Bioequivalence of Synthetic vs Natural Bioactive Compounds: Scientific Foundations, Methodologies, and Clinical Implications
This comprehensive review examines the scientific and regulatory framework for establishing bioequivalence between synthetic and natural bioactive compounds, a critical consideration for drug development professionals and researchers.
Bioequivalence of Synthetic vs Natural Bioactive Compounds: Scientific Foundations, Methodologies, and Clinical Implications
Abstract
This comprehensive review examines the scientific and regulatory framework for establishing bioequivalence between synthetic and natural bioactive compounds, a critical consideration for drug development professionals and researchers. The article explores fundamental differences in compound origin, structure, and complexity, alongside methodological approaches for bioavailability assessment including pharmacokinetic studies and advanced analytical techniques. It addresses significant challenges in ensuring therapeutic equivalence, including variability in natural sources, metabolic differences, and complex formulation requirements. Through comparative analysis of regulatory standards and clinical evidence, this work provides a rigorous foundation for evaluating interchangeability, offering strategic insights for developing safe, effective, and standardized bioactive therapies across pharmaceutical and nutraceutical domains.
Defining Bioequivalence and Bioactive Compound Diversity
Bioequivalence establishes that two products with the same active ingredient are therapeutically equivalent by demonstrating comparable rate and extent of drug availability at the site of action. For natural bioactive compounds and their synthetic counterparts, demonstrating bioequivalence presents unique scientific challenges. While small molecule synthetic drugs typically have well-defined chemical structures that enable straightforward bioequivalence testing, natural products often exist as complex mixtures whose full composition may not be completely characterized [1]. The fundamental principle governing this evaluation is that the human body responds to chemical structure, not the source of that structure [2]. When natural and synthetic versions are chemically identical ("nature-identical"), they are expected to behave identically in biological systems, though differences in impurities, chirality, or formulation can significantly impact their biological performance.
The assessment of rate and extent of availability involves sophisticated pharmacokinetic measurements and, when necessary, pharmacodynamic endpoint studies. For conventional chemical drugs, generic versions must demonstrate chemical identity and bioequivalence in healthy human subjects [1]. However, for more complex natural product-based therapeutics and biologics, the regulatory requirements are more stringent, often requiring a "totality of evidence" approach that integrates multiple analytical and biological methods to establish comparable safety and efficacy profiles [1].
Structural and Physicochemical Comparison
Comparative analysis of natural products (NPs) and synthetic compounds (SCs) reveals significant differences in their structural characteristics that can influence bioequivalence. A comprehensive time-dependent chemoinformatic analysis of over 186,000 natural products and an equal number of synthetic compounds provides quantitative insights into these distinctions [3].
Molecular Size and Complexity
Table 1: Physicochemical Properties of Natural vs. Synthetic Compounds
| Property | Natural Products | Synthetic Compounds | Analytical Implications |
|---|---|---|---|
| Molecular Weight | Larger and increasing over time [3] | Controlled range (often 100-1000 Da) [1] | Affects membrane permeability and bioavailability |
| Ring Systems | More rings, larger fused rings, increasing glycosylation [3] | More aromatic rings, stable 5-6 membered rings [3] | Impacts protein binding and metabolic stability |
| Structural Complexity | Higher complexity and structural diversity [3] | Governed by drug-like constraints (e.g., Rule of Five) [3] | Influences dissolution and absorption kinetics |
| Heavy Atoms | Higher counts, increasing over time [3] | Moderate counts with limited variation [3] | Affects distribution and elimination profiles |
Elemental Composition and Functional Groups
Natural products exhibit distinct elemental distributions, with higher oxygen content and specific functional group patterns compared to synthetic compounds, which contain more nitrogen atoms, sulfur atoms, and halogens [3]. These differences influence solubility characteristics, metabolic pathways, and ultimately the rate and extent of bioavailability. The structural evolution of synthetic compounds shows some influence from natural products but has not fully evolved in their direction, maintaining more constrained physicochemical properties governed by synthetic accessibility and drug-like criteria [3].
Regulatory Frameworks and Bioequivalence Standards
Small Molecule Drugs vs. Biologics
The regulatory requirements for demonstrating bioequivalence differ significantly between conventional small molecules and complex natural products or biologics. For small molecule drugs, generic versions must exhibit chemical identity and be bioequivalent in healthy human subjects, typically demonstrated through pharmacokinetic studies measuring rate (C~max~, T~max~) and extent (AUC) of availability [1]. This established pathway depends on the ability to fully characterize the chemical structure and establish pharmaceutical equivalence.
For natural product-based therapies and biological drugs, the regulatory framework is more complex. These products "are produced in living systems or are derived from biologic material" and "tend to be larger in size than chemically-derived drugs, can exhibit a variety of post-translational modifications, and can have activities that are dependent on specific conformations" [1]. The European Medicines Agency and US Food and Drug Administration have established specific pathways for biosimilar products (termed "subsequent entry biologics" or "biocomparables") that acknowledge the impossibility of exact replication of complex biological products [1].
The "Totality of Evidence" Approach
For complex natural products and biosimilars, regulators employ a risk-based "totality of evidence" approach that integrates multiple lines of evidence [1]. This includes:
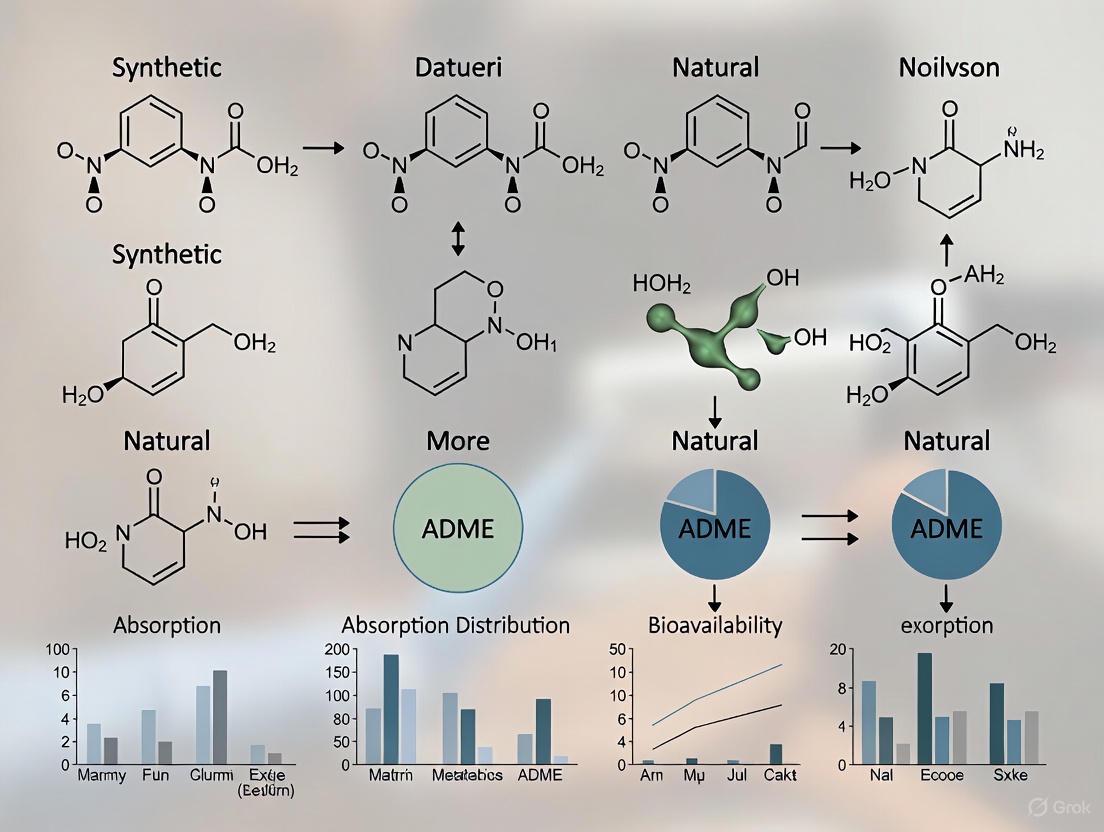
Diagram 1: Totality of Evidence Approach for Complex Products. This integrated strategy is required for natural products and biosimilars where conventional bioequivalence studies are insufficient [1].
Experimental Methodologies for Bioequivalence Assessment
Analytical Techniques for Structural Characterization
Establishing bioequivalence begins with comprehensive structural characterization using advanced analytical techniques:
Liquid Chromatography-Mass Spectrometry (LC-MS) provides high-resolution separation and identification of compounds in complex natural product mixtures. Modern ultra high pressure liquid chromatography systems coupled with high-resolution mass spectrometers enable crude plant extract profiling and metabolite identification [4]. Key parameters include: reversed-phase columns (C18, 1.7-1.8 μm particle size), water-acetonitrile gradients with 0.1% formic acid, and full-scan MS with data-dependent MS/MS fragmentation.
Nuclear Magnetic Resonance (NMR) Spectroscopy offers complementary structural information, particularly for stereochemistry and molecular conformation. The HPLC-PDA-HRMS-SPE-NMR platform integrates multiple techniques for definitive structural elucidation directly from crude extracts [4]. Standard experiments include ^1^H, ^13^C, COSY, HSQC, and HMBC NMR collected in appropriate deuterated solvents (methanol-d~4~, DMSO-d~6~).
Pharmacokinetic Study Design
For bioavailability assessment, well-controlled pharmacokinetic studies remain the gold standard:
Study Population: Typically 24-36 healthy adult volunteers under fasting conditions, with crossover design to minimize inter-subject variability. For natural products with known pharmacological effects, patient populations may be more appropriate.
Bioanalytical Method Validation: Fully validated methods per FDA/EMA guidelines assessing selectivity, sensitivity, linearity, accuracy, precision, and stability. For natural products, simultaneous quantification of multiple active constituents and metabolites may be required.
Pharmacokinetic Parameters: Primary endpoints include AUC~0-t~, AUC~0-∞~, and C~max~, with T~max~ as a secondary parameter. Bioequivalence is established if the 90% confidence intervals for the geometric mean ratios of test/reference products fall within 80-125% for AUC and C~max~.
In Vitro and Ex Vivo Models
Table 2: Experimental Models for Bioavailability Assessment
| Model System | Application | Key Parameters | Relevance to Natural Products |
|---|---|---|---|
| Caco-2 Cell Monolayers | Intestinal permeability | Apparent permeability (P~app~), efflux ratios | Predicts absorption of multiple constituents |
| Hepatocyte Cultures | Metabolic stability | Intrinsic clearance, metabolite identification | Accounts for complex metabolism |
| Plasma Protein Binding | Distribution characteristics | Free fraction, binding constants | Impacts volume of distribution |
| Biopharmaceutics Classification | Solubility and permeability | Dose number, dissolution rate | Guides formulation development |
Research Reagent Solutions for Bioequivalence Studies
Table 3: Essential Research Reagents for Bioequivalence Assessment
| Reagent/Category | Function | Application Notes |
|---|---|---|
| LC-MS Grade Solvents | Mobile phase preparation | Low UV cutoff, minimal background ions |
| Stable Isotope Standards | Internal standards for quantification | Deuterated or ^13^C-labeled analogs |
| Transwell Permeability Systems | In vitro absorption models | Caco-2, MDCK, PAMPA models |
| Human Liver Microsomes | Metabolic stability assessment | Cytochrome P450 phenotyping |
| Biorelevant Media | Dissolution testing | FaSSGF, FaSSIF, FeSSIF simulating gastrointestinal conditions |
| Cryopreserved Hepatocytes | Hepatic clearance prediction | Metabolic pathway identification |
| Plasma Protein Solutions | Protein binding studies | Human serum albumin, α-1-acid glycoprotein |
Bioequivalence Assessment Workflow
The comprehensive evaluation of bioequivalence between natural and synthetic bioactive compounds follows a structured methodology:
Diagram 2: Bioequivalence Assessment Workflow. This iterative process integrates in vitro and in vivo data to establish therapeutic equivalence [1].
Challenges and Future Perspectives
The demonstration of bioequivalence for natural products faces several significant challenges. Structural complexity increases with newly discovered natural products becoming "larger, more complex, and more hydrophobic over time" [3], creating analytical challenges for complete characterization. Multi-constituent preparations may contain multiple active compounds with synergistic or antagonistic effects that are not fully captured by measuring single marker compounds. Batch-to-batch variability in natural product sourcing contrasts with the highly controlled consistency achievable through synthetic production [2].
Emerging approaches to address these challenges include physiologically-based pharmacokinetic modeling to predict in vivo performance, biopharmaceutics tools for predicting absorption limitations, and pharmacometabolomics for comprehensive assessment of biological effects. The continuing evolution of analytical technologies, particularly in mass spectrometry and NMR, enables increasingly sophisticated characterization of complex natural products and their biological fates [4].
For drug development professionals, understanding these bioequivalence fundamentals is essential for bridging natural product research with contemporary drug development paradigms. The integration of advanced analytical methodologies with robust biological evaluation creates a framework for demonstrating therapeutic equivalence, enabling the rational development of both natural and synthetic bioactive compounds into safe and effective medicines.
The debate surrounding natural versus synthetic bioactive compounds is a foundational topic in pharmaceutical and nutraceutical research. For drug development professionals and scientists, the choice between these origins involves a complex trade-off between structural complexity, production scalability, and bioequivalence. Every ingredient, whether natural or synthetic, is fundamentally a chemical, and the human body responds to chemical structures rather than their sources [5]. This comprehensive guide objectively compares these two pathways by examining their distinct sources, structural characteristics, production methodologies, and experimental approaches for evaluation, providing researchers with critical data for informed decision-making in therapeutic development.
Natural bioactive compounds are directly extracted or derived from biological sources—plants, animals, marine organisms, or microorganisms [5] [6]. These compounds, including alkaloids, flavonoids, terpenoids, and phenolics, have evolved through natural selection, resulting in sophisticated chemical architectures [7]. In contrast, synthetically derived chemicals are produced through human-designed chemical processes in laboratory or industrial settings, either mimicking natural compounds ("nature-identical") or creating entirely novel structures not found in nature [5].
Comparative Analysis of Chemical Profiles
Table 1: Source and Structural Characteristics of Natural vs. Synthetic Bioactive Compounds
| Characteristic | Natural Bioactive Compounds | Synthetic Bioactive Compounds |
|---|---|---|
| Primary Sources | Plants, marine organisms, microorganisms, animals [6] [8] | Laboratories, industrial settings [5] |
| Structural Diversity | High chemical diversity; evolved through natural selection [7] | Can be nature-identical or novel structures [5] |
| Molecular Complexity | Elevated molecular complexity, higher sp³ carbon fractions, more stereocenters [9] [7] | Often simpler structures; complexity depends on design [9] |
| Structural Signature | Higher proportions of sp³-hybridized carbon atoms, increased oxygenation, lower halogen/nitrogen content [7] | Controlled structural parameters; potentially higher halogen content [5] |
| Batch-to-Batch Variability | Subject to natural variation (climate, soil, season) [5] | Highly controlled for consistency and purity [5] |
| Typical Impurities | Natural contaminants from complex biological matrices [5] | Process-related impurities, synthetic intermediates [5] |
Natural products distinguish themselves through their "privileged" structural characteristics, which include higher proportions of sp³-hybridized carbon atoms, increased oxygenation, and decreased halogen and nitrogen content compared to synthetic compounds [7]. This chemical richness is coupled with rigid molecular frameworks and lower lipophilicity (cLogP), traits that facilitate favorable interactions with challenging biological targets [7]. These structural advantages are evolutionary honed, as these molecules function as defense chemicals, signaling agents, and ecological mediators in their native contexts [7].
Production Methods and Technological Approaches
The production pipelines for natural and synthetic bioactive compounds diverge significantly, each with distinct technological requirements, advantages, and limitations.
Production Pathways for Natural and Synthetic Bioactives
Natural Compound Production
Natural compound production begins with sourcing biomass, followed by extraction using either conventional techniques (e.g., Soxhlet extraction, maceration) or modern green technologies including Ultrasound-Assisted Extraction (UAE), Microwave-Assisted Extraction (MAE), and Supercritical Fluid Extraction (SFE) [10] [11]. These advanced methods demonstrate improved efficiency in recovering bioactives while aligning with green chemistry principles through reduced solvent usage, lower energy consumption, and shorter processing times [10] [11]. Subsequent purification employs chromatographic techniques (HPLC, GC-MS) to isolate target compounds from complex biological matrices [8].
Synthetic Compound Production
Synthetic production utilizes chemical synthesis from petroleum-derived or plant-based feedstocks, or biocatalytic approaches using engineered enzymes or microorganisms [5] [12]. Chemical synthesis offers high flexibility for structural modification and analog generation, while biocatalysis leverages nature's synthetic machinery for stereoselective transformations under mild conditions [12]. Emerging hybrid approaches combine chemical and enzymatic steps (chemoenzymatic synthesis) to access complex molecules more efficiently than either method alone [12] [9].
Quantitative Production Metrics
Table 2: Production Method Comparison for Natural and Synthetic Compounds
| Production Aspect | Natural Production | Synthetic Production |
|---|---|---|
| Starting Materials | Plant/animal/microbial biomass [5] | Petroleum derivatives, plant-based feedstocks [5] |
| Extraction/Synthesis | UAE, MAE, SFE [10] | Chemical synthesis, fermentation, biocatalysis [5] [12] |
| Step Count (Complex Molecules) | Fewer biosynthetic steps [9] | High step counts (e.g., 7+ steps for sporothriolide) [9] |
| Scalability Challenges | Limited by biomass availability, seasonal variation [5] | Highly scalable but can be carbon-intensive [9] |
| Environmental Impact | Potential ecological damage from overharvesting [7] | High carbon emissions, energy consumption [9] |
| Purity Control | Variable purity, natural contaminants [5] | Highly controlled purity and consistency [5] |
| Stereochemical Control | Enzyme-controlled (high specificity) [12] | Requires chiral catalysts or resolution [12] |
Experimental Assessment and Bioequivalence
Evaluating the bioequivalence of natural and synthetic bioactive compounds requires rigorous experimental protocols assessing structural identity, biological activity, and pharmacological behavior.
Molecular Complexity Analysis
Quantitative complexity metrics enable direct comparison of natural and synthetic molecules and their production pathways. Key descriptors include molecular weight (MW), the fraction of sp³ hybridized carbon atoms (Fsp³), and complexity index (Cm) [9]. These parameters can be visualized in 3D plots to compare the efficiency of different synthetic strategies, with efficient pathways creating complex target molecules in fewer steps with more direct trajectories through this chemical space [9].
Protocol: Molecular Complexity Calculation
- Calculate Fsp³: Determine the ratio of sp³-hybridized carbon atoms to total carbon atoms [9]
- Determine Cm (Complexity Index): Calculate using the formula Cm = A + B - F, where A represents carbon atoms, B represents stereocenters, and F represents flexibility parameters [9]
- Plot in 3D Chemical Space: Create 3D plots parameterized by Fsp³, Cm, and MW to visualize and compare synthetic routes [9]
- Measure Chemical Distance: Calculate linear distance between intermediates using: Distance = √[(MW₂-MW₁)² + (Fsp³₂-Fsp³₁)² + (Cm₂-Cm₁)²] [9]
Bioequivalence Assessment Workflow
Experimental Protocols for Bioequivalence Testing
Protocol 1: Structural Identity Confirmation
- Chromatographic Analysis: Perform co-elution studies using HPLC/HPLC-MS to confirm identical retention times and mass spectra for natural and synthetic versions [8]
- Spectroscopic Characterization: Conduct comprehensive NMR (¹H, ¹³C, 2D) and HRMS analysis to verify structural identity [8]
- Stereochemical Analysis: Use chiral chromatography or circular dichroism to confirm identical stereochemistry for chiral compounds [12]
Protocol 2: Biological Activity Assessment
- In Vitro Target Engagement: Measure IC₅₀/EC₅₀ values against molecular targets using fluorescence-based or radiometric assays [7]
- Cellular Phenotypic Screening: Evaluate effects in relevant cell models (e.g., cytotoxicity, anti-inflammatory, antimicrobial activity) [7]
- Mechanism of Action Studies: Employ techniques like thermal shift assays, surface plasmon resonance, or CRISPR-based screening to confirm identical mechanisms [7]
Protocol 3: Pharmacokinetic Evaluation
- Bioavailability Assessment: Compare Cmax, Tmax, and AUC in appropriate animal models following oral and intravenous administration [8]
- Metabolite Profiling: Identify and compare metabolic products using LC-MS/MS in plasma, urine, and feces [8]
- Tissue Distribution Studies: Quantify compound levels in target tissues to confirm equivalent biodistribution [8]
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Tools for Natural vs. Synthetic Compound Research
| Tool/Category | Specific Examples | Research Application | Relevance to Origin |
|---|---|---|---|
| Extraction/Synthesis | UAE/MAE systems, bioreactors, chemical synthesis glassware | Obtaining target compounds from source or feedstocks [10] | Both, with technology variation |
| Separation & Analysis | HPLC/UPLC, GC-MS, LC-MS/MS, NMR spectroscopy | Purity assessment, structural elucidation [8] | Essential for both |
| Bioactivity Screening | HTS platforms, microplate readers, SPR instruments | Target engagement and potency assessment [7] | Critical for bioequivalence |
| Computational Tools | AntiSMASH, GNPS, molecular docking software | Pathway prediction, metabolite annotation [7] | Both origins |
| Cell-Based Assays | iPSCs, reporter cell lines, primary cells | Functional activity in biological systems [7] | Mechanism confirmation |
| Formulation Aids | Liposomes, nanoemulsions, solid lipid nanoparticles | Bioavailability enhancement [8] [13] | Addresses limitations of both |
The choice between natural and synthetic origins for bioactive compounds presents researchers with a multifaceted decision matrix rather than a simple binary selection. Natural products offer unparalleled structural complexity honed by evolution, often with privileged bioactivity profiles, but face challenges in sustainable sourcing and batch-to-batch consistency [9] [7]. Synthetic compounds provide superior production control, scalability, and purity but may lack the sophisticated structural features of natural counterparts and can involve carbon-intensive manufacturing processes [5] [9].
The emerging paradigm leverages the strengths of both approaches through hybrid strategies: using synthetic biology to optimize natural compound production, applying synthetic chemistry to diversify natural scaffolds, and utilizing biosynthetic pathways for complex steps coupled with chemical synthesis for diversification [12] [9]. For researchers, the critical determinant remains the demonstrated bioequivalence—structural, functional, and pharmacological—between natural and synthetic versions, rather than their origin. As technological advances in genomics, synthetic biology, and artificial intelligence continue to transform both fields, the distinction between natural and synthetic continues to blur, pointing toward an integrated future that maximizes the benefits of both approaches for drug discovery and development [7].
For researchers investigating the bioequivalence of synthetic versus natural bioactive compounds, understanding the regulatory framework established by the U.S. Food and Drug Administration (FDA) is fundamental. Bioequivalence (BE) studies are critical for demonstrating that a generic drug product performs in the same manner as the Reference Listed Drug (RLD) [14]. The FDA defines two products as bioequivalent when they are equal in the rate and extent to which the active pharmaceutical ingredient becomes available at the site(s) of drug action [15]. For generic drug approval, these studies provide the essential proof that the generic product matches the reference brand in terms of safety, efficacy, and quality, ensuring patients receive safe, effective, and interchangeable medicines [16].
The foundation of therapeutic equivalence rests on two key concepts: pharmaceutical equivalents and therapeutic equivalents. Pharmaceutical equivalents are drug products that contain identical amounts of the identical active drug ingredient in the identical dosage form and route of administration, meet identical compendial standards, but may differ in characteristics such as shape, scoring configuration, release mechanisms, packaging, and excipients [17]. Therapeutically equivalent products must be both pharmaceutical equivalents and bioequivalent, ensuring they can be expected to have the same clinical effect and safety profile when administered to patients under conditions specified in the labeling [17].
Quantitative Bioequivalence Standards
Statistical Criteria for Establishing Bioequivalence
The FDA employs rigorous statistical criteria to determine bioequivalence between generic and reference products. For most orally administered immediate-release solid oral dosage forms, the primary pharmacokinetic parameters assessed are the area under the concentration-time curve (AUC), which measures the extent of absorption, and the maximum concentration (Cmax), which measures the rate of absorption [16].
Table 1: Standard FDA Bioequivalence Criteria for Systemic Exposure Measures
| Parameter | Statistical Comparison | Acceptance Range | Study Design |
|---|---|---|---|
| AUC₀–t | Geometric mean ratio (Test/Reference) | 90% CI must fall within 80.00%-125.00% | Randomized, two-period, two-sequence crossover |
| AUC₀–∞ | Geometric mean ratio (Test/Reference) | 90% CI must fall within 80.00%-125.00% | Randomized, two-period, two-sequence crossover |
| Cmax | Geometric mean ratio (Test/Reference) | 90% CI must fall within 80.00%-125.00% | Randomized, two-period, two-sequence crossover |
These criteria apply to dosage forms intended for oral administration and to non-orally administered drug products where reliance on systemic exposure measures is suitable for documenting BE [18]. The 90% confidence intervals for the ratio of test-to-reference product pharmacokinetic parameters must fall entirely within the 80.00%-125.00% range, typically using a logarithmic transformation of the data [16].
Special Criteria for Narrow Therapeutic Index Drugs
For narrow therapeutic index (NTI) drugs, where small differences in dose or concentration can lead to serious therapeutic failures or adverse effects, the FDA applies stricter bioequivalence criteria. While specific harmonized criteria are still under development through the International Council for Harmonisation (ICH) M13 process, current approaches may include tighter confidence intervals, scaling approaches based within-subject variability, and point estimate constraints [19].
Recent research proposes alternative FDA BE criteria for NTI drugs that include "capping the minimum BE limits, applying alpha adjustment, and applying a point estimate constraint" [19]. This aligns with the ICH M13's goal of harmonizing BE standards globally and reflects the critical nature of NTI drugs where the balance between therapeutic efficacy and toxicity is particularly delicate.
Experimental Protocols and Methodologies
Standardized Study Designs
The FDA provides detailed recommendations for BE study designs to ensure generation of reliable and scientifically valid results. For most bioequivalence studies with pharmacokinetic endpoints, the agency recommends a randomized, two-period, two-sequence crossover design under both fasting and fed conditions where applicable [16].
Table 2: Key Elements of FDA Bioequivalence Study Protocols
| Study Component | Protocol Requirements | Scientific Rationale |
|---|---|---|
| Subject Selection | Healthy adult volunteers generally preferred; sufficient number to achieve adequate statistical power | Minimizes variability from disease states; ensures statistical validity |
| Study Conditions | Both fasting and fed conditions for applicable oral dosage forms | Accounts for food effects on drug absorption |
| Blood Sampling | Adequate sampling over time to define pharmacokinetic profile | Ensures accurate characterization of absorption and elimination phases |
| Bioanalytical Methods | Validated methods per Good Laboratory Practice (GLP) standards | Ensures reliability and reproducibility of concentration measurements |
| Statistical Analysis | Average bioequivalence using two one-sided tests procedure | Standard statistical approach for establishing equivalence |
Studies must be conducted according to Good Clinical Practice (GCP) and Good Laboratory Practice (GLP) standards to ensure the reliability and integrity of data [15] [16]. The FDA encourages sponsors to submit in vivo BE study protocols for review before beginning studies, particularly for complex products or novel methodologies [15].
Bioequivalence Establishment Pathways
The following diagram illustrates the key decision pathways and methodological considerations for establishing bioequivalence according to FDA standards, particularly highlighting the role of biowaivers and product-specific guidances.
Diagram 1: FDA Bioequivalence Assessment Pathway - This workflow outlines the key regulatory and scientific decision points for establishing bioequivalence, including biowaiver eligibility and study requirements.
Alternative Approaches: Biowaivers
The FDA may waive the requirement for in vivo BE studies (biowaivers) for certain generic products when in vitro approaches provide sufficient assurance of bioequivalence [15]. Categories of products potentially eligible for biowaivers include:
- Parenteral solutions intended for intravenous, subcutaneous, or intramuscular injection
- Oral solutions or other solubilized forms
- Topically applied solutions intended for local therapeutic effects
- Inhalant volatile anesthetic solutions
For a generic product to be considered for a biowaiver, it must generally contain the same active and inactive ingredients (Q1) in the same dosage form and concentration (Q2) and have the same pH and physico-chemical characteristics (Q3) as the approved Reference Listed Drug [15]. The ICH M13B guidance further describes scientific and technical aspects for supporting biowaivers for additional strengths of orally administered immediate-release solid oral dosage forms when in vivo BE has been demonstrated for at least one strength [20].
Essential Research Reagents and Materials
The Scientist's Toolkit for Bioequivalence Studies
Table 3: Essential Research Reagents and Materials for FDA-Compliant Bioequivalence Studies
| Reagent/Material | Function in BE Assessment | Regulatory Standards |
|---|---|---|
| Validated Bioanalytical Assays (LC-MS/MS) | Quantification of drug and metabolites in biological matrices | FDA Bioanalytical Method Validation Guidelines [15] |
| USP Calibration Standards | Reference materials for dissolution testing | USP General Chapter <711> Dissolution [21] |
| Biorelevant Dissolution Media | Simulate gastrointestinal conditions for in vitro release | Product-specific guidances [14] |
| Certified Reference Standards | Quantify active ingredient in test and reference products | 21 CFR 211.160 (cGLP) |
| Pharmacokinetic Modeling Software | Calculate AUC, Cmax, Tmax, and other parameters | FDA Statistical Guidance for Bioequivalence [18] |
Researchers must employ validated bioanalytical methods to generate reliable data for bioequivalence assessment. The FDA recommends submission of bioanalytical method validation reports for review prior to beginning pivotal BE studies [15]. For dissolution testing, which serves as a critical in vitro tool for predicting in vivo performance, the harmonized USP General Chapter <711> Dissolution provides standardized methodologies, though the FDA recommends mechanical calibration of dissolution apparatus rather than reliance on calibration tablets for GMP purposes [21].
Emerging Regulatory Trends and Complex Products
Product-Specific Guidance and Harmonization
The FDA issues product-specific guidances (PSGs) that provide detailed recommendations for developing generic versions of specific reference listed drugs [14]. These PSGs are developed and revised on a quarterly basis and describe the agency's current thinking on the most appropriate methodology for demonstrating bioequivalence for specific products [22]. For complex generic drug products—including those with complex active ingredients, formulations, routes of delivery, or dosage forms—the PSGs provide critical guidance on navigating uncertainty in the approval pathway [22].
The International Council for Harmonisation (ICH) is actively working to harmonize global bioequivalence standards through the M13 series of guidances. The recently drafted M13B guidance focuses on bioequivalence for immediate-release solid oral dosage forms, specifically addressing additional strengths biowaivers [20]. Simultaneously, scientific research continues to propose refined approaches for narrow therapeutic index drugs, aiming to balance statistical rigor with practical considerations for drug development [19].
Revision Categories for Product-Specific Guidances
The FDA categorizes revisions to PSGs based on their potential impact on generic drug development programs [22]:
- Critical revisions: Include additional BE studies necessary to establish BE reflecting a change in safety or effectiveness; impact all ANDAs including approved applications
- Major revisions: Include additional BE studies necessary to establish BE and support FDA approval (subcategorized as in vivo or in vitro major revisions)
- Minor revisions: Clarify study designs, provide less burdensome approaches, or add information on newly approved strengths without generally requiring additional studies
- Editorial revisions: Non-substantive changes such as updating references or correcting grammatical issues
This transparent categorization system helps generic drug developers anticipate potential changes to regulatory expectations and plan their development programs accordingly, particularly for products involving synthetic versus natural bioactive compounds where complexity may necessitate more frequent guidance updates.
The fundamental bioequivalence (BE) assumption is a cornerstone of modern pharmaceutical regulation, positing that if two drug products demonstrate equivalent pharmacokinetic (PK) profiles in the body, they will produce equivalent therapeutic outcomes. This principle enables the approval of generic small molecule drugs and biosimilar biological products without repeating large-scale clinical efficacy trials, thereby improving patient access to affordable medicines. BE studies bridge the gap between measured drug concentration-time profiles in biological fluids and the complex physiological processes that lead to a clinical effect.
This assumption rests on a critical chain of reasoning: equivalent PK parameters (the measure of what the body does to the drug) ensure equivalent pharmacodynamic (PD) effects (what the drug does to the body), which in turn produces equivalent clinical efficacy and safety. This review examines the experimental evidence supporting this critical linkage, with particular attention to the evolving context of natural product-based drug development, where complex mixtures and prodrug mechanisms may challenge traditional BE assessment frameworks.
Core Pharmacokinetic Parameters in Bioequivalence Assessment
Bioequivalence evaluation primarily relies on comparing key PK parameters that characterize the rate and extent of drug absorption into the systemic circulation. These parameters are derived from drug concentration measurements in plasma or blood over time following product administration.
Table 1: Key Pharmacokinetic Parameters in Bioequivalence Assessment
| PK Parameter | Definition | Relationship to Therapeutic Effect |
|---|---|---|
| AUC0-t | Area Under the concentration-time curve from zero to last measurable time point | Measures total drug exposure; correlates with efficacy and safety for most drugs |
| AUC0-∞ | Area Under the curve from zero to infinity | Represents complete total exposure; critical for drugs with long half-lives |
| Cmax | Maximum observed concentration | Indicates absorption rate; important for acute effects or concentration-dependent toxicity |
| Tmax | Time to reach Cmax | Reflects absorption speed; critical for drugs needing rapid onset |
Regulatory standards for BE typically require that the 90% confidence intervals for the geometric mean ratios (test/reference) of AUC and Cmax fall within the range of 80.00%-125.00% [23] [24]. For highly variable drugs with intra-individual variability ≥30%, reference-scaled average bioequivalence (RSABE) approaches may be applied [23].
Experimental Evidence: Case Studies Linking PK Equivalence to Clinical Outcomes
Small Molecule Drugs: Mycophenolate and Palbociclib Formulations
Recent studies on synthetic small molecule drugs provide robust evidence for the fundamental BE assumption. A 2025 randomized, replicated crossover study of enteric-coated mycophenolate sodium (EC-MPS) in healthy Chinese males established BE between generic and branded (Myfortic) formulations under both fasting and fed conditions [23]. The study design meticulously characterized PK parameters while also observing clinical tolerability.
Experimental Protocol:
- Design: Single-dose, open-label, four-period replicated crossover with 7-day washout
- Participants: 60 healthy Chinese male subjects
- Interventions: Single 180 mg oral dose of generic or branded EC-MPS
- PK Assessment: Plasma concentrations of mycophenolic acid quantified using validated LC-MS/MS; primary parameters (Cmax, AUC0-48, AUC0-inf) evaluated via non-compartmental analysis
- BE Determination: Reference-scaled average bioequivalence for highly variable parameters (CV ≥30%); average bioequivalence otherwise
- Clinical Correlation: 20 mild adverse events reported across both formulations; no serious AEs occurred, supporting equivalent safety profiles [23]
Similarly, a 2025 study of palbociclib tablets in healthy Chinese subjects demonstrated BE between generic and reference (Ibrance) formulations even under challenging gastric pH conditions created by rabeprazole pre-treatment [24]. This finding is clinically significant as cancer patients frequently require acid-reducing therapy.
Table 2: Bioequivalence Study Results for Synthetic Drugs
| Drug Product | Study Design | Geometric Mean Ratios (Test/Reference) | Clinical Correlation |
|---|---|---|---|
| Mycophenolate Sodium (Fasting) [23] | 4-period crossover (n=60) | Cmax: 99.00-111.00%AUC0-48: 98.00-106.00%AUC0-inf: 98.00-106.00% | Equivalent mild AE profile; no serious AEs |
| Mycophenolate Sodium (Fed) [23] | 4-period crossover (n=60) | Cmax: 119.74% (RSABE)AUC0-inf: 99.87% (RSABE) | Food delayed absorption but maintained BE |
| Palbociclib Tablets [24] | 2-period crossover with rabeprazole (n=64) | Cmax: 84.53-91.72%AUC0-t: 87.81-92.49%AUC0-∞: 87.59-92.03% | No serious AEs; well tolerated |
Biological Products: Biosimilar Monoclonal Antibodies
The fundamental BE assumption extends to complex biological products with the demonstration of PK equivalence for biosimilar monoclonal antibodies. The STELLAR-1 phase 1 study established three-way PK equivalence between Biocon's ustekinumab (Bmab-1200) and both EU-approved and US-licensed reference products in healthy subjects [25].
Experimental Protocol:
- Design: Randomized, double-blind, three-arm, parallel-design study over 20 weeks
- Participants: 258 healthy subjects (18-55 years) stratified by ethnicity, body weight, and gender
- Intervention: Single 45-mg subcutaneous injection
- Endpoints: Primary (AUC0-inf, Cmax); secondary (additional PK parameters, immunogenicity, safety)
- Results: All pairwise comparisons met equivalence criteria (90% CIs within 80-125%)
- Clinical Correlation: Similar safety profiles and immunogenicity across groups support the PK-PD-efficacy linkage for biologics [25]
Methodological Framework: Approaches for Establishing Bioequivalence
Study Designs and Statistical Approaches
Different methodological approaches support BE assessment throughout drug development:
BE Establishment Pathway
Advanced Modeling Approaches
Physiologically Based Pharmacokinetic (PBPK) Modeling integrates physiological parameters with drug-specific data to simulate ADME processes [26]. These models are increasingly used in regulatory submissions to support BE evaluation, particularly for:
- Formulation selection and optimization
- Predicting food effects
- Special population dosing
- Pediatric extrapolation [26]
Artificial Intelligence-Enhanced PBPK represents the cutting edge, using machine learning to predict PK parameters from structural formulas when experimental data are limited [27]. This approach is particularly valuable during early development phases of both synthetic and natural product-derived compounds.
Population PK (PopPK) Models enable model-informed precision dosing (MIPD) by quantifying variability in drug concentrations among individuals [28]. The predictive performance of these models is optimally evaluated using forecasting approaches that simulate real-world clinical use [28].
Natural Bioactive Products: Unique Challenges in Bioequivalence Assessment
Natural products present distinctive challenges for BE assessment due to their complex composition and potential prodrug mechanisms [29] [4]. Unlike synthetic compounds with well-defined active pharmaceutical ingredients, natural products often contain multiple constituents that may contribute to overall therapeutic effects.
The FDA and other regulatory agencies generally require identification of marker compounds or active constituents for BE evaluation of natural product-based drugs. However, the complex mixture nature of many natural products means that equivalent PK profiles for known markers may not fully capture potential differences in other bioactive constituents.
Experimental Considerations for Natural Products:
- Complex Mixtures: Multiple potentially active constituents with synergistic effects
- Prodrug Metabolism: Parent compounds may require metabolic activation
- Phytochemical Variation: Batch-to-batch consistency in complex botanical products
- Enteric Metabolism: Differential effects of gut microbiota on natural vs. synthetic compounds [30] [29]
Despite these challenges, technological advances in analytical methods (e.g., LC-MS/MS, NMR) and modeling approaches are strengthening the BE assessment framework for natural products [4].
The Scientist's Toolkit: Essential Reagents and Methods
Table 3: Key Research Reagents and Methods for Bioequivalence Studies
| Reagent/Method | Function in BE Assessment | Application Context |
|---|---|---|
| LC-MS/MS Systems | Quantification of drug and metabolite concentrations in biological matrices | Gold standard for PK parameter determination; essential for both synthetic and natural compounds [23] |
| Caco-2 Cell Models | Prediction of human intestinal absorption and permeability | Early development phase; estimates absorption rate constant (ka) and fraction absorbed [31] |
| Human Liver Microsomes/Hepatocytes | Prediction of metabolic clearance via IVIVE | Critical for projecting human clearance from in vitro data [31] |
| PBPK Modeling Software (GastroPlus, Simcyp) | Simulation of ADME processes in virtual populations | Formulation optimization, food effect prediction, special population dosing [26] [27] |
| Rabeprazole Pre-treatment | Induction of high gastric pH conditions | Assessment of BE under acid-reducing medication use; required for pH-dependent drugs like palbociclib [24] |
The fundamental bioequivalence assumption remains a scientifically valid and regulatory robust principle supported by extensive clinical evidence across diverse drug classes. The consistent demonstration that equivalent PK profiles predict equivalent clinical outcomes has enabled an efficient generic and biosimilar approval pathway that benefits global healthcare systems.
Ongoing scientific advances are strengthening this linkage through:
- More sophisticated study designs that evaluate BE under challenging clinical scenarios
- Enhanced analytical methods for complex natural products and biologics
- Advanced modeling approaches that improve prediction of clinical performance from PK data
As drug products grow more complex, particularly with the increasing development of natural product-derived therapeutics, the fundamental BE assumption will continue to evolve while maintaining its critical role in ensuring therapeutic equivalence for patients worldwide.
Natural products represent a cornerstone in drug discovery, with over 30% of prescribed medicines originating from flowering plants and more than 80% of populations in developing countries relying on traditional medicines predominately derived from herbal sources [29] [32]. These compounds, derived from plants, animals, and microbial resources, exhibit tremendous chemical diversity with superfluous potency for managing communicable and non-communicable diseases [29]. This very diversity, however, creates a fundamental challenge for standardization—the process of establishing consistent and reproducible quality parameters for natural product-based therapeutics.
The standardization paradox emerges from the tension between chemical complexity and therapeutic reproducibility. While natural products offer privileged chemical scaffolds with proven biological relevance, their inherent variability poses significant challenges for bioequivalence studies comparing natural and synthetic bioactive compounds [29] [6]. Low-income countries predominantly rely on natural products as primary health support, yet most herbal medicines are prescribed based on practical evidence and recommended in crude and semi-standardized forms, creating impediments for integration into contemporary medicinal practices [29]. This article examines the analytical frameworks and experimental approaches designed to navigate this complexity, enabling meaningful comparisons between natural and synthetic bioactive compounds within bioequivalence research.
Analytical Methodologies for Characterizing Complex Natural Matrices
Advanced Spectroscopic and Chromatographic Platforms
Modern natural product analysis employs sophisticated hyphenated techniques that combine separation and detection capabilities to address chemical complexity. The inherent chemical diversity of natural products has driven significant progress in analytical technologies, with hyphenated analytical platforms emerging as valuable tools for de novo identification, distribution, quantification, and authentication of constituents [33].
Chromatographic separation coupled with high-sensitivity detection forms the foundation of these approaches. Ultra-high-pressure liquid chromatography (UHPLC) provides enhanced resolution for crude plant extracts, while high-performance liquid chromatography (HPLC) systems enable quantification of biomarker compounds [32] [4]. When coupled with high-resolution mass spectrometry (HRMS) and nuclear magnetic resonance (NMR) spectroscopy, these platforms facilitate unambiguous structural elucidation directly from complex mixtures [4]. The Fourier-transform infrared spectroscopy (FTIR) technique further contributes to functional group identification and chemical fingerprinting [32].
Table 1: Core Analytical Techniques for Natural Product Standardization
| Technique | Application | Resolution/Sensitivity | Limitations |
|---|---|---|---|
| HPLC-PDA | Quantification of biomarker compounds | High resolution for separated compounds | Limited without authentic standards |
| LC-HRMS | Structural elucidation, metabolomics | High mass accuracy (<5 ppm) | Database dependencies |
| FTIR | Functional group identification | Rapid fingerprinting | Limited structural specificity |
| SEM with TLD | Microscopic structural analysis | High-resolution imaging | Surface characterization only |
Experimental Workflow for Comprehensive Phytochemical Characterization
A standardized methodology for natural product analysis begins with proper specimen collection and authentication, including voucher specimen deposition in recognized herbariums [32]. The process continues through multiple validation stages:
Sample Preparation and Macroscopic Evaluation: Plant material undergoes controlled drying and pulverization before storage in amber containers to prevent degradation. Macroscopic and organoleptic evaluation documents shape, texture, odor, taste, and appearance according to established pharmacognostic parameters [32].
Microscopic and Physicochemical Analysis: Microscopic investigations include transverse sectioning with staining techniques (e.g., toluidine blue) and scanning electron microscopy (SEM) with through-the-lens detectors for high-resolution structural details [32]. Physicochemical analyses determine ash values, moisture content, extractive values, foaming index, and swelling index—critical quality control parameters [32].
Fluorescence Characterization: Powdered plant material is treated with various reagents and examined under different wavelengths (natural daylight, UV at 254nm and 365nm) to generate unique fluorescence profiles that serve as identifying fingerprints [32].
Phytochemical Screening and Quantification: Preliminary qualitative analysis detects major compound classes (alkaloids, phenols, flavonoids, fixed oils) across different extraction solvents (ethanol, dichloromethane, n-hexane) [32]. Quantitative estimation employs the Folin-Ciocalteu method for total phenolic content and aluminum chloride colorimetry for total flavonoid content, with results expressed relative to standard compounds (gallic acid and quercetin) [32].
Figure 1: Experimental workflow for comprehensive phytochemical characterization of natural products, encompassing authentication, extraction, and analytical profiling.
Comparative Bioequivalence Assessment: Natural vs. Synthetic Bioactives
Methodological Framework for Bioequivalence Studies
Establishing bioequivalence between natural and synthetic bioactive compounds requires rigorous experimental design that accounts for the complex matrix effects in natural extracts. Pharmacological validation must encompass in-vivo and in-vitro studies evaluating cell cytotoxicity, cell-cell interactions, intracellular activity, gene expression, and metabolomic fingerprints [29]. These preclinical assessments provide robust evidence for the safe long-term utilization of natural medicines to treat diseases [29].
The standardization imperative addresses the economics of large-scale industrial production, shelf life, and distribution challenges that were not concerns when traditional practitioners prepared medicines individually according to patient needs [32]. Modern bioequivalence studies must apply rigorous scientific methodologies to ensure quality and lot-to-lot consistency while maintaining the chemical complexity that may contribute to therapeutic efficacy through synergistic effects [32].
Table 2: Key Methodological Considerations for Natural-Synthetic Bioequivalence Studies
| Parameter | Natural Products | Synthetic Compounds | Standardization Approach |
|---|---|---|---|
| Compound Definition | Complex mixtures with multiple actives | Single chemical entity | Biomarker quantification & chemical fingerprinting |
| Variability Source | Biological, environmental, processing | Synthetic process, purification | Strict quality control protocols |
| Synergistic Effects | Often present due to multi-component nature | Typically absent | Controlled extract ratios & enhanced characterization |
| Bioavailability | Influenced by plant matrix | More predictable | Pharmacokinetic studies with standardized formulations |
Analytical Validation and Quantification Protocols
Validation of analytical methods for natural product standardization requires demonstration of specificity, accuracy, precision, and robustness. The calibration curve approach quantifies total phenolic content (TPC) using gallic acid equivalents and total flavonoid content (TFC) using quercetin equivalents, establishing linearity across relevant concentration ranges (typically 20-100 μg/mL) [32].
Chromatographic fingerprinting employs thin-layer chromatography (TLC) for preliminary separation and Rf value calculation, while HPLC provides quantitative analysis of specific marker compounds [32]. Method validation must include determination of limit of detection (LOD), limit of quantification (LOQ), precision (repeatability and intermediate precision), and accuracy through recovery studies [33].
Advanced metabolomic approaches using LC-HRMS and multivariate statistical analysis can comprehensively capture the chemical complexity of natural products, enabling comparison of batch-to-batch consistency and detection of adulterants [4]. These methods facilitate the identification of chemical signatures responsible for therapeutic activity rather than focusing solely on single marker compounds.
Technological Innovations Addressing Standardization Challenges
Biotechnology and AI-Driven Solutions
Emerging technologies are revolutionizing natural product standardization by addressing historical bottlenecks. Biotechnological approaches including plant cell culture, microbial fermentation, and metabolic engineering enable more sustainable and scalable production of complex natural products [34] [6]. For instance, engineered yeast platforms can biomanufacture plant-inspired therapeutics like monoterpene indole alkaloids (MIAs) with improved pharmacological properties, overcoming the challenge of low extraction yields from natural sources (often below 0.001%) [34].
Artificial intelligence and machine learning accelerate compound identification and activity prediction. AI models trained on datasets linking molecular fingerprints with pharmacological properties can suggest structural modifications to optimize natural scaffolds for improved efficacy and bioavailability [34] [6]. These computational approaches significantly reduce the dependency on large-scale physical screening while enabling targeted exploration of chemical space around validated natural scaffolds [35].
Enhanced Analytical Capabilities
Modern spectroscopic and chromatographic technologies continue to evolve, addressing previous limitations in sensitivity and resolution. Hyphenated platforms such as LC-MS-NMR combine separation power with structural elucidation capabilities, enabling de novo identification of compounds directly from complex mixtures [33] [4]. Improvements in mass spectrometry instrumentation provide higher mass accuracy and resolution, supporting confident molecular formula assignment even for novel compounds [4].
Metabolic engineering represents another frontier in standardization, with researchers successfully engineering yeast cells to produce complex natural products like vinblastine through the insertion of extensive biosynthetic pathways (31 enzymatic reactions requiring approximately 100,000 DNA bases added to the yeast genome) [34]. This approach bypasses the biological variability associated with plant cultivation and enables consistent production of complex molecules that are difficult to synthesize chemically.
Figure 2: Integrated biotechnology and AI approach for standardized production of natural products, enabling consistent quality and enhanced properties.
The Scientist's Toolkit: Essential Research Reagents and Solutions
Successful standardization of natural products requires specialized reagents and reference materials carefully selected for their specific applications in phytochemical analysis and bioequivalence assessment.
Table 3: Essential Research Reagents for Natural Product Standardization
| Reagent/Solution | Application | Function | Technical Considerations |
|---|---|---|---|
| Folin-Ciocalteu Reagent | Total phenolic content quantification | Oxidation-reduction reaction with phenolics | Fresh preparation required; measures total phenolics not specific compounds |
| Aluminum Chloride (10%) | Total flavonoid content determination | Forms acid-stable complexes with C-4 keto group and C-3 or C-5 hydroxyl | Specific for flavones and flavonols; less reactive with other flavonoid subtypes |
| Toluidine Blue Stain | Microscopic section staining | Metachromatic staining for structural visualization | Differentiates cell types and tissues in transverse sections |
| Chloral Hydrate Solution | Powder microscopy | Clearing agent for tissue examination | Enhances visibility of cellular structures; requires careful handling |
| Standard Compounds (Gallic Acid, Quercetin) | Quantitative calibration | Reference standards for quantification | High-purity standards essential for accurate calibration curves |
| Chromatographic Solvents | TLC/HPLC analysis | Mobile phase components | HPLC-grade purity required; solvent systems optimized for target compounds |
The chemical diversity inherent in natural products presents both challenges and opportunities for standardization in the context of bioequivalence research. While complexity creates hurdles for reproducibility and quality control, it also represents a rich source of chemical scaffolds with validated biological relevance. Modern analytical technologies, including hyphenated chromatographic-spectroscopic platforms and AI-assisted compound identification, are progressively overcoming historical limitations in natural product characterization.
The future of natural product standardization lies in integrated approaches that combine advanced analytics with biotechnological production methods. By leveraging metabolic engineering and microbial biomanufacturing, researchers can achieve consistent production of complex natural compounds while reducing dependence on variable biological sources. Simultaneously, enhanced analytical capabilities enable comprehensive chemical profiling that captures the complexity of natural extracts rather than reducing them to single marker compounds.
For researchers and drug development professionals, this evolving landscape offers new frameworks for establishing meaningful bioequivalence between natural and synthetic bioactives. By adopting these technological advances and standardized methodologies, the scientific community can fully leverage the therapeutic potential of natural products while ensuring consistency, safety, and efficacy—ultimately bridging traditional knowledge with contemporary evidence-based medicine.
Natural products (NPs), or secondary metabolites, have served as the most successful source of potential drug leads throughout human history [36]. These compounds, produced by terrestrial plants, marine organisms, fungi, and bacteria, are not essential for the growth and development of the organism but often evolve as defense mechanisms or adaptations to the environment [36]. Historically, natural products have been used since ancient times and in folklore for treating numerous diseases, with the earliest records depicted on clay tablets in cuneiform from Mesopotamia (2600 B.C.) documenting oils from Cupressus sempervirens (Cypress) and Commiphora species (myrrh) which are still used today [36]. The profound influence of natural products continues in modern medicine, with analyses indicating that approximately half of all new drug approvals trace their structural origins to a natural product [37]. Between 1981 and 2019, 68% of approved small-molecule drugs were directly or indirectly derived from natural products [3]. This review provides a comprehensive comparison of natural and synthetic compounds, examining their structural properties, biological relevance, and experimental approaches to inform future drug discovery efforts.
Structural and Physicochemical Comparison
Historical Trajectories and Property Evolution
Table 1: Time-Dependent Evolution of Key Physicochemical Properties
| Property | Natural Products Trend | Synthetic Compounds Trend | Comparative Significance |
|---|---|---|---|
| Molecular Size | Consistent increase over time; recently discovered NPs tend to be larger [3] | Variation within limited range; constrained by synthesis technology and drug-like rules [3] | NPs generally larger than SCs; trend becomes more pronounced over time [3] |
| Ring Systems | Increasing numbers of rings, particularly non-aromatic and sugar rings; fewer ring assemblies indicating bigger fused rings [3] | Increase in aromatic rings; prevalence of five- and six-membered rings due to synthetic stability [3] | NPs feature more complex fused ring systems; SCs dominated by aromatic rings [3] |
| Stereocomplexity | Higher stereochemical content; greater number of stereocenters [37] | Lower stereochemical content; fewer stereocenters [37] | Increased complexity in NPs correlates with biological specificity and selectivity [37] |
| Hydrophobicity | Lower hydrophobicity (ALOGPs) despite larger size [37] | Generally higher hydrophobicity [37] | NPs maintain better solubility profiles despite structural complexity [38] |
| Chemical Diversity | Greater structural diversity and uniqueness; expanding chemical space [3] | Broader synthetic pathways but constrained structural diversity [3] | NPs occupy more diverse chemical space than SCs and drugs [37] |
Molecular Architecture and Drug-Like Properties
Natural products exhibit distinct structural features compared to synthetic compounds. NPs display greater three-dimensional complexity, measured by fraction of sp3 carbons (Fsp3) and stereocenter count [37]. They contain more oxygen atoms and fewer nitrogen atoms, while synthetic compounds show the opposite pattern [3] [37]. Notably, natural products frequently violate Lipinski's Rule of Five while remaining bioavailable, forming what has been described as a "parallel universe" of drug-like compounds [38]. This is possible because nature maintains low hydrophobicity and intermolecular H-bond donating potential when creating biologically active compounds with high molecular weight and numerous rotatable bonds [38].
Table 2: Structural and Biological Property Comparison Between Natural Products and Synthetic Compounds
| Parameter | Natural Products | Synthetic Compounds | Biological Implications |
|---|---|---|---|
| Fraction sp3 (Fsp3) | Higher (>0.5) [37] | Lower (<0.5) [37] | Correlated with improved clinical progression [37] |
| Aromatic Rings | Fewer aromatic rings [37] | More aromatic rings [3] [37] | Reduced flatness improves specificity [37] |
| Oxygen Content | Higher number of oxygen atoms [3] [37] | Lower number of oxygen atoms [3] [37] | Influences hydrogen bonding capacity [37] |
| Nitrogen Content | Fewer nitrogen atoms [3] [37] | Higher number of nitrogen atoms [3] [37] | Affects basicity and interaction patterns [37] |
| Biological Relevance | High; evolved to interact with biological targets [3] | Declining over time [3] | NPs access broader target space [37] |
Experimental Approaches and Methodologies
Modern Natural Product Library Development
The construction of chemically diverse natural product libraries requires strategic methodologies to maximize metabolite diversity. A bifunctional approach combining genetic barcoding with metabolomics has proven effective for assessing chemical diversity coverage [39].
Experimental Protocol: Library Development and Diversity Assessment
Sample Collection and Preparation: Environmental isolates are obtained through systematic collection programs (e.g., citizen-science-based soil collection). For fungi, samples are plated and strains exhibiting colony morphologies consistent with target taxa are selected [39].
Genetic Barcoding: Internal Transcribed Spacer (ITS) sequencing is performed to establish phylogenetic relationships. Sequences with >90% similarity to type strain data in GenBank are retained for further analysis [39].
Metabolome Profiling: Liquid chromatography-mass spectrometry (LC-MS) analysis is conducted to detect chemical features based on retention time and mass-to-charge ratio. Principal Coordinate Analysis (PCoA) helps identify chemical clusters [39].
Diversity Assessment: Chemical diversity coverage is quantified using feature accumulation curves, which measure the rate of new chemical feature discovery as more isolates are added to the library. This enables data-driven decisions about optimal library size [39].
Library Optimization: The relationship between phylogenetic clades and chemical clusters guides strategic inclusion of isolates from underrepresented chemical space, maximizing structural diversity while minimizing redundancy [39].
Advanced Analytical Techniques for Dereplication
Table 3: Essential Research Reagent Solutions for Natural Product Research
| Reagent/Technology | Function | Application Context |
|---|---|---|
| LC-HRMS-MS Systems | High-resolution metabolite profiling | Separation and identification of complex natural product mixtures [4] |
| NMR Spectroscopy | Structural elucidation | Determination of stereochemistry and complete molecular structure [4] |
| ITS Barcode Primers | Phylogenetic identification | Fungal identification and clade determination [39] |
| HPLC-UV/MS-SPE-NMR | Integrated isolation and characterization | Hyphenated system for rapid dereplication [4] |
| Global Natural Products Social Molecular Networking | Mass spectrometry data sharing and community curation | Structural analog identification and collaborative discovery [4] |
Modern natural product research employs advanced hyphenated techniques to accelerate compound identification:
- LC-HRMS-MS: Enables rapid dereplication through accurate mass measurement and fragmentation pattern analysis [4]
- HPLC-HRMS-SPE-NMR: Combined system that automates separation, purification, and structural elucidation, minimizing sample loss [4]
- Molecular Networking: Visualizes structural relationships between compounds within complex mixtures using mass spectrometry data [4]
Case Studies: Successful Clinical Translation
Historic Foundations to Modern Therapeutics
The trajectory from traditional natural medicines to modern drugs exemplifies the enduring value of natural products:
- Aspirin: Derived from salicin isolated from the bark of the willow tree Salix alba L. [36]
- Morphine: Isolated from Papaver somniferum L. (opium poppy) and first reported in 1803 [36]
- Artemisinin: Discovered by Youyou Tu (2015 Nobel Prize) from traditional Chinese medicine, now frontline antimalarial therapy [40] [41]
- Avermectins: Discovered by William C. Campbell and Satoshi Omura (2015 Nobel Prize), revolutionized treatment of parasitic diseases [41]
Impact on Drug Approval Trends
Analysis of new chemical entities (NCEs) approved between 1981-2010 reveals consistent influence of natural products, with approximately half of all small-molecule drugs tracing structural origins to natural products across all five-year intervals [37]. Natural product-based drugs occupy larger regions of chemical space and address a wider range of biological targets compared to completely synthetic drugs [37].
Future Perspectives and Concluding Remarks
Natural products continue to shape modern drug discovery, with technological advances including improved analytical tools, genome mining, and engineering strategies addressing previous challenges [4]. The unique structural features of natural products—increased three-dimensionality, stereocomplexity, and diverse ring systems—provide advantages in targeting challenging biological targets [3] [37]. As chemical diversity remains crucial for addressing emerging health challenges, including antimicrobial resistance, natural products offer expanding opportunities for drug discovery [4] [40]. The integration of modern analytical technologies with traditional knowledge presents a promising path for identifying next-generation therapeutics inspired by nature's chemical innovations [4] [39].
Assessment Methods and Production Technologies for Bioactive Compounds
Bioequivalence studies are fundamental to drug development, ensuring that generic drugs or different formulations of a product perform in the body similarly to a reference product. These studies rely on comparing key pharmacokinetic parameters that describe the rate and extent of drug absorption. For two products to be considered bioequivalent, they must exhibit comparable bioavailability, meaning the active ingredient is absorbed and becomes available at the site of action at a similar rate and extent. The core parameters used to establish this equivalence are the Area Under the Curve (AUC), the Maximum Concentration (Cmax), and the Time to Maximum Concentration (Tmax).
Regulatory agencies worldwide, such as the US Food and Drug Administration (FDA), require that the 90% confidence interval for the ratio of the geometric means of these parameters (test/reference) falls within a predefined range, typically 80% to 125% [42]. This statistical evaluation ensures that any difference between the two products is unlikely to have clinical significance. While this is sometimes misinterpreted as the generic containing 80-125% of the active ingredient, it actually pertains to the confidence interval of the pharmacokinetic ratios [42]. This review provides a detailed comparison of how AUC, Cmax, and Tmax are utilized in bioequivalence studies, with a specific focus on the context of natural and synthetic bioactive compounds.
Core Pharmacokinetic Parameters in Bioequivalence Assessment
Definition and Physiological Significance
The assessment of bioequivalence hinges on three primary pharmacokinetic parameters, each providing distinct insight into the drug's journey in the body.
Area Under the Curve (AUC): The AUC represents the total integrated drug exposure over time. It is calculated from the plasma drug concentration-time curve and is the primary measure of the extent of absorption [43]. A UC reflects how much of the drug ultimately reaches the systemic circulation. In bioequivalence studies, the parameters of interest are typically AUC from zero to the last measurable time point (AUC0–t) and AUC extrapolated to infinity (AUC0–∞) [43] [44].
Maximum Concentration (Cmax): Cmax is the peak plasma concentration observed after drug administration. It is a critical parameter for assessing the rate of absorption [43]. A drug's Cmax can influence both its therapeutic efficacy and its safety profile, particularly for substances with a narrow therapeutic index where high peak levels could cause toxicity.
Time to Maximum Concentration (Tmax): Tmax is the time taken to reach Cmax following drug administration. Like Cmax, it is an indicator of the absorption rate [45]. While Tmax is easier to interpret physiologically, it is generally observed with lower statistical precision than Cmax or AUC and is often considered a secondary parameter in bioequivalence testing [45].
Table 1: Summary of Key Pharmacokinetic Parameters in Bioequivalence Studies
| Parameter | Description | Primary Role in Bioequivalence | Regulatory Consideration |
|---|---|---|---|
| AUC | Area under the plasma concentration-time curve | Measures the extent of absorption; indicates total drug exposure | Primary parameter; 90% CI must be within 80-125% |
| Cmax | Maximum observed plasma concentration | Measures the rate of absorption; indicates peak drug exposure | Primary parameter; 90% CI must be within 80-125% |
| Tmax | Time to reach Cmax | Supports absorption rate assessment; indicates speed of drug arrival | Secondary parameter; typically assessed for clinical relevance rather than statistical equivalence |
Regulatory Standards and Statistical Evaluation
For a test product (e.g., a generic drug or a new formulation) to be deemed bioequivalent to a reference product, a randomized, crossover pharmacokinetic study is conducted. The 90% confidence intervals (CI) for the geometric mean ratios (test/reference) of AUC and Cmax must fall entirely within the bioequivalence range of 80% to 125% [42]. This means that the test product can be statistically shown to deliver drug exposure that is no less than 80% and no more than 125% of the reference product. In practice, for the entire 90% CI to meet this requirement, the mean values for the test and reference products must be very close, indicating that the actual variation between products is small [42].
The following diagram illustrates the standard workflow for a bioequivalence study, from design to regulatory conclusion.
Diagram 1: Standard Workflow for a Bioequivalence Study
Experimental Protocols in Bioequivalence Studies
Standardized Clinical Trial Design
The gold standard for assessing bioequivalence is a single-dose, randomized, crossover study in healthy volunteers. This design minimizes inter-subject variability by having each participant serve as their own control. A typical protocol involves:
- Ethics and Consent: The study must be approved by an independent ethics committee and conducted in accordance with international guidelines (e.g., ICH-GCP, Declaration of Helsinki). Written informed consent is obtained from all participants prior to enrollment [44].
- Subject Selection: Healthy volunteers, often within a specific age range (e.g., 18-40 or 18-55) and with a body mass index (BMI) within normal limits, are selected after medical screening [43] [44].
- Dosing and Washout: Participants are randomly assigned to receive either the test or reference formulation first. After administration, serial blood samples are collected over a period that covers the drug's absorption, distribution, and elimination phases (e.g., up to 84 hours for a long half-life drug) [43]. A washout period of at least 5-7 elimination half-lives separates the two treatment periods to ensure no drug carryover [44].
- Standardized Conditions: Studies are typically conducted under fasting conditions, with standardized meals served post-dose. Fluid intake is often controlled to minimize variability in drug absorption [44].
Analytical and Statistical Methods
- Bioanalysis: Plasma samples are analyzed using highly sensitive and specific methods, such as Ultra Performance Liquid Chromatography (UPLC) or Liquid Chromatography-Tandem Mass Spectrometry (LC-MS/MS) [43] [44]. These methods are validated to ensure accuracy, precision, and selectivity in measuring the drug's plasma concentration.
- Pharmacokinetic Analysis: Non-compartmental analysis is typically used to calculate the primary parameters: AUC0–t, AUC0–∞, and Cmax. Tmax is directly observed from the concentration-time data [44].
- Statistical Analysis for Bioequivalence: The calculated AUC and Cmax values are log-transformed and analyzed using analysis of variance (ANOVA). The 90% confidence intervals for the geometric mean ratios (test/reference) of AUC and Cmax are then derived. Bioequivalence is concluded if these intervals lie entirely within the 80-125% range [42] [44].
Table 2: Key Reagents and Materials for Bioequivalence Bioanalysis
| Reagent/Material | Function in the Experiment |
|---|---|
| Test and Reference Formulations | The pharmaceutical products being compared for bioequivalence. |
| LC-MS/MS or UPLC System | High-precision instrumentation for quantifying drug concentrations in biological samples (e.g., plasma) [43] [44]. |
| Validated Analytical Method | A protocol ensuring the bioanalytical assay is specific, accurate, precise, and reproducible over the expected concentration range. |
| Drug-Specific Standards & Internal Standards | Pure chemical standards used to calibrate the analytical instrument and correct for variability in sample preparation and analysis. |
| Healthy Human Volunteers | Study participants who provide the plasma samples for pharmacokinetic analysis after informed consent [43] [44]. |
Comparative Data: Bioequivalence in Practice
Case Studies of Synthetic Drugs
Recent bioequivalence studies provide clear examples of how pharmacokinetic parameters are applied. A study on rifapentine capsules, a synthetic antibiotic, compared test and reference formulations in healthy male volunteers. The results demonstrated bioequivalence, with the 90% confidence intervals for Cmax, AUC0-t, and AUC0-∞ all falling within the 80-125% range. The mean values for these parameters were closely aligned between the two formulations, confirming similar rates and extents of absorption [43].
Similarly, a study on a low-dose anagrelide capsule (0.5 mg), a synthetic drug for thrombocythemia, showed equivalent bioavailability. The mean AUC0–t was 4533.3 pg·h/mL for the test formulation versus 4515.0 pg·h/mL for the reference. The mean Cmax values were 1997.1 pg/mL and 2061.3 pg/mL, respectively. The point estimates for the ratios were 99.28% for AUC0–t and 94.37% for Cmax, well within the required bioequivalence range [44].
Considerations for Natural Bioactive Compounds
The assessment of natural bioactive compounds and nutraceuticals presents unique challenges. While formal bioequivalence studies are less common, research focuses on their bioavailability—how effectively the body absorbs and utilizes the active compounds.
- Structural Complexity: Natural products (NPs) are often larger and more complex than synthetic compounds (SCs), with higher molecular weight and more ring structures [3]. This structural complexity can impact solubility and permeability, directly influencing AUC and Cmax.
- Formulation Optimization: Studies explore how processing affects bioavailability. For instance, processed soybean flour showed reduced iron and oligosaccharides, potentially reducing side effects like flatulence without compromising the absorption of beneficial phytoalexins [46].
- Enhancing Bioavailability: Research investigates methods to improve the pharmacokinetics of natural compounds. A soluble complex of hesperetin-7-O-glucoside with β-cyclodextrin (HEPT7G/βCD) was developed to enhance its effects on vasodilation and skin blood flow, directly impacting its concentration-time profile [46].
- Source Equivalence: A study comparing chitosan-derived and biofermentation-derived glucosamine found they met bioequivalence standards, despite differing in their mean peak plasma concentration (Cmax) ratios. This suggests that different natural sources can produce bioequivalent supplements, with fermentation-derived products offering a sustainable alternative [46].
The following diagram summarizes the key structural and pharmacokinetic considerations when comparing natural and synthetic compounds.
Diagram 2: Natural vs. Synthetic Compounds: Structural & PK Considerations
The pharmacokinetic parameters AUC, Cmax, and Tmax are the cornerstone of bioequivalence assessment, providing a robust and standardized framework for ensuring that different drug formulations deliver the active ingredient in a comparable manner. The rigorous statistical requirement that the 90% confidence intervals for the ratios of AUC and Cmax fall within 80-125% guarantees that clinically significant differences in drug exposure are unlikely.
While the principles of bioequivalence are well-established for synthetic drugs, the evaluation of natural bioactive compounds introduces additional layers of complexity due to their intricate chemical structures and variable sources. However, the underlying goal remains the same: to understand and optimize the rate and extent of absorption to ensure consistent and effective therapeutic outcomes. As research continues to bridge the gap between traditional natural product use and modern evidence-based medicine, the precise measurement of AUC, Cmax, and Tmax will remain paramount in validating the bioavailability and therapeutic equivalence of both natural and synthetic compounds for researchers, scientists, and drug development professionals.
In clinical research, a crossover design is a repeated measurements design wherein each experimental unit (e.g., a patient) receives different treatments during different time periods, effectively crossing over from one treatment to another during the trial [47]. This stands in contrast to parallel designs, where patients are randomized to a single treatment throughout the trial duration [48]. The fundamental principle underlying crossover trials is that each subject serves as their own control, which removes inter-subject variability from treatment comparisons and increases statistical power [48] [49].
The simplest and most common crossover design is the 2-sequence, 2-period, 2-treatment (2×2) crossover design, often called the AB/BA design [48] [47]. In this design, subjects are randomly allocated to one of two sequence groups: the AB sequence (receiving treatment A first, then treatment B after a washout period) or the BA sequence (receiving treatment B first, then treatment A) [48]. This design is particularly valuable in bioequivalence studies, where the objective is to determine whether test and reference pharmaceutical formulations yield equivalent blood concentration levels [47] [50].
In the context of bioequivalence research on synthetic versus natural bioactive compounds, crossover designs offer significant advantages. Natural products and their structural analogues have historically made major contributions to pharmacotherapy, especially for cancer and infectious diseases [4]. The crossover design's ability to detect subtle differences between formulations with fewer subjects makes it ideally suited for comparing the pharmacokinetic profiles of natural products and their synthetic counterparts.
Advantages and Limitations of Crossover Designs
Key Advantages
Crossover designs offer several significant statistical and practical advantages over parallel group designs:
Increased Statistical Power and Efficiency: By comparing treatments within the same subject, crossover designs remove between-subject variability from the treatment effect estimate [48]. This typically allows researchers to obtain estimates with the same level of precision as parallel designs but with substantially fewer subjects [49] [47]. The reduced sample size requirement is particularly valuable when studying rare populations or expensive interventions.
Control for Confounding Variables: Since each participant serves as their own control, problems of comparability between study and control groups with regard to confounding variables (e.g., age, sex, metabolic status) are minimized [49]. This is especially important when comparing natural and synthetic compounds, as individual metabolic variations can significantly affect compound bioavailability and efficacy.
Ideal for Chronic Conditions: Crossover designs work well for chronic conditions such as asthma, diabetes, or stable cardiovascular diseases where there is no cure and treatments primarily alleviate symptoms or improve quality of life [47]. Many natural products are investigated for managing chronic conditions, making crossover designs particularly appropriate for this research domain.
Important Limitations and Considerations
Despite their advantages, crossover designs present several important limitations that must be addressed during study planning:
Carryover Effects: The main disadvantage of crossover designs is that carryover effects may be confounded with direct treatment effects [47]. A carryover effect occurs when the treatment from the previous period continues to influence the response in the current period [48]. Differential carryover effects (where carryover from treatment A differs from carryover from treatment B) present particularly serious challenges to interpretation [47].
Condition Stability Requirement: The crossover design requires that subject conditions remain stable throughout the study [48]. It is inappropriate for acute curable diseases or when symptoms disappear or are cured by treatment in the first period [48] [47]. This limitation is relevant when studying natural products with potential curative effects.
Washout Period Considerations: A sufficiently long washout period must be implemented between treatments to allow the effects of the previous treatment to subside [49]. For pharmaceutical products, the washout period is typically determined as a multiple of the drug's half-life [47]. If the washout period is too long, however, dropout rates may increase in the second period [48].
Table 1: Advantages and Disadvantages of Crossover Designs
| Advantages | Disadvantages |
|---|---|
| Increased statistical power | Potential carryover effects |
| Reduced sample size requirements | Requires stable chronic conditions |
| Control for confounding variables | Ethical concerns with multiple treatments |
| Direct within-subject comparisons | Complex statistical analysis |
| Ideal for bioequivalence studies | Missing data more problematic than in parallel designs |
Statistical Analysis and Modeling
Fundamental Statistical Model
The standard 2×2 crossover design can be described using a fundamental statistical model [48]:
Yijk = μ + Sik + Pj + Tj,k + Cj-1,k + eijk
Where:
Yijkis the response of the ith subject in the kth sequence at the jth periodμis the overall meanSikis the random effect of the ith subject in the kth sequencePjis the fixed effect of the jth periodTj,kis the direct fixed effect of the treatment in the jth period and kth sequenceCj-1,kis the carryover effect from the previous periodeijkis the random error term
This model includes both fixed effects (period, treatment, carryover) and random effects (subject, error), requiring specialized analytical approaches [48].
Analysis Workflow
The confirmatory analysis of crossover trials follows a specific workflow to ensure valid interpretation:
Pre-test for Carryover Effects: The first step involves testing for differential carryover effects using an unpaired t-test comparing the within-subject sums of responses from both periods between sequence groups [49]. The test statistic is calculated as:
T = (Mean(C(X)) - Mean(C(Y))) / (S_p * √(1/m + 1/n))
Where C(X) and C(Y) are within-subject sums for sequences AB and BA, m and n are sample sizes for each sequence, and S_p is the pooled standard deviation [49].
Treatment Effect Analysis: If carryover effects are negligible, treatment effects are tested using an unpaired t-test on the within-subject differences between periods [49]. For sequence AB (X), the differences are D_i(X) = X_1i - X_2i, and for sequence BA (Y), D_j(Y) = Y_1j - Y_2j. The test statistic follows the same structure as the carryover test but uses these within-subject differences [49].
Handling Complex Scenarios
In cases where significant differential carryover effects are detected, researchers must resort to analyzing only the first-period data, effectively converting the study to a parallel group design [49] [47]. This approach, however, results in a substantial loss of power and efficiency. Alternative strategies include using more complex crossover designs with more than two periods that allow separate estimation of carryover effects, though these require more complex implementation and analysis [47].
Sample Size Determination and Power Analysis
Fundamental Principles
Sample size determination for crossover trials follows principles similar to those for parallel designs but accounts for the reduced variance due to within-subject comparisons [51]. The key parameters for sample size calculation include:
- Expected difference (τ) between treatments A and B for the outcome measure, disregarding period effects [49]
- Measurement variance (σₑ²) expected to occur if the measurement procedure were repeated multiple times under identical conditions [49]
- Type I error (α), typically set at 5%
- Desired power (1-β), conventionally 80% or higher
For ethical reasons, studies should be sufficiently powered to demonstrate their objectives before initiation, though not all regulatory guidelines explicitly require power greater than 80% [50].
Regulatory Considerations
Regulatory requirements for sample size in bioequivalence studies vary across jurisdictions:
- Brazil, Japan, Mexico, Saudi Arabia, and the United States explicitly recommend calculations to ensure power greater than 80% [50]
- Many other countries (Argentina, Australia, Canada, EU, etc.) accept studies without this explicit requirement but maintain the 90% confidence interval approach [50]
- Brazil uniquely requires post-study power calculation, with studies rejected if post-study power is below 80% and variability between products is statistically different [50]
- Most regulators accept pilot studies without formal sample size calculations if they include at least 12 subjects (except Japan, which accepts only pivotal study data) [50]
Table 2: Sample Size Considerations in Bioequivalence Studies
| Regulatory Aspect | Requirements and Recommendations |
|---|---|
| Minimum sample size | Generally at least 12 subjects for pilot studies |
| Power requirement | Varies by jurisdiction (≥80% in some countries) |
| Type I error control | Maintained at 5% using 90% confidence intervals |
| Post-study power | Required in Brazil for study validation |
| Subject replacement | Generally allowed for pre-dose dropouts if pre-specified |
| Analysis set | All subjects completing per protocol should be included |
Application to Bioequivalence of Natural vs. Synthetic Compounds
Special Considerations for Natural Products
The application of crossover designs to bioequivalence studies comparing natural and synthetic bioactive compounds presents unique methodological considerations:
- Higher Variability: Natural products often exhibit higher variability in absorption and metabolism due to complex mixture composition, potentially requiring larger sample sizes or replicate designs [46] [4].
- Complex Pharmacokinetics: The pharmacokinetics of natural compounds can be more complex than synthetic drugs, potentially necessitating more frequent sampling or additional measurement time points [46] [52].
- Food Effects: Natural products may be more susceptible to food effects, requiring additional study arms or conditions to fully characterize bioavailability [46].
- Multiple Active Components: Unlike most synthetic drugs with single active ingredients, natural products often contain multiple bioactive compounds, complicating the selection of appropriate analytes for measurement [52] [4].
Case Studies and Applications
Recent research demonstrates the successful application of crossover designs in natural product bioequivalence research:
- A randomized clinical trial compared the pharmacokinetics of chitosan-derived and biofermentation-derived glucosamine using a crossover design, finding that while both types met bioequivalence standards, they differed in mean peak plasma concentration (Cmax) ratios [46].
- Studies on fermented garlic extract utilized crossover designs to demonstrate significant changes in vascular function parameters within 30-60 minutes post-consumption [46].
- Research on green tea bioactive compounds employed crossover designs to establish impacts on hormonal fluctuations and depression risk in postmenopausal women [46].
Regulatory and Standardization Framework
The International Pharmaceutical Regulators Programme (IPRP) Bioequivalence Working Group for Generics (BEWGG) has developed recommendations supporting global harmonization of bioequivalence study standards [50]. The resulting ICH M13A guideline, endorsed in December 2022, plays a crucial role in standardizing bioequivalence assessment for immediate-release solid oral dosage forms [50]. For natural products, regulatory standards continue to evolve as scientific understanding of their unique properties advances.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents and Materials for Crossover Bioequivalence Studies
| Reagent/Material | Function and Application |
|---|---|
| Standardized Natural Product Extracts | Ensure consistent composition and dosing of natural product test formulations |
| Synthetic Reference Compounds | Provide precisely characterized reference materials for comparison |
| Stable Isotope-Labeled Analogs | Serve as internal standards for precise bioanalytical measurements |
| Validated Bioanalytical Assays (LC-MS/MS) | Quantify drug concentrations in biological matrices with high sensitivity and specificity |
| Pharmacokinetic Software (e.g., WinNonlin) | Model concentration-time data and calculate key parameters (AUC, Cmax, Tmax) |
| Clinical Database Systems | Manage subject data, treatment sequences, and sampling timepoints |
| Randomization Systems | Ensure unbiased assignment to treatment sequences |
| Sample Processing Kits | Standardize plasma/serum separation and storage conditions |
Crossover designs offer a powerful methodological approach for bioequivalence studies comparing natural and synthetic bioactive compounds. Their enhanced statistical efficiency and ability to control for inter-individual variability make them particularly valuable in this research domain. However, careful attention to potential carryover effects, appropriate washout periods, and adequate sample size is essential for generating valid, interpretable results. As research on natural products continues to expand, with increasing recognition of their therapeutic potential [4], the proper application of crossover designs will play a crucial role in establishing robust scientific evidence for their bioavailability and bioequivalence relative to synthetic alternatives. The ongoing harmonization of regulatory standards through initiatives like ICH M13A further supports the generation of reliable, comparable data across the global scientific community.
Bioanalytical Method Validation for Compound Quantification
The rigorous validation of bioanalytical methods is a cornerstone in the development and evaluation of pharmaceuticals, ensuring the reliability of data used to make critical decisions. This process is paramount in the context of a broader thesis on the bioequivalence of synthetic versus natural bioactive compounds. Bioequivalence studies demand exceptionally high-quality data to demonstrate that a natural product and its synthetic counterpart, or a generic and a brand-name drug, exhibit comparable rate and extent of absorption. Even minor inconsistencies in the bioanalytical method can lead to incorrect bioequivalence conclusions, potentially preventing a safe and effective product from reaching the market or, conversely, allowing a non-equivalent product to be sold. Consequently, a thoroughly validated method is not merely a regulatory formality but a fundamental scientific necessity to ensure that comparative assessments of synthetic and natural bioactive compounds are accurate, reliable, and trustworthy [53] [29].
The global regulatory landscape for bioanalytical method validation is governed by several key guidelines, each with subtle but critical differences in their requirements. Major regulatory authorities, including the United States Food and Drug Administration (USFDA), the European Medicines Agency (EMA), Brazil's National Health Surveillance Agency (ANVISA), and Japan's Ministry of Health, Labour and Welfare (MHLW), have all established their own criteria [53]. Although these guidelines share a common foundation—originating from the seminal USFDA guidance issued in 2001—significant variations exist in their acceptance criteria and methodological specifics. Understanding these nuances is essential for researchers and drug development professionals aiming for global regulatory submission and acceptance, particularly when characterizing the complex pharmacokinetic profiles of natural bioactive products and their synthetic equivalents [30] [53].
Comparative Analysis of Global Validation Guidelines
A side-by-side comparison of the major guidelines reveals critical differences in scope, acceptance criteria, and specific recommendations. The following sections and tables summarize these requirements for key validation parameters.
Scope and Application of Guidelines
The applicability of various guidelines, while overlapping, has distinct focuses as outlined in the table below.
Table 1: Scope and Application of Bioanalytical Method Validation Guidelines
| Regulatory Authority | Document Release/Update | Primary Scope & Application | Notable Inclusions & Exclusions |
|---|---|---|---|
| USFDA | 2001 Guideline; 2013 Draft | Investigational New Drug (IND) Applications, New Drug Applications (NDA), Abbreviated New Drug Applications (ANDA). Preclinical studies (toxicology/pharmacology) [53]. | Applies to blood, plasma, serum, urine; GC, LC, and MS combinations. 2013 draft extended scope to Biological Licence Applications (BLAs) and biomarker concentration evaluation [53]. |
| EMA (Europe) | Effective February 2012 | Bioanalysis in animal toxicological studies and all clinical trial phases. Validation for Ligand Binding Assays (LBA) [53]. | Recommends performance in agreement with GLP principles for non-clinical studies. Excludes biomarker quantification for pharmacodynamic endpoints [53]. |
| ANVISA (Brazil) | 2003 (First); Amended 2012 | Bioanalytical methods using GC, HPLC, and MS combinations for drug quantification [53]. | Extended applicability to other matrices beyond blood, serum, plasma, and urine, which is lacking in other guidelines [53]. |
| MHLW (Japan) | 2013 Draft | Separate draft guidelines for low and high molecular weight drugs. Not restricted to a specific analytical technique [53]. | Recommends full validation for each species and matrix. Provides criteria for intra- and inter-laboratory precision for cross-validation [53]. |
Validation Parameters and Acceptance Criteria
The core of method validation lies in assessing specific parameters. The acceptance criteria for these parameters, while broadly similar, contain important variations between regulators, as detailed in the table below.
Table 2: Key Validation Parameters and Acceptance Criteria Across Guidelines
| Validation Parameter | USFDA (2001 & 2013 Draft) | EMA (2012) | ANVISA (2012) | MHLW (2013) |
|---|---|---|---|---|
| Accuracy & Precision | Within ±15% of nominal value for QC samples, except LLOQ (±20%) [53]. | Within ±15% of nominal value for QC samples, except LLOQ (±20%) [53]. | Within ±15% of nominal value for QC samples, except LLOQ (±20%) [53]. | Within ±15% of nominal value for QC samples, except LLOQ (±20%) [53]. |
| Calibration Curve | A specific number of standards should be used, including LLOQ. Not all standards need to be used in every run [53]. | A specific number of standards should be used, including LLOQ. Not all standards need to be used in every run [53]. | A specific number of standards should be used, including LLOQ. Not all standards need to be used in every run [53]. | A specific number of standards should be used, including LLOQ. Not all standards need to be used in every run [53]. |
| Lower Limit of Quantification (LLOQ) | Signal-to-noise ratio ≥ 5. Accuracy and precision within ±20% of nominal value [53]. | Signal-to-noise ratio ≥ 5. Accuracy and precision within ±20% of nominal value [53]. | Signal-to-noise ratio ≥ 5. Accuracy and precision within ±20% of nominal value [53]. | Signal-to-noise ratio ≥ 5. Accuracy and precision within ±20% of nominal value [53]. |
| Stability | Evaluation in matrix at room temperature, frozen, and freeze-thaw cycles [53]. | Evaluation in matrix at room temperature, frozen, and freeze-thaw cycles [53]. | Evaluation in matrix at room temperature, frozen, and freeze-thaw cycles [53]. | Evaluation in matrix at room temperature, frozen, and freeze-thaw cycles [53]. |
| Cross-Validation | Lacks detailed acceptance criteria [53]. | Accuracy within ±15%; difference between two methods ≤ ±20% of the mean for ≥67% of repeats [53]. | Lacks detailed acceptance criteria [53]. | Same as EMA, with additional consideration for intra- and inter-laboratory precision [53]. |
Experimental Protocols for Key Validation Experiments
This section provides detailed methodologies for conducting critical experiments in bioanalytical method validation, which are essential for generating defensible data for regulatory submission.
Protocol for Accuracy and Precision (Within-Run and Between-Run)
This experiment assesses the method's closeness to the true value (accuracy) and its reproducibility (precision) [53].
- Sample Preparation: Prepare a minimum of five replicates of Quality Control (QC) samples at three concentration levels (Low, Medium, High) spanning the calibration curve range, plus the Lower Limit of Quantification (LLOQ), in the biological matrix (e.g., plasma).
- Analysis: Analyze all QC samples within a single analytical run (for within-run accuracy/precision) and across three different analytical runs (for between-run accuracy/precision).
- Data Analysis:
- Accuracy: Calculate the mean measured concentration for each QC level. Accuracy is expressed as (Mean Measured Concentration / Nominal Concentration) × 100%.
- Precision: Calculate the relative standard deviation (RSD%) for each QC level. For within-run precision, use the five replicates from one run. For between-run precision, use the mean of each run's replicates across the three runs.
- Acceptance Criteria: The mean accuracy should be within 85–115% (100 ±15%) for all QC levels, except for the LLOQ, which is 80–120% (100 ±20%). The precision (RSD%) should not exceed 15% for all QC levels, and 20% for the LLOQ [53].
Protocol for Stability Assessment (Freeze-Thaw Stability)
This experiment determines the stability of the analyte in the matrix after undergoing repeated freeze-thaw cycles.
- Sample Preparation: Prepare QC samples at Low and High concentrations in the biological matrix.
- Freeze-Thaw Cycles: Store the samples at the intended storage temperature (e.g., -70°C or -20°C) for a minimum of 12 hours. Then, completely thaw the samples unassisted at room temperature. Once fully thawed, refreeze the samples under the same conditions for 12-24 hours. Repeat this cycle to generate stability data for a minimum of three freeze-thaw cycles.
- Analysis: After the final thaw cycle, analyze the stability samples alongside freshly prepared calibration standards and QC samples.
- Data Analysis: Calculate the mean measured concentration of the stability samples after each cycle. Compare this to the mean measured concentration of the freshly prepared QC samples (representing 0 cycles).
- Acceptance Criteria: The analyte is considered stable if the mean measured concentration after freeze-thaw cycles is within 85–115% of the nominal concentration or the comparison sample mean [53].
Protocol for Incurred Sample Reanalysis (ISR)
ISR is critical for demonstrating the method's reproducibility for study samples, as it can reveal matrix effects not present in spiked QC samples [53].
- Sample Selection: Select a representative number of incurred samples (samples from dosed subjects) from the study. Typically, 10% of samples or a minimum of 50 samples are selected, including samples near C~max~ and the elimination phase.
- Reanalysis: Reanalyze the selected incurred samples in a separate analytical run, under the same validated method conditions.
- Data Analysis: Calculate the percentage difference between the original concentration (C1) and the reanalyzed concentration (C2) for each sample using the formula: % Difference = [(C2 - C1) / Mean of C1 and C2] × 100.
- Acceptance Criteria: For at least 67% of the repeats, the percentage difference between the two values should be within ±20% of their mean [53].
Visualization of Validation Workflows and Strategic Approaches
The following diagrams, created using the specified color palette and contrast rules, illustrate the logical flow of the validation process and the strategic considerations for navigating regulatory differences.
Diagram 1: Bioanalytical Method Validation Workflow
Diagram 2: Strategic Approach to Global Validation
The Scientist's Toolkit: Essential Research Reagent Solutions
The successful development and validation of a bioanalytical method rely on a suite of critical reagents and materials. The following table details these essential components and their functions.
Table 3: Essential Research Reagents and Materials for Bioanalytical Method Validation
| Reagent / Material | Function & Role in Validation |
|---|---|
| Certified Reference Standard (Analyte) | The highly purified compound of interest, with a certified certificate of analysis. It is used to prepare calibration standards and is pivotal for demonstrating accuracy, selectivity, and for constructing the calibration curve [53]. |
| Stable Isotope-Labeled Internal Standard (IS) | A chemically identical analog of the analyte labeled with a stable isotope (e.g., Deuterium, ^13^C). It is added to all samples, standards, and QCs to correct for variability in sample preparation, matrix effects, and instrument response, thereby improving precision and accuracy [53]. |
| Control (Blank) Biological Matrix | The biological fluid (e.g., plasma, serum) from an untreated source. It is used to prepare calibration standards and QC samples, and is essential for demonstrating the method's selectivity by confirming the absence of interfering endogenous components at the retention times of the analyte and IS [53]. |
| Appropriate Anticoagulants | Chemicals (e.g., Heparin, EDTA) used to prevent the coagulation of blood samples. The choice of anticoagulant must be consistent and justified, as it can be a source of matrix variability and can affect analyte stability [53]. |
| Matrix-Specific Stability Additives | Reagents (e.g., enzyme inhibitors, antioxidants) added to the biological matrix to prevent the degradation of the analyte. Their use and concentration must be validated during stability experiments to ensure the integrity of samples before analysis [53]. |
| High-Purity Solvents & Reagents | HPLC/MS-grade solvents, water, and additives (e.g., formic acid, ammonium acetate) for mobile phase and sample preparation. High purity is critical to minimize chemical noise, reduce ion suppression/enhancement in MS, and ensure robust chromatographic performance [53]. |
Synthetic Biology and Metabolic Engineering for Compound Production
The pursuit of sustainable, scalable, and consistent production of bioactive compounds has catalyzed a significant shift from traditional plant extraction to engineered microbial systems. Within pharmaceutical and biofuel research, establishing bioequivalence—therapeutic equivalence despite different production origins—between natural plant-derived compounds and their synthetically biology-produced counterparts is a critical research frontier. This guide compares the performance of traditional natural extraction against modern synthetic biology platforms, focusing on technical parameters, experimental data, and methodological protocols relevant to researchers and drug development professionals.
Synthetic biology applies engineering principles to biology, designing and constructing novel biological systems for useful purposes. Metabolic engineering specifically rewires metabolic pathways in microorganisms to optimize the production of target compounds [54]. These approaches are revolutionizing production paradigms for high-value compounds, overcoming limitations of traditional plant-based extraction, such as low yields, resource-intensive cultivation, and chemical instability [55]. The core bioequivalence question is whether these different production methods yield molecules that are functionally identical in terms of purity, biological activity, and therapeutic effect.
Performance Comparison: Production Platforms and Key Metrics
The following tables provide a comparative analysis of different production systems based on key performance indicators, from feedstocks to final product yields.
Table 1: Comparison of Biofuel Production Generations by Feedstock, Technology, and Output [56]
| Generation | Feedstock Type | Technology | Yield (per ton feedstock) | Key Sustainability Metrics |
|---|---|---|---|---|
| First | Food crops (corn, sugarcane) | Fermentation, transesterification | Ethanol: 300–400 L | Competes with food supply; high land use |
| Second | Crop residues, lignocellulose | Enzymatic hydrolysis, fermentation | Ethanol: 250–300 L | Better land use; moderate GHG savings |
| Third | Algae | Photobioreactors, hydrothermal liquefaction | Biodiesel: 400–500 L | High GHG savings; scalability challenges |
| Fourth | GMOs, synthetic systems | CRISPR, electrofuels, synthetic biology | Varies (hydrocarbons, isoprenoids) | High potential; regulatory concerns |
Table 2: Comparative Analysis of Bioactive Compound Production Platforms [56] [34] [55]
| Platform Attribute | Traditional Plant Extraction | Microbial Cell Factories (E. coli, Yeast) | Engineered Algae/Fungi |
|---|---|---|---|
| Primary Feedstock | Agricultural plant biomass | Sugars, glycerol | CO₂, sunlight, wastewater |
| Exemplary Product/ Yield | Alstonine: < 0.001% extraction yield [34] | Vinblastine: 31-step pathway in yeast [34] | Fatty acids: 2.5-fold increase in Synechocystis [54] |
| Butanol (Biofuel) | N/A | 3-fold yield increase in engineered Clostridium spp. [56] | N/A |
| Xylose-to-Ethanol | N/A | ~85% conversion in S. cerevisiae [56] | N/A |
| Biodiesel | N/A | 91% conversion efficiency from lipids [56] | High lipid production potential |
| Production Timeline | Months to years (plant growth cycle) | Days to weeks (fermentation) | Weeks (cultivation) |
| Land Use Impact | High | Low | Very Low (non-arable land usable) |
| Process Control | Variable (climate-dependent) | Highly controlled & reproducible | Moderately controlled |
Experimental Protocols for Key Methodologies
Protocol 1: Engineering a Yeast Cell Factory for Complex Molecule Production
This protocol outlines the process for producing plant-inspired therapeutics, such as Monoterpene Indole Alkaloids (MIAs), in an engineered yeast chassis, as demonstrated by companies like Biomia [34].
- Objective: To engineer Saccharomyces cerevisiae for the heterologous production of a complex plant-derived bioactive compound (e.g., Alstonine or Vinblastine).
- Key Steps:
- Pathway Identification & Gene Selection: Identify the complete biosynthetic gene cluster (BGC) and enzymatic assembly line from the source plant. For MIAs, this involves genes encoding enzymes that turn amino acids and sugars into target molecules.
- DNA Assembly & Vector Construction: Clone the identified plant genes into expression vectors suitable for yeast. For extensive pathways (e.g., the 31-enzyme vinblastine pathway), this may involve assembling approximately 100,000 DNA bases into the yeast genome [34].
- Yeast Transformation & Genome Integration: Introduce the expression vectors into the yeast chassis using transformation techniques. Integrate the heterologous genes into the yeast genome and knock out competing native genes to optimize metabolic flux.
- Strain Cultivation & Fermentation: Cultivate the best-performing engineered yeast strains in bioreactors using scalable fermentation processes with defined media, typically using sugar as the primary carbon source.
- Product Extraction & Analysis: Harvest cells and extract the target compound from the fermentation broth. Quantify yield and purity using analytical techniques like High-Performance Liquid Chromatography (HPLC) and Mass Spectrometry (MS).
Protocol 2: CRISPR-Cas9 Mediated Pathway Engineering in Plants
This protocol describes using genome editing to enhance the production of Plant Natural Products (PNPs) directly in medicinal plants [55].
- Objective: To increase the yield and quality of a target PNP by performing precise genetic modifications in the host plant.
- Key Steps:
- Target Identification: Select key enzymes (e.g., rate-limiting enzymes) or transcription factors in the PNP's biosynthetic pathway as CRISPR targets.
- gRNA Design and Vector Construction: Design guide RNAs (gRNAs) with high specificity for the target gene sequence. Assemble the gRNA and Cas9 nuclease gene into a plant transformation vector.
- Plant Transformation: Introduce the CRISPR-Cas9 construct into plant cells via Agrobacterium tumefaciens-mediated transformation.
- Regeneration and Selection: Regenerate whole plants from the transformed cells on selective media. Screen for successful edits.
- Metabolite Profiling: Quantify the levels of the target PNP in edited plant lines compared to wild-type controls using HPLC or GC-MS. Assess for potential unintended metabolic consequences.
Visualizing Workflows and Pathways
The following diagrams, generated with Graphviz, illustrate the core logical and pathway relationships in synthetic biology production.
Microbial Biofactory Engineering Workflow
Metabolic Pathway Optimization Logic
The Scientist's Toolkit: Key Research Reagent Solutions
This table details essential materials and tools used in the development and optimization of microbial cell factories.
Table 3: Essential Reagents and Tools for Synthetic Biology and Metabolic Engineering
| Research Reagent / Tool | Function / Application | Specific Example / Context |
|---|---|---|
| CRISPR-Cas Systems | Precision genome editing for gene knock-outs, knock-ins, and transcriptional regulation in hosts. | Used to modify critical enzymes and transcription factors in plants to boost PNP yields [55]. |
| GoldenBraid (GB) / FungalBraid (FB) | Modular DNA assembly toolkit for standardized, interchangeable genetic parts. | FB toolkit adapted for filamentous fungi to streamline engineering for bioactive compound production [54]. |
| Biosensors | Real-time monitoring of specific metabolites, nutrients, or product concentrations during fermentation. | Employed with advanced analytics for bioprocess control to maintain optimal production conditions [57]. |
| Artificial Scaffold Systems | Spatial organization of enzymes to create metabolic channels, increasing reaction efficiency and reducing intermediate loss. | Protein- and nucleic acid-based scaffolds used in E. coli and yeast to increase titers of bioactive compounds [54]. |
| Machine Learning (ML) Platforms | AI-driven modeling to predict optimal DNA designs, enzyme performance, and fermentation parameters. | Used to correlate DNA-encoded assembly lines with production profiles in yeast [34] [54]. |
| Glycosyltransferases | Enzymes that attach sugar moieties to core compounds (glycosylation), altering their bioactivity, solubility, and stability. | UGT94D1 mutant used to glycosylate Reb D, producing Reb M2 with 92% yield [54]. |
The pursuit of bioequivalent synthetic bioactive compounds is a cornerstone of modern pharmaceutical and nutraceutical research. The choice of host system for heterologous production is pivotal, influencing the structural fidelity, biological activity, and scalability of these valuable molecules. While prokaryotic workhorses like Escherichia coli and established eukaryotic platforms like Saccharomyces cerevisiae have long dominated the landscape, emerging hosts like microalgae are challenging conventions with unique advantages. This guide provides an objective comparison of these three host systems—E. coli, yeast, and microalgae—synthesizing their performance data, experimental methodologies, and suitability for producing bioequivalent natural products.
The selection of a host organism is a primary determinant in the success of a biosynthetic project. Each system—E. coli, yeast, and microalgae—brings a distinct set of biological characteristics, advantages, and limitations to the process.
E. coli, a Gram-negative bacterium, is one of the most well-characterized prokaryotic systems. Its rapid growth, high yield, and extensive genetic toolset make it a default choice for many simple proteins and natural products [58]. However, its inability to perform post-translational modifications (PTMs) common in eukaryotes, such as glycosylation, and its tendency to form inclusion bodies with complex proteins, are significant drawbacks for producing sophisticated eukaryotic bioactives [58].
Saccharomyces cerevisiae (budding yeast) is a premier eukaryotic model organism. It offers the cellular machinery for basic PTMs, improved protein folding for complex eukaryotic proteins, and a generally recognized as safe (GRAS) status [59] [58]. Yeast synthetic biology has advanced to the point of enabling the design of complex synthetic microbial communities, allowing for a division of labor where different strains can be engineered to perform specialized metabolic tasks, thereby reducing the metabolic burden on any single strain [59]. Despite these strengths, yeast can hyperglycosylate proteins, leading to immunogenicity, and may lack the specific enzymes required for certain plant or animal-derived metabolic pathways [58].
Microalgae, particularly Chlamydomonas reinhardtii, represent a promising and sustainable eukaryotic platform. As photosynthetic organisms, they can be cultivated with minimal resources, requiring only 3.75% of the land area and 76% less water compared to soybean protein production, while fixing carbon dioxide [60]. Microalgae possess organelles that enable necessary eukaryotic PTMs but avoid the issue of hyperglycosylation seen in yeast [58]. They have been successfully engineered to produce a range of compounds, from high-value proteins to pigments and polyunsaturated fatty acids [60]. A key advantage is their ability to produce and secrete functional recombinant proteins, such as the reporter mVenus, without detrimental effects on cellular fitness, including growth and oxygen metabolism, even under varied environmental conditions [58]. This makes them suitable for controlled, localized therapeutic delivery systems [58]. The primary challenges lie in achieving stable nuclear genetic transformation and scaling up production in photobioreactors [60].
Table 1: Key Characteristics of Bioactive Compound Production Hosts
| Feature | E. coli | Yeast (S. cerevisiae) | Microalgae (C. reinhardtii) |
|---|---|---|---|
| Organism Type | Prokaryote | Eukaryote (Fungus) | Eukaryote (Photosynthetic) |
| Post-Translational Modifications | Limited or none | Basic glycosylation, risk of hyperglycosylation | Eukaryotic PTMs, avoids hyperglycosylation [58] |
| Typical Yield | High for simple proteins | Moderate to High | Actively being optimized; high for specific compounds [60] |
| Growth Rate | Very High (doubling ~20 min) | High (doubling ~90 min) | Moderate [58] |
| Resource Efficiency | High (fermentation) | High (fermentation) | Very High (low land/water use, CO₂ fixation) [60] |
| Key Advantage | Speed, cost, well-established tools | Eukaryotic machinery, GRAS status, synthetic communities [59] | Photosynthesis, eukaryotic PTMs, fitness unchanged post-engineering [58] |
| Key Disadvantage | No complex PTMs, inclusion bodies | Hyperglycosylation, limited pathway enzymes | Challenging nuclear transformation, scaling [60] |
Quantitative Comparison of Production Metrics
Direct comparative data is essential for evidence-based decision-making. The following table summarizes experimental performance data for the three host systems across various bioactive compounds, highlighting yields and relevant experimental conditions.
Table 2: Production Metrics for Bioactive Compounds Across Host Systems
| Bioactive Compound | Host System | Reported Yield/Activity | Key Experimental Condition | Citation |
|---|---|---|---|---|
| Recombinant Protein (mVenus) | Microalgae (C. reinhardtii) | Produced & secreted without detrimental effects on growth, cell size, or O₂ metabolism | Standard culture conditions; function maintained for 4 days at 22-37°C [58] | [58] |
| Polyunsaturated Fatty Acids (PUFAs) | Microalgae | Natural primary producers; commercial production of DHA and EPA achieved | Utilized as a renewable resource strategy; multiple strains developed [60] | [60] |
| Secondary Metabolites (e.g., Antibacterials) | Streptomyces sp. (Actinomycete) | Antibacterial, antioxidant, and anti-inflammatory activities confirmed | Isolated from mangrove sediment; optimized via RSM-CCD [61] | [61] |
| Synthetic Cooperation | Yeast (S. cerevisiae) | Stable co-cultures established via metabolic interdependence (e.g., amino acid exchange) | Engineered auxotrophic strains in selective medium [59] | [59] |
| Therapeutic Proteins | Mammalian Cells (CHO) | Fully functional, complex PTMs | Industry standard for complex biologics; used as a benchmark [58] | [58] |
Experimental Protocols for Host Engineering and Analysis
Robust and reproducible experimental protocols are the foundation of reliable research in metabolic engineering and synthetic biology. Below are detailed methodologies for key processes in utilizing these host systems.
Genetic Engineering of Microalgae
The transformation of microalgae like Chlamydomonas reinhardtii involves specific vectors and selection strategies.
- Plasmid Construction: Genetic constructs are assembled using toolkits like the Chlamydomonas MoClo. This involves combining plasmid backbones, promoters (e.g., synthetic promoter SAP11), coding sequences (e.g., mVenus), and terminators (e.g., from RuBisCO small subunit, RBCS2) using Type IIS restriction enzymes and T4 DNA ligase. To optimize transgene expression, endogenous introns are often incorporated into the coding sequences. For secreted proteins, a secretion peptide (e.g., pJP30) is placed at the N-terminus [58].
- Transformation and Selection: Vectors are transformed into cell-wall-deficient strains (e.g., UVM4) via methods such as electroporation or glass bead agitation. Selection of positive transformants is typically performed on solid Tris-Acetate-Phosphate (TAP) medium containing antibiotics like paromomycin, with resistance conferred by a marker like the APHVIII gene driven by a strong promoter (e.g., beta-Tubulin promoter) [58].
- Culture Conditions: Transformant strains are maintained photomixotrophically at 22±3°C in liquid or solid TAP medium under continuous white light with constant agitation. Cell density is monitored by measuring optical density at 550 nm (OD550) [58].
Media Optimization via Response Surface Methodology (RSM)
Optimizing culture conditions is critical for maximizing the yield of secondary metabolites, as demonstrated with actinomycetes.
- Strain Isolation and Screening: Potent microbial strains are first isolated from environmental samples (e.g., mangrove sediments) and selected based on primary screening for bioactivity (e.g., zone of inhibition against pathogenic bacteria) [61].
- One-Variable-at-a-Time (OVAT) Analysis: Initial media components (carbon source, nitrogen source, minerals, NaCl, pH, incubation time) are varied individually to identify their rough optimal ranges for metabolite production [61].
- RSM-Central Composite Design (CCD): A statistical model is designed with the key factors identified from OVAT (e.g., starch, yeast extract, NaCl, NH₄Cl) as independent variables. The antibacterial activity serves as the response variable (Y). A series of experiments are run as per the CCD matrix, and the data is fitted to a second-order polynomial equation. Analysis of Variance (ANOVA) is used to validate the model's significance and identify factors and interactions with the greatest impact on yield. The model then predicts the optimal combination of factors for maximum production [61].
Establishing Synthetic Microbial Consortia in Yeast
Engineering yeast communities allows for a division of labor in biosynthetic pathways.
- Design and Engineering: Two or more yeast strains are engineered to be auxotrophic for different essential metabolites (e.g., adenine and lysine). Each strain is further modified to overproduce the metabolite required by the other strain, without feedback inhibition [59].
- Co-culture and Validation: The engineered strains are co-inoculated into a selective medium that lacks both essential metabolites. The growth of the community is monitored over time. The proliferation of both strains is contingent on the metabolic exchange, demonstrating obligate mutualism (syntrophy). Control monocultures of each strain in the selective medium show no growth, confirming the dependency [59].
- Analysis: Population ratios and growth dynamics can be tracked using flow cytometry or by using differential markers. The stability of the consortium can be challenged by introducing "exploiter" cells or by varying initial population ratios [59].
Visualizing the Host Selection and Engineering Workflow
The following diagram outlines the logical decision-making process and key steps for selecting and engineering a host system for bioactive compound production.
The Scientist's Toolkit: Essential Research Reagents
Successful engineering and analysis of these host systems rely on a suite of specialized reagents and tools.
Table 3: Key Research Reagents and Their Applications
| Reagent / Tool | Function | Example Use Case |
|---|---|---|
| Type IIS Restriction Enzymes | Enable Golden Gate assembly (e.g., MoClo toolkits) for modular vector construction. | Assembling genetic circuits in microalgae and yeast [58]. |
| Tris-Acetate-Phosphate (TAP) Medium | Standard nutrient medium for the cultivation of microalgae like C. reinhardtii. | Maintaining and growing transformed microalgal strains [58]. |
| Paromomycin / APHVIII Marker | Antibiotic and corresponding resistance gene for selecting transformed cells. | Selecting for positive C. reinhardtii transformants on solid TAP plates [58]. |
| Response Surface Methodology (RSM) | Statistical technique for optimizing multiple process variables simultaneously. | Maximizing secondary metabolite yield in Streptomyces cultures [61]. |
| Fluorescent Reporter Proteins (e.g., mVenus) | Visual markers for tracking gene expression, protein localization, and secretion. | Confirming production and secretion of recombinant proteins in C. reinhardtii [58]. |
| Synthetic Promoters (e.g., SAP11) | Engineered DNA sequences providing strong, constitutive, or inducible transcription. | Driving high-level expression of transgenes in the microalgal nucleus [58]. |
| Auxotrophic Markers | Genes complementing a host's inability to synthesize an essential metabolite. | Creating synthetic, interdependent microbial consortia in yeast [59]. |
Bioequivalence (BE) assessment is a critical process in drug development, particularly for the approval of generic drugs. It serves as a surrogate for clinical trials to ensure that a generic drug product is therapeutically equivalent to its brand-name counterpart. The fundamental bioequivalence assumption states that if two drug products are shown to be bioequivalent, it is assumed that they will generally reach the same therapeutic effect [62]. This principle underpins regulatory approval pathways worldwide, allowing generic drugs to enter the market without repeating extensive clinical efficacy and safety trials.
The United States Food and Drug Administration (FDA) was authorized to approve generic drug products under the Drug Price Competition and Patent Term Restoration Act of 1984 [62]. This legislation established the current regulatory framework where generic manufacturers must demonstrate through bioavailability and bioequivalence studies that their products provide comparable systemic exposure to the reference listed drug. The 90% confidence interval and 80-125% bioequivalence range have become the cornerstone of this assessment, providing a standardized statistical approach to evaluate whether differences between drug products are clinically insignificant.
The Scientific Basis of the 80-125% Bioequivalence Range
Statistical and Pharmacokinetic Principles
The 80-125% range used in bioequivalence assessment is not arbitrary but is grounded in statistical principles related to the behavior of pharmacokinetic parameters. Key metrics such as maximum concentration (Cmax) and area under the concentration-time curve (AUC) are known to follow log-normal distributions [63] [62]. This means that while the raw data are skewed, taking the logarithmic transformation results in a normal distribution, which satisfies the assumptions required for parametric statistical testing.
When pharmacokinetic parameters are log-transformed, the 80-125% range becomes symmetrical around zero on the logarithmic scale. Specifically, the natural logarithm of 0.80 (80%) is -0.223, and the natural logarithm of 1.25 (125%) is +0.223, creating a symmetrical interval ±0.223 around the ideal ratio of 1.00 (0 on the log scale) [63]. This symmetry is crucial for the validity of the statistical tests used in bioequivalence assessment.
Clinical Significance of the 20% Difference
Regulatory bodies have determined that differences in systemic drug exposure up to 20% are not clinically significant for most drugs [63]. This decision was based on extensive scientific consideration of what constitutes a clinically relevant difference in drug exposure that would affect therapeutic outcomes. The 80-125% range represents 100% ± 20% when considered on the original scale, though the statistical testing occurs on the log-transformed data to maintain the normality assumption.
The 90% confidence interval requirement provides additional assurance about the consistency of the exposure matching. For bioequivalence to be concluded, the entire 90% confidence interval for the ratio of geometric means of the primary pharmacokinetic parameters must fall entirely within the 80-125% range [64]. This stringent requirement ensures that there is high confidence (90%) that the true population geometric mean ratio lies within the acceptable bounds, not just that the observed point estimate from the study falls within these limits.
Experimental Design and Methodologies for Bioequivalence Studies
Standard Bioequivalence Study Designs
Bioequivalence studies typically employ crossover designs where each participant receives both the test and reference formulations in random order, separated by an appropriate washout period [62]. The standard two-sequence, two-period (2×2) crossover design is most common, where subjects are randomly assigned to one of two sequences: test product followed by reference, or reference followed by test.
More complex designs are employed for specific situations. For highly variable drugs or narrow therapeutic index drugs, replicated crossover designs are often necessary. These may include:
- Three-period designs: RRT, RTR, or TRR (where T=Test, R=Reference)
- Four-period designs: RTRT or TRTR [65]
These replicated designs allow researchers to estimate within-subject variability for both formulations, which is essential for implementing specialized bioequivalence approaches such as reference-scaled average bioequivalence.
Statistical Analysis Protocol
The statistical analysis of bioequivalence studies follows a well-established protocol known as the two-one-sided tests (TOST) procedure [66]. This method tests two simultaneous hypotheses: that the test product is not significantly less bioavailable than the reference product, and that the test product is not significantly more bioavailable than the reference product.
The analysis involves several key steps:
- Log Transformation: Natural log transformation of the pharmacokinetic parameters (AUC and Cmax)
- Analysis of Variance: Performing ANOVA on the log-transformed data using a linear mixed effects model that accounts for sequence, period, and treatment effects as fixed factors, and subject within sequence as a random effect
- Point Estimate and Confidence Interval Calculation: Calculating the geometric mean ratio and its 90% confidence interval
- Decision Rule: Concluding bioequivalence if the entire 90% confidence interval falls within the bioequivalence limits of 80-125%
Table 1: Key Components of Bioequivalence Statistical Analysis
| Component | Description | Purpose |
|---|---|---|
| Log Transformation | Natural log transformation of AUC and Cmax | Addresses log-normal distribution of PK parameters |
| Linear Mixed Model | Statistical model accounting for sequence, period, treatment, and subject effects | Isolates treatment effect from other sources of variation |
| 90% Confidence Interval | Interval estimate for the true geometric mean ratio | Provides range of plausible values for the true ratio |
| Two-One-Sided Tests | Simultaneous testing of inferiority and superiority | Determines if confidence interval lies entirely within limits |
Advanced Bioequivalence Approaches for Special Drug Categories
Reference-Scaled Average Bioequivalence for Highly Variable Drugs
Highly variable drugs (HVDs) present a particular challenge for bioequivalence assessment due to their high within-subject variability (coefficient of variation ≥30%) [65]. For such drugs, demonstrating bioequivalence using the standard approach may require impractically large sample sizes. The reference-scaled average bioequivalence (RSABE) approach addresses this issue by scaling the bioequivalence limits according to the within-subject variability of the reference product.
The RSABE method allows widening of the acceptance limits in proportion to the variability observed with the reference product. The implementation varies between regulatory agencies:
- FDA: Permits RSABE for both AUC and Cmax when within-subject standard deviation (SWR) ≥0.294
- EMA: Permits RSABE only for Cmax when SWR ≥0.294, with AUC always evaluated using standard ABE [65]
The scaling approach uses the formula: (μT - μR)² / σ²WR ≤ θ, where θ is the scaled average BE limit [67]. This allows the acceptable range to widen as variability increases, making it feasible to demonstrate bioequivalence for highly variable drugs without requiring excessively large sample sizes.
Table 2: Bioequivalence Acceptance Criteria for Different Drug Categories
| Drug Category | Within-Subject CV | Regulatory Approach | Acceptance Criteria | Key Requirements |
|---|---|---|---|---|
| Standard Drugs | <30% | Average Bioequivalence (ABE) | 90% CI within 80-125% | Standard 2x2 crossover design, 90% CI for GMR |
| Highly Variable Drugs | ≥30% | Reference-Scaled Average Bioequivalence (RSABE) | Scaled limits based on variability | Replicated design, point estimate within 80-125% |
| Narrow Therapeutic Index Drugs | Any | Tightened ABE or RSABE with variability comparison | 90% CI within 90-111% (EMA) or scaled approach (FDA) | Replicated design, additional variability comparison |
Narrow Therapeutic Index Drugs
Narrow therapeutic index (NTI) drugs require special consideration in bioequivalence assessment due to the serious consequences of small differences in blood concentrations. For these drugs, regulatory agencies have implemented stricter criteria. Health Canada has tightened the average BE limits for critical dose drugs to 90.0-112.0%, while the European Medicines Agency recommends an acceptance interval of 90.00-111.11% for NTI drugs [67].
The approach for NTI drugs may include not only tightened average bioequivalence limits but also a comparison of within-subject variability between test and reference products. This ensures that the generic product does not exhibit greater variability than the reference product, which could increase the risk of adverse events or therapeutic failure in clinical use.
Application to Natural Bioactive Compounds Research
Bioequivalence Challenges for Natural Bioactive Compounds
The assessment of bioequivalence for natural bioactive compounds presents unique challenges compared to synthetic drugs. Natural compounds often have complex compositions, potential synergistic effects, and variable source materials that can affect their bioavailability [68]. Research on natural bioactive compounds in food preservation has highlighted their potential, but establishing bioequivalence for such compounds requires careful consideration of these factors.
Recent studies have explored innovative delivery systems for natural bioactive compounds, such as edible coatings containing synergistic combinations of compounds like anthocyanins and tea polyphenols [68]. These advanced formulations aim to enhance stability and bioavailability but complicate bioequivalence assessment due to their complex interactions and release profiles.
Methodological Considerations for Natural vs. Synthetic Compounds
When comparing natural and synthetic bioactive compounds, researchers must consider several methodological aspects in bioequivalence study design:
- Characterization of Test Product: Natural products may require more extensive characterization of active components and potential markers for bioavailability assessment
- Food Effects: Natural compounds often consumed as part of food matrices may have different absorption profiles compared to purified synthetic compounds
- Metabolite Profiling: Natural compounds may have complex metabolite profiles that need consideration in bioavailability assessment
- Synergistic Effects: Combination effects in natural extracts may require different endpoints for bioequivalence assessment
The fundamental statistical principles of the 90% confidence interval and 80-125% range remain applicable, but may require adaptation to address the specific characteristics of natural bioactive compounds.
Essential Research Tools and Reagent Solutions
Table 3: Key Research Reagent Solutions for Bioequivalence Studies
| Reagent/Equipment | Function in Bioequivalence Research | Application Context |
|---|---|---|
| Chromatography-Mass Spectrometry Systems | Quantification of drug concentrations in biological matrices | Bioanalytical method development and sample analysis |
| WinNonlin Software | Pharmacokinetic modeling and statistical analysis of BE data | Statistical analysis using FDA-compliant methods |
| Replicated Crossover Design Templates | Protocol development for highly variable or NTI drugs | Study design for RSABE approaches |
| Stabilized Emulsion Systems | Enhanced delivery of bioactive compounds | Improved bioavailability of natural bioactive compounds |
| Chitosan-based Edible Coatings | Delivery system for natural preservatives | Bioavailability enhancement of natural antimicrobials |
Workflow and Decision Pathways in Bioequivalence Assessment
The following diagram illustrates the key steps and decision points in planning and conducting a bioequivalence study, incorporating different approaches based on drug characteristics:
Bioequivalence Study Workflow and Method Selection
The 90% confidence interval and 80-125% bioequivalence range represent a scientifically grounded approach to ensuring therapeutic equivalence between drug products. While the fundamental statistical principles remain consistent across drug categories, advanced approaches such as reference-scaled average bioequivalence and tightened limits for narrow therapeutic index drugs have evolved to address specific challenges. The application of these methodologies to natural bioactive compounds requires careful consideration of their unique properties, but the underlying framework provides a robust basis for demonstrating comparable bioavailability. As research in both synthetic and natural bioactive compounds advances, bioequivalence assessment continues to adapt while maintaining its core statistical principles to ensure patient access to safe and effective medications.
In the global pharmaceutical landscape, establishing bioequivalence (BE) is a fundamental requirement for the approval of generic drugs. BE studies demonstrate that a generic product delivers the same amount of active ingredient into the bloodstream in the same time frame as the innovator (reference) product, ensuring therapeutic equivalence and patient safety [69]. However, conducting in vivo BE studies in humans is a resource-intensive process, requiring significant time, cost, and subject participation.
A biowaiver is a regulatory approval mechanism that waives the requirement for an in vivo BE study. Instead, approval is granted based on evidence of equivalence derived from other data, such as in vitro tests and comprehensive pharmaceutical quality data [69] [70]. The concept of biowaivers is crucial for enhancing the efficiency of drug development and regulatory review, thereby accelerating the availability of affordable medicines. This is particularly relevant in the context of research on natural versus synthetic bioactive compounds, where demonstrating bioequivalence can present unique challenges. This guide compares the regulatory pathways for biowaivers, detailing the specific scenarios where in vivo studies are not required and the experimental data needed to support such waivers.
Regulatory Frameworks for Biowaivers
Globally, regulatory harmonization efforts, led by bodies like the International Council for Harmonisation (ICH), have been instrumental in standardizing biowaiver criteria. The recently drafted ICH M13B guideline provides harmonized recommendations for waiving in vivo BE studies for additional strengths of immediate-release (IR) solid oral dosage forms when in vivo BE has already been established for at least one strength [20] [71] [72]. This facilitates the development of multi-strength drug products.
The following table summarizes the major regulatory frameworks and types of biowaivers available across key international authorities.
Table 1: Overview of Key Regulatory Frameworks for Biowaivers
| Regulatory Authority/Initiative | Key Guideline/Scope | Types of Biowaivers Addressed |
|---|---|---|
| International Council for Harmonisation (ICH) | M13B: Bioequivalence for IR Solid Oral Dosage Forms: Additional Strengths Biowaiver [20] | Additional strengths of IR solid oral dosage forms |
| World Health Organization (WHO) Prequalification of Medicines (PQT/MED) | General guidance on BE studies and biowaivers [69] | BCS-based biowaivers; Additional strength biowaivers |
| International Pharmaceutical Regulators Programme (IPRP) | Survey of biowaiver recommendations for various dosage forms [70] | Topical, ophthalmic, enemas, vaginal suppositories, and other non-oral dosage forms |
Beyond the well-defined pathways for oral dosage forms, many regulators also accept biowaivers for certain locally acting drug products. A 2025 survey from the International Pharmaceutical Regulators Programme (IPRP) indicates that for less complex dosage forms like topical solutions, ophthalmic solutions, and enemas, a common approach is to accept biowaivers if the test product is pharmaceutical equivalent (Q1, Q2) to the comparator and has comparable in vitro performance [70]. For example, Brazil and Argentina generally accept biowaivers for locally acting products not intended for systemic effects, provided they are Q1/Q2 equivalent and have comparable in vitro release profiles [70].
Table 2: Summary of Biowaiver Approaches for Select Non-Oral Dosage Forms (Based on IPRP Survey)
| Dosage Form | Country/Region | Key Biowaiver Criteria |
|---|---|---|
| Topical Products (e.g., solutions, gels) | Brazil, Argentina, Mexico | Pharmaceutical equivalence (Q1/Q2); Comparable in vitro release test (IVRT) [70] |
| Ophthalmic/Otic Solutions & Suspensions | Australia, Singapore, New Zealand | For non-systemic acting drugs; PK study may be required for systemic safety assessment [70] |
| Vaginal Solid Dosage Forms & Suppositories | IPRP participants | Case-by-case basis; Often requires Q1/Q2 and in vitro equivalence [70] |
The Biopharmaceutics Classification System (BCS) in Biowaivers
The Biopharmaceutics Classification System (BCS) is a scientific framework that provides a rationale for waiving in vivo BE studies for IR solid oral dosage forms. The BCS classifies drug substances based on their aqueous solubility and intestinal permeability [69].
- BCS Class I: High Solubility, High Permeability
- BCS Class II: Low Solubility, High Permeability
- BCS Class III: High Solubility, Low Permeability
- BCS Class IV: Low Solubility, Low Permeability
According to WHO and other major regulators, BCS-based biowaivers can be granted for BCS Class I and in some cases, Class III drug substances [69]. The underlying principle is that for these drugs, the rate and extent of absorption are primarily governed by their dissolution in the gastrointestinal fluid. Therefore, if two pharmaceutical products (e.g., a synthetic and a natural compound formulation) have very similar dissolution profiles under specific test conditions, they can be considered bioequivalent without the need for an in vivo study.
Table 3: Key Criteria for BCS-Based Biowaivers as per WHO Guidelines
| BCS Class | Solubility | Permeability | Eligibility for Biowaiver | Additional Requirements |
|---|---|---|---|---|
| I | High | High | Eligible | Rapid dissolution (85% in 30 minutes) in three pH media; Excipients should not affect absorption |
| II | Low | High | Not typically eligible for biowaiver | - |
| III | High | Low | Eligible (with considerations) | Very rapid dissolution (85% in 15 minutes); Excipients should not affect absorption or GI transit |
| IV | Low | Low | Not eligible for biowaiver | - |
The workflow for applying for a BCS-based biowaiver involves a systematic investigation of the drug substance and product, culminating in a formal application to the regulatory authority.
Case Study: Bioequivalence of Synthetic vs Natural Curcumin
The comparative analysis of natural and synthetic bioactive compounds presents a compelling application of bioequivalence principles. A 2014 study directly compared natural curcumin (nCUR) with synthetically manufactured curcumin (sCUR) using a combination of in vitro models, providing a robust template for establishing bioequivalence without an in vivo study [73].
Experimental Protocol and Methodology
The study employed an in vitro model of oral mucositis to test the anti-inflammatory and antimicrobial properties of both nCUR and sCUR [73].
- Test Substances: Natural CUR (purified from Curcuma longa, >65-70% CUR, >90% curcuminoids) and synthetic CUR (>99% pure, GRAS status) [73].
- Cell Line and Culture: Human pharyngeal epithelial cells (Detroit 562) were maintained in Eagle's minimal essential medium (MEM) with standard supplements [73].
- Bacterial Strains: Clinical isolates including Moraxella catarrhalis, Streptococcus pneumoniae, and non-typable Haemophilus influenzae [73].
- Key Assays and Procedures:
- Cytotoxicity Detection: Using a Cytotoxicity Detection Kit (LDH) to ensure CUR concentrations were not toxic to epithelial cells.
- Time-Kill Experiments: Bacteria were grown in broth with varying concentrations (20, 50, 100 μM) of nCUR or sCUR. Quantitative cultures were performed at 0, 60, 120, 180, and 240 minutes to compare antibacterial effects.
- Epithelial Cell Adherence Assays: Confluent Detroit cell monolayers were pre-incubated with nCUR or sCUR (0-200 μM). After washing, bacteria were added, and after incubation, the cells were washed, trypsinized, and cultured to quantify adherent bacteria.
- Epithelial Cell Invasion Assays: A gentamicin protection assay was used. Cells were exposed to CUR, infected with bacteria, and then treated with gentamicin to kill extracellular bacteria. The cells were then lysed, and the number of intracellular bacteria was determined via quantitative culture.
- Cytokine/Chemokine Secretion: Detroit cells were pre-incubated with CUR and then stimulated with live bacteria. Cell culture supernatants were analyzed for pro-inflammatory markers like IL-8 and IL-6 using ELISA and Luminex xMAP technology.
Key Findings and Data Comparison
The study demonstrated bioequivalence between nCUR and sCUR across all tested functional assays, supporting the premise that a highly purified synthetic version can be functionally equivalent to a natural extract [73].
Table 4: Summary of Experimental Results Comparing Natural and Synthetic Curcumin
| Experimental Model/Assay | Key Measured Endpoint | Result for nCUR | Result for sCUR | Conclusion on Equivalence |
|---|---|---|---|---|
| Bacterial Time-Kill | Reduction in colony-forming units (cfu) over time | Concentration-dependent killing | Concentration-dependent killing | Equivalent antibacterial effects [73] |
| Epithelial Cell Adherence | Proportion of bacteria adhering to cells | Significant inhibition of bacterial adherence | Significant inhibition of bacterial adherence | Equivalent inhibition of adherence [73] |
| Epithelial Cell Invasion | Number of intracellular bacteria post-gentamicin treatment | Significant reduction in bacterial invasion | Significant reduction in bacterial invasion | Equivalent inhibition of invasion [73] |
| Cytokine/Chemokine Secretion | Secretion of IL-8, IL-6 upon bacterial stimulus | Significant inhibition of pro-inflammatory secretion | Significant inhibition of pro-inflammatory secretion | Equivalent anti-inflammatory effect [73] |
The experimental workflow for this comparative study illustrates how multiple in vitro models can be integrated to build a compelling case for bioequivalence.
The Scientist's Toolkit: Essential Reagents and Materials
To conduct in vitro studies for bioequivalence assessment, particularly for natural and synthetic compounds, a specific set of research reagents and tools is required. The following table details key materials used in the featured curcumin study and their general functions in such research.
Table 5: Key Research Reagent Solutions for In Vitro Bioequivalence Studies
| Reagent / Material | Function / Application | Example from Curcumin Study |
|---|---|---|
| Cell Lines | Model systems for studying human cell interactions | Human pharyngeal epithelial cell line (Detroit 562) [73] |
| Culture Media & Supplements | Provide nutrients and environment for cell growth | Eagle's Minimal Essential Medium (MEM), Fetal Calf Serum (FCS), L-glutamine [73] |
| Test & Comparator Substances | The active compounds being compared for equivalence | Natural CUR (from Curcuma longa), Synthetic CUR (>99% pure) [73] |
| Bacterial Strains | Used in co-culture to model infection and test antimicrobial/anti-inflammation effects | Moraxella catarrhalis, Streptococcus pneumoniae, Haemophilus influenzae [73] |
| Viability/Cytotoxicity Kits | Quantify potential toxic effects of compounds on human cells | Cytotoxicity Detection Kit (LDH) [73] |
| Enzyme-Linked Immunosorbent Assay (ELISA) | Quantify specific protein biomarkers (e.g., cytokines) in cell supernatants | Commercial ELISA kit for Interleukin-8 (IL-8) [73] |
| Multiplex Immunoassay | Simultaneously quantify multiple protein biomarkers from a single sample | Luminex xMAP technology for 8-plex cytokine/chemokine panel [73] |
The pathway for obtaining biowaivers for in vivo BE studies is well-established for specific scenarios, primarily through the BCS-based and additional strength frameworks for IR solid oral dosage forms. Furthermore, regulatory convergence is growing for less complex non-oral dosage forms, as evidenced by international surveys [70]. The case study on curcumin demonstrates that for natural and synthetic bioactive compounds, a battery of rigorous in vitro assays—assessing critical functional endpoints like anti-inflammatory and antimicrobial activity—can provide compelling evidence for bioequivalence. This approach not only accelerates development but also reduces the ethical and financial burdens associated with clinical trials, facilitating the introduction of safe, effective, and affordable therapeutic alternatives.
Overcoming Bioequivalence Challenges in Complex Compounds
For researchers and drug development professionals, the bioequivalence of synthetic versus natural bioactive compounds presents a significant scientific challenge, primarily due to the inherent variability of natural sources. Unlike their synthetically produced counterparts, natural bioactive compounds are subject to fluctuations influenced by seasonal environmental conditions and geographical location, which can alter their chemical profile, concentration, and subsequent biological activity [4]. This variability poses substantial hurdles for the standardization, efficacy, and safety of therapeutics derived from natural products. In drug discovery, understanding and controlling for these factors is not merely an academic exercise but a critical component in ensuring batch-to-batch consistency, reproducible therapeutic outcomes, and ultimately, regulatory approval. This guide objectively compares the impact of these factors on natural product performance and outlines the experimental protocols essential for characterizing and mitigating this variability within bioequivalence research.
The Impact of Seasonal and Geographical Variability
The chemical composition of a natural product is a dynamic, rather than static, property. Seasonal and geographical factors can induce significant changes in the production of secondary metabolites, which are often the target bioactive compounds in drug discovery.
Seasonal Variability
Seasonal changes directly impact plant physiology and metabolism through factors such as temperature fluctuations, precipitation patterns, and solar radiation intensity.
- Evidence from Environmental Studies: Research on groundwater chemistry, which interacts closely with surface vegetation, demonstrates the profound effect of seasons. A study in a riverside groundwater resource area found that the principal components influencing water chemistry shifted dramatically between wet and dry seasons. Specifically, organic pollution from anthropogenic effects was a major factor in the wet season, while geogenic fluoride enrichment became dominant in the dry season [74]. This illustrates how seasonal hydrology and biogeochemical processes can alter the chemical environment, a dynamic that parallels the metabolic changes in plants.
- Climate Science Context: From a climate perspective, natural variability can cause fluctuations in short-term climate averages over years or decades. These variations can mask long-term trends, which is why climate scientists use a minimum of 30 years of data to draw conclusive findings about climate change [75]. Similarly, robust characterization of seasonal influences on natural products requires long-term, multi-seasonal sampling strategies to distinguish true seasonal trends from annual anomalies.
Geographical Variability
The geographical location, encompassing factors like soil composition, climate, and altitude, defines the phenotype of a natural source.
- Compositional Differences in Cultivars: While detailed geographical comparisons of drug candidates are often proprietary, the compositional diversity observed in commercial cultivars provides a compelling parallel. For instance, the Hass avocado cultivar is widely studied for its high oil content, whereas other cultivars like Fuerte and Bacon are valued for different attributes [11]. This genotypic and phenotypic diversity, shaped by cultivation in different regions, underscores the principle that geography and cultivar selection are critical determinants of chemical composition.
- Challenges in Natural Product Research: The screening of natural products for bioactive compounds is often challenging due to the vast concentration differences between various secondary metabolites within an extract [76]. These concentrations are, in turn, influenced by the geographical origin of the source material.
Comparative Data: Synthetic vs. Natural Bioactives and Analytical Techniques
The core challenge in bioequivalence is that a natural product is a complex mixture, while a synthetic drug is typically a single, pure chemical entity. The tables below summarize key comparative aspects.
Table 1: Key Variable Factors Influencing Natural vs. Synthetic Bioactive Compounds
| Factor | Impact on Natural Bioactive Compounds | Impact on Synthetic Bioactive Compounds |
|---|---|---|
| Seasonal Variation | Significant impact on metabolite yield and profile [74]. | Negligible impact; synthesis is controlled and independent of seasons. |
| Geographical Origin | Major impact due to soil, climate, and altitude [11]. | Negligible impact; production facility conditions are standardized. |
| Batch-to-Batch Consistency | Inherently variable; requires rigorous standardization [76]. | Highly consistent; controlled manufacturing process. |
| Chemical Complexity | Complex mixtures; multiple compounds with synergistic/antagonistic effects. | Defined single entity; simpler pharmacokinetic and pharmacodynamic profiles. |
| Regulatory Path for Approval | Often complex due to variability and identification of active moieties [4]. | Streamlined, with a well-defined Investigational New Drug (IND) application. |
Table 2: Analytical Techniques for Characterizing Natural Product Variability
| Technique | Application in Variability Assessment | Key Advantage | Experimental Consideration |
|---|---|---|---|
| HPLC-DAD/MS | Phytochemical characterization and fingerprinting of complex extracts [76]. | High-throughput separation coupled with preliminary identification. | Serves as the first-line tool for dereplication and profiling. |
| UHPLC-HRMS | Detailed metabolite profiling; precise molecular formula identification [76]. | Increased speed, sensitivity, and peak capacity over HPLC. | Essential for distinguishing between structurally similar metabolites from different sources. |
| HPLC-HRMS-SPE-NMR | Structural elucidation of bioactive components directly from a crude extract [76]. | Unifies separation, chemical identification, and structural determination. | Powerful for identifying novel active compounds without the need for lengthy isolation. |
| LC-NMR | Provides structural information on separated compounds. | Powerful for definitive structural elucidation. | Requires techniques like SPE to concentrate samples for sufficient sensitivity [76]. |
| High-Resolution Bioassay Profiling | Correlates biological activity (e.g., enzyme inhibition) with specific chromatographic peaks [76]. | Directly links chemical constituents to a biological effect in a complex mixture. | Critical for ensuring that seasonal/geographical changes do not diminish the desired bioactivity. |
Essential Experimental Protocols for Bioequivalence Research
To address natural source variability, researchers must adopt rigorous and sophisticated experimental protocols. The following are detailed methodologies cited in the literature for the chemical and biological assessment of natural products.
Protocol for High-Resolution Inhibition Profiling and HPLC-HRMS-SPE-NMR
This integrated protocol is designed to rapidly identify bioactive constituents from a complex natural extract while accounting for variability.
- Extract Preparation: Plant material is collected from different geographical locations and/or different seasonal time points. The dried, powdered material is defatted and extracted using an appropriate solvent (e.g., ethyl acetate) to obtain a crude extract [76].
- Microplate-Based High-Resolution Bioassay:
- Chromatographic Separation: A few hundred micrograms of the crude extract is separated using analytical-scale HPLC with a C18 column and a gradient elution (e.g., water-acetonitrile) [76].
- Fraction Collection: The eluate is collected into a 96-well microplate, generating dozens to hundreds of fractions that represent the separated chemical constituents of the extract.
- Bioassay Performance: Each fraction is tested for a specific biological activity (e.g., inhibition of hyaluronidase, α-glucosidase, or fungal plasma membrane H+-ATPase) [76].
- Profile Construction: The bioassay results are plotted against the retention time to generate a biochromatogram, which visually pinpoints the peaks responsible for the biological activity.
- Chemical Identification via HPLC-HRMS-SPE-NMR:
- Hyphenated Analysis: The crude extract is re-injected into an HPLC system coupled with a diode-array detector (DAD), a high-resolution mass spectrometer (HRMS), and a solid-phase extraction (SPE) unit. A small portion (e.g., 1%) of the flow is directed to the HRMS for accurate mass measurement, while the majority is diluted and trapped onto SPE cartridges [76].
- Sample Concentration: Multiple injections can be performed to concentrate sufficient material on the SPE cartridges.
- NMR Analysis: The trapped compounds are dried with nitrogen and subsequently eluted with a deuterated solvent directly into an NMR probe for structural determination [76].
Protocol for Phytochemical Characterization and Dereplication
This protocol is used for the initial chemical screening and quality control of natural products from variable sources.
- Sample Preparation: Extracts from different sources are prepared identically to ensure comparability.
- Ultra-High Performance Liquid Chromatography (UHPLC): The extracts are analyzed using UHPLC, which provides superior separation efficiency, speed, and resolution compared to conventional HPLC [76].
- High-Resolution Mass Spectrometry (HRMS): The UHPLC system is coupled to an HRMS instrument (e.g., Q-TOF or Orbitrap). This allows for the precise determination of the molecular mass and formula of the metabolites present in the extract, enabling the early identification of known compounds (dereplication) [76].
- Data Analysis: Chromatographic fingerprints and mass spectral data from different samples are compared using chemometric tools to identify significant chemical markers that correlate with geographical origin or harvest season.
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Reagents and Materials for Natural Product Variability Research
| Item | Function in Research | Application Note |
|---|---|---|
| C18 Reverse-Phase HPLC/UHPLC Columns | The workhorse for separating complex natural product extracts based on hydrophobicity. | Available in various particle sizes (<2µm for UHPLC) and dimensions to optimize resolution and speed [76]. |
| Deuterated NMR Solvents (e.g., Methanol-d4, Acetonitrile-d3) | Used for eluting compounds from SPE cartridges for NMR analysis without introducing interfering proton signals. | Critical for the HPLC-HRMS-SPE-NMR workflow to obtain high-quality spectra [76]. |
| Solid-Phase Extraction (SPE) Cartridges | To trap, concentrate, and clean up chromatographic peaks of interest from the HPLC eluent for subsequent NMR analysis. | A key component in hyphenated systems that bridge chromatography with NMR [76]. |
| Bioassay Reagents (e.g., Specific Enzymes, Substrates) | To test the biological activity of collected fractions in high-resolution profiling assays. | The choice is target-specific (e.g., hyaluronidase for necrosis inhibition studies) [76]. |
| Reference Standard Compounds | For method validation, calibration, and definitive identification of known compounds via co-chromatography and spectral matching. | Essential for ensuring the accuracy of quantitative and qualitative analyses across different sample batches. |
Visualizing the Research Workflow
The following diagram illustrates the integrated experimental workflow for identifying and characterizing bioactive natural products, from initial collection to final structural confirmation, while accounting for source variability.
The metabolic fate of a compound, whether a synthetic prodrug or a natural bioactive molecule, is a critical determinant of its therapeutic efficacy and safety. Understanding the differences in their activation and metabolic pathways is fundamental to drug design and the assessment of bioequivalence, particularly when comparing natural products with their synthetic analogs. This guide provides a detailed comparison of the metabolic handling of prodrugs and natural bioactive compounds, focusing on enzymatic activation, metabolic pathways, and the experimental approaches used to study them. This knowledge is essential for researchers and drug development professionals working to optimize lead compounds, develop targeted therapies, and establish therapeutic equivalence in the context of a growing interest in natural product-derived pharmaceuticals.
Fundamental Concepts: Prodrugs and Natural Bioactive Compounds
Prodrug Design and Activation
Prodrugs are defined as bioreversible, inactive derivatives of active drug molecules that undergo enzymatic or chemical transformation in vivo to release the pharmacologically active parent compound [77] [78] [79]. The primary objectives of prodrug design are to overcome limitations of the parent drug, such as poor solubility, inadequate permeability, rapid pre-systemic metabolism, lack of site-specificity, and toxicity [77] [78].
Activation Mechanisms: Prodrug activation occurs primarily through enzyme-mediated hydrolysis. Key enzymes involved include:
- Cytochrome P450 (CYP) isoforms: CYP2D6, CYP2C9, CYP2C19, CYP3A4 [79] [80].
- Hydrolases: Carboxylesterases, phosphatases, human valacyclovirase [77] [79].
- Transferases and Lyases [77].
The strategic design of prodrugs can be categorized into traditional and modern approaches. Traditional prodrugs aim to improve physicochemical properties like solubility and permeability, while modern prodrugs incorporate cellular and molecular parameters to enable targeted drug delivery [77].
Natural Bioactive Compounds and Metabolism
Natural Bioactive Compounds (NBCs) are secondary plant metabolites or synthetic equivalents recognized for their roles in health promotion, disease prevention, and therapeutic benefits [46]. Unlike prodrugs, NBCs are inherently bioactive, though they may be metabolized to compounds with altered activity profiles.
Key NBC Classes:
- Polyphenols and Flavonoids: Found in green tea, berries, and citrus; known for antioxidant, anti-inflammatory effects [46] [81].
- Alkaloids: Such as berberine, which improves triglyceride levels, fasting glucose, and blood pressure [81].
- Carotenoids: Present in carrots and tomatoes; protect against UV-induced skin damage and strengthen the intestinal barrier [46] [81].
Metabolic Handling: Xenobiotic metabolism of NBCs typically occurs in two phases. Phase I (e.g., oxidation, hydroxylation) introduces or unveils a functional group, while Phase II (e.g., glucuronidation, sulfation) involves conjugation to form more water-soluble, excretable metabolites [82]. The gut microbiome also plays a significant metabolic role for orally administered NBCs, producing metabolites with different bioactivities and toxicities [82].
Comparative Analysis of Activation and Metabolic Pathways
The following section provides a structured, data-driven comparison of the metabolic pathways for prodrugs and natural bioactive compounds.
Key Metabolic Enzymes and Their Roles
Table 1: Key Enzymes in Prodrug and Natural Bioactive Compound Metabolism
| Enzyme | Primary Role/Location | Impact on Prodrugs | Impact on Natural Bioactives |
|---|---|---|---|
| Cytochrome P450 (CYP) 2D6 | Liver; oxidative metabolism | Activates prodrugs (e.g., codeine to morphine, tamoxifen to endoxifen) [79] [80] | Involved in Phase I metabolism; genetic polymorphisms affect metabolite profiles [80] |
| Carboxylesterases | Liver, serum, tissues | Hydrolyzes ester-based promoieties (e.g., in POM prodrugs) [77] [83] | Can hydrolyze ester-containing natural compounds [82] |
| UDP-Glucuronosyltransferase (UGT) | Liver; Phase II conjugation | Can inactivate released parent drug [80] | Major enzyme for Phase II conjugation (e.g., glucuronidation of flavonoids) [82] |
| Microbial Esterases (e.g., GloB, FrmB) | Specific microbial species (e.g., S. aureus) [83] | Enable targeted antimicrobial prodrug activation [83] | Mediated by gut microbiome, altering bioavailability and activity [46] [82] |
Quantitative Comparison of Metabolic Parameters
Table 2: Quantitative Comparison of Metabolic Parameters
| Parameter | Prodrugs | Natural Bioactive Compounds |
|---|---|---|
| Representative Bioavailability Increase | Valacyclovir: 3-5 fold vs. acyclovir [77] | Berberine: Systematic review shows significant improvement in metabolic syndrome markers [81] |
| Impact of Genetic Polymorphism | CYP2D6 UM: ~16x higher morphine from codeine vs. PM [80] | Individual variation in metabolism and response, but less quantitatively defined for specific NBCs |
| Structural Influence on Permeability | ~35% of prodrug design goals target permeability enhancement [78] | Governed by rules like Lipinski's Rule of Five; NPs are typically larger and more complex [3] |
| Regulatory Status | ~13% of FDA-approved new molecular entities (2012-2022) [78] | Considered dietary supplements; evidence-based approach growing for disease management [46] |
Experimental Models for Metabolic Studies
Table 3: Models for Studying Metabolism
| Model System | Application in Prodrug Research | Application in Natural Bioactive Research |
|---|---|---|
| In Silico Methods | Predicting permeability via logP, molecular dynamics, machine learning [78] | Cheminformatic analysis of structural evolution and properties [3] |
| In Vitro Cell Cultures | Caco-2 cells for permeability (Papp) [78] | Cell line research on antioxidative, anticancer effects [46] |
| Human Liver Models | Studying enzymatic activation (CYP450, esterases) [82] | Studying Phase I and II metabolism [82] |
| Microbial Models (e.g., Cunninghamella fungi) | Limited application | Mimics mammalian Phase I/II metabolism; produces mammalian-equivalent metabolites for study [82] |
| Animal Models | In vivo efficacy and toxicity studies [83] | Studying physiological impacts (e.g., fortified foods in obese mice) [46] [81] |
| Randomized Controlled Trials (RCTs) | Clinical trials for FDA approval [77] | Used to establish efficacy in humans (e.g., berberine for metabolic syndrome) [81] |
Essential Research Reagent Solutions
Table 4: Key Reagents and Tools for Metabolic Pathway Research
| Research Reagent / Tool | Function in Metabolic Studies |
|---|---|
| Recombinant CYP Enzymes | Isolated study of specific cytochrome P450-mediated metabolic pathways for both prodrug activation and NBC metabolism [82]. |
| Cunninghamella spp. Cell Cultures | Microbial model to simulate mammalian metabolism of xenobiotics, particularly useful for predicting metabolites of natural and synthetic compounds [82]. |
| Caco-2 Cell Line | An in vitro model of the human intestinal epithelium used to assess passive permeability and transporter-mediated uptake of prodrugs and NBCs [78]. |
| Specific Enzyme Inhibitors | Chemical inhibitors (e.g., for esterases or specific CYP isoforms) used to delineate the contribution of specific enzymes to a compound's metabolic pathway [83]. |
| Human Liver Microsomes/S9 Fractions | Contain a full complement of human Phase I and II metabolizing enzymes, used for high-throughput metabolic stability and metabolite profiling studies [82]. |
| Metabolomics Services | Comprehensive analysis (untargeted/targeted) to identify and quantify metabolites, crucial for understanding the metabolic fate of both prodrugs and NBCs [79]. |
Metabolic Pathway and Experimental Workflow Visualization
Comparative Metabolic Pathways
Diagram 1: A comparison of the general metabolic pathways for synthetic prodrugs and natural bioactive compounds, highlighting key activation and deactivation steps.
Experimental Workflow for Metabolic Studies
Diagram 2: A generalized experimental workflow for characterizing the metabolic pathways of prodrugs and natural bioactive compounds, from initial screening to clinical validation.
The metabolic pathways of prodrugs and natural bioactive compounds, while distinct in their primary objectives, share common ground in their reliance on enzymatic systems for activation and elimination. Prodrugs are a deliberate engineering feat, designed to be activated in a controlled manner to overcome pharmaceutical and pharmacokinetic hurdles. In contrast, natural bioactive compounds are metabolized as xenobiotics, with their complex structures often leading to multiple metabolites with potential bioactivities. For researchers establishing bioequivalence between synthetic and natural bioactive compounds, this comparison underscores that identity in parent compound structure does not guarantee equivalence in metabolic fate or biological outcome. The choice of experimental models—from in silico predictions and in vitro systems to specialized microbial models and clinical trials—is critical for building a complete picture of a compound's metabolic profile. Understanding these parallel yet intersecting metabolic landscapes is fundamental to advancing rational drug design and accurately evaluating the therapeutic potential of both synthetic and natural products.
In pharmaceutical sciences, excipients and delivery systems are far from inert; they are foundational to transforming active pharmaceutical ingredients (APIs) into safe, stable, and efficacious medicines. This is particularly critical within bioequivalence research on synthetic versus natural bioactive compounds, where differences in formulation can significantly influence dissolution, absorption, and ultimately, therapeutic outcome. Excipients, defined as any substance other than the API intentionally included in a drug delivery system, fulfill vital roles as carriers, stabilizers, and enhancers of specific formulation characteristics [84] [85]. The complexity of modern drug development, driven by an increasing number of challenging, poorly soluble compounds, demands continuous innovation in these non-active components [86] [85]. This guide objectively compares the performance of various excipients and delivery systems, providing experimental data and methodologies central to advancing bioequivalence studies for natural and synthetic bioactives.
Excipient Limitations and Functional Challenges
Despite their utility, excipients present several inherent limitations that pose significant challenges in drug development and can profoundly impact bioequivalence studies.
- Compatibility and Stability Issues: Excipients can chemically or physically interact with APIs, leading to reduced potency, harmful byproducts, or phase separation. Thorough pre-formulation studies are essential to identify these risks early [87].
- Allergenicity and Toxicity Risks: Commonly considered inert, excipients like lactose, gluten, or specific preservatives can trigger adverse reactions in sensitive individuals. Prolonged use or high doses of others, such as polyethylene glycol, have been linked to toxicity [87].
- Patient-Specific and Regulatory Limitations: Excipients may not be suitable for all patient groups. Children and the elderly are more susceptible to adverse effects or may struggle with certain dosage forms. Furthermore, the lack of a rigorous, independent regulatory approval process for new excipients and global disparities in standards lead to inconsistencies in quality and safety, complicating international drug development [87] [85].
Table 1: Key Challenges in Excipient Use and Development
| Challenge Category | Specific Limitations | Impact on Formulation |
|---|---|---|
| Physicochemical | API-Excipient Incompatibility, Batch-to-Batch Variability | Compromised stability, reduced bioavailability, altered release kinetics [87]. |
| Biological & Safety | Allergenicity, Patient Population Suitability | Risk of adverse reactions, limitations in pediatric/geriatric formulations [87]. |
| Regulatory & Supply | Lack of Independent Approval, Global Disparities, Supply Chain Vulnerabilities | Increased development cost, delays, quality inconsistencies, drug shortages [87] [85]. |
| Performance in Advanced Systems | Incomplete Drug Release, Inability to Meet Precise Requirements | Failure to achieve controlled or targeted release, limiting therapeutic efficacy [87]. |
Advanced Drug Delivery Systems and Excipient Performance
Drug delivery systems (DDS) are technological formulations designed to transport APIs to specific target sites, maximizing therapeutic efficacy and minimizing off-target accumulation [88]. The evolution from simple pills to sophisticated controlled-release (CR) and nanoscale systems has been driven by the need to overcome physicochemical and biological barriers.
The Evolution of Drug Delivery
The journey began with simple coating technologies to mask taste, evolving in the mid-20th century with the introduction of Spansule technology, which used wax-coated beads to create sustained-release profiles [88]. The 1960s and 70s marked the birth of nanotechnology, with the discovery of liposomes and the development of the first drug-loaded nanoparticles [88]. Current, third-generation DDS focus on overcoming both physicochemical (e.g., poor solubility) and biological (e.g., systemic distribution) barriers to achieve targeted and controlled release [88].
The Critical Role of Excipients in Controlled Release
Controlled-release formulations, such as extended-release tablets, rely heavily on functional polymeric excipients to modulate API release. A prime example is hydroxypropyl methylcellulose (HPMC or hypromellose), used in hydrophilic matrix tablets. The CR mechanism involves critical steps: upon fluid contact, HPMC particles hydrate, swell, and coalesce to form a contiguous hydrogel layer around the tablet. This gel layer controls API release through a combination of diffusion and erosion [89].
Advanced excipient knowledge has shown that performance is not solely dependent on gel strength but on attributes like Powder Dissolution Temperature (PDT). HPMC grades with higher PDTs (e.g., K4M, above 50°C) hydrate more readily at physiological temperatures, forming a robust hydrogel and effectively modulating release, unlike methylcellulose which has a lower PDT and poorer performance [89]. Furthermore, HPMC particle size and viscosity grade are crucial. Smaller particles (45-125 μm) form a less porous hydrogel, slowing release, while higher viscosity grades slow hydrogel erosion, prolonging CR duration, especially for poorly soluble APIs [89].
Diagram Title: HPMC Controlled Release Mechanism
Comparative Performance Data: Excipients and Delivery Systems
Objective comparison of excipient performance is vital for rational formulation design. The following data summarizes key experimental findings from the literature.
Table 2: Performance Comparison of Selected Excipients and Delivery Systems
| Excipient / Delivery System | Functional Role | Key Performance Data | Experimental Context |
|---|---|---|---|
| HPMC (K4M, K100M) | Hydrophilic matrix former for CR [89]. | Smaller particles (45-125 μm) reduce API release rate vs. larger (125-355 μm). Higher viscosity grades prolong CR duration [89]. | Matrix tablets; API release studied via dissolution testing under USP conditions [89]. |
| Poly(NIPAm-co-DMA) | Novel polymeric excipient for solubility enhancement [86]. | 21x increase in mean AUC vs. crystalline drug. 3x higher oral bioavailability in rats vs. HPMCAS [86]. | Spray-dried solid dispersions of phenytoin; in vitro dissolution & in vivo PK study in rats [86]. |
| Co-processed Excipients | Multifunctional blends (e.g., filler-binder-disintegrant) [85]. | Simplify formulation to API + co-processed excipient + lubricant. Improve manufacturing efficiency [85]. | Direct compression trials; evaluation of tablet weight variability and dissolution profile [85]. |
| Red Blood Cell Camouflaged NPs | Nanoscale system for targeted delivery [88]. | Improved in vivo stability, reduced immunogenicity, enhanced targeting (preclinical data) [88]. | In vivo animal models; measurement of circulation half-life and target site accumulation [88]. |
Detailed Experimental Protocols for Formulation Research
To ensure reproducibility and validate performance claims, detailed methodologies are essential. The following protocols are adapted from key studies.
High-Throughput Polymer Screening for Solubility Enhancement
This protocol is designed to identify polymeric excipients that maintain drug supersaturation, a key strategy for enhancing oral bioavailability of poorly soluble compounds [86].
- Primary Materials: Drug candidate (e.g., Phenytoin), polymer library (e.g., synthesized via RAFT polymerization), phosphate-buffered saline (PBS), methanol, 96-well plates.
- Equipment: Automated liquid handler (e.g., Freedom EVO 200, Tecan), microplate reader, incubator maintained at 37°C.
- Procedure:
- Polymer Solution Preparation: Dissolve polymer candidates in PBS to a known concentration and dispense into a 96-well plate (0.912 mL/well).
- Solvent-Shift Supersaturation: Using the liquid handler, introduce a concentrated solution of the drug in methanol (2% v/v final volume) to each well containing pre-dissolved polymer and PBS.
- Incubation and Monitoring: Seal the plate and incubate at 37°C with continuous agitation. Monitor the drug concentration in the supernatant in triplicate wells over time (e.g., 180 minutes) using a microplate reader.
- Data Analysis: Calculate the area-under-the-dissolution-curve (AUC) for each polymer composition. Compare against a control (drug without polymer) and known benchmarks (e.g., HPMCAS) to identify leading candidates.
This non-sink (Sink Index ~0.09) precipitation inhibition assay rapidly identifies excipients capable of suppressing drug recrystallization, guiding the development of amorphous solid dispersions [86].
In Vitro Dissolution Testing of Controlled-Release Matrix Tablets
This protocol evaluates the release profile of APIs from hydrophilic matrix tablets, a standard for CR formulation development [89].
- Primary Materials: Manufactured matrix tablets (e.g., using HPMC as CR polymer), dissolution medium (e.g., 0.1 N HCl or pH 6.8 phosphate buffer), standard calibration solutions.
- Equipment: USP-compliant dissolution apparatus (paddle or basket), automated sampler, HPLC or UV-Vis spectrophotometer.
- Procedure:
- Apparatus Setup: Fill the dissolution vessel with a defined volume of medium, equilibrate to 37.0 ± 0.5 °C.
- Tablet Introduction: Place a single tablet in the vessel (or in a basket) and start the apparatus at a specified rotation speed (e.g., 50 rpm for paddles). This marks time zero.
- Sampling: Withdraw aliquots from a predetermined zone in the vessel at fixed time intervals (e.g., 1, 2, 4, 6, 8, 12, 18, 24 hours). Filter samples immediately to remove any suspended particles.
- Drug Quantification: Analyze the drug concentration in each sample using a validated analytical method (e.g., HPLC-UV). Compare against a standard curve.
- Release Kinetics Modeling: Plot the cumulative drug release (%) versus time. Fit the data to various mathematical models (e.g., zero-order, first-order, Higuchi) to understand the release mechanism.
This methodology directly assesses the impact of excipient properties (e.g., HPMC grade, particle size) on CR performance, a critical factor for ensuring bioequivalence.
The Scientist's Toolkit: Key Research Reagent Solutions
Successful formulation research relies on a suite of specialized reagents and materials. The following table details essential tools for investigating excipients and delivery systems.
Table 3: Essential Research Reagents and Materials for Formulation Science
| Reagent / Material | Core Function | Application Example |
|---|---|---|
| Hypromellose (HPMC) | Hydrophilic polymer for forming gel-based controlled-release matrix tablets [89]. | Investigating the effect of viscosity grade and particle size on API release kinetics in oral solid dosages [89]. |
| Hydroxypropyl Beta-Cyclodextrin (HPβCD) | Solubilizing agent that forms inclusion complexes with poorly soluble drugs [85]. | Enhancing the aqueous solubility and stability of synthetic or natural bioactive compounds in solution-based formulations [46]. |
| HPMC Acetate Succinate (HPMCAS) | Enteric polymer and precipitation inhibitor for solid dispersions [86]. | Enabling oral delivery of amorphous drugs by maintaining supersaturation in the gastrointestinal tract [86]. |
| Lipids (e.g., Phospholipids) | Structural components of nanocarriers like liposomes and solid lipid nanoparticles (SLNs) [88] [85]. | Developing targeted or parenteral delivery systems for chemotherapeutic agents or biopharmaceuticals [88]. |
| Co-processed Excipients | High-functionality blends designed to streamline manufacturing (e.g., direct compression) [85]. | Simplifying tablet formulation and improving production efficiency while maintaining consistent drug release profiles [85]. |
| RAFT Chain Transfer Agent | Mediates controlled radical polymerization for synthesizing well-defined polymeric excipients [86]. | High-throughput synthesis of custom polymer libraries with precise architectures for structure-property relationship studies [86]. |
The landscape of pharmaceutical formulation is intrinsically linked to the strategic deployment and continuous innovation of excipients and delivery systems. For researchers focused on the bioequivalence of synthetic and natural bioactive compounds, a deep understanding of these components is non-negotiable. The quantitative data, experimental protocols, and toolkit presented herein provide a foundation for objective comparison and rational formulation design. Overcoming challenges related to solubility, stability, and targeted release hinges on leveraging advanced excipient knowledge, from the nuanced chemistry of HPMC to the targeted potential of nanocarriers. Future progress will depend on collaborative efforts to streamline regulatory pathways and foster the development of novel, purpose-built excipients that can keep pace with the demands of modern API pipelines.
Highly Variable Drugs and Scaled Average Bioequivalence Criteria
Bioequivalence (BE) studies are fundamental to pharmaceutical development and regulation, performed to demonstrate in vivo that two pharmaceutically equivalent products are comparable in their rate and extent of absorption [90]. For systemically administered drugs, bioequivalence is primarily assessed using two key pharmacokinetic (PK) parameters: the maximum plasma concentration (Cmax), which reflects the rate of absorption, and the area under the plasma concentration-time curve (AUC), representing the extent of absorption [65]. The standard statistical approach, known as Average Bioequivalence (ABE), requires that the 90% confidence intervals for the geometric mean ratio (test product/reference product) for both Cmax and AUC fall entirely within the predefined acceptance range of 80% to 125% [65] [91].
A significant challenge arises with Highly Variable Drugs (HVDs), defined as drugs for which the within-subject variability (also called intra-subject variability) in Cmax and/or AUC is 30% or greater [90] [92] [91]. This high variability is often attributable to drug disposition characteristics such as extensive presystemic metabolism, low and variable oral bioavailability, or high lipophilicity [92] [91]. A survey of bioequivalence studies submitted to the U.S. Food and Drug Administration (FDA) from 2003 to 2005 found that approximately 20-31% of the drugs evaluated were highly variable, with about 60% of these due to drug substance pharmacokinetic characteristics [92].
For HVDs, the conventional ABE approach becomes problematic. High within-subject variability widens the 90% confidence interval, making it difficult to fall within the strict 80-125% limits without enrolling very large numbers of study subjects [65] [91]. Table 1 illustrates how sample size requirements escalate dramatically with increasing variability.
Table 1: Sample Size Requirements for Bioequivalence Studies (80% Power)
| Within-Subject %CV | GMR (%) | Sample Size for a Two-Way Crossover Study | Sample Size for a Four-Way Fully Replicated Crossover |
|---|---|---|---|
| 15 | 100 | 10 | 6 |
| 30 | 100 | 32 | 18 |
| 45 | 100 | 66 | 34 |
| 60 | 100 | 108 | 56 |
| 75 | 100 | 156 | 80 |
Data adapted from [91]. %CV: Coefficient of Variation; GMR: Geometric Mean Ratio.
This need for large sample sizes exposes more healthy volunteers to clinical trials, increases costs, and can deter the development of generic versions of HVDs, ultimately limiting patient access to affordable medications [91]. Furthermore, it has been observed that some HVDs fail to demonstrate bioequivalence even to themselves in a standard crossover study, questioning the appropriateness of "one-size-fits-all" BE limits for such products [91].
Scaled Average Bioequivalence: A Regulatory Solution
The Rationale and Evolution of RSABE
To address the challenges posed by HVDs, regulatory agencies have developed an alternative statistical method: Reference-Scaled Average Bioequivalence (RSABE). This approach was championed by the FDA's Office of Generic Drugs following recommendations from its advisory committee, which called for a "paradigm shift" for HVDs and suggested exploring reference scaling [91].
The fundamental principle of RSABE is to scale the bioequivalence acceptance limits based on the within-subject variability of the reference product. In essence, the permitted acceptance range widens as the variability of the reference product increases. This acknowledges that for a drug known to be highly variable, wider differences in PK measures between the test and reference products can be tolerated, as the reference product itself exhibits considerable variability from one administration to another in the same individual [65] [91]. This scaling reflects the inherent pharmacokinetic variability of the drug substance rather than penalizing it.
Key Regulatory Methodologies and Requirements
The implementation of RSABE, while similar in principle, varies between major regulatory agencies like the FDA and the European Medicines Agency (EMA). A critical requirement for both is the use of a replicated crossover study design, where each subject receives the reference product at least twice. This design is essential for obtaining a reliable estimate of the within-subject standard deviation of the reference product (sWR) [65]. Common designs include three-period (e.g., RRT, RTR, TRR) and four-period (e.g., RTRT, TRTR) studies.
Table 2: Comparison of FDA and EMA RSABE Criteria
| Parameter | Agency | sWR < 0.294 | sWR ≥ 0.294 |
|---|---|---|---|
| AUC | FDA | Standard ABE (CI 80-125%) | RSABE permitted; CI can be widened; Point estimate within 80-125% |
| EMA | Standard ABE (CI 80-125%) | Standard ABE (CI 80-125%) only | |
| Cmax | FDA | Standard ABE (CI 80-125%) | RSABE permitted; CI can be widened; Point estimate within 80-125% |
| EMA | Standard ABE (CI 80-125%) | RSABE permitted; CI can be widened up to 70-143%; Point estimate within 80-125% |
Data synthesized from [65]. sWR: within-subject standard deviation of the reference product. A CV of 30% corresponds to an sWR of 0.294.
The "scaling" in RSABE is derived from its statistical equations. While ABE uses fixed limits, RSABE scales the acceptance range. The FDA and EMA use different regulatory constants in their scaling formulae, leading to different widened limits at various variability levels, as shown in Table 3 [65].
Table 3: RSABE Acceptance Limits at Different Variability Levels
| Within-Subject CV (%) | sWR | EMA RSABE Limits | FDA RSABE Limits |
|---|---|---|---|
| < 30 | — | ABE method (80-125%) | ABE method (80-125%) |
| 30 | 0.294 | 80.00 – 125.00 | 76.94 – 129.97 |
| 40 | 0.385 | 74.62 – 134.02 | 70.89 – 141.06 |
| 50 | 0.472 | 69.84 – 143.19 | 65.58 – 152.48 |
Data adapted from [65]. Note: EMA applies a maximum widening to 69.84-143.19%.
Experimental Protocols for Implementing RSABE
Study Design and Population
A typical RSABE study for a highly variable drug is a single-dose, randomized, open-label, replicated crossover design conducted in a suitable population, most often healthy adult subjects [93]. For example, a study on agomelatine followed a randomized-sequence, four-way crossover design with a one-day washout period between doses [93]. Subjects are randomly assigned to a sequence of treatments, with each subject receiving the test product at least once and the reference product at least twice.
Key Pharmacokinetic Procedures
- Dosing and Sampling: After an overnight fast, subjects receive a single dose of either the test or reference formulation with water. Blood samples are collected at predetermined time points pre-dose and post-dose (e.g., at 0.25, 0.5, 1, 1.5, 2, 2.5, 3, 4, 6, 8, 12, and 24 hours) to adequately characterize the concentration-time profile [93].
- Bioanalytical Analysis: Plasma samples are separated via centrifugation and analyzed using a validated bioanalytical method, typically liquid chromatography coupled with tandem mass spectrometry (LC-MS/MS), to determine the concentration of the active drug and its metabolites [93].
- Pharmacokinetic Analysis: Non-compartmental methods using software like Phoenix WinNonlin are standard for calculating PK parameters. The primary parameters are:
- Cmax: The observed maximum plasma concentration.
- AUC0-t: The area under the plasma concentration-time curve from time zero to the last measurable time point, calculated by the linear trapezoidal rule.
- AUC0-∞: The area under the curve from time zero to infinity, calculated as AUC0-t + Ct/λz, where Ct is the last measurable concentration and λz is the elimination rate constant [93].
Statistical Analysis for RSABE
The statistical evaluation involves several steps and can be performed using specialized software or validated scripts in Phoenix WinNonlin [65]:
- Determine Eligibility for RSABE: Calculate the within-subject standard deviation (sWR) for the reference product for AUC and/or Cmax from the replicated study data. If sWR ≥ 0.294 (CV ≥ 30%), RSABE may be applied for that parameter.
- Apply the Scaled Criterion: For the FDA, bioequivalence is concluded if the following linearized criterion is met:
- Apply the Point Estimate Constraint: Regardless of scaling, the geometric mean ratio (GMR) for the test and reference products must fall within the conventional 80-125% range [65] [93].
Figure 1: Decision Flowchart for Reference-Scaled Average Bioequivalence (RSABE)
The Scientist's Toolkit: Essential Reagents and Software
Table 4: Key Research Reagent Solutions for Bioequivalence Studies
| Item | Function in BE Studies |
|---|---|
| Validated Reference Standard | The innovator's product (RLD) serves as the benchmark for comparing the test (generic) product. Its quality and handling are critical. |
| LC-MS/MS System | High-performance liquid chromatography coupled with tandem mass spectrometry is the gold standard for sensitive and specific quantification of drug and metabolite concentrations in biological matrices like plasma. |
| Stable Isotope-Labeled Internal Standards | Used in LC-MS/MS analysis to correct for sample preparation losses and matrix effects, ensuring analytical accuracy and precision. |
| Phoenix WinNonlin | Industry-standard software for pharmacokinetic and statistical analysis of bioequivalence data, including support for RSABE evaluation. |
| Clinical Trial Supplies | Includes drugs, placebos, and materials for sample collection (e.g., vacutainers, centrifuges, freezers) compliant with Good Clinical Practice (GCP). |
Bioequivalence in the Context of Synthetic vs. Natural Bioactive Compounds
The principles of bioequivalence and the challenges of high variability are highly relevant to the ongoing research on synthetic and natural bioactive compounds. While not all natural products are administered as oral dosage forms, for those that are (e.g., nutraceuticals, phytopharmaceuticals), demonstrating consistent pharmacokinetics is vital for ensuring their reliability and therapeutic effect [46].
Natural products often possess distinct molecular architectures compared to purely synthetic drugs. Cheminformatic analyses reveal that natural products and their derivatives typically exhibit greater three-dimensional complexity, higher stereochemical content (more chiral centers), lower hydrophobicity, and fewer aromatic rings [37] [38]. This complexity can influence their absorption, distribution, metabolism, and excretion (ADME) properties. For instance, some natural products violate Lipinski's Rule of Five yet are still orally bioavailable, potentially because their structures resemble biosynthetic intermediates or endogenous metabolites, allowing them to utilize active transport mechanisms [38].
These inherent characteristics can be a source of high variability. Factors such as extensive presystemic metabolism are a common cause of high variability for both synthetic and natural compounds [92]. Furthermore, the complex matrix of a natural product extract could lead to variable drug release and absorption, contributing to formulation-related variability [92]. Therefore, the RSABE approach is not only a solution for synthetic HVDs but also a potentially critical tool for the robust evaluation and development of reliable natural product-derived therapeutics, ensuring that patients receive consistent and predictable performance from these complex molecules.
Emerging Approaches and Future Directions
The field of bioequivalence for highly variable drugs continues to evolve. Beyond RSABE, researchers are exploring the application of advanced computational methods. One promising area is the use of Generative Artificial Intelligence (AI), specifically Variational Autoencoders (VAEs), to address the sample size problem [94].
VAEs are a type of neural network that can learn the underlying distribution of a dataset and generate new, synthetic data that mimics the original. In the context of BE studies, VAEs can be trained on a small, experimentally collected dataset and then used to "virtually" increase the sample size by generating additional, realistic PK profiles [94]. Simulation studies suggest that this AI-augmented approach, used with constant 80-125% limits, can achieve high statistical power even with less than half of the typically required human subjects, offering a potential pathway to reduce human exposure in clinical trials without compromising scientific rigor [94].
Protein glycosylation is one of the most ubiquitous and intricate forms of post-translational modification (PTM) in eukaryotic cells, profoundly influencing protein folding, stability, and function [95] [96]. This enzymatic process involves the covalent attachment of complex carbohydrate chains, known as glycans, to specific amino acid residues on proteins, creating a diverse repertoire of glycoproteins [95]. The process occurs primarily within the endoplasmic reticulum (ER) and Golgi apparatus, where a coordinated series of enzymatic reactions adds and trims sugar residues to produce mature glycoproteins [95] [96].
Glycosylation represents a critical interface in the bioequivalence discussion between synthetic and natural bioactive compounds. As a template-free process directed by complex enzyme machinery, it creates inherent structural heterogeneity that poses significant challenges for replicating in synthetic systems [95] [97]. Understanding these patterns and variants is essential for researchers and drug development professionals working with biologic therapeutics, as glycosylation can dramatically influence the pharmacokinetic properties, immunogenicity, and biological activity of protein-based drugs [97].
Major Types of Glycosylation and Their Structural Features
Protein glycosylation occurs in several major forms, each with distinct structural characteristics, biosynthetic pathways, and biological implications. The two most prevalent types are N-linked and O-linked glycosylation, while C-mannosylation and GPI-anchored proteins represent less common variants [96].
Table 1: Comparison of Major Glycosylation Types
| Glycosylation Type | Amino Acid Attachment Site | Initial Synthesis Location | Structural Features | Key Functions |
|---|---|---|---|---|
| N-glycosylation | Asparagine (Asn) within Asn-X-Ser/Thr consensus sequence (X ≠ Proline) [95] [96] | Endoplasmic Reticulum [95] | Common core structure (Asn-GlcNAc₂Man₃); classified into high mannose, complex, and hybrid subtypes [96] | Protein folding, quality control, intracellular trafficking, immune recognition [95] |
| O-glycosylation | Serine (Ser) or Threonine (Thr) [96] | Golgi apparatus [95] | No consensus sequence; mucin-type (O-GalNAc) and O-GlcNAc are most common [95] [96] | Cell-cell interaction, cell-matrix interactions, signaling regulation [96] |
| C-mannosylation | Tryptophan (Trp) within Trp-X-X-Trp motif [95] [96] | Endoplasmic Reticulum [95] | Attachment of α-mannopyranose via carbon-carbon bonds [95] | Less studied; implicated in protein secretion and stability [95] |
| GPI-anchored attachment | C-terminus of protein [96] | Endoplasmic Reticulum [96] | Glycan core links protein to phosphatidylinositol membrane anchor [96] | Membrane anchoring, protein localization, signal transduction [96] |
The following diagram illustrates the cellular localization and key stages of the major glycosylation pathways:
Experimental Approaches for Glycosylation Analysis
Methodologies for Structural Characterization
Advancements in analytical technologies have significantly enhanced our ability to characterize glycosylation patterns and structural variants. The following experimental protocols represent key approaches in the field:
Mass Spectrometry-Based Glycomics Protocol:
- Glycan Release: Release N-glycans using peptide-N-glycosidase F (PNGase F) or O-glycans via chemical methods (e.g., β-elimination) [4]
- Purification: Clean up released glycans using solid-phase extraction (graphitized carbon cartridges) or hydrophilic interaction liquid chromatography (HILIC) [4]
- Derivatization: Label glycans with fluorescent tags (e.g., 2-aminobenzamide) for detection or permethylate for enhanced mass spectrometry sensitivity [4]
- LC-MS/MS Analysis: Separate glycans using ultra-high performance liquid chromatography (UHPLC) coupled to high-resolution mass spectrometry [4]
- Data Interpretation: Use software tools (e.g., GlycoWorkbench) to interpret fragmentation spectra and determine glycan structures [4]
Glycoprotein-Specific Staining and Detection:
- Electrophoresis Separation: Separate glycoproteins using SDS-PAGE or 2D-gel electrophoresis [98]
- Membrane Transfer: Transfer proteins to PVDF or nitrocellulose membranes [98]
- Probe Incubation: Incubate with lectins (e.g., ConA for mannose, SNA for sialic acid) or glycan-specific antibodies [98]
- Signal Detection: Detect bound probes using chemiluminescence, fluorescence, or colorimetric substrates [98]
Metabolic Labeling Approach:
- Precursor Administration: Treat cells with modified sugar precursors (e.g., azido-labeled N-acetylmannosamine) [99]
- Incorporation Period: Allow 24-72 hours for metabolic incorporation into glycoproteins [99]
- Click Chemistry: Use copper-catalyzed azide-alkyne cycloaddition to attach detection tags [99]
- Visualization/Analysis: Detect labeled glycoproteins using fluorescence microscopy, flow cytometry, or mass spectrometry [99]
Research Reagent Solutions for Glycosylation Studies
Table 2: Essential Research Reagents for Glycosylation Analysis
| Reagent Category | Specific Examples | Research Application | Mechanism of Action |
|---|---|---|---|
| Glycosylation Inhibitors | Tunicamycin, 6-diazo-5-oxo-l-norleucine, Brefeldin A [99] | Studying N-glycosylation dependence, ER stress induction, disrupting Golgi trafficking [99] | Tunicamycin blocks GlcNAc phosphotransferase; Brefeldin A causes Golgi disintegration [99] |
| Glycosidase Inhibitors | Plant alkaloids (e.g., castanospermine, swainsonine), deoxynojirimycin [99] | Processing glycosidase inhibition, creating immature glycoforms, studying quality control [99] | Castanospermine inhibits α-glucosidase I; Swainsonine inhibits α-mannosidase II [99] |
| Metabolic Precursors | Modified mannosamine analogs, peracetylated N-azidoacetylgalactosamine [99] | Metabolic oligosaccharide engineering, chemoselective labeling, glycan imaging [99] | Incorporated into sialic acid residues enabling bioorthogonal chemistry [99] |
| Lectin Probes | Concanavalin A (ConA), Wheat Germ Agglutinin (WGA), Sambucus Nigra Lectin (SNA) [98] | Glycan profiling, histochemistry, flow cytometry, glycoprotein purification [98] | ConA binds mannose/glucose; WGA binds GlcNAc/sialic acid; SNA prefers α-2,6 sialic acid [98] |
| Enzymatic Tools | PNGase F, Endo H, O-Glycosidase, Sialidases [98] | Glycan release, structural analysis, glycosidase susceptibility testing [98] | PNGase F releases N-glycans; Endo H cleaves high mannose/hybrid N-glycans [98] |
Glycosylation in Therapeutic Protein Bioequivalence
Impact on Pharmacokinetics and Pharmacodynamics
The glycosylation status of therapeutic proteins significantly influences their bioequivalence profiles through multiple mechanisms. The following diagram illustrates how glycosylation affects the therapeutic efficacy of protein drugs:
For bioequivalence assessment between natural and synthetic compounds, several glycosylation-related parameters require careful evaluation:
Molecular Stability Enhancements:
- Structural Stability: Glycosylation stabilizes protein conformation through steric effects and hydrogen bonding, reducing aggregation propensity [97]
- Proteolytic Resistance: Glycans shield protease-sensitive sites, extending plasma half-life by reducing non-specific degradation [97]
- Colloidal Stability: Surface glycans improve solubility and reduce surface adsorption and precipitation [97]
Pharmacokinetic Modulations:
- Renal Clearance: Glycans increase hydrodynamic radius and molecular weight above the renal filtration threshold (~50 kDa) [97]
- Charge Effects: Negatively charged sialic acid residues retard filtration through charged glomerular basement membranes [97]
- Receptor-Mediated Clearance: Specific glycan patterns (e.g., terminal galactose) trigger asialoglycoprotein receptor-mediated hepatic clearance [97]
Comparative Analysis of Glycosylation in Production Systems
The bioequivalence of therapeutic glycoproteins is heavily influenced by the production system, as different expression hosts create distinct glycosylation patterns:
Table 3: Glycosylation Patterns Across Protein Production Systems
| Production System | N-glycan Profiles | O-glycan Profiles | Sialylation Patterns | Therapeutic Examples |
|---|---|---|---|---|
| Mammalian (CHO, HEK293) | Complex-type biantennary structures, core fucosylation, minimal α-Gal epitopes [97] | Core 1 and Core 2 O-glycans, sialylated mucin-type structures [97] | Moderate to high sialylation (N-glycolylneuraminic acid in some systems) [97] | Agalsidase beta (CHO), Alglucosidase alfa (CHO) [97] |
| Yeast Systems | High-mannose structures (Man₉-Man₁₃), hypermannosylation, phosphorylated mannoses [97] | Generally absent or significantly different from mammalian patterns | Absent or non-mammalian type sialylation | Limited therapeutic application due to immunogenicity |
| Insect Cells | Paucimannose structures (Man₃GlcNAc₂), minimal processing to complex-type, core fucosylation [97] | Limited O-glycosylation capacity, simpler structures compared to mammalian | Generally low or absent sialylation | Mainly used for research and vaccine production |
| Plant Systems | β(1,2)-xylose, α(1,3)-fucose epitopes, core fucosylation, plant-specific complex glycans [97] | Hydroxyproline-linked arabinogalactans, plant-specific structures | Generally low sialylation capacity | Emerging platform with immunogenicity challenges |
| Human Cell Lines | Most similar to native human patterns, including complex-type with bisecting GlcNAc, core and antenna fucosylation [97] | Human-like O-glycans including sialylated Core 1 and Core 2 structures | Human-type sialylation (N-acetylneuraminic acid) | Alpha 1-antitrypsin (human placenta) [97] |
Emerging Technologies and Future Directions
Glycoengineering Strategies
Advanced glycoengineering approaches are being developed to overcome challenges in creating bioequivalent glycosylation patterns:
Genome Editing Approaches:
- CRISPR-Cas9 mediated knockout of immunogenic glycosyltransferases (e.g., α-1,3-galactosyltransferase, N-glycolylneuraminic acid synthase) [97]
- Knock-in of human glycosyltransferase genes (e.g., β-1,4-galactosyltransferase, α-2,6-sialyltransferase) into production cell lines [97]
- Engineering of customized glycosylation pathways in non-mammalian systems for human-like glycoform production [97]
Chemical and Enzymatic Remodeling:
- In vitro enzymatic treatment with glycosidases and glycosyltransferases to convert glycan structures [97]
- Chemoenzymatic synthesis using purified glycosylation enzymes and synthetic sugar nucleotides [97]
- Post-production glycan modification using glycosyltransferase cascades and salvage pathways [97]
Analytical Technologies for Bioequivalence Assessment
Cutting-edge analytical methods are enhancing our ability to characterize glycosylation precisely:
High-Resolution Mass Spectrometry:
- Native MS for intact glycoprotein analysis preserving non-covalent interactions [4]
- Ion mobility separation for distinguishing glycoform isomers [4]
- Tandem MS with electron-based dissociation for detailed glycan structural analysis [4]
Multi-attribute Monitoring Methods:
- LC-MS workflows for simultaneous monitoring of multiple critical quality attributes [4]
- Automated data processing with bioinformatics tools for high-throughput glycan analysis [4]
- Implementation of quality-by-design principles for glycosylation characterization [4]
The continued advancement of glycosylation analysis and engineering technologies will play a pivotal role in establishing bioequivalence standards for synthetic versus natural bioactive compounds, ultimately enabling the development of more effective and consistent biotherapeutics.
The pursuit of cost-effective alternatives to brand-name medications has led to the development of two distinct categories: generic drugs and biosimilars. While both aim to increase accessibility and reduce healthcare costs, they differ fundamentally in their complexity, development pathways, and regulatory requirements. These differences stem from the inherent nature of the products they replicate: generics are copies of small-molecule chemical drugs, whereas biosimilars are versions of complex biological medicines derived from living organisms [100] [101].
Understanding these distinctions is crucial for researchers, drug development professionals, and healthcare providers involved in the development and utilization of these products. The complexity of biologic compounds introduces unique challenges in manufacturing, characterization, and regulatory approval that do not apply to conventional generics. This comparison guide examines the key differences between biosimilars and generics, supported by experimental data and analytical methodologies essential for demonstrating bioequivalence and biosimilarity in their respective regulatory frameworks [102] [101].
Comparative Analysis: Structural and Manufacturing Complexities
Molecular and Manufacturing Characteristics
The fundamental distinction between generics and biosimilars lies in the molecular size, structural complexity, and manufacturing processes of the products they replicate.
Table 1: Fundamental Characteristics of Generics versus Biosimilars
| Characteristic | Generic Drugs | Biosimilars |
|---|---|---|
| Molecular Size | Small molecular weight [101] | Large molecular weight [101] |
| Molecular Structure | Simple, well-defined [101] | Complex, heterogeneous [101] |
| Manufacturing Process | Chemical synthesis [100] [101] | Biological processes in living systems [100] [101] |
| Characterization | Easy to fully characterize [101] | Difficult to fully characterize [101] |
| Stability | Generally stable [100] [101] | Sensitive to storage conditions; often requires cold chain [100] |
Regulatory and Development Pathways
The regulatory approval processes for generics and biosimilars reflect their fundamental differences in complexity. Generic drugs are approved through an Abbreviated New Drug Application (ANDA) under the Federal Food, Drug, and Cosmetic Act, requiring demonstration of bioequivalence to the reference product [101]. In contrast, biosimilars are approved under section 351(k) of the Public Health Service Act, requiring a comprehensive data package demonstrating similarity to the reference product without clinically meaningful differences [103] [101].
Table 2: Development and Regulatory Pathways
| Parameter | Generic Drugs | Biosimilars |
|---|---|---|
| Development Time | ~2 years [100] | 7-8 years [100] |
| Development Cost | $1-4 million [100] | >$100 million [100] |
| Approval Pathway | ANDA [101] | 351(k) of PHS Act [101] |
| Clinical Studies Required | Generally not required [101] | Generally required [101] |
| Interchangeability | Automatically substitutable [100] | Requires additional demonstration [101] |
Analytical Methodologies and Experimental Protocols
Statistical Approaches for Demonstrating Similarity
The statistical framework for evaluating biosimilars differs significantly from that used for generics. While generics typically utilize bioequivalence studies with established confidence intervals, biosimilars employ a totality-of-the-evidence approach involving extensive structural, functional, and clinical comparisons [102] [101].
Equivalence Trial Design for Biosimilars: Biosimilar development typically uses equivalence trial designs with pre-specified equivalence margins. The statistical approach often employs the Two One-Sided Test (TOST) procedure to demonstrate that differences between the biosimilar and reference product remain within a predetermined acceptance range [102]. The hypothesis framework for TOST is:
- H₀: μ ≤ θL or μ ≥ θU (the treatment difference is outside the equivalence margin)
- H₁: θL < μ < θU (the treatment difference is within the margins) where θL and θU represent the lower and upper equivalence margins, and μ represents the analysis criterion [102].
The following diagram illustrates the statistical decision framework for biosimilar equivalence testing:
Comparative Clinical Study Design: Clinical studies for biosimilars typically employ randomized, parallel-group designs comparing the biosimilar to the reference product. Key parameters include:
- Primary Endpoints: Often pharmacokinetic parameters (AUC, Cmax) with equivalence margins typically set at 80-125% for geometric mean ratios [102]
- Secondary Endpoints: Efficacy measures, safety profiles, and immunogenicity assessment [101]
- Sample Size Calculation: Based on achieving sufficient power (typically 80-90%) to demonstrate equivalence within predefined margins [102]
Analytical Characterization Techniques
The analytical characterization of biosimilars requires an extensive battery of tests to demonstrate structural and functional similarity to the reference product, far exceeding the requirements for generics.
Table 3: Analytical Methods for Biosimilar Characterization
| Method Category | Specific Techniques | Parameters Assessed |
|---|---|---|
| Structural Analyses | Mass spectrometry, Circular dichroism, Amino acid sequencing, Peptide mapping | Primary structure, Higher-order structure, Post-translational modifications [101] |
| Functional Assays | Cell-based bioassays, Binding assays, Enzyme kinetics | Biological activity, Receptor binding, Mechanism of action [101] |
| Physicochemical Analyses | Chromatography, Electrophoresis, Spectroscopy | Purity, Impurity profiles, Aggregation [101] |
The following workflow illustrates the comprehensive analytical characterization required for biosimilar development:
Regulatory Standards and Evidence Requirements
The Totality of Evidence Approach
Biosimilar approval relies on a "totality of evidence" approach, where data from all stages of development collectively demonstrate that no clinically meaningful differences exist between the biosimilar and reference product [102] [101]. This comprehensive evaluation includes:
- Analytical Similarity: Extensive structural and functional characterization demonstrating high similarity to the reference product [101]
- Animal Studies: Assessment of toxicity and immunogenicity [101]
- Clinical Studies: Human PK/PD studies, comparative efficacy and safety studies, and immunogenicity assessment [101]
The FDA has recently moved to streamline biosimilar development by reducing unnecessary clinical testing requirements when sufficient analytical and functional data demonstrate similarity [103]. This recognizes that analytical methods have become increasingly sensitive in detecting product differences.
Interchangeability and Substitution
A critical regulatory distinction between generics and biosimilars lies in interchangeability. Generic drugs are automatically considered interchangeable and substitutable at the pharmacy level without prescriber intervention [100]. In contrast, biosimilars must undergo additional evaluation to be designated as interchangeable [101] [104].
Interchangeability Requirements for Biosimilars:
- Demonstration that the biosimilar produces the same clinical result as the reference product in any given patient [101]
- For products administered multiple times, evidence that switching between the reference and biosimilar does not increase safety risks or diminish effectiveness [101]
- Additional switching studies may be required to support interchangeability designation [101]
Research Reagents and Methodological Tools
Table 4: Essential Research Reagents for Biosimilar Development
| Reagent/Category | Function in Development | Application Examples |
|---|---|---|
| Reference Product | Serves as comparator for all analytical and functional comparisons | Source material for structural and functional analyses [101] |
| Cell-Based Bioassays | Measure biological activity and potency | Mechanism-of-action specific assays; proliferation, binding, signaling assays [101] |
| Characterized Cell Lines | Used in potency assays and functional assessments | Reporter gene assays, binding studies [101] |
| Antigen Reagents | Assess binding characteristics and immunogenicity | ELISA, surface plasmon resonance [101] |
| Mass Spectrometry Standards | Enable structural characterization | Peptide mapping, post-translational modification analysis [101] |
The complexity of biologic compounds fundamentally shapes the development pathway for biosimilars, creating requirements far more extensive than those for generic small-molecule drugs. While generics must demonstrate pharmaceutical equivalence and bioequivalence, biosimilars require comprehensive analytical, functional, and clinical characterization to establish similarity within an acceptable range of variability [100] [101].
For researchers and drug development professionals, these distinctions have significant implications for development timelines, costs, and technical requirements. The stepwise approach to biosimilar development—beginning with extensive analytical characterization and proceeding to targeted clinical evaluations—represents a more efficient pathway than full clinical development while still ensuring patient safety and product efficacy [102] [101].
As regulatory frameworks evolve to support more efficient biosimilar development [103], and as the market share of biosimilars continues to grow [105], understanding these complexities becomes increasingly important for advancing therapeutic options and improving patient access to essential biologic medicines.
For researchers and drug development professionals, navigating the global variation in bioequivalence (BE) requirements presents significant challenges in drug development and regulatory strategy. Bioequivalence studies are fundamental to demonstrating that generic drugs perform in the same manner as their reference products, yet harmonization remains incomplete across major regulatory jurisdictions. This landscape is particularly complex for developers working with natural bioactive compounds, which may face additional scrutiny compared to synthetic pharmaceuticals due to their inherent variability and complex composition.
The International Council for Harmonisation (ICH) has initiated crucial steps toward global alignment with the M13 series of guidelines. The recent ICH M13A guideline, which became effective in January 2025, supersedes parts of the European Medicines Agency's (EMA) previous BE guidance for immediate-release solid oral dosage forms [106]. Furthermore, the draft ICH M13B guideline, currently under consultation until October 2025, aims to provide harmonized criteria for waivers of in vivo BE studies for additional strengths where BE has been established for at least one strength [71] [107]. Despite these harmonization efforts, significant jurisdictional differences persist, especially for complex products like narrow therapeutic index drugs, modified-release formulations, and orally inhaled products, creating a complex regulatory environment for global drug development [108].
Global Regulatory Landscape: A Comparative Analysis
Current Status of Major Regulatory Agencies
The following table summarizes the recent regulatory updates and current BE requirements from major health authorities, highlighting the ongoing efforts toward harmonization and the areas where divergence remains.
Table 1: Recent Bioequivalence Regulatory Updates from Major Health Authorities
| Health Authority | Recent Update (2025) | Key Focus | Status & Implications |
|---|---|---|---|
| European Medicines Agency (EMA) | ICH M13A Implementation [106] | Immediate-Release Solid Oral Dosage Forms | Effective January 2025, superseding relevant parts of the previous EMA BE guideline. |
| U.S. Food and Drug Administration (FDA) | Draft ICH M13B Guidance [71] [107] | Additional Strengths Biowaiver | Draft under consultation; aims to harmonize criteria for waiving BE studies for additional strengths. |
| China NMPA | Revised Clinical Trial Policies [109] | Accelerating Drug Development | Effective September 2025; allows adaptive designs and aims to shorten trial approval timelines by ~30%. |
| Australia TGA | Adoption of ICH E9(R1) [109] | Estimands in Clinical Trials | Adopted September 2025, introducing the "estimand" framework for clearer trial design and analysis. |
| Health Canada | Revised Draft Biosimilar Guidance [109] | Biosimilar Biologic Drugs | Proposed removal of routine requirement for Phase III comparative efficacy trials (consultation closed Sept 2025). |
Persistent Areas of Divergence
While the ICH M13 series represents a significant step forward, the GBHI conference report identifies several areas where global requirements have not yet been fully aligned [108].
- Narrow Therapeutic Index (NTI) Drugs: A move toward harmonization is evident, with consensus on applying a mixed scale for the BE acceptance range depending on variability. However, differences remain in the statistical approaches for variability comparison and the selection of the regulatory constant.
- Orally Inhaled Drug Products (OIDPs): The regulatory approaches of the FDA and EMA "largely differ." The FDA employs a "weight-of-evidence" approach, while the EMA uses a stepwise approach. There is growing trust in using pharmacokinetic (PK) exposure data to predict comparable efficacy when these data reflect concentrations absorbed via the lung [108].
- Modified-Release (MR) Products: For BE demonstration of MR products, there is active discussion on using model-informed approaches to simulate steady-state profiles from single-dose data, potentially reducing the burden of multiple-dose studies [108].
Experimental Protocols for Bioequivalence Assessment
Adhering to regulatory requirements necessitates robust and well-defined experimental protocols. The following are generalized methodologies for key BE study types, reflecting current harmonized principles where they exist.
Standard Two-Period, Two-Treatment Crossover Design
This design remains a cornerstone for establishing BE for systemically acting drugs [110].
- Objective: To demonstrate that the rate and extent of absorption of a test product are not significantly different from those of the reference product under fasted conditions.
- Subjects: Typically involves healthy adult volunteers, with sample size justified by power calculation (often 80-90% power).
- Procedure:
- Period 1: Subjects are randomized to receive either the Test (T) or Reference (R) product.
- Washout: A washout period of at least 5 half-lives of the drug follows to ensure elimination.
- Period 2: Subjects receive the alternate treatment (R or T).
- Blood Sampling: Serial blood samples are collected pre-dose and at multiple time points post-dose to characterize the concentration-time profile fully.
- Bioanalytical Analysis: Plasma/serum samples are analyzed using a validated method (e.g., LC-MS/MS) to determine drug concentrations.
- Pharmacokinetic Analysis: Key parameters are calculated using non-compartmental analysis:
- AUC~0-t~: Area under the concentration-time curve from zero to the last measurable time point.
- AUC~0-∞~: Area under the concentration-time curve from zero to infinity.
- C~max~: Maximum observed concentration.
Population Bioequivalence (PBE) for In Vitro Data
For certain locally acting products like Orally Inhaled Respiratory Products (OIRPs), in vitro tests can support a BE determination.
- Objective: To compare the in vitro performance (e.g., delivered dose uniformity) of a test and reference product, accounting for both mean difference and variability [111].
- Sample Preparation: Multiple batches and units of both test and reference products are prepared according to their respective labels.
- In Vitro Testing: Using apparatuses such as impactors or dose units, critical quality attributes are measured (e.g., delivered dose, particle size distribution). A sufficient number of replicates are performed to support a statistical comparison.
- Statistical Analysis:
- The PBE approach is recommended by regulators for analyzing such in vitro data [111].
- The method tests a composite hypothesis that considers the mean difference between products and the difference in population variances.
- Current literature often assumes a log-normal distribution for the data, but research indicates that the assumption of the underlying distribution (normal vs. log-normal) can significantly impact the performance and conclusion of the PBE test, warranting careful consideration [111].
The Scientist's Toolkit: Key Reagents and Materials
Table 2: Essential Research Reagents and Materials for Bioequivalence Studies
| Item | Function in BE Research |
|---|---|
| Certified Reference Standard | Serves as the primary benchmark for quantifying the active pharmaceutical ingredient (API) in biological matrices; essential for method validation and sample analysis. |
| Stable Isotope-Labeled Internal Standard | Used in LC-MS/MS bioanalysis to correct for matrix effects, recovery losses, and instrument variability, ensuring analytical accuracy and precision. |
| Validated Bioanalytical Method (LC-MS/MS) | The core platform for quantifying drug concentrations in plasma/serum samples with high sensitivity and specificity, required to be validated per regulatory guidelines (e.g., FDA, EMA). |
| Blank Biological Matrix | Plasma or serum from untreated subjects, used for preparing calibration standards and quality control samples during bioanalytical method development and validation. |
| In Vitro Dissolution Apparatus (USP I, II, IV) | Used to assess and compare the drug release profile of the test and reference formulations, which can be critical for BCS-based biowaivers and quality control. |
Special Considerations for Natural vs. Synthetic Bioactives
The regulatory principles of BE apply equally to synthetic and natural bioactive compounds. However, the inherent properties of natural products can introduce specific challenges in meeting these standards.
- The Molecular Equivalence Principle: From a regulatory and biochemical perspective, "your body reacts to the chemical structure, not the source" [2]. If a natural bioactive and its synthetic counterpart are chemically identical, they are considered equivalent. The ICH M13B draft guideline, for example, focuses on the properties of the dosage form rather than the origin of the API [71].
- Challenges for Natural Bioactives:
- Complexity and Variability: Natural extracts are often complex mixtures, and their composition can vary based on source, season, and extraction method [2]. This poses a significant challenge in ensuring consistent quality and performance between batches, a fundamental requirement for BE.
- Impurity Profiles: The "risk" of natural ingredients can include "variable levels of active compounds" and potential "contaminants like heavy metals, pesticide residues, or microbial contamination" not typically present in well-controlled synthetic processes [2].
- Demonstrating Bioequivalence: A study on glucosamine highlights a practical example. Kang et al. found that while chitosan-derived and biofermentation-derived glucosamine met bioequivalence standards, they differed in their mean peak plasma concentration (Cmax) ratios [46]. This underscores that even when different sources of an active ingredient are deemed bioequivalent, subtle pharmacokinetic differences may exist, potentially related to formulation or minor impurities.
Visualizing Regulatory Pathways and Experimental Workflows
Regulatory Decision Pathway for Additional Strength Biowaiver
The following diagram visualizes the logical decision process for obtaining a biowaiver for additional drug strengths, as outlined in the draft ICH M13B guideline [71] [107].
Diagram 1: ICH M13B Biowaiver Decision Pathway
Standard Bioequivalence Study Workflow
This workflow outlines the key phases in the design, conduct, and analysis of a standard in vivo bioequivalence study, integrating elements from the described protocols and regulatory requirements.
Diagram 2: Bioequivalence Study Workflow
The global landscape of bioequivalence requirements is characterized by a dynamic tension between ongoing harmonization efforts and persistent jurisdictional variations. The advent of the ICH M13 series provides a more unified framework for immediate-release solid oral dosage forms, yet significant differences remain for complex drug products like NTI drugs and OIDPs [106] [108]. For developers, particularly those working with natural bioactive compounds, this necessitates a carefully tailored regulatory strategy. Success depends on early engagement with health authorities, a thorough understanding of region-specific guidance, and rigorous study design that accounts for the unique challenges of product variability. As regulatory science evolves, the increasing adoption of model-informed drug development and innovative statistical designs promises to further refine and, potentially, streamline the path to demonstrating bioequivalence across global markets.
Evidence-Based Evaluation and Regulatory Standards
The pursuit of bioactive compounds for therapeutic use presents a fundamental dichotomy: sourcing molecules from nature or creating them synthetically. This review examines the clinical evidence for the efficacy and safety of natural versus synthetic bioactive compounds, framed within the critical context of bioequivalence research. Natural products, derived from plants, animals, and microbial resources, have historically been a cornerstone of medicine, especially in low-income countries where over 80% of the population relies on traditional medicines for primary healthcare [29]. Contemporary drug development now leverages these natural templates, using rational drug design and semi-synthesis to create innovative therapeutic options [112]. Conversely, synthetic antioxidants and other wholly artificial compounds are developed to improve upon pharmacological properties, bioavailability, and targeted delivery [113]. For researchers and drug development professionals, the central challenge lies not only in identifying potent compounds but in establishing robust bioequivalence—demonstrating that natural and synthetic analogs share comparable therapeutic performance and safety profiles. This review synthesizes current experimental data and clinical evidence to objectively compare these two classes of bioactives, providing a foundational guide for future research and development.
Methodology for Evidence Collection and Analysis
This clinical evidence review was conducted through a systematic analysis of contemporary peer-reviewed literature, clinical trial reports, and comparative preclinical studies. The primary focus was on head-to-head studies directly comparing natural and synthetic bioactive compounds, with a particular emphasis on validated experimental protocols and standardized efficacy endpoints.
The analysis prioritized data from studies that detailed:
- Specific experimental models (e.g., in vivo animal models, in vitro cell-based assays, human clinical trials).
- Quantifiable efficacy metrics (e.g., IC50 values, reduction in symptom scores, microbial inhibition zones).
- Comprehensive safety and pharmacokinetic data (e.g., adverse event rates, bioavailability, half-life, clearance).
Studies employing crude or semi-standardized natural extracts without precise characterization of active constituents were excluded to ensure a rigorous comparison based on defined chemical entities. The ensuing tables and diagrams synthesize this filtered evidence to facilitate a cross-compound class comparison.
Comparative Efficacy Profiles: Experimental Data
The efficacy of bioactive compounds is evaluated across multiple stages, from initial in vitro screening to clinical trials in human populations. The data below summarizes key experimental findings comparing natural and synthetic bioactives.
Table 1: Comparative Efficacy in Preclinical and Clinical Models
| Compound / Class | Natural or Synthetic | Experimental Model | Efficacy Outcome | Key Findings & Mechanism |
|---|---|---|---|---|
| Artemisinin [40] | Natural (from Artemisia annua) | Clinical trials (Malaria) | Significant reduction in parasite load | Foundation of Artemisinin-based Combination Therapies (ACTs); direct anti-parasitic activity. |
| Synthetic Artemisinin Derivatives [40] | Semi-synthetic | Clinical trials (Malaria) | Comparable or improved efficacy vs. natural parent | Modified for improved pharmacokinetics and stability; used in ACTs to prevent resistance. |
| Alstonine [34] | Natural (MIA from plants) | Rodent models of schizophrenia | Reduction in disease symptoms | Demonstrated translational efficacy for mental health; basis for further optimization. |
| AI-Optimized Alstonine Analogues [34] | Semi-synthetic (AI-designed) | Rodent models of schizophrenia & pain | Superior efficacy to natural Alstonine | Improved pharmacological properties (e.g., brain penetration) via AI-driven structural optimization. |
| Edaravone [113] | Synthetic | Clinical practice (e.g., ischemic stroke) | Neuroprotective effects | One of the few synthetic antioxidants approved for clinical use; acts as a radical scavenger. |
| Dietary Antioxidants (e.g., Vitamin E) [113] | Natural | Human clinical trials (Cancer prevention) | Failed therapeutic benefits in some trials | Associated with adverse effects (e.g., increased risk of prostate cancer); ambiguous efficacy. |
| Ebselen [113] | Synthetic | Various disease models | Promising therapeutic potential | Mimics glutathione peroxidase activity; also acts as a NADPH oxidase (NOX) inhibitor. |
Analysis of Key Efficacy Trends
The experimental data reveals several critical trends. First, natural products often provide the initial bioactive scaffold, whose efficacy is confirmed in model systems, as seen with artemisinin and alstonine [34] [40]. However, subsequent semi-synthetic modification frequently yields derivatives with superior efficacy or optimized pharmacokinetic profiles. For instance, AI-driven optimization of the natural product alstonine resulted in lead molecules with proven superiority in rodent models of pain relief [34].
Second, the efficacy of synthetic compounds can be more targeted and potent, as exemplified by the synthetic antioxidant edaravone, which has achieved clinical success where many natural antioxidants have failed [113]. This highlights a key advantage of synthetic approaches: the ability to design molecules for specific mechanisms, such as inhibiting the NOX enzyme, a major source of pathological reactive oxygen species [113].
Comparative Safety and Tolerability Profiles
Safety and tolerability are paramount in drug development. The table below consolidates clinical and preclinical safety data for representative natural and synthetic bioactives.
Table 2: Comparative Safety and Tolerability Profiles
| Compound / Class | Natural or Synthetic | Safety Profile (Clinical/Preclinical) | Notable Adverse Effects & Risks |
|---|---|---|---|
| Artemisinin-based ACTs [40] | Natural & Semi-synthetic | Generally well-tolerated | Frontline malaria treatment; safety profile established through widespread clinical use. |
| Pyrimethamine + Sulfadiazine (Toxoplasmosis) [40] | Synthetic | Poorly tolerated | Adverse effects in up to 60% of patients; 45% require treatment discontinuation. |
| Nitazoxanide (Cryptosporidiosis) [40] | Synthetic | Ineffective in immunocompromised | Limited efficacy and safety in high-risk populations, highlighting a critical therapeutic gap. |
| Vitamin E Supplementation [113] | Natural | Failed safety in long-term use | Increased risk of prostate cancer in clinical trials, demonstrating potential risks of natural bioactives. |
| Synthetic Antioxidants (e.g., MitoQ10) [113] | Synthetic | Promising, but requires more study | Designed for improved safety and targeting (e.g., mitochondria); long-term clinical data still needed. |
| Ionophores & Anti-coccidials (Veterinary) [40] | Natural & Synthetic | Varied and context-dependent | Safety and efficacy are carefully managed in livestock to prevent resistance and toxicity. |
Analysis of Key Safety Trends
The safety data demonstrates that origin is not a reliable predictor of a compound's safety profile. Both natural and synthetic compounds can exhibit significant toxicity. For example, the natural product vitamin E is linked to serious adverse events like prostate cancer, while the synthetic combination therapy for toxoplasmosis has high rates of treatment-disrupting side effects [40] [113].
A principal advantage of synthetic approaches is the ability to engineer improved safety profiles. Techniques such as prodrug strategies, nanotechnology, polymer complexation, and targeted delivery systems are actively being employed to enhance the therapeutic index of synthetic bioactives, reducing off-target effects and toxicity [113]. This level of precise engineering is more challenging to achieve with complex, unmodified natural extracts.
Detailed Experimental Protocols for Key Comparisons
To ensure the reproducibility of comparative studies, this section outlines standardized protocols for evaluating bioactive compounds.
Protocol 1: In Vitro Antioxidant Activity and Cell Cytotoxicity Assay
This protocol is fundamental for establishing initial efficacy and safety parameters for antioxidants, both natural and synthetic [29] [113].
- Compound Preparation: Prepare serial dilutions of the test natural bioactive and its synthetic analogue in a suitable solvent (e.g., DMSO). Include a positive control (e.g., Trolox) and a negative control (solvent only).
- Antioxidant Activity Assessment:
- DPPH Scavenging Assay: Mix compound solutions with a methanolic DPPH solution. Incubate in the dark for 30 minutes. Measure absorbance at 517 nm. Calculate % radical scavenging activity.
- SOD Mimetic Activity: Use a cytochrome c reduction assay. Generate superoxide radicals (e.g., via xanthine/xanthine oxidase system) in the presence of cytochrome c and the test compound. Monitor the inhibition of cytochrome c reduction at 550 nm.
- Cell Cytotoxicity Assessment (MTT Assay):
- Culture relevant cell lines (e.g., HEK-293, HepG2) in 96-well plates.
- Treat cells with a range of compound concentrations for 24-48 hours.
- Add MTT reagent and incubate to allow formazan crystal formation.
- Solubilize crystals with DMSO and measure absorbance at 570 nm. Calculate cell viability and determine IC50 values.
- Data Analysis: Plot dose-response curves for both antioxidant and cytotoxic effects to establish a preliminary therapeutic window.
Protocol 2: In Vivo Efficacy Model for CNS Disorders
This protocol, inspired by contemporary drug discovery efforts, evaluates the translational efficacy of compounds for complex diseases like schizophrenia and pain [34].
- Animal Models: Use established rodent models (e.g., MK-801 or phencyclidine-induced model for schizophrenia; carrageenan-induced inflammatory pain model).
- Group Allocation: Randomize animals into groups (n=8-12): Vehicle control, Natural bioactive group (e.g., alstonine), Semi-synthetic optimized group (AI-derived analogue), and a positive control group (e.g., clozapine for schizophrenia).
- Dosing and Administration: Administer compounds intraperitoneally or orally at equimolar doses based on prior pharmacokinetic data.
- Behavioral Testing:
- For Schizophrenia Models: Conduct tests like prepulse inhibition (PPI) and open field test to assess sensorimotor gating and locomotor activity.
- For Pain Models: Assess mechanical allodynia (von Frey filaments) and thermal hyperalgesia (Hargreaves test) at baseline and post-treatment time points.
- Tissue Collection and Biomarker Analysis: Post-euthanasia, collect relevant tissues (e.g., brain regions, blood). Analyze biomarkers of oxidative stress (e.g., F2-isoprostanes, 8-OHdG) or inflammation (e.g., cytokine levels) to correlate efficacy with mechanism [113].
- Statistical Analysis: Use ANOVA with post-hoc tests to compare treatment groups against controls and against each other for superior efficacy.
Signaling Pathways and Workflow Visualization
The following diagrams illustrate the core pathways targeted by bioactives and the generalized workflow for their comparative development.
Diagram 1: Key Signaling Pathways in Bioactive Compound Action
Figure 1: Key signaling pathways in bioactive compound action. This diagram maps the primary pathological drivers (yellow) and their downstream effects (red) that are targeted by natural (green) and synthetic/semi-synthetic (blue, red) bioactive compounds. Arrows indicate the documented interactions and mechanisms of action, such as scavenging, inhibition, and modulation derived from the analyzed literature [114] [34] [113].
Diagram 2: Comparative Development Workflow
Figure 2: Comparative development workflow for natural and synthetic bioactives. This diagram contrasts the two primary development pathways. The natural product path (green) begins with sourcing and isolating compounds, while the synthetic path (blue) often starts with rational or AI-driven design, sometimes inspired by natural templates. Both paths converge on lead identification and optimization, with an increasing role for AI/ML feedback loops to enhance pharmacological properties, a key differentiator in modern drug development [29] [34] [115].
The Scientist's Toolkit: Essential Research Reagents and Solutions
The following table details key reagents and technologies critical for conducting the experiments described in this review.
Table 3: Key Research Reagents and Solutions for Bioactive Compound Evaluation
| Reagent / Technology | Function in Research | Application Example |
|---|---|---|
| DPPH (2,2-Diphenyl-1-picrylhydrazyl) | A stable free radical used to assess the radical scavenging activity of compounds in vitro. | Initial screening of antioxidant capacity for natural and synthetic compounds [113]. |
| MTT (3-(4,5-Dimethylthiazol-2-yl)-2,5-Diphenyltetrazolium Bromide) | A yellow tetrazole reduced to purple formazan in metabolically active cells; used to assay cell viability and proliferation. | Determining cytotoxicity (IC50) in cell lines after treatment with test bioactives [29]. |
| SOD/Catalase Mimetics (e.g., EUK compounds) | Synthetic low-molecular compounds mimicking endogenous antioxidant enzymes; used as experimental tools and therapeutic leads. | Comparing the activity of natural antioxidants to synthetic enzyme mimetics in models of oxidative stress [113]. |
| AI/ML Modeling Platforms | In silico tools to predict compound activity, optimize chemical structures, and explore structure-activity relationships (SAR). | Designing synthetic analogues of natural products (e.g., Alstonine) with improved efficacy and brain penetration [34]. |
| Engineered Yeast Cell Factories | Synthetic biology platforms for the biomanufacturing of complex natural products (e.g., alkaloids) without plant extraction. | Scalable production of plant-inspired drug candidates like monoterpene indole alkaloids for consistent testing and supply [34]. |
| Biomarkers of Oxidative Damage (e.g., 8-OHdG, F2-isoprostanes) | Measurable indicators of oxidative stress in biological samples, used to validate antioxidant mechanisms in vivo. | Correlating the therapeutic effect of a compound with a reduction in oxidative damage in preclinical and clinical studies [113]. |
The clinical evidence reviewed herein underscores that the distinction between natural and synthetic bioactive compounds is not a simple binary of efficacy or safety. Natural products provide an invaluable and historically validated source of chemical diversity and therapeutic potential, as exemplified by artemisinin [40]. However, they often face challenges related to complex purification, low yield, and suboptimal pharmacokinetics.
Synthetic and semi-synthetic strategies address these limitations by enabling the optimization of nature's blueprints. Through rational design, AI-driven modeling, and advanced biomanufacturing, synthetic approaches can enhance potency, improve safety profiles, and achieve scalable production [34] [113]. The future of bioactive compound development lies in the strategic convergence of these paradigms. Leveraging the structural inspiration from nature with the precision of synthetic chemistry and the predictive power of AI will be crucial for accelerating the discovery of the next generation of safe, effective, and bioequivalent therapeutics to address unmet medical needs.
The sourcing of bioactive compounds for pharmaceuticals and nutraceuticals presents a critical challenge in product development. Glucosamine, a fundamental building block for glycosaminoglycans in cartilage, exemplifies this challenge with its primary production methods: traditional extraction from chitosan in crustacean shells and modern biofermentation using microbial systems [116] [117]. This comparison guide examines the bioequivalence between these sources within the broader context of synthetic versus natural bioactive compound research.
For researchers and drug development professionals, understanding the pharmacokinetic profiles, experimental methodologies, and analytical approaches for comparing these sources is essential for formulation decisions. This analysis provides objective comparisons supported by experimental data, focusing specifically on the pharmacokinetic equivalence and technical considerations of each production method.
Pharmacokinetic Comparison: Experimental Data
Key Pharmacokinetic Parameters
A randomized, double-blind, cross-over study directly compared the pharmacokinetics of chitosan-derived and biofermentation-derived glucosamine sulfate 2KCl after a single 1500 mg oral dose in healthy subjects [116]. The results demonstrated notable similarities and differences:
Table 1: Pharmacokinetic Parameters of Glucosamine (1500 mg dose)
| Parameter | Chitosan-Derived | Biofermentation-Derived | Statistical Significance | Bioequivalence Assessment |
|---|---|---|---|---|
| AUC0-8h | Comparable | Comparable | No significant difference (p > 0.05) | Met bioequivalence criteria (90% CI within 0.8-1.25) |
| AUC0-∞ | Comparable | Comparable | No significant difference (p > 0.05) | Met bioequivalence criteria (90% CI within 0.8-1.25) |
| Cmax | Similar mean values | Similar mean values | No significant difference (p > 0.05) | Did not meet criteria (90% CI: 0.892-1.342) |
| Tmax | Comparable | Comparable | No significant difference | High within-subject variability observed |
| Terminal Half-life | Comparable | Comparable | No significant difference | High within-subject variability observed |
The study concluded that both glucosamine sources demonstrated equivalent systemic exposure based on AUC parameters, suggesting that biofermentation-derived glucosamine represents a viable alternative sourcing method [116].
Critical Analysis of Bioequivalence Study
A methodological critique of the primary bioequivalence study highlights several considerations for researchers [117]:
Table 2: Critical Assessment of Bioequivalence Study Methodology
| Methodological Aspect | Study Implementation | Critique/Consideration |
|---|---|---|
| Sample Size | 20 subjects (with 2 dropouts) | Small sample size (n=10 per group in first period) may underpower statistical analysis |
| Confidence Intervals | 90% CI used for bioequivalence | Conventional 95% CI might provide more rigorous assessment |
| Variability | Significant within-subject variability | High variability particularly affected Cmax comparisons |
| Equivalence Scope | AUC parameters showed equivalence | Tmax and terminal half-life failed to demonstrate full equivalence |
Experimental Protocols and Methodologies
Clinical Study Design
The foundational pharmacokinetic study employed a rigorous clinical design to minimize bias and confounding [116]:
- Design: Randomized, double-blind, single-dose, cross-over study
- Washout Period: 7 days between interventions to prevent carryover effects
- Participants: Healthy male and female adults under fasting conditions
- Intervention: Single dose of 1500 mg glucosamine sulfate 2KCl from either source
- Blood Sampling: Collected via intravenous catheter at 0, 10, 30 min, 1, 2, 3, 4, 6, and 8 hours post-administration
- Sample Processing: Plasma separation via centrifugation (1500× g, 10 min, 4°C) and storage at -80°C until analysis
Analytical Methodology: LC-MS/MS Quantification
The quantification of glucosamine in plasma samples required specialized techniques to address analytical challenges [116]:
- Instrumentation: Agilent 6460 triple quadrupole LC-MS/MS system with Agilent 1260 LC system
- Chromatography Column: Luna 3 μm CN 100 Å column (2.0 × 100 mm)
- Mobile Phase: 10 mM ammonium formate in water:acetonitrile (30:70 v/v)
- Flow Rate: 0.3 mL/min with 8.3 min total run time
- Critical Separation: Resolution of two anomeric forms of glucosamine (retention times ~3 and ~4 min) to prevent ion suppression from plasma matrix
- Mass Detection: ESI-positive mode with precursor-to-product ion transitions m/z 180.0→72.0 for glucosamine and m/z 268.3→116.2 for internal standard (metoprolol)
- Calibration Range: 0.1–10 μg/mL with LLOQ of 0.1 μg/mL
This methodological approach ensured precise quantification of glucosamine despite its existence in multiple isomeric forms and potential matrix effects.
Formulation Considerations
The glucosamine formulations for both sources were carefully standardized [116]:
- Dosage Form: Clear hypromellose hard-shell capsules containing 500 mg glucosamine sulfate
- Dosing: Three capsules administered together to achieve 1500 mg total dose
- Manufacturing: Prepared under cGMP conditions with separate production runs to prevent cross-contamination
- Excipients: No other active or inactive ingredients included in capsules
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Glucosamine Bioequivalence Studies
| Reagent/Instrument | Function/Application | Specific Examples/Properties |
|---|---|---|
| Glucosamine Standards | Reference standard for quantification and calibration | d-(+)-glucosamine hydrochloride; concentration range: 0.1-10 μg/mL for plasma [116] |
| Internal Standards | Normalization of analytical variability | Metoprolol (20 ng/mL in acetonitrile) [116] |
| LC-MS/MS System | Sensitive and specific quantification of glucosamine | Agilent 6460 triple quad; ESI-positive mode; MRM detection [116] |
| Chromatography Columns | Separation of glucosamine anomers from matrix | Luna 3 μm CN 100 Å column (2.0 × 100 mm) [116] |
| Chitosan | Absorption enhancer in formulation development | MW ~200 kDa; deacetylation degree 83%; enhances paracellular transport [118] |
| Mobile Phase Components | Liquid chromatography separation | 10 mM ammonium formate in water:acetonitrile (30:70 v/v) [116] |
| Sample Preparation Reagents | Protein precipitation and extraction | Acetonitrile with internal standard (200 μL:50 μL plasma ratio) [116] |
Metabolic Pathways and Experimental Workflows
Glucosamine Absorption and Metabolic Pathway
Diagram 1: Glucosamine Metabolic Pathway (79 characters)
The metabolic pathway illustrates the fate of oral glucosamine sulfate, which dissociates in gastric fluid before intestinal absorption [119]. The absorbed glucosamine enters systemic circulation and undergoes hepatic metabolism to key metabolites including glucosamine-6-sulfate (GlcN-6-S) and N-acetylglucosamine (GlcNAc), eventually distributing to target joint tissues [119].
Bioequivalence Study Workflow
Diagram 2: Bioequivalence Study Design (73 characters)
The experimental workflow outlines the cross-over design used to compare glucosamine sources, highlighting key elements including randomization, washout period, intensive blood sampling, and advanced analytical techniques [116].
Research Implications and Future Directions
Beyond strict bioequivalence, sourcing considerations present significant research implications:
- Sustainability: Biofermentation utilizes corn-based substrates, potentially offering a more sustainable production method compared to crustacean shell extraction [116] [117]
- Allergen Concerns: While shellfish allergies typically respond to flesh proteins rather than shell components, biofermentation provides an alternative for concerned consumers [117]
- Supply Chain Stability: Biofermentation may offer more consistent production yields independent of fishing industry fluctuations [116]
Formulation Strategies to Enhance Bioavailability
Research indicates that chitosan itself can significantly enhance glucosamine bioavailability when used as an excipient. Studies demonstrate:
- Permeability Enhancement: Chitosan increases glucosamine transport 1.9-4.0 fold in Caco-2 cell monolayers via reversible tight junction opening [118]
- In Vivo Validation: Glucosamine formulations with 0.5% (w/v) chitosan showed 2.8-fold increase in Cmax and 2.5-fold increase in AUC0-∞ in rat studies [118]
- Clinical Relevance: This enhancement strategy could address the bioavailability limitations observed in conventional glucosamine formulations
Research Gaps and Future Studies
Current literature reveals several areas requiring further investigation:
- Direct Clinical Outcomes: No studies directly compare the clinical efficacy (pain reduction, functional improvement) in osteoarthritis patients between sources
- Long-Term Safety: Limited long-term safety data specifically for biofermentation-derived glucosamine
- Metabolite Activity: Further research needed on the biological activity of glucosamine metabolites (GlcN-6-S, GlcNAc) [119]
- Quality Parameters: Standardization of quality metrics (purity, microbial limits) across different production methods [117]
For researchers and drug development professionals, these findings support the consideration of biofermentation-derived glucosamine as a pharmaceutically equivalent alternative to traditional crustacean-derived material, with particular relevance for sustainable sourcing initiatives and allergen-conscious formulations.
Regulatory frameworks established by the Food and Drug Administration (FDA) in the United States and the European Medicines Agency (EMA) in Europe are critical in ensuring the safety, efficacy, and quality of pharmaceutical products, including those derived from synthetic and natural bioactive compounds [120]. For drug development professionals, understanding the nuances between these agencies is essential for successful global market entry. Bioequivalence studies serve as a cornerstone for the approval of generic drugs and are equally relevant for demonstrating the therapeutic equivalence of natural bioactive compounds with complex compositions [121] [106]. These studies prove that a test product exhibits a comparable bioavailability profile to a reference product, ensuring similar clinical effects [106]. The evolving guidelines from the FDA and EMA reflect a continuous effort to adapt to scientific advancements, particularly with the ongoing ICH M13 harmonization initiative aiming to standardize global bioequivalence requirements [106] [122].
The comparison between synthetic and natural bioactive compounds adds a layer of complexity to bioequivalence assessments. Synthetic compounds often feature well-defined structures, while natural products are typically more complex, with greater molecular size, stereochemical complexity, and distinct physicochemical properties [37] [3]. Notably, approximately half of all new drug approvals trace their structural origins to a natural product, underscoring their importance in pharmacotherapy [37]. This guide provides a detailed, objective comparison of the FDA and EMA regulatory frameworks, focusing on bioequivalence requirements and their specific implications for synthetic versus natural bioactive compound research.
Agency Structures and Approval Pathways
The FDA and EMA exhibit fundamental structural differences that influence their regulatory processes. The FDA operates as a single entity under the Department of Health and Human Services, with key functions distributed between centers. The Center for Drug Evaluation and Research (CDER) evaluates drugs, generics, and many therapeutic biologics, while the Center for Biologics Evaluation and Research (CBER) oversees vaccines, blood products, and advanced therapies [120]. This centralized structure enables streamlined decision-making within the US market.
In contrast, the EMA operates as a coordinating body for the European Union's member states. Its scientific assessment of medicines involves two main committees: the Committee for Medicinal Products for Human Use (CHMP), which advises on benefit-risk and marketing approvals, and the Pharmacovigilance Risk Assessment Committee (PRAC), which monitors and assesses safety signals [120]. The EMA manages the centralized authorization procedure, which grants marketing authorization valid across all EU member states for selected products, particularly innovative medicines [120]. Some products may still follow national pathways with additional local requirements.
Table 1: Key Structural and Procedural Differences between FDA and EMA
| Feature | FDA (US) | EMA (EU) |
|---|---|---|
| Governance Structure | Single federal agency [120] | Network coordinating 27 member states [120] |
| Key Evaluation Bodies | CDER, CBER [120] | CHMP, PRAC [120] |
| Primary Approval Route | Single approval for entire US market [120] | Centralized procedure for EU-wide approval [120] |
| Typical Review Timelines | Standard: ~10 months; Priority: ~6 months [120] | Standard: ~210 days; Accelerated: ~150 days [120] |
| Accelerated Programs | Fast Track, Breakthrough Therapy [120] | PRIME (PRIority MEdicines) [120] |
Bioequivalence Study Requirements and Guidelines
Bioequivalence (BE) studies are fundamental for generic drug approval and are also critical for certain changes to innovator products. Both the FDA and EMA require robust, well-designed BE studies to ensure therapeutic equivalence. The general principle is to demonstrate that the 90% confidence interval for the ratio of the mean values for the primary pharmacokinetic parameters (AUC and C~max~) of the test versus reference product falls within the acceptance range of 80.00% to 125.00% [106].
The landscape of BE guidance is currently evolving significantly with the ICH M13 harmonization effort. The ICH M13A guideline for immediate-release solid oral dosage forms is set to supersede applicable parts of existing EMA guidelines, with an effective date of January 25, 2025 [106]. This initiative aims to create global uniformity in BE study design and data analysis. The ICH M13 series is planned to have three parts, with M13A covering general study considerations and M13B providing recommendations on obtaining biowaivers for additional strengths of a drug product where in vivo BE has been demonstrated for at least one strength [122].
A biowaiver allows for the approval of a drug without conducting an in vivo BE study under specific conditions. According to the draft ICH M13B guideline, a biowaiver for an additional strength may be accepted if the following criteria are met [122]:
- Pharmacokinetic linearity (dose proportionality) of the drug substance.
- Qualitatively identical and quantitatively proportional composition across different strengths.
- Similar in vitro dissolution profiles between the strength for which in vivo BE was demonstrated and the strength for which a waiver is requested.
For natural bioactive compounds, which often have complex compositions and may not follow standard solubility and permeability rules, the Biopharmaceutics Classification System (BCS)-based biowaivers present additional challenges. Appendix III of the EMA's previous guideline on BCS-based biowaivers has already been superseded by the ICH M9 guideline [106].
Table 2: Key Bioequivalence and Biowaiver Considerations
| Aspect | FDA Approach | EMA/ICH Approach |
|---|---|---|
| Primary BE Criteria | 90% CI for AUC and C~max~ within 80.00-125.00% | 90% CI for AUC and C~max~ within 80.00-125.00% [106] |
| Key Guideline | FDA-specific guidances on BE | Transitioning to ICH M13A (effective Jan 2025) [106] |
| Additional Strength Biowaiver | Based on proportionality and dissolution [122] | ICH M13B criteria: proportionality, similar dissolution, PK linearity [122] |
| BCS-based Biowaiver | Available for BCS Class I and III drugs | Governed by ICH M9 guideline [106] |
Comparative Analysis: Synthetic vs. Natural Bioactive Compounds
The intrinsic structural and physicochemical differences between synthetic and natural bioactive compounds have direct implications for their bioequivalence assessment and regulatory strategy.
Structural and Physicochemical Properties
Cheminformatic analyses reveal that natural products (NPs) and natural product-derived drugs occupy a larger and more diverse region of chemical space compared to completely synthetic drugs (S) [37] [3]. NPs and their derivatives tend to have:
- Higher Molecular Complexity: Greater number of stereocenters and a higher fraction of sp3 carbons (Fsp3), which is correlated with improved clinical success [37].
- Distinct Ring Systems: More complex ring assemblies with a higher proportion of non-aromatic rings, compared to the synthetic compounds' prevalence of aromatic rings [3].
- Altered Physicochemical Properties: Lower hydrophobicity (LogP), increased polarity, and fewer aromatic rings on average [37].
These properties can significantly influence a compound's absorption, distribution, metabolism, and excretion (ADME) profile, which is central to bioequivalence. For instance, the higher molecular weight and complexity of some natural products may pose challenges for oral bioavailability, a key factor in BE study design.
Implications for Bioequivalence Testing
The structural differences necessitate careful consideration during study design:
- Analytical Methods: The complex structure of natural products may require more sophisticated bioanalytical methods (e.g., LC-MS/MS) for accurate quantification of the active moiety and its metabolites in plasma.
- Food-Effect Studies: Natural compounds, especially those derived from food sources, might be more susceptible to food effects, potentially requiring specific BE studies under fed conditions.
- Demanding Bioequivalence: For certain natural products with high intra-subject variability, more complex study designs (e.g, replicate designs) may be necessary to demonstrate BE.
The regulatory framework acknowledges some of these challenges. For example, the EMA advises that for generic products using a different salt form or different pH-modifying excipients than the reference product, an additional BE study with concomitant treatment with an acid-reducing agent might be needed to establish bioequivalence [121]. This is particularly relevant for natural bioactive compounds whose solubility can be pH-dependent.
Experimental Protocols for Bioequivalence Assessment
A standard bioequivalence study for an immediate-release oral dosage form is a critical experiment that must be meticulously designed and executed. The following protocol outlines the core methodology referenced by regulatory standards [106].
Study Design and Population
- Design: A single-dose, randomized, two-period, two-sequence crossover design is most common for non-replicate studies. A replicate design may be required for highly variable drugs.
- Subjects: Generally conducted in healthy adult volunteers of both sexes, typically 18-55 years old, with a body mass index within the normal range. The number of subjects should be sufficient to provide adequate statistical power, often 12-36 participants.
- Inclusion/Exclusion Criteria: Subjects should be in good general health as confirmed by medical history, physical examination, and laboratory tests. Key exclusion criteria include a history of hypersensitivity to the drug, significant medical illness, smoking, and use of any other medication within a specified period before the study.
Procedures and Dosing
- Fasting/Fed State: Studies are usually performed under fasting conditions unless the product label indicates it should be taken with food, in which case a fed study is also required.
- Dosing and Washout: In each period, subjects receive a single dose of either the test or reference product with 240 mL of water. There must be a sufficient washout period (typically >5 half-lives of the drug) between the two dosing periods to ensure no carryover effect.
- Blood Sampling: Serial blood samples (e.g., venous) are collected in appropriate anticoagulant-containing tubes at pre-dose and at multiple time points post-dose to adequately characterize the plasma concentration-time profile. The sampling schedule should continue for at least three terminal half-lives of the drug.
Bioanalytical and Statistical Analysis
- Sample Analysis: Plasma is separated by centrifugation and stored frozen until analysis. Concentrations of the analyte (parent drug and/or metabolites, as appropriate) are determined using a fully validated bioanalytical method (e.g., HPLC-MS/MS) that is specific, sensitive, accurate, and precise.
- Pharmacokinetic Analysis: Non-compartmental analysis is standard. Key parameters calculated for each subject in each period include:
- AUC~0-t~: Area under the plasma concentration-time curve from zero to the last measurable concentration.
- AUC~0-∞~: Area under the curve from zero to infinity.
- C~max~: Maximum observed plasma concentration.
- T~max~: Time to reach C~max~.
- Statistical Analysis: An analysis of variance (ANOVA) is performed on the log-transformed AUC and C~max~ data. Bioequivalence is concluded if the 90% confidence interval for the ratio (Test/Reference) of the geometric means for both AUC and C~max~ falls entirely within the acceptance range of 80.00% to 125.00%.
BE Study Workflow: This diagram illustrates the sequential workflow of a standard two-period crossover bioequivalence study, from protocol finalization to statistical conclusion.
Visualization of Regulatory Pathways
Navigating the regulatory requirements for drug approval involves understanding the distinct yet sometimes overlapping pathways of the FDA and EMA. The following diagram synthesizes the key stages and decision points for a new small molecule drug, highlighting areas where bioequivalence data are crucial.
Drug Approval Pathways: This diagram outlines the parallel regulatory pathways for innovative drugs at the FDA and EMA, with a highlighted path for products requiring bioequivalence data.
The Scientist's Toolkit: Essential Reagents and Materials
Successfully conducting research and development under FDA and EMA frameworks, particularly for bioequivalence studies on complex compounds, requires a suite of specialized reagents and analytical solutions.
Table 3: Essential Research Reagent Solutions for Bioequivalence and Compound Analysis
| Reagent/Material | Primary Function | Application Context |
|---|---|---|
| Validated Bioanalytical Standards | Certified reference standards of the active pharmaceutical ingredient (API) and major metabolites for instrument calibration and method validation. | Quantifying drug concentrations in biological matrices (e.g., plasma) during PK studies for both synthetic and natural compounds [106]. |
| Stable Isotope-Labeled Internal Standards | (e.g., ^2^H, ^13^C-labeled analogs of the analyte) used to correct for matrix effects and variability in sample preparation and ionization in MS. | Essential for achieving the high precision and accuracy required for LC-MS/MS bioanalysis in BE studies [106]. |
| BCS Classification Kit | Standardized buffers and reagents for determining solubility and permeability, the key parameters for the Biopharmaceutics Classification System. | Assessing potential for BCS-based biowaivers, particularly challenging for natural products with complex chemistry [106]. |
| In Vitro Dissolution Apparatus | USP-compliant apparatus (e.g., baskets, paddles) and physiologically-relevant dissolution media (e.g., SGF, SIF). | Comparing dissolution profiles of test and reference products; critical for supporting biowaivers for additional strengths [122]. |
| HPLC/MS-MS Grade Solvents | Ultra-pure solvents (acetonitrile, methanol, water) with minimal impurities to prevent background noise and ion suppression. | Critical for robust and sensitive bioanalytical method performance during high-throughput sample analysis [106]. |
| Solid Phase Extraction (SPE) Cartridges | Chromatographic sorbents for selective extraction and purification of the analyte from complex biological samples like plasma. | Cleaning up samples to reduce matrix interference and improve the sensitivity and reliability of the analytical assay. |
The regulatory landscapes of the FDA and EMA, while distinct in structure and process, are converging on key scientific principles for demonstrating bioequivalence, as evidenced by the ICH M13 initiative [106] [122]. For researchers and drug development professionals, a deep understanding of both the commonalities and differences—such as the FDA's typically faster review timelines versus the EMA's multi-state coordination—is indispensable for strategic global planning [120].
The journey of a drug from concept to market is further complicated by the fundamental chemical differences between synthetic and natural bioactive compounds. Natural products offer unparalleled chemical diversity and have been the origin of nearly half of all small-molecule drugs [37]. However, their structural complexity, including greater molecular size, stereochemical content, and distinct ring systems, presents unique challenges for bioequivalence assessment [37] [3]. Mastering the interplay between compound characteristics and regulatory requirements, as detailed in this guide, empowers scientists to design more efficient development programs, leverage opportunities like biowaivers where appropriate, and ultimately accelerate the delivery of safe and effective therapies, whether synthetic or natural in origin, to patients worldwide.
Totality of Evidence Approach for Biosimilar Assessment
The totality of evidence approach represents the cornerstone regulatory and scientific framework for demonstrating that a biosimilar is highly similar to an approved reference product and has no clinically meaningful differences in terms of safety, purity, and potency [123] [124]. This comprehensive approach stands in stark contrast to the requirements for generic small-molecule drugs, reflecting the inherent complexity of biological medicines derived from living organisms [125]. Unlike generics, which must demonstrate bioequivalence through pharmaceutical equivalence and comparable pharmacokinetics, biosimilars are not exact replicas of their reference products but are instead highly similar versions that may have minor differences in clinically inactive components [124].
The foundation of this approach rests on a stepwise development process that begins with extensive analytical characterization and progresses through functional assays, nonclinical assessments, and targeted clinical studies [124]. Each step builds upon the previous one, with the goal of resolving any residual uncertainty about biosimilarity before advancing to the next phase [126]. This systematic framework acknowledges that "the process is the product" – meaning the specific manufacturing process defines the characteristics of a biologic, and biosimilar developers must reverse-engineer this process without access to the innovator's proprietary knowledge [125]. The totality of evidence approach has become increasingly refined as regulatory experience with biosimilars has grown, with recent expert consensus highlighting opportunities to streamline requirements further based on advancing analytical capabilities [127].
Analytical Characterization: The Foundation of Biosimilarity
Comprehensive Structural and Functional Analysis
Analytical studies form the cornerstone of the totality of evidence approach, providing the most sensitive assessment of similarity between a proposed biosimilar and its reference product [124]. These studies employ state-of-the-art technologies to characterize the structural and functional properties of both products in exquisite detail, with the understanding that "the analytical package serves as the foundation for the entire biosimilar development program" [126]. The goal is to demonstrate that the biosimilar falls within the quality range of the reference product, which itself may exhibit some batch-to-batch variability [126].
The analytical characterization encompasses multiple tiers of assessment, beginning with primary structure analysis and progressing through higher-order structure, post-translational modifications, and biological activity [123]. For the biosimilar AVT02 (an adalimumab biosimilar), analytical similarity assessments using mass spectrometry methods demonstrated an identical amino acid sequence to the reference product (Humira), along with high similarity in primary structure, post-translational modifications, and higher-order structural attributes [123]. Minor differences in some physiochemical attributes were noted but were determined not to impact biological activity or clinical performance [123].
Tiered Approach to Quality Attributes
A critical component of the analytical assessment is the classification of quality attributes based on their potential impact on safety and efficacy [126]. This risk-based approach categorizes attributes into three tiers:
- Tier 1: Attributes with known clinical relevance that are quantitatively compared using statistical equivalence testing
- Tier 2: Attributes with potential clinical impact that are evaluated using quality range approaches
- Tier 3: Attributes with lower risk that are assessed for visual similarity [126]
This tiered strategy ensures that resources are focused on the attributes most likely to impact clinical performance, while still providing comprehensive characterization of the entire molecule.
Table 1: Key Analytical Techniques in Biosimilar Assessment
| Analytical Category | Specific Methods | Parameters Assessed |
|---|---|---|
| Structural Characterization | Electrospray ionization mass spectrometry (ESI-MS), Circular dichroism, Nuclear magnetic resonance | Primary structure, higher-order structure, amino acid sequence |
| Physicochemical Properties | High-performance liquid chromatography, Capillary electrophoresis, Size-exclusion chromatography | Purity, molecular size, charge variants, aggregation |
| Functional Assays | Cell-based potency assays, Binding assays (ELISA, Surface plasmon resonance) | Mechanism of action, target binding, Fc receptor binding |
| Post-translational Modifications | Liquid chromatography-mass spectrometry, Glycan analysis | Glycosylation patterns, oxidation, deamidation |
Fingerprint-Like Similarity and Critical Quality Attributes
The concept of "fingerprint-like similarity" has emerged as an advanced approach to analytical comparison, representing the highest level of similarity achievable through state-of-the-art analytical techniques [126]. This approach utilizes the entire domain of each analytical technique to create a comprehensive multivariate assessment of similarity, going beyond individual quality attributes to evaluate the overall pattern of characteristics [126]. When fingerprint-like similarity is established across multiple orthogonal analytical methods, it provides powerful evidence that any remaining structural differences are unlikely to translate to clinical differences.
The identification of critical quality attributes is essential for focusing the comparative assessment on the characteristics most relevant to clinical performance [124]. These attributes are determined based on their potential impact on pharmacokinetics, pharmacodynamics, efficacy, and immunogenicity. For monoclonal antibodies like adalimumab, critical quality attributes typically include binding affinity to the target antigen, Fc receptor binding, complement-dependent cytotoxicity, antibody-dependent cell-mediated cytotoxicity, and glycosylation patterns [123] [124].
Clinical Development in Biosimilar Assessment
Stepwise Clinical Evaluation
The clinical development program for a biosimilar serves a fundamentally different purpose than that for a novel biologic. Rather than establishing standalone efficacy and safety, the goal is to confirm the absence of clinically meaningful differences between the biosimilar and reference product [124]. This confirmatory role means that the clinical program can be more targeted and efficient, building on the extensive analytical characterization that forms the foundation of the development program [123].
The clinical component typically progresses through three phases: pharmacokinetic studies, pharmacodynamic studies (when relevant biomarkers exist), and comparative clinical efficacy and safety studies [127]. The design of each phase is optimized to detect potential differences, with studies typically conducted in the most sensitive patient populations and using the most sensitive endpoints [124]. This approach maximizes the ability to identify any clinically meaningful differences should they exist, while minimizing unnecessary duplication of studies across multiple indications.
Clinical Study Design Considerations
Pharmacokinetic studies for biosimilars are typically conducted in healthy volunteers where feasible, as these populations provide less variable exposure data and are more sensitive for detecting potential differences [123] [124]. When healthy volunteers are not appropriate (e.g., for immunogenic products), patient populations are used instead. These studies employ highly sensitive designs to demonstrate equivalent exposure between the biosimilar and reference product.
Comparative clinical efficacy studies are typically conducted in one of the approved indications, selected based on sensitivity to detect potential differences in efficacy and safety [124]. For AVT02, the confirmatory clinical study was conducted in patients with moderate-to-severe chronic plaque psoriasis, which provided a sensitive model for detecting potential differences in clinical response [123]. These studies generally use equivalence margins that are clinically justified and sensitive enough to detect meaningful differences.
Table 2: Clinical Development Strategy for Biosimilars
| Study Type | Typical Design | Primary Endpoints | Purpose in Totality of Evidence |
|---|---|---|---|
| Pharmacokinetic Study | Randomized, single-dose or steady-state crossover or parallel design | AUC, Cmax | Demonstrate equivalent exposure between biosimilar and reference |
| Pharmacodynamic Study | Randomized, parallel design (when relevant biomarkers exist) | Biomarker response | Confirm similar biological effect on relevant pathway |
| Comparative Efficacy Study | Randomized, double-blind, parallel-group in sensitive indication | Clinical efficacy endpoint appropriate to indication | Confirm similar clinical effect and safety profile |
| Immunogenicity Assessment | Integrated throughout clinical program | Incidence and titer of anti-drug antibodies | Evaluate potential differences in immune response |
Extrapolation of Indications
A scientifically rigorous extrapolation process allows biosimilars to be approved for all indications of the reference product without conducting clinical trials in each individual condition [123]. This principle is supported by the understanding that the mechanism of action is fundamentally similar across indications when the same molecular entity is involved [124]. The justification for extrapolation rests on comprehensive analytical and functional data demonstrating similar mechanisms of action, along with clinical data in at least one indication that confirms similar clinical performance [123].
For AVT02, the demonstration of similar physicochemical properties, functional activities, and clinical performance in chronic plaque psoriasis supported extrapolation to all approved indications of the reference product, including rheumatoid arthritis, Crohn's disease, and other immune-mediated inflammatory conditions [123]. The scientific rationale for extrapolation must address the comparability of mechanism of action across indications and the potential relevance of any minor structural differences to each specific disease condition [124].
Regulatory Framework and Global Perspectives
Evolution of Regulatory Guidelines
The regulatory pathway for biosimilars was pioneered by the European Medicines Agency, which established the first comprehensive framework in 2004 [127]. This was followed by pathways in other jurisdictions, including Japan, the United States, and through the World Health Organization for global standards [127]. While each regulatory authority has its specific requirements, there is notable alignment in the fundamental scientific principles for establishing biosimilarity [127].
Recent years have seen significant evolution in regulatory thinking as experience with biosimilars has accumulated. There is growing recognition that analytical techniques have advanced to the point where they can detect extremely subtle differences, challenging the traditional role of comparative clinical efficacy studies [127] [125]. This has led to discussions about potentially streamlining requirements, with expert consensus increasingly questioning the necessity of comparative clinical efficacy studies when extensive analytical and functional similarity has been demonstrated [127].
Expert Consensus and Future Directions
A recent study employing a modified Nominal Group Technique with international regulators, academics, and industry representatives identified 16 high-consensus recommendations for streamlining biosimilar development [127]. The highest-rated recommendations included:
- Enhancing stakeholder education on science-based biosimilarity principles
- Promoting regulatory convergence through reliance mechanisms
- Reconsidering the requirement for comparative clinical efficacy studies
- Harmonizing reference product selection criteria globally
- Eliminating in vivo animal studies when scientifically justified [127]
These recommendations reflect a growing consensus that regulatory requirements should align more closely with current scientific knowledge and technological capabilities, potentially reducing development costs and timelines while maintaining the rigorous standards necessary to ensure patient safety [127].
Experimental Protocols and Methodologies
Analytical Similarity Assessment Protocol
The protocol for analytical similarity assessment follows a systematic approach to compare critical quality attributes of the biosimilar and reference product. For AVT02, this involved:
Primary Structure Analysis: Using mass spectrometry methods to confirm identical amino acid sequence and characterize post-translational modifications [123]
Higher-Order Structure Assessment: Employing techniques such as circular dichroism and nuclear magnetic resonance to evaluate secondary and tertiary structure [123]
Functional Characterization: Conducting cell-based bioassays to measure potency and binding assays to assess target engagement [123]
Purity and Impurity Profiling: Implementing chromatographic methods to quantify product-related substances and process-related impurities [126]
This comprehensive analytical package typically involves dozens of orthogonal methods capable of detecting subtle differences in product quality attributes. The results are evaluated using a tiered approach that applies appropriate statistical methods based on the criticality of each attribute [126].
Clinical Pharmacokinetic Study Protocol
The clinical pharmacokinetic study for a biosimilar follows a standardized protocol:
Study Design: Randomized, single-dose, crossover or parallel group design depending on the product characteristics [124]
Population: Healthy volunteers or patients, selected based on sensitivity to detect differences and immunogenicity risk [123]
Dosing: Single dose administered via the approved route, typically using the most sensitive dose for detecting differences [124]
Sampling: Intensive blood sampling over an appropriate time period to fully characterize the concentration-time profile [124]
Endpoints: Primary endpoints including AUC and Cmax, with predefined equivalence margins [124]
Immunogenicity Assessment: Monitoring for anti-drug antibodies throughout the study period [124]
This design maximizes the sensitivity for detecting potential differences in exposure between the biosimilar and reference product while controlling for variability.
Visualization of Biosimilar Development Pathway
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Tools for Biosimilar Assessment
| Research Tool Category | Specific Examples | Application in Biosimilar Development |
|---|---|---|
| Reference Standard | Innovator biologic from licensed source | Serves as benchmark for all comparative assessments |
| Cell-Based Assay Systems | Reporter gene assays, Primary cell cultures | Evaluate mechanism of action and biological activity |
| Binding Assay Reagents | Recombinant targets, Anti-idiotypic antibodies | Quantify target binding affinity and kinetics |
| Mass Spectrometry Kits | Trypsin digestion kits, Glycan labeling reagents | Characterize primary structure and post-translational modifications |
| Chromatography Columns | Size-exclusion, Ion-exchange, Reverse-phase columns | Separate and quantify product variants and impurities |
| Immunogenicity Reagents | Anti-drug antibody standards, Bridging ELISA components | Assess potential for unwanted immune responses |
The totality of evidence approach represents a scientifically rigorous framework that has successfully enabled the development and approval of biosimilars worldwide, increasing patient access to critical biologic therapies [123] [127]. This approach continues to evolve as analytical technologies advance and regulatory experience grows, with an increasing emphasis on the foundational analytical and functional comparisons that form the basis of biosimilarity [126] [125]. The future of biosimilar development will likely see further refinement of these requirements, potentially reducing the need for comparative clinical efficacy studies when state-of-the-art analytical techniques demonstrate fingerprint-like similarity [127]. This evolution promises to make biosimilar development more efficient while maintaining the rigorous standards necessary to ensure patient safety, ultimately benefiting healthcare systems and patients through increased access to affordable biologic therapies.
For researchers evaluating the bioequivalence of synthetic and natural bioactive compounds, pharmacokinetic (PK) data—which measures what the body does to a drug—has traditionally been the cornerstone of regulatory assessment. PK studies quantify the absorption, distribution, metabolism, and excretion of a compound, providing essential data on its concentration in biological fluids over time [128]. However, equivalent PK profiles between two compounds do not automatically guarantee equivalent biological effects. This is where pharmacodynamic (PD) endpoints become indispensable. PD measures what the drug does to the body, examining the biochemical and physiological effects of a compound, including receptor binding, downstream signaling, and ultimate therapeutic outcomes [128].
The limitation of relying solely on PK data is particularly pronounced when comparing natural bioactive compounds with their synthetic analogues or when evaluating complex multi-component formulations. Natural products often contain mixtures of active constituents, possess non-linear pharmacokinetics, or act through multiple simultaneous mechanisms that are not fully captured by measuring plasma concentrations alone [46] [4]. This article provides a comparative guide for researchers on the application of PD endpoints to demonstrate bioequivalence when PK parameters provide an incomplete picture of therapeutic equivalence.
The Scientific Rationale for PD Endpoints
The Hierarchy of Pharmacodynamic Effects
Clinical PD assessment provides evidence of a compound's mechanism of action (MOA) through a sequence of measurable biological events. Understanding this hierarchy is crucial for selecting appropriate PD endpoints [129] [130]:
- Primary (1°) PD Effects: The initial action of a drug on its biological target, providing proof of target engagement (e.g., reversible inhibition of Bcr-Abl kinase activity by imatinib) [129].
- Secondary (2°) PD Effects: Biochemical changes occurring immediately downstream of the intended molecular target (e.g., reduction in phospho-ERK levels after inhibition of Raf kinase activity) [129].
- Tertiary (3°) PD Effects: Subsequent cell biological or physiological responses (e.g., effects on cell cycle progression, apoptosis, or tumor shrinkage) [129].
When PK-PD Relationships Break Down
Several scenarios in natural and synthetic product development necessitate PD endpoints to establish true bioequivalence:
- Complex Mechanisms of Action: Natural products like curcumin and its synthetic analogue (2E,6E)-2,6-bis(2,3-dimethoxybenzylidine) cyclohexanone (DMCH) demonstrate different biological effects despite structural similarities. DMCH showed superior apoptosis induction in colon cancer cells compared to the parent compound, an important therapeutic difference not discernible through PK metrics alone [131].
- Non-Linear Tissue Distribution: A compound may achieve equivalent plasma concentrations but differ significantly in tissue penetration, particularly across challenging barriers like the blood-brain barrier [132].
- Prodrug Activation: Compounds requiring metabolic activation may show PK equivalence of the parent drug but differences in the formation and activity of active metabolites.
- Multi-Component Actions: Natural extracts like fermented garlic extract demonstrate vascular effects through nitrite conversion to nitric oxide, a complex mechanism requiring functional PD measurements of blood flow and blood pressure rather than mere concentration data [46].
Table 1: Scenarios Requiring PD Endpoints for Complete Bioequivalence Assessment
| Scenario | PK Limitation | Recommended PD Endpoint | Example |
|---|---|---|---|
| Complex Natural Formulations | Multiple active constituents with synergistic effects | Functional response biomarkers | Fermented garlic extract effects on cerebral blood flow [46] |
| Synthetic Analogues of Natural Products | Similar PK but different target potency | Target engagement markers | DMCH vs. curcumin apoptosis induction in colon cancer [131] |
| Compounds with Active Metabolites | Parent drug PK may not reflect active metabolite levels | Downstream pathway modulation | Hesperetin metabolite effects on skin blood flow [46] |
| Enzyme-Targeting Therapies | Substrate depletion not reflected in drug levels | Enzyme activity and substrate levels | L-glutaminase depletion of L-glutamine in cancer cells [131] |
Comparative Experimental Data: Natural vs Synthetic Bioactives
Direct Comparative Studies with PK/PD Correlations
Rigorous clinical trials increasingly incorporate both PK and PD endpoints to provide a more complete assessment of bioequivalence, particularly for natural products and their synthetic counterparts.
Table 2: Comparative PK/PD Profiles of Natural Products and Synthetic Analogues
| Compound Pair | PK Findings | PD Findings | Clinical Implications |
|---|---|---|---|
| Chitosan vs. Biofermentation-derived Glucosamine [46] | Met bioequivalence standards; differed in mean peak plasma concentration (Cmax) ratios | Equivalent therapeutic effects for osteoarthritis | Biofermentation-derived glucosamine represents a sustainable alternative |
| Curcumin vs. Synthetic DMCH [131] | Low bioavailability of curcumin; improved properties of DMCH | DMCH more effective in inducing apoptosis in colon cancer cells | Synthetic optimization overcame natural compound limitations |
| Hesperetin vs. HEPT7G/βCD complex [46] | Improved solubility with β-cyclodextrin complex | Significant increase in skin blood flow; restoration of peripheral skin temperature | Enhanced functional activity through synthetic modification |
| Thymol vs. Acetic Acid Thymol Ester [131] | Hydrophilic derivatives with improved cell permeability | Enhanced cytotoxic activity on colorectal cancer cells | Synthetic modification addressed bioavailability limitations |
Natural Products with In Vitro PD Evidence
Many natural compounds demonstrate compelling PD effects in preclinical models, providing a foundation for future comparative bioequivalence studies:
- Lesbicoumestan: Isolated from Lespedeza bicolor, this compound induced degradation of MALT1 protease and inhibited the NF-κB signaling pathway, demonstrating potent antileukemia activity in Jurkat cell models [131].
- Hirsutenone: A diarylheptanoid from Alnus sibirica showing significant NF-κB inhibitory ability and potent apoptosis induction in prostate cancer cell lines [131].
- Terretonin N and Butyrolactone I: Metabolites from the fungus Aspergillus terreus TM8 that promoted apoptosis in human prostate and ovarian cancer cells [131].
- Propionic Acid: A short-chain fatty acid produced by gut microbiota that suppressed cervical cancer cell viability by triggering both apoptosis and autophagy [131].
Essential Methodologies for PD Endpoint Analysis
Proof-of-Mechanism Studies in Early Clinical Development
Confirming a compound's mechanism of action in human subjects represents the foundational application of clinical PD assessment. Well-designed proof-of-mechanism studies incorporate several critical methodologies [129] [130]:
- Temporal PD Sampling: Measuring biomarker responses at multiple time points after compound administration to establish the duration of target modulation.
- Dose-Response Relationships: Correlating increasing dose levels with magnitude of PD effect to establish a therapeutic window.
- Tissue-Based Biomarkers: When possible, obtaining diseased tissue (e.g., tumor biopsies) to demonstrate direct target engagement in the relevant tissue compartment.
- Surrogate Tissue Analysis: When target tissue is inaccessible, identifying surrogate tissues (e.g., peripheral blood mononuclear cells) that may reflect PD activity in target tissues.
Advanced Analytical Technologies for PD Biomarker Assessment
Modern PD studies employ sophisticated analytical platforms to quantify biomarker responses with high sensitivity and specificity:
- Liquid Chromatography-Mass Spectrometry (LC-MS): Provides highly sensitive quantification of drug metabolites, protein phosphorylation, and other molecular PD biomarkers [4].
- Immunohistochemistry/Iimmunofluorescence: Enables spatial resolution of target engagement and modulation within tissue architecture, particularly valuable for tissue-based PD studies [130].
- Flow Cytometry: Permits single-cell analysis of PD responses in complex cell populations, especially valuable for immunomodulatory compounds [128].
- Molecular Imaging Techniques: Non-invasive methods like PET imaging can quantify target engagement in real-time in living subjects [130].
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Essential Research Tools for PD Endpoint Analysis
| Tool Category | Specific Technologies/Platforms | Research Application | Key Providers |
|---|---|---|---|
| PBPK/PBBM Modeling Software | GastroPlus X, Simcyp Simulator | Virtual prediction of human bioequivalence; simulation of drug absorption, distribution, metabolism [133] | Certara, Simulations Plus [133] |
| Bioanalytical Platforms | LC-MS Systems, Immunoassay Platforms | Quantification of drug concentrations, metabolite profiles, and protein biomarkers [128] [4] | Thermo Fisher Scientific [133] |
| Clinical PD Assay Services | GLP/GCP-compliant biomarker analysis | Regulatory-grade PD endpoint measurement across multiple matrices (serum, plasma, tissue) [128] | BioAgilytix, IQVIA, ICON plc [128] [134] |
| Biospecimen Procurement | Annotated clinical samples with PD data | Access to well-characterized human samples for biomarker validation [129] | Labcorp Drug Development, Charles River Laboratories [134] |
Regulatory and Practical Implementation Framework
Integrating PD Endpoints into Clinical Trial Design
Successful incorporation of PD biomarkers into bioequivalence studies requires strategic planning throughout the clinical development pipeline [130]:
- Phase 0 Trials: Utilize exploratory IND mechanisms to conduct microdose studies that provide early human PK and PD data, confirming target engagement before committing to large trials [130].
- Phase I Trials: Combine traditional safety assessment with PD biomarker measurements to identify the biologically effective dose (BED) rather than relying solely on the maximum tolerated dose (MTD) [130].
- Phase II/III Trials: Incorporate PD biomarkers as secondary endpoints to correlate target modulation with clinical efficacy, providing critical proof-of-concept data [130].
Navigating Regulatory Considerations
Global regulatory agencies have established frameworks for employing PD endpoints in bioequivalence assessments:
- FDA and EMA Guidance: Regulatory bodies increasingly accept model-informed drug development approaches, including PBPK modeling and simulation, to support bioequivalence determinations [133].
- Biomarker Qualification Programs: Regulatory pathways exist for qualification of PD biomarkers for specific contexts of use, enhancing their regulatory utility [130].
- The Biopharmaceutics Classification System (BCS): Provides a framework for biowaivers based on drug solubility and permeability characteristics, potentially reducing the need for in vivo studies in certain cases [69].
For researchers comparing synthetic and natural bioactive compounds, comprehensive bioequivalence assessment requires moving beyond traditional PK metrics to incorporate robust PD endpoints. The complex mechanisms of natural products, the subtle pharmacological differences between structural analogues, and the multi-faceted actions of complex formulations demand functional assessment of biological activity. By implementing the methodologies, technologies, and regulatory strategies outlined in this guide, researchers can generate more scientifically rigorous and clinically relevant evidence of therapeutic equivalence, ultimately ensuring that bioequivalent products deliver equivalent health outcomes.
The implementation of mandatory bioequivalence (BE) testing in China in 2016 represents a transformative regulatory intervention for the world's second-largest pharmaceutical market, which is dominated by generic drugs accounting for approximately 95% of its share [135]. This policy change occurred within a broader paradigm shift in China's pharmaceutical governance, transitioning from a traditional "command-control" model toward a comprehensive "lifecycle regulation" approach that balances drug safety, innovation, and accessibility [136]. For researchers investigating natural versus synthetic bioactive compounds, these regulatory developments establish a critical framework for validating the therapeutic equivalence and quality of generic products derived from both sources.
This article examines the impact of China's bioequivalence regulations through a scientific lens, providing comparative experimental data and methodologies relevant to drug development professionals. We objectively analyze the policy's effect on pharmaceutical firm behavior, research and development (R&D) investment, and resulting outcomes, while placing these findings within the broader context of global regulatory trends. The evidence demonstrates that regulatory mandates can significantly drive quality improvement in generic drugs, though with notable heterogeneity in implementation capacity across different types of firms and regions.
China's Regulatory Evolution and Bioequivalence Policy Framework
Historical Context and Regulatory Transformation
China's pharmaceutical regulatory system has evolved through four distinct phases [136]:
- Emergence (1949–1984): Characterized by reactive narcotics control and fragmented administrative decrees.
- Foundational (1985–2000): Marked by the first Drug Administration Law (1985) criminalizing counterfeit drugs and codifying production standards.
- Deepening Reform (2001–2018): Catalyzed by quality scandals and culminating in the 2016 announcement of mandatory BE testing.
- Lifecycle Regulation (2019–present): Institutionalized through the revised Drug Administration Law (2019) emphasizing proactive, risk-based oversight from R&D to post-market surveillance.
Prior to 2016, generic drugs in China faced weak regulatory oversight with no mandatory requirement for bioequivalence testing against innovator products, raising significant concerns about therapeutic effectiveness and patient safety [135]. The 2016 policy implemented a "stick-and-carrot" approach, requiring all generic oral drugs listed in the National Essential Medicine List and approved before 2007 (the "289 drug list") to successfully complete BE tests by 2018, while offering financial incentives and procurement priority for compliant firms [135].
Integration with Global Standards
Concurrently with domestic reforms, China's National Medical Products Administration (NMPA) has increasingly aligned with international standards, joining the International Council for Harmonisation (ICH) in 2017 and updating clinical pharmacology guidances to mirror those of the FDA and EMA [137]. This harmonization is particularly relevant for bioactive compound research, as it establishes consistent evidentiary requirements for both synthetic and natural product-derived therapeutics seeking market approval.
Table 1: Key Milestones in China's Pharmaceutical Regulatory Evolution
| Year | Regulatory Milestone | Significance for Bioequivalence & Drug Quality |
|---|---|---|
| 2015 | "Opinions on the Reform of Review and Approval Process for Drugs and Medical Devices" [138] | Initiated review process reforms reducing backlogs and encouraging innovation |
| 2016 | Announcement of mandatory bioequivalence testing [135] | Required generic drugs to pass BE tests against innovator reference products |
| 2017 | China joins ICH [137] | Began alignment of technical requirements with international standards |
| 2019 | Revised Drug Administration Law [136] | Institutionalized lifecycle regulation and risk-based oversight |
| 2019 | Vaccine Management Law [136] | Established end-to-end oversight for biological products |
| 2020 | Criminal Law Amendment (XI) [136] | Enhanced penalties for substandard and counterfeit drugs |
Impact Analysis: Quantitative Evidence from Regulation Implementation
Firm-Level Responses and R&D Investments
Empirical evidence from 122 publicly listed pharmaceutical firms in China reveals substantial behavioral changes following the regulatory mandate. Employing a difference-in-differences approach to analyze data from 2012-2022, researchers found that firms responded to the new regulations by significantly increasing their R&D investments by 20.7% on average [135]. This increased investment translated into tangible outputs, with the quality regulation leading to an average of 2.5 bioequivalence approvals per firm annually [135].
The policy impact, however, displayed significant heterogeneity across firm types. Larger firms and those with higher pre-regulation R&D capacity demonstrated greater increases in R&D investments and higher success rates in passing bioequivalence tests [135]. This variability suggests that regulatory mandates alone may be insufficient to ensure uniform quality improvement across the entire pharmaceutical sector, particularly for smaller firms with constrained resources and technical capabilities.
Table 2: Differential Impact of BE Regulations Across Firm Types
| Firm Characteristic | Impact on R&D Investment | Success in BE Test Approvals | Key Findings |
|---|---|---|---|
| Overall | Increased by 20.7% [135] | 2.5 approvals per firm annually [135] | Positive response to regulatory mandate |
| Large Firms | Greater increase [135] | Higher success rate [135] | Better resource capacity for compliance |
| High Pre-existing R&D Capacity | Greater increase [135] | Higher success rate [135] | Existing infrastructure accelerated adaptation |
| Firms in Wealthier Provinces | Greater increase [135] | Higher success rate [135] | Regional disparities in implementation |
| Private Companies | Typically higher R&D investment than SOEs [135] | Similar total number of successful BE tests as SOEs [135] | Different pathways to compliance |
Compliance Patterns and Strategic Prioritization
Analysis at the drug type level indicates that pharmaceutical firms strategically prioritized bioequivalence testing compliance based on regulatory deadlines and market potential [135]. Drugs facing stricter regulatory deadlines (such as the 289 drug type list requiring completion by 2018) or those with potentially higher economic returns (such as drug types prioritized for national procurement) received earlier attention and resources [135].
Despite these strategic efforts, completion rates remain incomplete. For drugs required to pass bioequivalence by 2018, only approximately half of the drug types had any generic drugs that passed the test [135]. This partial compliance underscores the implementation challenges of regulatory reforms, even when accompanied by incentives and deadlines.
Methodological Framework: Bioequivalence Assessment for Bioactive Compounds
Fundamental Principles and Regulatory Standards
Bioequivalence assessment provides the scientific foundation for establishing therapeutic equivalence between generic and reference products. According to regulatory definitions, bioavailability (BA) refers to "the rate and extent to which the active compound is absorbed from a drug and becomes available to the body," while bioequivalence (BE) represents "the absence of a significant difference in the rate and extent to which the active ingredient in an experimental drug and reference drug becomes available at the target site when administered at the same molar dose under similar conditions" [139].
The standard BE trial employs a randomized, crossover design with appropriate washout periods (typically at least 5 elimination half-lives) to ensure drug concentrations fall below the lower limit of quantification before administering the next treatment [139]. This design enables researchers to distinguish compound effects from other variables, providing robust evidence of therapeutic equivalence.
Core Pharmacokinetic Parameters and Statistical Criteria
Bioequivalence determination relies primarily on three pharmacokinetic parameters [139]:
- AUC (Area Under the Concentration-time curve): Reflects the total extent of drug exposure
- Cmax (Maximum Concentration): Indicates the peak concentration influenced by absorption rate
- Tmax (Time to Maximum Concentration): Represents the time taken to reach maximum concentration
For both the US FDA and EU EMA, two generic and reference drugs are considered bioequivalent when the 90% confidence interval (CI) for the log-transformed ratio of exposure measures (Cmax and AUC) falls entirely within the range of 80% to 125% [139]. This statistical standard ensures that differences in systemic exposure between generic and reference products do not exceed 20%, maintaining therapeutic equivalence.
Diagram 1: Bioequivalence Statistical Decision Pathway. This flowchart illustrates the key statistical decision process for establishing bioequivalence according to international regulatory standards.
Special Considerations for Natural vs. Synthetic Compounds
The evaluation of bioequivalence for natural bioactive compounds presents unique methodological challenges compared to synthetic chemicals. Natural products often contain complex mixtures of active constituents, potentially multiple mechanisms of action, and varying phytochemical profiles based on growing conditions, extraction methods, and processing techniques [46] [4]. These factors complicate the identification of appropriate biomarkers for pharmacokinetic studies and may necessitate additional evidence beyond standard BE parameters.
For instance, research on fermented garlic extract (FGE) has demonstrated enhanced vascular function through increased bioavailability of vascular nitric oxide, requiring specialized assessment of hemodynamic parameters beyond conventional pharmacokinetic measurements [46]. Similarly, studies on green tea bioactive compounds have evaluated effects on hormonal fluctuations and inflammatory markers in postmenopausal women, necessitating expanded endpoint selection [46].
Experimental Protocols for Bioequivalence Assessment
Standardized Clinical Trial Design
The following protocol outlines the core methodology for conducting bioequivalence studies compliant with international regulatory standards [139]:
Objective: To demonstrate bioequivalence between a test (generic) product and reference (innovator) product.
Design: Randomized, single-dose, laboratory-blinded, two-period, two-sequence crossover study with adequate washout period.
Participants:
- Healthy adult volunteers (typically 18-55 years)
- BMI between 18.5 and 30 kg/m²
- Normal health status confirmed by medical history, physical examination, and laboratory tests
- Sample size determined by statistical power calculation, accounting for potential dropouts
Procedures:
- Screening (Day -28 to -2): Informed consent, eligibility assessment
- Baseline (Day -1): Admission to clinical facility, standardization of diet and activity
- Treatment Period 1 (Day 1): Overnight fasting, administration of reference or test product with 240mL water, standardized meals throughout confinement period
- Washout Period: Based on 5 elimination half-lives (typically 5-10 days)
- Treatment Period 2 (Day n): Administration of alternate product following identical procedures
Blood Sampling:
- Pre-dose (0 hour)
- Multiple post-dose collections (e.g., 0.25, 0.5, 0.75, 1, 1.5, 2, 2.5, 3, 4, 5, 6, 8, 10, 12, 14, 16, 24, 36, 48 hours) based on drug pharmacokinetics
- Samples collected in appropriate anticoagulant tubes, processed to plasma, and stored at -70°C until analysis
Bioanalytical Method:
- Validated LC-MS/MS or HPLC method per FDA/EMA/NMPA guidelines
- Demonstration of specificity, sensitivity, linearity, accuracy, precision, and stability
Statistical Analysis:
- ANOVA on log-transformed AUC0-t, AUC0-∞, and Cmax
- Calculation of 90% geometric confidence intervals for test/reference ratios
- Bioequivalence concluded if 90% CIs for AUC and Cmax fall within 80-125%
Natural Product-Specific Methodological Adaptations
Research on natural bioactive compounds often requires methodological adaptations to account for their unique properties [46] [4]:
Multicomponent Analysis:
- Simultaneous quantification of multiple active constituents and metabolites
- Characterization of pharmacokinetic profiles for key marker compounds
- Assessment of potential synergistic effects
Specialized Endpoints:
- Functional biomarkers relevant to mechanism of action (e.g., antioxidant capacity, inflammatory markers)
- Metabolomic profiling to capture comprehensive bioavailability
- Pharmacodynamic measurements complementing pharmacokinetic data
Comparative Study Examples:
- Fermented Garlic Extract: Evaluation of blood pressure, carotid artery velocity, regional cerebral blood flow, and body surface temperature alongside nitrite bioavailability [46]
- Green Tea Bioactives: Assessment of depression scales, hormonal levels, and inflammatory indices in addition to catechins pharmacokinetics [46]
- Glucosamine Formulations: Comparison of pharmacokinetic parameters between chitosan-derived and biofermentation-derived glucosamine in osteoarthritis patients [46]
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Essential Research Reagents and Materials for Bioequivalence Studies
| Reagent/Material | Function in BE Research | Application Notes |
|---|---|---|
| Reference Standard | Provides comparator for BE assessment | Must be innovator product with verified quality and storage conditions |
| Analytical Reference Standards | Enables quantification of active compounds and metabolites | Certified purity with proper documentation for regulatory compliance |
| LC-MS/MS System | Gold standard for bioanalytical quantification of drugs in biological matrices | Requires full validation per FDA/EMA/NMPA guidelines |
| Stable Isotope-Labeled Internal Standards | Compensates for matrix effects and extraction efficiency variations in mass spectrometry | Essential for accurate bioanalytical quantification |
| Validated Bioanalytical Method | Ensures reliable, reproducible quantification of active compounds | Must demonstrate specificity, accuracy, precision, linearity, and stability |
| Pharmacokinetic Analysis Software | Calculates key PK parameters (AUC, Cmax, Tmax) from concentration-time data | WinNonlin, PK Solutions, or equivalent |
| Specialized Extraction Kits | Isolates target compounds from complex biological matrices | Critical for natural product analysis with multiple constituents |
China's implementation of mandatory bioequivalence regulation represents a significant case study in pharmaceutical regulatory reform, demonstrating both the potential and challenges of using policy interventions to drive quality improvement in generic drugs. The evidence shows a 20.7% increase in R&D investment and significant bioequivalence approval outputs following the regulation, confirming that regulatory mandates can effectively stimulate industry response [135].
The heterogeneous implementation across firm types and regions underscores the importance of complementary capacity-building measures, particularly for smaller manufacturers. For the global scientific community, these developments highlight the increasing regulatory alignment between China and international standards, facilitating more integrated global development strategies for both synthetic and natural bioactive compounds.
Future evolution in this field will likely include:
- Advanced analytical approaches for complex natural product mixtures
- Integration of real-world evidence to complement traditional BE studies
- Development of specialized frameworks for biologics and complex synthetic formulations
- Continued international harmonization of technical requirements and standards
As China continues its transition toward lifecycle regulation, the scientific community gains an increasingly robust framework for evaluating bioequivalence across diverse therapeutic modalities, ultimately strengthening the global generic drug infrastructure and ensuring patient access to high-quality medications regardless of their synthetic or natural origins.
Interchangeability is a regulatory designation that permits a biosimilar biological product to be substituted for its reference (originator) product at the pharmacy level without the intervention of the prescribing physician, a practice known as automatic substitution [140]. This concept is distinct from biosimilarity; while a biosimilar is approved after demonstrating it is highly similar to the reference product with no clinically meaningful differences, an interchangeable biosimilar must meet additional requirements to support switching without prescriber consultation [141] [142].
In the United States, the Biologics Price Competition and Innovation Act (BPCIA) of 2009 established the legal framework for biosimilar and interchangeable biological products [141]. The U.S. Food and Drug Administration (FDA) grants interchangeability status to a biosimilar if it can show that the product "can be expected to produce the same clinical result as the reference product in any given patient" and that "for a biological product that is administered more than once, the risk in terms of safety or diminished efficacy of alternating or switching between the biological product and the reference product is not greater than the risk of using the reference product without such alternation or switch" [140]. This designation is unique to the U.S. regulatory landscape—no other major health authority, including the European Medicines Agency, directly links interchangeability to automatic substitution without prescriber involvement [140].
Table: Global Regulatory Perspectives on Biosimilar Interchangeability
| Regulatory Authority | Position on Interchangeability | Implementation Responsibility |
|---|---|---|
| U.S. FDA | Designation permits automatic substitution at pharmacy level without prescriber intervention [140] | Individual states [140] |
| European Medicines Agency (EMA) | Considered a clinical decision; replacement requires prescriber involvement in switching [140] | Member states [140] |
| Health Canada | Authorization of a biosimilar is not a declaration of equivalence; interchangeability is not defined by the federal regulator [140] | Individual provinces and territories [140] |
| Japan PMDA | Not formally defined; considered a matter of clinical practice [140] | Physicians [140] |
Evolution of U.S. FDA Interchangeability Standards
The FDA's approach to demonstrating interchangeability has evolved significantly since the first biosimilar was approved in 2015. Initially, the FDA generally recommended that sponsors conduct switching studies to support an interchangeability designation [143]. These clinical studies were designed to evaluate safety and efficacy when patients alternate between a biosimilar and its reference product, with particular attention to immunogenicity risks [141].
In a major policy shift, the FDA issued updated draft guidance in June 2024 that eliminates the expectation for switching studies [143]. This change is based on accumulated scientific evidence and real-world experience. FDA researchers conducted a systematic review and meta-analysis that revealed "no differences in the risk of death, serious adverse events, and treatment discontinuations between participants who switched between biosimilars and reference products and participants who did not switch" [143]. The guidance states that for biosimilars approved to date, "the risk in terms of safety or diminished efficacy is insignificant following single or multiple switches between a reference product and a biosimilar product" [143].
This updated approach aligns the FDA's regulatory requirements with the existing science, recognizing that modern analytical tools can evaluate the structure and effects of biologic products with more precision and sensitivity than switching studies [143]. Of the 13 approved interchangeable biosimilars referenced in 2024, 9 were approved without additional clinical switching study data [143].
Table: Evolution of FDA Interchangeability Evidence Requirements
| Time Period | Key Requirements | Representative Examples |
|---|---|---|
| 2019 Guidance | Generally recommended switching studies to evaluate immunogenicity risks from multiple switches [142] | Early interchangeable designations based on switching study data |
| 2024 Updated Guidance | Switching studies generally not needed; reliance on analytical data and scientific justification [143] | Rezvoglar (insulin glargine-aglr): Interchangeability granted without switching study based on analytical and PK/PD data [144] |
Scientific Evidence Supporting Interchangeability
Systematic Review Evidence on Switching Safety
A comprehensive systematic literature review published in 2018 analyzed 57 studies reporting efficacy and/or safety data on switching between originator biologics and biosimilars [142]. The review included studies across multiple therapeutic areas, including rheumatology, gastroenterology, and dermatology. The majority of these studies (33 of 57 that included statistical analysis) "found no statistically significant differences between groups for main efficacy parameters," and "most studies reported similar safety profiles between groups" [142]. However, the authors noted important evidence gaps, including that most studies had fewer than 100 switched patients and limited long-term follow-up beyond one year [142].
The accumulated evidence from clinical experience has been sufficient to convince regulators that the risk profile of switching does not warrant special clinical studies. The FDA's 2024 guidance update reflects this assessment, stating that current evidence shows insignificant risk "following single or multiple switches between a reference product and a biosimilar product" [143].
Real-World Evidence and Clinical Experience
Real-world evidence has played a crucial role in demonstrating the safety of switching between reference products and biosimilars. For tumor necrosis factor (TNF) inhibitors used in managing immune-mediated inflammatory diseases, real-world studies have shown that "discontinuation rates have been shown to be higher in patients switched to biosimilars for non-medical reasons than in historical cohorts maintained on innovators," potentially due to negative patient attitudes (the "nocebo effect") rather than true pharmacological differences [140].
Despite these observations, there have not been widespread immunogenicity or safety concerns identified in real-world switching practice [144]. This growing body of evidence supports the scientific rationale for the FDA's updated approach to interchangeability.
Research Methodology: Evaluating Biosimilar Interchangeability
Experimental Framework for Interchangeability Assessment
The evaluation of biosimilar interchangeability requires a comprehensive analytical and clinical framework. The following workflow outlines the key methodological components for establishing interchangeability:
Key Methodological Approaches
Comparative Analytical Characterization: This foundational assessment employs state-of-the-art physicochemical and biological techniques to demonstrate high similarity between the biosimilar and reference product. Methodology includes:
- High-resolution mass spectrometry for structural characterization
- Nuclear magnetic resonance (NMR) spectroscopy for higher-order structure analysis
- Chromatographic methods (HPLC, UPLC) for purity and impurity profiling
- Cell-based bioassays for functional activity evaluation [104] [142]
Clinical Immunogenicity Assessment: This critical safety evaluation monitors the potential for unwanted immune responses to the biological product through:
- Standardized antibody detection assays for anti-drug antibodies (ADA)
- Neutralization assays for neutralizing antibodies (NAb)
- Longitudinal sampling throughout clinical trials
- Correlation analysis between immunogenicity and safety/efficacy outcomes [142]
Pharmacokinetic/Pharmacodynamic (PK/PD) Studies: These clinical trials compare systemic exposure and response parameters between the biosimilar and reference product using:
- Crossover or parallel study designs in healthy volunteers or patients
- Primary endpoints: AUC (area under the curve), Cmax (maximum concentration)
- Secondary endpoints: clinical response markers, safety parameters [142]
Comparative Analysis: Natural vs. Synthetic Bioactive Compounds
Clinical Success Rates
The interchangeability framework for biosimilars exists within the broader context of bioequivalence evaluation for both natural and synthetic compounds. Recent research has revealed significant differences in clinical development success rates between these categories.
A 2024 study analyzing clinical trial progression found that "the proportion of compounds from natural products (NPs) and hybrids significantly increases as compounds progress through clinical investigation, contrasting with a steady decline in the proportion of synthetic compounds" [145]. Specifically, synthetic compounds decreased from 65% of compounds in Phase I to 55.5% in Phase III, while natural products increased from approximately 20% to 26% over the same clinical trial phases [145].
Table: Clinical Trial Success Rates by Compound Type
| Clinical Trial Phase | Natural Products (%) | Hybrid Compounds (%) | Synthetic Compounds (%) |
|---|---|---|---|
| Phase I | ~20% (940/4749) | ~15% (724/4749) | 65% (3085/4749) |
| Phase III | ~26% (860/3356) | ~19% (632/3356) | 55.5% (1863/3356) |
| FDA-Approved Drugs | ~25% (1149/4749) | ~20% (895/4749) | ~25% (synthetic + other) |
Toxicity Profiles
The same study employed in vitro and in silico approaches to evaluate toxicity differences, finding that "NPs and their derivatives were less toxic alternatives to their synthetic counterparts" [145]. This reduced toxicity profile potentially contributes to the higher clinical success rates observed for natural products and their derivatives.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table: Key Research Reagents for Biosimilar Characterization
| Reagent/Material | Function in Interchangeability Assessment |
|---|---|
| Reference Biologic Standard | Serves as comparator for all analytical and functional comparisons; must be obtained from approved commercial sources [142] |
| Cell-Based Bioassay Systems | Evaluate biological activity and potency; typically use engineered cell lines responsive to the therapeutic target [142] |
| Mass Spectrometry Reagents | Enable structural characterization through peptide mapping, post-translational modification analysis, and higher-order structure assessment [104] |
| Immunogenicity Assay Components | Detect and characterize anti-drug antibodies; include antigen reagents, detection antibodies, and reference antibody controls [142] |
| Chromatography Columns | Separate and analyze product variants, aggregates, and impurities; various chemistries required for comprehensive profiling [142] |
Regulatory and Practical Implications
State Substitution Laws
While the FDA establishes the federal standards for interchangeability, the implementation of automatic substitution is governed by state laws [141]. All 50 states have enacted legislation regulating biosimilar substitution, with requirements that typically include:
- Physician notification when substitution occurs
- Patient notification in some jurisdictions
- Record-keeping requirements for pharmacists
- Potential limitations on substitution for certain clinical situations [141] [140]
These state-level variations create a complex regulatory landscape for interchangeable biosimilars. Additionally, current state laws generally permit substitution only between a reference product and an interchangeable biosimilar, not between different biosimilars of the same reference product [141].
Payer and Provider Considerations
For healthcare providers and payers, the interchangeability designation has practical implications despite its legal rather than clinical nature. Pharmacy Benefit Managers (PBMs) have generally treated biologics and biosimilars separately in formulary decisions, negotiating rebates with each manufacturer [141]. This means that even when an interchangeable biosimilar is available, "pharmacists must fill whichever version is preferred by a patient's insurance formulary" [141].
The commercial impact of interchangeability remains uncertain. As noted in recent analyses, "to date, formulary coverage has not consistently favored interchangeable biosimilar products" [144]. For provider-administered drugs, which are typically obtained directly by healthcare providers rather than dispensed through pharmacies, the interchangeability designation is largely irrelevant [144].
The regulatory standards for biosimilar interchangeability have evolved significantly, with the FDA's 2024 updated guidance eliminating the requirement for switching studies based on accumulated scientific evidence demonstrating the safety of switching between reference products and biosimilars [143]. This shift aligns regulatory requirements with the existing science, recognizing that modern analytical tools can accurately evaluate biologic products with precision potentially greater than clinical switching studies [143].
The evidence supporting interchangeability continues to grow, with systematic reviews and real-world experience demonstrating that biosimilars can be safely substituted for their reference products [142]. However, important considerations remain regarding state-level implementation, payer policies, and the need for ongoing pharmacovigilance to monitor long-term outcomes of automatic substitution.
The broader context of bioequivalence research shows that natural products and their derivatives demonstrate favorable clinical development trajectories compared to synthetic compounds, with higher success rates in later-stage clinical trials and potentially better toxicity profiles [145]. This evidence base supports the continued importance of natural products in drug discovery and development, alongside advances in biosimilar regulation.
Conclusion
Establishing bioequivalence between synthetic and natural bioactive compounds requires a multifaceted approach that integrates rigorous analytical methodologies, understanding of compound-specific challenges, and adherence to evolving regulatory standards. While synthetic biology and metabolic engineering offer promising pathways for sustainable production of standardized compounds, significant hurdles remain in addressing the inherent complexity and variability of natural products. The evidence suggests that successful demonstration of bioequivalence enables more accessible, affordable therapeutic options while maintaining safety and efficacy standards. Future research should focus on developing more sophisticated assessment frameworks for complex mixtures, advancing production technologies to enhance compound standardization, and establishing international harmonization of regulatory requirements. As synthetic biology and analytical technologies continue to evolve, they will undoubtedly transform our approach to bioequivalence assessment, potentially enabling more precise evaluation of therapeutic interchangeability for the benefit of global healthcare systems and patient populations.
References
- 1. Update on the safety and bioequivalence of biosimilars [https://pmc.ncbi.nlm.nih.gov/articles/PMC3684140/]
- 2. What's the risk? Synthetic vs natural chemical ingredients [https://cris.msu.edu/news/whats-the-risk/whats-the-risk-synthetic-vs-natural-chemical-ingredients/]
- 3. Time-Dependent Comparison of the Structural Variations ... [https://www.mdpi.com/1422-0067/25/21/11475]
- 4. Natural products in drug discovery: advances and ... [https://www.nature.com/articles/s41573-020-00114-z]
- 5. What's the Risk? Synthetic vs. Natural Chemical Ingredients [https://iit.msu.edu/news/2025-4-7-CRIS-trending-GRAS-loophole.html]
- 6. Comprehensive Insights into Natural Bioactive Compounds [https://pubmed.ncbi.nlm.nih.gov/41251190/]
- 7. Revitalizing natural products for sustainable drug Discovery [https://www.sciencedirect.com/science/article/abs/pii/S2352554125001809]
- 8. Natural sources of bioactive compounds: recent advances ... [https://www.sciencedirect.com/science/article/abs/pii/S096399692502191X]
- 9. Comparing total chemical synthesis and total biosynthesis ... [https://pubs.rsc.org/en/content/articlehtml/2025/np/d4np00015c]
- 10. Conventional and modern techniques for bioactive ... [https://www.sciencedirect.com/science/article/pii/S2468227624004514]
- 11. Bioactive Compounds, Technological Advances, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12346796/]
- 12. Grand challenges in chemical biology from the perspective ... [https://www.frontiersin.org/journals/chemical-biology/articles/10.3389/fchbi.2025.1731631/full]
- 13. Medicinal plants and human health: a comprehensive ... [https://link.springer.com/article/10.1007/s11101-025-10194-7]
- 14. Product-Specific Guidances for Generic Drug Development [https://www.fda.gov/drugs/guidances-drugs/product-specific-guidances-generic-drug-development]
- 15. Bioequivalence [https://www.fda.gov/animal-veterinary/abbreviated-new-animal-drug-applications/bioequivalence]
- 16. BA/BE Study Requirements for FDA Approval [https://credevo.com/articles/2025/06/15/ba-be-study-requirements-for-fda-approval-guidelines-global-locations-costs-quality-standards/]
- 17. Orange Book Preface [https://www.fda.gov/drugs/development-approval-process-drugs/orange-book-preface]
- 18. Bioequivalence Studies With Pharmacokinetic Endpoints ... [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/bioequivalence-studies-pharmacokinetic-endpoints-drugs-submitted-under-abbreviated-new-drug]
- 19. A Proposal for Alternative FDA Bioequivalence Criteria ... [https://pubmed.ncbi.nlm.nih.gov/41168569/]
- 20. M13B Bioequivalence for Immediate-Release Solid Oral ... [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/m13b-bioequivalence-immediate-release-solid-oral-dosage-forms-additional-strengths-biowaiver]
- 21. Dissolution and Bioequivalence [http://www.usp.org/sites/default/files/fda-exhibit/topics/dissolution.html]
- 22. Product-Specific Guidances for Generic Drug Development [https://www.fda.gov/drugs/guidances-drugs/upcoming-product-specific-guidances-generic-drug-product-development]
- 23. Pharmacokinetics and Bioequivalence of Mycophenolate ... [https://pubmed.ncbi.nlm.nih.gov/40959737/]
- 24. Bioequivalence of a Single Dose of Two Palbociclib ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1722151/full]
- 25. Pharmacokinetic equivalence and comparative safety ... [https://pubmed.ncbi.nlm.nih.gov/40331766/]
- 26. Physiologically Based Pharmacokinetic Modeling and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12541349/]
- 27. Prediction of pharmacokinetic/pharmacodynamic ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1578117/full]
- 28. Pharmacokinetic Model Comparisons: How We Do It and Why ... [https://blog.insight-rx.com/resources/pharmacokinetic-model-comparisons-methods]
- 29. Natural bioactive products as promising therapeutics [https://www.sciencedirect.com/science/article/pii/S0254629922002551]
- 30. Bioactive Natural and Synthetic Products in Human Health ... [https://www.mdpi.com/2072-6643/16/19/3265]
- 31. More Accurate Prediction of Human Pharmacokinetic ... [https://dmpkservice.wuxiapptec.com/articles/438-more-accurate-prediction-of-human-pharmacokinetic-parameters-for-small-molecule-compounds-methods-models-and-applications/]
- 32. Standardization of pharmacognostic characters and ... [https://www.nature.com/articles/s41598-025-94674-y]
- 33. A comprehensive review-current development in ... [https://www.sciencedirect.com/science/article/pii/S2211715625003248]
- 34. Nature's Most Promising Bioactives to Speed Up Evidence ... [https://www.bio-itworld.com/news/2025/08/19/nature-s-most-promising-bioactives-to-speed-up-evidence-based-drug-discovery]
- 35. The evolution of chemical collections and drug-like diversity [https://www.ddw-online.com/the-evolution-of-chemical-collections-and-drug-like-diversity-36277-202509/]
- 36. A Historical Overview of Natural Products in Drug Discovery [https://pmc.ncbi.nlm.nih.gov/articles/PMC3901206/]
- 37. Cheminformatic comparison of approved drugs from ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4607632/]
- 38. The impact of natural products upon modern drug discovery [https://www.sciencedirect.com/science/article/abs/pii/S1367593108000574]
- 39. Building Natural Product Libraries Using Quantitative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8547436/]
- 40. A review of natural products as a source of next-generation ... [https://www.nature.com/articles/s44259-025-00119-x]
- 41. A New Golden Age of Natural Products Drug Discovery [https://www.sciencedirect.com/science/article/pii/S0092867415015500]
- 42. Bioequivalence of generic drugs: a simple explanation for ... [https://pubmed.ncbi.nlm.nih.gov/26132680/]
- 43. Comparative study on the bioavailability and ... [https://pubmed.ncbi.nlm.nih.gov/39898756/]
- 44. Bioequivalence and Pharmacokinetics of Low-Dose ... [https://www.mdpi.com/2227-9059/13/8/1993]
- 45. Choice of characteristics and their bioequivalence ranges ... [https://pubmed.ncbi.nlm.nih.gov/7952792/]
- 46. Bioactive Natural and Synthetic Products in Human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11479150/]
- 47. Lesson 15: Crossover Designs [https://online.stat.psu.edu/stat509/book/export/html/749]
- 48. Considerations for crossover design in clinical study - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8342834/]
- 49. On the Proper Use of the Crossover Design in Clinical Trials [https://pmc.ncbi.nlm.nih.gov/articles/PMC3345345/]
- 50. The bioequivalence study design recommendations for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10993868/]
- 51. Power Analysis and Sample Size Determination ... [https://www.sciencedirect.com/science/article/pii/S0895398820300180]
- 52. Biological Activity of Natural and Synthetic Compounds [https://pmc.ncbi.nlm.nih.gov/articles/PMC9228419/]
- 53. Comparative assessment of bioanalytical method ... [https://www.sciencedirect.com/science/article/pii/S0731708516301819]
- 54. Editorial: Recent advances in application of synthetic ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2024.1517610/full]
- 55. Synthetic biology and metabolic engineering strategies in ... [https://www.sciencedirect.com/science/article/pii/S0926669025006065]
- 56. Synthetic biology and metabolic engineering paving the way ... [https://pubs.rsc.org/en/content/articlehtml/2025/ya/d5ya00118h]
- 57. Monitoring and Analyzing Process Parameters in ... [https://www.idbs.com/knowledge-base/monitoring-and-analyzing-process-parameters-in-bioprocessing/]
- 58. Effect of recombinant protein production and release on ... [https://jbioleng.biomedcentral.com/articles/10.1186/s13036-025-00525-9]
- 59. A new flavor of synthetic yeast communities sees the light [https://pmc.ncbi.nlm.nih.gov/articles/PMC11898667/]
- 60. Microalgae biofactories for animal based products [https://www.sciencedirect.com/science/article/abs/pii/S0924224425002912]
- 61. Optimization and characterization of bioactive secondary ... [https://bmcmicrobiol.biomedcentral.com/articles/10.1186/s12866-025-03763-5]
- 62. Bioavailability and Bioequivalence in Drug Development [https://pmc.ncbi.nlm.nih.gov/articles/PMC4157693/]
- 63. Where Did the 80-125% Bioequivalence Criteria Come ... [https://www.certara.com/blog/where-did-the-80-125-bioequivalence-criteria-come-from/]
- 64. Bioequivalence of Generic Drugs: A Simple Explanation ... [https://www.psychiatrist.com/jcp/bioequivalence-generic-drugs-simple-explanation-food/]
- 65. The Reference-scaled Average Bioequivalence (RSABE) ... [https://www.certara.com/blog/reference-scaled-average-bioequivalence-2/]
- 66. Sample size determination in bioequivalence studies using ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6783617/]
- 67. A Bioequivalence Approach for Generic Narrow ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4476992/]
- 68. Frontiers | Editorial: Natural in food... bioactive compounds [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1720905/full]
- 69. | WHO - Prequalification of Medical Products... Bioequivalence [https://extranet.who.int/prequal/medicines/bioequivalence]
- 70. A survey of regulatory recommendations for waivers of in vivo ... [https://www.frontierspartnerships.org/journals/journal-of-pharmacy-pharmaceutical-sciences/articles/10.3389/jpps.2025.14721/full]
- 71. M13B Bioequivalence for Immediate-Release Solid Oral ... [https://www.federalregister.gov/documents/2025/06/02/2025-09900/m13b-bioequivalence-for-immediate-release-solid-oral-dosage-forms-additional-strengths-biowaiver]
- 72. ICH Guideline M13B on bioequivalence for immediate-release ... [https://www.ema.europa.eu/en/ich-guideline-m13b-bioequivalence-immediate-release-solid-oral-dosage-forms-additional-strengths-biowaiver-scientific-guideline]
- 73. versus Synthetic curcumin: natural in an in vitro oral... bioequivalence [https://bmccomplementmedtherapies.biomedcentral.com/articles/10.1186/1472-6882-14-53]
- 74. and Spatial Seasonal of Anthropogenic and Variability ... Natural [https://www.mdpi.com/1660-4601/15/2/279]
- 75. – ClimateData.ca Natural Variability [https://climatedata.ca/resource/natural-variability/]
- 76. Comparison of analytical techniques for the identification ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5042860/]
- 77. for Improved Drug Delivery: Lessons Learned from Recently... Prodrugs [https://pmc.ncbi.nlm.nih.gov/articles/PMC7692606/]
- 78. Prodrug Approach as a Strategy to Enhance Drug Permeability [https://pmc.ncbi.nlm.nih.gov/articles/PMC11946379/]
- 79. and Their Active Metabolites - Creative Proteomics Prodrugs [https://www.creative-proteomics.com/resource/prodrugs-and-their-active-metabolites.htm]
- 80. Drug metabolizing enzyme activities versus genetic variances for drug... [https://clinicalproteomicsjournal.biomedcentral.com/articles/10.1186/1559-0275-8-12]
- 81. The Influence of Bioactive Compounds on Metabolic ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1703963/abstract]
- 82. Metabolism of natural and synthetic bioactive compounds ... [https://www.sciencedirect.com/science/article/abs/pii/S0045206823004625]
- 83. Structure-guided microbial targeting of antistaphylococcal prodrugs [https://elifesciences.org/articles/66657]
- 84. Excipients in drug delivery systems: A comprehensive ... [https://www.sciencedirect.com/science/article/pii/S093964112500013X]
- 85. Application Challenges and Examples of New Excipients in ... [https://www.americanpharmaceuticalreview.com/Featured-Articles/36925-Application-Challenges-and-Examples-of-New-Excipients-in-Advanced-Drug-Delivery-Systems/]
- 86. High-Throughput Excipient Discovery Enables Oral Delivery of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5084074/]
- 87. Excipients Limitations: Challenges in Drug Formulation and ... [https://www.openaccessjournals.com/articles/excipients-limitations-challenges-in-drug-formulation-and-delivery-18459.html]
- 88. Advances in drug delivery systems, challenges and future ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10320272/]
- 89. How Advanced Excipient Knowledge is Shaping the Future ... [https://drug-dev.com/controlled-release-how-advanced-excipient-knowledge-is-shaping-the-future-of-controlled-release-formulations/]
- 90. Evaluation of bioequivalence for highly variable drugs with ... [https://pubmed.ncbi.nlm.nih.gov/19817502/]
- 91. Implementation of a Reference-Scaled Average ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3475857/]
- 92. Highly Variable Drugs: Observations from Bioequivalence ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2751460/]
- 93. Implementation of a reference-scaled average ... [https://www.sciencedirect.com/science/article/pii/S2211383515001446]
- 94. Bioequivalence Studies of Highly Variable Drugs: An Old ... [https://www.mdpi.com/2076-3417/14/12/5279]
- 95. Glycosylation as an intricate post-translational modification ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12051319/]
- 96. Glycosylation: mechanisms, biological functions and ... [https://www.nature.com/articles/s41392-024-01886-1]
- 97. Glycosylation of Therapeutic Proteins: An Effective Strategy ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2805475/]
- 98. Post-translational modifications in proteins [https://pmc.ncbi.nlm.nih.gov/articles/PMC8040245/]
- 99. Natural and Synthetic Inhibitors of Glycosylation - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK20704/]
- 100. Biosimilar vs Generic Drugs: Key Differences in Healthcare [https://medpak.com/biosimilar-vs-generic-drugs/]
- 101. How Similar Are Biosimilars? What Do Clinicians Need to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5669137/]
- 102. Statistical Primer on Biosimilar Clinical Development - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5102275/]
- 103. FDA Moves to Accelerate Biosimilar Development and ... [https://www.fda.gov/news-events/press-announcements/fda-moves-accelerate-biosimilar-development-and-lower-drug-costs]
- 104. Biosimilars and interchangeability: Regulatory, scientific, ... [https://www.sciencedirect.com/science/article/pii/S0928098725002234]
- 105. Generics and Biosimiliars | Back to the Future [https://www.bbrown.com/us/insight/generics-and-biosimiliars-back-to-the-future/]
- 106. Investigation of bioequivalence - Scientific guideline [https://www.ema.europa.eu/en/investigation-bioequivalence-scientific-guideline]
- 107. ICH M13B Webinar: Navigating the Draft ... [https://www.fda.gov/drugs/news-events-human-drugs/ich-m13b-webinar-navigating-draft-ich-m13b-additional-strengths-biowaiver-guideline-09112025]
- 108. The Global Bioequivalence Harmonisation Initiative (GBHI) [https://www.sciencedirect.com/science/article/pii/S0928098725001289]
- 109. Regulatory Updates, September 2025 [https://www.caidya.com/resources/regulatory-updates-sept-2025/]
- 110. Performance Evaluation of Interim Analysis in ... [https://link.springer.com/article/10.1007/s43441-024-00664-z]
- 111. Performance properties of the population bioequivalence ... [https://pubmed.ncbi.nlm.nih.gov/24249218/]
- 112. IV Bio.Natural 2025 – Bioactive Natural Products Research ... [https://bionaturalconferences.com/]
- 113. Synthetic and semi-synthetic antioxidants in medicine and ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1599816/full]
- 114. Medicinal plants: bioactive compounds, biological activities ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12079674/]
- 115. The future of pharmaceuticals: Artificial intelligence in drug ... [https://www.sciencedirect.com/science/article/pii/S2095177925000656]
- 116. Pharmacokinetic Comparison of Chitosan-Derived and ... [https://www.mdpi.com/2072-6643/14/15/3213]
- 117. Vegan Glucosamine versus Crustacean ... [https://www.mjrheum.org/current-issue/newsid792/557/showfulltext792/1/showreferences792/1]
- 118. Bioavailability enhancement of glucosamine hydrochloride ... [https://www.sciencedirect.com/science/article/abs/pii/S0378517313005644]
- 119. Does Salt Form Matter? A Pilot Randomized, Double-Blind ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12348100/]
- 120. FDA vs EMA: Key Regulatory Differences in 2025 [https://pharmuni.com/2024/08/12/from-fda-to-ema-navigating-global-regulatory-requirements/]
- 121. Product-specific bioequivalence guidance [https://www.ema.europa.eu/en/human-regulatory-overview/research-development/scientific-guidelines/clinical-pharmacology-pharmacokinetics/product-specific-bioequivalence-guidance]
- 122. EMA publishes Draft of ICH M13B Guideline on ... [https://www.gmp-compliance.org/gmp-news/ema-publishes-draft-of-ich-m13b-guideline-on-bioequivalence]
- 123. The totality of evidence approach in the development ... [https://pubmed.ncbi.nlm.nih.gov/38250743/]
- 124. Developing the Totality of Evidence for Biosimilars: Regulatory ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5443883/]
- 125. The Art of Biosimilar Reverse Engineering: From Complex ... [https://www.drugpatentwatch.com/blog/the-art-of-biosimilar-reverse-engineering-from-complex-molecules-to-therapeutic-equivalence/?srsltid=AfmBOoq3NuUYNN_WdtaqBxoi7H_5l2QE2njM9nJ2APE39tU9wl2yRMJU]
- 126. Biosimilarity Assessments: The Totality of Evidence ... [https://www.bioprocessintl.com/product-characterization/biosimilarity-assessments-the-totality-of-evidence-framework]
- 127. Toward Regulatory Convergence and Streamlined ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12568798/]
- 128. The Difference Between Pharmacokinetics and ... [https://www.bioagilytix.com/blog/the-difference-between-pharmacokinetics-and-pharmacodynamics/]
- 129. Pharmacodynamic Endpoints as Clinical Trial Objectives to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5117459/]
- 130. Pharmacodynamic endpoints as clinical trial objectives to ... [https://www.sciencedirect.com/science/article/abs/pii/S0093775416300471]
- 131. Biological Activity of Natural and Synthetic Compounds [https://www.mdpi.com/1420-3049/27/12/3652]
- 132. What are Pharmacokinetic and Pharmacodynamic Studies? [https://www.als.net/news/what-are-pharmacokinetic-and-pharmacodynamic-studies/]
- 133. Studies Market Bioequivalence –2033 | Size, Trends & Forecast 2025 [https://www.datamintelligence.com/research-report/bioequivalence-studies-market]
- 134. Studies Market Size, Share & Forecast to 2030 Bioequivalence [https://www.researchandmarkets.com/report/bioequivalence]
- 135. The impact of bioequivalence regulation on ... [https://www.sciencedirect.com/science/article/abs/pii/S0277953625005738]
- 136. From Command-Control to Lifecycle Regulation: Balancing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11942016/]
- 137. Evolving drug regulatory landscape in China: A clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8301550/]
- 138. The rise of China's pharmaceutical industry from 2015–2024 [https://www.nature.com/articles/d41573-025-00102-1]
- 139. BE/BA in Phase 1 Clinical Trials: Insights and Guidelines [https://mmsholdings.com/perspectives/phase-1-clinical-trial-designs-be-ba-us-eu/]
- 140. The Automatic Substitution of Biosimilars: Definitions ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8107170/]
- 141. Biosimilar Interchangeability and Substitution in the US [https://www.ajmc.com/view/biosimilar-interchangeability-and-substitution-in-the-us-what-comes-next-]
- 142. Biosimilarity and Interchangeability: Principles and Evidence [https://pmc.ncbi.nlm.nih.gov/articles/PMC5814534/]
- 143. FDA updates guidance on interchangeability [https://www.fda.gov/drugs/drug-safety-and-availability/fda-updates-guidance-interchangeability]
- 144. Biosimilar Interchangeability: FDA Designation, Marketing ... [https://www.ipdanalytics.com/post/biosimilar-interchangeability-fda-designation-marketing-exclusivity-guidance-and-future-trends]
- 145. Natural Products Have Increased Rates of Clinical Trial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11287737/]