Statistical Adjustment for Total Energy Intake: A Foundational Guide for Robust Nutritional Epidemiology and Clinical Research
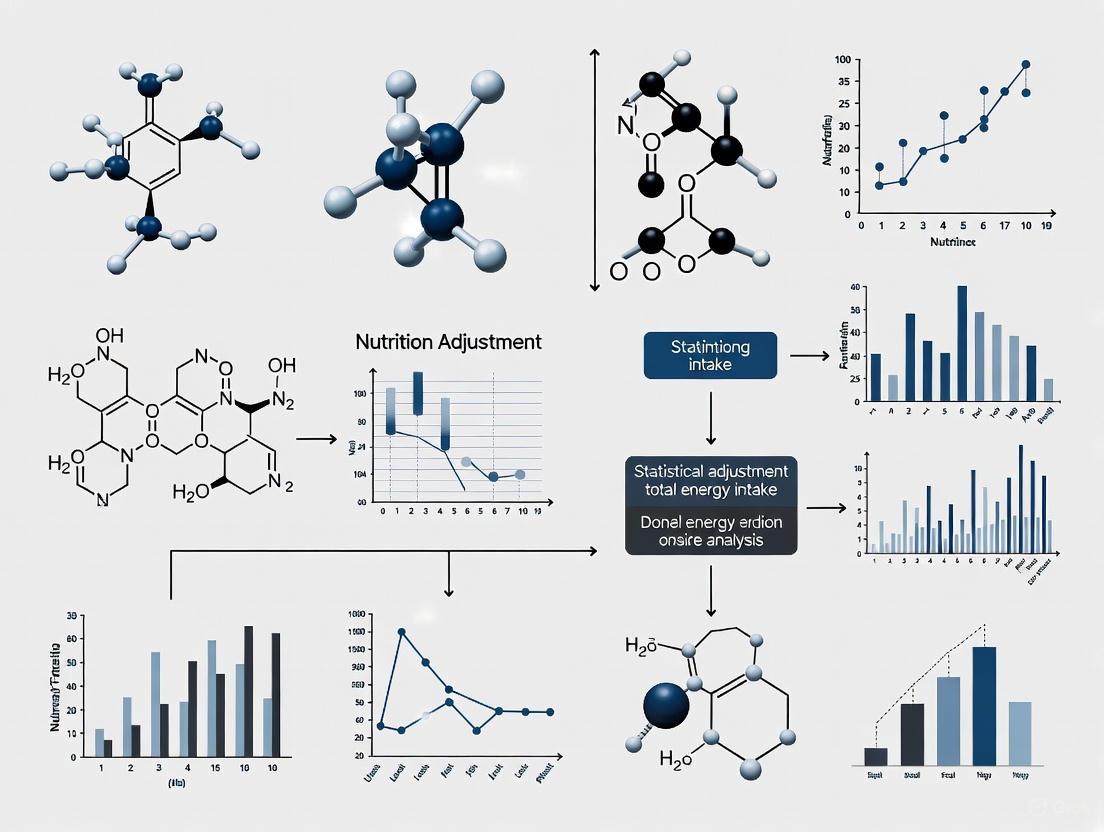
This article provides a comprehensive guide to the statistical adjustment of total energy intake, a critical methodological step for researchers and drug development professionals.
Statistical Adjustment for Total Energy Intake: A Foundational Guide for Robust Nutritional Epidemiology and Clinical Research
Abstract
This article provides a comprehensive guide to the statistical adjustment of total energy intake, a critical methodological step for researchers and drug development professionals. It covers the foundational rationale for energy adjustment to control for confounding and reduce extraneous variation in diet-disease association studies. The content explores established and novel methodological approaches, including the nutrient density and residual methods, and delves into troubleshooting pervasive issues like dietary misreporting, offering strategies for identification and correction using tools like the Goldberg cut-offs and doubly labeled water. Finally, it reviews validation techniques and comparative frameworks to assess the performance of different adjustment methods, equipping scientists with the knowledge to enhance the validity and reliability of their nutritional analyses.
Why Energy Adjustment is Non-Negotiable in Nutritional Research
Frequently Asked Questions (FAQs)
Q1: Why is adjusting for total energy intake so critical in nutritional research?
Failure to account for total energy intake can obscure true associations between nutrients and disease risk or even reverse the direction of an association. This is because intakes of most specific nutrients are correlated with total energy intake, creating confounding. Proper adjustment controls for this confounding, reduces extraneous variation, and helps predict the effect of realistic dietary interventions [1].
Q2: What are the primary methods for energy adjustment, and how do I choose?
Researchers commonly use four models, each with a different target estimand (the quantity being estimated). The choice depends on your specific research question [2].
The table below summarizes the core characteristics of each model:
| Model Name | Core Adjustment Method | Target Estimand | Key Interpretation |
|---|---|---|---|
| Standard Model | Includes both the nutrient and total energy intake as covariates. | Average Relative Causal Effect | Estimates the effect of substituting the nutrient for the weighted average of all other energy sources. |
| Energy Partition Model | Includes the nutrient and the energy from all other sources. | Total Causal Effect | Estimates the effect of adding the nutrient while holding all other energy sources constant. |
| Nutrient Density Model | Expresses the nutrient as a proportion of total energy (e.g., % of calories). | Obscure / Rescaled Relative Effect | Attempts to estimate a relative effect, but its interpretation is not straightforward. |
| Residual Model | Uses the residuals from a regression of the nutrient on total energy intake. | Average Relative Causal Effect | Mathematically identical to the Standard Model; it indirectly adjusts for total energy. |
Q3: My model is adjusted for total energy, but I still suspect confounding. Why?
This is a common limitation. Adjusting for a summary variable like total energy only partially accounts for confounding if the other individual dietary components have distinct effects on the outcome. This can introduce "composite variable bias." A more robust solution is the "all-components model," which simultaneously adjusts for all major dietary components. This approach can provide less biased estimates of both total and relative causal effects [2].
Q4: How can errors in measuring energy intake affect my results?
Energy intake is notoriously difficult to measure accurately. Dietary surveys, like 24-hour recalls, are often prone to substantial misreporting and tend to underestimate actual calorie intake [3]. This misreporting can introduce significant uncertainty and bias into your analysis, affecting the consistency and comparability of dietary assessment [3].
Troubleshooting Guides
Problem: Conflicting results between studies using different adjustment models.
Solution: This is often not a true conflict but a consequence of different models answering different questions.
- Diagnose the Cause: Identify the energy adjustment model used in each study. The Standard and Energy Partition models estimate different effects (substitution vs. addition) and should not be directly compared [2].
- Apply the Correct Interpretation: Refer to the table in FAQ A2. A study using the Standard Model answers: "What is the effect of increasing nutrient A while decreasing the average of all other nutrients to keep total energy constant?" A study using the Energy Partition Model answers: "What is the effect of adding more of nutrient A to the diet without changing anything else?" [2].
- Prevent in Meta-Analyses: When conducting systematic reviews or meta-analyses, ensure you do not inappropripool estimates from studies that used different models, as this can create the appearance of heterogeneity where none exists [2].
Problem: Determining the most accurate method to estimate energy requirements.
Solution: For population-level studies, consider moving beyond outdated factorial methods.
- Recommended Method: Use predictive equations for estimating energy requirements (EERs) derived from a comprehensive database of doubly labeled water (DLW) studies. The equations developed by the US National Academies of Sciences (2023) are considered current best practice [3].
- Implementation: These equations are differentiated by age, sex, and physical activity level and are dependent on age, height, and weight. Pair them with anthropometric data (body weight, height) to estimate energy requirements [3].
- Validation: This method has been validated against external DLW data and provides a proxy for energy intake that reflects observed anthropometric measures, bypassing some of the misreporting issues in dietary surveys [3].
The Scientist's Toolkit: Essential Reagents & Materials
The following table lists key components for a rigorous study investigating diet-disease relationships.
| Item | Function in Research |
|---|---|
| Validated Dietary Assessment Tool | To measure the exposure (e.g., 24-hour recalls, Food Frequency Questionnaires). Essential for collecting data on nutrient intake and total energy. |
| Doubly Labeled Water (DLW) | The gold-standard method for objectively measuring total energy expenditure in free-living individuals, used to validate energy intake data [3]. |
| Anthropometric Measurement Tools | To measure outcomes and confounders (e.g., calibrated scales, stadiometers, DEXA for body composition). Critical for assessing BMI, waist circumference, and fat-free mass [4]. |
| Causal Diagram (DAG) | A conceptual tool to map out hypothesized causal relationships between the nutrient, outcome, total energy, and other confounders. This is crucial for selecting appropriate adjustment variables [2]. |
| "All-Components" Model | A statistical model that simultaneously adjusts for intake of all major dietary components (protein, fat, carbohydrates, etc.) to provide a less biased estimate than models using only total energy [2]. |
Experimental Protocols & Data Presentation
Protocol 1: Assessing Energy Intake, Expenditure, and Balance in a Cohort
This retrospective cross-sectional design can be used to investigate associations between energy balance and health outcomes like obesity [4].
- 1. Participant Recruitment: Select participants using a multistage random sampling technique to ensure representativeness. Exclude pregnant or lactating individuals and those unable to provide consent [4].
- 2. Data Collection:
- Energy Intake: Collect dietary data via multiple, non-consecutive 24-hour dietary recalls. Calculate total energy and nutrient intake using a standardized food composition database [4].
- Anthropometry: Measure weight, height, and waist circumference using calibrated equipment following a strict protocol to calculate Body Mass Index (BMI) and identify abdominal obesity [4].
- Energy Expenditure: Calculate Total Energy Expenditure (TEE) as the sum of:
- Resting Energy Expenditure (REE): Estimate using predictive equations.
- Energy Expenditure of Activity (EEA): Assess using the WHO Global Physical Activity Questionnaire or accelerometers.
- Diet-Induced Thermogenesis: Typically estimated as a percentage (e.g., ~10%) of TEE [4].
- 3. Data Analysis:
- Calculate Energy Balance as:
Energy Intake - Total Energy Expenditure. - Use t-tests and ANOVA to compare numerical variables across groups.
- Employ logistic regression to evaluate factors associated with a positive energy balance [4].
- Calculate Energy Balance as:
Quantitative Data on Energy Intake and Imbalance
The following table summarizes key findings from recent global and cohort studies to provide context for expected values.
| Parameter | Study Population | Value (Mean ± SD or as stated) | Notes |
|---|---|---|---|
| Global Avg. Energy Intake (2020) | Global Population | 2160 kcal/day (95% CI: 2100 to 2210) | Estimated via anthropometric measures [3]. |
| Global Avg. Energy Imbalance (2020) | Global Population | +80 kcal/day (95% CI: 70 to 100) | Intake above requirements for healthy body weight [3]. |
| Total Energy Intake | Nigerian Young Adults (n=240) | 2416.0 ± 722.7 kcal/day [4] | |
| Total Energy Expenditure | Nigerian Young Adults (n=240) | 2195.5 ± 384.5 kcal/day [4] | |
| Resulting Energy Balance | Nigerian Young Adults (n=240) | +220.5 ± 787.3 kcal/day [4] | 68.8% of participants had a positive balance [4]. |
| Energy Balance with Obesity | Nigerian Adults with Obesity | +302.0 ± 1300.2 kcal/day [4] | Significantly higher than those without obesity. |
Model Relationships and Causal Pathways
Causal Diagram of Dietary Composition
Energy Adjustment Model Workflow
Troubleshooting Guides
Guide 1: Addressing Bias in Energy Intake Analysis
Problem: Inconsistent effect estimates for nutrient-outcome relationships across different statistical models.
Explanation: In nutritional research, individual dietary components are parts of a compositional whole. Total energy intake is a collider variable, meaning it is causally influenced by both your nutrient of interest and all other nutrients. Adjusting for it in statistical models can induce spurious associations if not handled properly [2].
Solution: Use the "all-components model" that simultaneously adjusts for all other dietary components instead of relying solely on total energy intake. This approach provides less biased estimates of both total and average relative causal effects [2].
Steps:
- Collect data on all major dietary components, not just your nutrient of interest
- In your regression model, include all dietary components simultaneously
- Avoid adjusting only for total energy intake, which creates collider bias
- Use directed acyclic graphs (DAGs) to map hypothesized causal relationships before analysis
Guide 2: Controlling for Extraneous Variation in Experimental Outcomes
Problem: Unmeasured variables affecting both your independent and dependent variables.
Explanation: Extraneous variables are any variables you're not investigating that can potentially affect your research outcomes. When these variables are associated with both your exposure and outcome, they become confounding variables that provide alternative explanations for your results [5].
Solution: Implement multiple control strategies at both design and analysis stages.
Steps:
- Randomization: Randomly assign participants to experimental conditions to evenly distribute extraneous variables [6]
- Elimination: Hold variables constant throughout the study (e.g., standardize laboratory conditions, use identical measurement protocols) [6]
- Statistical Control: Measure and adjust for extraneous variables in your analysis using regression or ANCOVA [5]
- Matching: Match participants across groups based on key extraneous variables
Guide 3: Forecasting Causal Effects from Observational Data
Problem: Needing to predict intervention effects without conducting randomized trials.
Explanation: Under certain conditions, longitudinal observational studies can forecast causal effects of hypothetical interventions using structural equation modeling and DAG-based approaches, even when the intervention hasn't been implemented [7].
Solution: Use cross-lagged panel models with proper causal identification assumptions.
Steps:
- Collect longitudinal data with multiple pre-intervention time points
- Specify a DAG representing your causal theory
- Use structural equation modeling to estimate parameters
- Apply the do-operator or related methods to simulate interventions
- Forecast post-intervention outcomes using the estimated model parameters
Frequently Asked Questions
Q: What's the difference between extraneous and confounding variables?
A: An extraneous variable is any variable you're not investigating that can potentially affect your dependent variable. A confounding variable is a specific type of extraneous variable that is associated with both your independent and dependent variables, creating spurious associations [5].
Q: Which energy adjustment method should I use in nutritional epidemiology?
A: Current research suggests the "all-components model" that simultaneously adjusts for all dietary components outperforms traditional approaches. The four common models estimate different causal quantities [2]:
- Standard model: Average relative causal effect (substitution effect)
- Energy partition model: Total causal effect
- Nutrient density model: Obscure interpretation attempting relative effect
- Residual model: Mathematically identical to standard model
Q: How can I distinguish between forecasting intervention effects and predicting outcomes?
A: Forecasting intervention effects involves estimating what would happen if you actively changed a variable, while prediction involves estimating future values under natural progression. Forecasting requires causal assumptions and methods like Pearl's do-calculus, while prediction can use purely associative patterns [7].
Q: What are the most effective ways to control extraneous variation?
A: The most effective approaches include [5] [6]:
- Randomization (balances all potential extraneous variables)
- Elimination (holding variables constant)
- Statistical control (measuring and adjusting in analysis)
- Matching (ensuring comparable groups)
- Blinding (reducing experimenter effects and demand characteristics)
Quantitative Data Tables
| Model Type | Target Estimand | Interpretation | Bias in Absence of Confounding | Key Limitation |
|---|---|---|---|---|
| Standard Model | Average relative causal effect | Substitution effect | Biased | Composite variable bias |
| Energy Partition Model | Total causal effect | Additive effect | Unbiased | Residual confounding when other nutrients have distinct effects |
| Nutrient Density Model | Obscure | Attempts relative effect rescaling | Biased | Difficult interpretation |
| Residual Model | Average relative causal effect | Substitution effect | Biased | Mathematically identical to standard model |
| All-Components Model | Total and relative effects | Both additive and substitution | Reduced bias | Requires complete dietary data |
| Control Method | Application Context | Effectiveness | Implementation Complexity | Key Considerations |
|---|---|---|---|---|
| Randomization | Experimental studies | High | Medium | Gold standard but not always ethical or feasible |
| Elimination | All study types | Medium-High | Low | Reduces generalizability |
| Statistical Control | Observational studies | Medium | High | Requires measurement of confounders |
| Matching | Observational studies | Medium | Medium | Can be computationally intensive |
| Blinding | Clinical trials | High | Low | Reduces experimenter and participant bias |
| Restriction | All study types | Medium | Low | Simplifies analysis but reduces sample size |
Experimental Protocols
Protocol 1: Implementing the All-Components Model for Energy Adjustment
Purpose: To estimate unbiased causal effects of individual dietary components on health outcomes.
Methodology:
- Collect dietary intake data for all major nutrient components
- Calculate total energy intake as the sum of all components
- Specify a directed acyclic graph (DAG) representing causal hypotheses
- Fit a multivariate regression model including all dietary components simultaneously:
Outcome ~ β₁Nutrient₁ + β₂Nutrient₂ + ... + βₖNutrientₖ + Covariates + ε - Interpret coefficients as the effect of increasing each nutrient while keeping all others constant
Validation: Test model assumptions including linearity, additivity, and error structure. Check for multicollinearity using variance inflation factors (VIF).
Protocol 2: Cross-Lagged Panel Design for Forecasting Intervention Effects
Purpose: To forecast causal effects of interventions using longitudinal observational data.
Methodology [7]:
- Collect repeated measures of exposure (X) and outcome (Y) variables at multiple time points
- Specify and estimate a cross-lagged panel model:
- Verify model fit using standard indices (CFI > 0.95, RMSEA < 0.06, SRMR < 0.08)
- Use the estimated parameters to forecast effects of hypothetical interventions using the do-operator
- Calculate forecasted mean, variance, and probability of outcomes falling within acceptable ranges
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Causal Inference Studies
| Item | Function | Application Example |
|---|---|---|
| DAGitty Software | Visualize and analyze causal diagrams | Identify minimal sufficient adjustment sets for confounding control |
| Structural Equation Modeling Software | Estimate complex causal models | Implement cross-lagged panel designs for forecasting intervention effects |
| Dietary Assessment Tools | Measure nutritional exposures | Collect comprehensive nutrient data for all-components models |
| Randomized Control Trial Protocols | Gold standard for causal inference | Establish true causal effects for validation of observational methods |
| Sensitivity Analysis Tools | Assess robustness to unmeasured confounding | E-value calculations and simulation-based methods |
| Directed Acyclic Graphs | Formalize causal assumptions | Visualize and test causal hypotheses before analysis |
The Energy-Nutrient-Disease Triad describes the interconnected relationship between chronic low energy availability, its subsequent impact on nutrient metabolism, and the development of multi-system physiological disorders. This framework, evolved from the Female Athlete Triad, now encompasses the broader syndrome known as Relative Energy Deficiency in Sport (REDs) [8] [9]. REDs occurs when an individual's energy intake is insufficient to support the energy expended by exercise, leaving inadequate energy to support the body's normal physiological functions [8]. This energy deficit triggers a cascade of endocrine adaptations that disrupt nutrient absorption and utilization, ultimately leading to impaired bone health, metabolic rate, immunity, and cardiovascular function [8] [10] [9].
Core Components of the Triad
The following diagram illustrates the interconnected, cyclical relationship between the three core components of the Energy-Nutrient-Disease Triad.
Low Energy Availability (LEA)
Low Energy Availability (LEA) is the cornerstone of the triad, defined as the state where dietary energy intake is insufficient to cover the cost of exercise expenditure, leaving inadequate energy to support homeostatic functions [9]. It is calculated as:
Energy Availability (EA) = (Energy Intake (kcal) - Exercise Energy Expenditure (kcal)) / Fat-Free Mass (kg) [9]
Chronic LEA is the primary etiological driver for the development of REDs [11]. An EA below 30 kcal/kg FFM/day is a commonly referenced threshold for LEA, though precise clinical cut-offs are still refined [12].
Nutrient and Metabolic Dysregulation
The body's response to LEA is a down-regulation of metabolic processes to conserve energy. This includes:
- Suppressed Resting Metabolic Rate (RMR): Measured RMR is often significantly lower than predicted values [9] [11].
- Hormonal Alterations: Marked reductions in triiodothyronine (T3), insulin-like growth factor-1 (IGF-1), and leptin, indicating a catabolic state [11].
- Menstrual Dysfunction: In females, hypothalamic suppression leads to reduced estrogen and progesterone production, causing functional hypothalamic amenorrhea or oligomenorrhea [10] [9].
- Micronutrient Deficiencies: Inadequate intake often leads to suboptimal levels of bone-supporting nutrients like Vitamin D, Calcium, and Iron [9].
Multi-System Disease Manifestations
Prolonged LEA and metabolic dysregulation lead to clinical disease manifestations across multiple systems [8]:
- Impaired Bone Health: Low estrogen and nutrient deficiencies result in decreased bone mineral density (BMD), osteopenia, osteoporosis, and a significantly elevated risk of stress fractures [8] [10].
- Endocrine and Reproductive Dysfunction: Includes menstrual irregularities and low libido [8].
- Immunological and Cardiovascular Compromise: Increased susceptibility to illness and potential long-term heart damage [8].
- Psychological Effects: Increased incidence of irritability, depression, and anxiety [8].
Common Methodological Challenges & Troubleshooting
Researchers studying the Energy-Nutrient-Disease Triad frequently encounter specific methodological issues. The following table outlines common problems and their solutions.
| Challenge | Potential Impact on Data | Troubleshooting Guide & Methodological Solutions |
|---|---|---|
| Inaccurate Energy Intake Assessment [13] [9] | Systematic under-reporting of food intake, leading to misclassification of LEA. | Use multiple dietary assessment tools (e.g., multiple 24-hr recalls + FFQ). Employ statistical correction using regression calibration where possible [13]. Incorporate objective biomarkers (e.g., plasma vitamin C for fruit/vegetable intake) as surrogate measures to correct for measurement error [13]. |
| Calculating Exercise Energy Expenditure (EEE) [9] | High variability in EEE estimation introduces significant error into the EA equation. | Utilize device-based measures (heart rate monitors, accelerometers, GPS) with individual calibration over self-report logs. For precision, use the adjusted EEE method: subtract resting metabolic rate during the exercise period from total exercise cost [9]. |
| Diagnosing REDs & Triad Severity [11] | Inconsistent use of biomarkers leads to challenges in comparing studies and accurately staging syndrome severity. | Adopt a standardized tool like the IOC REDs Clinical Assessment Tool-Version 2 (REDs CAT2) [11]. This provides a structured framework for assessing risk (from low to high) based on a combination of biomarkers, clinical symptoms, and performance metrics. |
| Biomarker Variability & Selection [11] | Lack of a single diagnostic biomarker; confusion over which markers are most informative. | Focus on a panel of biomarkers. The most frequently used and informative markers in research include Bone Mineral Density (BMD) via DEXA, hormones (T3, estradiol, testosterone), and hematological markers (ferritin, hemoglobin) [11]. |
Key Experimental Protocols
Protocol for Assessing Energy Availability and REDs Risk
This workflow provides a step-by-step guide for a comprehensive assessment of an individual's status within the Energy-Nutrient-Disease Triad.
1. Participant Screening & Questionnaires:
- Tools: Administer the Low Energy Availability in Females Questionnaire (LEAF-Q) to assess physiological symptoms and the Eating Disorder Examination Questionnaire (EDE-Q) or Brief EDs in Athletes Questionnaire (BEDA-Q) to evaluate disordered eating behaviors [9] [11].
- Purpose: Identifies at-risk individuals for further testing.
2. Dietary and Exercise Assessment:
- Dietary Intake: Collect at least 3 days of dietary intake (including at least one weekend day) using a detailed food diary or multiple 24-hour recalls. Data should be analyzed using validated nutritional software (e.g., ESHA Food Processor) [14] [9].
- Exercise Energy Expenditure (EEE): Record all exercise for the same days using a detailed log. EEE should be calculated using MET values from the Compendium of Physical Activities or, preferably, data from individual calibrated wearable devices [14] [9].
3. Body Composition Analysis:
- Method: Perform a Dual-Energy X-ray Absorptiometry (DEXA) scan to obtain accurate measurements of Fat-Free Mass (FFM), fat mass, and Bone Mineral Density (BMD) [14] [10].
- Application: FFM is used as the denominator in the EA equation. BMD Z-scores below -1.0 in athletes are considered indicative of low bone density [10].
4. Calculation of Energy Availability:
- Formula: Use the standard EA equation. Input total energy intake (from step 2), EEE (from step 2), and FFM (from step 3). Compare the result to established thresholds [9].
5. Biochemical & Hormonal Biomarker Analysis:
- Blood Collection: Conduct a fasted blood draw.
- Key Analytes:[
citation:4] [11]
- Hormones: Triiodothyronine (T3), luteinizing hormone (LH), follicle-stimulating hormone (FSH), estradiol (for females), testosterone, prolactin.
- Metabolic Markers: Resting Metabolic Rate (via indirect calorimetry if available).
- Nutrient Status: Iron panel (ferritin, transferrin), Vitamin D (25(OH)D), Calcium.
6. Synthesis and Diagnosis:
- Tool: Input all collected data (questionnaire scores, EA value, hormone levels, BMD results, clinical symptoms) into the IOC REDs CAT2 tool to determine the overall risk category (e.g., low, moderate, high) and guide management [11].
The Scientist's Toolkit: Essential Research Reagents & Materials
| Tool / Reagent | Primary Function in Research | Application Notes |
|---|---|---|
| Dual-Energy X-ray Absorptiometry (DEXA) [14] [10] | Gold-standard measurement of body composition (Fat-Free Mass) and Bone Mineral Density (BMD). | Critical for calculating EA denominator and diagnosing the bone health component of the triad. |
| Indirect Calorimeter [11] | Objective measurement of Resting Metabolic Rate (RMR) via oxygen consumption and carbon dioxide production. | Used to identify metabolic suppression (measured RMR << predicted RMR), a key sign of prolonged LEA. |
| Validated Questionnaires (LEAF-Q, EDE-Q) [9] [11] | Low-burden, initial screening for symptoms of LEA and disordered eating psychopathology. | Essential for large-scale cohort studies and identifying at-risk populations for further investigation. |
| Enzyme-Linked Immunosorbent Assay (ELISA) Kits | Quantification of specific biomarkers from blood, saliva, or urine samples (e.g., hormones like T3, estradiol, IGF-1). | Allows for high-throughput analysis of endocrine alterations associated with LEA. |
| Nutritional Analysis Software (e.g., ESHA Food Processor) [14] | Converts food record data into estimated intakes of energy, macronutrients, and micronutrients. | Standardizes dietary intake analysis. Must be used with up-to-date food composition databases. |
| Bioelectrical Impedance Analysis (BIA) [15] | Field-based assessment of body composition, providing estimates of fat mass and fat-free mass. | Less accurate than DEXA but more accessible. Can be useful for tracking longitudinal changes. |
Frequently Asked Questions (FAQs)
Q1: What is the critical distinction between the Female Athlete Triad and REDs? A: The Female Athlete Triad is a specific subset of REDs, focusing on three interrelated components in females: low energy availability, menstrual dysfunction, and low bone mineral density [8] [10]. REDs is a broader, more comprehensive syndrome that recognizes the multi-system physiological impairments caused by LEA and affects athletes of all genders [8] [9].
Q2: How can we statistically correct for the known measurement error in self-reported dietary data? A: This is a core challenge in nutritional epidemiology. Advanced statistical methods like regression calibration can be used [13]. This technique uses a reference measurement (e.g., data from a more detailed diet diary or a recovery biomarker like doubly labeled water for energy intake) in a subset of the cohort to estimate and correct for the bias in the main instrument (e.g., an FFQ) [13]. The use of surrogate biomarkers (e.g., plasma vitamin C, nitrogen) that correlate with intake can also be incorporated into measurement error models to improve accuracy [13].
Q3: Which blood biomarkers are considered most critical for diagnosing and monitoring REDs in a research setting? A: According to reviews of current methodologies, the most frequently utilized and informative biomarkers include [11]:
- Triiodothyronine (T3): A key marker of metabolic adaptation.
- Hormones for Menstrual Status: Luteinizing Hormone (LH), Follicle-Stimulating Hormone (FSH), and Estradiol in females; Testosterone in males.
- Bone Turnover Markers: Such as P1NP (formation) and CTX (resorption).
- Iron Panel: Ferritin and hemoglobin to assess for anemia, which can compound fatigue.
- Vitamin D (25-OH D): Crucial for bone health and often deficient.
Troubleshooting Guide: Statistical Models in Nutritional Research
This guide helps researchers identify and correct for common pitfalls in statistical models used in nutritional epidemiology, particularly when adjusting for total energy intake.
Q1: My model shows a significant effect of a nutrient, but I suspect it might be confounded by total energy intake. How can I investigate this?
Problem: A statistically significant result may be misleading if the model does not properly account for total energy intake, as overall diet can be a confounder [2].
Symptoms:
- The effect size of the nutrient changes substantially when total energy intake is added to the model.
- The direction of the association (positive/negative) reverses after adjustment.
- You know from existing literature that the nutrient is highly correlated with total energy intake in your study population.
Resolution: Follow this diagnostic workflow to identify the appropriate model and check for confounding:
Q2: After adjusting for baseline values in my analysis of change from baseline, the type I error rate seems inflated. What went wrong?
Problem: In pharmacogenomic (PGx) studies analyzing quantitative change, failing to adjust for baseline values can inflate type I error for genetic variants associated with the baseline trait [16] [17].
Symptoms:
- Anomalously high false-positive rates in your genome-wide association study (GWAS) of change from baseline.
- The baseline value of the trait is both associated with the genotype and is a predictor of the change from baseline (i.e., it acts as a mediator) [16] [17].
Resolution:
- Diagnose: Check if your baseline trait is associated with any genetic variants in your dataset. Also, verify the correlation between the baseline and the change-from-baseline values; a negative correlation is common [17].
- Act: The recommended primary analysis is to use a baseline-adjusted model to control for this mediator effect and maintain a correct type I error rate [16] [17]. If measurement error is still suspected of causing inflation, a baseline-unadjusted model can be run for diagnostic comparison [17].
Frequently Asked Questions (FAQs)
Q: What is the core consequence of using an unadjusted or incorrectly adjusted model? The primary consequence is biased estimation. This can either obscure a true association (leading to false negatives) or, more severely, reverse the direction of an association, creating a false positive for an effect that is the opposite of reality [2]. This heterogeneity in estimands can also invalidate meta-analyses if different studies use different adjustment methods [2].
Q: What is the "all-components model" and when should I use it? The "all-components model" is an approach that simultaneously adjusts for the intake of all other dietary components besides the one you are studying [2]. It is recommended to obtain less biased estimates of both the total causal effect and the average relative causal effect, as it avoids the residual confounding that can occur when using summary variables like total energy or remaining energy intake [2].
Q: In a PGx study, when might a baseline-unadjusted model have more power than an adjusted one? Simulations show that a baseline-unadjusted model may appear to have higher power when the genetic effect on the baseline trait is in the opposite direction from the genetic effect on the change from baseline [17]. However, this apparent power advantage comes at the cost of an inflated type I error rate if the baseline acts as a mediator, making the results unreliable [17].
The table below summarizes the four common models for energy adjustment, their target estimands, and interpretations, which is crucial for selecting the right one and avoiding erroneous conclusions [2].
| Model Name | Core Specification | Target Estimand | Key Interpretation | Primary Risk/Consequence of Misuse |
|---|---|---|---|---|
| Standard Model | Nutrient; Total Energy | Average Relative Causal Effect | Effect of substituting the nutrient for the weighted average of other energy sources [2]. | Biased estimates even without confounding; estimates a substitution effect, not a total effect [2]. |
| Energy Partition Model | Nutrient; Remaining Energy | Total Causal Effect | The total effect of increasing the nutrient while keeping all other intakes constant (an "additive" effect) [2]. | Unbiased only with no confounding or if all other nutrients have equal effects; otherwise, residual confounding [2]. |
| Nutrient Density Model | Nutrient/Total Energy | Obscure | Attempts to estimate a relative effect rescaled as a proportion of total energy [2]. | An obscure causal interpretation that makes results difficult to compare with other models [2]. |
| Residual Model | Residual of Nutrient ~ Total Energy | Mathematically identical to the Standard Model [2]. | Identical to the Standard Model—a substitution effect [2]. | Same as the Standard Model; provides no additional benefit [2]. |
Experimental Protocol: Comparing Energy Adjustment Models
Objective: To empirically demonstrate how different energy adjustment models can obscure or reverse the estimated effect of a specific nutrient (e.g., sugars) on a health outcome (e.g., fasting plasma glucose).
Methodology:
- Data Preparation: Utilize observational nutritional data with detailed dietary component intake and a measured health outcome.
- Model Fitting: Fit the four primary models (Standard, Energy Partition, Nutrient Density, Residual) to estimate the effect of the chosen nutrient [2].
- "All-Components" Model: As a more robust comparison, fit a model that includes the exposure nutrient and all other major dietary components simultaneously [2].
- Comparison & Analysis: Compare the estimated coefficient, direction, and statistical significance of the exposure nutrient across all five models.
Key Measurements & Outputs:
- Primary Output: A table of regression coefficients for the nutrient of interest from each model.
- Diagnostic Plot: A forest plot visualizing the point estimates and confidence intervals for the nutrient's effect across all models to easily see reversals or obscuring of effects.
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function in Analysis |
|---|---|
| Directed Acyclic Graphs (DAGs) | A visual tool to map out and identify potential confounding variables, like total energy intake, based on prior subject knowledge [2]. |
| Compositional Data Analysis | A set of statistical methods recognizing that dietary data are "parts of a whole," preventing spurious findings when analyzing individual nutrients [2]. |
| Monte Carlo Simulations | A computational algorithm used to evaluate model performance (e.g., type I error, power) under controlled, known conditions before applying them to real data [2] [16]. |
| All-Components Model | The statistical model that adjusts for all individual dietary components to provide a less biased estimate of a nutrient's effect [2]. |
Core Statistical Models and Practical Application Techniques
Frequently Asked Questions (FAQs)
FAQ 1: What is the core distinction between the Nutrient Density and Energy Partition models? The core distinction lies in their target causal effects. The Energy Partition model is used to estimate the total causal effect of a nutrient—the effect of increasing the intake of that specific nutrient while the intake of all other nutrients remains constant [2]. In contrast, the Nutrient Density model attempts to estimate an average relative causal effect (a "substitution" effect), which represents the effect of increasing the energy intake from the exposure nutrient while simultaneously decreasing the intake from all other energy sources to keep total energy constant [2].
FAQ 2: Why do different energy adjustment models produce different results for the same exposure and outcome? Different models produce different results because each one implies a different causal estimand [2]. The models are mathematically distinct and answer subtly different research questions. For instance, the Standard and Residual models estimate a substitution effect, whereas the Energy Partition model estimates a total effect. This fundamental difference in the target of inference naturally leads to variation in the estimated coefficients, and pooling these different estimands in meta-analyses can threaten the validity of the conclusions [2].
FAQ 3: When should I use the "all-components model" instead of a traditional model? The all-components model—which involves simultaneously adjusting for all other individual dietary components—is generally recommended when your goal is to obtain the least biased estimate of either the total causal effect or the average relative causal effect [2]. Traditional models that adjust for summary measures like total energy or remaining energy intake are susceptible to residual confounding and composite variable bias, which occurs because these aggregates combine multiple nutrients that likely have distinct effects on the outcome. The all-components model avoids this information loss [2] [18].
FAQ 4: How can I handle suspected measurement error in total energy intake? While detailed methodologies for handling measurement error are beyond the scope of this guide, it is a critical consideration. Be aware that errors in the measurement of total energy intake can propagate differently across the various adjustment models, potentially biasing the results. Sensitivity analyses specific to the chosen model are recommended to assess the robustness of your findings to potential measurement error [18].
Comparison of Energy Adjustment Models
The table below summarizes the key characteristics, interpretations, and performance of the four common energy intake adjustment models, plus the alternative all-components model.
Table 1: Characteristics of Statistical Models for Energy Intake Adjustment in Nutritional Research
| Model Name | Model Formulation Example | Target Causal Estimand | Key Interpretation | Performance & Key Considerations |
|---|---|---|---|---|
| Standard Model | Outcome ~ exposure + total_energy |
Average Relative Causal Effect [2] | Effect of substituting the exposure for a weighted average of all other energy sources [2]. | Mathematically identical to the residual model. Can be biased even without confounding [2] [18]. |
| Energy Partition Model | Outcome ~ exposure + remaining_energy |
Total Causal Effect [2] | Effect of increasing the exposure while holding all other energy intake constant (an "additive" effect) [2]. | Unbiased only with no confounding or if all other nutrients have equal effects on the outcome [2]. |
| Nutrient Density Model | Outcome ~ (exposure / total_energy) |
Attempts to estimate a rescaled Average Relative Causal Effect [2] | Effect of the exposure expressed as a proportion of total energy [2]. | Interpretation can be obscure. Performance depends on specific formulation [2]. |
| Residual Model | 1. exposure ~ total_energy 2. Outcome ~ residual_from_step_1 |
Average Relative Causal Effect [2] | Effect of the exposure after removing its linear association with total energy (a "substitution" effect) [2]. | Mathematically identical to the standard model. Provides biased estimates even without confounding [2]. |
| All-Components Model | Outcome ~ exposure + nutrient_2 + ... + nutrient_n |
Total Causal Effect (when all other components are adjusted for) [2] | Isolates the effect of the exposure by directly accounting for all other known dietary components [2]. | Provides less biased estimates of both total and relative effects by avoiding information loss from variable aggregation [2] [18]. |
Experimental Protocols & Methodologies
Protocol 1: Implementing and Comparing Energy Adjustment Models
This protocol outlines the steps for a simulation-based analysis to implement and compare the performance of different energy adjustment models, as described in the associated research [2] [18].
1. Research Reagent Solutions Table 2: Essential Components for Simulation-Based Analysis
| Component/Variable | Description/Function |
|---|---|
| Simulated Dietary Data | A dataset containing simulated values for key nutrients (e.g., sugars, carbohydrates, fibre, fats, protein) and an outcome variable (e.g., fasting plasma glucose) [18]. |
R Statistical Software |
The programming environment used for data simulation, model fitting, and analysis (e.g., version 4.0.3 or higher) [18]. |
| Total Energy Intake | A variable calculated as the sum of energy from all simulated nutrient components, including the exposure [2] [18]. |
| Remaining Energy Intake | A variable calculated as the sum of energy from all simulated nutrient components, excluding the exposure nutrient [2] [18]. |
| Model Comparison Script | Code to run the unadjusted, standard, energy partition, nutrient density, residual, and all-components models and store their exposure coefficient estimates [18]. |
2. Step-by-Step Workflow
Diagram 1: Model comparison workflow
- Step 1: Data Simulation. Simulate a base dataset with variables for multiple nutrients (e.g., non-milk extrinsic sugars as the exposure, carbohydrates, fibre, fats, protein) and a continuous health outcome (e.g., fasting plasma glucose). It is advisable to simulate data under two primary scenarios: one with and one without the presence of confounding by common causes of diet [18].
- Step 2: Variable Calculation. Create two key derived variables:
total_energy: The sum of energy intake from all nutrient sources, including the exposure.remaining_energy: The sum of energy intake from all nutrient sources excluding the exposure [18].
- Step 3: Model Fitting. Fit the following statistical models to the same simulated dataset:
- Unadjusted:
Outcome ~ exposure - Standard:
Outcome ~ exposure + total_energy - Energy Partition:
Outcome ~ exposure + remaining_energy - Nutrient Density:
Outcome ~ (exposure / total_energy)or a multivariable version with additional adjustment fortotal_energy. - Residual: First, regress
exposure ~ total_energyand save the residuals. Second, regressOutcome ~ these_residuals. - All-Components:
Outcome ~ exposure + nutrient_2 + nutrient_3 + ... + nutrient_n(adjusting for all other simulated nutrients individually) [2] [18].
- Unadjusted:
- Step 4: Results Extraction. For each fitted model, store the regression coefficient and standard error (or confidence interval) for the exposure variable.
- Step 5: Performance Comparison. Compare the estimated exposure coefficients across models against the known "true" effect size set during the simulation. Assess which models recover the true effect with minimal bias under different confounding scenarios [18].
Protocol 2: Validating a Nutrient Density Score with Diet Quality
This protocol describes how to develop and validate a hybrid nutrient density score against an independent measure of overall diet quality, such as the Healthy Eating Index (HEI-2015) [19].
1. Research Reagent Solutions Table 3: Essential Components for Nutrient Density Score Validation
| Component/Variable | Description/Function |
|---|---|
| NHANES Dietary Data | Publicly available, nationally representative dietary intake data from the National Health and Nutrition Examination Survey (What We Eat in America component) [19]. |
| FPED Database | The Food Patterns Equivalents Database used to convert reported foods into USDA food groups (e.g., whole grains, dairy, fruit) for HEI-2015 calculation [19]. |
| FNDDS Database | The Food and Nutrient Database for Dietary Studies, which provides the energy and nutrient values for foods reported in NHANES [19]. |
| HEI-2015 Score | The independent measure of diet quality, based on adherence to the Dietary Guidelines for Americans, used as the validation metric [19]. |
2. Step-by-Step Workflow
Diagram 2: Score validation process
- Step 1: Data Preparation. Obtain and prepare dietary intake data from NHANES. This includes filtering the dataset (e.g., excluding participants with incomplete data, pregnant or lactating individuals) and calculating the HEI-2015 score for each participant using the FPED and FNDDS databases [19].
- Step 2: Component Selection. Define a set of candidate nutrients to encourage (e.g., protein, fiber, potassium), nutrients to limit (e.g., saturated fat, added sugar, sodium), and MyPlate food groups to encourage (e.g., whole grains, dairy, fruits, nuts, and seeds) [19].
- Step 3: Model Formulation & Regression. Construct a large number of potential hybrid NRF (NRFh) models with different combinations of the candidate components. The general form is
NRFh(x.y.z) = NRx + MPy - LIMz, whereNRxis the sum of x beneficial nutrients,MPyis the sum of y beneficial food groups, andLIMzis the sum of z nutrients to limit [19]. Run iterative regression analyses for each potential NRFh model score against the HEI-2015 score. - Step 4: Model Selection. Identify the specific NRFh model (e.g., NRFh3.4.3 or NRFh4.3.3) that explains the highest proportion of variance (R²) in the HEI-2015 score [19].
- Step 5: Validation. Test the performance and significance of the final selected NRFh model across different population subgroups (e.g., by age, gender, race/ethnicity) to ensure its robustness [19].
The Scientist's Toolkit
Table 4: Key Research Reagents and Resources
| Tool / Resource | Function in Research | Example / Source |
|---|---|---|
| National Health and Nutrition Examination Survey (NHANES) | Provides nationally representative data on dietary intakes, health status, and anthropometric measures for analysis and model validation [20] [19]. | U.S. Centers for Disease Control and Prevention (CDC) National Center for Health Statistics [20]. |
| Food and Nutrient Database for Dietary Studies (FNDDS) | Provides the energy and nutrient values for foods and beverages reported in dietary surveys like NHANES, essential for calculating nutrient intakes [20] [19]. | U.S. Department of Agriculture (USDA) Agricultural Research Service [20]. |
| Food Patterns Equivalents Database (FPED) | Converts foods and beverages from FNDDS into USDA Food Patterns components (e.g., cup equivalents of fruit, ounce equivalents of whole grains), necessary for calculating diet quality scores like the HEI [20] [19]. | USDA Agricultural Research Service [20]. |
| Healthy Eating Index (HEI) | A validated, independent measure of overall diet quality used to assess compliance with dietary guidelines and validate nutrient profile models [19]. | USDA, National Cancer Institute [19]. |
| Doubly Labelled Water (DLW) Equations | The gold-standard method for estimating total energy expenditure. Predictive equations based on DLW studies provide the most accurate estimates of energy requirements for population studies [3]. | Committee on Dietary Reference Intakes for Energy (National Academies of Sciences, Engineering, and Medicine) [3]. |
| R Statistical Software | The primary programming environment for simulating nutritional data, implementing different adjustment models, and conducting statistical analyses [18]. | R Project (r-project.org) with necessary packages for simulation and regression analysis. |
In nutritional epidemiology, the residual method is a established statistical technique used to adjust for total energy intake when investigating the effects of specific nutrients or foods on health outcomes. This adjustment is crucial because individuals who consume more of any single dietary component typically have a higher overall energy intake, which is itself influenced by body size, metabolic efficiency, and physical activity. Without proper adjustment, observed associations may be confounded by these factors. The residual method provides a way to isolate the effect of a specific dietary component from the effect of total energy intake, thereby assessing the component's role in the context of overall diet composition.
Core Concept: What is the Residual Method?
The residual method is an energy adjustment approach where the energy-adjusted intake of a nutrient is represented by the residuals from a regression model. In this model, absolute nutrient intake serves as the dependent variable, and total energy intake is the independent variable. The resulting residuals represent the variation in nutrient intake that is uncorrelated with total energy intake, effectively providing a measure of nutrient intake independent of total caloric consumption [21].
This method is particularly valuable because it accounts for two key challenges in nutritional research:
- It controls for confounding by body size, metabolic efficiency, and physical activity, for which total energy intake often serves as a proxy [2] [21].
- It helps mitigate measurement error inherent in self-reported dietary data, especially from food frequency questionnaires (FFQs) [21].
Table 1: Key Terminology in Energy Adjustment
| Term | Definition | Application in Research |
|---|---|---|
| Residual Method | A statistical technique that uses residuals from a regression of nutrient intake on total energy intake to create an energy-adjusted variable [21]. | Isolates the effect of a specific nutrient from the effect of total energy intake. |
| Total Energy Intake | The total intake of calories from all dietary sources, including the nutrient of interest [2]. | Often used as a proxy for body size, metabolism, and physical activity. |
| Energy Partition Model | Adjusts for the remaining energy intake (calories from all sources excluding the exposure nutrient) [2]. | Aims to estimate the total causal effect of a nutrient. |
| Nutrient Density Model | Expresses the nutrient exposure as a proportion (percentage) of total energy intake [2] [21]. | Provides an intuitive measure of dietary composition. |
| Standard Model | Directly adjusts for total energy intake as a covariate in a regression model [2]. | Mathematically equivalent to the residual method but implemented differently. |
Step-by-Step Application Protocol
Step 1: Data Preparation and Assumption Checking
Before applying the residual method, ensure your dietary intake data has been collected using an appropriate instrument (e.g., FFQ, 24-hour recall) and has been cleaned. Check for the normality of the distribution for both the nutrient of interest and total energy intake. If the data are skewed, apply transformations (e.g., logarithmic, square root) to approximate a normal distribution, which satisfies a key assumption of linear regression [22].
Step 2: Model Specification and Regression
Run a simple linear regression model with the absolute intake of the nutrient or food group you are studying as the dependent variable (Y) and total energy intake as the independent variable (X).
The model is specified as:
Nutrient_i = β_0 + β_1 * Energy_i + ε_i
Where:
Nutrient_iis the absolute intake of the nutrient for individual iEnergy_iis the total energy intake for individual iβ_0is the regression interceptβ_1is the regression coefficient for energy intakeε_iis the error term, or residual, for individual i [21]
Step 3: Extracting the Residuals
The energy-adjusted values for the nutrient are the residuals (ε_i) from the regression model calculated in Step 2. Statistically, the residual for each individual is calculated as:
Residual_i = Observed Nutrient_i - Predicted Nutrient_i
Where the predicted nutrient intake is β_0 + β_1 * Energy_i [23] [21]. These residuals represent the difference between an individual's actual nutrient intake and the intake predicted by their total energy consumption. A positive residual indicates a higher-than-expected intake of the nutrient for a given energy intake, suggesting a diet denser in that nutrient.
Step 4: Utilizing the Adjusted Values in Downstream Analysis
The extracted residuals are now used as the exposure variable in your primary analysis model (e.g., a regression model with a health outcome as the dependent variable). Because these residuals are, by construction, uncorrelated with total energy intake, you do not need to adjust for energy again in the final model [24] [21].
The following diagram illustrates the logical workflow and statistical relationship at the heart of the residual method:
Comparison with Other Energy Adjustment Methods
The residual method is one of several approaches for energy adjustment. It is mathematically equivalent to the "standard model," which includes the nutrient and total energy intake as simultaneous covariates in a multivariate regression model targeting the health outcome [2]. However, it differs conceptually and computationally from other common techniques.
Table 2: Comparison of Common Energy Adjustment Methods
| Method | Underlying Concept | Target Estimand | Key Advantages | Key Limitations |
|---|---|---|---|---|
| Residual Method | Uses the part of nutrient variation uncorrelated with total energy [21]. | Average Relative Causal Effect (a "substitution" effect) [2]. | Produces a variable uncorrelated with energy for use in subsequent models. | The derived variable (residual) lacks intuitive units, making interpretation less straightforward [2]. |
| Standard Model | Includes both the nutrient and total energy as covariates in the outcome model [2]. | Average Relative Causal Effect (a "substitution" effect) [2]. | Simple to implement and interpret as a standard multivariate model. | Can be difficult to communicate that it estimates a substitution effect. |
| Energy Partition Model | Adjusts for energy from all other sources (excluding the nutrient of interest) [2]. | Total Causal Effect (an "additive" effect) [2]. | Aims to estimate the effect of adding the nutrient to the diet without changing other components. | Provides unbiased estimates only in absence of confounding or if all other nutrients have equal effects [2]. |
| Nutrient Density Model | Expresses the nutrient as a proportion of total energy (e.g., % of calories from fat) [2] [21]. | Attempts to estimate a relative effect, but its interpretation can be obscure [2]. | Intuitively represents diet composition; easy to calculate and understand. | Can be biased if total energy intake is associated with the outcome [2]. |
Troubleshooting and Frequently Asked Questions (FAQs)
FAQ 1: My residuals show a non-random pattern when plotted against predicted values. What does this mean?
A non-random pattern in your residuals (e.g., a funnel shape or a curved trend) indicates a violation of the linear regression assumptions. This could mean that the relationship between the nutrient and total energy intake is not linear. To address this, you can:
- Explore non-linear transformations (e.g., log, square root) of the nutrient and/or energy variables.
- Investigate the presence of outliers that may be unduly influencing the regression fit.
- Consider using non-parametric regression techniques, though these are less common in standard practice [25].
FAQ 2: How does the residual method help with measurement error in dietary assessment?
The residual method is particularly useful when using Food Frequency Questionnaires (FFQs), which cannot measure absolute energy intake accurately. It helps by assuming that individuals tend to misreport most foods and beverages in a similar direction and degree. By adjusting for total energy, the method partially corrects for this general tendency to under- or over-report, making the energy-adjusted nutrient values more reliable for diet-disease association analyses [21].
FAQ 3: When should I use the residual method versus the nutrient density method?
The choice of method should align with your research question.
- Use the residual method (or standard model) when your question is: "What is the effect of substituting a specific nutrient for the average of all other energy-contributing nutrients in the diet, while keeping total energy constant?" This is known as the "average relative causal effect" or "substitution effect" [2].
- Use the nutrient density method to simply describe the composition of the diet (e.g., the percentage of calories from saturated fat). However, be cautious as its causal interpretation in outcome models is less clear [2].
FAQ 4: The residual method and standard model are mathematically equivalent. Which one should I use in practice?
For simplicity and clarity in reporting, many researchers prefer the standard model. Including both the nutrient of interest and total energy intake as covariates in your final regression model for the health outcome is straightforward and avoids the extra step of creating and managing a residual variable. The results will be identical to those obtained using the two-step residual method [2] [24].
The Scientist's Toolkit: Essential Reagents for Dietary Pattern Analysis
Table 3: Key Methodological and Software Tools for Nutritional Analysis
| Tool Category | Example | Primary Function in Analysis |
|---|---|---|
| Dietary Assessment Instrument | Food Frequency Questionnaire (FFQ) [26] | Assesses habitual intake over a long-term period; cost-effective for large studies. |
| Dietary Assessment Instrument | 24-Hour Dietary Recall (24HR) [26] | Captures detailed recent intake (previous 24 hours); multiple non-consecutive recalls can estimate usual intake. |
| Statistical Software | SAS, R, STATA [27] [22] | Provides the computational environment for performing regression, calculating residuals, and implementing other energy adjustment models. |
| Validation Biomarker | Doubly Labeled Water (for energy) [28] | A recovery biomarker used as an objective reference to validate the accuracy of self-reported energy intake. |
| Validation Biomarker | Urinary Nitrogen (for protein) [28] | A recovery biomarker used as an objective reference to validate the accuracy of self-reported protein intake. |
Frequently Asked Questions (FAQs)
Q1: What is the fundamental purpose of adjusting for total energy intake in nutritional studies? Adjusting for total energy intake is crucial to account for confounding factors. An individual's overall food consumption level influences both their intake of specific nutrients and their health outcomes. Without this adjustment, it is difficult to determine whether an observed effect is due to a specific nutrient or simply the result of eating more food in general [29].
Q2: What are the primary statistical models for energy adjustment, and how do they differ? Researchers commonly use four main models, each with a different conceptual approach and interpretation [29]:
- The Standard Model: Adjusts for total energy intake as a covariate.
- The Nutrient Density Model: Expresses the nutrient intake as a proportion of total energy intake.
- The Residual Model: Uses the residuals from a regression of the nutrient intake on total energy intake.
- The Energy Partition Model: Adjusts for the energy intake from all other dietary components besides the nutrient of interest.
Q3: My model results change dramatically when I use different energy adjustment methods. Why does this happen, and which model should I trust? Different models estimate different causal effects, which explains why results can vary [29]. The "standard" and "residual" models estimate a substitution effect (e.g., the effect of replacing one nutrient with another while keeping total energy constant). The "energy partition" model estimates the total causal effect of the nutrient. The choice depends on your research question. There is no single "correct" model; the model must be selected based on the specific causal effect you wish to estimate [29].
Q4: How can I handle the issue of correlated dietary components (multicollinearity) in these models? Multicollinearity is a inherent challenge in nutritional data. To address this, the "all-components model" is recommended. This approach simultaneously includes all dietary components in the model, which can provide more accurate estimates of both total and average relative causal effects compared to the traditional four models [29].
Q5: A reviewer asked me to justify my choice of a nutrient density model (exposure per 1000 kcal) over other methods. How should I respond? You should explain that the nutrient density model attempts to estimate the average relative causal effect, rescaled as a proportion of total energy [29]. Justify your choice by aligning it with your research question—for instance, if your goal is to understand the effect of a nutrient's proportion in the diet, irrespective of total caloric intake. Acknowledge the model's limitations, particularly that its interpretation can be less straightforward than that of the standard or energy partition models [29].
Troubleshooting Common Experimental Issues
Problem 1: Inconsistent Associations with Health Outcomes
Issue: The association between a nutrient and a health outcome changes direction or significance depending on whether you analyze absolute intake or energy-adjusted intake.
Solution: This is a known phenomenon. For example, a study on greenhouse gas emissions (GHGE) of diets found that:
- Higher absolute GHGE (per day) was associated with higher daily intake of all micronutrients.
- However, when expressed per 1000 kcal, higher GHGE was linked to lower micronutrient intake [30].
Interpretation Guide:
| Analysis Type | What It Typically Measures |
|---|---|
| Absolute Intake (per day) | The association with the total volume of food consumed. |
| Energy-Adjusted Intake (per 1000 kcal) | The association with the composition or quality of the diet. |
Your interpretation must match your model. The choice of model is not merely statistical but fundamentally affects the scientific question being asked [30] [29].
Problem 2: Misreporting of Dietary Intake Skews Data
Issue: Self-reported dietary data from tools like Food Frequency Questionnaires (FFQs) are prone to measurement error, including under-reporting of total energy intake, which can bias your results [3] [31].
Solution and Validation Strategies:
- Use Biomarkers: When possible, validate intake reports with objective biomarkers. For example, serum cotinine can validate smoking status [32], and vitamin D levels can corroborate dietary reports.
- Anthropometric Proxies: Consider using methods that derive energy intake from measured body weight, height, and physical activity levels. This approach mirrors actual energy consumption and can be used to test the consistency of self-reported data [3].
- Comprehensive FFQ Reporting: If using an FFQ, report validation metrics beyond a single correlation coefficient. Provide exposure-specific validation details and a clear description of energy adjustment methodologies to improve transparency [31].
Issue: Combining national food availability data (which often overestimates intake) with individual-level dietary surveys (which often underestimate intake) leads to inconsistent findings.
Solution:
- Use a Bridging Metric: Employ estimates derived from anthropometry (body weight, height) as a consistent benchmark. These estimates are designed to align with trends in body weight and can help reconcile discrepancies between different data sources, such as food balance sheets and dietary surveys [3].
- Leverage National Datasets: For US-based research, use standardized data from the National Health and Nutrition Examination Survey (NHANES) and its component What We Eat in America (WWEIA). These datasets use 24-hour dietary recalls and standardized nutrient databases like the Food and Nutrient Database for Dietary Studies (FNDDS) and the Food Pattern Equivalents Database (FPED), ensuring internal consistency [20].
Key Experimental Protocols
Protocol 1: Implementing Energy Adjustment Models using NHANES Data
This protocol outlines how to apply different energy adjustment models using a standardized national dataset.
1. Data Source: Utilize the NHANES dataset, which includes 24-hour dietary recall data collected via the Automated Multiple Pass Method (AMPM) [32] [33]. 2. Key Variables:
- Exposure: Nutrient of interest (e.g., dietary choline [32]).
- Outcome: Health metric (e.g., Bone Mineral Density (BMD) [32]).
- Covariates: Total energy intake, demographic (age, sex, race), socioeconomic (Poverty-Income Ratio), and lifestyle factors (smoking status, physical activity) [32]. 3. Model Implementation: Fit a series of multivariate regression models with progressive adjustment [32]:
- Model 1: Adjusted for sex.
- Model 2: Additionally adjusted for age, BMI, and race.
- Model 3: Additionally adjusted for education, socioeconomic status, smoking, and physical activity.
- Model 4 (Fully Adjusted): Additionally adjusted for total energy intake and other relevant dietary components (e.g., calcium, vitamins). 4. Interpretation: Analyze how the coefficient for your nutrient of interest changes across models, noting the specific impact of adding total energy intake in the final model [32] [29].
Protocol 2: Assessing Diet Quality and Temporal Intake Patterns
This protocol measures the effect of meal timing and macronutrient quality, adjusted for total energy.
1. Data Preparation: Calculate the ratio of nutrient intake at dinner versus breakfast [33].
ΔRatio = (Nutrient at Dinner / Total Nutrient) - (Nutrient at Breakfast / Total Nutrient)
2. Exposure Variables: Create exposures for the difference in ratios (ΔRatio) for energy, high/low-quality carbohydrates, fats (saturated/unsaturated), and proteins (animal/plant) [33].
3. Outcome Variable: Obesity metrics (Body Mass Index, Waist Circumference) [33].
4. Statistical Analysis: Use multiple logistic and linear regression models, adjusting for total energy intake, age, sex, race, education, and other non-dietary confounders to isolate the effect of meal timing and composition [33].
Research Reagent Solutions: Essential Datasets and Tools
The following table lists key resources for conducting robust nutritional epidemiological research.
| Resource Name | Function & Application | Key Features |
|---|---|---|
| NHANES (WWEIA) [20] | Provides nationally representative data on food and nutrient consumption in the U.S. population. | Uses 24-hour dietary recall (gold standard); includes demographic, examination, and laboratory data. |
| FNDDS [20] | Provides the energy and nutrient values for foods and beverages reported in WWEIA, NHANES. | Contains data for energy and 64 nutrients for ~7,000 foods and beverages. |
| FPED [20] | Converts FNDDS foods into USDA Food Pattern components (e.g., fruits, vegetables, whole grains). | Allows researchers to assess adherence to dietary guideline recommendations. |
| Doubly Labeled Water (DLW) Database [3] | Provides measured data on total energy expenditure, used to validate equations for estimating energy requirements. | Considered a gold standard for measuring energy expenditure at the population level. |
Workflow and Conceptual Diagrams
The following diagram illustrates the decision pathway for selecting and implementing an appropriate energy adjustment model.
Diagram 1: Model Selection Workflow for Energy Adjustment
The following diagram outlines the steps for a robust analysis plan, from data collection to interpretation, emphasizing energy adjustment.
Diagram 2: Experimental Analysis Workflow
Frequently Asked Questions
Q1: What is the core challenge when adapting an RCT-like question to a cohort study in nutritional research?
The core challenge is reconciling the investigator-controlled intervention of an RCT with the observational nature of a cohort study. In an RCT, participants are randomly assigned to an intervention (e.g., a specific diet), which balances both known and unknown confounding factors across groups [34]. In a cohort study, researchers observe a naturally occurring exposure (e.g., habitual dietary intake) without any intervention [35] [34]. The primary methodological adaptation lies in using sophisticated statistical models to isolate the effect of a specific dietary component from the overall diet and other confounding factors, thereby approximating the causal question an RCT would ask [36] [2].
Q2: Why is adjusting for total energy intake so critical in observational studies of diet and disease?
Adjusting for total energy intake is fundamental for several reasons [37]:
- To Control for Confounding: Energy intake is correlated with physical activity, body size, and metabolic efficiency, which are themselves related to disease risk. Without adjustment, an association between a nutrient and a disease could be non-causal and merely reflect this shared link with total energy.
- To Reduce Extraneous Variation: Variation in nutrient intake resulting from differences in overall energy intake that are unrelated to disease risk can weaken true associations.
- To Model Realistic Interventions: Individuals changing their diet typically alter its composition without drastically changing their total energy intake (unless also changing physical activity or body weight). Energy adjustment helps predict the effect of such compositional changes [37].
Q3: What do the different energy adjustment models actually estimate?
Different models answer different research questions, which is a common source of confusion [2].
Table 1: Common Energy Adjustment Models and Their Interpretations
| Model Name | Statistical Approach | Target Estimand (What it Estimates) | Interpretation |
|---|---|---|---|
| Standard/Residual Model | Adjusts for total energy intake | Average Relative Causal Effect | The effect of substituting the exposure nutrient for a weighted average of all other energy sources [2]. |
| Energy Partition Model | Adjusts for energy from all other sources | Total Causal Effect | The effect of adding the exposure nutrient to the diet, keeping all else constant [2]. |
| Nutrient Density Model | Uses nutrient intake as a proportion of total energy | Rescaled Relative Effect | Attempts to estimate the relative causal effect, rescaled as a proportion of total energy; interpretation can be obscure [2]. |
| All-Components Model | Simultaneously adjusts for all other dietary components | Unconfounded Total or Relative Effect | Provides a less biased estimate of either effect by fully accounting for the diet's composition [2]. |
Q4: How can I implement a substitution analysis in a cohort study to mimic an RCT?
The "leave-one-out" method is a powerful approach for modeling isocaloric substitutions. This method mimics an RCT where one group receives calories from one source, and another group receives the same calories from a different source, with all else held constant [36].
For example, to model the substitution of SFA with PUFA, a Cox regression model would be specified as [36]:
Log(h(t; x)) = log(h0(t)) + β1PUFA + β2MUFA + β3Carbohydrates + β4Protein + β5Alcohol + β6Totalenergyintake + β7Confounders
In this model, the hazard ratio for β1 represents the estimated effect of replacing a specific amount of energy from SFA with an equivalent amount from PUFA.
Troubleshooting Guides
Issue 1: Misinterpretation of Model Estimates
- Problem: A researcher observes a null or counterintuitive association between a nutrient and a health outcome but has not considered the implicit question their model is asking.
- Solution:
- Clearly define your research question: Are you asking about adding a nutrient to the diet (a total effect) or replacing one nutrient with another (a substitution effect)?
- Select the statistical model that matches this question (refer to Table 1).
- For substitution effects, use the leave-one-out or all-components model to ensure the model is isocaloric and correctly specified [36] [2].
Issue 2: Dealing with Dietary Confounding and Collider Bias
- Problem: Energy intake is a collider variable, as it is a consequence of all individual nutrient intakes. Conditioning on it (by adjusting for it) can create spurious associations between the nutrients if they also share other common causes [2].
- Solution:
- The most robust method is to use the "all-components model", which includes all major dietary components (protein, fat, carbohydrates, etc.) in the same model. This provides a less biased estimate than adjusting for a summary variable like total energy or remaining energy [2].
- Be transparent about the limitations of your data and the potential for residual confounding.
Issue 3: Addressing Misreporting of Energy Intake
- Problem: Self-reported dietary data from tools like Food Frequency Questionnaires (FFQs) or dietary records are prone to systematic under- or over-reporting, which can severely bias results [38] [3].
- Solution:
- Internal Validation: If resources allow, use objective biomarkers like doubly labeled water (DLW) to measure total energy expenditure in a subset of the cohort to calibrate the self-reported intake data [38] [3].
- External Calibration: Use existing predictive equations and anthropometric data (body weight, height) to estimate energy intake required to sustain observed body weight and physical activity levels. This can serve as a complementary measure to assess and correct for misreporting in your primary data [3].
- Sensitivity Analyses: Conduct analyses excluding participants identified as extreme misreporters (e.g., those with implausible energy intake values) [36].
The Scientist's Toolkit: Key Research Reagents & Materials
Table 2: Essential Methodological Components for Dietary Adaptation Studies
| Item / Method | Function & Role in Analysis |
|---|---|
| Cohort Study with Dietary Data | Provides the foundational observational data. Requires detailed, prospectively collected dietary intake information, often via FFQs or dietary records [35]. |
| "Leave-One-Out" Model | The core statistical engine for performing isocaloric substitution analysis, allowing the investigator to model the effect of replacing one food or nutrient with another [36]. |
| All-Components Model | A more robust statistical approach that adjusts for all other dietary components simultaneously to minimize residual confounding from the overall diet composition [2]. |
| Doubly Labeled Water (DLW) | The gold-standard biomarker for total energy expenditure. Used to validate and calibrate self-reported energy intake data, addressing misreporting bias [38] [3]. |
| FADS1 Genotyping | An example of a tool for personalized nutrition research. Genetic variation (e.g., in the rs174550 SNP) can modify the association between fatty acid intake and health outcomes, allowing for stratified analyses [36]. |
Experimental Protocol: Implementing a Substitution Analysis
Aim: To estimate the effect of isocalorically replacing 5% of energy from Saturated Fatty Acids (SFA) with Polyunsaturated Fatty Acids (PUFA) on all-cause mortality in a large prospective cohort.
Step-by-Step Methodology:
- Cohort Definition: Identify your study population from a prospective cohort study (e.g., the ULSAM cohort) [36]. Exclude participants with prevalent disease at baseline and those with implausible energy intake reports.
- Exposure Assessment: Use baseline dietary intake data collected from a validated 7-day dietary record or a detailed FFQ. Compute daily intakes of all nutrients and foods.
- Model Specification: Use a multivariable Cox proportional hazards model. The model should be specified using the leave-one-out principle [36]:
Log(h(t; x)) = log(h0(t)) + β1PUFA + β2MUFA + β3Carbohydrates + β4Protein + β5Alcohol + β6Totalenergyintake + β7Confounders- Where all nutrients are expressed in units of 100 kcal.
- Confounder Adjustment: Include non-dietary confounders identified via a Directed Acyclic Graph (DAG), such as age, sex, smoking status, physical activity, and education level.
- Interpretation: The hazard ratio (HR) associated with
β1(PUFA) represents the effect of substituting 100 kcal of PUFA for 100 kcal of SFA. To express this for a 5% energy substitution, scale the coefficient appropriately.
The following diagram illustrates the logical workflow and key decision points in adapting an RCT-like question to a cohort study design using substitution analysis.
Identifying and Correcting for Pervasive Dietary Misreporting
The Prevalence and Impact of Energy Intake Misestimation
FAQs: Understanding Energy Intake Misestimation
What is energy intake misestimation and why is it a problem in nutritional research? Energy intake (EI) misestimation refers to the difference between reported and true energy intake from self-reported dietary data. All self-reported dietary intake data are characterized by such measurement error [39] [40]. This is problematic because error in estimating EI is relatively large compared to other dietary components, and since almost all foods and beverages contain energy, small errors in quantifying each item compound to significantly impact overall EI estimates [41]. This misestimation can distort observed associations between diet and disease, reduce statistical power to detect true associations, and lead to unreliable conclusions about diet-disease relationships [39] [40].
What proportion of research participants typically misreport their energy intake? Studies from large cohorts indicate a high prevalence of misreporting. Research from Alberta's Tomorrow Project found approximately 47-50% of participants were identified as misreporters of energy intake, depending on the statistical method used [39] [42] [40]. A global analysis suggests that misreporting in dietary surveys is substantial and structural, leading to underestimates of population-level energy intake [3].
Which foods and nutrients are most susceptible to misreporting? Research indicates that not all foods are misreported equally. Foods like cakes, pies, and savory snacks may be underestimated to a greater extent than others [41]. Omissions often include additions to foods like condiments, dressings, and ingredients in multi-component dishes (e.g., vegetables in salads and sandwiches) [43]. One validation study found tomatoes, mustard, peppers, cucumber, cheese, lettuce, and mayonnaise were among the most commonly omitted items [43].
How does misestimation affect dietary pattern analysis? The method used to handle energy intake misreporters significantly influences derived dietary patterns. Cluster analysis can identify different patterns (e.g., "Healthy," "Meats/Pizza," and "Sweets/Dairy"), but participant assignment to these patterns changes substantially depending on how misreporters are handled [39] [42]. These methodological differences can subsequently affect observed associations between dietary patterns and disease outcomes such as cancer risk [40].
Troubleshooting Guide: Methodological Approaches
Identifying Energy Intake Misreporters
Problem: Researchers need to identify implausible energy intake reports before conducting analyses.
Solution: Implement validated statistical methods to identify misreporters.
Table 1: Statistical Methods for Identifying Energy Intake Misreporters
| Method | Key Principle | Key Inputs Required | Performance Characteristics |
|---|---|---|---|
| Revised-Goldberg Method [39] [40] | Compares ratio of reported EI to Basal Metabolic Rate (BMR) against Physical Activity Level (PAL) | Age, sex, weight, height, reported EI, physical activity data | Sensitivity >92% compared to doubly labeled water [40]; Identified 47% as misreporters in ATP cohort [39] |
| Predicted Total Energy Expenditure (pTEE) Method [39] | Uses predicted total energy expenditure based on BMR and PAL | Age, sex, weight, height, reported EI, physical activity data | Identified 50% as misreporters in ATP cohort; considered most detailed statistical procedure [39] |
| Crude Cut-off Method [39] | Excludes participants reporting EI outside pre-defined range (e.g., <500 or >3,500 kcal/day) | Reported energy intake only | Not individualized; may exclude some plausible reports while missing some implausible ones [39] |
Experimental Protocol: Implementing the Revised-Goldberg Method
Calculate Basal Metabolic Rate (BMR) using the Mifflin equation [39] [40]:
BMR (kcal/day) = 9.99 * weight(kg) + 6.25 * height(cm) - 4.92 * age(years) + 166 * sex(males=1; females=0) - 161Calculate Physical Activity Level (PAL) as the ratio of total energy expenditure to BMR [39]. Energy expenditure can be derived from physical activity questionnaires capturing frequency, duration, and intensity of recreational, household, transport, and occupational activities [39].
Calculate the ratio of reported energy intake (rEI) to BMR.
Compare rEI:BMR ratio to PAL using established Goldberg cut-offs, which vary by activity level [40]. For example, for sedentary individuals: lower cut-off = 0.75270, upper cut-off = 2.07586 [40].
Classify participants:
- Under-reporters: rEI:BMR values below lower cut-off
- Plausible reporters: rEI:BMR values within cut-offs
- Over-reporters: rEI:BMR values above upper cut-off
Figure 1: Workflow for Identifying Energy Intake Misreporters Using the Revised-Goldberg Method
Addressing Misestimation in Data Analysis
Problem: How to handle identified misreporters in statistical analyses.
Solution: Various scenarios can be applied, each with different implications for results.
Table 2: Scenarios for Handling Energy Intake Misreporters in Analysis
| Scenario | Description | Impact on Dietary Pattern Analysis |
|---|---|---|
| Inclusion | Retain all misreporters in cluster analysis | Base case; includes all data but with inherent measurement error |
| Exclude Before (ExBefore) | Remove misreporters prior to completing cluster analysis | Changes composition of derived dietary patterns [39] |
| Exclude After (ExAfter) | Remove misreporters after completing cluster analysis | Substantially changes participant assignment to patterns compared to ExBefore [39] |
| Inclusion with Nearest Neighbor (InclusionNN) | Exclude misreporters before analysis but add them back to clusters using nearest neighbor method | Different pattern assignments compared to simple Inclusion [39]; Can influence observed diet-disease associations [40] |
Experimental Protocol: Comparing Handling Scenarios in Diet-Disease Analysis
Apply multiple scenarios (e.g., Inclusion, ExBefore, ExAfter, InclusionNN) to the same dataset when deriving dietary patterns through cluster analysis [39] [40].
Compare derived patterns using statistical indices of agreement (e.g., Hubert and Arabie's adjusted Rand Index, Kappa, Cramer's V). Values <0.8 indicate substantial differences between scenarios [39].
Analyze diet-disease associations using different pattern solutions. For example, in one study, significant associations between "Sweets/Dairy" pattern and all-cancer risk in women were observed in ExBefore but not all scenarios [40].
Report scenario comparisons transparently in methods and discussion sections, acknowledging how handling method might influence conclusions.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Resources for Energy Intake Misestimation Research
| Resource/Tool | Function | Application Context |
|---|---|---|
| Doubly Labeled Water (DLW) | Gold standard for measuring total energy expenditure; validation benchmark [40] | Validation studies; not feasible for large cohorts due to cost and burden [40] |
| Automated Multiple-Pass Method (AMPM) | Interviewer-administered 24-hour recall with probing questions to minimize omissions [43] | US NHANES surveys; improves completeness of dietary reporting [43] |
| ASA24 (Automated Self-Administered 24-h Recall) | Self-administered web-based 24-hour recall with memory prompts [43] | Large-scale studies; reduces respondent memory lapses through standardized probing [43] |
| myfood24 | Scientifically validated nutritional analysis software with extensive food composition database [44] | Diet tracking and assessment in research across multiple health conditions [44] |
| Physical Activity Questionnaires (e.g., PYTPAQ) | Assess domain-specific physical activity to calculate PAL [39] [40] | Essential input for revised-Goldberg and pTEE methods to estimate energy requirements [39] |
Figure 2: Methodological Framework for Energy Intake Assessment Research
In nutritional research, accurately measuring energy intake is fundamental to understanding energy balance, yet self-reported methods like 24-hour recalls are notoriously prone to measurement error [45]. The doubly labeled water (DLW) method serves as a gold standard for validating these instruments by providing an objective measure of total energy expenditure (TEE) in free-living individuals [46] [47]. By comparing reported energy intake to DLW-measured expenditure, researchers can quantify systematic errors, such as under-reporting, which is crucial for ensuring the validity of studies examining diet-disease relationships [45]. Framing this within the context of statistical adjustment for total energy intake, the DLW method provides the critical reference point needed to calibrate other dietary assessment tools and interpret findings from nutritional epidemiology accurately [2] [1].
Frequently Asked Questions (FAQs)
What is the Doubly Labeled Water method and why is it considered a gold standard?
The doubly labeled water method is a non-invasive, isotopic technique for measuring free-living total energy expenditure [46] [47]. It involves administering a dose of water labeled with stable, non-radioactive isotopes of hydrogen (²H) and oxygen (¹⁸O). After the dose equilibrates with the body's water pool, the differing elimination rates of ¹⁸O (lost as both water and carbon dioxide) and ²H (lost almost exclusively as water) are measured in bodily fluids like urine, saliva, or blood [48] [47]. The difference in these elimination rates is used to calculate the rate of carbon dioxide production (rCO₂), which is then converted to TEE using principles of indirect calorimetry [46] [47]. It is considered the gold standard because it is highly accurate (2-8% precision compared to room calorimetry), objective, and allows subjects to engage in their normal, daily activities without interference, unlike confined calorimetry methods [46] [47] [49].
How does DLW help in detecting error in self-reported energy intake?
In nutritional studies, energy intake is often assessed via self-report methods like 24-hour dietary recalls. These are susceptible to both random errors (reducing precision) and systematic errors like under-reporting (reducing accuracy) [45]. Since, in weight-stable individuals, total energy expenditure should equal energy intake, DLW provides a reference measure of true energy requirement [47]. A significant and consistent discrepancy where self-reported intake is lower than DLW-measured expenditure provides objective evidence of under-reporting at the group or individual level [45]. This allows researchers to statistically correct for this bias in epidemiologic analyses, strengthening the validity of observed associations between nutrient intake and health outcomes [45] [1].
What are the primary assumptions and limitations of the DLW method?
The DLW method relies on several key assumptions, and violations can introduce error [48]:
- Constant Body Water Pool: The volume of the body water pool is assumed to remain relatively constant (within ~3%) throughout the measurement period. Significant changes in hydration status can affect results.
- Constant Isotope Background: The natural background abundance of ²H and ¹⁸O in body water is assumed to remain stable. Changes due to dietary water sources or geographical relocation can introduce error if not accounted for [48] [49].
- No Isotope Re-entry: The isotopic tracers, once lost from the body, are assumed not to re-enter the body water pool.
- Known Respiratory Quotient: The calculation of energy expenditure from CO₂ production requires an assumption about the average respiratory quotient (RQ), often estimated from the diet's food quotient (FQ) [48].
A primary limitation is the high cost of the ¹⁸O-enriched water [46] [48]. Furthermore, the method measures total CO₂ production over a period (typically 1-3 weeks) and cannot provide minute-by-minute or day-by-day energy expenditure patterns [47].
What special situations require modifications to the standard DLW protocol?
Deviations from standard living conditions can alter background isotope levels or tracer elimination, requiring protocol adjustments [48]:
- Geographical Relocation or Change in Water/Diet Source: If a subject travels or changes their primary source of water and food during the study, the baseline isotope abundance can shift. In such cases, collecting an additional background sample after returning or a background sample from the new water source is recommended [48].
- Extreme Environmental Conditions: Exposure to very high or low temperatures or altitudes can increase fractionated water loss through the skin and lungs. While DLW has been validated at high altitudes, these conditions may require use of a specific fractionation factor (rGF) in the calculation models [48].
- Clinical Conditions: Conditions like renal failure, or episodes of vomiting or diarrhea, can affect water turnover and isotope elimination. It is best to delay dosing until the subject has recovered to a stable, normal state [48].
Troubleshooting Common Experimental Issues
| Problem | Potential Cause | Solution |
|---|---|---|
| High variability in final enrichment results | Insufficient number of post-dose samples; high day-to-day variation in water flux. | Use a multi-point sampling protocol (e.g., daily samples) instead of a two-point protocol to improve the precision of elimination rate calculations [49]. |
| Inaccurate Total Body Water (TBW) estimate | Single post-dose sample not representative of true plateau; sample collected before full equilibration. | Collect multiple post-dose samples (e.g., at 4, 5, and 6 hours); use the intercept method (back-extrapolation to time zero) instead of the plateau method to calculate dilution spaces [49]. |
| Drift in baseline isotope enrichment | Changes in the isotopic composition of consumed water/food during the study period [48] [49]. | Collect an additional post-study background sample. If using advanced laser spectroscopy (OA-ICOS), measure ¹⁷O to model and correct for background fluctuations in ²H and ¹⁸O [49]. |
| Under-reporting not detected | The study population is in positive energy balance (gaining weight). | Measure body weight at the start and end of the DLW period. Adjust the reference energy requirement from DLW-TEE for changes in body energy stores to accurately identify misreporting [45]. |
Key Experimental Protocols and Workflows
Standard DLW Administration and Sampling Protocol
The following is a typical "two-point" protocol for a human study [48]:
- Pre-Dose (Baseline):
- Collect a baseline urine sample (>20 mL) to determine background isotopic enrichment.
- Measure body weight.
- Dosing:
- Administer an oral dose of DLW. A typical dose is 0.09–0.12 g of ²H₂O and 0.18–0.23 g of H₂¹⁸O per kg of estimated total body water [48].
- Record the exact time of administration and the exact weight of the dose. Have the subject rinse the dose container with plain water and drink the rinse to ensure the full dose is consumed.
- Post-Dose Equilibration:
- Collect the first post-dose urine sample 4-6 hours after dosing. A second sample 5-6 hours post-dose is often recommended to confirm equilibration.
- Elimination Phase:
- The study concludes with the collection of final urine samples at the end of the measurement period (e.g., 7 or 14 days later). Samples should be collected at roughly the same time of day (± 3 hours) as the initial post-dose samples to minimize diurnal variation effects [48].
- Sample Handling:
- All urine samples should be sealed in airtight containers and frozen immediately after collection to prevent evaporation and isotopic fractionation.
Workflow: Using DLW to Validate a 24-Hour Recall Instrument
The following diagram illustrates the logical workflow for using DLW to detect and account for measurement error in self-reported dietary intake.
The Scientist's Toolkit: Essential Research Reagents & Materials
| Item | Function | Technical Specifications |
|---|---|---|
| ²H₂O (Deuterium Oxide) | Stable isotope tracer to label the body's hydrogen pool and track water loss. | Typically 99.8% Atom Percent Excess (APE). Dose: ~0.10 g/kg TBW [48] [49]. |
| H₂¹⁸O (¹⁸O-Labeled Water) | Stable isotope tracer to label the body's oxygen pool and track combined water and CO₂ loss. | Highly enriched (e.g., 98% APE). Dose: ~0.20 g/kg TBW. Using highly enriched ¹⁸O minimizes ¹⁷O interference [49]. |
| Isotope Ratio Mass Spectrometer (IRMS) | The traditional high-precision instrument for analyzing isotopic ratios (²H/¹H and ¹⁸O/¹⁶O) in urine, saliva, or blood samples [46]. | Provides high accuracy and precision but can be costly and require specialized operation. |
| Off-Axis Integrated Cavity Output Spectroscopy (OA-ICOS) | A modern laser-based spectroscopy technology for isotopic analysis. It allows for simultaneous measurement of δ²H, δ¹⁸O, and δ¹⁷O, which can be used to correct for background variation [49]. | Lower cost and easier to operate than IRMS, making multi-point sampling and ¹⁷O correction more feasible [49]. |
| Sterile Dosing Bottles & Filters | For preparing and administering the DLW dose. Sterile 0.22μm filters are used to sterilize the dose before administration [48]. | Prevents microbial contamination and ensures subject safety. |
| Airtight Sample Vials | For storing collected urine samples. | Prevents evaporation and isotopic fractionation prior to analysis. Samples must be frozen after collection [48]. |
Key Quantitative Data and Calculations
Equations for Calculating Energy Expenditure
The core calculation in DLW is the rate of CO₂ production (rCO₂). Below are commonly used equations [48] [47].
Table 1: Formulas for Calculating CO₂ Production and Energy Expenditure
| Calculation Step | Formula | Variables and Constants |
|---|---|---|
| Isotope Elimination Rates (k) | ( k = -(\ln(Ef) - \ln(Ei)) / \Delta t ) | k: Elimination rate (pools/day). E_i, E_f: Initial & final isotope enrichments above background. Δt: Time between samples (days) [48]. |
| CO₂ Production Rate (rCO₂) (Simplified) | ( rCO2 = 0.455 \times N \times (1.007kO - 1.041k_H) ) | N: Average pool size of body water (moles). k_O, k_H: Elimination rates for ¹⁸O and ²H. Constants correct for fractionation [48]. |
| CO₂ Production Rate (rCO₂) (Comprehensive) | ( rCO2 = (N/2.078)(1.01kO - 1.04kH) - 0.0246r{GF} ) | r_GF: Rate of fractionated water loss (transcutaneous & pulmonary). This is a more precise two-pool model equation [47]. |
| Total Energy Expenditure (TEE) | ( TEE = 22.4 \times (3.9 \times (\frac{rCO2}{RQ}) + 1.1 \times rCO2) \times \frac{4.184}{1000} ) | Converts rCO₂ (mol/day) to TEE (kcal/day). The Respiratory Quotient (RQ) is often estimated by the Food Quotient (FQ) of the diet [48]. |
Impact of Protocol Choices on Precision and Accuracy
A 2019 study compared different calculation approaches against the gold standard of a whole-room calorimeter [49].
Table 2: Impact of Sampling Protocol and Calculation on DLW Accuracy
| Protocol Feature | Comparison | Outcome on VCO₂ Measurement |
|---|---|---|
| Sampling Method | Multi-point (daily samples) vs. Two-point (start/end only) | Multi-point fitting improved average precision (4.5% vs. 6.0%) and accuracy (-0.5% vs. -3.0%) [49]. |
| Background Correction | Using ¹⁷O measurements to correct for background fluctuation vs. Standard single baseline. | Provided minor but additional improvements in precision (4.2% vs. 4.5%) and accuracy (0.2% vs. 0.5%) [49]. |
| Dilution Space Calculation | Intercept Method (back-extrapolation) vs. Plateau Method (using post-dose sample directly). | The optimal combination of approaches, which included the intercept method, yielded the best results, though the specific improvement was context-dependent [49]. |
Frequently Asked Questions (FAQs)
Q1: What is the core difference between the Revised-Goldberg and Predicted TEE methods for identifying misreporters?
A1: The core difference lies in their fundamental approach. The Revised-Goldberg method assesses the plausibility of reported Energy Intake (rEI) by comparing the ratio of rEI to Basal Metabolic Rate (BMR) against the Physical Activity Level (PAL), using confidence limits to identify misreporters [39]. In contrast, the Predicted Total Energy Expenditure (pTEE) method uses a predictive equation derived from Doubly Labeled Water (DLW) data to estimate an individual's expected TEE based on variables like weight, age, and sex. The reported EI is then compared directly to this predicted TEE value to determine plausibility [50] [39].
Q2: In a head-to-head comparison, which method identifies more energy intake misreporters?
A2: Studies directly comparing these methods have found that the Predicted TEE method identifies a significantly higher proportion of participants as misreporters. One large-scale analysis reported that the pTEE method identified misreporting in 50% of participants, compared to 47% identified by the Revised-Goldberg method [39].
Q3: Why is identifying energy intake misreporting critical for dietary pattern analysis?
A3: All self-reported dietary data contains measurement error, which compounds when estimating total energy intake [39]. Failure to account for misreporting can substantially alter the derived dietary patterns. Research shows that whether misreporters are included or excluded from cluster analysis changes the composition of the identified dietary patterns (e.g., "Healthy," "Meats/Pizza," "Sweets/Dairy"), leading to different and potentially erroneous conclusions about diet-disease relationships [39].
Q4: What are the practical implications of choosing one method over the other?
A4: The choice of method impacts the dataset's composition and subsequent analysis. The Revised-Goldberg method relies on estimated BMR and assumed activity levels, while the pTEE method uses a more direct TEE prediction from a large DLW database [50] [39]. The pTEE method is considered more detailed and may better detect subtle misreporting. However, the method you select should be clearly reported, as it influences which records are deemed plausible and can affect the reproducibility of your research [39].
Troubleshooting Common Experimental Issues
Issue 1: Inconsistent Identification of Misreporters Between Methods
- Problem: Your analysis identifies different sets of implausible reporters when using the Revised-Goldberg versus the Predicted TEE method, leading to uncertainty about which dataset to use.
- Solution: This is an expected outcome. The pTEE method generally identifies more misreporters [39].
- Action Plan:
- Conduct your primary analysis using the pTEE method, as it is based on a more contemporary and extensive DLW dataset [50] [39].
- Perform a sensitivity analysis by running your models with the dataset generated by the Revised-Goldberg method.
- Report results from both approaches and note any substantive differences in your conclusions. This transparency strengthens the validity of your findings.
- Action Plan:
Issue 2: Handling Misreporters in Dietary Pattern Analysis
- Problem: After identifying misreporters, it is unclear how to handle them in cluster analysis for dietary patterns.
- Solution: The strategy for handling misreporters significantly impacts results [39].
- Action Plan: Consider and report which of the following scenarios you employ:
ExBefore: Exclude misreporters before performing the cluster analysis.ExAfter: Exclude misreporters after performing the cluster analysis.InclusionNN: Exclude misreporters before clustering but add them back to the final cluster solution using a nearest neighbor method.
- Recommendation: Studies suggest that the
Inclusion(including all data without adjustment) andInclusionNNscenarios can yield substantially different dietary pattern assignments compared to exclusion-based methods. Testing multiple scenarios is recommended [39].
- Action Plan: Consider and report which of the following scenarios you employ:
Issue 3: Systematic Bias in Macronutrient Composition
- Problem: As the level of identified misreporting increases, the reported macronutrient composition of the diet becomes systematically biased, leading to spurious associations.
- Solution: This bias is a known consequence of misreporting and cannot be fully eliminated [50].
- Action Plan:
- Use the pTEE method to screen for implausible dietary reports.
- Statistically adjust for the degree of misreporting in your models, acknowledging that this adjustment rests on certain assumptions.
- Clearly state the potential for residual bias in the macronutrient-disease associations you report.
- Action Plan:
Protocol: Applying the Predicted TEE Method
The following workflow visualizes the step-by-step process for implementing the Predicted TEE method to identify misreporters in a research dataset.
Protocol: Applying the Revised-Goldberg Method
This diagram outlines the logical sequence for assessing energy intake plausibility using the Revised-Goldberg cut-off method.
Quantitative Data Comparison
Table 1: Key Comparative Metrics of Plausibility Assessment Methods
| Metric | Revised-Goldberg Method | Predicted TEE Method | Notes & Sources |
|---|---|---|---|
| Underlying Principle | Compares rEI:BMR ratio to PAL within confidence limits [39] | Compares rEI directly to TEE predicted from body metrics [50] [39] | |
| Typical Misreporters Identified | 47% of a cohort [39] | 50% of a cohort [39] | Variation expected based on population studied. |
| Sensitivity/Specificity (vs. DLW) | Reported sensitivity: 92%, specificity: 88% [39] | Considered a more detailed statistical procedure [39] | Performance metrics for pTEE vs. DLW are an area of ongoing research. |
| Primary Input Variables | rEI, Weight, Height, Age, Sex (for BMR), PAL [39] | rEI, Body Weight, Height, Age, Sex, Ethnicity, Elevation [50] | The pTEE method uses a more complex regression equation. |
| Impact on Dietary Patterns | Cluster composition changes significantly based on how misreporters are handled [39] | Cluster composition changes significantly based on how misreporters are handled [39] | Excluding vs. including misreporters alters the final dietary patterns identified. |
Table 2: Magnitude of Energy Intake Misreporting in National Surveys
| Survey | Measurement Technique | Average Underestimation of Energy Intake | Key Associated Factors | Source |
|---|---|---|---|---|
| UK National Diet &Nutrition Survey (NDNS) | Doubly Labeled Water (DLW) | 27% (95% CI: 25%, 28%) | Higher BMI, Older Age, Female Sex | [51] |
| Applied to NDNS & NHANES | Predicted TEE Equation | 27.4% misreporting rate | Systematic bias in macronutrient composition | [50] |
The Scientist's Toolkit: Essential Reagents & Materials
Table 3: Key Reagents and Materials for Energy Intake Assessment Research
| Item | Function / Application in Research |
|---|---|
| Doubly Labeled Water (DLW) | Considered the gold standard for validating self-reported energy intake by directly measuring total energy expenditure in free-living individuals. Used to derive and validate predictive TEE equations [50] [51]. |
| Validated Physical Activity Questionnaire (e.g., PYTPAQ) | A tool to collect data on frequency, duration, and intensity of various physical activities. Essential for calculating the Physical Activity Level (PAL) required for the Revised-Goldberg method [39]. |
| Food Frequency Questionnaire (FFQ) / 24-Hour Recall | Self-reported instruments to collect data on dietary intake. The raw data from these tools provides the "Reported Energy Intake (rEI)" which is evaluated for plausibility [39]. |
| Predictive TEE Equation | A published regression equation (e.g., from the IAEA DLW database) used to estimate an individual's total energy expenditure based on easily acquired variables like body weight, age, and sex. The core reagent for the pTEE method [50]. |
| BMR Prediction Equation (e.g., Mifflin-St Jeor) | A formula to estimate Basal Metabolic Rate using weight, height, age, and sex. A critical component for conducting the Revised-Goldberg assessment [39]. |
In nutritional epidemiology and research on total energy intake, reporting error poses a significant threat to data validity and subsequent conclusions. This technical support guide addresses how biological and demographic factors—specifically Body Mass Index (BMI), age, and sex—systematically influence the accuracy of self-reported dietary data. Understanding these biases is crucial for researchers conducting statistical adjustments in energy intake analysis, as unaddressed reporting errors can lead to attenuated effect estimates, reduced statistical power, and biased conclusions in both observational studies and clinical trials.
Recent research has quantified the substantial impact of reporting error on study outcomes. For instance, a 2025 analysis of the UK Biobank found that reporting inconsistencies can lead to a relative attenuation of approximately 21% in SNP heritability estimates for traits like childhood height [52]. This guide provides troubleshooting methodologies to identify, quantify, and correct for these biases within the context of energy intake research.
Quantitative Evidence: The Impact of Demographics on Reporting Error
How significantly do BMI, age, and sex affect self-reporting accuracy?
Reporting error is not random but varies systematically with participant demographics. Analyses of large datasets reveal distinct patterns:
Table 1: Impact of Demographic Factors on Reporting Error
| Demographic Factor | Impact on Reporting Error | Effect Size / Magnitude | Key Evidence |
|---|---|---|---|
| BMI | Positive correlation with reporting error | Not quantified in results | Higher BMI linked to less consistent self-reporting [52] |
| Age | Mixed effects based on outcome | Older age → ↑ reporting errorOlder age → ↑ participation | Conflicting influences depending on study context [52] |
| Sex | Significant differential effects | Women show ↓ reporting error for certain measures | Largest effect: mother's age at death (women substantially lower error) [52] |
| Education | Higher education → ↓ error | Negative correlation | More educated participants show more consistent reporting [52] |
Reporting error is widespread across nutritional research methodologies:
Table 2: Prevalence of Reporting Error in Research Contexts
| Research Context | Error Prevalence | Specific Examples | Data Source |
|---|---|---|---|
| UK Biobank Self-Reports | Present across all 33 assessed measures | Mean error estimate: 0.21 (scale 0-1) | [52] |
| Childhood Recall | Questionable repeatability | Childhood body size (R² = 0.47)Age at first facial hair (R² = 0.50) | [52] |
| Dietary Assessments | Substantial underestimation | 24-hour recalls and FFQs "substantially underestimate total calorie intake" | [3] |
| Food Availability Data | Overestimation tendency | Overestimates actual intake if not adjusted for waste | [3] |
Troubleshooting Guide: Methodologies for Detection and Correction
FAQ 1: How can I detect and quantify reporting error in my dietary dataset?
Issue: Researchers suspect systematic reporting errors in self-reported dietary data but lack objective measures to quantify them.
Solution: Implement these complementary methodological approaches:
1. Biomarker Validation Protocol
- Objective: Use objective biomarkers to calibrate self-reported intake data
- Procedure:
- Collect biospecimens (blood/urine) alongside dietary assessments
- Analyze for metabolites associated with specific dietary components
- Develop poly-metabolite scores to predict actual intake
- Example: NIH researchers identified hundreds of metabolites correlating with ultra-processed food intake and developed poly-metabolite scores that accurately differentiated between high-processed and unprocessed diets in clinical trial settings [53] [54]
- Application: These scores can be used to correct self-reported data or as complementary measures in large population studies
2. Repeated Measures Analysis
- Objective: Quantify reporting consistency across multiple assessments
- Procedure:
- Collect repeated measures of time-invariant phenotypes
- Calculate consistency metrics across measurement occasions
- Generate reporting error scores per participant
- Example: UK Biobank analysis assessed 33 time-invariant self-report measures across multiple occasions to compute reporting error scores [52]
3. Anthropometric Energy Intake Estimation
- Objective: Derive energy intake estimates independent of self-report
- Procedure:
- Use predictive equations based on doubly labeled water studies
- Apply equations to measured body weight, height, and physical activity data
- Compare self-reported intake with anthropometrically-derived estimates
- Example: Global analysis used this method to reveal systematic misreporting in dietary surveys and food availability statistics [3]
Figure 1: Workflow for Detecting and Correcting Reporting Error in Dietary Data
FAQ 2: What statistical adjustments are most effective for mitigating BMI-related reporting bias?
Issue: Participants with different BMI categories demonstrate varying reporting accuracy, potentially biasing energy intake associations.
Solution: Implement these statistical adjustments:
1. Measurement Error Models
- Protocol: Develop customized measurement error corrections that account for BMI-specific reporting patterns
- Implementation:
- Use validation sub-studies with objective intake measures (e.g., biomarkers, doubly labeled water)
- Estimate BMI-specific reporting functions
- Apply these functions to correct main study analyses
- Rationale: Since reporting error correlates with BMI, standard corrections may be insufficient without accounting for this relationship [52]
2. Multiple Imputation with Anthropometric Anchors
- Protocol: Use anthropometrically-derived energy intake estimates to inform imputation of missing or misreported data
- Implementation:
- Calculate energy requirements using established predictive equations (e.g., National Academies of Sciences equations)
- Use these as anchors in multiple imputation procedures
- Generate multiple complete datasets incorporating corrected values
- Rationale: Anthropometric measures provide objective references that are not subject to the same reporting biases as dietary recalls [3]
FAQ 3: How do I account for age and sex interactions in reporting error?
Issue: Reporting accuracy varies non-uniformly by age, sex, and their interaction, creating complex bias patterns.
Solution: Implement stratified and interaction-focused approaches:
1. Age-Period-Cohort Modeling
- Protocol: Disentangle age effects from cohort and period effects in longitudinal dietary data
- Implementation:
- Collect detailed demographic metadata including birth cohort
- Apply age-period-cohort statistical models
- Generate age-specific and cohort-specific reporting error corrections
- Evidence: UK Biobank analyses found reporting error varied as a function of both baseline age and follow-up time, with significant interaction effects [52]
2. Sex-Stratified Validation
- Protocol: Develop and apply sex-specific reporting error corrections
- Implementation:
- Conduct validation analyses separately for male and female participants
- Identify sex-specific correlates of reporting accuracy
- Apply differential corrections in final analyses
- Evidence: Significant sex-differential effects in reporting error were observed, with 75% of reporting error scores showing significant differences between men and women [52]
Figure 2: Demographic Bias Sources and Corresponding Methodological Solutions
The Researcher's Toolkit: Essential Methodologies and Reagents
Table 3: Research Reagent Solutions for Reporting Error Investigation
| Tool/Reagent | Function | Application Example | Technical Specifications |
|---|---|---|---|
| Poly-metabolite Scores | Objective biomarker-based intake assessment | Quantifying ultra-processed food consumption independent of self-report [53] [54] | Mass spectrometry-based metabolomic profiling of blood/urine samples |
| Doubly Labeled Water (DLW) | Gold-standard measurement of total energy expenditure | Validating self-reported energy intake against objective expenditure [3] | Isotope ratio mass spectrometry following ^2H and ^18O administration |
| Food Pattern Equivalents Database (FPED) | Standardized conversion of foods to dietary components | Converting food intake data to USDA Food Pattern components for consistency [20] | Converts ~7,000 foods to 37 food pattern components |
| Food and Nutrient Database for Dietary Studies (FNDDS) | Comprehensive nutrient composition database | Assigning nutrient values to foods reported in dietary recalls [20] | Contains energy and 64 nutrients for ~7,000 foods |
| Anthropometric Prediction Equations | Estimating energy requirements from physical measures | Deriving objective energy intake estimates independent of self-report [3] | NAS equations based on doubly labeled water database (n=8,600) |
Advanced Protocol: Biomarker-Based Validation Study
Objective:
To develop and validate objective biomarkers for assessing dietary intake, reducing reliance on error-prone self-reports.
Materials:
- Liquid chromatography-mass spectrometry (LC-MS) system
- Blood collection tubes (EDTA) and urine collection containers
- Dietary assessment tools (24-hour recalls, FFQs)
- Clinical trial facility for controlled feeding studies
Procedure:
Phase 1: Observational Discovery
- Recruit 700+ participants from existing cohort studies (e.g., IDATA Study)
- Collect detailed dietary data via multiple 24-hour dietary recalls
- Obtain concurrent blood and urine samples
- Perform untargeted metabolomic profiling
- Identify metabolites correlated with specific dietary components (e.g., ultra-processed foods)
Phase 2: Experimental Validation
- Conduct randomized controlled crossover feeding trial (n=20)
- Implement two controlled diet phases:
- High ultra-processed food diet (80% of energy)
- Zero ultra-processed food diet (0% of energy)
- Each phase: 2 weeks duration
- Collect biospecimens at end of each phase
- Validate ability of metabolite patterns to differentiate between dietary conditions
Phase 3: Score Development
- Apply machine learning algorithms to identify predictive metabolite patterns
- Develop poly-metabolite scores for blood and urine separately
- Validate scores in independent populations
- Test association with health outcomes (e.g., cancer, type 2 diabetes)
Expected Outcomes:
- Objective biomarker scores that can complement or replace self-reported dietary data
- Improved accuracy in assessing associations between diet and health outcomes
- Reduced bias from demographic influences on self-reporting [53] [54]
Addressing reporting error related to BMI, age, and sex requires a multifaceted methodological approach. The most effective strategy integrates multiple assessment methods: combining traditional self-reports with biomarker measurements, repeated assessments, and anthropometric estimation. Researchers should prioritize validation sub-studies that specifically examine demographic patterns in reporting accuracy and develop customized correction approaches for their target populations.
Implementation of these methodologies will significantly improve the validity of energy intake assessment in nutritional epidemiology, enhancing our ability to detect true diet-disease relationships and develop effective public health interventions. As research in this area advances, the development of standardized, demographically-sensitive correction methods will be essential for comparability across studies and populations.
Troubleshooting Guides
Handling Missing Data in Clinical Trials
Problem: A significant number of participants in a randomized controlled trial have dropped out, leading to missing outcome data. You are concerned this may bias the intent-to-treat analysis.
Solution: The appropriate strategy depends on the nature of the missing data and the assumptions you are willing to make [55] [56].
Step 1: Classify the Missing Data Mechanism First, theorize the mechanism behind the missing data, as this dictates the appropriate handling method [55] [57]. The three primary classifications are:
- Missing Completely at Random (MCAR): The probability of data being missing is unrelated to any observed or unobserved variables. An example is data loss due to a broken lab instrument [55].
- Missing at Random (MAR): The probability of data being missing is related to observed variables but not the unobserved missing values themselves. For example, dropout rates might be higher among a specific age group, which is fully recorded in your data [55].
- Missing Not at Random (MNAR): The probability of data being missing is related to the unobserved missing values. For instance, a participant experiencing severe side effects from a treatment may drop out and miss the final assessment because of that very outcome [55].
Step 2: Select a Handling Method Based on the Mechanism
- For MCAR, a complete case analysis can yield unbiased estimates, though with a loss of statistical power [55] [56].
- For MAR, preferred methods include Multiple Imputation or Maximum Likelihood estimation, as they use information from observed data to account for the missingness and provide less biased results compared to simple methods [55] [56] [58].
- For MNAR, no standard method can be definitively proven correct, as the mechanism is unverifiable. Sensitivity analyses are crucial to test how different MNAR assumptions impact the results [55] [56].
Step 3: Avoid Simple but Problematic Methods Methods like Last Observation Carried Forward (LOCF) or Baseline Observation Carried Forward (BOCF) are often criticized because they rely on unrealistic assumptions (e.g., no change after dropout) and can introduce significant bias [58].
Step 4: Perform Sensitivity Analyses Conduct analyses under different missing data assumptions (e.g., MAR vs. various MNAR scenarios) to assess the robustness of your primary conclusion [59]. This demonstrates to regulators and readers that your finding is not an artifact of a single, potentially flawed, method [59] [58].
Addressing Misreporting in Energy Intake (EI) Data
Problem: In nutritional research, you suspect that self-reported energy intake (EI) from food frequency questionnaires is inaccurate, potentially confounding the relationship between a nutrient of interest and a health outcome.
Solution: Implement methods to identify and account for implausible self-reported energy intake.
Step 1: Assess Plausibility of Reported Energy Intake (rEI) Compare rEI to an estimate of total energy expenditure (TEE). The gold standard for TEE is the doubly labeled water (DLW) method, but it is often prohibitively expensive [60]. Common alternatives include:
Step 2: Identify Misreporters Choose a method to classify participants as under-, over-, or plausible reporters.
- Crude Method: Exclude participants with rEI outside a pre-defined range (e.g., <500 or >3,500 kcal/day for women). This method is simple but not individualized and may misclassify people [60] [39].
- Individualized Methods:
- Revised-Goldberg Cut-off: Uses the ratio of rEI to BMR (rEI:BMR) and compares it to PAL, accounting for variation in rEI and BMR to create confidence limits for identifying misreporters [60] [39].
- Predicted TEE (pTEE) Method: Similar to the Goldberg method but uses the ratio of rEI to pTEE and incorporates different variance estimates [39]. Studies suggest the pTEE method may identify a higher proportion of misreporters [39].
Step 3: Address Misreporting in Analysis
- Exclusion: Remove identified misreporters from the analysis. The timing of exclusion (before or after deriving dietary patterns) can influence results [39].
- Statistical Adjustment: Include the ratio of rEI to TEE (rEI:TEE) as a covariate in your statistical models. This adjusts for the degree of misreporting continuously [60].
Step 4: Conduct Sensitivity Analyses Perform your primary analysis using different methods (e.g., revised-Goldberg vs. pTEE, exclusion vs. adjustment) to show whether the core findings remain consistent regardless of how misreporting is handled [39].
Frequently Asked Questions (FAQs)
Q1: What is the single most important thing I can do to handle missing data? The best strategy is prevention. Invest significant effort in trial design and conduct to minimize the amount of missing data from the outset. This includes designing user-friendly case report forms, ensuring adequate participant follow-up, and using effective patient retention strategies [55] [58].
Q2: What is a sensitivity analysis and why is it critical for clinical trials? A sensitivity analysis is "a series of analyses of a data set to assess whether altering any of the assumptions made leads to different final interpretations or conclusions" [59]. It is critical because it tests the robustness of your primary findings. If results remain consistent across different analytical assumptions (e.g., about missing data or protocol deviations), your conclusions are more credible to regulators like the FDA and EMA and to the scientific community [59].
Q3: When adjusting for total energy intake, what is the difference between the "standard" and "energy partition" models? These models estimate different causal effects and are not interchangeable [2].
- The "Standard Model" (adjusting for total energy intake) estimates the average relative causal effect. It answers: "What is the effect of increasing energy from one nutrient while simultaneously decreasing the average of all other nutrients to keep total energy constant?" This is a substitution effect [2].
- The "Energy Partition Model" (adjusting for energy from all other sources) estimates the total causal effect. It answers: "What is the effect of increasing energy from one nutrient while holding intake from all other nutrients constant?" This is an additive effect [2].
Q4: Is a complete case analysis ever acceptable? Yes, but only under very specific conditions. A complete case analysis can be valid when data are Missing Completely at Random (MCAR), as the complete cases represent a random subset of the original sample. However, since the MCAR assumption is often unrealistic, this method is generally not recommended as a primary analysis because it can lead to biased estimates and loss of statistical power [55] [56] [58].
Q5: How do I choose between single and multiple imputation for missing data? Multiple Imputation (MI) is almost always preferred over single imputation. Single imputation methods (e.g., mean imputation, LOCF) replace a missing value with one best guess, which ignores the uncertainty about the true value and artificially reduces data variability. MI creates multiple plausible datasets, analyzes them separately, and combines the results, thereby properly accounting for the uncertainty of the imputed values and leading to more accurate standard errors and statistical inferences [56] [57] [58].
Method Comparison Tables
Table 1: Comparison of Common Energy Intake Adjustment Models
| Model Name | Statistical Approach | Target Estimand | Key Interpretation |
|---|---|---|---|
| Standard Model [2] [1] | Adjusts for total energy intake | Average Relative Causal Effect | Effect of substituting the exposure nutrient for the weighted average of all other energy sources. |
| Energy Partition Model [2] | Adjusts for remaining energy intake (total minus exposure) | Total Causal Effect | Effect of adding the exposure nutrient while keeping all other energy sources constant. |
| Nutrient Density Model [2] | Exposure is rescaled as a proportion of total energy | Rescaled Average Relative Causal Effect | Obscure interpretation; attempts to estimate the substitution effect rescaled as a proportion of total energy. |
| Residual Model [2] | Uses the residual from regressing the nutrient on total energy | Mathematically identical to the Standard Model [2] | Same as the Standard Model: a substitution effect. |
| All-Components Model [2] | Simultaneously adjusts for all other dietary components | Total Causal Effect | Provides a less biased estimate of the total effect by avoiding the use of a summary variable (like total energy). |
Table 2: Comparison of Missing Data Mechanisms and Handling Methods
| Mechanism | Description | Impact on Analysis | Recommended Methods |
|---|---|---|---|
| MCAR (Missing Completely at Random) [55] [57] | Missingness is unrelated to any data. | Leads to loss of power but not bias. | Complete Case Analysis, Multiple Imputation. |
| MAR (Missing at Random) [55] [56] [57] | Missingness is related to observed data only. | Can cause bias if ignored. | Multiple Imputation, Maximum Likelihood, Inverse Probability Weighting. |
| MNAR (Missing Not at Random) [55] [56] | Missingness is related to the unobserved value itself. | Will cause bias; cannot be verified from the data. | Sensitivity Analyses (e.g., using selection models or pattern-mixture models). |
Experimental Protocols
Protocol for Implementing Multiple Imputation using Rubin's Rules
Multiple Imputation is a robust method for handling missing data under the MAR assumption. The following protocol outlines its implementation [58]:
- Specify the Imputation Model: Choose an appropriate model to impute (fill in) the missing values. This model should include variables related to the missingness and the outcome to improve accuracy. Predictive Mean Matching (PMM) is often used as it imputes values from similar observed data points [58].
- Generate Multiple Datasets: Run the imputation model multiple times (typically 5-20 times) to create
mnumber of complete datasets. Each dataset contains different plausible estimates for the missing values, reflecting the uncertainty about the true value [58]. - Analyze Each Dataset: Perform your planned statistical analysis (e.g., ANOVA, regression) separately on each of the
mcompleted datasets. - Pool the Results: Combine the results from the
manalyses using Rubin's rules [58]. This involves:- Pooling Parameter Estimates: Averaging the estimates (e.g., regression coefficients) across the
mdatasets. - Pooling Variances: Calculating the combined variance by averaging the within-imputation variances and adding the between-imputation variance, which accounts for the uncertainty due to the missing data.
- Pooling Parameter Estimates: Averaging the estimates (e.g., regression coefficients) across the
Protocol for Performing a Sensitivity Analysis on Missing Data
This protocol assesses how sensitive your trial's conclusions are to different assumptions about the missing data [59].
- Define the Primary Analysis: Start with your primary analysis, which should be based on a plausible assumption (commonly MAR, using a method like Multiple Imputation) [59].
- Specify Alternative Scenarios: Formulate alternative, clinically plausible scenarios for the missing data. For example:
- Tipping Point Analysis: Assume that all participants with missing data in the treatment group had a poor outcome (e.g., treatment failure), while all in the control group had a good outcome. Then, see if the treatment effect remains significant [59].
- MNAR-based Models: Use statistical models explicitly designed for MNAR data (e.g., selection models) to see how the results change under a defined "not at random" mechanism [55].
- Copy Reference (CR) Assumption: Assume that participants who dropped out of the treatment arm subsequently responded as if they were in the control/reference group [58].
- Re-analyze Data: Perform the same statistical test for each pre-specified scenario.
- Compare Results: Compare the results (e.g., effect sizes, p-values, confidence intervals) from all sensitivity analyses to the primary analysis. If the conclusion about the treatment's effectiveness does not change across the different scenarios, your result is considered robust [59].
Visualized Workflows
Missing Data Handling Strategy
Energy Intake Model Selection
Research Reagent Solutions
Table 3: Essential Methodological Tools for Data Handling
| Item Name | Type (Software/Method) | Primary Function |
|---|---|---|
| Multiple Imputation by Chained Equations (MICE) | Statistical Method / Software Package | A flexible multiple imputation procedure that handles variables of different types (continuous, binary, categorical) by using a series of regression models [57]. |
| Mixed Models for Repeated Measures (MMRM) | Statistical Model | A likelihood-based method for analyzing longitudinal data that provides unbiased estimates under the MAR assumption without imputation. Often recommended for primary analysis in clinical trials [58]. |
| Rubin's Rules | Statistical Formula | The standard set of rules for combining parameter estimates and variances from analyses performed on multiple imputed datasets [58]. |
| Directed Acyclic Graph (DAG) | Conceptual Tool | A graphical causal model that helps researchers visually map out and identify potential confounding variables, selection bias, and appropriate adjustment strategies, crucial for energy intake analysis [2]. |
| Sensitivity Analysis Plan | Study Protocol Component | A pre-specified plan in a statistical analysis protocol (SAP) that outlines the various scenarios and methods that will be used to test the robustness of the primary trial results [59]. |
Evaluating Method Performance and Comparative Frameworks
Frequently Asked Questions (FAQ)
Q1: What is the "gold standard" for measuring energy expenditure in free-living humans, and why is it used to validate dietary intake tools? The doubly labeled water (DLW) method is internationally recognized as the gold standard for measuring total energy expenditure (TEE) in free-living conditions [46] [61] [62]. It is based on measuring the differential elimination rates of stable isotopes (deuterium and oxygen-18) from body water after ingestion [46]. Because energy intake and expenditure are equal in weight-stable individuals, the DLW-measured TEE provides an objective benchmark to validate the accuracy of self-reported energy intake from tools like dietary recalls and food frequency questionnaires [61] [63] [64]. This helps researchers identify and quantify the pervasive issue of dietary misreporting [50].
Q2: My research uses predictive equations instead of direct DLW. How accurate are they? Predictive equations can be very useful, but their accuracy varies. A 2025 study evaluating new equations for older adults found that while they showed strong correlation with DLW-measured TEE at the group level, they had wide limits of agreement and high root mean square error at the individual level [62]. This means they should be used with caution for individual-level clinical decisions. Newer equations derived from large DLW databases (e.g., over 6,000 measurements) can predict TEE from weight, age, and sex, and are valuable for screening for misreporting in large dietary surveys [50] [3].
Q3: Why might energy intake from my 24-hour diet recalls be significantly lower than energy expenditure measured by DLW? It is common for 24-hour diet recalls to underreport energy intake. A 2022 study in Korean adults found that energy intake from 24-hour recalls was on average 12.0% lower than TEE measured by DLW, with under-prediction rates of 60.5% for all subjects [61]. A 2025 study also reported that 50% of recalls from older adults were classified as under-reported [63]. This underreporting is often attributed to challenges in estimating portion sizes, memory recall bias, and sometimes deliberate misreporting [50] [61].
Q4: I've found that increased physical activity doesn't lead to a corresponding increase in total energy expenditure. Is this possible? Yes, this aligns with the Constrained Total Energy Expenditure model [65]. This model suggests that in response to increased physical activity, the body may adapt metabolically by reducing energy expenditure on other physiological processes (such as basal metabolic rate, repair, or inflammatory activity), leading to a plateau in total daily energy expenditure, particularly at higher activity levels [65]. This contrasts with the traditional Additive model, which assumes a direct, linear increase in TEE with physical activity.
Troubleshooting Guides
Issue 1: Handling Suspected Dietary Misreporting in Cohort Studies
Problem: Data from food frequency questionnaires or 24-hour recalls is suspected to be widely misreported, potentially leading to spurious associations between diet and health outcomes.
Solution:
- Benchmark against predicted TEE: Use a predictive equation derived from DLW data to calculate expected TEE for each participant. For example, the equation from the International Atomic Energy Agency database uses body weight, height, age, sex, and ethnicity [50].
- Calculate reporting limits: Determine the 95% predictive limits for the expected TEE. Reported energy intake falling outside these limits can be flagged as implausible [50].
- Analyse bias: Be aware that misreporting is often non-random. Under-reporting is more common in individuals with higher BMI, and the degree of misreporting can systematically bias the apparent macronutrient composition of the diet [50] [63].
Issue 2: Validating a New Dietary Assessment Tool
Problem: You are testing a new mobile app or method for assessing dietary intake and need to validate its accuracy against an objective measure.
Solution:
- DLW Protocol: Administer doubly labeled water to participants and collect urine samples over a period of 7-14 days to measure TEE [61] [63].
- Concurrent Dietary Assessment: Have participants use the new dietary tool (e.g., a mobile app like SNAQ) and a traditional method (e.g., 24-hour recall) during the same period [64].
- Compare to Energy Expenditure: In weight-stable participants, compare the energy intake from the new tool to the TEE from DLW. Use statistical methods like Bland-Altman plots and paired t-tests to assess agreement and bias [64].
- Account for Energy Stores: For higher precision, calculate measured energy intake (mEI) as
mEI = TEE + ΔEnergy Stores, where changes in energy stores are derived from body composition scans (e.g., using QMR or DXA) at the start and end of the DLW period [63].
Issue 3: Interpreting Unexpected Relationships between Physical Activity and Total Energy Expenditure
Problem: Data shows that more physically active participants do not have a proportionally higher TEE, contradicting additive energy models.
Solution:
- Consider the Constrained Model: Recognize that a constrained relationship between physical activity and TEE is supported by ecological research. The body may compensate for increased activity energy costs by reducing expenditure on other metabolic processes [65].
- Analyze by Activity Level: Examine the relationship across the full spectrum of activity. The positive correlation between physical activity and TEE is often strongest at low activity levels and plateaus at higher activity levels [65].
- Control for Modulators: Include body fat percentage and activity intensity in your models, as these factors appear to modulate the metabolic response to physical activity [65].
Table 1: Common Predictive Equations for Energy Expenditure
| Equation Name / Source | Key Input Variables | Population Derived From | Reported Accuracy / Notes |
|---|---|---|---|
| IAEA Database Equation [50] | Body weight, height, age, sex, ethnicity, elevation | 6,497 individuals (age 4-96) | Explains 69.8% of variation in TEE. 95% predictive limits can screen for misreporting. |
| NASEM DRI Equations (2023) [3] | Age, sex, height, weight, physical activity level | 8,600 DLW values; validated on 5,056 participants | Differentiated by age, sex, and activity level. Used for population-level energy requirement estimates. |
| Porter et al. Equations [62] | Age-specific, includes resting energy expenditure | 1,657 older adults (>65 yrs) from 39 studies | For older adults; showed <10% bias at group level but wider individual limits of agreement. |
Table 2: Validation Studies of Dietary Assessment Tools vs. DLW
| Study & Tool | Population | Key Finding (Reported vs. Measured Energy) | Misreporting Rate |
|---|---|---|---|
| 24-hour Diet Recall [61] | 71 Korean adults (20-49 yrs) | Reported EI was 12.0% (317 kcal) lower than TEE-DLW. | Under-reporting: 60.5% of participants |
| SNAQ Mobile App [64] | 30 adult women with normal weight | Bias of -330 kcal/day vs. DLW (closer than 24HR's -543 kcal). | Not specified, but underestimation observed. |
| Dietary Recalls (Method Comparison) [63] | 39 older adults with overweight/obesity | 50% of recalls were under-reported using both standard and novel plausibility methods. | Under-reporting: 50% |
Detailed Protocol: Measuring TEE via Doubly Labeled Water
Principle: The method calculates CO2 production from the difference in elimination rates between deuterium (²H, leaves body as water) and oxygen-18 (¹⁸O, leaves as both water and CO2) [46].
Workflow:
- Dose Administration: The subject ingests a measured dose of DLW. A typical dose is 1.1 g per kg of body weight of water containing ²H₂O and H₂¹⁸O [61].
- Urine Sample Collection: Collect urine samples at:
- Isotopic Analysis: Analyze the urine samples using isotope ratio mass spectrometry to determine the enrichment of ²H and ¹⁸O [61].
- Calculation:
- Calculate the rate of CO2 production (rCO2) using the following formula [61]:
rCO2 (mol/day) = 0.4554 × Total Body Water × (1.007ko - 1.041kh)wherekoandkhare the elimination rates of ¹⁸O and ²H, respectively. - Convert rCO2 to TEE using the Weir equation [61] [63]:
TEE (kcal/day) = 3.9 × (rCO2) + 1.1 × (rCO2)This requires an assumed or measured respiratory quotient.
- Calculate the rate of CO2 production (rCO2) using the following formula [61]:
Detailed Protocol: Identifying Misreporting via Energy Balance
Principle: Objectively measured energy intake (mEI) is compared to self-reported energy intake (rEI) to classify reports as plausible, under-, or over-reported [63].
Workflow:
- Measure Components: Over a ~14-day period:
- Measure TEE using DLW.
- Measure changes in body energy stores (ΔES) via body composition scans (e.g., QMR, DXA) at start and end.
- Collect self-reported energy intake (rEI) via multiple 24-hour recalls.
- Calculate Measured Energy Intake (mEI):
mEI = TEE + ΔESwhere ΔES is derived from changes in fat mass and fat-free mass [63].
- Classify Reporting:
- Calculate the ratio
rEI / mEI. - Establish group-specific cut-offs (e.g., ±1 standard deviation from the mean ratio).
- Plausible reporters: Ratio within cut-off range.
- Under-reporters: Ratio below the lower cut-off.
- Over-reporters: Ratio above the upper cut-off [63].
- Calculate the ratio
The Scientist's Toolkit: Key Research Reagents & Materials
Table 3: Essential Research Reagents and Materials
| Item | Specification / Example | Primary Function in Research |
|---|---|---|
| Stable Isotopes | H₂¹⁸O (10% enriched); ²H₂O (99.9% enriched) [61] | Core component of DLW dose; used to trace water turnover and CO2 production. |
| Isotope Ratio Mass Spectrometer | e.g., Finnigan Delta Plus [61] | High-precision analysis of isotopic enrichment in biological samples (urine). |
| Body Composition Analyzer | Dual-Energy X-ray Absorptiometry (DXA) [66]; Quantitative Magnetic Resonance (QMR) [63] | Measures fat mass, lean mass, and bone mass; critical for calculating changes in energy stores. |
| Indirect Calorimeter | Vmax 229N system [66] | Measures resting energy expenditure (REE) via oxygen consumption and CO2 production. |
| Predictive Equations | NASEM DRI Equations (2023) [3]; IAEA-based equations [50] | Estimate energy requirements in lieu of direct DLW measurement, useful for large studies. |
| Bioelectrical Impedance Analysis (BIA) | Tetrapolar, single-frequency device (e.g., Quantum X) [66] | Estimates body composition (fat-free mass, fat mass) as an input for predictive equations. |
In nutritional epidemiology, dietary data is inherently compositional—the intake of different foods and nutrients sums to a total, most notably the total energy intake. This compositional nature means that increasing one component necessarily requires decreasing others if the total remains fixed. Consequently, adjusting for total energy intake becomes a fundamental methodological consideration when deriving dietary patterns and analyzing their health effects.
Different statistical approaches to energy adjustment estimate distinct causal effects and come with specific interpretations that are frequently misunderstood. This technical guide explores how these methodological choices influence dietary pattern derivation and provides troubleshooting support for researchers navigating these complex analytical decisions. Understanding these nuances is essential for producing valid, interpretable results that can effectively inform dietary guidelines and public health policy.
Core Energy Adjustment Methods: Theoretical Foundations
The Four Principal Models
Researchers commonly employ four statistical models to adjust for energy intake, each with different causal interpretations and mathematical properties [29]:
Table 1: Core Energy Adjustment Methods in Nutritional Research
| Model Name | Statistical Approach | Causal Estimand | Key Interpretation | Primary Limitations |
|---|---|---|---|---|
| Standard Model | Adjusts for total energy intake as a covariate | Average relative causal effect (substitution effect) | Effect of substituting one component for another while holding total energy constant | Biased estimates even without confounding |
| Energy Partition Model | Includes all dietary components without a reference | Total causal effect | Effect of changing the component while keeping all others constant | Unbiased only with no confounding or when all other nutrients have equal effects |
| Nutrient Density Model | Rescales exposure as proportion of total energy | Obscure interpretation | Attempts to estimate average relative causal effect rescaled as proportion of total energy | Problematic interpretation with variable totals |
| Residual Model | Uses residuals from regression of exposure on total energy | Mathematically identical to standard model | Same as standard model - substitution effect | Same limitations as standard model |
Compositional Data with Fixed vs. Variable Totals
A critical distinction in dietary analysis lies in whether the compositional total is fixed or variable [67]:
- Fixed Totals: The "whole" remains constant across observations (e.g., 24-hour time use, percentage of total energy)
- Variable Totals: The "whole" varies between units (e.g., total energy intake, total food weight)
This distinction profoundly affects analytical choices. With variable totals, the total must be explicitly included in models, whereas with fixed totals, it is implicit and cannot be included. Methods that perform well with one type may produce misleading results with the other [67].
Diagram 1: Decision Pathway for Energy Adjustment Methods
Troubleshooting Guide: Frequently Asked Questions
FAQ 1: Why do different energy adjustment methods produce substantially different effect estimates in my analysis?
Answer: This occurs because each method answers a different scientific question:
- The standard and residual models estimate substitution effects (the effect of replacing one dietary component with another while holding total energy constant) [29]
- The energy partition model estimates total effects (the effect of changing a dietary component while keeping all others constant) [29]
- The nutrient density model has an obscure interpretation but attempts to estimate effects rescaled as proportions of total energy [29]
Troubleshooting Steps:
- Precisely define your research question: Are you interested in substitution effects or total effects?
- Ensure your statistical model matches your conceptual question
- Consider using the "all-components model" that simultaneously adjusts for all dietary components, which can provide accurate estimates of both total and relative causal effects [29]
FAQ 2: How should I handle highly correlated dietary components in my pattern derivation?
Answer: High correlation between dietary components (multicollinearity) is expected in compositional data. Consider these approaches:
Solution Strategies:
- Use regularization techniques (e.g., graphical LASSO) as employed in Gaussian Graphical Models to improve model stability [68]
- Apply compositional data analysis (CoDA) methods that explicitly account for the compositional nature of dietary data [67]
- Consider network analysis approaches that can handle conditional dependencies between foods while accounting for correlations [68]
FAQ 3: My dietary pattern results are difficult to compare with previous literature. What reporting standards should I follow?
Answer: Inconsistent methodology application and reporting is a widespread challenge in dietary patterns research [69]. To improve comparability:
Reporting Checklist:
- Clearly document all subjective decisions in dietary pattern derivation (food grouping, number of factors retained, etc.)
- Report both food and nutrient profiles of identified patterns
- Provide quantitative information on food group contributions to patterns
- Use the Minimal Reporting Standard for Dietary Networks (MRS-DN) checklist if using network analysis [68]
- Follow standardized approaches like those used in the Dietary Patterns Methods Project for index-based methods [69]
FAQ 4: When should I use traditional dietary pattern methods versus newer network approaches?
Answer: The choice depends on your research question and data structure:
Table 2: Method Selection Guide: Traditional vs. Network Approaches
| Consideration | Traditional Methods (PCA, Factor Analysis, Cluster Analysis) | Network Analysis (GGMs, Mutual Information Networks) |
|---|---|---|
| Primary Strength | Reduces data complexity; identifies broad patterns | Maps complex interactions; reveals conditional dependencies |
| Research Question | "What broad patterns exist in this population?" | "How do specific foods interact and co-consume?" |
| Data Structure | Works well with normally distributed data | Can handle non-normal data with appropriate methods |
| Interpretation | Patterns represent correlated food groups | Edges represent conditional dependencies between foods |
| Key Limitations | Obscures food synergies; assumes relatively static patterns | Methodologically complex; requires careful model specification |
FAQ 5: How do I determine whether my compositional data has fixed or variable totals, and why does it matter?
Answer: The distinction profoundly affects analytical choices:
Identification Guide:
- Fixed Total: The sum is constant across all observations (e.g., percentage contributions to total energy, 24-hour time allocation)
- Variable Total: The sum differs between observations (e.g., absolute nutrient intakes, total energy intake)
Analytical Implications:
- With fixed totals, you cannot include the total as a covariate (it's implicit)
- With variable totals, you must include the total in your model [67]
- Using methods designed for fixed totals with variable totals (or vice versa) can produce severely biased estimates, particularly for larger reallocations [67]
Advanced Methodological Protocols
Protocol for Implementing Compositional Data Analysis (CoDA)
Compositional Data Analysis provides a robust framework for analyzing dietary data that respects its inherent structure [67]:
Step 1: Data Preparation
- Apply isometric log-ratio transformations to move data from simplex to Euclidean space
- Handle zeros using appropriate replacement strategies if necessary
Step 2: Model Specification
- For fixed totals: Use CoDA with implicit total constraint
- For variable totals: Close the data by dividing by total or condition on total
Step 3: Interpretation
- Interpret parameters as relative changes between components
- Use balance plots to visualize relative contributions
Protocol for Gaussian Graphical Models with Dietary Data
Gaussian Graphical Models (GGMs) are particularly valuable for exploring food co-consumption patterns [68]:
Step 1: Model Estimation
- Use graphical LASSO for network estimation with regularization
- Address non-normal data using Semiparametric Gaussian Copula Graphical Models (SGCGM) or log-transformations
Step 2: Network Visualization
- Nodes represent food groups or nutrients
- Edges represent conditional dependencies after controlling for all other nodes
Step 3: Validation
- Apply stability analysis using bootstrapping approaches
- Test robustness to different food grouping schemes
Table 3: Essential Analytical Resources for Dietary Pattern Research
| Resource Category | Specific Tools/Methods | Primary Application | Key References |
|---|---|---|---|
| Federal Data Sources | NHANES/WWEIA, FNDDS, FPED | Nationally representative dietary intake data | [20] |
| Energy Adjustment Methods | Standard, Partition, Density, Residual models | Adjusting for total energy intake | [29] |
| Compositional Data Analysis | Isometric log-ratios, CoDA | Analyzing data with fixed or variable totals | [67] |
| Network Analysis | Gaussian Graphical Models, Mutual Information Networks | Mapping food co-consumption patterns | [68] |
| Traditional Pattern Analysis | Principal Component Analysis, Factor Analysis, Cluster Analysis | Deriving broad dietary patterns | [69] |
| Reporting Standards | Minimal Reporting Standard for Dietary Networks (MRS-DN) | Standardizing network analysis reporting | [68] |
Diagram 2: Dietary Pattern Analysis Workflow
The derivation of dietary patterns is profoundly influenced by choices in energy adjustment methods. Rather than seeking a single "correct" approach, researchers should select methods aligned with their specific research questions, clearly communicate their analytical decisions, and employ multiple approaches when exploring complex dietary relationships. As methodological research advances, newer approaches like network analysis and compositional data analysis offer promising avenues for capturing the complex, synergistic nature of dietary intake, potentially revealing relationships that traditional methods might obscure. Through careful methodological selection, transparent reporting, and appropriate interpretation, researchers can generate more valid, comparable, and informative evidence to guide dietary recommendations and public health policy.
FAQs: Core Concepts and Methodologies
Q1: What is the primary limitation of using self-reported energy intake (EI) in research, and why are novel validation approaches needed?
Self-reported energy intake (SREI) from methods like dietary recalls and food frequency questionnaires is known to be highly inaccurate [70]. These methods are prone to substantial underreporting, often by hundreds of kilocalories per day, and the errors are not random but systematic, varying by factors like body mass index and age [70]. This level of inaccuracy can lead to spurious associations and flawed conclusions in nutritional research, making the development of objective validation methods not just beneficial but essential [70] [63].
Q2: How does the Energy Balance (EB) method provide an objective measure of energy intake?
The Energy Balance method calculates energy intake objectively using the principle of energy balance, which states that Energy Intake (EI) equals Total Energy Expenditure (TEE) plus the change in body energy stores (∆ES) [71]. The formula is: EI = TEE + ∆ES This approach bypasses self-reporting by:
- Measuring TEE using the doubly labeled water (DLW) technique, considered a gold standard.
- Quantifying ∆ES by measuring changes in body composition (Fat Mass and Fat-Free Mass) using precise methods like Dual-Energy X-Ray Absorptiometry (DXA) and applying known energy densities (9.5 kcal/g for fat and 1.0 kcal/g for fat-free mass) [71]. The calculated EI from this method provides a reference value against which self-reported intake can be validated [63].
Q3: In the context of statistical adjustment for total energy, what distinguishes the "energy partition model" from the "nutrient density model"?
When adjusting for total energy intake in nutritional research, different models estimate different effects [29]:
- The Energy Partition Model estimates the total causal effect of a nutrient. It includes all dietary components (e.g., carbohydrates, fat, protein) in the model as absolute intakes. However, it only provides unbiased estimates in the absence of confounding or when all other nutrients have equal effects on the outcome [29].
- The Nutrient Density Model rescales the nutrient exposure as a proportion of total energy intake (e.g., percentage of calories from fat). Its causal interpretation is often obscure, but it attempts to estimate an average relative causal effect rescaled as a proportion of total energy [29]. A more robust approach, termed the "all-components model," involves simultaneously adjusting for all dietary components to derive accurate estimates of both total and relative causal effects [29].
Q4: What are the key advantages of using the Energy Availability - Energy Balance (EAEB) method over traditional calculations?
The Energy Availability - Energy Balance (EAEB) method improves upon traditional calculations in several key ways [71]:
- Objective Intake Data: It replaces the error-prone self-reported energy intake with an objective calculation based on measured energy expenditure and changes in body energy stores.
- Reduced Participant Burden: It removes the need for participants to meticulously record all food consumption, which can itself alter eating behavior.
- Long-Term Assessment: It enables the assessment of energy availability over periods of weeks or months, which is more relevant for understanding chronic health consequences than the short-term (3-7 day) snapshots provided by traditional methods.
- Improved Accuracy: Studies have shown that EI calculated via the EB method aligns much more closely with total energy expenditure than self-reported EI, which can underestimate intake by an average of 20% [71].
Troubleshooting Guides
Guide 1: Addressing Misclassification of Self-Reported Energy Intake
Problem: A significant portion of self-reported dietary recalls are misclassified (under-reported or over-reported) when compared to measured energy requirements, leading to biased data [63].
Solution: Implement a two-method validation process using both measured Energy Expenditure (mEE) and measured Energy Intake (mEI).
Step-by-Step Procedure:
- Collect Data: For each participant, obtain:
- rEI: Self-reported Energy Intake from multiple (e.g., 3-6) non-consecutive 24-hour dietary recalls.
- mEE: Measured Energy Expenditure via the Doubly Labeled Water (DLW) method.
- Body Composition: Measure Fat Mass (FM) and Fat-Free Mass (FFM) at the beginning and end of the assessment period using a high-precision method like DXA or quantitative magnetic resonance (QMR) [63].
- Calculate mEI: Use the energy balance principle: mEI = mEE + ∆ES, where ∆ES is the change in energy stores calculated from changes in FM and FFM [63].
- Calculate Ratios and Set Cut-offs:
- Compute the ratios rEI:mEE (Method 1) and rEI:mEI (Method 2).
- For each method, establish group-specific cut-offs using the standard deviations of the ratios. Classify reports as:
- Plausible: Within ±1 SD of the mean ratio.
- Under-reported: < -1 SD of the mean ratio.
- Over-reported: > +1 SD of the mean ratio [63].
- Compare and Apply: Use both methods to identify misreported entries. Research suggests that using mEI (Method 2) may offer superior bias reduction and identify more over-reported entries than using mEE alone [63].
Table 1: Comparison of Validation Methods for Self-Reported Energy Intake
| Method | Comparison Metric | Key Assumption | Identified Challenge |
|---|---|---|---|
| Method 1 (Standard) | rEI vs. mEE (by DLW) | Participant is in energy balance during measurement [63]. | May misclassify reports during weight loss/gain [63]. |
| Method 2 (Novel) | rEI vs. mEI (by EB principle) | Accurate measurement of changes in body energy stores [63]. | Requires highly precise body composition analysis [71]. |
Guide 2: Selecting Statistical Models for Compositional Energy Intake Data
Problem: Dietary data are compositional—the parts (macronutrients) sum to a whole (total energy). Choosing an incorrect statistical model for such data can lead to severely misleading results, especially for larger nutrient substitutions [67].
Solution: Select a statistical model based on the research question and the nature of the compositional total (fixed or variable).
Decision Process and Models:
- Define the Research Question:
- Is the goal to model the effect of increasing one nutrient at the expense of another (an isocaloric substitution)?
- Or is it to model the total effect of a nutrient?
- Choose the Appropriate Model:
- For Isocaloric Substitution Effects: Use the "Leave-One-Out" (Isocaloric) Model.
Outcome = β₀ + β₁Nutrient₁ + β₂Nutrient₂ + ... + βₙ₋₁Nutrientₙ₋₁ + Total_Energy + e- Interpretation: Coefficient β₁ represents the effect of substituting one unit of
Nutrient₁for the omitted reference nutrient, while keeping total energy constant [67].
- For Total Causal Effects: Use the Energy Partition Model.
Outcome = β₀ + β₁Nutrient₁ + β₂Nutrient₂ + ... + βₙNutrientₙ + e- Interpretation: Coefficient β₁ represents the total effect of
Nutrient₁[29]. This model is unbiased only in the absence of confounding.
- For Complex Relative Relationships: Consider Compositional Data Analysis (CoDA) using isometric log-ratio transformations. This is a robust but complex method best applied when the relationships between dietary components are non-linear [67].
- For Isocaloric Substitution Effects: Use the "Leave-One-Out" (Isocaloric) Model.
Troubleshooting Tip: The performance of each model is highly dependent on the true underlying relationship in the data. Always explore the shape of the relationships before selecting a model. Using an incorrect parameterisation (e.g., a linear model for a log-ratio relationship) has more severe consequences for large nutrient reallocations (e.g., 100-kcal) than for 1-unit changes [67].
Experimental Protocols
Protocol: Validating Energy Intake via the Energy Balance Method
Purpose: To objectively determine a participant's energy intake over a sustained period (e.g., 2-4 weeks) for the purpose of validating self-reported dietary data or assessing long-term energy availability [71] [63].
Workflow Diagram:
Materials and Reagents: Table 2: Essential Research Reagents and Solutions
| Item | Function/Description | Key Consideration |
|---|---|---|
| Doubly Labeled Water (DLW) | A gold-standard, non-invasive method for measuring total energy expenditure in free-living individuals over 1-2 weeks [63]. | Contains stable isotopes ²H (deuterium) and ¹⁸O (oxygen-18). Requires isotope ratio mass spectrometry for analysis. |
| Dual-Energy X-Ray Absorptiometry (DXA) | A highly precise imaging technique for quantifying body composition (Fat Mass, Fat-Free Mass) [71]. | Preferred for its high precision and low measurement error, which is critical for accurately calculating ∆ES over longer periods [71]. |
| Quantitative Magnetic Resonance (QMR) | An alternative to DXA for body composition analysis, with high precision for detecting changes in fat mass [63]. | Can accommodate larger individuals and provides rapid measurements. |
| Isotope Ratio Mass Spectrometer | The analytical instrument used to measure the isotopic enrichment in urine samples from DLW studies [63]. | Essential for converting isotope dilution data into carbon dioxide production and, ultimately, total energy expenditure. |
Detailed Procedure:
- Baseline Measurements (Day 0):
- Perform a baseline body composition analysis using DXA or QMR. Measure body weight to the nearest 0.1 kg [63].
- Administer an oral dose of DLW according to established protocols (e.g., 1.68 g/kg body water of ¹⁸O and 0.12 g/kg of ²H₂O). Collect a pre-dose urine sample and samples 3-4 hours post-dose [63].
Free-Living Period (e.g., 14 days):
- Participants go about their normal lives. During this period, collect self-reported energy intake (rEI) data using multiple (e.g., 3-6) unannounced 24-hour dietary recalls to capture habitual intake [63].
Final Measurements (Day 14):
Laboratory Analysis & Calculations:
- TEE Calculation: Analyze urine samples using isotope ratio mass spectrometry. Calculate carbon dioxide production and then TEE using the Weir equation [63].
- ∆ES Calculation: Compute the change in body energy stores using the formula:
∆ES (kcal) = (ΔFM × 9500) + (ΔFFM × 1000), where ΔFM and ΔFFM are the changes in fat mass and fat-free mass in kilograms [71]. - mEI Calculation: Calculate the objective measure of energy intake:
mEI (kcal/day) = TEE (kcal/day) + [∆ES (kcal) / study duration (days)][71] [63].
Validation:
- Compare the self-reported energy intake (rEI) to the measured energy intake (mEI) to quantify reporting bias (under- or over-reporting) [63].
The Scientist's Toolkit: Key Reagents & Materials
Table 3: Essential Toolkit for Energy Intake Validation Studies
| Tool / Reagent | Primary Function | Application Note |
|---|---|---|
| Doubly Labeled Water (DLW) | Objective measurement of free-living Total Energy Expenditure (TEE) over 1-3 weeks [71] [63]. | Considered the gold standard. High cost for isotopes and analysis can be a limiting factor. |
| Dual-Energy X-Ray Absorptiometry (DXA) | High-precision measurement of body composition (fat mass, fat-free mass, bone mineral density) [71]. | Critical for accurately calculating changes in energy stores (∆ES). Low measurement error is essential. |
| Quantitative Magnetic Resonance (QMR) | Alternative technology for precise body composition analysis [63]. | Useful for populations with higher body weights. Provides rapid results. |
| Isotope Ratio Mass Spectrometer | Analyzes isotopic enrichment in biological samples (e.g., from DLW studies) [63]. | Specialized equipment typically located in core laboratory facilities. |
| Automated Self-Administered 24-Hour Recall (ASA24) | Tool for collecting self-reported dietary intake data with reduced interviewer burden [20]. | Aids in standardizing the collection of self-report data for comparison with objective measures. |
| Predictive Equations (e.g., NAS 2023) | Estimate Energy Requirements based on age, sex, weight, height, and physical activity level [3]. | Useful for large-scale population assessments or when direct measurement of TEE is not feasible. |
Troubleshooting Guides
Guide 1: Resolving Inconsistent Diet-Disease Associations
Problem: Researchers obtain conflicting results for the same nutrient-disease association when using different energy adjustment methods.
Explanation: Different energy adjustment methods estimate fundamentally different causal effects. The standard and nutrient density models estimate "substitution" effects (what happens when you increase one nutrient while decreasing others to keep total energy constant), while the energy partition model estimates the "total" effect of a nutrient (what happens when you increase the nutrient while keeping all other nutrients constant). These are different research questions with different answers [2].
Solution:
- Step 1: Clearly define your research question. Are you interested in the effect of adding more of a nutrient to the diet (total effect) or substituting it for other nutrients (relative effect)? [2]
- Step 2: For substitution effects, use the standard multivariate model (adjusting for total energy) or nutrient density method.
- Step 3: For total effects, use the energy partition model (adjusting for remaining energy intake) or the all-components model [2].
- Step 4: Always explicitly state which estimand you are targeting in your publications to avoid confusion.
Guide 2: Addressing Dietary Measurement Error
Problem: Self-reported dietary data contains substantial measurement error that attenuates diet-disease associations and may introduce bias [72] [73].
Explanation: All self-reported dietary intake data contain measurement error. Energy intake is particularly affected because errors in reporting each food compound when calculating totals. This error can be both systematic (e.g., underreporting of less healthy foods) and random [39] [73].
Solution:
- Step 1: Identify implausible energy reports using statistical methods like the revised-Goldberg or predicted total energy expenditure (pTEE) methods [39].
- Step 2: Apply energy adjustment to mitigate measurement error, as it assumes most foods are misreported similarly [21].
- Step 3: Consider using recovery biomarkers (e.g., doubly labeled water for energy) in validation subsamples when possible [74].
- Step 4: For dietary pattern analysis, consistently apply the same misreporting handling method across all analyses [39].
Frequently Asked Questions
Q1: Why is energy adjustment necessary in nutritional epidemiology studies?
Energy adjustment serves two primary purposes: (1) it accounts for the fact that people with different body sizes, metabolic efficiency, and physical activity levels have different energy requirements, thereby providing a measure of diet composition; and (2) it helps mitigate measurement error inherent in self-reported dietary data [21]. Without energy adjustment, observed associations between nutrients and disease may be confounded by total energy intake [1].
Q2: What are the main energy adjustment methods and when should I use each one?
Table 1: Comparison of Energy Adjustment Methods in Nutritional Epidemiology
| Method | Target Estimand | Interpretation | Key Strengths | Key Limitations |
|---|---|---|---|---|
| Standard Model | Average relative causal effect | Effect of increasing the nutrient while decreasing others to keep total energy constant | Intuitive; widely understood | Estimates substitution, not total effect [2] |
| Energy Partition Model | Total causal effect | Effect of increasing the nutrient while keeping other nutrients constant | Directly addresses "addition" questions | Susceptible to residual dietary confounding [2] |
| Nutrient Density Model | Rescaled relative effect | Effect expressed as proportion of total energy | Easy to interpret for macronutrients | Obscure causal interpretation [2] |
| Residual Model | Average relative causal effect | Mathematically identical to standard model | Removes correlation with energy | Difficult to interpret directly [2] [21] |
| All-Components Model | Both total and relative effects | Simultaneously estimates all component effects | Most comprehensive; reduces bias | Requires complete dietary data [2] |
Q3: How does measurement error in dietary assessment affect my results?
Measurement error in nutritional epidemiology can seriously distort findings in several ways [72] [73]:
- It typically attenuates (weakens) observed associations between dietary factors and disease
- It can distort dietary patterns derived by cluster or factor analysis
- Larger measurement errors cause more serious distortion, with consistency rates for dietary patterns ranging from 13.4% to 100% depending on the method [72]
- The impact varies by dietary pattern method - principal component factor analysis patterns with similar factor loadings and cluster analysis patterns with small clusters are more vulnerable [72]
Q4: What is the "all-components model" and why is it recommended?
The all-components model involves simultaneously adjusting for all dietary components in your analysis. This approach can provide less biased estimates of both total and average relative causal effects because it directly accounts for the compositional nature of dietary data, unlike methods that use summary variables like total energy or remaining energy, which can introduce "composite variable bias" [2].
Experimental Protocols
Protocol 1: Implementing Energy Adjustment Methods
Purpose: To properly adjust for total energy intake when analyzing the relationship between a specific nutrient and a health outcome.
Materials: Dietary dataset, statistical software (R, SAS, or Stata)
Procedure:
- Standard Multivariate Model:
- Fit a regression model:
Outcome ~ Nutrient + Total_Energy + Covariates - The coefficient for Nutrient represents the effect of increasing that nutrient while simultaneously decreasing other nutrients to keep total energy constant [2]
- Fit a regression model:
Nutrient Density Method:
Residual Method:
All-Components Model (Recommended):
- Include all major nutrient components in your model:
Outcome ~ Nutrient + Other_Nutrient_1 + Other_Nutrient_2 + ... + Other_Nutrient_N - This provides the most comprehensive adjustment [2]
- Include all major nutrient components in your model:
Protocol 2: Identifying and Handling Energy Intake Misreporters
Purpose: To identify participants with implausible energy intake reports and appropriately handle them in analysis.
Materials: Dietary data, anthropometric data, physical activity data
Procedure:
- Calculate Basal Metabolic Rate (BMR) using the Mifflin equation [39]:
- Men:
BMR = 9.99 × weight(kg) + 6.25 × height(cm) - 4.92 × age(y) + 5 - Women:
BMR = 9.99 × weight(kg) + 6.25 × height(cm) - 4.92 × age(y) - 161
- Men:
Apply Revised-Goldberg Method [39]:
- Calculate ratio of reported energy intake to BMR (rEI:BMR)
- Compare to physical activity level (PAL) categories
- Identify misreporters using 95% confidence limits of agreement
Apply Predicted Total Energy Expenditure (pTEE) Method [39]:
- Calculate total energy expenditure:
TEE = BMR × PAL - Compare reported energy intake to pTEE
- Classify based on predetermined cut-offs
- Calculate total energy expenditure:
Handle misreporters using one of these approaches:
- Exclusion: Remove before analysis (may introduce selection bias)
- Inclusion: Analyze all data regardless (may increase noise)
- Stratification: Analyze misreporters separately
- Statistical adjustment: Include misreporting status as covariate
Method Selection Workflow
The Scientist's Toolkit
Table 2: Essential Research Reagents for Energy Intake Analysis
| Tool/Reagent | Function | Application Notes |
|---|---|---|
| Revised-Goldberg Method | Identifies energy intake misreporters | Compares reported energy intake to basal metabolic rate and physical activity; 92% sensitivity, 88% specificity vs. doubly labeled water [39] |
| Predicted TEE Method | Alternative misreporter identification | Uses predicted total energy expenditure; may identify more misreporters than Goldberg method (50% vs 47%) [39] |
| Doubly Labeled Water | Gold standard for energy expenditure | Objective biomarker; prohibitively expensive for large studies [39] |
| All-Components Model | Comprehensive adjustment | Simultaneously adjusts for all dietary components; reduces bias from summary variables [2] |
| Food Frequency Questionnaire | Dietary assessment | Primary tool in large cohorts; requires energy adjustment to mitigate measurement error [21] |
| Physical Activity Questionnaires | Physical activity level estimation | Needed for misreporter identification methods; validated instruments recommended [39] |
Key Recommendations for Practitioners
Always energy-adjust nutrient intakes in observational studies to control for confounding and reduce measurement error [1] [21].
Select your adjustment method based on your research question, not convenience - different methods answer different questions [2].
Use the all-components model when possible for more accurate estimates of both total and relative causal effects [2].
Account for misreporting using statistical methods like revised-Goldberg or pTEE, and consistently apply your chosen approach [39].
Clearly report which energy adjustment method you used and interpret your findings accordingly to avoid contributing to contradictory literature [2].
Conclusion
Statistical adjustment for total energy intake is a foundational pillar for ensuring the integrity of nutritional epidemiology and clinical research. A thorough understanding of its rationale, coupled with the adept application of robust methods and a rigorous approach to identifying and correcting for dietary misreporting, is paramount. The choice of adjustment strategy can significantly influence the derived dietary patterns and the resulting associations with health outcomes. Future research must continue to refine validation techniques, develop standardized protocols for handling misreported data, and integrate these methods into the study of chronic diseases and healthy aging to inform effective public health guidelines and clinical interventions.
References
- 1. Adjustment for total energy intake in epidemiologic studies [https://pubmed.ncbi.nlm.nih.gov/9094926/]
- 2. Adjustment for energy intake in nutritional research [https://pmc.ncbi.nlm.nih.gov/articles/PMC8755101/]
- 3. Estimates of energy intake, requirements and imbalances ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12458847/]
- 4. Energy intake, expenditure and balance, and factors ... [https://bmcnutr.biomedcentral.com/articles/10.1186/s40795-022-00628-2]
- 5. Extraneous Variables | Examples, Types & Controls [https://www.scribbr.com/methodology/extraneous-variables/]
- 6. Experimental Designs As Variance Control [https://www.advanceinnovationgroup.com/blog/experimental-designs-as-variance-control]
- 7. Forecasting Causal Effects of Interventions versus Predicting ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9030387/]
- 8. Relative Energy Deficiency in Sport (REDs) [https://www.childrenshospital.org/conditions/reds]
- 9. Female Athlete Triad and Relative Energy Deficiency in ... [https://www.mdpi.com/2072-6643/16/3/359]
- 10. Female Athlete Triad - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK430787/]
- 11. A literature review of biomarkers used for diagnosis ... [https://www.frontiersin.org/journals/sports-and-active-living/articles/10.3389/fspor.2024.1375740/full]
- 12. Relative energy deficiency in sport [https://en.wikipedia.org/wiki/Relative_energy_deficiency_in_sport]
- 13. Using surrogate biomarkers to improve measurement error ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3824235/]
- 14. Intuitive Eating and the Female Athlete Triad in Collegiate ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12298869/]
- 15. Assessment of relative energy deficiency in sport and ... [https://www.sciencedirect.com/science/article/pii/S2667268524001281]
- 16. A statistical perspective on baseline adjustment in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9184591/]
- 17. A statistical perspective on baseline adjustment in ... [https://www.nature.com/articles/s41525-022-00303-2]
- 18. GitHub - georgiatomova/adjustment- energy -intake [https://github.com/georgiatomova/adjustment-energy-intake]
- 19. New Nutrient Rich Food Nutrient Density Models That ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2020.00107/full]
- 20. Data Analysis for the 2025 Guidelines Committee Report [https://www.dietaryguidelines.gov/2025-advisory-committee-report/data-analysis]
- 21. Learn More about Energy Adjustment [https://dietassessmentprimer.cancer.gov/learn/adjustment.html]
- 22. Adjustment of Observed Intake Data to Estimate the ... - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK221370/]
- 23. What Are Residuals in Statistics? Examples & Common ... [https://www.displayr.com/learn-what-are-residuals/]
- 24. Adjusting for energy intake in dietary pattern investigations ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2492394/]
- 25. 4.4 - Identifying Specific Problems Using Residual Plots [https://online.stat.psu.edu/stat462/node/120/]
- 26. Overview of Dietary Assessment Methods for Measuring ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8338737/]
- 27. A review of statistical methods for dietary pattern analysis [https://nutritionj.biomedcentral.com/articles/10.1186/s12937-021-00692-7]
- 28. Adjustments to Improve the Estimation of Usual Dietary ... [https://www.sciencedirect.com/science/article/pii/S0022316622131536]
- 29. Adjustment for energy intake in nutritional research [https://www.sciencedirect.com/science/article/pii/S000291652200123X]
- 30. Greenhouse gas emissions in relation to micronutrient ... [https://www.sciencedirect.com/science/article/pii/S0002916525001339]
- 31. the need for more rigorous reporting of food frequency ... [https://pubmed.ncbi.nlm.nih.gov/40810819/]
- 32. Association between dietary choline intake and bone ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12220277/]
- 33. The associations between evening eating and quality of ... [https://nutritionj.biomedcentral.com/articles/10.1186/s12937-025-01094-9]
- 34. Cohort studies and randomized controlled trials [https://www.hcplive.com/view/march-2006-glasser]
- 35. Overview of clinical study designs - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11009715/]
- 36. Substitution analyses of foods with varying fat quality and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10799108/]
- 37. Adjustment for total energy intake in epidemiologic studies [https://www.sciencedirect.com/science/article/pii/S0002916523177410]
- 38. Longitudinal changes in the accuracy of reported energy ... [https://www.sciencedirect.com/science/article/pii/S0002916522033342]
- 39. The effect of different methods to identify, and scenarios used to... [https://nutritionj.biomedcentral.com/articles/10.1186/s12937-021-00696-3]
- 40. Strategies to Address Misestimation of Energy Intake ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6893710/]
- 41. 4.3: Implications of measurement error for estimated dietary ... [https://med.libretexts.org/Bookshelves/Nutrition/Principles_of_Nutritional_Assessment_3e_(Gibson_et_al.)/04%3A_Measurement_Error_in_Dietary_assessment_(Chapter_5)/4.03%3A_Implications_of_measurement_error_for_estimated_dietary_intakes]
- 42. The effect of different methods to identify, and scenarios used to... [https://pubmed.ncbi.nlm.nih.gov/33964947/]
- 43. Measurement Error in Dietary assessment [https://nutritionalassessment.org/errors/]
- 44. myfood24 | Quick and Easy to Use Nutritional Analysis Software [https://www.myfood24.org/]
- 45. Measurement Errors in Dietary Assessment Using Self- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5683000/]
- 46. Doubly Labeled Water Is a Validated and Verified ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3985818/]
- 47. Doubly labelled water assessment of energy expenditure [https://pmc.ncbi.nlm.nih.gov/articles/PMC5486561/]
- 48. Special Considerations for Measuring Energy Expenditure ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4780846/]
- 49. Maximizing Precision and Accuracy of the Doubly Labeled ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7028494/]
- 50. Predictive equation derived from 6497 doubly labelled ... [https://www.nature.com/articles/s43016-024-01089-5]
- 51. Measurement error in total energy intake in the United ... [https://www.sciencedirect.com/science/article/pii/S000291652500588X]
- 52. The impact of self-report inaccuracy in the UK Biobank and ... [https://www.nature.com/articles/s41562-024-02061-w]
- 53. Diets high in ultra-processed foods, which are ... [https://www.nih.gov/news-events/news-releases/nih-researchers-develop-biomarker-score-predicting-diets-high-ultra-processed-foods]
- 54. Biomarker for Diets High in Ultra-processed Foods - NCI [https://dceg.cancer.gov/news-events/news/2025/biomarker-ultra-processed-foods]
- 55. Strategies for Dealing with Missing Data in Clinical Trials [https://pmc.ncbi.nlm.nih.gov/articles/PMC3767219/]
- 56. Handling missing data in clinical research [https://www.sciencedirect.com/science/article/pii/S0895435622002189]
- 57. Strategies for Handling Missing Values in Data Analysis [https://www.dasca.org/world-of-data-science/article/strategies-for-handling-missing-values-in-data-analysis]
- 58. Methodologies for Missing Data in Clinical Trials [https://www.quanticate.com/blog/missing-data-in-clinical-trials]
- 59. A tutorial on sensitivity analyses in clinical trials: the what, why ... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/1471-2288-13-92]
- 60. Examining Plausibility of Self-Reported Energy Intake Data [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2017.00045/full]
- 61. Comparison of total energy intakes estimated by 24-hour ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9523208/]
- 62. Evaluation of new predictive equations for energy ... [https://www.sciencedirect.com/science/article/pii/S0261561425001682]
- 63. Dietary misreporting: a comparative study of recalls vs energy ... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-025-02568-4]
- 64. Assessing daily energy intake in adult women: validity of a ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2023.1255499/full]
- 65. Constrained Total Energy Expenditure and Metabolic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4803033/]
- 66. Body composition, anthropometry, and resting energy ... [https://ojrd.biomedcentral.com/articles/10.1186/s13023-025-03912-z]
- 67. A comparison of methods for analysing compositional data ... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-025-02509-1]
- 68. Unveiling Dietary Complexity: A Scoping Review and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12567371/]
- 69. A Systematic Review of the Methods Used to Assess and ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2022.892351/full]
- 70. Energy Balance Measurement: When Something is Not ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4430460/]
- 71. Measurement of Energy Intake Using the Principle of Energy ... [https://sportsmedicine-open.springeropen.com/articles/10.1186/s40798-023-00558-8]
- 72. The impacts of measurement errors on a dietary pattern ... [https://www.sciencedirect.com/science/article/pii/S0002916522000569]
- 73. Impact on Nutrition Research and Adjustment for its Effects [https://prevention.cancer.gov/tools-resources/measurement-error-impact-nutrition-research-and-adjustment-its-effects]
- 74. Markers of the Validity of Reported Energy Intake [https://www.sciencedirect.com/science/article/pii/S0022316622157056]