Strategies to Improve Adherence to Dietary Weight Loss Interventions: A Research and Clinical Perspective
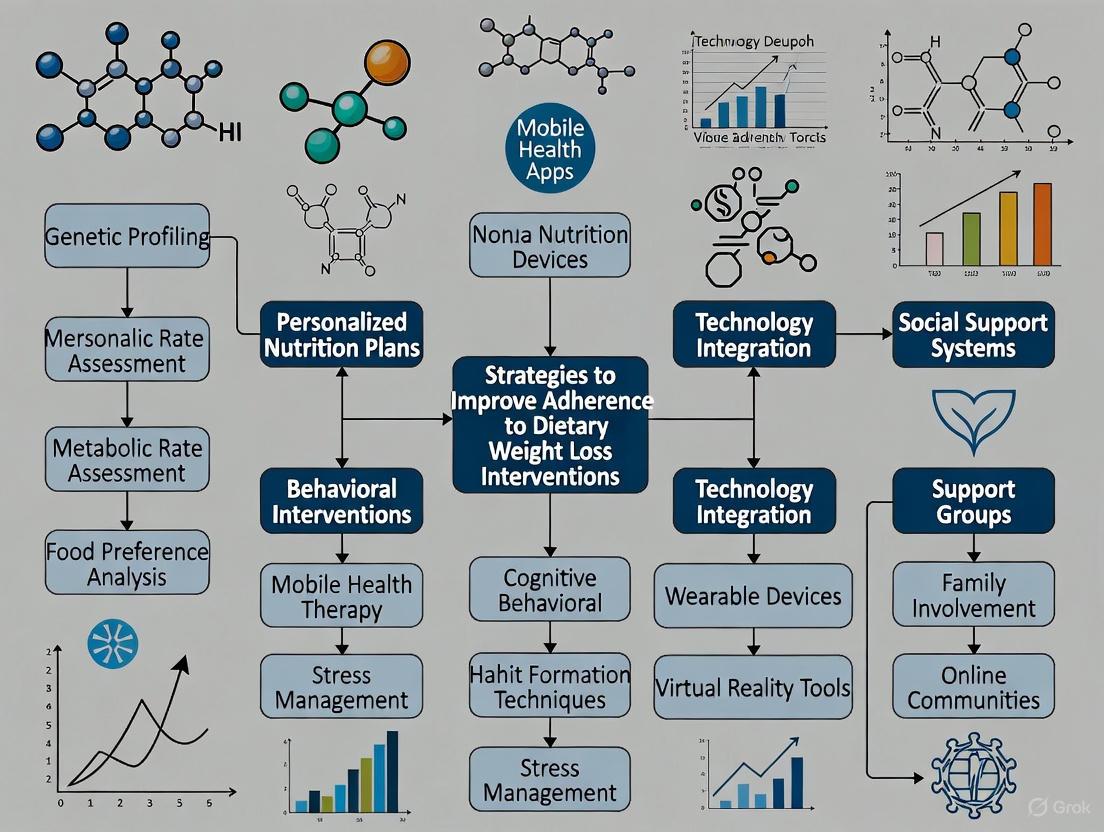
This article synthesizes current evidence and future directions for improving adherence in dietary weight loss interventions, a critical determinant of long-term success beyond specific macronutrient composition.
Strategies to Improve Adherence to Dietary Weight Loss Interventions: A Research and Clinical Perspective
Abstract
This article synthesizes current evidence and future directions for improving adherence in dietary weight loss interventions, a critical determinant of long-term success beyond specific macronutrient composition. Tailored for researchers, scientists, and drug development professionals, it explores the foundational evidence linking adherence to outcomes, methodological applications of behavioral and pharmacological strategies, troubleshooting for non-response and engagement decline, and validation through comparative efficacy studies. The scope encompasses behavioral techniques like self-monitoring and social support, emerging digital health technologies, and the integration of novel pharmacotherapies with lifestyle intervention, providing a comprehensive framework for enhancing the efficacy and sustainability of obesity treatments.
The Critical Link Between Dietary Adherence and Weight Loss Success
Frequently Asked Questions (FAQs)
1. What is the difference between adherence to a diet's composition and adherence to the behavior of self-monitoring? Adherence has two key components in weight loss research. The first is adherence to the prescribed dietary strategy (e.g., macronutrient goals). The second is adherence to the behavioral practices of the intervention, such as self-monitoring (e.g., recording food intake) [1] [2]. Research indicates that the combination of both high adherence to the diet and high adherence to self-monitoring is significantly more effective for weight loss than either factor alone [2].
2. Why do participants struggle to adhere to dietary interventions over time? Adherence declines due to several factors, including the increased drive to eat that accompanies energy restriction, the perceived burden of self-monitoring (especially dietary recording), and intervention fatigue [1] [3]. In digital interventions, challenges also include the timing and relevance of feedback messages, and a decline in engagement with digital tools [1] [4].
3. What are the most effective strategies to improve adherence? Evidence points to several key strategies:
- Supervision and Support: Interventions with supervised attendance and social support have significantly higher adherence rates than those without [5].
- Tailored Feedback: Providing personalized feedback on self-monitoring data can help sustain engagement, though its delivery must be optimized [1] [4].
- Dietary Focus: Programs focusing on dietary modification have shown better adherence than those focusing exclusively on exercise [5].
- Reducing Drive to Eat: Designing diets that help control hunger, such as those that induce ketosis, can improve adherence by addressing a key physical barrier [3].
4. How is adherence quantitatively measured in clinical trials? Adherence is measured using multiple metrics. The table below summarizes common methods and benchmarks based on clinical research:
Table 1: Quantitative Measures of Adherence in Dietary Weight Loss Trials
| Adherence Component | Measurement Method | Example Metric / Benchmark |
|---|---|---|
| Self-Monitoring of Diet | Digital food logs [1] | Recording ≥50% of daily calorie goals for ≥15 days/month [1] |
| Self-Monitoring of Weight | Smart scale data transmission [1] | Percentage of days with weight data recorded [1] |
| Self-Monitoring of Activity | Wearable device data [1] | Recording ≥500 steps per day [1] |
| Adherence to Diet Type | 24-hour dietary recalls [2] | Change in target macronutrient intake (e.g., net carbs for low-carb diets) [2] |
| Adherence to Diet Quality | Healthy Eating Index (HEI) scores [2] | An above-median improvement in HEI score [2] |
| Program Completion | Study retention data [5] | Overall adherence rate (meta-analysis average: 60.5%) [5] |
5. What are common pitfalls in designing adherence protocols, and how can they be avoided? Common pitfalls include high participant attrition, poor compliance with dietary requirements, and failure to maintain blinding [6] [7]. These can be mitigated by:
- Implementing a run-in period to assess participant motivation [6].
- Maintaining regular contact with participants, especially during control phases [6].
- Providing flexibility within the dietary requirements to accommodate preferences, potentially using herbs and spices to maintain acceptability [8].
- Using digital tools to reduce the burden of self-monitoring [1] [9].
Troubleshooting Guides
Challenge: Declining Self-Monitoring Engagement Over Time
Problem: Participants initially engage with self-monitoring tools (diet apps, wearables) but adherence drops significantly after the first few weeks or months [1] [4].
Investigation & Resolution:
- Step 1: Diagnose the Cause. Determine if the drop is due to burden, lack of feedback, or technical issues.
- Check: Analyze engagement data to see if the decline is correlated with a specific intervention phase or tool.
- Example: In the SMARTER trial, adherence to self-monitoring declined non-linearly over 12 months, but feedback helped slow the decline [1].
- Step 2: Optimize Feedback. Ensure feedback is timely, relevant, and non-generic.
- Protocol: Use a system like the SMARTER app, which delivered up to three tailored messages daily based on available self-monitoring data. Message libraries should be refreshed regularly to avoid desensitization [1].
- Step 3: Reduce Burden. Explore simplified self-monitoring methods.
- Protocol: As in the Spark trial, consider testing the necessity of multiple self-monitoring components (diet, steps, weight) to identify the minimal effective "package" that minimizes participant burden while maintaining efficacy [9].
Challenge: Poor Adherence to Prescribed Macronutrient Goals
Problem: Participants are not meeting their targets for calorie, carbohydrate, or fat intake, despite reporting compliance.
Investigation & Resolution:
- Step 1: Verify Data Quality. Assess the accuracy of dietary intake data.
- Step 2: Emphasize Diet Quality alongside Composition. Focus on food quality, not just macros.
- Protocol: As in the DIETFITS trial, categorize participants not just by adherence to low-carb or low-fat goals, but also by their improvement in Healthy Eating Index (HEI) scores. The greatest weight loss success was seen in the "High Quality/High Adherence" subgroups [2].
- Step 3: Incorporate Dietary Preferences. Tailor the diet to individual likes and cultural habits.
- Protocol: During the intervention design, develop culturally appropriate recipes that incorporate herbs and spices to maintain palatability and acceptability of healthier food options [8]. This improves long-term sustainability.
Challenge: High Attrition Rates in Long-Term Trials
Problem: A large percentage of participants drop out before the study concludes, threatening the validity of the results [6].
Investigation & Resolution:
- Step 1: Analyze Reasons for Dropout. Systematically collect data on why participants leave.
- Check: As done in the dairy intervention trial [6], conduct interviews or surveys with participants who drop out. Common reasons include inability to comply with the diet, health problems, and excessive time commitment.
- Step 2: Implement Retention Strategies. Proactively address common barriers.
- Protocol: Based on trial feedback, key strategies include [6]:
- Offering monetary compensation for completion.
- Sending reminder letters and phone calls before appointments.
- Providing nutritional counseling to help participants overcome hurdles (e.g., weight gain during a high-dairy phase).
- Minimizing the time commitment and number of in-person visits where possible.
- Protocol: Based on trial feedback, key strategies include [6]:
Experimental Protocols & Workflows
Protocol 1: Testing the Efficacy of Feedback on Self-Monitoring Adherence
This protocol is based on the SMARTER mobile health weight-loss trial [1].
1. Objective: To compare adherence to self-monitoring and behavioral goals between participants receiving automated feedback (SM+FB) and those in a self-monitoring only (SM-only) arm over 12 months.
2. Materials: Table 2: Key Research Reagent Solutions for Digital Adherence Trials
| Item | Function in the Experiment |
|---|---|
| Fitbit App (or equivalent) | Allows participants to record food intake and view nutrient values and daily summaries. |
| Wrist-worn Activity Tracker | Automatically collects physical activity data (e.g., steps) and syncs with a smartphone. |
| Smart Scale | Transmits weight data directly to the study database, providing an objective adherence measure. |
| Tailored Feedback Algorithm | Generates and delivers personalized messages to participants based on their incoming self-monitoring data. |
| 24-Hour Dietary Recall | A validated method used to verify and supplement self-reported dietary intake data from apps. |
3. Methodology:
- Participants: Adults with a BMI typically between 27-43 kg/m².
- Initial Session: All participants receive a single, one-on-one session with a dietitian to set goals and learn to use the digital tools.
- Randomization: Participants are randomized to SM+FB or SM-only.
- Intervention:
- SM-only group: Instructed to self-monitor diet, activity, and weight daily using the provided tools.
- SM+FB group: Performs the same self-monitoring but also receives up to three tailored feedback messages per day via a custom app. Message content is based on their data (e.g., "Calorie intake is above your goal, while fat grams are right on target.").
- Data Collection: Adherence is calculated monthly as the percentage of days participants meet the criteria for diet, activity, and weight self-monitoring. Weight is measured objectively.
4. Analysis:
- Use generalized linear mixed models to compare adherence patterns between groups over time.
- Examine the association between adherence measures and achieving ≥5% weight loss.
The workflow and key decision points for implementing and optimizing a feedback intervention are summarized in the diagram below:
Protocol 2: Isolating Active Ingredients of Self-Monitoring Using a Factorial Design
This protocol is based on the Spark trial, which employs the Multiphase Optimization Strategy (MOST) [9].
1. Objective: To examine the unique and combined weight loss effects of three self-monitoring strategies (tracking dietary intake, steps, and body weight) in a 6-month digital intervention.
2. Methodology:
- Design: A 2x2x2 full factorial randomized trial. This creates 8 experimental conditions, as each self-monitoring component (diet, steps, weight) is either present or absent.
- Participants: Adults with overweight or obesity.
- Intervention:
- All participants receive core intervention components (weekly lessons, action plans).
- Participants are randomized to one of the eight conditions, determining which self-monitoring tools they receive (e.g., a mobile app for diet, a wearable for steps, a smart scale for weight).
- For each assigned strategy, participants are instructed to self-monitor daily and receive a corresponding goal and automated feedback.
- Data Collection: Weight is measured objectively via a smart scale at baseline, 1, 3, and 6 months. Engagement is tracked as the percentage of days each self-monitoring activity is performed.
3. Analysis:
- The primary aim is to test the main effects of each of the three self-monitoring components and their interactions on 6-month weight change.
- This design identifies which components are "active ingredients" and whether any combinations have synergistic or antagonistic effects.
The following diagram illustrates the factorial design and optimization process:
Evidence Establishing Adherence as a Primary Predictor of Outcomes
Frequently Asked Questions (FAQs)
Q1: Why is adherence considered a more critical factor than the specific type of dietary intervention for weight loss success? Multiple randomized controlled trials have demonstrated that the degree of adherence to a dietary protocol is a stronger predictor of weight loss success than the macronutrient composition of the diet itself. A study comparing popular diets (Atkins, Zone, Ornish, and Weight Watchers) found a strong correlation between self-reported adherence and weight loss, with no significant association between the type of diet and the amount of weight lost [3]. Subsequent analysis of the DIETFITS randomized clinical trial confirmed that the most significant weight loss occurred in participants who combined both high dietary quality and high adherence to their assigned macronutrient-limiting diet (either low-fat or low-carbohydrate) [2].
Q2: What are the primary methodological challenges in measuring adherence in nutritional research, and how can they be overcome? Randomized controlled trials in nutrition (RCTNs) face two unique challenges: the influence of the participant's background diet and the accurate assessment of adherence [10]. Unlike pharmaceutical trials, participants are inevitably exposed to food components similar to the intervention through their regular diet. Furthermore, reliance on self-reported data (e.g., pill-taking questionnaires, dietary recalls) often leads to misclassification and overestimation of adherence [10] [11]. Overcoming these challenges involves:
- Using Validated Nutritional Biomarkers: Objective biomarkers can quantify systemic exposure to a dietary compound, providing unbiased data on both background diet and adherence [10] [12].
- Employing Electronic Monitoring: Digital tools, such as smart packaging, provide passive, precise measurement of dosing events, eliminating the bias inherent in self-reporting [13] [14].
Q3: How does adherence impact long-term weight maintenance after initial loss? Adherence is a critical determinant of long-term weight maintenance. Research shows that poor adherence during an active weight loss phase is a primary indicator of subsequent weight regain. One study found that individuals with high adherence to a low-energy diet regained only 50% of the lost weight after two years, whereas those with low adherence regained nearly all (99%) of it [3]. This underscores that the compensatory increase in the drive to eat that accompanies weight loss can undermine adherence, making strategies to manage hunger essential for long-term success [3].
Q4: What strategies can improve adherence to digital self-monitoring in behavioral weight loss programs? Sustaining engagement with digital self-monitoring (SM) tools during the maintenance phase is challenging. Key strategies include [15]:
- Understanding Patterns: Engagement is typically highest for exercise tracking and lowest for dietary tracking. Disengagement often occurs around 6-8 months into the program.
- Tailored Support: Individual characteristics, such as high weight-related information avoidance, predict a faster decline in dietary SM. Interventions can use this information to provide targeted support to at-risk participants at critical time points.
- Leveraging Data Sharing: Providing health coaches with access to participants' digital SM data allows for proactive support and has been shown to improve adherence and mitigate weight regain.
Troubleshooting Guides
Issue 1: Inaccurate Adherence Measurement Skewing Trial Outcomes
Problem: Reliance on subjective adherence measures (e.g., self-reports, pill counts) is introducing bias and noise into outcome data, making it difficult to establish a true efficacy signal [11] [13].
Solution: Implement objective, passive measurement technologies.
Step 1: Select the appropriate digital adherence technology.
- For oral solids: Utilize smart packaging like pill bottles or blister packs with integrated microchips that record the date and time of opening [13] [14].
- For other formulations: Explore digital solutions for injectables, inhalers, and creams that timestamp the activation event [14].
- For direct ingestion confirmation (Phase I): Consider "smart pills" with ingestible sensors, though scalability may be limited [13].
Step 2: Integrate the technology into the clinical supply chain. Work with a partner offering pre-qualified solutions to avoid lengthy vendor qualification processes, which can take 6-9 months [14].
Step 3: Utilize the rich dosing history data. Analyze the timestamp data to identify patterns of non-adherence (e.g., drug holidays, weekend skipping) and implement timely interventions. This data provides a causal pathway between medication intake, drug exposure, and treatment effects [13].
Issue 2: High Participant Drop-off and Non-Adherence in Long-Term Studies
Problem: Participant adherence decreases significantly over time, particularly in long-term trials, leading to loss of statistical power and potentially failed studies [16] [15] [14].
Solution: Proactively manage adherence through study design and participant engagement.
Step 1: Design the diet to control the physiological drive to eat. Consider dietary interventions that help manage hunger, such as ketogenic diets or very low-energy diets (VLEDs), which are associated with higher adherence and rapid, motivating weight loss [3].
Step 2: Tailor interventions to individual preferences. While ensuring nutritional adequacy, personalize dietary recommendations to a participant's food preferences to enhance long-term sustainability [3].
Step 3: Implement a data-driven feedback loop. Use data from digital adherence tools to:
- Provide participants with feedback on their adherence behavior to foster engagement [13].
- Enable investigators to monitor patterns, identify at-risk participants, and provide proactive, tailored support [13] [15].
- Allow sponsors to evaluate the impact of adherence on study outcomes in real-time [13].
Experimental Protocols & Data
Table 1: Key Methodologies from Cited Adherence Studies
| Study Focus | Adherence Measurement Method | Primary Outcome | Key Finding on Adherence |
|---|---|---|---|
| Bariatric Surgery (OBSERVE Study) [16] | Dietary Behavior Inventory-Surgery (DBI-S) questionnaire at multiple timepoints. | Percentage Total Weight Loss (%TWL) at 24 months. | A positive causal influence of dietary adherence on %TWL is hypothesized (Study ongoing, results pending). |
| Cocoa Flavanol RCT (COSMOS) [10] | Validated urinary biomarkers (gVLMB & SREMB). | Cardiovascular disease (CVD) events and mortality. | Biomarker-based analysis revealed 33% non-adherence (vs. 15% by self-report) and showed stronger treatment effects (e.g., Major CVD events HR: 0.48). |
| Medication Adherence (ARBITER 2) [11] | Pill count vs. 24-hour recall vs. refill history. | Adherence percentage to statin therapy. | Pill counts revealed significantly lower adherence (78.7%) than simpler methods and were sensitive to temporal changes. |
| Pediatric Multidisciplinary Program [17] | Adherence to lifestyle recommendations via questionnaire. | Change in BMI classification and Δ30BMI. | Adherence to breakfast recommendations was a significant predictor of moving to a lower weight class (aOR: 1.60). |
| Digital Self-Monitoring [15] | Days per month of tracking via digital tools. | Patterns of engagement during weight loss maintenance. | Only 21% of participants maintained high dietary self-monitoring; disengagement typically occurred at 7-8 months. |
Table 2: Research Reagent Solutions for Adherence Measurement
| Solution / Tool | Function / Description | Application Context |
|---|---|---|
| Validated Nutritional Biomarkers (e.g., gVLMB, SREMB) [10] | Objective, quantitative biomarkers in biofluids (e.g., urine, plasma) that measure systemic exposure to a specific nutrient or food compound. | RCTs targeting specific bioactive dietary components (e.g., flavanols, carotenoids). Corrects for background diet and misreported intake. |
| Dietary Guideline Index for Children & Adolescents (DGI-CA) [12] | A validated index score based on adherence to national dietary guidelines, assessing core food groups and discretionary foods. | Observational and intervention studies aiming to link overall diet quality with health outcomes in pediatric populations. |
| Electronic Monitoring Devices (e.g., MEMS Cap) [13] | Drug packaging (bottles, blisters) with microchips that passively record the date and time of opening. | Clinical trials (pharmaceutical and nutritional) where precise timing and patterns of supplement/medication intake are critical. |
| Smart Packaging Portfolio [14] | A suite of pre-qualified, digital packaging solutions for various formats (bottles, injectables, inhalers) that passively record dosing events. | Integrated into clinical supply chains to ensure GMP/GCP compliance and provide reliable adherence data without burdening the patient. |
| Digital Self-Monitoring Platforms [15] | Mobile apps and connected devices (e.g., digital scales, activity trackers) for tracking weight, diet, and exercise. | Behavioral weight loss interventions. Facilitates real-time monitoring and can be used to drive remote coaching interventions. |
Visualized Workflows and Pathways
Dietary Adherence Research Workflow
Impact of Adherence on Trial Outcomes
Frequently Asked Questions (FAQs)
FAQ 1: What are the primary biological mechanisms driving increased appetite during energy restriction? The increased drive to eat is largely mediated by hormonal changes that convey energy status to the brain. A key mechanism is the significant and often disproportionate reduction in circulating leptin, a hormone secreted by adipocytes in proportion to fat mass [18]. This decline in leptin promotes increased motivation to eat via down-regulation of anorexigenic neuropeptides (e.g., POMC, α-MSH) and up-regulation of orexigenic neuropeptides (e.g., NPY, AgRP) in the hypothalamus [18]. This system appears to be asymmetrical, with a much stronger defense against energy deficit than against overconsumption [18] [19].
FAQ 2: Is the counter-regulatory drive universal across different types of dietary interventions? While a heightened drive to eat is a common physiological response to energy deficit, its intensity can be influenced by the dietary strategy. Some evidence suggests that ketogenic diets, including those using Very Low Energy Diets (VLEDs), may help control the increased drive to eat, potentially due to the appetite-suppressing effects of ketosis [20]. Furthermore, emerging research indicates that the timing of energy intake, such as early time-restricted eating (eTRE), may offer additional benefits for improving metabolic outcomes compared to energy restriction alone, though its direct impact on the drive to eat requires further study [21].
FAQ 3: How can we accurately monitor and account for this biological response in clinical trials? Self-monitoring (SM) of diet, physical activity, and weight is a cornerstone behavioral strategy for assessing adherence. The use of digital tools (e.g., smartphone apps, wearable devices, smart scales) can reduce the burden of monitoring [1]. Research shows that higher adherence to self-monitoring is significantly associated with greater odds of achieving clinically meaningful weight loss (e.g., ≥5%) [1]. Accurately quantifying energy intake is complex; mathematical models that calculate metabolized energy intake using doubly labelled water and changes in body energy stores from Dual-Energy X-ray Absorptiometry (DEXA) can provide objective measures of adherence and help explain deviations from expected weight loss [20].
FAQ 4: What are the common pitfalls in trial design that fail to account for this biological drive? Common pitfalls include a lack of strategies to manage increased hunger, overly rigid dietary protocols that do not accommodate individual preferences, and insufficient monitoring of adherence. Trials that do not incorporate a run-in period to assess participant motivation and compliance potential, or that fail to maintain regular contact—especially during control phases—are at higher risk for attrition and poor adherence [6]. Providing flexibility within dietary requirements and ensuring the dietary intervention is acceptable and palatable to participants are key considerations for improving compliance [8] [6].
Troubleshooting Guides
Problem: High Attrition and Poor Dietary Adherence in Long-Term Interventions
| Potential Cause | Underlying Mechanism | Recommended Solution |
|---|---|---|
| Unmanaged Hunger | Physiological increase in orexigenic drive due to leptin decline and other hormonal cues [18]. | Consider dietary designs that help control hunger, such as ketogenic diets or VLEDs, which are associated with higher adherence and rapid, motivating weight loss [20]. |
| Dietary Inflexibility | Intervention conflicts with personal, cultural, or traditional food preferences, reducing acceptability [8]. | Tailor interventions to individual dietary preferences while meeting nutritional goals. Use herbs and spices to maintain palatability of healthier foods [20] [8]. |
| Burden of Self-Monitoring | Participant fatigue from manually and frequently recording food intake and other behaviors [1]. | Implement mHealth tools (apps, wearables, smart scales) to automate data collection and reduce participant burden [1]. |
| Insufficient Support | Lack of feedback or guidance, leading to loss of motivation and engagement [1] [6]. | Integrate regular, tailored feedback. Note: One study found remote feedback alone was insufficient for some; message content, timing, and relevance are critical [1]. |
Problem: Inaccurate Reporting of Energy Intake Blurring Intervention Efficacy
| Challenge | Solution | Experimental Protocol / Tool |
|---|---|---|
| Fluctuating Daily Intake | Poor adherence creates a gap between prescribed and actual energy intake, leading to a weight loss plateau [20]. | Use mathematical modeling of energy intake based on energy expenditure (from doubly labelled water) and change in energy stores (from DEXA) [20]. |
| Under-Reporting in Food Diaries | Self-reported data is often incomplete or inaccurate. | Combine self-report with objective biomarkers. In a provided-food study, quantify adherence by comparing provided food to calculated actual intake [20]. |
| Lack of Real-Time Data | Researchers cannot identify adherence issues as they occur. | Utilize a digital health infrastructure where participants use a designated app (e.g., Fitbit) and smart scale for real-time or daily monitoring of diet, activity, and weight [1]. |
Key Signaling Pathways in Appetite Regulation
The following diagram illustrates the core hypothalamic pathway through which energy restriction and falling leptin levels increase the drive to eat.
Experimental Protocols & Workflows
Protocol 1: Quantifying Adherence and Energy Intake in a Dietary Intervention
Objective: To objectively measure adherence to a prescribed diet and calculate actual metabolized energy intake in a weight loss trial [20].
Methodology:
- Participant Screening: Recruit overweight/obese adults. Exclude for conditions affecting energy balance (e.g., diabetes, use of weight-loss medications) [6].
- Baseline Assessment:
- Measure body composition via Dual-Energy X-ray Absorptiometry (DEXA).
- Measure total energy expenditure (TEE) over 7-14 days using the doubly labelled water (DLW) method.
- Intervention Phase:
- Provide all food to participants to control for dietary composition and prescribed energy intake.
- Instruct participants to maintain their usual physical activity levels.
- Adherence Monitoring:
- Endpoint Assessment (Post-Intervention):
- Repeat DEXA and DLW measurements.
- Data Analysis:
- Calculate Metabolized Energy Intake: Average energy intake over the intervention is calculated as: Energy Intake = TEE (from DLW) + Change in Body Energy Stores (from DEXA).
- Classify Adherence: Compare the calculated energy intake to the prescribed energy intake from provided food. Participants can be stratified into tertiles (e.g., high, medium, low adherers) based on this comparison [20].
Protocol 2: Testing a Feedback Intervention to Improve Self-Monitoring Adherence
Objective: To evaluate the efficacy of a mobile health (mHealth) feedback system in improving adherence to self-monitoring and behavioral goals over 12 months [1].
Methodology:
- Design: A two-arm randomized controlled trial (RCT).
- Participants: Adults with a BMI between 27-43 kg/m².
- Initial Session: All participants receive a single 90-minute, one-on-one session with a dietitian to set behavioral goals (calorie, fat, physical activity minutes) and receive training on digital self-monitoring tools [1].
- Digital Tool Provision:
- Diet: Smartphone app (e.g., Fitbit) for logging food intake.
- Physical Activity: Wrist-worn activity tracker (e.g., Fitbit Charge).
- Weight: Smart scale that transmits data daily.
- Intervention Arms:
- SM-Only Group: Self-monitors using the digital tools.
- SM+FB Group: Self-monitors and receives up to three tailored feedback messages per day via a custom app. Messages address diet, activity, and weekly weighing, and are based on uploaded self-monitoring data [1].
- Outcome Measures:
- Primary: Percent weight loss from baseline to 12 months.
- Secondary (Adherence):
- Diet SM Adherence: Percentage of days with ≥50% of daily calorie goal recorded.
- PA SM Adherence: Percentage of days with ≥500 steps recorded.
- Weight SM Adherence: Percentage of days with a weight measurement.
- Goal Adherence: Percentage of days meeting calorie, fat, and physical activity goals [1].
The Scientist's Toolkit: Research Reagent Solutions
| Item / Reagent | Function in Experimental Context |
|---|---|
| Doubly Labelled Water (DLW) | Gold-standard method for measuring total energy expenditure in free-living individuals over 1-2 weeks. Essential for calculating objective energy intake [20]. |
| Dual-Energy X-ray Absorptiometry (DEXA) | Precisely quantifies body composition (fat mass, fat-free mass). Used with DLW to calculate changes in body energy stores for determining metabolized energy intake [20]. |
| Leptin ELISA Kits | To quantify circulating leptin concentrations in serum/plasma as a biomarker of adipose-derived energy storage signals and to confirm the hormonal state of energy deficit [18]. |
| Validated Visual Analog Scales (VAS) | Subjectively measure components of appetite (hunger, desire to eat, fullness, prospective consumption) at specific timepoints to correlate with physiological measures [19]. |
| mHealth Digital Suite | Integrated system of apps, wearable activity trackers, and smart scales to facilitate low-burden, high-frequency self-monitoring and enable real-time data collection and feedback delivery [1]. |
| Standardized Food Provision | Providing all or key study foods to participants ensures strict control over dietary composition and energy intake, removing variability from self-selection and preparation [20]. |
Data Presentation: Key Quantitative Findings
Table 1: Impact of Dietary Adherence on Weight Loss Outcomes
| Study Design / Metric | High Adherers | Low Adherers | P-value |
|---|---|---|---|
| Low Energy Diet (LED) [20] | |||
| Average Energy Intake (kcal/day) | 644 ± 74 | 1573 ± 33 | < 0.001 |
| Rate of Weight Loss (g/day) | 126.5 ± 7.7 | 56.9 ± 2.7 | < 0.001 |
| mHealth Self-Monitoring [1] | |||
| Association with ≥5% Weight Loss (Odds) | Significantly Greater Odds | Significantly Lower Odds | < 0.05 |
| Outcome Measure | eTRE + ER Group | lTRE + ER Group | ER Alone Group |
|---|---|---|---|
| Body Mass Loss (kg) | -5.0 (-5.7, -4.3) | -4.4 (-5.2, -3.6) | -4.3 (-5.0, -3.6) |
| Fat Mass (%) | -1.2*† | -0.0* | -0.1† |
| Fasting Glucose (mmol/L) | -0.35* | -0.00* | -0.18 |
| Diastolic BP (mmHg) | -4* | -1 | -0 |
Values with the same symbol (, †) within a row are significantly different from each other.
Ketogenic Diets as a Strategy to Modulate Appetite and Physiology
For researchers investigating strategies to improve adherence to dietary weight loss interventions, the ketogenic diet (KD) presents a fascinating case study. This high-fat, very-low-carbohydrate diet aims to shift the body's metabolism into a state of nutritional ketosis, where fat-derived ketone bodies become the primary fuel source, replacing glucose [22]. This shift is associated with several physiological changes, including appetite modulation, which can influence dietary adherence. This technical support center provides an overview of the mechanisms, key experimental methodologies, and common research challenges related to studying the KD's effects on appetite and physiology.
Frequently Asked Questions (FAQs)
What are the core physiological mechanisms by which a ketogenic diet modulates appetite?
The KD influences appetite through multiple, interconnected hormonal and metabolic pathways. The primary mechanisms identified in the literature are summarized below.
- Table: Appetite Modulation Mechanisms of the Ketogenic Diet
| Mechanism | Physiological Basis | Key Biomarkers / Mediators |
|---|---|---|
| Hormonal Shifts | Increased satiety hormone release and altered hunger signaling [23] [24]. | ↑ Cholecystokinin (CCK), ↑ Glucagon-like peptide-1 (GLP-1); potential modulation of ghrelin [24]. |
| Ketone Body Effects | Direct appetite-suppressive effects of ketone bodies [24]. | Elevated Beta-Hydroxybutyrate (BHB). |
| Reduced Lipogenesis | Decreased fat storage creation and increased fat breakdown [25] [24]. | Lowered insulin levels promoting lipolysis. |
| Stable Glycaemia | Avoidance of blood glucose and insulin spikes, reducing hunger sensations [23]. | Lower glycemic variability, improved insulin sensitivity [23]. |
The following diagram illustrates the logical relationship between the KD, these physiological mechanisms, and the resulting appetite modulation.
What are the most significant challenges to adherence in ketogenic diet trials, and what mitigation strategies are effective?
Adherence is a critical, and often limiting, factor in KD research. Common challenges and potential solutions are detailed below.
- Table: Adherence Challenges and Mitigation Strategies in KD Research
| Challenge | Impact on Adherence | Evidence-Based Mitigation Strategy |
|---|---|---|
| Dietary Restrictiveness | High dropout rates; difficulty maintaining macronutrient targets [25] [26]. | Provide structured meal plans, recipes, and pantry guides [27]. Use modified KD approaches (e.g., Modified Atkins) with slightly more flexibility [24]. |
| Social & Dining Difficulties | Reduced quality of life; non-compliance in social settings [26]. | Incorporate behavioral counseling. Involve participants' family members in education sessions [27]. |
| "Keto Flu" & Side Effects | Early attrition during the adaptation period (1-2 weeks). | Forewarn participants. Ensure adequate electrolyte and fluid intake from the start. |
| Nutrient Quality Concerns | Long-term sustainability; potential for micronutrient deficiencies. | Emphasize a "well-formulated" KD with diverse, nutrient-dense whole foods and minimal dairy, if appropriate for the study design [27]. |
| Macronutrient Drift | Participants often consume more carbohydrates and less fat than the protocol requires, breaking ketosis [25]. | Implement frequent 24-hour dietary recalls or use a dedicated food-tracking mobile app (e.g., MyFitnessPal) with researcher monitoring [25] [27]. |
Experimental Protocols & Methodologies
Core Protocol for a 12-Week Ketogenic Diet Intervention
This protocol is adapted from recent feasibility studies in clinical populations and can be tailored for research on adherence [27].
- Primary Objective: To assess the feasibility, adherence, and physiological effects of a 12-week ketogenic diet intervention in adults with overweight or obesity.
- Participant Selection:
- Inclusion Criteria: Adults (age ≥18 years), BMI ≥25 kg/m², stable weight for 3 months prior.
- Exclusion Criteria: Significant heart disease, diabetes, kidney stones, gallstones, or pregnancy [27].
- Dietary Intervention:
- Macronutrient Goals: 70-80% of daily energy from fat, 15-20% from protein, 5-10% from carbohydrates (typically <50 g/day) [23] [27].
- Diet Composition: Focus on whole foods. The diet can be modified to limit dairy products, as high dairy intake has been associated with risks for certain conditions, potentially improving the diet's safety profile and acceptability [27].
- Support Structure: Weekly group or individual sessions for the first month, bi-weekly thereafter. Sessions include nutritional education, cooking guidance, and troubleshooting [27].
- Adherence Monitoring:
- Ketone Bodies: Measure capillary or serum Beta-Hydroxybutyrate (BHB) weekly. A level of 0.5 - 3.0 mM is typically indicative of nutritional ketosis [25] [27].
- Dietary Intake: Use a combination of 3-day weighed food records and a dedicated phone app for real-time tracking [25] [27].
- Participant Feedback: Conduct qualitative interviews or use structured questionnaires to assess acceptability and barriers [27].
The workflow for implementing and monitoring this protocol is outlined below.
Key Signaling Pathways for Investigation
The neurobiological pathways underlying appetite regulation on a KD are complex. Two key pathways for experimental investigation are:
Pathway 1: Gut-Brain Axis Signaling
- Mechanism: KD-induced changes in gut microbiome composition and subsequent production of microbial metabolites (e.g., short-chain fatty acids) can influence central appetite regulation via the vagus nerve [24].
- Experimental Measurement: 16S rRNA sequencing of fecal samples to assess microbiome changes; serum metabolomics for SCFA levels; functional MRI to assess brain activity in response to food cues.
Pathway 2: Central Nervous System (CNS) Neurotransmitter Balance
- Mechanism: Ketone bodies, particularly BHB, may increase central nervous system levels of the inhibitory neurotransmitter GABA and modulate glutamate receptors, leading to stabilized neural networks and potential appetite suppression [22] [24].
- Experimental Measurement: Magnetic resonance spectroscopy (MRS) to measure GABA and glutamate levels in the brain; assessment of behavioral correlates of appetite.
The Scientist's Toolkit
This section details essential reagents, assays, and equipment for conducting rigorous research on the ketogenic diet.
- Table: Key Research Reagents and Materials
| Item | Function / Application | Example Protocol / Notes |
|---|---|---|
| Beta-Hydroxybutyrate (BHB) Assay | Primary objective biomarker for verifying nutritional ketosis [25] [27]. | Use handheld ketone meters for capillary blood (frequent monitoring) or serum assays via ELISA/colorimetric kits for higher precision in lab settings. |
| Food Tracking Software | To quantify adherence to macronutrient targets and energy intake [25]. | Utilize apps like MyFitnessPal. Researchers should train participants and export data for analysis. 24-hour dietary recalls can supplement this data. |
| Dual-Energy X-ray Absorptiometry (DEXA) | To precisely measure changes in body composition (fat mass, lean mass, bone mass) [28]. | Perform scans at baseline and study endpoint. Critical for confirming that weight loss is primarily from fat mass, not muscle [28]. |
| Gut Microbiome Profiling Kits | To investigate the role of the gut-brain axis in appetite modulation [24]. | Collect fecal samples at baseline and endpoint. Use 16S rRNA gene sequencing or shotgun metagenomics for taxonomic and functional analysis. |
| Hormone Panels | To measure changes in appetite-related hormones [23] [24]. | Use multiplex ELISA or Luminex assays to profile GLP-1, CCK, ghrelin, leptin, etc., from fasting plasma samples. |
| Indirect Calorimetry | To measure resting energy expenditure and respiratory quotient (RQ), confirming a metabolic shift toward fat oxidation (lower RQ) [23]. | Conduct measurements in a fasted state under standardized conditions. A decreased RQ confirms increased fat utilization. |
Evidence-Based and Emerging Methodologies to Enhance Adherence
Technical Support Center: Troubleshooting Guides and FAQs
This section addresses common technical challenges researchers may encounter when implementing digital self-monitoring tools in dietary weight loss interventions.
Frequently Asked Questions (FAQs)
Q1: What is the optimal frequency of dietary self-monitoring for weight loss maintenance? A: Evidence suggests that self-monitoring at least three days per week may be helpful for long-term weight loss maintenance, but greater benefit is observed when self-monitoring five to six days per week. Daily monitoring is not always necessary for effectiveness, which can reduce participant burden [29].
Q2: Why might participants fail to engage with digital self-monitoring tools despite receiving feedback? A: Remotely delivered feedback alone can be insufficient to sustain engagement. Ineffectiveness may occur due to poor timing of message delivery, lack of engagement with the digital tools, or if the message content is not perceived as relevant to the participant at that moment [1].
Q3: How does the timeliness of self-monitoring entry affect data quality? A: Timely recording is crucial. Research using instrumented paper diaries (IPDs) found that the percentage of weight lost correlated significantly not only with the frequency of self-monitoring but also with the number of diary entries made close to the time of eating. Delayed or batched recording can introduce recall bias and reduce the opportunity for participants to take corrective action during the day [30].
Q4: What are common technical barriers to adopting digital self-monitoring tools in clinical research? A: Users often experience a mismatch between system usability and their technical competencies. The choice to adopt and integrate these tools depends on the perceived balance between the added benefits and the effort required to achieve them. Common technical issues include problems with software installation, connectivity, and data synchronization [31] [32].
Troubleshooting Common Technical Problems
| Problem Category | Specific Issue | Suggested Solution for Research Staff |
|---|---|---|
| Access & Authentication | Participant forgets login credentials [32] [33]. | Implement a self-service password reset portal. If unavailable, guide participants through identity verification via email or security questions. |
| Software & Application | Application fails to run or crashes [32]. | Guide participants to check software compatibility with their device OS, restart the application, reinstall the program, or check for and install software updates. |
| Hardware & Connectivity | Slow device performance [32] [33]. | Instruct participants to close unnecessary background applications, free up disk space, and run antivirus or anti-malware scans. |
| Unrecognized USB device (e.g., smart scale) [32]. | Advise participants to restart their computer, try a different USB port, and check for and update device drivers on their computer. | |
| Slow or lost internet connection [32] [33]. | Have participants restart their router and modem, check Wi-Fi signal strength, and move closer to the router or use a wired connection for stability. |
Experimental Protocols and Quantitative Data
This section summarizes key methodologies and findings from recent studies on self-monitoring adherence.
| Study & Focus | Participant Group | Core Intervention & Methodology | Key Quantitative Finding on Adherence |
|---|---|---|---|
| SMARTER Trial (2025) [1] | 502 adults with obesity; 80% female, 82% White. | 12-month mHealth trial; compared self-monitoring (SM) only vs. SM + tailored feedback (FB) on diet, activity, and weight. | - Adherence to SM and behavioral goals declined nonlinearly over time.- The SM+FB group showed a less steep decline than the SM-only group.- Higher adherence to diet, PA, and weight SM was associated with greater odds of achieving ≥5% weight loss. |
| UF Frequency Study (2024) [29] | 75 adults with overweight or obesity. | 3-month internet-based weight loss program; explored various thresholds for dietary self-monitoring. | - 3-4 days/week of self-monitoring supported weight loss maintenance.- 5-6 days/week of self-monitoring supported additional weight loss. |
| PREFER/IPD Study [30] | Sub-sample from an 18-month behavioral weight-loss program. | Used Instrumented Paper Diaries (IPDs) to electronically validate the timing and frequency of self-monitoring. | - Self-reported diary usage significantly exceeded electronically documented usage.- Percentage of weight lost correlated significantly with the frequency of IPD use (p=.001) and timely entries (p=.002). |
Detailed Methodology: The SMARTER mHealth Trial Protocol
The SMARTER trial provides a robust example of a digital self-monitoring intervention [1].
- Participant Training: All participants received one 90-minute, one-on-one in-person session with a dietitian. This session covered behavioral strategies for weight reduction, goal setting, and instruction on using the digital self-monitoring tools.
- Dietary Self-Monitoring: Participants used the Fitbit app to record food intake. Calorie goals were individualized based on baseline body weight.
- Physical Activity Monitoring: Participants used a wrist-worn Fitbit Charge 2 device synced with their smartphone. The goal was to gradually increase activity to 150 minutes/week by 12 weeks, with an ultimate goal of 300 minutes/week by 52 weeks.
- Weight Monitoring: Participants were instructed to weigh themselves daily using a study-provided smart scale that transmitted data to the study database.
- Feedback Intervention (SM+FB Group Only): The intervention group received up to three tailored feedback messages per day via a custom app. Messages were based on available self-monitoring data and addressed caloric, fat, and added sugar intake daily, and physical activity every other day. The message library was refreshed monthly to prevent desensitization.
Visualizing the mHealth Trial Workflow
The following diagram illustrates the integrated workflow of a digital self-monitoring intervention with feedback, as implemented in the SMARTER trial [1].
The Scientist's Toolkit: Key Research Reagents and Materials
The table below details essential tools and methodologies used in modern self-monitoring research for dietary weight loss interventions.
| Item / Tool | Function in Research | Application Notes |
|---|---|---|
| Instrumented Paper Diaries (IPDs) [30] | Objectively validates the timing and frequency of self-monitoring behaviors without participant awareness. | Critical for measuring true adherence and timeliness, overcoming the limitation of inflated self-reported data. |
| Digital Self-Monitoring Platform [1] [31] | Provides the infrastructure for participants to log diet, activity, and weight, and for researchers to collect and manage data. | Platforms like m-Path or commercial apps (e.g., Fitbit) are used. Ease of use is a major factor in participant adherence [31]. |
| Wearable Activity Tracker [1] | Automatically collects physical activity data (e.g., steps, active minutes), reducing participant burden. | Devices like the Fitbit Charge 2 can be synced with a study platform to provide objective PA data for analysis and feedback. |
| Smart Scale [1] | Transmits weight measurements wirelessly to a central database upon daily weighing. | Provides objective, frequent weight data without relying on participant self-report, enabling timely feedback. |
| Tailored Feedback Message Library [1] | A pre-written, dynamic set of messages used to provide automated, context-specific feedback to participants. | Message content, frequency, and timing must be carefully designed. The library should be refreshed periodically to maintain participant engagement. |
For researchers conducting dietary weight loss interventions, participant engagement with digital tools is a critical, yet often unstable, variable. Technical malfunctions and usability issues are not merely operational nuisances; they constitute significant sources of missing data and protocol deviations that can compromise study validity and power [1] [34]. Recent randomized controlled trials highlight that while higher adherence to self-monitoring via digital tools is associated with significantly greater odds of achieving ≥5% weight loss, maintaining this adherence is a persistent challenge [1] [35]. This technical support center provides targeted troubleshooting and methodologies to help research teams identify, mitigate, and preempt these technical barriers, thereby safeguarding data integrity and intervention efficacy.
Frequently Asked Questions (FAQs) for Research Teams
Q1: Our study participants are not receiving automated feedback messages. What could be the cause? A1: This is a common issue in mHealth trials. Based on recent studies, the causes can be multi-faceted [1] [34]:
- Message Delivery Failures: New FCC regulations (implemented March 2023) and carrier-level spam filters can automatically block legitimate study text messages, particularly those containing financial incentive information or high-frequency sends [34].
- Data Syncing Disruptions: Feedback algorithms often require recent self-monitoring data. If a participant's wearable (e.g., Fitbit) or smart scale has not synced data to the companion app, the system may lack the necessary information to trigger or tailor a message [1].
- Platform API Changes: In long-term studies, the discontinuation or update of application programming interfaces (APIs)—such as the MyFitnessPal-Fitbit integration—can sever data flow between devices and the central research platform, halting message delivery [34].
Q2: Why are we observing a steep, nonlinear decline in dietary self-monitoring adherence after the first few months? A2: The nonlinear decline in adherence is a well-documented pattern in digital weight loss trials. Research indicates this is rarely due to participant disinterest alone. Key technical and experiential factors include [1] [36]:
- User Interface Burden: Dietary logging remains a high-effort task. If the food database is difficult to search, barcode scanning is unreliable, or the app requires manual entry for complex meals, participant fatigue sets in.
- Lack of Perceived Relevance: Participants disengage if automated feedback messages are generic, ill-timed, or not perceived as personally relevant to their immediate challenges [1].
- Technical Friction: Frequent app crashes, slow loading times, and complex navigation menus directly lead to abandonment.
Q3: What are the most common points of failure in a system integrating wearables, smart scales, and an mHealth app? A3: The integrated system creates a chain that is only as strong as its weakest link. Common points of failure include [34] [37]:
- Device Pairing and Re-pairing: Bluetooth connections between wearables/apps and smartphones can be lost after operating system updates or app updates, requiring manual re-pairing.
- Scale Connectivity: "Smart" scales may fail to transmit data if Wi-Fi passwords are changed, the scale is moved to a new location with a weak signal, or its cellular data plan (for cellular models) expires [34].
- Data Sanitization: Raw data from consumer devices (e.g., step counts, active minutes) often requires cleaning and validation before it can be used for research purposes, a process prone to error [34].
Troubleshooting Guides
Connectivity and Data Flow Issues
Problem: Weight data from smart scales is not appearing in the study database. Solution: Follow this systematic diagnostic protocol to isolate the point of failure.
Diagnostic Steps:
- Verify Scale Power & Setup: Confirm the scale has charged batteries or is plugged in. Ensure it is on a hard, level surface; carpets can interfere with sensors and connectivity.
- Check Local Connectivity: Have the participant open the companion app on their phone while standing near the scale. If the data is present in the app but not the research portal, the issue is with the app-to-portal API. If data is missing from the app, the scale-to-phone connection has failed.
- Confirm Data Transmission: For Wi-Fi scales, ensure the home network password hasn't changed. For cellular scales (e.g., BodyTrace), confirm the embedded cellular plan is active [34].
- Check Research Platform API: Review study platform logs for API errors from the scale manufacturer's server, which may indicate a system-wide issue requiring developer intervention [34].
Automated Feedback Message Failure
Problem: The intervention group is not receiving tailored feedback messages based on their self-monitoring data. Solution: Investigate the message generation and delivery pipeline.
Table: Components of Feedback Message Failure Analysis
| Component to Check | Diagnostic Method | Potential Resolution |
|---|---|---|
| Data Availability | Check if recent, valid self-monitoring data exists in the database for the participant. | If no data, troubleshoot device syncing. If data exists, check algorithm logic. |
| Message Generation Algorithm | Review server-side logs for errors during message generation. Test algorithm with sample data. | Debug logic errors; ensure message library is correctly loaded and updated [1]. |
| Message Delivery Gateway | Check delivery status logs from SMS/email gateways. | Work with IT to register study numbers/mailers with carriers to avoid spam filtering [34]. |
| Participant Device | Confirm participants know how to view messages and that notifications are enabled. | Provide a simple guide for enabling app notifications on iOS and Android. |
Declining App Usability and Engagement
Problem: High initial usage followed by a rapid drop in app logins and feature use. Solution: Proactively assess and improve usability.
Protocol: Rapid Usability Assessment for Research Apps
- Method: Recruit a small sub-sample of participants (n=5-10) for a 20-minute structured interview and screen-sharing session.
- Tasks: Ask them to perform core tasks: log a meal, find a previous day's data, review a feedback message.
- Metrics: Measure effectiveness (task completion rate), efficiency (time on task), and satisfaction (post-task rating) [37].
- Analysis: Identify common points of friction (e.g., "too many clicks to log water," "can't find past weight graph"). The most frequently cited usability attributes to evaluate are outlined in the table below.
Table: Key Usability Attributes for mHealth Research Tools [37]
| Usability Attribute | Definition in Research Context | Evaluation Method |
|---|---|---|
| Satisfaction | The participant's perceived comfort and acceptability of using the app. | System Usability Scale (SUS); qualitative interviews. |
| Ease of Use | The degree to which the app can be used with minimal mental effort. | Task success rate; observation of user errors. |
| Perceived Usefulness | The participant's belief that the app will help them achieve their health goals. | Questionnaire; analysis of adherence correlates. |
| User Experience | The holistic experience of using the app, including emotional response. | Think-aloud protocols during task completion. |
| Effectiveness | The accuracy and completeness with which users achieve specified goals. | Data completeness metrics (e.g., % of days with diet logged). |
Experimental Protocols for Validating mHealth Tools
Before deploying a digital tool in a clinical trial, rigorous technical validation is required to ensure it functions as intended and is suitable for the target population.
Protocol: Technical Validation of Device Data Accuracy
Objective: To verify that data from consumer wearables and smart scales meets minimum accuracy thresholds for research purposes. Materials: Consumer device (e.g., Fitbit, Garmin), research-grade reference device (e.g., ActiGraph for activity, medical balance scale for weight), participant simulators (for controlled step testing). Methodology:
- Step Count Validation: Simultaneously mount the consumer wearable and reference device on a simulator or human participant. Program the simulator to execute a predefined series of steps (e.g., 1000 steps) at varying speeds. Record step counts from both devices [37].
- Weight Measurement Validation: Have a cohort of participants (n>30) weigh themselves sequentially on the smart scale and a calibrated medical scale. Record weights from both devices across a range of body masses.
- Data Analysis: Calculate intraclass correlation coefficients (ICCs) and mean absolute percentage errors (MAPE) between the consumer and research-grade devices. Establish a pre-defined acceptability threshold (e.g., ICC > 0.80, MAPE < 5% for steps).
Protocol: Piloting the End-to-End Data Pipeline
Objective: To ensure all components of the digital intervention—from device data capture to feedback message delivery—work cohesively before study launch. Materials: Full tech stack (devices, apps, central database, messaging system), pilot participants (n=10-15), data monitoring dashboard. Methodology:
- Scripted Scenario Testing: Pilot participants follow a scripted 3-day protocol of activities: daily self-weighing, food logging, and wearing an activity tracker.
- Data Flow Monitoring: Use the research dashboard to track the arrival of all expected data points in the central database.
- Message Trigger Verification: Confirm that the predefined self-monitoring data triggers the correct tailored feedback messages, which are delivered to participants' devices on schedule [1] [34].
- Troubleshooting Documentation: Log all failures (e.g., data not syncing, message not sent) and document their root causes and resolutions. This log becomes a primary resource for the study's technical support team.
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Digital "Reagents" for mHealth Adherence Research
| Item / Platform | Function in Research | Key Considerations |
|---|---|---|
| Fitbit Charge / Sense Series | Wrist-worn accelerometer for capturing physical activity and sleep data. | Ease of use for participants; robust API for data extraction; battery life can impact continuous wear [1] [34]. |
| BodyTrace Cellular Scale | Transmits weight data directly via cellular networks, bypassing participant Wi-Fi. | Eliminates a major connectivity barrier; requires an active cellular service plan [34]. |
| MyFitnessPal / Fitbit App Food Database | Provides the nutrient database for dietary self-monitoring. | Database comprehensiveness affects logging burden; API stability is a known risk factor [34]. |
| Log2Lose-style Platform | A customizable platform for automating data collection, incentive processing, and participant messaging. | Critical for managing complex, fully remote trials; requires adaptable software and continuous technical support [34]. |
| System Usability Scale (SUS) | A standardized 10-item questionnaire for assessing the perceived usability of a system. | Provides a quick, reliable metric to compare usability across different versions of a research app [37]. |
This technical support center provides researchers and scientists with troubleshooting guides and FAQs to address common challenges in experiments focused on personalized nutrition for improving adherence to dietary weight loss interventions.
Frequently Asked Questions
Q1: What is the core difference between traditional dietary advice and personalized nutrition? Traditional dietary advice offers a "one-size-fits-all" approach, assuming uniform metabolism across populations. In contrast, personalized nutrition tailors interventions based on an individual's unique genetic, epigenetic, microbiome, and real-time metabolic data to improve efficacy and adherence [38].
Q2: Which genetic variants are most relevant for personalizing carbohydrate and fat intake? Common genetic variations studied for dietary response include SNPs in genes like FTO and TCF7L2, which are linked to obesity and glucose metabolism. For instance, individuals with specific PPARG polymorphisms may respond better to a Mediterranean diet rich in monounsaturated fats [38] [39]. The table below summarizes key genetic factors.
| Gene | Associated Function | Dietary Implication | Key Reference |
|---|---|---|---|
| FTO | Risk of obesity & impaired glucose metabolism [38] | May benefit from tailored carbohydrate intake [38] | de Toro‐Martín et al. (2017) |
| TCF7L2 | Glucose metabolism [38] | May benefit from tailored carbohydrate intake [38] | de Toro‐Martín et al. (2017) |
| PPARG | Fat metabolism & adipocyte differentiation | Carriers may see superior weight loss on a high-monounsaturated fat diet [38] | Ferguson et al. (2016) |
| APOA2 | Lipid metabolism | Associated with higher obesity risk with high saturated fat intake; recommendation to reduce [38] | Lagoumintzis and Patrinos (2023) |
| MTHFR | Folate metabolism [39] | Variants (e.g., C677T) can lead to folic acid deficiency; requires supplementation [39] | - |
Q3: How can the gut microbiome be leveraged for personalized nutrition? The gut microbiome plays a critical role in nutrient absorption and metabolic health. Species like Akkermansia muciniphila are associated with improved insulin sensitivity. Diets can be personalized based on an individual's microbiome composition; for example, individuals with higher levels of beneficial bacteria may respond better to high-fiber interventions, which enhance short-chain fatty acid production [38].
Q4: What are the primary technical and ethical challenges in PN research? Key challenges include:
- Data Privacy: Managing sensitive genetic and health data [38].
- Clinical Validation: The need for robust, large-scale randomized controlled trials to substantiate efficacy [38] [39].
- Accessibility and Cost: Ensuring these strategies are accessible beyond a specific subgroup to have a widespread population health impact [38] [40].
Q5: What is the role of digital health technologies in modern PN studies? Digital tools are transformative for implementing and studying PN. Continuous Glucose Monitors (CGMs), AI-driven meal planning apps, and mobile health platforms enable dynamic dietary adjustments and real-time monitoring of adherence and metabolic parameters [38]. These tools facilitate the creation of Adaptive Personalized Nutrition Advice Systems (APNAS) that use dynamic data to guide both the "what" and "how" of dietary change [40].
Experimental Protocol Guide
Protocol: A Workflow for a Genetically-Informed Dietary Intervention Study
This protocol outlines a methodology for designing a weight loss intervention that incorporates nutrigenetic data.
1. Participant Genotyping & Group Allocation
- Method: Collect DNA samples (e.g., via saliva) from participants. Use genotyping arrays or targeted sequencing to identify relevant SNPs (e.g., in FTO, TCF7L2, PPARG) [38] [39].
- Troubleshooting: Ensure informed consent explicitly covers genetic analysis. Use standard DNA extraction kits and follow manufacturer protocols for optimal yield.
- Group Allocation: Randomize participants into a control group (general dietary advice) and an intervention group (genetically-tailored advice).
2. Baseline Phenotypic & Behavioral Assessment
- Clinical Measures: Collect baseline data on BMI, body composition (DEXA/BIA), and fasting blood markers (glucose, insulin, lipids) [38].
- Dietary & Behavioral Assessment: Use validated tools like 3-day food records or 24-hour recalls. Assess psycho-behavioral traits (e.g., eating behavior, motivation) via questionnaires [40].
3. Formulation & Delivery of Personalized Recommendations
- Algorithm Development: Create an algorithm that matches genetic profiles (from Step 1) to specific dietary prescriptions. For example, assign a lower glycemic load diet to carriers of certain TCF7L2 variants [38].
- Recommendation Delivery: Deliver advice via a dietitian or a digital platform. Digital apps can provide real-time feedback and nudges to enhance adherence [38].
4. Adherence & Outcome Monitoring
- Monitoring Adherence: Use digital food-tracking apps and, if feasible, objective biomarkers (e.g., CGM data, plasma fatty acid profiles) to track compliance [38] [40].
- Outcome Measurement: The primary outcome is often adherence rate (%) or weight loss (kg). Secondary outcomes include changes in body fat %, blood pressure, and glycemic markers [38].
Logical Workflow of a Personalized Nutrition Study
The Scientist's Toolkit: Key Research Reagents & Materials
The following table details essential materials and tools for conducting state-of-the-art personalized nutrition research.
| Item Name | Function / Application | Example / Specification |
|---|---|---|
| Genotyping Array | Identifies single nucleotide polymorphisms (SNPs) associated with nutrient metabolism and disease risk [38] [39]. | Targets variants in genes like FTO, TCF7L2, MTHFR [38]. |
| 16S rRNA Sequencing Kit | Profiling gut microbiome composition to inform personalized pre/probiotic and fiber recommendations [38]. | Differentiates taxa such as Akkermansia muciniphila [38]. |
| Continuous Glucose Monitor (CGM) | Captures real-time, dynamic blood glucose data to understand individual postprandial responses to different foods [38] [40]. | - |
| Body Composition Analyzer | Precisely measures outcomes like body fat percentage, a more sensitive metric than body weight alone [38]. | DEXA Scan or Bioelectrical Impedance Analysis (BIA) device. |
| Dietary Assessment Platform | Digital tool for collecting high-frequency dietary intake data and monitoring adherence [38] [40]. | Mobile health applications with barcode scanners. |
| AI / Machine Learning Algorithm | Integrates multi-omics (genetic, microbiome), clinical, and behavioral data to generate and optimize personalized dietary plans [38] [40]. | - |
Nutrigenetics: From Gene to Dietary Advice
Frequently Asked Questions
What constitutes a 'structured support system' in weight loss research? Structured support systems are organized, methodical approaches designed to improve adherence and outcomes in dietary weight loss interventions. They primarily encompass two key elements: medically supervised weight management programs (MSWMPs) that provide clinical oversight and a structured curriculum [41], and social support mechanisms that leverage relationships with family, friends, or peers to encourage healthy eating and physical activity behaviors [42] [43].
Are short-term interventions effective for achieving significant weight loss? Yes, meta-analyses of randomized controlled trials (RCTs) demonstrate that multicomponent lifestyle interventions lasting 6 months or less can produce significant weight loss. A 2024 systematic review found a pooled mean difference in weight change of -2.59 kg (95% CI, -3.47 to -1.72) compared to control groups [44]. This suggests short-term programs can be a viable option, potentially improving enrollment and retention.
Which sources of social support are most impactful for weight management? Longitudinal studies indicate that different sources of support influence different behaviors [42]:
- Friend and Coworker Support: Most associated with improved healthy eating behaviors.
- Family Support: Most associated with improved physical activity behaviors. Conversely, family social undermining for healthy eating (e.g., bringing unhealthy foods) is significantly associated with weight gain [42].
How can cognitive modeling address the challenge of dietary self-monitoring adherence? The Adaptive Control of Thought-Rational (ACT-R) cognitive architecture can model and predict adherence dynamics. This computational framework simulates human cognitive processes like goal pursuit and habit formation over time. Model-based analyses can qualitatively test the impact of different intervention strategies, such as showing that tailored feedback combined with intensive support sustains goal pursuit and behavioral practice [4].
Troubleshooting Guides
Problem: Declining Adherence to Dietary Self-Monitoring
Issue: Participant engagement with self-monitoring tools (e.g., food diaries, apps) wanes over time, a common challenge in long-term interventions [4].
Solution: Implement a multi-faceted support strategy based on cognitive modeling and behavioral theory.
Experimental Protocol: Dynamic ACT-R Modeling for Adherence [4]
- Objective: To develop a prognostic model for dietary self-monitoring adherence and simulate the effects of different support interventions.
- Methodology:
- Participant Assignment: Assign participants to one of three groups: basic self-management, tailored feedback, or intensive support.
- Data Collection: Collect longitudinal self-monitoring data (e.g., daily logins, food entries) over a minimum of 21 days.
- Cognitive Modeling: Use the ACT-R architecture to model adherence. The model incorporates:
- Declarative Memory: Chunks of knowledge about self-monitoring.
- Procedural Memory: Production rules for executing self-monitoring behavior.
- Subsymbolic Calculations: Computes activation levels for memory retrieval and utility for rule selection.
- Model Validation: Evaluate model performance using Root Mean Square Error (RMSE) to compare predicted vs. actual adherence.
- Intervention Simulation: Use the validated model to simulate and analyze the effects of varying support mechanisms on long-term adherence trends.
The workflow below illustrates the technical process of using cognitive modeling to understand and improve adherence.
Problem: Weight Loss Plateau
Issue: A participant experiences a state of little or no weight change after a period of active progress, typically for six weeks or more [45].
Solution: A holistic reassessment to identify and address underlying physiological and behavioral factors.
Experimental Protocol: Systematic Plateau Analysis [45] [46]
- Objective: To identify the physiological and behavioral determinants of a weight loss plateau and implement a targeted corrective strategy.
- Methodology:
- Reassess Baseline & Goals: Re-evaluate the participant's current dietary intake, physical activity level, and routine against their initial baseline. Confirm goal realism (e.g., 1 lb/week weight loss) [45].
- Audit Holistic Pillars: Systematically investigate key areas that impact metabolism and adherence:
- Sleep: Assess duration and quality. Sleep deprivation can decrease metabolism and increase hunger hormones [45].
- Stress: Evaluate perceived stress levels and management techniques. Chronic stress elevates cortisol, which can impair metabolism and promote emotional eating [45].
- Nutritional Deficiencies: Check for deficiencies in common micronutrients (e.g., Vitamin D, zinc, magnesium) or macronutrients (e.g., protein) that can cause low energy and hinder progress [46].
- Support System: Conduct an "inner circle inventory" to determine if the participant's close social contacts support or undermine their health goals [45].
- Adjust Energy Balance: Based on the reassessment, create a corrective action plan. This may involve:
The following decision tree provides a structured approach to diagnosing the root causes of a weight loss plateau.
Table 1: Weight Loss Outcomes from Structured Programs
| Program / Study Type | Duration | Sample Size | Weight Change from Baseline (kg) | Key Findings | Source |
|---|---|---|---|---|---|
| Medically Supervised Program (MSWMP) | 5 Years | 2,777 (with 5-yr data) | -6.4 kg (SE = 0.29) at 5 years | 35.2% achieved ≥10% weight loss at 5 years. | [41] |
| Short-Term Multicomponent Interventions (Meta-Analysis) | ≤6 Months | 14 RCTs (Pooled) | Pooled MD: -2.59 kg (95% CI: -3.47 to -1.72) | Effective for significant short-term loss; may improve enrollment. | [44] |
| Social-Support-Based Interventions (Meta-Analysis) | Varies (End of Intervention) | 24 RCTs (n=4,919) | Significant effect vs. control (p=0.04) | Effect significant at end of intervention and at 3- and 6-month follow-ups. | [43] |
This table summarizes longitudinal associations between specific sources of support/undermining and weight change over 24 months [42].
| Source & Type of Influence | Behavior Targeted | Association with Weight Change (β coefficient) | Statistical Significance (p-value) |
|---|---|---|---|
| Friend Support | Healthy Eating | β = -0.15 | p < 0.05 |
| Coworker Support | Healthy Eating | β = -0.11 | p < 0.05 |
| Family Support | Physical Activity | β = -0.032 | p < 0.05 |
| Family Social Undermining | Healthy Eating | β = +0.12 | p = 0.0019 |
β coefficient interpretation: A negative β indicates weight reduction; a positive β indicates weight gain.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Methodological Components for Adherence Research
| Research "Reagent" (Method/Tool) | Function / Purpose in the "Experiment" |
|---|---|
| ACT-R Cognitive Architecture | A computational framework to model and simulate the cognitive processes (goal pursuit, habit formation) underlying adherence dynamics over time [4]. |
| Social Support & Undermining Survey (Sallis) | A validated 23-item instrument to quantify perceived support and social undermining for healthy eating and physical activity from family, friends, and coworkers [42]. |
| Medically Supervised Program (MSWMP) Protocol | A standardized, multi-phase (meal replacement, transition, maintenance) intervention protocol to deliver structured, clinically supervised weight management [41]. |
| Digital Self-Monitoring Platform | A technology (e.g., mobile app) to collect continuous, fine-grained data on user dietary behaviors and adherence, enabling dynamic analysis [4]. |
| Holistic Pillar Assessment Framework | A structured protocol to audit key lifestyle factors (sleep, stress, nutrition, support system) that can confound weight loss outcomes and adherence [45] [46]. |
Troubleshooting Guide: Common Adherence Barriers and Research Interventions
Table 1: Adherence Barriers and Proposed Mitigation Strategies for Research Protocols
| Adherence Barrier | Evidence from Clinical/Real-World Studies | Proposed Experimental Mitigation Strategy |
|---|---|---|
| Gastrointestinal (GI) Side Effects | Most common adverse effects; nausea, diarrhea, vomiting, constipation [47] [48] [49]. Often dose-dependent and transient [50]. | Implement a forced, slow titration schedule in study design. Protocol to include prophylactic patient education on dietary modification (e.g., low-fat meals) and scheduled antiemetic use. |
| Patient Discontinuation & Non-Persistence | Real-world study: 46.3% persistence at 180 days; 32.3% at 1 year [51]. Another study: 22% discontinuation at 6 months [52]. | Integrate specialty pharmacy support for proactive follow-ups. Design trials with remote monitoring, dose adjustment support, and structured check-ins at high-risk periods (e.g., 3, 6, 9 months). |
| Access & Affordability Barriers | High drug cost leads to access issues; 54% of adults report difficulty affording therapy [53]. Insurance barriers (step therapy, prior authorization) cause delays [53]. | Incorporate a dedicated research coordinator to manage prior authorizations. Pre-screen participants for insurance coverage and integrate patient assistance programs into study protocols. |
| Management of Weight Regain | Observation of weight regain after treatment discontinuation is a key clinical concern [47]. | Design trials to include a combination therapy arm (e.g., GLP-1 RAs with behavioral therapy) and a structured tapering/discontinuation protocol to study rebound effects. |
| Aspiration Risk & Anesthesia | Delayed gastric emptying linked to increased aspiration risk during anesthesia [47] [48]. | Establish a mandatory pre-procedure drug withholding protocol (e.g., 1-week washout) for study participants undergoing elective anesthesia or endoscopy. |
Frequently Asked Questions (FAQs) for Clinical Research Design
Q1: What are the most critical safety signals to monitor in long-term trials involving GLP-1 RAs for weight management?
A: While early concerns about pancreatic and thyroid cancer have been largely attenuated by recent evidence [47], vigilant monitoring is recommended for:
- Gallbladder and Biliary Disorders: Recognized as potential risks [47] [48].
- Acute Pancreatitis: Although rare, it remains a serious adverse event to monitor [48] [49].
- Renal Function: Emerging real-world evidence suggests an increased risk of kidney conditions; routine monitoring of kidney function is essential [49].
- Psychiatric Safety: Requires ongoing investigation, though some studies indicate potential benefits for conditions like suicidal ideation and substance abuse [47] [49].
Q2: What is the expected magnitude of weight loss for different GLP-1 RAs, to help set realistic endpoints?
A: Weight loss efficacy varies significantly between agents. In clinical trials, placebo-corrected weight loss is approximately 5% with liraglutide, 12% with semaglutide, and 18% with the dual GLP-1/GIP receptor agonist tirzepatide [48]. The weight loss for GLP-1 RAs as a class typically ranges from 15% to 20% in many clinical trials [47].
Q3: How can research protocols address the high real-world discontinuation rates to improve data integrity?
A: Integrate adherence-supporting interventions directly into the study design. This includes:
- Specialty Pharmacy Models: Utilize health system specialty pharmacies (HSSPs) integrated with electronic health records to streamline access, provide patient education, and offer proactive follow-up [53].
- Data-Driven Tracking: Implement technology to monitor refill adherence and intervene early when barriers arise [53].
- Managing Expectations: Provide comprehensive patient education on expected results and side effect management to preempt frustration [53].
Q4: What are the key considerations for designing a dietary intervention study alongside GLP-1 RA pharmacotherapy?
A: The mechanisms of GLP-1 RAs—slowing gastric emptying and promoting satiety [54]—directly impact nutritional intake. Protocols should:
- Adapt Dietary Counseling: Tailor nutritional advice to mitigate GI side effects, emphasizing small, frequent meals and low-fat content.
- Monitor Lean Mass: As reductions in lean mass accompany weight loss [47], study designs should include body composition analysis (e.g., DXA scans) to assess the impact of combined dietary and pharmacologic interventions.
- Time Meals and Dosing: Consider the interaction between drug administration and meal timing to optimize tolerability and adherence to the dietary intervention.
Experimental Protocols for Adherence Research
Protocol: Assessing a Multicomponent Adherence Intervention
Objective: To evaluate the efficacy of an integrated specialty pharmacy support model on 12-month persistence and adherence to GLP-1 RA therapy in a research cohort.
Methodology:
- Design: Randomized Controlled Trial (RCT).
- Participants: Adults with obesity without diabetes, initiating GLP-1 RA therapy.
- Intervention Arm: Participants receive support from a health system specialty pharmacy (HSSP). This includes:
- A dedicated pharmacist to navigate prior authorization and secure financial assistance [53].
- Initial education on injection technique, side effect management, and realistic outcome expectations [53].
- Proactive, scheduled follow-ups at 2, 4, 8, 12, 26, and 52 weeks for dose adjustment and side-effect management [53].
- Data-driven tracking of prescription refills with timely interventions [53].
- Control Arm: Participants receive usual care (standard prescription processing and brief provider counseling).
- Primary Outcome: Proportion of participants persistent (gap in therapy ≤60 days) at 12 months [51].
- Secondary Outcomes: Proportion of participants with PDC ≥80% [51], change in body weight, and incidence of GI adverse events.
Protocol: Evaluating Weight Regain Post-Discontinuation
Objective: To characterize the pattern and magnitude of weight regain after discontinuation of GLP-1 RAs and test the efficacy of a maintenance dietary intervention.
Methodology:
- Design: A multi-phase, interventional study.
- Phase 1 (Lead-in): All participants receive a standardized GLP-1 RA therapy for 36 weeks to achieve weight stabilization.
- Phase 2 (Randomized Discontinuation): Participants are randomized into two groups:
- Group A (Continued Pharmacotherapy): Continues the GLP-1 RA.
- Group B (Structured Discontinuation): Discontinues the GLP-1 RA and initiates a structured maintenance protocol, which could include a combination of intensive behavioral therapy, tailored dietary plans, or other anti-obesity medications [47].
- Assessments: Body weight, body composition (lean mass), appetite scores, and metabolic parameters are measured at baseline, week 36 (discontinuation), and then at regular intervals for one year.
- Endpoint: Difference in mean weight regain from week 36 to week 88 between groups.
Signaling Pathways and Experimental Workflows
GLP-1 Receptor Agonist Signaling Pathway
Patient Adherence Challenge and Support Workflow
Research Reagent Solutions
Table 2: Key GLP-1 RAs and Research Applications
| Research Reagent | Primary Indications | Key Research Applications in Adherence/Obesity | Notable Characteristics |
|---|---|---|---|
| Liraglutide (Saxenda, Victoza) | Obesity, T2D | Study of cardiovascular outcomes (LEADER trial), real-world persistence patterns [51] [52]. | Once-daily injection; lower 1-year persistence (19.2%) in real-world studies [51]. |
| Semaglutide (Wegovy, Ozempic, Rybelsus) | Obesity, T2D, CVD risk reduction | Gold comparator for weight loss efficacy (SELECT, STEP trials), research on organ protection (FLOW kidney trial) [47] [55] [52]. | Once-weekly injection or daily oral pill; higher 1-year persistence (47.1% for Ozempic) [51]. |
| Tirzepatide (Zepbound, Mounjaro) | Obesity, T2D | Investigating superior efficacy vs. selective GLP-1 RAs, dual-agonist mechanisms (SURPASS-CVOT) [47] [52]. | Once-weekly injection; GLP-1/GIP dual receptor agonist; highest weight loss in class [48]. |
| Oral GLP-1 RAs (e.g., Rybelsus, Danuglipron) | T2D, (under investigation for obesity) | Research on adherence advantages of oral formulations, pharmacokinetics, and combination therapies [55]. | Small molecules; offer convenience and potential for fixed-dose combinations with other agents [55]. |
Identifying and Overcoming Barriers to Sustained Adherence
Addressing the Universal Challenge of Declining Engagement Over Time
Declining engagement over time presents a fundamental challenge in dietary weight loss interventions, significantly impacting data quality and intervention efficacy in research settings. Studies consistently demonstrate that adherence rates to weight loss programs average approximately 60.5%, with dropout rates reaching up to 68.5% after one year in multidisciplinary programs [5] [56]. This engagement decay follows a predictable pattern, with dropout rates accelerating from 21.3% at two months to 44.4% at six months, and ultimately 68.5% at twelve months in residential obesity treatment programs [56]. For researchers and drug development professionals, understanding and mitigating this decline is crucial for maintaining statistical power and validity in clinical trials investigating weight management therapeutics.
The relationship between engagement and outcomes is unequivocal. Research on digital behavior change interventions demonstrates that higher engagement levels—measured through metrics like meal logging, article reading, and self-weighing—directly correlate with superior weight loss outcomes [57]. Participants who consistently track dietary intake achieve significantly greater weight loss (-9.99 pounds) compared to inconsistent trackers, with consistent engagement facilitating linear weight loss throughout intervention periods [58]. This evidence underscores that declining engagement represents not merely an attrition problem but a fundamental confounding variable that can compromise research integrity and therapeutic efficacy assessment.
Quantitative Engagement Metrics: Evidence from Clinical Research
Table 1: Documented Engagement and Dropout Rates in Weight Management Interventions
| Intervention Type | 2-Month Dropout | 6-Month Dropout | 12-Month Dropout | Key Engagement Predictors |
|---|---|---|---|---|
| Multidisciplinary Residential Program [56] | 21.3% | 44.4% | 68.5% | Higher baseline BMI, uric acid levels, white blood cell count |
| Digital Behavior Change Intervention (Noom) [57] | N/A | N/A | Retention: 60.32%* | Meal logging, article reading, self-weighing, coach messaging |
| Supervised Attendance Programs [5] | N/A | N/A | Adherence: 60.5% (overall) | Supervision, social support, dietary focus (vs. exercise only) |
*Calculated from reported data: 39.68% high weight loss + 42.11% moderate weight loss at 33-52 weeks.
Table 2: Engagement-Outcome Relationships in Digital Weight Management
| Engagement Metric | Impact on Weight Loss Outcomes | Temporal Pattern |
|---|---|---|
| Dietary Tracking Consistency [58] | Consistent trackers (>66% days): -9.99 lbs; Rare trackers (<33% days): significantly less weight loss | Linear relationship for consistent trackers; nonlinear for inconsistent trackers |
| Meal Logging [57] | Significantly associated with moderate (5-10%) and high (≥10%) weight loss vs. stable weight | Maintained significance from 9-16 weeks through 33-52 weeks |
| Article Reading [57] | Positive association with weight loss outcomes across all time periods | Stronger association in early intervention phases (9-16 weeks) |
| Self-Weighing [57] | Predictive of successful weight loss (≥5% body weight) | Maintained significance throughout 52-week intervention |
Troubleshooting Guide: Addressing Common Engagement Scenarios
FAQ 1: How can researchers identify participants at risk of early dropout?
Evidence-Based Protocol: Implement baseline screening for established predictor factors. Research indicates that participants with higher baseline BMI, elevated uric acid levels, and increased white blood cell counts demonstrate significantly higher dropout rates at 2-month follow-ups [56]. Additionally, patients who lose a higher percentage of fat mass during initial intervention phases may be at increased risk of subsequent dropout, possibly due to diminished motivation once initial goals are achieved [56].
Methodology:
- Collect comprehensive baseline measures including BMI, body composition (via DXA), and biochemical markers (uric acid, WBC)
- Establish risk stratification protocol using these parameters
- Implement enhanced support mechanisms for high-risk participants
- Monitor early weight loss patterns, as rapid initial success may predict later disengagement
FAQ 2: Which intervention components most effectively sustain long-term engagement?
Evidence-Based Protocol: Prioritize supervised attendance, social support integration, and dietary-focused interventions. Meta-analytical evidence demonstrates that supervised attendance programs achieve 65% higher adherence rates than unsupervised interventions (RR 1.65) [5]. Programs incorporating social support mechanisms show 29% improved adherence (RR 1.29), while dietary-focused interventions maintain 27% better adherence than exercise-only programs (RR 1.27) [5].
Methodology:
- Implement regular supervised check-ins (weekly initially, transitioning to biweekly)
- Incorporate structured social support components (group sessions, peer matching)
- Focus intervention content on dietary modification rather than exclusive exercise emphasis
- Utilize digital tools for between-session monitoring and support
FAQ 3: What specific engagement metrics should researchers monitor to predict intervention success?
Evidence-Based Protocol: Track multidimensional engagement metrics including self-monitoring behaviors, educational engagement, and social interaction. Research on digital interventions identifies seven key metrics: (1) number of articles read, (2) meals logged, (3) steps recorded, (4) messages to coach, (5) exercise logged, (6) weigh-ins, and (7) days with at least one meal logged per week [57]. These metrics collectively provide a comprehensive engagement profile that predicts weight loss success.
Methodology:
- Implement automated tracking systems for specified engagement metrics
- Establish threshold values for each metric (e.g., ≥3 days with meal logging/week)
- Monitor patterns rather than absolute values (consistency over intensity)
- Create engagement dashboards for real-time participant monitoring
FAQ 4: How can researchers address the logistical barriers to engagement?
Evidence-Based Protocol: Optimize referral processes, initial assessments, and logistical support. Qualitative research reveals that referrer knowledge about program specifics significantly influences early engagement [59]. Participants value detailed information during referral that accurately shapes expectations. Additionally, the initial consultation experience serves as a critical motivational opportunity, with participants desiring person-centered assessments rather than perfunctory system-focused evaluations [59].
Methodology:
- Develop comprehensive referrer education materials detailing program specifics
- Implement personalized initial assessments exploring individual needs and preferences
- Offer flexible scheduling options accommodating work and family commitments
- Provide transportation support or telehealth alternatives for geographic barriers
Conceptual Framework for Engagement Sustainability
Research Reagent Solutions: Essential Methodological Components
Table 3: Core Methodological Components for Engagement Research
| Research Component | Function in Engagement Studies | Implementation Example |
|---|---|---|
| Digital Tracking Platforms | Enable real-time monitoring of engagement metrics | Mobile applications for meal logging, step counting, and educational content access [57] |
| Doubly Labeled Water Method | Quantifies metabolized energy intake to objectively measure dietary adherence | Validation of self-reported dietary intake in energy restriction studies [20] |
| Dual-Energy X-Ray Absorptiometry (DXA) | Measures body composition changes to correlate with engagement levels | Assessment of fat mass, fat-free mass, and visceral adipose tissue changes in response to intervention adherence [56] |
| Hierarchical Linear Modeling (HLM) | Statistical approach to model engagement patterns over time | Analysis of weight loss trajectories in relation to dietary tracking consistency [58] |
| Semi-Structured Interview Protocols | Qualitative assessment of engagement barriers and facilitators | Investigation of patient experiences with referral processes and initial consultations [59] |
Experimental Protocol: Measuring Engagement in Weight Loss Trials
Standardized Protocol for Multidimensional Engagement Assessment
Objective: To comprehensively measure and analyze participant engagement in dietary weight loss interventions across multiple dimensions and timepoints.
Materials:
- Digital or paper-based food tracking system (e.g., food journals, mobile apps)
- Self-monitoring tools (weighing scales, pedometers)
- Educational content delivery platform
- Communication channels for coach/practitioner interaction
- Data collection system for engagement metrics
Procedure:
- Baseline Assessment (Week 0)
- Collect demographic, anthropometric, and biochemical data
- Establish individual goals and preferences
- Provide training on self-monitoring procedures
Engagement Monitoring (Weekly)
- Track seven core metrics: articles read, meals logged, steps recorded, messages to coach, exercise logged, weigh-ins, and days with ≥1 meal logged [57]
- Implement consistency thresholds: <33% days = rare tracker; 33-66% = inconsistent tracker; >66% = consistent tracker [58]
- Monitor engagement patterns rather than isolated data points
Data Analysis
- Employ Hierarchical Linear Modeling to account for individual trajectories
- Correlate engagement metrics with weight loss outcomes
- Identify predictive factors for disengagement
- Conduct qualitative analysis of withdrawal reasons
Intervention Adjustment
- Implement tailored support based on engagement patterns
- Address identified barriers through protocol modifications
- Enhance successful engagement strategies
Validation Measures:
- Objective adherence validation through doubly labeled water method where feasible [20]
- Correlation of self-reported metrics with physiological outcomes
- Comparison of engagement patterns across participant subgroups
This comprehensive approach enables researchers to systematically address the universal challenge of declining engagement, enhancing both the scientific rigor of weight management research and the practical effectiveness of dietary interventions.
Adaptive Interventions for Early Non-Responders
Diagnostic Criteria and Early Identification
What are the defining criteria for an "Early Non-Responder" in a weight loss intervention? An "Early Non-Responder" is typically defined as an individual who fails to lose a specific threshold amount of weight during the initial 1 to 2 months of a behavioral weight loss program [60]. The specific thresholds used in research vary, commonly ranging from 0.5% to 3% of initial body weight [60]. On average, this classification applies to about one-quarter to one-third of participants in a standard program [60]. Failure to meet these early benchmarks is significant, as these individuals are 3 to 11 times less likely to achieve a clinically significant weight loss (typically ≥5% of body weight) long-term [60].
Table 1: Common Early Non-Response Criteria and Associated Long-Term Outcomes
| Early Time Point | Weight Loss Threshold | Likelihood of Achieving Clinically Significant WL | Proportion of Participants |
|---|---|---|---|
| 1-2 Months | < 0.5% - 3% of initial body weight | 3 to 11 times less likely [60] | ~25-33% (Early Non-Responders) [60] |
| 1-2 Months | ≥ 0.5% - 3% of initial body weight | Significantly more likely | ~67-75% (Early Responders) |
What is the evidence that early weight loss predicts long-term success? Secondary analyses of multiple weight loss trials have consistently shown that the amount of weight lost within the first few months of treatment is a strong predictor of post-treatment and longer-term weight loss outcomes [60]. This relationship has been observed across different types of interventions (individual, group-based, internet-delivered) and in populations both with and without type 2 diabetes [60]. For example, data from the Look AHEAD trial demonstrated that an individual's weight change trajectory at 1 month was predictive of their weight loss at 1, 4, and even 8 years [60].
Intervention Protocols and Rescue Strategies
What is an Adaptive Intervention (AI) and how can it rescue early non-responders? An Adaptive Intervention (AI) is a sequence of pre-specified decision rules that guide how to alter the type, dosage, or delivery of treatment over time based on an individual's evolving needs and response status [61]. In the context of weight loss, an AI provides a methodological framework to "rescue" early non-responders by intensifying or changing their treatment. This approach allows all participants to start with a standard, often less intensive intervention, with additional resources being reserved for and directed toward those who show a poor initial response [60] [61].
What are Stepped-Care approaches, a specific type of Adaptive Intervention? Stepped-care is a specific type of adaptive intervention where all participants begin with a low-intensity, first-line treatment [60]. At a pre-defined decision point (e.g., after 1 month), each participant's response is evaluated against a pre-set criterion (e.g., ≥5 lbs weight loss). Those who meet or exceed the criterion (responders) continue with the initial treatment. Those who do not meet the criterion (non-responders) are "stepped up" to a more intensive, supplemental, or alternative treatment [60] [61]. This strategy helps to allocate costly resources more efficiently.
Figure 1: A Stepped-Care Adaptive Intervention Workflow for Weight Loss.
What critical questions must be addressed when designing an Adaptive Intervention? Researchers must answer several key questions when developing an AI [61]:
- Timing: When is the optimal time to define non-response and intervene? (e.g., 5 weeks vs. 10 weeks)
- Treatment Option: For non-responders, what is the best subsequent treatment? (e.g., augmenting vs. switching the initial intervention)
- Tailoring Variables: Should the initial treatment or the rescue strategy be individualized based on baseline patient characteristics (e.g., comorbidities, emotional eating history)?
- Decision Rules: What specific metrics (e.g., weight loss, adherence data) and thresholds best differentiate responders from non-responders?
Methodological Toolkit and Experimental Design
What is a Sequential Multiple Assignment Randomized Trial (SMART)? A Sequential Multiple Assignment Randomized Trial (SMART) is a special type of experimental design developed explicitly for building optimal adaptive interventions [61]. In a SMART, participants are randomly assigned to different treatment options at multiple decision stages over time, mimicking the clinical decision-making process in an AI. This design allows researchers to compare different adaptation rules (e.g., "When to intervene?" and "What to offer non-responders?") within a single trial, providing rigorous data to inform the decision rules in an AI [61].
Figure 2: A Generic SMART Design for Optimizing an Adaptive Intervention.
Table 2: The Scientist's Toolkit: Key Components of a SMART for Weight Loss
| Component | Function & Role in Intervention Development | Example from Weight Loss Research |
|---|---|---|
| Decision Stages | Timepoints in the trial where a decision about treatment is made. | Stage 1: Start of intervention. Stage 2: After 5 weeks of initial treatment. |
| Treatment Options | The different types, dosages, or delivery modes of intervention available at each stage. | Option A: Individual Behavioral Therapy (IBT). Option B: IBT + Meal Replacements. |
| Tailoring Variables | Measured variables used to individualize treatment at a decision point. Can be baseline or intermediate. | Intermediate: Early weight loss (e.g., <5 lbs at 5 weeks). Baseline: History of emotional eating. |
| Decision Rule | The formalized rule linking tailoring variables to treatment options. | "IF weight loss <5 lbs at Week 5, THEN augment IBT with Meal Replacements." |
Troubleshooting Guide: Common Scenarios in Adaptive Intervention Research
Scenario: High participant attrition after being identified as an early non-responder.
- Problem: Participants who are labeled "non-responders" may become discouraged and drop out.
- Solution: Frame the step-up in treatment positively as a "personalized adjustment" rather than a failure. Implement proactive motivational support from interventionists at the time of re-assessment. The protocol should emphasize that non-response is common and that the new treatment is specifically chosen to help them overcome their initial challenges [60].
Scenario: Uncertainty in defining the optimal early weight loss threshold.
- Problem: The literature uses a range of thresholds (0.5%-3%), making it difficult to select one for a specific study.
- Solution: Conduct a pilot study or analyze existing data to establish a threshold that best predicts poor long-term outcomes in your target population. Consider using multiple metrics, such as combining a weight loss threshold (e.g., <2%) with adherence data (e.g., <80% self-monitoring completion) to define non-response more robustly [60].
Scenario: The "rescue" intervention for non-responders is not effective.
- Problem: The supplemental treatment provided to non-responders fails to re-engage them and initiate weight loss.
- Solution: Use a SMART design to empirically test different rescue strategies (e.g., augmenting vs. switching treatments) before launching a large-scale trial. Ensure the rescue intervention addresses potential barriers that caused initial non-response, such as poor adherence, lack of satiety, or unmet psychological needs [61].
Scenario: How to handle participants with poor adherence in the initial phase?
- Problem: It is unclear whether early non-response is due to the intervention's inefficacy or the participant's non-adherence.
- Solution: Define non-response criteria that incorporate both weight loss and adherence metrics. For participants with very poor adherence, consider a separate decision rule that addresses adherence barriers (e.g., additional counseling, simplifying self-monitoring) before changing the core dietary intervention [60].
Troubleshooting Guide: Resolving Common mHealth Adherence Challenges
This guide addresses frequent challenges researchers encounter when designing feedback mechanisms for dietary weight loss interventions.
Problem 1: Decline in User Self-Reporting Adherence Over Time
- Symptom: User engagement with diet tracking features drops significantly after the initial weeks of a study.
- Explanation: User motivation can wane over time, leading to incomplete dietary data, a phenomenon known as "missing events" [62].
- Solution:
- Implement Cue-Based Prompting: Introduce fixed reminders to record meals. One study using two fixed reminders saw a higher rate of logged meals compared to versions with one or no reminders [62].
- Allow for Addendums: Enable users to log meals after the eating event has occurred. This accommodates situations where immediate logging is inconvenient [62].
- Incorporate Gamification: A comparative study of two app versions found that the one with gamification features achieved significantly higher user adherence and a superior System Usability Scale score (80.67, ranked A) than the version without it [63].
Problem 2: User Failure to Personalize Generic Feedback
- Symptom: Users ignore or disengage with automated feedback messages, rendering them ineffective.
- Explanation: Generic feedback does not account for individual user preferences, progress, or context, leading to reduced perceived relevance and impact [64].
- Solution:
- Deploy Recommender Systems (RS): Use software tools that leverage machine learning to offer personalized suggestions based on past user preferences and behaviors [64].
- Ground Design in Behavioral Theory: Incorporate constructs from established theories like Social Cognitive Theory (SCT), such as self-monitoring, goal-setting, and building self-efficacy, to make feedback more impactful [64] [65].
- Utilize a "Toolbox" Strategy: Develop a range of personalized treatment recommendations based on objective user data (e.g., weight change, dietary logs) to guide and maintain behavior change [65].
Problem 3: Low Engagement with Dietary Logging Interface
- Symptom: Users find the process of inputting dietary data burdensome, resulting in poor data quality or drop-out.
- Explanation: High data-entry burden and poor user experience are key barriers to sustained app engagement [64] [62].
- Solution:
- Diversify Input Methods: Instead of relying solely on text, allow for photo, voice, or video inputs of diet information to reduce effort [66].
- Optimize System Usability: Ensure the app interface is intuitive. High usability scores are correlated with better adherence [63].
- Integrate Automated Sensors: Use Bluetooth-enabled devices (e.g., smart scales, activity trackers) to automatically collect objective data like body weight and physical activity, reducing the manual reporting burden on users [63] [65].
Frequently Asked Questions (FAQs) for Researchers
Q1: What is the optimal timing for delivering feedback in a dietary mHealth intervention? Feedback should be as temporally contiguous to the user's action as possible. Learning theory suggests that timely feedback based on objective data results in superior behavior change [65]. For example, the SmartLoss platform utilizes remote devices to collect body weight and exercise information "in near real time to facilitate timely behavior change" [65].
Q2: Which behavior change techniques (BCTs) are most effective for improving adherence in dietary apps? Evidence supports a combination of BCTs. A scoping review of mobile-based dietary interventions found that while all included studies used self-monitoring, other effective techniques included personalized feedback, gamification, goal reviews, and social support [66]. The integration of gamification with other BCTs has been shown to specifically boost adherence for self-reporting lifestyle data [63].
Q3: How can we accurately measure adherence to the mHealth intervention itself? Adherence is multi-faceted and should be measured beyond just study drop-out. Key metrics include [62]:
- Momentary Adherence: Compare the number of user-reported eating events to normative expected events (e.g., 3-4 episodes per day).
- Logging Trajectories: Analyze the stability of recorded events over the study duration to identify declines.
- Self-Reported Missing Events: Use interviews or daily questionnaires to ask users directly about missed logs and their reasons.
Q4: What are the primary reasons users fail to log their meals? Common reasons are competing activities and technical issues, whereas situational barriers are less frequently reported [62]. This highlights the importance of a low-burden, technically robust logging process.
Experimental Protocols for Key Cited Studies
Protocol 1: Evaluating the Impact of Gamification on Adherence This methodology is derived from a study that quantified the effect of adding gamification to an mHealth app [63].
- Participant Recruitment: Recruit two groups of users without specific health conditions.
- App Development: Develop two versions of an mHealth app.
- Version A: Includes common BCT categories (e.g., self-monitoring, feedback, goal setting).
- Version B: Includes all features of Version A, plus gamification features (e.g., rewards, badges, challenges).
- Intervention: Assign one user group to Version A and the other to Version B for a set period (e.g., 1-2 months).
- Data Collection: Collect the following metrics:
- Primary Outcome: Adherence, defined as the "percentage of days active".
- Secondary Outcomes: System Usability Scale (SUS) score; user expectations and feedback.
- Analysis: Compare adherence rates and SUS scores between the two groups to isolate the effect of gamification.
Protocol 2: Assessing "Missing Events" in Mobile Dietary Assessments This protocol uses a synopsis of three indicators to approximate the rate of missing eating events [62].
- Study Design: Conduct an event-based Ecological Momentary Assessment (EMA) study over multiple days (e.g., 8 days).
- App Features: Equip the mobile diet app with features like fixed reminders, an addendum function (for logging after the fact), and an option to report skipped meals.
- Data Collection and Analysis:
- Normative Comparison: Calculate the ratio of reported eating events to the socially normative expected number (e.g., 3 meals + 1 snack per day).
- Logging Trajectory: Use multilevel models to analyze the logging rate of meals and snacks over time to identify significant declines.
- Recalled Missing Events: Conduct semi-structured interviews or daily questionnaires to ask participants how many events they missed and why.
- Synthesis: Triangulate the results from all three indicators to get a comprehensive view of adherence and its drivers.
Visualization of mHealth Feedback Optimization
The diagram below illustrates the logical workflow for optimizing feedback in an mHealth intervention to improve dietary adherence.
Adherence Optimization Workflow
Research Reagent Solutions: Essential mHealth Tools
The table below catalogs key tools and methodologies used in advanced mHealth research for dietary interventions.
| Item Name | Function in Research | Example Application |
|---|---|---|
| Event-Based EMA | A research method where participants initiate a report each time a predefined event (e.g., an eating event) occurs [62]. | Used to capture dietary intake in real-time, reducing memory bias associated with retrospective recalls [62]. |
| Bluetooth-Enabled Sensors | Peripheral devices (e.g., smart scales, activity trackers) that automatically and wirelessly transmit objective data to the mHealth app [63] [65]. | Automates collection of body weight and physical activity data, reducing user burden and improving data accuracy [65]. |
| Recommender Systems (RS) | Software tools using machine learning to provide users with personalized recommendations based on their past preferences and behaviors [64]. | Used in weight management apps to suggest personalized foods or exercises, enhancing user engagement and decision-making [64]. |
| System Usability Scale (SUS) | A standardized, reliable tool for measuring the perceived usability of a system or application [63]. | Provides a quantitative score to compare the usability of different app versions (e.g., with/without gamification) [63]. |
| Behavior Change Techniques (BCTs) | A consolidated taxonomy of theory-based interventions for changing behavior. Common categories include self-monitoring, feedback, and goals and planning [66] [63]. | Serves as a "building block" for designing the active components of an mHealth intervention to promote dietary change [63]. |
Nutritional Strategies to Mitigate Side Effects of Pharmacotherapy
Troubleshooting Guides
Guide 1: Addressing Severe Caloric Restriction and Malnutrition Risk
Problem: Patients on GLP-1 receptor agonists or dual GIP/GLP-1 receptor agonists are experiencing severe caloric restriction (<800 kcal/day), leading to fatigue, nutrient deficiencies, and potential treatment discontinuation.
Root Cause: Excessive appetite suppression from pharmacotherapy mechanism of action, particularly during initial titration phase, sometimes exacerbated by gastrointestinal side effects.
Solutions:
- Implement structured meal timing: Recommend 5-6 small, nutrient-dense meals throughout the day rather than 3 large meals
- Enhance dietary energy density: Add healthy fats (avocado, olive oil, nuts) and lean proteins to meals without increasing volume
- Monitor nutritional biomarkers: Track micronutrient levels (iron, B12, vitamin D) regularly to identify deficiencies early
- Use oral nutritional supplements: Provide high-protein, high-calorie supplements between meals to boost intake without affecting satiety
Expected Outcome: Improved caloric intake to >1200 kcal/day, reduced fatigue, maintained treatment adherence, and prevention of nutrient deficiencies.
Guide 2: Managing Lean Body Mass Loss
Problem: Significant loss of lean body mass (up to 45% of total weight loss in some trials) during obesity pharmacotherapy, increasing risk of sarcopenia and metabolic slowdown.
Root Cause: Rapid weight loss without adequate protein intake or resistance exercise stimulus to preserve muscle mass.
Solutions:
- Increase protein intake: Target 1.0-1.5 g/kg of ideal body weight per day, distributed evenly across meals
- Implement timed protein supplementation: Provide 15-30g high-quality protein (whey, casein, or plant-based) within 30 minutes of resistance exercise
- Incorporate resistance training: Prescribe progressive resistance exercise 2-3 times per week targeting major muscle groups
- Consider branched-chain amino acids: Supplement with leucine-rich sources to stimulate muscle protein synthesis
Expected Outcome: Improved ratio of fat mass to lean mass loss (targeting >75% fat mass loss), maintained metabolic rate, and preserved physical function.
Guide 3: Counteracting Gastrointestinal Side Effects
Problem: Nausea, vomiting, diarrhea, or constipation interfering with dietary intake and medication adherence.
Root Cause: Delayed gastric emptying and altered gastrointestinal motility from GLP-1 receptor activation.
Solutions:
- Modify food texture: Offer soft, moist, easy-to-digest foods (smoothies, soups, stews) during symptomatic periods
- Adjust meal composition: Reduce high-fat, spicy, and high-fiber foods during acute symptoms
- Implement hydration strategies: Encourage small, frequent sips of water, electrolyte solutions, or ginger tea
- Time medication with food: Administer pharmacotherapy with small meals to reduce gastrointestinal irritation
Expected Outcome: Reduced gastrointestinal symptoms, improved dietary tolerance, and maintained pharmacotherapy adherence.
Frequently Asked Questions
Q1: What are the most critical nutritional deficiencies to monitor during obesity pharmacotherapy?
The highest risk deficiencies include protein, iron, B vitamins, vitamin D, calcium, and zinc. Regular monitoring of serum biomarkers every 3-6 months is recommended, with more frequent assessment in high-risk populations (older adults, those with pre-existing deficiencies, or individuals with pronounced appetite suppression). Proactive supplementation should be considered based on baseline status and dietary intake patterns [67].
Q2: How can dietary strategies help mitigate the loss of lean body mass observed with GLP-1 receptor agonists?
Strategic protein timing is essential—distributing 25-30g of high-quality protein across 3-4 meals daily appears most effective for stimulating muscle protein synthesis. Combining this protein distribution with progressive resistance exercise 2-3 times per week provides the synergistic stimulus needed to preserve lean mass. Essential amino acid supplementation, particularly leucine, may provide additional benefit for older adults or those with low baseline muscle mass [67].
Q3: What dietary approaches improve long-term adherence to weight loss medications?
Evidence supports several key strategies: implementing structured meal plans to reduce decision fatigue, using portion-controlled foods during initial treatment phases, incorporating regular self-monitoring through food logging, and providing ongoing nutritional counseling. Digital tools that provide feedback on dietary patterns can enhance adherence, though content relevance and delivery timing must be optimized for sustained engagement [1].
Q4: Are there specific dietary patterns that enhance the efficacy of obesity pharmacotherapy?
Emerging research suggests minimally processed diets following healthy dietary guidelines (like the UK Eatwell Guide) may enhance weight loss outcomes compared to ultra-processed diets, even with similar macronutrient profiles. The UPDATE trial found significantly greater weight loss (-2.06% vs -1.05%) and fat mass reduction on a minimally processed diet following the same dietary guidelines as the ultra-processed comparator diet [68].
Q5: How does cognitive-behavioral therapy complement nutritional strategies during pharmacotherapy?
CBT addresses weight self-stigma and maladaptive eating behaviors that impair dietary adherence. Group-based CBT specifically has shown promise in reducing internalized weight stigma and improving eating self-efficacy, which may enhance adherence to prescribed nutritional interventions. This psychological support is particularly valuable for populations disproportionately affected by weight stigma [69].
Table 1: Body Composition Changes in Obesity Pharmacotherapy Trials
| Trial | Medication | Total Weight Loss | Lean Mass Loss | % of Total as Lean Mass |
|---|---|---|---|---|
| STEP 1 [67] | Semaglutide 2.4 mg | -15.3 kg (-14.9%) | -6.9 kg (-13.2%) | 45.1% |
| SURMOUNT-1 [67] | Tirzepatide | -22.5% | Not reported | 25.7% |
| SUSTAIN-8 [67] | Semaglutide | -5.3 kg (-6.0%) | -2.3 kg (-4.5%) | 43.4% |
Table 2: Dietary Intervention Effects on Body Composition (UPDATE Trial) [68]
| Outcome Measure | Minimally Processed Diet | Ultra-Processed Diet | Between-Diet Difference | P-value |
|---|---|---|---|---|
| Weight Change (%) | -2.06% | -1.05% | -1.01% | 0.024 |
| Fat Mass Change (kg) | -1.69 kg | -0.71 kg | -0.98 kg | 0.004 |
| Body Fat Percentage | -1.24% | -0.48% | -0.76% | 0.010 |
| Visceral Fat Rating | -0.68 | -0.27 | -0.41 | 0.008 |
Table 3: Adherence Predictors of Weight Loss Success [1]
| Adherence Measure | Odds Ratio for ≥5% Weight Loss | Statistical Significance |
|---|---|---|
| Diet Self-Monitoring | 2.34 | P<0.001 |
| Physical Activity Self-Monitoring | 1.87 | P<0.01 |
| Weight Self-Monitoring | 2.15 | P<0.001 |
| Calorie Goal Adherence | 2.42 | P<0.001 |
| Physical Activity Goal Adherence | 1.92 | P<0.01 |
Experimental Protocols
Protocol 1: Nutritional Assessment and Monitoring Framework for Pharmacotherapy Trials
Purpose: To systematically evaluate nutritional status, body composition changes, and dietary adherence during obesity pharmacotherapy studies.
Materials:
- Dual-energy X-ray absorptiometry (DXA) scanner for body composition
- Standardized food diary application or platform
- Bioelectrical impedance analysis (BIA) device
- Blood collection equipment for nutritional biomarkers
- Validated food frequency questionnaire
Methodology:
- Baseline Assessment (Week 0):
- Conduct DXA scan for fat mass, lean mass, and bone density
- Collect fasting blood for nutritional biomarkers (iron studies, B12, folate, 25-OH vitamin D, calcium, zinc)
- Administer 3-day weighed food record or digital food diary
- Complete BIA measurement as rapid assessment tool
Interim Monitoring (Weeks 4, 12, 24):
- Repeat BIA measurements for body composition trends
- Analyze 24-hour dietary recalls for macronutrient and micronutrient intake
- Assess gastrointestinal side effects using validated scale (e.g., GSRS)
- Evaluate protein intake specifically using food diary data
Endpoint Assessment (Week 52):
- Repeat all baseline measurements (DXA, nutritional biomarkers, comprehensive dietary assessment)
- Calculate lean mass to fat mass loss ratio
- Identify participants with >30% lean mass loss for targeted interventions
Quality Control: Standardize DXA calibration procedures, train staff in dietary assessment methods, implement data validation checks for food records.
Protocol 2: Integrated CBT and Nutritional Support Intervention
Purpose: To evaluate the combined effect of cognitive-behavioral therapy and structured nutritional support on dietary adherence during obesity pharmacotherapy.
Materials:
- CBT manual for weight self-stigma reduction
- Standardized nutritional counseling materials
- Weight Self-Stigma Questionnaire (WSSQ)
- Digital food monitoring platform
- Body composition tracking tools
Methodology:
- Screening and Recruitment (Week -2):
- Identify participants with obesity (BMI 30-40 kg/m²) and elevated weight self-stigma (WSSQ ≥36)
- Obtain informed consent and baseline measurements
Randomization (Week 0):
- Assign to intervention (CBT + nutritional support) or control (nutritional support only) using computer-generated randomization sequence
- Stratify by baseline BMI category and weight self-stigma score
Intervention Phase (Weeks 1-12):
- Experimental Group: Receive 12 weekly 90-minute group CBT sessions plus individualized nutritional counseling
- Control Group: Receive individualized nutritional counseling only
- Both groups: Receive standard obesity pharmacotherapy per protocol
Assessment Points (Weeks 0, 4, 8, 12):
- Evaluate dietary adherence through body composition changes (avoiding self-report bias)
- Administer psychological assessments (WSSQ, Weight Bias Internalization Scale, General Health Questionnaire)
- Measure anthropometric indices (weight, BMI, body composition)
Outcome Measures: Primary: Dietary adherence measured by body composition changes; Secondary: Weight self-stigma scores, anthropometric changes, treatment retention rates.
Visualizations
Nutrient-Pharmacotherapy Interaction Pathways
Dietary Adherence Support Framework
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Research Reagent Solutions for Nutritional Pharmacotherapy Studies
| Reagent/Material | Function/Application | Example Use Cases |
|---|---|---|
| Dual-energy X-ray Absorptiometry (DXA) | Gold-standard body composition analysis | Quantifying lean mass vs fat mass changes in pharmacotherapy trials |
| Bioelectrical Impedance Analysis (BIA) | Rapid body composition assessment | Frequent monitoring of fluid balance and body composition trends |
| Digital Food Diary Platforms | Real-time dietary intake assessment | Tracking macronutrient/micronutrient intake and adherence patterns |
| Validated Psychological Questionnaires | Weight stigma and mental health assessment | Measuring WSSQ, Weight Bias Internalization Scale, eating behavior |
| Standardized Oral Nutritional Supplements | Controlled nutritional supplementation | Providing consistent protein/calorie supplementation between meals |
| Wearable Activity Monitors | Physical activity quantification | Objective measurement of activity levels and energy expenditure |
| Point-of-Care Biomarker Testing | Rapid nutritional status assessment | Quick assessment of iron, vitamin D, B12 status during study visits |
| Cognitive-Behavioral Therapy Manuals | Standardized psychological intervention | Implementing reproducible CBT protocols for weight stigma reduction |
Core Concepts & Quantitative Evidence
The preservation of lean mass during weight loss is critical, as its loss can compromise metabolic health and physical function. The following table summarizes the key quantitative findings on the role of protein intake in muscle mass maintenance.
Table 1: Protein Intake Recommendations for Muscle Mass Preservation
| Population | Recommended Protein Intake | Key Effect on Muscle Mass | Key Effect on Muscle Strength/Function | Primary Source |
|---|---|---|---|---|
| Adults with Overweight/Obesity during Weight Loss | >1.3 g/kg/day | Significantly prevents decline [70]. | No significant preventive effect on strength or physical function [70]. | Systematic Review & Meta-analysis [70] |
| <1.0 g/kg/day | Higher risk of decline [70]. | |||
| Physically Active Individuals & Athletes | 1.4 - 2.0 g/kg/day | Sufficient for building/maintaining muscle mass [71]. | Mixed effects on maximal strength; context-dependent [71]. | ISSN Position Stand [71] |
| Elderly Females with Sarcopenia | 1.2 g/kg/day | Significant improvement in muscle mass composition vs. 0.8 g/kg/day [72]. | Improved handgrip strength and knee flexion [72]. | Randomized Controlled Trial [72] |
Detailed Experimental Protocols
Protocol 1: Evaluating Protein Intake in Elderly Females with Sarcopenia
This 12-week RCT provides a model for investigating the impact of varying protein doses on muscle mass composition in a clinical population [72].
- 1. Participant Recruitment:
- Population: Elderly females (e.g., 60-75 years).
- Condition: Sarcopenia, diagnosed per criteria from the Asian Working Group for Sarcopenia (AWGS): handgrip strength <18 kg, low knee flexion strength, and low muscle cross-sectional area [72].
- Exclusion Criteria: Kidney disease, autoimmune disorders affecting muscles [72].
- 2. Study Design & Intervention:
- Randomization: Participants are randomly assigned to groups using a computer-generated sequence with concealed allocation [72].
- Control Group (NP): Normal protein diet (0.8 g/kg body weight/day).
- Intervention Group (MHP): Moderately high protein diet (1.2 g/kg body weight/day).
- Diet Structure: Both groups follow an energy-restricted diet (e.g., 1,800 kcal/day). Fat intake is kept constant, while carbohydrate intake is adjusted to accommodate the higher protein percentage in the MHP group [72].
- Blinding: A single-blind design is used where participants are unaware of their group assignment [72].
- 3. Outcome Measures (Baseline & 12-weeks):
- Anthropometrics: Body mass, BMI, waist circumference, fat mass (via Bioelectrical Impedance Analysis) [72].
- Muscle Function:
- Muscle Composition:
- Magnetic Resonance Imaging (MRI): Using a 3T scanner to obtain cross-sectional images of thigh and calf muscles. Analyze for Muscle Cross-Sectional Area (MCSA) and fat infiltration [72].
- 4. Adherence Monitoring: Use 24-hour dietary recalls on different days to confirm adherence to the prescribed diet [72].
- 5. Statistical Analysis: Perform using SPSS. Use paired sample t-tests for within-group (baseline vs. post-intervention) and independent t-tests for between-group comparisons at a significance level of p < 0.05 [72].
Protocol 2: Investigating Combined Diet and Exercise Strategies
The ADAPT trial exemplifies a complex design to test sequential interventions for weight loss, which can be adapted to include lean mass outcomes [73].
- 1. Participant Recruitment: Adults with overweight/obesity (BMI ≥27) and prediabetes [73].
- 2. Adaptive Intervention Design (Sequential Multiple Assignment Randomized Trial - SMART):
- Stage 1 (All Participants): Randomize to one of two hypocaloric diets (e.g., Reduced-Carbohydrate vs. High-Carbohydrate) for 4 weeks [73].
- Stage 2 (For Non-Responders): Define "non-response" (e.g., <2.5% weight loss at week 4). Re-randomize non-responders to augment their diet with a second strategy, such as:
- Time-Restricted Eating (TRE)
- Structured Exercise Counseling [73].
- 3. Outcome Measures (Baseline, Week 4, Week 16):
- Primary: Body weight.
- Secondary: Glycemic control markers (fasting glucose, HbA1c), body composition (lean mass should be a key measure via DEXA).
- 4. Data Analysis: Compare outcomes between initial diet groups and between second-stage strategies among non-responders.
Troubleshooting Common Research Challenges
Table 2: Frequently Asked Questions (FAQ) for Researchers
| Question | Evidence-Based Insight & Solution |
|---|---|
| What is the minimum effective protein dose to prevent muscle loss during weight loss? | Evidence indicates that a protein intake below 1.0 g/kg/day is associated with a higher risk of muscle mass decline. The threshold for increasing muscle mass during weight loss is above 1.3 g/kg/day [70]. |
| Why does higher protein intake sometimes fail to improve muscle strength in trials? | Studies consistently show that while protein intake helps preserve muscle mass, it does not consistently improve muscle strength or physical function on its own [70] [74]. Strength gains are primarily driven by resistance training, which should be a core component of the intervention [74]. |
| How can we improve participant adherence to self-monitoring in digital weight loss studies? | Adherence to self-monitoring (diet, activity, weight) declines nonlinearly over time. Tailored feedback and intensive support can slow this decline. Higher adherence to self-monitoring is strongly associated with greater odds of achieving ≥5% weight loss [1]. Cognitive modeling suggests feedback and support enhance the "goal pursuit" mechanism for sustaining behavior [4]. |
| Is high protein intake safe for our study population? | For healthy, exercising individuals, intakes of 1.4-2.0 g/kg/day are safe and not detrimental to kidney function or bone metabolism [75] [71]. Caution is advised for individuals with pre-existing renal insufficiency [75]. |
| What are the emerging pharmacological strategies for preserving lean mass? | Preclinical research shows that GLP-1 receptor agonist-induced muscle loss may be mitigated by blocking specific ligands like GDF8 (myostatin) and activin A. This blockade can prevent muscle loss and even increase fat loss in obese animal models, presenting a potential future combination therapy [76]. |
The Scientist's Toolkit: Research Reagents & Materials
Table 3: Essential Materials for Body Composition and Muscle Function Research
| Item | Function in Research | Example Application / Note |
|---|---|---|
| Dual-Energy X-ray Absorptiometry (DEXA) | Gold standard for quantifying total body lean mass, fat mass, and bone mineral density non-invasively [77]. | Used to track changes in lean body mass (LBM) and appendicular lean mass (ALM) as primary outcomes in intervention studies [77]. |
| Magnetic Resonance Imaging (MRI) | Provides high-resolution, precise measurements of muscle cross-sectional area (MCSA) and fat infiltration within muscle (muscle quality) [72]. | Can be applied to specific muscle groups (e.g., thigh, calf) for detailed analysis of muscle composition changes [72]. |
| Bioelectrical Impairment Analysis (BIA) | Provides a rapid, portable, and low-cost estimate of body composition (body fat and lean mass) [72]. | Useful for large-scale studies or frequent monitoring where DEXA/MRI is impractical; though less accurate than DEXA [72]. |
| Hydraulic Hand Dynamometer | Objective measure of upper body muscle strength, a key indicator of overall muscle function and a diagnostic criterion for sarcopenia [72]. | Follow standardized protocols (e.g., 3 maximum squeezes with dominant hand, record highest value) [72]. |
| Isokinetic Dynamometer | Gold standard for measuring lower body muscle strength (e.g., knee flexion/extension) under controlled conditions [72] [77]. | Provides highly reliable data on peak torque and power, critical for assessing functional lower limb strength [77]. |
| High-Quality Protein Sources (Whey, Casein, Soy) | Used in supplementation studies to ensure consistent, quality protein intake. Rapidly digested proteins rich in essential amino acids (especially leucine) are most effective at stimulating Muscle Protein Synthesis (MPS) [71]. | Dose per serving should aim for 0.25 g/kg or 20-40 g of protein, containing 700-3000 mg of leucine for optimal MPS stimulation [71]. |
| Smart Scales & Activity Monitors | Enable passive, remote collection of weight and physical activity data, reducing participant burden and allowing for real-time feedback in mHealth interventions [1]. | Facilitates the study of adherence dynamics to self-monitoring behaviors, a key variable in intervention success [1] [4]. |
Visualizing Pathways and Workflows
Protein & Exercise Signaling for Muscle Synthesis
Adaptive Trial Design for Weight Loss
Evaluating Comparative Efficacy and Validating New Approaches
Quantitative Data on Adherence Rates and Health Impacts
The tables below summarize key quantitative findings from recent meta-analyses and studies on adherence rates and their consequences.
Table 1: Meta-Analysis Findings on Adherence and Mortality in Chronic Disease
| Health Condition | Adherence Level | Impact on All-Cause Mortality (Hazard Ratio, HR) | Impact on Cardiovascular Mortality (HR) | Source Meta-Analysis Details |
|---|---|---|---|---|
| Cardiovascular Diseases (CVDs) | Persistent Nonadherence | Significantly higher risk [78] | Significantly higher risk [78] | 9 cohorts, 226,203 patients, mean age 66.1, follow-up to 5 years [78] |
| Hypertension | Poor Adherence (<80%) | HR: 1.32 (1.14, 1.51), p<0.001 [79] | HR: 1.61 (1.43, 1.78), p<0.001 [79] | 12 cohort studies, 2,198,311 patients [79] |
Table 2: General Adherence Statistics and Consequences
| Category | Statistic | Details |
|---|---|---|
| General Adherence Rates | ~50% | Proportion of patients on chronic medications who adhere to treatment plans [80]. |
| Therapeutic Threshold | 80% | Minimum adherence level typically required for optimal therapeutic outcomes [80]. |
| Health Consequences | 125,000 | Estimated annual deaths in the U.S. linked to medication nonadherence [80] [81]. |
| 10%-25% | Proportion of U.S. hospital and nursing home admissions linked to nonadherence [81]. | |
| Financial Impact | $100-$300 billion | Potential annual U.S. healthcare cost savings from improved medication adherence [80]. |
Experimental Protocols for Adherence Research
This section outlines methodologies from key studies quantifying adherence.
Protocol: Meta-Analysis of Adherence Trajectories and Clinical Outcomes
This protocol is based on a 2025 systematic review and meta-analysis investigating how different adherence patterns over time affect patients with cardiovascular diseases (CVDs) [78].
- 1. Research Question & Registration: Define the association between medication adherence trajectories and clinical outcomes (e.g., mortality, MACE) in CVD patients. Pre-register the study protocol on a platform like PROSPERO (CRD42023456395) [78].
- 2. Search Strategy:
- Databases: Search Cochrane Library, PubMed, Embase, CINAHL, and Web of Science from inception to current date without language restrictions [78].
- Keywords: Combine terms for CVD (e.g., "Coronary Disease," "Acute Coronary Syndrome") with terms for adherence (e.g., "Medication Adherence," "Patient Compliance") and study design [78].
- 3. Study Selection:
- Inclusion Criteria: Longitudinal cohort studies in adult CVD patients (≥18 years) that report association between ≥2 adherence trajectories and clinical outcomes with a quantifiable relative risk measure [78].
- Exclusion Criteria: Studies with incomplete data, reviews, meta-analyses, and meeting abstracts [78].
- Process: Use dual-reviewer screening of titles/abstracts and full texts, with conflicts resolved by a third reviewer [78].
- 4. Data Extraction: Use a piloted, standardized form to extract data including author, year, country, sample size, cohort type, CVD type, mean age, adherence definition, follow-up duration, and outcome data (Hazard Ratios with confidence intervals) [78].
- 5. Risk of Bias Assessment: Assess quality of included cohort studies using the Newcastle-Ottawa Scale (NOS) [78].
- 6. Data Synthesis & Analysis:
- Statistical Analysis: Pool hazard ratios (HRs) and 95% confidence intervals (CIs) using random-effects models. Assess heterogeneity with the I² statistic [78].
- Adherence Measurement: The proportion of days covered (PDC) is a common metric. Group-based trajectory modeling (GBTM) is used to identify distinct longitudinal adherence patterns (e.g., persistent adherence, persistent nonadherence, gradual decline/increase) [78].
- Sensitivity Analysis: Perform leave-one-out analysis and meta-regression to test robustness and explore sources of heterogeneity [78].
Protocol: Digital Monitoring of Dietary Adherence in Behavioral Weight Loss
This protocol is based on digital health trials like the SMARTER study, which investigated adherence to self-monitoring (SM) of diet, physical activity, and weight [1] [4].
- 1. Study Design: A randomized controlled trial (RCT) comparing intervention groups (e.g., self-monitoring only vs. self-monitoring with personalized feedback) over a defined period (e.g., 12 months) [1].
- 2. Participants: Recruit adults meeting specific criteria (e.g., BMI 27-43 kg/m², willingness to improve lifestyle) [1].
- 3. Intervention Components:
- Digital Self-Monitoring Tools: Provide participants with:
- Behavioral Goals: Set individualized daily calorie, fat, and physical activity minute goals [1].
- Feedback Mechanism (Intervention Group): Develop a system to deliver tailored, automated feedback messages based on logged data, addressing calorie intake, nutrient balance, and progress toward goals [1].
- 4. Data Collection & Adherence Metrics:
- Calculate adherence percentages daily and average monthly [1].
- Diet SM Adherence: Defined as recording ≥50% of daily calorie goal in the app for a minimum number of days (e.g., ≥15 days/month) [1].
- Physical Activity SM Adherence: Defined as recording a minimum step count (e.g., ≥500 steps/day) [1].
- Weight SM Adherence: Defined as having daily weight data transmitted from the smart scale [1].
- Goal Adherence: Calculate the percentage of days adherent to calorie, fat, and activity goals out of days with valid self-monitoring data [1].
- 5. Outcome Measurement: The primary outcome is often percent weight loss from baseline. Association between adherence metrics and achieving clinically significant weight loss (e.g., ≥5%) is analyzed using statistical models like generalized linear mixed models [1].
Visual Workflow: Adherence Research Pathway
The diagram below outlines the core logical workflow for conducting research on dietary adherence.
Table 3: Essential Resources for Dietary Adherence Research
| Category / Item | Specific Examples & Functions | Key Considerations & Citations |
|---|---|---|
| Adherence Measurement Tools | ||
| Digital Food Logging App | Fitbit app, MyFitnessPal, custom apps. Function: Enables real-time dietary self-monitoring, key for calculating adherence. | High participant burden; requires clear instructions and technical support [1] [4]. |
| Activity & Weight Trackers | Wrist-worn activity tracker (e.g., Fitbit), Smart Scale. Function: Passively or semi-passively collects physical activity and weight data. | Can sync with apps to reduce manual entry and provide objective adherence measures [1]. |
| Adherence Questionnaires | Dietary Behavior Inventory-Surgery (DBI-S). Function: Validated instrument to measure adherence to post-surgical dietary guidelines efficiently. | Useful for longitudinal studies and conditions with specific dietary protocols [16]. |
| Pharmacy/Database Metrics | Proportion of Days Covered (PDC), Medication Possession Ratio (MPR). Function: Objective calculation of medication adherence from refill records. | Common in pharmaco-epidemiological studies; PDC ≥80% is a standard cutoff for "good" adherence [78] [79]. |
| Intervention Components | ||
| Tailored Feedback System | Automated, algorithm-driven messages based on user-logged data. Function: Provides personalized guidance to improve adherence and outcomes. | Message content, timing, and relevance are critical for effectiveness [1] [4]. |
| SIMPLE Framework | Mnemonic for adherence strategies: Simplifying regimens, Imparting knowledge, Modifying beliefs, Patient communication, Leaving bias, Evaluating adherence. | A conceptual framework for designing multi-component adherence interventions [81]. |
Frequently Asked Questions (FAQs) for Researchers
Q1: What is the minimum adherence level considered "good" for achieving therapeutic outcomes in chronic disease interventions?
- A: For many chronic conditions, including cardiovascular disease and hypertension, an adherence level of at least 80% is generally considered the threshold required to achieve the best possible therapeutic outcomes [80] [79]. This is often measured using metrics like the Proportion of Days Covered (PDC) [79].
Q2: Our digital weight-loss study shows a rapid decline in app usage for diet logging after the first few months. What strategies can improve sustained engagement?
- A: This is a common challenge. Evidence suggests that tailored, automated feedback based on user-logged data can help slow the decline in engagement compared to self-monitoring alone [1]. Furthermore, modeling studies indicate that combining this tailored feedback with intensive support (e.g., emotional social support) may lead to more sustained goal pursuit and behavioral practice over time [4]. The content, frequency, and timing of messages must be carefully designed to maintain relevance [1].
Q3: When analyzing adherence data, what are the advantages of using group-based trajectory modeling over simple average adherence?
- A: Traditional static measures (e.g., average adherence over a fixed period) fail to capture the dynamic nature of adherence behavior. Group-based trajectory modeling identifies distinct longitudinal patterns (e.g., "persistent adherence," "gradual decline," "persistent nonadherence") within a population [78]. This is crucial because these patterns have vastly different clinical impacts; for example, one meta-analysis found that "persistent nonadherence" was associated with a significantly higher risk of mortality and cardiovascular events compared to "persistent adherence," while "gradually declining adherence" showed an intermediate risk [78].
Q4: How significant is the impact of medication nonadherence on patient mortality and healthcare costs?
- A: The impact is substantial. Recent meta-analyses and reviews consistently show that poor adherence to medications for conditions like hypertension and CVD increases the risk of all-cause mortality by 32% and cardiovascular mortality by over 60% [79]. In the United States, medication nonadherence is a factor in approximately 125,000 deaths annually and is associated with up to 25% of all hospitalizations [80] [81]. The potential savings from improving adherence are estimated to be between $100-300 billion annually in healthcare costs [80].
Comparative Effectiveness of Dietary, Behavioral, and Pharmacological Strategies
The comparative effectiveness of weight-management strategies is fundamentally moderated by participant adherence. Across dietary, behavioral, and pharmacological interventions, suboptimal adherence remains a primary barrier to achieving clinically significant outcomes in research settings and clinical practice. This technical support resource synthesizes current evidence on strategies to improve adherence to dietary weight loss interventions, providing researchers with practical methodologies, troubleshooting guides, and analytical frameworks for designing robust clinical trials. The content focuses specifically on optimizing adherence measurement and intervention within the context of obesity research, addressing the critical gap between efficacy under ideal conditions and effectiveness in real-world applications.
Comparative Effectiveness Tables: Quantitative Outcomes Across Modalities
Table 1: Weight Loss Outcomes from Behavioral Interventions over 24 Months [82]
| Intervention Group | Mean Weight Change (kg) | % Achieving ≥5% Weight Loss | Key Intervention Components |
|---|---|---|---|
| Control (Self-Directed) | -0.8 kg | 18.8% | Brief advice only |
| Remote Support Only | -4.6 kg (P<0.001) | 38.2% | Telephone, email, and website support; motivational interviewing |
| In-Person Support | -5.1 kg (P<0.001) | 41.4% | Remote support plus face-to-face group and individual sessions |
Table 2: Key Characteristics of Featured Experimental Protocols [82] [83] [73]
| Trial Feature | Behavioral POWER Trial [82] | CBT for Weight Self-Stigma [83] | ADAPT Trial (SMART Design) [73] |
|---|---|---|---|
| Population | 415 adults, BMI 36.6, ≥1 CV risk factor | 120 adult women, BMI 30-40 | 83 adults, BMI ≥27, with prediabetes |
| Duration | 24 months | 12 weeks | 16 weeks |
| Experimental Groups | 1. Remote support2. In-person support3. Control | 1. CBT + diet2. Diet only | 1. HC diet → non-responders → TRE or Exercise2. RC diet → non-responders → TRE or Exercise |
| Primary Adherence/Outcome Measures | Weight change; % achieving ≥5% weight loss | Adherence assessed via FM/FFM changes; WSSQ scores | Weight loss; glycemic control markers |
Experimental Protocols: Detailed Methodologies
Objective: To determine the effectiveness of two behavioral weight-loss interventions—one with and one without in-person contact—in obese patients with at least one cardiovascular risk factor.
Population: 415 obese adults (mean age 54.0 years, 63.6% women, 41.0% black) with a mean BMI of 36.6, recruited from six primary care practices.
Intervention Components:
- Theoretical Framework: Social cognitive theory with behavioral self-management approaches.
- Coach Role: Used motivational interviewing techniques to help participants set weight-related goals, self-monitor behaviors, increase self-efficacy, and solve problems.
- Web-based Support: Study-specific website with learning modules, self-monitoring tools for weight, calorie intake, and exercise, and automated progress feedback.
- Contact Schedule:
- Months 1-3: Weekly contact (remote group: 12 calls; in-person group: 9 group sessions + 3 individual sessions).
- Months 4-6: Monthly contact (remote group: 1 call/month; in-person group: 3 sessions/month).
- Months 7-24: Remote group continued monthly calls; in-person group had two monthly contacts.
- Re-engagement Protocol: Automated email after 7-10 days without website login; telephone call after 14 days of inactivity.
Outcome Measures: Weight change from baseline at 24 months; percentage of participants losing ≥5% of initial body weight.
Objective: To assess the effectiveness of a group-based cognitive-behavioral therapy intervention in mitigating weight self-stigma and enhancing adherence to a weight-loss diet in adult women with obesity.
Population: 120 adult women with BMI between 30-40 kg/m², aged 18-50 years, with confirmed weight self-stigma (WSSQ score ≥36).
Intervention Design:
- Randomization: 1:1 allocation to either CBT plus personalized diet or diet-only control group.
- CBT Protocol: 12 weekly online group therapy sessions, each 1.5 hours duration.
- Assessment Points: Baseline, 4, 8, and 12 weeks.
- Adherence Measurement: Objectively assessed via changes in fat mass (FM) and fat-free mass (FFM) to avoid self-report bias.
- Secondary Measures: Weight Self-Stigma Questionnaire (WSSQ), Weight Bias Internalization Scale, General Health Questionnaire.
Objective: To investigate adaptive treatment strategies for weight loss in adults with overweight/obesity and prediabetes using a Sequential Multiple Assignment Randomized Trial (SMART) design.
Population: 83 adults with BMI ≥27 and prediabetes.
Adaptive Protocol:
- Stage 1 (Weeks 1-4): All participants randomized to either reduced carbohydrate (RC) or high carbohydrate (HC) calorie-restricted diet.
- Stage 2 (Weeks 5-16): Participants classified as "non-responders" (<2.5% weight loss at week 4) were re-randomized to augment their diet with either time-restricted eating (TRE) or exercise counseling.
- Outcome Measures: Weight loss at week 16; changes in fasting glucose, A1c, fasting insulin, and quantitative insulin sensitivity check index.
Conceptual Framework: Understanding Adherence Barriers
Troubleshooting Guides & FAQs
FAQ 1: How can we effectively address weight self-stigma that undermines dietary adherence in clinical trials?
Evidence-Based Solution: Implement group-based Cognitive Behavioral Therapy (CBT) specifically targeting weight self-stigma [83].
- Protocol Details: 12 weekly online group therapy sessions (1.5 hours each) focusing on identifying and restructuring faulty beliefs and thought patterns related to weight.
- Mechanism of Action: CBT helps participants internalize societal stereotypes about obesity less, reducing feelings of shame and unfavorable self-assessments that interfere with dietary adherence.
- Outcome Measures: Use validated Weight Self-Stigma Questionnaire (WSSQ) and Weight Bias Internalization Scale; assess adherence objectively through body composition changes (fat mass/fat-free mass) rather than self-report.
- Implementation Tip: Focus on women with obesity (BMI 30-40) who experience disproportionately higher rates of weight self-stigma.
FAQ 2: What intervention delivery methods optimize adherence while maintaining scientific rigor?
Evidence-Based Solution: Remote support interventions can achieve comparable outcomes to in-person delivery [82].
- Key Findings: Remote support (phone, email, website) achieved -4.6 kg weight loss vs. -5.1 kg for in-person support over 24 months, with no significant difference between groups.
- Critical Components:
- Regular motivational interviewing by trained coaches
- Self-monitoring tools with automated feedback
- Structured re-engagement protocols for participants with declining adherence
- Primary care provider reinforcement during routine visits
- Technical Specification: Implement automated email reminders after 7-10 days of website inactivity; personal telephone follow-up after 14 days of non-use.
FAQ 3: How should we structure information presentation to maximize participant understanding and implementation?
Evidence-Based Solution: Optimize information length and incorporate implementation intentions for participants with poorer planning skills [84].
- Experimental Evidence: Brief strategy explanations (mean adherence 74%) showed a small but consistent advantage over detailed explanations (mean adherence 69%).
- Implementation Intentions: Use "if-then" planning ("If situation X occurs, then I will do Y") particularly effective for participants with poorer planning skills.
- Practical Application:
- Present core strategy information concisely
- Incorporate planning exercises for all participants
- Assess planning skills at baseline for potential stratification
- Use brief, lay-friendly measures to reduce participant burden
Evidence-Based Solution: Implement Sequential Multiple Assignment Randomized Trial (SMART) designs with early non-responder identification [73].
- Protocol Specification: Assess initial weight loss at 4 weeks; define non-response as <2.5% weight loss.
- Adaptive Strategies: Augment initial dietary prescription with either time-restricted eating (TRE) or exercise counseling for non-responders.
- Critical Finding: Early non-responders achieved less weight loss despite augmented interventions, suggesting need for more intensive rescue strategies (e.g., meal provisions, supervised exercise).
- Design Consideration: Build adaptive interventions into trial structure with pre-specified decision rules for non-response.
FAQ 5: How can we enhance adherence to prescribed dietary patterns in free-living settings?
Evidence-Based Solution: Address key barriers identified through qualitative research on real-world implementation [85].
- Key Facilitators:
- Simplicity and versatility of dietary approach
- Non-obsessive, non-dieting mindset
- Supportive environment
- Common Barriers:
- Hunger and food cravings
- Conflicting social eating occasions
- Obsessive mindset during initial stages
- Participant-Driven Strategies:
- Build flexibility into dietary protocols
- Develop coping strategies for social situations
- Frame intervention as long-term lifestyle rather than short-term diet
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Assessments for Adherence Research
| Tool/Assessment | Function/Purpose | Example Application | Key References |
|---|---|---|---|
| Weight Self-Stigma Questionnaire (WSSQ) | Measures internalized weight bias and self-stigma | Identify participants with high stigma for targeted CBT intervention | [83] |
| COM-B Model Framework | Identifies Capability, Opportunity, and Motivation barriers | Qualitative analysis of adherence challenges; intervention design | [85] |
| Implementation Intention Protocols | "If-then" planning to bridge intention-behavior gap | Improve adherence in participants with poor planning skills | [84] |
| Automated Re-engagement Algorithms | Systematic protocol for re-engaging participants | Email after 7-10 days inactivity; call after 14 days | [82] |
| Sequential Multiple Assignment Randomized Trial (SMART) | Adaptive trial design for non-responders | Rescue strategies for participants failing initial intervention | [73] |
| Body Composition Analysis (FM/FFM) | Objective adherence assessment | Avoid self-report bias in dietary adherence measurement | [83] |
| Motivational Interviewing Protocols | Patient-centered counseling technique | Coach-participant interactions to enhance motivation | [82] [86] |
Adaptive Intervention Workflow
Core Concepts: Cognitive Modeling & Prognostics for Self-Monitoring
This section clarifies the fundamental concepts that form the basis of validating digital tools for dietary interventions.
What is cognitive modeling in the context of dietary self-monitoring? Cognitive modeling involves using computational simulations to represent the mental processes that underpin human behavior. In dietary interventions, these models help explain and predict how participants manage their food intake by simulating cognitive mechanisms like goal pursuit and habit formation [87]. For example, the Adaptive Control of Thought-Rational (ACT-R) architecture is a neurocognitive architecture that can dynamically model a participant's adherence to self-monitoring of dietary behaviors over time [87].
What are prognostic models for self-monitoring adherence? Prognostic models are tools designed to forecast future outcomes. In this field, they predict a participant's likelihood of adhering to self-monitoring protocols, such as logging their food intake. The ultimate goal is to develop models that can self-monitor their own predictive performance and auto-update when their accuracy drifts, ensuring they remain valid across different participant groups and time periods [88]. This is crucial for providing timely and accurate support.
Why is validation important for these models? Validation ensures that a cognitive or prognostic model is accurate, reliable, and useful in real-world settings. Without proper validation, there is a risk that the model's predictions will be misleading, which could compromise the effectiveness of a dietary intervention and the validity of the research findings [88]. Key performance aspects to validate include:
- Discrimination: The model's ability to distinguish between adherent and non-adherent participants.
- Calibration: The agreement between the model's predicted probabilities of adherence and the observed adherence rates.
Implementation Guide: Protocols & Reagents
This section provides detailed methodologies for key experiments and lists essential "research reagents" for the field.
Experimental Protocol: Modeling Adherence with ACT-R
This protocol outlines the steps for developing a cognitive model to forecast adherence to dietary self-monitoring [87].
- Data Collection and Preparation: Gather fine-grained self-monitoring data (e.g., daily food log entries) from a digital behavioral weight loss program. Participant data should include assignment to different intervention groups (e.g., self-management, tailored feedback, intensive support).
- Define Model Parameters: Within the ACT-R framework, operationalize the cognitive mechanisms. This involves defining the "activation" of memory chunks (influenced by the frequency and recency of self-monitoring) and the "utility" of production rules (which are updated based on rewards from executing self-monitoring actions) [87].
- Model Training: Use the collected data to train the ACT-R model, allowing it to learn the utility of different behaviors based on the sequence of self-monitoring actions.
- Model Performance Evaluation: Validate the model by comparing its predictions against actual adherence data. Calculate error metrics such as Root Mean Square Error (RMSE) to quantify performance. For example, an RMSE of 0.084-0.099 across different intervention groups indicates a good fit [87].
- Mechanism Visualization and Analysis: Analyze the model to visualize the relative contribution of cognitive mechanisms like goal pursuit and habit formation over the intervention period. This helps explain why adherence changes.
Experimental Protocol: Establishing an Auto-Updating Prognostic Model
This protocol describes how to create a prognostic model that maintains its accuracy over time through automatic updates [88].
- Initial Model Development: Train an initial prognostic model (e.g., using logistic regression or a gradient-boosted decision tree algorithm) on a development cohort of patient data. Identify key predictors of the outcome (e.g., 28-day survival, adherence behavior).
- Prospective Performance Monitoring: Continuously run the model on new, incoming data (a prospective validation cohort). Monitor its performance, specifically watching for calibration drift, where the model's predictions gradually become less aligned with observed outcomes.
- Define Update Triggers: Establish a pre-defined performance threshold that will trigger a model update. For example, an Integrated Calibration Index (ICI) greater than 0.03 can be set as the trigger [88].
- Execute Model Update: When triggered, update the model using a sliding window of the most recent data (e.g., the latest 2,000 patient records). The update can be a full model retraining or a simpler logistic recalibration which adjusts the model's intercept and slope to correct its probability outputs [88].
- Validation of Updated Model: Confirm that the updated model shows significantly improved calibration on the subsequent data without loss of discrimination, ensuring the update was successful.
Research Reagent Solutions
The table below details key computational tools and their functions in this field.
| Item Name | Function/Application |
|---|---|
| ACT-R Cognitive Architecture | A hybrid (symbolic-subsymbolic) computational framework used to model the cognitive processes underlying human behavior, such as goal pursuit and habit formation in dietary self-monitoring [87]. |
| Extreme Gradient Boosting (XGBoost) | A machine learning algorithm based on gradient boosted decision trees, useful for developing high-performance prognostic models that can handle complex, non-linear relationships in data [88]. |
| Logistic Regression with LASSO | A statistical modeling technique used for binary outcome prediction (e.g., adherence vs. non-adherence). The LASSO penalization helps select the most relevant predictors from a larger set, creating a more parsimonious model [88]. |
| Sliding Window Update Framework | A method for model updating that uses only the most recent data within a defined window, ensuring the model adapts to recent trends and maintains calibration over time [88]. |
Validation & Troubleshooting Framework
Performance Benchmarking Tables
Table 1: Performance Metrics for Cognitive Modeling (ACT-R) Based on modeling dietary self-monitoring adherence over 21 days [87].
| Intervention Group | Sample Size (n) | Root Mean Square Error (RMSE) |
|---|---|---|
| Self-Management | 49 | 0.099 |
| Tailored Feedback | 23 | 0.084 |
| Intensive Support | 25 | 0.091 |
Table 2: Impact of Auto-Updating on Prognostic Model Calibration Comparison of a static model versus an auto-updating model for predicting 28-day survival in a clinical context. A lower ICI indicates better calibration [88].
| Model Type | Integrated Calibration Index (ICI) | Notes |
|---|---|---|
| Static Model (No Updates) | 0.119 | Significant calibration drift occurs over time. |
| Auto-Updating Model | 0.014 - 0.021 | Calibration is significantly maintained and improved. |
Frequently Asked Questions (FAQs)
Q: My prognostic model's performance is degrading over time. What is the most common cause and how can I fix it? A: The most common cause is calibration drift, often due to changes in participant characteristics, adherence patterns, or external factors. To fix this, implement an auto-updating framework. Continuously monitor a performance metric like the Integrated Calibration Index (ICI) and trigger a model update (e.g., logistic recalibration) when a threshold is exceeded [88].
Q: In my cognitive model, the influence of the 'habit formation' mechanism seems to diminish in the later stages of the intervention. Is this expected? A: Yes, this has been observed. Research using ACT-R to model dietary self-monitoring found that the goal pursuit mechanism remained dominant throughout, while the impact of habit formation weakened later on. This suggests that for finite behavioral interventions like a 21-day program, conscious goal-directed effort may be a stronger driver of adherence than automated habits [87].
Q: What types of behavioral strategies should my model encourage to maximize long-term weight loss? A: Your model should prioritize strategies related to Planned Eating and Food Purchasing. A secondary analysis of a weight loss trial found that greater use of strategies in these domains was significantly associated with greater weight loss at one year, whereas the sheer number of strategies used was not [89].
Q: How much data do I need to perform a valid model update? A: The required data volume can vary. One validated framework used a sliding window of 2,000 patient records, incrementing at intervals of 500 new records, to perform effective updates. The key is to balance having enough data for stable parameter estimation with the need for the model to be responsive to recent changes [88].
Workflow Visualization
Model Update Workflow
Cognitive Model Structure
Frequently Asked Questions (FAQs)
Q1: What is the fundamental relationship between adherence and weight loss success? Research consistently demonstrates that the degree of adherence to an intervention is a more critical determinant of weight loss success than the specific type of diet prescribed. A strong curvilinear relationship (r = 0.60) has been found between self-reported dietary adherence and the amount of weight lost, with no significant association between diet type and weight loss outcomes [3]. Furthermore, better adherence during the active weight loss phase predicts superior weight maintenance at two years [3].
Q2: After discontinuing pharmacotherapy, how much weight regain typically occurs? Weight regain is common and varies significantly by drug class. A 2025 meta-analysis quantified the magnitude of this effect, showing that after treatment cessation, semaglutide showed the highest weight regain, followed by exenatide, orlistat, and liraglutide [90]. This underscores obesity as a chronic condition requiring long-term management strategies [90].
Q3: What is the typical timeline for weight regain after a lifestyle intervention ends? Evidence indicates that weight regain often begins approximately 36 weeks after the conclusion of a structured intervention. Some patients may experience a complete return to their baseline weight within about one year (approximately 40-48 weeks) [91]. This highlights a critical window for implementing maintenance strategies.
Q4: Which intervention components are most strongly associated with better adherence? Pooled analyses from multiple studies reveal that several factors significantly improve adherence rates:
- Supervised Attendance: Interventions with supervised attendance have 65% higher adherence than those without (Rate Ratio [RR] 1.65) [5].
- Social Support: The presence of social support improves adherence by 29% (RR 1.29) [5].
- Dietary Focus: Programs focusing on dietary modification alone have 27% better adherence than those focusing exclusively on exercise (RR 1.27) [5].
Q5: What physiological mechanisms contribute to weight regain after weight loss? Recent research has identified several physiological factors that create a biological pressure to regain weight, independent of the weight loss method (lifestyle, pharmacological, or surgical) [92]. Key areas of investigation include an "obesity immune memory" in adipose tissue, alterations in the gut microbiome that promote energy harvest, the proportion of fat-free mass lost during weight loss, and persistent changes in hypothalamic activity and appetite-related hormones that increase hunger [92].
Troubleshooting Guides
Problem 1: High Attrition and Non-Adherence in Clinical Trials
Issue: Participants are dropping out of a weight loss study or demonstrating poor adherence to the prescribed protocol.
Solution: Implement a multi-faceted strategy to support participant engagement.
Step 1: Enhance Supervision and Accountability.
- Action: Structure the intervention to include regular, supervised check-ins, either in-person or via telehealth.
- Rationale: Supervised attendance is one of the strongest predictors of adherence, with a 65% higher adherence rate compared to unsupervised programs [5].
Step 2: Integrate Structured Social Support.
Step 3: Utilize Early Adherence to Predict Long-Term Outcomes.
- Action: Monitor adherence metrics (e.g., self-monitoring compliance, session attendance, weight loss) closely within the first 4-8 weeks.
- Rationale: Early non-response can predict long-term difficulties. One study found that participants who were non-responders (<2.5% weight loss at week 4) achieved less weight loss at 16 weeks even after being re-randomized to augmented interventions like time-restricted eating or exercise [94]. This allows for the timely application of adaptive trial designs or rescue strategies.
Problem 2: Significant Weight Regain After Intervention Discontinuation
Issue: Participants successfully lose weight during the active intervention phase but regain a substantial amount after the study concludes.
Solution: Plan for long-term weight maintenance from the outset of the study.
Step 1: Design a Tapering Protocol, Not an Abrupt Stop.
- Action: For pharmacological trials, consider a dose-tapering phase rather than immediate cessation. For behavioral trials, gradually reduce the intensity of support (e.g., moving from weekly to bi-weekly to monthly check-ins).
- Rationale: Abrupt discontinuation of medications like semaglutide leads to significant regain, as the body's physiological drivers of weight rebound are left unopposed [90] [92]. A tapered withdrawal may help the body adapt gradually.
Step 2: Incorporate Behavioral Maintenance Strategies.
- Action: Actively train participants in skills for long-term maintenance, such as self-monitoring, problem-solving for high-risk situations, and relapse prevention.
- Rationale: Interventions that foster self-regulatory skills are cited as key facilitators of adherence. Providing maintenance counseling, even monthly, can delay weight regain [93] [91].
Step 3: Address Physiological Adaptations.
- Action: Consider strategies that mitigate the physiological drive to regain weight, such as incorporating exercise to preserve fat-free mass or exploring dietary patterns that enhance satiety (e.g., ketogenic diets).
- Rationale: A higher percentage of lost fat-free mass is inversely correlated with the amount of weight regained. Exercise has been shown to result in a more favorable body composition during maintenance compared to pharmacotherapy alone [92].
Experimental Protocols & Data
Key Quantitative Data on Adherence and Regain
Table 1: Meta-Analysis of Weight Regain After Discontinuation of Anti-Obesity Pharmacotherapy [90]
| Pharmacological Agent | Mean Weight Regain (kg) (95% CI) | Heterogeneity (I²) |
|---|---|---|
| Semaglutide | -5.15 (-5.27 to -5.03) | 99.7% |
| Exenatide | -3.06 (-3.91 to -2.22) | 41.7% |
| Liraglutide | -1.50 (-2.41 to -0.26) | 93.3% |
| Orlistat | -1.66 (-2.75 to -0.58) | 98.1% |
Table 2: Factors Improving Adherence to Weight Loss Interventions [5]
| Factor | Adherence Rate Ratio (RR) (95% CI) | Impact on Adherence |
|---|---|---|
| Supervised Attendance | 1.65 (1.54 - 1.77) | 65% higher adherence |
| Social Support | 1.29 (1.24 - 1.34) | 29% higher adherence |
| Dietary Focus (vs. Exercise Only) | 1.27 (1.19 - 1.35) | 27% higher adherence |
| Overall Adherence Rate | 60.5% (53.6 - 67.2) | - |
Protocol: Assessing Adherence and Its Correlates in a Dietary Weight Loss Trial
Objective: To quantitatively and qualitatively measure participant adherence and identify key barriers and facilitators.
Methodology:
- Participant Screening & Recruitment: Recruit adults with overweight or obesity. Obtain informed consent.
- Baseline Assessment:
- Anthropometrics: Weight, height, BMI.
- Biomarkers: Fasting blood glucose, lipids, appetite hormones (e.g., leptin, ghrelin) [92].
- Psychosocial Questionnaires: Assess readiness for change, self-efficacy, and perceived barriers using validated tools like the Weight Loss Behavior-Stage of Change Scale or readiness rulers [95].
- Intervention Phase (e.g., 12-16 weeks):
- Prescribe a standardized dietary intervention (e.g., Mediterranean diet, reduced carbohydrate).
- Quantitative Adherence Measures:
- Self-Monitoring: Participants log food intake daily via a digital app or diary [3].
- Biomarker Analysis: Use ketone levels in urine or blood for ketogenic diets as an objective adherence measure [3].
- Doubly Labeled Water (Gold Standard): In a sub-study, calculate energy intake to verify self-reported data [3].
- Qualitative Adherence Measures (Mid-point):
- Conduct structured interviews or focus groups to explore perceived barriers (e.g., time, cost, social situations) and facilitators (e.g., social support, perceived health benefits) [93].
- Endpoint Assessment (Week 12-16): Repeat all baseline anthropometric and biomarker measurements.
- Follow-Up Phase (e.g., 1 year): Track weight periodically to assess weight maintenance and regain. Correlate with adherence metrics from the active phase [91].
Workflow: Analyzing Adherence Data
The following diagram illustrates the logical workflow for collecting and analyzing adherence data within a clinical study.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Tools for Adherence Research
| Item / Tool | Function in Research | Example Use Case |
|---|---|---|
| Doubly Labeled Water (DLW) | Objective gold-standard measurement of total energy expenditure, allowing for calculation of metabolized energy intake and verification of dietary self-reports [3]. | Quantifying adherence levels in a low-energy diet study by comparing reported intake to actual energy intake [3]. |
| WebPlotDigitizer | Software to extract numerical data from published graphs and figures in existing literature. | Digitizing weight regain curves from previous meta-analyses for secondary analysis or power calculations [90]. |
| Behavior Change Technique (BCT) Taxonomy | A standardized classification system of active ingredients designed to change behavior. Used to code and replicate intervention components [93]. | Ensuring precise reporting of a trial's "active ingredients" (e.g., "goal setting," "self-monitoring") to understand which techniques best improve adherence. |
| Readiness Rulers & Stage of Change Scales | Validated psychometric instruments to assess a participant's motivation, confidence, and readiness to engage in behavior change [95]. | Tailoring intervention intensity at baseline and understanding how baseline motivation correlates with subsequent adherence. |
| Critical Appraisal Skills Programme (CASP) Checklist | A tool for methodologically assessing the quality of qualitative research studies during systematic reviews [93]. | Evaluating the rigor of included studies in a systematic review of qualitative barriers and facilitators to adherence. |
| Dual-Energy X-Ray Absorptiometry (DXA) | Precisely measures body composition (fat mass, fat-free mass). The proportion of fat-free mass lost is a potential predictor of weight regain [92]. | Tracking body composition changes during weight loss to investigate its relationship with post-intervention weight regain [92]. |
Cost-Effectiveness and Scalability of Integrated Adherence Strategies
For researchers and scientists investigating dietary weight loss, patient adherence remains a critical yet often sub-optimally addressed factor in trial design and implementation. Suboptimal adherence is a pervasive challenge globally, contributing to suboptimal treatment results, higher rates of complications, and substantial healthcare expenditures [96]. In obesity research, long-term weight management represents the greatest challenge, with traditional approaches facing significant limitations in scalability, personalisation, and long-term adherence rates [97]. Between a third and a half of prescribed medicines for long-term conditions are not taken as intended, and this figure is likely comparable for complex dietary interventions [98]. The financial impact is staggering, with poor medication adherence alone costing an estimated $100-300 billion annually in the US [99]. This technical guide provides evidence-based troubleshooting strategies to enhance adherence within weight loss research protocols, focusing on cost-effectiveness and scalability for implementation across diverse populations.
Frequently Asked Questions: Core Adherence Concepts for Researchers
Q1: What is the operational difference between "adherence" and related terms like "compliance" and "persistence"?
- Adherence emphasizes a collaborative approach where the patient actively participates in their treatment plan, aligning with patient-centered care principles. It refers to the extent to which a patient follows prescribed therapeutic recommendations [96].
- Compliance traditionally implied a more passive role for the patient, who was expected to follow healthcare provider instructions without deviation [96].
- Persistence refers to the duration of time a patient continues the treatment as prescribed, without discontinuation. Both adherence and persistence are necessary to achieve therapeutic goals, but they focus on different aspects of patient behavior [96].
Q2: What are the primary categories of adherence barriers I should account for in my study design?
Medication non-adherence might be categorized into intentional and unintentional, a framework applicable to dietary interventions [96]:
- Intentional non-adherence occurs when a patient consciously decides not to follow the prescribed regimen due to factors such as perceived ineffectiveness, fear of side effects, or mistrust.
- Unintentional non-adherence results from forgetfulness, confusion about the treatment regimen, or financial barriers.
A more comprehensive framework considers five dimensions of adherence [100]:
- Patient-related: Health literacy, forgetfulness, alternative therapies, denial of diagnosis
- Therapy-related: Complexity, side effects, treatment duration
- Healthcare system/team-related: Access to care, communication, clinician burnout
- Condition-related: Symptom severity, mental health, multiple comorbidities
- Sociodemographic: Income, social support, housing status
Q3: Which adherence assessment methodologies are most suitable for different research budgets and designs?
Table: Adherence Assessment Methodologies for Research Studies
| Method Category | Specific Methods | Strengths | Limitations | Cost Level |
|---|---|---|---|---|
| Direct Methods | Biochemical assays, drug levels in bodily fluids | High accuracy | Invasive, costly, may not reflect timing | High |
| Indirect Objective Methods | Electronic monitoring systems, prescription refill records, digital health usage data | More reliable than self-report, provides patterns | Requires technology infrastructure, privacy considerations | Medium-High |
| Indirect Subjective Methods | Patient self-reports, standardized questionnaires (e.g., Morisky Medication Adherence Scale) | Low cost, easy to implement | Prone to social desirability and recall biases | Low |
| Clinical Outcome Measures | Biomarkers (HbA1c, blood pressure), weight measurements, clinical events | Objective health outcomes | Can be influenced by factors beyond adherence | Variable |
Q4: Which adherence interventions demonstrate the strongest evidence for cost-effectiveness and scalability?
Systematic reviews and meta-analyses have identified several intervention approaches with demonstrable effectiveness [98]:
- Pharmacist-delivered interventions were more effective in improving adherence than interventions delivered by others [98]
- Face-to-face interventions are more effective than non-face-to-face methods, particularly when delivered in pharmacy settings rather than patients' homes [98]
- Fixed-dose combination formulations ('polypills') improved adherence in majority of studies [98]
- SMS/prompting mechanisms were associated with small yet significant improvements in adherence versus standard care [98]
- Team-based care and well-functioning patient-centered medical homes are associated with better adherence and risk factor control [100]
Troubleshooting Guide: Common Adherence Scenarios in Weight Loss Trials
Scenario 1: Declining Adherence Over Study Duration
Problem: Adherence rates tend to decline over time. Approximately 21% of patients stop taking their medicines within just three months, and this number jumps to 44% by six months [99]. This "white-coat effect" sees adherence temporarily improving around clinic visits but dropping significantly between visits [99].
Recommended Solutions:
- Implement ongoing support mechanisms rather than single educational interventions. Healthcare providers should coordinate care and communicate regularly about patient progress [99] [101].
- Use regular adherence assessments throughout the study, not just at baseline and endpoint. Regular assessment of patient adherence by itself can help patients stick to their treatment plans [99].
- Incorporate maintenance-phase interventions specifically designed to address declining motivation over time. Recent findings indicate that pragmatic implementation of an automated online behavioral obesity treatment program with active maintenance phase led to significant weight loss at 12- and 24 months [102].
Scenario 2: Complex Intervention Protocols Leading to Poor Implementation
Problem: Complex treatment regimens, including multiple dietary components, supplement schedules, and behavior modifications, can overwhelm participants and reduce adherence.
Recommended Solutions:
- Simplify intervention protocols by adjusting timing, frequency, and complexity to create more manageable routines. When possible, recommend once-daily dosing or consolidated protocols, which show remarkable improvement in consistency [99].
- Match intervention schedules to participants' daily activities (like meals or bedtime) so it becomes part of their routine rather than an additional burden [99].
- Use adherence aids like medication boxes, alarms, and electronic devices to help patients remember protocol components [99].
- Break complex regimens into sequential stages rather than implementing all components simultaneously [99].
Scenario 3: Digital Health Tools With Suboptimal Engagement
Problem: Digital therapeutics and mobile health applications show promise but often suffer from declining user engagement over time [97].
Recommended Solutions:
- Incorporate patient engagement modules comparable to excipients in a drug, designed to enhance patients' interaction with the software [35].
- Implement personalized, adaptive content that evolves based on participant progress and engagement patterns. The DEMETRA study found that participants who used a digital therapeutic app for at least 40% of the expected time achieved significantly greater weight loss (-7.02 kg vs -3.50 kg) compared to less engaged users [35].
- Use multicomponent digital strategies that combine self-monitoring, educational content, and behavioral therapy rather than single-function applications [35] [102].
- Include gamification elements and regular content refreshes to maintain interest and motivation [102].
Scenario 4: Socioeconomic and Access Barriers in Diverse Populations
Problem: Socioeconomic status is one of the most significant predictors of adherence. Patients with lower income levels often struggle with intervention costs and accessibility [96].
Recommended Solutions:
- Systematically identify cost barriers during screening and study design. Create an environment where participants feel comfortable discussing financial concerns [99].
- Implement cost reduction strategies such as providing study materials at no cost, offering transportation assistance, or compensating for time and travel [99] [103].
- Use technology to reduce access barriers through telemedicine, remote monitoring, and digital communication to minimize clinic visits [104].
- Partner with community organizations to enhance support networks and resource access for participants [103].
Experimental Protocols: Key Adherence Methodologies
Protocol 1: Multidimensional Adherence Assessment Strategy
Purpose: To comprehensively evaluate adherence across multiple domains using a combination of objective and subjective measures.
Materials Needed:
- Electronic monitoring devices (if applicable)
- Standardized adherence questionnaires (e.g., Morisky Medication Adherence Scale)
- Biomarker assessment tools (e.g., blood assays, body composition measures)
- Digital tracking platform (e.g., mobile app, web portal)
Procedure:
- Baseline Assessment: Administer adherence questionnaires, collect demographic and socioeconomic data, assess health literacy, and establish baseline biomarkers.
- Continuous Monitoring: Implement electronic or digital monitoring of protocol adherence throughout the study period.
- Regular Check-ins: Conduct brief adherence assessments at regular intervals (e.g., biweekly or monthly) using simplified measures.
- Endpoint Evaluation: Collect final adherence measures and biomarkers, comparing to baseline and intermediate timepoints.
- Barrier Identification: For participants with suboptimal adherence, conduct structured interviews to identify specific barriers.
Implementation Considerations:
- Allocate sufficient budget for adherence monitoring technologies
- Train research staff in adherence assessment protocols
- Plan for data management and analysis of multiple adherence measures
Protocol 2: Technology-Enhanced Adherence Support System
Purpose: To leverage digital health tools to support participant adherence through reminders, monitoring, and engagement.
Materials Needed:
- Mobile health application with reminder functionality
- Backend dashboard for research team monitoring
- Communication platform for participant-team interactions
- Data integration system for combining adherence data with outcomes
Procedure:
- Platform Selection: Choose or develop a digital health platform appropriate for your intervention and population.
- Participant Onboarding: Provide comprehensive training on technology use, with technical support availability.
- Personalized Reminder Setup: Collaborate with participants to establish optimal reminder timing and frequency.
- Engagement Protocol: Implement a systematic approach for research team monitoring of participant engagement, with predefined escalation procedures for disengagement.
- Data Integration: Automate collection of adherence data from the digital platform into your research database.
- Feedback Mechanism: Provide participants with regular feedback on their adherence patterns and progress.
Implementation Considerations:
- Ensure ADA compliance and accessibility for diverse populations
- Establish data privacy and security protocols
- Plan for technical support and troubleshooting resources
Adherence Strategy Implementation Workflow
Research Reagent Solutions: Essential Tools for Adherence Research
Table: Key Methodologies and Tools for Adherence Research
| Tool/Methodology | Primary Function | Implementation Considerations | Evidence Level |
|---|---|---|---|
| Digital Adherence Monitoring | Electronic tracking of protocol implementation | Requires technology infrastructure; consider accessibility for diverse populations | Strong for medication adherence [99] [104]; emerging for dietary interventions |
| Standardized Adherence Questionnaires | Subjective assessment of adherence behaviors | Low cost; prone to social desirability bias; should be combined with objective measures | Established for medications [96]; requires validation for dietary protocols |
| Biomarker Verification | Objective validation of adherence through physiological measures | Cost variable; must align with intervention targets (e.g., specific nutrient levels) | Gold standard when available and appropriate |
| Mobile Health Platforms | Remote support, reminders, and engagement | Implementation cost; technical support requirements; data security | Growing evidence in weight management [35] [102] |
| Implementation Science Frameworks | Systematic approach to implementing evidence-based practices | Requires training in specific frameworks; enhances generalizability | Critical for scaling successful interventions [101] |
Cost-Effectiveness Analysis of Adherence Strategies
Table: Comparative Analysis of Adherence Strategy Attributes
| Strategy Category | Relative Cost | Scalability Potential | Evidence Strength | Key Implementation Factors |
|---|---|---|---|---|
| Simplified Protocols | Low | High | Strong [99] [100] | Requires careful protocol design; minimal ongoing costs |
| Digital Health Tools | Medium-High | High | Moderate-Strong [35] [97] [102] | Initial development costs; technical support infrastructure |
| Team-Based Care | High | Medium | Strong [99] [101] | Workforce training; role definition; communication systems |
| Patient Education | Low-Medium | High | Moderate [99] [103] | Health literacy adaptation; culturally appropriate materials |
| Reminder Systems | Low | High | Strong [104] [98] | Personalization; frequency optimization; technology access |
| Behavioral Interventions | Medium | Medium | Moderate [103] [102] | Staff training; session frequency; participant engagement |
The most successful approaches typically combine multiple strategies tailored to specific adherence barriers and population characteristics. Future research should prioritize long-term evaluation of emerging technologies and the development of tailored strategies to improve adherence across diverse patient populations [96]. Strengthening adherence is not only crucial for individual patient outcomes, but also for enhancing the sustainability and efficiency of healthcare systems and research initiatives [96].
Conclusion
The evidence consistently underscores that dietary adherence, more than any specific diet type, is the cornerstone of successful and sustainable weight loss. A multi-faceted approach is essential, integrating personalized nutrition, technology-enabled self-monitoring, structured social support, and, where appropriate, pharmacotherapy to address the complex physiological and behavioral barriers to adherence. For researchers and drug development professionals, future directions must focus on the development of dynamic, adaptive interventions that can preemptively address adherence lapses. Key priorities include refining just-in-time adaptive interventions (JITAIs) through advanced cognitive modeling, elucidating the mechanisms by which new pharmacotherapies influence dietary behavior and adherence, and designing rigorous long-term studies that combine optimized lifestyle support with pharmaceutical agents to achieve synergistic, sustained health outcomes.
References
- 1. Adherence to self‐monitoring and behavioral goals is ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11897847/]
- 2. Original Research Article Association of dietary adherence ... [https://www.sciencedirect.com/science/article/pii/S0002916523662355]
- 3. Strategies to Improve Adherence to Dietary Weight Loss ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5618052/]
- 4. Exploring the Dynamics of Dietary Self-Monitoring ... [https://www.jmir.org/2025/1/e65431]
- 5. Weight loss intervention adherence and factors promoting ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4990387/]
- 6. Long-term dietary intervention trials - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC3453508/]
- 7. Common Limitations and Challenges of Dietary Clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8453651/]
- 8. Perspective: Key Considerations When Developing and ... [https://www.sciencedirect.com/science/article/pii/S0022316624004759]
- 9. Optimizing Self-Monitoring in a Digital Weight Loss ... [https://www.researchprotocols.org/2025/1/e75629]
- 10. The overlooked impact of background diet and adherence ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12199553/]
- 11. How should we measure medication adherence in clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2374934/]
- 12. A Dietary Guideline Adherence Score Is Positively ... [https://www.sciencedirect.com/science/article/pii/S0022316622085960]
- 13. The Era of Digital adherence measurement in clinical trials [https://aardexgroup.com/digital-adherence-measurement-in-clinical-trials/]
- 14. Smart packaging advances quality in clinical trials [https://www.patheon.com/us/en/insights-resources/blog/smart-packaging-advances-clinical-trial-adherence-and-accuracy.html]
- 15. Patterns and Predictors of Engagement With Digital Self ... [https://mhealth.jmir.org/2023/1/e45057]
- 16. Investigating the influence of adherence to dietary ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12434788/]
- 17. Predictors of Weight Reduction in a Multidisciplinary ... [https://www.mdpi.com/2072-6643/17/18/3015]
- 18. Energy Metabolism and Appetite Control - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK453149/]
- 19. The Control of Food Intake in Humans - Endotext - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK278931/]
- 20. Strategies to Improve Adherence to Dietary Weight Loss ... [https://www.mdpi.com/2076-328X/7/3/44]
- 21. Randomized Control Trials Early time-restricted eating with ... [https://www.sciencedirect.com/science/article/pii/S0261561425000950]
- 22. Investigating the Therapeutic Potential of the Ketogenic Diet in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11990313/]
- 23. Ketogenic Diets for Body Weight Loss: A Comparison with ... [https://www.mdpi.com/2072-6643/17/6/965]
- 24. Therapeutic effects of ketogenic diets on physiological and ... [https://www.explorationpub.com/Journals/eff/Article/101079]
- 25. Adherence to ketogenic diet in lifestyle interventions ... [https://www.nature.com/articles/s41387-023-00246-2]
- 26. Keto's collapse: The end of a diet era [https://www.foodnavigator.com/Article/2025/09/11/keto-diet-decline-what-it-means-for-the-food-industry/]
- 27. A mixed methods feasibility study of a ketogenic diet as ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12325006/]
- 28. The impact of a ketogenic diet on weight loss, metabolism ... [https://www.sciencedirect.com/science/article/pii/S2589004224025161]
- 29. How much self-monitoring for weight loss is enough? [https://phhp.ufl.edu/2024/06/06/how-much-self-monitoring-for-weight-loss-is-enough/]
- 30. Using Instrumented Paper Diaries to Document Self ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2435095/]
- 31. Understanding Appropriation of Digital Self-Monitoring Tools ... [https://humanfactors.jmir.org/2025/1/e60096/]
- 32. 50 Most Common IT Support Problems and Their Solutions [https://itadon.com/blog/50-most-common-it-support-problems-and-their-solutions/]
- 33. 16 Most Common Helpdesk Problems and How to Solve ... [https://www.alert-software.com/blog/the-most-common-helpdesk-problems-and-how-to-solve-them]
- 34. Randomized Controlled Digital Health Trial [https://formative.jmir.org/2025/1/e70842]
- 35. Effectiveness of a Digital Therapy on 6-Month Weight Loss in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12587017/]
- 36. A systematic review of influences on engagement with ... [https://www.nature.com/articles/s41366-025-01811-8]
- 37. Attributes, Methods, and Frameworks Used to Evaluate ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11031706/]
- 38. Personalized Nutrition in the Era of Digital Health [https://pmc.ncbi.nlm.nih.gov/articles/PMC12474561/]
- 39. Current insights into genome-based personalized nutrition ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2024.1346144/full]
- 40. Data in Personalized Nutrition: Bridging Biomedical ... [https://www.sciencedirect.com/science/article/pii/S2161831325000134]
- 41. Real-World Effectiveness of a Medically Supervised Weight ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5798936/]
- 42. The influence of family, friend, and coworker social support ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4435839/]
- 43. The effectiveness of social-support-based weight-loss ... [https://www.nature.com/articles/s41366-024-01468-9]
- 44. Weight Loss in Short-Term Interventions for Physical ... [https://www.cdc.gov/pcd/issues/2024/23_0347.htm]
- 45. 3 Steps To Help Nutrition Coaches Troubleshoot A Clients ... [https://growyournutritionbusiness.com/steps-to-help-nutrition-coaches-troubleshoot-a-clients-weight-loss-plateau/]
- 46. 3 Steps to Fix Any Diet Problem [https://www.precisionnutrition.com/fix-any-diet-problem]
- 47. The expanding role of GLP-1 receptor agonists [https://pmc.ncbi.nlm.nih.gov/articles/PMC12303005/]
- 48. Weight loss outcomes, tolerability, side effects, and risks [https://www.sciencedirect.com/science/article/pii/S2667368124000299]
- 49. Study identifies benefits, risks linked to popular weight-loss ... [https://medicine.washu.edu/news/study-identifies-benefits-risks-linked-to-popular-weight-loss-drugs/]
- 50. Adverse Effects of GLP-1 Receptor Agonists - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5397288/]
- 51. Real-world persistence and adherence to glucagon-like ... [https://pubmed.ncbi.nlm.nih.gov/38717042/]
- 52. An Update on GLP‐1 Receptor Agonists - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12371248/]
- 53. Addressing GLP-1 Access and Adherence Challenges with ... [https://shieldshealthsolutions.com/glp1-access-adherence-specialty-pharmacy/]
- 54. Glucagon-like peptide-1 receptor: mechanisms and ... [https://www.nature.com/articles/s41392-024-01931-z]
- 55. Current Insights, Advantages and Challenges of Small ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11966775/]
- 56. Two, Six, and Twelve-Month Dropout Rate and Predictor ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2022.851802/full]
- 57. The Relationship Between Weight Loss Outcomes and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8663454/]
- 58. The Effect of Adherence to Dietary Tracking on Weight Loss [https://pmc.ncbi.nlm.nih.gov/articles/PMC5568610/]
- 59. The influence of referral, initial assessment, and logistical ... [https://www.sciencedirect.com/science/article/abs/pii/S1871403X25001218]
- 60. Initial Weight Loss Response as an Indicator for Providing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5789799/]
- 61. Introduction to SMART designs for the development of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4167891/]
- 62. Occurrence of and Reasons for “Missing Events” in Mobile ... [https://mhealth.jmir.org/2020/10/e15430]
- 63. An approach to boost adherence to self-data reporting in ... [https://bmcmedinformdecismak.biomedcentral.com/articles/10.1186/s12911-024-02833-4]
- 64. Recommender systems use in weight management ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11791383/]
- 65. Smartloss: A Personalized Mobile Health Intervention for ... [https://mhealth.jmir.org/2016/1/e18/]
- 66. Mobile-Based Interventions for Dietary Behavior Change ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6360385/]
- 67. Unintended Consequences of Obesity Pharmacotherapy [https://pmc.ncbi.nlm.nih.gov/articles/PMC12157928/]
- 68. Ultraprocessed or minimally processed diets following ... [https://www.nature.com/articles/s41591-025-03842-0]
- 69. Investigating the effect of a cognitive-behavioral therapy ... [https://trialsjournal.biomedcentral.com/articles/10.1186/s13063-025-09113-0]
- 70. Enhanced protein intake on maintaining muscle mass ... [https://www.sciencedirect.com/science/article/abs/pii/S2405457724001761?utm_source=chatgpt.com]
- 71. International Society of Sports Nutrition Position Stand: protein ... [https://jissn.biomedcentral.com/articles/10.1186/s12970-017-0177-8]
- 72. Role of protein intake in maintaining muscle mass ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1547325/full]
- 73. Adaptive dietary and exercise strategies for weight loss in ... [https://www.sciencedirect.com/science/article/pii/S0002916525004514]
- 74. Preserving Healthy Muscle during Weight Loss [https://www.sciencedirect.com/science/article/pii/S2161831322006810]
- 75. International Society of Sports Nutrition position stand: protein ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2117006/]
- 76. GDF8 and activin A blockade protects against GLP-1- ... [https://pubmed.ncbi.nlm.nih.gov/40360507/]
- 77. Effects of protein supplementation on muscle mass, muscle ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11978179/]
- 78. Medication adherence trajectories and clinical outcomes in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12061002/]
- 79. The link between adherence to antihypertensive medications ... [https://bmccardiovascdisord.biomedcentral.com/articles/10.1186/s12872-025-04538-6]
- 80. 35+ Latest Patient Adherence Statistics for 2025 [https://www.dialoghealth.com/post/patient-adherence-statistics]
- 81. Strategies to Enhance Patient Adherence: Making it Simple [https://pmc.ncbi.nlm.nih.gov/articles/PMC1681370/]
- 82. Comparative Effectiveness of Weight-Loss Interventions in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4074540/]
- 83. Investigating the effect of a cognitive-behavioral therapy ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12461973/]
- 84. Effects of Information Length and Implementation Intentions on ... [https://mhealth.jmir.org/2025/1/e65260]
- 85. Navigating challenges and adherence in time‐restricted ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12401815/]
- 86. Counseling Patients With Obesity - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK589679/]
- 87. Exploring the Dynamics of Dietary Self-Monitoring Adherence ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12064973/]
- 88. Development and validation of self-monitoring auto ... [https://www.nature.com/articles/s41467-022-34646-2]
- 89. Use of Cognitive and Behavioral Strategies During a ... [https://www.sciencedirect.com/science/article/pii/S2212267223001661]
- 90. Rebound or Retention: A Meta-Analysis of Weight Regain ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12535773/]
- 91. Understanding weight regain after a nutritional weight loss ... [https://www.sciencedirect.com/science/article/abs/pii/S2405457722002017]
- 92. Physiology of Weight Regain after Weight Loss [https://pmc.ncbi.nlm.nih.gov/articles/PMC11958498/]
- 93. Barriers and facilitators to diet, physical activity and lifestyle ... [https://ijbnpa.biomedcentral.com/articles/10.1186/s12966-023-01424-2]
- 94. Adaptive dietary and exercise strategies for weight loss in ... [https://pubmed.ncbi.nlm.nih.gov/40763896/]
- 95. Comprehensive Behavioral Modification and Counseling ... [https://www.ncbi.nlm.nih.gov/books/NBK618378/]
- 96. Enhancing Therapy Adherence: Impact on Clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11766829/]
- 97. Artificial intelligence for obesity management: A review of ... [https://www.sciencedirect.com/science/article/pii/S2451847625000776]
- 98. Improving medication adherence in the community [https://link.springer.com/article/10.1007/s11096-025-01885-4]
- 99. 11 Effective Strategies for Improving Medication Adherence ... [https://www.dialoghealth.com/post/strategies-for-improving-medication-adherence-in-patients]
- 100. Scalable strategies for improving adherence in adults with ... [https://www.explorationpub.com/Journals/em/Article/1001298]
- 101. Healthcare provider interventions to support medication ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12322503/]
- 102. Beyond weight loss: digital therapeutic for behavioral ... [https://www.frontiersin.org/journals/digital-health/articles/10.3389/fdgth.2025.1671649/full]
- 103. Medication management: strategies for enhancing ... [https://www.asteroidhealth.com/blog/medication-management-strategies-for-enhancing-compliance]
- 104. Technology-integrated nursing interventions to improve ... [https://bmcnurs.biomedcentral.com/articles/10.1186/s12912-025-03796-1]