Bioactive Compounds and the Gut Microbiota: Mechanisms, Therapeutic Applications, and Future Directions in Precision Medicine
This article synthesizes current research on the intricate interplay between dietary bioactive compounds and the gut microbiota, a dynamic interface critical for human health.
Bioactive Compounds and the Gut Microbiota: Mechanisms, Therapeutic Applications, and Future Directions in Precision Medicine
Abstract
This article synthesizes current research on the intricate interplay between dietary bioactive compounds and the gut microbiota, a dynamic interface critical for human health. Aimed at researchers, scientists, and drug development professionals, it explores the foundational mechanisms by which polyphenols, fibers, and other bioactives modulate microbial ecology and metabolite production. The scope extends to methodological advances in studying these interactions, the challenges of individual variability and drug-microbiome interactions (pharmacomicrobiomics), and the validation of these relationships in therapeutic contexts for conditions like inflammatory diseases, metabolic disorders, and cancer. The review concludes by highlighting the transformative potential of leveraging these insights for developing targeted, microbiome-informed therapies and precision nutrition strategies.
The Gut-Microbiota Interface: How Bioactive Compounds Shape Our Microbial Ecosystem
Dietary bioactive compounds are secondary metabolites derived from plant-based foods that exert significant effects on human health beyond basic nutrition, primarily through their modulation of the gut microbiota. These compounds, which include polyphenols, flavonoids, dietary fibers, and carotenoids, escape digestion in the upper gastrointestinal tract and reach the colon, where they are metabolized by the residing microbial communities. This biotransformation process produces a myriad of bioactive metabolites that influence host physiology, immune function, and metabolic pathways. Understanding the structural diversity, dietary sources, and microbial metabolism of these compounds is fundamental to advancing gut microbiota research and developing targeted nutritional interventions for chronic disease prevention and management. This technical guide provides a comprehensive overview of these key dietary bioactives, with emphasis on their classification, sources, and analytical approaches for researchers and drug development professionals.
Polyphenols
Definition and Classification
Polyphenols constitute a large family of naturally occurring phenols characterized by the presence of multiple phenolic rings with hydroxyl groups [1]. They are abundant in plants and structurally diverse, with molecular weights typically ranging from 500 to 4000 Daltons [1]. The White–Bate-Smith–Swain–Haslam (WBSSH) definition characterizes polyphenols as moderately water-soluble compounds with more than 12 phenolic hydroxyl groups and 5–7 aromatic rings per 1000 Da [1]. According to Quideau's more inclusive definition, polyphenols are compounds derived from the shikimate/phenylpropanoid and/or polyketide pathways, featuring more than one phenolic unit without nitrogen-based functions [1].
Polyphenols are classified into four principal categories based on their chemical structure: phenolic acids, flavonoids, stilbenes, and lignans [1] [2]. This classification reflects their biosynthetic origins and structural complexity, which directly influence their bioavailability and physiological effects.
Table 1: Major Classes of Polyphenols and Their Characteristics
| Class | Subclasses | Representative Compounds | Structural Features |
|---|---|---|---|
| Phenolic Acids | Hydroxybenzoic acids, Hydroxycinnamic acids | Caffeic acid, Ferulic acid | C1-C6 and C3-C6 backbones [2] |
| Flavonoids | Flavonols, Flavanols, Flavanones, Anthocyanins, Isoflavones | Quercetin, Catechin, Cyanidin, Daidzein | C6-C3-C6 skeleton with varying oxidation states [2] |
| Stilbenes | - | Resveratrol | C6-C2-C6 structure with two phenyl groups connected by a two-carbon methylene bridge [2] |
| Lignans | - | Secoisolariciresinol | Phenylpropane dimers [2] |
Polyphenols are widely distributed in the plant kingdom, with particularly high concentrations found in fruits, vegetables, cereals, beans, tea, coffee, honey, and red wine [2]. The most abundant polyphenols are the condensed tannins, found in virtually all families of plants, often concentrated in leaf tissue, epidermis, bark layers, flowers, and fruits [1]. Total phenolic content in plant tissues typically ranges from 1% to 25% of dry green leaf mass, varying widely depending on plant species, tissue type, and environmental conditions [1].
Bioavailability of polyphenols is generally low, with a large proportion of dietary polyphenols remaining unabsorbed along the gastrointestinal tract [2]. Their complicated structures and high molecular weights limit absorption in the small intestine, resulting in accumulation in the large intestine where they undergo extensive biotransformation by gut microbiota into bioactive, low-molecular-weight phenolic metabolites [2]. This microbial metabolism is crucial for unlocking the health-promoting effects of polyphenols.
Table 2: Major Dietary Sources of Polyphenols
| Food Category | Specific Sources | Dominant Polyphenol Types |
|---|---|---|
| Fruits | Berries, apples, grapes, pears, cherries | Flavonols, anthocyanins, flavanols, phenolic acids |
| Vegetables | Onions, kale, broccoli, tomatoes, parsley | Flavonols, flavones, phenolic acids |
| Beverages | Tea, coffee, red wine | Flavanols, flavonols, phenolic acids |
| Cereals & Legumes | Soybeans, whole grains | Isoflavones, phenolic acids, lignans |
| Nuts & Seeds | Flaxseed, almonds | Lignans, phenolic acids |
Experimental Protocols for Polyphenol Analysis
Extraction Methodologies
Efficient extraction is critical for accurate polyphenol analysis. Conventional solvent extraction remains the most widely used approach, with the choice of solvent depending on the polyphenol classes of interest [1]. Common protocols include:
- Solvent Selection: Water, methanol, methanol/formic acid, methanol/water/acetic or formic acid mixtures are typically employed. The polarity of the solvent should match the target polyphenols [1].
- Advanced Extraction Techniques: Ultrasonic extraction, heat reflux extraction, microwave-assisted extraction, critical carbon dioxide, high-pressure liquid extraction, and immersion extractors using ethanol have been developed to improve efficiency and reduce solvent consumption [1].
- Optimization Parameters: Extraction conditions including temperature, duration, solvent-to-solid ratio, particle size, and solvent concentration must be optimized for different raw materials [1].
Analysis and Quantification
- Separation Techniques: High-performance liquid chromatography (HPLC), especially reversed-phase liquid chromatography (RPLC), is the gold standard for polyphenol separation [1].
- Detection Methods: Diode array detectors coupled with mass spectrometry (MS) provide both structural identification and quantification capabilities [1].
- Quantification Approaches: Volumetric titration using permanganate as an oxidizing agent can quantify tannin content [1]. Colorimetric methods include the Porter's assay for specific polyphenol classes and the Folin-Ciocalteu reaction for total phenol content, with results expressed as gallic acid equivalents [1].
- Antioxidant Capacity Assays: The Trolox equivalent antioxidant capacity (TEAC) assay using ABTS radical cation, diphenylpicrylhydrazyl (DPPH), oxygen radical absorbance capacity (ORAC), and ferric reducing ability of plasma (FRAP) assays are commonly employed [1].
Flavonoids
Structural Classification and Properties
Flavonoids represent the largest subclass of polyphenols, with over 10,000 identified structures [3]. They share a common C6-C3-C6 skeleton consisting of two aromatic rings (A and B) connected by a three-carbon bridge that forms an oxygenated heterocycle (C ring) [3]. This basic structure allows for extensive structural variation through different substitution patterns, degrees of unsaturation, and oxidation states of the C ring.
Flavonoids are classified into seven major subclasses based on these structural modifications: flavones, flavonols, flavanones, isoflavonoids, flavanols, anthocyanins, and chalcones [3] [4]. Each subclass possesses distinct chemical properties that influence their biological activities, bioavailability, and microbial metabolism.
Table 3: Major Subclasses of Flavonoids and Their Characteristics
| Subclass | Structural Features | Representative Compounds | Key Dietary Sources |
|---|---|---|---|
| Flavonols | 3-hydroxyflavone backbone with a double bond between C2 and C3 | Quercetin, Kaempferol, Myricetin | Onions, kale, broccoli, apples, tea [5] [3] |
| Flavones | No substitution at C3 position | Apigenin, Luteolin | Parsley, celery, chamomile, mint [3] |
| Flavanones | Saturated C ring with no double bond between C2 and C3 | Naringenin, Hesperetin | Citrus fruits and peels [5] [3] |
| Isoflavonoids | B-ring attached at C3 position of C-ring | Genistein, Daidzein | Soybeans, legumes [5] [3] |
| Flavanols | Hydroxyl group at C3, no double bond between C2 and C3 | Catechin, Epicatechin | Tea, cocoa, apples, grapes [5] [3] |
| Anthocyanins | Flavylum cation structure, exist as glycosides | Cyanidin, Delphinidin | Berries, red grapes, red cabbage [5] [3] |
| Chalcones | Open-chain structure with no heterocyclic C ring | Phloretin, Arbutin | Tomatoes, pears, strawberries [5] |
Biosynthesis Pathways
Flavonoids are synthesized through the phenylpropanoid pathway, which originates from the aromatic amino acid phenylalanine [3]. The pathway involves a series of enzymatic reactions that sequentially modify the basic phenylpropanoid skeleton:
- Initial Conversion: Phenylalanine is converted to cinnamic acid by phenylalanine ammonia-lyase (PAL).
- Hydroxylation: Cinnamic acid undergoes hydroxylation to form p-coumaric acid.
- Activation: Formation of p-coumaroyl-CoA by 4-coumarate:CoA ligase.
- Core Structure Formation: Condensation of p-coumaroyl-CoA with three molecules of malonyl-CoA by chalcone synthase produces the first flavonoid, naringenin chalcone.
- Structural Diversification: Chalcone isomerase catalyzes the formation of the flavanone naringenin, which serves as the central intermediate for the biosynthesis of all other flavonoid classes through the action of various enzymes including hydroxylases, reductases, and glycosyltransferases.
This biosynthetic pathway is highly conserved across plant species, though the specific flavonoid profiles vary considerably depending on genetics, developmental stage, and environmental conditions.
Interaction with Gut Microbiota
The bidirectional interaction between flavonoids and gut microbiota represents a crucial aspect of their bioactivity. Most dietary flavonoids are poorly absorbed in the small intestine due to their glycosylated forms and complex structures, with approximately 90-95% reaching the colon [4]. Here, they undergo extensive microbial metabolism through three primary mechanisms:
- Deglycosylation: Removal of sugar moieties by bacterial glycosidases such as β-glucosidase, enhancing absorption.
- Ring Cleavage: Breakdown of the heterocyclic C ring producing various phenolic acids and other metabolites.
- Modification Reactions: Including dehydroxylation, demethylation, and decarboxylation.
These microbial transformations produce bioactive metabolites with enhanced absorption and diverse physiological effects. Simultaneously, flavonoids modulate the composition and function of gut microbiota, often promoting the growth of beneficial bacteria (e.g., Bifidobacterium, Lactobacillus) while inhibiting potential pathogens [4]. This reciprocal relationship significantly influences host health through multiple pathways, including strengthening intestinal barrier function, modulating immune responses, and regulating metabolic processes.
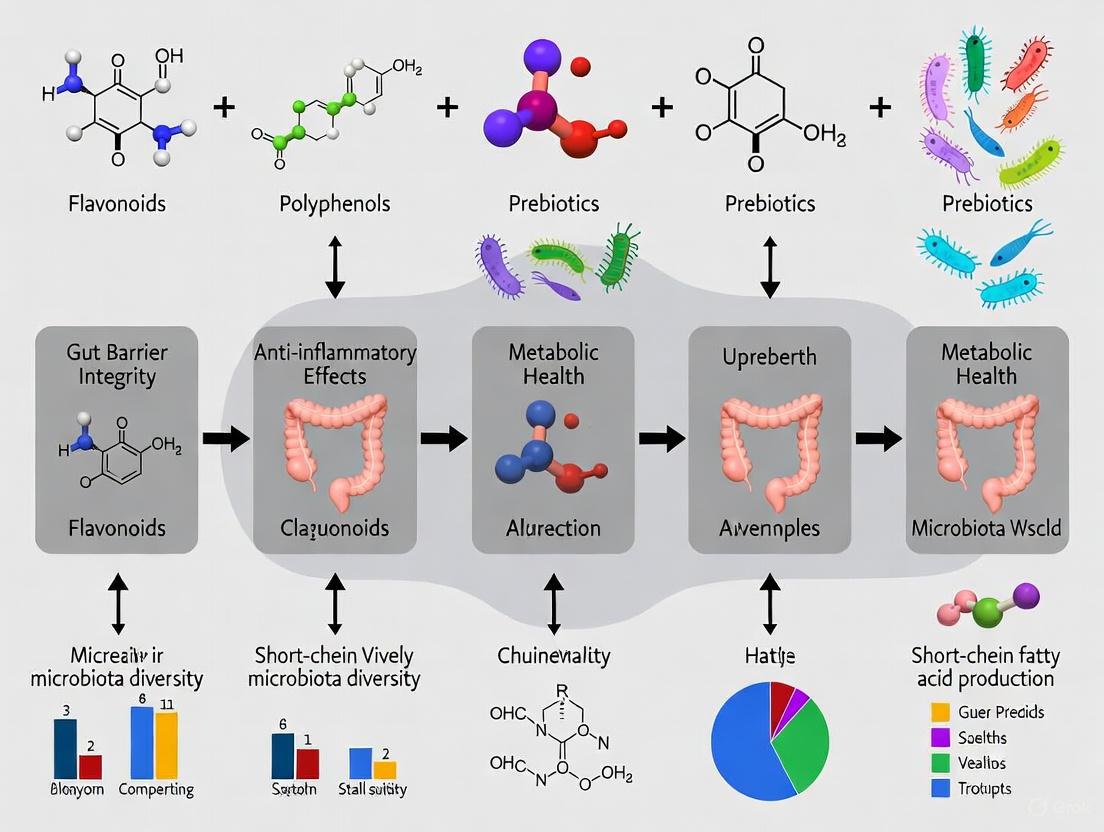
Diagram 1: Bidirectional Interaction Between Flavonoids and Gut Microbiota. This diagram illustrates how dietary flavonoids interact with gut microbiota, leading to the production of bioactive metabolites and modulation of microbial communities, ultimately influencing host health.
Dietary Fibers
Definition and Classification
Dietary fiber encompasses carbohydrate polymers with ten or more monomeric units that are resistant to hydrolysis by human endogenous enzymes and absorption in the small intestine [6]. This definition has been expanded to include indigestible oligosaccharides with 3-9 monomeric units, recognizing their similar physiological effects [6]. The traditional binary classification of soluble versus insoluble fiber is increasingly recognized as insufficient for predicting physiological effects, leading to proposals for more comprehensive frameworks that consider additional properties such as backbone structure, water-holding capacity, structural charge, fiber matrix, and fermentation rate [7].
Based on physiological properties and monomeric unit polymerization, dietary fibers are classified into three main types:
- Nonstarch Polysaccharides (NSPs): Include cellulose, hemicellulose, pectins, inulin, and various hydrocolloids with monomeric units ≥10 [6].
- Resistant Starches (RS): Classified into RS1 (physically inaccessible), RS2 (ungelatinized granular starch), RS3 (retrograded starch), RS4 (chemically modified), and RS5 (amylose-lipid complex) [6].
- Resistant Oligosaccharides (ROS): Include fructo-oligosaccharides (FOS), galacto-oligosaccharides (GOS), and xylo-oligosaccharides (XOS) with 3-9 monomeric units [6].
Fermentation by Gut Microbiota and Health Implications
Dietary fibers escape digestion in the upper gastrointestinal tract and undergo fermentation by colonic microbiota, producing beneficial metabolites including short-chain fatty acids (SCFAs) such as acetate, propionate, and butyrate [6]. The extent and rate of fermentation depend on fiber characteristics including degree of polymerization, particle size, solubility, and viscosity [6]. Fibers with low polymerization degrees are degraded more rapidly, while soluble, viscous fibers exhibit slower fermentation patterns [6].
The specific microbial metabolism of dietary fibers depends on the presence of carbohydrate-active enzymes (CAZymes), primarily glycoside hydrolases (GHs) and polysaccharide lyases (PLs), which vary across bacterial taxa [6]. This fiber-specific fermentation leads to selective stimulation of beneficial microbes, contributing to host health through multiple mechanisms:
- SCFA Production: Butyrate serves as the primary energy source for colonocytes, propionate regulates gluconeogenesis and satiety, and acetate influences cholesterol metabolism and lipogenesis.
- Microbial Diversity: Fiber fermentation promotes microbial richness and functional diversity, associated with improved metabolic health.
- Barrier Function: SCFAs enhance intestinal barrier integrity through upregulation of tight junction proteins.
- Immunomodulation: Fiber-derived metabolites regulate immune cell function and inflammatory responses.
Global dietary fiber intake ranges from 15-26 g/day, generally below recommended levels of 20-35 g/day [6]. This "fiber gap" has significant implications for gut microbiota composition and function, contributing to the increasing prevalence of non-communicable diseases including obesity, type 2 diabetes, and cardiovascular disorders [6].
Table 4: Dietary Fiber Classification, Sources, and Microbial Fermentation Characteristics
| Fiber Type | Subtypes & Examples | Primary Food Sources | Fermentation Characteristics | Primary Health Effects |
|---|---|---|---|---|
| Nonstarch Polysaccharides | Cellulose, Hemicellulose, Pectins, Inulin | Whole grains, vegetables, fruits, legumes | Varies from slow (cellulose) to rapid (inulin) fermentation | Stool bulking, SCFA production, prebiotic effects |
| Resistant Starches | RS1-RS5 (based on structure and source) | Legumes, unripe bananas, cooked and cooled potatoes, whole grains | Generally slow to moderate fermentation | Butyrate production, improved insulin sensitivity, enhanced satiety |
| Resistant Oligosaccharides | FOS, GOS, XOS | Chicory root, onions, leeks, asparagus, soybeans | Rapid and selective fermentation | Selective stimulation of bifidobacteria and lactobacilli, enhanced mineral absorption |
Carotenoids
Chemistry and Classification
Carotenoids are isoprenoid polyenes comprising approximately 750 naturally occurring pigments synthesized by plants, algae, and photosynthetic bacteria [8]. Their structure consists of isoprene (C5) units connected head-to-tail, forming symmetrical molecules typically containing 40 carbon atoms (tetraterpenoids) [9]. The extensive system of conjugated double bonds in the polyene chain is responsible for their characteristic yellow, orange, and red colors and their ability to absorb light in the UV-visible spectrum [9].
Carotenoids are broadly classified into two main categories:
- Carotenes: Hydrocarbon carotenoids without oxygen atoms (e.g., β-carotene, α-carotene, lycopene).
- Xanthophylls: Oxygenated derivatives containing hydroxyl, methoxy, epoxy, keto, or carboxy functional groups (e.g., lutein, zeaxanthin, astaxanthin, β-cryptoxanthin) [9] [8].
Carotenoids also differ in their terminal groups, which can be acyclic, monocyclic, or bicyclic. The most common dietary carotenoids include α-carotene, β-carotene, β-cryptoxanthin, lutein, zeaxanthin, and lycopene [8]. Among these, α-carotene, β-carotene, and β-cryptoxanthin function as provitamin A carotenoids that can be converted by the body to retinol, whereas lutein, zeaxanthin, and lycopene lack provitamin A activity [8].
Absorption, Metabolism, and Microbial Interactions
Carotenoid absorption is a complex process that requires release from the food matrix and incorporation into mixed micelles in the presence of dietary fat (minimum 3-5 g per meal) [8]. Food processing and cooking enhance carotenoid bioavailability by disrupting the food matrix [8]. Within enterocytes, carotenoids are absorbed via both passive diffusion and active transport through membrane transporters including Scavenger Receptor-class B type I (SR-BI), Cluster Determinant 36 (CD36), and Niemann-Pick C1 like intracellular transporter 1 (NPC1L1) [8].
Metabolic fate within enterocytes differs between provitamin A and nonprovitamin A carotenoids:
- Provitamin A Carotenoids: May be cleaved by β-carotene 15,15'-oxygenase 1 (BCO1) to produce retinal, which is further converted to retinol or retinoic acid, or by β-carotene 9',10'-oxygenase 2 (BCO2) to produce apocarotenals [8].
- Nonprovitamin A Carotenoids: Primarily cleaved by BCO2 [8].
The conversion efficiency of provitamin A carotenoids to retinol is influenced by vitamin A status, regulated through the intestine-specific homeobox (ISX) transcription factor that modulates expression of SR-BI and BCO1 [8]. Genetic polymorphisms in genes involved in carotenoid absorption, transport, and metabolism contribute to substantial interindividual variability in carotenoid status [8].
While carotenoid metabolism has traditionally been viewed as a host-centric process, emerging evidence indicates significant roles for gut microbiota in carotenoid biotransformation. Microbial enzymes may cleave carotenoids, producing bioactive metabolites such as apocarotenoids, and modulate carotenoid absorption efficiency through interactions with host absorption pathways.
Experimental Protocols for Carotenoid Analysis
Extraction Methods
Carotenoid extraction requires careful optimization due to their susceptibility to degradation during processing:
- Solvent Selection: Nonpolar solvents (hexane, petroleum ether) for carotenes; polar solvents (acetone, ethanol, methanol) for xanthophylls [9]. Ethanol and acetone are preferred for algal samples with high water content [9].
- Cell Disruption: Mechanical methods (homogenization, grinding) or enzymatic approaches to facilitate carotenoid release [9].
- Advanced Techniques: Microwave-assisted extraction, ultrasound-assisted extraction, supercritical fluid extraction, and pressurized liquid extraction improve efficiency and reduce solvent use [9].
- Saponification: Alkaline hydrolysis removes chlorophylls, lipids, and esters that interfere with analysis, though it should be omitted for alkali-sensitive carotenoids like astaxanthin and fucoxanthin [9].
Analysis and Quantification
- Spectrophotometric Methods: UV/Vis spectrophotometry for rapid determination of total carotenoid content based on specific absorption maxima [9].
- Chromatographic Techniques: High-performance liquid chromatography (HPLC) with UV/Vis or mass spectrometric detection for separation and quantification of individual carotenoids [9].
- Additional Techniques: Fourier transform infrared spectroscopy (FTIR) and nuclear magnetic resonance (NMR) for structural elucidation [9].
The Scientist's Toolkit: Essential Research Reagents and Methodologies
Research Reagent Solutions
Table 5: Essential Reagents and Materials for Bioactive Compound Research
| Reagent/Material | Application | Function | Technical Considerations |
|---|---|---|---|
| Methanol/Acetone with Acid Modifiers | Polyphenol and Flavonoid Extraction | Solvent system for efficient extraction of various phenolic compounds | Acid modifiers (formic/acetic acid) improve stability and recovery of acidic phenolics [1] |
| Hexane/Ethanol Solvent Systems | Carotenoid Extraction | Sequential extraction of nonpolar and polar carotenoids | Hexane for carotenes; ethanol for xanthophylls; consider safety and environmental impact [9] |
| Folin-Ciocalteu Reagent | Total Phenolic Content Assay | Oxidizing agent for colorimetric quantification of phenolics | Results expressed as gallic acid equivalents; interference from reducing agents [1] |
| DPPH/ABTS+ Radicals | Antioxidant Capacity Assessment | Stable radicals for measuring free radical scavenging activity | Results expressed as Trolox equivalents; different mechanisms of action [1] |
| β-Glucosidase Enzymes | Flavonoid Bioavailability Studies | Simulates intestinal deconjugation of flavonoid glycosides | Critical for assessing bioaccessibility; microbial sources often used [4] |
| Carbohydrate-Active Enzymes (CAZymes) | Dietary Fiber Characterization | Specific enzymes for fiber structure analysis | Glycoside hydrolases (GHs) and polysaccharide lyases (PLs) for fiber degradation studies [6] |
| Sodium/ Potassium Hydroxide in Methanol | Carotenoid Saponification | Alkaline hydrolysis for removal of interfering compounds | Omit for alkali-sensitive carotenoids; potential degradation issues [9] |
| C18 Solid-Phase Extraction Cartridges | Sample Clean-up | Purification and concentration of analytes prior to analysis | Removes interfering compounds; improves chromatographic performance [1] |
Advanced Methodological Approaches
In Vitro Fermentation Models
- Batch Culture Systems: Simple, high-throughput screening of microbial metabolism using fecal inocula in anaerobic conditions.
- Continuous Culture Models: Multi-stage systems (e.g., TIM-2, SHIME) simulating different colonic regions with more physiological relevance.
- Analytical Endpoints: SCFA analysis by GC-FID, microbial composition by 16S rRNA sequencing, metabolite profiling by LC-MS.
Omics Technologies
- Metagenomics: Reveals microbial community structure and genetic potential for bioactive compound metabolism.
- Metatranscriptomics: Identifies actively expressed genes involved in compound biotransformation.
- Metabolomics: Comprehensive profiling of microbial metabolites derived from dietary bioactives.
- Integration: Multi-omics approaches provide systems-level understanding of diet-microbiota-host interactions.
The intricate relationships between dietary bioactive compounds (polyphenols, flavonoids, dietary fibers, and carotenoids) and gut microbiota represent a frontier in nutritional science with profound implications for human health and disease management. The structural diversity of these compounds dictates their bioavailability, microbial metabolism, and ultimate physiological effects. As research in this field advances, sophisticated analytical approaches and model systems are enabling deeper understanding of the mechanisms underlying these interactions. Future research directions should focus on personalized nutrition approaches that account for interindividual variability in microbiota composition and function, the development of targeted delivery systems to enhance bioactive compound efficacy, and the integration of multi-omics technologies to unravel the complex networks connecting diet, microbiota, and host physiology. For researchers and drug development professionals, mastering the fundamental concepts and methodologies presented in this guide provides a critical foundation for advancing this rapidly evolving field and developing evidence-based nutritional interventions for gut microbiota modulation.
The human gut microbiota, a complex ecosystem of bacteria, archaea, viruses, and eukaryotes, encodes over 3 million genes—far exceeding the human genome. This review delineates the composition and function of the gut microbiota, framing it as a critical metabolic organ that biotransforms dietary components, synthesizes essential metabolites, and modulates host physiology. Within the context of bioactive compounds research, we explore how diet-derived phytochemicals, prebiotics, and other bioactives interact with microbial communities to influence host health. We present standardized methodologies for microbial profiling, quantitative data on core microbial associations with disease, and visualizations of key metabolic pathways. This synthesis aims to equip researchers and drug development professionals with advanced tools and frameworks for leveraging gut microbiota modulation in therapeutic interventions.
The human gastrointestinal tract hosts a dynamic community of trillions of microorganisms, collectively known as the gut microbiota. This community encodes a metabolic repertoire vastly exceeding human hepatic capabilities, with its gene set—the gut microbiome—estimated at approximately 3 million genes, 150 times larger than the human genome [10]. This "second genome" functions as an invisible organ [11], essential for nutrient extraction, vitamin synthesis, and metabolic regulation. The microbiota's composition remains relatively stable yet exhibits plasticity in response to dietary bioactive compounds, medications, and other environmental factors [12] [11]. Its metabolic output, including short-chain fatty acids (SCFAs), vitamins, and bile acid derivatives, profoundly influences local and systemic host physiology through intricate gut-organ axes, including the gut-brain, gut-liver, and gut-immune pathways [13] [12].
Composition and Core Functions of the Gut Microbiota
Microbial Composition and Enterotypes
The healthy human gut microbiota is dominated by six major bacterial phyla: Bacillota (formerly Firmicutes), Bacteroidota (formerly Bacteroidetes), Pseudomonadota (Proteobacteria), Actinomycetota, Verrucomicrobiota, and Fusobacteria [12]. Bacteroidota and Bacillota typically constitute the majority of the microbial community. At the species level, certain microbial members are consistently prevalent and abundant across populations, forming a core microbiota believed to be crucial for maintaining gut homeostasis [14]. Enterotype analysis often classifies the human gut microbiome into distinct community types, frequently characterized by dominance of either Bacteroides or Prevotella [15].
Table 1: Core Gut Microbiota and Key Functional Roles
| Microbial Taxon | Category | Relative Abundance/Prevalence | Primary Functional Role |
|---|---|---|---|
| Phocaeicola vulgatus [15] | Bacterial Species | High Abundance | Polysaccharide fermentation |
| Faecalibacterium prausnitzii [16] | Bacterial Species | Prevalent & Abundant | Butyrate production, anti-inflammatory |
| Akkermansia muciniphila [13] [16] | Bacterial Species | Prevalent | Mucin degradation, gut barrier integrity |
| Roseburia spp. [10] [16] | Bacterial Genus | ~2.7% average abundance [15] | Butyrate production from dietary fiber |
| Bifidobacterium [16] | Bacterial Genus | Variable | SCFA production, pathogen exclusion |
| Lactic Acid Bacteria (LAB) [17] | Functional Group | Variable | Bioactive metabolite production (e.g., organic acids) |
Central Metabolic Functions
The gut microbiota performs fundamental metabolic processes essential for host health:
- Nutrient Fermentation: Saccharolytic fermentation of undigested dietary carbohydrates, primarily dietary fibers, produces SCFAs (acetate, propionate, butyrate) and gases [10].
- Biosynthesis: The microbiota synthesizes essential vitamins (e.g., Vitamin K, B vitamins) and amino acids for the host [12] [16].
- Biotransformation: It metabolizes host-derived compounds, such as bile acids, and dietary xenobiotics, including plant polyphenols, significantly altering their bioavailability and bioactivity [18] [11].
The Gut Microbiota as a Metabolic Organ
Metabolism of Dietary Nutrients and Bioactive Compounds
The gut microbiota acts as a critical interface for the metabolism of dietary components, particularly those inaccessible to human digestive enzymes.
Carbohydrate Metabolism: The fermentation of microbiota-accessible carbohydrates (MACs) is a primary metabolic function. SCFAs, the key fermentation products, serve multiple roles: butyrate is the primary energy source for colonocytes and has anti-cancer properties, propionate regulates gluconeogenesis and satiety, and acetate is involved in cholesterol metabolism and lipogenesis [10]. The specificity of SCFA production is outlined in Table 2.
Table 2: Primary Bacterial Metabolites and Their Systemic Effects
| Metabolite | Primary Producers | Key Physiological Functions | Impact of Bioactive Compounds |
|---|---|---|---|
| Butyrate | Faecalibacterium prausnitzii, Roseburia spp., Eubacterium rectale [10] | Colonocyte energy source, anti-inflammatory, HDAC inhibition [10] [16] | Prebiotics (e.g., resistant starch) increase butyrate producers [16] |
| Propionate | Bacteroides species, Negativicutes [10] | Hepatic gluconeogenesis, satiety signaling [10] | Influenced by dietary fiber composition |
| Acetate | Many bacteria (e.g., Bifidobacterium) [10] | Cholesterol metabolism, lipogenesis, cross-feeding [10] | Produced by fermentative LAB [17] |
| Equol | Adlercreutzia equolifaciens [16] | Antioxidant, estrogenic properties | Derived from soy isoflavone metabolism by specific bacteria |
Protein Metabolism: When carbohydrate availability is low, gut bacteria can utilize proteins and amino acids for energy, producing metabolites like branched-chain fatty acids, ammonia, and phenolic compounds, which can be detrimental in high concentrations [10].
Metabolism of Bioactive Compounds: Dietary bioactive compounds, such as polyphenols from berries and cocoa, rely extensively on gut microbiota for activation. These compounds are often metabolized into more bioavailable forms by bacterial enzymes, enhancing their health benefits [18] [16]. For instance, specific bacteria like Adlercreutzia equolifaciens convert soy isoflavones into equol, a potent antioxidant [16]. Furthermore, microalgae-derived bioactive compounds (polysaccharides, peptides) have emerged as promising modulators of gut microbial composition and function [19].
Key Metabolic Pathways and Interactions
The following diagram illustrates the central metabolic pathways through which the gut microbiota processes dietary inputs and generates bioactive metabolites that influence host health.
Methodologies for Gut Microbiota Research
Profiling and Quantification Techniques
Advanced molecular techniques are essential for characterizing the gut microbiota's composition and functional potential.
- Metagenomic Next-Generation Sequencing (mNGS): This discovery-oriented approach allows for comprehensive analysis of all microbial genes in a sample, enabling taxonomic profiling and functional inference [14] [15]. A large-scale meta-analysis of 6,314 metagenomes demonstrated its power in identifying disease-associated microbial signatures across multiple studies [15]. However, mNGS is costly, requires sophisticated bioinformatics, and lacks standardization [14].
- Quantitative PCR (qPCR): For targeted, rapid quantification of specific bacterial taxa, qPCR is a highly effective method. A recently developed panel of 45 qPCR assays targeting gut core microbes allows for absolute quantification with high sensitivity (limit of detection: 0.1-1.0 pg/µL DNA) and strong correlation with mNGS results (Pearson’s r = 0.87) [14]. This method is ideal for tracking dynamic changes of key microbes in individuals over time [14].
Experimental Workflow for Microbiota Analysis
The following diagram outlines a standardized workflow for a gut microbiota study, from sample collection to data interpretation.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for Gut Microbiota Studies
| Reagent / Material | Function in Research | Example Application |
|---|---|---|
| QIAamp DNA Mini Kit [14] | High-quality genomic DNA extraction from fecal samples or bacterial cultures. | Standardized DNA preparation for downstream qPCR or NGS. |
| Species-Specific qPCR Primers [14] | Quantitative detection and enumeration of specific gut bacterial taxa (e.g., core microbes). | Tracking abundance of A. muciniphila or F. prausnitzii in intervention studies. |
| MetaPhlAn4 Database [15] | Reference database for taxonomic profiling of metagenomic sequencing data. | Identifying microbial community composition from mNGS data in population studies. |
| SYBR Green Master Mix [14] | Fluorescent dye for real-time detection of amplified DNA in qPCR assays. | Enabling quantification of target bacteria in qPCR reactions. |
| Gnotobiotic Mouse Models [13] [14] | Animals with defined microbiota, allowing for causal studies of microbial function. | Investigating the impact of a defined human microbial community on host physiology. |
Implications for Drug Development and Therapeutic Interventions
The recognition of the gut microbiota as a metabolic organ has profound implications for pharmacology and drug development. The microbiota can directly and indirectly modulate drug function by affecting drug absorption, metabolism, bioavailability, and toxicity—a phenomenon termed "pharmacomicrobiomics" [11]. Key mechanisms include:
- Biotransformation of Drugs: Gut bacterial enzymes can chemically modify drugs, altering their pharmacokinetics and pharmacodynamics [11].
- Modulation of Host Metabolism: Microbiota-derived metabolites like SCFAs can influence the expression of host drug-metabolizing enzymes in the liver [11].
- Impact on Mucosal Barrier: The microbiota affects the integrity of the gut mucosal barrier, which in turn influences oral drug absorption [11].
These interactions present both challenges and opportunities. Understanding an individual's gut microbiota composition could inform personalized drug dosing and selection. Furthermore, targeted modulation of the gut microbiota using prebiotics (e.g., specific fibers, microalgae-derived compounds [19] [16]), probiotics (e.g., specific lactic acid bacteria strains [17]), and faecal microbiota transplantation (FMT) [13] represents a novel therapeutic avenue for managing metabolic, inflammatory, and other microbiota-associated disorders.
The human gut microbiota, a complex ecosystem of bacteria, fungi, viruses, and protozoa, plays an indispensable role in maintaining host health by influencing metabolism, immune function, and disease protection [20]. The composition and function of this microbial community are profoundly shaped by various modifiable factors, with diet being the most significant [20]. Within our diet, bioactive compounds—non-nutrient food constituents with biological activity—serve as critical mediators of the host-microbiota interface [20]. These compounds, including polyphenols, dietary fibers, and antimicrobial phytochemicals, exert profound effects on microbial ecology through multifaceted mechanisms. This whitepaper delineates the direct and indirect pathways through which dietary bioactives modulate gut microbial communities, promoting beneficial bacteria while inhibiting pathogenic species, with implications for therapeutic development and clinical practice. Understanding these mechanisms provides a scientific foundation for developing targeted nutritional interventions to maintain gut eubiosis and prevent dysbiosis-associated diseases.
Direct Mechanisms of Microbial Modulation
Bioactive compounds directly influence gut microbiota through specific biochemical interactions that either enhance beneficial bacterial populations or directly inhibit pathogens.
Direct Antimicrobial Action Against Pathogens
Many plant-derived bioactive compounds exert direct antibacterial effects against pathogenic bacteria through well-characterized mechanisms (Table 1). These compounds target fundamental cellular structures and processes essential for bacterial survival and virulence.
Table 1: Direct Antimicrobial Mechanisms of Selected Bioactive Compounds
| Bioactive Compound | Source | Target Pathogens | Primary Mechanism of Action |
|---|---|---|---|
| Catechins (e.g., EGCG) | Green tea, cocoa | E. coli, Salmonella spp. | Inhibits bacterial DNA gyrase and dihydrofolate reductase [20] |
| Bacteriocins | Probiotic bacteria (e.g., Lactococcus lactis) | Various intestinal pathogens | Forms pores in bacterial membranes; acts as signaling molecules [21] |
| Allicin | Garlic | E. coli, Staphylococcus aureus | Inhibits biofilm formation; disrupts cellular functions [22] |
| Chitosan | Shellfish exoskeletons | E. coli, Salmonella typhi | Disrupts cell membrane integrity [23] |
| Flavonoids | Various plants | Staphylococcus aureus, E. coli | Disrupts bacterial cell membranes and inhibits biofilm formation [22] |
| Alkaloids (e.g., Berberine) | Various plants | Methicillin-resistant S. aureus (MRSA) | Targets nucleic acid synthesis and compromises cell wall integrity [22] |
| Terpenes (e.g., Carvacrol, Thymol) | Oregano, thyme | Foodborne pathogens | Disrupts cellular functions and enhances membrane permeability [22] |
Polyphenols such as catechins from green tea inhibit bacterial enzymes critical for DNA replication and folate synthesis, effectively suppressing pathogenic bacterial growth [20]. Similarly, bacteriocins—ribosomally synthesized antimicrobial peptides produced by probiotic bacteria—create pores in bacterial membranes, leading to cell death [21]. Plant antimicrobials including flavonoids, alkaloids, and terpenes disrupt cell membrane integrity, impede cell wall and protein synthesis, and prevent biofilm formation, ultimately causing bacterial cell death [22]. These direct antimicrobial properties provide a mechanistic basis for using bioactives as natural alternatives to synthetic antimicrobials, particularly in addressing antimicrobial resistance (AMR) [22].
Selective Promotion of Beneficial Bacteria
Bioactive compounds selectively enhance beneficial bacterial populations through prebiotic effects and metabolic support:
Prebiotic Fibers and Oligosaccharides: Non-digestible dietary components like inulin, oligosaccharides, and d-Tagatose selectively stimulate the growth and activity of beneficial bacteria such as Bifidobacterium and Lactobacillus [24] [25]. These compounds resist host digestion and serve as fermentable substrates for commensal bacteria, promoting their proliferation and metabolic activity [24].
Polyphenol Metabolism: Many dietary polyphenols have low bioavailability in the upper gastrointestinal tract, with 90-95% reaching the colon intact [20]. Gut microbiota metabolize these complex polyphenols into bioavailable metabolites through reactions including dehydroxylation, decarboxylation, and aromatic ring cleavage [20]. This metabolic relationship creates a symbiotic association where certain bacterial taxa obtain energy while generating beneficial metabolites for the host.
Synbiotic Combinations: Strategic combinations of prebiotics and probiotics demonstrate synergistic effects on gut microbiota. Prebiotics provide specialized substrates for probiotics, enhancing their survival and functionality within the competitive gut environment [24].
The following diagram illustrates the direct mechanisms through which bioactive compounds modulate gut microbiota:
Indirect Mechanisms of Microbial Modulation
Beyond direct antimicrobial effects, bioactives influence gut microbiota through complex host-mediated pathways that alter the gut environment and immune responses.
Enhancement of Gut Barrier Function
Bioactive compounds strengthen intestinal barrier integrity through multiple mechanisms:
Tight Junction Protein Regulation: Bioactive compounds such as hesperidin from citrus fruits enhance the expression of tight junction proteins including occludin and zonula occludens-1 (ZO-1) in intestinal epithelial cells [20]. This fortification of the epithelial barrier reduces bacterial translocation and systemic inflammation.
Mucosal Barrier Support: Compounds like chitosan have been shown to improve intestinal mucosal barrier function and regulate the expression of tumor necrosis factor-alpha (TNF-α) and tight junction proteins in colitis models [25].
Immune-Mediated Barrier Protection: By modulating host immune responses, bioactives create an intestinal environment less conducive to pathogen colonization while supporting commensal species.
Immunomodulation
The intestinal immune system maintains a delicate balance between tolerance to commensals and defense against pathogens. Bioactive compounds modulate this balance through several pathways:
Cytokine Regulation: Compounds like quercetin reduce pro-inflammatory cytokine production by modulating NF-κB and mitogen-activated protein kinase (MAPK) signaling pathways in intestinal epithelial cells [20]. Similarly, pistachio consumption reduces protein levels of TNF-α and IL-1β in serum and adipose tissue [25].
Immune Cell Differentiation: Certain polyphenols influence dendritic cell function and promote regulatory T cell differentiation through increased interleukin-10 (IL-10) production, fostering an anti-inflammatory environment [20].
Innate Immune Activation: Some microbial metabolites derived from bioactive compounds directly influence pattern recognition receptors on immune cells, fine-tuning inflammatory responses.
Metabolic Byproducts and Signaling Molecules
Beneficial gut bacteria ferment dietary bioactives to produce metabolites that profoundly influence host physiology and microbial ecology (Table 2).
Table 2: Key Microbial Metabolites Derived from Bioactive Compounds and Their Functions
| Metabolite | Producing Bacteria | Health Effects | Mechanisms |
|---|---|---|---|
| Short-Chain Fatty Acids (Butyrate, Propionate, Acetate) | Faecalibacterium prausnitzii, Roseburia spp., Bifidobacterium | Energy for colonocytes, anti-inflammatory, anti-tumor [21] | Lower colonic pH, inhibit pathogens, enhance barrier function [20] |
| Bile Acid Derivatives | Various gut microbes | Lipid digestion, glucose metabolism [26] | Activation of nuclear receptors (FXR, TGR5) [20] |
| Tryptophan Metabolites | Multiple species | Immune regulation, gut barrier maintenance [20] | Aryl hydrocarbon receptor activation [20] |
| Lactic Acid | Lactobacillus species | Lowers pH, inhibits pathogens [21] | Creates unfavorable environment for acid-sensitive pathogens [21] |
Short-chain fatty acids (SCFAs)—including acetate, propionate, and butyrate—are produced through bacterial fermentation of dietary fibers and resistant starches [21]. These metabolites lower colonic pH, inhibiting pH-sensitive pathogens while promoting acid-tolerant commensals [20]. Butyrate serves as the primary energy source for colonocytes and exhibits anti-inflammatory and anti-tumor properties [21]. Other microbial metabolites such as bile acid derivatives and tryptophan intermediates influence host metabolism and immune function through specific receptor interactions [20].
The following diagram illustrates the indirect pathways through which bioactives influence gut microbiota:
Experimental Approaches and Methodologies
Investigating bioactive-microbiota interactions requires sophisticated experimental models and analytical techniques.
In Vitro Screening Methods
Initial assessment of antimicrobial activity typically employs standardized in vitro assays:
Disk Diffusion Method: This classic technique involves impregnating filter paper disks with test compounds, placing them on agar plates inoculated with target pathogens, and measuring inhibition zones after incubation. Studies testing chitosan, EGCG, and garlic against E. coli and Salmonella typhi used this method with 50μL of 0.5%, 1%, and 2% solutions applied to 8mm discs [23].
Broth Dilution Methods: Minimum inhibitory concentration (MIC) determinations using serial dilutions of bioactive compounds in liquid culture provide quantitative data on antimicrobial potency.
Biofilm Assays: Specific assays quantify inhibition of biofilm formation—a key virulence mechanism—addressing challenges in food processing and clinical infections [22].
In Vivo and Ex Vivo Models
Animal models and human studies provide physiological context for bioactive effects:
Animal Studies: Rodent models allow investigation of complex host-microbe interactions. For example, studies with pistachio consumption demonstrated reduced Firmicutes/Bacteroidetes ratio and increased abundance of beneficial genera like Parabacteroides, Lactobacillus, and Anaeroplasma in mice [25].
Human Intervention Trials: Randomized controlled trials provide clinically relevant data. A study with orange juice consumption for two months significantly increased anaerobic bacteria and lactobacilli in healthy human subjects [20].
Ex Vivo Fecal Cultures: In vitro fermentation systems inoculated with human fecal microbiota simulate colonic conditions. Studies with different inulin-type fructans demonstrated prebiotic-specific increases in Bacteroides, Bifidobacterium, and Faecalibacterium [25].
Analytical Methods
Advanced analytical techniques characterize microbial community changes and metabolic outputs:
16S rRNA Gene Sequencing: Profiling bacterial communities before and after interventions identifies taxonomic shifts. Chemogenetic activation of hypothalamic POMC neurons revealed rapid, anatomically-specific changes in duodenal microbiota composition within 2-4 hours [26].
Metabolomics: Mass spectrometry-based profiling of microbial metabolites (SCFAs, bile acids, tryptophan derivatives) in feces, serum, and tissues connects microbial changes to functional outcomes [20].
Transcriptomics and Proteomics: RNA sequencing and protein analysis identify host pathways affected by bioactive-microbiota interactions, such as NF-κB and MAPK signaling in inflammation [20].
The following workflow represents a standardized experimental approach for evaluating bioactive effects on gut microbiota:
Research Reagent Solutions
The following table provides essential research tools for investigating bioactive-microbiota interactions:
Table 3: Essential Research Reagents for Studying Bioactive-Microbiota Interactions
| Reagent Category | Specific Examples | Research Applications | Key Functions |
|---|---|---|---|
| Prebiotics | Inulin, 1-kestose, Actilight, galactooligosaccharides [25] | Prebiotic specificity studies; microbial enrichment | Selective stimulation of beneficial bacteria; SCFA production |
| Probiotic Strains | Lactobacillus spp., Bifidobacterium spp., Saccharomyces boulardii [21] | Mechanistic studies; therapeutic applications | Direct introduction of beneficial species; bacteriocin production |
| Antimicrobial Compounds | Chitosan, EGCG, allicin, bacteriocins [23] [22] | Pathogen inhibition assays; biofilm studies | Membrane disruption; enzyme inhibition; biofilm prevention |
| Culture Media | Nutrient agar, Luria-Bertani medium, specialized fermentation media [23] | Microbial cultivation; fermentation studies | Support bacterial growth; simulate gut conditions |
| Analytical Standards | SCFA mixes, bile acids, phenolic metabolites [20] | Metabolite quantification; method validation | Calibration; identification of microbial metabolites |
| Molecular Biology Kits | 16S rRNA sequencing kits, RNA isolation kits, cytokine assays [26] [25] | Community analysis; host response measurement | Taxonomic profiling; gene expression; inflammation assessment |
Bioactive compounds modulate gut microbiota through an intricate network of direct and indirect mechanisms that collectively shape microbial ecology and function. Direct mechanisms include selective antimicrobial activity against pathogens and nutritional support for beneficial species, while indirect pathways involve enhancement of gut barrier function, immunomodulation, and production of microbial metabolites that influence host physiology. The therapeutic potential of these compounds is particularly relevant in addressing modern health challenges including antimicrobial resistance, metabolic diseases, and inflammation-related disorders. Future research should prioritize human clinical trials, personalized nutrition approaches accounting for interindividual microbiota variability, and systematic investigation of synergistic effects between different bioactive compounds. As our understanding of these mechanisms deepens, targeted modulation of gut microbiota through dietary bioactives represents a promising frontier in nutritional science and therapeutic development.
The human gut microbiota functions as a metabolic organ, converting dietary components into a diverse array of bioactive molecules that profoundly influence host physiology and disease susceptibility. Among these microbial metabolites, short-chain fatty acids (SCFAs), bile acids (BAs), and tryptophan derivatives represent three critical classes that mediate host-microbe communication through specialized molecular pathways [27] [28]. These microbiota-dependent metabolites (MDMs) serve as essential signaling molecules at the interface between prokaryotic and eukaryotic cells, regulating fundamental processes including immune cell differentiation, epithelial barrier integrity, metabolic homeostasis, and neuroendocrine signaling [27]. The structural diversity of these metabolites enables them to engage specific host receptors—including G protein-coupled receptors (GPCRs), nuclear receptors, and ligand-activated transcription factors—thereby orchestrating complex transcriptional and epigenetic programs across tissues [28]. This technical guide comprehensively details the biosynthetic pathways, molecular mechanisms, and research methodologies for these critical microbial metabolites, providing a foundational resource for advancing targeted therapeutic interventions in human health and disease.
Short-Chain Fatty Acids (SCFAs)
Production and Biosynthesis
Short-chain fatty acids are fatty acids with 1-6 carbon atoms, primarily produced from microbial fermentation of undigested dietary fibers in the colon and cecum [27]. The three most abundant SCFAs in the intestine are acetate (C2), propionate (C3), and butyrate (C4), which typically occur in a molar ratio of approximately 3:1:1 in healthy individuals [28]. Their production exhibits significant regional variation within the gastrointestinal tract, with total SCFA concentration substantially higher in the colon (ranging from 80±11 mmol/kg in the descending colon to 131±9 mmol/kg in the cecum) compared to the terminal ileum (13±6 mmol/kg) [27]. Following production, SCFAs are absorbed into the bloodstream via passive diffusion or carrier-mediated transport (primarily through monocarboxylate transporters MCT1 and SMCT1), though significant hepatic metabolism ensures only a small fraction reaches peripheral tissues [27]. Plasma concentrations in human peripheral venous blood are estimated at 19–146 μM for acetate, 1–13 μM for propionate, and 1–12 μM for butyrate [27].
SCFA biosynthesis pathways demonstrate notable microbial species specificity:
- Acetate is produced from pyruvate via acetyl-CoA or through the Wood-Ljungdahl pathway by various intestinal bacteria including Akkermansia muciniphila, Bacteroides spp., and Bifidobacterium spp. [27].
- Propionate is synthesized through three distinct pathways: succinate, acrylate, and propanediol pathways by specific microorganisms like Bacteroides spp. and Salmonella spp. [27].
- Butyrate is formed from two acetyl-CoA molecules through two enzymatic routes involving bacteria such as Anaerostipes spp., Roseburia spp., and Coprococcus eutactus [27] [28].
The intestinal pH plays a critical regulatory role in SCFA synthesis by shaping microbial composition and modulating enzyme activity. For instance, at pH 5.5, butyrate-producing bacteria such as Faecalibacterium prausnitzii become dominant, whereas at pH 6.5, genera including Bacteroides and Bifidobacterium preferentially produce acetate and propionate [28].
Mechanisms of Action and Immunomodulatory Roles
SCFAs exert their biological effects through three primary mechanisms: (1) serving as cellular energy substrates; (2) inhibiting histone deacetylases (HDACs); and (3) activating G protein-coupled receptors (GPCRs) including GPR41 (FFAR3), GPR43 (FFAR2), and GPR109A (HCAR2) [27] [28]. While early research suggested that SCFA-sensing GPCRs were predominantly expressed in innate immune populations (macrophages, dendritic cells, and intestinal Tregs) with minimal expression in conventional T lymphocytes, subsequent studies have demonstrated functional GPCR expression on differentiated effector T cells, revealing direct SCFA-GPCR signaling crosstalk [27].
The immunomodulatory effects of SCFAs include:
- Enhancing regulatory T cell (Treg) differentiation and function through HDAC inhibition and GPR43 activation [28].
- Reinforcing intestinal barrier integrity via upregulation of tight junction proteins [29] [28].
- Modulating inflammatory responses in macrophages and dendritic cells through HDAC inhibition and GPCR signaling [27] [28].
- Enhancing CD8+ T cell cytotoxicity and altering T cell memory potential [27].
Table 1: SCFA Concentrations in Biological Compartments
| SCFA | Colonic Concentration (mmol/kg) | Plasma Concentration (μM) | Primary Producing Bacteria |
|---|---|---|---|
| Acetate | 70-140 (proximal colon) [28] | 19-146 [27] | Akkermansia muciniphila, Bacteroides spp., Bifidobacterium spp. [27] |
| Propionate | 20-70 (distal colon) [28] | 1-13 [27] | Bacteroides spp., Phascolarctobacterium succinatutens, Veillonella spp. [27] [28] |
| Butyrate | 20-70 (distal colon) [28] | 1-12 [27] | Faecalibacterium prausnitzii, Anaerostipes spp., Roseburia spp., Coprococcus eutactus [27] [28] |
Figure 1: SCFA Biosynthesis and Immunomodulatory Mechanisms
Bile Acids
Production and Microbial Modification
Bile acids are synthesized by hepatocytes through cholesterol oxidation, resulting in primary bile acids including cholate (CA) and chenodeoxycholate (CDCA) [27]. These primary BAs are conjugated with glycine or taurine in the liver, rendering them more hydrophilic, and subsequently secreted into the intestinal lumen to facilitate nutrient digestion, transport, and absorption [27] [28]. Approximately 95% of conjugated primary BAs are reabsorbed in the terminal ileum and returned to the liver via enterohepatic circulation, while the remaining 5% undergo extensive microbial transformation in the cecum and colon into secondary bile acids [27].
Microbial transformation of BAs involves five key reactions:
- Deconjugation: The initial and crucial step mediated by bile salt hydrolases (BSHs) found in many bacteria including Bacteroides spp., Bifidobacterium, and Lactobacillus [27] [28].
- Dehydroxylation: Primarily carried out by anaerobic bacteria such as Clostridium, essential for converting primary BAs into secondary BAs like deoxycholic acid (DCA) and lithocholic acid (LCA) [27].
- Oxidation: Conversion of BAs to oxo-BAs mediated by position-specific hydroxysteroid dehydrogenases (HSDHs) [27].
- Epimerization: Requires coordinated effort of different HSDHs (e.g., 7α-HSDH and 7β-HSDH) [27].
- Re-conjugation: Recently identified fifth microbial modification producing novel BA amidates independent of glycine or taurine, such as phenylalanocholic acid and tyrosocholic acid [27].
Signaling Mechanisms and Biological Functions
BAs and their derivatives engage with specific receptors including the farnesoid X receptor (FXR), pregnane X receptor (PXR), vitamin D receptor (VDR), and G protein-coupled bile acid receptor 1 (GPBAR1, also known as TGR5) [27] [28]. Through these receptors, BAs regulate diverse physiological processes:
- Metabolic homeostasis: FXR activation regulates glucose and lipid metabolism [28] [30].
- Immune modulation: Secondary BAs influence the immune phenotype of hepatic Kupffer cells and modulate inflammasome activation through FXR and TGR5 signaling [28].
- Gastrointestinal function: BAs impact gut barrier function, motility, and mucosal immunity [30].
- Carcinogenesis: Increased levels of certain secondary bile acids, such as deoxycholic acid (DCA), are associated with genotoxic stress and pro-oncogenic signaling cascades in gastrointestinal cancers [28] [31].
Table 2: Primary and Secondary Bile Acids: Production and Receptors
| Bile Acid Type | Examples | Production/Modification | Primary Receptors | Biological Functions |
|---|---|---|---|---|
| Primary BAs | Cholate (CA), Chenodeoxycholate (CDCA) | Synthesized in liver from cholesterol [27] | FXR, PXR [27] [28] | Nutrient digestion and absorption [27] |
| Secondary BAs | Deoxycholic acid (DCA), Lithocholic acid (LCA) | Microbial dehydroxylation of primary BAs [27] | FXR, TGR5, VDR [27] [28] | Immune modulation, metabolic regulation [28] |
| Re-conjugated BAs | Phenylalanocholic acid, Tyrosocholic acid | Microbial re-conjugation independent of glycine/taurine [27] | Not specified | Emerging roles in host signaling [27] |
Figure 2: Bile Acid Metabolism and Signaling Pathways
Tryptophan Derivatives
Production and Biosynthetic Pathways
Tryptophan is an essential amino acid obtained from dietary protein that reaches the colon, where it undergoes extensive microbial metabolism into various bioactive indole derivatives [27] [32]. In the human body, tryptophan is metabolized via three main pathways: the kynurenine (Kyn) pathway, the serotonin (5-hydroxytryptamine) pathway, and the indole pathway, with microorganisms primarily utilizing the indole pathway to generate various derivatives [27] [32].
Key microbial tryptophan metabolites and their producing organisms include:
- Indole-3-propionic acid (IPA) and indole-3-lactic acid (ILA): Produced by Clostridium sporogenes (with the fldC subunit being indispensable for IPA biosynthesis) and Peptostreptococcus species including P. russellii, P. anaerobius, and P. stomatis [27].
- Indolealdehyde (IAld) and ILA: Generated by Lactobacillus species [27].
- Indoleacrylic acid (IA): Produced by Peptostreptococcus species [27].
- Kynurenine (Kyn) and serotonin: Some microorganisms can produce these metabolites and their downstream products such as 3-hydroxyanthranilic acid (3-HAA) and 3-hydroxykynurenine (3-H-Kyn) [27].
The average serum concentrations of microbial indole derivatives are estimated to be 60-80 μM for IPA and indolepyruvic acid and 0-20 μM for IAA and ILA in mice [27]. In humans, mean concentrations in healthy adults have been reported as 227 ng/ml for IAA, 191.1 ng/ml for IPA, and 31.5 ng/ml for ILA [27].
Biological Activities and Health Implications
Tryptophan-derived metabolites function as bioactive compounds that facilitate communication between bacteria and the host mainly by binding to specific receptors like the aryl hydrocarbon receptor (AhR) and pregnane X receptor (PXR) [27] [28] [32]. These interactions mediate diverse physiological effects:
- Mucosal defense enhancement: IPA enhances mucosal defense mechanisms through activation of the AhR-IL-22 signaling pathway [28].
- Immune regulation: Tryptophan metabolites help maintain the equilibrium between Tregs and Th17 cells, with insufficient AhR ligand availability increasing the risk of autoimmune disorders [28].
- Antioxidant and anti-inflammatory activities: Tryptamine and IPA demonstrate potent antioxidant and anti-inflammatory properties that may protect against age-related diseases [32].
- Gut-brain axis modulation: Tryptophan metabolites serve as crucial mediators in gut-brain communication, influencing neuronal function and potentially affecting neuropsychiatric conditions [33] [32].
Table 3: Microbial Tryptophan Metabolites and Their Functions
| Metabolite | Producing Microbes | Primary Receptors | Concentrations | Biological Functions |
|---|---|---|---|---|
| Indole-3-propionic acid (IPA) | Clostridium sporogenes, Peptostreptococcus spp. [27] | AhR, PXR [27] [28] | 191.1 ng/ml (human serum) [27] | Antioxidant, enhances mucosal defense [28] [32] |
| Indole-3-lactic acid (ILA) | Clostridium sporogenes, Lactobacillus spp. [27] | AhR [27] | 31.5 ng/ml (human serum) [27] | Immune modulation [27] |
| Indolealdehyde (IAld) | Lactobacillus spp. [27] | AhR [27] | Not specified | Mucosal immunity [27] |
| Kynurenine (Kyn) | Various microorganisms [27] | AhR [27] | Not specified | Immune regulation [27] |
Figure 3: Tryptophan Metabolism and Biological Functions
Experimental Approaches and Research Methodologies
Analytical Techniques for Metabolite Quantification
Accurate measurement of microbial metabolites requires sophisticated analytical platforms that can handle complex biological matrices while providing sufficient sensitivity and specificity:
- Gas Chromatography-Mass Spectrometry (GC-MS): Widely employed for SCFA analysis due to its ability to separate and quantify these volatile fatty acids [31]. Sample preparation typically involves acidification followed by liquid-liquid extraction or solid-phase microextraction.
- Liquid Chromatography-Mass Spectrometry (LC-MS): The preferred method for analyzing tryptophan derivatives and bile acids due to its superior sensitivity for semi-volatile and non-volatile metabolites [31]. Reverse-phase chromatography with C18 columns coupled to tandem mass spectrometry enables simultaneous quantification of multiple metabolite classes.
- Nuclear Magnetic Resonance (NMR) Spectroscopy: Useful for untargeted metabolite profiling and structural elucidation of novel microbial metabolites [31]. While less sensitive than MS-based methods, NMR provides complementary structural information without extensive sample preparation.
Genetic Manipulation of Microbial Producers
Elucidating the specific contributions of microbial genes to metabolite production requires targeted genetic approaches:
- CRISPR-Cas Systems: Enable precise gene knockouts in model gut bacteria such as Bacteroides thetaiotaomicron and Clostridium sporogenes to validate gene functions in SCFA and tryptophan derivative biosynthesis [27]. For example, the fldC subunit in C. sporogenes has been identified as indispensable for IPA biosynthesis through genetic approaches [27].
- Heterologous Expression: Biosynthetic genes from difficult-to-culture microbes can be expressed in model organisms like E. coli or Lactococcus lactis to confirm enzyme functions and reconstitute metabolic pathways [27].
In Vitro and Ex Vivo Model Systems
Several experimental models facilitate the study of host-microbe metabolic interactions:
- In vitro Bioreactors: Sophisticated continuous-culture systems that simulate different regions of the gastrointestinal tract, allowing controlled investigation of microbial metabolite production under varying environmental conditions [27].
- Intestinal Organoids: Three-dimensional structures derived from intestinal stem cells that recapitulate key aspects of intestinal epithelium physiology, enabling study of host-metabolite interactions in a human-derived system [30]. Filtered fecal supernatants from different donor populations can be applied to organoids to assess effects on enterocyte proliferation and maturation [30].
- Gnotobiotic Mouse Models: Germ-free animals colonized with defined microbial communities permit causal inference between specific microbes, their metabolites, and host phenotypes [30].
Table 4: Research Reagent Solutions for Microbial Metabolite Research
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| Analytical Standards | Deuterated SCFAs (d3-acetate), Stable isotope-labeled tryptophan derivatives, Certified bile acid standards | Quantification via GC-MS/LC-MS, Method validation [31] |
| Recombinant Receptors | Human FXR, TGR5, AhR, GPR43 | Receptor-ligand binding assays, Signaling studies [27] [28] |
| Genetic Tools | CRISPR-Cas systems for Bacteroides and Clostridium, Shuttle vectors for lactic acid bacteria | Microbial gene manipulation, Pathway engineering [27] |
| Cell-based Assays | Reporter cell lines (AhR-luciferase), Primary immune cell cultures, Intestinal organoids | Functional validation of immunomodulatory effects [27] [30] |
| Enzyme Inhibitors | HDAC inhibitors (Trichostatin A), BSH inhibitors, HSDH inhibitors | Mechanistic studies of metabolite actions [27] [28] |
The intricate metabolic interplay between gut microbes and their human host represents a fundamental biological dialogue maintained through chemical signaling molecules. SCFAs, bile acids, and tryptophan derivatives exemplify how structurally diverse microbial metabolites engage specialized host receptor systems to regulate immunity, metabolism, and tissue homeostasis. Current research continues to unravel the complexity of these interactions, revealing novel microbial transformations—such as the recently discovered re-conjugation of bile acids—and clarifying the molecular mechanisms through which these metabolites influence health and disease [27]. Emerging technologies including spatial metabolomics, synthetic biology, and AI-driven predictive modeling are poised to accelerate discovery in this field, enabling the development of targeted therapeutic strategies that leverage the gut microbiome's metabolic potential [28]. Future research directions should focus on establishing comprehensive metabolite-receptor interaction networks, validating clinical biomarkers, and developing precision interventions that account for interindividual variation in microbial metabolic capacity. As our understanding of these critical microbial metabolites deepens, they offer promising avenues for novel diagnostic and therapeutic approaches across a spectrum of conditions including inflammatory disorders, metabolic diseases, cancer, and age-related pathologies.
The gastrointestinal tract represents a critical interface between the external environment and the internal milieu, with its integrity being paramount for systemic health. This whitepaper delineates the sophisticated structure of the gut barrier, its dynamic interplay with the commensal microbiota, and the subsequent priming of the host immune system. Within the context of bioactive compounds research, we examine how dietary and microbial-derived factors modulate these relationships. The document provides a detailed analysis of core gut microbiota constituents, standardized methodologies for assessing barrier integrity and immune responses, and visualizes key signaling pathways. Furthermore, we present a curated toolkit of research reagents and solutions to support experimental replication and innovation in the field of mucosal immunology and gut microbiome research.
The intestinal epithelium, a single-cell layer covering a surface of over 300 m², serves as a primary physical and immunological barrier [34]. It is constantly exposed to a vast array of dietary antigens and a dense community of commensal microorganisms, collectively known as the gut microbiota, which contains over 10¹⁴ microorganisms and a gene repertoire (the microbiome) 10-fold larger than the human genome [34] [35]. The functional integrity of this barrier is not static but is dynamically regulated by complex interactions between host cells, microbial metabolites, and dietary components [34] [36]. Compromised barrier function, often referred to as "leaky gut," is characterized by increased intestinal permeability and has been associated with a spectrum of gastrointestinal and systemic disorders, including inflammatory bowel disease (IBD), irritable bowel syndrome (IBS), food allergies, obesity, diabetes, and neurological conditions [34] [35] [37]. A foundational understanding of the gut barrier's composition and function is essential for developing interventions aimed at preserving systemic health.
Architectural and Functional Composition of the Intestinal Barrier
The gut barrier is a multi-layered system comprising chemical, physical, and immunological components that function in concert to maintain homeostasis.
Cellular and Junction Protein Complexes
The intestinal epithelium is a rapidly self-renewing tissue, with stem cells giving rise to various specialized lineages: enterocytes (nutrient absorption), goblet cells (mucus secretion), enteroendocrine cells (hormone production), and Paneth cells [34]. Paneth cells, located in the small intestinal crypts, secrete antimicrobial peptides (AMPs) such as α-defensins, which are crucial for shaping the microbiota and defending against pathogens [34] [35].
The paracellular space between epithelial cells is sealed by the junctional protein complex, which includes tight junctions (TJs), adherens junctions, and desmosomes [34]. Tight junctions, primarily composed of proteins like claudin (CLDN) and occludin (OCLN), are dynamic structures that regulate the selective passage of ions, water, and solutes, while preventing the translocation of harmful luminal substances [34] [38]. Pro-inflammatory cytokines, such as TNF-α and IFN-γ, can dysregulate the expression of these junctional proteins, initiating a vicious cycle of increased permeability and inflammation [34].
Biochemical and Immunological Defense Layers
- The Mucus Layer: Goblet cells secrete gel-forming mucins, primarily MUC2, which form a bilayered structure in the colon. The outer layer is colonized by microbiota, while the inner layer is largely sterile and prevents direct contact between bacteria and the epithelium [34] [35]. This mucus barrier is not merely a physical shield; it also constrains the immunogenicity of intestinal antigens by imprinting dendritic cells (DCs) in an anti-inflammatory state [35].
- Secretory Immunoglobulin A (sIgA): The gut-associated lymphoid tissue (GALT) produces sIgA, which is transcytosed across the epithelium into the lumen. sIgA neutralizes pathogens and toxins and helps maintain host-commensal mutualism by coating bacteria and limiting their epithelial adhesion and invasion [34] [35].
- Antimicrobial Peptides (AMPs): Paneth cell-derived AMPs, including defensins and cathelicidins, provide innate immune defense by directly killing or inhibiting the growth of microbes, thereby contributing to the regulation of microbial community composition [35].
Table 1: Core Components of the Intestinal Barrier and Their Functions
| Barrier Component | Key Elements | Primary Function |
|---|---|---|
| Cellular Epithelium | Enterocytes, Goblet cells, Paneth cells | Nutrient absorption, mucus secretion, AMP production |
| Junctional Complex | Claudins, Occludin, ZO-1 | Regulation of paracellular permeability |
| Mucus Layer | Mucins (e.g., MUC2) | Physical separation of microbes from epithelium |
| Immunological Agents | sIgA, Antimicrobial Peptides (AMPs) | Pathogen neutralization, microbial population control |
Gut Microbiota and Immune System Cross-Talk
The gut microbiota is indispensable for the proper development and function of the host immune system. Germ-free (GF) animal models have been instrumental in revealing the profound immunodeficiency associated with the absence of microbial colonization [35].
Microbiota in Immune Development and Education
Early-life colonization is a critical period for immune maturation. The microbiota educates the host immune system by driving the development of gut-associated lymphoid tissues (GALT), including Peyer's patches [34] [35]. Key immune cells are primed by microbial signals:
- T Helper 17 (Th17) Cells: These pro-inflammatory cells are absent in GF mice and can be induced by specific commensals like segmented filamentous bacteria (SFB) [35].
- Regulatory T (Treg) Cells: Certain microbial products, such as Polysaccharide A (PSA) from Bacteroides fragilis, promote the differentiation of Treg cells, which are vital for sustaining immune tolerance and preventing aberrant inflammation [35].
- Immunoglobulin A (IgA): Microbial colonization stimulates the production of IgA, which is significantly reduced in GF animals [35].
Recognition and Signaling Pathways
The innate immune system uses Pattern Recognition Receptors (PRRs), including Toll-like receptors (TLRs) and NOD-like receptors (NLRs), to detect conserved Microbial-Associated Molecular Patterns (MAMPs).
- TLR Signaling: For instance, TLR5 recognizes bacterial flagellin. Signaling through TLRs is involved not only in host defense but also in maintaining epithelial integrity and regulating the composition of the commensal microbiota [35].
- Anti-inflammatory Pathways: PSA from B. fragilis is recognized by a TLR2/TLR1 heterodimer in cooperation with Dectin-1. This signaling cascade activates the PI3K pathway, inactivating GSK3β and leading to CREB-dependent expression of anti-inflammatory genes [35].
The following diagram illustrates the core signaling pathways in microbiota-immune system crosstalk:
Diagram 1: Microbiota-Immune Signaling Pathways. MAMPs from microbiota engage PRRs on host cells, activating pro-inflammatory (NFkB) or anti-inflammatory pathways. Microbial metabolites like SCFAs also directly strengthen the barrier and modulate immune cells.
Quantitative Profiling of Gut Core Microbiota: Methodological Frameworks
Accurate quantification of gut microbiota is vital for understanding its role in health and disease. While metagenomic next-generation sequencing (mNGS) is a powerful discovery tool, its limitations—including cost, turnaround time, and lack of standardization—hinder wide clinical application [14].
Absolute vs. Relative Quantification
A critical advancement in the field is the shift from relative to absolute quantitative analysis. Relative quantification, which expresses the abundance of a microbe as a proportion of the total sequenced community, can be misleading. For example, a decrease in one species' relative abundance might not reflect an actual decrease in its absolute numbers but rather an increase in another species [39]. Absolute quantification measures the true, concrete number of each microbial target, providing a more accurate picture of the microbial community [39]. A 2025 study on berberine highlighted that conclusions about drug-induced microbial changes drawn from absolute and relative quantification methods can differ significantly, underscoring the importance of absolute quantification for evaluating drug effects [39].
Quantitative Real-Time PCR (qPCR) Assay Panel
To address the need for rapid and precise quantification, a panel of 45 quantitative real-time PCR (qPCR) assays targeting gut core microbes with high prevalence and/or abundance has been developed [14]. This method offers a streamlined alternative to mNGS for targeted analysis.
- Primer Design: Species-specific genetic markers and primers were selected through comprehensive comparative genomic analysis. For 31 of the 45 core microbes, novel specific primers were designed to ensure high specificity [14].
- Performance Metrics: The established qPCR assays demonstrate high sensitivity, with a limit of detection ranging from 0.1 to 1.0 pg/µL of genomic DNA. The method showed strong consistency with mNGS (Pearson’s r = 0.8688, P < 0.0001) when analyzing the abundance of selected bacteria in human fecal samples [14].
- Application: This qPCR system enables simple, rapid (1-2 hours), and quantitative tracking of dynamic changes in core microbes, providing a valuable tool for understanding their role in health and disease [14].
Table 2: Key Methodologies for Gut Microbiota and Barrier Integrity Assessment
| Methodology | Key Feature | Application in Gut Research | Performance/Output |
|---|---|---|---|
| Absolute Quantitative Metagenomics | Measures total microbial load | Accurately evaluates drug effects on microbiota; overcomes limitations of relative abundance data [39] | Reveals true bacterial count changes; critical for pharmacological studies |
| qPCR Assay Panel | Targets 45 core gut microbes | Rapid, specific quantification of known bacterial targets; tracking dynamic changes in individuals [14] | LOD: 0.1-1.0 pg/µL; High correlation with mNGS (r=0.87) |
| Germ-Free (GF) Animal Models | Complete absence of microorganisms | Studies on microbiota's role in immune system development and barrier function [35] | Reveals immunodeficiency and underdeveloped lymphoid tissues in GF animals |
| ELISA & Cytokine Profiling | Quantifies protein biomarkers | Measures inflammatory cytokines (e.g., TNF-α, IL-6) in serum and colon tissue [39] | Quantifies systemic and local inflammatory responses; DAI scoring |
| Histological Examination (H&E Staining) | Visualizes tissue morphology | Assesses epithelial damage, crypt architecture, and immune cell infiltration [39] | Histopathological scoring (0-4 scale) for colitis severity |
The Scientist's Toolkit: Research Reagent Solutions
The following table catalogues essential reagents and models used in advanced gut barrier and microbiota research, as derived from the cited experimental protocols.
Table 3: Essential Research Reagents and Models
| Reagent / Model | Function / Application | Example Use Case |
|---|---|---|
| Dextran Sodium Sulfate (DSS) | Chemical inducer of colitis | Induces ulcerative colitis in mouse models for studying barrier disruption and inflammation [39] |
| Berberine (BBR) | Natural alkaloid with antimicrobial and anti-inflammatory properties | Ameliorates DSS-induced colitis; modulates gut microbiota composition; used at 0.2 g/mL in mouse studies [39] |
| Sodium Butyrate (SB) | Microbial metabolite (SCFA) | Enhances intestinal barrier function; reduces inflammation; used at 2.85 g/L in mouse studies [39] |
| PacBio Sequel II System | Full-length 16S rRNA gene sequencing | Provides high-resolution taxonomic profiling of gut microbiota; avoids amplification biases [39] |
| Specific Pathogen-Free (SPF) Mice | Standardized animal model | Host for experimental colonization and intervention studies; ensures defined baseline microbiota [39] |
| ELISA Kits (e.g., for TNF-α, IL-6) | Quantification of inflammatory cytokines | Measures cytokine levels in serum and colon homogenates to assess systemic and local immune responses [39] |
| FcRn Receptor | Mediates selective IgG transcytosis | Studied in rodent models to understand passive immune transfer and epithelial transport mechanisms [38] |
Concluding Perspectives
The integrity of the gut barrier and its sophisticated dialogue with the commensal microbiota form the bedrock of systemic immunity and health. The emergence of advanced quantitative techniques, particularly absolute quantification, is refining our understanding of how dietary bioactive compounds and microbial metabolites precisely modulate this interface. Future research must focus on translating these mechanistic insights into targeted therapeutic strategies that can restore and maintain barrier integrity in a wide range of communicable and non-communicable diseases. The experimental frameworks and tools detailed herein provide a roadmap for researchers and drug development professionals to navigate this complex, yet critically important, biological system.
From Bench to Bedside: Research Methods and Therapeutic Applications of Microbiota-Modulating Bioactives
The human gut microbiome, a complex ecosystem of bacteria, archaea, fungi, and viruses, significantly influences host physiology through metabolic, immunological, and neurological pathways [40]. Disruptions in this ecosystem, known as dysbiosis, are linked to pathologies including inflammatory bowel disease (IBD), obesity, type 2 diabetes (T2D), and neurodegenerative disorders [41] [40]. Advancing our understanding of this system, particularly the impact of bioactive compounds (BCs), requires the integrated application of advanced analytical techniques. Metagenomics, metabolomics, and culturomics have emerged as cornerstone methodologies for exploring microbial diversity, functional capacity, and host-microbe interactions. This technical guide delineates how these technologies, especially when used synergistically, are revolutionizing gut microbiota research by enabling the discovery of novel biomarkers, therapeutic targets, and mechanistic insights into the effects of dietary and therapeutic BCs, thereby paving the way for personalized microbiome-informed medicine [41] [42].
Core Analytical Techniques in Gut Microbiota Research
Metagenomics: Decoding Microbial Blueprints
Metagenomics involves the direct sequencing and analysis of genetic material recovered directly from environmental or clinical samples, bypassing the need for cultivation. This approach provides unparalleled insights into the taxonomic composition and functional gene repertoire of microbial communities [41].
- Methodologies: Two primary strategies are employed:
- Shotgun Metagenomics: Whole-genome sequencing of all DNA in a sample. This method facilitates strain-level identification, reconstruction of microbial genomes, and profiling of metabolic pathways and antimicrobial resistance (AMR) genes [41] [40]. For instance, mNGS (metagenomic Next-Generation Sequencing) has been successfully applied to cerebrospinal fluid for unbiased pathogen detection [41].
- 16S rRNA Gene Sequencing: Amplification and sequencing of the conserved 16S rRNA gene to profile taxonomic composition. While cost-effective for diversity studies, its resolution is often limited to the genus level and it provides inferential, rather than direct, functional data [43].
- Advanced Applications: Long-read sequencing technologies (e.g., Oxford Nanopore, PacBio) are overcoming limitations of short-read sequencing by resolving repetitive genomic elements and enabling complete genome assembly from complex samples, which is crucial for studying mobile genetic elements like plasmids [40].
Metabolomics: Profiling Microbial Chemical Output
Metabolomics focuses on the comprehensive analysis of small-molecule metabolites, providing a direct readout of microbial functional activity and its interaction with the host [44]. The gut microbiota produces a vast array of metabolites, including short-chain fatty acids (SCFAs), bile acids, and neurotransmitters, which play critical roles in health and disease [45].
- Analytical Platforms:
- Mass Spectrometry (MS) is prized for its high sensitivity, selectivity, and broad dynamic range. Common configurations include:
- Nuclear Magnetic Resonance (NMR) Spectroscopy: A highly reproducible and quantitative technique that requires minimal sample preparation, though it generally offers lower sensitivity than MS [44].
- Approaches: The field is divided into targeted analysis (quantifying specific classes of metabolites) and untargeted analysis (providing a global snapshot of the metabolome) [44].
Culturomics: Reviving the Uncultured Majority
Culturomics employs high-throughput cultivation under diverse conditions, combined with rapid identification (often via MALDI-TOF MS or sequencing), to isolate and characterize previously uncultured microorganisms [43]. It is essential for moving beyond correlative observations to mechanistic, functional validation.
- Core Principle: The use of extensive variations in culture conditions to mimic the native gut environment, thereby coaxing "unculturable" microbes to grow [47] [48]. It is estimated that a significant proportion of species in the Unified Human Gastrointestinal Genome database remain uncultured [43].
- Strategic Media Composition: Success hinges on optimizing growth conditions. Key modifications include [43] [48]:
- Carbon Sources: Using complex dietary fibers (inulin, pectin) and mucin to favor specialized microbes.
- Bioactive Compounds: Adding compounds like caffeine, polyphenols, or alkaloids to selectively modulate community growth.
- Physicochemical Conditions: Adjusting pH, temperature, and oxygen levels.
- Inhibitors and Selectors: Using bile acids, SCFAs, and antibiotics to inhibit fast-growing taxa and enrich for target organisms.
Integrated Multi-Omic Workflows and Experimental Protocols
The true power of these techniques is realized through their integration, creating a holistic view of the gut ecosystem from genetic potential to biochemical activity and culturable isolates.
A Representative Multi-Omic Workflow
The following diagram illustrates a synergistic workflow for investigating the impact of bioactive compounds on the gut microbiota.
Detailed Protocol for Metagenome-Guided Culturomics
The following protocol, adapted from Armetta et al. (2025), details the steps for targeted enrichment of gut microbes using bioactive compounds [47] [48].
Objective: To selectively enrich for specific gut microbial taxa and functions using a base growth medium modified with bioactive compounds.
Materials:
- Stool Samples: Collected from donors and processed anaerobically.
- Base Medium: Commercial Gifu Anaerobic Medium (GAM), modified with hemin, vitamin K1, and antioxidants [48].
- Bioactive Compounds: A library of compounds for media modification (e.g., caffeine, polyphenols, bile acids, antibiotics, SCFAs, complex carbohydrates) [48] [42].
- Anaerobic Chamber: For oxygen-free cultivation of gut anaerobes [43].
Procedure:
- Sample Preparation: Homogenize fresh stool samples in an anaerobic environment using a suitable buffer (e.g., phosphate-buffered saline).
- Media Modification: Prepare the base medium. Supplement with pre-determined concentrations of bioactive compounds from the library. For instance:
- Inoculation and Cultivation: Spread the homogenized stool sample onto Petri dishes containing the modified media. Incubate plates anaerobically at 37°C (or other optimized temperatures) for a specified period (e.g., 24-72 hours).
- Biomass Harvesting: After observing colony growth, scrape the biomass from the entire plate for community-level analysis.
- DNA Extraction and Sequencing: Extract microbial DNA from the harvested biomass. Perform deep whole-metagenome sequencing (e.g., Illumina shotgun sequencing).
- Data Analysis:
- Taxonomic Analysis: Compare the taxonomic profile of the cultured community against the original stool sample metagenome to identify enriched or depleted taxa.
- Functional Analysis: Assess the enrichment of specific metabolic pathways (e.g., dopamine metabolism, SCFA production) in the cultured community [47] [48].
Multi-Omic Integration for Biomarker Discovery
The diagram below outlines a protocol for discovering diagnostic biomarkers for conditions like cerebral infarction by correlating microbial features with blood metabolites [46].
Data Presentation: Techniques and Applications
Quantitative Profiles of Core Techniques
The following table summarizes the key characteristics, outputs, and applications of the three core techniques discussed.
Table 1: Comparative Analysis of Core Advanced Analytical Techniques
| Technique | Primary Analytical Target | Key Technologies/Platforms | Example Outputs | Strengths | Key Applications in Bioactive Compound Research |
|---|---|---|---|---|---|
| Metagenomics | Microbial DNA from a community | Illumina/Nanopore/PacBio sequencing; Bioinformatic pipelines (QIIME2, MG-RAST) | Taxonomic profiles; Functional gene catalogues; Antimicrobial Resistance (AMR) genes | Culture-independent; Comprehensive view of genetic potential; High-resolution strain tracking | Identifying microbial signatures altered by BCs; Predicting shifts in metabolic pathways (e.g., SCFA production) [41] [40] |
| Metabolomics | Small-molecule metabolites | LC-MS, GC-MS, NMR | Metabolite concentrations; Metabolic pathway activity; Biomarker panels | Direct functional readout; High sensitivity; Can reflect host and microbial activity | Quantifying microbial-derived metabolites (e.g., bile acids, indoles); Validating predicted functional shifts from metagenomics [44] [45] |
| Culturomics | Live microbial cells | High-throughput culture; Diverse growth media; MALDI-TOF MS/Rapid sequencing for ID | Pure microbial isolates; Defined culture collections; Phenotypic data (e.g., substrate utilization) | Enables functional validation and mechanistic studies; Recovers novel organisms | Targeted enrichment of microbes stimulated/inhibited by BCs; Providing isolates for downstream experimentation [47] [43] |
Impact of Bioactive Compounds in Culturomics Experiments
The selective effect of different bioactive compounds and conditions on cultured microbial communities is quantifiable. The table below summarizes findings from a culturomics study that tested 50 different modifications [48].
Table 2: Selective Impact of Media Modifications on Cultured Gut Microbiota
| Media Modification Category | Example Modifications | Observed Impact on Cultured Community |
|---|---|---|
| Bioactive Compounds (Alkaloids) | Caffeine | Enhanced enrichment of taxa associated with healthier subjects (e.g., Lachnospiraceae, Oscillospiraceae, Ruminococcaceae) [48] |
| Complex Carbohydrates | Inulin, Pectin | Robust biomass yield; Supported growth of specialized fiber-degrading taxa [48] |
| Bile Acids | Taurocholic Acid (TCA), Deoxycholic Acid (DCA) | TCA: Enhanced culturability of spore-forming bacteria. DCA: Led to lower phylogenetic diversity [48] |
| Antibiotics | Vancomycin, Chloramphenicol | Increased phylogenetic diversity by suppressing dominant taxa. Clindamycin, Tetracycline: Reduced phylogenetic diversity [48] |
| Physicochemical Conditions | pH 4, 10X Medium Dilution | pH 4: Associated with increased phylogenetic diversity. Dilution: Aided in recovering a higher diversity of unique species [48] |
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful implementation of the described protocols relies on a suite of essential reagents and materials.
Table 3: Key Research Reagent Solutions for Integrated Microbiome Studies
| Item | Specific Examples | Function/Application |
|---|---|---|
| Base Cultivation Media | Gifu Anaerobic Medium (GAM), Brain Heart Infusion (BHI), Fastidious Anaerobe Broth | Serves as a nutritional foundation for growing gut microbes; Often requires modification for optimal diversity [43] [48] |
| Media Additives & Selective Agents | Hemin, Vitamin K1, Bile Acids (e.g., TCA, DCA), Antibiotics (e.g., Vancomycin), Short-Chain Fatty Acids (e.g., Butyrate) | Promotes growth of fastidious anaerobes; Selectively enriches for or inhibits specific microbial groups based on their metabolic capabilities and tolerances [43] [48] |
| Bioactive Compound Library | Caffeine, Polyphenols (e.g., Quercetin, Resveratrol), Alkaloids, Dietary Fibers (Inulin, Pectin) | Used to investigate the prebiotic, inhibitory, or modulatory effects of dietary and therapeutic compounds on gut microbial composition and function [48] [42] |
| DNA/RNA Extraction Kits | E.Z.N.A. Stool DNA Kit | Efficiently and reliably extracts high-quality microbial nucleic acids from complex sample matrices like stool for downstream sequencing [46] |
| Chromatography & Separation | UHPLC columns, GC columns, Solid-Phase Extraction (SPE) cartridges | Separates complex mixtures of metabolites from biofluids (serum, urine, fecal water) prior to mass spectrometry analysis, reducing ion suppression and improving detection [44] [45] |
| Anaerobic Cultivation Systems | Anaerobic chambers (e.g., with gas mix of N₂/CO₂/H₂), Anaerobic jars | Creates and maintains an oxygen-free environment essential for the survival and growth of obligate anaerobic gut bacteria, which constitute the majority of the gut microbiota [43] |
The confluence of metagenomics, metabolomics, and culturomics is fundamentally advancing our capacity to decipher the complex interplay between bioactive compounds and the gut microbiome. Metagenomics provides the blueprint of microbial potential, metabolomics offers a dynamic snapshot of functional output, and culturomics brings elusive microbes into the laboratory for definitive experimentation. This integrated, multi-optic framework is transforming gut microbiome research from a descriptive, correlative science into a mechanistic and predictive discipline. It accelerates the discovery of novel therapeutic targets, diagnostic biomarkers, and a deeper understanding of how diet and therapeutics can be harnessed to manipulate the microbiome for improved human health. As these technologies continue to evolve—driven by long-read sequencing, artificial intelligence, and increasingly sophisticated culturing techniques—they promise to unlock personalized microbiome-based interventions with unprecedented precision.
The human gut microbiome, often termed the "forgotten organ" or "second genome," possesses metabolic capabilities that significantly expand the host's ability to process bioactive compounds from herbal medicines and dietary sources [49] [50]. With 100 times more metabolic capacity than the liver and encoding approximately 5 million genes—far surpassing the human gene count—this complex ecosystem plays a crucial role in determining the efficacy, bioavailability, and toxicity of natural products [51] [50]. The field of pharmacomicrobiomics has emerged as a natural extension of pharmacogenomics to study how microbiome variations influence drug response and disposition, particularly relevant for herbal compounds that undergo extensive microbial processing [51] [52].
This review explores the mechanistic basis of gut microbiota-mediated biotransformation of herbal and dietary compounds, focusing on enzymatic transformations, key microbial players, and experimental approaches for researchers investigating this rapidly evolving frontier. Understanding these processes is essential for drug development professionals seeking to harness microbiome capabilities for enhancing therapeutic efficacy and reducing adverse effects.
Fundamental Mechanisms of Microbial Biotransformation
Key Biotransformation Reactions
Gut microbiota employ diverse enzyme systems to transform herbal compounds through specific biochemical reactions that fundamentally alter their chemical properties and bioactivity [50] [53]. The table below summarizes the primary transformation types and their functional consequences.
Table 1: Major Biotransformation Reactions Mediated by Gut Microbiota
| Reaction Type | Chemical Process | Key Microbial Enzymes | Functional Outcome |
|---|---|---|---|
| Hydrolysis | Cleavage of glycosidic bonds | β-Glucosidase, β-glucuronidase, α-rhamnosidase | Enhanced bioavailability of aglycones |
| Reduction | Nitro→amine, sulfoxide→sulfide, azo bond cleavage | Nitroreductase, azoreductase | Prodrug activation, toxicity modulation |
| Decarboxylation | Removal of carboxyl groups | Decarboxylases | Altered compound lipophilicity |
| Dehydroxylation | Removal of hydroxyl groups | Dehydroxylases | Modified receptor binding affinity |
| Demethylation | Removal of methyl groups | Demethylases | Altered metabolic pathways |
| Dihydroxylation | Addition of hydroxyl groups | Dihydroxylases | Enhanced solubility properties |
Microbial Enzymatic Pathways
The gut microbiota performs direct enzymatic transformations that convert parent compounds into metabolites with altered pharmacological properties [49] [53]. These microbial enzymes include glucosidases, reductases, lyases, and transferases that significantly expand the metabolic repertoire available to the host [53]. For instance, β-glucuronidases produced by Escherichia coli catalyze the hydrolysis of baicalin to its more bioactive aglycone form, baicalein, which demonstrates enhanced anti-inflammatory and antioxidant effects through inhibition of Nrf2-ARE and NF-κB signaling pathways [53]. Similarly, feruloyl esterases from Bifidobacterium animalis, Lactobacillus reuteri, and other species hydrolyze chlorogenic acid to caffeic acid, which demonstrates hepatoprotective effects by increasing Nrf2 transcription [53].
Key Microbial Taxa and Their Metabolic Capabilities
Primary Biotransforming Bacteria
Specific bacterial genera possess specialized enzymatic capabilities for transforming different classes of herbal compounds. The table below highlights key microbial taxa and their documented transformation activities.
Table 2: Key Gut Microbes and Their Biotransformation Capabilities
| Microbial Taxon | Enzyme Systems | Herbal Substrates | Resulting Metabolites |
|---|---|---|---|
| Escherichia coli | β-Glucuronidase, Curcumin reductase | Baicalin, Curcumin | Baicalein, Dihydrocurcumin, Tetrahydrocurcumin |
| Bifidobacterium spp. | Feruloyl esterase, β-Glucosidase | Chlorogenic acid, Ginsenosides | Caffeic acid, Compound K |
| Lactobacillus spp. | Feruloyl esterase, β-Glucosidase | Chlorogenic acid, Various glycosides | Caffeic acid, Aglycones |
| Bacteroides spp. | α-L-Rhamnosidase, β-Glucuronidase | Rutin, Various flavonoids | Quercetin-3-O-glucoside, Aglycones |
| Eubacterium spp. | β-Glucosidase | Glycyrrhizin | 18β-Glycyrrhetinic acid |
| Streptococcus spp. | β-Glucosidase | Glycyrrhizin | 18β-Glycyrrhetinic acid |
Structural Modifications and Pharmacological Consequences
Microbial biotransformation typically converts polar compounds with low bioavailability into smaller, less polar, and more lipophilic metabolites with enhanced absorption characteristics [50]. For example, glycoside hydrolysis represents one of the most significant microbial transformations, where flavonoid glycosides with limited intestinal absorption are converted to their more bioavailable aglycone forms [54] [50]. Similarly, gut microbial β-glucosidases transform glycyrrhizin from licorice into 18β-glycyrrhetinic acid, which exhibits enhanced anti-inflammatory activity [53]. These transformations often unlock the therapeutic potential of herbal compounds that would otherwise demonstrate limited efficacy due to poor absorption.
Experimental Approaches for Studying Microbial Biotransformation
Methodological Framework
Investigating gut microbiota-mediated biotransformation requires integrated approaches that combine in vitro systems with in vivo validation. The following experimental workflow provides a systematic framework for studying these complex interactions.
Essential Research Reagents and Methodologies
The table below outlines key research reagents and methodologies essential for investigating microbial biotransformation of herbal compounds.
Table 3: Research Reagent Solutions for Microbial Biotransformation Studies
| Category | Specific Reagents/Methods | Research Application | Technical Considerations |
|---|---|---|---|
| Bacterial Cultures | Specific strains (E. coli, Bifidobacterium, Lactobacillus), Anaerobic culture systems | In vitro transformation studies, Enzyme characterization | Maintain anaerobic conditions; Use defined media for reproducible results |
| Enzyme Assays | β-Glucosidase, β-Glucuronidase, Nitroreductase activity kits | Quantifying specific enzymatic activities | Standardize against positive controls; Measure kinetics parameters |
| Analytical Instruments | UPLC-Q-TOF-MS, LC-MS/MS, GC-MS | Metabolite identification and quantification | High resolution needed for structural elucidation; Use authentic standards |
| Animal Models | Germ-free mice, Antibiotic-treated mice, Humanized microbiota mice | In vivo validation of microbial role | Control for cage effects; Consider inter-individual microbiota variation |
| Omics Technologies | Metagenomics, Metabolomics, Metatranscriptomics | Comprehensive pathway analysis | Integrate multiple data types; Apply appropriate bioinformatics tools |
| Cell-based Assays | Caco-2 cells, HepG2 cells, Primary hepatocytes | Absorption and toxicity screening | Validate with multiple cell lines; Use physiologically relevant concentrations |
Advanced Analytical Techniques
Metabolomics approaches, particularly ultra-performance liquid chromatography coupled with quadrupole time-of-flight mass spectrometry (UPLC-Q-TOF-MS), have become indispensable for identifying and characterizing microbial metabolites of herbal compounds [50]. These techniques enable researchers to track the metabolic fate of parent compounds and identify novel microbial metabolites with potential bioactivity. Integrated multi-omics approaches that combine metagenomics (for microbial composition), metatranscriptomics (for gene expression), and metabolomics (for metabolic profiling) provide comprehensive insights into the complex interactions between herbal medicines and gut microbiota [54] [51]. These methodologies allow researchers to connect specific microbial taxa and their enzymatic activities with the transformation of herbal compounds and subsequent pharmacological effects.
Implications for Drug Discovery and Precision Medicine
The understanding of gut microbiota-mediated biotransformation opens new avenues for drug discovery and development [54] [52]. By identifying specific microbial enzymes responsible for activating herbal compounds, researchers can develop enzyme-based bioprocessing systems for large-scale production of bioactive metabolites [53]. Furthermore, the emerging field of pharmacomicrobiomics offers potential for personalizing herbal medicine interventions based on an individual's gut microbiome composition [51] [52]. Clinical studies have demonstrated that inter-individual variation in gut microbiota significantly influences drug metabolism and efficacy, suggesting that modulating the gut microbiome through probiotics, prebiotics, or fecal microbiota transplantation could optimize therapeutic outcomes [51] [52].
The bidirectional interaction between herbal medicines and gut microbiota represents a promising frontier for developing novel therapeutic strategies that harness the metabolic power of the human microbiome. As research in this field advances, we anticipate increased integration of microbiome considerations into drug development pipelines and clinical practice, ultimately enabling more precise and effective use of herbal and dietary compounds for maintaining human health and treating disease.
The human gut microbiota, a complex community of microorganisms, has emerged as a central regulator of systemic health and disease. Through the continuous production of bioactive compounds, it influences physiological processes far beyond the gastrointestinal tract, forming critical communication axes such as the gut-brain, gut-liver, and gut-heart pathways [17]. Modern lifestyle factors can disrupt this delicate ecosystem, leading to dysbiosis that is increasingly implicated in the pathogenesis of a spectrum of chronic diseases [17]. This whitepaper examines the compelling evidence for therapeutic strategies that target or are influenced by the gut microbiota across four major disease areas: inflammatory bowel disease (IBD), obesity, diabetes, and cardiovascular diseases (CVD). By synthesizing recent advances and detailed methodological approaches, we provide researchers and drug development professionals with a technical framework for developing microbiota-informed therapeutics.
Inflammatory Bowel Disease (IBD)
Pathophysiology and Gut Microbiota Interactions
IBD, encompassing Crohn's disease (CD) and ulcerative colitis (UC), is characterized by chronic inflammation of the gastrointestinal tract. Its pathogenesis involves a complex interplay of genetic predisposition, environmental triggers, and dysregulated immune responses to gut microbiota [55]. Key genetic mutations identified in IBD, such as those affecting NOD2 and ATG16L1, impair innate immune recognition of bacterial components and disrupt autophagy pathways, leading to inadequate handling of intestinal bacteria and persistent inflammation [55]. The composition and function of the gut microbiome are fundamentally altered in IBD patients, with noted reductions in microbial diversity and weakened mucosal barriers that normally protect against commensal microorganism attack [55].
Advanced Therapeutic Modalities
Biological Agents and Small Molecules
Recent years have witnessed significant advancements in IBD therapeutics, moving beyond conventional aminosalicylates and corticosteroids to targeted biological agents and small molecules.
Table 1: Advanced Pharmacotherapies for Inflammatory Bowel Disease
| Therapy Class | Representative Agents | Mechanism of Action | Efficacy (Induction/Maintenance) | Key Clinical Trial Findings |
|---|---|---|---|---|
| Anti-TNF | Infliximab | Neutralizes tumor necrosis factor-alpha | Remission rates of 40%-69% in IBD patients [55] | Reduced colectomy rates to 10% at 54 weeks [55] |
| Anti-integrin | Vedolizumab | Blocks α4β7 integrin, inhibiting T-cell migration to gut mucosa | Remission rates of 40%-69% in IBD patients [55] | Gut-selective mechanism with minimal systemic immunosuppression |
| IL-12/23 Inhibitor | Ustekinumab | Targets IL-12 and IL-23 shared p40 subunit | Approved for moderate to severe UC [56] | Effective in patients failing anti-TNF therapy |
| JAK Inhibitors | Tofacitinib, Upadacitinib | Blocks Janus kinase signal transduction | Approved for moderate to severe UC [56] | Small molecule with oral administration |
| S1P Receptor Modulators | Ozanimod, Etrasimod | Sequesters lymphocytes in lymphoid tissue | Approved for moderate to severe UC [56] | Reduces lymphocyte migration to inflammatory sites |
The 2025 ACG UC Guideline update emphasizes treat-to-target with endoscopic improvement (Mayo Endoscopic Score [MES] 0 or 1) as a key treatment goal to achieve sustained steroid-free remission and prevent hospitalizations and surgery [56]. Therapeutic drug monitoring (TDM) is recommended to optimize dosing of biologics and minimize immunogenicity.
Microbiota-Targeted Interventions
Fecal Microbiota Transplantation (FMT) has emerged as a promising therapy for UC, with trials reporting 87.1% clinical remission at 48 weeks compared to 66.7% in the placebo group, along with higher endoscopic and histological remission rates [55]. A trial on multidonor-intensive FMT found a 27% clinical remission rate at week 8, significantly higher than the 8% observed in the placebo group [55]. The proposed mechanism involves restoration of a healthy microbial community, enhancement of short-chain fatty acid production, and improved gut barrier integrity.
Specific probiotic strains, particularly lactic acid bacteria (LAB), demonstrate significant potential for IBD management. Weissella confusa Wc1982 was shown to alleviate colitis in mice by suppressing pro-inflammatory cytokines while enriching Akkermansia muciniphila, a mucin-degrading bacterium with anti-inflammatory properties [17]. Similarly, Lactobacillus reuteri SBC5-3 suppressed NF-κB and MAPK signaling pathways in porcine epithelial cells, reducing inflammation [17].
Experimental Protocols for IBD Research
Protocol 1: Evaluating Anti-Colitis Efficacy of Microbial Strains
- Animal Model: Use 8-10 week old C57BL/6 mice with dextran sulfate sodium (DSS)-induced colitis.
- Intervention: Administer candidate bacterial strain (e.g., Weissella confusa Wc1982) at 1×10^9 CFU/day orally for 14 days.
- Disease Activity Index (DAI): Monitor daily for weight loss, stool consistency, and fecal blood.
- Histopathological Analysis: Collect colon tissue for H&E staining; score for inflammatory cell infiltration, crypt damage, and ulceration.
- Cytokine Profiling: Measure colonic TNF-α, IL-6, IL-1β, and IL-10 levels by ELISA.
- Microbiota Analysis: Perform 16S rRNA sequencing of fecal samples to assess microbial community changes.
- Statistical Analysis: Compare treated vs. control groups using one-way ANOVA with Tukey's post-hoc test [17].
Protocol 2: FMT Clinical Trial for UC
- Donor Screening: Comprehensive pathogen testing per FDA guidelines.
- Patient Selection: Adults with mild-moderate UC (Mayo score 4-10) despite 5-ASA therapy.
- Study Design: Randomized, double-blind, placebo-controlled trial.
- Intervention: Intensive multidonor FMT via colonoscopy at baseline and enemas subsequently for 8 weeks.
- Primary Endpoint: Clinical remission at week 8 (Mayo score ≤2 with no subscore >1).
- Secondary Endpoints: Endoscopic remission (MES 0-1), histological healing, and microbiome engraftment by shotgun metagenomics [55].
Obesity
Neuroendocrine Regulation of Energy Balance
Obesity arises from a chronic energy imbalance where intake exceeds expenditure, regulated by complex signaling along the gut-adipose-brain axis [57]. The hypothalamic arcuate nucleus (ARC) contains orexigenic neurons secreting neuropeptide Y (NPY) and agouti-related peptide (AgRP) that increase appetite, while anorexigenic neurons release pro-opiomelanocortin (POMC) derivatives that promote satiety [57]. Peripheral signals from the gut, including ghrelin (hunger-promoting), cholecystokinin (CCK), glucagon-like peptide-1 (GLP-1), and peptide YY (PYY) (satiety-promoting), integrate with central nervous system circuits to modulate food intake behavior [57].
Pharmacological Targeting of Incretin Pathways
Revolutionary advances in obesity pharmacotherapy have emerged with agents targeting incretin hormones.
Table 2: Anti-Obesity Medications Targeting Incretin Pathways
| Medication | Mechanism of Action | Formulation and Dosing | Weight Loss Efficacy | Common Adverse Events |
|---|---|---|---|---|
| Liraglutide | GLP-1 receptor agonist | Subcutaneous, 3.0 mg daily | 7-8% total body weight loss [57] | Nausea, vomiting, diarrhea, constipation |
| Semaglutide (Wegovy) | GLP-1 receptor agonist | Subcutaneous, 2.4 mg weekly | 14.9% total body weight loss at 68 weeks [58] | GI adverse events, gallbladder disease |
| Tirzepatide (Zepbound) | GLP-1 and GIP receptor dual agonist | Subcutaneous, 5-15 mg weekly | 20.9% total body weight loss at 72 weeks [58] | GI adverse events (nausea, diarrhea, vomiting) |
| Oral Semaglutide | GLP-1 receptor agonist | Oral, daily (dose varies) | Comparable to injectable semaglutide [58] | GI adverse events |
The Institute for Clinical and Economic Review (ICER) has assigned a rating of "A" for injectable semaglutide, oral semaglutide, and tirzepatide, indicating high certainty of substantial net benefit compared with lifestyle modifications alone [58]. Tirzepatide produces more weight loss than semaglutide but with some uncertainty about comparative cardiovascular benefits [58].
Microbiome-Mediated Mechanisms in Obesity
Gut microbiota composition differs significantly between obese and lean individuals, with specific microbial taxa influencing energy harvest, fat storage, and inflammation. Translational research has demonstrated that Bifidobacterium longum APC1472 exhibits anti-obesity effects in both healthy individuals with overweight/obesity and mouse models [33]. This strain attenuates the enduring effects of early-life high-fat high-sugar diet, including food intake dysregulation and hypothalamic molecular alterations [33]. Dietary supplementation with prebiotics like fructooligosaccharides (FOS) and galactooligosaccharides (GOS) can similarly modulate these pathways, potentially by increasing production of short-chain fatty acids (SCFAs) that influence satiety signaling and energy metabolism.
Experimental Protocols for Obesity Research
Protocol 1: Evaluating Anti-Obesity Effects of Microbial Strains
- Animal Model: Use C57BL/6 mice fed high-fat diet (45-60% kcal from fat) for 8-12 weeks.
- Intervention: Administer candidate probiotic strain (e.g., Bifidobacterium longum APC1472) at 1×10^9 CFU/day orally.
- Body Composition: Measure body weight weekly; assess fat and lean mass by EchoMRI at endpoint.
- Food Intake: Monitor daily caloric consumption using automated feeding monitors.
- Metabolic Parameters: Conduct oral glucose tolerance test (OGTT) and insulin tolerance test (ITT); measure serum lipids, leptin, and ghrelin.
- Gene Expression: Analyze hypothalamic expression of NPY, AgRP, POMC, and CART by qRT-PCR.
- Microbiota Analysis: Perform 16S rRNA sequencing of cecal content [33].
Protocol 2: Clinical Trial for Obesity Pharmacotherapy
- Study Design: Randomized, double-blind, placebo-controlled trial.
- Participants: Adults with BMI ≥30 kg/m² or ≥27 kg/m² with ≥1 weight-related comorbidity.
- Intervention: Once-weekly subcutaneous semaglutide 2.4 mg or tirzepatide 5-15 mg vs. placebo for 68-72 weeks.
- Primary Endpoint: Percentage change in body weight from baseline.
- Secondary Endpoints: Proportion achieving ≥5%, ≥10%, ≥15% weight loss; changes in cardiometabolic risk factors; patient-reported outcomes.
- Safety Monitoring: Comprehensive assessment of gastrointestinal and other adverse events [57] [58].
Diabetes
Therapeutic Evolution in Diabetes Management
Diabetes management has evolved from simple insulin replacement to sophisticated approaches that leverage gut-derived signals and advanced technologies. The American Diabetes Association's 2025 Standards of Care incorporate substantial updates, including broader use of continuous glucose monitors (CGM) for adults with type 2 diabetes on non-insulin therapies, expanded guidance on GLP-1 receptor agonists for cardiorenal benefits beyond weight loss, and emphasis on personalized nutrition approaches [59].
Technological and Biological Solutions
Artificial pancreas systems, integrating continuous glucose monitoring with automated insulin delivery, represent the cutting edge of type 1 diabetes management. These systems aim to mimic physiological insulin secretion through closed-loop algorithms that adjust insulin delivery based on real-time sensor glucose values [60]. While technological challenges remain, including accuracy of subcutaneous glucose sensors and delays in subcutaneous insulin absorption, practical options are expected within the next decade [60].
Islet cell transplantation offers a biological solution for type 1 diabetes, with the Edmonton protocol demonstrating initial success. However, challenges persist with limited donor tissue availability, declining graft survival over time, and toxicity of immunosuppressive regimens [60]. Research into alternative beta cell sources, including differentiation of stem cells and reprogramming of somatic cells, shows promise for overcoming these limitations [60].
Microbiome-Diabetes Interactions
The gut microbiome influences diabetes pathogenesis through multiple mechanisms, including modulation of inflammation, bile acid metabolism, and production of metabolites that affect insulin sensitivity. Personalized nutrition approaches recognize that individual microbial makeup determines response to dietary interventions. For instance, women possessing gut microbes that convert soy isoflavones to equol experience a 75% greater reduction in menopausal symptoms when supplemented with isoflavones compared to those lacking these species [33]. This principle extends to diabetes management, where interindividual variability in microbiome composition may determine responses to specific dietary patterns and prebiotic interventions.
Cardiovascular Diseases
Cardiovascular Benefits of Anti-Obesity Therapies
The cardiovascular benefits of newer anti-obesity medications extend beyond weight loss, demonstrating direct protective effects on cardiac tissue and metabolic processes. Clinical trials show that these medications can reduce the risk of major adverse cardiovascular events by up to 20% in patients with obesity and preexisting cardiovascular conditions [61].
The SUMMIT trial demonstrated that tirzepatide significantly reduced cardiovascular outcomes in patients with obesity-related heart failure with preserved ejection fraction (HFpEF). Cardiovascular death or worsening heart failure occurred in 9.9% of tirzepatide patients versus 15.3% of placebo patients (hazard ratio [HR], 0.62), with worsening heart failure reported in 8.0% of tirzepatide patients and 14.2% of controls (HR, 0.54) [61]. A cardiac magnetic resonance imaging substudy showed that tirzepatide therapy led to reduced left ventricular mass and pericardiac adipose tissue compared with placebo, changes that paralleled weight loss and may contribute to the reduction in heart failure events [61].
Inflammation as a Therapeutic Target
The recognition of inflammation as a critical participant in cardiac disease progression has opened new therapeutic avenues. Building on the CANTOS trial with the IL-1β inhibitor canakinumab, emerging research explores more complex inflammatory pathways [61]. Common inflammatory pathways participate in the pathogenesis of multiple acute and chronic diseases, suggesting potential for therapies with interdisciplinary benefit [61].
Microbiome-Cardiovascular Connections
The gut microbiome influences cardiovascular health through multiple mechanisms, including production of trimethylamine N-oxide (TMAO) from dietary precursors, modulation of systemic inflammation, and metabolism of bile acids that affect lipid homeostasis. Specific lactic acid bacteria (LAB) demonstrate lipid-lowering effects through bile salt hydrolase activity and SCFA production. Lacticaseibacillus paragasseri HM018, derived from breast milk, improved lipid and bile acid metabolism in hypercholesterolemic rats, while Levilactobacillus brevis RAMULAB54 from fermented sugarcane juice showed hypoglycemic and hypolipidemic effects through activation of PPAR-γ [17].
Integrating Therapeutic Strategies: The Gut Microbiota Link
Common Pathways and Cross-Disease Applications
The gut microbiota serves as a unifying element across these therapeutic areas, with microbial metabolites and components influencing disease processes through shared pathways. Short-chain fatty acids (acetate, propionate, butyrate) produced by microbial fermentation of dietary fiber exert anti-inflammatory effects through G-protein coupled receptor (GPCR) activation and histone deacetylase inhibition, relevant to IBD, obesity, diabetes, and CVD [17]. Bile acid metabolism by gut bacteria influences lipid homeostasis, glucose regulation, and inflammation through FXR and TGR5 signaling [17]. Tryptophan metabolism by microbial enzymes generates aryl hydrocarbon receptor ligands that modulate immune responses and barrier function [17].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Gut Microbiota-Disease Investigations
| Reagent/Category | Function/Application | Examples/Specific Products |
|---|---|---|
| Gut-on-a-Chip Systems | Microfluidic devices mimicking intestinal microenvironment for host-microbe interaction studies | Emulate intestinal villi structure with fluid flow and mechanical strain |
| Gnotobiotic Animal Models | Germ-free animals colonized with defined microbial communities for causal studies | Germ-free mice, rats; defined microbial consortia (e.g., Altered Schaedler Flora) |
| Anaerobic Culture Systems | Maintaining and cultivating oxygen-sensitive gut microbes | Anaerobic chambers, gas-packed systems, pre-reduced media |
| Multi-Omics Platforms | Comprehensive analysis of microbiome-host interactions | 16S rRNA sequencing, shotgun metagenomics, metabolomics, metatranscriptomics |
| Pathway Reporters | Monitoring specific microbial metabolic activities in real-time | GFP/luciferase-based biosensors for bile acid metabolism, SCFA production |
| Organoid Cultures | 3D stem cell-derived structures modeling intestinal epithelium | Intestinal organoids from human biopsies for host-pathogen interaction studies |
| Neuroactive Compound Assays | Screening for microbial production of neurotransmitters | ELISA, LC-MS for GABA, serotonin, dopamine, norepinephrine |
Visualizing Key Pathways and Workflows
Gut-Brain Axis Signaling in Obesity
IBD Therapeutic Development Workflow
The convergence of evidence across IBD, obesity, diabetes, and cardiovascular diseases reveals the gut microbiota as a fundamental modulator of therapeutic response and disease pathogenesis. Future research directions should prioritize:
Precision Microbiome Engineering: Developing personalized microbial consortia based on individual microbial genetics, host factors, and disease characteristics.
Mechanistic Deep-Diving: Elucidating precise molecular mechanisms by which microbial metabolites influence host pathways across organs.
Advanced Delivery Systems: Creating technologies for targeted delivery of microbial therapeutics to specific intestinal niches.
Longitudinal Monitoring: Implementing continuous microbiome surveillance to track therapeutic efficacy and disease progression.
Cross-Disease Biomarkers: Identifying universal microbial signatures predictive of treatment response across related conditions.
The integration of microbiota-focused strategies with established therapeutic modalities represents the next frontier in managing complex chronic diseases, offering the potential for more effective, personalized, and sustainable clinical outcomes.
The human gut microbiota, a complex ecosystem of trillions of microorganisms, plays a fundamental role in regulating host digestion, immunity, metabolism, and overall health [62] [63]. Bioactive compounds that modulate this microbial community offer promising therapeutic strategies for managing various diseases. This whitepaper provides an in-depth technical analysis of three key microbiota-targeting approaches: probiotics (live beneficial microorganisms), prebiotics (substrates selectively utilized by host microorganisms), and postbiotics (preparations of inanimate microorganisms and/or their components) [62] [64]. Within the context of a broader thesis on the impact of bioactive compounds on gut microbiota research, this review synthesizes current scientific evidence, mechanistic insights, experimental methodologies, and emerging applications, framing them as integrated biotic strategies for advancing human health and disease management.
Definitions, Mechanisms, and Key Components
Probiotics
Probiotics are defined as "live microorganisms that, when administered in adequate amounts, confer a health benefit on the host" [64]. They function through multiple mechanisms including competitive exclusion of pathogens, enhancement of gut epithelial barrier integrity, immunomodulation, and production of bioactive metabolites like short-chain fatty acids (SCFAs) [63] [65]. Common probiotic genera include Lactobacillus, Bifidobacterium, and the yeast Saccharomyces boulardii [62]. Emerging research focuses on next-generation probiotics (NGPs) and live biotherapeutic products (LBPs), which are designed for enhanced specificity and function in precision medicine applications [66] [65].
Prebiotics
Prebiotics are "a substrate that is selectively utilized by host microorganisms conferring a health benefit" [67] [64]. They primarily consist of non-digestible carbohydrates such as fructooligosaccharides (FOS), galactooligosaccharides (GOS), inulin, and human milk oligosaccharides (HMOs) [67]. Their mechanism of action involves selectively stimulating the growth and/or activity of beneficial gut bacteria (e.g., Bifidobacterium, Lactobacillus), leading to increased production of SCFAs, enhanced mineral absorption, and improved immune function [67] [63]. Recent research has expanded the prebiotic concept to include emerging candidates like polyphenols and microbial polysaccharides [68] [67].
Postbiotics
According to the International Scientific Association of Probiotics and Prebiotics (ISAPP), a postbiotic is a "preparation of inanimate microorganisms and/or their components that confers a health benefit on the host" [64]. This definition includes inactivated microbial cells (intact or broken) and their components, with or without metabolites [69] [64]. Key components include cell wall fragments (peptidoglycans, teichoic acids), surface proteins, and metabolites like SCFAs, organic acids, and antimicrobial peptides [69]. Advantages over probiotics include improved stability, easier storage and transportation, and reduced risks for immunocompromised individuals [69] [70]. The ISAPP definition does not require that the progenitor strain be a probiotic, allowing for development of novel postbiotics from microbes whose live forms may raise safety concerns (e.g., Akkermansia muciniphila) [70].
Quantitative Evidence of Health Benefits
Table 1: Documented Health Benefits of Probiotics, Prebiotics, and Postbiotics
| Biotic Category | Specific Strain/Substance | Health Benefit | Model System | Key Outcomes | Reference |
|---|---|---|---|---|---|
| Probiotic | Lactiplantibacillus plantarum CNTA 628 | Modulates lipid metabolism | C. elegans | >18% fat reduction; improved healthspan & oxidative stress resistance | [71] |
| Probiotic | Kluyveromyces lactis JSA 18 | Anti-obesity effects | HFD-fed mice | Reduced weight gain, liver/fat indexes, hyperlipidemia, serum triglycerides | [68] |
| Postbiotic | Heat-killed Pediococcus acidilactici GQ01 (G1PB) | Attenuates hyperuricemia | Mouse model | Reduced blood uric acid, creatinine; inhibited XOD activity; upregulated kidney ABCG2 | [68] |
| Postbiotic | Cell-free supernatant from fermented milk | Protection from infection | Mouse model | Protected mice from Salmonella infection | [69] |
| Prebiotic | Human Milk Oligosaccharides (HMOs) | Modulates infant gut microbiota | In vitro fermentation | Increased beneficial Bifidobacterium; production of acetate | [68] |
| Prebiotic | Inulin, FOS, GOS | Improves metabolic health | Human Clinical Trials | Enhanced SCFA production, improved glucose homeostasis, increased satiety | [67] |
Table 2: Evidence for Immune and Gut Barrier Effects
| Mechanistic Action | Probiotics | Prebiotics | Postbiotics |
|---|---|---|---|
| Pathogen Inhibition | Competitive exclusion; antimicrobial production [63] | - | Direct antibacterial activity [69] |
| Gut Barrier Strengthening | Enhances tight junction integrity [63] | Increases SCFA production (butyrate) [65] | Upregulates tight junction gene expression [70] |
| Immunomodulation | Increases anti-inflammatory cytokines (IL-10); decreases pro-inflammatory (TNF-α) [68] [63] | Modulates immune responses via SCFAs [63] | Induces anti-inflammatory cytokines; trains immune system [69] [63] |
| Microbiota Modulation | Increases beneficial bacteria; decreases pathobionts [63] | Selectively stimulates Bifidobacterium, Lactobacillus [67] | Increases beneficial SCFAs; restores healthy microbiota structure [68] [69] |
Experimental Protocols and Methodologies
Protocol for Evaluating Anti-Allergic Effects of Probiotics
This protocol is based on the study by Xu et al. using Lactobacillus kefiranofaciens ZW3 in an ovalbumin (OVA)-induced allergic mouse model [68].
- Animal Model: Female BALB/c mice (6-8 weeks old).
- Sensitization: Intraperitoneally inject with 20 µg of OVA adsorbed in 2 mg of aluminum hydroxide on day 0 and day 14.
- Probiotic Administration: Orally administer ZW3 (e.g., 1x10^9 CFU/day) daily for 28 days. The allergy group receives saline.
- Challenge: On days 21, 23, and 25, orally challenge with 50 mg of OVA.
- Sample Collection: On day 28, collect blood (for serum), spleens (for cytokine analysis), and intestinal contents (for microbiota analysis).
- Outcome Measures:
- Allergy Scores: Monitor for diarrhea, scratching, and lethargy after OVA challenge.
- Serum Immunoglobulins: Measure OVA-specific IgE (OVA-sIgE) levels using ELISA.
- Cytokine Profiling: Quantify Th1 (IFN-γ, IL-2) and Th2 (IL-4, IL-5, IL-10) cytokines in splenocyte culture supernatants or serum via ELISA or multiplex immunoassay.
- Microbiota Analysis: Analyze cecal or fecal content using 16S rRNA gene sequencing to assess changes in microbial composition (e.g., Muribaculaceae, Ruminococcaceae, Lachnospiraceae).
Protocol for Optimizing and Screening GABA-Producing Probiotics
This protocol is adapted from Cai et al. for screening high Gamma-aminobutyric acid (GABA)-producing Lactiplantibacillus plantarum strains from Chinese Paocai [68].
- Strain Screening:
- Inoculate candidate strains in MRS broth supplemented with monosodium glutamate (MSD, e.g., 5 g/L) as a GABA precursor.
- Incubate anaerobically at 37°C for 48-72 hours.
- Centrifuge cultures and filter the supernatant through a 0.22 µm membrane.
- Quantify GABA production using High-Performance Liquid Chromatography (HPLC) with a UV or fluorescence detector after derivatization.
- Optimization via Response Surface Methodology (RSM):
- Identify Critical Factors: Use a one-factor-at-a-time approach to identify key variables affecting GABA yield (e.g., initial pH, incubation temperature, MSD concentration, fermentation time).
- Design Experiment: Employ a central composite design (CCD) or Box-Behnken design to create an experimental matrix.
- Run Experiments and Model Fitting: Conduct fermentation runs as per the design and measure GABA yield. Fit the data to a quadratic polynomial model.
- Validation: Perform a verification experiment under the optimal conditions predicted by the model to validate the GABA yield (e.g., ~1158 mg/L for Lp. plantarum FRT7).
Protocol for Assessing the Efficacy of Postbiotics in Hyperuricemia
Based on the study by Ren et al. on Pediococcus acidilactici GQ01 and its heat-killed postbiotic G1PB [68].
- Animal Model: Establish a hyperuricemic mouse model, e.g., by oral administration of potassium oxonate and uric acid.
- Postbiotic Administration: Orally administer the postbiotic preparation (e.g., heat-killed bacteria, 1x10^9 cells/day or equivalent) daily for an intervention period (e.g., 2-3 weeks).
- Sample Collection: Collect blood (for serum) and tissues (liver, kidney) at the end of the study.
- Outcome Measures:
- Biochemical Markers: Measure serum uric acid, creatinine, and urea nitrogen levels using commercial assay kits.
- Enzyme Activity: Assess the activity of key enzymes in uric acid metabolism, such as xanthine oxidase (XOD) and adenosine deaminase (ADA), in liver homogenates or serum.
- Gene Expression Analysis: Isolate RNA from kidney and liver tissues. Use quantitative real-time PCR (qRT-PCR) to analyze the expression of transporters and enzymes (e.g., kidney ABCG2, URAT1, GLUT9; liver XOD).
- Gut Microbiota and SCFAs: Analyze fecal microbiota via 16S rRNA sequencing and quantify SCFA levels (acetic, propionic, butyric acid) in cecal contents or feces using GC or LC-MS.
Visualization of Pathways and Workflows
Probiotic and Postbiotic Immunomodulation
The following diagram illustrates the key mechanisms by which probiotics and postbiotics modulate the host immune system and strengthen the gut barrier.
Prebiotic Mechanism of Action
This diagram outlines the mechanism by which prebiotics selectively modulate the gut microbiota to confer health benefits.
Experimental Workflow for Probiotic/Postbiotic Efficacy
This workflow depicts a generalized experimental pipeline for evaluating the efficacy of probiotic or postbiotic interventions, from in vitro studies to mechanistic analysis.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents and Materials
| Reagent/Material | Function/Application | Examples / Technical Notes |
|---|---|---|
| Probiotic Strains | Live microbes for intervention studies; progenitor for postbiotics. | Lactobacillus spp., Bifidobacterium spp., Saccharomyces boulardii, Next-Generation Probiotics (NGPs) like Akkermansia muciniphila [66] [65] [70]. |
| Prebiotic Substrates | Selective growth substrates for beneficial gut bacteria. | Fructooligosaccharides (FOS), Galactooligosaccharides (GOS), Inulin, Human Milk Oligosaccharides (HMOs) [68] [67]. |
| Cell Culture Media | For in vitro propagation of strains and cell lines. | MRS broth (for lactobacilli), M17 broth (for streptococci), BHI; Cell culture media for epithelial (Caco-2) and immune (e.g., THP-1) cell lines [69] [71]. |
| Inactivation Equipment | Preparation of postbiotic samples. | Heat (autoclave, water bath), High-Pressure Processing (HPP), Ultrasound, Radiation equipment. Method choice impacts functionality [64] [70]. |
| Encapsulation Materials | Enhance probiotic stability and targeted delivery. | Calcium alginate, gelatin, carrageenan, chitosan. Used in microencapsulation to protect viability during storage and GI transit [68] [71]. |
| Anaerobic Workstation | Culture oxygen-sensitive gut microbes. | Essential for working with strict anaerobes (e.g., Faecalibacterium prausnitzii) to maintain viability and function [65] [70]. |
| ELISA Kits | Quantify proteins, cytokines, immunoglobulins. | Commercial kits for OVA-sIgE, cytokines (IL-4, IL-10, IFN-γ, TNF-α), metabolic markers (insulin, leptin) in serum/cell supernatants [68] [63]. |
| qRT-PCR Systems | Analyze gene expression of host/microbe. | Quantify expression of host genes (e.g., ABCG2, URAT1, tight junctions) and bacterial genes using specific primers and probes [68] [65]. |
| HPLC & GC-MS | Quantify metabolites and SCFAs. | HPLC for GABA, bile acids; GC-MS for SCFAs (acetate, propionate, butyrate) in fecal/cecal content or culture supernatant [68] [65]. |
| 16S rRNA Sequencing Reagents | Profiling gut microbiota composition. | Kits for DNA extraction from fecal samples, primers for 16S rRNA gene (V3-V4 region), sequencing platforms (Illumina MiSeq) [68] [65]. |
The integration of probiotics, prebiotics, and postbiotics represents a sophisticated, multi-layered strategy for modulating gut microbiota and influencing host health. The field is moving beyond generic formulations toward personalized nutrition and precision medicine [66]. Advances in microbiome profiling, metabolomics, and genetic engineering are enabling the development of next-generation probiotics and tailored symbiotic combinations designed to correct individual-specific dysbiosis [66] [65]. Furthermore, the emergence of postbiotics addresses critical challenges associated with live microorganisms, offering enhanced stability and safety for broader applications in functional foods and pharmaceuticals [69] [70]. Future research will focus on elucidating detailed molecular mechanisms, standardizing production processes, and conducting robust clinical trials to validate the efficacy of these biotic strategies, solidifying their role in advancing gut microbiome research and therapeutic applications.
This case study investigates the demonstrated capacity of specific lactic acid bacteria (LAB) strains to modulate host inflammatory responses and lipid metabolism. Framed within a broader thesis on the impact of bioactive compounds on gut microbiota research, this analysis synthesizes findings from recent in vitro and in vivo studies. It details the mechanistic roles of LAB-derived bioactive metabolites, presents quantitative efficacy data in structured tables, and outlines standardized experimental protocols. The evidence underscores the potential of targeted LAB strains as novel therapeutic interventions for managing chronic metabolic and inflammatory diseases, providing a scientific foundation for future research and development in the field of pharmacobiotics.
The gut microbiota constitutes a complex ecosystem of microorganisms that engage in a symbiotic relationship with the host, playing a pivotal role in regulating immunity, strengthening the intestinal epithelium, and maintaining metabolic homeostasis [17]. Lactic acid bacteria (LAB), a diverse group of Gram-positive, non-sporulating bacteria, are of particular interest due to their established presence in fermented foods and the human gastrointestinal tract [72]. Beyond their traditional role in food preservation, many LAB strains are recognized for their probiotic functionalities, influencing host physiology through direct interaction with host cells and via the production of bioactive compounds [17] [73].
Within the framework of gut microbiota research, LAB are increasingly investigated as live biotherapeutics. Their ability to produce short-chain fatty acids (SCFAs), bacteriocins, and neuroactive compounds like γ-aminobutyric acid (GABA) positions them as key modulators of the microbiota-gut-brain axis and systemic metabolism [72]. The recent reclassification of the Lactobacillus genus into more specific genera (e.g., Lacticaseibacillus, Lactiplantibacillus) has further refined our understanding of their strain-specific functions [17]. This case study delves into the scientific evidence for selected LAB strains, focusing on their anti-inflammatory and lipid-lowering properties, thereby illustrating the profound impact of microbial bioactive compounds on human health.
Results: Efficacy Data of LAB Strains
Anti-inflammatory Effects
The anti-inflammatory potential of specific LAB strains has been demonstrated in various models of colitis and immune cell assays. The following table summarizes key findings from recent studies.
Table 1: Summary of Anti-inflammatory Effects of Specific LAB Strains
| LAB Strain | Model System | Key Anti-inflammatory Outcomes | Mechanistic Insights |
|---|---|---|---|
| Weissella confusa Wc1982 | Murine Colitis Model | Alleviated colitis symptoms; suppressed pro-inflammatory cytokines; enriched Akkermansia muciniphila [17]. | Immunomodulation via cytokine suppression and beneficial microbiota modulation. |
| Lacticaseibacillus reuteri SBC5-3 | Porcine Epithelial Cells | Suppressed NF-κB and MAPK signaling pathways [17]. | Inhibition of key pro-inflammatory signaling cascades. |
| Ligilactobacillus salivarius CGMCC17718 | Heat-stressed Mice | Enhanced antioxidative capacity [17]. | Reduction of oxidative stress, a key driver of inflammation. |
| Lactiplantibacillus plantarum SY6 | In Vitro & Cheese Model | Produced bacteriocins and organic acids with antimicrobial activity [74]. | Pathogen exclusion via direct antimicrobial action. |
Lipid-Lowering Effects
Numerous studies have confirmed the role of specific LAB strains in regulating lipid metabolism, often via the activity of microbial bile salt hydrolases (BSH) and the production of SCFAs. The quantitative results are consolidated in the table below.
Table 2: Summary of Lipid-Lowering Effects of Specific LAB Strains
| LAB Strain / Product | Model System | Key Lipid-Lowering Outcomes | Proposed Primary Mechanism |
|---|---|---|---|
| Lacticaseibacillus paragasseri HM018 (from breast milk) | Hypercholesterolaemic Rats | Improved lipid and bile acid metabolism [17]. | Modulation of bile acid metabolism and hepatic lipid pathways. |
| LAB-Fermented Chinese Cabbage Roots | Experimental Animal Models | Lowered cholesterol and triglyceride levels [75]. | Upregulation of hepatic cholesterol catabolism; downregulation of lipogenesis genes. |
| Levilactobacillus brevis RAMULAB54 (from fermented sugarcane juice) | In Vivo Study | Hypoglycaemic and hypolipidaemic effects [17]. | Activation of PPAR-γ signaling. |
| Lactococcus lactis subsp. lactis G423 | Broilers | Improved lipid metabolism [17]. | SCFA production and BSH activity. |
| Lactiplantibacillus plantarum L-27-2 & Pediococcus lactis L-14-1 | Murine Model | Cholesterol-lowering effects [17]. | Bile salt hydrolase (BSH) activity impacting cholesterol metabolism. |
Experimental Protocols
To ensure reproducibility and provide a practical guide for researchers, this section outlines detailed methodologies for key experiments cited in this case study.
Protocol for Assessing Anti-inflammatory Effects in Monocytic Cell Lines
This protocol is adapted from studies investigating plant-derived bioactives and can be applied to evaluate LAB-derived metabolites [76].
Cell Culture and Differentiation:
- Maintain human monocytic cell lines (e.g., U-937 or THP-1) in RPMI-1640 medium supplemented with 10% Fetal Bovine Serum (FBS) and 1% antibiotic-antimycotic solution at 37°C in a 5% CO₂ atmosphere.
- Induce differentiation into macrophage-like cells by treating with Phorbol 12-myristate 13-acetate (PMA) (e.g., 100 nM for 48 hours).
Treatment:
- Differentiated cells are treated with the LAB-derived compound of interest (e.g., cell-free supernatant, purified metabolite) for a predetermined period.
- A positive control for inflammation (e.g., Lipopolysaccharides - LPS) and a negative control (vehicle only) should be included.
Gene Expression Analysis:
- Extract total RNA from treated cells using a commercial kit.
- Perform quantitative Real-Time PCR (qRT-PCR) to measure the expression of key inflammatory markers (e.g., TNF-α, IL-6, IL-1β) and anti-inflammatory markers (e.g., IL-4). Use stable reference genes like GAPDH for normalization [76].
Protein Expression Analysis:
- Isolate total protein from cell lysates.
- Determine protein expression levels of key targets (e.g., LOX-5, MPO, TNF-α) via Western Blot analysis using specific primary and HRP-conjugated secondary antibodies [76].
Molecular Docking (In Silico):
- To predict compound-protein interactions, conduct molecular docking studies using software such as AutoDock Vina. Assess the binding affinity of the bioactive compound to human target proteins like IL-4, 5-Lipoxygenase (LOX-5), Myeloperoxidase (MPO), and TNF-α [76].
Protocol for Evaluating Lipid-Lowering Effects in Animal Models
This protocol synthesizes methods from hypercholesterolemic rodent studies [17] [75].
Animal Model Induction and Grouping:
- Utilize male/female rodents (e.g., C57BL/6 mice or Sprague-Dawley rats). Induce hyperlipidemia by feeding a high-fat, high-cholesterol diet for 6-8 weeks.
- Randomly assign animals to experimental groups: (i) Normal diet control, (ii) High-fat diet control, (iii) High-fat diet + LAB strain (administered via oral gavage at a defined CFU/day), (iv) High-fat diet + positive control drug (e.g., atorvastatin).
Sample Collection:
- At the end of the intervention period, collect blood samples after fasting for the analysis of serum lipids (Total Cholesterol, LDL-C, HDL-C, Triglycerides).
- Euthanize animals and dissect liver tissue for lipid content analysis and histopathological examination (e.g., Oil Red O staining).
Biochemical and Molecular Analyses:
- Serum Lipid Profiling: Measure cholesterol and triglyceride levels in serum using commercial enzymatic kits.
- Gene Expression in Liver Tissue: Analyze the expression of genes involved in lipid metabolism (e.g., PPAR-γ, HMG-CoA reductase, CYP7A1) in liver tissue via qRT-PCR.
- Bile Salt Hydrolase (BSH) Activity: Assess BSH activity of the LAB strain in vitro using a glycocholate-deconjugation assay.
Mechanisms of Action: Pathways and Metabolites
The beneficial effects of LAB are mediated through a complex interplay of microbial metabolites and the modulation of host signaling pathways.
Anti-inflammatory Mechanisms
LAB and their metabolites alleviate inflammation by suppressing critical pro-inflammatory signaling cascades and enhancing the gut barrier. A key mechanism involves the inhibition of the NF-κB and MAPK pathways, as demonstrated by Lacticaseibacillus reuteri SBC5-3 in porcine epithelial cells [17]. This inhibition leads to reduced production of cytokines like TNF-α and IL-6. Furthermore, specific LAB strains can downregulate enzymes pivotal to the inflammatory response, such as 5-Lipoxygenase (LOX-5) and Myeloperoxidase (MPO), thereby reducing the production of leukotrienes and reactive oxygen species (ROS) [76]. The integrity of the intestinal barrier is also fortified by LAB, which upregulate proteins like mucin-2 (MUC-2), preventing the translocation of pro-inflammatory molecules [77].
Figure 1: LAB Anti-inflammatory Signaling Pathways. This diagram illustrates how LAB intake leads to the production of metabolites that act through multiple parallel mechanisms—including inhibition of NF-κB/MAPK signaling, downregulation of inflammatory enzymes, enhancement of the gut barrier, and modulation of the gut microbiota—to collectively reduce inflammation.
Lipid-Lowering Mechanisms
LAB modulate lipid homeostasis via a multi-pronged approach. A central mechanism involves the enzyme bile salt hydrolase (BSH), which deconjugates bile acids in the gut, leading to their excretion and forcing the liver to utilize circulating cholesterol to synthesize new bile acids, thereby reducing serum cholesterol [17]. LAB also ferment dietary fiber to produce short-chain fatty acids (SCFAs) like acetate, propionate, and butyrate. These SCFAs can influence hepatic lipid metabolism by downregulating lipogenesis genes and upregulating genes involved in cholesterol catabolism and bile acid synthesis, as seen with fermented cabbage roots [75]. Furthermore, certain strains, like Levilactobacillus brevis RAMULAB54, activate the PPAR-γ nuclear receptor, a master regulator of lipid and glucose metabolism [17].
Figure 2: LAB Lipid-Lowering Metabolic Pathways. This diagram outlines the key mechanisms by which LAB lower lipids, including BSH-mediated bile acid excretion, SCFA-driven modulation of hepatic gene expression, and activation of PPAR-γ signaling.
The Scientist's Toolkit: Essential Research Reagents
The following table details key reagents and materials essential for conducting research on the anti-inflammatory and lipid-lowering properties of LAB, as derived from the cited methodologies.
Table 3: Research Reagent Solutions for LAB Functional Analysis
| Reagent / Material | Function / Application | Experimental Example |
|---|---|---|
| Human Monocytic Cell Lines (U-937, THP-1) | In vitro model for studying immune cell differentiation and inflammatory responses [76]. | Differentiation into macrophages with PMA to test LAB metabolite effects on inflammatory pathways. |
| Phorbol 12-Myristate 13-Acetate (PMA) | Chemical inducer of monocyte-to-macrophage differentiation [76]. | Used to activate U-937 or THP-1 cells prior to treatment with LAB compounds. |
| Lipopolysaccharides (LPS) | Potent inflammatory stimulant; positive control in inflammation assays [76]. | Used to trigger an inflammatory response in cell models to test the anti-inflammatory efficacy of LAB. |
| Specific Antibodies (anti-IL-4, anti-TNF-α, anti-LOX-5, anti-MPO) | Detection and quantification of protein expression levels via Western Blot [76]. | Analyzing the expression of key inflammatory markers in cell lysates after treatment. |
| qRT-PCR Reagents & Primers | Quantitative analysis of gene expression for inflammatory and metabolic markers [17]. | Measuring mRNA levels of cytokines (e.g., TNF-α, IL-6) or metabolic genes (e.g., PPAR-γ, CYP7A1). |
| High-Fat Diet (HFD) | Induction of hyperlipidemia and obesity in rodent models [17] [75]. | Creating an in vivo model to test the lipid-lowering efficacy of LAB interventions. |
| Enzymatic Kits for Lipid Profiling | Quantitative measurement of total cholesterol, LDL-C, HDL-C, and triglycerides in serum [75]. | Assessing the impact of LAB supplementation on blood lipid parameters in animal studies. |
| Bile Salt Hydrolase (BSH) Assay Kit | In vitro measurement of BSH activity in LAB strains [17]. | Screening LAB strains for their potential cholesterol-lowering mechanism. |
This case study provides compelling evidence that specific lactic acid bacteria strains, through their bioactive compounds and metabolites, function as potent modulators of inflammation and lipid metabolism. The data synthesized here, derived from robust in vitro and in vivo models, highlight mechanisms such as the inhibition of NF-κB signaling, downregulation of pro-inflammatory enzymes, BSH activity, and SCFA production. The detailed experimental protocols and curated research toolkit offer a valuable resource for scientists aiming to validate and build upon these findings. Within the broader context of bioactive compound research, this analysis solidifies the role of selected LAB as promising, safe, and multi-targeted agents for the prevention and management of metabolic syndrome, cardiovascular diseases, and chronic inflammatory disorders, paving the way for their integration into future therapeutic and functional food strategies.
Navigating Complexity: Challenges in Bioavailability, Personalization, and Drug-Microbiota Interactions
The efficacy of orally administered bioactive compounds and pharmaceutical drugs is fundamentally constrained by their bioavailability, which encompasses the proportion of a substance that enters circulation to exert its biological effects. Traditional pharmacokinetic models have primarily focused on host physiology, but a paradigm shift is occurring with the recognition of the gut microbiota as a central mediator of bioavailability. The complex ecosystem of microorganisms in the human gastrointestinal tract possesses a diverse enzymatic arsenal that can extensively modify ingested compounds, transforming them into metabolites with altered bioactivity, solubility, and absorption characteristics. This microbial metabolism represents both a challenge and an opportunity: while it can inactivate some compounds, it can also activate prodrugs, enhance the bioavailability of poorly absorbed substances, and generate novel bioactive metabolites that underlie the therapeutic effects of many natural products. Within the broader thesis on the impact of bioactive compounds on gut microbiota research, this review synthesizes current understanding of the specific mechanisms through which gut microbes influence compound efficacy, providing researchers and drug development professionals with experimental frameworks and strategic insights for leveraging this relationship to overcome the persistent challenge of low bioavailability.
Mechanisms of Microbial Influence on Bioavailability
The gut microbiota influences the bioavailability of oral compounds through three primary interconnected mechanisms: direct enzymatic transformation, modulation of host drug transport systems, and alteration of gastrointestinal properties. Each mechanism represents a potential intervention point for enhancing compound efficacy.
Direct Enzymatic Transformation
Microbial enzymes catalyze biotransformations that fundamentally alter the chemical structure and properties of dietary compounds and pharmaceuticals [78]. These transformations include:
Prodrug Activation: Many compounds are administered as inactive prodrugs that require enzymatic conversion to their active forms. Gut microbiota express enzymes such as azoreductases, β-glucuronidases, and nitroreductases that perform this activation [78]. For example, the anti-inflammatory drug sulfasalazine is activated by microbial azoreductases to release mesalazine (5-ASA) in the colon [78]. Similarly, lovastatin's bioavailability and pharmacological effects decrease with antibiotic co-treatment, indicating microbial involvement in its activation [78].
Metabolic Interconversion: Gut microbes transform compounds into metabolites with different absorption profiles. A key example is the conversion of the alkaloid berberine to its absorbable form, dihydroberberine, by microbial enzymes, significantly enhancing its bioavailability [78]. Microbial metabolism of glucosinolates from cruciferous vegetables into bioactive isothiocyanates like sulforaphane represents another critical activation pathway [79].
Enterohepatic Recirculation Modulation: Microbial β-glucuronidases can deconjugate compounds that have been glucuronidated by the host liver, allowing their reabsorption and prolonging their systemic exposure [78]. This process affects drugs like mycophenolic acid and indomethacin, whose bioavailability decreases when antibiotics are administered [78].
Table 1: Microbial Enzymes Involved in Compound Biotransformation
| Enzyme Class | Example Enzymes | Substrates Affected | Bioavailability Impact |
|---|---|---|---|
| Azoreductases | Bacterial azoreductase | Sulfasalazine, Prontosil | Prodrug activation [78] |
| β-Glucuronidases | GUS enzymes | Mycophenolic acid, Indomethacin | Enterohepatic recirculation [78] |
| Glycosidases | β-Glucosidase | Glucosinolates, Flavonoid glycosides | Aglycone release [36] [79] |
| Nitroreductases | Oxygen-insensitive nitroreductase | Nitro-containing prodrugs | Prodrug activation [78] |
| Bile salt hydrolases | BSH enzymes | Bile acid conjugates | Altered lipid solubility [78] |
Modulation of Drug Transport Systems
The gut microbiota indirectly influences compound bioavailability by regulating the expression and function of intestinal drug transporters [78]. Through their metabolites, particularly secondary bile acids and short-chain fatty acids (SCFAs), gut microbes can:
- Modulate P-glycoprotein (P-gp) Expression: SCFAs like butyrate have been shown to influence the expression of P-gp, an efflux transporter that limits the absorption of many drugs [78].
- Affect Bile Acid-Dependent Transport: Microbial transformation of primary bile acids to secondary forms alters their signaling through nuclear receptors like FXR, which regulates the expression of various transport proteins [78].
- Influence Tight Junction Permeability: Microbial metabolites can modify the integrity of intestinal tight junctions, thereby affecting paracellular transport of compounds [78].
Alteration of Gastrointestinal Environment
The gut microbiota creates a distinctive biochemical environment that influences compound solubility and stability [78] [80]. Key modifications include:
- pH Modulation: Microbial fermentation of indigestible carbohydrates produces SCFAs that lower colonic pH, potentially affecting the ionization and solubility of compounds [80].
- Bile Acid Metabolism: Microbes transform primary bile acids into secondary forms through deconjugation and dehydroxylation, altering the solubilizing capacity of the bile acid pool and thereby affecting the absorption of lipophilic compounds [78].
- Mucus Layer Modification: Certain bacteria degrade and modify the mucus layer, potentially changing drug access to the intestinal epithelium [80].
Experimental Models for Studying Microbial Bioavailability Enhancement
Accurately assessing microbial contributions to bioavailability requires integrated experimental approaches that span in vitro systems, ex vivo models, and in vivo validation.
In Vitro Digestion and Fermentation Models
In vitro systems provide controlled, reproducible platforms for dissecting specific microbial contributions to compound metabolism:
- Artificial Gastrointestinal Digestion Systems: These systems simulate gastric and intestinal digestion phases to assess compound stability and bioaccessibility under physiological conditions [81]. Parameters such as pH, digestive enzymes, and mixing patterns are carefully controlled to mimic human digestion.
- Caco-2 Cell Monolayers: This human colon adenocarcinoma cell line differentiates into enterocyte-like cells and serves as a standard model for predicting intestinal absorption [81]. When combined with microbial metabolism, it provides insights into absorption of microbial metabolites.
- Colonic Fermentation Models: Laboratory simulations of colonic fermentation using fecal inocula enable researchers to track compound transformation by complex microbial communities over time [81]. These systems can be operated in batch or continuous modes to simulate different retention times.
Figure 1: Experimental Workflow for Assessing Microbial Bioavailability Enhancement
Gnotobiotic Animal Models
Gnotobiotic animals (germ-free animals colonized with defined microbial communities) provide powerful platforms for establishing causal relationships between specific microbes and bioavailability outcomes [78] [80]. Key applications include:
- Microbial Transplantation Studies: Fecal microbiota transplants from human donors to germ-free animals allow researchers to study how inter-individual microbial variations affect drug metabolism and bioavailability.
- Targeted Microbial Manipulation: Antibiotic cocktail treatments and pseudo-germ-free models help elucidate microbial contributions by comparing outcomes in microbiota-depleted versus conventional animals [78]. Studies with antibiotics have demonstrated substantially altered bioavailability for drugs like amlodipine, nifedipine, and aspirin [78].
- Genetic Manipulation of Microbes: Isogenic microbial strains differing in specific metabolic genes can be used to pinpoint enzymatic activities responsible for observed biotransformations.
Table 2: Key Research Reagent Solutions for Microbial Bioavailability Studies
| Research Tool | Function/Application | Examples/Specifications |
|---|---|---|
| Simulated Gastrointestinal Fluids | In vitro digestion models | Gastric juice (pH 2.0), Intestinal fluid (pH 6.5-7.5) [81] |
| Caco-2 Cell Line | Intestinal absorption model | Human colon adenocarcinoma cells, 21-day differentiation [81] |
| Transwell/Insert Systems | Paracellular transport assessment | Permeable supports for Caco-2 monolayer formation [81] |
| Anaerobic Chamber | Oxygen-free microbial culture | Maintains <1 ppm O₂ for obligate anaerobe cultivation [81] |
| Fecal Inoculum Preparation | Colonic fermentation studies | Fresh or frozen fecal samples in anaerobic medium [81] |
| UPLC-MS/MS Systems | Metabolite quantification | High-sensitivity detection of compounds and metabolites [78] |
| Germ-free Rodent Models | In vivo microbiota function | Mice/rats devoid of all microorganisms [78] [80] |
| Antibiotic Cocktails | Microbiota depletion | Broad-spectrum combinations (e.g., ampicillin, neomycin, vancomycin) [78] |
| 16S rRNA Sequencing | Microbial community analysis | Identification and quantification of bacterial taxa [78] |
| Metagenomic Sequencing | Functional gene analysis | Shotgun sequencing of microbial community DNA [78] |
Case Studies: Microbial Enhancement of Bioavailability
Selenium Metabolism
The essential trace element selenium demonstrates complex interactions with gut microbiota that significantly influence its bioavailability [81]. Different selenium species undergo specific microbial transformations:
- Selenite and Selenate Reduction: Gut microbes reduce inorganic selenium compounds to elemental selenium or selenide, which serves as a precursor for selenoprotein synthesis [81].
- Selenocyanate and Semethylselenocysteine Conversion: These organic selenium compounds are metabolized by gut microbiota to selenomethionine (SeMet), a highly bioavailable form [81].
- Selenosugar Production: Gut microbiota in normal rats convert selenium to 1β-methylseleno-N-acetyl-D-galactosamine, the major urinary selenosugar [81].
The bioavailability of different selenium forms varies considerably, with studies reporting relative bioavailability of selenite at 55.5–100%, selenate at 34.7–94%, and SeMet at 22–330% [81]. This variation underscores the importance of considering microbial metabolism when evaluating selenium supplementation strategies.
Glucosinolate Activation
Glucosinolates from cruciferous vegetables represent a compelling case of complete microbial dependency for bioactivity [79]. These sulfur-containing glucosides are converted to bioactive isothiocyanates like sulforaphane through a multi-step process:
- Myrosinase-Mediated Hydrolysis: Although plant-derived myrosinase can initiate this conversion in the upper GI tract, microbial thioglucosidases in the colon perform this function when plant myrosinase is denatured by cooking or inactivated by gastric conditions [79].
- Bioavailability Limitations: The limited and variable bioavailability of glucosinolates and isothiocyanates remains a key challenge, with high inter-individual variability linked to differences in gut microbiota composition [79].
- Intervention Strategies: Approaches to enhance bioavailability include co-administration with myrosinase-rich foods, utilization of specific bacterial strains with high thioglucosidase activity, and development of specialized formulations that protect compounds until they reach the colon [79].
Polyphenol Biotransformation
Dietary polyphenols, including flavonoids, phenolic acids, and tannins, undergo extensive microbial metabolism that dictates their bioavailability and health effects [82] [36]:
- Glycoside Deglycosylation: Most dietary polyphenols exist as glycosides that require microbial glycosidases for removal of sugar moieties before absorption [36].
- Ring Fission and Demethylation: The complex polyphenol structures are broken down into simpler phenolic acids through microbial ring cleavage and demethylation reactions [36].
- Lactone Hydrolysis: Ellagitannins are converted to urolithins through microbial hydrolysis and lactonization, with different individuals classified as urolithin metabotypes based on their capacity to produce these metabolites [36].
Figure 2: Microbial Activation Pathway for Dietary Polyphenols
Implications for Drug Development and Personalized Medicine
Understanding microbial influences on bioavailability has profound implications for pharmaceutical development and clinical practice:
Microbiome-Informed Drug Development
The pharmaceutical industry is increasingly incorporating microbiome considerations into drug development pipelines:
- Early-Stage Screening: Compounds are screened for susceptibility to microbial metabolism using in vitro systems with human fecal incubations [78].
- Targeted Prodrug Design: Drugs can be designed to require specific microbial enzymes for activation, enabling targeted colonic delivery and reduced systemic side effects [78]. The bacteria-directed enzyme prodrug therapy (BDEPT) approach represents an advanced application of this principle [78].
- Formulation Strategies: Delivery systems can be engineered to protect compounds from gastric conditions and control their release in specific gut regions based on microbial ecology [78].
Personalized Medicine Approaches
Interindividual variation in gut microbiota composition contributes to differential treatment responses, supporting personalized approaches:
- Microbiome-Based Dosing: Future clinical practice may incorporate microbiome profiling to predict drug metabolism capacity and optimize dosing regimens [79].
- Prebiotic and Probiotic Coadministration: Specific microbial strains or growth substrates can be administered to enhance the bioavailability of particular drugs [78] [36]. For example, probiotic supplementation with Lactobacillus and Bifidobacterium species can modulate microbial enzyme activities relevant to drug metabolism [82].
- Microbiome Biomarkers: Identification of microbial signatures associated with favorable or adverse drug responses could guide treatment selection and improve therapeutic outcomes [79].
The gut microbiota represents an essential consideration in overcoming the challenge of low bioavailability for orally administered compounds. Through direct enzymatic transformation, modulation of host transport systems, and alteration of the gastrointestinal environment, microbial communities significantly influence the bioavailability and efficacy of both pharmaceutical compounds and dietary bioactives. The case studies of selenium, glucosinolates, and polyphenols illustrate the diverse mechanisms through which microbes enhance compound efficacy, while experimental models provide researchers with tools to investigate these interactions.
Future research directions should focus on elucidating specific microbial genes and enzymes responsible for key biotransformations, developing standardized in vitro systems that better recapitulate in vivo conditions, and conducting larger clinical trials that incorporate microbiome analysis to understand interindividual variability. As our understanding of host-microbe-drug interactions deepens, we can anticipate more sophisticated approaches to leveraging microbial metabolism for enhanced bioavailability, including engineered microbial therapeutics, precision formulations targeting specific gut regions, and microbiome-informed personalized medicine strategies that optimize therapeutic outcomes based on an individual's microbial metabolic capacity.
The efficacy of nutritional and therapeutic interventions is not uniform across individuals. A growing body of evidence underscores that inter-individual variability in response to dietary components, particularly bioactive compounds, is modulated by a complex interplay of host genetics, baseline gut microbiota composition, and prior dietary exposures. This in-depth technical guide synthesizes current research to elucidate the mechanisms underlying this variability, highlighting that pre-intervention microbial community structures, such as Prevotella-rich versus Bacteroides-rich enterotypes, can profoundly determine the outcome of fiber-based interventions. Furthermore, host genetic factors, including those influencing lactose metabolism and sucrase-isomaltase activity, create a metabolic backdrop that interacts with microbial functional capacity. This whitepaper provides a detailed analysis of key experimental protocols, quantitative findings, and emerging methodologies like absolute quantitative metagenomics, which is critical for moving beyond relative abundance data. The integration of these factors is paving the way for sophisticated, predictive models in precision nutrition and drug development, enabling researchers to account for this variability from the initial design stages of clinical trials and intervention strategies.
The human gut microbiome represents a vast and complex ecosystem whose composition and function are shaped by numerous host and environmental factors. While diet is a major modulator of this ecosystem, emerging evidence consistently reveals that identical dietary interventions elicit highly heterogeneous responses across different individuals [83]. This inter-individual variability often obscures consistent results between studies and complicates the perceived efficacy of dietary interventions aimed at modulating the gut microbiota for human health benefits [83]. The central thesis of this whitepaper is that a tripartite framework—encompassing host genetics, baseline microbiota composition, and dietary history—serves as the primary determinant of an individual's response to bioactive compounds and other dietary interventions. Understanding and addressing this variability is no longer a secondary consideration but a fundamental prerequisite for advancing the field of gut microbiota research, particularly in the context of developing targeted therapies and personalized nutritional strategies. This document provides a technical deep-dive into the evidence, mechanisms, and methodologies essential for navigating this complexity.
The Dominant Role of Baseline Microbiota Composition
The initial structure of an individual's gut microbiota is a powerful predictor of how that ecosystem will respond to a dietary perturbation. This concept moves beyond simple measures of diversity to include specific taxonomic and functional configurations that pre-determine metabolic capacity.
Enterotype-Driven Responses to Dietary Fiber
A pivotal double-blind, randomized, controlled pilot trial demonstrated this principle with striking clarity. The study investigated the effects of resistant starch (RS)-rich unripe banana flour (UBF) and inulin on the gut microbiota of 48 healthy adults [84] [85]. Prior to the intervention, baseline clustering analysis revealed two distinct microbial constellations in the participants:
- Cluster P: Characterized by a high abundance of the genus Prevotella.
- Cluster B: Dominated by bacteria from the genus Bacteroides.
The response to the six-week intervention was entirely contingent on this baseline classification [84] [85]. As detailed in the results, only participants in the Prevotella-rich cluster (Cluster P) who consumed UBF exhibited significant and global shifts in their microbiota composition (weighted Unifrac Beta diversity, PERMANOVA p = 0.007) and substantial functional changes, with 533 KEGG orthologs significantly altered [84] [85]. Inulin induced only modest changes (19 KOs) in Cluster P, and remarkably, neither fiber intervention had a significant effect on the global microbiota of individuals in the Bacteroides-rich cluster (Cluster B) [84] [85]. This demonstrates that the pre-existing microbial community structure can render an intervention effective, marginally effective, or largely ineffective.
Table 1: Key Findings from the Enterotype-Driven Fiber Intervention Study
| Parameter | Prevotella-Rich (Cluster P) | Bacteroides-Rich (Cluster B) |
|---|---|---|
| Alpha Diversity | Higher richness (Chao1, p=0.0072) and phylogenetic diversity (Faith's PD, p=0.0056) | Lower richness and phylogenetic diversity |
| Response to RS (UBF) | Significant global microbiota shifts & major functional changes (533 KOs, FDR < 0.05) | No significant effects observed |
| Response to Inulin | Modest functional modulation (19 KOs) | No significant effects observed |
| Key Taxa | Prevotella copri, Prevotella stercorea, Sutterella, Ruminococcus | Bacteroides ovatus, B. plebeius, B. uniformis, Alistipes indistinctus |
Microbiome Diversity and Stability
The stability of the gut ecosystem in the face of dietary change is also influenced by its initial diversity. A 2023 controlled feeding study found that the gut microbiota of individuals with higher initial microbiome diversity was less susceptible to modulation following short-term dietary changes [86]. This suggests that a highly diverse ecosystem is more resilient, a property that must be accounted for when designing interventions, as the potential for change may be greater in individuals with lower baseline diversity.
The Influence of Host Genetics
While the microbiota is a plastic entity, the host's genetic background provides a fixed landscape that constrains and guides microbial ecology and the host's metabolic response to diet.
Genetic Modulation of Diet-Microbiota-Health Axis
Research using inbred mouse strains has provided controlled, experimental evidence for the role of host genetics. When four genetically distinct mouse strains (A/J, C57BL/6J, FVB/NJ, and NOD/ShiLtJ) were fed four different human-relevant diets (Mediterranean, Japanese, Ketogenic, and Western), the effect of diet on gut microbiota composition (α-diversity, β-diversity, and specific taxa abundance) was significantly modified by the host's genetic background [87]. For instance, the C57BL/6J strain was found to be more susceptible to diet-induced alterations in gut microbiota compared to the other strains [87]. Moreover, the same diet could have divergent effects on host metabolic health depending on the underlying genetics; the Ketogenic diet, for example, induced poor glucose tolerance in NOD/ShiLtJ mice, an effect not observed in other strains [87]. This demonstrates a complex, three-way interaction where host genetics modulates how diet alters the microbiota, which in turn influences host health.
Specific Genetic Loci Influencing Microbial Metabolism
Human studies have begun to pinpoint specific genetic loci that interact with diet to shape the microbiota. A notable example involves the LCT-MCM6 locus, which regulates lactose tolerance [87]. Lactose-intolerant individuals (without a functional LCT gene) who regularly consumed dairy products were found to have increased abundance of Bifidobacterium compared to lactose-intolerant individuals who avoided dairy [87]. This illustrates a direct gene-diet interaction shaping microbial abundance. Similarly, genetic variation in the sucrase-isomaltase (SI) gene can predispose individuals to carbohydrate maldigestion, influencing symptoms and potentially shaping the colonic microbial community that ferests these undigested carbohydrates [33].
Methodological Considerations for Advanced Research
Accurately measuring and interpreting intervention-driven changes in the microbiome requires sophisticated methodologies that move beyond standard practices.
Absolute vs. Relative Quantification
A critical methodological advancement is the shift from relative to absolute quantitative metagenomic analysis. Standard 16S rRNA gene sequencing generates relative abundance data, where the proportion of one taxon is dependent on the abundances of all others. This can be misleading, as a change in relative abundance does not necessarily reflect a change in the absolute number of a microorganism [88].
Absolute quantitative sequencing, which uses internal spike-in standards to determine the actual number of microbial cells, provides a more accurate picture. A 2025 study on the effects of berberine and metformin in mice found that while some relative quantitative results contradicted the absolute sequencing data, the latter was more consistent with the actual microbial community composition [88]. For instance, both methods showed an upregulation of Akkermansia, but absolute quantification provided a true measure of its abundance change independent of shifts in other community members [88]. This approach is vital for accurately evaluating the modulatory effects of drugs and bioactive compounds on the microbiome.
The Impact of Prior Diet and Lead-in Periods
The dietary context immediately preceding an intervention—the "lead-in diet"—can significantly alter the host's response. A longitudinal study demonstrated that a 13-day lead-in diet reflecting the average Canadian intake (CanDiet) influenced the gut microbiome and branched-chain fatty acid (BCFA) response to a subsequent 3-day Mediterranean diet (MedDiet) intervention [86]. Specifically, the reduction in BCFAs following the MedDiet was more pronounced when the MedDiet was preceded by the CanDiet [86]. This highlights the importance of controlling for recent dietary history in clinical trials, as the same intervention can yield different results based on the participants' immediate prior nutritional status.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Research Reagents and Materials for Investigating Diet-Microbiota-Host Interactions
| Reagent / Material | Function / Application | Example from Literature |
|---|---|---|
| Spike-in Internal Standards | Artificially synthesized DNA sequences added to samples before DNA extraction and sequencing to enable absolute quantitative microbial abundance measurement. | Used in Accu16S absolute quantification sequencing to determine true microbial loads, correcting biases of relative abundance data [88]. |
| Standardized Diet Matrices | Controlled, defined diets used in intervention studies (human or animal) to eliminate variability from self-reported intake and ensure consistent nutritional delivery. | Used in controlled feeding studies (e.g., MedDiet, CanDiet, defined mouse diets) to precisely test the effect of specific dietary patterns [87] [86]. |
| 16S rRNA Gene Primers | Oligonucleotides designed to amplify hypervariable regions of the bacterial 16S rRNA gene for taxonomic profiling of microbial communities. | Primer pair 27F/1492R used for full-length 16S sequencing on PacBio Sequel II platform to assess microbiota composition [88]. |
| LC-MS/MS Platforms | (Liquid Chromatography with Tandem Mass Spectrometry) Used for high-sensitivity quantification of host and microbial metabolites, including lipid mediators and SCFAs. | Employed to quantify plasma endocannabinoidome mediators (e.g., AEA, 2-AG) and fatty acids in dietary intervention studies [86]. |
Integrated Pathways and Experimental Workflows
The following diagrams synthesize the core concepts and methodological approaches discussed in this whitepaper into clear visual workflows.
Determinants of Inter-individual Variability
Absolute Quantification Sequencing Workflow
The paradigm of nutritional science and microbiota research is irrevocably shifting from a one-size-fits-all approach to a framework that embraces and deciphers human heterogeneity. The evidence is clear: inter-individual variability in response to dietary bioactive compounds is not noise to be averaged out, but a central signal determined by the triumvirate of baseline microbiota, host genetics, and dietary context. Future research must integrate these factors into its experimental DNA, employing rigorous methodologies like absolute quantification and controlled lead-in diets. The ultimate goal is the development of robust, predictive models that can stratify individuals based on their genetic and microbial profiles, enabling truly effective personalized nutrition and microbiome-targeted therapies that finally deliver on the promise of improved human health.
Pharmacomicrobiomics has emerged as a transformative discipline that investigates the intricate relationships between variations in the gut microbiome and individual responses to pharmaceutical agents [89]. This field represents a natural extension of pharmacogenomics, recognizing that the gut microbiome—often termed the "second genome"—contributes significantly to the extensive variability observed in drug efficacy and safety profiles [52]. The human gut hosts a complex ecosystem of over 100 trillion microorganisms encoding approximately 5 million genes, far surpassing the human gene count and providing immense metabolic capacity that directly interfaces with pharmaceutical compounds [51]. This microbial community functions as a virtual endocrine organ with the capability to directly metabolize drugs, produce bioactive metabolites that modulate host pathways, and influence the expression and activity of human drug-metabolizing enzymes [90] [49].
The clinical implications of pharmacomicrobiomics are particularly relevant for precision medicine, as interindividual variability in drug response poses significant challenges across therapeutic areas [51]. While pharmacogenomics has explained some variability, human genetic factors account for only 20-95% of variation depending on the drug, leaving substantial unexplained differences in drug pharmacokinetics and pharmacodynamics [51]. The gut microbiome represents a crucial missing piece in this puzzle, with growing evidence demonstrating that microbiome-mediated effects can determine therapeutic success or failure for numerous drug classes, including chemotherapeutic agents, immunosuppressants, and cardiovascular drugs [89] [91]. This whitepaper examines the fundamental mechanisms of drug-microbiome interactions, explores relevant clinical applications, details experimental methodologies, and discusses the integration of pharmacomicrobiomics into the broader context of bioactive compound research and drug development.
Fundamental Mechanisms of Drug-Microbiome Interactions
Direct Microbial Metabolism of Pharmaceuticals
The gut microbiota directly interfaces with pharmaceutical compounds through an extensive repertoire of microbial enzymes that catalyze biotransformations distinct from host metabolism. These direct interactions can substantially alter drug bioavailability, activity, and toxicity profiles [49].
Table 1: Direct Microbial Biotransformation Reactions and Representative Drugs
| Reaction Type | Representative Drugs | Microbial Enzymes/Processes | Functional Consequences |
|---|---|---|---|
| Reductive Metabolism | Azo drugs (sulfasalazine, prontosil), nitro compounds (clonazepam, nitrazepam) | Azo- and nitroreductases from Clostridia and Eubacterium species [49] | Prodrug activation; Toxicity generation |
| Hydrolytic Reactions | Conjugates (glucuronides, sulfates) | Microbial β-glucuronidases, sulfatases [49] | Enterohepatic recirculation; Drug toxicity (e.g., GI toxicity of irinotecan) |
| Decarboxylation | Amino acid analogs, levodopa | Bacterial decarboxylases | Reduced drug bioavailability; Altered pharmacokinetics |
| Dehydroxylation | Bile acids, catechol-containing drugs | Bacterial dehydroxylases | Altered drug solubility and absorption |
| Dealkylation | Caffeine, theophylline | Microbial demethylases | Metabolite formation with altered activity |
| Dehalogenation | Chloramphenicol, halogenic compounds | Bacterial dehalogenases | Toxic metabolite generation (bone marrow suppression) |
The most extensively characterized direct microbial biotransformations include reductive metabolism and hydrolytic reactions [49]. Azo reduction is essential for activating prodrugs like sulfasalazine, which requires bacterial azo reduction in the colon to release the active 5-aminosalicylic acid moiety for treating inflammatory bowel disease [49]. Conversely, nitroreduction of drugs like nitrazepam and clonazepam produces amine metabolites that may contribute to teratogenicity and other adverse effects [49]. Hydrolytic reactions are particularly significant for glucuronide conjugates that are excreted in bile; microbial β-glucuronidases can deconjugate these metabolites, reactivating the parent compound and facilitating enterohepatic recirculation. This process underlies the dose-limiting gastrointestinal toxicity of irinotecan, where bacterial β-glucuronidase activity regenerates the toxic SN-38 compound in the gut lumen [49].
Indirect Modulation of Drug Metabolism
Beyond direct biotransformation, gut microbiota indirectly influence drug disposition through multiple host-mediated mechanisms [51]. These include:
Modulation of host drug-metabolizing enzymes: Microbial metabolites such as short-chain fatty acids (SCFAs), secondary bile acids, and polyamines can regulate the expression and activity of hepatic cytochrome P450 enzymes and phase II conjugation systems [90]. Butyrate and other SCFAs have been shown to modulate hepatic CYP3A4 and CYP2E1 expression through epigenetic mechanisms and nuclear receptor signaling [51].
Regulation of intestinal barrier function: Microbial metabolites help maintain intestinal epithelial integrity, thereby influencing drug absorption. SCFAs, particularly butyrate, enhance tight junction function and mucin production, potentially limiting systemic exposure to microbiota-modified drug metabolites [17] [36].
Immune system modulation: Gut microbiota profoundly shape host immune responses, which can subsequently influence drug pharmacology, particularly for immunomodulatory agents [52]. Microbial-directed immune polarization affects the therapeutic efficacy of cancer immunotherapies and anti-inflammatory drugs [52].
Microbial metabolite-drug competition: Bacterially derived metabolites may compete with drugs for host metabolic enzymes or transporters, potentially altering drug clearance rates and metabolic patterns [49].
Clinical Applications and Therapeutic Implications
Cancer Therapeutics and Immunotherapy
The intersection of pharmacomicrobiomics and oncology represents one of the most advanced applications of this field, with compelling evidence linking gut microbiome composition to immunotherapy outcomes [52]. The efficacy of immune checkpoint inhibitors (ICIs), including anti-PD-1, anti-PD-L1, and anti-CTLA-4 antibodies, demonstrates significant dependence on an individual's gut microbial ecology [52] [51]. Clinical studies have identified specific bacterial taxa associated with improved ICI responses, with Akkermansia muciniphila, Faecalibacterium prausnitzii, and various Bifidobacterium species consistently correlated with enhanced therapeutic efficacy and prolonged progression-free survival [52]. The mechanisms underlying these associations involve microbiota-mediated priming of dendritic cells, enhanced antigen presentation, and subsequent potentiation of tumor-specific T-cell responses [52].
These findings have prompted clinical trials exploring microbiome-based interventions to improve cancer treatment outcomes. Fecal microbiota transplantation (FMT) from ICI-responsive patients to non-responders has demonstrated promise in restoring therapeutic sensitivity in refractory melanoma patients [52]. Additionally, specific probiotic formulations and defined bacterial consortia are under investigation as adjunctive therapies to enhance ICI efficacy [89]. The bidirectional nature of drug-microbiome interactions is evident in oncology, as chemotherapeutic agents themselves can induce significant shifts in gut microbial composition, potentially creating feedback loops that influence subsequent treatment cycles [51].
Immunosuppressive Therapy in Transplantation
Pharmacomicrobiomics has profound implications for transplant medicine, where narrow therapeutic indices and significant interpatient variability characterize immunosuppressive regimens [91]. The calcineurin inhibitor tacrolimus exemplifies these interactions, exhibiting substantial pharmacokinetic variability that cannot be fully explained by host genetic factors in CYP3A5 and ABCB1 [91]. Emerging evidence indicates that gut microbiota contribute to this variability through direct metabolic transformations of tacrolimus and indirect modulation of host metabolism [91]. Specific gut bacterial taxa, including Faecalibacterium and members of the Lachnospiraceae family, correlate with tacrolimus dosing requirements, while gut microbiome-derived tacrolimus metabolites with potentially altered immunosuppressive activity have been identified [91].
Similarly, the enteric-coated formulation of mycophenolate mofetil undergoes extensive microbial processing that significantly influences its pharmacokinetic profile [91]. Microbial β-glucuronidases in the gut lumen catalyze the deconjugation of mycophenolic acid glucuronide, facilitating enterohepatic recirculation and contributing to characteristic secondary plasma concentration peaks [91]. This microbial metabolic activity has direct clinical implications, as variations in gut microbiome composition may explain the unpredictable gastrointestinal toxicity that frequently complicates mycophenolate therapy [91].
Table 2: Clinical Evidence for Microbiome-Drug Interactions in Transplantation
| Immunosuppressant | Nature of Interaction | Clinical Consequences | Key Microbial Taxa/Enzymes |
|---|---|---|---|
| Tacrolimus | Direct metabolism; Altered bioavailability | Unexplained PK variability; Potential altered efficacy [91] | Faecalibacterium, Lachnospiraceae; Bacterial CYP analogs |
| Mycophenolate Mofetil | Enterohepatic recirculation via deconjugation | GI toxicity; Altered exposure profiles [91] | Microbial β-glucuronidases |
| Corticosteroids | Indirect immunomodulation | Varied anti-inflammatory response | SCFA-producing bacteria |
| Azathioprine/6-MP | Potential direct metabolism | Unexplained efficacy/toxicity variations | Microbial thiopurine metabolizing enzymes |
Cardiovascular and Metabolic Drugs
The gut microbiome significantly influences the disposition and activity of various cardiovascular and metabolic medications [51]. The cardiac glycoside digoxin provides a historical example, where its inactivation by the gut bacterium Eggerthella lenta reduces therapeutic efficacy in approximately 10% of patients [49]. This biotransformation involves the bacterial cytochrome-containing operon that reduces digoxin to inactive dihydrodigoxin, with inactivation rates modifiable by dietary protein intake that affects bacterial metabolism [49]. The antiplatelet agent clopidogrel represents another clinically significant interaction, as gut microbial composition influences the metabolic activation of this prodrug through both direct microbial metabolism and microbial modulation of host liver enzyme activity [51].
For metformin, the first-line therapy for type 2 diabetes, the gut microbiome mediates both efficacy and gastrointestinal side effects [51]. Metformin administration alters gut microbial composition, enriching for SCFA-producing bacteria and Akkermansia muciniphila, which may contribute to its glucose-lowering effects through enhanced gut peptide secretion and reduced inflammation [51]. Simultaneously, metformin-induced shifts in microbial bile acid metabolism potentially contribute to its characteristic gastrointestinal adverse effects [51].
Experimental Methodologies in Pharmacomicrobiomics
Core Technical Approaches
Investigating drug-microbiome interactions requires integrated methodological approaches that characterize microbial community structure, function, and metabolic output [92] [91].
Table 3: Essential Methodologies for Pharmacomicrobiomics Research
| Methodology | Key Applications | Technical Considerations | Limitations |
|---|---|---|---|
| 16S rRNA Sequencing | Bacterial identification and community structure analysis; Alpha and beta diversity metrics [91] | Targets hypervariable regions; Low cost; High coverage | Limited taxonomic resolution (species/strain); Functional inference only |
| Shotgun Metagenomics | Comprehensive taxonomic profiling; Functional gene annotation; Pathway analysis [91] | Whole-genome sequencing; Higher resolution | Increased computational demands; Higher cost |
| Metatranscriptomics | Assessment of microbial gene expression; Active metabolic pathways | RNA-based; Functional activity assessment | Technical challenges in RNA stabilization |
| Metabolomics | Detection of microbial metabolites; Drug biotransformation products | Mass spectrometry; NMR spectroscopy; Direct functional readout | Challenging metabolite source attribution |
| Culturomics | Isolation of novel bacterial species; Functional validation | High-throughput culture techniques; Reference strains | Majority of gut microbes uncultured |
| Gnotobiotic Models | Mechanistic studies; Causality establishment | Germ-free animals; Defined microbial consortia | Limited host physiology relevance |
The 16S rRNA sequencing approach remains widely used for initial characterization of microbial community structure due to its cost-effectiveness and comprehensive reference databases [91]. This method amplifies and sequences hypervariable regions of the bacterial 16S ribosomal RNA gene, allowing taxonomic classification and calculation of diversity metrics such as alpha diversity (within-sample diversity) and beta diversity (between-sample dissimilarity) [91]. However, functional inferences from 16S data remain limited, prompting implementation of shotgun metagenomics, which sequences all microbial DNA in a sample and provides higher taxonomic resolution while enabling reconstruction of metabolic pathways [91].
Functional assessments are enhanced through metatranscriptomics (microbial gene expression), metaproteomics (protein expression), and metabolomics (metabolite profiling) [92]. Each approach contributes complementary information, with metabolomics providing the most direct functional readout of microbial activities through identification and quantification of small molecule metabolites, including drug transformation products [92]. Integration of these multi-omics datasets represents the current state-of-the-art for comprehensively characterizing drug-microbiome interactions [51].
In Vitro and In Vivo Models
Experimental models of varying complexity facilitate mechanistic studies of pharmacomicrobiomics interactions:
In vitro fermentation systems (e.g., batch cultures, chemostats, gut simulators) enable controlled investigation of drug metabolism by defined microbial communities or fecal samples [92]. These systems allow high-throughput screening of drug-microbiome interactions under anaerobic conditions mimicking the gut environment [92].
Gnotobiotic mouse models, particularly germ-free animals colonized with defined human microbial communities, provide powerful in vivo platforms for establishing causal relationships between specific microbial taxa and drug metabolism [51]. These models demonstrate that gut microbiota are necessary for both metabolic activation of prodrugs like sulfasalazine and for toxicity manifestations of drugs like irinotecan [49].
Humanized mouse models, where germ-free mice are colonized with human fecal microbiota, enable studies of interindividual variability in drug response attributable to differences in human microbiome composition [51].
Conventional animal models with antibiotic depletion or microbiota-targeted interventions help elucidate microbiome contributions to drug disposition and effects, though species-specific microbial differences limit direct human extrapolation [92].
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagents and Resources for Pharmacomicrobiomics
| Reagent/Resource | Primary Function | Application Notes |
|---|---|---|
| Anaerobic Culture Media | Maintenance and growth of obligate anaerobic gut bacteria | Essential for in vitro metabolism studies; Requires anaerobic chambers or systems |
| Defined Microbial Consortia | Controlled colonization of gnotobiotic models | Enables mechanistic studies of specific microbial functions |
| 16S rRNA Primers | Amplification of bacterial taxonomic markers | Selection of hypervariable region affects taxonomic resolution |
| Reference Genomes | Taxonomic classification and functional annotation | Curated databases (e.g., GTDB, NCBI) essential for accurate analysis |
| Metabolomics Standards | Quantification and identification of microbial metabolites | Includes stable isotope-labeled compounds for tracking biotransformations |
| β-Glucuronidase Inhibitors | Specific blockade of microbial deconjugation reactions | Helps distinguish host vs. microbial metabolism (e.g., irinotecan studies) |
| Therapeutic Drug Monitoring Kits | Precise quantification of drug concentrations | Essential for correlating microbiome features with PK parameters |
| Bile Salt Supplements | Simulation of intestinal conditions for in vitro studies | Affects microbial composition and drug solubility/metabolism |
Integration with Bioactive Compounds Research
The field of pharmacomicrobiomics intersects significantly with research on dietary bioactive compounds, particularly (poly)phenols, creating bidirectional relationships that influence both drug and food component metabolism [93]. Many phytochemicals undergo extensive microbial metabolism that generates bioactive derivatives with altered pharmacological properties, while simultaneously shaping gut microbial ecology in ways that subsequently influence drug metabolism [93] [36].
The concept of "(poly)phenol metabotypes" provides a framework for understanding interindividual variability in microbial metabolism of dietary compounds and its implications for drug response [93]. These metabotypes classify individuals based on their capacity to convert specific (poly)phenols into characteristic metabolites:
- Equol producers versus non-producers for soy isoflavone metabolism
- Urolithin metabotypes A, B, and 0 for ellagitannin metabolism from pomegranates and berries
- Complex isoflavone metabotypes that extend beyond simple producer/non-producer dichotomies [93]
These metabotypes reflect underlying differences in gut microbial ecology that may concurrently influence drug metabolism capacity [93]. For instance, individuals harboring microbial communities capable of extensive (poly)phenol metabolism may also exhibit enhanced metabolic processing of certain pharmaceutical compounds, representing a potential intersection between dietary and pharmaceutical metabolism [93].
Lactic acid bacteria (LAB) represent a particularly significant group of microbes that bridge dietary and pharmaceutical domains [17]. LAB and their bioactive compounds demonstrate substantial impacts on gut microbiota composition and function, with documented abilities to influence lipid metabolism, immune regulation, and intestinal barrier integrity [17]. These microbial modulations create systemic effects that indirectly influence drug pharmacokinetics and pharmacodynamics through mechanisms including:
- Modulation of host inflammatory status, potentially altering drug target expression
- Enhancement of intestinal barrier function, affecting drug absorption
- Production of microbial metabolites that compete with or modulate host drug metabolism pathways
- Modification of bile acid profiles that influence solubility and absorption of lipophilic drugs [17]
Future Perspectives and Clinical Translation
The translation of pharmacomicrobiomics from basic research to clinical practice faces several challenges but offers significant opportunities for advancing precision medicine. Key considerations for clinical implementation include:
- Standardization of methodologies for microbiome analysis across laboratories to enable comparable results and established reference ranges [93]
- Development of predictive models that integrate microbiome data with pharmacogenomic and clinical variables to forecast individual drug responses [51]
- Validation of microbiome-based biomarkers for drug selection and dosing through prospective clinical trials [89]
- Establishment of regulatory frameworks for evaluating microbiome-related drug interactions and approving microbiome-based therapeutics [89]
Intervention strategies leveraging pharmacomicrobiomics principles are already emerging in clinical development:
- Targeted probiotics containing strains with specific metabolic capabilities (e.g., β-glucuronidase inhibitors for irinotecan toxicity prevention) [89]
- Prebiotic interventions designed to shape microbial communities toward favorable metabolic profiles for specific drug therapies [93]
- Fecal microbiota transplantation to restore therapeutic drug responsiveness, as demonstrated in immunotherapy-resistant melanoma patients [52]
- Microbiome-informed drug design that incorporates microbial metabolism considerations during pharmaceutical development [90] [89]
The ongoing expansion of pharmacomicrobiomics research will increasingly illuminate the complex interplay between our microbial inhabitants and pharmaceutical interventions, ultimately enabling more predictive, personalized, and effective therapeutic strategies that account for both human and microbial contributions to drug disposition and activity.
The investigation into the impact of bioactive compounds on gut microbiota represents one of the most dynamic frontiers in nutritional science and therapeutic development. Within this field, probiotics and prebiotics have emerged as promising interventions for modulating the gut ecosystem to promote human health. However, a critical methodological challenge has consistently complicated the interpretation of clinical trial results: the failure to adequately account for participants' background diet as a key confounding variable. Diet plays a fundamental role in shaping both host gastrointestinal function and microbiota features, exerting a significant influence on prebiotic and probiotic efficacy [94]. The inherent individuality of gut microbiome composition—where twins share only 34% of gut microbes and unrelated individuals share 30%—further underscores the necessity of controlling for dietary variables that may contribute to this variability [33].
Recognizing this gap, international experts have issued recommendations calling for researchers to systematically collect data on participants' background diets as part of future probiotic and prebiotic trials [94]. This technical guide examines the rationale for treating diet as a confounder, provides evidence-based methodological frameworks for its assessment and control, and offers practical tools for implementing these approaches in clinical research design. By addressing this persistent methodological shortcoming, researchers can enhance the validity, reproducibility, and clinical relevance of trials investigating microbiota-targeted interventions.
The Scientific Rationale: How Diet Influences Intervention Outcomes
Mechanisms of Dietary Interference
Background diet influences probiotic and prebiotic efficacy through multiple interconnected mechanisms. Diet directly shapes the gut microbial community structure and function, creating an ecological context that determines whether introduced organisms or substrates will thrive or fail to establish [94]. The macronutrient and micronutrient composition of habitual intake affects the gut environment, including pH, transit time, and bile acid profiles, all of which impact the survival, colonization, and metabolic activity of probiotics [33]. Additionally, dietary components directly interact with probiotic organisms, influencing their gene expression, metabolic pathways, and functional outputs independently of population-level compositional changes [94].
The relationship between diet and intervention response is perhaps most evident in the context of bioactive compound metabolism. A compelling example presented at NeuroGASTRO 2025 demonstrated that women with gut microbial communities capable of converting soy isoflavones to equol experienced a 75% greater reduction in menopausal symptoms when supplemented with isoflavones compared to those lacking these specific microbial species [33]. This finding illustrates how background diet interacts with host microbiota to determine intervention efficacy, with significant implications for personalized nutrition approaches.
Evidence from Clinical Studies
Recent meta-analyses and clinical trials provide quantitative evidence of how diet confounds intervention outcomes. A 2025 meta-analysis of 29 randomized controlled trials examining probiotics, prebiotics, and synbiotics in older adults found significant heterogeneity in microbial response that may be attributable to unmeasured dietary factors [95]. The analysis demonstrated that prebiotic supplementation significantly increased Bifidobacterium abundance (SMD = 1.09), while probiotics had a more modest effect (SMD = 0.40), suggesting that the existing microbial environment and nutritional context differentially affect various intervention types [95].
Table 1: Effects of Probiotics, Prebiotics, and Synbiotics on Gut Microbiota and Inflammatory Markers in Older Adults (Based on 2025 Meta-Analysis of 29 RCTs)
| Intervention | Outcome Measure | Effect Size (SMD) | Beneficial Changes |
|---|---|---|---|
| Prebiotics | Bifidobacterium abundance | 1.09 | Significant increase |
| Prebiotics | IL-10 levels | 0.61 | Anti-inflammatory increase |
| Prebiotics | IL-1β levels | -0.39 | Pro-inflammatory reduction |
| Probiotics | Bifidobacterium abundance | 0.40 | Moderate increase |
| Probiotics | Microbial diversity (Shannon index) | 0.76 | Diversity improvement |
| Synbiotics | Lactobacillus casei abundance | 0.75 | Specific strain enhancement |
| Synbiotics | TNF-α levels | -0.36 | Pro-inflammatory reduction |
| Synbiotics | Acetic acid levels | 0.62 | SCFA production enhancement |
| Synbiotics | Valeric acid levels | 0.50 | SCFA production enhancement |
Beyond direct nutritional effects, dietary patterns also influence intervention adherence and response through practical mechanisms. Research presented at NeuroGASTRO 2025 highlighted that patients following restrictive dietary protocols like the low FODMAP diet for irritable bowel syndrome face challenges including the "misalignment between food preferences and beliefs and dietary regimen, difficulties in puzzling the ingredients to whole meals, not knowing where to find reliable sources of information online, and the burden of preparing their own meals" [33]. These factors directly impact adherence and consequently confound measurement of intervention efficacy.
Methodological Framework for Dietary Assessment and Control
Ten Recommendations for Improved Trial Design
A recent Perspective paper in Nature Microbiology provides a comprehensive framework for addressing dietary confounding in prebiotic and probiotic trials [94]. The international expert panel developed ten specific recommendations covering study design, conduct, and reporting:
Table 2: Essential Methodological Recommendations for Diet-Responsive Trial Design
| Domain | Key Recommendations | Implementation Guidance |
|---|---|---|
| Pre-Trial Design | 1. Define primary outcome related to mechanism | Select outcomes aligned with hypothesized diet-microbe interactions |
| 2. Justify choice of probiotic/prebiotic | Base selection on previous evidence of diet-dependent effects | |
| 3. Consider dietary context as inclusion criterion | Stratify or select participants based on relevant dietary patterns | |
| Dietary Assessment | 4. Record baseline dietary intake | Use validated FFQs, 24-hour recalls, or food diaries |
| 5. Monitor dietary changes during trial | Track dietary adherence and changes throughout study period | |
| 6. Measure relevant food-related biomarkers | Include objective biomarkers to complement self-reported data | |
| Analysis & Reporting | 7. Statistically adjust for dietary intake | Include dietary variables as covariates in primary analysis |
| 8. Perform subgroup analyses by diet | Explore effect modification by dietary patterns or nutrients | |
| 9. Report dietary assessment methods | Detail tools, timing, and metrics in methods section | |
| 10. Interpret findings in dietary context | Discuss how background diet may have influenced results |
Dietary Assessment Methodologies
Implementing these recommendations requires careful selection of dietary assessment methods appropriate to the research context. The choice of assessment tool should be guided by the specific research question, resources available, and particular dietary components of interest:
Food Frequency Questionnaires (FFQs) provide comprehensive data on habitual intake over extended periods and are particularly valuable for identifying overall dietary patterns and estimating intake of specific bioactive compounds. Their lower respondent burden supports use in longer trials, though they are less precise for quantifying exact intakes.
24-Hour Dietary Recalls offer more detailed quantitative data on recent intake and can be administered repeatedly throughout a trial to capture day-to-day variability. Multiple recalls (at least 2-3) across different time points are needed to estimate habitual intake.
Food Diaries/Records provide the most detailed information on actual consumption, including food preparation methods and timing. These are particularly valuable when investigating nutrient-intervention interactions but require substantial participant literacy and commitment.
Dietary Biomarkers offer objective measures that complement self-reported data, helping to address systematic reporting errors. Relevant biomarkers might include plasma fatty acids, carotenoids, or metabolites derived from specific food components.
The timing and frequency of dietary assessment should capture both baseline habitual intake (to identify pre-existing patterns that may modify intervention response) and changes during the intervention period (to identify potential dietary shifts that may confound outcomes). For trials longer than 4 weeks, repeated assessments are essential to account for potential dietary changes during the study period.
Experimental Protocols and Analytical Approaches
Integrated Workflow for Diet-Aware Trials
The following diagram illustrates a comprehensive experimental workflow that incorporates dietary assessment throughout the trial process:
Statistical Considerations for Dietary Confounding
Appropriate statistical approaches are essential for addressing dietary confounding in trial analysis. The following methods should be considered:
Covariate adjustment incorporates dietary variables as covariates in primary outcome models, requiring careful selection of which dietary factors to adjust for based on biological plausibility and preliminary evidence.
Stratified analysis examines intervention effects within subgroups defined by baseline dietary characteristics, which is particularly valuable for identifying effect modification by diet.
Mediation analysis helps disentangle whether intervention effects operate through dietary changes or directly on outcomes.
Principal component analysis of dietary data can reduce multiple correlated dietary variables into composite scores that capture major patterns of intake.
Each approach has specific assumptions and limitations that must be considered in the analysis plan. Covariate adjustment, while powerful, assumes a consistent linear relationship between the dietary variable and outcome across intervention groups. Stratified analysis avoids this assumption but reduces statistical power. The analysis plan should be finalized before data collection and clearly documented in the trial protocol.
Table 3: Research Reagent Solutions for Diet-Responsive Microbiome Studies
| Category | Specific Tools/Reagents | Function/Application |
|---|---|---|
| Dietary Assessment | Food Frequency Questionnaires (FFQ) | Assess habitual dietary intake and patterns |
| 24-Hour Dietary Recall Protocols | Capture detailed recent food consumption | |
| Food Diary Templates | Record real-time food intake and preparation methods | |
| Biological Sampling | Fecal Collection Kits with stabilizers | Preserve microbial DNA/RNA for composition analysis |
| Blood Collection Tubes (EDTA, serum) | Measure nutritional biomarkers and inflammatory markers | |
| Short-Chain Fatty Acid (SCFA) Analysis Kits | Quantify microbial metabolic products | |
| Microbiome Analysis | DNA Extraction Kits optimized for stool | Isolate high-quality microbial genetic material |
| 16S rRNA Gene Sequencing Primers | Profile bacterial community composition | |
| Shotgun Metagenomics Sequencing Services | Assess functional potential of microbial communities | |
| Intervention Materials | Characterized Probiotic Strains (e.g., Bifidobacterium longum APC1472) | Well-defined test organisms with documented effects [33] |
| Defined Prebiotics (e.g., inulin, FOS, GOS) | Selective substrates for beneficial microbes [33] [95] | |
| Synbiotic Formulations | Combined probiotic-prebiotic preparations [95] | |
| Data Integration | Dietary Analysis Software (e.g., NDSR, GloboDiet) | Convert food intake to nutrient composition data |
| Microbiome Analysis Pipelines (QIIME 2, mothur) | Process and analyze sequencing data | |
| Statistical Software (R, SAS, STATA) | Implement complex models incorporating dietary variables |
Case Studies and Evidence-Based Examples
Successful Implementation Models
Recent research provides compelling examples of how accounting for dietary context strengthens trial design and interpretation. A study presented at NeuroGASTRO 2025 demonstrated that Bifidobacterium longum APC1472 exhibited anti-obesity effects in otherwise healthy individuals with overweight/obesity, with unpublished findings in mice showing that microbiota-targeted interventions with this strain or fructooligosaccharides and galactooligosaccharides could "attenuate the enduring effects of early-life high-fat high-sugar, including food intake dysregulation and hypothalamic molecular alterations" [33]. This carefully controlled study illustrates the importance of considering background diet in both experimental models and human trials.
Research on quercetin, a flavonoid with prebiotic properties, further demonstrates the complex interplay between dietary compounds, gut microbiota, and health outcomes. A 2025 study developed a dietary fiber-based hybrid-hydrogel microparticle formulation of quercetin (FQ-35) that effectively restored gut microbial diversity in an antibiotic-induced dysbiosis rat model, demonstrating "significant enrichment of beneficial taxa such as Lactobacillus and Bacteroides" alongside cognitive improvement [96]. This sophisticated delivery system highlights how the matrix and formulation of bioactive compounds—fundamentally dietary factors—significantly influence their effects on the gut microbiome.
Consequences of Neglecting Dietary Context
Conversely, failures to account for dietary context have led to inconsistent results and controversial conclusions in the literature. The 2025 meta-analysis of probiotics, prebiotics, and synbiotics in older adults noted substantial heterogeneity in outcomes across studies, which the authors partially attributed to "inconsistent study designs, small sample sizes, and varying patient responses" [95]—factors that inevitably include unmeasured dietary variation.
Research on inflammatory bowel diseases (IBD) further illustrates this challenge. While certain probiotic formulations such as single-strain preparations consisting of Lactobacillus, or mixed-strain combinations of Lactobacillus and Bifidobacterium, have proven effective in improving clinical, immunological, and symptomatic aspects of IBD [97], these findings remain inconclusive due to methodological inconsistencies across studies. The failure to standardize and account for background diet represents a significant limitation in this evidence base.
Integrating comprehensive dietary assessment and control strategies into probiotic and prebiotic trial design is no longer optional but essential for advancing the field. The methodological frameworks presented in this guide provide a roadmap for researchers to address dietary confounding through appropriate study design, rigorous assessment methods, and sophisticated statistical approaches. As the field progresses, emerging technologies including continuous dietary monitoring apps, multi-omics integration, and machine learning approaches offer promising avenues for more precisely characterizing diet-intervention interactions.
The increasing recognition that "diet can affect the efficacy of prebiotics and probiotics through changes in the gut microbiome and in the metabolism and expression of genes of the probiotic" [33] underscores the fundamental importance of these methodological considerations. By implementing the recommendations outlined in this guide, researchers can generate more reliable, reproducible, and clinically meaningful evidence regarding the health effects of probiotics, prebiotics, and other microbiota-targeted interventions.
The concept of "gut health" extends beyond the absence of gastrointestinal disease, encompassing the effective functioning of the digestive system, a balanced gut microbiome, robust barrier integrity, and appropriate immune status. Within research on bioactive compounds—such as polyphenols, prebiotics, and specific probiotics—measuring the success of interventions requires a multi-faceted approach using objective, quantitative biomarkers. This whitepaper synthesizes the core metrics, advanced methodologies, and experimental protocols essential for evaluating how dietary bioactives modulate the gut ecosystem to improve host health. It highlights the critical importance of controlling for confounders and adopting quantitative profiling to move beyond compositional data toward clinically meaningful findings.
The gut microbiome is a key mediator of human health, influencing everything from metabolism and immunity to brain function [82]. The scientific pursuit of defining "gut health" is therefore intrinsically linked to understanding the state of the gut microbiota. Bioactive compounds (BCs), including polyphenols, omega-3 fatty acids, and prebiotic fibers, are nutritional components that can positively influence this system. Their primary modes of action include directly modulating microbial composition, supporting the production of beneficial microbial metabolites like short-chain fatty acids (SCFAs), reinforcing the gut barrier, and reducing systemic inflammation [82] [18] [98].
However, assessing the efficacy of these interventions presents a significant challenge. The gut microbiome is highly individualized and influenced by numerous confounding factors such as transit time, diet, and host physiology [33] [99]. Consequently, a robust framework of scientific metrics and biomarkers is required to move from observational associations to causative mechanisms and validated health outcomes. This guide details the core and advanced biomarkers, experimental protocols, and analytical tools necessary for rigorous research in this field.
Core Biomarkers and Metrics for Assessing Gut Health
Evaluating gut health and the impact of bioactive compounds relies on a multi-parametric approach. The following table summarizes the primary categories of biomarkers and their significance.
Table 1: Core Biomarker Categories for Gut Health Assessment
| Category | Specific Biomarkers | Physiological Significance | Association with Bioactives |
|---|---|---|---|
| Microbial Composition & Diversity | Alpha-diversity (Shannon Index, ASVs), Beta-diversity (PCoA), Relative abundance of key taxa (e.g., Faecalibacterium, Bifidobacterium, Akkermansia) [100] [99] | Indicator of ecosystem richness and stability; reduced diversity linked to dysbiosis and metabolic disease [100]. | Prebiotics (inulin) and polyphenols can increase diversity and enrich beneficial genera [33] [82]. |
| Microbial Metabolic Output | Short-Chain Fatty Acids (SCFAs: acetate, propionate, butyrate), Tryptophan metabolites, Branched-Chain Amino Acids (BCAAs) [82] [101] | SCFAs maintain gut barrier, regulate immunity; Butyrate is a primary energy source for colonocytes [82]. Reduced butyrate is noted in ME/CFS [101]. | Seaweed polysaccharides, dietary fiber fermented by microbiota increase SCFA production [102]. Polyphenols influence tryptophan pathways [101]. |
| Gut Barrier Integrity & Inflammation | Plasma/Fecal Zonulin, Lipopolysaccharide (LPS), Fecal Calprotectin [103] [99] | Measures of "leaky gut" and intestinal inflammation. Calprotectin is a direct marker of neutrophil activity in the gut [99]. | Polyphenol-rich diets can reduce intestinal permeability and pro-inflammatory mediators [33]. |
| Systemic & Metabolic Health | HOMA-IR, HbA1c, C-reactive Protein (CRP) [100] | Surrogates for insulin resistance, glycemic control, and systemic inflammation; strongly correlated with gut microbiome diversity [100]. | BCs like omega-3 PUFAs and polyphenols aim to alleviate obesity-associated inflammation and metabolic dysfunction [18]. |
The relationships between these biomarker categories and the effects of bioactive compounds can be visualized as a functional pathway. The following diagram illustrates the sequence from intervention to physiological outcome.
Figure 1: Functional pathway of bioactive compounds. Bioactive compounds from the diet are metabolized by the gut microbiota, leading to increased production of health-promoting metabolites like butyrate, which in turn drive key physiological improvements in gut health.
Advanced Biomarkers and Integrated Multi-Omics Approaches
Moving beyond standard metrics, advanced techniques and biomarkers are providing a deeper, more mechanistic understanding of intervention effects.
- Quantitative Microbiome Profiling (QMP): Moving from relative to absolute abundance measurements is critical. QMP, which combines 16S rRNA sequencing with flow cytometry, reveals true microbial loads and has shown that well-established disease associations (e.g., with Fusobacterium nucleatum) can become non-significant after controlling for confounders like transit time and inflammation [99].
- Bacterial DNA in Blood: Emerging evidence suggests bacterial DNA in the blood could serve as a biomarker for a compromised gut barrier and may help identify individuals most likely to benefit from protective dietary interventions [33].
- Gut-Brain Axis Modules: A novel bioinformatics approach involves mapping microbial genomic capacity for producing or degrading neuroactive compounds into Gut-Brain Modules (GBMs). This allows researchers to quantify the potential of a microbiome to influence host neurology and psychiatry, beyond just taxonomic identification [33].
- Artificial Intelligence for Biomarker Discovery: AI models like BioMapAI are now being used to integrate massive, multi-omics datasets (gut metagenomics, plasma metabolomics, immune cell profiles). This approach has achieved high accuracy (e.g., 90%) in distinguishing patients with complex conditions like myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) from healthy controls by linking specific microbial and metabolic disruptions to symptom clusters [101].
Essential Experimental Protocols and Methodologies
Robust experimental design is paramount for generating reliable data on bioactive interventions.
Confounder Control and Cohort Design
Failing to account for key variables can lead to spurious results. Studies must rigorously control for:
- Transit Time: A primary driver of microbiota composition, often proxied by stool moisture content [99].
- Intestinal Inflammation: Measured via fecal calprotectin [99].
- Host Genetics: Variations in genes like sucrase-isomaltase (SI) can predispose individuals to carbohydrate maldigestion and confound responses to dietary interventions like the low FODMAP diet [33].
- BMI, Age, and Medication Use: These are significant covariates that must be recorded and statistically adjusted for [100] [99].
Protocol for a Longitudinal Intervention Study
A typical workflow for a clinical trial investigating a bioactive compound is outlined below.
Figure 2: Workflow for a longitudinal intervention study. This protocol emphasizes comprehensive baseline and endpoint sampling to capture changes in the microbiome and host physiology in response to a bioactive intervention.
Detailed Methodological Notes:
- Stool Sample Processing: For QMP, use of 16S rRNA gene sequencing (e.g., V4 region with 515F/806R primer set) combined with flow cytometry for absolute cell count is recommended [99]. DNA extraction should be performed with standardized kits (e.g., MO-BIO PowerSoil DNA isolation kit) with inclusion of artificial community and extraction blank controls [100].
- SCFA Analysis: Quantification of SCFAs from stool is typically performed using gas chromatography-mass spectrometry (GC-MS).
- Immune and Metabolic Profiling: Plasma samples can be analyzed using flow cytometry for immune cell subsets (e.g., MAIT cells) and mass spectrometry-based metabolomics platforms for compounds like tryptophan and benzoate [101].
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Research Reagents and Tools for Gut Health Studies
| Reagent / Tool | Function & Application | Example Use Case |
|---|---|---|
| 16S rRNA Gene Sequencing | Profiling microbial community composition and structure. Primer set 515F/806R targets the V4 hypervariable region [100]. | Baseline characterization of cohort microbiome and monitoring shifts post-intervention. |
| Shotgun Metagenomics | Unbiased sequencing of all genetic material in a sample; allows for functional potential analysis (e.g., Gut-Brain Modules) [33]. | Investigating the genetic capacity of the microbiome to produce specific neuroactive or anti-inflammatory metabolites. |
| Fecal Calprotectin ELISA Kit | Quantitatively measure intestinal inflammation from stool samples [99]. | A key covariate to control for; also a primary outcome measure in IBD-related studies. |
| Gas-Sensing Capsule | An emerging technology to measure intraluminal hydrogen concentrations in real-time, assessing colonic fermentation of fibers [33]. | Objectively determining the fermentation kinetics of a prebiotic fiber or bioactive compound in the human colon. |
| BioMapAI / Deep Neural Networks | AI platforms for integrating multi-omics data (microbiome, metabolome, immune profiles) to identify complex biomarkers [101]. | Identifying novel, predictive biomarker signatures for complex conditions like ME/CFS or for stratifying patient responses to interventions. |
Defining and measuring gut health requires a sophisticated, multi-dimensional approach that integrates microbial ecology, host biochemistry, and immunology. For researchers investigating bioactive compounds, success is no longer just about reporting a change in bacterial relative abundance. It hinges on demonstrating a causal link between the intervention, a shift toward a healthier microbial ecosystem (verified by QMP and confounder control), a corresponding change in functional metabolites, and a tangible improvement in host physiological markers. By adopting the advanced metrics, rigorous protocols, and integrated tools outlined in this whitepaper, the scientific community can generate the high-quality evidence needed to validate the role of bioactives in promoting gut health and translating these findings into personalized nutritional strategies.
Evidence and Efficacy: Validating Health Claims and Comparing Intervention Strategies
The investigation of how bioactive compounds influence human health through gut microbiota modulation represents a frontier in nutritional and pharmaceutical sciences. A fundamental challenge in this field lies in effectively bridging deep mechanistic understanding, often derived from animal models, with clinically relevant outcomes from human studies. Animal models provide a foundational platform for exploring the complex mechanisms through which diet-derived compounds, such as peptides and fibers, interact with the gut ecosystem and host physiology [104] [105]. These models enable controlled interventions and detailed tissue-level analyses that are rarely feasible in human trials. However, the ultimate validation of these mechanisms requires corroboration through human studies, which capture the full complexity of human genetics, lifestyle, and long-term health outcomes [106]. This article examines the strategic integration of both approaches to advance the development of microbiota-targeted therapies, focusing specifically on the context of bioactive compounds.
Comparative Analysis of Research Approaches
The following table summarizes the core strengths, limitations, and primary applications of animal and human research models in gut microbiota studies.
Table 1: Comparative Analysis of Research Models in Gut Microbiota Studies
| Aspect | Animal Models | Human Studies |
|---|---|---|
| Mechanistic Depth | Enable detailed investigation of molecular pathways, signaling cascades, and host-microbe interactions in specific tissues [105] [107]. | Limited to peripheral biofluids (blood, urine) and fecal samples; indirect mechanistic inference [33]. |
| Environmental Control | High control over genetics, diet, environment, and microbiota (e.g., gnotobiotic models) [104]. | Limited control over diet, lifestyle, genetics, and medication use; many confounding factors [33]. |
| Temporal Resolution | Longitudinal sampling from multiple tissues, including intestinal mucosa and organs [105]. | Typically relies on pre- and post-intervention sampling of accessible biofluids. |
| Physiological Relevance | Species-specific differences in genetics, metabolism, gut anatomy, and immune function may limit direct translation [106]. | Directly relevant to human physiology and disease states. |
| Interventional Flexibility | Permits testing of novel compounds and invasive procedures not yet approved for humans [108]. | Constrained by ethical and safety regulations; limited to approved compounds and non-invasive sampling. |
| Primary Application | Hypothesis generation, mechanistic elucidation, and preliminary efficacy/safety testing [104] [108]. | Validation of efficacy, safety, and clinical relevance in the target population [33]. |
Experimental Workflows for Corroborative Research
A synergistic research program strategically employs both animal and human models at different stages of investigation. The diagram below outlines a typical workflow for validating the effects of a bioactive compound.
Figure 1: Integrated Workflow for Translational Research on Bioactive Compounds
Detailed Experimental Protocol: Preclinical Animal Study
Objective: To evaluate the efficacy and mechanism of a marine-derived bioactive peptide (e.g., from octopus or scallop) in alleviating induced colitis [108].
- Animal Model Selection: Typically, C57BL/6 mice or Sprague-Dawley rats (8-10 weeks old) are used. Their well-characterized immune systems and genetic uniformity make them suitable for inflammatory models.
- Colitis Induction: Colitis is induced by administering 2-3% (w/v) Dextran Sulfate Sodium (DSS) in the drinking water for 5-7 days. Control groups receive normal water.
- Compound Administration: The marine peptide (e.g., 50-200 mg/kg body weight) or a vehicle control is administered daily via oral gavage. This can begin before (preventive model) or after (therapeutic model) DSS exposure.
- Sample Collection and Analysis:
- Clinical Phenotyping: Daily monitoring of disease activity index (weight loss, stool consistency, fecal blood).
- Tissue Collection: Upon sacrifice, colonic tissue is collected for:
- Histopathology: Scoring of inflammation, crypt damage, and immune cell infiltration (H&E staining).
- Molecular Analysis: Expression of tight junction proteins (ZO-1, occludin) via immunohistochemistry or qPCR; measurement of pro-inflammatory cytokines (TNF-α, IL-1β, IL-6) via ELISA.
- Microbiota Analysis: Fecal samples are collected for 16S rRNA gene sequencing to assess microbial diversity and specific taxon changes (e.g., Lactobacillus, Lachnospiraceae) [108].
Detailed Experimental Protocol: Human Clinical Trial
Objective: To validate the impact of a β-glucan prebiotic on gut microbiota composition and systemic inflammatory markers in overweight humans [33] [109].
- Study Design: Randomized, double-blind, placebo-controlled trial (the gold standard).
- Participant Recruitment: Overweight/obese but otherwise healthy adults (e.g., n=80, BMI 25-35). Participants are stratified by age and sex and randomized to intervention or placebo groups.
- Intervention: The intervention group receives a daily dose of β-glucan (e.g., 3-5 g from oat or yeast), while the control group receives an iso-caloric placebo (e.g., maltodextrin) for 8-12 weeks.
- Data and Sample Collection:
- Baseline and Endpoint Measurements: Body composition, fasting blood glucose, lipids.
- Biospecimen Collection:
- Blood: For measuring inflammatory markers (e.g., C-reactive protein, cytokines) and metabolic hormones (e.g., GLP-1).
- Stool: For 16S rRNA metagenomic sequencing, SCFA analysis via GC-MS, and calprotectin (gut inflammation marker).
- Dietary Records: 3-day food diaries to monitor and control for background dietary intake [33].
- Data Analysis: Primary outcomes include changes in microbial diversity (e.g., Shannon index), abundance of beneficial bacteria (e.g., Bifidobacterium, Faecalibacterium), and SCFA levels. Secondary outcomes include changes in inflammatory and metabolic markers.
Corroborating Mechanistic Pathways: From Animals to Humans
A key mechanistic pathway through which bioactive compounds exert their effect is the modulation of the gut-immune axis. The following diagram illustrates a core mechanism, identified in animal studies and validated in humans, for how certain compounds reduce inflammation.
Figure 2: Core Gut-Immune Mechanism of Bioactive Compounds
This pathway, demonstrated in animal models [105] [108], finds support in human studies. For instance, β-glucan fermentation by gut bacteria increases SCFA levels, which correlates with improved gut barrier function and reduced inflammation in human cohorts [109]. Similarly, the anti-inflammatory effects of specific probiotics, such as Bifidobacterium longum APC1472, in mitigating obesity-related low-grade inflammation, were first identified in mice and successfully translated to humans [33].
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table catalogues key reagents and materials essential for conducting the experiments described in the protocols above.
Table 2: Essential Research Reagents and Solutions for Gut Microbiota Studies
| Reagent / Material | Function / Application | Examples / Specifications |
|---|---|---|
| Dextran Sulfate Sodium (DSS) | Chemical inducer of colitis in rodent models, disrupting the colonic epithelium and triggering inflammation. | Molecular weight: 36,000-50,000 Da; typically administered at 2-5% (w/v) in drinking water [108]. |
| Bioactive Compounds | The intervention being tested (prebiotics, peptides, etc.). | β-Glucans from oats/yeast (≥95% purity); marine peptides from octopus/scallop (hydrolyzed, low molecular weight) [109] [108]. |
| ELISA Kits | Quantification of specific proteins (cytokines, hormones) in serum, tissue homogenates, or cell culture supernatants. | Kits for TNF-α, IL-6, IL-1β, GLP-1; require a microplate reader for detection. |
| DNA/RNA Extraction Kits | Isolation of high-quality nucleic acids from complex samples like stool or intestinal tissue for sequencing. | Kits optimized for soil/fecal samples (e.g., QIAamp PowerFecal Pro DNA Kit); must inhibit RNases for RNA work [105]. |
| 16S rRNA Sequencing Reagents | Profiling the composition and diversity of the gut microbiota. | Primers targeting hypervariable regions (e.g., V3-V4); PCR master mix; sequencing platform (Illumina MiSeq) [33] [110]. |
| Short-Chain Fatty Acid (SCFA) Standards | Calibration and quantification of SCFA concentrations in fecal or cecal content using GC-MS or LC-MS. | Certified reference standards for acetate, propionate, butyrate, etc., in known concentrations. |
| Antibodies for Immunostaining | Visualization and localization of specific proteins in tissue sections (e.g., intestinal mucosa). | Validate primary antibodies for tight junction proteins (anti-ZO-1, anti-occludin); species-specific fluorescent secondary antibodies [108]. |
The journey from mechanistic insight to clinical application in gut microbiota research is not a linear path but an iterative dialogue between animal models and human studies. Animal models provide the necessary resolution to deconstruct complex host-microbe-diet interactions and propose definitive molecular mechanisms. Human studies, in turn, ground these discoveries in physiological reality, validating their relevance and identifying potential confounders like diet, genetics, and environment [33]. The future of this field lies in developing more sophisticated, humanized animal models and employing multi-omics technologies in both domains to create a unified and causally understood picture. This integrative approach is paramount for successfully translating the promise of bioactive compounds into effective, evidence-based nutritional and therapeutic strategies.
The human gut microbiota, a complex ecosystem of microorganisms, plays a critical role in maintaining host health by regulating digestion, metabolism, and immune function [82] [111]. Disruption of this ecosystem, known as dysbiosis, has been linked to a wide range of disorders, including inflammatory bowel disease, metabolic syndrome, neurodegenerative diseases, and cancer [112] [82] [113]. Dietary intervention represents a primary strategy for modulating the gut microbiota, with bioactive compounds such as polyphenols, dietary fibers, and specific probiotic strains standing at the forefront of scientific research [20]. These components interact with the gut microbiota through distinct yet sometimes complementary mechanisms, influencing microbial composition and function to confer health benefits.
This review provides a comparative analysis of the efficacy of three major classes of bioactive compounds: polyphenols, known for their prebiotic-like modulation of microbial populations; dietary fibers, which serve as fermentable substrates for beneficial bacteria; and specific probiotic strains, which introduce live microorganisms to the gut environment. Framed within a broader thesis on the impact of bioactive compounds on gut microbiota research, this article synthesizes current evidence from preclinical and clinical studies, summarizes quantitative data in structured tables, and details essential experimental protocols for researchers and drug development professionals. The goal is to offer a technical guide that illuminates the mechanisms, outcomes, and research methodologies central to this dynamic field.
Mechanisms of Action and Comparative Efficacy
Polyphenols: Prebiotic Modulators of Microbial Ecology
Polyphenols are secondary metabolites found abundantly in plant-based foods such as fruits, vegetables, tea, coffee, and wine [114] [115]. Their chemical structure, characterized by phenolic rings, allows for diverse biological activities, including antioxidant and anti-inflammatory properties [82]. A key feature of polyphenols is their low bioavailability in the upper gastrointestinal tract; approximately 90-95% reach the colon intact, where they are metabolized by the gut microbiota [112] [20]. This bidirectional relationship—where polyphenols shape the microbiota and the microbiota transforms polyphenols into bioactive metabolites—underpins their mechanism of action.
- Microbial Modulation: Polyphenols selectively enrich beneficial bacterial genera such as Bifidobacterium, Lactobacillus, Faecalibacterium, Roseburia, and Akkermansia [112] [82] [20]. Concurrently, they inhibit the growth of pathogenic bacteria, including Clostridia, Helicobacter, and Escherichia coli [112] [20]. For instance, the flavonoid quercetin increases the abundance of Bifidobacterium and Lactobacillus while reducing Enterococcus and Fusobacterium [20].
- Key Metabolites and Health Effects: Microbial metabolism of polyphenols yields bioactive compounds like urolithins (from ellagitannins) and phenolic acids, which have anti-inflammatory effects [116]. These metabolites, along with the modulation of the microbiota itself, contribute to improved gut barrier function by enhancing the expression of tight junction proteins (e.g., occludin, ZO-1) [20]. The resulting reduction in systemic inflammation and oxidative stress is implicated in alleviating symptoms of neurodegenerative diseases (NDDs), metabolic disorders, and cancer [112] [82] [113].
Dietary Fibers: Fuel for Microbial Fermentation
Dietary fibers (DFs) are non-digestible carbohydrates that resist digestion in the upper GI tract and serve as primary substrates for microbial fermentation in the colon [116] [111]. The U.S. FDA defines them as "non-digestible soluble and insoluble carbohydrates (with three or more monomeric units) and lignin" that confer physiological benefits [111]. Their health effects are largely mediated through the production of short-chain fatty acids (SCFAs).
- SCFA Production and Microbial Cross-Feeding: The fermentation of DFs by gut bacteria produces SCFAs, primarily acetate, propionate, and butyrate, in an approximate ratio of 3:1:1 [116]. Butyrate serves as the primary energy source for colonocytes, enhances gut barrier function, and possesses anti-inflammatory properties [116]. Propionate is involved in gluconeogenesis and also exhibits anti-inflammatory effects, while acetate is a substrate for butyrate production and influences cholesterol metabolism [116]. This fermentation process often involves cross-feeding, where different bacterial species sequentially degrade complex fibers [116].
- Microbial Producers and Health Implications: DF fermentation enriches SCFA-producing genera such as Faecalibacterium, Roseburia, Eubacterium, and Bifidobacterium [116] [113]. Increased SCFA levels are associated with reduced gut inflammation, strengthened intestinal barrier integrity, and improved metabolic outcomes [116] [111]. In the context of breast cancer, DF intake correlates with beneficial microbial changes and influences estrogen metabolism through the gut estrobolome, potentially modulating cancer risk [113].
Specific Probiotic Strains: Live Microbial Interventions
Probiotics are defined as "live microorganisms that, when administered in adequate amounts, confer a health benefit to the host" [117]. They are not classified as bioactive compounds but are a critical intervention in gut microbiota management. Their effects are strain-specific and dose-dependent.
- Mechanisms of Action: Probiotics exert benefits through multiple mechanisms, including competitive exclusion of pathogens, enhancement of gut barrier function, modulation of the host immune system, and production of antimicrobial substances [117].
- Clinical Efficacy on GI Symptoms: An umbrella meta-analysis of multiple RCTs demonstrated that probiotic supplementation significantly reduces the risk of several gastrointestinal symptoms, including diarrhea (RR 0.44), nausea (RR 0.59), bloating (RR 0.74), and epigastric pain (RR 0.71) [117]. The analysis found that multi-strain formulations and shorter intervention durations (≤ 2–4 weeks) were often associated with more pronounced effects [117]. Specific strains like Bifidobacterium longum APC1472 have shown promise in attenuating obesity-related metabolic parameters and regulating food intake in both animal models and humans [33] [117].
Synergistic Interactions
Emerging research highlights the synergistic effects of combining different bioactives, particularly DFs and polyphenols [111]. These interactions can occur through covalent bonds (e.g., in lignin-polyphenol complexes) or non-covalent interactions (e.g., between pectin and anthocyanins) [111]. Such combinations can enhance the bioavailability of polyphenols and lead to greater production of SCFAs and other beneficial metabolites compared to either component alone, offering promising avenues for functional food development [111].
Table 1: Comparative Analysis of Bioactive Classes: Mechanisms and Efficacy
| Feature | Polyphenols | Dietary Fibers | Specific Probiotic Strains |
|---|---|---|---|
| Primary Mechanism | Prebiotic-like modulation; metabolized into bioactive compounds by microbiota [112] [114] | Fermentation substrate for SCFA production [116] [111] | Direct introduction of live microbes; competitive exclusion; immune modulation [117] |
| Key Microbial Changes | ↑ Bifidobacterium, Lactobacillus, Akkermansia, Faecalibacterium [112] [82]↓ Clostridia, Helicobacter [112] | ↑ Faecalibacterium, Roseburia, Eubacterium, Bifidobacterium [116] [113] | Strain-specific; general increase in beneficial populations [117] |
| Key Metabolites | Urolithins, phenolic acids [116] | Short-chain fatty acids (Acetate, Propionate, Butyrate) [116] | Strain-dependent (e.g., bacteriocins, vitamins) [117] |
| Primary Health Benefits | Antioxidant, anti-inflammatory, improved gut barrier, neuroprotection [112] [82] | Gut barrier integrity, anti-inflammatory, metabolic regulation (e.g., insulin sensitivity) [116] [111] | Alleviation of GI symptoms (diarrhea, nausea, bloating) [117] |
| Representative Efficacy Data | Improved memory/motor function in animal models of NDDs [112] | SCFA production in a ~3:1:1 ratio (Acetate:Propionate:Butyrate) [116] | Reduced risk of diarrhea (RR 0.44) and nausea (RR 0.59) [117] |
Experimental Protocols for Gut Microbiota Research
In Vivo Assessment in Animal Models
Protocol: Evaluating Polyphenol Efficacy in a Neurodegenerative Disease (NDD) Model
- Objective: To investigate the effects of a polyphenol intervention on gut microbiota composition, microbial metabolites, and disease pathology in a transgenic Alzheimer's disease (AD) mouse model.
- Animal Model: APP/PS1 transgenic mice (e.g., n=10-12 per group, male, 16 weeks old) [112].
- Intervention: Test group receives a specific polyphenol (e.g., Chlorogenic Acid - CGA at 80 mg/kg) via oral gavage daily for 16 weeks. Control groups receive vehicle [112].
- Sample Collection:
- Fecal Samples: Collected at baseline, midpoint, and endpoint for 16S rRNA sequencing and microbial metabolite analysis (e.g., SCFAs via GC-MS) [112].
- Blood Plasma: For measuring inflammatory cytokines (e.g., IL-1β, TNF-α) via ELISA [112].
- Brain and Intestinal Tissues: Post-sacrifice for immunohistochemical analysis of amyloid-beta plaques and gut barrier integrity (e.g., ZO-1 staining) [112].
- Behavioral Tests: Conduct Morris water maze for cognitive assessment and rotarod test for motor function at the end of the intervention [112].
- Data Analysis: Correlate changes in microbial abundance (e.g., increased Bacteroidetes, decreased Prevotella) with biochemical, pathological, and behavioral outcomes [112].
Clinical Trial Design for Probiotic Efficacy
Protocol: Umbrella Meta-Analysis of Probiotics for Gastrointestinal Symptoms
- Objective: To provide a comprehensive evaluation of the effects of probiotics on gastrointestinal disorders (diarrhea, nausea, bloating) by synthesizing existing meta-analyses of RCTs [117].
- Search Strategy: Conduct a systematic literature search in PubMed, Scopus, Web of Science, and Google Scholar up to a specified date (e.g., June 2024) using keywords: "(Probiotic...) AND (diarrhea OR nausea OR bloating...) AND (Meta-analysis...)" [117].
- Inclusion Criteria (PICO):
- Population (P): Adults.
- Intervention (I): Probiotics.
- Comparison (C): Control or placebo.
- Outcome (O): Gastrointestinal disorder incidence (diarrhea, nausea, etc.) [117].
- Data Extraction and Quality Assessment:
- Extract risk ratios (RR) and 95% confidence intervals (CIs) for each symptom.
- Assess methodological quality of included meta-analyses using the AMSTAR 2 tool [117].
- Statistical Analysis: Pool effect sizes using a random-effects model. Conduct subgroup analyses based on intervention duration and probiotic strain formulation [117].
Visualization of Key Pathways and Workflows
Gut-Brain Axis Signaling Pathway
This diagram illustrates the mechanistic pathways through which dietary bioactives influence host physiology via the gut microbiota, particularly in the context of the gut-brain axis.
Diagram 1: Bioactive-Gut-Brain Signaling Pathway
Experimental Workflow for Preclinical Studies
This flowchart outlines a standardized experimental workflow for evaluating bioactive compounds in animal models.
Diagram 2: Preclinical Study Experimental Workflow
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Research Reagents for Gut Microbiota Studies
| Reagent / Material | Function / Application | Example Usage |
|---|---|---|
| SYRCLE's Risk of Bias Tool | A dedicated tool for assessing the risk of bias in animal studies. Covers sequence generation, blinding, outcome reporting, etc. [112] | Used in systematic reviews of animal studies to evaluate methodological quality and potential biases [112]. |
| AMSTAR 2 (Assessing Methodological Quality of Systematic Reviews 2) | A critical appraisal tool for evaluating the quality of systematic reviews that include randomized or non-randomized studies. [117] | Employed in umbrella meta-analyses to grade the confidence in the results of included meta-analyses [117]. |
| 16S rRNA Gene Sequencing Reagents | Primers targeting hypervariable regions (e.g., V3-V4), DNA extraction kits, and sequencing platforms (Illumina). For taxonomic profiling of gut microbiota. [112] | Used to analyze fecal DNA and determine changes in microbial community structure (e.g., alpha/beta diversity, taxonomic abundance) in response to an intervention [112]. |
| Gas Chromatography-Mass Spectrometry (GC-MS) | An analytical technique for separating and quantifying volatile and semi-volatile compounds. Ideal for measuring SCFA levels in fecal or cecal content. [116] | Used to quantify concentrations of acetate, propionate, and butyrate as primary readouts of dietary fiber fermentation [116]. |
| Enzyme-Linked Immunosorbent Assay (ELISA) Kits | Pre-coated plates and reagents for quantifying specific proteins (e.g., cytokines, gut barrier markers) in biological fluids like plasma or tissue homogenates. [112] | Used to measure plasma levels of pro-inflammatory cytokines (e.g., IL-1β, TNF-α, IL-6) to assess systemic inflammatory status [112]. |
| Specific Probiotic Strains (e.g., Bifidobacterium longum APC1472) | Commercially available, well-characterized bacterial strains for use in interventional studies, often in lyophilized form. [33] [117] | Administered in clinical or preclinical trials to investigate their specific effects on metabolic parameters, food intake regulation, or GI health [33] [117]. |
The comparative analysis of polyphenols, dietary fibers, and specific probiotic strains reveals distinct yet complementary roles in modulating the gut microbiota to promote host health. Polyphenols act as sophisticated modulators of microbial ecology, dietary fibers provide fundamental fuel for beneficial fermentation, and probiotics offer direct microbial intervention. The efficacy of each class is highly dependent on factors such as chemical structure, dosage, duration of intervention, and the initial composition of the individual's gut microbiota.
Future research must prioritize well-designed human clinical trials to translate promising preclinical findings into validated applications. The exploration of synergistic combinations, particularly between dietary fibers and polyphenols, represents a promising frontier for developing targeted nutritional strategies and functional foods. Furthermore, the integration of multi-omics technologies and personalized nutrition approaches will be crucial for advancing this field, enabling the development of precise, microbiota-targeted interventions for the prevention and management of a wide spectrum of diseases.
The human gut microbiome, a complex ecosystem of trillions of microorganisms, has emerged as a pivotal regulator of human health and disease. Its influence extends far beyond the gastrointestinal tract, modulating systemic inflammation, immune responses, and therapeutic efficacy for conditions including inflammatory bowel disease (IBD) and cancer. Acting through metabolic reprogramming, immune modulation, and microenvironment remodeling, specific microbial taxa and their metabolites can either enhance or hinder conventional drug outcomes [118]. This creates a compelling rationale for integrating microbiota-targeted interventions with established pharmaceutical paradigms.
The thesis that bioactive compounds—from dietary components to defined 'biotics'—can strategically modulate this microbial community to improve clinical outcomes is supported by a growing body of evidence. This whitepaper provides an in-depth technical analysis of the mechanisms underlying microbiome-drug interactions, summarizes quantitative evidence for synergistic potential, and outlines rigorous experimental methodologies for exploring this frontier. The goal is to equip researchers and drug development professionals with the tools to advance a new class of combinatorial therapies that harness the power of the microbiome.
Mechanisms of Interaction: How Microbes Modulate Drug Efficacy and Toxicity
The gut microbiota influences host physiology and drug action through multiple, interconnected mechanistic pathways. Understanding these mechanisms is essential for designing rational synergistic strategies.
Key Mechanistic Pathways
Microbial Metabolite Signaling: Gut microbes produce a vast array of metabolites that serve as critical signaling molecules. Short-chain fatty acids (SCFAs) like butyrate, propionate, and acetate, produced from dietary fiber fermentation, provide energy for colonocytes, enhance gut barrier integrity, and exert potent immunomodulatory effects. Butyrate, for instance, inhibits histone deacetylase (HDAC) and NF-κB signaling, reducing the production of pro-inflammatory cytokines such as IL-12 and IFN-γ [116]. This anti-inflammatory milieu can potentiate therapies for IBD and mitigate inflammatory adverse events from cancer treatments.
Enzymatic Drug Metabolism: The microbiome encodes a vast repertoire of enzymes that can directly metabolize pharmaceuticals, altering their bioavailability and efficacy. For example, bacterial β-glucuronidase can reactivate the toxic metabolite of the chemotherapeutic drug irinotecan, leading to severe diarrhea. Conversely, microbial cytidine deaminase has been implicated in the inactivation of gemcitabine, contributing to drug resistance in pancreatic and colorectal cancers [118].
Systemic Immune Modulation: The gut microbiome is essential for proper immune system development and function. Specific commensal bacteria can enhance anti-tumor immunity by promoting the infiltration of CD8+ T-cells into tumors and activating dendritic cells. For instance, Bifidobacterium species have been shown to improve the efficacy of PD-L1 checkpoint inhibitors in melanoma models by enhancing T-cell effector functions [118]. In IBD, promoting SCFA-producing bacteria like Faecalibacterium prausnitzii helps reinforce intestinal barrier function and suppress aberrant immune activation [33] [116].
Tumor Microenvironment (TME) Remodeling: Intratumoral and gut-resident microbes can reshape the TME. Fusobacterium nucleatum has been associated with colorectal cancer progression, while certain bacteria can increase PD-L1 expression on tumor cells and modulate the STING pathway, thereby altering the susceptibility to immunotherapy [118].
The following diagram illustrates the core signaling pathways through which gut microbiota and their metabolites influence host health and therapy response, particularly in the contexts of IBD and cancer.
Quantitative Evidence: Comparative Analysis of Interventions
The therapeutic potential of microbiota-targeted interventions is demonstrated by their ability to improve clinical metrics in IBD and cancer, either as monotherapies or in combination with conventional drugs. The tables below synthesize quantitative data from recent research, highlighting the synergistic potential.
Table 1: Microbiota-Targeted Interventions in Inflammatory Bowel Disease (IBD)
| Intervention Type | Specific Example | Key Microbiota/Metabolite Changes | Clinical Outcomes & Synergy Potential |
|---|---|---|---|
| Prebiotics (Fibers) | Psyllium, Inulin-type Fructans [33] | Increases SCFA producers (Faecalibacterium, Roseburia); Raises fecal SCFA (butyrate) levels [116]. | Improves constipation symptoms; synergy with 5-ASAs by reducing inflammation. |
| Probiotics | Multi-strain probiotics, Bifidobacterium lactis [33] | Modulates microbial community; enhances gut barrier integrity. | Reduces disease activity in mild-moderate UC; may maintain remission. |
| Postbiotics | Bacterial lysates, SCFA formulations [33] | Directly provides bioactive molecules (e.g., butyrate). | Attenuates intestinal inflammation; potential to reduce steroid dependency. |
| Fecal Microbiota Transplantation (FMT) | Healthy donor stool [118] | Increases microbial diversity; restores beneficial taxa. | ~30% efficacy in inducing remission in refractory UC; resets microbial ecology. |
| Dietary Patterns | High-fiber, Polyphenol-rich (e.g., Green-Mediterranean) [116] | Enriches Faecalibacterium, Eubacterium, Roseburia; increases plasma urolithins. | Reduces inflammatory markers (e.g., CRP); synergistic with biologics. |
Table 2: Microbiota-Targeted Interventions in Cancer Therapy
| Intervention Type | Specific Example | Key Microbiota/Metabolite Changes | Clinical Outcomes & Synergy Potential |
|---|---|---|---|
| Probiotics | Lactobacillus rhamnosus [118] | Mitigates radiation-induced dysbiosis; reduces pro-inflammatory cytokines (IL-1β). | Significantly reduces radiation-induced diarrhea [118]. |
| Probiotics in Immunotherapy | Bifidobacterium longum APC1472 [33] | Attenuates food intake dysregulation; modulates hypothalamic molecular alterations. | Anti-obesity effects; potential synergy with immunotherapy via metabolic health. |
| FMT in Immunotherapy | Healthy donor FMT + PD-1 inhibitors [118] | Enriches immunogenic bacteria; enables donor strain engraftment. | 65% response rate in advanced melanoma (20% CR); reverses anti-PD-1 resistance. |
| Prebiotics in Chemotherapy | Fructooligosaccharides (FOS)/Galactooligosaccharides (GOS) [33] | Supports growth of beneficial Bifidobacterium; increases SCFA production. | Preclinical data shows attenuation of enduring effects of early-life poor diet. |
| Engineered Bacteria | Lactobacillus strains engineered to deliver therapeutics [119] | Local production of anti-inflammatory cytokines or enzyme inhibitors in gut. | Preclinical: Targeted delivery to tumor microenvironment reduces off-target effects. |
Table 3: Impact of Microbiome on Conventional Drug Efficacy and Toxicity
| Conventional Drug | Condition | Microbiome Interaction | Impact on Therapy |
|---|---|---|---|
| Immune Checkpoint Inhibitors (e.g., anti-PD-1) | Melanoma, Cancers | Presence of Bifidobacterium species enhances dendritic cell activation and CD8+ T-cell infiltration [118]. | Enhanced Efficacy: Improved response rates and survival in patients with favorable microbiota. |
| 5-Fluorouracil (5-FU) | Colorectal Cancer | Bacteroides fragilis metabolizes 5-FU, altering its bioavailability [118]. | Reduced Efficacy/Resistance: Microbial metabolism can decrease drug activity. |
| Irinitotecan | Colorectal Cancer | Gut bacterial β-glucuronidase reactivates drug metabolite, causing severe diarrhea [118]. | Increased Toxicity: Dose-limiting toxicity driven by microbial enzyme activity. |
| Oxaliplatin (OXP) | Colorectal Cancer | Modulates ileal microbiota to enhance local anti-tumor immune responses [118]. | Enhanced Efficacy: Efficacy is partially microbiota-dependent. |
| Trastuzumab | HER2+ Breast Cancer | Low abundance of Bifidobacterium & Prevotella linked to non-response [118]. | Reduced Efficacy: Antibiotic depletion of microbiota impairs drug efficacy in models. |
Experimental Protocols: Methodologies for Validating Synergy
To rigorously investigate the synergy between microbiota-targeted interventions and conventional drugs, well-designed experimental workflows are essential. The following section details key methodologies cited in recent literature.
Predicting Metabolite Responses Using Deep Learning (McMLP Protocol)
The McMLP (Metabolite response predictor using coupled Multilayer Perceptrons) model is a deep-learning approach designed to predict an individual's metabolite response to a dietary intervention based on their baseline gut microbiome profile [120]. This is crucial for personalizing interventions.
- Objective: To predict post-intervention (endpoint) metabolite concentrations (e.g., SCFAs) using pre-intervention (baseline) microbial composition and dietary intervention strategy as inputs.
- Workflow:
- Input Data Preparation:
- Baseline Data: Collect baseline fecal samples for 16S rRNA or shotgun metagenomic sequencing (to get species-level relative abundances) and metabolomic profiling (e.g., via LC-MS for targeted SCFA quantification).
- Dietary Intervention: Encode the intervention strategy (e.g., binary for presence/absence of a fiber, or numeric for dose).
- Data Transformation: Apply Centered Log-Ratio (CLR) transformation to microbial relative abundances and log10 transformation to metabolite concentrations.
- Model Architecture (Two-Step):
- Step 1 (MLP₁): A multilayer perceptron (MLP) with ReLU activation functions takes the baseline microbiota, baseline metabolome, and dietary intervention as input to predict the endpoint microbial composition.
- Step 2 (MLP₂): A second MLP takes the predicted endpoint microbiota, the baseline metabolome, and the dietary intervention as input to predict the endpoint metabolomic profile.
- Training and Validation: The model is trained on a subset of the data from a dietary intervention study. The first MLP is trained using the actual endpoint microbiome data, but the second MLP is trained using only the predicted endpoint microbiome from MLP₁ to maintain consistency with the application phase. Performance is evaluated on a held-out test set using metrics like the Spearman correlation coefficient between predicted and true metabolite values [120].
- Input Data Preparation:
The DOT script below visualizes this two-step prediction workflow.
Assessing Synergy in Preclinical Cancer Models
This protocol evaluates whether a microbiota-targeted intervention (e.g., a probiotic) enhances the anti-tumor efficacy of an immune checkpoint inhibitor (ICI) in a mouse model.
- Objective: To determine if co-administration of a probiotic synergistically improves the response to anti-PD-1 therapy.
- Workflow:
- Animal Grouping: Inoculate immunocompetent mice with syngeneic tumor cells (e.g., MC38 colon carcinoma). Randomize mice into four treatment groups (n=8-10/group):
- Group 1: Vehicle control (oral gavage + IgG IP).
- Group 2: Probiotic only (e.g., Bifidobacterium longum via oral gavage).
- Group 3: Anti-PD-1 antibody only (intraperitoneal injection).
- Group 4: Probiotic + anti-PD-1 antibody.
- Monitoring and Sample Collection:
- Monitor tumor volume 2-3 times weekly by caliper measurement.
- Collect fecal samples at baseline, during, and at endpoint for microbiome analysis (16S sequencing).
- At endpoint, harvest tumors, spleen, and blood.
- Endpoint Analyses:
- Tumor Immunophenotyping: Digest tumor tissue to create a single-cell suspension. Analyze tumor-infiltrating lymphocytes (TILs) by flow cytometry, focusing on CD45⁺CD8⁺ T-cells, CD4⁺FoxP3⁺ T-regs, and markers of activation (e.g., IFN-γ, Granzyme B).
- Cytokine Profiling: Measure serum or tumor homogenate levels of cytokines (e.g., IFN-γ, TNF-α, IL-6) by ELISA or multiplex immunoassay.
- Microbiome Analysis: Process fecal DNA and sequence the 16S rRNA V4 region. Analyze for differences in alpha/beta diversity and specific taxon abundances (e.g., Bifidobacterium) between groups.
- Animal Grouping: Inoculate immunocompetent mice with syngeneic tumor cells (e.g., MC38 colon carcinoma). Randomize mice into four treatment groups (n=8-10/group):
- Statistical Analysis: Compare tumor growth curves (repeated measures ANOVA) and final tumor weights/endpoint metrics (one-way ANOVA with post-hoc test). A significant reduction in tumor volume and increase in cytotoxic T-cells in the combination group versus either monotherapy demonstrates synergy [118].
This table catalogs key reagents, tools, and computational resources essential for conducting research at the intersection of the microbiome and therapeutic intervention.
Table 4: Key Research Reagent Solutions
| Tool / Reagent | Function / Purpose | Specific Examples & Notes |
|---|---|---|
| Deep Metagenomic Sequencing | Provides high-resolution, strain-level analysis of the entire gut microbiome community. | Shotgun sequencing (used in ZOE's PREDICT studies [121]) is preferred over 16S rRNA for functional gene analysis. |
| Gnotobiotic Mouse Models | Allows study of host-microbe interactions in a controlled, germ-free environment. | Essential for establishing causality. Can be colonized with defined microbial communities (e.g., humanized microbiota). |
| GC-MS / LC-MS Platforms | Quantification of microbial metabolites in fecal, serum, or tumor samples. | GC-MS is standard for SCFA quantification. LC-MS is used for broader metabolomic profiling, including bile acids and polyphenol metabolites [116]. |
| Flow Cytometry Panels | Comprehensive immunophenotyping of immune cells in blood, spleen, and tumor microenvironment. | Panels should include markers for T-cells (CD3, CD4, CD8), T-regs (FoxP3), activation (CD69, ICOS), and exhaustion (PD-1, LAG-3). |
| McMLP Software | Deep learning tool to predict personalized metabolite responses to dietary interventions. | Outperforms traditional machine learning (Random Forest) in predicting SCFA responses, enabling precision nutrition design [120]. |
| GA-map Dysbiosis Test | Standardized assay to assess and quantify the degree of microbiome dysbiosis. | Provides a validated dysbiosis index, useful as a biomarker in patient stratification [33]. |
| Engineered Probiotic Strains | Precise delivery of therapeutic payloads (e.g., enzymes, cytokines) to the gut niche. | e.g., Lactobacillus strains engineered to produce anti-inflammatory IL-10 or degrade inflammatory mediators [119]. |
The evidence for synergistic interplay between microbiota-targeted interventions and conventional drugs is compelling and points toward a new paradigm in managing complex diseases like IBD and cancer. The integration of prebiotics, probiotics, postbiotics, and FMT with pharmaceuticals holds the promise of enhanced efficacy, reduced toxicity, and the overcoming of drug resistance. However, significant challenges remain, including high interindividual variability, the need for more robust clinical trials that control for background diet [33], and the development of standardized, high-evidence microbial signatures for patient stratification.
Future research must focus on elucidating causal mechanisms, moving beyond correlation. This will involve sophisticated computational models like McMLP for prediction [120], advanced drug delivery systems for precise microbiome modulation [119], and large-scale, longitudinal studies that integrate multi-omics data. The ultimate goal is the realization of truly personalized medicine, where a patient's microbiome composition informs the selection of both the conventional drug and the optimal biotic partner to achieve the best possible clinical outcome.
The integration of genomic, metabolomic, and clinical data represents a paradigm shift in gut microbiota research, enabling comprehensive validation of bioactive compound effects on host physiology. Multi-omics integration moves beyond single-layer analyses to provide a systems-level understanding of how dietary components and microbial metabolites influence human health through complex host-microbe interactions. This technical guide explores established and emerging methodologies for multi-omics data generation, processing, integration, and validation, with specific applications to studying bioactive compounds and their functional impacts on the gut microbiome and host systems. We detail experimental workflows, computational frameworks, and validation strategies that researchers can implement to generate robust, translatable findings in nutritional science, pharmacobiology, and therapeutic development.
The human gut microbiota constitutes a complex ecosystem of bacteria, fungi, parasites, and viruses that enter symbiotic relationships with host cells, playing crucial roles in pathogen protection, intestinal epithelium development, and immune system regulation [17]. Bioactive compounds derived from dietary sources or produced by commensal bacteria, including lactic acid bacteria (LAB), can significantly influence this ecosystem through multiple molecular pathways. These microbial metabolites enter host circulation and influence distant body systems through various gut-organ axes, including the gut-microbiota-brain, gut-liver, and gut-bone pathways [17].
Multi-omics approaches are particularly valuable for validating the effects of bioactive compounds because they simultaneously capture changes across multiple biological layers—from genetic potential to metabolic output—within the same experimental framework. This integrated perspective is essential for moving beyond correlation to establish causal mechanisms in microbiome research. As technological advancements have reduced costs for high-throughput data generation, researchers can now collect large-scale datasets across genomic, transcriptomic, proteomic, metabolomic, and epigenomic layers, enabling unprecedented insights into the molecular interactions associated with complex diseases and therapeutic interventions [122].
The fundamental challenge in multi-omics integration lies in addressing the high dimensionality and heterogeneity of the resulting datasets while extracting biologically meaningful patterns. Successful integration requires specialized computational methods that can accommodate different data types, scales, and structures while accounting for technical variability and batch effects. When properly executed, multi-omics integration provides a powerful framework for biomarker discovery, patient stratification, and guiding therapeutic interventions [122].
Multi-Omics Experimental Design and Methodologies
Core Omics Layers and Their Applications
Table 1: Core omics technologies for validating bioactive compound effects
| Omics Layer | Analytical Platforms | Key Outputs | Relevance to Bioactive Compounds |
|---|---|---|---|
| Genomics | Whole-genome sequencing, SNP arrays, GSA | Genetic variants, SNP profiles, ancestry | Host genetic predisposition to metabolite response, microbial genetic potential |
| Metabolomics | LC-MS, GC-MS, NMR | Metabolite identification and quantification | Direct measurement of bioactive compounds and their metabolic products |
| Microbiomics | 16S rRNA sequencing, shotgun metagenomics | Microbial composition, functional potential | Changes in microbial communities in response to interventions |
| Proteomics | LC-MS/MS, affinity-based arrays | Protein identification and quantification | Host and microbial protein expression changes |
| Epigenomics | Bisulfite sequencing, ChIP-seq | DNA methylation patterns, histone modifications | Regulatory changes induced by microbial metabolites |
| Clinical Data | Laboratory tests, imaging, surveys | Physiological and phenotypic measurements | Correlation of molecular changes with health outcomes |
Experimental Workflows for Multi-Omics Studies
Well-designed multi-omics studies follow structured workflows that ensure data quality and integration capability. The general workflow encompasses study design, sample processing, data generation, computational integration, and biological validation [123]. For studies investigating bioactive compounds, key considerations include longitudinal sampling to capture temporal dynamics, appropriate control groups, and standardized processing protocols to minimize technical variation.
Figure 1: Experimental workflow for multi-omics studies of bioactive compounds, showing parallel processing of different molecular layers from sample collection through data integration and validation.
Sample Collection and Preparation Protocols
Proper sample collection and processing are critical for generating high-quality multi-omics data. For gut microbiota studies focused on bioactive compounds, the following protocols are recommended:
- Fecal Sample Collection: Collect fresh fecal samples in sterile containers with stabilizers (e.g., RNAlater for transcriptomics, specific preservatives for metabolomics). Immediately freeze at -80°C. For metabolomic analysis, snap-freezing in liquid nitrogen is preferred to preserve labile metabolites.
- Blood Collection: Draw blood into appropriate collection tubes (EDTA for plasma, serum separator tubes for serum). Process within 30 minutes of collection. Separate into plasma/serum, buffy coat (for genomic DNA), and red blood cells. Aliquot and store at -80°C.
- Tissue Biopsies: For animal or human intestinal biopsies, collect using standardized surgical procedures. Rinse with saline to remove luminal content. Divide samples for different omics analyses if sufficient material is available.
For multi-omics studies, it is essential to align sampling times across omics layers and maintain consistent processing protocols throughout the study to minimize technical variability. Documenting detailed metadata, including time of collection, processing delays, and storage conditions, is crucial for downstream analysis and interpretation [123].
Computational Integration Methods and Data Analysis
Data Preprocessing and Quality Control
Before integration, each omics dataset requires specialized preprocessing to ensure data quality and comparability. Key steps include:
Genomic Data Processing: For host genomics, process raw sequencing data through quality filtering, adapter trimming, alignment to reference genomes, variant calling, and annotation. For microbiome data, process 16S rRNA sequences through denoising, chimera removal, and amplicon sequence variant (ASV) calling, or process shotgun metagenomic data through quality control, host sequence removal, and taxonomic/functional profiling [123].
Metabolomic Data Processing: Process raw mass spectrometry data through peak detection, retention time alignment, ion annotation, and compound identification using reference databases. Apply quality control measures including pooled quality control samples, internal standards, and blank subtraction to account for technical variation [123].
Critical preprocessing considerations for multi-omics integration include:
- Batch effect correction using ComBat or other statistical methods
- Missing value imputation using k-nearest neighbors or random forest approaches
- Data normalization to account for technical variability (e.g., median normalization, probabilistic quotient normalization)
- Data transformation (e.g., log transformation, variance stabilizing transformation) to approximate normal distributions
- Data scaling (e.g., mean-centering, unit variance scaling) to make variables comparable across platforms [123]
Multi-Omics Integration Approaches
Multi-omics data can be integrated at different stages of analysis, each with distinct advantages and limitations:
Figure 2: Multi-omics integration approaches, showing the continuum from early to late integration methods with their characteristic features.
Early Integration (A Priori): Combines raw or preprocessed data from multiple omics layers into a single matrix before analysis. Requires measurements from the same biospecimens and careful scaling to ensure equal contribution from each platform. Methods include concatenation-based approaches followed by multivariate analysis [123].
Intermediate Integration: Simultaneously models multiple omics datasets while preserving their distinct nature. Includes methods like:
- Multiple Factor Analysis (MFA): Identifies common structures across datasets
- Joint Non-negative Matrix Factorization (jNMF): Decomposes multiple matrices into shared and specific components
- Multi-Omics Factor Analysis (MOFA): Discovers latent factors that explain variation across multiple omics layers [123]
Late Integration (A Posteriori): Analyzes each omics dataset separately, then integrates the results. Includes:
- Pathway enrichment integration: Combines enriched pathways from separate omics analyses
- Network-based integration: Constructs networks for each omics type, then integrates them into multi-layer networks
- Machine learning integration: Uses results from one omics analysis to inform analysis of another layer [123] [122]
Network-Based Integration Approaches
Network-based methods are particularly powerful for multi-omics integration as they provide a holistic view of relationships among biological components in health and disease [122]. These approaches represent molecular entities as nodes and their relationships as edges, enabling the identification of key regulators and functional modules.
For bioactive compound studies, network integration can reveal how specific compounds influence cross-omics interaction networks and identify key driver molecules that mediate their effects. Implementation typically involves:
- Constructing individual omics networks (co-expression, correlation, or interaction networks)
- Integrating networks using methods like similarity-based fusion or multi-layer network approaches
- Identifying multi-omics modules and hub nodes
- Annotating modules with functional information and correlating with phenotypes
Validation Strategies and Statistical Frameworks
Validation Protocols for Multi-Omics Findings
Robust validation is essential for establishing the biological significance of multi-omics discoveries. A tiered validation approach includes:
Technical Validation: Confirm analytical measurements using orthogonal platforms. For genomic findings, validate using different sequencing technologies or PCR-based methods. For metabolomic discoveries, confirm compound identities using purified standards and tandem mass spectrometry.
Biological Validation: Establish functional relevance using experimental models:
- In vitro systems: Cell culture models (e.g., Caco-2, HT-29 for intestinal studies) to test direct effects
- Animal models: Gnotobiotic mice, humanized microbiota models to validate host-microbe interactions
- Organ-on-a-chip systems: Microphysiological systems that mimic human intestinal environment
Clinical Validation: Translate findings to human populations through:
- Independent cohort studies: Validate biomarkers in different populations with similar characteristics
- Interventional trials: Test predictions through targeted dietary interventions or supplementation
- Longitudinal tracking: Monitor stability of multi-omics signatures over time [124]
Statistical Frameworks for Multi-Omics Studies
Appropriate statistical methods are crucial for robust multi-omics analysis. Key considerations include:
Multiple Testing Correction: Account for the high dimensionality of multi-omics data using false discovery rate (FDR) control rather than family-wise error rate. Commonly used methods include Benjamini-Hochberg procedure and Storey's q-value.
Power and Sample Size: Ensure adequate statistical power through sample size calculations specific to multi-omics studies. While challenging due to the high dimensionality, power calculations can be based on the expected effect sizes of key variables or through simulation studies [125].
Confounding Adjustment: Address potential confounders including age, sex, BMI, batch effects, and population stratification through inclusion in statistical models or using regression-based adjustment before analysis.
Table 2: Validation metrics for multi-omics models of bioactive compound effects
| Validation Type | Statistical Approach | Interpretation | Application Example |
|---|---|---|---|
| Discriminatory Power | Area Under ROC Curve (AUC) | 0.5 (random) - 1.0 (perfect) | Distinguishing responders from non-responders to bioactive compounds |
| Calibration | Hosmer-Lemeshow test | p > 0.05 indicates good fit | Agreement between predicted and observed clinical outcomes |
| Stability | Bootstrap resampling | Consistency of selected features across resampled datasets | Robustness of microbial biomarkers across subpopulations |
| Prospective Validation | Sensitivity, Specificity | Performance in independent cohort | Real-world performance of multi-omics signature |
| Temporal Validation | Intraclass Correlation | 0-1 (poor to excellent consistency) | Stability of multi-omics profiles over time [124] |
Applications to Bioactive Compounds and Gut Microbiota Research
Case Studies: Multi-Omics Validation of Bioactive Compound Effects
Lactic Acid Bacteria and Metabolic Health: Multi-omics approaches have validated the beneficial effects of specific LAB strains on host metabolism. For example, integrative analysis revealed that Lacticaseibacillus paragasseri HM018 from human breast milk improved lipid and bile acid metabolism in hypercholesterolemic rats, with metabolomic profiling showing changes in bile acid composition and genomic analysis identifying modulated expression of lipid-regulating genes [17]. Similarly, Levilactobacillus brevis RAMULAB54 from fermented sugarcane juice demonstrated hypoglycemic and hypolipidemic effects through activation of PPAR-γ, validated through combined genomic (gene expression), metabolomic (short-chain fatty acids), and clinical (glucose, lipid measurements) data [17].
Polyphenol-Rich Dietary Patterns: Multi-omics integration has elucidated mechanisms underlying the health benefits of polyphenol-rich diets. A study combining metabolomic profiling of polyphenol metabolites with microbiome sequencing and host inflammatory markers demonstrated that a polyphenol-rich dietary pattern reduced intestinal permeability and lowered pro-inflammatory gut bacteria-derived mediators [33]. Metagenomic sequencing further identified specific bacterial taxa involved in polyphenol metabolism, while metabolomic analysis quantified resulting bioactive metabolites in circulation.
Bifidobacterium and Immune Function: Integrated multi-omics approaches have validated the immunomodulatory effects of Bifidobacterium longum APC1472 in overweight/obese individuals. The study combined clinical parameters (body weight, food intake), inflammatory markers, metabolomic profiling of microbial metabolites, and metagenomic sequencing of gut microbiota, demonstrating attenuation of endocrine and behavioral alterations associated with obesity [33].
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Essential research reagents and platforms for multi-omics studies of bioactive compounds
| Category | Essential Items | Function and Application |
|---|---|---|
| Sample Collection | RNAlater, PAXgene Blood RNA tubes, Streck Cell-Free DNA Blood Collection Tubes | Stabilize nucleic acids for transcriptomic and genomic analyses |
| DNA/RNA Extraction | QIAamp DNA Stool Mini Kit, RNeasy PowerMicrobiome Kit, MagMAX Microbiome Ultra Nucleic Acid Isolation Kit | High-quality nucleic acid extraction from complex samples |
| Metabolite Extraction | Methanol:Water:Chloroform, Oasis HLB Solid Phase Extraction Cartridges | Comprehensive metabolite extraction for untargeted metabolomics |
| Sequencing | Illumina NovaSeq, PacBio Sequel, Oxford Nanopore GridION | Genomic, metagenomic, and transcriptomic profiling |
| Mass Spectrometry | Q-Exactive HF, TripleTOF 6600, Orbitrap Fusion Lumos | High-resolution metabolomic and proteomic profiling |
| Bioinformatics | QIIME 2, mothur, XCMS Online, MetaboAnalyst 5.0, mixOmics | Data processing, statistical analysis, and integration |
| Cell Culture Models | Caco-2, HT-29, SH-SY5Y, primary intestinal organoids | In vitro validation of bioactive compound effects |
| Animal Models | Germ-free mice, humanized microbiota mice, genetically engineered models | In vivo validation of mechanisms and efficacy |
Future Directions and Implementation Challenges
Emerging Technologies and Methodologies
The field of multi-omics research continues to evolve rapidly, with several emerging technologies promising to enhance studies of bioactive compounds and gut microbiota:
Single-Cell Multi-Omics: Technologies like scRNA-seq combined with metabolomic or proteomic profiling at single-cell resolution will enable unprecedented resolution in understanding how bioactive compounds affect specific cell types within complex tissues like the intestinal epithelium.
Spatial Multi-Omics: Spatial transcriptomics and metabolomics platforms allow researchers to preserve spatial context while measuring multiple molecular layers, revealing how gut microbiota and their metabolites influence tissue organization and microenvironments.
Longitudinal Multi-Omics Sampling: Advanced sampling technologies including capsule-based gut samplers and continuous monitoring devices will enable dense longitudinal data collection, capturing dynamic responses to bioactive compounds over time.
AI-Driven Integration: Machine learning and deep learning approaches are increasingly being applied to multi-omics data, with graph neural networks showing particular promise for integrating heterogeneous biological data and predicting personalized responses to bioactive compounds [123] [122].
Implementation Challenges and Solutions
Despite considerable advances, several challenges remain in implementing robust multi-omics studies:
Data Heterogeneity: The different scales, distributions, and types of multi-omics data present integration challenges. Solutions include developing specialized normalization methods and using ensemble approaches that combine multiple integration strategies.
Sample Requirements: Comprehensive multi-omics profiling often requires substantial biological material, which can be limiting for certain sample types. Miniaturized protocols and low-input technologies are addressing this limitation.
Computational Resources: Large-scale multi-omics studies require significant computational infrastructure and expertise. Cloud-based platforms and user-friendly workflows are making multi-omics more accessible to non-computational researchers.
Biological Interpretation: Translating integrated multi-omics findings into mechanistic insights remains challenging. Enhanced pathway databases, network analysis tools, and functional validation frameworks are improving interpretability.
Standardization and Reproducibility: Inconsistent protocols and reporting hinder reproducibility and comparison across studies. Adoption of FAIR (Findable, Accessible, Interoperable, Reproducible) principles and reporting standards like MIAME (Microarray), MSI (Metabolomics), and MIAPE (Proteomics) is addressing these issues [123].
Multi-omics integration represents a powerful framework for validating the effects of bioactive compounds on gut microbiota and host physiology. By simultaneously interrogating genomic, metabolomic, and clinical data layers, researchers can move beyond correlation to establish causal mechanisms and identify key molecular players in the host-microbe dialogue. The methodologies and validation strategies outlined in this technical guide provide a roadmap for implementing robust multi-omics approaches that generate biologically meaningful and clinically translatable findings. As technologies advance and computational methods mature, multi-omics integration will play an increasingly central role in precision nutrition, therapeutic development, and personalized health interventions targeting the gut microbiome.
The human gut microbiome, a complex ecosystem of trillions of microorganisms, is increasingly recognized as a pivotal factor in human health and disease. Within this realm, the emergence of next-generation probiotics (NGPs) and engineered microbial therapeutics represents a paradigm shift, moving from conventional probiotic supplementation to the precise manipulation of gut microbiota for therapeutic purposes [126]. This evolution is intrinsically linked to a deeper understanding of how bioactive compounds influence microbial communities and host physiology. Driven by advances in synthetic biology, genomics, and bioinformatics, these innovative therapeutic strategies are transitioning from concept to clinical reality, offering novel solutions for a range of chronic conditions including cancer, metabolic disorders, and inflammatory bowel diseases [127] [128] [129].
This whitepaper provides a technical evaluation of NGPs and engineered microbial therapeutics, framing their development within the broader context of bioactive compound research. It is structured to guide researchers and drug development professionals through the latest advances, core methodologies, and future directions of this rapidly advancing field.
Next-Generation Probiotics: From Identification to Therapeutic Application
Defining Next-Generation Probiotics
Next-generation probiotics are live microorganisms, identified through comparative microbiota analyses, that confer a health benefit when administered in adequate amounts [126]. Unlike traditional probiotics (e.g., Lactobacillus and Bifidobacterium species), which have a long history of use primarily as food ingredients, NGPs are often derived from previously unexplored microbial genera and are developed specifically for pharmaceutical applications [126]. Key differentiators include their origin from next-generation sequencing studies, a well-defined mode of action, and their status as live biotherapeutic products (LBPs) subject to pharmaceutical regulations [126].
Identification, Characterization, and Validation
The pipeline for developing NGPs involves a multi-stage process of identification, characterization, and functional validation to ensure safety and efficacy.
Identification and Isolation: Potential NGP strains are initially identified through 16S rRNA gene sequencing and bioinformatic analysis of microbiota compositions from healthy versus diseased individuals [126]. This allows for the targeted isolation of strains associated with a healthy state. Advanced techniques like terminal restriction fragment length polymorphism (T-RFLP) and analysis of the 16S to 23S intergenic spacer region provide higher resolution for distinguishing between prokaryotic species [126].
In Vitro Characterization: Isolated strains undergo rigorous in vitro screening. This includes:
- Antagonistic Activity Assays: Co-culture experiments to evaluate the strain's ability to inhibit the growth of pathogenic organisms [126].
- Immunomodulatory Assays: Measuring the production of cytokines and the activation of immune cells to determine immunomodulatory potential [126].
- Adhesion Assays: Using organoids, intestinal tissue cultures, or biopsies to assess the strain's ability to adhere to intestinal epithelium, a prerequisite for persistence and colonization [126].
- Simulated Gut Models: Employing artificial stomach and intestinal fluids to study survival, growth, and metabolism under conditions that approximate the human gastrointestinal tract [126].
In Vivo Validation and Omics Integration: Promising candidate strains are advanced to in vivo testing in animal models of disease to evaluate their efficacy in reducing pathogen colonization, modulating inflammation, and other therapeutic endpoints [126]. The process is further refined using advanced omics technologies. Transcriptomics, proteomics, and metabolomics are used to identify biomarkers of efficacy and elucidate mechanisms of action [126].
Table 1: Key Differences Between Traditional and Next-Generation Probiotics
| Aspect | Traditional Probiotics | Next-Generation Probiotics |
|---|---|---|
| Origin | Limited species (e.g., Lactobacillus, Bifidobacterium) with a long history of use | Diverse, newly isolated genera/species from advanced microbiome analyses |
| Development | Top-down screening from healthy individuals | Comparative analysis of healthy vs. diseased microbiota |
| Safety Profile | Long history of safe use | New and require extensive toxicological studies |
| Primary Application | Food ingredients or supplements | Live biotherapeutic products (LBPs) or drugs |
| Regulatory Path | Dietary supplement regulation | Pharmaceutical clinical trials (PK/PD studies) |
| Strain Specificity | Health benefits are often species-specific | Health benefits are highly strain-specific |
The following diagram illustrates the multi-stage workflow for the identification and development of novel NGP strains:
Diagram 1: NGP Development Workflow
Engineered Microbial Therapeutics: Programming Bacteria for Precision Medicine
Synthetic Biology Tools for Engineering
The application of synthetic biology enables the creation of engineered bacteria that function as "living therapeutics" or "living robots" for targeted drug delivery [127]. Key technological advancements facilitate this programming:
CRISPR-Cas Systems: This genome editing tool is central to microbial engineering due to its high precision, efficiency, and scalability [130]. The CRISPR-Cas9 system, involving a Cas9 protein and a single-guide RNA (sgRNA), introduces double-strand breaks at specific genomic locations, allowing for precise mutations, deletion of inhibitory elements, or integration of novel biosynthetic pathways [130]. Derivatives like CRISPR interference (CRISPRi) and CRISPR activation (CRISPRa) allow for fine-tuned modulation of gene expression without altering the DNA sequence, useful for activating dormant biosynthetic gene clusters in species like Streptomyces to discover novel antibiotics [130].
Programmable Gene Circuits and Biosensors: Synthetic gene circuits can be designed to dynamically control therapeutic functions. These include environment-responsive triggers that enable bacteria to sense local disease-specific cues (e.g., low oxygen in tumors, inflammatory signals) and subsequently release a therapeutic payload [127].
Targeting and Safety Mechanisms
For in vivo applications, precision targeting and robust safety controls are paramount.
- Targeting Strategies: Engineered bacteria can be directed to disease sites using surface adhesion molecules or by exploiting microenvironmental cues, enabling them to home to specific tissues like tumors [127].
- Biosafety Control Systems: To address the risk of uncontrolled bacterial spread, built-in safety mechanisms are essential. These include suicide genetic circuits (or "kill-switches") that induce bacterial cell death upon completion of the therapeutic task or in response to an external signal, and auxotrophy designs that make the bacteria dependent on externally supplied nutrients not available in the environment [127].
Table 2: Engineering Tools and Their Applications in Microbial Therapeutics
| Technology/Strategy | Key Function | Therapeutic Application Example |
|---|---|---|
| CRISPR-Cas9 | Precise gene editing and pathway optimization | Enhancing insulin production in E. coli [130] |
| CRISPRi/CRISPRa | Targeted gene repression or activation | Activating dormant antibiotic pathways in Streptomyces [130] |
| Synthetic Gene Circuits | Conditionally control therapeutic output | Drug release in response to tumor microenvironment cues [127] |
| Surface Modifications | Enhance tissue-specific targeting | Adhesion molecules for targeting tumors [127] |
| Suicide Genetic Circuits | Prevent uncontrolled bacterial proliferation | Biocontainment strategy for environmental release [127] |
Impact on Host Health and Therapeutic Applications
Mechanisms of Action
NGPs and engineered microbes exert their therapeutic effects through multiple synergistic mechanisms:
- Production of Bioactive Compounds: They can synthesize beneficial molecules, such as short-chain fatty acids (SCFAs), directly at the disease site. Butyrate, for example, is a key SCFA with anti-inflammatory properties and a crucial energy source for colonocytes [131].
- Competitive Exclusion of Pathogens: NGPs can outcompete pathogenic bacteria for nutrients and adhesion sites, restoring a healthy microbial balance [126].
- Modulation of Host Immunity: These therapeutics can directly interact with host immune cells, promoting anti-inflammatory responses (e.g., increasing regulatory T-cells) or activating immune pathways against cancer cells [127] [126].
- Reinforcement of Gut Barrier: Certain NGPs, such as Akkermansia muciniphila, contribute to the integrity of the gut barrier, preventing the translocation of harmful substances and reducing systemic inflammation [132] [126].
Key Therapeutic Areas
- Oncology: Engineered microbes are being developed to target tumors, where they can locally produce anti-cancer agents, minimizing systemic side effects [127]. Furthermore, the gut microbiome is linked to cancer therapy responses. Specific gut microbiota signatures are associated with KRAS mutations in colorectal cancer (CRC), and machine learning models using these microbial profiles can predict KRAS mutation status, offering potential diagnostic tools [133].
- Metabolic and Inflammatory Disorders: NGPs show promise in treating metabolic syndrome, inflammatory bowel disease (IBD), and other chronic inflammatory conditions by modulating the gut microbiome and host metabolism [127] [128] [129]. For instance, Faecalibacterium duncaniae is recognized for its anti-inflammatory properties [132].
- Infectious Diseases: Engineered probiotics can produce antimicrobial peptides (bacteriocins) or other compounds that directly inhibit the growth of pathogens, offering a novel approach to combat infections [128] [126].
The diagram below illustrates the core mechanisms by which NGPs and engineered microbes exert their therapeutic effects on the host:
Diagram 2: Core Therapeutic Mechanisms
Experimental Methodologies and Research Toolkit
A robust technical toolkit is essential for advancing research in NGPs and engineered microbial therapeutics. The following table details key reagents and methodologies used in this field.
Table 3: Essential Research Reagent Solutions and Methodologies
| Research Tool / Reagent | Function / Application | Example Use Case |
|---|---|---|
| 16S rRNA Gene Sequencing Kits | Profiling and identifying microbial community composition | Identifying differential gut microbiota between KRAS mutant and wild-type CRC patients [133] |
| DNA Extraction Kits (e.g., MOBIO PowerSoil) | Isolation of high-quality microbial DNA from complex samples (stool, mucosa) | Preparing fecal samples for 16S rRNA sequencing to study gut microbiota signatures [134] [133] |
| In Vitro Colon Fermentation Models | Simulating human colonic conditions to study microbial metabolism | Investigating the impact of seaweed phenolics on microbial composition and SCFA production [131] |
| CRISPR-Cas9 Systems & gRNA | Precise genomic modification of microbial strains | Engineering E. coli for enhanced recombinant protein production [130] |
| Selective Culture Media (e.g., MRS, M17) | Isolation and cultivation of specific probiotic strains (e.g., lactic acid bacteria) | Studying growth characteristics and metabolite production of isolated NGP strains [126] |
| Artificial Stomach/Intestinal Fluids | Simulating GI tract conditions for survival and efficacy testing | Evaluating probiotic survival during passage through the gastrointestinal tract [126] |
| Cytokine Detection Assays (ELISA/MSD) | Quantifying immune markers to assess immunomodulatory effects | Measuring IL-10, TNF-α levels in cell culture supernatants after NGP co-culture [126] |
Quantitative Data from Key Studies
Recent studies have generated crucial quantitative data illustrating the interactions between bioactive compounds, the microbiome, and therapeutic interventions.
Table 4: Selected Quantitative Findings from Gut Microbiota Studies
| Study Focus | Key Quantitative Findings | Reference |
|---|---|---|
| Gut Microbiota in Colorectal Polyps | - ACE and Chao indexes were higher in normal mucosa and polyp tissues than in fecal samples (P < 0.05).- Fusobacterium abundance in normal mucosa was significantly higher in healthy individuals than in the polyp group. | [134] |
| Seaweed Phenolics & Colonic Fermentation | - Durvillaea potatorum showed highest total phenolic content at 8 h (3.14 mg GAE/g).- Phyllospora comosa significantly elevated SCFAs (acetic, butyric, isovaleric acid) at 12 h of fermentation. | [131] |
| KRAS Mutation & Microbiota in CRC | - Machine learning (Random Forest) model using 26 KRAS-associated gut microbiota achieved "qualified efficacy" in predicting KRAS mutation status. - Bifidobacterium spp. showed a significant positive correlation with mast cell infiltration. | [133] |
Emerging Trends and Challenges
The future of NGPs and engineered microbial therapeutics is being shaped by several converging trends:
- Personalized Nutrition and Medicine: The integration of gut microbiota profiling will enable the identification of individuals who will benefit most from specific NGPs, paving the way for personalized functional foods and biotherapeutics tailored to an individual's microbial signature [129].
- Artificial Intelligence and Machine Learning: AI and ML are playing an increasingly vital role in predicting metabolic network interactions, optimizing bioprocesses, and even automating genome editing to accelerate drug discovery and strain development [130].
- Postbiotics and Membrane Vesicles: Research is expanding beyond live bacteria to include non-viable microbial components, or postbiotics. Membrane vesicles (MVs)—nanosized extracellular structures secreted by bacteria—are a promising class of postbiotics. These MVs, derived from NGPs like Akkermansia muciniphila, are rich in bioactive molecules and can modulate immune responses and gut barrier integrity, offering a potentially safer alternative to live biologics [132].
- Regulatory and Production Hurdles: Translating these technologies to the clinic faces significant challenges. NGPs and engineered microbes are subject to stringent pharmaceutical regulations, requiring extensive preclinical and clinical testing to demonstrate safety and efficacy [126]. Furthermore, scaling up production while maintaining consistency and viability presents a major bottleneck for industrial application [130].
Next-generation probiotics and engineered microbial therapeutics represent a frontier in medical science, merging insights from microbiome research with the precision of synthetic biology. Their development is deeply interwoven with the study of bioactive compounds, which serve both as tools for modulating the gut ecosystem and as products of the engineered microbes themselves. For researchers and drug development professionals, navigating this field requires a multidisciplinary grasp of genomics, microbial ecology, genetic engineering, and immunology. While challenges in safety, production scale-up, and regulatory approval remain, the continued integration of advanced technologies like AI and CRISPR, coupled with a deeper understanding of host-microbe interactions, holds the promise of delivering a new class of powerful, personalized therapeutics for a wide spectrum of diseases.
Conclusion
The evidence unequivocally positions dietary bioactive compounds as powerful modulators of the gut microbiota, with far-reaching implications for host physiology and disease prevention. The bidirectional relationship—where bioactives shape the microbiome and the microbiome, in turn, metabolizes these compounds into active mediators—forms a critical axis for health. Future research must pivot towards large-scale, well-controlled human studies that integrate multi-omics data to decode the precise mechanisms and immense personal variability. For biomedical and clinical research, the path forward lies in harnessing these insights to develop novel, microbiota-targeted therapeutics and personalized nutrition plans. The convergence of pharmacomicrobiomics and nutritional science promises a new era in precision medicine, where diet and drugs are tailored to an individual's unique microbial fingerprint to optimize therapeutic outcomes and mitigate adverse effects [citation:5].
References
- 1. Polyphenol [https://en.wikipedia.org/wiki/Polyphenol]
- 2. Dietary Polyphenol, Gut Microbiota, and Health Benefits [https://pmc.ncbi.nlm.nih.gov/articles/PMC9220293/]
- 3. A Review of Classification, Biosynthesis, Biological ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10343696/]
- 4. The Interaction between Flavonoids and Intestinal Microbes [https://pmc.ncbi.nlm.nih.gov/articles/PMC9857828/]
- 5. Top Foods High in Flavonoids [https://www.webmd.com/diet/foods-high-in-flavonoids]
- 6. Dietary Fiber Intake and Gut Microbiota in Human Health - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9787832/]
- 7. Beyond soluble and insoluble: A comprehensive ... [https://www.sciencedirect.com/science/article/pii/S0963996925001802]
- 8. Carotenoids | Linus Pauling Institute | Oregon State University [https://lpi.oregonstate.edu/mic/dietary-factors/phytochemicals/carotenoids]
- 9. Algal Carotenoids : Chemistry, Sources , and Application - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10379930/]
- 10. Gut microbiota functions: metabolism of nutrients and other ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5847071/]
- 11. Gut microbiota as an “invisible organ” that modulates the ... [https://www.sciencedirect.com/science/article/pii/S0753332219352758]
- 12. Frontiers | Understanding dysbiosis and resilience in the human gut microbiome: biomarkers, interventions, and challenges [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1559521/full]
- 13. Frontiers | The human gut microbiota is associated with host lifestyle: a comprehensive narrative review [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1549160/full]
- 14. Quantitative and dynamic profiling of human gut core ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11208268/]
- 15. A population-scale analysis of 36 gut microbiome studies ... [https://www.nature.com/articles/s41522-024-00567-9]
- 16. Frontiers | Unveiling roles of beneficial gut bacteria and optimal diets for health [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1527755/full]
- 17. Editorial: Lactic acid bacteria and their bioactive compounds [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1720803/full]
- 18. Interplay Between Dietary Bioactive Compounds and Gut ... [https://pubmed.ncbi.nlm.nih.gov/40367957/]
- 19. The impact of microalgae-derived bioactive compounds on ... [https://www.sciencedirect.com/science/article/abs/pii/S2214799325000955]
- 20. Reinventing gut health: leveraging dietary bioactive ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2024.1491821/full]
- 21. Bioactive molecules of probiotic bacteria and their ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6656846/]
- 22. Plant Antimicrobial Compounds and Their Mechanisms of ... [https://www.mdpi.com/2076-3417/15/7/3516]
- 23. The inhibitory effect of natural bioactives on the growth ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2849034/]
- 24. Mechanisms of microbiota modulation: Implications for health ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11081615/]
- 25. Molecular Mechanisms of Bioactive Nutrients Promoting ... [https://www.mdpi.com/1422-0067/24/18/13731]
- 26. Rapid modulation of gut microbiota composition by ... [https://www.nature.com/articles/s42255-025-01280-3]
- 27. Microbiota-dependent metabolites – New engine for T cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12218545/]
- 28. Immunomodulatory role of gut microbial metabolites [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1675065/full]
- 29. Evolving Dynamics of Fermented Food Microbiota and the Gut ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12249264/]
- 30. Mechanisms and implications of the gut microbial ... [https://www.nature.com/articles/s44324-025-00066-1]
- 31. Gut microbial metabolites: Shaping future diagnosis and ... [https://www.sciencedirect.com/science/article/pii/S1043661824003189]
- 32. Microbiota-derived tryptophan metabolism: Impacts on ... [https://www.sciencedirect.com/science/article/pii/S0531556523002401]
- 33. Nutrition & microbiome research highlights NeuroGASTRO ... [https://www.gutmicrobiotaforhealth.com/nutrition-and-microbiome-research-highlights-from-neurogastro-2025/]
- 34. Bioactive Compounds in Food as a Current Therapeutic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8401766/]
- 35. Interaction between microbiota and immunity in health and ... [https://www.nature.com/articles/s41422-020-0332-7]
- 36. The role of phytochemicals in modulating the gut microbiota [https://www.sciencedirect.com/science/article/pii/S2590097825000060]
- 37. Microbiota in health and diseases [https://www.nature.com/articles/s41392-022-00974-4]
- 38. The Immature Gut Barrier and Its Importance in ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2020.01153/full]
- 39. Absolute Quantitative Metagenomic Analysis Provides ... [https://www.mdpi.com/2218-273X/15/3/400]
- 40. Frontiers | Enhanced metagenomic strategies for elucidating the... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1626002/full]
- 41. Gut microbiome metagenomics in clinical practice [https://pmc.ncbi.nlm.nih.gov/articles/PMC12562794/]
- 42. Exploring Bioactive Compounds and the Gut Microbiota [https://www.mdpi.com/2076-3425/13/8/1226]
- 43. Advances in Culturomics Research on the Human Gut ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11091661/]
- 44. Gut Microbiota Profiling: Metabolomics Based Approach to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4960240/]
- 45. Therapeutic evaluation of gut microbiota-derived ... [https://www.sciencedirect.com/science/article/pii/S305078712500054X]
- 46. and metabolomics to evaluate the potential role of Metagenomics ... gut [https://bmcmicrobiol.biomedcentral.com/articles/10.1186/s12866-025-04259-y]
- 47. Metagenome-guided culturomics for the targeted enrichment of gut ... [https://pubmed.ncbi.nlm.nih.gov/39809763/]
- 48. Metagenome-guided culturomics for the targeted ... [https://www.nature.com/articles/s41467-024-55668-y]
- 49. Gut Microbiome Interactions with Drug Metabolism, Efficacy ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5718288/]
- 50. Gut microbiota: A potential enhancing factor for the ... [https://www.sciencedirect.com/science/article/pii/S0367326X25001959]
- 51. Drug-microbiota interactions: an emerging priority for ... [https://www.nature.com/articles/s41392-023-01619-w]
- 52. Pharmacomicrobiomics: The Role of the Gut Microbiome in ... [https://www.sciencedirect.com/science/article/pii/S0016508525007553]
- 53. Potential roles of gut microbes in biotransformation ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2022.956378/full]
- 54. Gut Microbiota-Mediated Biotransformation of Medicinal ... [https://www.mdpi.com/2571-8800/7/3/20]
- 55. Advancements in Immunomodulatory Therapies for IBD and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12336292/]
- 56. The updated 2025 ACG guidelines to manage adult ... [https://gi.org/journals-publications/ebgi/alkazzi_aug2025/]
- 57. Pharmacotherapy for Obesity: Recent Updates - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12456317/]
- 58. Institute for Clinical and Economic Review Publishes ... [https://icer.org/news-insights/press-releases/institute-for-clinical-and-economic-review-publishes-evidence-report-on-treatments-for-obesity/]
- 59. The American Diabetes Association Releases Standards of ... [https://diabetes.org/newsroom/press-releases/american-diabetes-association-releases-standards-care-diabetes-2025]
- 60. Diabetes treatment in 2025: can scientific advances keep ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3498849/]
- 61. Cover Story | Transformative Trends in CV Medicine For 2025 [https://www.acc.org/latest-in-cardiology/articles/2025/01/01/42/cover-story-transformative-trends-in-cv-medicine-for-2025]
- 62. Probiotics, prebiotics, and postbiotics in health and disease [https://pmc.ncbi.nlm.nih.gov/articles/PMC10625129/]
- 63. Unveiling the therapeutic symphony of probiotics ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2024.1355542/full]
- 64. The International Scientific Association of Probiotics and ... [https://www.nature.com/articles/s41575-021-00440-6]
- 65. Gut microbiome engineering with probiotics: current trends ... [https://link.springer.com/article/10.1007/s42452-025-07622-w]
- 66. The role of probiotics in personalized therapeutics [https://www.sciencedirect.com/science/article/pii/S2950194625002651]
- 67. Recent advances in prebiotics: Classification, mechanisms, ... [https://www.sciencedirect.com/science/article/pii/S266683352500142X]
- 68. Probiotics, Prebiotics, Synbiotics, Postbiotics, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12346543/]
- 69. Current research status and trends in the bioactivity of ... [https://www.frontiersin.org/journals/food-science-and-technology/articles/10.3389/frfst.2025.1692683/full]
- 70. Postbiotics in the medical field under the perspective of the ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2023.1239745/full]
- 71. Probiotics, Prebiotics, Postbiotics: From Mechanisms to ... [https://www.mdpi.com/journal/applsci/special_issues/707M0P3X5U]
- 72. The Metabolites Produced by Lactic Acid Bacteria and ... [https://www.mdpi.com/2311-5637/11/7/378]
- 73. Lactic Acid Bacteria: An Inexhaustible Source of Scientific ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11899038/]
- 74. Impact of lactic acid bacteria coculture on the quality ... [https://www.sciencedirect.com/science/article/pii/S0022030225008070]
- 75. Lactic Acid Bacteria Fermented Cabbage Cuts Lipids [https://bioengineer.org/lactic-acid-bacteria-fermented-cabbage-cuts-lipids/]
- 76. Bioactive compounds in the modulation of oxidative stress ... [https://www.nature.com/articles/s41598-025-16505-4]
- 77. The Influence of Bioactive Compounds on Metabolic ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1703963/abstract]
- 78. The influence of the gut microbiota on the bioavailability of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8343123/]
- 79. Bioavailability, Human Metabolism, and Dietary ... [https://pubmed.ncbi.nlm.nih.gov/40870788/]
- 80. Mechanisms and implications of the gut microbial modulation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12441142/]
- 81. Gut microbiota: a new perspective for bioavailability of ... [https://www.nature.com/articles/s41538-025-00589-3]
- 82. Exploring Bioactive Compounds and the Gut Microbiota - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10452544/]
- 83. Interindividual variability in gut microbiota and host ... [https://pubmed.ncbi.nlm.nih.gov/29190368/]
- 84. Baseline intestinal microbiota composition influences ... [https://www.nature.com/articles/s41522-025-00817-4]
- 85. Baseline intestinal microbiota composition influences ... [https://pubmed.ncbi.nlm.nih.gov/41198696/]
- 86. The diet rapidly and differentially affects the gut microbiota ... [https://microbiomejournal.biomedcentral.com/articles/10.1186/s40168-023-01469-2]
- 87. Gut microbiota and host genetics modulate the effect of ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2022.896348/full]
- 88. Absolute quantitative metagenomic analysis reveals ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12403899/]
- 89. Microbiome-driven precision medicine: advancing drug ... [https://pubmed.ncbi.nlm.nih.gov/40388258/]
- 90. Interactions between the intestinal microbiota and drug ... [https://www.sciencedirect.com/science/article/pii/S0006295225000711]
- 91. Pharmacomicrobiomics: immunosuppressive drugs and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11327386/]
- 92. Tutorial: Microbiome studies in drug metabolism - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9747132/]
- 93. (Poly)phenol-gut microbiota interactions and their impact ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12147749/]
- 94. Design and reporting of prebiotic and probiotic clinical ... [https://isappscience.org/resource/design-and-reporting-of-prebiotic-and-probiotic-clinical-trials-in-the-context-of-diet-and-the-gut-microbiome/]
- 95. Effects of probiotics, prebiotics, and synbiotics on gut ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12482033/]
- 96. Quercetin hybrid-hydrogel microparticles modulate gut ... [https://www.nature.com/articles/s41598-025-26608-7]
- 97. The role of probiotics, prebiotics, and synbiotics in ... [https://www.frontiersin.org/journals/systems-biology/articles/10.3389/fsysb.2025.1561047/full]
- 98. Modulation of gut microbiota by bioactive compounds for ... [https://www.sciencedirect.com/science/article/pii/S0753332222005376]
- 99. Microbiome confounders and quantitative profiling ... [https://www.nature.com/articles/s41591-024-02963-2]
- 100. Markers of metabolic health and gut microbiome diversity [https://pmc.ncbi.nlm.nih.gov/articles/PMC8245388/]
- 101. Gut microbiome may predict invisible chronic fatigue ... [https://www.jax.org/news-and-insights/2025/july/gut-microbiome-may-predict-invisible-chronic-fatigue-syndrome-and-long-covid]
- 102. Gut microbiota targeted interventions for immune function [https://www.sciencedirect.com/science/article/pii/S1756464625000386]
- 103. Tracking a dysregulated gut-brain axis with biomarkers of ... [https://www.sciencedirect.com/science/article/pii/S2666144619300097]
- 104. Frontiers | Comparative Perspectives and Translational Models in... [https://www.frontiersin.org/research-topics/72419/comparative-perspectives-and-translational-models-in-eating-behavior-insights-from-animal-models-and-human-studies]
- 105. Gut microbiome and health: mechanistic insights - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8995832/]
- 106. Appropriateness of Animal for Models Disease Studying Human [https://www.news-medical.net/life-sciences/How-Appropriate-are-Animal-Models-for-Studying-Human-Disease.aspx]
- 107. systems biology between Comparative and human ... animal models [https://pubmed.ncbi.nlm.nih.gov/23572365/]
- 108. Bio-Active Peptides from Marine Sources [https://www.mdpi.com/1422-0067/26/21/10508]
- 109. Mechanistic insights into β-glucans and gut microbiota ... [https://link.springer.com/article/10.1007/s44187-025-00503-6]
- 110. Global research trends in gut microbiota and cellular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12364940/]
- 111. The mutual effect of dietary fiber and polyphenol on gut ... [https://www.sciencedirect.com/science/article/abs/pii/S0144861725003224]
- 112. The effects of polyphenols on gut microbial metabolites and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12632128/]
- 113. Associations between dietary fiber, the gut microbiota, and ... [https://www.sciencedirect.com/science/article/pii/S2667268525000397]
- 114. Polyphenols—Gut Microbiota Interrelationship: A Transition to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8747136/]
- 115. Dietary polyphenols maintain human health through ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1710088/full]
- 116. Gut microbiome-mediated health effects of fiber and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12425962/]
- 117. Probiotics and gastrointestinal disorders: an umbrella meta ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12183855/]
- 118. Focus on gut microbes: new direction in cancer treatment - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12427127/]
- 119. Strategic modulation of the gastrointestinal microbiome to ... [https://www.sciencedirect.com/science/article/pii/S1359644625002417]
- 120. Predicting metabolite response to dietary intervention ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11742956/]
- 121. Whitepaper: The gut microbiome [https://zoe.com/whitepapers/gut-microbiome?srsltid=AfmBOorUyr2wVDBOIvfvZPHQviElrWlTs85z52kzcNpMAKTH-6pzy1OR]
- 122. Integrating Multi-Omics Data: Methods and Applications in ... [https://www.sciencedirect.com/science/article/pii/S2215017X25000657]
- 123. Metabolomics and Multi-Omics Integration - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC7281435/]
- 124. Multi-omic integration sets the path for early prevention ... [https://www.nature.com/articles/s41525-025-00491-7]
- 125. Multi-omics analyses develop and validate the optimal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12078830/]
- 126. Next-Generation Probiotics as Novel Therapeutics for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10972033/]
- 127. advances in engineered bacteria for targeted in vivo ... [https://www.sciencedirect.com/science/article/pii/S2090123225008239]
- 128. Recent advances of engineered probiotics for therapeutic ... [https://www.sciencedirect.com/science/article/pii/S2693125725000408]
- 129. Danone could leverage next -gen probiotics to formulate superior... [https://www.dairyreporter.com/Article/2025/02/04/danone-could-leverage-next-gen-probiotics-to-formulate-superior-functional-foods/]
- 130. Engineering Useful Microbial Species for Pharmaceutical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11944651/]
- 131. Bioactive phenolic compounds from Australian seaweeds ... [https://www.nature.com/articles/s41598-025-04689-8]
- 132. Membrane vesicles produced by next - generation from the... probiotics [https://pubmed.ncbi.nlm.nih.gov/40888419/]
- 133. Identification of KRAS mutation-associated gut in... microbiota [https://pmc.ncbi.nlm.nih.gov/articles/PMC11064510/]
- 134. Frontiers | Gut signatures in tissues of the colorectal polyp... microbiota [https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2022.1054808/full]