Energy Efficiency in Continuous Dietary Monitoring: Technologies, Applications, and Clinical Validation for Metabolic Research
This article examines the critical role of continuous dietary monitoring in understanding human energy metabolism and its application in clinical research and drug development.
Energy Efficiency in Continuous Dietary Monitoring: Technologies, Applications, and Clinical Validation for Metabolic Research
Abstract
This article examines the critical role of continuous dietary monitoring in understanding human energy metabolism and its application in clinical research and drug development. It explores the foundational science of energy balance, the current landscape of digital and biomarker-based monitoring technologies, and strategies for optimizing data accuracy and patient adherence. A comparative analysis validates the efficacy of these tools for managing metabolic diseases, with a specific focus on their utility in weight management, diabetes research, and the evaluation of emerging therapeutics like GLP-1 receptor agonists. The synthesis provides a roadmap for researchers and drug development professionals to leverage these tools for robust, data-driven nutritional science.
The Science of Energy Balance and the Imperative for Continuous Monitoring
Fundamental Concepts and Definitions
Energy Balance is the state achieved when the energy consumed as food and drink (Energy Intake) equals the total energy expended by the body (Energy Expenditure) over a defined period. A positive energy balance (intake > expenditure) leads to weight gain, while a negative energy balance (intake < expenditure) results in weight loss [1] [2].
Energy Intake (EI) is the total energy provided by the macronutrients (carbohydrates, fats, proteins, and alcohol) consumed in the diet.
Energy Expenditure (EE) is the total energy an individual utilizes each day, comprising several components [3] [2]:
- Resting Energy Expenditure (REE) or Basal Metabolic Rate (BMR): The energy required to maintain fundamental physiological functions at rest. This is the largest component of total daily energy expenditure [2].
- Thermic Effect of Food (TEF) or Diet-Induced Thermogenesis (DIT): The energy cost of digesting, absorbing, and storing consumed nutrients [2].
- Activity Energy Expenditure (AEE): The energy cost of physical activity, which can be further divided into:
- Exercise Activity Thermogenesis (EAT): Energy expended during voluntary exercise.
- Non-Exercise Activity Thermogenesis (NEAT): Energy expended for all other physical activities, such as walking, talking, and fidgeting [2].
Adaptive Thermogenesis (AT) is a physiological adaptation characterized by a change in energy expenditure that is independent of changes in body composition (fat mass and fat-free mass) or physical activity levels. During weight loss, it manifests as a reduction in energy expenditure beyond what is predicted, thereby conserving energy and opposing further weight loss [4].
Key Quantitative Values of Energy Expenditure Components
Table 1: Typical contribution of different components to total daily energy expenditure in sedentary individuals.
| Component of Expenditure | Typical Contribution (%) | Description |
|---|---|---|
| Basal Metabolic Rate (BMR) | 60-75% | Energy for core bodily functions at rest [2] |
| Thermic Effect of Food (TEF) | ~10% | Energy cost of processing food (adjusted for thermic effect) [4] |
| Non-Exercise Activity Thermogenesis (NEAT) | Highly variable | Energy from spontaneous daily activities [2] |
Frequently Asked Questions (FAQs) and Troubleshooting
FAQ 1: In our dietary intervention study, we observe that weight loss plateaus despite maintained caloric restriction. Is this a methodological error or an expected physiological response?
Answer: This is an expected physiological response, largely driven by Adaptive Thermogenesis. As individuals lose weight, their body resists further weight loss through several mechanisms [2] [4]:
- Decreased Resting Energy Expenditure: A reduction in REE occurs that is greater than what would be expected from the loss of fat and fat-free mass alone [4].
- Increased Metabolic Efficiency: The body becomes more efficient at utilizing energy, thereby reducing overall energy expenditure.
- Potential Hormonal Changes: Changes in hormones like leptin and ghrelin can increase hunger and reduce energy expenditure.
Troubleshooting Guide:
- Confirm Phenomenon: Measure REE via indirect calorimetry before and after weight loss and compare it to predicted values based on new body composition to quantify adaptive thermogenesis [4].
- Adjust Energy Prescription: Recognize that a fixed caloric intake will not produce continuous linear weight loss. Energy intake targets may need to be recalculated periodically based on the new, lower energy expenditure.
- Manage Expectations: Inform study participants that weight loss plateaus are a normal part of the process and not necessarily a sign of non-adherence.
FAQ 2: What are the primary sources of measurement error when calculating energy balance in free-living human subjects?
Answer: Accurately measuring all components of energy balance is notoriously challenging. The main sources of error are [5]:
- Energy Intake Measurement: Self-reported dietary intake (e.g., 24-hour recalls, food diaries) is frequently subject to under-reporting and misrepresentation, making it the most unreliable component in energy balance equations.
- Energy Expenditure Measurement: While the Doubly Labeled Water (DLW) method is the gold standard for measuring Total Energy Expenditure (TEE) in free-living individuals, it has limitations. It requires sophisticated equipment for analysis, is expensive, and its accuracy can be influenced by the estimate of the food quotient used in calculations [3] [5].
- Body Composition Measurement: Predictive equations for body composition based on anthropometrics (like skinfold thickness) can have large individual-level errors compared to gold-standard methods like the 4-component model, leading to inaccurate estimates of energy stores [5].
Troubleshooting Guide:
- Mitigate Intake Error: Use multiple, non-consecutive 24-hour recalls administered by trained interviewers. When possible and ethically permissible, provide all food to participants to achieve precise intake data [3] [5].
- Validate Expenditure: Ensure DLW measurements are conducted with strict protocol adherence, including background urine samples and proper dose administration [3].
- Use Gold-Standard Body Comp: For high-precision studies, use DXA or a 4-component model instead of predictive equations to track changes in fat and fat-free mass [3].
FAQ 3: Are there new technologies that can automate and improve the accuracy of dietary intake monitoring?
Answer: Yes, the field of Automatic Dietary Monitoring (ADM) is rapidly evolving to address the limitations of self-report. Emerging technologies include [6]:
- Wearable Bio-Sensors: Devices like the
iEatwrist-worn sensor use bio-impedance to detect unique electrical patterns created by hand-to-mouth gestures and interactions with food and utensils, allowing for recognition of food intake activities and types. - Acoustic Sensors: Wearable microphones (e.g., on the neck) can detect sounds associated with chewing and swallowing.
- Image-Based Methods: Smartphone applications that use photos to identify foods and estimate portion sizes.
Troubleshooting Guide:
- Contextual Limitations: Bio-impedance wearables may struggle to differentiate between foods with similar electrical properties. Acoustic sensors can be affected by ambient noise.
- Validation is Key: Any new ADM technology must be validated against established methods (e.g., weighed food records) in the specific population of interest before use in research [6].
- Multi-Sensor Approach: The highest accuracy may be achieved in the future by combining data from multiple sensors (e.g., inertial measurement units for gesture recognition and acoustic sensors for swallowing detection).
Experimental Protocols for Key Measurements
Protocol 1: Measuring Adaptive Thermogenesis in a Clinical Trial
This protocol is based on a study investigating the effects of probiotics on adaptive thermogenesis during continuous energy restriction [4].
1. Objective: To determine whether an intervention (e.g., probiotic supplementation) attenuates adaptive thermogenesis induced by a hypocaloric diet in adults with obesity.
2. Study Design:
- Type: Randomized, double-blind, placebo-controlled clinical trial.
- Population: Adult males with obesity (BMI 30.0–39.9 kg/m²), weight-stable.
- Intervention:
- Control Group (CERPLA): Continuous Energy Restriction (CER) + Placebo.
- Intervention Group (CERPRO): Continuous Energy Restriction (CER) + Probiotic.
- Dietary Protocol:
- CER set at 30% below Total Daily Energy Expenditure (TDEE).
- TDEE calculated as: [Measured REE × Physical Activity Factor (1.5)] + Thermic Effect of Food (10%) [4].
3. Key Measurements and Methods:
- Resting Energy Expenditure (REE): Measured via indirect calorimetry after an overnight fast at baseline and after the intervention.
- Body Composition: Assessed using DXA or other precise methods at baseline and post-intervention to measure changes in Fat Mass (FM) and Fat-Free Mass (FFM).
- Calculation of Adaptive Thermogenesis:
- Step 1: Predict REE at follow-up using a regression equation derived from baseline data, incorporating the new FFM and FM.
- Step 2: Calculate adaptive thermogenesis as: REE (measured) - REE (predicted).
- A significant negative value (e.g., -129 ± 169 kcal) indicates the presence of adaptive thermogenesis [4].
Protocol 2: Comprehensive Energy Balance Assessment (POWERS Study Model)
This protocol outlines the methodology for a longitudinal study of the weight-reduced state [3].
1. Objective: To understand physiological contributors to weight regain by examining energy intake and expenditure phenotypes before and after behavioral weight loss.
2. Study Design:
- Type: Longitudinal cohort study.
- Population: Adults with obesity (BMI 30-<40 kg/m²).
- Phases:
- Weight Loss: Supervised behavioral intervention until ≥7% weight loss.
- Weight-Reduced State: Follow-up with no intervention support at 4 months (T4) and 12 months (T12).
- Crucial Requirement: Weight stability is required immediately before baseline (pre-weight loss) and post-weight loss (T0) measurement periods.
3. Key Measurements and Timelines: Table 2: Measurement schedule for the POWERS study design [3].
| Measurement | Baseline (BL) | Post-WL (T0) | 4-Month FU (T4) | 12-Month FU (T12) |
|---|---|---|---|---|
| Body Weight & Composition (DXA) | Yes | Yes | Yes | Yes |
| Total Energy Expenditure (DLW) | Yes | Yes | Yes | Yes |
| Resting Energy Expenditure | Yes | Yes | Yes | Yes |
| Energy Intake (Serial DLW) | Yes | Yes | Yes | Yes |
| 24-Hour Food Recalls | Yes | Yes | Yes | Yes |
| Muscle Efficiency | Yes | Yes | Not specified | Not specified |
4. Methodological Details:
- Doubly Labeled Water (DLW) for TEE & EI:
- Participants receive an oral dose of H218O and D2O.
- Urine samples are collected at baseline, over a 14-day period, and analyzed for isotope elimination rates.
- CO2 production is calculated, and TEE is derived using an established equation.
- Energy Intake is calculated as an average over the 14-day period from changes in body energy stores (measured by DXA) plus TEE [3].
- Energy Expenditure Components: Resting Energy Expenditure (REE) is measured by indirect calorimetry. Non-Resting Energy Expenditure (NREE) is calculated as TEE - REE [3].
Essential Research Reagents and Materials
Table 3: Key materials and equipment for energy balance research.
| Item | Function in Research | Example / Specification |
|---|---|---|
| Doubly Labeled Water (DLW) | Gold-standard method for measuring total energy expenditure in free-living individuals over 1-2 weeks [3]. | H218O (10 atom % excess) and D2O (5 atom % excess) [3]. |
| Dual-Energy X-ray Absorptiometry (DXA) | Precisely measures body composition (fat mass, fat-free mass, bone mass) to calculate energy stores [3]. | - |
| Indirect Calorimetry System | Measures resting energy expenditure and substrate utilization by analyzing oxygen consumption and carbon dioxide production [2] [4]. | - |
| Stable Isotope Analyzer | Analyzes isotope enrichment in biological samples (e.g., urine) for DLW studies [3]. | Off-axis integrated cavity output spectroscopy [3]. |
| Bio-impedance Sensor (Research) | Emerging tool for automatic dietary monitoring by detecting gestures and food interactions via electrical impedance [6]. | e.g., iEat wearable with electrodes on each wrist [6]. |
| Current Transformers (CTs) | For industrial energy monitoring; measure electrical current in conductors for facility energy audits [7]. | - |
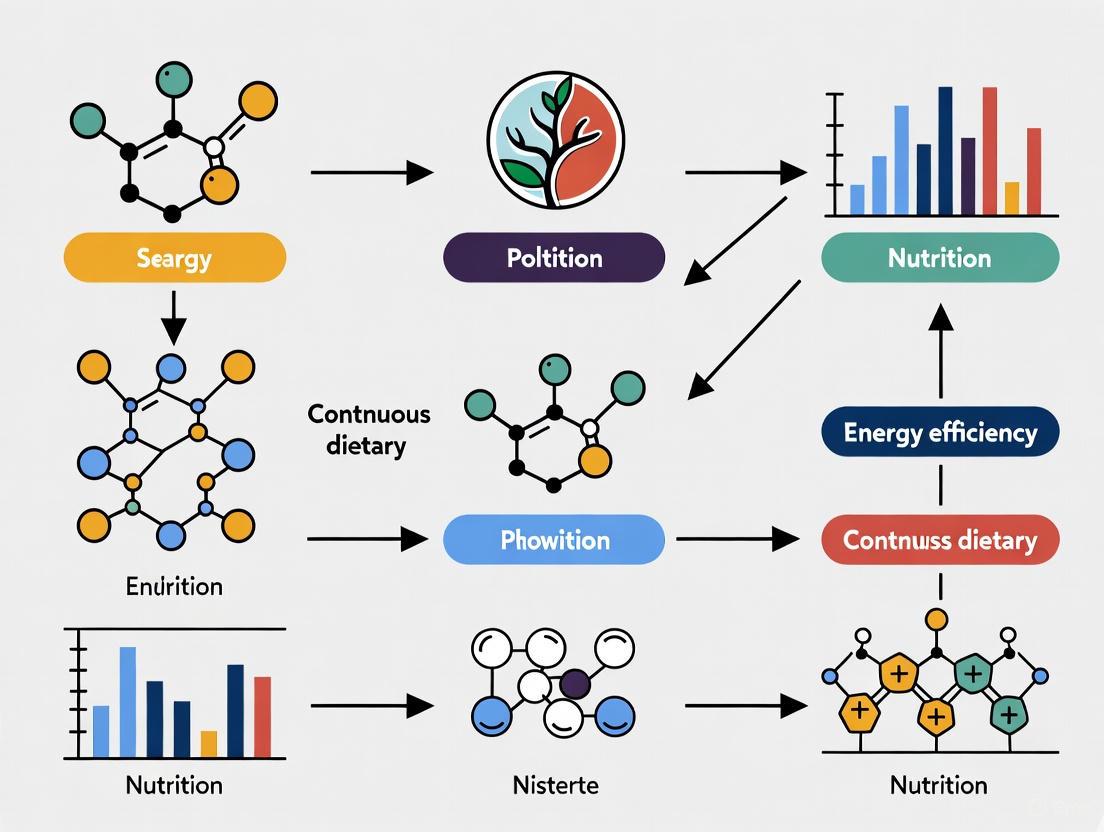
Visualizing Energy Balance and Experimental Workflow
Energy Balance and Adaptive Thermogenesis
Diagram 1: The human energy balance system. A negative energy balance (weight loss) can trigger Adaptive Thermogenesis, which reduces Energy Expenditure, creating a physiological counter-response that favors weight regain.
Adaptive Thermogenesis Measurement Protocol
Diagram 2: Workflow for a clinical trial measuring adaptive thermogenesis. The key calculation involves comparing measured REE post-intervention to the REE predicted from the new body composition.
The Limitations of Traditional Dietary Assessment Methods
Accurate dietary assessment is fundamental to nutrition research, public health monitoring, and the development of evidence-based dietary guidelines [8]. However, traditional methods for measuring dietary intake are notoriously challenging and subject to significant measurement error, which poses a substantial impediment to scientific progress in the fields of obesity and nutrition research [8] [9]. These limitations are particularly critical when investigating energy efficiency and conducting continuous dietary monitoring, as inaccuracies in core intake data can compromise the entire research endeavor. This technical support center outlines the specific limitations of traditional dietary tools, provides troubleshooting guidance for researchers encountering these issues, and details protocols for mitigating error in dietary assessment experiments.
FAQ: Core Concepts for Researchers
Q1: What are the primary categories of traditional dietary assessment methods? Traditional methods can be broadly categorized into retrospective and prospective tools [10]. Retrospective methods, such as 24-hour recalls and Food Frequency Questionnaires (FFQs), rely on a participant's memory of past intake. Prospective methods, primarily food records or diaries, require the participant to record all foods and beverages as they are consumed [8] [10].
Q2: Why is the assessment of energy intake uniquely challenging? Energy intake is tightly regulated by physiological controls, resulting in low between-person variation after accounting for weight and demographic variables [11]. Furthermore, the deviations from energy balance that lead to clinically significant weight changes are very small (on the order of 1-2% of daily intake), meaning that assessment tools require extreme precision to detect these differences, a level of accuracy that current self-report methods typically fail to achieve [11].
Q3: What is the "gold standard" for validating energy intake assessment? The Doubly Labeled Water (DLW) method is considered the reference method for measuring total energy expenditure (TEE) in free-living, weight-stable individuals [12]. It provides an objective measure against which self-reported energy intake can be validated, as in a state of energy balance, intake should equal expenditure [12].
Q4: How does participant burden affect dietary data quality? Participant burden is a major source of error. High burden can lead to non-participation bias, where certain population groups are underrepresented, and a decline in data quality over the recording period [8] [10]. In food records, burden often causes reactivity, where participants alter their usual diet—either by choosing simpler foods or by eating less—because they are required to record it [8] [10].
Troubleshooting Guide: Common Experimental Issues & Solutions
Table 1: Limitations and Methodological Solutions in Dietary Assessment
| Problem Area | Specific Issue | Signs to Detect the Issue | Corrective & Preventive Actions |
|---|---|---|---|
| Measurement Error | Systematic under-reporting of energy intake [12]. | Reported energy intake is significantly lower than Total Energy Expenditure from DLW; implausibly low energy intake relative to body weight [11] [12]. | Use multiple, non-consecutive 24-hour recalls to capture day-to-day variation [8]. Integrate recovery biomarkers (e.g., DLW, urinary nitrogen) to quantify and adjust for measurement error [8] [12]. |
| Participant Reactivity | Participants change diet during monitoring [10]. | A marked decline in reported intake or complexity of foods recorded after the first day of a multi-day food record. | Use unannounced 24-hour recalls to capture intake without prior warning [8]. For food records, include a run-in period to habituate participants to the recording process. |
| Nutrient Variability | High day-to-day variability in nutrient intake obscures habitual intake [8]. | High within-person variation for nutrients like Vitamin A, Vitamin C, and cholesterol, making a few days of records non-representative [8]. | Increase the number of short-term assessments (e.g., multiple 24HRs over different seasons) and use statistical adjustment (e.g., the National Cancer Institute's method) to estimate usual intake [8]. |
| Study Design Complexity | Difficulty defining an appropriate control group in Dietary Clinical Trials (DCTs) [13]. | Lack of a well-formulated placebo for dietary interventions; high collinearity between dietary components [13]. | Carefully match control and intervention groups for key confounders. Use a sham intervention or wait-list control where possible. Account for collinearity in the statistical analysis plan [13]. |
Experimental Protocols for Method Validation
Protocol 1: Controlled Feeding Study for Validation Against True Intake
This protocol validates a dietary assessment method by comparing estimated intake to known, weighed intake under controlled conditions [14].
- Participant Recruitment & Randomization: Recruit a sufficient sample size (e.g., N=150+) representing the target population. Randomize participants to different feeding days or menus to account for order and menu effects [14].
- Food Preparation & Serving: Prepare all meals and beverages in a metabolic kitchen. Weigh all food and beverage items using high-precision digital scales before serving. Use a crossover design where participants consume different controlled meals on separate days [14].
- Dietary Intake Estimation: On the day following the controlled feeding, administer the dietary assessment method being validated (e.g., an automated 24-hour recall like ASA24 or Intake24) [14].
- Data Analysis: Compare the estimated energy and nutrient intakes from the dietary tool to the true, weighed intakes. Calculate the mean difference (bias) and the limits of agreement. Use linear mixed models to assess differences among methods while accounting for repeated measures [14].
Protocol 2: Validation Against the Doubly Labeled Water (DLW) Method
This protocol assesses the validity of self-reported Energy Intake (EI) in free-living individuals [12].
- Baseline Assessment: Measure participant height, weight, and body composition. Collect a baseline urine sample.
- DLW Administration: Administer a dose of doubly labeled water (²H₂¹â¸O) based on the participant's body weight according to standardized equations [12].
- Urine Collection: Collect urine samples over a period of 7-14 days to account for day-to-day variation in physical activity. The specific collection schedule (e.g., daily, on days 1, 7, and 14) depends on the study protocol [12].
- Dietary Assessment: During the DLW measurement period, administer the self-report dietary method(s) under investigation (e.g., 7-day food record, multiple 24-hour recalls) [12].
- Laboratory & Data Analysis: Analyze urine samples for isotopic enrichment to calculate Total Energy Expenditure (TEE). In weight-stable individuals, TEE is equivalent to energy intake. Compare self-reported EI to TEE from DLW to determine the degree of misreporting (under- or over-reporting) [12].
Visualization of Method Selection & Error Pathways
Diagram 1: Dietary Assessment Method Selection
Diagram 2: Error Pathways in Traditional Self-Report
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Tools for Advanced Dietary Assessment Research
| Item | Function & Application | Key Considerations |
|---|---|---|
| Doubly Labeled Water (DLW) | Objective measurement of total energy expenditure in free-living individuals; serves as a reference method for validating self-reported energy intake [12]. | Extremely expensive and requires specialized laboratory equipment for isotopic analysis. Not feasible for large-scale studies. |
| Recovery Biomarkers | Objective biomarkers (e.g., urinary nitrogen for protein, urinary potassium/sodium) used to validate the intake of specific nutrients and quantify measurement error [8]. | Exist for only a limited number of nutrients (energy, protein, sodium, potassium). Collection of 24-hour urine samples can be burdensome. |
| Automated Self-Administered 24-Hour Recall (ASA24) | A web-based tool that automatically administers a 24-hour dietary recall, reducing interviewer burden and cost [8] [14]. | May not be feasible for all study populations (e.g., those with low literacy or limited internet access). |
| Image-Assisted Dietary Assessment | Uses photos of food pre- and post-consumption to aid in portion size estimation and food identification, reducing reliance on memory [14] [9]. | Requires standardization of photography protocols. Potential issues with image quality and participant compliance in capturing images. |
| Wearable Sensors (e.g., iEat) | Emerging technology using bio-impedance or other sensors to automatically detect food intake gestures and potentially identify food types, minimizing participant burden [6]. | Still in developmental stages. Accuracy for nutrient estimation and performance in real-world, unstructured environments needs further validation [6] [9]. |
| 5-(1-Methyl-4-Piperidyl)5H-Dibenzo | 5-(1-Methyl-4-Piperidyl)5H-Dibenzo, CAS:3967-32-6, MF:C21H23NO, MW:305.4 g/mol | Chemical Reagent |
| 3-[4-(Benzyloxy)phenyl]aniline | 3-[4-(Benzyloxy)phenyl]aniline|CAS 400744-34-5 | 3-[4-(Benzyloxy)phenyl]aniline is a biphenyl aniline derivative for research use only. It serves as a key synthetic intermediate. Purity ≥96%. For Research Use Only. Not for human use. |
The Rise of Preventative Medicine and Personalized Nutrition
Technical Support Center: Troubleshooting Guides and FAQs
This technical support center addresses common challenges in continuous dietary monitoring research, with a specific focus on optimizing energy efficiency in experimental protocols. The guidance is designed for researchers, scientists, and drug development professionals.
Frequently Asked Questions (FAQs)
Q1: What are the primary reasons for participant discontinuation in long-term Continuous Glucose Monitoring (CGM) studies, and how can we mitigate them? Participant discomfort and device burden are leading causes of CGM discontinuation [15]. Mitigation requires a multi-pronged approach:
- Device Selection: Choose newer-generation CGM sensors with smaller form factors and improved adhesives to minimize skin irritation and physical burden [15].
- Participant Training: Provide comprehensive education on proper sensor attachment and management. Setting realistic expectations about the initial feeling of wearing a device can improve long-term adherence.
- Data Feedback: Implement protocols to prevent information overload. Instead of providing raw, continuous data streams, use software that offers simplified, actionable insights and summary reports [15].
Q2: Our research app's high energy consumption is limiting data collection periods. What features are the biggest energy drains? Energy consumption in health apps is significantly influenced by specific functionalities. A comparative analysis of popular apps identified key contributors [16].
- High-Impact Features: Frequent push notifications, continuous GPS tracking, and high app complexity (e.g., real-time AI-driven recommendations) are statistically significant drivers of energy use [16].
- Optimization Strategy: To extend battery life, design study protocols that minimize the frequency of location pings and use efficient data syncing schedules (e.g., batch syncing instead of real-time). Where possible, use native app features over cross-platform frameworks, which can be less energy-efficient [16].
Q3: How can we validate the accuracy of digital dietary assessment tools in our trials? Validation is crucial for scientific rigor. The guiding principles for Personalized Nutrition (PN) implementation emphasize using validated diagnostic methods and measures [17].
- Reference Methods: Cross-validate new digital tools (e.g., image-based food recognition apps) against established reference methods, such as doubly labeled water for energy expenditure or weighed food records for intake [18].
- Portion Size Estimation: This is a major source of error. Utilize tools that incorporate reference images or 3D modeling to enhance the accuracy of portion size estimates provided by participants [18].
- Data Quality: Ensure the nutrient database powering your app or software is frequently updated and comprehensive to ensure data quality and relevance [17].
Troubleshooting Common Experimental Challenges
Challenge 1: High Variability in Glycemic Response Data
- Problem: Significant inter-individual variability in postprandial glucose responses makes it difficult to identify clear patterns or effects of interventions [19] [20].
- Solution: Do not rely on glucose data alone. Implement a multi-omics personalization approach. Develop algorithms that integrate CGM data with other individual-specific information such as gut microbiome composition (e.g., abundance of Akkermansia muciniphila), lipid profiles, and dietary habits to better predict and explain responses [19] [20]. The study by Zeevi et al. demonstrated that integrated models significantly outperform predictions based on single parameters.
Challenge 2: Participant Adherence to Personalized Dietary Protocols
- Problem: Participants struggle to adhere to prescribed personalized diets over the 18-week duration of a trial, confounding results [20].
- Solution:
- User-Friendly Tools: Provide participants with an intuitive app that offers clear, easy-to-understand food scores and simple guidance, rather than complex nutritional data [17] [20].
- Gamification and Feedback: Incorporate elements of behavioral science, such as personalized nudges, goal setting, and positive feedback, to maintain engagement [19]. Studies show that self-reported adherence is significantly higher in groups using a structured, app-based personalized program compared to those receiving standard static advice [20].
Challenge 3: Managing and Interpreting Large, Multimodal Datasets
- Problem: Integrating data from CGMs, wearable activity trackers, microbiome sequencing, and food logs creates massive, complex datasets that are challenging to analyze.
- Solution: Leverage advanced computational techniques. Artificial intelligence (AI) and machine learning (ML) models are essential for analyzing this vast amount of data to develop algorithms that can predict an individual's response to a specific food or diet [19] [21]. Cloud-based research platforms, like the one used in the Nutrition for Precision Health (NPH) study, are critical for managing and processing this information [21].
Experimental Protocols for Energy-Efficient Research
Protocol 1: Assessing Energy Consumption of Digital Monitoring Tools
Objective: To quantitatively evaluate and compare the energy efficiency of different mHealth apps and wearable devices used in dietary monitoring research.
Methodology:
- Baseline Measurement: Measure the device's energy consumption (in milliwatt-hours) over a set period while the app is installed but not in active use. This establishes a baseline for background processes [16].
- Feature-Specific Testing: Conduct controlled scenarios that trigger specific app features:
- Logging: Measure energy used while a participant logs a standardized meal.
- Syncing: Measure energy consumed during a data synchronization event.
- GPS/Notifications: Activate location tracking and push notifications and measure the subsequent energy drain [16].
- Data Analysis: Use regression modeling to quantify the impact of each feature on total energy consumption. The model can be structured as:
Energy Consumption = β₀ + βâ‚(Notification Frequency) + β₂(GPS Use) + β₃(App Complexity) + ε[16].
Energy Impact of Common mHealth App Features
| Feature | Impact on Energy Consumption | Optimization Strategy |
|---|---|---|
| Push Notifications | Statistically significant increase (P value = .01) [16] |
Batch notifications; reduce frequency during low-engagement periods. |
| GPS Tracking | Statistically significant increase (P value = .05) [16] |
Use geofencing for location triggers instead of continuous tracking. |
| App Complexity / Real-time AI | Statistically significant increase (P value = .03); can consume up to 30% more energy [16] |
Offload complex processing to cloud servers; optimize algorithms. |
| Background Data Syncing | Can account for up to 40% of total energy use [16] | Schedule syncing for periods of device charging or high battery. |
Protocol 2: A Multi-Parameter Personalized Nutrition Trial
Objective: To evaluate the efficacy of a multi-level personalized dietary program (PDP) on cardiometabolic health outcomes compared to standard dietary advice.
Methodology (Adapted from the ZOE METHOD Study) [20]:
- Participant Characterization: At baseline, collect:
- Genotype: Focus on SNPs relevant to metabolism (e.g., FTO, TCF7L2) [19].
- Phenotype: Measure postprandial glucose and triglyceride responses to standardized test meals [20].
- Microbiome: Analyze gut microbiota composition via 16S rRNA sequencing [19] [20].
- Clinical Biomarkers: HbA1c, LDL-C, TG, body weight, waist circumference.
- Intervention: Randomize participants into two groups:
- PDP Group: Receive dietary advice via an app-based program that integrates all baseline data to generate personalized food scores.
- Control Group: Receive standard, general dietary advice (e.g., USDA Guidelines) [20].
- Duration: 18-week intervention period.
- Endpoint Analysis: Re-measure all clinical biomarkers from baseline. Perform statistical analysis (e.g., ITT analysis) to compare changes between groups.
Key Reagent Solutions for Personalized Nutrition Research
| Research Reagent | Function in Experiment |
|---|---|
| Continuous Glucose Monitor (CGM) | Measures interstitial glucose levels continuously to assess glycemic variability and postprandial responses [19] [15]. |
| Standardized Test Meals | Used in challenge tests to elicit a standardized metabolic response for comparing inter-individual variability [17] [20]. |
| DNA Microarray / SNP Genotyping Kit | Identifies genetic variations (e.g., in FTO, PPARG) that influence an individual's response to nutrients like fats and carbohydrates [19]. |
| 16S rRNA Sequencing Reagents | Profiles the gut microbiome composition to identify bacterial species (e.g., A. muciniphila) associated with dietary fiber metabolism and insulin sensitivity [19]. |
| Multiplex ELISA Kits | Allows simultaneous measurement of multiple cardiometabolic biomarkers from a single serum/plasma sample (e.g., TG, LDL-C, insulin) [20]. |
Visualized Workflows and Pathways
Diagram: Multi-Omics Data Integration in Personalized Nutrition
Diagram: Energy Consumption in mHealth App Ecosystem
Key Biomarkers and Metabolic Parameters for Continuous Tracking
Fundamental Biomarker Classification for Nutritional Research
Categories of Nutritional Biomarkers
In nutritional studies, biomarkers are systematically classified into three primary categories based on their function and the information they provide. This classification is critical for designing experiments and interpreting data related to energy metabolism and dietary exposure [22].
Biomarkers of Exposure serve as objective indicators of nutrient intake, overcoming limitations inherent in self-reported dietary assessments such as recall bias and portion size estimation errors. These include direct measurements of food-derived compounds in biological samples [23]. Example biomarkers in this category include alkylresorcinols (whole-grain intake), proline betaine (citrus exposure), and daidzein (soy intake) [23].
Biomarkers of Status measure the concentration of nutrients in biological fluids or tissues, or the urinary excretion of nutrients and their metabolites. These biomarkers aim to reflect body nutrient stores or the status of tissues most sensitive to depletion. Examples include serum ferritin for iron status and plasma zinc for zinc status [22].
Biomarkers of Function assess the functional consequences of nutrient deficiency or excess, providing greater biological significance than static concentration measurements. These are subdivided into:
- Functional Biochemical Biomarkers: Measure activity of nutrient-dependent enzymes or presence of abnormal metabolites (e.g., erythrocyte transketolase activity for thiamine status) [22].
- Functional Physiological/Behavioral Biomarkers: Assess outcomes related to health status such as immune function, growth, cognition, or response to vaccination [22].
Table 1.1: Classification of Nutritional Biomarkers with Examples
| Biomarker Category | Primary Function | Representative Examples | Sample Type |
|---|---|---|---|
| Exposure | Objective assessment of food/nutrient intake | Alkylresorcinols, Proline betaine, Daidzein | Plasma, Urine |
| Status | Measurement of body nutrient reserves | Nitrogen, Ferritin, Plasma zinc | Urine, Serum, Plasma |
| Function | Assessment of functional consequences | Enzyme activity assays, Immune response, Cognitive tests | Blood, Urine, Functional tests |
Context of Use Framework for Biomarker Validation
The Context of Use (COU) is defined as "a concise description of the biomarker's specified use" and includes both the biomarker category and its intended application in research or development. Establishing a clear COU is essential because it determines the statistical analysis plan, study populations, and acceptable measurement variance [24].
The BEST (Biomarkers, EndpointS, and other Tools) resource categorizes biomarkers as:
- Diagnostic: Identify presence or absence of a condition
- Monitoring: Track disease status or response to intervention
- Pharmacodynamic/Response: Show biological response to therapeutic intervention
- Predictive: Identify likelihood of response to specific treatment
- Prognostic: Identify likelihood of clinical event
- Safety: Indicate likelihood of adverse event
- Susceptibility/Risk: Identify potential for developing condition [24]
For continuous dietary monitoring research, the COU framework ensures biomarkers are validated specifically for their intended application in tracking metabolic parameters, which is fundamental to generating reliable, reproducible data.
Key Metabolic Parameters for Continuous Tracking
Core Metabolic Health Markers
Metabolic health is quantitatively assessed through five primary clinical markers that reflect the body's energy processing efficiency. These markers provide crucial insights into metabolic syndrome risk and overall physiological function [25] [26].
Blood Glucose Levels represent circulating sugar primarily from dietary intake. Maintaining stable levels is critical for metabolic homeostasis. Optimal fasting levels are generally below 100 mg/dL, with variability being as significant as absolute values. Continuous Glucose Monitors (CGMs) enable real-time tracking of glucose fluctuations in response to dietary interventions, physical activity, and sleep patterns [25].
Triglycerides are a form of dietary fat stored in fat tissue and circulating in blood. Elevated levels (>150 mg/dL) correlate with cardiovascular disease risk and metabolic dysfunction. Factors influencing triglyceride levels include high sugar intake, alcohol consumption, and physical inactivity [25] [26].
HDL Cholesterol functions as "good cholesterol" that transports LDL away from arteries. Optimal levels are ≥60 mg/dL, with low values increasing cardiovascular risk. Unlike other markers, higher HDL is generally desirable, influenced by factors including smoking, sedentary behavior, and diet composition [25] [26].
Blood Pressure measures arterial force during heart contraction (systolic) and relaxation (diastolic). Healthy values are at or below 120/80 mmHg. Chronic elevation increases risks for cardiovascular disease, stroke, and vascular dementia. Influential factors include sodium intake, stress management, and physical activity levels [25] [26].
Waist Circumference quantifies abdominal fat deposition, specifically indicating visceral fat surrounding organs. Healthy measurements are <40 inches (men) and <35 inches (non-pregnant women). This marker independently predicts metabolic disease risk beyond overall body weight [25] [26].
Table 2.1: Core Metabolic Health Markers and Their Clinical Ranges
| Metabolic Marker | Optimal Range | Risk Threshold | Primary Significance | Influencing Factors |
|---|---|---|---|---|
| Blood Glucose (Fasting) | <100 mg/dL | ≥100 mg/dL | Energy processing, Diabetes risk | Diet, Exercise, Sleep, Stress |
| Triglycerides | <150 mg/dL | ≥150 mg/dL | Cardiovascular risk | Sugar intake, Alcohol, Activity |
| HDL Cholesterol | ≥60 mg/dL | <40 mg/dL | Reverse cholesterol transport | Smoking, Exercise, Diet |
| Blood Pressure | ≤120/80 mmHg | >130/80 mmHg | Cardiovascular strain | Sodium, Stress, Activity |
| Waist Circumference | <40" (M), <35" (F) | ≥40" (M), ≥35" (F) | Visceral fat accumulation | Diet, Exercise, Genetics |
Advanced Nutritional Biomarkers for Continuous Monitoring
Beyond the core metabolic panel, numerous specialized biomarkers provide targeted information about specific dietary exposures and nutritional status. These biomarkers are particularly valuable for validating dietary interventions and understanding nutrient bioavailability [23].
Food Intake Biomarkers include:
- Alkylresorcinols: Metabolites indicating whole-grain wheat and rye consumption, measurable in plasma [23]
- Proline Betaine: Marker for citrus fruit intake, detectable in urine following consumption [23]
- Daidzein and Genistein: Phytoestrogens indicating soy product consumption, measurable in urine and plasma [23]
- Carotenoids: Plant pigment compounds reflecting fruit and vegetable intake, quantifiable in plasma/serum [23]
Nutrient Status Biomarkers include:
- Homocysteine: Functional biomarker of one-carbon metabolism and folate status [23]
- Erythrocyte Fatty Acid Composition: Status marker for essential fatty acids including EPA and DHA [23]
- Creatinine and Nitrogen: Urinary markers of protein intake and muscle metabolism [23]
These biomarkers enable researchers to objectively verify dietary compliance in intervention studies and correlate specific food exposures with metabolic outcomes, providing advantages over traditional food frequency questionnaires and dietary recalls.
Experimental Protocols for Biomarker Validation
Analytical Validation Methodology
Diagram 1: Analytical Validation Workflow for Biomarker Assays
Analytical validation establishes that a biomarker detection method meets acceptable performance standards for sensitivity, specificity, accuracy, precision, and other relevant characteristics using specified technical protocols [24]. This process validates the technical performance of the assay itself, independent of its clinical usefulness.
Key Steps in Analytical Validation:
- Define Performance Specifications: Establish target values for sensitivity, specificity, accuracy, and precision based on the biomarker's Context of Use [24]
- Protocol Standardization: Develop detailed specimen collection, handling, storage, and analysis procedures to minimize technical variability [22]
- Inter- and Intra-Assay Validation: Determine coefficient of variation across multiple runs and within single assays
- Linearity and Recovery: Establish assay performance across expected physiological range
- Stability Studies: Evaluate biomarker stability under various storage conditions and timeframes
Clinical Validation Methodology
Clinical validation establishes that a biomarker "acceptably identifies, measures, or predicts the concept of interest" for its specified Context of Use [24]. This process evaluates the biomarker's performance and usefulness as a decision-making tool.
Clinical Validation Protocol Components:
- Study Population Selection: Recruit participants representing the intended use population, considering age, sex, health status, and relevant comorbidities [24]
- Reference Standard Comparison: Compare biomarker performance against accepted reference standards (clinical outcome assessments, established diagnostic tools, or postmortem pathology) [24]
- Longitudinal Assessment: For monitoring biomarkers, implement repeated measures over time to establish relationship to disease progression or intervention response [24]
- Confounding Factor Documentation: Record medications, supplements, hormonal status, physical activity, health status, and other factors that may influence biomarker levels [22]
- Statistical Analysis Plan: Develop analysis strategy aligned with Context of Use, including determination of effect sizes, confidence intervals, and decision thresholds [24]
Troubleshooting Guides and FAQs
Common Experimental Challenges and Solutions
Issue: High Intra-Individual Variability in Biomarker Measurements
- Potential Causes: Diurnal variation, recent dietary intake, inconsistent fasting status, biological rhythms [22] [27]
- Solutions: Standardize collection times across participants, implement controlled fasting protocols, collect multiple samples over time, account for menstrual cycle phases in female participants [22]
Issue: Inconsistency Between Self-Reported Intake and Biomarker Data
- Potential Causes: Underreporting in dietary assessments, limitations in food composition tables, inter-individual differences in nutrient bioavailability [23]
- Solutions: Use multiple dietary assessment methods, include biomarker measurements to validate intake data, account for food preparation and processing methods that affect nutrient bioavailability [23]
Issue: Influence of Inflammation on Nutritional Biomarkers
- Potential Causes: Acute infection, inflammatory disorders, obesity, recent physical trauma triggering acute-phase response [22]
- Solutions: Measure C-reactive protein (CRP) and alpha-1-acid glycoprotein (AGP) to detect inflammation, apply statistical correction methods (e.g., BRINDA), exclude participants with active inflammatory conditions [22]
Issue: Discrepancy Between Different Sample Types (e.g., Plasma vs. Urine)
- Potential Causes: Different elimination kinetics, varying metabolic pathways, compartmental distribution differences
- Solutions: Establish sample-type specific reference ranges, understand pharmacokinetic profiles of target biomarkers, standardize sample type across study [28]
Frequently Asked Questions
Q: How often should biomarker measurements be repeated in continuous monitoring studies? A: Measurement frequency depends on the biomarker's biological half-life and physiological variability. Short-lived biomarkers (e.g., glucose) may require continuous or daily monitoring, while stable biomarkers (e.g., HbA1c) may only need monthly assessment. Consider the research question, biomarker kinetics, and practical constraints when determining frequency [22] [27].
Q: What is the difference between 'normal' ranges and 'optimal' ranges for biomarkers? A: 'Normal' ranges are statistical constructs derived from population data, typically representing the 95% central interval of a reference population. 'Optimal' ranges represent values associated with the lowest disease risk and best health outcomes, which often fall within narrower windows than general population norms [27].
Q: When should liquid biopsies versus tissue biopsies be used for biomarker assessment? A: Liquid biopsies are less invasive and provide systemic information but may have lower sensitivity for detecting certain biomarkers, particularly with low disease burden or specific alteration types. Tissue biopsies remain the gold standard for initial diagnosis and can detect histological changes, but carry higher procedural risks. The choice depends on the specific biomarkers, clinical context, and research objectives [28].
Q: How can researchers address the energy efficiency requirements of continuous monitoring systems? A: Implement IoT-based ecosystems with ultra-low consumption sensors, optimize data transmission protocols to minimize power use, utilize edge processing to reduce continuous data streaming, and select monitoring equipment with high energy efficiency ratings [29].
Q: What are the key considerations for selecting biomarkers for nutritional intervention studies? A: Choose biomarkers with appropriate responsiveness to the intervention timeframe, established analytical validity, relevance to the biological pathways being modified, practical measurement requirements, and well-characterized confounding factors. Combining exposure, status, and functional biomarkers provides comprehensive assessment [23] [22].
Research Reagent Solutions and Essential Materials
Table 5.1: Essential Research Materials for Biomarker Analysis
| Reagent/Material | Function/Application | Technical Considerations |
|---|---|---|
| Next-Generation Sequencing (NGS) Kits | Comprehensive genomic biomarker testing for multiple targets simultaneously | Should include DNA and RNA sequencing capabilities; essential for detecting fusions/rearrangements [28] |
| Liquid Biopsy Collection Systems | Non-invasive sampling for circulating biomarkers | Balance between sensitivity and specificity; optimal for point mutations but may miss complex alterations [28] |
| Continuous Glucose Monitoring Systems | Real-time tracking of glucose dynamics | Provide continuous data on glucose variability and responses to interventions; superior to single-point measurements [25] |
| Standard Reference Materials | Quality control and assay calibration | Certified reference materials with known biomarker concentrations essential for analytical validation [24] |
| Stabilization Buffers/Preservatives | Maintain biomarker integrity during storage/transport | Specific to biomarker type (e.g., protease inhibitors for protein biomarkers, RNAlater for RNA) [22] |
| Immunoassay Reagents | Quantification of protein biomarkers | Include appropriate antibodies with demonstrated specificity; consider cross-reactivity potential [27] |
| Mass Spectrometry Standards | Absolute quantification of metabolites | Isotope-labeled internal standards for precise measurement of small molecules and metabolites [23] |
Energy-Efficient Monitoring Technologies
Implementing continuous biomarker monitoring requires careful consideration of energy requirements, particularly for long-term studies and remote monitoring applications [29].
IoT-Based Monitoring Ecosystems enable real-time data collection while optimizing power consumption through:
- Ultra-low consumption sensors for temperature, humidity, and environmental monitoring [29]
- Configurable data transmission intervals to balance temporal resolution with battery life [29]
- Edge processing capabilities to reduce continuous data streaming requirements [29]
System Architecture Considerations for energy-efficient monitoring:
- Sensor Selection: Choose sensors with appropriate power requirements for the monitoring context
- Data Transmission: Utilize low-power communication protocols (e.g., LoRaWAN, Bluetooth LE)
- Power Sourcing: Evaluate battery, solar, or wired power options based on deployment location and duration
- Data Processing: Implement algorithms to minimize redundant data collection and transmission
Diagram 2: Energy-Efficient Data Flow for Continuous Monitoring Systems
Linking Dietary Patterns to Energy Metabolism and Chronic Disease
## Foundational Knowledge: Dietary Patterns and Health
This section provides evidence-based summaries of dietary patterns relevant to metabolic health and chronic disease prevention.
What does the current evidence say about the effectiveness of major dietary patterns for Metabolic Syndrome (MetS)?
A 2025 network meta-analysis of 26 randomized controlled trials provides a direct comparison of six dietary patterns for managing MetS. The key findings on their effectiveness for specific outcomes are summarized in the table below [30].
Table 1: Ranking of Dietary Patterns for Specific Metabolic Syndrome Components
| Metabolic Component | Most Effective Diet | Key Comparative Finding |
|---|---|---|
| Reducing Waist Circumference | Vegan Diet | Best for reducing waist circumference and increasing HDL-C levels [30]. |
| Lowering Blood Pressure | Ketogenic Diet | Highly effective in reducing both systolic and diastolic blood pressure [30]. |
| Lowering Triglycerides (TG) | Ketogenic Diet | Highly effective for triglyceride reduction [30]. |
| Regulating Fasting Blood Glucose | Mediterranean Diet | Highly effective in controlling fasting blood glucose [30]. |
| Increasing HDL-C | Vegan Diet | Ranked as the best choice for increasing "good" cholesterol [30]. |
What are the core features of the Mediterranean, DASH, and Plant-Predominant diets?
Table 2: Appraisal of Common Dietary Patterns for Chronic Disease
| Dietary Pattern | Core Features | Evidence Summary for Chronic Disease | Practical Considerations |
|---|---|---|---|
| Mediterranean Diet | High in fruits, vegetables, whole grains, olive oil, nuts, legumes; moderate fish/poultry; low red meat [31] [32]. | Strong evidence for cardiovascular risk reduction, anti-inflammatory and antioxidant effects [31] [32]. | Flexible and adaptable to cultural preferences; can use frozen produce for budget [31]. |
| DASH Diet | Emphasizes fruits, vegetables, whole grains, lean protein; rich in potassium (4,700 mg/day); limits sodium (1,500 mg/day) [31] [30]. | Significant improvements in blood pressure, metabolic syndrome, and lipid profiles [31] [30]. | Contraindicated for patients with kidney disease due to high potassium; budget-friendly with staples like beans/oatmeal [31]. |
| Plant-Predominant Diets | Spectrum from vegetarian (no meat) to vegan (no animal products) [31]. | Reduced cholesterol, blood pressure, and risk of certain cancers [31]. | Risk of iron deficiency; focus on whole foods (beans, lentils, greens) over processed alternatives [31]. |
## The Scientist's Toolkit: Dietary Monitoring Technologies
This section details the methodologies and tools for objective dietary intake monitoring, a cornerstone of energy efficiency in nutrition research.
What are the key technology-assisted methods for dietary assessment, and how accurate are they?
A 2022 randomized crossover feeding study compared the accuracy of four technology-assisted 24-hour dietary recall (24HR) methods against objectively measured true intake [14].
Table 3: Accuracy of Technology-Assisted Dietary Assessment Methods
| Assessment Method | Description | Mean Difference in Energy Estimation vs. True Intake | Key Findings |
|---|---|---|---|
| ASA24 | Automated Self-Administered Dietary Assessment Tool [14]. | +5.4% [14] | Estimated average intake with reasonable validity [14]. |
| Intake24 | An online 24-hour dietary recall system [14]. | +1.7% [14] | Most accurate for estimating the distribution of energy and protein intake in the population [14]. |
| mFR-TA | Mobile Food Record analyzed by a trained analyst [14]. | +1.3% [14] | Estimated average intake with reasonable validity [14]. |
| IA-24HR | Interviewer-administered recall using images from a mobile Food Record app [14]. | +15.0% [14] | Overestimated energy intake significantly [14]. |
| Glycidyl caprate | Glycidyl caprate, CAS:26411-50-7, MF:C13H24O3, MW:228.33 g/mol | Chemical Reagent | Bench Chemicals |
| 1,4-Bis(4-bromophenyl)-1,4-butanedione | 1,4-Bis(4-bromophenyl)-1,4-butanedione, CAS:2461-83-8, MF:C16H12Br2O2, MW:396.07 g/mol | Chemical Reagent | Bench Chemicals |
What are the emerging sensor-based methods for Automatic Dietary Monitoring (ADM)?
Beyond traditional recalls, research is focused on automated, sensor-based systems to reduce user burden and improve accuracy [33] [6].
- Vision-Based Methods: Use cameras and computer vision for food recognition, portion size estimation, and intake action detection. Challenges include occlusion, privacy concerns, and variable computational efficiency [33].
- Wearable Bio-Impedance Sensors: Systems like iEat use wrist-worn electrodes to measure impedance changes caused by dynamic circuits formed between the body, utensils, and food during eating. This method can recognize intake activities (e.g., cutting, drinking) and classify food types [6].
- Other Wearables & Smart Objects: These include smart utensils with inertial measurement units (IMUs), neckbands with microphones to detect chewing/swallowing, and smart trays with pressure sensors [33] [6].
Diagram 1: Dietary assessment workflow.
## Experimental Protocols & Methodologies
This section provides detailed protocols for key experiments and methodologies cited in this field.
Detailed Protocol: Controlled Feeding Study for Validating Dietary Assessment Tools
This protocol is based on the design used to generate the data in Table 3 [14].
- Objective: To compare the accuracy of energy and nutrient intake estimation of multiple technology-assisted dietary assessment methods relative to true intake in a controlled setting.
- Design: Randomized crossover feeding study.
- Participants: Recruit ~150 participants, representing a mix of genders, with mean age around 32 and mean BMI around 26 kg/m² [14].
- Feeding Day:
- Randomize participants to one of several separate feeding days.
- Provide participants with standardized breakfast, lunch, and dinner.
- Weigh all foods and beverages provided and any leftovers unobtrusively to establish the "true intake" with high precision [14].
- Dietary Recall:
- On the day following the feeding day, participants are randomized to complete a 24-hour dietary recall using one of the technology-assisted methods under investigation (e.g., ASA24, Intake24, mFR-TA, IA-24HR) [14].
- Data Analysis:
- Calculate the difference between the true intake (from weighed food) and the estimated intake (from the recall tool) for energy and multiple nutrients.
- Use linear mixed models to assess the statistical significance of the differences among methods.
- Report mean differences, confidence intervals, and variances [14].
Detailed Protocol: Wearable Bio-Impedance for Dietary Activity Monitoring (iEat System)
This protocol outlines the methodology for using wearable impedance sensors, as described in the iEat study [6].
- Objective: To automatically detect food intake activities and classify food types using a wrist-worn bio-impedance sensor.
- Hardware Setup:
- Use a wearable device with a single bio-impedance sensing channel.
- Attach one electrode to each wrist of the participant. A two-electrode configuration is sufficient for detecting dynamic impedance changes [6].
- Data Collection:
- Conduct experiments in a realistic, everyday table-dining environment.
- Participants consume multiple meals, performing activities like cutting, drinking, and eating with utensils or hands.
- The impedance sensor continuously measures the electrical impedance across the body. Dynamic circuits formed between hands, utensils, food, and the mouth cause unique temporal patterns in the impedance signal [6].
- Signal Processing and Modeling:
- The system relies on the variation in impedance signals, not absolute values.
- An abstracted human-food interaction circuit model is used to interpret the signal changes.
- A lightweight, user-independent neural network model is trained to classify the signal patterns into specific activities (cutting, drinking, etc.) and food types [6].
- Performance Evaluation:
- Evaluate the system using metrics like macro F1 score for activity recognition and food classification on a dataset of multiple meals from numerous volunteers [6].
## Research Reagent Solutions
Table 4: Essential Tools for Dietary Monitoring Research
| Item / Solution | Function in Research | Example / Note |
|---|---|---|
| Automated 24HR Systems | Enable scalable, self-administered dietary data collection for population surveillance. | ASA24, Intake24 [14]. |
| Wrist-Worn Bio-Impedance Sensor | Detects dietary activities and food types via dynamic electrical circuit changes caused by body-food-utensil interactions. | The iEat wearable system [6]. |
| Neck-Worn Acoustic Sensor | Monitors ingestion sounds (chewing, swallowing) for intake detection and food recognition. | AutoDietary system [6]. |
| Smart Utensils & Objects | Directly monitor interaction with food via integrated sensors (e.g., IMU, pressure). | Smart forks (IMU), smart dining trays (pressure sensors) [33] [6]. |
| Computer Vision Algorithms | Automate food recognition, segmentation, and volume estimation from images or video. | Used in Vision-Based Dietary Assessment (VBDA); requires RGB or depth-sensing cameras [33]. |
| Professional Diet Analysis Software | Analyze nutrient composition of recipes, menus, and diets for clinical or research purposes. | Nutritionist Pro software [34]. |
Diagram 2: Bio-impedance sensing principle.
## Frequently Asked Questions (FAQs)
Q1: In our research on Metabolic Syndrome, which dietary pattern should we recommend as an intervention for the best overall outcomes?
Based on a recent network meta-analysis, the Vegan, Ketogenic, and Mediterranean diets show more pronounced effects for ameliorating MetS, but the choice depends on the primary outcome [30]. For overall profile improvement, a Mediterranean diet is a strong candidate due to its proven benefits in regulating blood glucose, improving lipid profiles, and reducing cardiovascular risk through anti-inflammatory and antioxidant mechanisms [30] [32]. The best diet is ultimately the one participants can adhere to long-term, considering cultural, personal, and socioeconomic factors [31].
Q2: Our validation study found significant over-reporting of energy intake with image-assisted interviewer recalls. What might be the cause, and what are more accurate alternatives?
Your finding is consistent with controlled validation studies. Research shows the Image-Assisted Interviewer-Administered 24HR (IA-24HR) method can overestimate energy intake by approximately 15% compared to true, weighed intake [14]. This could be due to participant or interviewer bias in describing portion sizes even with image aids. For more accurate population-level averages, consider Intake24, ASA24, or the mobile Food Record analyzed by a trained analyst (mFR-TA), which showed mean differences of only +1.7%, +5.4%, and +1.3% respectively [14]. If estimating the distribution of intake in your population is important, Intake24 was found to be the most accurate for that specific task [14].
Q3: We are developing a wearable for dietary monitoring. What is an emerging sensing modality that moves beyond traditional inertial measurement units (IMUs)?
An emerging and promising modality is bio-impedance sensing. Systems like iEat use electrodes on each wrist to measure impedance changes created by dynamic circuits formed between the body, metal utensils, and conductive food items during eating activities [6]. This method can recognize specific activities (e.g., cutting, drinking) and classify food types based on unique temporal signal patterns, offering a novel approach that is different from gesture-based IMU recognition [6].
Q4: What are the major practical challenges and sources of bias when applying vision-based dietary monitoring in free-living conditions?
Key challenges include [33]:
- Occlusion: Food items often obscure each other, making identification and volume estimation difficult.
- Privacy: Continuous video or image capture raises significant user privacy concerns.
- Variable Image Quality: Performance is highly dependent on lighting conditions and camera stability.
- Computational Efficiency: Running complex food recognition algorithms in real-time on mobile devices is challenging.
- Practicality: Requiring users to capture images of every meal can be burdensome and lead to non-adherence.
Digital and Biomarker Tools for Precision Dietary Data Collection
Commercial Continuous Glucose Monitors (CGMs) for Metabolic Research
FAQs: Utilizing CGMs in Research Settings
Q1: How can CGMs be applied in research involving healthy adult populations? CGM systems are valuable tools for investigating glucose dynamics in response to various stimuli in healthy adults. Research applications include studying the metabolic impact of nutritional interventions, understanding the effects of physical activity on glucose regulation, examining the relationship between psychological stress and glucose levels, and establishing normative glucose profiles for different demographics. Key metrics often analyzed include Time in Range (TIR), mean 24-hour glucose, and glycemic variability indices [35].
Q2: What are the primary technical challenges when using CGMs in experiments? Common technical issues researchers may encounter include:
- Signal Loss: The receiver or smart device is too far from the transmitter, or physical barriers (walls, metal) disrupt the Bluetooth connection [36] [37].
- Sensor Failure: Sensors can fail due to applicator malfunction, accidental knocks, or expiration of the sensor session (typically 10-14 days for most models) [36] [37].
- Skin Irritation: Adhesives can cause skin reactions, potentially affecting participant compliance [36].
- Data Gaps: Temporary "Brief Sensor Issue" or "No Readings" alerts can create interruptions in the continuous data stream [37].
Q3: What methodologies ensure data accuracy in CGM-based studies? To ensure data quality, researchers should:
- Strictly follow manufacturer instructions for sensor application [36].
- Clean the application site with an alcohol wipe to ensure proper adhesion [36].
- Be aware of the inherent time delay (typically a few minutes) between blood glucose and interstitial fluid glucose readings, especially during periods of rapidly changing glucose levels [35].
- Use blood glucose meter (BGM) measurements to verify CGM readings when values are questionable or do not match clinical symptoms [37].
Q4: How is CGM data interpreted for participants without diabetes? Studies establishing normative values show that healthy, nondiabetic, normal-weight individuals typically spend about 96% of their time in a glucose range of 70 to 140 mg/dL. The mean 24-hour glucose for these populations is approximately 99 ± 7 mg/dL (5.5 ± 0.4 mmol/L) [35]. Deviations from these baselines, such as increased time above 140 mg/dL, can be a focus of research [35].
Troubleshooting Guides
Signal Loss and Connectivity Issues
A Signal Loss alert means the display device is not receiving data from the sensor.
- Potential Cause 1: Excessive distance or physical obstacles between the sensor and receiver/smart device.
- Resolution: Ensure the devices are within 6 meters of each other without obstructive barriers. Keep the display device's Bluetooth enabled and the Dexcom app (or other manufacturer app) open [37].
- Potential Cause 2: Low battery or power-saving mode on the smart device.
- Potential Cause 3: Water on or around the sensor.
- Resolution: While most sensors are water-resistant, water can temporarily disrupt signal transmission. Dry the area thoroughly [36].
Sensor Application and Failure
- Potential Cause 1: Improper sensor application or applicator malfunction.
- Resolution: Do not reuse a sensor. For applicator malfunctions, contact the manufacturer for a replacement and return the faulty unit if requested [36].
- Potential Cause 2: Sensor becomes dislodged.
- Resolution: Ensure the skin is clean, dry, and free of lotions before application. For studies where activity may loosen sensors, consider using approved liquid adhesives or overlay patches to improve retention [36].
- Potential Cause 3: Sensor session has ended or transmitter battery is depleted.
- Resolution: Sensor sessions are finite (e.g., 10 days for Dexcom G6). Transmitters also have a lifespan (e.g., ~3 months for Dexcom G6). Adhere to manufacturer-specified lifetimes and replace components as needed [37].
The table below summarizes key normative CGM data for healthy, non-diabetic adults, which can serve as a baseline for research comparisons [35].
Table 1: Normative CGM Metrics for Healthy, Non-Diabetic Adults
| Metric | Average Value | Significance in Research |
|---|---|---|
| Time in Range (TIR)(70-140 mg/dL) | 96% | Primary endpoint for assessing glycemic stability; a decrease may indicate impaired glucose regulation. |
| Mean 24-h Glucose | 99 ± 7 mg/dL(5.5 ± 0.4 mmol/L) | Provides a central tendency measure for overall glucose exposure. |
| Time <70 mg/dL(Hypoglycemia) | ~15 minutes per day | Establishes a baseline for normal, brief fluctuations into low glucose levels. |
| Time >140 mg/dL(Hyperglycemia) | ~30 minutes per day | Establishes a baseline for normal, brief postprandial spikes. |
Experimental Protocols
Protocol: Assessing Glycemic Response to Nutritional Interventions
Objective: To evaluate the impact of specific foods or meals on postprandial glucose dynamics in a research cohort.
Materials:
- Commercial CGM system (e.g., Dexcom G7, FreeStyle Libre 3)
- Standardized test meals
- Blood glucose meter (BGM) for calibration/validation
- Data collection platform (e.g., smartphone app, manufacturer's cloud software)
Methodology:
- Baseline Period: Record a minimum of 24 hours of CGM data under the participant's habitual diet to establish a personal baseline.
- Test Meal Administration: After an overnight fast, participants consume the standardized test meal within a fixed time window (e.g., 15 minutes).
- Data Recording: CGM data is collected continuously for a minimum of 2 hours postprandially. Participants should log meal start time and any symptoms.
- Activity Control: Participants should remain sedentary during the 2-hour postprandial observation period.
- Data Analysis: Calculate the glucose Area Under the Curve (AUC), peak glucose value, and time to peak for the test meal. Compare these metrics against the baseline or between different test meals [35] [38].
Protocol: Evaluating the Effect of Physical Activity on Glucose Stability
Objective: To quantify the impact of different exercise modalities (e.g., HIIT vs. steady-state cardio) on glycemic control.
Materials:
- CGM system
- Heart rate monitor or fitness tracker
- Equipment for prescribed exercise (treadmill, stationary bike, etc.)
Methodology:
- Pre-Exercise Baseline: Ensure participants begin the exercise session with stable glucose levels (not in a hypoglycemic or hyperglycemic state).
- Exercise Intervention: Participants perform a prescribed exercise protocol at a specific time of day (e.g., post-absorptive state or postprandial).
- Real-Time Monitoring: Record CGM and heart rate data throughout the exercise session and during the recovery period (e.g., 24 hours).
- Data Analysis: Analyze the change in glucose levels during and immediately after exercise. Assess the duration and magnitude of any post-exercise hypoglycemic events and observe the effect on overall 24-hour glycemic variability [35] [38].
Research Reagent Solutions
Table 2: Essential Materials for CGM-Based Metabolic Research
| Item | Function in Research |
|---|---|
| Commercial CGM System(e.g., Dexcom G7, Abbott Libre 3) | Core device for continuous, ambulatory measurement of interstitial glucose levels. Provides the primary data stream for analysis [35] [38]. |
| Skin Adhesive & Barrier Wipes(e.g., Liquid adhesive, barrier films) | Ensures sensor retention for the entire study duration and manages skin reactions to preserve participant compliance and data integrity [36]. |
| Blood Glucose Meter (BGM) & Test Strips | Provides fingerstick capillary blood samples for validation of CGM readings during critical time points or when CGM values are questionable [37]. |
| Data Visualization & Analysis Software(e.g., Manufacturer cloud platforms, R, Python) | Enables aggregation, visualization, and statistical analysis of CGM data (e.g., TIR, AUC, glycemic variability) [35]. |
| Standardized Test Meals | Provides a controlled nutritional stimulus for studying postprandial glucose metabolism and allows for comparison across participants and studies [35] [38]. |
Experimental Workflow and Data Interpretation
The following diagram illustrates a generalized workflow for a CGM-based metabolic study, from participant screening to data interpretation.
CGM Research Workflow
Signaling Pathways in Glucose Regulation
The diagram below outlines the core physiological pathways that govern blood glucose levels, which are the foundation for interpreting CGM data.
Glucose Homeostasis Pathways
Mobile Applications for Diet Self-Monitoring and Nutrient Analysis
Troubleshooting Guides and FAQs
Q1: Our research participants are underreporting nutrient intake, particularly sodium and calcium, when using mobile diet apps. What methodologies can improve data accuracy?
A: Underreporting is a common challenge. A pre-post intervention study using the Diet-A mobile application demonstrated significant decreases in reported sodium (p=0.04) and calcium (p=0.03) intake, suggesting systematic underreporting rather than actual dietary change [39]. To improve accuracy:
- Implement 24-hour recall validation: Collect data using 24-hour dietary recalls pre- and post-intervention to establish baseline accuracy metrics and identify reporting patterns [39].
- Multi-modal data entry: Enable both voice and text input to reduce recording burden, which was cited by >70% of participants as a significant barrier to consistent logging [39].
- Strategic prompting: Use timed pop-up notifications at logical intervals (e.g., 11:00 AM for breakfast, 3:00 PM for lunch, 8:00 PM for dinner) to prompt meal recording without relying on participant memory [39].
- Photographic reinforcement: Include functionality to take food photos as memory aids for later data entry when immediate logging isn't feasible [39].
Q2: How can we maintain participant engagement with diet tracking applications throughout long-term studies to prevent data attrition?
A: Maintaining engagement requires addressing both technical and behavioral factors:
- Reduce recording burden: Implement voice-to-text functionality and simplified portion size selection (e.g., proportion of pre-specified serving sizes) rather than requiring manual weight/volume entries [39].
- Provide immediate feedback: Develop systems that display real-time nutrient intake comparisons to dietary reference standards, giving participants personal insights that reinforce continued use [39].
- Minimize user effort: Utilize barcode scanners and extensive food databases to simplify food logging [40].
- Address participant mindset: In studies using CGM integration, some participants reported that continuous monitoring amplified negative feelings about food, highlighting the need for psychological support components in prolonged interventions [41].
Q3: What integration methods exist between continuous glucose monitoring (CGM) systems and dietary self-monitoring applications to optimize energy efficiency in data collection?
A: Effective CGM-diet integration can create more energy-efficient data collection paradigms by reducing participant burden and automating data capture:
- Real-time feedback systems: Research shows that integrating CGM data with nutrition therapy significantly increased whole-grain (p=0.02) and plant-based protein intake (p=0.02) while improving sleep efficiency by 5% (p=0.02) through automated data synthesis [42].
- Standardized interpretation frameworks: Implement simplified approaches like the "1, 2, 3 method" (tracking glucose before and after meals) and "yes/less framework" for food choices, which help participants understand CGM data without technical expertise [41].
- Unified data platforms: Systems that automatically align dietary intake with glycemic responses eliminate redundant manual data entry and correlation analysis, significantly reducing the computational energy required for post-hoc analysis [41].
- Visual data integration: Combine CGM metrics with food intake timelines using intuitive graphics and simplified messaging to enhance comprehension while minimizing cognitive load and engagement time [41].
Q4: What technical support infrastructure ensures reliable operation of dietary monitoring applications in research settings?
A: A robust support system is essential for research continuity:
- Multi-channel support: Implement in-app chat for immediate assistance, email support for complex queries, and knowledge bases for self-service troubleshooting [43] [44].
- Prioritized response protocol: Categorize issues into critical (app functionality), important (user experience), and routine (general inquiries), with target response times of 15-30 minutes for critical issues [43].
- Proactive monitoring: Use analytics to identify common points of failure in the data recording workflow and implement preventive fixes through regular updates [44].
- Comprehensive training: Ensure research staff are proficient in both technical troubleshooting and communicating with participants about data recording challenges [43].
Experimental Protocols for Dietary Monitoring Research
Protocol 1: Validation of Mobile Application Against Traditional Dietary Assessment Methods
Objective: To compare nutrient intake data from mobile applications against 24-hour dietary recalls.
Methodology:
- Recruit participants meeting study criteria (e.g., n=33 as in Diet-A study) [39]
- Collect baseline demographic data and smartphone proficiency metrics
- Administer 24-hour dietary recalls pre-intervention by trained interviewers
- Implement mobile application with voice/text input and portion size selection
- Conduct post-intervention 24-hour dietary recalls
- Analyze differences using statistical methods (e.g., general linear model repeated measures)
Energy Efficiency Consideration: This protocol reduces long-term resource expenditure by validating the more scalable mobile method against the resource-intensive interview method.
Protocol 2: Integrated CGM and Nutrition Intervention Framework
Objective: To assess the impact of real-time CGM feedback on dietary quality and sleep efficiency.
Methodology (adapted from Basiri et al., 2025) [42]:
- Randomize participants to treatment (unblinded CGM) or control (blinded CGM) groups
- Provide individualized nutrition recommendations tailored to energy needs for both groups
- Equip treatment group with real-time CGM access with nutrition-focused interpretation guides
- Assess dietary intake using ASA24 recall or equivalent automated system
- Measure sleep quality through validated instruments
- Analyze outcomes via appropriate statistical tests with p<0.05 significance threshold
Energy Efficiency Consideration: This protocol leverages continuous automated glucose monitoring to reduce the need for frequent laboratory blood draws and manual dietary assessment.
Research Workflow Visualization
Dietary App Validation Workflow
CGM-Nutrition Integration Data Flow
Research Reagent Solutions
Table: Essential digital tools for dietary monitoring research
| Research Tool | Function | Research Application |
|---|---|---|
| MyFitnessPal | Extensive food database with barcode scanning and macro/micronutrient tracking [40] | Validation studies comparing app-generated data to traditional dietary assessment methods |
| Cronometer | Detailed micronutrient tracking with verified food database [40] | Research requiring comprehensive vitamin and mineral intake analysis |
| Continuous Glucose Monitors (Dexcom G7) | Real-time glucose monitoring with smartphone integration [41] | Studies examining relationships between dietary intake and glycemic response |
| Diet-A Platform | Customizable research application with voice input and timed prompts [39] | Feasibility studies and interventions requiring reduced participant burden |
| ASA24 Automated System | Automated self-administered 24-hour dietary recall system [42] | Validation standard for mobile application dietary assessment accuracy |
| UNITE Intervention Materials | Nutrition-focused CGM initiation materials with simplified messaging [41] | Standardized protocols for CGM-diet integration studies |
Wearable Sensors and Devices for Tracking Energy Expenditure
Troubleshooting Guides
Guide 1: Addressing Inaccurate Energy Expenditure Estimates
Problem: Your wearable system is providing inaccurate estimates of energy expenditure (EE), particularly during high-intensity or time-varying activities.
Explanation: Many commercial devices and research prototypes show a tendency to underestimate energy expenditure at high intensities (e.g., >10 METs) and during non-steady-state activities, which can constitute a significant portion of daily movement [45] [46]. This often occurs because algorithms are trained on limited data or rely on sensors (like wrist-worn accelerometers or heart rate monitors) that do not fully capture the biomechanics of lower-limb activities [45] [46].
Solution Steps:
- Sensor Placement Verification: Ensure inertial measurement units (IMUs) are securely placed on the shank and thigh of the subject. Research indicates that lower-limb kinematics distinguish activities better than wrist or trunk kinematics and converge more quickly than physiological signals like heart rate [46].
- Algorithm and Training Data Audit: Verify that the classification model has been trained on data that includes the specific activities causing inaccuracy. Holding out running conditions from training, for example, can lead to significant estimation errors when running data is encountered [46].
- Ground Truth Validation: Cross-validate your system's output against a ground-truth method, such as indirect calorimetry (respirometry), during steady-state conditions to quantify the device's bias and error [46].
Guide 2: Managing Excessive Energy Consumption of the Wearable System
Problem: The battery life of your wearable sensor platform is too short for prolonged data collection, limiting its usefulness in long-term, real-world dietary monitoring studies.
Explanation: Continuous sensor data acquisition, processing, and wireless transmission are significant drains on battery power. This is a critical design challenge for wearable technology [47].
Solution Steps:
- Implement Episodic Sampling: Adopt a context-aware sensing technique where context classification occurs only at specific time instances. Between these episodes, place the sensors in a low-power sleep mode. One study demonstrated that an Additive-Increase/Multiplicative-Decrease (AIMD) algorithm can reduce energy consumption by 85% with only a 5% loss in classification accuracy [47].
- Utilize Ultra-Low-Power Components: Select system components, such as microcontrollers based on Sub-threshold Power Optimized Technology (SPOT), designed for minimal energy consumption in active and idle modes [48].
- Employ Edge Computing: Process data locally on the wearable device to reduce the need for constant, energy-intensive wireless transmission to a cloud or central server [49] [50].
Guide 3: Resolving Connectivity and Data Integrity Issues
Problem: The wearable device experiences intermittent connectivity, leading to incomplete datasets or corrupted data packets.
Explanation: In an IoT-assisted wearable platform, reliable data flow from the sensor to the endpoint is crucial. Delays or dropouts can result in data loss and inadequate information for end-users [51].
Solution Steps:
- Check Protocol Efficiency: Ensure the device uses low-energy communication protocols like Bluetooth Low Energy (BLE) and that the firmware is configured to maximize sleep intervals between data bursts [48] [50].
- Inspect Intermediate Layer Performance: If using a cloud or edge computing architecture, verify that this intermediary layer is functioning correctly. A well-designed edge layer can decrease delay and establish more reliable communications [51].
- Signal Strength Monitoring: Implement a system log to record signal strength during transmissions. This can help identify if data loss is correlated with physical movement into areas with poor connectivity.
Frequently Asked Questions (FAQs)
FAQ 1: What are the primary energy source options for wearable sensors, and how do they compare? While batteries are the most common power source, energy harvesting technologies are emerging alternatives. The table below summarizes key options [52]:
| Energy Source | Typical Output/Performance | Key Advantages | Key Limitations |
|---|---|---|---|
| Lithium-ion Batteries | Working Voltage: ~3.7V [52] | Mature technology, high energy density [52] | Finite lifespan, contains toxic substances [52] |
| Solar Cells | Varies with light intensity [52] | Can continuously recharge in suitable environments [52] | Intermittent power source, depends on ambient light [52] |
| Thermoelectric Generators | Varies with temperature gradient (ΔT) [52] | Utilizes body heat [52] | Low power density [52] |
| Biofuel Cells | Varies with fuel concentration [52] | Uses biological fluids as fuel [52] | Low power density, complex operation [52] |
| Triboelectric Generators | Varies with motion intensity [52] | Harvests energy from body movement [52] | Requires consistent motion [52] |
FAQ 2: My device is accurate in lab settings but fails in free-living conditions. Why? This is often due to the device's inability to generalize to activities not well-represented in its training data. Laboratory experiments often consist of steady-state activities, whereas real-life involves frequent time-varying activities (e.g., short bouts of walking, transitioning between activities) [46]. Furthermore, algorithms trained on a specific subject group may not perform well on new subjects with different physiologies or movement styles [46]. Ensure your model is trained on a diverse dataset that includes a wide range of activities and subject demographics.
FAQ 3: What is the most accurate method for validating energy expenditure estimates from my wearable system? The gold-standard method for validating total daily energy expenditure in free-living situations is the doubly labeled water (DLW) method [45] [46]. For validation under controlled laboratory conditions, indirect calorimetry (IC), which measures oxygen consumption, is the reference method [45] [46]. Note that IC requires a face mask, which can interfere with natural behavior.
FAQ 4: How can I improve the energy efficiency of an AI-powered wearable? AI and machine learning can be power-intensive. To mitigate this:
- Use On-Device AI: Employ optimized, lightweight models for local processing on the wearable (edge computing) instead of continuous cloud streaming [50].
- Data Prioritization: Compress and prioritize data transmission based on context or urgency [50].
- Energy-Aware Scheduling: Integrate scheduling that limits computationally heavy AI tasks when the battery is low [50].
Experimental Protocols & Data
Protocol 1: Validation of Energy Expenditure Estimates
Objective: To validate the accuracy of a wearable sensor system's energy expenditure estimates against a gold-standard reference method.
Methodology:
- Subject Preparation: Fit subjects with the wearable sensor system (e.g., IMUs on shank and thigh) and the ground truth equipment.
- Activity Protocol: Subjects perform a series of activities covering a range of intensities and types. A typical protocol includes [46]:
- Steady-state walking at multiple speeds (e.g., 3, 5, 7 km/h)
- Running
- Stair ascent and descent
- Stationary cycling
- Time-varying activities (e.g., intervals of walking and running)
- Data Collection:
- Data Analysis: Calculate the absolute and relative error between the wearable system's estimate and the ground truth for each activity and across the entire protocol.
Protocol 2: Evaluating Energy Efficiency of a Sensing Algorithm
Objective: To quantify the energy savings achieved by an energy-efficient sensing algorithm like episodic sampling.
Methodology:
- Baseline Measurement: Deploy the wearable system with continuous sensing and data processing enabled. Measure the total energy consumption (or battery drain rate) over a fixed period or until a specific task is completed.
- Intervention Measurement: Deploy the same system under identical conditions, but with the energy-efficient algorithm (e.g., episodic sampling with AIMD control) activated [47].
- Comparison: Calculate the percentage reduction in energy consumption. One study using episodic sampling reported an 85% reduction in energy use with a minimal impact on performance [47].
Quantitative Performance Comparison of Estimation Methods
The following table summarizes errors reported for different energy expenditure estimation methods when evaluated with new subjects [46]:
| Estimation Method | Sensor Placement | Cumulative Error (across common activities) |
|---|---|---|
| Wearable System (Data-Driven Model) | Shank and Thigh (IMUs) | 13% [46] |
| Standard Smartwatch | Wrist | 42% [46] |
| Activity-Specific Smartwatch | Wrist | 44% [46] |
Research Reagent Solutions
| Item Name | Function/Application in Research |
|---|---|
| Inertial Measurement Unit (IMU) | Measures motion kinematics (acceleration, angular rotation). Critical for capturing body movement, especially on the lower limbs, to estimate activity-related energy expenditure [46]. |
| Ultra-Low-Power Microcontroller | The core processing unit of the wearable device. Selecting an energy-efficient model (e.g., based on SPOT technology) is fundamental to extending operational lifetime [48]. |
| Electrochemical Biosensors | Used to detect biochemical markers in biofluids (e.g., sweat glucose, lactate). Relevant for multi-modal monitoring that combines metabolic data with energy expenditure [52]. |
| Energy Management Unit | A hardware/software interface that enables real-time energy monitoring and dynamic power control of sensors and wireless interfaces, allowing for on-demand activation [47]. |
| Bluetooth Low Energy (BLE) Module | Provides wireless connectivity for data transmission with minimal power consumption, essential for maintaining device portability and battery life [48] [50]. |
System Architecture and Workflow Visualizations
Energy-Efficient Wearable System Architecture
Episodic Sampling Algorithm Workflow
Integrating Digital Platforms for Nutritionists and Clinical Researchers
Frequently Asked Questions (FAQs)
Q1: What are the primary sensor-based methods for automatic dietary monitoring (ADM) in free-living individuals? ADM systems are broadly categorized into wearable sensors and smart objects. Wearable devices, such as wrist-worn bio-impedance sensors or neck-borne microphones, offer portability and continuous monitoring by detecting dietary-related gestures or physiological signals like swallowing [6]. Smart objects, including instrumented utensils, trays, or bottles, directly interact with food and can precisely capture intake actions but may be less practical for sustained, unattended use [6]. Vision-based methods use cameras and computer vision algorithms for high-accuracy food recognition, but they can face challenges with privacy, computational efficiency, and variable lighting conditions [33].
Q2: What technical challenges are commonly encountered with vision-based intake monitoring? Researchers deploying vision-based systems often face several technical hurdles [33]:
- Occlusion: Food items or utensils can be hidden from the camera's view.
- Variable Lighting Conditions: Changes in ambient light can affect image quality and the performance of food recognition algorithms.
- Computational Efficiency: Processing image or video data in real-time requires significant computational resources.
- Privacy Concerns: Continuous visual monitoring raises data privacy issues for participants.
- Practicality: Ensuring consistent camera angle and coverage in real-world, free-living settings can be difficult.
Q3: How can energy efficiency be improved in continuous dietary monitoring systems? Energy efficiency is critical for the sustained use of wearable dietary sensors. Key strategies include:
- Using Low-Power Sensors: Selecting sensing modalities like bio-impedance, which can be implemented with low-power electronics [6].
- On-Device, Lightweight Processing: Deploying lightweight neural network models on the wearable device itself to process data locally, reducing the energy cost of continuous wireless data transmission to a central server [6].
- Sensor Fusion Logic: Developing intelligent algorithms that activate high-power sensors (e.g., a camera) only when a low-power primary sensor (e.g., an accelerometer) detects a potential intake event.
Q4: What performance metrics can be expected from current automated dietary monitoring technologies? Performance varies by technology and task. The table below summarizes example metrics from recent research:
| Technology | Task | Reported Performance | Citation |
|---|---|---|---|
| Wearable Bio-Impedance (iEat) | Recognizing 4 food intake activities | Macro F1 score: 86.4% | [6] |
| Wearable Bio-Impedance (iEat) | Classifying 7 food types | Macro F1 score: 64.2% | [6] |
| High-Fidelity Neck Microphone | Recognizing food intake (7 food types) | Accuracy: 84.9% | [6] |
| Smart Dining Tray | Classifying 8 intake activities | Accuracy: 94.6% | [6] |
| AI/Computer Vision | Food classification and nutrient detection | Accuracy: >99% (in controlled settings) | [53] |
Troubleshooting Guides
Issue: Poor Classification Accuracy in Wearable Sensor Data
Problem: A wearable dietary monitor (e.g., based on bio-impedance or motion) is yielding low F1 scores or accuracy when classifying eating activities or food types.
Possible Causes and Solutions:
- Signal Artifacts from Non-Dietary Movements
- Cause: Arm movements unrelated to eating (e.g., gesturing, scratching) can create impedance or motion patterns that mimic eating.
- Solution: Implement a secondary classification layer to filter out "idle" activities. Collect more diverse training data that includes common non-eating activities to improve the model's discrimination.
Insufficient User-Independent Training Data
- Cause: The machine learning model was trained on too few subjects and has not learned to generalize across a population with different physiologies and movement patterns.
- Solution: Re-train the model using a user-independent validation strategy. Ensure the training dataset encompasses data from a larger and more diverse cohort of participants.
Suboptimal Sensor Placement or Contact
- Cause: For bio-impedance sensors, poor electrode-skin contact can lead to noisy, unreliable signals.
- Solution: Standardize and document the exact sensor placement protocol. Use electrodes that ensure consistent skin contact and instruct participants on proper wearing techniques.
Issue: High False Positive Rate in Vision-Based Intake Detection
Problem: A vision-based system frequently labels non-eating actions (e.g., hand touching face, talking) as food intake events.
Possible Causes and Solutions:
- Limited Context in Frame Analysis
- Cause: The algorithm is analyzing individual frames or short clips without considering the temporal context that defines an eating gesture (e.g., hand moving toward mouth with an utensil, then returning).
- Solution: Employ temporal deep learning models like Long Short-Term Memory (LSTM) networks that can analyze video sequences to distinguish the full trajectory of an eating gesture from other hand-to-face movements [53].
- Inadequate Training Dataset
- Cause: The training dataset for the computer vision model lacks sufficient negative examples (i.e., videos of people not eating but performing similar actions).
- Solution: Augment the training dataset with a wide variety of negative examples. Utilize data augmentation techniques to artificially expand the dataset and improve model robustness.
Experimental Protocols for Key Methodologies
Protocol 1: Dietary Activity Recognition Using Wrist-Worn Bio-Impedance Sensing
This protocol outlines the methodology for using bio-impedance wearables to detect food intake activities, as exemplified by the iEat system [6].
1. Hypothesis: Dynamic changes in bio-impedance signals measured across the wrists can be used to automatically and reliably classify specific food intake activities.
2. Materials and Setup:
- Device: A wearable device with a bio-impedance analyzer in a two-electrode configuration.
- Electrode Placement: One electrode is worn on each wrist.
- Data Acquisition: The device continuously measures the electrical impedance across the body. The signal is sampled at a frequency sufficient to capture dynamic changes (e.g., 10-100 Hz).
3. Experimental Procedure:
1. Recruit participants according to the study's inclusion/exclusion criteria.
2. Fit participants with the wrist-worn sensors and verify signal integrity.
3. Conduct a structured meal session in a controlled, everyday dining environment. Participants should use standard metal utensils.
4. Simultaneously record the bio-impedance signal and a synchronized video feed for ground truth annotation.
5. Annotate the video data to label the start and end times of target activities: Cutting, Drinking, Eating with a Fork, Eating with Hand, and Idle.
4. Data Analysis: 1. Pre-process the raw impedance signal (filtering, normalization). 2. Segment the continuous signal into windows corresponding to the annotated activities. 3. Extract relevant features (e.g., statistical features, frequency-domain features) from each segment. 4. Train a lightweight, user-independent neural network (e.g., a compact convolutional network) using the features and ground truth labels. 5. Evaluate model performance using macro F1 score and accuracy on a held-out test set.
Diagram 1: Bio-impedance activity recognition workflow.
Protocol 2: Food Recognition and Volume Estimation Using Computer Vision
This protocol describes a standard pipeline for using deep learning and computer vision for dietary assessment from food images [53].
1. Hypothesis: Deep Convolutional Neural Networks (CNNs) can accurately classify food types and estimate portion sizes from images taken in real-world conditions.
2. Materials and Setup:
- Imaging Device: A standard smartphone camera or a dedicated RGB/Depth camera.
- Reference Object: A checkerboard or a fiducial marker of known dimensions placed next to the food for scale.
- Computing Infrastructure: A workstation with a GPU for model training and inference.
3. Experimental Procedure: 1. Data Collection: Capture images of food items before and after consumption. Ensure varied lighting conditions and angles to build a robust dataset. 2. Ground Truth Labeling: Manually label images with food type, and if required, perform precise weighing of food items to obtain true volume/mass. 4. Pre-processing: Apply standardization techniques like resizing, normalization, and data augmentation (rotation, brightness adjustment).
4. Data Analysis: 1. Food Recognition: Train a CNN (e.g., ResNet, Vision Transformer) or a multi-level attention network on the labeled dataset for food classification. 2. Portion Size Estimation: * Use the reference object to calibrate the image and estimate the food's volume via 3D reconstruction or depth mapping. * Train a regression model to map image features (e.g., pixel area, shape descriptors) to the known food mass/volume. 3. Model Validation: Report top-1 and top-5 classification accuracy, and mean absolute percentage error for volume estimation.
Diagram 2: Computer vision dietary assessment workflow.
The Scientist's Toolkit: Key Research Reagent Solutions
| Item | Function in Dietary Monitoring Research |
|---|---|
| Wrist-worn Bio-impedance Sensor | Measures changes in electrical impedance across the body to detect food-handling and ingestion activities based on dynamic circuit formation [6]. |
| Neck-worn Acoustic Sensor | Captures sounds associated with chewing and swallowing for intake detection and food type classification [6]. |
| Inertial Measurement Unit (IMU) | Tracks motion and orientation of wrists or utensils to identify specific dietary gestures (e.g., scooping, bringing to mouth) [6]. |
| RGB-D Camera | Captures both color images and depth information, crucial for food recognition and accurate portion size/volume estimation [33]. |
| Continuous Glucose Monitor (CGM) | Provides real-time, interstitial glucose measurements to link dietary intake with individual metabolic responses, a key input for personalized nutrition [19]. |
| Pre-trained CNN Models (e.g., YOLOv8) | Enables rapid development and deployment of accurate food recognition and detection systems from images [53]. |
| [4-(2-Morpholinoethoxy)phenyl]methylamine | [4-(2-Morpholinoethoxy)phenyl]methylamine | 95% | C13H20N2O2 |
| 1-(5-Bromopyridin-2-yl)piperidin-4-ol | 1-(5-Bromopyridin-2-yl)piperidin-4-ol, CAS:149806-52-0, MF:C10H13BrN2O, MW:257.13 g/mol |
FAQs: Technical Guidance for Researchers
FAQ 1: What are the key considerations when selecting a population biomarker for Wastewater-Based Epidemiology (WBE)?
Choosing a robust biomarker is critical for accurate population-level estimation. The table below summarizes the core selection criteria and performance of various biomarker types.
Table 1: Comparison of Biomarker Types for Population Estimation in WBE
| Biomarker Category | Example Biomarkers | Key Selection Criteria | Performance & Considerations |
|---|---|---|---|
| Chemical Biomarkers | Cimetidine, Metformin, Cotinine [54] | Low temporal variability, human-linked origin, stable in sewage [54] | High performance. Chemicals like cimetidine show excellent correlation with population size and low spatiotemporal variability [54]. |
| Genetic Biomarkers | Human mitochondrial DNA (mtDNA) [55] | Human-specific, quantitative, stable for rapid detection [55] | Moderate performance. Can be quantitatively monitored but are generally outperformed by chemical markers for population size estimation [54]. |
| Viral Markers & Nutrients | Ammonium, Orthophosphate [54] | Correlation with human load | Not recommended. Suffer from high temporal variability, leading to unreliable population estimates [54]. |
FAQ 2: How can I troubleshoot epigenetic biomarker analysis from non-invasive samples like blood or saliva?
A common challenge is ensuring that the identified epigenetic marks are truly representative of the exposure or disease state. The following workflow is recommended for robust analysis:
- Select Technologically-Validated Markers: Begin with epigenetic markers that have been rigorously validated. For example, hypomethylation of
AHRR(cg05575921) can predict current smoking status with an Area Under the Curve (AUC) > 0.99, and a panel of CpG sites can discriminate heavy alcohol drinkers from non-drinkers with an AUC > 0.90 [56]. - Account for Temporal Dynamics: Recognize that epigenetic marks can revert. For instance, methylation status of alcohol-related markers begins to revert to baseline after enforced abstinence [56]. The timing of sample collection is therefore crucial.
- Use a Multi-Marker Panel: Relying on a single CpG site can be error-prone. Combining several markers into a panel significantly increases the discriminatory accuracy and reliability of the test [56].
FAQ 3: What are the energy efficiency advantages of using a wearable bio-impedance device for dietary monitoring over traditional methods?
Traditional dietary monitoring methods like 24-hour recalls or smart utensils often require significant user intervention or dedicated hardware. A wearable bio-impedance sensor like the iEat system offers a more energy-efficient and passive monitoring paradigm [6].
- Principle of Operation: The device measures impedance between two wrist-worn electrodes. During dining activities, dynamic circuit variations occur (e.g., through hands, mouth, utensils, and food), creating unique temporal patterns in the impedance signal [6].
- Energy Efficiency Advantage: This method is inherently low-power because it leverages the body's existing conductive properties and the natural interaction with food and utensils. It eliminates the need for energy-intensive external instrumented devices (e.g., smart trays, specialized utensils) and complex video-based systems, enabling sustained, all-day monitoring with minimal battery consumption [6].
Troubleshooting Common Experimental Issues
Issue 1: High Variability in Population Size Estimates from Wastewater
- Problem: Estimates of the population size in a catchment area are inconsistent.
- Solution:
- Calibrate Locally: Population biomarker performance can vary by region. Always calibrate and validate your chosen biomarker (e.g., cimetidine) against local census data at the country or region level [54].
- Avoid Seasonal Markers: Do not use substances with strong seasonal usage trends (e.g., antihistamines, anti-inflammatories) as population markers [54].
- Pre-concentrate Samples: For genetic biomarkers like mtDNA, integrate a filter to remove solids and simultaneously perform DNA extraction and enrichment to improve the limit of detection [55].
Issue 2: Low Accuracy in Classifying Food Types with Wearable Sensors
- Problem: A wearable dietary monitor fails to accurately distinguish between different food types.
- Solution:
- Leverage Characteristic Impedance Patterns: The key is to analyze the unique impedance variation patterns caused by different foods. The electrical properties (
Zf) of various foods (e.g., a piece of vegetable vs. meat) will alter the overall impedance of the human-food circuit in distinct ways [6]. - Refine the Model: Ensure your classification model is trained on a robust dataset captured in real-life dining environments. User-independent models can then be developed to recognize these food-specific patterns with higher accuracy [6].
- Leverage Characteristic Impedance Patterns: The key is to analyze the unique impedance variation patterns caused by different foods. The electrical properties (
Experimental Protocols
Protocol 1: Rapid "Sample-to-Answer" Detection of Genetic Biomarkers from Wastewater
This protocol is adapted from a study demonstrating the detection of human mitochondrial DNA (mtDNA) from raw wastewater [55].
- Sample Collection: Collect a composite raw wastewater sample.
- Sample Preparation: Pass the sample through an integrated filter to remove solid impurities. This filter also functions to extract and enrich DNA directly from the sample.
- Isothermal Amplification: Perform Loop-Mediated Isothermal Amplification (LAMP) targeting the human-specific mtDNA sequence. This step is carried out at a constant temperature (e.g., 60-65°C), eliminating the need for a high-energy thermal cycler.
- Detection: Use a low-cost lateral flow test strip to visualize the amplified LAMP products.
- Analysis: The entire process, from sample to result, takes approximately 45 minutes and can be performed on-site with minimal intervention [55].
Protocol 2: Metagenomic Sequencing for Antimicrobial Resistance (AMR) Surveillance in Wastewater
This protocol outlines the workflow for profiling antibiotic resistance genes (ARGs) from wastewater to monitor population health [57] [58].
- Sample Collection: Collect composite wastewater samples from the inlet of wastewater treatment plants or specific sources (e.g., nursing homes, schools).
- DNA Extraction: Concentrate microbial biomass from wastewater, followed by genomic DNA extraction using a commercial kit.
- Library Preparation & Sequencing: Prepare metagenomic sequencing libraries from the extracted DNA and sequence them using a high-throughput platform (e.g., Illumina PE150).
- Bioinformatic Analysis:
- Quality Control: Trim adapters and assess read quality using tools like Trimmomatic and FastQC.
- Assembly: Assemble quality-filtered reads into contigs using an assembler like Skesa.
- Gene Identification: Use specialized pipelines (e.g., NCBI AMR Finder Plus) to identify and characterize ARGs, virulence factors, and plasmid replicons from the assembled contigs [57].
- Data Interpretation: Correlate the diversity and abundance of ARGs with the source population (e.g., age group, geographic location) to assess public health risks [58].
Research Reagent Solutions
Table 2: Essential Materials for Genetic/Epigenetic and Wastewater Biomarker Research
| Item | Function/Application | Examples / Notes |
|---|---|---|
| CHROMagar ESBL | A selective chromogenic medium for culturally isolating ESBL-producing E. coli from complex samples like wastewater [57]. | Used in AMR surveillance studies to screen for specific resistant bacteria before genomic analysis [57]. |
| LAMP Assay Kits | For rapid, isothermal amplification of nucleic acid biomarkers in field-deployable settings [55]. | Enables "sample-to-answer" detection of genetic targets (e.g., mtDNA) without complex lab infrastructure [55]. |
| DNA Methylation Analysis Kits | For processing blood or saliva DNA to identify exposure-associated epigenetic markers [56]. | Includes bisulfite conversion kits and targeted sequencing or pyrosequencing assays for specific CpG sites (e.g., in AHRR, F2RL3) [56]. |
| Solid-Phase Extraction (SPE) Cartridges | Sample preparation for the analysis of chemical biomarkers in wastewater [59]. | Hydrophilic-lipophilic balance (HLB) phases are commonly used to concentrate analytes from the aqueous matrix prior to LC-MS analysis [59]. |
| Bio-Impedance Sensing Circuit | The core sensing unit for wearable dietary monitoring devices [6]. | Typically deployed in a two-electrode configuration on the wrists to measure dynamic impedance changes during eating [6]. |
Schematic: Wastewater-Based Epidemiology for Public Health
The following diagram illustrates the integrated workflow of using wastewater analysis for population-level health assessment, demonstrating the energy-efficient advantage of pooling community data.
Overcoming Data Accuracy and Adherence Challenges in Research Settings
Addressing Variability in Data Collection and Patient-Reported Intake
Troubleshooting Guides & FAQs
FAQ 1: What are the primary sources of variability in self-reported dietary intake data, and how can we mitigate them?
Variability and inaccuracies in self-reported data are notorious challenges in dietary monitoring [8]. The primary sources of error and their mitigations are summarized below.
| Source of Variability | Description | Mitigation Strategies |
|---|---|---|
| Memory Reliance | Participant forgetfulness leads to under-reporting or misreporting of foods consumed [8]. | Use 24-hour recalls on recent, non-consecutive days; leverage technology like image-based records to reduce reliance on memory [8] [18]. |
| Portion Size Estimation | Participants are often poor at estimating the volume or weight of consumed food and beverages [18]. | Implement tools with reference images (e.g., coins, cards) or use image-based methods with portion size estimation algorithms [18] [33]. |
| Social Desirability Bias | Participants may alter their reported intake to what they perceive as more socially acceptable [18]. | Use automated, self-administered tools (e.g., ASA-24) to reduce interviewer bias and emphasize data confidentiality [8]. |
| Participant Reactivity | The act of monitoring can cause individuals to change their usual dietary patterns [8] [18]. | Use less obtrusive methods like passive sensing or 24-hour recalls (which query past intake) rather than pre-conceived food records [8]. |
| Day-to-Day Variation | A person's diet can vary significantly from one day to the next [8]. | Collect multiple days of data, including both weekdays and weekends, and use statistical adjustments to estimate usual intake [8]. |
FAQ 2: How can emerging technologies make continuous dietary monitoring more energy-efficient and less burdensome?
Current research is shifting from purely self-reported methods to more passive, sensor-based technologies. These aim to reduce user burden and improve the objectivity and energy efficiency of data collection [18] [33]. The following workflow illustrates how these technologies can be integrated for continuous monitoring.
FAQ 3: What methodologies should I use to validate a new dietary intake monitoring tool against established techniques?
Validation is critical for adopting any new monitoring tool. The table below compares common validation methodologies, moving from least to most rigorous.
| Method | Description | Application & Considerations |
|---|---|---|
| Comparison with Self-Report | Compare the new tool's results against a traditional method like a Food Record or 24-hour recall [8]. | Subject to same biases as self-report. Useful for initial feasibility studies but does not confirm accuracy. |
| Concentration Biomarkers | Compare reported intake of a nutrient (e.g., Vitamin C) with its corresponding biomarker level in blood or urine [8]. | Does not directly measure intake "recovery," but a correlation can support the validity of the tool for ranking individuals. |
| Recovery Biomarkers | Use objective biomarkers where nearly 100% of the consumed nutrient is recovered in urine (e.g., nitrogen for protein, doubly labeled water for energy) [8]. | Considered the "gold standard" for validating energy, protein, sodium, and potassium intake. Logistically complex and expensive. |
| Direct Observation | Use controlled feeding studies or continuous observation in a lab setting as the ground truth [33]. | Provides highly accurate validation data but lacks ecological validity as it does not reflect real-world conditions. |
The Scientist's Toolkit: Research Reagent Solutions
The following table details essential "research reagents"—both methodological and technological—for the field of continuous dietary monitoring.
| Item / Solution | Function in Dietary Monitoring Research |
|---|---|
| 24-Hour Dietary Recall (24HR) | A structured interview to capture all foods/beverages consumed in the previous 24 hours. Serves as a benchmark for short-term intake assessment [8]. |
| Recovery Biomarkers (e.g., Doubly Labeled Water) | Objective, biological measurements used to validate the accuracy of self-reported energy and protein intake without relying on participant memory [8]. |
| Inertial Measurement Units (IMUs) | Wearable sensors (accelerometers, gyroscopes) that detect and classify specific intake gestures (e.g., hand-to-mouth movements) for passive monitoring [18] [33]. |
| Convolutional Neural Networks (CNNs) | A class of deep learning algorithms critical for automating the analysis of dietary images, including food recognition and portion size estimation [33]. |
| Automated Self-Administered 24HR (ASA-24) | A web-based tool that automates the 24-hour recall process, reducing interviewer burden and cost while standardizing data collection [8]. |
| 4-(2-Bromomethylphenyl)benzonitrile | 4-(2-Bromomethylphenyl)benzonitrile |
| 5-(thiophen-2-yl)-1H-indole | 5-(Thiophen-2-yl)-1H-indole|CAS 144104-54-1 |
Strategies for Improving Long-Term Participant Adherence to Monitoring
Frequently Asked Questions (FAQs)
Q1: Why is long-term participant adherence critical in dietary monitoring research? Successful completion of research and the validity of its findings depend heavily on retaining participants throughout the study period. Poor adherence can lead to significant cost overruns, time delays, and introduce biases that threaten the credibility of the results [60].
Q2: What are the most common challenges to participant adherence? Challenges are multifaceted and include participant migration, perceived or real adverse events, lack of trust, socioeconomic barriers, and interference from family or physicians not involved in the study. In digital remote studies, the burden of frequent study visits and active tasks can also lead to disengagement [60] [61].
Q3: How can we address the burden of dietary data collection to improve adherence? Leveraging technology-assisted dietary assessment methods can improve accuracy and reduce participant burden. Methods like automated 24-hour dietary recalls (ASA24, Intake24) and mobile food records have shown reasonable validity in estimating energy and nutrient intake compared to observed intake, making the process less intrusive for participants [14].
Q4: Are there specific participant characteristics associated with better adherence? Yes, research has shown that older age is significantly associated with longer retention in studies. Furthermore, in remote digital studies, the type of smartphone and recruitment site can also influence how long participants remain engaged and contribute data [61].
Q5: What is a key psychological factor in keeping participants engaged? The quality of the relationship between the research staff and the participant is a vital factor for success. Personalized care, including listening to a participant's problems and ensuring they can contact the study team at any time, has been shown to improve retention [60].
Troubleshooting Guides
Problem 1: High Drop-out Rates in Long-Term Monitoring
Symptoms: Participants stop attending scheduled visits, fail to submit data, or become unresponsive to communication attempts [60].
| Diagnostic Step | Corrective Action |
|---|---|
| Identify signs of disengagement early (e.g., missed visits, impatience) [60]. | Implement proactive appointment reminders via phone, email, or cards [60]. |
| Analyze demographic and baseline data for retention risk factors [61]. | Assign a dedicated study coordinator to build rapport and provide a "listening ear" [60]. |
| Assess participant burden and logistical barriers [60]. | Offer reasonable travel reimbursement and consider meal vouchers, with approval from the Ethics Committee [60]. |
Diagram 1: Participant Engagement Workflow
Problem 2: Inaccurate or Incomplete Dietary Data Collection
Symptoms: Large discrepancies in reported energy intake, missing data points, or poor compliance with dietary reporting protocols [14].
| Diagnostic Step | Corrective Action |
|---|---|
| Compare estimated energy intake from different dietary assessment methods against controlled feeding data [14]. | Select a validated, technology-assisted method like Intake24 or ASA24 that balances accuracy and user burden [14]. |
| Evaluate if the chosen statistical model for energy adjustment aligns with the research question [62]. | Use the "all-components model" which simultaneously adjusts for all dietary components to reduce confounding for both total and relative causal effect estimands [62]. |
| Investigate user-friendliness of dietary reporting tools. | Provide clear instructions and technical support for dietary apps or recall tools to ensure proper use. |
Diagram 2: Dietary Data Validation Pathway
Summarized Quantitative Data on Adherence
Table 1: Participant Retention Rates in Long-Term Clinical and Digital Studies This table summarizes retention rates from various studies, demonstrating that high retention is achievable with targeted strategies [60] [61].
| Study / Trial Name | Context | Number of Participants | Retention Rate (%) |
|---|---|---|---|
| PIONEER 6 [60] | Clinical Trial | 3,418 | 100 |
| LEADER [60] | Clinical Trial | 9,340 | 97 |
| DEVOTE [60] | Clinical Trial | 7,637 | 98 |
| RADAR-MDD (Phone-Active) [61] | Remote Digital Study (43 weeks) | 614 | 54.6 |
| RADAR-MDD (Fitbit-Passive) [61] | Remote Digital Study (43 weeks) | 614 | 67.6 |
Table 2: Accuracy of Technology-Assisted Dietary Assessment Methods This table compares the accuracy of different dietary intake estimation methods against true intake, a key factor in selecting a low-burden, valid tool for participants [14]. Values represent the mean percentage difference between true and estimated energy intake.
| Dietary Assessment Method | Mean Difference from True Intake (%) |
|---|---|
| IA-24HR (Image-Assisted Interviewer-Administered 24HR) | 15.0% |
| ASA24 (Automated Self-Administered 24HR) | 5.4% |
| Intake24 | 1.7% |
| mFR-TA (mobile Food Record-Trained Analyst) | 1.3% |
Experimental Protocols for Key Cited Studies
Protocol 1: Implementing a Participant Retention Strategy
Objective: To achieve high long-term participant adherence (≥95%) in a clinical or observational monitoring study [60].
- Pre-Recruitment Planning: Integrate retention strategies into the study protocol design. Secure ethical approval for incentives and communication plans [60].
- Team Structure: Appoint a dedicated Study Coordinator or National Study Coordinator. Define their primary responsibility as building rapport, tracking adherence, and acting as the first point of contact for participants [60].
- Participant Onboarding: During informed consent, clearly articulate the participant's value to the study. Establish communication channels, including a 24-hour contact number for the study team [60].
- Ongoing Engagement:
- Communication: Implement a system of proactive appointment reminders (calls, emails, cards) [60].
- Incentives: Provide travel reimbursement or meal vouchers at each visit, as approved by the Ethics Committee [60].
- Feedback: Use newsletters to update participants on the study's progress and highlight their contribution [60].
- Monitoring and Intervention: Continuously monitor for signs of disengagement (e.g., missed visits). Proactively reach out to at-risk participants to understand and address challenges [60].
Protocol 2: Validating Dietary Assessment Methods for Energy Intake
Objective: To accurately estimate energy and nutrient intake using technology-assisted methods in a remote monitoring context [14].
- Study Design: A randomized crossover controlled feeding study is the gold standard for validation [14].
- Controlled Feeding: Participants consume breakfast, lunch, and dinner prepared and unobtrusively weighed by the research team to establish "true intake" [14].
- Dietary Recall: The following day, participants are randomized to complete a 24-hour dietary recall using one of several technology-assisted methods (e.g., ASA24, Intake24, mobile Food Record) [14].
- Data Analysis: Compare the estimated energy and nutrient intakes from the dietary assessment tools to the true intake from the controlled feeding. Assess accuracy using mean differences and variances [14].
- Energy Adjustment in Analysis: For data analysis, use the "all-components model" to adjust for energy intake by simultaneously including all dietary components in the statistical model to reduce confounding [62].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Remote Dietary Monitoring Research
| Item | Function |
|---|---|
| Validated Dietary Assessment Platform (e.g., ASA24, Intake24) | Enables automated, self-administered 24-hour dietary recalls, reducing staff burden and facilitating remote data collection with reasonable accuracy [14]. |
| Wearable Activity Tracker (e.g., Fitbit) | Collects passive data on physical activity and sleep, which can provide contextual behavioral information and may be shared for longer periods than active survey data [61]. |
| Secure Data Collection Platform | A scalable backend system to handle high-fidelity, multimodal data streams from smartphones and wearables while ensuring participant data privacy [61]. |
| Participant Relationship Management (PRM) System | A centralized system for tracking participant interactions, scheduling reminders, and logging communications to facilitate personalized follow-up and build rapport [60]. |
| Phenyl 2-(phenylthio)phenylcarbamate | Phenyl 2-(phenylthio)phenylcarbamate, CAS:111974-73-3, MF:C19H15NO2S, MW:321.4 g/mol |
| N-ACETYLAMINOMETHYLPHOSPHONATE | N-ACETYLAMINOMETHYLPHOSPHONATE, CAS:57637-97-5, MF:C3H8NO4P, MW:153.07 g/mol |
Algorithmic and Analytical Methods for Enhancing Data Reliability
Core Data Reliability Concepts in Dietary Monitoring
In the context of energy-efficient continuous dietary monitoring research, data reliability refers to the trustworthiness and consistency of data collected across its entire lifecycle. For research on energy efficiency in continuous dietary monitoring, ensuring data reliability is paramount, as unreliable data can corrupt analyses, lead to flawed insights, and cause resources to be wasted on erroneous pathways [63] [64].
Data Reliability vs. Data Quality: While related, these concepts are distinct. Data quality is a broader umbrella that encompasses various dimensions, including reliability. Key dimensions include [65] [66]:
- Accuracy: The degree to which data correctly represents the real-world values or events it is intended to model (e.g., a correctly logged food item and its accurate portion size).
- Completeness: The extent to which all required data is present without gaps or missing values (e.g., a full day of dietary logging instead of only a single meal).
- Consistency: Ensures that data values are coherent and compatible across different datasets, systems, or time periods.
- Timeliness: Data must be up-to-date and relevant for analysis when used. Outdated information can lead to incorrect conclusions.
- Uniqueness: The absence of duplicate records in a dataset, which can skew analysis by over-representing specific data points.
Data Reliability vs. Data Validity: Data reliability focuses on the consistency and repeatability of data across different observations. Data validity, in contrast, concerns the accuracy and integrity of the data, ensuring it is formatted correctly and measures what it is intended to measure. You can have a highly reliable data collection process that yields consistent results, but if the data being collected is not valid, the end result will still be low-quality [63].
Troubleshooting Common Data Reliability Issues
This section addresses specific data reliability challenges encountered in dietary monitoring research, providing root causes and actionable solutions.
FAQ 1: How can I mitigate user-induced reporting biases in subjective dietary data?
- Issue: Traditional dietary assessment methods like 24-hour recalls and Food Frequency Questionnaires (FFQs) rely on self-reporting, which is susceptible to recall bias, social desirability bias, and misunderstanding of portion sizes. These biases produce data that may not reflect true consumption patterns [67].
- Solution:
- Incorporate Objective Biomarkers: Integrate metabolic biomarkers from blood or urine samples to objectively validate self-reported intake. For example, biomarkers related to lipid metabolism, liver function, and metabolic factors have been pivotal in discriminating between dietary patterns like pro-Mediterranean and pro-Western diets [67].
- Leverage AI-Assisted Tools: Utilize mobile applications that employ image recognition, barcode scanning, and machine learning to reduce reliance on memory and subjective portion estimation. These tools can improve the accuracy and objectivity of data collection [68] [69].
FAQ 2: What is the minimum data collection period needed for a reliable estimate of usual nutrient intake?
- Issue: Day-to-day variability in food intake can obscure true dietary patterns, making it challenging to determine a sufficient data collection period without overburdening participants [68].
- Solution:
- Follow Evidence-Based Guidelines: Research based on large digital cohorts indicates that the minimum number of days required varies by nutrient [68]:
- 1-2 days: Sufficient for water, coffee, and total food quantity.
- 2-3 days: Adequate for most macronutrients (carbohydrates, protein, fat) to achieve good reliability.
- 3-4 days: Generally required for micronutrients and food groups like meat and vegetables.
- Optimize Day Selection: Data collection should ideally be non-consecutive and include at least one weekend day, as intake patterns for energy, carbohydrates, and alcohol often differ on weekends [68].
- Follow Evidence-Based Guidelines: Research based on large digital cohorts indicates that the minimum number of days required varies by nutrient [68]:
FAQ 3: Which application features significantly increase energy consumption, and how can this be managed?
- Issue: The energy efficiency of continuous monitoring is compromised by certain app functionalities, which can drain device batteries and disrupt long-term monitoring [70].
- Solution:
- Identify High-Consumption Features: Key contributors to elevated energy consumption in mobile health (mHealth) apps include frequent notifications, continuous GPS use, and high app complexity with real-time syncing and background activities [70].
- Implement Energy-Aware Design:
- Optimize the frequency of push notifications and background data syncing.
- Use GPS services adaptively rather than continuously.
- Simplify app interfaces and workflows to reduce computational load.
FAQ 4: How can I handle missing or incomplete dietary data effectively?
- Issue: Datasets often have missing values due to non-response, technical errors, or participant dropout, which can compromise data completeness and analytic validity [67] [64].
- Solution:
- Apply Robust Imputation Strategies: For parameters with less than 20% missingness, replace missing values with the median of the available data. For higher rates of missingness, consider more advanced imputation techniques or exclusion, depending on the variable's importance [67].
- Establish Data Validation Rules: Implement real-time validation during data entry to flag missing critical fields, reducing the incidence of incomplete records from the outset [66].
Experimental Protocols for Ensuring Data Reliability
Protocol for Developing a Predictive Biomarker Algorithm
This methodology details the creation of a computational algorithm to classify dietary patterns using biochemical markers, enhancing objectivity [67].
- Participant Recruitment & Data Collection: Recruit a sufficient sample size (calculation based on expected correlation coefficients). Collect data through:
- Comprehensive clinical examinations and lifestyle questionnaires.
- Biochemical Sampling: Collect fasting blood samples for a full profile (e.g., hematology, metabolites, enzymes, vitamins).
- Dietary Assessment: Administer a 72-hour dietary recall and a validated Food Frequency Questionnaire (FFQ).
- Data Preprocessing & Imputation: Address missing values in biochemical data. Exclude biomarkers with >20% missingness. For others, use median imputation for missing values in the remaining parameters [67].
- Dietary Pattern Clustering: Use statistical clustering methods (e.g., k-means) on the 72-hour recall data, factoring in sex, age, and BMI, to identify distinct dietary patterns (e.g., pro-Mediterranean vs. pro-Western).
- Biomarker Selection: Employ elastic net regression on the biochemical data to identify the most predictive biomarkers (e.g., those related to lipid metabolism, liver function) that are significantly associated with the identified dietary clusters.
- Algorithm Construction & Validation: Construct computational algorithms (e.g., a main algorithm and a simplified, clinically feasible version) using the selected biomarkers. Validate the model's predictive capability using metrics such as the ROC curve (target: >0.9) and precision-recall curve (target: >0.8) [67].
Protocol for Energy Consumption Profiling of mHealth Apps
This protocol provides a method to quantify and analyze the energy consumption of dietary tracking applications [70].
- App Selection: Select a representative sample of popular mHealth apps based on criteria such as number of downloads, user ratings, and functional complexity.
- Baseline Measurement: Measure the baseline energy consumption of each app in an idle state (not in active use) to establish a benchmark.
- Feature-Specific Scenario Testing: Design and execute test scenarios that trigger specific, common app features:
- Logging a meal (using camera and image processing).
- Syncing data with a cloud server or wearable device.
- Using GPS for location-based logging.
- Receiving and interacting with push notifications.
- Energy Measurement: Use advanced power consumption frameworks to measure energy use in milliwatt-hours (mWh) for each scenario. Employ metrics like "energy-per-function" and "energy-per-user-interaction" for granular understanding [70].
- Statistical Analysis:
- Perform descriptive statistics to reveal variability in app energy consumption.
- Use ANOVA to verify the critical role of different features and user engagement.
- Apply regression modeling (e.g.,
energy consumption = β₀ + βâ‚*notification frequency + β₂*GPS use + β₃*app complexity + ε) to quantify the effects of specific factors on energy use [70].
Reference Tables and Data Summaries
Table 1: Factors Contributing to mHealth App Energy Consumption
This table summarizes key findings on what drives energy use in dietary apps, informing more efficient design choices. [70]
| Factor | Impact on Energy Consumption | Statistical Significance (P-value) |
|---|---|---|
| Notification Frequency | Significant positive correlation | 0.01 |
| GPS Use | Significant positive correlation | 0.05 |
| App Complexity (Real-time features, background sync) | Significant positive correlation | 0.03 |
| User Interaction & Engagement | Major source of observed variance | Confirmed via ANOVA |
Table 2: Minimum Days Required for Reliable Dietary Intake Estimation
This table provides evidence-based guidance on data collection duration for different nutrients, balancing reliability and participant burden. [68]
| Nutrient / Food Group | Minimum Days for Reliable Estimation (r ≥ 0.8) | Notes |
|---|---|---|
| Water, Coffee, Total Food Quantity | 1-2 days | Most quickly estimable. |
| Carbohydrates, Protein, Fat | 2-3 days | Most macronutrients. |
| Micronutrients, Meat, Vegetables | 3-4 days | Generally required. |
| Recommendation | 3-4 non-consecutive days, including one weekend day | Optimizes for most nutrients and accounts for weekly variation. |
Workflow and System Diagrams
Data Reliability Workflow
Data Reliability Management Workflow
Energy-Aware Algorithm Design
Energy-Aware Algorithm Framework
The Scientist's Toolkit: Essential Reagents & Materials
Table 3: Key Research Reagent Solutions for Reliable Dietary Monitoring Studies
| Item | Function & Application in Research |
|---|---|
| Validated FFQs & 24-Hour Recall Protocols | Standardized tools for collecting self-reported dietary intake data. Provides a baseline for comparison with objective measures and is essential for initial dietary pattern clustering [67] [71]. |
| Biochemical Assay Kits | Kits for analyzing metabolic biomarkers in blood/urine (e.g., lipid panels, liver enzymes, specific nutrient metabolites). Used for objective validation of dietary intake and as inputs for predictive algorithms [67]. |
| Mobile Health (mHealth) Application | A digital tool for dietary tracking, ideally with image recognition, barcode scanning, and AI-based food identification. Reduces recall bias and enables continuous, detailed data collection with timestamps [68] [69]. |
| Energy Profiling Software | Frameworks and tools (e.g., Android's Battery Historian) for measuring the energy consumption of software applications. Critical for quantifying the energy efficiency of dietary monitoring apps and identifying optimization targets [70]. |
| Machine Learning Libraries | Software libraries (e.g., scikit-learn, TensorFlow) containing implementations of algorithms for regression, classification, and clustering. Used to build predictive models of dietary patterns and analyze complex biomarker data [67] [72]. |
| Statistical Analysis Software | Platforms (e.g., R, Python with pandas/statsmodels) capable of performing advanced statistical analyses, including linear mixed models, ANOVA, and intraclass correlation coefficients. Necessary for analyzing variability, determining minimum days, and validating results [70] [68]. |
Ensuring Data Interoperability and Secure Management in Clinical Trials
This technical support center provides troubleshooting guides and FAQs for researchers managing data in clinical trials, with a specific focus on energy-efficient systems for continuous dietary monitoring.
Frequently Asked Questions (FAQs)
Data Interoperability & Standards
Q: What standards should we use to ensure dietary monitoring data from wearables is interoperable with clinical systems? A: For US-based research, the United States Core Data for Interoperability (USCDI) provides a standardized set of health data classes and elements for nationwide interoperability. When transmitting data from dietary monitors to electronic health records (EHRs), you should map your data elements to relevant USCDI classes. As of July 2024, USCDI v4 includes 20 new data elements and one new data class, providing expanded structure for health data exchange [73]. Always ensure your data formats align with the latest USCDI version to maintain compliance and seamless data flow.
Q: How can we improve the completeness of demographic data in our research databases? A: Incomplete demographic data is a common issue that hampers health equity research. To improve this:
- Implement validation rules: Set system-level checks that require key fields (e.g., race, gender) to be populated before form submission.
- Automate data exchange: Ensure your EHR and research systems are configured to exchange demographic data seamlessly, not just clinical information. One analysis of immunization data found that while immunization data was exchanged, patient demographic information often was not [74].
- Monitor completeness: Regularly run reports to quantify missing data, similar to Florida's COVID-19 reporting which showed 10.6% missing race data in vaccinated populations [74]. Use these metrics to target improvement efforts.
Data Security & Compliance
Q: What are the essential data security measures for digital clinical trials? A: Core security measures include [75]:
- Data encryption: Encrypt data both in transit (TLS/SSL) and at rest (AES-256 or equivalent).
- Role-based access control (RBAC): Limit system access based on user roles and responsibilities.
- Audit trails: Automatically record who accessed or modified data, when, and what changes were made.
- Multi-factor authentication (MFA): Require more than just passwords for system access.
- Regular security audits: Conduct periodic assessments to identify vulnerabilities.
Q: What compliance frameworks are most critical for clinical trial data? A: Key frameworks include [75]:
- ICH-GCP (Good Clinical Practice): Global standard for ethical and scientific trial conduct.
- 21 CFR Part 11: FDA regulation for electronic records and electronic signatures.
- HIPAA: US regulation for health data privacy and security.
- GDPR: EU law governing personal data processing and transfer.
Energy Efficiency in Dietary Monitoring
Q: Which features of continuous dietary monitoring apps most significantly impact energy consumption? A: Research on mobile health (mHealth) apps identifies these key energy consumption factors [70]:
- GPS Use: Continuous location tracking significantly increases energy drain.
- Notification Frequency: Frequent alerts and push notifications consume substantial energy.
- App Complexity: Advanced features like real-time monitoring and AI-driven recommendations can increase energy consumption by up to 30% compared to simpler apps [70].
- Background Activities: Unnoticed background processes like continuous data syncing can account for up to 40% of an app's total energy consumption [70].
Q: What strategies can optimize energy use in continuous dietary monitoring applications? A: To enhance energy efficiency [70]:
- Use adaptive brightness settings and device energy-saving modes, which can extend battery life by up to 20%.
- Batch process data and synchronize at intervals rather than using continuous real-time transmission.
- Leverage software-defined networking for energy optimization in mobile cloud computing, which can decrease energy use by up to 25%.
- Consider cross-platform frameworks carefully, as they can significantly increase energy consumption compared to native apps [70].
Troubleshooting Guides
Problem: High Energy Consumption in Dietary Monitoring Wearables
Symptoms: Short battery life, device overheating, incomplete data collection during long monitoring periods.
Resolution Protocol:
- Profile Energy Usage: Measure baseline energy consumption (typically 150-310 milliwatt-hours for mHealth apps) and identify peaks [70].
- Analyze Feature Impact: Use the regression model: Energy consumption = β₀ + β₠× notification frequency + β₂ × GPS use + β₃ × app complexity + ε [70].
- Implement Optimizations:
- Reduce GPS sampling frequency when precise location isn't critical.
- Batch notifications and process data in chunks rather than continuously.
- Disable non-essential background processes, especially during idle periods.
Prevention: During study design, conduct energy impact assessments for all monitoring features and set energy budgets for different functions.
Problem: Data Silos Between Dietary Monitoring Devices and Clinical Databases
Symptoms: Inability to automatically transfer data, manual data entry requirements, inconsistent data across systems.
Resolution Protocol:
- Map Data Elements: Create a crosswalk between your device's output data and USCDI data classes (e.g., "food intake events" to "Patient Care Interventions") [73].
- Implement APIs: Use standardized APIs for data exchange rather than custom integrations.
- Validate Data Flow: Test with sample data to ensure completeness and accuracy during transfer.
- Centralize Storage: Create a unified data repository that harmonizes information from all sources [76].
Prevention: Select monitoring devices with demonstrated interoperability capabilities and standardize data formats across your research portfolio.
Energy Monitoring Experimental Workflow
The following diagram illustrates the experimental workflow for profiling and optimizing energy usage in a dietary monitoring system, integrating both device-level and data management considerations:
Quantitative Energy Consumption Data
Table: Energy Consumption Factors in Mobile Health Applications [70]
| Factor | Impact on Energy Consumption | Statistical Significance (P-value) |
|---|---|---|
| Notification Frequency | Significant increase | 0.01 |
| GPS Use | Significant increase | 0.05 |
| App Complexity | Moderate to significant increase | 0.03 |
| Background Data Syncing | Accounts for up to 40% of total consumption | Not specified |
| Real-time Monitoring Features | Up to 30% higher than simpler apps | Not specified |
Research Reagent Solutions
Table: Essential Materials for Bio-Impedance Dietary Monitoring Research [6]
| Item | Function in Research |
|---|---|
| Wrist-worn Electrodes (Pair) | Measures bio-impedance signals across the body during dining activities. One electrode is placed on each wrist. |
| Bio-impedance Sensor | Quantifies impedance variation caused by dynamic circuit changes during hand-to-mouth gestures and food interactions. |
| Signal Processing Unit | Converts raw impedance data into analyzable signals for activity and food type recognition. |
| Lightweight Neural Network Model | Classifies food intake activities and types from impedance patterns in real-life dining environments. |
| Metal Utensils (Fork, Knife) | Forms conductive circuit bridges between hands, food, and mouth during eating activities. |
| Data Logging Platform | Records temporal impedance signal patterns for subsequent analysis and model training. |
Mitigating Bias and Ensuring Equity in Digital Monitoring Tools
A technical support guide for researchers in continuous dietary monitoring
Frequently Asked Questions
What does "bias" mean in the context of a digital monitoring tool? Bias occurs when a system produces systematically prejudiced results that unfairly disadvantage specific groups of users [77]. In your research, this could mean a tool that accurately tracks the dietary intake of one demographic group but performs poorly for another, potentially skewing your study results.
Couldn't poor performance just be a technical glitch, not actual bias? Not all performance variations constitute bias. Sometimes, outcomes accurately reflect real-world distributions [78]. The key is to conduct a thorough analysis to determine if differences stem from a technical flaw, unrepresentative training data, or a genuine phenomenon. For example, if your tool struggles with identifying a specific food type across all users, it is likely a technical issue. If it fails only for certain user demographics, it may be biased.
Why should energy-efficient research models care about algorithmic bias? Mitigating bias is crucial for research integrity and energy efficiency. A biased model that requires constant recalibration or produces errors that need manual correction wastes computational resources and energy. A fair, well-functioning model operates more efficiently and reliably, supporting sustainable research practices [77] [78].
My model is accurate overall. Do I still need to check for biased outcomes? Yes. High overall accuracy can mask significant performance disparities across different user groups [77]. A dietary monitoring tool might be 95% accurate overall but could be failing for 30% of users from a particular background. Comprehensive bias testing is essential.
Troubleshooting Guide
| Problem & Symptom | Root Cause | Solution |
|---|---|---|
| Model Performance Disparity: High error rates for specific participant demographics (e.g., age, skin tone) [77]. | Biased Training Data: Unrepresentative dataset lacking diversity [77] [78]. | 1. Audit Dataset: Analyze training data demographic representation.2. Augment Data: Collect more data from underrepresented groups.3. Apply Techniques: Use re-sampling or re-weighting methods. |
| Unexplained Output Drift: Model performance degrades over time with new participants. | Historical Bias: Model learned and perpetuates societal biases from historical data [77]. | 1. Identify Proxies: Find and remove features correlating with protected attributes.2. Pre-process Data: Use algorithms to remove bias from labels.3. Post-process: Adjust model outputs to ensure fairness. |
| Inconsistent Feature Recognition: Tool inaccurately tracks specific foods or actions for some users. | Measurement Bias: Inconsistent data collection methods or environmental factors [77]. | 1. Standardize Protocols: Ensure consistent data collection settings (lighting, sensors).2. Diverse Testing: Test in real-world environments used by all participant groups. |
| Failed Fairness Audit: Tool shows discriminatory outcomes in fairness metrics. | Algorithmic Design Bias: Optimization goals lack fairness constraints [77]. | 1. Implement Fairness Metrics: Define and embed metrics (e.g., demographic parity).2. Re-train Model: Incorporate fairness constraints into the learning process. |
Experimental Protocol for Bias Testing
This protocol provides a methodology for auditing a digital monitoring tool for bias, a critical step before deploying it in research.
1. Define Protected Groups and Metrics
- Protected Groups: Identify participant subgroups for testing (e.g., based on skin tone, age, gender, cultural background) [77] [78].
- Performance Metrics: Select metrics for evaluation (e.g., accuracy, false positive rate, false negative rate).
2. Curate a Diverse Test Set
- Assemble a test dataset with balanced representation from all protected groups.
- Ensure ground truth labels are accurate and consistently applied.
3. Execute Stratified Evaluation
- Run the model on the entire test set.
- Calculate performance metrics for each protected subgroup separately.
- Compare metrics across subgroups to identify significant disparities.
4. Analyze Results and Mitigate
- Root Cause Analysis: For any discovered disparity, investigate the cause (e.g., data, features, algorithm).
- Implement Mitigations: Apply solutions from the troubleshooting guide.
- Re-test: Validate mitigation effectiveness with a fresh validation dataset.
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function |
|---|---|
| Diverse, Representative Datasets | Serves as the foundational material for training and testing; ensures the model learns from a population it will serve [77] [78]. |
| Bias Auditing Framework | A set of metrics and statistical tools used to diagnose and quantify bias in model outcomes across participant subgroups [77]. |
| Fairness-Aware Algorithms | Specialized algorithms (e.g., adversarial debiasing, reweighting) act as reagents to remove or reduce unwanted bias from models during training [77]. |
| Multi-Demographic Test Set | A controlled substance for validation; provides the ground truth to verify model performance and fairness across all target groups before deployment [77] [78]. |
Data Presentation: WCAG Color Contrast Standards for Visualization
Adhering to accessibility standards like the Web Content Accessibility Guidelines (WCAG) ensures your research visualizations are legible to all colleagues, including those with low vision or color blindness [79] [80]. The tables below summarize the minimum contrast ratios.
| Text Type | Minimum Ratio (AA) | Enhanced Ratio (AAA) |
|---|---|---|
| Small Text (below 18pt) | 4.5:1 | 7:1 |
| Large Text (18pt+ or 14pt+bold) | 3:1 | 4.5:1 |
Source: Based on WCAG 2.1 guidelines [80].
| Element Type | Minimum Ratio (AA) |
|---|---|
| User Interface Components | 3:1 |
| Graphical Objects (e.g., icons) | 3:1 |
Source: Based on WCAG 2.1 Non-Text Contrast requirement [80].
Workflow Diagram for Bias Mitigation
The following diagram illustrates the logical workflow for integrating bias mitigation into the development of a digital monitoring tool.
Clinical Efficacy and Comparative Analysis of Monitoring Approaches
Validating Digital Monitoring for Weight Management and Obesity Research
This technical support center provides troubleshooting and methodological guidance for researchers validating digital monitoring tools in weight management and obesity research, with a focus on energy-efficient practices.
Frequently Asked Questions
What are the core self-monitoring strategies tested in contemporary digital weight loss trials? Modern trials often investigate a core set of three self-monitoring strategies: tracking dietary intake, physical activity (steps), and body weight [81]. Research is focused on identifying the optimal combination of these strategies to maximize weight loss while minimizing participant burden, using frameworks like the Multiphase Optimization Strategy (MOST) [81].
My study participants show declining engagement with self-monitoring apps over time. Is this normal and how can it be addressed? Yes, a decline in engagement is a common challenge [81]. This can be due to time demands, perceived burden, or waning novelty [81]. To address this:
- Prioritize Active Ingredients: Use optimization trial results to include only the most effective (active) self-monitoring components, reducing unnecessary effort [81].
- Leverage Digital Tools: Utilize commercially available digital tools like mobile apps and wearables that offer immediate feedback and portability, which can enhance engagement [81].
- Focus on Adherence: Studies show that participants who are adherent to app use achieve significantly greater weight loss, highlighting the importance of designing interventions that promote sustained engagement [82].
How can I accurately assess real-world dietary intake in my cohort study? Ecological Momentary Assessment (EMA) is a validated approach that captures dietary data in real-time to reduce recall bias [83]. Key protocols include:
- Event-Contingent: Participants report all foods and beverages at each eating occasion.
- Signal-Contingent: Participants are prompted at random or fixed intervals to record their consumption. These methods can be used alone or in combination, often via smartphones, to capture the complexity of food intake in a participant's natural environment [83].
We are using smart scales. What are common sources of measurement error? To ensure data quality from smart scales, instruct participants to:
- Use the scale on a hard, level surface (soft rugs can affect accuracy).
- Ensure the scale is reset to zero before each reading, especially after moving it.
- Weigh themselves at the same time each day, without clothing, for consistent results [84].
- Stand still, with feet not hanging off the scale, as leaning can cause inaccurate readings [84].
Troubleshooting Guides
Problem: Inconsistent or Noisy Weight Data from Smart Scales
Potential Causes and Solutions:
- Cause 1: Scale placed on an uneven or soft surface (e.g., carpet).
- Solution: Ensure the scale is used on a firm, flat surface [84].
- Cause 2: Scale not calibrated after being moved or having its battery replaced.
- Solution: Recalibrate the scale by tapping the center or corner to trigger the zero-reset function. Wait for zeros to appear on the display before weighing [84].
- Cause 3: Participant technique (e.g., leaning, feet off the platform).
- Solution: Standardize weighing protocol: stand still with feet fully on the scale platform [84].
- Cause 4: Low battery.
- Solution: Replace with a fresh battery according to the manufacturer's instructions [84].
Problem: Low Participant Adherence to Digital Self-Monitoring
Potential Causes and Solutions:
- Cause 1: Excessive participant burden from tracking too many metrics.
- Solution: Implement findings from optimization trials like Spark. Use a factorial design to identify the minimal set of effective self-monitoring components (e.g., perhaps tracking only diet and weight is as effective as tracking diet, weight, and steps), thereby reducing burden [81].
- Cause 2: Lack of intuitive feedback or perceived usefulness.
- Solution: Utilize digital therapeutics (DTx) that provide automated, personalized feedback and goal setting. Evidence suggests that higher engagement with comprehensive DTx apps is linked to greater weight loss [82].
- Cause 3: Waning motivation over time.
- Solution: Incorporate behavioral design elements such as gamification, weekly learning modules, and digital health coaching to maintain engagement, as seen in recent DTx studies [85].
Key Experimental Protocol: The Spark Optimization Trial
The following diagram illustrates the design of the Spark trial, which uses a factorial design to optimize self-monitoring components.
Objective: To examine the unique and combined (interaction) effects of three self-monitoring strategies on 6-month weight change [81].
Design: A 6-month, fully digital, optimization-randomized clinical trial using a 2 × 2 × 2 full factorial design [81].
Participants: 176 US adults with overweight or obesity [81].
Intervention Components:
- Core Components: All participants received weekly lessons and action plans informed by Social Cognitive Theory [81].
- Experimental Components: Participants were randomized into one of eight conditions, receiving between 0 and 3 of the following self-monitoring strategies [81]:
- Dietary Intake Tracking: Using a mobile app.
- Step Tracking: Using a wearable activity tracker.
- Body Weight Tracking: Using a smart scale.
- For each assigned strategy, participants received a corresponding goal and weekly automated feedback [81].
Outcomes:
- Primary: Weight change from baseline to 6 months (assessed via smart scale) [81].
- Secondary: Changes in BMI, caloric intake, diet quality, physical activity, health-related quality of life, and engagement [81].
The table below summarizes key quantitative findings from recent clinical trials investigating digital monitoring and therapeutic interventions for weight management.
| Trial (Year) | Intervention | Duration | Key Weight-Related Outcomes | Other Key Findings |
|---|---|---|---|---|
| DEMETRA (2025) [82] | DTxO App (personalized diet, exercise, behavioral support) vs. Placebo App (logging only). | 6 months | No significant difference between groups overall. Adherent DTxO users: -7.02 kg (vs. -3.50 kg for adherent placebo). | Adherence to app use was significantly associated with greater weight loss. |
| Lifeness DTx (2025) [85] | Full DTx app with program & coaching vs. limited app. | 12 weeks | No significant change in body weight. Waist circumference: -3.4 cm in intervention group. | Improvements in eating behavior (disinhibition) and quality of life, independent of weight loss. |
| CGM + Nutrition (2025) [42] | Individualized Nutrition Therapy with real-time CGM feedback vs. blinded CGM. | 8 weeks | Not primary focus. | Significant increase in whole-grain and plant-based protein intake. Improved sleep efficiency. |
The Scientist's Toolkit: Research Reagent Solutions
This table details essential digital tools and methodologies for setting up energy-efficient continuous monitoring research.
| Item / Solution | Function in Research | Example / Key Feature |
|---|---|---|
| Commercial Digital Health Platforms | Provides an integrated, validated system for delivering interventions and collecting self-monitoring data (diet, activity, weight). | Platforms like that used in the Spark trial offer mobile apps, wearable tracker integration, and smart scale connectivity [81]. |
| Ecological Momentary Assessment (EMA) | A real-time data capture method to assess dietary intake and behaviors in natural environments, reducing recall bias and improving validity [83]. | Can be implemented via smartphone using event-contingent (patient-initiated at eating occasions) or signal-contingent (researcher-prompted) protocols [83]. |
| Continuous Glucose Monitors (CGM) | Provides real-time, objective data on glycemic responses to diet. Used to provide biofeedback and validate dietary adherence in nutrition studies [42] [41]. | Sensors like Dexcom G7; used in interventions to help participants link food choices to glucose levels [41]. |
| Multiphase Optimization Strategy (MOST) | An engineering-inspired framework for building efficient, effective multicomponent interventions by identifying "active ingredients" [81]. | Used in the Spark trial to determine which self-monitoring components are essential for weight loss, allowing for a more efficient, less burdensome final intervention [81]. |
| Digital Therapeutics (DTx) | Evidence-based, software-driven interventions to prevent, manage, or treat a medical disorder. Often certified as medical devices [82]. | Apps like DTxO and Lifeness that include personalized plans, behavioral therapy, and clinician dashboards to support obesity management [82] [85]. |
In energy efficiency research for continuous dietary monitoring, selecting appropriate data collection tools is paramount. The two primary methodologies are Continuous Glucose Monitoring (CGM) and Traditional Dietary Logs, which differ fundamentally in their data structure, collection mechanisms, and resource requirements. CGM systems automatically capture interstitial glucose readings at regular intervals (typically every 5 minutes), generating up to 288 data points per day for a continuous, high-temporal-resolution physiological stream [86] [87]. In contrast, traditional dietary logs rely on periodic self-reporting through methods like 24-hour recalls, food frequency questionnaires (FFQs), and food records, which are inherently episodic and subject to human memory and reporting biases [8] [88]. This fundamental distinction in data collection approaches creates significant differences in the energy investment required for data acquisition, processing, and analysis within research environments. Understanding these methodological characteristics is essential for designing energy-efficient nutritional studies that balance data richness with practical resource constraints.
Technical Comparison of Data Characteristics
The table below summarizes the core technical differences between CGM data and traditional dietary logs from a research perspective, with implications for energy efficiency in study design.
Table 1: Technical Characteristics of Dietary Monitoring Methodologies
| Characteristic | CGM Data | Traditional Dietary Logs |
|---|---|---|
| Data Structure | Continuous time-series data | Episodic, self-reported entries |
| Temporal Resolution | High (5-minute intervals) | Low (daily or per-meal) |
| Data Volume | High (~1,440 readings daily) [86] | Low to moderate (text/numeric entries) |
| Primary Data Type | Objective physiological measurements | Subjective behavioral reporting |
| Key Metrics | Time-in-Range, glycemic variability, glucose management indicator [86] | Nutrient estimates, food groups, portion sizes [8] |
| Completeness | Prone to technical gaps (sensor errors) [89] | Prone to reporting gaps (participant non-compliance) [8] |
| Resource-Intensive Processing | Signal processing, imputation for missing data [89] | Coding, nutrient analysis, recall validation [8] |
This technical comparison reveals that CGM systems generate substantially larger datasets with objective physiological measurements, while traditional dietary logs produce smaller but more complex datasets requiring significant human interpretation. The energy investment required for each method varies accordingly, with CGM demanding more computational resources for data processing and traditional logs requiring more human analytical resources for data coding and validation.
Experimental Protocols for Integrated Data Collection
Simultaneous CGM and Dietary Logging Protocol
To conduct a comparative analysis of CGM data versus traditional dietary logs, researchers should implement a standardized protocol for simultaneous data collection:
Participant Recruitment and Training: Recruit participants representing the target population (e.g., individuals with prediabetes, type 2 diabetes, or healthy controls). Conduct training sessions on properly using CGM devices and accurately completing dietary logs. For dietary assessment, training should include portion size estimation and prompt recording [8].
Device Configuration and Deployment: Apply CGM sensors according to manufacturer specifications, typically on the back of the upper arm. Initialize devices and ensure proper connectivity with companion apps. For CGM placement consistency, note that research has shown variations of up to 3.7 mg/dL between different arm placements [15].
Parallel Data Collection Period: Implement a 10-14 day monitoring period during which participants wear CGM devices while simultaneously completing detailed food records. This duration captures weekly variation while minimizing participant burden [8].
Data Synchronization: Timestamp all dietary entries and synchronize with CGM data using a common time framework. Utilize digital platforms that automatically timestamp entries to enhance synchronization accuracy.
Quality Control Checks: Perform daily data checks for both CGM (signal loss, sensor errors) and dietary logs (completeness, plausibility). Implement protocols for addressing data gaps, such as prompted recall for missing meals or imputation methods for CSignal loss [89].
Data Integration and Analysis Workflow
The following diagram illustrates the experimental workflow for comparative analysis of CGM and dietary log data:
Diagram 1: Experimental Data Collection Workflow
This integrated workflow enables researchers to systematically compare the data characteristics, resource requirements, and complementary insights from both methodologies, with particular attention to the energy efficiency of continuous versus episodic monitoring approaches.
Troubleshooting Technical Challenges
CGM Data Quality Issues
Table 2: Troubleshooting CGM Data Collection Problems
| Problem | Possible Causes | Solutions | Energy Efficiency Impact |
|---|---|---|---|
| Signal Loss | Sensor detachment, wireless interference, device out of range | Secure with additional adhesive, ensure proper device proximity, implement gap imputation algorithms [89] | High computational resources needed for data reconstruction |
| Physiological Gaps | Sensor compression during sleep, hydration issues | Educate participants on optimal wear positions, monitor hydration | Manual intervention required, reducing automation efficiency |
| Data Anomalies | Sensor error, electromagnetic interference, manufacturing issues | Implement validation checks, outlier detection algorithms [86] | Computational overhead for real-time data quality monitoring |
| Missing CGM Data | Early sensor failure, participant removal | Pre-plan sensor replacement protocol, establish criteria for data completeness [89] | Resource waste from incomplete datasets requiring replacement |
Dietary Log Data Quality Issues
Table 3: Troubleshooting Dietary Log Collection Problems
| Problem | Possible Causes | Solutions | Energy Efficiency Impact |
|---|---|---|---|
| Under-Reporting | Social desirability bias, forgetfulness, portion size underestimation | Use multiple pass 24-hour recall, provide portion size aids, incorporate biomarkers [8] | Increased researcher time for data validation and cleaning |
| Over-Reporting | Misunderstanding of instructions, inclusion of non-consumed items | Training with examples, use of food imagery validation | Computational resources for inconsistency detection |
| Missing Meal Data | Participant burden, non-compliance | Implement prompted recalls, meal-time notifications | Manual follow-up required, reducing efficiency |
| Inaccurate Timing | Poor recall, delayed logging | Use time-stamped digital entry, meal-time notifications | Computational alignment challenges with CGM data |
Frequently Asked Questions (FAQs)
Methodology Questions
Q1: What is the minimum CGM wear time required for reliable pattern analysis? A: For reliable daily pattern analysis, a minimum of 10-14 days of CGM data is recommended, as this captures weekly variations in diet and activity patterns. For assessment of glycemic variability, studies suggest at least 5-7 days of data are necessary [86] [15].
Q2: How many days of dietary records are needed to compare with CGM data? A: Research indicates that 4-7 days of food records (including weekdays and weekends) provide reasonable estimates of usual intake for comparison with CGM metrics. For nutrient estimates with high day-to-day variability (e.g., Vitamin A, cholesterol), more days are needed [8].
Q3: What are the key considerations for temporal alignment of CGM and dietary data? A: Precise timestamping is essential. Account for the 15-20 minute physiological lag between blood glucose and interstitial glucose measurements. Implement automated timestamping in digital food logs to minimize human error in recording times [86].
Technical Implementation Questions
Q4: How should researchers handle missing CGM data in analysis? A: Establish pre-specified criteria for data completeness (e.g., ≥70% of expected data points). For minor gaps (<2 hours), imputation methods like linear interpolation can be used. For larger gaps, consider sensitivity analyses excluding participants with substantial missing data [89].
Q5: What approaches validate the accuracy of self-reported dietary data? A: While no perfect validation exists, approaches include: (1) comparing reported energy intake to estimated energy requirements, (2) using recovery biomarkers (doubly labeled water for energy, urinary nitrogen for protein), and (3) checking for internal consistency across multiple reporting days [8] [88].
Q6: How can researchers address participant burden in combined CGM and dietary assessment? A: Implement user-friendly digital tools for dietary tracking, provide adequate training, use intermittent sampling protocols where appropriate, and consider incentive structures that reward data completeness rather than specific dietary behaviors [8].
Research Reagent Solutions
Table 4: Essential Research Materials for Comparative Studies
| Item | Function | Technical Specifications | Energy Efficiency Considerations |
|---|---|---|---|
| RT-CGM Systems (Dexcom G7, FreeStyle Libre 3) | Continuous glucose data collection | 5-minute readings, 10-14 day wear, Bluetooth connectivity [87] | Higher initial cost but reduced participant burden for data collection |
| Digital Dietary Assessment Platforms (ASA-24, Glooko) | Streamlined dietary data collection | Nutrient database integration, portion size imagery, automated coding [8] [90] | Reduced manual coding time but requires computational resources |
| Data Integration Platforms | Synchronize CGM and dietary timestamps | Custom API development, timestamp alignment algorithms | Significant development resources but enables automated processing |
| Statistical Software Packages (R, Python with specialized libraries) | Advanced time-series analysis | Functional data analysis, mixed-effects models [86] | Computational intensity varies by analytical approach |
| Data Validation Tools | Quality control checks | Automated outlier detection, completeness reports [89] | Pre-processing investment improves overall analysis efficiency |
The comparative analysis of CGM data and traditional dietary logs reveals significant trade-offs between methodological approaches in continuous dietary monitoring research. CGM provides objective, high-temporal-resolution physiological data but requires substantial computational resources for processing and analysis. Traditional dietary logs offer direct behavioral insights but demand significant human resources for collection, coding, and validation. The most energy-efficient research designs strategically combine both methodologies, leveraging their complementary strengths while implementing the troubleshooting strategies and technical protocols outlined in this guide. As digital health technologies evolve, emerging approaches like automated food recognition and integration with wearable activity trackers promise to further enhance the energy efficiency of comprehensive dietary monitoring studies [87] [90]. Researchers should select methodologies based on their specific research questions, resource constraints, and the particular balance of physiological versus behavioral data required for their scientific objectives.
The Role of Monitoring in Nutritional Support for GLP-1 Agonist Therapies
Scientific Rationale for Nutritional Monitoring in GLP-1 Agonist Therapy
Why is nutritional monitoring critical for patients on GLP-1 agonist therapies? GLP-1 receptor agonists (GLP-1RAs) have revolutionized the treatment of type 2 diabetes and obesity, with benefits extending to cardiovascular, renal, and metabolic health [91] [92]. However, a significant clinical challenge associated with their use is the composition of weight loss; studies indicate that lean body mass can account for 15-40% of the total weight loss experienced by patients on these therapies [93]. This loss of muscle mass is detrimental to long-term metabolic health and physical function. Furthermore, these medications work by delaying gastric emptying and increasing satiety, which can naturally lead to reduced food intake and potential nutrient deficiencies if not carefully managed [94]. Therefore, meticulous nutritional monitoring is not adjunctive but fundamental to preserving muscle mass, ensuring adequate nutrient intake, and optimizing the quality of weight loss and overall therapeutic outcomes.
Key Monitoring Technologies and Methodologies
What are the primary technologies for monitoring dietary intake in clinical research? Accurate dietary assessment is essential for understanding diet-health relationships, yet day-to-day variability in intake complicates the identification of usual consumption patterns [68]. The table below summarizes the key technological approaches for dietary monitoring in a research context, aligned with the goal of energy-efficient data collection.
Table 1: Technologies for Dietary Intake Monitoring in Research
| Technology/Method | Key Function | Data Output | Considerations for Energy Efficiency |
|---|---|---|---|
| AI-Assisted Food Tracking Apps (e.g., MyFoodRepo) | Log meals via image, barcode, or manual entry; uses AI for food classification and nutrient estimation [68] [53]. | Detailed data on macro/micronutrients, food groups, and meal timing. | Reduces participant burden, enabling longer tracking with less energy expenditure per data point. Cloud-based processing offloads computational energy cost from the device. |
| Image-Based Dietary Assessment | Uses Convolutional Neural Networks (CNNs) and computer vision for automatic food identification and portion size estimation [53]. | Objective records of food consumption with classification accuracy often >85-90% [53]. | Automates manual annotation tasks, significantly reducing the researcher time and energy required for data analysis. |
| Continuous Nutrient Sensors (Emerging) | Biosensors designed to detect biomarkers like phenylalanine to track muscle breakdown or protein intake in real-time [93]. | Continuous, real-time data on metabolic status related to protein balance. | Provides high-frequency data without requiring user input, minimizing participant interaction energy. Enables proactive versus reactive interventions. |
| Digital Food Frequency Questionnaires (FFQs) | Digitized versions of traditional FFQs to capture habitual intake. | Estimates of usual intake over a longer period. | Streamlines data collection and analysis, but potential for recall bias remains. Less energy intensive for the participant than daily tracking. |
What is the minimum data collection required for reliable dietary assessment? Efficient research design requires minimizing participant burden while collecting meaningful data. A 2025 digital cohort study determined the minimum number of days needed to reliably estimate usual intake for various nutrients, which is critical for designing energy-efficient monitoring protocols [68].
Table 2: Minimum Days for Reliable Dietary Intake Estimation
| Nutrient/Food Group | Minimum Days for Reliability (r > 0.8) | Notes |
|---|---|---|
| Water, Coffee, Total Food Quantity | 1-2 days | Can be assessed most rapidly. |
| Macronutrients (Carbohydrates, Protein, Fat) | 2-3 days | Foundation for energy and macronutrient balance monitoring. |
| Micronutrients, Meat, Vegetables | 3-4 days | Requires a slightly longer observation window. |
| General Recommendation | 3-4 non-consecutive days, including at least one weekend day | This strategy accounts for weekly variation and is more efficient than consecutive day logging [68]. |
Experimental Protocols for Muscle Mass Preservation
What are the key experimental methodologies for investigating muscle preservation during GLP-1RA therapy? Research into mitigating muscle loss combines pharmacological interventions with precise body composition monitoring. The following workflow outlines a protocol from a landmark clinical trial, the BELIEVE study, which investigated a combination therapy for preserving lean mass [93].
Diagram 1: BELIEVE Trial Experimental Workflow
What were the key findings of the BELIEVE trial? The BELIEVE Phase 2b trial demonstrated that the combination of semaglutide and bimagrumab was significantly more effective than either drug alone. The results highlight the importance of monitoring body composition, not just total weight.
Table 3: Key Outcomes from the BELIEVE Phase 2b Trial
| Treatment Group | Total Body Weight Loss | Composition of Weight Loss | Key Finding |
|---|---|---|---|
| Semaglutide + Bimagrumab | -22.1% | 92.8% from fat mass | Superior fat loss and lean mass preservation. |
| Semaglutide Alone | -15.7% | 71.8% from fat mass | Significant weight loss, but a substantial portion was lean mass. |
| Bimagrumab Alone | -10.8% | 100% from fat mass | Resulted in a 2.5% increase in total lean mass. |
| Placebo | N/A | N/A | Control for comparison. |
Troubleshooting Common Research Challenges
FAQ 1: How can we address the common issue of under-reporting dietary intake in study participants? Under-reporting, particularly correlated with higher BMI, is a major data quality challenge [68].
- Solution: Implement AI-assisted tools that simplify tracking (e.g., photo-based logging) to reduce participant burden and improve accuracy [68] [53]. The MyFoodRepo app, for example, showed high adherence, with 76.1% of entries logged through photographs, which minimizes manual effort and potential misrepresentation [68].
- Protocol Adjustment: Use the minimum days estimation (Table 2) to design shorter, more intensive tracking bursts (3-4 days including a weekend) rather than prolonged, burdensome logging that increases fatigue and under-reporting [68].
FAQ 2: Our research aims to monitor protein intake to prevent muscle loss. What is the most efficient method? Ensuring adequate protein intake is a key strategy for muscle preservation [93].
- Current Method: Utilize AI-powered dietary apps with extensive food databases to estimate protein intake from logged meals. This provides a reasonable proxy for intake.
- Emerging Technology: A novel continuous protein sensor has been developed as a proof-of-concept. This biosensor uses a DNA-based aptamer to detect phenylalanine, a biomarker released during muscle breakdown or after protein ingestion. This technology promises objective, real-time data on protein metabolism, moving beyond crude intake estimates [93].
FAQ 3: How do we account for variability in individual glycemic responses when assessing a diet's effectiveness alongside GLP-1RAs? GLP-1RAs themselves modulate glycemic response, making personalized nutrition critical.
- Solution: Integrate Continuous Glucose Monitors (CGMs) with dietary tracking apps. AI algorithms can then model the interaction between the specific GLP-1RA therapy, the meal composition, and the patient's unique postprandial glycemic response. Reinforcement learning techniques have been shown to reduce glycemic excursions by up to 40% by creating dynamic, personalized feedback loops [53].
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 4: Key Reagents and Materials for Nutritional Support Research
| Item | Function/Application in Research |
|---|---|
| GLP-1 Receptor Agonists (e.g., Semaglutide, Tirzepatide) | The foundational therapeutic agent under investigation for its metabolic effects [91] [94]. |
| Activin Type II Receptor Inhibitors (e.g., Bimagrumab) | Investigational monoclonal antibody used to block pathways that inhibit muscle growth, thereby preserving lean mass [93]. |
| AI-Powered Dietary Assessment Platform (e.g., MyFoodRepo) | Software tool for collecting, processing, and analyzing detailed dietary intake data with minimal participant burden [68]. |
| Dual-Energy X-ray Absorptiometry (DEXA) | Gold-standard method for precisely monitoring changes in body composition (fat mass, lean mass, bone density) throughout the study [93]. |
| Continuous Glucose Monitor (CGM) | Device for tracking interstitial glucose levels continuously, providing data on glycemic variability and response to meals [53]. |
| Biomarker Assay Kits (e.g., for Phenylalanine) | Laboratory kits for validating and cross-referencing data from emerging continuous nutrient sensors [93]. |
| Standardized Portion Size Databases | Critical reference data for converting food images or descriptions into quantitative nutrient estimates, ensuring consistency across the dataset [68]. |
Cost-Benefit and ROI of Continuous Monitoring in Clinical Workflows
Technical Support Center: FAQs & Troubleshooting
Q1: What are the most common financial pitfalls when implementing a continuous monitoring system for a clinical research study?
A: The most common financial pitfalls include underestimating data preparation costs and overlooking ongoing maintenance expenses. Data preparation and cleaning can consume up to 60% of the original project budget, a cost that is frequently overlooked during initial planning [95]. Furthermore, organizations often fail to account for the costs of continuous system monitoring, software updates, and the clinical staff time required to manage the alerts and data generated by the system [96]. To avoid this, ensure your budget includes a dedicated line item for data preparation and a sustained operational budget for software maintenance and clinical oversight.
Q2: Our research team is experiencing "alert fatigue" from the continuous monitoring system. How can we adjust the system to reduce noise without compromising data integrity?
A: Alert fatigue is a common human-factor challenge. To address it, refine your system's alerting protocols to prioritize contextual and actionable alerts. Configure the system's thresholds to suppress low-priority notifications and only flag significant deviations from baseline measurements [97]. Furthermore, instead of delivering all alerts to the entire team, use the system's routing capabilities to direct specific types of alerts (e.g., technical issues vs. participant data anomalies) to the appropriate research team member (e.g., data scientist vs. clinical investigator) [98]. This streamlines communication and ensures critical information reaches the right person without overwhelming everyone.
Q3: We are encountering interoperability issues between our new monitoring devices and the existing Electronic Health Record (EHR) system. What steps should we take?
A: Interoperability is a frequent technology-related barrier [96]. First, verify that all your devices and software platforms support modern data standards like HL7 and FHIR APIs, which are designed for healthcare data exchange [99]. If the technical specifications are compatible, the issue may lie in the implementation. Work with your IT team or vendor to perform thorough integration testing in a non-clinical environment before full deployment. A phased rollout, starting with a single device or unit, can help identify and resolve interoperability issues on a small scale before they affect the entire study [99].
Q4: How can we quantitatively demonstrate the ROI of a continuous dietary monitoring system to our funding body?
A: To build a compelling ROI case, focus on metrics that capture both cost savings and value generation. Track and report on the following:
- Cost Avoidance: Quantify the reduction in data errors or protocol deviations that would have required costly corrective actions or extended the study timeline.
- Operational Efficiency: Measure the reduction in time research staff spend on manual data collection and entry, allowing them to focus on higher-value tasks [97] [100].
- Value-Based Outcomes: If applicable, document how continuous monitoring improved the quality or reliability of your research data, leading to more robust findings [101]. Present these metrics in the context of the initial investment, including hardware, software, and implementation costs [95].
Quantitative Data Analysis
The financial justification for continuous monitoring hinges on understanding both the initial investment and the potential returns. The following tables summarize key cost and revenue data.
Table 1: Implementation Cost Breakdown for AI-Driven Monitoring Systems
This table outlines the investment required for different types of AI systems relevant to clinical monitoring workflows.
| System Type | Estimated Implementation Cost | Key Cost Drivers | Implementation Timeline |
|---|---|---|---|
| Predictive Analytics / ML Models [95] | $100,000 - $200,000 | Data collection & preparation, integration with legacy EHR systems. | 3-6 months |
| Generative AI / LLM Implementation [95] | $150,000 - $500,000+ | Model customization, regulatory compliance (e.g., HIPAA), computational resources. | 6-12+ months |
| Computer Vision (Imaging) [95] | $180,000 - $400,000+ | Neural network complexity, data annotation, validation. | 6-12 months |
| Custom Deep Learning Solutions [95] | $200,000 - $500,000+ | Specialized expertise, high-performance computing, extensive testing. | 6-12+ months |
Table 2: Operational Savings and Revenue Potential from Monitoring Systems
This table summarizes the documented financial benefits and savings from various monitoring and automation technologies.
| Monitoring Application | Documented Savings / Revenue | Context & Notes |
|---|---|---|
| Hospital Energy Monitoring [102] | 25-35% reduction in energy costs | For a 200,000 sq. ft. facility, this equates to $225,000-$315,000 in annual savings. |
| Remote Patient Monitoring (RPM) [101] | $110-$140 monthly revenue per patient (Medicare) | Well-run RPM programs can achieve gross margins of 60-80% after operational costs. |
| AI in Diagnosis [95] | ~$1,600 daily savings per hospital (Year 1) | Savings grow significantly over time, reaching ~$17,800 daily by Year 10. |
| Workflow Automation [97] | Reduces administrative spending | Addresses the 15-30% of U.S. healthcare spending ($285B-$570B) that is administrative. |
Experimental Protocols for Dietary Monitoring Research
Protocol 1: Establishing a Cost-Benefit Framework for a Dietary Monitoring Study
Objective: To systematically evaluate the financial costs and scientific benefits of implementing a continuous dietary monitoring system in a longitudinal cohort study.
Methodology:
- Cost Accounting: Itemize all initial and ongoing costs using Table 1 as a guide. Key items include:
- Hardware: Wearable sensors, data loggers, and communication modules.
- Software: Data platform licenses, AI/analytics modules, and cloud storage fees.
- Personnel: Time for system setup, data management, and result interpretation.
- Indirect Costs: Overhead for electricity and administrative support.
- Benefit Quantification: Define and measure key outcome metrics:
- Data Quality: Compare the frequency of data gaps or errors against a control period of manual tracking.
- Research Efficiency: Track the reduction in time spent by researchers on data cleaning and validation.
- Scientific Value: Assess if continuous data leads to novel findings or higher-quality publications.
- ROI Calculation: Calculate the Return on Investment using the formula: ROI = (Net Benefits / Total Costs) x 100. Net Benefits are the monetary value of the quantified benefits (e.g., staff time saved, grant value of higher-impact research) minus the total costs from Step 1.
Protocol 2: Integrating Continuous Monitoring Data with Clinical Workflows
Objective: To seamlessly integrate data from continuous dietary monitors into a standard Electronic Health Record (EHR) system to support clinical research.
Methodology:
- Interoperability Assessment: Confirm that the monitoring device and the EHR support common data standards like FHIR (Fast Healthcare Interoperability Resources) to ensure seamless data transfer [99].
- Workflow Mapping: Diagram the current clinical workflow without the monitor. Identify the optimal point where the monitored data should be presented to the researcher or clinician to avoid disruption [98].
- Pilot Integration: Conduct a small-scale pilot with a limited number of study participants.
- Use API interfaces to establish a secure data pipeline from the monitoring platform to the EHR [99].
- Configure data dashboards within the EHR to display summarized trends and critical alerts from the dietary data.
- Validation and Refinement: Check data fidelity post-transfer to ensure no corruption or loss. Gather feedback from research staff on the usability and clinical relevance of the integrated data and refine the display and alert settings accordingly [96].
System Workflow Visualization
The following diagram illustrates the key stages, challenges, and benefits involved in implementing a continuous monitoring system, connecting the concepts discussed in the FAQs and protocols.
The Scientist's Toolkit: Research Reagent Solutions
This table details essential non-hardware components required for establishing and running a continuous monitoring system in a research context.
Table 3: Key Research Reagents and Solutions for Continuous Monitoring
| Item | Function in Research Context |
|---|---|
| Data Interoperability Standards (HL7/FHIR) | The essential "protocol" for ensuring different software systems (e.g., monitoring devices, EHRs, analytics platforms) can communicate and exchange data seamlessly [99]. |
| Cloud Analytics Platform | Provides the scalable computational environment for storing, processing, and analyzing large, continuous streams of monitoring data. Enables machine learning and real-time analytics [102]. |
| Predictive Analytics / ML Models | Software tools that learn from historical monitoring data to identify patterns, predict future outcomes (e.g., participant non-adherence), and flag anomalies [95]. |
| Change Management Framework | A structured methodology for preparing and supporting research staff in adopting new monitoring technologies, crucial for overcoming resistance and ensuring proper system use [99] [96]. |
| ROI Calculation Model | A tailored financial model (e.g., a spreadsheet with defined formulas) used to track costs, quantify benefits, and demonstrate the financial viability and impact of the monitoring system [101] [95]. |
Conclusion
Continuous dietary monitoring represents a paradigm shift in nutritional science, moving from static self-reporting to dynamic, data-rich profiling of individual energy metabolism. The integration of CGMs, digital applications, and wearable devices provides researchers with unprecedented insights into the links between diet, energy expenditure, and health outcomes. For drug development, these tools are indispensable for objectively assessing the efficacy of nutritional interventions and emerging pharmacotherapies like GLP-1 agonists, ensuring that nutritional support is optimized to prevent deficiencies and maximize therapeutic outcomes. Future directions must focus on standardizing data protocols, advancing non-invasive biomarkers, and leveraging artificial intelligence to translate complex monitoring data into actionable, personalized nutritional guidance for improved public health and clinical care.
References
- 1. Information about Energy Balance - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK20371/]
- 2. The Human Energy Balance: Uncovering the Hidden ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11854607/]
- 3. The Physiology Of the WEight Reduced State (POWERS ... [https://www.nature.com/articles/s41366-025-01935-x]
- 4. Can probiotics influence adaptive thermogenesis induced ... [https://www.sciencedirect.com/science/article/abs/pii/S0022316625005322]
- 5. Challenges in measuring energy balance and body ... [https://www.nature.com/articles/s41430-023-01286-8]
- 6. iEat: automatic wearable dietary monitoring with bio- ... [https://www.nature.com/articles/s41598-024-67765-5]
- 7. Energy Monitoring | Short Guide to ... [https://www.iox-connect.com/benefits-of-energy-monitoring]
- 8. Overview of Dietary Assessment Methods for Measuring ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8338737/]
- 9. Narrative Review of New Methods for Assessing Food and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6116053/]
- 10. Dietary Assessment Methods For the Athlete: Pros and ... [https://www.gssiweb.org/sports-science-exchange/article/sse-150-dietary-assessment-methods-for-the-athlete-pros-and-cons-of-different-methods]
- 11. Can energy intake and expenditure (energy balance ... - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK565800/]
- 12. Validity of Dietary Assessment Methods When Compared ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2019.00850/full]
- 13. Common Limitations and Challenges of Dietary Clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8453651/]
- 14. Accuracy of energy and nutrient intake estimation versus ... [https://www.sciencedirect.com/science/article/pii/S0002916524004568]
- 15. Overcoming barriers in continuous glucose monitoring : Challenges ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12057385/]
- 16. Evaluating the Energy Efficiency of Popular US Smartphone ... [https://humanfactors.jmir.org/2024/1/e58311/]
- 17. Perspective: Guiding Principles for the Implementation of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7442375/]
- 18. Opportunities and Challenges of Technology Tools in Dietary ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8803491/]
- 19. Personalized Nutrition in the Era of Digital Health [https://pmc.ncbi.nlm.nih.gov/articles/PMC12474561/]
- 20. Effects of a personalized nutrition program on ... [https://www.nature.com/articles/s41591-024-02951-6]
- 21. Moving past 'one-size-fits-all' diet recommendations [https://news.northwestern.edu/stories/2024/11/moving-away-from-one-size-fits-all-diet-recommendations]
- 22. Nutritional assessment - Biomarkers [https://nutritionalassessment.org/biomarkers/]
- 23. Biomarkers of Nutrition and Health: New Tools for New ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6567133/]
- 24. Biomarker Program FAQs [https://www.ninds.nih.gov/current-research/focus-tools-topics/biomarkers-research/biomarker-program-faqs]
- 25. 5 Key Metabolic Markers: What They Mean for Your Health [https://www.nutrisense.io/blog/metabolic-markers-you-should-know?srsltid=AfmBOorHqtZ9SxG0gV3rKxzu1XSedqkaZZm_dlt9uFEgVFnIUss6N9eM]
- 26. The 5 Markers of Metabolic Health and How to Manage Them [https://www.veri.co/learn/metabolic-health-markers?srsltid=AfmBOorWAxT58VOQn9A4t-ATmF95Cwhk7KGJOMl2zOe28KOlLvMsPJXc]
- 27. The Complete Guide to Biomarker Testing [https://superpower.com/library/guide-to-biomarker-testing?srsltid=AfmBOoozYBc1Wr_DX7CrY8npZ0Jqoaw3CITyI_hZ0jzReodv6tsWjLNY]
- 28. Navigating Biomarker Testing: Frequently Asked Questions [https://www.lung.org/lung-health-diseases/lung-disease-lookup/lung-cancer/symptoms-diagnosis/biomarker-testing/biomarker-faqs]
- 29. Is IoT monitoring key to improve building energy efficiency? ... [https://www.sciencedirect.com/science/article/abs/pii/S0378778823001123]
- 30. Network meta-analysis of the effects of different dietary ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1634545/full]
- 31. Integrative Nutrition for Chronic Disease [https://www.indwes.edu/articles/2025/11/integrative-nutrition-chronic-disease-what-research-really-says.html]
- 32. Mediterranean diet in the targeted prevention and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11147989/]
- 33. Vision-Based Methods for Food and Fluid Intake Monitoring [https://pmc.ncbi.nlm.nih.gov/articles/PMC10346353/]
- 34. Nutritionist Proâ„¢ | FAQs [https://nutritionistpro.com/faqs/]
- 35. Continuous Glucose Monitoring in Healthy Adults—Possible ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8915088/]
- 36. CGM Troubleshooting: Quick Fixes for Diabetes Devices [https://beyondtype1.org/cgm-troubleshooting-diabetes-tips/]
- 37. Common Issues and Troubleshooting Tips [https://www.dexcom.com/en-gb/blog/troubleshoot-common-dexcom-issues-and-alerts]
- 38. CGM for Non-Diabetics: Optimize Your Metabolic Health [https://thrombosis.org/patients/patient-articles/continuous-glucose-monitoring-for-non-diabetics-a-new-frontier-in-metabolic-health-optimization]
- 39. Use of a Mobile for Application - Self Intake... Monitoring Dietary [https://pmc.ncbi.nlm.nih.gov/articles/PMC5537862/]
- 40. Best Apps for Nutrition Tracking in 2025 | ROUVY [https://rouvy.com/blog/best-apps-for-nutrition-tracking]
- 41. “Now I can see it works!†Perspectives on Using a Nutrition ... [https://diabetes.jmir.org/2025/1/e67636]
- 42. Effects of Individualized Nutrition Therapy and Continuous ... [https://pubmed.ncbi.nlm.nih.gov/40362826/]
- 43. 7 Proven Strategies for Handling Mobile App Support ... [https://thisisglance.com/blog/7-proven-strategies-for-handling-mobile-app-support-requests]
- 44. The Ultimate Guide to Mobile App Customer Support [2025] [https://document360.com/blog/mobile-app-customer-support/]
- 45. Monitoring Energy Expenditure Using a Multi-Sensor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5714893/]
- 46. Sensing leg movement enhances wearable monitoring of ... [https://www.nature.com/articles/s41467-021-24173-x]
- 47. Episodic Sampling: Towards Energy-efficient Patient ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5019958/]
- 48. 4 Steps to Choose an Energy-Efficient Semiconductor for ... [https://ambiq.com/blog/4-steps-to-choose-an-energy-efficient-semiconductor-for-wearables/]
- 49. From sensing to energy savings: A comprehensive survey ... [https://www.sciencedirect.com/science/article/pii/S2352864824001627]
- 50. Why energy-efficient wellness wearables matter for health ... [https://www.ignitec.com/insights/why-energy-efficient-wellness-wearables-matter-for-scaleable-health-tech-innovation/]
- 51. Design of an energy-efficient IOT device-assisted wearable ... [https://www.sciencedirect.com/science/article/pii/S2665917423002647]
- 52. Energy Solutions for Wearable Sensors: A Review - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8197793/]
- 53. Artificial intelligence in personalized nutrition and food ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1636980/full]
- 54. Multi-biomarker approach for estimating population size in ... [https://www.sciencedirect.com/science/article/pii/S004313542401426X]
- 55. Monitoring Genetic Population Biomarkers for Wastewater- ... [https://pubmed.ncbi.nlm.nih.gov/28814081/]
- 56. Epigenetic Biomarkers for Environmental Exposures and ... [https://www.mdpi.com/1660-4601/17/4/1181]
- 57. Wastewater based genomic surveillance key to population ... [https://www.nature.com/articles/s41598-025-91516-9]
- 58. Wastewater-based surveillance reveals distinct resistome ... [https://www.sciencedirect.com/science/article/abs/pii/S0269749125013235]
- 59. Identification of biomarkers in wastewater-based epidemiology [https://pmc.ncbi.nlm.nih.gov/articles/PMC8591405/]
- 60. Strategies for participant retention in long term clinical trials [https://pmc.ncbi.nlm.nih.gov/articles/PMC10003583/]
- 61. Long-term participant retention and engagement patterns ... [https://www.nature.com/articles/s41746-023-00749-3]
- 62. Adjustment for energy intake in nutritional research [https://pmc.ncbi.nlm.nih.gov/articles/PMC8755101/]
- 63. What Is Data Reliability? | IBM [https://www.ibm.com/think/topics/data-reliability]
- 64. How to Improve the Reliability of Your Data in 11 Easy Steps [https://atlan.com/how-to-improve-the-reliability-of-your-data/]
- 65. 6 Pillars of Data Quality and How to Improve Your Data [https://www.ibm.com/products/tutorials/6-pillars-of-data-quality-and-how-to-improve-your-data]
- 66. 5 Effective Strategies to Enhance Your Data Accuracy [https://data-sleek.com/blog/strategies-to-enhance-data-accuracy/]
- 67. Translational Algorithms for Technological Dietary Quality ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11597732/]
- 68. Minimum days estimation for reliable dietary intake ... [https://www.nature.com/articles/s41430-025-01644-8]
- 69. Validity and accuracy of artificial intelligence-based dietary ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12229984/]
- 70. Evaluating the Energy Efficiency of Popular US Smartphone ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11127174/]
- 71. Data Analysis for the 2025 Guidelines Committee Report [https://www.dietaryguidelines.gov/2025-advisory-committee-report/data-analysis]
- 72. An effective tool for monitoring and ensuring food safety ... [https://www.sciencedirect.com/science/article/abs/pii/S0308814625006429]
- 73. United States Core Data for Interoperability (USCDI) [https://www.healthit.gov/isp/united-states-core-data-interoperability-uscdi]
- 74. FAQs | Interoperability Standards Platform (ISP) [https://www.healthit.gov/isp/faqs]
- 75. Clinical Trial Compliance and Data Security [https://www.mahalo.health/insights/clinical-trial-compliance-and-data-security]
- 76. Common Data Management Challenges and Solutions [https://rivery.io/data-learning-center/data-management-challenges/]
- 77. Bias in AI | Examples, Causes & Mitigation Strategies 2025 [https://kodexolabs.com/bias-in-ai/]
- 78. Addressing AI bias: a human-centric approach to fairness [https://www.ey.com/en_us/insights/emerging-technologies/addressing-ai-bias-a-human-centric-approach-to-fairness]
- 79. Elements must meet minimum color contrast ratio thresholds [https://dequeuniversity.com/rules/axe/4.8/color-contrast]
- 80. Color contrast - Accessibility - MDN Web Docs - Mozilla [https://developer.mozilla.org/en-US/docs/Web/Accessibility/Guides/Understanding_WCAG/Perceivable/Color_contrast]
- 81. Optimizing Self-Monitoring in a Digital Weight Loss ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12504904/]
- 82. Effectiveness of a Digital Therapy on 6-Month Weight Loss ... [https://www.jmir.org/2025/1/e72054]
- 83. A Systematic Review of Ecological Momentary Assessment ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6893429/]
- 84. Product FAQs | Health o Meter [https://www.healthometer.com/product-faqs.html]
- 85. Beyond weight loss: digital therapeutic for behavioral ... [https://www.frontiersin.org/journals/digital-health/articles/10.3389/fdgth.2025.1671649/full]
- 86. CGM Data Analysis 2.0: Functional Data Pattern Recognition and Artificial Intelligence Applications - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12356821/]
- 87. State of the Global CGM Market: 2025 [https://sequenex.com/state-of-the-global-cgm-market/]
- 88. Improving dietary data collection tools for better nutritional ... [https://www.sciencedirect.com/science/article/pii/S2666990022000180]
- 89. Hidden Statistical Challenges of Continuous Glucose ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12623221/]
- 90. 13 Best Glucose Monitoring Apps of 2025 - Nutrisense Journal [https://www.nutrisense.io/blog/best-blood-sugar-apps]
- 91. Current Perspectives on GLP-1 Agonists in Contemporary ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12511252/]
- 92. Glucagon-like peptide-1 receptor: mechanisms and ... [https://www.nature.com/articles/s41392-024-01931-z]
- 93. New GLP-1 Therapies Enhance Quality of Weight Loss by ... [https://diabetes.org/newsroom/press-releases/new-glp-1-therapies-enhance-quality-weight-loss-improving-muscle-0]
- 94. Glucagon-Like Peptide-1 Receptor Agonists - StatPearls - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK551568/]
- 95. What Is The Cost of AI in Healthcare in 2025? [https://riseapps.co/cost-of-ai-in-healthcare/]
- 96. Artificial intelligence adoption challenges from healthcare ... [https://www.sciencedirect.com/science/article/pii/S092575352500253X]
- 97. Why 2025 is the Year for Healthcare Workflow Automation [https://csicompanies.com/why-2025-is-the-year-healthcare-finally-gets-workflow-automation-right/]
- 98. Why Workflow Chaos Is Undermining Care [https://medcitynews.com/2025/05/why-workflow-chaos-is-underming-care-and-what-providers-can-do-about-it/]
- 99. Overcoming EHR Implementation Challenges: A 2025 ... [https://helpsquad.com/overcoming-ehr-implementation-challenges/]
- 100. Top 5 Healthcare Challenges in 2025 [+ Strategies to ... [https://ccdcare.com/resource-center/healthcare-challenges/]
- 101. Remote Patient Monitoring Revenue Models Compared ... [https://sovdoc.com/remote-patient-monitoring-revenue-models-compared-2025/]
- 102. Hospital Energy Monitoring: Cut Facility Costs 30% [https://envigilance.com/healthcare/energy-monitoring/]