Colonic Fermentation of Undigested Food: Mechanisms, Metabolites, and Therapeutic Applications in Human Health
This article provides a comprehensive review of the colonic fermentation of undigested dietary components, a critical process shaping human metabolic health.
Colonic Fermentation of Undigested Food: Mechanisms, Metabolites, and Therapeutic Applications in Human Health
Abstract
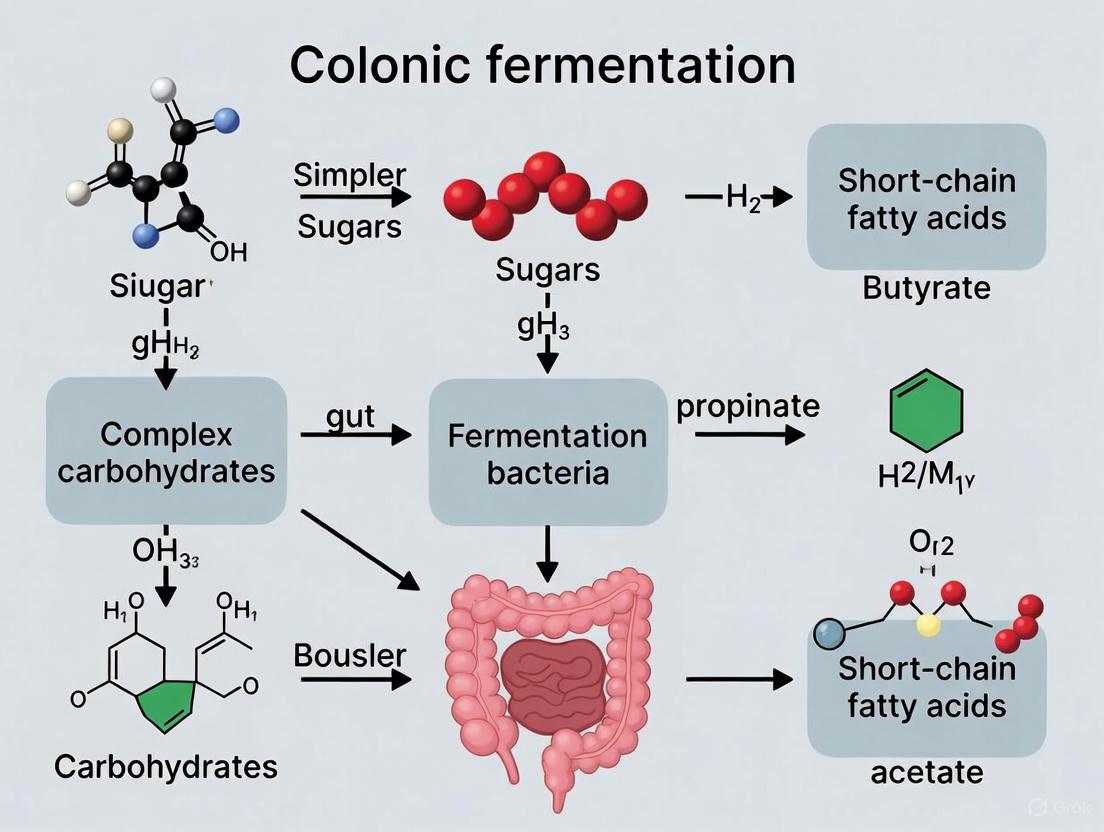
This article provides a comprehensive review of the colonic fermentation of undigested dietary components, a critical process shaping human metabolic health. It explores the foundational science of gut microbiota transforming fibers and resistant starches into key metabolites like short-chain fatty acids (SCFAs). The scope extends to established in vitro methodologies, such as the INFOGEST model, for studying these processes, and examines the challenges in translating research into targeted interventions. Finally, it synthesizes clinical evidence and comparative data on how fermented foods and specific microbial consortia modulate colonic fermentation, offering insights for developing microbiome-based therapeutics for conditions like colorectal cancer, metabolic disorders, and gastrointestinal diseases. This resource is tailored for researchers, scientists, and drug development professionals seeking to harness colonic fermentation for precision medicine.
The Gut as a Bioreactor: Unraveling the Science of Colonic Fermentation
The traditional view of digestion as a process governed solely by host-derived enzymes has been fundamentally redefined. Current scientific understanding reveals that intestinal metabolism is a complex, cooperative endeavor between the host and the vast community of microorganisms residing in the gastrointestinal tract—the gut microbiota [1]. This symbiotic relationship facilitates the breakdown of dietary components and xenobiotics through intricate and dynamic interactions between host epithelial cells and gut microbes [2]. Disruptions in this fragile equilibrium can lead to metabolic and gastrointestinal diseases, highlighting the profound significance of this host-microbe symbiosis for human health [2]. This whitepaper provides an in-depth technical overview of the core mechanisms governing intestinal metabolism and host-microbe relationships, framed within the context of colonic fermentation research.
The gut microbiota contributes a vast enzymatic repertoire that complements host capabilities, particularly in the fermentation of undigested food components that reach the colon. This collaborative processing generates a diverse array of metabolic products, including short-chain fatty acids (SCFAs), which serve as crucial energy sources and signaling molecules that influence systemic health [1] [3]. Understanding this sophisticated host-microbe symbiosis is essential for researchers and drug development professionals seeking to develop targeted interventions for metabolic disorders, inflammatory conditions, and other microbiota-associated diseases.
Core Concepts and Terminologies
Fundamental Definitions
- Intestinal Metabolism: The metabolic processes exclusively occurring within the intestines that facilitate the breakdown and absorption of dietary nutrients and xenobiotics, entailing a multifaceted interaction between the host and gut bacteria [2]. These processes include nutrient sensing, digestion, absorption, energy harvesting, detoxification, and immunomodulation.
- Host-Microbe Symbiosis: A mutually beneficial relationship between the host organism and the gut microbiota, where both parties derive advantages from coexistence, including metabolic cooperation, immune education, and niche specialization [4].
- Colonic Fermentation: The anaerobic breakdown of undigested dietary components, primarily nondigestible carbohydrates, by gut microbiota in the colon, producing SCFAs, gases, and other metabolites [3] [4].
- Gut Metabolome: The cumulative metabolites produced by intestine-specific metabolic processes, both host and microbe-derived, which regulate intestinal immunometabolic homeostasis [2].
- Microbiota-Accessible Carbohydrates (MACs): Complex dietary components, primarily fibers and resistant starches, that resist host enzyme digestion in the upper GI tract and become available for microbial fermentation in the colon [4].
Conceptual Models of Host-Microbe Metabolic Cooperation
Two primary frameworks describe the enzymatic interaction between host and microbiota in the gut ecosystem [1]:
- The "Duet" Model: Represents sequential or complementary enzymatic activities where host enzymes initiate digestion and microbial enzymes complete it, or vice versa. For example, salivary and pancreatic amylases hydrolyze starch to maltose and oligosaccharides, which are subsequently fermented by microbial glycoside hydrolases into SCFAs in the colon.
- The "Orchestra" Model: Envisions a highly coordinated, multi-layered interaction where host and microbial enzymes operate in a spatially and temporally regulated manner with complex feedback loops. An exemplary orchestra interaction involves bile acids secreted by the liver being modified by microbial bile salt hydrolases, which subsequently modulate bile acid signaling via nuclear receptors (FXR, TGR5), influencing host metabolism and immune responses.
Key Metabolic Processes in Host-Microbe Symbiosis
Carbohydrate Fermentation and SCFA Production
The fermentation of nondigestible carbohydrates represents a fundamental metabolic cooperation between host and microbiota. While host enzymes effectively digest simple sugars and easily accessible starches, complex dietary fibers resist host enzymatic degradation and reach the colon intact [4]. Here, gut microbiota—particularly species belonging to Bacteroides, Roseburia, Faecalibacterium, and Bifidobacterium—deploy an extensive arsenal of carbohydrate-active enzymes (CAZymes) to break down these complex substrates [1].
The principal products of this saccharolytic fermentation are short-chain fatty acids (SCFAs), primarily acetate, propionate, and butyrate, typically present in molar ratios ranging from 3:1:1 to 10:2:1 [3]. These SCFAs serve distinct but complementary physiological roles:
- Butyrate: Serves as the primary energy source for colonocytes, exhibits anti-inflammatory properties, and regulates gene expression through inhibition of histone deacetylases [3].
- Propionate: Transferred to the liver where it participates in gluconeogenesis and satiety signaling through interaction with GPR41 and GPR43 receptors [3].
- Acetate: The most abundant SCFA, serves as an essential co-factor for microbial cross-feeding and influences cholesterol metabolism and central appetite regulation [3].
Table 1: Primary Short-Chain Fatty Acids and Their Physiological Roles
| SCFA | Primary Producers | Receptors | Major Physiological Functions | Dysregulation Implications |
|---|---|---|---|---|
| Butyrate | Faecalibacterium prausnitzii, Lachnospiraceae, Roseburia spp. | GPR109a, GPR41 | Primary energy source for colonocytes; anti-inflammatory; histone deacetylase inhibitor; promotes gut barrier function | Reduced levels associated with IBD, colitis, and metabolic syndrome |
| Propionate | Bacteroides spp., Negativicutes, some Clostridium clusters | GPR41, GPR43 | Hepatic gluconeogenesis precursor; satiety signaling; cholesterol synthesis regulation | Impaired glucose homeostasis; disrupted energy balance |
| Acetate | Many commensal bacteria including Bifidobacterium spp. | GPR43 | Substrate for other bacteria; cholesterol metabolism and lipogenesis; central appetite regulation | Altered microbial composition; metabolic dysfunction |
Protein and Amino Acid Metabolism
When carbohydrate availability is limited, gut microbiota shift toward proteolytic fermentation, breaking down dietary and endogenous proteins that escape host digestion [3]. Specific Bacteroidetes and Firmicutes species ferment amino acids, producing both SCFAs and various potentially detrimental metabolites:
- Propionate production from aspartate, alanine, threonine, and methionine [3]
- Butyrate production from glutamate, lysine, histidine, cysteine, serine, and methionine [3]
- Generation of branched-chain fatty acids, ammonia, amines, phenols, and indoles
This metabolic flexibility allows the microbiota to maintain metabolic activity during periods of dietary carbohydrate restriction, though excessive proteolytic fermentation has been associated with mucosal inflammation and gut barrier dysfunction.
Bile Acid Metabolism
Bile acid transformation represents a quintessential example of host-microbe co-metabolism. Primary bile acids synthesized in the liver from cholesterol are conjugated to glycine or taurine before secretion into the intestine [1]. Gut microbes, particularly Clostridium and Bacteroides species, express bile salt hydrolases (BSH) that deconjugate these primary bile acids [2]. Further microbial modifications generate a diverse array of secondary bile acids that function as important signaling molecules through activation of nuclear receptor FXR and membrane receptor TGR5, influencing lipid metabolism, glucose homeostasis, and immune function [2] [1].
Bioactivation of Dietary Phytochemicals
Gut microbiota significantly expand the host's metabolic capabilities by transforming dietary polyphenols and other phytochemicals into more bioavailable and active metabolites [1]. For instance, microbial communities convert glucoraphanin from cruciferous vegetables into isothiocyanate sulforaphane, a potent antioxidant and chemopreventive compound [1]. Similarly, complex polyphenols from fruits, vegetables, and tea undergo microbial biotransformation into simpler phenolic acids with enhanced bioavailability and biological activity, substantially contributing to their documented health benefits.
Table 2: Microbial Metabolic Capabilities and Health Implications
| Metabolic Process | Key Bacterial Taxa | Major Products | Health Implications | Associated Pathways |
|---|---|---|---|---|
| Fiber Fermentation | Faecalibacterium, Roseburia, Bacteroides, Bifidobacterium | SCFAs (acetate, propionate, butyrate) | Gut health, reduced inflammation, improved glucose metabolism | GPR41, GPR43 signaling |
| Bile Acid Transformation | Clostridium, Bacteroides | Secondary bile acids | Lipid digestion, vitamin absorption, metabolic regulation | FXR, TGR5 signaling |
| Vitamin Synthesis | Bacteroides, Bifidobacterium | Vitamins K, B12, others | Coagulation, energy production, neural function | Various metabolic pathways |
| Polyphenol Metabolism | Lactobacillus, Bifidobacterium | Bioactive phenolic compounds | Antioxidant, anti-inflammatory effects | Antioxidant response elements |
| Choline Metabolism | Desulfovibrio, Bacteroides | TMA, TMAO | Cardiovascular risk modulation | Conversion to TMA/TMAO |
| Tryptophan Metabolism | Escherichia, Bacteroides | Indole derivatives | Immune function, gut barrier integrity | Aryl hydrocarbon receptor |
Methodologies for Studying Host-Microbe Metabolic Interactions
Experimental Models and Systems
Research into host-microbe symbiosis employs a hierarchical approach utilizing multiple complementary model systems, each with distinct advantages and limitations for investigating specific aspects of intestinal metabolism.
In Vitro Systems
- Batch Culture Fermenters: Simple, reproducible systems using fecal inocula in defined media to study specific metabolic pathways under controlled conditions [3]. Useful for preliminary screening of substrate utilization and metabolite production.
- Continuous Culture Gut Models: Multi-chambered systems (e.g., SHIME, TIM-2) that simulate different regions of the human gastrointestinal tract, maintaining complex microbial communities for extended periods [3]. These models enable investigation of microbial community dynamics and metabolic responses to dietary interventions.
- Intestinal Organoids: Three-dimensional structures derived from intestinal stem cells that recapitulate key aspects of intestinal architecture and function [2]. As demonstrated by Dougherty et al., treatment of organoids with filtered fecal supernatants from infants revealed that microbial metabolites promote enterocyte proliferation and maturation, indicating that varied microbiota generates metabolites facilitating intestinal epithelial development [2].
In Vivo Models
- Germ-Free (GF) Mice: Raised in sterile isolators without any microorganisms, providing a blank slate for assessing microbial contributions to intestinal metabolism [2]. GF mice exhibit substantially altered intestinal development and metabolism compared to conventional counterparts, highlighting the essential role of microbiota in digestive processes [2].
- Human Microbiota-Associated (HMA) Mice: Germ-free mice colonized with human donor microbiota, enabling investigation of specific microbial communities in a controlled animal model [3].
- Antibiotic-Treated Mice: Animals treated with broad-spectrum antibiotics to deplete gut microbes, resulting in altered luminal metabolite profiles, mucosal metabolic signaling, and colonocyte transcriptome and metabolism [2]. This model helps elucidate the metabolic consequences of microbial depletion.
Analytical Approaches
- Metagenomics: High-throughput sequencing of total microbial DNA to determine taxonomic composition and genetic potential of the gut microbiome [3]. Reveals the presence of genes encoding specific metabolic enzymes.
- Metatranscriptomics: RNA sequencing to assess actively expressed genes and metabolic pathways under different physiological conditions [1].
- Metabolomics: Comprehensive profiling of metabolites in fecal, luminal, or systemic samples using mass spectrometry or NMR spectroscopy [1] [3]. Directly measures the metabolic output of host-microbe interactions.
- Targeted Functional Gene Analysis: Primer-based approaches targeting key metabolic genes (e.g., for butyrate synthesis pathways) to enumerate functional microbial groups beyond phylogenetic identification [3].
Detailed Experimental Protocol: SCFA Production from Dietary Fiber Fermentation
Objective: To quantify and characterize short-chain fatty acid production from microbial fermentation of specific nondigestible carbohydrates using an in vitro batch culture system.
Materials and Reagents:
- Anaerobic workstation (e.g., Coy Laboratory Products)
- Phosphate-buffered saline (PBS, pH 7.4)
- Defined medium for gut microbiota (e.g., YCFA or similar)
- Substrate carbohydrates (e.g., fructo-oligosaccharides, arabinoxylan, resistant starch)
- Fresh fecal samples from healthy human donors (collected anaerobically)
- Gas chromatography system with flame ionization detector (GC-FID) or mass spectrometer (GC-MS)
- DNA/RNA extraction kits
- PCR reagents for functional gene analysis
Procedure:
- Sample Collection and Preparation: Collect fresh fecal samples from healthy human donors (n=minimum 5) under anaerobic conditions. Homogenize samples in pre-reduced PBS (1:10 w/v) and filter through sterile mesh to remove large particles.
- Inoculum Preparation: Combine equal volumes of filtered fecal slurry from multiple donors to create a pooled inoculum. Alternatively, maintain donor-specific inocula for personalized response assessment.
- Fermentation Setup: In anaerobic chamber, aliquot 10 mL of defined medium into sterile fermentation vessels. Add test substrates at physiological concentrations (e.g., 1% w/v). Include negative controls (no substrate) and positive controls (known fermentable carbohydrate).
- Inoculation and Incubation: Inoculate vessels with 1 mL of fecal slurry (final concentration 10% v/v). Seal vessels with butyl rubber stoppers to maintain anaerobiosis. Incubate at 37°C with constant agitation (150 rpm) for 24-48 hours.
- Sample Collection: At predetermined timepoints (e.g., 0, 6, 12, 24, 48h), aseptically remove 1 mL aliquots for:
- SCFA analysis: Centrifuge at 13,000 × g for 10 min, collect supernatant, acidify with 1% formic acid, store at -80°C until analysis
- Microbial composition: Pellet cells for DNA extraction and 16S rRNA gene sequencing
- Functional gene expression: Preserve samples in RNA stabilization reagent for transcriptomic analysis
- SCFA Analysis by GC-FID:
- Derivatize samples with N-methyl-N-(tert-butyldimethylsilyl)trifluoroacetamide
- Separate using DB-FFAP column (30 m × 0.25 mm × 0.25 μm)
- Employ temperature program: 80°C for 1 min, ramp to 120°C at 10°C/min, then to 240°C at 20°C/min, hold for 5 min
- Quantify acetate, propionate, butyrate, and branched-chain fatty acids against external calibration standards
- Microbial Community Analysis:
- Extract DNA using commercial kits with bead-beating step
- Amplify V4 region of 16S rRNA gene with dual-indexed primers
- Sequence on Illumina MiSeq platform (2×250 bp)
- Process data using QIIME2 or similar pipeline
- Functional Gene Quantification:
- Design primers targeting key butyrate synthesis genes (but, buk) and propionate pathways
- Perform quantitative PCR with SYBR Green chemistry
- Normalize to 16S rRNA gene copies
Data Analysis:
- Calculate SCFA production rates and yields relative to substrate consumed
- Determine correlations between specific microbial taxa and metabolite production
- Assess changes in microbial diversity (α- and β-diversity metrics)
- Integrate metabolite production with functional gene abundance
The Scientist's Toolkit: Essential Research Reagents and Models
Table 3: Essential Research Materials for Investigating Host-Microbe Symbiosis
| Category | Specific Reagents/Models | Key Applications | Technical Considerations |
|---|---|---|---|
| In Vitro Models | SHIME (Simulator of Human Intestinal Microbial Ecosystem), TIM-2, Intestinal organoids | Study of microbial community dynamics, substrate utilization, host-microbe interactions | Requires specialized equipment; organoids need stem cell isolation and 3D culture expertise |
| Animal Models | Germ-free mice, Human microbiota-associated mice, Antibiotic-treated mice | Investigation of causal relationships in host-microbe interactions | GF facilities expensive; HMA mice require human donor screening; antibiotic cocktails must be validated |
| Molecular Biology Tools | 16S rRNA gene primers (V3-V4 region), Metagenomic sequencing kits, RNA stabilization reagents | Microbial community profiling, functional potential assessment, gene expression studies | Primer selection affects taxonomic resolution; rapid RNA preservation critical for accurate transcriptomics |
| Metabolite Analysis | GC-MS/FID systems, LC-MS platforms, NMR spectroscopy | Quantification of SCFAs, bile acids, neurotransmitters, other microbial metabolites | Derivatization often needed for volatile compounds; authentic standards required for quantification |
| Specialized Reagents | Defined media for gut microbiota (YCFA), Bile acid standards, SCFA calibration mixes | Cultivation of fastidious anaerobes, metabolite identification and quantification | Media must be pre-reduced for anaerobic work; standard purity critical for accurate quantification |
| Cell Culture Systems | Caco-2 cells, HT-29-MTX cells, Primary intestinal epithelial cells | Assessment of host responses to microbial metabolites, barrier function studies | Differentiation time varies; primary cells have limited lifespan and donor variability |
Signaling Pathways in Host-Microbe Communication
The continuous dialogue between gut microbiota and the host occurs through multiple sophisticated signaling pathways that translate microbial metabolic activities into host physiological responses. Three particularly significant pathways include SCFA receptor signaling, bile acid receptor activation, and enterocrine signaling.
SCFA Signaling Through G-Protein Coupled Receptors
SCFAs produced through microbial fermentation act as signaling molecules primarily through the G-protein coupled receptors (GPCRs) GPR41 (FFAR3) and GPR43 (FFAR2) [2] [3]. Butyrate also signals through GPR109a. Receptor activation triggers intracellular cascades that influence numerous physiological processes:
- GPR43 Activation: Predominantly by acetate and propionate, leading to enhanced expression of peptide YY (PYY) and glucagon-like peptide-1 (GLP-1), promoting satiety and glucose homeostasis [3].
- GPR41 Activation: Primarily by propionate, resulting in sympathetic nervous system modulation and energy expenditure regulation [3].
- GPR109a Activation: By butyrate, inducing anti-inflammatory responses in colonic macrophages and dendritic cells, and promoting regulatory T-cell differentiation [3].
Bile Acid Signaling Through Nuclear Receptors
Microbial transformation of primary bile acids into secondary bile acids creates potent signaling molecules that activate the nuclear farnesoid X receptor (FXR) and membrane receptor TGR5 [2] [1]. These signaling pathways exert profound effects on host metabolism:
- FXR Activation: Regulates bile acid synthesis, lipid metabolism, and glucose homeostasis through modulation of gene expression networks in the liver and intestine [1].
- TGR5 Activation: Stimulates GLP-1 secretion in intestinal L-cells, enhances energy expenditure in brown adipose tissue, and exerts neuroprotective effects [1].
Microbial Influence on Enterocrine Signaling
Gut microbes significantly influence the production of enterocrine hormones through multiple direct and indirect mechanisms [2]. Microbial metabolites including SCFAs, secondary bile acids, and indole derivatives stimulate enteroendocrine cells to secrete hormones such as GLP-1, PYY, and serotonin (5-HT), which regulate gastrointestinal motility, appetite, glucose homeostasis, and mood [2].
Implications for Drug Development and Therapeutic Interventions
The intricate metabolic interplay between host and microbiota presents numerous promising targets for therapeutic intervention in metabolic, inflammatory, and neoplastic diseases.
Microbiota-Targeted Therapeutics
- Next-Generation Probiotics: Moving beyond traditional Lactobacillus and Bifidobacterium strains to include species such as Akkermansia muciniphila (mucin degradation), Faecalibacterium prausnitzii* (butyrate production), and defined consortia targeting specific metabolic deficiencies [5].
- Prebiotic Strategies: Targeted supplementation with specific nondigestible carbohydrates (e.g., arabinoxylan oligosaccharides, resistant starch, fructo-oligosaccharides) to selectively stimulate growth of beneficial taxa and enhance production of health-promoting metabolites like butyrate [5] [4].
- Synbiotic Approaches: Rational combinations of prebiotics and probiotics designed to work synergistically, such as pairing Bifidobacterium strains with fructo-oligosaccharides that they efficiently utilize [6].
- Postbiotic Formulations: Administration of microbial metabolites themselves (e.g., SCFAs, secondary bile acids) or inactivated microbial cells to bypass the need for live microorganisms while still delivering beneficial effects [1].
Precision Nutrition Approaches
The understanding that individuals harbor unique microbial communities with distinct metabolic capabilities enables development of personalized nutritional strategies [5]. This includes dietary recommendations tailored to an individual's microbial composition and functional capacity, potentially determined through metagenomic sequencing and metabolomic profiling [5]. For instance, individuals with high abundance of Bacteroides species may respond differently to dietary interventions than those dominated by Prevotella, allowing for more effective, personalized dietary recommendations for metabolic disease management.
Drug Metabolism Considerations
The gut microbiota significantly influences the metabolism and efficacy of numerous pharmaceutical compounds, opening avenues for microbiome-informed drug development [2] [1]. Strategies include:
- Screening new chemical entities for microbial metabolism
- Developing microbiome-compatible formulations that maintain efficacy despite microbial transformation
- Considering an individual's microbial metabolic capacity when prescribing drugs subject to significant microbial metabolism
- Utilizing microbial enzymes for targeted drug activation in the colon
The paradigm of intestinal metabolism has evolved from a host-centric process to a sophisticated collaborative system between host and microbiota. This host-microbe symbiosis, particularly through colonic fermentation of undigested food components, profoundly influences not only gastrointestinal health but also systemic metabolic homeostasis, immune function, and even neurological processes. The intricate enzymatic cooperation between host and microbiota—conceptualized as both "duet" and "orchestra"—generates a diverse metabolome that serves as a key interface between diet, microbiota, and host physiology.
Ongoing research in this field continues to unravel the complex mechanisms underlying host-microbe metabolic interactions, providing unprecedented opportunities for therapeutic intervention. From next-generation probiotics and precision nutrition to microbiome-informed drug development, leveraging this symbiotic relationship holds tremendous promise for addressing the growing burden of metabolic, inflammatory, and neoplastic diseases. As methodologies advance and our understanding deepens, targeting the gut microbiota and its metabolic output will undoubtedly play an increasingly prominent role in both preventive medicine and therapeutic strategies.
The human colonic microbiota, a complex ecosystem comprising over 1000 bacterial species, possesses an extensive metabolic repertoire that is distinct from but complementary to mammalian enzymes [3]. This microbial community plays an indispensable role in host health through the fermentation of undigested dietary components, primarily driven by specific functional groups including lactic acid bacteria (LAB) and butyrate-producing bacteria [3] [7]. The metabolic activities of these key microbial players result in the production of short-chain fatty acids (SCFAs)—particularly acetate, propionate, and butyrate—which exert profound effects on host physiology, including energy homeostasis, anti-inflammatory responses, and anti-carcinogenic activity [3] [8]. Understanding the intricate relationships between these microbial groups, their metabolic cross-feeding, and the environmental factors that shape their activities is fundamental to advancing research in colonic fermentation and its implications for human health and disease [7].
The human colon hosts a diverse microbial community dominated by four main bacterial phyla: Firmicutes, Bacteroidetes, Actinobacteria, and Proteobacteria [8]. Within this ecosystem, specific functional groups perform specialized metabolic roles in the breakdown of undigested food components that escape host digestion in the upper gastrointestinal tract [3]. The colonic microbiota's gene set, or microbiome, is estimated at approximately 3 million genes—150 times larger than the human genome—providing an extensive enzymatic capability that complements human physiology [3].
Research comparing germ-free and conventional animals, along with in vitro human fecal incubations, has demonstrated the critical importance of these microbial communities in host metabolism [3]. The microbial fermentation of dietary fibers and resistant starches represents a fundamental process for energy harvest in the colon, with the metabolic outputs having systemic effects on host health [3] [7]. More recently, evidence has accumulated implicating the gut microbiota in various conditions including obesity, diabetes, inflammatory bowel disease (IBD), and irritable bowel syndrome (IBS) [3]. This review will focus on the key microbial players involved in these processes, with particular emphasis on lactic acid bacteria as primary fermenters and butyrate-producing bacteria as critical contributors to gut health.
Key Microbial Players and Their Metabolic Pathways
Lactic Acid Bacteria: Primary Fermenters
Lactic acid bacteria (LAB), including genera such as Lactobacillus, Streptococcus, Lactococcus, and Pediococcus, typically belong to the Firmicutes and Actinobacteria phyla [9]. These bacteria are often considered primary fermenters, capable of initiating the breakdown of dietary carbohydrates into intermediate products including lactate, acetate, and ethanol [3]. In traditional fermented foods, these same bacterial groups drive the fermentation process and may act as probiotics when consumed, potentially inhibiting pathogenic microorganisms and contributing to host gut health [9].
LAB play a crucial role in shaping the gut environment through acid production, which lowers pH and creates selective pressure for other microbial community members [7]. However, lactate is typically present at negligible levels in adult feces due to extensive utilization by other bacteria, except in certain pathological conditions such as ulcerative colitis where it can be detected in significantly higher amounts [3]. This observation highlights the importance of metabolic cross-feeding relationships between LAB and other bacterial groups in maintaining gut homeostasis.
Butyrate-Producing Bacteria: Key Health-Promoting Metabolites
Butyrate-producing bacteria are predominantly found within the Firmicutes phylum, including some Lachnospiraceae and Faecalibacterium prausnitzii [3]. Butyrate is arguably the most important SCFA for human health, serving as the primary energy source for colonocytes and exhibiting anti-cancer activity through its ability to induce apoptosis of colon cancer cells and regulate gene expression by inhibiting histone deacetylases [3]. There is also evidence that butyrate can activate intestinal gluconeogenesis via a cAMP-dependent mechanism with beneficial effects on glucose and energy homeostasis [3].
Butyrate production occurs mainly through two metabolic pathways identified by Louis and colleagues [3]. Genomic analyses have revealed that butyrate production capability is distributed across multiple bacterial taxa without strict phylogenetic consistency, necessitating functional gene approaches rather than 16S rRNA analysis alone to enumerate these important bacterial groups [3]. Butyrate can be produced directly from carbohydrate fermentation or through cross-feeding interactions where bacteria utilize intermediates such as lactate and acetate produced by other community members [7].
Cross-Feeding Dynamics and Metabolic Interactions
Cross-feeding represents a fundamental ecological principle within gut microbial communities, where metabolic products of one bacterium serve as substrates for another. These interactions significantly influence the final SCFA profile and overall gut environment [3]. For example, lactate produced by Bifidobacterium longum during growth on fructo-oligosaccharides (FOS) completely disappears in co-culture with Eubacterium hallii, replaced by significant butyrate production—despite the fact that E. hallii alone cannot utilize the carbohydrate substrate [3].
Similarly, growth of Roseburia intestinalis on FOS is stimulated by acetate, and in co-culture with B. longum, growth of R. intestinalis is delayed until sufficient acetate produced by B. longum accumulates in the growth medium [3]. These cross-feeding relationships create metabolic interdependence among gut microbes, contributing to community stability and functional redundancy.
Table 1: Key Microbial Functional Groups in Colonic Fermentation
| Microbial Group | Representative Genera | Primary Metabolic Outputs | Functional Role |
|---|---|---|---|
| Lactic Acid Bacteria (LAB) | Lactobacillus, Streptococcus, Lactococcus, Pediococcus | Lactate, acetate, ethanol [3] [9] | Primary fermentation, pH reduction, pathogen inhibition [9] |
| Butyrate Producers | Faecalibacterium, Roseburia, Eubacterium, Lachnospiraceae members | Butyrate, acetate, CO₂ [3] [7] | Colonocyte energy source, anti-inflammatory, anti-carcinogenic [3] |
| Acetate Producers | Many bacterial groups including Bifidobacterium | Acetate [3] | Universal metabolite, precursor for butyrogenesis, cholesterol metabolism [3] |
| Propionate Producers | Bacteroides, Negativicutes, some Clostridium | Propionate, acetate, succinate [3] | Gluconeogenesis, satiety signaling [3] |
| Lactate-Utilizing Bacteria | Eubacterium hallii, Anaerositpes caccae | Butyrate, propionate [7] | Lactate conversion to other SCFAs, pH regulation [7] |
Quantitative Analysis of Microbial Metabolites
Short-Chain Fatty Acid Profiles and Ratios
The three most abundant SCFAs detected in feces are acetate, propionate, and butyrate, normally present in molar ratios ranging from 3:1:1 to 10:2:1 [3]. These ratios are consistent with values observed within the intestine in sudden death victims [3]. Each of these primary SCFAs performs distinct roles in human physiology:
Acetate: The most abundant SCFA, serves as an essential co-factor/metabolite for the growth of other bacteria (e.g., Faecalibacterium prausnitzii requires acetate for growth) [3]. Within the human body, acetate is transported to peripheral tissues and used in cholesterol metabolism and lipogenesis, and recent evidence from mouse studies indicates it plays a significant role in central appetite regulation [3].
Propionate: Serves as an energy source for epithelial cells and is transported to the liver where it participates in gluconeogenesis [3]. It is increasingly recognized as an important molecule in satiety signaling due to interaction with gut receptors (GPR41 and GPR43, also known as FFAR3 and FFAR2), which may activate intestinal gluconeogenesis [3].
Butyrate: Forms the key energy source for human colonocytes and has potential anti-cancer activity [3]. Butyrate also regulates gene expression by inhibiting histone deacetylases and activates intestinal gluconeogenesis via a cAMP-dependent mechanism [3].
The Butyrate Shift Phenomenon
Recent analyses of human volunteer studies have established that the proportions of SCFAs in fecal samples significantly shift toward butyrate as the overall concentration of SCFAs increases [7]. This "butyrate shift" has important implications for gut health, as butyrate plays a key role in maintaining colonic epithelium and exhibits anti-inflammatory effects [7]. Multiple factors may contribute to this phenomenon, including:
- Selection for butyrate-producing bacteria by certain types of dietary fiber
- Additional butyrate formation from lactate and acetate via cross-feeding
- Impact of decreased pH in the proximal colon as SCFA concentrations increase [7]
A mildly acidic pH has been shown to significantly impact microbial competition and the stoichiometry of butyrate production, creating conditions that favor butyrate-producing bacteria [7].
Table 2: Short-Chain Fatty Acid Characteristics and Physiological Roles
| SCFA | Typical Molar Ratio | Primary Producers | Major Physiological Roles | Health Implications |
|---|---|---|---|---|
| Acetate | 60% (3-10 in ratio) [3] | Many bacterial groups [3] | Cholesterol metabolism, lipogenesis, appetite regulation [3] | Essential co-factor for other bacteria; peripheral tissue metabolism [3] |
| Propionate | 20% (1-2 in ratio) [3] | Bacteroides species, Negativicutes, some Clostridium [3] | Gluconeogenesis, satiety signaling [3] | GPR41/43 activation; intestinal gluconeogenesis activation [3] |
| Butyrate | 20% (1 in ratio) [3] | Faecalibacterium prausnitzii, Lachnospiraceae, Roseburia [3] | Colonocyte energy, histone deacetylase inhibition, apoptosis induction [3] | Anti-cancer, anti-inflammatory, energy homeostasis [3] [7] |
Experimental Models and Methodologies
In Vitro Fermentation Models
Studying variations in the gut microbiota via in vivo methods is often restricted for ethical and safety reasons, making in vitro digestion models valuable tools for investigating the effects of food on the microbiome and related metabolite production [9]. These models range from complex automated dynamic systems to simple static models, all aiming to mimic human and animal digestion. Protocols validated by the INFOGEST static digestion and fermentation model are widely recommended for studying the characteristics of food matrices [9].
The INFOGEST model can be used to complement outcomes from advanced dynamic computerized models such as the Simulator of Human Intestinal Microbial Ecosystem (SHIME) and the TNO Intestinal Model (TIM) [9]. These systems allow researchers to investigate microbial community dynamics and metabolite production under controlled conditions that simulate different regions of the gastrointestinal tract.
Methodological Workflow for In Vitro Colonic Fermentation
The following diagram illustrates a typical experimental workflow for studying microbial fermentation using in vitro models:
Experimental Workflow for In Vitro Fermentation
This workflow typically begins with stool sample collection from human donors, followed by treatment preparation (e.g., test substrates, positive controls like fructooligosaccharides, and negative controls like sterile water) [9]. Samples undergo simulated digestion using the INFOGEST protocol before anaerobic incubation for 24 hours with stool inoculum [9]. Post-incubation, genomic DNA is extracted for bacterial composition analysis via 16S rRNA gene sequencing of the V3-V4 hypervariable region, while supernatants are collected for SCFA analysis using gas chromatography or mass spectrometry techniques [9].
Molecular and 'Omics Approaches
Advanced molecular techniques have revolutionized our ability to study gut microbial communities and their functional capacities. While 16S rRNA gene sequencing provides information about bacterial composition, it reveals little about metabolic activities [3]. Targeted approaches focusing on key metabolic genes offer more functional insights.
Primers designed against key genes in butyrate and propionate production pathways can help enumerate functional groups of bacteria in different cohorts [3]. This functional gene approach may prove more useful than 16S rRNA analysis alone for understanding fluctuations in metabolic activities. Additionally, metagenomic screening of bacterial genomes has identified numerous species containing butyrate production pathways, with no consistency within families, further supporting the need for functional rather than purely phylogenetic analyses [3].
Butyrate Signaling and Host Interactions
Butyrate and other SCFAs exert profound effects on host physiology through multiple signaling pathways. The following diagram illustrates key molecular mechanisms through which butyrate influences host cellular processes:
Butyrate Signaling Pathways and Host Mechanisms
Butyrate regulates the expression of 5-20% of human genes through multiple mechanisms [8]. In colonic cell lines, at low concentrations (0.5 mM), 75% of the upregulated genes are dependent on ATP citrate lyase activity, while at high concentrations (5 mM), this proportion reverses, with 75% becoming independent of this enzyme [8]. This concentration-dependent shift in gene regulation mechanisms underscores the complexity of butyrate's effects on host cellular processes.
Through their capacity to modulate gene expression, SCFAs play pivotal roles in regulating critical cellular processes including proliferation and differentiation, highlighting their importance in maintaining tissue homeostasis, supporting development, and potentially influencing disease progression [8].
Research Reagent Solutions for Microbial Fermentation Studies
Table 3: Essential Research Reagents for Colonic Fermentation Studies
| Reagent Category | Specific Examples | Experimental Function | Research Applications |
|---|---|---|---|
| Digestive Enzymes | Porcine pepsin (P6887), Porcine pancreatin (P7545), Human salivary amylase (A1031) [9] | Simulate human gastrointestinal digestion in INFOGEST model [9] | In vitro digestion preceding colonic fermentation [9] |
| Bile Salts & Digestive Components | Sodium taurodeoxycholate, Bovine blood hemoglobin, Trichloroacetic acid [9] | Emulate intestinal environment for lipid digestion and protein breakdown [9] | Physiological relevance in digestion models [9] |
| SCFA Standards | Acetate, propionate, isobutyrate, butyrate, formate, lactate standards [9] | Quantitative calibration for chromatographic analysis of fermentation products [9] | SCFA quantification via GC/MS or HPLC [9] |
| Prebiotic Controls | Fructooligosaccharides (F8052), Peptone from potatoes [9] | Positive control substrates for microbial fermentation studies [9] | Comparison of test substrates to known fermentable compounds [9] |
| Biochemical Assays | 3,5-dinitrosalicylic acid, Maltose standard, Phosphocreatine disodium salt [9] | Quantification of carbohydrate utilization and metabolic activity [9] | Monitoring fermentation progress and microbial activity [9] |
| Buffer Systems | Sodium phosphate buffer, Sodium hydroxide, Hydrochloric acid [9] | pH control and maintenance of physiological conditions during fermentation [9] | Environmental parameter control in fermentation systems [9] |
The intricate relationships between lactic acid bacteria, butyrate producers, and other microbial functional groups in the human colon represent a sophisticated metabolic network with profound implications for human health. Understanding the key microbial players involved in colonic fermentation of undigested food components—from primary fermenters like lactic acid bacteria to butyrate-producing specialists—provides crucial insights for developing targeted nutritional interventions and therapeutic strategies.
The experimental methodologies outlined, including in vitro fermentation models and molecular approaches, offer powerful tools for investigating these complex microbial communities and their metabolic outputs. As research advances, the "butyrate shift" phenomenon and the critical roles of cross-feeding relationships underscore the importance of considering microbial ecology and community dynamics rather than focusing solely on individual bacterial species.
Future research directions should include further elucidation of the specific mechanisms underlying microbial cross-feeding, the development of more sophisticated in vitro models that better capture the spatial and temporal dynamics of the colonic environment, and translational studies exploring how manipulation of these key microbial players can be leveraged for improving human health and treating disease.
The human colon represents a critical interface where diet, microbial ecology, and host physiology converge through the process of colonic fermentation. This anaerobic process, primarily mediated by the complex consortium of gut microbiota, transforms indigestible dietary components, notably dietary fiber, into short-chain fatty acids (SCFAs)—predominantly acetate, propionate, and butyrate. These bacterial metabolites exert profound effects on human health, influencing everything from colonic integrity and immune function to systemic metabolism [10] [11]. Over recent centuries, a marked decrease in dietary fiber intake has driven detrimental alterations in the gut microbiota, contributing to the global epidemic of obesity, type 2 diabetes, and other metabolic disorders [12]. Understanding the precise metabolic pathways from fiber to SCFAs is therefore not only a fundamental scientific pursuit but also a venture with significant implications for therapeutic development and nutritional interventions. This whitepaper delineates the current scientific understanding of these pathways, framed within the context of colonic fermentation research, to provide researchers and drug development professionals with a comprehensive technical guide to this critical field.
Dietary Fiber: Definitions, Types, and Intake
Classification of Dietary Fibers
Dietary fiber comprises carbohydrate polymers that resist hydrolysis by human endogenous enzymes and absorption in the small intestine [12]. The official definition has evolved to include oligosaccharides, recognizing their similar physiological activities to traditional fibers [12]. Based on physiological properties and monomeric unit (MU) polymerization, dietary fibers are classified into three primary types, each with distinct structures and sources [12]:
- Non-Starch Polysaccharides (NSPs) (MU ≥ 10): Include cellulose, hemicellulose, pectins, inulin, and various hydrocolloids.
- Resistant Starches (RS) (MU ≥ 10): Categorized as RS1 (physically inaccessible, e.g., in milled grains), RS2 (ungelatinized, e.g., raw potatoes, green bananas), RS3 (retrograded, e.g., cooked and cooled potatoes), RS4 (chemically modified), and RS5 (amylose-lipid complexes).
- Resistant Oligosaccharides (ROS) (MU: 3–9): Include fructo-oligosaccharides (FOS), galacto-oligosaccharides (GOS), and xylo-oligosaccharides (XOS).
The chemical structure, solubility, degree of polymerization, and viscosity of these fibers are critical determinants of their fermentability and the specificity of bacterial degradation in the colon [12] [11].
Global Intake Levels and Recommendations
Table 1: Global Dietary Fiber Intake Levels and Official Recommendations
| Region | Average Intake (g/day) | Recommended Intake (g/day) | Key Reference |
|---|---|---|---|
| China | 17.6 (Women), 19.4 (Men) | 25-30 (Overall) | Chinese Dietary Reference Intake (2017) [12] |
| Japan | 18.0 (Women), 19.9 (Men) | 18 (Women), 21 (Men) | National Health and Nutrition Survey in Japan (2019) [12] |
| USA | 15.2 (Women), 18.1 (Men) | 25 (Women), 38 (Men) | Dietary Guidelines for Americans (2020-2025) [12] |
| Australia | 21.1 (Women), 24.8 (Men) | 28 (Women), 38 (Men) | Australian Health Survey (2011-2012) [12] |
| European Union | ~25 (Overall) | 30 (Overall) | EFSA Scientific Opinion (2010) [12] |
Globally, average dietary fiber intake ranges from 15 to 26 g/day, consistently falling below the recommended levels of 20 to 38 g/day established in most countries [12]. Discrepancies in intake and recommendations are influenced by factors such as dietary habits, body size, and tolerance to high-fiber diets [12]. The widespread failure to meet recommended intake levels underscores a significant modifiable factor in the global burden of non-communicable diseases.
The Gut Microbiota and Fermentation Machinery
The human colon harbors a dense and diverse ecosystem of over 1000 microbial species, dominated by the phyla Firmicutes, Bacteroidetes, Actinobacteria, and Proteobacteria [11]. This community's collective genome encodes a vast repertoire of carbohydrate-active enzymes (CAZymes), such as glycoside hydrolases (GHs) and polysaccharide lyases (PLs), which far exceed the host's endogenous digestive capabilities [12]. The ability of specific bacterial taxa to utilize particular dietary fibers is genetically predetermined, depending on whether their genomes encode the necessary enzymes, carbohydrate-binding proteins, and transporters [11].
Bacterial fermentation is an anaerobic process wherein these microbes break down complex carbohydrates into SCFAs, gases (H₂, CH₄, CO₂), and other metabolites [11]. The rate and extent of fermentation are influenced by the fiber's properties (e.g., solubility, particle size) and the gut transit time [10]. Soluble fibers (e.g., inulin, pectins, β-glucans) are generally fermented more rapidly than insoluble fibers (e.g., cellulose) [11]. This intricate interplay between substrate and microbe ultimately dictates the quantity and profile of SCFAs produced.
Figure 1: Core Pathway of Microbial Fermentation of Dietary Fiber to SCFAs. NSPs: Non-Starch Polysaccharides; RS: Resistant Starch; ROS: Resistant Oligosaccharides; CAZymes: Carbohydrate-Active Enzymes; GHs: Glycoside Hydrolases; PLs: Polysaccharide Lyases.
Metabolic Pathways of SCFA Production
The saccharolytic fermentation of dietary fiber primarily yields three major SCFAs: acetate (C2), propionate (C3), and butyrate (C4). These acids account for over 90-95% of the SCFAs produced, with minor amounts of valerate, hexanoate, and branched-chain fatty acids (BCFAs) derived from protein fermentation [11]. The metabolic pathways for their synthesis are distinct and often carried out by different bacterial specialists.
- Acetate Production: Acetate is the most abundant SCFA in the colon. It is produced through the Wood-Ljungdahl pathway by many obligate anaerobes, including Bacteroides and Bifidobacterium species. This pathway also serves as a key hydrogen sink, maintaining anaerobic conditions.
- Propionate Production: Propionate is generated via multiple pathways, with the succinate pathway (common in Bacteroidetes), the acrylate pathway (used by some Firmicutes like Coprococcus catus), and the propanediol pathway (which ferments deoxy sugars like rhamnose or fucose) being the most significant.
- Butyrate Production: Butyrate is a primary energy source for colonocytes. It is synthesized mainly through the butyryl-CoA: acetate CoA-transferase pathway, employed by key butyrate producers such as Faecalibacterium prausnitzii and Eubacterium rectale, which convert two molecules of acetate into one of butyrate.
The specific SCFA profile resulting from fermentation is highly dependent on the dietary fiber substrate, as different fibers selectively enrich for bacterial taxa that possess the requisite pathways [11] [13].
Table 2: SCFA Production from Different Dietary Substrates in In Vitro Fermentation (72h)
| Substrate | Acetate | Propionate | Butyrate | Key Microbial Shifts | Reference |
|---|---|---|---|---|---|
| Mycoprotein | High | High (delayed) | Moderate | Enrichment of Bacteroides ovatus, B. uniformis | [13] |
| Oat Bran | High (rapid) | High (rapid) | Lower | Enrichment of Bifidobacterium longum, B. adolescentis | [13] |
| Chicken | Moderate | Moderate | High (delayed) | Minimal change; small increase in Alistipes | [13] |
| Inulin | Increased | Increased (in YA) | Increased (44% in inaccessible pool) | Not Specified | [14] |
Experimental Models for Studying Colonic Fermentation
In Vitro Fermentation Models
In vitro models are indispensable tools for studying the fermentation of specific substrates without the ethical and financial constraints of human or animal trials. They allow for controlled, dynamic sampling and quantitative measurement of metabolites [11].
Static Batch Fermentation: This is a closed system in sealed tubes or reactors, inoculated with single bacterial strains or mixed fecal microbiota from humans or animals. It is simple and requires less inoculum but can inhibit bacterial growth due to nutrient limitation and metabolite accumulation over time [11]. A typical protocol involves:
- Inoculum Preparation: Fresh fecal samples from healthy donors are homogenized in an anaerobic buffer (e.g., phosphate-buffered saline) under a constant flow of CO₂ or N₂ to maintain anaerobiosis.
- Substrate Incubation: The substrate of interest is added to a fermentation vessel containing a defined nutritional medium and the fecal inoculum.
- Sampling: Headspace gases and liquid samples are collected at predetermined time points (e.g., 0, 4, 8, 24, 48, 72 h) for analysis of SCFAs (via GC-MS or HPLC), microbial composition (via 16S rRNA sequencing or MetaPhlAn), and other metabolites [11] [13].
Dynamic Multi-Stage Continuous Systems: These systems (e.g., the Simulator of the Human Intestinal Microbial Ecosystem - SHIME) use multiple, sequentially connected vessels to simulate the different physiological conditions of the proximal, transverse, and distal colon. They are more complex but offer greater stability and a more accurate representation of the colonic environment by continuously adding fresh media and removing microbial suspensions and metabolites [11].
In Vivo and Clinical Methodologies
Human studies are crucial for validating findings from in vitro models. Recent advances have enabled more precise measurement of SCFA kinetics in vivo.
- Stable Tracer Methodology: A cutting-edge approach involves intravenous administration of [U-¹³C]-labeled SCFAs followed by serial blood draws. Compartmental modeling of plasma tracer enrichments and concentrations measured by gas chromatography-mass spectrometry (GC-MS) allows for the calculation of SCFA production rates in both accessible (systemic circulation) and inaccessible (potentially intestinal) pools [14]. A recent randomized controlled trial used this method to demonstrate that inulin supplementation increased butyrate production by 44% in an inaccessible intestinal pool [14].
- Wireless Motility Capsule (WMC): This ambulatory device measures pH, temperature, and pressure as it traverses the gastrointestinal tract. A characteristic pH drop identifies the ileo-caecal junction, and a low caecal pH serves as a non-invasive, inverse surrogate biomarker for excessive SCFA production and fermentation, which has been linked to symptoms of irritable bowel syndrome (IBS) [15].
Figure 2: Integrated Experimental Workflow for SCFA Research. The workflow shows parallel in vitro and in vivo approaches converging on analytical measurement and data modeling.
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Reagents and Materials for SCFA Fermentation Research
| Reagent/Material | Function & Application in Research | Key Context |
|---|---|---|
| Specific Dietary Fibers(e.g., Inulin, FOS, β-Glucans) | Used as controlled fermentation substrates to study structure-function relationships and selective bacterial growth. | [14] [11] [13] |
| Stable Isotope Tracers(e.g., [U-¹³C]-SCFAs) | Enable precise kinetic studies of SCFA production, turnover, and distribution in vivo via GC-MS. | [14] |
| Anaerobic Chamber/Gassing Kit | Creates and maintains a strict anaerobic environment (e.g., with CO₂/N₂/H₂ mix) essential for cultivating gut microbiota. | [16] [11] |
| Chromatography Standards(Pure SCFAs for GC/LC) | Required for calibrating instruments (GC-MS, HPLC) to accurately identify and quantify SCFA concentrations. | [14] [13] |
| DNA/RNA Extraction Kits(Optimized for stool) | Facilitate the analysis of microbial community composition and gene expression via 16S rRNA sequencing and metagenomics. | [13] |
| Pre-defined Media(for gut microbiota) | Provides standardized nutritional support for microbial growth in in vitro fermentation models. | [16] [11] |
Implications for Drug Metabolism and Therapeutics
The gut microbiome, through its metabolic activities including SCFA production, is a key modifier of drug metabolism and efficacy. The colon is a site of significant drug-microbiome interaction, especially for poorly soluble orally administered drugs or drugs that reach the colon via biliary excretion [16].
- Microbial Drug Metabolism: Gut microbiota encode enzymes that can directly metabolize drugs, altering their bioavailability and toxicity. An ex vivo fermentation screening platform identified that 5 out of 12 tested drugs (sulfasalazine, sulfinpyrazone, sulindac, nizatidine, and risperidone) were biotransformed by human gut microbiota [16]. Sulfasalazine is a canonical example of a prodrug designed to be activated by gut bacterial azoreductases into active 5-aminosalicylic acid (5-ASA) and sulfapyridine [16].
- SCFAs as Therapeutic Modulators: SCFAs, particularly butyrate, influence host health at multiple levels. Butyrate is a primary energy source for colonocytes, helps maintain gut barrier integrity, and has anti-inflammatory and anti-carcinogenic properties, partly through its role as a histone deacetylase (HDAC) inhibitor [10]. This has therapeutic implications for conditions like inflammatory bowel disease and colorectal cancer. Furthermore, SCFAs can indirectly influence drug response by modulating host physiology, immune function, and systemic metabolism [17].
The metabolic pathways converting dietary fiber to SCFAs represent a cornerstone of the symbiotic relationship between the host and the gut microbiota. The type and structure of dietary fiber dictate the rate of fermentation, the resulting SCFA profile, and the subsequent physiological effects. Advanced in vitro models and sophisticated in vivo techniques, such as stable isotope tracers, are unraveling the complex kinetics and health impacts of these critical metabolites. For researchers and drug development professionals, a deep understanding of these pathways is increasingly vital. The gut microbiome and its metabolites are now recognized as significant variables influencing drug pharmacokinetics, efficacy, and safety. Future research will likely focus on designing targeted dietary interventions and novel therapeutics that leverage these pathways—for instance, by developing fibers with specific fermentation properties or by manipulating the microbiota to optimize SCFA production—to prevent and treat a wide spectrum of metabolic, inflammatory, and neoplastic diseases.
The gut metabolome represents the complete set of small molecule metabolites present in the gastrointestinal tract, constituting a dynamic interface between host physiology, dietary components, and the gut microbiota. This complex mixture arises from both host-derived metabolic processes and the biochemical activities of trillions of resident microorganisms. In the context of colonic fermentation of undigested food components, the gut metabolome serves as a functional readout of microbial activity and host-microbe interactions [18] [19]. The intricate chemical dialogue between microbial metabolites and host signaling pathways fundamentally influences gastrointestinal health, systemic metabolism, and disease susceptibility [20] [18].
Understanding the precise origins and functional consequences of these metabolites provides critical insights for developing targeted therapeutic interventions. This technical guide comprehensively defines microbial and host-derived metabolites within the gut ecosystem, detailing their sources, measurement methodologies, and functional significance for researchers and drug development professionals.
Core Concepts in Gut Metabolome Composition
Origins and Classification of Gut Metabolites
The gut metabolome comprises molecules originating from distinct sources, each contributing to the overall metabolic landscape:
- Host-Derived Metabolites: Synthesized by human biochemical pathways, these include digestive enzymes, bile acids, mucins, and other secretions essential for nutrient processing and gut homeostasis [18] [19].
- Microbiota-Derived Metabolites: Produced by gut microorganisms through fermentation of dietary components or transformation of host secretions. These include short-chain fatty acids (SCFAs), tryptophan catabolites, and secondary bile acids [20] [19].
- Diet-Derived Metabolites: Originating directly from food sources, including undigested carbohydrates, fibers, polyphenols, and other complex compounds that serve as substrates for microbial metabolism [19] [21].
Table 1: Major Classes of Microbial-Derived Metabolites and Their Microbial Producers
| Metabolite Class | Specific Metabolites | Producing Bacterial Species/Genera | Primary Dietary Substrates |
|---|---|---|---|
| Short-Chain Fatty Acids (SCFAs) | Acetate, Propionate, Butyrate | Bacteroides spp., Bifidobacterium spp., Prevotella spp., Faecalibacterium prausnitzii, Roseburia spp., Blautia hydrogenotrophica, Clostridium spp. [20] | Dietary fiber, resistant starch [21] |
| Tryptophan Catabolites | Indole, IAA, IPA, IAld, Tryptamine | Clostridium sporogenes, Bacteroides ovatus, Enterococcus faecalis, Lactobacillus spp., Ruminococcus gnavus [20] | Dietary tryptophan [20] |
| Bile Acid Metabolites | Lithocholic acid, Deoxycholic acid, Ursodeoxycholic acid | Multiple species expressing bile salt hydrolases (BSHs) and 7α-hydroxysteroid dehydrogenase (7α-HSDH) [20] [19] | Primary bile acids (host-derived) [20] |
Quantitative Distribution and Compartmentalization
The distribution and concentration of metabolites vary significantly between gut compartments and systemic circulation. A recent comparative study of paired fecal and blood metabolomes revealed critical insights:
- Fecal vs. Blood Metabolome Correlations: Phenotypic correlations between paired fecal and blood metabolites are generally low (correlation coefficients: 0.05 ± 0.12), with only 8 of 132 metabolites showing significant correlations (coefficients >0.3) [22].
- Microbiome Explainability: Fecal metabolites show substantially higher predictability from gut microbiome composition (mean correlation coefficient: 0.40±0.15) compared to blood metabolites (mean correlation coefficient: 0.09±0.11) [22].
- Well-Predicted Metabolites: Based on taxonomic composition, 98 fecal metabolites were well-predicted (correlation coefficient >0.3), including SCFAs, bile acids, and phenylpropanoic acids, while only 10 blood metabolites met this threshold [22].
Table 2: Experimental Approaches for Distinguishing Metabolite Origins
| Experimental Approach | Core Methodology | Key Findings | Advantages/Limitations |
|---|---|---|---|
| Antibiotic-mediated Microbiome Depletion [19] | Administration of non-absorbable antibiotics (vancomycin, neomycin) + polyethylene glycol purge; comparison of pre- vs. post-depletion metabolomes | 2,856 microbial products decreased post-depletion; 1,057 microbial substrates increased post-depletion; 2,496 diet-derived metabolites identified | Gold standard for identifying microbiome-dependent metabolites; cannot distinguish direct vs. indirect microbial effects |
| Controlled Feeding Studies [19] | Subjects randomized to defined diets (omnivore vs. enteral nutrition); metabolomic profiling across diet groups | In depleted microbiome: 162 omnivore-derived metabolites identified vs. 2496 when considering intact microbiome | Isolates diet-derived metabolites; reveals microbiome's role in diet metabolism; requires strict dietary control |
| Germ-Free vs. Conventionalized Models [18] | Comparison of metabolite profiles between germ-free and conventionally colonized animals | Altered secondary bile acids, SCFAs, and indole derivatives in germ-free animals | Provides causal evidence for microbial contribution; limited translational relevance to humans |
Methodologies for Gut Metabolome Characterization
Experimental Workflows for Metabolite Origin Determination
Diagram 1: Experimental workflow for distinguishing metabolite origins through microbiome depletion. LC-MS: Liquid Chromatography-Mass Spectrometry; GC-MS: Gas Chromatography-Mass Spectrometry.
Analytical Techniques for Metabolite Quantification
Targeted Metabolomics for Absolute Quantification:
- Short-Chain Fatty Acid Analysis: Acidification with hydrochloric acid, extraction with diethyl ether, derivatization with N-tert-butyldimethylsilyl-N-methyltrifluoroacetamide, and detection using gas chromatography with flame ionization detection (GC-FID) [23]. Quantification against standard solutions of acetate, propionate, and butyrate with 2-ethyl butyric acid as internal standard.
- Bile Acid Profiling: Liquid chromatography-tandem mass spectrometry (LC-MS/MS) with multiple reaction monitoring for primary, secondary, and conjugated bile acids. Identification based on retention time matching to pure standards and characteristic fragmentation patterns [20] [19].
Untargeted Metabolomics for Comprehensive Discovery:
- High-resolution mass spectrometry (HRMS) coupled with reverse-phase and hydrophilic interaction liquid chromatography (HILIC) to maximize metabolite coverage. Data processing using XCMS, MZmine, or similar platforms for peak picking, alignment, and annotation [19].
- Metabolite identification using reference standards when available, or putative annotation based on accurate mass, isotopic pattern, and fragmentation spectra against databases such as HMDB, METLIN, and MassBank.
Computational Integration with Microbial Communities
Genome-Scale Metabolic Modeling (GEMs):
- MICOM Platform: Uses flux balance analysis under mass steady-state assumptions to predict microbial metabolite production as fluxes (units of concentration per time) [23]. Constraints based on dietary compound availability and microbial community composition.
- AGORA2 Metabolic Reconstructions: Resource of genome-scale metabolic models for human gut microbes, enabling in silico prediction of SCFA production from defined nutritional inputs [23].
Machine Learning Approaches:
- LOCATE (Latent variables Of miCrobiome And meTabolites rElations): Treats microbiome-metabolome relations as equilibria of complex interactions, using a latent representation to predict host condition [24]. Demonstrates superior performance for predicting metabolite concentrations from microbiome composition compared to linear models.
- Random Forest Regression: Applied to predict metabolite abundances from taxonomic composition or microbial pathways, with performance evaluation through cross-validation [22].
The Scientist's Toolkit: Essential Research Reagents & Platforms
Table 3: Key Research Reagent Solutions for Gut Metabolome Studies
| Reagent/Platform | Specific Product Examples | Primary Application | Technical Considerations |
|---|---|---|---|
| Antibiotics for Microbiome Depletion | Vancomycin, Neomycin (non-absorbable) | Selective reduction of gut microbial load to identify microbiome-derived metabolites [19] | Requires polyethylene glycol purge for complete clearance; confirm depletion via 16S rRNA quantification |
| Chromatography Columns | HILIC, C18 reverse-phase | Separation of polar and non-polar metabolites prior to mass spectrometry | Column choice dramatically impacts metabolite coverage; requires method optimization |
| Metabolite Standards | SCFA mixtures, bile acid panels, isotopically labeled internal standards (e.g., 13C-acetate) | Absolute quantification of targeted metabolites; quality control | Use deuterated/internal standards for quantification accuracy; purity >95% recommended |
| DNA Extraction Kits | MOBIO PowerSoil, QIAamp DNA Stool Mini Kit | Concurrent microbiome analysis from same fecal samples | Extraction method significantly impacts microbial community profiles; maintain consistency |
| In Silico Modeling Platforms | MICOM, AGORA2 reconstructions | Prediction of community-level metabolite production from genomic data [23] | Accuracy varies by dietary context; better performance with complex carbohydrates vs. other compounds |
| 16S rRNA Gene Primers | V3-V4 (341F/806R), other hypervariable region targets | Taxonomic profiling of microbial communities | V region selection introduces bias; V3-V4 most common but may miss specific taxa [25] |
Functional Significance of Key Metabolite Classes
Signaling Pathways and Host Receptors
Diagram 2: Key microbial metabolite classes and their signaling pathways. SCFAs: Short-Chain Fatty Acids; GPCR: G-Protein Coupled Receptor; Tregs: Regulatory T cells; tMacs: Tolerogenic Macrophages; LCA: Lithocholic Acid; DCA: Deoxycholic Acid; FXR: Farnesoid X Receptor; TGR5: G Protein-coupled Bile Acid Receptor; I3A: Indole-3-Aldehyde; IAld: Indole-3-Aldehyde; IPA: Indole-3-Propionic Acid; AHR: Aryl Hydrocarbon Receptor.
Impact on Intestinal and Systemic Homeostasis
The functional effects of gut microbial metabolites extend from local intestinal processes to systemic physiological regulation:
- Immune Cell Differentiation: SCFAs promote differentiation and function of immunosuppressive cells including regulatory T cells (Tregs), tolerogenic macrophages (tMacs), and tolerogenic dendritic cells (tDCs), while inhibiting inflammatory cells such as inflammatory Macs (iMacs) and Th17 cells [20].
- Intestinal Barrier Function: Butyrate serves as the primary energy source for colonocytes, enhancing epithelial barrier integrity through upregulation of tight junction proteins and promoting mucus production [20] [18].
- Systemic Metabolic Regulation: Secondary bile acids and SCFAs influence glucose homeostasis and energy metabolism through activation of FXR and GPCR receptors, impacting hepatic gluconeogenesis, insulin sensitivity, and energy expenditure [20] [18].
- Gut-Brain Axis Communication: Microbial metabolites including SCFAs, tryptamine, and indole derivatives modulate enteric nervous system function and influence central processes through vagal afferent signaling [18].
Implications for Therapeutic Development
The strategic manipulation of gut microbial metabolites presents promising avenues for therapeutic intervention:
- Microbiome-Informed Dietary Interventions: Baseline microbiota composition (e.g., Prevotella-rich vs. Bacteroides-rich enterotypes) determines response to dietary fiber interventions, suggesting personalized nutritional approaches [21].
- Metabolite-Based Biomarker Discovery: Specific microbial metabolites, including secondary bile acids and indole derivatives, show promise as diagnostic and prognostic biomarkers for cardiometabolic diseases, inflammatory bowel disease, and colorectal cancer [22] [19].
- Targeted Microbial Consortia: Defined communities of metabolite-producing bacteria (e.g., butyrate-producing consortia) represent a novel therapeutic modality for restoring metabolic deficiencies in dysbiotic states [20] [21].
- Enzyme-Targeted Inhibitors: Selective inhibition of microbial enzymes (e.g., bile salt hydrolases) offers precision approaches to modulate metabolite pools without broad-spectrum microbiome disruption [20].
The gut metabolome represents a rich source of biological insight and therapeutic potential, with advanced methodologies now enabling precise dissection of microbial and host contributions to this complex chemical environment. Integration of multi-omics datasets with computational modeling and controlled intervention studies continues to accelerate our understanding of how microbial metabolites shape human health and disease.
The colon represents a critical interface where host physiology and the gut microbiota interact through the fermentation of undigested food components. This process is not merely digestive but is fundamental to maintaining host health, influencing everything from local barrier integrity to systemic immunity. Colonic fermentation of dietary fibers and resistant starches by gut microbes produces short-chain fatty acids (SCFAs), which serve as key signaling molecules and energy sources [26] [27]. These metabolites and others directly modulate the integrity of the intestinal epithelial barrier (IEB) and the more recently discovered gut vascular barrier (GVB) [28] [18]. Disruption of these barriers, often described as "leaky gut," facilitates the translocation of bacteria and inflammatory molecules into systemic circulation, contributing to various pathological conditions [28] [29] [30]. This whitepaper synthesizes current research to provide an in-depth technical guide on how colonic fermentation products impact host physiology, with a specific focus on barrier function, immune regulation, and systemic signaling pathways relevant to researchers and drug development professionals.
Colonic Fermentation and Key Microbial Metabolites
The colon harbors a complex microbial ecosystem that ferments non-digestible carbohydrates and other dietary substrates. The metabolic output of this fermentation is highly dependent on the structural characteristics of the dietary inputs and the composition of the microbial community [26] [27].
- Resistant Starch (RS) Fermentation: The fermentative behavior of RS and its resulting SCFA profile are dictated by structural domains such as amylose-to-amylopectin ratio, granular morphology, and crystalline type [26]. For instance, high-amylose, B-type crystalline RS selectively enriches for butyrate-producing bacteria (e.g., Ruminococcus and Bifidobacterium), thereby enhancing butyrate production. Conversely, retrograded RS may promote Bacteroides and alter the acetate-to-propionate ratio [26].
- SCFA Production and Functions: SCFAs, primarily acetate, propionate, and butyrate, are the most studied fermentation metabolites. Butyrate serves as the primary energy source for colonocytes, maintains epithelial barrier integrity, and possesses potent anti-inflammatory properties, including histone deacetylase (HDAC) inhibition [26]. Propionate is involved in gluconeogenesis and cholesterol synthesis in the liver, while acetate enters systemic circulation to influence appetite regulation and peripheral tissues [26] [18].
- Other Bioactive Metabolites: Beyond SCFAs, microbial fermentation of proteins and amino acids can produce metabolites like branched-chain fatty acids (BCFAs), biogenic amines, hydrogen sulfide (H2S), and ammonia, which in excess can be detrimental to barrier health [27]. Conversely, fermentation of dietary polyphenols and yeast-derived β-glucans/MOS yields metabolites with anti-inflammatory and barrier-protective effects [31].
Table 1: Key Microbial Metabolites and Their Physiological Roles in Host Physiology
| Metabolite | Primary Microbial Producers | Key Physiological Roles | Impact on Barriers & Immunity |
|---|---|---|---|
| Butyrate | Ruminococcus, Bifidobacterium, Faecalibacterium prausnitzii | Primary energy source for colonocytes, HDAC inhibition, anti-inflammatory [26] | Enhances tight junction proteins (ZO-1), reduces inflammation, supports GVB integrity [28] [26] |
| Propionate | Bacteroides, Phascolarctobacterium | Gluconeogenesis precursor, cholesterol metabolism, immune cell regulation [26] | Binds to GPCRs (GPR41/43) on immune cells, exerts anti-inflammatory effects [26] [18] |
| Acetate | Many saccharolytic bacteria (e.g., Bifidobacterium) | Substrate for systemic metabolism, lipogenesis, cross-feeding other bacteria [26] [31] | Contributes to mucus layer viscosity, supports overall epithelial health [28] |
| Yeast β-Glucans/MOS Metabolites | Microbes utilizing yeast cell walls | Immunomodulation, pathogen agglutination [31] | Increases IL-10 production, improves transepithelial electrical resistance (TEER) [31] |
The Multi-Layered Intestinal Barrier System
The intestine is protected by a sophisticated, multi-layered barrier system that is profoundly influenced by microbial metabolites.
The Intestinal Epithelial Barrier (IEB)
The IEB is a continuous monolayer of intestinal epithelial cells (IECs) bound together by tight junction (TJ) proteins like Zonula Occludens-1 (ZO-1) and claudins [28] [30]. A critical component is the mucus layer, secreted by goblet cells, which physically separates the luminal microbiota from the epithelium [28] [30]. The cellular hierarchy of the IEB is maintained within the colonic crypts, which house LGR5+ stem cells that give rise to all mature epithelial lineages, including colonocytes, goblet cells, and enteroendocrine cells [30]. The balance between proliferation, differentiation, and extrusion is regulated by signaling pathways such as WNT, Notch, and BMP [30].
The Gut Vascular Barrier (GVB)
Beyond the IEB lies the GVB, a specialized endothelial barrier that controls the passage of molecules and bacteria from the gut lamina propria into the portal circulation and systemic organs [28]. Structurally analogous to the blood-brain barrier, the GVB is composed of endothelial cells sealed by tight junctions, supported by pericytes and enteric glial cells [28]. Its integrity is regulated by the canonical Wnt/β-catenin signaling pathway. Activation of this pathway promotes a sealed barrier, while its disruption, as seen during Salmonella infection, leads to upregulation of Plasmalemma Vesicle-Associated Protein-1 (PV1) and increased vascular permeability, facilitating bacterial dissemination to the liver and spleen [28]. GVB dysfunction has been implicated in the pathogenesis of non-alcoholic fatty liver disease (NAFLD), alcoholic liver disease, and colorectal cancer metastasis [28].
Experimental Models for Assessing Barrier Integrity and Immunity
Investigating host-microbe interactions requires robust in vitro and in vivo models. Below are detailed protocols for key methodologies.
In Vivo Model: Assessing Probiotic Effects in a Murine Infection Model
Objective: To evaluate the efficacy of a multi-strain probiotic formulation (MPF) in preserving intestinal barrier integrity against Salmonella typhimurium challenge [28].
Materials:
- Animals: C57BL/6J mice.
- Test Material: Multi-strain probiotic (e.g., Lactobacillus rhamnosus LR32, Bifidobacterium lactis BL04, Bifidobacterium longum BB536).
- Pathogen: Salmonella enterica serovar Typhimurium strain SL3261AT (attenuated, mCherry-labeled).
- Key Reagents: Formaldehyde, OCT compound, anti-ZO-1 antibody, anti-PV1 antibody, Alcian Blue/PAS stain, collagenase D, LB agar with chloramphenicol.
Methodology:
- Pretreatment: Administer MPF (e.g., 10^8 CFUs/strain) daily to mice via oral gavage for 10 days.
- Infection: Orally infect pretreated and control mice with Salmonella (10^9–10^11 CFU).
- Tissue Collection: Euthanize mice 6-16 hours post-infection. Aseptically remove the colon and ileum.
- Bacterial Translocation Assay:
- Digest colon tissue with collagenase D.
- Lyse cells and plate homogenates on chloramphenicol-containing LB agar.
- Quantify Salmonella CFUs after overnight culture to assess systemic translocation [28].
- Histological & Immunofluorescence Analysis:
- Fix tissues in formaldehyde or PLP buffer for immunofluorescence.
- Embed in paraffin for H&E staining (to assess villus/crypt morphology) and Alcian Blue/PAS staining (to quantify acid/neutral mucins in the mucus layer).
- For immunofluorescence, embed tissues in OCT and section. Stain with antibodies against ZO-1 (for IEB integrity) and PV1 (for GVB integrity). Quantify fluorescence intensity [28].
In Vitro Model: Colon-on-a-Plate with Host Cell Co-Culture
Objective: To study the prebiotic potential of test compounds and assess their fermentation products on host barrier integrity and immune response in vitro [31].
Materials:
- Fecal Inoculum: From human or animal donors (e.g., dogs with IBD for disease-specific models).
- Test Products: e.g., Biolex MB40 (MOS and β-glucan) or Leiber Beta-S (purified β-glucan).
- Nutritional Medium: e.g., Nutritional blend PD03 (ProDigest) to simulate colon environment.
- Host Cell Co-Culture: Caco-2 cells (human colorectal adenocarcinoma cells for epithelium) and THP-1 cells (monocytic cells for immunity).
- Key Reagents: Anaerobic workstation, 24-well deep-well plates, transepithelial electrical resistance (TEER) measurement equipment, ELISA kits for cytokines (e.g., IL-10).
Methodology:
- Fermentation Phase:
- In an anaerobic workstation, inoculate wells of a 24-deep-well plate containing nutritional medium with a fecal suspension.
- Supplement wells with the test prebiotic or leave as a blank control.
- Incubate for 48 hours to allow for microbial fermentation [31].
- Metabolite Analysis:
- Collect supernatant post-fermentation.
- Analyze SCFA concentrations (acetate, propionate, butyrate) using techniques like gas chromatography (GC) or high-performance liquid chromatography (HPLC).
- Perform 16S rRNA gene sequencing on the fermentate to assess shifts in microbial composition [31].
- Host Cell Assay:
- Culture Caco-2 cells on transwell inserts to form a confluent, differentiated monolayer. Add THP-1 cells to the basolateral compartment.
- Apply the fermented supernatant from step 1 to the apical side of the Caco-2 monolayer.
- Induce inflammation (e.g., with TNF-α) to disrupt barrier integrity.
- Barrier Integrity Assessment: Measure Transepithelial Electrical Resistance (TEER) over time to quantify barrier strength.
- Immune Response Assessment: Collect basolateral media and measure anti-inflammatory cytokine IL-10 production via ELISA [31].
- Fermentation Phase:
Key Research Findings and Data Synthesis
Research using the aforementioned models has generated quantitative data on how dietary components and microbes influence host physiology.
Table 2: Quantitative Effects of Interventions on Barrier Integrity and Immunity
| Intervention / Condition | Experimental Model | Key Quantitative Outcomes | Interpretation & Mechanistic Insight |
|---|---|---|---|
| Multi-Strain Probiotic (MPF) [28] | In vivo murine Salmonella infection | - Preserved ZO-1 expression- Reduced PV1 upregulation- Significant reduction in Salmonella translocation to colon tissue- Maintained mucus layer thickness (Alcian Blue/PAS) | MPF protects both IEB and GVB from pathogen-induced damage via maintaining tight junctions and Wnt/β-catenin-dependent GVB sealing. |
| Yeast β-Glucan/MOS (Biolex MB40) [31] | In vitro Colon-on-a-plate (dog IBD microbiota) & Caco-2/THP1 co-culture | - Significantly increased acetate & propionate vs. blank- Increased microbial diversity & biomass- Protected against inflammation-induced TEER reduction- Significantly increased IL-10 production | Fermentation of prebiotics modulates microbiota, increasing SCFAs that directly improve barrier function and exert anti-inflammatory effects via IL-10. |
| High-Amylose Maize RS (Type 2) [26] | In vivo human & animal studies | - Selectively increases butyrate-producing bacteria (e.g., Ruminococcus)- Leads to higher fecal butyrate concentrations- Associated with improved epithelial integrity markers | B-type crystalline structure of RS resists digestion, enabling slow fermentation in the colon, selectively stimulating butyrogenic microbes. |
| Ulcerative Colitis (UC) [29] | Population-based meta-analysis (Human) | - Pooled CRC incidence: 1.47 per 1000 person-years- Standardized Incidence Ratio (SIR) for CRC: 2.48- SIR with extensive colitis: 3.95 | Chronic inflammation in UC disrupts mucosal and epithelial barriers, creating a pro-carcinogenic environment and significantly increasing colorectal cancer risk. |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Models for Investigating Gut Barrier Physiology
| Reagent / Model | Specific Example | Function & Application in Research |
|---|---|---|
| Probiotic Formulations | Multi-strain probiotic (L. rhamnosus LR32, B. lactis BL04, B. longum BB536) [28] | Used in in vivo models to investigate protective effects against pathogen-induced barrier disruption and to elucidate mechanisms of IEB and GVB fortification. |
| Prebiotic Substrates | Biolex MB40 (MOS & β-glucan), Leiber Beta-S (β-glucan) [31] | Applied in in vitro fermentation models to study how specific fibers modulate microbial composition and SCFA production, and subsequent effects on host cells. |
| Specific Antibodies | Anti-ZO-1, Anti-PV1, Anti-MUC2 [28] [30] | Critical for immunofluorescence staining and Western blotting to visualize and quantify the expression and localization of key barrier proteins in tissue sections or cell cultures. |
| Cell Lines | Caco-2, HT-29, THP-1 [31] | Caco-2/HT-29 form polarized monolayers for TEER and permeability studies. THP-1 is a monocyte model for co-culture studies of immunomodulation. |
| In Vitro Fermentation Systems | Colon-on-a-plate, SIMGI, SHIME [31] | Sophisticated bioreactors that simulate the human colon environment, allowing for controlled, longitudinal study of test compound fermentation and microbiota shifts. |
| Pathogen Strains | Salmonella typhimurium SL3261AT (mCherry-labeled) [28] | Genetically modified, attenuated strains enable safe and trackable investigation of barrier breach, bacterial translocation, and host-pathogen interactions. |
Signaling Pathways Linking Metabolites to Host Physiology
The effects of microbial metabolites are largely mediated through specific host signaling pathways.
Wnt/β-catenin Signaling in Barrier Integrity
The Wnt/β-catenin pathway is a master regulator of both epithelial homeostasis in the crypt and the integrity of the GVB [28] [30]. In the colonic crypt, Wnt signaling is crucial for the maintenance and proliferation of LGR5+ stem cells [30]. At the GVB, endothelial β-catenin activation promotes a sealed barrier, while its inhibition leads to PV1 upregulation and increased vascular permeability [28]. Butyrate and other SCFAs can influence this pathway, contributing to its barrier-strengthening effects.
Diagram 1: Wnt/β-catenin signaling in barrier integrity.
SCFA Signaling via GPCRs in Immunity and Metabolism
SCFAs (acetate, propionate, butyrate) exert widespread effects by activating specific G-protein coupled receptors (GPCRs), such as GPR43 (FFAR2) and GPR41 (FFAR3), which are expressed on various cell types including intestinal epithelial cells (IECs) and immune cells [26] [18]. This signaling is pivotal for maintaining metabolic and immune homeostasis.
Diagram 2: SCFA signaling through GPCRs.
The colonic fermentation of undigested food components is a cornerstone of host physiology, directly impacting gut barrier integrity, immune function, and systemic signaling. The evidence is clear that microbial metabolites, particularly SCFAs, reinforce the multi-layered intestinal barrier (IEB and GVB) and modulate immune responses via specific signaling pathways like Wnt/β-catenin and GPCRs. Disruption of this delicate equilibrium is a hallmark of gastrointestinal and systemic diseases, including IBD, NAFLD, and colorectal cancer [28] [29] [18].
Future research should focus on the precision design of functional foods and next-generation probiotics. By tailoring the structural properties of prebiotics like resistant starch, it is possible to direct fermentation towards desired SCFA profiles and microbial populations, offering a targeted nutritional strategy for health maintenance and disease intervention [26]. Furthermore, integrating advanced in silico modeling with the sophisticated in vitro and in vivo protocols outlined here will accelerate our understanding of diet-microbiota-host interactions, paving the way for personalized nutrition and novel therapeutic agents aimed at fortifying the gut barrier and modulating systemic immunity.
Tools and Models: Investigating Colonic Fermentation from In Vitro to Clinical Trials
The study of colonic fermentation, the process by which gut microbiota metabolize undigested food components into bioactive metabolites, is crucial for understanding human nutrition, health, and disease. In vitro digestion models provide indispensable tools for this research, enabling scientists to simulate the complex environment of the human gastrointestinal tract under controlled and reproducible conditions. The development of the INFOGEST standardized static in vitro digestion method represents a significant advancement in the field, addressing previous challenges with protocol variability that impeded cross-comparison of research findings [32] [33]. This harmonized framework, coupled with sophisticated bioreactor systems that model colonic fermentation, has accelerated research into how undigested food components, particularly proteins and fibers, are metabolized by the gut microbiome to produce metabolites such as short-chain fatty acids (SCFAs) that influence host health [9] [34].
This technical guide examines the INFOGEST protocol, explores advanced bioreactor technologies for simulating colonic conditions, and presents practical methodologies for researching the colonic fermentation of undigested food components, with particular emphasis on protein fermentation metabolites and their potential health implications.
The INFOGEST Standardized Static Digestion Method
The INFOGEST static digestion method was developed through international collaboration to create a harmonized protocol simulating human gastrointestinal digestion based on physiologically inferred conditions [32] [33]. This method provides a standardized framework for the oral, gastric, and small intestinal phases of digestion, using consistent pH levels, electrolyte compositions, enzyme activities, and digestion times to enable reproducible results across laboratories [35] [33].
Core Protocol Parameters and Procedures
The INFOGEST method outlines specific conditions for each digestive phase, with key parameters summarized in Table 1 below.
Table 1: Key Parameters of the INFOGEST Static Digestion Protocol
| Digestion Phase | Duration | pH | Key Enzymes | Enzyme Activity | Typical Ionic Composition |
|---|---|---|---|---|---|
| Oral | 2 minutes | 7.0 | α-amylase | 150 U/mL | Simulated Salivary Fluid (SSF) |
| Gastric | 2 hours | 3.0 | Pepsin | 2000 U/mL | Simulated Gastric Fluid (SGF) |
| Small Intestinal | 2 hours | 7.0 | Pancreatin, Bile salts | Various | Simulated Intestinal Fluid (SIF) |
For the oral phase, the method recommends mixing solid foods (approximately 5g) with simulated salivary fluid (SSF) containing α-amylase at a 1:1 ratio (v/w) for 2 minutes at 37°C [32]. For solid foods, a mechanical mincer is suggested to simulate chewing, reducing food particles to approximately 2mm to mimic the bolus formation that occurs in vivo [32] [35].
The gastric phase utilizes simulated gastric fluid (SGF) with porcine pepsin at an activity of 2000 U/mL of gastric contents, maintained at pH 3.0 for 2 hours at 37°C [32] [33]. The recommendation for phosphatidylcholine (0.17 mM) in vesicular form addresses lipid digestion considerations, though gastric lipase is not included in the standard protocol due to limited availability and affordability of enzymes with correct pH and site specificity [32].
In the small intestinal phase, samples are mixed with simulated intestinal fluid (SIF) containing pancreatin and bile salts, maintained at pH 7.0 for 2 hours at 37°C [32] [35]. This phase completes the simulation of upper gastrointestinal tract digestion, producing chyme that can subsequently be used for colonic fermentation studies.
Adaptation for Special Populations
The INFOGEST consortium has developed variations of the standard protocol to simulate digestion in specific populations, including infants and older adults [35]. These adaptations adjust enzyme activities, pH values, and digestion times to reflect the physiological differences in these populations, such as decreased gastric acid secretion and digestive enzyme activity in older adults [35]. This is particularly relevant for colonic fermentation research, as altered digestion in the upper GI tract significantly affects the substrates available for microbial metabolism in the colon.
Advanced Bioreactor Systems for Colonic Fermentation
While static models like INFOGEST effectively simulate upper GI digestion, dynamic bioreactor systems provide more physiologically relevant environments for studying colonic fermentation by incorporating continuous flow, pH control, and anaerobic conditions that better mimic the in vivo colonic environment [36].
Complex Dynamic Models
Advanced bioreactor systems have been developed to simulate the dynamic conditions of the human colon, with several models offering multi-compartmental designs that replicate the distinct environments of different colonic regions:
Table 2: Advanced Bioreactor Systems for Simulating Colonic Fermentation
| Bioreactor System | Key Features | Applications in Colonic Fermentation Research |
|---|---|---|
| SHIME (Simulator of Human Intestinal Microbial Ecosystem) | Multi-compartment system simulating stomach to distal colon; controls pH, temperature, nutrient supply, transit time, and anaerobic atmosphere | Protein fermentation studies; microbial metabolite production; probiotic survival [34] [36] |
| TIM-2 (TNO Intestinal Model) | Represents colonic conditions with characteristic motility patterns; incorporates water absorption | Drug metabolization; bacterial composition analysis; SCFA production [36] |
| MimiCol3 | Dynamic colon model with multiple parallel vessels; automated pH and redox potential control; anaerobic conditions with nitrogen gassing | Simultaneous testing under identical conditions; sulfasalazine degradation; bacterial growth studies [36] |
These systems maintain complex microbial communities similar to those found in the human colon, dominated by five primary phyla: Bacteroidetes, Firmicutes, Actinobacteria, Proteobacteria, and Verrucomicrobia, with the first two accounting for more than 90% of the bacteria [36]. The MimiCol3 model, for instance, operates with a volume of 150mL to simulate the ascending colon (in vivo volume: 170 ± 40mL), maintains a pH range of 6.2 ± 0.25, and uses a shaking motion at 100rpm to ensure homogeneous distribution and optimized bacterial growth under anaerobic conditions [36].
Experimental Workflow for Colonic Fermentation Studies
The following diagram illustrates a typical integrated experimental workflow combining the INFOGEST protocol with advanced bioreactors for colonic fermentation research:
Diagram 1: Integrated experimental workflow for colonic fermentation studies
This workflow demonstrates how the INFOGEST-digested material serves as input for colonic fermentation systems, enabling researchers to study the production of microbial metabolites such as SCFAs, branched-chain fatty acids (BCFAs), ammonia, and various tryptophan derivatives under controlled conditions [9] [34].
Research Applications and Methodologies
Investigating Protein Fermentation in the Colon
Advanced in vitro models have been particularly valuable for studying protein fermentation in the colon, a process that produces both beneficial and potentially harmful metabolites. Research using the SHIME system has demonstrated that different protein sources yield distinct fermentation profiles, with zein and whey potentially producing the highest levels of ammonia and BCFAs in the proximal colon, while whey and pigeon peas may result in the highest levels of H₂S [34]. These findings are significant as they highlight how dietary protein selection might influence colonic metabolite production, with potential implications for gut health.
The relationship between amino acid precursors in ileal digesta and their fermentation metabolites has been systematically investigated using these systems. Studies have found that the relative changes in most metabolites positively correlate with their amino acid precursors in ileal digesta, and ammonia production serves as a good predictor for the production of other metabolites in both proximal and distal colon vessels [34]. Furthermore, indole production has been strongly associated with oxindole, 5-HT, and tryptamine, as well as the sum of tryptophan metabolites in the distal colon [34].
Assessing Traditional Fermented Foods
In vitro models have also been employed to evaluate how traditional fermented foods (TFFs) influence gut microbiota composition and metabolic activity. A recent study investigating Mabisi, a traditional Zambian fermented dairy product, used the INFOGEST protocol for initial digestion followed by in vitro colon fermentation with stool samples from both consumers and non-consumers of Mabisi [9]. The research demonstrated that Mabisi supplementation increased beneficial bacteria such as Pediococcus in both consumers and non-consumers, but the gut microbiota of regular consumers showed greater resilience, with limited changes in community composition compared to non-consumers [9]. Non-consumers exhibited higher production of SCFAs including acetate, butyrate, formate, and succinate after Mabisi exposure, suggesting that regular consumption may lead to microbial adaptation [9].
Essential Research Reagents and Materials
Successful implementation of in vitro digestion and colonic fermentation studies requires specific reagents and specialized equipment, as detailed in Table 3.
Table 3: Essential Research Reagents for In Vitro Digestion and Colonic Fermentation Studies
| Reagent/Equipment | Specification/Function | Research Application |
|---|---|---|
| Porcine Pepsin | EC 3.4.23.1, 2000 U/mL gastric contents | Protein hydrolysis in gastric phase [32] |
| Pancreatin | Porcine-derived, contains mixture of digestive enzymes | Simulates pancreatic secretions in small intestine [32] |
| Bile Salts | Porcine bile extract or synthetic salts | Lipid emulsification in small intestinal phase [32] |
| α-amylase | Human salivary Type IX-A, 150 U/mL SSF | Starch digestion in oral phase [32] |
| Schaedler Broth | Nutrient-rich medium for anaerobic bacteria | Supports microbial growth in colonic fermentation [36] |
| 16S rRNA Sequencing | Analysis of hypervariable regions (V3-V4) | Determines microbial community composition [9] [36] |
| GC-MS/HPLC | Gas Chromatography-Mass Spectrometry / High-Performance Liquid Chromatography | Quantification of SCFAs, BCFAs, and other metabolites [9] [34] |
The diagram below illustrates the architecture of an advanced bioreactor system like the MimiCol3, showing the integration of sensors and control systems that maintain physiological conditions:
Diagram 2: Advanced bioreactor system architecture with control mechanisms
Current Challenges and Future Directions
Despite significant advancements, current in vitro digestion and colonic fermentation models face several limitations. Static models like INFOGEST cannot fully replicate the complex dynamic physiology of the human GI tract, including gradual acidification in the stomach, continuous nutrient delivery, and sophisticated motility patterns [37] [35]. Even advanced dynamic models have difficulty accurately simulating the complex interplay between different regions of the colon and the host's immune and endocrine systems [36].
Future developments are likely to focus on creating more sophisticated multi-compartmental systems that better simulate the distinct environments of different colonic regions (ascending, transverse, and descending colon), each with specific pH ranges, microbial populations, and metabolic functions [36]. There is also growing interest in developing population-specific models that simulate the digestive and microbial environments of specific populations, including infants, older adults, and individuals with gastrointestinal diseases [37] [35]. These advancements would enable more personalized nutrition research and product development.
Integration of in vitro models with in vivo validation and in silico modeling represents another promising direction. Combining data from in vitro systems with computational models can help predict in vivo outcomes more accurately and identify the most critical parameters controlling colonic fermentation processes [37] [35]. This integrated approach will enhance the predictive power of in vitro systems and reduce the need for extensive animal and human trials.
As these technologies continue to evolve, in vitro digestion models and advanced bioreactors will play an increasingly important role in understanding the complex relationships between diet, gut microbiota, and human health, particularly in the context of colonic fermentation of undigested food components.
Anaerobic Incubation and Simulating the Colonic Environment
The human colon is a highly complex biological niche hosting trillions of bacteria that exist in symbiosis with the colon epithelium [38]. This bacterial community, known as the microbiota, includes at least 500–1,000 different species, predominantly obligate anaerobes [38]. The paramount challenge in creating physiologically relevant colonic models lies in replicating the strict anaerobic environment while simultaneously supporting the metabolic interactions between host cells, commensal microbiota, and dietary components. In vitro fermentation systems that model the human gastrointestinal tract allow for the investigation of microbial communities with precise control of various physiological parameters while decoupling confounding factors from the human host [39]. The critical importance of maintaining oxygen levels below 1% is underscored by the fact that the gut microbiota is predominantly composed of strict anaerobes, with Bacteroidetes and Firmicutes representing the two dominant bacterial phyla in healthy individuals [8]. Disruption of this anaerobic environment leads to dysbiosis, characterized by decreased microbial diversity and outgrowth of Proteobacteria, which has been linked to various inflammatory and metabolic diseases [8].
Table 1: Key Physiological Parameters of the Human Colon Environment
| Parameter | Physiological Range | Functional Significance |
|---|---|---|
| Oxygen Level | <1% [38] | Essential for obligate anaerobe survival and function |
| pH | 5.5-7.0 (varying along segments) [39] | Affects microbial enzyme activity and community composition |
| Temperature | 37°C [39] | Maintains physiological metabolic rates |
| Transit Time | 30-48 hours [39] | Determines nutrient availability and microbial growth |
| Shear Stress | 0.1-0.6 dyn/cm² [38] | Mimics fluid mechanical forces on mucosal surfaces |
Technological Solutions for Anaerobic Incubation
Advanced Anaerobization Systems
Traditional approaches to maintaining anaerobic conditions have relied on nitrogen containers or passive diffusion through oxygen-permeable materials like polydimethylsiloxane (PDMS) [38]. However, these methods are equipment-intensive, slow, and limit experimental accessibility. A novel approach utilizes an anaerobization unit (AU) that enables online deoxygenation of media via liquid-to-liquid gas diffusion [38]. This system exploits the fast diffusion of oxygen through silicone rubber and the highly oxygen-attractant properties of antioxidant liquids. An ultrathin silicone tube is coiled within a container filled with a strong aqueous antioxidant solution, allowing passing liquid media to be rapidly depleted of dissolved oxygen before reaching the culture chamber. This innovation maintains stable oxygen levels below 1% for several days without compromising epithelial cell viability and eliminates the need for complex gas chambers [38].
The Mini Colon Model (MiCoMo) represents another significant advancement—a low-cost, benchtop multi-bioreactor system that simulates the human colon environment with physiologically relevant conditions while operating independently of an anaerobic chamber [39]. Each 30-mL working volume reactor is equipped with automated pH, temperature, and fluidic control, with anoxia maintained through N₂ sparging that also serves as the mixing mechanism. Validation experiments confirmed MiCoMo's ability to support the growth of strict anaerobes including Clostridium beijerinckii and Bacteroides fragilis, with the system demonstrating no oxygen leakage over 24-hour operational periods [39].
Diagram 1: Integrated anaerobization and bioreactor system for colonic simulation. The anaerobization unit deoxygenates media before entry, while N₂ sparging maintains anoxic conditions.
Comparative Analysis of Anaerobic Cultivation Systems
Table 2: Comparison of Anaerobic In Vitro Colon Model Systems
| System Type | Oxygen Control Mechanism | Working Volume | Key Advantages | Reported O₂ Levels |
|---|---|---|---|---|
| Anaerobic Flow Model [38] | Online deoxygenation via liquid-to-liquid gas diffusion | Not specified | Stand-alone system, no gas chambers required, compatible with physiological shear stress | <1% for several days |
| Mini Colon Model (MiCoMo) [39] | N₂ sparging, independent of anaerobic chamber | 30 mL | Low-cost, automatic pH/temperature control, fast stabilization (<5 days) | Anoxic conditions validated with resazurin |
| Organ-on-Chip with Nitrogen Box [38] | Encapsulation in nitrogen-filled container | Microfluidic channels | Enables co-culture with human epithelium, physiological 3D architecture | <1% for up to 3 days |
| Multi-stage Systems (e.g., SHIME) [39] | Complex gas control in multi-chamber setup | Liter-scale | Mimics different GI tract segments, well-established | Varies by segment |
Methodological Framework for Colonic Fermentation Research
Experimental Protocols for Anaerobic Co-culture
The establishment of long-term co-culture of intestinal epithelial cells with obligate anaerobic bacteria requires meticulous protocol implementation. The following methodology, adapted from recent advances [38], enables sustained colonization of live intestinal epithelium by anaerobic bacteria:
Dual Flow Chamber (DFC) Setup:
- Mount two Ibidi sticky slides back-to-back with a thin, porous, transparent polyester membrane in between to create apical and basolateral flow channels
- Use oxygen-impermeable hard plastic materials rather than gas-permeable PDMS to prevent oxygen leakage
- Culture intestinal epithelial cells (e.g., Caco-2) on the membrane to maturity (typically 7 days) before introducing anaerobic bacteria
Media Anaerobization and Flow Parameters:
- Implement an anaerobization unit with silicone tubing (0.99 mm luminal diameter, 0.31 mm wall thickness, ≥150 cm length) coiled in antioxidant solution
- Set flow rate to 320 µl/min to generate physiological shear stress of 0.3 dyn/cm² while maintaining oxygen exit levels below 1%
- Maintain pH at 6.7 ± 0.1 through automated control systems [39]
Inoculation and Sampling:
- Introduce anaerobic bacteria (e.g., Clostridioides difficile, Bacteroides fragilis) to the apical channel once epithelial barrier is established
- Conduct sampling under controlled conditions to minimize oxygen exposure
- Monitor oxygen levels at critical points: AU exit, DFC inlet, and DFC outlet
In Vitro Fermentation of Food Components
The INFOGEST static digestion model protocol 2.0 provides a standardized framework for studying the colonic fermentation of undigested food components [9]. This method enables investigation of how dietary particles, particularly from plant foods, impact microbial community composition and metabolic output:
Sample Preparation:
- Subject food components to simulated oral, gastric, and intestinal digestion prior to colonic fermentation
- For plant food particles, consider both particle size and chemical composition as critical variables affecting fermentation outcomes [40]
- Use fructooligosaccharides (FOS) as a positive control and sterile water as a negative control in experimental designs
Fermentation Conditions:
- Inoculate with fecal microbiota from appropriate donor populations (considering factors like prior dietary exposure)
- Maintain strict anaerobic conditions (≥97% N₂, 3% H₂) throughout the fermentation period
- Incubate at 37°C for 24 hours with continuous agitation [9]
Analytical Endpoints:
- Quantify short-chain fatty acid (SCFA) production (acetate, propionate, butyrate) via GC-MS or HPLC
- Analyze microbial community composition through 16S rRNA gene sequencing of the V3–V4 hypervariable region
- Assess specific bacterial taxa of interest through targeted qPCR or fluorescence in situ hybridization
Diagram 2: Experimental workflow for colonic fermentation of dietary components, from particle preparation to metabolic output analysis.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents for Anaerobic Colonic Fermentation Studies
| Reagent/Material | Specification | Functional Role | Application Example |
|---|---|---|---|
| Silicone Tubing [38] | 0.99 mm luminal diameter, 0.31 mm wall thickness | Oxygen permeability enables liquid-to-liquid gas diffusion in anaerobization units | Media deoxygenation before bioreactor entry |
| Antioxidant Solution [38] | Aqueous solution with strong oxygen-attractant properties | Chemical oxygen scavenging in anaerobization units | Maintaining media oxygen levels <1% |
| Porous Polyester Membrane [38] | Thin, transparent, track-etched | Supports epithelial cell growth while allowing nutrient diffusion | Creating apical-basolateral compartments in flow chambers |
| Fructooligosaccharides (FOS) [9] | ≥99% purity, from chicory | Prebiotic positive control in fermentation studies | Stimulating growth of beneficial bacteria |
| Resazurin Solution [39] | 1 mg·L⁻¹ in pre-reduced PBS | Anaerobic indicator (colorless when reduced, pink when oxidized) | Validation of anoxic conditions in bioreactors |
| Short-Chain Fatty Acid Standards [9] | Acetate, propionate, butyrate, etc. | Quantification of microbial metabolic output | GC-MS or HPLC calibration for SCFA analysis |
| Anaerobic Culture Media [41] | Supplemented with peptides and B vitamins [42] | Supports fast growth of auxotrophic lactic acid bacteria | Enrichment of specific microbial functional groups |
Analytical Approaches for Microbial Community and Metabolic Profiling
Microbial Community Assessment
Advanced sequencing technologies have revolutionized our ability to characterize complex microbial communities in colonic models. Shotgun metagenomics enables comprehensive taxonomic profiling and functional gene analysis, as demonstrated in studies of fermented food ecosystems where 485 high-quality bacterial metagenome-assembled genomes (MAGs) were obtained from 69 water kefir samples [43]. For more targeted analysis, 16S rRNA gene sequencing of the V3–V4 hypervariable region provides cost-effective community composition data, particularly useful for longitudinal studies tracking community dynamics in response to dietary interventions [9].
Stability metrics are essential for validating model performance. The Bray-Curtis similarity index effectively quantifies day-to-day community variations, with established systems like MiCoMo demonstrating average daily similarity of 0.81 ± 0.10 after a short stabilization period of 3–5 days [39]. Additional diversity measures including the Shannon Index (reported as 3.17 ± 0.65 in validated systems) provide insights into microbial diversity retention from original fecal inoculum [39].
Metabolic Output Analysis
Short-chain fatty acid (SCFA) quantification serves as a primary functional readout for colonic fermentation efficiency. The main SCFAs produced include acetate, propionate, and butyrate in an approximate ratio of 60:20:20 mM/kg in the human colon [8]. These microbial metabolites serve crucial roles in host health: butyrate as the primary energy source for colonocytes with demonstrated anti-cancer and anti-inflammatory properties; acetate and propionate as regulators of glucose metabolism and immune function [8].
Modern analytical approaches employ gas chromatography-mass spectrometry (GC-MS) or high-performance liquid chromatography (HPLC) for precise SCFA quantification. In studies investigating traditional fermented foods, SCFA profiling has revealed significantly higher production in naive consumers compared to regular consumers, highlighting the adaptive nature of gut microbial communities [9]. Beyond SCFAs, comprehensive volatilomic analysis provides insights into aroma compounds and other microbial metabolites that influence both sensory properties and potential health impacts of fermentation products [43].
The field of anaerobic incubation and colonic environment simulation has evolved dramatically from simple batch cultures to sophisticated systems that maintain oxygen levels below 1% while supporting complex host-microbe interactions. The development of standalone anaerobization technologies and miniaturized bioreactor platforms has addressed critical limitations of earlier models, enabling more physiologically relevant studies of colonic fermentation processes. These advances come at a crucial time when understanding the intricate relationships between diet, gut microbiota, and human health has become a research priority.
Future directions will likely focus on further integration of host elements including immune components and enteric nervous system representations, creating even more complete models of the colonic environment. Additionally, the application of multi-omics approaches—combining metagenomics, metabolomics, and volatilomics—will provide unprecedented insights into the functional outcomes of microbial fermentation. As these systems become more accessible and cost-effective, they will play an increasingly vital role in screening therapeutic interventions, evaluating functional food components, and elucidating the mechanisms underlying diet-microbiota-host interactions in health and disease.
The colonic fermentation of undigested food components by the gut microbiota produces short-chain fatty acids (SCFAs), which exert profound effects on host health. Investigating this process requires a multifaceted analytical approach. This technical guide details the integrated application of 16S rRNA gene sequencing for microbial community profiling and complementary techniques for SCFA quantification. We provide a critical evaluation of these methodologies, present standardized protocols, and discuss advanced functional genomic techniques that move beyond inference to directly characterize microbial activity. This resource is designed to equip researchers and drug development professionals with the foundational knowledge to design robust studies exploring the diet-microbiota-host axis.
The human colon hosts a complex microbial ecosystem that ferments undigested dietary components, primarily dietary fibers, to produce a range of metabolites, most notably short-chain fatty acids (SCFAs)—acetate, propionate, and butyrate. These SCFAs are not merely waste products; they are critical signaling molecules that influence host metabolism, immune function, and gut homeostasis [44] [45]. The precise relationship between microbial community structure and its metabolic output is a central focus in nutritional science and functional food development.
Analytical characterization of this system rests on two pillars: comprehensive profiling of the microbial community and accurate quantification of the resultant SCFAs. For years, 16S ribosomal RNA (rRNA) gene sequencing has been the cornerstone of microbial ecology, providing a detailed census of the taxa present in a complex sample. However, this approach primarily offers taxonomic inference, and its limitations must be understood. As Segal and colleagues emphasize, "Functional characterization of the lower airway microbiota through metatranscriptome identify metabolically active organisms capable of producing metabolites with immunomodulatory capacity such as SCFAs" [46]. This highlights that while 16S sequencing is powerful for community profiling, functional insights often require complementary, multi-omics approaches.
Core Analytical Techniques
16S rRNA Gene Sequencing for Microbial Community Analysis
The 16S rRNA gene is a highly conserved bacterial marker that contains variable regions, allowing for taxonomic classification. The standard workflow involves DNA extraction, PCR amplification of target regions, library preparation, high-throughput sequencing, and bioinformatic analysis.
Key Methodological Considerations:
- Primer Selection: The choice of primers targeting hypervariable regions (e.g., V3-V4) is critical for coverage and specificity. Studies optimized for full-length 16S rRNA gene sequencing using MinION technology have compared primer sets, such as 27F/1492R versus GM3/GM4, with the latter providing broader bacterial recognition [47].
- PCR Optimization: The number of PCR amplification cycles and the choice of DNA polymerase significantly impact results. Excessive cycles (e.g., >25) can introduce PCR bias, while polymerases like LongAmp Hot Start Taq are often recommended for long amplicons [47].
- Sequencing Technology: While short-read sequencing (Illumina) is common, full-length 16S sequencing using long-read technologies (Oxford Nanopore's MinION, PacBio) improves taxonomic resolution, sometimes to the species level [47].
- Bioinformatic Workflows: The selection of analysis pipelines (e.g., BugSeq, EPI2ME-16S, QIIME2) and reference databases (e.g., SILVA, Greengenes) influences taxonomic classification accuracy and correlation with expected microbial abundances [47].
Table 1: Key Reagents and Tools for 16S rRNA Gene Sequencing
| Research Reagent/Tool | Function/Explanation | Exemplary Products/Citations |
|---|---|---|
| DNA Extraction Kit | Isolates microbial genomic DNA from complex samples (feces, digesta). | PowerSoil DNA Isolation Kit [48] |
| 16S rRNA Primers | PCR amplification of specific hypervariable regions for sequencing. | 27F/1492R, GM3/GM4 [47]; Bakt341F/Bakt805R (V3-V4) [49] |
| DNA Polymerase | Enzymatic amplification of target gene regions. | LongAmp Hot Start Taq [47] |
| Sequencing Platform | High-throughput determination of DNA sequences. | Illumina MiSeq [49]; Oxford Nanopore MinION [47] |
| Bioinformatics Pipeline | Processing raw sequences into taxonomic units and diversity metrics. | QIIME2 [49], BugSeq [47], RiboSnake [49] |
Quantifying Microbial Metabolites: Short-Chain Fatty Acids (SCFAs)
SCFAs are the functional readout of bacterial fermentation. Accurate quantification is essential for linking microbial communities to host physiology.
Primary Quantification Technique: Gas Chromatography (GC) GC is the gold standard for SCFA quantification due to its high sensitivity and resolution.
- Protocol Overview: Sample supernatants (from fecal material or fermentation broth) are acidified, often with metaphosphoric acid, to protonate the SCFAs. The sample is then injected into a GC system equipped with a capillary column (e.g., a polar stationary phase) and a flame ionization detector (FID) [44] [50] [48].
- Data Analysis: Concentrations of acetate, propionate, butyrate, and other SCFAs are determined by comparing peak areas to those of known external standards.
Alternative and Complementary Methods:
- Mass Spectrometry (MS): Coupling GC to MS provides superior specificity and sensitivity, allowing for the identification and quantification of SCFAs and other metabolites in complex mixtures [46].
- Rectal Dialysis Bag Method: This in vivo technique measures SCFA absorption rates in human subjects. A dialysis bag containing a known SCFA solution is inserted into the rectum; absorption is calculated based on the concentration change over time (e.g., 30 minutes) [44].
Table 2: Core Methodologies for SCFA Measurement
| Method | Principle | Key Steps | Applications |
|---|---|---|---|
| Gas Chromatography (GC) | Separates volatile SCFAs based on affinity for the stationary phase, with detection via FID. | 1. Acidification of sample.2. Centrifugation.3. Injection into GC system.4. Quantification vs. standards. | In vitro fermentation [50] [48]; Faecal SCFA measurement [44] |
| GC-Mass Spectrometry | Combines separation by GC with precise molecular identification by MS. | Similar to GC, with MS as the detector. | Targeted metabolomics; verification of SCFA identity [46] |
| Rectal Dialysis Bag | Measures in vivo SCFA absorption from the colon using a semi-permeable membrane. | 1. Insert bag with SCFA solution.2. Incubate 30 min.3. Analyze concentration change. | Human clinical studies on SCFA flux [44] |
Integrated Experimental Workflows
A major research challenge is correlating microbial composition from 16S data with SCFA production. The following workflows outline standard approaches for in vitro and in vivo studies.
1In VitroFermentation Models
In vitro batch culture fermentation is a controlled system to study the direct impact of dietary substrates on gut microbiota.
- Inoculum Preparation: Fresh fecal samples from healthy donors are homogenized in anaerobic phosphate-buffered saline (PBS) to create a 10% (w/v) slurry. The slurry is briefly centrifuged at low speed (e.g., 300 rpm) to remove large particulate matter.
- Fermentation Medium: A defined, anaerobic medium such as Yeast Extract-Casein Hydrolysate-Fatty Acids (YCFA) or a similar Basal Nutrient Medium (BNM) is used. This medium supports the growth of a wide range of gut bacteria.
- Experimental Setup: The test substrate (e.g., a specific dietary fiber, HMO, or functional food extract at 8 mg/mL [50]) is added to the medium. A control group contains only the medium and inoculum.
- Incubation: The fermentation is carried out in airtight serum bottles under a nitrogen (N₂) atmosphere to maintain anaerobiosis. Bottles are incubated at 37°C with constant agitation for a set period (typically 24 hours).
- Sample Collection: Aliquots are collected at various time points (e.g., 0, 3, 6, 12, 24 h). Samples are centrifuged, and the supernatants and pellets are stored at -80°C for subsequent SCFA and microbial analysis, respectively.
Moving Beyond Relative Abundance: Absolute Quantification
A critical limitation of standard 16S sequencing is that it generates relative abundance data, where an increase in one taxon necessitates an apparent decrease in others. This can mask true biological changes.
Solution: Integrating Absolute Quantification [45]
- Method: Combine 16S rRNA sequencing with quantitative PCR (qPCR) or flow cytometry to determine the total bacterial load.
- Calculation: Absolute abundance for a specific taxon = (Total bacterial count) × (Relative abundance of that taxon from 16S data).
- Significance: This approach reveals true microbial growth dynamics. For instance, a study fermenting dietary fibers found that the absolute abundance of SCFA-producing genera like Faecalibacterium, Roseburia, and Anaerostipes showed a strong positive correlation with butyrate production—a relationship that was not apparent from relative abundance data alone [45].
Advanced Techniques and Functional Correlations
Bridging the Gap from Correlation to Causation
While 16S sequencing can correlate taxa with SCFA levels, it cannot confirm which organisms are metabolically active or responsible for production. Advanced functional techniques address this.
- This technique sequences the total RNA (metatranscriptome) in a community, revealing which genes are actively being expressed.
- Application: It directly identifies active microbial metabolism and pathways, such as those for SCFA production. Research has shown that functional evaluations based on inferred metagenomes from 16S data can be dissimilar from direct measurements of activity via metatranscriptomics [46]. This is crucial for understanding the functional reality behind taxonomic shifts.
Resuscitation of Uncultured Bacteria [52]
- Many gut bacteria are unculturable, posing a challenge for functional validation.
- Innovative Approach: SCFAs themselves have been identified as potential resuscitation factors that can promote the isolation and growth of previously uncultured marine bacteria, suggesting a potential role in breaking microbial dormancy in various environments [52].
Temporal Dynamics and Data Modeling
Microbial communities and their metabolites are not static; they exhibit dynamic fluctuations in response to diet and host circadian rhythms.
Capturing Daily Oscillations:
- Studies in animal models (e.g., pigs) show that feed intake, colonic nutrient substrates (starch, cellulose), microbial populations, and SCFA levels undergo significant diurnal oscillations [53]. For example, acetate, propionate, butyrate, and valerate may peak during the dark phase, while branched SCFAs like isobutyrate peak in the light phase [53].
Modeling Microbial Shifts with Machine Learning:
- Simple statistical methods can fail to reliably distinguish significant microbial shifts from normal temporal fluctuations.
- Advanced Modeling: Long Short-Term Memory (LSTM) networks, a type of recurrent neural network, have outperformed other models (e.g., ARIMA, Random Forest) in predicting bacterial abundance trajectories and identifying significant outlier changes in time-series data from human gut and environmental microbiomes [49]. This allows for the development of early-warning systems to detect critical community disruptions.
The integrated analysis of microbial communities via 16S rRNA sequencing and SCFA profiling is a powerful paradigm for studying colonic fermentation. However, researchers must be cognizant of the inherent limitations of inferred data. The field is moving towards a more comprehensive and causal understanding through:
- The adoption of absolute quantification to reveal true microbial growth.
- The application of functional genomics (e.g., metatranscriptomics) to move beyond correlation to activity.
- The use of sophisticated modeling approaches to decipher complex temporal dynamics.
For drug development and functional food research, this multi-pronged, evidence-based toolkit is indispensable for rationally designing interventions that target the gut microbiome to produce defined, health-promoting metabolic outcomes, such as elevated SCFA production.
Within the framework of research on the colonic fermentation of undigested food components, probiotics, prebiotics, and synbiotics have emerged as pivotal tools for developing functional foods aimed at enhancing human health. These substances directly modulate the composition and function of the gut microbiota, leading to the production of bioactive metabolites such as short-chain fatty acids (SCFAs) through bacterial fermentation [3]. The growing understanding of microbial ecology and host-microbe interactions is driving rapid innovation in the food industry, with applications expanding beyond traditional fermented dairy products into plant-based beverages, baked goods, and snack foods [54] [55]. This whitepaper provides an in-depth technical examination of the mechanisms, efficacy, and development methodologies for these ingredients, with a specific focus on their role within the context of colonic fermentation processes and their implications for health and disease prevention.
Definitions, Classifications, and Mechanisms of Action
Core Definitions and Categories
Probiotics: Live microorganisms which when administered in adequate amounts confer a health benefit on the host [56]. Common strains include Lactobacillus, Bifidobacterium, Saccharomyces boulardii, and Bacillus coagulans [56]. To be classified as a probiotic, a strain must be non-pathogenic, non-toxic, adequately characterized, and proven to confer documented health benefits [57].
Prebiotics: Non-digestible food components that selectively stimulate the growth and/or activity of beneficial microorganisms in the colon [56] [58]. Traditional prebiotics include fructooligosaccharides (FOS), galactooligosaccharides (GOS), xylooligosaccharides (XOS), and inulin, while emerging categories include certain polyphenols and human milk oligosaccharides (HMOs) [56] [58].
Synbiotics: Combinations of probiotics and prebiotics that act synergistically, where the prebiotic compound selectively favors the probiotic organism [56]. These formulations are designed to improve the survival and implantation of live microbial supplements in the gastrointestinal tract [56].
Molecular Mechanisms and Pathways in Colonic Fermentation
The primary mechanism of action for these functional ingredients occurs through the modulation of colonic fermentation processes. Upon reaching the colon, prebiotics and probiotic metabolites serve as substrates for saccharolytic bacterial fermentation, resulting in the production of SCFAs, primarily acetate, propionate, and butyrate [3].
The diagram below illustrates the core pathways through which probiotics, prebiotics, and synbiotics influence human physiology via gut microbiota modulation.
The metabolic pathways of SCFA production are highly specific and involve complex cross-feeding mechanisms between different bacterial species. For instance, lactate produced by Bifidobacterium longum during growth on FOS can be utilized by Eubacterium hallii to produce butyrate, despite E. hallii being unable to directly metabolize the initial carbohydrate substrate [3]. Some bacteria, such as Roseburia inulinivorans, can completely alter their fermentation products based on substrate availability, switching from butyrate to propionate production when fucose is available as an energy source [3].
Health Benefits and Clinical Evidence
Documented Health Benefits and Mechanisms
The health benefits of probiotics, prebiotics, and synbiotics are extensive and supported by growing clinical evidence. These benefits are mediated through multiple mechanisms, including pathogen inhibition, intestinal barrier reinforcement, immunomodulation, and the production of beneficial metabolites [56] [59].
Table 1: Documented Health Benefits of Probiotics, Prebiotics, and Synbiotics
| Health Area | Reported Benefits | Proposed Mechanisms | Example Strains/Components |
|---|---|---|---|
| Gastrointestinal Health | Prevention of diarrhea, constipation, inflammatory bowel disease relief [56] | Pathogen inhibition, barrier function enhancement, SCFA production [59] | Lactobacillus rhamnosus GG, FOS, GOS [56] |
| Metabolic Health | Anti-obesity effects, improved lipid profiles, hyperuricemia management [54] | Downregulation of lipid synthesis genes (PPAR-γ, SREBP-1), inhibition of xanthine oxidase [54] | Kluyveromyces lactis JSA 18, Pediococcus acidilactici GQ01 [54] |
| Immunity & Allergy | Reduced allergic symptoms, immune modulation [54] | Shift from Th2 to Th1 cytokine profile (increased IFN-γ, decreased IL-4, IL-5) [54] | Lactobacillus kefiranofaciens ZW3 [54] |
| Brain-Gut Axis | Mood regulation, cognitive support, stress resilience [57] | Neurotransmitter production (e.g., GABA), vagus nerve signaling, inflammatory pathway regulation [54] [57] | Lactiplantibacillus plantarum FRT7 (GABA producer) [54] |
Quantitative Clinical Outcomes
Recent studies provide quantitative data on the efficacy of specific probiotic strains and prebiotic compounds. The table below summarizes key findings from clinical and preclinical investigations.
Table 2: Quantitative Efficacy Data from Selected Studies
| Intervention | Study Model | Key Quantitative Outcomes | Reference |
|---|---|---|---|
| Lactobacillus kefiranofaciens ZW3 | OVA-induced allergic mice | ↓ allergy scores, ↓ serum OVA-sIgE, ↓ IL-4, IL-5, IL-10; ↑ IFN-γ, IL-2 [54] | [54] |
| Kluyveromyces lactis JSA 18 | High-fat diet mice | Reduced weight gain, liver/fat indexes, hyperlipidemia, serum triglycerides, and liver enzymes (ALT/AST) [54] | [54] |
| Pediococcus acidilactici GQ01 & postbiotic G1PB | Hyperuricemia mice | Reduced blood uric acid, creatinine, urea nitrogen; upregulated kidney ABCG2; downregulated URAT1/GLUT9 [54] | [54] |
| Kakadu Plum Powder (Prebiotic) | In vitro colonic fermentation (48h) | Significantly increased SCFA concentrations and antioxidant activity (FRAP) [60] | [60] |
| Human Milk Oligosaccharides (HMOs) | In vitro infant fecal fermentation (24h) | B. infantis-dominant strain produced significantly higher acetic acid than B. breve-dominant strain (p = 0.000) [50] | [50] |
Experimental Models and Methodologies for Studying Colonic Fermentation
1In VitroFermentation Models
In vitro digestion and colonic fermentation models offer a rapid, cost-effective method for preliminary assessment of the functional potential of food components and their impacts on gut health [54]. These systems range from simple batch cultures to more sophisticated continuous culture models that simulate the different regions of the human colon [3] [50].
The experimental workflow for conducting in vitro colonic fermentation studies typically follows a systematic process, as illustrated below.
Batch cultures are widely utilized due to their operational convenience and ability to quickly assess the intestinal microbiota's capacity to utilize specific carbon sources [50]. For instance, the YCFA (yeast extract–casein hydrolysate–fatty acids) medium has demonstrated capability to culture the majority of intestinal microbiota, maintaining approximately 93% consistency with native fecal microorganisms based on metagenomic sequencing [50].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents for Colonic Fermentation Studies
| Reagent/Material | Function/Application | Example Use Case |
|---|---|---|
| YCFA Medium | Anaerobic culture medium supporting growth of diverse gut microbiota [50] | In vitro fermentation of HMOs and other prebiotics using human fecal inocula [50] |
| Human Milk Oligosaccharides (HMOs) | Model prebiotic substrates for infant gut microbiota studies [50] | Investigating strain-specific utilization by Bifidobacterium species (e.g., 2'-FL, 3'-SL, 6'-SL, LNT, LNnT) [50] |
| Alginate-Based Encapsulation Systems | Protect probiotic viability during digestion and controlled release in colon [54] | Calcium alginate-gelatin beads for Lactobacillus rhamnosus GG delivery in fermented black goji berry beverages [54] |
| PBS or Saline Solution | Diluent for preparing fecal bacterial suspensions [50] | Creating 10% (w/v) fecal homogenates for inoculation in fermentation systems [50] |
| qPCR Assays & Primers | Quantification of specific bacterial taxa and functional genes [3] [50] | Enumeration of 10 different Bifidobacterium species in HMO fermentation studies [50] |
| Gas Chromatography (GC) System | Quantification of SCFAs (acetate, propionate, butyrate) [3] [50] | Monitoring SCFA production in fecal fermentation samples over time [50] |
Formulation Technologies and Industrial Applications
Encapsulation and Delivery Systems
A significant challenge in functional food development is maintaining the viability and stability of probiotics during processing, storage, and gastrointestinal transit. Encapsulation technologies have been developed to address these challenges. Research demonstrates that calcium alginate encapsulation combined with hydrocolloids significantly improves the viability of Lactobacillus rhamnosus GG compared to alginate alone [54].
Specific findings show that:
- Calcium alginate–gelatin beads showed the highest level of probiotic survival after simulated digestion.
- Calcium alginate–carrageenan beads best preserved viability when co-digested with milk.
- Co-ingestion with milk enhanced total phenolic content retention across all bead types, as milk macronutrients protected polyphenols during digestion [54].
Synbiotic Formulation Strategies
The rational design of synbiotics requires careful selection of probiotic-prebiotic pairs based on demonstrated synergistic relationships. For instance, certain Bifidobacterium strains exhibit superior growth on specific HMOs, with B. infantis-dominant strains producing significantly higher acetic acid from HMO degradation compared to B. breve-dominant strains [50]. This strain-specific substrate utilization highlights the importance of targeted synbiotic development rather than arbitrary combinations of probiotics and prebiotics.
Future Perspectives and Research Directions
Despite significant advances, several challenges and research gaps remain in the field. Current studies primarily focus on bioactivity, with significant gaps persisting in production methods and food interactions for functional food development [54]. Further validation is needed to substantiate bioactivity claims, especially for functional food applications [54].
Future research priorities include:
- Personalized nutrition approaches based on individual microbiota composition [58]
- Advanced encapsulation technologies for enhanced probiotic protection and targeted release
- Standardized protocols for in vitro and in vivo assessment of efficacy
- Long-term clinical studies to validate health claims and establish dietary recommendations
- Exploration of novel prebiotic sources and probiotic strains with specific health benefits
The continued investigation of the colonic fermentation of undigested food components will undoubtedly yield new insights and opportunities for developing more effective and targeted functional foods in the future.
The human gastrointestinal tract is home to a complex community of trillions of microbes that profoundly influence host health through intricate metabolic networks. The process of colonic fermentation, where gut microbes metabolize undigested food components, produces a diverse array of bioactive metabolites that can modulate host physiological processes [3] [18]. When this delicate ecological balance is disrupted—a state known as dysbiosis—it is associated with a range of infectious, metabolic, and chronic diseases [61]. This understanding has catalyzed the development of microbiome-based therapeutics, with Live Biotherapeutic Products (LBPs) emerging as a promising new class of drugs designed to restore healthy microbial function [61] [62].
Unlike conventional pharmaceuticals, LBPs consist of live organisms—typically bacteria—that exert their therapeutic effect through colonization, community integration, and metabolic modulation [61]. The development pathway for these products requires specialized approaches that bridge microbial ecology, gnotobiotic technology, and clinical translation. This whitepaper provides a comprehensive technical guide to the pipeline for translating fundamental research on colonic fermentation into clinically effective LBPs, with specific methodologies and tools for researchers and drug development professionals.
Foundational Science: Colonic Fermentation and Microbial Metabolism
The therapeutic rationale for LBPs is fundamentally rooted in the metabolic capacity of the gut microbiota. During colonic fermentation, dietary components that escape upper gastrointestinal digestion—primarily complex carbohydrates and proteins—become substrates for microbial metabolism [3] [18]. This process generates key metabolites that influence host health:
- Short-chain fatty acids (SCFAs): Acetate, propionate, and butyrate are the primary SCFAs produced through bacterial fermentation of dietary fiber [3]. Butyrate serves as the primary energy source for colonocytes and possesses anti-inflammatory properties, while propionate and acetate influence gluconeogenesis and satiety signaling through G-protein coupled receptors (GPCRs) such as GPR41 and GPR43 [3] [18].
- Bioactive peptides and amino acid derivatives: Bacterial metabolism of dietary proteins can produce both beneficial and detrimental metabolites. For instance, certain species can convert aromatic amino acids into immune-modulatory compounds, while others produce toxic metabolites like genotoxic cyclodipeptides associated with carcinogenesis [63] [64].
- Secondary metabolites: Plant polyphenols and other phytochemicals are transformed into more bioavailable compounds with enhanced bioactivity through microbial metabolism [65].
The composition and function of the microbial community directly determine the metabolic output of colonic fermentation. Bacterial cross-feeding—where metabolic intermediates produced by one species become substrates for another—creates ecological networks that influence community stability and function [3]. For example, Faecalibacterium prausnitzii depends on acetate produced by other bacteria for growth, while lactate produced by bifidobacteria can be converted to butyrate by species like Eubacterium hallii [3]. These metabolic relationships are crucial considerations when designing synthetic microbial communities for therapeutic applications.
Synthetic Community Design Strategies for LBPs
A critical step in LBP development is the design and assembly of defined microbial consortia. Current approaches move beyond traditional probiotics by incorporating species native to the human gut with specific functional attributes [61]. Four primary strategies guide the rational design of synthetic communities:
Table 1: Synthetic Microbial Community Design Strategies
| Design Strategy | Description | Key Example | Application |
|---|---|---|---|
| Fecal Derivation | Isolation of strains from complex fecal communities that recapitulate desired phenotypes | RePOOPulate (33 strains) [61] | Recurrent C. difficile infection |
| Feature-Guided | Selection based on specific genomic, metabolic, or immunologic features | hCom2 (119 strains) [61] | Enterohemorrhagic E. coli infection |
| Model-Based | Computational prediction of community structure and function | 94 consortia of diverse sizes [61] | Immune modulation |
| Experimentally-Guided | Iterative testing and refinement based on phenotypic screens | GUT-103 (17 strains) [61] | Inflammatory Bowel Disease |
Feature-Guided Design Methodology
The feature-guided approach represents one of the most sophisticated strategies for consortium development. The following protocol outlines the key steps:
Identify Correlative Features: Conduct cross-sectional comparative analyses (e.g., healthy vs. diseased subjects) using metagenomic sequencing and metabolomic profiling to identify microbial taxa and functional pathways associated with the desired phenotype [61] [63].
Strain Isolation and Characterization:
- Inoculate selective media targeting taxa of interest from donor samples under anaerobic conditions (2-5% H₂, 5-10% CO₂, balance N₂) [61] [63].
- Isplicate single colonies and expand in liquid culture.
- Genomically sequence isolates and screen for key functional genes (e.g., SCFA production pathways, bile acid metabolism, immunomodulatory properties) [3].
- Characterize metabolic output using HPLC-MS/MS to quantify SCFAs and other metabolites [63].
Community Assembly:
- Combine strains based on complementary functional attributes and known cross-feeding relationships.
- Assess community stability and function using in vitro culture systems before advancing to animal models.
The resulting defined consortia offer significant advantages over fecal transplants, including reproducible manufacturing, elimination of pathogen risk, and the ability to conduct mechanistic studies using "knockout" communities where specific strains are systematically omitted [61].
Preclinical Models for LBP Validation
Preclinical validation of LBP candidates requires specialized models that can evaluate both microbial ecology and host physiological responses. The following experimental systems provide complementary approaches:
Table 2: Preclinical Models for LBP Development
| Model System | Key Features | Applications | Limitations |
|---|---|---|---|
| In Vitro Gut Models | Controlled physicochemical parameters; high-throughput capability | Initial screening of colonization, community dynamics, and metabolic output | Lack host biological systems |
| Gnotobiotic Mice | Germ-free or defined microbiota; controllable host genetics | Mechanistic studies of host-microbe interactions; community assembly rules | Altered immune physiology; simplified microbiota |
| Antibiotic-Treated Mice | Depleted endogenous microbiota; intact host biology | Evaluation of colonization resistance; therapeutic efficacy | Incomplete microbiota ablation; variable results |
| Disease-Specific Models | Chemically-induced or genetic disease models | Therapeutic efficacy in disease context | May not fully recapitulate human pathology |
Gnotobiotic Mouse Model Protocol
Gnotobiotic mice represent the gold standard for evaluating synthetic community assembly and host response:
Animal Preparation:
- Maintain germ-free C57BL/6J mice in flexible film isolators with autoclaved food, water, and bedding.
- Verify germ-free status through regular culturing (aerobic and anaerobic) and 16S rRNA gene PCR of fecal samples.
Community Inoculation:
- Prepare synthetic community by combining equal volumes (e.g., 10⁸ CFU/mL each strain) of overnight cultures in pre-reduced anaerobic PBS.
- Administer 200µL of consortium via oral gavage to 6-8 week old mice.
- Monitor colonization dynamics through longitudinal fecal sampling (days 1, 3, 7, 14, 21 post-inoculation).
Phenotypic Assessment:
- Analyze microbial engraftment and community structure via 16S rRNA gene sequencing and strain-specific qPCR.
- Quantify microbial metabolites in feces and serum using HPLC-MS/MS.
- Assess host responses through histology, immune profiling (flow cytometry of mesenteric lymph nodes, lamina propria), and transcriptomic analysis of intestinal tissues.
The Altered Schaedler Flora (ASF), an 8-member defined community, has served as an important model minimal microbiome for establishing these methodological approaches [61].
Pathway: Microbial Metabolite Signaling
The following diagram illustrates a key mechanism by which microbial metabolites from colonic fermentation influence host physiology, which can be evaluated in preclinical models:
Clinical Translation and Regulatory Considerations
The successful transition from preclinical models to clinical application requires careful attention to manufacturing, regulatory pathways, and clinical trial design. As of 2025, the microbiome therapeutics market has gained significant momentum with regulatory approvals for recurrent Clostridioides difficile infection (rCDI) paving the way for broader applications [62].
LBP Manufacturing and Quality Control
Manufacturing of LBPs presents unique challenges compared to traditional drugs:
- Strain Banking: Create Master Cell Banks (MCBs) and Working Cell Banks (WCBs) under controlled conditions with comprehensive genomic and phenotypic characterization.
- Fermentation Process: Optimize growth conditions for each strain individually to maximize yield and functionality while maintaining genetic stability.
- Formulation and Delivery: Develop cryopreservation formulations that maintain viability; utilize enteric coatings for oral delivery to protect against gastric acidity.
- Quality Control: Implement rigorous testing for identity (genomic sequencing), purity (absence of contaminants), potency (functional assays), and viability (CFU counts).
Clinical Pipeline and Trial Design
The current LBP pipeline encompasses over 240 candidates across various development stages, with gastrointestinal disorders remaining the primary indication while expansion into metabolic, autoimmune, and oncologic diseases accelerates [62].
Table 3: Select Live Biotherapeutic Products in Clinical Development (2025)
| Product / Company | Indication | Composition | Mechanism of Action | Development Stage |
|---|---|---|---|---|
| Vowst (SER-109) | rCDI | Purified Firmicutes spores | Recolonizes gut, restores bile acid metabolism, outcompetes C. difficile | Approved (FDA) |
| VE303 (Vedanta) | rCDI | Defined 8-strain bacterial consortium | Promotes colonization resistance and bile acid metabolism | Phase III |
| VE202 (Vedanta) | Ulcerative colitis | 8-strain consortium | Induces regulatory T-cell responses and anti-inflammatory metabolites | Phase II |
| MRx0518 (4D Pharma) | Oncology (solid tumors) | Single-strain Bifidobacterium longum | Activates innate and adaptive immunity | Phase I/II |
| SYNB1934 (Synlogic) | Phenylketonuria | Engineered E. coli Nissle | Expresses phenylalanine ammonia lyase to convert phenylalanine | Phase II |
Clinical trial design for LBPs requires special considerations:
- Patient Stratification: Incorporate microbiome-based biomarkers to identify patients most likely to respond to treatment.
- Dosing Rationale: Determine dosing based on colonization kinetics and metabolic activity rather than traditional pharmacokinetics.
- Endpoint Selection: Include both clinical endpoints and microbial endpoints (engraftment, metabolic changes, ecological impact).
- Control Groups: Utilize appropriate placebo controls that account for potential nutritional components in LBPs.
Emerging Technologies and Future Directions
The next generation of LBPs will leverage advanced technologies for enhanced precision and functionality:
Microbiome-Active Drug Delivery Systems (MADDS)
MADDS represent an innovative approach that exploits microbial stimuli for site-specific therapeutic release [66]. These systems respond to microbial enzymes, metabolites, or environmental conditions to trigger drug activation in the gastrointestinal tract, enabling more targeted delivery of small molecules, biologics, and even LBPs themselves.
Engineered Microbial Therapeutics
Synthetic biology approaches are being used to design microbes with enhanced therapeutic capabilities. Examples include:
- Sensor-effector systems: Bacteria engineered to detect disease-associated metabolites and produce therapeutic responses in real-time.
- CRISPR-based antimicrobials: Phages engineered with CRISPR systems to selectively eliminate antibiotic-resistant pathogens [62].
- Metabolic engineering: Microbes designed to produce and deliver therapeutic molecules directly in the gut environment.
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagents for LBP Development
| Reagent / Tool | Function | Application Examples |
|---|---|---|
| Gnotobiotic Mouse Facilities | Provides controlled environment for studying host-microbe interactions without confounding microbial influences | Evaluation of synthetic community assembly; host immune response to defined consortia |
| Anaerobic Chamber | Creates oxygen-free environment for cultivating obligate anaerobic gut bacteria | Strain isolation and characterization; in vitro community modeling |
| HPLC-MS/MS Systems | Quantifies microbial metabolites (SCFAs, bile acids, neurotransmitters) | Functional assessment of microbial communities; pharmacodynamic biomarker analysis |
| Strain-Specific qPCR Assays | Enables precise quantification of individual consortium members in complex samples | Engraftment and persistence monitoring in animal models and clinical trials |
| Genome-Scale Metabolic Models | Computational prediction of community metabolic networks and interactions | Rational design of synthetic communities with desired metabolic output |
The development pathway from preclinical models to Live Biotherapeutic Products represents a paradigm shift in therapeutic intervention, moving from targeting host pathways to modifying the gut ecosystem. The process begins with careful design of synthetic microbial communities based on insights from colonic fermentation research, proceeds through rigorous validation in gnotobiotic and disease models, and culminates in clinical trials with specialized endpoints that account for microbial ecology.
As the field advances, key challenges remain, including understanding the principles governing stable colonization, predicting individual responses to microbial therapeutics, and optimizing manufacturing processes for complex living drugs. The integration of synthetic biology, advanced delivery systems, and computational ecology will drive the next generation of LBPs with enhanced precision and efficacy for a wide range of diseases beyond the gastrointestinal tract.
Challenges and Refinements in Modulating Colonic Fermentation for Health
Addressing Inter-Individual Variability in Microbial Composition and Response
In the context of colonic fermentation of undigested food components, inter-individual variability in gut microbial composition presents a fundamental challenge for developing targeted nutritional and therapeutic strategies. While diet significantly influences microbial metabolism, even identical dietary intake results in substantial variations in gut microbiome composition and function between individuals [67]. This variability stems from a complex interplay of host physiology, environmental factors, and microbial ecosystem dynamics that collectively shape individual microbial signatures.
Understanding these drivers is particularly crucial for research on colonic fermentation, where microbial communities transform undigested dietary components into metabolites with far-reaching health implications. The "fermentome" – the complex system of diet, symbiont bacteria, and volatile gases produced through fermentation – varies significantly between individuals and has direct impacts on colonic and metabolic health [68]. This technical guide examines the key factors underlying inter-individual variability and provides methodologies for addressing these challenges in research settings.
Key Drivers of Inter-Individual Variability
Host Physiological Factors
Gut Transit Time and Luminal pH Whole-gut and segmental transit times account for substantial variation in microbiome composition between healthy individuals. Research using wireless motility capsules has demonstrated that longer transit times correlate with increased microbial protein degradation and methane production, while metabolites from carbohydrate fermentation show negative correlations with gut passage time [67]. The median values of segmental transit times measured in healthy populations include:
- Gastric emptying time (GET): 4.8 hours (range 3.1-6.2 hours)
- Whole-gut transit time (WGTT): 23.3 hours (range 12.4-72.3 hours)
- Colonic transit time (CTT): 13.6 hours (range 2.1-63.5 hours)
- Small-bowel transit time (SBT): 5.1 hours (range 2.5-10.3 hours) [67]
Luminal pH variations along the gastrointestinal tract further influence microbial composition, with acidic environments inhibiting certain bacterial taxa while favoring acid-tolerant species [67]. These physiological parameters exhibit significant inter-individual differences that persist over time, contributing to stable personal microbiome signatures.
Gut Environmental Stability Daily sampling reveals that individuals exhibit varying degrees of fluctuation in gut environmental factors. The coefficient of intra-individual variation ranges observed in healthy adults include:
- Faecal pH: 0.3-8.1%
- Bristol Stool Form Scale (BSS): 0-57.8%
- Stool frequency: 0-73.1%
- Stool moisture: 2.2-24%
- Microbial load: 7.6-72.7% [67]
Notably, participant identity explains a significant proportion of variation in day-to-day fluctuations of all gut environmental factors, indicating that gut environment stability is itself an individual characteristic [67].
Microbial Community Variation by Niche
The gastrointestinal tract contains distinct microbial niches with different community structures. Luminal microbes are predominantly anaerobic and play key roles in fermentation and metabolism of luminal contents, while mucosal-associated bacteria may be more involved with immune functions [69]. Sampling methodology significantly influences microbial community assessment, with substantial taxa differences observed between rectal swab, stool, and mucosal samples [69].
Table 1: Microbial Community Variations by Sampling Method
| Sample Type | Characteristics | Key Taxa Variations | Functional Differences |
|---|---|---|---|
| Stool | Primarily luminal bacteria; more transient communities | Higher abundance of anaerobic fermentative bacteria | Enhanced carbohydrate metabolism and fermentation pathways |
| Rectal Swab | Combination of luminal and mucosal bacteria | Intermediate between stool and mucosal samples | Mixed functional profile |
| Mucosal Biopsy | Adherent mucosal communities; less diverse | Enriched for bacteria adapted to mucus layer | Increased involvement in immune modulation |
Whole-genome metagenome shotgun sequencing reveals that while swab samples are closer to stool samples than mucosal samples, all KEGG functional Level 1 and Level 2 pathways differ significantly across sample types [69]. This highlights the importance of standardized sampling protocols when comparing results across studies.
Methodological Approaches for Assessing Variability
In Vitro Fermentation Models
Model Systems for Protein Fermentation In vitro models allow systematic investigation of fermentation potential across different protein sources while controlling for inter-individual variability. Using ileal digesta from pigs as a substrate (collecte in accordance with DIAAS determination protocols) with human fecal inoculum enables assessment of undigested dietary protein fermentation [70].
Significant variations exist in fermentation kinetic parameters between different protein sources:
- Maximum gas production rate (Rmax) ranges from 15.5 ± 0.7 mL/h for wheat bran-derived proteins to 24.5 ± 0.9 mL/h for oatmeal-derived proteins
- Time to reach cumulative gas production from substrate (TGPs) varies from 14.7 ± 0.7 hours for egg-derived proteins to 27.6 ± 7.1 hours for mushroom-derived proteins [70]
When categorized into food groups ('animal protein', 'grains', 'legumes', 'fungi, algae and microorganisms', and 'others'), no significant differences emerge in fermentation kinetic parameters, suggesting substantial variability within categories [70].
Traditional Fermented Food Assessment The INFOGEST static digestion model protocol 2.0 provides a standardized approach for evaluating how traditional fermented foods (TFFs) modulate gut microbiota from different donor populations [9]. This method involves:
- Anaerobic incubation of stool samples with digested food substrates for 24 hours
- 16S rRNA gene sequencing of the V3-V4 hypervariable region to determine microbial communities
- SCFA measurement as a proxy for gut microbiota functionality
Studies using this approach demonstrate that baseline consumption history significantly influences microbial responses. Non-consumers of Mabisi (a traditional Zambian fermented dairy product) exhibit greater shifts in gut microbiota composition and more pronounced increases in SCFA production compared to regular consumers, highlighting how prior dietary exposure shapes microbial resilience [9].
Longitudinal Study Designs
Multi-Omics Profiling Comprehensive assessment of inter-individual variability requires longitudinal studies integrating multiple data types. A 9-day observational trial with 61 healthy adults demonstrated that:
- Individual identity explains >50% of inter-individual variations in quantitative microbiome profiles, urine metabolomes, and fecal metabolomes
- Sampling day explains only 6.7% of urine metabolome variation on average and does not significantly explain day-to-day variations in gut microbiome or fecal metabolome [67]
Distance-based redundancy analysis reveals that stool moisture and fecal pH explain 3.5% and 2.5% of intra-individual variations in gut microbiome, respectively, while dietary components show no significant explanatory power for daily fluctuations [67].
Table 2: Key Experimental Approaches for Addressing Inter-Individual Variability
| Methodology | Application | Key Parameters | Considerations |
|---|---|---|---|
| Wireless Motility Capsules | Measure segmental transit times and pH | Gastric emptying, small bowel and colonic transit times, luminal pH | Provides direct physiological measurements; capsule retention can occur |
| Multi-omics Profiling | Link microbiome composition with metabolic output | 16S rRNA sequencing, LC-MS metabolomics, quantitative microbiome profiling | Reveals functional relationships; requires specialized analytical capabilities |
| In Vitro Fermentation Models | Assess substrate fermentability | Gas production kinetics, SCFA profiles, microbial composition changes | Controls for confounding variables; may not fully replicate in vivo conditions |
| Longitudinal Sampling | Capture intra-individual variation | Daily stool moisture, pH, BSS, microbial load | Identifies personal baselines; resource-intensive for large cohorts |
Analytical Framework for Data Integration
Statistical Approaches
Permutational multivariate analysis of variance (PERMANOVA) enables quantification of variance components attributable to different factors. For microbiome data, this approach can partition variation into inter-individual, intra-individual, and technical components [67]. Distance-based redundancy analysis (db-RDA) further identifies specific environmental factors explaining microbiome and metabolome variations.
Linear regression analysis of fermentation kinetic parameters between human and porcine-derived inoculum shows correlation only for Rmax (R² = 0.78, P < 0.01) and TGPs (R² = 0.17, P < 0.05), underscoring the importance of inoculum source selection for human health predictions [70].
Data Management and FAIR Principles
Implementing FAIR (Findable, Accessible, Interoperable, Reusable) data principles ensures research on inter-individual variability can be effectively integrated across studies. The ODAM (Open Data for Access and Mining) approach provides a framework for structuring experimental data tables with embedded metadata, facilitating combined analysis of multiple data types [71]. Key considerations include:
- Standardizing structural metadata describing how data tables are organized
- Providing unambiguous definitions of all elements with links to community-approved ontologies
- Using open interoperability standards like Frictionless datapackage for data dissemination
Proper data management is particularly crucial for heterogeneous datasets capturing inter-individual variability, as it enables meta-analyses across study populations and conditions.
Research Reagent Solutions
Table 3: Essential Research Reagents and Materials
| Reagent/Material | Function/Application | Examples/Specifications |
|---|---|---|
| Wireless Motility Capsule (SmartPill) | Measure segmental transit times and pH in vivo | Records pH, temperature, pressure; determines GET, SBT, CTT |
| Faecal Inoculum Preservation Solution | Maintain microbial viability for in vitro studies | Phosphate buffered saline with 10% glycerol; stored under CO₂ |
| N-free Buffer for Fermentation | Create nitrogen-limiting conditions for protein fermentation studies | Supplemented with easily fermentable carbohydrates (maltose, pectin, xylose, soluble potato starch) |
| INFOGEST Digestive Reagents | Simulate human gastrointestinal digestion in vitro | Porcine pepsin (P6887), human salivary amylase (A1031), porcine pancreatin (P7545), rabbit gastric extract |
| SCFA Analysis Standards | Quantify short-chain fatty acid production | Acetate, propionate, isobutyrate, butyrate, formate, lactate standards for calibration |
| DNA Isolation Kits | Extract microbial DNA from complex samples | E.Z.N.A. Stool DNA kit with optional 95°C incubation for Gram-positive bacteria lysis |
Experimental Workflows and Relationships
Workflow for Assessing Inter-Individual Variability: This diagram outlines the comprehensive approach to studying inter-individual variability in microbial composition and response, integrating host factor assessment with multiple experimental methodologies and data analysis approaches.
Addressing inter-individual variability in microbial composition and response requires integrated methodological approaches that account for host physiology, environmental exposures, and microbial ecosystem dynamics. Standardized protocols for in vitro fermentation, multi-omics profiling, and longitudinal sampling provide powerful tools for disentangling the complex factors contributing to individual microbial signatures. By implementing robust experimental designs and analytical frameworks, researchers can advance our understanding of colonic fermentation processes and develop targeted strategies that account for the substantial inter-individual differences observed in human populations.
Overcoming Hurdles in LBP Manufacturing and Standardization
Live Biotherapeutic Products (LBPs) represent a novel class of biologics that utilize stabilized live organisms, such as bacteria, for the treatment or prevention of diseases, many of which are linked to microbial dysbiosis [72]. The development of these products is gaining significant momentum, propelled by well-defined regulatory pathways in regions like the United States and European Union, advancements in oral delivery technologies, and a growing understanding of disease areas associated with the human microbiome [73]. The central hypothesis underpinning LBP therapeutics is that restoring a healthy microbial balance can mitigate or reverse associated health conditions [72].
This therapeutic approach is intrinsically connected to the science of colonic fermentation. The colon acts as a natural fermenting chamber, where undigested food components are metabolized by resident bacteria [68]. This complex process, sometimes referred to as the 'fermentome', involves the production of various metabolites, including short-chain fatty acids (SCFAs) and volatile organic compounds (VOCs), which have direct effects on colonocytes and broader gut neural and metabolic functions [68]. The intimate relationship between the gut microbiota and host health means that LBPs are uniquely positioned to modulate this colonic environment for therapeutic benefit. However, the path from concept to clinic is fraught with technical and standardization challenges that must be systematically addressed.
Key Manufacturing Challenges in LBP Development
The manufacturing of LBPs presents a unique set of hurdles distinct from those of conventional small-molecule drugs or even traditional biologics. These challenges stem from the fundamental nature of LBPs as living, often anaerobic, entities.
Upstream Process Development
The viability and stability of LBPs begin with the upstream manufacturing process. A primary challenge lies in the optimization of media composition and critical process parameters like pH, dissolved oxygen, and temperature to maximize cell density [72]. Many beneficial microbes are strict anaerobes, requiring specialized, oxygen-free fermentation systems to maintain viability and functionality [74]. Furthermore, the growth requirements and yields can vary significantly between different microbial strains, making the development of a universal process impractical. Advanced fermentation strategies, such as fed-batch or biostat-controlled processes, are often necessary to achieve higher biomass, and the fermentation process can affect the final output at a logarithmic scale [72].
Downstream Stabilization and Formulation
Following fermentation, the next critical hurdle is stabilizing the live microbes to ensure they remain metabolically active until they reach the patient. Moisture removal is correlated with improved shelf life, typically achieved through lyophilization (freeze-drying) or spray drying [72]. The presence of cryoprotectants and osmo-protectants, such as sucrose, trehalose, inulin, and skim milk, is critical to reduce crystal formation during freezing and prevent damage to cell membranes [72]. The ratio of biomass to cryoprotectant is a key determinant of microbial preservation.
For topical or oral applications, the dried powders must be incorporated into a delivery matrix. Aqueous formulations can compromise microbial stability, making non-aqueous formulations better suited for many applications [72]. The final product must balance the need to keep the therapeutic microbes "happy and healthy" with the requirement to prevent the growth of unwanted contaminants, often necessitating innovations in packaging that allow for mixing at the point of application [72].
Quality Control and Analytical Challenges
Unlike chemical drugs, the potency of an LBP is tied to the viability and metabolic activity of living organisms. This introduces significant challenges in batch-to-batch consistency and quality control [73]. Characteristics such as strain viability, purity (ensuring the absence of contaminants), and potency must be rigorously monitored and controlled. The main challenges stemming from manufacturing include process upscaling, batch-to-batch variability, and differences in growth yields and strain characteristics [73]. Establishing robust and predictive analytical methods that can accurately reflect the biological activity of these complex products remains a significant hurdle for the field.
Table 1: Key Manufacturing Challenges and Potential Mitigation Strategies
| Manufacturing Stage | Core Challenges | Potential Solutions & Technologies |
|---|---|---|
| Upstream Processing | Strain-specific growth requirements; Oxygen sensitivity for anaerobes; Low biomass yields | Specialized anaerobic fermentation systems; Advanced process control (e.g., fed-batch); Optimized growth media [72] [74] |
| Downstream Processing & Stabilization | Maintaining microbial viability during drying; Sensitivity to moisture and oxygen; Long-term shelf-life | Lyophilization/Spray drying with cryoprotectants (e.g., trehalose, inulin); Oxygen-impermeable packaging; Inert atmosphere (N2) headspace [72] |
| Formulation & Delivery | Incompatibility with traditional preservatives; Stability in delivery matrices (e.g., creams, capsules) | Non-aqueous formulations; Encapsulation technologies; Point-of-use reconstitution systems [72] |
| Quality Control & Standardization | Batch-to-batch variability; Defining and measuring potency/purity; Complex microbial characterization | Development of strain-specific potency assays; Metagenomic quality checks; Real-time viability monitoring platforms [73] [74] |
Standardization and Regulatory Pathways
The establishment of standardized protocols and clear regulatory guidelines is paramount for the successful translation of LBPs from research to clinical application.
Evolving Regulatory Frameworks
The growth in LBP production can be attributed in part to well-defined regulatory pathways in regions such as the US and EU [73]. Regulatory bodies require strict adherence to Chemical, Manufacturing, and Control (CMC) requirements to ensure product quality and safety. Specialized Contract Development and Manufacturing Organizations (CDMOs) are increasingly offering integrated regulatory services, including consulting and CMC documentation support, which are critical for successful Investigational New Drug (IND) filings and Biologics License Application (BLA) approvals in this novel field [74].
The Imperative for Standardized Experimental Models
In the research and development phase, standardized in vitro models are essential for reliably evaluating LBP functionality and its impact on colonic fermentation. The INFOGEST static digestion model is a widely recognized and validated protocol for simulating human gastrointestinal digestion, providing a reproducible foundation for pre-clinical studies [9].
The following workflow diagram illustrates the application of this model in LBP research, connecting key manufacturing stages to functional assessment in a standardized colonic fermentation system.
A key application of this model is testing the hypothesis that an individual's prior exposure to a microbial product influences the resilience of their gut ecosystem. For instance, research on Mabisi, a traditional fermented food, demonstrated that the gut microbiota of regular consumers exhibited greater resilience, with limited changes in community composition upon re-exposure, compared to non-consumers [9]. This type of standardized assessment is crucial for predicting LBP efficacy.
The Scientist's Toolkit: Essential Reagents and Materials
The following table details key reagents and materials essential for conducting standardized in vitro LBP and colonic fermentation research, based on established protocols [9].
Table 2: Key Research Reagent Solutions for In Vitro LBP Fermentation Studies
| Reagent/Material | Function/Application | Specific Examples |
|---|---|---|
| Digestive Enzymes | Simulate human gastrointestinal digestion to assess LBP survival and activity. | Porcine pepsin (for gastric phase), Porcine pancreatin (for intestinal phase) [9] |
| Bile Salts | Critical for mimicking the solubilizing and antimicrobial environment of the small intestine. | Sodium taurodeoxycholate [9] |
| Culture/Media Components | Provide nutrients for supporting the growth of both the LBP and the complex donor microbiota during fermentation. | Peptone from potatoes, Soluble potato starch, Fructooligosaccharides (FOS - as a positive control) [9] |
| SCFA & Metabolite Standards | Calibration and quantification of microbial metabolic output via Gas Chromatography (GC) or HPLC. | Acetate, Propionate, Butyrate, Lactate, Succinate standards [9] |
| DNA Extraction & Sequencing Kits | Analyze shifts in microbial community composition and structure in response to LBP. | Kits for 16S rRNA gene amplification & sequencing (e.g., V3–V4 hypervariable region) [9] [75] |
| Cryoprotectants | Protect microbial viability during freeze-drying (lyophilization) of LBP samples. | Sucrose, Trehalose, Inulin, Skim Milk [72] |
The LBP field is poised for extraordinary expansion, with the associated CDMO market projected to grow from USD 0.08 billion in 2025 to USD 1.11 billion by 2035, reflecting a compound annual growth rate (CAGR) of 30.1% [74]. This growth is underpinned by technological innovations in anaerobic bioprocessing, such as automated anaerobic handling systems and real-time viability monitoring platforms, which enhance product quality and manufacturing consistency [74].
While the market is currently dominated by applications for C. difficile infection, the future lies in therapeutic expansion into inflammatory bowel disease (IBD), metabolic diseases, and beyond [74]. Success in these complex areas will depend on our ability to overcome the inherent manufacturing and standardization hurdles discussed. This will require a unified approach that synchronizes activities from strain selection through to final product stability, leveraging cross-disciplinary collaboration and advanced technologies like artificial intelligence to strengthen the link between upstream and downstream operations [72]. The continued maturation of regulatory pathways, coupled with a deeper scientific understanding of the "fermentome," will be essential to fully realize the potential of LBPs in modulating colonic fermentation for human health.
The resilience of the gut microbiota—its ability to resist and recover from perturbation—is a cornerstone of gastrointestinal health. Utilizing the comparative responses of consumers versus non-consumers to specific foods provides a powerful experimental model to elucidate the mechanisms underlying this resilience. This whitepaper synthesizes recent findings from in vitro colonic fermentation studies to demonstrate that prior dietary exposure establishes a stabilized microbial community capable of mitigating compositional shifts upon re-introduction of a substrate. The non-consumer gut microbiota, in contrast, exhibits greater plasticity and metabolic responsiveness, offering strategic pathways for targeted microbial modulation in nutritional science and therapeutic development.
The human colon hosts a complex ecosystem where undigested food components are metabolized by the resident microbiota. A key outcome of this colonic fermentation is the production of short-chain fatty acids (SCFAs) like acetate, propionate, and butyrate, which are crucial for gut barrier integrity, immune modulation, and systemic health [76] [77]. The concept of "microbial resilience" describes the capacity of this gut ecosystem to maintain its structural and functional stability in the face of dietary perturbations [78].
The consumer vs. non-consumer study model serves as a pristine experimental framework for isolating the effects of dietary exposure. Research on traditional fermented foods (TFFs) is particularly revealing, as these foods introduce both live microorganisms and pre-formed bioactive metabolites [9] [76]. A core hypothesis in this field is that chronic consumption of a specific food component leads to the development of a microbial community that is adapted and resilient to that component, thereby showing a muted response upon subsequent exposure compared to a naïve microbiota [9]. This principle is foundational for developing personalized nutritional strategies aimed at enhancing gut health through directed microbial modulation.
Conceptual Framework: The Consumer vs. Non-Consumer Model
The differential response between consumers and non-consumers hinges on fundamental ecological principles applied to the gut microenvironment.
- Microbial Adaptation and Selection: Regular consumption of a food product, such as a fermented food, consistently introduces specific microbial taxa and substrates. This repeated exposure acts as a selective pressure, enriching for bacterial species that can efficiently utilize these resources. The resulting community is pre-adapted to the food, leading to stability upon re-exposure [9] [76].
- Metabolic Priority and Cross-Feeding: The established microbiota in consumers possesses the necessary enzymatic machinery for the primary breakdown of familiar substrates. This can lead to efficient cross-feeding networks, where the metabolic byproducts of one bacterium become the nutrients for another, creating a stable, interdependent consortium that is resistant to invasion or major shifts [77].
- The Non-Consumer as a Model of Plasticity: The gut microbiota of non-consumers lacks this specific adaptation. When exposed to a novel substrate, the community undergoes significant structural reorganization as different taxa compete for the new resource. This lack of prior adaptation manifests as greater shifts in both composition and metabolic output, providing a clear window into the substrate's intrinsic modulatory potential [9].
The following diagram illustrates the conceptual framework and hypothesized outcomes of this model.
Experimental Insights from a Mabisi Fermentation Model
A seminal 2025 study by Nyati et al. provides a compelling case study that directly tests the consumer/non-consumer model using Mabisi, a traditional Zambian fermented dairy product [9] [79].
Detailed Experimental Protocol
The methodology offers a robust template for in vitro research in this domain.
- Sample Collection and Donor Classification: Stool samples were obtained from Zambian children (aged 6-12 months) classified as either Mabisi consumers or non-consumers via questionnaire. Critically, no donor had received antibiotics in the preceding 30 days [9].
- In Vitro Digestion and Fermentation: The study employed the INFOGEST static digestion model (protocol 2.0) to simulate upper gastrointestinal tract digestion of three treatments:
- Mabisi (test substrate)
- Fructooligosaccharides (FOS) (positive control)
- Sterile water (negative control) The digested treatments were then subjected to anaerobic incubation with a fecal slurry from the donors for 24 hours under conditions simulating the colon [9].
- Downstream Analysis:
The workflow of this experiment is detailed below.
Key Quantitative Findings
The data from the Mabisi study clearly demonstrate the divergent responses between the two groups. The following table summarizes the core quantitative findings.
Table 1: Key Experimental Outcomes from Mabisi In Vitro Fermentation [9] [79]
| Metric | Mabisi Consumers | Mabisi Non-Consumers | Interpretation |
|---|---|---|---|
| Beta Diversity Shift (vs. negative control) | R² = 0.07, p-adj = 0.375 (Non-significant) | R² = 0.08, p-adj = 0.05 (Significant) | Consumers' microbiota composition remained stable; non-consumers' composition significantly changed. |
| Pediococcus Abundance | Increased | Increased | Mabisi consistently enriches this beneficial genus, regardless of consumption history. |
| Total SCFA Production | Lower | Significantly Higher | The non-consumer microbiota exhibited a more pronounced metabolic response, producing more SCFAs. |
| Acetate, Butyrate, Formate, Succinate | Lower | Higher | Non-consumers produced significantly higher levels of these key SCFAs. |
The Scientist's Toolkit: Essential Reagents and Models
To replicate and advance research in this field, scientists require a specific set of validated tools and reagents. The following table details essential components of the experimental toolkit, as evidenced by the reviewed literature.
Table 2: Key Research Reagent Solutions for In Vitro Colonic Fermentation Studies
| Item | Function & Rationale | Example from Literature |
|---|---|---|
| INFOGEST Model | A standardized, static in vitro digestion protocol that simulates the oral, gastric, and small intestinal phases to generate physiologically relevant digesta. | Used to pre-digest Mabisi before colonic fermentation [9]. |
| TIM-2 (TNO Intestinal Model) | A dynamic, computer-controlled in vitro colon simulator that maintains a stable, complex microbiota and allows for real-time monitoring of metabolism. | Used to study yeast-based protein and fermented ketchup [80] [81]. |
| Fructooligosaccharides (FOS) | A well-characterized, rapidly fermentable positive control substrate to validate the metabolic activity of the fecal inoculum in an experiment. | Served as a positive control in the Mabisi study [9]. |
| 16S rRNA Sequencing (V3-V4) | A standard molecular technique for profiling the composition and structure of complex microbial communities, allowing for beta-diversity analysis. | Used to determine microbial communities in Mabisi and fiber studies [9] [78]. |
| GC-MS for SCFAs | Gas Chromatography-Mass Spectrometry is the gold-standard method for the precise identification and quantification of SCFAs and other microbial metabolites. | Used to measure acetate, propionate, butyrate, etc. [80] [82]. |
| N-Free Fermentation Buffer | Creates a nitrogen-limiting environment in vitro, forcing the microbiota to ferment the provided proteinaceous test substrate for nitrogen, allowing kinetic studies. | Used in protein fermentation kinetic studies with ileal digesta [70]. |
Implications for Research and Development
The insights from the consumer/non-consumer model have profound implications for designing future studies and developing interventions.
- Informing Clinical Trial Design: The model underscores the necessity of stratifying study participants based on baseline dietary habits. Failure to account for prior consumption history can obscure true treatment effects, as seen in the muted SCFA response in Mabisi consumers [9].
- Personalized Nutritional Strategies: Understanding that an individual's microbial resilience is shaped by their dietary history enables a more personalized approach. For a desired metabolic outcome like butyrate production, a specific dietary intervention may be most effective for individuals with a "non-consumer" type microbiota for that component [78] [77].
- Pathway to Microbial Therapeutics: The non-consumer microbiota's plasticity identifies it as a prime target for dietary interventions aimed at rapid microbial modulation. This principle can be leveraged to design functional foods or synbiotic formulations intended to correct dysbiosis by introducing novel, beneficial taxa or metabolites to which the community is not adapted [83] [76] [81].
The consumer vs. non-consumer model provides a critical lens through which to view and optimize gut microbial resilience. Evidence from advanced in vitro studies demonstrates that chronic dietary exposure fosters a stabilized, resilient microbiota, while naïve microbiota exhibit functional plasticity. This dichotomy is not merely observational but is quantifiable through metrics of community composition and metabolic output, particularly SCFA production. For researchers and drug development professionals, integrating this paradigm into experimental design and data interpretation is essential. It paves the way for more nuanced, effective, and personalized nutritional and therapeutic strategies aimed at harnessing the gut microbiome to improve human health. Future work should focus on defining the specific microbial taxa and functional genes that underpin this resilience, further bridging the gap between observational correlation and mechanistic causation.
Navigating Regulatory Pathways for Microbiome-Based Therapeutics
The human colon is a primary site of dynamic interaction between the host and the gut microbiota, where the fermentation of undigested food components generates a complex array of microbial metabolites with significant local and systemic health implications. Research on colonic fermentation of undigested food components provides the fundamental scientific basis for developing microbiome-based therapies (MbTs). This in-depth technical guide explores the regulatory pathways for these innovative products, framed within the context of colonic fermentation science. For researchers and drug development professionals, understanding this regulatory landscape is crucial for successfully translating laboratory findings on microbial metabolites, such as short-chain fatty acids (SCFAs), into approved therapies. The intended use of a finished product is the primary determinant of its regulatory status, governing whether a substance will be regulated as a food, supplement, or medicinal product [84].
The Spectrum of Microbiome-Based Therapies
Microbiome-based therapies encompass a diverse continuum of products, ranging from minimally manipulated whole ecosystems to highly characterized single strains. This spectrum is categorized based on the level of manipulation and characterization of the microbial material.
Table: Spectrum of Microbiome-Based Therapies
| Therapy Category | Description | Level of Characterization | Key Regulatory Considerations |
|---|---|---|---|
| Microbiota Transplantation (MT) | Transfer of minimally manipulated microbial community from a human donor to a recipient [84]. | Low | Donor screening, pathogen transmission risk [84]. |
| Donor-Derived Microbiome-Based Medicinal Products | Whole or highly complex ecosystems from human microbiome samples with industrial manufacturing [84]. | Medium | Control of complex starting material, batch-to-batch consistency [84]. |
| Rationally Designed Ecosystem-Based Medicinal Products | Dozens of strains co-fermented to form a controlled ecosystem; produced from clonal cell banks [84]. | Medium-High | Process validation, potency tests, functional characterization [84]. |
| Live Biotherapeutic Products (LBPs) | Single strain or mixture of strains grown separately and blended; produced from clonal cell banks [84]. | High | Thorough strain characterization, defined mechanism of action [84]. |
The donor or origin of the microbiome sample plays a varying role in the risk-benefit assessment across this spectrum. For MTs, the donor is critically important, whereas for LBPs, the impact of the original donor is minimized due to the high level of strain characterization and control [84].
European Regulatory Framework for Microbiome-Based Therapies
The European regulatory landscape for MbTs is evolving, with the recent Regulation on Substances of Human Origin (SoHO) introducing key changes to address these innovative products. The following diagram illustrates the core regulatory concepts and pathways.
The intended use of a product is a key determinant of its regulatory status. Products intended for the prevention or treatment of disease must be registered as medicinal products. The European Medicines Agency (EMA) and national drug authorities assess a drug candidate's quality, safety, and efficacy within the intended population [84]. The recent SoHO regulation provides a framework for substances of human origin, including microbiota for transplantation [84].
Regulatory Science and Future Challenges
The field of regulatory science has emerged to develop new tools, standards, and methodologies for evaluating innovative products like MbTs. According to the EMA, regulatory science encompasses the scientific disciplines applied to the quality, safety, and efficacy assessment of medicinal products throughout their lifecycle [84]. Key future challenges include:
- Harmonizing Terminology: There is a pressing need to clarify and harmonize terminology for products like "faecal microbiota-based medicinal products" to ensure consistency between regulators, academia, and industry [84].
- Batch-to-Batch Consistency: For complex products involving co-fermentation of multiple strains, maintaining consistent quality between batches remains a significant challenge for manufacturers [84].
- Characterization and Potency Testing: Establishing robust methods for characterizing complex microbial ecosystems and developing meaningful potency tests are critical for regulatory approval [84].
In Vitro Colonic Fermentation Models: Informing Therapeutic Development
In vitro colonic fermentation models are indispensable tools for studying diet-microbiota interactions and providing the scientific evidence required for MbT development. These models allow researchers to investigate how undigested food components are metabolized by the gut microbiota and influence microbial community structure and function.
Table: Common In Vitro Colonic Fermentation Models
| Model Type | Key Features | Applications | Examples |
|---|---|---|---|
| Static Batch Fermentation | Simple, anaerobic incubation of fecal inoculum with substrate for fixed time (e.g., 24-48 h) [82] [9]. | Screening substrate effects on microbiota composition and SCFA production [9]. | INFOGEST static model [23] [9]. |
| Dynamic Multi-Compartment Models | Multiple connected compartments simulating different gut regions; continuous flow [85] [86]. | Long-term studies of microbial ecology, nutrient utilization [86]. | TIM-2, SHIME [86]. |
| Advanced Simulation Reactors | Incorporate peristalsis, absorption, and biofilm formation [86]. | Studying the impact of mechanical forces and colonization [86]. | Simulation Colon Reactor (SCR) [86]. |
The experimental workflow for a static in vitro batch fermentation, commonly used in foundational research for MbTs, is outlined below.
Key Analytical Methods for Functional Assessment
To generate robust data for regulatory dossiers, specific analytical methods are employed to assess the functional output of colonic fermentation:
- Short-Chain Fatty Acid (SCFA) Quantification: A key functional readout. Organic acids are acidified, extracted with diethyl ether, derivatized, and detected using gas chromatography (GC) with a flame ionization detector (FID). Quantification is performed using standard solutions of acetate, propionate, and butyrate [23].
- Microbiota Composition Analysis: The hypervariable region (V3-V4) of the 16S rRNA gene is sequenced using an Illumina MiSeq platform. The DADA2 pipeline is used for denoising, chimera removal, and inferring amplicon sequence variants, which are assigned taxonomy using the SILVA database [23] [9].
The Scientist's Toolkit: Essential Research Reagents and Materials
The table below details essential reagents and materials used in a typical in vitro colonic fermentation experiment, which provides the foundational data for MbT development.
Table: Essential Research Reagents for In Vitro Colonic Fermentation
| Reagent/Material | Function/Description | Example from Literature |
|---|---|---|
| Fecal Inoculum | Source of human gut microbiota; typically pooled from multiple screened donors to represent a community [9]. | Pooled fecal inoculum from weaning infants or consumers/non-consumers of a specific food [23] [9]. |
| Nutritional Medium | Provides base nutrients and maintains osmotic balance for microbial growth during fermentation. | Phosphate buffer supplemented with host-secreted compounds (mucin, bile acids) and minimal nutrients [23]. |
| Substrates for Fermentation | Test compounds (e.g., prebiotics, putative therapeutics) whose impact on microbiota is being studied. | Flavan-3-ols (monomers/oligomers), traditional fermented foods (Mabisi), complementary foods [82] [9] [23]. |
| Digestive Enzymes | For in vitro digestion of food matrices prior to fermentation to mimic upper GI tract conditions. | Porcine pepsin, pancreatin, human salivary amylase, rabbit gastric extract (as per INFOGEST protocol) [9]. |
| SCFA Standards | Certified reference materials for quantifying microbial metabolite production via chromatography. | Standard solutions of acetate, propionate, butyrate, formate, lactate, etc. [23] [9]. |
| Redox Indicator | Visual indicator of anaerobic conditions essential for the growth of obligate anaerobes. | Resazurin [82]. |
| Oxygen Scavenger | Maintains strict anaerobic environment in the fermentation vessel. | L-cysteine hydrochloride [82]. |
Successfully navigating the regulatory pathways for microbiome-based therapies requires an integrated strategy that combines robust scientific evidence from colonic fermentation research with a deep understanding of the evolving regulatory frameworks in Europe and beyond. The translation of research on the colonic fermentation of undigested food components into approved therapies hinges on the careful classification of the product, the intended use claims, and the ability to demonstrate consistent quality, safety, and efficacy through well-controlled studies. As regulatory science for these complex products continues to mature, close collaboration between researchers, developers, and regulators will be essential to unlock the full potential of microbiome-based therapies for human health.
The field of nutrition is undergoing a fundamental transformation, shifting from generalized population-level dietary advice toward dynamic, data-driven frameworks powered by artificial intelligence (AI). This paradigm shift is particularly relevant within the context of colonic fermentation research, where inter-individual variability in gut microbiota composition and function significantly influences nutritional outcomes. Personalized nutrition is defined as the adaptation of dietary recommendations based on individual-level variability in biology, behavior, and environment [87]. This approach represents a critical advancement in addressing chronic conditions such as obesity, diabetes, and cardiovascular diseases, where standardized dietary interventions often fail to achieve clinically meaningful outcomes [87].
The integration of AI with nutrigenomics and multi-omics approaches has accelerated the implementation of personalized nutrition strategies, providing more precise, individualized insights into dietary needs and health outcomes [87]. Meanwhile, research on the colonic fermentation of undigested food components provides the essential scientific foundation for understanding the mechanisms through which diet influences host physiology. The gut microbiota, a complex community of microorganisms primarily inhabiting the human large intestine, plays a crucial role in human health by fermenting undigested food components and producing metabolites such as short-chain fatty acids (SCFAs) that offer numerous benefits to the host [88]. AI serves as the critical bridge that translates insights from colonic fermentation research into actionable, personalized dietary recommendations.
AI Methodologies for Personalized Nutrition
Machine Learning and Deep Learning Approaches
AI technologies, particularly machine learning (ML) and deep learning (DL), facilitate the extraction of actionable insights from complex health and dietary datasets [87]. These technologies enable the implementation of personalized nutrition through several key approaches:
Adaptive Dietary Planning: Supervised models such as multilayer perceptrons (MLPs) and long short-term memory (LSTM) networks have been employed to predict postprandial glycemic responses, lipid fluctuations, and weight dynamics, thereby transforming user-specific parameters into personalized, actionable dietary recommendations [87]. Unsupervised methods like k-means clustering and principal component analysis (PCA) support phenotype-driven stratification for targeted interventions [87].
Reinforcement Learning: Reinforcement learning (RL) algorithms, such as Deep Q-Networks and Policy Gradient methods, enable continuous personalization via feedback loops from behavioral and physiological data (e.g., continuous glucose monitoring), reducing glycemic excursions by up to 40% [87].
Image-Based Dietary Assessment: Advancements in DL, especially convolutional neural networks (CNNs), have significantly enhanced the accuracy and efficiency of dietary assessment tools. CNN-based models have consistently achieved classification accuracies above 85% across standard datasets, automating tasks such as food image classification, portion size estimation, and nutrient content prediction [87].
Deep Generative Models: Novel AI-based nutrition recommendation methods leverage deep generative networks and sophisticated loss functions to generate highly accurate personalized weekly meal plans. These systems model user-specific information and align the network with well-defined nutritional rules through the use of variational autoencoders to robustly model anthropometric measurements and medical conditions [89].
Table 1: AI Techniques and Their Applications in Personalized Nutrition
| AI Technique | Specific Methods | Nutrition Application | Reported Performance |
|---|---|---|---|
| Deep Learning | CNNs, Vision Transformers | Food image classification and nutrient detection | >90% accuracy in fine-grained food identification [87] |
| Reinforcement Learning | Deep Q-Networks, Policy Gradient methods | Dynamic dietary adjustment based on continuous glucose monitoring | 40% reduction in glycemic excursions [87] |
| Generative Models | Variational Autoencoders | Personalized weekly meal plan generation | High accuracy in energy intake alignment [89] |
| Natural Language Processing | ChatGPT, LLMs | Meal variety expansion and dietary advice | Increased meal variety and generalization capabilities [89] |
Integration of Large Language Models
The introduction of Large Language Models (LLMs) and more specifically ChatGPT has sparked new opportunities in personalized nutrition. Leveraging its low complexity, high speed, and extensive pool of meals drawn from the web, ChatGPT can be used to make dietary recommendations to users [89]. When combined with traditional nutrition recommendation systems that achieve increased accuracy through expert knowledge and validated nutritional guidelines, LLMs can significantly expand meal databases for improved accuracy and generalization ability [89]. However, initial investigations of the safety and credibility of LLM-provided meal recommendations have unveiled that they can be prone to errors, emphasizing the need for expert-guided validation systems [89].
Figure 1: AI-Nutrition Integration Framework. This diagram illustrates the continuous feedback loop between data collection, AI modeling, personalized intervention, and health outcomes assessment, informed by core disciplines including colonic fermentation research.
Colonic Fermentation: The Foundation for Personalization
Gut Microbiota as a Key Determinant of Nutritional Response
The relationship between the gut microbiota, metabolic disorders, and diet has become increasingly evident, particularly through understanding the mechanisms linking gut microbiota with obesity in animal models and clinical trials [90]. The gut microbiota starts seeding during birth and largely develops during the first 3 years of life, with its composition influenced by multiple factors including mode of delivery, feeding method, environment, diet, immune system, antimicrobial agents, medications, hygiene, and climatic conditions [90]. These factors contribute to significant variations in gut microbiota between individuals, which in turn lead to differential responses to dietary interventions.
Research has revealed that the responses of individuals to dietary inputs vary remarkably, therefore no single diet can be suggested to every individual [90]. These variations are attributed to differences in the microbiome and host characteristics. While the inherent nature of host-derived factors makes them difficult to modulate, diet can more easily shape the microbiome, potentially influencing human physiology through modulation of digestion, absorption, mucosal immune response, and the availability of bioactive compounds [90]. This understanding positions the microbiota as an attractive target for dietary intervention, as it can be modified relatively easily in terms of composition and general functions.
Short-Chain Fatty Acids as Key Microbial Metabolites
Short-chain fatty acids (SCFAs), including acetate, propionate, and butyrate, are crucial microbial metabolites produced through the colonic fermentation of undigested food components, particularly dietary fibers and resistant starch [91]. These SCFAs offer numerous benefits to the host, including maintaining colonic barrier integrity, serving as an energy source for colonocytes, and exerting neuroprotective effects [91]. The production levels of different SCFAs vary based on individual gut microbiota composition and the specific dietary compounds available for fermentation.
Table 2: Key Short-Chain Fatty Acids and Their Health Implications
| SCFA Type | Primary Producers | Health Benefits | Measurement Techniques |
|---|---|---|---|
| Acetate | Bacteroidetes, Akkermansia | Energy source, cholesterol metabolism, cross-feeding with other bacteria | Gas chromatography with flame ionization detection [9] [91] |
| Propionate | Bacteroidetes, Firmicutes | Glucose metabolism, satiety signaling, cholesterol synthesis inhibition | Gas chromatography with flame ionization detection [9] [91] |
| Butyrate | Firmicutes (Roseburia, Faecalibacterium) | Primary energy source for colonocytes, anti-inflammatory, anti-carcinogenic | Gas chromatography with flame ionization detection [9] [91] |
Experimental Models for Studying Diet-Microbiota Interactions
In Vitro Fermentation Models
In vitro models offer a convenient and ethical alternative to in vivo studies for investigating nutrient-gut microbiome interactions, facilitating easy sampling and controlled experimental conditions [88]. Among these, continuous multistaged in vitro fermentation models, which simulate different sections of the human gastrointestinal tract (e.g., proximal colon, transverse colon, and distal colon), provide a more accurate representation of the human gut environment compared to single-batch fermentation [88]. Various configurations of these multistaged models have been developed and widely employed in studies examining the effects of dietary compounds on the gut microbiome.
The INFOGEST static digestion model is a highly recommended protocol for studying the characteristics of food matrices [9]. This model can be used to complement the outcomes of advanced dynamic computerized models such as the Simulator of the Human Intestinal Microbial Ecosystem (SHIME) and TNO in vitro model of the colon (TIM-2) [9]. A specific application of this protocol involves digesting food samples using the INFOGEST static digestion model before anaerobic incubation with stool samples for 24 hours to assess effects on gut microbiota composition and SCFA production [9].
Figure 2: In Vitro Fermentation Workflow. This experimental workflow outlines the key steps from sample collection through digestion, fermentation, and multi-modal analysis of microbial composition and metabolic outputs.
Mathematical Modeling of Microbial Communities
Mathematical models show promise as complementary tools to reduce the cost and time of microbiota investigations [91]. Various models have been proposed to investigate diet-colonic microbiota interactions, including kinetic-based, agent-based, and genome-scale metabolic models (GEMs) [91]. GEMs use metabolic reconstructions, a mathematical representation of a microorganism's metabolism, and flux balance analysis (FBA) to predict microbial metabolite production as fluxes (units of concentration per time).
Metagenome-scale community metabolic models (MGCMs) extend this concept to microbial communities [91]. Among MGCMs, the Microbial Community model (MICOM) stands out for its user-friendly approach, extensive documentation, and pre-made workflows that range from data preparation to visualization [91]. MICOM is based on FBA under a mass steady-state assumption, representing the exponential phase of microbial growth, during which growth rates remain constant. Fluxes of microbial metabolites are calculated as the solution to a constrained linear programming problem, integrating the biochemical reactions performed by the microbial community, assuming no accumulation of substrates in the system, to maximize microbial community biomass [91].
However, a recent study assessing the accuracy of MICOM in predicting microbial SCFA production in real-life feeding scenarios for weaning infants found that the model exhibited overall poor accuracy, with only a weak, significant correlation between measured and predicted acetate production (r = 0.17, p = 0.03) [91]. The agreement between predicted and measured SCFA production improved for samples primarily composed of plant-based foods: acetate exhibited a moderate positive correlation (r = 0.31, p = 0.005), and butyrate a trend toward a weak positive correlation (r = 0.21, p = 0.06) [91]. These findings suggest that the model is better suited for predicting the influence of complex carbohydrates on the colonic microbiota than for other dietary compounds.
Research Reagent Solutions for Colonic Fermentation Studies
Table 3: Essential Research Reagents for Diet-Microbiota Interaction Studies
| Reagent Category | Specific Examples | Function/Application | Experimental Context |
|---|---|---|---|
| Fermentation Media | Gifu Anaerobic Medium (GAM), Simulated Ileal Effluent Medium (SIEM) | Provides nutrients for microbial growth during in vitro fermentation | Used in continuous multistaged in vitro fermentation models [88] |
| Dietary Substrates | Fructooligosaccharides (FOS), Polyphenols, Resistant Starch | Test compounds for evaluating microbial metabolic responses | Positive controls in fermentation experiments [88] [9] |
| Enzymes for Digestion | Porcine pepsin (P6887), Human salivary amylase (A1031), Porcine pancreatin (P7545) | Simulate gastrointestinal digestion in INFOGEST protocol | Critical components of static in vitro digestion models [9] |
| SCFA Standards | Acetate, Propionate, Butyrate, Isobutyrate standards | Calibration and quantification of microbial metabolites | Essential for gas chromatography analysis of fermentation products [9] [91] |
| DNA Extraction Kits | Commercially available microbiome DNA isolation kits | Microbial community analysis through 16S rRNA sequencing | Enables taxonomic profiling of fermented samples [9] |
| Metabolic Modeling Tools | MICOM, AGORA2 metabolic reconstructions | In silico prediction of microbial metabolite production | Computational approaches complementing experimental methods [91] |
Integrated AI and Diagnostic Applications in Research
Clinically Validated AI Systems
Several AI-powered personalized nutrition systems have undergone clinical validation with demonstrated efficacy in chronic disease management. For instance, the RxFood platform has been clinically tested, showing that after 3 months of use, children with type 1 diabetes managed in a quaternary diabetes center demonstrated improved ability to carb count and lower A1c (0.8% improvement compared to the control group) [92]. This platform uses AI to assess patients' daily eating habits through picture-based food entry and provides evidence-based, baseline dietary assessment using advanced analytics [92].
In a randomized control trial, this technology generated a cost savings of over $1000 per person per year, creating a 5x return on investment [92]. The system incorporates the latest in AI and sensor technology while meeting PHIPA/HIPAA standards for data protection [92]. This demonstrates how AI-driven personalized nutrition can deliver both clinical benefits and economic value in healthcare systems.
Interventional Studies on Traditional Fermented Foods
Research on traditional fermented foods provides valuable insights into how dietary exposures modulate gut microbiota resilience and metabolic outputs. A study on Mabisi, a traditional Zambian fermented dairy food product, assessed the effect of exposure on gut microbiota and SCFA production in stool samples of consumers and non-consumers [9]. The study found that Mabisi supplementation increased Pediococcus in both consumers and non-consumers compared to sterile water [9].
After treatment with Mabisi, the gut microbiota of consumers showed greater resilience, with limited changes in community composition compared to non-consumers, as indicated by beta diversity (Mabisi consumers: R² = 0.07, p-adjusted = 0.375; Mabisi non-consumers: R² = 0.08, p-adjusted = 0.05) relative to their respective negative controls [9]. Non-consumers were associated with higher production of SCFAs, including acetate, butyrate, formate and succinate, compared to Mabisi consumers [9]. This demonstrates how regular consumption of fermented foods may contribute to a more stable gut ecosystem that is less susceptible to perturbation.
The integration of AI technologies with advanced diagnostics and colonic fermentation research represents the frontier of personalized nutrition. This multidisciplinary approach enables the transition from static, population-level dietary models to dynamic, data-informed frameworks tailored to individual needs [87]. The gut microbiota serves as a crucial interface between diet and host physiology, with its composition and metabolic outputs providing valuable biomarkers for personalization.
Future research directions should focus on enhancing the accuracy of mathematical models predicting diet-microbiota interactions, particularly for mixed diets and diverse population groups [91]. Additionally, further clinical validation of AI-powered nutrition systems across various disease states and demographic groups will be essential for establishing evidence-based guidelines for implementation [92] [93]. As these technologies evolve, attention must be paid to addressing challenges related to algorithmic transparency, data privacy, and equitable access to ensure that advancements in personalized nutrition benefit diverse populations [87].
The synergy between AI, diagnostics, and colonic fermentation research holds immense potential for developing more effective, targeted nutritional interventions that can modulate host-microbiota interactions to prevent and control metabolic disorders [90]. By bridging advanced computational approaches with fundamental nutritional science, researchers can unlock new possibilities for personalized health optimization through dietary means.
Evidence and Efficacy: Clinical Outcomes and Comparative Analyses of Fermentation Modulators
Within the broader research on colonic fermentation of undigested food components, the clinical validation of interventions aimed at improving gastrointestinal wellbeing and bowel function represents a critical translational step. This whitepaper provides an in-depth technical guide to recent meta-analytical evidence and validated methodologies for assessing gastrointestinal outcomes in both healthy populations and clinical cohorts. The complex interaction between undigested food components, gut microbiota, and host physiological responses necessitates rigorous clinical validation frameworks to establish efficacy of therapeutic interventions. As research in colonic fermentation progresses, the need for standardized, validated assessment tools and clearly demonstrated therapeutic outcomes becomes increasingly important for drug development professionals seeking to translate basic science findings into clinically meaningful applications.
Research indicates that gastrointestinal symptoms are remarkably common even in healthy populations, with one retrospective cross-sectional study of more than 52,000 healthy participants finding that 54% reported experiencing at least one GI symptom within the past seven days [94]. The impact of these symptoms on quality of life has driven the development of validated assessment tools and the clinical evaluation of various interventions, particularly probiotics and dietary modifications, which are thought to influence the colonic fermentation process.
Validated Clinical Assessment Methodologies
Digestion-associated Quality of Life Questionnaire (DQLQ)
The Digestion-associated Quality of Life Questionnaire (DQLQ) represents a significant advancement in clinical assessment tools specifically designed for healthy populations experiencing GI symptoms. Unlike generic quality of life instruments, the DQLQ was developed to be sensitive to the physical and mental well-being changes that may occur due to GI symptoms in individuals without diagnosed gastrointestinal disorders [94].
Development and Validation: The DQLQ was developed through a rigorous process beginning with a 24-item questionnaire generated after an extensive review of QOL questionnaires and GI symptom assessment literature, with input from experienced GI researchers. Through focus groups comprised of healthy adults experiencing GI-related symptoms and variability analysis, the instrument was refined to a final 9-item questionnaire [94]. The validation study demonstrated favorable internal consistency reliability (Cronbach's α = 0.84, McDonald's ω = 0.84) and test-retest reliability (ICC = 0.89) in a sample of 594 healthy undergraduate students aged 18-30 years [94].
Table 1: Psychometric Properties of the DQLQ Questionnaire
| Validation Parameter | Result | Sample Size | Interpretation |
|---|---|---|---|
| Internal Consistency (Cronbach's α) | 0.84 | n=594 | Favorable |
| Test-Retest Reliability (ICC) | 0.89 | n=273 | High agreement |
| Convergent Validity (GSRS correlation) | r=0.54 | n=594 | Good correlation |
| Divergent Validity (Stress correlation) | r=0.13, p<0.005 | n=592 | Appropriate divergence |
| Divergent Validity (Bowel satisfaction) | r=0.18, p<0.001 | n=592 | Appropriate divergence |
Clinical Applications: The DQLQ has been shown to be responsive to changes in GI symptoms, making it suitable for interventional studies assessing how nutritional supplements, dietary modifications, or other interventions impact digestion-associated quality of life [94]. Its validation in a population experiencing academic stress further supports its utility in detecting changes in GI-related QOL under conditions known to exacerbate gastrointestinal symptoms.
Assessing Positive Psychological Well-being in IBS Populations
A systematic review examining relationships between positive psychological well-being (PPWB) and clinical characteristics in Irritable Bowel Syndrome (IBS) revealed that individuals with IBS have consistently lower levels of various PPWB constructs compared to healthy populations [95]. This research is particularly relevant to clinical validation as it highlights the importance of assessing multidimensional factors in gastrointestinal disorders.
The review, which included 22 articles with a total of 4,285 participants with IBS, found that individuals with IBS had lower levels of resilience, positive affect, self-efficacy, and emotion regulation capabilities compared to healthy controls [95]. Furthermore, greater PPWB was associated with superior physical, psychological, and health-related quality of life outcomes, suggesting that interventions targeting these psychological constructs may improve overall clinical outcomes in IBS patients.
Meta-Analytical Evidence on Therapeutic Interventions
Probiotic Efficacy for Gastrointestinal Symptoms
A comprehensive umbrella meta-analysis conducted in 2025 evaluated the effects of probiotic supplementation on various gastrointestinal disorders, synthesizing evidence from multiple earlier meta-analyses [96]. The findings demonstrate significant beneficial effects across multiple GI symptoms.
Table 2: Probiotic Efficacy for Gastrointestinal Symptoms Based on Umbrella Meta-Analysis
| Symptom | Risk Ratio (95% CI) | P-value | Number of Meta-Analyses Included |
|---|---|---|---|
| Diarrhea | 0.44 (0.37-0.52) | <0.001 | 12 |
| Nausea | 0.59 (0.49-0.60) | <0.001 | 8 |
| Epigastric Pain | 0.71 (0.56-0.87) | <0.001 | 5 |
| Bloating | 0.74 (0.64-0.84) | <0.001 | 7 |
| Taste Disturbance | 0.55 (0.36-0.75) | <0.001 | 3 |
Subgroup Analyses: The umbrella meta-analysis revealed more pronounced effects in studies with shorter intervention durations (≤2-4 weeks) and with multi-strain probiotic formulations, particularly for diarrhea and epigastric pain [96]. This finding has important implications for clinical trial design in drug development, suggesting that optimal probiotic interventions may differ depending on the target symptom.
Methodological Considerations: Despite the promising findings, the authors noted moderate to high heterogeneity and generally low methodological quality among several included meta-analyses, highlighting the need for more rigorous clinical trials in this field [96]. The assessment using AMSTAR 2 tools indicated that only 4 of the 12 included meta-analyses were of high quality, while the remainder were rated as low quality [96].
Experimental Models and Methodologies
In Vitro Fermentation Models
Protein Fermentation Kinetics: Recent research has investigated the fermentation potential of undigested dietary proteins using an in vitro model with human faecal inoculum [70]. This methodology allows for the systematic investigation of protein fermentation kinetics, which is relevant to understanding the colonic fermentation of undigested food components. The study utilized ileal digesta collected from pigs as substrates, representing the undigested protein that normally enters the human colon [70].
The experimental protocol involved:
- Preparation of pooled ileal digesta samples containing approximately 10mg nitrogen
- Utilization of human faecal inoculum from healthy donors
- Incubation in sealed bottles with nitrogen-free buffer supplemented with easily fermentable carbohydrates
- Continuous monitoring of gas production using the method described by Cone et al. (1996; 2005)
- Mathematical modeling of cumulative gas production to determine fermentation kinetics parameters [70]
Traditional Fermented Foods Research: The INFOGEST static digestion model has been applied to study the effects of traditional fermented foods on gut microbiota composition and metabolic activity [9]. This protocol involves:
- Subjecting food samples to simulated gastrointestinal digestion
- Anaerobic incubation with fecal microbiota from consumers and non-consumers
- 16S rRNA sequencing to assess microbial community changes
- Short-chain fatty acid (SCFA) measurement as a functional outcome [9]
Advanced Digestibility Models
The TIM-1 (TNO Gastro-Intestinal Model) digestion system has been employed to assess protein digestibility and amino acid bio-accessibility [80]. This dynamic model more closely mimics human physiological conditions compared to static models. The standard protocol includes:
- A 5-hour digestion simulation with continuous monitoring
- Sequential collection of dialysate and ileal effluent samples
- Quantification of total nitrogen and free amino acids
- Subsequent colon fermentation using the Colon-on-a-Plate batch system [80]
Experimental Workflows and Signaling Pathways
Clinical Validation Workflow for GI Interventions
Clinical Validation Workflow for GI Interventions
In Vitro Fermentation Assessment Pathway
In Vitro Fermentation Assessment Pathway
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents and Materials for GI Clinical Research
| Item | Function/Application | Example Sources |
|---|---|---|
| DQLQ Questionnaire | Assesses digestion-associated quality of life in healthy individuals | [94] |
| GSRS (Gastrointestinal Symptom Rating Scale) | Measures GI symptom severity across multiple domains | [94] |
| Human Faecal Inoculum | Provides human gut microbiota for in vitro fermentation studies | [70] [9] |
| INFOGEST Static Digestion Model | Simulates human gastrointestinal digestion in vitro | [9] |
| TIM-1 System (TNO Gastro-Intestinal Model) | Dynamic model for assessing protein digestibility and bioaccessibility | [80] |
| N-Free Buffer with Carbohydrates | Creates nitrogen-limiting environment for protein fermentation studies | [70] |
| 16S rRNA Sequencing Reagents | Analyzes microbial community composition | [9] |
| GC-MS Equipment | Quantifies short-chain fatty acids and microbial metabolites | [80] |
| AMSTAR 2 Tool | Assesses methodological quality of systematic reviews and meta-analyses | [96] |
The clinical validation of interventions targeting gastrointestinal wellbeing and bowel function requires a multidisciplinary approach incorporating validated patient-reported outcomes, controlled intervention studies, and appropriate experimental models. The evidence from recent meta-analyses indicates that probiotic interventions can significantly reduce multiple GI symptoms, though methodological limitations in existing studies highlight the need for more rigorous clinical trials.
Future research in this field should focus on:
- Standardizing assessment methodologies across clinical trials
- Elucidating the mechanisms linking colonic fermentation of specific food components to clinical outcomes
- Developing targeted interventions based on individual microbiota composition and fermentation patterns
- Integrating positive psychological interventions with gastrointestinal treatments for improved overall outcomes
The continuing advancement of in vitro digestion and fermentation models, coupled with rigorously validated clinical assessment tools, provides a robust foundation for translating basic research on colonic fermentation into clinically meaningful interventions for improving gastrointestinal wellbeing and bowel function.
Within the context of colonic fermentation research, fermented foods represent a critical interface between diet and the gut ecosystem. These foods contribute both live microorganisms and undigested food components that undergo further microbial metabolism in the colon, producing metabolites with local and systemic biological effects. This technical review examines the fundamental differences between traditional and industrial fermentation processes and their distinct impacts on gut microbiota composition and function, providing researchers with methodological frameworks for continued investigation in this field.
Defining Fermented Food Categories
Traditional Fermented Foods
Traditional fermented foods (TFFs) are characterized by spontaneous fermentation processes driven by complex, endogenous microbial communities. These foods are typically produced under non-pasteurized conditions using various vessels at ambient temperatures over 1-3 days [9]. The fermentation is driven by naturally occurring lactic acid bacteria (LAB) and yeasts, leading to the development of unique sensory, microbial, and nutritional properties [9]. Examples include Mabisi (a Zambian fermented dairy product), kimchi, sauerkraut, and traditional kefir.
Industrial Fermented Foods
Industrial fermented foods undergo controlled, standardized processes often using selected starter cultures to ensure consistency and safety. Production typically occurs in specialized equipment with strict temperature and humidity control. These processes often include pasteurization and may involve steps that reduce microbial diversity, such as filtration or preservation treatments. Examples include commercial yogurt, pasteurized sauerkraut, and mass-produced kombucha.
Table 1: Fundamental Characteristics of Traditional vs. Industrial Fermentation Processes
| Characteristic | Traditional Fermentation | Industrial Fermentation |
|---|---|---|
| Microbial Inoculum | Spontaneous; complex endogenous communities | Defined starter cultures; limited diversity |
| Production Environment | Ambient conditions; variable vessels | Controlled bioreactors; standardized conditions |
| Process Control | Minimal; relies on empirical knowledge | Highly controlled parameters (pH, temperature) |
| Microbial Diversity | High; includes LAB, yeasts, acetobacter | Lower; dominated by specific starter strains |
| Post-processing | Typically none; live microbes retained | Often pasteurized, filtered, or preserved |
| Examples | Mabisi, traditional kimchi, artisanal kefir | Commercial yogurt, pasteurized sauerkraut |
Impact on Gut Microbiota Composition
Microbial Diversity and Resilience
Clinical evidence demonstrates that diets rich in fermented foods enhance gut microbial diversity. A landmark Stanford study found that a 10-week high-fermented food diet significantly increased microbiome diversity, with stronger effects from larger servings [97]. This diversity increase is clinically relevant as low microbiome diversity has been linked to obesity and diabetes [97].
The gut microbiota of regular consumers of traditional fermented foods exhibits greater resilience. An in vitro study using stool samples from consumers and non-consumers of Mabisi found that after treatment with Mabisi, the gut microbiota of consumers showed limited changes in community composition compared to non-consumers, indicating enhanced ecological stability [9]. This suggests that regular consumption modulates the gut ecosystem toward a more stable state resistant to perturbation.
Taxonomic Shifts and Microbial Enrichment
Traditional fermented foods introduce diverse microbial taxa to the gut ecosystem. 16S rRNA sequencing reveals that TFFs consistently contain Firmicutes and Actinobacteria phyla, with beneficial genera including Lactobacillus, Streptococcus, Lactococcus, Pediococcus, and Bifidobacterium [9]. In vitro fermentation experiments demonstrate that traditional fermented products like Mabisi significantly increase Pediococcus in both consumers and non-consumers [9].
Industrial fermented foods with defined starter cultures typically produce more limited taxonomic changes, primarily enriching for the specific strains contained in the product. The reduction in microbial diversity through industrial processing limits their capacity to introduce novel taxa to the gut ecosystem.
Table 2: Microbial Taxa Associated with Traditional Fermented Food Consumption
| Taxonomic Level | Associated Microbes | Potential Functional Significance |
|---|---|---|
| Phylum | Firmicutes, Actinobacteria | Foundation of diverse gut ecosystem |
| Genus | Lactobacillus, Streptococcus | Lactic acid production; pathogen inhibition |
| Genus | Lactococcus, Pediococcus | Bioactive metabolite production |
| Genus | Bifidobacterium | Enhanced gut barrier function |
| Species | Varies by food product | Specific functional adaptations |
Metabolic Output and Colonic Fermentation
Short-Chain Fatty Acid Production
Short-chain fatty acids (SCFAs) including acetate, propionate, and butyrate are key microbial metabolites produced during colonic fermentation that serve as energy sources for colonocytes, fortify gut barrier integrity, modulate inflammatory responses, and regulate metabolism [98].
Research indicates that traditional fermented foods promote greater SCFA production. In vitro colon fermentation models demonstrate that non-consumers of traditional fermented foods like Mabisi show significantly higher production of SCFAs including acetate, butyrate, formate, and succinate compared to regular consumers when exposed to these foods [9]. This suggests that naive gut microbiomes undergo more substantial metabolic reprogramming when introduced to traditional fermented foods.
Bioactive Metabolite Profile
Beyond SCFAs, traditional fermentation generates diverse bioactive compounds including bacteriocins (e.g., nisin, plantaricin), bioactive peptides with antihypertensive and antimicrobial properties, exopolysaccharides (EPSs) with prebiotic and immunomodulatory properties, and modified polyphenolic compounds with enhanced bioavailability [98].
These fermentation-derived metabolites directly influence host physiology. For example, bioactive peptides derived from milk proteins in fermented dairy products exhibit antihypertensive, antioxidant, immunomodulatory, and antimicrobial properties [98]. Similarly, microbial biotransformation of plant-derived polyphenols in products such as kombucha, tempeh, and miso yields smaller, more bioavailable metabolites with improved antioxidant, antimicrobial, and anti-inflammatory effects [98].
Methodological Approaches for Investigating Fermentation Impacts
In Vitro Digestion and Fermentation Models
In vitro models provide controlled systems for investigating the fermentation potential of undigested food components. The INFOGEST static digestion model protocol 2.0 is widely used to simulate human gastrointestinal digestion before anaerobic incubation with fecal samples [9]. This protocol involves simulated oral, gastric, and intestinal phases using standardized enzymes and conditions to mimic physiological digestion.
More complex dynamic models like the TIM-1 (TNO Gastro-Intestinal Model) and TIM-2 (colon model) systems offer advanced simulation of human digestion, incorporating parameters such as transit time, pH gradients, and continuous absorption [80]. These systems allow for precise monitoring of digestibility and metabolite production throughout the digestive process.
Diagram 1: In vitro fermentation workflow for comparing traditional and industrial fermented foods
Analytical Approaches for Metabolite Characterization
Comprehensive characterization of fermentation products requires multiple analytical techniques. Gas chromatography-mass spectrometry (GC-MS) enables quantification of SCFAs and other volatile organic compounds [9]. Untargeted metabolomics approaches like liquid chromatography-revolutionary ambient ionization mass spectrometry (LA-REIMS) provide broad metabolite profiling [80]. Sequencing of the hypervariable region (V3-V4) of the 16S rRNA gene allows microbial community analysis, while shotgun metagenomics offers strain-level resolution and functional gene assessment [9].
Research Reagent Solutions for Fermentation Studies
Table 3: Essential Research Reagents for Investigating Fermented Food-Gut Microbiota Interactions
| Reagent/Category | Specific Examples | Research Application | Function |
|---|---|---|---|
| Digestive Enzymes | Porcine pepsin (P6887), Porcine pancreatin (P7545), Human salivary amylase (A1031) | In vitro digestion simulation | Mimic physiological digestion of food matrices |
| Fermentation Substrates | Fructooligosaccharides (F8052), Soluble potato starch (S2630), Pectin (P9135) | Positive controls for fermentation assays | Validate microbial metabolic activity |
| SCFA Standards | Acetate, propionate, butyrate, isobutyrate, formate, lactate standards | Metabolite quantification (GC-MS) | Calibration and identification of microbial metabolites |
| Buffer Components | Sodium phosphate buffer (P4922), Sodium taurodeoxycholate (904236) | Physiological simulation | Maintain pH and biological relevance |
| DNA Extraction Kits | Commercially available microbiome DNA isolation kits | Microbial community analysis | Extract high-quality DNA for sequencing |
| Culture Media Components | Peptone from potatoes (83059), Bovine blood hemoglobin (H2500) | Microbial growth support | Provide nutrients for diverse microbiota |
Mechanistic Pathways of Host-Microbe Interaction
The consumption of fermented foods influences host physiology through multiple interconnected pathways. Bioactive metabolites produced during fermentation and subsequent colonic fermentation modulate immune function, enhance gut barrier integrity, and regulate systemic metabolism.
Diagram 2: Mechanistic pathways of fermented food impact on host physiology
Traditional and industrial fermented foods exert distinct effects on gut microbiota composition and function through their differential microbial complexity, metabolite profiles, and impact on colonic fermentation. Traditional fermentation processes support diverse microbial ecosystems that introduce higher taxonomic diversity to the gut and promote ecological resilience. Industrial processes, while ensuring safety and consistency, typically yield products with reduced microbial complexity and more limited effects on gut microbial ecology.
Future research should prioritize standardized characterization of fermented food microbiomes, validation of mechanistic pathways in relevant human populations, and development of personalized nutrition approaches based on individual microbial ecology. The integration of multi-omics technologies with well-designed clinical studies will advance our understanding of how different fermented foods influence the gut microbiome and human health, ultimately informing evidence-based dietary recommendations and functional food development.
The human gut microbiome, a complex ecosystem of microorganisms, plays a pivotal role in human health through its metabolic activities, particularly the colonic fermentation of undigested dietary components. This process yields short-chain fatty acids (SCFAs) and other metabolites that are crucial for host health. When this ecosystem is disrupted—often by antibiotics—pathogens like Clostridioides difficile can proliferate, leading to recurrent C. difficile infection (rCDI), a significant clinical challenge. Traditional approaches like fecal microbiota transplantation (FMT), while effective, face challenges in consistency and safety. Defined microbial consortia, comprising specific, clonally derived bacterial strains, represent a novel therapeutic class that addresses these limitations by offering a standardized, reproducible, and mechanistically grounded approach to microbiome restoration [99] [100] [101].
This technical guide provides an in-depth analysis of two leading defined bacterial consortium candidates: Vedanta Biosciences' VE303 and Seres Therapeutics' VOWST (also known as SER-109 or VOS). We examine their development, mechanisms of action, and the experimental evidence supporting their use, placing their efficacy firmly within the context of microbial ecology and the restoration of a protective colonic fermentation profile.
Vedanta's VE303: A Defined Consortium for rCDI Prevention
VE303 is an orally administered, defined bacterial consortium consisting of eight commensal Clostridia strains. These strains were rationally selected from Vedanta's proprietary library of bacteria isolated from healthy human donors. A key differentiator of VE303's manufacturing process is that it is produced from pure, clonal bacterial cell banks. This method bypasses the need for direct sourcing of donor fecal material, ensuring a standardized drug product with consistent composition, potency, and improved scalability compared to donor-derived treatments [99] [101].
Clinical Evidence and Engraftment Dynamics
The clinical development of VE303 underscores the importance of proper colonization. A Phase 1a/b study in healthy volunteers established that VE303 was safe and well-tolerated. Critically, it demonstrated that vancomycin pretreatment followed by multi-day dosing was the optimal regimen for achieving durable colonization of VE303 strains, with some strains persisting for up to one year post-dosing [99].
The subsequent Phase 2 CONSORTIUM study in patients at high risk for rCDI yielded compelling efficacy data. Patients receiving the high-dose VE303 regimen showed an over 80% reduction in the odds of CDI recurrence by Week 8 compared to placebo, translating to a 31.7% absolute risk reduction [101]. This clinical success was underpinned by robust pharmacodynamic responses.
Table 1: Key Efficacy and Engraftment Findings from VE303 Clinical Studies
| Study Parameter | Phase 1 Findings (Healthy Volunteers) | Phase 2 Findings (rCDI Patients) |
|---|---|---|
| Safety & Tolerability | Safe and well-tolerated at all doses tested [99] | Acceptable safety profile [101] |
| Optimal Dosing Regimen | Multiple days of dosing after vancomycin pretreatment [99] | High dose for 14 days after antibiotics [101] |
| Strain Engraftment | Durable colonization observed for up to 1 year [99] | Superior strain colonization at 14 days; long-term engraftment [101] |
| Clinical Efficacy | Not Applicable | >80% odds reduction in rCDI vs. placebo [101] |
| Microbiome Impact | Promotion of a microbiota community providing colonization resistance [99] | Early restoration of microbiota and beneficial metabolites [101] |
Mechanism of Action: Multi-faceted Restoration
Mechanistic analyses from the Phase 2 study revealed that VE303's efficacy is mediated through multiple, interconnected pathways, as illustrated in the workflow below.
The diagram above shows the multi-faceted mechanism of action for VE303. Analyses of fecal samples identified that three of the VE303 strains were significantly associated with non-recurrence of CDI. Furthermore, several VE303 strains were linked to beneficial metabolic changes within the first two weeks of treatment. This suggests VE303 acts by directly establishing a protective community that outcompetes pathogens, and indirectly by synthesizing metabolites and facilitating the recovery of the indigenous gut microbiome [101].
Seres' VOWST (SER-109): A Firmicutes-Spore Based Approach
VOWST (VOS) is an orally administered microbiome therapeutic approved for the prevention of rCDI. It consists of a preparation of Firmicutes spores purified from healthy donor stool. Unlike VE303's defined set of eight clonal strains, VOWST is characterized as a purified microbiome therapeutic derived from donor material but processed to consist primarily of bacterial spores [100].
Impact on Antimicrobial Resistance and Microbiome Remodeling
The efficacy of VOWST was established in the phase 3 ECOSPOR III trial, which showed a significant reduction in rCDI rates (12% for VOWST vs. 40% for placebo) [100]. A key post-hoc analysis of this trial provided profound insights into a secondary benefit of microbiome remodeling: the reduction of antimicrobial resistance genes (ARGs).
At baseline, patients with rCDI had a significantly elevated abundance of ARGs compared to a healthy cohort, correlated with a microbiota dominated by Proteobacteria and depleted in Firmicutes. Following VOWST treatment, there was a marked and rapid decline in the total ARG abundance compared to placebo. This reduction was driven by a dramatic microbiome shift: a depletion of Proteobacteria and a reciprocal repletion of spore-forming Firmicutes [100]. This study provides proof-of-concept that microbiome therapeutics can be a novel approach to combatting the global health crisis of antimicrobial resistance.
Table 2: Key Findings from VOWST (SER-109) ECOSPOR III Analysis
| Parameter | Baseline (rCDI Patients) | Post-VOWST Treatment | Placebo Group |
|---|---|---|---|
| Clinical rCDI Rate | Qualifying CDI episode | 12% [100] | 40% [100] |
| ARG Abundance | Significantly elevated vs. healthy [100] | Greater decline vs. placebo (p=0.003) [100] | Less pronounced change |
| Proteobacteria Abundance | High (Median: 25-29%) [100] | Marked reciprocal reduction [100] | Less pronounced change |
| Spore-Forming Firmicutes | Depleted [100] | Repleted [100] | Less pronounced change |
| Key Association | Proteobacteria & non-spore-forming Firmicutes abundance positively correlated with ARGs [100] | Spore-forming Firmicutes abundance negatively correlated with ARGs [100] | Not Reported |
Comparative Analysis: Mechanisms and Metabolites
While both VE303 and VOWST aim to prevent rCDI by restoring a protective microbiome, their compositions and precise mechanisms differ, as summarized in the table below.
Table 3: Comparative Analysis of VE303 and VOWST
| Feature | Vedanta's VE303 | Seres' VOWST (SER-109/VOS) |
|---|---|---|
| Therapeutic Type | Defined Bacterial Consortium | Purified Microbiome Therapeutic |
| Composition | 8 clonal commensal Clostridia strains [99] | Firmicutes spores purified from donor stool [100] |
| Manufacturing | Grown from pure clonal cell banks; no donor dependency [101] | Derived from donated human stool material [100] |
| Proposed Primary Mechanism | Direct engraftment and competitive exclusion; production of beneficial metabolites; community restoration [101] | General repletion of spore-forming Firmicutes; suppression of Proteobacteria; reduction of ARG carriage [100] |
| Key Metabolites Linked to Efficacy | Increased SCFAs and secondary bile acids [102] | Increased SCFAs (e.g., butyrate) [100] |
| Clinical Stage | Phase 3 (Fast Track designation) [101] | Phase 3 (Approved) [100] |
A common thread linking both therapeutics is their impact on the colonic fermentation landscape. Both consortia are designed to shift the gut environment from one that favors pathogens to one that supports commensal, health-promoting bacteria. This is achieved partly through the production of SCFAs like acetate, butyrate, and propionate. These metabolites serve as an energy source for colonocytes, improve gut barrier function, and exert anti-inflammatory effects [100] [102]. Furthermore, the restoration of secondary bile acid metabolism, which is inhibitory to C. difficile germination, is another critical mechanism shared by these and other beneficial microbes [102].
Experimental Protocols for Consortium Evaluation
The development of microbial consortia therapeutics relies on a suite of standardized experimental protocols to assess their safety, engraftment, and biological activity.
Protocol 1: Assessing Strain Engraftment and Microbiota Composition
Objective: To evaluate the colonization success of administered consortium strains and their impact on the overall gut microbiota structure in stool samples from clinical trial subjects.
Methodology:
- Sample Collection: Stool samples are collected from participants at baseline and at multiple timepoints post-dosing (e.g., weeks 1, 2, 8, and 24) using standardized collection kits like OMNIgene Gut tubes [102].
- DNA Extraction: Microbial community DNA is extracted from stool samples using commercial kits, such as the MagAttract PowerMicrobiome DNA/RNA EP kit [102].
- Metagenomic Sequencing: DNA libraries are prepared (e.g., with Nextera XT kits) and sequenced on high-throughput platforms (e.g., Illumina NovaSeq) to a depth of tens of millions of microbial reads per sample [100] [102].
- Bioinformatic Analysis:
- Taxonomic Profiling: Tools like MetaPhlAn2 or MetaPhlAn3 are used with curated genomic databases to determine species-level relative abundance [100] [102].
- Strain Tracking: For defined consortia like VE303, unique genetic signatures of the administered strains are used to track their presence and relative abundance over time, distinguishing them from closely related indigenous strains [99] [101].
Protocol 2: Functional Metabolite Profiling
Objective: To quantify changes in the concentration of microbially derived metabolites, such as SCFAs, in response to consortium administration.
Methodology:
- Sample Collection and Preparation: Stool samples are collected in specialized metabolite-preserving tubes (e.g., OMNImet GUT). Metabolites are extracted from stool or from in vitro fermentation supernatants [102] [50].
- Gas Chromatography-Mass Spectrometry (GC-MS):
- The extracted samples are derivatized if necessary to increase volatility.
- Samples are separated using gas chromatography and detected/quantified using mass spectrometry [50].
- Quantification is achieved by comparing peak areas to standard curves of known SCFA concentrations (acetate, propionate, butyrate, etc.) [50].
- Data Integration: Metabolite data are integrated with taxonomic data from sequencing to identify correlations between specific consortium members and metabolic outputs.
The Scientist's Toolkit: Essential Research Reagents
The following table details key reagents and tools essential for researching microbial consortia and their functions.
Table 4: Essential Research Reagents for Microbial Consortia Investigation
| Reagent / Tool | Function / Application | Example Use Case |
|---|---|---|
| OMNIgene Gut OMR-200 | Stabilizes microbial DNA in stool samples at ambient temperature for transport and storage [102]. | Standardized collection of clinical stool samples for longitudinal metagenomic studies. |
| MagAttract PowerMicrobiome DNA/RNA Kit | Simultaneous isolation of high-quality microbial DNA and RNA from complex samples like stool [102]. | Preparation of nucleic acids for downstream metagenomic and metatranscriptomic sequencing. |
| MetaPhlAn (Microbial Profiler) | Bioinformatics tool for profiling microbial community composition from metagenomic sequencing data [100] [102]. | Tracking taxonomic changes in patient microbiota and quantifying engraftment of exogenous strains. |
| ShortBRED | Bioinformatics pipeline for identifying and quantifying protein family abundances (e.g., ARGs) in metagenomic data [100]. | Profiling the antimicrobial resistance potential (resistome) of the microbiome pre- and post-treatment. |
| Comprehensive Antibiotic Resistance Database (CARD) | A curated resource of ARGs, their products, and associated antibiotics [100]. | Serves as a reference database for ARG identification and annotation in metagenomic analyses. |
| YCFA Medium | A specialized culture medium designed to support the growth of a wide diversity of gut anaerobes [50]. | Used in in vitro fermentation models to cultivate fecal inocula and test the utilization of substrates by microbiota. |
| TIM-1 System | A dynamic, multi-compartmental in vitro model of the human stomach and small intestine [80]. | Used to study the digestibility and bio-accessibility of compounds (e.g., proteins, therapeutics) before colonic fermentation. |
VE303 and VOWST exemplify the successful translation of microbial ecology principles into targeted, efficacious therapeutics. They demonstrate that a deep understanding of colonic fermentation and the metabolic outputs of key bacterial taxa is paramount for designing interventions against dysbiosis-related diseases. While VOWST represents a pioneering approved therapy derived from purified Firmicutes spores, VE303 showcases the next generation of rationally designed, defined consortia manufactured from clonal cell banks. The evidence from their clinical development solidifies the premise that microbial consortia can restore colonization resistance against pathogens like C. difficile and, importantly, reduce the reservoir for antimicrobial resistance. This field is poised for growth, with these case studies providing a robust framework for the development of consortia for a wider range of conditions, including inflammatory bowel disease, metabolic disorders, and beyond.
The colonic fermentation of undigested food components is a critical process at the intersection of nutrition, gut microbiology, and human pathophysiology. This whitepaper examines the therapeutic potential of targeting this process in colorectal cancer (CRC), inflammatory bowel disease (IBD), and metabolic syndrome. Through the lens of current research, we explore how microbial metabolites, including short-chain fatty acids (SCFAs) and sphingolipids, modulate host immune responses, epithelial integrity, and carcinogenic pathways. We present quantitative data from recent studies, detailed experimental methodologies for investigating colonic fermentation, and visualizations of key signaling pathways. The findings underscore the promise of dietary interventions, microbiota modulation, and sphingolipid-centric therapies as innovative strategies for disease management and prevention, offering a roadmap for future drug development and clinical applications.
Colonic fermentation represents a fundamental host-microbe interaction where undigested dietary components, primarily fibers and polyphenols, are metabolized by the gut microbiota into a spectrum of bioactive compounds. This process is not merely digestive but is a central modulator of systemic health and disease. Within the framework of a broader thesis on colonic fermentation research, this whitepaper details how the products and processes of fermentation are intrinsically linked to the pathogenesis and potential treatment of CRC, IBD, and metabolic syndrome. The gut microbiome, often described as a microbial organ, encodes metabolic capabilities far exceeding the human genome, and its output is heavily influenced by dietary input [103]. Disruption of this ecological balance, known as dysbiosis, is a hallmark of these chronic diseases, characterized by a reduction in beneficial bacteria and an increase in pro-inflammatory and pro-carcinogenic species [103]. This document synthesizes current evidence for therapeutic interventions—from fermented foods to targeted sphingolipid modulators—that aim to restore microbial equilibrium and correct dysfunctional host signaling, thereby outlining a path from mechanistic understanding to clinical application for researchers and drug development professionals.
Molecular Mechanisms and Signaling Pathways
Gut Microbiota, Dysbiosis, and Carcinogenesis
The gut microbiota plays a paradoxical role in colorectal cancer, with certain commensals exerting protective effects while others drive tumorigenesis. Dysbiosis promotes a pro-carcinogenic environment through chronic inflammation, immune dysregulation, and direct genotoxic effects [103]. Specific bacterial species are implicated in CRC pathogenesis: Fusobacterium nucleatum (F. nucleatum), frequently detected in CRC tissues, promotes cancer cell proliferation, inhibits anti-tumor immunity, and is associated with reduced survival [104] [103]. Enterotoxigenic Bacteroides fragilis (ETBF) and polyketide synthases-positive Escherichia coli also inhibit antitumor immunity [104]. The "driver-passenger" model explains this dynamic, where bacterial "drivers" initiate carcinogenesis, and "passengers" later proliferate in the favorable tumor microenvironment [104].
These pathogens activate multiple oncogenic signaling pathways. F. nucleatum adhesin A interacts with E-cadherin, activating the β-catenin pathway [104]. Pro-tumorigenic bacteria can also hyperactivate the WNT-β-catenin pathway and trigger the release of pro-inflammatory cytokines like IL-17 and TNF [104]. Chronic inflammation, a key player in CRC development, is fueled by factors that activate the transcription factor NF-κB [104]. Conversely, beneficial bacteria such as Akkermansia muciniphila and Lactobacillus plantarum can promote antitumor immunity [104].
Sphingolipid Metabolism in IBD and CRC
Sphingolipids are a class of bioactive lipids that regulate critical cellular processes including apoptosis, proliferation, senescence, and inflammation. The balance between ceramide (Cer), which promotes apoptosis and differentiation, and sphingosine-1-phosphate (S1P), which drives proliferation and inflammation, is vital for maintaining intestinal homeostasis [105]. Altered sphingolipid metabolism is a hallmark of both IBD and CRC. Studies of colon tissues from CRC patients show significant upregulation of genes related to sphingolipid metabolism, including acid ceramidase (ASAH1), sphingosine kinases 1 and 2 (SPHK1, SPHK2), and S1P receptors 1 and 4 (S1PR1, S1PR4) [105]. The central role of the Cer-S1P axis makes it a promising therapeutic target.
- Ceramide Synthases (CerS): Different CerS isoforms, with their preference for generating ceramides of specific acyl chain lengths, play distinct roles. For instance, mice lacking CerS2 were more susceptible to DSS-induced colitis, whereas global loss of CerS4 exacerbated colitis-associated cancer (CAC) [105]. Interestingly, loss of CerS4 in T cells alone reduced neutrophil infiltration, highlighting the cell-specific nature of these effects.
- Ceramidases (CDase): These enzymes degrade ceramide to sphingosine. Patients with IBD exhibit higher levels of acid ceramidase (aCDase) in colon biopsies [105]. Genetically engineered mouse models demonstrate that loss of neutral ceramidase (nCDase) or alkaline ceramidase 3 (ACER3) increases susceptibility to colitis, and ACER3 loss increases CAC tumor burden [105].
Quantitative Data Synthesis
Therapeutic Outcomes of Fermented Food Interventions
Table 1: Meta-Analysis of Fermented Food Impact on Gastrointestinal Wellbeing (2025 Systematic Review & Meta-Analysis) [106]
| Outcome Measure | Mean Difference (MD) / Standardized MD (SMD) | 95% Confidence Interval | P-value | I² (Heterogeneity) |
|---|---|---|---|---|
| Stool Frequency | MD 0.60 | [0.04, 1.16] | 0.04 | 74% |
| Stool Consistency (BSFS) | MD 0.25 | [0.03, 0.47] | 0.03 | 72% |
| Gastrointestinal Symptoms | SMD -0.60 | [-1.05, -0.15] | 0.009 | 90% |
| Intestinal Transit Time | MD -13.65 | [-21.88, -5.43] | 0.001 | 95% |
Table 2: Impact of Traditional Fermented Food (Mabisi) on Gut Microbiota and SCFA Production (2025 In Vitro Study) [9]
| Parameter | Observation in Mabisi Consumers | Observation in Mabisi Non-Consumers | Interpretation |
|---|---|---|---|
| Microbial Resilience | Limited changes in community composition (R² = 0.07, p-adj = 0.375) | Significant shifts in community composition (R² = 0.08, p-adj = 0.05) | Consumers' microbiota is more stable and resilient to Mabisi exposure. |
| SCFA Production | Lower production of acetate, butyrate, formate, and succinate. | Higher production of acetate, butyrate, formate, and succinate. | Non-consumers show a more pronounced, adaptive response to a novel fermented food. |
| Beneficial Genera | Increase in Pediococcus. | Increase in Pediococcus. | Mabisi introduces beneficial bacteria regardless of consumption history. |
Experimental Protocols for Colonic Fermentation Research
In Vitro INFOGEST Static Digestion and Fermentation Model
The INFOGEST model is a widely validated, consensus protocol for simulating human gastrointestinal digestion. Its application in studying the effects of food on the microbiome is highly recommended [9]. The following methodology is adapted from a 2025 study investigating the effects of a traditional fermented food, Mabisi, on gut microbiota [9].
1. Sample Preparation and Treatment Allocation:
- Test Food: The food of interest (e.g., Mabisi, other fermented foods, or plant food particles).
- Positive Control: A substrate known to be fermented by gut microbiota, such as Fructooligosaccharides (FOS).
- Negative Control: Sterile water or a non-fermentable buffer.
2. In Vitro Digestion (INFOGEST Protocol 2.0): Subject the treatments to a three-stage static digestion simulating oral, gastric, and intestinal phases. Key reagents include:
- Oral Phase: Human salivary amylase in simulated salivary fluid.
- Gastric Phase: Porcine pepsin and rabbit gastric extract in simulated gastric fluid.
- Intestinal Phase: Porcine pancreatin and bile salts (e.g., sodium taurodeoxycholate) in simulated intestinal fluid.
3. Colonic Fermentation:
- Inoculum Preparation: Prepare a fecal slurry from fresh stool samples from human donors (e.g., consumers and non-consumers of the test food). The donors should not have taken antibiotics for at least 30 days prior.
- Anaerobic Incubation: Mix the digested food samples with the fecal slurry in an anaerobic workstation. Flush the headspace with an anaerobic gas mix (e.g., N₂:CO₂:H₂). Incubate at 37°C for a set period (e.g., 24 hours) with constant agitation.
4. Post-Fermentation Analysis:
- Microbial Community Analysis: Centrifuge aliquots to collect microbial pellets. Extract genomic DNA and perform 16S rRNA gene sequencing (e.g., of the V3-V4 hypervariable region) to determine shifts in microbial composition.
- Short-Chain Fatty Acid (SCFA) Analysis: Collect supernatant from fermented samples. Analyze SCFA content (e.g., acetate, propionate, butyrate, formate, succinate) using techniques like gas chromatography (GC) or high-performance liquid chromatography (HPLC).
- Other Metabolites: Target other bacterial metabolites, such as sphingolipids or bile acids, using liquid chromatography-mass spectrometry (LC-MS).
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagent Solutions for Colonic Fermentation and Therapeutic Research
| Reagent / Material | Function & Application in Research | Example from Literature |
|---|---|---|
| INFOGEST Simulated Fluids | Standardized buffers for in vitro oral, gastric, and intestinal digestion to ensure physiological relevance and reproducibility. | Used to digest Mabisi prior to colonic fermentation [9]. |
| Fructooligosaccharides (FOS) | A prebiotic positive control in fermentation experiments, known to stimulate the growth of beneficial bacteria and SCFA production. | Served as a positive control in the Mabisi in vitro fermentation study [9]. |
| Porcine Pepsin & Pancreatin | Digestive enzymes used in the gastric and intestinal phases, respectively, of the INFOGEST protocol to break down food matrices. | Key components of the in vitro digestion process [9]. |
| Bile Salts (e.g., Sodium Taurodeoxycholate) | Emulsify fats and are critical for simulating the intestinal environment during in vitro digestion. | Part of the intestinal phase simulation [9]. |
| Sphingolipid Modulators | Analogues, inhibitors, and modulators (e.g., of SPHK, CerS, S1PRs) to probe the therapeutic potential of the sphingolipid pathway. | Discussed as therapeutic targets for IBD and CRC [105]. |
| SCFA Standards | Pure chemical standards (e.g., acetate, propionate, butyrate) for calibrating analytical equipment to quantify SCFAs from fermentation samples. | Acetate, propionate, butyrate, and formate standards were used for quantification [9]. |
The traditional understanding of the gut-brain axis has evolved into a more complex model encompassing bidirectional communication between the gut microbiota, the central nervous system, and metabolic pathways. This whitepaper examines the systemic effects mediated by colonic fermentation of undigested food components, focusing on the role of microbial metabolites as key signaling molecules. Evidence from recent studies indicates that short-chain fatty acids (SCFAs) and other bacterial fermentation products exert profound influence on neuroimmune function, metabolic homeostasis, and barrier integrity throughout the body. This review synthesizes current mechanistic insights, presents quantitative data on microbial metabolites, details experimental methodologies, and discusses therapeutic implications for drug development targeting gut-derived signaling pathways.
The human gastrointestinal tract hosts a complex ecosystem of approximately 100 trillion microbial cells, whose genetic capacity (the microbiome) exceeds the human genome by nearly 150-fold [107]. Colonic fermentation of undigested dietary components represents a crucial metabolic interface between host and microbiota, generating bioactive metabolites that influence systemic physiology far beyond the gastrointestinal tract. The conceptual framework of the gut-brain axis has expanded to incorporate immune and metabolic signaling, forming a comprehensive gut-immune-brain-metabolic axis [108].
SCFAs—primarily acetate, propionate, and butyrate—are the most extensively studied metabolites derived from bacterial fermentation of dietary fiber [3]. These molecules serve not only as local energy sources but also as potent signaling molecules that impact brain function, immune regulation, and metabolic processes [107] [3]. Understanding the systemic effects of these gut-derived signals is essential for developing novel therapeutic interventions for neurological, psychiatric, and metabolic disorders.
Mechanisms of Systemic Signaling
Microbial Metabolite Production and Distribution
The colonic fermentation of indigestible carbohydrates produces SCFAs in a characteristic molar ratio of approximately 3:1:1 for acetate:propionate:butyrate, though this can range from 60:20:20 mM/kg in the human colon to as wide as 10:2:1 depending on dietary composition and microbial community structure [3] [8]. Butyrate serves as the primary energy source for colonocytes, propionate is largely metabolized in the liver, and acetate reaches the highest systemic concentrations, distributing throughout the body including across the blood-brain barrier [107] [3].
Table 1: SCFA Characteristics and Systemic Distribution
| SCFA Type | Primary Producing Bacteria | Typical Colonic Concentration | Systemic Concentration | Major Systemic Roles |
|---|---|---|---|---|
| Acetate | Bifidobacterium spp., Akkermansia muciniphila, Bacteroides spp. | 60-70% of total SCFAs | 100-200 µM (peripheral) | Cholesterol metabolism, lipogenesis, central appetite regulation |
| Propionate | Bacteroides spp., Akkermansia muciniphila, Negativicutes | 15-20% of total SCFAs | 1-15 µM (peripheral) | Hepatic gluconeogenesis, satiety signaling |
| Butyrate | Faecalibacterium prausnitzii, Eubacterium rectale, Roseburia spp. | 10-15% of total SCFAs | 1-15 µM (peripheral) | Primary energy source for colonocytes, anti-inflammatory, anti-cancer properties |
Cross-feeding mechanisms between bacterial species significantly influence final SCFA profiles. For instance, lactate produced by Bifidobacterium longum during fructo-oligosaccharide fermentation can be utilized by Eubacterium hallii to produce butyrate [3]. Similarly, Roseburia intestinalis depends on acetate produced by other bacteria for optimal growth on prebiotic substrates [3].
Signaling Pathways and Molecular Targets
SCFAs exert systemic effects through multiple molecular mechanisms, primarily via G protein-coupled receptor (GPCR) activation and epigenetic modulation through histone deacetylase (HDAC) inhibition [107] [108].
GPCR Signaling: SCFAs are endogenous ligands for free fatty acid receptors FFAR2 (GPR43) and FFAR3 (GPR41). FFAR2 is highly expressed in immune cells, intestinal epithelium, and adipocytes, while FFAR3 shows predominant expression in the peripheral nervous system and endothelial cells of the blood-brain barrier [107]. Receptor activation triggers intracellular signaling cascades that modulate immune cell function, hormone secretion, and neuronal activity.
HDAC Inhibition: Butyrate is a particularly potent HDAC inhibitor, regulating the expression of 5-20% of human genes through epigenetic mechanisms [8]. This activity influences critical cellular processes including proliferation, differentiation, and apoptosis, with implications for cancer prevention and neurodevelopment.
The following diagram illustrates the key signaling pathways through which gut microbial metabolites, particularly SCFAs, exert systemic effects:
Impact on Brain Structure and Function
The gut microbiota significantly influences brain development and function through multiple interconnected pathways. Germ-free animals demonstrate substantial alterations in brain morphology, including impaired blood-brain barrier integrity, altered microglial maturation and function, and reduced neurogenesis [109]. Microglia, the resident immune cells of the central nervous system, are particularly sensitive to microbial signals, with SCFAs playing essential roles in their maturation and functional programming [107].
The microbiota-gut-brain axis modulates synaptic plasticity, neuronal morphology, and myelination processes through direct effects on oligodendrocytes and indirect mechanisms involving immune activation [109]. These structural changes have functional consequences for behavior, cognition, and vulnerability to neurological diseases.
Quantitative Analysis of Microbial Metabolites
Systemic concentrations of gut-derived metabolites vary considerably based on production, absorption, and tissue-specific metabolism. The following table summarizes key quantitative data on microbial metabolites with systemic effects:
Table 2: Quantitative Analysis of Gut Microbial Metabolites
| Metabolite Class | Specific Metabolites | Production Site | Systemic Concentration Range | Blood-Brain Barrier Permeability | Key Functions |
|---|---|---|---|---|---|
| Short-Chain Fatty Acids | Acetate, Propionate, Butyrate | Cecum > Proximal Colon > Distal Colon | Acetate: 100-200 µM; Propionate/Butyrate: 1-15 µM | Yes (Acetate > Propionate > Butyrate) | HDAC inhibition, GPCR activation, energy metabolism |
| Neurotransmitters | GABA, Serotonin, Dopamine | Gut lumen (microbial production) | Varies by compound; Serotonin: predominantly peripheral | Limited direct transfer | Vagus nerve activation, modulation of CNS function |
| Bile Acid Derivatives | Secondary bile acids (deoxycholate, lithocholate) | Small intestine, colon | Varies by individual and diet | Limited data | FXR, TGR5 receptor activation, cholesterol metabolism |
The concentration gradient of SCFAs along the gastrointestinal tract follows a distinct pattern: cecum > proximal colon > distal colon [107]. Only 5-10% of produced SCFAs are excreted in feces, with the majority absorbed by colonic epithelial cells or entering portal circulation [107]. In brain tissue, physiological concentrations of acetate range from 17-19 pmol/mg, while cerebrospinal fluid concentrations show wider variation (acetate: 0-171 mM, propionate: 0-6 mM, butyrate: 0-2.8 mM) [107].
Methodologies for Investigating Gut-Brain-Metabolic Axes
Experimental Models and Manipulation Approaches
Research into gut-brain-metabolic axes employs specialized models to dissect causal relationships and mechanistic pathways. The following experimental approaches represent cornerstone methodologies in the field:
Germ-Free (GF) Animal Models: GF animals are raised in sterile isolators with no exposure to microorganisms, allowing investigation of physiological development in the absence of microbiota [108] [109]. These models demonstrate the essential role of microbiota in neurodevelopment, immune maturation, and metabolic programming. Key findings from GF studies include altered stress responses, neurotransmitter levels, and neurodevelopmental outcomes [108].
Protocol 1: Establishing GF Mouse Colonies
- Maintain breeding pairs in flexible film isolators with sterile air supply
- Sterilize all food, water, and bedding through autoclaving (121°C for 45 minutes)
- Regularly monitor sterility through bacterial and fungal culture of fecal samples
- Conduct experiments within isolators or using specialized transfer equipment
Microbiota Depletion with Antibiotics: Broad-spectrum antibiotic cocktails administered via drinking water effectively deplete gut microbiota, creating a model of microbiota disruption without the developmental adaptations seen in GF models [18].
Protocol 2: Antibiotic-Induced Microbiota Depletion
- Prepare antibiotic cocktail containing ampicillin (1 mg/mL), vancomycin (0.5 mg/mL), neomycin (1 mg/mL), and metronidazole (1 mg/mL)
- Administer in drinking water ad libitum for 3-4 weeks
- Include control group receiving normal drinking water
- Verify depletion through 16S rRNA sequencing of fecal samples
Fecal Microbiota Transplantation (FMT): FMT involves transferring fecal material from a donor to a recipient animal, enabling investigation of causal relationships between specific microbiota compositions and host phenotypes [110].
Protocol 3: Fecal Microbiota Transplantation in Rodents
- Collect fresh fecal pellets from donor animals and suspend in sterile saline (100 mg/mL)
- Homogenize by vortexing and centrifuge at low speed (800 × g for 3 minutes) to remove large particles
- Administer 200 µL of supernatant to recipient animals via oral gavage daily for 5-7 days
- Allow 2-3 weeks for microbial engraftment before phenotypic assessment
Metabolite Measurement and Analysis
Accurate quantification of microbial metabolites is essential for understanding gut-brain communication. The following methodologies represent gold-standard approaches:
Short-Chain Fatty Acid Quantification: Gas chromatography-mass spectrometry (GC-MS) and liquid chromatography-mass spectrometry (LC-MS) enable precise measurement of SCFA concentrations in biological samples including feces, blood, and brain tissue [107].
Protocol 4: SCFA Extraction and Measurement by GC-MS
- Homogenize fecal samples (100 mg) in 1 mL of acidified water (pH 2-3)
- Add internal standards (e.g., deuterated SCFAs)
- Extract SCFAs using diethyl ether or ethyl acetate
- Derivatize with N-tert-butyldimethylsilyl-N-methyltrifluoroacetamide (MTBSTFA)
- Analyze by GC-MS with a capillary column (e.g., DB-5MS)
- Quantify using standard curves for acetate, propionate, and butyrate
Microbial Community Profiling: 16S rRNA gene sequencing and shotgun metagenomics provide comprehensive characterization of microbial community structure and functional potential.
Protocol 5: 16S rRNA Gene Sequencing for Gut Microbiota Analysis
- Extract genomic DNA from fecal samples using bead-beating protocols
- Amplify hypervariable regions (e.g., V3-V4) with barcoded primers
- Purify amplicons and quantify using fluorometric methods
- Sequence on Illumina platform (MiSeq or NovaSeq)
- Process sequences using QIIME 2 or Mothur pipelines
- Analyze microbial diversity, composition, and predicted functions
The following diagram illustrates a comprehensive experimental workflow for investigating the gut-brain-metabolic axes:
The Scientist's Toolkit: Essential Research Reagents
Table 3: Research Reagent Solutions for Gut-Brain Axis Investigation
| Reagent Category | Specific Products/Compounds | Research Application | Key Considerations |
|---|---|---|---|
| SCFA Receptor Modulators | FFAR2/FFAR3 agonists (acetate, propionate); FFAR2 antagonist (CATPB); FFAR3 antagonist (AR420626) | Mechanistic studies of SCFA signaling | Receptor specificity; concentration-dependent effects |
| HDAC Inhibitors | Sodium butyrate, trichostatin A, valproic acid | Epigenetic regulation studies | Butyrate has broad HDAC inhibitory activity; selectivity varies |
| Microbiota Manipulation Tools | Broad-spectrum antibiotics (ampicillin, vancomycin, neomycin, metronidazole); probiotics (Lactobacillus, Bifidobacterium strains) | Creating dysbiosis models; testing microbial interventions | Antibiotic regimens vary by study; probiotic effects are strain-specific |
| Biological Sample Collection | RNAlater for tissue; specialized fecal collection tubes with stabilizers | Preserving sample integrity for multi-omics | Different stabilizers needed for DNA, RNA, and metabolites |
| Analytical Standards | Deuterated SCFAs (d3-acetate, d5-propionate, d7-butyrate); SCFA calibration mixes | Quantitative metabolomics by GC-MS/MS or LC-MS/MS | Essential for accurate quantification in complex matrices |
Implications for Drug Development and Therapeutic Interventions
The gut-brain-metabolic axis presents novel targets for therapeutic intervention across neurological, psychiatric, and metabolic disorders. Several promising approaches have emerged from preclinical and clinical studies:
Microbiome-Targeted Therapies: Probiotics, prebiotics, and synbiotics offer potential for modulating gut-brain communication. Specific bacterial strains, including certain Lactobacillus and Bifidobacterium species, demonstrate ability to improve hippocampal BDNF-TrkB signaling, enhance neurogenesis, and support myelination processes [109]. Fecal microbiota transplantation represents a more comprehensive approach for reshaping microbial communities, with demonstrated benefits in animal models of substance use disorders and preliminary human trials in alcohol use disorder [111].
Drug-Induced Dysbiosis Considerations: Commonly prescribed medications including metformin, statins, proton-pump inhibitors, NSAIDs, and antidepressants significantly impact gut microbiota composition, potentially contributing to both therapeutic and adverse effects [112] [113]. Understanding these drug-microbiome interactions is crucial for optimizing therapeutic outcomes and minimizing unintended consequences, particularly in patients receiving polypharmacy.
Metabolite-Based Therapeutics: Direct administration of SCFAs or development of receptor-targeted compounds represents a promising approach for harnessing gut-brain signaling. Preclinical evidence indicates that SCFA administration can modulate microglial function, reduce neuroinflammation, and influence reward pathways relevant to substance use disorders [111].
The gut-brain and metabolic axes represent an integrated signaling network with profound implications for systemic health and disease. Colonic fermentation of undigested food components generates bioactive metabolites that influence distant organs including the brain through immune, neural, and endocrine pathways. Advanced methodological approaches continue to elucidate the complex mechanisms underlying these systemic effects, providing novel targets for therapeutic intervention in neurological, psychiatric, and metabolic disorders. Future research should focus on translating mechanistic insights into targeted interventions that leverage the gut-brain-metabolic axis for improved patient outcomes.
Conclusion
The colonic fermentation of undigested food is a cornerstone of human health, directly influencing gastrointestinal function, immune regulation, and systemic metabolism. The synthesis of foundational science, advanced methodological tools, and clinical evidence underscores its profound therapeutic potential. Future research must focus on standardizing interventions, validating strain-specific mechanisms of action, and integrating high-resolution multi-omics data with artificial intelligence. This will enable the transition from a one-size-fits-all approach to precise microbiome engineering, paving the way for novel diagnostics, targeted live biotherapeutic products, and effective personalized nutrition strategies to prevent and treat a wide spectrum of chronic diseases.
References
- 1. Coordinated Host–Microbiome Enzymatic Interplay in Gut ... [https://www.mdpi.com/2218-273X/15/8/1151]
- 2. Mechanisms and implications of the gut microbial modulation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12441142/]
- 3. Gut microbiota functions: metabolism of nutrients and other ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5847071/]
- 4. Nondigestible carbohydrates and gut microbiota [https://www.cambridge.org/core/journals/animal-nutriomics/article/nondigestible-carbohydrates-and-gut-microbiota-a-dynamic-duo-in-host-defense/20011CC577E9DC2B9FC7D3E2D1695D7A]
- 5. How Gut Microbiome Science Is Reshaping Our Diet [https://www.sciencedirect.com/science/article/pii/S0022316625005383]
- 6. The interaction between various food components and ... [https://pubs.rsc.org/en/content/articlehtml/2025/fo/d4fo04430d]
- 7. Why does increased microbial fermentation in the human ... [http://aimspress.com/article/doi/10.3934/microbiol.2024016?viewType=HTML]
- 8. Food, Nutrition, and Gut Health: Mechanisms Explained [https://esmed.org/food-nutrition-and-gut-health-mechanisms-explained/]
- 9. In vitro colon fermentation of a traditional fermented food using ... [https://pubs.rsc.org/en/content/articlehtml/2025/fo/d5fo01627d]
- 10. Colonic health: fermentation and short chain fatty acids - PubMed [https://pubmed.ncbi.nlm.nih.gov/16633129/]
- 11. In vitro colonic fermentation of dietary fibers [https://www.sciencedirect.com/science/article/pii/S0924224418307878]
- 12. Dietary Fiber Intake and Gut Microbiota in Human Health - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9787832/]
- 13. Colonic in vitro fermentation of mycoprotein promotes shifts ... [https://www.nature.com/articles/s42003-024-05893-4]
- 14. Short-chain fatty acid kinetics and concentrations are ... [https://pubmed.ncbi.nlm.nih.gov/40274191/]
- 15. Caecal pH is a biomarker of excessive colonic fermentation [https://pmc.ncbi.nlm.nih.gov/articles/PMC4009533/]
- 16. An Ex Vivo Fermentation Screening Platform to Study Drug ... [https://www.sciencedirect.com/science/article/abs/pii/S0090955624055661]
- 17. Short-chain fatty acids (SCFAs) in gut health: Implications for drug metabolism and therapeutics - ScienceDirect [https://www.sciencedirect.com/science/article/pii/S2590097825000205]
- 18. Mechanisms and implications of the gut microbial ... [https://www.nature.com/articles/s44324-025-00066-1]
- 19. Distinguishing diet- and microbe-derived metabolites in the ... [https://microbiomejournal.biomedcentral.com/articles/10.1186/s40168-025-02258-9]
- 20. Gut-Microbiota-Derived Metabolites Maintain Gut and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10000530/]
- 21. Baseline intestinal microbiota composition influences ... [https://www.nature.com/articles/s41522-025-00817-4]
- 22. Comparison of fecal and blood metabolome reveals ... [https://www.nature.com/articles/s41467-023-36256-y]
- 23. Mathematical models of the colonic microbiota [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1623418/full]
- 24. Gut microbiome-metabolome interactions predict host condition [https://microbiomejournal.biomedcentral.com/articles/10.1186/s40168-023-01737-1]
- 25. Comparing Published Gut Microbiome Taxonomic Data ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8740627/]
- 26. Key structural domains of resistant starch and their role in ... [https://www.sciencedirect.com/science/article/abs/pii/S0268005X25009749]
- 27. Dietary patterns influencing the human colonic microbiota ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1591341/full]
- 28. A multi-strain probiotic formulation preserves intestinal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12332529/]
- 29. Colorectal cancer risk in ulcerative colitis: an updated ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12150054/]
- 30. The Colonic Crypt: Cellular Dynamics and Signaling ... [https://www.mdpi.com/2073-4409/14/18/1428]
- 31. In vitro fermentation of yeast cell walls (mannan ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0322877]
- 32. InfoGest Consensus Method - The Impact of Food ... - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK500165/]
- 33. The harmonized INFOGEST in vitro digestion method [https://www.sciencedirect.com/science/article/pii/S0963996915302751]
- 34. Exploring in vitro production of colonic microbial ... [https://www.sciencedirect.com/science/article/pii/S0308814625038841]
- 35. A Review on In Vitro Evaluation of Chemical and Physical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12027026/]
- 36. An Advanced Bioreactor Simulating Dynamic Physiological ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9146976/]
- 37. A review of in-vitro digestibility models on diverse foods ... [https://link.springer.com/article/10.1007/s44187-025-00454-y]
- 38. An anaerobic in vitro flow model for studying interactions at ... [https://www.nature.com/articles/s41522-025-00800-z]
- 39. The Mini Colon Model: a benchtop multi-bioreactor system ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9291644/]
- 40. Factors affecting plant food particle behaviour during in ... [https://www.sciencedirect.com/science/article/pii/S0924224424004783]
- 41. Advances in in vitro cultivation techniques for ... [https://www.sciencedirect.com/science/article/abs/pii/S0734975025000813]
- 42. Selecting for lactic acid producing and utilising bacteria in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7187302/]
- 43. The core microbiomes and associated metabolic potential ... [https://www.nature.com/articles/s42003-025-07808-3]
- 44. Evidence for Greater Production of Colonic Short Chain ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3970979/]
- 45. Absolute abundance values reveal microbial shifts and co ... [https://www.sciencedirect.com/science/article/abs/pii/S0268005X21008389]
- 46. Functional lower airways genomic profiling of the microbiome to... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8643072/]
- 47. Optimized bacterial community characterization through full ... [https://bmcmicrobiol.biomedcentral.com/articles/10.1186/s12866-024-03208-5]
- 48. The in vitro fermentation of compound oral liquid by human ... [https://pubs.rsc.org/en/content/articlehtml/2022/ra/d2ra05053f]
- 49. Distinguishing critical microbial community shifts from ... [https://www.nature.com/articles/s41598-025-01781-x]
- 50. An In Vitro Colonic Fermentation Study of the Effects ... [https://www.mdpi.com/2304-8158/13/6/921]
- 51. Microbial community and functional shifts across ... [https://www.sciencedirect.com/science/article/pii/S0301479724036697]
- 52. Short-chain fatty acids ( SCFAs ) as potential resuscitation factors that... [https://link.springer.com/article/10.1007/s42995-023-00187-w]
- 53. Daily fluctuation of colonic microbiome in response to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10632506/]
- 54. Probiotics, Prebiotics, Synbiotics, Postbiotics, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12346543/]
- 55. Probiotics, Prebiotics, Synbiotics, Postbiotics, and ... [https://www.mdpi.com/2304-8158/14/15/2613]
- 56. Probiotics, prebiotics and synbiotics- a review - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4648921/]
- 57. A comprehensive overview of the effects of probiotics ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1651965/full]
- 58. Recent advances in prebiotics: Classification, mechanisms, ... [https://www.sciencedirect.com/science/article/pii/S266683352500142X]
- 59. Unveiling the role of functional foods with emphasis on ... [https://www.sciencedirect.com/science/article/pii/S1756464624003396]
- 60. In-vitro colonic fermentation of Kakadu plum (Terminalia ... [https://www.sciencedirect.com/science/article/pii/S0308814624007064]
- 61. Design and application of synthetic human gut microbial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12622336/]
- 62. Human Microbiome Market & Therapeutic Pipeline 2025 [https://www.strategicmarketresearch.com/blogs/human-microbiome-market-clinical-trials-pipeline]
- 63. A new gut pathogenic bacteria and its metabolites promote ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12416176/]
- 64. Review Dietary protein and the intestinal microbiota [https://www.sciencedirect.com/science/article/pii/S2589004222015851]
- 65. Fermentation: A Boon for Production of Bioactive ... [https://www.mdpi.com/1420-3049/23/10/2560]
- 66. Microbiome-active drug delivery systems (MADDS) [https://www.sciencedirect.com/science/article/pii/S0169409X25002054]
- 67. Gut physiology and environment explain variations in human gut microbiome composition and metabolism | Nature Microbiology [https://www.nature.com/articles/s41564-024-01856-x]
- 68. Colonic fermentation – More than meets the nose [https://www.sciencedirect.com/science/article/abs/pii/S0306987709002977]
- 69. Inter-niche and inter-individual variation in gut microbial community assessment using stool, rectal swab, and mucosal samples | Scientific Reports [https://www.nature.com/articles/s41598-018-22408-4]
- 70. In vitro fermentation potential of diet-derived ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12303725/]
- 71. Making experimental data tables in the life sciences more FAIR [https://pmc.ncbi.nlm.nih.gov/articles/PMC7736789/]
- 72. Common Manufacturing Challenges For LBP Formulations [https://www.bioprocessonline.com/doc/common-manufacturing-challenges-for-lbp-formulations-0001]
- 73. Live Biotherapeutic Products Whitepaper 2025 [https://novotech-cro.com/whitepapers/live-biotherapeutic-products-whitepaper-2025]
- 74. Live Biotherapeutic Products & Microbiome CDMO Market [https://www.factmr.com/report/live-biotherapeutic-products-microbiome-cdmo-market]
- 75. Noninvasive, microbiome-based diagnosis of inflammatory ... [https://www.nature.com/articles/s41591-024-03280-4]
- 76. Evolving Dynamics of Fermented Food Microbiota and the ... [https://www.mdpi.com/2304-8158/14/13/2361]
- 77. Why does increased microbial fermentation in the human ... [https://www.aimspress.com/article/doi/10.3934/microbiol.2024016?viewType=HTML]
- 78. The gut microbiota of healthy individuals remains resilient ... [https://www.nature.com/articles/s41598-024-72673-9]
- 79. In vitro colon fermentation of a traditional ... [https://pubmed.ncbi.nlm.nih.gov/40891083/]
- 80. In vitro human gastrointestinal digestibility and colonic ... [https://www.sciencedirect.com/science/article/pii/S0963996925004351]
- 81. Gut microbiota modulatory capacity of fermented ketchup in ... [https://www.sciencedirect.com/science/article/pii/S0963996924008718]
- 82. Optimization of an In Vitro Colonic Fermentation [https://pmc.ncbi.nlm.nih.gov/articles/PMC12232328/]
- 83. The multi-unit in vitro colon model to assess gut ecological ... [https://www.sciencedirect.com/science/article/pii/S096399692401648X]
- 84. The regulatory framework for microbiome-based therapies [https://www.nature.com/articles/s41522-025-00683-0]
- 85. In Vitro Simulation of Human Colonic Fermentation [https://www.mdpi.com/2076-3417/11/17/8135]
- 86. In-vitro dynamic fermentation simulation colon reactor for ... [https://www.sciencedirect.com/science/article/abs/pii/S1369703X23000724]
- 87. Artificial intelligence in personalized nutrition and food ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12325300/]
- 88. Personalized nutrition studies of human gut microbiome ... [https://www.sciencedirect.com/science/article/pii/S0271531725000193]
- 89. AI nutrition recommendation using a deep generative ... [https://www.nature.com/articles/s41598-024-65438-x]
- 90. Personalized nutrition, microbiota, and metabolism: A triad for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9623024/]
- 91. Mathematical models of the colonic microbiota [https://pmc.ncbi.nlm.nih.gov/articles/PMC12507599/]
- 92. RxFood - evidence-based, AI powered personalized nutrition [https://rxfood.com/]
- 93. A Scoping Review of Artificial Intelligence for Precision ... [https://www.sciencedirect.com/science/article/pii/S2161831325000341]
- 94. Validation of a novel quality of life questionnaire [https://pmc.ncbi.nlm.nih.gov/articles/PMC8962596/]
- 95. Review article Positive psychological well-being and ... [https://www.sciencedirect.com/science/article/abs/pii/S016383432300004X]
- 96. Probiotics and gastrointestinal disorders: an umbrella meta ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12183855/]
- 97. Fermented-food diet increases microbiome diversity ... [https://med.stanford.edu/news/all-news/2021/07/fermented-food-diet-increases-microbiome-diversity-lowers-inflammation.html]
- 98. Fermented Foods as Functional Systems: Microbial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12249102/]
- 99. Colonization of the live biotherapeutic product VE303 and ... [https://www.sciencedirect.com/science/article/pii/S1931312822001469]
- 100. Impact of a Purified Microbiome Therapeutic on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11006105/]
- 101. VE303 receives Fast Track designation for ... [https://www.vedantabio.com/press-release/vedanta-biosciences-receives-fast-track-designation-for-ve303-and-presents-phase-2-data-at-digestive-disease-week/]
- 102. Safety and efficacy of a defined bacterial consortium ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11841841/]
- 103. Dysbiosis and colorectal cancer: conducive factors, biological ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12203119/]
- 104. The impact of fermented foods and microbiota modulation ... [https://gulhanemedj.org/articles/the-impact-of-fermented-foods-and-microbiota-modulation-on-colorectal-cancer/gulhane.galenos.2025.59672]
- 105. Therapeutic Potential for Sphingolipids in Inflammatory Bowel ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10887199/]
- 106. Impact of fermented foods consumption on gastrointestinal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12549620/]
- 107. Elucidating the specific mechanisms of the gut-brain axis [https://pmc.ncbi.nlm.nih.gov/articles/PMC12093714/]
- 108. decoding the gut–immune–brain axis in health and disease [https://www.nature.com/articles/s41423-025-01333-3]
- 109. Exploring the microbiota-gut-brain axis: impact on ... [https://www.frontiersin.org/journals/neuroanatomy/articles/10.3389/fnana.2025.1504065/full]
- 110. Microbiota–gut–brain axis and its therapeutic applications ... [https://www.nature.com/articles/s41392-024-01743-1]
- 111. The Gut Microbiome and Drug Addiction: An Emerging Link [https://asm.org/articles/2023/april/the-gut-microbiome-and-drug-addiction-an-emerging]
- 112. Potential effects of the most prescribed drugs on ... [https://pubmed.ncbi.nlm.nih.gov/38244807/]
- 113. Review Potential effects of the most prescribed drugs on ... [https://www.sciencedirect.com/science/article/pii/S0361923024000169]