Mechanisms of Lipid-Soluble Vitamin Absorption: From Cellular Pathways to Clinical Applications
This comprehensive review synthesizes current understanding of lipid-soluble vitamin (A, D, E, K) absorption mechanisms for research scientists and drug development professionals.
Mechanisms of Lipid-Soluble Vitamin Absorption: From Cellular Pathways to Clinical Applications
Abstract
This comprehensive review synthesizes current understanding of lipid-soluble vitamin (A, D, E, K) absorption mechanisms for research scientists and drug development professionals. We explore foundational physiological pathways, methodological approaches for studying absorption, troubleshooting for malabsorption conditions, and validation through clinical and comparative studies. The article examines emerging concepts including gut microbiota interactions, genetic polymorphisms affecting transport proteins, and advanced formulation strategies to overcome absorption barriers, providing a translational framework connecting basic science to therapeutic applications.
Cellular and Physiological Pathways of Lipid-Soluble Vitamin Uptake
The absorption of dietary lipids and fat-soluble vitamins is a complex, multistep process orchestrated by the gastrointestinal tract, primarily within enterocytes. This process is essential for whole-body lipid and energy homeostasis and involves intricate interactions between bile salts for solubilization, intracellular trafficking mechanisms within enterocytes, and the assembly and secretion of chylomicrons [1] [2]. Dysregulation of this machinery contributes to dyslipidemia and increases the risk of atherosclerotic cardiovascular disease [1]. This whitepaper provides an in-depth technical guide on the core components of this system—enterocytes, bile salts, and chylomicron assembly—framed within the context of lipid-soluble vitamin absorption research. It is structured to aid researchers, scientists, and drug development professionals by summarizing quantitative data, detailing experimental protocols, and visualizing key pathways and workflows.
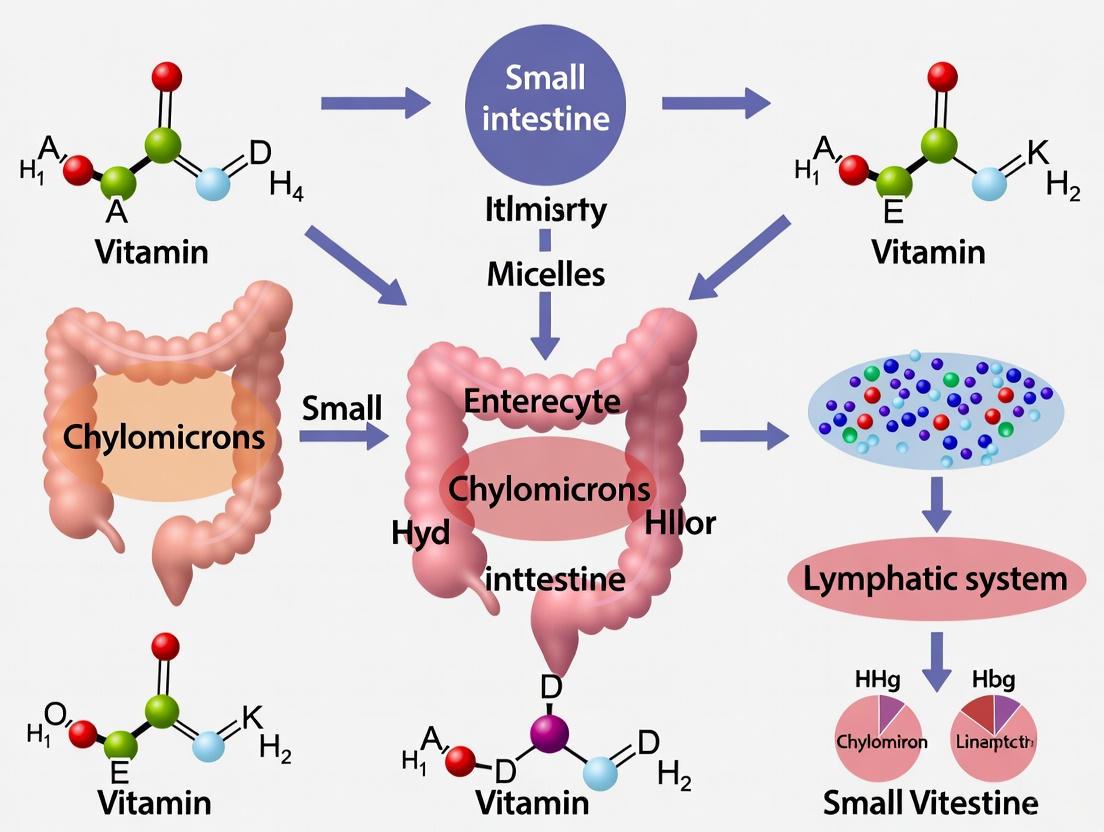
The efficient digestion and absorption of dietary lipids, including triacylglycerols (TAGs), phospholipids, sterols, and fat-soluble vitamins (A, D, E, and K), are critical for maintaining energy homeostasis and supporting vital physiological functions [2]. The process can be broadly divided into three phases: 1) intraluminal digestion and solubilization, which relies on lipases and bile salts; 2) cellular uptake and processing within enterocytes; and 3) packaging and export via chylomicrons into the lymphatic system and circulation [1] [2] [3].
The enterocyte serves as the central processing unit, where resynthesized lipids are assembled into chylomicrons, large TAG-rich lipoprotein particles [4]. Beyond triglycerides, this pathway is also the principal route for the absorption of lipid-soluble vitamins, which rely on their incorporation into chylomicrons for systemic delivery [3]. Understanding this machinery is paramount for developing therapeutic strategies to modulate lipid absorption and address associated metabolic disorders.
Core Machinery and Molecular Components
Enterocytes: The Central Processing Unit
Enterocytes, the predominant epithelial cells lining the small intestine, are equipped with specialized structures and molecular machinery to handle lipid absorption [5].
- Cellular Specialization: The apical membrane of enterocytes is composed of a brush border of microvilli, dramatically increasing the surface area available for nutrient uptake [5].
- Key Absorptive Functions:
Bile Salts: Essential Solubilizing Agents
Bile salts, synthesized in the liver and secreted into the duodenum, are critical for the efficient absorption of lipids and fat-soluble vitamins.
- Emulsification and Micelle Formation: Bile salts act as biological detergents, emulsifying dietary fat into fine lipid droplets and forming mixed micelles with the products of lipid hydrolysis (e.g., fatty acids, monoacylglycerols) and fat-soluble vitamins [2]. This process is indispensable for presenting hydrophobic molecules to the enterocyte's brush border membrane.
- Clinical Evidence: The critical nature of bile is highlighted by significantly decreased lipid absorption rates in individuals with bile fistulas, where the duodenal concentration of bile acids is greatly reduced [2].
The Chylomicron Assembly Line within Enterocytes
The assembly and secretion of chylomicrons (CMs) is a multistep process within enterocytes, requiring precise coordination of apolipoproteins, enzymes, and transport proteins.
Table 1: Key Molecular Components in Chylomicron Assembly
| Component | Type/Classification | Primary Function in Chylomicron Pathway |
|---|---|---|
| Apolipoprotein B-48 (apoB48) | Structural Protein | A truncated form of apoB100; essential structural component of the chylomicron particle; lipidates during translation to form a primordial lipoprotein [3]. |
| Microsomal Triglyceride Transfer Protein (MTP) | Lipid Transfer Protein | Transfers lipids to nascent apoB48 in the endoplasmic reticulum (ER) lumen; critical for proper folding of apoB48 and formation of pre-chylomicron particles [1] [3]. |
| CD36/FAT | Fatty Acid Transporter | Facilitates uptake of fatty acids; plays a regulatory role in CM formation by inducing key proteins like MTP and FABP; involved in post-assembly transport [1] [2]. |
| Fatty Acid Binding Protein (FABP) | Intracellular Carrier | Binds fatty acids and monoacylglycerols intracellularly; facilitates their trafficking to the ER for re-esterification; FABP1 also initiates the budding of pre-chylomicron transport vesicles (PCTVs) from the ER [1] [2]. |
| Monoacylglycerol Acyltransferase (MGAT) & Diacylglycerol Acyltransferase (DGAT) | Enzymes | Catalyze the resynthesis of triglycerides from absorbed fatty acids and monoacylglycerols via the monoacylglycerol pathway, which accounts for ~80% of intestinal TAG synthesis [2]. |
| SNARE Complex (e.g., VAMP7, Syntaxin-5) | Vesicle Docking/Fusion Machinery | Mediates the fusion of Pre-Chylomicron Transport Vesicles (PCTVs) with the Golgi apparatus, enabling the maturation of chylomicrons [1]. |
- Uptake and Resynthesis: Products of lipid digestion (fatty acids, 2-monoacylglycerols) are taken up by enterocytes via passive diffusion and protein-mediated transport (e.g., CD36) [2]. Inside the cell, they are bound to FABPs and transported to the ER. Within the smooth endoplasmic reticulum (SER), TAGs are resynthesized predominantly via the MGAT and DGAT pathway [4].
- Primordial Particle Formation: In the ER membrane, nascent apoB48 is lipidated by MTP, forming a dense, primordial lipoprotein particle. This step prevents the intracellular degradation of apoB48 [3].
- Core Expansion and Pre-CM Formation: The primordial particle is expanded into a triglyceride-rich pre-chylomicron through the addition of a large bolus of lipid, potentially from lumenal lipid droplets or via direct transfer [3].
- Vesicular Transport to Golgi: Pre-chylomicrons are packaged into specialized Pre-Chylomicron Transport Vesicles (PCTVs). The budding of PCTVs from the ER is facilitated by FABP1 and CD36, and the vesicles are directed to the Golgi by the vesicle-SNARE protein VAMP7 [1].
- Golgi Maturation and Secretion: At the Golgi, PCTVs fuse via the SNARE complex (VAMP7, Syntaxin-5), releasing the pre-CM into the Golgi lumen for final maturation (e.g., glycosylation of apoB48, addition of apoAIV) [1]. Mature CMs are then transported in secretory vesicles to the basolateral membrane, exocytosed into the lamina propria, and subsequently enter the lymphatic lacteals for systemic distribution [1].
The diagram below illustrates the sequential stages of chylomicron assembly within an enterocyte.
Quantitative Data in Lipid-Soluble Vitamin Absorption
Understanding the absorption of lipid-soluble vitamins (FSVs) is a key application of the core gastrointestinal machinery. The following table summarizes quantitative and mechanistic data related to their absorption.
Table 2: Quantitative and Mechanistic Data on Fat-Soluble Vitamin Absorption
| Vitamin | Key Absorption Characteristics | Associated Transport Proteins/Pathways | Molecular Interaction with Membrane (from MD Simulations) |
|---|---|---|---|
| Vitamin A (Retinol) | Absorbed via chylomicron pathway; its ester, retinyl ester, is packaged into CMs [3]. | Retinol-binding protein; Chylomicron pathway dependent on MTP [3]. | Hydroxyl group at the tail; highest structural flexibility and diffusion coefficient; plugs head group into hydrocarbon core of lipid bilayer [6]. |
| Vitamin E (α-Tocopherol) | Major pathway: secretion with chylomicrons. A secondary pathway involves secretion with HDLs, important when chylomicron assembly is defective [7]. | MTP-dependent for chylomicron pathway; HDL pathway is MTP-independent [7]. | Hydroxyl at the head group; moves through one leaflet and stabilizes in the opposite leaflet; forms hydrogen bonds with phosphate group of DPPC [6]. |
| Vitamin K (Phylloquinone) | Absorbed similarly to other dietary lipids [6]. | Intestinal scavenger receptors; Chylomicron pathway [6]. | No hydroxyl group; stabilizes near phosphate group without H-bonding; precise tilting angle of 120°; low diffusion coefficient suggests high retention in gel-phase membranes [6]. |
| Vitamin D | Absorbed in the duodenum [5]. | Chylomicron pathway [5]. | Information not specified in search results. |
Experimental Protocols for Investigating Absorption Pathways
To study the complex process of lipid and vitamin absorption, researchers employ a range of in vitro, ex vivo, and in vivo models. Below are detailed methodologies for key experiments cited in this field.
Protocol: Investigating Vitamin E Transport Pathways Using Primary Enterocytes
This protocol is adapted from the work published in the Journal of Lipid Research and is used to delineate the dual pathways of vitamin E absorption [7].
Objective: To characterize the mechanisms of α-tocopherol uptake and secretion in primary enterocytes and identify the contribution of chylomicron vs. HDL pathways.
Materials:
- Primary Enterocytes: Isolated from rat or mouse small intestine.
- Radioactive Tracer: [³H]α-tocopherol.
- Lipid Supplements: Oleic acid complexed with bovine serum albumin (BSA), lipid mixtures (e.g., taurocholate, monoolein, fatty acids).
- MTP Inhibitor: e.g., CP-346086 or BMS-197636.
- Cell Culture Medium: Dulbecco's Modified Eagle Medium (DMEM) or equivalent, supplemented with fatty acid-free BSA.
- Ultracentrifugation Equipment: For separation of lipoprotein density classes.
- Scintillation Counter: For quantifying radioactivity.
Methodology:
- Cell Isolation and Culture: Isolate primary enterocytes from the small intestine of rats or mice. Culture the cells in an appropriate medium.
- Uptake Phase: Incubate enterocytes with [³H]α-tocopherol for up to 1 hour to allow for cellular uptake. The medium can be varied:
- Group A (No Lipid): Medium alone.
- Group B (With Lipid): Medium supplemented with lipids and oleic acid to stimulate chylomicron assembly.
- Secretion Phase: After uptake, wash the cells to remove extracellular tracer. Incubate the cells with fresh medium to allow for secretion of the incorporated vitamin E.
- To test the role of MTP, include a treatment group where a specific MTP inhibitor is added during the secretion phase.
- To test the HDL pathway, include a group where exogenous HDL is added to the secretion medium.
- Lipoprotein Separation and Analysis: Collect the secretion medium. Separate different lipoprotein classes (chylomicrons/VLDL, IDL/LDL, HDL) via sequential ultracentrifugation at their characteristic densities.
- Quantification: Measure the radioactivity of [³H]α-tocopherol in each lipoprotein fraction and within the cells using a scintillation counter.
- Data Analysis: Calculate the proportion of secreted vitamin E associated with each lipoprotein pathway. Compare secretion profiles under different conditions (with/without lipids, with/without MTP inhibition, with/without HDL).
Protocol: Molecular Dynamics (MD) Simulations of Vitamin Absorption into Lipid Bilayers
This computational protocol is based on studies that investigate the molecular interactions of fat-soluble vitamins with membranes [6].
Objective: To determine the distribution, orientation, and dynamics of retinol, α-tocopherol, and phylloquinone within a model phospholipid bilayer.
Materials:
- Simulation Software: GROMACS, AMBER, NAMD, or similar MD simulation package.
- Force Field Parameters: CHARMM36, AMBER Lipid21, or other compatible force fields for lipids and small molecules.
- Molecular Structures:
- Membrane: A pre-equilibrated bilayer of 128 Dipalmitoylphosphatidylcholine (DPPC) molecules.
- Ligands: 3D coordinate files for retinol, α-tocopherol, and phylloquinone.
- Solvent Model: Explicit water model, e.g., SPC (Simple Point Charge) or TIP3P.
- Computational Resources: High-performance computing (HPC) cluster.
Methodology:
- System Setup:
- Obtain the initial structure of the DPPC bilayer.
- Place one vitamin molecule in the aqueous phase, approximately 41 Å from the bilayer center along the z-axis.
- Solvate the entire system (bilayer + vitamin) in a box of explicit water molecules.
- Add ions (e.g., Na⁺, Cl⁻) to neutralize the system's charge and achieve a physiological salt concentration.
- Energy Minimization: Perform energy minimization (e.g., using steepest descent algorithm) to remove any steric clashes and relax the system.
- Equilibration:
- Conduct a short simulation (e.g., 100-200 ps) in the NVT ensemble (constant Number of particles, Volume, and Temperature) to stabilize the temperature.
- Follow with a longer simulation (e.g., 1 ns) in the NPT ensemble (constant Number of particles, Pressure, and Temperature) to stabilize the pressure and density of the system.
- Production Run: Perform a long, unbiased MD simulation (e.g., 100 ns or more) under NPT conditions. Trajectories are saved at regular intervals for analysis.
- Trajectory Analysis:
- Distribution and Localization: Calculate the density profile of the vitamin along the bilayer axis (z-axis) to identify its favorable binding site.
- Orientation: Analyze the tilt angle of the vitamin molecule relative to the lipid bilayer.
- Interactions: Identify hydrogen bonds and other non-covalent interactions between the vitamin and lipid headgroups (e.g., phosphate groups).
- Dynamics: Calculate the mean-squared displacement (MSD) to determine the diffusion coefficient of the vitamin within the membrane.
The workflow for this computational approach is visualized below.
The Scientist's Toolkit: Essential Research Reagents and Models
This section details key reagents, models, and tools essential for experimental research in the field of intestinal lipid and fat-soluble vitamin absorption.
Table 3: Key Research Reagent Solutions for Lipid Absorption Studies
| Reagent / Model | Category | Specific Function / Application |
|---|---|---|
| Caco-2 Cell Line | In Vitro Model | Differentiated human colon adenocarcinoma cells; model human intestinal epithelium for studying uptake, intracellular trafficking, and polarized secretion of lipids and vitamins [6] [7]. |
| Primary Enterocytes | Ex Vivo Model | Enterocytes freshly isolated from rodent intestine; provide a more physiologically relevant model than cell lines, retaining native expression of transporters and metabolic enzymes [7]. |
| MTP Inhibitors | Pharmacological Tool | Compounds like CP-346086; used to inhibit MTP activity, thereby blocking the assembly and secretion of apoB-containing lipoproteins (chylomicrons) to study their necessity for lipid/vitamin absorption [7] [3]. |
| CD36/FAT Knockout Mice | Genetic Model | Mice with targeted deletion of the Cd36 gene; used to study the role of this fatty acid transporter in lipid sensing, CM formation, and post-assembly transport [1] [2]. |
| SNARE Complex Inhibitors | Molecular Tool | Proteins or peptides that disrupt SNARE complex formation (e.g., targeting Syntaxin-Binding Protein 5); used to probe the mechanisms of PCTV fusion with the Golgi apparatus [1]. |
| Radiolabeled Tracers | Tracking Reagent | e.g., [³H]α-tocopherol, [¹⁴C]triolein; used to quantitatively track the uptake, intracellular fate, and secretion of specific lipids and vitamins in experimental models [7]. |
| Dipalmitoylphosphatidylcholine | Model Membrane | A synthetic phospholipid used to form well-defined lipid bilayers for biophysical studies, such as Molecular Dynamics simulations, to investigate vitamin-membrane interactions [6]. |
The gastrointestinal absorption machinery, centered on enterocytes, bile salts, and chylomicron assembly, represents a highly efficient and regulated system for the assimilation of dietary lipids and fat-soluble vitamins. The process, from luminal solubilization to basolateral secretion, involves a cascade of coordinated events mediated by specific proteins, enzymes, and vesicular transport systems. Ongoing research continues to elucidate critical regulatory nodes, including post-assembly mechanisms and the role of intestinal lymphatics [1]. A deep understanding of this machinery not only advances fundamental biological knowledge but also provides a foundation for developing novel therapeutic interventions targeting dyslipidemia, cardiovascular disease, and disorders of fat-soluble vitamin absorption.
The absorption of lipophilic compounds, including drugs and essential micronutrients, is a complex process governed by their solubility in the gastrointestinal environment and their subsequent incorporation into absorbable mixed micelles. This whitepaper delineates the critical roles that dietary lipids and bile acid secretion play in modulating the bioaccessibility and bioavailability of lipid-soluble vitamins and poorly water-soluble drugs. The dissolution and solubilization of these compounds are contingent upon the presence of dietary fat, which stimulates biliary secretion, and the physicochemical properties of the lipids themselves. Through an examination of recent in vitro, in silico, and in vivo studies, this guide provides a mechanistic overview of the absorption pathways, summarizes quantitative findings on factors influencing bioavailability, and presents standardized experimental protocols for preclinical assessment. The insights herein are intended to inform researchers and drug development professionals in the design of more effective lipid-based formulations and nutritional interventions.
The oral bioavailability of lipid-soluble vitamins (A, D, E, and K) and Biopharmaceutics Classification System (BCS) Class II/IV drugs is intrinsically limited by their poor aqueous solubility. Their absorption is not a passive process but is an active cascade mediated by the co-consumption of dietary lipids and the subsequent secretion of bile acids [8] [9]. This process can be conceptualized in two primary stages: first, the solubilization of the compound within the lipid phase of the digesta, and second, its enzymatic lipolysis and incorporation into mixed micelles composed of bile acids and phospholipids, which enable transport to the enterocyte surface [10] [11].
The gastrointestinal tract represents a dynamic physiological environment where the food matrix, lipid composition (solid vs. liquid), and the bile acid pool interact to determine the ultimate bioavailability of a lipophilic substance. Emerging research underscores that this process is further modulated by the gut microbiome, which enzymatically alters the bile acid landscape, and by dietary components such as soluble fibers, which can profoundly impact micelle formation and stability [9] [11]. This guide synthesizes current research on these mechanisms, providing a technical foundation for leveraging these principles in scientific and industrial applications.
Core Mechanisms: Lipids, Bile, and the Aqueous Boundary Layer
The Lipid Catalyst: Dietary Fat as a Solubilization Vehicle
Dietary lipids serve as the initial hydrophobic solvent for lipophilic compounds within the gut. The type of lipid—categorized by its physical state (solid vs. liquid) and fatty acid chain length—plays a determinative role in the efficiency of this process.
- Liquid vs. Solid Lipids: Liquid lipids, such as triolein (TO), are generally more effective at enhancing bioavailability compared to solid lipids like tristearin (TS). This is attributed to the more complete and rapid lipolysis of liquid lipids, which readily releases fatty acids and monoglycerides that integrate into mixed micelles. Solid lipids, in contrast, may undergo only partial lipolysis and can act as inert carriers, neither significantly aiding nor impeding the dissolution and absorption of associated drugs like griseofulvin [8] [10].
- Stimulation of Biliary and Pancreatic Secretions: The presence of fat in the duodenum is a potent physiological trigger for the release of bile from the gallbladder and pancreatic enzymes. This is a critical step, as bile acids are indispensable for the formation of mixed micelles [11].
Bile Acids: The Gateway to Absorption
Bile acids are biological surfactants synthesized from cholesterol in the liver and conjugated to glycine or taurine. Their primary function in absorption is the solubilization of lipolytic products (e.g., fatty acids, monoglycerides) and lipophilic compounds into mixed micelles.
- Enterohepatic Circulation: Bile acids undergo efficient enterohepatic circulation, a process where they are recycled from the ileum back to the liver, ensuring a constant pool is available for lipid absorption [11]. This circulation is modulated by the gut microbiome via enzymes like bile salt hydrolase (BSH), which deconjugates primary bile acids, influencing their solubility, function, and reabsorption kinetics [11].
- Mixed Micelle Formation: Mixed micelles are molecular aggregates that ferry lipophilic content through the unstirred aqueous boundary layer adjacent to the intestinal epithelium. This transport is essential for bringing compounds like fat-soluble vitamins into direct contact with the apical membrane of enterocytes for absorption [6] [9].
The following diagram illustrates the enterohepatic circulation of bile acids and their critical role in the absorption of lipophilic compounds.
Molecular-Scale Interactions at the Enterocyte Membrane
At the cellular level, absorption involves the spontaneous penetration of lipophilic molecules into the phospholipid bilayer of the enterocyte. Molecular dynamics (MD) simulations reveal that the specific chemical structure of a compound dictates its orientation and dynamics within the membrane.
- Retinol (Vitamin A): With a hydroxyl (-OH) group at the tail of its structure, retinol exhibits high structural flexibility and a broad tilt angle within the dipalmitoylphosphatidylcholine (DPPC) bilayer. It plugs its head group into the hydrocarbon core, demonstrating a high diffusion coefficient [6].
- α-Tocopherol (Vitamin E): Also possessing a hydroxyl group, but at its head group, α-tocopherol moves through one leaflet of the membrane and stabilizes in the opposite leaflet, facilitated by hydrogen bonding with phosphate groups [6].
- Phylloquinone (Vitamin K1): Lacking a hydroxyl group, phylloquinone stabilizes near the phosphate groups of the membrane without hydrogen bond formation. It penetrates at a precise tilting angle of 120° and has a low diffusion coefficient, suggesting higher retention in gel-phase membranes [6].
Quantitative Data on Factors Influencing Bioaccessibility
The efficiency with a lipophilic compound is released from its matrix and incorporated into micelles (its bioaccessibility) is quantitatively influenced by various dietary and physiological factors. The tables below summarize key experimental findings.
Table 1: Impact of Dietary Fibers on Carotenoid Bioaccessibility (In Vitro Digestion Model) [9]
| Dietary Fibre Type | Solubility | β-Carotene Bioaccessibility (% Change) | Lutein Bioaccessibility (% Change) | Lycopene Bioaccessibility (% Change) | Primary Mechanism of Action |
|---|---|---|---|---|---|
| Pectin | Soluble/Gelling | ▼ 38.5% (from 29.1% to 17.9%) | ▼ 55.4% (from 58.3% to 26.0%) | ▼ 25.0% (from 7.2% to 5.4%) | Increased viscosity, entrapment |
| Alginate | Soluble/Gelling | ▼ 59.5% (from 29.1% to 11.8%) | No significant impact | ▼ 43.1% (from 7.2% to 4.1%) | Increased viscosity, reduced lipid digestion |
| Guar Gum | Soluble/Gelling | No significant impact | No significant impact | ▼ 33.3% (from 7.2% to 4.8%) | Increased viscosity, reduced micelle size |
| Cellulose | Insoluble | No significant impact | No significant impact | No significant impact | No gelation, minimal effect |
| Resistant Starch | Insoluble | No significant impact | No significant impact | No significant impact | No gelation, minimal effect |
Table 2: Influence of Lipid Type on Drug Bioavailability (In Vivo Porcine Model) [8] [10]
| Parameter | Solid Lipid (Tristearin, TS) | Liquid Lipid (Triolein, TO) |
|---|---|---|
| Lipolysis Extent | Partial | Near-complete |
| Drug Adsorption | Negligible griseofulvin adsorption | N/A |
| Gastric Emptying | Faster in fasted state | Fed-state kinetics |
| Overall Bioavailability | No significant positive or negative effect | Enhanced for many lipophilic compounds |
| Proposed Mechanism | Inert carrier due to partial lipolysis | Efficient production of micelle-forming lipids |
Table 3: Association between Dietary Live Microbe Intake and Serum Fat-Soluble Vitamin Levels (NHANES Population Study) [12]
| Serum Vitamin | Low Intake Group (Reference) | Medium-High (MedHi) Intake Group (Adjusted Change) |
|---|---|---|
| Vitamin A | Baseline | + 0.17 μg/dL (95% CI: 0.04, 0.30) |
| Vitamin D | Baseline | + 0.36 nmol/L (95% CI: 0.22, 0.51) |
| Vitamin E | Baseline | + 4.65 μg/dL (95% CI: 1.91, 7.39) |
| Mechanistic Link | Gut microbiota modulation of bile acid metabolism, absorption pathways, and vitamin receptor expression. |
Experimental Protocols for Preclinical Assessment
In Vitro Lipolysis Model
This protocol is adapted from studies investigating the impact of solid and liquid lipids on drug dissolution [8] [10].
Objective: To simulate the gastrointestinal lipolysis of a lipid-based formulation and measure the bioaccessibility of a co-administered lipophilic compound.
Materials:
- Simulated Intestinal Fluids (FeSSIF): Prepared according to established recipes, containing bile salts and phospholipids.
- Lipase Enzyme Preparation: Porcine pancreatic extract (e.g., 250 U/mg).
- Calcium Ion Solution: (e.g., 0.5 M CaCl₂) to stimulate lipase activity and precipitate fatty acids.
- pH-Stat Titrator: To automatically maintain pH and record the consumption of NaOH, which is proportional to free fatty acid release.
- Ultracentrifuge: For separation of the micellar phase.
Methodology:
- Initial Mixture: The lipid formulation containing the drug/vitamin is dispersed in FeSSIF under controlled temperature (37°C) and agitation.
- Lipolysis Initiation: Porcine pancreatin extract is added to the mixture to initiate digestion. The pH is automatically maintained at 6.5 using a pH-stat titrator with 0.2-0.6 M NaOH.
- Calcium Addition: A controlled volume of CaCl₂ solution is added incrementally to precipitate liberated fatty acids and drive the lipolysis reaction forward.
- Termination and Separation: After a set digestion period (e.g., 30-60 minutes), the reaction is stopped by adding a lipase inhibitor (e.g., Orlistat) or by ultracentrifugation (e.g., 40,000 rpm for 1 hour).
- Analysis: The aqueous phase (containing mixed micelles) is carefully sampled. The concentration of the drug/vitamin in this micellar phase is quantified via HPLC-UV/FLD or LC-MS/MS. Bioaccessibility is calculated as: (Mass in micellar phase / Total mass in digestion vessel) × 100%.
Molecular Dynamics (MD) Simulation of Membrane Absorption
This protocol is derived from computational studies of fat-soluble vitamin absorption into lipid bilayers [6].
Objective: To investigate the molecular-level interactions, orientation, and diffusion of a lipophilic compound within a model phospholipid bilayer.
Materials:
- Software: GROMACS, AMBER, or NAMD.
- Force Fields: CHARMM36, GROMOS, or similar, with parameters for lipids and the compound of interest.
- Model Membrane: A pre-equilibrated bilayer of a specific phospholipid (e.g., 128 DPPC molecules).
- Ligand Structure: 3D molecular structure file of the vitamin/drug (e.g., from PubChem).
Methodology:
- System Setup:
- Place the ligand molecule approximately 40 Å from the center of the pre-equilibrated DPPC bilayer along the z-axis.
- Solvate the entire system (bilayer + ligand) in an explicit solvent model (e.g., SPC water) within a periodic boundary box.
- Add ions (e.g., Na⁺, Cl⁻) to neutralize the system and achieve physiological ionic strength.
- Energy Minimization: Use the steepest descent algorithm to remove steric clashes and bad contacts in the initial structure.
- Equilibration:
- Perform a short NVT simulation (constant Number of particles, Volume, and Temperature) to stabilize the system temperature at 310 K.
- Conduct a longer NPT simulation (constant Number of particles, Pressure, and Temperature) to achieve the correct density and stabilize the bilayer structure.
- Production Run: Execute a long-term MD simulation (e.g., 100-500 ns) with a 2-fs time step, saving trajectory data at regular intervals.
- Trajectory Analysis:
- Root Mean Square Deviation (RMSD): Assess the stability of the ligand and bilayer.
- Density Profiles: Plot the probability distribution of specific atoms (e.g., ligand head group, phosphate groups of DPPC) along the bilayer normal (z-axis) to determine location.
- Hydrogen Bonding: Analyze the formation and lifetime of H-bonds between the ligand and lipid head groups.
- Diffusion Coefficient: Calculate the mean square displacement of the ligand within the bilayer to assess its mobility.
The workflow for the molecular-level investigation of vitamin absorption is outlined below.
The Scientist's Toolkit: Key Research Reagents and Models
Table 4: Essential Reagents and Models for Investigating Lipid-Soluble Compound Absorption
| Reagent / Model | Function and Application | Key Characteristics |
|---|---|---|
| Tristearin (TS) & Triolein (TO) | Model solid and liquid lipids for studying the impact of lipid physical state on lipolysis and bioavailability [8] [10]. | TS: Solid triglyceride (C18:0). TO: Liquid triglyceride (C18:1). |
| Sodium Taurodeoxycholate (NaTDC) | A common bile salt used in simulated intestinal fluids (e.g., FaSSIF/FeSSIF) for in vitro dissolution and lipolysis studies [8]. | Conjugated primary bile acid; provides critical micelle-forming capacity. |
| Porcine Pancreatin Extract | Source of digestive enzymes, including lipase, for in vitro lipolysis experiments [10] [9]. | Contains a physiologically relevant mix of enzymes; activity must be standardized (e.g., 250 U/mg). |
| DPPC Bilayer | A model phospholipid membrane for Molecular Dynamics (MD) simulations to study molecule-membrane interactions [6]. | Dipalmitoylphosphatidylcholine; well-characterized and widely used in computational studies. |
| Caco-2 Cell Line | Human colon adenocarcinoma cell line that differentiates into enterocyte-like cells; a standard model for intestinal permeability screening. | Forms polarized monolayers with tight junctions and expresses relevant transporters. |
| Swine (Porcine) Model | In vivo model for preclinical bioavailability and food-effect studies due to physiological similarities to humans in GI tract and bile secretion [8] [10]. | Similar gallbladder anatomy, bile acid composition, and dietary habits to humans. |
The critical interdependence between dietary lipids, bile acid secretion, and the absorption of lipid-soluble compounds is a cornerstone of nutritional science and drug development. Evidence confirms that liquid lipids typically promote greater bioavailability than solid lipids via more complete lipolysis, and that the bile acid-driven formation of mixed micelles is the non-negotiable gateway to absorption for these compounds. Furthermore, external factors, particularly soluble gel-forming dietary fibers, can significantly impair bioaccessibility by altering the physicochemical environment of the gut.
Future research directions should focus on a more granular understanding of the gut microbiome's role, particularly through enzymes like bile salt hydrolase (BSH), in shaping the host's bile acid profile and its subsequent effect on the absorption of not only vitamins but also lipophilic drugs [11]. The application of advanced models, including the porcine in vivo model and sophisticated in silico MD simulations, will continue to be invaluable. Integrating these insights will empower the rational design of next-generation lipid-based drug delivery systems and precision nutrition strategies aimed at optimizing the health benefits of lipid-soluble bioactive compounds.
The biological activity of lipid-soluble vitamins (A, D, E, and K) is entirely contingent upon sophisticated intracellular processing mechanisms that govern their activation, transport, and functional integration into cellular metabolism. Unlike their water-soluble counterparts, these vitamins leverage lipid-mediated pathways and complex enzymatic cascades to transform from dietary precursors into potent signaling molecules, antioxidants, and gene regulators [13] [14]. For researchers and drug development professionals, a precise understanding of these mechanisms—including the specific transport proteins such as scavenger receptor class B type I (SR-BI), CD36, and Niemann-Pick C1-like 1 (NPC1L1), and the enzymes that catalyze their activation—is paramount [13]. Disruptions in these processes are linked to diverse pathologies, from neurological disorders to cancer, highlighting their potential as therapeutic targets [13] [15]. This whitepaper delineates the core principles of intracellular processing for lipid-soluble vitamins, framed within contemporary research on their absorption and metabolism, and provides a toolkit of experimental methodologies for their investigation.
Core Mechanisms of Intracellular Processing
Transport Proteins and Cellular Uptake
Following absorption, lipid-soluble vitamins are distributed to target cells via chylomicrons and other lipoproteins [14]. Their cellular uptake is mediated by specific transport proteins that ensure targeted delivery and bioavailability.
Table 1: Key Transport Proteins for Lipid-Soluble Vitamins
| Vitamin | Key Transport Proteins | Cellular Uptake Mechanism | Tissue Specificity/Notes |
|---|---|---|---|
| Vitamin A | SR-BI, CD36 [13] | Receptor-mediated endocytosis; lipid-mediated pathways [13] [14] | Critical for retinal function and cellular differentiation. |
| Vitamin D | SR-BI, CD36 [13] | Lipid-mediated pathways; carrier proteins in intestinal membrane [13] [16] | Liver and kidneys are primary sites for enzymatic activation [16]. |
| Vitamin E | SR-BI, CD36, NPC1L1 [13] | Lipid-mediated pathways; targeted by tocopherol transfer protein (TTP) in liver [13] [14] | TTP mutations cause vitamin E deficiency [14]. |
| Vitamin K | SR-BI, CD36, NPC1L1 [13] | Lipid-mediated pathways [13] | Gut microbiota synthesizes vitamin K2 [13] [14]. |
The role of these transporters is crucial for cellular homeostasis. For instance, the tocopherol transfer protein (TTP) in the liver specifically incorporates α-tocopherol (vitamin E) into lipoproteins for distribution to other tissues, and mutations in the TTP gene can lead to vitamin E deficiency [14].
Enzymatic Activation Pathways
Once inside the cell, most lipid-soluble vitamins must undergo enzymatic transformation to become biologically active.
- Vitamin A (Retinol): Retinol is converted to its active form, all-trans retinoic acid, within the cell. This process involves a two-step oxidation: first, retinol is oxidized to retinal by enzymes like alcohol dehydrogenases (ADHs), and then retinal is oxidized to retinoic acid by retinaldehyde dehydrogenases (RALDHs) [14]. All-trans retinoic acid functions as a ligand for nuclear retinoic acid receptors (RARs), which heterodimerize with retinoid X receptors (RXRs) to act as transcription factors for genes governing cell differentiation, proliferation, and development [14].
- Vitamin D (Cholecalciferol): Vitamin D requires a two-step hydroxylation for activation. The first hydroxylation occurs in the liver, catalyzed by the cytochrome P450 enzyme CYP2R1 (25-hydroxylase), which converts vitamin D to 25-hydroxyvitamin D [25(OH)D], the major circulating form and primary indicator of vitamin D status [14] [16]. The second hydroxylation occurs primarily in the kidneys, mediated by CYP27B1 (1α-hydroxylase), which produces the biologically active hormone 1,25-dihydroxyvitamin D [1,25(OH)2D], or calcitriol [14] [16]. This active form binds to the vitamin D receptor (VDR) in the nucleus, regulating gene expression involved in calcium and phosphate homeostasis, immune function, and cell growth [16].
The following diagram illustrates the sequential enzymatic activation pathway of vitamin D, from its precursor form to the active hormone that regulates gene expression.
- Vitamin E: The primary active form, α-tocopherol, itself functions as a potent antioxidant, protecting polyunsaturated fatty acids in cell membranes from oxidative damage [14]. While not activated by a complex enzymatic pathway, its incorporation into cellular membranes is a critical step mediated by transport proteins.
- Vitamin K: Vitamin K acts as a cofactor for the enzyme γ-glutamyl carboxylase, which catalyzes the post-translational carboxylation of glutamate residues to form gamma-carboxyglutamate (Gla) in specific proteins [14]. This modification is essential for the activation of clotting factors (II, VII, IX, X) and proteins involved in bone metabolism [14]. During this reaction, vitamin K hydroquinone is oxidized to vitamin K epoxide, which is then recycled back to its active form by vitamin K epoxide reductase [14].
Experimental Protocols for Investigating Processing Mechanisms
Protocol 1: CRISPR/Cas9-Mediated Gene Editing to Elucidate Transporter Function
This protocol is adapted from studies investigating the role of genes like SDR42E1 in vitamin D absorption and sterol metabolism [15].
Objective: To create a knock-in model of a gene of interest (e.g., SDR42E1) in a colorectal cell line (e.g., HCT116) to study its impact on vitamin D-related pathways.
Materials:
- HCT116 cells (or other relevant cell line)
- eSpCas9-2A-GFP (PX458) plasmid
- Donor DNA template containing the target mutation (e.g., nonsense variant p.Q30*) and a puromycin resistance cassette
- Lipofectamine 3000 transfection reagent
- Puromycin antibiotic
- Materials for RNA sequencing and proteomic analysis
Methodology:
- Guide RNA (gRNA) Design and Plasmid Construction: Design a gRNA specific to the exon of the target gene (e.g., exon 3 of
SDR42E1). Co-transfect HCT116 cells with the Cas9/gRNA plasmid and the donor DNA template using Lipofectamine 3000. - Selection and Cloning: After 48 hours, subject the cells to puromycin selection for two weeks to eliminate non-transfected cells. Isolate single-cell clones and expand them.
- Validation of Editing:
- Genotypic Validation: Perform polymerase chain reaction (PCR) and Sanger sequencing on genomic DNA from the clones to confirm the successful integration of the mutation.
- Phenotypic Validation: Confirm the loss of protein expression via Western blotting and immunofluorescence using a target-specific antibody.
- Functional Assays:
- Cell Viability: Assess the impact of the gene knock-in on cell viability using assays like MTT or CellTiter-Glo over 5-7 days.
- Transcriptomic and Proteomic Analysis: Extract total RNA and protein from wild-type and knock-in cells. Perform RNA sequencing and quantitative proteomic profiling (e.g., via LC-MS/MS) to identify differentially expressed genes and proteins. Pathway analysis can reveal disruptions in sterol absorption and cancer signaling pathways.
- Rescue Experiments: Transiently transfect the knock-in cells with a wild-type version of the gene to confirm the reversal of observed phenotypic effects.
Protocol 2: Cryo-EM Structural Analysis of Vitamin Transporters
This protocol outlines the process for determining the high-resolution structure of a human vitamin transporter, such as a riboflavin transporter, in complex with its substrate [17].
Objective: To determine the atomic structure of a human riboflavin transporter (RFVT2 or RFVT3) in different conformational states to understand the mechanism of riboflavin recognition and transport.
Materials:
- HEK293T cells
- Plasmid encoding the target transporter (e.g., RFVT2 or RFVT3)
- Plasmid for GFP-nanobody fiducial marker fusion
- [¹³C]riboflavin for functional assays
- Detergent for membrane protein purification
- Grids for cryo-EM sample preparation
Methodology:
- Construct Engineering and Expression: Fuse a GFP-nanobody fiducial marker to the target transporter (e.g., between E228-P262 for RFVT2) to create a larger complex for improved cryo-EM particle alignment. Express the engineered construct in HEK293T cells.
- Functional Validation of Construct: Perform transport assays to ensure the engineered construct retains wild-type function. Incubate transfected cells with [¹³C]riboflavin and measure accumulation using quantitative mass spectrometry. Determine kinetic parameters (Km, Vmax) at different pH levels to confirm pH-dependent activity profile.
- Membrane Protein Purification: Solubilize the transporter from cell membranes using a suitable detergent. Purify the protein via affinity and size-exclusion chromatography in the presence of riboflavin.
- Cryo-EM Grid Preparation and Data Collection: Apply the purified protein sample to cryo-EM grids, vitrify them in liquid ethane, and collect a large dataset of micrographs using a high-end cryo-electron microscope.
- Image Processing and Model Building:
- Use software (e.g., RELION, cryoSPARC) for 2D classification, 3D classification, and refinement to generate high-resolution 3D density maps.
- Build an atomic model of the transporter into the density map, manually fitting amino acid side chains and the riboflavin ligand.
- Refine the model against the map and validate its geometry.
The workflow for this structural biology approach is outlined below.
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Research Reagent Solutions for Vitamin Processing Studies
| Reagent / Material | Function / Application | Example from Search Results |
|---|---|---|
| CRISPR/Cas9 System | Targeted gene editing to create knock-in/knockout models for functional genomics. | Used to introduce a nonsense variant (p.Q30*) in the SDR42E1 gene in HCT116 cells [15]. |
| Specialized Cell Lines | Models for studying tissue-specific absorption and metabolism. | HCT116 colorectal carcinoma cell line for intestinal vitamin D studies [15]. HEK293T cells for heterologous protein expression [17]. |
| Isotope-Labeled Vitamins | Tracers for quantitative uptake assays and metabolic flux studies. | [¹³C]riboflavin used in transport assays to measure accumulation via quantitative mass spectrometry [17]. |
| Tagging Systems for Structural Biology | Fiducial markers to facilitate structure determination of small membrane proteins. | GFP-nanobody fusion used to increase particle size and contrast for cryo-EM analysis of RFVTs [17]. |
| Pathway Analysis Software | Bioinformatics tools for interpreting omics data from transcriptomic and proteomic studies. | Used to identify dysregulation in sterol absorption and cancer signaling pathways in SDR42E1-deficient cells [15]. |
Quantitative Data in Vitamin Research
Table 3: Summary of Key Quantitative Data on Vitamins
| Vitamin | Recommended Dietary Allowance (RDA) for Adults | Circulating Form & Half-Life | Deficiency Threshold (Serum) | Toxicity Level (Serum) |
|---|---|---|---|---|
| Vitamin A | Male: 900 µg; Female: 800 µg [13] | Retinol [14] | < 0.70 µmol/L [14] | > 3.5 µmol/L [14] |
| Vitamin D | 15 µg (600 IU) [13] | 25-hydroxyvitamin D [25(OH)D]; ~2-3 weeks [16] | < 20 ng/mL (50 nmol/L) [16] | > 100 ng/mL (risk of hypercalcemia) [14] |
| Vitamin E | 15 mg [13] | α-tocopherol [14] | < 5 µg/mL (Adults) [14] | Not well established [13] |
| Vitamin K | Male: 120 µg; Female: 90 µg [13] | Phylloquinone (K1), Menaquinone (K2) [14] | Prolonged Prothrombin Time (PT) [14] | Rare; no common toxicity [13] |
The intracellular processing of lipid-soluble vitamins represents a finely tuned interface of biophysics, biochemistry, and cell biology. The precise mechanisms of transport protein-mediated uptake and multi-step enzymatic activation are fundamental to their function as essential signaling molecules and cofactors. Contemporary research, leveraging advanced tools from gene editing to high-resolution structural biology, continues to unravel the complexity of these pathways and their profound impact on health and disease. The experimental frameworks and reagents detailed in this whitepaper provide a foundation for further investigation, which is crucial for developing targeted nutritional interventions and novel therapeutic strategies aimed at modulating these critical metabolic pathways.
The absorption and metabolism of lipid-soluble vitamins (A, D, E, and K) represent a complex physiological process influenced by dietary intake, environmental factors, and genetic predisposition. While the fundamental pathways of absorption—including micelle formation, chylomicron packaging, and lymphatic transport—are well-established, significant interindividual variation exists in the efficiency of these processes [14]. A critical source of this variation lies in genetic polymorphisms, subtle DNA sequence variations that occur frequently within populations and can exert modest but biologically significant effects on gene function [18]. This whitepaper explores the genetic regulation of lipid-soluble vitamin absorption by focusing on key polymorphisms in four pivotal genes: the Vitamin D Receptor (VDR), the Vitamin D Binding Protein (GC), the Vitamin K Epoxide Reductase Complex (VKORC1), and Beta-Carotene Oxygenase 1 (BCO1). Understanding these genetic determinants is paramount for advancing personalized nutrition and developing targeted therapeutic strategies, moving beyond a one-size-fits-all approach to a more precise, mechanism-based framework.
Core Genes and Polymorphisms
Vitamin D Receptor (VDR)
The VDR gene, located on chromosome 12q13.11, encodes a nuclear receptor that, upon activation by its ligand calcitriol (1,25-dihydroxyvitamin D), forms a heterodimer with the Retinoid X Receptor (RXR). This complex regulates the transcription of numerous genes involved in calcium and phosphate metabolism, immune function, and cellular proliferation [18]. Several polymorphisms in the VDR gene have been extensively studied for their impact on vitamin D responsiveness and disease risk.
- FokI (rs10735810): This C>T transition in exon 2 creates an alternative start codon, resulting in a truncated VDR protein (424 amino acids versus 427 for the "f" allele). The shorter "F" variant is associated with increased transcriptional activity and a better response to vitamin D supplementation [19].
- TaqI (rs731236): A silent T>C polymorphism in exon 9. The variant "t" allele (presence of the TaqI restriction site) has been associated with a better response to vitamin D supplementation in meta-analyses [19].
- BsmI (rs1544410) & ApaI (rs7975232): These linked polymorphisms in intron 8 do not alter the amino acid sequence of the VDR protein but may influence mRNA stability. Meta-analyses show no significant association between the BsmI and ApaI polymorphisms and the response to vitamin D supplementation [19].
Vitamin D Binding Protein (GC)
The GC gene encodes the Vitamin D Binding Protein (DBP), the primary plasma carrier for vitamin D metabolites. DBP is crucial for the transport and stabilization of vitamin D in circulation and modulates its delivery to target tissues [20]. The GC gene is highly polymorphic, with two common missense variants defining the major isoforms:
- rs7041: This G>T polymorphism results in an amino acid change (Asp→Glu) and defines the
GC1F(T allele) andGC1S(G allele) isoforms. - rs4588: This C>A polymorphism results in an amino acid change (Thr→Lys) and defines the
GC1S(C allele) andGC2(A allele) isoforms.
These polymorphisms significantly influence the concentration and affinity of DBP in plasma, thereby affecting the bioavailability of vitamin D metabolites. Specific haplotypes are associated with varying baseline levels of circulating 25-hydroxyvitamin D [20].
Vitamin K Epoxide Reductase Complex (VKORC1)
The VKORC1 gene encodes the catalytic subunit of the vitamin K epoxide reductase complex, an essential enzyme that recycles vitamin K. This recycling is critical for the continuous gamma-carboxylation of vitamin K-dependent proteins, which are involved in coagulation (e.g., prothrombin) and bone metabolism (e.g., osteocalcin) [14] [21].
- rs9923231 (c.-1639G>A): This promoter polymorphism is the most extensively studied variant in
VKORC1. The A allele is associated with reducedVKORC1gene expression, leading to lower levels of the functional enzyme. This makes individuals more sensitive to vitamin K antagonists like warfarin, as less drug is required to inhibit the already reduced enzyme activity [22] [23]. This SNP accounts for approximately 20-25% of the variance in warfarin dosing requirements [22]. - rs61742245 (Asp36Tyr): This polymorphism has been associated with partial or complete resistance to vitamin K antagonists, requiring unusually high doses to achieve a therapeutic anticoagulant effect [21].
Beta-Carotene Oxygenase 1 (BCO1)
The BCO1 gene encodes the enzyme responsible for the central cleavage of provitamin A carotenoids, such as beta-carotene, into retinal (vitamin A aldehyde) in the intestine and liver [24] [20]. This is the key step in converting dietary carotenoids to bioactive vitamin A.
- rs12934922: A common polymorphism in
BCO1is associated with reduced enzymatic activity. Individuals carrying the variant allele exhibit a lower efficiency in converting beta-carotene to retinol, leading to higher fasting levels of beta-carotene and lower levels of vitamin A in the blood [20]. This genetic variation contributes to the substantial population variability observed in the vitamin A yield from plant-based diets.
Table 1: Key Polymorphisms Affecting Lipid-Soluble Vitamin Absorption and Metabolism
| Gene | Polymorphism | Major/Minor Allele | Functional Consequence | Clinical/Physiological Impact |
|---|---|---|---|---|
| VDR | FokI (rs10735810) | C (F) / T (f) | Alters start codon; shorter, more active protein (F) | The FF genotype is associated with a better response to vitamin D supplementation [19]. |
| VDR | TaqI (rs731236) | T (T) / C (t) | Silent mutation in exon 9 | The variant (Tt+tt) genotype is associated with a better response to vitamin D supplementation [19]. |
| GC | rs7041 | G / T | Determines GC1S/GC1F isoforms; affects DBP affinity/levels | Influences baseline 25-hydroxyvitamin D levels and bioavailability [20]. |
| GC | rs4588 | C / A | Determines GC1S/GC2 isoforms; affects DBP affinity/levels | Influences baseline 25-hydroxyvitamin D levels and bioavailability [20]. |
| VKORC1 | rs9923231 | G / A | Reduced gene expression; less functional enzyme | Increased sensitivity to warfarin; lower therapeutic dose requirement [22] [23]. |
| BCO1 | rs12934922 | A / T | Reduced enzymatic cleavage activity | Decreased conversion of beta-carotene to retinal; higher beta-carotene, lower vitamin A levels [20]. |
Molecular and Physiological Impact
The polymorphisms described in Section 2 exert their influence through diverse molecular mechanisms, ultimately shaping an individual's physiological response to lipid-soluble vitamins.
The VDR FokI polymorphism directly alters the structure of the receptor protein. The shorter "F" variant is believed to be a more potent transactivator of target genes. This translates to a system that is more responsive to a given level of vitamin D, explaining why individuals with the FF genotype show a greater increase in serum 25-hydroxyvitamin D levels after supplementation compared to those with the ff genotype [19]. In contrast, the VKORC1 rs9923231 polymorphism acts at the regulatory level. The A allele leads to reduced transcription of the VKORC1 gene, resulting in a lower basal amount of the enzyme available for vitamin K recycling [22]. When a vitamin K antagonist like warfarin is administered, it more readily inhibits the limited enzyme pool, producing a pronounced anticoagulant effect at a standard dose.
The GC polymorphisms affect the transport and reservoir function of the vitamin D system. Different DBP isoforms have varying affinities for vitamin D metabolites, which influences the fraction of free, bioavailable hormone versus the protein-bound fraction. This can affect the delivery of vitamin D to target tissues and its overall metabolic clearance rate [20]. Finally, BCO1 polymorphisms directly impact nutritional biochemistry. A less active BCO1 enzyme, as seen with the rs12934922 variant, creates a functional bottleneck. Dietary beta-carotene is less efficiently converted to vitamin A, leading to its accumulation and reduced retinol synthesis. This has significant implications for populations relying on plant-based sources for their vitamin A requirements [24] [20].
Table 2: Summary of Physiological Impact and Research Considerations
| Gene | Key Physiological Role | Impact of Significant Polymorphism | Primary Tissue/Cell Type |
|---|---|---|---|
| VDR | Genomic signaling; regulation of calcium homeostasis, immune function, cell differentiation. | Altered transcriptional response to 1,25(OH)2D; differences in bone density, immune response, and cancer risk [19] [18]. | Intestine, Bone, Kidney, Immune Cells |
| GC | Transport and stabilization of vitamin D metabolites in circulation. | Altered baseline 25(OH)D levels and vitamin D bioavailability; potential association with disease risk [20]. | Liver (synthesis), Plasma |
| VKORC1 | Recycling of vitamin K for activation of coagulation and bone proteins. | Altered sensitivity to vitamin K antagonists (warfarin); potential impact on baseline gamma-carboxylation status [21] [22]. | Liver, Bone |
| BCO1 | Conversion of provitamin A carotenoids (e.g., β-carotene) to retinal (Vitamin A). | Reduced vitamin A synthesis from plant sources; variability in provitamin A bioavailability [24] [20]. | Intestinal Enterocytes, Liver |
Experimental and Methodological Approaches
Research into the genetic regulation of vitamin absorption relies on robust methodologies for genotyping, functional validation, and clinical assessment.
Genotyping Techniques
- Polymerase Chain Reaction-Restriction Fragment Length Polymorphism (PCR-RFLP): This traditional method involves amplifying the target gene region containing the polymorphism, followed by digestion with a restriction enzyme that cuts the DNA only in the presence (or absence) of the variant. The resulting fragment patterns are visualized by gel electrophoresis to determine the genotype. This method was used in several of the
VDRstudies included in the meta-analysis [19]. - Sanger Sequencing: Considered the gold standard for validating genetic variants, this technique determines the exact nucleotide sequence of a DNA fragment. It is highly accurate but can be more costly and lower throughput than other methods. It was utilized for confirming
VKORC1polymorphisms in the case reports of warfarin resistance [21]. - Real-Time PCR (qPCR) and Advanced Arrays: Modern high-throughput approaches use TaqMan allele-specific probes or genotyping arrays that can simultaneously assay hundreds of thousands of SNPs across the genome. These methods are essential for genome-wide association studies (GWAS) that have identified novel genetic contributors to warfarin dose response, such as polymorphisms in
CYP4F2[22].
Functional and Clinical Assessment
- Vitamin Status Biomarkers: The functional impact of polymorphisms is assessed by measuring specific biomarkers before and after an intervention.
- Vitamin D: Serum 25-hydroxyvitamin D is the best indicator of overall vitamin D status [14].
- Vitamin K: Functional status is often assessed indirectly via Prothrombin Time (PT)/International Normalized Ratio (INR) for coagulation, or by measuring levels of undercarboxylated osteocalcin in bone [14] [25].
- Vitamin A: Serum retinol levels and the relative proportion of beta-carotene can indicate
BCO1activity [20].
- Clinical Outcome Measures: For
VDR, studies correlate genotypes with Bone Mineral Density (BMD) or fracture risk [25]. ForVKORC1, the primary outcome is the stable therapeutic warfarin dose or the time-in-therapeutic INR range [22] [23]. - In Vitro Studies: Cell culture models (e.g., transfected cell lines) are used to study the mechanistic impact of a polymorphism, such as measuring the transcriptional activity of different
VDRFokI variants in response to calcitriol [18].
Figure 1: Vitamin D Metabolic and Signaling Pathway. The diagram illustrates the activation of vitamin D and its genomic action via the VDR/RXR heterodimer. The location where the FokI polymorphism impacts the system is highlighted in red.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Genetic and Functional Studies
| Reagent / Assay | Specific Example / Kit | Function in Research |
|---|---|---|
| DNA Extraction Kit | QIAamp DNA Blood Mini Kit (Qiagen) | High-quality genomic DNA isolation from whole blood or buccal swabs for downstream genotyping. |
| PCR-RFLP Reagents | Thermo Scientific FastDigest Restriction Enzymes (e.g., TaqI, FokI) | Amplification and allele-specific digestion of target gene sequences for cost-effective genotyping. |
| TaqMan Genotyping Assay | Applied Biosystems TaqMan Drug Metabolism Genotyping Assays | High-throughput, real-time PCR-based allele discrimination for specific SNPs (e.g., CYP2C9*2, *3, VKORC1). |
| Vitamin D ELISA | DIAsource 25-OH Vitamin D TOTAL ELISA | Quantification of total serum 25-hydroxyvitamin D levels to correlate genotype with vitamin D status. |
| Vitamin K HPLC-MS/MS | - | High-performance liquid chromatography with tandem mass spectrometry for precise quantification of vitamin K isoforms (K1, MK-4, MK-7) in plasma or tissues. |
| BCO1 Activity Assay | In vitro cleavage assay with β-carotene substrate and recombinant BCO1 variants. | Measurement of enzymatic kinetics to determine the functional impact of BCO1 polymorphisms on provitamin A conversion. |
Discussion and Future Directions
The study of polymorphisms in VDR, GC, VKORC1, and BCO1 provides a powerful mechanistic framework for understanding the heritable component of lipid-soluble vitamin absorption and metabolism. The evidence clearly demonstrates that common genetic variations can significantly alter protein function, nutrient status, and response to supplementation and medication. This knowledge is foundational to the field of precision nutrition, where dietary recommendations and therapeutic interventions can be tailored to an individual's genetic makeup.
Future research must focus on integrating these genetic factors with other critical dimensions. A key consideration is the distinction between nutrients from whole foods versus supplemental forms, as their metabolic effects and health outcomes may differ substantially [25]. Furthermore, gene-environment interactions and gene-diet interactions are crucial; the phenotypic expression of a genetic variant often depends on contextual factors like overall dietary patterns, sun exposure (for vitamin D), and the use of medications [18]. For instance, the effect of VKORC1 genotype is only manifest upon administration of a vitamin K antagonist.
Future studies should prioritize several areas:
- Long-Term Clinical Outcomes: Moving beyond intermediate biomarkers like serum nutrient levels to harder endpoints such as fracture risk for vitamin D or cancer incidence.
- System-Level Integration: Investigating how polymorphisms in these different genes interact with each other (e.g.,
VDRandGC) to jointly influence vitamin D physiology. - Functional Characterization: Continued work is needed to fully elucidate the molecular mechanisms by which non-coding polymorphisms (e.g.,
VKORC1rs9923231) exert their effects. - Diverse Populations: Expanding research beyond predominantly European ancestries to ensure the global applicability of genetic findings.
In conclusion, the genetic regulation of lipid-soluble vitamin absorption is a sophisticated and multi-layered system. A deep understanding of polymorphisms in VDR, GC, VKORC1, and BCO1 equips researchers and clinicians with the insights needed to decode interindividual variability, paving the way for more effective and personalized healthcare strategies.
The small intestine, a highly specialized organ system primarily responsible for nutrient absorption, is anatomically and functionally segmented into three distinct parts: the duodenum, jejunum, and ileum [5]. This structural specialization enables efficient processing and uptake of diverse nutrients, with each segment exhibiting unique cellular architectures, membrane compositions, and molecular transport mechanisms optimized for specific dietary components. Within the context of lipid-soluble vitamin absorption research, understanding these regional differentiations is crucial for elucidating the complex absorption mechanisms of vitamins A, D, E, and K, and for developing targeted therapeutic interventions for malabsorption syndromes.
The gastrointestinal tract's wide range of functions includes nutrient absorption after the breakdown of carbohydrates, proteins, fats, vitamins, and minerals, all essential for energy production, growth, and cellular maintenance [5]. This review systematically examines the comparative anatomy of duodenal, jejunal, and ileal absorption sites, with particular emphasis on their specialized roles in lipid-soluble vitamin assimilation and the experimental methodologies employed in this field of research.
Anatomical Segmentation and Regional Specializations
Macroscopic Organization
The small intestine exhibits progressive anatomical specialization along its approximately 9-meter length, with each segment demonstrating distinct structural and functional characteristics [5]:
Duodenum: The proximal segment measuring approximately 30 cm (1 foot) in length, which receives the food-acid mixture from the stomach (chyme) along with secretions from the liver, pancreas, and gallbladder [5].
Jejunum: The middle segment measuring approximately 244 cm (8 feet) in length, characterized by prominent circular folds (valves of Kerckring) and villi that maximize absorptive surface area [5] [26].
Ileum: The most distal segment measuring approximately 150-350 cm (5-11.5 feet) in length, distinguished by the presence of Peyer's patches and terminating at the ileocecal valve [5] [27] [26].
Table 1: Anatomical and Functional Characteristics of Small Intestinal Segments
| Parameter | Duodenum | Jejunum | Ileum |
|---|---|---|---|
| Length | ~30 cm (1 foot) [5] | ~244 cm (8 feet) [5] | ~150-350 cm (5-11.5 feet) [5] [27] |
| Primary Absorptive Functions | Iron, calcium, phosphorus, magnesium, copper, selenium, thiamin, riboflavin, niacin, biotin, folate, fat-soluble vitamins A, D, E, K [5] | Lipids (as glycerol and free fatty acids), amino acids, thiamine, riboflavin, niacin, pantothenate, biotin, folate, pyridoxine, ascorbic acid, calcium, phosphorus, magnesium, iron, zinc, chromium, manganese, molybdenum, lipids, monosaccharides, small peptides, fat-soluble vitamins A, D, E, K [5] | Bile salts, vitamin B12, ascorbic acid, folate, cobalamin, vitamin D, vitamin K, magnesium [5] [27] |
| Specialized Structures | Brunner's glands, prominent circular folds [5] | Well-developed circular folds, long villi [5] [26] | Peyer's patches, less prominent circular folds [27] [26] |
| pH Environment | Acidic (receives gastric chyme) [5] | Neutral to slightly alkaline [5] | Neutral to slightly alkaline [5] |
| Lymphoid Tissue | Limited | Moderate | Extensive (Peyer's patches) [26] |
Microanatomical Specializations
Brush Border Architecture
The luminal surface of all three intestinal segments features a brush border composed of microvilli, which are approximately 100 nanometers in diameter and vary in length from 100 to 2,000 nanometers [28]. These tightly packed cytoplasmic projections dramatically increase the apical surface area of enterocytes, facilitating efficient nutrient absorption. The brush border membrane anchors various digestive enzymes as integral membrane proteins, positioning them near specific transporters for prompt absorption of digested nutrients [28].
Research on brush border assembly during development reveals that microvilli formation is a rapid, coordinated process that dramatically expands the digestive and absorptive surface area before the completion of villi maturation [29]. Gene expression studies of microvilli structural components show distinct patterns for Plastin 1 (which bundles and binds actin cores to the terminal web), Ezrin, and Myo1a (both actin core-cell membrane cross-linkers), suggesting sophisticated regulation of brush border assembly and function [29].
Cellular Composition
The intestinal epithelium comprises several specialized cell types that contribute to its absorptive and immunologic functions:
Enterocytes: The predominant cells responsible for nutrient absorption, featuring extensive microvilli on their apical surface [5].
Goblet cells: Scattered between enterocytes, these cells produce alkaline mucus that protects the gastrointestinal lining from shearing forces and acidic secretions [5].
Enteroendocrine cells: Responsible for secreting various hormones including ghrelin, cholecystokinin, glucagon-like peptide 1, and peptide YY, which regulate digestion and nutrient absorption [5].
Microfold (M) cells: Specialized epithelial cells overlying Peyer's patches that sample antigens from the intestinal lumen for immune surveillance [5] [26].
Paneth cells: Located in the crypts, these cells secrete antimicrobial peptides and proteins that regulate gut microbiota and inflammation [5].
The distribution and density of these specialized cell types vary along the length of the small intestine, contributing to segment-specific functional capabilities.
Region-Specific Absorption Mechanisms
Duodenal Absorption Specializations
The duodenum serves as the primary site for mineral absorption and the initial phase of lipid-soluble vitamin uptake. Its unique position immediately distal to the stomach allows it to receive highly acidic chyme, which is subsequently neutralized by pancreatic and biliary secretions to create an optimal environment for nutrient assimilation [5].
The duodenum absorbs most of the iron, calcium, phosphorus, magnesium, copper, selenium, and multiple B vitamins (thiamin, riboflavin, niacin, biotin, folate), in addition to the fat-soluble vitamins A, D, E, and K [5]. The absorption of fat-soluble vitamins occurs through a sophisticated process involving incorporation into micelles - lipid clusters with hydrophobic groups internally and hydrophilic groups externally - which depends on bile secretion and pancreatic enzymes [14]. Following absorption into enterocytes, fat-soluble vitamins are packaged into chylomicrons and secreted into the lymphatic system before entering the bloodstream [14].
Jejunal Absorption Specializations
The jejunum represents the principal site for absorption of dietary lipids, amino acids, and monosaccharides, facilitated by its extensive surface area resulting from well-developed circular folds and long villi [5] [26]. The jejunal enterocytes possess highly specialized transport mechanisms for nutrient uptake:
Lipid Absorption: Dietary triglycerides are broken down into monoglycerides and free fatty acids that incorporate into mixed micelles with bile salts. These micelles transport lipid components to the enterocyte brush border where passive diffusion occurs. Within the enterocyte, resynthesis of triglycerides takes place, followed by incorporation into chylomicrons for transport via lymphatic circulation [5].
Protein Absorption: Peptides and amino acids are transported across the brush border membrane via specific carrier-mediated mechanisms, including sodium-dependent and sodium-independent transport systems [5].
Carbohydrate Absorption: Monosaccharides (glucose, galactose, fructose) are absorbed through active transport (SGLT1 transporter) and facilitated diffusion (GLUT5 transporter) mechanisms [5].
Experimental studies in diabetic rat models have demonstrated that jejunal morphology and brush border membrane composition are dynamically regulated in response to dietary modifications and metabolic states [30]. These adaptations include alterations in villus height and brush border membrane enzyme activities (sucrase and alkaline phosphatase), as well as changes in membrane phospholipid composition, particularly in response to variations in dietary carbohydrate content [30].
Ileal Absorption Specializations
The ileum exhibits several unique absorptive specializations, particularly for vitamin B12 and bile acids, despite its less permeable lining and slower peristaltic contractions compared to proximal segments [27]. The ileum contains specific receptors for vitamin B12-intrinsic factor complexes and bile salts that are exclusively present in its lining [27] [26].
Vitamin B12 Absorption: The process of vitamin B12 absorption involves a sophisticated multi-step mechanism. In the stomach, dietary B12 is released from protein complexes and binds to R-protein (cobalophilin, haptocorrin). In the small intestine, pancreatic enzymes liberate B12 from R-protein, allowing it to bind to intrinsic factor produced by gastric parietal cells. This B12-intrinsic factor complex then travels to the ileum, where specific receptors mediate its uptake into enterocytes [31]. The absorbed B12 subsequently binds to transcobalamin II for transport in the bloodstream [31].
Bile Salt Absorption: The ileum efficiently reabsorbs approximately 95% of conjugated bile salts through specific active transport mechanisms, facilitating enterohepatic circulation [27]. This recycling process is essential for maintaining adequate bile salt pools for efficient lipid digestion and absorption.
Immunological Specialization: The ileum contains abundant lymphoid follicles (Peyer's patches) that constitute an important component of gut-associated lymphoid tissue (GALT) [26]. M cells within the follicle-associated epithelium sample luminal antigens and deliver them to antigen-presenting cells, initiating appropriate immune responses [26].
Experimental Models and Methodologies
In Vivo Animal Models
Streptozotocin-induced diabetic rats have been extensively utilized to investigate the effects of metabolic disorders and dietary interventions on intestinal morphology and function [30]. The following protocol outlines a representative experimental approach:
Animal Model Development:
- Induce hyperglycemia in experimental rats via streptozotocin administration
- Maintain control and diabetic animals for 2 weeks on defined diets varying in carbohydrate, essential fatty acid, cholesterol, or protein content
- Implement strict glycemic monitoring throughout the study period
Tissue Collection and Processing:
- Euthanize animals at predetermined timepoints
- Rapidly excise jejunal segments and flush with ice-cold physiological buffer
- Process tissue for:
- Morphological analysis (villus height measurements)
- Brush border membrane isolation and compositional analysis
- Enzyme activity assays (sucrase, alkaline phosphatase)
- Membrane lipid composition analysis
Analytical Techniques:
- Histological examination using light and electron microscopy
- Spectrophotometric enzyme activity measurements
- Lipid extraction and chromatographic separation
- Statistical analysis of diet-induced and diabetes-related alterations
This experimental paradigm has demonstrated that dietary manipulations produce significant changes in jejunal morphology and brush border membrane composition in both control and diabetic animals, including alterations in villus height and membrane enzyme activities [30]. Furthermore, brush border membrane phospholipids show specific modifications in response to variations in dietary carbohydrate and protein content, with differential effects observed between control and diabetic states [30].
Brush Border Assembly Studies
Research on intestinal brush border assembly during the peri-hatch period in chickens has provided insights into the developmental regulation of microvilli formation and maturation [29]. The experimental methodology includes:
Developmental Time Course Analysis:
- Sample small intestines at multiple developmental stages (prehatch ages 17E and 19E, day of hatch, and posthatch days 1, 3, 7, and 10)
- Process tissues for morphological, molecular, and gene expression analyses
Morphological Assessments:
- Scanning electron microscopy (SEM) for detailed microvilli visualization
- Light microscopy for general histological evaluation
- Quantitative measurements of microvilli length, villi length, microvilli amplification factor, and total enterocyte surface area
Molecular Analyses:
- Real-Time qPCR analysis of microvilli structural genes (Plastin 1, Ezrin, Myo1a)
- Correlation of gene expression patterns with morphological development
These investigations have revealed that microvilli assembly is a rapid, coordinated process that dramatically expands the digestive and absorptive surface area before the completion of villi maturation [29]. The expression patterns of microvilli structural genes portray diverse developmental regulation, suggesting complex control mechanisms underlying brush border formation [29].
Research Reagent Solutions
Table 2: Essential Research Reagents for Intestinal Absorption Studies
| Reagent/Category | Specific Examples | Research Application | Experimental Function |
|---|---|---|---|
| Animal Models | Streptozotocin-induced diabetic rats [30] | Metabolic studies | Models diabetes-induced alterations in intestinal morphology and function |
| Broiler embryos and chicks [29] | Developmental studies | Investigates brush border assembly during peri-hatch development | |
| Histological Tools | Scanning electron microscopy (SEM) [29] | Morphological analysis | High-resolution visualization of microvilli structure |
| Light microscopy [29] | General histology | Tissue structure evaluation and villi measurements | |
| Molecular Biology Reagents | Real-Time qPCR assays [29] | Gene expression analysis | Quantification of microvilli structural gene expression (Plastin 1, Ezrin, Myo1a) |
| Enzyme Activity Assays | Sucrase activity measurement [30] | Brush border function | Assessment of brush border membrane digestive capacity |
| Alkaline phosphatase assay [30] | Membrane integrity | Evaluation of brush border membrane organization and function | |
| Membrane Analysis Methods | Lipid extraction and chromatography [30] | Membrane composition | Analysis of brush border membrane phospholipid and cholesterol content |
| Dietary Formulations | Defined carbohydrate, protein, fat diets [30] | Nutritional studies | Investigation of diet-induced intestinal adaptations |
Visualization of Inter-segmental Relationships and Experimental Approaches
Nutrient Absorption Specialization by Intestinal Segment
Experimental Workflow for Intestinal Absorption Research
Implications for Lipid-Soluble Vitamin Absorption Research
The segmental specializations of the small intestine have profound implications for understanding the absorption mechanisms of lipid-soluble vitamins (A, D, E, and K). These vitamins share common absorption pathways that depend on adequate bile secretion, pancreatic function, and micelle formation, primarily occurring in the duodenum and jejunum [14]. However, specific aspects of their metabolism exhibit segmental preferences:
Vitamin A: Absorbed primarily in the duodenum and jejunum as retinol, with involvement in epithelial cell differentiation and proliferation throughout the intestinal tract [14].
Vitamin D: Undergoes complex activation involving hepatic and renal hydroxylation, with absorption of dietary vitamin D occurring mainly in the proximal small intestine [14].
Vitamin E: As the principal lipid-soluble antioxidant, vitamin E (α-tocopherol) absorption occurs predominantly in the jejunum, with specific tocopherol transfer proteins facilitating its incorporation into lipoproteins in the liver [14].
Vitamin K: Absorbed via both dietary sources (phylloquinone) in the proximal intestine and microbial synthesis (menaquinone) in the colon, with efficient jejunal uptake mechanisms [14].
Research on intestinal segmental specializations provides critical insights for developing targeted drug delivery systems, designing therapeutic interventions for malabsorption syndromes, and understanding the pathophysiology of gastrointestinal disorders that disproportionately affect specific intestinal regions.
The duodenum, jejunum, and ileum exhibit distinct anatomical and functional specializations that enable efficient nutrient processing and absorption along the gastrointestinal tract. The duodenum serves as the primary site for mineral and initial lipid-soluble vitamin absorption, the jejunum as the main site for dietary macronutrient assimilation, and the ileum as a specialized region for vitamin B12 uptake, bile salt reabsorption, and immunological surveillance. These segmental differentiations reflect evolutionary adaptations that maximize digestive efficiency while maintaining immune competence. Contemporary research methodologies, including animal models of metabolic disease, detailed morphological analyses, and molecular techniques, continue to elucidate the complex interplay between intestinal structure and function, with significant implications for understanding lipid-soluble vitamin absorption and developing targeted therapeutic approaches for gastrointestinal disorders.
Advanced Methodologies for Studying and Enhancing Vitamin Absorption
The study of how substances are processed by the body relies heavily on pharmacokinetic (PK) modeling, a mathematical discipline that quantifies the absorption, distribution, metabolism, and excretion (ADME) of compounds [32]. For researchers investigating lipid-soluble vitamins (A, D, E, and K), selecting the appropriate pharmacokinetic model is paramount to understanding their complex behavior in vivo. These vitamins share challenging biopharmaceutical properties, including poor water solubility and absorption processes that are intimately tied to dietary lipid metabolism [33]. Unlike water-soluble compounds, their absorption involves digestion, enterocyte uptake, intracellular re-esterification, and packaging into lipoproteins for transport primarily via the lymphatic system, bypassing first-pass hepatic metabolism initially [34]. This intricate pathway presents unique challenges for predicting their bioavailability and tissue distribution.
Pharmacokinetic models range from simple mathematical constructs that view the body as a single homogeneous unit to highly complex physiologically-based frameworks that mirror the actual anatomy and physiology of the organism [35] [36]. The core purpose of these models is to simplify the body's complexity by grouping tissues and fluids with similar pharmacokinetic properties into "compartments" [32]. This review provides a comprehensive technical guide to these modeling approaches, with specific application to the study of lipid-soluble vitamins, aiming to equip researchers with the knowledge to select optimal models for their investigative needs.
Traditional Pharmacokinetic Models: Foundations and Principles
Core Compartmental Model Architectures
The compartmental approach is a foundational method in pharmacokinetics, simplifying the body into one or more hypothetical spaces where drug distribution is assumed to be uniform [36]. These models are classified based on their complexity and the number of compartments required to accurately describe the drug's concentration-time profile.
One-Compartment Model: This is the simplest model, which assumes the body acts as a single, homogeneous unit where the drug distributes instantaneously and uniformly [35] [32]. After administration, the drug concentration declines mono-exponentially due to elimination. While simple and useful for preliminary analysis, its major limitation is the failure to account for distribution phases, making it unsuitable for drugs that do not rapidly equilibrate throughout the body [32].
Two-Compartment Model: This model provides a more realistic representation by dividing the body into a central compartment (blood and highly perfused tissues like the heart and liver) and a peripheral compartment (less-perfused tissues such as muscle and fat) [35] [32]. The plasma concentration-time curve following intravenous administration exhibits a distinct biphasic decline: a rapid distribution phase where the drug distributes from the central compartment to the peripheral compartment, followed by a slower elimination phase where the drug is removed from the body [32].
Three-Compartment Model: For drugs with complex distribution patterns, a three-compartment model may be necessary. This model further divides the peripheral compartment into two sections: one representing highly perfused tissues and another representing scarcely perfused or deep tissues [32]. This allows the model to capture an additional, slower distribution phase, providing a more accurate fit for drugs that exhibit tri-exponential decline [35].
Non-Compartmental Analysis (NCA): As a model-independent approach, NCA does not assume a specific compartmental structure [35] [36]. It uses statistical moments theory to calculate key PK parameters such as area under the curve (AUC), clearance (CL), and half-life directly from the plasma concentration-time data [35]. Its simplicity and minimal assumptions make NCA valuable in early drug development stages; however, it is less powerful for simulating scenarios outside the studied dosing regimen [35].
Comparative Analysis of Traditional Models
Table 1: Characteristics of Traditional Pharmacokinetic Models.
| Model Type | Structural Assumption | Key Advantages | Key Limitations | Suitability for Lipid-Soluble Vitamins |
|---|---|---|---|---|
| One-Compartment | Single, homogeneous body compartment [32] | Simple, cost-efficient, straightforward calculation [32] | Oversimplified; ignores distribution phase; limited applicability [32] | Low; cannot model complex distribution into adipose tissue |
| Two-Compartment | Central (blood, well-perfused organs) and Peripheral (poorly-perfused tissues) compartments [35] [32] | More accurate; accounts for distribution phase; wider applicability [32] | Increased complexity and data requirements [32] | Moderate; can model initial distribution but may miss deep tissue kinetics |
| Three-Compartment | Central, shallow peripheral, and deep peripheral compartments [32] | High accuracy for complex PK; models multi-phase distribution [32] | Computationally difficult; requires extensive data [32] | High; suitable for modeling long-term storage in deep tissue reservoirs |
| Non-Compartmental (NCA) | No structural assumptions; data-driven [35] | Simple, minimal assumptions, useful for initial PK screening [37] | Limited predictive power for new dosing regimens [35] | Medium; useful for deriving basic parameters (AUC, half-life) from in vivo studies |
Advanced Modeling Approaches: PBPK and Integrative Frameworks
Physiologically-Based Pharmacokinetic (PBPK) Modeling
PBPK models represent a paradigm shift from traditional compartmental models. Instead of hypothetical spaces, they structure the model around real human (or animal) physiology, with compartments representing specific organs and tissues (e.g., liver, gut, adipose, muscle) interconnected by the circulatory system [36] [38]. These models incorporate a wealth of prior knowledge, including:
- Physiological parameters: Organ volumes, blood flow rates, and tissue composition [38].
- Drug-specific physicochemical properties: Solubility, partition coefficient, and protein binding [38].
- System-specific parameters: Expression levels of metabolizing enzymes or transport proteins [38].
A key process in these models is the description of drug distribution into tissues, often using a perfusion rate-limited model, where the rate of distribution is governed by tissue blood flow (QT), tissue volume (VT), and the tissue-to-plasma partition coefficient (KPT) [38]. The differential equation for a non-eliminating tissue in such a model is:
VT × dCT/dt = QT × (CA - CT / KPT) [38]
Where CT is the tissue drug concentration and CA is the arterial blood drug concentration.
Population PK and In Vitro-In Vivo Correlation (IVIVC)
- Population Pharmacokinetics (PopPK): This approach analyzes variability in drug concentrations within a target population. It uses nonlinear mixed-effects models to identify and quantify sources of variability (e.g., demographics, genetics, organ function) and their impact on PK parameters [37] [36]. This is crucial for personalized medicine, especially for lipidsoluble vitamins whose absorption can be highly variable [37].
- In Vitro-In Vivo Correlation (IVIVC): For lipid-based formulations (LBFs) of poorly soluble drugs like lipidsoluble vitamins, establishing a predictive link between in vitro performance and in vivo bioavailability is a major challenge [33]. IVIVC aims to develop a mathematical relationship between an in vitro property (e.g., dissolution or digestion rate) and a relevant in vivo response (e.g., absorption rate or extent) [33]. Successful IVIVCs can reduce development time and serve as a surrogate for bioequivalence studies. The levels of IVIVC include:
- Level A: Point-to-point correlation between in vitro dissolution and in vivo absorption, which is the most informative [33].
- Level B: Comparison of mean in vitro dissolution time and mean in vivo residence time.
- Level C: Correlation of a single dissolution time point to a PK parameter (e.g., AUC).
- Multiple Level C: Correlation at several time points [33].
Experimental Models for Studying Lipid-Soluble Vitamin Absorption
In Vivo and Ex Vivo Systems
Understanding the absorption of lipid-soluble vitamins requires robust experimental models that can capture the complexity of the process, which includes digestion, uptake by enterocytes, intracellular processing, and transport via lipoproteins [34].
In Vivo Models: These models, particularly rodents, are the cornerstone of absorption research as they preserve the integrated physiology of the whole organism [34].
- Lymph Fistula Model (Lymph Duct Cannulation): Considered the "gold standard" for studying intestinal lipid transport, this surgical model involves cannulating the mesenteric or thoracic lymph duct [34]. This allows for the direct collection of intestinal lipoproteins (chylomicrons and VLDL) before they enter the systemic bloodstream, providing uncontaminated insight into the transport phase of lipid-soluble vitamins [34]. The procedure has been refined for use in conscious rodents, with lipid emulsions infused intraduodenally to maintain physiological lymph flow and enable kinetic analysis [34].
- Portal Vein Cannulation: While most large lipoproteins enter the lymphatics, smaller VLDLs can bypass this route and enter the portal circulation directly [34]. Cannulation of the portal vein allows researchers to quantify this alternative transport pathway.
Ex Vivo Models: These use intact intestinal segments outside the body, offering a controlled environment to study specific absorption mechanisms while maintaining some tissue integrity [34].
In Vitro and In Silico Systems
In Vitro Models: These provide high experimental control for mechanistic studies.
- Cell Cultures: Models like Caco-2 cell monolayers (a human colon adenocarcinoma line) are widely used as a model of the human intestinal epithelium to study vitamin uptake and transport [6] [33].
- In Vitro Lipolysis Models: These apparatuses simulate the digestion of lipid-based formulations in the gastrointestinal tract by adding pancreatic enzymes and bile salts. The rate and extent of lipolysis, as well as drug precipitation, can be monitored and are often used to try to establish IVIVC [33].
In Silico Models: Computational approaches are increasingly important.
- Molecular Dynamics (MD) Simulations: As highlighted in the study on vitamins A, E, and K1, MD simulations can provide atomic-level insights into how these vitamins spontaneously penetrate and interact with phospholipid bilayers, revealing details about their orientation, hydrogen bonding, and diffusion within the membrane that are inaccessible to experimental methods [6].
Table 2: Key Experimental Protocols for Lipid-Soluble Vitamin Research.
| Protocol | Core Methodology | Key Measurable Outputs | Application in Lipid-Soluble Vitamin Research |
|---|---|---|---|
| Lymph Fistula Model [34] | Surgical cannulation of the mesenteric/thoracic lymph duct in rodents; intraduodenal infusion of lipid/vitamin emulsion. | - Kinetics of vitamin appearance in lymph- Vitamin association with chylomicrons vs. VLDL- Total lymphatic recovery of administered dose. | Gold-standard for studying the primary transport route for vitamins A, D, E, and K. |
| In Vitro Lipolysis [33] | Simulation of GI digestion using a pH-stat titrator, enzymes (pancreatin), and bile salts in a biorelevant medium. | - Rate and extent of lipid digestion- Pattern of vitamin precipitation/solubilization in digestive phases. | Evaluating performance of lipid-based formulations; understanding formulation-dependent absorption. |
| Molecular Dynamics (MD) Simulation [6] | Atomic-scale computer simulation of vitamins within a model phospholipid (e.g., DPPC) bilayer over nanoseconds. | - Preferred location & orientation in the bilayer- Tilting angle (e.g., 120° for phylloquinone)- Hydrogen-bonding interactions & diffusion coefficients. | Mechanistic study of initial absorption step: passive permeation through the enterocyte membrane. |
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Research Reagent Solutions for Pharmacokinetic and Absorption Studies.
| Item | Function/Application | Example in Context |
|---|---|---|
| Dipalmitoylphosphatidylcholine (DPPC) | A synthetic phospholipid used to create a standardized model of the cell membrane for MD simulations and permeability studies [6]. | Used in MD simulations to study the absorption orientation and dynamics of retinol, α-tocopherol, and phylloquinone in a lipid bilayer [6]. |
| Caco-2 Cell Line | A human colon carcinoma cell line that, upon differentiation, exhibits enterocyte-like properties, forming a polarized monolayer with tight junctions. | A standard in vitro model for predicting intestinal permeability and uptake of compounds, including lipid-soluble vitamins [6] [33]. |
| Stable Isotope-Labeled Vitamins | (e.g., ^2H, ^13C) Non-radioactive tracers that allow for precise tracking of the administered vitamin's metabolic fate using mass spectrometry. | Enables quantitative tracking of vitamin absorption, distribution, and metabolism in complex biological matrices without radioactive hazards. |
| Pancreatin & Bile Salts | Critical components of in vitro lipolysis models. Pancreatin provides digestive enzymes (lipase, colipase), while bile salts emulsify lipids. | Used to simulate the intraluminal digestion of lipid-based drug formulations, predicting their in vivo performance [33]. |
| Apolipoprotein B (ApoB) Assays | Immunoassays to quantify ApoB, the primary structural protein of chylomicrons and VLDL. | Used to measure intestinal lipoprotein secretion in lymph fistula models or cell culture studies, correlating it with vitamin transport [34]. |
Visualizing Model Relationships and Experimental Workflows
Hierarchy of Pharmacokinetic Models
This diagram illustrates the conceptual relationships and progression from the most physiologically detailed to the simplest pharmacokinetic models.
Lipid-Soluble Vitamin Absorption and Modeling Workflow
This flowchart outlines the key physiological stages of lipid-soluble vitamin absorption and links them to the most relevant experimental and computational models used for investigation.
The pharmacokinetic assessment of lipid-soluble vitamins demands a sophisticated toolkit of modeling approaches, each with distinct strengths. Traditional compartmental models offer a simplified, efficient framework for describing plasma concentration-time profiles, while PBPK models provide a more physiologically realistic platform for predicting tissue distribution and extrapolating across populations. The choice of model is not a matter of selecting the "best" one, but rather the most fit-for-purpose. A simple NCA may suffice for initial screening, whereas a full PBPK model may be necessary to understand the complex distribution of vitamin A into the liver or vitamin E into adipose tissue.
The future of modeling in this field lies in integration. Combining insights from atomic-scale MD simulations, which reveal the fundamental interactions between vitamins and membranes [6], with data from gold-standard in vivo models like the lymph fistula [34], will enable the development of more robust PBPK models. Furthermore, the application of population PK approaches will be crucial for understanding and predicting the significant inter-individual variability in the absorption of these essential nutrients, ultimately guiding personalized nutritional and therapeutic strategies.
The efficacy of orally administered bioactive compounds, including lipid-soluble vitamins, is fundamentally constrained by their inherent biopharmaceutical challenges. These challenges include poor aqueous solubility, low permeability across intestinal membranes, and instability in the gastrointestinal environment [39] [40]. A significant proportion of new therapeutic candidates fall into the Biopharmaceutics Classification System (BCS) Class II (low solubility, high permeability) or Class IV (low solubility, low permeability), which severely limits their oral bioavailability [39] [41]. Consequently, high doses are often required to achieve therapeutic effects, which can lead to side effects and reduced patient compliance [39].
Nanocarrier delivery systems have emerged as a transformative strategy to overcome these barriers. These systems, typically smaller than 100 nanometers, leverage their high surface area-to-volume ratio and the ability to be engineered with specific surface properties to enhance the delivery efficiency of encapsulated payloads [39] [42]. For research on lipid-soluble vitamin absorption, nanocarriers offer a powerful tool to investigate and ameliorate the complex mechanisms governing their uptake, transport, and systemic availability. By enhancing solubility, providing protection from degradation, and facilitating transport across mucosal barriers, nanocarriers can significantly improve the bioavailability of these essential nutrients [43] [44].
This whitepaper provides an in-depth technical guide to nanocarrier systems, focusing on their design principles, mechanisms of action, and experimental methodologies relevant to advancing research on lipid-soluble vitamin absorption.
Nanocarrier Types and Their Impact on Bioavailability
Various nanocarrier systems have been developed, each with unique structural and functional characteristics that address specific biopharmaceutical challenges. The selection of a nanocarrier type is crucial for optimizing the delivery of lipid-soluble vitamins.
Table 1: Classification and Mechanisms of Common Nanocarrier Systems
| Nanocarrier Type | Composition | Key Mechanism of Action | Reported Bioavailability Enhancement |
|---|---|---|---|
| Polymeric Nanoparticles | Biodegradable polymers (e.g., PLGA, Chitosan) [45] [41] | Protection from degradation; controlled release; mucoadhesion or mucus penetration [45] [44] | High drug loading capacity, sustained release profiles [41] |
| Lipid-Based Nanoparticles | Lipids (triglycerides), surfactants, emulsifiers [39] [46] | Enhanced solubilization in GI tract; stimulation of lymphatic transport [39] | Piperine-loaded SLNs: 2.5-fold increase [47] |
| Nanoemulsions | Oil, water, surfactant (e.g., Tween) [39] | Increased surface area for dissolution; improved membrane permeability [39] | Resveratrol nanoemulsion: 3.2-fold relative bioavailability [47] |
| Liposomes | Phospholipids forming bilayered vesicles [47] | Encapsulation of hydrophilic and lipophilic compounds; fusion with cellular membranes [47] | Curcumin-loaded liposomes: 9-fold increase in oral bioavailability [47] |
| Nanogels/Nanomatrices | Cross-linked hydrophilic polymers [41] | Swell to retain large amounts of water; enhance solubility and stability [41] | High drug loading for both hydrophobic/hydrophilic drugs [41] |
The core mechanism by which these nanocarriers enhance bioavailability begins with increasing the solubility and dissolution rate of the encapsulated compound, which is the initial step for absorption [39] [41]. Furthermore, they protect their payload from harsh gastric pH and enzymatic degradation [47] [40]. Their small size and modifiable surfaces enable them to navigate the mucus layer and increase residence time at the absorption site, thereby improving the potential for epithelial uptake [45] [44].
Overcoming the Mucus Barrier: Design and Mechanisms
The mucus layer coating the gastrointestinal tract is a major barrier to nanocarrier delivery. It acts as a physical filter and a biochemical trap, rapidly clearing foreign particles [45] [44]. This barrier is particularly relevant for the absorption of lipid-soluble vitamins, as their uptake sites are located beneath this layer. The design of nanocarriers that can efficiently penetrate this barrier is therefore paramount.
The permeability of nanoparticles through mucus is governed by their interaction with mucin, the primary glycoprotein component. These interactions include steric hindrance, electrostatic interactions, hydrophobic interactions, and hydrogen bonding [44]. Optimizing the physicochemical properties of nanocarriers can minimize adhesive interactions and promote diffusion.
Table 2: Impact of Nanoparticle Properties on Mucus Penetration
| Property | Impact on Mucus Penetration | Optimal Design Strategy |
|---|---|---|
| Size | Small size avoids size filtration by the mucus mesh. | Diameters less than the average mucus mesh size (approx. 100 nm) are ideal [45] [44]. |
| Surface Charge | Cationic surfaces bind strongly to anionic mucin; highly anionic surfaces may also be trapped. | Neutral or weakly anionic surfaces minimize electrostatic interaction. Zwitterionic coatings are highly effective [45] [44]. |
| Surface Hydrophilicity | Hydrophobic surfaces undergo unfavorable hydrophobic interactions with mucin. | Grafting with hydrophilic polymers like polyethylene glycol (PEG) creates a hydration layer that reduces mucoadhesion [45] [44]. |
| Shape | Spherical particles may be trapped more easily than elongated shapes in some cases. | Rod-shaped nanoparticles have demonstrated superior penetration compared to spherical ones in certain studies [44]. |
| Stiffness | The effect is complex and context-dependent. | Semi-elastic stiffness may be favorable for mucus penetration [44]. |
The following diagram illustrates the key nanoparticle properties and biological factors that determine success in traversing the mucus barrier.
Mucus Penetration Factors
Advanced strategies involve designing "mucus-penetrating particles" (MPPs) by coating them with dense layers of PEG or other hydrophilic polymers, which effectively shield the core particle from interactions with mucin fibers [45] [44]. Conversely, "mucoadhesive particles" can be designed to prolong residence time at specific sites, which is useful for local drug delivery.
Experimental Protocols for Nanocarrier Evaluation
Robust experimental protocols are essential for the development and characterization of nanocarriers for lipid-soluble vitamin delivery. The following sections detail key methodologies.
Protocol: Preparation of Polysaccharide-Based Nanocarriers
This protocol outlines the preparation of nanocarriers using biopolymers like chitosan or starch, which are known for their biocompatibility and ability to enhance stability and bioavailability [43].
- Polymer Dissolution: Dissolve the selected polysaccharide (e.g., 0.2% w/v chitosan) in an aqueous acid solution (e.g., 1% v/v acetic acid) under magnetic stirring until fully dissolved.
- Bioactive Loading: Disperse or dissolve the lipid-soluble vitamin (e.g., vitamin D3 or a carotenoid) in an appropriate organic solvent (e.g., ethanol). For hydrophobic bioactives, this step often follows the next step for nanoemulsion-based encapsulation.
- Nanoparticle Formation:
- Ionic Gelation (for Chitosan): Add a cross-linking agent, such as tripolyphosphate (TPP) solution (0.1% w/v), dropwise to the chitosan solution under constant stirring. Nanoparticles form spontaneously via electrostatic interaction.
- Emulsion Cross-linking: For hydrophobic compounds, create an oil-in-water emulsion by homogenizing the oil phase (containing the vitamin) with the aqueous polymer solution. Subsequently, add a cross-linker (e.g., glutaraldehyde) to solidify the droplets.
- Self-Assembly: Alternatively, induce nanoparticle self-assembly by adjusting the pH or solvent polarity.
- Purification: Separate the formed nanoparticles from free drug and solvents by centrifugation (e.g., 15,000 rpm for 30 minutes) and wash repeatedly. Purification can also be achieved using dialysis or gel filtration chromatography.
- Lyophilization: Resuspend the nanoparticle pellet in a cryoprotectant solution (e.g., 5% w/v mannitol) and lyophilize to obtain a stable powder for long-term storage.
Protocol: Evaluating Mucus Permeation In Vitro
This experiment assesses the ability of nanocarriers to penetrate mucus, a critical step for intestinal absorption.
- Mucus Preparation: Isolate porcine intestinal mucus from a local slaughterhouse. Centrifuge at 15,000 × g for 30 minutes to remove insoluble debris. Use the supernatant as the native mucus model.
- Diffusion Setup: Use a vertical diffusion cell apparatus. Place a membrane filter (e.g., 0.45 μm pore size) between the donor and receiver chambers. Carefully layer 500 μL of the fresh mucus onto the membrane in the donor chamber.
- Sample Application: Apply the fluorescently labeled nanocarrier suspension (e.g., equivalent to 1 mg/mL of the cargo) on top of the mucus layer in the donor chamber.
- Sampling: The receiver chamber contains a buffer (e.g., PBS, pH 7.4) maintained at 37°C with continuous stirring. At predetermined time intervals (e.g., 0.5, 1, 2, 4 h), withdraw aliquots from the receiver chamber and replace with fresh buffer.
- Analysis: Quantify the amount of nanocarriers that permeated through the mucus layer using a fluorescence spectrophotometer. Calculate the apparent permeability coefficient (P_app) and compare it against a control (e.g., a solution of the free fluorescent dye).
Protocol: Assessing Bioavailability in a Preclinical Model
This in vivo protocol measures the ultimate enhancement in systemic exposure achieved by the nanocarrier formulation.
- Animal Grouping: Divide rodents (e.g., Sprague-Dawley rats) into at least two groups (n=6-8): a control group receiving the free vitamin suspension and a test group receiving the vitamin-loaded nanocarrier formulation. Dose based on body weight.
- Dosing and Sampling: Administer the formulations orally via gavage. Collect blood samples from the retro-orbital plexus or tail vein into heparinized tubes at pre-determined time points (e.g., 0, 0.25, 0.5, 1, 2, 4, 8, 12, 24 h).
- Sample Processing: Centrifuge blood samples immediately to separate plasma. Store plasma at -80°C until analysis.
- Bioanalytical Quantification: Extract the vitamin from plasma samples using liquid-liquid extraction. Quantify the plasma concentration using a validated analytical method, typically High-Performance Liquid Chromatography (HPLC) coupled with UV or mass spectrometry (MS) detection.
- Pharmacokinetic Analysis: Plot plasma concentration versus time curves. Use non-compartmental analysis to determine key pharmacokinetic parameters: Maximum plasma concentration (C~max~), Time to reach C~max~ (T~max~), and Area under the curve (AUC). A significant increase in AUC and C~max~, and/or a decrease in T~max~, indicates enhanced bioavailability [47] [46].
The workflow below summarizes the key stages from formulation to efficacy assessment.
Experimental Workflow
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table details key reagents, materials, and instruments essential for research into nanocarrier-mediated delivery of lipid-soluble vitamins.
Table 3: Essential Research Reagents and Tools
| Category/Item | Specific Examples | Function/Application |
|---|---|---|
| Polymeric Materials | PLGA, Chitosan, Chondroitin sulfate, Sodium alginate, Polyvinyl pyrrolidone (PVP) [41] | Form the core matrix of nanoparticles; provide biocompatibility and controlled release. |
| Lipidic Excipients | Triglycerides, Phospholipids (for liposomes), Poloxamers, Tweens (e.g., Tween 80) [39] [41] | Form lipid nanoparticles, nanoemulsions, and liposomes; act as surfactants and stabilizers. |
| Cross-linkers & Stabilizers | Tripolyphosphate (TPP), Glutaraldehyde, Mannitol, Trehalose [41] [43] | Cross-link polymer chains to form stable nanoparticles; act as cryoprotectants during lyophilization. |
| Characterization Instruments | Dynamic Light Scattering (DLS), HPLC-UV/MS, Transmission Electron Microscope (TEM) [46] | Measure particle size/zeta potential; quantify drug content and release; visualize nanoparticle morphology. |
| In Vitro Models | Caco-2 cell lines, Porcine intestinal mucus, Dialysis membranes, Vertical diffusion cells [45] [44] | Simulate intestinal epithelium for permeability studies; serve as a native mucus barrier for permeation tests. |
Nanocarrier delivery systems represent a sophisticated and highly promising approach to overcoming the fundamental challenges associated with the delivery of lipid-soluble vitamins and other poorly bioavailable compounds. Through rational design that targets specific barriers—such as low solubility with lipid-based systems, instability with protective polymer matrices, and poor mucosal penetration with surface-engineered nanoparticles—researchers can profoundly enhance the absorption and therapeutic efficacy of these molecules. The experimental frameworks and tools outlined in this whitepaper provide a foundation for advancing this critical field of research. As nanotechnology continues to evolve, its integration into nutritional science and pharmaceutical development promises to unlock a deeper understanding of absorption mechanisms and lead to more effective formulations for improving human health.
The human gut microbiome, a complex ecosystem of trillions of microorganisms, exerts profound influence on host physiology, including the absorption and metabolism of essential nutrients. Within the specific context of lipid-soluble vitamin absorption research, targeted modulation of this microbiota presents a promising therapeutic avenue. Lipid-soluble vitamins (A, D, E, and K) are essential for numerous bodily functions, including vision, bone health, antioxidant defense, and coagulation. Their absorption is a complex process that depends on adequate digestive function, biliary secretion, and intestinal integrity. Emerging evidence indicates that the gut microbiota plays a pivotal role in regulating the bioavailability of these vitamins through both direct and indirect mechanisms [48] [49]. This technical guide provides an in-depth examination of three primary microbiota modulation strategies—probiotics, postbiotics, and live microbial interventions—framing their mechanisms and applications within the specific framework of enhancing lipid-soluble vitamin absorption for researchers and drug development professionals.
Defining the Intervention Strategies
Probiotics
Probiotics are defined as "live microorganisms that, when administered in adequate amounts, confer a health benefit on the host" [50] [51]. To be classified as a probiotic, a microorganism must be non-pathogenic, genetically stable, and survive transit through the gastrointestinal tract [51]. Common probiotic strains include lactic acid bacteria (LAB) such as Lactobacillus, Lactococcus, and Bifidobacterium genera, as well as the yeast Saccharomyces boulardii [50] [52] [51]. These microbes are sourced from fermented foods or the gut microbiota of humans and animals and can be consumed as pure formulations or as components of fermented foods like yogurt and cheese [50] [51].
Postbiotics
In contrast, postbiotics are "preparations of inanimate microorganisms and/or their components that confer a health benefit on the host" [53] [50] [54]. This definition, established by the International Scientific Association of Probiotics and Prebiotics (ISAPP), encompasses a range of non-viable microbial materials, including heat-killed cells, cell fragments, and microbial metabolites such as short-chain fatty acids (SCFAs), bacteriocins, extracellular polysaccharides, and cell wall components like peptidoglycans and teichoic acids [53] [50]. Key advantages of postbiotics over their live counterparts include enhanced safety profile—particularly for immunocompromised individuals—greater stability during storage and processing, and the absence of risks associated with live bacteria, such as the transfer of antibiotic resistance genes [53] [50].
Live Microbial Interventions
This category extends beyond traditional probiotics to include advanced therapeutic interventions utilizing live microbes. A prominent example is Fecal Microbiota Transplantation (FMT), which involves transferring processed fecal matter from a healthy donor to a recipient to restore a healthy gut microbial community [55]. Furthermore, the field is being revolutionized by CRISPR-based genetic engineering of probiotic strains, such as Escherichia coli Nissle 1917, to introduce targeted genetic modifications that enhance their therapeutic potential, for instance, by enabling the degradation of antibiotic resistance genes in the gut [52].
Table 1: Comparative Analysis of Microbiota Modulation Strategies
| Characteristic | Probiotics | Postbiotics | Live Microbial Interventions |
|---|---|---|---|
| Definition | Live microorganisms | Inanimate microorganisms and/or their components | Broad range, including advanced probiotics and FMT |
| Key Components | Live Lactobacillus, Bifidobacterium, S. boulardii | Cell fragments, SCFAs, bacteriocins, organic acids | Engineered probiotic strains, donor microbiota |
| Primary Mechanisms | Competitive exclusion, immunomodulation, barrier enhancement | Receptor interaction, immune regulation, metabolic pathway modulation | Microbiome restoration, targeted delivery of therapeutic functions |
| Stability | Lower; requires viability control | High; resistant to environmental conditions | Variable; depends on formulation and host engraftment |
| Safety Profile | Good; caution in immunocompromised | High; suitable for vulnerable populations | Higher risk; requires stringent donor screening |
| Key Advantages | Direct interaction with host and microbiota | Standardized dosage, improved safety, convenient storage | Potent and durable restoration of microbial ecology |
Mechanisms of Action in Lipid-Soluble Vitamin Absorption
The interplay between microbiota-based interventions and the host is multifaceted, involving several direct and indirect pathways that can significantly influence the absorption of lipid-soluble vitamins.
Direct Modulation of the Gut Environment
Probiotics and postbiotics directly influence the intestinal lumen's conditions. Certain probiotic strains produce bile salt hydrolases (BSH), which deconjugate bile acids [49]. This process alters the bile acid pool, potentially enhancing the micellar solubilization of lipid-soluble vitamins, a critical step preceding their absorption. Furthermore, microbial metabolites, particularly the SCFAs acetate, propionate, and butyrate produced from dietary fiber fermentation, can lower intestinal pH. This acidification may improve the solubility and bioavailability of certain lipid-soluble vitamins [48] [49]. Some bacteria are also capable of synthesizing vitamin K and certain B vitamins, contributing directly to the host's vitamin status [48] [49].
Enhancement of Intestinal Barrier Function
The integrity of the intestinal epithelium is paramount for the efficient absorption of lipids and lipid-soluble vitamins. Probiotics and postbiotics strengthen this barrier through multiple mechanisms. They promote the increased production of mucins by goblet cells, forming a protective gel layer [51]. More directly, they upregulate the expression of tight junction proteins (e.g., occludin, ZO-1), which reduces paracellular permeability and prevents the leakage of absorbed nutrients [51]. The SCFA butyrate serves as a primary energy source for colonocytes, promoting epithelial cell health and proliferation, which is essential for maintaining a robust absorptive surface [49] [51].
Immunomodulation and Systemic Metabolism
A significant portion of the health benefits conferred by these interventions is mediated through immune system regulation. They interact with gut immune cells, such as dendritic cells and macrophages, and gut-associated lymphoid tissue (GALT), often promoting a shift towards an anti-inflammatory cytokine profile (e.g., increased IL-10, decreased TNF-α) [51] [56]. This reduction in local and systemic inflammation is crucial, as chronic inflammatory states can impair intestinal absorption and disrupt metabolic homeostasis, indirectly affecting the utilization of lipid-soluble vitamins [55] [56]. Butyrate, for instance, has been shown to activate the GPR109A receptor on immune cells, promoting anti-inflammatory responses [56].
Diagram 1: Mechanisms of Microbiota Modulation in Vitamin Absorption
Experimental Protocols for Efficacy Assessment
In Vitro Model of Vitamin Absorption
Objective: To screen the efficacy of probiotic strains or postbiotic preparations on the uptake of lipid-soluble vitamins using a simulated intestinal epithelium. Methodology:
- Cell Culture: Utilize human intestinal epithelial cell lines (e.g., Caco-2) cultured on permeable transwell inserts to form a polarized monolayer with tight junctions. Confirm monolayer integrity by measuring transepithelial electrical resistance (TEER) regularly [49].
- Intervention: Apply the test intervention (live probiotics, postbiotic supernatant, or purified metabolites) to the apical compartment. For probiotics, a common multiplicity of infection (MOI) of 10:1 to 100:1 (bacteria:cells) is used. For postbiotics, protein content (e.g., 0.1-1.0 mg/mL) can be used for standardization.
- Vitamin Dosing: After a pre-treatment period (e.g., 24 hours), add lipid-soluble vitamins (e.g., vitamin D3 or E acetate) dissolved in a mixed micellar solution to the apical medium to mimic post-prandial conditions.
- Sampling and Analysis: Collect basolateral media after a set incubation period (e.g., 2-6 hours). Quantify vitamin concentration using high-performance liquid chromatography (HPLC) with UV or mass spectrometry detection. Normalize results to cellular protein content or TEER values.
In Vivo Assessment in Vitamin-Deficient Models
Objective: To evaluate the ability of interventions to restore vitamin status and related physiological markers in a live animal model. Methodology:
- Animal Model: Employ rodent models (e.g., mice or rats) rendered deficient in a specific lipid-soluble vitamin (e.g., vitamin A or D) through a defined diet.
- Study Design: Randomize animals into groups: (1) Deficient control, (2) Intervention group (oral gavage or dietary supplementation with probiotic/postbiotic), (3) Positive control (vitamin supplementation). The intervention period typically lasts 4-8 weeks.
- Sample Collection: At endpoint, collect blood via cardiac puncture for serum vitamin analysis (by HPLC). Euthanize animals and dissect tissues (liver, intestine) for vitamin quantification and gene expression analysis.
- Outcome Measures: Primary outcomes are serum and hepatic vitamin levels. Secondary outcomes can include gene expression of vitamin transporters and receptors, histology of intestinal villi, and markers of immune status.
Analyzing Gut Microbiota Composition
Objective: To characterize changes in the gut microbial community structure following intervention. Methodology:
- DNA Extraction: Extract total genomic DNA from fecal or intestinal content samples using a commercial kit designed for stool samples.
- 16S rRNA Gene Sequencing: Amplify the hypervariable regions (e.g., V3-V4) of the bacterial 16S rRNA gene and perform high-throughput sequencing on an Illumina MiSeq or similar platform.
- Bioinformatic Analysis: Process raw sequences using QIIME 2 or Mothur to cluster sequences into operational taxonomic units (OTUs) or amplicon sequence variants (ASVs). Analyze alpha-diversity (within-sample richness) and beta-diversity (between-sample community differences). Use statistical models like LEFSe to identify taxa significantly associated with the intervention [52].
Table 2: Key Analytical Techniques in Vitamin Absorption Research
| Technique | Measurement Target | Application in Research | Key Considerations |
|---|---|---|---|
| High-Performance Liquid Chromatography (HPLC) | Concentration of specific vitamins (A, D, E, K) in serum, tissues, or basolateral media | Gold standard for quantifying vitamin absorption and status | Requires specialized columns and detectors; high sensitivity and specificity |
| Transepithelial Electrical Resistance (TEER) | Integrity and permeability of intestinal epithelial monolayers | Assess the impact of interventions on gut barrier function in real-time | Non-destructive; allows for longitudinal monitoring in cell culture models |
| 16S rRNA Gene Sequencing | Composition and relative abundance of bacterial taxa in a community | Profiling gut microbiota changes in response to intervention | Identifies taxonomy but not direct function; requires bioinformatics expertise |
| Gas Chromatography-Mass Spectrometry (GC-MS) | Microbial metabolites, particularly SCFAs (acetate, propionate, butyrate) | Linking microbial metabolic activity to host physiological outcomes | Quantitative and highly sensitive; requires metabolite extraction |
| Quantitative PCR (qPCR) | Gene expression of host transporters, receptors, or tight junction proteins | Understanding molecular mechanisms of absorption at the host level | Requires high-quality RNA and specific primer/probe sets |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Microbiota and Vitamin Studies
| Reagent / Material | Function & Utility | Example Application |
|---|---|---|
| Caco-2 Cell Line | A human colorectal adenocarcinoma cell line that differentiates into enterocyte-like cells, forming a polarized monolayer with functional tight junctions. | In vitro model for studying vitamin transport and gut barrier function [49]. |
| Transwell Permeable Supports | Polyester or polycarbonate membrane inserts for cell culture, allowing separate access to apical and basolateral compartments. | Culturing Caco-2 monolayers for vitamin uptake and transport assays [49]. |
| Mixed Micellar Solution | An in vitro simulation of intestinal micelles, typically containing bile salts, monoolein, and fatty acids. | Solubilizing lipid-soluble vitamins for absorption studies in cell culture models. |
| Bile Salt Hydrolase (BSH) Activity Assay Kit | Measures the enzymatic activity of BSH, which deconjugates bile acids and influences lipid absorption. | Screening probiotic strains for their potential to modify the host bile acid pool [49]. |
| 16S rRNA Metagenomic Sequencing Kit | Provides reagents for amplifying and preparing the bacterial 16S rRNA gene for high-throughput sequencing. | Profiling the composition of gut microbiota in animal models or human subjects pre- and post-intervention [52]. |
| Recombinant Engineered Probiotic Strains | Probiotics (e.g., E. coli Nissle 1917) genetically modified using CRISPR-Cas systems to express or knock out specific functions. | Investigating the role of specific bacterial genes or pathways in vitamin absorption (e.g., vitamin synthesis genes) [52]. |
Diagram 2: Experimental Workflow for Vitamin Absorption Research
The strategic modulation of the gut microbiota through probiotics, postbiotics, and advanced live microbial interventions represents a sophisticated and promising approach to enhancing the absorption of lipid-soluble vitamins. The mechanisms are multifaceted, involving direct modulation of the intestinal environment, reinforcement of the epithelial barrier, and systemic immunomodulation. For researchers in this field, a combination of robust in vitro screening models and physiologically relevant in vivo studies, supported by modern 'omics' technologies, is essential for elucidating these complex interactions. As the field progresses, the integration of genetically engineered microbial strains and well-characterized postbiotic formulations holds significant potential for developing targeted nutritional and therapeutic strategies to address vitamin deficiencies and improve human health.
The efficacy of interventions involving lipid-soluble vitamins (A, D, E, and K) is critically dependent on their successful absorption and systemic availability. This whitepaper explores the development and application of a panel of biochemical biomarkers to serve as functional indicators of absorption for these vitamins. Specifically, we evaluate the utility of bone turnover markers (BTMs)—undercarboxylated osteocalcin (ucOC), procollagen type I N-terminal propeptide (P1NP), and C-terminal telopeptide of type I collagen (β-CTX-I)—alongside lipid peroxidation markers to provide a sophisticated, mechanistic window into the biological activity of absorbed vitamins. Framed within a broader thesis on lipid-soluble vitamin absorption research, this guide provides drug development professionals with the technical foundation and experimental protocols necessary to deploy these biomarkers in preclinical and clinical studies.
Biomarker Profiles and Physiological Context
Bone Turnover Markers (BTMs) as Indicators of Vitamin K and D Status
Bone is a dynamic tissue that undergoes constant remodeling, a process reflected in the systemic concentrations of BTMs. The International Osteoporosis Foundation (IOF) and the International Federation of Clinical Chemistry and Laboratory Medicine (IFCC) have designated P1NP and β-CTX-I as reference markers for bone formation and resorption, respectively [57] [58]. Their clinical utility, however, extends to assessing the biological impact of vitamins that regulate bone metabolism.
- P1NP (Procollagen type I N-terminal propeptide): A formation marker, P1NP is a cleavage product released during the synthesis of type I collagen, the primary organic constituent of bone matrix. Its serum concentration reflects the rate of osteoblast-mediated bone formation [57].
- β-CTX-I (β-isomerized C-terminal telopeptide of type I collagen): A resorption marker, β-CTX-I is a degradation product generated during the osteoclastic breakdown of type I collagen. Its level in serum or plasma is a measure of bone resorption rate [57].
- ucOC (Undercarboxylated osteocalcin): Osteocalcin is a vitamin K-dependent protein produced by osteoblasts. Its biological activity in bone mineralization depends on vitamin K-mediated γ-carboxylation. Elevated levels of the uncarboxylated form (ucOC) are a functional indicator of vitamin K deficiency [25] [59]. Furthermore, ucOC has been implicated in glucose metabolism, with prospective studies showing that increases in ucOC are associated with improved insulin sensitivity (decreased HOMA-IR) [59].
Lipid Peroxidation Markers as Indicators of Vitamin E Antioxidant Status
The absorption of vitamin E (α-tocopherol) can be gauged indirectly through its primary function as a chain-breaking antioxidant in lipid membranes. Its efficacy in preventing the peroxidation of polyunsaturated fatty acids (PUFAs) can be quantified by measuring specific secondary oxidation products.
- Malondialdehyde (MDA): One of the most studied secondary products of lipid peroxidation, MDA is a highly reactive and mutagenic dialdehyde. It is frequently measured via its reaction with thiobarbituric acid (TBARS assay), though more specific methods like LC-MS/MS are recommended for accurate quantification [60].
- 4-Hydroxy-2-nonenal (4-HNE): A toxic aldehyde generated from the peroxidation of omega-6 fatty acids, 4-HNE is a key mediator of oxidative stress and can form adducts with proteins, affecting their function. Its concentration serves as a sensitive marker of lipid peroxidation intensity [60].
- Lipid Hydroperoxides (LOOH): These are the primary products of the lipid peroxidation propagation phase and represent the initial oxidative damage to PUFAs [60].
Quantitative Biomarker Data and Reference Intervals
The clinical and research interpretation of biomarker data requires an understanding of reference intervals and typical responses to interventions. The tables below summarize key quantitative data.
Table 1: Selected Reference Intervals for Key Bone Turnover Markers in Postmenopausal Women
| Biomarker | Population | Reported Reference Interval | Notes |
|---|---|---|---|
| P1NP | Postmenopausal Women | Varies by study and population [57] | A systematic review found a lack of uniformity in reporting reference intervals across 29 studies. |
| β-CTX-I | Postmenopausal Women | Varies by study and population [57] | Standardized, population-specific reference intervals are needed. |
Table 2: Effects of Vitamin D Supplementation on Bone Turnover Markers in Deficient Subjects
| Study Population | Intervention | Change in P1NP | Change in β-CTX-I | Notes |
|---|---|---|---|---|
| Adults with vitamin D deficiency (Baseline 34.0 nmol/L) [61] | 20,000 IU/week for 4 months | Significant decrease (Delta: -1.2 μg/L) | No significant change | The effect was more pronounced in subjects with high baseline PTH. |
| Multi-ethnic immigrant population (Baseline 29 nmol/L) [62] | 10 or 25 μg/day for 16 weeks | No significant change (MD: -1.2 μg/L) | No significant change (MD: -0.005 μg/L) | Supplementation increased 25(OH)D and decreased PTH, but did not affect BTMs. |
Table 3: Lipid Peroxidation Markers and Their Significance
| Marker | Chemical Nature | Significance as an Absorption Indicator | Preferred Assay |
|---|---|---|---|
| Malondialdehyde (MDA) | Reactive dialdehyde | Most popular marker; indicates overall peroxidation load of omega-3/6 PUFAs [60]. | LC-MS/MS (for specificity) |
| 4-HNE | Reactive aldehyde | Most toxic product; indicates significant oxidative stress and tissue damage [60]. | GC-MS, HPLC |
| Lipid Hydroperoxides (LOOH) | Primary oxidation product | Direct measure of the initial peroxidation reaction [60]. | FOX assay, HPLC |
Signaling Pathways and Biomarker Interrelationships
The biomarkers discussed are integral components of specific biological pathways. The following diagrams, generated using DOT language, illustrate the key pathways involving vitamin K and E.
Vitamin K-Dependent Bone-Carboxylation Pathway
This pathway illustrates the role of vitamin K in bone matrix protein carboxylation and how ucOC serves as a functional absorption and status marker.
Vitamin E Antioxidant Function and Peroxidation Pathway
This diagram depicts the antioxidant role of absorbed vitamin E in mitigating lipid peroxidation, the formation of peroxidation markers, and their downstream effects.
Experimental Protocols for Biomarker Analysis
Protocol: Assessing Vitamin K Status via ucOC and BTMs
This protocol outlines a longitudinal study design to evaluate vitamin K absorption and efficacy using bone-related biomarkers.
- Objective: To determine the bioavailability and biological activity of an orally administered vitamin K supplement by monitoring changes in ucOC and BTMs.
- Study Population: Postmenopausal women or elderly men, after an overnight fast.
- Sample Collection: Serum or plasma samples at baseline, 4 weeks, and 12 weeks. Samples for β-CTX-I require strict fasting and collection before 10:00 a.m. to minimize diurnal variation [57] [58].
- Intervention: Daily oral dose of Vitamin K (e.g., phylloquinone or menaquinone).
- Biomarker Analysis:
- ucOC: Measure using ELISA or specific immunoassays. A significant decrease in ucOC levels post-intervention indicates successful absorption and biological utilization for protein carboxylation [25] [59].
- P1NP & β-CTX-I: Analyze using automated, standardized immunoassays (e.g., electrochemiluminescence). The IOF/IFCC recommends these as reference BTMs. A reduction in both markers may indicate an overall suppression of bone turnover, which can be a positive outcome in high-turnover states [57] [58] [61].
- Data Interpretation: Successful vitamin K absorption is primarily confirmed by a reduction in %ucOC. Concurrent changes in P1NP and β-CTX-I provide insight into the compound's broader effect on bone metabolism.
Protocol: Evaluating Vitamin E Bioavailability via Lipid Peroxidation Markers
This protocol uses a challenge model to assess if absorbed vitamin E is functionally active in combating oxidative stress.
- Objective: To establish the functional antioxidant status following vitamin E supplementation by measuring lipid peroxidation markers before and after an oxidative challenge.
- Study Population: Healthy adults or populations with elevated oxidative stress.
- Study Design: Randomized, placebo-controlled trial. Baseline fasting blood samples are collected.
- Intervention: Daily oral vitamin E (e.g., RRR-α-tocopherol) for a minimum of 8 weeks.
- Oxidative Challenge (Optional): At the end of the supplementation period, an ex vivo challenge of serum or isolated LDL with a pro-oxidant (e.g., copper sulfate or AAPH) can be performed.
- Biomarker Analysis:
- MDA: Quantify using LC-MS/MS for high specificity. A reduced post-supplementation MDA level, especially after an oxidative challenge, indicates effective antioxidant activity of the absorbed vitamin E [60].
- 4-HNE: Measure using GC-MS or HPLC. A decrease in 4-HNE adducts or free serum levels signifies protection against severe lipid peroxidation [60].
- Lipid Hydroperoxides (LOOH): Use the ferrous oxidation-xylenol orange (FOX) assay or HPLC to measure primary oxidation products.
- Data Interpretation: Effective absorption and biological activity of vitamin E are demonstrated by a significant attenuation in the rise of lipid peroxidation markers following the challenge compared to placebo.
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Reagents and Assays for Biomarker Analysis
| Item | Function/Application | Examples & Notes |
|---|---|---|
| Standardized P1NP Assay | Quantifying bone formation rate. | Automated immunoassays recognized by the IOF/IFCC [57] [58]. |
| Standardized β-CTX-I Assay | Quantifying bone resorption rate. | Automated immunoassays. Requires standardized patient preparation (fasting, morning draw) [57] [58]. |
| ucOC-Specific ELISA | Differentiating and quantifying undercarboxylated osteocalcin. | Commercial kits available that use antibodies specific to the uncarboxylated form. |
| LC-MS/MS System | Gold-standard for specific quantification of MDA and other peroxidation products. | Provides high specificity over traditional TBARS assays [60]. |
| GC-MS System | Sensitive detection and quantification of volatile aldehydes like 4-HNE. | |
| SPC Water Model | Molecular dynamics simulations for studying vitamin-membrane interactions. | Used in computational studies to model the absorption of fat-soluble vitamins like phylloquinone [6]. |
| DPPC Lipid Bilayer | In silico model for studying vitamin absorption mechanisms. | A computational model to investigate the location and orientation of vitamins during membrane penetration [6]. |
The study of drug absorption mechanisms is a cornerstone of pharmaceutical development, particularly for compounds with complex bioavailability pathways such as lipid-soluble vitamins. Understanding the interplay between in vitro models, which provide controlled mechanistic insights, and in vivo systems, which capture full physiological complexity, is essential for advancing predictive capabilities in drug development. Research on lipid-soluble vitamins (A, D, E, and K) provides an excellent framework for exploring these relationships, as their absorption involves intricate processes including micellar solubilization, chylomicron incorporation, lymphatic transport, and complex intracellular trafficking [25] [63]. These vitamins share absorption pathways with many lipophilic drugs, making them valuable model compounds for investigating broader principles of lipid-soluble compound absorption.
The fundamental challenge in absorption modeling lies in bridging the gap between simplified, controlled in vitro systems and the complex, dynamic in vivo environment. For lipid-soluble vitamins, this is further complicated by their dependence on dietary fat, bile secretion, and metabolic transformations that influence their bioavailability [63] [6]. Recent advances in experimental models and computational approaches have enhanced our ability to simulate these processes, yet significant limitations remain in fully recapitulating the human gastrointestinal environment and its impact on absorption kinetics [64] [65]. This review systematically examines the current landscape of absorption models, their applications in drug development, and their specific relevance to lipid-soluble vitamin research, with the aim of providing researchers with a comprehensive framework for model selection and interpretation.
Current Experimental Models: A Comparative Analysis
In Vitro Models and Their Applications
In vitro models provide controlled, reproducible systems for investigating specific aspects of absorption mechanisms without the complexity of whole organisms. These models range from simple cell monolayers to more complex co-culture systems that better mimic intestinal physiology.
Cell-based models represent the most widely used approach for initial absorption screening. The Caco-2 cell line, derived from human colon adenocarcinoma, spontaneously differentiates into a polarized monolayer exhibiting microvilli, tight junctions, and various transport proteins characteristic of small intestinal enterocytes [65]. This model has been extensively employed to study the absorption mechanisms of lipid-soluble vitamins, including their passive diffusion, carrier-mediated transport, and metabolic processing. For instance, molecular dynamics simulations using phosphatidylcholine bilayers have revealed how structural features of vitamins A, E, and K1 influence their orientation and movement across lipid membranes, with retinol showing the highest structural flexibility and diffusion coefficient [6]. Similarly, MDCK cells serve as an alternative renal epithelial model, though their relevance to intestinal absorption is more limited [65].
Advanced in vitro systems have emerged to address limitations of simple monolayer cultures. Co-culture models incorporating mucus-producing cells (e.g., HT29-MTX), M-cells, or immune cells provide a more physiologically relevant microenvironment that influences compound permeability and metabolism [64]. The HepaRG cell line, which exhibits highly differentiated hepatic functions, has proven valuable for studying vitamin D metabolism and enterolepatic recycling [64]. For lipid-soluble vitamins, which undergo complex intracellular processing and incorporation into chylomicrons, these advanced systems offer insights beyond simple transmembrane passage.
Table 1: Comparison of Primary In Vitro Models for Absorption Studies
| Model Type | Advantages | Limitations | Applications in Lipid-Soluble Vitamin Research |
|---|---|---|---|
| Caco-2 Monolayer | Low cost, easy standardization, high throughput screening for permeability | Lack of mucus layer, limited metabolic enzyme expression, does not fully represent human enterocytes | Study of transmembrane passive diffusion; transport mechanisms; drug-vitamin interactions |
| MDCK Cells | Rapid growth, well-formed tight junctions | Canine origin with potential species differences in transporter expression | Rapid screening of passive transcellular transport; paracellular pathway assessment |
| HepaRG Cells | Highly differentiated hepatic functions, relevant cytochrome P450 expression | Limited applicability for intestinal absorption | Metabolism and toxicity studies of vitamin derivatives; metabolic activation |
| Co-culture Systems | Better physiological relevance; inclusion of multiple cell types | More complex culture requirements; variable reproducibility | Study of mucus penetration; vitamin uptake in presence of different intestinal cell types |
In Vivo and Ex Vivo Models
In vivo models provide the full physiological context for absorption studies, including the influence of gastrointestinal motility, blood flow, neural and endocrine regulation, and enterolepatic circulation. Whole animal studies, typically conducted in rodents or larger species, remain the gold standard for evaluating overall bioavailability and identifying systemic distribution patterns [65]. For lipid-soluble vitamins, in vivo models have been essential for understanding how dietary factors, genetic polymorphisms, and pathological conditions influence absorption efficiency. Recent compartmental modeling of postprandial plasma retinyl ester kinetics in humans has demonstrated how sophisticated pharmacokinetic analysis of in vivo data can quantify vitamin A absorption efficiency, with studies reporting absorption rates of 72-81% in healthy adults [66].
Ex vivo and in situ models offer intermediate complexity between cell cultures and whole animals. These systems maintain intact intestinal architecture, including the epithelial barrier, transporters, and enzymatic activity, while allowing better experimental control than in vivo models [65]. The everted gut sac technique, intestinal perfusion models (e.g., single-pass intestinal perfusion), and using chamber apparatus have been particularly valuable for investigating region-specific absorption of lipid-soluble vitamins along the gastrointestinal tract.
Table 2: In Vivo and Ex Vivo Models for Absorption Studies
| Model Type | Advantages | Limitations | Applications in Lipid-Soluble Vitamin Research |
|---|---|---|---|
| Whole Animal Models | Full physiological context; long-term studies possible; systemic responses | High cost; ethical concerns; species differences; inter-individual variability | Bioavailability assessment; dose-response relationships; tissue distribution studies |
| Ex Vivo Intestinal Tissue | Retention of intestinal structure and function; direct observation possible | Limited tissue viability; absence of systemic factors; altered microenvironment | Mechanistic studies of vitamin transport; carrier-mediated uptake; metabolism during absorption |
| In Situ Perfusion Models | Maintains blood flow and neural connections; better preserves tissue viability | Technically challenging; anesthesia effects; limited experimental duration | Regional absorption differences; kinetics of vitamin uptake; influence of luminal factors |
Methodologies and Experimental Protocols
Protocol for Caco-2 Transwell Transport Studies
The Caco-2 model remains a cornerstone for in vitro absorption studies, with standardized protocols ensuring reproducibility across laboratories. The following protocol outlines the key steps for assessing compound transport, with specific considerations for lipid-soluble vitamins:
Cell Culture and Differentiation: Plate Caco-2 cells at a density of 1×10^5 cells/cm² on collagen-coated polyester membrane Transwell inserts (3.0 μm pore size). Maintain cells in DMEM supplemented with 10% fetal bovine serum, 1% non-essential amino acids, 100 U/mL penicillin, and 100 μg/mL streptococcus at 37°C in 5% CO₂. Change media every 2-3 days for 21-28 days to allow full differentiation [65].
Monolayer Integrity Validation: Measure transepithelial electrical resistance (TEER) using an epithelial voltohmmeter, accepting values >300 Ω·cm² for differentiated monolayers. Confirm integrity by assessing apparent permeability (Papp) of marker compounds: lucifer yellow (<1×10^-6 cm/s) for paracellular pathway and propranolol (>1×10^-5 cm/s) for transcellular passive diffusion [65].
Experimental Setup for Lipid-Soluble Compounds: Prepare test solutions containing the lipid-soluble vitamin (e.g., 10-100 μM) in fasted-state simulated intestinal fluid (FaSSIF) or fed-state simulated intestinal fluid (FeSSIF) to mimic physiological solubilization conditions. Add to the apical compartment (donor) while the basolateral compartment (receiver) contains protein-containing buffer (e.g., 4% BSA) to accept transported compounds [6].
Sampling and Analysis: Collect samples from the receiver compartment at predetermined time points (e.g., 30, 60, 90, 120 min) and replace with fresh buffer. Analyze samples using HPLC-MS/MS for sensitive quantification of vitamin compounds and their metabolites. Calculate apparent permeability (Papp) using the formula: Papp = (dQ/dt)/(A×C₀), where dQ/dt is the transport rate, A is the membrane surface area, and C₀ is the initial donor concentration [6] [65].
Data Interpretation: For lipid-soluble vitamins, compare transport rates under different solubilization conditions and in the presence of transport inhibitors to elucidate specific absorption mechanisms. Molecular dynamics simulations can complement these studies by providing atomic-level insights into vitamin-membrane interactions [6].
Protocol for In Vivo Absorption Studies
In vivo studies provide critical validation for findings from in vitro systems. The following protocol describes a controlled feeding study design for quantifying lipid-soluble vitamin absorption in humans:
Subject Preparation and Baseline Assessment: Recruit subjects according to institutional ethical guidelines. After an overnight fast, collect baseline blood samples for determination of fasting vitamin levels. For vitamin A absorption studies, measure baseline retinyl esters as these reflect recent intake rather than stored vitamin [66].
Controlled Dose Administration: Administer a precise dose of the vitamin (e.g., 1.91 μmol unlabeled vitamin A) with a standardized breakfast containing a specific amount of fat (e.g., 7 g canola oil mixed with 145 g fat-free yogurt) to ensure consistent micelle formation and absorption. Maintain controlled feeding conditions with standardized snacks and meals throughout the study period [66].
Serial Blood Sampling: Collect blood samples at frequent intervals (e.g., every 30 minutes for 8 hours) to capture the absorption kinetics. For retinyl esters, which appear in circulation specifically from newly absorbed vitamin A, this provides a direct measure of absorption efficiency without interference from endogenous stores [66].
Compartmental Modeling: Analyze the time-course data using sophisticated modeling approaches. Develop a physiologically realistic compartmental model (e.g., 12 compartments with 10 adjustable parameters) to describe the absorption, distribution, and clearance processes. Use software such as Simulation, Analysis and Modeling (SAAM) to fit the model to experimental data and estimate absorption parameters [66].
Validation and Refinement: Validate model predictions against independent measures of vitamin status or using stable isotope techniques. Refine the model structure and parameters based on these comparisons to improve predictive accuracy [66].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions for Absorption Studies
| Reagent/Material | Function/Application | Considerations for Lipid-Soluble Vitamin Research |
|---|---|---|
| Caco-2 Cell Line | Human intestinal epithelial model for permeability screening | Requires 21-28 day differentiation; demonstrates relevant transport proteins for vitamins |
| Simulated Intestinal Fluids (FaSSIF/FeSSIF) | Mimic physiological solubilization conditions | Critical for lipid-soluble vitamins requiring micellar incorporation for absorption |
| Transwell Inserts | Permeable supports for cell culture creating apical and basolateral compartments | Standard 3.0 μm pore size, various diameters available; collagen coating improves cell attachment |
| Transepithelial Electrical Resistance (TEER) Meter | Monitors monolayer integrity and tight junction formation | Essential quality control; values >300 Ω·cm² indicate acceptable monolayer integrity |
| LC-MS/MS Systems | Sensitive quantification of vitamins and metabolites | Enables detection of low concentrations; can distinguish different vitamers (e.g., D2 vs D3) |
| Vitamin Reference Standards | Quantification and metabolite identification | Must include relevant metabolites (e.g., 25-OH-D3 for vitamin D studies) |
| Specific Transport Inhibitors | Elucidation of absorption mechanisms | Examples: bile acid transporters inhibitors for studying vitamin D absorption |
| Radiolabeled Vitamins (³H, ¹⁴C) | Tracing absorption and distribution pathways | Requires specialized handling facilities; provides unparalleled sensitivity for mass balance studies |
Advanced Applications and Integration Approaches
In Vitro-In Vivo Correlation (IVIVC) and Modeling Approaches
The establishment of correlations between in vitro dissolution/release profiles and in vivo pharmacokinetic parameters represents a significant advancement in predictive absorption modeling. IVIVC allows researchers to use in vitro data as a surrogate for in vivo bioavailability studies, particularly for quality control and formulation optimization [67]. For lipid-soluble vitamins, which often require specialized delivery systems to overcome solubility limitations, IVIVC provides a valuable tool for evaluating formulation performance.
Three levels of IVIVC are recognized in regulatory guidance:
- Level A: Point-to-point correlation between in vitro dissolution and in vivo absorption, representing the highest level of predictive capability. This approach can support biowaivers for formulation changes and is most preferred by regulatory agencies [67].
- Level B: Uses statistical moment analysis to compare mean in vitro dissolution time with mean in vivo residence or absorption time. While useful for formulation development, it offers limited predictive power for actual plasma profiles [67].
- Level C: Establishes a single-point relationship between a dissolution parameter (e.g., t50%) and a pharmacokinetic parameter (e.g., Cmax or AUC). This provides limited but potentially useful early development insights [67].
Model-Informed Drug Development (MIDD) represents a more comprehensive approach to integrating in vitro and in vivo data. MIDD employs quantitative models, including physiologically based pharmacokinetic (PBPK) modeling, population PK/PD analysis, and quantitative systems pharmacology (QSP), to predict in vivo performance based on in vitro inputs [68]. For lipid-soluble vitamins, PBPK models can incorporate specific absorption processes such as micellar solubilization, enterocyte uptake, chylomicron incorporation, and lymphatic transport, providing a mechanistic framework for predicting bioavailability under different physiological conditions [68].
Emerging Technologies and Future Directions
Several emerging technologies show promise for addressing current limitations in absorption modeling:
Microphysiological Systems (MPS), including organ-on-a-chip platforms, offer more physiologically relevant environments by incorporating fluid flow, mechanical stimulation, and multi-tissue interactions. These systems can potentially replicate the intestinal lumen, epithelial barrier, and underlying vasculature in a more realistic manner than static cultures [64] [65].
Stem cell-derived intestinal models using induced pluripotent stem cells (iPSCs) enable the generation of human intestinal tissues with patient-specific characteristics. These models potentially capture genetic polymorphisms that influence vitamin absorption and metabolism, supporting personalized nutrition and medicine approaches [64].
Advanced imaging techniques such as high-resolution in vivo microscopy and molecular imaging provide unprecedented views of absorption processes at the cellular and subcellular levels. For lipid-soluble vitamins, these techniques can visualize intracellular trafficking, metabolic conversion, and incorporation into chylomicrons [65].
Molecular dynamics simulations offer atomic-level insights into the interactions between lipid-soluble vitamins and biological membranes. Recent simulations have revealed how structural features of vitamins A, E, and K influence their orientation and movement within lipid bilayers, with specific hydroxyl groups mediating hydrogen bonding with phospholipid head groups [6].
Visualizing Model Applications and Relationships
The following diagram illustrates the strategic integration of different absorption models in drug development and their specific applications for lipid-soluble vitamin research:
Strategic Integration of Absorption Models in Drug Development
The experimental workflow for investigating lipid-soluble vitamin absorption typically follows a tiered approach that progresses from simple screening models to increasingly complex systems:
Tiered Workflow for Vitamin Absorption Research
In vitro and in vivo absorption models each offer distinct advantages and limitations that must be carefully considered within the context of specific research questions. For lipid-soluble vitamin research, the integration of data from multiple models—from molecular dynamics simulations that reveal atomic-level membrane interactions to human clinical trials that capture full physiological complexity—provides the most comprehensive understanding of absorption mechanisms. The ongoing development of more sophisticated in vitro systems, including microphysiological platforms and stem cell-derived intestinal models, promises to enhance the predictive power of preclinical studies while reducing the reliance on animal models. Similarly, advances in computational approaches, particularly PBPK modeling and IVIVC, are improving our ability to translate in vitro findings into accurate predictions of in vivo performance. For researchers investigating lipid-soluble vitamin absorption, a strategic combination of these tools, guided by careful consideration of their respective strengths and limitations, offers the most promising path toward advancing both basic understanding and clinical applications.
Overcoming Absorption Barriers: Clinical Challenges and Formulation Solutions
Malabsorption syndromes represent a complex array of conditions characterized by impaired nutrient assimilation, arising from disruptions in the meticulously coordinated processes of digestion, absorption, and transport. Within the specific context of lipid-soluble vitamin (A, D, E, K) research, understanding these syndromes is paramount, as their absorption is intrinsically linked to the efficient processing of dietary fats [69] [70]. The pathophysiological mechanisms underlying these syndromes provide critical insights for developing targeted therapeutic and diagnostic strategies.
This whitepaper delineates the impact of gastrointestinal disorders, liver diseases, and surgical resections on nutrient absorption, with a specialized focus on the mechanisms governing lipid-soluble vitamin assimilation. The interdependent processes of fat digestion and absorption—reliant on pancreatic enzymes, bile acids, and intact mucosal and lymphatic function—are frequently compromised in these conditions, leading to characteristic deficiencies and their associated clinical sequelae [69] [71]. The objective is to furnish researchers and drug development professionals with a consolidated, technical resource that bridges clinical pathophysiology with experimental methodology.
Pathophysiological Framework and Clinical Impact
The absorption of nutrients occurs in three distinct phases: luminal, mucosal, and post-absorptive. Malabsorption syndromes are classified based on which of these stages is disrupted [69].
Table 1: Phases of Nutrient Absorption and Associated Dysfunction
| Physiological Phase | Core Function | Impact of Dysfunction on Lipid-Soluble Vitamins | Exemplary Conditions |
|---|---|---|---|
| Luminal Phase | Mechanical mixing & chemical digestion by enzymes [69]. | Impaired solubilization & hydrolysis of dietary fats, preventing release of fat-soluble vitamins from food matrix [71]. | Exocrine Pancreatic Insufficiency (EPI), Chronic Pancreatitis, Cystic Fibrosis [69] [71]. |
| Mucosal Phase | Absorption across intestinal mucosa [69]. | Defective uptake of packaged vitamins within mixed micelles [70]. | Celiac Disease, Crohn's Disease, Whipple's Disease [69]. |
| Post-Absorptive Phase | Nutrient transport via intact blood supply & lymphatic system [69]. | Disrupted packaging into chylomicrons & transport into circulation [69]. | Intestinal Lymphangiectasia, Surgical Resection affecting lymphatics, Severe Liver Disease [69] [70]. |
Impact of Specific Etiologies
Gastrointestinal Disorders: Conditions like Celiac disease and Crohn's disease cause mucosal injury and inflammation, directly compromising the absorptive surface area of the small intestine [69]. This damage impairs the critical mucosal phase of absorption. Furthermore, Small Intestinal Bacterial Overgrowth (SIBO), a common comorbidity in motility disorders or blind loop syndromes, leads to bacterial deconjugation of bile acids. This deconjugation renders bile acids ineffective for micelle formation, which is essential for fat and fat-soluble vitamin absorption [69].
Liver and Biliary Tract Diseases: The liver is the primary site for bile acid synthesis. Liver disease, particularly hepatic cirrhosis, reduces bile acid synthesis [69]. Cholestasis, characterized by impaired bile flow, prevents the delivery of these essential bile acids to the intestinal lumen [69] [70]. Without adequate bile, the emulsification and micellar solubilization of lipids and lipid-soluble vitamins fails, leading to steatorrhea and vitamin deficiencies [70].
Surgical Resections: Surgical resection of the small intestine reduces the total absorptive surface area, leading to a condition known as short bowel syndrome [69]. The specific consequences depend on the site of resection. Resection of the terminal ileum is particularly detrimental as it disrupts the enterohepatic circulation of bile salts, leading to a permanent reduction in the bile acid pool and subsequent fat malabsorption [70]. The ileum is also the exclusive site for vitamin B12 absorption, making deficiencies common post-resection [70].
Diagram: Malabsorption Pathways Impacting Lipid-Soluble Vitamins
Quantitative Analysis and Market Drivers
The growing recognition and diagnosis of malabsorption disorders are reflected in the expanding market for diagnostic and therapeutic solutions. The global malabsorption syndrome market serves as a proxy for disease burden and research interest.
Table 2: Global Malabsorption Syndrome Market Analysis and Forecasts
| Metric | Current Value (2023-2025) | Projected Value (2032-2033) | Compound Annual Growth Rate (CAGR) | Primary Drivers |
|---|---|---|---|---|
| Overall Market Size | USD 3.1 - 3.66 Billion [72] [73] | USD 5.65 - 5.88 Billion [72] [73] | 6.9% - 7.0% [72] [73] | Rising disease prevalence, advanced diagnostics, novel drug formulations [72] [73]. |
| Dominant Product Segment | Celiac Disease (45% share in 2025) [73] | N/A | (Informed by market share) | Growing disease awareness & improved diagnostic accuracy [73]. |
| Fastest-Growing Region | Asia-Pacific [72] [74] | USD 1.54 Billion (2033) [74] | 8.3% [74] | Large & aging populations, improving healthcare infrastructure, changing lifestyles [72]. |
| North America Market Share | 38% (Largest regional share) [74] | USD 2.16 Billion (2033) [74] | 5.94% [74] | Established healthcare infrastructure, high healthcare expenditure, advanced technologies [72]. |
The increasing prevalence of causative disorders is a key market and research driver. Celiac disease, once considered rare, is now recognized as a common genetic disorder with a global prevalence of approximately 1% [73]. Similarly, the incidence of Crohn's disease is steadily growing worldwide, linked to changes in lifestyle and dietary patterns [73]. This rising patient pool creates an urgent need for more refined research models and targeted therapies, particularly for complex macronutrient and lipid-soluble vitamin malabsorption.
Experimental Models and Methodologies
Research into malabsorption syndromes and lipid-soluble vitamin absorption employs a range of in vitro and ex vivo models to dissect cellular mechanisms and screen therapeutic compounds.
Key Research Reagent Solutions
Table 3: Essential Research Reagents for Investigating Lipid-Soluble Vitamin Absorption
| Research Reagent / Tool | Core Function in Experimental Models | Specific Application Example |
|---|---|---|
| Caco-2 Cell Line | Human colon adenocarcinoma cell line that spontaneously differentiates into enterocyte-like monolayers [70]. | Gold-standard in vitro model for studying passive and active transport of compounds, including lipid-soluble vitamins, across the intestinal epithelium. |
| Pancreatic Lipase & Colipase | Enzymes critical for the luminal hydrolysis of dietary triglycerides into absorbable monoglycerides and fatty acids [71]. | Used in simulated digestion models to study the luminal phase of fat digestion and its necessity for liberating lipid-soluble vitamins from the food matrix. |
| Synthetic Bile Salts | Surfactants that form micelles, solubilizing lipolytic products and lipid-soluble vitamins for diffusion to the enterocyte brush border [70]. | Essential component of biorelevant simulated intestinal fluids (e.g., FaSSIF/FeSSIF) to study micellar incorporation and uptake of vitamins A, D, E, and K. |
| Chylomicron Secretion Assay | Measures the assembly and secretion of chylomicrons by intestinal cells post-prandially [69]. | Critical for investigating the post-absorptive phase; used to assess the impact of drugs or disease states on the packaging and transport of lipid-soluble vitamins into lymphatics. |
| Serum & Fecal Markers | Analytical standards for vitamins and their metabolites (e.g., 25-OH Vitamin D), fecal elastase, acid steatocrit. | Used to validate in vivo efficacy of interventions in animal models or human samples, quantifying the functional outcome of absorption. |
Detailed Experimental Protocol: Micellar Uptake in a Caco-2 Model
This protocol outlines a standard method for investigating the mucosal uptake of a lipid-soluble vitamin (e.g., Vitamin D3) under different bile acid conditions, simulating a healthy versus cholestatic state.
Workflow: Investigating Mucosal Uptake of Lipid-Soluble Vitamins
Materials:
- Caco-2 cell line (ATCC)
- DMEM culture medium with fetal bovine serum and non-essential amino acids
- Collagen-coated Transwell inserts (e.g., 12-well, 1.12 cm² surface area, 3.0 µm pore size)
- Vitamin D3 (cholecalciferyl) standard
- Synthetic bile salts (e.g., sodium taurocholate)
- Monoolein
- Oleic acid
- Hanks' Balanced Salt Solution (HBSS) with 10 mM HEPES, pH 7.4
- LC-MS/MS system for analysis
Methodology:
- Cell Culture and Differentiation: Plate Caco-2 cells at a density of 1 × 10⁵ cells/cm² on the apical side of collagen-coated Transwell inserts. Culture for 21-23 days, changing the medium every 2-3 days, to allow full differentiation into a polarized monolayer with tight junctions. Confirm monolayer integrity by measuring transepithelial electrical resistance (TEER) > 300 Ω·cm².
- Micelle Formulation:
- Normal Micelles (Control): Dissolve Vitamin D3 with monoolein and oleic acid in chloroform. Evaporate the solvent under nitrogen to form a thin film. Rehydrate the film with HBSS-HEPES buffer containing a physiologically relevant concentration of synthetic bile salts (e.g., 10 mM sodium taurocholate). Sonicate and vortex to form mixed micelles [70].
- Bile Acid-Deficient Micelles (Test): Prepare identically but omit the bile salts from the HBSS-HEPES rehydration buffer.
- Transport Study: On the day of the experiment, wash the Caco-2 monolayers with pre-warmed HBSS-HEPES. Add the micellar solutions (e.g., 0.5 mL) to the apical donor compartment and fresh HBSS-HEPES (e.g., 1.5 mL) to the basolateral acceptor compartment. Incubate at 37°C with orbital shaking.
- Sample Collection: At predetermined time points (e.g., 30, 60, 90, 120 minutes), withdraw the entire volume from the basolateral compartment and replace with fresh pre-warmed buffer. At the end of the experiment, also collect the apical solution and lyse the cells with methanol or RIPA buffer.
- Bioanalytical Quantification: Quantify the concentration of Vitamin D3 in all collected samples (apical, basolateral, cellular) using a validated Liquid Chromatography with tandem mass spectrometry (LC-MS/MS) method. This provides high sensitivity and specificity.
- Data Analysis: Calculate the Apparent Permeability (Papp) using the formula: Papp = (dQ/dt) / (A × C₀), where dQ/dt is the steady-state flux rate (mol/s), A is the surface area of the membrane (cm²), and C₀ is the initial donor concentration (mol/mL). Compare the Papp values and cumulative transport of Vitamin D3 between the normal and bile acid-deficient conditions to quantify the impact of bile salts on uptake.
Advanced Research and Future Directions
Molecular and "Omics" Approaches
Contemporary research extends beyond physiological models to molecular and ecological investigations. Proteogenomic analysis is being used to characterize novel enzymes, such as reductive dehalogenases (RDases) in bacteria, which have implications for environmental bioremediation and understanding microbial metabolism in the gut [75]. Furthermore, metagenomic sequencing of enrichment cultures from diverse environments allows for the discovery of novel bacterial populations and their metabolic capabilities, shedding light on the complex syntrophy interactions within the gut microbiome that may influence host nutrition and disease states [75].
Drug Development and Therapeutic Strategies
The malabsorption syndrome market is evolving with several key strategic focuses:
- Personalized Medicine: Development of targeted therapies for specific sub-populations, such as refractory celiac disease, where there are currently no approved pharmacological treatments [73]. Targeting mucosal healing through immune modulation is a key research avenue.
- Novel Formulations: Investment in drug formulations with improved absorption and targeted delivery systems, including enzyme replacement therapies and bile acid supplements [73].
- Digital Health Integration: Companies are utilizing digital tools for remote patient monitoring and adherence tracking, which can improve clinical trial efficiency and real-world outcomes [73].
A significant challenge and opportunity lie in the high complexity and diverse nature of malabsorption disorders, which makes targeted drug development difficult. Economic factors and the high cost of advanced therapies can also limit accessibility, presenting a barrier that future innovations must address [72].
This technical guide examines the mechanistic pathways through which bile acid sequestrants, antacids, and anticoagulants interfere with nutrient absorption and drug efficacy, with particular focus on fat-soluble vitamin metabolism. Through detailed analysis of molecular interactions, quantitative data synthesis, and experimental methodology documentation, this review provides researchers and drug development professionals with evidence-based insights into these clinically significant interactions. The content is framed within the broader context of lipid-soluble vitamin absorption research, highlighting critical gaps in current understanding and proposing standardized methodologies for future investigation.
Drug-nutrient interactions represent a significant challenge in therapeutic management, particularly for chronic conditions requiring long-term pharmacotherapy. These interactions occur through multiple mechanisms including altered gastrointestinal absorption, changes in metabolic pathways, and interference with physiological processes essential for nutrient utilization. Understanding these mechanisms is paramount for researchers developing new therapeutic agents and clinicians managing patients on complex medication regimens. The narrow therapeutic index of many drugs, including anticoagulants, increases the clinical significance of these interactions, where even minor alterations in bioavailability can substantially impact therapeutic outcomes and patient safety.
Within this landscape, the absorption and metabolism of fat-soluble vitamins (A, D, E, and K) are particularly vulnerable to pharmaceutical interference. These vitamins share common absorption pathways dependent on bile acid secretion, pancreatic enzymes, and chylomicron formation, making them susceptible to disruption by drugs that alter gastrointestinal environment or bile acid dynamics. This review systematically examines three major drug classes with well-documented nutrient interaction profiles, focusing on mechanistic pathways, clinical consequences, and methodological approaches for investigating these interactions within lipid-soluble vitamin research frameworks.
Bile Acid Sequestrants
Mechanisms of Action and Therapeutic Applications
Bile acid sequestrants, including colesevelam, colestipol, and cholestyramine, are polymeric compounds that bind bile acids in the intestinal lumen, forming insoluble complexes that are excreted in feces [76]. This mechanism depletes the bile acid pool from the enterohepatic circulation, resulting in compensatory hepatic conversion of cholesterol to bile acids. The subsequent reduction in hepatic cholesterol upregulates hepatic LDL receptors, increasing LDL clearance from blood and reducing serum cholesterol concentrations [76]. Beyond their primary indication for hypercholesterolemia management, bile acid sequestrants demonstrate therapeutic benefits for type 2 diabetes mellitus (improving glycemic control), bile acid malabsorption diarrhea, and pruritus associated with partial biliary obstruction [76].
The molecular structure of bile acid sequestrants contains multiple positive charges that interact ionically with negatively charged bile acids. This binding is pH-dependent and occurs throughout the gastrointestinal tract. Colesevelam was specifically engineered with higher affinity for bile acids compared to earlier agents, allowing for lower dosing and potentially reduced side effects [76]. The sequestration process disrupts the formation of micelles, which are essential for the solubilization and absorption of dietary lipids and fat-soluble vitamins, establishing the foundation for their nutrient interaction profile.
Interference with Fat-Soluble Vitamin Absorption
Bile acid sequestrants impair the absorption of fat-soluble vitamins by multiple complementary mechanisms. The primary pathway involves disruption of micelle formation through bile acid binding, which reduces the solubilization of dietary lipids and fat-soluble vitamins essential for their absorption [76] [77]. Additionally, direct binding interactions may occur between the sequestrant polymer and vitamin molecules, further reducing their bioavailability [78]. With chronic administration, this can lead to clinically significant deficiencies, particularly of vitamins A, D, E, and K.
The extent of vitamin malabsorption varies by specific sequestrant, dosage, and treatment duration. Research indicates that folate supplementation may be particularly necessary during long-term therapy, as cholestyramine has been documented to bind folate polyglutamates and decrease absorption of folate from food [78]. Although other nutrient levels often remain within normal ranges, the potential for deficiency necessitates monitoring and potential supplementation in high-risk populations.
Table 1: Quantitative Effects of Bile Acid Sequestrants on Fat-Soluble Vitamin Status
| Vitamin | Mechanism of Interference | Clinical Consequences | Management Strategies |
|---|---|---|---|
| Vitamin A | Reduced micelle formation; possible direct binding | Decreased serum retinol; potential night vision impairment | Separate supplementation by ≥4 hours; monitor serum levels |
| Vitamin D | Impaired solubilization and absorption | Reduced 25-hydroxyvitamin D; potential bone metabolism effects | Vitamin D supplementation with temporal separation |
| Vitamin E | Disruption of lipid absorption pathway | Decreased α-tocopherol levels; reduced antioxidant capacity | Supplement with vitamin E; monitor in long-term therapy |
| Vitamin K | Binding of vitamin K; reduced absorption | Potential prolonged PT/INR; bleeding risk with warfarin | Consistent dietary intake; monitor coagulation parameters |
Experimental Protocols for Investigating Sequestrant-Vitamin Interactions
In Vitro Binding Assays: To quantify the binding affinity between bile acid sequestrants and fat-soluble vitamins, prepare solutions of individual vitamins (A, D, E, K) in simulated intestinal fluid (pH 6.8) with taurocholate to mimic fed state conditions. Add increasing concentrations of each bile acid sequestrant (0-10 mg/mL) and incubate at 37°C with constant agitation for 2 hours. Separate bound and free fractions using ultrafiltration centrifugation (10,000 × g, 15 minutes). Quantify vitamin concentrations in supernatant using HPLC with UV/Vis or MS detection. Calculate binding constants using Scatchard or Langmuir isotherm analysis [76] [78].
Caco-2 Cell Absorption Studies: Culture Caco-2 cells on Transwell inserts until fully differentiated (21 days). Pre-treat with therapeutic concentrations of bile acid sequestrants (0.5-2 mg/mL) in fasted or fed state simulated intestinal fluids for 30 minutes. Apply vitamin-containing solutions to apical compartment. Sample from basolateral compartment at timed intervals over 2 hours. Analyze vitamin content using LC-MS/MS. Measure transepithelial electrical resistance (TEER) before and after experiments to monitor barrier integrity. This model quantifies the direct effect of sequestrants on vitamin transport across intestinal epithelium [78].
Animal Model of Chronic Administration: Administer therapeutic equivalents of bile acid sequestrants to rodent models (e.g., Sprague-Dawley rats) via oral gavage for 4-12 weeks. Include control groups receiving vehicle alone. Monitor food intake and body weight weekly. Collect serum monthly for vitamin quantification (HPLC-MS/MS). At endpoint, analyze tissue vitamin concentrations (liver, adipose). Assess functional outcomes: bone density (vitamin D status), coagulation parameters (vitamin K status), and vision tests (vitamin A status). This longitudinal design characterizes the progression of deficiency states [76] [78].
Antacids
Pharmacological Properties and Clinical Use
Antacids are basic compounds containing aluminum, calcium, magnesium, or sodium salts that neutralize gastric hydrochloric acid, increasing intragastric pH [79]. This activity provides symptomatic relief in GERD, peptic ulcer disease, and dyspepsia. Beyond acid neutralization, certain antacids demonstrate additional therapeutic properties: aluminum hydroxide binds phosphate in the GI tract, making it useful for hyperphosphatemia management in renal failure, while calcium salts can serve as calcium supplementation [79].
The acid-neutralizing capacity varies among antacid formulations, with magnesium and aluminum hydroxide combinations providing rapid and sustained effects. The duration of action is typically 30-60 minutes when taken on an empty stomach, extending to 2-3 hours when taken after meals due to delayed gastric emptying. These pH-altering properties directly and indirectly influence drug and nutrient bioavailability through multiple mechanisms that extend throughout the gastrointestinal tract.
Mechanisms of Nutrient Interference
Antacids impact nutrient absorption through three primary mechanisms: pH-dependent solubility alterations, direct complexation, and gastrointestinal motility changes. The increased gastric pH can reduce the dissolution of pH-dependent compounds and alter ionization states, affecting passive diffusion across enterocytes. Divalent and trivalent cations in antacids (Al³⁺, Ca²⁺, Mg²⁺) can form insoluble complexes with minerals and some vitamins, preventing their absorption [78] [79]. Additionally, aluminum-containing antacids may decrease fluoride absorption, while magnesium-containing formulations can influence manganese bioavailability [78].
The clinical significance of these interactions depends on antacid composition, dosage, timing relative to food/nutrient intake, and treatment duration. For example, chronic use of aluminum-containing antacids may cause hypophosphatemia at high doses, particularly with low dietary phosphorus intake [78]. Similarly, magnesium-containing antacids can result in hypermagnesemia in patients with impaired renal function due to reduced mineral excretion [78].
Table 2: Nutrient Interactions with Common Antacid Formulations
| Nutrient | Interacting Antacid | Interaction Mechanism | Clinical Management |
|---|---|---|---|
| Iron | Aluminum/magnesium hydroxide | Reduced solubility at increased pH; complex formation | Separate administration by ≥2 hours; consider ascorbic acid co-administration |
| Folate | Various antacids | Slight impairment of synthetic folic acid absorption | Temporal separation of ≥3 hours between administration |
| Calcium | Magnesium-containing | Competitive absorption; altered motility | Monitor calcium status with chronic use |
| Phosphate | Aluminum hydroxide | Insoluble aluminum phosphate formation | Particularly concerning with high doses and low dietary intake |
| Fluoride | Aluminum-containing | Decreased absorption | Separate administration by ≥2 hours |
Methodologies for Investigating Antacid-Nutrient Interactions
pH-Dependent Solubility Studies: Prepare simulated gastric fluid (pH 1.2) and intestinal fluid (pH 6.8) according to USP specifications. Add nutrients of interest (iron, calcium, folate, etc.) at physiological concentrations with and without therapeutic concentrations of antacids. Incubate at 37°C with continuous agitation. Sample at predetermined time points (5, 15, 30, 60, 120 minutes). Filter samples (0.45 μm) and analyze soluble fraction using appropriate analytical methods (AAS for minerals, HPLC for vitamins). Compare dissolution profiles with and without antacids to quantify pH-mediated effects on bioavailability [78] [79].
Complexation Binding Studies: Utilize isothermal titration calorimetry (ITC) to directly measure binding constants between antacid cations (Al³⁺, Ca²⁺, Mg²⁺) and anionic forms of nutrients. Prepare solutions in physiological buffers at relevant pH values. Titrate nutrient solutions into antacid suspensions while measuring heat changes. Calculate binding stoichiometry and affinity constants from thermograms. Complement with FTIR and NMR spectroscopy to characterize complex structures. These techniques elucidate molecular-level interactions that reduce nutrient bioavailability [79].
Clinical Absorption Studies: Employ randomized crossover designs in healthy volunteers or patient populations. Administer single doses of test nutrients with and without co-administered antacids after appropriate washout periods. Utilize stable isotope-labeled nutrients (e.g., ⁵⁷Fe, ⁴⁴Ca) when possible to track absorption independently from endogenous stores. Collect serial blood samples over 24-72 hours. Measure area under the curve (AUC), maximum concentration (Cmax), and time to maximum concentration (Tmax) for nutrient pharmacokinetics. These human studies provide clinically relevant absorption data [78] [79].
Anticoagulants
Vitamin K Antagonists and Nutrient Interactions
Vitamin K antagonists (VKAs) like warfarin exert their anticoagulant effect by inhibiting vitamin K epoxide reductase (VKOR), preventing the recycling of vitamin K and thereby reducing the γ-carboxylation of vitamin K-dependent clotting factors (II, VII, IX, X) [80]. This mechanism creates a direct dependency on dietary vitamin K intake, where fluctuations can significantly alter anticoagulation status. The narrow therapeutic index of VKAs amplifies the clinical significance of these interactions, requiring consistent vitamin K consumption to maintain international normalized ratio (INR) within target range [80].
Genetic polymorphisms in VKORC1 and CYP2C9 significantly influence warfarin sensitivity and metabolism, contributing to interindividual variability in dose requirements and interaction susceptibility. Drugs that induce or inhibit CYP2C9 or CYP3A4 further complicate management by altering warfarin clearance [80]. Understanding these interconnected pathways is essential for predicting and managing clinically significant interactions with VKAs.
Direct Oral Anticoagulants and Emerging Interaction Profiles
Direct oral anticoagulants (DOACs) including dabigatran, rivaroxaban, apixaban, and edoxaban target specific coagulation factors (Factor Xa or thrombin) rather than vitamin K metabolism [80]. While theoretically less susceptible to dietary vitamin K fluctuations, DOACs are subject to interactions involving transport proteins, particularly P-glycoprotein (P-gp) and breast cancer resistance protein (BCRP). Inhibitors or inducers of these transporters can significantly alter DOAC plasma concentrations, potentially leading to under-anticoagulation (thrombotic risk) or over-anticoagulation (bleeding risk) [80].
The interaction profiles vary among DOACs due to differences in their dependence on specific metabolic pathways. For instance, rifampicin (a strong CYP3A4 and P-gp inducer) decreases plasma levels of all DOACs, while verapamil (a P-gp inhibitor) increases dabigatran and edoxaban exposure [80]. Understanding these distinct profiles is crucial for appropriate DOAC selection in patients taking multiple medications.
Table 3: Clinically Significant Drug-Nutrient Interactions with Anticoagulants
| Anticoagulant | Interacting Substance | Interaction Mechanism | Clinical Effect | Management |
|---|---|---|---|---|
| Warfarin | Vitamin K-rich foods (spinach, kale) | Competitive inhibition of VKOR | Reduced anticoagulant effect | Consistent daily intake |
| Warfarin | Grapefruit juice | CYP3A4 inhibition | Increased warfarin levels | Avoid concurrent use |
| Warfarin | Mango | Unknown mechanism | Enhanced anticoagulant effect | Monitor INR closely |
| Dabigatran | P-gp inducers (St. John's Wort) | Increased efflux transport | Reduced drug levels | Avoid combination |
| Rivaroxaban | P-gp/BCRP inhibitors (ketoconazole) | Decreased efflux transport | Increased drug exposure | Avoid with strong inhibitors |
| All DOACs | High-fat meals | Altered dissolution/absorption | Variable effect on bioavailability | Take with consistent food relation |
Experimental Framework for Investigating Anticoagulant-Nutrient Interactions
In Vitro CYP and Transporter Inhibition Assays: Use human liver microsomes or recombinant CYP enzymes (CYP2C9, CYP3A4) to assess metabolic inhibition. Incubate anticoagulants with nutrient extracts or specific dietary compounds at physiological concentrations. Monitor metabolite formation using LC-MS/MS. For transporter studies, use polarized cell lines (MDCK, Caco-2) overexpressing P-gp or BCRP. Measure directional flux of anticoagulants with and without nutrient compounds to determine transporter inhibition potential. These high-throughput screens identify potential interactions before clinical investigation [80].
Animal Pharmacokinetic-Pharmacodynamic Studies: Administer anticoagulants to rodent models with and without co-administered nutrients or dietary supplements. Collect serial blood samples for pharmacokinetic analysis (plasma drug concentrations) and pharmacodynamic assessment (coagulation parameters: PT/INR for warfarin, anti-Factor Xa activity for Xa inhibitors, thrombin time for dabigatran). Include groups with genetic modifications relevant to human polymorphisms (VKORC1, CYP2C9) to model interindividual variability. These controlled in vivo studies establish causality and mechanism [80].
Clinical Interaction Studies with Dietary Interventions: Conduct controlled crossover trials in healthy volunteers or stable patients. Implement standardized diets with low, medium, and high content of interacting nutrients (e.g., vitamin K). Administer fixed anticoagulant doses during each dietary phase. Employ stable isotope-labeled vitamins to trace pharmacokinetics. Measure anticoagulant pharmacokinetic parameters, vitamin levels, and coagulation markers. Utilize pharmacogenomic testing to stratify participants by VKORC1 and CYP2C9 genotype. These studies provide definitive evidence for dietary recommendations [80] [25].
Research Reagent Solutions
Table 4: Essential Research Reagents for Investigating Drug-Nutrient Interactions
| Reagent/Category | Specific Examples | Research Application | Key Function in Experimental Design |
|---|---|---|---|
| In Vitro Digestion Models | Simulated gastric/intestinal fluids (USP), TIM-1 system, Caco-2 cells | Screening drug-nutrient interactions | Reproduces gastrointestinal environment for absorption studies |
| Analytical Standards | Stable isotope-labeled vitamins (d6-vitamin D, 13C-vitamin K), certified reference materials | Quantification of vitamins and drugs | Enables precise measurement using LC-MS/MS; distinguishes endogenous vs. administered compounds |
| Cell-Based Transport Systems | MDCK-MDR1, Caco-2, transfected HEK293 cells | Transporter interaction studies | Express specific transport proteins (P-gp, BCRP) to study absorption mechanisms |
| Animal Models | Cypor (cytochrome P450-humanized), Vkorc1 mutant mice, germ-free models | In vivo interaction studies | Models human metabolism and genetics; elucidates microbiome role in interactions |
| Molecular Biology Tools | VKORC1 polymorphism genotyping kits, CYP2C9 sequencing panels, siRNA libraries | Pharmacogenomic studies | Identifies genetic modifiers of drug-nutrient interactions |
| Coagulation Assays | PT/INR, anti-Factor Xa chromogenic assays, thrombin generation tests | Pharmacodynamic assessment | Measures functional anticoagulant effect in interaction studies |
Integrated Mechanisms and Visualization
The drug-nutrient interactions discussed share common physiological pathways despite their distinct primary mechanisms. The gastrointestinal tract serves as the primary interface for these interactions, with hepatic metabolism and transport proteins providing secondary modification sites. The following diagram illustrates the integrated mechanisms through which bile acid sequestrants, antacids, and anticoagulants interfere with nutrient absorption and utilization, with particular emphasis on fat-soluble vitamin pathways:
Integrated Drug-Nutrient Interaction Pathways
The visualization above illustrates the sequential processes of fat-soluble vitamin absorption and utilization, with specific intervention points for each drug class. Antacids primarily alter the gastric environment, affecting pH-dependent dissolution and initial digestion. Bile acid sequestrants disrupt micelle formation in the intestinal lumen, impairing solubilization of fat-soluble vitamins. Anticoagulants target the hepatic vitamin K cycle, directly interfering with the physiological activity of vitamin K. This integrated representation highlights how these drug classes target different points along the same physiological pathway, collectively contributing to potential nutrient deficiencies and therapeutic complications.
This analysis demonstrates that bile acid sequestrants, antacids, and anticoagulants each employ distinct yet complementary mechanisms that interfere with fat-soluble vitamin absorption and utilization. The clinical significance of these interactions depends on multiple factors including dosage, treatment duration, patient genetics, and nutritional status. Understanding these mechanisms is essential for optimizing therapeutic outcomes while minimizing adverse nutritional consequences.
Future research should prioritize several key areas: (1) development of novel formulations that maintain therapeutic efficacy while reducing nutrient interaction potential; (2) personalized medicine approaches incorporating pharmacogenomic testing to identify high-risk patients; (3) standardized protocols for assessing drug-nutrient interactions during drug development; and (4) longitudinal studies examining the cumulative effects of chronic medication use on nutritional status. Addressing these research gaps will enhance patient safety and therapeutic efficacy for medications with significant nutrient interaction potential.
The investigation into lipid-soluble vitamin absorption presents a fundamental dichotomy in nutritional science: the complex, synergistic delivery of vitamins via whole foods versus the targeted, concentrated delivery of isolated supplements. Vitamins A, D, E, and K, by their nature, rely on fat-soluble pathways and co-ingested dietary lipids for absorption, packaging into micelles, and ultimate cellular uptake. Pharmacological dosing with isolated vitamins bypasses the natural food matrix, potentially altering bioavailability, kinetics, and physiological effects. This whitepaper delineates the critical mechanisms governing these divergent absorption pathways, synthesizing current research to provide a technical framework for researchers and drug development professionals. Understanding these principles is paramount for developing effective nutritional interventions, fortified foods, and pharmaceutical formulations that account for the intricate biology of nutrient assimilation.
Fundamental Mechanisms of Lipid-Soluble Vitamin Absorption
The absorption of fat-soluble vitamins (FSVs) is a complex process intrinsically linked to dietary fat digestion and is governed by a sequence of physiological events.
- Digestive Liberation: Within the stomach and small intestine, FSVs are liberated from the food matrix through mechanical and enzymatic action. The presence of dietary fat stimulates the release of bile acids from the gallbladder and pancreatic lipase, initiating the digestion of triglycerides into free fatty acids and monoglycerides.
- Micellarization: Bile acids emulsify lipid digestion products, forming mixed micelles. These micelles are critical for the solubilization of hydrophobic FSVs, allowing them to traverse the unstirred water layer adjacent to the intestinal enterocytes.
- Cellular Uptake & Processing: FSVs enter enterocytes via passive diffusion or specific transporter proteins. Inside the cell, they are incorporated into chylomicrons—large lipoprotein particles.
- Systemic Distribution: Chylomicrons are secreted into the lymphatic system and subsequently enter the bloodstream, delivering FSVs to the liver and peripheral tissues.
The efficiency of this entire cascade is highly dependent on the presence of dietary fat and the specific structure of the vitamin and its food source. Interindividual variation in digestive capacity, bile acid production, and genetic factors in transporter expression further modulate absorption efficacy, presenting significant challenges for standardized dosing [81] [82].
Table 1: Key Processes in Lipid-Soluble Vitamin Absorption
| Process Stage | Key Components | Function in Absorption |
|---|---|---|
| Digestive Liberation | Dietary Fat, Pancreatic Lipase, Gastric/Intestinal Enzymes | Releases vitamins from the food matrix and facilitates fat digestion. |
| Micellar Solubilization | Bile Acids, Phospholipids, Lipid Digestion Products | Encapsulates hydrophobic vitamins for aqueous transport to enterocytes. |
| Cellular Uptake | Enterocytes, Passive Diffusion, Specific Transporters (e.g., for Vitamins A, D) | Mediates cellular entry of vitamins from the intestinal lumen. |
| Systemic Distribution | Chylomicrons, Lymphatic System, Liver, Carrier Proteins (e.g., RBP, LDL) | Packages and transports vitamins to the liver and peripheral tissues. |
The efficacy of vitamin delivery is highly contingent on its form and delivery vehicle. The following tables provide a comparative analysis of these two paradigms, highlighting differences in bioaccessibility, influencing factors, and clinical implications.
Table 2: Bioaccessibility and Efficacy: Dietary vs. Supplemental Forms
| Parameter | Dietary Sources (Synergistic Matrix) | Supplemental Forms (Pharmacological Dosing) |
|---|---|---|
| Bioaccessibility | Enhanced by co-nutrients; e.g., MLCTs increased Vit. A bioaccessibility by 15.67% [83]. | Highly variable; dependent on formulation (oil-filled softgels vs. dry tablets). |
| Key Influencing Factors | Food matrix structure, type and amount of dietary fat, cooking/processing methods. | Delivery form (oil, powder, emulsion), presence of synthetic excipients. |
| Nutrient Synergies | Direct; e.g., carotenoids with tocopherols and phospholipids in whole foods [84]. | Indirect/absent; requires deliberate formulation (e.g., composite antioxidants [85]). |
| Kinetic Profile | Gradual, sustained release aligned with digestive processes. | Typically rapid, high-concentration spike; dependent on supplement form. |
| Clinical Implications | Supports physiological homeostasis; lower risk of toxicity. | Potent for correcting deficiency; risk of pro-oxidative effects at high doses [85]. |
Table 3: Research Insights into Matrix and Formulation Effects
| Study Focus | Experimental Finding | Research Implication |
|---|---|---|
| Structured Lipids (MLCT) | MLCT with sn-2 DHA achieved 88.51% intestinal FFA release, outperforming physical lipid mixes (78.44%) [83]. | The covalent structure of triglycerides, not just their fatty acid profile, is a critical determinant of digestibility and vitamin carrier efficacy. |
| Composite Antioxidants | A ternary blend (EQ+BHT+Citric Acid) provided superior, temperature-resilient protection against lipid peroxidation vs. single antioxidants [85]. | Synergistic antioxidant systems mimic food-based protection, overcoming limitations like volatility and pro-oxidative thresholds of single compounds. |
| Vitamin K Forms | Vitamin K2 from fermented foods (e.g., natto) demonstrated stronger bone-protective effects compared to pharmacological vitamin K1 [25]. | The chemical form (vitamer) and its dietary source (whole food vs. isolated) can lead to distinct pharmacokinetics and clinical outcomes. |
Experimental Protocols for Assessing Bioaccessibility
Robust in vitro methodologies are essential for deconstructing the mechanisms of vitamin absorption. The following protocols are standardized for investigating matrix and formulation effects.
Protocol 1: In Vitro Digestion Model for Bioaccessibility
This protocol simulates the human gastrointestinal tract to quantify the micellarized fraction of a vitamin available for absorption.
- Apparatus: pH-stat titrator, shaking water bath, centrifuge.
- Reagents: Simulated salivary fluid (SSF), simulated gastric fluid (SGF), simulated intestinal fluid (SIF), pancreatin, bile extracts, digestive enzymes (e.g., pepsin, lipase).
- Procedure:
- Oral Phase: Mix the test sample (food or supplement) with SSF for 2 minutes at 37°C.
- Gastric Phase: Adjust to pH 3.0 with HCl, add pepsin in SGF, and incubate for 1-2 hours with constant agitation.
- Intestinal Phase: Raise pH to 7.0 with NaHCO₃, add pancreatin and bile extracts in SIF, and incubate for 2 hours. Maintain pH stat with NaOH to monitor free fatty acid release.
- Sample Analysis: Centrifuge the intestinal digest (e.g., 10,000 x g, 45 min) to isolate the aqueous micellar phase. Analyze the vitamin content in this supernatant via HPLC-UV/FLD to determine bioaccessibility percentage [83].
Protocol 2: Evaluating Antioxidant Protection in Feed/Food Models
This protocol assesses the synergistic protection of vitamins against oxidation during storage, relevant for product stability.
- Design: A basal diet/feed containing oxidized oil serves as a negative control (CON). Experimental groups supplement the basal diet with single (e.g., BHT, EQ) or composite antioxidants.
- Accelerated Storage: Subject samples to thermal stress (e.g., 120°C for 2 h) followed by ambient storage. Collect triplicate samples at regular intervals over 10 weeks.
- Oxidative Stability Markers:
- Primary Oxidation: Peroxide Value (PV), Conjugated Dienes (CD).
- Secondary Oxidation: p-Anisidine Value (p-AV), Malondialdehyde (MDA) via TBARS assay.
- Integrated Indices: TOTOX value [2(PV) + p-AV].
- Antioxidant Capacity: DPPH/ABTS radical scavenging assays, total antioxidant capacity kits [85].
- Data Interpretation: Compare the rate of oxidation marker increase and retention of antioxidant capacity between single and composite systems to quantify synergy.
Visualization of Pathways and Workflows
The following diagrams, generated with Graphviz DOT language, illustrate the core experimental workflow and the mechanistic pathway of enhanced vitamin absorption via structured lipids.
Experimental Workflow for Bioaccessibility Assessment
Mechanism of Enhanced Absorption via Structured Lipids
The Scientist's Toolkit: Essential Research Reagents and Materials
This section details critical reagents, materials, and model systems used in advanced research on lipid-soluble vitamin absorption and stability.
Table 4: Key Research Reagent Solutions
| Reagent / Material | Function & Application in Research | Key Characteristics |
|---|---|---|
| Synthetic Lipids (e.g., MLCT) | Model system for studying the impact of triglyceride structure on digestibility and vitamin carrier efficiency [83]. | Pre-defined fatty acid regio-specificity (e.g., sn-2 LCFA); high purity (>95%). |
| Composite Antioxidant Blends | Mimic food-based synergistic protection; used to inhibit lipid peroxidation in fat-containing feeds, foods, and supplements during storage studies [85]. | Combines radical scavengers (BHT, EQ) with metal chelators (Citric Acid); optimized ratios. |
| Simulated Digestive Fluids (SSF, SGF, SIF) | Key components of in vitro digestion models to simulate the chemical environment of the human GI tract [83]. | Defined electrolyte, enzyme, and bile salt composition; pH-statable. |
| sn-1,3 Specific Lipases | Enzymatic catalysts for synthesizing structured triglycerides or for studying regioselective hydrolysis during digestion [83]. | High regioselectivity; immobilization compatible for re-use. |
| Differentiated Caco-2 Cell Line | An in vitro model of the human intestinal epithelium for studying vitamin uptake, transport, and metabolism [81]. | Forms polarized monolayers with tight junctions; expresses relevant transporters. |
The choice between dietary sources and supplemental forms of lipid-soluble vitamins is not merely a matter of potency but one of physiological context and mechanism. The synergistic food matrix offers a naturally optimized delivery system where lipids, absorption enhancers, and antioxidants work in concert to regulate bioaccessibility and metabolic fate. In contrast, pharmacological dosing provides a powerful tool for addressing deficiency states but must be applied with an understanding of its altered kinetic profile and potential for non-physiological effects. The future of nutritional science and therapeutic development lies in leveraging the principles of the food matrix to engineer smarter, more effective supplements and functional foods. This requires a deep mechanistic understanding, facilitated by the robust experimental protocols and model systems detailed herein, to bridge the gap between traditional nutrition and modern pharmaceutical science.
The absorption and metabolism of lipid-soluble vitamins (LSVs)—A, D, E, and K—represent a complex physiological process governed by specific transport proteins, receptors, and enzymatic pathways. Within the context of mechanisms governing LSV absorption research, it is now evident that genetic variability constitutes a fundamental determinant of interindividual differences in vitamin status. Genetic polymorphisms in genes encoding critical components of LSV transport and activation pathways can significantly alter their bioavailability, cellular utilization, and overall physiological efficacy [13] [86]. The emerging field of nutritional genomics aims to decipher these relationships to move beyond one-size-fits-all supplementation strategies.
This paradigm shift is supported by genome-wide association studies (GWAS), which have provided unprecedented insights into the genetic architecture underlying circulating vitamin status biomarkers. These studies confirm that vitamin status is a complex polygenic trait, influenced by numerous genetic variants interacting with dietary and environmental factors [86]. Understanding these mechanisms is paramount for researchers and drug development professionals seeking to develop targeted interventions that can overcome genetic limitations in LSV absorption and metabolism, thereby optimizing nutritional status and supporting disease prevention strategies in specific genetic subgroups.
Key Genetic Polymorphisms Affecting Lipid-Soluble Vitamin Status
Vitamin Transport and Metabolism Pathways
The absorption and cellular distribution of LSVs depend on a sophisticated network of specialized transport proteins, contrasting sharply with the passive diffusion model historically assumed. Transport proteins such as scavenger receptor class B type I (SR-BI), CD36, and Niemann-Pick C1-like 1 (NPC1L1) are integral to the uptake of LSVs, integrating their absorption with core lipid metabolic pathways [13]. Defects in these transporters are linked to diverse metabolic disorders, highlighting their physiological significance beyond mere nutrient absorption.
Following absorption, LSVs are subject to enzymatic activation—a process particularly critical for vitamins A and D. For instance, beta-carotene 15,15'-monooxygenase (BCO1) is the key enzyme responsible for converting dietary beta-carotene into active vitamin A (retinal). Genetic variants in the BCO1 gene can profoundly reduce the efficiency of this conversion, meaning individuals carrying these variants may not effectively derive vitamin A from plant-based carotenoid sources and may require pre-formed retinol from animal products or targeted supplementation [87]. Similarly, variations in genes encoding vitamin D binding protein (GC) and enzymes involved in the vitamin D hydroxylation pathway (e.g., CYP2R1, CYP27B1) influence individual vitamin D status and response to supplementation [86].
Significant Gene Variants and Their Functional Impact
Research has identified several key genetic polymorphisms that directly impact LSV status by altering the function of proteins involved in their transport, activation, or cellular signaling.
Table 1: Key Genetic Polymorphisms Affecting Lipid-Soluble Vitamin Status
| Vitamin | Gene | Function of Encoded Protein | Impact of Polymorphism |
|---|---|---|---|
| Vitamin A | BCO1 | Converts beta-carotene to retinal [87] | Reduced conversion efficiency; may necessitate pre-formed vitamin A intake [87] |
| Vitamin D | GC (Group-specific component) | Major vitamin D binding and transport protein [86] | Altered circulating levels of 25-hydroxyvitamin D [86] |
| Vitamin D | CYP2R1 | Key enzyme for 25-hydroxylation of vitamin D [86] | Reduced enzyme activity, leading to lower circulating 25(OH)D levels [86] |
| Vitamin D | VDR (Vitamin D Receptor) | Nuclear receptor mediating vitamin D signaling [25] | Modifies tissue response to vitamin D; associated with bone metabolism and disease risk [25] |
| Vitamin K | VKORC1 | Enzyme complex involved in vitamin K cycle [25] | Alters vitamin K activity and requirements; critical for anticoagulant drug response [25] |
The clinical relevance of these polymorphisms is substantial. For example, polymorphisms in the VKORC1 gene not only influence vitamin K status but also determine individual sensitivity to warfarin, a vitamin K antagonist anticoagulant [25]. This underscores the critical intersection of pharmacogenomics and nutritional science in personalized medicine. Furthermore, genetic variation in the VDR gene can modulate the pleiotropic effects of vitamin D on immune function, cell proliferation, and bone mineralization, explaining heterogeneous responses to uniform vitamin D supplementation protocols in both research and clinical settings [25].
Analytical Methodologies for Assessing Vitamin-Related Genetics
Genome-Wide Association Studies (GWAS) and Biobank Data
The advent of large-scale genome-wide association studies (GWAS) has revolutionized the identification of genetic loci associated with vitamin status. This hypothesis-free approach involves genotyping hundreds of thousands to millions of single nucleotide polymorphisms (SNPs) across the genomes of a large study population and testing for statistical associations with specific biomarkers of vitamin status, such as serum 25-hydroxyvitamin D for vitamin D or retinol-binding protein for vitamin A [86]. This method has successfully identified numerous novel loci beyond candidate genes, revealing the polygenic nature of vitamin status.
The utility of GWAS is greatly amplified by access to large biobank-scale resources like the UK Biobank (UKBB), which combine genetic data with detailed phenotypic and biochemical information from hundreds of thousands of participants [86]. The statistical power of these studies allows for the detection of common genetic variants with modest effects, providing a more comprehensive map of the genetic architecture of LSV status. Subsequent analyses, such as Mendelian randomization (MR), leverage these genetic associations to infer causal relationships between vitamin status and health outcomes, helping to triangulate evidence from sometimes inconclusive randomized controlled trials [86].
Functional Validation and Mechanistic Studies
While GWAS identifies statistical associations, functional studies are required to establish the biological mechanisms. In vitro and in vivo models are employed to characterize the functional consequences of identified genetic variants. For transporter genes, this involves experiments to measure uptake efficiency of specific vitamers in cell lines overexpressing wild-type versus variant transporters [13] [88]. The effect of a polymorphism on enzyme kinetics (e.g., for BCO1 or CYP enzymes) can be determined by expressing the variant protein and measuring its catalytic activity and affinity for substrates.
Advanced analytical chemistry techniques are crucial for quantifying vitamers and their metabolites. Liquid chromatography–tandem mass spectrometry (LC-MS/MS) is the state-of-the-art method for the precise quantification of various vitamers of vitamin D (D2, D3, 25-OH-D2, 25-OH-D3) and vitamin A (retinol, retinal, retinyl esters) in biological samples [88]. The availability of certified reference materials (CRMs) is essential for method validation and ensuring analytical accuracy across laboratories [88]. These functional and analytical tools form the cornerstone of translational research, bridging the gap between genetic association and physiological understanding.
Table 2: Essential Research Reagents and Methodologies for Vitamin Genetics Research
| Reagent/Method | Category | Specific Application/Function | Key Consideration |
|---|---|---|---|
| LC-MS/MS | Analytical Method | Quantification of specific vitamers and metabolites in serum/tissues [88] | Requires vitamer-specific standards and optimized separation protocols [88] |
| Certified Reference Materials (CRMs) | Quality Control | Method validation and standardization (e.g., NIST SRM 968e for fat-soluble vitamins) [88] | Essential for cross-study comparability and data reliability [88] |
| GWAS Genotyping Arrays | Genetic Tool | Genome-wide SNP profiling for association discovery [86] | Imputation to reference panels increases genomic coverage; power depends on sample size [86] |
| Recombinant Vitamin Transporters | Research Reagent | Functional characterization of variant proteins in cell-based uptake assays [13] | Enables direct measurement of kinetic parameters (Km, Vmax) for wild-type vs. mutant [13] |
| Mendelian Randomization | Statistical Method | Assesses potential causal effects of vitamin status on disease outcomes [86] | Uses genetic variants as instrumental variables to limit confounding [86] |
Visualizing the Research Workflow
The following diagram illustrates the integrated workflow from genetic discovery to clinical application in LSV research.
Figure 1: From Gene Discovery to Personalized Nutrition
A Pathway-Centric Visualization of Vitamin A Metabolism
The metabolic pathway of vitamin A, from dietary intake to cellular function, is a prime example of how genetic variation impacts nutrient status. The following diagram details key genes involved in this pathway where polymorphisms can alter individual requirements.
Figure 2: Genetic Regulation of Vitamin A Metabolism
Future Directions and Clinical Translation
The future of personalized supplementation lies in the development of integrated polygenic scores that aggregate the effects of multiple genetic variants across relevant pathways to provide a more comprehensive genetic propensity score for an individual's LSV status and requirements [86]. Furthermore, research must move beyond main genetic effects to explore gene-by-environment (GxE) interactions, where factors such as gut microbiota composition, overall diet, and medication use modulate the impact of genetic polymorphisms [25] [12]. For instance, the dietary intake of live microbes has been associated with increased serum levels of LSVs, suggesting the gut microbiome may interact with host genetics to determine vitamin status [12].
The ultimate goal is to translate this genetic knowledge into clinically actionable tools. This requires rigorous intervention studies testing the efficacy of genotype-guided supplementation recommendations compared to standard approaches. Key challenges include establishing cost-effectiveness, ensuring ethical implementation to avoid genetic determinism, and integrating genetic data with other biomarkers and lifestyle factors to create truly personalized and effective nutritional strategies for optimizing lipid-soluble vitamin status and improving long-term health outcomes.
Aging induces a complex set of physiological alterations that significantly impair the absorption of lipid-soluble vitamins. These changes span the entire gastrointestinal (GI) tract, encompassing diminished digestive enzyme activity, reduced bile acid availability, and alterations in intestinal morphology and function. For researchers and drug development professionals, understanding these mechanisms is paramount for designing innovative formulation strategies that can overcome these barriers. This whitepaper synthesizes current research on the physiological basis of age-related absorption decline and details cutting-edge experimental methodologies for investigating these changes. Furthermore, it outlines advanced compensatory formulation technologies, including self-emulsifying drug delivery systems (SEDDS), nanoemulsions, and prodrug approaches, which are critical for enhancing the bioavailability of lipid-soluble vitamins and active pharmaceutical ingredients (APIs) in the geriatric population.
Aging is characterized by a progressive decline in the functional capacity of multiple organ systems, including the gastrointestinal tract. This decline is driven by a combination of cellular hallmarks of aging, such as genomic instability, epigenetic alterations, and loss of proteostasis [89]. In the context of lipid-soluble vitamin absorption, these changes manifest as a progressive impairment of the intricate processes of digestion, absorption, and assimilation. The significance of this issue is magnified by the fact that deficiencies in vitamins A, D, E, and K are linked to a spectrum of age-related conditions, including osteoporosis, immune dysfunction, cognitive decline, and cardiovascular diseases [90] [91]. For pharmaceutical scientists, the aging GI tract presents a unique set of challenges. The absorption of lipid-soluble compounds is particularly vulnerable to age-associated changes in gastric, pancreatic, and hepatic function, necessitating a deep physiological understanding to devise effective countermeasures. This document frames the problem of age-related absorption decline within the broader research landscape of lipid-soluble vitamin absorption, highlighting key physiological targets and the advanced formulation strategies being developed to address them.
Physiological Mechanisms of Absorption Decline
The process of lipid-soluble vitamin absorption is a multi-stage operation that is systematically compromised by aging. The following sections detail the physiological alterations at each key step.
Decline in Digestive Enzyme Function
The initial phase of lipid digestion is hampered by an age-related reduction in the activity and output of key digestive enzymes.
- Gastric Lipase: A significant negative correlation exists between age and gastric lipase activity [92]. This decline can be exacerbated by conditions highly prevalent in the elderly, such as chronic atrophic gastritis and the widespread use of proton pump inhibitors, which reduce gastric acid secretion—a factor critical for optimal gastric lipase stability and function [92].
- Pancreatic Lipase: The pancreas undergoes morphological changes with age, including atrophy and steatosis, particularly noted at age thresholds of 40 and 60 years [92]. Concurrently, its exocrine function declines, leading to a marked reduction in the concentration, secretion volume, and activity of pancreatic lipase. Studies indicate a decline in lipase output by approximately 45% in older adults compared to younger individuals [92]. One proposed mechanism is the accumulation of unfolded, non-functional enzymes due to an age-related decrease in proteasome activity (e.g., reduced Psmb5), which affects the synthesis and secretion of effective lipases [92].
Alterations in Bile Acid Physiology
Bile acids are critical for the emulsification of dietary lipids and the formation of mixed micelles, which are essential for the absorption of lipid-soluble vitamins.
- Reduced Bile Acid Pool and Reabsorption: Aging is associated with a consistent decline in bile acid levels [92]. In the fasting state, plasma bile acid concentrations are lower in older men, and postprandial bile acid responses are significantly weaker in the elderly. This is linked to reduced reabsorption in the ileum, evidenced by higher fecal bile acid concentrations in older adults. The underlying mechanism involves the reduced gene expression of the apical sodium-dependent bile acid transporter (Asbt), the primary transporter regulating bile acid uptake in the intestinal apical membrane [92].
Changes in Intestinal Absorption and Metabolism
Even after digestion and emulsification, the ability of the intestinal wall to absorb nutrients is compromised.
- Reduced Triglyceride and Increased Cholesterol Absorption: Research indicates an overall reduction in triglyceride absorption capacity with age, potentially due to morphological changes in the small intestine [92] [93]. Paradoxically, cholesterol absorption appears to increase [92] [93].
- Impaired Enterocyte Uptake and Lymphatic Transport: Age-related changes in the expression and function of specific transporters and receptors on enterocytes likely contribute to absorption decline, though the exact mechanisms for lipid-soluble vitamins are still under investigation. Furthermore, alterations in lymphatic function, the primary transport route for absorbed lipids and lipid-soluble vitamins, may also play a role.
Table 1: Summary of Key Age-Related Physiological Changes Impacting Lipid-Soluble Vitamin Absorption
| Physiological Process | Specific Age-Related Change | Impact on Lipid-Soluble Vitamin Absorption |
|---|---|---|
| Gastric Digestion | Decreased gastric lipase activity; increased prevalence of atrophic gastritis and hypochlorhydria [92] [94] | Reduced initial hydrolysis of lipid-based matrices, impairing subsequent processing. |
| Pancreatic Function | Atrophy; reduced secretion and activity of pancreatic lipase [92] | Incomplete digestion of dietary triglycerides, limiting the release of lipids and lipid-soluble vitamins for incorporation into micelles. |
| Bile Acid Physiology | Reduced bile acid pool and ileal reabsorption; decreased expression of Asbt transporter [92] | Impaired formation of mixed micelles, reducing the aqueous solubility and absorption of lipid-soluble vitamins. |
| Intestinal Morphology/Function | Reduced absorptive surface area; potential alterations in transporter expression and lymphatic function [92] [95] | Diminished capacity for uptake and transport of absorbed lipids and vitamins into systemic circulation. |
Experimental Protocols for Investigating Absorption Mechanisms
To study these complex physiological changes and evaluate the efficacy of novel formulations, robust and sophisticated experimental models are required.
In Vitro Digestion and Permeability Models
- Protocol: Simulated Gastrointestinal Digestion System (SGIDS)
- Objective: To simulate the sequential pH, enzymatic, and surfactant conditions of the senior GI tract for evaluating API or vitamin release from formulations.
- Materials:
- Methodology:
- Gastric Phase: The test formulation is introduced to gastric simulation fluid (pH ~3 for aged stomach, potentially adjusted higher for hypochlorhydria) containing reduced gastric lipase and pepsin. Incubate with continuous agitation for 1 hour.
- Intestinal Phase: The gastric chyme is transferred to intestinal simulation fluid (pH 6.5-7) containing reduced concentrations of pancreatic lipase and age-mimetic bile salts.
- Analysis: Samples are taken at timed intervals. The digested material is often further subjected to permeability studies using Caco-2 cell monolayers or artificial membranes (PAMPA) to predict intestinal absorption.
In Vivo and Preclinical Animal Models
- Protocol: Pharmacokinetic Study in Aged Rodent Models
- Objective: To characterize the pharmacokinetic (PK) profile and relative bioavailability of a novel lipid-soluble vitamin formulation in aged versus young rodents.
- Materials:
- Aged rodents (e.g., 20-24 month old rats or mice) and young controls (e.g., 2-3 month old)
- Test formulation and control (e.g., standard oil solution)
- Surgical equipment for cannulation (e.g., jugular vein for serial blood sampling)
- LC-MS/MS system for quantitative analysis of the vitamin or API in plasma
- Methodology:
- Dosing and Sampling: Animals are fasted overnight and administered the test or control formulation via oral gavage. Serial blood samples are collected over a 24-48 hour period.
- Bioanalysis: Plasma concentrations of the vitamin/API are determined using a validated LC-MS/MS method.
- PK Analysis: Non-compartmental analysis is performed to determine key parameters: C~max~ (maximum concentration), T~max~ (time to C~max~), AUC~0-t~ (area under the concentration-time curve, a measure of total absorption), and t~1/2~ (elimination half-life). A significant increase in AUC and C~max~ in aged rats treated with the novel formulation compared to the control indicates enhanced bioavailability.
Clinical and Population Study Methods
- Protocol: Analysis of NHANES Data for Age-Dependent Nutrient Levels
- Objective: To establish correlation between aging and blood concentrations of lipid-soluble vitamins in a large, representative human population.
- Data Source: National Health and Nutrition Examination Survey (NHANES) datasets [90].
- Methodology:
- Data Stratification: Subject data is stratified into age decades (e.g., 20-30, 30-40, ..., 60-70 years).
- Data Cleaning: Application of rigorous cleaning algorithms (e.g., modified Horn algorithm) to remove outliers and exclude subjects with confounding factors (smoking, high alcohol use, certain medical treatments) [90].
- Statistical Analysis: Bootstrap techniques with Bonferroni adjustment are used to compare vitamin levels (A, D, E) across age groups and establish age-specific reference ranges [90].
Table 2: Key Research Reagents and Materials for Studying Age-Related Absorption
| Research Reagent / Material | Function in Experimental Protocol | Justification for Age-Related Modeling |
|---|---|---|
| Porcine Pancreatic Lipase (Reduced Concentration) | To simulate pancreatic digestion in in vitro models (SGIDS). | Mimics the documented age-related decline in pancreatic lipase secretion and activity [92]. |
| Gastric Lipase (Reduced Concentration) | To simulate gastric lipid digestion in in vitro models. | Accounts for the negative correlation between age and gastric lipase activity [92]. |
| Bile Salts (Reduced Concentration) | To act as surfactants for micelle formation in intestinal phase simulations. | Represents the smaller bile acid pool and reduced reabsorption observed in the elderly [92]. |
| Aged Rodent Models (e.g., 24-month old rats) | As in vivo models for pharmacokinetic and bioavailability studies. | Their physiological changes (e.g., reduced pancreatic function, altered body composition) mirror those in aging humans [92] [94]. |
| Caco-2 Cell Line | A human colon adenocarcinoma cell line that differentiates into enterocyte-like monolayers for permeability screening. | Provides a high-throughput model for predicting passive and active transport across the human intestinal epithelium. |
| NHANES Laboratory Data | Provides real-world, population-level data on vitamin status and biomarkers. | Allows for correlation of chronological age with biochemical status, controlling for various confounders [90]. |
Compensatory Formulation Strategies
To circumvent the physiological barriers outlined above, several advanced formulation strategies have been developed.
- Lipid-Based Formulations (LBFs): This category includes Self-Emulsifying Drug Delivery Systems (SEDDS) and nanoemulsions. These formulations are composed of lipids, surfactants, and co-surfactants that, upon mild agitation in the GI fluids, form fine emulsions or microemulsions (droplet size < 300 nm for SEDDS, and < 100 nm for SMEDDS). This process presents the lipid-soluble vitamin in a pre-dissolved state and in a small droplet size, effectively bypassing the slow and inefficient dissolution step and reducing the reliance on the patient's compromised digestive physiology [92] [93]. The large surface area of the resulting droplets facilitates rapid interaction with enterocytes and absorption via the lymphatic system, which can reduce first-pass metabolism.
- Prodrug Approaches: Chemical modification of a lipid-soluble vitamin to create a more water-soluble prodrug (e.g., esterification with a hydrophilic moiety) can enhance its absorption via the aqueous intestinal environment and passive diffusion. Once absorbed, esterases in the gut wall or plasma hydrolyze the prodrug, releasing the active vitamin.
- Nanosuspensions and Nanoparticles: For crystalline vitamins, reducing the particle size to the nano-scale (e.g., 200-800 nm) via techniques like wet milling or high-pressure homogenization can dramatically increase the surface area available for dissolution, according to the Noyes-Whitney equation. This can significantly improve the dissolution rate and extent, leading to higher bioavailability.
- Enzyme and Bile Acid Supplementation: Co-formulating lipid-soluble vitamins with digestive enzymes (e.g., lipases) or bile acids (e.g., taurocholate) is a direct strategy to compensate for the age-related deficits in these endogenous components, thereby restoring the efficiency of the digestive and absorptive process.
Visualization of Experimental Workflows
The following diagrams illustrate key experimental and physiological concepts described in this whitepaper.
In Vitro Digestion Model Workflow
Vitamin Absorption Pathway in Aging
The challenge of age-related decline in lipid-soluble vitamin absorption is multifaceted, rooted in specific physiological degradations across the digestive system. For the research and pharmaceutical development community, a mechanistic understanding of these changes—from reduced enzyme activity to altered bile acid kinetics—provides a clear roadmap for innovation. The experimental protocols and models discussed herein are critical tools for quantifying these phenomena and evaluating the efficacy of advanced formulations. The promising strategies of lipid-based delivery systems, nano-formulations, and prodrugs represent a proactive and targeted approach to ensure adequate nutrient delivery and therapeutic efficacy in the rapidly growing geriatric population. Future research must continue to refine these strategies, validate them in clinically relevant models, and translate them into effective products that promote healthy aging.
Clinical Validation and Comparative Analysis of Absorption Enhancement Strategies
This whitepaper synthesizes findings from recent population studies utilizing National Health and Nutrition Examination Survey (NHANES) data to elucidate the relationship between dietary live microbial intake and serum concentrations of fat-soluble vitamins. Evidence indicates that live microbe consumption is associated with significantly higher levels of vitamins A, D, and E and may mediate health outcomes such as reduced obesity risk through vitamin-dependent pathways. This analysis provides technical guidance on the experimental protocols, data interpretation, and mechanistic frameworks relevant to researchers investigating microbiome-nutrient interactions in the context of lipid-soluble vitamin absorption.
The absorption of lipid-soluble vitamins (A, D, E, and K) is a complex process inherently dependent on adequate fat digestion, biliary secretion, and intestinal uptake. Emerging research posits the gut microbiota as a critical modifier of this process, influencing host vitamin status through direct synthesis, competition for substrates, and alteration of gastrointestinal environments [82]. While mechanistic studies in animal models have demonstrated microbial involvement in vitamin metabolism, population-level evidence has historically been limited.
The National Health and Nutrition Examination Survey (NHANES) provides a robust platform for investigating these relationships in a free-living, nationally representative population. By applying standardized dietary classification protocols to NHANES data, researchers can quantify habitual intake of live microbes and examine correlations with biochemical indicators of vitamin status, thereby offering unique insights into real-world absorption dynamics. This whitepaleper synthesizes key findings from this emerging body of literature and details the methodologies enabling these discoveries, framing them within the broader thesis of understanding mechanistic pathways of lipid-soluble vitamin absorption.
Core NHANES Findings: Quantitative Data Synthesis
Analysis of cross-sectional NHANES data has revealed consistent, significant associations between the consumption of foods containing medium and high levels of live microbes and improved status of several fat-soluble vitamins.
Table 1: Summary of Key NHANES Studies on Live Microbial Intake and Vitamin Status
| Study Focus | Population (NHANES Cycles) | Exposure Metric | Key Vitamin Association Findings | Mediated Health Outcomes |
|---|---|---|---|---|
| Live Microbes & FSVs [12] [96] | 27,668 adults (1999-2002, 2005-2006, 2009-2018) | MedHi intake (Continuous, log-transformed) | • Vitamin A: ↑ 0.17 μg/dL (95% CI: 0.04, 0.30)• Vitamin D: ↑ 0.36 nmol/L (95% CI: 0.22, 0.51)• Vitamin E: ↑ 4.65 μg/dL (95% CI: 1.91, 7.39) | Reduced prevalence of low serum FSV levels |
| Live Microbes, Vitamin D, & Obesity [97] [98] | 18,099 adults (2007-2018) | MedHi intake (Categorical) | Serum Vitamin D identified as a significant mediator | Mediated Proportions:• BMI: 14.6%• Waist Circumference: 12.5%• Obesity: 13.0%• Abdominal Obesity: 12.5% |
| Live Microbes & Metabolic Health [99] | 15,175 adults (1999-2016) | High live microbe intake (vs. Low) | Not a primary focus | Reduced Odds of Metabolic Syndrome:OR: 0.79 (95% CI: 0.69, 0.91) |
The data demonstrate a dose-response relationship, where higher intake of live dietary microbes is associated with a favorable shift in population-level serum vitamin concentrations and a concomitant reduction in the risk of vitamin insufficiency and related metabolic diseases.
Experimental Protocols: Detailed Methodologies for Population-Level Analysis
The reproducibility of NHANES-based findings relies on strict adherence to standardized protocols for data collection, variable construction, and statistical analysis.
Dietary Live Microbe Classification Protocol
The foundational step in this research is the systematic classification of live microbial content in foods, a protocol established by Marco et al. [99].
- Data Source: USDA Food and Nutrient Database for Dietary Studies (FNDDS) food codes from 24-hour dietary recall interviews.
- Expert Panel: A consensus panel of at least four experts in microbiology and nutrition classifies each food item.
- Classification Tiers:
- Low (Lo): Foods with < 10⁴ colony-forming units per gram (CFU/g). Includes most heat-treated or processed foods.
- Medium (Med): Foods with 10⁴ – 10⁷ CFU/g. Includes many raw fruits and vegetables (e.g., carrots, cabbage).
- High (Hi): Foods with > 10⁷ CFU/g. Primarily includes fermented dairy products like yogurt, kefir, and certain aged cheeses [98] [99].
- Exposure Variable Construction:
- Categorical: Participants are grouped by diet type: "Low" (only Lo foods), "Moderate" (Med, but no Hi foods), "High" (any Hi foods).
- MedHi Intake: A composite continuous variable representing the total gram weight of all Med and Hi category foods consumed.
Biomarker and Outcome Measurement Protocols
- Serum Vitamin D Quantification:
- Method: Ultra-high-performance liquid chromatography–tandem mass spectrometry (LC-MS/MS).
- Analytes: 25-hydroxyvitamin D3 (25OHD3), 3-epi-25-hydroxyvitamin D3, and 25-hydroxyvitamin D2 (25OHD2).
- Total 25(OH)D: Sum of 25(OH)D3 and 25(OH)D2 concentrations. Quality control complies with the Clinical Laboratory Improvement Act (CLIA) standards [98].
- Obesity and Metabolic Syndrome Definitions:
- Obesity: Body Mass Index (BMI) ≥ 30 kg/m².
- Abdominal Obesity: Waist circumference >102 cm (men) or >88 cm (women) [98].
- Metabolic Syndrome (MetS): Defined per National Cholesterol Education Program-Adult Treatment Panel III (NCEP-ATP III) criteria, encompassing waist circumference, triglycerides, HDL-C, blood pressure, and fasting glucose [99].
Statistical Analysis Workflow
The analytical approach can be visualized as a multi-stage process for evaluating exposure-outcome associations and mediating pathways.
Diagram 1: Data analysis workflow for NHANES studies.
- Model Adjustment: Analyses employ weighted multivariate regression models to account for NHANES's complex survey design. Covariates are typically adjusted in stages:
- Model 1: Crude, unadjusted.
- Model 2: Adjusted for basic demographics (age, sex, race).
- Model 3: Fully adjusted for demographics, socioeconomic status (PIR, education), lifestyle (smoking, physical activity), laboratory values, and relevant dietary factors (e.g., total energy intake, dietary vitamin intake) [97] [99].
- Mediation Analysis: To test if serum vitamin D explains the live microbe-obesity link, formal mediation analysis is conducted using statistical methods like the Sobel test, quantifying the proportion of the total effect that is mediated [97] [98].
Proposed Mechanistic Pathways and Research Implications
The observed population-level associations are supported by plausible biological mechanisms rooted in the gut microbiome's role as a metabolic organ. The following diagram integrates findings from population studies with known mechanistic insights from the literature.
Diagram 2: Proposed mechanisms linking live microbes to vitamin status.
The gut microbiota influences fat-soluble vitamin status through several interconnected pathways:
- Bile Acid Metabolism: Gut bacteria modify bile acids, which are essential for micelle formation and the solubilization of lipid-soluble vitamins, thereby enhancing their absorption [12] [82].
- Gut Barrier Function: A healthy microbiota, supported by live dietary microbes, helps maintain intestinal epithelial integrity. This reduces systemic inflammation and may create a more favorable environment for nutrient absorption [99].
- Direct Microbial Synthesis and Activation: Certain gut bacterial species possess the capacity to synthesize vitamins like vitamin K2 and various B vitamins. Furthermore, microbial enzymes may participate in the activation of vitamin precursors [100].
- Systemic Signaling: Microbial metabolites, particularly short-chain fatty acids (SCFAs) from fiber fermentation, can influence systemic metabolic homeostasis and cellular responses to vitamins [100].
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table details key reagents and resources central to conducting and extending research in this field.
Table 2: Key Research Reagent Solutions for Investigating Microbe-Vitamin Interactions
| Reagent / Resource | Function / Application | Example Use in Context |
|---|---|---|
| LC-MS/MS Systems | Gold-standard quantification of serum vitamin D metabolites and other fat-soluble vitamins. | Precise measurement of 25(OH)D, 25(OH)D2, and 25(OH)D3 in NHANES biospecimens [98]. |
| Standardized 24-Hour Dietary Recall Protocols (USDA FNDDS) | Provides comprehensive, codified dietary intake data for population studies. | Foundation for classifying individual food items into live microbe categories (Lo, Med, Hi) [99]. |
| Gnotobiotic Mouse Models | Enables study of host-microbiome interactions in a controlled, germ-free environment. | Validating causal roles of specific bacteria in drug and vitamin metabolism, as seen in dexamethasone metabolism studies [100]. |
| High-Throughput Mass Spectrometry | Enables untargeted metabolomics to identify novel microbe-derived metabolites. | Used to identify 868 candidate drug metabolites produced by gut bacteria in vitro, a approach applicable to vitamin metabolites [100]. |
| Custom Bacterial Culture Media (Anaerobic) | Supports the growth of fastidious anaerobic gut bacteria for in vitro assays. | Culturing the 76 diverse human gut bacterial strains screened for drug-metabolizing capacity [100]. |
Population studies leveraging NHANES data have established a significant and consistent correlation between dietary live microbial intake and improved serum status of fat-soluble vitamins A, D, and E. These associations are biologically plausible, supported by mechanistic research illustrating the gut microbiome's profound influence on vitamin absorption, metabolism, and systemic function. The methodologies outlined—from standardized dietary classification and precise biomarker quantification to sophisticated statistical mediation analysis—provide a robust framework for continued investigation. Future research should prioritize longitudinal designs and integrate multi-omics technologies to move beyond correlation and definitively establish causality, ultimately informing targeted dietary interventions and microbiome-based therapeutics to optimize vitamin status and human health.
The Grading of Recommendations, Assessment, Development, and Evaluations (GRADE) framework provides a systematic approach for rating evidence quality and strength of recommendations in healthcare. This technical guide examines the application of GRADE to bone health research, with particular focus on moving beyond bone mineral density (BMD) as a surrogate endpoint toward fracture risk and bone quality assessments. Within the context of lipid-soluble vitamin research, we analyze how factors affecting vitamin absorption—including gut microbiota, genetic polymorphisms, and delivery systems—influence the certainty of evidence for bone health outcomes. We present structured methodologies for evaluating clinical studies, quantitative data summaries, experimental protocols for assessing vitamin bioavailability, and key signaling pathways. This whitepaper equips researchers and drug development professionals with frameworks for robust evidence assessment that acknowledges the complexity of bone physiology and the multifaceted mechanisms of fat-soluble vitamin action.
The GRADE (Grading of Recommendations, Assessment, Development, and Evaluations) framework represents a systematic, transparent approach for grading the quality (or certainty) of evidence and strength of healthcare recommendations [101] [102]. Unlike earlier hierarchical systems that primarily considered study design, GRADE employs a nuanced methodology that acknowledges the complexity of evidence assessment across multiple domains. The framework emphasizes the importance of patient-important outcomes, requiring explicit evaluation of the balance between desirable and undesirable effects, values and preferences, and resource use [102].
In bone health research, traditional reliance on BMD as a primary endpoint has created significant evidence assessment challenges. While BMD measurement via dual-energy X-ray absorptiometry (DXA) remains the gold standard for osteoporosis diagnosis, substantial evidence indicates it is an imperfect surrogate for fracture risk [103] [104]. Approximately 45% of postmenopausal women have osteoporosis and 43.5% have osteopenia, yet over half of women with osteoporosis receive no active pharmacologic treatment—a concerning care gap partially attributable to overreliance on BMD thresholds [103]. Furthermore, many fragility fractures occur in individuals with osteopenic T-scores (between -1.0 and -2.5), highlighting that BMD alone inadequately captures bone fragility [103] [104].
The integration of GRADE methodology becomes particularly crucial when evaluating interventions involving fat-soluble vitamins (A, D, E, and K), where absorption kinetics, genetic variability in transport and metabolism, and nutrient-nutrient interactions significantly impact clinical outcomes [25] [105]. This whitepaper explores the application of GRADE to bone health outcomes beyond BMD, with special consideration of the mechanistic complexities inherent in fat-soluble vitamin research.
Limitations of Bone Mineral Density as a Surrogate Endpoint
The Diagnostic and Predictive Limitations of BMD
Bone mineral density (BMD) as measured by DXA has served as the cornerstone of osteoporosis diagnosis and fracture risk assessment for decades, with the World Health Organization defining osteoporosis as a T-score of ≤ -2.5 at the lumbar spine or hip [103]. However, compelling evidence reveals significant limitations in its predictive capacity. Epidemiological data demonstrate that a substantial proportion of fragility fractures occur in individuals with BMD values above the osteoporosis threshold, with studies indicating that up to one-third of women over age 50 will experience an osteoporotic fracture during their lifetime regardless of BMD classification [103]. This diagnostic gap has stimulated the development of complementary assessment tools that better capture bone quality aspects beyond mere mineral density.
The pathophysiological basis for this discrepancy lies in the multifaceted nature of bone strength, which encompasses not only bone density but also bone microarchitecture, turnover rate, mineralization degree, and microdamage accumulation. Postmenopausal estrogen deficiency triggers accelerated osteoclast genesis and bone turnover, culminating in net bone mass loss and structural deterioration that extends beyond what BMD alone can detect [103]. This complex pathophysiology explains why individuals with similar BMD measurements may exhibit dramatically different fracture susceptibilities.
Advanced Assessment Modalities Beyond BMD
The Trabecular Bone Score (TBS) has emerged as a valuable tool that addresses BMD limitations by indirectly analyzing bone microarchitecture from lumbar spine DXA images [104]. TBS provides a texture index that correlates with trabecular characteristics independently of BMD, offering insights into bone quality that significantly enhance fracture risk prediction. Clinical validations demonstrate that when TBS is integrated into FRAX calculations, fracture risk prediction becomes significantly more accurate across age groups, sexes, and ethnicities [104]. Particularly noteworthy is the strong association between low TBS values and increased fracture risk in secondary osteoporosis conditions including diabetes, chronic kidney disease, and long-term glucocorticoid therapy, even when BMD values appear normal [104].
Table 1: Comparison of Bone Assessment Modalities
| Assessment Tool | Parameters Measured | Strengths | Limitations |
|---|---|---|---|
| BMD (DXA) | Areal bone mineral density (g/cm²) | Gold standard for osteoporosis diagnosis; Strong predictor of fracture risk in population studies | Does not capture bone microarchitecture; Limited prediction for individual fracture risk |
| TBS | Trabecular microarchitecture texture index | Independent of BMD; Enhances fracture risk prediction; Identifies high-risk patients with normal BMD | Derived from DXA image; Limited to lumbar spine assessment |
| FRAX | 10-year probability of major osteoporotic fracture | Incorporates clinical risk factors; Accessible without BMD | Without BMD, less accurate; Does not incorporate falls risk |
| FRAX + TBS | Enhanced fracture risk prediction | Superior to FRAX alone; Accounts for bone quality | Requires specialized software |
The clinical impact of incorporating these advanced assessment modalities is substantial. Research confirms that over 1,500 peer-reviewed studies validate TBS as an independent predictor of fragility fractures, leading to its inclusion in more than 30 national and international guidelines [104]. This evolution in assessment paradigms underscores the necessity of moving beyond BMD as a standalone endpoint in both clinical practice and research settings, particularly when evaluating interventions that may differentially affect bone density versus bone quality.
GRADE Methodology Framework
Fundamental Principles of Evidence Assessment
The GRADE framework employs a structured, transparent process for rating the quality of evidence and developing recommendations. As outlined in the GRADE handbook, the approach begins by defining the health care question in terms of the population of interest, alternative management strategies, and all patient-important outcomes [101]. Systematic reviews are conducted to identify relevant studies, and the evidence is summarized for each outcome. The certainty of evidence is then assessed across five domains that may lead to rating down the evidence (risk of bias, inconsistency, indirectness, imprecision, and publication bias) and three domains that may lead to rating up the evidence (large magnitude of effect, dose-response gradient, and effect of plausible residual confounding) [101] [102].
A distinctive strength of GRADE is its explicit acknowledgment that evidence quality represents a continuum rather than discrete categories. The framework nevertheless employs four certainty ratings—high, moderate, low, and very low—to facilitate decision-making. These ratings reflect the extent to which one can be confident that an estimate of effect is correct [101]. In the context of bone health and fat-soluble vitamin research, this systematic approach is particularly valuable for navigating complex evidence landscapes where multiple biological systems interact.
Evidence to Decision Framework
The final stage of the GRADE process involves moving from evidence to recommendations through the Evidence to Decision (EtD) framework [102]. This structured approach considers multiple criteria including balance of benefits and harms, certainty of evidence, values and preferences, resource use, equity, acceptability, and feasibility. Recommendations are classified as either strong or conditional (weak), reflecting the degree of confidence that the desirable consequences of an intervention outweigh the undesirable consequences [102]. For bone health interventions, this necessitates careful consideration of fracture risk reduction benefits versus potential treatment harms, costs, and patient burden.
Diagram 1: GRADE Evidence Assessment Workflow
Application of GRADE to Bone Health Outcomes
Critical and Important Outcomes in Bone Health
When applying GRADE methodology to bone health interventions, appropriate outcome selection is paramount. Fracture incidence represents the definitive patient-important outcome, as fractures directly impact morbidity, mortality, quality of life, and healthcare costs [25]. However, practical considerations including study duration, sample size requirements, and cost often necessitate the use of surrogate and intermediate outcomes. The table below categorizes bone health outcomes according to their importance in GRADE assessments.
Table 2: Bone Health Outcomes for GRADE Evaluation
| Outcome Category | Specific Outcomes | Importance in GRADE | Considerations for Fat-Soluble Vitamin Research |
|---|---|---|---|
| Patient-Important | Vertebral, hip, non-vertebral fractures | Critical | Must demonstrate direct impact; Long-term studies required |
| Surrogate | BMD (spine/hip), TBS | Important | Susceptible to indirectness; Require validation against fractures |
| Biochemical | Bone turnover markers (CTX, P1NP), ucOC | Important | Mechanism insight; High variability; Confounded by multiple factors |
| Functional | Quality of life, mobility, pain | Critical | Patient-centered; May not be specific to bone health |
| Safety | Hypercalcemia, nephrolithysis, other AEs | Critical | Particularly relevant for vitamin D interventions |
Rating Certainty for Bone-Specific Interventions
Applying GRADE domains to bone health research requires special consideration of field-specific methodological challenges. For risk of bias, particular attention should be paid to blinding difficulties in lifestyle interventions and potential outcome measurement bias in fracture adjudication. The inconsistency domain must acknowledge that bone response to interventions varies substantially by skeletal site, menopausal status, baseline nutrient status, and comorbidities. Indirectness is particularly relevant when evaluating fat-soluble vitamin interventions, as effects may differ based on chemical form (D2 vs. D3), administration timing, co-nutrient availability, and individual absorption capacity [105] [106].
Regarding imprecision, sample size requirements for fracture outcomes are substantial, often necessitating meta-analyses to detect clinically important effects. For BMD outcomes, the minimal clinically important difference (typically 3-5% at the hip) should inform precision assessments. Publication bias is a recognized concern in nutritional research, where small studies with null results often remain unpublished.
The certainty of evidence for fat-soluble vitamin interventions may be rated up for a demonstrated dose-response gradient in bone outcomes, or for a large magnitude of effect in high-risk populations. For instance, vitamin D supplementation demonstrates a more pronounced anti-fracture effect in individuals with baseline deficiency than in replete populations [106].
Fat-Soluble Vitamins and Bone Metabolism: Mechanistic Insights
Absorption Kinetics and Physiological Roles
Fat-soluble vitamins (A, D, E, and K) exhibit complex absorption, transport, and activation pathways that significantly influence their biological activity on bone tissue. These vitamins share common absorption mechanisms requiring bile salts and pancreatic enzymes for incorporation into mixed micelles, followed by uptake into intestinal enterocytes and incorporation into chylomicrons for transport via the lymphatic system [105]. This absorption pathway creates substantial interindividual variability based on genetic factors, digestive function, dietary composition, and gut microbiota status.
Vitamin D exists in two primary forms—ergocalciferol (D2) from plant sources and cholecalciferol (D3) from animal sources and cutaneous synthesis—with both forms requiring sequential hydroxylation in the liver (to 25-hydroxyvitamin D) and kidney (to 1,25-dihydroxyvitamin D) for full activation [105] [106]. The resulting hormone regulates gene transcription in target tissues including intestine, bone, and kidney, critically influencing calcium homeostasis and bone metabolism. Vitamin K functions as a cofactor for γ-glutamyl carboxylase, which activates osteocalcin—a protein essential for bone mineralization [25]. Vitamin A and its metabolites influence bone remodeling through effects on osteoblast and osteoclast differentiation, though the relationship appears U-shaped with both deficiency and excess associated with poor bone outcomes [105].
Factors Modifying Vitamin Bioavailability
Multiple factors influence the bioavailability and biological activity of fat-soluble vitamins relevant to bone health:
- Genetic polymorphisms in genes encoding vitamin D receptor (VDR), vitamin K epoxide reductase complex (VKORC1), and carotenoid oxygenases (BCO1) significantly modify individual responses to vitamin intake [25]
- Gut microbiota composition influences bile acid metabolism, lipid absorption pathways, and vitamin receptor expression, all critical for fat-soluble vitamin absorption [12]
- Dietary factors including concurrent fat intake, presence of fat-soluble vitamin antagonists, and food matrix effects modify bioavailability [105]
- Pharmaceutical interactions with drugs that affect lipid absorption or vitamin metabolism (e.g., statins, orlistat, warfarin) can substantially impact vitamin status [25]
Recent population-based evidence indicates that dietary intake of live microbes is positively associated with serum levels of vitamins A, D, and E, suggesting a potentially important role for gut microbiota in maintaining adequate vitamin status for bone health [12].
Diagram 2: Fat-Soluble Vitamin Absorption & Metabolism
Experimental Protocols for Assessing Bone Health Outcomes
Methodologies for Clinical Trial Endpoints
Robust assessment of bone health outcomes in clinical trials requires standardized methodologies across multiple domains. For fracture outcomes, clearly defined adjudication procedures using radiologic confirmation are essential, with pre-specified categorization of fracture types (vertebral, non-vertebral, hip) and trauma level (fragility vs. non-fragility). BMD measurement should follow ISCD (International Society for Clinical Densitometry) guidelines for DXA acquisition and analysis, with quality control procedures including phantom scanning and cross-calibration in multi-center trials [103]. TBS analysis should be performed using validated software (e.g., TBS Osteo Advanced) on lumbar spine DXA images, with appropriate consideration of technical limitations including high BMI artifacts [104].
Biochemical marker assessment requires strict standardization of sampling conditions (fasting status, time of day, seasonal variation) and analytical methods. Recommended bone turnover markers include procollagen type I N-terminal propeptide (P1NP) for formation and C-terminal telopeptide of type I collagen (CTX) for resorption, with undercarboxylated osteocalcin (ucOC) providing specific information about vitamin K status [25]. For vitamin status assessment, liquid chromatography-tandem mass spectrometry (LC-MS/MS) represents the gold standard for 25-hydroxyvitamin D measurement, while high-performance liquid chromatography (HPLC) methods are preferred for vitamins A, E, and K assessment [12].
Advanced Methodologies for Mechanistic Studies
Research on fat-soluble vitamin mechanisms requires specialized methodologies to address absorption and metabolic complexities:
- Stable isotope tracer techniques enable quantitative assessment of vitamin absorption, distribution, and conversion to active metabolites
- Enteroid models derived from human intestinal stem cells provide physiologically relevant systems for studying absorption mechanisms
- Genotyping platforms for polymorphisms in VDR, GC, CYP2R1, VKORC1, and BCO1 allow stratification by genetic determinants of vitamin status
- Microbiome sequencing (16S rRNA and metagenomic) characterizes microbial communities that influence vitamin bioavailability
- Nanoformulation approaches address delivery challenges by improving solubility, stability, and targeted delivery of fat-soluble vitamins [105]
These advanced methodologies strengthen the mechanistic component of intervention studies, potentially increasing the certainty of evidence by elucidating biological pathways and explaining heterogeneous treatment effects.
Research Reagent Solutions for Bone Health and Vitamin Studies
Table 3: Essential Research Reagents and Materials
| Reagent Category | Specific Examples | Research Application | Technical Considerations |
|---|---|---|---|
| Vitamin Standards | Certified reference materials for 25(OH)D3, 25(OH)D2, retinol, α-tocopherol, phylloquinone | LC-MS/MS quantification; Assay calibration | Ensure isotopic purity for stable isotope tracers; Verify stability with proper storage |
| Immunoassays | ELISA kits for P1NP, CTX, osteocalcin forms, vitamin D binding protein | Bone turnover assessment; Vitamin transport evaluation | Prefer automated platforms for high-throughput studies; Validate against reference methods |
| Cell Culture Systems | Osteoblast/osteoclast cell lines; Human primary bone cells; Enteroid cultures | Mechanistic studies; Absorption modeling | Use physiologically relevant differentiation conditions; Consider donor characteristics for primary cells |
| Genotyping Assays | TaqMan assays for VDR (FokI, BsmI), VKORC1, GC, CYP2R1 polymorphisms | Pharmacogenomic analyses; Stratification factors | Validate in target population; Consider haplotype structures in diverse populations |
| Microbiome Tools | 16S rRNA sequencing primers; DNA extraction kits for stool; Microbial culture media | Gut-microbiota interactions | Standardize collection and storage; Include appropriate contamination controls |
| Animal Models | Ovariectomized rodents; Vitamin D receptor knockout mice; Zebrafish bone models | Preclinical efficacy testing | Consider species differences in vitamin metabolism; Control for dietary vitamin content |
Quantitative Data Synthesis and Evidence Profiles
Evidence Profile Development
GRADE evidence profiles provide structured summaries of effect estimates and certainty assessments for each critical outcome. For bone health interventions, these profiles should include both absolute and relative effect measures, with particular attention to baseline risk stratification since intervention benefits are typically greater in high-risk populations. The following exemplar data illustrate how vitamin D supplementation effects vary across outcomes and population characteristics.
Table 4: Exemplary Evidence Profile for Vitamin D Supplementation in Postmenopausal Women
| Outcome | Relative Effect (95% CI) | Absolute Risk in Controls | Absolute Risk with Intervention | Certainty |
|---|---|---|---|---|
| Hip fracture | RR 0.80 (0.72-0.89) | 20 per 1000 | 16 per 1000 | Moderate¹ |
| Vertebral fracture | RR 0.66 (0.54-0.81) | 50 per 1000 | 33 per 1000 | Moderate¹ |
| Any non-vertebral fracture | RR 0.86 (0.78-0.94) | 150 per 1000 | 129 per 1000 | Moderate¹ |
| BMD change (hip) | MD 2.3% (1.8-2.8) | - | - | High |
| Serum 25(OH)D | MD 28 nmol/L (24-32) | - | - | High |
| Hypercalcemia | RR 1.55 (1.02-2.35) | 5 per 1000 | 8 per 1000 | Moderate² |
¹Rated down for imprecision due to wide confidence intervals ²Rated down for indirectness due to population differences
Contextualizing Evidence for Decision-Making
When applying GRADE to fat-soluble vitamin interventions, several contextual factors require consideration. First, the baseline nutritional status of the population significantly modifies treatment effects, with deficient individuals demonstrating greater responsiveness. Second, the chemical form (D2 vs. D3), dosage regimen (daily vs. bolus), and administration timing (with meals) influence efficacy. Third, co-nutrient status (particularly calcium, magnesium, and vitamin K) may modify bone responses to vitamin D supplementation.
For researchers and guideline developers, these nuances necessitate careful specification of the population, intervention, comparator, and outcomes (PICO) framework. Evidence assessments should explicitly state assumptions about baseline status, intervention characteristics, and companion nutrients. When meta-analyses combine studies with importantly different implementations, the certainty of evidence may need rating down for indirectness.
The application of GRADE methodology to bone health outcomes requires moving beyond traditional surrogate endpoints like BMD to incorporate fracture incidence, bone quality assessments, and patient-centered outcomes. For fat-soluble vitamin research, this entails careful consideration of absorption kinetics, genetic modifiers, nutrient interactions, and microbiota influences that contribute to heterogeneous treatment effects. By employing structured evidence assessment frameworks, standardized experimental protocols, and comprehensive outcome measurement, researchers can generate higher certainty evidence to inform clinical practice and public health guidelines. The continuing evolution of bone assessment technologies and nutritional science methodologies promises to further refine our understanding of how fat-soluble vitamins influence skeletal health across diverse populations.
This technical review examines the comparative efficacy of natural vitamin K2, specifically menaquinone-7 (MK-7) derived from Bacillus subtilis natto, against pharmacological vitamin K1 (phylloquinone) formulations. Within the broader context of lipid-soluble vitamin absorption research, we analyze fundamental differences in pharmacokinetics, bioavailability, and physiological efficacy that underlie their distinct clinical applications. Evidence synthesized from clinical trials and mechanistic studies demonstrates that natto-derived MK-7 exhibits superior bioavailability and sustained activity in extrahepatic tissues compared to K1, with significant implications for cardiovascular, bone, and cognitive health beyond traditional coagulation roles. This assessment provides researchers and drug development professionals with critical insights for designing targeted interventions leveraging the unique properties of each vitamer.
Vitamin K encompasses a group of fat-soluble vitamers essential for the post-translational modification of vitamin K-dependent proteins (VKDPs). These compounds share a common 2-methyl-1,4-naphtoquinone ring structure but differ in their side chains, which determine their pharmacokinetic properties and tissue distribution [107]. The two primary natural forms are phylloquinone (vitamin K1) and menaquinones (vitamin K2), which exhibit distinct sources, bioavailability, and biological activities [107].
Table 1: Fundamental Characteristics of Vitamin K Forms
| Parameter | Vitamin K1 (Phylloquinone) | Vitamin K2 (Menaquinone-7) |
|---|---|---|
| Primary Source | Photosynthetic plants (leafy greens, plant oils) [107] | Bacterial synthesis (Bacillus subtilis natto) [108] |
| Side Chain Structure | Phytyl side chain (4 isoprenoid units, one unsaturated) [107] | Polyisoprenyl side chain (7 isoprenoid units, all unsaturated) [107] |
| Dietary Contribution | ~75-90% of total vitamin K intake [107] | Minor dietary contribution, but high bioavailability [108] |
| Absorption Efficiency | 5-10% from vegetables [108] | Nearly complete absorption [108] |
| Industrial Production | Chemical synthesis [109] | Microbial fermentation using Bacillus subtilis [108] |
Vitamin K1 serves as the primary dietary form obtained from leafy green vegetables and plant oils, while vitamin K2 represents a group of compounds (MK-4 through MK-13) synthesized by anaerobic bacteria [107]. MK-4 can be synthesized from K1 in humans and animals, while longer-chain menaquinones (MK-5 to MK-13) are primarily produced by bacteria, with MK-7 being particularly abundant in natto, a traditional Japanese fermented soybean food [107] [108]. The structural differences between these vitamers significantly impact their absorption, transport, and tissue distribution, ultimately influencing their physiological efficacy.
Pharmacokinetic Profiles and Bioavailability
Clinical investigations directly comparing the pharmacokinetic properties of vitamin K1 and natto-derived MK-7 reveal substantial differences that underlie their distinct biological activities.
Absorption and Serum Kinetics
Table 2: Comparative Pharmacokinetic Parameters of K1 and MK-7
| Pharmacokinetic Parameter | Synthetic Vitamin K1 | Natto-derived MK-7 |
|---|---|---|
| Peak Serum Concentration (Tmax) | 4 hours post-intake [109] | 4 hours post-intake [109] |
| Elimination Half-life | Short (~1-2 hours) [109] | Very long (~72 hours) [109] |
| Serum Accumulation | Minimal accumulation | 7- to 8-fold higher accumulation during prolonged intake [109] |
| Area Under Curve (AUC) | Reference value | 106.407 ± 73.794 μg·h/mL (HyperCelle formulation) [110] |
| Maximum Concentration (Cmax) | Reference value | 3.038 ± 2.184 μg/mL (HyperCelle formulation) [110] |
Both vitamin K1 and MK-7 are absorbed effectively, reaching peak serum concentrations approximately 4 hours after oral administration [109]. The critical distinction emerges in their elimination kinetics: MK-7 demonstrates a substantially longer half-life resulting in more stable serum levels and significant accumulation during prolonged intake [109]. This prolonged circulation time enables MK-7 to maintain sustained activity in extrahepatic tissues, a property less pronounced with rapidly cleared K1.
Bioavailability Enhancement Strategies
Recent advances in formulation technology have significantly improved the bioavailability of MK-7. The HyperCelle nanoencapsulation method produces spherical nanoparticles with a well-defined core-shell structure (average diameter 321.4 nm) that enhance water dispersibility (>90%) compared to conventional powdered formulations [110]. This technology significantly increases both AUC and Cmax values compared to non-encapsulated MK-7, demonstrating the potential of advanced delivery systems to optimize the pharmacokinetic profile of this lipophilic compound [110].
Figure 1: Comparative Pharmacokinetic Pathways of Vitamin K1 and MK-7
Molecular Mechanisms of Action
The fundamental mechanism of action for both vitamin K1 and K2 involves serving as essential cofactors for the γ-carboxylation of vitamin K-dependent proteins (VKDPs). This post-translational modification converts specific glutamate residues to γ-carboxyglutamate (Gla), enabling these proteins to bind calcium and undergo conformational activation [107] [111].
Vitamin K-Dependent Proteins and Tissue Distribution
Table 3: Key Vitamin K-Dependent Proteins and Their Functions
| VKDP | Primary Tissue Location | Physiological Function | Relative Activation by K1 vs K2 |
|---|---|---|---|
| Coagulation Factors (II, VII, IX, X) | Liver | Blood coagulation | Equally activated by K1 and K2 [111] |
| Protein C & Protein S | Liver | Anticoagulation regulation | Equally activated by K1 and K2 [111] |
| Osteocalcin | Bone | Bone mineralization | MK-7 induces more complete carboxylation [109] |
| Matrix Gla Protein (MGP) | Vascular smooth muscle | Inhibits vascular calcification | MK-7 more effective due to sustained availability [111] |
| Gla-Rich Protein (GRP) | Cartilage, vascular | Inhibits ectopic calcification | MK-7 more effective due to sustained availability [110] |
While both vitamers activate the γ-carboxylation system, their efficacy differs significantly between hepatic and extrahepatic tissues. In hepatic tissues, both K1 and K2 effectively activate coagulation factors. However, in extrahepatic tissues, MK-7 demonstrates superior efficacy due to its longer half-life and greater bioavailability, enabling more sustained activation of proteins like osteocalcin in bone and matrix Gla protein in the vascular system [109] [111].
Figure 2: Differential Activation of Vitamin K-Dependent Proteins by K1 and MK-7
Experimental Methodologies for Efficacy Assessment
Clinical Protocol for Bioavailability Assessment
Study Design: Randomized, double-blind, controlled, parallel-group clinical trial [110]
Participants: Healthy adults aged 20-29 years with BMI 18.5-30.0 kg/m²
Interventions:
- Test formulation: HyperCelle Vitamin K2 (nanoencapsulated MK-7)
- Control formulation: Conventional powdered MK-7 without nanoparticle processing
- Single oral dose administration after fasting
Sample Collection and Analysis:
- Blood sampling at baseline, 6, 10, 24, and 72 hours post-administration
- Plasma separation via centrifugation at 3000 rpm for 15 minutes at 4°C
- MK-7 quantification using HPLC with UV detection
- Pharmacokinetic parameters calculation: AUC, Cmax, Tmax, elimination half-life
Statistical Analysis:
- Comparison of AUC and Cmax between groups using Student's t-test
- Significance threshold set at p < 0.05
Protocol for Assessment of Biochemical Efficacy
Study Design: Comparative clinical trial over 6-week supplementation [109]
Participants: Healthy volunteers
Interventions:
- Group 1: Synthetic vitamin K1 supplements
- Group 2: Natto-derived MK-7 supplements (equivalent doses)
Primary Endpoints:
- Serum vitamin K species concentration (marker of absorption)
- Osteocalcin carboxylation status (functional biomarker)
- Undercarboxylated osteocalcin (ucOC) levels
- Ratio of carboxylated to undercarboxylated osteocalcin
Analytical Methods:
- Serum vitamin K quantification using HPLC
- Osteocalcin carboxylation status via ELISA or RIA
- Statistical comparison of carboxylation efficacy between groups
Comparative Efficacy in Physiological Systems
Bone Health and Osteocalcin Carboxylation
Clinical evidence demonstrates that MK-7 induces more complete carboxylation of osteocalcin compared to vitamin K1 [109]. In a direct comparison study, circulating undercarboxylated osteocalcin (a marker for hip fracture risk) decreased significantly more with MK-7 supplementation than with K1 [112]. While both forms improved the ratio between carboxylated and undercarboxylated osteocalcin, the curve for K1 reached a clear plateau, whereas MK-7 continued to show increasing efficacy after six weeks of administration [112]. This sustained activation of osteocalcin by MK-7 contributes to improved bone mineralization and reduced fracture risk.
Cardiovascular Health and Vascular Calcification
Matrix Gla Protein (MGP) is a potent inhibitor of vascular calcification that requires vitamin K-dependent activation. The superior bioavailability and sustained serum levels of MK-7 result in more effective activation of MGP compared to K1 [111]. Through this mechanism, MK-7 plays a critical role in maintaining vascular elasticity and reducing arterial stiffness—key factors in cardiovascular health and cognitive function [111]. Arterial stiffness, measured by pulse wave velocity (PWV), is strongly associated with cognitive impairment, and MK-7's efficacy in mitigating vascular calcification represents a crucial mechanism linking vascular health to brain health [111].
Potential Neuroprotective Effects
Emerging research suggests that vitamin K2 may play a role in brain health through multiple mechanisms. By reducing arterial stiffness and improving cerebral blood flow, MK-7 may help preserve cognitive function [111]. The brain, with its high-flow, low-resistance vascular system, is particularly vulnerable to damage from arterial stiffness, which has been associated with age-related cerebral changes, including atrophy and small vessel disease [111]. These mechanisms position MK-7 as a potential neuroprotective agent, though more research is needed to fully elucidate its role in cognitive health.
Research Reagent Solutions
Table 4: Essential Research Materials for Vitamin K Investigation
| Reagent/Material | Specifications | Research Application |
|---|---|---|
| Natto-derived MK-7 | High-purity extract from Bacillus subtilis natto fermentation; ≥1% MK-7 concentration [110] | Reference standard for bioavailability and efficacy studies |
| HyperCelle Formulation | Nanoencapsulated MK-7 (321.4 nm diameter, PI: 0.210); spray-dried powder with dextrin/maltodextrin [110] | Bioavailability enhancement studies; nanoparticle delivery system research |
| Vitamin K1 Standard | Synthetic phylloquinone; pharmaceutical grade [109] | Comparative pharmacokinetic studies; control substance for efficacy trials |
| HPLC-UV System | Reverse-phase C18 column; UV detection at 248-270 nm [110] | Quantification of vitamin K species in plasma and tissues |
| Anti-ucOC Antibodies | Monoclonal or polyclonal specific for undercarboxylated osteocalcin | Assessment of vitamin K functional status in bone metabolism |
| Dynamic Light Scattering | Detection range: 0.1 nm to 10 μm; temperature control at 25°C [110] | Nanoparticle characterization and quality control |
| Transmission Electron Microscope | Operation at 80 kV; magnification 100,000x [110] | Visualization of nanoencapsulation structure and integrity |
Clinical Implications and Therapeutic Considerations
The distinct pharmacokinetic and functional properties of natto-derived MK-7 versus pharmacological K1 formulations necessitate careful consideration in clinical applications. While vitamin K1 remains effective for addressing coagulation-related deficiencies, MK-7 demonstrates superior efficacy for extrahepatic applications, particularly in bone and cardiovascular health [109] [111]. This differential efficacy has important implications for patients on oral anticoagulant therapy, as supplements providing 50 μg/d or more of MK-7 may interfere with anticoagulant treatment in a clinically relevant way [109].
Future research should focus on elucidating the precise dosage requirements for specific health outcomes, understanding genetic factors that influence vitamin K metabolism, and developing targeted delivery systems that optimize the bioavailability and tissue-specific delivery of each vitamer [25]. The emerging evidence supporting vitamin K2's role in broader physiological functions, including cognitive health, underscores the need for continued investigation into the therapeutic potential of natto-derived MK-7 beyond its established roles in bone and cardiovascular health [111].
The absorption, metabolism, and physiological effects of fat-soluble vitamins A and D differ significantly based on their source—whether from whole foods or supplemental forms. This whitepaper examines the distinct safety and toxicity profiles of dietary versus supplemental vitamin A and D within the broader context of lipid-soluble vitamin absorption mechanisms. We synthesize current evidence on the differential risks, integrating quantitative toxicity thresholds, molecular absorption studies, and clinical outcomes. For researchers and drug development professionals, this analysis provides critical insights for designing safer therapeutic formulations and nutritional interventions, emphasizing that supplemental forms pose substantially higher toxicity risks due to pharmacological dosing, altered bioavailability, and absence of synergistic food matrices that modulate natural absorption kinetics.
Vitamins A and D, while essential for numerous physiological processes including vision, bone metabolism, and immune function, exhibit a narrow therapeutic index, making their safety profile a critical research focus [113] [114]. The source of intake—dietary versus supplemental—is a fundamental determinant of their pharmacokinetics and potential for toxicity [25]. Dietary vitamins exist within complex food matrices, often accompanied by other nutrients and compounds that modulate their absorption and bioactivity. In contrast, supplements typically deliver isolated, high-potency compounds that bypass natural regulatory mechanisms [25] [115].
Understanding these differential risks requires a foundation in the mechanisms of lipid-soluble vitamin absorption. These vitamins follow absorption pathways similar to other dietary lipids, requiring bile acid solubilization and formation of chylomicrons for transport into the lymphatic system and systemic circulation [6] [106]. The molecular structure of each vitamin dictates its specific interaction with the intestinal epithelium and subsequent metabolic fate. Recent molecular dynamics simulations reveal that vitamins A and E spontaneously penetrate the lipid bilayer, with their hydroxyl groups forming hydrogen bonds with phosphate groups of phospholipids, a process critical for their absorption efficiency [6]. This technical review examines how these fundamental absorption mechanisms diverge between natural and supplemental sources, creating distinct toxicological landscapes for each vitamin.
Vitamin A Safety Parameters
Table 1: Vitamin A (Retinol) Safety and Toxicity Parameters
| Parameter | Dietary Sources | Supplemental Sources | Toxicity Threshold |
|---|---|---|---|
| Recommended Daily Allowance (RAE) | 700-900 μg/day for adults [113] | Same as dietary | Upper Limit (UL): 3,000 μg/day [113] |
| Common Sources | Liver, eggs, dairy, fish (preformed); carrots, sweet potatoes (provitamin A) [113] | Isolated retinol, retinyl esters | Acute Toxicity: >100,000 μg [113] |
| Bioavailability Modulators | Food matrix, dietary fats, other carotenoids [25] | Often administered without modulators | Chronic Toxicity: >8,000 μg/day [113] |
| Toxic Forms | Preformed vitamin A from animal sources [113] | All preformed vitamin A supplements | Provitamin A carotenoids unlikely [113] |
| Key Toxicity Concerns | Hepatic steatosis, fibrosis, cirrhosis [114] | Teratogenicity, osteoporosis, hypercalcemia [113] [115] | Bone mineral density effects at ~2x RDA [115] |
Vitamin D Safety Parameters
Table 2: Vitamin D (Cholecalciferol) Safety and Toxicity Parameters
| Parameter | Dietary Sources | Supplemental Sources | Toxicity Threshold |
|---|---|---|---|
| Recommended Daily Allowance | 600-800 IU/day (15-20 μg) [116] | Same as dietary | Upper Limit (UL): 4,000 IU/day [117] |
| Common Sources | Fatty fish, egg yolks, fortified foods [116] [117] | Isolated D2 (ergocalciferol) or D3 (cholecalciferol) | Toxicity Level: >10,000 IU/day typically required [116] |
| Bioavailability Modulators | Dietary fat, healthy gastrointestinal tract [106] | Formulation (oil vs. powder), co-administered fats | Toxic Serum 25(OH)D: >150 ng/mL (375 nmol/L) [116] |
| Endogenous Production | Significant source via UV-B exposure [116] [106] | Not applicable | Sun exposure does not cause toxicity [117] |
| Key Toxicity Concerns | Extremely rare from dietary sources [117] | Hypercalcemia, nephrolithiasis, renal failure [116] [117] | Hypercalcemia primary concern [117] |
Molecular Absorption Mechanisms and Toxicological Implications
The differential toxicity between dietary and supplemental vitamins A and D originates in their distinct absorption pathways and molecular interactions with intestinal structures.
Vitamin A Absorption Dynamics
Dietary vitamin A exists primarily as retinyl esters from animal sources and provitamin A carotenoids from plants. These forms require enzymatic hydrolysis in the intestinal lumen before absorption. Retinol subsequently incorporates into mixed micelles with bile acids and other dietary lipids, a process that naturally limits absorption capacity [113]. Molecular dynamics simulations reveal that retinol spontaneously penetrates the lipid bilayer, leveraging its hydroxyl group to form hydrogen bonds with phosphate groups of dipalmitoylphosphatidylcholine (DPPC) membranes. This interaction enables high structural flexibility and a broad tilt angle toward the lipid membrane, facilitating its absorption [6].
Supplemental preformed vitamin A, often administered as retinyl palmitate or retinol, bypasses the natural release kinetics from food matrices. This results in rapid absorption of pharmacological doses that can overwhelm the liver's storage capacity in hepatic stellate cells [114]. When capacity is exceeded, retinoids spill into systemic circulation, causing oxidative stress, mitochondrial dysfunction, and activation of apoptotic pathways [114]. The saturable absorption of dietary provitamin A carotenoids provides inherent protection against toxicity, as conversion to retinol decreases with increasing doses [113].
Vitamin D Absorption and Regulation
Vitamin D absorption occurs primarily in the small intestine via passive diffusion facilitated by incorporation into mixed micelles [106]. Unlike vitamin A, vitamin D undergoes minimal pre-absorptive processing. Molecular studies indicate that its hydroxyl group facilitates membrane integration, though with different orientation dynamics compared to retinol [6]. The critical distinction between dietary and supplemental vitamin D lies in the dose-response relationship and regulatory control.
Endogenous vitamin D synthesis from sun exposure is self-regulating through cutaneous feedback mechanisms, preventing toxicity [116] [117]. Dietary vitamin D from natural foods rarely provides sufficient amounts to cause toxicity due to low concentration levels [117]. However, high-potency supplements bypass these natural controls, leading to direct absorption of pharmacological doses. This saturates vitamin D-binding proteins, increases free 1,25(OH)2D concentrations, and disrupts calcium homeostasis, resulting in hypercalcemia—the hallmark of vitamin D toxicity [116].
Experimental Models and Methodologies
Molecular Dynamics Simulations
Protocol Title: Molecular Dynamics Simulation of Fat-Soluble Vitamin Absorption into Lipid Bilayers [6]
Objective: To investigate the distribution, location, orientation, and dynamics of retinol (vitamin A), α-tocopherol (vitamin E), and phylloquinone (vitamin K1) within a dipalmitoylphosphatidylcholine (DPPC) bilayer membrane.
Methodology Details:
- System Preparation: Initial structure of DPPC consisting of 128 molecules as a lipid bilayer was obtained from the MOOSE database. One vitamin molecule was placed in the center of the x-axis exterior of the lipid bilayer, located 41 Å from the bilayer center along the z-axis.
- Solvation Model: SPC (Single-Point Charge) parameters were used as the explicit solvent model.
- Simulation Parameters: Three-dimensional periodic boundary conditions were applied. Energy minimization was performed using the steepest descent method for 10,000 steps. Systems were equilibrated for 100 ps in the NVT ensemble followed by 100 ps in the NPT ensemble at 1 bar.
- Production Run: All systems were simulated for 100 ns using the GROMACS package with CHARMM36 force field.
- Analysis: Binding orientations, favorable binding sites, hydrogen bonding interactions, and diffusion coefficients were calculated. The angle distribution profiles indicating molecular orientation inside the DPPC bilayer were analyzed.
Key Findings: Retinol showed the highest structural flexibility and diffusion coefficient, plugging its head group into the hydrocarbon core. The hydroxyl group of retinol and tocopherol formed hydrogen bonds with the phosphate group of DPPC, which was essential for their absorption behavior.
Clinical Monitoring Protocol
Protocol Title: Targeted Vitamin D Supplementation with Biochemical Monitoring [118]
Objective: To achieve and maintain optimal vitamin D levels (40-80 ng/mL) through personalized dosing while preventing toxicity.
Methodology Details:
- Participant Selection: Adults with heart disease and previous heart attack.
- Baseline Assessment: Serum 25(OH)D and calcium levels measured in all participants.
- Intervention Group: Received vitamin D supplementation with doses adjusted every three months based on serum levels.
- Dose Titration: Starting dose of 5,000 IU/day for 52% of participants with levels below 40 ng/mL. Doses were reduced or stopped if vitamin D levels exceeded 80 ng/mL or if hypercalcemia occurred.
- Safety Monitoring: Regular checks of both vitamin D and calcium levels to prevent toxicity. Co-administration of vitamin D with calcium was avoided in participants with tendency toward hypercalcemia.
- Duration: Average follow-up of 4.2 years.
Key Findings: Personalized dosing requiring >5,000 IU/day in most participants reduced heart attack risk by 52% without inducing toxicity, demonstrating that high-dose supplementation can be safe with appropriate monitoring.
Research Reagent Solutions
Table 3: Essential Research Reagents for Studying Fat-Soluble Vitamin Absorption
| Reagent/Material | Specifications | Research Function |
|---|---|---|
| DPPC Bilayer | Dipalmitoylphosphatidylcholine, 128 molecules [6] | Model membrane system for molecular dynamics simulations |
| SPC Water Model | Single-Point Charge parameters [6] | Explicit solvent model for hydration in simulation systems |
| CHARMM36 Force Field | Chemistry at HARvard Macromolecular Mechanics [6] | Parameter set for molecular dynamics simulations |
| Caco-2 Cell Line | Human colon adenocarcinoma cell line [6] | In vitro model of human intestinal epithelium |
| Liquid Chromatography-Tandem Mass Spectrometry | Fully validated technique [12] | Quantitative assessment of serum vitamin concentrations |
| Vitamin D Binding Protein | Specific carrier protein [116] | Study vitamin D transport and bioavailability |
Clinical Implications and Pathological Outcomes
Vitamin A Toxicity Manifestations
Vitamin A toxicity presents distinct pathological profiles based on source and exposure duration. Chronic toxicity from supplemental use manifests primarily in hepatic and skeletal systems. The liver, as the primary storage organ, experiences progressive damage beginning with hepatic steatosis and advancing to fibrosis and cirrhosis [114]. Histopathological examination reveals vacuolar degeneration, hepatocellular ballooning, and activation of hepatic stellate cells, which transform into myofibroblasts driving collagen production [114]. Molecular mechanisms involve oxidative stress from reactive oxygen species generation, apoptosis through mitochondrial dysfunction, and dysregulated signaling pathways including TGF-β and NF-κB [114].
Skeletal effects include bone resorption and hypercalcemia, with osteoporosis and hip fracture risk associated with intakes only twice the RDA [115]. Teratogenic effects represent a particularly severe risk of supplemental vitamin A during pregnancy, with isotretinoin increasing fetal malformation risk by 25-fold through toxic effects on neural crest cells and disruption of axial patterning gene expression [113].
Vitamin D Toxicity Mechanisms
Vitamin D toxicity primarily manifests as hypercalcemia due to its fundamental role in calcium homeostasis [116]. Excessive 25(OH)D and free 1,25(OH)2D concentrations enhance intestinal calcium absorption and osteoclastic bone resorption, overwhelming renal clearance capacity [116]. Clinical presentations include gastrointestinal symptoms (nausea, vomiting, constipation), neurological symptoms (confusion, apathy), renal impairment (polyuria, nephrolithiasis), and cardiovascular abnormalities (shortened QT interval, arrhythmias) [116].
The management of vitamin D toxicity involves cessation of supplementation, intravenous hydration with isotonic saline, and in severe cases, corticosteroids or bisphosphonates to lower serum calcium levels [116]. Critical to prevention is recognizing that toxicity typically requires doses exceeding 10,000 IU/day for prolonged periods, with serum 25(OH)D concentrations >150 ng/mL [116].
The safety profiles of vitamins A and D differ fundamentally between dietary and supplemental sources, with supplemental forms posing substantially higher toxicity risks due to pharmacological dosing, absence of natural food matrices, and bypassing of regulatory absorption controls. Vitamin A toxicity from supplements manifests in hepatic, skeletal, and teratogenic effects at doses only moderately above nutritional requirements, while vitamin D toxicity primarily causes hypercalcemia through disruption of calcium homeostasis. Molecular absorption studies reveal that specific structural features govern vitamin-membrane interactions, providing insights for designing safer formulations. Future research should focus on developing biomarkers for early toxicity detection, personalized risk assessment considering genetic polymorphisms in vitamin metabolism, and establishing refined dietary guidelines that account for the distinct bioactivity and toxicity of natural versus supplemental sources. For drug development professionals, these findings underscore the importance of considering source-dependent toxicity in therapeutic design and the necessity of biochemical monitoring during high-dose interventions.
This technical guide addresses the critical challenge of validating functional endpoints in clinical research focused on lipid-soluble vitamins. While traditional biomarkers like serum vitamin levels provide useful pharmacokinetic data, they frequently correlate poorly with clinically meaningful health outcomes. This whitepaper establishes a framework for implementing and validating three core functional endpoints—fracture risk, immune function, and quality of life measures—within the specific context of fat-soluble vitamin absorption and metabolism research. We present standardized experimental protocols, quantitative data synthesis, and mechanistic pathways to enhance the rigor, regulatory acceptance, and clinical relevance of future studies in this field. The integration of these patient-centered endpoints is essential for truly understanding the therapeutic impact of vitamins A, D, E, and K on human health.
Research on fat-soluble vitamins (FSVs)—including vitamins A, D, E, and K—has traditionally relied heavily on circulating serum levels as primary endpoints. While these biochemical measures provide valuable absorption data, they represent insufficient proxies for functional health outcomes. A significant limitation in the current literature is the lack of distinction between dietary intake and supplemental forms, which may have profoundly different biological effects due to synergistic actions with other food components [25]. Furthermore, genetic polymorphisms in genes such as VDR, GC, and VKORC1 can alter individual responses to FSVs, necessitating functional validation that accounts for this variability [25].
The validation of functional endpoints is particularly crucial for demonstrating the real-world efficacy of FSV interventions. As noted in a recent critique, many studies "primarily emphasized bone mineral density (BMD) as a clinical endpoint, but BMD alone is an imperfect surrogate for fracture risk" [25]. This whitepaper addresses this methodological gap by providing technical guidance for implementing three validated functional endpoint categories—fracture risk, immune parameters, and quality of life measures—within the mechanistic framework of lipid-soluble vitamin absorption research.
Quantitative Data Synthesis: Functional Endpoints in Clinical Research
Table 1: Functional Endpoint Measurements in Clinical Studies Involving Fat-Soluble Vitamins
| Endpoint Category | Specific Measure | Population | Results/Values | Clinical Significance |
|---|---|---|---|---|
| Bone Health/Fracture Risk | Incident Non-vertebral Fractures (36 months) | Seniors ≥70 years (DO-HEALTH Trial) [119] | Primary endpoint; results pending | Direct measure of fracture risk prevention |
| Bone Mineral Density (BMD) - Lumbar Spine | Patients with combined Vitamin D & K supplementation [120] | Notable increase reported | Surrogate marker for bone strength | |
| Undercarboxylated Osteocalcin (ucOC) | Patients with Vitamin D & K supplementation [120] | Significant decrease | Functional biomarker of vitamin K activity in bone | |
| Physical Function & QoL | SF-12 Physical Domain Score | Lower limb fracture patients [121] | 39.9 ± 9.5 points | Significantly impaired vs. population norms |
| SF-12 Mental Domain Score | Lower limb fracture patients [121] | 48.6 ± 10.9 points | Indicative of mental health impact | |
| Timed Up and Go (TUG) Test | Lower limb fracture patients [121] | 12.3 ± 3.3 seconds | Objective functional mobility measure | |
| 10-Meter Walk Test | Lower limb fracture patients [121] | 1.6 ± 0.3 m/s | Quantitative gait speed assessment | |
| Immune Function | Infection Rate (any) | Seniors ≥70 years (DO-HEALTH Trial) [119] | Primary endpoint; results pending | Clinically relevant immune competence measure |
| CIN1 Regression Rate | Bi-weekly cholecalciferol (50,000 IU) recipients [122] | 84.6% (vs. lower control) | Direct measure of cervical lesion improvement | |
| Neutrophil-to-Lymphocyte Ratio (NLR) | Preclinical and early clinical studies [122] | Reduced with Vitamin D | Potential biomarker of immune modulation |
Table 2: Biomarkers and Analytical Methods for Endpoint Validation
| Biomarker Category | Specific Analyte | Detection Method | Association with Functional Outcome | Technical Considerations |
|---|---|---|---|---|
| Bone Turnover | Beta-CrossLaps (CTX) | Immunoassay [119] | Bone resorption marker; predicts fracture risk | Circadian variation requires standardized sampling |
| P1NP (Procollagen Type I N-terminal Propeptide) | Immunoassay [119] | Bone formation marker; treatment monitoring | Less circadian variation than CTX | |
| Undercarboxylated Osteocalcin (ucOC) | ELISA/HPLC [25] [120] | Functional vitamin K status; bone quality | Correlates with fracture risk independently of BMD | |
| Immune Function | 25-hydroxyvitamin D [25(OH)D] | Liquid Chromatography-Tandem Mass Spectrometry (LC-MS/MS) [12] | Vitamin D status; correlates with infection risk | Gold standard method; preferred over immunoassays |
| Inflammatory Cytokines (IL-6, CRP) | Immunoassay [119] | Systemic inflammation; predicts morbidity | Acute phase reactants; non-specific | |
| Immune Cell Subsets (Treg, Th1, Th17) | Flow Cytometry [122] | Cervical TIME profiling; immune competence | Requires fresh samples; complex standardization | |
| Global Health | Vitamin A (Retinol) | HPLC [12] | Deficiency impairs innate/adaptive immunity | Homeostatically controlled; insensitive to stores |
| Vitamin E (α-Tocopherol) | HPLC [12] | Antioxidant capacity; immune cell membrane integrity | Circulating levels do not always reflect tissue status |
Experimental Protocols for Endpoint Assessment
Fracture Risk Assessment Protocol
Objective: To evaluate the efficacy of fat-soluble vitamin interventions on reducing fracture incidence and improving bone quality metrics beyond traditional BMD measurements.
Methodology:
- Study Population: Community-dwelling seniors ≥70 years old, with ≥40% having a history of low-trauma falls to enrich the population with at-risk individuals [119].
- Study Design: Randomized, double-blind, placebo-controlled trial with 2×2×2 factorial design (e.g., DO-HEALTH trial) to test individual and combined effects of interventions [119].
- Intervention Duration: Minimum 3-year follow-up to capture sufficient fracture events for statistical power.
- Primary Endpoint: Incident non-vertebral fractures confirmed by radiography or medical reports [119].
- Secondary Endpoints:
- Hip fracture incidence
- New vertebral fractures assessed by vertebral morphometry in a subset with yearly DXA measurements
- Rate of falls (any low trauma fall, injurious falls) assessed every 3 months
- Biomarker Support:
Quality Control: Centralized adjudication of all fracture endpoints by blinded radiologists; standardized DXA protocols across multiple sites; batch analysis of biomarkers to minimize inter-assay variability.
Immune Function Validation Protocol
Objective: To quantify the effects of fat-soluble vitamin supplementation on clinically relevant immune outcomes and associated biomarkers.
Methodology:
- Study Population: Adults with specific immune challenges (e.g., persistent high-risk HPV infection for cervical immunity studies) [122].
- Intervention: For cervical immunity, biweekly cholecalciferol at 50,000 IU for 6 months with monitoring of 25(OH)D levels [122].
- Primary Clinical Endpoints:
- Secondary Immunological Endpoints:
- Neutrophil-to-lymphocyte ratio (NLR) as a systemic inflammation marker [122]
- T-cell polarization (Th1, Th17, Treg) in target tissues
- Dendritic cell maturation status and antigen-presenting capacity
- Biomarker Correlates:
Technical Considerations: For cervical immunity studies, single-cell RNA sequencing and spatial transcriptomics are recommended to profile the tumor immune microenvironment (TIME) and identify VitD-VDR axis effects on immune cell populations [122].
Quality of Life and Functional Capacity Protocol
Objective: To measure the impact of fat-soluble vitamin interventions on patient-reported outcomes and physical performance.
Methodology:
- Study Population: Patients with conditions affecting functional status (e.g., lower limb fracture patients) [121].
- Assessment Timeline: Baseline, 6 months, 12 months, and annually thereafter to track recovery trajectories.
- Physical Performance Measures:
- Patient-Reported Outcomes:
- Return-to-Work Status: Document occupational reintegration as a functional milestone [121].
Data Analysis: Decision tree models can identify predictors of functional recovery (e.g., hospital stay length, fracture characteristics) and return to work [121].
Signaling Pathways and Mechanistic Insights
Vitamin D-Calcium-Bone Signaling Axis
Diagram 1: Vitamin D signaling pathway linking to fracture risk
This pathway illustrates the mechanistic connection between vitamin D absorption and bone health outcomes. The active metabolite calcitriol binds to VDR, forming a heterodimer with RXR that regulates gene expression via vitamin D response elements (VDREs) [123]. This genomic signaling upregulates calcium transport proteins (e.g., TRPV6, calbindin) that mediate intestinal calcium absorption [123]. The resulting increase in calcium availability supports bone mineralization, which functionally translates to reduced fracture risk—a validated endpoint superior to BMD measurements alone [25].
Vitamin D and K Synergy in Calcium Homeostasis
Diagram 2: Vitamins D and K synergy in calcium regulation
This diagram illustrates the complementary roles of vitamins D and K in directing calcium to skeletal tissues and away from soft tissues. Vitamin D enhances intestinal calcium absorption, while vitamin K activates calcium-binding proteins through γ-carboxylation [120]. Osteocalcin requires vitamin K-dependent activation to bind calcium effectively in bone, thus supporting bone mineralization and reducing fracture risk [25] [120]. Simultaneously, matrix Gla protein (MGP) depends on vitamin K to inhibit calcium deposition in arteries, thereby connecting these vitamins to cardiovascular outcomes [120]. This synergy exemplifies why functional endpoints like fracture incidence and arterial health provide more comprehensive efficacy assessment than serum vitamin levels alone.
The Scientist's Toolkit: Essential Research Reagents and Methodologies
Table 3: Essential Research Reagents and Methodologies for Endpoint Validation
| Category | Reagent/Kit | Specific Function | Application Context |
|---|---|---|---|
| Biomarker Analysis | LC-MS/MS Kit for 25(OH)D | Gold-standard quantification of vitamin D status [12] | All studies requiring precise vitamin D status assessment |
| ELISA for Undercarboxylated Osteocalcin (ucOC) | Functional biomarker of vitamin K status in bone [25] | Bone quality assessment in vitamin K intervention studies | |
| Multiplex Cytokine Panel (IL-6, CRP, etc.) | Quantification of inflammatory mediators [119] | Immune function studies, inflammatory response monitoring | |
| Cell Culture & Tissue | Caco-2 TC-7 Cell Line | Model of human intestinal epithelium for absorption studies [6] | Mechanistic studies of vitamin absorption pathways |
| Primary Human Keratinocytes | Target cells for vitamin D effects on epithelial barriers [122] | Skin and cervical immunity research | |
| Molecular Biology | VDR Antibody for IHC | Detection of vitamin D receptor expression in tissues [122] | Mechanistic studies of vitamin D responsiveness |
| scRNA-Seq Kit (10X Genomics) | Single-cell transcriptomic profiling of immune microenvironments [122] | Comprehensive TIME analysis in cervical lesions | |
| Functional Assays | Short Physical Performance Battery (SPPB) | Standardized assessment of physical function [119] | Functional mobility outcome in clinical trials |
| SF-12 or SF-36 Health Survey | Validated patient-reported quality of life measure [121] | Multicenter trials requiring standardized QoL assessment |
The validation of functional endpoints represents a paradigm shift in fat-soluble vitamin research, moving beyond biochemical markers to clinically meaningful outcomes. Fracture risk, immune competence, and quality of life measures provide comprehensive assessment of vitamin efficacy that directly reflects patient experience and health status. The experimental protocols and methodological frameworks presented in this whitepaper enable researchers to design studies that capture the functional benefits of FSVs while elucidating their mechanisms of action. As the field advances, integrating these endpoints with emerging technologies like single-cell sequencing and molecular dynamics simulations [6] will further enhance our understanding of how fat-soluble vitamins promote human health at both molecular and systemic levels.
Conclusion
The absorption of lipid-soluble vitamins represents a complex interplay of physiological mechanisms, genetic factors, gut microbiota interactions, and formulation science. Future research must prioritize clinically relevant endpoints over surrogate markers, incorporate pharmacogenomic insights for personalized nutrition, and develop advanced delivery systems that account for the synergistic effects of whole foods. The integration of microbiome science with pharmaceutical development presents promising avenues for overcoming absorption barriers, particularly for patient populations with malabsorption conditions. As research advances, a more nuanced understanding of these mechanisms will enable targeted interventions that optimize vitamin status for disease prevention and therapeutic applications across diverse genetic and clinical populations.
References
- 1. Regulation of Chylomicron Secretion: Focus on Post ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6396431/]
- 2. Intestinal lipid absorption - PMC - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC2692399/]
- 3. Intestinal Lipid Absorption and Lipoprotein Formation - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4265799/]
- 4. Intracellular events in the assembly of chylomicrons ... [https://www.sciencedirect.com/science/article/pii/S0022227520319660]
- 5. Physiology, Nutrient Absorption - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK597379/]
- 6. Absorption study of fat-soluble vitamins into ... [https://www.sciencedirect.com/science/article/abs/pii/S1093326324002298]
- 7. Mechanisms involved in vitamin E transport by primary ... [https://www.sciencedirect.com/science/article/pii/S0022227520424903]
- 8. The impact of solid and liquid lipids and their lipolysis on ... [https://www.sciencedirect.com/science/article/pii/S0928098725003525]
- 9. Negative impact of soluble, gel-forming dietary fibres on the ... [https://pubs.rsc.org/en/content/articlehtml/2025/fo/d5fo01844g]
- 10. The impact of solid and liquid lipids and their lipolysis on ... [https://pubmed.ncbi.nlm.nih.gov/41173288/]
- 11. New insights into microbial bile salt hydrolases [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1513541/full]
- 12. The association between the serum fat-soluble vitamins (A, ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1593461/full]
- 13. Transporters in vitamin uptake and cellular metabolism [https://pmc.ncbi.nlm.nih.gov/articles/PMC12121362/]
- 14. Biochemistry, Fat Soluble Vitamins - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK534869/]
- 15. SDR42E1 modulates vitamin D absorption and cancer ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2025.1585859/full]
- 16. The Power of Vitamin D: Is the Future in Precision Nutrition ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11054101/]
- 17. Structure and transport mechanism of human riboflavin ... [https://www.nature.com/articles/s41467-025-59255-7]
- 18. The Relevance of Vitamin D Receptor (VDR) Gene ... [https://ar.iiarjournals.org/content/29/9/3511]
- 19. Vitamin D Receptor (VDR) Gene Polymorphisms Modify ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8780067/]
- 20. How to Read your Lifecode report [https://thesourdoughschool.com/how-to-read-your-lifecode-report/]
- 21. VKORC1 polymorphisms and complete resistance to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10962563/]
- 22. Warfarin Dosing and VKORC1/CYP2C9: Overview, Clinical ... [https://emedicine.medscape.com/article/1733331-overview]
- 23. Warfarin sensitivity - Genetics [https://medlineplus.gov/genetics/condition/warfarin-sensitivity/]
- 24. Carotenoids Diet: Digestion, Gut Microbiota Modulation, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10220829/]
- 25. Regarding: the role of fat-soluble vitamins A, D, E, and K in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12529735/]
- 26. Ileum: Anatomy, histology, composition, functions [https://www.kenhub.com/en/library/anatomy/the-ileum]
- 27. Ileum | Small Intestine, Digestion & Absorption [https://www.britannica.com/science/ileum]
- 28. Brush border [https://en.wikipedia.org/wiki/Brush_border]
- 29. Intestinal brush border assembly during the peri-hatch ... [https://www.sciencedirect.com/science/article/pii/S0032579121004247]
- 30. Diets alter jejunal morphology and brush border ... [https://pubmed.ncbi.nlm.nih.gov/3567735/]
- 31. Vitamin B12 Absorption [https://veganhealth.org/vitamin-b12/vitamin-b12-absorption/]
- 32. What Is Compartment Modelling in Pharmacokinetics? [https://www.cusabio.com/c-21197.html?srsltid=AfmBOoovVLwedAGasQrstARIbsgHJc2OPs4KBwKVD-mkC4FCAMybJgFG]
- 33. Improving In Vitro–In Vivo Correlation (IVIVC) for Lipid ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12567226/]
- 34. Guide for Selecting Experimental Models to Study Dietary ... [https://www.mdpi.com/2072-6643/17/23/3644]
- 35. Pharmacokinetics & Compartmental Modeling [https://www.allucent.com/resources/blog/compartmental-modeling-pharmacokinetics]
- 36. What models are used in in vivo pharmacokinetics studies? [https://synapse.patsnap.com/article/what-models-are-used-in-in-vivo-pharmacokinetics-studies]
- 37. Statistical analysis and reporting of clinical pharmacokinetic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9372427/]
- 38. A compatibility evaluation between the physiologically ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2022.964049/full]
- 39. Advances in Nanotechnology for Enhancing the Solubility and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11070169/]
- 40. Nanoparticle tools for maximizing oral drug delivery - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12172155/]
- 41. Overview of nanoparticulate strategies for solubility ... [https://www.sciencedirect.com/science/article/abs/pii/S0024320522000017]
- 42. The Advancement and Obstacles in Improving the Stability ... [https://pubmed.ncbi.nlm.nih.gov/38409730/]
- 43. Nanocarriers based on polysaccharides for improving the ... [https://www.sciencedirect.com/science/article/pii/S2666893923000671]
- 44. Overcoming the mucus barrier: Optimization design of ... [https://www.sciencedirect.com/science/article/abs/pii/S0168365925009150]
- 45. Nanoparticle-Mediated Strategies for Enhanced Drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10610050/]
- 46. Promising Nanocarriers to Enhance Solubility and ... [https://www.mdpi.com/1420-3049/27/18/6070]
- 47. Advancement in nanocarrier-mediated delivery of herbal ... [https://link.springer.com/article/10.1007/s13659-025-00550-7]
- 48. Probiotics enhance vitamin absorption in the intestine [https://pubmed.ncbi.nlm.nih.gov/40553040/]
- 49. Mechanisms and implications of the gut microbial modulation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12441142/]
- 50. Postbiotics: an insightful review of the latest category in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12317891/]
- 51. A Review of the Influence of Prebiotics, Probiotics ... [https://www.mdpi.com/2077-0383/14/11/3673]
- 52. Probiotics and Synbiotics: Applications, Benefits, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11910042/]
- 53. Current research status and trends in the bioactivity of ... [https://www.frontiersin.org/journals/food-science-and-technology/articles/10.3389/frfst.2025.1692683/full]
- 54. Comprehensive insights into postbiotics: Bridging the gap ... [https://www.sciencedirect.com/science/article/pii/S3050843625000253]
- 55. Insights into the Role of Gut Microbiota Modulation in ... [https://www.sciencedirect.com/science/article/abs/pii/S0014299925009641]
- 56. The gut microbiome, immune modulation, and cognitive ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1529958/full]
- 57. Update on the role of bone turnover markers ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12064614/]
- 58. Joint consensus highlights the role of bone turnover ... [https://www.osteoporosis.foundation/news/joint-consensus-highlights-role-bone-turnover-markers-osteoporosis-diagnosis-and-management]
- 59. Total and undercarboxylated osteocalcin predict changes ... [https://www.sciencedirect.com/science/article/pii/S0002916523026126]
- 60. Lipid Peroxidation: Production, Metabolism, and Signaling ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4066722/]
- 61. Effects of vitamin D supplementation on bone turnover ... [https://www.sciencedirect.com/science/article/pii/S8756328219301309]
- 62. Effect of vitamin D3-supplementation on bone markers ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5365165/]
- 63. Differences in the absorption and metabolism of vitamin D ... [https://www.sciencedirect.com/science/article/abs/pii/S0960076025000469]
- 64. Key Challenges and Opportunities Associated with the Use of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5027328/]
- 65. Advances and challenges in research methods on oral ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12449861/]
- 66. Pilot Studies to Determine Vitamin A Absorption Using ... [https://pubmed.ncbi.nlm.nih.gov/41232774/]
- 67. CMC Perspectives of In Vitro / In Vivo Correlation (IVIVC) ... [https://premier-research.com/perspectives/cmc-perspectives-of-in-vitro-in-vivo-correlation-ivivc-in-drug-development/]
- 68. Advancing drug development with “Fit-for-Purpose” modeling ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12436579/]
- 69. Malabsorption Syndromes - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK553106/]
- 70. Malabsorption [https://iffgd.org/gi-disorders/malabsorption/]
- 71. Small and Large Intestine (I): Malabsorption of Nutrients [https://www.mdpi.com/2072-6643/13/4/1254]
- 72. Malabsorption Syndrome Market Size, Share, and Growth ... [https://www.skyquestt.com/report/malabsorption-syndrome-market]
- 73. Malabsorption Syndrome Market Size Opportunities 2025- ... [https://www.coherentmi.com/industry-reports/malabsorption-syndrome-market]
- 74. Global Malabsorption Syndrome Market Report 2025 ... [https://www.cognitivemarketresearch.com/malabsorption-syndrome-market-report]
- 75. Comparative proteogenomics reveals ecological and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12016555/]
- 76. Antilipemic Agent Bile Acid Sequestrants - StatPearls - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK549906/]
- 77. Bile acid sequestrant drugs (drug interactions) [https://www.ebsco.com/research-starters/nutrition-and-dietetics/bile-acid-sequestrant-drugs-drug-interactions]
- 78. Drug-Nutrient Interactions | Linus Pauling Institute [https://lpi.oregonstate.edu/mic/drug-nutrient-interactions]
- 79. Antacids - StatPearls - NCBI Bookshelf - NIH [https://www.ncbi.nlm.nih.gov/books/NBK526049/]
- 80. The Significance of Drug—Drug and Drug—Food ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5889806/]
- 81. Fat-soluble vitamins: updated review of their role and ... [https://nutritionandmetabolism.biomedcentral.com/articles/10.1186/s12986-022-00696-y]
- 82. Fat-Soluble Vitamins A, D, E, and K: Review of the ... [https://www.mdpi.com/2077-0383/13/13/3641]
- 83. Enhancing the bioaccessibility of lipid-soluble nutrients ... [https://www.sciencedirect.com/science/article/pii/S0023643825014161]
- 84. Synergistic effects produced by certain antioxidants in ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1558597/full]
- 85. A Comparative Study on Oxidative Stability of Lipids ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12382763/]
- 86. Understanding the Genetic Architecture of Vitamin Status ... [https://www.sciencedirect.com/science/article/pii/S2161831324001789]
- 87. Vitamins DNA Wellness Report [https://sequencing.com/marketplace/vitamins-dna-analysis-genetic-report?srsltid=AfmBOop9LZKb7Vtm2-2pDeJ98hk3Lkxs7XZnLgnArxOPIXNCfUj3nXAG]
- 88. Challenges to Quantify Total Vitamin Activity - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC6776468/]
- 89. Aging and aging-related diseases: from molecular ... [https://www.nature.com/articles/s41392-022-01251-0]
- 90. Age-dependent changes in fat- and water-soluble vitamins—National Health and Nutrition Examination Surveys study - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9641218/]
- 91. Exploring the link between fat-soluble vitamins and aging-associated immune system status: a literature review | Immunity & Ageing | Full Text [https://immunityageing.biomedcentral.com/articles/10.1186/s12979-025-00501-3]
- 92. The Roles of Lipid Metabolism in the Pathogenesis of Chronic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10420821/]
- 93. Impact of age-related alterations in lipid metabolism on ... [https://www.news-medical.net/news/20230808/Impact-of-age-related-alterations-in-lipid-metabolism-on-general-health.aspx]
- 94. Influence of Ageing on the Pharmacodynamics and Pharmacokinetics of Chronically Administered Medicines in Geriatric Patients: A Review | Clinical Pharmacokinetics [https://link.springer.com/article/10.1007/s40262-024-01466-0]
- 95. Nutritional and lifestyle management of the aging journey [https://pmc.ncbi.nlm.nih.gov/articles/PMC9903079/]
- 96. The association between the serum fat-soluble vitamins ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12342190/]
- 97. Exploring the mediating role of serum vitamin D in the link ... [https://pubmed.ncbi.nlm.nih.gov/40948872/]
- 98. Exploring the mediating role of serum vitamin D in the link ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1588700/full]
- 99. Association of dietary live microbes and nondietary ... [https://www.nature.com/articles/s41598-024-83971-7]
- 100. Mapping human microbiome drug metabolism by gut ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6597290/]
- 101. GRADE handbook [https://gradepro.org/handbook]
- 102. Introduction to the GRADE tool for rating certainty in ... [https://www.sciencedirect.com/science/article/pii/S2213398423002713]
- 103. Beyond Bone Mineral Density: Real-World Fracture Risk ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12346389/]
- 104. TBS Osteo Advanced is transforming bone health ... [https://www.medimaps.ai/insights-tbs-osteo-advanced-is-transforming-bone-health-assessment/?utm_source=social%20media&utm_medium=social&utm_campaign=Blog_insights]
- 105. Pharmacokinetics of vitamin dosage forms: A complete overview [https://pmc.ncbi.nlm.nih.gov/articles/PMC10804103/]
- 106. Vitamin D: recent advances, associated factors, and its role ... [https://www.nature.com/articles/s41538-025-00460-5]
- 107. Vitamin K: Metabolism, Genetic Influences, and Chronic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12173841/]
- 108. Review: Bacterially produced vitamin K2 and its potential to ... [https://www.sciencedirect.com/science/article/abs/pii/S0924224424001377]
- 109. Vitamin K-containing dietary supplements: comparison of synthetic vitamin K1 and natto-derived menaquinone-7 - PubMed [https://pubmed.ncbi.nlm.nih.gov/17158229/]
- 110. Oral bioavailability enhancement of MK-7 from natto extract ... [https://applbiolchem.springeropen.com/articles/10.1186/s13765-025-01043-4]
- 111. The role of vitamin K2 in cognitive impairment [https://www.frontiersin.org/journals/aging-neuroscience/articles/10.3389/fnagi.2024.1527535/full]
- 112. Natto vitamin K2 superior to vitamin K? [https://www.nutraingredients.com/Article/2004/03/24/Natto-vitamin-K2-superior-to-vitamin-K/]
- 113. Vitamin A Toxicity - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK532916/]
- 114. Vitamin A toxicity and hepatic pathology - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC12400428/]
- 115. The acute and chronic toxic effects of vitamin A [https://www.sciencedirect.com/science/article/pii/S0002916523292710]
- 116. Vitamin D Toxicity - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK557876/]
- 117. Vitamin D toxicity: What if you get too much? [https://www.mayoclinic.org/healthy-lifestyle/nutrition-and-healthy-eating/expert-answers/vitamin-d-toxicity/faq-20058108]
- 118. Heart attack risk halved in adults with heart disease taking ... [https://newsroom.heart.org/news/heart-attack-risk-halved-in-adults-with-heart-disease-taking-tailored-vitamin-d-doses]
- 119. Trial [https://do-health.eu/about/trial/]
- 120. The Science Behind Taking Vitamin and K Together D [https://www.rupahealth.com/post/the-science-behind-taking-vitamin-d-and-k-together-for-enhanced-health-outcomes]
- 121. Evaluation of functionality and quality of life in patients with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12374052/]
- 122. Vitamin D, immune microenvironment, and cervical lesions [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1688910/full]
- 123. Calcitriol - StatPearls - NCBI Bookshelf - NIH [https://www.ncbi.nlm.nih.gov/books/NBK526025/]