Mechanistic Links Between Dietary Patterns and Chronic Disease: From Molecular Pathways to Therapeutic Innovation
This article synthesizes current scientific evidence on the biological mechanisms through which dietary patterns influence chronic disease risk, tailored for researchers, scientists, and drug development professionals.
Mechanistic Links Between Dietary Patterns and Chronic Disease: From Molecular Pathways to Therapeutic Innovation
Abstract
This article synthesizes current scientific evidence on the biological mechanisms through which dietary patterns influence chronic disease risk, tailored for researchers, scientists, and drug development professionals. It explores foundational pathways like hyperinsulinemia and inflammation, examines methodological approaches for studying diet-disease interactions, addresses complexities such as food-drug interactions and research biases, and provides a comparative analysis of the protective efficacy of major dietary patterns like the MIND, DASH, and Mediterranean diets. The review aims to inform the integration of nutritional science into targeted therapeutic strategies and precision medicine frameworks.
Core Biological Pathways: How Diet Modulates Chronic Disease Risk
Hyperinsulinemia, characterized by elevated circulating insulin levels, has emerged as a critical pathophysiological mechanism linking modern dietary patterns to the development of major chronic diseases. As obesity and metabolic syndrome reach epidemic proportions globally, with insulin resistance affecting an estimated 51% of the population in developed and developing countries, the role of hyperinsulinemia as a unifying driver of chronic disease requires urgent research attention [1]. This whitepaper synthesizes current evidence demonstrating how dietary patterns promote hyperinsulinemia, which in turn serves as a central mechanism initiating and propagating multiple disease processes, including type 2 diabetes, cardiovascular disease, and cancer [2] [1] [3].
The evolutionary conservation of insulin and insulin-like growth factor signaling pathways underscores their fundamental role in metabolism, growth, and longevity [4]. In contemporary populations, chronic consumption of pro-hyperinsulinemic diets generates a persistent state of elevated insulin that dysregulates these ancient pathways, creating a permissive environment for disease development. This review examines the mechanistic evidence connecting hyperinsulinemia to major chronic diseases, provides detailed experimental methodologies for investigating these relationships, and outlines key signaling pathways that represent potential therapeutic targets for researchers and drug development professionals.
Dietary Patterns and Hyperinsulinemia: Epidemiological and Clinical Evidence
Strong evidence from multiple large-scale prospective cohorts demonstrates that specific dietary patterns significantly influence hyperinsulinemia risk and subsequent chronic disease development. Research using empirically-derived dietary indices has identified distinct patterns that directly impact insulinemic and inflammatory responses.
Table 1: Dietary Patterns and Their Association with Chronic Disease Risk
| Dietary Pattern | Key Components | Biomarker Impact | Disease Risk Association |
|---|---|---|---|
| Hyperinsulinemic (High EDIH) | Red meat, processed meat, poultry, refined grains, sugar-sweetened beverages [5] | ↑ C-peptide, ↑ HOMA-IR, ↑ triglycerides, ↓ HDL-C, ↓ adiponectin [5] | Major chronic disease HR: 1.42-1.72 [2] |
| Pro-inflammatory (High EDIP) | Red meat, processed meat, refined grains, high-energy beverages [5] | ↑ CRP, ↑ IL-6, ↑ TNF-αR2, ↑ triglycerides [5] | Strong association with T2D, CVD, cancer [5] |
| Low Insulinemic (Low EDIH) | Wine, whole fruit, coffee, green leafy vegetables [5] | ↓ C-peptide, ↓ HOMA-IR, ↑ HDL-C, ↑ adiponectin [5] | Major chronic disease HR: 0.58-0.80 [2] |
| Western Pattern | Soft drinks, refined grains, pastries, corn tortillas [6] | ↑ Fasting glucose, ↓ HDL-C, ↑ triglycerides [6] | MetS OR: 1.56 (95% CI: 1.31-1.88) [6] |
| High-Fiber Nutrient-Dense | Vegetables, fruits, whole grains, fish [7] | Improved glucose metabolism, lipid profiles [7] | Reduced T2DM risk [7] |
Data from the Women's Health Initiative (n=35,360 postmenopausal women) demonstrated that the Empirical Dietary Index for Hyperinsulinemia (EDIH) and Empirical Dietary Inflammatory Pattern (EDIP) significantly associated with altered concentrations of 25 of 40 biomarkers examined, including insulin resistance, inflammation, endothelial dysfunction, and dyslipidemia markers [5]. The hyperinsulinemic dietary pattern increased homeostatic model assessment for insulin resistance (HOMA-IR) by +8%, C-reactive protein by +7.8%, and reduced HDL cholesterol by -2.4% [5].
A prospective study of 205,852 healthcare professionals followed for up to 32 years demonstrated that participants with low-insulinemic dietary patterns had the largest risk reduction for incident major cardiovascular disease, type 2 diabetes, and cancer as a composite outcome, with hazard ratios comparing the 90th with the 10th percentile of dietary pattern scores ranging from 0.58 to 0.80 [2]. Notably, the low insulinemic (HR = 0.58, 95% CI = 0.57, 0.60) and low inflammatory (HR = 0.61, 95% CI = 0.60, 0.63) diets demonstrated the most substantial protective effects [2].
Hyperinsulinemia as a Unifying Pathogenic Mechanism
Molecular Pathways Linking Hyperinsulinemia to Chronic Disease
Hyperinsulinemia exerts its pathogenic effects through multiple interconnected molecular pathways that create a permissive environment for chronic disease development. The underlying mechanisms involve complex interactions between insulin signaling pathways, inflammatory processes, and cellular growth regulation.
Under insulin resistance conditions, the phosphoinositide-3 kinase (PI3-K) dependent metabolic pathway becomes specifically impaired, while the mitogen-activated protein kinase (MAPK)-dependent pathway remains sensitive to insulin or becomes overstimulated by compensatory hyperinsulinemia [1]. This imbalance creates a pathophysiological state where the metabolic actions of insulin are diminished while the growth-promoting and inflammatory effects are disproportionately enhanced [1] [4].
The PI3-K pathway primarily mediates insulin's metabolic actions, including regulation of glucose metabolism in muscle, adipose tissue, and liver, as well as nitric oxide (NO) production by endothelial and vascular smooth muscle cells [1]. When this pathway is impaired, NO production decreases, leading to endothelial dysfunction. Concurrent overstimulation of the MAPK pathway promotes secretion of endothelin-1 (ET-1), a potent vasoconstrictor, and stimulates mitogenic and proliferative actions that can contribute to cancer development [1] [4].
Tissue-Specific Pathogenic Mechanisms
Cardiovascular System
Hyperinsulinemia promotes cardiovascular damage through multiple mechanisms. It induces hyperactivation of the sympathetic nervous system and stimulates renal sodium reabsorption, contributing to hypertension [1]. The PI3-K/MAPK pathway imbalance creates endothelial dysfunction through reduced NO and increased ET-1 production, establishing a pro-atherogenic environment [1]. Persistent hyperinsulinemia also promotes atherogenic dyslipidemia characterized by elevated triglycerides, reduced HDL cholesterol, and increased small, dense LDL particles [1] [8].
Cancer Development
Hyperinsulinemia contributes to carcinogenesis through both direct and indirect mechanisms. Insulin acts as a growth factor for epithelial cells, binding to insulin receptors (INSR) and insulin-like growth factor-1 receptors (IGF-1R) to activate the MAPK and PI3-K signaling pathways that stimulate cell proliferation and inhibit apoptosis [3] [4]. A prospective cohort study demonstrated that hyperinsulinemia (defined as fasting insulin ≥10 μU/mL) was associated with significantly higher cancer mortality among nonobese participants without diabetes (adjusted HR 1.89, 95% CI 1.07-3.35) [3].
Recent research has elucidated tissue-specific mechanisms, such as in pancreatic cancer where hyperinsulinemia acts via acinar insulin receptors to initiate pancreatic cancer by increasing digestive enzyme production and inflammation [9]. This mechanism demonstrates how organ-specific insulin signaling can create a permissive microenvironment for carcinogenesis.
Metabolic Dysregulation and Type 2 Diabetes
Hyperinsulinemia initially compensates for insulin resistance but eventually leads to β-cell exhaustion and apoptosis through ER stress and oxidative damage [4]. The persistent lipid abnormalities associated with hyperinsulinemic states, particularly elevated triglycerides and reduced HDL-C, further exacerbate insulin resistance and glucose intolerance [8]. This creates a vicious cycle where hyperinsulinemia begets further metabolic dysfunction.
Experimental Models and Research Methodologies
Dietary Pattern Assessment and Validation
The following methodology details the approach used to develop and validate empirical dietary patterns for hyperinsulinemia research, as implemented in large cohort studies [5]:
Food Frequency Questionnaire (FFQ) Administration
- Utilize a validated semi-quantitative FFQ with 122+ food items
- Assess dietary intake over preceding 3-month period
- Collect data on portion sizes using standardized instruments (e.g., food photographs, standard serving sizes)
- Convert consumption frequencies to daily intake values (servings/day)
Dietary Pattern Calculation
- Calculate Empirical Dietary Index for Hyperinsulinemia (EDIH) scores using 18 weighted food groups
- Food groups promoting hyperinsulinemia: red meat, processed meat, poultry, refined grains, sugar-sweetened beverages
- Food groups reducing hyperinsulinemia: wine, whole fruit, coffee, green leafy vegetables
- Compute overall EDIH score as weighted sum of food group intakes
Biomarker Validation
- Collect fasting blood samples
- Measure insulin-related biomarkers: C-peptide, insulin, glucose, HOMA-IR
- Measure inflammatory biomarkers: CRP, IL-6, TNF-αR2
- Measure lipid biomarkers: triglycerides, HDL-C, LDL-C, total cholesterol
- Use linear regression to assess associations between dietary patterns and biomarkers, adjusting for potential confounders (age, BMI, physical activity, smoking, etc.)
Table 2: Key Methodological Approaches in Hyperinsulinemia Research
| Method Category | Specific Techniques | Key Applications | Advantages/Limitations |
|---|---|---|---|
| Dietary Assessment | FFQ, 24-hour recalls, dietary records | Establishing dietary patterns linked to hyperinsulinemia | FFQ efficient for large cohorts but subject to recall bias [5] |
| Insulin Resistance Measurement | HOMA-IR, TyG index, euglycemic clamp | Quantifying insulin resistance and β-cell function | HOMA-IR practical for epidemiology; clamp gold standard but resource-intensive [1] |
| Biomarker Profiling | Multiplex immunoassays, ELISA, clinical chemistry | Comprehensive metabolic phenotyping | Enables pattern analysis across multiple biological pathways [5] |
| Genetic Manipulation | Tissue-specific knockout mice (e.g., acinar Insr knockout) | Establishing causal mechanisms | Demonstrates tissue-specific insulin effects [9] |
| Cell Culture Models | Primary acinar cells, cancer cell lines | Elucidating molecular mechanisms | Controlled environment but may not fully recapitulate in vivo physiology [9] |
In Vivo Models of Hyperinsulinemia-Disease Relationships
Recent innovative approaches have established causal relationships between hyperinsulinemia and disease development:
Pancreatic Cancer Model [9]
- Utilize KrasG12D-expressing mice as pancreatic cancer model
- Generate acinar cell-specific insulin receptor knockout (InsrΔacinar)
- Expose to high-fat diet to induce hyperinsulinemia
- Monitor PanIN formation and progression
- Measure digestive enzyme production and local inflammation
- Assess insulin signaling pathway activation in acinar cells
Mechanistic Findings: Insulin receptor loss in acinar cells did not affect glucose metabolism but prevented hyperinsulinemia-driven pancreatic intraepithelial neoplasia (PanIN) formation, demonstrating that direct insulin action on acinar cells via insulin receptors is necessary for obesity-driven pancreatic cancer initiation [9].
Research Reagents and Methodological Solutions
Table 3: Essential Research Reagents for Hyperinsulinemia Mechanisms Investigation
| Reagent/Category | Specific Examples | Research Application | Key Function |
|---|---|---|---|
| Dietary Assessment Tools | WHI FFQ, NHS FFQ [5] | Dietary pattern characterization | Validated instruments for quantifying food intake |
| Biomarker Assays | C-peptide ELISA, CRP immunoassay, insulin ELISA [5] | Biomarker quantification | Objective measures of insulin response and inflammation |
| Genetic Models | KrasG12D mice, Insr floxed mice [9] | Tissue-specific mechanism studies | Enable conditional gene knockout in specific cell types |
| Cell Culture Systems | Primary acinar cells, pancreatic cancer cell lines [9] | In vitro mechanism studies | Permit controlled manipulation of insulin signaling |
| Metabolic Phenotyping | HOMA-IR calculation, TyG index [1] | Insulin resistance assessment | Practical indices correlating with gold-standard measures |
| Pathological Assessment | Histology for PanIN classification [9] | Disease progression monitoring | Standardized cancer precursor identification |
The evidence synthesized in this whitepaper establishes hyperinsulinemia as a central mechanistic pathway linking modern dietary patterns to increased risk of diabetes, cardiovascular disease, and cancer. The bidirectional relationship between specific dietary components and hyperinsulinemia creates a self-reinforcing cycle that drives chronic disease pathogenesis through multiple molecular mechanisms.
Priority research directions include:
- Developing targeted interventions to disrupt the hyperinsulinemia-disease pathway
- Elucidating tissue-specific insulin signaling mechanisms in different disease contexts
- Establishing optimal dietary patterns for hyperinsulinemia reduction across diverse populations
- Investigating the potential of insulin-lowering strategies for cancer prevention and treatment
The profound impact of hyperinsulinemia on multiple disease states highlights the urgent need for continued mechanistic research and therapeutic development in this area. Research efforts should prioritize understanding the nuanced relationships between dietary factors, insulin dynamics, and disease-specific pathological processes to enable more effective prevention and treatment strategies for the growing burden of hyperinsulinemia-related chronic diseases.
Chronic, low-grade inflammation is a fundamental pathological process underlying a wide spectrum of non-communicable diseases, including cardiovascular diseases, cancer, neurodegenerative disorders, and diabetes [10]. Dietary components exert a profound influence on systemic inflammation, acting through complex interactions with immune signaling pathways, the gut microbiome, and cellular aging processes [11] [10]. The inflammatory potential of diet is not merely the sum of individual nutrient effects but represents a synergistic interplay of bioactive compounds that can either promote or resolve inflammatory states [10]. Understanding these mechanisms is critical for developing targeted nutritional strategies to mitigate chronic disease risk and progression.
Emerging evidence from large-scale cohort studies and clinical trials demonstrates that dietary patterns significantly influence inflammatory status and clinical outcomes across diverse populations. Research utilizing data from the UK Biobank, the Nurses' Health Study, and the Health Professionals Follow-Up Study has established robust associations between pro-inflammatory diets and increased incidence of major brain disorders, reduced healthy aging, and worse survival outcomes in conditions such as stage III colon cancer [11] [12] [13]. Conversely, anti-inflammatory dietary patterns consistently associate with preserved cognitive function, physical capacity, mental health, and longevity [12]. This whitepaper synthesizes current evidence on the mechanisms linking dietary components to inflammatory pathways and provides methodological guidance for research in nutritional immunology.
Quantitative Evidence: Dietary Patterns and Health Outcomes
Table 1: Association of Dietary Patterns with Health Outcomes from Recent Large-Scale Studies
| Health Outcome | Dietary Pattern/Index | Population | Effect Size (Highest vs. Lowest Adherence) | Reference |
|---|---|---|---|---|
| Healthy Aging | Alternative Healthy Eating Index (AHEI) | 105,015 US adults | OR: 1.86 (95% CI: 1.71-2.01) | [12] |
| Overall Survival in Stage III Colon Cancer | Anti-inflammatory vs. Pro-inflammatory Diet | 1,625 patients | 87% higher risk of death with pro-inflammatory diet | [13] [14] |
| Dementia Risk | MIND Diet | 166,916 UK Biobank participants | HR: 0.87 (95% CI: 0.77-0.98) | [11] |
| Depression Risk | MIND Diet | 166,916 UK Biobank participants | HR: 0.77 (95% CI: 0.71-0.82) | [11] |
| Physical Component of HRQOL | Anti-inflammatory Diet | 3,294 adults with chronic disease | SMD: 0.17 (95% CI: 0.06-0.27) | [15] |
| Combined Diet and Exercise on Survival | Anti-inflammatory Diet + High Physical Activity | Stage III colon cancer patients | 63% lower risk of death | [13] [16] |
Table 2: Inflammatory Biomarkers and Their Association with Dietary Patterns
| Biomarker | Dietary Assessment | Association | Study Population | Reference |
|---|---|---|---|---|
| White Blood Cell (WBC) Count | HEI-2015 (per unit increase) | Inverse association | 19,110 NHANES participants | [10] |
| Neutrophil-to-Lymphocyte Ratio (NLR) | DII (pro-inflammatory diet) | Positive association | 19,110 NHANES participants | [10] |
| High-sensitivity CRP | eADI-17 (per 4.5-point increase) | 12% lower concentration | 4,432 Swedish men | [17] |
| IL-6 | eADI-17 (per 4.5-point increase) | 6% lower concentration | 4,432 Swedish men | [17] |
| TNF-R1 | eADI-17 (per 4.5-point increase) | 8% lower concentration | 4,432 Swedish men | [17] |
| Systemic Immune-Inflammation Index (SII) | HEI-2015 vs. DII | HEI-2015: inverse; DII: positive | 19,110 NHANES participants | [10] |
Methodological Approaches for Dietary Inflammation Research
Major Dietary Indices and Their Applications
Nutritional epidemiology employs several validated indices to quantify the inflammatory potential of diets:
Empirical Dietary Inflammatory Pattern (EDIP): Calculated as a weighted sum of 18 food groups (9 pro-inflammatory and 9 anti-inflammatory). Pro-inflammatory foods include red meat, processed meats, refined grains, and sugary drinks, while anti-inflammatory foods include coffee, tea, dark yellow vegetables, and leafy greens [13] [14]. EDIP has been validated against inflammatory biomarkers including IL-6, TNF-R1, TNF-R2, and hsCRP [17].
Dietary Inflammatory Index (DII): Developed based on literature and population data, the DII quantitatively assesses the pro- and anti-inflammatory potential of food intake using 45 food parameters scored according to their effects on six inflammatory markers (IL-1β, IL-4, IL-6, IL-10, TNF-α, and CRP) [10] [18]. A DII score > 0 indicates a pro-inflammatory diet, while < 0 indicates an anti-inflammatory diet.
Empirical Anti-inflammatory Diet Index (eADI): A recently developed index based on multiple inflammatory biomarkers (hsCRP, IL-6, TNF-R1, TNF-R2). The eADI-17 includes 17 food groups (11 with anti-inflammatory potential, 6 with pro-inflammatory potential) with clear scoring criteria (tertiles of consumption corresponding to 0, 0.5, and 1 point) [17].
Healthy Eating Index-2015 (HEI-2015): Assesses overall diet quality through 13 components (9 adequacy, 4 moderation) with scores from 0-100. Higher scores indicate better diet quality and are inversely associated with inflammatory markers [10].
Experimental Protocols for Assessing Diet-Inflammation Relationships
Protocol 1: Development and Validation of Empirical Dietary Indices
Based on the methodology described by [17] for developing the eADI-17:
Study Population: Recruit a sufficiently large cohort (e.g., n > 4,000) with diverse dietary habits. Exclude participants with acute inflammatory conditions (e.g., hsCRP > 20 mg/L) or implausible energy intake reports.
Dietary Assessment: Administer a validated food frequency questionnaire (FFQ) with comprehensive food items (≥ 145 items). The FFQ should capture frequency of consumption using predefined categories (never/seldom to ≥ 3 times per day).
Biomarker Measurement: Collect fasting blood samples and analyze multiple inflammatory biomarkers including hsCRP (using high-sensitivity immunonephelometric assays), IL-6, TNF-R1, and TNF-R2 (using proteomic panels such as Olink Proteomics).
Statistical Analysis:
- Randomly split the cohort into Discovery and Replication groups.
- In the Discovery group, apply feature selection methods (e.g., 10-fold Lasso regression) to identify food groups most correlated with inflammatory biomarkers.
- Construct the dietary index by summing scores of selected food groups (tertiles of consumption: 0, 0.5, 1 point).
- Validate in the Replication group using multivariable-adjusted linear regression models to examine associations between the dietary index and inflammatory biomarkers.
Protocol 2: Assessing Diet-Cancer Survival Relationships
Based on the CALGB/SWOG 80702 trial analysis [13] [14]:
Study Population: Enroll patients with confirmed stage III colon cancer after surgical resection. Record demographic and clinical characteristics (age, sex, ECOG performance status, cancer stage).
Dietary Assessment: Administer food frequency questionnaires at baseline (e.g., 6 weeks post-randomization) and at follow-up intervals (e.g., 14-16 months). Calculate EDIP scores based on 18 food groups.
Physical Activity Assessment: Collect data on exercise habits using validated questionnaires. Categorize activity levels (e.g., high activity: ≥ 9 MET hours/week equivalent to walking at 2-3 mph for 1 hour approximately 3 times/week).
Outcome Measures: Track overall survival and disease-free survival over extended follow-up (multiple years). Use Cox proportional hazards models to assess associations between dietary patterns and survival, adjusting for potential confounders.
Additional Analyses: Investigate effect modification by anti-inflammatory medications (e.g., celecoxib), although the CALGB/SWOG 80702 trial found no significant influence of celecoxib on the diet-survival relationship [16].
Mechanistic Pathways Linking Diet to Inflammation
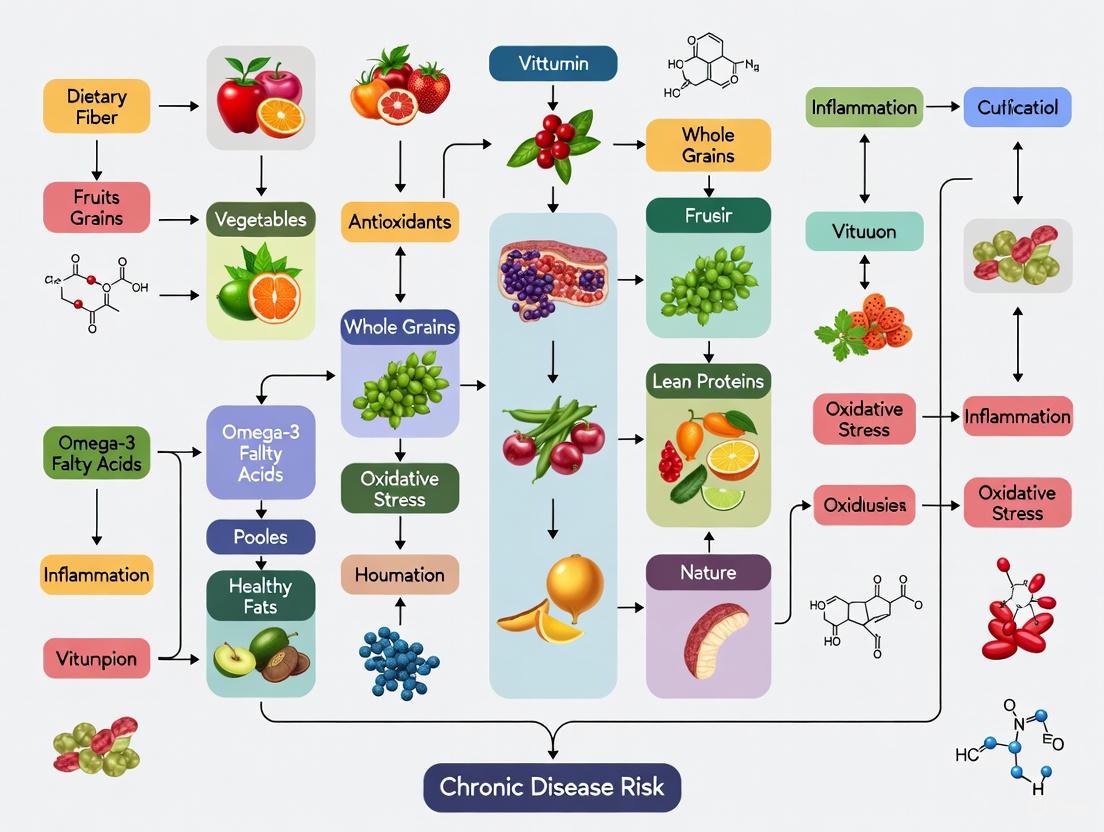
Diagram 1: Mechanistic Pathways of Dietary Inflammation. This diagram illustrates the proposed biological pathways through which pro- and anti-inflammatory dietary components influence systemic inflammation and chronic disease risk, incorporating findings from multi-omics analyses [11].
Multi-Omics Insights into Dietary Inflammation
Recent multi-omics analyses have elucidated specific biological pathways mediating the relationship between diet and inflammation:
Metabolic Signature Mediation: A favorable metabolic signature explains substantial proportions of reduced risk for stroke (60.63%), depression (38.97%), and anxiety (26.06%) associated with the MIND diet [11]. These metabolites likely include gut microbiome-derived short-chain fatty acids from fiber fermentation, as well as polyphenol metabolites with anti-inflammatory properties.
Biological Aging Pathways: Slower biological aging significantly mediates the reduced risk of dementia (19.40%) associated with anti-inflammatory dietary patterns [11]. This suggests that anti-inflammatory diets may attenuate epigenetic aging processes and cellular senescence, potentially through reducing oxidative stress and DNA damage.
Proteomic Alterations: Anti-inflammatory diets associate with favorable profiles of inflammation-related proteins including adipokines, acute-phase proteins, and inflammatory cytokines that collectively reduce systemic inflammation [17].
The Scientist's Toolkit: Essential Research Reagents and Methodologies
Table 3: Research Reagent Solutions for Dietary Inflammation Studies
| Reagent/Resource | Function/Application | Example Specifications | Key References |
|---|---|---|---|
| Food Frequency Questionnaire (FFQ) | Assess habitual dietary intake | 145+ food items; validated against dietary recalls | [17] |
| Olink Proteomics Panels | Quantify inflammatory proteins | CVD II/III panels; measure IL-6, TNF-R1, TNF-R2 | [17] |
| High-Sensitivity CRP Assay | Measure chronic inflammation | Latex-enhanced immunonephelometric assay; detection limit <0.1 mg/L | [17] |
| Dietary Inflammatory Index (DII) Calculator | Quantify dietary inflammatory potential | 45 food parameters; scores based on effects on 6 inflammatory markers | [10] [18] |
| EDIP Calculation Algorithm | Classify pro-/anti-inflammatory diets | 18 food groups with weighted scores | [13] [14] |
| Metabolomics Profiling Platforms | Identify metabolic signatures of diet | LC-MS/MS; covers ~1,000+ metabolites | [11] |
| Epigenetic Aging Clocks | Assess biological aging | DNA methylation arrays; measures Phenotypic Age Acceleration | [11] |
The evidence synthesized in this whitepaper demonstrates that dietary patterns significantly influence inflammatory pathways through multiple biological mechanisms, with consequential effects on chronic disease risk and progression. Anti-inflammatory dietary patterns, characterized by abundant fruits, vegetables, whole grains, nuts, legumes, and healthy fats, consistently associate with reduced inflammatory biomarkers, better health-related quality of life, improved survival in conditions such as colon cancer, and enhanced healthy aging trajectories.
Future research should prioritize several key areas: (1) elucidating the precise molecular mechanisms through which dietary components influence inflammatory signaling using multi-omics approaches; (2) conducting randomized controlled trials to establish causal relationships between dietary interventions and inflammatory outcomes in diverse populations; (3) developing personalized anti-inflammatory dietary recommendations based on genetic, metabolic, and microbiome profiles; and (4) investigating the synergistic effects of diet and pharmacological anti-inflammatory agents on disease outcomes. As dietary inflammation research advances, it holds significant promise for developing targeted nutritional strategies to mitigate the global burden of chronic inflammatory diseases.
The progressive functional decline characteristic of biological ageing is the primary risk factor for most chronic, non-communicable diseases (NCDs) [19]. Within geroscience, the objective has shifted from merely extending lifespan to maximising healthspan—the period of life spent in good physical, cognitive, and mental health [19]. Among various modifiable factors, nutrition emerges as a potent modulator of the rate of biological ageing and resilience against NCDs [19]. This whitepaper explores the pivotal role of metabolic signatures as biomarkers of ageing and examines how dietary patterns influence these signatures to modulate biological ageing trajectories and disease risk, providing a technical guide for researchers and drug development professionals.
Metabolic Signatures as Biomarkers of Ageing
Defining Metabolic Signatures of Ageing
Metabolites, the small molecules produced by metabolic processes, serve as sensitive indicators of physiological state and can provide a real-time snapshot of biological age. Research from the Long Life Family Study (LLFS) analysed 408 plasma metabolites and identified 308 metabolites associated with chronological age, 258 that change over time, 230 associated with extreme longevity, and 152 associated with mortality risk [20]. Network analysis revealed that essential fatty acids, particularly linoleic and gamma-linolenic acids, play a critical role in connecting lipid metabolism with other metabolic processes during ageing [20].
Muscle-Specific Metabolic Signatures in Ageing
Skeletal muscle metabolomics offers unique insights into ageing processes. A non-targeted metabolomics study on murine gastrocnemius muscle identified 50 metabolites that consistently distinguish healthy from unhealthy ageing trajectories, termed the 'Advanced Age Muscle-Enriched Metabolite Set' (AAMEMS) [21]. This signature includes 18 metabolites commonly reduced under unhealthy ageing (e.g., arginine, lysine) and 32 metabolites increased (including various ceramides and short-chain acylcarnitines) [21]. The most significant associations were found with oxidative stress and nutrient sensing pathways, highlighting their central role in musculoskeletal ageing [21].
Table 1: Key Metabolite Classes in Ageing and Their Associations
| Metabolite Class | Association with Unhealthy Ageing | Primary Ageing Hallmarks Involved | Potential Dietary Modulators |
|---|---|---|---|
| Long-chain Acylcarnitines | Decreased [21] | Mitochondrial Dysfunction, Oxidative Stress | Carnitine, Omega-3 Fatty Acids |
| Arginine & Lysine | Decreased [21] | Deregulated Nutrient Sensing, Stem Cell Dysfunction | High-Quality Protein, Plant-Based Diets |
| Ceramides | Increased [21] | Chronic Inflammation, Oxidative Stress | Low Saturated Fat, High Fiber |
| Short-chain Acylcarnitines | Increased [21] | Mitochondrial Dysfunction | Caloric Restriction, Exercise |
| Essential Fatty Acids | Altered Profiles [20] | Chronic Inflammation, Genomic Instability | Omega-3 Rich Foods, Mediterranean Diet |
Dietary Modulation of Metabolic Signatures
Neuroprotective Dietary Patterns
Large-scale prospective cohort studies have comprehensively compared dietary patterns for brain health. A study using UK Biobank data (N=166,916) evaluated ten dietary patterns and found the MIND (Mediterranean-DASH Intervention for Neurodegenerative Delay) diet demonstrated the broadest neuroprotective effects [22]. Over a median follow-up of 10.5 years, adherence to the MIND diet was significantly associated with reduced risk of dementia (HR=0.87), stroke (HR=0.89), depression (HR=0.77), and anxiety (HR=0.82), but not Parkinson's disease (HR=0.94) [22]. These findings were validated in the U.S. Health and Retirement Study (n=4,496) and the Chinese Longitudinal Healthy Longevity Survey (n=9,099) [22].
Multi-Omics Mediation of Dietary Effects
The protective mechanisms of the MIND diet were elucidated through multi-omics analyses, revealing that:
- A favourable metabolic signature mediated 60.63% of the reduced stroke risk, 38.97% of reduced depression risk, and 26.06% of reduced anxiety risk [22].
- Slower biological ageing significantly mediated 19.40% of the reduced dementia risk [22].
- Structural equation modeling confirmed the overall protective pathway linking the MIND diet to better brain health via these mediators [22].
Conversely, ultra-processed food (UPF) intake was associated with increased risk for dementia (HR=1.40), Parkinson's disease (HR=1.26), depression (HR=1.42), and anxiety (HR=1.26) through detrimental changes in these same metabolic and ageing pathways [22].
Table 2: Association of Dietary Patterns with Healthy Ageing Odds (from Prospective Cohorts)
| Dietary Pattern | Acronym | Odds Ratio for Healthy Ageing | Primary Health Domains Benefitted |
|---|---|---|---|
| Alternative Healthy Eating Index | AHEI | ~2.00 (Strongest Association) [19] | Cognitive, Physical, and Mental Function |
| Mediterranean Diet | aMED | Increased [19] | Cognitive Function, Cardiovascular Health |
| Dietary Approaches to Stop Hypertension | DASH | Increased [19] | Cardiovascular Health, Metabolic Function |
| Planetary Health Diet Index | PHDI | Increased [19] | Systemic Health, Environmental Sustainability |
| MIND Diet | MIND | Significant Risk Reduction for Dementia, Stroke, Depression, Anxiety [22] | Brain Health, Neuropsychiatric Disorders |
Methodologies for Assessing Metabolic Signatures in Aging Research
Experimental Workflow for Muscle Metabolomics
The following diagram outlines a standardised workflow for skeletal muscle metabolomics in ageing studies:
Computational Analysis of Microbiome-Metabolite Interactions
The STELLA algorithm provides a computational framework for deriving metabolite spectra from microbiome data [23]:
- Input: 16S rRNA sequencing data from fecal samples.
- Pathway Mapping: Uses MACADAM and METACYC databases to retrieve metabolic pathways for each operational taxonomic unit (OTU).
- Stoichiometric Modeling: Considers reaction stoichiometry and directionality to assign production/consumption scores.
- Abundance Weighting: Weights pathway contributions according to OTU abundance.
- Output: Estimated metabolite concentrations for each patient.
Validation against experimental metabolomic data from autism spectrum disorder studies showed strong predictive accuracy (F₁ score=0.67) [23]. Batch effect removal via singular value decomposition is critical when merging datasets from different sources [23].
Research Reagent Solutions
Table 3: Essential Research Reagents for Ageing Metabolomics
| Reagent/Resource | Function/Application | Example Use in Ageing Research |
|---|---|---|
| UPLC-MS/MS Systems | High-resolution metabolite separation and quantification | Non-targeted metabolomics on skeletal muscle; quantification of 427 metabolites in murine studies [21] |
| Epigenetic Clock Panels | DNA methylation-based biological age estimation | Tracking intervention efficacy; distinguishing chronological vs. biological age (e.g., Horvath, GrimAge clocks) [19] |
| MACADAM & METACYC Databases | Metabolic pathway curation and stoichiometric modeling | Predicting microbiome-derived metabolites using computational approaches like STELLA [23] |
| Cohort Biobanks | Large-scale human biological samples with multi-omics data | Validation of metabolic signatures (e.g., UK Biobank, Long Life Family Study) [22] [20] |
| Standardized Dietary Indices | Quantifying adherence to neuroprotective diets | Assessing MIND, AHEI, DASH, and other dietary patterns in cohort studies [19] [22] |
Metabolic signatures provide a powerful lens through which to quantify biological ageing and evaluate the efficacy of nutritional interventions. The integration of metabolomic data with other omics technologies reveals the mechanistic pathways through which dietary patterns like the MIND diet exert their neuroprotective effects, largely by modulating specific metabolic pathways and slowing the pace of biological ageing. Future research should focus on standardising metabolite nomenclature, incorporating longitudinal dietary data, and translating these findings into targeted nutritional therapeutics for promoting healthspan and mitigating age-related disease risk.
The gut-brain axis (GBA) represents a complex, bidirectional communication network linking the gastrointestinal tract with the central nervous system, with profound implications for neurological health and cognitive function. This whitepaper synthesizes current evidence on dietary modulation of the GBA, examining mechanisms through which nutritional patterns influence neuroinflammation, oxidative stress, and neuronal signaling. Drawing from recent clinical studies and emerging molecular research, we analyze how specific dietary components and patterns affect gut microbiota composition, microbial metabolite production, and subsequent brain health outcomes. The therapeutic potential of microbiota-targeted nutritional interventions for cognitive disorders, mental health conditions, and neurodegenerative diseases is examined, with specific consideration for research methodologies and biomarker assessment. This analysis provides a framework for integrating nutritional strategies into neurological drug development and precision medicine approaches for brain disorders.
The gut-brain axis comprises an extensive communication network facilitating constant interaction between the central nervous system (CNS) and the enteric nervous system through multiple parallel pathways including neural, endocrine, immune, and metabolic signaling routes [24]. This bidirectional system integrates brain and gut functions, with the gut microbiota—a diverse ecosystem of microorganisms residing in the gastrointestinal tract—serving as a critical modulator of this interface [25]. The conceptualization of the GBA has evolved beyond simple brain-gut communication to recognize the microbiota as a key regulator of this system, often described as the microbiota-gut-brain axis.
The significance of the GBA extends to numerous neurological and psychiatric conditions. Research indicates that imbalances in gut microbial communities (dysbiosis) can disrupt GBA signaling, potentially contributing to inflammation and neurotransmitter disturbances implicated in depression, anxiety, and cognitive disorders [24]. The gut microbiota influences brain function through multiple mechanisms: production of neurotransmitters and neuroactive metabolites; regulation of immune responses; modulation of the hypothalamic-pituitary-adrenal (HPA) axis; and maintenance of intestinal barrier integrity [25]. The vagus nerve, a primary neural pathway between the gut and brain, facilitates direct communication that can modulate brain activity and behaviors associated with anxiety and mood [24].
Diet represents one of the most potent modulators of the gut microbiota composition and function, thereby serving as a primary intervention point for influencing the GBA [25]. Nutritional neuroscience has emerged as a discipline focused on understanding how dietary components and patterns influence brain function and mental health through their effects on the GBA [26]. This whitepaper examines the mechanisms underlying dietary influences on the GBA and their implications for cognitive function and mental health within the broader context of chronic disease risk mechanisms.
Molecular Mechanisms of Gut-Brain Communication
Neural and Endocrine Pathways
The GBA utilizes multiple sophisticated communication channels to maintain gut-brain homeostasis. The vagus nerve serves as a direct neural pathway, transmitting gut-derived signals to brain regions involved in emotion regulation, stress response, and cognition [24]. Gut microbes and their metabolites can activate vagal afferents through enteroendocrine cells, influencing central neurotransmitter systems. This neural pathway represents the most direct route for gut-brain signaling.
The endocrine system facilitates GBA communication through the HPA axis, the body's primary stress response system. The gut microbiota regulates HPA axis development and function, with dysbiosis potentially leading to HPA axis dysregulation and increased susceptibility to stress-related disorders [24]. Gut microbes influence circulating levels of cortisol and other stress hormones, which in turn can modulate gut permeability and microbial composition, creating a feedback loop.
The immune system provides another crucial communication channel, with gut microbes continuously interacting with intestinal immune cells. This interaction regulates systemic levels of pro-inflammatory and anti-inflammatory cytokines that can cross the blood-brain barrier (BBB) and influence neuroinflammation [24]. Dysbiosis can trigger immune activation, leading to increased circulating pro-inflammatory cytokines that compromise BBB integrity and promote neuroinflammation associated with various neurological and psychiatric conditions.
Microbial Metabolites and Signaling Molecules
Gut microbiota produce numerous neuroactive compounds that significantly influence brain function:
- Short-chain fatty acids (SCFAs): including butyrate, acetate, and propionate, are produced through microbial fermentation of dietary fiber. SCFAs strengthen the intestinal barrier, reduce systemic inflammation, and can cross the BBB to influence microglia function and neuroinflammation [24]. Butyrate particularly demonstrates histone deacetylase inhibitor activity, influencing gene expression in neural cells.
- Neurotransmitters: Gut bacteria synthesize numerous neurotransmitters including gamma-aminobutyric acid (GABA), serotonin, dopamine, and norepinephrine [26]. Notably, approximately 90% of the body's serotonin is synthesized in the gut under microbial influence [24].
- Tryptophan metabolites: As the precursor to serotonin, tryptophan metabolism is heavily influenced by gut microbiota through the kynurenine and serotonin pathways, with implications for serotonin availability in the brain [24].
- Bile acids: Microbial-modified bile acids function as signaling molecules that can influence host metabolism and neuroinflammation through activation of nuclear receptors.
Table 1: Key Microbial Metabolites in Gut-Brain Signaling
| Metabolite | Primary Producers | Neurological Effects | Research Implications |
|---|---|---|---|
| Short-chain fatty acids (Butyrate, Acetate, Propionate) | Faecalibacterium prausnitzii, Roseburia, Eubacterium, Bifidobacterium | Reduce neuroinflammation, strengthen blood-brain barrier, support microglia function, influence epigenetic regulation | Potential therapeutic for neurodegenerative diseases; biomarker for fiber fermentation |
| GABA (Gamma-aminobutyric acid) | Lactobacillus, Bifidobacterium | Primary inhibitory neurotransmitter; regulates anxiety, stress response, sleep | Psychobiotic development for anxiety disorders |
| Serotonin | Enterochromaffin cells (microbiota-regulated) | Mood regulation, appetite, sleep, cognitive functions | Understanding SSRIs microbiota interactions; depression therapeutics |
| Secondary bile acids | Bacteroides, Clostridium, Lactobacillus | FXR and TGR5 receptor activation; neuroinflammation modulation | Metabolic disorder-neurodegeneration link |
Figure 1: Gut-Brain Axis Communication Pathways. This diagram illustrates the primary mechanisms through which dietary components influence brain function via the gut microbiota and multiple signaling pathways.
Barrier Systems and Their Regulation
The GBA involves critical barrier systems that regulate molecule passage between compartments:
- Intestinal barrier: A single layer of epithelial cells with tight junctions that selectively permits nutrient absorption while restricting pathogen translocation. Gut microbes and their metabolites, particularly SCFAs, regulate intestinal barrier integrity. Dysbiosis can increase intestinal permeability ("leaky gut"), allowing bacterial components like lipopolysaccharide (LPS) to enter circulation and trigger systemic inflammation [24].
- Blood-brain barrier: A specialized endothelial structure that protects the brain from circulating toxins and pathogens. Systemic inflammation resulting from gut dysbiosis can compromise BBB integrity, permitting entry of pro-inflammatory molecules and immune cells into the brain [24]. SCFAs have been shown to support BBB function through effects on tight junction proteins.
These barrier systems represent critical intervention points for dietary influences on the GBA, with specific nutritional components demonstrating protective effects on both intestinal and BBB integrity.
Dietary Patterns and Their Impact on Gut-Brain Signaling
Mediterranean and MIND Diets
The Mediterranean diet (MeDi) is characterized by high consumption of fruits, vegetables, legumes, whole grains, nuts, and olive oil; moderate intake of fish and poultry; and low consumption of red meat and processed foods. This dietary pattern has demonstrated significant neuroprotective effects across multiple studies [27]. Research indicates that MeDi adherence is associated with a 30-40% reduced risk of Alzheimer's disease and improved cognitive function [28]. The protective mechanisms include enhanced microbial diversity, increased SCFA production, reduced neuroinflammation, and attenuation of oxidative stress.
The MIND diet (Mediterranean-DASH Intervention for Neurodegenerative Delay) specifically targets brain health, emphasizing green leafy vegetables, berries, nuts, whole grains, and limited intake of saturated fats and processed foods [28]. A recent 5-year prospective cohort study comparing both diets found that higher adherence to either diet was associated with significantly better cognitive scores (p < 0.0001), lower amyloid-beta, tau, and neurofilament light chain (NfL) levels, and reduced inflammatory markers (CRP, IL-6, TNF-α) [28]. The MIND diet demonstrated a slightly stronger association with cognitive protection than the Mediterranean diet.
Table 2: Quantitative Outcomes of Mediterranean vs. MIND Diet Adherence (5-Year Study)
| Biomarker/Cognitive Measure | Mediterranean Diet High Adherence | MIND Diet High Adherence | Low Adherence (Control) | P-value |
|---|---|---|---|---|
| MMSE Score Change | -0.8 ± 0.3 points | -0.5 ± 0.2 points | -2.9 ± 0.5 points | < 0.0001 |
| MoCA Score Change | -1.1 ± 0.4 points | -0.7 ± 0.3 points | -3.5 ± 0.6 points | < 0.0001 |
| Amyloid-β (Aβ42/40) | 325 ± 45 pg/mL | 355 ± 38 pg/mL | 215 ± 52 pg/mL | < 0.0001 |
| Tau Protein | 85 ± 12 pg/mL | 78 ± 10 pg/mL | 125 ± 18 pg/mL | < 0.0001 |
| Neurofilament Light Chain | 28 ± 6 pg/mL | 25 ± 5 pg/mL | 42 ± 8 pg/mL | < 0.0001 |
| C-reactive Protein | 2.1 ± 0.5 mg/L | 1.8 ± 0.4 mg/L | 4.5 ± 0.9 mg/L | < 0.0001 |
Plant-Based and High-Fiber Diets
Plant-based diets rich in fruits, vegetables, legumes, and whole grains promote microbial diversity and SCFA production through several mechanisms:
- Dietary fiber serves as a primary substrate for microbial fermentation, leading to SCFA production. High-fiber diets increase the abundance of SCFA-producing bacteria including Bifidobacteria, Lactobacilli, Faecalibacterium prausnitzii, and Roseburia species [24]. These microbial shifts correlate with improved cognitive performance and reduced neuroinflammation.
- Polyphenols from plant foods exhibit prebiotic-like effects, promoting beneficial bacteria while inhibiting potential pathogens [25]. Regular consumption of polyphenol-rich foods (berries, green tea, dark chocolate, olive oil) is associated with enhanced cognitive function, potentially through antioxidant and anti-inflammatory mechanisms.
- Plant-based proteins from legumes and nuts support beneficial microbes compared to animal proteins, which may promote bile-tolerant bacteria associated with inflammation [24].
Intervention studies demonstrate that shifts toward plant-based dietary patterns can induce measurable changes in microbial composition within weeks, with corresponding improvements in cognitive parameters, particularly in executive function and memory domains [27].
Western and High-Fat Diets
In contrast to plant-rich diets, Western dietary patterns characterized by high consumption of processed foods, saturated fats, refined sugars, and low fiber content have consistently demonstrated negative effects on gut-brain signaling:
- Reduced microbial diversity: Western diets decrease overall microbial richness and diversity, potentially leading to the extinction of beneficial microbes [25]. This diversity loss reduces functional redundancy and ecosystem resilience.
- Increased intestinal permeability: High-fat and high-sugar diets can disrupt tight junction proteins, increasing LPS translocation and systemic inflammation [24].
- Altered microbial metabolism: Western diets shift microbial metabolism toward production of potentially harmful metabolites including trimethylamine-N-oxide (TMAO), associated with cardiovascular and neurological risks [24].
- Neuroinflammation: Diet-induced systemic inflammation promotes microglial activation and neuroinflammation, potentially accelerating neurodegenerative processes [29].
The detrimental effects of Western diets on the GBA provide a mechanistic explanation for epidemiological associations between these dietary patterns and increased risk of depression, cognitive decline, and neurodegenerative diseases.
Experimental Models and Research Methodologies
Human Study Designs and Biomarker Assessment
Research investigating diet-GBA-brain interactions employs multiple methodological approaches:
Clinical Trial Designs:
- Randomized controlled trials (RCTs): The gold standard for establishing causal relationships between dietary interventions and neurological outcomes. Recent RCTs have implemented dietary interventions ranging from 8 weeks to 24 months with detailed assessment of microbiota composition, microbial metabolites, inflammatory markers, and cognitive measures [28].
- Cohort studies: Large prospective cohorts (e.g., 5-year study with 1500 participants) provide longitudinal data on dietary patterns, microbiome changes, and cognitive trajectories [28].
- Cross-over studies: Particularly valuable for nutritional interventions due to ability to control for inter-individual variability.
Biomarker Assessment:
- Microbiome analysis: 16S rRNA sequencing for taxonomic classification; shotgun metagenomics for functional potential; metabolomics for microbial metabolite profiling.
- Inflammatory markers: CRP, IL-6, TNF-α measured in blood and sometimes CSF [28].
- Neurodegeneration biomarkers: Amyloid-β, tau, neurofilament light chain (NfL) in blood and CSF [28].
- Cognitive assessment: Standardized instruments including MMSE, MoCA, and specialized neuropsychological batteries.
Figure 2: Experimental Workflow for Dietary Intervention Studies. This diagram outlines the standard methodology for clinical trials investigating diet-gut-brain interactions, from participant screening through multi-omics analysis.
Animal Models and Mechanistic Studies
Animal models provide critical insights into causal mechanisms underlying diet-GBA interactions:
- Germ-free models: Animals raised without microorganisms enable investigation of microbiota necessity for normal brain development and function.
- Microbiota transplantation: Fecal microbiota transplantation from human donors to germ-free animals allows demonstration of causal relationships between microbial communities and behavioral phenotypes.
- Genetic models: Transgenic models of neurodegenerative diseases (e.g., Alzheimer's, Parkinson's) permit investigation of dietary interventions on disease progression.
- Pharmacological interventions: Receptor antagonists, enzyme inhibitors, and other pharmacological tools help elucidate molecular mechanisms.
Standardized behavioral tests in animal models include forced swim test (depression-like behavior), open field test (anxiety-like behavior), Morris water maze (spatial learning and memory), and novel object recognition (recognition memory).
Research Reagents and Methodological Tools
Table 3: Essential Research Reagents for Gut-Brain Axis Investigations
| Reagent/Category | Specific Examples | Research Applications | Technical Considerations |
|---|---|---|---|
| DNA Extraction Kits | QIAamp PowerFecal Pro, DNeasy PowerLyzer PowerSoil | Microbiome profiling, 16S rRNA sequencing, metagenomics | Standardization critical for cross-study comparisons; controls for contamination |
| 16S rRNA Primers | 515F/806R (V4 region), 27F/338R (V1-V2) | Bacterial identification and relative abundance | Primer selection influences taxonomic resolution; validation with mock communities |
| ELISA Kits | Amyloid-β (Thermo Fisher KHB3481), Tau (R&D Systems DTA00), NfL (Peninsula Laboratories 42-1001) | Quantification of neurodegeneration biomarkers in blood/CSF | Consider sensitivity (pg/mL range) and dynamic range; batch variation controls |
| Cytokine Panels | Multiplex assays for CRP, IL-6, TNF-α, IL-1β | Inflammation monitoring in serum, plasma, CSF | High-sensitivity assays required for subtle inflammatory changes |
| SCFA Analysis | GC-MS, LC-MS platforms | Quantification of microbial metabolites (butyrate, acetate, propionate) | Sample collection critical (immediate freezing); internal standards required |
| Cell Culture Models | Caco-2 (intestinal barrier), SH-SY5Y (neuronal), BV-2 (microglial) | Mechanistic studies of barrier function, neuroinflammation | Limitations in representing complex in vivo microenvironment |
| Gnotobiotic Equipment | Isolators, sterile housing | Research with germ-free, defined microbiota animals | Technical expertise required; contamination monitoring essential |
Analytical Platforms and Omics Technologies
Advanced analytical platforms enable comprehensive investigation of diet-GBA interactions:
- Metagenomic sequencing: Shotgun sequencing provides strain-level taxonomic resolution and functional gene annotation, enabling reconstruction of microbial metabolic pathways.
- Metabolomics: Mass spectrometry-based platforms (GC-MS, LC-MS) quantify microbial metabolites (SCFAs, neurotransmitters, bile acids) in feces, blood, and sometimes CSF.
- Metatranscriptomics: RNA sequencing of microbial communities reveals functionally active metabolic pathways responding to dietary interventions.
- Proteomics: Mass spectrometry-based quantification of host and microbial proteins in various biofluids.
- Multi-omics integration: Computational approaches integrating data from multiple platforms to construct comprehensive models of diet-microbiota-host interactions.
Therapeutic Applications and Clinical Translation
Nutritional Interventions for Cognitive Disorders
Dietary approaches show promise for preventing and managing cognitive decline:
- MIND and Mediterranean diets: Long-term adherence associates with slower cognitive decline and reduced Alzheimer's disease pathology [28]. The 5-year prospective study demonstrated that both diets significantly preserved cognitive function, with the MIND diet showing marginally superior effects [28].
- Ketogenic diets: Very low-carbohydrate, high-fat diets may benefit neurological conditions by providing alternative energy substrates, reducing oxidative stress, and modulating gut microbiota [30].
- Polyphenol supplementation: Interventions with specific polyphenol-rich foods (berries, green tea, cocoa) demonstrate improvements in memory, executive function, and neuroplasticity markers [27].
- Omega-3 fatty acids: DHA and EPA supplementation shows particular benefit in individuals with low baseline levels, reducing neuroinflammation and supporting neuronal membrane integrity [31].
Psychobiotics and Microbial Therapeutics
Psychobiotics—probiotics and prebiotics with mental health benefits—represent a promising therapeutic approach:
- Probiotic strains: Specific strains of Lactobacillus and Bifidobacterium demonstrate anti-anxiety and antidepressant effects in clinical trials, potentially through GABA production, HPA axis modulation, and inflammation reduction [24].
- Prebiotics: Non-digestible fibers (FOS, GOS, resistant starch) selectively promote beneficial bacteria, indirectly influencing brain function through SCFA production and immune modulation [25].
- Synbiotics: Combinations of probiotics and prebiotics designed to work synergistically.
- Postbiotics: Bacterial-derived products including SCFAs, cell wall fragments, and other bioactive molecules.
Clinical translation requires consideration of individual factors including baseline microbiota composition, host genetics, diet, and environmental exposures. Personalized nutrition approaches that account for these variables may enhance therapeutic efficacy.
The gut-brain axis represents a fundamental pathway through which diet influences neurological health and cognitive function. Evidence from mechanistic studies, animal models, and human interventions consistently demonstrates that dietary patterns significantly modulate gut microbiota composition and function, with consequent effects on neuroinflammation, neurotransmitter systems, and neuronal integrity. Mediterranean and MIND diets, rich in plant foods, fiber, and polyphenols, promote microbial diversity and SCFA production, correlating with improved cognitive outcomes and reduced neurodegeneration biomarkers.
Future research priorities include:
- Long-term intervention studies: Extending beyond 2 years to establish durable effects of dietary patterns on cognitive trajectories.
- Personalized nutrition approaches: Integrating multi-omics data with clinical phenotypes to predict individual responses to dietary interventions.
- Mechanistic elucidation: Further delineation of molecular pathways linking specific microbial metabolites to brain function.
- Intervention timing: Determining critical periods for dietary interventions across the lifespan.
- Microbiome-targeted therapeutics: Developing novel psychobiotics, prebiotics, and microbial metabolites as adjunctive therapies for neurological and psychiatric conditions.
The integration of nutritional strategies with neurological drug development holds promise for enhancing therapeutic outcomes in brain disorders. As research methodologies advance and our understanding of diet-GBA interactions deepens, targeted nutritional interventions may become established components of comprehensive approaches to brain health maintenance and neurological disease treatment.
Research Methods and Translational Applications in Nutrition Science
Prospective cohort studies represent the gold standard research design in observational nutritional epidemiology for investigating the complex relationships between long-term dietary patterns and chronic disease risk. These studies collect extensive data on a large group of healthy individuals and follow them forward in time to observe how exposures, such as dietary habits, correlate with the subsequent development of diseases. The Nurses' Health Study (NHS), Health Professionals Follow-Up Study (HPFS), and UK Biobank exemplify this methodology, having generated pivotal evidence that informs our understanding of diet-disease relationships through their massive scale, long-term follow-up, and comprehensive data collection protocols [32] [12].
The fundamental strength of these designs lies in their ability to establish temporal sequence—dietary exposure is assessed before disease onset, minimizing recall bias that plagues case-control studies. When conducted with rigorous methodology, including repeated dietary assessments, validation substudies, and careful control for confounding variables, these studies can provide compelling evidence about the role of diet in chronic disease development. Their large sample sizes enable sufficient statistical power to detect modest associations and examine effect modification across population subgroups, while their prospective nature allows for the investigation of multiple disease outcomes simultaneously from the same baseline data [32] [33].
Key Findings: Dietary Patterns and Chronic Disease Risk
Large-scale prospective cohorts have consistently demonstrated that specific dietary patterns significantly influence the risk of major chronic diseases, including cardiovascular disease, cancer, type 2 diabetes, and overall mortality. The evidence from these studies has evolved from focusing on single nutrients to comprehensive dietary patterns that better reflect how people actually eat and the potential synergistic effects of foods.
Dietary Patterns and Cancer Risk
The association between dietary patterns and cancer risk has been extensively investigated in prospective cohorts. Evidence from the REGARDS cohort, which followed 22,041 participants over a 10-year observation period, identified significant associations between dietary patterns and cancer mortality [34]. The study derived five empirical dietary patterns through factor analysis: Convenience (Chinese and Mexican foods, pasta, pizza), Plant-based (fruits, vegetables), Southern (added fats, fried foods, sugar-sweetened beverages), Sweets/Fats (sugary foods), and Alcohol/Salads (alcohol, green-leafy vegetables, salad dressing) [34].
Greater adherence to the Southern dietary pattern was associated with a 67% increased risk of cancer mortality (HR: 1.67; 95% CI: 1.32–2.10) compared to those with lowest adherence [34]. This pattern was especially detrimental among White participants (HR: 1.59; 95% CI: 1.22–2.08). Conversely, the Convenience (HR: 0.73; 95% CI: 0.56–0.94) and Plant-based (HR: 0.72; 95% CI: 0.55–0.93) dietary patterns were associated with approximately 28% reduced risk of cancer mortality, though these protective associations were observed primarily among White participants [34].
A recent umbrella review of meta-analyses including 74 meta-analyses from 30 articles evaluated the strength of evidence linking dietary patterns to cancer risk [35]. The analysis identified convincing evidence that adherence to the 2007 World Cancer Research Fund/American Institute for Cancer Research (WCRF/AICR) dietary recommendations was associated with lower risk of all cancers (RR = 0.93, 95% CI: 0.92, 0.95 per 1-unit score increase) [35]. Similarly, prudent diets (RR = 0.89, 95% CI: 0.85, 0.93) and vegetable-fruit-soybean diets (RR = 0.87, 95% CI: 0.83, 0.92) demonstrated convincing evidence for breast cancer risk reduction [35].
The Million Women Study, encompassing 542,778 UK women with 12,251 incident colorectal cancer cases over 16.6 years, provided particularly insightful diet-wide association analyses [36]. Alcohol consumption demonstrated the strongest positive association with colorectal cancer risk (RR per 20 g/day = 1.15, 95% CI: 1.09–1.20), while calcium intake showed the strongest inverse association (RR per 300 mg/day = 0.83, 95% CI: 0.77–0.89) [36]. Red and processed meat intake was positively associated with colorectal cancer risk (RR per 30 g/day = 1.08, 95% CI: 1.03–1.12), though this association was weaker than those observed for alcohol and calcium [36].
Dietary Patterns and Healthy Aging
Recent evidence from the NHS and HPFS, with up to 30 years of follow-up, has examined dietary patterns in relation to healthy aging, defined as surviving to 70 years free of major chronic diseases and maintaining intact cognitive, physical, and mental health [12]. Among 105,015 participants, only 9,771 (9.3%) achieved healthy aging, highlighting the importance of identifying modifiable factors like diet that promote healthspan [12].
The study examined eight dietary patterns, finding that higher adherence to all patterns was associated with greater odds of healthy aging, with odds ratios comparing the highest to lowest quintiles ranging from 1.45 (95% CI: 1.35–1.57) for the healthful plant-based diet index to 1.86 (95% CI: 1.71–2.01) for the Alternative Healthy Eating Index [12]. When the healthy aging threshold was shifted to 75 years, the Alternative Healthy Eating Index showed an even stronger association (OR: 2.24, 95% CI: 2.01–2.50) [12].
Specific dietary components demonstrated distinct relationships with healthy aging domains. Higher intakes of fruits, vegetables, whole grains, unsaturated fats, nuts, legumes, and low-fat dairy were consistently associated with greater odds of healthy aging, whereas trans fats, sodium, sugary beverages, and red/processed meats were inversely associated [12]. Added unsaturated fat intake was particularly associated with surviving to age 70 years and maintaining intact physical and cognitive function [12].
Comparative Effectiveness of Dietary Patterns
Research directly comparing multiple dietary patterns within the same population provides valuable evidence for understanding their relative effectiveness for chronic disease prevention. A comprehensive analysis of 205,852 healthcare professionals from the NHS, NHS II, and HPFS followed for up to 32 years assessed two mechanism-based diets and six diets based on dietary recommendations in relation to major chronic disease—a composite outcome of incident major cardiovascular disease, type 2 diabetes, and cancer [33].
The study demonstrated that participants with low insulinemic (HR: 0.58, 95% CI: 0.57–0.60), low inflammatory (HR: 0.61, 95% CI: 0.60–0.63), or diabetes risk-reducing diets (HR: 0.70, 95% CI: 0.69–0.72) had the largest risk reduction for the composite endpoint [33]. These findings suggest that dietary patterns associated with markers of hyperinsulinemia and inflammation may be particularly informative for future dietary guidelines aimed at chronic disease prevention [33].
Table 1: Association Between Dietary Patterns and Chronic Disease Risk in Major Prospective Cohorts
| Dietary Pattern | Chronic Disease Outcome | Risk Estimate (Highest vs. Lowest Adherence) | Cohort |
|---|---|---|---|
| Alternative Healthy Eating Index | Healthy Aging | OR: 1.86 (95% CI: 1.71–2.01) | NHS, HPFS [12] |
| Healthful Plant-Based Diet | Healthy Aging | OR: 1.45 (95% CI: 1.35–1.57) | NHS, HPFS [12] |
| Southern Pattern | Cancer Mortality | HR: 1.67 (95% CI: 1.32–2.10) | REGARDS [34] |
| Plant-Based Pattern | Cancer Mortality | HR: 0.72 (95% CI: 0.55–0.93) | REGARDS [34] |
| Low Insulinemic Diet | Major Chronic Disease* | HR: 0.58 (95% CI: 0.57–0.60) | NHS, HPFS, NHS II [33] |
| WCRF/AICR Recommendations | All Cancers | RR: 0.93 (95% CI: 0.92–0.95) per 1-unit | Umbrella Review [35] |
*Composite of incident major cardiovascular disease, type 2 diabetes, and cancer
Methodological Protocols in Prospective Cohort Studies
Dietary Assessment Methods
Prospective cohort studies employ standardized, validated dietary assessment tools to capture habitual intake. The NHS and HPFS utilize semi-quantitative food frequency questionnaires (FFQs) administered every 2-4 years to assess dietary intake over the preceding year [33] [12]. These FFQs typically include 130-150 food items with standard portion sizes and frequency categories ranging from "never or less than once per month" to "6+ times per day" [12]. The repeated measures allow for calculation of cumulative averages that better represent long-term dietary patterns and reduce measurement error.
The UK Biobank employs multiple assessment methods, including a touchscreen food frequency questionnaire at baseline and a web-based 24-hour dietary assessment tool (Oxford WebQ) for subsequent assessments [37]. The Oxford WebQ collects data on consumption of up to 206 types of foods and 32 types of drinks during the previous 24 hours, providing more detailed recent intake data [37]. This multi-method approach enhances the comprehensiveness of dietary exposure assessment.
Table 2: Dietary Assessment Methods in Major Prospective Cohorts
| Assessment Method | Frequency of Administration | Key Components | Validation Studies |
|---|---|---|---|
| Semi-Quantitative FFQ (NHS/HPFS) | Every 2-4 years | 130-150 food items, standard portion sizes, 9 frequency categories | Comparison with diet records and biomarkers [33] |
| Touchscreen FFQ (UK Biobank) | Baseline | Common food groups, intake frequencies | Comparison with 24-hour recalls [37] |
| Oxford WebQ 24-hour Recall (UK Biobank) | Multiple timepoints | 206 foods, 32 drinks, previous 24-hour intake | Comparison with biomarkers [37] |
| Block 98 FFQ (REGARDS) | Baseline | 110 food items, frequency and portion size | Comparison with 24-hour recalls [34] |
Outcome Ascertainment
Chronic disease outcomes are ascertained through multiple complementary methods to ensure completeness. In the NHS and HPFS, participants report diagnoses on biennial questionnaires, which are then confirmed through medical record review by physicians blinded to exposure status [12]. Mortality outcomes are identified through the National Death Index, state vital statistics records, and reports from family members [12]. Specific endpoints like cancer are confirmed through pathology reports, while cardiovascular events undergo additional review using standard criteria like the MONICA protocol.
The UK Biobank utilizes linkage to national health registries, including hospital episode statistics, cancer registries, and death registries, providing comprehensive capture of disease endpoints [37] [36]. This linkage approach minimizes loss to follow-up and enables complete ascertainment of hard endpoints. The REGARDS cohort employs semi-annual telephone follow-up, proxy reports, and linkages with the Social Security Death Index and National Death Index, with cause of death adjudicated by expert committees [34].
Statistical Analysis Approaches
Prospective cohort studies employ sophisticated statistical methods to account for potential confounding and test the robustness of associations. Multivariable Cox proportional hazards models are standard for analyzing time-to-event data, with careful adjustment for known confounders including age, sex, body mass index, physical activity, smoking status, alcohol intake, and total energy intake [33] [34] [12]. Additional adjustments are made for socioeconomic factors, family history of diseases, and menopausal status (in women-specific analyses).
More advanced methods include:
- High-dimensional Fixed Effects (HDFE) models: Used in UK Biobank analyses to control for numerous occupational, regional, and ethnicity-related fixed effects that might confound diet-disease relationships [37].
- Mendelian Randomization: Employed to strengthen causal inference using genetic variants as instrumental variables for dietary exposures [37] [36].
- Factor and Cluster Analysis: Used to derive empirical dietary patterns from the dietary data itself, as seen in the REGARDS cohort analysis [34].
- Bayesian Age-Period-Cohort models: Implemented for projecting future disease burden based on current trends [38].
Research Workflow in Prospective Cohort Studies
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Methodological Components for Prospective Diet-Disease Research
| Research Component | Function | Implementation Examples |
|---|---|---|
| Validated FFQs | Assess habitual dietary intake | Semi-quantitative FFQs with portion sizes [33] |
| Biobanking | Storage of biological samples for future analysis | UK Biobank's collection of blood, urine, saliva [37] |
| Biomarker Measurements | Objective measures of nutritional status | Serum 25(OH)D for vitamin D status [39] |
| Genetic Data | Enable Mendelian randomization approaches | Genotyping arrays in UK Biobank [37] |
| Covariate Databases | Control for potential confounding | Standardized demographic, clinical, lifestyle data [32] |
| Statistical Code | Implement complex adjustment and modeling | R, STATA, SAS packages for survival analysis [38] |
Biological Mechanisms Linking Diet to Chronic Disease Risk
Prospective cohort studies have contributed significantly to understanding the biological pathways through which dietary patterns influence chronic disease risk. Several key mechanisms have emerged from these investigations:
Insulinemic and Inflammatory Pathways
The NHS and HPFS analyses have demonstrated that dietary patterns associated with lower insulinemic and inflammatory potential provide the strongest protection against major chronic diseases [33]. The empirical dietary index for hyperinsulinemia (EDIH) and empirical dietary inflammatory pattern (EDIP) represent mechanism-based scores derived from plasma biomarkers of insulin resistance (C-peptide) and inflammation (IL-6, CRP, TNFαR2) [33]. Diets high in sugar-sweetened beverages, processed meats, and other high-glycemic foods activate these pathways, promoting cellular environments favorable to cancer development, atherosclerosis, and metabolic dysfunction.
Aging-Related Pathways
UK Biobank research has identified multiple aging-related pathways modulated by dietary factors, including telomere length maintenance, phenotypic age acceleration, and brain structure preservation [37]. Plant-based food consumption correlates with increased telomere length and reduced phenotypic age, while animal-based food intake shows opposite associations [37]. Mendelian randomization analyses suggest causal benefits of carbohydrate intake for reducing phenotypic age and increasing whole-brain grey matter volume [37].
Key Biological Pathways Linking Diet to Chronic Disease Risk
Global Burden and Future Projections
Analyses from the Global Burden of Disease Study 2021 provide critical context for understanding the population-level impact of dietary risk factors on chronic disease burden worldwide [38]. From 1990 to 2021, global age-standardized mortality rates and disability-adjusted life year rates associated with dietary factors decreased by approximately one-third for neoplasms and cardiovascular diseases [38].
The specific dietary risk factors vary by socioeconomic development level. In high sociodemographic index regions, neoplasm-related deaths show stronger correlation with diets high in red meat, while cardiovascular disease burden is primarily linked to low-grain diets, and diabetes burden associates with increased processed meat intake [38]. In low sociodemographic index regions, diets low in vegetables show the strongest association with neoplasm-related mortality, while diets low in fruits significantly impact cardiovascular disease and diabetes burden [38].
Projections through 2030 indicate continued declines in mortality from neoplasms and cardiovascular diseases attributable to dietary factors, but a slight increase in diabetes mortality rates [38]. These trends highlight the evolving challenge of diet-related chronic diseases and the need for targeted interventions across different global contexts.
Prospective cohort designs leveraging large-scale studies like the NHS, HPFS, and UK Biobank have fundamentally advanced our understanding of how dietary patterns influence chronic disease risk and healthy aging. The consistent evidence from these studies demonstrates that dietary patterns emphasizing plant-based foods, unsaturated fats, whole grains, and lean protein sources while minimizing red and processed meats, sugary beverages, and refined carbohydrates offer significant protection against major chronic diseases and promote healthy aging.
The methodological rigor of these studies—including repeated dietary assessments, comprehensive outcome ascertainment, sophisticated statistical adjustment, and incorporation of biomarker and genetic data—provides a robust foundation for public health recommendations and clinical guidelines. Future research should continue to leverage these rich resources to examine dietary patterns in diverse populations, understand biological mechanisms, and inform personalized nutrition approaches that maximize healthspan and reduce the global burden of chronic diseases.
The application of omics technologies has revolutionized nutritional science by providing unprecedented insights into the molecular mechanisms linking dietary patterns to chronic disease risk. Metabolomics and microbiome analysis serve as complementary approaches that bridge the gap between dietary exposure and physiological outcomes, revealing the complex interplay of microbial communities and their metabolic products that modulate human health. These technologies capture the functional readout of the host-microbiome interface, where dietary components are transformed into bioactive metabolites that influence host physiology through multiple signaling pathways. The integration of these data layers provides a systems biology framework for moving beyond correlation to establish causal mechanisms in diet-disease relationships, offering potential for targeted therapeutic interventions and personalized nutrition strategies that disrupt disease pathways at their metabolic origins.
Analytical Methodologies in Metabolomics and Microbiome Research
Metabolomic Profiling Technologies
Metabolomic analysis employs two primary analytical platforms: mass spectrometry (MS) and nuclear magnetic resonance (NMR) spectroscopy. MS-based approaches, particularly when coupled with liquid chromatography (LC) or gas chromatography (GC), offer high sensitivity and the ability to characterize thousands of metabolites simultaneously. The Nightingale Health platform represents a high-throughput 1H-NMR approach that profiles 249 metabolites primarily in energy and lipid metabolism pathways, providing absolute quantification with high reproducibility [40]. In contrast, untargeted MS platforms like that used in the ATBC Study can measure over 1,300 metabolites, including chemically identified compounds spanning amino acids, lipids, carbohydrates, and xenobiotics, providing broader coverage of the metabolome [41].
Table 1: Key Analytical Platforms in Metabolomics
| Platform | Metabolite Coverage | Key Strengths | Common Applications |
|---|---|---|---|
| LC-MS/MS | 1,000+ metabolites | High sensitivity, structural information | Untargeted discovery, complex biomarker profiling |
| GC-MS | 500-1,000 metabolites | Reproducible separation, compound libraries | Metabolic pathways, volatile compounds |
| 1H-NMR (Nightingale) | 249 metabolites | Absolute quantification, high throughput | Large cohort studies, lipid and energy metabolism |
| FIA-MS/MS (Biocrates p500) | 630 metabolites | Targeted quantification, validated assays | Ceramides, acylcarnitines, bile acids |
Sample preparation protocols vary by platform but typically involve protein precipitation using organic solvents (e.g., methanol or acetonitrile) for MS-based approaches, while NMR requires minimal sample preparation. Quality control measures include the use of pooled quality control samples, internal standards, and blinded replicate samples to monitor technical variation, with intraclass correlation coefficients typically exceeding 0.85 for robust metabolites [41].
Microbiome Analysis Techniques
Microbiome analysis has evolved from culture-based methods to high-throughput sequencing approaches that provide comprehensive taxonomic and functional characterization. 16S rRNA gene sequencing remains the most widely used method for taxonomic profiling, providing information on microbial community structure through amplification of hypervariable regions. Shotgun metagenomic sequencing offers superior resolution at the species level and enables reconstruction of metabolic potential by sequencing all genetic material in a sample.
More recently, multi-omics integration has emerged as a powerful approach for understanding host-microbiome interactions. This includes metatranscriptomics (microbial gene expression), metaproteomics (microbial protein expression), and metabolic modeling to predict functional capabilities. Constraint-based metabolic modeling of the microbiome, using tools like MicrobiomeGS2 and BacArena, reconstructs genome-scale metabolic networks to predict reaction fluxes and metabolite exchanges between microbial species and with the host [42].
Experimental Workflows
The standard workflow for integrated microbiome-metabolome studies begins with proper sample collection and preservation. For metabolomics, fasting blood samples are collected and processed to serum or plasma, with immediate freezing at -70°C to preserve metabolite integrity. For microbiome analysis, stool samples are typically flash-frozen or stored in stabilization buffers to preserve microbial community structure and genetic material.
Diagram 1: Integrated Omics Analysis Workflow
Downstream data processing involves peak identification and alignment for metabolomics, and quality filtering, OTU clustering, and taxonomy assignment for microbiome data. Statistical analysis typically employs both univariate (linear models, correlation analysis) and multivariate (PCA, PLS-DA) approaches to identify features associated with dietary exposures or disease states, followed by pathway enrichment analysis to place findings in biological context.
Dietary Patterns and Their Molecular Signatures
Established Dietary Patterns and Health Outcomes
Multiple dietary patterns have been systematically studied using omics technologies to elucidate their mechanistic foundations. The Alternative Healthy Eating Index (AHEI), Alternative Mediterranean Diet (aMED), and Mediterranean-DASH Intervention for Neurodegenerative Delay (MIND) diet have demonstrated strong associations with healthy aging, with odds ratios for healthy aging ranging from 1.45 to 1.86 when comparing highest to lowest adherence quintiles [12]. These patterns share common features including emphasis on plant-based foods, unsaturated fats, and dietary fiber, while limiting red and processed meats, sodium, and sugary beverages.
Long-term prospective studies including the Nurses' Health Study and Health Professionals Follow-Up Study with up to 30 years of follow-up have shown that adherence to these dietary patterns is associated with significantly greater likelihood of healthy aging, defined as survival to 70 years with intact cognitive, physical, and mental health and absence of major chronic diseases [12]. The associations between diet quality and healthy aging appear stronger in women, smokers, and individuals with higher BMI, suggesting potential personalized approaches to dietary recommendations.
Metabolomic Signatures of Dietary Patterns
Metabolomic profiling has identified distinct molecular signatures associated with healthy dietary patterns. In the Alpha-Tocopherol, Beta-Carotene Cancer Prevention (ATBC) Study, the HEI-2010, aMED, WHO Healthy Diet Indicator (HDI), and Baltic Sea Diet (BSD) were associated with 23, 46, 23, and 33 metabolites respectively, with the lysolipid and xenobiotic pathways most strongly associated with diet quality [41]. These metabolite signatures reflect the specific components used to score adherence to each pattern, such as fruit, vegetables, whole grains, fish, and unsaturated fats.
Table 2: Metabolite Classes Associated with Healthy Dietary Patterns
| Metabolite Class | Specific Metabolites | Dietary Correlates | Biological Significance |
|---|---|---|---|
| Lipids | Tri/di-glycerides, lyso/phosphatidylcholine | Unsaturated fats, whole grains | Membrane integrity, signaling |
| Amino Acids | Branched-chain amino acids | Plant proteins, fish | Insulin sensitivity, muscle metabolism |
| Bile Acids | Primary and secondary bile acids | Dietary fiber, fats | Lipid absorption, signaling |
| Ceramides | Ceramide species | Saturated fats, calories | Insulin resistance, apoptosis |
| Fatty Acids | Acylcarnitines | Meat, dairy, energy metabolism | Mitochondrial function |
| Indoles | Tryptophan metabolites | Protein sources, gut microbiota | Neurotransmitter precursors |
| Sphingomyelins | Sphingomyelin species | Eggs, meat, dairy | Cell signaling, membrane structure |
In the Baltimore Longitudinal Study of Aging, higher adherence to MDS, MIND, and AHEI dietary patterns was associated with 218, 236, and 278 metabolites respectively, with 127 common metabolites spanning multiple classes including lipids, amino acids, bile acids, and sphingomyelins [43]. These metabolomic signatures explained 28-38% of the variance in dietary patterns and mediated up to 61% of the association between diet and frailty, providing molecular evidence for the biological effects of diet on aging-related decline.
Microbiome Signatures of Dietary Patterns
Dietary patterns exert profound effects on the composition and function of the gut microbiome. Plant-based diets rich in fiber promote microbial taxa capable of polysaccharide degradation, including Prevotella and Clostridia clusters IV and XIVa, which ferment indigestible carbohydrates to short-chain fatty acids (SCFAs) such as acetate, propionate, and butyrate [44]. These SCFAs serve as energy sources for colonocytes and exert anti-inflammatory effects through regulation of immune cell function and gene expression.
In contrast, animal-based diets high in fat and protein select for bile-tolerant bacteria and promote proteolytic fermentation with increased production of branched-chain fatty acids (BCFA) from amino acid degradation [44]. These diets also increase microbial metabolism of choline and L-carnitine to trimethylamine (TMA), which is subsequently oxidized in the liver to trimethylamine N-oxide (TMAO), a metabolite associated with increased cardiovascular disease risk.
The gut microbiome exhibits remarkable plasticity in response to dietary changes, with rapid shifts in microbial composition and function observed within 24-48 hours of dietary modification [44]. However, long-term dietary patterns establish stable microbial enterotypes that may determine individual responses to dietary interventions and influence disease risk trajectories.
Host-Microbiome Metabolic Interactions in Health and Disease
Metabolic Cross-Talk in Homeostasis
The gut microbiome functions as a metabolic interface that transforms dietary components and host-derived metabolites into signaling molecules that regulate host physiology. This host-microbiome metabolic cross-talk involves reciprocal exchange of metabolites that influence energy homeostasis, immune function, and neuroendocrine signaling [45].
Microbial metabolites with established host effects include short-chain fatty acids (acetate, propionate, butyrate) from fiber fermentation; secondary bile acids from modification of host primary bile acids; tryptophan catabolites including indole derivatives; and neuroactive metabolites such as gamma-aminobutyric acid (GABA) and serotonin [46] [45]. These microbial metabolites regulate host processes through interaction with specific receptors (e.g., GPR41, GPR43, TGR5, AHR) and modulation of epigenetic marks that influence gene expression.
Diagram 2: Host-Microbiome Metabolic Cross-Talk
The gut microbiome also functions as a virtual endocrine organ through production of hormones and neurotransmitters that mimic host signaling molecules, including production of GABA, serotonin precursors, and dopamine metabolites that can influence host neural function and behavior through the gut-brain axis [45].
Dysregulation in Chronic Disease
Dysregulation of host-microbiome metabolic interactions has been implicated in the pathogenesis of multiple chronic diseases, including inflammatory bowel disease (IBD), major depressive disorder (MDD), and cardiometabolic disorders. In IBD, metabolic modeling of densely phenotyped patient cohorts has revealed concomitant changes in NAD, amino acid, one-carbon, and phospholipid metabolism in both host tissues and the microbiome [42].
Specifically, inflamed intestinal tissue in IBD patients shows elevated tryptophan catabolism that depletes circulating tryptophan and impairs NAD biosynthesis, while reduced transamination reactions disrupt nitrogen homeostasis and polyamine/glutathione metabolism [42]. The suppressed one-carbon cycle in patient tissues alters phospholipid profiles due to limited choline availability, with simultaneous microbiome shifts in NAD, amino acid and polyamine metabolism exacerbating these host metabolic imbalances.
In major depressive disorder, metabolome-wide association studies have identified disturbances in energy and lipid metabolism, with specific alterations in the tricarboxylic acid cycle (decreased citrate, increased pyruvate) and lipoprotein subclasses (decreased HDL, increased VLDL) [40]. These metabolic shifts are consistent with the differential composition of gut microbiota observed in MDD patients, particularly changes in Clostridiales, Proteobacteria/Pseudomonadota, and Bacteroidetes/Bacteroidota, suggesting that gut dysbiosis may contribute to the metabolic manifestations of depression.
Methodological Protocols for Key Experiments
Metabolome-Wide Association Study (MWAS) Protocol
Metabolome-wide association studies represent a powerful approach for identifying metabolic signatures associated with dietary patterns or disease states. The following protocol outlines the key steps for conducting a MWAS:
Sample Preparation: Collect fasting blood samples in EDTA or heparin tubes. Process within 2 hours to isolate plasma or serum. Aliquot and store at -80°C. For analysis, thaw samples on ice and precipitate proteins using cold methanol or acetonitrile (2:1 solvent-to-sample ratio). Centrifuge and collect supernatant for analysis [41].
Metabolite Profiling: Utilize targeted (e.g., Nightingale Health NMR, Biocrates p500) or untargeted (LC-MS, GC-MS) platforms. For untargeted LC-MS, use reversed-phase chromatography with C18 columns and positive/negative electrospray ionization with mass resolution >30,000. Include quality control samples (pooled reference plasma) every 10-15 injections to monitor instrument performance [41] [40].
Data Preprocessing: For MS data, perform peak detection, alignment, and integration using software such as XCMS or Progenesis QI. For NMR data, apply phase correction, baseline correction, and chemical shift alignment. Normalize data using probabilistic quotient normalization or internal standards. Replace values below detection limit with imputed values (e.g., half minimum value) [40].
Statistical Analysis: Conduct log transformation and Pareto scaling to normalize data. For association analysis, use linear regression models adjusting for age, sex, BMI, technical covariates, and multiple testing (false discovery rate < 0.05). For mediation analysis, assess whether metabolites mediate the diet-disease association using causal inference tests [40] [43].
Microbiome-Metabolic Modeling Protocol
Constraint-based metabolic modeling enables prediction of metabolic fluxes in microbial communities and their interactions with the host. The following protocol outlines the approach for integrating microbiome data with metabolic models:
Metagenomic Data Processing: Quality filter raw sequencing reads using Trimmomatic or similar tools. Perform taxonomic profiling using MetaPhlAn2 or mOTU2. For functional profiling, align reads to reference genomes or catalogs (e.g., IGC) using Bowtie2 or BWA [42].
Metabolic Network Reconstruction: Map metagenomic data to reference genome-scale metabolic models from resources such as the Human Metabolic Atlas or AGORA. Reconstruct community metabolic models using tools like MicrobiomeGS2 or mgPipe that integrate individual organism models [42].
Flux Balance Analysis: Define community objective functions (e.g., biomass production, butyrate production). Apply constraints based on nutrient availability from dietary data. Calculate optimal flux distributions using linear programming solvers (CPLEX, Gurobi). For dynamic simulation, use agent-based modeling approaches (BacArena) [42].
Host-Microbiome Integration: Integrate microbial metabolite exchange predictions with host metabolic models (Recon3D) to predict systemic effects. Validate predictions using measured serum metabolomics data and assess correlation between predicted and measured metabolite levels [42].
Research Reagent Solutions and Essential Materials
Table 3: Essential Research Reagents and Materials for Diet-Microbiome-Metabolome Studies
| Category | Specific Reagents/Platforms | Function/Application |
|---|---|---|
| Sample Collection | EDTA/heparin blood collection tubes, stool DNA/RNA stabilizers, liquid nitrogen | Sample integrity preservation for different analyte types |
| Metabolomics | Methanol, acetonitrile (HPLC/MS grade), deuterated internal standards, Biocrates p500 kit, Nightingale Health NMR platform | Metabolite extraction, quantification, and profiling |
| Microbiome | DNeasy PowerSoil Pro Kit, Illumina sequencing kits, MetaPhlAn2 database, AGORA model resource | DNA extraction, sequencing, taxonomic profiling, metabolic modeling |
| Data Analysis | XCMS Online, MetaboAnalyst 5.0, QIIME 2, Cobrapy, R packages (vegan, mixOmics) | Data preprocessing, statistical analysis, integration |
| Reference Materials | NIST SRM 1950 (plasma), ZymoBIOMICS Microbial Community Standard | Quality control, method validation |
The integration of metabolomics and microbiome analysis provides a powerful framework for deciphering the mechanisms through which dietary patterns influence chronic disease risk. These omics technologies move beyond correlation to reveal the functional interactions between diet, gut microbes, and host physiology, identifying specific metabolic pathways that mediate dietary effects on health outcomes.
Future research directions include the development of dynamic models that capture the temporal relationships between dietary exposures, microbial ecological dynamics, and metabolic responses; the application of single-cell omics to resolve cellular heterogeneity in host responses; and the implementation of intervention studies that test causal mechanisms identified through observational omics profiling. As these technologies mature and become more accessible, they hold promise for advancing personalized nutrition approaches that leverage individual microbial and metabolic characteristics to optimize dietary recommendations for chronic disease prevention and healthy aging.
In nutritional epidemiology and chronic disease mechanisms research, dietary pattern indices have emerged as critical tools for quantifying exposure to complex dietary exposures that single-nutrient approaches often miss. These indices provide standardized metrics for evaluating how overall eating patterns influence disease risk pathways, offering superior predictive power for chronic disease outcomes compared to isolated food or nutrient analyses. The Alternative Healthy Eating Index (AHEI), reverse Empirical Dietary Index for Hyperinsulinemia (rEDIH), reverse Empirical Dietary Index for Inflammation (rEDIP), and Mediterranean-DASH Intervention for Neurodegenerative Delay (MIND) diet represent four rigorously validated indices that capture distinct biological pathways relevant to chronic disease pathogenesis. Their application extends from observational research to clinical trials and drug development, where they help identify dietary modifiers of treatment efficacy and disease progression.
The fundamental premise underlying these indices is that foods and nutrients act synergistically within biological systems, making dietary patterns more informative than individual components for understanding disease mechanisms. These indices transition research from a reductionist focus on single nutrients to a holistic approach that better reflects actual eating behaviors and their integrated effects on metabolic, inflammatory, and neurobiological pathways. For researchers and drug development professionals, understanding the construction, application, and biological relevance of these indices is essential for designing robust studies on dietary influences on chronic disease risk and progression.
Comprehensive Index Specifications and Scoring Methodologies
Component Structures and Scoring Criteria
Each dietary pattern index comprises distinct components selected for their established relationships with specific disease pathways, with scoring algorithms that transform dietary intake data into standardized quantitative metrics.
Table 1: Component Comparison of Major Dietary Pattern Indices
| Index | Number of Components | Key Emphasis Areas | Scoring Range | Primary Biological Targets |
|---|---|---|---|---|
| AHEI-2010 | 11 components | Foods/nutrients predictive of chronic disease risk | 0-110 | Cardiovascular disease, diabetes, cancer |
| rEDIH | 18 food groups | Dietary insulinemic potential | Continuous (reverse scored) | Hyperinsulinemia, metabolic dysfunction |
| rEDIP | 39 food groups | Dietary inflammatory potential | Continuous (reverse scored) | Chronic inflammation, inflammatory diseases |
| MIND | 15 components | Neuroprotective foods | 0-15 | Cognitive decline, neurodegeneration |
The AHEI-2010 was specifically designed to capture dietary factors most predictive of chronic disease risk, updating earlier versions with additional evidence-based components [47]. It includes 11 components scored from 0-10, with total scores ranging from 0 (non-adherence) to 110 (perfect adherence). Components include vegetables, fruits, whole grains, sugar-sweetened beverages, nuts and legumes, red/processed meat, trans fats, long-chain omega-3 fats, polyunsaturated fatty acids, sodium, and alcohol [47]. Each component is scored according to established criteria, with intermediate intake levels receiving proportional scores.
The MIND diet score comprises 15 components focusing specifically on neuroprotective foods, with 10 brain-healthy food groups (green leafy vegetables, other vegetables, nuts, berries, beans, whole grains, fish, poultry, olive oil, and wine) and 5 brain-unhealthy groups (red meats, butter and margarine, cheese, pastries and sweets, and fast/fried food) [48]. Each component is scored 0, 0.5, or 1 point based on adherence to criteria, with total scores ranging from 0-15 [48]. The scoring system specifically emphasizes foods with demonstrated neuroprotective properties, with particularly strong weighting for green leafy vegetables and berries.
The rEDIH and rEDIP indices employ distinct methodological approaches as empirically-derived indices. Unlike the a priori design of AHEI and MIND, these indices were developed using reduced rank regression to identify dietary patterns most predictive of specific biomarkers - plasma C-peptide for EDIH (insulin secretion) and inflammatory biomarkers (IL-6, CRP, TNFαR2) for EDIP [12]. The "reverse" scoring (rEDIH, rEDIP) indicates that higher scores reflect lower insulinemic or inflammatory potential, representing more favorable dietary patterns. These indices comprise weighted contributions from multiple food groups based on their empirical relationships with these biomarkers.
Dietary Assessment Methodologies and Data Transformation
Implementation of these indices requires standardized dietary assessment and data processing protocols. The most common assessment methods include:
- Food Frequency Questionnaires (FFQs): Validated FFQs provide comprehensive data on habitual intake across multiple food groups and are the primary tool for calculating dietary pattern scores in large cohort studies [47]. The Harvard FFQ, used in the Nurses' Health Study and Health Professionals Follow-up Study, has been extensively validated for this purpose.
- 24-Hour Recalls: Increasingly used in population studies like NHANES, with the average of multiple recalls providing a reasonable estimate of usual intake [49]. The USDA Automated Multiple-Pass Method enhances accuracy of recall data.
- Food Records: While providing detailed intake data, these require high participant burden and are less practical for large studies [50].
Following data collection, food intake quantities are transformed into index-specific components using standardized algorithms. For AHEI, components are generally adjusted for energy intake using density-based approaches (per 1000 kcal) [47]. The MIND diet uses tertile-based scoring for some components, where participants receive 1, 0.5, or 0 points based on their ranking within the population distribution for each food group [48].
Diagram 1: Dietary Pattern Index Development Workflow (53 characters)
Health Outcome Associations and Epidemiological Evidence
Chronic Disease Risk Reduction Across Multiple Organ Systems
Strong epidemiological evidence supports the association between higher adherence to these dietary patterns and reduced risk of multiple chronic diseases, with each index demonstrating particular strengths for specific health outcomes.
Table 2: Health Outcome Associations of Dietary Pattern Indices
| Index | Strongest Evidence Base | Key Epidemiological Findings | Population Studies |
|---|---|---|---|
| AHEI | Healthy aging, chronic disease prevention | 86% higher odds of healthy aging (highest vs. lowest quintile); 16-19% reduced chronic disease risk | NHS, HPFS, NHANES [12] [47] |
| rEDIH | Metabolic diseases, healthy aging | Strong association with healthy aging (OR~1.8); strongest association with freedom from chronic diseases | NHS, HPFS [12] |
| rEDIP | Inflammatory conditions, physical function | Significant association with intact physical function | NHS, HPFS [12] |
| MIND | Neurodegenerative diseases, liver health | 27% reduced dementia risk; associations with MASLD severity | UK Biobank, Clinical cohorts [51] [48] |
The AHEI has demonstrated particularly robust associations with healthy aging, defined as survival to 70 years free of major chronic diseases with intact cognitive, physical, and mental health. In pooled analyses from the Nurses' Health Study and Health Professionals Follow-Up Study (n=105,015), participants in the highest AHEI quintile had 1.86 times greater odds (95% CI: 1.71-2.01) of healthy aging compared to the lowest quintile [12]. The AHEI showed the strongest association with intact mental health (OR: 2.03, 95% CI: 1.92-2.15) and physical function (OR: 2.30, 95% CI: 2.16-2.44) among all indices studied [12].
The MIND diet has shown particular efficacy for cognitive outcomes. In the UK Biobank study (n=131,209), higher MIND diet adherence was associated with a 27% reduced dementia risk (HR: 0.73) over a median 13.5-year follow-up [51]. Recent evidence also extends these benefits to hepatic health, with a cross-sectional study of 450 MASLD patients demonstrating that each 1-unit increase in MIND score was associated with significant reductions in HOMA-IR (β=-2.11), CRP (β=-2.12), and LPS (β=-8.52), suggesting broad metabolic and anti-inflammatory benefits [48].
The rEDIH and rEDIP indices offer unique value for targeting specific metabolic pathways. The rEDIH showed the strongest association with freedom from chronic diseases among healthy aging domains (OR: 1.75, 95% CI: 1.65-1.87) [12], highlighting its relevance for metabolic disease prevention. The rEDIP, while showing slightly weaker overall associations with healthy aging, demonstrated significant relationships with inflammatory pathways relevant to multiple chronic conditions.
Comparative Performance Across Population Subgroups
The effectiveness of these dietary patterns varies across population subgroups, with important implications for targeted interventions. Evidence suggests stronger protective associations for AHEI, MIND, and Mediterranean-style patterns in women compared to men, with significant interaction terms (P interaction: 0.0226 to <0.0001) [12]. Similarly, enhanced benefits have been observed among smokers, individuals with BMI >25 kg/m², and those with lower physical activity levels [12]. These differential effects highlight the importance of considering population characteristics when applying these indices in research or clinical guidance.
For cognitive outcomes specifically, the protective associations of the MIND and Mediterranean diets appear more pronounced in older adults (≥60 years), women, non-obese individuals, and ApoEε4 non-carriers [51]. This stratification offers valuable insights for targeting dietary interventions to populations most likely to benefit.
Research Implementation Protocols
Experimental Workflows for Index Application
Implementation of dietary pattern indices in research settings requires standardized protocols to ensure consistency and reproducibility across studies. The following workflow outlines key steps for proper application:
Diagram 2: Research Implementation Workflow (44 characters)
For cohort studies and clinical trials, dietary data should be collected at baseline and periodically throughout follow-up to account for dietary changes. The NHS and HPFS exemplify this approach with dietary assessments every 4 years [47]. Analysis typically involves categorizing participants into quintiles or tertiles of adherence for each index, with comprehensive adjustment for potential confounders including age, sex, BMI, physical activity, smoking status, energy intake, and socioeconomic factors [12] [49].
For mechanistic studies, mediation analyses can elucidate biological pathways linking dietary patterns to health outcomes. In MASLD research, the Simpson diversity index was identified as a partial mediator of the relationship between MIND diet adherence and liver health indicators, suggesting gut microbiota involvement in the diet-liver axis [48]. Similar approaches can be applied to inflammatory biomarkers for rEDIP or metabolic markers for rEDIH.
Essential Research Reagents and Methodological Tools
Table 3: Research Reagent Solutions for Dietary Pattern Implementation
| Research Tool Category | Specific Examples | Research Application | Technical Considerations |
|---|---|---|---|
| Validated Dietary Assessment Instruments | Harvard FFQ, Oxford WebQ, ASA24 | Standardized dietary data collection | Selection depends on population, culture, and resources [47] [51] |
| Food Composition Databases | USDA Food Patterns Equivalents Database (FPED), metric adaptations (mHEI) | Food group and component quantification | Metric adaptations needed for international applications [52] |
| Biomarker Assay Kits | C-peptide, IL-6, CRP, TNFαR2, LPS, TMAO | Validation of mechanistic pathways | Essential for empirical indices and mediation analyses [12] [48] |
| Statistical Analysis Packages | R, SAS, STATA with nutritional epidemiology macros | Data transformation and index calculation | Custom programming required for complex scoring algorithms |
| Cognitive Assessment Tools | CERAD, Animal Fluency, DSST | Neurodegenerative outcome assessment | Standardized protocols essential for comparability [49] |
Application in Chronic Disease Mechanisms Research and Drug Development
Elucidating Biological Pathways in Disease Pathogenesis
These dietary pattern indices serve as powerful tools for investigating the biological mechanisms through which diet influences chronic disease risk and progression. Each index captures distinct aspects of dietary influence on physiological systems:
The rEDIP index specifically targets inflammatory pathways, providing insights into how dietary patterns modulate systemic inflammation. The original EDIP was developed based on plasma biomarkers of inflammation (IL-6, CRP, TNFαR2) [12], making it particularly valuable for research on inflammatory diseases, including cardiometabolic disorders, certain cancers, and autoimmune conditions. The reverse scoring (rEDIP) allows researchers to quantify the anti-inflammatory potential of overall diets.
The rEDIH index offers a unique approach to studying metabolic regulation through dietary influences on insulin secretion. Developed using plasma C-peptide concentrations as the response variable [12], this index captures the collective insulinemic effect of dietary patterns, providing insights into dietary contributors to hyperinsulinemia, insulin resistance, and related metabolic disorders.
The MIND diet integrates neuroprotective dietary components, emphasizing foods rich in polyphenols, antioxidants, and anti-inflammatory compounds that may cross the blood-brain barrier or exert indirect effects through the gut-brain axis [48]. The significant associations between MIND adherence and gut microbiota composition (Simpson diversity index, Firmicutes-to-Bacteroidetes ratio) highlight the potential role of microbial mediators in diet-brain relationships [48].
The AHEI provides a comprehensive assessment of overall diet quality based on current understanding of chronic disease prevention, making it particularly valuable for studies of multi-system health outcomes like healthy aging [12].
Applications in Pharmaceutical Research and Clinical Trial Design
In drug development contexts, dietary pattern indices offer valuable tools for several applications:
- Stratification Factors: These indices can identify patient subgroups with different dietary exposures that might modify drug efficacy or adverse event profiles.
- Covariate Adjustment: Including dietary pattern scores in statistical models helps control for dietary confounding when assessing treatment effects.
- Combined Intervention Studies: Dietary indices provide outcome measures for trials testing pharmaceutical-dietary combination approaches, particularly relevant for metabolic, inflammatory, and neurodegenerative diseases.
- Mediation Analyses: These indices help elucidate whether dietary improvements represent mechanisms through which lifestyle interventions exert their effects.
The robust association between the MIND diet and dementia risk (27% reduction) [51] suggests potential applications in neurodegenerative disease drug development, either as complementary lifestyle approaches or for identifying populations that might respond differently to pharmacological interventions.
Dietary pattern indices represent sophisticated tools for quantifying complex dietary exposures in chronic disease research. The AHEI, rEDIH, rEDIP, and MIND scores each offer unique strengths for investigating different physiological pathways and health outcomes. Their standardized scoring systems enable consistent application across studies, while their established associations with clinical outcomes validate their utility in both observational research and clinical trials.
For researchers and drug development professionals, understanding the construction, application, and interpretation of these indices is essential for designing robust studies of diet-disease relationships. The continued refinement of these tools, including cultural adaptations and metric system conversions [52], will further enhance their global applicability. As precision nutrition advances, these indices may also be refined to identify subgroup-specific optimal eating patterns, potentially enhancing their effectiveness for both prevention and adjunctive therapy across the spectrum of chronic diseases.
Nutritional epidemiology faces a fundamental challenge: while observational studies readily identify associations between diet and health, establishing definitive causal relationships remains methodologically complex. The field is criticized for its inability to provide plausible information on the causal effects of diet on health and disease outcomes, which is essential for both scientific understanding and guiding public policies [53]. Although most public dietary guidelines globally have arrived at similar conclusions, they continue to rely strongly on observational studies, which produce the lowest-quality data with perceivable but also unidentifiable confounding and with very limited, if any, opportunities to assess direct causality [53]. The inherent limitations of randomized controlled trials (RCTs) in nutrition research—including multifactorial dietary components, long latency periods for chronic disease outcomes, low compliance, high dropout rates, and the frequent impossibility of blinding—create a methodological gap that demands sophisticated causal inference approaches [53].
The transition from observed associations to validated causal pathways requires rigorous methodological frameworks that can account for the complex interplay between dietary exposures, confounding factors, mediating mechanisms, and health outcomes. This technical guide provides researchers with a comprehensive overview of established and emerging causal inference methods, with specific application to the challenges of nutritional epidemiology and chronic disease risk mechanism research.
Causal Criteria and Theoretical Foundations
Fundamental Causal Criteria in Nutritional Epidemiology
Making nutrition recommendations involves complex judgments about the balance between benefits and risks associated with a nutrient or food. Causal criteria are central features of such judgments but are not sufficient alone [54]. The current practice, methods, and theory of causal inference permit flexibility in the choice of criteria, their relative priority, and the rules of inference assigned to them. At a minimum, the set of criteria includes consistency, strength of association, dose response, plausibility, and temporality [54].
The specific interpretation of these criteria in nutritional epidemiology includes several key considerations. Consistency across study designs is compelling when the studies are of high quality and are not subject to biases. Strength of association is considered positive when there is a statistically significant risk estimate with a >20% increase or decrease in risk. A statistically significant linear or otherwise regularly increasing dose-response trend reinforces the judgment in favor of a recommendation. A plausible hypothesis likewise reinforces a recommendation, although the rules of inference for biological evidence are highly variable and depend on the situation. Temporality in nutrition recommendations involves consideration of the extent to which a dietary factor affects disease onset or progression [54]. Evidence supporting these criteria provides a strong basis for making a nutrition recommendation, given due consideration of the balance between presumed benefits and presumed harms.
Table 1: Causal Criteria in Nutritional Epidemiology
| Criterion | Interpretation in Nutritional Epidemiology | Evidentiary Standard |
|---|---|---|
| Consistency | Agreement across different study designs and populations | Compelling when high-quality studies free of major biases show consistent effects |
| Strength of Association | Magnitude of effect size | >20% increase or decrease in risk considered clinically meaningful |
| Dose Response | Monotonic relationship between exposure and outcome | Statistically significant linear or nonlinear trend reinforcing causality |
| Plausibility | Biological mechanism supporting the relationship | Variable rules of inference depending on mechanistic evidence |
| Temporality | Sequence of exposure preceding outcome | Consideration of effects on disease onset versus progression |
Directed Acyclic Graphs (DAGs) for Causal Modeling
Directed Acyclic Graphs (DAGs) provide a formal framework for representing causal assumptions and identifying confounding factors that must be addressed in analytical models. DAGitty is a browser-based environment for creating, editing, and analyzing causal diagrams, with a focus on minimizing bias in empirical studies in epidemiology and other disciplines [55]. The software implements algorithms for identifying appropriate sets of covariates to adjust for in order to obtain unbiased effect estimates.
The diagram below illustrates a basic causal DAG for nutritional epidemiology research, depicting relationships between dietary patterns, potential confounders, mediating biomarkers, and chronic disease outcomes:
Causal DAG for Nutritional Epidemiology Research
This DAG illustrates how socioeconomic status and genetic predisposition act as confounders, potentially influencing both dietary patterns and chronic disease risk, while mediating biomarkers represent potential biological mechanisms through which diet affects disease outcomes.
Advanced Causal Inference Methods
Mendelian Randomization: Principles and Applications
Mendelian randomization (MR) has emerged as a powerful method for strengthening causal inference in nutritional epidemiology. MR is a form of instrumental variable analysis that uses genetic variants as proxies for modifiable exposures to assess causal effects on outcomes [53]. The fundamental principles and prerequisites for univariable Mendelian randomization analysis are based on three key axioms: (i) the genetic variant(s) must associate with the exposure; but (ii) not with either known or unknown confounders; and (iii) there should be no pathway from the genetic variant(s) to the outcome that does not include the exposure of interest [53].
The workflow for implementing MR studies involves specific steps from genetic instrument selection to causal effect estimation, as illustrated below:
Mendelian Randomization Analysis Workflow
In nutritional epidemiology, however, the interpretation of the genetic component of predominantly environmental traits, such as dietary intake, is complicated and prone to various caveats. Dietary habits are highly correlated both with each other and with non-dietary traits, suggesting that any single dietary phenotype may represent a broader diet and lifestyle, for example, with confounding links to obesity and socioeconomic status [53]. Methodological challenges including inevitable genetic pleiotropy and weak instruments further complicate the quest for robust findings.
Multivariable Extensions and Causal Mediation Analysis
Multivariable Mendelian randomization (MVMR) extends the basic MR framework to address multiple related exposures simultaneously, providing particular value in nutritional epidemiology where dietary factors are often correlated [53]. This approach retains the benefits of using genetic instruments for causal inference while allowing for estimation of direct and indirect effects through mediating pathways.
Table 2: Mendelian Randomization Applications in Nutritional Epidemiology
| Application Type | Key Features | Nutritional Epidemiology Examples |
|---|---|---|
| Univariable MR | Single exposure analyzed using genetic instruments | Effect of circulating vitamin C on coronary heart disease using SLC23A1 gene variants [53] |
| Multivariable MR (MVMR) | Multiple correlated exposures analyzed simultaneously | Dietary patterns rather than single foods or nutrients [53] |
| MR Mediation Analysis | Decomposition of direct and indirect effects | Assessment of physiological mediators between diet and chronic disease [53] |
| Two-Step MR | Exposure effect on mediator, then mediator on outcome | Dietary factors → biomarkers → disease outcomes [53] |
MVMR has been applied to study the potential causal associations of dietary patterns with over a hundred circulating biomarkers analyzed by nuclear magnetic resonance (NMR) metabolomics. These analyses identified more than 400 potentially causal links between food and biomarkers, with replication of some previous findings (e.g., increased oily fish consumption and higher circulating docosahexaenoic acid concentrations) and new causal findings such as various food effects on apolipoprotein B-containing lipoprotein particles [53].
Experimental Protocols and Methodological Implementation
Prospective Cohort Studies for Dietary Pattern Analysis
Large-scale prospective cohort studies with long-term follow-up provide the foundational evidence for assessing associations between dietary patterns and chronic disease outcomes. The protocol for such studies typically includes:
Population Recruitment and Baseline Assessment: Studies such as the Nurses' Health Study (NHS), Health Professionals Follow-up Study (HPFS), and NHS II enroll tens to hundreds of thousands of participants [33] [12]. Comprehensive baseline data collection includes demographic characteristics, medical history, lifestyle factors, and anthropometric measurements. Diet is typically assessed using validated food frequency questionnaires (FFQs) that capture usual dietary intake over the preceding year.
Dietary Pattern Operationalization: Multiple dietary patterns are derived from FFQ data, including mechanism-based diets (e.g., low insulinemic, low inflammatory) and diets based on dietary recommendations (e.g., Alternative Healthy Eating Index, Mediterranean-style, Dietary Approaches to Stop Hypertension) [33]. Participants receive scores reflecting their adherence to each pattern, with higher scores indicating better alignment with the ideal pattern.
Outcome Ascertainment: During follow-up periods extending up to 30 years, outcome data are collected through repeated questionnaires, medical record review, and linkage with disease registries [12]. Composite endpoints may include major chronic diseases (cardiovascular disease, type 2 diabetes, and cancer) [33] or multidimensional healthy aging outcomes encompassing cognitive, physical, and mental health, plus freedom from chronic diseases [12].
Statistical Analysis: Cox proportional hazards models are used to calculate hazard ratios (HRs) for disease outcomes comparing different levels of dietary pattern adherence, while logistic regression models estimate odds ratios (ORs) for healthy aging outcomes [33] [12]. Multivariable models adjust for potential confounders including age, body mass index, physical activity, smoking status, and other lifestyle factors.
Global Burden of Disease Analytical Framework
The Global Burden of Disease (GBD) Study provides a systematic approach to quantifying the population-level impact of dietary risk factors on chronic disease burden:
Risk Factor Definition: The GBD framework evaluates 15 diet-related risk factors, including "Diet high in processed meat," "Diet high in red meat," "Diet high in sodium," "Diet high in sugar-sweetened beverages," "Diet high in trans fatty acids," and diets low in protective factors such as fruits, vegetables, whole grains, nuts, seeds, and omega-3 fatty acids [38].
Theoretical Minimum Risk Exposure Level (TMREL): For each dietary factor, a TMREL is established representing the optimal intake level that minimizes risk [38]. Population exposure distributions are compared against these TMRELs to calculate population attribution fractions (PAFs).
Burden Calculation: The disease burden attributable to dietary risks is quantified through deaths and disability-adjusted life years (DALYs), which combine years of life lost due to premature mortality with years lived with disability [38]. Age-standardized rates facilitate comparisons across populations and over time.
Trend Analysis and Projection: Joinpoint regression models analyze trends in age-standardized mortality rates (ASMR) and age-standardized DALY rates (ASDR) over time [38]. Bayesian age-period-cohort models project future burden through 2030, informing policy planning and evaluation.
Key Research Findings and Quantitative Evidence
Dietary Patterns and Chronic Disease Risk
Large-scale prospective evidence demonstrates that adherence to healthy dietary patterns is consistently associated with reduced risk of major chronic diseases. In studies following 205,852 healthcare professionals for up to 32 years, adherence to a healthy diet was generally associated with a lower risk of major chronic disease, defined as a composite outcome of incident major cardiovascular disease, type 2 diabetes, and cancer [33]. Hazard ratios comparing the 90th to 10th percentile of dietary pattern scores ranged from 0.58 to 0.80, with participants following low insulinemic (HR 0.58, 95% CI 0.57, 0.60), low inflammatory (HR 0.61, 95% CI 0.60, 0.63), or diabetes risk-reducing diets (HR 0.70, 95% CI 0.69, 0.72) showing the largest risk reduction [33].
Table 3: Dietary Patterns and Chronic Disease Risk: Hazard Ratios from Prospective Cohorts
| Dietary Pattern | Chronic Disease Composite HR (90th vs 10th percentile) | Cardiovascular Disease HR | Type 2 Diabetes HR | Cancer HR |
|---|---|---|---|---|
| Low Insulinemic | 0.58 (0.57, 0.60) | 0.60 (0.57, 0.63) | 0.43 (0.41, 0.46) | 0.73 (0.71, 0.75) |
| Low Inflammatory | 0.61 (0.60, 0.63) | 0.63 (0.60, 0.66) | 0.51 (0.48, 0.53) | 0.72 (0.70, 0.74) |
| Diabetes Risk-Reducing | 0.70 (0.69, 0.72) | 0.73 (0.70, 0.76) | 0.54 (0.52, 0.57) | 0.83 (0.80, 0.85) |
| Alternative Healthy Eating Index | 0.77 (0.75, 0.79) | 0.74 (0.71, 0.77) | 0.70 (0.67, 0.73) | 0.87 (0.85, 0.90) |
| Mediterranean-style | 0.80 (0.78, 0.82) | 0.78 (0.75, 0.82) | 0.78 (0.74, 0.81) | 0.88 (0.85, 0.91) |
Dietary Patterns and Healthy Aging
Beyond disease-specific outcomes, dietary patterns show significant associations with multidimensional healthy aging. After up to 30 years of follow-up in studies of 105,015 participants, higher adherence to all dietary patterns was associated with greater odds of healthy aging, defined according to measures of cognitive, physical and mental health, plus living to 70 years free of chronic diseases [12]. The multivariable-adjusted odds ratios for the highest quintile versus the lowest ranged from 1.45 (95% CI 1.35-1.57) for the healthful plant-based diet to 1.86 (95% CI 1.71-2.01) for the Alternative Healthy Eating Index [12].
When examining associations with individual healthy aging domains, higher adherence to all dietary patterns was associated with all individual domains. For intact cognitive health, ORs ranged from 1.22 to 1.65; for intact physical function, 1.38 to 2.30; for intact mental health, 1.37 to 2.03; for being free of chronic diseases, 1.32 to 1.75; and for surviving to age 70 years, 1.33 to 2.17 [12].
Global Burden of Diet-Related Chronic Diseases
Analysis of the Global Burden of Disease Study 2021 data reveals significant population-level impacts of dietary risk factors on chronic disease mortality and disability. From 1990 to 2021, global age-standardized mortality rates and DALY rates associated with dietary factors decreased by approximately one-third for neoplasms and cardiovascular diseases [38]. The leading dietary risk factors vary by disease and region: in high sociodemographic index (SDI) regions, neoplasm-related deaths show stronger correlation with dietary factors, particularly high red meat intake, while in cardiovascular diseases, the leading dietary factors are low-grain diets, and in diabetes, increased intake of processed meat [38]. In low-SDI regions, diets low in vegetables show the strongest association with neoplasm-related mortality, while diets low in fruits are significantly linked to CVD and diabetes burden [38].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Essential Research Reagents and Materials for Nutritional Epidemiology
| Research Tool | Specification/Function | Application in Causal Inference |
|---|---|---|
| Validated Food Frequency Questionnaires (FFQs) | Semi-quantitative assessment of habitual dietary intake | Exposure assessment in prospective cohort studies; operationalization of dietary patterns [33] [12] |
| Genetic Variant Panels | Pre-selected SNPs associated with dietary intake or nutrient metabolism | Instrumental variables in Mendelian randomization studies [53] |
| Biomarker Assays | Objective measures of nutrient status (e.g., plasma vitamins, fatty acids) | Validation of dietary assessment; mediation analysis in causal pathways [53] |
| NMR Metabolomics Platforms | High-throughput profiling of circulating metabolites | Identification of mediating biomarkers in diet-disease relationships [53] |
| Causal Diagram Software (DAGitty) | Browser-based environment for creating and analyzing causal diagrams | Identification of appropriate covariate adjustment sets; minimization of bias [55] |
| Statistical Software Packages (R, Stata) | Implementation of specialized causal inference methods | Mendelian randomization, mediation analysis, propensity score methods |
| GBD Data Exchange (GHDx) | Repository of global burden of disease data | Population-level assessment of diet-related disease burden [38] |
The progression from association to causation in nutritional epidemiology requires meticulous application of causal inference frameworks, with each method contributing unique strengths for addressing specific methodological challenges. Directed Acyclic Graphs provide formal frameworks for articulating and testing causal assumptions, while Mendelian randomization approaches leverage genetic instruments to reduce confounding. Multivariable extensions and causal mediation analyses enable researchers to decompose complex pathways linking dietary patterns to chronic disease outcomes through biological mediators.
The consistent evidence from large prospective cohorts demonstrating substantial risk reductions for major chronic diseases and enhanced odds of healthy aging with adherence to healthy dietary patterns—particularly those emphasizing plant-based foods, with moderate inclusion of healthy animal-based foods—provides a strong evidentiary base for dietary guidance [33] [12]. Future research should continue to refine causal inference methods, with particular attention to addressing pleiotropy in genetic studies, integrating multi-omics data to elucidate biological mechanisms, and accounting for complex temporal relationships between dietary exposures and health outcomes across the life course.
Navigating Complexities: From Food-Drug Interactions to Research Pitfalls
Pharmacokinetic food-drug interactions represent a critical area of study in clinical pharmacology and drug development, significantly influencing the therapeutic efficacy and safety profile of numerous medications. Within this domain, the cytochrome P450 (CYP450) enzyme system serves as the primary catalyst for the oxidative biotransformation of an estimated 70-80% of all clinically used drugs [56]. These enzymes constitute a superfamily of hemoproteins that are predominantly expressed in hepatocytes and enterocytes, positioning them as a fundamental determinant of first-pass metabolism and oral drug bioavailability [56]. The interaction between dietary constituents and CYP enzymes can precipitate clinically significant alterations in drug plasma concentrations, potentially leading to subtherapeutic outcomes or dose-dependent adverse events.
Understanding these interactions is particularly relevant within the broader context of dietary patterns and chronic disease risk mechanisms. Modern dietary practices incorporate an increasingly diverse array of bioactive compounds from edible plants, herbal supplements, and processed foods, many of which possess the capacity to modulate metabolic enzyme activity [57]. The mechanisms underpinning these interactions are multifaceted, involving direct enzyme inhibition, induction of gene expression, and complex nutrient-nutrient interactions that collectively determine the net effect on drug disposition. This review synthesizes current evidence on food-mediated modulation of CYP450 function, with particular emphasis on quantitative assessment of interaction magnitude, elucidation of underlying molecular mechanisms, and implications for personalized therapeutic approaches in diverse patient populations.
Enzyme Classification and Genetic Architecture
The cytochrome P450 system encompasses a diverse superfamily of monooxygenase enzymes characterized by the presence of a heme-iron center that catalyzes the insertion of one oxygen atom from molecular oxygen into relatively inert substrate molecules [56]. This superfamily is organized into families and subfamilies based on amino acid sequence homology, with the CYP1, CYP2, and CYP3 families representing the primary mediators of xenobiotic metabolism in humans [56]. The human genome encodes 57 functional CYP genes distributed across 18 families and 44 subfamilies, giving rise to more than 50 distinct isoenzymes with varying substrate specificities and regulatory mechanisms [56].
The most pharmacologically significant CYP isoforms include CYP3A4/5, CYP2D6, CYP2C9, CYP2C19, and CYP1A2, which collectively account for the majority of phase I drug metabolism [56]. These enzymes demonstrate considerable genetic polymorphism, particularly CYP2D6 and CYP2C19, contributing to well-characterized interindividual variability in drug response. However, genetic variation alone cannot explain the extensive population-level heterogeneity observed in drug metabolism, highlighting the importance of extrinsic factors such as dietary components that can modulate enzyme activity through inhibition, induction, or mechanism-based inactivation.
Tissue Distribution and Physiological Role
While CYP450 enzymes are ubiquitously expressed throughout the body, their highest concentration and metabolic capacity reside in hepatocytes, with secondary significant expression in intestinal epithelial cells [56]. This anatomical distribution establishes sequential metabolic barriers that collectively determine the systemic bioavailability of orally administered drugs. Hepatic CYP enzymes constitute the dominant site of drug clearance for most therapeutics, while intestinal CYP3A4 contributes significantly to presystemic extraction, often exceeding 50% for certain substrates [56].
The fundamental reaction catalyzed by CYP enzymes involves monooxygenation, typically incorporating a single oxygen atom into the substrate molecule while reducing the second oxygen atom to water via NADPH-cytochrome P450 reductase [56]. This process generally increases substrate hydrophilicity, facilitating subsequent phase II conjugation and eventual biliary or renal elimination. Beyond their role in xenobiotic detoxification, select CYP isoforms participate in critical endogenous metabolic pathways, including steroidogenesis, bile acid biosynthesis, and vitamin D activation, establishing this enzyme system as a crucial interface between metabolism and homeostasis.
Food-Drug Interactions: Mechanisms and Clinical Consequences
Direct Enzyme Inhibition
The most rapid and mechanistically straightforward food-drug interactions involve direct inhibition of CYP enzymes by dietary constituents. This process typically occurs through competitive or non-competitive binding at the enzyme's active site, immediately reducing metabolic capacity for co-administered drug substrates. The clinical manifestations are most pronounced for drugs with narrow therapeutic indices, where even modest alterations in clearance can precipitate toxicity or therapeutic failure.
Table 1: Dietary Inhibitors of Major CYP Enzymes and Affected Drug Substrates
| CYP Enzyme | Dietary Inhibitor | Source | Affected Drug Substrates | Magnitude of Interaction |
|---|---|---|---|---|
| CYP3A4 | Bergamottin, Dihydroxybergamottin | Grapefruit, Seville orange, Pomelo | Felodipine, Simvastatin, Cyclosporine, Carbamazepine | ↑ AUC 1.5-3.0 fold [56] |
| CYP3A4 | Ellagitannins, Anthocyanins | Pomegranate, Cranberry | Tolbutamide, Warfarin | ↑ AUC 1.3-1.8 fold [56] |
| CYP1A2 | Flavonoids (Apigenin, Luteolin) | Chamomile tea, Celery, Parsley | Theophylline, Caffeine, Clozapine | ↑ AUC 1.2-1.5 fold [57] |
| CYP2C9 | Sulfur compounds | Garlic, Onion | Warfarin, Phenytoin, NSAIDs | ↑ AUC 1.3-1.7 fold [57] |
| CYP2D6 | Flavonoids (Quercetin, Naringenin) | Grapefruit, St. John's Wort | Codeine, Tramadol, Tricyclic antidepressants | Mild to moderate inhibition [57] |
Grapefruit juice represents the most extensively characterized example of dietary CYP inhibition, with documented interactions involving more than 85 medications [56]. The furanocoumarins bergamottin and 6',7'-dihydroxybergamottin irreversibly inactivate CYP3A4 through mechanism-based inhibition, forming covalent adducts with the enzyme's apoprotein that effectively reduce intestinal CYP3A4 content by up to 70% for 24-72 hours post-ingestion [56]. This interaction demonstrates distinctive dose-dependency and interindividual variability based on baseline CYP3A4 expression, with the greatest relative impact observed in individuals with high intrinsic CYP3A4 activity.
Enzyme Induction and Transcriptional Upregulation
In contrast to acute inhibition, certain dietary components can enhance drug metabolism through induction of CYP gene expression. This process typically involves activation of nuclear receptors such as pregnane X receptor (PXR), constitutive androstane receptor (CAR), or aryl hydrocarbon receptor (AhR), leading to increased transcription of target CYP genes and subsequent enzyme synthesis. The temporal course of induction is characteristically delayed, requiring several days to reach maximal effect and persisting for a similar duration following discontinuation of the inducing agent.
Table 2: Dietary Inducers of Cytochrome P450 Enzymes
| Dietary Inducer | Nuclear Receptor | CYP Enzymes Induced | Representative Affected Drugs | Time Course |
|---|---|---|---|---|
| Hyperforin (St. John's Wort) | PXR | CYP3A4, CYP2C9 | Cyclosporine, Irinotecan, Warfarin | 7-14 days [56] |
| Polycyclic Aromatic Hydrocarbons (Grilled Meat) | AhR | CYP1A1, CYP1A2, CYP1B1 | Theophylline, Olanzapine | Days [56] |
| Isothiocyanates (Cruciferous Vegetables) | AhR, Nrf2 | CYP1A1, CYP1A2 | Clozapine, Fluvoxamine | Days to weeks [57] |
| Resveratrol (Red Grapes, Peanuts) | PXR, CAR | CYP3A4, CYP2C9 | Calcium channel blockers, Statins | Days [57] |
| Capsaicin (Chili Peppers) | PXR, CAR | CYP3A4, CYP2C9 | Saquinavir, Verapamil | Days [58] |
St. John's Wort (Hypericum perforatum) exemplifies clinically significant CYP induction, with hyperforin activating PXR at concentrations achievable through standard supplementation [56]. This interaction reduces the systemic exposure of numerous drugs, including a 40-60% decrease in cyclosporine AUC that has resulted in documented organ transplant rejection [56]. Similarly, polycyclic aromatic hydrocarbons formed during high-temperature cooking of meat products activate the AhR pathway, potentially accelerating the metabolism of CYP1A2 substrates such as theophylline and clozapine [56]. The magnitude of induction varies substantially based on genetic polymorphisms in both the nuclear receptors and target CYP genes, dietary preparation methods, and concomitant exposure to other inducing agents.
Transport Protein Interactions
Beyond direct effects on metabolic enzymes, numerous dietary components modulate drug transporter function, particularly P-glycoprotein (P-gp) and multidrug resistance-associated proteins (MRPs) that govern drug absorption and elimination. These transporters frequently exhibit overlapping substrate specificity with CYP3A4, creating complementary barriers to drug bioavailability that can be simultaneously modulated by dietary constituents.
Table 3: Effects of Dietary Components on Drug Transport Proteins
| Dietary Component | Transport Protein | Effect | Experimental Model | Clinical Consequence |
|---|---|---|---|---|
| Piperine (Black Pepper) | P-gp | Inhibition | LS-180V cells [58] | ↑ Bioavailability of digoxin, fexofenadine |
| Capsaicin (Chili Peppers) | P-gp, MRP1, MRP3 | Inhibition & Increased mRNA expression | LS-180V cells [58] | Altered chemotherapeutic drug disposition |
| Genistein, Daidzein (Soy) | P-gp | Stimulation | LS-180V cells [58] | ↓ Bioavailability of P-gp substrates |
| Curcumin (Turmeric) | P-gp | Complex modulation | LS-180V cells [58] | Variable effects on chemotherapeutic agents |
| Sesamin (Sesame) | P-gp, MRP1 | Inhibition & Increased mRNA expression | LS-180V cells [58] | Potential ↑ drug absorption |
Experimental evidence from vinblastine-resistant human colon carcinoma cells (LS-180V cells) demonstrates that piperine, capsaicin, and sesamin significantly inhibit P-gp-mediated efflux, increasing intracellular accumulation of fluorescent P-gp substrates such as rhodamine 123 [58]. Conversely, the soy isoflavones genistein and daidzein stimulate P-gp-mediated efflux, potentially reducing the oral bioavailability of concomitant medications [58]. Interestingly, chronic exposure (48-hour pretreatment) to sesamin significantly increased MDR1 mRNA expression without corresponding changes in P-gp protein levels or function, suggesting complex transcriptional and post-transcriptional regulation [58]. Similar pretreatment with capsaicin, daidzein, and piperine significantly increased mRNA levels of MRP1 and MRP3, highlighting the potential for dietary components to modulate multiple transport pathways simultaneously [58].
Experimental Methodologies for Investigating Food-Drug Interactions
In Vitro Approaches
Table 4: Experimental Models for Assessing Food-Drug Interactions
| Methodology | Key Components | Applications | Advantages | Limitations |
|---|---|---|---|---|
| Human liver microsomes | CYP enzymes, NADPH regeneration system | Metabolic stability, Reaction phenotyping, Enzyme inhibition kinetics | Maintain native enzyme conformation and partnerships | Lacks cellular context and transporter interplay |
| Recombinant CYP enzymes | Individual CYP isoforms, Cytochrome P450 reductase, Cytochrome b5 | Enzyme-specific metabolic activity, Inhibition screening | High specificity for individual CYP isoforms | Non-physiological enzyme ratios and environment |
| Primary human hepatocytes | Functional CYP enzymes, Uptake/efflux transporters, Nuclear receptors | Enzyme induction potential, Integrated metabolism and transport | Maintain physiological enzyme and transporter interplay | Limited availability, Donor variability, Rapid dedifferentiation |
| Caco-2 cell monolayers | Differentiated enterocytes, Apical and basolateral compartments, Expressed transporters | Intestinal absorption, Transporter inhibition, First-pass metabolism prediction | Model of intestinal barrier with functional efflux transporters | Lack of mucus layer, Variable expression of metabolic enzymes |
| LS-180V cells (Vinblastine-resistant colon carcinoma) | Overexpressed P-gp, MRP transporters | Transporter inhibition assays, Transcriptional regulation studies | Specific model for P-gp and MRP interactions | Cancer cell line with abnormal regulatory mechanisms |
In vitro characterization typically begins with enzyme-based screening systems to identify direct inhibition. Human liver microsomes or recombinant CYP enzymes are incubated with prototype substrate probes, specific inhibitory metabolites, and appropriate cofactors. Reaction velocity is measured via liquid chromatography-tandem mass spectrometry (LC-MS/MS) detection of metabolite formation, with IC50 or Ki values calculated from concentration-response relationships [58]. Mechanism-based inactivation is distinguished from reversible inhibition through time- and NADPH-dependent loss of enzyme activity, with kinact and KI parameters derived from these analyses.
For induction assessment, freshly isolated or cryopreserved primary human hepatocytes represent the gold standard model, as they maintain functional expression of nuclear receptors and responsive CYP genes. Cells are exposed to test compounds for 48-72 hours, with mRNA quantification by RT-qPCR and corresponding enzyme activity measurements using selective metabolic probes [58]. The LS-180V cell line, a vinblastine-resistant human colon carcinoma subline, provides a specialized model for investigating P-gp and MRP interactions, allowing simultaneous assessment of transporter function and mRNA expression in response to dietary components [58].
In Vivo and Clinical Evaluation
Clinical investigation of food-drug interactions follows standardized protocols, typically employing randomized, crossover designs in healthy volunteers. Participants receive a single dose of a probe drug (e.g., midazolam for CYP3A4, caffeine for CYP1A2) following administration of the dietary component of interest versus control condition, with intensive blood sampling over the drug's elimination phase. Primary pharmacokinetic parameters include area under the concentration-time curve (AUC), maximum plasma concentration (Cmax), time to Cmax (Tmax), and elimination half-life (t1/2).
The FDA guidance categorizes food effects based on the magnitude of change in these parameters, with a >20% difference in AUC or Cmax generally considered clinically relevant. Special consideration is given to the physical properties of food, including volume, viscosity, pH, and temperature, which can independently alter gastrointestinal physiology and drug absorption kinetics [59]. Emerging approaches incorporate physiologically based pharmacokinetic (PBPK) modeling to integrate in vitro data and predict clinical interaction magnitude, potentially reducing the need for extensive clinical trials [59].
Research Reagent Solutions for Food-Drug Interaction Studies
Table 5: Essential Research Reagents for Food-Drug Interaction Investigations
| Reagent/Cell Line | Manufacturer/ Source | Primary Application | Key Features |
|---|---|---|---|
| Human liver microsomes | Corning Life Sciences, XenoTech LLC | CYP inhibition and metabolic stability studies | Pooled from multiple donors, Characterized CYP activities |
| Cryopreserved human hepatocytes | BioIVT, Lonza | CYP induction and transporter studies | Viable cells retaining metabolic competence and transporter function |
| Caco-2 cell line | ATCC HTB-37 | Intestinal permeability and efflux transport | Forms polarized monolayers with functional P-gp expression |
| LS-180V cell line | Japanese Collection of Research Bioresources Cell Bank | P-gp and MRP transporter assays | Vinblastine-selected with high P-gp and MRP expression [58] |
| P450-Glo CYP450 Assays | Promega Corporation | High-throughput CYP inhibition screening | Luminescent substrates for major CYP isoforms |
| BD BioCoat CYP Induction System | Corning Life Sciences | Standardized CYP induction assessment | Optimized plating and induction protocols |
| Transwell Permeability Supports | Corning Incorporated | Caco-2 and similar transport studies | Polycarbonate membranes for monolayer formation |
Signaling Pathways in CYP450 Regulation by Dietary Components
The molecular pathways through which dietary components modulate CYP450 expression primarily involve ligand-activated nuclear receptors that function as transcription factors. As illustrated in the diagram above, lipophilic dietary compounds capable of crossing plasma membranes bind to and activate nuclear receptors such as PXR, CAR, or AhR in the hepatocyte cytoplasm or nucleus [56]. Following ligand binding, these receptors heterodimerize with retinoid X receptor (RXR) and translocate to the nucleus, where they bind specific response elements (e.g., phenobarbital-responsive enhancer module [PBREM] for CAR, xenobiotic-responsive element [XRE] for AhR) in the promoter regions of target CYP genes [56]. This binding recruits coactivator complexes that initiate chromatin remodeling and assembly of the transcriptional machinery, ultimately increasing CYP mRNA and protein synthesis.
The time course of enzyme induction reflects this multi-step process, with detectable mRNA increases typically occurring within 4-8 hours and maximal protein expression requiring 48-72 hours of continuous exposure [56]. The corresponding increase in metabolic capacity develops proportionally, potentially resulting in significantly enhanced drug clearance that may persist for several days after discontinuation of the inducing agent due to the relatively slow turnover of CYP proteins.
The intricate interplay between dietary components and the cytochrome P450 system represents a formidable challenge in predicting drug response and optimizing therapeutic outcomes. The substantial interindividual variability in the magnitude of these interactions reflects the complex interplay between genetic determinants, environmental exposures, and dietary patterns. As global dietary practices continue to evolve and incorporate novel bioactive compounds, the potential for previously unrecognized food-drug interactions will correspondingly increase.
Future research directions should prioritize the development of integrated models that incorporate quantitative prediction of food-drug interactions based on dietary composition, cooking methods, and consumption patterns. The application of physiologically based pharmacokinetic modeling, coupled with enhanced understanding of transporter-enzyme interplay, promises to improve the extrapolation of in vitro data to clinical outcomes [59]. Additionally, personalized nutrition approaches that account for genetic polymorphisms in both metabolic enzymes and nuclear receptors may eventually enable tailored dietary recommendations for patients receiving critical medications with narrow therapeutic indices.
From a public health perspective, increased awareness of clinically significant food-drug interactions among healthcare providers and patients remains essential for preventing adverse events. Particular attention should be directed toward vulnerable populations, including the elderly, those with polypharmacy, and individuals with specific dietary practices that involve regular consumption of potent CYP modulators. Through continued mechanistic research and translational application of findings, the systematic understanding of food-drug interactions will contribute substantially to the broader goals of personalized medicine and chronic disease risk mitigation.
Nutritional research stands as a critical field for public health policy development, particularly in understanding the relationship between dietary patterns and chronic disease risk mechanisms. Despite its importance, the discipline faces a triad of fundamental methodological challenges that threaten the validity and utility of its findings: confounding, bias, and reproducibility issues. Recent analyses reveal that nutritional epidemiology relies heavily on "relatively weak methods including simple observational designs and substandard measurements," despite low internal validity and other sources of bias [60]. The field has been characterized by some critics in extreme terms, with questions raised about its very validity, while others defend current practices, creating a contentious scientific landscape [60]. This methodological crisis has tangible consequences; for instance, a 2024 evaluation of systematic reviews used to inform the Dietary Guidelines for Americans found "critical methodological weaknesses," with all included reviews judged to be of "critically low quality" [61]. Within the context of dietary patterns and chronic disease risk research, these challenges become particularly pronounced due to the complex, multifactorial nature of both exposures and outcomes, the long latency periods of disease development, and the intricate biological pathways involved. This technical guide examines these core challenges through a rigorous methodological lens, providing researchers with frameworks to strengthen study design, measurement, and analysis in nutrition science.
Core Methodological Challenges in Nutrition Research
Confounding: Untangling Causal Pathways
Confounding represents a fundamental challenge in nutritional epidemiology, where external variables distort the true relationship between dietary exposures and health outcomes. The complex interplay between diet, lifestyle, socioeconomic factors, and genetics creates a web of potential confounders that can generate spurious associations or mask true effects. In observational studies of dietary patterns and chronic disease, key confounders include socioeconomic status (SES), educational attainment, health consciousness, access to healthcare, and environmental factors—all of which correlate with both dietary choices and health outcomes [12] [60]. For example, in studies examining the Mediterranean diet and healthy aging, participants in the highest adherence quintile were "more likely to have a higher SES, use multivitamins, have a higher level of physical activity and slightly lower body mass index (BMI); they were also less likely to have a history of depression compared to the lowest quintile" [12]. These systematic differences introduce confounding that must be addressed through methodological and statistical approaches.
Table 1: Common Confounders in Dietary Patterns and Chronic Disease Research
| Confounder Category | Specific Variables | Chronic Disease Applications | Adjustment Methods |
|---|---|---|---|
| Socioeconomic Factors | Income, education, occupation, food security | All chronic diseases | Stratification, multivariate adjustment, propensity scoring |
| Lifestyle Factors | Physical activity, smoking status, alcohol consumption, sleep patterns | Cardiovascular disease, diabetes, cancer | Multivariate models, restriction, regression calibration |
| Psychological Factors | Depression, stress, cognitive function | Mental health disorders, cognitive decline | Measurement and adjustment, sensitivity analyses |
| Environmental Factors | Food accessibility, neighborhood characteristics, environmental toxins | Obesity, metabolic syndrome, inflammation | Multilevel modeling, geographic adjustment |
| Genetic Predisposition | Polygenic risk scores, family history | All chronic diseases with genetic components | Family-based designs, genomic control |
Traditional adjustment methods often prove insufficient for several reasons: residual confounding persists when confounders are measured imperfectly; over-adjustment occurs when intermediate variables on the causal pathway are controlled for; and many unknown confounders remain unmeasured [60]. The limitations of conventional approaches are exemplified in large cohort studies where "cohort studies were noted to be more prone to residual confounding, and the variables included in the statistical models had significant consequences for the direction and magnitude of associations estimated" [62]. Furthermore, nutritional research faces the challenge of "over-adjustment or failure to recognize unrecoverable selection bias" when constructing statistical models [62].
Bias: Systemic Distortions in Nutritional Evidence
Bias permeates multiple stages of nutritional research, from initial study conception through final interpretation and dissemination. Unlike random error, bias introduces systematic distortions that can persistently mislead scientific understanding. A critical yet underrecognized form is "investigator bias," defined as "acts of omission or commission that arise from ignorance, hubris or excessive attachment to beliefs" [62]. This bias influences what research questions are pursued, how hypotheses are tested, and how results are interpreted and disseminated. Ernst and Canter further define it as "bias resulting from a conflict of interest arising from passionate beliefs held by the investigators," which extends beyond financial conflicts to include deeply held theoretical or personal commitments to specific nutritional paradigms [62].
Table 2: Major Bias Categories in Nutritional Research
| Bias Type | Definition | Impact on Evidence | Remedial Approaches |
|---|---|---|---|
| Investigator Bias | Bias from investigators' passionate beliefs or conflicts beyond financial | Shapes research questions, methods, interpretation, dissemination | Blind data analysis, protocol registration, adversarial collaboration |
| Measurement Error | Non-differential or differential error in exposure assessment | Attenuates true effect sizes or introduces directional bias | Biomarkers, recovery biomarkers, measurement error models |
| Selection Bias | Systematic differences between participants and target population | Compromises external validity, introduces confounding | Incident vs. prevalent designs, careful recruitment, weighting methods |
| Recall Bias | Differential accuracy in dietary recall by case status | Distorts exposure-disease associations in case-control studies | Prospective designs, memory aids, biomarker calibration |
| Publication Bias | Selective publication of statistically significant results | Overestimates true effect sizes in meta-analyses | Prospective registration, gray literature searches, statistical corrections |
Measurement error represents a particularly pernicious form of bias in nutritional research. The field relies heavily on self-reported dietary data through food frequency questionnaires, 24-hour recalls, and food records, all of which contain substantial measurement error [63]. These errors are typically "non-differential," meaning they are independent of the outcome, which generally attenuates effect estimates toward the null and reduces statistical power [63]. The basic measurement error model can be represented as:
$$X^* = \alpha0 + \alphaX X + e$$
Where $X^*$ is the measured exposure, $X$ is the true exposure, $\alpha0$ represents location bias, $\alphaX$ represents scale bias, and $e$ represents random error [63]. In nutritional epidemiology, this error structure becomes increasingly complex when examining dietary patterns rather than single nutrients, as patterns represent multidimensional exposures with correlated components.
Additional biases emerge throughout the research process. Investigator bias can manifest as "asking questions no one wants or needs answers for," including "retesting globally well-proven hypotheses" without clear justification or pursuing research with minimal practical implications [62]. Selection bias occurs when study participants differ systematically from the target population, compromising external validity. Publication bias favors the dissemination of statistically significant or "positive" findings, creating distorted evidence landscapes that overestimate true effects.
Reproducibility and Transparency Deficits
The reproducibility crisis affecting many scientific disciplines has particularly pronounced manifestations in nutritional research. Recent evaluations of systematic reviews conducted to inform dietary guidelines reveal critical weaknesses in methodological quality and reporting transparency. A 2024 assessment of Nutrition Evidence Systematic Review (NESR) team products used for the Dietary Guidelines for Americans identified "critical methodological weaknesses," with all included systematic reviews judged to be of "critically low quality" according to AMSTAR 2 criteria [61]. The evaluation found that only 74% of PRISMA 2020 checklist items and 63% of PRISMA-S (search extension) checklist items were satisfactorily fulfilled [61]. When reproduction was attempted, researchers "could not reproduce searches within a 10% margin of the original results," indicating substantial reproducibility deficits in core evidence synthesis products that inform national nutrition policy [61].
The landscape of randomized controlled trials (RCTs) in nutrition reveals similar transparency concerns. A metaresearch analysis of 1,068 nutrition- and diet-related RCT protocols published between 2012-2022 found that while protocol publication is increasing, "the support and mention of relevant reporting guidelines by journals and researchers, respectively, remain far from ideal" [64]. Only 32.1% of protocols mentioned SPIRIT (Standard Protocol Items: Recommendations for Interventional Trials), 27.8% mentioned CONSORT, and a mere 1.9% mentioned TIDieR (Template for Intervention Description and Replication) [64]. This lack of adherence to reporting guidelines compromises the transparency, reproducibility, and utility of nutrition RCTs.
Advanced Methodological Approaches
Strengthening Study Designs Beyond Ordinary Association Tests
Moving beyond simple observational designs represents the most promising pathway toward more reliable nutritional epidemiology. The heavy reliance on Ordinary Association Tests (OATs)—defined as "observational studies on samples of individuals in which the sole or primary means of controlling for potential confounding factors is inclusion of measures of some potential confounding factors as covariates in statistical models"—has been identified as a fundamental limitation [60]. While OATs have utility for hypothesis generation, they constitute poor tests of causal hypotheses. Several design approaches can strengthen causal inference in nutritional research:
Negative Control Exposure Studies: This design uses "control" exposures that share similar confounding structures with the primary exposure but have no plausible biological effect on the outcome. For example, when studying sugar-sweetened beverage consumption and diabetes risk, an artificial sweetener exposure group might serve as a negative control under certain assumptions. Discrepancies between primary and negative control analyses reveal residual confounding.
Within-Person Studies: Leveraging repeated measurements within individuals over time, such as N-of-1 trials or crossover designs, effectively controls for all time-invariant confounding characteristics. This approach is particularly valuable for studying short-term effects of dietary interventions on biomarkers, though it requires careful consideration of carryover effects and period effects.
Instrumental Variable Methods: This approach uses a variable (the instrument) that influences exposure but is independent of confounders. Mendelian randomization represents a prominent application in nutritional epidemiology, using genetic variants as instruments to strengthen causal inference about nutrition-disease relationships.
Regression Discontinuity Designs: These exploit arbitrary thresholds in assignment mechanisms to create quasi-experimental variation. For example, studying health outcomes in populations just above versus just below eligibility cutoffs for nutrition assistance programs can provide less confounded effect estimates.
Enhanced Measurement and Analytical Techniques
Addressing measurement error requires sophisticated approaches beyond conventional statistical adjustment. Recovery biomarkers represent the gold standard for addressing measurement error in nutritional epidemiology, allowing for quantitative assessment of intake for certain nutrients and foods. Doubly labeled water for energy intake and 24-hour urinary sodium, potassium, and nitrogen for sodium, potassium, and protein intakes, respectively, provide objective measures that can be used to calibrate self-reported data [63]. The resulting measurement error models enable correction for systematic and random errors in dietary assessment.
Measurement error correction methods include:
Regression Calibration: This method uses a calibration study to estimate the relationship between true intake and reported intake, then uses this relationship to adjust relative risk estimates in the main study. This approach requires that the error in the main study and calibration study is the same and requires careful consideration of transportability between populations.
Multiple Imputation: This approach treats true intake as missing data and uses multiple imputation methods to generate plausible values based on biomarker data and other correlates.
Method of Moments: This statistical approach uses the moments of the observed data to estimate the parameters of the measurement error model and adjust effect estimates accordingly.
Beyond measurement error, analytical approaches to address confounding have evolved substantially. Directed acyclic graphs (DAGs) provide formal frameworks for identifying minimal sufficient adjustment sets and avoiding over-adjustment bias. Quantitative bias analysis enables researchers to quantify how strong an unmeasured confounder would need to be to explain away an observed association. Machine learning approaches can help identify complex nonlinear confounding patterns without strong parametric assumptions, though they require careful implementation to avoid overfitting.
Protocols for Reproducible Nutrition Science
Establishing rigorous, predefined protocols represents a cornerstone for enhancing reproducibility in nutritional research. Protocol registration and publication mitigate investigator bias and selective reporting while promoting methodological transparency. The SPIRIT (Standard Protocol Items: Recommendations for Interventional Trials) and TIDieR (Template for Intervention Description and Replication) guidelines provide structured frameworks for comprehensive protocol development [64]. For systematic reviews, PROSPERO registration and adherence to PRISMA-P (Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols) ensure methodological rigor and transparency.
Key elements of reproducible nutrition research protocols include:
Pre-specified Analysis Plans: Detailed statistical analysis plans (SAPs) that define primary and secondary outcomes, covariate selection criteria, missing data handling, and sensitivity analyses before data analysis begins. These plans prevent p-hacking and selective reporting of statistically significant results.
Blinded Data Analysis: Implementing procedures where investigators remain unaware of exposure or outcome status during data cleaning, variable transformation, and model development phases. This approach reduces conscious and unconscious manipulation of analytical decisions to produce desired results.
Comprehensive Search Strategies: For evidence syntheses, detailed documentation of search strategies across multiple databases with explicit inclusion/exclusion criteria enables reproducibility. The PRISMA-S (Search) extension provides specific guidance for transparent reporting of literature searches [61].
Data and Code Sharing: Making deidentified data and analytical code publicly available facilitates independent verification of findings and enables meta-analytical approaches.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Methodological Tools for Robust Nutritional Epidemiology
| Tool Category | Specific Tools/Techniques | Primary Function | Application Context |
|---|---|---|---|
| Measurement Error Correction | Recovery biomarkers (doubly labeled water, 24h urine), concentration biomarkers | Quantify and correct for systematic and random measurement error | All observational studies using self-reported diet |
| Causal Inference Methods | Mendelian randomization, propensity score methods, marginal structural models | Strengthen causal inference given unmeasured confounding | Etiological research on diet-disease relationships |
| Study Design Templates | N-of-1 trials, crossover designs, pragmatic trials | Control for between-person confounding through design rather than analysis | Intervention studies, personalized nutrition |
| Reporting Guidelines | SPIRIT, CONSORT, TIDieR, PRISMA, STROBE | Ensure comprehensive and transparent research reporting | All study protocols, manuscripts, systematic reviews |
| Data Analysis Frameworks | Directed acyclic graphs (DAGs), multiple imputation, quantitative bias analysis | Identify sufficient adjustment sets, handle missing data, quantify bias | Statistical analysis planning and interpretation |
| Laboratory Biomarkers | Metabolomic profiles, inflammatory markers, oxidative stress measures | Objective assessment of biological pathways and intermediate outcomes | Mechanistic studies, intervention efficacy assessment |
The challenges of confounding, bias, and reproducibility in nutritional research are substantial but not insurmountable. Addressing these issues requires a fundamental shift from reliance on simple observational designs with ordinary association tests toward more methodologically sophisticated approaches that strengthen causal inference. The field must move beyond defense of the status quo and embrace constructive criticism and methodological innovation. As one analysis concludes, "Changing the status quo will require ongoing, unflinching scrutiny of research questions, practices, and reporting—and a willingness to admit that 'good enough' is no longer good enough" [60]. This evolution is particularly critical for research on dietary patterns and chronic disease risk mechanisms, where public health implications are substantial. By implementing strengthened designs, improved measurement, robust analytical techniques, and enhanced transparency practices, nutritional epidemiology can overcome its current methodological challenges and provide more reliable evidence to inform both clinical practice and public policy.
The one-diet-fits-all paradigm is increasingly inadequate for addressing the global burden of chronic diseases. This whitepaper examines the complex interplay between genetic factors, gut microbiome composition, and socioeconomic determinants that modulate individual responses to diet and chronic disease risk. We synthesize evidence from nutrigenetic, microbiomic, and population-level studies to elucidate mechanisms underlying variable disease susceptibility and propose a framework for integrating multi-omic data with socioeconomic considerations in nutrition research. Experimental protocols for assessing gene-nutrient interactions, microbiome assemblage, and social determinants of health are detailed alongside visualization of key biological pathways. The findings underscore that equitable implementation of personalized nutrition requires addressing structural barriers to health alongside biological heterogeneity.
Chronic diseases represent the primary cause of global morbidity and mortality, with approximately 90% of the $4.1 trillion annual U.S. healthcare expenditure attributed to their management and treatment [65]. Traditional nutritional epidemiology has established broad associations between dietary patterns and disease risk, but these population-level recommendations fail to account for significant interindividual variation in response to dietary interventions [66]. The transition to personalized nutrition is driven by understanding that individuals respond differently to nutrients based on their unique genetic makeup, gut microbiome composition, and life circumstances [67].
The conceptual framework for personalized nutrition rests on the principle that chronic disease phenotypes emerge from complex interactions between genetic susceptibility, environmental exposures, and social determinants [68]. This relationship can be represented as: Genotype + Environment + (Genotype × Environment) = Metabolic Phenotype [68]. The environment includes not only dietary exposures but also socioeconomic factors that constrain food choices and access to healthcare [69] [65]. Advancements in multi-omic technologies have enabled precise characterization of these interactions, revealing mechanisms through which nutrients influence gene expression, protein synthesis, and metabolic processes [68].
This technical guide examines the biological mechanisms through which genetic and microbiome diversity modulate dietary response and disease risk, while addressing how socioeconomic factors create structural barriers to implementing equitable personalized nutrition strategies. By integrating experimental approaches from nutrigenetics, microbiomics, and social epidemiology, we provide a comprehensive framework for advancing research on dietary patterns and chronic disease risk mechanisms.
Genetic Diversity in Nutrient Response
Fundamental Principles of Nutrigenetics
Nutrigenetics examines how specific genetic variants, particularly single nucleotide polymorphisms (SNPs), modulate individual responses to dietary components and influence nutrient requirements [70]. These genetic variations can affect the metabolism of lipids, carbohydrates, and micronutrients, creating differential susceptibility to nutrition-related diseases even with identical dietary intake [70]. More than 600 genes and DNA regions have been associated with human obesity through genome-wide association studies (GWAS), revealing the polygenic nature of most chronic disease risk [68].
Table 1: Key Genetic Variants Influencing Response to Dietary Components
| Gene | Polymorphism | Nutrient Interaction | Physiological Effect | Chronic Disease Association |
|---|---|---|---|---|
| FTO | rs9939609 | Energy intake | Increased obesity susceptibility | Type 2 diabetes, obesity [70] |
| TCF7L2 | rs7903146 | Wholegrain intake | Impaired glucose metabolism | Type 2 diabetes [70] |
| APOA2 | 2265T>C | Saturated fat intake | Increased BMI | Obesity, cardiovascular disease [70] |
| MC4R | rs17782313 | Mediterranean diet adherence | Modulated diabetes risk | Type 2 diabetes, obesity [70] |
| MTHFR | C677T | Folic acid supplementation | Altered homocysteine metabolism | Cardiovascular disease [70] |
| PPARG | Pro12Ala | Monounsaturated fat intake | Improved insulin sensitivity | Type 2 diabetes, metabolic syndrome [67] |
Experimental Protocols for Nutrigenetic Research
Protocol 1: Genotype-Guided Dietary Intervention Study
Participant Selection and Genotyping: Recruit approximately 500-1000 adults with prediabetes or metabolic syndrome. Collect buccal swabs or blood samples for DNA extraction. Genotype for key variants (FTO rs9939609, TCF7L2 rs7903146, APOA2 265T>C, MC4R rs17782313, PPARG Pro12Ala) using TaqMan SNP Genotyping Assays or genome-wide arrays.
Randomization and Intervention: Randomize participants to control (standard dietary advice) or genotype-guided group. For the genotype-guided group:
- FTO risk allele carriers: prescribe reduced energy diet (500 kcal deficit) with macronutrient distribution of 30% protein, 30% fat, 40% carbohydrate
- TCF7L2 risk allele carriers: implement low-glycemic index diet (<55 GI) with high fiber intake (>35g/day)
- PPARG Ala12 carriers: prescribe Mediterranean-style diet high in monounsaturated fats (20% of total energy)
Outcome Measures: Assess at baseline, 3, 6, and 12 months:
- Primary outcomes: fasting glucose, HbA1c, HOMA-IR, body weight
- Secondary outcomes: lipid profile, inflammatory markers (CRP, IL-6), adipokines
- Dietary adherence: 3-day food records and plasma fatty acid composition
Statistical Analysis: Use intention-to-treat analysis with linear mixed models to test genotype×diet interaction effects on metabolic outcomes, adjusting for age, sex, and baseline BMI.
Protocol 2: Cellular Models for Nutrient-Gene Interaction Studies
Cell Culture: Utilize human hepatocyte (HepG2) and adipocyte (3T3-L1) cell lines. Culture in DMEM with 10% FBS and 1% penicillin-streptomycin at 37°C with 5% CO₂.
Genetic Manipulation: Perform CRISPR/Cas9 editing to introduce risk variants (e.g., FTO rs9939609) in isogenic cell lines. Validate edits by Sanger sequencing and assess expression by qRT-PCR.
Nutrient Stimulation: Treat cells with:
- Physiological concentrations of fatty acids (palmitate, oleate) complexed to BSA
- Glucose gradients (5-25mM) to mimic normoglycemia to hyperglycemia
- Amino acid mixtures representing high vs. low protein diets
Outcome Measures:
- Gene expression: RNA-seq for transcriptomic profiling
- Metabolic phenotyping: Seahorse Analyzer for mitochondrial respiration
- Signaling pathways: Western blot for insulin signaling (p-AKT/AKT), mTOR pathway
- Lipid accumulation: Oil Red O staining and quantification
Figure 1: Nutrient-Gene Interactions Influencing Metabolic Phenotype. Genetic variants modulate transcriptional responses to nutrients, influencing metabolic pathways and chronic disease risk.
Gut Microbiome as a Modulator of Dietary Response
Microbiome Assembly and Dietary Programming
The gut microbiome undergoes dynamic development during early life, with diet playing a critical role in its assembly and function. The initial infant microbiota is primarily characterized by exposure to maternal stool during vaginal birth, establishing a foundation for microbial succession [71]. Human milk oligosaccharides (HMOs) from breast milk selectively promote Bifidobacterium species, which produce aromatic lactic acids that modulate immune development [71]. The "weaning reaction" period, marked by rapid diversification of the gut microbiome during introduction to solid foods, represents a critical window for immune development that has lifelong implications for disease susceptibility [71].
Dietary patterns throughout life continuously shape microbiome composition. Low-fiber diets reduce microbial diversity in a transgenerational manner, with effects becoming irreversibly established within two generations [71]. Highly processed foods, dairy desserts, and unhealthy meats promote gut species associated with elevated biomarkers for chronic diseases, whereas diverse plant-based diets support microbial profiles linked to reduced disease risk [72].
Table 2: Diet-Microbiome Interactions in Chronic Disease Pathogenesis
| Dietary Component | Microbial Changes | Metabolic Consequences | Disease Associations |
|---|---|---|---|
| Dietary Fiber | ↑ Faecalibacterium, ↑ A. muciniphila | ↑ SCFA production, improved insulin sensitivity | Reduced obesity, T2D risk [71] [67] |
| Human Milk Oligosaccharides | ↑ Bifidobacterium, ↑ Lactobacillus | Immune regulation, pathogen exclusion | Reduced allergy, asthma [71] |
| Low-Fiber Diet | ↓ Diversity, ↓ SCFA producers | Impaired gut barrier, inflammation | Obesity, inflammatory diseases [71] |
| Polyunsaturated Fats | ↑ Beneficial clusters | Reduced inflammation | Cardiovascular protection [72] |
| Processed Foods | ↑ Enterobacteriaceae | Increased endotoxemia, inflammation | Metabolic syndrome, T2D [72] |
Experimental Protocols for Microbiome Research
Protocol 1: Microbiota-Directed Complementary Food (MDCF) Intervention
Participant Recruitment: Enroll children (12-18 months) with moderate acute malnutrition. Exclude those with severe infections, congenital disorders, or antibiotic use within 4 weeks.
Baseline Assessment:
- Anthropometrics: weight-for-length z-score (WLZ), mid-upper arm circumference
- Microbiome: Fecal samples for 16S rRNA sequencing and metagenomics
- Plasma biomarkers: Inflammatory markers (CRP, IL-6), growth factors (IGF-1)
Intervention Formulation: Develop MDCFs containing specific blends of dietary fibers (e.g., chickpea, banana, peanut) optimized to promote growth-promoting microbiota.
Study Design: Randomized, controlled trial with 2-month intervention:
- Intervention group: MDCF (2 feedings/day)
- Control group: Ready-to-use therapeutic food (RUTF)
Outcome Measures:
- Primary: Change in WLZ
- Secondary: Microbiota composition, plasma proteome, growth factors
Analytical Methods:
- Microbiome: 16S rRNA sequencing (V4 region), QIIME2 pipeline
- Metabolomics: LC-MS for fecal and plasma metabolites
- Proteomics: LC-MS/MS for plasma proteins
Protocol 2: Gnotobiotic Mouse Models for Diet-Microbiome Interactions
Animal Models: Use germ-free (GF) C57BL/6 mice (8-10 weeks old). Maintain in flexible film isolators with autoclaved food, water, and bedding.
Microbial Transplantation:
- Prepare fecal slurries from human donors with contrasting diets (traditional high-fiber vs. Westernized)
- Administer via oral gavage (200μl/mouse) to GF recipients
- Include sham-treated GF controls
Dietary Interventions: After colonization, randomize to:
- High-fiber diet (15% diverse fibers)
- Low-fiber Western diet (5% cellulose)
- Customized fiber blends
Sample Collection:
- Weekly fecal samples for microbiome
- Serum for metabolomics (SCFAs, bile acids)
- Tissues post-sacrifice: liver, adipose, colon for transcriptomics
Host Phenotyping:
- Glucose tolerance test (week 4)
- Body composition (EchoMRI)
- Systemic inflammation (serum cytokines)
- Gut barrier function (FITC-dextran assay)
Figure 2: Diet-Microbiome-Immune Interactions in Chronic Disease. Dietary patterns shape gut microbiome composition and function, influencing host immunity and disease susceptibility through microbial metabolite production.
Socioeconomic Determinants of Dietary Patterns and Health Equity
Structural Barriers to Healthy Nutrition
Socioeconomic status (SES) creates significant disparities in chronic disease prevalence through multiple mechanisms. Research demonstrates that Zip Code Tabulation Areas (ZCTAs) with the highest chronic disease prevalence show significantly greater socioeconomic disadvantages, including lower household income, lower educational attainment, and higher uninsured rates [65]. These areas also face substantial barriers to healthcare access, including lower rates of car ownership and longer travel distances to medical facilities [65].
Behavioral factors, including diet quality, account for a substantial proportion of the association between neighborhood SES and health outcomes—77.4% for type 2 diabetes, 46.3% for major cardiovascular disease, and 42.8% for total mortality [69]. However, characterizing dietary behaviors as purely individual choices overlooks structural constraints. For populations with limited economic resources, affordability and convenient access often become the primary determinants of food selection rather than nutritional quality [65].
Table 3: Socioeconomic Determinants of Chronic Disease Risk
| Socioeconomic Factor | Association with Chronic Disease | Mechanistic Pathways | Intervention Implications |
|---|---|---|---|
| Educational Attainment | Less than high school education: 2x odds of diabetes [65] | Health literacy, employment opportunities, income | Community-based nutrition education programs |
| Household Income | Strong inverse correlation with multiple chronic conditions [65] | Food affordability, healthcare access, stress | Economic policies, SNAP enhancements |
| Neighborhood Resources | Longer distances to healthcare: higher disease prevalence [65] | Healthcare access, food environment, built environment | Mobile health clinics, telehealth expansion |
| Food Environment | Limited healthy food access: higher obesity rates [65] | Food deserts, food swamps, transportation barriers | Supermarket initiatives, farmers' markets |
| Health Insurance | Uninsured status: reduced preventive care [65] | Delayed diagnosis, medication adherence | Insurance expansion, safety-net programs |
Methodological Approaches for Socioeconomic Research
Protocol 1: Geospatial Analysis of Food Environment and Disease Prevalence
Data Collection:
- Chronic disease prevalence: CDC PLACES dataset (ZCTA-level)
- Socioeconomic data: American Community Survey (median income, poverty, education)
- Food environment: USDA Food Access Research Atlas (food deserts)
- Healthcare resources: AHA Survey (hospital services), CMS (FQHC locations)
Geospatial Mapping:
- Create composite chronic disease score (0-20) based on prevalence quartiles for 10 conditions
- Classify ZCTAs into low (≤6), moderate (7-13), and high (≥14) prevalence
- Perform hotspot analysis using Getis-Ord Gi* statistic to identify disease clusters
Statistical Analysis:
- Multilevel models examining ZCTA-level predictors of disease prevalence
- Path analysis to test mediators between SES and health outcomes
- Quantile regression to examine relationships across disease prevalence distribution
Equity Assessment:
- Calculate concentration indices for disease burden by SES
- Identify ZCTAs with both high poverty and high disease burden for targeted interventions
Protocol 2: Community-Engaged Intervention for Food Desert Zones
Community Partnership: Establish community advisory board with representation from residents, local organizations, and healthcare providers.
Mixed-Methods Assessment:
- Quantitative: Food environment audit using NEMS tool, health surveys
- Qualitative: Focus groups on food acquisition challenges, preferred solutions
Intervention Co-Design: Develop multifaceted approach including:
- Mobile produce market with SNAP/EBT acceptance
- Nutrition education programs tailored to local food preferences
- Community kitchen programs for cooking skills
Evaluation Framework:
- Primary outcomes: Fruit/vegetable consumption, food security status
- Secondary outcomes: Self-rated health, clinical biomarkers
- Process measures: Program participation, satisfaction, sustainability
Integration Framework and Research Applications
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Research Resources for Personalized Nutrition Studies
| Category | Specific Tools/Assays | Research Applications | Technical Considerations |
|---|---|---|---|
| Genomic Analysis | GWAS arrays (Illumina Global Screening Array), TaqMan SNP genotyping, Whole genome sequencing | Nutrigenetic discovery, genetic risk scores | Sample size requirements, multiple testing correction, population stratification |
| Microbiome Profiling | 16S rRNA sequencing (V4 region), Shotgun metagenomics, Metatranscriptomics | Microbial community structure, functional potential | Sampling stability, DNA extraction standardization, bioinformatic pipelines |
| Metabolomic Platforms | LC-MS (untargeted), GC-MS (SCFAs), NMR spectroscopy | Metabolic phenotyping, food intake biomarkers | Compound identification, quantification, batch effects |
| Digital Monitoring | Continuous glucose monitors, Mobile food recording apps, Wearable activity sensors | Real-time diet-response phenotyping | Data integration, participant burden, privacy considerations |
| Social Determinants | Area Deprivation Index, Food Environment Index, American Community Survey data | Socioeconomic contextual factors | Geographic scale, temporal alignment, multidimensional indices |
Multi-Omic Integration for Precision Nutrition
The most significant advances in personalized nutrition will come from integrating multiple data types to capture the complexity of gene-diet-environment interactions. Studies incorporating genotyping, microbiome sequencing, metabolomic profiling, and dietary assessment can create comprehensive models predicting individual responses to dietary interventions [67]. Digital health technologies, including continuous glucose monitors and AI-driven dietary assessment tools, provide dynamic data on metabolic responses to nutritional intake [67].
However, equitable implementation requires addressing socioeconomic barriers that limit access to personalized nutrition approaches. Developing low-cost assessment tools, ensuring diverse representation in research, and creating scalable implementation models are essential for translating scientific advances into public health impact [66]. Future research should prioritize intervention studies that simultaneously address biological and social determinants of health.
Figure 3: Integrated Framework for Personalized Nutrition Research. Multi-omic data integration enables personalized dietary recommendations, while socioeconomic context modulates implementation and effectiveness.
Personalized nutrition represents a paradigm shift from one-diet-fits-all approaches to targeted strategies that account for genetic, microbiome, and socioeconomic diversity. Gene-nutrient interactions, such as those involving FTO and TCF7L2 polymorphisms, demonstrate how genetic variation creates differential responses to dietary components [70]. The gut microbiome serves as a dynamic interface between diet and host physiology, with early life assembly and dietary patterns throughout life shaping microbial communities that influence disease risk [71]. Socioeconomic factors create structural constraints that limit healthy food access and healthcare resources, contributing to geographic disparities in chronic disease prevalence [65].
Advancing this field requires methodologically rigorous approaches that integrate multi-omic data with social determinants of health. The experimental protocols outlined in this whitepaper provide frameworks for investigating these complex interactions across biological and social dimensions. Future research should prioritize diverse participant recruitment, development of culturally appropriate interventions, and implementation science to translate personalized nutrition into equitable health improvements. By simultaneously addressing biological heterogeneity and socioeconomic barriers, the field can realize the full potential of personalized nutrition to reduce the global burden of chronic diseases.
Dietary interventions are fundamental to preventing and managing chronic diseases. While the debate on the optimal dietary pattern continues, a compelling body of evidence suggests that long-term adherence, rather than the specific type of diet, is the primary determinant of successful health outcomes [73]. The degree to which an individual 'sticks' to a diet is strongly associated with weight loss success and the reduction of chronic disease risk over both short and long terms [73]. This whitepaper synthesizes current evidence on dietary adherence, exploring the biological, behavioral, and personalized strategies that enhance long-term maintenance. It provides a framework for researchers and drug development professionals to conceptualize adherence not merely as a behavioral outcome, but as a central physiological and mechanistic variable in nutritional science and chronic disease risk mitigation. The focus extends beyond weight management to encompass broader health outcomes, including cardiometabolic health, healthy aging, and the delay of chronic disease onset [33] [12].
The Evidence Base: Linking Adherence to Health Outcomes
Adherence as a Predictor of Success
Evidence from multiple study designs confirms that adherence is a more critical factor for success than the specific macronutrient composition of a diet. A curvilinear association has been demonstrated between self-reported dietary adherence and weight loss, with no independent association found for diet type itself [73]. This relationship holds across diverse dietary patterns, from very low-carbohydrate to very low-fat regimens [73]. Furthermore, mathematical modeling of energy intake fluctuations indicates that poor adherence is the primary driver of the weight loss plateau typically observed around six months into an intervention [73].
Long-term cohort studies reinforce the importance of adherence for chronic disease prevention. Research involving over 200,000 healthcare professionals followed for up to 32 years demonstrated that adherence to healthy dietary patterns was consistently associated with a lower risk of major chronic diseases, including cardiovascular disease, type 2 diabetes, and cancer [33]. The risk reduction was most pronounced for diets associated with lower insulinemic and inflammatory responses [33].
Quantifying the Impact of Dietary Patterns on Healthy Aging
The association between dietary adherence and multidimensional health outcomes is exemplified by research on healthy aging. A 2025 study examining data from the Nurses' Health Study and the Health Professionals Follow-Up Study defined "healthy aging" as survival to 70 years free of major chronic diseases, with intact cognitive, physical, and mental health [12]. The study evaluated eight dietary patterns and found that higher adherence to each was associated with significantly greater odds of achieving healthy aging after up to 30 years of follow-up [12].
Table 1: Association Between Dietary Patterns and Odds of Healthy Aging
| Dietary Pattern | Odds Ratio (Highest vs. Lowest Quintile) | 95% Confidence Interval |
|---|---|---|
| Alternative Healthy Eating Index (AHEI) | 1.86 | 1.71 - 2.01 |
| Reverse Empirical Dietary Index for Hyperinsulinemia (rEDIH) | 1.83 | 1.68 - 1.99 |
| Alternative Mediterranean Diet (aMED) | 1.79 | 1.65 - 1.95 |
| Planetary Health Diet Index (PHDI) | 1.73 | 1.59 - 1.88 |
| DASH Diet | 1.66 | 1.53 - 1.80 |
| MIND Diet | 1.62 | 1.49 - 1.76 |
| Reverse Empirical Dietary Inflammatory Pattern (rEDIP) | 1.60 | 1.47 - 1.74 |
| Healthful Plant-Based Diet Index (hPDI) | 1.45 | 1.35 - 1.57 |
The AHEI showed the strongest association, while all patterns demonstrated significant benefits, underscoring that sustained adherence to a variety of healthful dietary patterns can promote well-being in aging populations [12].
Biological Mechanisms Linking Adherence to Health Outcomes
Counter-Regulatory Physiological Responses to Weight Loss
A significant biological barrier to dietary adherence is the body's compensatory response to energy restriction. Weight loss triggers a cascade of physiological adaptations that collectively oppose the maintenance of reduced body weight. A key component is the increase in the drive to eat, or hunger, which is driven by hormonal changes including alterations in ghrelin, leptin, and peptide YY [73]. This heightened appetite is a major contributor to attrition from weight loss programs and the inability to maintain weight loss [73]. The degree of hunger experienced during energy restriction has been shown to predict subsequent weight regain [73].
Mechanistic Pathways of Dietary Patterns
Different dietary patterns may influence adherence and health outcomes through distinct biological pathways. The Mediterranean diet (MedDiet), for instance, is associated with a wide range of health benefits, particularly for cardiovascular disease (CVD). The biomolecular mechanisms contributing to its long-term effects are multifaceted [74].
Table 2: Key Biological Mechanisms of the Mediterranean Diet
| Mechanism | Biological Process | Key Components in MedDiet |
|---|---|---|
| Lipid-Lowering Effects | Reduces LDL-C, improves HDL function, modulates triglycerides. | Monounsaturated fats (olive oil), polyunsaturated fats (nuts), fiber. |
| Anti-Inflammatory Effects | Downregulates pro-inflammatory cytokines (e.g., TNF-α, IL-6). | Polyphenols (olive oil, red wine), omega-3 fatty acids (fish), antioxidants (fruits, vegetables). |
| Antioxidant Effects | Reduces oxidative stress and cellular damage. | Vitamins C & E, carotenoids, polyphenols. |
| Improved Endothelial Function | Enhances nitric oxide bioavailability, reduces blood pressure. | Polyphenols, healthy fats, fiber. |
| Prevention of Platelet Aggregation | Reduces risk of thrombotic events. | Omega-3 fatty acids, polyphenols. |
Diets associated with lower empirical dietary indices for hyperinsulinemia (EDIH) and inflammation (EDIP) show the strongest inverse associations with chronic disease risk, suggesting that modulating insulinemic and inflammatory pathways is a critical mechanism through which dietary patterns exert their effects [33]. This provides a mechanistic rationale for personalizing dietary prescriptions based on an individual's metabolic phenotype.
Figure 1: Biological Pathways of the Mediterranean Diet. This diagram illustrates the key mechanistic pathways through which adherence to the Mediterranean diet influences chronic disease risk and promotes healthy aging.
Evidence-Based Strategies to Enhance Dietary Adherence
Dietary Design to Mitigate Physiological Drivers of Non-Adherence
One strategy to improve adherence involves designing diets that help control the increased drive to eat that accompanies weight loss. Ketogenic diets, including Very-Low-Calorie Ketogenic Diets (VLCKD), may promote satiety and reduce hunger, potentially through the appetite-suppressing effects of ketone bodies [73] [75]. While effective for short-term weight loss, the long-term sustainability and risks of such restrictive diets require careful consideration [75]. Alternatively, emphasizing high-quality foods common to many healthy patterns—such as fruits, vegetables, whole grains, and nuts—can improve satiety and nutrient density, supporting adherence and overall health [12] [76].
Personalization and Tailoring of Interventions
Tailoring dietary interventions to individual preferences, cultural backgrounds, and nutritional requirements is a cornerstone of improving adherence [73] [76]. The 2020 review by Kim emphasized that there is no single best strategy for weight management, and interventions should be individualized based on patient preferences [75]. This includes flexibility in macronutrient distribution, provided an overall energy deficit is maintained [76]. Personalization also extends to accommodating socioeconomic constraints, for example, by incorporating frozen vegetables and legumes to make patterns like the MedDiet and DASH more affordable and practical [77].
Promoting Exploration and Dietary Variety
Promoting dietary variety within a healthy framework can enhance long-term adherence. A 2024 randomized controlled trial demonstrated that participants exposed to a fixed, large menu of healthy options explored a wider array of foods and sustained higher adherence to the Mediterranean diet six months post-intervention, compared to those receiving a new small menu each week [78]. This suggests that early presentation of a wide array of options can increase dietary exploration, helping individuals discover healthy foods they find rewarding, which supports long-term habit formation [78].
Structured Self-Monitoring and Behavioral Support
Self-monitoring of food intake is a key strategy for improving adherence [73]. Regular follow-ups with healthcare professionals, such as dietitians, have been proven to prevent weight regain and help maintain a 5–10% weight loss for up to two years [76]. Combining nutritional therapy with behavioral interventions, such as cognitive behavioral therapy (CBT) and motivational interviewing, improves adherence and facilitates long-term maintenance [76]. This highlights the need for a multidisciplinary, ongoing support system rather than a one-time prescription.
Experimental Protocols for Adherence Research
Protocol: A Fixed-Menu Intervention to Promote Dietary Exploration
This protocol is based on the RCT by Shavit et al. (2024) that tested the effect of menu structure on exploration and adherence [78].
- Objective: To investigate whether a fixed, diverse menu of healthy options promotes greater long-term dietary adherence and exploration compared to a rotating menu.
- Population: Adults seeking to improve dietary quality.
- Intervention:
- Randomization: Participants are randomly assigned to one of two groups for a 6-week intervention:
- Fixed Menu Group: Receives the same extensive menu weekly, listing numerous healthy options (e.g., 20-30 items).
- Changing Menu Group: Receives a new, small menu each week (e.g., 5-7 items).
- Menu Design: All menus are designed to align with a target dietary pattern (e.g., Mediterranean diet). Menus include meal suggestions and recipes.
- Post-Intervention Phase: After 6 weeks, both groups are given the same set of menu suggestions and followed for 6 months.
- Randomization: Participants are randomly assigned to one of two groups for a 6-week intervention:
- Data Collection:
- Primary Outcome (Adherence): Assessed using a validated dietary adherence screener (e.g., the 14-item I-MEDAS for MedDiet) at baseline, end of intervention, 3 months, and 6 months.
- Primary Outcome (Exploration): The number of different healthy food items tried each week, collected via weekly self-reports during the intervention.
- Covariates: Demographic data, food neophobia score, and baseline dietary habits.
- Analysis: Independent t-tests to compare exploration between groups. Repeated-measures ANCOVA to analyze adherence scores over time, controlling for baseline scores and covariates.
Protocol: Assessing Biological Mechanisms in Dietary Trials
This protocol outlines the measurement of key physiological mediators in dietary intervention studies.
- Objective: To quantify the changes in insulinemic, inflammatory, and appetite-regulatory pathways in response to different dietary patterns.
- Population: Participants enrolled in a dietary intervention trial.
- Biological Sampling and Analysis:
- Blood Samples: Collected after an overnight fast at baseline, mid-point, and end of the intervention.
- Insulinemia: Measure fasting insulin and C-peptide. Calculate HOMA-IR.
- Inflammation: Measure high-sensitivity C-reactive protein (hs-CRP), interleukin-6 (IL-6), and tumor necrosis factor-alpha (TNF-α).
- Appetite Hormones: Measure leptin, ghrelin, peptide YY (PYY), and glucagon-like peptide-1 (GLP-1).
- Urine Collection: 24-hour urine collection to estimate sodium intake (a proxy for dietary compliance) and nitrogen excretion (a proxy for protein intake).
- Blood Samples: Collected after an overnight fast at baseline, mid-point, and end of the intervention.
- Functional Measures:
- Energy Expenditure: Measured via indirect calorimetry at rest and after meals.
- Appetite Sensations: Assessed using visual analogue scales (VAS) at multiple timepoints after a standardized test meal.
- Data Integration: Use mediation analysis to determine the proportion of the diet's effect on clinical outcomes (e.g., weight loss, blood pressure) that is explained by changes in these biological mediators.
Figure 2: Fixed-Menu Intervention Workflow. This diagram outlines the experimental workflow for a randomized controlled trial investigating the effect of menu structure on dietary exploration and long-term adherence.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Tools for Dietary Adherence Research
| Tool / Reagent | Function / Application | Example Use Case |
|---|---|---|
| Validated Food Frequency Questionnaires (FFQs) | Assess habitual dietary intake over an extended period. | Evaluating long-term adherence to a prescribed dietary pattern in cohort studies [33] [12]. |
| Dietary Adherence Screeners (e.g., I-MEDAS) | Rapid, specific assessment of adherence to a target diet (e.g., Mediterranean). | Primary outcome measure in intervention trials [78]. |
| Multiplex Immunoassay Panels | Simultaneous quantification of multiple biomarkers (e.g., inflammatory cytokines, appetite hormones). | Mechanistic studies to link dietary adherence to changes in physiological pathways [33] [74]. |
| Doubly Labeled Water (²H₂¹⁸O) | Gold-standard measurement of total energy expenditure in free-living individuals. | Objectively verifying energy intake and calculating metabolized energy to quantify adherence [73]. |
| Standardized Test Meals | A controlled meal used to assess postprandial metabolic and hormonal responses. | Measuring physiological responses like insulinemia, inflammation, and satiety hormones in a standardized setting [73]. |
| Food Neophobia Scale | Quantifies an individual's reluctance to try novel foods. | As a covariate or effect modifier in studies of dietary exploration and variety [78]. |
Optimizing long-term dietary adherence requires a multi-faceted approach that integrates biological, behavioral, and personalized strategies. The evidence is clear: the sustainability of a dietary pattern is as important as its theoretical efficacy. Future research and clinical practice must move beyond a one-size-fits-all approach and leverage strategies that mitigate physiological counter-responses, personalize dietary recommendations, promote enjoyable exploration of healthy foods, and provide ongoing support. For researchers in chronic disease mechanisms, understanding and measuring the mediators through which diets exert their effects—such as insulinemia and inflammation—is crucial. The ultimate goal is to translate this knowledge into practical, personalized interventions that empower diverse populations to maintain health-promoting dietary behaviors for a lifetime, thereby reducing the global burden of chronic disease.
Evidence Synthesis: Comparative Efficacy of Dietary Patterns for Disease Prevention
Dietary patterns represent a holistic approach to understanding the relationship between nutrition and health, moving beyond the study of individual nutrients or foods. Within the context of chronic disease prevention, three dietary patterns have garnered significant scientific interest for their potential protective effects: the Mediterranean Diet (MedDiet), the Dietary Approaches to Stop Hypertension (DASH) diet, and the Mediterranean-DASH Intervention for Neurodegenerative Delay (MIND) diet. While these patterns share common principles, they differ in their specific emphases and proposed mechanisms of action. This technical review provides a systematic, evidence-based comparison of these dietary patterns, focusing on their efficacy in preventing neurological, metabolic, and cardiovascular disorders, with particular attention to the biological mechanisms underlying their protective effects. The analysis is situated within the broader research landscape of dietary patterns and chronic disease risk mechanisms, providing critical insights for researchers, scientists, and drug development professionals investigating nutritional interventions and their pathophysiological targets.
Comparative Analysis of Protective Effects Across Disease States
Neuroprotective Effects and Dementia Risk Reduction
The protective effects of the MIND, Mediterranean, and DASH diets against neurological disorders, particularly dementia, have been extensively investigated in large-scale cohort studies and meta-analyses. A comprehensive study using the UK Biobank cohort (N=166,916) with a median follow-up of 10.5 years directly compared ten dietary patterns and found that the MIND diet demonstrated the broadest neuroprotective effects [11]. Adherence to the MIND diet was significantly associated with reduced risk of dementia (HR=0.87, 95% CI=0.77–0.98), stroke (HR=0.89, 95% CI=0.81–0.98), depression (HR=0.77, 95% CI=0.71–0.82), and anxiety (HR=0.82, 95% CI=0.76–0.88), but not Parkinson's disease (HR=0.94, 95% CI=0.80–1.11) [11].
A systematic review and meta-analysis of 12 studies involving 14 cohorts specifically investigated the associations between these three dietary patterns and dementia risk in elderly individuals [79]. The analysis revealed that the MIND diet showed the most robust protective effect against dementia (HR=0.78, 95% CI=0.68–0.89), followed by the DASH diet (HR=0.80, 95% CI=0.60–1.06), and the Mediterranean diet (HR=0.85, 95% CI=0.71–1.03) [79]. Subgroup analysis indicated that the Mediterranean diet demonstrated stronger protective effects (HR=0.72, 95% CI=0.55–0.93) when the follow-up duration was 10 years or less [79].
Further validating these findings, a 5-year prospective cohort study comparing the long-term neuroprotective effects of the Mediterranean and MIND diets in 1,500 participants (750 healthy controls, 750 Alzheimer's disease patients) found that higher adherence to both diets was associated with significantly better cognitive scores (p<0.0001), lower amyloid-beta, tau, and neurofilament light chain (NfL) levels, and reduced inflammatory markers (CRP, IL-6, TNF-α) [28]. The MIND diet showed a slightly stronger association with cognitive protection than the Mediterranean diet in this direct comparison [28].
Table 1: Comparative Neuroprotective Effects of Dietary Patterns
| Dietary Pattern | Dementia Risk Reduction | Cognitive Performance | Stroke Risk Reduction | Other Neuropsychiatric Benefits |
|---|---|---|---|---|
| MIND Diet | HR=0.78 (0.68-0.89) [79] | Strong association (p<0.0001) [28] | HR=0.89 (0.81-0.98) [11] | Reduced depression, anxiety [11] |
| Mediterranean Diet | HR=0.85 (0.71-1.03) [79] | Significant association (p<0.0001) [28] | Not specifically reported | Limited consistent evidence |
| DASH Diet | HR=0.80 (0.60-1.06) [79] | Not specifically reported | Not specifically reported | Limited consistent evidence |
Cardiovascular and Metabolic Protection
The Mediterranean diet has demonstrated substantial cardioprotective effects across multiple studies. A cumulative analysis of prospective cohort studies and randomized controlled trials reported a strong inverse correlation between Mediterranean diet adherence and cardiovascular morbidity and mortality (RR=0.71; 95% CI=0.65–0.78) [74]. The landmark PREDIMED trial, a large-scale randomized controlled intervention trial, demonstrated that following a personalized Mediterranean diet pattern supplemented with extra virgin olive oil or nuts decreased cardiovascular events by 30% compared to a control low-fat diet [74].
The DASH diet was originally developed to address hypertension and has shown significant efficacy in blood pressure reduction. Recent research has extended its applications to multidimensional integrated prevention and treatment of diabetes and its complications [80]. A clinical trial led by Johns Hopkins researchers developed a modified version (DASH4D) that is lower in carbohydrates and higher in unsaturated fats, specifically for type 2 diabetes patients [81]. The study found that participants consuming the DASH4D diet had blood glucose levels on average 11 mg/dL lower than when eating a standard diet and remained in the optimal blood glucose range for an extra 75 minutes per day, effects considered clinically meaningful for reducing long-term diabetic complications [81].
Table 2: Cardiovascular and Metabolic Benefits of Dietary Patterns
| Dietary Pattern | Cardiovascular Risk Reduction | Blood Pressure Effects | Glycemic Control | Other Metabolic Benefits |
|---|---|---|---|---|
| MIND Diet | Not specifically reported | Not specifically reported | Not specifically reported | Not specifically reported |
| Mediterranean Diet | RR=0.71 (0.65-0.78) [74] | Significant reductions in systolic and diastolic BP [74] | Moderate effect | Lipid-lowering, anti-inflammatory effects [74] |
| DASH Diet | Not specifically reported | Significant reductions in systolic and diastolic BP [80] | Clinically meaningful improvement [81] | Reduces diabetic nephropathy risk [80] |
Effects on Healthy Aging and Chronic Disease Prevention
A comprehensive study examining dietary patterns in relation to healthy aging using data from the Nurses' Health Study (1986-2016) and the Health Professionals Follow-Up Study (1986-2016) evaluated eight dietary patterns and their association with healthy aging, defined according to measures of cognitive, physical, and mental health, as well as living to 70 years free of chronic diseases [12]. After up to 30 years of follow-up, higher adherence to all dietary patterns was associated with greater odds of healthy aging. The Alternative Healthy Eating Index showed the strongest association (OR=1.86, 95% CI=1.71–2.01), followed by the Mediterranean diet, while the healthful plant-based diet showed the weakest association (OR=1.45, 95% CI=1.35–1.57) [12].
When examining associations with individual healthy aging domains, higher adherence to all dietary patterns was associated with all individual domains. For intact cognitive health, the Planetary Health Diet Index showed the strongest association (OR=1.65, 95% CI=1.57–1.74), while for intact physical function and intact mental health, the Alternative Healthy Eating Index showed the strongest associations (OR=2.30, 95% CI=2.16–2.44 and OR=2.03, 95% CI=1.92–2.15, respectively) [12].
Mechanistic Pathways and Biological Underpinnings
Multi-Omics Mechanisms of Neuroprotection
The UK Biobank study employed a four-way decomposition model with multi-omics data as mediators to explore the biological mechanisms underlying the observed neuroprotective effects [11]. The analyses revealed that the MIND diet's protective effects were mediated through several key pathways. A favorable metabolic signature explained a substantial proportion of the reduced risk for stroke (proportion mediated=60.63%), depression (38.97%), and anxiety (26.06%) [11]. Furthermore, slower biological aging significantly mediated the reduced risk of dementia (19.40%) [11]. A structural equation model confirmed the overall protective pathway linking the MIND diet to better brain health via these mediators.
The 5-year prospective cohort study on Alzheimer's disease patients provided additional mechanistic insights, demonstrating that higher adherence to both the Mediterranean and MIND diets was associated with lower amyloid-beta, tau, and neurofilament light chain (NfL) levels, and reduced inflammatory markers (CRP, IL-6, TNF-α) [28]. Specific micronutrients, including polyphenols, omega-3 fatty acids, and B vitamins, were correlated with improved cognitive performance, suggesting their potential role in the observed neuroprotection [28].
Cardiovascular and Metabolic Mechanisms
The Mediterranean diet's cardioprotective effects are mediated through multiple biomolecular mechanisms, including lipid-lowering effects, prevention of inflammation, platelet aggregation, and oxidative stress [74]. The diet's rich content of polyphenols and monounsaturated or polyunsaturated fatty acids contributes to these beneficial effects, with particular emphasis on improved endothelial function and blood pressure regulation [74].
The DASH diet's efficacy in diabetes management stems from its multi-target metabolic effects, including optimizing blood glucose homeostasis, reducing hemoglobin A1c (HbA1c), improving insulin sensitivity and insulin resistance, regulating lipid metabolism, and inhibiting oxidative stress and inflammation [80]. For diabetic nephropathy specifically, the DASH diet significantly reduces urinary albumin excretion rate (UAER) and serum creatinine levels while improving estimated glomerular filtration rate (eGFR), indicating a direct renal protective effect independent of age, baseline renal function, and glycemic control level [80].
Experimental Methodologies and Research Protocols
Key Methodological Approaches in Dietary Pattern Research
Cohort Study Designs: Large-scale prospective cohorts form the foundation of evidence on dietary patterns and chronic disease risk. The UK Biobank study exemplifies this approach, analyzing data from 166,916 participants enrolled between April 2009 and June 2012, with a median follow-up of 10.5 years [11]. Similarly, the Nurses' Health Study and Health Professionals Follow-Up Study have provided decades of longitudinal data on dietary patterns and healthy aging outcomes [12]. These studies employ repeated dietary assessments, typically using validated food frequency questionnaires (FFQs), to capture long-term dietary habits and reduce measurement error.
Randomized Controlled Trials: The PREDIMED trial represents the gold standard in dietary intervention research, randomly assigning participants to Mediterranean diet supplemented with extra virgin olive oil, Mediterranean diet supplemented with nuts, or a control low-fat diet to assess cardiovascular outcomes [74]. More recently, the DASH4D CGM study utilized a randomized crossover design where 89 participants with type 2 diabetes consumed prepared meals following either the DASH4D diet or a standard diet for 5-week periods, with continuous glucose monitoring to assess glycemic control [81]. This crossover design enhanced statistical power despite the moderate sample size by comparing participants with themselves under different diet conditions.
Systematic Reviews and Meta-Analyses: These methodologies provide quantitative syntheses of existing evidence. The systematic review on dietary patterns and dementia risk followed PRISMA guidelines, identified 12 studies involving 14 cohorts, and pooled hazard ratios using random-effects models to compare the protective effects of the three dietary patterns [79]. Similarly, the review of Mediterranean diet and autoimmune diseases employed MOOSE guidelines and computed pooled effect sizes using random-effects models expressed as risk ratios, hazard ratios, or odds ratios [82].
Assessment Tools and Biomarker Measurement
Dietary Adherence Assessment: Research on dietary patterns relies on validated tools to quantify adherence. The Mediterranean Diet Adherence Screener (MEDAS, 4-15 scale) and MIND Diet Score (4-15 scale) are commonly used instruments [28]. These are typically administered alongside food frequency questionnaires and 24-hour dietary recalls to enhance accuracy.
Biomarker Analysis: Advanced biomarker measurement is critical for understanding mechanistic pathways. The 5-year prospective study on Alzheimer's disease employed comprehensive biomarker analysis, including:
- Amyloid-beta (Aβ42/40 levels) measured using Thermo Fisher Scientific ELISA Kit
- Tau Protein Levels measured using R&D Systems assays
- Neurofilament Light Chain (NfL) measured using Peninsula Laboratories kits
- Inflammatory markers (CRP, IL-6, TNF-α) measured using commercially available eBioscience kits [28]
Neuroimaging and Genetic Analysis: Structural MRI for hippocampal volume and cortical thickness provides objective measures of neurodegeneration [28]. Genetic analysis, particularly APOE-ε4 status determination via polymerase chain reaction (PCR), helps identify potential effect modification by genetic predisposition [28].
Table 3: Research Reagent Solutions for Dietary Pattern Studies
| Research Tool Category | Specific Examples | Application & Function |
|---|---|---|
| Dietary Assessment Tools | Mediterranean Diet Adherence Screener (MEDAS) [28], MIND Diet Score [28], Food Frequency Questionnaires (FFQ) [12], 24-hour dietary recall [28] | Quantifies adherence to specific dietary patterns and assesses nutrient intake |
| Neurological Biomarkers | Amyloid-beta (Aβ42/40) ELISA kits [28], Tau protein assays [28], Neurofilament Light Chain (NfL) kits [28] | Measures Alzheimer's disease pathology and neuronal damage |
| Inflammatory Markers | High-sensitivity CRP, IL-6, TNF-α immunoassays [28], INFLA score [11] | Quantifies systemic and neuroinflammation |
| Metabolic Assays | Continuous glucose monitoring systems [81], HbA1c, insulin sensitivity indices (HOMA-IR) [80] | Assesses glycemic control and metabolic health |
| Omics Technologies | Metabolomic profiling [11], Proteomic analysis [11], Genotyping (APOE-ε4) [28] | Identifies molecular mechanisms and effect modification |
The head-to-head comparison of the MIND, Mediterranean, and DASH diets reveals distinct protective profiles against chronic diseases. The MIND diet demonstrates superior neuroprotective effects, particularly for dementia, cognitive decline, and neuropsychiatric disorders, with multi-omics analyses identifying metabolic signatures and biological aging as key mediating pathways. The Mediterranean diet shows broad-spectrum benefits for cardiovascular health and healthy aging, with strong evidence supporting its anti-inflammatory and antioxidant properties. The DASH diet exhibits specialized efficacy for hypertension, glycemic control, and diabetes-related complications, particularly diabetic nephropathy.
These differential protective profiles suggest that dietary pattern recommendations could be tailored to individual risk profiles. For brain health and neurodegenerative disease prevention, the MIND diet appears most promising. For comprehensive cardiovascular protection and healthy aging, the Mediterranean diet shows robust efficacy. For metabolic disorders, hypertension, and diabetic complications, the DASH diet offers targeted benefits. The overlapping components of these diets—emphasis on plant-based foods, healthy fats, and limited processed foods—suggest shared fundamental principles for chronic disease prevention, while their distinctive features may optimize protection for specific organ systems and disease pathways.
Future research should prioritize randomized controlled trials to establish causality, further elucidate molecular mechanisms through multi-omics approaches, and explore personalized nutrition strategies based on genetic predisposition, metabolic characteristics, and individual risk factors. The integration of dietary pattern research into chronic disease prevention frameworks holds significant promise for developing targeted nutritional interventions that complement pharmacological approaches in the management of complex chronic diseases.
Dietary pattern analysis has evolved from guideline-based indices to empirically derived, mechanism-based scores. This review systematically compares the Alternative Healthy Eating Index (AHEI) and healthful Plant-Based Diet Index (hPDI)—developed from dietary guidelines and health outcomes—against the reversed empirical dietary index for hyperinsulinemia (rEDIH) and reversed empirical dietary inflammatory pattern (rEDIP), derived to directly predict biomarkers of insulin resistance and inflammation. We evaluate their construction methodologies, biological pathways, and efficacy in chronic disease prevention across multiple large-scale cohort studies. Evidence indicates that while all four patterns associate with reduced disease risk, mechanism-based diets (rEDIH/rEDIP) demonstrate particular potency for specific conditions, including certain cancers and cardiometabolic diseases, offering refined targets for nutritional interventions and drug development research.
Dietary patterns represent the cumulative effects of overall food and nutrient intake, offering a more comprehensive approach to understanding diet-disease relationships than single-nutrient studies. Two distinct paradigms have emerged: guideline-based diets and mechanism-based diets.
Guideline-based diets like AHEI and hPDI are primarily grounded in prior evidence linking specific food groups to health outcomes. The AHEI was developed based on foods and nutrients predictive of chronic disease risk, while hPDI emphasizes healthful plant foods. In contrast, mechanism-based diets like rEDIH and rEDIP employ empirical methods to create patterns directly predictive of specific physiological processes—hyperinsulinemia and chronic inflammation—that are established drivers of chronic disease pathogenesis.
The reversal of original EDIH and EDIP scores (to rEDIH and rEDIP) allows consistent interpretation where higher scores indicate healthier patterns, enabling direct comparison with AHEI and hPDI. This review synthesizes evidence from recent large-scale prospective cohorts to evaluate their comparative utility for chronic disease prevention research.
Methodological Foundations: From Concept to Index
Guideline-Based Dietary Indices
Alternative Healthy Eating Index (AHEI)
The AHEI was developed to address limitations in the original Healthy Eating Index, specifically targeting foods and nutrients predictive of chronic disease risk. The index comprises 11 components scored from 0 (worst) to 10 (best) [83]. The scoring criteria are summarized in Table 1.
healthful Plant-Based Diet Index (hPDI)
The hPDI classifies 18 food groups into three categories: healthful plant foods (positive scoring), less healthful plant foods (negative scoring), and animal foods (negative scoring) [83]. Participants receive quintile-based scores for each food group, with higher overall scores indicating greater consumption of healthful plant foods.
Mechanism-Based Dietary Indices
Empirical Dietary Index for Hyperinsulinemia (rEDIH)
The original EDIH was developed using reduced rank regression to identify dietary patterns most predictive of plasma C-peptide, a marker of insulin secretion [83]. The dietary pattern was derived from food group intake as predictors and fasting plasma C-peptide as the response variable. The resulting pattern represents a dietary score highly correlated with hyperinsulinemia. For consistent interpretation, the score is reversed (rEDIH), whereby higher scores indicate a lower insulinemic potential.
Empirical Dietary Inflammatory Pattern (rEDIP)
The EDIP was developed using reduced rank regression with plasma inflammatory biomarkers (IL-6, CRP, TNFαR2) as response variables [83]. The resulting pattern represents a dietary score predictive of systemic inflammation. The reversed score (rEDIP) allows higher values to indicate anti-inflammatory potential.
Table 1: Composition and Scoring of Dietary Indices
| Dietary Index | Development Method | Key Components | Scoring Approach |
|---|---|---|---|
| AHEI | Based on foods/nutrients associated with chronic disease risk | Fruits, vegetables, whole grains, nuts, legumes, LCPUFA; Red/processed meats, sugar-sweetened beverages, trans fat, sodium | 0-10 points per component; Maximum 110 points |
| hPDI | Based on healthful plant food consumption | Whole grains, fruits, vegetables, nuts, legumes, tea/coffee; Fruit juices, sweetened beverages, refined grains, sweets/desserts | Quintile-based scoring; Positive scores for healthful plants, reverse for animal foods |
| rEDIH | Reduced rank regression predicting plasma C-peptide | Soup, tomato, poultry, low-energy beverages, cream soup; Coffee, high-energy beverages, whole fruits, wine | Food group weights based on relationship to hyperinsulinemia |
| rEDIP | Reduced rank regression predicting inflammatory biomarkers (IL-6, CRP, TNFαR2) | Processed meat, red meat, fish, other vegetables; Green leafy vegetables, snack foods, pizza, wine | Food group weights based on relationship to inflammation |
Comparative Methodological Considerations
The fundamental methodological distinction lies in the derivation approach. Guideline-based indices (AHEI, hPDI) apply pre-specified, hypothesis-driven frameworks based on existing epidemiological evidence. Mechanism-based indices (rEDIH, rEDIP) employ data-driven, agnostic approaches to maximize prediction of specific physiological pathways.
Validation approaches also differ substantially. AHEI and hPDI are validated against future health outcomes, while rEDIH and rEDIP are first validated against biomarker concentrations, then subsequently tested against disease endpoints. This fundamental difference in construction leads to variations in the food groupings and scoring weights, as illustrated in the following development workflow:
Biological Pathways and Mechanisms
Insulin Signaling and Metabolic Regulation (rEDIH Focus)
The rEDIH targets dietary patterns that minimize postprandial insulin secretion, directly addressing the pathway where hyperinsulinemia drives metabolic dysfunction. The identified pattern influences insulin signaling through multiple interconnected mechanisms:
Nutrient-Specific Effects: The pattern emphasizes foods with low insulinemic demand, including specific whole fruits, coffee, and wine, while reducing foods that stimulate disproportionate insulin secretion relative to their carbohydrate content [33].
Mitochondrial Function: Reduced insulin secretion decreases mTOR activation, enhancing mitochondrial biogenesis and metabolic flexibility. This process is mediated through SIRT1 activation and AMPK signaling pathways.
Inflammatory Crosstalk: Hyperinsulinemia potentiates NF-κB signaling, creating a feed-forward loop between metabolic and inflammatory dysfunction. The rEDIH pattern appears to disrupt this cycle by reducing primary insulin stimulation.
Immunomodulatory Pathways (rEDIP Focus)
The rEDIP targets the NF-κB signaling cascade, a master regulator of inflammatory gene expression. The empirically-derived food pattern influences multiple points in this pathway:
Cytokine Regulation: The pattern reduces production of pro-inflammatory cytokines (IL-6, TNF-α) while potentially enhancing anti-inflammatory mediators (adiponectin, IL-10).
Immune Cell Signaling: Bioactive components in the pattern modulate TLR4 receptor sensitivity and subsequent intracellular signaling, reducing neutrophil infiltration and macrophage polarization toward pro-inflammatory phenotypes.
Inflammasome Regulation: Emerging evidence suggests the pattern may inhibit NLRP3 inflammasome activation, reducing IL-1β and IL-18 production.
The following diagram illustrates the key biological pathways targeted by these dietary patterns:
Comparative Pathway Activation
While all four dietary patterns influence overlapping biological processes, their primary mechanisms differ substantially. AHEI operates through broader nutritional adequacy and metabolic optimization, while hPDI emphasizes fiber-mediated microbiota changes and phytonutrient effects. The mechanism-based patterns target more specific physiological drivers: rEDIH directly addresses insulin secretory demand, while rEDIP specifically modulates inflammatory signaling cascades.
Efficacy in Chronic Disease Prevention: Comparative Evidence
Healthy Aging Outcomes
Recent evidence from over 105,000 participants followed for 30 years in the Nurses' Health Study and Health Professionals Follow-Up Study provides direct comparison of these dietary patterns for promoting healthy aging, defined as surviving to age 70 years free of major chronic diseases and with intact cognitive, physical, and mental health [12] [84].
Table 2: Associations Between Dietary Patterns and Healthy Aging (Highest vs. Lowest Quintile)
| Dietary Pattern | Odds Ratio (95% CI) | Population Attributable Fraction | Domain-Specific Strengths |
|---|---|---|---|
| AHEI | 1.86 (1.71-2.01) | Highest overall benefit | Strongest for physical and mental health |
| rEDIH | 1.83 (1.68-1.99) | Comparable to AHEI | Strongest for freedom from chronic diseases |
| rEDIP | 1.65 (1.52-1.79) | Moderate benefit | Balanced protection across domains |
| hPDI | 1.45 (1.35-1.57) | Modest benefit | Weakest association among patterns |
The AHEI demonstrated the strongest overall association with healthy aging, nearly doubling the odds compared to the lowest adherence quintile [12] [84]. Notably, the association strengthened when the healthy aging threshold was shifted to age 75 years, with AHEI showing an odds ratio of 2.24 (95% CI: 2.01-2.50). The rEDIH performed comparably well, while hPDI showed the most modest association among the four patterns.
Chronic Disease Prevention
In analyses of major chronic diseases (cardiovascular disease, type 2 diabetes, and cancer) across three US cohorts followed for up to 32 years, mechanism-based diets demonstrated particular efficacy [33]. The hazard ratios comparing the 90th to 10th percentile of dietary pattern scores were 0.58 (95% CI: 0.57-0.60) for rEDIH, 0.61 (95% CI: 0.60-0.63) for rEDIP, compared to 0.70 (95% CI: 0.69-0.72) for the diabetes risk reduction diet and 0.80 for AHEI.
Site-Specific Cancer Prevention
For digestive system cancers, a comprehensive analysis of over 213,000 participants revealed nuanced differential efficacy [83]. While all patterns showed inverse associations with overall digestive system cancer risk, mechanism-based diets demonstrated particular strength for specific cancer types:
Stomach Cancer: rEDIH (HR: 0.64, 95% CI: 0.47-0.87) and rEDIP (HR: 0.53, 95% CI: 0.39-0.72) showed particularly strong inverse associations.
Liver Cancer: AHEI (HR: 0.49, 95% CI: 0.36-0.68) showed the strongest association among all patterns, with rEDIH and rEDIP demonstrating more modest protective associations.
Colorectal Cancer: All patterns showed approximately 10-20% risk reduction with no clear superiority between approaches.
Brain Health Outcomes
For neurological and psychiatric disorders, the MIND diet (not directly compared here) has shown particular efficacy [11]. However, mechanism-based diets demonstrate relevance through their impact on biological aging, where slower biological aging mediated 19.40% of the reduced dementia risk associated with healthy dietary patterns [11].
Research Applications and Methodological Toolkit
Cohort Study Implementation
Implementation of these dietary patterns in research settings requires specific methodological approaches, as demonstrated in the foundational cohort studies [12] [33] [83]:
Dietary Assessment: All major studies used validated semi-quantitative food frequency questionnaires (FFQs) with 130+ items, administered every 4 years to capture long-term dietary habits.
Covariate Adjustment: Comprehensive multivariate adjustment for non-dietary factors includes age, energy intake, physical activity, BMI, smoking status, alcohol consumption, family history of chronic diseases, medication use, and socioeconomic factors.
Statistical Analysis: Most studies use Cox proportional hazards models with time-varying cumulative averages of dietary scores to account for dietary changes over time and reduce measurement error.
Table 3: Essential Research Reagents and Methodological Components
| Research Component | Specifications | Research Application |
|---|---|---|
| Food Frequency Questionnaire (FFQ) | 130+ food items, validated against diet records | Primary dietary data collection; correlation coefficients: 0.53-0.66 for nutrients, 0.63-0.66 for foods |
| Biomarker Assays | C-peptide (for EDIH validation); IL-6, CRP, TNFαR2 (for EDIP validation) | Validation of mechanism-based dietary patterns; assessment of biological pathway engagement |
| Cohort Datasets | Nurses' Health Study, Health Professionals Follow-up Study, UK Biobank | Validation across diverse populations with long-term follow-up |
| Statistical Algorithms | Reduced rank regression, Cox proportional hazards models, time-varying covariate analysis | Pattern development and risk association analysis |
Biomarker Integration in Research Protocols
Advanced research applications incorporate multi-omics approaches to elucidate mechanisms [85] [86]:
Epigenetic Clocks: GrimAge and PhenoAgeAccel assessment to quantify biological aging modulation.
Metabolomic Profiling: LC-MS platforms to identify food-derived metabolites and endogenous metabolic shifts.
Proteomic Analysis: Multiplexed assays to quantify inflammatory mediators and signaling proteins.
Microbiome Sequencing: 16S rRNA and shotgun metagenomics to characterize microbial community changes.
Discussion and Research Implications
The comparative evidence indicates that mechanism-based and guideline-based dietary patterns offer complementary strengths for chronic disease prevention research. Guideline-based patterns (AHEI) demonstrate robust associations with multidimensional healthy aging outcomes, while mechanism-based patterns (rEDIH/rEDIP) show particular efficacy for specific disease endpoints and stronger risk reduction for cardiometabolic diseases.
The differential performance across disease endpoints suggests distinct applications for these patterns in research settings. AHEI may be preferred for studies of multidimensional healthy aging, while rEDIH and rEDIP offer advantages for research on metabolic diseases, inflammation-driven conditions, and certain site-specific cancers.
From a drug development perspective, mechanism-based diets provide valuable insights into targetable physiological pathways. The success of rEDIH and rEDIP in predicting disease risk validates hyperinsulinemia and inflammation as critical intervention targets, offering nutritional blueprints for pharmaceutical development.
Limitations and Research Gaps
Current evidence has several limitations: predominantly observational design, potential residual confounding, measurement error in dietary assessment, and population homogeneity in major cohorts (primarily health professionals of European ancestry). Future research should prioritize randomized controlled trials, diverse populations, integration of multi-omics biomarkers, and investigation of gene-diet interactions.
Both guideline-based and mechanism-based dietary patterns provide valuable frameworks for chronic disease prevention research. The AHEI demonstrates superior performance for multidimensional healthy aging, while rEDIH and rEDIP offer targeted efficacy for metabolic and inflammatory diseases. The empirical development approach of mechanism-based diets provides stronger biological plausibility and pathway-specific insights, representing a promising direction for nutritional epidemiology and preventive medicine research. Future studies integrating these patterns with advanced biomarkers and diverse populations will further refine their applications in both public health and clinical practice.
The rising global prevalence of neurological and psychiatric disorders presents a critical public health challenge, with approximately 60 million individuals currently living with dementia worldwide—a figure projected to rise to 150 million by 2050 [87]. Similarly, depression affects over 350 million people globally, representing a nearly 20% increase over the past decade [88]. Within this context, dietary patterns have emerged as significant modifiable risk factors capable of influencing brain health through multiple biological pathways. This technical review synthesizes current evidence on the associations between dietary patterns and the risk of dementia, depression, and anxiety, with a specific focus on validated outcomes, mechanistic pathways, and methodological considerations for research and drug development professionals.
The analysis of dietary patterns, as opposed to individual nutrients or foods, provides a more comprehensive approach to understanding the complex interplay between nutrition and brain health. Dietary pattern analysis accounts for synergistic effects among food components and better reflects real-world eating behaviors, thereby offering more clinically relevant insights for therapeutic development [89]. This review examines the evidence linking specific dietary patterns to neurological outcomes, explores underlying biological mechanisms, details methodological approaches for dietary assessment, and identifies key gaps in current research paradigms.
Dietary Patterns and Dementia Risk: Evidence and Mechanisms
Epidemiological Evidence and Clinical Outcomes
Adherence to healthy dietary patterns has been consistently associated with improved cognitive function and reduced dementia risk in large-scale epidemiological studies. Research demonstrates that healthy dietary patterns are generally associated with a 20-42% lower risk of major chronic diseases, including those affecting brain health [33]. A diet rich in legumes, meat, vegetables, and fruits has been shown to reduce the likelihood of cardiometabolic cognitive impairment comorbidity by 59% compared to diets rich in milk and eggs with low grain intake [90]. These findings align with prospective cohort data showing that dietary patterns emphasizing high-quality foods, plant-based components, and adherence to established dietary recommendations confer significant neuroprotective benefits [33].
Table 1: Dietary Patterns Associated with Reduced Dementia Risk
| Dietary Pattern | Risk Reduction | Population Studied | Key Components | Proposed Primary Mechanisms |
|---|---|---|---|---|
| Healthy Dietary Patterns | 20-42% lower risk of major chronic diseases [33] | 205,852 healthcare professionals [33] | Plant-based foods, high-quality nutrients | Reduced inflammation, modified gut microbiome, preserved cerebral microstructure [87] |
| Legume-Meat-Vegetable-Fruit Rich | 59% less likely to have cardiometabolic cognitive impairment comorbidity [90] | Older adults from NHANES [90] | Legumes, vegetables, fruits, meat | Improved cardiometabolic parameters, reduced systemic inflammation |
| Low Insulinemic Diet | HR: 0.58 (95% CI: 0.57, 0.60) for chronic diseases [33] | NHS, NHS II, HPFS cohorts [33] | Foods associated with lower insulin response | Reduced hyperinsulinemia, preserved cerebral energetics [87] |
| Low Inflammatory Diet | HR: 0.61 (95% CI: 0.60, 0.63) for chronic diseases [33] | NHS, NHS II, HPFS cohorts [33] | Anti-inflammatory foods | Lower neuroinflammation, reduced amyloid-β load [87] |
Neuroprotective Mechanisms of Dietary Components
The neuroprotective effects of healthy dietary patterns operate through multiple interconnected biological mechanisms. Diets low in inflammatory potential and with reduced insulinemic response demonstrate particularly strong associations with reduced risk of major chronic diseases, including those affecting brain health [33]. These patterns exert protective effects through systemic mechanisms including improved cardiometabolic health, reduced inflammation, modified gut microbiome composition and metabolism, and slower pace of aging [87]. Brain-specific mechanisms include lower amyloid-β load, reduced brain atrophy, and preserved cerebral microstructure and energetics [87].
Plant-derived polyphenols, including flavonoids, phenolic acids, stilbenes, and lignans, represent particularly promising bioactive compounds with multimodal neuroprotective properties. These compounds demonstrate potent antioxidant properties that neutralize reactive oxygen species (ROS) in the brain, thereby reducing oxidative stress—a key contributor to neurodegenerative pathology [91]. Beyond their antioxidant effects, polyphenols modulate inflammation, enhance neuronal survival, support neurogenesis, and protect mitochondrial function [91] [92]. Specific polyphenolic compounds such as epigallocatechin gallate (EGCG) from green tea and resveratrol from red wine have shown particular promise in modulating pathways relevant to neurodegenerative diseases [91].
Diagram 1: Multimodal Mechanisms Linking Dietary Patterns to Neuroprotection. This diagram illustrates the systemic and brain-specific pathways through which healthy dietary patterns exert neuroprotective effects, based on evidence from Shannon et al. [87].
Dietary Patterns and Affective Disorders: Differential Outcomes for Depression and Anxiety
Evidence for Depression Risk Reduction
The association between dietary patterns and depression reveals a complex picture with important methodological considerations. Recent meta-analyses of prospective studies indicate that the strength of evidence supporting dietary interventions for depression prevention varies significantly based on assessment methods and population characteristics [93]. Bayesian meta-analyses reveal that associations are evident when depression is self-reported but not when clinically diagnosed, suggesting potential measurement issues or different underlying biological mechanisms [93].
The Healthy Eating Index-2015 (HEI-2015), which assesses adherence to dietary guidelines, demonstrates a significant negative correlation with depression (OR = 0.99, 95% CI: 0.98-1.00, p = 0.002) [88]. Compared to the lowest HEI-2015 quartile, the highest quartile shows a 34% reduction in depression risk (OR = 0.66, 95% CI: 0.50-0.87, p = 0.003) [88]. Importantly, mediation analysis indicates that body mass index (BMI) partially mediates the relationship between HEI-2015 and depression, accounting for approximately 6.39% of the total effect (p < 0.0001) [88]. SHapley Additive exPlanations (SHAP) analysis identifies added sugars, whole fruits, and saturated fats as key HEI-2015 components influencing depression risk, with added sugars and whole fruits reducing risk and saturated fats increasing it [88].
Table 2: Dietary Patterns and Depression Risk: Quantitative Outcomes
| Dietary Pattern/Index | Outcome Measure | Effect Size (OR, HR, or d) | Population/Study Characteristics | Evidence Strength |
|---|---|---|---|---|
| HEI-2015 (Highest vs. Lowest Quartile) | Depression risk (PHQ-9 ≥10) | OR = 0.66 (95% CI: 0.50-0.87) [88] | 11,091 NHANES participants | Strong in general populations |
| Mediterranean Diet | Self-reported symptoms | OR = 0.91 (95% CI: 0.88-0.96) [93] | Meta-analysis of prospective studies | Anecdotal to moderate |
| Dietary Interventions (Treatment RCTs) | Depression improvement | d = -0.80 (95% CI: -1.46 to -0.14) [93] | Patient samples | Anecdotal to moderate, low internal validity |
| Dietary Interventions (Prevention RCTs) | Depression incidence | Strong evidence for null association [93] | Non-patient samples | Strong evidence for no effect |
| Fish/DHA/EPA/Omega-3 | Postpartum depression | OR = 0.84 (95% CI: 0.78-0.91) [93] | Postpartum women | Moderate for specific population |
Anxiety and Stress Outcomes
Evidence linking dietary patterns to anxiety and stress reveals more targeted associations, particularly in clinical populations with comorbid conditions. In patients with type 2 diabetes, adherence to a healthy dietary pattern is associated with a significantly lower risk of stress (OR: 0.31, 95% CI: 0.13-0.72, P-trend=0.002), though no significant associations were observed for anxiety or depression in this population [94].
Research involving individuals living with HIV provides additional insights into anxiety-specific dietary relationships. In this population, distinct dietary patterns have been identified through factor analysis, including the egg-dairy pattern, livestock-meat pattern, whole grain pattern, and vegetable-fruit pattern [89]. Participants in the highest quartile of the egg-dairy pattern exhibited significantly lower odds of anxiety symptoms (OR = 0.60; 95% CI: 0.36 to 0.99) compared to those in the lowest quartile [89]. This pattern highlights the potential for targeted dietary interventions in specific clinical populations, even when broader population-level associations may be less clear.
Mechanistic Pathways Linking Diet to Affective Disorders
The biological pathways connecting dietary patterns to affective disorders involve complex interactions between inflammatory processes, oxidative stress, and neuroendocrine function. Diets with high inflammatory potential, as measured by the Dietary Inflammatory Index (DII), are associated with elevated inflammatory markers that may promote depressive symptoms by increasing neuroinflammation or activating central immune pathways [88]. Chronic inflammation represents a key shared pathway through which poor dietary patterns may influence both depression and dementia risk [92].
The gut-brain axis emerges as another critical pathway, with dietary patterns influencing gut microbiota composition and subsequent production of neuroactive metabolites [88]. The Dietary Index for Gut Microbiota (DI-GM) assesses intake of prebiotic and probiotic foods, as well as components like fiber and polyphenols that modulate gut bacteria and potentially alleviate depressive symptoms through this pathway [88]. Additionally, the Composite Dietary Antioxidant Index (CDAI) estimates overall dietary antioxidant intake, which may protect neural health by reducing oxidative stress—a known factor in the development of depression [88].
Diagram 2: Integrated Pathways Linking Diet to Affective Disorders. This diagram illustrates the biological and psychosocial pathways through which dietary patterns may influence depression and anxiety risk, incorporating evidence from multiple studies [93] [89] [88].
Methodological Framework: Dietary Assessment and Research Design
Dietary Pattern Assessment Methodologies
Research on diet and brain health employs diverse methodological approaches for dietary assessment, each with distinct strengths and limitations. The following experimental protocols represent commonly used methodologies in nutritional neuroscience research:
24-Hour Dietary Recall Protocol:
- Application: Used in NHANES and large cohort studies to calculate dietary indices including HEI-2015, DII, DI-GM, and CDAI [88]
- Procedure: Trained interviewers conduct two non-consecutive 24-hour dietary recalls using standardized automated data collection systems
- Timeline: First recall conducted in-person, second assessment via telephone 3-10 days later
- Data Processing: Nutrient composition determined using USDA Food Patterns Equivalent Database and Food and Nutrition Database for Dietary Studies
- Analysis: Intake calculated as average of both recalls; single recall used if only one available
Food Frequency Questionnaire (FFQ) Protocol:
- Application: Used in cross-sectional studies to assess habitual dietary intake over extended periods [89]
- Structure: Semi-quantitative FFQ with predefined food items and standardized portion sizes
- Timeframe: Typically assesses consumption over previous month or year
- Validation: Often validated against biomarkers or multiple 24-hour recalls in specific populations
- Analysis: Factor analysis (principal component analysis) used to derive dietary patterns; varimax rotation applied to simplify structure
Dietary Pattern Scoring Methodologies:
- Healthy Eating Index-2015: Assesses adherence to Dietary Guidelines for Americans using multiple components (total fruits, whole fruits, total vegetables, greens and beans, whole grains, dairy, total protein foods, seafood and plant proteins, fatty acids, refined grains, sodium, added sugars, saturated fats) [88]
- Dietary Inflammatory Index: Computed based on 26 nutrients with positive scores indicating pro-inflammatory effects and negative scores indicating anti-inflammatory effects [88]
- Empirical Dietary Patterns: Derived using reduced rank regression to explain variation in biomarkers like C-peptide (insulinemic pattern) or inflammatory markers (inflammatory pattern) [33]
Outcome Assessment and Statistical Approaches
Standardized assessment of neurological and psychiatric outcomes is critical for valid comparison across studies. Common assessment methods include:
Cognitive Function Assessment:
- Comprehensive test batteries including Consortium to Establish a Registry for Alzheimer's disease test, Animal Fluency test, and Digit Symbol Substitution test [90]
- Global cognitive scores computed through normalization and averaging of individual test scores
- Cut-points established based on population distributions (e.g., lowest quartile indicating cognitive impairment)
Depression and Anxiety Assessment:
- Patient Health Questionnaire-9 (PHQ-9) for depression severity screening [88] [90]
- Hospital Anxiety and Depression Scale (HADS) with subscales for anxiety (HADS-A) and depression (HADS-D) [89]
- Established cut-offs (PHQ-9 ≥10, HADS subscale ≥8) for case identification
Advanced Statistical Approaches:
- Bayesian meta-analysis to evaluate strength of evidence for diet-depression relationships [93]
- Mediation analysis to quantify indirect effects (e.g., BMI mediation of diet-depression relationship) [88]
- Machine learning approaches (SHapley Additive exPlanations) to identify influential dietary components [88]
- Latent class analysis to identify subtypes of multiple chronic conditions [90]
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Methodologies and Tools for Diet-Brain Health Research
| Research Tool | Application | Key Features | Implementation Considerations |
|---|---|---|---|
| 24-Hour Dietary Recall | Dietary assessment in cohort studies [88] | Standardized automated data collection; Multiple non-consecutive days | Requires trained interviewers; USDA databases for nutrient calculation |
| Food Frequency Questionnaire (FFQ) | Habitual dietary intake assessment [89] | Semi-quantitative; Validated for specific populations | Factor analysis for pattern derivation; Memory-dependent |
| Healthy Eating Index-2015 | Diet quality assessment [88] | 13 components aligned with Dietary Guidelines | Allows comparison to national recommendations; Sensitive to dietary changes |
| Dietary Inflammatory Index | Inflammatory potential of diet [88] | Based on 26 food parameters; Positive/negative scores indicate pro/anti-inflammatory effects | Requires complete nutrient data; Validated against inflammatory biomarkers |
| Patient Health Questionnaire-9 | Depression screening [88] [90] | 9 items corresponding to DSM-IV criteria; Scores 0-27 | Cut-off ≥10 for clinical depression; Good sensitivity/specificity |
| Hospital Anxiety and Depression Scale | Anxiety and depression symptoms [89] | 14 items with subscales for anxiety and depression | Minimizes somatic item bias; Validated in medical populations |
| Principal Component Analysis | Dietary pattern derivation [89] | Factor analysis with varimax rotation; Eigenvalue >1 criterion | Simplifies complex dietary data; Enables pattern-based analysis |
| Bayesian Meta-Analysis | Evidence synthesis [93] | Evaluates strength of evidence for associations | Provides evidence gradation beyond frequentist approaches |
The evidence reviewed demonstrates that dietary patterns significantly influence brain health outcomes, with particularly robust data supporting the role of healthy dietary patterns in reducing dementia risk. For affective disorders, associations appear more nuanced, with stronger evidence for self-reported symptoms than clinically diagnosed depression, and population-specific effects for anxiety. The methodological toolkit for diet-brain research has advanced substantially, incorporating sophisticated dietary assessment methods, validated outcome measures, and complex statistical approaches that account for mediation and interaction effects.
Future research should prioritize several key areas: (1) intervention studies with longer follow-up periods to establish causal relationships; (2) improved standardization of depression assessment to reconcile disparities between self-reported and clinically diagnosed outcomes; (3) investigation of bioavailability and formulation strategies to overcome limitations in polyphenol bioavailability [91]; and (4) personalized nutrition approaches that account for genetic, metabolic, and microbiome factors influencing individual responses to dietary patterns. For drug development professionals, dietary patterns represent promising complementary approaches that may enhance the efficacy of pharmacological interventions through modification of underlying inflammatory, oxidative, and metabolic pathways implicated in both neurodegenerative and affective disorders.
The Global Burden of Disease (GBD) Study, coordinated by the Institute for Health Metrics and Evaluation (IHME), represents the most comprehensive effort to quantify health loss across locations and over time [95]. Within this framework, dietary risk factors have emerged as critical modifiable determinants of non-communicable diseases (NCDs), which account for approximately 74% of all deaths worldwide [96]. The GBD 2021 study systematically estimated the burden of diseases, injuries, and risk factors for 204 countries and territories and selected subnational locations, producing estimates of 15 dietary risks and their attributable burden from 1990-2021 [97]. This technical guide examines the attributable risk of specific dietary factors across diverse economies, providing researchers and drug development professionals with methodological insights, quantitative assessments, and experimental frameworks for understanding diet-disease mechanisms in varied socioeconomic contexts.
The economic development of nations, quantified through the Socio-demographic Index (SDI), profoundly influences dietary patterns and associated disease burdens. Countries experience distinct nutrition transitions characterized by shifting consumption patterns as economies develop. Low-SDI regions often face challenges related to inadequate intake of protective foods like fruits, vegetables, and whole grains, while middle- and high-SDI regions increasingly contend with overconsumption of processed meats, sugar-sweetened beverages, and other energy-dense, nutrient-poor foods [38] [98]. Understanding these stratified patterns is essential for developing targeted interventions and for drug development professionals seeking to contextualize disease pathogenesis across global markets.
Methodological Framework: GBD Dietary Risk Assessment
The GBD 2021 study employs a standardized comparative risk assessment framework to quantify the proportion of disease-specific burden attributable to each dietary risk factor [99] [96]. The main analytical inputs include: (1) the intake distribution of each dietary factor across populations; (2) the effect size of the dietary factor on disease endpoints derived from meta-analyses of epidemiological studies; and (3) the theoretical minimum risk exposure level (TMREL), defined as the level of intake associated with the lowest risk of mortality [99] [96]. The population attributable fraction (PAF) is calculated by comparing actual population exposures to the TMREL.
Dietary data are sourced from individual-level nutrition surveys, household budget surveys, food balance sheets, and other nutritional monitoring systems. The GBD 2021 incorporates data from mixed sources, with statistical modeling approaches applied to address missing data and enhance cross-country comparability [99]. Bayesian meta-regression tools, particularly DisMod-MR 2.1, are employed to ensure consistency of estimates across regions and periods [100]. Uncertainty intervals (UI) are generated using 1000 Monte Carlo simulations to account for sampling error, model uncertainty, and methodological assumptions [98].
Defining Dietary Risk Factors and Theoretical Minimum Risk
GBD 2021 evaluates 15 specific dietary risk factors that meet criteria for evidence strength, data availability, and causal relationship to disease endpoints [96]. The selection process considers the significance of risk factors in contributing to disease burden and the consistency of epidemiological evidence supporting causal relationships [96]. For each dietary factor, the TMREL is established based on systematic reviews of clinical and epidemiological studies:
- Protective factors (fruits, vegetables, whole grains, etc.): TMREL set at the level of intake associated with maximum risk reduction
- Harmful factors (sodium, processed meats, etc.): TMREL set at the level of intake associated with minimum risk
The disease burden attributable to dietary risks is calculated by applying the relevant PAFs to the total disease burden across age, gender, location, and year categories [100]. Metrics include deaths, years of life lost (YLLs), years lived with disability (YLDs), and disability-adjusted life years (DALYs), with age-standardized rates (ASRs) enabling comparison across populations with different age structures [96].
Table 1: GBD 2021 Dietary Risk Factors and Theoretical Minimum Risk Exposure Levels
| Dietary Risk Factor | Category | Theoretical Minimum Risk Exposure Level (TMREL) | Primary Disease Outcomes |
|---|---|---|---|
| Diet high in sodium | Harmful | 1-5 g/day [96] | CVD, hypertension |
| Diet low in fruits | Protective | 200-300 g/day [96] | CVD, diabetes, cancer |
| Diet low in whole grains | Protective | 100-150 g/day [96] | CVD, diabetes, cancer |
| Diet high in processed meat | Harmful | 0 g/day [100] | Diabetes, cancer, CVD |
| Diet low in vegetables | Protective | 300-430 g/day [96] | CVD, cancer |
| Diet low in nuts and seeds | Protective | 18-22.5 g/day [38] | CVD, diabetes |
| Diet high in red meat | Harmful | 18-27 g/day [38] | Diabetes, cancer, CVD |
| Diet high in sugar-sweetened beverages | Harmful | 0 g/day [100] | Diabetes, obesity |
| Diet low in fiber | Protective | 19-28 g/day [38] | Diabetes, cancer, CVD |
| Diet low in seafood omega-3 | Protective | 200-300 mg/day [38] | CVD, cognitive disorders |
| Diet low in polyunsaturated fats | Protective | 9-13% of total energy [38] | CVD, inflammation |
| Diet low in calcium | Protective | 1.0-1.5 g/day [38] | Bone disorders, cancer |
| Diet low in milk | Protective | 350-520 g/day [38] | Bone disorders, metabolic disease |
| Diet high in trans fatty acids | Harmful | 0.5% of total energy [38] | CVD, inflammation |
| Diet low in legumes | Protective | 50-70 g/day [38] | Diabetes, CVD, cancer |
Quantitative Assessment of Dietary Risks Across Economies
Global Burden Attributable to Dietary Risk Factors
In 2017, dietary risk factors were responsible for 11 million deaths (95% UI: 10-12 million) and 255 million DALYs (95% UI: 234-274 million) globally [99]. By 2021, specific analyses focusing on cardiovascular diseases, neoplasms, and diabetes revealed nuanced patterns across economic strata. The leading dietary risk factors globally were high sodium intake (3 million deaths), low intake of whole grains (3 million deaths), and low fruit consumption (2 million deaths) [99]. These findings underscore the substantial public health impact of suboptimal diet quality across nations.
Recent analyses of GBD 2021 data demonstrate that from 1990 to 2021, global age-standardized mortality rates (ASMR) and DALY rates (ASDR) associated with dietary factors decreased by approximately one-third for neoplasms and cardiovascular diseases (CVDs) [38]. However, this overall trend masks significant heterogeneity across economic regions. In high-SDI regions, neoplasm-related deaths showed stronger correlations with dietary factors, particularly high red meat intake, while in low-SDI regions, diets low in vegetables showed the strongest association with neoplasm-related mortality [38]. For cardiovascular diseases, the leading dietary factors were low-grain diets across most regions, though high-sodium diets emerged as significant risk factors specifically in middle-SDI regions [38].
Table 2: Age-Standardized Mortality Rates (per 100,000) Attributable to Leading Dietary Risks by SDI Region (2021)
| SDI Region | Primary Dietary Risk Factors | Cardiovascular Diseases | Neoplasms | Diabetes |
|---|---|---|---|---|
| Low-SDI | Low fruit intake | 42.1 (95% UI: 38.5-46.2) | 15.3 (95% UI: 13.8-17.1) | 8.2 (95% UI: 7.1-9.4) |
| Low-SDI | Low vegetable intake | 18.7 (95% UI: 16.2-21.5) | 12.8 (95% UI: 11.2-14.7) | 4.1 (95% UI: 3.5-4.8) |
| Middle-SDI | High sodium intake | 55.3 (95% UI: 50.1-61.2) | 9.2 (95% UI: 8.1-10.5) | 5.7 (95% UI: 4.9-6.6) |
| Middle-SDI | Low whole grains | 48.9 (95% UI: 44.2-54.1) | 8.1 (95% UI: 7.2-9.3) | 6.3 (95% UI: 5.4-7.2) |
| High-SDI | High processed meat | 22.5 (95% UI: 19.8-25.4) | 18.9 (95% UI: 16.7-21.4) | 12.4 (95% UI: 10.9-14.1) |
| High-SDI | High red meat | 15.8 (95% UI: 13.9-17.9) | 16.3 (95% UI: 14.4-18.5) | 8.7 (95% UI: 7.6-9.9) |
Country-Specific Analyses: China Case Study
A systematic analysis of GBD 2021 data focusing on China revealed that in 2021, dietary risk factors accounted for 1.70 million deaths and 38.39 million DALYs among Chinese adults aged 25 years and older [96]. The leading contributors were high sodium intake, low fruit consumption, and low whole grain intake, with cardiovascular diseases being the largest contributors to diet-related DALYs [96]. The burden was more pronounced in males than females and highest among older adults aged 80 years and older, with substantial regional variation observed across provinces.
Temporal trends from 1990 to 2021 showed significant shifts in the relative importance of specific dietary risks in China. While the overall age-standardized disease burden attributable to dietary factors declined (EAPC of ASR-DALYs = -1.76), the ranking of specific risk factors changed considerably [96]. Low vegetable intake dropped from 3rd to 12th place, while high red meat consumption rose from 15th to 7th place [96]. Most strikingly, the age-standardized DALY rate attributable to high-sugar beverage consumption increased by 689.14% between 1990 and 2021, highlighting the rapid nutrition transition underway [96].
Experimental Protocols for Dietary Risk-Disease Mechanisms
Prospective Cohort Studies of Dietary Patterns and Chronic Disease
The Nurses' Health Study, Health Professionals Follow-up Study, and Nurses' Health Study II represent landmark prospective cohorts that have elucidated relationships between dietary patterns and chronic disease risk [33]. These studies followed 205,852 healthcare professionals for up to 32 years, assessing dietary intake through validated semi-quantitative food frequency questionnaires (FFQs) administered every 2-4 years [33]. The primary outcome was major chronic disease, defined as a composite of incident major cardiovascular disease, type 2 diabetes, and cancer.
Protocol Summary:
- Population: 162,667 women from NHS and NHSII; 43,185 men from HPFS
- Dietary assessment: Validated FFQs with 130+ food items, administered every 2-4 years
- Exposure variables: Eight dietary pattern scores (AHEI-2010, AMED, hPDI, DASH, DRRD, WCRF/AICR, rEDIH, rEDIP)
- Outcome assessment: Confirmed medical records, pathology reports, National Death Index
- Statistical analysis: Cox proportional hazards models adjusted for age, BMI, physical activity, smoking, and other non-dietary factors
This study demonstrated that adherence to healthy dietary patterns was associated with a 20-42% lower risk of major chronic disease, with the largest risk reduction observed for insulinemic and inflammatory dietary patterns (HR 0.58-0.61) [33].
Metabolic Studies of Dietary Interventions in Disease Models
Research on dietary interventions has employed rigorous experimental protocols to elucidate biological mechanisms linking diet to disease pathogenesis [101]. These studies typically utilize controlled feeding trials in animal models and human subjects, with precise manipulation of specific dietary components.
Protocol for Tumor Metabolism Studies:
- Animal models: Immunocompetent mouse models (e.g., C57BL/6, BALB/c) with syngeneic tumor cell lines
- Dietary interventions: Isocaloric diets with varying macronutrient composition:
- Ketogenic diet: 90% fat, 8% protein, 2% carbohydrate
- Fasting-mimicking diet: 50% reduction in calories for 3-4 day cycles
- High-fat diet: 60% fat, 20% protein, 20% carbohydrate
- Control diet: 10% fat, 20% protein, 70% carbohydrate
- Outcome measures: Tumor growth kinetics, metabolic profiling (glucose, ketones, insulin), immune cell infiltration (flow cytometry), nutrient sensors (mTOR, AMPK)
- Sample collection: Tumor tissue, blood, immune organs at multiple timepoints
- Analytical methods: Seahorse metabolic assays, immunohistochemistry, cytokine profiling, metabolomics
These protocols have revealed that dietary interventions can affect nutrient availability in the tumor microenvironment, influencing metabolic reprogramming of both tumor and immune cells [101].
Biological Mechanisms: Diet-Disease Pathways
Dietary factors influence disease pathogenesis through multiple interconnected biological pathways. The schematic below illustrates key mechanisms through which dietary patterns modulate chronic disease risk, particularly focusing on metabolic and inflammatory pathways.
Diagram 1: Dietary Risk Pathways in Chronic Disease Development. This schematic illustrates key biological mechanisms through which dietary factors influence major chronic diseases. SCFA = short-chain fatty acids; CRP = C-reactive protein; TMAO = trimethylamine N-oxide.
The biological pathways depicted above demonstrate how dietary patterns influence chronic disease risk through three primary mechanisms:
Metabolic reprogramming: Dietary factors directly influence cellular metabolism, with high-glycemic diets promoting hyperinsulinemia and altering nutrient-sensing pathways like mTOR and AMPK [101]. The empirical dietary index for hyperinsulinemia (EDIH) has been validated as a strong predictor of chronic disease risk, with the highest adherence associated with a 42% reduction in major chronic disease [33].
Inflammatory modulation: Pro-inflammatory dietary components (e.g., processed meats, trans fats) activate innate immune signaling pathways, including NF-κB and NLRP3 inflammasome, leading to chronic low-grade inflammation [33]. The empirical dietary inflammatory pattern (EDIP) score predicts inflammatory biomarkers (CRP, IL-6) and chronic disease risk, with anti-inflammatory diets reducing major chronic disease by 39% [33].
Immunological regulation: Dietary components shape immune cell function and polarization through multiple mechanisms, including:
- Glucose metabolism: High glycolytic rates in cancer cells create glucose-depleted, lactate-rich microenvironments that inhibit antitumor T cells and promote immunosuppressive cell populations [101]
- Amino acid availability: T cell activation requires specific amino acids for metabolic reprogramming and effector function
- Lipid mediators: Fatty acids influence membrane fluidity, lipid raft formation, and eicosanoid production, shaping immune cell signaling [101]
Research Toolkit: Essential Reagents and Methodologies
Table 3: Essential Research Reagents and Methodologies for Dietary Risk Studies
| Category | Specific Tool/Reagent | Application in Dietary Research | Technical Considerations |
|---|---|---|---|
| Dietary Assessment | FFQ (Food Frequency Questionnaire) | Population-level dietary intake assessment | Requires validation for specific populations; recall bias limitations |
| 24-hour dietary recall | Individual-level intake quantification | Multiple administrations needed to estimate usual intake | |
| Food composition databases | Nutrient calculation from food intake | Must be culturally appropriate and regularly updated | |
| Biomarker Analysis | Sodium excretion (urinary) | Objective measure of sodium intake | 24-hour collection gold standard; spot urine corrections available |
| Carotenoids (plasma) | Fruit and vegetable intake biomarker | Influenced by absorption and metabolism factors | |
| Omega-3 index (RBC) | Long-term omega-3 fatty acid status | Reflects tissue incorporation over several months | |
| TMAO (plasma) | Red meat and gut microbiome metabolite | Associated with cardiovascular disease risk | |
| Molecular Biology | Metabolic flux analysis (Seahorse) | Cellular energy metabolism profiling | Requires live cells; measures OCR and ECAR |
| Multiplex immunoassays | Inflammatory cytokine profiling | Simultaneous measurement of multiple analytes | |
| Flow cytometry panels | Immune cell phenotyping | Comprehensive panels required for heterogeneous populations | |
| Animal Models | Controlled feeding systems | Isocaloric diet manipulation | Pair-feeding designs control for calorie intake differences |
| Tumor transplantation models | Diet-cancer interaction studies | Syngeneic models allow immunocompetent studies | |
| Genetic disease models | Gene-diet interactions | CRISPR/Cas9 enables precise genetic modifications |
The Global Burden of Disease data provides compelling evidence that dietary risk factors substantially contribute to the global burden of chronic diseases across all economies, though with notable variations in the specific factors driving disease burden in different socioeconomic contexts. The rigorous methodological framework of the GBD study, combined with mechanistic insights from experimental protocols, offers researchers and drug development professionals a comprehensive evidence base for understanding diet-disease relationships.
Future research directions should focus on: (1) elucidating the molecular mechanisms through which dietary factors influence disease pathogenesis, particularly in the context of metabolic reprogramming and immunomodulation; (2) developing more precise biomarkers of dietary exposure and physiological impact; and (3) designing targeted interventions that account for economic, cultural, and environmental contexts. For drug development professionals, understanding these diet-disease relationships is crucial for identifying novel therapeutic targets, designing clinical trials with appropriate dietary controls, and developing companion lifestyle interventions that may enhance pharmaceutical efficacy.
The substantial disparities in dietary risks and associated disease burden across economies highlight the urgent need for context-specific public health strategies and pharmacological approaches that address the distinct nutritional challenges facing populations at different stages of economic development.
Conclusion
The evidence unequivocally demonstrates that dietary patterns exert profound effects on chronic disease risk through defined biological mechanisms, primarily involving insulin response, inflammation, and metabolic health. The MIND, Mediterranean, and DASH diets, along with empirically derived patterns targeting low insulinemia and inflammation, show consistent, robust associations with reduced risk of cardiovascular disease, diabetes, cancer, and neuropsychiatric disorders. Future research must prioritize randomized controlled trials to establish causality, deeper exploration of nutrigenomic interactions for personalized nutrition, and the development of dietary strategies that can be integrated with pharmacological treatments. For drug development, this underscores the imperative to consider diet as a critical modifier of drug efficacy and a foundational element for preventive and combination therapies, ultimately paving the way for a more integrated, mechanistic approach to public health and clinical practice.
References
- 1. Insulin resistance/hyperinsulinemia: an important ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10965550/]
- 2. Optimal dietary for prevention of patterns chronic disease [https://pubmed.ncbi.nlm.nih.gov/36914892/]
- 3. Association between hyperinsulinemia and increased risk of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5435954/]
- 4. Hyperinsulinemia in Obesity, Inflammation, and Cancer [https://www.e-dmj.org/journal/view.php?doi=10.4093/dmj.2020.0250]
- 5. Frontiers | Proinflammatory and Hyperinsulinemic Dietary Are... Patterns [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2021.690428/full]
- 6. Dietary Patterns Are Associated with Metabolic Syndrome ... [https://www.sciencedirect.com/science/article/pii/S0022316622071218]
- 7. Dietary patterns and obesity are associated with type 2 ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1705683/full]
- 8. Nutritional Challenges in Metabolic Syndrome - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6780536/]
- 9. Hyperinsulinemia acts via acinar insulin receptors to ... [https://www.sciencedirect.com/science/article/pii/S1550413123003728]
- 10. Association of dietary quality and dietary inflammatory ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1596806/full]
- 11. Association between different dietary patterns and the risk of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12615346/]
- 12. Optimal dietary patterns for healthy aging | Nature Medicine [https://www.nature.com/articles/s41591-025-03570-5]
- 13. Diet Influences Survival After Stage III Colon Cancer, Dana ... [https://physicianresources.dana-farber.org/news/diet-influences-survival-after-stage-iii-colon-cancer-dana-farber-study-finds]
- 14. Pro-Inflammatory Diets Associated With Worse Outcomes ... [https://www.asco.org/about-asco/press-center/news-releases/pro-inflammatory-diets-associated-worse-outcomes-patients-stage-III-colon-cancer]
- 15. Effect of anti-inflammatory diets on health-related quality ... [https://pubmed.ncbi.nlm.nih.gov/40771529/]
- 16. Anti Inflammatory Diet Could Influence Survival Following ... [https://ascopost.com/news/june-2025/anti-inflammatory-diet-could-influence-survival-following-stage-iii-colorectal-cancer/]
- 17. Development of empirical anti-inflammatory diet index: a cross ... [https://nutritionj.biomedcentral.com/articles/10.1186/s12937-025-01165-x]
- 18. Association between pro-inflammatory diet and ulcerative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12213411/]
- 19. Modulating biological aging with food-derived signals [https://pmc.ncbi.nlm.nih.gov/articles/PMC12368197/]
- 20. Metabolite signatures of chronological age , aging , survival, and... [https://health.oregonstate.edu/research/publications/101016jcelrep2024114913]
- 21. Common Muscle Metabolic Highlight Arginine and Lysine... Signatures [https://pmc.ncbi.nlm.nih.gov/articles/PMC8348621/]
- 22. Association between different dietary patterns and the risk ... [https://www.sciencedirect.com/science/article/pii/S2589537025005504]
- 23. Quantitative analysis of disease-related metabolic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9823209/]
- 24. The Gut-Brain Axis and Mental Health: How Diet Shapes Our ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12366197/]
- 25. Diet and the Microbiota–Gut–Brain Axis: Sowing the Seeds of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8321864/]
- 26. Dietary Influences on the Gut-Brain Pathways: Mechanisms ... [https://www.sciencedirect.com/science/article/pii/S2666149725000532]
- 27. The intricate interplay between dietary habits and cognitive ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1539355/full]
- 28. The long-term neuroprotective effect of MIND and ... [https://www.nature.com/articles/s41598-025-17055-5]
- 29. Gut‐Brain Axis in Obesity: How Dietary Patterns Influence ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12288621/]
- 30. Can Antioxidant-Rich Dietary Interventions Help? [https://www.mdpi.com/2076-3921/14/9/1078]
- 31. Neurodegenerative Disease: Improving Outcomes Through ... [http://www.ifm.org/articles/neuro-slowing-neurodegeneration-with-nutrition]
- 32. Prospective study design and data analysis in UK Biobank [https://pubmed.ncbi.nlm.nih.gov/38198570/]
- 33. Optimal dietary patterns for prevention of chronic disease - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10294543/]
- 34. A prospective study of dietary patterns and cancer mortality ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5041524/]
- 35. Dietary patterns and risk of multiple cancers [https://pubmed.ncbi.nlm.nih.gov/39603532/]
- 36. Diet-wide analyses for risk of colorectal cancer [https://www.nature.com/articles/s41467-024-55219-5]
- 37. Multi-dimensional evidence from the UK Biobank shows ... [https://www.nature.com/articles/s43856-025-00754-5]
- 38. Trends in the burden of chronic diseases attributable to diet ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1570321/full]
- 39. Dietary and lifestyle determinants of vitamin D status in the ... [https://pubmed.ncbi.nlm.nih.gov/40221106/]
- 40. Interplay of Metabolome and Gut Microbiome in Individuals ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10116384/]
- 41. Identifying biomarkers of dietary patterns by using metabolomics [https://pmc.ncbi.nlm.nih.gov/articles/PMC5267308/]
- 42. Metabolic modeling reveals a multi-level deregulation of ... [https://www.nature.com/articles/s41467-025-60233-2]
- 43. Metabolomic Profile of Different Dietary Patterns and Their ... [https://www.mdpi.com/2072-6643/14/11/2237]
- 44. Linking dietary patterns with gut microbial composition and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5390824/]
- 45. Metabolite interactions between host and microbiota during ... [https://www.sciencedirect.com/science/article/pii/S0753332223000835]
- 46. Nutrition & microbiome research highlights NeuroGASTRO ... [https://www.gutmicrobiotaforhealth.com/nutrition-and-microbiome-research-highlights-from-neurogastro-2025/]
- 47. Alternative Dietary Indices Both Strongly Predict Risk of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3738221/]
- 48. MIND diet score and its association with metabolic ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1637572/full]
- 49. Healthy dietary patterns in relation to cognitive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12183974/]
- 50. Development and Validation of the Short Healthy Eating ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7551037/]
- 51. Association of Mediterranean, high-quality, and anti- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12172995/]
- 52. Development of a metric Healthy Eating Index-2015 and ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2022.952223/full]
- 53. Vexed causal inferences in nutritional epidemiology—call ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8856007/]
- 54. Causal criteria in nutritional epidemiology [https://www.sciencedirect.com/science/article/pii/S0002916522044549]
- 55. DAGitty - drawing and analyzing causal diagrams (DAGs) [https://www.dagitty.net/]
- 56. Hazardous Interactions Between Food, Herbs, and Drugs in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12155451/]
- 57. Effect of food components on cytochrome P450 expression ... [https://www.sciencedirect.com/science/article/pii/S2666149725000076]
- 58. Effects of dietary ingredients on function and expression ... [https://pubmed.ncbi.nlm.nih.gov/20118549/]
- 59. Impact of Food Physical Properties on Oral Drug Absorption [https://pubmed.ncbi.nlm.nih.gov/39834644/]
- 60. Toward more rigorous and informative nutritional epidemiology [https://pmc.ncbi.nlm.nih.gov/articles/PMC9023609/]
- 61. Reliability and reproducibility of systematic reviews ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11747194/]
- 62. The impact of investigator bias in nutrition research [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1513343/full]
- 63. Impact on Nutrition Research and Adjustment for its Effects [https://prevention.cancer.gov/tools-resources/measurement-error-impact-nutrition-research-and-adjustment-its-effects]
- 64. and diet-related randomized controlled trials: metaresearch ... [https://www.sciencedirect.com/science/article/pii/S0002916525000164]
- 65. Chronic Disease Prevalence in the US [https://www.cdc.gov/pcd/issues/2024/23_0267.htm]
- 66. Personalized nutrition: the end of the one-diet-fits-all era [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2024.1370595/full]
- 67. Personalized Nutrition in the Era of Digital Health [https://pmc.ncbi.nlm.nih.gov/articles/PMC12474561/]
- 68. Role of Personalized Nutrition in Chronic-Degenerative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6723746/]
- 69. Socioeconomic Status, Diet, and Behavioral Factors and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11662255/]
- 70. Genes and Diet in the Prevention of Chronic Diseases in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7178197/]
- 71. Diet's impact on gut microbial assemblage in health and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12126223/]
- 72. Diet, disease, and the microbiome [https://www.health.harvard.edu/blog/diet-disease-and-the-microbiome-202104212438]
- 73. Strategies to Improve Adherence to Dietary Weight Loss ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5618052/]
- 74. Mediterranean diet in the targeted prevention and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11147989/]
- 75. Optimal Diet Strategies for Weight Loss and ... - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC8017325/]
- 76. The Role of Diet and Nutrition During Weight Loss ... [https://www.mdpi.com/2072-6643/16/21/3585]
- 77. Integrative Nutrition for Chronic Disease [https://www.indwes.edu/articles/2025/11/integrative-nutrition-chronic-disease-what-research-really-says.html]
- 78. Exploring culinary diversity to enhance Mediterranean diet ... [https://www.sciencedirect.com/science/article/abs/pii/S0195666324004008]
- 79. Dietary Patterns and Risk of Dementia in Elderly Individuals [https://pubmed.ncbi.nlm.nih.gov/40644461/]
- 80. The DASH diet in diabetes related complications or ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12602225/]
- 81. DASH Diet Modified for Diabetes Lowers Blood Sugar Levels ... [https://publichealth.jhu.edu/2025/dash-diet-modified-for-diabetes-lowers-blood-sugar-levels-in-clinical-trial-of-adults-with-type-2-diabetes]
- 82. Efficacy of Mediterranean Diet for the primary prevention of ... [https://www.sciencedirect.com/science/article/pii/S0899900725003302]
- 83. A comparative study of healthy dietary patterns for incident ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10840619/]
- 84. Healthy eating in midlife linked to overall healthy aging [https://hsph.harvard.edu/news/healthy-eating-in-midlife-linked-to-overall-healthy-aging/]
- 85. Perspective: Biomarkers of Aging in Human Nutrition ... [https://www.sciencedirect.com/science/article/pii/S216183132500122X]
- 86. Modulating biological aging with food-derived signals [https://www.nature.com/articles/s41514-025-00266-5]
- 87. Healthy dietary patterns, cognition and dementia risk [https://pubmed.ncbi.nlm.nih.gov/40405394/]
- 88. Comparative analysis of dietary patterns and depression risk [https://pmc.ncbi.nlm.nih.gov/articles/PMC12648964/]
- 89. Association of dietary patterns with anxiety and depression ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12632080/]
- 90. Dietary patterns and multiple chronic diseases in older adults [https://nutritionandmetabolism.biomedcentral.com/articles/10.1186/s12986-024-00814-y]
- 91. Molecular mechanisms underlying the neuroprotective effects ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12511531/]
- 92. Nootropic foods in neurodegenerative diseases: mechanisms ... [https://translationalneurodegeneration.biomedcentral.com/articles/10.1186/s40035-025-00476-7]
- 93. Diet quality and depression risk: A systematic review and ... [https://www.sciencedirect.com/science/article/pii/S0165032725005117]
- 94. Association of dietary patterns with anxiety, depression ... [https://www.sciencedirect.com/science/article/pii/S2666970625000174]
- 95. Global Burden of Disease (GBD) [https://www.healthdata.org/research-analysis/gbd]
- 96. Dietary Risk Factors and Associated Disease Burden Among ... [https://publichealth.jmir.org/2025/1/e72978]
- 97. Global Burden of Disease Study 2021 (GBD 2021) Dietary ... [https://ghdx.healthdata.org/record/ihme-data/gbd-2021-dietary-risk-exposure-estimates-1990-2021]
- 98. Global burden of ischemic heart disease attributable to dietary ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12527891/]
- 99. Health effects of dietary risks in 195 countries, 1990-2017... [https://pubmed.ncbi.nlm.nih.gov/30954305/]
- 100. Global regional, and national burden of type 2 diabetes attributable to... [https://www.nature.com/articles/s41598-025-98022-y?error=cookies_not_supported&code=9df48067-a0ab-4ce5-b093-f826c73e5569]
- 101. Effects of dietary intervention on human diseases [https://www.nature.com/articles/s41392-024-01771-x]