Enhancing Dietary Intervention Compliance: Self-Monitoring Techniques, Optimization Strategies, and Clinical Validation
This article synthesizes current evidence on self-monitoring as a cornerstone of behavioral dietary interventions for researchers and drug development professionals.
Enhancing Dietary Intervention Compliance: Self-Monitoring Techniques, Optimization Strategies, and Clinical Validation
Abstract
This article synthesizes current evidence on self-monitoring as a cornerstone of behavioral dietary interventions for researchers and drug development professionals. It explores the foundational role of self-monitoring in weight management and health outcomes, examines traditional and emerging digital methodologies, and analyzes key challenges such as adherence decay. The content provides a comparative analysis of optimization frameworks like the Multiphase Optimization Strategy (MOST) and validation evidence from recent clinical trials, including the role of feedback and cognitive modeling. This review aims to inform the development of more effective, data-driven, and personalized dietary monitoring strategies for clinical and research applications.
The Critical Role of Self-Monitoring in Dietary Interventions and Weight Management
Self-Monitoring as a Cornerstone of Behavioral Weight Loss Programs
Self-monitoring (SM) of dietary behaviors is a foundational component of most behavioral weight loss programs, widely recognized for its effectiveness in promoting healthy behavior changes and improving health outcomes [1] [2]. As overweight and obesity rates continue to escalate globally—with 43% of adults classified as overweight and 16% as obese in 2022—the economic and health burdens necessitate effective intervention strategies [1]. The core premise of dietary self-monitoring operates on principles of self-regulation, enabling individuals to enhance awareness of their eating behaviors in relation to dietary goals in real-time, thereby facilitating behavior change through a phenomenon known as reactivity [3]. Despite its established efficacy, adherence to self-monitoring protocols tends to decline over time due to the labor-intensive nature of traditional methods and the absence of efficient passive recording systems [1] [4]. This technical guide examines the mechanisms, efficacy, and implementation methodologies of dietary self-monitoring within weight loss interventions, with particular emphasis on digital innovations and tailored support systems that enhance long-term adherence.
Theoretical Foundations and Mechanisms of Action
Cognitive Architecture of Self-Monitoring
The Adaptive Control of Thought-Rational (ACT-R) cognitive architecture provides a robust computational framework for modeling adherence dynamics in dietary self-monitoring. ACT-R integrates physical, neurophysiological, behavioral, and cognitive mechanisms into a unified model consisting of symbolic and subsymbolic systems [1]. The architecture operates through several key mechanisms:
- Activation: Determines the accessibility of knowledge chunks in declarative memory, influenced by base-level activation (frequency of access) and spreading activation (contextual relationships)
- Retrieval: Selects and activates specific knowledge chunks from declarative memory, with probability influenced by activation level
- Learning: Calculates the utility of production rules through repeated execution and reward accumulation
- Selection: Chooses which production rule to execute based on utility values [1]
Within weight management interventions, ACT-R modeling reveals that goal pursuit mechanisms typically remain dominant throughout the intervention period, while the influence of habit formation mechanisms often diminishes during later stages [1] [2]. This cognitive framework enables researchers to simulate and predict adherence patterns under various intervention conditions, providing valuable insights for program optimization.
Metacognitive Foundations
Effective self-monitoring relies heavily on accurate metacognitive monitoring—the ability to evaluate one's own comprehension and performance. Research indicates that monitoring accuracy is essential for appropriate regulatory actions in learning and behavior change [5]. The construction-integration model of text comprehension proposes that learners construct mental representations at multiple levels: surface level (word encoding), text-based level (propositional connections), and situation-model level (deep understanding through integration with prior knowledge) [5]. Interventions that prompt learners to utilize situation-model cues rather than surface-level cues significantly enhance monitoring accuracy, ultimately supporting more effective self-regulation of health behaviors [6] [5].
Efficacy and Adherence Dynamics
Quantitative Adherence Metrics
Recent studies employing computational modeling and trajectory analysis have yielded significant insights into self-monitoring adherence patterns. The ACT-R modeling approach has demonstrated strong predictive capability for dietary self-monitoring behaviors across different intervention frameworks, with root mean square error (RMSE) values indicating high model precision [1] [2].
Table 1: ACT-R Model Performance Across Intervention Groups
| Intervention Group | Sample Size | RMSE Value | Dominant Cognitive Mechanism |
|---|---|---|---|
| Self-management | 49 | 0.099 | Goal pursuit |
| Tailored feedback | 23 | 0.084 | Goal pursuit |
| Intensive support | 25 | 0.091 | Goal pursuit |
Data-driven trajectory modeling using group-based trajectory modeling (GBTM) has identified distinct participant subgroups with differing adherence patterns and weight loss outcomes [4]. Studies reveal that a "Higher SM Group" demonstrating consistent self-monitoring behaviors achieves significant weight loss and maintained glycemic control, while a "Lower SM Group" with consistently low adherence shows minimal clinical improvements [4]. Notably, these subgroups exhibit significantly different SM adherence levels as early as the second week of intervention, highlighting the critical importance of early engagement.
Adherence Determinants and Barriers
Table 2: Key Facilitators and Barriers to Self-Monitoring Adherence
| Facilitators | Barriers |
|---|---|
| Acceptance of SM technologies | Forgetfulness |
| Perceived SM benefits | Burdensome SM process |
| Positive problem-solving skills | Technical inaccuracies |
| Tailored feedback | Discouragement from challenges |
| Social and emotional support | Time-consuming food entry |
Qualitative analyses across multiple studies have consistently identified several thematic categories influencing self-monitoring adherence [4]. Acceptance toward SM technologies emerges as a critical facilitator, particularly when participants perceive tools as accurate and easy to use. The presence of automatic syncing functionality significantly enhances technology acceptance and regular use [4]. Participants across adherence levels recognize SM benefits, describing it as "positive feedback" that aids in diet and physical activity behavior changes [4].
However, significant barriers persist. Both responders and non-responders cite individual challenges (forgetfulness) and technical issues (inaccurate food databases, time-consuming entry processes) as impediments to consistent monitoring [4]. The distinction between adherence groups manifests primarily in their responses when facing SM barriers. Responders demonstrate positive problem-solving approaches to overcome challenges, while non-responders often become discouraged and disengage from monitoring activities [4].
Digital Self-Monitoring Interventions
Technological Modalities and Implementation
Digital technologies have transformed dietary self-monitoring by enhancing accessibility, convenience, and precision. Modern implementations typically utilize:
- Mobile applications providing real-time tracking capabilities
- Mobile-optimized websites ensuring cross-platform compatibility
- Wearable devices enabling passive data collection
- Automated feedback systems delivering personalized guidance [1] [3]
Research indicates that digital self-monitoring adherence significantly surpasses traditional paper-based methods, primarily through reducing participant burden and enabling immediate data recording [1]. A proof-of-concept trial examining digital dietary self-monitoring for children reported participants tracked intake on 23.6 ± 4.6 of 28 days, with 69.3% ± 45.1% of items recorded on the day of intake [3].
Reinforcement Strategies for Enhanced Engagement
Positive reinforcement (PR) techniques have demonstrated significant potential for improving self-monitoring adherence, particularly in pediatric populations. Two primary reinforcement modalities have been investigated:
- Caregiver praise: A social reinforcer providing social acceptance and encouragement
- Gamification: A token reinforcer utilizing points, badges, or "leveling up" that can be exchanged for rewards [3]
Recent research indicates that automated gamification (implemented on 20.8 ± 12.3 of 28 days) was delivered more consistently than caregiver praise (implemented on 12.2 ± 5.8 of 28 days), suggesting that automation provides advantages for immediate, consistent, and convenient reinforcement [3]. This consistent delivery aligns with established principles of effective reinforcement, which emphasize immediacy and reliability [3].
Experimental Protocols and Methodologies
ACT-R Modeling Protocol for Adherence Prediction
The development of prognostic models for dietary self-monitoring adherence using ACT-R architecture involves a structured methodology:
Participant Recruitment and Group Assignment
Data Collection and Variable Definition
- Collect daily self-monitoring data over 21-day intervention periods
- Define predictor and outcome variables as adjacent elements in self-monitoring sequences
- Record frequency, timing, and completeness of dietary entries [1]
Model Implementation and Validation
Diagram Completion Intervention for Metacognitive Monitoring
Enhancing monitoring accuracy through diagram completion interventions follows an established protocol:
Intervention Design
Implementation Protocol
- Participants study texts followed by delayed diagram completion (minimum 30-minute delay)
- Participants complete diagrams by filling missing causal relationships
- Provide performance standards (correctly completed diagrams) as feedback in experimental conditions [6]
Assessment and Analysis
Research Reagents and Methodological Tools
Table 3: Essential Research Solutions for Self-Monitoring Intervention Studies
| Research Tool | Function/Application | Example Implementation |
|---|---|---|
| ACT-R Cognitive Architecture | Computational modeling of adherence dynamics and cognitive mechanisms | Prognostic model development for dietary self-monitoring adherence [1] [2] |
| Group-Based Trajectory Modeling (GBTM) | Identification of participant subgroups with distinct adherence patterns | Classification of Higher SM and Lower SM groups based on longitudinal adherence [4] |
| Causal Diagram Completion Tasks | Generation of situation-model cues to enhance metacognitive monitoring accuracy | Intervention to improve monitoring accuracy in text comprehension [6] [5] |
| Digital Self-Monitoring Logs | Mobile-optimized platforms for real-time dietary tracking | 4-week monitoring of fruits, vegetables, snacks, and sugar-sweetened beverages [3] |
| Positive Reinforcement Systems | Implementation of reward structures to enhance self-monitoring adherence | Automated gamification and caregiver praise delivery protocols [3] |
Self-monitoring remains an indispensable component of effective behavioral weight loss interventions, with digital technologies and computational modeling approaches offering unprecedented opportunities to enhance adherence and outcomes. The integration of cognitive architectures like ACT-R provides sophisticated frameworks for understanding and predicting adherence dynamics, while diagram completion interventions and reinforcement strategies address fundamental cognitive and motivational mechanisms. Future research should prioritize several key areas:
- Extended Intervention Durations: Explore sustained adherence mechanisms beyond short-term interventions to support long-term weight maintenance [1] [2]
- Social Cognitive Integration: Incorporate social cognitive factors more comprehensively into dynamic models to capture nuanced behavioral compliance insights [1]
- Adaptive Intervention Frameworks: Develop dynamic models capable of informing just-in-time adaptive interventions that respond to individual adherence patterns [1] [4]
- Individualized Reinforcement Schedules: Investigate optimal reinforcement timing and methodologies tailored to individual differences and response patterns [7] [3]
As digital technologies continue to evolve, their integration with established behavioral principles and cognitive frameworks will undoubtedly yield increasingly sophisticated and effective self-monitoring interventions, ultimately enhancing their impact on global obesity prevention and management efforts.
Linking Self-Monitoring Adherence to Improved Health and Weight Loss Outcomes
Self-monitoring of dietary intake is widely recognized as the cornerstone of behavioral weight loss interventions [8]. This adherence is positively correlated with significant improvements in health behaviors and physiological outcomes, including successful weight loss and long-term weight maintenance [1]. However, participant adherence to these self-monitoring practices often wanes over time due to their labor-intensive nature and the absence of efficient passive recording methods [1]. Within the broader thesis of dietary intervention compliance research, understanding and enhancing the dynamics of self-monitoring adherence is paramount. This guide synthesizes current research and quantitative models to provide researchers and drug development professionals with a detailed framework for analyzing adherence and developing more effective, data-driven interventions.
Quantitative Evidence and Data Synthesis
Empirical evidence consistently demonstrates a significant association between the frequency of self-monitoring and successful weight loss outcomes [8]. Recent studies have begun to quantify the specific thresholds of adherence required to achieve and maintain weight loss.
Table 1: Association Between Self-Monitoring Adherence and Weight Loss Outcomes
| Study / Intervention Type | Sample Size & Groups | Self-Monitoring Metric | Key Quantitative Finding on Weight Loss |
|---|---|---|---|
| Digital Behavioral Weight Loss Program (ACT-R Model) [1] [2] | Total N=97• Self-management (n=49)• Tailored feedback (n=23)• Intensive support (n=25) | Model adherence over 21 days (Root Mean Square Error) | • Self-management RMSE: 0.099• Tailored feedback RMSE: 0.084• Intensive support RMSE: 0.091 |
| Internet-Based Weight Loss Program [9] | n=75 adults with overweight/obesity | Days per week of dietary self-monitoring | • 3-4 days/week: Supports weight loss maintenance.• 5-6 days/week: Supports additional weight loss. |
| Internet Behavior Therapy [8] | n=46 | Number of online diaries submitted | Correlation between diaries submitted and weight loss: r = -0.50, p=0.001 |
| 8-Week Descriptive Study [8] | n=59 | Therapist ratings of self-monitoring consistency | Correlation between consistency and weight change: r = -0.35, p<0.007 |
Furthermore, research into the cognitive mechanisms underlying adherence reveals distinct patterns. One study visualized the contributions of goal pursuit and habit formation mechanisms, finding that goal pursuit remained dominant throughout a 21-day intervention, while the influence of habit formation diminished in the later stages [1]. This suggests that long-term adherence may rely more on conscious, goal-directed effort than on automaticity, a crucial insight for designing sustained interventions.
Experimental Protocols and Methodologies
Protocol: ACT-R Modeling of Adherence Dynamics
This protocol outlines the procedure for developing a prognostic computational model to analyze adherence dynamics, as described in recent research [1].
- 1. Objective: To develop a prognostic model for adherence to self-monitoring of dietary behaviors using the Adaptive Control of Thought-Rational (ACT-R) cognitive architecture and to qualitatively investigate adherence dynamics and the impact of various interventions.
- 2. Participant Recruitment:
- Population: Target adults who express a willingness to improve their lifestyle.
- Assignment: Randomly assign participants to one of three intervention groups:
- Group 1: Self-management. Participants use self-monitoring tools with minimal external support.
- Group 2: Tailored feedback. Participants receive personalized nutritional feedback based on their logged data.
- Group 3: Intensive support. Participants receive tailored feedback combined with emotional social support.
- 3. Intervention Delivery:
- Utilize a digital platform (e.g., mobile application) for self-monitoring of dietary behaviors.
- The tailored feedback allows participants to compare their dietary behaviors with healthy standards.
- Emotional social support is characterized by emotional communication, care, and understanding, potentially delivered via support groups or coach communication [1].
- 4. Data Collection & Modeling:
- Duration: Collect self-monitoring adherence data over a minimum of 21 days.
- Cognitive Modeling: Use the ACT-R architecture to model adherence.
- The model focuses on two key cognitive mechanisms: goal pursuit and habit formation.
- Predictor and outcome variables are defined as adjacent elements in the sequence of self-monitoring behaviors.
- The model simulates how declarative memory (chunks) and procedural memory (production rules) are retrieved and updated based on activation and utility, respectively [1].
- 5. Data Analysis:
- Model Performance: Evaluate the model using Mean Square Error, Root Mean Square Error (RMSE), and goodness-of-fit statistics.
- Mechanistic Analysis: Visualize the contributions of the goal pursuit and habit formation mechanisms over time to analyze adherence patterns.
- Group Comparison: Analyze differences in model parameters and mechanistic contributions between the three intervention groups to assess the impact of tailored feedback and social support.
Protocol: Determining the Dose-Response Relationship
This protocol is based on research aimed at establishing frequency thresholds for effective self-monitoring [9].
- 1. Objective: To identify the frequency of dietary self-monitoring required for successful weight loss maintenance and additional weight loss.
- 2. Study Design: Prospective analysis of data from a three-month, internet-based behavioral weight loss program.
- 3. Participants: 75 adults with overweight or obesity.
- 4. Data Collection:
- Monitor and record the frequency of dietary self-monitoring (days per week) throughout the program and into the maintenance phase.
- Track weight loss outcomes objectively.
- 5. Data Analysis:
- Explore various thresholds for dietary self-monitoring.
- Correlate specific frequency ranges (e.g., 1-2, 3-4, 5-7 days per week) with weight loss maintenance and continued weight loss.
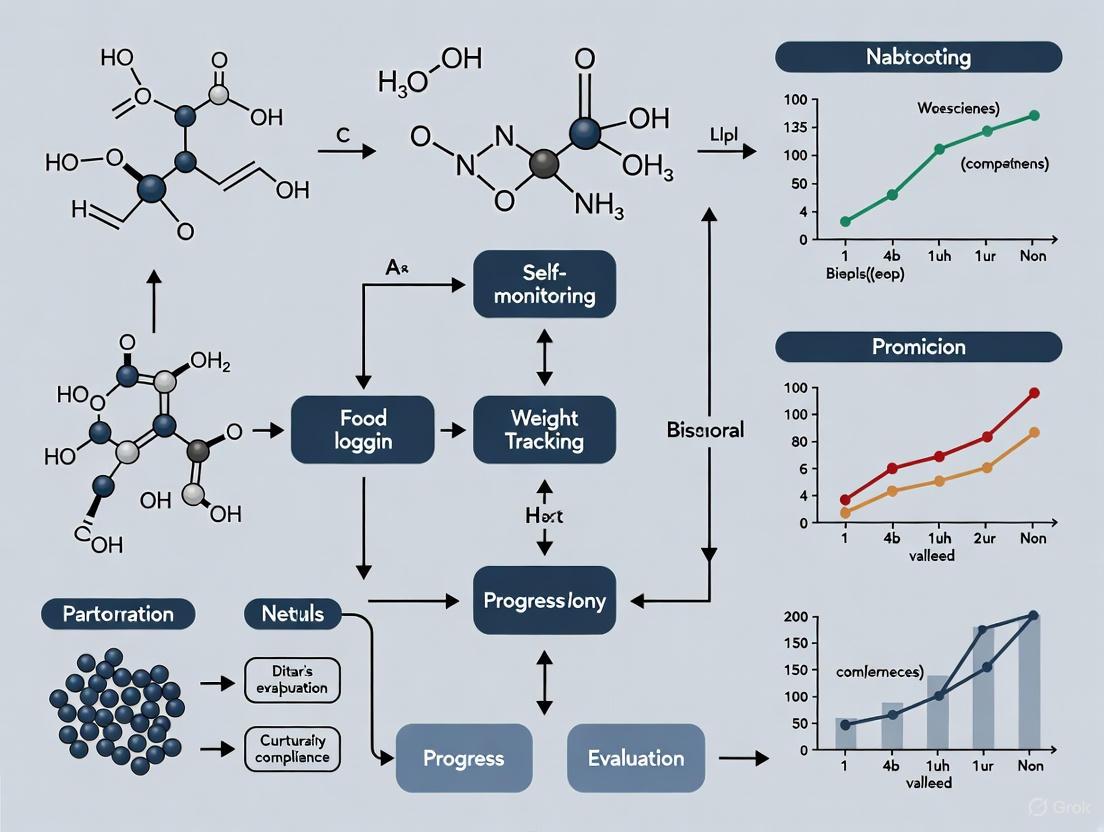
Visualizing Logical Relationships and Workflows
The following diagrams, generated with Graphviz, illustrate the core concepts and workflows discussed in this guide.
Cognitive & Behavioral Model of Adherence
ACT-R Modeling Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials and Digital Tools for Self-Monitoring Research
| Item / Solution | Function in Research | Specific Examples / Notes |
|---|---|---|
| Digital Self-Monitoring Platform | Core tool for participants to log dietary intake and for researchers to collect continuous, fine-grained data. | Mobile applications or web-based diaries; superior adherence compared to paper-based methods [1]. |
| Computational Cognitive Architecture (ACT-R) | Framework for developing prognostic models of adherence dynamics by simulating human cognitive processes like memory retrieval and rule utility [1]. | Open-source cognitive architecture; can be used to model the tension between goal pursuit and habit formation. |
| Tailored Feedback Algorithm | Generates personalized nutritional feedback for participants based on their logged data, enhancing engagement and goal pursuit. | Allows participants to compare their behaviors with healthy standards, providing directly relevant information [1]. |
| Social Support Integration Module | A structured system for delivering emotional social support within the digital platform to mitigate self-regulatory depletion. | Can include support groups, coach messaging, or forums; characterized by emotional communication and understanding [1]. |
| Color Contrast Analyzer | Ensures that all text and graphical elements in research tools and visualizations meet WCAG 2 AA contrast ratio thresholds for accessibility. | Critical for inclusive study design; minimum ratio of 4.5:1 for small text and 3:1 for large text [10] [11]. |
Understanding the Global Challenge of Overweight and Obesity
Overweight and obesity represent a critical global health crisis, characterized by excessive fat deposits that can impair health. According to the World Health Organization (WHO), this complex chronic disease has reached pandemic proportions, with 1 in 8 people worldwide living with obesity in 2022. The global prevalence of obesity among adults has more than doubled since 1990, while adolescent obesity has quadrupled, creating unprecedented public health challenges and economic burdens across healthcare systems worldwide [12].
This escalating epidemic is not confined to high-income nations. Low- and middle-income countries face a double burden of malnutrition, where undernutrition coexists with rising obesity rates, often within the same communities and households. The economic impacts are staggering, with global costs of overweight and obesity predicted to reach US$3 trillion per year by 2030 and more than US$18 trillion by 2060 if no effective interventions are implemented [12]. Understanding the dynamics of this crisis and developing evidence-based interventions, particularly those leveraging dietary self-monitoring techniques, is paramount for researchers and healthcare professionals seeking to reverse these trends.
Epidemiological Landscape: Quantifying the Crisis
The global scale of overweight and obesity requires precise quantification to inform public health policy and intervention strategies. The following tables summarize key epidemiological data that illustrate the scope and distribution of this health challenge.
Table 1: Global Prevalence of Overweight and Obesity (2022) [12]
| Population Group | Overweight Prevalence | Obesity Prevalence | Affected Population |
|---|---|---|---|
| Adults (18+ years) | 43% (2.5 billion) | 16% (890 million) | Total: 2.5 billion |
| Children (5-19 years) | 20% (390 million) | 8% (160 million) | Total: 390 million |
| Children (<5 years) | Not specified | 35 million | Not applicable |
Table 2: Regional Variation in Adult Overweight Prevalence (2022) [12]
| WHO Region | Prevalence of Overweight |
|---|---|
| African Region | 31% |
| South-East Asia Region | 31% |
| Region of the Americas | 67% |
| Global Average | 43% |
The World Obesity Federation's 2025 Atlas projects that these trends will continue their alarming trajectory, with the total number of adults living with obesity expected to increase by more than 115% between 2010 and 2030, rising from 524 million to 1.13 billion [13]. This projection underscores the urgent need for effective interventions. Furthermore, the majority of countries lack sufficient plans and policies to address rising obesity levels, with only 7% of countries having health systems adequately prepared to manage this crisis [13].
Etiology and Health Consequences
Multifactorial Causes
Obesity pathogenesis involves complex interactions between environmental, psychosocial, genetic, and physiological factors. The fundamental energy imbalance—where energy intake consistently exceeds energy expenditure—manifests within what researchers term "obesogenic environments" [12]. These environments are characterized by structural factors that limit the availability of healthy, sustainable food at affordable prices, coupled with lack of safe opportunities for physical mobility integrated into daily life. In a subgroup of patients, single major etiological factors can be identified, including medications, underlying diseases, immobilization, iatrogenic procedures, and monogenic diseases or genetic syndromes [12].
Health Consequences and Comorbidities
The health risks associated with overweight and obesity are extensive and well-documented. In 2021, higher-than-optimal BMI caused an estimated 3.7 million deaths from noncommunicable diseases (NCDs), including cardiovascular diseases, diabetes, cancers, neurological disorders, chronic respiratory diseases, and digestive disorders [12]. Childhood and adolescent obesity not only affect immediate health but are associated with greater risk and earlier onset of various NCDs, with significant adverse psychosocial consequences, including stigma, discrimination, and bullying that affect school performance and quality of life [12].
Dietary Self-Monitoring: A Cornerstone Intervention
Theoretical Foundations and Implementation
Dietary self-monitoring represents a cornerstone of behavioral obesity treatment, grounded in self-regulation theory which posits that self-evaluation and self-reinforcement are necessary for behavior change [14]. This technique requires individuals to maintain awareness of their dietary actions, thereby supporting the development of self-regulation skills. As a behavior change technique, self-monitoring functions by increasing self-awareness of one's actions and the conditions under which they occur, helping to bridge the "intention-behaviour gap" that individuals often experience when attempting to modify dietary patterns [15].
Traditional dietary self-monitoring involves comprehensive recording of all foods and beverages consumed, typically using paper logs where participants look up nutrient content and calculate total intake. However, this approach is labor-intensive and adherence decreases over time, prompting researchers to develop innovative implementation strategies [14]. Current self-monitoring formats include:
- Paper-based records: Traditional food diaries and journals
- Digital platforms: Websites and applications (e.g., MyFitnessPal)
- Mobile applications: Smartphone-based tracking tools
- Hybrid approaches: Combination of digital and personal support
Table 3: Dietary Self-Monitoring Implementation Characteristics [14]
| Implementation Aspect | Options | Considerations |
|---|---|---|
| Format | Paper, website, mobile app, phone | Mobile apps show superior adherence to paper-based tools |
| Intensity | All intake vs. specific components | Higher intensity tracks complete diet; lower intensity focuses on specific behaviors/foods |
| Frequency | Real-time, daily, intermittent | More frequent monitoring associated with better outcomes but potential lower adherence |
| Feedback | Automated, personal, none | Tailored feedback enhances engagement and effectiveness |
The Adherence Challenge and Innovative Solutions
Despite its established efficacy, adherence to dietary self-monitoring remains a significant challenge. Evidence indicates that adherence decreases within the first three to five weeks for paper-based tools and during the fourth to ninth week for mobile applications [15]. This decline is primarily driven by the complexity and time-consuming nature of current tools, which often require numeracy, health literacy, and technological skills that may not be universally available.
Innovative approaches are emerging to address these adherence challenges. The plate-based approach, as exemplified by the iCANPlateTM mobile application, represents a promising alternative to traditional itemized tracking [15]. This method utilizes a visual representation of a plate divided according to the Canada Food Guide (half vegetables and fruits, one-quarter protein, one-quarter whole grains), allowing users to record meals by adjusting proportions rather than counting calories or specifying serving sizes. This simplified approach reduces cognitive burden and may enhance long-term adherence, particularly for populations with varying levels of health literacy [15].
Digital technologies offer significant advantages for self-monitoring adherence, including date and time stamps, instant feedback, and reminder signals that reduce the self-monitoring burden [15]. A 2025 study exploring the dynamics of dietary self-monitoring adherence in a digital behavioral weight loss program utilized the Adaptive Control of Thought-Rational (ACT-R) cognitive architecture to model adherence patterns [1]. The findings indicated that tailored feedback combined with intensive support significantly improved adherence, with the goal pursuit mechanism remaining dominant throughout the intervention period across all study groups [1].
Experimental Protocols and Methodologies
Systematic Review Methodology for Self-Monitoring Strategies
To evaluate the effectiveness of dietary self-monitoring implementation strategies, researchers have conducted systematic reviews following rigorous methodological protocols [14]:
Search Strategy:
- Comprehensive searches across eight databases (Ovid MEDLINE, Ovid EMBASE, Ovid PsycINFO, Cochrane Library, PubMed, Web of Science, EBSCOhost CINAHL)
- No language restrictions but restricted to human subjects
- Grey literature searches in Embase for conference materials, dissertations, and unpublished studies
- Reference searches within included articles
Study Selection Criteria:
- Population: Adults with overweight/obesity
- Intervention: Weight loss interventions incorporating dietary self-monitoring as a behavior change technique
- Comparators: Control groups with usual care, wait list, or distinct interventions without identical self-monitoring procedures
- Outcomes: Weight loss as primary outcome
- Study Design: RCTs, experimental, longitudinal designs
Data Extraction and Quality Assessment:
- General study characteristics (author, year, country, design, sample size)
- Self-monitoring implementation details (platform, recording processes, feedback mechanisms)
- Adherence metrics and intensity of dietary reporting
- Risk of bias assessment using appropriate tools
Nutritional Intervention Protocol for Adolescent Athletes
A 12-week evidence-based nutritional intervention program developed for adolescent athletes exemplifies the integration of self-monitoring within a comprehensive behavioral change framework [16]. This protocol employs the 5 A's behavioral change model (Assess, Advise, Agree, Assist, Arrange) combined with motivational interviewing techniques:
Phase 1: Assessment (Week 1)
- Collect baseline anthropometric measurements (height, weight, BMI, body composition)
- Administer questionnaires on nutritional knowledge, eating habits, water intake, sleep time
- Complete 3-day food records to establish baseline nutrient intake
- Identify specific nutritional problems (e.g., insufficient energy intake, inadequate carbohydrate consumption, vitamin deficiencies)
Phase 2: Group Education Sessions (Weeks 1-12)
- Four 40-minute group sessions covering:
- Basic nutrition concepts (regular eating intervals, hydration, healthy body image)
- Basic food skills (meal planning, cooking skills, nutrient enhancement, food safety)
- Performance nutrition (fueling before, during, and after exercise)
- Performance enhancement (body composition optimization, supplement safety)
Phase 3: Individualized Counseling (Weeks 2-11)
- Four 20-30 minute individual counseling sessions implementing the 5 A's model:
- Assess: Nutritional status, dietary habits, nutrient intake
- Advise: Specific information on health risks and benefits of change
- Agree: Collaborative goal-setting based on participant interest and confidence
- Assist: Identify barriers, strategies, problem-solving techniques
- Arrange: Follow-up plan through visits, phone calls, reminders
Phase 4: Ongoing Support (Weeks 1-12)
- Regular phone calls and mobile messages for reinforcement
- Continuous monitoring of self-reported dietary intake
- Adjustment of goals based on progress and challenges
Personal Health Support Model for Hypertension Management
The Personal Health Support Model (PHSM) represents an advanced computational approach to dietary intervention that incorporates self-monitoring principles for managing obesity-related conditions such as hypertension [17]. This model integrates multiple methodologies:
Analytic Hierarchy Process (AHP):
- Structures user preferences into a hierarchy
- Assigns appropriate weights through pairwise comparisons
- Focuses on DASH diet principles and lifestyle choices
Fuzzy Multi-Choice Goal Programming (FMCGP):
- Associates each nutritional goal with multiple aspiration levels
- Captures flexible and ambiguous nature of individual dietary preferences
- Ensures clinically appropriate and personally tailored dietary plans
Nonlinear Multi-Segment Goal Programming (NLMSGP):
- Captures nonlinear effects of food consumption
- Incorporates both quantity and timing of food intake
- Uses vector-based coefficients for accurate representation
This integrated model generates personalized daily dietary menus and lifestyle recommendations based on individual factors including gender, age, activity level, and dietary preferences, while adhering to clinical guidelines for hypertension management [17].
Visualization of Key Processes and Relationships
Dietary Self-Monitoring Adherence Dynamics
Diagram 1: Self-Monitoring Adherence Dynamics
5 A's Behavioral Model with Motivational Interviewing
Diagram 2: 5 A's Behavioral Change Model
Research Reagents and Tools
Table 4: Essential Research Reagents and Methodological Tools
| Tool/Reagent | Function/Application | Implementation Example |
|---|---|---|
| ACT-R Cognitive Architecture | Computational modeling of adherence dynamics; simulates goal pursuit and habit formation mechanisms | Modeling dietary self-monitoring adherence over 21-day interventions; predicting long-term adherence patterns [1] |
| 24-Hour Dietary Recall (24HR) | Assessment of individual intake over previous 24 hours; multiple recalls capture habitual intake | Automated Self-Administered 24HR (ASA-24) reduces interviewer burden; collects multiple non-consecutive day recalls [18] |
| Food Frequency Questionnaire (FFQ) | Assessment of usual intake over extended periods; categorizes food frequency consumption | Semi-quantitative FFQs query portion sizes and frequency; population-specific adaptations for different cultural contexts [18] |
| Digital Self-Monitoring Platforms | Mobile applications and websites for real-time dietary tracking; reduces burden of traditional methods | iCANPlateTM application using plate-based approach; MyFitnessPal for traditional itemized tracking [15] |
| Recovery Biomarkers | Objective validation of self-reported dietary data; measures energy, protein, sodium, potassium | Doubly labeled water for energy expenditure; urinary nitrogen for protein intake; sodium and potassium as objective intake measures [18] |
| FMCGP/NLMSGP Models | Computational optimization of personalized dietary plans; handles multi-criteria decision making | Personal Health Support Model for hypertension management; generates tailored DASH diet recommendations [17] |
The global challenge of overweight and obesity requires multifaceted intervention strategies, with dietary self-monitoring emerging as a critical component of effective behavioral treatments. Current evidence indicates that simplified approaches, such as plate-based monitoring, digital technologies, and personalized feedback systems, can significantly enhance adherence to self-monitoring protocols and improve weight loss outcomes. The integration of computational modeling, cognitive architectures, and advanced behavioral frameworks offers promising avenues for developing more effective, personalized interventions that can be scaled to address this pressing global health crisis. Future research should focus on extending intervention durations to explore sustained adherence mechanisms, integrating social cognitive factors to capture behavioral compliance insights, and adapting dynamic models to inform just-in-time adaptive interventions for broader applications [1].
Social Cognitive Theory (SCT), pioneered by Albert Bandura, provides a comprehensive framework for understanding how people acquire and maintain behavioral patterns, making it particularly relevant for dietary intervention compliance research [19]. This theory posits that human functioning results from a dynamic, reciprocal interaction between personal cognitive factors, behavioral patterns, and environmental influences—a concept known as triadic reciprocal causation or reciprocal determinism [20]. Within this triad, self-regulation emerges as a central mechanism through which individuals exercise control over their thoughts, feelings, and actions to achieve desired goals [19].
When applied to dietary interventions, SCT helps explain the psychological processes that facilitate or hinder adherence to nutritional guidelines. Self-regulation enables individuals to set dietary goals, monitor their food intake, and adjust their behavior in alignment with their health objectives [21]. Research consistently demonstrates that self-regulation capacity is a critical determinant of successful dietary behavior change and long-term maintenance [22]. This technical guide examines the core constructs of SCT and self-regulation, their operationalization in dietary research, and their application for improving compliance in nutritional interventions.
Core Theoretical Constructs and Mechanisms
Reciprocal Determinism in Dietary Contexts
Reciprocal determinism describes the continuous, mutual interaction between three distinct factors: personal/cognitive, behavioral, and environmental [20]. In dietary contexts, these interactions create complex feedback loops that either support or undermine intervention compliance.
- Personal/Cognitive Factors: These include nutrition knowledge, dietary self-efficacy, outcome expectations, and self-regulatory capacity. For example, an individual's belief in their ability to resist unhealthy foods (self-efficacy) influences their dietary choices [23].
- Behavioral Factors: These encompass specific dietary behaviors, such as food recording, meal timing, and macronutrient composition. Successful behaviors (e.g., achieving daily fruit and vegetable targets) reinforce positive cognitive factors.
- Environmental Factors: These include the physical environment (e.g., home food availability), social context (e.g., family eating patterns), and structural factors (e.g., access to healthy foods) [21].
The dynamic interplay between these factors means that change in one component inevitably influences the others. For instance, nutritional education (targeting cognitive factors) can increase healthy food purchasing (behavior), which subsequently alters the home food environment [20].
Self-Regulation: Components and Subfunctions
Self-regulation represents the executive function through which individuals manage their goal-directed behaviors [24]. In dietary contexts, effective self-regulation involves three interconnected subprocesses:
- Self-Observation: Systematic monitoring of one's food intake, often through food diaries, digital tracking, or mindful eating practices [24].
- Self-Judgment: Comparing monitored behavior against personal dietary standards or goals (e.g., evaluating daily food consumption against recommended nutritional guidelines).
- Self-Reaction: Implementing corrective actions when discrepancies between actual and desired eating behaviors are detected, and engaging in self-reinforcement when goals are achieved [24].
These subprocesses function cyclically, creating an ongoing feedback system that enables individuals to adjust their dietary behaviors in response to changing circumstances and progress toward goals.
Self-Efficacy and Outcome Expectations
Self-efficacy refers to an individual's confidence in their ability to successfully execute behaviors required to produce specific outcomes [23]. In dietary contexts, this encompasses beliefs about one's capability to perform specific nutrition-related behaviors, such as resisting tempting foods, preparing healthy meals, or maintaining dietary records [22]. Research demonstrates that self-efficacy significantly predicts adherence to dietary self-monitoring and healthy eating patterns [23].
Outcome expectations represent the anticipated consequences of performing specific dietary behaviors [20]. These expectations include:
- Physical outcomes (e.g., weight loss, improved energy)
- Social outcomes (e.g., approval from healthcare providers)
- Self-evaluative outcomes (e.g., feelings of pride or self-satisfaction)
The motivational power of outcome expectations depends on both the perceived likelihood of the outcome and the value placed upon it by the individual.
Quantitative Evidence: SCT Constructs and Dietary Outcomes
Empirical research has consistently demonstrated significant relationships between SCT constructs and dietary behaviors across diverse populations. The following tables summarize key quantitative findings from recent studies.
Table 1: Influence of SCT Domains on Physical Activity and Dietary Behavior in Type-2 Diabetes Patients (N=225) [23]
| SCT Domain | Correlation with Physical Activity | Correlation with Dietary Behavior | Significance Level |
|---|---|---|---|
| Self-Efficacy | r = .41 | Not Significant | p < .001 |
| Self-Regulation | r = .44 | r = .44 | p < .001 |
| Social Support | r = .35 | r = .35 | p < .001 |
| Outcome Expectancy | r = .33 | r = .33 | p < .05 |
Table 2: Contextual Factors Influencing Healthy Eating Self-Regulation (N=892) [21]
| Contextual Factor | Effect on Self-Regulation | Statistical Significance |
|---|---|---|
| Meal Moment (Breakfast vs. Dinner) | Higher at breakfast (Estimate = -0.08) | p < .001 |
| Location (Home vs. Out-of-Home) | Higher at home (Estimate = -0.08) | p < .001 |
| Tiredness | Negative influence (Estimate = 0.04) | p < .001 |
| Distractedness | Negative influence (Estimate = 0.07) | p < .001 |
| Intrinsic Motivation (Between-Individual) | Positive influence (Estimate = 0.19) | p < .001 |
| Self-Efficacy (Between-Individual) | Positive influence (Estimate = 0.41) | p < .001 |
Table 3: Association Between Self-Regulation of Eating Behavior (SREB) and Health Outcomes in Saudi Arabian Adults (N=651) [22]
| Outcome Variable | Association with SREB | Statistical Significance |
|---|---|---|
| Generalized Anxiety Disorder (GAD) | Negative correlation (β = -0.13) | p < .001 |
| Body Mass Index (BMI) | Negative correlation (β = -0.10) | p = 0.01 |
| Daily Fruit Consumption | Positive association (OR = 2.90) | p = 0.003 |
| Regular Breakfast Consumption | Positive association (OR = 1.64) | p = 0.04 |
Experimental Protocols and Methodologies
Longitudinal Observational Study on Self-Regulation Fluctuations
Objective: To investigate within-individual variability in healthy eating self-regulation across different meal moments and contexts [21].
Participants: 892 adults (Mean age = 44.3 ± 12.7 years).
Design:
- Within-subjects observational study with 9 repeated measurements over 3 weeks.
- Data collection occurred three times weekly before meal moments.
- Participants reported self-regulation levels, tiredness, distractedness, social context, and physical environment.
Measures:
- Self-regulation of healthy eating: Assessed via self-report before meals.
- Within-individual predictors: Meal moment, tiredness, distractedness, social environment, physical location.
- Between-individual predictors: Self-efficacy, intrinsic motivation, perception of social and physical opportunity (measured at baseline).
Statistical Analysis: Random intercept and slopes model accounting for both within-individual and between-individual variables.
Digital Behavioral Weight Loss Program with ACT-R Modeling
Objective: To develop a prognostic model for adherence to dietary self-monitoring using the Adaptive Control of Thought-Rational (ACT-R) cognitive architecture [1].
Participants: 97 adults in a digital weight loss program.
Intervention Groups:
- Self-management group (n=49)
- Tailored feedback group (n=23)
- Intensive support group (n=25)
Procedure:
- 21-day intervention focusing on goal pursuit and habit formation mechanisms.
- ACT-R architecture simulated human cognitive processes including activation, retrieval, learning, and selection.
- Model performance evaluated using mean square error, root mean square error (RMSE), and goodness of fit.
Key ACT-R Mechanisms:
- Activation: Calculation of chunk activation level based on frequency and recency of access.
- Retrieval: Selection of knowledge chunks from declarative memory based on activation levels.
- Learning: Calculation of production rule utility through repeated execution and reward accumulation.
- Selection: Choice of which production rule to execute based on utility values.
Self-Regulation Strategy Training Intervention
Objective: To evaluate the effectiveness of situation-based strategies and cognitive reappraisal for promoting healthy eating behaviors [25].
Participants: 360 adults.
Design: Longitudinal intervention with assessment of short-term (2 weeks) and long-term (2 months) effects.
Experimental Conditions:
- Situation-based strategy training targeting healthy foods
- Situation-based strategy training targeting unhealthy foods
- Cognitive reappraisal training targeting healthy foods
- Cognitive reappraisal training targeting unhealthy foods
- Control group (no training)
Measures:
- Food cravings (healthy and unhealthy foods)
- Resistance to unhealthy foods
- Actual consumption of unhealthy foods
- Transfer effects across food categories
Visualization of Theoretical Mechanisms
Observational Learning Processes in Dietary Contexts
Bandura identified four cognitive processes that must occur for observational learning to successfully take place [20]. These processes are particularly relevant when individuals learn healthy eating behaviors through observation of role models, healthcare providers, or peers.
Self-Regulatory Feedback Loop in Dietary Management
The self-regulation process in dietary management operates through a continuous feedback cycle where individuals monitor, evaluate, and adjust their eating behaviors in relation to their dietary goals [24].
Research Reagent Solutions: Essential Materials for SCT Dietary Research
Table 4: Essential Research Instruments and Their Applications in SCT Dietary Studies
| Research Instrument | Function | Example Application |
|---|---|---|
| Self-Regulation of Eating Behavior Questionnaire (SREBQ-5) | Assesses cognitive, emotional, and behavioral processes in eating control [22] | Measuring capacity to regulate food intake according to personal goals in Saudi Arabian population study [22] |
| Social Cognitive Theory Questionnaire for Physical Activity & Dietary Behavior | Evaluates four SCT domains: self-efficacy, self-regulation, social support, and outcome expectancy [23] | Examining correlations between SCT domains and physical activity/dietary behavior in type-2 diabetes patients [23] |
| Health-Promoting Lifestyle Profile II (HPLP-II) | Measures health-promoting behaviors across six subscales, including nutrition and physical activity [23] | Assessing dietary habits and physical activity patterns in conjunction with SCT constructs [23] |
| Adaptive Control of Thought-Rational (ACT-R) Architecture | Computational implementation of cognitive processes for behavioral modeling [1] | Simulating adherence to dietary self-monitoring and evaluating intervention effectiveness in digital weight loss program [1] |
| Digital Food Recording Tools | Enable real-time tracking of dietary intake and eating patterns [1] | Facilitating self-monitoring component of self-regulation in behavioral weight loss interventions [1] |
Social Cognitive Theory and self-regulation constructs provide robust theoretical frameworks for understanding and improving dietary intervention compliance. The empirical evidence demonstrates significant relationships between SCT domains (particularly self-efficacy and self-regulation) and successful dietary outcomes across diverse populations [23] [22]. Contextual factors, including meal timing, location, and cognitive state, significantly influence self-regulatory capacity and should be considered in intervention design [21].
Future research should extend intervention durations to explore sustained adherence mechanisms and further integrate social cognitive factors into dynamic computational models [1]. The development of just-in-time adaptive interventions based on SCT principles represents a promising approach for enhancing dietary compliance through personalized support [1]. Additionally, research should examine the neural mechanisms underlying dietary self-regulation to further elucidate the biological substrates of successful behavior change.
For researchers and drug development professionals, incorporating SCT-based interventions that target self-regulatory skills, enhance self-efficacy, and modify outcome expectations can significantly improve adherence to dietary protocols in clinical trials and therapeutic interventions. The methodological approaches and assessment tools outlined in this guide provide a foundation for rigorously evaluating these intervention components.
The Persistent Challenge of Adherence Decay Over Time
Adherence decay, the decline in participant engagement with intervention requirements over time, presents a fundamental challenge in clinical and behavioral nutrition research. This phenomenon is particularly pronounced in dietary interventions where self-monitoring—the systematic observation and recording of one's own food intake—is a cornerstone behavioral strategy [14]. Despite the established efficacy of self-monitoring for initiating weight loss and improving dietary patterns, maintaining consistent participant engagement remains difficult [14] [1]. The labor-intensive nature of traditional tracking methods and the waning of initial motivation frequently undermine long-term compliance [14] [26]. Understanding the dynamics, underlying mechanisms, and potential mitigations for adherence decay is therefore critical for developing more effective and sustainable dietary interventions. This guide examines the current evidence and proposes structured methodologies for addressing this persistent issue within research contexts.
Quantitative Evidence of Adherence Decay
Empirical studies across diverse populations and intervention types consistently report suboptimal and declining adherence rates, underscoring the pervasiveness of this challenge.
Table 1: Adherence Rates Across Different Health Contexts
| Health Context | Population | Adherence Metric | Rate | Source |
|---|---|---|---|---|
| Hypertension Management | Rural adults in Northeast China | Medication Adherence | 73.7% | [27] |
| Hypertension Management | Rural adults in Northeast China | Behavioral Adherence (e.g., lifestyle changes) | 29.3% | [27] |
| Hypertension Management | Rural adults in Northeast China | Dietary Adherence | 10.5% | [27] |
| DASH Diet | US Hypertensive Adults | Adherence to Dietary Recommendations | 19.4% | [27] |
| Multiple Health Behaviors | Chinese Adults (CKB Cohort) | Adherence to 6 key health behaviors | 0.7% | [27] |
The data in Table 1 reveals a clear hierarchy, with pharmacological adherence being more manageable for patients than sustained dietary or comprehensive lifestyle changes [27]. This highlights the particular difficulty of maintaining long-term behavioral modification.
In digital weight loss interventions, the relationship between self-monitoring engagement and outcomes is well-documented. A systematic review found that the majority of studies using both high- and low-intensity self-monitoring strategies demonstrated statistically significant weight loss compared to control groups [14]. However, this review also noted that participant adherence to these strategies typically declines over time because the practice is often perceived as labor-intensive and heavily reliant on continuous internal motivation [14].
Experimental Protocols for Investigating Adherence
To systematically study and combat adherence decay, researchers are employing rigorous experimental designs. The following protocols detail key methodological approaches.
Protocol 1: Factorial Randomized Trial for Optimizing Self-Monitoring (Spark Trial)
This protocol is designed to identify the "active ingredients" of self-monitoring [26].
- Objective: To examine the unique and combined weight loss effects of three self-monitoring strategies: tracking dietary intake, tracking steps, and tracking body weight.
- Study Design: A 6-month, fully digital weight loss intervention using a 2 × 2 × 2 full factorial design. This creates eight experimental conditions to which participants are randomized.
- Participants: US adults with overweight or obesity (N=176).
- Intervention: For each assigned self-monitoring strategy, participants are instructed to self-monitor daily using commercially available digital tools (a mobile app, wearable activity tracker, and smart scale). They receive a corresponding goal and weekly automated feedback. All participants receive core intervention components, including weekly lessons and action plans informed by Social Cognitive Theory.
- Data Collection: Assessments occur at baseline, 1, 3, and 6 months. The primary outcome is weight change, measured objectively via a smart scale. Engagement is operationalized as the percentage of days self-monitoring occurs during the 6-month intervention.
Protocol 2: Cognitive Modeling of Adherence Dynamics
This protocol uses computational modeling to understand the cognitive mechanisms behind self-monitoring behavior [1].
- Objective: To develop a prognostic model for adherence to dietary self-monitoring using the Adaptive Control of Thought-Rational (ACT-R) cognitive architecture and to qualitatively investigate adherence dynamics.
- Study Design: Model development study using data from a digital behavioral weight loss program (Health Diary for Lifestyle Change). Participants were assigned to one of three groups: self-management, tailored feedback, or intensive support.
- Modeling Framework: The ACT-R architecture simulates human cognitive processes, focusing on two key mechanisms for self-monitoring adherence:
- Goal Pursuit: A conscious, effortful process driven by rewards and feedback.
- Habit Formation: An automatic process that strengthens with repeated behavior in a consistent context.
- Data Analysis: The model tracks adherence over 21 days, evaluating model performance using metrics like root mean square error (RMSE). The mechanistic contributions of goal pursuit and habit formation are visualized to analyze patterns.
Protocol 3: Pilot Feasibility Study for a Digital Nutrition Intervention
This protocol focuses on initial feasibility and acceptability before a larger-scale trial [28].
- Objective: To evaluate the feasibility and acceptability of a 4-week digital nutrition intervention to promote healthy and sustainable diets.
- Study Design: A pilot single-arm pre-post intervention study.
- Participants: 32 young adults (18–25 years) who are students or staff at Deakin University, Australia, and have low legume and nut intakes.
- Intervention: Delivery of the intervention via the Deakin Wellbeing mobile application for 4 weeks.
- Primary Outcomes: Feasibility (measured by retention rate) and acceptability (measured by engagement and user experience).
- Secondary Outcomes: Changes in sustainable food literacy, legume and nut intakes, and overall adherence to a healthy and sustainable diet.
Visualizing the Cognitive Mechanisms of Adherence
The ACT-R model provides a framework for understanding the cognitive processes that underlie self-monitoring behavior. The diagram below illustrates the interaction between the goal pursuit and habit formation systems, and how interventions can influence these systems to improve adherence.
Diagram 1: Cognitive Model of Adherence Dynamics
This diagram illustrates the two primary cognitive systems governing adherence. The Goal Pursuit System is dominant in the early and middle stages of an intervention, driven by conscious effort and reinforced by strategies like tailored feedback and social support [1]. The Habit Formation System strengthens with repeated behavior but often requires more time to become stable. Adherence decay occurs when the influence of the goal system wanes due to motivational depletion or high cognitive load, before robust habits have been formed [1].
The Researcher's Toolkit: Key Reagents and Materials
Table 2 outlines essential digital and methodological "reagents" for implementing and studying dietary self-monitoring interventions.
Table 2: Research Reagent Solutions for Dietary Self-Monitoring Studies
| Item Name | Category | Function in Research |
|---|---|---|
| Deakin Wellbeing App | Digital Platform | A mobile application used as a delivery vehicle for intervention content and a tool to collect engagement metrics [28]. |
| Commercial Diet Tracking App | Digital Tool | Enables digital self-monitoring of dietary intake; allows researchers to test the effect of this strategy versus control conditions [26]. |
| Wearable Activity Tracker | Digital Tool | Enables self-monitoring of physical activity (e.g., steps); used to isolate the effect of this self-monitoring component [26]. |
| Smart Scale | Digital Tool | Provides objective weight data and facilitates self-monitoring of body weight with minimal participant effort [26]. |
| ACT-R Cognitive Architecture | Computational Model | A modeling framework to simulate and analyze the dynamic cognitive processes (goal pursuit vs. habit formation) behind adherence patterns [1]. |
| Standardized Questionnaires | Assessment Tool | Used to measure constructs like sustainable food literacy, knowledge, attitudes, and intentions at multiple time points [28] [27]. |
| 24-Hour Dietary Recalls | Assessment Tool | A detailed dietary assessment method used to validate self-reported food intake and measure changes in specific food groups (e.g., nuts, legumes) [28]. |
Adherence decay is a multifaceted problem driven by behavioral, cognitive, and contextual factors. Tackling it requires a move from traditional "treatment package" approaches to optimized, personalized strategies. Research indicates that leveraging digital tools for reduced-burden self-monitoring, providing tailored feedback, and understanding the distinct cognitive pathways of goal pursuit and habit formation are promising directions. Future work should focus on extending intervention durations to study long-term habit stability, integrating real-time social cognitive data into dynamic models, and developing just-in-time adaptive interventions that can proactively deliver support when the risk of disengagement is predicted to be high [1]. By systematically applying these experimental protocols and leveraging the outlined research toolkit, scientists can develop more potent and durable dietary interventions.
Digital Tools, Cognitive Modeling, and Practical Application Frameworks
The Shift from Paper-Based to Digital Self-Monitoring Tools
The accuracy of dietary intake assessment is a cornerstone of nutritional epidemiology and compliance research in clinical trials for drug development. Self-monitoring, the systematic observation and recording of one's own behaviors, is a critical technique for collecting this data [29]. For years, paper-based diaries were the standard tool for this purpose. However, the digital transformation has introduced a paradigm shift towards mobile applications and wearable technology, offering new possibilities for data quality, participant engagement, and real-time intervention [30] [31]. This shift is particularly relevant within dietary intervention compliance research, where the precision of dietary exposure data directly impacts the validity of findings on a drug's efficacy or a health intervention's outcomes. This guide provides researchers and drug development professionals with a technical overview of this transition, summarizing quantitative evidence, detailing experimental methodologies, and presenting essential tools for implementing digital self-monitoring in rigorous scientific studies.
Quantitative Comparison: Paper-Based vs. Digital Tools
Empirical studies have directly compared the acceptability, adherence, and effectiveness of paper-based and digital self-monitoring tools. The data, summarized in the table below, reveal a nuanced landscape where digital tools are not universally superior but offer distinct advantages for specific demographics and outcomes.
Table 1: Key Findings from Comparative Studies on Self-Monitoring Tools
| Study & Population | Intervention Comparison | Acceptability & Adoption | Adherence & Effectiveness | Reported Challenges |
|---|---|---|---|---|
| Office Workers in Sri Lanka [30](Non-randomized trial, n=123) | Mobile application vs. paper-based tool for dietary intake. | 19.5% overall preferred mobile app. Significantly higher acceptance among younger, unmarried workers without children (p < 0.05). | No significant difference in adherence over 3 months or in the change to healthy dietary intake between groups. | Demographic factors (age, marital status) significantly influence acceptance of digital tools. |
| National Weight Control Registry (NWCR) [32](Survey, n=794; adults maintaining weight loss) | Technology (apps/websites) vs. paper-based methods for self-monitoring. | "Regain" group (gained ≥2.3kg) was more interested in technology for tracking weight and diet (p<0.01) than the "maintain" group. | Both groups used technology, but the "regain" group reported more negative feelings (guilt, discouragement) associated with tracking technology use (p<0.001). | Digital tools can be associated with negative emotional byproducts in certain populations, potentially affecting long-term compliance. |
| Systematic Review of Physical Activity [31](19 studies included) | Technology-assisted self-monitoring (e.g., fitness trackers, email feedback) vs. non-technological methods. | Fitness trackers were the most popular type of technology used. Technology reduced user response effort for self-recording. | Combined self-monitoring and technology interventions were effective at increasing physical activity across multiple populations. | The review highlighted the need for identifying the most effective methodologies for lasting behavior change. |
Experimental Protocols for Dietary Self-Monitoring Research
For researchers designing studies to evaluate self-monitoring tools, the following detailed methodologies provide a framework for rigorous experimentation. These protocols are adapted from recent peer-reviewed studies.
Protocol 1: Comparing Dietary Intervention Delivery Methods
This protocol is based on a non-randomized trial comparing a mobile application to a paper-based tool [30].
- Objective: To assess the acceptability and effectiveness of a mobile application versus a paper-based tool for monitoring dietary intake and promoting healthy eating.
- Population: Office workers identified as being in the preparation, action, or maintenance stages of the Trans-Theoretical Model (TTM) of behavior change. Exclusion criteria include jobs involving physical exertion and being on special dietary plans.
- Tool Development (Mobile App):
- Phase 1 (Design): Conduct an extensive literature review to identify evidence-based behavior change techniques (BCTs). Common effective BCTs include goal setting, self-monitoring, and providing information from credible sources [30].
- Phase 2 (Expert Consultation): Engage a panel of local experts in behavioral science, nutrition, and mobile health to refine the tool's layout and operationalize dietary portions and servings.
- Phase 3 (Software Development & Testing): Develop the application and conduct pre-testing and piloting in a non-study setting to refine functionality and user experience.
- Study Design: Non-randomized, open-label trial with two parallel arms (mobile app vs. paper-based). Participants self-select their preferred intervention method.
- Data Collection:
- Baseline: Collect socio-demographic data, general health status, and dietary behaviors via a self-administered questionnaire. Measure height and weight.
- Follow-up: Monitor adherence to the self-monitoring tool for three months.
- Outcome Assessment (3 months): The primary outcome is the progressive change in the stage of change (TTM). The secondary outcome is the change from unhealthy to healthy dietary intake, assessed via 24-hour dietary recall.
- Analysis: Compare outcomes between the two groups using appropriate statistical tests (e.g., chi-square for categorical data, t-tests for continuous data).
Protocol 2: Evaluating Dietary Guidelines in a Specific Population
This protocol outlines a qualitative approach to understanding the cultural acceptability of standardized dietary patterns, which is crucial for designing compliant digital tools [33].
- Objective: To explore the acceptability, perceptions, and cultural relevance of three U.S. Dietary Guidelines (USDG) dietary patterns (Healthy US, Mediterranean, Vegetarian) among African American adults.
- Population: Adults who self-identify as African American, with a BMI between 25-49.9 kg/m² and exhibiting ≥3 risk factors for type 2 diabetes.
- Intervention Structure:
- Duration: 12-week randomized controlled feeding trial.
- Components: Participants are randomized to one of the three USDG dietary patterns. All groups receive the same structure: weekly nutrition classes via Zoom, cooking demonstrations, behavioral strategies from the Diabetes Prevention Program, and use of the MyPlate app for tracking.
- Support: Weekly food samples are provided.
- Qualitative Data Collection:
- Method: Conduct focus group discussions (FGDs) upon completion of the intervention. Separate FGDs are held for each dietary pattern group.
- Tool: Use a semi-structured focus group guide developed based on Social Cognitive Theory and the Designing Culturally Relevant Intervention Development Framework. Questions probe self-efficacy, facilitators, barriers, and cultural tailoring needs.
- Analysis: Transcribe FGDs verbatim and analyze them thematically using a constant comparative method in qualitative data analysis software (e.g., NVivo).
- Outcome: Thematic insights into barriers, facilitators, and necessary adaptations to enhance cultural relevance and program adherence.
Workflow and System Architecture for Digital Self-Monitoring
The integration of digital self-monitoring into research involves a structured workflow from tool selection to data utilization. The diagram below illustrates this process and the logical architecture of a digital self-monitoring system.
Diagram 1: Dietary Assessment Research Workflow
The system architecture for a digital self-monitoring tool is built on a user-facing application and a researcher-facing data platform, as shown below.
Diagram 2: System Architecture for Digital Self-Monitoring
The Researcher's Toolkit: Essential Reagents and Materials
Implementing self-monitoring studies requires a suite of "research reagents"—both digital and methodological. The following table details these essential components.
Table 2: Essential Research Reagents for Self-Monitoring Studies
| Item Name | Type | Specifications & Functions | Key Considerations for Research |
|---|---|---|---|
| Mobile Health Application | Software | A smartphone app for real-time dietary logging, often incorporating Behavior Change Techniques (BCTs) like goal setting and self-monitoring [30]. | Must be based on evidence-based BCTs and validated dietary assessment methods. Requires pre-testing and piloting. |
| Wearable Activity Tracker | Hardware/Software | Devices (e.g., Fitbit, accelerometers) that automatically track physical activity metrics like step count, heart rate, and sleep duration [31]. | Superior reliability and data richness compared to older tools like pedometers. Allows unobtrusive data collection. |
| Paper-Based Food Diary | Analog Tool | The traditional standard for dietary assessment, involving handwritten records of all food and beverages consumed. | Serves as an active comparator in studies. Prone to recall bias and back-filling, but has high familiarity. |
| 24-Hour Dietary Recall | Methodological Tool | A structured interview to capture detailed dietary intake from the previous 24 hours, often used as a reference method for validation [30]. | Can be used to validate the data collected from primary self-monitoring tools (paper or digital). |
| Focus Group Guide | Methodological Tool | A semi-structured questionnaire based on theoretical frameworks (e.g., Social Cognitive Theory) to gather qualitative data on user experience and cultural acceptability [33]. | Essential for understanding the "why" behind quantitative results and for tailoring interventions to specific populations. |
| Best Practice Guidelines (DIET@NET) | Methodological Framework | A set of expert-consensus guidelines for selecting and implementing Dietary Assessment Tools (DATs) in health research [34]. | Provides a structured, 4-stage process (Define, Investigate, Select, Implement) to minimize measurement error and strengthen study design. |
The shift from paper-based to digital self-monitoring tools represents a significant evolution in dietary intervention compliance research. While digital tools offer profound advantages in data richness, real-time feedback, and reduced user burden, the evidence indicates that a one-size-fits-all approach is not optimal. Success depends on a nuanced strategy that considers the target population's demographic and psychological characteristics, employs rigorous tool development and validation protocols, and remains aware of potential emotional byproducts of tracking. For researchers and drug development professionals, leveraging best practice guidelines and selecting the appropriate "research reagents" are critical steps in harnessing the power of digital self-monitoring to generate high-quality, reliable data on dietary compliance and intervention efficacy.
Adaptive Control of Thought-Rational (ACT-R) for Modeling Adherence Dynamics
Dietary self-monitoring is a cornerstone of behavioral weight loss programs, widely recognized for its effectiveness in promoting healthy behavior changes and improving health outcomes [2] [1]. However, participant adherence to self-monitoring of dietary behaviors tends to wane over time due to the labor-intensive nature of the approach and the absence of efficient passive recording methods [1] [35]. This adherence decay presents a significant challenge for researchers and clinicians seeking to optimize interventions for chronic conditions where dietary management is crucial.
The Adaptive Control of Thought-Rational (ACT-R) cognitive architecture offers a novel computational framework for modeling the dynamics of dietary adherence, simulating human cognitive processes to predict and explain how adherence patterns evolve throughout interventions [2] [1]. By leveraging ACT-R's mechanisms of goal pursuit and habit formation, researchers can move beyond descriptive, cross-sectional analyses to dynamic computational models that capture the fine-grained temporal relationships between interventions and behavioral outcomes [1] [35]. This approach represents a significant advancement in computational behavioral science, enabling more personalized and adaptive dietary interventions.
Theoretical Foundations of the ACT-R Architecture
ACT-R is a hybrid cognitive architecture that integrates physical, neurophysiological, behavioral, and cognitive mechanisms into a unified computational model [1] [35]. It operates through two interconnected systems: a symbolic system representing declarative and procedural knowledge, and a subsymbolic system managing the activation and utility of these knowledge structures through mathematical computations.
Architectural Components
The symbolic system comprises multiple modules, with the central procedural module serving as the core component that integrates all other modules [1] [35]. Each module corresponds to a specific brain region and interacts with associated buffers to retrieve and store information. The architecture posits two primary types of memory: (1) "chunks" residing in the declarative module, characterized by an "activation" attribute influenced by retrieval time, frequency, and recentness of access, and (2) "production rules" located in the procedural module, consisting of conditional statements ("if") and corresponding actions ("then") with a "utility" attribute determining execution likelihood [1].
The subsymbolic system governs operations within modules through four fundamental computational processes outlined in Table 1 below.
Table 1: Core Computational Mechanisms in ACT-R's Subsymbolic System
| Mechanism | Description | Equation | Parameters |
|---|---|---|---|
| Activation | Calculates the activation level of a chunk, comprising base-level activation and spreading activation | ( Ai = Bi + \sumj Wj S_{ji} ) | ( A ): activation level; ( B ): base-level activation; ( S ): spreading activation; ( t_i ): time since ith access; ( d ): decay rate |
| Retrieval | Selects and activates knowledge chunks from declarative memory | ( Pi = \frac{1}{1 + e^{-(Ai - \tau)/s}} ) | ( P_r ): probability of retrieval; ( \tau ): retrieval threshold; ( s ): activation noise |
| Learning | Calculates the utility of production rules through reward accumulation | ( Ui(n) = Ui(n-1) + \alpha[Ri(n) - Ui(n-1)] ) | ( U ): utility of production rule; ( \alpha ): learning rate; ( R ): reward for rule execution |
| Selection | Chooses which production rule to execute based on utility values | ( Pi = \frac{e^{Ui/t}}{\sumj e^{Uj/t}} ) | ( P_s ): probability of selection; ( t ): temperature parameter |
Visualizing the ACT-R Framework for Dietary Adherence
The following diagram illustrates how ACT-R modules and mechanisms interact to model dietary self-monitoring behavior:
Diagram 1: ACT-R Architecture for Dietary Adherence
Experimental Implementation: Modeling Dietary Self-Monitoring
Study Design and Participant Allocation
A recent study implemented ACT-R modeling to analyze adherence dynamics in a digital behavioral weight loss program called Health Diary for Lifestyle Change (HDLC) [1] [35]. The study recruited adults expressing willingness to improve their lifestyle and assigned them to one of three intervention groups with varying support levels. Participant distribution and model performance metrics across these groups are summarized in Table 2 below.
Table 2: Participant Allocation and ACT-R Model Performance Metrics
| Intervention Group | Sample Size | Root Mean Square Error (RMSE) | Key Adherence Findings |
|---|---|---|---|
| Self-management | 49 participants | 0.099 | Baseline adherence with minimal external support |
| Tailored Feedback | 23 participants | 0.084 | Improved adherence through personalized nutritional feedback |
| Intensive Support | 25 participants | 0.091 | Enhanced adherence via combined feedback and social support |
| Total Sample | 97 participants | - | Goal pursuit remained dominant throughout intervention |
The modeling data captured adherence to self-monitoring of dietary behaviors over 21 days, with predictor and outcome variables defined as adjacent elements in the sequence of self-monitoring behaviors [2]. Model performance was evaluated using mean square error, root mean square error (RMSE), and goodness of fit measures, demonstrating ACT-R's capacity to effectively capture adherence trends across all intervention conditions [2] [1].
Experimental Protocol for ACT-R Implementation
Researchers implementing ACT-R modeling for dietary adherence dynamics should follow this detailed methodological workflow:
Diagram 2: ACT-R Experimental Implementation Workflow
Step 1: Participant Recruitment and Group Assignment
- Recruit adults expressing willingness to improve lifestyle behaviors
- Randomize participants into intervention groups (e.g., self-management, tailored feedback, intensive support)
- Obtain ethical approval and informed consent [1] [35]
Step 2: Digital Monitoring Infrastructure Setup
- Implement mobile application for dietary self-monitoring
- Configure data collection protocols for daily dietary tracking
- Establish database infrastructure for behavioral data storage [1]
Step 3: Behavioral Data Collection
- Collect daily self-monitoring data over 21-day intervention period
- Record frequency and completeness of dietary logging
- Time-stamp all participant interactions with monitoring system [2]
Step 4: ACT-R Model Parameterization
- Define declarative memory chunks for self-monitoring knowledge
- Specify production rules for goal pursuit and habit formation behaviors
- Set initial activation values and utility parameters based on theoretical priors [1] [35]
Step 5: Model Training and Validation
- Fit ACT-R parameters to observed adherence patterns
- Validate model using cross-validation techniques
- Calculate goodness-of-fit metrics (RMSE, MSE) [2]
Step 6: Adherence Trend Analysis
- Visualize adherence trajectories across intervention groups
- Identify critical drop-points in self-monitoring behavior
- Compare observed versus predicted adherence patterns [2] [1]
Step 7: Mechanism Contribution Assessment
- Quantify relative contributions of goal pursuit versus habit formation
- Analyze how mechanism dominance shifts throughout intervention
- Assess intervention impact on cognitive mechanisms [2]
Key Findings and Quantitative Results
Adherence Dynamics and Mechanism Dominance
The ACT-R modeling revealed crucial insights about the cognitive mechanisms underlying dietary self-monitoring adherence. Across all intervention groups, the goal pursuit mechanism remained dominant throughout the entire intervention period, whereas the influence of the habit formation mechanism diminished during later stages [2] [1]. This finding suggests that conscious goal-directed behavior, rather than automated habits, primarily drives adherence to dietary self-monitoring in digital interventions.
Notably, interventions providing tailored feedback and higher levels of social support were associated with greater goal pursuit and more sustained behavioral practice [2] [35]. The visualization below illustrates the dynamic relationship between these cognitive mechanisms and intervention components:
Diagram 3: Mechanism-Intervention Relationships
Comparative Effectiveness of Intervention Strategies
The ACT-R modeling approach enabled quantitative comparison of different intervention strategies through their effects on cognitive mechanisms and adherence outcomes. Table 3 presents a comprehensive comparison of adherence patterns across support levels, synthesizing findings from multiple studies [2] [36] [37].
Table 3: Comparative Analysis of Dietary Intervention Support Strategies
| Intervention Characteristic | Self-Management Only | Tailored Feedback | Intensive Support | JITAI Approaches |
|---|---|---|---|---|
| Adherence Decline Pattern | Steep nonlinear decline | Gradual decline | Moderate decline | Context-dependent |
| Primary Cognitive Mechanism | Goal pursuit (depletion over time) | Goal pursuit (sustained) | Goal pursuit (enhanced) | Situation-specific mechanism activation |
| Key Active Components | Daily self-monitoring | Personalized nutritional feedback | Combined feedback + social support | Real-time risk detection + tailored messages |
| Typical RMSE in ACT-R Models | 0.099 | 0.084 | 0.091 | Not formally modeled with ACT-R |
| Long-term Sustainability | Low | Moderate | High | Potentially high (requires validation) |
| Implementation Complexity | Low | Moderate | High | Very high |
Implementing ACT-R modeling for dietary adherence research requires specific methodological tools and computational resources. Table 4 catalogues essential research reagents and their functions for developing and testing ACT-R models of dietary adherence behavior.
Table 4: Research Reagent Solutions for ACT-R Adherence Modeling
| Resource Category | Specific Tool/Technique | Function in ACT-R Implementation |
|---|---|---|
| Cognitive Architecture | ACT-R Framework (Python/Common Lisp) | Core cognitive modeling infrastructure simulating human thought processes |
| Data Collection Platforms | Mobile EMA (Ecological Momentary Assessment) | Real-time capture of dietary behaviors and contextual factors |
| Behavioral Tracking | Digital dietary self-monitoring apps | Passive and active recording of food intake and nutritional data |
| Intervention Delivery Systems | Tailored feedback algorithms | Personalized nutritional messaging based on individual adherence patterns |
| Social Support Infrastructure | Structured peer support platforms | Facilitation of emotional and informational support among participants |
| Analytical Frameworks | RMSE, MSE, goodness-of-fit metrics | Quantification of model accuracy in predicting adherence patterns |
| Model Visualization Tools | Graphviz, matplotlib | Creation of mechanism diagrams and adherence trajectory plots |
| Statistical Analysis Environment | R, Python (pandas, sci-kit learn) | Data preprocessing, parameter estimation, and hypothesis testing |
Research Implications and Future Directions
The application of ACT-R modeling to dietary adherence dynamics represents a significant advancement in computational behavioral science, offering unprecedented granularity in understanding how cognitive mechanisms respond to different intervention strategies [2] [1]. This approach enables researchers to move beyond descriptive accounts of adherence patterns to computational simulations that can predict individual trajectories and identify critical intervention points.
Future research should prioritize three key directions:
Extended Intervention Durations: Current modeling has focused on short-term (21-day) interventions. Extending these models to capture sustained adherence mechanisms over months or years is essential for understanding long-term behavior maintenance [2].
Integration of Social Cognitive Factors: Future ACT-R models should incorporate social cognitive constructs (e.g., self-efficacy, social support) to more comprehensively capture the determinants of behavioral compliance [2] [35].
Dynamic Adaptive Interventions: The ultimate application of ACT-R modeling lies in informing just-in-time adaptive interventions (JITAIs) that dynamically adjust support based on real-time adherence risk assessments [2] [38]. These systems could use ACT-R-based predictions to deliver tailored interventions at moments of highest vulnerability to non-adherence.
The integration of ACT-R modeling with emerging digital technologies represents a promising frontier for enhancing dietary adherence in both research and clinical practice, potentially leading to more effective, personalized interventions for weight management and chronic disease prevention.
Self-monitoring stands as a cornerstone technique in behavioral interventions, particularly within the realm of obesity treatment and dietary compliance research. It functions through a self-regulatory cycle where individuals observe and record their own behaviors, compare these behaviors against set goals, and adjust their actions accordingly to reduce the discrepancy between their current state and their goals [39]. This process is fundamentally rooted in self-regulation theories, including Social Cognitive Theory and Control Theory [39] [40]. Among the various behaviors that can be tracked, the triad of dietary intake, physical activity, and body weight has emerged as the core set of self-monitoring domains in behavioral weight loss interventions [39]. The digital transformation of healthcare has provided new tools—such as mobile apps, wearable activity trackers, and smart scales—that can automate aspects of this process, potentially reducing participant burden and improving adherence [39] [1]. This whitepaper delves into the technical specifications, experimental protocols, and mechanistic underpinnings of these core domains, providing researchers and drug development professionals with a rigorous framework for their application in clinical and research settings.
Domain-Specific Methodologies and Evidence
Dietary Intake Self-Monitoring
Dietary self-monitoring is a critical behavior change technique for initiating and sustaining dietary modifications [40] [41]. Traditional methodologies often involve the detailed itemization of all consumed foods and beverages, with subsequent tracking of energy content (calories) or specific nutrients [14]. This high-intensity approach, while effective, is often labor-intensive, leading to declining adherence over time [14] [1].
Evolution of Methodologies:
- High-Intensity Tracking: Requires recording all daily food and beverage intake, often using paper logs or digital apps, with participants looking up nutrient content [14].
- Low-Intensity Tracking: Focuses on monitoring only specific dietary components or behaviors, such as fruit and vegetable consumption or intake of sugar-sweetened beverages, to reduce participant burden [14].
- Plate-Based Methodologies: A simplified approach that conforms to visual food guides. Tools like the
iCANPlateapp or a printablePlate Toolrequire users to estimate and record the proportional composition of their meals on a virtual plate, typically with half the plate dedicated to vegetables and fruits, a quarter to protein, and a quarter to whole-grain foods [40] [41].
Evidence Base: A systematic review found that both higher and lower-intensity dietary self-monitoring strategies demonstrate statistically significant weight loss in intervention groups compared to control groups, though variability in adherence measures complicates direct comparison [14]. Qualitative studies on plate-based methods reveal key facilitators, including simplicity, quick completion time, and increased awareness of dietary habits [40] [41]. However, barriers include a lack of precision, difficulty in categorizing mixed foods, and challenges recording foods not present in the guide [41].
Physical Activity Self-Monitoring
Self-monitoring of physical activity typically involves tracking the volume and/or intensity of movement, with step counting being one of the most prevalent and simplified methods [39].
Methodologies:
- Wearable Technology: Devices like commercial activity trackers (e.g., Fitbit, Garmin) automatically monitor and record steps, distance traveled, active minutes, and sometimes heart rate.
- Digital Logging: Participants manually log physical activity sessions (e.g., type, duration, intensity) in mobile applications or web-based portals.
- Protocol Integration: In digital interventions, participants are typically instructed to wear the device daily and sync it with a companion app. The intervention platform often provides a daily step goal and automated, tailored feedback on progress [39].
Body Weight Self-Monitoring
Regular self-weighing provides feedback on the aggregate outcome of dietary and physical activity behaviors, reinforcing the self-regulatory cycle [39].
Methodologies:
- Smart Scales: Bluetooth or Wi-Fi-enabled scales that automatically transmit weight measurements to a smartphone app or web database upon weighing, removing the need for manual entry and reducing measurement error [39].
- Manual Tracking: Participants record their weight in a paper diary or digital spreadsheet.
- Protocol Integration: Participants are often instructed to weigh themselves at a consistent frequency (e.g., daily, weekly) using the provided smart scale. The resulting data stream allows for longitudinal tracking and objective assessment of the primary outcome in weight loss trials [39].
Table 1: Summary of Core Self-Monitoring Domains and Implementation Characteristics
| Domain | Core Metric | Common Tools | Intensity & Burden | Key Challenges |
|---|---|---|---|---|
| Dietary Intake | Energy intake, food groups, meal composition | Paper logs, mobile apps (e.g., MyFitnessPal), plate-based tools (e.g., iCANPlate) | High (itemization) to Low (plate-method) | High burden of detailed tracking; classification inaccuracy; adherence decline |
| Physical Activity | Step count, active minutes, energy expenditure | Wearable activity trackers (e.g., Fitbit), smartphone sensors | Low (with wearables) | Device charging; consistent wear |
| Body Weight | Mass (kg or lbs) | Smart scales, digital scales | Low | Psychological impact of fluctuations; objective data collection |
Quantitative Data Synthesis from Key Studies
The empirical evidence supporting self-monitoring is robust, though the optimal combination of strategies is still under investigation. The following table synthesizes findings from key studies and reviews.
Table 2: Quantitative Data and Outcomes from Self-Monitoring Research
| Study / Review | Design | Primary Outcome Related to Self-Monitoring | Key Findings |
|---|---|---|---|
| Spark Trial (PMC12504904) [39] | Optimization RCT (6-month, N=176) | Weight change from baseline to 6 months | Awaited (Data collection completed June 2025). Aims to identify "active ingredients" among tracking diet, steps, and weight. |
| Systematic Review (PMC8928602) [14] | Systematic Review (59 studies) | Weight loss | Majority of studies using high- and low-intensity dietary self-monitoring demonstrated significant weight loss vs. control. |
| Yu et al. (JMIR 2025) [1] | Modeling Study (N=97) | Adherence to dietary self-monitoring over 21 days | ACT-R model effectively captured adherence trends (RMSE: 0.084-0.099). Tailored feedback and social support associated with more sustained practice. |
| Kheirmandparizi et al. (PLoS One 2023) [40] | Qualitative Focus Groups (N=96) | Perceptions of a plate-based app | Participants liked the simplicity and promotion of self-awareness. Concerns included insufficient food classifications and difficulty conceptualizing proportions. |
Experimental Protocols for Optimization Trials
The Spark trial protocol serves as a state-of-the-art template for investigating the core self-monitoring domains [39].
Protocol: Spark Optimization Randomized Clinical Trial
1. Objective: To examine the unique and combined (interaction) effects of three self-monitoring strategies (tracking dietary intake, steps, and body weight) on 6-month weight change in adults with overweight or obesity [39].
2. Study Design:
- Design Type: A 2 × 2 × 2 full factorial randomized controlled trial.
- Conditions: Eight experimental conditions, enabling the isolation of main effects and interaction effects for each self-monitoring component.
- Randomization: Participants are randomly assigned to one of the eight conditions, which dictate which of the three self-monitoring strategies they are instructed to perform [39].
3. Participant Population:
- Sample Size: N = 176.
- Criteria: US adults with overweight or obesity [39].
4. Intervention Components:
- Core Components: All participants receive weekly lessons and action plans informed by Social Cognitive Theory.
- Experimental Components:
- Dietary Tracking: Instruction to self-monitor daily dietary intake via a commercial mobile app, with a corresponding daily calorie goal and automated feedback.
- Step Tracking: Instruction to wear a commercial activity tracker daily and monitor steps, with a daily step goal and automated feedback.
- Weight Tracking: Instruction to self-weigh daily using a provided smart scale with automated data transmission [39].
5. Data Collection and Outcomes:
- Primary Outcome: Objectively assessed weight change via smart scale from baseline to 6 months.
- Secondary Outcomes: Changes in BMI, caloric intake, diet quality, physical activity, and health-related quality of life at 1, 3, and 6 months.
- Engagement: The percentage of days of self-monitoring during the 6-month intervention is operationalized and its relation to weight change is analyzed [39].
The logical structure and workflow of this optimization trial is delineated in the diagram below.
Theoretical Models and Mechanistic Pathways
Understanding the cognitive and behavioral mechanisms that underpin self-monitoring is crucial for optimizing interventions.
The Self-Regulatory Feedback Loop
At its core, self-monitoring enables a continuous feedback loop for behavior regulation, as explained by Control Theory [39] [40]. The following diagram illustrates this cyclical process.
Cognitive Architecture of Adherence: The ACT-R Model
Computational cognitive models like the Adaptive Control of Thought-Rational (ACT-R) architecture provide a fine-grained, dynamic framework for analyzing adherence. A 2025 study used ACT-R to model adherence to dietary self-monitoring over 21 days, focusing on goal pursuit and habit formation mechanisms [1].
Table 3: Key Mechanisms in the ACT-R Cognitive Architecture for Self-Monitoring
| Mechanism | Description | Role in Self-Monitoring Adherence |
|---|---|---|
| Activation | Calculates the activation level of a "chunk" (e.g., memory of tracking). Comprises base-level activation (frequency of access) and spreading activation (context). | Explains how recent and frequent self-monitoring makes the behavior more salient and easily recalled. |
| Retrieval | The process of selecting a knowledge chunk from memory. Probability of retrieval is a function of its activation. | Determines the likelihood a participant will remember to self-monitor at the appropriate time. |
| Learning | Calculates the utility of production rules (if-then statements) through repeated execution and reward accumulation. | Captures how the perceived benefit (or cost) of self-monitoring is reinforced over time. |
| Selection | The system's process of choosing which production rule to execute based on their utility values. | Models the decision-making process that leads to either engaging in or skipping self-monitoring. |
The dynamic interplay between the goal-directed and habitual systems that govern self-monitoring behavior can be visualized as follows.
The Researcher's Toolkit: Key Reagents and Materials
For researchers designing self-monitoring studies, particularly in digital interventions, a standardized set of "research reagents" is essential.
Table 4: Essential Research Reagents and Materials for Digital Self-Monitoring Studies
| Item / Solution | Specification / Example | Primary Function in Research |
|---|---|---|
| Commercial Mobile App | Apps like MyFitnessPal or Lose It! | Provides the platform for dietary self-monitoring, including large food databases and calorie/nutrient tracking. |
| Wearable Activity Tracker | Devices like Fitbit, Garmin, or Apple Watch | Automates the collection of physical activity data (e.g., steps, active minutes) and provides a data stream for analysis. |
| Smart Scale | Bluetooth/Wi-Fi enabled scales (e.g., Withings, Fitbit Aria) | Enables objective, frequent weight measurement with automated data transmission, reducing manual entry error. |
| Tailored Feedback Algorithm | Automated, rule-based or AI-driven feedback system | Generates personalized messages based on comparing self-monitored data to goals, a key element of the self-regulatory loop. |
| Adherence Metrics | Percentage of days tracked; Consistency over time | Serves as a key process variable to measure engagement with the self-monitoring intervention and correlate with outcomes. |
| Qualitative Interview Guides | Semi-structured questions based on frameworks like COM-B | Used in mixed-methods studies to elucidate user perceptions, barriers, and facilitators related to self-monitoring tools. |
Leveraging the Multiphase Optimization Strategy (MOST) to Identify Active Ingredients
The Multiphase Optimization Strategy (MOST) is a comprehensive framework for developing, optimizing, and evaluating behavioral interventions that draws upon principles from engineering, statistics, and behavioral science [42] [43]. Traditional randomized controlled trials (RCTs) treat interventions as "bundled" packages, making it difficult to identify which components are actually responsible for observed effects [42] [44]. In contrast, MOST employs a systematic process to empirically identify intervention components that positively contribute to desired outcomes under real-life constraints, thereby building interventions that are not only effective but also efficient and cost-effective [43] [44].
MOST is particularly valuable in the context of dietary self-monitoring research, where interventions typically consist of multiple interacting components such as tracking platforms, feedback mechanisms, and support systems [14] [1]. Without a structured approach like MOST, researchers cannot definitively assess which aspects of an intervention can be reduced or replaced, or whether there are synergistic or antagonistic interactions between components [44]. This guide provides researchers with the methodological foundation and practical protocols for applying MOST to identify the "active ingredients" in dietary self-monitoring interventions.
The THREE Phases of MOST
The MOST framework consists of three sequential phases: Preparation, Optimization, and Evaluation [43]. Each phase addresses distinct research questions and employs specific methodological approaches.
Phase 1: Preparation
The Preparation Phase establishes the conceptual and practical foundation for optimization [43]. Key activities in this phase include:
- Conceptual Model Development: Creating a conceptual model that outlines the hypothesized mechanisms of change and intervention components [43].
- Pilot Testing: Conducting preliminary studies to assess feasibility, finalize implementation details, and identify potential "core components" [42] [43].
- Outcome Identification: Determining what outcomes should be optimized (e.g., effectiveness, efficiency, cost) [43].
- Component Selection: Identifying a finite set of intervention components (both program and delivery components) with theoretical basis for inclusion [42].
For dietary self-monitoring research, this phase would involve specifying the various self-monitoring components to be tested, such as tracking platforms (paper, website, mobile app), intensity levels (recording all intake versus specific components), frequency of monitoring, and feedback mechanisms [14].
Phase 2: Optimization
The Optimization Phase uses randomized experimentation to identify which components contribute meaningfully to desired outcomes and should be retained in the final intervention [42] [43]. This phase typically employs factorial designs that allow researchers to test multiple components simultaneously and efficiently [42].
In the context of dietary self-monitoring, a factorial experiment might investigate different combinations of self-monitoring components, such as:
- Tracking modality (paper vs. digital app)
- Monitoring intensity (complete diet vs. specific foods)
- Feedback type (personalized vs. generic)
- Support mechanisms (professional vs. peer support)
The results of this phase enable researchers to make empirically-based decisions about which components to include in the optimized intervention, potentially based on statistical significance, effect size thresholds, or cost-effectiveness considerations [42].
Phase 3: Evaluation
The Evaluation Phase involves testing the optimized intervention, consisting of the components identified in the Optimization Phase, in a standard randomized controlled trial (RCT) [42]. This phase addresses questions such as:
- Is the optimized intervention efficacious as a package?
- Is the intervention effect large enough to justify investment in broader implementation?
- How does the optimized intervention compare to existing alternatives?
For dietary self-monitoring research, this would involve comparing the optimized self-monitoring intervention against an appropriate control condition to determine its overall efficacy for improving dietary behaviors and related health outcomes [42] [14].
Table 1: Key Phases of the Multiphase Optimization Strategy (MOST)
| Phase | Primary Objective | Key Activities | Output |
|---|---|---|---|
| Preparation | Establish foundation for optimization | Conceptual model development, pilot testing, outcome identification, component selection | Set of candidate intervention components with theoretical basis |
| Optimization | Identify active components | Randomized experimentation using factorial designs, component effect estimation | Optimized intervention consisting of empirically-selected components |
| Evaluation | Test optimized intervention | Standard RCT comparing optimized intervention to control | Evidence of efficacy for the optimized intervention package |
Applying MOST to Dietary Self-Monitoring Research
Dietary self-monitoring is a cornerstone of behavioral interventions for weight management and chronic disease prevention, yet implementation approaches vary widely [14] [1]. MOST provides a rigorous methodology for identifying the most effective and efficient self-monitoring strategies.
Key Components of Dietary Self-Monitoring Interventions
Dietary self-monitoring interventions typically comprise multiple components that can be optimized using MOST:
- Self-Monitoring Modality: Traditional paper diaries, websites, mobile applications, or wearable devices [14]
- Monitoring Intensity: Comprehensive tracking of all dietary intake versus focused monitoring of specific dietary components or behaviors [14]
- Feedback Mechanisms: Personalized feedback, automated messages, or provider guidance [45] [1]
- Support Systems: Professional support, peer support, or self-guided approaches [45] [1]
- Reminder Schedules: Frequency and timing of prompts to self-monitor [1]
Research indicates that digital self-monitoring tools generally achieve better adherence than traditional paper-based methods, and that tailored feedback combined with emotional support can significantly enhance engagement [1].
Optimal Self-Monitoring Frequency
Identifying the necessary frequency of self-monitoring is an ideal optimization question. A recent study found that self-monitoring at least three days per week may be helpful for long-term weight loss maintenance, with greater benefit observed when self-monitoring five to six days per week [9]. This type of evidence can inform the specification of component levels in a MOST optimization phase.
Adherence Patterns and Predictors
Understanding adherence dynamics is crucial for optimizing self-monitoring interventions. Research using the Adaptive Control of Thought-Rational (ACT-R) cognitive architecture has demonstrated that goal pursuit mechanisms remain dominant throughout interventions, while habit formation influences tend to diminish in later stages [1]. Studies have identified distinct engagement patterns, with "consistent engagers" more likely to be older, more educated, and married or living with a partner [46].
Table 2: Key Components for Optimization in Dietary Self-Monitoring Interventions
| Component Category | Specific Components | Example Levels | Evidence Base |
|---|---|---|---|
| Tracking Platform | Modality | Paper, website, mobile app | Digital tools show superior adherence to paper [1] |
| Monitoring Protocol | Intensity | All intake, specific foods/beverages | Both high- and low-intensity can support weight loss [14] |
| Frequency | Daily, 3-4 days/week, 5-6 days/week | 3-4 days/week for maintenance; 5-6 days/week for loss [9] | |
| Feedback System | Type | Personalized, automated, none | Personalized feedback enhances engagement [45] [1] |
| Source | Professional, peer, automated | Professional feedback often most effective [45] | |
| Support Mechanisms | Type | Professional, peer, self-guided | Combined support strategies enhance adherence [1] |
| Format | Individual, group, mixed | Group formats provide social support [45] |
Experimental Protocols for MOST in Dietary Self-Monitoring
This section provides detailed methodological protocols for implementing MOST in dietary self-monitoring research.
Screening Phase Protocol: Factorial Experiment for Component Selection
Objective: To efficiently identify which of several self-monitoring components meaningfully contribute to adherence and effectiveness.
Design: A full or fractional factorial design with 2-5 factors (components), each with 2-4 levels [42].
Sample Size Calculation:
- For a 2^4 factorial design (4 components, each with 2 levels): 128-256 participants
- For a 2^5 factorial design (5 components, each with 2 levels): 160-320 participants
- Calculations should account for anticipated effect sizes (typically small to medium for behavioral components) and desired power (typically 80-90%)
Procedure:
- Recruit participants meeting inclusion criteria (e.g., adults with overweight/obesity, specific medical conditions)
- Randomly assign participants to experimental conditions representing different combinations of components
- Implement intervention with exact protocol for each condition
- Collect outcome data at baseline, throughout intervention, and post-intervention
Primary Outcomes:
- Adherence to self-monitoring (percentage of days with monitoring completed)
- Dietary change (e.g., DASH score, fruit/vegetable consumption, energy intake)
- Clinical outcomes (weight, blood pressure, glycemic control)
Data Analysis:
- Use factorial ANOVA to estimate main effects and interaction effects
- Apply multiple comparison corrections as appropriate
- Consider cost-effectiveness in component selection decisions
Refining Phase Protocol: Identifying Optimal Component Dosage
Objective: To fine-tune the selected components, particularly regarding optimal dosage parameters.
Design: Randomized experiment focusing on dosage variations of components identified in screening phase.
Example Protocol for Monitoring Frequency Optimization:
- Recruit participants who have completed initial weight loss phase
- Randomize to different self-monitoring frequency conditions:
- Condition 1: 1-2 days per week
- Condition 2: 3-4 days per week
- Condition 3: 5-6 days per week
- Condition 4: Daily monitoring
- Provide identical self-monitoring tools and support across conditions
- Maintain intervention for 6-12 months to assess weight maintenance
Outcomes: Weight change, monitoring adherence, participant burden, cost-effectiveness
Analysis: Dose-response modeling, linear mixed effects models
Confirming Phase Protocol: RCT of Optimized Intervention
Objective: To evaluate the efficacy of the optimized self-monitoring intervention package.
Design: Standard two-arm RCT comparing optimized intervention to appropriate control.
Procedure:
- Recruit new sample of participants
- Randomize to optimized intervention or control condition
- Control condition could include:
- Education only
- Minimal intervention
- Standard care
- Alternative active intervention
- Implement protocol with careful attention to treatment fidelity
- Collect outcome data at baseline, post-intervention, and follow-up periods
Primary Outcome: Clinically relevant outcome (e.g., weight loss, HbA1c reduction, blood pressure improvement)
Secondary Outcomes: Dietary behaviors, adherence metrics, cost-effectiveness, mediators and moderators
Analysis: Intent-to-treat analysis using appropriate statistical models (ANCOVA, mixed models)
Diagram: MOST Workflow for Dietary Self-Monitoring
The following diagram illustrates the complete MOST workflow applied to dietary self-monitoring research:
MOST Workflow for Dietary Self-Monitoring
Diagram: Component Selection Decision Logic
The following diagram presents the decision logic for selecting intervention components during the Optimization Phase:
Component Selection Decision Logic
Research Reagent Solutions for MOST Implementation
Successful implementation of MOST in dietary self-monitoring research requires specific methodological tools and approaches. The following table details essential "research reagents" for designing and executing MOST studies.
Table 3: Research Reagent Solutions for MOST in Dietary Self-Monitoring Research
| Research Reagent | Function | Implementation Examples |
|---|---|---|
| Factorial Experimental Designs | Enables efficient testing of multiple components simultaneously | Full factorial, fractional factorial, or sequential designs to evaluate self-monitoring components [42] |
| Component Specification Framework | Provides systematic approach for defining and categorizing intervention components | Behavior Change Technique Taxonomy (BCTTv1) to classify active ingredients [45] [47] |
| Adherence Measurement Tools | Quantifies engagement with self-monitoring protocols | Digital tracking of app usage, automated adherence metrics, latent class growth modeling to identify engagement patterns [1] [46] |
| Cognitive Architecture Models | Models mechanisms of behavior change and adherence dynamics | Adaptive Control of Thought-Rational (ACT-R) to simulate goal pursuit and habit formation processes [1] |
| Cost-Effectiveness Analysis Methods | Evaluates economic efficiency of components | Cost per unit of behavior change, incremental cost-effectiveness ratios for different component combinations [43] |
| Multilevel Statistical Models | Analyzes nested data and longitudinal patterns | Linear mixed models for repeated measures, growth curve models for adherence trajectories [1] [46] |
Optimization Outcomes and Decision Making
The ultimate goal of applying MOST to dietary self-monitoring research is to develop interventions that are effective, efficient, and scalable. This requires careful consideration of optimization outcomes and decision rules.
Decision Criteria for Component Selection
Several criteria can inform decisions about which components to include in the optimized intervention:
- Effect Size: Components demonstrating clinically meaningful effects on primary outcomes should be prioritized [42]
- Statistical Significance: Traditional significance thresholds (p < 0.05) or more lenient thresholds (p < 0.20) may be used depending on the study's goals [42]
- Cost-Effectiveness: Components providing substantial benefit at reasonable cost should be favored [43]
- Interactions: Components that show synergistic effects with other valuable components may be included even if main effects are modest [42]
Expected Outcomes from Optimized Self-Monitoring Interventions
Research suggests that optimized dietary self-monitoring interventions can yield:
- Improved Adherence: Digital interventions with personalized feedback show adherence rates between 63% and 85.5% [45]
- Enhanced Effectiveness: AI-generated dietary interventions have demonstrated a 39% reduction in IBS symptom severity and a 72.7% diabetes remission rate [48]
- Sustainable Engagement: Continued self-monitoring at optimal frequencies (3-6 days/week) supports long-term weight maintenance [9]
By systematically applying the MOST framework to dietary self-monitoring research, investigators can develop more potent, efficient, and scalable interventions that maximize public health impact while conserving resources.
The Impact of Tailored Feedback and Social Support Mechanisms
The global prevalence of overweight and obesity presents a critical public health challenge, with these conditions significantly elevating the risk of diabetes, cardiovascular diseases, and imposing substantial economic burdens on healthcare systems worldwide [35]. Within behavioral weight loss interventions, self-monitoring of dietary behaviors is widely recognized as a cornerstone strategy for promoting healthy behavior changes and improving health outcomes [35]. However, participant adherence to self-monitoring tends to wane over time due to the labor-intensive nature of the approach and the absence of efficient passive recording methods [35]. This technical whitepaper examines two pivotal mechanisms for enhancing adherence within dietary interventions: tailored feedback and social support mechanisms. Framed within a broader thesis on self-monitoring techniques for dietary intervention compliance, this analysis synthesizes current evidence on how these components quantitatively impact adherence dynamics and weight loss outcomes, providing researchers and drug development professionals with methodological insights for optimizing intervention design.
Theoretical Foundations and Adherence Dynamics
Cognitive Architecture of Self-Monitoring
The Adaptive Control of Thought-Rational (ACT-R) cognitive architecture provides a robust computational framework for modeling adherence to self-monitoring of dietary behaviors. ACT-R integrates physical, neurophysiological, behavioral, and cognitive mechanisms into a unified model, simulating human cognitive processes through symbolic and subsymbolic systems [35]. The symbolic system comprises modules with associated buffers for information retrieval and storage, while the subsymbolic system manages operations through activation, retrieval, learning, and selection mechanisms [35]. Within dietary interventions, ACT-R modeling focuses particularly on two core mechanisms: goal pursuit and habit formation.
Recent research utilizing ACT-R has demonstrated that across various intervention groups, the goal pursuit mechanism remains dominant throughout the intervention period, whereas the influence of the habit formation mechanism typically diminishes during later stages [35]. This finding has profound implications for intervention design, suggesting that sustained goal-oriented strategies may be more effective than relying solely on habit formation. The presence of tailored feedback and higher levels of social support are associated with enhanced goal pursuit and more sustained behavioral practice [35], indicating that these components directly influence the cognitive mechanisms underlying adherence.
Visualizing the Cognitive-Behavioral Framework
The following diagram illustrates the cognitive-behavioral framework of dietary self-monitoring adherence, integrating ACT-R mechanisms with intervention components:
Quantitative Evidence and Empirical Findings
Efficacy of Tailored Feedback Mechanisms
Table 1: Impact of Tailored Feedback on Dietary Behaviors and Weight Loss Outcomes
| Study Design | Population | Intervention Components | Key Metrics | Results |
|---|---|---|---|---|
| ACT-R Modeling Study [35] | 97 adults in digital weight loss program | Self-management vs. tailored feedback vs. intensive support | RMSE of adherence trends, mechanism dominance | Tailored feedback group: RMSE 0.084; greater goal pursuit influence vs. self-management (RMSE 0.099) |
| Smartphone App Intervention [49] | Caregivers and children in Kenya | Consumption tracking with tailored messaging vs. no feedback | Minimum dietary diversity attainment | Children's likelihood of meeting threshold increased by 23 percentage points with feedback |
| Online Weight Loss Intervention [50] | 61 Chinese adults | Quantitative and qualitative self-monitoring with weekly feedback | Weight change (kg and percentage) | Average loss of 2.52 kg (3.99% of initial weight); timeliness of self-monitoring predicted success |
| Factorial RCT (Spark Trial) [26] | 176 US adults with overweight/obesity | Tracking diet, steps, and weight with automated feedback | Weight change at 6 months, engagement patterns | Study completed 2025; results forthcoming on optimal self-monitoring combinations |
Social Support Mechanisms and Combined Interventions
Table 2: Efficacy of Social Support and Combined Intervention Approaches
| Intervention Type | Social Support Format | Adherence Outcomes | Weight-Related Outcomes | Participant Engagement |
|---|---|---|---|---|
| Online Group Counseling [50] | Closed WeChat groups (8-12 participants) with peer communication | Higher timeliness and frequency of self-monitoring | 20/61 participants achieved >5% weight loss ("Excellent" group) | Excellent group reported significantly more qualitative self-monitoring entries |
| Digital Behavioral Weight Loss [35] | Intensive support condition with emotional social support | Sustained behavioral practice throughout intervention period | Not specifically reported | Greater goal pursuit throughout intervention period |
| Health Diary for Lifestyle Change [35] | Support groups among participants | Long-term healthy lifestyle maintenance | Weight loss success enhancement | Social support mitigated effects of self-regulatory depletion |
Experimental Protocols and Methodologies
ACT-R Modeling Protocol for Adherence Dynamics
The ACT-R modeling approach provides a rigorous methodology for predicting adherence to self-monitoring of dietary behaviors. The following workflow details the implementation protocol:
Implementation Details: The modeling protocol utilizes the ACT-R architecture to simulate cognitive processes over a 21-day intervention period [35]. The symbolic system employs chunks (in declarative memory) with activation attributes influenced by retrieval time, frequency, and recentness of access. Production rules (in procedural memory) are characterized by utility attributes, with rules matching buffer conditions and having highest utility being most likely to execute [35]. The subsymbolic system manages operations through computational processes including activation, retrieval, learning, and selection. Model performance is evaluated using mean square error, root mean square error (RMSE), and goodness of fit metrics, with mechanistic contributions visualized to analyze adherence patterns and intervention impacts [35].
Smartphone Application Intervention with Regression Discontinuity
A rigorous protocol for testing tailored feedback impacts was implemented through the Mbiotisho smartphone application in Samburu County, Kenya [49]:
Participant Recruitment: 189 caregivers meeting inclusion criteria (primary caregiver for child 6-48 months, working with designated Community Health Volunteers, no plans to move outside county) were recruited through stratified random sampling from four community health units [49].
Training Protocol: Participants completed a 9-day training program on smartphone use, nutritional concepts (food groups and suggested consumption), and application operation. Training included 3 days of home practice by caregivers [49].
Data Collection: Caregivers recorded consumption of 16 food groups based on FAO guidelines using 24-hour recall separately for themselves and their child participants. Parallel data collection was performed monthly by Community Health Volunteers during home visits [49].
Intervention Rollout: The child feedback feature was delayed until December 15, 2019 (six weeks after data collection began), creating natural treatment and control conditions for regression discontinuity analysis. Caregiver feedback was added later in response to participant requests [49].
Feedback Content: Messages were communicated through series of screens with images and audio in the local language, describing recommended benchmarks and simple assessment of caregiver-submitted records. Child feedback provided age-appropriate WHO recommendations on daily breastfeeding frequency and dietary diversity, while caregiver feedback focused on consumption of animal source foods, dark green leafy vegetables, and Vitamin A rich fruits and vegetables [49].
Multiphasic Optimization Strategy (MOST) Framework
The Spark trial exemplifies an advanced methodological approach for identifying active intervention components through a factorial randomized design [26]:
Experimental Design: 2 × 2 × 2 full factorial design with 8 experimental conditions testing three self-monitoring strategies (dietary intake, steps, and body weight) in all possible combinations [26].
Participant Population: 176 US adults with overweight or obesity recruited between September 2023 and November 2024, with data collection completed in June 2025 [26].
Intervention Structure: All participants received core intervention components including weekly lessons and action plans informed by Social Cognitive Theory. For each assigned self-monitoring strategy, participants received corresponding goals and weekly automated feedback delivered via commercial digital tools [26].
Assessment Schedule: Objective weight measurement via smart scale at baseline, 1, 3, and 6 months; secondary outcomes include BMI, caloric intake, diet quality, physical activity, and health-related quality of life [26].
Engagement Metrics: Patterns of engagement operationalized as percentage of days of self-monitoring during the 6-month intervention; qualitative interviews conducted with participant subsets to elucidate engagement factors [26].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Methodological Components for Dietary Intervention Compliance Research
| Research Component | Function & Purpose | Implementation Examples |
|---|---|---|
| ACT-R Computational Architecture | Models cognitive processes underlying adherence; predicts adherence dynamics through goal pursuit and habit formation mechanisms | Hybrid symbolic-subsymbolic system; models chunk activation and production rule utility; quantifies mechanism dominance [35] |
| Digital Self-Monitoring Platforms | Enables real-time tracking of dietary behaviors; reduces retrospective recall error; facilitates automated feedback | Mbiotisho app (Kenya); Bohee Health app (China); Commercial apps with 24-hour recall capabilities [49] [50] |
| Tailored Feedback Algorithms | Generates personalized comparisons between behavior and guidelines; enhances salience of performance gaps | Automated messaging comparing consumption to WHO/FAO standards; traffic light labeling systems; personalized recommendation engines [49] |
| Social Support Infrastructure | Mitigates self-regulatory depletion; provides emotional communication and accountability | Closed online groups (WeChat); Support groups among participants; Intensive support conditions with emotional reinforcement [35] [50] |
| Multiphase Optimization Strategy (MOST) | Identifies active intervention components; eliminates inactive elements to reduce participant burden | 2×2×2 factorial designs; component isolation experiments; preparation-optimization-evaluation pipeline [26] |
| Regression Discontinuity Design | Establishes causal inference in absence of randomized trials; leverages phased implementation schedules | Delayed feature rollout (e.g., 6-week feedback delay); natural cut-point creation for treatment assignment [49] |
The integration of tailored feedback and social support mechanisms within dietary self-monitoring interventions demonstrates significant potential for enhancing adherence and improving weight loss outcomes. Current evidence indicates that tailored feedback operates primarily through strengthening goal pursuit mechanisms, with ACT-R modeling showing RMSE values of 0.084 for tailored feedback groups compared to 0.099 for self-management approaches [35]. Social support functions to mitigate self-regulatory depletion and sustain behavioral practice over time, particularly in digital intervention contexts. Methodological innovations such as the MOST framework, ACT-R computational modeling, and regression discontinuity designs provide robust approaches for identifying active intervention components and optimizing their implementation. Future research directions should include extending intervention durations to explore sustained adherence mechanisms, integrating additional social cognitive factors to capture behavioral compliance insights, and adapting dynamic models to inform just-in-time adaptive interventions [35]. For researchers and drug development professionals, these findings underscore the importance of incorporating both tailored feedback and social support structures into dietary intervention frameworks to maximize adherence and clinical outcomes.
Overcoming Adherence Barriers and Implementing Optimization Strategies
Self-monitoring stands as a cornerstone of effective behavioral obesity treatment and dietary intervention compliance, involving the systematic tracking of dietary intake, physical activity, and body weight [26]. This technique is firmly grounded in self-regulation theories, including Social Cognitive Theory and Control Theory, which posit that behavior change occurs through a cyclical process of goal setting, self-monitoring, feedback, and behavioral adjustment [26]. Within digital health interventions, self-monitoring serves as a critical mechanism for promoting adherence to dietary guidelines and facilitating weight management [1]. However, despite its established efficacy, engagement with self-monitoring protocols frequently declines over time due to several persistent barriers [26] [1]. Understanding these barriers—specifically patient burden, accessibility challenges, and waning novelty—is essential for researchers and drug development professionals seeking to optimize dietary intervention frameworks and improve long-term compliance outcomes. This technical guide examines these barriers within the context of dietary intervention compliance research, providing methodological insights and experimental approaches for identifying and addressing these challenges in clinical and research settings.
Core Barrier Framework: Burden, Accessibility, and Waning Novelty
Research consistently identifies three primary categories of barriers that impede consistent self-monitoring in dietary interventions. These barriers operate across individual, environmental, and intervention levels, creating complex challenges for long-term adherence [51].
Perceived Burden
Perceived burden represents one of the most significant barriers to self-monitoring adherence, encompassing the time demands, effort, and complexity associated with tracking behaviors [26] [51]. In focus groups examining barriers to dietary recommendations, patients consistently reported that dietary modifications were perceived as considerably more burdensome than medication regimens, with strict weight-loss diets rated as similarly burdensome to insulin therapy [52]. This burden manifests particularly in dietary self-monitoring, which requires literate, motivated populations and can lead to reactivity—where participants change their usual dietary patterns either for ease of recording or due to social desirability biases [18]. The labor-intensive nature of dietary self-monitoring, especially without efficient passive recording methods, directly contributes to declining adherence over time [1].
Accessibility Challenges
Accessibility barriers encompass both physical and technical limitations that prevent consistent self-monitoring. At the individual level, these include constraints related to literacy and numeracy [26], while at the environmental level, cost factors consistently emerge as significant barriers across diverse populations [52]. Digital accessibility presents particular challenges, including compatibility with organizational infrastructure, access to necessary equipment, and technical support requirements [53]. Research in childcare centers identified that the "changes needed in team interactions" subdomain scored lowest as a potential barrier to adopting digital health interventions, indicating that organizational workflow integration presents significant accessibility challenges [53]. This is particularly problematic for interventions targeting geographically, racially, and ethnically heterogeneous populations who are underrepresented in traditional obesity treatment research despite being disproportionately burdened by obesity [26].
Waning Novelty
The phenomenon of waning novelty describes the gradual decline in engagement with self-monitoring tools as initial enthusiasm diminishes and the repetitive nature of tracking sets in [26]. This barrier is especially prevalent in digital interventions, where engagement often follows a pattern of initial high use followed by gradual decline [1] [54]. The dynamic analysis of dietary self-monitoring adherence reveals that while goal pursuit mechanisms remain dominant throughout interventions, the influence of habit formation mechanisms typically diminishes in later stages without adequate support structures [1]. This novelty effect is particularly challenging in adolescent populations, where digital interventions frequently lose impact after just a few weeks despite initial engagement [54]. Maintaining engagement requires strategic intervention design that incorporates evolving feedback mechanisms, adaptive goal structures, and varied content delivery to combat the predictable decline in novelty.
Table 1: Barrier Classification Framework in Dietary Self-Monitoring
| Barrier Category | Subtypes | Affected Populations | Impact Level |
|---|---|---|---|
| Perceived Burden | Time demands, complexity, cognitive load, rigidity of schedule | Highly variable by literacy, motivation levels; especially challenging in Type 2 diabetes populations [52] | Individual level |
| Accessibility Challenges | Cost, technical infrastructure, literacy/numeracy constraints, social support deficits | Low socioeconomic groups, rural populations, older adults, culturally diverse groups [26] [52] | Environmental level |
| Waning Novelty | Engagement decline, habit formation failure, repetitive tracking fatigue | Adolescents, digital native populations, those with high initial engagement [1] [54] | Intervention level |
Quantitative Assessment: Measuring Barrier Impact
Understanding the prevalence and impact of self-monitoring barriers requires robust quantitative assessment methodologies. Research across diverse populations provides insight into the measurable effects of these barriers on intervention adherence and outcomes.
Burden Metrics and Measurement
The perceived burden of dietary self-monitoring can be quantified using standardized rating scales that compare different treatment modalities. One study employing a 7-point burden rating scale found significant differences between interventions, with moderate diet interventions rated as a greater burden than oral agents (median burden score 1 vs. 0, P = 0.001) but less burdensome than insulin therapy [52]. Particularly revealing was the finding that strict weight-loss diets were rated as similarly burdensome to insulin therapy (median burden score 4 vs. 4, P = NS), highlighting the significant perceived burden of intensive dietary monitoring [52]. Despite this burden, self-reported adherence was much higher for both pills and insulin than for moderate diet interventions, indicating that burden directly impacts compliance.
Adherence Decline Patterns
The quantitative measurement of adherence patterns provides compelling evidence for the waning novelty effect. Research on digital dietary self-monitoring reveals distinct engagement trajectories, with studies reporting adherence rates between 63% and 85.5% for interventions incorporating personalized feedback and gamification elements [54]. However, these rates typically decline over intervention periods, with one study noting that SMS-based interventions initially showed improvement in eating habits, but these effects were not maintained long-term according to intention-to-treat analysis [54]. The dynamic modeling of self-monitoring adherence using the Adaptive Control of Thought-Rational (ACT-R) cognitive architecture has quantified this decline, demonstrating how goal pursuit and habit formation mechanisms evolve differently throughout intervention periods [1].
Adoption Intentions and Barriers
Quantitative assessment of organizational adoption intentions for digital health interventions reveals specific barrier profiles. In a national sample of Australian childcare centers, 58.9% (229/389) demonstrated high intentions to adopt digital health interventions to support dietary guideline implementation [53]. When assessed using the Nonadoption, Abandonment, Scale-up, Spread, and Sustainability (NASSS) framework, the "changes needed in team interactions" subdomain scored lowest (mean 3.52, SD 1.30), indicating a significant organizational barrier, while "organization's capacity to innovate" scored highest (mean 5.25, SD 1.00), indicating a potential enabler [53]. Regression analysis identified that ease of the adoption decision (P<.001) and identifying work and individuals involved in implementation (P=.001) were significantly associated with high intentions to adopt digital health interventions.
Table 2: Quantitative Metrics for Self-Monitoring Barrier Assessment
| Metric Category | Specific Measures | Data Collection Methods | Associated Barriers |
|---|---|---|---|
| Burden Assessment | 7-point burden rating scales, time expenditure logs, cognitive load measures | Structured surveys, time-motion studies, ecological momentary assessment | Perceived burden [52] |
| Adherence Tracking | Percentage of days with self-monitoring, completion rates of food records, engagement metrics from digital platforms | Mobile health apps, wearable device data, self-report diaries, 24-hour recalls | Waning novelty, perceived burden [26] [1] |
| Adoption Intentions | Technology Acceptance Model constructs, NASSS framework subdomains, organizational readiness scales | Cross-sectional surveys, structured interviews, pre-implementation assessments | Accessibility challenges, perceived burden [53] |
Methodological Approaches: Experimental Protocols for Barrier Investigation
Rigorous experimental designs are essential for investigating self-monitoring barriers and testing potential mitigation strategies. Several sophisticated methodological approaches have emerged in recent research.
The Spark Trial: Multiphase Optimization Strategy (MOST)
The Spark trial exemplifies an advanced methodological approach to identifying active ingredients in self-monitoring interventions while accounting for participant burden [26] [39]. This optimization-randomized clinical trial employs a 2 × 2 × 2 full factorial design with 8 experimental conditions to examine the unique and combined weight loss effects of three self-monitoring strategies (tracking dietary intake, steps, and body weight). The protocol involves 176 US adults with overweight or obesity randomized to receive 0-3 self-monitoring strategies in a 6-month fully digital weight loss intervention [26].
Experimental Protocol: For each assigned strategy, participants self-monitor daily via commercially available digital tools (mobile app, wearable activity tracker, and smart scale) and receive corresponding goals (e.g., daily calorie goal) with weekly automated feedback [26]. All participants receive core intervention components, including weekly lessons and action plans informed by Social Cognitive Theory. Assessments occur at baseline, 1, 3, and 6 months, with weight assessed objectively via smart scale [26]. The primary aim tests the main effects of the three self-monitoring components and their interactions on weight change from baseline to 6 months, while secondary outcomes include changes in BMI, caloric intake, diet quality, physical activity, and health-related quality of life [26]. This factorial design enables researchers to disentangle the effects of individual self-monitoring components and identify potential antagonistic interactions where burdensome components may undermine engagement with other elements.
ACT-R Cognitive Architecture Modeling
The Adaptive Control of Thought-Rational (ACT-R) cognitive architecture provides a computational framework for modeling adherence dynamics to dietary self-monitoring [1]. This approach simulates human cognitive processes to model adherence over time, focusing specifically on the mechanisms of goal pursuit and habit formation.
Experimental Protocol: The modeling framework utilizes data from digital behavioral weight loss programs with participants assigned to different intervention groups (e.g., self-management, tailored feedback, and intensive support) [1]. Predictor and outcome variables are defined as adjacent elements in the sequence of dietary self-monitoring behaviors. The ACT-R architecture, comprising symbolic and subsymbolic systems, models chunk activation in declarative memory based on frequency and recency of access, with activation calculated as A = B + S, where B represents base-level activation and S represents spreading activation [1]. The probability of chunk retrieval is modeled as Pr = 1/(1+e-(A-τ)/s), where τ is the retrieval threshold and s represents activation noise [1]. Production rule utilities are learned through repeated execution, with utility calculated as U = U0 + α(R - U0), where α is the learning rate and R is the reward [1]. This approach allows researchers to simulate and predict adherence patterns and test the potential impact of different intervention strategies before implementation.
Qualitative Systematic Review Methodology
A comprehensive qualitative systematic review following Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines provides a methodological framework for synthesizing participant-reported barriers across multiple studies [51].
Experimental Protocol: The review process involves searching multiple databases (Google Scholar, Cochrane Reviews, Medline, PubMed, and Web of Science) using appropriate Boolean operators and truncation [51]. Studies are screened according to predefined inclusion and exclusion criteria, with quality assessment conducted using the Critical Appraisal Skills Programme (CASP) checklist for qualitative research [51]. Thematic analysis is performed on extracted data using inductively derived themes organized within an adapted Socio-Ecological Model at individual, environment, and intervention levels [51]. This methodology enables researchers to identify consistent barrier patterns across diverse interventions and populations, providing a comprehensive understanding of the perceived challenges to dietary self-monitoring adherence.
Diagram 1: Barrier-Methodology Mapping Framework (76x76px)
The Scientist's Toolkit: Research Reagent Solutions
Investigating barriers to dietary self-monitoring requires specific methodological tools and assessment frameworks. The following research reagents represent essential components for designing rigorous studies in this domain.
Table 3: Essential Research Reagents for Barrier Investigation
| Research Reagent | Function/Application | Implementation Example |
|---|---|---|
| NASSS Framework | Assesses individual, organizational, and contextual barriers to technology adoption in healthcare settings | Identifying that "changes needed in team interactions" subdomain scores lowest as barrier to digital health adoption (mean 3.52, SD 1.30) [53] |
| ACT-R Cognitive Architecture | Computational modeling of cognitive processes underlying self-monitoring adherence dynamics | Modeling goal pursuit and habit formation mechanisms in dietary self-monitoring with RMSE values of 0.084-0.099 across intervention groups [1] |
| 24-Hour Dietary Recalls | Gold-standard dietary assessment method minimizing memory burden and reactivity | Multiple Automated Self-Administered 24-hour recalls (ASA-24) collected on non-consecutive days to assess dietary intake [18] |
| Factorial RCT Designs | Isolates active intervention components and identifies component interactions | 2 × 2 × 2 factorial design testing 3 self-monitoring strategies in 8 conditions to identify essential components [26] |
| Behavior Change Technique Taxonomy | Standardized classification of active intervention components | Identifying goal setting, feedback, social support as most effective BCTs for adolescent engagement [54] |
The systematic investigation of barriers to dietary self-monitoring—particularly burden, accessibility, and waning novelty—requires sophisticated methodological approaches and assessment frameworks. The research protocols and tools outlined in this technical guide provide researchers and drug development professionals with robust methods for identifying and addressing these critical challenges. The integration of optimization trials, computational modeling, and qualitative synthesis approaches offers a comprehensive framework for advancing the science of dietary intervention compliance. Future research should focus on developing adaptive intervention systems that dynamically respond to individual barrier profiles, ultimately enhancing the effectiveness and sustainability of dietary self-monitoring in diverse populations.
Within the framework of dietary intervention compliance research, self-monitoring is widely recognized as a cornerstone of successful behavior change. The data generated through self-monitoring, however, achieves its maximum impact only when paired with strategic feedback. This technical guide provides an in-depth analysis of feedback optimization parameters—content, timing, frequency, and delivery mode—to enable researchers to design more effective dietary intervention protocols. Evidence consistently demonstrates that incorporating feedback significantly enhances intervention outcomes; for instance, physical activity interventions with feedback provision were found to be more effective than those without (d=0.29, 95% CI [0.16;0.43]) [55]. Nevertheless, the specific characteristics that constitute optimal feedback remain inadequately defined across the literature. This whitepaper synthesizes current evidence and methodological approaches to address this critical research gap, with particular emphasis on applications in clinical trials and efficacy studies where dietary adherence directly influences primary outcome validity.
Theoretical Foundations of Feedback in Behavior Change
Feedback operates within several established behavioral theoretical frameworks. Within Social Cognitive Theory, feedback provides positive reinforcement for successful goal attainment, offers insight into potential barriers, and supports problem-solving and effective development of future goals [55]. Supportive Accountability Theory further posits that interventionist support, often delivered through feedback, is essential for promoting engagement with health behavior change interventions [55].
The Capability, Opportunity, Motivation-Behaviour (COM-B) model and the Theoretical Domains Framework (TDF) provide systematic approaches for identifying behavioral determinants that feedback can target [28] [56]. These frameworks help researchers pinpoint specific barriers to dietary adherence (e.g., lack of knowledge, low self-efficacy, environmental constraints) and select appropriate feedback strategies to address them. The Behaviour Change Wheel (BCW) then links these behavioral analysis to appropriate intervention functions, including feedback-based strategies [28].
Feedback is formally categorized within the Behavior Change Technique (BCT) Taxonomy v1 as a distinct technique. Two primary feedback types are recognized:
- Feedback on behavior: "Monitor and provide informative or evaluative feedback on performance of the behavior (e.g., form, frequency, duration, intensity)" [55]
- Feedback on outcomes: "Monitor and provide feedback on the outcome of performance of the behavior" [55]
The following diagram illustrates how these theoretical elements integrate within a comprehensive feedback system for dietary interventions:
Critical Dimensions of Feedback Optimization
Feedback Content and Personalization
Feedback content varies significantly in complexity, from basic confirmation of self-monitoring completion to personalized nutritional guidance. Research indicates that personalized feedback may confer approximately a 2 kg benefit over interventions that do not provide personalized feedback in weight management studies [55]. Personalization extends beyond simply inserting the participant's name; effective personalized feedback references specific participant data, aligns with individual goals, and addresses unique barriers.
The Dashboard for Improving Sustainable Healthy (DISH) food choices exemplifies an advanced approach to feedback content, leveraging nudge and traffic-light labels to enable consumers to compare and envision the potential environmental, nutritional, and health impacts of their food choices before purchasing [57]. This multi-dimensional feedback system presents complex information in an immediately accessible format.
Digital interventions increasingly employ artificial intelligence to generate adaptive feedback content. One systematic review found that interventions incorporating personalized feedback showed adherence rates between 63% and 85.5% among adolescents, with notable improvements in dietary habits [45]. The most effective feedback content includes:
- Specific comparison between current behavior and targets
- Actionable suggestions for improvement
- Positive reinforcement for successes
- Problem-solving guidance for challenges
Feedback Timing and Frequency
The timing of feedback delivery significantly influences its effectiveness. Just-in-time feedback represents an ideal approach, providing input when individuals are most receptive to it, though the implementation challenges are substantial [55]. Different feedback schedules serve distinct purposes:
Table 1: Feedback Timing and Frequency Approaches
| Approach | Description | Evidence of Effectiveness | Best Applications |
|---|---|---|---|
| Immediate/Real-time | Provided instantly after self-monitoring entry | Limited direct evidence; theoretically strong for habit formation | Simple dietary behaviors; digital tracking apps |
| Daily Summary | Consolidated feedback on daily patterns | Associated with weight loss success when tracking ≥2 eating occasions [58] | Establishing initial adherence patterns |
| Weekly Review | Comprehensive analysis of weekly trends | Commonly used in effective interventions [45] | Longer-term pattern recognition |
| Adaptive Scheduling | Frequency adjusts based on participant engagement | Shown to improve maintenance in computational models [1] | Sustaining engagement over time |
The optimal feedback frequency balances intervention effectiveness with participant burden. Evidence suggests that daily feedback may be particularly important during initial intervention phases when participants are establishing self-monitoring habits, with potential transition to less frequent feedback as interventions progress [1].
Feedback Delivery Mode
Feedback delivery channels should align with intervention context and participant characteristics. Digital platforms offer diverse delivery options, each with distinct advantages:
Table 2: Feedback Delivery Modes and Implementation Considerations
| Delivery Mode | Technical Requirements | Strength of Evidence | Implementation Notes |
|---|---|---|---|
| In-app Messaging | Mobile application with notification system | Strong for engagement [45] | Enables immediate, context-specific feedback |
| Human-generated Comments | Trained staff for feedback generation | Personalized feedback may confer ~2kg benefit [55] | Resource-intensive; scalability challenges |
| Algorithm-generated Messages | Automated feedback algorithms | Comparable effectiveness to human feedback in some studies [55] | Enables scalability; requires sophisticated programming |
| Multimedia Formats | Video/audio capabilities | Video interventions improve adherence outcomes [59] | Enhances accessibility and engagement |
| Traffic-light Systems | Color-coded display interfaces | DISH system improved sustainable choices [57] | Simplifies complex information for quick decisions |
The distinction between human-generated versus algorithm-generated feedback represents a critical consideration for research design. While some studies report no significant differences in outcomes between these approaches [55], human-generated feedback may offer advantages in complex clinical scenarios, whereas algorithm-generated feedback provides superior scalability for large trials.
Methodological Protocols for Feedback Research
Experimental Design for Feedback Optimization
Robust experimental designs are essential for isolating the effects of feedback parameters. The following protocol outlines a comprehensive approach to testing feedback efficacy in dietary interventions:
Research Design: Randomized controlled trials with factorial designs enable researchers to test multiple feedback parameters simultaneously. For example, a 2x2x2 design might investigate: personalization (personalized vs. generic) x timing (daily vs. weekly) x delivery mode (human vs. algorithm) [55].
Participant Recruitment: Target population should reflect the intended application context. For dietary interventions, key inclusion criteria often include: age 18-65, BMI ≥25, ownership of smartphone/tablet, and willingness to self-monitor diet [58]. Exclusion criteria typically include conditions affecting weight (uncontrolled thyroid conditions), history of eating disorders, and recent significant weight loss [58].
Intervention Protocol:
- Baseline Assessment: Collect demographic, anthropometric, and dietary data (multiple 24-hour recalls or food frequency questionnaires) [18]
- Randomization: Use computerized random-number generators with allocation concealment [58]
- Self-monitoring Implementation: Participants track dietary intake using assigned method (e.g., calorie-tracking app, photo-based app, wearable device) [58]
- Feedback Manipulation: Systematically vary feedback parameters according to experimental condition
- Outcome Assessment: Measure adherence, dietary changes, and weight outcomes at predetermined intervals
Standardized Measures:
- Adherence to self-monitoring: Defined as number of days with ≥2 eating occasions tracked [58]
- Dietary intake: Multiple 24-hour recalls provide least biased intake estimates [18]
- Weight outcomes: Measured in light street clothes without shoes using calibrated digital scales [58]
The following workflow diagram illustrates the experimental process for feedback optimization studies:
Adherence Measurement Protocols
Defining and measuring adherence precisely is fundamental to feedback research. Evidence indicates that defining adherence as "the number of days participants tracked at least two eating occasions" explains the most variance in weight loss at 6 months (R²=0.27; P<0.001) [58]. The following table outlines core adherence metrics:
Table 3: Adherence Measurement Methods in Dietary Interventions
| Adherence Metric | Operational Definition | Data Collection Method | Strengths | Limitations |
|---|---|---|---|---|
| Days with tracking | Number of days with any self-monitoring | Automated digital collection | Objective; comparable across methods | Doesn't reflect completeness |
| Eating occasions tracked | Number of meals/snacks recorded | Automated digital collection | Captures detail of monitoring | Varies by eating pattern |
| ≥2 eating occasions/day | Days with ≥2 recorded eating occasions | Automated digital collection | Optimal predictor of weight loss [58] | May not reflect total intake |
| Energy tracking completeness | Percentage of estimated needs tracked | Algorithm calculation | Reflects thoroughness of tracking | Requires estimation of needs |
| Protocol adherence | Adherence to specific dietary targets | Self-report + biomarkers | Measures actual dietary change | More resource-intensive |
Digital platforms enable continuous adherence monitoring, allowing researchers to identify patterns such as the typical decline in self-monitoring after approximately 10 weeks [58]. This detailed monitoring enables just-in-time adaptive interventions that can address adherence declines proactively.
Advanced Analytical Approaches
Computational Modeling of Adherence Dynamics
The Adaptive Control of Thought-Rational (ACT-R) cognitive architecture provides a sophisticated framework for modeling adherence dynamics. ACT-R integrates physical, neurophysiological, behavioral, and cognitive mechanisms into a computational model to simulate how feedback influences self-monitoring behavior over time [1].
Key ACT-R mechanisms relevant to feedback include:
- Activation: Determines memory accessibility based on frequency and recency of use
- Retrieval: Selects knowledge chunks from declarative memory based on activation levels
- Learning: Calculates production rule utility through repeated execution and reward accumulation
- Selection: Chooses which production rule to execute based on utility values [1]
Research using ACT-R modeling has demonstrated that the goal pursuit mechanism remains dominant throughout interventions, while the influence of habit formation diminishes in later stages [1]. This suggests that feedback should increasingly target goal-based motivation as interventions progress.
Personalization Algorithms
Advanced personalization approaches move beyond simple rule-based systems to incorporate multiple individual factors. The Personal Health Support Model (PHSM) exemplifies this approach by integrating:
- Analytic Hierarchy Process (AHP): Structures user preferences into a hierarchy and assigns weights through pairwise comparisons
- Fuzzy Multi-Choice Goal Programming (FMCGP): Accommodates diverse dietary and lifestyle preferences with multiple aspiration levels
- Nonlinear Multi-Segment Goal Programming (NLMSGP): Optimizes dietary plans considering timing and quantity of food intake [17]
This integrated approach significantly outperforms conventional dietitian-led approaches in user satisfaction, engagement, and perceived effectiveness [17].
Table 4: Essential Research Reagents and Tools for Feedback Implementation
| Tool Category | Specific Tools/Platforms | Primary Function | Implementation Considerations |
|---|---|---|---|
| Self-monitoring Platforms | FatSecret, MealLogger, Bite Counter | Dietary intake tracking | Compatibility with feedback systems; data export capabilities |
| Feedback Delivery Systems | Custom web dashboards, DISH system, SMS platforms | Delivering feedback to participants | Integration with monitoring platforms; personalization capabilities |
| Adherence Analytics | Custom algorithms, ACT-R modeling, statistical packages | Analyzing adherence patterns | Definition of adherence metrics; handling of missing data |
| Personalization Engines | PHSM, rule-based systems, machine learning algorithms | Tailoring feedback content | Balance of complexity and interpretability; validation requirements |
| Outcome Assessment Tools | ASA-24, FFQs, biomarker assays | Measuring dietary and health outcomes | Resource requirements; validity for specific populations |
Optimizing feedback in dietary interventions requires meticulous attention to content, timing, frequency, and delivery mode. Evidence suggests that personalized, regular feedback that tracks multiple eating occasions provides the strongest foundation for adherence and weight outcomes. Nevertheless, significant research gaps remain.
Priority research directions include:
- Long-term adherence mechanisms: Most current evidence comes from short-term studies (<6 months)
- Just-in-time adaptive interventions: Developing algorithms to deliver feedback at optimal moments
- Integration of multi-modal data: Combining dietary tracking with physiological, environmental, and psychological data
- Standardized adherence metrics: Establishing consensus definitions for adherence across different tracking methodologies
- Hybrid human-algorithm feedback systems: Determining the optimal balance between automated and human-delivered feedback
As digital health technologies continue to evolve, feedback optimization will play an increasingly critical role in maximizing the efficacy of dietary interventions across diverse populations and settings. Researchers should prioritize transparent reporting of feedback parameters and adherence outcomes to facilitate evidence synthesis across studies.
Dietary intervention compliance remains a significant challenge in clinical research and public health. The efficacy of any nutritional guideline or pharmaceutical treatment is contingent upon consistent patient adherence, yet long-term compliance is often poor. Within this context, positive reinforcement has emerged as a critical mechanism for sustaining health behavior change. This whitepaper examines two distinct modalities of positive reinforcement: algorithm-driven gamification and interpersonal caregiver praise. Framed within the broader thesis of self-monitoring techniques for dietary compliance research, this analysis provides researchers and drug development professionals with a rigorous comparison of underlying mechanisms, efficacy evidence, and methodological protocols for these two approaches. We synthesize current empirical data to elucidate how these reinforcement strategies can be integrated into clinical trials and behavioral intervention designs to improve patient outcomes and data quality.
Theoretical Frameworks and Mechanisms of Action
The psychological and neurocognitive foundations of gamification and caregiver praise diverge significantly, informing their distinct applications and predicted outcomes.
Gamification: Engineered Reinforcement Systems
Gamification is formally defined as "the application of game-design elements in non-game contexts" to motivate and shape behavior [60] [61]. In digital health interventions, gamification operates through structured reinforcement schedules embedded within self-monitoring platforms:
- Mechanistic Components: Gamification systems implement tangible game mechanics including points systems, badges, leaderboards, and progress visualizations that provide immediate, quantifiable feedback on performance [62]. These elements are strategically layered to trigger reward pathways through perceived achievement and status recognition.
- Theoretical Underpinnings: Effective gamification draws from Self-Determination Theory (addressing autonomy, competence, and relatedness) and Social Cognitive Theory (emphasizing observational learning and self-efficacy) [60]. The Adaptive Control of Thought-Rational (ACT-R) cognitive architecture provides a computational framework for modeling how goal pursuit and habit formation mechanisms interact during gamified self-monitoring, with goal pursuit remaining dominant throughout intervention periods [1] [2].
Caregiver Praise: Relational Reinforcement Dynamics
Caregiver praise represents an interpersonal reinforcement modality rooted in social bonding and authority recognition:
- Social-Cognitive Foundations: Caregiver influence operates primarily through modeling behaviors, where children observe and internalize dietary behaviors demonstrated by caregivers [63]. This process is facilitated through emotional communication and expressed approval that reinforces compliant behaviors.
- Environmental Scaffolding: Beyond verbal praise, caregivers create supportive environments through controlled food availability and structured meal routines that make compliance easier to achieve and maintain [63]. The relational context amplifies the reinforcement value of praise, particularly in pediatric and adolescent populations.
Table 1: Core Mechanisms of Action Comparison
| Mechanism | Gamification | Caregiver Praise |
|---|---|---|
| Primary Reinforcement Type | Engineered, algorithm-driven | Relational, interpersonal |
| Theoretical Foundations | Self-Determination Theory, Social Cognitive Theory, ACT-R architecture | Social Learning Theory, Attachment Theory |
| Key Behavioral Components | Points, badges, leaderboards, progress visualizations | Verbal affirmation, modeling, environmental control |
| Temporal Dynamics | Immediate, consistent feedback loops | Variable, context-dependent reinforcement |
| Scalability | Highly scalable through digital platforms | Labor-intensive, limited by caregiver availability |
Quantitative Evidence and Comparative Efficacy
Recent meta-analyses and systematic reviews provide robust evidence for the differential effects of gamification and caregiver involvement on dietary and health outcomes.
Gamification Intervention Outcomes
A 2024 meta-analysis of 16 randomized controlled trials (N=7,472 children and adolescents) demonstrated that gamification interventions significantly increased moderate-to-vigorous physical activity (SMD 0.15, 95% CI 0.01 to 0.29; P=.04) and reduced BMI (SMD 0.11, 95% CI 0.05 to 0.18; P<.001) [60]. However, the same analysis found no significant improvements in sedentary behavior, vigorous physical activity, or daily step counts, indicating targeted rather than universal effects.
For dietary outcomes specifically, a 2021 systematic review and meta-analysis found that gamification interventions significantly increased nutritional knowledge scores (MD 0.88, 95% CI 0.05-1.75) and fruit and vegetable consumption [64]. The data suggest gamification is particularly effective for cognitive components of dietary compliance rather than solely behavioral metrics.
Caregiver Involvement Outcomes
A Cochrane review of 23 trials (N≈12,192 children) examined the added value of caregiver components to dietary and physical activity interventions [65]. The analysis found that interventions with caregiver involvement demonstrated a small but significant reduction in children's sugar-sweetened beverage consumption (SMD -0.28, 95% CI -0.44 to -0.12) compared to child-only interventions. However, for most other dietary intake measures (saturated fat, sodium, fruit and vegetable consumption) and physical activity outcomes, the addition of caregiver components did not yield statistically significant improvements.
Observational research in low-income Appalachian communities provides complementary evidence that specific caregiver practices—particularly modeling healthy eating (Beta=1.02; p=0.04 for vegetable consumption) and healthful home food availability (Beta=0.06; p=0.002 for fruit consumption)—significantly predict child dietary behaviors [63].
Table 2: Comparative Efficacy Metrics from Meta-Analyses
| Outcome Measure | Gamification Effects | Caregiver Involvement Effects |
|---|---|---|
| Physical Activity (MVPA) | SMD 0.15* (P=.04) [60] | MD 1.81 min/d (NS) [65] |
| BMI Reduction | SMD 0.11* (P<.001) [60] | Not reported |
| Fruit/Vegetable Consumption | Increased significantly [64] | MD 0.38 servings/d (NS) [65] |
| Nutritional Knowledge | MD 0.88* (95% CI 0.05-1.75) [64] | Not assessed |
| Sugar-Sweetened Beverages | Not assessed | SMD -0.28 (95% CI -0.44 to -0.12) [65] |
Note: SMD = Standardized Mean Difference; MD = Mean Difference; NS = Not Statistically Significant; *p<0.05, p<0.01, *p<0.001
Methodological Protocols and Experimental Designs
Gamification Intervention Protocols
The Spark Trial protocol exemplifies rigorous methodology for testing gamification components in dietary interventions [26]. This optimization randomized clinical trial employs a 2×2×2 full factorial design to isolate the effects of three self-monitoring strategies: dietary intake tracking, step counting, and weight monitoring. Participants (N=176 adults with overweight/obesity) are randomized to receive 0-3 of these self-monitoring strategies within a 6-month digital intervention, with all participants receiving core Social Cognitive Theory-informed components including weekly lessons and action plans.
Key measurement intervals occur at baseline, 1, 3, and 6 months, with the primary outcome being weight change. The protocol emphasizes engagement patterns (percentage of days with self-monitoring) as a key process variable and uses commercially available digital tools (mobile apps, wearable activity trackers, smart scales) to enhance ecological validity and scalability.
Caregiver Praise Measurement Approaches
The Shop Smart Tennessee study provides a methodological template for quantifying caregiver influence [63]. This cross-sectional analysis of 178 caregiver-child dyads in low-income Appalachian communities employed validated instruments including:
- Caregider Modeling Scales: Assessing the importance caregivers place on modeling healthy eating and frequency of these behaviors.
- Home Food Availability Inventories: Documenting availability of both healthy and less healthy food options in the household.
- Dietary Recall Measures: Using interviewer-administered surveys to assess child dietary intake.
Regression analyses controlled for demographic covariates to isolate the effects of specific caregiver practices on child dietary outcomes, with a focus on modeling behaviors, caregiver dietary intake, and home food environment factors.
Integration Framework and Research Applications
The following diagram illustrates the dynamic interaction between gamification systems and caregiver praise within dietary self-monitoring interventions:
Intervention Integration Framework
This framework demonstrates how both reinforcement systems operate through distinct but potentially complementary psychological mechanisms to influence dietary compliance outcomes.
Table 3: Research Reagents and Assessment Tools for Compliance Studies
| Tool Category | Specific Instrument | Research Application |
|---|---|---|
| Digital Platforms | Commercial mobile apps (MyFitnessPal), Wearable activity trackers (Fitbit), Smart scales | Enable real-time self-monitoring and gamification implementation; provide objective adherence metrics [26] [62] |
| Behavioral Assessments | Caregider Modeling Scales, Home Food Availability Inventory, 24-hour dietary recalls | Quantify caregiver practices and environmental factors; assess dietary intake outcomes [63] |
| Cognitive Architecture Models | Adaptive Control of Thought-Rational (ACT-R) | Computational modeling of goal pursuit and habit formation dynamics in self-monitoring [1] [2] |
| Theoretical Frameworks | Social Cognitive Theory, Self-Determination Theory, Behavior Change Techniques (BCT) Taxonomy | Inform intervention design and identify active ingredients of behavior change [60] [26] |
| Optimization Methodologies | Multiphase Optimization Strategy (MOST), Factorial RCT designs | Efficiently test multiple intervention components and their interactions [26] |
The evidence synthesized in this whitepaper indicates that gamification and caregiver praise represent distinct but potentially complementary approaches to enhancing dietary intervention compliance. Gamification demonstrates efficacy through engineered reinforcement systems that sustain goal pursuit behavior, particularly in digital self-monitoring contexts. Caregiver praise, while more limited in its standalone effects, shows targeted benefits for specific outcomes like reducing sugar-sweetened beverage consumption and modeling healthy eating behaviors.
For researchers designing clinical trials and behavioral interventions, key considerations include:
- Target Population: Gamification may be more effective for technologically-literate adolescents and adults, while caregiver components remain relevant for younger children and populations with strong family structures.
- Intervention Goals: For cognitive outcomes (knowledge) and physical activity, gamification shows stronger evidence; for specific dietary changes, combined approaches may be optimal.
- Methodological Rigor: Employing optimization frameworks (MOST) and cognitive architecture models (ACT-R) can enhance the precision and efficacy of reinforcement-based interventions.
Future research should prioritize personalized reinforcement strategies that match intervention components to individual characteristics and preferences, as well as hybrid models that strategically combine algorithmic and interpersonal reinforcement to maximize dietary compliance across diverse populations.
Addressing Insufficient Intervention Dose and Participant Disengagement
Table 1: Core Challenges in Dietary Intervention Adherence
| Challenge Category | Specific Manifestations | Impact on Intervention Dose |
|---|---|---|
| Behavioral Adherence | Steep decline in self-monitoring over time; Disengagement from digital tools [36] [66] | Reduces actual received dose and compromises data quality. |
| Technical & Methodological | Lack of consensus on defining adherence metrics; Inefficient feedback delivery systems [58] [36] | Hampers accurate measurement of dose and timely intervention. |
| Psychological & Social | Low self-efficacy; Weight-related information avoidance; Lack of family support [67] [66] | Diminishes perceived value and acceptability of the intervention. |
Insufficient intervention dose and participant disengagement present formidable challenges in clinical nutrition research, fundamentally threatening the internal validity of trials and the real-world efficacy of dietary interventions. The cornerstone of behavioral dietary interventions, dietary self-monitoring, is notoriously susceptible to rapid decline in adherence. Studies consistently show that engagement with self-monitoring tools, whether digital or paper-based, drops precipitously, with fewer than half of participants actively tracking after 10 weeks in many interventions [58]. This disengagement creates a significant gap between the protocol-defined intervention dose and the participant-received dose, potentially leading to null findings and inaccurate conclusions about an intervention's true effectiveness. This guide synthesizes recent evidence to provide researchers with a strategic framework for diagnosing, preventing, and addressing these critical issues, with a specific focus on interventions utilizing self-monitoring for dietary compliance.
Quantifying the Problem: Data on Disengagement
Understanding the scale and trajectory of disengagement is the first step toward addressing it. The data reveal a consistent pattern of decline across various intervention types and populations.
Table 2: Documented Rates of Disengagement in Dietary Interventions
| Study Context / Population | Key Adherence Findings | Temporal Trend |
|---|---|---|
| General Behavioral Weight Loss (SMARTER mHealth Trial, N=502) [36] | Adherence to self-monitoring and behavioral goals declined non-linearly over a 12-month period. | Steady decline, with feedback groups showing slower rates of disengagement. |
| Weight Loss Maintenance (BWL Program, N=72) [66] | During maintenance, high adherence (≥50% of days/month) was observed for 61% for exercise, 40% for weight, and only 21% for diet. | Steep decline for diet and weight tracking; exercise adherence dropped later. |
| Adolescent Digital Interventions (Systematic Review) [45] | Mixed results on long-term effectiveness; many interventions lose impact after a few weeks. | Challenging to sustain engagement and impact long-term. |
| Mobile Self-Monitoring (Two 6-month RCTs, N=124) [58] | Fewer than half the sample continued tracking after Week 10. All adherence methods showed rapid decline. | Rapid initial decline, with low persistence past 10 weeks. |
A critical insight from the data is that the method of defining adherence itself influences the observed outcomes. In weight loss interventions, defining adherence as the number of days participants tracked at least two eating occasions explained the most variance in weight loss (R²=0.27, P<0.001), outperforming other metrics such as tracking any intake or tracking a minimum calorie threshold [58]. This highlights the need for standardized, meaningful adherence metrics.
Key Barriers and Facilitators of Engagement
A deep understanding of the factors that hinder or promote adherence is essential for designing robust interventions. These factors span psychological, social, and technical domains.
Barriers to Engagement
- Lack of Knowledge and Skills: Pregnant women with GDM reported barriers including insufficient knowledge of pregnancy nutrition and a lack of skills in dietary management [67].
- Psychological Factors: Low disease risk perception, negative experiences with dietary interventions, and low self-efficacy significantly hinder adherence [67]. Furthermore, weight-related information avoidance (the tendency to avoid unwanted weight-related info) predicts a faster rate of decrease in dietary self-monitoring [66].
- Social and Environmental Factors: Limited support from family members is a commonly cited barrier [67].
- Technical and Burden-Related Factors: The labor-intensive nature of self-monitoring is a primary driver of disengagement, especially with methods that require extensive manual entry [1] [14].
Facilitators of Engagement
- Trust and Professional Support: High trust in professional support is a key facilitator of adherence [67].
- Positive Perception of Benefits: A positive perception of dietary management benefits encourages sustained engagement [67].
- Tailored Feedback and Social Support: Interventions incorporating tailored feedback and emotional social support demonstrate higher adherence and more sustained behavioral practice [1] [45].
- Reduced-Burden Digital Tools: Digital tools that simplify self-monitoring (e.g., via food databases, barcode scanners, or passive tracking) can improve initial engagement [66].
Experimental Protocols and Intervention Strategies
Drawing from recent clinical trials and reviews, this section outlines specific, experimentally-validated methodologies to combat disengagement.
Protocol: COM-B Model for Qualitative Diagnosis
- Objective: To identify context-specific barriers and facilitators to dietary adherence from the participant's perspective [67].
- Methods:
- Participant Recruitment: Recruit a purposive sample with maximum variation in demographics (age, parity, education, etc.) from the target population.
- Data Collection: Conduct face-to-face, semi-structured interviews guided by the COM-B model. Example questions include: "What factors pose challenges to adherence?" and "What forms of support have you received?" [67].
- Data Analysis: Use directed content analysis to map interview transcripts onto the COM-B components (Capability, Opportunity, Motivation).
- Outcome Application: The identified themes (e.g., "lack of nutritional knowledge" as a Capability barrier) directly inform the selection of targeted BCTs for the intervention.
Protocol: ACT-R Modeling for Dynamic Engagement Forecasting
- Objective: To computationally model and predict adherence to self-monitoring of dietary behaviors, allowing for the testing of intervention strategies in silico [1].
- Methods:
- Data Input: Use fine-grained, longitudinal self-monitoring data (e.g., daily logins, food entries) from a digital behavioral program.
- Modeling Framework: Employ the Adaptive Control of Thought-Rational (ACT-R) cognitive architecture. This model simulates the interplay between goal pursuit and habit formation over time.
- Intervention Simulation: The model can simulate how variations in support (e.g., tailored feedback, social support) influence the trajectory of adherence.
- Outcome Application: The model identifies critical points of disengagement and predicts which participants are at highest risk, enabling proactive, just-in-time adaptive interventions [1].
Protocol: Integrating Multi-Component BCTs
- Objective: To sustain engagement through a combination of evidence-based Behavior Change Techniques (BCTs) [45].
- Methods: Implement a core package of BCTs delivered via digital tools:
- Self-Monitoring: Provide easy-to-use digital tools for tracking diet (e.g., photo-based apps, calorie counters).
- Goal Setting: Collaboratively set specific, measurable, achievable, relevant, and time-bound (SMART) dietary goals.
- Personalized Feedback: Provide automated, tailored feedback on progress. For example: "Your calorie intake is above your goal, while fat grams are right on target. Take a moment to plan ahead for tomorrow." [36].
- Social Support: Incorporate elements of social communication, care, and understanding, potentially through facilitated group interactions [1] [45].
- Prompts/Cues: Use push notifications or SMS reminders to encourage self-monitoring and reinforce habits [45].
- Outcome Measurement: Track adherence metrics (e.g., days with ≥2 eating occasions tracked) and weight loss or other primary health outcomes.
Diagram 1: A comprehensive workflow for addressing insufficient intervention dose, from problem diagnosis to solution implementation and outcome evaluation.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Tools and Reagents for Dietary Adherence Research
| Tool / Reagent | Function in Research | Example Application / Note |
|---|---|---|
| COM-B Model Framework [67] | A theoretical framework for diagnosing barriers to behavior change. | Used to structure qualitative interviews and analyze data to identify Capability, Opportunity, and Motivation barriers. |
| ACT-R Cognitive Architecture [1] | A computational modeling system for simulating human cognitive processes and predicting adherence. | Models the dynamics between goal pursuit and habit formation to forecast disengagement points. |
| Standardized Adherence Metric (≥2 eating occasions/day) [58] | An objective, validated metric for defining and quantifying self-monitoring adherence. | Serves as a primary outcome variable; strongly correlated with weight loss success. |
| Behavior Change Technique (BCT) Taxonomy v1 [45] | A standardized taxonomy of 93 hierarchical techniques for changing behavior. | Ensures consistent reporting and implementation of techniques like "goal setting" and "self-monitoring." |
| Digital Self-Monitoring Platform (e.g., Fitbit app, FatSecret) [36] [58] | Enables objective, remote, and detailed tracking of participant dietary intake. | Reduces burden compared to paper diaries and allows for real-time data collection and feedback. |
| Tailored Feedback Message Library [36] | A pre-written, dynamic set of messages responding to participant self-monitoring data. | Messages are tailored to available data (e.g., calorie intake, fat intake) and rotated to prevent desensitization. |
Addressing insufficient intervention dose is not a single-action task but requires a continuous, multi-faceted strategy integrated throughout the research lifecycle. By moving from a reactive to a proactive stance—using diagnostic frameworks like COM-B, predictive tools like ACT-R modeling, and engaging intervention components like tailored feedback and social support—researchers can significantly mitigate the risk of participant disengagement. The ultimate goal is to close the gap between the intervention as designed and the intervention as delivered, thereby ensuring that the efficacy of dietary strategies can be accurately evaluated and effectively translated into real-world health benefits. Future research must continue to refine dynamic adherence metrics and explore the optimal timing and content of just-in-time adaptive interventions to sustain engagement in the long term.
Framework for Evidence-Based Appraisal of Monitoring Procedures
Within dietary intervention compliance research, self-monitoring represents a cornerstone methodology for capturing habitual dietary intake and assessing adherence to prescribed nutritional regimens. The accurate appraisal of monitoring procedures is therefore critical to ensuring the validity of intervention outcomes in clinical and public health research. A wide variety of methods are available to assess dietary intake, each with distinct strengths, weaknesses, and sources of potential error or bias [68]. This technical guide provides a structured framework for the evidence-based appraisal of these monitoring procedures, enabling researchers to select, implement, and evaluate methods that will yield the highest-quality dietary data possible within practical and financial constraints [68].
The adoption and sustained implementation of evidence-based monitoring innovations in real-world healthcare and research settings face significant challenges, with studies estimating that only 23% of interventions are maintained 2 years after implementation [69]. Implementation science frameworks, such as the Consolidated Framework for Implementation Research (CFIR), offer methodologies to equip practitioners with tools to identify and address the contextual factors that influence implementation success [69]. This guide integrates these principles to support the rigorous appraisal of monitoring procedures across diverse research contexts.
Core Dietary Monitoring Methods and Characteristics
Dietary assessment involves collecting information on foods and drinks consumed over a specified time, which is then coded and processed to compute intakes of energy, nutrients, and other dietary constituents using food composition tables [68]. The most commonly used methods include Food Frequency Questionnaires (FFQs), 24-hour recalls, and food records/diaries, each with distinct methodological approaches, cognitive demands, and resource requirements.
Table 1: Core Dietary Self-Monitoring Methods and Technical Characteristics
| Method | Primary Function | Temporal Scope | Data Collection Approach | Participant Burden | Analytical Processing |
|---|---|---|---|---|---|
| Food Frequency Questionnaire (FFQ) | Capture habitual dietary intake | Long-term (typically past year) | Predefined food list with frequency response options | Low to moderate (dependent on length/complexity) | Automated coding and analysis |
| 24-Hour Recall | Detailed capture of recent intake | Short-term (previous 24 hours) | Structured interview or self-administered automated system | Moderate per administration | Traditionally labor-intensive coding; automated for electronic versions |
| Food Record/Diary | Real-time recording of intake | Variable (typically 3-7 consecutive days) | Real-time recording at time of consumption | High (continuous recording effort) | Labor-intensive coding; automated for electronic systems |
Food Frequency Questionnaires (FFQs)
FFQs include defined lists of foods and drinks for which participants indicate their typical frequency of consumption over a specified period in the past (usually the past year) [68]. Frequency responses are typically in a closed-ended multiple-choice format. Semi-quantified FFQs use individual or standard portion sizes to estimate food quantities. While participant burden is generally lower than other methods, FFQs challenge participants with complex cognitive tasks including recall over extended periods, estimating average intake over time, and conceptualizing consumption relative to specified portion amounts [68].
24-Hour Recalls
The 24-hour recall captures detailed dietary intake over a 24-hour period, including descriptions of foods and beverages, amounts, brand information (if relevant), and preparation methods [68]. The multiple pass 24-hour recall is now in widespread use, consisting of several passes designed to aid memory: an uninterrupted quick list of consumed items, detailed probes querying food characteristics and amounts, a forgotten food list, and a thorough review [68]. Ideally, the recall day is unannounced to reduce the likelihood of changes in habitual dietary intake.
Food Records or Diaries
Food records are intended to be completed by study participants at the time of consumption in real time for a specific period, typically three to seven consecutive days [68]. Recording can occur on paper or within electronic automated systems, with portion sizes either weighed (weighed diary) or estimated using food models, images, or standard household measures (non-weighed diary) [68]. The estimation of portion size reduces participant burden but is less precise compared with weighing.
Appraisal Framework Implementation
The evidence-based appraisal of monitoring procedures requires systematic evaluation across multiple domains. The framework presented below adapts implementation science principles to address the specific challenges of dietary assessment methods.
Table 2: Evidence-Based Appraisal Framework for Dietary Monitoring Procedures
| Appraisal Domain | Critical Evaluation Factors | Validation Metrics | Common Methodological Limitations |
|---|---|---|---|
| Validity | Comparison against recovery biomarkers or reference method; population-specific validation | Correlation coefficients; attenuation factors; calibration studies | Differential bias by population subgroups; measurement error structure |
| Reliability | Test-retest reliability; internal consistency; day-to-day variability assessment | Intra-class correlation coefficients; Cohen's kappa; within-to-between person variance ratios | Seasonality effects; learning effects with repeated administration |
| Feasibility | Participant acceptance; completion rates; resource requirements; staff training needs | Recruitment rates; adherence percentages; cost per completed assessment | High attrition in long-term monitoring; literacy and numeracy requirements |
| Measurement Error | Systematic under-/over-reporting; portion size estimation error; food composition table limitations | Biomarker studies; doubly labeled water; urinary nitrogen | Social desirability bias; memory recall limitations; coding inaccuracies |
Implementation Science Framework
The Consolidated Framework for Implementation Research (CFIR) provides a meta-theoretical framework that synthesizes constructs from multiple behavioral and implementation theories to enable holistic evaluation of implementation [69]. The CFIR organizes determinants into five domains that influence implementation outcomes: (1) innovation characteristics (the monitoring procedure itself), (2) outer setting (the broader environment), (3) inner setting (the research context), (4) individuals involved, and (5) implementation process (activities and strategies used) [69].
The systematic application of the CFIR enables implementers to identify context-specific factors that serve as barriers and enablers to successful implementation of monitoring procedures. This knowledge allows research teams to adapt monitoring innovations, tailor implementation strategies, and assess progress, thereby improving implementation outcomes and enhancing the overall quality of dietary data collection [69].
Process Mapping for Implementation Optimization
Process flow diagrams (process maps) serve as valuable tools for supporting the implementation of evidence-based monitoring procedures in new research settings [70]. These visual tools describe individual process steps and their sequence, identify responsibility assignments, clarify process scope, and distinguish branching points and subsequent steps [70].
Process mapping offers multiple benefits for implementing dietary monitoring procedures, including understanding local system complexity, engaging stakeholders with relevant perspectives, designing interventions through collective problem solving, and establishing monitoring and measurement protocols [70]. These maps are particularly useful for complex interventions involving coordination across multiple research team roles and responsibilities.
Diagram 1: Dietary Monitoring Implementation Workflow
Emerging Technologies and Methodological Innovations
Recent technological advances have transformed dietary monitoring methodologies, offering potential advantages over traditional approaches, including faster and less error-prone data processing [68]. Interactive conversational agents (CAs) and other artificial intelligence tools provide real-time, personalized dietary assessment and feedback, maintaining ongoing engagement with research participants [71].
Technology-Enhanced Monitoring Approaches
Studies evaluating interactive conversational agents for dietary behavior change report improvements in specific dietary components, including significant increases in fruit and vegetable consumption (P=.04 and P=.005 in separate studies) and enhanced adherence to the Mediterranean diet at 6 weeks with gains maintained at 12 weeks [71]. Additional benefits include improved nutritional knowledge, modest weight loss, and decreased waist circumference (-2.1 cm, 95% CI -3.5 to 0.7; P=.003) in one randomized controlled trial [71].
Technology-based methods address several limitations of traditional dietary assessment, including enhanced personalization, real-time feedback, reduced participant burden through automated coding, and continuous engagement through interactive interfaces [71]. However, challenges remain including unnatural conversation styles in CAs, simplistic content, limited perceived usefulness, and variable impacts on different nutrient intakes [71].
Diagram 2: Technology-Enhanced Monitoring Evolution
Research Reagent Solutions for Dietary Monitoring
The implementation of robust dietary monitoring procedures requires specific methodological tools and resources. The table below details essential "research reagents" for establishing evidence-based dietary assessment protocols.
Table 3: Essential Research Reagent Solutions for Dietary Monitoring Research
| Research Reagent | Primary Function | Technical Specifications | Implementation Considerations |
|---|---|---|---|
| Validated FFQ Instruments | Assessment of habitual dietary intake | Population-specific food lists; standardized portion sizes; frequency response categories | Requires validation for specific population; resource-intensive development |
| Multiple-Pass 24-Hour Recall Protocols | Detailed capture of recent intake | Structured interview guides; portion size estimation aids; standardized probing questions | Interviewer training requirements; multiple non-consecutive days needed for usual intake |
| Electronic Food Composition Databases | Conversion of food intake to nutrient values | Country-specific nutrient profiles; recipe calculation algorithms; brand-specific variations | Regular updates required; completeness for local foods varies |
| Portion Size Estimation Aids | Quantification of food amounts consumed | Standardized household measures; food models; image-based portion guides | Population-specific validation needed; influences estimation accuracy |
| Dietary Biomarker Panels | Objective validation of self-reported intake | Recovery biomarkers (doubly labeled water, urinary nitrogen); concentration biomarkers | Cost-prohibitive for large studies; technical expertise required |
| Technology-Enhanced Assessment Platforms | Automated dietary data collection | Mobile applications; conversational agents; image-based food recognition | Digital literacy requirements; algorithm validation necessary |
Methodological Protocols for Validation Studies
Protocol for Validation Against Recovery Biomarkers
Objective: To validate self-reported dietary intake from monitoring procedures against objective recovery biomarkers.
Materials: Doubly labeled water for energy expenditure measurement; urinary nitrogen for protein intake assessment; standardized self-monitoring tools (FFQ, 24-hour recalls, or food records); biological sample collection kits; laboratory analysis equipment.
Procedure:
- Recruit participant sample representative of target population
- Administer self-monitoring instrument according to standardized protocol
- Collect biological samples for biomarker analysis within same time period
- Analyze biological samples using established laboratory methods
- Calculate energy and protein intake from biomarker data
- Compare self-reported intake with biomarker-derived estimates
- Calculate correlation coefficients and calibration factors
- Assess differential bias across participant characteristics
Validation Metrics: Pearson or Spearman correlation coefficients; attenuation factors; de-attenuated correlation coefficients; Bland-Altman plots of agreement [68].
Protocol for Technology-Enhanced Monitoring Evaluation
Objective: To evaluate the validity and feasibility of technology-enhanced dietary monitoring methods.
Materials: Mobile application or conversational agent platform; traditional dietary assessment method for comparison; usability questionnaires; participant engagement metrics.
Procedure:
- Develop or select technology platform with defined features
- Recruit participants and randomize to assessment methods
- Implement monitoring protocol with equivalent timeframes
- Collect parallel dietary data using technology and traditional methods
- Assess participant engagement through usage metrics
- Administer usability and acceptability questionnaires
- Compare dietary outputs between methods
- Analyze cost-effectiveness and resource requirements
Evaluation Metrics: Usability scores (e.g., System Usability Scale); participant adherence rates; inter-method correlation; qualitative feedback on user experience [71].
The evidence-based appraisal of monitoring procedures requires multidimensional evaluation across validity, reliability, feasibility, and measurement error domains. Implementation science frameworks such as the CFIR provide structured approaches for identifying contextual factors that influence implementation success of dietary assessment methods [69]. Process mapping techniques offer valuable visualization tools for optimizing implementation workflows and identifying potential barriers in research settings [70].
Emerging technologies, including interactive conversational agents and automated dietary assessment platforms, show promising potential to address limitations of traditional methods through enhanced personalization, real-time feedback, and reduced participant burden [71]. However, these innovations require rigorous validation against established biomarkers and reference methods to ensure measurement accuracy.
The framework presented in this guide provides researchers with a structured approach for selecting, implementing, and evaluating dietary monitoring procedures that will yield the highest-quality data for dietary intervention compliance research. By systematically applying these appraisal principles, researchers can enhance the validity of intervention outcomes and advance the field of nutritional science.
Clinical Evidence, Comparative Efficacy, and Validation Frameworks
Meta-Analysis Evidence on Self-Monitoring Effectiveness for Behavior Change
Self-monitoring stands as a cornerstone of behavioral obesity treatment, integral to the self-regulation process outlined by Social Cognitive and Control Theories [39]. This process involves a cyclical pattern of goal setting, self-monitoring, feedback, and behavioral adjustment to achieve desired outcomes [39]. Within fully digital weight loss interventions, self-monitoring consistently demonstrates a positive correlation with weight loss success, yet adherence frequently declines over time due to perceived burden and time demands [39] [1]. This technical guide synthesizes meta-analysis evidence and contemporary research to elucidate the efficacy of self-monitoring for dietary behavior change, providing methodologies and frameworks for researchers developing compliance interventions.
Quantitative Evidence Synthesis
Meta-analyses of randomized controlled trials (RCTs) provide robust evidence for the effect of remotely delivered, standalone self-monitoring interventions on dietary behavior change.
Table 1: Meta-Analysis of Remotely Delivered Self-Monitoring Interventions on Dietary Behavior
| Study Reference | Number of Studies & Participants | Intervention Type | Control Condition | Standardized Mean Difference (SMD) | 95% Confidence Interval | P-value |
|---|---|---|---|---|---|---|
| Teasdale et al. (2018) [72] | 26 studies (N=21,262) | Self-monitoring or Tailored Feedback | Various control groups | 0.17 | 0.10, 0.24 | < 0.0001 |
The meta-analysis by Teasdale et al. demonstrated a statistically significant, though small, positive effect on dietary behavior from self-regulatory methods [72]. The substantial heterogeneity (I² = 0.77) indicates significant variation in study results, underscoring the need to examine specific intervention components and methodologies to optimize effectiveness [72].
Key Experimental Protocols and Methodologies
The Spark Trial: Optimizing Self-Monitoring Components
The Spark trial represents a state-of-the-art methodological approach, employing the Multiphase Optimization Strategy (MOST) to identify "active ingredients" in self-monitoring [39].
- Objective: To examine the unique and combined weight loss effects of three self-monitoring strategies: tracking dietary intake, steps, and body weight [39].
- Study Design: A 6-month, fully digital, optimization-randomized clinical trial using a 2 × 2 × 2 full factorial design. This resulted in eight experimental conditions to which participants were randomized [39].
- Participants: 176 US adults with overweight or obesity [39].
- Intervention Components:
- Core Components: All participants received weekly lessons and action plans informed by Social Cognitive Theory [39].
- Experimental Components: Participants were randomized to receive between 0 and 3 of the following self-monitoring strategies, each with a corresponding goal and automated feedback [39]:
- Dietary Intake Tracking: Daily self-monitoring via a mobile app.
- Step Tracking: Daily self-monitoring via a wearable activity tracker.
- Body Weight Tracking: Daily self-monitoring via a smart scale.
- Primary Outcome: Weight change from baseline to 6 months, assessed objectively via a smart scale [39].
- Analysis Plan: The primary aim involves testing the main effects of the three self-monitoring components and their interactions on weight change [39].
Modeling Adherence Dynamics with ACT-R
A novel study developed a prognostic model for dietary self-monitoring adherence using the Adaptive Control of Thought-Rational (ACT-R) cognitive architecture to simulate human cognitive processes [1].
- Objective: To model adherence to dietary self-monitoring over 21 days, focusing on goal pursuit and habit formation mechanisms [1].
- Study Design & Participants: 97 participants in a digital behavioral weight loss program were assigned to one of three groups: self-management, tailored feedback, or intensive support [1].
- ACT-R Architecture:
- Symbolic System: Includes declarative and procedural modules. "Chunks" in declarative memory have an "activation" level, while "production rules" in procedural memory have a "utility" value [1].
- Subsymbolic System: Manages operations through four key mechanisms [1]:
- Activation: Calculates a chunk's activation level based on frequency and recency of access.
- Retrieval: Selects knowledge chunks based on their activation level.
- Learning: Calculates the utility of production rules based on rewards from repeated execution.
- Selection: Chooses which production rule to execute based on utility.
- Model Performance: The model effectively captured adherence trends, with Root Mean Square Error (RMSE) values of 0.099 (self-management), 0.084 (tailored feedback), and 0.091 (intensive support) [1].
- Key Finding: Visualized results indicated the goal pursuit mechanism remained dominant throughout the intervention across all groups, while the habit formation mechanism diminished in later stages [1].
Diagram 1: ACT-R Model of Adherence
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials and Digital Tools for Self-Monitoring Research
| Item Category | Specific Example | Primary Function in Research |
|---|---|---|
| Digital Self-Monitoring Platforms | Commercial Mobile Apps | Enable daily tracking of dietary intake; often include large food databases and nutrient calculations [39] [1]. |
| Wearable Activity Trackers | Commercial Wearables (e.g., Fitbit, Garmin) | Provide objective, continuous measurement of step counts and physical activity levels [39]. |
| Objective Weight Measurement Tools | Smart Scales | Allow for objective, frequent weight measurement at home; data can be automatically synced for research analysis [39]. |
| Conceptual Frameworks | Multiphase Optimization Strategy (MOST) | An engineering-inspired framework for building, optimizing, and evaluating multicomponent behavioral interventions [39]. |
| Cognitive Modeling Architectures | Adaptive Control of Thought-Rational (ACT-R) | A computational model simulating human cognitive processes to analyze and predict behavioral adherence dynamics [1]. |
| Theory-Based Intervention Components | Social Cognitive Theory (SCT) | Informs the development of intervention content, such as weekly lessons and action plans targeting self-regulation and outcome expectations [39]. |
Conceptual and Analytical Workflows
The research process for optimizing self-monitoring interventions can be structured using modern frameworks like MOST, which systematically builds effective interventions.
Diagram 2: MOST Framework Process
The meta-analytic evidence confirms that self-monitoring is a statistically significant, though modestly effective, component of dietary behavior change interventions [72]. Current research frontiers are moving beyond simple efficacy questions to focus on optimization—identifying the essential components and their interactions to maximize outcomes while minimizing participant burden [39]. The application of engineering-inspired frameworks like MOST and sophisticated cognitive modeling with ACT-R provides researchers with a powerful toolkit to deconstruct the "black box" of complex behavioral interventions [39] [1]. Future work should prioritize extending intervention durations to understand sustained adherence, integrating social cognitive factors into dynamic models, and leveraging these models to develop just-in-time adaptive interventions that can respond to individual patterns of engagement in real-time [1].
Within the escalating global challenge of obesity, the development of effective, scalable behavioral interventions is a critical public health priority. Self-monitoring (SM) constitutes a cornerstone of behavioral weight loss treatment, grounded in self-regulation theory which posits that behavior change necessitates self-evaluation and self-reinforcement [14] [1]. The evolution of mobile health (mHealth) technologies has transformed the delivery of these interventions, enabling real-time monitoring and feedback. This in-depth technical guide provides a comparative analysis of two pivotal research initiatives—the SMART and SMARTER trials—framed within a broader thesis on self-monitoring techniques for dietary intervention compliance research. It synthesizes experimental protocols, quantitative outcomes, and methodological frameworks to inform researchers, scientists, and drug development professionals in the design of efficacious, digitally-enabled health interventions.
Theoretical Foundations and Key Concepts
The Self-Regulation Framework
At the core of both SMART and SMARTER trials is Kanfer’s theory of self-regulation, a process comprising three distinct stages: self-monitoring, self-evaluation, and self-reinforcement [73]. Successful self-regulation depends on the fidelity, consistency, and temporal proximity of self-monitoring to the target behavior [73]. This theoretical basis is complemented by elements of Social Cognitive Theory, particularly the concept of reciprocal determinism—the continuous bi-directional influence between environment, behaviors, and personal cognitions [73]. Self-efficacy, a key component of Social Cognitive Theory, is enhanced through the establishment of specific, proximal goals and the use of feedback to attribute success to individual efforts [73].
Methodological Frameworks: MOST and SMART Designs
The Multiphase Optimization Strategy (MOST) is a comprehensive framework for developing, optimizing, and evaluating interventions [74]. The Sequential Multiple-Assignment Randomized Trial (SMART) is an experimental design used within the MOST framework for optimizing adaptive interventions [74]. A SMART design is particularly useful for determining the best sequencing of intervention components or for tailoring interventions based on an individual's response, making it well-suited for complex behavioral interventions.
The SMARTER Trial: Design and Protocol
Study Design and Participant Recruitment
The SMARTER (Self-Monitoring and Feedback for Weight Loss) trial was a single-site, randomized controlled trial conducted in southwestern Pennsylvania from August 2018 to March 2021 [75] [76]. The study randomized 502 adults with overweight or obesity (BMI 27-43 kg/m²) to one of two groups: (1) self-monitoring alone (SM, n=251) or (2) self-monitoring plus tailored feedback messages (SM+FB, n=251) [75] [76]. Participants were mostly female (80%), White (83%), with an average age of 45±14.4 years and average BMI of 33.7±4.0 kg/m² [75] [76].
Recruitment utilized multiple strategies including a research registry (Pitt+Me), university email announcements, mailings, social media, and community fliers [73]. Inclusion criteria required participants to be ≥18 years old, own a smartphone with a data plan, have a BMI between 27-43 kg/m², and successfully complete a 5-day electronic food diary during a run-in period [73] [76]. Exclusion criteria included conditions requiring physician-supervised diet and exercise, physical limitations precluding moderate-intensity physical activity, pregnancy, serious mental illness, alcohol abuse, or current participation in other weight loss programs [73] [76].
Intervention Protocol and Components
All participants received a 90-minute, one-on-one, in-person behavioral weight loss counseling session with a dietitian addressing core concepts of standard behavioral treatment [75] [76]. This session included instruction on using the provided digital tools: a Fitbit Charge 2 tracker for physical activity monitoring, a smart scale for daily self-weighing, and the Fitbit app for dietary self-monitoring [75] [76].
Dietary Goals: Calorie goals were prescribed based on baseline body weight and sex: women <200 lbs: 1,200 kcal/day, women ≥200 lbs: 1,500 kcal/day; men <200 lbs: 1,500 kcal/day, men ≥200 lbs: 1,800 kcal/day [75] [76]. Fat gram goals approximated 25% of the calorie goal [76].
Physical Activity Goals: Participants were prescribed a gradual increase in physical activity from ≥150 min/week of moderate-to-vigorous physical activity (MVPA) at week 1 to ≥300 min/week by week 42, maintained until study end at 52 weeks [75].
Feedback Mechanism (SM+FB Group Only): Participants in the SM+FB group downloaded an investigator-developed smartphone app that delivered up to three tailored feedback messages daily [75] [73]. Messages were triggered by an algorithm that read self-monitoring data from the integrated system (Awesome Data Acquisition Method - ADAM) [75]. The algorithm randomly sent prompts during morning, afternoon, and evening hours; if participants opened the prompt within an hour, a real-time feedback message tailored to their data appeared [75]. Physical activity was addressed in 3-4 messages per week, diet was addressed daily, and weight was addressed weekly [75].
Data Collection and Adherence Metrics
Data were collected through multiple digital tools integrated via the ADAM system, which downloaded daily data from the Fitbit server through its Application Programming Interface [75].
Physical Activity Adherence: Valid physical activity data were defined as having ≥4 days/week with ≥500 steps/day, indicating device wear [75]. Weekly MVPA minutes were computed by summing fairly active and very active minutes (based on MET cut-points), dividing by days with valid data, and multiplying by 7 [75].
Dietary Adherence: Participants were considered adherent to dietary self-monitoring if they recorded ≥50% of their daily calorie goal in the Fitbit app [75].
Weight Monitoring Adherence: Daily self-weighing constituted adherence to weight monitoring goals [75].
Table 1: Key Digital Tools and Metrics in the SMARTER Trial
| Component | Tool/Platform | Adherence Metric | Frequency |
|---|---|---|---|
| Physical Activity Monitoring | Fitbit Charge 2 tracker | ≥500 steps/day (device wear) | Daily |
| Dietary Self-Monitoring | Fitbit app | Recording ≥50% of daily calorie goal | Daily |
| Weight Monitoring | Smart scale | Daily weight measurement | Daily |
| Feedback Delivery | Investigator-developed SMARTER app | Opening prompt within 1 hour | Up to 3x/day |
| Data Integration | Awesome Data Acquisition Method (ADAM) | N/A | Continuous |
Quantitative Outcomes and Predictive Insights
Primary Efficacy Results
At 12 months, retention was 78.5% (n=394/502) and similar between groups (SM+FB: 80.5%; SM: 76.5%) [76]. Both groups achieved significant percent weight loss from baseline (SM+FB: -2.12%, 95% CI -3.04% to -1.21%, P<.001; SM: -2.39%, 95% CI -3.32% to -1.47%; P<.001), with no statistically significant difference between groups (-0.27%; 95% CI -1.57% to 1.03%; P=.68) [76]. Clinically significant weight loss (≥5%) was achieved by 26.3% (66/251) of the SM+FB group and 29.1% (73/251) of the SM group (P=.49) [76].
Predictors of Adherence and Engagement
A secondary analysis using machine learning methods identified several predictors of long-term adherence to the physical activity goal (≥150 min/week of MVPA over 52 weeks) [75]. The most important predictor was adherence to the PA goal in the first week of the intervention [75]. Additional factors associated with higher long-term PA goal adherence included greater opening of feedback messages, older age, male gender, higher education, being single, and not having obstructive sleep apnea [75].
Engagement with the feedback system was significantly associated with outcomes. A 1% increase in feedback messages opened was associated with a 0.10% greater percent weight loss at 12 months (b=-0.10; 95% CI -0.13 to -0.07; P<.001) and with a 0.12% greater percentage of days adherent to the calorie goal per month (b=0.12; 95% CI 0.07-0.17; P<.001) [76].
Table 2: Predictors of Physical Activity Goal Adherence in the SMARTER Trial
| Predictor Category | Specific Factor | Association with PA Goal Adherence |
|---|---|---|
| Short-term Intervention Response | PA goal adherence in first week | Strongest positive predictor |
| Engagement Metrics | Higher percentage of FB messages opened | Positive association |
| Sociodemographic Factors | Older age | Positive association |
| Male gender | Positive association | |
| Higher education | Positive association | |
| Being single | Positive association | |
| Clinical Factors | No obstructive sleep apnea | Positive association |
Advanced Analytical Approaches and Modeling
Machine Learning in Behavioral Prediction
The SMARTER trial applied machine learning methods to identify predictors of long-term physical activity goal adherence from a pool of 25 explanatory variables [75]. This approach represented an advancement in behavioral intervention research by enabling the identification of complex, non-linear relationships between participant characteristics, early intervention response, and long-term outcomes.
Cognitive Architecture Modeling of Adherence Dynamics
Recent research has employed the Adaptive Control of Thought-Rational (ACT-R) cognitive architecture to model adherence dynamics in digital behavioral weight loss programs [1]. ACT-R is a hybrid cognitive architecture consisting of symbolic and subsymbolic systems that simulate human cognitive processes, focusing on mechanisms of goal pursuit and habit formation [1].
In a study modeling dietary self-monitoring adherence over 21 days across three intervention groups (self-management, tailored feedback, and intensive support), the ACT-R model effectively captured adherence trends with root mean square error values of 0.099, 0.084, and 0.091 respectively [1]. The model revealed that across all groups, the goal pursuit mechanism remained dominant throughout the intervention, while the influence of the habit formation mechanism diminished in later stages [1]. The presence of tailored feedback and higher levels of social support were associated with greater goal pursuit and more sustained behavioral practice [1].
The Researcher's Toolkit: Essential Methodological Components
Table 3: Research Reagent Solutions for Digital Dietary Interventions
| Component | Function | Implementation Example |
|---|---|---|
| Commercial Wearable Trackers | Objective physical activity monitoring | Fitbit Charge 2 for MVPA tracking [75] |
| Smartphone Applications | Dietary self-monitoring platform | Fitbit app for food intake logging [76] |
| Smart Scales | Automated weight data collection | Bluetooth-enabled scales for daily self-weighing [73] |
| Tailored Feedback Algorithms | Automated, personalized message delivery | Algorithm reading SM data and selecting messages from library [73] |
| Integrated Data Systems | Centralized data collection from multiple sources | Awesome Data Acquisition Method (ADAM) [75] |
| Cognitive Architecture Models | Computational modeling of behavior change dynamics | ACT-R for simulating goal pursuit and habit formation [1] |
Discussion and Research Implications
The comparative analysis of the SMARTER trial findings reveals several critical insights for dietary intervention compliance research. The absence of significant differences in weight loss between the SM+FB and SM-only groups suggests that the use of commercially available digital self-monitoring tools alone can produce clinically significant weight loss in over 25% of participants [76]. This finding has important implications for the scalability and dissemination of weight loss interventions, as digital self-monitoring tools are increasingly accessible to the general population.
The predictive value of first-week physical activity adherence for long-term success highlights the importance of early engagement and the potential for early identification of participants who may require additional support [75]. Furthermore, the association between feedback message engagement and improved outcomes, even in the absence of between-group differences, points to the potential of within-group engagement as a critical moderator of intervention success [76].
From a methodological perspective, the application of machine learning and cognitive architecture models represents a significant advancement in the analysis of behavioral interventions. These approaches enable researchers to move beyond static, cross-sectional analyses to dynamic modeling of behavior change processes over time [75] [1]. The ACT-R model's demonstration that goal pursuit remains dominant throughout the intervention, while habit formation diminishes, provides valuable insight for intervention design, suggesting that sustained goal-focused strategies may be more effective than relying on habit formation alone [1].
For drug development professionals, these findings highlight the potential of digital tools to support medication adherence and provide real-time monitoring of lifestyle factors that may interact with pharmacological treatments. The methodologies and insights from the SMARTER trial can inform the design of comprehensive treatment approaches that integrate pharmacological and behavioral components.
Future research should focus on strategies to enhance engagement with digital tools, particularly among populations identified as having lower adherence (e.g., younger participants, women) [75]. Additionally, extending the duration of interventions and modeling efforts will be crucial for understanding long-term adherence mechanisms and developing sustainable weight maintenance strategies.
Validating Self-Monitoring as a Mediator of Weight Loss Outcomes
Self-monitoring stands as a cornerstone of behavioral weight loss interventions, yet its specific role as a mechanistic pathway mediating the effect of other intervention components on weight outcomes requires rigorous validation. This whitepaper synthesizes current evidence from clinical trials and computational modeling studies to establish self-monitoring adherence as a validated mediator in the causal pathway between behavioral interventions and weight loss success. We present quantitative data demonstrating that the positive effect of intervention components like tailored feedback is significantly mediated through improved self-monitoring adherence, with mediation accounting for approximately 36-49% of total effects in key trials. Methodological protocols for establishing mediation are detailed, including the use of cognitive architectures for dynamic modeling of adherence mechanisms. The findings underscore that self-monitoring functions not merely as a complementary strategy but as a critical mediating variable that must be explicitly targeted and measured in dietary intervention compliance research.
Within behavioral obesity treatment, self-monitoring of dietary intake, physical activity, and weight is widely recognized as a central component of effective interventions [8] [77]. The theoretical foundation posits that self-monitoring enables behavior change through increased awareness of current behaviors and progress toward goals, drawing from self-regulation theory which suggests self-monitoring precedes self-evaluation and self-reinforcement [8]. While numerous studies have established a correlation between self-monitoring and weight loss, a more nuanced understanding of its role as a causal mechanism has emerged in recent years.
The mediation hypothesis proposes that self-monitoring adherence serves as a key pathway through which other intervention components (e.g., feedback, social support, digital tools) exert their effects on weight loss outcomes. This represents a shift from viewing self-monitoring as merely an active ingredient to understanding it as a mediating variable that explains how or why an intervention works [78] [79]. Establishing mediation requires demonstrating that: (1) the intervention affects the proposed mediator (self-monitoring adherence), (2) the intervention affects the outcome (weight loss), (3) the mediator affects the outcome when controlling for the intervention, and (4) the effect of the intervention on the outcome reduces when controlling for the mediator [78].
This whitepaper synthesizes evidence validating self-monitoring as a mediator, detailing experimental protocols for mediation testing, and providing methodological guidance for researchers investigating compliance mechanisms in dietary interventions.
Quantitative Evidence for Self-Monitoring as a Mediator
Clinical Trial Evidence
The SMART randomized clinical trial provides direct evidence for self-monitoring adherence as a mediator between feedback frequency and weight loss [78] [79]. In this study, 210 participants were assigned to one of three self-monitoring methods: paper diary (PD), personal digital assistant (PDA), or PDA with daily tailored feedback (PDA+FB). The trial objectively measured self-monitoring adherence as the proportion of sessions where participants recorded at least 50% of their weekly calorie goal.
Table 1: Mediation Analysis Results from the SMART Trial [78]
| Relationship | Effect Type | Effect Size | Statistical Significance |
|---|---|---|---|
| Feedback frequency → Weight loss | Total effect | β = -1.93% | P < 0.05 |
| Feedback frequency → Self-monitoring adherence | Path A | β = 16.8% | P < 0.001 |
| Self-monitoring adherence → Weight loss (controlling for feedback) | Path B | β = -0.07% | P < 0.05 |
| Feedback frequency → Weight loss (controlling for self-monitoring) | Direct effect (C') | β = -0.82% | P = 0.31 |
| Feedback frequency → Weight loss through self-monitoring | Indirect effect | β = -1.11% | P < 0.05 |
The mediation analysis revealed that the initial significant effect of feedback frequency on weight loss was no longer significant after controlling for self-monitoring adherence, indicating complete mediation [78]. The indirect effect through self-monitoring adherence was statistically significant, confirming that daily feedback improved weight loss primarily by increasing self-monitoring adherence.
Further evidence comes from a systematic review of self-monitoring in weight loss, which found consistent associations between self-monitoring and weight loss across 22 studies, though the authors noted methodological limitations in establishing causal mediation pathways in earlier research [8].
Dynamic Modeling of Adherence Mechanisms
Recent research has employed computational modeling to understand the dynamic mechanisms through which self-monitoring operates. A 2025 study used the Adaptive Control of Thought-Rational (ACT-R) cognitive architecture to model adherence to dietary self-monitoring over 21 days [1] [2]. The study involved 97 participants across three intervention groups: self-management, tailored feedback, and intensive support.
Table 2: ACT-R Model Performance in Predicting Self-Monitoring Adherence [1]
| Intervention Group | Sample Size | Root Mean Square Error (RMSE) | Dominant Cognitive Mechanism |
|---|---|---|---|
| Self-management | 49 | 0.099 | Goal pursuit |
| Tailored feedback | 23 | 0.084 | Goal pursuit |
| Intensive support | 25 | 0.091 | Goal pursuit |
The ACT-R model effectively captured adherence trends, demonstrating that goal pursuit mechanisms remained dominant throughout the intervention, while habit formation diminished in later stages [1]. The presence of tailored feedback and social support was associated with greater goal pursuit and more sustained behavioral practice, revealing the cognitive pathways through which these interventions influence self-monitoring adherence.
The visualization below illustrates the cognitive architecture and workflow for modeling self-monitoring adherence:
Cognitive Architecture of Self-Monitoring Adherence. This diagram illustrates how interventional components influence cognitive mechanisms to drive behavioral outcomes, with self-monitoring adherence functioning as a key mediator toward weight loss.
Experimental Protocols for Mediation Testing
Randomized Clinical Trial Design
The SMART trial protocol provides a robust methodological framework for testing self-monitoring mediation [78] [79]. The study employed a randomized clinical design with three self-monitoring conditions:
- Paper Diary (PD) Group: Participants recorded dietary intake and physical activity using paper diaries with no daily feedback.
- Personal Digital Assistant (PDA) Group: Participants used PDAs with dietary and activity software but no daily feedback.
- PDA with Feedback (PDA+FB) Group: Participants used PDAs with software plus daily tailored feedback messages.
The standard behavioral intervention was consistent across groups, emphasizing reduced energy intake, increased energy expenditure, and behavioral changes delivered through 20 group sessions over six months [78]. Self-monitoring adherence was objectively verified at each session as recording at least 50% of the weekly calorie goal.
Measurement and Analysis Protocols
The measurement of proposed mediators requires careful operationalization:
- Self-Monitoring Adherence Metric: Calculated as the proportion of sessions where participants met the 50% calorie recording threshold (number of adherent sessions / total sessions) [78].
- Weight Measurement: Assessed in-person using digital scales with standardized procedures (lightweight clothing, no shoes).
- Statistical Mediation Analysis: Performed using the Preacher and Hayes simple mediation macro with Sobel test via bootstrapping, which tests both the direct effect of the intervention on weight loss and the indirect effect through self-monitoring adherence [78].
For handling missing data due to attrition, the SMART trial applied a conservative approach of adding 0.3 kg/month to the last recorded weight to account for potential weight regain [78].
Cognitive Modeling Approach
The ACT-R cognitive architecture provides a novel methodological approach for modeling the dynamic mechanisms of self-monitoring adherence [1]. The protocol involves:
- Data Collection: Participants engage in a digital behavioral weight loss program with continuous monitoring of self-monitoring behaviors.
- Model Development: The ACT-R architecture simulates human cognitive processes through symbolic and subsymbolic systems, with modules corresponding to specific brain regions.
- Parameter Definition:
- Activation: Calculation of chunk activation level based on frequency and recency of access.
- Retrieval: Probability-based selection of knowledge chunks from declarative memory.
- Learning: Calculation of production rule utility based on repeated execution and rewards.
- Selection: Process of choosing which production rule to execute based on utility values.
- Model Validation: Performance evaluated using mean square error, root mean square error, and goodness of fit measures comparing predicted versus actual adherence patterns.
This approach allows researchers to simulate and analyze how different intervention components influence cognitive mechanisms and subsequent adherence behaviors over time.
Research Reagent Solutions for Mediation Studies
Table 3: Essential Methodological Components for Self-Monitoring Mediation Research
| Research Component | Function in Mediation Studies | Exemplars from Literature |
|---|---|---|
| Digital Self-Monitoring Platforms | Enable objective adherence tracking with timestamped data | Personal Digital Assistants (PDAs) with dietary software [78]; Mobile applications with automated feedback [26] |
| Cognitive Modeling Architectures | Simulate dynamic adherence mechanisms and intervention pathways | Adaptive Control of Thought-Rational (ACT-R) framework [1] |
| Statistical Mediation Packages | Test indirect effects and quantify mediation proportions | Preacher and Hayes mediation macro with bootstrapping [78]; Sobel test implementation in SAS/R |
| Objective Adherence Metrics | Provide standardized, quantifiable mediator variables | Percentage of sessions with ≥50% calorie goal recorded [78]; Daily self-monitoring consistency scores |
| Multiphase Optimization Strategy (MOST) | Systematically identify active intervention components | Factorial designs testing self-monitoring combinations [26] |
Discussion and Research Implications
The validation of self-monitoring as a mediator of weight loss outcomes has significant implications for dietary intervention compliance research and practice. The evidence demonstrates that self-monitoring adherence serves as a critical pathway through which other intervention strategies exert their effects, explaining why components like tailored feedback and social support improve weight loss outcomes.
For pharmaceutical and behavioral researchers, these findings suggest that intervention potency can be enhanced by specifically targeting self-monitoring adherence rather than treating it as one of many equivalent components. The methodological approaches detailed herein provide robust protocols for future studies seeking to validate mechanistic pathways in health behavior interventions.
Future research directions should focus on: (1) extending intervention durations to explore sustained adherence mechanisms, (2) integrating social cognitive factors to capture behavioral compliance insights, and (3) adapting dynamic models to inform just-in-time adaptive interventions [1] [2]. Additionally, studies in more diverse populations are needed to enhance generalizability, as prior research has predominantly focused on White female participants [8].
The optimization of self-monitoring strategies through frameworks like the Multiphase Optimization Strategy (MOST) represents a promising approach for identifying the most effective combination of self-monitoring components while minimizing participant burden [26]. As digital health interventions continue to evolve, understanding and leveraging the mediating role of self-monitoring will be essential for developing maximally efficient and effective weight loss interventions.
Self-monitoring is a cornerstone of behavioral interventions for diet and health, grounded in self-regulation theory which posits that behavior change occurs through a cyclical process of goal setting, self-monitoring, feedback, and action planning [26] [36]. This technical assessment examines the fundamental distinction between objective and subjective self-monitoring methodologies within dietary intervention compliance research.
Objective tools quantify behaviors through recorded phenomena, such as wearable devices that track physical activity or smart scales that measure weight [80]. Subjective tools rely on individual self-report through methods like food diaries, questionnaires, and digital food logs [18] [80]. Research reveals a significant discordance between these measurement approaches. In obstructive sleep apnea patients, for instance, 64.1% reported poor subjective sleep quality via the Pittsburgh Sleep Quality Index, while only 12.8% exhibited poor objective sleep efficiency measured by polysomnography, with no significant correlation between these measures [81]. Similarly, in cognitive functioning research, a comprehensive umbrella review found only a weak pooled correlation (r = 0.14) between subjective and objective cognition across neuropsychiatric conditions [82].
This guide provides researchers and drug development professionals with a technical framework for selecting, implementing, and evaluating self-monitoring tools in dietary intervention studies, with emphasis on methodological considerations for compliance research.
Comparative Analysis: Technical Specifications and Performance Metrics
Table 1: Technical Specifications of Self-Monitoring Tools
| Parameter | Objective Tools | Subjective Tools |
|---|---|---|
| Data Collection Method | Automated sensing technology (wearables, smart scales, bite counters) [58] [80] | Self-report (digital apps, paper diaries, questionnaires, 24-hour recalls) [18] [80] |
| Primary Output | Behavioral metrics (step counts, weight, bite counts) [58] [36] | Perceived behaviors (estimated intake, frequency, quality) [18] [14] |
| Memory Dependency | Minimal [80] | High (specific or generic memory) [18] |
| Reactivity Potential | Low to moderate [18] | High (social desirability bias, change for ease of recording) [18] |
| Implementation Cost | Higher (device costs) [58] | Lower (potentially cost-effective for large samples) [18] |
| Participant Burden | Variable (device wear) [58] | High (literacy, motivation, time) [18] [14] |
| Contextual Adaptation | Limited without customization [80] | Can be tailored to specific populations [80] |
Table 2: Performance Characteristics in Dietary Research
| Characteristic | Objective Tools | Subjective Tools |
|---|---|---|
| Measurement Error Type | Primarily random error [18] | Systematic error (under-reporting, social desirability) [18] |
| Energy Reporting Accuracy | Less biased for energy intake (via recovery biomarkers) [18] | Pervasive under-reporting, especially with BMI [18] |
| Nutrient Capture Precision | Limited to specific parameters | Comprehensive nutrient databases [18] |
| Adherence Definition | Device-based (e.g., ≥500 steps/day) [36] | Behavior-based (e.g., ≥2 eating occasions tracked) [58] |
| Adherence Decline Pattern | Technology abandonment [36] | Motivational decline over time [58] [14] |
| Correlation with Weight Loss | Strong (e.g., self-weighing) [26] [36] | Strong (diet tracking frequency) [58] [14] |
Methodological Protocols for Dietary Self-Monitoring Research
Defining and Measuring Adherence
The operational definition of adherence significantly impacts research outcomes. In weight loss interventions, the number of days participants tracked at least two eating occasions explained the most variance in weight loss at 6 months (R²=0.27, p<0.001) [58]. This definition outperformed other metrics such as total days tracked or number of eating occasions tracked.
Digital monitoring protocols should specify:
- Minimum tracking frequency: Daily tracking of ≥2 eating occasions provides optimal predictive value [58]
- Data completeness threshold: ≥50% of daily calorie goals recorded constitutes adherent diet self-monitoring [36]
- Persistent non-adherence definition: The last day before adherence to upcoming days declines to <25-50% [58]
Experimental Designs for Self-Monitoring Research
Factorial designs enable researchers to isolate active intervention components. The Spark trial employs a 2×2×2 full factorial design to test three self-monitoring strategies (dietary intake, steps, and weight) both individually and in combination [26]. This approach, based on the Multiphase Optimization Strategy (MOST), identifies which components meaningfully contribute to weight loss outcomes and which can be eliminated to reduce participant burden [26].
Comparative effectiveness trials have demonstrated that:
- Digital tracking methods (apps, wearables) produce superior adherence to paper-based methods [1] [14]
- Tailored feedback combined with intensive support sustains engagement [1]
- Adherence declines nonlinearly over time, with fewer than half of participants still tracking after 10 weeks [58]
Cognitive Architecture Modeling
The Adaptive Control of Thought-Rational (ACT-R) cognitive architecture provides a computational framework for modeling adherence dynamics. This hybrid architecture consists of symbolic (declarative and procedural modules) and subsymbolic (activation, retrieval, learning, selection) systems that simulate human cognitive processes [1].
ACT-R modeling of dietary self-monitoring adherence over 21 days revealed that the goal pursuit mechanism remains dominant throughout interventions, while the habit formation mechanism diminishes in later stages [1]. This modeling approach achieved strong fit with observed data (RMSE values: 0.084-0.099 across intervention groups) [1].
Table 3: Research Reagent Solutions for Self-Monitoring Studies
| Tool Category | Specific Examples | Research Application | Technical Considerations |
|---|---|---|---|
| Objective Monitoring Devices | Wearable bite counters (Bite Counter) [58], Accelerometers [80], Smart scales [26] [36] | Quantifying intake bites, physical activity, weight | Bite counter accuracy: within-individual correlation between energy consumed and bites = 0.53 [58] |
| Digital Tracking Platforms | Commercial apps (Fitbit, FatSecret, MealLogger) [58] [36], Custom applications (SMARTER app) [36] | Dietary self-monitoring with automated feedback | Integration with study informatics infrastructure required [36] |
| Subjective Assessment Tools | Pittsburgh Sleep Quality Index (PSQI) [81], Food Frequency Questionnaires (FFQs) [18], 24-hour dietary recalls [18] | Measuring perceived sleep quality, habitual intake, recent consumption | PSQI showed no correlation with objective sleep efficiency in OSA patients [81] |
| Adherence Analytics | Latent class growth modeling [46], ACT-R cognitive modeling [1], Generalized linear mixed modeling [36] | Identifying engagement trajectories, simulating cognitive processes, analyzing adherence patterns | Latent class analysis identified "consistent engagers" and "disengagers" in app usage [46] |
| Feedback Systems | Tailored message libraries, Algorithmic feedback delivery [36], Crowdsourced rating systems [58] | Providing personalized intervention support | Message libraries should be refreshed monthly to prevent desensitization [36] |
Implementation Framework and Best Practices
Engagement Sustainability Protocols
Long-term engagement with self-monitoring remains a significant challenge. Research indicates adherence to diet self-monitoring steeply declines over time, with fewer than half of participants continuing beyond 10 weeks [58]. The SMARTER trial demonstrated that feedback interventions can moderate this decline, with the feedback group showing less reduction in adherence compared to the self-monitoring only group [36].
Effective engagement strategies include:
- Tailored nutritional feedback: Allows participants to compare behaviors with healthy standards [1]
- Emotional social support: Mitigates self-regulatory depletion [1]
- Multi-modal digital tools: Reduce burden through apps, wearables, and smart scales [36]
- Dynamic message systems: Updated regularly to maintain relevance [36]
Contextual Adaptation Framework
Tool selection must consider cultural, economic, and technological contexts. In Low- and Middle-Income Countries (LMICs), 94% of adolescent diet and physical activity studies used subjective tools, but only 39% employed tools validated for their specific contexts [80]. This highlights the critical need for contextual adaptation and validation rather than direct tool transfer from high-income countries.
Objective and subjective self-monitoring tools offer complementary rather than interchangeable insights for dietary intervention compliance research. Objective tools provide less biased behavioral measures but face technological and cost barriers, while subjective tools capture perceived behaviors and are more scalable but susceptible to systematic reporting errors.
The optimal self-monitoring framework combines objective verification with subjective context, tailored to specific research questions, populations, and resources. Future research directions should focus on:
- Developing more sophisticated cognitive models of adherence behavior
- Creating adaptive intervention systems that respond to real-time engagement patterns
- Validating context-specific tools for diverse populations
- Establishing standardized metrics for cross-study comparison
Researchers should select tools based on explicit theoretical links to targeted mechanisms rather than convenience, with acknowledgement that each method captures distinct aspects of the complex behavior change process.
The Spark trial represents a significant methodological advancement in behavioral obesity treatment research by employing the Multiphase Optimization Strategy (MOST) framework to isolate the active ingredients of self-monitoring. This fully digital, optimization-randomized clinical trial utilized a 2×2×2 factorial design to disentangle the unique and combined effects of tracking dietary intake, steps, and body weight on 6-month weight change among adults with overweight or obesity [83] [26] [39]. Unlike traditional treatment package paradigms that bundle multiple self-monitoring strategies, this protocol systematically evaluates which components meaningfully contribute to weight loss outcomes and which represent unnecessary patient burden. The trial's findings have substantial implications for designing efficient, scalable digital interventions that maximize weight loss while minimizing participant effort.
Self-monitoring stands as one of the most robust predictors of successful weight loss in behavioral obesity treatment [26] [39]. Traditional digital weight loss interventions frequently bundle multiple self-monitoring strategies—typically tracking dietary intake, physical activity, and body weight—into a single treatment package [39]. While effective, this bundled approach makes it impossible to determine whether all components are necessary or if some constitute "inactive ingredients" that add participant burden without meaningful clinical benefit [83] [26]. This gap is particularly relevant for digital interventions, where engagement frequently declines over time due to tracking burden [26] [39].
The Spark trial protocol addresses this fundamental limitation by applying the MOST framework, an engineering-inspired approach for building and optimizing behavioral interventions [26] [39]. The preparation phase identified self-monitoring as a critical intervention component requiring optimization, leading to the current optimization phase that tests the unique and combined effects of three self-monitoring strategies. A subsequent evaluation phase will test the newly optimized intervention against a comparator in a traditional randomized controlled trial [39].
Methodological Framework
Trial Design and Structure
The Spark trial employed a full factorial design with eight experimental conditions to test all possible combinations of three self-monitoring components [83] [39]. This rigorous approach enables researchers to examine both main effects and potential interaction effects among components.
Table 1: Spark Trial 2×2×2 Factorial Design Matrix
| Experimental Condition | Dietary Tracking | Steps Tracking | Weight Tracking |
|---|---|---|---|
| 1 | No | No | No |
| 2 | No | No | Yes |
| 3 | No | Yes | No |
| 4 | No | Yes | Yes |
| 5 | Yes | No | No |
| 6 | Yes | No | Yes |
| 7 | Yes | Yes | No |
| 8 | Yes | Yes | Yes |
Participant Characteristics and Recruitment
The trial enrolled 176 U.S. adults with overweight or obesity, with recruitment occurring from September 2023 to November 2024 [83] [39]. All study procedures were conducted fully remotely, enhancing scalability and reach while reducing barriers to participation for geographically, racially, and ethnically diverse populations who are often underrepresented in traditional obesity treatment research [26] [39].
Core Intervention Components
All participants received foundational behavioral intervention components regardless of their randomization assignment [83] [26] [39]:
- Weekly lessons informed by Social Cognitive Theory
- Action planning guidance to promote healthy eating and physical activity
- Digital tools for self-monitoring based on experimental condition assignment
Self-Monitoring Components and Implementation
For each assigned self-monitoring strategy, participants received specific implementation protocols [83] [26] [39]:
Dietary Intake Tracking: Participants used a mobile application to log all foods and beverages consumed daily, with a corresponding daily calorie goal and weekly automated feedback on performance.
Steps Tracking: Participants used a wearable activity tracker to monitor daily steps, with a corresponding step goal and weekly automated feedback on progress.
Body Weight Tracking: Participants used a smart scale to measure body weight daily, with weekly automated feedback on weight change patterns.
Assessment Protocols and Outcome Measures
Primary and Secondary Outcomes
The trial employed a comprehensive assessment protocol with multiple data collection timepoints to capture both primary and secondary outcomes [83] [39].
Table 2: Spark Trial Assessment Schedule and Outcome Measures
| Assessment Timepoint | Primary Outcomes | Secondary Outcomes | Data Collection Method |
|---|---|---|---|
| Baseline | Weight | BMI, caloric intake, diet quality, physical activity, health-related quality of life | Smart scale, self-report, digital tracking |
| 1 Month | - | Weight change, self-monitoring engagement | Smart scale, digital platform data |
| 3 Months | - | Weight change, self-monitoring engagement | Smart scale, digital platform data |
| 6 Months | Weight change from baseline | All secondary outcomes, engagement patterns, moderators | Smart scale, self-report, digital platform data |
Engagement Metrics
Self-monitoring engagement was operationally defined as the percentage of days participants engaged in each assigned tracking behavior during the 6-month intervention [83] [39]. This objective measurement approach, facilitated by digital tools, provided robust data on adherence patterns over time.
Embedded Experimental Components
The protocol included several innovative methodological features [83] [39]:
- Moderator analyses to identify subgroups that might benefit more from specific self-monitoring strategies
- Qualitative interviews with a participant subset to elucidate factors impacting engagement and its relationship to weight loss
- Embedded experiment testing a self-directed web-based orientation session's impact on 6-month trial retention
Technical Implementation and Workflow
The Spark trial implemented a sophisticated digital infrastructure to support the fully remote intervention and data collection. The following workflow diagram illustrates the experimental protocol and assessment procedures.
Diagram 1: Spark Trial Experimental Workflow
Research Reagent Solutions and Digital Infrastructure
The Spark trial utilized a comprehensive suite of digital tools and methodological components to implement the fully remote self-monitoring intervention.
Table 3: Essential Research Reagents and Digital Tools
| Research Component | Function in Spark Trial | Implementation Details |
|---|---|---|
| Commercial Mobile App | Dietary intake self-monitoring | Enabled daily logging of foods and beverages with calorie calculation [26] [39] |
| Wearable Activity Tracker | Physical activity self-monitoring | Automated steps tracking with daily synchronization [83] [39] |
| Smart Scale | Body weight self-monitoring | Objective weight assessment with automated data transmission [83] [39] |
| Automated Feedback System | Personalized performance feedback | Weekly algorithm-generated feedback based on self-monitoring data [26] [39] |
| Digital Platform | Intervention delivery and assessment | Hosted weekly lessons, action plans, and data collection forms [83] [26] |
| Remote Consent and Enrollment | Participant onboarding | Fully digital process enabling nationwide recruitment [39] |
Analytical Framework
Primary Analytical Approach
The primary aim of the Spark trial is to test the main effects of the three self-monitoring components and their interactions on weight change from baseline to 6 months [83] [39]. The factorial design enables detection of both synergistic and antagonistic interactions between components:
- Synergistic interactions occur when combined components result in better outcomes than expected based on main effects alone
- Antagonistic interactions occur when combined components result in worse outcomes than expected based on main effects alone [39]
Engagement and Moderator Analyses
Secondary analyses examine the relationship between self-monitoring engagement and weight change, with engagement operationalized as the percentage of days participants engaged in each assigned tracking behavior [83] [39]. Moderator analyses explore whether specific participant subgroups benefit more from particular self-monitoring strategies, potentially informing personalized intervention approaches.
Implications for Dietary Intervention Compliance Research
The Spark trial protocol represents a paradigm shift in how researchers conceptualize and implement self-monitoring in behavioral interventions. By moving beyond the traditional treatment package approach, this methodology enables precise identification of essential intervention components [83] [26] [39]. For dietary intervention compliance research specifically, the findings will help determine which tracking strategies are necessary to promote adherence and which may be unnecessarily burdensome.
The fully remote implementation demonstrates the feasibility of conducting rigorous optimization trials in real-world settings, enhancing ecological validity and scalability [26] [39]. The digital infrastructure developed for Spark provides a template for future researchers seeking to implement similar remote assessment and intervention protocols.
As obesity treatment increasingly moves to digital platforms, the Spark trial's findings will inform the development of more efficient, engaging, and effective interventions that maximize weight loss outcomes while respecting participant burden [83] [39]. This approach has particular relevance for reaching populations who have historically been underrepresented in behavioral obesity research but disproportionately affected by obesity and its complications.
Conclusion
Self-monitoring remains an indispensable, evidence-based component of dietary interventions, with its efficacy firmly established in promoting weight loss and health behavior change. The integration of digital tools has significantly reduced the burden of self-monitoring, while cognitive architectures like ACT-R and optimization frameworks like MOST provide sophisticated methods for analyzing and enhancing adherence dynamics. Future directions must focus on developing just-in-time adaptive interventions, integrating social cognitive factors into dynamic models, and personalizing strategies based on individual patient characteristics and real-time adherence data. For biomedical and clinical research, this underscores the imperative to move beyond monolithic intervention packages toward optimized, efficient, and sustainable self-monitoring protocols that maximize adherence and clinical outcomes while minimizing participant burden.
References
- 1. Exploring the Dynamics of Dietary Self-Monitoring ... [https://www.jmir.org/2025/1/e65431]
- 2. Exploring the Dynamics of Dietary Self-Monitoring ... [https://pubmed.ncbi.nlm.nih.gov/40279647/]
- 3. Enhancing Child Digital Dietary Self-Monitoring via ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12610852/]
- 4. Decoding heterogeneity in data-driven self-monitoring ... [https://bmcdigitalhealth.biomedcentral.com/articles/10.1186/s44247-024-00115-7]
- 5. Exploring the use of metacognitive monitoring cues ... [https://link.springer.com/article/10.1007/s10459-023-10309-9]
- 6. The role of feedback on students' diagramming: Effects ... [https://www.sciencedirect.com/science/article/pii/S0361476X23001054]
- 7. Self-Monitoring Intervention for Adolescents and Adults ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9952041/]
- 8. Self-Monitoring in Weight Loss: A Systematic Review of the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3268700/]
- 9. How much self-monitoring for weight loss is enough? [https://phhp.ufl.edu/2024/06/06/how-much-self-monitoring-for-weight-loss-is-enough/]
- 10. Elements must meet minimum color contrast ratio thresholds [https://dequeuniversity.com/rules/axe/4.8/color-contrast]
- 11. Color contrast - Accessibility - MDN Web Docs - Mozilla [https://developer.mozilla.org/en-US/docs/Web/Accessibility/Guides/Understanding_WCAG/Perceivable/Color_contrast]
- 12. Obesity and overweight [https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight]
- 13. World Obesity Atlas 2025 [https://www.worldobesity.org/resources/resource-library/world-obesity-atlas-2025]
- 14. A systematic review of the use of dietary self-monitoring in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8928602/]
- 15. Perceptions of self-monitoring dietary intake according to a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10683993/]
- 16. Development of an Evidence-based Nutritional Intervention ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6823648/]
- 17. Qualitative and quantitative analysis of the dietary ... [https://www.sciencedirect.com/science/article/abs/pii/S0360835225004322]
- 18. Overview of Dietary Assessment Methods for Measuring ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8338737/]
- 19. Social Cognitive Theory (SCT) [https://thedecisionlab.com/reference-guide/psychology/social-cognitive-theory]
- 20. Albert Bandura's Social Cognitive Theory [https://www.simplypsychology.org/social-cognitive-theory.html]
- 21. Context matters: Self‐regulation of healthy eating at different ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9291911/]
- 22. Increased self-regulation of eating behavior is associated ... [https://www.frontiersin.org/journals/psychology/articles/10.3389/fpsyg.2024.1480812/full]
- 23. Applying social cognitive theory to predict physical activity and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8801595/]
- 24. Self-Regulation Training Enhances Dietary Self-Efficacy ... [https://www.sciencedirect.com/science/article/abs/pii/S0002822301002498]
- 25. Training self-regulation to promote healthy eating [https://www.sciencedirect.com/science/article/pii/S0195666325004635]
- 26. Optimizing Self-Monitoring in a Digital Weight Loss ... [https://www.researchprotocols.org/2025/1/e75629]
- 27. Analysis of Adherence Status and Influencing Factors Among ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12049249/]
- 28. Feasibility of an online nutrition intervention to improve ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12414212/]
- 29. The CBT Technique That's Overlooked, Undervalued, And ... [https://www.psychologytools.com/articles/the-cbt-technique-thats-overlooked-undervalued-and-essential-why-is-self-monitoring-so-important]
- 30. Paper-based and mobile application-based self-monitoring ... [https://bmcdigitalhealth.biomedcentral.com/articles/10.1186/s44247-024-00109-5]
- 31. The Use of Self-Monitoring and Technology to Increase ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7490310/]
- 32. Differences in Self-Monitoring Technology Use and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12425467/]
- 33. Perceptions of the Three Dietary Patterns of the 2020– ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12608769/]
- 34. DIET@NET: Best Practice Guidelines for dietary assessment ... [https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-017-0962-x]
- 35. Exploring the Dynamics of Dietary Self-Monitoring Adherence ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12064973/]
- 36. Adherence to self‐monitoring and behavioral goals is ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11897847/]
- 37. Physical activity and diet just-in-time adaptive intervention ... [https://www.nature.com/articles/s41746-025-01844-3]
- 38. Optimizing a Just-in-Time Adaptive Intervention to Improve ... [https://www.researchprotocols.org/2021/12/e33568/]
- 39. Optimizing Self-Monitoring in a Digital Weight Loss ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12504904/]
- 40. Perceptions of self-monitoring dietary intake according to a ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0294652]
- 41. A Qualitative Evaluation of a Plate-Method Dietary Self- ... [https://www.sciencedirect.com/science/article/pii/S2475299123247988]
- 42. The Multiphase Optimization Strategy (MOST) and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2062525/]
- 43. Using the Multiphase Optimization Strategy (MOST ... - Trials [https://trialsjournal.biomedcentral.com/articles/10.1186/s13063-019-3853-y]
- 44. Applying the Multiphase Optimization Strategy for ... [https://www.sciencedirect.com/science/article/pii/S0885392420308861]
- 45. Digital dietary interventions for healthy adolescents: A ... [https://www.sciencedirect.com/science/article/pii/S0261561425000135]
- 46. Patterns of Engagement With an Application-Based Dietary ... [https://www.sciencedirect.com/science/article/pii/S2773065422000359]
- 47. The effectiveness of mobile app-based interventions in ... [https://ijbnpa.biomedcentral.com/articles/10.1186/s12966-025-01823-7]
- 48. Artificial Intelligence Applications to Personalized Dietary ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12193492/]
- 49. Impacts of consumption tracking and tailored feedback on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12100978/]
- 50. Why more successful? An analysis of participants' self ... [https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-024-17848-9]
- 51. and facilitators to Barriers , physical activity and lifestyle behavior... diet [https://ijbnpa.biomedcentral.com/articles/10.1186/s12966-023-01424-2]
- 52. to following Barriers recommendations in Type 2 diabetes dietary [https://pubmed.ncbi.nlm.nih.gov/15606688/]
- 53. Journal of Medical Internet Research - Barriers and Enablers to... [https://www.jmir.org/2020/11/e22036/]
- 54. Digital dietary interventions for healthy adolescents [https://www.sciencedirect.com/science/article/abs/pii/S0261561425000135]
- 55. Impact of feedback generation and presentation on self ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10765525/]
- 56. Exploring how researchers consider nutrition trial design and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11685074/]
- 57. An experimental design and implementation protocol for ... [https://www.sciencedirect.com/science/article/pii/S2215016125000913]
- 58. Defining Adherence to Mobile Dietary Self-Monitoring and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6856872/]
- 59. Interventions to enhance adherence to dietary advice for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4900876/]
- 60. Effectiveness of Gamification Interventions to Improve ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12445784/]
- 61. The Use of Gamification in the Self-Management of Patients ... [https://games.jmir.org/2023/1/e39019]
- 62. Gamification in Healthcare: Use Cases, Trends, and ... [https://www.uptech.team/blog/gamification-in-healthcare]
- 63. Caregiver Feeding Practices as Predictors for Child Dietary ... [https://www.mdpi.com/2072-6643/13/8/2773]
- 64. Gamification for the Improvement of Diet, Nutritional Habits, ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8308535/]
- 65. Caregiver involvement in interventions for improving children's ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6956675/]
- 66. Patterns and Predictors of Engagement With Digital Self ... [https://mhealth.jmir.org/2023/1/e45057]
- 67. Factors Influencing Adherence to Dietary Interventions ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12335251/]
- 68. Dietary assessment toolkits: an overview - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6368251/]
- 69. Implementation science in nutrition practice: A review of the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12590315/]
- 70. Optimizing process flow diagrams to guide implementation of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10689519/]
- 71. Interactive Conversational Agents to Improve Dietary ... [https://www.jmir.org/2025/1/e78220]
- 72. Systematic review and meta - analysis of remotely delivered... [https://pubmed.ncbi.nlm.nih.gov/29529158/]
- 73. The SMARTER Trial: Design of a trial testing tailored mHealth ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7269678/]
- 74. What is the difference between MOST and SMART ... [https://cadio.org/what-is-the-difference-between-most-and-smart-how-are-they-related/]
- 75. Identifying Predictors of Adherence to the Physical Activity Goal [https://pmc.ncbi.nlm.nih.gov/articles/PMC10106377/]
- 76. the SMARTER Randomized Clinical Trial [https://www.jmir.org/2022/7/e38243/]
- 77. Self-Monitoring of Weight as a Weight Loss Strategy [https://link.springer.com/article/10.1007/s12170-024-00746-5]
- 78. Self-Monitoring as a Mediator of Weight Loss in the SMART ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3529986/]
- 79. Self-monitoring as a mediator of weight loss in the SMART ... [https://pubmed.ncbi.nlm.nih.gov/22936524/]
- 80. Assessing adolescent diet and physical activity behaviour ... [https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-022-13160-6]
- 81. Comparison of Subjective and Objective Sleep Quality in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12340704/]
- 82. The association between subjective and objective ... [https://www.sciencedirect.com/science/article/pii/S0272735825001151]
- 83. Optimizing Self-Monitoring in a Digital Weight Loss ... [https://pubmed.ncbi.nlm.nih.gov/40986860/]