Correlating Continuous Glucose Monitoring with Food Intake: From Foundational Science to Clinical Endpoints in Drug Development
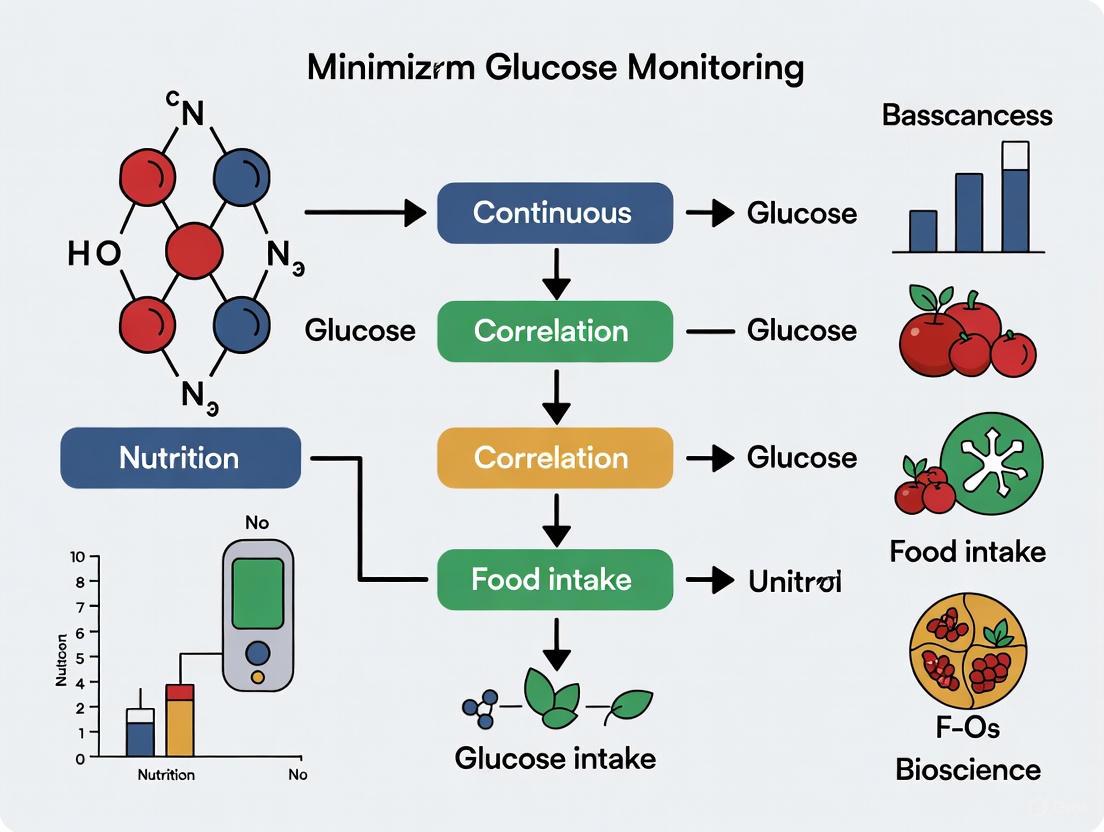
This article synthesizes the latest evidence on the application of Continuous Glucose Monitoring (CGM) for correlating food intake with glycemic responses, tailored for researchers and drug development professionals.
Correlating Continuous Glucose Monitoring with Food Intake: From Foundational Science to Clinical Endpoints in Drug Development
Abstract
This article synthesizes the latest evidence on the application of Continuous Glucose Monitoring (CGM) for correlating food intake with glycemic responses, tailored for researchers and drug development professionals. It explores the foundational principles of glucose dynamics, examines advanced methodological approaches like Functional Data Analysis (FDA) for modeling postprandial trajectories, and reviews the use of CGM-derived endpoints like Time in Range (TIR) in clinical trials. The content further addresses the critical evaluation of CGM device performance and the optimization of dietary interventions, providing a comprehensive resource for integrating CGM data into biomedical research and therapeutic development.
Understanding Glucose Dynamics: The Physiological Basis of Food-Induced Glycemic Responses
Core Principles of Postprandial Glucose Metabolism in Health and Disease
Postprandial glucose metabolism represents a critical physiological process wherein the body regulates blood sugar levels following food intake. Effective control of postprandial glucose responses (PPGR) is essential for managing the progression of type 2 diabetes mellitus (T2DM) and overall metabolic health [1] [2]. The global epidemic of T2DM, affecting approximately 537 million people worldwide, underscores the urgent need to understand these core principles [3]. Postprandial glucose excursions contribute significantly to elevated glycated hemoglobin (HbA1c) levels and are independently associated with increased risk of cardiovascular complications, neuropathy, and kidney damage [3]. Recent advances in continuous glucose monitoring (CGM) technology have revolutionized our ability to study these metabolic processes in real-time, providing unprecedented insights into the complex interplay between dietary factors, physiological mechanisms, and individual variability in glucose regulation [4] [3] [5].
Physiological Mechanisms of Postprandial Glucose Regulation
Key Metabolic Pathways
The regulation of postprandial glucose involves multiple integrated physiological processes across various tissues and organ systems. Following carbohydrate ingestion, the breakdown of complex carbohydrates into monosaccharides enables intestinal absorption, primarily as glucose, which enters the bloodstream and triggers a cascade of metabolic responses [6]. Insulin secretion from pancreatic β-cells represents the primary hormonal response, facilitating glucose uptake into insulin-sensitive tissues including skeletal muscle, adipose tissue, and liver. Simultaneously, incretin hormones such as GLP-1 and GIP amplify glucose-dependent insulin secretion while inhibiting glucagon release and delaying gastric emptying.
Skeletal muscle constitutes the major site for postprandial glucose disposal, accounting for approximately 70-80% of ingested glucose clearance under normal physiological conditions. The process is mediated by insulin-stimulated translocation of GLUT4 glucose transporters to the cell surface. Concurrently, the liver suppresses endogenous glucose production and enhances glycogen synthesis. These coordinated processes normally limit postprandial glucose excursions to a peak of <140 mg/dL within 30-60 minutes after eating, returning to baseline within 2-3 hours.
Disrupted Mechanisms in Disease States
In insulin-resistant states such as T2DM, these regulatory mechanisms become compromised at multiple levels. Peripheral tissues, particularly skeletal muscle, exhibit reduced sensitivity to insulin, impairing glucose disposal. Hepatic insulin resistance fails to adequately suppress endogenous glucose production, resulting in continued glucose output despite elevated postprandial glucose levels. Additionally, pancreatic β-cell dysfunction leads to impaired, delayed, or insufficient insulin secretion relative to the glucose load. These defects collectively result in exaggerated and prolonged postprandial hyperglycemia, which further contributes to glucotoxicity and progressive metabolic deterioration [3].
Recent research has highlighted that the entire musculature normally accounts for only about 15% of the oxidative metabolism of glucose when sitting inactive, despite being the body's largest lean tissue mass [6]. This suggests that methods capable of elevating oxidative muscle metabolism could be advantageous to complement other lifestyle and pharmacological approaches whose mechanisms of action are limited to non-oxidative metabolic pathways.
The following diagram illustrates the core pathways of postprandial glucose regulation in health and their dysregulation in disease states:
Experimental Approaches for Investigating Postprandial Glucose Metabolism
Continuous Glucose Monitoring Methodologies
Continuous glucose monitoring (CGM) has emerged as a transformative technology for investigating postprandial glucose metabolism in both research and clinical settings. CGM devices measure glucose concentrations in the interstitial fluid at regular intervals (typically every 5-15 minutes), providing high-resolution temporal data on glucose fluctuations [3]. This comprehensive profiling enables researchers to capture postprandial glucose peaks, excursion duration, and glucose variability that would be missed with conventional intermittent blood sampling.
Standard CGM-derived metrics for assessing postprandial glucose metabolism include:
- Postprandial glucose peak: The maximum glucose level reached after meal consumption
- Incremental Area Under the Curve (iAUC): The net increase in glucose above baseline following a meal
- Time in Range (TIR): The percentage of time glucose levels remain within a target range (typically 70-180 mg/dL)
- Mean Amplitude of Glycemic Excursions (MAGE): A measure of glycemic variability
- 24-hour mean glucose: The average glucose concentration across a full day [4] [5]
Recent research has demonstrated significant correlations between various CGM metrics and dietary factors. A study in healthy adults found significant positive moderate correlations between glycemic load and several CGM metrics including area under the curve (ρ = 0.40), relative amplitude (ρ = 0.40-0.42), and standard deviation (ρ = 0.41) in time windows of 2-4 hours postprandially [7].
Personalized Nutrition Approaches
Substantial interindividual variability in postprandial glucose responses to identical foods has driven the development of personalized nutrition approaches. Research has shown that no two individuals share the same dietary and temporal predictors of PPG excursions [3]. This variability stems from differences in biological factors (insulin sensitivity, gut microbiota composition, genetic variations), food properties (food structure, nutrient composition), and behavioral contexts (meal timing, eating rate, physical activity patterns) [2].
N-of-1 trial designs have emerged as a powerful methodology for investigating this individual variability. These trials determine individual responses to specific interventions through prospective, randomized crossover designs conducted either on individual patients or a series of patients [1] [2]. A prototypical N-of-1 trial protocol for testing PPGR to various staple foods involves:
- Randomizing participants to receive different test foods (e.g., white rice, germ rice, brown rice, rice noodles, pasta) three times in a randomized order
- Using CGM to track PPGR at 5-minute intervals
- Standardizing available carbohydrate content across test meals (typically 50g)
- Maintaining consistent accompanying foods and meal timing
- Applying Bayesian analysis at both individual and group levels to assess PPGR [2]
Machine learning approaches have further advanced personalized predictions of PPG excursions. Personalized models trained on individual CGM data, with or without manually-logged meal information, can predict PPG excursions with average F1-scores of 75.88% [3]. These models enable identification of individual "vulnerability states" - periods of heightened susceptibility to PPG excursions - which can inform just-in-time adaptive interventions (JITAIs) for glycemic control.
The following workflow diagram illustrates the experimental approach for personalized postprandial glucose research:
Quantitative Data on Dietary Interventions and Postprandial Glucose Responses
Carbohydrate-Restricted Diets
Meta-analytic evidence demonstrates that carbohydrate-restricted diets (CRDs) significantly improve 24-hour mean blood glucose in patients with T2DM (d = -0.51, 95% CI: -0.88 to -0.14, p < 0.05) [4]. Exploratory trend analysis suggests a positive correlation between intervention duration and the magnitude of 24-hour mean glucose reduction, with longer interventions (≥1 year) potentially yielding greater benefits, though this requires confirmation through longer-term randomized controlled trials [4].
Table 1: Effects of Carbohydrate-Restricted Diets on Glucose Metrics in T2DM
| Intervention Type | Duration | Participants | Effect on 24-h Mean Glucose | Other Significant Findings |
|---|---|---|---|---|
| Low-carbohydrate diets (≤45% energy from carbs) | 6 days to 6 months | 301 (pooled) | Standardized mean difference: -0.51 (95% CI: -0.88 to -0.14) | Trend toward greater improvement with longer duration |
| Very-low-carbohydrate diets (<26% energy from carbs) | Varies | Subset of above | Generally larger effects | Improved β-cell function and insulin sensitivity |
Diet Quality and Carbohydrate Composition
Beyond carbohydrate quantity, diet quality and carbohydrate composition significantly influence postprandial glucose profiles. Data from the Framingham Heart Study demonstrates that higher overall diet quality and better carbohydrate quality are associated with favorable CGM-derived metrics [5]. Specifically, replacing 5% of energy intake from protein with equivalent energy from carbohydrates was associated with a 0.97 mg/dL higher CGM mean glucose (SE = 0.47; P = 0.04) [5].
Notably, consuming a diet with more than 1g of fiber for every approximately 9g of carbohydrates was associated with 7-10% lower time spent above 140 mg/dL compared with higher carb-to-fiber ratios in individuals with prediabetes (P-trend < 0.001) [5]. This highlights the importance of considering carbohydrate quality rather than merely quantity in dietary interventions for glucose management.
Table 2: Association of Diet Quality and Carbohydrate Composition with CGM Metrics
| Dietary Factor | Population | Key Associations with CGM Metrics | Effect Size |
|---|---|---|---|
| Overall Diet Quality | Normoglycemic (n=385) | Stronger associations with favorable CGM measures | More pronounced in normoglycemia |
| Carbohydrate-to-Fiber Ratio | Prediabetes (n=292) | Higher ratio associated with increased time >140 mg/dL | 7-10% reduction with ratio <~9:1 |
| Carbohydrate Substitution | Overall (n=677) | Replacing protein with carbohydrates increased mean glucose | 0.97 mg/dL increase per 5% energy |
Physical Activity Interventions
Brief interruptions to prolonged sitting, known as "exercise snacks," acutely attenuate postprandial glucose and insulin responses in adults with obesity [8]. Meta-analysis of 17 trials (261 unique participants) showed that versus uninterrupted sitting, activity breaks reduced glucose iAUC (SMD = -0.49, 95% CI: -0.85 to -0.14) and insulin iAUC (SMD = -0.26, 95% CI: -0.50 to -0.03) [8]. Exploratory subgroup analyses suggested larger effects with higher-frequency (≤30-minute) and short-bout (≤3-minute) interruptions and with walking or simple resistance activities.
Different types of physical activity induce distinct physiological processes that either oppose or enhance postprandial glucose tolerance [6]. Methods capable of elevating oxidative muscle metabolism, such as specialized soleus muscle activity, may be particularly advantageous as they complement other lifestyle and pharmacological approaches whose mechanisms of action are limited to non-oxidative metabolic pathways [6].
Research Reagent Solutions Toolkit
Table 3: Essential Research Materials and Technologies for Postprandial Glucose Studies
| Research Tool | Specification/Model | Primary Research Application | Key Performance Metrics |
|---|---|---|---|
| Continuous Glucose Monitor | Dexcom G7 or equivalent | Real-time glucose measurement in interstitial fluid | 5-15 minute sampling intervals; MARD <9% |
| CGM Data Analysis Software | "cgmanalysis" R package or equivalent | Calculation of glycemic variability metrics | Computes iAUC, MAGE, CONGA, TIR, etc. |
| Standardized Test Meals | Varies by protocol (e.g., 50g available carbohydrate) | Controlled nutrient challenge for PPGR assessment | Precise macronutrient composition |
| Dietary Assessment Tools | Digital food diaries, image-assisted methods | Tracking dietary intake and timing | Correlation with CGM metrics (ρ = 0.40-0.45) |
| Physical Activity Monitors | Research-grade accelerometers | Quantifying activity patterns and energy expenditure | MET estimation, sedentary time quantification |
| Machine Learning Frameworks | Python Scikit-learn, R caret | Personalized PPG excursion prediction | F1-score for prediction (~75.88%) |
Detailed Experimental Protocols
N-of-1 Trial Protocol for Staple Food Testing
This protocol systematically evaluates individual postprandial glucose responses to different carbohydrate-rich staple foods using a randomized, crossover N-of-1 design [2].
Materials and Setup:
- CGM device with 5-minute sampling capability
- Standardized test meals with 50g available carbohydrate portions
- Digital food scales and preparation guidelines
- Meal timing and contextual factor logging system
Test Diet Composition:
- Staple foods: White rice (143g), germ rice (175g), brown rice (173g), rice noodles (198g), pasta (178g) - portions adjusted to provide 50g available carbohydrates
- Accompanying foods: 150g scrambled eggs with tomatoes, 50g cucumber, 200mL milk (consistent across tests)
- Nutritional analysis: Verify macronutrient composition through certified laboratory analysis
Experimental Procedure:
- Participant screening: Recruit adults with T2DM (age 18-70 years) diagnosed for ≥3 months, on stable lifestyle intervention or single hypoglycemic medication
- Baseline assessment: Collect demographic data, medical history, anthropometric measurements
- Randomization sequence: Generate computerized randomization schedule for the 5 test diets across 3 periods (15 test days total)
- Test day protocol:
- Overnight fast of 10-12 hours
- Baseline CGM reading pre-meal
- Test meal consumption within 20 minutes under supervision
- CGM monitoring for 3-5 hours postprandially
- Standardized physical activity and medication patterns across test days
- Data collection: Capture CGM data at 5-minute intervals, document meal timing, self-reported symptoms, and contextual factors
Statistical Analysis:
- Calculate primary outcome (postprandial blood glucose peak) and secondary outcomes (iAUC, time to peak, time to return to baseline)
- Apply Bayesian hierarchical models for individual and group-level inference
- Conduct sensitivity analyses adjusting for potential confounding factors (medication timing, prior physical activity, sleep quality)
Protocol for Exercise Snack Interventions
This protocol examines the acute effects of brief activity breaks on postprandial glucose metabolism in adults with obesity [8].
Experimental Conditions:
- Control condition: Uninterrupted sitting
- Intervention conditions: Interruptions of sitting every 30 minutes with 2-5 minutes of light-to-moderate activity (walking or simple resistance exercises)
Outcome Measures:
- Co-primary outcomes: Glucose iAUC and insulin iAUC
- Secondary outcomes: Total AUC, mean glucose and insulin levels, glucose and insulin peaks
Standardized Procedures:
- Pre-test standardization: 48-hour control of diet and physical activity prior to testing
- Test meal: Standardized mixed meal (e.g., 75g carbohydrate, 25g protein, 15g fat)
- Blood sampling: Frequent venous blood samples (every 15-30 minutes) for 2-3 hours postprandially
- Activity protocols: Precisely timed activity breaks with standardized intensity and duration
- Data analysis: Calculate iAUC using the trapezoidal method above baseline; compare conditions using linear mixed models with participant as random effect
This systematic approach enables rigorous investigation of the dose-response relationships between activity interruption patterns and postprandial metabolic outcomes.
CGM as a Tool for Behavioral Modification and Lifestyle Guidance
Continuous Glucose Monitoring (CGM) has transcended its original purpose as a passive glucose tracking tool for diabetes management, emerging as a dynamic technology for motivating behavioral modification and guiding lifestyle choices. By providing real-time, visual feedback on how nutrition, physical activity, and other daily behaviors impact glycemic responses, CGM serves as a powerful catalyst for behavior change [9]. This application note details the quantitative evidence, underlying behavioral mechanisms, and practical protocols for utilizing CGM as an intervention tool in research and clinical practice, framing its use within the broader context of food intake correlation research.
Quantitative Evidence: CGM Metrics and Behavioral Outcomes
The efficacy of CGM-driven interventions is supported by a growing body of quantitative research linking specific CGM metrics to dietary components and behavioral changes. The tables below summarize key findings from recent studies.
Table 1: Correlations between CGM Metrics and Dietary Components in a Healthy Cohort (n=48) [10]
| Dietary Component | Correlated CGM Metric(s) | Correlation Coefficient (ρ) | Statistical Significance |
|---|---|---|---|
| Glycemic Load (GL) | Relative Amplitude (4-hour window) | 0.42 | P < .0004 |
| Standard Deviation (4-hour window) | 0.41 | P < .0004 | |
| Variance (4-hour window) | 0.43 | P < .0004 | |
| Carbohydrates | Standard Deviation (24-hour) | 0.45 | P < .0004 |
| Variance (24-hour) | 0.44 | P < .0004 | |
| Mean Amplitude of Glycemic Excursions (MAGE) | 0.40 | P < .0004 |
Table 2: Effects of Carbohydrate-Restricted Diets (CRDs) on 24-Hour Mean Glucose in T2DM (Meta-Analysis) [4]
| Parameter | Summary of Findings |
|---|---|
| Overall Effect | Significant improvement in 24-h mean blood glucose (d = -0.51, 95% CI: -0.88 to -0.14, p < 0.05) |
| Intervention Duration | Exploratory trend analysis suggested a positive correlation between longer intervention duration and greater magnitude of glucose reduction. |
| Conclusion | CRDs may improve 24-h MBG in T2DM patients, with longer durations potentially yielding greater benefits. |
Table 3: Self-Reported Behavioral Changes in CGM Users (Survey of n=40 Users) [11]
| Behavioral Change | Percentage of Users Reporting Change |
|---|---|
| Overall healthier lifestyle | 90% |
| Modified food choices | 87% |
| Noticed how food affects glucose | 87.5% |
| Increased physical activity | 42.5% |
| More likely to walk/be active after seeing glucose rise | 47.5% |
Mechanism of Action: The CGM-Driven Feedback Loop
CGM facilitates behavior change through a continuous feedback loop, transforming abstract dietary choices into tangible, visual outcomes. The process can be summarized in the following workflow, which illustrates how CGM data leads to sustained behavioral modification.
Experimental Protocols for CGM-Based Behavioral Research
Protocol: Investigating the Diet-Glucose Relationship in Free-Living Populations
This protocol is adapted from studies that successfully correlated CGM metrics with dietary intake in free-living conditions [10] [5] [12].
Objective: To quantify the relationship between meal composition (macronutrients, glycemic load) and subsequent glycemic responses in a target population.
Materials: See "Research Reagent Solutions" below. CGM devices should be selected based on required data accessibility (blinded vs. unblinded) and approval for use in the target population (e.g., FDA-cleared for over-the-counter use in non-insulin using populations) [13].
Procedure:
- Participant Recruitment & Sensor Application: Recruit participants according to inclusion/exclusion criteria (e.g., adults with or without diabetes). Apply CGM sensor according to manufacturer's instructions.
- Dietary Recording: Participants concurrently record all food and beverage intake for a minimum of 3 days. Preferred methods include:
- Image-assisted Dietary Log: Use of a wearable camera (e.g., eButton) [12] or smartphone to capture images of all meals and snacks.
- Digital Food Diary: Utilization of a mobile app to log food type, estimated portion size, and timing.
- Data Collection Period: Maintain simultaneous CGM wear and dietary recording for a target of 10-14 days to capture intra-individual variability [12].
- Data Processing & Analysis:
- CGM Data: Extract standard glycemic metrics (e.g., mean glucose, TIR, TAR, TBR, GV, MAGE) using analysis packages (e.g.,
cgmanalysisR package) [5]. - Dietary Data: Convert food logs into quantitative nutritional data (energy, carbs, protein, fat, fiber, glycemic load).
- Statistical Analysis: Employ linear mixed models to account for repeated measures within individuals. Correlate dietary components (independent variables) with CGM metrics (dependent variables).
- CGM Data: Extract standard glycemic metrics (e.g., mean glucose, TIR, TAR, TBR, GV, MAGE) using analysis packages (e.g.,
Protocol: A Nutrition-Focused CGM Initiation Intervention
This protocol is based on the "Using Nutrition to Improve Time in Range (UNITE)" study, which integrated evidence-based nutrition guidance with CGM initiation [14].
Objective: To evaluate the impact of a structured, nutrition-focused educational session during CGM initiation on subsequent food-related behaviors and glycemic outcomes.
Materials: CGM device and companion app; NFA educational materials (e.g., interactive slides, one-page CGM nutrition guide) emphasizing a "1, 2, 3 approach" (check glucose before, 1-2 hours after meals) and a "yes/less framework" for food choices [14].
Procedure:
- Baseline & Recruitment: Recruit eligible participants (e.g., non-insulin-using T2D adults). Collect baseline HbA1c and demographic data.
- Session 1 - CGM Initiation & Education (60 mins, in-person):
- Apply the CGM sensor.
- Deliver the NFA curriculum using the prepared materials. Key messages include:
- Defining glucose goals (TIR >70%, TBR <4%).
- Teaching the "1, 2, 3" method for discovering personal postprandial responses.
- Introducing the "yes/less" food choice framework to align eating patterns with evidence-based nutrition guidance.
- Free-Living Phase (14 days): Participants use the CGM in real-time. They are encouraged to actively review their data before and after meals.
- Session 2 - Data Review & Reinforcement (30 mins, remote):
- Review the participant's ambulatory glucose profile (AGP) report.
- Discuss patterns and link high or low glucose events to specific meals or behaviors.
- Problem-solve and reinforce nutrition messages from Session 1.
- Outcome Assessment (2-month endpoint):
- Quantitative: Analyze CGM metrics (TIR, GV) from the final 2 weeks of the study.
- Qualitative: Conduct semi-structured interviews to understand user experience, perceived behavior change, and intervention receipt [14].
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Materials and Tools for CGM-Based Behavioral Research
| Item Category | Specific Examples & Functions |
|---|---|
| CGM Systems | Dexcom G7/Freestyle Libre: For real-time, unblinded data collection. Blinded Pro versions: For objective endpoint assessment without participant behavior influence. Stelo Glucose Biosensor: An over-the-counter CGM indicated for non-insulin using adults to understand lifestyle impacts [13]. |
| Dietary Assessment Tools | eButton: A wearable, automatic camera that captures food images, reducing self-reporting burden and bias [12]. Digital Food Diaries (Apps): Log food intake, timing, and portion sizes. Dietitian-Led 24-hr Recall: Validated method for reconstructing dietary intake and calculating nutrient composition and glycemic load [10]. |
| Data Analysis Software | cgmanalysis R Package: A standardized tool for batch-processing CGM data and calculating a wide array of glycemic metrics (Mean glucose, TIR, MAGE, etc.) [5]. Functional Data Analysis (FDA) Software (R, MATLAB): For analyzing entire postprandial glucose trajectories instead of scalar summaries, revealing time-dependent effects of diet [15]. |
| Educational & Visualization Aids | Ambulatory Glucose Profile (AGP) Report: The international standard report for visualizing CGM data, using color-coding (Green=TIR, Red=TBR) for quick pattern recognition [16]. Nutrition-Focused Approach (NFA) Guides: Simplified materials (e.g., "yes/less" framework) to help users connect CGM data with evidence-based food choices [14]. |
Cardiovascular and Metabolic Outcomes of Carbohydrate-Restricted Diets
Table 1: Composite findings from meta-analyses on cardiovascular and metabolic outcomes.
| Outcome Measure | Effect of CRDs | Magnitude of Change (SMD or Mean Difference) | Certainty of Evidence |
|---|---|---|---|
| Triglycerides | Significant reduction | SMD: −15.11 mg/dL (CI: −18.76, −11.46) [17] [18] | High |
| HDL Cholesterol | Significant increase | SMD: +2.92 mg/dL (CI: 2.10, 3.74) [17] [18] | High |
| LDL Cholesterol | Modest increase | SMD: +4.81 mg/dL (CI: 2.58, 7.05) [17] [18] | High |
| Systolic Blood Pressure | Significant reduction | SMD: −2.05 mmHg (CI: −3.13, −0.96) [17] [18] | High |
| 24-h Mean Blood Glucose (T2D) | Significant reduction | d = −0.51 (CI: −0.88, −0.14) [4] [19] | Moderate |
| HOMA-IR | Significant reduction | SMD: −0.54 (CI: −0.75, −0.33) [20] | High |
| C-Reactive Protein (CRP) | Significant reduction | SMD: −0.48 (CI: −0.75, −0.21) [17] | High |
Body Composition and Dose-Response Weight Loss
Table 2: Impact on body composition and dose-response weight loss effects.
| Parameter | Effect of CRDs | Details / Dose-Response | Source |
|---|---|---|---|
| Body Weight | Significant reduction | Each 10% decrease in carb intake reduced body weight by 0.64 kg (6-month) and 1.15 kg (12-month) [21] | |
| Optimal Long-Term Intake | Non-linear effect | Greatest weight reduction at ~30% carbohydrate intake in follow-ups >12 months [21] | |
| All Body Composition Markers | Significant reductions | Includes body fat percentage, waist circumference, and fat mass [17] | |
| Ketogenic Diet Trade-off | Greatest weight loss | But associated with greater increases in LDL and total cholesterol vs. moderate-carb diets [17] [18] |
Experimental Protocols for Research and Clinical Application
Protocol 1: 6-Month Medically-Supervised Ketogenic Diet Program (MSKDP) with CGM
This protocol is adapted from a randomized clinical trial evaluating CGM versus BGM during a carbohydrate-restricted nutrition intervention [22].
- Objective: To evaluate the effects of a virtual, medically supervised ketogenic diet program on glycemic control, medication use, and weight in adults with Type 2 Diabetes (T2D) over 6 months.
- Population: Adults with T2D (e.g., mean HbA1c ~8.1%, mean duration ~9.7 years) [22].
- Intervention Arm (CGM):
- Diet: Medically supervised ketogenic diet program. Macronutrient composition is not fully detailed but implies a significant reduction in carbohydrates.
- Monitoring: Use of Continuous Glucose Monitoring (CGM) for real-time glucose feedback.
- Support: Virtual program with remote supervision.
- Medication Management: Protocol for insulin and/or other diabetes medication de-intensification based on glucose data.
- Control Arm (BGM):
- Diet: Identical medically supervised ketogenic diet program.
- Monitoring: Use of Blood Glucose Monitoring (BGM) with finger-stick checks.
- Support & Medication Management: Identical to the CGM arm.
- Primary Outcomes:
- Glycemic Control: Time in Range (TIR 70-180 mg/dL), HbA1c.
- Diabetes Medication Effect Score (MES).
- Body Weight.
- Carbohydrate and Energy Intake (via dietary recalls).
- Key Findings: Both CGM and BGM arms achieved significant and equivalent improvements from baseline: TIR increased from ~61-63% to ~87-88%, HbA1c decreased by ≥1.3%, and participants experienced clinically meaningful weight loss with significant medication de-intensification [22].
Protocol 2: Time-Restricted Eating (TRE) with Low-Carbohydrate Diet for Insulin-Using T2D
This protocol is designed for insulin-using patients, a population often excluded from such interventions due to hypoglycemia risk [23].
- Objective: To assess the safety and feasibility of a combined low-carbohydrate and time-restricted eating protocol in adults with T2D who use insulin.
- Population: Insulin-using adults with T2D (e.g., ages 49-77) [23].
- Intervention:
- Dietary Pattern: Low-carbohydrate (≤30 grams per day) combined with Time-Restricted Eating (TRE).
- Eating Window: Two meals per day within a self-selected 6- to 8-hour window.
- Core Component: A proactive, structured insulin titration protocol to reduce hypoglycemia risk. Baseline total daily insulin is typically reduced by 30-50% upon initiation.
- Monitoring & Safety:
- Close glucose monitoring (BGM or CGM).
- Documentation of symptomatic and biochemical hypoglycemic events (e.g., glucose <70 mg/dL).
- Outcomes:
- Primary: Hypoglycemic events requiring medical care; adherence to the timed eating protocol.
- Secondary: Daily insulin use, HbA1c, Body Mass Index (BMI), blood pressure, and quality-of-life metrics.
- Key Findings: The protocol was demonstrated to be feasible and safe. After 6 months, average daily insulin use decreased significantly (by 62.2 units), with 74% of participants discontinuing insulin entirely. No episodes of severe hypoglycemia occurred, and significant improvements were seen in BMI and systolic blood pressure [23].
Signaling Pathways and Metabolic Workflows
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential materials and tools for research on carbohydrate-restricted diets and glucose monitoring.
| Tool / Reagent | Primary Function in Research | Specific Application Example |
|---|---|---|
| Continuous Glucose Monitor (CGM) | Measures interstitial glucose concentrations nearly continuously (e.g., every 5 minutes), providing high-resolution data on 24-hour mean blood glucose, time-in-range, and glycemic variability [4] [22]. | Core device for correlating food intake (macronutrient composition and timing) with glycemic excursions in real-world settings [22]. |
| Beta-Hydroxybutyrate (BHB) Meter | Quantifies blood ketone concentrations, serving as an objective biomarker of adherence to a ketogenic diet and confirming a state of nutritional ketosis [20]. | Differentiating metabolic effects of ketogenic vs. non-ketogenic low-carbohydrate diets. |
| Standardized Biochemical Assays | Measurement of key metabolic biomarkers from blood samples, including HbA1c, lipid profiles (TG, HDL-C, LDL-C), and inflammatory markers (CRP, TNF-α, sICAM-1) [17] [24] [25]. | Evaluating comprehensive cardiovascular and metabolic outcomes in response to dietary intervention. |
| Dietary Assessment Platform | Tools for collecting and analyzing participant dietary intake, such as 24-hour dietary recalls or food frequency questionnaires, to verify compliance with macronutrient targets [22]. | Quantifying actual carbohydrate, fat, and protein intake to ensure internal validity and analyze dose-response relationships [21]. |
| Insulin & HOMA-IR Assays | Precise measurement of fasting insulin and glucose for calculating Homeostatic Model Assessment of Insulin Resistance (HOMA-IR), a key metric of metabolic health [20] [24]. | Assessing the impact of carbohydrate restriction on underlying insulin sensitivity, independent of glycemia. |
Within continuous glucose monitoring (CGM) and food intake correlation research, a central challenge is distinguishing true, biologically meaningful individual differences from transient fluctuations caused by measurement variability or temporary physiological states. Research into individual differences requires accurately quantifying among-individual variation in the trait in question, a process that depends on standardized, repeatable measurement protocols [26]. The dynamic nature of human physiology means that multiple measurements are required to estimate a stable central tendency from a dynamic system [27]. This Application Note provides detailed methodologies for quantifying individual variability in glycemic responses, framing these protocols within the broader context of personalized nutrition and metabolic drug development.
Quantitative Data on Individual Glycemic Variability
Table 1: Key CGM-Derived Metrics for Quantifying Individual Glycemic Variability
| Metric Category | Specific Metric | Description | Research Significance | Representative Association |
|---|---|---|---|---|
| Average Glucose | 24-hour Mean Blood Glucose (MBG) | Average glucose concentration over 24 hours [4]. | Primary outcome for dietary interventions; reflects overall glycemic control. | CRDs show a significant improvement (d = -0.51, 95% CI: -0.88 to -0.14) [4]. |
| Glycemic Variability | Mean Amplitude of Glycemic Excursions (MAGE) | Average height of excursions that exceed one standard deviation from the mean [5]. | Captures postprandial swings and glucose instability. | Associated with overall diet quality and carbohydrate quality [5]. |
| Coefficient of Variation (CV) | Standard deviation of glucose values divided by the mean glucose (expressed as a percentage) [5]. | Indicator of glucose stability; lower CV suggests greater stability. | ||
| Continuous Overall Net Glycemic Action (CONGA-1) | Glycemic variability over a 1-hour interval [5]. | Measures intra-day variability. | ||
| Mean of Daily Differences (MODD) | Average of absolute differences between glucose values at the same time on successive days [5]. | Measures day-to-day variability. | ||
| Time-in-Range | % Time >140 mg/dL | Percentage of time spent above the hyperglycemic threshold [5]. | Direct measure of hyperglycemic exposure. | In prediabetes, higher fiber intake and lower carb-to-fiber ratio are associated with 7-10% lower time >140 mg/dL [5]. |
Table 2: Influence of Dietary Factors on Glycemic Metrics
| Dietary Factor | Effect on Glycemic Metrics | Notes on Individual Variability |
|---|---|---|
| Carbohydrate-Restricted Diets (CRDs) | Significant improvement in 24-hour MBG [4]. | Effect size may correlate with intervention duration; exploratory analysis suggests greater benefits with longer durations [4]. |
| Carbohydrate Substitution | Replacing 5% energy from protein with carbohydrate associated with a 0.97 mg/dL higher CGM mean glucose [5]. | Highlights the impact of macronutrient composition independent of overall energy intake. |
| Carbohydrate Quality (Fiber, Carb-to-Fiber Ratio) | Higher quality associated with favorable CGM measures, including lower time above range and reduced variability [5]. | Associations are typically more pronounced in individuals with normoglycemia compared to those with prediabetes [5]. |
| Overall Diet Quality (HEI, aMED, DASH) | Higher scores are associated with favorable CGM-derived measures [5]. | Suggests comprehensive dietary patterns can influence glycemic variability. |
Experimental Protocols for Standardized Challenges
Dynamic In Vitro Interference Testing of CGM Sensors
Purpose: To validate CGM sensor performance and identify measurement variability introduced by interfering substances under controlled, dynamic conditions [28].
Key Materials:
- CGM Sensors: Dexcom G6 (user-calibrated) and Freestyle Libre 2 (factory-calibrated) sensors.
- Macrofluidic Test Bench: A 3D-printed solid block with a fluidic channel (e.g., 2 mm × 10 mm × 500 mm), housing sensor needles [28].
- Fluid Delivery System: High-Pressure Liquid Chromatography (HPLC) pumps for generating programmable gradients of glucose and interferents in phosphate-buffered saline (PBS) [28].
- Reference Analyzer: YSI 2300 Stat Plus for reference glucose measurements [28].
Procedure:
- Setup: Place at least three sensors from each CGM system on the test bench. Initiate device operation according to manufacturers' instructions [28].
- Calibration: Calibrate user-calibrated sensors (e.g., Dexcom G6) at a stable glucose level (e.g., 120 mg/dL) against the reference method [28].
- Glucose Gradient Test:
- Start with a stable glucose level (e.g., 100 mg/dL) for 30 minutes.
- Increase glucose to a higher level (e.g., 300 mg/dL) at a controlled rate (e.g., 2 mg/dL/min).
- Maintain the high level for 30 minutes.
- Return to the baseline level at the same controlled rate.
- Maintain the baseline for a final 30 minutes [28].
- Substance Interference Test:
- Stabilize the system at a fixed glucose concentration (e.g., 200 mg/dL).
- Superimpose a gradient of the test interferent (e.g., acetaminophen, xylose, maltose) from 0 to a target concentration over 30 minutes.
- Maintain the peak interferent concentration for 30 minutes.
- Reduce the interferent back to 0 mg/dL over 30 minutes [28].
- Data Collection: Record sensor readings and collect outflow samples for reference measurement at least every 10 minutes throughout all experiments [28].
- Analysis: For user-calibrated sensors, interference is defined as a >20% difference between reference and sensor readings at maximal interferent concentration. For factory-calibrated sensors, calculate the "Bias Over Baseline" (BOB) [28].
Protocol for Assessing Diet-Glycemia Associations in Cohort Studies
Purpose: To cross-sectionally evaluate associations between diet composition/quality and CGM-derived glycemic metrics in free-living populations, accounting for individual variability [5].
Key Materials:
- Cohort: A well-characterized population-based cohort (e.g., Framingham Heart Study).
- CGM Devices: Participants wear a CGM sensor for a minimum of 3 days.
- Dietary Records: Multiple self-reported dietary records (e.g., ≥2 days), analyzed for nutrient composition and diet quality indices.
Procedure:
- Participant Selection: Include adults with and without diabetes. Exclude participants with insufficient CGM wear time or dietary data [5].
- Data Collection:
- Collect CGM data for the specified period.
- Collect dietary intake data concurrently or within a close timeframe.
- Gather covariate data (e.g., age, sex, BMI, glycemic status).
- CGM Data Processing: Calculate glycemic traits (MBG, MAGE, CV, CONGA, MODD, Time-in-Range) using standardized packages (e.g.,
cgmanalysisR package) [5]. - Dietary Data Processing: Calculate dietary indices (Healthy Eating Index, Alternate Mediterranean Diet Score, etc.), carbohydrate intake, fiber intake, and carb-to-fiber ratios [5].
- Statistical Analysis:
- Use multivariable linear regression models to assess relationships between dietary exposures and CGM outcomes, adjusting for covariates.
- Perform subgroup analyses stratified by glycemic status (normoglycemia vs. prediabetes/diabetes).
- Model macronutrient substitution effects (e.g., replacing protein with carbohydrate).
- Visualize adjusted group differences across quartiles of diet quality metrics [5].
Visualization of Workflows and Relationships
Diagram 1: Diet-Glycemia Association Study Workflow
Diagram 2: Sources of Variability in CGM Research
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Reagents and Equipment for CGM Variability Research
| Item | Function/Description | Example Use in Protocol |
|---|---|---|
| Continuous Glucose Monitor (CGM) | Device that measures glucose concentrations in interstitial fluid at regular intervals (e.g., every 5 minutes) [28] [5]. | Core device for capturing dynamic glycemic data in free-living or clinical settings. Examples: Dexcom G6, Freestyle Libre 2 [28]. |
| High-Pressure Liquid Chromatography (HPLC) Pumps | Generate precise, programmable gradients of glucose and potential interferents in a buffer solution [28]. | Essential for dynamic in vitro testing of CGM sensors under controlled fluidic conditions [28]. |
| Reference Glucose Analyzer (e.g., YSI Stat) | Provides high-precision reference measurements for blood glucose levels against which CGM sensor accuracy is calibrated and validated [28] [29]. | Used for calibrating sensors during in vitro tests and for verifying glucose levels during clamp studies [28] [29]. |
| Macrofluidic Test Bench | A custom housing that provides a stable fluidic environment for testing multiple CGM sensors in parallel in vitro [28]. | Used for standardized interference testing, allowing for controlled flow rates and sensor placement [28]. |
| Glucose Clamp Equipment | A method to maintain blood glucose at a specified level through variable dextrose infusion, based on frequent blood measurements [29]. | Creates a highly standardized metabolic challenge to quantify individual physiological responses under fixed conditions [29]. |
| Indirect Calorimetry Metabolic Cart | Measures oxygen consumption and carbon dioxide production to determine resting energy expenditure and fuel utilization (respiratory exchange ratio) [29]. | Provides complementary metabolic data during glycemic challenges to understand underlying energy substrate use. |
| Sympathetic Microneurography Setup | Directly records sympathetic nerve activity directed to muscle beds, a measure of neural output from the brain [29]. | Used to investigate neural contributions to individual glycemic variability, particularly during induced hypoglycemia. |
Advanced Analytics and CGM Endpoints in Clinical Research and Trials
Continuous Glucose Monitoring (CGM) generates dense, time-series data, providing an unparalleled view of glycemic dynamics. Traditional research and clinical practice often reduce these rich trajectories to scalar summaries, such as the 2-hour area under the curve (AUC) or peak glucose [30] [15]. While useful, these summaries inevitably discard critical temporal information, potentially overlooking when and how dietary components exert their effects. This application note details how Multilevel Functional Data Analysis (FDA) addresses this limitation, preserving the full, continuous nature of postprandial glucose responses (PPGRs) to yield deeper biological insights. Framed within a broader thesis on CGM and food intake correlation, this protocol provides a practical guide for researchers aiming to implement these advanced analytical techniques in nutritional studies and drug development.
Application Notes: Insights from FDA of the AEGIS Data
Applying multilevel FDA to data from the A Estrada Glycation and Inflammation Study (AEGIS) reveals nuanced physiological responses that scalar metrics cannot capture [30] [15]. The core advantage of FDA is its ability to model how dietary effects evolve over the entire postprandial window.
Table 1: Temporal Effects of Dietary Components on Postprandial Glucose Trajectories
| Dietary Component | Effect on Glucose Trajectory | Timing of Maximum Effect |
|---|---|---|
| Dietary Fiber | Blunts (reduces) the glucose response | After 90 minutes [15] |
| Fats | Reduces the early glucose rise | Within 50 minutes [15] |
| Fruit Component | Induces a higher initial glycemic peak, followed by a subsequent glucose-lowering effect | Peak at initial phase, lowering thereafter [31] |
| Alcohol Component | Associated with an initial hypoglycemic effect | Early postprandial phase [31] |
| Large Meals (High Starch/Dairy) | Significantly higher glucose levels throughout the 6-hour window | Entire 6-hour period [31] |
Furthermore, FDA effectively partitions variability in glucose responses. Analyses show that individuals with prediabetes exhibit greater day-to-day fluctuations in their postprandial trajectories compared to their normoglycemic counterparts, who display more consistent, subject-specific trends [30] [15]. This stratification of variability is crucial for identifying metabolic phenotypes and personalizing interventions.
Table 2: Subject Characteristics in the AEGIS Cohort (FDA Analysis Subset)
| Variable | Normoglycemic (N=319) | Prediabetes (N=58) |
|---|---|---|
| Age (years) | 44.6 (13.7) | 58.7 (12.0) |
| Weight (kg) | 73.7 (14.3) | 83.0 (19.6) |
| HbA1c (%) | 5.25 (0.25) | 5.86 (0.20) |
| Dinner Carbs (g) | 59.9 (40.5) | 53.7 (37.5) |
| Dinner Fats (g) | 30.1 (23.8) | 25.7 (22.3) |
Experimental Protocols
Protocol: CGM Data Collection and Preprocessing for FDA
Objective: To collect high-quality, time-matched CGM and meal data suitable for multilevel functional analysis. Background: CGM devices measure interstitial glucose every few minutes, creating a dense, smooth, and hierarchical functional output [30] [32].
Materials:
- Real-time or professional CGM systems (e.g., Enlite sensor with iPro recorder).
- Standardized protocols for meal logging (e.g., dietitian-assisted reconstruction).
- Computing environment with FDA capabilities (e.g., R with
fdapace,refundpackages).
Procedure:
- Participant Preparation: Fit participants with a CGM sensor. For blinded studies, use professional CGM; for interventional studies, real-time CGM is appropriate.
- Meal Recording: Instruct participants to record all food and drink intake, including precise timing and detailed description of portion sizes. For "dinner" analysis, ensure consistent meal type labeling.
- Data Collection: Collect data over a period sufficient to capture multiple meals per individual (e.g., 6-7 days).
- Data Extraction:
- For each recorded meal, extract the CGM data for a defined postprandial window (e.g., 6 hours) starting from the reported mealtime.
- Compile individual-level covariates (e.g., age, BMI, HbA1c) and meal-level covariates (e.g., grams of carbohydrates, fats, protein, fiber).
- Trajectory Alignment: Align all extracted postprandial trajectories to a common time scale (t=0 at meal start). This creates the fundamental unit of analysis: a set of smooth glucose curves.
Protocol: Implementing Multilevel Functional Principal Component Analysis (MFPCA)
Objective: To identify and characterize the dominant modes of variability in the hierarchical postprandial glucose data. Background: MFPCA decomposes variation in the glucose curves into between-subject and within-subject (meal-to-meal) components, revealing major patterns of response [30].
Procedure:
- Smoothing: Smooth the raw, discrete CGM measurements for each meal trajectory to create continuous functions using basis functions (e.g., B-splines).
- Covariance Estimation: Estimate the covariance structure of the curves at two levels:
- Between-Subject Covariance: Captures variability in average response curves between different individuals.
- Within-Subject Covariance: Captures variability between different meals within the same individual.
- Eigenanalysis: Perform eigenanalysis on the estimated covariance operators to obtain functional principal components (FPCs) at each level.
- Level 1 FPCs: Represent the main patterns of variation from meal to meal within a person.
- Level 2 FPCs: Represent the main patterns of variation between different people.
- Interpretation: Examine the FPCs to understand patterns of variability. For example, an FPC might represent a component of variability associated with the magnitude of the glucose peak, while another might be associated with the speed of decline.
Figure 1: MFPCA analysis workflow for hierarchical glucose data.
Protocol: Implementing Function-on-Scalar Regression (FoSR)
Objective: To model the relationship between scalar predictors (e.g., diet, patient characteristics) and the entire functional glucose response. Background: FoSR allows the effect of a predictor to vary over time, showing when a factor is significantly associated with the glucose trajectory [15].
Procedure:
- Model Specification: Construct a multilevel FoSR model. The model can be conceptually represented as:
Glucose_Curve(t) = β_Age(t)*Age + β_Carbs(t)*Carbs + ... + Z_subject(t) + ε(t)where eachβ(t)is a functional coefficient, andZ_subject(t)is a subject-specific random intercept function. - Coefficient Estimation: Estimate the functional coefficients
β(t)and their confidence bands. This reveals how the effect of a predictor (e.g., fiber) changes throughout the postprandial period. - Inference & R² Extension: Test the null hypothesis that
β(t) = 0for all time pointst. Calculate the extended functional R² metric to quantify the proportion of variance explained by the predictors in the model [15].
Figure 2: Logical flow of FoSR model from inputs to inference.
The Scientist's Toolkit
Table 3: Essential Research Reagent Solutions for CGM-FDA Studies
| Item / Solution | Function / Application Note |
|---|---|
| Continuous Glucose Monitor | Provides high-frequency interstitial glucose measurements. Use research-grade devices for accuracy. The AEGIS study used Enlite sensors with iPro recorders [30]. |
| Structured Meal Logging Protocol | Ensures accurate and quantifiable dietary data. Requires dietitian support for reconstruction and nutrient estimation using standardized software (e.g., Dietowin) [32]. |
| Multilevel Functional PCA (MFPCA) | A statistical method implemented in R to decompose variability in hierarchical functional data, identifying dominant between- and within-subject variation patterns [30] [33]. |
| Function-on-Scalar Regression (FoSR) | A regression framework that models an entire curve (output) against scalar inputs (e.g., nutrient grams). It is key for identifying time-varying associations [30] [15]. |
| Functional R² Metric | An extension of the standard R² to quantify the explanatory power of predictors on functional outcomes, critical for model selection in FoSR [15]. |
Core Glycemic Metrics and Their Clinical Significance
The interpretation of Continuous Glucose Monitoring (CGM) data relies on a standardized set of glycemic metrics that provide a comprehensive picture of glucose control beyond traditional measures like HbA1c. These metrics address HbA1c's limitations by capturing glucose variability, hypoglycemia, and hyperglycemia that would otherwise go undetected [34].
Table 1: International Consensus on Core CGM Metrics
| Metric | Definition | Clinical Target (Most Adults) | Interpretation & Clinical Relevance |
|---|---|---|---|
| Time in Range (TIR) | Percentage of time glucose is between 70 and 180 mg/dL [35] [34] | ≥70% [35] [34] | Strongly associated with reduced risk of microvascular and macrovascular complications [34]. Represents daily time spent in the target zone. |
| Time Below Range (TBR) | Percentage of time glucose is <70 mg/dL (Level 1) and <54 mg/dL (Level 2) [34] | <4% (<70 mg/dL); <1% (<54 mg/dL) [34] | Key safety metric. Quantifies hypoglycemia risk, which is critical for treatment adjustments [34]. |
| Time Above Range (TAR) | Percentage of time glucose is >180 mg/dL (Level 1) and >250 mg/dL (Level 2) [34] | <25% (>180 mg/dL); <5% (>250 mg/dL) [34] | Reflects hyperglycemia burden and long-term complication risk [34]. |
| Mean Glucose | The average glucose value over the monitoring period [34] | N/A | Provides a quick summary of overall control but lacks detail on highs/lows [34]. |
| Glucose Management Indicator (GMI) | An estimate of A1C (%) based on mean CGM glucose [34] | N/A | Helps bridge CGM data with lab A1C. Discrepancies can indicate high variability or hemoglobin issues [34]. |
| Coefficient of Variation (CV) | Measure of glucose variability (Standard Deviation/Mean Glucose) [34] | ≤36% [34] | Predictor of hypoglycemia risk. Indicates glucose stability; lower values mean steadier control [34]. |
These metrics form the foundation for a modern, dynamic approach to diabetes management, enabling clinicians and researchers to assess safety, stability, and progress toward individualized goals [34].
Advanced Analytical Frameworks: CGM Data Analysis 2.0
While traditional summary statistics (CGM Data Analysis 1.0) are practically useful, they can oversimplify complex glucose patterns. The field is now advancing towards "CGM Data Analysis 2.0," which uses more sophisticated methods to extract deeper insights from dense time-series data [36].
Table 2: Evolution of CGM Data Analysis Methods
| Feature | Traditional Statistical Analysis (CGM 1.0) | Functional Data Analysis (FDA) | Machine Learning (ML) & Artificial Intelligence (AI) |
|---|---|---|---|
| Approach | Visual inspection and summary statistics [36] | Statistical modeling of the entire CGM time series as a dynamic curve [36] | Predictive modeling and pattern classification using advanced algorithms [36] |
| Data Used | Aggregated metrics (e.g., TIR, mean glucose) [36] | Each complete CGM trajectory treated as a mathematical function [36] | Large CGM datasets, often combined with other data (EHR, lifestyle) [36] |
| Primary Purpose | Identify obvious trends and patterns for clinical use [36] | Quantify and model complex temporal dynamics and phenotypes [36] | Predict future glucose levels, classify metabolic subphenotypes, and optimize therapy automatically [36] |
| Key Insight | The shape of the glucose curve reflects underlying pathophysiology and patient behaviors [36] | FDA outperforms traditional methods by modeling glucose as a dynamic process, revealing patterns like weekday-weekend differences [36] | ML/AI can integrate CGM data with other parameters for real-time, adaptive interventions, such as in closed-loop systems [36] |
Furthermore, research is identifying independent components of glucose dynamics that may have distinct clinical implications. A 2025 study proposed that value (average glucose levels), variability (fluctuations), and autocorrelation (the degree to which subsequent glucose readings are predictable from previous ones) are three independent factors, with autocorrelation being a novel predictor of coronary plaque vulnerability [37]. The relationship between these components and their clinical implications can be visualized as follows:
Experimental Protocols for Food Intake Correlation Research
Correlating CGM metrics with food intake requires meticulous experimental design to isolate the effect of nutrition from other confounding variables. The following protocol provides a framework for such investigations.
Protocol: Assessing Individual Glycemic Response to Food
Objective: To quantify the impact of specific foods or meals on glycemic parameters (TIR, TAR, glucose spikes) in a target population (e.g., individuals with Type 2 Diabetes).
Materials & Reagents:
- CGM Devices: Real-time CGM sensors (e.g., Dexcom G7) with a minimum wear time of 14 days and ≥70% data availability [14] [34].
- Standardized Test Meals: Precisely formulated meals with known macronutrient composition. For carbohydrate-restricted diet (CRD) studies, "low-carbohydrate" is defined as ≤45% of total energy and "very-low-carbohydrate" as <26% [38].
- Data Platform: Software capable of generating Ambulatory Glucose Profile (AGP) reports and exporting high-resolution time-series data [36].
- Dietary Log: A digital or paper-based tool for participants to meticulously record food type, quantity, and timestamps.
Procedure:
- Baseline Period (3-5 days): Participants wear CGM and log all food intake without any dietary intervention. This establishes individual baseline glucose patterns (mean glucose, CV, TIR).
- Intervention Period (≥6 weeks): Participants adhere to the prescribed dietary intervention (e.g., CRD) [38]. The duration should be sufficient to detect meaningful trends, as longer interventions may show greater benefits [38].
- Meal Challenge Tests (Optional): At predetermined points, participants consume a standardized test meal. CGM data is analyzed for the 3-hour postprandial period to calculate the area under the curve (AUC) and peak glucose value.
- Data Integration: Synchronize CGM data timestamps with dietary log entries.
- Outcome Analysis:
- Calculate primary outcomes: Change in 24-hour mean blood glucose and TIR from baseline to end-of-study [38] [39].
- Analyze secondary outcomes: Change in TAR, TBR, CV, and fasting glucose [39].
- For meal-specific analysis, aggregate glucose responses to similar meal types to identify personal triggers.
This experimental workflow, from participant recruitment to data analysis, is outlined below:
Nutrition-Focused Approach (NFA) for CGM Initiation
Qualitative research suggests that pairing CGM initiation with evidence-based nutrition guidance improves user engagement and leads to positive behavior changes [14]. A proposed 2-session intervention can be implemented as follows:
Session 1 (In-Person Initiation, 60 minutes):
- CGM Application: Apply sensor and train on device operation (scanning, app use).
- Set Glucose Goals: Explain target range (70-180 mg/dL) and the objective of >70% TIR [14].
- Introduce the "1, 2, 3 Approach":
- Check glucose before a meal.
- Check glucose 2 hours after a meal.
- Learn how your body responds to different foods and portions [14].
- Provide "Yes/Less" Framework: Use simple visual aids to guide food choices toward non-starchy vegetables and reduce foods with added sugars, aligning with evidence-based nutrition [14].
Session 2 (Remote Review, 30 minutes, ~14 days later):
- Review AGP Report: Discuss overall patterns in TIR, TAR, and TBR.
- Identify Personal Triggers: Use daily graphs to correlate high glucose excursions with specific meals or activities.
- Empower Discovery Learning: Support participants in deriving their own insights from the data to promote sustainable behavior change [14].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for CGM-Food Correlation Research
| Item | Function/Application in Research | Example/Notes |
|---|---|---|
| Real-time CGM System | Continuous measurement of interstitial glucose every 5-15 minutes; provides the core time-series data. | Dexcom G7 [14]; Ensure devices have API access for raw data export. |
| Professional CGM | Blinded CGM for short-term observational studies where patient behavior should not be altered. | Often used in clinical settings for 1-2 week profiles. |
| Ambulatory Glucose Profile (AGP) Report | Standardized visualization tool for summarizing 14 days of CGM data into a single, interpretable 24-hour profile [36]. | Key for clinical interpretation and identifying temporal patterns [36]. |
| Data Analysis Software | Platform for advanced statistical analysis, Functional Data Analysis, and machine learning modeling. | SAS, STATA, R, Python; Custom scripts for FDA and ML [40] [38] [36]. |
| Structured Dietary Intervention | A controlled diet to test a specific hypothesis regarding macronutrients (e.g., CRDs) on glycemic outcomes. | Meals should be fully provided or closely monitored [38]. "Low-carbohydrate" is ≤45% total energy [38]. |
| Digital Dietary Logging App | For precise tracking of food intake, portion sizes, and meal timings to correlate with CGM traces. | Critical for ensuring data synchronization and accuracy in free-living studies. |
The design of clinical trials for metabolic therapies and nutritional interventions is undergoing a significant transformation, moving beyond the traditional reliance on glycated hemoglobin (HbA1c). Continuous glucose monitoring (CGM) has emerged as a powerful technology providing unprecedented granularity in capturing glycemic dynamics [41]. This paradigm shift is particularly relevant for research investigating the correlation between food intake and glycemic response, where CGM endpoints offer a nuanced understanding of how dietary interventions affect glucose metabolism in real-world settings.
The adoption of CGM in clinical research has accelerated substantially following international standardization efforts, with time in range (TIR) emerging as a particularly valuable endpoint that complements or potentially supplants HbA1c in certain trial designs [41] [42]. For researchers investigating food intake correlations, CGM provides the temporal resolution necessary to link specific dietary exposures to postprandial glycemic responses, enabling more precise quantification of nutritional interventions [10]. This application note examines the trends in CGM adoption as a primary endpoint in clinical trials and provides detailed experimental protocols for implementing CGM in studies focused on food intake correlation research.
Quantitative Analysis of CGM Adoption Trends
Analysis of ClinicalTrials.gov Data
A comprehensive analysis of ClinicalTrials.gov records from 2012 to 2023 reveals a significant expansion in the use of CGM endpoints in clinical research [41]. The data, summarized in Table 1, demonstrates striking growth patterns across study phases, populations, and funding sources when comparing the six-year periods before and after the publication of the first international CGM consensus guidelines in 2017.
Table 1: Adoption Trends of CGM Endpoints in Clinical Trials (2012-2023)
| Category | Period 1 (2012-2017) | Period 2 (2018-2023) | Change | P-value |
|---|---|---|---|---|
| Total Studies | 121 | 194 | +60.3% | <0.01 |
| Phase 2 Studies | 31 | 70 | +125.8% | <0.01 |
| Phase 3 Studies | 13 | 35 | +169.2% | <0.01 |
| Adult-Only Population | 109 | 153 | +40.4% | 0.05 |
| Pediatric-Inclusive Population | 12 | 41 | +241.7% | <0.01 |
| Industry-Funded Studies | 37 | 66 | +78.4% | <0.05 |
| Non-Industry-Funded Studies | 60 | 108 | +80.0% | <0.01 |
| Studies with TIR as Endpoint | 13 | 42 | +222.4% | <0.01 |
| Studies with MAGE as Endpoint | 14 | 4 | -71.3% | <0.01 |
The data reveals several noteworthy trends. First, the overall adoption of CGM endpoints increased significantly (60.3%) in the period following guideline standardization, with particularly dramatic growth in Phase 2 and Phase 3 clinical trials [41]. Second, while adult populations continue to dominate clinical research, studies including pediatric populations have increased substantially (241.7%), indicating expanding application of CGM across patient demographics [41]. Third, the adoption of CGM has been driven by both industry and non-industry sponsors, with both categories showing similar robust growth (78.4% and 80.0%, respectively) [41].
Perhaps most notably, the analysis reveals a dramatic shift in the specific CGM metrics preferred by researchers. The use of time in range (TIR) as an endpoint increased by 222.4%, while the use of mean amplitude of glycemic excursions (MAGE) decreased by 71.3% [41]. This shift reflects the research community's alignment with internationally standardized metrics that have demonstrated clinical relevance and correlation with long-term outcomes [42].
CGM Endpoint Adoption Across Indications
The application of CGM endpoints has expanded beyond traditional diabetes populations. While studies of type 1 diabetes (T1DM) and type 2 diabetes (T2DM) increased by 55.8% and 26.9%, respectively, studies of non-diabetes indications increased by a remarkable 233.3% in the post-2018 period [41]. This expansion reflects growing recognition of the role glycemic variability plays in various metabolic conditions and the utility of CGM in assessing nutritional and therapeutic interventions across diverse populations.
For research correlating food intake with glycemic response, this expansion is particularly significant, as CGM enables researchers to study glucose dynamics in non-diabetic populations, including those with prediabetes, obesity, or other metabolic risk factors [10] [43]. The ability to capture subtle glycemic variations in response to dietary interventions in these populations provides valuable insights for preventive strategies and early interventions.
Standardized CGM Metrics and Endpoints for Clinical Research
Internationally Consensus-Endorsed Metrics
The international consensus statement on CGM metrics for clinical trials provides clear recommendations for standardized data collection and reporting [42]. These recommendations have been endorsed by major professional organizations including the American Diabetes Association, European Association for the Study of Diabetes, and several other international bodies. The consensus emphasizes that CGM data should be collected using devices with adequate accuracy and that studies should report specific core metrics to enhance comparability across trials.
Table 2: Standardized CGM Metrics for Clinical Trials of Dietary Interventions
| Metric Category | Specific Metrics | Target/Definition | Relevance to Food Intake Research |
|---|---|---|---|
| Time in Ranges | Time in Range (TIR) | 70-180 mg/dL (3.9-10.0 mmol/L) | Primary endpoint for overall dietary efficacy |
| Time Above Range (TAR) | >180 mg/dL (>10.0 mmol/L) | Identifies hyperglycemic responses to meals | |
| Time Below Range (TBR) | <70 mg/dL (<3.9 mmol/L) | Safety metric for aggressive interventions | |
| Glycemic Variability | Coefficient of Variation (CV) | ≤36% | Measure of glucose stability throughout day |
| Standard Deviation (SD) | Individualized | Absolute measure of glucose fluctuations | |
| Acute Response Metrics | Area Under Curve (AUC) | 0-4 hours postprandial | Quantifies total glycemic impact of meals |
| Glucose Excursion | Peak - baseline amplitude | Measures magnitude of postprandial spike | |
| Time to Peak (TTP) | Time from meal to maximum glucose | Kinetics of glucose absorption | |
| Glucose Recovery Time to Baseline (GRTB) | Time to return to pre-meal levels | New metric for metabolic resilience [43] |
For food intake correlation research, the consensus recommends capturing meal-related data through standardized time-blocks (e.g., 3-4 hour postprandial windows) and using appropriate metrics such as area under the curve (AUC) and glucose excursion to quantify meal-related glycemic responses [42]. The emerging metric of Glucose Recovery Time to Baseline (GRTB) shows particular promise for assessing metabolic resilience in response to dietary challenges [43].
Advanced Metrics for Nutritional Research
Beyond the core metrics, specialized CGM-derived parameters offer additional insights for food intake correlation studies:
- Postprandial Glucose Response: Defined as the incremental AUC over a 2-4 hour period following meal consumption [10]. This metric directly quantifies the glycemic impact of specific foods or meals.
- Meal Glucose Response Profile: A comprehensive assessment including time to peak, peak glucose value, and recovery time to baseline [43]. This provides kinetic information about glucose metabolism following food intake.
- Inter-day Variability: Assesses consistency of glycemic responses to similar meals across different days, which may reflect underlying metabolic flexibility [10].
These advanced metrics enable researchers to move beyond simple averages and capture the dynamic nature of glycemic responses to dietary interventions, providing a more comprehensive understanding of how specific nutritional approaches affect glucose metabolism.
Experimental Protocols for CGM in Food Intake Research
Core Protocol for CGM Deployment and Data Collection
Objective: To establish standardized methodology for deploying CGM systems in clinical trials investigating correlations between food intake and glycemic responses.
Materials:
- Factory-calibrated CGM systems (e.g., FreeStyle Libre, Dexcom G6/G7, Medtronic Guardian)
- Data extraction software/cloud platforms
- Standardized data collection forms for meal timing and composition
- Adhesive overlays or securement devices as needed
Procedure:
- Sensor Placement: Apply CGM sensor to posterior upper arm or abdomen according to manufacturer instructions, ensuring proper adhesion and site rotation from previous placements.
- Run-in Period: Allow a minimum 2-hour sensor warm-up period followed by a 24-hour run-in period before formal data collection to ensure sensor stability [44].
- Data Collection Period: Maintain continuous CGM wear for a minimum of 14 days to capture adequate data for meaningful pattern analysis [45]. For nutritional interventions, extend collection to cover the entire intervention period plus baseline.
- Meal Documentation: Implement precise meal documentation including:
- Exact meal start time
- Detailed food composition (weighed or estimated using standardized methods)
- Macronutrient content (carbohydrate, protein, fat grams)
- Glycemic load calculation where applicable
- Data Extraction: Download CGM data at least weekly during extended trials and at study conclusion using manufacturer-specific software.
- Data Quality Assessment: Verify that CGM active time exceeds 70% during each analysis period [45]. Exclude periods of sensor failure or extended calibration.
Endpoint Calculation:
- Calculate primary endpoints (e.g., TIR, mean glucose) over the entire study period for overall intervention effects
- Calculate meal-specific endpoints (e.g., postprandial AUC, glucose excursion) for individual meal responses
- Perform subgroup analyses by time of day (nocturnal vs. daytime) where relevant to research question
Specialized Protocol for Controlled Meal Challenges
Objective: To assess glycemic responses to standardized test meals under controlled conditions, eliminating variability in meal composition and timing.
Materials:
- CGM systems as above
- Standardized test meals with precisely controlled macronutrient composition
- Food scales and preparation facilities
- Activity monitors to control for physical activity confounding
Procedure:
- Baseline Period: Collect 3 days of baseline CGM data with ad libitum diet to establish individual glycemic patterns.
- Test Meal Preparation: Prepare standardized test meals with identical composition, portion size, and presentation for all participants. Macronutrient composition should be verified by laboratory analysis where possible.
- Test Meal Administration: Administer test meals after an overnight fast of 10-12 hours, with meal consumption completed within 15 minutes.
- Postprandial Monitoring: Collect CGM data for a minimum of 4 hours postprandially with participants remaining in a controlled setting with limited physical activity.
- Comparison Meals: Utilize crossover design where participants receive different test meals on separate days in randomized order.
- Data Analysis: Calculate postprandial metrics including AUC, peak glucose, time to peak, and glucose recovery time to baseline.
Endpoint Calculation:
- Primary: Incremental AUC (0-4 hours) for comparison between test meals
- Secondary: Peak glucose concentration, time to peak, and glucose recovery time to baseline
- Exploratory: Glycemic variability metrics during postprandial period
This protocol was successfully implemented in the CGM-HYPE study, which demonstrated significant differences in glucose responses to various dietary challenges in healthy young adults [43].
Protocol for Free-Living Food Intake Correlation Studies
Objective: To correlate CGM data with self-selected food intake under free-living conditions, capturing real-world dietary behaviors.
Materials:
- CGM systems as above
- Digital food diary application or structured paper food records
- Food photography aids (standard reference objects) if using photographic documentation
- Carbohydrate counting references
Procedure:
- Participant Training: Train participants in detailed food recording using chosen methodology, emphasizing portion size estimation and timing accuracy.
- Data Collection Period: Implement simultaneous CGM wear and food recording for a minimum of 10 days to capture variability across different days [10].
- Food Recording Methodology:
- Record all food and beverages consumed with precise timing
- Estimate portion sizes using household measures or food scales
- Document macronutrient composition using food database or nutrition labels
- Include description of food preparation methods
- Data Synchronization: Time-synchronize CGM data with food intake records using standardized time stamps.
- Meal Identification: Define postprandial windows (typically 2-4 hours) following each eating occasion.
- Statistical Correlation: Apply linear mixed models to account for repeated measures within individuals when correlating dietary components with glycemic responses.
Analytical Approach:
- Calculate correlation coefficients between dietary parameters (glycemic load, carbohydrate content) and CGM metrics (postprandial AUC, peak glucose)
- Develop prediction models for glycemic response based on meal composition
- Assess inter-individual variability in responses to similar meals
This approach was validated in a 2025 study that demonstrated moderate correlations between glycemic load and CGM metrics including area under the curve, standard deviation, and variance in healthy adults [10].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Materials for CGM Food Intake Correlation Studies
| Category | Specific Items | Research Function | Implementation Considerations |
|---|---|---|---|
| CGM Systems | Factory-calibrated CGM (Dexcom G7, FreeStyle Libre 3) | Continuous glucose data collection | Select based on accuracy requirements, connectivity needs, and wear duration |
| Data Acquisition | CGM proprietary software, Cloud data platforms, API interfaces | Raw data extraction and storage | Ensure compatibility with data management plan and regulatory requirements |
| Dietary Assessment | Digital food diaries, Food scale, Photographic aids, Nutrient database | Precise documentation of food intake | Standardize methodology across all study participants and sites |
| Meal Standardization | Test meal ingredients, Food preparation facilities, Packaging materials | Controlled meal challenges | Maintain consistency in composition, preparation, and presentation |
| Reference Analytics | HbA1c point-of-care devices, Laboratory HbA1c services, Standardized laboratories | Validation against traditional endpoints | Schedule collections to align with CGM wear periods |
| Data Analysis | Statistical software (R, SAS, Python), Custom scripts for CGM metrics, Data visualization tools | Endpoint calculation and visualization | Pre-specify analytical approach in statistical analysis plan |
Implementation Framework and Multidisciplinary Considerations
Successful implementation of CGM endpoints in clinical trials requires careful attention to operational considerations. A pilot implementation study demonstrated the effectiveness of a multidisciplinary approach involving primary care physicians, certified diabetes care and education specialists, and clinical pharmacists [46]. This model improved patient access to CGM technology and enhanced the interpretation of CGM data in clinical practice, with significant improvements in time in range and HbA1c outcomes [46].
For nutritional research specifically, incorporating a nutrition-focused approach during CGM initiation has shown positive results. Qualitative research revealed that participants who received nutrition-focused CGM initiation materials were better able to make food-related decisions aligned with evidence-based nutrition recommendations [14]. This approach emphasized simple frameworks such as monitoring glucose before and after meals and adjusting food choices using a "yes/less" framework for healthier options [14].
The integration of CGM into clinical trials of dietary interventions represents a significant advancement in nutritional science, providing objective, continuous data on glycemic responses to food intake. By implementing standardized protocols and metrics, researchers can generate comparable, high-quality evidence regarding the effects of nutritional interventions on glucose metabolism across diverse populations.
Linking Meal Composition and Timing to Continuous Glucose Profiles
Continuous Glucose Monitoring (CGM) has revolutionized the assessment of glycemic responses by providing high-frequency, real-time interstitial glucose measurements, typically every 5 minutes [38]. For researchers and drug development professionals, understanding how dietary factors—specifically meal composition and timing—influence these continuous glucose profiles is critical for developing targeted nutritional interventions and metabolic therapeutics. This document synthesizes current evidence and methodologies for correlating dietary intake with CGM-derived metrics, providing a structured framework for research design and data interpretation in both clinical and free-living settings.
The physiological basis for linking diet to glucose profiles stems from multiple interconnected mechanisms. Postprandial glucose responses are influenced by meal carbohydrate quantity and quality, with fiber content significantly modulating absorption rates [5]. Furthermore, circadian regulation of metabolic processes means that identical meals consumed at different times of day elicit divergent glycemic responses due to intrinsic variations in insulin sensitivity, glucose tolerance, and pancreatic function throughout the 24-hour cycle [47] [48]. Advanced analytical approaches, including functional data analysis and machine learning, now enable researchers to move beyond traditional summary statistics to identify nuanced patterns in CGM data that reflect both physiological status and behavioral influences [36].
The Impact of Meal Composition on Glucose Profiles
Carbohydrate Restriction and Quality
Carbohydrate intake represents the primary dietary determinant of postprandial glucose excursions. Meta-analyses of randomized controlled trials demonstrate that carbohydrate-restricted diets (CRDs) significantly improve 24-hour mean blood glucose (MBG) in individuals with type 2 diabetes (T2D) [38]. The magnitude of improvement appears positively correlated with intervention duration, suggesting potential adaptive mechanisms.
Beyond quantity, carbohydrate quality significantly influences glycemic responses. Research from the Framingham Heart Study indicates that carbohydrate quality, particularly the carbohydrate-to-fiber ratio, is strongly associated with favorable CGM-derived metrics [5]. A ratio exceeding approximately 9:1 (grams of carbohydrate to grams of fiber) is associated with significantly greater time spent above the glucose target range (>140 mg/dL) in individuals with prediabetes.
Table 1: Effects of Carbohydrate Modification on CGM-Derived Metrics
| Dietary Intervention | Population | Key CGM Findings | Effect Size | Reference |
|---|---|---|---|---|
| Carbohydrate Restriction (≤45% energy from carbs) | T2D (7 studies, n=301) | ↓ 24-hour mean blood glucose | d = -0.51 (CI: -0.88 to -0.14) | [38] |
| Improved Carb Quality (Carb:Fiber ratio <9:1) | Prediabetes | ↓ Time >140 mg/dL | 7-10% reduction | [5] |
| Macronutrient Substitution (5% energy from protein to carbs) | Without diabetes | ↑ CGM mean glucose | +0.97 mg/dL | [5] |
Comprehensive Diet Quality
Overall dietary patterns, beyond isolated nutrients, significantly associate with glycemic variability. Higher scores on established diet quality indices—including the Healthy Eating Index (HEI), Alternate Healthy Eating Index (AHEI), Dietary Approaches to Stop Hypertension (DASH), and Alternate Mediterranean Diet (aMED)—correlate with more favorable CGM metrics, including lower mean glucose and reduced glycemic variability [5]. These associations are typically more pronounced in individuals with normoglycemia, suggesting that dietary interventions may be most effective in early metabolic dysfunction stages.
The Chrononutrition Dimension: Meal Timing Effects
Eating Schedule and Circadian Alignment
Meal timing independently influences glycemic control, likely through alignment or misalignment with circadian rhythms. A cross-over trial in young adult males demonstrated that a late eating schedule (meals at 12:00, 17:00, and 23:00) significantly increased 24-hour mean interstitial glucose concentrations compared to an early schedule (meals at 08:30, 13:30, and 19:30)—99.2 ± 4.6 mg/dL versus 91.2 ± 2.9 mg/dL (P = 0.003) [48]. This effect persisted when comparing equivalent time elapsed since first meal, suggesting true circadian influences beyond simply clock time.
Epidemiological evidence from NHANES (n=7,619) corroborates these experimental findings, showing that every hour later that eating commences is associated with approximately 0.6% higher fasting glucose and 3% higher HOMA-IR (both p < 0.001) [47]. Notably, eating duration alone was not significantly associated with these metabolic measures after adjusting for timing, highlighting the critical importance of when—not just how long—eating occurs within the 24-hour cycle.
Table 2: Impact of Meal Timing on Glycemic Measures
| Timing Factor | Study Design | Population | Key Metabolic Findings | Reference |
|---|---|---|---|---|
| Late vs. Early Eating Schedule | Randomized cross-over trial | Young adult males (n=8) | ↑ 24-h mean glucose: 99.2 vs 91.2 mg/dL (P=0.003) | [48] |
| Later Eating Start Time | Cross-sectional (NHANES) | Adults (n=7,619) | ↑ Fasting glucose (+0.6%/hour) ↑ HOMA-IR (+3%/hour) | [47] |
| Eating Duration | Cross-sectional (NHANES) | Adults (n=7,619) | No significant association after adjustment for timing | [47] |
Potential Mechanisms
The circadian system regulates glucose metabolism through multiple pathways. Pancreatic β-cell responsiveness to glucose, intestinal glucose absorption efficiency, and peripheral tissue insulin sensitivity all exhibit diurnal variations [47]. Mistimed feeding can desynchronize peripheral clocks in metabolic tissues from the central pacemaker, leading to impaired glucose tolerance even without changes in nutrient composition or quantity [48].
Advanced CGM Data Analysis Methodologies
From Traditional Metrics to Advanced Analytics
Traditional CGM analysis focuses on summary statistics including time in range (TIR: 3.9-10.0 mmol/L or 70-180 mg/dL), time above range (TAR: >10.0 mmol/L or >180 mg/dL), time below range (TBR: <3.9 mmol/L or <70 mg/dL), mean glucose, and coefficient of variation (CV) [49]. While these metrics provide valuable clinical endpoints, they oversimplify the dynamic, time-dependent nature of glucose fluctuations [36].
Advanced analytical approaches now enable more nuanced investigation:
- Functional Data Analysis: Treats CGM trajectories as continuous mathematical functions rather than discrete measurements, allowing identification of subtle temporal patterns and phenotypes [36].
- Machine Learning: Algorithms can predict future glycemic trends, classify metabolic subphenotypes, and automatically detect ingestive activity from CGM patterns [50] [36].
- Automated Meal Detection: CGM-based approaches for automatic detection of eating events show promise for objective dietary assessment, with detection times ranging from 9.0 to 45.0 minutes in research settings [50].
Diagram 1: CGM Data Analysis Workflow (47 characters)
Experimental Protocols for Diet-CGM Correlation Research
Standardized Meal Timing Studies
Objective: To investigate the effect of meal timing on 24-hour glycemic control independent of nutritional composition.
Protocol:
- Design: Randomized, controlled, cross-over trial with washout period [48]
- Participants: Recruit homogeneous sample (e.g., 8-20 participants) to control for confounding variables
- Intervention Conditions:
- Early eating schedule: Meals at 08:30, 13:30, and 19:30
- Late eating schedule: Meals at 12:00, 17:00, and 23:00
- Dietary Control: Provide isocaloric meals with identical macronutrient composition (e.g., 55% carbohydrate, 15% protein, 30% fat) for both conditions
- CGM Data Collection: Use research-grade CGM devices with simultaneous activation in all participants
- Primary Outcome: 24-hour mean interstitial glucose concentration measured by CGM
- Analysis: Compare glucose profiles using both clock time and time elapsed since first meal
Considerations: Control for prior sleep-wake patterns, physical activity, and light exposure, which may influence circadian physiology [48].
Carbohydrate Manipulation Studies
Objective: To quantify the effect of carbohydrate restriction and quality on 24-hour mean blood glucose.
Protocol:
- Design: Parallel-group or cross-over randomized controlled trial [38]
- Participants: Adults with T2D; exclude those with conditions affecting glucose metabolism
- Intervention:
- Experimental: Carbohydrate-restricted diet (≤45% energy from carbohydrates)
- Control: Conventional diabetes diet (46-60% energy from carbohydrates)
- Duration: Minimum 6 weeks based on meta-analytic findings of duration effects [38]
- Dietary Adherence: Provide all meals or key foods (≥30% energy) to ensure compliance [38]
- CGM Protocol: Continuous glucose monitoring for at least 3-5 days at baseline and end-of-intervention
- Primary Outcome: Change in 24-hour mean blood glucose
- Secondary Outcomes: Time-in-range, glycemic variability (coefficient of variation), postprandial glucose excursions
Considerations: Monitor potential confounding factors including medication changes, body weight fluctuations, and physical activity patterns [38].
Free-Living Diet Assessment with CGM
Objective: To examine associations between habitual diet composition/quality and glycemic metrics in community-based cohorts.
Protocol:
- Design: Observational cohort or cross-sectional study [5]
- Participants: Community-dwelling adults with and without dysglycemia
- Dietary Assessment:
- Multiple 24-hour dietary recalls (minimum 2 non-consecutive days)
- Diet quality indices: HEI, AHEI, DASH, or aMED scores
- Carbohydrate quality metrics: fiber intake, carbohydrate-to-fiber ratio
- CGM Assessment: Minimum 3 days of CGM data with ≥70% device active time [49]
- Covariate Assessment: Demographics, BMI, medication use, sleep duration, physical activity
- Statistical Analysis:
- Multivariable linear regression for continuous CGM outcomes
- Least-squares means across quartiles of dietary exposures
- Stratification by glycemic status (normoglycemia, prediabetes, diabetes)
Considerations: Account for potential reverse causality where glucose patterns may influence dietary choices rather than vice versa [5].
The Scientist's Toolkit: Essential Research Solutions
Table 3: Key Research Reagents and Technologies
| Tool Category | Specific Examples | Research Application | Technical Considerations |
|---|---|---|---|
| CGM Devices | Professional/Blinded CGM, Personal CGM, Flash Glucose Monitoring | Continuous glucose assessment in clinical and free-living settings | Research-grade devices allow blinded data collection; personal devices provide real-time feedback [49] |
| Dietary Assessment | 24-hour dietary recalls, Food frequency questionnaires, Digital food photography | Quantification of nutritional intake and diet quality | Multiple non-consecutive days needed to account for day-to-day variability [5] |
| Meal Detection Algorithms | CGM-only approaches, CGM + auxiliary sensor inputs | Automated detection of ingestive activity for objective dietary assessment | Performance varies (sensitivity 21-100%); detection times range 9-45 minutes [50] |
| Data Analysis Platforms | "cgmanalysis" R package, Commercial AGP software, Custom machine learning pipelines | Standardized calculation of CGM-derived metrics | Functional data analysis requires statistical expertise but provides deeper pattern insights [36] |
| Chrononutrition Assessment | Time-stamped dietary recalls, Eating window calculation, Circadian alignment measures | Quantification of meal timing and eating patterns | Define behavioral day (e.g., 4:00 a.m. start) to account for late-night eating [47] |
Diagram 2: Research Design Framework (44 characters)
Integrating CGM technology with precise dietary assessment enables researchers to move beyond static glycemic measures to dynamic, time-based understanding of how nutritional factors influence metabolic health. The evidence synthesized herein indicates that both meal composition—particularly carbohydrate quantity and quality—and meal timing independently and collectively influence continuous glucose profiles. Methodological advancements in CGM data analysis, including functional data analysis and machine learning approaches, offer unprecedented opportunities to identify nuanced metabolic phenotypes and personalize dietary interventions. For drug development professionals, these approaches facilitate more precise assessment of metabolic interventions and their interaction with dietary patterns. Standardized protocols incorporating controlled meal timing, macronutrient manipulation, and advanced CGM analytics will strengthen the evidence base for chrononutrition and personalized nutrition approaches to metabolic health.
Addressing Technical and Intervention Challenges for Robust Data Generation
Continuous Glucose Monitoring (CGM) systems have revolutionized diabetes management by providing real-time insights into glucose fluctuations, thereby enabling improved glycemic control [51]. For researchers, particularly those investigating correlations between food intake and glucose response, understanding the performance characteristics of these devices is paramount. The analytical accuracy of a CGM is a critical determinant of its reliability in detecting postprandial glucose excursions and subtle metabolic variations.
The Mean Absolute Relative Difference (MARD) is the most widely adopted metric for quantifying CGM accuracy [52]. It represents the average percentage difference between the CGM sensor readings and a reference glucose value. A lower MARD indicates superior accuracy, with values below 10% generally considered indicative of good clinical performance [53] [52]. However, MARD is a complex parameter influenced by numerous factors including study design, glucose range, and sensor algorithm, and should not be used as the sole performance metric [52].
This application note provides a structured framework for evaluating CGM performance, summarizing the latest comparative accuracy data, detailing essential experimental protocols, and outlining the core technological components relevant to metabolic research.
Performance Metrics and Comparative Device Analysis
Key Performance Metrics for CGM Evaluation
When evaluating CGM systems for research, several metrics beyond the overall MARD provide a more complete picture of device performance, especially in the context of food intake studies where dynamic glucose changes are expected.
- MARD (Mean Absolute Relative Difference): The primary accuracy metric, calculated as the average of the absolute percentage differences between CGM readings and reference values [52]. It is a measure of the total system performance (sensor + algorithm) rather than the sensor element alone.
- Accuracy Across Glucose Ranges: Sensor performance can vary significantly across hypoglycemic, normoglycemic, and hyperglycemic ranges. This is crucial for studies examining postprandial hyperglycemia or reactive hypoglycemia [54].
- Precision during Glucose Dynamics: The ability of the sensor to accurately track rapidly changing glucose levels, a key requirement for assessing meal responses [54].
- First-Day Accuracy: Some sensors exhibit reduced accuracy during the initial wear period, which must be accounted for in study designs involving short-term dietary interventions [54].
- Parkes Error Grid Analysis: A clinical risk analysis that categorizes measurement errors based on their potential to cause clinically significant misinterpretation, with Zones A and B representing clinically acceptable readings [55].
Comparative Analysis of Leading CGM Systems
Recent head-to-head studies provide critical insights into the performance of contemporary CGM devices. A 2025 study by Eichenlaub et al. compared three major systems under controlled conditions, revealing distinct performance profiles [54].
Table 1: Overall Accuracy (MARD) from Head-to-Head Comparative Study (Eichenlaub et al., 2025)
| CGM System | Overall MARD vs. Lab Reference (YSI) | MARD vs. Fingerstick Meter | Low Glucose Detection Rate |
|---|---|---|---|
| Dexcom G7 | 12.0% | ~9.7-10.1% | 80% |
| FreeStyle Libre 3 | 11.6% | ~9.7-10.1% | 73% |
| Medtronic Simplera | 11.6% | 16.6% | 93% |
Table 2: Performance Across Different Glucose Ranges and Conditions
| CGM System | Performance in High Glucose | Performance during Rapid Changes | First-Day Accuracy (MARD) |
|---|---|---|---|
| Dexcom G7 | Excellent, closely tracks post-meal spikes | Maintains steady performance | ~12.8% |
| FreeStyle Libre 3 | Excellent, closely tracks post-meal spikes | Maintains steady performance | ~10.9% (most stable) |
| Medtronic Simplera | Less reliable, sometimes misses actual highs | Struggles during fast glucose rises | ~20.0% (improves after) |
Furthermore, next-generation devices in development show continued improvement. A new 15-day Dexcom G7 sensor has demonstrated an overall MARD of 8.0% in a prospective multicenter study, improving upon the 8.2% MARD of the currently available 10-day G7 [55] [56]. This sensor also maintained high accuracy across all glucose ranges, with a MARD of 8.2% in the hypoglycemic range (54-69 mg/dL) and 7.4% in the severe hyperglycemic range (>250 mg/dL) [55].
For research requiring long-term implantation, the Eversense 365 system offers a 365-day wear time with a reported MARD of 8.8% [57].
Experimental Protocols for CGM Validation
A robust validation protocol is essential for generating reliable CGM data in a research setting. The following methodology is adapted from recent high-quality clinical studies [54] [55].
Protocol 1: Head-to-Head CGM Accuracy Comparison
This protocol is designed for the comparative evaluation of multiple CGM systems under controlled conditions, ideal for validating devices before their use in food-intake correlation studies.
Objective: To compare the accuracy and performance of multiple CGM systems simultaneously in a cohort of subjects with diabetes.
Study Population:
- Participants: Adults with type 1 or type 2 diabetes (e.g., n=24-130, based on study scale) [54] [55].
- Inclusion Criteria: Stable diabetes management, willingness to attend multiple in-clinic sessions.
- Exclusion Criteria: Conditions that could interfere with sensor placement or glucose measurements.
Materials & Equipment:
- CGM systems for comparison (e.g., Dexcom G7, FreeStyle Libre 3, Medtronic Simplera).
- Laboratory-grade reference glucose analyzer (e.g., Yellow Springs Instrument/YSI 2300 Stat Plus) [55] [56].
- Standard fingerstick glucose meters (e.g., Contour Next) for secondary comparison [54].
- Materials for controlled glycemic manipulation (standardized meals, insulin, exercise equipment).
Procedure:
- Sensor Deployment: All participants simultaneously wear each CGM sensor on the upper arm according to manufacturers' instructions for a defined period (e.g., up to 15 days). Sensor replacement should follow their respective approved wear durations [54].
- In-Clinic Sessions: Participants undergo multiple (e.g., 3-4) in-clinic sessions of 7-13 hours duration on different days (e.g., days 2, 5, and 15) to assess accuracy across the sensor's life [54] [55].
- Reference Sampling: During sessions, venous blood is drawn frequently (every 10-15 minutes) and immediately analyzed using the laboratory reference device to establish "true" glucose values [55].
- Glucose Manipulation: Glucose levels are manipulated through standardized meals, insulin dosing, or controlled exercise to generate data across a wide glycemic range (hypo-, normo-, and hyperglycemia) and at different rates of change [54] [55].
- Data Pairing: CGM readings are time-matched with the reference values taken within a 5-minute window for analysis [55].
Data Analysis:
- Calculate the overall MARD for each system against the primary reference.
- Stratify MARD by glucose range (hypoglycemic, normoglycemic, hyperglycemic).
- Perform Parkes Error Grid analysis to assess clinical risk.
- Analyze accuracy during periods of rapid glucose change (>2 mg/dL/min).
- Compare low and high glucose alert accuracy (e.g., percentage of true alerts).
Protocol 2: Assessing CGM Performance in a Simulated Hospital Workflow
This protocol evaluates the practical efficiency of CGM systems in a controlled, clinical-style environment, relevant for research conducted in inpatient settings or clinical research units.
Objective: To compare the time efficiency and staff perception of flash glucose monitoring (DIGM) versus traditional finger-prick testing.
Study Population:
- Participants: Healthcare professionals (e.g., nurses, allied health staff, n=25) familiar with standard glucose monitoring [58].
Materials & Equipment:
- High-fidelity medical mannequin.
- Flash glucose monitoring system (e.g., FreeStyle Libre).
- Standard finger-prick glucose testing kit.
- Video recording equipment for time-motion analysis.
- Structured perception survey (5-point Likert scale).
Procedure:
- Training: All participants receive standardized training on the application and use of the DIGM system.
- Simulated Tasks: Each participant performs three key tasks on the mannequin in a simulated clinical environment:
- Task A: Apply a flash glucose sensor.
- Task B: Scan the sensor to obtain a glucose reading.
- Task C: Perform a complete finger-prick test.
- Timing: Video recordings are used to extract the precise time taken for each task, including setup, measurement, and documentation [58].
- Survey: Participants complete a survey immediately after the simulation to assess their perception of the two methods regarding workflow efficiency, patient comfort, and infection control [58].
Data Analysis:
- Compare mean task durations using paired statistical tests (e.g., paired t-test or Wilcoxon signed-rank test).
- Calculate projected time savings per patient per day based on a typical number of glucose checks.
- Analyze survey responses to quantify staff preference and perceived benefits.
Signaling Pathways and Core Technology
Biochemical Sensing Pathway of CGM Systems
At their core, most CGM sensors operate via an electrochemical sensing mechanism. The following diagram illustrates the generalized biochemical pathway that translates interstitial glucose concentration into a measurable electrical signal.
Diagram 1: CGM Electrochemical Sensing Pathway.
The process begins when glucose from the interstitial fluid diffuses into the sensor membrane. The core reaction is catalyzed by the enzyme Glucose Oxidase (GOx). GOx converts glucose and oxygen into gluconolactone and hydrogen peroxide (H₂O₂). The H₂O₂ is then oxidized at the surface of a platinum-based working electrode, releasing electrons and generating a proportional electrical current. This current is measured by the sensor's transmitter. Finally, a proprietary algorithm processes this raw signal, applying calibration and smoothing filters to account for factors like the physiological lag between blood and interstitial fluid glucose and sensor-specific characteristics, ultimately outputting a calibrated glucose value [52].
Experimental Workflow for CGM Validation Studies
A rigorous validation study requires a structured workflow to ensure reliable and comparable results. The following diagram outlines the key phases from planning to data analysis.
Diagram 2: CGM Validation Study Workflow.
The Scientist's Toolkit: Essential Research Reagents and Materials
For researchers designing CGM validation or food-intake correlation studies, specific materials and tools are essential for generating high-quality, reproducible data.
Table 3: Essential Research Reagents and Materials for CGM Studies
| Item | Function/Application | Examples/Specifications |
|---|---|---|
| Laboratory Glucose Analyzer | Provides the primary reference ("gold standard") for glucose concentration against which CGM accuracy is measured. | Yellow Springs Instrument (YSI) 2300 Stat Plus [55] [56] |
| Standardized Fingerstick Meter | Provides a secondary, clinically relevant comparison method for CGM readings in ambulatory settings. | Contour Next meter [54] |
| CGM Systems Under Investigation | The devices being evaluated or used as the primary data collection tool in the research study. | Dexcom G7, FreeStyle Libre 3, Medtronic Guardian 4, Eversense 365 [54] [57] [59] |
| Materials for Controlled Glycemic Manipulation | Used to induce controlled glucose fluctuations across a wide range, testing sensor performance under dynamic conditions. | Standardized meal tests, intravenous insulin/dextrose protocols, controlled exercise equipment [54] [55] |
| Data Logging and Synchronization System | Critical for accurately time-matching CGM readings with reference blood draws and other experimental events (e.g., meal intake). | Dedicated clinical trial software, timestamped electronic case report forms (eCRFs) |
The evolving landscape of CGM technology offers researchers powerful tools for investigating glucose metabolism and food intake correlations. While MARD remains a vital benchmark for device selection, a comprehensive evaluation must consider performance across glycemic ranges, during dynamic changes, and throughout the sensor's wear period. The experimental protocols and methodological considerations outlined in this document provide a foundation for rigorous CGM validation, ensuring that the data generated in research settings is both accurate and clinically meaningful. As sensor technology continues to advance—with improvements in wear time, initial accuracy, and algorithm sophistication—their potential to unlock deeper insights into metabolic health grows accordingly.
Within the burgeoning field of continuous glucose monitoring (CGM) and food intake correlation research, the precise design of dietary interventions is paramount for generating robust, translatable scientific evidence. The integration of CGM data provides an unprecedented, high-resolution view of glycemic responses, allowing researchers to move beyond traditional endpoints like HbA1c and capture dynamic fluctuations in glucose control [39] [5]. This application note details evidence-based protocols and methodologies for optimizing key elements of dietary intervention design—duration, adherence monitoring, and macronutrient control—specifically for research correlating CGM metrics with nutritional intake.
Quantitative Evidence Base for Intervention Design
Recent meta-analyses and clinical trials provide critical data to inform the expected effect sizes and necessary parameters for dietary studies utilizing CGM. The tables below synthesize key quantitative findings relevant to researchers in designing their own investigations.
Table 1: Glycemic and Anthropometric Outcomes from a Meta-Analysis of CGM-Guided Lifestyle Interventions in T2D [39]
| Outcome Measure | Mean Difference (MD) | 95% Confidence Interval (CI) | Certainty of Evidence (GRADE) |
|---|---|---|---|
| HbA1c (%) | -0.46 | -0.71, -0.22 | Moderate |
| Time in Range (TIR), % | +7.18 | +2.77, +11.58 | Moderate |
| Time Above Range (TAR), % | -7.32 | -12.98, -1.66 | Moderate |
| Fasting Glucose (mg/dL) | -7.86 | -15.06, -0.65 | Moderate |
| Body Weight (kg) | -2.06 | -3.74, -0.38 | Moderate |
| Mean CGM Glucose (mg/dL) | -11.57 | -22.58, -0.56 | Low |
| Glucose Standard Deviation (mg/dL) | -4.06 | -6.54, -1.58 | Low |
Table 2: Impact of Specific Dietary Interventions on CGM-Measured Glycemia [4] [60]
| Dietary Intervention | Population | Key CGM Findings | Notes |
|---|---|---|---|
| Carbohydrate-Restricted Diets (CRDs) | T2D (7 studies, n=301) | Overall improvement in 24-h mean blood glucose (d = -0.51, CI: -0.88 to -0.14). | Exploratory trend suggests greater benefits with longer intervention duration [4]. |
| Modified DASH (DASH4D) | T2D (n=89) | Average glucose reduced by 11 mg/dL; Time in Range increased by 75 min/day. | Effect was more pronounced in participants with baseline HbA1c >8%, who gained ~3 hours in TIR per day [60]. |
Detailed Experimental Protocols
This section provides a step-by-step methodology for implementing a controlled dietary intervention with integrated CGM, drawing from successful clinical trial designs.
Protocol: Controlled Crossover Trial of a Modified Dietary Pattern
- Source Model: DASH4D CGM Study [60].
- Objective: To evaluate the efficacy of a modified DASH diet (DASH4D) versus a standard diet on glycemic control in adults with Type 2 Diabetes.
- Population: Adults with T2D. The original study (n=89) had a mean age of 64 years, with 67% female and 88% African American participants.
Design:
- Type: Randomized, controlled, crossover trial.
- Duration: 20 weeks total, comprising four 5-week dietary periods.
- Interventions: Participants consume, in random order:
- Low-sodium DASH4D diet
- High-sodium DASH4D diet
- Low-sodium standard diet
- High-sodium standard diet
- Key Feature: This design compares participants to themselves under different conditions, reducing inter-individual variability and enhancing statistical power.
Methodology:
- Meal Provision: All meals are prepared and provided to participants by a metabolic kitchen for the duration of the study to ensure strict adherence to macronutrient and micronutrient targets.
- CGM Deployment: Participants wear a blinded or unblinded CGM device (e.g., Dexcom G6/G7, Abbott FreeStyle Libre Pro) throughout the study. The specific CGM brand and model should be consistent for all participants.
- Data Collection Points: CGM data is actively collected and analyzed during weeks 3 and 4 of each 5-week dietary period to allow for metabolic adaptation.
- Outcome Measures:
- Primary: Mean CGM glucose, Time in Range (TIR 70-180 mg/dL).
- Secondary: Time Above Range (TAR >180 mg/dL), glycemic variability (Standard Deviation-SD, Coefficient of Variation-CV), time below range (TBR <70 mg/dL).
Protocol: Implementing a Nutrition-Focused CGM (NFA) Initiative
- Source Model: UNITE (Using Nutrition to Improve Time in Range) Study [14].
- Objective: To understand how a nutrition-focused approach during CGM initiation influences patient perspectives and food-related behaviors.
- Population: Non-insulin using adults with T2D.
Design:
- Type: Qualitative interview study embedded within a randomized clinical trial.
- Duration: 2-month intervention with post-study interviews.
Methodology:
- Structured Sessions:
- Session 1 (In-Person, 60-min): Initiate CGM (e.g., Dexcom G7) and deliver NFA materials. The materials use simple imagery and messaging to teach a "1, 2, 3 approach": check glucose (1) before eating, (2) 2 hours after eating, and (3) around activity to learn the body's response. A "yes/less" framework guides food choices toward evidence-based options.
- Session 2 (Remote, 30-min, ~Day 14): Review retrospective CGM data (e.g., Ambulatory Glucose Profile - AGP report) with the participant, focusing on linking glucose patterns to food choices.
- Data Collection: Conduct semi-structured qualitative interviews post-intervention. Use a rapid matrix analysis approach with a priori coding based on fidelity frameworks (e.g., NIH fidelity framework) to assess:
- Intervention Receipt: Understanding and perceptions of the NFA materials.
- Intervention Enactment: How CGM data was used to make food-related decisions and what specific changes were made.
- Structured Sessions:
Visualizing the Research Workflow
The diagram below outlines the logical workflow for a comprehensive CGM-food intake correlation study, integrating core experimental components.
The Scientist's Toolkit: Research Reagent Solutions
For researchers embarking on CGM-food correlation studies, the following tools and datasets are essential for ensuring data quality and reproducibility.
Table 3: Essential Research Tools for CGM-Food Intake Studies
| Item / Resource | Function / Application | Example from Literature |
|---|---|---|
| Blinded Professional CGM | Measures glucose at regular intervals (e.g., 5-15 min) without displaying data to the participant, preventing behavior modification during data collection. | Abbott FreeStyle Libre Pro [61] |
| Unblinded Personal CGM | Provides real-time glucose data to the participant; used in behavioral interventions where immediate feedback is part of the study design. | Dexcom G6 / G7 [14] [61] |
| Multimodal Datasets | Provide benchmark data for algorithm development and validation. The CGMacros dataset includes CGM, macronutrients, food images, and activity data from healthy, pre-diabetic, and T2D participants [61]. | CGMacros Dataset [61] |
| Structured Meal Provision | The gold standard for controlling macronutrient and calorie intake. Meals are designed by research dietitians and prepared in a metabolic kitchen [60]. | DASH4D Trial [60] |
| Digital Diet Logging Tools | Enable participants to self-report food intake in free-living settings. Tools can include barcode scanners, photo-based logging, and integrated nutrient databases. | MyFitnessPal App [61] |
| Activity Trackers | Monitor physical activity, a key confounder of glycemic variability. Data (e.g., METs) is used to adjust statistical models. | Fitbit Smartwatch [61] |
| Nutrition-Focused Education Materials | Standardized tools (e.g., slide decks, one-page guides) used to educate participants on linking CGM data with food choices, ensuring consistent intervention delivery. | UNITE Study "Yes/Less" Framework [14] |
The following tables consolidate key quantitative findings from recent studies on discrepancies within Continuous Glucose Monitoring (CGM) systems and between CGM systems and blood glucose measurements.
Table 1: Discrepancies Between Current Displayed (CUR) and Auto-Logged (AL) CGM Values [62] This table summarizes the systematic differences between the two primary data streams provided by the FreeStyle Libre 3 (FSL3) system.
| Glycaemic Range (by AL) | Mean Difference (CUR - AL) ± SD (mg/dL) | 5th - 95th Percentile of Differences (mg/dL) | Frequency of Differences > ±10 mg/dL |
|---|---|---|---|
| Overall | -1.2 ± 6.4 | -11 to +10 | ~10% |
| Hypoglycaemia (<70 mg/dL) | -3.1 ± 2.6 | -8 to +1 | Not Reported |
| Euglycaemia (70–180 mg/dL) | -1.9 ± 6.3 | -11 to +9 | Not Reported |
| Hyperglycaemia (>180 mg/dL) | 0.4 ± 7.0 | -10 to +12 | Not Reported |
Table 2: Display Error Characteristics and Point Accuracy of FSL3 Data Streams [62] This table details the conditions under which display errors occur and the accuracy of each data stream compared to capillary blood glucose reference measurements.
| Parameter | Auto-Logged (AL) Values | Current Displayed (CUR) Values |
|---|---|---|
| Overall MARD vs. Capillary Reference | 9.7% | 10.1% |
| MARD in Hypoglycaemia | Higher than overall MARD | Higher than overall MARD |
| Display Error Rate | Not Applicable | 3.9% of retrieval attempts |
| Glucose Level during Display Errors | +91.9 mg/dL higher than during successful retrievals | Not Applicable |
| Rate of Change during Display Errors | Mean absolute RoC +1.52 mg/dL/min higher | Not Applicable |
Table 3: Glycemic Outcomes from Carbohydrate-Restricted Diets (CRDs) in T2DM [4] This table presents results from a meta-analysis on the effect of CRDs on 24-hour mean blood glucose (MBG) in patients with Type 2 Diabetes (T2DM).
| Outcome Measure | Result (Effect Size) | Statistical Significance | Context |
|---|---|---|---|
| 24-hour MBG | d = -0.51 (95% CI: -0.88 to -0.14) | p < 0.05 | Improved with CRDs |
| Correlation: Intervention Duration & MBG Reduction | Positive correlation suggested | Not Reported | Longer duration associated with greater benefit |
| HbA1c Reduction (Context from other meta-analyses) | 3.7 mmol/L greater reduction vs. high-carbohydrate diets | Not Reported | Cited for context in introduction [4] |
Experimental Protocols
Protocol for Characterizing CGM Data Stream Discrepancies
This protocol is derived from a post-hoc analysis of a clinical performance evaluation study [62].
- Objective: To quantitatively characterize systematic differences between auto-logged (AL) and current displayed (CUR) values in the FreeStyle Libre 3 CGM system and to identify conditions associated with display errors.
- Study Population: Adults with diabetes mellitus. The source study included 24 participants [62].
- Materials:
- FreeStyle Libre 3 CGM sensors.
- Android-based smart device with the FSL3 application installed.
- Reference glucose measurement systems: Venous glucose analyzers (e.g., YSI 2300 STAT PLUS) and capillary blood glucose monitoring system (e.g., Contour Next).
- Procedure:
- Sensor Deployment: Participants wear the FSL3 sensor for a 15-day period.
- In-Clinic Sessions: Conduct three in-clinic sessions with induced glycaemic excursions (e.g., on study days 2, 5, and 15).
- Data Collection During Sessions:
- Retrieve CUR values every 15 minutes by study personnel opening the smartphone application. Document each attempt as 'Successful' (value displayed) or 'Display Error' (error message shown).
- Measure reference capillary and venous blood glucose every 15 minutes in parallel.
- Data Export: Export AL and CUR timestamps and glucose readings using the manufacturer's data management platform after the study.
- Data Analysis:
- Preprocessing: Align paired CUR and AL values within a ±5-minute window for 'Successful' retrievals.
- Discrepancy Analysis: Calculate descriptive statistics (mean, SD) for the pointwise differences (CUR - AL) overall and stratified by glycaemic range (hypo-, eu-, hyperglycaemia). Use Wilcoxon signed-rank test for paired differences.
- Accuracy Analysis: Calculate the Mean Absolute Relative Difference (MARD) for both AL and CUR values against capillary blood glucose references.
- Display Error Analysis: Use linear mixed-effects models to assess associations between display errors and variables like glucose level and rate of change (RoC), with participant ID as a random effect.
Protocol for an N-of-1 Trial on Personalized Postprandial Glucose Responses
This protocol outlines a method to investigate interindividual variability in response to different foods [2].
- Objective: To identify staple foods that most effectively stabilize postprandial blood glucose for individual patients with T2DM using an N-of-1 trial design.
- Study Population: Adults aged 18-70 years with a T2DM diagnosis for ≥3 months, managed by lifestyle alone or stable single hypoglycemic drug [2].
- Materials:
- Continuous Glucose Monitor (CGM).
- Pre-portioned test meals (see Table 4 for examples).
- Standardized documentation tools (e.g., smartphone app, logbook).
- Procedure:
- Study Design: A single-center, randomized, crossover N-of-1 trial consisting of 3 periods. Each period comprises 5 test days.
- Test Meals: Provide 5 different test diets for breakfast in a randomized order. The variable component is the staple food, portioned to provide 50g of available carbohydrates. All other meal components (e.g., 150g scrambled eggs with tomatoes, 50g cucumber, 200mL milk) remain consistent [2].
- Glucose Monitoring: Use CGM to track interstitial glucose at 5-minute intervals. The primary outcome is the postprandial blood glucose peak.
- Participant Compliance: Participants maintain medication logs. Adherence is verified via telephone follow-ups.
- Data Analysis: Conduct Bayesian analysis at both the individual and group levels to determine the posterior probability of different PPGRs to each staple food for each participant.
Signaling Pathways and Workflow Visualizations
CGM Data Streams & Research Analysis Workflow
The following diagram illustrates the workflow for collecting, processing, and analyzing different data streams from a CGM system to characterize discrepancies, as outlined in the experimental protocol [62].
N-of-1 Trial Design for Personalized Nutrition
This diagram outlines the structure of an N-of-1 trial designed to investigate individual postprandial glucose responses to different staple foods [2].
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Materials for CGM and Food Intake Correlation Research This table lists key reagents, technologies, and tools required for conducting research in the field of continuous glucose monitoring and its correlation with nutritional interventions.
| Item | Function / Application in Research |
|---|---|
| FreeStyle Libre 3 CGM | Provides the two primary data streams (AL and CUR) for analyzing internal discrepancies and accuracy against reference methods [62]. |
| Capillary Blood Glucose Monitor (e.g., Contour Next) | Serves as a primary reference method for validating CGM accuracy during in-clinic sessions, as per recent IFCC WG-CGM recommendations [62]. |
| Venous Glucose Analyzer (e.g., YSI 2300) | Provides a high-accuracy reference measurement for blood glucose in controlled laboratory settings [62]. |
| Data Management Platform (e.g., Abbott's) | Essential for exporting auto-logged (AL) CGM data for retrospective trend analysis and calculation of standardized CGM metrics [62]. |
| Standardized Test Meals | Critical for investigating postprandial glucose responses. Meals are designed with a fixed available carbohydrate content (e.g., 50g) to ensure comparability [2]. |
| Python Data Science Libraries (pandas, NumPy, SciPy, statsmodels) | Used for data preprocessing, statistical analysis (e.g., Wilcoxon signed-rank test), and advanced modeling (e.g., linear mixed-effects models) of CGM data [62]. |
| N-of-1 Trial Framework | A research design used to assess individual, rather than group-average, responses to dietary interventions like different staple foods, highlighting interindividual variability [2]. |
Within the specific context of continuous glucose monitoring (CGM) research correlated with food intake, data integrity is the cornerstone of generating valid, reproducible, and clinically meaningful insights. CGM devices provide a dynamic stream of glucose measurements, offering an unprecedented opportunity to understand the glycemic impact of dietary interventions [4] [5]. However, the fidelity of this data can be compromised by various artifacts and technical confounders, which pose a significant threat to the accuracy of food-intake correlation studies. This document outlines application notes and standardized protocols to help researchers identify, manage, and prevent these issues, thereby ensuring the collection of high-quality CGM data.
Understanding CGM Data and Potential Artifacts
Key CGM Metrics for Nutritional Research
For research linking diet to glycemic response, several CGM-derived metrics are of paramount importance. The 24-hour mean blood glucose (MBG) provides an overall picture of glycemic control, while Time in Range (TIR), typically defined as the percentage of readings between 70-180 mg/dL, serves as a key outcome for assessing the effectiveness of dietary patterns [63]. The Glucose Management Indicator (GMI) offers an estimate of HbA1c, and the Coefficient of Variation (CV) is a critical measure of glycemic variability, where a CV ≤ 36% is considered stable [63].
Table 1: Key CGM Metrics for Nutritional Studies
| Metric | Definition | Research Significance | Target/Standard |
|---|---|---|---|
| Time in Range (TIR) | % of readings 70-180 mg/dL [63] | Primary outcome for diet effect | >70% [63] |
| Mean Blood Glucose | Average glucose over 24 hours [4] | Overall glycemic status | Study-dependent |
| Coefficient of Variation (CV) | Measure of glycemic variability [63] | Indicates glucose stability | ≤36% [63] |
| Time Above Range (TAR) | % of readings >250 mg/dl (L1: 181-250 mg/dL) [63] | Identifies hyperglycemia | Minimize |
| Time Below Range (TBR) | % of readings <70 mg/dL (L1: 54-69 mg/dL) [63] | Identifies hypoglycemia risk | Minimize |
Artifacts in CGM data can arise from multiple sources:
- Signal Integrity: While modern CGM sensors (e.g., FreeStyle Libre) have been shown to maintain functionality and data integrity after exposure to common radiologic procedures like CT, X-ray, and MRI, their presence during imaging requires documentation as a potential, though low-risk, confounder [64].
- Physiological Factors: Sensor placement, local inflammation, and compression on the sensor site can lead to erroneous readings that do not reflect systemic glucose levels.
- User-Dependent Factors: Improper sensor insertion, failure to calibrate (if required), and premature sensor failure introduce significant noise.
- Data Handling Artifacts: Incomplete data extraction, improper synchronization of device timestamps with food intake logs, and failure to meet minimum data completeness thresholds (e.g., <70% of data from a 14-day period) can render a dataset unusable for robust analysis [63].
Protocols for Ensuring High-Quality CGM Data Collection
A standardized protocol is essential to minimize artifacts and ensure consistency across study participants and timepoints.
Pre-Study Sensor Validation and Participant Training
- Sensor Lot Verification: Document sensor model and lot numbers. Prior to study initiation, verify that all sensors are functional and from validated batches.
- Standardized Participant Training: Conduct hands-on training for participants on proper sensor insertion, use of the reader/app, and basic troubleshooting. Emphasize the importance of avoiding compression on the sensor and documenting any off-body times.
Data Collection and Integrity Monitoring Workflow
The following workflow outlines the critical steps for managing CGM data throughout a nutritional study.
Data Quality Assessment and Inclusion Criteria
Upon data collection, researchers must systematically assess its quality against predefined benchmarks before inclusion in analysis.
Table 2: CGM Data Quality Assessment Criteria
| Criterion | Minimum Standard | Action for Non-Compliance |
|---|---|---|
| Wear Time | ≥14 days recommended [63] | Extend data collection period if possible. |
| Sensor Active % | ≥70% of data from recommended wear period [63] | Exclude periods with significant gaps. |
| Glycemic Variability | CV ≤ 36% [63] | Investigate for physiological vs. technical causes. |
| Correlation with Food Logs | Timestamps for ≥90% of reported meals | Reconcile logs with participant. |
The Scientist's Toolkit: Research Reagent Solutions
The following table details essential materials and digital tools required for conducting rigorous CGM-based nutritional research.
Table 3: Essential Research Reagents and Tools
| Item | Function/Application | Specifications/Notes |
|---|---|---|
| Professional CGM System | Core device for continuous interstitial glucose measurement. | Select factory-calibrated or user-calibrated models based on protocol. Ensure regulatory approval for research use. |
| Standardized Food Logging Tool | Digital platform for participants to record food type, quantity, and time of consumption. | Critical for timestamp synchronization with CGM data. Should include a nutrient database. |
| Data Extraction & FHIR API | Standardized method for retrieving raw and summary CGM data from devices and apps. | HL7 FHIR implementation guides (e.g., CGM Data Submission Bundle profile) provide a framework for structured data transfer [65]. |
| Statistical Analysis Software | For processing CGM data streams and performing correlation analyses with nutritional variables. | R (e.g., cgmanalysis package [5]), Python, or other specialized platforms. |
| Data Visualization Platform | To generate standardized reports like the Ambulatory Glucose Profile (AGP) for qualitative and quantitative assessment [63]. | Aids in pattern recognition and data quality inspection. |
Maintaining data integrity in CGM-based food intake correlation research demands a meticulous, proactive, and standardized approach. By understanding potential artifacts, implementing rigorous pre-study validation, adhering to a structured data collection workflow, and employing robust quality assessment criteria, researchers can significantly enhance the reliability and validity of their findings. These protocols provide a foundation for generating high-quality evidence that can truly illuminate the complex relationship between diet and glycemic physiology.
Validating CGM Efficacy and Comparing Dietary and Technological Interventions
The following table summarizes the key quantitative findings from a recent systematic review and meta-analysis on the use of Continuous Glucose Monitoring (CGM) to guide lifestyle choices, with a focus on nutrition, in the management of Type 2 Diabetes (T2D) [39] [66].
Table 1: Meta-Analysis Results of CGM-Guided Lifestyle Interventions on Glycemic and Anthropometric Outcomes
| Outcome Measure | Number of RCTs | Pooled Effect Estimate (MD) | 95% Confidence Interval | Certainty of Evidence (GRADE) |
|---|---|---|---|---|
| HbA1c (%) | 20 | -0.46% | -0.71, -0.22 | Moderate |
| Time in Range (TIR), 70-180 mg/dL (%) | 20 | +7.18% | +2.77, +11.58 | Moderate |
| Time Above Range (TAR), >180 mg/dL (%) | 20 | -7.32% | -12.98, -1.66 | Moderate |
| Fasting Glucose (mg/dL) | 20 | -7.86 mg/dL | -15.06, -0.65 | Moderate |
| Body Weight (kg) | 20 | -2.06 kg | -3.74, -0.38 | Moderate |
| Mean CGM Glucose (mg/dL) | 20 | -11.57 mg/dL | -22.58, -0.56 | Low |
| Glucose Standard Deviation (mg/dL) | 20 | -4.06 mg/dL | -6.54, -1.58 | Low |
Abbreviations: MD, Mean Difference; RCTs, Randomized Controlled Trials; TIR, Time in Range; TAR, Time Above Range. [39]
Experimental Protocols & Methodologies
Core Protocol for CGM-Guided Lifestyle Intervention Trials
The evidence supporting CGM efficacy is derived from RCTs where the intervention involved two key components [39]:
- CGM Device Use: Utilization of a CGM device (real-time, intermittently-scanned, or professional) with a duration ranging from a single episode to continuous use throughout the intervention period.
- Structured Feedback and Education: Delivery of guidance intended to modify food or nutrition choices. This could be part of a dedicated nutrition intervention or a multicomponent lifestyle education program. Feedback was provided by healthcare professionals (e.g., diabetes specialists, dietitians) via handouts, live education sessions, or integrated digital platforms.
Visual Workflow: CGM-Guided Lifestyle Intervention Protocol
Protocol for Investigating CGM-Diet Correlations
For research focused on the direct correlation between CGM data and food intake, the following methodology, as implemented in the CGMacros dataset, provides a robust framework [61]:
Visual Workflow: Multimodal Data Collection for CGM-Diet Correlation
Key Methodological Details:
- CGM Data Processing: CGM data from devices with different sampling rates (e.g., 5-min and 15-min) are often linearly interpolated to a uniform rate (e.g., 1-min) for analysis [61].
- Macronutrient Correlation: Studies analyze the relationship between meal Glycemic Load (GL) or carbohydrate content and CGM metrics like Area Under the Curve (AUC), Standard Deviation (SD), and Mean Amplitude of Glycemic Excursions (MAGE) over specific postprandial windows (2-4 hours) [10].
- Dietary Control: To reduce variability, some studies provide standardized meals with known macronutrient profiles for specific meals (e.g., breakfast, lunch), while allowing participant-selected dinners to assess free-living conditions [61].
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials and Tools for CGM-Based Nutrition Research
| Item / Solution | Function / Application in Research | Example Products / Sources |
|---|---|---|
| Continuous Glucose Monitors (CGM) | Measures interstitial glucose concentrations at regular intervals to capture glycemic variability and postprandial responses. | Abbott FreeStyle Libre Pro, Dexcom G6 Pro [61] |
| Activity & Heart Rate Monitors | Quantifies physical activity and energy expenditure, a critical confounder in glucose metabolism analysis. | Fitbit Sense, other research-grade accelerometers [61] |
| Digital Food Logging Platforms | Enables detailed self-reporting of food intake, portion sizes, and timestamps for correlation with CGM data. | MyFitnessPal, other dietary tracking mobile apps [61] |
| Standardized Meal Kits | Provides meals with precisely known macronutrient composition to control for dietary variability and establish clear dose-response relationships. | Custom-prepared shakes, meals from commercial restaurants (e.g., Chipotle) [61] |
| CGM-Diet Correlation Datasets | Publicly available datasets for algorithm development and validation without requiring new clinical trials. | CGMacros dataset (includes CGM, macronutrients, activity, images) [61] |
| Key CGM Metrics for Analysis | Quantitative descriptors of glycemic control, variability, and response to meals. | Time in Range (TIR), Time Above Range (TAR), AUC, MAGE, Glucose Standard Deviation (SD) [39] [10] |
Comparative Effectiveness of Different Dietary Patterns on 24-Hour Mean Glucose
The following tables synthesize key quantitative findings from recent research on the relationship between dietary patterns, macronutrient composition, meal timing, and 24-hour mean glucose levels.
Table 1: Impact of Dietary Composition and Restriction on 24-Hour Mean Glucose
| Dietary Pattern / Intervention | Study Population | Key Effect on 24-h Mean Glucose & Glycemic Variability | Effect Size / Correlation | Citation |
|---|---|---|---|---|
| Carbohydrate-Restricted Diet (CRD) | Adults with T2DM (7 studies, n=301) | Significant improvement in 24-hour mean blood glucose. | Pooled effect size (d) = -0.51 (95% CI: -0.88 to -0.14) [38] | |
| High Carbohydrate Intake | Adults with Normoglycemia (n=14) | Higher carbohydrate intake predicted greater glucose variability (GV) and mean amplitude of glycemic excursions (MAGE). | MAGE: β=0.9, SE=0.4, p=0.02GV: β=0.4, SE=0.2, p=0.04 [67] | |
| High-Protein & High-Carbohydrate Pattern | T2DM Patients (n=2,984) | Significantly associated with increased risk of cardiovascular disease (CVD), a key complication of poor glycemic control. | Adjusted OR for CVD: 2.89 (95% CI: 2.11–3.96) [68] | |
| Modern Dietary Pattern (High in red meats) | General Adult Population (n=3,137) | Positively associated with high blood glucose. | Structural Equation Model: β=0.127, p<0.05 [69] | |
| Glycemic Load (GL) & Carbohydrate Intake | Healthy Adults (n=48) | Moderate positive correlation with postprandial CGM metrics. | GL vs. Variance (4h): ρ=0.43Carbs vs. SD (24h): ρ=0.45 [10] |
Table 2: Impact of Meal Timing Patterns on Glucose Variability
| Meal Timing Variable | Study Population | Key Effect on Glucose Variability (GV) | Effect Size | Citation |
|---|---|---|---|---|
| Later Eating Midpoint | Adults with Dysglycemia (n=26) | Predicts lower glucose variability. | β = -2.3, SE=1.0, p=0.03 [67] | |
| Later Last Eating Occasion | Adults with Normoglycemia (n=14) | Predicts higher glucose variability. | β = 1.5, SE=0.6, p=0.04 [67] | |
| Intermittent Glucose Ingestion (30-min apart) | Healthy Adults (n=3) | Minimizes the peak postprandial blood glucose level compared to bolus ingestion. | Experimentally validated model prediction [70] |
Experimental Protocols
Protocol for Free-Living Dietary and CGM Observational Study
This protocol outlines the methodology for investigating associations between diet, meal patterns, and glucose levels under real-world conditions [67].
1. Participant Recruitment and Grouping:
- Recruit adults into distinct glycemic groups: Dysglycemia (D-GLYC) (e.g., prediabetes or T2D) and Normoglycemia (N-GLYC) based on HbA1c or fasting glucose criteria.
- Exclude individuals with confounding conditions such as shift work, sleep disorders, or use of medications that severely impact glucose metabolism (other than metformin).
2. Baseline Assessments:
- Obtain anthropometric measurements (height, weight, BMI) in duplicate or triplicate while participants wear light clothing.
- Measure blood pressure in triplicate after a 10-minute seated rest.
3. Continuous Glucose Monitoring (CGM):
- Use a professional CGM system (e.g., Abbott Freestyle Libre Pro).
- Insert the sensor on the non-dominant upper arm.
- Initiate data collection from 4:00 a.m. the day after insertion to allow for sensor equilibrium. Collect data for a continuous 2-week period.
- Process CGM data using specialized software (e.g., EasyGV v8.6) to extract key endpoints:
- 24-hour Mean Glucose
- Mean Amplitude of Glycemic Excursions (MAGE)
- Largest Amplitude of Glycemic Excursions (LAGE)
- Standard Deviation (SD) of glucose as a marker of Glucose Variability (GV).
4. Dietary Intake Assessment:
- Instruct participants to complete multiple (e.g., up to six) non-consecutive 24-hour dietary recalls, including at least one weekend day, using a validated automated self-administered tool (e.g., ASA24).
- Collect data on caloric intake, grams of carbohydrates, protein, fat, sugar, and fiber.
5. Meal Pattern Logging:
- Equip participants with a smartphone application (e.g., myCircadianClock mCC app) to capture time-stamped photographs of all caloric intake in real time.
- Define an Eating Occasion (EO) as any instance of caloric consumption.
- Calculate meal timing parameters from the logged data:
- Eating Window: The interval containing 95% of all EOs.
- First and Last EO: Time of the first and last caloric intake.
- Eating Midpoint: The median timepoint between the first and last EO.
6. Statistical Analysis:
- Employ general linear models to test associations.
- Use meal timing and dietary composition variables (and their standard deviations) as predictors.
- Use glucose variables (mean glucose, MAGE, LAGE, GV) as dependent variables.
- Adjust models for total caloric intake and key nutrients.
Protocol for Optimizing Meal Ingestion Pattern to Minimize Glucose Excursions
This protocol uses a mathematical modeling approach to design and validate a glucose ingestion pattern that minimizes postprandial glycemia [70].
1. Preliminary Data Collection for Model Fitting:
- Recruit healthy volunteers.
- On separate days, administer oral glucose challenges in different patterns:
- Bolus ingestion: Rapid consumption of different glucose doses (e.g., 25g, 50g, 75g).
- Continuous ingestion: Consumption of the same doses over a prolonged period (e.g., 2 hours).
- Collect frequent blood samples to measure time-course data for blood glucose, insulin, C-peptide, GIP, and GLP-1 over a 4-hour period.
2. Mathematical Model Construction and Selection:
- Develop a system of ordinary differential equations representing the blood glucose control system, incorporating the roles of insulin and incretins (GIP, GLP-1).
- Create model variants with different mechanisms of incretin action (independent vs. cooperative with glucose).
- Fit all model variants to the individual subject's time-course data.
- Select the best-fitting model for each subject using a statistical criterion (e.g., Akaike Information Criterion - AIC).
3. Inverse Problem Solving for Pattern Optimization:
- Using the validated subject-specific model, solve the inverse problem.
- Define the objective function as minimizing the peak value of the blood glucose response.
- Computationally predict the optimal temporal pattern of glucose ingestion that achieves this objective.
4. Experimental Validation:
- Administer the predicted optimal glucose ingestion pattern (e.g., intermittent ingestion 30 minutes apart) to the same subjects.
- Measure the blood glucose response and compare the peak value against those from standard bolus and continuous ingestion patterns.
Signaling Pathways and Experimental Workflows
Pathway: Blood Glucose Regulation by Incretins
This diagram illustrates the physiological pathway by which orally ingested glucose stimulates insulin secretion through incretin hormones, a key mechanism for managing postprandial glucose levels [70].
Workflow: Free-Living CGM & Diet Correlation Study
This workflow outlines the sequence of procedures for a comprehensive observational study investigating links between diet and glucose metrics in a free-living context [67] [10].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Tools for CGM-Diet Correlation Research
| Item / Solution | Function / Application in Research | Exemplar Products / Methods (from Search Results) |
|---|---|---|
| Professional CGM System | Measures interstitial glucose concentrations every 5-15 minutes for up to 14 days, providing high-resolution data for calculating 24-h mean glucose and variability metrics. | Abbott Freestyle Libre Pro [67] |
| Automated Dietary Assessment Tool | Collects self-reported dietary intake data in a standardized, structured format to calculate nutrient composition and energy intake. | ASA24 (Automated Self-Administered 24-hour Dietary Assessment Tool) [67] |
| Image-Assisted Dietary Logging App | Captures real-time, time-stamped visual records of all caloric intake to objectively determine meal timing and eating window duration with high temporal precision. | myCircadianClock (mCC) App [67] |
| Glycemic Variability Analysis Software | Processes raw CGM data to compute established metrics of glucose control and variability, such as MAGE and standard deviation. | EasyGV Software (v8.6) [67] |
| Mathematical Modeling Framework | Used to construct and fit physiological models of glucose-insulin-incretin dynamics and to solve inverse problems for optimizing nutritional interventions. | Custom ODE Models (e.g., for predicting optimal ingestion patterns) [70] |
| Statistical Analysis Software | Performs complex statistical modeling, including general linear models and logistic regression, to test associations between dietary predictors and glucose outcomes. | SAS, IBM SPSS, STATA, R [67] [68] [38] |
Continuous Glucose Monitoring (CGM) technology has revolutionized diabetes management by providing real-time, dynamic glucose readings, enabling both patients and researchers to observe glycemic fluctuations with unprecedented detail. Factory-calibrated CGM sensors represent a significant advancement, eliminating the need for user calibration through fingerstick tests and thereby reducing management burden while improving accuracy by removing user-induced calibration errors [71]. The integration of CGM data with food intake correlation research provides invaluable insights into personalized nutrition strategies and glycemic response patterns [5] [10]. For researchers and pharmaceutical professionals, understanding the precise performance characteristics of leading factory-calibrated systems is fundamental to designing robust nutritional studies and developing effective diabetes interventions. This application note provides a comprehensive, evidence-based comparison of the latest factory-calibrated CGM sensors, with a specific focus on their application in nutritional research and dietary intervention studies.
Performance Comparison of Leading Factory-Calibrated CGM Systems
FreeStyle Libre 2 Plus and Libre 3 Plus Systems
The FreeStyle Libre 2 Plus and Libre 3 Plus systems feature an updated 15-day sensor design with minimized vitamin C interference [71]. A substantial prospective multicenter study evaluated these systems in 332 participants aged 2 years and older with type 1 or type 2 diabetes.
Quantitative Accuracy Data: The table below summarizes the key performance metrics from the clinical evaluation.
Table 1: Performance Metrics of FreeStyle Libre 2 Plus/3 Plus Systems
| Participant Group | Sample Size (with paired data) | Comparator Method | MARD (%) | % within ±20 mg/dL/20% | Hypoglycemia Performance (% within ±15 mg/dL) |
|---|---|---|---|---|---|
| Adults | 149 | YSI 2300 | 8.2% | 94.2% | 97.1% |
| Pediatric (6-17 years) | 124 | YSI 2300 | 8.1% | 94.0% | 98.0% |
| Pediatric (2-5 years) | 12 | SMBG | 11.2% | 86.6% | Not Reported |
The study employed glycemic manipulation in participants aged 11 years and older to achieve glucose levels across the sensor's measurement range (<70 mg/dL and >300 mg/dL), providing robust accuracy assessment during clinically challenging glycemic events [71]. The systems demonstrated excellent performance in the hypoglycemic range, which is critical for patient safety.
Comparative Sensor Architecture and Research Implications
The FreeStyle Libre systems utilize wired enzyme technology with glucose oxidase [71]. The sensor design was improved to reduce available electrode area for electrochemical oxidation of potential interfering compounds, thereby enhancing specificity.
The Libre 3 Plus sensor shares the same sensor element as the Libre 2 Plus but features a smaller on-body form factor [71]. This design consistency means performance data for the Libre 2 Plus is representative of the Libre 3 Plus system, an important consideration for researchers selecting monitoring equipment for nutritional studies.
Experimental Protocols for CGM Accuracy Validation
Reference Standardized Protocols for CGM Validation
The methodology cited in the FreeStyle Libre 2 Plus study provides a robust template for designing CGM validation protocols in nutritional research [71].
Table 2: Key Elements of CGM Validation Protocol
| Protocol Component | Specification | Research Application Notes |
|---|---|---|
| Study Design | Prospective, multicenter | Ensures generalizable results across diverse populations. |
| Participants | Inclusion of adults and pediatrics (age 2+); T1D and T2D | Captures age-specific and diabetes-type-specific performance. |
| In-clinic Sessions | Up to three 10-hour sessions per adult participant | Covers beginning, early middle, late middle, and end of sensor wear. |
| Comparator Measurement | YSI 2300 for venous blood; SMBG for pediatrics 2-5 years | Laboratory-standard reference method. |
| Blood Sampling Frequency | Every 15 minutes (standard); every 5 minutes when glucose <70 or >250 mg/dL | Increased sampling during glycemic extremes enhances accuracy assessment. |
| Glycemic Manipulation | Controlled food intake and insulin administration to achieve <70 or >300 mg/dL for ~1 hour | Generates data across full measurement range, which is essential for comprehensive validation. |
| Data Pairing | Sensor value closest in time to YSI blood draw (±5 minutes) | Standardizes temporal alignment for comparison. |
CGM Data Analysis in Nutritional Research
For nutritional studies utilizing CGM data, several standardized metrics and analytical approaches are essential:
- Mean Absolute Relative Difference (MARD): Calculated as the absolute value of the average percent difference between paired sensor and comparator glucose values [71].
- Consensus Error Grid Analysis: Categorizes clinical accuracy of paired glucose points across glucose ranges [71].
- Time-in-Range (TIR) Analysis: Percentage of time spent in target glucose range (typically 70-180 mg/dL) [10] [14].
- Postprandial Glycemic Response (PPGR): Calculated as incremental area under the curve (AUC) 2 hours after meals [72].
- Glycemic Variability Metrics: Includes Mean Amplitude of Glycemic Excursions (MAGE), Continuous Overall Net Glycemic Action (CONGA), and standard deviation of glucose values [10].
CGM Applications in Food Intake Correlation Research
Correlating CGM Metrics with Dietary Intake
The integration of CGM in nutritional science enables researchers to move beyond traditional glycemic indices to personalized glycemic response analysis. A study investigating correlations between CGM metrics and glycemic load (GL) or daily macronutrient consumption in 48 healthy participants found significant positive moderate correlations between GL and several CGM metrics [10].
Table 3: CGM Metrics Correlated with Dietary Parameters in Research
| Dietary Parameter | Correlated CGM Metric(s) | Correlation Strength (ρ) | Time Window |
|---|---|---|---|
| Glycemic Load (GL) | Area Under Curve (AUC) | 0.40 | 2 hours |
| Glycemic Load (GL) | Relative Amplitude | 0.40-0.42 | 3-4 hours |
| Glycemic Load (GL) | Standard Deviation (SD) | 0.41 | 4 hours |
| Glycemic Load (GL) | Variance | 0.43 | 4 hours |
| Carbohydrate Intake | Standard Deviation (SD) | 0.45 | 24 hours |
| Carbohydrate Intake | Variance | 0.44 | 24 hours |
| Carbohydrate Intake | MAGE | 0.40 | 24 hours |
These correlations demonstrate that CGM can provide objective data for estimating dietary intake, particularly valuable for overcoming limitations of self-reported food diaries [10].
Nutritional Intervention Studies Using CGM
Research utilizing CGM to monitor dietary interventions shows promising applications:
- Carbohydrate-Restricted Diets: A 2025 meta-analysis of seven studies found that carbohydrate-restricted diets (CRDs) significantly improved 24-hour mean blood glucose in patients with T2DM (effect size d = -0.51), with longer intervention durations correlating with greater benefits [38].
- Personalized Nutrition: Studies demonstrate marked interindividual differences in postprandial glucose response to identical meals, highlighting the potential for CGM-guided personalized dietary recommendations [72].
- Nutrition-Focused CGM Initiation: Research indicates that pairing nutrition information with CGM initiation helps individuals with type 2 diabetes make beneficial food choices aligned with evidence-based nutrition guidance [14].
Advanced Applications: CGM and AI Integration in Nutritional Research
Machine Learning for Predictive Glucose Modeling
The integration of artificial intelligence with CGM data creates powerful tools for nutritional research:
- Large Sensor Models: Transformer-based foundation models pretrained on massive CGM datasets (e.g., 1.6 million CGM records) can predict glucose readings with high accuracy (48.51% reduction in RMSE for 1-hour horizon prediction) [73].
- Meal Detection Algorithms: AI can identify complex patterns in CGM data to detect meal consumption and predict postprandial glucose responses based on nutritional content [74].
- Personalized Intervention Planning: Machine learning models can analyze individual glycemic responses to different foods, enabling truly personalized nutrition plans [72].
Experimental Workflow for CGM-Based Nutritional Studies
The following diagram illustrates a comprehensive research workflow integrating CGM with nutritional assessment:
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Essential Materials for CGM-Based Nutritional Research
| Item | Specification | Research Application |
|---|---|---|
| Factory-Calibrated CGM Systems | FreeStyle Libre 2 Plus/3 Plus or equivalent | Primary glucose data collection; ensure consistent performance without user calibration. |
| Clinical Reference Analyzer | YSI 2300 STAT Plus or equivalent | Gold-standard venous glucose measurement for validation studies. |
| Standardized Meal Kits | Precisely formulated macronutrient composition | Controlled nutritional challenges for PPGR assessment. |
| Digital Dietary Assessment Tools | Smartphone apps with nutrient databases | Accurate real-time food logging and nutrient analysis. |
| Activity Monitors | Research-grade accelerometers (e.g., ActiGraph) | Quantification of physical activity energy expenditure as glucose confounding factor. |
| Data Integration Platform | Custom software for temporal alignment of CGM, diet, and activity data | Synchronization of multi-modal datasets for comprehensive analysis. |
| Statistical Analysis Software | R, Python with specialized packages (e.g., 'cgmanalysis' R package) | Standardized CGM metric extraction and statistical modeling [5]. |
Factory-calibrated CGM sensors, particularly the FreeStyle Libre 2 Plus and Libre 3 Plus systems, demonstrate high accuracy (MARD 8.1-8.2% in adults and children) with reliable performance across glycemic ranges, making them suitable for clinical research and nutritional studies [71]. The integration of these sensors in dietary research enables objective assessment of glycemic responses to nutritional interventions, providing valuable insights beyond traditional glycemic indices. Standardized experimental protocols, including appropriate comparator methods and glycemic manipulation techniques, are essential for generating valid, generalizable results. The growing integration of AI and machine learning with CGM data further enhances the potential for personalized nutrition approaches, creating new opportunities for precision medicine in diabetes management.
Continuous Glucose Monitoring (CGM) is transitioning from a tool for diabetes management to a valuable technology for metabolic research in healthy populations and athletes. This shift necessitates the development and validation of more nuanced metrics to describe individual glucose responses to specific lifestyle stimuli, such as food intake, exercise, and stress [75] [76]. Traditional CGM metrics like time-in-range (TIR) and average glucose, while useful for aggregated data overviews, offer limited utility for analyzing discrete physiological events [76]. This Application Note details the validation and application of novel kinetic parameters, with a focus on the Glucose Recovery Time to Baseline (GRTB), for use in research correlating CGM data with food intake and other interventions. These metrics provide a standardized framework for quantifying dynamic glucose responses, enabling deeper insights into metabolic health and the impact of nutritional and lifestyle interventions [75].
Research under standardized conditions has quantified glucose responses using several key metrics. The following table summarizes typical values observed in healthy young adults under various controlled interventions, providing a reference for expected outcomes.
Table 1: Quantitative Glucose Response Metrics to Standardized Interventions in Healthy Young Adults
| Intervention Type | Glucose Excursion (mg/dL) | Maximum Glucose (cmax) | GRTB (minutes) | AUC₀–₄ (mg/dL·h) | Time to Max Glucose (tmax, minutes) |
|---|---|---|---|---|---|
| Anaerobic Exercise | 28.7 ± 21.46 [76] | Data not specified | Data not specified | Data not specified | Data not specified |
| Aerobic Exercise | 8.8 ± 4.91 [76] | Data not specified | Data not specified | Data not specified | Data not specified |
| Carbohydrate-Rich Food | 161.4 ± 15.59 [76] | Data not specified | Data not specified | Data not specified | Data not specified |
| Psychosocial Stress (TSST) | Significant increase (p=0.0113) [75] | Data not specified | Data not specified | Data not specified | Data not specified |
Table 2: Correlation of CGM Metrics with Glycemic Load (GL) and Carbohydrate Intake
| CGM Metric | Correlation with Meal GL (ρ) | Correlation with 24h Carbohydrate Intake (ρ) | Observation Window |
|---|---|---|---|
| Area Under the Curve (AUC) | 0.40 [10] | Not specified | 2 hours |
| Relative Amplitude | 0.42 [10] | Not specified | 4 hours |
| Standard Deviation (SD) | 0.41 [10] | 0.45 [10] | 4 hours / 24 hours |
| Variance | 0.43 [10] | 0.44 [10] | 4 hours |
| Mean Amplitude of Glycemic Excursions (MAGE) | Not specified | 0.40 [10] | 24 hours |
Experimental Protocol for Validating GRTB and Kinetic Parameters
The following protocol is adapted from the CGM-HYPE study, an exploratory clinical trial designed to provide reference data on glucose responses in healthy young adults [75] [76].
Study Design and Participant Selection
- Design: A single-arm, exploratory, interventional clinical trial with each participant serving as their own control.
- Participants: Recruit healthy, young adults (e.g., aged ≥18 and <40 years) with a BMI between 18.5 and 30 kg/m² and normal glucose tolerance confirmed by a fasting blood glucose <100 mg/dL and a 2h-OGTT <140 mg/dL [76].
- Exclusion Criteria: Smokers, individuals with diabetes, eating disorders, cognitive or physical impairments, or any chronic disease affecting glucose metabolism. Exclude those taking drugs with metabolic effects (e.g., glucocorticoids) [76].
Equipment and Reagents
Table 3: Research Reagent Solutions and Essential Materials
| Item | Specification / Example | Primary Function in Protocol |
|---|---|---|
| CGM System | FreeStyle Libre 3 (MARD: 7.8%) [76] | Measures interstitial glucose concentrations continuously every 1-15 minutes. |
| Glucometer | ContourNext [76] | Provides capillary blood glucose measurements for point-of-care verification (e.g., fasting glucose, OGTT). |
| Standardized Challenges | High-carbohydrate food, Aerobic exercise, Anaerobic exercise, Trier Social Stress Test (TSST) [75] | Serve as controlled, repeatable stimuli to elicit measurable glucose responses. |
| Data Logging Tools | Electronic food diary, Activity log [76] | For precise timestamping of interventions and participant activities. |
| CGM Data Analysis Software | Custom scripts (e.g., in R or Python) or commercial AGP software | To extract raw CGM data and compute kinetic metrics (AUC, GRTB, etc.). |
Procedural Workflow
- Sensor Deployment: Apply a CGM sensor (e.g., FreeStyle Libre 3) to the upper arm according to the manufacturer's instructions. The sensor should be worn for a sufficient period to establish baseline patterns (e.g., 14 days) [76].
- Baseline Establishment: Calculate the individual's Continuous Glucose Baseline (24h-CGB). Evidence suggests using the 40th percentile of CGM data from the previous 24 hours provides a robust and generalizable estimate of basal glucose levels at any time of day, superior to a single fasting measurement [77].
- Standardized Interventions: Over the monitoring period, participants complete a series of standardized challenges, each followed by a 4-hour observational window [75] [76].
- Dietary Challenge: Consume a meal with a defined macronutrient composition (e.g., rich in carbohydrates).
- Exercise Challenges: Perform controlled sessions of aerobic (e.g., steady-state running) and anaerobic (e.g., high-intensity interval training) exercise.
- Stress Challenge: Administer the Trier Social Stress Test (TSST) to induce psychobiological stress.
- Data Annotation: Participants meticulously log the start time of each intervention. For dietary challenges, the type and amount of food (carbohydrates, proteins, fats) must be recorded [76].
- Data Extraction and Metric Calculation: For each intervention, extract the CGM data for the 4-hour post-challenge period. Calculate the following metrics relative to the pre-challenge baseline (24h-CGB) [75] [76]:
- AUC₀–₄: The total area under the glucose curve from 0 to 4 hours.
- Max Glucose (cmax): The highest glucose value recorded.
- Glucose Excursion: The numerical difference between cmax and the baseline.
- Time to Max Glucose (tmax): The time from the start of the intervention until cmax is reached.
- Glucose Recovery Time to Baseline (GRTB): The time required for glucose levels to first return to and stabilize at the pre-challenge baseline level after the excursion.
Data Analysis and Validation
- Use appropriate statistical tests (e.g., repeated measures ANOVA, paired t-tests) to compare metric values across different intervention types [75] [76].
- Validate the GRTB metric by assessing its correlation with other established metrics (e.g., AUC, glucose excursion) and its sensitivity in differentiating between intervention types (e.g., anaerobic vs. aerobic exercise) [75].
Visualization of Metric Analysis Workflow
The diagram below outlines the logical workflow for processing CGM data to calculate and interpret the kinetic parameters, including GRTB.
The Glucose Recovery Time to Baseline (GRTB), alongside other kinetic parameters like AUC, cmax, and tmax, provides a powerful and standardized methodology for quantifying dynamic glucose responses in nutritional and metabolic research [75]. The experimental protocol outlined here offers a validated framework for applying these metrics to investigate the impact of diet, physical activity, and stress on glucose metabolism in both healthy and clinical populations. The adoption of a continuous glucose baseline (24h-CGB) further enhances the robustness of incremental calculations [77]. This toolkit enables researchers and drug development professionals to move beyond static glycemic measures, facilitating a more detailed understanding of individual metabolic phenotypes and the efficacy of interventions.
Conclusion
The integration of CGM with food intake data provides an unprecedented, high-resolution view of glycemic physiology, offering powerful tools for both clinical research and drug development. Foundational studies confirm that CGM is effective for guiding lifestyle interventions and capturing significant responses to dietary challenges. Methodological advances, particularly Functional Data Analysis, allow for a more nuanced understanding of postprandial glucose regulation beyond traditional scalar metrics. The validation of CGM through meta-analyses and its growing acceptance as a primary endpoint in clinical trials underscore its reliability and clinical relevance. Future directions should focus on standardizing analytical approaches across studies, establishing the prognostic value of novel CGM metrics for long-term outcomes, and further exploring personalized nutrition strategies based on individual glycemic phenotypes to inform next-generation therapies.
References
- 1. Protocol of a series of N-of-1 trials for exploring ... [https://www.sciencedirect.com/science/article/pii/S2475299125030379]
- 2. Protocol of a Series of N-of-1 trials for Exploring ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12639426/]
- 3. Predicting postprandial glucose excursions to personalize ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12271334/]
- 4. The effects of carbohydrate-restricted diets on 24-h mean ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12537420/]
- 5. Associations of diet composition and quality with ... [https://www.sciencedirect.com/science/article/pii/S0002916525004435]
- 6. Physiological processes induced by different types of ... [https://pubmed.ncbi.nlm.nih.gov/40687587/]
- 7. Continuous Glucose Measurements for Diet Monitoring in ... [https://pubmed.ncbi.nlm.nih.gov/40792561/]
- 8. Acute effects of exercise snacks on postprandial glucose ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1708301/full]
- 9. Leveraging continuous glucose monitoring as a catalyst for ... [https://ijbnpa.biomedcentral.com/articles/10.1186/s12966-024-01622-6]
- 10. Continuous Glucose Measurements for Diet Monitoring in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12343543/]
- 11. Continuous Glucose Monitoring As a Behavior Modification ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7164990/]
- 12. Experience of Using Wearable Devices for Dietary ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12490776/]
- 13. Stelo Wearable Glucose Biosensor | OTC CGM | Stelo by ... [https://www.stelo.com/en-us?srsltid=AfmBOopX4-rwPV8YXYEtPYbz8E7_RHTbm9tReUW_Lbv2nc05fGGLB5e_]
- 14. “Now I can see it works!” Perspectives on Using a Nutrition ... [https://diabetes.jmir.org/2025/1/e67636]
- 15. Functional Data Analysis of Postprandial Continuous ... [https://arxiv.org/html/2405.14690v2]
- 16. More Green, Less Red: How Color Standardization May ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8875060/]
- 17. Effects of carbohydrate-restricted diets and macronutrient ... [https://www.sciencedirect.com/science/article/pii/S0002916525005283]
- 18. Effects of carbohydrate-restricted diets and macronutrient ... [https://pubmed.ncbi.nlm.nih.gov/40935153/]
- 19. The effects of carbohydrate-restricted diets on 24-h mean ... [https://pubmed.ncbi.nlm.nih.gov/41127101/]
- 20. Carbohydrate-restricted diet types and macronutrient ... [https://www.sciencedirect.com/science/article/pii/S0261561425002535]
- 21. Effect of carbohydrate restriction on body weight in overweight ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10731359/]
- 22. Effects of Continuous Glucose Monitoring Versus Blood ... [https://www.sciencedirect.com/science/article/pii/S1530891X25008985]
- 23. Feasibility Study of a Low-Carbohydrate/Time-Restricted ... [https://pubmed.ncbi.nlm.nih.gov/38436633/]
- 24. Dietary carbohydrate restriction improves insulin sensitivity ... [https://pubmed.ncbi.nlm.nih.gov/24176230/]
- 25. Dietary carbohydrate restriction improves insulin sensitivity ... [https://www.sciencedirect.com/science/article/abs/pii/S0271531713001863]
- 26. A standardized method for quantifying consistent individual ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5493478/]
- 27. Challenges in measuring individual differences of brain function [https://pmc.ncbi.nlm.nih.gov/articles/PMC12319922/]
- 28. Laboratory Protocol and Pilot Results for Dynamic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10899833/]
- 29. Equipment for Experimental Protocols [https://www.medschool.umaryland.edu/davislab/research-facilities/equipment-for-experimental-protocols/]
- 30. Multilevel functional data analysis modeling of human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11142320/]
- 31. Divergent hypoglycemic and hyperglycemic responses to ... [https://www.sciencedirect.com/science/article/pii/S0261561424004175]
- 32. Reproducibility of continuous glucose monitoring results ... [https://www.nature.com/articles/s41598-023-40949-1]
- 33. Modeling continuous glucose monitoring (CGM) data ... [https://www.semanticscholar.org/paper/Modeling-continuous-glucose-monitoring-(CGM)-data-Gaynanova-Punjabi/d563aeb34f3fd92e0137d8280422c7b08955c968]
- 34. Core Glycemic Metrics Explained. TIR, TBR, TAR, GMI, CV, ... [https://www.adces.org/education/danatech/glucose-monitoring/continuous-glucose-monitors-(cgm)/glycemic-metrics--an-overview]
- 35. CGM & Time in Range [https://diabetes.org/about-diabetes/devices-technology/cgm-time-in-range]
- 36. CGM Data Analysis 2.0: Functional Data Pattern Recognition ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12356821/]
- 37. Three components of glucose dynamics – value, variability ... [https://elifesciences.org/reviewed-preprints/102860/reviews]
- 38. The effects of carbohydrate-restricted diets on 24-h mean ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1670022/full]
- 39. Continuous Glucose Monitoring to Guide Lifestyle Choices ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12536011/]
- 40. Evaluation of a Continuous Glucose Monitoring Based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12579156/]
- 41. The Application of Continuous Glucose Monitoring Endpoints in Clinical Research: Analysis of Trends and Review of Challenges - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11603422/]
- 42. Continuous glucose monitoring and metrics for clinical trials: an international consensus statement - PubMed [https://pubmed.ncbi.nlm.nih.gov/36493795/]
- 43. An exploratory clinical trial | PLOS Digital Health [https://journals.plos.org/digitalhealth/article?id=10.1371/journal.pdig.0001087]
- 44. Design of a randomized cross-over study evaluating effects of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10041710/]
- 45. Interpreting Continuous Glucose Monitoring (CGM) Data [https://ade.adea.com.au/interpreting-continuous-glucose-monitoring-cgm-data/]
- 46. JMIR Diabetes - Continuous Glucose Monitoring in Primary Care: Multidisciplinary Pilot Implementation Study [https://diabetes.jmir.org/2025/1/e69061]
- 47. Associations between Timing and Duration of Eating and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9919634/]
- 48. Delayed Eating Schedule Raises Mean Glucose Levels in ... [https://www.sciencedirect.com/science/article/pii/S0022316622137703]
- 49. How to analyse CGM data: A structured and practical ... [https://diabetesonthenet.com/journal-diabetes-nursing/how-analyse-cgm-data-structured-and-practical-approach/]
- 50. Continuous glucose monitoring for automatic real-time ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10804456/]
- 51. Transformative Advances in Continuous Glucose ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12007415/]
- 52. Benefits and Limitations of MARD as a Performance Parameter for... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7189145/]
- 53. LIFE: Improved chemistry successfully tested in... — TradingView News [https://www.tradingview.com/news/reuters.com,2025-02-04:newsml_MFNbjKKPh:0-life-improved-chemistry-successfully-tested-in-sensor/]
- 54. SNAQ - Blog [https://www.snaq.ai/blog/cgm-accuracy-comparison-2025-dexcom-g7-vs-freestyle-libre-3-vs-medtronic-simplera]
- 55. Next-generation CGM with 15-day sensor improves upon previous... [https://www.healio.com/news/endocrinology/20250324/nextgeneration-cgm-with-15day-sensor-improves-upon-previous-generations-accuracy]
- 56. Dexcom’s 15-day CGM Adds Wear Time, Accuracy to Current G7 [https://www.medscape.com/viewarticle/dexcoms-15-day-cgm-adds-wear-time-accuracy-current-g7-2025a10006y3]
- 57. 5 Best Continuous Glucose Monitors for 2025 : Most Accurate Devices... [https://www.type1strong.org/blog-post/5-best-continuous-glucose-monitors-for-2025]
- 58. Comparing glucose monitoring methods: efficiency insights ... [https://www.frontiersin.org/journals/clinical-diabetes-and-healthcare/articles/10.3389/fcdhc.2025.1517161/full]
- 59. CGM Device Comparison [https://pro.aace.com/cgm/toolkit/cgm-device-comparison]
- 60. DASH Diet Modified for Diabetes Lowers Blood Sugar Levels ... [https://publichealth.jhu.edu/2025/dash-diet-modified-for-diabetes-lowers-blood-sugar-levels-in-clinical-trial-of-adults-with-type-2-diabetes]
- 61. a pilot scientific dataset for personalized nutrition and diet ... [https://www.nature.com/articles/s41597-025-05851-7]
- 62. Discrepancies between current displayed and auto‐logged ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12587223/]
- 63. CGM l Interpreting Patient Data l danatech [https://www.adces.org/education/danatech/glucose-monitoring/continuous-glucose-monitors-(cgm)/cgms-in-professional-practice/interpreting-cgm-patient-data]
- 64. Safety and Functional Integrity of Continuous Glucose ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10658671/]
- 65. Artifacts Summary - Continuous Glucose Monitoring v1.0.0 [https://build.fhir.org/ig/HL7/cgm/artifacts.html]
- 66. Continuous Glucose Monitoring to Guide Lifestyle Choices ... [https://pubmed.ncbi.nlm.nih.gov/41109846/?utm_source=FeedFetcher&utm_medium=rss&utm_campaign=None&utm_content=0VA3dou2iwoJ-0iNw6nHb_mbTQWBx4eCDN-S3AIHrOp&fc=None&ff=20251023170332&v=2.18.0.post22+67771e2]
- 67. Diet and Meal Pattern Determinants of Glucose Levels ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11085124/]
- 68. Using Multiple Statistical Methods to Derive Dietary Patterns ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9381206/]
- 69. The Relationship between Dietary Patterns and High Blood ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9570980/]
- 70. Logical design of oral glucose ingestion pattern minimizing ... [https://www.nature.com/articles/s41540-019-0108-1]
- 71. Accuracy of a 15-day Factory-Calibrated Continuous ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11977615/]
- 72. Use of Machine Learning to Predict Individual Postprandial ... [https://www.researchprotocols.org/2025/1/e59308]
- 73. A large sensor foundation model pretrained on continuous ... [https://www.nature.com/articles/s44401-025-00039-y]
- 74. Continuous glucose monitoring combined with artificial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12146165/]
- 75. under standardised conditions... Continuous Glucose Monitoring [https://pubmed.ncbi.nlm.nih.gov/41237124/]
- 76. Continuous Glucose Monitoring under standardised ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12617953/]
- 77. Defining a Continuous Glucose Baseline to assess ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10425768/]