Bridging the Gap: A Comprehensive Guide to In Vitro-In Vivo Correlation (IVIVC) Models in Drug Development
This article provides a comprehensive examination of In Vitro-In Vivo Correlation (IVIVC) models, which establish predictive relationships between a drug's laboratory dissolution and its in vivo pharmacokinetic behavior.
Bridging the Gap: A Comprehensive Guide to In Vitro-In Vivo Correlation (IVIVC) Models in Drug Development
Abstract
This article provides a comprehensive examination of In Vitro-In Vivo Correlation (IVIVC) models, which establish predictive relationships between a drug's laboratory dissolution and its in vivo pharmacokinetic behavior. Aimed at researchers and drug development professionals, the content explores foundational principles, methodological approaches for building robust correlations, strategies for troubleshooting complex formulations, and frameworks for regulatory validation. By synthesizing current research and regulatory perspectives, this guide serves as a critical resource for leveraging IVIVC to streamline formulation optimization, reduce development costs, support bioequivalence assessments, and accelerate the translation of drug products from the lab to the clinic.
Understanding IVIVC: Core Concepts, Regulatory Definitions, and Correlation Levels
In the realm of pharmaceutical development, In Vitro-In Vivo Correlation (IVIVC) serves as a critical scientific bridge, connecting a drug's laboratory performance to its behavior in the human body. Regulatory authorities recommend establishing IVIVC models for most modified-release dosage forms to streamline development and enhance formulation strategies [1]. According to the United States Pharmacopeia (USP), IVIVC is defined as "the establishment of a rational relationship between a biological property, or a parameter derived from a biological property produced by a dosage form, and a physicochemical property or characteristic of the same dosage form" [2]. In parallel, the Food and Drug Administration (FDA) provides a more application-oriented definition, describing IVIVC as "a predictive mathematical model describing the relationship between an in vitro property of a dosage form and a relevant in vivo response" [2] [1]. While the USP emphasizes establishing a rational relationship between broadly defined properties, the FDA specifically focuses on the predictive capability of the mathematical model for in vivo performance.
The primary advantage of IVIVC lies in its ability to provide a mechanism for evaluating how changes in in vitro drug release affect in vivo drug absorption. This predictive capability can reduce the need for certain clinical bioequivalence studies, supporting more ethical research and accelerating development timelines [1]. Furthermore, IVIVC enhances understanding of drug product characteristics, facilitates broader acceptance criteria, and helps optimize formulation stability throughout the product lifecycle [1].
Regulatory Framework and Correlation Levels
Comparative Analysis of USP and FDA Perspectives
The following table summarizes the key distinctions between the USP and FDA perspectives on IVIVC:
Table 1: Comparison of USP and FDA Perspectives on IVIVC
| Aspect | USP Perspective | FDA Perspective |
|---|---|---|
| Core Definition | Establishment of a rational relationship between a biological property and a physicochemical property [2]. | A predictive mathematical model between an in vitro property and a relevant in vivo response [2] [1]. |
| Primary Emphasis | Broad relationship establishment, including various biological and physicochemical parameters [2]. | Predictive capability and model application for bioavailability/bioequivalence assessments [1]. |
| In Vivo Response | Can be any "biological property produced by a dosage form" [2]. | Typically plasma drug concentration, amount absorbed, or other PK parameters (e.g., Cmax, AUC) [2] [1]. |
| Regulatory Application | General standard for relationship establishment [2]. | Supports biowaivers, sets dissolution specifications, and justifies formulation changes [1]. |
Levels of IVIVC and Their Regulatory Acceptance
Regulatory guidelines recognize multiple levels of IVIVC, which differ in complexity, predictive power, and regulatory utility. The most common categories are Levels A, B, and C.
Table 2: Levels of IVIVC and Their Regulatory Implications
| Level | Definition | Predictive Value | Regulatory Acceptance & Use Cases |
|---|---|---|---|
| Level A | A point-to-point correlation between in vitro dissolution and in vivo absorption [1]. | High – predicts the full plasma concentration-time profile [1]. | Most preferred by FDA; supports biowaivers and major formulation changes. Requires ≥2 formulations with distinct release rates [1]. |
| Level B | A statistical correlation using mean in vitro and mean in vivo parameters [2] [1]. | Moderate – does not reflect individual pharmacokinetic curves [1]. | Less robust; usually requires additional in vivo data. Not suitable for quality control specifications [1]. |
| Level C | A correlation between a single in vitro time point and one pharmacokinetic parameter (e.g., Cmax, AUC) [2] [1]. | Low – does not predict the full PK profile [1]. | Least rigorous; not sufficient for biowaivers or major changes. May support early development insights [1]. |
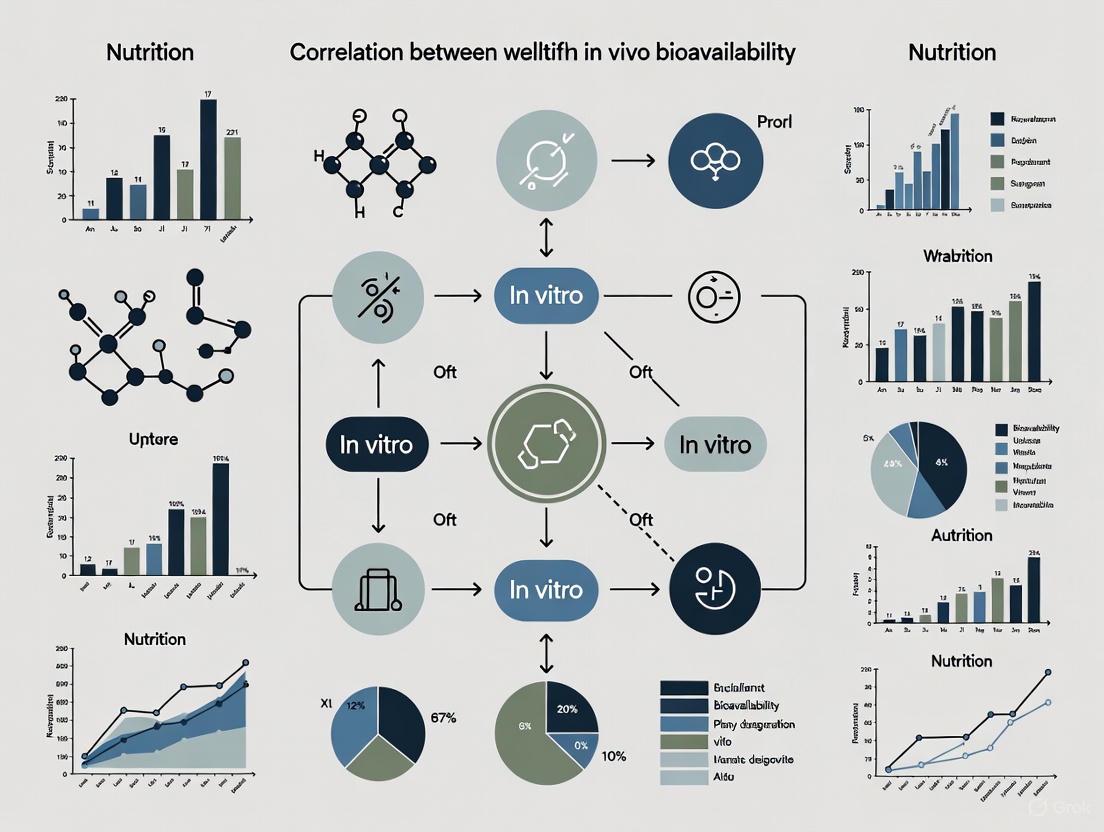
Diagram 1: IVIVC Levels and Predictive Value Hierarchy
Experimental Protocols for IVIVC Development
Development of Level A IVIVC for Extended-Release Tablets
A robust Level A IVIVC was successfully developed for lamotrigine extended-release (ER) 300 mg tablets, establishing patient-centric quality standards for dissolution. The systematic approach involved multiple experimental and computational phases [3].
Materials and Methods:
- Formulations: Marketed lamotrigine ER tablets (Lamictal XR 300 mg) as reference, with in-house manufactured slow, medium, and fast-release formulations for IVIVC validation [3].
- Dissolution Testing: Comprehensive dissolution profiling using USP Apparatus II (paddle) and III (reciprocating cylinder) under various conditions, including biorelevant and standard compendial media with different pH levels and hydrodynamic parameters [3].
- Analytical Techniques: HPLC analysis of dissolution samples with validated methods to determine lamotrigine concentration [3].
- PBPK Modeling: Development and verification of a physiologically based pharmacokinetic (PBPK) model using plasma lamotrigine profiles from intravenous solution and oral immediate-release tablets. Model verification showed accurate prediction of Cmax and AUC with confidence levels exceeding 95% [3].
Key Experimental Workflow: The experimental workflow for establishing a predictive IVIVC involves multiple interconnected stages, as illustrated below:
Diagram 2: Comprehensive IVIVC Development Workflow
Results and Validation: The study demonstrated that dissolution in standard compendial media using USP Apparatus II established a robust Level A IVIVC. The model passed both internal and external validation criteria with prediction errors below 10%, confirming its predictive capability. Using these dissolution conditions, patient-centric quality standards (PCQS) were successfully derived as ≤10% release at 2 h, ≤45% at 6 h, and ≥80% at 18 h [3].
Universal In Vivo Predictive Dissolution Method for Immediate-Release Tablets
For acyclovir immediate-release tablets, a universal in vivo predictive dissolution (IPD) method was developed using a mini-vessel/mini-paddle apparatus, guided by computational simulations in a PBPK model [4].
Materials and Methods:
- Formulations: Acyclovir IR tablets (200 mg and 800 mg strengths), including reference (Zovirax) and generic products [4].
- Dissolution Apparatus: Miniaturized version of USP Type II apparatus with 135 mL or 150 mL volumes, compared with standard USP Type II apparatus with 900 mL volume [4].
- Dissolution Media: Hydrochloric acid, pH 2.0, at varying stirring rates (100, 125, 150 rpm) [4].
- PBPK Modeling: Adaptation of a previously built PBPK model for acyclovir IR tablets in GastroPlus software, incorporating optimized effective permeability values and transporter-mediated kinetics [4].
Experimental Findings: The research revealed that dissolution of 800 mg acyclovir tablets in 900 mL of media largely overpredicted observed plasma profiles due to poor resemblance of non-sink conditions in the human lumen. Conversely, dissolution in the mini-vessel filled with 135 mL of HCl, pH 2.0, at 150 rpm produced accurate predictions of plasma profiles without affecting successful predictions with the lowest strength tablets. This method was validated through in-human and virtual bioequivalence studies, confirming its predictive potential as a universal IPD method for acyclovir immediate-release tablets [4].
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Essential Materials and Equipment for IVIVC Studies
| Tool/Reagent | Function in IVIVC Development | Application Example |
|---|---|---|
| USP Apparatus II (Paddle) | Standard dissolution apparatus for oral dosage forms under controlled hydrodynamic conditions [3]. | Dissolution testing of lamotrigine ER tablets in compendial media [3]. |
| USP Apparatus III (Reciprocating Cylinder) | Alternative dissolution apparatus with different hydrodynamics, useful for establishing bio-relevant conditions [3]. | Comparative dissolution profiling of lamotrigine ER tablets [3]. |
| Mini-Vessel/Mini-Paddle Apparatus | Miniaturized dissolution apparatus with smaller volumes (135-150 mL) to better simulate physiological conditions [4]. | Development of IPD method for acyclovir 800 mg tablets under non-sink conditions [4]. |
| Biorelevant Media | Dissolution media simulating gastrointestinal fluids (e.g., FaSSIF, FeSSIF) to enhance physiological relevance [3]. | Evaluation of dissolution characteristics under simulated fasted and fed states [3]. |
| PBPK Modeling Software | Computational platform (e.g., GastroPlus) for developing and verifying physiologically based pharmacokinetic models [3] [4]. | Prediction of plasma concentration-time profiles and virtual bioequivalence studies [3] [4]. |
| HPLC-MS/MS Systems | Advanced analytical instrumentation for precise quantification of drug concentrations in dissolution samples and biological matrices [4]. | Bioanalysis of acyclovir in plasma samples from bioequivalence trials [4]. |
Applications and Future Perspectives
IVIVC continues to evolve beyond traditional oral dosage forms, expanding into complex delivery systems. For lipid-based formulations (LBFs), IVIVC development presents unique challenges due to the complex interplay of digestion, permeation, and dynamic solubilization processes [2]. Similarly, for long-acting injectables (LAIs) based on poly(lactide-co-glycolide), IVIVC establishment requires consideration of drastically different circumstances compared to oral formulations, including month-long release durations and more complex release mechanisms [5].
The future of IVIVC is increasingly intertwined with advanced modeling approaches and emerging technologies. The convergence of artificial intelligence-driven modeling platforms, microfluidics, organ-on-a-chip systems, and high-throughput screening assays holds immense potential for augmenting the predictive power and scope of IVIVC studies [1]. Furthermore, the integration of IVIVC with Quality by Design (QbD) frameworks and model-informed drug development (MIDD) approaches enables the establishment of clinically relevant dissolution specifications that better account for variability in patient physiology and drug absorption [3] [4]. These advancements are paving the way for more personalized drug therapies while simultaneously accelerating drug development timelines.
In vitro-in vivo correlation (IVIVC) is a pivotal scientific framework in pharmaceutical development, defined as a predictive mathematical model that describes the relationship between an in vitro property of a dosage form (typically the rate or extent of drug dissolution) and a relevant in vivo response (such as plasma drug concentration or amount absorbed) [1] [6]. The primary objective of establishing an IVIVC is to use in vitro drug release profiles as a surrogate for in vivo performance, enabling researchers to predict how a drug will behave in patients based on laboratory dissolution data [1]. This approach streamlines drug development, enhances formulation strategies, supports regulatory decisions, and can reduce the need for certain clinical bioequivalence studies [1].
The U.S. Food and Drug Administration (FDA) formalized the modern classification system for IVIVC in its 1997 guidance "Extended Release Oral Dosage Forms: Development, Evaluation, and Application of In Vitro/In Vivo Correlations," which remains the definitive regulatory guidance on the topic [1]. This classification establishes a hierarchy of correlation levels—A, B, C, and Multiple Level C—categorized by their complexity, predictive power, and regulatory utility [1] [7]. Level A represents the most robust and predictive correlation, while Level C provides the most limited relationship. Understanding this hierarchy is essential for researchers, scientists, and drug development professionals seeking to optimize formulations and meet regulatory requirements for modified-release dosage forms.
The IVIVC Hierarchy: Levels and Regulatory Applications
The IVIVC hierarchy consists of distinct levels of correlation that differ significantly in their mathematical approaches, predictive capabilities, and regulatory acceptance. The following sections provide a detailed explanation of each level, including their definitions, methodologies, and applications within drug development.
Figure 1: IVIVC Hierarchy and Data Relationships. This diagram illustrates the fundamental relationships between in vitro data and in vivo parameters for each level of IVIVC, showing decreasing predictive power from Level A to Level C.
Level A Correlation: The Gold Standard
Level A correlation represents the highest and most informative category of IVIVC, establishing a point-to-point relationship between in vitro dissolution and in vivo absorption rates [1] [7]. This model is constructed by comparing the percentage of drug dissolved in vitro with the percentage of drug absorbed in vivo at corresponding time points, creating a direct correlation where in vitro dissolution rate serves as a surrogate for in vivo performance [7].
The mathematical foundation of Level A correlation typically involves deconvolution techniques to derive the in vivo absorption profile. Common approaches include:
- Wagner-Nelson method: Suitable for one-compartment models
- Loo-Riegelman method: Applicable to two-compartment models
- Model-independent deconvolution: Uses a reference formulation to determine the input function [7]
For a valid Level A correlation, regulatory guidelines typically require development using at least two formulations with different release rates (e.g., slow, medium, and fast) [1]. However, in specific cases where formulation changes are minimal, a single formulation may be acceptable. The predictive performance of the model is evaluated using internal validation, where prediction errors for key pharmacokinetic parameters (AUC and Cmax) should not exceed 10% on average, with no individual prediction error exceeding 15% [7].
Level A correlation provides the highest regulatory value and can support:
- Biowaivers for major formulation changes
- Changes in manufacturing site, method, or raw material supplies
- Minor formulation modifications
- Different product strengths using the same formulation [1] [7]
Level B Correlation: Statistical Moment Analysis
Level B correlation utilizes the principles of statistical moment analysis, comparing the mean in vitro dissolution time (MDTvitro) to either the mean residence time (MRT) or mean in vivo dissolution time (MDTvivo) [7]. This approach uses the entire dissolution and plasma concentration dataset but does not establish a point-to-point relationship between in vitro and in vivo profiles [1].
While Level B correlation incorporates complete in vitro and in vivo data, it represents a less predictive approach than Level A because different in vivo plasma concentration curves can produce similar mean residence time values [7]. Consequently, Level B correlation does not uniquely reflect the actual shape of the in vivo plasma concentration curve and cannot predict the complete drug absorption profile [1].
Due to these limitations, Level B correlation has limited regulatory utility and is generally not sufficient to justify biowaivers or support significant post-approval changes (SUPAC) without additional in vivo data [1] [7]. It may serve as an intermediate tool during formulation development but lacks the predictive precision required for definitive regulatory decisions.
Level C and Multiple Level C Correlations
Level C correlation establishes a single-point relationship between one dissolution time point (e.g., t50%, t90%) and one pharmacokinetic parameter (such as AUC, Cmax, or Tmax) [1] [7]. This represents the simplest and least informative form of IVIVC, as it only identifies a partial relationship between absorption and dissolution without reflecting the complete shape of the plasma concentration-time curve [7].
Multiple Level C correlation expands on the basic Level C approach by correlating one or several pharmacokinetic parameters with the amount of drug dissolved at multiple time points throughout the dissolution profile [7]. This multi-point approach should include at least three dissolution time points covering the early, middle, and late stages of the dissolution profile to provide a more comprehensive assessment than single-point Level C correlation [7].
While Multiple Level C correlation offers more information than single-point Level C, both approaches have limited regulatory applications:
- Level C may aid in formulation selection during early development stages
- Multiple Level C may potentially support biowaivers if established over the entire dissolution profile and with appropriate pharmacokinetic parameters [7]
- Neither approach alone is sufficient to predict the complete in vivo performance of drug products [1]
Table 1: Comprehensive Comparison of IVIVC Levels
| Aspect | Level A | Level B | Level C | Multiple Level C |
|---|---|---|---|---|
| Definition | Point-to-point correlation between in vitro dissolution and in vivo absorption [1] [7] | Statistical moment analysis comparing mean in vitro dissolution time with mean in vivo residence/time [1] [7] | Single-point relationship between one dissolution time point and one PK parameter [1] [7] | Relationship between PK parameters and drug dissolved at several time points [7] |
| Predictive Value | High – predicts full plasma concentration-time profile [1] | Moderate – does not reflect individual PK curves [1] | Low – does not predict full PK profile [1] | Moderate – more predictive than Level C but less than Level A [7] |
| Mathematical Basis | Deconvolution (Wagner-Nelson, Loo-Riegelman) [7] | Statistical moment analysis [7] | Linear regression between single parameters [7] | Multivariate regression between multiple parameters [7] |
| Data Utilization | Uses entire dissolution and plasma profile [7] | Uses entire dissolution and plasma profile [7] | Uses limited data points [7] | Uses multiple but not complete data points [7] |
| Regulatory Acceptance | Most preferred; supports biowaivers and major changes [1] | Less robust; usually requires additional in vivo data [1] | Least rigorous; not sufficient for biowaivers [1] | May support biowaivers if correlation is strong [7] |
| Primary Applications | Surrogate for bioequivalence, SUPAC changes, setting dissolution specifications [1] [7] | Limited regulatory use, primarily for internal development [1] | Early formulation screening and development [7] | Formulation optimization with more insight than Level C [7] |
Experimental Protocols for IVIVC Development
Developing a robust IVIVC requires carefully designed experiments and systematic data analysis. The following section outlines standardized protocols for establishing different levels of correlation, with particular emphasis on Level A IVIVC as the regulatory gold standard.
Formulation Development and In Vitro Testing
The initial stage involves creating formulations with intentionally varied release rates to provide the necessary data range for correlation development.
- Formulation Design: Develop at least two or three formulations with distinct drug release rates (typically slow, medium, and fast) [1] [7]. These formulations should differ only in the critical factors affecting release rate (e.g., polymer composition, excipient ratios, coating thickness) while maintaining similar composition otherwise.
- In Vitro Dissolution Testing:
- Use biorelevant dissolution media that simulate gastrointestinal conditions (e.g., pH 1.2, 4.5, 6.8, or FaSSIF/FeSSIF) [8]
- Employ appropriate apparatus such as USP I (basket), USP II (paddle), or USP IV (flow-through cell) based on dosage form characteristics [8]
- Ensure sink conditions and demonstrate discriminatory power between formulations with different release rates [8]
- For extended-release formulations, aim for a dissolution profile where ≥80% drug release occurs over 12-24 hours [8]
In Vivo Pharmacokinetic Studies
Conduct pharmacokinetic studies in human subjects or appropriate animal models to characterize the in vivo performance of each formulation.
- Study Design: Implement a single-dose, randomized crossover study comparing test formulations with different release rates and including an immediate-release reference product for deconvolution [7]
- Subject Selection: Enroll healthy adult volunteers (typically n=12-36) following ethical guidelines and good clinical practice standards
- Sample Collection: Obtain frequent blood samples (e.g., 0, 0.5, 1, 2, 4, 6, 8, 12, 16, 24, 36, 48 hours) to adequately characterize the plasma concentration-time profile [7]
- Bioanalytical Methods: Use validated HPLC-MS/MS or HPLC-UV methods to quantify drug concentrations in plasma samples with appropriate precision and accuracy [7]
Data Analysis and Model Development
The core of IVIVC development involves mathematical manipulation of in vitro and in vivo data to establish predictive relationships.
- Pharmacokinetic Analysis: Calculate key PK parameters including AUC, Cmax, and Tmax using non-compartmental analysis [7]
- Deconvolution: Apply model-dependent (Wagner-Nelson for one-compartment; Loo-Riegelman for two-compartment) or model-independent deconvolution methods to determine the in vivo absorption time course [7]
- Correlation Establishment:
- For Level A: Plot fraction absorbed in vivo versus fraction dissolved in vitro to establish point-to-point correlation [7]
- Apply time-scaling approaches (e.g., Levy's plot) if in vitro and in vivo timescales differ [7]
- For Level B: Calculate and compare mean dissolution time (MDT) in vitro with mean residence time (MRT) in vivo [7]
- For Level C/Multiple Level C: Perform regression analysis between dissolution parameters (e.g., t50%, t90%) and PK parameters (AUC, Cmax) [7]
Model Validation
Assess the predictive performance of the IVIVC model using internal validation techniques.
- Prediction Validation: Use the established IVIVC model to predict in vivo pharmacokinetic profiles from in vitro dissolution data [7]
- Acceptance Criteria: Evaluate prediction errors for Cmax and AUC; according to regulatory standards, mean prediction error should be ≤10% and individual prediction error should be ≤15% [7]
- For Level A correlation, if these criteria are met, the model can support biowaivers for post-approval changes without additional clinical studies [7]
Figure 2: IVIVC Development Workflow. This flowchart outlines the systematic process for developing and validating IVIVC models, from initial formulation design through to regulatory application.
The Scientist's Toolkit: Essential Reagents and Materials
Establishing a robust IVIVC requires specific reagents, equipment, and methodologies. The following table details essential materials and their functions in IVIVC development.
Table 2: Essential Research Reagent Solutions for IVIVC Studies
| Reagent/Material | Function/Application | Specifications/Standards |
|---|---|---|
| Dissolution Apparatus | Simulates gastrointestinal conditions to measure drug release rate [8] | USP Apparatus I (basket), II (paddle), or IV (flow-through cell) [8] |
| Biorelevant Dissolution Media | Mimics physiological conditions of GI tract for predictive dissolution testing [8] | pH 1.2 (gastric), pH 4.5-6.8 (intestinal), FaSSIF/FeSSIF (fasted/fed state) [8] |
| Reference Standards | Bioanalytical method calibration and validation for drug quantification [7] | Certified reference materials with known purity and stability |
| HPLC-MS/MS Systems | Quantification of drug concentrations in biological samples (plasma) [7] | Validated methods with appropriate sensitivity, precision, and accuracy |
| Cryopreserved Hepatocytes | Metabolic stability assessment for IVIVE (in vitro-in vivo extrapolation) [9] | Species-specific (human, mouse, rat) with viability >70% [9] |
| Transwell Systems (Caco-2) | Assessment of drug permeability in early development [9] | Cell monolayer integrity with appropriate tightness markers [9] |
| Physicochemical Property Assays | Determination of key parameters affecting absorption (solubility, log P, pKa) [6] | Kinetic solubility, shake-flask method, potentiometric titration |
The hierarchy of IVIVC correlations provides a structured framework for relating in vitro drug release to in vivo performance, with each level offering distinct advantages and limitations. Level A correlation stands as the gold standard for regulatory applications, enabling biowaivers and supporting formulation changes without additional clinical studies. Level B offers limited utility despite using complete datasets, while Level C and Multiple Level C serve primarily in early development stages. The successful implementation of IVIVC requires careful experimental design, appropriate statistical analysis, and rigorous validation. When properly established, particularly with Level A correlation, IVIVC significantly enhances formulation development efficiency, reduces animal and human testing, and strengthens regulatory submissions—ultimately accelerating the delivery of quality drug products to patients.
In the pursuit of efficient drug development, the establishment of a predictive in vitro-in vivo correlation (IVIVC) is paramount. An IVIVC is defined as a predictive mathematical model describing the relationship between an oral dosage form's in vitro property (typically the rate or extent of drug dissolution) and a relevant in vivo response (such as plasma drug concentration or amount absorbed) [6]. The primary objective of developing an effective IVIVC is to enable the prediction of in vivo drug performance based on in vitro behavior, thereby reducing the need for extensive clinical studies and accelerating the development of robust drug products [6].
The efficacy of this correlation heavily depends on a thorough understanding of a drug's fundamental physicochemical properties. Among these, solubility, pKa, and particle size play disproportionately critical roles. They collectively govern the journey of an active pharmaceutical ingredient (API) from its release from the dosage form to its dissolution in the gastrointestinal fluids and subsequent absorption across the intestinal membrane. For poorly water-soluble drugs (PWS), which constitute more than 50% of commercially available oral drugs and an even higher percentage of new chemical entities, these factors become the primary determinants of bioavailability [10] [11]. This review objectively examines the experimental data and mechanistic roles of these three key properties in the context of IVIVC, providing a comparative framework for researchers in drug development.
Solubility: The Fundamental Prerequisite for Absorption
Mechanistic Role in Bioavailability
Solubility is the concentration of a drug in a saturated solution at a specific temperature and pH, representing the maximum amount of drug that can remain dissolved in the gastrointestinal (GI) fluid. It is the foundational step in the drug absorption cascade, as a drug must be in solution to permeate the intestinal wall [6]. The critical nature of solubility is captured in the Noyes-Whitney equation (Equation 1), which models dissolution rate [6].
Equation 1: Noyes-Whitney Dissolution Equation [ \frac{dM}{dt} = \frac{D \times S \times (Cs - Cb)}{h} ] Where:
- ( \frac{dM}{dt} ): Dissolution rate
- ( D ): Diffusion coefficient of the drug
- ( S ): Surface area of the drug particle
- ( C_s ): Drug solubility in the dissolution medium
- ( C_b ): Drug concentration in the bulk medium at time t
- ( h ): Thickness of the diffusion layer
This equation illustrates that the dissolution rate is directly proportional to the drug's solubility (( Cs )). Under sink conditions (( Cb ) is negligible), the equation simplifies further, highlighting that the dissolution rate is directly driven by solubility [6]. The Maximum Absorbable Dose (MAD) model (Equation 2) further quantifies the direct relationship between solubility and the potential for oral absorption [6].
Equation 2: Maximum Absorbable Dose (MAD) [ MAD = S \times K_a \times SIWV \times SITT ] Where:
- ( S ): Solubility at pH 6.5 (mg/mL)
- ( K_a ): Intestinal absorption rate constant (min⁻¹)
- ( SIWV ): Small intestinal water volume (≈ 250 mL)
- ( SITT ): Small intestinal transit time (≈ 3 hours)
Experimental Data and Comparison
Table 1: Impact of Solubility on Key Bioavailability Parameters
| Solubility Class | Typical Dose Number (D₀) | Expected Absorption Efficiency | Key Formulation Challenges |
|---|---|---|---|
| High Solubility | D₀ < 1 | High and consistent absorption; IVIVC often straightforward | Chemical stability, controlled release |
| Low Solubility | D₀ > 1 | Highly variable, incomplete absorption; complex IVIVC | Enhancing dissolution, maintaining supersaturation, preventing precipitation |
The Dose Number (D₀) is a key parameter that relates the dose to solubility, calculated as the ratio of dose concentration to solubility [6]. A dose number greater than 1 indicates that the drug dose is insufficiently soluble to dissolve completely in the available GI fluid volume, signaling potential bioavailability problems.
Standard Experimental Protocols
Shake-Flask Method is the standard for equilibrium solubility measurement.
- Preparation: An excess of the drug is added to a vial containing the dissolution medium (e.g., simulated gastric or intestinal fluid).
- Equilibration: The vial is sealed and shaken at a constant temperature (e.g., 37°C) for a sufficient time (typically 24-72 hours) to reach equilibrium.
- Separation: The solution is filtered or centrifuged to separate undissolved solid.
- Quantification: The concentration of the drug in the saturated supernatant is quantified using a validated analytical method, such as UV spectrophotometry or High-Performance Liquid Chromatography (HPLC).
- pH Profiling: The process is repeated across a physiologically relevant pH range (1.2 to 7.5) to understand pH-dependent solubility.
pKa: The Master of Ionization and pH-Dependent Behavior
Mechanistic Role in Bioavailability
The acid dissociation constant (pKa) determines the pH at which a molecule is 50% ionized. This is critically important because the unionized form of a drug typically exhibits higher membrane permeability than its ionized counterpart, a principle known as the pH-partition hypothesis [6]. The human GI tract possesses a significant and dynamic pH gradient, ranging from highly acidic in the stomach (pH ~1.5) to neutral in the small intestine (pH ~6.5) and more basic in the colon (pH ~7-8) [6]. As a drug transits through these different environments, its pKa dictates its ionization state, thereby influencing both its solubility and permeability in a reciprocal manner.
The fraction of a drug that is unionized can be calculated using the Henderson-Hasselbalch equation:
- For weak acids: ( \text{pH} = \text{pKa} + \log\left(\frac{[\text{Ionized}]}{[\text{Unionized}]}\right) )
- For weak bases: ( \text{pH} = \text{pKa} + \log\left(\frac{[\text{Unionized}]}{[\text{Ionized}]}\right) )
A weakly basic drug with a pKa of 4.5 will be highly ionized (and thus more soluble) in the stomach but will become largely unionized (and more permeable) upon entering the small intestine. This interplay is a major source of complexity in developing IVIVCs, as dissolution tests at a single pH may not accurately reflect the in vivo environment [6].
Experimental Data and Comparison
Table 2: Impact of pKa and Ionization Class on Drug Absorption
| Ionization Class | Absorption Site (pH) | Primary Limiting Factor | IVIVC Consideration |
|---|---|---|---|
| Weak Acid (pKa 3-5) | Stomach (pH 1-3) | Permeability in intestine (ionized form) | Dissolution media must reflect gastric pH |
| Weak Base (pKa 6-8) | Small Intestine (pH 6-8) | Solubility in intestine (precipitation risk) | Biphasic dissolution may be necessary |
| Amphoteric | Varies with pH | Complex solubility/permeability profile | Requires multi-pH dissolution profiling |
Standard Experimental Protocols
Potentiometric Titration is a standard method for pKa determination.
- Setup: A known amount of the drug compound is dissolved in a container of water or a water-co-solvent mixture, maintained at a constant temperature (25°C) and ionic strength.
- Titration: For a basic compound, a strong acid (e.g., HCl) is added incrementally. For an acidic compound, a strong base (e.g., NaOH) is used.
- Measurement: After each addition of titrant, the pH of the solution is measured precisely.
- Calculation: The pKa value is determined from the resulting titration curve by identifying the pH at the half-equivalence point or by using specialized software that performs a non-linear regression analysis on the data.
Particle Size: Engineering the Surface Area for Dissolution
Mechanistic Role in Bioavailability
Particle size directly influences the available surface area (S) for dissolution, as defined in the Noyes-Whitney equation. Reducing particle size increases the surface area-to-volume ratio, thereby enhancing the dissolution rate [6] [12]. This principle is the foundation for several formulation strategies aimed at improving the bioavailability of poorly water-soluble drugs. The relationship is not always linear, however, as very small particles (< 1-10 µm) can be susceptible to aggregation, which can counteract the benefits of increased surface area [12].
For drugs with very low solubility and high dose, micronization or nanosizing can be transformative. Nanoparticles not only increase surface area but can also lead to a transient increase in saturation solubility due to the Ostwald-Freundlich equation, further driving dissolution [12]. The success of drug delivery via particle size reduction depends heavily on the anatomical and biological barriers of the administration route, with different optimal size ranges for crossing the GI epithelium, skin, or blood-brain barrier [12].
Experimental Data and Comparison
Table 3: Impact of Particle Size Reduction on Bioavailability
| Particle Size Category | Typical Size Range | Key Mechanism | Reported Bioavailability Outcome |
|---|---|---|---|
| Macroscopic (Conventional) | > 100 µm | Standard dissolution | Baseline absorption; often low for BCS Class II/IV drugs |
| Micronized | 1 µm - 100 µm | Increased surface area (S) | Moderate improvement (e.g., 1.5 to 3-fold increase) |
| Nanosized | < 1 µm | Increased S + potential for increased saturation solubility | Significant improvement (e.g., 5 to 10-fold increase or more) |
Standard Experimental Protocols
Laser Diffraction Particle Size Analysis is a widely used technique.
- Dispersion: A representative sample of the drug powder is dispersed in a suitable medium (often a surfactant solution to prevent aggregation) and circulated through the measurement cell.
- Measurement: The sample is passed through a laser beam. The particles scatter light at an angle that is inversely related to their size.
- Detection: A detector array measures the intensity of light scattered at multiple angles.
- Analysis: Using optical models (like Mie Theory or Fraunhofer Approximation), the instrument software calculates the volume-based particle size distribution from the light scattering data, reporting metrics such as D10, D50 (median), and D90.
Integrated Workflow and Research Toolkit
The following diagram illustrates the logical sequence of experiments and the interconnected roles of solubility, pKa, and particle size in the early-stage development of an oral drug product, framed within the IVIVC context.
Diagram: Integrated workflow for IVIVC-focused physicochemical profiling.
Table 4: The Scientist's Toolkit: Essential Reagents and Materials for Key Experiments
| Research Reagent / Material | Primary Function | Application in Protocol |
|---|---|---|
| Simulated Gastric/Intestinal Fluids (e.g., FaSSIF, FeSSIF) | Biorelevant dissolution media mimicking the pH, buffer capacity, and surface-active components of GI fluids. | Solubility and dissolution testing under physiologically predictive conditions [10]. |
| Potentiometric Titrator | Automated system for precise addition of acid/base and measurement of solution pH. | High-throughput and accurate determination of pKa values. |
| Laser Diffraction Particle Sizer | Instrument for rapid, high-resolution measurement of particle size distributions. | Quality control and R&D for APIs and formulated products. |
| High-Performance Liquid Chromatography (HPLC) System | Analytical instrument for separating and quantifying chemical compounds in a mixture. | Quantifying drug concentration in saturated solutions (solubility) and dissolution samples. |
| Lipid-Based Excipients (e.g., Medium-Chain Triglycerides, Labrasol) | Formulation components that enhance solubilization and supersaturation of poorly soluble drugs. | Used in lipid-based formulation strategies to improve bioavailability [10]. |
The physicochemical triumvirate of solubility, pKa, and particle size forms the bedrock of predictive IVIVC models for oral drug absorption. Solubility sets the absolute limit for the amount of drug available for absorption. The pKa governs the dynamic, pH-dependent interplay between a drug's solubility and its permeability across the intestinal membrane. Particle size is a critical engineering parameter that can be manipulated to overcome solubility-limited dissolution.
A robust IVIVC cannot be established by considering these factors in isolation. As demonstrated by the experimental data and protocols, their effects are deeply intertwined. The future of IVIVC development lies in integrated, systems-based approaches that quantitatively model these concurrent processes. This includes leveraging advanced in silico tools and multi-compartmental, biorelevant dissolution models that can simulate the complex journey of a drug—particularly a poorly water-soluble one—through the changing environment of the gastrointestinal tract. A deep, mechanistic understanding of these key physicochemical factors is, therefore, not merely an academic exercise but a practical necessity for the efficient development of safe and effective oral drug products.
For drug development professionals, predicting a drug's in vivo performance from in vitro data is a critical challenge. The establishment of a robust in vitro-in vivo correlation (IVIVC) is a central goal, serving as a predictive mathematical model between an in vitro property and a relevant in vivo response [6]. Success hinges on a deep understanding of key biopharmaceutical properties that govern a drug's journey through the body. This guide provides a comparative analysis of three fundamental properties—permeability, partition coefficient (LogP), and absorption potential (AP)—by examining their theoretical bases, experimental protocols, and roles in predicting absorption. Mastery of these properties allows researchers to better navigate the complexities of drug development, from early candidate screening to formulating successful dosage forms.
Theoretical Foundations and Interrelationships
The absorption of an orally administered drug is a complex process contingent upon its dissolution and its ability to permeate the gastrointestinal membrane. The Biopharmaceutics Classification System (BCS) provides a foundational framework that categorizes drug substances based on two of these key properties: solubility and intestinal permeability [13]. Permeability, LogP, and Absorption Potential are intrinsically linked quantitative descriptors that provide a multi-faceted prediction of a drug's absorption profile.
- Permeability: This measures the rate at which a drug molecule crosses a biological membrane, a prerequisite for systemic absorption. The transcellular permeability (Pm) of a compound is defined by the relationship:
Pm = (Kp × Dm) / Lm, where Kp is the membrane-water partition coefficient, Dm is the membrane diffusivity, and Lm is the membrane thickness [6]. High permeability is a key characteristic of BCS Class I and II drugs. - LogP (Octanol-Water Partition Coefficient): This is a measure of a drug's lipophilicity, defined as the ratio of its concentration in octanol to its concentration in water at equilibrium. It quantifies the molecule's preference for a lipid-like environment over an aqueous one. In general, a bell-shaped distribution exists between absorption and LogP, with compounds having LogP between 0 and 3 typically exhibiting high permeability [6].
- Absorption Potential (AP): This parameter represents a more integrated approach. Developed by Dressman et al., it combines lipophilicity, ionization, and dose-solubility considerations into a single metric:
AP = log[(P × Fun) / D0], where P is the partition coefficient, Fun is the fraction of unionized drug at pH 6.5, and D0 is the dose number (ratio of dose concentration to solubility) [6]. Studies indicate that AP correlates well with the fraction of drug absorbed.
The following diagram illustrates the logical and experimental relationships between these core properties and the ultimate in vivo outcome they aim to predict.
Comparative Analysis of Key Properties
The following table provides a direct, data-driven comparison of these three critical properties, summarizing their definitions, optimal ranges, and their respective roles in IVIVC.
Table 1: Comparative Overview of Critical Biopharmaceutical Properties
| Property | Definition & Measurement | Optimal Range for High Oral Absorption | Role in IVIVC & BCS |
|---|---|---|---|
| Permeability | Rate of membrane crossing. Measured via experimental models (e.g., Caco-2 cells) or predicted via algorithms [14] [6]. | High permeability is required for BCS Class I and III. A good correlation exists between Caco-2 permeability and human fraction absorbed [14]. | Serves as a direct input for mechanistic absorption models. Critical for classifying drug permeability according to BCS and for justifying biowaivers [13]. |
| LogP | Logarithm of the partition coefficient of the unionized drug in an octanol-water system. A measure of lipophilicity [6]. | Generally between 0 and 3. Values outside this range (e.g., < -1.5 or > 4.5) often indicate lower membrane permeability [6]. | Used as an early screening tool for permeability prediction. Informs formulation strategies, especially for BCS Class II and IV drugs where solubility is low [13]. |
| Absorption Potential (AP) | A composite parameter: AP = log[(P * Fun) / D0]. It integrates lipophilicity, ionization, and dose-solubility [6]. |
Higher values correlate with a higher fraction of drug absorbed. The relationship is sigmoidal, allowing for quantitative absorption estimates. | Provides a more holistic pre-formulation assessment than LogP or solubility alone, helping to identify potential absorption issues early in development. |
Experimental Protocols and Methodologies
Caco-2 Cell Permeability Assay
The Caco-2 cell model is a gold standard in vitro system for predicting passive intestinal drug absorption in humans [14].
- Principle: Caco-2 cells are human colon adenocarcinoma cells that, upon differentiation, form a monolayer with tight junctions and express brush border enzymes, mimicking the intestinal epithelium. The apparent permeability coefficient (Papp) is determined by measuring the rate of drug transport from the donor compartment (apical) to the receiver compartment (basolateral).
- Detailed Protocol:
- Cell Culture: Grow Caco-2 cells to confluence on porous membrane filters in transwell plates. Culture for 21 days to ensure full differentiation and polarization.
- Experiment Setup: Prepare drug solution in a suitable transport buffer (e.g., Hanks' Balanced Salt Solution, HBSS, at pH 7.4). Add the solution to the donor compartment (apical for A→B transport, basolateral for B→A transport). The receiver compartment contains blank buffer.
- Incubation: Maintain the system at 37°C with gentle agitation. Sample from the receiver compartment at predetermined time points (e.g., 30, 60, 90, 120 minutes) and replace with fresh buffer.
- Analysis: Quantify the drug concentration in the samples using a validated analytical method (e.g., HPLC-UV, LC-MS/MS).
- Calculations: Calculate the Papp (cm/s) using the formula:
Papp = (dQ/dt) / (A * C0), where dQ/dt is the steady-state flux, A is the surface area of the membrane, and C0 is the initial donor concentration.
- Data Interpretation: A Papp value > 1 × 10⁻⁶ cm/s typically indicates high permeability and is correlated with >90% absorption in humans [14]. Drugs like naproxen, propranolol, and diltiazem exhibit high Papp, while cimetidine and chlorothiazide show low Papp, correlating with their lower human absorption [14].
Determination of LogP
- Principle: LogP is most accurately determined using the shake-flask method, where the drug is partitioned between immiscible octanol and aqueous phases (typically buffer at pH 7.4).
- Detailed Protocol:
- Partitioning: Pre-saturate n-octanol and aqueous buffer with each other. Add the drug to the system in a sealed vial and shake vigorously to reach equilibrium.
- Separation and Analysis: Centrifuge the vial to separate the two phases. Carefully sample from each phase and analyze the drug concentration in each using a suitable method (e.g., UV spectrophotometry, HPLC).
- Calculation: LogP = log10 (Concentrationinoctanol / Concentrationinwater).
Calculation of Absorption Potential (AP)
- Principle: The AP is a calculated value that integrates several experimentally determined properties [6].
- Methodology:
- Determine Input Parameters:
- P: The octanol-water partition coefficient (from 4.2).
- Fun: The fraction of unionized drug at pH 6.5. Calculated from the drug's pKa using the Henderson-Hasselbalch equation.
- D0: The dose number. Calculated as
Dose (mg) / [Solubility at pH 6.5 (mg/mL) * 250 mL]. The volume of 250 mL is an estimate for small intestinal water volume [6].
- Calculation: Input the determined parameters into the equation:
AP = log[(P × Fun) / D0].
- Determine Input Parameters:
The Scientist's Toolkit: Essential Research Reagents
Successful experimental assessment of these properties relies on specific reagents and model systems. The following table details key solutions and materials required for the protocols described above.
Table 2: Essential Reagents and Materials for Permeability and Property Screening
| Reagent / Material | Function and Application | Key Considerations |
|---|---|---|
| Caco-2 Cell Line | A widely accepted in vitro model of the human intestinal mucosa for permeability screening [14]. | Requires rigorous cell culture practices and 21-day differentiation to form a valid barrier with functional tight junctions. |
| Transwell Plates | Permeable supports that allow for the growth of cell monolayers and separate apical and basolateral compartments for transport studies. | Pore size (e.g., 0.4 μm, 3.0 μm) and membrane material (e.g., polycarbonate, polyester) must be selected based on the experimental goal. |
| HBSS (Hanks' Balanced Salt Solution) | A standard physiological buffer used as the transport medium in permeability assays. It provides essential ions and nutrients to maintain cell viability during the experiment. | Often requires pH adjustment (e.g., to 6.5 and 7.4) with HEPES or MES buffer to simulate different gastrointestinal regions. |
| n-Octanol & Aqueous Buffers | The two-phase solvent system used in the shake-flask method for the experimental determination of the LogP. | Critical to pre-saturate both phases with each other to prevent volume shifts and achieve a stable equilibrium. |
Permeability, LogP, and Absorption Potential are not isolated metrics but interconnected pillars in the predictive science of biopharmaceutics. While LogP offers a simple estimate of lipophilicity, and permeability provides a direct measure of membrane transit, the Absorption Potential synthesizes these with solubility and ionization to deliver a more robust, holistic forecast of a drug's absorbability. A thorough, comparative understanding of these properties—their theoretical basis, their experimental determination, and their integration into models like the BCS—is indispensable for modern drug development. This knowledge empowers scientists to make informed decisions, from selecting promising drug candidates to developing formulations that ensure reliable in vivo performance, thereby strengthening the vital bridge between in vitro data and clinical outcomes.
The journey of an oral drug from ingestion to systemic circulation is a complex process governed by a dynamic interplay between the drug's properties and the physiological environment of the human gastrointestinal (GI) tract. A drug's bioavailability is profoundly influenced by variable factors such as gastrointestinal pH, transit times, and prandial state (fed versus fasted conditions). Food ingestion affects the oral bioavailability of more than 40% of drugs approved since 2010, creating significant challenges for predicting in vivo performance from in vitro data [15]. For drugs with a low therapeutic index, this fast-fed variability can lead to acute toxicities or therapeutic failure, endangering patient lives [16]. This guide objectively compares the capabilities of contemporary experimental models in incorporating these critical physiological realities, providing a framework for selecting appropriate tools in drug development research.
Physiological Factors Governing Oral Drug Absorption
Gastrointestinal pH and Fed-State Dynamics
The pH environment within the GI tract exhibits significant variability both between individuals and between fasted and fed states, particularly impacting drugs with pH-dependent solubility.
- Fasted State Gastric pH: Typically ranges between pH 1 and 2.5 [6] [15].
- Fed State Gastric pH: Can increase to pH 4-5 after a meal due to the buffering capacity of food, gradually returning to fasted state levels over several hours [16] [15].
- Intestinal pH: In the fasted state, duodenal pH ranges from approximately 5.0 to 6.5, while in the fed state, it initially decreases due to acidic chyme from the stomach before returning to near fasted-state levels through pancreatic bicarbonate secretion [16].
These pH shifts alter the ionization state of weakly acidic and basic drugs according to the pH-partition hypothesis, thereby influencing their absorption flux [16]. For instance, weakly acidic drugs become more ionized in the higher pH of the fed state, which can affect their membrane permeability.
Gastrointestinal Transit Times
GI transit time is a critical determinant for drugs with limited dissolution rates or site-specific absorption.
Table 1: Gastrointestinal Transit Parameters in Fasted and Fed States
| GI Segment | Length (m) | Surface Area (m²) | Fasted State Transit Time | Fed State Transit Time |
|---|---|---|---|---|
| Stomach | 0.2 | 0.2 | <30 minutes (liquids) [16] | Up to 120 minutes or more [16] |
| Small Intestine | 7.3 | ~200 | 3-4 hours [16] [17] | Similar to fasted state [17] |
| Colon | 1.5 | 3 | 15-48 hours [16] | Not significantly influenced by food [17] |
In the fasted state, gastric emptying is regulated by the Migrating Myoelectric Complex (MMC), a cyclical pattern of electromechanical activity that clears indigestible solids from the stomach every 1.5-2 hours [16] [17]. Food ingestion disrupts the MMC, replacing it with digestive motility patterns that delay gastric emptying, particularly for solid dosage forms [17]. The caloric content of food directly influences this delay, with higher caloric meals prolonging gastric residence time [17].
Food Effects on Drug Solubility and Permeability
Food-induced physiological changes create complex effects on drug absorption:
- Bile Secretion: Fed state promotes bile secretion, leading to micelle formation that can solubilize lipophilic drugs (positive food effect) but potentially trap drugs and reduce free fraction available for absorption [18].
- Luminal Fluid Volume: Increased fluid volume in fed state can enhance dissolution, particularly for poorly soluble drugs [15].
- Splanchnic Blood Flow: Postprandial increase in blood flow may enhance the absorption of high-permeability drugs [15].
- Transporter/Enzyme Interactions: Food components (e.g., grapefruit juice) can inhibit intestinal CYP3A4 metabolism and drug transporters like P-glycoprotein, increasing bioavailability of susceptible drugs [15].
Diagram 1: Food Effect on Drug Absorption Pathways
Comparison of Experimental Models for Absorption Prediction
Different model systems offer varying capabilities for incorporating physiological factors in drug absorption prediction.
Table 2: Capability Comparison of Absorption Prediction Models
| Model System | GI pH Control | Transit Time Simulation | Fed/Fast State Modeling | Throughput | Human Relevance | Key Limitations |
|---|---|---|---|---|---|---|
| In Vitro Dissolution with IVIVC [6] [1] | Moderate (using biorelevant media) | Limited (time points only) | Moderate (different media) | High | Moderate | Does not capture permeability or metabolism |
| Caco-2 Monolayers [19] | Limited | None | Limited | Medium | Moderate (altered expression of transporters/enzymes) | Limited expression of human transporters and metabolic enzymes |
| SPIP (Rat) [20] | Good (controlled perfusate) | Partial (flow rate control) | Good (dosing with/without food) | Low | Good (correlates with human Peff) | Surgical model, species differences |
| Gut-on-a-Chip (MPS) [19] | Good | Good (fluid flow control) | Good (media switching) | Low-medium | High (human cells, physiological shear stress) | Technically complex, low throughput |
| PBPK Modeling [21] [18] | Excellent (parameterizable) | Excellent (computational) | Excellent (integrated parameters) | Very High (once established) | Excellent (human data integration) | Requires extensive validation |
In Vitro - In Vivo Correlation (IVIVC) Approaches
IVIVC establishes predictive mathematical relationships between in vitro dissolution and in vivo absorption, with regulatory applications for biowaivers [6] [1].
- Level A IVIVC: Point-to-point correlation representing the highest level of correlation, most preferred by regulatory agencies for supporting biowaivers [1].
- Level B IVIVC: Uses statistical moments (mean dissolution time vs. mean residence time), less useful for predicting in vivo profiles [1].
- Level C IVIVC: Correlates single dissolution time point with pharmacokinetic parameter (e.g., Cmax, AUC), useful in early development but insufficient for biowaivers [1].
The predictive power of IVIVC is enhanced using biorelevant media (FaSSGF, FaSSIF, FeSSIF) that simulate fasted and fed state gastrointestinal conditions, including pH, buffer capacity, and bile salt composition [18].
Advanced Microphysiological Systems (Gut-on-a-Chip)
The novel gut MPS/Fluid3D-X system represents a significant advancement in predicting human drug absorption by incorporating key physiological features [19].
Diagram 2: Gut MPS Experimental Workflow
This system utilizes human induced pluripotent stem cell-derived small intestinal epithelial cells (hiSIECs) that form polarized epithelial structures with functional drug transporters (P-gp, BCRP) and metabolic enzymes (CYP3A4) [19]. The Fluid3D-X device features a polyethylene terephthalate (PET) construction that prevents drug adsorption issues encountered with polydimethylsiloxane (PDMS) chips [19]. Validation studies demonstrated accurate prediction of intestinal metabolic extraction (e.g., Fg=0.64 for midazolam vs. clinical value of 0.55) [19].
In Situ Perfusion Models (SPIP)
The Single-Pass Intestinal Perfusion (SPIP) model is an FDA-recognized method for studying regional intestinal permeability [20].
- Experimental Setup: Anesthetized rats undergo surgical isolation of intestinal segments with cannulation for controlled perfusion while maintaining blood and lymph supply [20].
- Key Parameters: Calculates effective permeability (Peff) and fraction absorbed (Fa), with demonstrated correlation to human permeability values [20].
- Fed/Fast State Modeling: Can be modified by including food components in perfusate or pre-treating animals with food [20].
The SPIP model provides direct measurement of drug permeability while avoiding the complicating factors of hepatic first-pass metabolism, enabling isolation of intestinal absorption processes [20].
Experimental Protocols for Physiological Absorption Studies
Biorelevant Dissolution Testing Under Fed and Fasted Conditions
Purpose: To simulate the in vivo dissolution of solid oral dosage forms under physiologically relevant GI conditions [6] [18].
Protocol:
- Prepare biorelevant media: FaSSGF (fasted state simulated gastric fluid) and FaSSIF-V2 (fasted state simulated intestinal fluid) for fasted conditions; FeSSIF-V2 (fed state simulated intestinal fluid) for fed conditions [18].
- For immediate-release products: Begin dissolution in FaSSGF (pH 1.2-1.6) for 30-60 minutes, then transfer to FaSSIF-V2 (pH 6.5) [18].
- Use USP Apparatus II (paddles) at 50 rpm with media volumes of 300 mL for gastric phase and 500 mL for intestinal phase [18].
- Maintain temperature at 37°C ± 0.5°C throughout the experiment.
- Sample at predetermined time points (e.g., 5, 10, 15, 30, 45, 60 minutes), filter immediately, and analyze drug concentration.
- Perform tests in triplicate to ensure reproducibility.
Data Analysis: Compare dissolution profiles between fed and fasted media and correlate with clinical food effect data when available [18].
Protocol for Assessing Enterohepatic Circulation with Fed-State Considerations
Purpose: To predict pharmacokinetics of drugs undergoing enterohepatic circulation with consideration of fed-state physiology [18].
Protocol:
- Select model drugs with known EHC (e.g., meloxicam, ezetimibe) with different solubility characteristics [18].
- Determine solubility ratio in FeSSIF-V2/FaSSIF-V2 to assess drug entrapment in bile micelles.
- Develop PBPK model incorporating gallbladder compartment with meal-triggered emptying.
- For reabsorption process, adjust permeability rate constant based on free fraction ratio (accounting for drug sequestration in bile micelles).
- Validate model by comparing predicted and observed plasma concentration-time profiles using Mean Absolute Percentage Error (MAPE) [18].
Key Consideration: For drugs solubilized by bile micelles (e.g., ezetimibe), compensating the permeation rate constant based on free fraction ratio significantly improves prediction accuracy [18].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagents for GI Absorption Studies
| Reagent/Material | Function | Application Examples | Physiological Relevance |
|---|---|---|---|
| FaSSIF/FeSSIF Media [18] | Simulates intestinal fluid composition in fasted and fed states | Dissolution testing, solubility measurements | Contains physiological bile salts and phospholipids at relevant concentrations |
| hiSIECs [19] | Human intestinal epithelial cells from induced pluripotent stem cells | Gut-on-a-chip models, permeability studies | Maintains drug transporter and metabolic enzyme expression similar to human intestine |
| PET Microfluidic Devices [19] | Platform for gut MPS with minimal compound adsorption | Advanced in vitro absorption models | Enables fluid flow mimicking peristalsis; prevents compound loss |
| PBPK Software Platforms (e.g., PK-Sim, Simcyp) [21] | Integrates physiological parameters to predict absorption | IVIVC, food effect prediction, formulation optimization | Incorporates population variability and system-specific parameters |
| Permeability Marker Compounds [20] | Reference standards for permeability classification | SPIP studies, Caco-2 validation | Enables BCS-based permeability classification (e.g., metoprolol-high, atenolol-low) |
The accurate prediction of oral drug absorption requires careful consideration of the dynamic physiological environment of the human gastrointestinal tract. While traditional models like IVIVC and SPIP provide valuable frameworks for understanding drug absorption, emerging technologies like gut-on-a-chip systems offer more comprehensive integration of critical factors such as GI pH, transit times, and fed/fast state variability. The selection of an appropriate model system should be guided by the specific research question, stage of development, and resources available. As these technologies continue to evolve, their integration with PBPK modeling and artificial intelligence promises to further enhance our ability to predict human oral bioavailability with greater precision, ultimately streamlining drug development and ensuring more predictable clinical outcomes.
Building Predictive Models: From In Vitro Tools to In Vivo Projections
Selecting Biorelevant Dissolution Apparatus and Media
The establishment of a robust in vitro-in vivo correlation (IVIVC) is a critical goal in modern drug development, serving as a predictive mathematical model that describes the relationship between an in vitro property of a dosage form and a relevant in vivo response [2] [1]. For orally administered drugs, biorelevant dissolution testing represents a fundamental component of this correlation, as it aims to simulate in vivo dissolution conditions within the gastrointestinal tract [22]. Unlike traditional dissolution methods that may employ simple aqueous buffers, biorelevant dissolution utilizes media that closely mimic the composition, surface tension, and solubilizing properties of human gastric and intestinal fluids under both fasted and fed states [22] [23]. The primary objective of selecting appropriate apparatus and media is to generate in vitro data that can reliably predict in vivo performance, thereby streamlining formulation development, reducing development costs, and potentially supporting regulatory submissions for biowaivers [1].
The Biopharmaceutics Classification System (BCS) provides a framework for understanding the challenges associated with different drug substances, particularly BCS Class II (low solubility, high permeability) and Class IV (low solubility, low permeability) compounds [2]. For these challenging molecules, conventional dissolution methods often fail to establish meaningful IVIVCs because they do not adequately replicate the complex physiological environment of the human GI tract, including dynamic pH changes, the presence of bile components, phospholipids, and digestive enzymes [2] [23]. This article provides a comprehensive comparison of available biorelevant dissolution apparatus and media, supported by experimental data, to guide researchers in selecting the most appropriate tools for predicting in vivo performance.
Comparison of Dissolution Apparatus
The United States Pharmacopeia (USP) standardizes several dissolution apparatuses that are commonly used in biorelevant testing. USP Apparatus II (paddle apparatus) is the most widely implemented system for conventional and biorelevant dissolution studies due to its simplicity and well-characterized hydrodynamics [22] [24]. The apparatus consists of a cylindrical vessel containing the dissolution medium maintained at 37°C, with a paddle that rotates at a controlled speed to provide gentle agitation. This system is particularly valuable for evaluating immediate-release solid oral dosage forms under biorelevant conditions [22].
USP Apparatus III (reciprocating cylinder) offers an alternative hydrodynamic environment that more closely simulates the mechanical stresses and changing physiological conditions experienced by a dosage form as it transits through the gastrointestinal tract [25]. This apparatus features a set of glass tubes containing the dosage form that move vertically within vessels filled with dissolution media. The agitation rate is controlled by the number of dips per minute (dpm), with studies demonstrating that approximately 5 dpm produces hydrodynamic conditions equivalent to USP Apparatus II at 50 rpm [25]. A comparative study evaluating USP Apparatus II and III for immediate-release products of both highly soluble drugs (metoprolol and ranitidine) and poorly soluble drugs (acyclovir and furosemide) found that with appropriate agitation rates, Apparatus III can produce similar dissolution profiles to Apparatus II while offering the advantage of mimicking the changing physiochemical conditions of the GI tract [25].
Apparatus Selection Guide
The selection of an appropriate dissolution apparatus depends on the specific drug properties, formulation characteristics, and the objectives of the dissolution study. The following table provides a comparative overview of the two primary apparatuses used in biorelevant dissolution testing:
Table 1: Comparison of Key Dissolution Apparatus for Biorelevant Testing
| Apparatus Type | Key Features | Hydrodynamic Characteristics | Optimal Applications | Limitations |
|---|---|---|---|---|
| USP Apparatus II (Paddle) | Simple design, well-established method [22] [24] | Laminar flow dependent on paddle rotation speed (typically 50-75 rpm) [22] | Immediate-release formulations, quality control testing, comparative dissolution studies [22] | Potential for cone formation, limited ability to simulate GI tract physiology [25] |
| USP Apparatus III (Reciprocating Cylinder) | Ability to transfer between different media, simulates GI transit [25] | Vertical agitation controlled by dips per minute (5-25 dpm) [25] | Extended-release formulations, dosage forms requiring pH changes, simulating fasted/fed state transitions [25] | More complex operation, potential for incomplete dissolution observed with some poorly soluble drugs [25] |
For specialized applications, particularly with lipid-based formulations, additional in vitro tools such as lipolysis assays may be necessary to account for the complex interplay of digestion, permeation, and dynamic solubilization that occurs in vivo [2]. These systems incorporate digestive enzymes and bile components to better simulate the intestinal environment where lipid digestion significantly influences drug release and absorption.
Comparison of Biorelevant Media
Composition and Physiological Relevance
Biorelevant media are specifically designed to simulate the composition and physicochemical properties of human gastrointestinal fluids under both fasted and fed states. These media contain bile salts, phospholipids, and other components that create a solubilizing environment similar to that encountered by a drug product in vivo [22]. The following table summarizes the key biorelevant media and their compositions:
Table 2: Comparison of Key Biorelevant Dissolution Media
| Medium | Prandial State | Simulated GI Fluid | pH | Key Components | Primary Applications |
|---|---|---|---|---|---|
| FaSSGF | Fasted [22] | Gastric [22] | 1.6 [22] | 3F Powder + FaSSGF Buffer [22] | Simulates gastric dissolution in fasted state [22] |
| FaSSIF | Fasted [22] | Small Intestinal [22] | 6.5 [22] | 3F Powder + FaSSIF Buffer [22] | Standard fasted state intestinal dissolution [22] |
| FeSSIF | Fed [22] | Small Intestinal [22] | 5.0 [22] | 3F Powder + FeSSIF Buffer [22] | Standard fed state intestinal dissolution [22] |
| FaSSIF-V2 | Fasted [22] | Small Intestinal [22] | 6.5 [22] | FaSSIF-V2 Powder + FaSSIF-V2 Buffer [22] | Updated fasted state formula [22] |
| FeSSIF-V2 | Fed [22] | Small Intestinal [22] | 5.8 [22] | FeSSIF-V2 Powder + FeSSIF-V2 Buffer [22] | Updated fed state formula [22] |
The critical difference between biorelevant and traditional media lies in their solubilizing capacity. Traditional phosphate buffers lack the mixed micelles present in intestinal fluids, which can lead to misleading results, particularly for poorly soluble drugs that may exhibit supersaturation in vivo [23]. As demonstrated in the gefitinib case study, traditional phosphate buffer resulted in rapid drug precipitation, while biorelevant media (FaSSIF) maintained the drug in a supersaturated state, more accurately reflecting the in vivo behavior [23].
Media Selection Strategy
The selection of appropriate biorelevant media should be guided by the anticipated in vivo conditions and the properties of the drug substance. For compounds with pH-dependent solubility, a sequential testing approach that simulates GI transit (e.g., starting with FaSSGF followed by transfer to FaSSIF or FeSSIF) may be necessary to fully capture the dissolution and precipitation behavior [23]. For drugs administered with food, fed-state media (FeSSIF, FeSSIF-V2) are essential to evaluate potential food effects on dissolution and absorption [22].
The updated versions of biorelevant media (FaSSIF-V2 and FeSSIF-V2) offer improved physiological relevance compared to their predecessors, with revised buffer capacities and osmolarity that better match human intestinal fluids [22]. When possible, these updated media should be prioritized for IVIVC development, particularly during later stages of formulation development where predictive accuracy is critical.
Experimental Protocols and Methodologies
Standard Biorelevant Dissolution Protocol
A comprehensive biorelevant dissolution experiment follows a systematic approach to ensure generated data is reproducible and biologically relevant:
Apparatus Setup: Use USP Apparatus II (paddle) or Apparatus III according to study objectives. For USP Apparatus II, set vessel volume to 500-1000 mL and maintain temperature at 37±0.5°C [22] [23].
Medium Preparation: Prepare fresh biorelevant media using standardized powders and buffers according to manufacturer specifications. For fed-state simulations, ensure appropriate reconstitution and equilibration [22].
Dosage Form Introduction: Place the dosage form in the vessel containing the appropriate medium. For two-stage experiments, begin with gastric medium (FaSSGF) [23].
Sampling Schedule: Withdraw samples at predetermined time points (e.g., 5, 10, 15, 20, 30, 45, 60, 90, 120 minutes) using syringes equipped with glass microfibre filters (13mm, 0.45μm) [22]. Use a fresh filter at each time point to prevent adsorption artifacts and halt the dissolution process effectively.
Sample Analysis: Analyze drug concentration in samples using validated HPLC methods with UV (DAD or PDA) detection. Employ preliminary filter adsorption studies to confirm that sampling methodology does not artificially influence results [22].
Data Processing: Calculate cumulative drug release and plot dissolution profiles for comparison between test and reference formulations.
Two-Stage Dissolution Protocol for GI Transit Simulation
For compounds whose solubility varies with pH, a two-stage dissolution experiment better simulates the transition from stomach to intestinal environment:
Gastric Phase: Conduct dissolution in FaSSGF (pH 1.6) for 60 minutes using USP Apparatus II at 50 rpm [23].
Intestinal Phase Transition: Without removing the dosage form, carefully add a concentrated buffer solution (e.g., FaSSIF Converter Buffer Concentrate) to adjust pH to intestinal conditions (pH 6.5) while maintaining sink conditions [23].
Intestinal Phase Monitoring: Continue dissolution for an additional 120 minutes, sampling at appropriate intervals to monitor for potential precipitation or supersaturation behavior [23].
Data Analysis: Compare the resulting dissolution profile with that obtained using traditional phosphate buffer to identify differences in precipitation behavior that might significantly impact in vivo performance prediction [23].
Case Study: Gefitinib Two-Stage Dissolution
Experimental Design and Results
A compelling case study demonstrating the critical importance of media selection involves the tyrosine kinase inhibitor gefitinib (250 mg dose) [23]. This study directly compared two-stage dissolution using biorelevant media (FaSSGF → FaSSIF) versus traditional phosphate buffer in a physiologically-structured experiment.
The results revealed dramatic differences in dissolution behavior between the two media systems. Gefitinib completely dissolved during the first hour in FaSSGF (pH 1.6) under both conditions. However, upon transition to the intestinal phase, stark contrasts emerged:
Table 3: Gefitinib Dissolution Behavior in Different Media
| Medium System | Gastric Phase (60 min) | Intestinal Phase (120 min) | Supersaturation Maintenance |
|---|---|---|---|
| Biorelevant Media | Complete dissolution in FaSSGF [23] | No significant precipitation; drug remained in metastable supersaturated state [23] | Maintained throughout intestinal phase [23] |
| Traditional Phosphate Buffer | Complete dissolution in FaSSGF [23] | Rapid drug precipitation observed [23] | No supersaturation maintained [23] |
Implications for IVIVC
The gefitinib case study highlights several critical considerations for IVIVC development:
Predictive Accuracy: Traditional phosphate buffer provided a potentially misleading prediction of in vivo behavior by failing to maintain supersaturation, which could have led to underestimation of bioavailability [23].
Physiological Relevance: The biorelevant media, containing mixed micelles of bile salts and phospholipids, more accurately simulated the in vivo intestinal environment where supersaturation is often maintained through interaction with physiological surfactants [23].
Formulation Decision-Making: Reliance on traditional media might have prompted unnecessary formulation optimization for gefitinib, whereas biorelevant testing correctly indicated that the drug would likely remain bioavailable despite the pH shift in the intestine [23].
This case study substantiates the value of biorelevant media in predicting supersaturation and precipitation behaviors—critical phenomena for BCS Class II compounds that significantly influence in vivo absorption [2] [23].
Essential Research Reagents and Materials
Implementing biorelevant dissolution requires specific reagents and materials to ensure physiological relevance and experimental consistency. The following table catalogues essential solutions and their functions:
Table 4: Essential Research Reagent Solutions for Biorelevant Dissolution
| Reagent/Material | Function | Application Examples |
|---|---|---|
| 3F Powder | Base powder for preparing FaSSGF, FaSSIF, and FeSSIF media [22] | Standard biorelevant medium preparation for fasted and fed states [22] |
| FaSSIF-V2 Powder | Base powder for updated FaSSIF-V2 medium [22] | Improved fasted state simulation with updated buffer capacity and osmolarity [22] |
| FeSSIF-V2 Powder | Base powder for updated FeSSIF-V2 medium [22] | Improved fed state simulation [22] |
| Various Buffer Concentrates (FaSSGF Buffer, FaSSIF Buffer, FeSSIF Buffer, etc.) | Provide appropriate pH and ionic strength for specific GI regions [22] | Media reconstitution for regional GI simulation [22] |
| Glass Microfibre Filters (0.45μm) | Sample filtration to separate undissolved drug while minimizing adsorption [22] | Sampling at predetermined time points during dissolution experiments [22] |
| FaSSIF Converter Buffer Concentrate | pH adjustment from gastric to intestinal conditions in two-stage experiments [23] | Transition from FaSSGF to FaSSIF during GI transit simulation [23] |
Decision Framework for Apparatus and Media Selection
The following workflow diagrams provide visual guidance for selecting appropriate dissolution apparatus and media based on research objectives and drug substance properties:
Diagram 1: Apparatus and Media Selection Workflow
Diagram 2: IVIVC Level and Media Requirement Relationship
The selection of appropriate dissolution apparatus and media is fundamental to establishing meaningful in vitro-in vivo correlations that can reliably predict drug product performance in vivo. As demonstrated through comparative data and case studies, biorelevant media consistently outperform traditional phosphate buffers in predicting dissolution behavior, particularly for BCS Class II and IV compounds where solubilization and supersaturation phenomena significantly influence absorption [22] [23]. The choice between USP Apparatus II and III should be guided by formulation characteristics and the need to simulate GI transit conditions, with Apparatus III offering advantages for modified-release formulations and compounds whose solubility is highly dependent on physiological position [25].
The continued evolution of biorelevant dissolution methodologies—including the development of more physiologically accurate media and apparatus that better simulate GI hydrodynamics—promises to enhance IVIVC predictability further [2] [1]. As pharmaceutical scientists increasingly work with challenging drug molecules exhibiting poor solubility, the strategic selection of dissolution apparatus and media will remain crucial for efficient formulation development and successful regulatory outcomes.
The successful development of oral drug products, particularly for poorly water-soluble compounds, hinges on accurately predicting how a formulation will behave in the human body. Within this framework, advanced in vitro tools have been developed to simulate the complex physiological processes of digestion and absorption. Two critical components in this predictive arsenal are in vitro lipolysis assays, which model the digestion of lipid-based formulations, and cellular permeability studies, such as those employing Caco-2 cell monolayers, which assess a drug's ability to cross the intestinal barrier. This guide objectively compares the performance, applications, and limitations of these key technologies and their emerging alternatives, framing the discussion within the essential research objective of establishing a robust correlation between in vitro and in vivo bioavailability models [26] [6] [27].
Comparative Analysis of Permeability Models
A critical step in predicting oral absorption is assessing a drug's permeability across the intestinal mucosa. The following table compares the primary in vitro models used for this purpose.
Table 1: Comparison of Key Permeability Models Used in Drug Development
| Model | Principle & Characteristics | Predictive Performance & Applications | Key Advantages & Limitations |
|---|---|---|---|
| Caco-2 Cells [28] | Derived from human colorectal adenocarcinoma; spontaneously differentiate into enterocyte-like monolayers over 21 days. | Considered the gold standard; shows good correlation with human absorption data for passive diffusion and transporter-mediated flux [29] [30]. | Advantages: Most physiologically relevant model; expresses a wide array of intestinal transporters.Limitations: Long culture time (21 days); significant lab-to-lab variability due to differences in culture conditions and passage number [30] [28]. |
| MDCK-MDR1 Cells [28] | Madin-Darby canine kidney cells genetically modified to overexpress the human P-glycoprotein (P-gp) efflux transporter. | Useful for identifying compounds that are P-gp substrates; may not always correctly rank in vivo formulation performance [26]. | Advantages: Rapid culture (3-5 days); highly reproducible; excellent for efflux transporter studies.Limitations: Less complex transporter expression than Caco-2; non-human origin [28]. |
| PAMPA [29] | Non-cell-based parallel artificial membrane permeability assay; uses a lipid-impregnated filter to mimic the phospholipid bilayer. | Effectively models passive transcellular diffusion; can be optimized (e.g., A-PAMPA) to achieve good concordance with Caco-2 for BCS classification [29]. | Advantages: High-throughput, low-cost, and no cell culture required.Limitations: Lacks transporters and paracellular pathway; cannot model active transport or metabolism [29]. |
| Artificial Membranes (LiDo) [26] [27] | Lecithin-in-dodecane membrane immobilized on a PVDF filter; used in conjunction with lipolysis assays. | Shown to accurately reproduce the in vivo rank-order of drug exposure from lipid-based formulations, performing similarly to Caco-2 in some setups [26] [27]. | Advantages: Cell-free; resistant to lipolysis conditions; simple and cost-effective for passive diffusion screening.Limitations: Does not capture biological processes like active transport or metabolism [27]. |
Methodology and Experimental Protocols
The In Vitro Lipolysis-Permeation Assay
The lipolysis-permeation assay is an advanced tool designed to simultaneously simulate the digestion of a lipid-based formulation and the absorption of the drug. The following diagram and protocol outline the core workflow.
Diagram 1: Lipolysis-Permeation Assay Workflow (Title: Lipolysis Permeation Setup)
Detailed Protocol [26] [27] [31]:
- Lipolysis Setup: The lipid-based formulation (LBF) is dispersed in a digestion chamber containing fasted-state simulated intestinal fluid (FaSSIF) at 37°C. The pH is maintained using a pH-stat titrator.
- Initiation of Digestion: Porcine pancreatin extract (or a purified lipase like Palatase 20,000 L [31]) is added to the chamber to initiate the digestion of triglycerides, releasing free fatty acids.
- Real-time Monitoring: The concentration of the drug (e.g., fenofibrate) in the digestion chamber can be monitored in real-time using in-line UV probes [31] or by withdrawing samples at scheduled time points for HPLC analysis. This allows tracking of supersaturation and precipitation events.
- Simultaneous Permeation: An absorption membrane (e.g., Caco-2 monolayer, MDCK monolayer, or artificial LiDo membrane [26]) separates the digestion chamber from a receiver chamber containing a buffer like Acceptor Sink Buffer.
- Sample Analysis: Samples are taken from both the digestion and receiver chambers over time. The drug concentration in the receiver chamber is used to calculate the apparent permeability coefficient (Papp), which serves as an indicator of absorption potential.
Caco-2 Permeability Assay
The Caco-2 assay is a well-established method for predicting intestinal absorption.
- Cell Culture: Caco-2 cells are cultured on permeable filter supports (e.g., Transwell inserts) for 21 days to allow full differentiation into a polarized monolayer with tight junctions.
- Integrity Check: The integrity of the monolayer is verified before the experiment by measuring the transepithelial electrical resistance (TEER) or the permeability of a paracellular marker like Lucifer Yellow [27].
- Experiment: The drug compound is added to the apical compartment (donor), which represents the intestinal lumen. The basolateral compartment (receiver) is sampled over time, typically up to 2 hours.
Analysis: Drug concentration in the samples is quantified (e.g., by HPLC-MS) to calculate the apparent permeability (Papp) using the following equation:
Papp = (dQ/dt) / (A × C₀)
Where dQ/dt is the transport rate, A is the membrane surface area, and C₀ is the initial donor concentration.
In Vitro-In Vivo Correlation (IVIVC): A Critical Framework
The ultimate goal of using advanced in vitro tools is to establish a predictive in vitro-in vivo correlation (IVIVC). This is a mathematical model that describes the relationship between an in vitro property (e.g., dissolution rate, permeation rate) and a relevant in vivo response (e.g., plasma drug concentration, amount absorbed) [6] [1].
Table 2: Levels and Regulatory Utility of In Vitro-In Vivo Correlation (IVIVC) [6] [1]
| Level | Definition | Predictive Value | Regulatory Acceptance |
|---|---|---|---|
| Level A | A point-to-point correlation between the in vitro dissolution/release and the in vivo absorption rate. | High – predicts the full plasma concentration-time profile. | Most preferred by regulatory agencies; can support biowaivers for formulation and process changes. |
| Level B | Uses statistical moments to compare the mean in vitro dissolution time to the mean in vivo residence or absorption time. | Moderate – does not reflect the actual shape of the in vivo profile. | Less common and less useful for regulatory purposes. |
| Level C | Correlates a single dissolution time point (e.g., % dissolved in 1 hour) with a single pharmacokinetic parameter (e.g., AUC or Cmax). | Low – represents a single point, not the entire profile. | Least rigorous; may be useful in early development but insufficient for biowaivers. |
Research demonstrates the pursuit of IVIVC for these models. For instance, the LiDo artificial membrane in a lipolysis-permeation setup provided a similar rank-order of fenofibrate exposure as seen in landrace pigs, demonstrating a Level A correlation for that specific case [26]. However, achieving a robust and generalizable IVIVC remains challenging, as no single in vitro method can perfectly predict the complex human in vivo environment [32].
Essential Research Reagents and Materials
The following table lists key reagents and materials essential for conducting the experiments described in this guide.
Table 3: Key Research Reagent Solutions for Lipolysis and Permeability Studies
| Reagent / Material | Function and Application | Example Usage |
|---|---|---|
| Caco-2 Cells | Human-derived cell line that forms an intestinal epithelial model for permeability and transport studies [30] [28]. | Cultured on Transwell inserts for 21 days to create a differentiated monolayer for permeability assays. |
| Porcine Pancreatin | A crude extract of digestive enzymes, including lipases, used to simulate intestinal digestion in vitro [26] [27]. | Added to the digestion chamber to initiate lipolysis of lipid-based formulations. |
| Lecithin-in-Dodecane (LiDo) | Artificial membrane-forming solution used in PAMPA and lipolysis-permeation assays to model passive transcellular diffusion [26] [27]. | Impregnated onto PVDF filters to create a cell-free absorption barrier in lipolysis-permeation setups. |
| Simulated Intestinal Fluids (e.g., FaSSIF) | Biorelevant media designed to mimic the pH, buffer capacity, and bile salt/phospholipid composition of human intestinal fluid [26] [27]. | Used as the dispersion medium in lipolysis assays to create a physiologically relevant environment. |
| Transwell Inserts | Permeable filter supports (e.g., polycarbonate, PVDF) that allow for the growth of cell monolayers and measurement of compound flux [27] [28]. | The physical scaffold for culturing Caco-2 or MDCK cells and for assembling artificial membranes. |
The landscape of advanced in vitro tools for predicting drug absorption is diverse, with each model offering distinct advantages. Caco-2 cells remain the gold standard for comprehensive permeability assessment due to their biological relevance, while MDCK-MDR1 cells provide a robust, high-throughput system for efflux transporter studies. For lipid-based formulations, the integration of in vitro lipolysis with permeation measurements, using either cellular monolayers or increasingly validated artificial membranes (LiDo), represents a significant step towards more biorelevant performance evaluation. The choice of tool should be guided by the specific research question, the compound's properties, and the need for throughput versus biological complexity. Ultimately, the continued refinement of these models and their integration into a structured IVIVC framework are paramount for enhancing the efficiency and success rate of modern drug development.
In the field of pharmaceutical research, the development of predictive mathematical models that correlate in vitro drug dissolution with in vivo pharmacokinetic performance is crucial for efficient drug development. This correlation, known as in vitro-in vivo correlation (IVIVC), plays a fundamental role in formulation development, optimization, and regulatory approval of drug products, particularly for modified-release dosage forms [33]. Among the various methodologies available for establishing IVIVCs, deconvolution- and convolution-based approaches represent two fundamentally distinct modeling philosophies. These techniques enable researchers to bridge the gap between laboratory dissolution tests and clinical performance, ultimately reducing the need for extensive clinical trials [34] [35].
The ongoing scientific discourse centers on which approach provides more accurate predictions of in vivo performance based on in vitro data. While regulatory guidelines have traditionally emphasized deconvolution-based methods, recent advances in computational power and physiological understanding have increased the adoption of convolution-based techniques [36] [35]. This comparison guide examines the technical foundations, experimental applications, and predictive performance of both methodologies within the context of modern drug development.
Theoretical Foundations
Deconvolution-Based Modeling
Deconvolution is a mathematical process that derives the in vivo drug input rate from plasma concentration-time data [37] [38]. This approach operates on the principle of determining the unknown input function of a system when the output and system characteristics are known.
Fundamental Principle: Deconvolution calculates the cumulative amount and fraction of drug absorbed over time using pharmacokinetic profile data and known reference information [37]. It treats the body as a linear system where the observed plasma concentration represents the output resulting from the drug input process convoluted with the disposition function.
Key Assumptions: Traditional deconvolution methods assume linear, time-invariant drug disposition [37] [38]. They typically require first-order absorption and preclude saturable (non-linear) absorption or clearance processes. An important limitation is the assumption that terminal oral plasma concentration-time points are independent of drug absorption, which effectively ignores colonic absorption [38].
Methodological Variations:
- Model-dependent methods (Wagner-Nelson for one-compartment models; Loo-Riegelman for multi-compartment models) utilize mass balance equations among different pharmacokinetic compartments [38].
- Model-independent numerical deconvolution applies linear systems analysis without presuming a specific compartmental model [37] [38].
Mechanistic Deconvolution: An advanced approach that incorporates physiological parameters and specific drug properties (solubility, permeability, logP, pKa) to provide a more comprehensive understanding of drug dissolution and absorption, including site-dependent regional absorption and first-pass extraction [38].
Convolution-Based Modeling
Convolution-based modeling takes the inverse approach, directly predicting in vivo plasma concentrations from in vitro dissolution data using the convolution integral.
Fundamental Principle: Convolution models the relationship between in vitro release and plasma concentrations in a single stage, directly predicting the plasma concentration-time course [36]. The fundamental equation describes the plasma concentration at time t as the convolution integral of the input rate function and the unit impulse response:
Cp(t) = ∫f(τ) × UIR(t-τ)dτ[39]where Cp is plasma concentration, f is the drug input rate, and UIR is the unit impulse response function [39].
Key Assumptions: Convolution assumes linearity and time-invariance of the disposition process but does not necessarily require the strict absorption assumptions of deconvolution [36] [39].
Methodological Advantages: This approach directly models the relationship between measured quantities (in vitro release and plasma drug concentrations) rather than indirectly calculated values [36]. It focuses on predicting conventional bioequivalence metrics and can be constructed without requiring intravenous, oral solution, or immediate-release reference doses in all cases [36].
Extended Applications: Advanced convolution models incorporate time-scaling functions and bioavailability sub-models to account for differences between in vitro and in vivo release rates and variations in absorption extent [40].
The diagram below illustrates the fundamental differences in workflow between deconvolution and convolution approaches:
Methodological Comparison
Technical Implementation
The practical implementation of deconvolution and convolution approaches differs significantly in terms of data requirements, computational procedures, and analytical workflows.
Table 1: Technical Implementation Comparison
| Aspect | Deconvolution-Based Approach | Convolution-Based Approach |
|---|---|---|
| Primary Data Input | Plasma concentration-time data for test and reference formulations [37] | In vitro dissolution data and unit impulse response parameters [40] |
| Mathematical Foundation | Numerical deconvolution or mass-balance equations (Wagner-Nelson, Loo-Riegelman) [38] | Convolution integral [39] |
| Reference Requirement | Requires IV, oral solution, or IR reference dose [37] [38] | Can be implemented without reference dose in some cases [36] |
| Software Tools | WinNonlin Phoenix [33], GastroPlus [33] | Pumas [40], NONMEM [39], GastroPlus [33] |
| Output Generated | In vivo drug release/absorption profile [37] | Predicted plasma concentration-time profile [39] |
| Validation Metrics | Prediction error for C~max~ and AUC [33] | Prediction error for C~max~ and AUC [40] |
Experimental Protocols
Deconvolution Workflow Protocol
The standard protocol for implementing deconvolution-based IVIVC follows these key stages:
Unit Impulse Response (UIR) Determination:
- Obtain mean concentration-time data following administration of an immediate-release formulation [33]
- For model-dependent methods, fit the UIR parameters using compartmental modeling (1-compartment for Wagner-Nelson; 2- or 3-compartment for Loo-Riegelman) [38]
- For numerical deconvolution, define the UIR using exponential terms with coefficients (A) and exponents (α) [37]
In Vivo Release Calculation:
IVIVC Model Development:
Model Validation:
Convolution Workflow Protocol
The standard protocol for convolution-based IVIVC involves these sequential steps:
Dissolution Model Development:
Unit Impulse Response Characterization:
Input Function Specification:
Plasma Profile Prediction:
Bioavailability Considerations:
The following diagram illustrates a specific convolution-based implementation for a complex modified-release formulation:
Case Studies and Experimental Data
Direct Comparison Study: MK-0941 Formulations
A comprehensive study directly compared both IVIVC approaches for MK-0941, a BCS Class III development candidate, formulated as matrix tablets and multiparticulates with three distinct release rates each [33].
Deconvolution Implementation: Researchers employed a two-stage linear regression model with differential absorption scaling factors to account for regional-dependent absorption observed approximately 5-6 hours after administration [33]. The model included parameters for absorption scaling (AbsScale1, AbsScale2), time scaling (Tscale), change time (Tchange), and cutoff time (Tcutoff) [33].
Convolution Implementation: Using GastroPlus Advanced Compartmental Absorption and Transit (ACAT) model, researchers incorporated physiological parameters, drug-specific properties (pKa, logP, solubility), and optimization of absorption scaling factors [33]. The "CR: integral tablet" and "CR: Dispersed" models were designated for matrix and multiparticulate formulations, respectively [33].
Performance Results: Both approaches demonstrated acceptable prediction accuracy according to regulatory standards [33].
Table 2: Prediction Performance for MK-0941 IVIVC Models [33]
| Formulation Type | IVIVC Approach | Average %PE AUC | Average %PE C~max~ |
|---|---|---|---|
| Matrix Tablets | Deconvolution/Convolution-Based | <10% | <15% |
| Multiparticulate Formulations | Deconvolution/Convolution-Based | <10% | <15% |
Diltiazem Extended-Release Products
A 2022 study evaluated convolution and deconvolution approaches for predicting pharmacokinetic parameters of diltiazem extended-release products using Flow-Through Cell (USP IV) dissolution testing [35].
Experimental Design: Researchers tested ER gel-matrix tablets against a market product (Tildiem Retard) using open- and closed-loop configurations of the FTC apparatus [35]. In vitro release showed ≥75% of diltiazem released after 6 hours (open-loop) and 12 hours (closed-loop) [35].
IVIVC Establishment: Linear correlation between fraction-dissolved and fraction-absorbed was achieved using the FTC open-loop setup [35].
Predictive Performance: The convolution-based approach demonstrated superior discriminative ability in predicting diltiazem in vivo PK parameters (C~max~, AUC~0-t~, AUC~0-∞~) with minimal prediction error compared to the deconvolution-based approach [35]. The study established a successful convolution-based methodology for predicting diltiazem pharmacokinetics from individual in vitro data [35].
Complex Modified-Release Case: Methylphenidate HCl
A novel convolution-based IVIVC model was developed for JORNAY PM, a methylphenidate hydrochloride delayed-release and extended-release capsule featuring complex dual coating technology [40].
Methodology: Researchers implemented a convolution integral approach incorporating time-scaling and bioavailability sub-models [40]. The model characterized disposition using a one-compartment model with first-order absorption and linear elimination derived from immediate-release data [40].
Model Refinement: The basic IVIVC model was refined by including a quadratic polynomial relationship between time to 50% drug dissolution in vitro and relative bioavailability between formulations [40].
Validation Results: Prediction errors for C~max~ and AUC~0-∞~ met FDA expectations for both internal and external validation, supporting the model's use for post-approval manufacturing changes [40].
Application Scenarios and Limitations
Ideal Application Contexts
Each modeling approach offers distinct advantages in specific pharmaceutical development scenarios:
Deconvolution is preferred when:
Convolution is advantageous for:
- Complex modified-release systems with non-linear absorption [40] [39]
- Scenarios where reference formulations are unavailable [36]
- Projecting bioequivalence metrics during formulation development [36]
- Compounds with regional-dependent absorption or flip-flop kinetics [33] [39]
- Model-informed drug development integrating dissolution-PK-PD relationships [39]
Limitations and Challenges
Both approaches present specific limitations that researchers must consider:
Deconvolution Limitations:
- Assumes linearity and time-invariance, which may not reflect complex physiological processes [38]
- Limited accuracy when absorption changes along the GI tract (regional-dependent absorption) [33] [34]
- Requires administration of reference formulation (IV, oral solution, or IR) [37] [38]
- Model-dependent methods assume specific compartmental structures that may not reflect true distribution [38]
- Struggles with compounds exhibiting flip-flop kinetics [39]
Convolution Limitations:
The Scientist's Toolkit
Successful implementation of IVIVC modeling approaches requires specific computational tools and methodological resources:
Table 3: Essential Research Tools for IVIVC Modeling
| Tool Category | Specific Solutions | Application Context |
|---|---|---|
| Software Platforms | WinNonlin Phoenix [37], GastroPlus [33], Simcyp [33], PK-Sim [33], Intellipharm [33], NONMEM [39], Pumas [40] | Deconvolution analysis, absorption PBPK modeling, convolution implementation, population PK/PD modeling |
| Dissolution Apparatus | Flow-Through Cell (USP IV) [35], USP Apparatus II (Paddle) [35] | In vitro release testing under various hydrodynamic conditions |
| Analytical Methods | HPLC/UV spectroscopy [35], Mass spectrometry [41] | Drug quantification in dissolution media and biological samples |
| Mathematical Functions | Weibull function [33], Sigmoid-Emax model [40], First-order kinetics [34] | Modeling dissolution profiles and drug input rates |
Deconvolution and convolution approaches represent complementary methodologies for establishing IVIVCs in pharmaceutical development. The selection between these techniques should be guided by specific compound characteristics, formulation properties, and development objectives.
Deconvolution maintains its position as the established regulatory standard for linear systems with predictable absorption patterns, providing a direct mathematical relationship between in vitro dissolution and in vivo absorption [33] [38]. Conversely, convolution offers enhanced flexibility for complex drug delivery systems, enabling direct prediction of plasma profiles and supporting model-informed drug development without always requiring reference data [36] [39].
The emerging trend in pharmaceutical development points toward a synergistic implementation of both approaches, leveraging their respective strengths based on specific development phase requirements. As demonstrated in the MK-0941 case study, both methodologies can yield bioequivalent predictions when appropriately implemented, with prediction errors meeting regulatory standards [33]. The continued evolution of computational tools and physiological understanding will further enhance the application of both deconvolution and convolution approaches in accelerating drug development while maintaining rigorous scientific standards.
Application in Formulation Optimization and Quality by Design (QbD)
In modern pharmaceutical development, the integration of In Vitro-In Vivo Correlation (IVIVC) within the Quality by Design (QbD) framework represents a paradigm shift from empirical quality testing to scientifically-driven quality assurance. This powerful combination enables formulators to establish clinically relevant product specifications and optimize drug formulations with a clear understanding of how critical process parameters and material attributes influence therapeutic performance [1] [42]. IVIVC provides a predictive mathematical model describing the relationship between an in vitro property of a dosage form (typically dissolution rate) and its in vivo performance (such as plasma drug concentration), while QbD offers a systematic approach for designing formulations and manufacturing processes to consistently deliver the intended product performance [6] [42]. This synergistic approach moves pharmaceutical development beyond the traditional "test-and-fail" methodology toward a proactive strategy where quality is built into the product through thorough scientific understanding.
The fundamental value of this integration lies in its ability to link formulation variables to clinical outcomes, thereby creating a direct pathway for developing patient-centric drug products. By establishing robust correlations between laboratory dissolution data and human pharmacokinetic profiles, researchers can significantly reduce the need for costly and time-consuming clinical bioequivalence studies during formulation optimization and post-approval changes [1]. This review comprehensively examines the application of IVIVC within QbD, comparing traditional versus QbD-based formulation approaches, detailing experimental protocols for correlation development, and presenting quantitative data that demonstrates the enhanced predictive capability and regulatory efficiency achieved through this integrated methodology.
Comparative Analysis: Traditional vs. QbD-Based Formulation Development
Fundamental Differences in Development Philosophy
The transition from traditional pharmaceutical development to QbD-based approaches represents a fundamental shift in how drug products are designed, optimized, and manufactured. Traditional pharmaceutical development typically relies on empirical methods and limited understanding of cause-and-effect relationships within the manufacturing process [43]. This approach often involves one-factor-at-a-time experimentation, fixed manufacturing processes without accounting for inherent variability, and primary focus on end-product testing to ensure compliance with predetermined specifications [43]. The traditional method provides limited understanding of why a product meets quality standards and offers little flexibility for process adjustments without regulatory complications.
In contrast, the QbD approach utilizes scientific principles and data analysis to proactively understand and control the entire manufacturing process, leading to built-in quality [43]. This systematic method begins with predefined objectives that emphasize product and process understanding based on sound science and quality risk management [42]. Under QbD, manufacturers identify characteristics critical to quality from the patient's perspective, translate them into critical quality attributes (CQAs), and establish how formulation and manufacturing variables affect these CQAs to consistently deliver drug products that meet patient needs [42]. The approach allows for flexible manufacturing within a defined "design space" while maintaining consistent quality through implementation of effective control strategies [43].
IVIVC as a Cornerstone of QbD Implementation
The incorporation of IVIVC within QbD provides a crucial bridge between formulation development and clinical performance. IVIVC enables predictive modeling of in vivo behavior based on in vitro data, which aligns perfectly with QbD's objective of designing quality into products rather than merely testing for it [1]. When successfully developed and validated, IVIVC models can serve as surrogates for in vivo bioequivalence studies, support biowaivers, establish clinically meaningful dissolution specifications, and guide formulation optimization throughout the product lifecycle [1] [6].
The regulatory advantages of this integrated approach are substantial. A validated IVIVC can provide scientifically sound evidence for biowaivers and product consistency, potentially reducing regulatory burden while enhancing product understanding [1]. This is particularly valuable for modified-release dosage forms, where IVIVC is recommended by regulatory authorities to evaluate how changes in formulation or manufacturing affect in vivo drug absorption [1]. The integration of IVIVC within QbD creates a comprehensive framework for developing robust, patient-centric drug products with well-understood clinical performance.
Table 1: Key Differences Between Traditional and QbD-Based Formulation Approaches
| Aspect | Traditional Approach | QbD-Based Approach |
|---|---|---|
| Development Basis | Empirical, trial-and-error [43] | Scientific, data-driven understanding [43] |
| Process Flexibility | Fixed manufacturing process [43] | Flexible within established design space [43] |
| Quality Focus | End-product testing [43] | Quality built into development and manufacturing [43] |
| IVIVC Role | Limited, primarily for specifications | Central, for predictive modeling and design space [1] |
| Regulatory Strategy | Compliance with specifications [43] | Risk-based control strategy [42] |
| Post-approval Changes | Often require new BE studies [1] | Easier within design space with IVIVC support [1] [43] |
Core Elements of QbD and Their Integration with IVIVC
Systematic Framework for Quality Assurance
The successful implementation of QbD with IVIVC relies on several interconnected elements that form a comprehensive framework for quality assurance. According to ICH guidelines, the core elements of pharmaceutical QbD include: (1) a Quality Target Product Profile (QTPP) that identifies the critical quality attributes (CQAs) of the drug product; (2) product design and understanding including identification of critical material attributes (CMAs); (3) process design and understanding including identification of critical process parameters (CPPs); (4) a control strategy; and (5) process capability and continual improvement [42]. The QTPP serves as the foundation of this framework—it is a prospective summary of the quality characteristics of a drug product that ideally will be achieved to ensure the desired quality, taking into account safety and efficacy [42].
Within this structured approach, IVIVC provides critical linkages between material attributes, process parameters, and clinical performance. For oral extended-release formulations, dissolution behavior typically represents a CQA that directly impacts drug absorption and therapeutic efficacy [1] [3]. Through IVIVC development, researchers can quantitatively relate dissolution profiles (in vitro performance) to pharmacokinetic parameters (in vivo performance), thereby establishing a scientific basis for defining clinically relevant dissolution specifications [3]. This patient-focused approach to specification setting represents a significant advancement over traditional methods based solely on batch history and manufacturing capability.
Risk Assessment and Control Strategies
A essential component of QbD implementation is systematic risk assessment to identify and evaluate potential risks to product quality throughout development and manufacturing [43]. Common methodologies include Failure Mode and Effects Analysis (FMEA), Ishikawa (fishbone) diagrams, and Fault Tree Analysis [43]. These tools help prioritize factors requiring further investigation and control based on their potential impact on CQAs. IVIVC enhances risk assessment by providing a mechanistic understanding of how formulation and process variables affect clinical performance, enabling more accurate identification of truly critical parameters.
The knowledge gained through risk assessment and IVIVC development directly informs the establishment of a control strategy—a planned set of controls derived from current product and process understanding that ensures process performance and product quality [42] [43]. For formulations with validated IVIVC, the control strategy may include real-time release testing using dissolution methods that are predictive of in vivo performance, potentially reducing the need for end-product testing [43]. This represents a more efficient and scientifically advanced approach to quality assurance compared to traditional methods that rely heavily on final product testing.
Table 2: Core QbD Elements and Their Integration with IVIVC
| QbD Element | Definition | IVIVC Integration |
|---|---|---|
| Quality Target Product Profile (QTPP) | Prospective summary of quality characteristics ensuring safety and efficacy [42] | Defines target in vivo performance linked to dissolution [44] |
| Critical Quality Attributes (CQAs) | Physical, chemical, biological properties within appropriate limits to ensure product quality [42] | Dissolution profile as key CQA predictive of in vivo performance [1] |
| Critical Material Attributes (CMAs) | Physical, chemical properties of materials affecting product quality [42] | Particle size, polymorphism, excipient grades affecting dissolution [42] |
| Critical Process Parameters (CPPs) | Process parameters affecting CQAs [42] | Compression force, granulation time impacting dissolution profile [43] |
| Design Space | Multidimensional combination of input variables proven to ensure quality [43] | Ranges of CMAs/CPPs maintaining bioequivalent dissolution profiles [3] |
| Control Strategy | Planned controls derived from product and process understanding [42] | Dissolution specifications predictive of in vivo performance [1] |
Experimental Framework for IVIVC Development in QbD
Methodological Approaches and Technical Considerations
The development of a predictive IVIVC within a QbD framework requires careful experimental design and execution. The regulatory guidance provided by the FDA's "Extended Release Oral Dosage Forms: Development, Evaluation, and Application of In Vitro/In Vivo Correlations" remains the foundational document for IVIVC development, outlining approaches for model development, evaluation of predictability, and application as a surrogate for in vivo bioequivalence studies [1]. A critical first step involves selecting appropriate formulations with distinct release rates—typically slow, medium, and fast-releasing formulations—to establish a meaningful correlation space [1].
The biorelevant dissolution method development represents another crucial aspect of IVIVC establishment. As demonstrated in the lamotrigine extended-release case study, dissolution testing should employ various apparatus (USP II & III) and media (biorelevant, non-bio relevant) with different compositions, pH levels, and hydrodynamics to identify the most biopredictive conditions [3]. For BCS Class II drugs like lamotrigine, where dissolution is often rate-limiting for absorption, the selection of dissolution method becomes particularly important for achieving a predictive IVIVC [3]. The use of physiologically based pharmacokinetic (PBPK) modeling can further enhance IVIVC development by providing a mechanistic framework for integrating dissolution data with physiological factors affecting drug absorption [3].
Levels of Correlation and Their Applications
IVIVC models are categorized into different levels based on their complexity and predictive capability. Level A correlation, the most comprehensive and regulatory preferred approach, represents a point-to-point relationship between in vitro dissolution and in vivo absorption [1]. This level provides the highest predictive capability for the full plasma concentration-time profile and can support biowaivers for major formulation changes [1]. Level A IVIVC development typically involves deconvolution techniques to determine the in vivo absorption time course, which is then correlated with in vitro dissolution data.
Level B correlation utilizes statistical moments analysis, comparing mean in vitro dissolution time to mean in vivo residence or absorption time [1]. While this approach provides a useful statistical comparison, it does not reflect the actual shape of the plasma concentration-time curve and therefore offers limited predictive capability [1]. Level C correlation, the simplest form, establishes a single-point relationship between a dissolution parameter (e.g., t50%) and a pharmacokinetic parameter (e.g., Cmax or AUC) [1]. This level provides the least rigorous correlation and is insufficient for supporting biowaivers, though it can offer valuable insights during early development stages [1].
Diagram 1: IVIVC Development Workflow in QbD Framework. This workflow illustrates the systematic process for developing and implementing IVIVC within Quality by Design, from initial planning through model application for establishing clinically relevant specifications.
Case Study: QbD-Based Formulation Optimization of Cinacalcet Nanoparticles
Systematic Formulation Design and Optimization
A comprehensive example of QbD-based formulation optimization with IVIVC elements is demonstrated in the development of cinacalcet hydrochloride polymeric nanoparticles [44]. The researchers began by defining a Quality Target Product Profile (QTPP) that included enhanced oral bioavailability, sustained release characteristics, and appropriate particle size distribution [44]. From the QTPP, they identified Critical Quality Attributes (CQAs) including particle size, zeta potential, and drug release profile, which would significantly impact the drug product's bioavailability and therapeutic performance [44].
The experimental approach employed statistical design of experiments for systematic formulation optimization. Initial screening utilized a Taguchi design with 7 factors at 2 levels to identify significant variables affecting CQAs [44]. This was followed by more comprehensive optimization using a Box-Behnken Design (BBD) with 3 factors and 3 levels to characterize nonlinear relationships and interaction effects between the critical formulation variables: drug-polymer ratio, stabilizer concentration, and stirring speed [44]. This systematic approach allowed the researchers to efficiently identify the optimal formulation parameters while developing a thorough understanding of the design space.
Enhanced Bioavailability Through QbD Optimization
The success of this QbD-based optimization was confirmed through both in vitro characterization and in vivo pharmacokinetic studies. The optimized cinacalcet nanoparticle formulation demonstrated significantly enhanced bioavailability compared to pure drug suspension, with AUC and Cmax values increasing by approximately 3-fold and 2.9-fold, respectively [44]. This dramatic improvement in bioavailability directly resulted from the careful control of critical material attributes and process parameters identified through the systematic QbD approach.
The case study further highlights the value of risk-based development in pharmaceutical formulation. By identifying potential failure modes early in development and implementing appropriate control strategies, the researchers developed a robust nanoparticle formulation that maintained stability and critical quality attributes throughout the recommended shelf life [44]. Although this particular study did not establish a full IVIVC, the correlation between in vitro characterization and enhanced in vivo performance demonstrates the fundamental principle underlying IVIVC development within a QbD framework.
Table 3: Experimental Data from QbD-Based Cinacalcet Nanoparticle Optimization [44]
| Formulation Parameter | Low Level | Medium Level | High Level | Impact on CQAs |
|---|---|---|---|---|
| Drug:PLGA Ratio (mg) | 1:1 | 1:2 | 1:3 | Significant impact on drug release rate and entrapment efficiency |
| Poloxamer-188 Concentration (% w/v) | 0.5 | 1.0 | 1.5 | Critical for particle size control and stability |
| Stirring Speed (rpm) | 5000 | 10000 | 15000 | Affected particle size distribution and aggregation |
| Cumulative % Drug Release (Q24) | 65% | 82% | 78% | Optimized formulation showed sustained release profile |
| Particle Size (nm) | 215 | 186 | 253 | Target range 150-250 nm for enhanced absorption |
| Zeta Potential (mV) | -28.4 | -32.6 | -25.8 | Adequate for colloidal stability |
Advanced Applications: Establishing Patient-Centric Quality Standards
Integration of PBPK Modeling and IVIVC
The most advanced application of IVIVC within QbD involves combining Level A correlation with Physiologically Based Pharmacokinetic (PBPK) modeling to establish patient-centric quality standards [3]. This integrated approach was successfully demonstrated in the development of lamotrigine extended-release tablets, where researchers used a verified PBPK model combined with IVIVC to define dissolution specifications that ensured consistent in vivo performance [3]. The methodology involved developing multiple IVIVC models using different dissolution conditions and deconvolution approaches to identify the most biopredictive method.
The lamotrigine case study exemplifies how computational approaches can enhance traditional IVIVC development. The researchers developed and verified a PBPK model using intravenous and immediate-release clinical data, then applied this model to simulate plasma concentration profiles for various extended-release formulations with different dissolution characteristics [3]. The optimal IVIVC model, established using a second-order polynomial and two-compartment Loo-Riegelman deconvolution, passed both internal and external validation criteria with prediction errors below 10%, demonstrating high predictive accuracy [3].
Regulatory Applications and Bioequivalence Assessment
The integration of IVIVC with PBPK modeling enables more scientifically advanced regulatory applications, including the justification of clinically relevant dissolution specifications and the assessment of virtual bioequivalence [3]. For lamotrigine extended-release tablets, this approach supported the establishment of patient-centric quality standards of ≤10% release at 2 h, ≤45% at 6 h, and ≥80% at 18 h, which were demonstrated to ensure consistent in vivo performance through PBPK simulations [3]. This methodology provides a robust framework for setting dissolution specifications based on clinical relevance rather than merely batch history.
The ability to predict virtual bioequivalence using IVIVC-PBPK models offers significant advantages for managing post-approval changes and scale-up activities [3]. Rather than conducting additional clinical studies for every formulation or process change, manufacturers can use validated models to demonstrate that proposed changes remain within the "safe space" of bioequivalence [3]. This application is particularly valuable for Quality by Design implementation, as it provides a scientific basis for establishing design spaces and control strategies that ensure consistent clinical performance despite normal variability in manufacturing.
Diagram 2: Integrated IVIVC-PBPK Modeling Framework. This diagram illustrates the relationship between input data, modeling components, and output applications when combining IVIVC with PBPK modeling to establish patient-centric quality standards.
Essential Research Reagents and Materials for IVIVC-QbD Studies
The successful implementation of IVIVC within QbD requires specific research reagents, analytical tools, and experimental systems. The following table summarizes key materials and their functions in supporting correlation development and validation studies.
Table 4: Essential Research Reagents and Materials for IVIVC-QbD Studies
| Category | Specific Examples | Function in IVIVC-QbD |
|---|---|---|
| Polymeric Carriers | PLGA, Poloxamer-188, PEG [44] | Control drug release rates; create formulations with varying release profiles for IVIVC development |
| Dissolution Apparatus | USP Apparatus II (Paddle), USP Apparatus III (Reciprocating Cylinder) [3] | Generate in vitro release profiles under various hydrodynamic conditions and media compositions |
| Biorelevant Media | Fasted State Simulated Intestinal Fluid (FaSSIF), Fed State Simulated Intestinal Fluid (FeSSIF) [3] | Simulate physiological conditions for more biopredictive dissolution testing |
| Analytical Instruments | Ultrafast Liquid Chromatography (UFLC), UV-Vis Spectroscopy, Dynamic Light Scattering [44] | Quantify drug concentration, characterize particle size, zeta potential, and other CQAs |
| Statistical Software | Design Expert, other DoE applications [44] | Design experiments, analyze data, optimize formulations, and define design space |
| Modeling Software | PBPK platforms, IVIVC modeling tools [3] | Develop and validate correlation models; simulate in vivo performance |
The integration of IVIVC within the QbD framework represents a significant advancement in pharmaceutical development methodology, enabling a more scientific, efficient, and patient-centric approach to formulation optimization and quality assurance. This synergistic combination allows researchers to establish meaningful relationships between formulation variables, in vitro performance, and clinical outcomes, thereby building quality into drug products through fundamental understanding rather than merely testing for compliance. The comparative analysis presented in this review demonstrates clear advantages of the QbD-IVIVC approach over traditional methods, including enhanced predictive capability, reduced development timelines, more flexible regulatory pathways, and ultimately, better assurance of consistent therapeutic performance for patients.
Despite these demonstrated benefits, regulatory experience indicates that the overall acceptance rate of IVIVC submissions remains approximately 40%, highlighting the technical challenges in developing robust, predictive correlations [45]. Common issues include inappropriate selection of formulations for correlation development, inadequate richness of data, and failure to investigate reasons for poor predictability [45]. Future advances in this field will likely involve greater incorporation of mechanistic modeling approaches, improved biopredictive dissolution methods, and enhanced computational tools that further strengthen the scientific basis for correlation development. As pharmaceutical manufacturing continues to evolve toward more sophisticated and patient-focused paradigms, the integration of IVIVC within QbD will play an increasingly vital role in ensuring that quality medicines consistently deliver their intended clinical performance.
In the pursuit of more efficient drug development, In Vitro-In Vivo Correlation (IVIVC) has emerged as a pivotal scientific approach that enables researchers to use laboratory data as a surrogate for clinical studies. Regulatory authorities, including the U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA), recognize IVIVC as "a predictive mathematical model describing the relationship between an in vitro property of a dosage form (usually the rate or extent of drug release) and an in vivo response" such as plasma drug concentration or amount absorbed [1] [6] [46]. This correlation forms the scientific basis for a biowaiver—a regulatory provision that allows for the waiver of in vivo bioequivalence (BE) studies under specific conditions [47]. For modified-release dosage forms, IVIVC provides a mechanism to evaluate the impact of in vitro dissolution changes on in vivo drug absorption, enabling scientists to predict bioavailability without conducting additional clinical trials [1].
The fundamental value of IVIVC in securing biowaivers lies in its ability to establish a predictive relationship that can substitute for certain otherwise required in vivo studies [1]. Once a validated IVIVC model has been established, it serves as a tool for bioavailability and bioequivalence assessments using existing in vitro dissolution data, thereby reducing the need for clinical bioequivalence studies involving human subjects [1]. This approach is particularly valuable for assessing the impacts of post-approval manufacturing changes, alterations in manufacturing sites, and issues with individual manufactured lots without incurring the costs associated with repeating in vivo bioequivalence studies [1].
Levels of IVIVC: Correlation Hierarchies and Regulatory Acceptance
The United States Pharmacopeia (USP) and regulatory guidelines recognize multiple levels of IVIVC, which differ significantly in their complexity, predictive power, and regulatory acceptance [1]. Understanding these hierarchies is crucial for selecting the appropriate correlation strategy for biowaiver applications.
Table: Levels of IVIVC and Their Regulatory Implications
| Aspect | Level A | Level B | Level C |
|---|---|---|---|
| Definition | Point-to-point correlation between in vitro dissolution and in vivo absorption | Statistical correlation using mean in vitro and mean in vivo parameters | Correlation between a single in vitro time point and one PK parameter |
| Predictive Value | High – predicts the full plasma concentration-time profile | Moderate – does not reflect individual PK curves | Low – does not predict the full PK profile |
| Regulatory Acceptance | Most preferred by FDA; supports biowaivers and major formulation changes | Less robust; usually requires additional in vivo data | Least rigorous; not sufficient for biowaivers alone |
| Common Applications | Regulatory submissions for extended-release formulations; biowaiver requests | Early development screening | Early development insights; supporting data |
Level A represents the most comprehensive correlation, establishing a point-to-point relationship between in vitro dissolution and in vivo absorption [1] [46]. This level is considered the gold standard for regulatory submissions as it predicts the entire in vivo time course from dissolution data and can support biowaivers for major formulation and manufacturing changes [1]. Level B correlation utilizes statistical moment analysis, comparing mean in vitro dissolution time to mean in vivo dissolution time or mean residence time [1] [46]. While it uses all available in vitro and in vivo data, it does not reflect the actual shape of the plasma concentration-time curve and therefore has limited utility for biowaiver applications [1]. Level C correlation establishes a single-point relationship between a dissolution parameter (e.g., time for 50% dissolution) and a pharmacokinetic parameter (e.g., AUC or Cmax) [1] [46]. This approach provides less comprehensive correlation and is generally insufficient for biowaiver requests alone, though it can be valuable during early formulation development [1].
Table: Advanced IVIVC Approaches for Complex Formulations
| Correlation Type | Definition | Utility for Biowaivers |
|---|---|---|
| Multiple Level C | Correlates one or several PK parameters to the amount of drug dissolved at several time points | Can support biowaivers if it correlates dissolution at all time points that affect in vivo performance [46] |
| IVIVR | Qualitative rank-order relationship between in vitro dissolution and in vivo input | Mainly used for formulation development guidance rather than regulatory biowaivers [48] |
The selection of an appropriate IVIVC level depends on the specific context of use, with Level A being the most widely accepted for regulatory submissions and biowaiver requests for extended-release oral dosage forms [1]. The FDA's guidance document "Extended Release Oral Dosage Forms: Development, Evaluation, and Application of In Vitro/In Vivo Correlations" remains the primary source of regulatory guidance on IVIVC, outlining how to develop an IVIVC model, evaluate its predictability, and apply it as a surrogate for in vivo BE studies [1].
Experimental Framework for IVIVC Development
Fundamental Methodological Approaches
Developing a robust IVIVC requires a systematic experimental approach that integrates dissolution testing with pharmacokinetic analysis. The process typically involves three stages of mathematical manipulation: constructing a functional relationship between input (in vitro dissolution) and output (in vivo dissolution), establishing a structural relationship using collected data, and parameterizing the unknowns in the structural model [6]. Two primary mathematical approaches are employed in IVIVC development:
The Deconvolution Method: This two-stage approach involves determining the in vivo absorption or dissolution time course from plasma concentration data, followed by comparison of the fraction of drug absorbed to the fraction of drug dissolved [46]. The Wagner-Nelson method is used for one-compartment models, while the Loo-Riegelman method is applied for two-compartment models [3].
The Convolution Method: This approach compares the predicted plasma concentrations from the model directly with those observed from the in vivo study [46]. Based on the principle of superposition, this method uses the input function (dissolution profile) and the unit impulse response (pharmacokinetics of the drug) to predict plasma concentrations.
A critical requirement for IVIVC model development is testing formulations with different release rates. Regulatory guidance typically requires at least two, but preferably three, formulations with distinct release rates (e.g., slow, medium, and fast) to establish a correlation [1]. The formulations should differ significantly in their in vitro release characteristics, ideally by at least 10% in the percentage dissolved across the profiles [46].
Key Considerations in Model Development
Several critical factors must be considered during IVIVC development to ensure a biopredictive correlation:
Physicochemical Properties: Drug solubility, pKa, salt forms, and particle size significantly influence dissolution and absorption [6]. The Noyes-Whitney dissolution equation provides a fundamental mechanistic approach to model dissolution, where dM/dt = D × S × (Cs - Cb)/h, with M being the amount dissolved, D the diffusion coefficient, S the surface area, h the diffusion layer thickness, and Cs and Cb representing drug solubility and bulk concentration, respectively [6].
Biopharmaceutical Properties: Drug permeability plays a major role in absorption, with parameters such as octanol-water partition coefficient (logP), absorption potential (AP), and polar surface area (PSA) providing valuable insights [6]. Permeability (Pm) can be estimated using the equation Pm = Kp × Dm/Lm, where Kp is the membrane-water partition coefficient, Dm is the membrane diffusivity, and Lm is the membrane thickness [6].
Physiological Factors: GI pH gradients, transit times, and fluid volumes significantly impact in vivo performance [6]. These factors are particularly important for drugs with pH-dependent solubility and for specialized formulations such as lipid-based systems [2].
The following workflow outlines the key decision points and processes in establishing a regulatory-grade IVIVC:
Essential Research Reagents and Materials for IVIVC Studies
Successful IVIVC development requires carefully selected reagents, equipment, and methodologies. The following toolkit outlines critical components for establishing a regulatory-acceptable correlation:
Table: Research Reagent Solutions for IVIVC Development
| Category | Specific Items | Function and Importance |
|---|---|---|
| Dissolution Apparatus | USP Apparatus II (Paddle) and III (Reciprocating Cylinder) | Simulates gastrointestinal hydrodynamics; USP II is most common for Level A IVIVC [3] |
| Dissolution Media | Biorelevant media (e.g., FaSSGF, FaSSIF), standard compendial buffers (pH 1.2-7.4) | Mimics physiological conditions; standard compendial media may be biopredictive for some APIs [3] |
| Analytical Instruments | HPLC systems with validated methods, UV-Vis spectrophotometers | Quantifies drug dissolution profiles with accuracy and precision |
| Modeling Software | PBPK/PBBM platforms, IVIVC-specific tools (e.g., Phoenix WinNonlin) | Enables deconvolution, convolution, and statistical analysis of in vitro-in vivo relationships |
| Reference Standards | Pharmacopeial reference standards (e.g., Lamotrigine USP standard) | Ensures analytical method validity and quantitative accuracy [3] |
| Test Formulations | ER tablets with fast, medium, and slow release rates | Provides necessary dissolution profile variability for correlation development [3] |
For specialized formulations such as lipid-based drug delivery systems (LBFs), additional specific reagents may be required, including lipid excipients (oils, surfactants, co-surfactants), and in vitro lipolysis models to simulate lipid digestion [2]. The Lipid Formulation Classification System (LFCS) categorizes LBFs into four types (I-IV) based on composition and dispersion properties, with Type I being simple oily solutions and Type IV containing only surfactants and co-solvents without traditional lipids [2].
Regulatory Framework and Application Strategies
Current Regulatory Landscape
The regulatory framework for IVIVC is well-established for conventional extended-release formulations but continues to evolve for complex drug products. The 1997 FDA guidance "Extended Release Oral Dosage Forms: Development, Evaluation, and Application of In Vitro/In Vivo Correlations" remains the foundational document, providing detailed recommendations for IVIVC development, evaluation, and application in regulatory submissions [1]. Both the FDA and EMA guidelines outline the requirements for IVIVC model development, assessment of predictability, internal and external validation processes, and the use of IVIVC to establish dissolution specifications and support biowaivers [46].
The Biopharmaceutics Classification System (BCS) provides a scientific framework for biowaiver considerations, with BCS Class I (high solubility, high permeability) and Class III (high solubility, low permeability) drugs being most favored for biowaiver applications [47]. Recent developments have seen the World Health Organization (WHO) expand biowaiver acceptance criteria to consider all BCS classes, though conservative approaches remain for BCS Class II and IV drugs [47].
Validation Requirements and Acceptance Criteria
For regulatory acceptance, IVIVC models must undergo rigorous validation to demonstrate predictive capability. The FDA guidance specifies two types of validation:
Internal Validation: Uses the same data set from which the correlation was derived, with prediction errors for Cmax and AUC not exceeding 10% on average, and no individual formulation exceeding 15% [3] [46].
External Validation: Uses an independent data set not used in model development, with the same acceptance criteria of ≤10% average prediction error and ≤15% for individual formulations [3].
A successfully validated Level A IVIVC can support biowaivers for various scenarios, including:
- Higher, lower, or new strengths for the same formulation [1]
- Post-approval manufacturing changes (equipment, process, manufacturing site) [1]
- Complete waiver of bioequivalence studies for certain ANDAs [1]
Case Study: Lamotrigine Extended-Release Tablets
A recent study demonstrates the practical application of IVIVC for establishing patient-centric quality standards for lamotrigine extended-release 300 mg tablets [3]. This case exemplifies the integration of IVIVC with physiologically based pharmacokinetic (PBPK) modeling to support biowaiver applications without extensive clinical trials.
The research team developed a robust Level A IVIVC using verified PBPK models and optimized dissolution methods [3]. The PBPK model was initially developed and verified using plasma lamotrigine profiles following administration of intravenous solution and oral immediate-release tablets, achieving accurate prediction of Cmax and AUC with confidence levels exceeding 95% [3]. Various IVIVC models were investigated using dissolution data of fast, medium, and slow ER lamotrigine 300 mg tablets manufactured in-house, with optimal correlations obtained using a second-order polynomial and a two-compartment Loo-Riegelman deconvolution approach [3].
The study demonstrated that dissolution in standard compendial media using USP Apparatus II established a Level A IVIVC that passed both internal and external validation criteria with prediction errors below 10% [3]. Based on this validated model, the researchers established patient-centric quality standards for dissolution of ≤10% release at 2 h, ≤45% at 6 h, and ≥80% at 18 h [3]. This approach provided a reliable method for assessing product performance and supported the establishment of clinically relevant dissolution specifications without additional clinical studies.
Challenges and Future Perspectives
Despite its significant advantages, IVIVC development faces several challenges that vary by formulation type. For conventional extended-release formulations, the main hurdles include achieving adequate formulation differentiation and developing biopredictive dissolution methods [6]. For more complex systems such as lipid-based formulations (LBFs), additional complications arise from the dynamic processes of lipid digestion, micelle formation, and potential lymphatic transport [2]. Case studies with fenofibrate, cinnarizine, and other lipophilic drugs have demonstrated limited predictability, with some analyses failing to distinguish between formulations administered in fasted or fed states or to correlate in vitro lipolysis data with in vivo performance [2].
The future of IVIVC is closely tied to technological advancements and modeling sophistication. The integration of artificial intelligence (AI) and machine learning (ML) shows promise for analyzing complex datasets and improving prediction accuracy [1]. Physiologically Based Biopharmaceutics Modeling (PBBM) represents another significant advancement, combining IVIVC with physiological parameters such as organ perfusion rates, tissue distribution kinetics, and metabolic pathways for more precise human drug simulations [1] [48]. However, surveys indicate that around two-thirds of PBBM submissions to regulatory agencies were rejected, primarily due to inadequate model parametrization, insufficient validation, lack of agreement on proposed validation criteria, and use of non-biopredictive dissolution methods [48]. These statistics highlight the need for continued refinement of modeling approaches and clearer regulatory expectations.
Looking ahead, the convergence of advanced technologies such as AI-driven modeling platforms, microfluidics, organ-on-a-chip systems, and high-throughput screening assays holds immense potential for augmenting the predictive power and scope of IVIVC studies [1]. By embracing these technological advancements synergistically with traditional development methodologies, pharmaceutical researchers can unlock new frontiers in precision pharmacology and personalized drug therapies while simultaneously accelerating drug development timelines [1].
Overcoming IVIVC Challenges for Complex Formulations and Modalities
Navigating the IVIVC Gap in Lipid-Based Formulations (SEDDS, SNEDDS)
The development of robust in vitro-in vivo correlations (IVIVC) is a critical yet challenging goal in the pharmaceutical sciences, particularly for lipid-based formulations like Self-Emulsifying Drug Delivery Systems (SEDDS) and Self-Nanoemulsifying Drug Delivery Systems (SNEDDS). These complex formulations enhance the oral bioavailability of poorly water-soluble drugs (BCS Class II and IV) through multiple mechanisms, including enhanced solubilization, lymphatic transport, and inhibition of efflux transporters [2] [49]. However, their dynamic in vivo behavior, involving digestion, permeation, and solubilization processes, creates significant obstacles for predicting in vivo performance from standard in vitro tests [2] [50]. While IVIVCs are well-established for conventional controlled-release formulations where dissolution is the rate-limiting step, the establishment of IVIVC for lipid-based formulations has proven more difficult due to the complex interplay of formulation components with gastrointestinal physiology [2]. This guide objectively compares the IVIVC performance of SEDDS and SNEDDS, examining the experimental methodologies and data that highlight both the progress and persistent challenges in this field.
Formulation and IVIVC Performance Comparison
SEDDS and SNEDDS are isotropic mixtures of oils, surfactants, and co-solvents that spontaneously form emulsions or nanoemulsions upon contact with gastrointestinal fluids [51] [49]. The key distinction lies in the droplet size post-emulsification: SEDDS typically form emulsions with droplet sizes above 100-200 nm, while SNEDDS form nanoemulsions with droplet sizes generally below 100-200 nm [51] [52]. This difference in colloidal structure significantly influences their biopharmaceutical performance and the resulting IVIVC challenges.
Table 1: Comparative Analysis of SEDDS and SNEDDS Characteristics Relevant to IVIVC Development
| Characteristic | SEDDS | SNEDDS |
|---|---|---|
| Typical Droplet Size | 100-300 nm [51] | < 100-200 nm [51] [52] |
| Interfacial Area | Lower | Higher, leading to faster drug release rates [52] |
| Drug Solubilization Capacity | Moderate | Potentially higher due to smaller droplet size [52] |
| Predicted Absorption | Good, but more variable | Enhanced and more consistent [52] |
| IVIVC Complexity | High, prone to precipitation | High, but may offer more predictable absorption |
| Common In Vitro Challenges | Poor predictability of traditional dissolution tests; requires lipolysis models [2] | Similar challenges, though smaller size may improve correlation with permeation |
The primary advantage of SNEDDS lies in their superior surface-to-volume ratio, which can lead to faster drug release rates and more consistent absorption profiles compared to conventional SEDDS [52]. However, both systems face substantial IVIVC challenges because their performance depends not merely on dissolution but on complex dynamic processes including lipid digestion, micellar solubilization, and interaction with biliary secretions [2] [50]. Case studies highlight these difficulties: research on fenofibrate LBFs in rats failed to establish a correlation between in vitro dispersion data and in vivo performance, while a review of pH-stat lipolysis models found only 50% of eight studied drugs correlated well with in vivo data [2].
Experimental Protocols for IVIVC Development
Standardized Dispersion and Emulsification Tests
The initial assessment of SEDDS/SNEDDS performance involves characterizing self-emulsification properties. The standard protocol involves adding the formulation to a dissolution apparatus or beaker containing medium (often 500 mL) at 37°C under gentle agitation (typically 50-100 rpm) [51]. The time until a transparent or slightly bluish emulsion forms is recorded, with an ideal system achieving self-emulsification within 3 minutes [51]. The resulting emulsion is then characterized for droplet size (by dynamic light scattering), polydispersity index (PDI, indicating size distribution), and zeta potential (indicating surface charge and physical stability) [52].
In Vitro Lipolysis Models
Traditional dissolution tests frequently fail to predict the in vivo performance of LBFs because they do not account for lipid digestion [2] [50]. Lipolysis models that simulate the gastrointestinal environment have emerged as more physiologically relevant tools. The experimental workflow involves placing the formulation in a thermostated vessel (37°C) containing digestion buffer (often with Tris-maleate) and simulated intestinal fluids [2]. The pH is maintained by an automated pH-stat titrator that records the consumption of sodium hydroxide, which neutralizes free fatty acids liberated during digestion by added pancreatic lipase/colipase [2] [50]. Samples are collected at timed intervals and ultracentrifuged to separate different phases (aqueous, oily, pellet) for drug quantification, helping to identify potential precipitation issues [2].
Permeation and Absorption Studies
Following dissolution and digestion testing, permeation studies using models like Caco-2 cell monolayers or artificial membranes help predict intestinal absorption. For formulations containing non-ionic surfactants (common in SNEDDS), additional mechanistic studies may assess P-glycoprotein (P-gp) inhibition or tight junction modulation that could enhance permeability [52]. The most critical validation comes from in vivo pharmacokinetic studies in animal models (typically rats or dogs) or humans, measuring key parameters including maximum plasma concentration (Cmax), time to reach Cmax (Tmax), and area under the curve (AUC) [2] [52].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Research Reagents and Equipment for SEDDS/SNEDDS IVIVC Studies
| Category/Item | Function/Purpose | Examples/Specifications |
|---|---|---|
| Lipid Excipients | Oil phase for drug solubilization | Medium-chain triglycerides (e.g., Captex), Long-chain triglycerides (e.g., Soybean oil), Semi-synthetic oils (e.g., Labrafil M1944CS) [51] [53] |
| Surfactants | Stabilize emulsion droplets, reduce interfacial tension | Non-ionic surfactants (e.g., Cremophor EL/RH40, Tween 80, Labrasol) [51] [53] |
| Co-surfactants/Co-solvents | Enhance emulsification, improve drug loading | Transcutol HP, Propylene Glycol, Polyethylene Glycol 400 (PEG 400) [51] [53] |
| Digestion Reagents | Simulate intestinal environment for lipolysis studies | Pancreatic lipase/colipase, Taurocholate salts, Calcium chloride, Tris-maleate buffer [2] [50] |
| Analytical Instruments | Characterize formulation properties and performance | Dynamic Light Scattering (DLS) for droplet size/PDI, Zeta Potential Analyzer, HPLC for drug quantification, pH-Stat Titrator [2] [52] |
Correlation Levels and Current Limitations
The U.S. Food and Drug Administration (FDA) recognizes different levels of IVIVC, with Level A representing the most informative correlation, directly linking the in vitro dissolution rate to the in vivo input rate [2]. Level B compares mean in vitro dissolution time to mean in vivo residence time, while Level C correlates a single dissolution time point with a pharmacokinetic parameter (e.g., AUC or Cmax) [2]. For complex lipid-based systems, achieving Level A correlations has proven difficult, with many studies only achieving Level C or qualitative Level D correlations [2]. For instance, in development of cinnarizine LBFs, researchers observed precipitation during in vitro lipolysis that did not translate to differences in in vivo performance in dogs, permitting only a Level D (qualitative) correlation [2].
The limitations of current IVIVC approaches for lipid-based systems stem from several factors: physiological variability between preclinical species and humans, non-linear absorption mechanisms, and the formulation-dependent nature of the correlations [2]. Furthermore, traditional in vitro models often fail to fully replicate the complex dynamics of the human gastrointestinal tract, including the continuous removal of digestion products and drug permeation across the intestinal epithelium [50].
The development of predictive IVIVCs for SEDDS and SNEDDS remains a significant challenge in pharmaceutical sciences. While SNEDDS generally offer advantages in terms of smaller droplet size, larger interfacial area, and potentially more predictable absorption profiles compared to SEDDS, both systems face substantial correlation hurdles due to their complex digestion and absorption mechanisms. Current research focuses on developing more sophisticated in vitro models that better simulate gastrointestinal physiology, particularly integrated digestion-permeation systems [2] [50]. Furthermore, the emergence of in silico modeling approaches, including physiologically based pharmacokinetic (PBPK) modeling and artificial intelligence (AI)-driven formulation design, shows promise for improving IVIVC predictability [2] [54] [53]. As these advanced tools evolve, coupled with standardized experimental protocols and comprehensive datasets, the pharmaceutical industry moves closer to reliably bridging the IVIVC gap for lipid-based formulations, ultimately accelerating the development of effective products for poorly water-soluble drugs.
In vitro lipolysis models are widely used in pharmaceutical development to predict the in vivo performance of lipid-based drug delivery systems (LbDDS). These tests simulate human gastrointestinal conditions to assess how formulations will behave during digestion, with the goal of reducing costly and time-consuming animal and human studies [50]. The establishment of a predictive in vitro-in vivo correlation (IVIVC) is considered a valuable tool for formulation optimization and regulatory evaluation [55] [1].
However, despite careful model development, there are notable instances where in vitro lipolysis data fails to accurately predict in vivo outcomes. This article examines a specific case study involving fenofibrate-loaded lipid-based formulations where traditional in vitro lipolysis models provided misleading predictions of in vivo performance, and explores the experimental methodologies and potential reasons behind this disconnect.
Case Study: Fenofibrate-Loaded Lipid-Based Formulations
Experimental Formulations and Design
Thomas et al. (2014) conducted a comprehensive investigation comparing the in vitro lipolysis performance and in vivo bioavailability of various fenofibrate formulations in a minipig model [56] [57]. The researchers prepared multiple formulations containing an identical dose of 200 mg fenofibrate:
- SNEDDS (75% drug load): Self-nanoemulsifying drug delivery system with drug load at 75% of solubility capacity
- Super-SNEDDS (150% drug load): Supersaturated SNEDDS with drug load at 150% of solubility capacity, prepared using heating/cooling cycles
- SNEDDS suspension (150% drug load): Contained saturated solution plus suspended fenofibrate
- Lipanthyl 200 M: Commercial micronized fenofibrate formulation as reference
The study aimed to evaluate two key in vitro performance indicators: drug solubilization during digestion and the maximum supersaturation ratio (SRM), which represents the ratio of theoretical drug concentration to drug solubility in the aqueous phase during digestion [56].
In Vitro Lipolysis Methodology
The in vitro lipolysis protocol simulated human gastrointestinal conditions through a two-step process [56]:
- Gastric Phase (pH 2): Formulations were initially exposed to simulated gastric conditions
- Intestinal Phase (pH 6.5): The digestion process continued in simulated intestinal fluid
The lipolysis conditions specifically utilized porcine bile salts and pancreatic lipase extract to match the minipig model used for the subsequent in vivo study. Samples were collected throughout the process to analyze drug concentration in different phases (aqueous, pellet, and oily phases) using HPLC methods. The area under the solubilization-time curves (AUCin vitro) during the intestinal step was calculated for each formulation.
In Vivo Study Protocol
The in vivo evaluation employed a minipig model with the following experimental design [56]:
- Animal Model: Minipigs (consistent with the porcine-derived enzymes used in vitro)
- Dosing: All formulations contained identical 200 mg fenofibrate doses
- Analysis: Plasma concentration of fenofibrate over time was measured
- Endpoint: Area under the plasma concentration-time curve (AUCin vivo) was calculated for bioavailability assessment
Results: The In Vitro-In Vivo Disconnect
In Vitro Performance Rankings
Based on the in vitro lipolysis data, the formulations demonstrated distinct performance characteristics, allowing for the following rank-order classification [56]:
Table 1: In Vitro Lipolysis Performance of Fenofibrate Formulations
| Formulation | Drug Load | Physical State | In Vitro Performance Ranking | Supersaturation Ratio (SRM) | Precipitation Tendency |
|---|---|---|---|---|---|
| SNEDDS | 75% | Dissolved | 1 (Best) | <3 | Low |
| Super-SNEDDS | 150% | Dissolved (supersaturated) | 2 | >3 | High |
| SNEDDS Suspension | 150% | Partially suspended | 2 | >3 | High |
| Lipanthyl 200 M | Commercial | Micronized crystalline | 3 (Worst) | N/A | N/A |
The in vitro data indicated a clear rank-order of performance: SNEDDS (75% drug load) > super-SNEDDS = SNEDDS suspension > Lipanthyl. Researchers observed an increased likelihood of drug precipitation when the maximum supersaturation ratio exceeded SRM > 3, which occurred with both the super-SNEDDS and SNEDDS suspension formulations [56].
In Vivo Performance Results
Contrary to the in vitro predictions, the in vivo study in minipigs revealed strikingly different results [56] [57]:
Table 2: Comparison of In Vitro and In Vivo Performance
| Formulation | Expected In Vivo Performance (Based on In Vitro Data) | Actual In Vivo Performance (Minipig Model) | Key Findings |
|---|---|---|---|
| SNEDDS | Highest bioavailability | Equivalent to other LbDDS | No advantage over higher-load formulations |
| Super-SNEDDS | Reduced due to precipitation | Equivalent to other LbDDS | Precipitation did not reduce bioavailability |
| SNEDDS Suspension | Reduced due to precipitation | Equivalent to other LbDDS | Suspended drug did not impair absorption |
| Lipanthyl 200 M | Lowest bioavailability | Lowest bioavailability | Consistent with expectations |
The critical finding was that the mean plasma concentration over time curves of all lipid-based formulations (LbDDS) were comparable, regardless of the initial physical state of the drug or the observed precipitation during in vitro lipolysis [56]. Most significantly, statistical analysis revealed no correlation between the area under the solubilization-time curves (AUCin vitro) of the intestinal step and the actual in vivo AUCin vivo [56] [57].
Analysis of the In Vitro-In Vivo Disconnect
Potential Explanations for the Predictive Failure
Several factors may explain why the in vitro lipolysis model failed to predict the in vivo performance in this case study:
Nature of Precipitated Drug: Unlike some other drugs (cinnarizine, simvastatin, halofantrine) that precipitate in amorphous form during in vitro lipolysis, fenofibrate has been shown to precipitate in its crystalline form [56]. However, the physical characteristics and redispersion properties of the precipitate in vivo may differ from in vitro conditions.
Absorption Kinetics: The in vivo environment may allow for more rapid absorption of dissolved drug before extensive precipitation occurs, or the precipitated drug may redissolve more readily under continuous absorption conditions.
Model Limitations: Traditional in vitro models may not adequately capture the dynamic nature of gastrointestinal processes, including the continuous removal of drug through absorption, changes in bile salt concentration, and the role of intestinal motility [50].
Supersaturation Maintenance: Excipients in the formulations may help maintain supersaturation in vivo through mechanisms not replicated in the in vitro model.
Advanced Research Reagent Solutions
Table 3: Essential Research Reagents for Lipolysis Studies
| Reagent / Material | Function in Lipolysis Studies | Application Notes |
|---|---|---|
| Porcine Pancreatic Lipase | Digestible lipid excipient hydrolysis | ≥3× USP activity; matches porcine physiology models |
| Porcine Bile Extract | Emulsification of lipid digestion products | 68% purity; critical for micelle formation |
| Calcium Chloride | Cofactor for lipase activity; binds liberated fatty acids | Concentration affects digestion kinetics |
| Candida Antarctica Lipase A | Alternative lipase source for method development | Used in novel lipolysis models [31] |
| Palatase 20000 L | Purified liquid lipase for real-time analysis | Comparable to porcine pancreatin [31] |
| Sodium Taurodeoxycholate | Synthetic bile salt for standardized conditions | Reduces variability of natural bile extracts |
| 4-Bromobenzeneboronic Acid (BBBA) | Lipase inhibitor for sample quenching | Stops digestion at specific timepoints |
This case study demonstrates a significant instance where in vitro lipolysis models failed to predict the in vivo performance of fenofibrate-loaded lipid-based formulations. The data clearly shows that drug precipitation observed during in vitro lipolysis did not translate to reduced bioavailability in vivo, challenging the conventional interpretation of in vitro precipitation parameters.
These findings highlight the need for cautious interpretation of in vitro lipolysis data and suggest potential limitations in using supersaturation ratios and solubilization profiles as primary predictors of in vivo performance for certain drug formulations. Future work should focus on developing more sophisticated in vitro models that better capture the complex in vivo environment, particularly the dynamic interplay between digestion, precipitation, and absorption processes.
The continued refinement of in vitro lipolysis models remains crucial for optimizing lipid-based drug delivery systems, but researchers should remain aware of their potential limitations and complement in vitro data with appropriate in vivo validation studies, especially when making critical formulation decisions.
Unique Hurdles for Long-Acting Injectables (LAIs) and PLGA-Based Systems
Poly(lactic-co-glycolic acid) (PLGA) is a cornerstone polymer in the development of long-acting injectable (LAI) and implantable drug products. Approved by the U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA), PLGA is celebrated for its biocompatibility, biodegradability, and tunable properties, making it one of the preferred inactive ingredients for complex formulations [58] [59]. PLGA-based LAI products are designed to extend drug release over periods ranging from weeks to months, enabling reduced dosing frequency, improved therapeutic efficacy, and enhanced patient compliance [58]. Since the introduction of the first PLGA-based product, Lupron Depot, in 1989, over 25 such drug products have received regulatory approval [58]. These systems are particularly vital for managing chronic conditions such as prostate cancer, schizophrenia, and diabetes [58] [59].
Despite their clinical success and the fact that many have lost patent protection, the development of generic versions of these complex drug products has proven exceptionally difficult. The scarcity of generic PLGA-based LAIs underscores the profound technical and regulatory challenges inherent in replicating their complex formulation and manufacturing processes [58]. This guide objectively compares the hurdles faced by PLGA-based systems against the broader LAI landscape, with a specific focus on the critical context of establishing a correlation between in vitro release data and in vivo bioavailability.
Fundamental Challenges in LAI and PLGA-Based System Development
Complexity of Formulation and Manufacturing
The development of any LAI is a complex endeavor, but PLGA-based systems present additional unique layers of difficulty. A primary challenge is the intricate interplay between the physicochemical properties of the drug and the polymer, which dictates critical performance outcomes like drug loading, release kinetics, and stability [60]. For PLGA systems, key polymer attributes—including molecular weight, lactide-to-glycolide (L:G) ratio, end-group chemistry, and blockiness—directly influence the degradation period and drug release profile, which can range from months to years [59].
The manufacturing process itself introduces significant variability. Methods such as emulsion solvent evaporation, spray drying, and hot melt extrusion are commonly used [58]. However, minor alterations in process parameters (e.g., homogenization speed, solvent evaporation rate) can lead to major differences in critical quality attributes like particle size, porosity, and drug distribution within the polymer matrix [58]. This sensitivity complicates scale-up and consistent production. Furthermore, the drug encapsulation process must be meticulously controlled to achieve high encapsulation efficiency while maintaining the stability of the active pharmaceutical ingredient (API) [61]. The complexity is such that even with qualitative and quantitative (Q1/Q2) sameness in formulation, generic manufacturers may fail to achieve bioequivalence due to differences in the manufacturing process [58].
The Critical Hurdle of In Vitro-In Vivo Correlation (IVIVC)
A central challenge for all LAIs, and a particularly acute one for PLGA-based systems, is establishing a predictive In Vitro-In Vivo Correlation (IVIVC). The goal of IVIVC is to create a predictive mathematical model between the rate and extent of drug release measured in the laboratory (in vitro) and the drug's absorption profile in the human body (in vivo) [1].
Traditional in vitro models, often simplistic 2D cell cultures or standard dissolution apparatuses, frequently fail to accurately recapitulate the complex physiological environment these systems encounter upon administration [62]. For PLGA systems, the complex, multi-stage degradation mechanism—involving hydration, initial degradation, constant degradation (often with autocatalysis), and final solubilization—is difficult to replicate in a test tube [59]. The lack of a standardized, biorelevant compendial method for in vitro release testing of PLGA LAIs creates a significant barrier. Without it, it is challenging to compare different formulations robustly or to use in vitro data as a reliable surrogate for in vivo bioequivalence, which is a requirement for generic approval [58] [1].
Table 1: Levels of IVIVC and Their Regulatory Acceptance
| Level | Definition | Predictive Value | Regulatory Acceptance |
|---|---|---|---|
| Level A | Point-to-point correlation between in vitro dissolution and in vivo absorption. | High – predicts the full plasma concentration–time profile. | Most preferred by FDA; supports biowaivers for major formulation changes [1]. |
| Level B | Statistical correlation using mean in vitro and mean in vivo parameters. | Moderate – does not reflect individual pharmacokinetic curves. | Less robust; usually requires additional in vivo data [1]. |
| Level C | Correlation between a single in vitro time point and one PK parameter (e.g., Cmax, AUC). | Low – does not predict the full PK profile. | Least rigorous; not sufficient for biowaivers [1]. |
Comparative Analysis of PLGA System Performance and Data
This section provides an objective comparison of PLGA-based systems, highlighting their performance against alternative delivery approaches and illustrating the key variable of release kinetics.
Table 2: Experimental Drug Release Profile Comparison: PLGA NPs vs. Free Drugs
| Formulation | Drug(s) Encapsulated | Cumulative Release at 96h | Cumulative Release of Free Drug at 8h | Key Experimental Findings |
|---|---|---|---|---|
| Cur-Que-Pip-PLGA NPs [61] | Curcumin (Cur), Quercetin (Que), Piperine (Pip) | Cur: 26.9%, Que: 57.5%, Pip: 98% | 92.1% (Cur), 94.8% (Que), 96.6% (Pip) | Demonstrated significant sustained-release effect and enhanced stability for hydrophobic compounds. |
| PLGA-based Microspheres [58] | Various (e.g., Leuprolide, Risperidone) | Varies by formulation (sustained over 1-6 months) | Not Applicable (requires continuous administration) | Enabled extended dosing intervals from weeks to months, improving patient compliance. |
The data in Table 2 underscores the primary function of PLGA systems: to provide sustained release. The co-loaded nanoparticle study [61] vividly demonstrates how PLGA can drastically slow the release of hydrophobic drugs compared to their free forms. Furthermore, commercial products [58] validate the ability of these systems to achieve release over periods of months, a feat not possible with conventional formulations.
Table 3: Impact of PLGA Physicochemical Properties on Release Kinetics
| PLGA Property | Impact on Drug Release and Degradation | Experimental Evidence |
|---|---|---|
| Molecular Weight (MW) | Higher MW generally correlates with slower degradation and more prolonged drug release [59]. | Tunable MW allows release duration to be tailored from months to years [59]. |
| Lactide:Glycolide (L:G) Ratio | A higher lactide ratio (e.g., 75:25) leads to a slower degradation rate compared to a 50:50 ratio [59]. | Commercial products (e.g., Lupron Depot) use specific L:G ratios to control release duration (1-6 months) [58]. |
| End-Group Chemistry | Acid-capped PLGA degrades faster than ester-capped (end-capped) PLGA due to autocatalytic hydrolysis [59]. | Used to fine-tune the degradation profile and match desired release kinetics. |
| Particle Size | Smaller particles have a larger surface area-to-volume ratio, potentially leading to faster initial drug release [60]. | A critical quality attribute monitored during manufacturing to ensure consistent release profiles. |
Essential Experimental Protocols
Protocol for Preparing PLGA Nanoparticles via Emulsification-Solvent Evaporation
The emulsification-solvent evaporation method is a widely used technique for formulating PLGA-based nanoparticles [61] [63].
- Preparation of Organic Phase: Dissolve 200 mg of PLGA polymer (e.g., 50:50 ratio, MW 55,000) and the active pharmaceutical ingredient(s) (e.g., Curcumin, Quercetin, Piperine at a mass ratio of 1:1:0.2) in 3 mL of an organic solvent mixture, typically dichloromethane and acetone (4:1 v/v) [61].
- Preparation of Aqueous Phase: Prepare an aqueous surfactant solution, commonly 5 mL of 2% polyvinyl alcohol (PVA).
- Emulsification: Slowly add the organic phase dropwise into the aqueous PVA solution under continuous magnetic stirring to form a coarse oil-in-water (o/w) emulsion. Subsequently, sonicate the mixture in an ice bath (e.g., at 40% amplitude for 5 minutes) to form a fine emulsion with reduced nanoparticle size.
- Solvent Evaporation: Transfer the fine emulsion into a larger volume of a dilute surfactant solution (e.g., 10 mL of 0.5% PVA). Stir the suspension magnetically for approximately 3 hours at room temperature to allow the organic solvent to evaporate, solidifying the nanoparticles.
- Collection and Washing: Centrifuge the nanoparticle suspension first at 5000 rpm for 15 minutes to remove large aggregates, then at 15,000 rpm for 30 minutes at 4°C to pellet the nanoparticles. Wash the pellet with distilled water three times to remove residual solvent and surfactant.
- Lyophilization: Re-suspend the final nanoparticles and freeze-dry them at -20°C for storage and further characterization [61].
Protocol for In Vitro Drug Release Testing
A standard protocol for assessing drug release from PLGA systems is critical for IVIVC development.
- Sample Incubation: Place a precise amount of the drug-loaded PLGA formulation (e.g., 10 mg of nanoparticles) into a dialysis membrane tube or directly into a release medium.
- Release Medium: Use Phosphate-Buffered Saline (PBS) at pH 7.4 to simulate physiological conditions. Maintain the system at 37°C under continuous, gentle agitation [64] [61].
- Sampling: At predetermined time points (e.g., 2, 4, 8, 24, 48, 96 hours, and longer for extended-release systems), withdraw a small aliquot of the release medium.
- Replenishment: Immediately replace the withdrawn volume with fresh, pre-warmed PBS to maintain sink conditions.
- Drug Quantification: Analyze the collected samples using a validated analytical technique, such as High-Performance Liquid Chromatography (HPLC), to determine the cumulative percentage of drug released over time [61].
Advanced and Emerging Solutions
Machine Learning (ML) and Artificial Intelligence (AI)
The "trial-and-error" paradigm in LAI development is being disrupted by data-driven approaches. Machine learning models can predict drug release profiles by learning from complex datasets that incorporate descriptors of the drug, polymer, and formulation parameters.
- Algorithm Application: Studies have shown that models like Light Gradient Boosting Machine (LGBM) can predict fractional drug release from polymeric LAIs with high accuracy [60]. Neural network-based models like "DrugNet" have also demonstrated a stronger ability to fit complex, nonlinear drug release data from PLGA systems compared to traditional semi-empirical models like Korsmeyer-Peppas and Weibull [64].
- Workflow: These models use inputs such as drug molecular weight, LogP, polymer molecular weight, L:G ratio, drug loading, and particle size to forecast release curves, significantly accelerating formulation design and reducing experimental burden [64] [60].
Advanced In Vitro and In Silico Models
To improve IVIVC, researchers are moving beyond traditional models.
- Advanced In Vitro Models: Tools like Organs-on-Chips (e.g., Liver Chips) are microfluidic devices lined with living human cells that better mimic human organ physiology and disease states. These models have shown superior performance in predicting drug-induced liver injury compared to animal models [62] [65].
- In Silico and PBPK Modeling: The integration of IVIVC with Physiologically Based Pharmacokinetic (PBPK) modeling creates a more precise simulation of human drug absorption, distribution, metabolism, and excretion [1]. The FDA's Fit-for-Purpose Initiative and the Critical Path Institute are working to establish pathways for the regulatory acceptance of these New Approach Methodologies (NAMs) [65].
The Scientist's Toolkit: Key Research Reagents and Materials
Table 4: Essential Materials for PLGA-Based LAI Research
| Reagent/Material | Function in Research | Specific Example |
|---|---|---|
| PLGA Polymer | The biodegradable backbone of the delivery system; properties determine release kinetics. | PLGA (50:50 lactide:glycolide, acid end-group, MW 55,000) [61]. |
| Polyvinyl Alcohol (PVA) | A surfactant/stabilizer used in emulsion-based methods to control particle size and prevent aggregation. | 2% w/v aqueous PVA solution used as the continuous phase [61]. |
| Dichloromethane (DCM) | An organic solvent for dissolving PLGA and hydrophobic drugs in the emulsification process. | Used in a 4:1 v/v ratio with acetone to form the organic phase [61]. |
| Phosphate Buffered Saline (PBS) | The standard in vitro release medium; simulates physiological pH and osmolarity. | PBS pH 7.4, 37°C, used for drug release studies [64] [61]. |
| Targeting Ligands | Molecules (e.g., antibodies, peptides) conjugated to the nanoparticle surface for active targeting. | Used on PEGylated PLGA NPs for targeted cancer therapy [63]. |
| Polyethylene Glycol (PEG) | Used for "PEGylation" to create a stealth corona, reducing immune clearance and prolonging circulation. | PEG-lipid conjugates used to form PEG corona on PLGA NPs [63]. |
Addressing Discrepancies in Lipid Nanoparticle (LNP) Development for Nucleic Acids
The development of Lipid Nanoparticles (LNPs) has revolutionized the delivery of nucleic acid therapeutics, as evidenced by the successful deployment of mRNA vaccines. However, a significant challenge persists in bridging the gap between in vitro performance and in vivo efficacy, creating a major bottleneck in the translational pipeline [66]. Establishing a reliable in vitro-in vivo correlation (IVIVC) is critical for accelerating the development and optimization of LNP formulations, yet emerging studies consistently highlight substantial discrepancies between experimental models and clinical outcomes [66] [67]. This discrepancy delays the translation of promising experimental findings into clinical applications, underscoring the need for a more holistic understanding of LNP behavior across biological systems.
The core of the problem lies in the complex biological journey of LNPs. While in vitro studies provide valuable initial data on cellular uptake and transfection efficiency in controlled environments, they often fail to capture the multifaceted interactions LNPs encounter in living organisms [66] [68]. Factors such as stability in biological fluids, formation of a protein corona, biodistribution patterns, and cellular trafficking pathways can dramatically alter LNP performance in ways that are not predicted by standard in vitro assays [68] [69]. This review systematically compares the performance of LNP formulations across experimental models, provides supporting experimental data, and analyzes the underlying causes of IVIVC discrepancies to guide more predictive LNP development.
Composition and Structure of LNPs: Foundation for Performance
LNPs are sophisticated delivery systems typically composed of four key lipid components, each playing a distinct role in encapsulation, stability, and delivery efficiency [70] [71] [72].
- Ionizable Cationic Lipids: Constituting approximately 50% of the lipid mixture, these lipids are neutral at physiological pH (7.4) but become positively charged in acidic environments. This unique property enables efficient RNA encapsulation during formulation (at low pH) while reducing toxicity in the bloodstream. Following cellular uptake, protonation in the acidic endosomal environment (pH ~6.5) facilitates endosomal escape, a critical step for nucleic acid delivery [70] [71].
- Phospholipids (e.g., DSPC, DOPE): Typically comprising about 10% of the formulation, these structural lipids enhance bilayer stability and contribute to cellular uptake and fusion processes [70] [71].
- Cholesterol: Making up approximately 38.5% of the mixture, cholesterol integrates into the lipid bilayer and enhances its structural integrity and stability. It improves encapsulation efficiency and facilitates membrane fusion, aiding in cellular delivery [70] [71].
- PEGylated Lipids: Representing a small proportion (1.5-2%), PEG-lipids play a crucial role in controlling nanoparticle size during formulation, preventing aggregation, and reducing rapid clearance by the immune system, thereby extending circulation time [70] [71] [73].
The specific combination and molar ratios of these components determine critical quality attributes (CQAs) of LNPs, including particle size, polydispersity index (PDI), zeta potential, and encapsulation efficiency [66] [71]. These CQAs are essential for the biological performance and reproducibility of LNP formulations, influencing their behavior in both in vitro and in vivo settings.
Experimental Methodologies for LNP Formulation and Characterization
LNP Formulation Using Microfluidics
Microfluidic mixing has emerged as the gold standard for LNP production, enabling the precise and reproducible generation of nanoparticles with low polydispersity and high encapsulation efficiency [70] [71]. The standard protocol involves:
- Preparation of Lipid and RNA Phases: The lipid mixture (ionizable lipid, phospholipid, cholesterol, and PEG-lipid) is dissolved in an organic solvent, typically ethanol. The nucleic acid cargo (e.g., mRNA) is prepared in an acidic aqueous buffer, such as citrate or acetate buffer (pH 4) [66] [71].
- Rapid Mixing: Using a microfluidic device (e.g., NanoAssemblr), the aqueous and organic phases are mixed at a controlled flow rate ratio (typically 3:1 aqueous-to-organic) and a defined total flow rate. This rapid mixing in micro-channels facilitates efficient nanoparticle self-assembly through a nucleation-growth process [66] [71].
- Purification and Buffer Exchange: Following formulation, the LNP suspension is dialyzed or subjected to Tangential Flow Filtration (TFF) against a neutral pH buffer, such as phosphate-buffered saline (PBS). This critical step removes the organic solvent and free, unencapsulated RNA, adjusts the pH to physiological conditions for stability and application, and concentrates the final LNP product [71].
Characterization of Critical Quality Attributes
Comprehensive characterization is essential for understanding LNP performance and variability.
- Physicochemical Properties: Particle size, polydispersity index (PDI), and zeta potential are typically measured using Dynamic Light Scattering (DLS). Well-formulated LNPs for nucleic acid delivery generally exhibit a size range of 70-100 nm, a PDI below 0.2, and a near-neutral zeta potential [66] [71] [73].
- Encapsulation Efficiency: This is most commonly determined using a modified RiboGreen assay. The fluorescence of the RNA-binding dye RiboGreen is measured before and after LNP disruption with a detergent (e.g., Triton X-100). The difference between the total RNA (after disruption) and free RNA (before disruption) indicates the amount of encapsulated RNA [73]. Recent studies emphasize calculating encapsulation efficiency relative to the input RNA concentration (EEinput%) rather than the traditional ratio of encapsulated to total RNA in the sample (EE%), as the latter can be artificially inflated by the degradation of unencapsulated RNA during processing [73].
Comparative Performance Analysis: In Vitro vs. In Vivo Discrepancies
Case Study: Ionizable Lipids and Protein Expression
A systematic evaluation of four LNP formulations, identical except for their ionizable lipid components (SM-102, ALC-0315, MC3, and C12-200), revealed significant IVIVC discrepancies [66] [67]. The following table summarizes the key findings:
Table 1: Comparative Performance of LNPs with Different Ionizable Lipids
| Ionizable Lipid | In Vitro Protein Expression | In Vivo Protein Expression | Vaccine Efficacy (In Vivo) |
|---|---|---|---|
| SM-102 | Significantly higher (p<0.05) in immortalized and immune cells [66] | High, no significant difference from ALC-0315 [66] | Strong immune response, no significant differences among formulations [66] |
| ALC-0315 | Lower than SM-102 [66] | High, no significant difference from SM-102 [66] | Strong immune response, no significant differences among formulations [66] |
| MC3 | Lower than SM-102 [66] | Lower expression levels [66] | Strong immune response, no significant differences among formulations [66] |
| C12-200 | Lower than SM-102 [66] | Lower expression levels [66] | Strong immune response, no significant differences among formulations [66] |
This data clearly demonstrates that in vitro transfection efficiency does not reliably predict in vivo protein expression levels. While SM-102 showed superior performance in cell cultures, its in vivo efficacy was comparable to ALC-0315. Furthermore, all formulations elicited similarly strong immune responses in vivo, despite their differences in protein expression, indicating that vaccine efficacy involves complex immunological mechanisms beyond mere expression levels [66].
Impact of RNA Cargo Size on Encapsulation
The relationship between RNA cargo size and encapsulation efficiency is another critical factor in LNP development. A careful characterization of benchmark LNP formulations revealed important insights and a crucial methodological consideration regarding encapsulation calculation [73].
Table 2: Encapsulation Efficiency vs. RNA Cargo Size in Benchmark Formulations
| RNA Cargo Type | Representative Length | Traditional EE% | EEinput% (vs. Input RNA) |
|---|---|---|---|
| Antisense Oligo (ASO) | 10 bases | >85% | <50% |
| siRNA | 21 base pairs | >85% | <50% |
| RNA Aptamer | 96 bases | >85% | <50% |
| mRNA | 996 bases | >85% | <50% |
| mRNA | 1929 bases | >85% | <50% |
The data demonstrates that the traditional calculation of encapsulation efficiency (EE%) can be misleading, consistently showing high values (>85%) across all cargo sizes. In contrast, the calculation based on the input RNA (EEinput%) reveals that less than 50% of the initial RNA is successfully encapsulated in the final product [73]. This discrepancy is critical for formulation optimization and cost-effectiveness, particularly for expensive RNA therapeutics. Furthermore, the study found that LNP size was not strongly influenced by the cargo size, a counterintuitive finding that highlights the complex nature of LNP self-assembly [73].
Mechanisms Underlying IVIVC Discrepancies
The Protein Corona Effect
Upon administration into biological fluids, LNPs are immediately coated by biomolecules, primarily proteins, forming a "protein corona" that redefines their biological identity [68] [69]. This corona significantly alters LNPphysicochemical properties and directly impacts delivery efficiency.
Recent research using quantitative, label-free mass spectrometry-based proteomics has identified specific proteins consistently enriched in the LNP corona, including vitronectin, C-reactive protein, and alpha-2-macroglobulin [69]. The formation of this corona has a direct and profound impact on LNP function:
- Mismatch Between Uptake and Expression: Surprisingly, certain corona proteins can increase cellular uptake of LNPs by up to five-fold without a corresponding increase in mRNA expression. This suggests that the protein corona can alter intracellular trafficking routes, potentially directing LNPs toward lysosomal degradation pathways instead of facilitating endosomal escape [69].
- Compromised Endosomal Escape: The protein corona may create a physical barrier or alter the LNP's fusogenic properties, hindering the ability of the ionizable lipids to interact with endosomal membranes and mediate the release of the nucleic acid payload into the cytosol [69].
The following diagram illustrates how the protein corona influences the cellular delivery pathway of LNPs, often leading to divergent outcomes between in vitro and in vivo environments:
Diagram: Protein Corona Impact on LNP Delivery Efficiency
Stability in Biological Fluids
The stability of RNA-LNPs in biological fluids is a crucial, yet often overlooked, factor governing their in vivo performance [68]. The interplay between LNP stability and instability is a delicate balance: excessive stability can prevent the release of the nucleic acid cargo at the target site, while premature instability leads to degradation and loss of activity before reaching the target cells.
Key factors influencing LNP stability include lipid composition, particle surface properties, and interactions with proteins in physiological conditions [68]. For instance, the density and structure of PEG-lipids can significantly influence protein adsorption and subsequent stability. Strategies to enhance stability, such as the use of shielding lipids or PEGylation, must be carefully optimized to ensure that stability does not come at the cost of reduced cargo delivery efficiency [68].
The Scientist's Toolkit: Essential Research Reagents and Solutions
The following table details key reagents and materials essential for LNP research, based on formulations and methodologies cited in the literature [66] [71] [73].
Table 3: Essential Research Reagents for LNP Formulation and Characterization
| Reagent / Material | Function / Role | Examples / Specifications |
|---|---|---|
| Ionizable Lipids | Bind and encapsulate RNA; facilitate endosomal escape | SM-102, ALC-0315, DLin-MC3-DMA (MC3), C12-200 [66] [73] |
| Phospholipids | Provide structural integrity to the LNP bilayer | DSPC, DOPE, DOPC [66] [73] |
| PEGylated Lipids | Control particle size, prevent aggregation, enhance stability | ALC-0159, DMG-PEG2000, DMPE-PEG2000 [66] [73] |
| Sterols | Enhance bilayer stability and packing | Cholesterol [66] [73] |
| Microfluidic Instrument | Enables reproducible, scalable LNP formation with high encapsulation efficiency | NanoAssemblr Ignite [66] [71] |
| Analytical Tools: DLS | Measures hydrodynamic size, PDI, and zeta potential | Z-average size, PDI < 0.2 [71] [73] |
| Analytical Tools: RiboGreen Assay | Quantifies RNA encapsulation efficiency | Critical to calculate EEinput% relative to input RNA [73] |
| Analytical Tools: TEM | Visualizes LNP morphology and structure | Cryo-TEM, Negative Stain EM [71] |
The journey of LNPs from in vitro benches to in vivo applications is fraught with challenges arising from the complex biological interactions that are not fully captured by conventional cellular assays. The discrepancies in performance, as evidenced by the divergent outcomes for different ionizable lipids and the significant impact of the protein corona, underscore the limitations of relying solely on in vitro data for formulation optimization. A more holistic approach, incorporating advanced characterization of LNP stability in biological fluids, a deeper understanding of protein corona formation and its functional consequences, and the adoption of more predictive in vitro models that better simulate in vivo conditions, is essential for improving IVIVC. By integrating these factors into the LNP development workflow, researchers can bridge the current correlation gap and accelerate the clinical translation of next-generation nucleic acid therapeutics.
Strategies for Time Scaling and Accelerated In Vitro Release Testing
In the development of extended-release drug products, particularly parenteral dosage forms such as long-acting injectables (LAIs), in vitro release testing (IVRT) serves as a critical bridge between formulation development and clinical performance. These dosage forms are designed to release active pharmaceutical ingredients over periods ranging from weeks to months, making real-time in vitro testing impractical for timely formulation screening and quality control [74]. The pursuit of predictive in vitro-in vivo correlation (IVIVC) models represents a cornerstone of modern pharmaceutical development, enabling scientists to forecast a drug's in vivo performance based on laboratory dissolution data [6]. Time scaling and accelerated release testing methodologies have emerged as powerful strategies to compress these extended release profiles into practically manageable timeframes while maintaining biopredictive capabilities [75] [76].
The fundamental challenge lies in the inherent discrepancy between the prolonged in vivo release duration of these formulations and the practical necessities of industrial product development. Accelerated IVRT methods aim to shorten testing times from months to days or hours through strategic modification of critical parameters such as temperature, hydrodynamics, sink conditions, and apparatus configuration [74]. Concurrently, time scaling provides the mathematical framework to translate these accelerated in vitro profiles back to their corresponding in vivo timescales, enabling meaningful correlation and prediction [77] [75]. This guide systematically compares the current methodological approaches, their experimental implementations, and their respective applications within the broader context of IVIVC model development.
Comparative Analysis of Time Scaling and Accelerated Release Testing Approaches
The table below provides a structured comparison of the primary methodologies employed for time scaling and accelerated release testing of extended-release parenteral dosage forms.
Table 1: Comparison of Time Scaling and Accelerated In Vitro Release Testing Strategies
| Strategy | Core Principle | Typical Applications | Key Advantages | Recognized Limitations |
|---|---|---|---|---|
| Inverse Release Function (IRF) Approach [77] | Mathematically closed function providing time-to-time links; uses complete dataset from all in vitro and in vivo time points. | Level A IVIVC for extended-release oral and parenteral formulations. | High predictive capacity; nearly negligible prediction errors for Cmax reported; mathematically robust. | Requires high-quality in vivo absorption data for model development. |
| Multi-Method Accelerated IVRT Strategy [75] [76] | Employs separate, optimized USP Apparatus 2 methods to characterize distinct release phases (initial burst, intermediate, terminal). | Complex long-acting injectables (LAIs), including combination products. | Provides complete release profile in <48 hours; successfully predicts in vivo performance over 75 days; high reproducibility. | Requires development and validation of multiple methods; may need preclinical data for time scaling. |
| Apparatus & Condition Modification [74] | Acceleration via parameters like increased agitation, temperature, surfactant use, or altered hydrodynamics. | Polymeric microspheres, lipid microparticles, in situ forming implants. | Utilizes compendial (USP) equipment; highly customizable for specific formulation properties. | Risk of altering release mechanism; requires demonstration of bio-relevance. |
| Bio-relevant Adapter Systems [78] | Uses specialized adapters (e.g., Teflon, Glass slide) to control depot shape and environment, mimicking in vivo conditions. | In situ forming implants. | Generates highly reproducible data; controls critical attributes like surface-to-volume ratio and water uptake. | Method development can be complex and formulation-specific; not a compendial standard. |
Experimental Protocols for Key Methodologies
The Inverse Release Function (IRF) Protocol for Time Scaling
The IRF approach addresses a fundamental challenge in Level A IVIVC: the lack of coincident times of similar release in vitro and in vivo. The protocol establishes a direct functional relationship between the in vitro and in vivo timescales [77].
- Objective: To develop a point-to-point correlation between the percent dissolved in vitro and the percent absorbed in vivo, enabling prediction of the entire in vivo absorption time course from in vitro dissolution data.
- Procedure: A minimum of two formulations with different release rates (e.g., slow, medium, fast) are tested. The in vivo absorption profile is typically obtained via deconvolution of plasma concentration-time data. The IRF model is then fitted to determine the function that maps in vitro time to its corresponding in vivo time for equivalent percent release.
- Key Output: A mathematical model that allows for the time scaling of any in vitro profile from the same drug product family to predict its in vivo absorption profile.
Multi-Method Accelerated IVRT for Long-Acting Injectables
This strategy uses two distinct USP Apparatus 2 (paddle) methods to characterize different phases of drug release from an LAI suspension within a drastically shortened timeframe [75] [76].
- Objective: To predict the preclinical in vivo performance of single-agent and combination LAI suspension products over 75 days using IVRT methods that take 48 hours or less.
- Apparatus: USP Apparatus 2 with specific modifications.
- Procedure Overview:
- Method for Initial & Intermediate Phases: The formulation is introduced into the dissolution vessel using a suspension cup. A moderate agitation rate (e.g., 50-75 rpm) is applied to maintain a constant, low surface area exposure of the suspension to the release media, mimicking the initial depot formation and subsequent release.
- Method for Terminal Phase: The formulation is exposed to a high initial paddle speed (e.g., 150-250 rpm). This high shear disperses the suspension particulates throughout the media, creating a high cumulative surface area that enables rapid drug release, effectively accelerating the slow terminal phase.
- Time Scaling & IVIVC: The release profiles from both accelerated methods are independently time-scaled to reflect the in vivo timescale (e.g., 1800 hours). Level A IVIVCs are then developed separately for each method and Active Pharmaceutical Ingredient (API) using in vivo absorption profiles derived from preclinical (e.g., rat) pharmacokinetic data [75].
Bio-Relevant Adapter Method for In-Situ Forming Implants
This protocol addresses the unique challenges of testing in situ forming implants, which exhibit complex release mechanisms and are difficult to test reproducibly [78].
- Objective: To generate reproducible, bio-relevant in vitro release profiles for in situ forming implants to enable the development of a Level A IVIVC.
- Apparatus: USP Apparatus 2 equipped with a custom-designed adapter (e.g., Glass slide adapter, GF/F-Teflon adapter).
- Procedure: The liquid formulation is injected into the adapter, which is then immersed in the release medium. The adapter physically constrains the formulation, controlling its shape (and thus its surface-to-volume ratio) during the solidification process and subsequent release. This controlled environment mimics key in vivo attributes, such as limited water uptake and mechanical confinement, leading to a release profile that more closely matches the in vivo absorption profile [78].
- Key Insight: The surface-to-volume ratio and water uptake of the formed depot are identified as critical attributes that must be mimicked in vitro to achieve a successful IVIVC for these systems.
Workflow and Relationship Diagrams
The following diagram illustrates the logical workflow for developing and applying an accelerated IVRT strategy with time scaling for IVIVC.
The diagram above outlines the core process for leveraging accelerated IVRT. The critical integration point is the application of time scaling, which acts as the bridge between the compressed in vitro timescale and the extended in vivo timescale, enabling the establishment of a predictive Level A IVIVC [77] [75].
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful implementation of the strategies described herein relies on a set of key materials and instruments. The following table details these essential components and their functions.
Table 2: Essential Research Reagents and Materials for Accelerated IVRT Development
| Item | Function / Relevance | Application Notes |
|---|---|---|
| USP Apparatus 2 (Paddle) [74] [75] | Standard dissolution apparatus adapted for parenteral formulations; provides controlled hydrodynamics and temperature. | Often modified with accessories like suspension cups or custom adapters to handle different dosage forms. |
| Specialized Adapters(Teflon, Glass Slide) [78] | Control the shape and environment of depot-forming systems (e.g., in situ implants) to mimic in vivo conditions and ensure reproducibility. | Critical for achieving bio-relevant release profiles for implants by controlling surface-to-volume ratio and water uptake. |
| Biorelevant Release Media [74] [75] | Aqueous buffers, often with surfactants (e.g., Cremophor EL) to maintain sink conditions and simulate physiological environment. | Composition (pH, ionic strength, surfactants) is optimized to accelerate release without changing the fundamental mechanism. |
| Degradable Polymers(e.g., PLGA, PLA) [74] [78] | The primary formulation component for many extended-release systems (microspheres, implants); its properties dictate release kinetics. | Polymer attributes (MW, L/G ratio, end-cap) are Critical Quality Attributes (CQAs) that must be controlled for consistent performance. |
| HPMC Capsules [75] | A method for standardized introduction of suspension formulations into the dissolution vessel, improving reproducibility. | Helps minimize variability associated with manual sample introduction in early method development. |
The strategic implementation of accelerated in vitro release testing coupled with robust time scaling methodologies represents a paradigm shift in the development of complex extended-release drug products. As evidenced by the comparative data and experimental protocols, approaches like the multi-method IVRT strategy for LAIs and the bio-relevant adapter systems for implants demonstrate that it is possible to compress months of release into days of testing while retaining predictive power for in vivo performance [75] [76] [78]. The mathematical rigor of the Inverse Release Function approach further enhances the precision of these predictions by establishing a direct, point-to-point correlation [77].
The successful application of these strategies directly supports the broader thesis of IVIVC by providing a reliable and efficient means to correlate in vitro drug release with in vivo bioavailability. This not only accelerates formulation screening and optimization but also strengthens quality control paradigms. The ongoing integration of these methods with advanced modeling techniques, including PBPK and AI-driven analytics, promises to further refine their predictive accuracy and expand their applicability across the pharmaceutical development landscape [1]. Ultimately, the adoption of these sophisticated in vitro tools empowers scientists to make data-driven decisions earlier in the development process, reducing the regulatory burden and accelerating the delivery of advanced drug products to patients.
Ensuring Predictive Power: Model Validation, Regulatory Standards, and Case Analyses
In vitro-in vivo correlation (IVIVC) is defined by the U.S. Food and Drug Administration (FDA) as a predictive mathematical model describing the relationship between an in vitro property of a dosage form and a relevant in vivo response [6]. For a model to be considered valid and reliable for regulatory purposes, it must undergo rigorous validation, primarily through internal and external predictivity evaluations [1] [3]. These evaluations determine whether the IVIVC model can accurately forecast in vivo performance based on in vitro dissolution data, which is critical for supporting biowaivers and reducing the need for extensive clinical studies [1]. This guide compares the application of these evaluations across different drug development scenarios, providing a framework for researchers and scientists to achieve regulatory compliance.
Experimental Protocols for IVIVC Development and Validation
The development and validation of a Level A IVIVC—the most preferred by the FDA—follows a structured process. The core workflow, from formulation to model validation, is illustrated below.
Core Experimental Methodology
The establishment of a robust IVIVC requires carefully designed experiments and specific analytical procedures.
- Formulation and In Vitro Dissolution: A minimum of two or three formulations with different release rates (e.g., slow, medium, fast) are developed [1]. Dissolution testing is performed using apparatus such as USP II (paddle) or USP III (bio-relevant apparatus) under various conditions, including different pH levels and media compositions (e.g., biorelevant media simulating fed or fasted states) to generate distinct in vitro release profiles [3].
- In Vivo Data Generation: The same formulations are administered in a clinical study, typically in a cross-over design, to obtain plasma concentration-time profiles [6]. Key pharmacokinetic (PK) parameters like AUC (area under the curve) and Cmax (maximum concentration) are calculated.
- Mathematical Model Construction: The in vivo absorption or dissolution time course is determined from the PK data using mathematical techniques like deconvolution (e.g., the Wagner-Nelson method for one-compartment models or the Loo-Riegelman method for two-compartment models) [3] [79]. A point-to-point relationship is then established between the in vitro dissolution and the in vivo dissolution/absorption [1].
Internal and External Predictivity Evaluation Protocols
The validation of the IVIVC model hinges on two main types of predictability assessments, with a specific quantitative benchmark for success.
- Internal Predictivity Evaluation: This is an internal validation step. The established IVIVC model is used to predict the PK profiles of the formulations that were originally used to create the model. The predicted AUC and Cmax values are compared to the actual observed clinical values [1] [3]. The percent prediction error (%PE) is calculated for each parameter as follows:
%PE = [(Observed Value - Predicted Value) / Observed Value] × 100[79]. - External Predictivity Evaluation: This is a more rigorous, external validation step. It involves using a new formulation batch or a formulation with a different release rate that was not part of the initial model development set [3] [79]. The IVIVC model predicts this new formulation's in vivo performance, and the %PE is calculated similarly. Successful external validation strongly supports the model's robustness and predictive capability.
The FDA's validation criteria require that the average %PE for both Cmax and AUC should be 10% or less, and no individual %PE should exceed 15% [1] [3]. If these criteria are met, the model is considered predictive and can be used for setting dissolution specifications and requesting biowaivers.
Performance Data Comparison: Case Studies in IVIVC Validation
The following table summarizes the outcomes of internal and external predictivity evaluations from published case studies, illustrating the application of FDA validation criteria.
Table 1: Comparison of IVIVC Predictivity Performance Across Case Studies
| Drug Compound | Dosage Form | Study Type | % PE (Cmax) | % PE (AUC) | FDA Criteria Met? | Key Findings & Experimental Notes |
|---|---|---|---|---|---|---|
| Lamotrigine [3] | Extended-Release Tablets | Internal & External Validation | < 10% | < 10% | Yes | Used USP Apparatus II and standard compendial media. Model passed both internal and external validation. |
| Progesterone [79] | Vaginal Ring | Internal Validation | < 7% at most time points | < 2% for AUC(0-408h) | Yes | A population modeling approach was used. For AUC(0-408h), %PE was <2% for each dose. |
| Progesterone [79] | Vaginal Ring | External Validation | < 10% after 264h | < 3% at end of experiment | Yes | Model predictability was assessed by leaving out 375 mg data as an external dataset. |
| Fenofibrate [2] | Lipid-Based Formulations | Correlation Attempt | N/R | N/R | No | In vitro dispersion data failed to distinguish between LBFs in fasted/fed states in rats. No correlation identified. |
| Cinnarizine [2] | Lipid-Based Formulations | Correlation Attempt | N/R | N/R | No | Only a qualitative Level D correlation was obtained. Observed precipitation in vitro but not in vivo. |
Abbreviations: % PE: Percent Prediction Error; N/R: Not Reported, or specific %PE not available due to failed correlation.
The Scientist's Toolkit: Essential Reagents and Materials
Developing and validating an IVIVC requires a combination of specialized instrumentation, software, and biochemical reagents.
Table 2: Key Research Reagent Solutions for IVIVC Studies
| Item | Function in IVIVC | Application Example |
|---|---|---|
| USP Dissolution Apparatus II (Paddle) & III (Bio-relevant) [3] | To simulate the drug release from the solid dosage form under controlled conditions of pH, agitation, and fluid dynamics. | Used with lamotrigine ER tablets to generate biopredictive dissolution profiles in compendial media [3]. |
| Biorelevant Dissolution Media (e.g., FaSSIF, FeSSIF) [80] | To more accurately mimic the composition and surface-active properties of human intestinal fluids under fasted and fed conditions, improving in vivo predictability. | Employed in PBPK modeling to predict food effect on drug absorption for lipophilic compounds [80]. |
| PBPK Modeling Software (e.g., GastroPlus, Simcyp) [3] [80] | To create a physiologically based pharmacokinetic (PBPK) model that simulates drug absorption, distribution, metabolism, and excretion, integrating in vitro dissolution as an input. | A verified PBPK model was crucial for establishing a Level A IVIVC and patient-centric quality standards for lamotrigine ER [3]. |
| In Vitro Lipolysis Assay [2] | To model the digestion of lipid-based formulations (LBFs) in the gastrointestinal tract, which is critical for predicting the performance of LBFs for poorly water-soluble drugs. | Used to study fenofibrate and other BCS Class II drugs, though predictability can be variable and challenging [2]. |
Achieving a successful IVIVC that meets FDA validation criteria is a cornerstone of modern, efficient drug development. As demonstrated by the case studies, success hinges on a systematic approach: developing multiple formulations with varying release rates, employing biopredictive dissolution methods, and rigorously testing the model's internal and external predictability against the strict %PE benchmarks. While straightforward for many extended-release formulations, significant challenges remain for complex systems like lipid-based formulations, where dynamic processes such as digestion and permeation complicate predictability [2]. The ongoing integration of advanced tools like PBPK modeling and population-based analysis is steadily enhancing the power and regulatory acceptance of IVIVC, paving the way for its broader application in justifying biowaivers and ensuring product quality [3] [79].
Common Deficiencies in IVIVC Submissions for Generic Drug Applications (ANDA)
An in vitro-in vivo correlation (IVIVC) is a predictive mathematical model describing the relationship between an in vitro property of a dosage form (typically the rate or extent of drug dissolution or release) and a relevant in vivo response (generally plasma drug concentration or amount of drug absorbed) [81] [6]. For generic drug development, the primary objective of establishing an IVIVC is to serve as a surrogate for human bioequivalence (BE) studies, potentially reducing the number of BE studies required during the initial approval process and for certain scale-up and post-approval changes (SUPAC) [81] [82]. Despite the publication of the FDA IVIVC Guidance for Extended Release Oral Dosage Forms in September 1997, which provides a regulatory framework for development, evaluation, and application of IVIVCs, deficiencies in IVIVC submissions remain a significant challenge in the Abbreviated New Drug Application (ANDA) review process [81] [82]. An analysis of internal FDA databases from January 1996 to December 2014 revealed that only 14 ANDA submissions for proposed generic oral extended-release (ER) drug products contained IVIVC data, and most were not acceptable, with only one submission including adequate information to enable completion of the BE review within the first review cycle [81]. This guide examines the common deficiencies, provides comparative performance data, and outlines methodological approaches to strengthen IVIVC submissions.
Analysis of IVIVC Submission Deficiencies: Patterns and Prevalence
The Division of Bioequivalence within the FDA's Office of Generic Drugs consistently identifies specific deficiency patterns in IVIVC submissions. The remarkably low number of ANDA submissions containing IVIVC data (only 14 over an 18-year period) highlights the technical challenges associated with developing robust correlations [81]. The majority of these submissions contained inadequacies that prevented regulatory acceptance, underscoring the need for improved scientific approaches and regulatory alignment.
Quantitative Analysis of IVIVC Submission Outcomes
Table 1: Analysis of IVIVC Submissions in ANDAs (1996-2014)
| Submission Characteristic | Number of ANDAs | Percentage of Total |
|---|---|---|
| Total ANDAs with IVIVC data | 14 | 100% |
| Acceptable IVIVCs | 1 | 7.1% |
| Unacceptable IVIVCs | 13 | 92.9% |
| IVIVCs for pre-approval changes | 9 | 64.3% |
| IVIVCs for post-approval changes | 4 | 28.6% |
| IVIVCs to guide formulation development | 1 | 7.1% |
Table 2: Common Deficiency Categories in IVIVC Submissions
| Deficiency Category | Specific Deficiencies | Impact on Review |
|---|---|---|
| Model Development | Lack of point-to-point correlation; Inadequate formulation selection; Improper deconvolution methods | Precludes establishment of Level A IVIVC |
| Predictability Evaluation | Insufficient internal validation; External prediction errors >15%; Inappropriate statistical methods | Unable to verify model predictive performance |
| Data Analysis | Use of mean data masking variability; Improper time-scaling; Failure to account for flip-flop kinetics | Compromises correlation strength and reliability |
| Regulatory Application | Attempted biowaiver without validated model; Setting dissolution specs without IVIVC justification | Cannot support requested regulatory relief |
Experimental Protocols for Robust IVIVC Development
Formulation Selection and Design
A foundational requirement for developing a predictive IVIVC is the use of appropriate formulations with varying release rates. According to regulatory expectations, a minimum of two formulations with different release rates (e.g., slow, medium, and fast) should be developed and tested to establish a meaningful correlation [1]. These formulations should differ only in the critical manufacturing variables or release-controlling excipients that affect drug release rate, while maintaining similarity in all other qualitative and quantitative aspects. For extended-release products, this typically involves varying the polymer type, polymer concentration, or other release-modifying excipients to achieve distinctly different in vitro dissolution profiles that bracket the intended commercial formulation profile.
In Vitro Dissolution Method Development
The development of a biorelevant dissolution method is critical for establishing a predictive IVIVC. The experimental protocol should include:
- Apparatus Selection: Standard compendial apparatus (USP I [basket] or USP II [paddle]) should be evaluated for suitability, with justification for any deviations [81].
- Medium Composition: Multiple media covering the physiological pH range (e.g., 0.1N HCl, pH 4.5-7.4 buffers) should be investigated, with particular attention to biorelevant media for poorly soluble drugs [3].
- Hydrodynamic Conditions: Appropriate agitation speeds (typically 50-100 rpm for paddle, 100-150 rpm for basket) that maintain sink conditions and avoid coning should be established.
- Sampling Time Points: Sufficient time points to fully characterize the dissolution profile (early, middle, and late stages) should be included [1].
For lipid-based formulations and other complex delivery systems, conventional dissolution tests may fail to predict in vivo performance, necessitating the use of in vitro digestion models that more closely simulate gastrointestinal physiology [50].
In Vivo Study Design
The pharmacokinetic studies should employ a crossover design with adequate sample size to characterize the absorption profile of each formulation. Key considerations include:
- Reference Formulation: An oral solution, suspension, or immediate-release formulation with known bioavailability should be used as the reference for deconvolution, unless an IV reference is available [83].
- Sampling Frequency: Frequent blood sampling, particularly during the absorption phase, to adequately capture the concentration-time profile.
- Subject Selection: Healthy adult volunteers under standardized conditions (fasting/fed) as appropriate for the drug product.
Data Analysis and Model Development
The core IVIVC model development involves establishing a point-to-point relationship between in vitro dissolution and in vivo input rate. The methodological steps include:
- Determine In Vivo Absorption/Release Time Course: The Wagner-Nelson method (for one-compartment drugs) or Loo-Riegelman method (for two-compartment drugs) is typically employed for this deconvolution process [3].
- Establish Correlation Function: Develop a mathematical relationship (linear or nonlinear) between the fraction dissolved in vitro and the fraction absorbed in vivo.
- Predict In Vivo Profiles: Using the established IVIVC model, predict the plasma concentration-time profiles for the formulations used in model development.
- Evaluate Predictability: Calculate the percent prediction error (%PE) for C~max~ and AUC according to regulatory standards, where %PE = [(Observed - Predicted)/Observed] × 100 [1].
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Essential Research Reagents and Materials for IVIVC Studies
| Item | Specification/Function | Application Notes |
|---|---|---|
| Dissolution Apparatus | USP Apparatus I (Basket) or II (Paddle) | Standardized hydrodynamics; compendial compliance [81] |
| Biorelevant Dissolution Media | Fasted State Simulated Intestinal Fluid (FaSSIF), Fed State Simulated Intestinal Fluid (FeSSIF) | Enhanced predictability for BCS Class II drugs [3] |
| Analytical Reference Standards | USP-grade drug substance; certified purity | Quantification of dissolution and plasma concentrations |
| Deconvolution Software | Phoenix WinNonlin, MATLAB, or similar | Wagner-Nelson/Loo-Riegelman methods for absorption calculation [83] |
| Chromatographic Systems | HPLC/UPLC with UV/PDA/MS detection | Bioanalysis of plasma samples; dissolution sample analysis |
| Physiologically-Based Pharmacokinetic (PBPK) Software | GastroPlus, Simcyp Simulator, PK-Sim | Advanced IVIVC development and extrapolation [84] [3] |
Regulatory Framework and Application Strategies
The FDA IVIVC Guidance establishes clear expectations for correlation levels, with Level A IVIVC being the most preferred for regulatory applications as it represents a point-to-point relationship between in vitro dissolution and in vivo absorption [1] [85]. Level A correlations can support biowaivers for:
- Higher or Lower Strengths: When all strengths are qualitatively similar, have the same release mechanism, and exhibit similar in vitro dissolution profiles [81].
- Post-Approval Changes: Certain SUPAC changes where the IVIVC validates that dissolution profiles remain within established boundaries that ensure bioequivalence [81].
- Dissolution Specifications: Setting clinically relevant dissolution specifications that ensure batch-to-batch consistency and product quality [81] [3].
The high deficiency rate in IVIVC submissions for generic drug applications underscores the technical complexity of developing robust in vitro-in vivo correlations. Successful submissions share several key characteristics: they employ scientifically sound experimental designs with appropriate formulation variants, use biorelevant dissolution methods that accurately reflect the in vivo release environment, apply proper statistical and mathematical approaches for model development and validation, and clearly demonstrate predictability within established regulatory thresholds. Furthermore, successful submissions comprehensively address the regulatory context for the intended application, whether for supporting dissolution specifications, justifying biowaivers for formulation changes, or bridging between product strengths. As IVIVC methodologies continue to evolve with advances in PBPK modeling, artificial intelligence, and more sophisticated in vitro systems, the pharmaceutical industry's ability to develop predictive correlations is expected to improve significantly [1] [84] [3]. By addressing the common deficiency patterns outlined in this guide and employing robust scientific approaches, generic drug developers can enhance the quality of IVIVC submissions, potentially accelerating regulatory approval and bringing quality generic medicines to patients more efficiently.
In vitro-in vivo correlation (IVIVC) is a critical biopharmaceutical tool defined as a predictive mathematical model describing the relationship between an in vitro property of a dosage form (typically the rate or extent of drug dissolution or release) and a relevant in vivo response (such as plasma drug concentration or amount of drug absorbed) [6]. The establishment of a robust IVIVC plays a pivotal role in modern drug development by serving as a surrogate for bioequivalence studies, supporting biowaivers, setting dissolution specifications, and reducing development costs and time [1] [86].
Despite its recognized value, successful development and regulatory acceptance of IVIVCs remains challenging. This guide provides a comparative analysis of successful and unsuccessful IVIVC case studies, examining the critical factors that differentiate them and offering practical methodologies for researchers and drug development professionals.
IVIVC Success and Failure Landscape
The pharmaceutical industry's experience with IVIVC reveals a significant gap between attempted and successful correlations. A comprehensive survey of IVIVC development within the pharmaceutical industry indicated that while most companies acknowledge the importance of IVIVC throughout drug development stages, the approach seems underutilized in regulatory submissions [87]. An analysis of Abbreviated New Drug Applications (ANDAs) for generic oral extended-release (ER) drug products from 1996-2014 found that only 14 submissions contained IVIVC data, with most being deemed unacceptable. Only one ANDA submission included adequate IVIVC information enabling completion of bioequivalence review within the first review cycle [81].
| Purpose of IVIVC | Dosage Form | Number of ANDAs | Number Acceptable |
|---|---|---|---|
| Change in dissolution method/specifications | ER Tablets | 1 | 0 |
| Level 3 site manufacturing change | ER Tablets | 1 | 0 |
| Waiver for lower strengths | ER Tablets | 1 | 1 |
| Waiver for higher strengths | ER Tablets with enteric coat | 2 | 0 |
| Support dissolution method | ER Tablets | 1 | 0 |
| Batch-to-batch variation | ER Tablets with pellets | 3 | 1 |
| Change in dissolution specifications | ER Capsules | 1 | 1 |
| Change in dissolution specifications | ER Capsules with beads/pellets | 1 | 0 |
| Challenge failed BE study | ER Tablets | 1 | 0 |
Levels of IVIVC and Regulatory Acceptance
The U.S. Food and Drug Administration (FDA) recognizes different levels of IVIVC, which vary in their complexity and predictive power [1]. Understanding these categories is essential for selecting the appropriate approach for a given development program.
| Aspect | Level A | Level B | Level C |
|---|---|---|---|
| Definition | Point-to-point correlation between in vitro dissolution and in vivo absorption. | Statistical correlation using mean in vitro and mean in vivo parameters. | Correlation between a single in vitro time point and one PK parameter. |
| Predictive Value | High – predicts the full plasma concentration-time profile. | Moderate – does not reflect individual PK curves. | Low – does not predict the full PK profile. |
| Regulatory Acceptance | Most preferred; supports biowaivers and major formulation changes. | Less robust; usually requires additional in vivo data. | Least rigorous; not sufficient for biowaivers alone. |
| Use Case | Requires ≥2 formulations with distinct release rates; most common for regulatory submissions. | Compares mean dissolution time with mean residence/absorption time; not for quality control. | May support early development insights but requires supplementation. |
Level A IVIVC is the most preferred for regulatory submissions due to its high predictive capability, while Level C and multiple Level C correlations can provide valuable early development insights but are generally insufficient for biowaivers without supplemental data [81] [1].
Successful IVIVC Case Study: Lamotrigine Extended-Release Tablets
A recent successful case study established a Level A IVIVC for lamotrigine extended-release (ER) 300 mg tablets with the objective of developing patient-centric quality standards (PCQS) for dissolution. Lamotrigine ER serves as an ideal model formulation for BCS Class IIb drugs where dissolution rate limits absorption [3].
Experimental Methodology
Formulations: The study utilized marketed lamotrigine ER tablets (Lamictal XR 300 mg) as the reference formulation, alongside in-house manufactured fast, medium, and slow release lamotrigine ER 300 mg tablets for IVIVC validation [3].
Dissolution Testing: Multiple dissolution conditions were systematically evaluated using USP Apparatus II and III with various media including biorelevant media and standard compendial media at different pH levels to identify the most biopredictive conditions [3].
PBPK Model Development: A physiologically based pharmacokinetic (PBPK) model was developed and verified using plasma lamotrigine profiles following intravenous solution and oral immediate-release tablet administration. Model verification demonstrated accurate prediction of Cmax and AUC with confidence levels exceeding 95% [3].
IVIVC Model Development: Multiple IVIVC models were investigated using dissolution data from the fast, medium, and slow ER formulations. Optimal IVIVC was obtained using a second-order polynomial and a two-compartment Loo-Riegelman deconvolution approach [3].
Key Success Factors
- Systematic Dissolution Method Selection: Comprehensive evaluation of multiple dissolution conditions identified that standard compendial media using USP Apparatus II established a Level A IVIVC [3].
- Robust PBPK Modeling: The PBPK model was rigorously validated with clinical data, providing a solid foundation for predicting in vivo performance [3].
- Proper Formulation Design: The use of formulations with different release rates (slow, medium, fast) provided the necessary data range for establishing a meaningful correlation [3].
- Statistical Validation: The IVIVC model passed both internal and external validation criteria with prediction errors below 10%, meeting regulatory standards for predictability [3].
Outcomes and Applications
The successful IVIVC enabled establishment of patient-centric quality standards for dissolution (≤10% release at 2 h, ≤45% at 6 h, and ≥80% at 18 h), demonstrating that PCQS can be established using verified PBPK and validated IVIVC models without extensive clinical studies [3].
Unsuccessful IVIVC Case Studies
Lipid-Based Formulations (LBFs)
Lipid-based formulations present unique challenges for IVIVC development due to complex processes including lipid digestion, dynamic solubilization, and permeation enhancement that are not captured by traditional dissolution tests [88].
Case Study - Fenofibrate LBFs: A study evaluating four different LBFs using in vitro dispersion data failed to establish a correlation with in vivo performance in rats. The in vitro tests could not distinguish between formulations administered in fasted versus fed states, and no meaningful IVIVC could be established despite testing multiple formulations [88].
Case Study - pH-Stat Lipolysis Models: An evaluation of eight drugs studied using pH-stat lipolysis devices found that only half correlated well with in vivo data, indicating significant limitations in predicting in vivo performance for LBFs using this method [88].
Mirabegron Modified Release Formulations
Mirabegron MR formulations present challenges due to non-linear absorption characteristics that complicate conventional IVIVC approaches. A study attempting conventional IVIVC methodologies failed to obtain adequate correlation due to the inability to account for dissolution and absorption mechanisms in the physiological environment, particularly the non-linear absorption processes [89].
While researchers eventually developed a physiologically based biopharmaceutics model (PBBM) that enabled Level A IVIVC for mirabegron, the conventional approach failed because it did not adequately consider luminal drug concentration-dependent membrane permeation and required specialized modeling of in vivo dissolution using zero-order rate equations [89].
Common Failure Patterns
Analysis of unsuccessful IVIVC attempts reveals several recurring themes:
- Physiological Complexity: Failure to account for complex in vivo processes such as lipid digestion, non-linear absorption, or region-dependent permeability [89] [88].
- Inadequate In Vitro Methods: Use of dissolution methods that lack biopredictiveness for the specific formulation technology [3] [88].
- Improper Data Treatment: Common pitfalls include incorrect use of mean versus individual data, improper handling of lag times, and failure to account for flip-flop pharmacokinetics [83].
- Formulation Limitations: Attempting IVIVC for formulations where drug release is not the rate-limiting step in absorption [6] [83].
Comparative Analysis: Critical Success Factors
Table 3: Key Differentiators Between Successful and Unsuccessful IVIVC Attempts
| Factor | Successful IVIVC | Unsuccessful IVIVC |
|---|---|---|
| Formulation Strategy | Use of ≥2 formulations with different release rates; drug release is rate-limiting step | Single formulation; dissolution not rate-limiting; complex formulations (e.g., LBFs) |
| In Vitro Methods | Biopredictive dissolution methods; systematic method development | Conventional compendial methods without biopredictive verification |
| Physiological Factors | Accounted for in model (GI pH, transit times, permeability) | Oversimplified or ignored physiological variables |
| Modeling Approach | Level A with proper deconvolution; PBPK integration when needed | Level C or multiple Level C without full profile prediction |
| Validation | Internal and external validation with prediction errors <10-15% | Inadequate validation or high prediction errors |
| Drug Properties | BCS Class I/III for ER products; Class II with dissolution-limited absorption | Non-linear absorption; extensive first-pass metabolism; complex transport |
Experimental Design and Methodological Considerations
IVIVC Development Workflow
The following diagram illustrates the critical steps in developing a robust IVIVC, integrating lessons from both successful and unsuccessful case studies:
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Key Research Reagents and Materials for IVIVC Development
| Item | Function in IVIVC | Application Notes |
|---|---|---|
| Dissolution Apparatus (USP I, II, III) | Provides controlled hydrodynamic conditions for drug release testing | USP II (paddle) most common; USP III (bio-relevant) for specialized applications [3] |
| Biorelevant Media (FaSSGF, FaSSIF, FeSSIF) | Simulates gastrointestinal fluids composition and pH | Essential for BCS Class II/IV drugs; improves biopredictiveness [3] |
| PBPK Modeling Software | Predicts in vivo PK profiles from in vitro data | Enables IVIVC for complex absorption patterns; requires verification [3] [89] |
| Statistical Packages | Model development and validation | Calculate prediction errors; internal/external validation [3] [83] |
| Analytical Instruments (HPLC, UV-Vis) | Quantifies drug concentration in dissolution samples | Validated methods with sufficient sensitivity and specificity [3] |
The comparative analysis of successful and unsuccessful IVIVC case studies reveals clear patterns that can guide future development efforts. Successful IVIVCs typically involve systematic approach to dissolution method development, proper formulation design with multiple release rates, integration of advanced modeling tools like PBPK when needed, and rigorous validation against clinical data. In contrast, failed IVIVCs often result from oversimplified in vitro methods that lack biopredictiveness, inadequate consideration of physiological complexity, and attempts to correlate formulations where dissolution is not the rate-limiting step in absorption.
For researchers developing IVIVCs, particularly for challenging compounds, the emerging integration of physiologically-based modeling, biorelevant dissolution testing, and quality by design principles offers promising approaches to overcome historical limitations and increase the success rate of these valuable correlations.
The Role of IVIVC in Scale-Up and Post-Approval Changes (SUPAC)
In vitro-in vivo correlation (IVIVC) is defined by the U.S. Food and Drug Administration (FDA) as a predictive mathematical model describing the relationship between an in vitro property of a dosage form and a relevant in vivo response [6]. Typically, the in vitro property is the rate or extent of drug dissolution or release, while the in vivo response is the plasma drug concentration or amount of drug absorbed [6] [81]. The establishment of a meaningful IVIVC serves as a critical biopharmaceutical tool that can provide a surrogate for bioequivalence studies, improve product quality, and reduce regulatory burden during pharmaceutical development [6].
Scale-Up and Post-Approval Changes (SUPAC) guidelines provide recommendations to sponsors of new drug applications who intend, during the post-approval period, to change components or composition, site of manufacture, scale-up/scale-down of manufacture, or manufacturing process and equipment [90]. These regulatory frameworks recognize that approved drug products may undergo changes for various reasons, including increased batch size, alterations in drug product constituents, manufacturing process improvements, and shifts in manufacturing sites [91].
The convergence of IVIVC and SUPAC creates a powerful paradigm in pharmaceutical development and regulation. A validated IVIVC model can significantly streamline the SUPAC process by providing a scientific justification for predicting the in vivo impact of manufacturing changes without additional clinical studies [1] [81]. This integration offers substantial benefits in reducing development timelines, minimizing animal and human testing, and maintaining product quality throughout the product lifecycle.
Levels of IVIVC and Their Regulatory Significance
The FDA recognizes different levels of IVIVC, each with distinct characteristics and regulatory implications [1] [81]. Understanding these categories is essential for selecting the appropriate correlation strategy for SUPAC applications.
Table: Levels of In Vitro-In Vivo Correlation (IVIVC)
| Level | Definition | Predictive Value | Regulatory Acceptance | Use Cases in SUPAC |
|---|---|---|---|---|
| Level A | Point-to-point correlation between in vitro dissolution and in vivo absorption [1]. | High – predicts the full plasma concentration-time profile [1]. | Most preferred by FDA; supports biowaivers and major formulation changes [1]. | SUPAC changes requiring bioequivalence assessment; setting dissolution specifications [81]. |
| Level B | Statistical correlation using mean in vitro and mean in vivo parameters [1]. | Moderate – does not reflect individual pharmacokinetic curves [1]. | Less robust; usually requires additional in vivo data [1]. | Limited SUPAC applications; not suitable for quality control specifications [1]. |
| Level C | Correlation between a single in vitro time point and one pharmacokinetic parameter [1]. | Low – does not predict the full PK profile [1]. | Least rigorous; not sufficient for biowaivers or major changes [1]. | Early development insights; supporting evidence for SUPAC [1]. |
| Multiple Level C | Expands Level C to correlate multiple dissolution time points with pharmacokinetic parameters [81]. | Moderate – more comprehensive than single point [81]. | Useful for regulatory purposes when Level A is not feasible [81]. | Justifying certain post-approval changes [81]. |
The hierarchy of IVIVC levels directly corresponds to their utility in SUPAC applications. Level A correlations are considered the most informative and are the primary type used to support biowaivers for post-approval changes [1] [81]. This level of correlation allows for the prediction of the entire in vivo time course from in vitro data, providing high confidence in assessing the impact of formulation or manufacturing changes. In contrast, Level B and Level C correlations provide progressively less precise predictions and are generally insufficient as standalone evidence for significant SUPAC submissions, though they can provide valuable supportive data and are useful during formulation development [1].
Experimental Protocols for IVIVC Development
Developing a robust IVIVC requires systematic experimentation that encompasses dissolution testing, in vivo data collection, and mathematical modeling.
In Vitro Dissolution Method Development
The foundation of a predictive IVIVC lies in developing a biorelevant dissolution method that can discriminate between different release rates while maintaining physiological relevance. Key considerations include:
- Apparatus Selection: Both USP Apparatus II (paddle) and USP Apparatus III (bio-relevant conditions) are commonly employed. The selection depends on the drug and formulation characteristics [3].
- Media Composition: The use of biorelevant media that simulate gastrointestinal fluids (e.g., Fast State Simulated Intestinal Fluid) is critical for predicting in vivo performance, particularly for poorly soluble drugs [3].
- Hydrodynamic Conditions: Proper adjustment of agitation speed to mimic physiological conditions without creating unrealistic turbulence [3].
- Sampling Points: Sufficient time points should be selected to adequately characterize the dissolution profile shape, typically including early, middle, and late phases of release [81].
For extended-release formulations like lamotrigine ER tablets, a robust Level A IVIVC was established using dissolution testing in standard compendial media with USP Apparatus II, with specifications set at ≤10% release at 2 h, ≤45% at 6 h, and ≥80% at 18 h [3].
In Vivo Data Collection and Analysis
The in vivo component of IVIVC development requires careful study design and data analysis:
- Study Population: Typically conducted in healthy human volunteers under fasted or fed conditions, depending on the intended clinical use.
- Formulation Selection: For Level A IVIVC, a minimum of two formulations with different release rates (e.g., slow, medium, fast) should be tested to establish a meaningful correlation [1].
- Pharmacokinetic Analysis: Blood samples are collected at predetermined time points, and plasma concentrations are analyzed to determine key PK parameters including C~max~, T~max~, and AUC [81].
- Deconvolution Methods: Mathematical techniques such as the Wagner-Nelson method for one-compartment models or Loo-Riegelman method for two-compartment models are used to determine the in vivo absorption time course [3].
Model Development and Validation
The correlation between in vitro and in vivo data is established through mathematical modeling:
- Correlation Plotting: In vitro dissolution time is plotted against in vivo absorption time, often using linear or polynomial functions [3].
- Predictability Evaluation: The developed model must be validated by predicting the in vivo performance of formulations not used in model development [81].
- Acceptance Criteria: For internal validation, the average absolute percent prediction error (%PE) for C~max~ and AUC should be ≤10%, and each formulation's %PE should not exceed 15% [81].
Essential Research Reagents and Materials for IVIVC Studies
Successful IVIVC development requires specific reagents, equipment, and methodologies. The following table outlines key research solutions essential for conducting robust IVIVC studies.
Table: Essential Research Reagents and Materials for IVIVC Studies
| Category | Specific Items | Function in IVIVC Development | Example Applications |
|---|---|---|---|
| Dissolution Apparatus | USP Apparatus I (Basket), II (Paddle), III (Bio-relevant) [3] | Simulate drug release under controlled hydrodynamic conditions | Discriminating between formulations with different release rates [3] |
| Dissolution Media | 0.1 N HCl, phosphate buffers (pH 6.8), biorelevant media (FaSSIF) [3] [81] | Simulate gastrointestinal environments for predictive dissolution | Establishing biopredictive dissolution methods [3] |
| Analytical Instruments | HPLC systems, UV-Vis spectrophotometers | Quantify drug concentration in dissolution samples and biological fluids | Determining dissolution profiles and plasma concentration curves [3] |
| Reference Standards | USP reference standards [3] | Ensure accuracy and reproducibility of analytical methods | Method validation and quality control during testing [3] |
| Software Tools | PBPK modeling platforms, statistical packages | Develop and validate mathematical models, perform deconvolution | Establishing Level A correlations, predicting in vivo performance [3] |
The selection of appropriate research reagents and methodologies should be guided by the specific drug characteristics and formulation type. For BCS Class II drugs (low solubility, high permeability), where dissolution is rate-limiting, the use of biorelevant media that simulate intestinal fluids becomes particularly important for establishing a predictive IVIVC [3]. Similarly, for extended-release formulations, the dissolution method must adequately characterize the entire release profile with sufficient time points to capture early, middle, and late phases of drug release [81].
Applications of IVIVC in SUPAC
The integration of IVIVC into SUPAC processes provides substantial scientific and regulatory advantages across multiple aspects of pharmaceutical development and post-approval management.
Regulatory Applications and Biowaivers
The primary application of IVIVC in SUPAC is to support biowaiver requests for bioequivalence studies that would otherwise be required for certain manufacturing changes [81]. According to FDA assessments, IVIVCs have been successfully used to justify:
- Site Manufacturing Changes: Level 3 manufacturing site changes for Class I drugs [81].
- Non-Proportional Formulations: Waivers for lower or higher strengths that are not proportionally similar to the bio-batch [81].
- Dissolution Method Changes: Modifications to dissolution methods and specifications while maintaining product quality [81].
- Formulation Changes: Certain changes in components or composition that might otherwise require clinical validation [1].
A survey of ANDA submissions revealed that out of 14 submissions containing IVIVC data, 4 were submitted in support of postapproval changes, 9 supported preapproval changes, and 1 was used to guide the development of the to-be-marketed formulation [81]. This distribution highlights the significant role of IVIVC throughout the product lifecycle, particularly during scale-up and post-approval phases.
Formulation Optimization and Quality Control
Beyond regulatory compliance, IVIVC provides powerful tools for formulation optimization and robust quality control strategies:
- Setting Clinically Relevant Specifications: IVIVC enables the establishment of dissolution specifications that are directly linked to in vivo performance, creating patient-centric quality standards [3].
- Reducing Batch Rejections: By defining a "safe space" for dissolution profiles, manufacturers can reduce batch rejections while ensuring therapeutic equivalence [3].
- Quality by Design (QbD) Integration: IVIVC can be integrated into the QbD framework to establish clinically meaningful specifications and control strategies [1].
- Troubleshooting Manufacturing Variability: When batch-to-batch variability occurs, IVIVC helps determine whether the variations are clinically significant [1].
For lamotrigine ER tablets, researchers established a Level A IVIVC that enabled the development of patient-centric quality standards without extensive clinical trials, demonstrating how IVIVC can streamline both development and post-approval changes [3].
Challenges and Future Perspectives
Despite its significant advantages, the implementation of IVIVC in SUPAC faces several challenges that impact its development, accuracy, and applicability.
Current Limitations
Several factors can limit the successful development and application of IVIVC:
- Physiological Variability: Human gastrointestinal physiology exhibits significant inter-individual variability, complicating predictions [2].
- Formulation Dependence: IVIVC is formulation-dependent; a correlation established for one formulation may not apply to others [2].
- Complex Drug Properties: Drugs with nonlinear absorption, significant first-pass metabolism, or active transport mechanisms are more difficult to correlate [2].
- Low Success Rate: FDA reviews revealed that only one out of 14 ANDA submissions with IVIVC data contained adequate information for approval within the first review cycle [81].
For complex formulations like lipid-based drug delivery systems, establishing IVIVC presents additional challenges due to the dynamic processes of lipid digestion, micelle formation, and lymphatic transport that are not easily captured by traditional dissolution tests [2]. Case studies on fenofibrate and cinnarizine highlighted instances where in vitro lipolysis data failed to predict in vivo performance, underscoring the need for more sophisticated models [2].
Emerging Technologies and Future Directions
Advanced technologies are being developed to enhance the predictive power of IVIVC:
- PBPK Modeling Integration: Combining IVIVC with physiologically based pharmacokinetic modeling creates more robust predictive tools for evaluating SUPAC changes [3].
- Artificial Intelligence: AI-driven analytics can analyze complex datasets to uncover patterns and improve prediction accuracy [1].
- Advanced In Vitro Models: Microfluidic systems and organ-on-a-chip technologies offer more physiologically relevant environments for dissolution testing [1].
- Machine Learning Applications: ML algorithms can help identify critical formulation and manufacturing parameters that impact in vivo performance [1].
The convergence of these advanced technologies with traditional IVIVC methodologies holds promise for expanding the application of IVIVC in SUPAC, particularly for complex dosage forms that currently present correlation challenges. As these approaches mature, they may enable more widespread implementation of IVIVC to support post-approval changes while maintaining assurance of product quality and performance.
IVIVC plays an indispensable role in the SUPAC framework by providing a scientific foundation for predicting the in vivo impact of manufacturing changes. The integration of well-established Level A correlations into regulatory submissions can significantly reduce the need for additional bioequivalence studies, streamlining post-approval changes while maintaining product quality and performance. Despite challenges in development and implementation, particularly for complex dosage forms, advances in PBPK modeling, biorelevant dissolution methods, and computational approaches continue to enhance the predictive power and regulatory acceptance of IVIVC. As pharmaceutical manufacturing evolves and lifecycle management becomes increasingly important, the strategic application of IVIVC in SUPAC will remain a critical component of efficient drug development and regulatory compliance.
The pursuit of accurate predictions of human pharmacokinetics, particularly the correlation between in vitro assays and in vivo bioavailability, remains a central challenge in drug development. Traditional reliance on animal models and isolated in vitro systems has been hampered by high costs, ethical concerns, and poor translatability to human outcomes [92]. Today, a powerful technological triad is emerging to address these limitations: Physiologically Based Pharmacokinetic (PBPK) modeling, Artificial Intelligence (AI), and Organ-on-a-Chip (OOC) platforms. This guide objectively compares the performance of these integrated technologies against traditional methods, providing experimental data and protocols to underscore their transformative potential in defining a new paradigm for in vitro-in vivo correlation (IVIVC).
Technology Performance Comparison: Integrated vs. Traditional Approaches
The table below provides a quantitative and qualitative comparison of the emerging integrated framework against conventional methodologies across key performance metrics.
Table 1: Performance Comparison of Traditional vs. Integrated Technologies in Bioavailability Prediction
| Feature | Traditional Methods (Animal Studies, Isolated Assays) | Integrated PBPK-AI-OOC Framework |
|---|---|---|
| Predictive Accuracy for Human PK | Often poor; cited as cause for ~16% of Phase I failures [92] | High; demonstrated clinical translatability (e.g., midazolam bioavailability prediction within clinical range) [92] |
| Key Supporting Data | Historical high attrition rates in clinical phases [92] | Peer-reviewed case studies (e.g., Abbas et al., 2025) showing accurate parameter estimation [92] |
| Regulatory Acceptance | Established but being phased out (e.g., FDA Modernization Act 2.0) [92] | Growing; PBPK used in 26.5% of FDA new drug approvals (2020-2024), particularly for DDI and special populations [93] |
| Ethical Considerations | High reliance on animal testing | Reduces and replaces animal studies [92] |
| Data Richness & Mechanism | Often limited, phenomenological | High, mechanistic; provides insights into saturation, non-linear behavior, and individual parameters (e.g., CLint, Papp) [92] |
| Cost & Time Efficiency | High cost and long duration [94] | Potential for significant reduction via virtual simulations and optimized experimental design [94] [92] |
Experimental Protocols for Technology Integration
The following detailed methodologies are cited from validation studies demonstrating the successful integration of these tools.
Protocol: Establishing IVIVR using PBPK for Vaginal Drug Products
This protocol, derived from a study on progesterone intravaginal rings, outlines the use of PBPK to develop an in vitro-in vivo relationship (IVIVR) [95].
- Objective: To develop and validate an IVIVR that simulates in vivo drug release from measured in vitro release profiles and to assess virtual bioequivalence (VBE).
- Materials & Methods:
- PBPK Platform: The Mechanistic Vaginal Absorption & Metabolism (MechVAM) model within the Simcyp Simulator was used [95].
- In Vitro Data: Measured in vitro release profiles of progesterone from intravaginal rings.
- Model Verification: The PBPK model was first verified by simulating clinical data from progesterone vaginal gel and ring formulations.
- IVIVR Development: The verified model was used to correlate in vitro release rates with simulated in vivo absorption.
- VBE Assessment: The validated IVIVR was applied to simulate clinical trials for two different progesterone rings, and the VBE results were compared with actual bioequivalence study outcomes [95].
- Key Outputs: A validated IVIVR for predicting in vivo performance and an established "dissolution safe space" (defined as -7.36% to +9.40% mg/day release) for post-approval changes [95].
Protocol: Integrating OOC with In Silico Modeling for Oral Bioavailability
This protocol is based on a peer-reviewed workflow for predicting the oral bioavailability of midazolam using a Gut/Liver-on-a-chip and computational modeling [92].
- Objective: To accurately estimate human oral bioavailability (F) and key ADME parameters from a single OOC experiment.
- Materials & Methods:
- OOC System: CN Bio's PhysioMimix Multi-organ Gut/Liver MPS.
- Experimental Procedure: Midazolam was introduced to the gut compartment. Samples were taken over 72 hours from both gut and liver compartments to measure concentration changes as the drug was absorbed and metabolized [92].
- Computational Modeling: A mathematical model describing drug movement was developed and fitted to the experimental data. Using Bayesian methods, key parameters were estimated with confidence intervals:
- CLint,liver & CLint,gut: Intrinsic clearance by liver and gut.
- Papp: Apparent permeability.
- Er: Efflux ratio.
- Bioavailability Calculation: The fractions absorbed (Fa), escaping gut metabolism (Fg), and escaping liver metabolism (Fh) were calculated from the model outputs. Oral bioavailability was estimated as F = Fa × Fg × Fh [92].
- Key Outputs: Estimated oral bioavailability of midazolam within the clinically observed range and a set of mechanistic ADME parameters for PBPK modeling [92].
Visualization of the Integrated Workflow
The following diagram, generated using DOT language, illustrates the logical workflow and data flow of the integrated system.
Diagram Title: Integrated Workflow for Bioavailability Prediction
The Scientist's Toolkit: Essential Research Reagent Solutions
The table below details key materials and tools essential for implementing the described integrated approach.
Table 2: Key Research Reagent Solutions for Integrated ADME Studies
| Item / Solution | Function / Description | Example Use Case |
|---|---|---|
| PhysioMimix Gut/Liver MPS | A microphysiological system (organ-on-a-chip) that co-cultures primary human gut and liver tissues to study intestinal absorption and hepatic metabolism in a dynamic, interconnected environment [92]. | Investigating first-pass metabolism and bioavailability of orally administered drugs like midazolam [92]. |
| Simcyp Simulator | A leading PBPK software platform with extensive physiological and genetic population libraries, used for predicting human pharmacokinetics, drug-drug interactions, and special population dosing [95] [96] [93]. | Establishing IVIVR for vaginal rings and simulating virtual bioequivalence [95]. |
| Bioavailability Assay Kit | All-in-one kits that provide the necessary hardware, consumables, and assay protocols to run specific MPS experiments, reducing the barrier to adoption [92]. | Standardized assessment of drug absorption and metabolism in the Gut/Liver model. |
| AI-Powered Digital Twin Generator | Software that uses AI to create virtual patient models simulating disease progression, which can be used as synthetic control arms in clinical trials [94]. | Reducing the size and cost of control arms in Phase III trials, especially in areas like Alzheimer's disease [94]. |
| PBPK Model Libraries | Curated databases within PBPK software containing population-specific parameters (e.g., for pediatrics, geriatrics, specific ethnicities, and organ impairment) [97] [96]. | Simulating drug exposure in vulnerable populations where clinical trials are ethically challenging or difficult. |
Quantitative Impact and Regulatory Adoption
The integration of these technologies is not merely theoretical but is having a tangible impact on drug development, as evidenced by regulatory submissions.
Table 3: PBPK Model Applications in FDA-Approved New Drugs (2020-2024) [93]
| Application Domain | Frequency (%) | Key Context |
|---|---|---|
| Drug-Drug Interaction (DDI) Assessment | 81.9% | The dominant application, primarily for enzyme-mediated (e.g., CYP3A4) and transporter-mediated (e.g., P-gp) interactions [93]. |
| Dosing in Organ Impairment | 7.0% | Guides dosing recommendations for patients with hepatic or renal impairment without requiring dedicated clinical trials [93]. |
| Pediatric Dosing Prediction | 2.6% | Leverages physiological differences to extrapolate adult data to pediatric populations [93]. |
| Overall Use in FDA Submissions | 26.5% | 65 of 245 new drug applications from 2020-2024 included PBPK models as pivotal evidence, with the highest use in Oncology (42%) [93]. |
The synergistic integration of PBPK modeling, AI, and Organ-on-a-Chip technologies represents a definitive frontier in drug development. As demonstrated by the experimental data and performance comparisons, this framework offers a more accurate, mechanistic, and human-relevant path to establishing robust in vitro-in vivo relationships. By leveraging OOC for high-quality human data generation, AI for parameter optimization and insight extraction, and PBPK for holistic human system prediction, researchers can de-risk development, reduce animal testing, and accelerate the delivery of safer and more effective therapeutics to patients.
Conclusion
The establishment of a robust IVIVC is a cornerstone of modern, efficient drug development, providing a critical bridge between laboratory data and clinical performance. Success hinges on a deep understanding of a drug's physicochemical and biopharmaceutical properties, the selection of biorelevant in vitro methods, and the application of sound mathematical modeling. While significant challenges remain—particularly for complex modalities like lipid-based systems, long-acting injectables, and LNPs—emerging technologies such as PBPK modeling, artificial intelligence, and advanced tissue-mimicking systems offer promising pathways to enhance predictive accuracy. By systematically addressing the foundational, methodological, and validation principles outlined in this article, researchers can harness the full potential of IVIVC to reduce animal and human testing, accelerate timelines, set clinically relevant specifications, and ultimately deliver safe and effective therapeutics to patients faster.
References
- 1. CMC Perspectives of In Vitro / In Vivo Correlation (IVIVC) ... [https://premier-research.com/perspectives/cmc-perspectives-of-in-vitro-in-vivo-correlation-ivivc-in-drug-development/]
- 2. Improving In Vitro–In Vivo Correlation (IVIVC) for Lipid ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12567226/]
- 3. Development of in vitro-in vivo correlation for establishing ... [https://www.sciencedirect.com/science/article/abs/pii/S0939641125002516]
- 4. Development of a Universal In Vivo Predictive Dissolution ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12505258/]
- 5. In vitro-in vivo correlation (IVIVC) development for long- ... [https://www.sciencedirect.com/science/article/abs/pii/S0168365924007661]
- 6. In vitro-In vivo Correlation: Perspectives on Model Development [https://pmc.ncbi.nlm.nih.gov/articles/PMC3099258/]
- 7. Four Levels of In-Vitro-In-Vivo Correlation | PPT [https://www.slideshare.net/slideshow/four-levels-of-invitroinvivo-correlation/55840876]
- 8. In Vitro–In Vivo Correlation (IVIVC) for SR Dosage Forms [https://pharmalesson.com/in-vitro-in-vivo-correlation-ivivc-for-sr-dosage-forms/]
- 9. a tailored approach to optimize DMPK properties of PROTACs [https://pubs.rsc.org/en/content/articlehtml/2025/md/d4md00854e?page=search]
- 10. Lipid-associated Oral Delivery: Mechanisms and Analysis of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5082615/]
- 11. Successful oral delivery of poorly water-soluble drugs both ... [https://www.sciencedirect.com/science/article/pii/S0928098719302301]
- 12. The effect of particle size on drug bioavailability in various ... [https://www.sciencedirect.com/science/article/pii/S2773216923000296]
- 13. The Biopharmaceutics Classification System: Subclasses for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4112588/]
- 14. Link between drug absorption solubility and permeability ... [https://www.sciencedirect.com/science/article/pii/S0022354915507041]
- 15. Food effects on gastrointestinal physiology and drug ... [https://www.sciencedirect.com/science/article/abs/pii/S1347436722000453]
- 16. Fast-Fed Variability: Insights into Drug Delivery, Molecular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9505616/]
- 17. Gastrointestinal Transit - an overview [https://www.sciencedirect.com/topics/biochemistry-genetics-and-molecular-biology/gastrointestinal-transit]
- 18. Importance of Considering Fed-State Gastrointestinal ... [https://link.springer.com/article/10.1007/s11095-024-03669-3]
- 19. 新型gut MPS/Fluid3D-X系统精准洞察药物肠道吸收,点亮 ... [https://news.bioon.com/article/95f485891ed9.html]
- 20. 在体单向肠灌流(SPIP)模型在口服药物肠道吸收研究中的应用 [https://dmpkservice.wuxiapptec.com/cn/blogs/153-id/]
- 21. 基于胃肠道生理模型的口服药物吸收预测 [https://manu41.magtech.com.cn/Jweb_clyl/CN/Y2010/V15/I6/656]
- 22. Biorelevant Dissolution Experiments [https://biorelevant.com/biorelevant-dissolution/buy/]
- 23. Gefitinib two stage dissolution comparison (Biorelevant vs ... [https://biorelevant.com/learning_center/gefitinib-two-stage-dissolution-comparison-biorelevant-vs-non-biorelevant/]
- 24. Dissolution and Drug Release Tests [https://www.usp.org/small-molecules/dissolution]
- 25. Evaluation of USP apparatus 3 for dissolution testing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2751286/]
- 26. Comparison of Cellular Monolayers and an Artificial ... [https://www.sciencedirect.com/science/article/pii/S0022354921004780]
- 27. Suitability of Artificial Membranes in Lipolysis-Permeation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7239831/]
- 28. Comparison of MDCK-MDR1 and Caco-2 Cell-Based ... [https://www.creative-bioarray.com/support/comparison-of-mdck-mdr1-and-caco-2-cell-based-permeability-assays.htm]
- 29. Comparison of Drug Permeabilities and BCS Classification [https://pmc.ncbi.nlm.nih.gov/articles/PMC2844511/]
- 30. Quantitative analysis of lab-to-lab variability in Caco-2 ... [https://www.sciencedirect.com/science/article/abs/pii/S0939641116305264]
- 31. Developing an in vitro lipolysis model for real-time analysis ... [https://www.sciencedirect.com/science/article/pii/S0928098723003093]
- 32. Evaluation of In Vitro Tools to Predict the In Vivo Absorption ... [https://www.sciencedirect.com/science/article/pii/S0022354922001575]
- 33. Comparison of Deconvolution-Based and Absorption ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4627461/]
- 34. Deconvolution and IVIVC: Exploring the Role of Rate-Limiting ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4779109/]
- 35. Convolution- and Deconvolution-Based Approaches for ... [https://link.springer.com/article/10.1208/s12249-022-02361-2]
- 36. Convolution-based approaches for in vivo-in vitro ... [https://pubmed.ncbi.nlm.nih.gov/9269483/]
- 37. Deconvolution [https://onlinehelp.certara.com/phoenix/8.2/topics/deconv.htm]
- 38. Level A IVIVC Deconvolution - GastroPlus® Documentation [https://gastroplus.slp-software.com/scientific-principles-guide/GPX.2/level-a-ivivc-deconvolution]
- 39. Convolution-based approach for modeling the ... [https://link.springer.com/article/10.1007/s10928-022-09835-7]
- 40. Novel convolution-based In vitro-In vivo correlation (IVIVC) ... [https://www.page-meeting.org/Abstracts/novel-convolution-based-in-vitro-in-vivo-correlation-ivivc-model-with-time-scaling-and-bioavailability-sub-models-for-jornay-pm-a-methylphenidate-hydrochloride-delayed-release-and-extended-r/]
- 41. The Deconvolution Revolution: Strategies for Target ... [https://momentum.bio/content/the-deconvolution-revolution-strategies-for-target-identification/]
- 42. Understanding Pharmaceutical Quality by Design - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4070262/]
- 43. What is Quality by Design for Optimization of Finished ... [https://www.zimlab.in/blog-posts/what-is-quality-by-design-qbd-for-optimization-of-finished-formulations]
- 44. QbD-based Formulation Optimization and Characterization of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8430414/]
- 45. Regulatory Experience with In Vivo In Vitro Correlations ... [https://pubmed.ncbi.nlm.nih.gov/27480319/]
- 46. IVIVC modelling can speed up the drug development process [https://www.biopharmaservices.com/blog/ivivc-modelling-can-speed-up-the-drug-development-process/]
- 47. Biowaiver based on biopharmaceutics classification system [https://www.sciencedirect.com/science/article/pii/S2773216923000181]
- 48. Development of a Physiologically Based Biopharmaceutics ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12135060/]
- 49. Self-Emulsifying Drug Delivery Systems (SEDDS) [https://pubmed.ncbi.nlm.nih.gov/39861711/]
- 50. In vitro and in vivo correlation for lipid-based formulations [https://www.sciencedirect.com/science/article/pii/S2211383521000976]
- 51. From Liquid SNEDDS to Solid SNEDDS: A Comprehensive ... [https://link.springer.com/article/10.1208/s12248-025-01167-x]
- 52. Comparative Study of Snedds and Sedds for Enhancing ... [https://www.orientjchem.org/vol41no4/comparative-study-of-snedds-and-sedds-for-enhancing-oral-delivery-of-vildagliptin/]
- 53. Quality by Design and In Silico Approach in SNEDDS ... [https://www.mdpi.com/1999-4923/17/6/701]
- 54. A dataset of formulation compositions for self-emulsifying ... [https://www.nature.com/articles/s41597-023-02812-w]
- 55. In Vitro-In Vivo Correlation for Complex Non-Oral Drug Products [https://pmc.ncbi.nlm.nih.gov/articles/PMC4739855/]
- 56. In Vitro Lipolysis Data Does Not Adequately Predict the In ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4012058/]
- 57. In vitro lipolysis data does not adequately predict the in ... [https://pubmed.ncbi.nlm.nih.gov/24687210/]
- 58. Challenges and Complications of Poly(lactic-co-glycolic acid) [https://pmc.ncbi.nlm.nih.gov/articles/PMC8955085/]
- 59. Recent Applications of PLGA in Drug Delivery Systems [https://www.mdpi.com/2073-4360/16/18/2606]
- 60. Machine learning models to accelerate the design of ... [https://www.nature.com/articles/s41467-022-35343-w]
- 61. Synthesis and performance optimization of multi-bioactive ... [https://www.nature.com/articles/s41598-025-25043-y]
- 62. Advanced In Vitro Models: Opportunities and Challenges ... [https://www.lek.com/insights/hea/us/ei/advanced-vitro-models-opportunities-and-challenges-drug-development]
- 63. PEGylated PLGA nanoparticles: unlocking advanced ... [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-025-02410-x]
- 64. The Prediction of the In Vitro Release Curves for PLGA-Based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12030581/]
- 65. Beyond Animals: Revolutionizing Drug Discovery with Human ... [https://wyss.harvard.edu/news/beyond-animals-revolutionizing-drug-discovery-with-human-relevant-models/]
- 66. Exploring the Challenges of Lipid Nanoparticle Development [https://pmc.ncbi.nlm.nih.gov/articles/PMC12031360/]
- 67. Exploring the Challenges of Lipid Nanoparticle Development [https://pubmed.ncbi.nlm.nih.gov/40333261/]
- 68. Investigating the stability of RNA-lipid nanoparticles in ... [https://www.sciencedirect.com/science/article/pii/S0168365925001683]
- 69. Protein corona formed on lipid nanoparticles compromises ... [https://www.nature.com/articles/s41467-025-63726-2]
- 70. A complete guide to understanding Lipid nanoparticles (LNP) [https://insidetx.com/resources/reviews/complete-guide-to-understanding-lipid-nanoparticles-lnp/]
- 71. Lipid Nanoparticles (LNPs): A complete guide for researchers [https://ozbiosciences.com/blog/lipid-nanoparticles-lnps-a-complete-guide-for-researchers-n107]
- 72. Review Lipid nanoparticles: Composition, formulation, and ... [https://www.sciencedirect.com/science/article/pii/S2329050125000580]
- 73. A careful look at lipid nanoparticle characterization [https://www.nature.com/articles/s41598-024-52685-1]
- 74. Accelerated in vitro release testing methods for extended ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3408959/]
- 75. Accelerated and Biopredictive In Vitro Release Testing ... [https://www.sciencedirect.com/science/article/abs/pii/S0022354924000571]
- 76. Accelerated and Biopredictive In Vitro Release Testing ... [https://pubmed.ncbi.nlm.nih.gov/38369022/]
- 77. Time Scaling for In Vitro-In Vivo Correlation: the Inverse ... [https://pubmed.ncbi.nlm.nih.gov/30159772/]
- 78. In vivo correlation models for in situ forming drug implants [https://www.sciencedirect.com/science/article/abs/pii/S0168365924004188]
- 79. In vitro-in vivo correlation (IVIVC) population modeling for ... [https://www.page-meeting.org/default.asp?abstract=8581]
- 80. Predictive Performance of Physiologically Based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5824104/]
- 81. Applications of In Vitro–In Vivo Correlations in Generic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4476988/]
- 82. Applications of In Vitro-In Vivo Correlations in Generic Drug ... [https://pubmed.ncbi.nlm.nih.gov/25896303/]
- 83. In vitro–In Vivo Correlations: Tricks and Traps - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3385821/]
- 84. A Perspective on Model-Informed IVIVC for Development of ... [https://link.springer.com/article/10.1007/s11095-023-03572-3]
- 85. In vitro–in vivo correlation for complex non-oral drug products [https://www.sciencedirect.com/science/article/abs/pii/S0168365915301528]
- 86. In vivo–In Vitro correlation (IVIVC) in drug development [https://wjarr.com/content/vivo%E2%80%93-vitro-correlation-ivivc-drug-development-bridging-preclinical-and-clinical-outcomes]
- 87. A survey on IVIVC/IVIVR development in the ... [https://www.sciencedirect.com/science/article/abs/pii/S0928098717301069]
- 88. Improving In Vitro–In Vivo Correlation (IVIVC) for Lipid- ... [https://www.mdpi.com/1999-4923/17/10/1310]
- 89. in vivo correlation of modified release oral formulations ... [https://www.sciencedirect.com/science/article/pii/S0939641124003059]
- 90. SUPAC-IR: Immediate-Release Solid Oral Dosage Forms ... [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/supac-ir-immediate-release-solid-oral-dosage-forms-scale-and-post-approval-changes-chemistry]
- 91. Scale-Up and Postapproval Changes in Orally Inhaled ... [https://pubmed.ncbi.nlm.nih.gov/39648823/?utm_source=FeedFetcher&utm_medium=rss&utm_campaign=None&utm_content=16koWIt7v5kNs8rDlsDGcQuYlCswHLvXS02M7qn1ETDmPUMcie&fc=None&ff=20241215171215&v=2.18.0.post9+e462414]
- 92. Blog | Integrating in silico tools with Organ-on-a-chip [https://cn-bio.com/integrating-in-silico-tools-with-organ-on-a-chip-to-advance-adme-studies/]
- 93. The Evolution and Future Directions of PBPK Modeling in ... [https://www.mdpi.com/1999-4923/17/11/1413]
- 94. How AI will reshape pharma in 2025 [https://www.drugtargetreview.com/article/154981/how-ai-will-reshape-pharma-by-2025/]
- 95. Demonstration of in vitroin vivo relationship (IVIVR) and ... [https://www.sciencedirect.com/science/article/abs/pii/S0022354925005003]
- 96. Application of Physiologically-Based Pharmacokinetic (PBPK ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12334468/]
- 97. Applications of PBPK Modeling to Estimate Drug Metabolism ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12473325/]