alkaline phosphatase) and natural antimicrobial peptides [39].
Integration with AI and Machine Learning
The combination of high-throughput Caco-2 screening data with artificial intelligence is revolutionizing predictive toxicology and pharmacokinetics. Message Passing Neural Networks (MPNNs) with contrastive learning are being trained on molecular structures and their corresponding Caco-2 permeability data to predict the absorption potential of novel compounds with high accuracy [43]. These models can identify critical molecular substructures that influence permeability, providing valuable insights for medicinal chemists during the molecule optimization process. Similarly, AI-PBPK models leverage this data to simulate a drug's concentration-time profile in humans, enabling more informed decision-making in early drug development [44].
The Caco-2 cell culture model remains an indispensable tool for simulating intestinal absorption, effectively bridging the gap between simple bioaccessibility measurements and costly human bioavailability studies. Its robustness, reproducibility, and physiological relevance have cemented its role in both regulatory science and industrial R&D. While the standard model provides excellent predictions of permeability and transporter effects, ongoing innovations—such as the engineering of metabolically competent cells and the development of complex 3D biomimetic co-cultures—continuously expand its predictive power. As these advanced models are integrated with cutting-edge computational approaches like AI and PBPK modeling, the ability to rapidly and accurately forecast the in vivo fate of molecules from their in vitro profile will only improve, streamlining the development of safer and more effective drugs and nutraceuticals.
Diagrams
Diagram 1: Caco-2 Permeability Assay Workflow
Diagram Title: Caco-2 Assay Steps
Diagram 2: CYP3A4-Expressing Caco-2 Cell Mechanism
Diagram Title: Engineered Cell Mechanism
Within pharmaceutical development, precisely defining the journey of a drug from administration to its site of action is crucial for evaluating product performance. Two key concepts, bioaccessibility and bioavailability, form the foundation of this understanding, yet they represent distinct stages in the process. Bioaccessibility refers to the fraction of a compound that is released from its dosage form and becomes dissolved in the gastrointestinal fluids, making it potentially available for absorption. In contrast, bioavailability is defined as the proportion of the administered drug that reaches the systemic circulation intact and is thus available to exert its therapeutic effect at the target site [32]. The gold standard for assessing bioavailability in humans is the in vivo bioequivalence (BE) study.
These studies are not merely academic exercises; they are a regulatory cornerstone. For generic immediate-release solid oral dosage forms, international harmonized guidelines from the International Council for Harmonisation (ICH), specifically the ICH M13A and the draft ICH M13B guidances, provide the framework for demonstrating bioequivalence [45] [46]. These studies ensure that a generic drug product delivers the same therapeutic performance as its innovator counterpart, thereby protecting patient safety and efficacy while promoting competition and access to medicines.
The Regulatory Framework for Bioequivalence
Global regulatory authorities have established clear pathways for demonstrating bioequivalence, with a strong trend toward international harmonization to streamline drug development.
ICH Harmonized Guidelines
The ICH M13A guideline, which supersedes regional guidances like the European Medicines Agency's (EMA) previous guideline, outlines the scientific and technical aspects of BE study design and data analysis for immediate-release (IR) solid oral dosage forms [45]. This harmonization reduces duplicative clinical studies and standardizes marketing application submissions on a global scale [46]. The subsequent draft guideline, ICH M13B, provides further criteria for waiving in vivo BE studies for additional strengths of a drug product when in vivo BE has already been demonstrated for at least one strength [46]. This is known as a biowaiver.
Key Regulatory Considerations
Regulatory guidelines specify rigorous requirements for BE studies. The foundational principle is that two products are considered bioequivalent if the 90% confidence intervals for the ratio of the population means of the test (T) and reference (R) products for key pharmacokinetic parameters fall entirely within the acceptance range of 80.00% to 125.00% [46]. The primary endpoints are typically the area under the plasma concentration-time curve (AUC), which reflects the extent of absorption, and the maximum plasma concentration (C~max~), which reflects the rate of absorption.
Table 1: Key Regulatory Guidelines for Bioequivalence (as of 2025)
| Guideline | Issuing Authority | Scope & Focus | Key Update/Feature |
|---|---|---|---|
| ICH M13A (Final) [45] | ICH (International) | BE for IR solid oral dosage forms; study design & data analysis. | Harmonized global standard for non-replicate study designs. |
| ICH M13B (Draft) [46] | ICH (International) | BE for additional strengths of IR forms; biowaiver criteria. | Allows waivers for in vivo studies for certain additional strengths. |
| Expedited Programs for Regenerative Medicine (Draft) [47] | FDA CBER | Cell/gene therapies for serious conditions. | Details use of expedited pathways (e.g., RMAT) and innovative trial designs. |
| Revised Clinical Trial Policies [47] | China NMPA | Streamlining clinical trial processes in China. | Allows adaptive designs and aims to shorten approval timelines by ~30%. |
Methodologies for In Vivo Bioequivalence Assessment
The design, conduct, and analysis of a BE study are meticulously controlled to ensure the results are reliable and meaningful.
Standard Study Design and Protocol
The most common design for a bioequivalence study is a single-dose, randomized, crossover design in healthy adult volunteers. In this design, each subject receives both the test and the reference product in separate dosing periods, with a washout period in between that is sufficiently long to eliminate any carry-over effect of the previous dose. The study protocol must rigorously define inclusion/exclusion criteria, the conditions of dosing (e.g., after an overnight fast), and the schedule for blood sample collection to accurately characterize the plasma concentration-time profile.
Key Pharmacokinetic Parameters and Statistical Analysis
Blood samples collected over time are analyzed to determine the drug's plasma concentration. From this data, the key pharmacokinetic parameters are calculated:
- AUC~0-t~: Area under the plasma concentration-time curve from zero to the last measurable time point.
- AUC~0-∞~: Area under the curve from zero to infinity, representing total drug exposure.
- C~max~: The maximum observed plasma concentration.
Statistical analysis is performed on the log-transformed values of AUC and C~max~. Analysis of variance (ANOVA) is used, and the 90% confidence interval for the geometric mean ratio (T/R) of these parameters must fall within the 80-125% range to conclude bioequivalence.
Table 2: Core Components of a Standard In Vivo Bioequivalence Study
| Component | Standard Approach | Purpose & Rationale |
|---|---|---|
| Study Design | Randomized, single-dose, two-period, two-sequence crossover. | Each subject acts as their own control, minimizing inter-subject variability. |
| Subjects | Healthy adult volunteers (typically n=18-36). | Homogeneous population reduces variability; ethics favor healthy subjects for generic BE. |
| Administration | Fasting or fed state, as specified, with 240 mL of water. | Standardizes conditions affecting gastrointestinal transit and dissolution. |
| Blood Sampling | Serial sampling pre-dose and at multiple time points post-dose. | Enables accurate characterization of the concentration-time profile for PK analysis. |
| Key PK Parameters | AUC~0-t~, AUC~0-∞~, C~max~. | Quantify the extent and rate of absorption into the systemic circulation. |
| Statistical Analysis | ANOVA on log-transformed data; 90% CI for T/R ratio. | Standard statistical method to demonstrate equivalence within defined bounds. |
Experimental Workflow Visualization
The following diagram illustrates the standard workflow for conducting an in vivo bioequivalence study, from protocol design through to regulatory submission.
The Scientist's Toolkit: Key Reagents and Materials
Conducting high-quality in vivo research and bioanalysis requires a suite of specialized materials and reagents to ensure data integrity and reproducibility.
Table 3: Essential Research Reagent Solutions for Bioequivalence Studies
| Reagent / Material | Primary Function | Application Context |
|---|---|---|
| Validated Bioanalytical Method | To accurately and precisely quantify drug concentrations in biological matrices (e.g., plasma). | Liquid Chromatography with Mass Spectrometry (LC-MS/MS) is the gold standard for PK sample analysis. |
| Stable-Labeled Internal Standards | To correct for variability in sample preparation and ionization efficiency during LC-MS/MS analysis. | Essential for achieving high-precision bioanalytical data for pharmacokinetic calculations. |
| Anticoagulants (e.g., K₂EDTA) | To prevent blood samples from clotting post-collection. | Used in blood collection tubes for plasma preparation prior to bioanalysis. |
| Standardized Blank Matrices | To create calibration standards and quality control samples for the bioanalytical assay. | Drug-free plasma from the same species as the study subjects (human) is used. |
| Stable, GMP-Manufactured Dosage Forms | To serve as the Test and Reference products for administration. | Ensures product quality and consistency are maintained throughout the clinical study. |
Interrelationship of Bioaccessibility, Bioavailability, and Bioequivalence
The pathway from oral drug administration to therapeutic action is a multi-stage process, and understanding the relationship between its components is critical. Bioaccessibility is a prerequisite for bioavailability; a drug must first be dissolved and accessible in the gut before it can be absorbed. However, high bioaccessibility does not guarantee high bioavailability, as factors at the absorption and metabolic stages can limit the amount of drug reaching the systemic circulation. In vivo bioequivalence studies serve as the ultimate functional test, measuring the net result of all these processes for two products.
The following diagram maps this logical sequence and the relationship between these core concepts.
Advanced Concepts and Future Directions
The field of bioequivalence assessment is evolving, with regulatory science adapting to new therapeutic modalities and leveraging efficiencies from data science.
Innovative Trial Designs for Small Populations: For rare diseases and advanced therapies like cell and gene products, regulators encourage novel trial designs. The FDA has issued draft guidance recommending flexible statistical approaches and surrogate endpoints to demonstrate effectiveness in small patient populations [47]. This is complemented by "umbrella" trial designs, which evaluate multiple targeted therapies for a single disease or related diseases under a single master protocol, increasing efficiency and enabling personalized medicine strategies [48].
Leveraging In Vivo Data Science: Best practices in data science are being applied to in vivo experimentation to maximize the value of generated data. This includes organizing data at the smallest experimental unit with rich metadata, using unique identifiers, and sharing data according to FAIR principles (Findable, Accessible, Interoperable, Reusable). Aggregating in vivo data from multiple studies can help identify unrecognized trends and improve statistical power [49].
The Role of Ex Vivo Models in Development: While in vivo human studies remain the gold standard for regulatory approval, ex vivo models like organ baths continue to provide critical functional data during drug discovery. These systems, which measure parameters like tissue contraction and relaxation, help validate drug efficacy and safety in a physiologically relevant context before proceeding to human trials, thereby helping to reduce attrition rates [50].
Overcoming Barriers: Strategies to Enhance Bioaccessibility and Bioavailability
In the realm of nutrition and pharmaceutical sciences, bioaccessibility and bioavailability represent two critical sequential phases in the journey of a dietary compound from ingestion to physiological utilization. Bioaccessibility refers to the fraction of a compound that is released from its food matrix during digestion and becomes available for intestinal absorption [32]. It specifically describes the proportion of a nutrient that is solubilized within the gastrointestinal tract and capable of crossing the intestinal lumen [14]. Bioavailability, however, encompasses the complete pathway, representing the proportion of an ingested nutrient that is absorbed, metabolized, and ultimately reaches systemic circulation for utilization in physiological functions or storage [32] [51].
This distinction is crucial for researchers and drug development professionals because a compound may be highly bioaccessible yet exhibit poor bioavailability due to extensive pre-systemic metabolism, poor cellular uptake, or rapid elimination [52]. The interplay between these concepts forms the foundation for understanding how dietary components and pharmaceutical compounds interact, and how these interactions can be modulated to enhance therapeutic outcomes.
Key Dietary Inhibitors of Bioavailability
Numerous dietary components can significantly reduce the bioavailability of bioactive compounds and pharmaceuticals through various mechanisms. The table below summarizes the most clinically significant inhibitors.
Table 1: Key Dietary Bioavailability Inhibitors
| Inhibitor Class | Specific Compounds/Factors | Primary Mechanisms | Affected Nutrients/Drugs |
|---|---|---|---|
| Antinutritional Factors | Phytic acid, oxalates, tannins, saponins [51] | Chelation of minerals, complex formation with proteins and starches, enzyme inhibition [51] | Iron, zinc, calcium, magnesium, proteins [51] [37] |
| Dietary Fiber | Total dietary fiber (TDF), especially insoluble varieties [51] | Physical entrapment, increased viscosity, reduced diffusion, binding minerals [51] | Minerals, polyphenols, various pharmaceuticals [51] |
| Polyphenols | Tannins, flavonols with catechol/pyrogallol groups [32] | Complexation with minerals, inhibition of digestive enzymes, interaction with drug transporters [32] | Iron, certain pharmaceuticals, proteins [32] |
| Competitive Minerals | Calcium, iron, copper [37] | Competition for shared transport systems (e.g., ZIP and DMT1 transporters) [37] | Zinc, iron, other divalent cations [37] |
| Food Processing Components | Thermal degradation products, Maillard reaction products [32] | Chemical modification, destruction of sensitive compounds, altered digestibility [32] | Heat-labile vitamins, phenolic compounds [32] |
The negative correlation between total phenolic content (TPC) and mineral bioavailability demonstrates this inhibitory relationship. In iron-biofortified lentils, higher TPC was directly correlated with reduced iron bioavailability as measured by Caco-2 cell ferritin formation [51]. Similarly, total dietary fiber (TDF) content showed a negative correlation with mineral bioavailability across multiple mineral species [51].
Dietary Enhancers and Bioavailability Promotion Strategies
Conversely, numerous dietary components and processing strategies can enhance bioavailability. These enhancers operate through diverse mechanisms including improved solubility, protection from degradation, and enhanced absorption.
Table 2: Key Dietary Bioavailability Enhancers
| Enhancer Category | Specific Strategies/Compounds | Primary Mechanisms | Affected Nutrients/Drugs |
|---|---|---|---|
| Processing Techniques | Fermentation, boiling, germination [51] | Reduction of antinutritional factors, breakdown of cell wall structures, release of bound compounds [51] | Minerals, polyphenols, bioactive compounds [51] |
| Macronutrient Carriers | Proteins, peptides, phospholipids, edible lipids [32] [37] | Solubilization of hydrophobic compounds, formation of mixed micelles, enhanced membrane permeability [32] | Lipophilic pharmaceuticals, carotenoids, fat-soluble vitamins [32] |
| Novel Delivery Systems | Nanoencapsulation, emulsions, liposomes, solid lipid nanoparticles [32] [53] | Protection from degradation, targeted release, improved cellular uptake, enhanced stability [32] [53] | Polyphenols, omega-3 fatty acids, sensitive bioactive compounds [53] |
| Specific Enhancer Compounds | Amino acids (especially cysteine and methionine), organic acids [37] | Chelation forming absorbable complexes, reducing precipitation, maintaining reduced state (Fe²⁺, Zn²⁺) [37] | Zinc, iron, other minerals [37] |
| Synergistic Food Matrices | Oil-added purees, lipid-rich meals [32] | Stimulation of bile secretion, enhanced micelle formation, increased solubilization [32] | Carotenoids, fat-soluble vitamins, lipophilic drugs [32] |
Fermentation has demonstrated particularly impressive enhancements, with fermented lentil flour showing significantly higher iron bioavailability (69.4%) compared to boiled lentil flour, as evidenced by increased Caco-2 cell ferritin formation [51]. Similarly, nanoencapsulation techniques significantly improve the bioavailability and therapeutic effectiveness of polyphenols by enhancing their stability and absorption [53].
Molecular Mechanisms of Mineral Interactions
The intestinal absorption of essential minerals involves complex transport systems that become points of competition and interaction.
The diagram illustrates the competitive relationships at major transport pathways. ZIP transporters serve as a key competition point for divalent cations like zinc, iron, and copper [37]. This competition explains why high doses of iron supplements can impair zinc absorption and vice versa. Simultaneously, amino acid transporters provide an enhancement pathway for mineral-amino acid complexes (such as ZnAA), which bypass the competitive ZIP transporter system [37].
Experimental Models for Assessing Bioaccessibility and Bioavailability
In Vitro Digestion Models
In vitro digestion simulations provide a controlled, reproducible system for initial bioaccessibility screening.
Protocol: Two-Phase In Vitro Digestion with Dialysis [54]
- Gastric Phase: Sample incubation with pepsin in HCl solution (pH 2.0-3.0) for 1-2 hours at 37°C with continuous agitation
- Intestinal Phase: Adjustment to pH 7.0-7.5 followed by addition of pancreatin and bile salts, incubation for 2-4 hours
- Bioaccessibility Assessment: Placement in dialysis tubing (12 kDa molecular weight cut-off) to separate absorbable fraction
- Sample Analysis: Application of HPLC-MS/MS or atomic absorption spectrometry to quantify compounds in dialysate
The bioaccessible fraction is calculated as: (Compound concentration in dialysate / Initial compound concentration in sample) × 100%
Cellular Absorption Models
The Caco-2 cell model, derived from human colon adenocarcinoma, spontaneously differentiates into enterocyte-like cells and expresses relevant transport proteins.
Protocol: Caco-2 Cell Bioavailability Assay [51]
- Cell Culture: Maintenance in DMEM with 10% fetal bovine serum, 1% antibiotic-antimycotic at 37°C, 5% CO₂
- Differentiation: Seeding in transwell inserts at density of 1×10⁵ cells/insert, culture for 14-21 days to form polarized monolayer
- TEER Measurement: Regular monitoring of transepithelial electrical resistance to verify monolayer integrity
- Dosing: Application of bioaccessible fraction from in vitro digestion to apical compartment
- Absorption Period: Incubation for 2-4 hours at 37°C
- Bioavailability Assessment: Measurement of ferritin formation (for iron) via ELISA or compound quantification in basolateral medium via HPLC-MS
Table 3: Research Reagent Solutions for Bioavailability Studies
| Research Reagent | Function/Application | Example Usage |
|---|---|---|
| Caco-2 Cell Line | Human intestinal absorption model [51] | Permeability studies, transporter activity, mineral bioavailability (via ferritin formation) [51] |
| Transwell Inserts | Permeable supports for cell culture | Creating polarized intestinal cell monolayers for transport studies [51] |
| TIM System | Computer-controlled gastrointestinal simulator [54] | Dynamic digestion modeling with peristalsis, pH regulation, enzyme addition [54] |
| Dialysis Tubing | Molecular weight-based separation | Simulating intestinal absorption barrier in bioaccessibility studies [54] |
| Specific ELISA Kits | Protein quantification | Measuring ferritin formation in Caco-2 cells as iron bioavailability indicator [51] |
Advanced Model Systems
Physiologically Based Pharmacokinetic (PBPK) Modeling integrates in vitro and in vivo data to predict absorption, distribution, metabolism, and excretion [55]. These computational tools are particularly valuable for predicting drug-drug and drug-nutrient interactions by simulating how inhibitors or inducers affect pharmacokinetics through interactions with enzymes (e.g., CYPs) and transporters (e.g., P-glycoprotein) [55].
The Gastro-Intestinal Model (TIM), a sophisticated computer-controlled system that simulates peristaltic movements, pH regulation, and digestive enzyme incorporation, represents one of the most advanced platforms for predicting bioaccessibility [54].
Impact of Gut Microbiota on Bioavailability
The gut microbiota represents a crucial factor in bioavailability that traditional models often overlook. Gut microbes compete with the host for certain nutrients, including selenium, but also enhance the bioavailability of other compounds through metabolic transformations [14].
The gut microbiota significantly modulates polyphenol bioavailability. Most dietary polyphenols are complex structures that require microbial transformation into absorbable metabolites [52]. Specific bacterial strains such as Lactiplantibacillus spp. and Bifidobacterium spp. increase in abundance with polyphenol consumption and contribute to this biotransformation [52]. Simultaneously, polyphenols positively modulate the gut microbiota composition, creating a reciprocal relationship that enhances the bioavailability and health effects of these compounds [52].
The interplay between dietary inhibitors and enhancers represents a critical frontier in nutritional science and drug development. Understanding these interactions requires a multifaceted approach that considers:
- The chemical speciation of compounds and their interaction with the food matrix
- The processing methods that alter bioaccessibility
- The host factors including transport systems and gut microbiota
- The compound interactions at absorption and metabolic sites
Future research directions should focus on:
- Developing standardized in vitro-in vivo correlation (IVIVC) models for more accurate bioavailability prediction
- Exploring personalized nutrition approaches based on individual differences in absorption and metabolism
- Advancing nano-delivery systems to overcome bioavailability barriers
- Investigating gut microbiota-mediated biotransformation of bioactive compounds
The strategic application of this knowledge enables researchers and pharmaceutical developers to optimize formulations, anticipate interactions, and maximize the therapeutic efficacy of both dietary bioactives and pharmaceutical compounds.
In nutritional sciences and drug development, understanding the journey of a nutrient or active compound from food ingestion to its final physiological utilization is paramount. This journey is critically governed by two distinct but sequential concepts: bioaccessibility and bioavailability.
- Bioaccessibility refers to the fraction of a nutrient that is released from the food matrix and becomes accessible for intestinal absorption. It encompasses the processes of digestion—the breakdown of food into releasable compounds—and their subsequent solubilization within the gastrointestinal chyme [56].
- Bioavailability, however, is a broader term. It describes the proportion of an ingested nutrient that is not only absorbed but also reaches the systemic circulation, is distributed to tissues and organs, and is ultimately utilized for normal physiological functions [7] [56].
The food matrix (FM), defined as the physical domain that contains and interacts with specific food constituents, is a critical factor influencing both these parameters [57]. It can be viewed as a physical domain that contains and/or interacts with specific constituents of a food, providing functionalities and behaviors which are different from those exhibited by the components in isolation or a free state [57]. The complex interactions within the food matrix can either inhibit or enhance the release, transformation, and absorption of bioactive compounds and drugs, making it a central consideration in the design of functional foods and nutraceuticals.
The Food Matrix: Classification and Components
Food matrices are structured systems that can be classified based on their physical and structural properties. The major types of matrices found in foods are summarized in the table below.
Table 1: Classification of Major Food Matrix Types
| Matrix Type | Key Characteristics | Common Examples |
|---|---|---|
| Liquid Matrices | Homogeneous fluids where nutrients are dissolved or suspended. | Fruit juices, milk, soups [56] |
| Emulsion Matrices | Dispersion of two immiscible liquids (e.g., oil and water), stabilized by emulsifiers. | Milk, mayonnaise, salad dressings [56] |
| Semi-Solid Matrices | Systems with intermediate rheological properties between solids and liquids. | Yogurt, purees, gels [56] |
| Cellular Matrices | Intact plant or animal tissue structures where nutrients are compartmentalized within cells. | Raw fruits, vegetables, muscle meat [56] |
| Polymer Network Matrices | Systems with interconnected biopolymer chains (proteins, polysaccharides) forming a 3D network. | Bread, cheese, protein gels [56] |
| Fibrous Matrices | Composed of aligned, elongated structural components. | Muscle meat, celery stalks [56] |
The composition of these matrices—namely proteins, carbohydrates, lipids, and minerals—directly determines the bioavailability of embedded nutrients. For instance, dietary fiber can bind to polyphenols and minerals, potentially reducing their bioaccessibility, while lipids are crucial for the absorption of fat-soluble vitamins [7] [56]. The physical structure of the matrix acts as a primary barrier; nutrients entrapped within intact cellular structures, like those in raw carrots, are far less accessible than those in processed or homogenized foods [56].
Impact of Processing on the Food Matrix and Nutrient Release
Food processing techniques deliberately alter the food matrix, with significant consequences for nutrient release. The following diagram illustrates the general workflow for analyzing these impacts.
Thermal Processing
Thermal treatments are among the most common processing methods, and their effects are dualistic.
- Positive Effects: Heat application can disrupt plant and animal cell walls, breaking down cellular compartments and dietary fiber, which enhances the release of bound nutrients. For example, the bioavailability of carotenoids, such as lycopene in tomatoes, is significantly higher in cooked and processed products compared to raw fruits because heat disrupts the chromoplast membranes in which they are stored [56].
- Negative Effects: Conversely, high temperatures degrade heat-labile nutrients. Water-soluble vitamins, particularly Vitamin C and B vitamins (thiamine, folate), are highly sensitive to heat and can be significantly degraded during processes like blanching, pasteurization, and canning [58] [59]. The extent of loss depends on time, temperature, and the presence of oxygen.
Non-Thermal and Mechanical Processing
Non-thermal methods and physical techniques can modify the food matrix with less damage to heat-sensitive compounds.
- High-Pressure Processing (HPP): This method inactivates microorganisms with minimal heat, thereby better preserving the content and activity of thermolabile vitamins and phytochemicals compared to thermal pasteurization [58].
- Mechanical Processing: Techniques such as cutting, homogenization, and milling physically break down the structural integrity of the food matrix. For instance, grinding whole grains into flour disrupts the fibrous bran, making embedded minerals more accessible, though it may also increase the rate of oxidation and nutrient degradation during storage [56].
- Encapsulation: This is a deliberate processing technique used to create a protective barrier around sensitive nutrients like vitamins. Systems such as liposomes, emulsions, and spray-dried microcapsules protect against environmental factors during storage and control the release of the core material during digestion. For example, liposomes and oleogels can provide over 80% stability for vitamin C, while emulsion-based systems allow more than 70% stability for vitamin A [2]. Spray-dried microcapsules can enhance the bioavailability of vitamin B12 up to 1.5-fold, and nano-delivery systems can enhance the cellular transport of vitamin D up to five-fold [2].
Table 2: Impact of Common Processing Methods on Nutrient Bioaccessibility
| Processing Method | Effect on Food Matrix | Impact on Nutrient | Typical Change in Bioaccessibility/Bioavailability |
|---|---|---|---|
| Blanching & Boiling | Cell wall softening, leaching of water-soluble compounds into cooking water. | Loss of water-soluble vitamins (B, C). | Reduction of water-soluble vitamins by 20-40% due to leaching [58]. |
| Steaming & Microwaving | Disruption of cellular structures with minimal water contact. | Better retention of water-soluble vitamins. | Higher retention of Vitamin C compared to boiling [58]. |
| Canning | Severe thermal treatment, leading to extensive cell wall breakdown. | Degradation of heat-labile vitamins. | Can lead to >50% loss of Vitamin C [58]. |
| Fermentation | Breakdown of macromolecules by microbial activity, formation of new compounds. | Synthesis of some B vitamins; increase in bioactive peptides. | Can improve mineral bioavailability by reducing phytate content [56]. |
| Milling & Refining | Removal of outer bran and germ layers of cereals. | Loss of dietary fiber, vitamins, and minerals. | Significantly reduces the content of B vitamins and iron unless fortified [58]. |
| High-Pressure Processing | Inactivation of microbes with minimal effect on covalent bonds. | Preservation of heat-sensitive vitamins and pigments. | Up to 95% retention of Vitamin C compared to 60-80% in thermal processing [58]. |
| Encapsulation | Creates a protective wall material around sensitive nutrients. | Protects vitamins from degradation during storage and digestion. | Can enhance vitamin bioavailability by 2- to 8-fold, depending on the formulation [2]. |
Impact of Storage Conditions on Nutrient Stability
After processing, storage conditions play a critical role in determining the shelf life and nutritional quality of food. The stability of nutrients during storage is influenced by environmental factors that drive chemical degradation and physical changes.
- Temperature: Elevated temperatures accelerate the rate of chemical reactions, including the degradation of vitamins. Frozen storage (−18°C and below) generally preserves nutrients effectively, though some loss can occur during frozen storage due to ice crystal formation and solute concentration [58] [60].
- Light: Exposure to light, especially ultraviolet light, is a major factor in the degradation of photolabile nutrients. Riboflavin (Vitamin B2) and Vitamin A are particularly susceptible. Using opaque or light-blocking packaging is a common strategy to mitigate these losses [59].
- Oxygen: The presence of oxygen leads to the oxidation of unsaturated fats, fat-soluble vitamins (A, D, E), and Vitamin C. This results in rancidity and loss of vitamin activity. Technologies like vacuum packaging, modified atmosphere packaging (flushing with nitrogen or carbon dioxide), and the addition of antioxidants are employed to control oxidative degradation [59].
The interaction of these factors is complex. For example, the stability of encapsulated vitamins is highly dependent on the wall material used, with proteins being promising carriers that protect against environmental factors and gastrointestinal digestion conditions [2].
Experimental Protocols for Assessing Bioaccessibility and Bioavailability
Robust experimental models are essential for quantifying the food matrix effect. The scientific community employs a combination of in vitro and in vivo methodologies.
In Vitro Digestion Models
In vitro simulations are widely used to predict bioaccessibility. They are reproducible, avoid ethical concerns, and allow for high-throughput screening.
Detailed Protocol: Standardized Static In Vitro Digestion Model
This protocol is adapted from methods commonly used in the studies cited and represents a general approach for simulating human gastrointestinal digestion [2] [56] [12].
- Sample Preparation: The food sample is homogenized to a consistent particle size. A precise mass is weighed for digestion.
- Oral Phase:
- Simulated Salivary Fluid (SSF) is prepared, containing electrolytes and alpha-amylase.
- The sample is mixed with SSF at a defined ratio (e.g., 1:1 w/v).
- The pH is adjusted to 7.0, and the mixture is incubated for 2 minutes at 37°C with constant agitation.
- Gastric Phase:
- Simulated Gastric Fluid (SGF) is prepared, containing electrolytes and pepsin.
- The oral bolus is combined with SGF.
- The pH is adjusted to 3.0 using HCl.
- The mixture is incubated for 2 hours at 37°C with constant agitation.
- Intestinal Phase:
- Simulated Intestinal Fluid (SIF) is prepared, containing electrolytes, pancreatin, and bile salts.
- The gastric chyme is mixed with SIF.
- The pH is adjusted to 7.0 using NaOH.
- The mixture is incubated for 2 hours at 37°C with constant agitation.
- Bioaccessible Fraction Collection:
- After intestinal digestion, the mixture is centrifuged (e.g., at 10,000 x g, 30 min, 4°C).
- The supernatant, representing the bioaccessible fraction where nutrients are solubilized and ready for absorption, is collected and filtered.
- The nutrient content in this fraction is quantified using analytical techniques like HPLC (High-Performance Liquid Chromatography) or MS (Mass Spectrometry) and compared to the original content in the undigested sample to calculate bioaccessibility [12].
Cellular Uptake Assays (e.g., Caco-2 Model)
To further assess intestinal absorption, the bioaccessible fraction from the in vitro digestion can be applied to human cell lines.
Detailed Protocol: Caco-2 Cell Absorption Assay
The Caco-2 cell line, derived from human colon adenocarcinoma, spontaneously differentiates into enterocyte-like cells and is a gold standard model for predicting intestinal permeability [7] [12].
- Cell Culture: Caco-2 cells are maintained in standard culture flasks with DMEM medium supplemented with fetal bovine serum (FBS), non-essential amino acids, and antibiotics at 37°C in a 5% CO₂ atmosphere.
- Seeding on Transwell Inserts: Cells are seeded onto porous polyester membrane inserts (e.g., 3.0 µm pore size) placed in multi-well plates. This creates an apical (top, representing gut lumen) and basolateral (bottom, representing blood side) compartment.
- Cell Differentiation: The culture medium is changed every 2-3 days for 21 days until the cells form a confluent, differentiated monolayer with well-developed tight junctions. Transepithelial Electrical Resistance (TEER) is regularly measured to confirm monolayer integrity.
- Treatment with Bioaccessible Fraction: The culture medium is removed. The bioaccessible fraction (from Step 5.1), diluted in a suitable buffer, is added to the apical compartment. Fresh buffer is added to the basolateral compartment.
- Incubation and Sampling: The plate is incubated for a set period (e.g., 2-4 hours) at 37°C. Samples are collected from the basolateral compartment at specific time points.
- Analysis: The transported nutrient or compound in the basolateral samples is quantified (e.g., via HPLC-MS). The apparent permeability coefficient (Papp) is calculated to quantify the absorption rate. Intracellular concentrations can also be measured to assess uptake and metabolism, as demonstrated in studies on luteolin glucosides [12].
In Vivo Studies
In vivo studies in animals or humans provide the most direct measure of bioavailability, as they account for the full complexity of absorption, metabolism, distribution, and excretion.
Key Methodologies:
- Plasma Kinetics: Blood samples are collected at multiple time points after ingestion of the test food. The concentration-time curve (AUC - Area Under the Curve) of the nutrient or its metabolites in plasma or serum is measured, providing a direct measure of bioavailability [2].
- Stable Isotope Tracers: The test nutrient is labeled with a non-radioactive stable isotope (e.g., ^13C). The appearance and kinetics of this tracer in blood, urine, or feces are monitored using mass spectrometry. This method, used in studies of vitamins like B12 and β-carotene, allows for precise tracking of the specific ingested dose without interference from body pools [2].
- Ileostomy Studies: In volunteers with an ileostomy, the ileal effluent (digesta that has passed through the small intestine) can be collected and analyzed. This allows for direct measurement of the amount of a nutrient that was not absorbed, providing highly accurate data on absorption/bioavailability in the small intestine.
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Reagents and Materials for Food Matrix and Bioavailability Research
| Research Tool / Reagent | Function and Application in Research |
|---|---|
| Simulated Digestive Fluids (SSF, SGF, SIF) | Standardized solutions of electrolytes and enzymes (e.g., pepsin, pancreatin, bile salts) used to replicate the biochemical environment of the human GI tract in in vitro models [2] [56]. |
| Caco-2 Cell Line | A human colon adenocarcinoma cell line that differentiates into enterocyte-like cells. It is a critical model for studying intestinal transport, absorption kinetics, and drug/nutrient interactions [7] [12]. |
| Transwell Inserts | Permeable supports with a polyester membrane used for culturing Caco-2 cells as a polarized monolayer. Essential for measuring transepithelial transport and permeability [12]. |
| HPLC-MS Systems | High-Performance Liquid Chromatography coupled with Mass Spectrometry. The gold standard for the separation, identification, and precise quantification of specific nutrients, metabolites, and bioactive compounds in complex mixtures like food digesta and biological fluids [12]. |
| Stable Isotope Tracers | Non-radioactive isotopes (e.g., ^13C, ^2H) used to label nutrients. They allow for the precise tracking of the fate of the ingested dose in in vivo studies, distinguishing it from endogenous body pools [2]. |
| Encapsulation Materials | Wall materials such as whey protein isolates, maltodextrin, chitosan, Arabic gum, and lipids used to fabricate delivery systems (liposomes, emulsions) for studying and enhancing nutrient stability and bioavailability [2]. |
| DPPH Radical | (2,2-Diphenyl-1-picrylhydrazyl) A stable free radical used in spectrophotometric assays to measure the in vitro antioxidant capacity of food digesta and extracts [60] [12]. |
The food matrix is an integral and dynamic component that dictates the ultimate nutritional value of food. Its interaction with processing and storage conditions creates a complex interplay that either enhances or diminishes the bioaccessibility and bioavailability of nutrients. A deep understanding of these relationships, powered by robust experimental protocols and advanced analytical tools, is fundamental for researchers and drug development professionals. This knowledge is crucial for designing next-generation functional foods, optimizing dietary recommendations, and developing effective nutraceuticals where controlled release and predictable bioavailability are key to efficacy.
Advanced formulation technologies are revolutionizing therapeutic delivery by addressing the critical challenge of ensuring that active compounds not only reach the systemic circulation but also exert their intended biological effects. This whitepaper provides an in-depth technical analysis of nanoencapsulation and lipid-based drug delivery systems, framed within the essential context of bioaccessibility and bioavailability. For researchers and drug development professionals, the document details the mechanisms by which these advanced systems enhance drug solubility, protect payloads from degradation, and facilitate targeted delivery. It further presents standardized experimental protocols for evaluating performance, visualizes key cellular pathways and workflows, and catalogues essential research reagents. The insights herein aim to guide the rational design of next-generation formulations that maximize therapeutic potential by systematically overcoming biological barriers.
The efficacy of any bioactive compound, whether a small-molecule drug or a dietary nutrient, is fundamentally governed by its journey through the body. Two parameters are pivotal in this journey: bioaccessibility and bioavailability. Precise understanding of their definitions and differences is critical for rational formulation design [32].
- Bioaccessibility refers to the proportion of an ingested compound that is released from its food or formulation matrix and becomes soluble and accessible for intestinal absorption during digestion. It encompasses the processes of release and dissolution in the gastrointestinal tract [32].
- Bioavailability, in contrast, is a broader term describing the fraction of the administered compound that reaches the systemic circulation intact and is thereby available for delivery to the tissues and organs where it can exert its biological activity. This process includes absorption, metabolism, distribution, and eventual utilization [32].
The relationship is sequential: a compound must first be bioaccessible before it can become bioavailable. Many promising therapeutic agents have low water solubility and are vulnerable to degradation by enzymes, acids, and other conditions in the gastrointestinal tract, leading to exceedingly low bioaccessibility and, consequently, poor bioavailability [32]. Advanced formulation technologies, specifically nanoencapsulation and lipid-based systems, are engineered to intervene at these critical stages, protecting the payload and enhancing its release and absorption profile.
Nanoencapsulation Technologies
Nanoencapsulation involves entrapping active ingredients within nanocarriers (NCs), typically ranging from 1 to 1000 nanometers. This technology offers unparalleled control over the release, distribution, and stability of therapeutic agents [61] [62].
Types of Nanocarriers and Their Synthesis
Table 1: Classification and Synthesis Methods of Prominent Nanocarriers
| Nanocarrier Type | Composition | Key Synthesis Methods | Drug Loading Mechanism |
|---|---|---|---|
| Liposomes | Phospholipid bilayers forming spherical vesicles [61]. | Polycarbonate membrane extrusion; High-pressure homogenization; Reversed-phase evaporation; Sonication [61]. | Passive (hydration of lipid film with drug); Active (pH gradient across pre-formed liposomes) [61]. |
| Polymeric Nanoparticles | Biodegradable polymers (e.g., PLGA, PLA) [62]. | Nano-precipitation; Emulsion-solvent evaporation; Microfluidics [62]. | Encapsulation within the polymer matrix or adsorption onto the surface. |
| Solid Lipid Nanoparticles (SLNs) | Solid lipids at room and body temperature [63]. | High-pressure homogenization; Microemulsion templating [63]. | Incorporation into the solid lipid matrix. |
| Nanostructured Lipid Carriers (NLCs) | Blended solid and liquid lipids [63]. | High-pressure homogenization [63]. | Accommodation in the imperfections of the hybrid lipid matrix. |
| Dendrimers | Highly branched, tree-like polymeric structures [61]. | Divergent or convergent synthesis [61]. | Covalent conjugation to surface groups or physical encapsulation in interior voids. |
Mechanisms for Enhancing Bioaccessibility and Bioavailability
Nanoencapsulation improves the biological fate of drugs through several concurrent mechanisms [61] [62] [64]:
- Protection from Degradation: The nanocarrier acts as a physical barrier, shielding encapsulated drugs from enzymatic degradation and harsh pH conditions in the gastrointestinal tract [61].
- Enhanced Solubility and Dissolution: By presenting the drug in a nano-sized or pre-dissolved state, NCs dramatically increase the surface area for dissolution, overcoming limitations of low water solubility [64].
- Prolonged Circulation and Targeted Delivery: Surface modification with hydrophilic polymers like polyethylene glycol (PEG) creates a "stealth" effect, reducing recognition and clearance by the mononuclear phagocyte system (MPS) and prolonging systemic circulation [61]. Furthermore, ligands (e.g., antibodies, peptides) can be grafted onto the NC surface for active targeting to specific cells or tissues [61].
- Facilitated Cellular Uptake: Nanoscale particles are more readily internalized by cells via endocytic pathways, promoting drug absorption across intestinal epithelia [64].
The following diagram illustrates the primary mechanisms of nano-drug delivery and cellular uptake.
Lipid-Based Drug Delivery Systems
Lipid-based drug delivery systems (LBDDS) leverage the biocompatibility and solubilizing properties of lipids to enhance the oral bioavailability of poorly water-soluble drugs. They are classified by their composition and behavior upon dispersion [65] [66].
Lipid Formulation Classification System (LFCS)
The Lipid Formulation Classification System (LFCS) is a critical framework for formulators, categorizing systems based on their composition and potential performance in vivo [65].
Table 2: The Lipid Formulation Classification System (LFCS)
| Formulation Type | Composition | Characteristics on Dispersion | Advantages | Disadvantages |
|---|---|---|---|---|
| Type I | Oils without surfactants (e.g., tri-, di-, monoglycerides) [65]. | Non-dispersing; requires digestion [65]. | GRAS status; simple; excellent capsule compatibility [65]. | Poor solvent capacity unless drug is highly lipophilic [65]. |
| Type II | Oils and water-insoluble surfactants [65]. | Forms SEDDS without water-soluble components; turbid o/w dispersion (0.25–2 μm) [65]. | Unlikely to lose solvent capacity on dispersion [65]. | Turbid dispersion; may require digestion for optimal absorption [66]. |
| Type III | Oils, surfactants, and cosolvents (water-insoluble and soluble) [65]. | Forms SEDDS/SMEDDS; clear or almost clear dispersion [65]. | Drug absorption may occur without digestion [65]. | Potential loss of solvent capacity on dispersion [65]. |
| Type IV | Water-soluble surfactants and cosolvents [65]. | Disperses to form a micellar solution [65]. | Good solvent capacity for many drugs [65]. | High risk of drug precipitation on dispersion; not digestible [65]. |
SEDDS: Self-Emulsifying Drug Delivery Systems; SMEDDS: Self-Microemulsifying Drug Delivery Systems; GRAS: Generally Recognized As Safe
Mechanisms of Enhanced Absorption
LBDDS enhance bioavailability through several interconnected mechanisms [65] [66]:
- Maintenance of Solubilization: By delivering the drug in a pre-dissolved state and promoting the formation of fine colloidal droplets (e.g., microemulsions), LBDDS maintain the drug in a solubilized state throughout the gastrointestinal tract, which is a prerequisite for absorption [66].
- Stimulation of Intestinal Lymphatic Transport: Dietary lipids and some lipidic formulations promote the assembly and secretion of chylomicrons, which can shuttle highly lipophilic drugs directly into the lymphatic system, bypassing first-pass metabolism [65].
- Alteration of Intestinal Permeability: Certain lipidic excipients can transiently and reversibly alter the permeability of the intestinal mucosa, enhancing the absorption of drugs that would otherwise have poor permeability [65].
- Supersaturation: Supersaturated lipid-based formulations (e.g., supersaturated SEDDS) create a metastable, high-energy state of the drug in the gut, generating a large driving force for absorption. The inclusion of precipitation inhibitors (e.g., HPMC, PVP) is often critical to sustain this state long enough for absorption to occur [66].
Experimental Protocols for Assessing Bioaccessibility and Bioavailability
Robust in vitro and in vivo models are essential for predicting the performance of advanced formulations.
In Vitro Bioaccessibility Assessment Using Simulated Gastrointestinal Digestion
This protocol is adapted from methods used to evaluate dietary bioactives and lipids [32] [37].
Objective: To determine the fraction of a drug that is released from its formulation and solubilized in the simulated intestinal fluid, making it accessible for absorption.
Materials:
- Simulated Gastric Fluid (SGF)
- Simulated Intestinal Fluid (SIF)
- Pancreatin extract (source of digestive enzymes)
- Bile salts
- pH-stat titrator or pH meter
- Water bath with shaking, maintained at 37°C
- Centrifuge and ultracentrifugation/filtration units (e.g., 50 kDa molecular weight cut-off)
Procedure:
- Gastric Phase: The formulation (containing a known dose of drug) is introduced into SGF. The pH is adjusted, and pepsin may be added. The mixture is incubated for a defined period (e.g., 1 hour) at 37°C with continuous agitation.
- Intestinal Phase: The gastric chyme is mixed with SIF. The pH is adjusted, and pancreatin and bile salts are added to simulate the fed or fasted state. This mixture is incubated for a further 2 hours at 37°C.
- Sampling and Separation: At the end of the intestinal phase, an aliquot of the digest is centrifuged at high speed (e.g., 40,000 RPM) or filtered through a membrane with a molecular weight cut-off that separates micelles and other small colloidal structures from undissolved particles.
- Analysis: The drug content in the bioaccessible fraction (the supernatant or filtrate) is quantified using a validated analytical method, such as High-Performance Liquid Chromatography (HPLC). Bioaccessibility (%) is calculated as (Amount of drug in bioaccessible fraction / Total drug amount in formulation) × 100 [32] [37].
In Vivo Bioavailability Study in Rodent Models
Objective: To determine the pharmacokinetic profile and absolute or relative bioavailability of a drug from a novel formulation compared to a reference standard.
Materials:
- Animal model (e.g., Sprague-Dawley rats)
- Test formulation and reference standard (e.g., intravenous solution and oral suspension)
- Catheters for serial blood sampling
- HPLC system coupled with Mass Spectrometry (LC-MS/MS)
Procedure:
- Dosing and Grouping: Animals are randomly assigned to test and control groups. The test group receives the novel formulation orally, while the control group receives an intravenous bolus of the drug for absolute bioavailability calculation.
- Serial Blood Sampling: Blood samples (e.g., 0.2 mL) are collected via a catheter at predetermined time points post-administration (e.g., 0, 0.25, 0.5, 1, 2, 4, 8, 12, 24 hours).
- Sample Processing: Plasma is separated from blood cells by centrifugation.
- Bioanalysis: Drug concentration in plasma is determined using a sensitive and specific LC-MS/MS method.
- Pharmacokinetic Analysis: The plasma concentration-time data are analyzed using non-compartmental methods to determine key parameters: Area Under the Curve (AUC), maximum plasma concentration (C~max~), and time to C~max~ (T~max~). Bioavailability (F) is calculated as: F (%) = (AUC~oral~ × Dose~IV~) / (AUC~IV~ × Dose~oral~) × 100 [61].
The workflow for a comprehensive formulation assessment, from in vitro testing to in vivo validation, is outlined below.
The Scientist's Toolkit: Essential Research Reagents and Models
Successful research in this field relies on a suite of specialized reagents, cell models, and analytical techniques.
Table 3: Key Research Reagent Solutions for Formulation Development
| Reagent / Model | Function and Application | Specific Examples |
|---|---|---|
| Lipids (Various HLB) | Core structural and functional excipients. Low HLB (<10) for oil phases; High HLB (>10) for emulsification [65]. | Low HLB: Soy phosphatidylcholine, Sorbitan monooleate. High HLB: Polysorbate 80 (Tween 80), Polyoxyl 40 hydrogenated castor oil (Cremophor RH40) [65]. |
| Biodegradable Polymers | Form the matrix for nano/microparticles, enabling controlled release [62]. | Poly(lactic-co-glycolic acid) (PLGA), Poly(lactic acid) (PLA) [62]. |
| Precipitation Inhibitors | Prevent drug crystallization in supersaturated formulations, maintaining a high driving force for absorption [66]. | Hydroxypropyl methylcellulose (HPMC), Polyvinylpyrrolidone (PVP) [66]. |
| Caco-2 Cell Line | A human colon adenocarcinoma cell line that differentiates into enterocyte-like monolayers. The gold standard for in vitro prediction of intestinal permeability [37]. | Used in transwell assays to measure apparent permeability (P~app~) [37]. |
| Simulated Intestinal Fluids | Biorelevant media mimicking the composition of human intestinal fluids for in vitro digestion and dissolution testing [66]. | Fasted State Simulated Intestinal Fluid (FaSSIF), Fed State Simulated Intestinal Fluid (FeSSIF) [66]. |
Nanoencapsulation and lipid-based delivery systems represent a paradigm shift in formulation science, moving beyond simple delivery to intelligent design that controls the biological fate of active compounds. By understanding and leveraging the principles of bioaccessibility and bioavailability, researchers can strategically select and engineer these systems to overcome the specific challenges associated with each drug candidate. The continued refinement of predictive in vitro models, coupled with a deeper understanding of in vivo absorption pathways and the development of novel functional excipients, will further accelerate the creation of advanced, effective, and patient-centric medicines.
In the realm of nutritional science and drug development, understanding the journey of a bioactive compound from ingestion to physiological action is paramount. This journey is quantitatively described by two distinct but related concepts: bioaccessibility and bioavailability.
Bioaccessibility refers to the fraction of an ingested compound that is released from its food matrix and becomes soluble in the gastrointestinal tract, thus becoming potentially available for intestinal absorption [67] [68]. It is primarily dependent on processes of digestion and release. Bioavailability, however, is a broader term encompassing the fraction of the ingested nutrient that is not only absorbed but also becomes available for utilization in normal physiological functions or for storage [32] [68]. Bioavailability depends on bioaccessibility, absorption by intestinal cells, transport to systemic circulation, and eventual distribution to tissues and organs.
This whitepaper utilizes three critical models—zinc, iron, and dietary polyphenols—to explore the factors influencing these parameters and the strategies employed to optimize them for improved human health and pharmaceutical efficacy.
Zinc: Bioaccessibility and Bioavailability Optimization
Absorption Pathways and Key Influencing Factors
Zinc is an essential trace element, critical for the function of approximately 300 enzymes and involved in immune response, gene expression, and neuro-modulation [69] [7]. Its absorption occurs primarily in the duodenum and jejunum via saturable, carrier-mediated processes involving two major transporter families: the Zrt, Irt-like protein (ZIP) family, which imports zinc into enterocytes, and the ZnT transporters, which export it into the systemic circulation [69] [7]. Intracellular zinc homeostasis is regulated by zinc-binding metallothioneins.
Table 1: Factors Influencing Zinc Bioavailability
| Factor Category | Specific Factor | Effect on Zinc Bioavailability |
|---|---|---|
| Dietary Inhibitors | Phytic Acid | Strongly negative; forms insoluble complexes with Zn [67] [7] |
| Cellulose | Negative; limits absorption [67] | |
| Iron & Copper | Negative; competitive inhibition for absorption transporters [67] [7] | |
| Dietary Enhancers | Proteins & Amino Acids | Positive; can form absorbable complexes and use amino acid transporters [7] |
| Organic Zinc Forms | Positive; e.g., zinc diglycinate shows higher bioaccessibility than inorganic salts [67] | |
| Physiological Regulators | Individual Zinc Status | Absorption efficiency increases during deficiency [67] [69] |
| Intestinal Mucus | Acts as a buffer, storing and slowly releasing zinc [7] |
Case Study: Bioaccessibility of Zinc from Dietary Supplements
A recent in vitro study investigating ten different zinc supplements on the Polish market revealed significant variations in bioaccessibility and compliance with labeling [67].
Experimental Protocol:
- Objective: To determine the potential relative bioaccessibility of Zn from supplements differing in pharmaceutical form, content, and chemical form.
- Digestion Model: A simulated in vitro digestion model mimicking human gastric and intestinal conditions.
- Analysis: Zinc content and bioaccessibility were quantified using Flame Atomic Absorption Spectrometry (FAAS). The method was validated for linearity (R² = 0.998), recovery (109%), and accuracy [67].
Table 2: Bioaccessibility and Content of Zinc from Various Supplement Forms [67]
| Supplement Form | Chemical Form | Declared Zn Content | Bioaccessibility (%) | Notes |
|---|---|---|---|---|
| DS1 | Zinc Bisglycinate | 25 mg | ~9.4% | Highest bioaccessibility |
| DS2 | Zinc Bisglycinate | 10 mg | Data in range | High bioaccessibility |
| DS9 | Zinc Bisglycinate | 30 mg | Data in range | High bioaccessibility |
| DS4 | Zinc Picolinate | 15 mg | ~7.5% | Moderate bioaccessibility |
| DS5 | Zinc Citrate | 25 mg | Data in range | Moderate bioaccessibility |
| DS6 | Zinc Methionine | 30 mg | Data in range | Moderate bioaccessibility |
| DS7 | Zinc Gluconate | 24.6 mg | Data in range | Moderate bioaccessibility |
| DS3 | Zinc Sulphate | 30 mg | ~1.1% | Lowest bioaccessibility |
Key Findings:
- The bioaccessibility of zinc from the supplements varied widely, ranging from 1.1% to 9.4% [67].
- Zinc diglycinate (bisglycinate) demonstrated the highest bioaccessibility, whereas zinc sulphate showed the lowest [67].
- In 9 out of 10 products, the actual determined zinc content exceeded the declared value by up to 161%, and five supplements exceeded the tolerable upper intake level (UL) [67].
This case study highlights that the chemical form of a mineral in a supplement is a critical factor for its release and potential absorption, and it underscores the importance of quality control in manufacturing.
Iron: Navigating Bioavailability Challenges
Bioavailability of Heme vs. Non-Heme Iron
Iron deficiency is the most prevalent mineral deficiency worldwide [70] [68]. A core challenge is its bioavailability, which is heavily influenced by its dietary form. Iron in food exists as:
- Heme iron: Found in animal-based foods (meat, poultry, seafood); typically exhibits higher absorption (∼15-35%) due to specific uptake mechanisms [68].
- Non-heme iron: Found in plant-based foods (cereals, legumes, vegetables) and some animal tissues; absorption is lower (∼5-12%) and highly influenced by dietary factors [68].
Case Study: Enhancing Iron Bioavailability from Plant-Based Matrices
A 2025 study investigated the effects of different polyphenols on the iron bioavailability from potato protein–iron complexes, a model for plant-based iron fortification [71].
Experimental Protocol:
- Complex Formation: Potato protein (PP) was complexed with iron to create PP-Fe complexes.
- Polyphenol Intervention: Three polyphenols—gallic acid, caffeic acid, and quercetin—were added to the complexes at different molar ratios (0.5:1 to 3:1, polyphenol:complex).
- In Vitro Digestion: Samples underwent simulated gastrointestinal digestion (gastric and small intestinal phases).
- Bioavailability Assessment: Iron bioavailability was measured using the Caco-2 cell model, where ferritin formation in the cells is a proxy for iron uptake and utilization [71].
Key Findings:
- The impact of polyphenols was highly dependent on their structure and concentration.
- Quercetin was most effective, maintaining nearly 100% iron release during digestion and enhancing ferritin formation in Caco-2 cells at a 1:1 ratio.
- Gallic acid only increased iron uptake (ferritin formation) at a high 3:1 ratio.
- All polyphenols increased protein hydrolysis in the gastric phase, but only quercetin improved it in the small intestine, facilitating better iron release [71].
This study demonstrates that strategic selection of dietary components, such as specific polyphenols, can modulate the food matrix to enhance, rather than inhibit, the bioavailability of non-heme iron.
Polyphenols: The Gut Microbiota Axis
The Dual Role of Polyphenols
Dietary polyphenols are bioactive compounds with antioxidant, anti-inflammatory, and anticancer properties [72]. However, their health benefits are intrinsically linked to their bioavailability, which is often low due to limited absorption in the small intestine. A significant portion of ingested polyphenols reaches the colon, where they are metabolized by the gut microbiota. This creates a bidirectional relationship: polyphenols modulate the microbial composition, and the microbiota transforms polyphenols into more bioavailable metabolites [72].
Optimization via Micro-Encapsulation
To overcome the challenges of low stability and bioaccessibility, micro-encapsulation has emerged as a promising strategy. This technology involves coating polyphenols (or other bioactives) within a protective wall material, which can:
- Protect the core compound from degradation during processing and storage.
- Mask undesirable tastes.
- Control release at the specific site in the gastrointestinal tract for optimal absorption [70] [72]. For instance, encapsulation in thermo-resistant modified starch has been shown to effectively protect iron and limit its interaction with inhibitory food components [70].
Essential Methodologies for Assessment
In Vitro Models for Bioaccessibility and Bioavailability
In vitro methods are vital for rapid, cost-effective screening, avoiding the complexities and ethical considerations of human trials [67] [68].
Table 3: Key In Vitro Methods for Assessing Bioaccessibility/Bioavailability
| Method | Principle | Key Application | Advantages |
|---|---|---|---|
| Solubility | Measures the fraction of a compound solubilized after simulated digestion. | Initial screening of bioaccessibility. | Simplicity and low cost [68]. |
| Dialysability | Uses a membrane to separate the soluble fraction, simulating passive absorption. | Estimation of the fraction available for uptake [68]. | Accounts for some absorption barriers. |
| Caco-2 Cell Model | Utilizes human colon adenocarcinoma cells differentiated into enterocyte-like cells to study uptake and transport. | Gold-standard in vitro model for assessing bioavailability [73] [68] [71]. | Provides cellular and molecular insights on absorption. |
| INFOGEST | A standardized, international static in vitro digestion method. | Simulates gastric and small intestinal digestion for consistent bioaccessibility data [68]. | High inter-laboratory reproducibility. |
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagent Solutions for Bioaccessibility/Bioavailability Studies
| Reagent / Material | Function in Experimentation | Exemplary Use Case |
|---|---|---|
| Caco-2 Cell Line | A human epithelial cell line that differentiates into enterocyte-like cells; used to model intestinal absorption and transport. | Measuring ferritin formation as an indicator of iron bioavailability [73] [71]. |
| Simulated Digestive Fluids | Chemically defined solutions mimicking saliva, gastric, and intestinal secretions (enzymes, salts, bile acids). | In vitro digestion models (e.g., INFOGEST) to study compound release from food matrix [67] [68]. |
| Atomic Absorption Spectrometry (AAS) | Analytical technique for quantifying specific mineral elements (e.g., Zn, Fe) at trace concentrations. | Determining the zinc content and its bioaccessible fraction in digested samples [67]. |
| Transwell / Permeable Supports | Inserts with a porous membrane that allow for co-culture of cells and separate apical and basolateral compartments. | Studying the transport of compounds across the Caco-2 cell monolayer [69]. |
| Spray Dryer (e.g., Büchi B-290) | Equipment used for microencapsulation via spray-drying, creating powder-based encapsulates. | Producing encapsulated ferrous sulphate or lactate using a starch suspension as the wall material [70]. |
Pathways and Workflows: A Visual Synthesis
Pathway of Dietary Zinc Absorption
The following diagram illustrates the key molecular and cellular players in zinc absorption within the intestinal epithelium.
Workflow for In Vitro Bioaccessibility & Bioavailability Assessment
This flowchart outlines a standard experimental protocol for evaluating the bioaccessibility and bioavailability of a dietary bioactive, integrating digestion models with cellular assays.
The optimization of bioaccessibility and bioavailability is a multifaceted challenge at the intersection of nutrition, food science, and pharmacology. The case studies of zinc, iron, and polyphenols provide powerful models that illustrate core principles:
- The chemical form of a mineral (e.g., zinc diglycinate vs. sulphate) is a primary determinant of its bioaccessibility.
- The food matrix and dietary context can be strategically engineered to enhance bioavailability, as demonstrated by the use of specific polyphenols to improve iron uptake from plant proteins.
- Advanced technologies like microencapsulation offer robust solutions to protect bioactive compounds and target their release.
- Standardized in vitro methodologies, particularly those incorporating cellular models like Caco-2, are indispensable tools for efficient and mechanistic screening.
A deep understanding of the bioaccessibility-bioavailability cascade, from the lumen to systemic circulation, is therefore fundamental for developing effective nutritional interventions and pharmaceutical formulations, ultimately bridging the gap between dietary intake and physiological benefit.
Ensuring Efficacy: Validation, Regulatory Standards, and Comparative Analysis
This technical guide provides an in-depth analysis of the 80/125 rule, the cornerstone regulatory criterion for establishing bioequivalence of generic drugs. Within the broader context of bioaccessibility and bioavailability research, we examine the statistical foundation, regulatory application, and methodological protocols governing this fundamental principle. Designed for researchers and drug development professionals, this whitepaper synthesizes current regulatory standards with practical experimental considerations, offering structured data visualization and analytical frameworks to navigate the complex bioequivalence landscape.
In pharmaceutical development, understanding the journey of an active pharmaceutical ingredient (API) from administration to systemic circulation is crucial and is defined by several key parameters. Bioaccessibility refers to the fraction of a compound that is released from its food or dosage form and becomes available for intestinal absorption; it represents the compound's solubility and stability under gastrointestinal conditions. Bioavailability (BA), defined by the FDA as "the extent and rate to which the active drug ingredient or active moiety from the drug product is absorbed and becomes available at the site of drug action," encompasses the subsequent processes of absorption, distribution, metabolism, and excretion [74]. When comparing two drug products, typically a generic (test) versus a brand-name (reference) product, bioequivalence (BE) is established if they exhibit no significant difference in the rate and extent of absorption when administered under similar conditions [75] [74].
The Fundamental Bioequivalence Assumption underpins regulatory approval of generics: if two drug products are shown to be bioequivalent, it is assumed they will achieve the same therapeutic effect and are therefore therapeutically equivalent [74]. This principle allows generic manufacturers to submit an Abbreviated New Drug Application (ANDA), relying on the innovator's established safety and efficacy data, rather than conducting duplicative clinical trials [74] [76]. The 80/125 rule serves as the primary statistical tool for verifying this assumption.
The Statistical and Regulatory Basis of the 80/125 Rule
Historical Evolution and Clinical Justification
The 80/125 rule emerged from decades of regulatory refinement. Initially, bioequivalence was assessed using the ±20 rule, which concluded equivalence if the average bioavailability of the test formulation fell within ±20% of the reference [74] [77]. This approach was abandoned due to a critical flaw: it could theoretically allow two generic products (A and B) to differ from each other by as much as 40% while both being deemed equivalent to the reference product [75].
In 1986, an FDA Bioequivalence Hearing concluded that "differences of less than 20% in AUC and Cmax between products in normal subjects are unlikely to be clinically significant in patients" [77]. This expert judgment, noting that clinical studies often struggle to detect even 50-100% differences in dose, formed the clinical basis for the current rule [77]. The 80/125 rule was subsequently adopted, requiring that the 90% confidence interval for the ratio of geometric means of primary pharmacokinetic parameters fall entirely within 80-125% [74].
Log-Normal Distribution and Statistical Symmetry
The selection of 80-125%, rather than 80-120%, stems from the log-normal distribution of pharmacokinetic parameters like AUC (area under the concentration-time curve, measuring extent of absorption) and Cmax (maximum concentration, measuring rate of absorption) [78] [75]. These parameters are naturally bounded at zero and positively skewed, but their log-transformations approximate a normal distribution, satisfying the assumptions of conventional statistical tests [78].
A symmetrical ±20% range on a linear scale becomes asymmetrical around 1.0 (representing perfect equivalence). However, applying this variance to the log-transformed data creates statistical symmetry, which is essential for valid hypothesis testing.
Table 1: Transformation Between Linear and Logarithmic Scales
| Test/Reference Ratio (Linear) | Percentage | Natural Log (ln) of Ratio |
|---|---|---|
| 0.8 | 80% | -0.223 |
| 0.9 | 90% | -0.105 |
| 1.0 | 100% | 0 |
| 1.1 | 110% | 0.095 |
| 1.2 | 120% | 0.182 |
| 1.25 | 125% | 0.223 |
As shown in Table 1, the natural log of 0.8 (80%) is -0.223 and the natural log of 1.25 (125%) is +0.223. This creates a perfectly symmetrical interval [-0.223, +0.223] on the log scale, corresponding to the 80-125% interval on the linear scale [78]. The statistical assessment uses the Two One-Sided Tests (TOST) procedure to demonstrate that the true difference is neither too low (less than 80%) nor too high (more than 125%) [79].
Regulatory Framework and Study Design
The Bioequivalence Study Protocol
Demonstrating bioequivalence requires a well-controlled study, typically employing a randomized, crossover design with healthy volunteers [75] [74]. The standard design is a two-sequence, two-period crossover, where each subject receives both the test and reference formulations in randomly assigned order, separated by a washout period [74]. This design eliminates inter-subject variability from the formulation comparison.
Key pharmacokinetic blood samples are collected at predetermined times following each dose. The resulting concentration-time profiles are used to calculate AUC (extent of absorption) and Cmax (rate of absorption) [75] [77]. The statistical analysis is performed on the log-transformed AUC and Cmax values.
Table 2: Key Components of a Standard Bioequivalence Study
| Study Element | Standard Protocol | Regulatory Purpose |
|---|---|---|
| Study Design | Randomized, two-period, two-sequence crossover | Minimizes variability; each subject serves as their own control |
| Subjects | Healthy adult volunteers (typically 18-55) | Homogeneous population reduces variability; ethical considerations |
| Primary Endpoints | AUC0-t, AUC0-∞ (extent of absorption), Cmax (rate of absorption) | Surrogate measures for clinical effect |
| Statistical Analysis | 90% Confidence Interval (CI) for the geometric mean ratio (Test/Reference) of log-transformed PK parameters | To conclude bioequivalence, the entire 90% CI must lie within 80-125% |
| Acceptance Criterion | 90% CI fully within 80.00% to 125.00% | Ensures with high probability that the true mean difference is not clinically significant |
Clarifying a Common Misconception
A prevalent misunderstanding is that the 80-125% rule applies to the absolute drug content in the generic product. This is incorrect [75]. The rule applies specifically to the 90% confidence interval of the ratio of geometric means of the pharmacokinetic parameters (AUC and Cmax) from a clinical study [75]. Because the entire confidence interval must fall within the limits, the actual mean PK values of the generic are forced to be very close to the reference. An FDA study found that the mean difference for AUC values between approved test and reference products was only about 3.5%, with the vast majority differing by less than 5% [75].
Methodological Toolkit for Researchers
Experimental Workflow and Signaling Pathways
The following diagram illustrates the complete experimental workflow for a bioequivalence study, from design to regulatory conclusion.
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Key Research Reagent Solutions for Bioequivalence Studies
| Reagent / Material | Critical Function in Bioequivalence Assessment |
|---|---|
| Reference Listed Drug (RLD) | The approved brand-name product serving as the comparator; essential for establishing the benchmark for rate and extent of absorption. |
| Test Formulation | The generic drug product under investigation; must be pharmaceutically equivalent to the RLD in dosage form, strength, and route of administration. |
| Validated Bioanalytical Assay | (e.g., LC-MS/MS) Quantifies drug concentrations in plasma/serum samples over time. Must be selective, sensitive, accurate, and precise. |
| Stabilized Blood Collection Tubes | Used for serial pharmacokinetic sampling; anticoagulants (e.g., K2EDTA) and preservatives prevent analyte degradation pre-analysis. |
| Clinical Database & Statistical Software | Manages subject data and performs statistical analysis (TOST procedure) for calculating the 90% confidence interval of the geometric mean ratio. |
Sample Size Determination
Sample size planning is critical for a successful BE study. It is typically based on a power calculation using the within-subject coefficient of variation (CV%) for the primary PK endpoints and the expected geometric mean ratio (GMR), which is often assumed to be 1.00 (true equivalence) or 1.05 [80]. As shown in Table 4, higher variability requires a larger sample size to achieve the standard 80% or 90% power.
Table 4: Example Sample Sizes for a 2x2 Crossover BE Study (90% Power, GMR=1.00)
| Within-Subject CV% | Sample Size (Total) | Within-Subject CV% | Sample Size (Total) |
|---|---|---|---|
| 10% | ~ 12 | 25% | ~ 54 |
| 15% | ~ 22 | 30% | ~ 76 |
| 20% | ~ 36 | 35% | ~ 102 |
Newer methods, such as calculating statistical assurance, have been proposed to account for uncertainty in the true T/R-ratio, providing an average probability of success over a distribution of potential ratios rather than for a single assumed value [80].
The 80/125 rule remains a robust, statistically sound foundation for ensuring therapeutic equivalence between generic and innovator drugs. Its derivation from the log-normal distribution of pharmacokinetic parameters and the requirement that the entire 90% confidence interval must lie within the bioequivalence limits provide a high degree of assurance that approved generic products will perform clinically like their reference counterparts. For researchers and drug development professionals, a precise understanding of this rule—distinguishing it from misconceptions about absolute content and appreciating its embedded statistical rigor—is essential for successfully navigating the regulatory landscape. As science advances, methodologies continue to evolve, but the 80/125 rule endures as a critical benchmark in making safe, effective, and affordable medicines available to the public.
Correlating In Vitro Data with In Vivo Outcomes
In the development of new drugs and functional foods, a critical challenge lies in accurately predicting in vivo performance based on laboratory data. This process hinges on understanding two distinct but sequential concepts: bioaccessibility, the release of compounds from a matrix into a form accessible for absorption, and bioavailability, the fraction that reaches systemic circulation and becomes available at the site of action [81] [18]. The establishment of an In Vitro-In Vivo Correlation (IVIVC) creates a predictive mathematical model linking in vitro drug release profiles with relevant in vivo responses, typically plasma drug concentration or amount absorbed [82] [83]. For researchers and drug development professionals, a robust IVIVC is not merely an academic exercise; it provides a mechanism for evaluating in vivo drug absorption based on in vitro dissolution, thereby streamlining development, enhancing formulation strategies, supporting regulatory decisions, and reducing the need for extensive clinical bioequivalence studies [83].
Defining the Foundational Concepts: Bioaccessibility and Bioavailability
Precise terminology is essential for describing the complex journey of a compound from ingestion to physiological action. The following diagram illustrates the sequential relationship and key differentiators between bioaccessibility and bioavailability.
Figure 1. The Sequential Pathway from Ingestion to Action. This diagram visualizes the critical distinction between bioaccessibility and bioavailability in the absorption pathway.
As shown in Figure 1, bioaccessibility describes the fraction of a compound that is released from its food or drug matrix and becomes soluble in the gastrointestinal tract, thus being potentially available for absorption [81] [68]. It is primarily governed by processes such as dissolution, digestion, and the physical breakdown of the matrix. For instance, the cell wall in plant-based foods can act as a significant physical barrier, limiting nutrient release and thus bioaccessibility [81] [68].
In contrast, bioavailability is a subsequent step, referring to the proportion of the ingested substance that is absorbed, passes through the intestinal mucosa, and reaches the systemic circulation intact, from where it can be transported to its site of action [18]. Bioavailability depends not only on bioaccessibility but also on factors such as membrane permeability, metabolism in the gut wall and liver, and tissue distribution [82]. In nutrition, a key example is non-haem iron from plants, which must be released from the food matrix (bioaccessibility) and then reduced from ferric (Fe³⁺) to ferrous (Fe²⁺) state before it can be absorbed by enterocytes, resulting in lower overall bioavailability compared to haem iron from animal sources [68].
Key Factors Influencing the Correlation
Developing a predictive IVIVC model requires a systematic consideration of the factors that govern drug dissolution and absorption. These can be categorized into three main groups.
Physicochemical Properties
The inherent properties of the drug substance itself are primary determinants of its dissolution behavior. These include:
- Solubility and Dissolution Rate: Governed by the Noyes-Whitney equation (dM/dt = D × S × (Cs - Cb)/h), dissolution is the prerequisite for absorption [82]. The Maximum Absorbable Dose (MAD) model provides an initial guide, calculated as MAD = S × Ka × SIWV × SITT, where S is solubility, Ka is the absorption rate constant, SIWV is small intestinal water volume (~250 mL), and SITT is small intestinal transit time (~3 hours) [82].
- Ionization Constant (pKa): This determines the drug's solubility and absorption across the pH gradients of the GI tract, which ranges from pH 1-2 in the stomach to 7-8 in the colon, according to the pH-partition hypothesis [82].
- Particle Size and Salt Form: A reduction in particle size increases surface area and can enhance dissolution rate. The selection of salt form can also significantly impact dissolution characteristics [82].
Biopharmaceutical Properties
These properties influence the movement of the drug across biological membranes:
- Permeability: The transcellular permeability (Pm) is defined as Pm = (Kp × Dm) / Lm, where Kp is the membrane-water partition coefficient, Dm is membrane diffusivity, and Lm is membrane thickness [82].
- Lipophilicity: Often represented by the octanol-water partition coefficient (log P), it is a key indicator of membrane permeability. Compounds with log P values between 0 and 3 generally exhibit high permeability, while those with values below -1.5 or above 4.5 have lower permeability, often forming a bell-shaped relationship with absorption [82].
- Other Predictive Parameters: Absorption Potential (AP = log(P × Fun / D₀)) and Polar Surface Area (PSA) are other useful measures for predicting passive transport through membranes [82].
Physiological Properties
The physiological environment of the human body adds another layer of complexity:
- GI pH and Transit Time: The dynamic pH environment and variable gastric emptying times (~1 hour for liquids, ~2-3 hours for solids) significantly affect drug solubility, stability, and the extent of release [82].
- Presence of Food and Other Components: Food intake can alter the physiological environment, while specific dietary components can act as inhibitors (e.g., phytates, tannins, calcium) or enhancers (e.g., ascorbic acid, proteins/amino acids) of absorption [7] [68].
Levels and Regulatory Framework of IVIVC
Regulatory authorities like the FDA and EMA have outlined specific levels of IVIVC, which differ in their complexity and predictive power [83] [84]. The following table summarizes the key characteristics of these levels.
Table 1: Levels of In Vitro-In Vivo Correlation (IVIVC) as Defined by Regulatory Guidance
| Aspect | Level A | Level B | Level C |
|---|---|---|---|
| Definition | A point-to-point correlation between in vitro dissolution and the in vivo input rate (e.g., absorption profile) [83] [84]. | A statistical correlation using means of in vitro dissolution time and in vivo residence or absorption time [83]. | A single point correlation relating one dissolution time point (e.g., t50%) to one pharmacokinetic parameter (e.g., Cmax or AUC) [83]. |
| Predictive Value | High; can predict the entire plasma concentration-time profile and is the most preferred for regulatory submissions [83]. | Moderate; does not reflect the actual in vivo plasma concentration curve shape [83]. | Low; does not predict the full PK profile and is considered the least rigorous [83]. |
| Regulatory Acceptance | Most preferred by FDA/EMA; can support biowaivers for major formulation and process changes [83]. | Less robust; usually requires additional in vivo data to support any claims [83]. | Least rigorous; not sufficient for biowaivers alone, but can provide early development insights [83]. |
| Common Use Case | Typically requires data from ≥2 formulations with different release rates (e.g., slow, medium, fast) [83]. | Not commonly used for product quality control or setting dissolution specifications [83]. | Multiple Level C (correlating several dissolution time points to PK parameters) can be more useful than a single point [83]. |
The primary regulatory guidance is provided in the FDA's "Extended Release Oral Dosage Forms: Development, Evaluation, and Application of In Vitro/In Vivo Correlations" (September 1997) [83]. A validated Level A IVIVC can be used to set dissolution specifications and, crucially, to obtain biowaivers, which allow for a surrogate of in vivo bioequivalence studies for certain post-approval changes, saving significant time and resources [83].
Experimental Protocols for Establishing IVIVC
Establishing a robust IVIVC is a multi-stage process that integrates laboratory testing, clinical data, and mathematical modeling. The workflow below outlines the key stages involved.
Figure 2. IVIVC Development and Validation Workflow. This diagram outlines the critical stages for building a predictive in vitro-in vivo correlation model.
In Vitro Dissolution Testing
The first step involves selecting appropriate in vitro tests that mimic physiological conditions [85]. Dissolution testing is central to this, where the drug release profile is measured over time in a dissolution apparatus. Key considerations include:
- Biorelevant Media: Using dissolution media that simulate the pH, composition, and surface tension of fluids in different segments of the GI tract (stomach, small intestine) [82] [83].
- Hydrodynamic Conditions: Adjusting agitation speed to replicate the fluid dynamics and motility patterns of the human GI tract [85].
- For Nutrients - Simulated Gastrointestinal Digestion: The INFOGEST method is a standardized international static in vitro simulation of gastric and intestinal digestion widely used in food science to assess bioaccessibility [68]. This protocol typically involves sequential incubation with simulated gastric and intestinal fluids containing relevant enzymes (e.g., pepsin, pancreatin) and salts under controlled pH and time conditions [68].
In Vivo Study and Data Analysis
The next step is to conduct in vivo studies, typically in human subjects, to determine the pharmacokinetic profile of the drug (e.g., C~max~, T~max~, AUC) [85]. For nutrients, this may involve measuring plasma concentrations or using isotopic tracers to assess absorption [7]. The collected in vivo data is then analyzed, often using deconvolution techniques, to determine the time-course of in vivo drug absorption or dissolution [82]. This in vivo absorption profile becomes the key endpoint for correlation with the in vitro dissolution data.
Model Development and Validation
A mathematical model is developed to establish a functional relationship between the input (in vitro dissolution) and the output (in vivo absorption) [82] [85]. This can range from simple linear correlations (for Level C) to more complex non-linear models (for Level A). The final and critical stage is model validation, where the predictability of the IVIVC is tested by comparing the PK parameters predicted by the model against those observed from a new in vivo study (often with a different formulation) [83] [85]. A model is considered validated if the prediction error for key parameters like AUC and C~max~ is within a predefined acceptable limit (e.g., ≤10%) [83].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Reagents and Materials for IVIVC and Bioavailability Research
| Reagent / Material | Function and Application in Research |
|---|---|
| Caco-2 Cell Line | A human colon adenocarcinoma cell line that, upon differentiation, exhibits enterocyte-like properties. It is a gold-standard in vitro model for predicting intestinal permeability and active transport of drugs and nutrients [7] [68]. |
| Simulated Gastrointestinal Fluids | Chemically defined solutions that mimic the composition, pH, and bile salt content of gastric and intestinal fluids. They are essential for conducting biorelevant dissolution and bioaccessibility studies (e.g., using the INFOGEST protocol) [68]. |
| Transwell / Permeability Assay Systems | Multi-compartment cell culture plates used with Caco-2 cells to measure the transport of a compound from the apical (intestinal lumen) to the basolateral (bloodstream) side, quantifying its apparent permeability (Papp) [68]. |
| Dialyzability Setups | Apparatuses incorporating a dialysis membrane with a specific molecular weight cutoff. They are used to separate the soluble, low-molecular-weight fraction of a compound (the bioaccessible fraction) from the larger, undigested matrix during in vitro digestion simulations [68]. |
| Specific Enzymes (e.g., Pepsin, Pancreatin) | Digestive enzymes added to simulated fluids to catalyze the hydrolysis of proteins, carbohydrates, and lipids, which is a critical step in the release of compounds from the food or drug matrix [81] [68]. |
Challenges and Future Perspectives
Despite its significant value, establishing a robust IVIVC faces considerable challenges. Biological variability among individuals, complex drug release mechanisms, and intricate food matrices can lead to poor correlation [84] [86]. A multicentre analysis on biomaterials for bone regeneration surprisingly revealed no significant overall correlation between in vitro and in vivo outcomes, highlighting the inadequacy of some current in vitro models [86]. Furthermore, IVIVC development is particularly difficult for drugs with low solubility or complex absorption pathways, such as those in BCS Class II and IV [84].
Future advancements are focused on leveraging technology to overcome these hurdles. The integration of Physiologically Based Pharmacokinetic (PBPK) modeling combines IVIVC with organ perfusion rates and tissue distribution kinetics for more precise human simulations [83]. Artificial Intelligence and Machine Learning are being used to analyze complex datasets, uncover hidden patterns, and improve prediction accuracy [83] [84]. Finally, the development of more sophisticated in vitro models, such as microfluidics and organ-on-a-chip systems, aims to better mimic human physiology and improve the predictive power of in vitro testing [83].
Within nutrition and pharmaceutical sciences, accurately predicting the physiological utilization of bioactive compounds requires a clear distinction between two fundamental concepts: bioaccessibility and bioavailability. Bioaccessibility refers to the fraction of a compound that is released from its food matrix and becomes soluble in the gastrointestinal tract, making it potentially available for intestinal absorption [34] [68]. It represents the maximum amount that could be absorbed. In contrast, bioavailability describes the proportion of an ingested nutrient that is ultimately absorbed, metabolized, and reaches the systemic circulation for utilization by tissues and organs [87] [88]. Essentially, for a compound to be bioavailable, it must first be bioaccessible.
This distinction is critical for researchers and drug development professionals, as a nutrient or drug may be fully released from the food matrix (high bioaccessibility) yet poorly absorbed across the intestinal epithelium (low bioavailability) due to various physiological barriers [68]. The methodologies used to assess these two parameters are, therefore, inherently different. This guide provides a comparative analysis of the primary experimental approaches, detailing their advantages, limitations, and appropriate applications within modern research.
The assessment of bioaccessibility and bioavailability typically employs a hierarchy of models, ranging from simple in vitro simulations to complex in vivo human trials. Figure 1 illustrates the standard workflow and the relationship between these key methodologies.
Core Methodological Workflow
Diagram Title: Bioaccessibility & Bioavailability Assessment Workflow
As shown in Figure 1, the process begins with simulating gastrointestinal digestion to determine the bioaccessible fraction. This is often a prerequisite for subsequent steps aiming to quantify the bioavailable fraction, which involves absorption and metabolism [68] [89].
In Vitro Methodologies for Bioaccessibility
In vitro methods simulate human gastrointestinal conditions to estimate the fraction of a compound released from the food matrix. These are cost-effective, high-throughput screening tools.
Primary In Vitro Protocols
The most recognized protocol is the INFOGEST static simulation method, which provides a standardized framework for simulating oral, gastric, and intestinal digestion phases [68] [90]. A typical protocol involves the following steps:
- Oral Phase: The sample is mixed with simulated salivary fluid (SSF) and incubated for a short period (e.g., 2 minutes) at 37°C, often including α-amylase.
- Gastric Phase: Simulated gastric fluid (SGF) and pepsin are added. The pH is reduced to 3.0, and the mixture is incubated for a set time (e.g., 2 hours) at 37°C with constant agitation.
- Intestinal Phase: Simulated intestinal fluid (SIF), pancreatin, and bile salts are added. The pH is adjusted to 7.0, and incubation continues (e.g., 2 hours) at 37°C [68] [90].
Following digestion, the bioaccessible fraction is separated from the solid residue, typically via centrifugation or filtration. For lipophilic compounds like carotenoids and zinc, the fraction incorporated into mixed micelles is considered bioaccessible and can be isolated by ultracentrifugation [89] [91].
Research Reagent Solutions for In Vitro Digestion
Table 1: Essential Reagents for In Vitro Gastrointestinal Models
| Reagent / Component | Function in Simulation | Example from Literature |
|---|---|---|
| Simulated Salivary Fluid (SSF) | Mimics ionic composition of saliva; initiates starch digestion. | Contains electrolytes; often includes α-amylase [90]. |
| Pepsin | Gastric protease that hydrolyzes proteins in the stomach phase. | Porcine pepsin is commonly used (e.g., Sigma P7000) [91]. |
| Pancreatin | A mixture of pancreatic enzymes (amylase, protease, lipase) for intestinal digestion. | Used in the intestinal phase to simulate pancreatic secretion [91]. |
| Bile Salts | Emulsify lipids and form mixed micelles for solubilizing lipophilic compounds. | Porcine bile extracts are standard (e.g., Sigma B8631) [89] [91]. |
| Dialyzation Membranes | Act as a synthetic intestinal barrier to separate low-molecular-weight compounds. | Used in dialyzability methods to estimate bioaccessibility [68]. |
| Caco-2 Cell Lines | Human colon adenocarcinoma cells that differentiate into enterocyte-like monolayers. | Used in bioavailability models to study intestinal uptake and transport [37] [68]. |
Methodologies for Assessing Bioavailability
Bioavailability assessment requires models that account for intestinal absorption and metabolism.
In Vitro Bioavailability Models
The Caco-2 cell model is a widely used in vitro system for predicting intestinal permeability. Differentiated Caco-2 cells form a polarized monolayer with tight junctions and express brush border enzymes and transporters found in the human small intestine [37] [68]. The experimental protocol involves:
- Growing and differentiating Caco-2 cells on permeable filters for 2-3 weeks.
- Applying the bioaccessible fraction (from in vitro digestion) to the apical compartment.
- Measuring the rate and amount of the compound that appears in the basolateral compartment over time, which represents the fraction absorbed [68].
In Vivo and Clinical Methods
In vivo methods provide the most direct measure of bioavailability but are resource-intensive.
- Animal Models: Studies in rodents or other animals allow for the direct measurement of nutrient concentrations in blood, plasma, or specific tissues over time. Post-mortem, tissues can be analyzed for nutrient accumulation [37].
- Human Clinical Trials: The gold standard for bioavailability. This involves dosing human subjects and frequently collecting blood samples to create a concentration-time curve for the compound or its metabolites in the plasma. The use of stable isotopes as tracers can precisely track absorption and distribution [37] [87].
Comparative Analysis: Advantages and Limitations
Each methodology offers distinct benefits and suffers from specific constraints. The choice of method depends on the research question, stage of development, and available resources.
Table 2: Comparative Analysis of Bioaccessibility and Bioavailability Methodologies
| Methodology | Key Advantage | Primary Limitation | Typical Application |
|---|---|---|---|
| In Vitro Digestion (e.g., INFOGEST) | High-throughput, cost-effective, ethical, standardized protocol, no inter-individual variability [68] [90]. | Oversimplified physiology; lacks absorption step; static vs. dynamic peristalsis [34] [68]. | Initial screening of food formulations, processing techniques, and ingredient interactions [90] [91]. |
| Caco-2 Cell Model | Provides mechanistic insight on absorption and transport; more physiologically relevant than digestion alone [37] [68]. | Does not fully replicate mucus layer, microbiome, or systemic metabolism; lengthy cell differentiation time [68]. | Studying transporter-mediated uptake, permeability, and the effects of enhancers/inhibitors [37]. |
| In Vivo (Animal) Studies | Provides full pharmacokinetic data (ADME); allows for tissue distribution analysis [37]. | Ethical concerns; high cost; interspecies differences may not translate to humans [37]. | Preclinical safety and efficacy testing; mechanistic studies requiring tissue analysis. |
| Human Clinical Trials | Gold standard for human bioavailability; accounts for full human physiology including microbiome [87]. | Extremely high cost and complexity; ethical constraints; significant inter-individual variability [87] [88]. | Final validation of nutrient bioavailability or drug bioequivalence. |
Quantitative Data from Comparative Studies
The practical differences between these methodologies are evident in quantitative results. For instance, a study on caffeine in beverages found a high bioaccessibility of 83-112% across different drinks, meaning nearly all consumed caffeine was released during digestion. However, its bioavailability (the amount actually absorbed) was lower, ranging from 52% to 79% [87]. This discrepancy highlights the critical importance of distinguishing between release from the matrix and actual absorption.
Similarly, research on zinc has demonstrated that its bioavailability is highly dependent on dietary factors. While inorganic zinc salts like zinc oxide are commonly used, organic forms such as zinc complexes with amino acids show better absorption, as they can utilize amino acid transporters in the intestine [37].
Emerging Trends and Advanced Techniques
The field of bioavailability assessment is evolving with the integration of advanced technologies.
- Artificial Intelligence (AI) and Machine Learning (ML): AI models are being trained to predict the bioavailability of compounds by analyzing large datasets encompassing molecular structures, food matrix effects, and results from in vitro and in vivo studies. This can help prioritize compounds for testing and reduce reliance on extensive laboratory experiments [92].
- Enhanced Delivery Systems: To overcome low bioavailability, research is focused on designing novel delivery systems. Nanostructured carriers, such as liposomes, nanoemulsions, and biopolymeric nanoparticles, can protect bioactive compounds during digestion and enhance their solubility and absorption [93] [89].
- Non-Thermal Processing: Techniques like high-hydrostatic pressure extraction (HHPE) and ultrasound-assisted extraction (UAE) are shown to improve the extraction yield and bioaccessibility of carotenoids and antioxidants from food matrices, as demonstrated in studies on red lobster by-products and dill juice [90] [91].
A comprehensive understanding of the advantages and limitations of each methodology is paramount for designing robust research in nutritional and pharmaceutical sciences. The synergistic use of in vitro bioaccessibility methods as a rapid screening tool, followed by more complex in vitro bioavailability models and ultimately validated through targeted in vivo studies, represents a powerful and efficient strategy. As emerging technologies like AI and advanced delivery systems continue to mature, they promise to further refine our ability to predict and enhance the bioavailability of bioactive compounds, ultimately leading to more effective nutraceuticals and pharmaceuticals.
The Fundamental Bioequivalence Assumption in Drug Development
The development of generic drugs operates on a foundational scientific principle that allows for the substitution of a brand-name drug with a generic version without compromising safety or efficacy. This principle, the Fundamental Bioequivalence Assumption, posits that if two drug products (a test generic and a reference brand-name) deliver the same concentration of the active pharmaceutical ingredient (API) to the systemic circulation over the same time period, they will produce the same therapeutic effect. This assumption enables generic manufacturers to forego lengthy and costly repeat clinical trials, relying instead on demonstrating comparable pharmacokinetic profiles. Central to understanding this principle is the precise differentiation between bioaccessibility and bioavailability. Bioaccessibility refers to the fraction of a nutrient or compound that is released from the food or drug matrix and becomes available for intestinal absorption, encompassing processes of release and solubilization within the gastrointestinal tract [13] [18]. In contrast, bioavailability is a broader term referring to the proportion of the ingested substance that reaches the systemic circulation and is thus available for utilization at the site of physiological activity [18]. For a drug, this includes not only absorption but also subsequent processes of metabolism, distribution, and bioactivity [18]. The bioequivalence assumption effectively bridges these concepts, asserting that equivalent bioavailability, as demonstrated through measured plasma concentrations, guarantees equivalent therapeutic outcome.
The Scientific and Regulatory Pillars of Bioequivalence
Quantitative Criteria for Demonstration
Regulatory agencies worldwide, including the FDA and EMA, have established strict, quantitative criteria to confirm bioequivalence. These criteria are applied to pharmacokinetic parameters derived from measuring drug concentrations in the plasma of human subjects over time. The core parameters and the standards for comparison are detailed in the table below.
Table 1: Key Pharmacokinetic Parameters and Regulatory Criteria for Bioequivalence Studies
| Pharmacokinetic Parameter | Definition | Regulatory Acceptance Range |
|---|---|---|
| AUC0-t | Area Under the plasma Concentration-time curve from zero to the last measurable time point, representing total exposure. | 90% Confidence Interval (CI) must fall within 80.00% - 125.00% [45] |
| AUC0-∞ | Area Under the Curve from zero to infinity, representing total exposure with extrapolation. | 90% CI must fall within 80.00% - 125.00% [45] |
| Cmax | Maximum observed plasma concentration, indicating the rate of absorption. | 90% CI must fall within 80.00% - 125.00% [45] |
The rigorous requirement that the 90% confidence intervals for these primary metrics fall entirely within the 80-125% range provides strong statistical assurance that the test and reference products do not differ significantly in their rate and extent of absorption. This statistical comparison is the cornerstone of the bioequivalence assumption.
The Role of In Vitro Models and Bioaccessibility
In vitro gastrointestinal models are pivotal tools in early development for predicting the in vivo performance of drug formulations. They are used to study digestibility (the breakdown of complex nutrients) and bioaccessibility (the fraction released from the food/drug matrix for absorption) [13] [94]. While in vitro bioaccessibility is often used as an indicator of in vivo bioavailability, the terminology in scientific literature has been inconsistent, leading to confusion [13]. A standardized understanding clarifies that bioaccessibility is the result of combined processes like physical release and solubilization in the gut, whereas bioavailability encompasses the entire journey from ingestion to systemic availability [13]. For a drug, high bioaccessibility is a prerequisite for high bioavailability, but it does not guarantee it, as factors like intestinal permeability and first-pass metabolism can further limit systemic availability.
Experimental Methodologies for Establishing Bioequivalence
Standard Clinical Bioequivalence Study Design
The most direct method for establishing bioequivalence is through a well-controlled clinical pharmacokinetic study. The standard protocol involves:
- Study Design: A randomized, balanced, single-dose, two-treatment, two-period, two-sequence crossover design is most frequently employed [45]. This design minimizes intersubject variability by having each subject serve as their own control.
- Subject Selection: Studies typically enroll healthy adult volunteers of both sexes, often in a fasted state, though fed-state studies are required for drugs whose absorption is affected by food.
- Procedure: In each period, subjects receive either the test (T) or reference (R) formulation. Blood samples are collected at predetermined intervals over a period sufficient to characterize the complete concentration-time profile (typically at least three terminal half-lives).
- Bioanalytical Analysis: Plasma samples are analyzed using a validated specific and sensitive analytical method, such as Liquid Chromatography with tandem Mass Spectrometry (LC-MS/MS), to determine the concentration of the API.
- Pharmacokinetic and Statistical Analysis: The primary parameters (AUC0-t, AUC0-∞, Cmax) are calculated using non-compartmental analysis (NCA). An analysis of variance (ANOVA) is performed, and the 90% confidence intervals for the geometric mean ratio (T/R) of these parameters are calculated.
Advanced and Emerging Methodologies
For complex drug products or to reduce human testing, advanced methodologies are increasingly used.
- In Vitro Studies: For some drugs, in vitro studies comparing dissolution profiles can support a biowaiver, especially for drugs classified under the Biopharmaceutics Classification System (BCS) as highly soluble and highly permeable (BCS Class I) [95] [45].
- Virtual Bioequivalence (VBE): This in silico approach uses Physiologically Based Pharmacokinetic (PBPK) modeling to simulate drug absorption, distribution, metabolism, and excretion. The VBEToolbox R package, for example, integrates in vitro data (e.g., dissolution, skin permeation) to train mechanistic models and virtually determine the study size needed to demonstrate bioequivalence, reducing the need for human trials [96].
- Model-Informed Drug Development (MIDD): MIDD is a broader framework that uses quantitative tools like PBPK, Population PK (PPK), and Exposure-Response (ER) modeling to inform drug development [97]. These "fit-for-purpose" models help optimize formulations and predict bioequivalence outcomes by providing data-driven insights across the development lifecycle [97].
Diagram 1: Standard BE Study Workflow
The Scientist's Toolkit: Essential Reagents and Models
Table 2: Key Reagents and Models in Bioequivalence and Formulation Research
| Tool/Reagent | Function/Description | Application in BE & Development |
|---|---|---|
| In Vitro Dissolution Apparatus | Equipment that simulates gastrointestinal conditions to measure drug release rate from the solid dosage form. | Critical for quality control, formulation screening, and supporting biowaiver requests. |
| LC-MS/MS System | Highly sensitive and specific analytical instrumentation for quantifying drug concentrations in biological matrices (e.g., plasma). | Gold standard for bioanalysis in PK studies; essential for generating AUC and Cmax data. |
| Simulated Gastric/Intestinal Fluids | Chemically defined fluids mimicking the pH and composition of human gastrointestinal juices. | Used in dissolution and in vitro digestion models to predict in vivo bioaccessibility. |
| PBPK Modeling Software | Computational platforms (e.g., GastroPlus, Simcyp, VBEToolbox) for mechanistic simulation of ADME processes. | Enables Virtual Bioequivalence (VBE), formulation optimization, and trial design [97] [96]. |
| Caco-2 Cell Lines | A human colon adenocarcinoma cell line that differentiates to form a monolayer with properties of small intestinal epithelium. | In vitro model for predicting intestinal permeability of drug compounds. |
| Artificial Intelligence/Machine Learning (AI/ML) | Computational techniques to analyze large datasets for prediction and optimization. | Used to predict ADME properties, optimize formulation composition, and streamline clinical trial design [97] [95]. |
Economic and Regulatory Context
The bioequivalence paradigm is the engine of the generic drug industry, which is projected to grow to over $926 billion by 2034 [98]. This growth is fueled by the "patent cliff," a phenomenon where blockbuster drugs lose market exclusivity, creating a massive transfer of market value—often $200-$300 billion in annual revenues become vulnerable in a given period [98]. The subsequent entry of generics, which can be 80-90% cheaper than their branded counterparts, saved the U.S. healthcare system an estimated $445 billion in 2023 alone [98]. This economic reality is underpinned by a complex intellectual property battlefield where generic manufacturers use reverse engineering to decode the innovator product's formulation and manufacturing process, navigating "patent thickets" to bring affordable medicines to market [98]. Regulatory harmonization, such as the ICH M13A guideline, further standardizes BE practices globally, promoting efficient drug development and approval [97] [45].
Diagram 2: Economic & Regulatory Drivers
The Fundamental Bioequivalence Assumption remains a scientifically valid and economically critical pillar of modern pharmaceutical regulation. By relying on robust pharmacokinetic comparisons, it ensures that generic drugs are therapeutically equivalent to their brand-name counterparts, thereby fostering competition and expanding patient access to affordable medicines. The field continues to evolve with the integration of more sophisticated in silico tools like PBPK modeling and AI, which promise to further refine bioequivalence assessments and streamline the development of complex generic products. A precise understanding of the underlying concepts of bioaccessibility and bioavailability is essential for researchers and regulators to accurately interpret data from both in vitro and in vivo studies, ensuring the continued safety and efficacy of generic medicines worldwide.
Conclusion
A precise understanding of the distinction between bioaccessibility and bioavailability is non-negotiable for predicting the efficacy of bioactive compounds and drugs. This synthesis underscores that bioavailability is the ultimate determinant of physiological impact, integrating the prerequisite of bioaccessibility. The future of biomedical research lies in refining predictive in vitro models, developing smarter formulation technologies that navigate biological barriers, and strengthening the regulatory bridge between compound absorption and clinical therapeutic equivalence. Embracing these interconnected concepts is pivotal for advancing the development of effective nutraceuticals and pharmaceuticals.
References
- 1. In-Vitro Dynamic Bioaccessibility and Bioavailability as Key ... [https://www.mdpi.com/2076-3417/15/17/9417]
- 2. Stability, bioaccessibility and bioavailability of vitamins in ... [https://www.sciencedirect.com/science/article/abs/pii/S0308814625027037]
- 3. Comparative assessment of polyphenol stability, bioactivity ... [https://www.nature.com/articles/s41598-025-13104-1]
- 4. Section 1 - LADME Scheme [https://www.rxkinetics.com/pktutorial/1_2.html]
- 5. Bioactive component:The four steps of Bioavailability [https://www.biofortis.fr/2018/08/07/bioactive-componentthe-four-steps-of-bioavailability/]
- 6. Oral bioavailability of bioactive compounds; modulating ... [https://pubmed.ncbi.nlm.nih.gov/37096550/]
- 7. Dietary Zn—Recent Advances in Studies on Its ... [https://www.mdpi.com/1420-3049/30/13/2742]
- 8. Pharmacokinetics and Pharmacodynamics in Drug ... [https://amsbiopharma.com/pk-pd-studies-drug-development-adme/]
- 9. Reviews Pharmacokinetics in Drug Discovery [https://www.sciencedirect.com/science/article/abs/pii/S0022354916324832]
- 10. Drug discovery and development: introduction to the ... [https://www.frontiersin.org/journals/drug-discovery/articles/10.3389/fddsv.2023.1201419/full]
- 11. Quantitative Systems Pharmacology: A Framework for Context [https://pmc.ncbi.nlm.nih.gov/articles/PMC4996481/]
- 12. Differences in in vitro bioavailability, bioaccessibility, and ... [https://pubmed.ncbi.nlm.nih.gov/39967112/]
- 13. Terminology in the context of in vitro food digestion studies [https://www.sciencedirect.com/science/article/pii/S0308814625016759]
- 14. Gut microbiota: a new perspective for bioavailability of ... [https://www.nature.com/articles/s41538-025-00589-3]
- 15. The Bioavailability of Drugs—The Current State ... [https://www.mdpi.com/1420-3049/28/24/8038]
- 16. Trust your gut: Bioavailability and bioaccessibility of dietary ... [https://www.sciencedirect.com/science/article/pii/S2665927122000028]
- 17. What is the Difference Between Bioavailability Bioaccessibility ... [https://www.foodwasterecovery.group/what-is-the-difference-between-bioavailability-bioaccessibility-and-bioactivity-of-food-components/]
- 18. What is the Difference Between Bioavailability ... [https://www.linkedin.com/pulse/what-difference-between-bioavailability-bioactivity-food-galanakis]
- 19. Drug Absorption - StatPearls - NCBI Bookshelf - NIH [https://www.ncbi.nlm.nih.gov/books/NBK557405/]
- 20. Bioavailability of bioactive food compounds: a challenging ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3575927/]
- 21. Drug Absorption - Clinical Pharmacology [https://www.merckmanuals.com/professional/clinical-pharmacology/pharmacokinetics/drug-absorption]
- 22. Impact of gastrointestinal physiology on drug absorption in ... [https://www.sciencedirect.com/science/article/pii/S0928098720300695]
- 23. Bioavailability and bioaccessibility of food bioactive ... [https://pubmed.ncbi.nlm.nih.gov/33337033/]
- 24. Trust your gut: Bioavailability and bioaccessibility of dietary ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8787780/]
- 25. INFOGEST static in vitro simulation of gastrointestinal food ... [https://pubmed.ncbi.nlm.nih.gov/30886367/]
- 26. InfoGest Consensus Method - The Impact of Food ... - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK500165/]
- 27. INFOGEST [https://www.bio-cat.com/infogest/]
- 28. Application of the INFOGEST Protocol Using the BioXplorer ... [https://helgroup.com/application-notes/application-of-the-infogest-protocol-for-automated-digestion-simulation/?srsltid=AfmBOoocqdKCI9BaVCc7bZGFfpDl0giTbCqyREkldaKVQCD0AlmWVh_r]
- 29. Assessment of the bioaccessibility and bioavailability ... [https://www.sciencedirect.com/science/article/abs/pii/S2212429223002869]
- 30. Applications of the INFOGEST In Vitro Digestion Model to ... [https://pubmed.ncbi.nlm.nih.gov/36446138/]
- 31. Application of In Vitro Digestion Models in the Evaluation ... [https://www.mdpi.com/2304-8158/13/13/2135]
- 32. Evaluation of bioaccessibility and bioavailability of dietary ... [https://www.sciencedirect.com/science/article/abs/pii/S2212429224018595]
- 33. Application of in vitro bioaccessibility and bioavailability ... [https://www.frontiersin.org/journals/physiology/articles/10.3389/fphys.2012.00317/full]
- 34. Bioaccessibility study for toxic and essential elements in ... [https://www.sciencedirect.com/science/article/abs/pii/S2949824425002721]
- 35. In Vitro Bioaccessibility and Speciation of Toxic and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12428530/]
- 36. In Vitro Assessment of the Physiologically Relevant Oral ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10386267/]
- 37. Dietary Zn—Recent Advances in Studies on Its ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12251316/]
- 38. Insights from in vitro exploration of factors influencing iron ... [https://www.sciencedirect.com/science/article/pii/S0733521020307918]
- 39. Biomimetic culture substrates for modelling homeostatic ... [https://www.nature.com/articles/s41467-025-59459-x]
- 40. Generation of tetracycline-controllable CYP3A4-expressing ... [https://www.nature.com/articles/s41598-021-91160-z]
- 41. Articles Optimization of Drug-Drug Interaction Study Design ... [https://www.sciencedirect.com/science/article/abs/pii/S0090955624097435]
- 42. An In Vitro Digestion/Caco-2 Cell Culture System ... [https://www.sciencedirect.com/science/article/pii/S0022316623031127]
- 43. Prediction of blood–brain barrier and Caco-2 permeability ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12051285/]
- 44. Prediction of pharmacokinetic/pharmacodynamic ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1578117/full]
- 45. Investigation of bioequivalence - Scientific guideline [https://www.ema.europa.eu/en/investigation-bioequivalence-scientific-guideline]
- 46. M13B Bioequivalence for Immediate-Release Solid Oral ... [https://www.federalregister.gov/documents/2025/06/02/2025-09900/m13b-bioequivalence-for-immediate-release-solid-oral-dosage-forms-additional-strengths-biowaiver]
- 47. Regulatory Updates, September 2025 [https://www.caidya.com/resources/regulatory-updates-sept-2025/]
- 48. In Vivo Gene Editing for Rare Diseases Begins with ... [https://www.insideprecisionmedicine.com/topics/precision-medicine/in-vivo-gene-editing-for-rare-diseases-begins-with-umbrella-clinical-trial/]
- 49. Eleven quick tips to unlock the power of in vivo data science [https://pmc.ncbi.nlm.nih.gov/articles/PMC12005514/]
- 50. The Enduring Value of Organ Baths in Modern Drug ... [https://www.reprocell.com/blog/biopta/the-enduring-value-of-organ-baths-in-modern-drug-discovery]
- 51. Impact of dietary components and processing on mineral ... [https://www.sciencedirect.com/science/article/abs/pii/S0963996925017855]
- 52. Bioaccessibility and Bioavailability of Diet Polyphenols and ... [https://www.mdpi.com/1422-0067/24/4/3813]
- 53. Functional Foods Enriched With Bioactive Compounds [https://pmc.ncbi.nlm.nih.gov/articles/PMC12501769/]
- 54. Influence of Diet on the Bioaccessibility of Active ... [https://www.mdpi.com/1420-3049/30/22/4429]
- 55. Navigating Drug–Drug Interactions in Clinical Drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12454681/]
- 56. The influence of food matrix on the stability and ... [https://www.sciencedirect.com/science/article/abs/pii/S2949824423002021]
- 57. The food matrix: implications in processing, nutrition and ... [https://pubmed.ncbi.nlm.nih.gov/30040431/]
- 58. Food processing and nutrition [https://www.betterhealth.vic.gov.au/health/healthyliving/food-processing-and-nutrition]
- 59. Nutrient Loss During Food Preservation [https://www.auctoresonline.org/article/nutrient-loss-during-food-preservation]
- 60. The Effects of Storage on Quality and Nutritional Values ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6770199/]
- 61. Nanoencapsulation for drug delivery - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4464443/]
- 62. Nanoencapsulation in Drug Delivery: Everything You Need ... [https://oakwoodlabs.com/nanoencapsulation-in-drug-delivery-everything-you-need-to-know/]
- 63. The future of lipid-based drug delivery systems [https://www.cas.org/resources/cas-insights/future-lipid-drug-delivery]
- 64. The Mechanism of Nano-drug Delivery [https://link.springer.com/article/10.1007/s40495-019-00205-5]
- 65. Lipid-Based Drug Delivery Systems - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4590796/]
- 66. Lipid based formulations as supersaturating oral delivery ... [https://www.sciencedirect.com/science/article/pii/S0928098723001860]
- 67. Comparison of the Potential Relative Bioaccessibility of Zinc Supplements—In Vitro Studies - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10300733/]
- 68. A Narrative Review: In-vitro Methods for Assessing Bio- ... [https://www.frontiersin.org/journals/sustainable-food-systems/articles/10.3389/fsufs.2021.727533/full]
- 69. A Guide to Human Zinc Absorption: General Overview and Recent Advances of In Vitro Intestinal Models - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7146416/]
- 70. Comparison Study of Iron Bioaccessibility from Dietary ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6412228/]
- 71. Effects of polyphenols on the functional properties ... [https://www.sciencedirect.com/science/article/abs/pii/S0308814625021831]
- 72. Bioaccessibility and Bioavailability of Diet Polyphenols and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9961503/]
- 73. Impact of dietary components and processing on mineral ... [https://pubmed.ncbi.nlm.nih.gov/41214957/]
- 74. Bioavailability and Bioequivalence in Drug Development [https://pmc.ncbi.nlm.nih.gov/articles/PMC4157693/]
- 75. The 80-125% Bioequivalence Rule [https://www.pharmacytimes.com/view/debunking-a-common-pharmacy-myth-the-80-125-bioequivalence-rule]
- 76. Navigating the Regulatory Labyrinth: Compliance ... [https://www.drugpatentwatch.com/blog/compliance-challenges-in-generic-drug-development-lessons-learned/?srsltid=AfmBOoou9qVIGU2meHLJdNIFzEv7vnIgTeiHq2zwysZkTwtI4F2LnkOl]
- 77. The-History-of-the-FDA-80-125-Rule-for-Bioequivalence-of ... [https://aesnet.org/abstractslisting/the-history-of-the-fda-80-125-rule-for-bioequivalence-of-generic-drugs-including-aeds]
- 78. Where Did the 80-125% Bioequivalence Criteria Come ... [https://www.certara.com/blog/where-did-the-80-125-bioequivalence-criteria-come-from/]
- 79. Online Bioequivalence Study Sample Size Calculator [https://www.biostatistics.ca/online-bioequivalence-study-sample-size-calculator/]
- 80. Sample size determination in bioequivalence studies using ... [https://pubmed.ncbi.nlm.nih.gov/31276603/]
- 81. Bioaccessibility and associated concepts: Need for a ... [https://www.sciencedirect.com/science/article/abs/pii/S0924224424000499]
- 82. In vitro-In vivo Correlation: Perspectives on Model Development [https://pmc.ncbi.nlm.nih.gov/articles/PMC3099258/]
- 83. CMC Perspectives of In Vitro / In Vivo Correlation (IVIVC) ... [https://premier-research.com/perspectives/cmc-perspectives-of-in-vitro-in-vivo-correlation-ivivc-in-drug-development/]
- 84. In vivo–In Vitro correlation (IVIVC) in drug development [https://wjarr.com/content/vivo%E2%80%93-vitro-correlation-ivivc-drug-development-bridging-preclinical-and-clinical-outcomes]
- 85. How is in vitro–in vivo correlation (IVIVC) established? [https://synapse.patsnap.com/article/how-is-in-vitroE28093in-vivo-correlation-ivivc-established]
- 86. A surprisingly poor correlation between in vitro and in vivo ... [https://pubmed.ncbi.nlm.nih.gov/27215739/]
- 87. How much consumed caffeine is actually absorbed? ... [https://www.sciencedirect.com/science/article/pii/S0308814625028778]
- 88. Understanding Bioavailability: Maximizing the Potential of ... [https://www.openaccessjournals.com/articles/understanding-bioavailability-maximizing-the-potential-of-medications-and-nutrients-16657.html]
- 89. Improving the Bioaccessibility and Bioavailability of ... [https://www.mdpi.com/2076-3921/11/10/1931]
- 90. an in vitro digestion approach [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1666391/full]
- 91. Enhanced Bioaccessibility of Carotenoids, Antioxidants ... [https://www.mdpi.com/2227-9717/13/1/10]
- 92. Artificial intelligence-enhanced bioavailability studies [https://www.sciencedirect.com/science/article/abs/pii/S0924224425003395]
- 93. Bioavailability Enhancement and Formulation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11859484/]
- 94. Terminology in the context of in vitro food digestion studies [https://pubmed.ncbi.nlm.nih.gov/40288343/]
- 95. Bioequivalence Studies Market Size, Share, Trends 2025- ... [https://www.metatechinsights.com/industry-insights/bioequivalence-studies-market-2262]
- 96. An Open-Source Framework for Virtual Bioequivalence ... [https://pubmed.ncbi.nlm.nih.gov/40990143/]
- 97. Advancing drug development with “Fit-for-Purpose” modeling ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12436579/]
- 98. From Brand to Generic: Comprehensive Reverse ... [https://www.drugpatentwatch.com/blog/from-brand-to-generic-comprehensive-reverse-engineering-methodologies-in-drug-development/?srsltid=AfmBOorPqph9GSGBANKiVCtAa7teAH8ybCABa5lRsiR0Djx6O1IbD9D9]