Bridging the Data Gap: A Research Framework for Consistent Nutrient Comparisons in Organic vs Conventional Agriculture
This article addresses the critical lack of consistency in studies comparing the nutrient profiles of organic and conventional foods, a significant hurdle for researchers, scientists, and drug development professionals.
Bridging the Data Gap: A Research Framework for Consistent Nutrient Comparisons in Organic vs Conventional Agriculture
Abstract
This article addresses the critical lack of consistency in studies comparing the nutrient profiles of organic and conventional foods, a significant hurdle for researchers, scientists, and drug development professionals. We explore the foundational reasons for conflicting evidence, from heterogeneous study designs to unmeasured confounding variables. The piece then outlines robust methodological frameworks, including standardized nutrient profiling systems and precision nutrition tools, to enhance data quality. It further provides strategies for troubleshooting common experimental biases and validates approaches through comparative analysis of existing models. The goal is to equip the scientific community with a unified framework to generate reliable, comparable data that can inform clinical research and public health policy.
Deconstructing the Controversy: Why Organic vs. Conventional Nutrient Data Remains Inconclusive
Frequently Asked Questions (FAQs) on Research Consistency
FAQ 1: What is the current state of evidence regarding nutritional differences between organic and conventional foods? The body of evidence presents a complex picture without a consensus on general superiority. A comprehensive systematic review from 2024, which analyzed 147 scientific articles encompassing 656 comparative analyses, found that:
- 41.9% of comparisons showed no significant difference.
- 29.1% of comparisons found significant differences.
- 29.0% of comparisons had divergent results (where some studies reported significant differences while others did not) [1]. This indicates that claims of nutritional advantages are highly specific to the food type and nutritional parameter being studied, rather than being universally applicable [1].
FAQ 2: What are the primary methodological sources of inconsistency in study results? Inconsistencies often arise from several key methodological variables:
- Study Duration & Soil History: Short-term studies may not capture long-term soil and crop dynamics. The initial health and organic matter content of the soil at the experiment's start can significantly influence results [2].
- Nutrient Management Systems: Comparisons are confounded by the type of organic inputs used (e.g., farmyard manure, compost, biofertilizers) and the specific practices of the conventional system used as a control [2] [3].
- Analytical Focus: Variations exist in the specific nutritional properties (macronutrients, micronutrients, antioxidants, pesticide residues) and food types analyzed, making cross-study comparisons difficult [1] [4].
- Post-Harvest Handling: Differences in the time to analysis, storage conditions, and transportation of samples can affect the measured nutrient content [5].
FAQ 3: How can researchers better account for soil health in their experimental designs? Soil health is a critical confounding variable. Key parameters to monitor throughout the experiment include:
- Soil Organic Carbon (SOC) and Soil Organic Matter (SOM): Fundamental indicators of soil fertility.
- Microbial Population and Diversity: Measures the soil's biological activity.
- Soil Enzymatic Activities: Indicators of functional soil processes like nutrient cycling [2]. Integrating these soil health metrics with crop nutrient data allows for a more nuanced interpretation of why nutritional differences may or may not occur.
FAQ 4: What are the proven health benefits linked to organic food consumption? While nutritional content may be comparable, health benefits are often linked to reduced exposure to synthetic inputs. Evidence suggests that organic food consumption:
- Is associated with fewer cases of non-Hodgkin lymphoma (NHL) [6] [5].
- May reduce risks of pregnancy complications and pre-eclampsia, likely due to lower pesticide exposure [5].
- Can lead to a reduction in obesity and body mass index (BMI) [6]. It is crucial to note that these observed benefits may be influenced by broader lifestyle factors common among consistent organic consumers [5].
FAQ 5: What is the typical yield trade-off in organic systems, and how does it affect research interpretations? A meta-analysis on organic farming in Bangladesh revealed a yield reduction of 5-34% compared to conventional methods [3]. This is a critical factor to consider when designing studies and interpreting data, as it relates to the broader debate on the trade-offs between nutritional quality, environmental sustainability, and productivity. Some integrated systems show that initial yield penalties can decrease over time with improved soil health [2].
Quantitative Data Synthesis
The following tables synthesize key quantitative findings from recent meta-analyses and systematic reviews to provide a clear, comparative overview of the evidence base.
Table 1: Statistical Overview of Comparative Nutritional Analyses
| Category of Finding | Percentage of Comparisons | Number of Comparisons (Out of 656) | Interpretation |
|---|---|---|---|
| No Significant Difference | 41.9% | 275 | No consistent evidence of superiority for either system in these parameters [1]. |
| Significant Differences | 29.1% | 191 | Highlights context-specific advantages, dependent on crop and nutrient [1]. |
| Divergent Results | 29.0% | 190 | Underscores methodological inconsistencies and high variability in the research field [1]. |
Table 2: Documented Health Outcomes Associated with Organic Food Consumption
| Health Outcome | Associated Effect | Notes / Potential Mechanism |
|---|---|---|
| Cancer Risk | Reduction in non-Hodgkin lymphoma (NHL) risk [6] [5]. | Linked to reduced exposure to synthetic pesticides like glyphosate [6]. |
| Maternal & Fetal Health | Reduced risks of pregnancy complications and impaired fetal development [5]. | Associated with lower maternal pesticide exposure [5]. |
| Body Weight | Reduction in obesity and body mass index (BMI) [6]. | Correlational; may be influenced by overall healthier lifestyle choices [6]. |
Table 3: Soil Health Improvements Under Organic Management
| Soil Health Parameter | Documented Improvement | Source / Context |
|---|---|---|
| Soil Microbial Activity | Increase of 32-84% [3]. | Meta-analysis of organic farming studies. |
| Soil Organic Carbon (SOC) | Increase of up to 15.2% [2]. | Field experiment with integrated organic amendments. |
| Soil Organic Matter (SOM) | Increase of up to 14.7% [2]. | Field experiment with integrated organic amendments. |
| Available Nutrients (N, P, K, etc.) | Increase of 10.7-36.6% [2]. | Field experiment with integrated organic amendments. |
Experimental Protocols & Workflows
Protocol 1: Integrated Field Trial for Soil and Crop Nutrient Analysis
This protocol is designed to systematically compare the long-term effects of organic and conventional systems on both soil health and crop nutritional quality.
Detailed Methodology:
- Experimental Design: Establish a Randomized Complete Block Design (RCBD) with a minimum of three replications to account for field variability [2].
- Treatment Structure:
- T1 (Conventional Control): 100% Recommended Dose of Fertilizers (RDF) using synthetic sources [2].
- T2 (Basic Organic): 100% Recommended Dose of Nitrogen (RDN) through Farmyard Manure (FYM) [2].
- T3-T7 (Integrated Organic): Combinations of FYM (e.g., 50%, 75%, 100% RDN), Plant Growth-Promoting Rhizobacteria (PGPR), and foliar sprays like panchagavya [2].
- Soil Sampling & Analysis: Collect soil samples (0-15 cm depth) at baseline and after each cropping cycle. Analyze for:
- Plant Sampling & Analysis: Harvest crops at physiological maturity. Analyze for:
- Data Collection Period: Conduct the experiment over a minimum of three consecutive years to observe trends and mitigate seasonal variations [2].
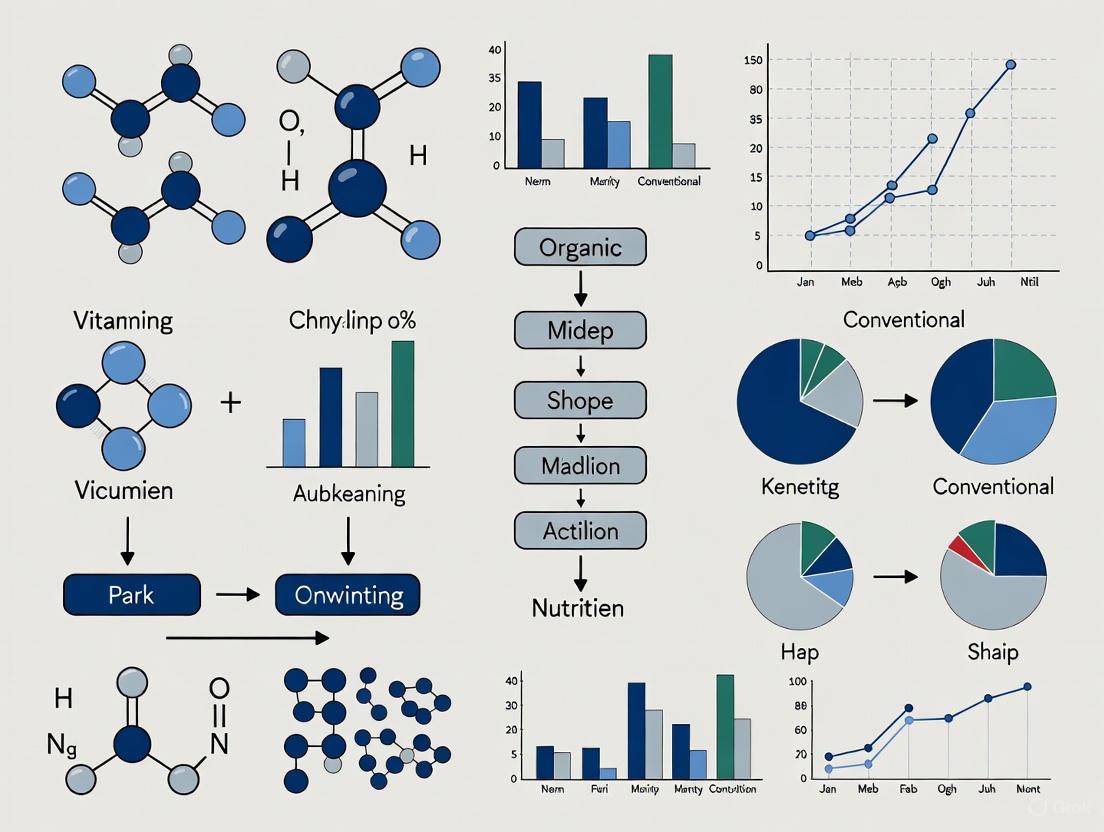
The workflow for this experimental protocol is summarized in the following diagram:
Protocol 2: Systematic Review for Evidence Synthesis
This protocol outlines a rigorous methodology for conducting systematic reviews and meta-analyses on organic vs. conventional research, aiming to reduce bias and enhance reproducibility.
Detailed Methodology:
- Protocol Registration: Prospectively register the review protocol on an international platform like PROSPERO (CRD42024512893) to enhance transparency and reduce reporting bias [7].
- Search Strategy: Develop a comprehensive search strategy using PRISMA 2020 guidelines [7]. Search multiple electronic databases (e.g., PubMed/MEDLINE, Scopus, Web of Science) with predefined inclusion criteria.
- Study Screening & Selection: Systematically screen records (title/abstract, then full-text) against the inclusion criteria. Document the flow of studies and reasons for exclusions [7].
- Data Extraction & Quality Assessment: Use standardized data extraction forms. Assess the quality and risk of bias in individual studies using validated tools (e.g., RoB 2, ROBINS-I, Newcastle–Ottawa Scale) [7].
- Data Synthesis: Perform a random-effects meta-analysis where appropriate, as heterogeneity is expected. Quantify heterogeneity using I² statistics. Assess publication bias using funnel plots and Egger's test [7].
The workflow for this evidence synthesis protocol is summarized below:
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Materials and Reagents for Comparative Studies
| Item / Reagent | Function in Experiment | Application Notes |
|---|---|---|
| Farmyard Manure (FYM) | A primary source of organic matter and slow-release nutrients. Improves soil structure, water retention, and microbial activity [2]. | Quality can vary; should be well-composted and characterized for nutrient content before application. |
| Plant Growth-Promoting Rhizobacteria (PGPR) | Biofertilizers that enhance plant nutrient uptake via biological nitrogen fixation, phosphorus solubilization, and production of growth-promoting substances [2]. | Strain selection is critical; must be compatible with the crop and soil conditions. |
| Panchagavya | An indigenous liquid formulation used as a foliar spray to enhance plant immunity, soil microbial activity, and nutrient assimilation efficiency [2]. | Typically applied as a 3% foliar spray at critical growth stages [2]. |
| Cover Crop Seeds (e.g., Clover, Rye) | Used to maintain soil cover, prevent erosion, fix nitrogen (legumes), improve soil structure, and enhance nutrient cycling [4]. | Species selection depends on the cropping system and climate. |
| Solvents & Standards for HPLC/GC-MS | Used for the extraction and quantification of specific bioactive compounds (e.g., polyphenols, vitamins) and pesticide residues in plant tissues [6] [4]. | Requires high-purity grades and calibrated standards for accurate quantification. |
| Culture Media for Soil Microbiology | Used to isolate, enumerate, and identify soil microbial populations (bacteria, fungi, actinomycetes) to assess biological soil health [2]. | Different media are required for different microbial groups. |
Troubleshooting Guide & FAQs
This technical support center provides guidance for researchers on controlling critical variables that can compromise the validity of studies comparing organic and conventional agricultural systems, with a focus on nutrient composition research.
Frequently Asked Questions
FAQ 1: How significant are soil properties in skewing crop nutrient data, and what is the most critical factor to control? Soil properties are a primary source of experimental skew. Soil thinning (topsoil loss) is the dominant degradation factor affecting yield and, by extension, nutrient concentration. A meta-analysis of black soil regions established that a topsoil removal depth of 5 cm is the critical threshold, beyond which crop yields are significantly reduced [8]. Yield reduction from soil thinning (-27%) exceeds that from nutrient depletion (-20%) or soil structure degradation (-6%) [8]. This directly impacts nutrient density per unit of yield.
Table 1: Impact of Soil Degradation Types on Crop Yield [8]
| Degradation Type | Average Yield Reduction | Key Contributing Factors |
|---|---|---|
| Soil Thinning | 27% | Topsoil removal depth, Soil Organic Matter (SOM), Total Soil Nitrogen (STN) |
| Nutrient Depletion | 20% | Depletion of soil organic matter and essential nutrients |
| Soil Structure Degradation | 6% | Breakdown of soil aggregates, soil compaction |
Experimental Protocol for Controlling Soil Variables:
- Site Selection & Baseline Analysis: Select paired plots (organic & conventional) with similar soil types. Conduct pre-experiment soil analysis to determine baseline levels of Soil Organic Matter (SOM), Total Nitrogen (STN), Available Phosphorus, bulk density, and pH [8] [9].
- Monitor Thickness: Measure and ensure comparable topsoil depth across all study plots, noting that differences greater than 5 cm can be a significant confounder [8].
- Long-Term Monitoring: In long-term studies, track changes in these soil properties annually, as factors like experimental duration and fertilizer types can alter soil chemistry and physics over time, indirectly affecting yield and nutrient content [8].
FAQ 2: To what extent does crop variety, rather than farming system, influence nutritional outcomes? Crop variety can be a more significant determinant of nutrient content than the farming system itself. Controlled environment studies demonstrate that genetic differences between varieties can lead to statistically significant variations in nutraceutical properties, while the difference between a common and a hybrid variety grown under identical conditions can be negligible [10].
Table 2: Effect of Cultivar on Bioactive Compounds in a Controlled Environment [10]
| Plant Crop | Varieties Compared | Key Findings on Nutraceutical Properties |
|---|---|---|
| Spinach | Virofly vs. Acadia F1 | No statistically significant differences in antioxidant activity, phenolic content, flavonoids, and photosynthetic pigments were found between the common (Virofly) and hybrid (Acadia F1) varieties. |
| Grapes | Khalili vs. Halwani | The two cultivars showed significantly different responses to the same NPK, Selenium, and Silicon dioxide treatments for traits like cluster length, cluster weight, and total sugar levels. |
Experimental Protocol for Controlling Crop Variety:
- Variety Selection: Use the same genetic cultivar for both organic and conventional arms of the experiment. If this is not feasible, use multiple, well-matched varieties in a balanced design to account for genetic variation.
- Controlled Assessment: When evaluating the effect of a farming practice on a specific nutrient profile, first screen multiple varieties under uniform, controlled conditions (e.g., in a Plant Factory with Artificial Lighting - PFAL) to establish baseline genetic variability [10].
- Documentation: Clearly report the specific cultivars used in all study publications to enable accurate cross-study comparisons and replication.
FAQ 3: What post-harvest handling factors pose the greatest risk to data integrity in nutritional studies? Post-harvest losses (PHL) severely skew results by reducing the edible mass and nutritional value of food before it can be analyzed or consumed [11]. For fruits and vegetables, losses can reach 30-50% along the value chain [11]. The stages of highest loss vary by crop but commonly include threshing/cleaning, transport, and storage [12]. These losses decrease the availability of essential nutrients in the food system, directly impacting measurements of nutritional security [11].
Table 3: Documented Post-Harvest Losses for Key Crops in Niger [12]
| Crop | Reported Loss Rate (Declarative) | Objectively Measured Loss Rate | Stages of Highest Loss |
|---|---|---|---|
| Cowpea | 19.0% | 14.1% | Threshing, cleaning, transport, drying |
| Maize | 16.7% | 19.5% | Threshing, cleaning, transport, drying |
| Sorghum | 17.1% | 14.2% | Threshing, cleaning, transport, drying |
| Millet | 12.5% | 15.7% | Threshing, cleaning, transport, drying |
Experimental Protocol for Standardizing Post-Harvest Handling:
- Define a Standard Operating Procedure (SOP): Establish a strict, documented protocol for harvesting, handling, transporting, and storing samples for all study arms. This includes defining temperature conditions, handling procedures, and time intervals.
- Simulate Value Chain Stages: For a comprehensive assessment, measure key nutritional compounds at multiple points: immediately after harvest, after simulated transport, and after a defined storage period.
- Use Appropriate Technologies: Implement proven loss-reduction technologies consistently. For durable cereals and legumes, hermetic storage bags are widely effective. For perishables, storage structures that maintain temperatures below ambient are critical [13].
Visualizing Research Workflows and Variable Interactions
The following diagrams map the key variables and experimental workflows discussed in this guide.
Diagram 1: Key Variables Affecting Nutrient Research
Diagram 2: Robust Experimental Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Materials and Methods for Controlled Experiments
| Item / Method | Function / Purpose | Application Example |
|---|---|---|
| Hermetic Storage Bags | Creates an oxygen-depleted, modified atmosphere that kills pests and suppresses mold growth, significantly reducing storage losses. | Storing grains and pulses in post-harvest intervention studies to maintain quality and minimize nutrient degradation [13]. |
| Pan American Health Organization Nutrient Profile Model (PAHO-NPM) | A profiling tool to objectively classify the "healthiness" of food products based on their nutrient composition, beyond simple nutrient comparisons. | Assessing and reporting the overall nutritional quality of organic and conventional processed foods in a standardized way [14]. |
| Core Sampler | A metal cylinder driven into the soil to extract an undisturbed sample for determining soil bulk density, a key indicator of soil structure and health. | Measuring soil compaction and porosity as part of the baseline soil analysis in experimental plots [8] [9]. |
| Controlled Environment (PFAL) | Plant Factory with Artificial Lighting allows for the precise control of temperature, humidity, light spectrum, and nutrients, eliminating environmental variability. | Studying the intrinsic effect of crop variety on nutraceutical properties without the confounding effects of field conditions [10]. |
| Walkley-Black Method | A wet-chemical oxidation procedure for determining the percentage of organic carbon in soil, a critical metric for soil fertility. | Quantifying Soil Organic Matter (SOM) during the initial site characterization and throughout long-term studies [9]. |
For researchers investigating the compositional differences between organic and conventional foods, the landscape extends far beyond macronutrients. Significant, yet often inconsistent, variations are reported in the concentrations of secondary metabolites like antioxidants, and in the levels of environmental contaminants such as heavy metals and pesticide residues. This technical guide addresses the key methodological challenges in this field and provides standardized protocols to enhance the consistency, reliability, and comparability of future research.
Table 1: Summary of Compositional Differences Between Organic and Conventional Crops from Meta-Analyses
| Compound Category | Specific Compound | Median Difference (Organic vs. Conventional) | Key References |
|---|---|---|---|
| Antioxidants & Polyphenolics | Total Polyphenolics | + 18% to +69% | [15] [16] |
| Flavanones | +69% | [15] | |
| Anthocyanins | +51% | [15] | |
| Stilbenes | +28% | [15] | |
| Flavonols | +50% | [15] | |
| Toxic Heavy Metals | Cadmium (Cd) | -48% | [15] [16] |
| Pesticide Residues | Incidence on Crops | 4x lower frequency | [16] |
Table 2: Summary of Associated Health Outcomes from Observational Studies
| Health Outcome | Association with Higher Organic Food Intake | Key References |
|---|---|---|
| Non-Hodgkin Lymphoma | Reduced incidence | [17] [5] |
| Pregnancy & Fetal Development | Fewer complications and improved development (linked to reduced pesticide exposure) | [5] |
| Allergic Sensitization | Reduced incidence | [17] |
| Infertility | Reduced incidence | [17] |
| Metabolic Syndrome | Reduced incidence | [17] |
Troubleshooting Common Research Inconsistencies
FAQ 1: Why do studies on antioxidant levels in organic vs. conventional crops show such high variability?
Answer: Variability often stems from agronomic and environmental factors that are not adequately controlled.
- Root Cause: Differences are linked to specific agronomic practices. The absence of chemical pesticides forces plants to increase production of defensive secondary metabolites, including polyphenolics [15]. Furthermore, the shift from soluble mineral fertilizers (conventional) to slow-release organic fertilizers (organic) alters soil nutrient dynamics and stress responses, significantly affecting gene and protein expression patterns related to secondary metabolism [15].
- Solution: Implement strict control and reporting of the following variables:
- Fertilizer Type & Regimen: Document the type (e.g., manure, compost), nitrogen content, and application schedule.
- Crop Variety: Use identical genotypes in comparative trials.
- Soil Health Metrics: Measure and report soil organic matter, microbial biomass, and biodiversity.
- Post-Harvest Handling: Standardize time to analysis, storage conditions, and processing methods.
FAQ 2: How can we reliably assess the health implications of lower-level, chronic pesticide exposure via diet?
Answer: The limitation of current regulatory standards, which are based on Maximum Residue Levels (MRLs) for single pesticides, is a key factor.
- Root Cause: Pesticide approval processes typically do not require safety testing for complex mixtures or formulations [17]. Conventional crops often contain multiple pesticide residues simultaneously, creating a "cocktail effect" that is not captured by individual MRL assessments [17].
- Solution: In clinical and cohort studies, move beyond simply measuring the presence or absence of residues. Employ:
- Biomarker Monitoring: Use urine or blood samples to quantify specific pesticide metabolites (e.g., pyrethroid or organophosphate breakdown products) as a direct measure of internal exposure and bioavailability [18].
- Mixture Toxicology Models: Develop and apply experimental models that test the synergistic or additive effects of common pesticide combinations found in the food supply.
FAQ 3: Why do some large-scale reviews conclude there are no significant nutritional benefits to organic food?
Answer: This often results from differing study methodologies and inclusion criteria, particularly the conflation of nutrient composition studies with direct health outcome studies.
- Root Cause: Early systematic reviews were limited by a small number of available studies, especially long-term human dietary interventions [17] [16]. Conclusions based solely on macronutrient (protein, fat, carbohydrate) content often obscure differences in micronutrients and contaminants [1].
- Solution: Design studies with a holistic compositional approach. Focus on:
- Whole-Diet Substitution: Use long-term interventions where the entire diet is replaced with certified organic counterparts to detect measurable health impacts [17].
- Beyond Macronutrients: Prioritize the analysis of bioactive compounds (antioxidants) and contaminants (Cd, pesticides) linked to chronic disease pathways [15] [18].
Standardized Experimental Protocols
Protocol 1: Quantifying Polyphenolics in Plant Tissues
1. Sample Preparation:
- Homogenization: Flash-freeze plant material in liquid N₂ and homogenize to a fine powder using a ceramic mortar and pestle or a laboratory-grade mixer mill.
- Extraction: Weigh 1.0 g of homogenate. Add 10 mL of acidified methanol (e.g., 1% HCl/methanol) or another suitable solvent (e.g., 70% aqueous acetone) for comprehensive polyphenol extraction. Sonicate for 20 minutes at room temperature, then centrifuge at 10,000 x g for 15 minutes.
- Filtration: Collect the supernatant and filter through a 0.45 μm PTFE or nylon syringe filter prior to chromatographic analysis.
2. HPLC-DAD/MS Analysis:
- Instrumentation: High-Performance Liquid Chromatography system coupled with a Diode Array Detector (DAD) and Mass Spectrometer (MS).
- Column: Reversed-phase C18 column (e.g., 250 mm x 4.6 mm, 5 μm).
- Mobile Phase: (A) Water with 0.1% Formic Acid; (B) Acetonitrile with 0.1% Formic Acid.
- Gradient: 5% B to 95% B over 40-60 minutes, followed by a column wash and re-equilibration.
- Detection: Use DAD for quantification at characteristic wavelengths (e.g., 280 nm for flavan-3-ols, 360 nm for flavonols). Use MS for definitive compound identification based on mass-to-charge ratio (m/z) and fragmentation patterns.
3. Data Quantification:
- Quantify individual compounds using external calibration curves of authentic standards. Express results as μg per g of fresh or dry weight.
Protocol 2: Monitoring Pesticide Exposure in Human Subjects
1. Study Design:
- Intervention: A 24-week randomized, controlled crossover trial is recommended [18]. Participants replace their conventional diet with a certified organic diet for a set period, followed by a washout period and a return to their conventional diet.
- Control: Maintain a consistent cohort on a conventional diet for comparison.
2. Biospecimen Collection:
- Urine Sampling: Collect first-morning void urine samples from participants at baseline, weekly during the intervention, and post-washout.
- Storage: Aliquot samples and store immediately at -80°C to prevent analyte degradation.
3. LC-MS/MS Analysis for Pesticide Metabolites:
- Analytes: Target specific metabolites of common pesticides (e.g., 3-phenoxybenzoic acid for pyrethroids; dialkyl phosphates for organophosphates).
- Sample Prep: Thaw samples on ice. Dilute 1:1 with a buffer. Use solid-phase extraction (SPE) or dilute-and-shoot protocols for clean-up and pre-concentration.
- Instrumentation: Liquid Chromatography-Tandem Mass Spectrometry (LC-MS/MS).
- Quantification: Use isotope-labeled internal standards for each target metabolite to ensure analytical precision and accuracy. Report results as μg of metabolite per g of creatinine.
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Key Reagents and Materials for Comparative Food Composition Studies
| Item Name | Function/Application | Technical Specifications & Notes |
|---|---|---|
| Certified Organic & Conventional Reference Materials | Essential for method validation and calibration. Provides a known baseline for compositional analysis. | Must be sourced from the same crop variety, harvest year, and geographical region to control for confounding variables. |
| Stable Isotope-Labeled Internal Standards (e.g., ¹³C-labeled pesticide metabolites) | Used in LC-MS/MS for highly accurate quantification. Corrects for matrix effects and analyte loss during sample preparation. | Critical for achieving publication-grade data in complex biological matrices like urine or plant extracts. |
| Reverse-Phase C18 HPLC Columns | The workhorse for separating complex mixtures of antioxidants, polyphenols, and pesticide residues. | Standard dimensions: 250 mm x 4.6 mm, 5 μm particle size. UHPLC columns (sub-2 μm) offer higher resolution and faster analysis. |
| Solid-Phase Extraction (SPE) Cartridges | Clean-up and pre-concentration of analytes from complex sample matrices (e.g., urine, food extracts). | Various sorbents available (C18, HLB). Select based on the chemical properties of the target analytes to maximize recovery and reduce interference. |
| Authentic Phytochemical Standards (e.g., Quercetin, Cyanidin, Resveratrol) | Used to create calibration curves for the identification and absolute quantification of specific antioxidants. | Purity should be ≥95% (HPLC grade). Store according to manufacturer specifications to maintain stability. |
Technical Support Center
Frequently Asked Questions (FAQs)
FAQ 1: What are the most critical confounding factors when comparing organic and conventional diets in human studies?
The most significant confounding factors stem from the difficulty in accurately assessing dietary intake and the inherent differences between people who choose organic versus conventional foods [19] [17].
- Dietary Assessment Limitations: All methods for measuring what people eat (e.g., 24-hour recalls, food frequency questionnaires) have weaknesses. These include poor memory, underreporting of disliked foods like alcohol, and an inability to correctly estimate portion sizes. Furthermore, a single 24-hour recall does not capture an individual's habitual diet, which is what matters for chronic disease risk [19].
- Systematic Consumer Differences: Studies show that regular organic food consumers are often more health-conscious, have higher educational attainment and income, are more physically active, and are more likely to follow plant-based or whole-food diets. These lifestyle and socioeconomic factors are independently linked to better health outcomes and can easily confound observed health differences [17] [20].
- The "Healthy Consumer" Bias: An individual's current diet may not reflect their past diet, and recall of past diet can be influenced by their present habits and beliefs. This makes case-control studies investigating diet and disease particularly susceptible to bias [19].
FAQ 2: How can I control for the "healthy consumer" effect in my observational study design?
Controlling for this effect requires meticulous study design and statistical analysis.
- Measure and Adjust: Collect extensive data on potential confounders, including:
- Use Propensity Score Matching: This statistical technique can help create a comparison group of conventional consumers who are similar to the organic consumers across all measured confounding variables.
- Longitudinal Cohort Designs: Prospective studies that enroll participants before disease develops and follow them over time are more robust than case-control studies for this type of research [21].
FAQ 3: My intervention trial requires participants to switch to an organic diet. What practical challenges should I anticipate?
Dietary intervention trials face specific hurdles related to compliance and study design.
- Cost and Accessibility: Organic foods are often more expensive and less available, which can be a barrier for participants and increase the cost of the study [20].
- Blinding Difficulty: It is challenging to blind participants to their dietary assignment, which may lead to placebo or nocebo effects.
- Defining the Intervention: The "organic" intervention must be clearly defined, typically requiring the use of certified organic foods, and the control diet must be matched in every way except for the production method [17].
- Appropriate Duration: Short-term studies may only capture immediate changes (e.g., reduction in pesticide urine biomarkers) but miss long-term health outcomes. Determining the required length to see a physiological effect is a key design challenge [17] [22].
FAQ 4: How does day-to-day variation in an individual's diet impact my results, and how can I account for it?
Day-to-day variation is a major source of error that can obscure true dietary patterns [19].
- The Problem: An individual's intake of foods and nutrients varies widely from day to day. A single 24-hour recall may miss commonly eaten foods simply because they were not consumed on that specific day.
- The Solution: Increase the number of dietary assessment days. The number needed for a moderately accurate estimate of habitual intake varies by nutrient but can sometimes exceed 30 days. Using food frequency questionnaires (FFQs) designed to capture habitual intake over a longer period (months or a year) is another common, though less precise, approach [19].
Troubleshooting Guides
Problem: An observed health benefit from organic food consumption disappears after adjusting for socioeconomic status and lifestyle factors.
- Diagnosis: This strongly suggests that the observed association was not causal but was instead confounded by the "healthy consumer" effect. The health benefit was likely driven by the overall healthier profile of people who choose organic food, not the organic food itself [17] [20].
- Solution:
- Re-evaluate Your Model: Ensure you have collected and adjusted for all relevant confounding variables. Consider using more sophisticated statistical methods like propensity score analysis.
- Design for the Future: For future studies, consider a long-term, whole-diet substitution trial where participants are randomly assigned to receive either organic or conventional diets, thereby minimizing the self-selection bias [17].
Problem: Urine biomarker data shows high variability between participants on the same diet regime.
- Diagnosis: This is expected due to interindividual variation in metabolism, pharmacokinetics, and baseline microbiome composition. Personalization is a key feature of diet-microbiome interactions; the same food can be metabolized differently by different people [22].
- Solution:
- Longitudinal Sampling: Take multiple samples from the same individual over time to define their personalized response, rather than relying on a single time point [22].
- Increase Sample Size: Ensure your study has enough participants to capture and account for the range of human variability.
- Control Diet Pre-sampling: In intervention studies, provide participants with a standardized diet for a few days before sample collection to reduce noise from recent dietary intake [22].
Problem: A study finds no compositional differences between organic and conventional foods, but other literature claims there are.
- Diagnosis: Inconsistencies can arise from methodological differences in food sampling, chemical analysis, and statistical modeling. Factors like crop variety, soil type, weather, and harvest timing can also cause natural variation that obscures production method effects [19] [20].
- Solution:
- Review the Protocol: Critically examine the methodologies of the conflicting studies. Were the foods grown in controlled conditions or purchased from the market? Were they analyzed in the same lab using the same methods?
- Check for Systematic Reviews: Rely on large-scale systematic reviews and meta-analyses, which pool data from multiple studies to provide a more definitive conclusion than any single study can [17] [20].
- Focus on Consistent Trends: Look for patterns across the literature. For example, some meta-analyses consistently report higher antioxidant concentrations and lower cadmium levels in organic crops, even if individual studies disagree [17].
Methodological Protocols & Data Presentation
Table 1: Key Confounding Factors and Mitigation Strategies in Organic vs. Conventional Diet Studies
| Confounding Factor | Impact on Research | Recommended Mitigation Strategy |
|---|---|---|
| Socioeconomic Status | Organic consumers often have higher income/education, which correlates with better health. | Measure and statistically adjust for income, education, and occupation [17] [20]. |
| Overall Diet Quality | Organic consumers may eat more fruits, vegetables, and whole grains, and less processed food. | Assess and control for overall dietary patterns (e.g., Mediterranean diet score) and food group intake [17] [20]. |
| Lifestyle Factors | Organic consumers are often more physically active and less likely to smoke. | Collect data on physical activity, smoking status, and alcohol use for use as covariates [17]. |
| Health Consciousness | Greater attention to personal health leads to behaviors that improve outcomes, independent of diet. | Use validated questionnaires to measure health consciousness and include in analysis [20]. |
| Body Mass Index (BMI) | BMI is a strong independent risk factor for many diseases and can be a confounder. | Measure and adjust for BMI at baseline and, in long-term studies, over time [17]. |
Table 2: Comparison of Dietary Intake Assessment Methods [19]
| Method | Description | Key Advantages | Key Limitations |
|---|---|---|---|
| 24-Hour Recall | Interviewer asks participant to recall all food/beverages consumed in the previous 24 hours. | Low participant burden; does not alter eating behavior. | Relies on memory; single day not representative of usual intake; prone to under-reporting. |
| Food Record/Diary | Participant records all foods/beverages as they are consumed, often with weighed amounts. | More detailed and accurate than recall; multiple days possible. | High participant burden; can alter habitual diet ("reactivity"); requires high motivation. |
| Food Frequency Questionnaire (FFQ) | Participant reports how often they consumed a fixed list of foods over a long period (e.g., past year). | Captures habitual intake; efficient for large studies. | Portion size estimates are imprecise; memory decay over long periods; fixed food list may not capture all items. |
| Food Supply Data | Estimates national consumption based on food production + imports - exports. | Useful for international comparisons and tracking trends. | Does not account for waste or individual intake; only provides population-level averages. |
Experimental Protocol: Designing a Controlled Feeding Trial to Isolate Production Method Effects
Objective: To determine the effect of a diet made from certified organic ingredients versus a conventional diet on specific health biomarkers, while controlling for diet composition and confounding factors.
Key Materials & Reagents:
- Certified Organic Foodstuffs: All intervention foods must be sourced from certified organic producers.
- Conventional Control Foodstuffs: Sourced to be of the same variety and type as the organic foods.
- Food Composition Database: For nutritional analysis and meal matching (e.g., USDA FoodData Central).
- Biomarker Assay Kits: Validated kits for measuring outcomes of interest (e.g., pesticide metabolites, nutritional biomarkers, oxidative stress markers).
Procedure:
- Participant Recruitment & Screening: Recruit healthy participants and screen for willingness to consume all provided study foods. Exclude those with allergies or dietary restrictions that would interfere with the diet.
- Randomization & Blinding: Randomly assign participants to the Organic Diet group or the Conventional Diet group. Implement single-blinding where possible (e.g., participants are not told which diet they are receiving, though complete blinding is difficult).
- Diet Design & Preparation:
- Develop a standardized 7-day rotating menu.
- Prepare identical meals for both groups, differing only in the production method (organic vs. conventional) of the ingredients.
- Control for all other variables: use the same recipes, cooking methods, and portion sizes.
- Food Provision: Provide all meals and snacks to participants for the duration of the intervention period (e.g., 2 weeks to 3 months).
- Compliance Monitoring: Use multiple methods to monitor compliance, such as daily check-ins, returned food containers, and periodic 24-hour recalls.
- Biological Sampling: Collect biological samples (e.g., blood, urine, feces) at baseline, at regular intervals during the intervention, and at the end of the study.
- Sample Analysis: Analyze samples for target biomarkers using standardized, validated laboratory protocols [23].
Visual Workflows and Pathways
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Reagents and Materials for Diet-Microbiome and Nutritional Studies
| Item | Function in Research | Example Application |
|---|---|---|
| Certified Organic Reference Materials | Serves as the verified organic intervention material in controlled feeding studies. | Used as the primary ingredient in meals for the organic arm of a clinical trial [17]. |
| Pesticide Metabolite ELISA Kits | Quantifies specific pesticide breakdown products in urine or blood serum. | Measuring changes in pesticide exposure biomarkers in participants before and after an organic diet intervention [17]. |
| DNA/RNA Extraction Kits | Isolates high-quality genetic material from microbial samples (e.g., stool). | Profiling the gut microbiome composition of study participants to investigate diet-microbiome interactions [22]. |
| Short-Chain Fatty Acid (SCFA) Assay Kits | Measures concentrations of microbially produced fatty acids (e.g., acetate, propionate, butyrate) in fecal or blood samples. | Assessing functional changes in the gut microbiome in response to different dietary regimes [22]. |
| Food Composition Database | Provides standardized nutrient profile data for thousands of food items. | Calculating the nutritional content of study diets and ensuring the organic and conventional arms are matched for macronutrients and key micronutrients [24] [25]. |
| Nutrient Profiling Model | A algorithm to score the overall nutritional quality of foods or diets. | Controlling for overall diet quality as a confounding variable in observational studies comparing organic and conventional consumers [25]. |
Implementing Rigorous Frameworks: Standardized Methods for Reliable Food Composition Analysis
Leveraging Validated Nutrient Profiling Models (NPS) for Objective Food Quality Assessment
Frequently Asked Questions (FAQs)
Q1: What is a Nutrient Profiling Model (NPM), and why is its validation critical for research?
A1: A Nutrient Profiling Model (NPM) is a science-based tool that classifies or ranks foods based on their nutritional composition to assess their healthfulness [26] [27]. Validation is the process of testing how well the model's ratings correlate with real-world health outcomes. Using a validated model is crucial for research integrity, as it ensures that the conclusions drawn about a food's quality are supported by scientific evidence and not just the arbitrary output of an algorithm [26] [28]. For instance, a model with strong criterion validity has been shown in studies that higher-rated foods are linked to a lower risk of chronic diseases [28].
Q2: Which NPMs have the strongest scientific validation for predicting health outcomes?
A2: Based on a systematic review and meta-analysis, several NPMs have been assessed for their criterion validity. The following table summarizes the current validation evidence for key models [28]:
| Nutrient Profiling System (NPS) | Level of Criterion Validation Evidence | Key Health Outcomes Linked to Higher Diet Quality (Where Available) |
|---|---|---|
| Nutri-Score | Substantial | Lower risk of cardiovascular disease, cancer, and all-cause mortality. |
| Food Standards Agency (FSA-NPS) | Intermediate | Evidence exists but is less extensive than for Nutri-Score. |
| Health Star Rating (HSR) | Intermediate | Evidence exists but is less extensive than for Nutri-Score. |
| Food Compass | Intermediate | Evidence exists but is less extensive than for Nutri-Score. |
| Nutrient-Rich Food (NRF) Index | Intermediate | Evidence exists but is less extensive than for Nutri-Score. |
Q3: My research compares organic and conventional foods. Are some NPMs better suited for this purpose?
A3: The choice of NPM is critical in organic vs. conventional studies. Systematic reviews have found that significant nutritional differences between organic and conventional foods are not universal but are highly dependent on the specific food type and nutrient being analyzed [29] [30]. Therefore, you should select a model with high content validity that incorporates a wide range of relevant nutrients. A model that only considers a few "negative" nutrients (e.g., sugar, sodium, saturated fat) may miss subtle differences in beneficial nutrients (e.g., certain minerals, polyphenols) that could be influenced by production methods [31]. The model should be transparent and its algorithm publicly available to ensure the reproducibility of your findings [31].
Q4: What are common sources of error when applying an NPM in an experimental setting?
A4: Common experimental issues include:
- Inaccurate Input Data: The quality of the NPM output is entirely dependent on the accuracy of the nutrient composition data entered. Reliable data must come from rigorous chemical analysis using validated methods, not just estimated from packaging [32].
- Improper Sample Preparation: Inconsistent sample preparation techniques can alter the nutrient composition of the food being tested, leading to erroneous profiling results [32].
- Misapplication of the Model: Using a model outside its intended scope (e.g., applying a general model to a specific food category for which it wasn't designed) can produce invalid classifications [26] [31].
Troubleshooting Common Experimental Issues
Issue 1: Inconsistent or Unreliable Nutrient Composition Data
Problem: Results from the NPM are inconsistent with nutritional expectations, potentially due to poor-quality input data.
Solution: Implement a rigorous protocol for generating and handling nutrient composition data.
Experimental Protocol for Food Composition Analysis:
- Representative Sampling: Ensure the food sample is a true representative of the bulk material being studied. Use appropriate quartering or riffling techniques for solid foods [32].
- Standardized Sample Preparation:
- Validated Analytical Methods:
- Total Protein: Prefer the Enhanced Dumas method over traditional Kjeldahl, as it is faster, does not require toxic chemicals, and can be automated [32].
- Total Fat: For complex matrices, Microwave-Assisted Extraction (MAE) offers a faster, more efficient, and less solvent-consuming alternative to traditional Soxhlet extraction [32].
- Dietary Fibre: Utilize integrated assay kits (e.g., Rapid Integrated Total Dietary Fibre (RITDF)) that combine multiple official methods for greater accuracy and potential cost savings [32].
- Data Quality Control: All analytical methods should follow Good Laboratory Practice (GLP) and, where possible, use methods endorsed by international organizations like AOAC International to ensure reliability and reproducibility [32].
Issue 2: The Chosen NPM Fails to Detect Relevant Nutritional Differences
Problem: In an organic vs. conventional comparison study, the selected NPM shows no difference, but you hypothesize there may be differences in micronutrients or phytochemicals.
Solution: Employ advanced, non-targeted analytical techniques to build a comprehensive nutrient profile and consider using or developing an NPM that incorporates a wider range of beneficial components.
Experimental Protocol for Non-Targeted NMR Metabolomics:
This technique provides a holistic "fingerprint" of a food's metabolome, capturing subtle variations that targeted methods might miss [33].
- Sample Preparation: Extract metabolites using a standardized solvent (e.g., buffer solution in D₂O). The process must be identical for all samples to ensure comparability [33].
- NMR Measurement: Use optimized and agreed-upon acquisition parameters. The 1D NOESY-presat pulse sequence is often used for aqueous extracts to suppress the water signal. The Carr-Purcell-Meiboom-Gill (CPMG) pulse sequence can be used to highlight low-molecular-weight metabolites [33].
- Data Processing: Process the Free Induction Decay (FID) signals by applying Fourier Transform (FT), phase correction, and baseline correction. Normalize the spectra to a internal standard, such as DSS [33].
- Data Analysis: Use multivariate statistical analysis (e.g., Principal Component Analysis - PCA) on the processed spectral data to identify metabolite patterns that differentiate sample groups (e.g., organic vs. conventional) [33].
The Scientist's Toolkit: Essential Research Reagents & Materials
The following table details key materials and instruments essential for generating high-quality data for nutrient profiling.
| Item | Function / Relevance in Nutrient Profiling Research |
|---|---|
| Halogen Moisture Analyzer | Determines moisture content rapidly and accurately, which is critical for expressing all other nutrient data on a consistent dry-weight basis [32]. |
| Microwave-Assisted Extraction (MAE) System | Extracts components like fat efficiently from complex food matrices with reduced solvent use and time compared to traditional methods [32]. |
| NMR Spectrometer | The core instrument for non-targeted metabolomics. It provides a highly reproducible and comprehensive fingerprint of a food's molecular composition, ideal for detecting subtle differences and ensuring authenticity [33]. |
| Internal Standard (e.g., DSS for NMR) | A compound of known concentration added to samples to provide a reference point for quantitative analysis and spectral normalization, ensuring data comparability across different runs and instruments [33]. |
| Integrated Dietary Fibre Assay Kit | Provides a streamlined and accurate method for quantifying total dietary fibre by combining several official methods into a single test [32]. |
| Certified Reference Materials (CRMs) | Samples with known nutrient concentrations used to calibrate instruments and validate analytical methods, ensuring the accuracy and traceability of all generated data [32]. |
Frequently Asked Questions (FAQs)
FAQ 1: What is the fundamental difference between a criterion-validated system like the FSA-NPS and a simple, unvalidated checklist for classifying food quality? A criterion-validated system undergoes rigorous scientific testing to ensure it measures what it intends to measure. The FSA-NPS, which underpins the Nutri-Score, has been evaluated for three key types of validity, as recommended by the WHO [34]:
- Content Validity: Its ability to correctly rank foods according to their healthfulness across the entire food supply [34] [35].
- Convergent Validity: Its alignment with national food-based dietary guidelines. Studies have assessed its consistency with French dietary guidelines, though further adaptations may be needed for other European countries [34].
- Predictive Validity: Its ability, when applied to population dietary data, to predict disease risk. Prospective cohort studies have shown that diets composed of foods with worse FSA-NPS scores are associated with higher risks of overall cancer, as well as specific cancers like colon-rectum and lung cancer [36].
An unvalidated checklist lacks this evidence base, leading to potential misclassification and unreliable results in comparative studies.
FAQ 2: Our research involves comparing the nutritional quality of organic versus conventional foods. How can the FSA-NPS algorithm be integrated into our study design to improve consistency? You can use the FSA-NPS as a standardized, quantitative tool to score and compare products from both production systems. This addresses a key challenge in the field, as systematic reviews have found "no evidence of a difference in nutrient quality between organically and conventionally produced foodstuffs" when using simple nutrient comparisons [30]. The FSA-NPS provides a holistic profile.
- Data Collection: For each food item in your study, collect the nutritional data required by the FSA-NPS algorithm per 100g or 100ml: energy, saturated fat, total sugars, sodium, protein, fiber, and the percentage of fruits, vegetables, legumes, and nuts [34] [35].
- Calculation: Apply the FSA-NPS algorithm to calculate a single score for each product. A lower score indicates better nutritional quality [34].
- Comparison: Statistically compare the mean FSA-NPS scores between the organic and conventional product groups. This provides an objective, validated metric for overall nutritional quality comparison, moving beyond isolated nutrient comparisons.
FAQ 3: We applied the FSA-NPS algorithm and found that some results appear counter-intuitive (e.g., a traditional product scores poorly). Does this invalidate the system? Not necessarily. This scenario often highlights a key principle: the system is designed for public health guidance, not to endorse all traditional or "natural" products.
- Check the Algorithm's Scope: The FSA-NPS is designed for "across-the-board" comparison of all packaged and processed foods [34]. It may correctly identify products high in energy, saturated fats, sugars, or salt, even if they are traditional [37].
- Confirm Your Inputs: Double-check that the nutritional composition data for your products is accurate and that you have correctly applied the algorithm's specific modifications for categories like beverages, cheeses, and added fats [35].
- Contextualize Findings: Acknowledge that the system focuses on nutritional quality for chronic disease prevention. A product's cultural value or "natural" status does not automatically equate to a high nutritional quality within this specific framework [38].
FAQ 4: A reviewer has questioned the real-world effectiveness of the Nutri-Score system, citing publication bias. How should we address this in our manuscript? Acknowledge this ongoing scientific debate and present a balanced view based on the available evidence.
- Cite Supporting Evidence: Reference studies that demonstrate the label's effectiveness in laboratory and simulated shopping environments, such as its superior ability to help consumers rank products by nutritional quality compared to other labels [35].
- Acknowledge Limitations: Note that a recent systematic review found limited real-life impact on purchasing behavior and that effect sizes can be small, particularly for products in the middle (C, D) categories [39].
- Discuss Bias Concerns: Cite analyses that report a potential publication bias, where a large majority of studies supporting Nutri-Score are carried out by its developers, while a majority of independently conducted studies show unfavorable results [40]. Clearly state the affiliations of the studies you cite to ensure transparency.
Troubleshooting Guides
Issue: Inconsistent Application of the FSA-NPS Algorithm to Composite Foods
| Symptoms | Possible Causes | Recommended Solutions |
|---|---|---|
| Wide variation in scores for similar composite foods (e.g., pizzas, sandwiches). | • Inaccurate estimation of the Fruits, Vegetables, Legumes, and Nuts (FVLN) component, which is a key "positive" element in the algorithm [35]. | • Do not estimate FVLN from nutritional proxies. Instead, obtain the precise percentage (by weight) from the product manufacturer or use detailed recipe-based calculations. |
| • Misapplication of the specific algorithm rules for borderline food categories. | • Consult the specific technical guides for the adapted FSA-NPS (FSAm-NPS). Adhere to the distinct rules for beverages, cheeses, and added fats [34] [35]. | |
| • Use of generic nutritional data that does not match the specific product formulation. | • Source product-specific data from food composition databases or direct chemical analysis where feasible, especially for key variables like fiber and sodium. |
Issue: Low Discriminatory Power in Specific Food Subgroups
| Symptoms | Possible Causes | Recommended Solutions |
|---|---|---|
| All products within a narrow category (e.g., different brands of white bread) receive similar or identical scores. | • The nutritional composition of products within the category is genuinely very similar. | • Acknowledge the finding. The system may be working correctly, indicating a market segment with little nutritional variation. Report the lack of discrimination as a result. |
| • The algorithm's resolution is insufficient for making fine distinctions within very homogeneous, low-quality categories. | • Supplement the FSA-NPS analysis with additional, more specific nutrient analyses (e.g., free sugars vs. total sugars, specific fatty acid profiles) that are relevant to your research question [17]. | |
| • The product category is outside the system's optimal design scope (e.g., single-ingredient, unprocessed foods). | • Contextualize the results. For basic ingredients (e.g., fresh fruits, vegetables, plain meat), the primary differentiator may be the presence of pesticide residues or other non-nutritional factors, which FSA-NPS does not capture [41] [17]. |
Experimental Protocols
Protocol: Validating a Nutrient Profiling System for Comparative Studies
This protocol outlines the key steps for establishing the content and convergent validity of a profiling system, based on the validation framework of the FSA-NPS/Nutri-Score [34] [35].
Objective: To determine if a nutrient profiling system correctly ranks foods by healthfulness (content validity) and aligns with independent dietary guidance (convergent validity).
Materials:
- Research Reagent Solutions: See the detailed table in Section 4.
- Software: Statistical analysis software (e.g., R, SPSS, SAS), data visualization tools.
- Primary Input: A comprehensive food composition database representing the food supply under study (e.g., a national database or a study-specific database of analyzed samples).
Methodology:
- Food Sampling & Data Collection:
- Assemble a representative sample of foods from the relevant food supply. The sample should cover all major food groups and subgroups.
- For each food, compile accurate data for all nutrients and components required by the profiling algorithm.
Calculation of Profile Scores:
- Apply the algorithm to each food item to compute its nutritional quality score.
Content Validity Assessment:
- Analysis: Examine the distribution of scores within and across pre-defined food groups (e.g., grains, dairy, meats, composite foods).
- Expected Outcome: The system should demonstrate a gradient of scores. For example, in the Nutri-Score validation, fruits and vegetables were predominantly classified in the healthier categories (A/B), while fats and sugars were concentrated in the less healthy categories (D/E) [35]. A system that fails to create such discrimination has poor content validity.
Convergent Validity Assessment:
- Analysis: Compare the system's classifications with official national dietary guidelines. Categorize foods as "Recommended" (to be consumed frequently), "Neutral," or "Limit" (to be consumed in moderation) based on the guidelines.
- Expected Outcome: A statistically significant majority of foods classified as "Recommended" by the guidelines should receive favorable scores from the profiling system, and vice-versa [34] [35].
Workflow Diagram: System Validation and Application
The diagram below illustrates the logical workflow for validating and applying a criterion-validated system like the FSA-NPS in a research study, such as comparing organic and conventional foods.
The Scientist's Toolkit: Research Reagent Solutions
This table details the core components required to implement the FSA-NPS algorithm in a research setting.
| Research Reagent / Material | Function in the Experiment | Technical Specifications & Considerations |
|---|---|---|
| Nutritional Composition Database | Provides the primary input data for calculating the FSA-NPS score for each food item. | • Must contain data per 100g/100ml for: energy (kJ), saturated fat (g), total sugars (g), sodium (mg), protein (g), fiber (g).• Critical: Must include or allow estimation of Fruits, Vegetables, Legumes, and Nuts (FVLN) as a percentage of total weight [35]. |
| FSA-NPS / FSAm-NPS Algorithm | The core computational formula that integrates positive and negative nutritional components into a single score. | • Use the officially documented and updated algorithm (e.g., the FSAm-NPS used for Nutri-Score) [34] [37].• Note specific rules for product categories like beverages, cheeses, and fats [35]. |
| Food Classification Framework | Allows for the analysis of score distributions within and across homogeneous food groups. | • Use a standardized system like the EUROFIR classification (e.g., "grain product" -> "breakfast cereals") to ensure consistent grouping and meaningful interpretation of results [35]. |
| Laboratory Analysis Kits | For generating primary nutritional data when reliable database information is unavailable. | • Required for analyzing: Dietary Fiber, Specific Sugar Profiles, Saturated Fatty Acids, and Sodium content. Essential for primary data collection in intervention studies [41]. |
| Statistical Analysis Software | To perform significance testing on score differences between groups and to assess the discriminatory power of the system. | • Used for tests like ANOVA (to compare mean FSA-NPS scores between organic and conventional groups) and Chi-Square (to compare distributions across nutritional classes) [35]. |
Designing Long-Term, Whole-Diet Substitution Trials to Assess Clinically Relevant Health Outcomes
Troubleshooting Common Challenges in Dietary Trials
FAQ: What are the most significant threats to the viability of long-term dietary intervention trials?
High attrition rates and difficulties maintaining participant compliance are major threats to trial viability. One 12-month dairy intervention trial reported a 49.3% attrition rate, fundamentally threatening the study's statistical power. The primary factors contributing to dropout included: inability to comply with dietary requirements (27.0%), health problems or medication changes (24.3%), and excessive time commitment (10.8%) [42].
FAQ: How can we mitigate participant dropout in long-term studies?
Implementing a run-in period before randomization helps assess participant motivation, commitment, and availability. Maintaining regular contact during control phases, minimizing time commitment, providing flexibility with dietary requirements, and facilitating positive experiences also improve retention. Stringent monitoring of diet through logs and regular check-ins can further enhance adherence [42].
FAQ: What biases are particularly problematic in dietary trials?
Dietary trials are susceptible to several unique biases. Selection bias occurs when participants with certain dietary habits or beliefs are more likely to enroll. Compliance bias emerges when pre-existing diet beliefs and behaviors influence a participant's ability to adhere to the protocol. Participant expectancy effects can shape clinical responses based on prior knowledge of the intervention. Dietary collinearity presents another challenge, where changing one dietary component leads to compensatory changes in others, confounding results [43].
Methodological Guidance for Robust Trial Design
FAQ: What are the key considerations when choosing a mode of dietary intervention delivery?
The choice of delivery method involves trade-offs between precision, adherence, cost, and real-world applicability. The table below compares the primary approaches:
| Delivery Method | Key Advantages | Key Limitations | Best Suited For |
|---|---|---|---|
| Feeding Trials (Providing all food) | High precision; Excellent adherence control; Direct compensation for dietary collinearity [43] | High cost; Limited real-world applicability; Logistically complex [43] | Highly controlled efficacy studies with sufficient budget [43] |
| Dietary Counseling (Guiding food choices) | High clinical applicability; Lower cost; Respects personal preferences [43] | Variable adherence; Imprecise intervention; Difficult to control for collinearity [43] | Pragmatic effectiveness trials and clinical practice translation [43] |
| Hybrid Approaches (Combining methods) | Balances control and practicality; Can improve adherence | Still faces some limitations of both methods | Trials needing moderate control with better real-world application |
FAQ: How can we improve dietary adherence and acceptability in long-term trials?
Incorporating cultural and taste preferences is crucial. Using herbs and spices can maintain the acceptability of healthier food options without adding excessive saturated fat, sodium, or sugar. Providing detailed recipes and preparation methods improves intervention reproducibility and translatability. Collaboration with specialist dietitians allows for personalization based on food preferences, cultural and religious practices, and socioeconomic restrictions while maintaining nutritional adequacy [43] [44].
FAQ: What design aspects are critical for a robust whole-diet substitution trial?
- Crossover vs. Parallel Design: Crossover designs (where participants act as their own controls) reduce required sample size but risk carryover effects and require careful consideration of washout periods [42] [43].
- Control Group Selection: A well-designed control diet is essential. For organic versus conventional comparisons, this may involve matching for all variables except the farming method [43].
- Blinding: While full blinding is challenging in dietary trials, partial blinding (e.g., to the study hypothesis) and using neutral language can mitigate expectancy effects [43].
- Outcome Measurement: Use high-quality, clinically relevant, and validated endpoints. For microbiome-related outcomes, consider the rapidity of diet-induced changes and substantial temporal variability [43].
Experimental Protocols for Diet-Metabolic Health Assessments
Protocol: Assessing Cardiometabolic and Cognitive Health Outcomes in a 12-Month Dietary Intervention
This protocol is adapted from a published 12-month, randomised, two-way crossover study [42].
1. Participant Recruitment and Screening:
- Target Population: Recruit overweight/obese adults (BMI ≥25 kg/m²) with habitually low intake of the food of interest (e.g., <2 dairy servings/day).
- Exclusion Criteria: Include current smokers, pre-existing metabolic diseases (diabetes, CVD, liver/renal disease), food allergies/intolerances related to the intervention, use of medications affecting outcomes, and pregnancy.
- Recruitment Strategies: Utilize local newspaper advertisements, public noticeboards, and television segments to reach potential volunteers [42].
2. Baseline and Follow-up Assessments: Conduct comprehensive assessments at baseline, 6 months, and 12 months.
- Anthropometry & Body Composition: Measure body weight, waist circumference, and percentage total and abdominal body fat (via DEXA).
- Blood Pressure & Biochemistry: Assess systolic/diastolic blood pressure and analyze fasting plasma glucose, triglycerides, HDL, LDL, and total cholesterol.
- Metabolic Rate: Measure resting metabolic rate by indirect calorimetry.
- Vascular Health: Assess arterial compliance via pulse wave velocity.
- Cognitive Function: Administer a battery of neuropsychological tests (approx. 1-1.5 hours) assessing processing speed, attention, memory, executive function, etc [42].
3. Dietary Intervention Delivery:
- High-Intake Phase: Provide participants with all required intervention foods (e.g., 4 servings/day) weekly or fortnightly. Use coolers and ice bricks for transport. Provide verbal and written serving size instructions.
- Low-Intake (Control) Phase: Instruct participants to limit intake to habitual low levels (e.g., 1 serving/day). Do not provide food during this phase.
- Dietary Compliance Monitoring: Use daily food logs during the high-intake phase. Offer nutritional counseling to help participants incorporate intervention foods without increasing total energy intake [42].
4. Data Collection and Monitoring:
- Dietary Intake: Collect 3-day weighed food records, food frequency questionnaires, and 3-day physical activity diaries at each assessment point.
- Participant Retention: Send reminder letters 2 weeks before assessments and make reminder phone calls the week prior. Follow a strict protocol (max. 3 calls + 1 letter) for non-attendance before considering withdrawal [42].
Diagram: 12-Month Crossover Trial Workflow for Whole-Diet Intervention
The Researcher's Toolkit: Essential Reagents & Materials
Research Reagent Solutions for Dietary Intervention Trials
| Item/Category | Function/Purpose | Specific Examples & Notes |
|---|---|---|
| Dietary Assessment Tools | To quantify habitual intake and monitor compliance during the trial. | 3-day weighed food records [42], Food Frequency Questionnaires (FFQs) [42], 24-hour dietary recalls. |
| Food Provision System | To ensure consistent quality and dosage of the intervention diet. | Cooler bags, ice bricks for transport [42], standardized food portions. |
| Anthropometry Kit | To measure body composition changes as primary/secondary outcomes. | DEXA for body fat [42], stadiometer, calibrated scales, waist circumference tape. |
| Phlebotomy & Blood Analysis | To assess cardiometabolic biomarkers. | Fasting blood samples for glucose, lipids (HDL, LDL, triglycerides) [42]. |
| Cognitive Assessment Batteries | To evaluate cognitive health outcomes. | Neuropsychological tests for memory, attention, executive function [42]. |
| Physical Activity Monitors | To control for confounding from energy expenditure. | 3-day physical activity diaries [42], accelerometers. |
Logical Framework for Designing a Dietary Substitution Trial
Diagram: Logical Flow for Trial Design Decision-Making
This technical support center provides troubleshooting and methodological guidance for researchers integrating Dried Blood Spot (DBS) testing and metabolic profiling into nutritional studies. The content is specifically framed to support investigations aimed at improving consistency in comparing the biological effects of organic versus conventional foods. The following FAQs, protocols, and data summaries are designed to address key experimental challenges.
Frequently Asked Questions (FAQs) and Troubleshooting
1. How does the metabolic coverage of DBS compare to plasma, and is it suitable for detecting nutritional biomarkers?
While DBS samples contain whole blood (including blood cells), they typically yield a lower number of detectable metabolites (~700-900) compared to plasma (~1200) [45]. However, all major metabolic pathways and over 95% of the sub-pathways detectable in plasma are also covered by DBS analysis [45]. DBS is particularly well-suited for detecting certain nutritional and inflammatory markers, including:
- Carbohydrates from nucleotide sugars and glycolysis.
- Amino acids related to glutathione metabolism.
- Nucleotides in purine metabolism.
- Cofactors and vitamins such as NAD+.
- Inflammatory markers like eicosanoids and docosanoids [45]. Well-characterized metabolic signatures of disease and dietary intake identified in plasma are generally maintained in DBS, making it a valid matrix for nutritional biomonitoring [45].
2. What are the critical factors affecting metabolite stability in DBS samples, and how can we mitigate them?
Metabolite stability is highly dependent on storage temperature and the chemical nature of the metabolite [46]. Temperature has a more significant impact than storage duration, with warmer conditions accelerating degradation [45].
- Stable Metabolites: 69 metabolites, including 15 lipids, 9 amino acids, and 8 carbohydrates, have been shown to remain stable (RSD < 15%) for 21 days even at temperatures up to 40°C [46].
Unstable Metabolites: Certain classes are highly susceptible to degradation, particularly at higher temperatures. These include:
Mitigation Strategies:
- Consistent Handling: Process all samples (cases and controls) identically [45].
- Optimal Storage: Store and ship samples at -80°C in gas-impermeable bags with desiccant packs. This is the best practice for preserving a wide range of metabolites [45].
- Rapid Analysis or Equilibration: If cold chain is broken, note that most stability changes occur rapidly and stabilize after about three weeks. Metabolon recommends not analyzing samples until they have been stored for at least three weeks post-collection to allow metabolite levels to equilibrate [45].
3. Our study involves remote, at-home sample collection. What are the best practices for DBS collection to ensure data quality?
Successful at-home collection is feasible but requires clear protocols for participants [45].
- Improve Blood Flow: Instruct participants to drink water 30 minutes before collection and keep their hands warm with their hand below waist level before and during collection [45].
- Spot Size: Allow a large blood droplet to form (close to dripping) before application. A single spot should be larger than 7 mm in diameter. Do not "milk" the finger, as this can cause hemolysis [45].
- Spotting: Apply only one droplet per designated circle on the DBS card. If a spot seems too small, wait for a larger droplet and use the next circle. Two full spots are typically required for a comprehensive metabolomic analysis [45].
4. From a precision nutrition standpoint, how can metabolomic data objectively improve comparisons between organic and conventional diets?
Self-reported dietary data is prone to significant inaccuracies [47]. Metabolomics provides an objective snapshot of an individual's nutritional status, capturing the complex biological response to dietary intake beyond what questionnaires can achieve [48] [47].
- Biomarkers of Food Intake: Metabolites can distinguish between dietary patterns.
- Metabotyping: Individuals can be grouped based on their metabolic phenotype (metabotype), which influences their response to dietary interventions [47]. This can help stratify study populations to reduce inter-individual variability and identify subgroups that may respond differently to organic or conventional diets. For example, individuals with "unfavorable" baseline metabotypes may show the greatest metabolic improvement from a dietary intervention [47].
Key Experimental Data for Study Design
Table 1: Metabolite Stability in DBS Under Various Storage Conditions
Data derived from multi-platform untargeted metabolomics analysis (based on [46]).
| Metabolite Category | Stability at 4°C (21 days) | Stability at 25°C (21 days) | Stability at 40°C (21 days) | Key Notes |
|---|---|---|---|---|
| Amino Acids | Mostly Stable | Stable (<14 days) | Becomes Unstable (>14 days) | Chemical transformations at high temps [46]. |
| Phosphatidylcholines (PCs) | Variable | Unstable | Unstable | Major driver of profile separation; susceptible to hydrolysis/oxidation [46]. |
| Triglycerides (TAGs) | Variable | Unstable | Unstable | Major driver of profile separation; susceptible to hydrolysis/oxidation [46]. |
| LysoPCs | Stable | Increased Intensity | Increased Intensity | Elevated intensities observed at higher temperatures [46]. |
| Carbohydrates | Stable | Variable | Variable | Instability observed over 14 days at 25°C & 40°C [46]. |
| Nucleotides, Peptides, SMs | Stable | Stable | Stable | Generally stable across temperature ranges [46]. |
| Number of Stable Metabolites (of 353) | 188 | 130 | 81 | 69 metabolites stable across all three temperatures [46]. |
Table 2: DBS vs. Plasma for Metabolomic Analysis
A comparison of matrix properties and suitability for nutritional studies (based on [45]).
| Parameter | Dried Blood Spot (DBS) | Venous Plasma/Serum |
|---|---|---|
| Sample Volume | Low (finger-prick) | High (venipuncture) |
| Collection | Minimally invasive; suitable for remote, self-collection | Invasive; requires trained phlebotomist |
| Transport/Storage | Stable at ambient temp for many metabolites; easy shipping [47] | Requires cold chain (refrigeration/frozen) |
| Metabolite Coverage | ~700-900 metabolites [45] | ~1200 metabolites [45] |
| Pathway Coverage | >95% of plasma sub-pathways [45] | Standard for biomarker discovery |
| Key Strengths | Ideal for longitudinal & remote studies; good for cellular metabolites (e.g., purines, NAD+) [45] | Higher metabolite coverage; traditional gold standard |
| Key Limitations | Susceptible to oxidation of certain lipids; hematocrit effects can be a factor [45] | Logistically complex and expensive for large-scale studies |
Detailed Experimental Protocols
Protocol 1: Validated Workflow for DBS Metabolomic Analysis in Nutritional Studies
This protocol is adapted from established LC-HRMS workflows for exposomic and metabolomic analysis [49].
1. Sample Collection:
- Material: Use standardized filter paper cards (e.g., Whatman 903 Protein Saver Card) [45].
- Procedure: Follow best practices for finger-prick collection as outlined in the FAQ section. Ensure complete saturation of spots and air-dry for a minimum of 3 hours at room temperature without stacking or exposing to direct heat sources [45].
2. Sample Storage and Transportation:
- Place dried cards in gas-impermeable zip-lock bags with a desiccant pack.
- For optimal preservation of the broadest metabolome, store at -80°C immediately [45]. If simulating postal delivery, define consistent conditions (e.g., 21 days at 25°C) and ensure all samples from a case-control set are treated identically [46] [45].
3. Metabolite Extraction:
- Punching: Remove a defined punch (e.g., 3-6 mm) from the center of each DBS spot.
- Extraction Solvent: Use a pre-optimized single-phase solvent system like methanol with 0.1% formic acid, which has demonstrated acceptable recoveries (60-140%) and reproducibility (median RSD ~18%) for a wide panel of xenobiotics and endogenous metabolites [49].
- Procedure: Add a known volume of internal standard mixture in extraction solvent to the punch. Vortex mix vigorously for 1 minute, then shake for 30 minutes at room temperature. Centrifuge and transfer the supernatant for analysis [49].
4. LC-HRMS Analysis:
- Chromatography: Employ reversed-phase (C18) UHPLC separation with a water/acetonitrile gradient, suitable for a broad range of hydrophilic and hydrophobic compounds.
- Mass Spectrometry: Use a high-resolution mass spectrometer (e.g., Q-TOF or Orbitrap) operating in both positive and negative electrospray ionization (ESI) modes with data-independent acquisition (DIA) to fragment all ions.
5. Data Processing and Integration:
- Process raw data using untargeted metabolomics software for peak picking, alignment, and compound identification against authentic standard libraries where possible.
- For nutritional studies, focus on known food-derived metabolites and dietary biomarkers (e.g., betaine for fruits/vegetables, TMAO for meat/fish) to objectively assess dietary patterns and their biological effects [47].
Protocol 2: A Multi-Omics Integration Pipeline for Precision Nutrition
This pipeline outlines steps for integrating multi-omics data to stratify populations for nutritional intervention, such as organic versus conventional diet studies [50].
1. Sample Collection:
- Collect DBS, saliva, or urine from participants. DBS is ideal for its simplicity and suitability for remote collection [47].
2. Multi-Omics Data Generation:
- Genomics: Perform whole-genome or exome sequencing (DNA-seq) to identify genetic variants (SNPs) [50].
- Transcriptomics: Isolate RNA and perform RNA-seq to analyze gene expression patterns [50].
- Proteomics & Metabolomics: Use LC-MS/MS on DBS or other biofluids to profile protein and metabolite levels [50].
3. Data Preprocessing and Quality Control:
- Genomics/Transcriptomics: Use tools like FastQC for quality control and Trimmomatic for adapter trimming. Align sequences to a reference genome using BWA (DNA) or STAR (RNA) [50].
- Proteomics/Metabolomics: Process raw LC-MS/MS data. Perform filtration, normalization, and imputation of missing values using methods like
MissForestormice[50]. Conduct differential expression analysis with tools likelimma[50].
4. Multi-Omics Data Integration and Functional Analysis:
- Integrate processed datasets from all omics layers.
- Perform functional enrichment analysis (Gene Ontology, KEGG pathways) to identify biological processes and pathways significantly associated with different dietary groups or metabotypes [50].
5. Population Stratification and Intervention:
- Use clustering algorithms on the integrated multi-omics data to identify distinct metabotypes within the study population [47].
- Develop and deliver tailored dietary interventions (e.g., specific organic/conventional food recommendations) based on the identified metabotypes to test for consistent biological responses [50] [47].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Reagents and Materials for DBS-Based Nutritional Metabolomics
This table lists critical components for setting up and running DBS metabolomics studies.
| Item | Function/Description | Example Products / Notes |
|---|---|---|
| DBS Collection Cards | Specially designed filter paper for consistent blood absorption and drying. | Whatman 903 Protein Saver Card [45]. |
| Desiccant Packs | Absorbs moisture during storage to protect sample integrity. | Silica gel desiccant. Must be included in storage bags [45]. |
| Gas-Impermeable Bags | Protects DBS cards from humidity and oxygen during storage/transport. | Zip-lock bags with low oxygen permeability [45]. |
| Internal Standards (IS) | Isotopically-labeled compounds added to correct for extraction and instrument variability. | IS mixture should cover multiple chemical classes (e.g., stable isotope-labeled amino acids, lipids, vitamins). |
| LC-HRMS System | Platform for separating and detecting thousands of metabolites. | UHPLC coupled to Q-TOF or Orbitrap mass spectrometer [49]. |
| Metabolite Libraries | Databases for compound identification and annotation. | Commercially available or custom libraries of authentic standards. |
| Bioinformatics Software | Tools for raw data processing, statistical analysis, and pathway mapping. | XCMS, MetaboAnalyst, DESeq2, limma [50]. |
Overcoming Research Pitfalls: Strategies to Mitigate Bias and Enhance Data Reproducibility
Controlling for Socioeconomic and Lifestyle Confounders in Observational Cohort Studies
Why is controlling for confounders critical in observational studies comparing organic and conventional food consumption? In observational studies, where researchers do not assign exposures, confounding bias is a significant threat to internal validity. A confounder is a variable that is a common cause of both the exposure (e.g., organic food consumption) and the outcome (e.g., a health measure). If not properly accounted for, it can lead to underestimating, overestimating, or even reversing the true effect size, producing misleading conclusions about the relationship between organic diets and health [51].
What are the typical confounders in organic vs. conventional food research? Individuals who regularly consume organic food often differ systematically from those who do not. Common confounders include [17] [20]:
- Socioeconomic Factors: Higher income and education levels are strongly associated with increased organic food purchases.
- Lifestyle Factors: Organic consumers are more likely to be health-conscious, physically active, have a higher ratio of plant to animal foods, and are less likely to smoke. Failure to adequately adjust for these factors can create a false association where the observed health benefits are actually due to a privileged socioeconomic status and healthier overall lifestyle, rather than the organic diet itself.
Troubleshooting Guides & FAQs
Confounder Adjustment Methods
FAQ: What is the most appropriate method to adjust for multiple confounders when investigating several dietary factors?
Problem: A study aims to examine the specific associations of three factors (organic diet, physical activity, and non-smoking status) with a health outcome. The analyst includes all three factors in a single multivariable model.
Issue Identified: This approach, known as mutual adjustment, is a common pitfall. It might lead to "overadjustment bias" because some of these factors (e.g., physical activity) may not be confounders but rather mediators or colliders in the relationship between organic diet and health. This can transform the estimated effect of organic diet from a total effect to a direct effect, potentially providing a misleading interpretation [51].
Solution: The recommended method is to adjust for potential confounders specific to each risk factor-outcome relationship separately. This requires building multiple multivariable regression models, one for each exposure of interest [51].
Table: Comparison of Confounder Adjustment Methods in Multi-Factor Studies
| Adjustment Method | Description | Potential Issue | Appropriateness |
|---|---|---|---|
| Separate Adjustment (Recommended) | A separate model is built for each risk factor, adjusting only for its unique set of confounders. | Requires careful identification of confounders for each specific relationship. | High |
| Mutual Adjustment | All studied risk factors are included in a single multivariable model. | Can cause overadjustment bias if factors are mediators, leading to misleading effect estimates [51]. | Low |
| Identical Adjustment | All risk factors are adjusted for the same set of confounders in separate models. | May adjust for non-confounders for some factors (unnecessary adjustment) or miss key confounders for others (insufficient adjustment) [51]. | Low |
Experimental Protocol for Confounder Adjustment
Protocol: A Step-by-Step Workflow for Robust Confounder Control
- Define the Causal Question: Precisely specify the primary exposure (e.g., level of organic food consumption) and outcome (e.g., incidence of non-Hodgkin lymphoma).
- Construct a Conceptual Diagram: Use a Directed Acyclic Graph (DAG) to map the assumed causal relationships between exposure, outcome, and all other relevant variables (see diagram below).
- Identify Confounders: Based on the DAG, select the set of variables that meet the definition of a confounder for your specific exposure-outcome relationship [51].
- Select Adjustment Method:
- For studies exploring multiple risk factors, use the separate adjustment method [51].
- For a single primary exposure, include all identified confounders in the final regression model.
- Collect and Measure Data: Ensure high-quality data collection for all confounders. Consider using validated questionnaires for lifestyle factors (see "Scientist's Toolkit" below).
- Execute Statistical Analysis: Perform the regression analysis (e.g., Cox regression for time-to-event data) and report effect estimates (e.g., Hazard Ratios) with confidence intervals.
Causal Pathways Between Diet and Health
Data Collection & Measurement
FAQ: How can I accurately measure complex lifestyle confounders like "health consciousness"?
Problem: A study uses a single, non-validated question to assess overall "health consciousness," leading to misclassification and residual confounding.
Issue Identified: Insufficient adjustment occurs when confounder measurement is inadequate, failing to fully remove confounding bias. Crude measures of complex constructs introduce noise and weaken the ability to control for their effect [51].
Solution: Use validated, multi-item instruments or composite scores to reliably capture complex lifestyle and socioeconomic confounders.
Table: Essential Tools for Measuring Key Confounders
| Research Reagent / Tool | Function | Application in Organic Food Studies |
|---|---|---|
| Food Frequency Questionnaire (FFQ) | Assesses habitual dietary intake over time. | Quantifies overall diet quality and level of organic food consumption. Can be used to calculate scores like the Mediterranean Diet Score [52]. |
| International Physical Activity Questionnaire (IPAQ) | Measures levels of physical activity. | Controls for the confounding effect of exercise, which is linked to better diet quality and health outcomes [52]. |
| Validated Mindfulness Scale | Assesses traits like mindful or intuitive eating. | Controls for the psychological aspect of food choice, as mindfulness is positively associated with healthier dietary patterns [52]. |
| Socioeconomic Status (SES) Index | A composite measure often combining income, education, and occupation. | More robustly controls for socioeconomic privilege than any single metric, a major confounder in organic diet research [20]. |
Workflow for Robust Confounder Control
This technical support center provides troubleshooting guides and FAQs to help researchers address specific issues encountered during experiments comparing organic and conventional foods, ultimately improving consistency in this field of research.
Troubleshooting Guides
Guide 1: Unexplained High Variability in Nutrient Analysis Results
Problem Identification: Measured nutrient levels (e.g., polyphenols, antioxidants) show unexpectedly high variance between samples that were expected to be similar.
List Possible Causes:
- Sample Contamination: From tools, containers, or the environment.
- Inconsistent Sample Handling: Variations in washing, drying, or storage temperature.
- Degraded Reagents: Antibodies or assay chemicals stored improperly or used past expiration.
- Instrument Calibration: Spectrophotometer or HPLC not properly calibrated.
- Operator Error: Slight variations in protocol execution by different lab personnel.
Data Collection & Elimination:
- Review Controls: Check if positive and negative controls yielded expected results. If controls are abnormal, the issue is likely with the reagents or instruments [53].
- Audit Equipment & Storage: Verify calibration records for all instruments. Check storage conditions and expiration dates for all reagents [54].
- Review Lab Notebooks: Compare detailed notes from different technicians to identify any inadvertent deviations from the standardized protocol [54].
Experimentation & Identification:
- Re-run a subset of samples using a fresh batch of common reagents to test for reagent degradation.
- Have a single, experienced technician re-prepare and analyze samples with the highest and lowest variances to isolate operator error.
- The cause is identified once a specific change (e.g., using new reagents) returns results to the expected variance range.
Guide 2: PCR-Based Analysis Fails or Produces Inconsistent Data
Problem Identification: Failure to detect PCR products or inconsistent band intensities on agarose gels when analyzing genetic material from food samples.
List Possible Causes:
- DNA Template Quality: Degraded or low-concentration DNA from samples.
- PCR Master Mix Issues: Problems with Taq polymerase, MgCl₂, buffer, dNTPs, or primers.
- PCR Equipment & Procedure: Malfunctioning thermocycler or errors in cycling parameters.
Data Collection & Elimination:
- Run Controls: A positive control (using a known good DNA vector) indicates whether the PCR Master Mix and thermocycler are functioning. If the positive control works, the problem is likely the sample DNA [53].
- Check Reagents: Confirm the PCR kit has not expired and was stored at the correct temperature [53].
Experimentation & Identification:
- Test DNA Templates: Run sample DNA on a gel to check for degradation and measure concentration spectrophotometrically [53].
- If DNA is intact and concentrated, test different primer annealing temperatures or MgCl₂ concentrations in the Master Mix.
- The cause is identified as poor DNA quality if samples are degraded, or a suboptimal reagent concentration if adjustments restore consistent amplification.
Frequently Asked Questions (FAQs)
Q1: What is the core difference between standardization and harmonization in our context? A1: Standardization is the ideal approach. It requires a clearly defined measurand (the specific nutrient or compound being measured) and establishes traceability to a higher-order reference method or a pure substance defined by the International System of Units (SI) [55]. Harmonization is a practical alternative used when standardization isn't possible due to ill-defined measurands or a lack of reference methods. It achieves agreement among different measurement procedures by tracing them to a reference system agreed upon by convention [55]. For many complex nutritional compounds, harmonization is the more feasible goal.
Q2: How can we improve the reproducibility of our cell-based assays (e.g., for cytotoxicity)? A2: Key strategies include [56] [57]:
- Standardize Cellular Systems: Use defined cell lines with low passage numbers or primary cells from inbred animal strains. Record genetic background and preparation procedures meticulously.
- Control Culture Conditions: Document and maintain consistency in temperature, pH, CO₂ levels, and serum batches.
- Detailed Protocol Documentation: Record lot numbers for all reagents, especially antibodies, as their quality can vary significantly between batches.
- Automate Data Processing: Use computer programs for normalization and analysis to reduce arbitrary or biased manual processing.
Q3: Our team is getting conflicting results from similar experiments. How do we align our methods? A3: This is a common challenge in collaborative research. The solution is to develop and adhere to a Standardized Experimental Protocol [58]:
- Define Variables Clearly: Explicitly document independent (e.g., food type), dependent (e.g., antioxidant level), and controlled variables (e.g., grinding method, solvent).
- Create a Comprehensive Protocol: Write a detailed, step-by-step procedure covering material preparation, equipment calibration, environmental conditions, data collection, and record-keeping.
- Train All Personnel: Ensure every team member is thoroughly trained on the protocol and understands the importance of strict adherence.
- Implement Quality Monitoring: Use control samples in every run to check for accuracy and precision over time.
The following table consolidates quantitative findings from systematic reviews comparing organic and conventional foods, highlighting the nuanced nature of the evidence.
Table 1: Summary of Comparative Analyses from Systematic Reviews
| Review Focus | Number of Comparative Analyses | Analyses Showing Significant Difference | Analyses Showing Divergent/Conflicting Results | Analyses Showing No Significant Difference | Key Findings |
|---|---|---|---|---|---|
| Health Outcomes (2019) [17] | 35 studies included | Associated with reduced incidence of infertility, birth defects, allergic sensitisation, non-Hodgkin lymphoma, etc. | Not specified in results | Not specified in results | Evidence base does not allow a definitive statement on health benefits. Growing number of observational studies link organic intake with demonstrable health benefits. |
| Nutritional Content (2024) [1] | 656 | 191 (29.1%) | 190 (29.0%) | 275 (41.9%) | No generalizable nutritional superiority of organic over conventional foods. Claims of advantages are specific to particular food types and nutritional parameters. |
Detailed Experimental Protocols
Protocol 1: Standardized Sampling of Plant-Based Foods for Nutrient Analysis
Objective: To ensure consistent and representative collection of fruit, vegetable, and grain samples from both organic and conventional farming systems for subsequent laboratory analysis.
Field Selection & Replication:
- Select multiple farms (at least 5 per production type) with similar soil types, climate conditions, and comparable cultivars to minimize confounding factors [17].
- Within each farm, identify multiple sampling plots (e.g., 1m x 1m for crops) in a randomized block design.
Sampling Procedure:
- Timing: Harvest samples at the same commercial maturity stage.
- Method: Collect a composite sample from each plot. For plants, take edible portions from multiple randomly selected plants. Use clean, gloves hands or sterilized tools to avoid contamination.
- Replication: Collect a minimum of three independent biological replicates per farm.
Post-Harvest Handling & Transport:
- Process samples immediately in the field or temporarily store on ice.
- Place samples in pre-labeled, sterile containers.
- Transport to the lab in a cooled container and begin processing or flash-freeze in liquid nitrogen for long-term storage at -80°C.
Protocol 2: Quantitative Immunoblotting for Protein-Based Nutrient Detection
Objective: To accurately quantify specific proteins (e.g., allergenic proteins, enzymes) in food samples with high reproducibility.
Sample Preparation:
- Homogenize frozen tissue under liquid nitrogen to a fine powder.
- Lyse the powder in a standardized, chilled lysis buffer with protease inhibitors.
- Centrifuge to clarify the lysate and determine the protein concentration of the supernatant using a standardized assay (e.g., Bradford assay).
- Normalization: Dilute all samples to the same protein concentration with lysis buffer.
Gel Electrophoresis and Immunoblotting:
- Load an equal volume of each normalized sample onto a pre-cast SDS-PAGE gel. Include a molecular weight ladder and a calibrated positive control on every gel.
- After electrophoresis, transfer proteins to a PVDF membrane.
- Blocking: Incubate membrane in a standardized blocking buffer for 1 hour.
Antibody Incubation and Detection:
- Primary Antibody: Incubate with the target-specific primary antibody (lot number documented) at a pre-optimized dilution overnight at 4°C.
- Washing: Wash the membrane with TBST buffer 3 times for 5 minutes each.
- Secondary Antibody: Incubate with a standardized, HRP-conjugated secondary antibody for 1 hour at room temperature.
- Washing: Repeat the washing step.
- Detection: Develop the blot using a standardized chemiluminescent substrate and image with a digital imager. Ensure the image is not saturated.
Data Processing:
- Use automated image analysis software to quantify band intensities.
- Normalize the intensity of the target band to a loading control (e.g., a housekeeping protein) on the same membrane.
- Normalize the resulting ratio to the calibrated positive control included on the gel to allow for inter-blot comparisons [57].
Workflow and Relationship Diagrams
Standardization Verification Workflow
Systematic Troubleshooting Process
The Scientist's Toolkit
Table 2: Essential Research Reagent Solutions for Food Nutrient Analysis
| Item | Function in Experiment |
|---|---|
| Lysis Buffer (with Protease Inhibitors) | Extracts and solubilizes proteins from complex food matrices while preventing their degradation by proteases. |
| Protein Standard (e.g., BSA) | Serves as a calibrated reference in assays (e.g., Bradford) to determine the total protein concentration of sample lysates, enabling normalization. |
| Primary & Secondary Antibodies | Enable specific detection and quantification of target proteins (e.g., specific allergenic proteins) through techniques like ELISA or Western Blot. |
| PCR Master Mix | A pre-mixed solution containing Taq polymerase, dNTPs, MgCl₂, and buffer necessary for the amplification of specific DNA sequences from samples. |
| Certified Reference Materials (CRMs) | Samples with a certified concentration of a specific analyte (e.g., a specific vitamin or heavy metal). Used to validate the accuracy and calibration of analytical methods [55]. |
Frequently Asked Questions (FAQs)
Q1: Why is achieving high statistical power particularly challenging in studies comparing nutrient levels in organic versus conventional crops? Achieving high power is difficult due to the inherent variability in agricultural data. Key challenges include:
- High Field Variability: Natural variations in soil composition, microclimates, and weather across different field sites and growing seasons significantly affect nutrient content, increasing data variance [59].
- Complex System Comparisons: Organic and conventional systems differ in more than just pesticide use; variations in crop varieties, rotation diversity, and specific management adaptations can all influence nutritional outcomes, introducing confounding factors [60] [6].
- Moderate Effect Sizes: The nutritional differences between organic and conventional produce, such as elevated levels of certain minerals or vitamins, are often moderate rather than dramatic. Detecting these smaller effects reliably requires a larger sample size to avoid Type II errors (false negatives) [6].
Q2: What are the primary factors I must consider when calculating sample size for such studies? Your sample size calculation should be based on:
- Expected Effect Size (d): The magnitude of the difference you expect to find. Use estimates from prior meta-analyses or pilot studies. For example, if you are investigating the reported higher levels of iron or vitamin C in organic foods, use those differences to inform your effect size [6].
- Desired Statistical Power (1-β): The probability of correctly rejecting a false null hypothesis. A power of 0.80 (or 80%) is a common standard, meaning you have an 80% chance of detecting an effect if it truly exists.
- Significance Level (α): The risk of a Type I error (false positive) you are willing to accept, typically set at 0.05.
- Underlying Variance (σ²): The expected variability in the nutrient data. You can estimate this from previous similar studies or pilot data. Higher variance demands a larger sample size.
Q3: A previous study found no significant nutrient difference, but the effect size was notable. What might have gone wrong? This scenario often points to an underpowered study. The researchers likely failed to reject a false null hypothesis (Type II error). The sample size was probably too small to detect the meaningful effect size that was present. To prevent this, always conduct an a priori sample size calculation and report the achieved power for the critical effect sizes in your results [6].
Q4: How can I manage variability from different farms or growing seasons in my study design? Incorporate these factors directly into your experimental design:
- Blocking: Group experimental units by known sources of variation, such as "farm" or "soil type." This allows you to account for and remove the variability these factors introduce, giving a clearer view of the treatment effect.
- Randomization: Randomly assign treatments (organic, conventional) within each block to ensure that any unmeasured confounding variables are equally distributed across groups.
- Multi-Season Studies: Conduct the experiment over multiple growing seasons to capture and account for annual climatic variability, thereby strengthening the generalizability of your findings [60].
Q5: How do I determine an appropriate effect size for my sample size calculation? Do not simply guess. Use one of these evidence-based approaches:
- Pilot Study: Conduct a small-scale version of your experiment to get preliminary estimates of the mean difference and variance.
- Literature Review: Perform a meta-analysis or systematic review of existing published work to find reported effect sizes for the nutrient you are studying.
- Minimum Clinically Important Difference (MCID): Define the smallest difference in nutrient level that would be considered biologically or nutritionally significant, even if it is statistically significant.
Troubleshooting Guides
Problem: Inconsistent or conflicting results between your study and previously published literature.
| Potential Cause | Diagnostic Steps | Solution |
|---|---|---|
| Underpowered Study | Calculate the achieved statistical power of your study post-hoc for the critical effect sizes of interest. | If power is low (<0.80), plan a follow-up study with a larger, calculated sample size. Clearly state this limitation in your publication. |
| Unaccounted-for Confounding Variables | Audit your protocol for variables like specific crop cultivars, soil pH, organic matter content, or harvest timing that were not controlled. | Use a multivariate statistical model (e.g., ANCOVA) to control for these confounders. In future studies, employ a blocked design and record these variables meticulously. |
| High Within-Group Variance | Calculate the standard deviation and coefficient of variation for your treatment groups. Compare them to values in similar studies. | Increase sample size to compensate for high variance. Standardize laboratory protocols for nutrient analysis to reduce measurement error. |
Problem: Failing to achieve statistical significance (p > 0.05) for a seemingly large mean difference.
| Potential Cause | Diagnostic Steps | Solution |
|---|---|---|
| Excessively Noisy Data | Plot your raw data to visualize the spread and overlap between groups. Check for outliers that may be inflating variance. | Re-check data for entry errors. Consider if outlier removal is statistically justified. Focus on reducing measurement error in future iterations. |
| Inadequate Sample Size | Perform a sensitivity analysis to determine what effect size your study was powered to detect. | If the observed effect size is larger than the detectable effect, the study was underpowered. Use the observed effect and variance from this study to accurately power the next one. |
| Non-Normal Data Distribution | Use normality tests (e.g., Shapiro-Wilk) or inspect Q-Q plots for your outcome variables. | Apply an appropriate data transformation (e.g., log, square root). Alternatively, use non-parametric statistical tests. |
Table 1: Relative Crop Yields in Organic vs. Conventional Systems (8-Year Study) [60]
| Crop | Organic Yield (as % of Conventional Non-Bt) | Organic Yield (as % of Conventional Bt) |
|---|---|---|
| Cotton | 93% | 82% |
| Soybean | 102% | Not Applicable |
| Wheat | 77% | Not Applicable |
Table 2: Reported Nutritional Differences and Health Impacts [6]
| Metric | Finding in Organic Systems | Notes / Context |
|---|---|---|
| Iron | Higher levels | Compared to conventional counterparts. |
| Magnesium | Higher levels | Compared to conventional counterparts. |
| Vitamin C | Higher levels | Compared to conventional counterparts. |
| Obesity & BMI | Reduction associated with consumption | Based on observational studies. |
| Cancer Risk | Reduction in non-Hodgkin lymphoma (NHL) and colorectal cancers | Associated with reduced pesticide exposure. |
Experimental Protocols for Robust Nutrient Comparison
Protocol 1: Designing a Multi-Site, Multi-Season Field Trial
- Site Selection: Select multiple paired farms (organic and conventional) with similar soil types and climatic zones to act as blocks.
- Treatment Definition: Clearly document all management practices for each system (e.g., approved pesticides/fertilizers, tillage practices, irrigation schedules) [6].
- Random Sampling: Within each farm and field, collect plant samples from randomly selected locations at the same maturity stage.
- Sample Preparation: Use standardized, validated methods for washing, peeling (if applicable), and compositing samples before laboratory analysis.
- Laboratory Analysis: Utilize validated analytical methods (e.g., HPLC, ICP-MS) to quantify nutrient and potential contaminant levels. Perform all analyses in duplicate or triplicate [61].
Protocol 2: A Priori Sample Size Calculation
- Define Parameters: Establish your α (e.g., 0.05), desired power (1-β, e.g., 0.80 or 80%), and the statistical test (e.g., two-independent samples t-test).
- Determine Effect Size (d): Based on a literature review, select the minimum biologically important difference. For example, you might target detecting a 10% difference in vitamin C content.
- Estimate Variance (σ²): Use the pooled standard deviation from previous studies on the same crop and nutrient.
- Calculate Sample Size: Use statistical software (e.g., G*Power, R, PASS) or standard formulas to compute the required sample size per group. For example, to detect a moderate effect (d = 0.5) with 80% power at α=0.05, you would need approximately 64 samples per group (organic vs. conventional).
Methodology and Workflow Visualizations
The Scientist's Toolkit: Research Reagent & Material Solutions
Table 3: Essential Materials for Nutrient Comparison Research
| Item | Function / Application |
|---|---|
| High-Performance Liquid Chromatography (HPLC / UPLC) | Separation and quantification of specific organic compounds, such as vitamins (e.g., Vitamin C) and phenolic compounds, in plant samples [61]. |
| Inductively Coupled Plasma Mass Spectrometry (ICP-MS) | Highly sensitive elemental analysis to measure mineral content (e.g., Iron, Magnesium, Zinc) and potential heavy metal contaminants in digested plant tissue [61]. |
| Validated Analytical Methods | Laboratory protocols that have been proven to be accurate, precise, specific, and reproducible for the specific analyte-matrix combination, ensuring data reliability for regulatory and publication purposes [61]. |
| Stable Isotope Tracers | Used to track the uptake and assimilation of specific nutrients from the soil into the plant, helping to elucidate mechanistic differences between farming systems. |
| Standard Reference Materials (SRMs) | Certified plant tissue materials with known analyte concentrations. Used to calibrate instruments and verify the accuracy and precision of the entire analytical process. |
Blinding and Randomization Protocols in Clinical Trials to Minimize Investigator and Participant Bias
Troubleshooting Guides
Guide 1: Troubleshooting Randomization Implementation
Problem: Group Imbalance in Small Sample Size Trials
- Background: Simple randomization in small trials often leads to significant group size or prognostic factor imbalances, reducing statistical power [62]. In studies with 40 subjects, the probability of allocation ratio imbalance can be as high as 52.7% [62].
- Solution: Implement block randomization with varying block sizes of 4 or more to maintain balance while preventing prediction of future assignments [62] [63]. For trials with multiple important prognostic factors, use stratified randomization within defined strata [62].
- Prevention: During planning, calculate probability of imbalance based on sample size and use restrictive randomization for studies with fewer than 200 participants [62].
Problem: Selection Bias in Unblinded Allocation
- Background: When investigators can predict upcoming treatment assignments, they may consciously or unconsciously enroll patients they believe are better suited for that treatment, introducing selection bias [63].
- Solution: Maintain strict allocation concealment using centralized interactive response systems (IWRS/IRT) that release assignment only after participant enrollment [64]. Ensure the randomization team operates independently from those involved in participant recruitment [64].
- Verification: Conduct periodic audits to ensure allocation concealment procedures are followed consistently across all trial sites [64].
Problem: Accidental Unblinding Through System Patterns
- Background: Use of fixed block sizes or poorly implemented allocation systems can allow investigators to decipher randomization patterns, compromising blinding [62] [63].
- Solution: Use multiple random block sizes and ensure block sizes are not disclosed to site personnel [62] [64]. Implement robust randomization systems that conceal patterns through complex algorithms [63].
- Documentation: Clearly document randomization methods, including software used, block sizes, and stratification factors, while maintaining necessary blinding of operational staff [64].
Guide 2: Troubleshooting Blinding Challenges
Problem: Blinding Difficulty with Complex Interventions
- Background: Complex interventions (e.g., behavioral therapies, surgical procedures, nutrient delivery systems) present inherent blinding challenges due to their distinctive components and implementation requirements [65]. A recent survey found 91% of researchers agreed that complex interventions pose significant challenges to adequate blinding [65].
- Solution: When full blinding is impossible, implement partial blinding of outcome assessors, data managers, and statisticians [66] [67]. Use sham procedures or placebos that mimic active interventions when ethically and practically feasible [66] [67].
- Alternative Approaches: For objectively measurable outcomes, use centralized assessment of complementary investigations and clinical examinations by blinded evaluators [66].
Problem: Detection Bias in Outcome Assessment
- Background: Non-blinded outcome assessors may generate exaggerated effect sizes, with studies showing inflated hazard ratios by 27% and odds ratios by 36% on average [66].
- Solution: Implement independent blinded endpoint adjudication committees for objective events and independent assessors for performance tests who are not involved in intervention delivery [67] [65].
- Verification: Test blinding success by asking blinded personnel to guess treatment allocations; significant correct guessing indicates compromised blinding [67].
Problem: Participant-Reported Bias (PROMs)
- Background: Patient-Reported Outcome Measures (PROMs) cannot produce blinded data when participants know their treatment allocation, potentially overestimating treatment effects [65].
- Solution: Combine PROMs with blinded outcome assessments to provide objective anchors [65]. Use active placebos that mimic expected side effects to reduce participant bias [66].
- Documentation: Transparently report limitations of unblinded PROMs in publications and consider them as secondary rather than primary outcomes when possible [65].
Frequently Asked Questions (FAQs)
Q1: What is the fundamental difference between allocation concealment and blinding?
- Answer: Allocation concealment prevents selection bias during recruitment and randomization by keeping upcoming group assignments secret until the moment of assignment. Blinding (or masking) prevents performance and detection bias after randomization by withholding information about assigned interventions from various trial participants until the experiment is complete [66] [67].
Q2: When is stratified randomization particularly important?
- Answer: Stratified randomization is crucial when known prognostic factors significantly influence outcomes. In nutrient comparison research, this might include factors like participant age, baseline nutritional status, or metabolic markers. It ensures balanced distribution of these factors across treatment groups, especially in small trials where chance imbalances are more likely [62] [63].
Q3: How can we maintain blinding when interventions are visibly different?
- Answer: Use double-dummy techniques where each group receives both an active and placebo intervention [66]. For example, in comparing organic vs conventional nutrients, both groups might receive similar-looking products with variations only in the source material. Additionally, have different personnel handle intervention preparation versus administration and use opaque packaging [67].
Q4: What should we do when complete blinding is impossible?
- Answer: When complete blinding is unattainable, blind as many individuals as possible, particularly outcome assessors and statisticians [67] [65]. Standardize all other aspects of care and data collection to minimize differential treatment. Use objective outcomes whenever possible and document the limitations transparently [67].
Q5: How do we determine appropriate block sizes for randomization?
- Answer: Block sizes should be multiples of the number of treatment groups and large enough to prevent prediction (typically 4 or more) [62]. Use multiple random block sizes to enhance concealment. Balance the need for group balance with the risk of unmasking allocation patterns, especially in small trials or multi-center studies [63] [64].
Quantitative Data Tables
Table 1: Randomization Method Comparison
| Method | Best Use Case | Balance Control | Prediction Risk | Statistical Properties |
|---|---|---|---|---|
| Simple Randomization | Large trials (n>200) [62] | Low - high imbalance probability in small samples [62] | Low | Valid tests but potentially underpowered with imbalances [63] |
| Block Randomization | Small to medium trials, sequential recruitment [62] [63] | High - maintains balance within blocks [62] | Moderate with fixed blocks, Low with varying blocks [62] | Preserves type I error when properly implemented [63] |
| Stratified Randomization | Trials with known important prognostic factors [62] [63] | High for known factors within strata [62] | Low to Moderate depending on design | Increases power by controlling for prognostic covariates [63] |
| Adaptive Randomization | Trials with accumulating evidence or many prognostic factors [62] [64] | Variable - depends on algorithm [64] | Low | Complex analysis; may require randomization-based tests [63] |
Table 2: Impact of Lack of Blinding on Effect Size Exaggeration
| Unblinded Group | Impact on Effect Size | Primary Bias Type | Evidence Source |
|---|---|---|---|
| Participants | Subjective outcomes exaggerated by 0.56 standard deviations [66] | Performance bias [66] [67] | Systematic review of 250 RCTs from 33 meta-analyses [67] |
| Outcome Assessors | 27% exaggerated hazard ratios (time-to-event) [66] | Detection bias [66] [67] | Meta-analysis on observer bias [66] |
| Outcome Assessors | 36% exaggerated odds ratios (binary outcomes) [66] | Detection bias [66] [67] | Meta-analysis on observer bias [66] |
| Outcome Assessors | 68% exaggerated pooled effect size (measurement scales) [66] | Detection bias [66] [67] | Meta-analysis on observer bias [66] |
| All Unblinded | 17% larger odds ratios in unblinded vs blinded trials [67] | Performance and detection bias [67] | Systematic review of 250 RCTs [67] |
Experimental Protocols
Protocol 1: Implementing Stratified Block Randomization
Purpose: To achieve balanced treatment groups while controlling for important prognostic factors in nutrient comparison research.
Materials: Secure randomization system (e.g., IWRS/IRT), predefined stratification factors, allocation schedule.
Procedure:
- Identify Stratification Factors: Select 2-3 key prognostic factors (e.g., age group, BMI category, baseline nutrient levels) that significantly impact outcomes [62] [63].
- Define Blocks: Determine appropriate block sizes (multiple of treatment groups, typically 4-8) and use multiple varying block sizes to enhance concealment [62] [64].
- Generate Allocation Schedule: Create separate randomization schedules for each stratum using computer-generated random numbers [64].
- Implement Concealment: Use centralized interactive response technology to assign treatments only after participant enrollment and stratification data collection [64].
- Document and Archive: Securely store randomization schedules with restricted access; maintain complete documentation for reproducibility [64].
Troubleshooting: If too many strata result in sparse cells, reduce stratification factors or use minimization approach for small samples [62].
Protocol 2: Blinding Outcome Assessors in Nutrient Studies
Purpose: To minimize detection bias when interventions cannot be fully blinded to participants and investigators.
Materials: Independent assessors, standardized assessment protocols, data collection forms that conceal treatment allocation.
Procedure:
- Recruit Independent Assessors: Hire or train assessors who have no role in intervention delivery and are unaware of study hypotheses [67] [65].
- Standardize Assessments: Develop detailed, objective assessment protocols with clear criteria for all measurements [67].
- Conceal Treatment Information: Remove all treatment identifiers from assessment forms and equipment; use neutral labeling [66] [67].
- Coordinate Assessments: Schedule assessments to prevent accidental unblinding through participant comments or environmental cues [65].
- Test Blinding Success: Periodically ask assessors to guess treatment allocation to test blinding effectiveness [67].
Validation: Compare assessments between blinded and unblinded assessors if feasible; use duplicate assessments to measure agreement [67].
Research Reagent Solutions
Essential Materials for Implementation
| Item | Function | Implementation Example |
|---|---|---|
| Interactive Response Technology (IRT) | Automated real-time treatment allocation while maintaining concealment [64] [68] | Centralized web-based system for multi-center trials |
| Allocation Sealed Envelopes | Emergency access to treatment assignment while maintaining routine concealment [64] | Opaque, sequentially numbered envelopes for emergency unblinding |
| Active and Placebo Preparations | Physically identical interventions to maintain participant and investigator blinding [66] [67] | Identical-looking organic and conventional nutrient preparations with placebos |
| Blinded Assessment Equipment | Tools modified to conceal treatment-specific information during outcome measurement [67] | Laboratory equipment with masked labels and automated output |
| Secure Electronic Database | Storage of randomization schedules with access controls to prevent unauthorized unblinding [64] | Password-protected, encrypted databases with audit trails |
Methodological Diagrams
Bias Control in Clinical Trials
Bias Types and Control Methods
Benchmarking Evidence: Validating Methodologies and Cross-Comparing Global Research Findings
Frequently Asked Questions
Q1: What is the primary challenge in linking a nutrition pattern score (NPS) or diet quality to hard health endpoints? The main challenge is measurement error in dietary exposure data. Self-reported intake from tools like Food Frequency Questionnaires (FFQs) is prone to both random error (e.g., day-to-day variation) and systematic error (e.g., misreporting). This error can attenuate the observed associations between diet and disease, making real effects harder to detect or biasing them toward a null finding [69] [70].
Q2: Our study found a weak association between an unhealthy NPS and cancer risk. Is the diet truly low-risk, or could measurement error be masking the effect? It is very possible that measurement error is causing an attenuation effect. In regression analysis, error in the biomarker or exposure variable (like your NPS) typically biases the estimated effect (e.g., hazard ratio) toward 1.0 (the null). A weak observed association could be a substantially stronger true association that has been diluted by imprecise measurement [70].
Q3: What is the gold-standard study design for establishing that a dietary pattern causes a health outcome? A double-blind Randomized Controlled Trial (RCT) is the gold standard for determining causation. However, long-term dietary RCTs for hard endpoints like cardiovascular disease (CVD) or cancer are often not feasible due to the need for a large sample size, long duration, high cost, and difficulty in maintaining participant adherence and blinding [69]. When RCTs are not possible, prospective cohort studies are the preferred observational design, as they minimize recall and selection bias by assessing diet in healthy participants and following them over time for disease onset [69].
Q4: How can we statistically correct for measurement error in our NPS? A common approach is to use data from a validation substudy. In this substudy, a more precise dietary assessment method (e.g., multiple 24-hour recalls or biomarker data) is collected from a portion of your cohort. The relationship between the NPS (from the FFQ) and the more precise measure is used to calculate a reliability ratio, which can then be used to correct the attenuation in the main analysis [70].
Q5: We want to validate our NPS against a clinical outcome. What are key considerations for the biomarker we choose? An ideal biomarker should have analytical validity (a reliable and reproducible assay), clinical validity (it accurately predicts the disease state of interest), and be measurable from an easily accessible specimen (e.g., blood). The biomarker's intended use (e.g., risk prediction, diagnosis, prognosis) must be defined early, and the study must be designed to avoid biases in patient selection and specimen analysis [71].
Troubleshooting Guides
Problem: Inconsistent or non-significant findings when associating NPS with cancer or CVD mortality.
| Potential Issue | Diagnostic Steps | Recommended Solution |
|---|---|---|
| Measurement Error in NPS | Review the correlation between your dietary assessment tool (e.g., FFQ) and more precise measures from validation studies. | Use statistical correction methods such as regression calibration, which requires a validation substudy with a more precise dietary measure to quantify and adjust for the error [69] [70]. |
| Inadequate Control for Confounding | Check if key confounders (e.g., smoking, physical activity, socioeconomic status, total energy intake) are missing from your statistical model. | Perform multivariate regression with careful adjustment for all relevant confounders. Consider stratified analyses or restricting to a more homogeneous subgroup to reduce residual confounding [69]. |
| Insufficient Statistical Power | Conduct a power analysis to determine if your sample size and number of incident disease cases are sufficient to detect a realistic effect size. | Increase sample size by forming or joining a consortium to pool data from multiple cohorts. This also allows for assessing heterogeneity across different populations [69]. |
| Misclassification of Diet Patterns | Evaluate if your NPS algorithm correctly categorizes complex dietary intakes. Compare with data-driven methods like clustering. | Consider using machine learning approaches, such as stacked generalization or causal forests, which can better model complex, synergistic interactions between dietary components and account for heterogeneity [72]. |
Problem: The diagnostic performance (e.g., AUC) of my biomarker for predicting disease is lower than expected.
| Potential Issue | Diagnostic Steps | Recommended Solution |
|---|---|---|
| Measurement Error in Biomarker | Assess the assay's precision and the within-subject variability of the biomarker. Check the correlation between research assays and clinical-grade assays. | Account for measurement error in your estimates of diagnostic efficacy (e.g., AUC, sensitivity, specificity). Statistical correction methods exist that can provide a less biased estimate of the true diagnostic performance [70]. |
| Single Biomarker is Insufficient | Evaluate if the disease pathophysiology involves multiple pathways that cannot be captured by a single molecule. | Develop a panel of multiple biomarkers. Using continuous values for each biomarker and incorporating variable selection techniques in model estimation can improve panel performance over a single marker [71]. |
Experimental Protocols for Key Methodologies
Protocol 1: Prospective Cohort Study for Linking Diet to Hard Endpoints This is a foundational design for investigating the relationship between NPS-classified diets and the incidence of diseases like CVD and cancer [73] [69].
- Cohort Recruitment: Enroll a large number of participants (e.g., >100,000) who are free of the diseases of interest at baseline.
- Baseline Assessment:
- Dietary Exposure: Collect detailed dietary intake using a validated Food Frequency Questionnaire (FFQ), 24-hour recalls, or dietary records. Use this data to compute the NPS for each participant.
- Covariate Data: Systematically collect data on potential confounders, including age, sex, BMI, smoking status, physical activity, medical history, and socioeconomic status.
- Biospecimen Collection: Collect and archive blood, urine, or other samples for future biomarker analysis.
- Follow-up: Actively and continuously follow the entire cohort for a long period (often many years) to ascertain incident disease cases.
- Outcome Ascertainment: Identify and confirm new cases of CVD, cancer, or other endpoints through linkage with cancer registries, death indices, and rigorous medical record review.
- Statistical Analysis: Use multivariate Cox proportional hazards regression to estimate hazard ratios (HRs) and 95% confidence intervals (CIs) for the association between the NPS and disease risk, adjusting for identified confounders.
Protocol 2: Statistical Correction for Dietary Measurement Error This protocol outlines how to correct for attenuation bias using a validation substudy [70].
- Main Cohort: Obtain dietary data from an FFQ for all participants to calculate the NPS.
- Validation Substudy: Select a random subset of the main cohort (e.g., 5-10%). For this subset, collect detailed dietary data using a more precise instrument, such as:
- Multiple (e.g., 3-4) non-consecutive 24-hour dietary recalls.
- Biomarkers of intake (e.g., doubly labeled water for energy, urinary nitrogen for protein).
- Modeling the Relationship: Statistically model the relationship between the "true" habitual intake (estimated from the precise measures in the substudy) and the reported NPS (from the FFQ).
- Correction Calculation: Use the parameters from this model (e.g., the reliability ratio) to correct the hazard ratios for the diet-disease association observed in the main cohort analysis.
The Scientist's Toolkit: Essential Research Reagents & Materials
| Item | Function in Research |
|---|---|
| Validated Food Frequency Questionnaire (FFQ) | A practical tool to assess habitual dietary intake over a long period (e.g., the past year) in large epidemiological cohorts. It is used to calculate the NPS [69]. |
| Biobanked Biospecimens | Archived samples (serum, plasma, urine, DNA) collected at baseline from cohort participants. These are crucial for later measuring predictive or nutrient biomarkers to validate dietary patterns or understand biological mechanisms [71] [70]. |
| Dietary Biomarkers (e.g., Doubly Labeled Water, Urinary Nitrogen) | Objective measures used to validate self-reported dietary data. They help quantify and correct for measurement error in energy and protein intake, respectively [70]. |
| Multistate Modeling | A statistical technique used to analyze complex disease pathways. For example, it can model transitions from health to a first chronic disease (e.g., cancer) and then to multimorbidity (e.g., cancer and cardiometabolic disease), providing a more nuanced view of diet-disease relationships [73]. |
| Machine Learning Algorithms (e.g., Causal Forests) | Advanced, flexible computational methods used to model complex, non-linear, and synergistic interactions between multiple dietary components. They can also identify heterogeneity in how diet affects different population subgroups [72]. |
Experimental Workflow & Data Analysis Pathways
The following diagram illustrates the core workflow for validating a dietary pattern against hard health endpoints, integrating key steps from cohort design to data analysis and accounting for major challenges like measurement error.
Nutrient profiling (NP) is defined as the science of classifying or ranking foods according to their nutritional composition for reasons related to preventing disease and promoting health [26]. In the context of research comparing organic and conventional foods, NP models provide an essential standardized methodology to objectively evaluate and compare nutritional quality, moving beyond simple single-nutrient comparisons to a more comprehensive assessment.
Globally, numerous NP models have been developed, with one systematic review identifying 387 different models [26]. This proliferation creates challenges for researchers seeking consistent methodologies. This technical support center addresses these challenges by providing detailed protocols for implementing three prominent models—FSANZ (Food Standards Australia New Zealand), Nutri-Score, and PAHO (Pan American Health Organization)—within experimental research frameworks.
FSANZ (Food Standards Australia New Zealand) Nutrient Profiling Scoring Criterion (NPSC)
The FSANZ model was developed to regulate health claims on food products [74]. Foods with an FSANZ-NPSC score of >4 are not permitted to make health claims [74]. The model uses a scoring system based on nutrients and food components per 100g or 100ml.
Basis and Adaptations: The FSANZ model was adapted from the UK Ofcom model, which was originally developed to define foods permitted for marketing to children [26]. Research has demonstrated "near perfect" agreement (κ=0.89) between FSANZ and the validated Ofcom reference model, with only 5.3% discordant classifications [26] [75].
Nutri-Score
Nutri-Score is an interpretive front-of-pack labeling system that assigns foods a color-coded score from A (dark green) to E (red) [26] [74]. The system is designed to help consumers quickly identify the nutritional quality of food products at the point of purchase.
Relationship to Other Models: Like FSANZ, Nutri-Score was also adapted from the UK Ofcom model [74]. Validation studies show it has "near perfect" agreement (κ=0.83) with the Ofcom model, with 8.3% discordant classifications [26] [75]. Research has indicated potential for using Nutri-Score to restrict health claims on foods, similar to FSANZ [74].
PAHO (Pan American Health Organization) Nutrient Profile Model
The PAHO model was developed as a tool for governments to identify unhealthy products and implement public policies to discourage their consumption [76]. Unlike other models, it defines products as excessive in critical nutrients based on percentage of energy from sugars, fats, saturated fats, trans fats, and sodium, rather than using a scoring system [26] [76].
Philosophical Approach: The PAHO model is considered one of the strictest profiling systems and is specifically designed to address the obesity and non-communicable disease epidemic in the Americas [76] [77]. It defines when products are high in critical nutrients based on WHO Population Nutrient Intake Goals adjusted according to energy requirements [76].
Table 1: Key Characteristics of Profiling Models
| Characteristic | FSANZ | Nutri-Score | PAHO |
|---|---|---|---|
| Region of Origin | Australia/New Zealand | France | Americas |
| Primary Purpose | Regulate health claims | Front-of-pack labeling | Multiple policy applications |
| Reference Amount | 100g or 100ml | 100g | % energy of food |
| Food Categories | 3 | 2 | 5 |
| Nutrients/Components Considered | 7 | 7 | 6 |
| Outcome Type | Continuous score & dichotomous | Score classes (A-E) | Dichotomous (excessive/not) |
| Basis/Adaptation | Adapted from UK Ofcom | Adapted from UK Ofcom | Based on WHO population goals |
Table 2: Validation Results Compared to Ofcom Reference Model
| Model | Agreement (κ statistic) | Agreement Level | Discordant Classifications |
|---|---|---|---|
| FSANZ | 0.89 | Near perfect | 5.3% |
| Nutri-Score | 0.83 | Near perfect | 8.3% |
| PAHO | 0.28 | Fair | 33.4% |
Experimental Protocols and Implementation
Data Collection and Preparation Protocol
Essential Research Reagent Solutions:
- Nutritional Composition Database: Comprehensive database with values per 100g/ml for energy, saturated fat, total sugar, sodium, protein, fiber, and fruit/vegetable/nut/legume (FVNL) content [26]
- Food Categorization Framework: Standardized system for classifying foods into relevant categories (varies by model) [26]
- Reference Value Guide: Document outlining model-specific reference values and daily intake recommendations [78]
- Standardized Conversion Tools: Utilities for converting between serving sizes and 100g/ml reference amounts [26]
Step 1: Data Collection Collect complete nutritional information for all food products in your study. Essential nutrients vary by model but typically include:
- Energy (kJ or kcal)
- Saturated fat (g)
- Total sugars (g)
- Sodium (mg or mg)
- Protein (g)
- Dietary fiber (g)
- FVNL content (%) [26]
Step 2: Food Categorization Categorize each food product according to the specific requirements of each model:
- FSANZ: 3 food categories
- Nutri-Score: 2 food categories (foods and beverages)
- PAHO: 5 food categories [26]
Step 3: Standardize Reference Amounts Convert all nutrient values to standardized reference amounts:
- FSANZ and Nutri-Score: 100g or 100ml
- PAHO: Percentage of energy from food [26]
FSANZ NPSC Calculation Protocol
Step 1: Calculate 'A' Points (Baseline Points) Assign points based on energy (kJ), saturated fat (g), total sugar (g), and sodium (mg) content per 100g. Higher points indicate less favorable nutritional content.
Step 2: Calculate 'B' Points (Modifying 'A' Points) Assign points based on favorable components: fruit, vegetable, nut, legume (FVNL) content (%), protein (g), and fiber (g) [26].
Step 3: Calculate Final Score Final NPSC Score = A Points - B Points
Step 4: Apply Category-Specific Thresholds
- For foods in Category 1 (non-specific): If NPSC score ≤4, product may make health claims
- For foods in Category 2 (specific categories): If NPSC score ≤28, product may make health claims [74]
Nutri-Score Calculation Protocol
Step 1: Calculate 'A' Points (Unfavorable Nutrients) Assign points (0-10) for energy (kJ), saturated fat (g), total sugar (g), and sodium (mg) per 100g.
Step 2: Calculate 'C' Points (Favorable Nutrients) Assign points (0-5) for favorable components: FVNL content (%), protein (g), and fiber (g) [26].
Step 3: Calculate Final Score Final Score = A Points - C Points
Step 4: Assign Nutri-Score Letter and Color
- A (Dark Green): -1 to -5 points (best nutritional quality)
- B (Light Green): 0 to 2 points
- C (Yellow): 3 to 10 points
- D (Orange): 11 to 18 points
- E (Red): ≥19 points (lowest nutritional quality) [74]
PAHO Classification Protocol
Step 1: Calculate Nutrient Content as Percentage of Energy For each critical nutrient, calculate the percentage of total energy:
- Total sugars (% energy)
- Total fats (% energy)
- Saturated fats (% energy)
- Trans fats (% energy) [76]
Step 2: Compare to PAHO Thresholds A product is classified as having "excessive" amounts of critical nutrients if it exceeds ANY of these thresholds:
- Total sugars: ≥10% of total energy
- Total fats: ≥30% of total energy
- Saturated fats: ≥10% of total energy
- Trans fats: ≥1% of total energy
- Sodium: Based on absolute amounts per 100g/product, adjusted for energy density [76] [77]
Step 3: Final Classification
- Not excessive: Product does not exceed any thresholds
- Excessive: Product exceeds at least one threshold [76]
Troubleshooting Guide: Frequently Asked Questions
Model Selection and Application
Q1: Which model is most appropriate for research comparing organic versus conventional foods?
A: The choice depends on your research objectives:
- For comprehensive nutritional quality assessment: Use FSANZ or Nutri-Score as they provide continuous scores allowing for statistical comparisons [26] [75]
- For identifying products with excessive levels of critical nutrients: Use PAHO model [76] [77]
- For consumer-facing research: Nutri-Score provides intuitive visual output [74]
- For regulatory alignment: Choose based on your target region or policy context
Q2: How do I handle discrepancies between model classifications for the same food product?
A: Classification discrepancies are common, particularly between stricter models like PAHO and more permissive models [26] [77]. In your research:
- Report results from multiple models to provide comprehensive analysis
- Acknowledge that different models serve different purposes
- Consider your research question when interpreting discrepant results
- Note that FSANZ and Nutri-Score show high agreement (80% in one study) due to common origins [74]
Technical Implementation Issues
Q3: How should I handle missing nutrient data in my analysis?
A: Implement a standardized approach:
- For mandatory nutrients (energy, saturated fat, sugars, sodium): Exclude products with missing data
- For optional nutrients (fiber, protein): Use conservative estimates (assign 0g if missing) or exclude from favorable nutrient calculation
- Document all assumptions in your methodology section
- Consider sensitivity analyses to test the impact of missing data
Q4: What reference amount should I use when products have different serving sizes?
A: Standardize to 100g or 100ml for all products when applying FSANZ or Nutri-Score models [26]. For PAHO, calculate percentage of energy, which naturally standardizes for different serving sizes [76].
Interpretation and Validation
Q5: How can I validate the NP model classifications in my research?
A: Several validation approaches exist:
- Indicator foods method: Use a small number of foods previously identified as "healthy" or "unhealthy" by nutrition professionals and assess whether NP classifications agree [77]
- Construct validity: Test whether foods classified as healthy by the NPS create healthy diets as defined by independent dietary quality indices [77]
- Calibration: Compare classifications with those from a validated NPS designed for similar purposes [77]
Q6: Why does PAHO classify more products as "excessive" compared to other models?
A: PAHO uses stricter thresholds based directly on WHO Population Nutrient Intake Goals and is specifically designed to identify products with excessive levels of critical nutrients [76] [77]. Validation studies show PAHO has fair agreement (κ=0.28) with the Ofcom model and 33.4% discordant classifications [26].
Table 3: Troubleshooting Common Implementation Challenges
| Challenge | Symptoms | Solution | Prevention |
|---|---|---|---|
| Inconsistent Categorization | Same product classified differently across models | Create model-specific categorization protocols | Pre-classify all products using each model's guidelines |
| Missing Nutrient Data | Inability to calculate complete scores | Implement standardized imputation or exclusion criteria | Verify data completeness during collection phase |
| Serving Size Variations | Incorrect nutrient density calculations | Standardize all values to 100g/ml before calculation | Extract raw nutrient data rather than relying on serving-based information |
| Discrepant Results | Contradictory classifications between models | Report multiple model outcomes with interpretation framework | Pre-define primary model based on research question |
Research Reagent Solutions
Table 4: Essential Materials for Nutrient Profiling Research
| Research Reagent | Function | Implementation Example |
|---|---|---|
| Standardized Food Composition Database | Provides complete nutrient profiles for analysis | Use national food composition databases or commercial nutritional analysis software |
| Model-Specific Calculation Algorithms | Ensures accurate implementation of each profiling system | Develop validated spreadsheets or scripts for FSANZ, Nutri-Score, and PAHO calculations |
| Food Categorization Framework | Enables proper application of category-specific thresholds | Create decision trees for each model's food categorization system |
| Reference Value Guide | Provides context for interpreting scores and classifications | Compile document with model-specific reference values and threshold justifications |
| Validation Food Set | Tests model implementation against known classifications | Curate subset of foods with pre-determined classifications for system validation |
Data Collection and Management Framework
Standardized Data Collection Protocol:
- Nutrient Data Extraction Form: Structured template capturing all required nutrients for each profiling model
- Product Categorization Guide: Decision trees for consistent food categorization across research team members
- Quality Control Checklist: Verification steps to ensure data accuracy and completeness
- Data Transformation Scripts: Automated tools for converting between different units and reference amounts
This technical support resource provides researchers with standardized methodologies for implementing three prominent nutrient profiling models. By following these protocols, researchers can generate consistent, comparable data on the nutritional quality of organic versus conventional food products, contributing to more robust and reproducible research in this field.
Frequently Asked Questions (FAQs)
Planning and Protocol Development
Q1: What is the primary purpose of a systematic review in validating health outcomes? A systematic review provides a consolidated, unbiased summary of all available evidence on a specific health outcome. It uses predefined, methodical search and selection criteria to minimize bias, thereby validating whether reported outcomes are consistent and reliable across multiple independent studies. This is crucial for informing healthcare policy, clinical decision-making, and identifying gaps for future research [79].
Q2: How should I define the scope of my systematic review? A clearly defined scope is critical. Use the PICOS framework (Population, Intervention, Comparator, Outcome, Study design) established a priori to guide your review's boundaries [79]. For example:
- Population: Adult patients with relapsed or refractory Diffuse Large B-Cell Lymphoma (DLBCL) [79].
- Intervention: Chimeric Antigen Receptor (CAR) T-cell therapy.
- Comparator: Standard salvage chemotherapy or other novel therapies.
- Outcomes: Health-Related Quality of Life (HRQOL) and health state utility values.
- Study Design: Published clinical trials, observational studies, and economic evaluations.
Q3: What common pitfalls should I avoid during the planning phase?
- Vague PICOS criteria: This leads to inconsistent study selection and potential bias.
- Unregistered protocol: Registering your protocol (e.g., on PROSPERO) enhances transparency and reduces risk of reporting bias [80].
- Ignoring the existing landscape: Conduct a preliminary literature scan to ensure your review is not redundant and can address a genuine evidence gap [79].
Search Strategy and Study Selection
Q4: How can I ensure my literature search is comprehensive and reproducible? Your search strategy should be developed by an experienced information specialist and peer-reviewed using tools like the Peer Review of Electronic Search Strategies (PRESS) checklist [79]. The strategy must be documented with full syntax and adapted across multiple databases (e.g., Ovid MEDLINE, Embase, Cochrane Library) [79].
Q5: What is the standard process for screening studies? Screening should be performed by two independent reviewers to minimize error and bias [79]. The process is typically done in two stages in a systematic review software platform:
- Title and Abstract Screening: Initial assessment against PICOS criteria.
- Full-Text Review: Detailed evaluation of potentially relevant studies, with reasons for exclusion meticulously recorded [79].
Q6: My search yielded an unmanageable number of results. How can I refine it? Refine your PICOS criteria. Consider narrowing the Population (e.g., a specific lymphoma subtype), Intervention, or Study Design. Use more specific database filters (e.g., by publication type) while being cautious not to omit relevant studies.
Data Extraction and Quality Assessment
Q7: What key data should be extracted from included studies? Create a standardized data extraction form. Essential items include [79] [80]:
- Study identifiers and characteristics (author, year, design).
- PICOS details for each study.
- Results for primary and secondary outcomes (e.g., mean utility values, HRQOL scores).
- Key conclusions and funding sources.
Q8: How is the quality of evidence assessed? Quality assessments should be performed in accordance with health technology assessment guidelines, such as those from the National Institute for Health and Care Excellence (NICE) [79]. Use validated tools appropriate to the study design (e.g., Cochrane Risk of Bias tool for randomized trials) and have at least two reviewers assess each study independently.
Data Synthesis and Interpretation
Q9: When is a meta-analysis appropriate? A meta-analysis is appropriate when the included studies are sufficiently homogeneous in terms of PICOS. If studies are too heterogeneous in design, outcomes, or populations, a descriptive synthesis is the valid and preferred approach, as was the case in a recent lymphoma PROMS review [80].
Q10: How should I handle heterogeneity among studies? First, investigate the potential sources of clinical and methodological heterogeneity. If a meta-analysis is performed, use statistical measures (e.g., I² statistic) to quantify inconsistency. If heterogeneity is high, a subgroup analysis or sensitivity analysis can help explore the reasons, but a descriptive summary is often the most appropriate course [80].
Troubleshooting Common Experimental Challenges
Encountering Heterogeneity and Inconsistent Reporting
A primary challenge in systematic reviews is the heterogeneity in how outcomes are measured and reported across studies. The table below summarizes common problems and solutions.
| Problem | Symptom | Solution |
|---|---|---|
| Outcome Measure Heterogeneity | Studies use different instruments to measure the same construct (e.g., HRQOL measured with EORTC QLQ-C30, FACT-Lym, EQ-5D) [79] [80]. | * Document all instruments used.* Report results by instrument type; do not combine in analysis.* Acknowledge this as a limitation for direct comparison. |
| Inconsistent Reporting of Results | Key outcomes like PROs are collected in trials but not reported in the primary publication [80]. | * Search for supplementary materials, clinical trial registries, and regulatory agency reports.* Contact the corresponding authors for data.* Clearly note the discrepancy between planned and reported outcomes. |
| Variable Follow-up Times | Studies report outcomes at different time points (e.g., 3, 6, 12 months), making synthesis difficult. | * Predefine the primary time point of interest in your protocol.* If feasible, group results into short-, medium-, and long-term follow-ups.* Use the most representative time point for each study in your summary. |
Ensuring Validity and Avoiding Bias
| Problem | Symptom | Solution |
|---|---|---|
| Selection Bias | The included studies do not represent the full spectrum of relevant evidence. | * Use a comprehensive, multi-database search strategy.* Include gray literature (e.g., conference abstracts, theses).* Have a transparent, dual-reviewer process for study selection [79]. |
| Confirmation Bias | Interpreting results in a way that confirms pre-existing beliefs. | * Pre-specify hypotheses and methods for synthesis in your protocol.* Involve multiple team members in data interpretation.* Consider the strength of evidence for all findings, not just significant ones. |
| Poor Quality of Included Studies | The body of evidence is dominated by studies with high risk of bias. | * Conduct a rigorous quality assessment for every included study.* Incorporate quality ratings into the interpretation of results (e.g., perform a sensitivity analysis excluding high-risk studies).* Clearly state that conclusions are limited by the quality of primary studies. |
Key Experiment Protocols
Protocol for a Systematic Review on Health Outcomes
This protocol outlines the core methodology for conducting a robust systematic review, adaptable to outcomes like HRQOL in lymphoma or biomarkers in metabolic syndrome.
1. Objective Formulation: Clearly state the research question using PICOS [79]. 2. Protocol Registration: Register the review protocol on a platform like PROSPERO [80]. 3. Search Strategy: * Develop search syntax in consultation with an information specialist. * Perform PRESS peer review of the search strategy [79]. * Execute searches across multiple bibliographic databases and gray literature sources. * Document all search dates and strategies fully. 4. Study Selection: * Use a two-stage screening process (title/abstract, then full-text) in software like DistillerSR [79]. * Employ two independent reviewers; resolve conflicts via consensus or a third reviewer [79]. 5. Data Extraction: * Use a piloted, standardized data extraction form. * Extract data in duplicate to ensure accuracy. 6. Quality Assessment: * Assess the risk of bias of included studies using appropriate tools (e.g., Cochrane RoB 2, NIH Quality Assessment Tool). * Perform assessments independently by two reviewers. 7. Data Synthesis: * If studies are homogeneous, perform a meta-analysis. * If heterogeneity is too high, perform a descriptive synthesis, summarizing findings in tables and narrative [80]. 8. Report Writing: * Report the review according to the PRISMA (Preferred Reporting Items for Systematic reviews and Meta-Analyses) guidelines [80].
Protocol for Validating a New Prognostic Index
This protocol is based on studies that develop and validate clinical tools, such as the International Metabolic Prognostic Index (IMPI) for lymphoma.
1. Cohort Definition: * Define clear inclusion/exclusion criteria for the patient population (e.g., r/r LBCL, available pre-treatment PET/CT) [81]. 2. Cohort Splitting: * Divide the total cohort into a Development Cohort (for model creation and threshold identification) and an independent Validation Cohort (for testing the model's performance) [81]. 3. Variable Selection and Model Building: * Select candidate predictor variables based on clinical relevance and prior evidence (e.g., metabolic tumor volume, age, disease stage) [81]. * In the development cohort, use statistical methods (e.g., maximally selected rank statistics, Cox regression) to identify optimal cut-off values and derive model coefficients [81]. 4. Model Validation: * Apply the newly developed model and its cut-offs to the independent validation cohort without modification. * Use Kaplan-Meier survival curves and log-rank tests to assess the model's ability to discriminate between risk groups for outcomes like Progression-Free Survival (PFS) and Overall Survival (OS) [81]. 5. Multivariate Analysis: * Perform a multivariable Cox regression in the validation cohort to confirm the model is an independent predictor of outcome after adjusting for other known prognostic factors [81].
Visualizing Systematic Review Workflows and Methodologies
Systematic Review Workflow
Prognostic Model Development & Validation
The Researcher's Toolkit: Essential Reagents & Materials
The following table details key tools and resources used in the featured systematic reviews and clinical studies.
| Research Reagent / Tool | Function & Application |
|---|---|
| PICOS Framework | A structured tool used to formulate a focused research question and define eligibility criteria for a systematic review (Population, Intervention, Comparator, Outcomes, Study design) [79]. |
| PRISMA Guidelines | An evidence-based minimum set of items for reporting in systematic reviews and meta-analyses. Used to ensure transparent and complete reporting of the review process [80]. |
| EORTC QLQ-C30 | A validated, core 30-item questionnaire developed to assess the health-related quality of life of cancer patients. Frequently used as a Patient-Reported Outcome Measure (PROM) in oncology trials [79] [80]. |
| EQ-5D-5L | A standardized, non-disease-specific instrument for measuring generic health status. It provides a simple descriptive profile and a single index value for health status, useful for health economic evaluations [79] [80]. |
| Cochrane Risk of Bias Tool (RoB 2) | A structured tool for assessing the risk of bias in the results of randomized trials. It is a critical component of the quality assessment phase in a systematic review. |
| Metabolic Tumor Volume (MTV) | A quantitative imaging biomarker derived from 18FDG-PET/CT scans. It measures the total volume of metabolically active tumor and is a key prognostic factor in lymphoma research, used in tools like the IMPI [81]. |
| Kaplan-Meier Estimator | A non-parametric statistic used to estimate the survival function from lifetime data. Essential for visualizing and comparing time-to-event outcomes (e.g., PFS, OS) between patient groups in clinical research [81]. |
| Cox Proportional Hazards Model | A regression model commonly used for investigating the association between survival time and one or more predictor variables. Used in multivariable analysis to confirm a factor's independent prognostic value [81]. |
Frequently Asked Questions
Q1: Our study found no significant nutritional differences between organic and conventional foods. Could methodological limitations be responsible? Yes, this is a common challenge. Inconsistent findings often stem from methodological variations rather than an actual absence of differences. Key factors include:
- Variable Control: Differences in crop variety, soil type, climate, harvest timing, and post-harvest handling between studies can obscure true effects. Failing to control these introduces significant noise [6] [82].
- Confounding Variables: Consumer lifestyle factors (e.g., overall diet, physical activity) are often stronger determinants of health outcomes than food type alone, making it difficult to isolate the effect of organic food consumption [6].
- Short Study Durations: Many clinical trials are too short to detect the long-term, cumulative health impacts of differences in pesticide residue or antioxidant intake [6].
- Analytical Scope: A narrow focus on a limited set of nutrients may miss broader patterns. One systematic review found significant differences in only 29% of comparisons, with 42% showing no difference, highlighting the inconsistency that plagues the field [1].
Q2: How can we improve the consistency of nutrient composition analysis in our research? Standardizing protocols is crucial for improving cross-study comparability.
- Matched Pair Design: Source organic and conventional produce from farms in the same geographical region with similar soil and climate conditions to control for environmental variability [82].
- Blinded Analysis: Ensure laboratory technicians are blinded to the sample group (organic or conventional) during nutrient and chemical analysis to prevent unconscious bias.
- Multi-Parameter Assessment: Move beyond basic macronutrients. Include analyses for secondary metabolites (e.g., polyphenols, antioxidants), pesticide residues, and heavy metals to build a more comprehensive profile [1] [82].
- Standardized Sampling: Define and adhere to strict protocols for sampling edible portions, preparation, and laboratory analysis to ensure consistency across different research groups [1].
Q3: What are the primary methodological challenges when linking organic food consumption to human health outcomes like reduced cancer risk? Establishing a direct causal link is exceptionally complex.
- Residual Confounding: In cohort studies, observed health benefits (e.g., reduced risk of non-Hodgkin lymphoma) may be partially attributed to other health-conscious behaviors common among regular organic food consumers [6].
- Exposure Assessment: Accurately quantifying long-term dietary exposure and pesticide residue intake is difficult, often relying on self-reported data which can be unreliable [6].
- Complex Biological Pathways: The health benefits of organic food may result from the synergistic effect of reduced harmful substance intake and increased beneficial nutrient intake, a relationship that is not linear and hard to model [6].
Troubleshooting Common Experimental Issues
| Problem | Possible Cause | Solution |
|---|---|---|
| Inconsistent nutrient results between sample replicates. | Inhomogeneous sample material or improper sample preparation. | Implement a rigorous homogenization protocol for the entire edible portion of the plant. Document the specific preparation method (e.g., fresh, frozen, freeze-dried) as it affects nutrient concentration [82]. |
| No significant difference in primary macronutrients (e.g., protein, fiber). | The production system may have a greater impact on secondary metabolites than on primary macronutrients. | Expand the analytical panel to include polyphenolic compounds, antioxidant capacity (FRAP, DPPH), and vitamin C, where differences are more frequently reported [1] [82]. |
| High variation in antioxidant readings within a group. | The antioxidant content in plants is highly sensitive to environmental stress. Variations in sunlight, water, and pest pressure on the farm can cause large standard deviations. | Increase sample size to account for high biological variability. Record and statistically control for agronomic variables where possible [82]. |
| Difficulty interpreting the public health significance of findings. | A statistically significant difference in a nutrient level may not translate to a biologically meaningful health impact. | Contextualize results by comparing the magnitude of difference to established dietary intake recommendations or known biological effect thresholds. |
The following table summarizes quantitative findings from key studies, illustrating the variability and specific areas where differences are often detected.
Table 1: Nutritional Comparison Between Organic and Conventional Production
| Food Item | Nutrient/Analyte | Conventional Mean | Organic Mean | Significant Difference? | Notes & Source |
|---|---|---|---|---|---|
| Allium Vegetables (Garlic, Leek, Onion) | Total Polyphenols | Lower | Higher | Yes (p<0.05) | Consistent trend across garlic, leek, and red/yellow onion [82]. |
| Vitamin C | Lower | >50% Higher | Yes (p<0.001) | Organic red onion had the highest content [82]. | |
| Antioxidant Capacity (FRAP/DPPH) | Lower | Higher | Yes | Confirmed higher antioxidant potential in organic samples [82]. | |
| Minerals (Ca, Mg, Fe, Zn, Cu, Mn) | Lower | Higher | Yes | All analyzed organic vegetables were more mineral-abundant [82]. | |
| Crude Protein | Variable | Variable | Inconsistent | Higher in conventional garlic/leek; higher in organic onion [82]. | |
| Various Fruits & Vegetables | Iron, Magnesium, Vitamin C | Lower | Higher | Inconsistent | Trend identified, but evidence is not conclusive across all studies [6]. |
| (Systematic Review) | Any Nutritional Parameter | - | - | Only in 29.1% of comparisons | 41.9% of analyses showed no significant difference [1]. |
Detailed Experimental Protocols
Protocol 1: Assessing Antioxidant Capacity and Polyphenolic Content in Allium Vegetables
This protocol is adapted from a study that found significant differences between organic and conventional production systems [82].
Sample Preparation:
- Source matched pairs of organic and conventional vegetables (e.g., garlic, leek, onion) from comparable growing regions.
- Clean and separate the edible portions. Homogenize the plant material thoroughly using a commercial food processor. For dry weight analysis, a sub-sample should be freeze-dried.
Extraction of Bioactive Compounds:
- Weigh 1.0 g of fresh homogenate (or 0.2 g of freeze-dried powder) into a centrifuge tube.
- Add 10 mL of acidified methanol (e.g., 80% methanol, 1% HCl). Vortex vigorously for 1 minute.
- Sonicate the mixture for 15 minutes in an ultrasonic water bath, then centrifuge at 10,000 x g for 10 minutes at 4°C.
- Carefully transfer the supernatant to a new vial. The extract can be used immediately or stored at -80°C for subsequent analysis.
Analysis of Total Polyphenolic Content (TPC):
- Method: Folin-Ciocalteu assay.
- Procedure: In a microplate or cuvette, combine:
- 20 µL of the sample extract (or standard Gallic Acid solution for the calibration curve).
- 100 µL of Folin-Ciocalteu reagent (diluted 1:10 with water).
- After 5 minutes, add 80 µL of sodium carbonate solution (7.5% w/v).
- Incubate in the dark for 60 minutes at room temperature.
- Measure the absorbance at 765 nm. Express results as mg Gallic Acid Equivalents (GAE) per 100 g of fresh weight.
Analysis of Antioxidant Capacity:
- FRAP (Ferric Reducing Antioxidant Power) Assay:
- Prepare the FRAP working reagent by mixing acetate buffer (300 mM, pH 3.6), TPTZ solution (10 mM in 40 mM HCl), and FeCl₃·6H₂O solution (20 mM) in a 10:1:1 ratio.
- Combine 180 µL of FRAP reagent with 20 µL of sample extract or standard (FeSO₄·7H₂O).
- Incubate for 10 minutes at 37°C and measure absorbance at 593 nm. Results are expressed as µmol Fe²⁺ equivalents per g fresh weight.
- DPPH (2,2-diphenyl-1-picrylhydrazyl) Radical Scavenging Assay:
- Dilute a stock DPPH solution in methanol to an absorbance of ~1.0 at 515 nm.
- Mix 100 µL of sample extract with 100 µL of the DPPH solution.
- Incubate in the dark for 30 minutes and measure the decrease in absorbance at 515 nm. Calculate the percentage of radical scavenging activity relative to a methanol blank.
- FRAP (Ferric Reducing Antioxidant Power) Assay:
Protocol 2: Systematic Review Methodology for Nutritional Comparisons
This protocol outlines the methodology used in large-scale systematic reviews to assess the overall evidence [1].
Literature Search & Screening:
- Databases: Search major scientific databases (e.g., PubMed, Scopus, Web of Science) using a structured search string with keywords: ("organic" OR "conventional") AND ("nutritional value" OR "mineral content" OR "antioxidant" OR "polyphenol") AND (fruit OR vegetable OR cereal).
- Inclusion/Exclusion Criteria: Pre-define criteria based on publication date (e.g., last 25 years), language, and requirement for direct side-by-side comparison of organic and conventional foods.
- Process: The search results are screened by title and abstract, followed by a full-text review of eligible articles. The process should be performed by at least two independent reviewers to minimize bias.
Data Extraction:
- Create a standardized data extraction form. For each study, record: food type, specific nutrient/compound analyzed, analytical method, sample size, mean values for organic and conventional, standard deviation, and p-value.
- Each unique nutrient-food pair from a study is treated as a single "comparative analysis."
Data Synthesis & Categorization:
- Statistical Analysis: Based on the data reported in the primary studies, comparative analyses are categorized as:
- Significant Difference: The primary study reported a statistically significant difference (p < 0.05).
- No Significant Difference: The primary study reported no statistically significant difference.
- Divergent Results: Different studies on the same food-nutrient pair reported conflicting significant and non-significant results.
- Summary Statistics: Calculate the proportion and number of comparative analyses that fall into each category to provide a quantitative overview of the evidence.
- Statistical Analysis: Based on the data reported in the primary studies, comparative analyses are categorized as:
Experimental Workflow Visualization
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents and Kits for Nutritional Quality Analysis
| Item | Function/Application |
|---|---|
| Folin-Ciocalteu Reagent | Determination of total polyphenolic content via colorimetric reaction with phenolic compounds. |
| DPPH (2,2-diphenyl-1-picrylhydrazyl) | A stable free radical used to assess antioxidant capacity through a radical scavenging assay. |
| FRAP (Ferric Reducing Antioxidant Power) Reagent | Contains TPTZ and Fe³⁺; measures the reducing ability of antioxidants by detecting reduced Fe²⁺. |
| Methanol & Acetone (HPLC Grade) | High-purity solvents for the extraction of a wide range of bioactive compounds, including polyphenols and vitamins. |
| Standard Compounds (Gallic Acid, Quercetin, Ascorbic Acid) | Used to create calibration curves for the quantitative analysis of polyphenols, flavonoids, and Vitamin C. |
| ICP-MS/OES Sample Prep Kits | Kits for digesting and preparing plant tissue samples for multi-element mineral analysis. |
Conclusion
Achieving consistency in organic versus conventional nutrient comparisons is not merely an academic exercise but a prerequisite for translating agricultural research into meaningful biomedical and clinical applications. By adopting the standardized methodological frameworks, rigorous validation processes, and troubleshooting strategies outlined in this article, the research community can move beyond the current state of contradictory findings. Future research must prioritize long-term, whole-diet interventions and leverage emerging technologies in precision nutrition to understand the individual health impacts of food production methods. This will ultimately provide the robust, high-quality evidence base needed to inform drug development, refine dietary guidelines, and shape effective public health policies for chronic disease prevention.
References
- 1. Are organics more nutritious than conventional foods? A ... [https://www.sciencedirect.com/science/article/pii/S2405844024043196]
- 2. Organic farming for a sustainable future: soil and yield ... [https://www.frontiersin.org/journals/sustainable-food-systems/articles/10.3389/fsufs.2025.1564945/full]
- 3. Assessing the Potential and Limitations of Organic Farming ... [https://www.sciencedirect.com/science/article/pii/S2667010025002653]
- 4. Regenerative Organic Agriculture and Human Health [https://pmc.ncbi.nlm.nih.gov/articles/PMC12108233/]
- 5. Organic foods: Are they safer? More nutritious? [https://www.mayoclinic.org/healthy-lifestyle/nutrition-and-healthy-eating/in-depth/organic-food/art-20043880]
- 6. A Comprehensive Analysis of Organic Food [https://pmc.ncbi.nlm.nih.gov/articles/PMC10814746/]
- 7. A Comprehensive Systematic Review of Dynamic Nutrient ... [https://www.mdpi.com/2304-8158/14/21/3625]
- 8. Soil thinning dominates crop yield reduction among ... [https://www.sciencedirect.com/science/article/abs/pii/S116103012500190X]
- 9. Analysis of soil properties and wheat yield in relation to ... [https://www.nature.com/articles/s41598-025-96550-1]
- 10. Journal of Applied Horticulture Selected Contents of Year ... [https://www.horticultureresearch.net/abstract.php?a=2025]
- 11. Study protocol: post-harvest losses of fruits and vegetables ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12490541/]
- 12. A new report sheds light on losses across agricultural ... [https://www.fao.org/in-action/agrisurvey/news/news-detail/a-new-report-sheds-light-on-losses-across-agricultural-and-agrifood-value-chains-in-niger/en]
- 13. The evidence on crop postharvest loss reduction ... [https://www.sciencedirect.com/science/article/pii/S0022474X25001869]
- 14. Nutritional Description of Organic and Conventional Food ... [https://www.mdpi.com/2072-6643/15/8/1876]
- 15. Higher antioxidant and lower cadmium concentrations and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4141693/]
- 16. New study finds significant differences between organic ... [https://www.cambridge.org/core/blog/2014/07/13/new-study-finds-significant-differences-between-organic-and-non-organic-food/]
- 17. A Systematic Review of Organic Versus Conventional Food ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7019963/]
- 18. Can organic farming improve the soil properties, food ... [https://www.sciencedirect.com/science/article/abs/pii/S2949824424001733]
- 19. Methodological Considerations in Evaluating the Evidence [https://www.ncbi.nlm.nih.gov/books/NBK218763/]
- 20. Evaluating Nutritional Value and Impact on Human Health [https://www.mdpi.com/2304-8158/13/2/208]
- 21. Understanding Nutritional Epidemiology and Its Role in ... [https://www.sciencedirect.com/science/article/pii/S2161831322006196]
- 22. A Guide to Diet-Microbiome Study Design [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2020.00079/full]
- 23. Protocols & Troubleshooting Guides [https://www.rndsystems.com/resources/protocols-troubleshooting-guides]
- 24. Methodology for the Review and Update of Nutrient Criteria ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9218624/]
- 25. Nutrient Profiling Can Help Identify Foods of Good ... [https://www.sciencedirect.com/science/article/pii/S0022316622098273]
- 26. Comparison of nutrient profiling models for assessing the nutritional quality of foods: a validation study - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6137431/]
- 27. Nutrient Profile Models Position Paper [https://www.advocacyincubator.org/program-areas/food-and-nutrition-2/nutrient-profile-models-position-paper]
- 28. Criterion validation of nutrient profiling systems: a systematic review and meta-analysis - ScienceDirect [https://www.sciencedirect.com/science/article/pii/S0002916523661878]
- 29. Are organics more nutritious than conventional foods? A ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10987935/]
- 30. Nutritional quality of organic foods: a systematic review [https://www.sciencedirect.com/science/article/pii/S0002916523265636]
- 31. Perspective: How to Develop Nutrient Profiling Models ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8166553/]
- 32. Recent Techniques in Nutrient Analysis for Food ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7582643/]
- 33. Validating NMR-based non-targeted methods and fostering ... [https://www.sciencedirect.com/science/article/abs/pii/S0079656525000068]
- 34. The Nutri-Score algorithm: Evaluation of its validation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9421047/]
- 35. Performance of the Front-of-Pack Nutrition Label Nutri ... [https://www.mdpi.com/2072-6643/12/5/1303]
- 36. Nutritional quality of food as represented by the FSAm-NPS ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6143197/]
- 37. The Nutri-Score nutrition label : justifications, scientific basis ... [https://nutriscore.blog/2025/10/31/the-nutri-score-nutrition-label-justifications-scientific-basis-user-guide-benefits-limitations-deployment-and-update/]
- 38. A comparison of organic-certified versus non ... [https://www.sciencedirect.com/science/article/abs/pii/S019566632100605X]
- 39. Nutri-Score effectiveness in improving consumers' nutrition ... [https://www.sciencedirect.com/science/article/pii/S0899900725001984]
- 40. Publication bias and Nutri-Score: A complete literature ... [https://www.sciencedirect.com/science/article/pii/S2213434424000069]
- 41. Some Differences in Nutritional Biomarkers are Detected ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6397420/]
- 42. Long-term dietary intervention trials - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC3453508/]
- 43. Optimal Design of Clinical Trials of Dietary Interventions in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9169766/]
- 44. Perspective: Key Considerations When Developing and ... [https://www.sciencedirect.com/science/article/pii/S0022316624004759]
- 45. Metabolon's Validation of Dried Blood Spot (DBS) Cards ... [https://www.metabolon.com/blog/metabolons-validation-of-dried-blood-spot-dbs-cards-for-metabolomics-analysis/]
- 46. Evaluation of metabolite stability in dried blood spot stored ... [https://www.nature.com/articles/s41598-024-82041-2]
- 47. Precision nutrition – Unlocking health through metabolomics [https://biocrates.com/precision-nutrition-through-metabolomics/]
- 48. Role of metabolomics in the delivery of precision nutrition [https://www.sciencedirect.com/science/article/pii/S2213231723002094]
- 49. Dried blood spots analysis for targeted and non- ... [https://www.sciencedirect.com/science/article/pii/S0160412025005653]
- 50. Precision nutrition: Is tailor‑made dietary intervention a reality ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11956147/]
- 51. Confounder adjustment in observational studies investigating ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11881322/]
- 52. Lifestyle-Related Factors for Improving Diet Quality [https://www.mdpi.com/2072-6643/17/3/448]
- 53. How to be a Better Troubleshooter in Your Laboratory [https://www.goldbio.com/blogs/articles/how-to-be-a-better-troubleshooter?srsltid=AfmBOopKqyD_W7d27EDVcmZekII8bdXmssiPZLb08cei6lhgq7PSG48k]
- 54. Troubleshooting Protocols - Biological Sciences: Summer ... [https://guides.library.cmu.edu/biologicalsciencesSRI/troubleshooting]
- 55. Current practices and challenges in the standardization and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5004491/]
- 56. Teaching troubleshooting skills to graduate students - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11407763/]
- 57. Standardizing experimental protocols [https://www.sciencedirect.com/science/article/abs/pii/S0958166908000773]
- 58. How can you standardize experimental conditions? [https://www.linkedin.com/advice/3/how-can-you-standardize-experimental-conditions-lmfxf]
- 59. The Design and Testing of a Field Operations Visualizer [https://www.mdpi.com/2624-7402/6/4/264]
- 60. Long-term economic and yield comparison of organic ... [https://www.sciencedirect.com/science/article/pii/S1161030125003107]
- 61. Pharma Quality Control Strategies for Drug Development ... [https://biotech-spain.com/en/articles/pharma-quality-control-strategies-for-drug-development-and-regulatory-compliance/]
- 62. Randomization in clinical studies - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6547231/]
- 63. A roadmap to using randomization in clinical trials [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-021-01303-z]
- 64. A Guide to Randomisation in Clinical Trials [https://www.quanticate.com/blog/randomisation-in-clinical-trials]
- 65. Navigating blinding challenges in complex intervention trials [https://trialsjournal.biomedcentral.com/articles/10.1186/s13063-025-09223-9]
- 66. Blinding in Clinical Trials: Seeing the Big Picture - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8308085/]
- 67. Blinding: Who, what, when, why, how? - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2947122/]
- 68. Randomization & Blinding in Clinical Research Trials - Castor [https://www.castoredc.com/blog/randomization-clinical-trials/]
- 69. Diet and Cardiovascular Disease: Advances and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5844273/]
- 70. Biomarker data with measurement error in medical research [https://pmc.ncbi.nlm.nih.gov/articles/PMC11305697/]
- 71. Biomarker Discovery and Validation: Statistical Considerations [https://pmc.ncbi.nlm.nih.gov/articles/PMC8012218/]
- 72. Machine learning can improve the development of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9378580/]
- 73. Consumption of ultra-processed foods and risk ... [https://www.sciencedirect.com/science/article/pii/S2666776223001904]
- 74. Nutri-Score and health claims: a comparative analysis of ... [https://www.cambridge.org/core/journals/proceedings-of-the-nutrition-society/article/nutriscore-and-health-claims-a-comparative-analysis-of-the-nutrient-profile-of-foods-making-health-claims-in-supermarkets-in-ireland/A7F35209E3AB469ED6CA20D991ADF551]
- 75. Comparison of nutrient profiling models for assessing the ... [https://pubmed.ncbi.nlm.nih.gov/30015603/]
- 76. Nutrient Profile Model [https://www.paho.org/en/nutrient-profile-model]
- 77. Comparative Analysis of the Classification of Food ... [https://www.mdpi.com/2072-6643/10/6/737]
- 78. Defining Energy-Dense, Nutrient-Poor Food and Drinks ... [https://www.mdpi.com/2072-6643/14/7/1477]
- 79. A Systematic Literature Review of Health-Related Quality of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10883903/]
- 80. Patient-Reported Outcome Measures (PROMS) in ... [https://www.mdpi.com/1718-7729/32/5/265]
- 81. Optimization and validation of the international metabolic ... [https://www.nature.com/articles/s41408-025-01338-1]
- 82. Nutritional value and antioxidant capacity of organic and ... [https://www.nature.com/articles/s41598-022-23497-y]