The Calorie Counting Conundrum: A Critical Analysis of Wearable Technology Accuracy for Biomedical Research
This article provides a critical evaluation of the accuracy and validity of wearable devices for tracking energy expenditure (EE), tailored for researchers and drug development professionals.
The Calorie Counting Conundrum: A Critical Analysis of Wearable Technology Accuracy for Biomedical Research
Abstract
This article provides a critical evaluation of the accuracy and validity of wearable devices for tracking energy expenditure (EE), tailored for researchers and drug development professionals. It synthesizes current evidence from meta-analyses and validation studies, revealing significant error margins in EE measurement that can exceed 25%. The scope covers foundational accuracy benchmarks, methodological considerations for integrating wearables into clinical and research protocols, strategies for troubleshooting inherent device limitations, and a comparative analysis of validation frameworks. The discussion focuses on the implications of these findings for interpreting data in clinical trials, epidemiological studies, and patient monitoring, offering a roadmap for the rigorous application of consumer wearables in scientific contexts.
Establishing the Baseline: Current Evidence on Wearable Calorie Tracking Accuracy
The accurate measurement of energy expenditure (EE) is fundamental to research in areas including metabolism, pharmacology, and public health. With the proliferation of wearable activity monitors in both consumer and research settings, quantifying the systemic error in these devices' EE estimates has become a critical endeavor. This guide objectively compares the EE measurement performance of major wearable devices against criterion measures, framing the findings within the broader thesis of accuracy validation for wearable calorie tracking research. The data presented herein, drawn from recent meta-analyses and validation studies, provides researchers with a quantitative basis for device selection and data interpretation.
Comparative Performance of Wearable Devices
Meta-analytic data reveals a consistent pattern across wearable devices: while they provide a practical means of estimating EE, their accuracy is substantially lower than for other metrics like heart rate or step count. The table below summarizes the quantitative findings from large-scale analyses.
Table 1: Meta-Analytic Summary of Wearable Device Accuracy for Energy Expenditure and Related Metrics
| Device / Analysis Focus | Mean Bias (EE) | Limits of Agreement (EE) | Mean Absolute Percent Error (MAPE) | Key Findings on EE Accuracy |
|---|---|---|---|---|
| Fitbit (Combined-Sensing Models) [1] | -2.77 kcal/min | -12.75 to 7.41 kcal/min | Not Reported | Devices are likely to underestimate EE; accuracy may be unacceptable for some research purposes [1]. |
| Apple Watch [2] [3] | 0.30 kcal/min [3] | -2.09 to 2.69 kcal/min [3] | 27.96% [2] | Provides the strongest accuracy among consumer devices, but error rate is still high [2] [4]. |
| Archon Alive 001 [5] | Not Reported | Not Reported | 29.3% | Considered sufficient for monitoring exercise intensity but insufficient for clinical assessment [5]. |
| Garmin [4] | Not Reported | Not Reported | ~48.05% (Moderate Accuracy) | Identified as one of the least accurate for measuring calories burned [4]. |
| Actigraph (Research-Grade) [6] | No significant difference (SMD = 0.01) | Not Reported | Not Reported | Can be used for assessing total PAEE, but has limited validity for specific activity intensities [6]. |
| Comparative Metric | Mean Bias (Heart Rate) | Limits of Agreement (Heart Rate) | Mean Absolute Percent Error (MAPE) for Heart Rate | Mean Absolute Percent Error (MAPE) for Step Count |
|---|---|---|---|---|
| Fitbit [1] | -2.99 bpm | -23.99 to 18.01 bpm | Not Reported | Not Reported |
| Apple Watch [2] [3] | -0.12 bpm [3] | -11.06 to 10.81 bpm [3] | 4.43% [2] | 8.17% [2] |
| Archon Alive 001 [5] | -3.33 bpm | -31.55 to 24.90 bpm | Not Reported | 3.46% |
This systemic error in EE estimation is notably greater than for other common metrics. One large-scale meta-analysis of various brands found that while heart rate tracking showed strong accuracy (76.35%) and step count moderate accuracy (68.75%), the accuracy for energy expenditure was the lowest, at just 56.63% [4]. This underscores the particular challenge EE measurement presents for wearable algorithms.
Detailed Experimental Protocols and Methodologies
The quantitative findings in the previous section are derived from rigorous validation protocols. Understanding these methodologies is essential for researchers to critically evaluate the data and design their own validation studies.
Laboratory-Based Structured Protocols
The most common approach for high-quality validation involves controlled laboratory settings where wearable device outputs can be compared to criterion-standard measures.
- Criterion Measures for EE: Indirect Calorimetry (IC) is the most frequently used criterion measure for EE. It estimates energy expenditure by measuring respiratory gas exchange (oxygen consumption and carbon dioxide production) using a metabolic analyzer such as the PNOĒ [5]. Doubly Labeled Water (DLW) is another gold standard for measuring total daily energy expenditure in free-living conditions, though it is less common in single-activity validation studies [1] [6].
- Criterion Measures for Heart Rate: An electrocardiogram (ECG) is the gold standard for heart rate validation. Research-grade chest strap systems (e.g., Polar H7/Polar OH1) are also used as reliable reference measures [1] [5] [7].
- Criterion Measures for Step Count: Direct observation (manual count by a researcher, often verified by video recording) serves as the primary criterion for step count [1] [5].
- Standardized Activity Protocols: Participants typically perform a series of structured activities while wearing the devices and the criterion equipment. A common treadmill protocol includes:
- Walking at varying speeds (e.g., 3, 4, and 5 km/h) [5].
- Running (e.g., 8 km/h) [5].
- Each stage lasts a set duration (e.g., 3 minutes) with rest periods in between.
- Other protocols may include graded cycling exercises and resistance training to assess device performance across different activity types and intensities [7].
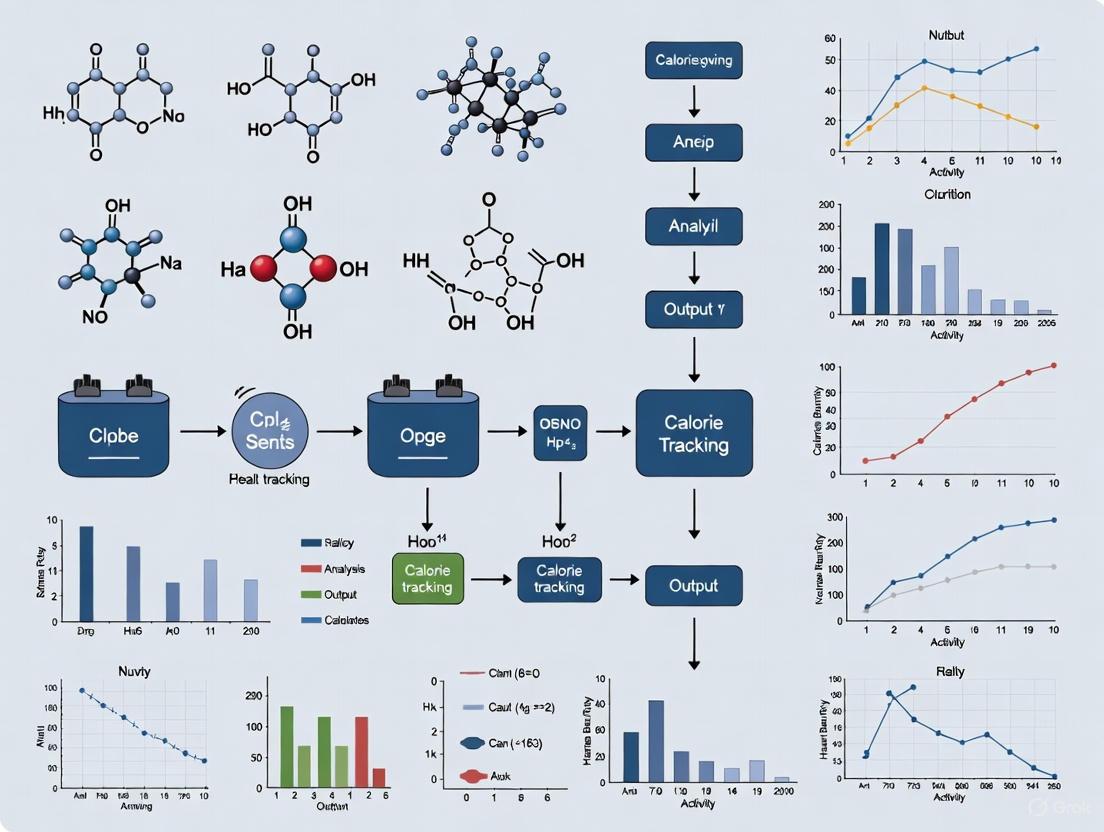
The following diagram illustrates a typical laboratory validation workflow.
Free-Living and Special Population Protocols
To complement laboratory studies, researchers also validate devices in free-living conditions and specific clinical populations, which introduces new challenges and considerations.
- Objective: To assess device performance in real-world environments and in populations whose movement patterns may differ from healthy adults (e.g., patients with lung cancer who often have slower gait speeds) [8].
- Protocol: Participants wear multiple devices (e.g., consumer-grade Fitbit Charge 6 and research-grade ActiGraph LEAP/activPAL) simultaneously for an extended period (e.g., 7 days) [8].
- Criterion Measures: In the absence of direct observation, data from research-grade devices is often used as a proxy criterion for comparison with consumer-grade devices. Surveys on health-related quality of life and symptom burden are administered to control for confounding factors [8].
The Researcher's Toolkit: Essential Reagents and Materials
The following table details key equipment and methodologies used in the validation of wearable activity monitors.
Table 2: Key Research Reagent Solutions for Wearable Validation Studies
| Item / Solution | Primary Function in Validation | Specific Examples |
|---|---|---|
| Indirect Calorimetry System | Serves as the criterion measure for Energy Expenditure (EE) by analyzing respiratory gases. | PNOĒ metabolic analyzer [5]; Medical-grade metabolic carts [6]. |
| Electrocardiogram (ECG) | Provides gold-standard measurement of heart rate for validating optical heart rate sensors. | 12-lead clinical ECG [9]; Single-lead ECG integrated into some wearables (e.g., Apple Watch) [9]. |
| Research-Grade Accelerometer | Used as a benchmark for validating step count and physical activity intensity in research settings. | Actigraph wGT3x-BT [5]; ActiGraph LEAP [8]. |
| Photoplethysmography (PPG) Reference | Provides a validated reference for optical heart rate monitoring. | Polar OH1 [5]; Polar H7 chest strap [7]. |
| Direct Observation / Video Recording | Serves as the criterion measure for validating step count and activity type. | Manual counting with a hand tally [5]; Video recording with subsequent blinded annotation [8]. |
| Standardized Treadmill | Provides a controlled environment for administering structured activity protocols at precise speeds. | Freemotion, iFIT, or other calibrated treadmills [5]. |
| Bland-Altman Analysis | A key statistical method for assessing agreement between the wearable device and the criterion measure. | Used to calculate mean bias and 95% Limits of Agreement (LoA) [1] [5] [3]. |
| Mean Absolute Percentage Error (MAPE) | A standard metric for quantifying accuracy as a percentage of error. | Calculated as the average of absolute errors divided by actual values [2] [5]. |
Meta-analytic evidence quantifies a significant systemic error in the energy expenditure estimates provided by wearable devices, with most exhibiting a mean absolute percent error between 27% and 48%. This error is markedly larger than that for heart rate or step count. While consumer devices like the Apple Watch show relatively stronger performance, and research-grade tools like the Actigraph are valid for assessing total physical activity energy expenditure, all devices have limitations. The accuracy of EE measurement is influenced by the type of physical activity, the device model, and user demographics. Researchers must therefore incorporate these known errors into their study design and interpretation, utilizing wearable EE data as a useful but approximate indicator rather than a definitive measure.
Wearable activity monitors have become integral tools in health and fitness, offering users insights into their physical activity, cardiovascular function, and energy expenditure. For researchers and clinicians, understanding the comparative accuracy of these devices across different metrics is crucial for interpreting data, designing studies, and making clinical recommendations. This guide objectively compares the performance of wearable devices in tracking steps, heart rate, and calories, framing the analysis within the broader context of accuracy validation for wearable calorie tracking research. The analysis synthesizes findings from recent validation studies, details experimental methodologies, and provides resources to support further scientific investigation.
A consistent pattern emerges from recent validation studies: the accuracy of wearable devices varies significantly depending on the metric being measured. Step counting and heart rate monitoring demonstrate notably higher accuracy compared to the estimation of energy expenditure.
- Step Count: This is generally the most reliable metric, with high-fidelity devices like the Apple Watch and Archon Alive tracker showing mean absolute percentage errors (MAPE) of approximately 3-8% under controlled conditions [2] [5]. This high accuracy is attributed to the well-established use of accelerometers to detect rhythmic arm movements associated with walking and running.
- Heart Rate: Heart rate tracking also shows good agreement with gold-standard measures, such as electrocardiogram (ECG) and chest straps. Studies report percentage errors around 4-5% for devices like the Apple Watch, and Intraclass Correlation Coefficients (ICC) of 75.8% for affordable trackers like the Archon Alive [2] [5] [10]. The underlying photoplethysmography (PPG) technology, while effective, can be influenced by motion and device fit.
- Calories Burned (Energy Expenditure): This is the least accurate metric, with errors substantially higher than for steps or heart rate. Meta-analyses and validation studies consistently report MAPE values around 28-30% for this metric [2] [5] [11]. The high error rate stems from the indirect nature of the calculation, which relies on proprietary algorithms that estimate a complex physiological process from a limited set of inputs like heart rate and movement.
Comparative Performance Data
The following tables summarize quantitative data on device accuracy from recent scientific studies.
Table 1: Summary of Device Accuracy Across Key Metrics from Recent Studies
| Device / Study | Step Count Accuracy (MAPE) | Heart Rate Accuracy | Calorie Expenditure Accuracy (MAPE) | Citation |
|---|---|---|---|---|
| Apple Watch (Meta-analysis) | 8.17% (MAPE) | 4.43% (MAPE) | 27.96% (MAPE) | [2] [11] |
| Archon Alive 001 | 3.46% (MAPE vs. hand tally) | ICC: 75.8% (vs. Polar OH1) | 29.3% (MAPE vs. PNOĒ) | [5] |
| Actigraph wGT3x-BT | 31.46% (MAPE vs. hand tally) | Not Reported in Study | Not Reported in Study | [5] |
| Corsano CardioWatch (Pediatric) | Not Reported in Study | 84.8% of readings within 10% of Holter ECG | Not Reported in Study | [10] |
| Hexoskin Smart Shirt (Pediatric) | Not Reported in Study | 87.4% of readings within 10% of Holter ECG | Not Reported in Study | [10] |
Table 2: Impact of External Factors on Metric Accuracy
| Factor | Impact on Step Count | Impact on Heart Rate | Impact on Calorie Expenditure |
|---|---|---|---|
| Activity Type/Speed | Accuracy decreases at very slow walking speeds [5] [8]. | Accuracy decreases during high-intensity movement [10]. | Inaccurate across walking, running, cycling, and mixed-intensity workouts [2]. |
| Population | Gait impairments (e.g., in lung cancer patients) can reduce accuracy [8]. | Accuracy lower in children with higher, more variable heart rates [10]. | Individual factors (age, weight, metabolism) not fully captured by algorithms [12]. |
| Device Grade | Consumer-grade (e.g., Archon) can outperform research-grade (e.g., Actigraph) in specific protocols [5]. | Research-grade and medically certified devices may offer higher reliability for clinical applications [10] [8]. | Proprietary algorithms vary significantly between brands; no consumer device is highly accurate [2] [13]. |
Detailed Experimental Protocols
To critically assess the data presented in comparison tables, an understanding of the underlying experimental methodologies is essential. The following are detailed protocols from key studies cited in this guide.
Protocol 1: Validation of an Affordable Fitness Tracker
This 2025 study validated the Archon Alive 001 against criterion measures in a controlled laboratory setting [5].
- Objective: To assess the validity of the Archon Alive 001 for measuring step count, heart rate, and energy expenditure.
- Participants: Approximately 35 adults with a BMI between 18-25 kg/m² and no chronic diseases or mobility restrictions.
- Criterion Measures:
- Step Count: Manual hand tally.
- Heart Rate: Polar OH1 (a validated PPG heart rate monitor).
- Energy Expenditure: PNOĒ metabolic analyzer (portable cardio-metabolic analyzer of breath).
- Protocol: Participants walked or ran on a treadmill at four set speeds: 3, 4, 5, and 8 kilometers per hour. Each stage lasted 3 minutes with a 1-minute break in between. The Archon Alive and Actigraph wGT3x-BT were worn on the non-dominant wrist, while the Polar OH1 was worn on the upper arm. The PNOĒ was fastened to the participant's back, with the participant breathing through a Hans Rudolph mask.
- Data Analysis: Mean Absolute Percentage Error (MAPE) was calculated for step count and calorie expenditure against the criterion. For heart rate, Intraclass Correlation Coefficient (ICC) and Bland-Altman analysis (including bias and limits of agreement) were used to compare the Archon Alive with the Polar OH1.
Protocol 2: A Meta-Analysis of Apple Watch Accuracy
This 2025 study from the University of Mississippi provides a high-level overview of Apple Watch performance based on a synthesis of existing research [2] [11].
- Objective: To evaluate the accuracy of the Apple Watch in measuring energy expenditure, heart rate, and step counts across different user demographics and activities.
- Methodology (Meta-analysis): Researchers identified and systematically reviewed 56 individual studies that compared Apple Watch data to trusted reference tools. The analysis specifically evaluated how accuracy varied by age, health status, Apple Watch version, and type of physical activity (e.g., walking, running, cycling).
- Data Analysis: The core of the analysis was the calculation of the mean absolute percent error (MAPE), a standard measure of accuracy, for each of the three key metrics across the aggregated studies.
Protocol 3: Validation of Wearables in a Pediatric Clinical Population
This 2025 study assessed the accuracy of two wearables in a pediatric cardiology cohort, highlighting the importance of validation in specific populations [10].
- Objective: To assess the heart rate accuracy and validity of the Corsano CardioWatch bracelet and the Hexoskin smart shirt in children with congenital heart disease or suspected arrhythmias.
- Participants: 31 participants for the CardioWatch and 36 for the Hexoskin shirt (mean age ~13 years).
- Criterion Measure: 24-hour Holter electrocardiogram (ECG), the gold standard for ambulatory heart rate monitoring.
- Protocol: Participants were equipped with the Holter ECG and both wearables simultaneously for a 24-hour free-living period. They were encouraged to maintain their normal daily routine but refrain from showering and swimming.
- Data Analysis: Accuracy was defined as the percentage of heart rate readings from the wearables that fell within 10% of the concurrent Holter ECG values. Agreement was further assessed using Bland-Altman analysis. Subgroup analyses were conducted based on factors like BMI, age, time of wearing, and accelerometry-measured bodily movement.
Experimental Workflow and Logical Relationships
The following diagram illustrates the standard workflow and logical relationships involved in validating a wearable device's metrics, as demonstrated by the protocols above.
The Scientist's Toolkit: Key Research Reagents and Materials
For researchers aiming to replicate or design validation studies, the following table details essential equipment and their functions as derived from the cited protocols.
Table 3: Essential Materials for Wearable Validation Research
| Item | Function in Validation Research | Example from Search Results |
|---|---|---|
| Criterion Measure for Energy Expenditure | Provides a gold-standard measurement of calorie burn/energy expenditure via gas analysis for validating wearable estimates. | PNOĒ metabolic analyzer [5]. |
| Criterion Measure for Heart Rate | Provides a gold-standard measurement of heart rate and rhythm for validating optical heart rate sensors. | Holter ECG [10] & Polar OH1 chest strap/armband [5]. |
| Criterion Measure for Step Count | Provides a ground-truth measure of steps taken during controlled trials. | Manual hand tally [5]. |
| Controlled Activity Generator | Allows for standardized, repeatable physical activities at various intensities to test device performance across a range of metabolic demands. | Freemotion T10.8 Treadmill [5]. |
| Research-Grade Activity Monitor | Serves as a benchmark device, often used in public health research, for comparison with consumer-grade trackers. | Actigraph wGT3x-BT [5] [8]. |
| Data Analysis Software | Used for processing raw data and conducting specialized statistical analyses to quantify agreement and error. | ActiLife (for Actigraph data) [5]; Statistical packages for Bland-Altman, ICC, MAPE [5] [10]. |
The collective evidence indicates a clear hierarchy in the accuracy of metrics provided by consumer wearable devices. Steps and heart rate can be measured with a reasonable degree of confidence for general tracking and trend analysis, making them suitable for a wide range of research applications. In contrast, energy expenditure (calorie burn) remains an inaccurate metric, with errors too high for precise scientific or clinical use. Researchers and professionals should therefore prioritize devices with strong validation data for steps and heart rate, treat calorie estimates with significant caution, and always consider the target population and specific use case when selecting and implementing wearable technology in studies.
The accuracy of calorie measurements from wearable devices is not a fixed value but a variable dependent on a complex interplay of factors. For researchers and professionals in drug development and clinical sciences, understanding these variables is critical when considering the use of consumer wearables in research protocols or health interventions. This guide objectively compares the performance of various wearable devices, framing their accuracy within the broader thesis of validation research. The data reveals that accuracy is predominantly influenced by the type and intensity of physical activity performed by the user, as well as their individual demographic characteristics. A synthesis of current studies indicates that while some metrics like heart rate can be measured with reasonable reliability, energy expenditure (EE) remains a significant challenge, with even the best-performing devices showing considerable error rates [14] [15]. This analysis provides a structured comparison of device performance, detailed experimental methodologies from key studies, and essential resources for the validation of wearable calorie tracking.
Quantitative Data Comparison of Wearable Devices
The tables below summarize the accuracy of various commercial wearable devices for measuring energy expenditure (calories burned), heart rate, and step count, as reported in validation studies. This data allows for a direct, objective comparison of device performance across key metrics.
Table 1: Overall Accuracy of Wearables by Metric (WellnessPulse Analysis)
| Metric | Cumulative Accuracy | Notes on Variation |
|---|---|---|
| Heart Rate (HR) | 76.35% | Most accurate metric; Apple Watch showed highest accuracy (86.31%) [4]. |
| Step Count (SC) | 68.75% | Accuracy can drop for non-ambulatory movements [4]. |
| Energy Expenditure (EE) | 56.63% | Least accurate metric; highly variable across devices and activities [4]. |
Table 2: Device-Specific Error Rates for Key Metrics
| Device Brand | Energy Expenditure (EE) Error | Heart Rate (HR) Error | Step Count (SC) Error |
|---|---|---|---|
| Apple Watch | MAPE: -6.61% to 53.24% [16]Overall Accuracy: 71.02% [4] | Underestimation: ~1.3 BPM during exercise [16]Overall Accuracy: 86.31% [4] | Error: 0.9-3.4% [16]Overall Accuracy: 81.07% [4] |
| Fitbit | MAPE: ~0.44 [15]Error: 14.8% [16]Overall Accuracy: 65.57% [4] | Underestimation: ~9.3 BPM during exercise [16]Overall Accuracy: 73.56% [4] | Error: 9.1-21.9% [16]Overall Accuracy: 77.29% [4] |
| Garmin | Error: 6.1-42.9% [16]Overall Accuracy: 48.05% [4] | Error: 1.16-1.39% [16] | Error: 23.7% [16]Overall Accuracy: 82.58% [4] |
| Samsung Gear S3 | MAPE: Up to 0.44 [15] | MAPE from 0.04 (at rest) to 0.34 [15] | Data not reported in analysis |
| Polar | Error: 10-16.7% [16]Overall Accuracy: 50.23% [4] | Error: 2.2% (upper arm) [16] | Overall Accuracy: 53.21% [4] |
Detailed Experimental Protocols
To critically assess the data from wearables, understanding the underlying validation methodologies is essential. The following are detailed protocols from two key studies that exemplify rigorous device testing.
Protocol 1: Multi-Device Validation Under Semi-Naturalistic Conditions
A 2018 comparative study by Lei et al. evaluated the validity of several mainstream wearable devices under various physical activities [15].
- Objective: To evaluate the accuracy of multiple wearable devices in measuring heart rate, steps, distance, energy consumption, and sleep duration across different activity states.
- Subjects: 44 healthy subjects were recruited for the study.
- Devices & Comparators: Each subject simultaneously wore six devices: Apple Watch 2, Samsung Gear S3, Jawbone Up3, Fitbit Surge, Huawei Talk Band B3, and Xiaomi Mi Band 2. Two smartphone apps (Dongdong and Ledongli) were also included.
- Activity Protocol: Subjects performed activities in various states:
- Resting: To establish baseline heart rate.
- Walking: To simulate light-to-moderate activity.
- Running: For high-intensity dynamic movement.
- Cycling: For non-ambulatory exercise.
- Sleeping: For sleep duration tracking.
- Gold Standard Measures:
- Heart Rate: Manually measured (likely via electrocardiogram or palpation).
- Steps & Distance: Manually counted and measured.
- Energy Expenditure: Measured via oxygen consumption (indirect calorimetry).
- Sleep Duration: Manually recorded.
- Data Analysis: The Mean Absolute Percentage Error (MAPE) was calculated for each device and metric against the gold standard. The study found high accuracy for heart rate, steps, distance, and sleep (MAPE ~0.10), but poor accuracy for energy consumption (MAPE up to 0.44) [15].
Protocol 2: Systematic Review and Meta-Analysis Methodology
A 2020 systematic review in PMC provides a broader overview of device accuracy by synthesizing data from 158 publications [14].
- Objective: To examine the validity and reliability of commercial wearables in measuring step count, heart rate, and energy expenditure.
- Search Strategy: Comprehensive searches were conducted in PubMed, Embase, and SPORTDiscus up to May 2019. The strategy used controlled vocabulary and text words related to wearables, validity, and specific brands.
- Eligibility Criteria:
- Included studies using consumer-grade wearables (e.g., Apple, Fitbit, Garmin).
- Focused on studies examining reliability or validity of step count, heart rate, or energy expenditure.
- Excluded studies with fewer than 10 participants and those focusing on research-grade devices.
- Data Extraction & Synthesis: Researchers extracted key study characteristics and outcome data, including correlation coefficients, percentage differences, and MAPE values. Where possible, group percentage error was calculated to standardize comparisons across studies.
- Key Findings:
- In laboratory settings, Fitbit, Apple Watch, and Samsung were most accurate for steps.
- Heart rate accuracy was variable, with Apple Watch and Garmin being most accurate.
- No brand was accurate for measuring energy expenditure [14].
Visualizing Influencing Factors on Accuracy
The diagram below illustrates the logical relationship between the key influencing factors (activity type, intensity, and demographics) and their combined impact on the accuracy of calorie measurements in wearable devices.
The Scientist's Toolkit: Key Research Reagents & Materials
For researchers designing validation studies for wearable devices, the following table details essential equipment and their functions, as derived from the cited experimental protocols.
Table 3: Essential Materials for Wearable Validation Research
| Item | Function in Validation Research |
|---|---|
| Indirect Calorimeter | Considered the "gold standard" for measuring energy expenditure. It calculates calories burned by measuring oxygen consumption and carbon dioxide production [15]. |
| Electrocardiogram (ECG) | Serves as the gold standard for heart rate measurement. Provides a medical-grade reference to which optical heart rate sensors from wearables are compared [4]. |
| Research-Grade Actigraph | Provides high-fidelity, validated data on step count and movement acceleration, often used as a benchmark for consumer-grade activity trackers [14]. |
| Manual Step Counter/Tally | Used for direct, observable counting of steps during controlled walking or running protocols, providing a simple and accurate ground truth [15]. |
| Gold Standard Sleep Polysomnography (PSG) | The comprehensive reference method for validating sleep metrics tracked by wearables, measuring brain waves, eye movement, muscle activity, and more [16]. |
Wearable fitness trackers have become ubiquitous in both consumer and clinical settings. However, for researchers and scientists relying on this data, a significant gap exists between the number of devices on the market and those that have undergone rigorous, peer-reviewed validation. This guide objectively compares the validation status of various wearable devices and details the experimental methodologies used to assess their accuracy.
The Scale of the Validation Gap
The market for wearable fitness trackers is expanding rapidly, projected to grow from USD 35.8 billion in 2025 to USD 144.8 billion by 2035 [17]. Despite this proliferation, a relatively small fraction of commercially available devices have been scientifically validated.
The table below quantifies this validation gap, synthesizing data from a large-scale 2024 living umbrella review of systematic reviews [18].
Table 1: Peer-Reviewed Validation Status of Commercial Wearable Devices
| Metric | Findings | Source |
|---|---|---|
| Total Commercially Available Wearables | 310 devices released to date | [18] |
| Devices Validated for ≥1 Biometric | ~11% (approximately 34 devices) | [18] |
| Total Possible Biometric Outcomes | All measurable metrics (e.g., HR, EE, sleep) across all devices | [18] |
| Validated Biometric Outcomes | ~3.5% of total possible outcomes | [18] |
This comprehensive review highlights a critical challenge for the research community: the vast majority of wearable devices and the data they produce lack independent, peer-reviewed assessment against accepted reference standards [18].
Accuracy of Validated Metrics by Device Type
For the subset of devices that have been validated, accuracy varies significantly by the biometric being measured and the specific device model. The following tables summarize key accuracy metrics for common tracking domains.
Table 2: Accuracy of Heart Rate and Step Count Tracking
| Device / Study Focus | Heart Rate Accuracy (MAPE or Mean Bias) | Step Count Accuracy (MAPE or Mean Bias) | Source |
|---|---|---|---|
| Apple Watch (Meta-Analysis) | Mean Bias: -0.12 bpm; MAPE: 4.43% | Mean Bias: -1.83 steps/min; MAPE: 8.17% | [2] [3] |
| Various Wearables (Umbrella Review) | Mean Absolute Bias: ±3% | Mean Absolute Percentage Error: -9% to 12% | [18] |
| Multiple Brands (2018 Study) | MAPE range: 12%-34% (varies by brand/activity) | MAPE range: 1%-42% (varies by brand/activity) | [15] |
Table 3: Accuracy of Energy Expenditure and Other Metrics
| Device / Study Focus | Energy Expenditure (Calories) Accuracy | Other Metrics | Source |
|---|---|---|---|
| Apple Watch (Meta-Analysis) | Mean Bias: 0.30 kcal/min; MAPE: 27.96% | N/A | [2] [3] |
| Various Wearables (Umbrella Review) | Mean Bias: -3 kcal/min (range: -21.27% to 14.76%) | Aerobic Capacity (VO₂max): Overestimation by 9.83%-15.24%Sleep: Tends to overestimate total sleep time (MAPE >10%) | [18] |
| Multiple Brands (2018 Study) | MAPE up to 44% (varies by brand/activity) | Sleep Duration: High accuracy (MAPE ~0.10) | [15] |
The data consistently shows that while heart rate and step count are generally measured with reasonable accuracy, energy expenditure (calorie burn) is a particularly challenging metric for all wearable devices, with error rates often exceeding what is considered clinically valid [2] [18] [15]. Newer models show a trend of gradual improvement, and recent research is developing more accurate algorithms for specific populations, such as individuals with obesity [2] [19].
Experimental Protocols for Validating Wearables
To critically assess validation studies, researchers must understand the standard experimental protocols and reference standards used. The following workflow diagram outlines a typical validation study design.
Participant Recruitment and Instrumentation
Studies typically recruit a cohort of healthy adult subjects, though recent research increasingly focuses on specific clinical populations (e.g., individuals with obesity) [19]. Sample sizes vary, with smaller studies involving around 20-50 participants [15] [19] and larger meta-analyses synthesizing data from hundreds of thousands of individuals [18]. Participants are simultaneously fitted with the consumer wearable device(s) under test and the research-grade reference equipment.
Controlled Activity Protocol
A critical phase involves subjects performing a structured set of activities while being monitored. This protocol is designed to assess device performance across different physiological states and movement patterns. A typical protocol includes:
- Resting State: To establish baselines for heart rate and metabolic rate.
- Ambulatory Activities: Such as walking and running at controlled speeds, often on a treadmill.
- Cycling: Using stationary bikes.
- Activities of Daily Living: And, in more recent studies, free-living conditions, sometimes with body cameras for ground truth annotation [15] [19].
Gold Standard Reference Measures
The accuracy of wearable devices is judged by comparing their data outputs to those from accepted gold standard clinical and research tools. The table below lists key reference methods.
Table 4: Research Reagent Solutions for Validation Studies
| Resource / Tool | Function in Validation | Example Use Case |
|---|---|---|
| Metabolic Cart | Measures oxygen consumption (VO₂) and carbon dioxide production (VCO₂) to calculate Energy Expenditure via indirect calorimetry. Considered a gold standard. | Used as criterion measure for validating calorie burn estimates during rest and various physical activities [19]. |
| Electrocardiogram (ECG) | Provides clinical-grade measurement of heart rate and heart rhythm. | Used as a reference for validating optical heart rate sensors on wearable devices [15] [12]. |
| Manually Counted Steps | Provides a ground-truth measure of step count. | Serves as a simple, accurate reference for validating pedometer functions during walking/running protocols [15]. |
| Polysomnography (PSG) | Comprehensive sleep study tracking brain waves, blood oxygen, heart rate, breathing, and eye/leg movements. | Used as a gold standard for validating wearable-derived sleep stage and sleep duration data [18]. |
| Actigraphy | A research-grade activity monitor, often worn on the wrist or hip. | Sometimes used as a higher-grade benchmark against which consumer devices are compared [12]. |
Data Processing and Statistical Analysis
Data from the wearable devices and reference standards are time-synchronized and processed. Common statistical measures used to report validity include:
- Mean Absolute Percentage Error (MAPE): The average absolute percentage difference between the device and the reference standard.
- Mean Bias: The average difference between the device and the reference standard, indicating systematic over- or under-estimation.
- Limits of Agreement (LoA): Often derived from Bland-Altman analysis, showing the range within which 95% of the differences between the two measurement methods lie [3].
- Intraclass Correlation Coefficient (ICC): Measures the reliability or consistency between the device and the gold standard measurements.
The Scientist's Toolkit
For researchers incorporating wearable data into clinical trials or scientific studies, understanding the components of a robust validation framework is essential. The following table details key resources.
Table 5: Essential Research Toolkit for Wearable Validation
| Tool / Resource Category | Specific Examples | Critical Function |
|---|---|---|
| Gold Standard Reference Devices | Metabolic cart, ECG, Polysomnography system | Provide the criterion measure against which consumer device accuracy is judged [15] [19]. |
| Standardized Validation Protocols | INTERLIVE Network recommendations, FIMS global standards | Ensure consistency, comparability, and rigor across different validation studies [18]. |
| Open-Source Algorithms & Software | Northwestern's dominant-wrist algorithm for obesity | Enable transparency, replication, and improvement of data processing methods, especially for underrepresented groups [19]. |
| Living Evidence Syntheses | "Living" umbrella reviews (e.g., [18]) | Provide continuously updated assessments of device accuracy in a rapidly evolving market, crucial for informed decision-making. |
| Data Privacy & Security Framework | Institutional review board (IRB) protocols, data anonymization tools | Protect sensitive participant health data collected by wearables, a major ethical and legal requirement [12] [20]. |
The wearable device market is characterized by a significant validation gap, with only an estimated 11% of devices validated for at least one biometric outcome [18]. For the devices that have been assessed, accuracy is highly metric-dependent, with heart rate and step counts being generally reliable, while energy expenditure measurements often contain substantial errors. Researchers must prioritize the use of devices and metrics with established validity for their specific population of interest and must be critical consumers of validation literature, paying close attention to the experimental protocols and reference standards used. The development of standardized validation frameworks and living evidence syntheses is crucial to bridge this gap and ensure that wearable-generated data meets the rigorous standards required for scientific and clinical application.
From Data to Discovery: Methodological Frameworks for Research Applications
Standardized Protocols for Validating Wearables in Specific Populations
The accuracy of data from wearable devices is not uniform; it varies significantly across different biometric outcomes and is highly dependent on the specific population being studied. For researchers and drug development professionals, employing standardized validation protocols is paramount to ensuring that wearable-generated endpoints are reliable, clinically meaningful, and fit for purpose in clinical trials and scientific studies. This guide objectively compares the performance of various wearables and details the experimental methodologies essential for their rigorous validation.
Quantitative Accuracy of Wearable Devices
The table below summarizes the accuracy of consumer wearables for various biometric measures, as synthesized from systematic reviews and primary validation studies. This data serves as a benchmark for comparing device performance.
Table 1: Accuracy of Wearable Devices for Key Biometric Measures
| Biometric Measure | Device(s) Tested | Reference Standard | Accuracy Metric | Reported Performance | Context & Population |
|---|---|---|---|---|---|
| Step Count | Archon Alive 001 [5] | Manual hand tally | Mean Absolute Percentage Error (MAPE) | 3.46% MAPE | Controlled treadmill walking (3-8 kph) in healthy adults [5] |
| Actigraph wGT3x-BT [5] | Manual hand tally | Mean Absolute Percentage Error (MAPE) | 31.46% MAPE | Controlled treadmill walking (3-8 kph) in healthy adults [5] | |
| Heart Rate (HR) | Corsano CardioWatch [21] | Holter ECG | Bias (BPM); 95% LoA | -1.4 BPM; -18.8 to 16.0 | 24-hour free-living, children with heart disease [21] |
| Hexoskin Smart Shirt [21] | Holter ECG | Bias (BPM); 95% LoA | -1.1 BPM; -19.5 to 17.4 | 24-hour free-living, children with heart disease [21] | |
| Archon Alive 001 [5] | Polar OH1 | ICC; Bias (BPM) | ICC 75.8%; -3.33 BPM | Controlled treadmill walking and running [5] | |
| Calorie Expenditure | Archon Alive 001 [5] | PNOĒ metabolic analyzer | Mean Absolute Percentage Error (MAPE) | 29.3% MAPE | Controlled treadmill walking and running [5] |
| Heart Rate (General) | Various Consumer Wearables [18] | Clinical-grade devices | Mean Absolute Bias | ± 3% | Synthesis of 24 systematic reviews [18] |
| Aerobic Capacity (VO₂max) | Various Consumer Wearables [18] | Clinical gas analysis | Overestimation | 9.83% - 15.24% | Synthesis of 24 systematic reviews [18] |
| Sleep Measurement | Various Consumer Wearables [18] | Polysomnography | Tendency to Overestimate | MAPE > 10% | Synthesis of 24 systematic reviews [18] |
Detailed Experimental Protocols for Validation
A robust validation protocol must define the context of use, population, and rigorous methodology against an accepted reference standard.
Protocol for Validating Heart Rate in Pediatric Cardiology
This protocol is based on a prospective cohort study validating two wearables in children with heart disease [21].
- Objective: To assess the accuracy and patient satisfaction of the Corsano CardioWatch (wristband) and Hexoskin smart shirt in children with congenital heart disease or suspected arrhythmias.
- Population: 31-36 pediatric participants (mean age ~13 years) indicated for 24-hour Holter monitoring [21].
- Reference Standard: 24-hour Holter electrocardiogram (ECG), applied by a certified nurse [21].
- Device Setup:
- CardioWatch: Worn tightly on the non-dominant wrist, connected via Bluetooth to a smartphone for data syncing [21].
- Hexoskin Shirt: Appropriate size selected based on chest circumference. Electrode transmission gel applied for better signal conduction. Holter electrodes were placed strategically to avoid interference with the shirt's electrodes [21].
- Procedure: Participants wore all three devices (Holter, CardioWatch, Hexoskin) simultaneously for a 24-hour free-living period. They were encouraged to maintain their normal routine but avoid showering and swimming. A symptom and activity diary was maintained [21].
- Data Analysis:
- Accuracy: Defined as the percentage of heart rate measurements within 10% of Holter values. Agreement was assessed using Bland-Altman analysis (bias and 95% Limits of Agreement) [21].
- Subgroup Analysis: Accuracy was analyzed based on factors like BMI, age, time of wearing, and heart rate zone [21].
- Patient Satisfaction: Measured using a 5-point Likert scale questionnaire and compared to satisfaction with the Holter monitor [21].
The following workflow diagrams the key stages of this pediatric validation protocol:
Protocol for Validating Step Count and Calorie Expenditure
This protocol outlines a controlled laboratory study to validate an affordable fitness tracker's core metrics [5].
- Objective: To assess the validity of the Archon Alive 001 for step count, heart rate, and energy expenditure during treadmill walking and running.
- Population: Healthy adults (BMI 18-25 kg/m²) with no contraindications to exercise [5].
- Reference Standards:
- Device Placement: The Archon Alive and Actigraph (used for step count comparison) were randomized on the non-dominant wrist. The Polar OH1 was placed on the upper arm [5].
- Treadmill Protocol: Participants completed stages at 3, 4, 5, and 8 km/h, each lasting 3 minutes with 1-minute rest intervals [5].
- Data Analysis:
- Step Count: Mean Absolute Percentage Error (MAPE) was calculated relative to hand tally. A MAPE ≤ 3% was considered clinically irrelevant. Multivariate analysis of variance (MANCOVA) assessed the effect of speed and demographics on accuracy [5].
- Heart Rate: Intraclass Correlation Coefficient (ICC) and Bland-Altman analysis (bias, 95% LoA) against the Polar OH1 [5].
- Calorie Expenditure: MAPE and correlation (r) against the PNOĒ analyzer [5].
The Scientist's Toolkit: Research Reagent Solutions
For researchers designing validation studies, the following table details essential materials and their functions.
Table 2: Essential Materials for Wearable Validation Studies
| Item Name | Function in Validation | Example Use Case |
|---|---|---|
| Holter Electrocardiogram (ECG) | Gold standard for ambulatory heart rate and rhythm monitoring [21]. | Validating wearable heart rate and arrhythmia detection in clinical populations [21]. |
| Portable Metabolic Analyzer (e.g., PNOĒ) | Gold standard for measuring energy expenditure (calories) via gas analysis [5]. | Validating calorie expenditure algorithms in wearables during controlled exercise [5]. |
| Research-Grade Accelerometer (e.g., ActiGraph) | Objective measure of physical activity and step count; considered a criterion device in research [5]. | Benchmarking the step count and activity intensity accuracy of consumer wearables [5]. |
| Photoplethysmography (PPG) Sensor (e.g., Polar OH1) | Provides validated heart rate data from a wearable form factor [5]. | Serving as a reference for optical heart rate sensors in consumer wristbands [5]. |
| Medical-Grade Biosensor (e.g., Everion) | Provides aggregated, validated accelerometer and physiological data for continuous monitoring [22]. | Calibrating less accurate but more unobtrusive ambient sensor systems (e.g., passive infrared sensors) [22]. |
Navigating the Regulatory and Validation Pathway
Integrating wearables into clinical research requires adherence to a rigorous regulatory and scientific pathway to ensure data quality and regulatory compliance.
- Context of Use (COU) is Critical: The FDA and other regulators require that validation be performed for the specific context of use. A device validated for general wellness tracking is not automatically qualified for use as a clinical trial endpoint [23] [24].
- Analytical and Clinical Validation: The validation process has two key stages [23] [24]:
- Analytical Validation: Does the device measure the physiological parameter accurately and reliably? This is tested against a reference standard in a controlled setting.
- Clinical Validation: Does the measurement correlate with a clinically meaningful endpoint or outcome in the target population?
- Global Regulatory Considerations: The regulatory landscape is fragmented. The FDA's Digital Health Innovation Action Plan and the EMA's framework emphasize data quality, security, and clinical validation. Multinational trials must navigate regional variations, including GDPR compliance in Europe and local certification requirements in Asia-Pacific countries [24].
The diagram below illustrates the key stages a wearable must pass through to be deemed suitable for clinical research.
Key Considerations for Specific Populations
- Pediatric and Young Adult Populations: A scoping review revealed that wearable studies in pediatric oncology primarily use devices like ActiGraph and Fitbit to monitor physical activity and sleep, often as data collection tools rather than active interventions [25]. Validation in children is crucial as their higher, more variable heart rates and activity patterns differ significantly from adults [21].
- Older Adults: This population may prefer unobtrusive, contactless monitoring systems (e.g., passive infrared sensors) due to discomfort or difficulty with wearable devices. A promising strategy is to use wearable biosensors for initial calibration of these ambient systems to improve their accuracy for quantifying in-home physical activity [22].
In conclusion, the journey toward standardized validation is ongoing. While significant variability in device accuracy persists [18], the research community is moving toward more rigorous, population-specific testing frameworks. By adhering to detailed experimental protocols and understanding the regulatory pathway, researchers can confidently leverage wearable technology to generate high-quality, clinically relevant data.
Integrating Wearable EE Data with Gold-Standard Measures (e.g., Indirect Calorimetry)
The accurate measurement of energy expenditure (EE) is fundamental to research in metabolism, nutrition, and exercise physiology. While wearable fitness trackers have democratized access to personal activity data, their integration with gold-standard measures like indirect calorimetry remains crucial for validating and improving their accuracy in research settings. Energy expenditure consists of three components: resting energy expenditure (approximately 60%), physical activity energy expenditure (PAEE, approximately 30%), and diet-induced thermogenesis (approximately 10%) [26]. For researchers and drug development professionals, understanding the alignment between consumer-grade wearable data and laboratory standards is essential for determining appropriate applications of these devices in clinical trials and physiological studies.
The historical progression of EE assessment methodologies reveals a continuous evolution toward less invasive, more practical solutions. From the initial emergence of calorimeters in the late 18th century to the steady development of standardized equations throughout the 20th century, the field has now entered an intelligent era characterized by machine learning and computer vision applications [26]. This review examines the current state of integrating wearable EE data with established reference standards, providing researchers with a critical analysis of methodological approaches, accuracy assessments, and practical implementation frameworks.
Gold-Standard Measures for Energy Expenditure Validation
Established Reference Methodologies
Research validating wearable energy expenditure data relies on several established gold-standard measures, each with distinct advantages and limitations:
Indirect Calorimetry: This method estimates energy expenditure by measuring oxygen consumption (VO₂) and carbon dioxide production (VCO₂) [27] [26]. It is considered one of the most accurate approaches for estimating EE because it directly reflects metabolic activity [27] [26]. Portable systems such as the PNOĒ metabolic analyzer enable measurements during physical activity, making them particularly valuable for validating wearable devices under controlled conditions [5].
Doubly Labelled Water (DLW) Technique: This approach uses stable isotopes to measure total daily energy expenditure over extended periods (typically 1-2 weeks) in free-living conditions [26]. While considered a gold standard for free-living total energy expenditure measurement, it is not suitable for assessing EE during single exercise sessions [26].
Direct Calorimetry: This method quantifies metabolic rate by precisely measuring heat loss through a calorimeter [26]. Although highly accurate, its application is limited by high costs, technical complexity, and the need for controlled laboratory conditions [26].
Comparative Framework for Validation Studies
When designing validation protocols, researchers should consider the appropriate reference standard based on the research question:
Table 1: Gold-Standard Methods for Energy Expenditure Validation
| Method | Primary Application | Advantages | Limitations |
|---|---|---|---|
| Indirect Calorimetry | Short-duration exercise validation | High accuracy for discrete activities; measures substrate utilization | Limited to controlled settings; equipment can be cumbersome |
| Doubly Labelled Water | Free-living total energy expenditure | Captures real-world activity patterns over time | Expensive; cannot provide exercise-specific data |
| Direct Calorimetry | Fundamental metabolic research | Considered the most accurate method | Highly specialized equipment; impractical for most validation studies |
Accuracy Assessment of Consumer Wearables
Quantitative Performance Across Metrics
Recent validation studies reveal significant variation in the accuracy of consumer wearables across different metrics. A comprehensive meta-analysis of 45 scientific studies examining commonly used fitness trackers found that these devices demonstrate markedly different performance levels depending on the metric being measured [4].
Table 2: Overall Accuracy of Fitness Trackers by Metric Type
| Metric | Average Accuracy | Performance Classification | Top Performing Device |
|---|---|---|---|
| Heart Rate | 76.35% | Strong | Apple Watch (86.31%) |
| Step Count | 68.75% | Moderate | Garmin (82.58%) |
| Energy Expenditure | 56.63% | Moderate | Apple Watch (71.02%) |
The overall cumulative accuracy across HR, SC, and EE metrics provided by analyzed fitness trackers is moderate, ranging between 62.09% and 73.53%, with an average score of 67.40% for accuracy [4]. This analysis highlights the particular challenge wearables face in measuring energy expenditure, a complex physiological process influenced by multiple individual factors.
Device-Specific Performance Analysis
Research comparing specific wearable devices against gold standards provides granular insights into their performance characteristics:
Apple Watch: In a meta-analysis of 56 studies, Apple Watches demonstrated a mean absolute percent error of 4.43% for heart rate and 8.17% for step counts, while the error for energy expenditure was significantly higher at 27.96% [2]. This inaccuracy was observed across all types of users and activities tested, including walking, running, cycling, and mixed-intensity workouts [2].
Archon Alive 001: A 2025 validation study comparing this affordable tracker (under $45) found it had a Mean Absolute Percentage Error (MAPE) of 3.46% for step count compared to manual hand tally, demonstrating high accuracy for this metric [5]. However, for total calorie expenditure, the device showed 29.3% MAPE relative to PNOĒ metabolic analyzer, indicating moderate accuracy for energy expenditure [5].
General Performance Trends: Newer wearable models generally show improved accuracy over earlier versions, with a "noticeable trend of gradual improvements over time" as manufacturers refine their sensors and algorithms [2]. However, the fundamental challenge of accurately estimating energy expenditure remains, with even the best-performing devices showing significant error margins compared to gold-standard measures.
Methodological Approaches for Integration and Validation
Experimental Protocols for Device Validation
Robust validation studies employ standardized protocols to assess wearable device performance under controlled conditions:
Treadmill Protocols: Studies typically have participants walk or run on treadmills at varying speeds (e.g., 3, 4, 5, and 8 km/h) while simultaneously wearing the consumer wearable and being connected to reference equipment such as portable gas analyzers [5]. Each stage typically lasts 3-5 minutes with rest intervals between stages to allow for equipment adjustments [5].
Comparative Metrics: Researchers calculate Mean Absolute Percentage Error (MAPE), Intraclass Correlation Coefficient (ICC), and Bland-Altman analysis to assess agreement between devices [5]. MAPE ≤3% is generally considered clinically irrelevant, providing a benchmark for acceptable performance [5].
Free-Living Validation: For assessing real-world performance, researchers combine doubly labelled water with wearable data collection over extended periods (typically 7-14 days) to capture a more comprehensive picture of device performance outside laboratory settings.
Emerging Technical Approaches
Recent research has explored innovative methods to enhance the accuracy of energy expenditure estimation:
Personalized Machine Learning Models: A 2025 study developed person-specific and group-level models using the Random Forest algorithm, analyzing 7 combinations of 4 biomarkers across 1 to 16 body locations [28]. Personalized models achieved significantly higher accuracy (2% MAPE) compared to generalized models (16.5%-28% MAPE) but were more sensitive to sensor placement and data availability [28].
Multi-Sensor Data Fusion: The highest accuracy in personalized EE prediction is achieved when combining movement-based, thermal, and cardiovascular data [28]. While accelerometry alone performs well, adding physiological inputs, particularly skin temperature, improves accuracy, especially for females [28].
Real-Time Energy Expenditure Estimation: The RTEE method integrates a Deep Q-Network-based activity intensity coefficient inference network with a modified energy consumption prediction algorithm to estimate energy expenditure based on real-time variations in the user's heart rate measurements [27]. This approach adapts conventional EE estimation formulas with a reinforcement learning component to improve real-time prediction accuracy.
The following diagram illustrates the typical experimental workflow for validating wearable energy expenditure data against gold-standard measures:
Experimental Validation Workflow for Wearable EE Data
Research Reagent Solutions: Essential Tools for EE Validation
Table 3: Essential Research Equipment for Wearable Validation Studies
| Equipment Category | Specific Examples | Research Function | Key Features |
|---|---|---|---|
| Reference Metabolic Systems | PNOĒ metabolic analyzer, Douglas bag systems, Portable gas analyzers | Provides criterion measure for energy expenditure via indirect calorimetry | Measures oxygen consumption (VO₂) and carbon dioxide production (VCO₂) to calculate EE [5] |
| Research-Grade Accelerometers | Actigraph wGT3x-BT | Serves as intermediate standard for physical activity assessment | Validated 3-dimensional accelerometer commonly used in research settings [5] |
| Heart Rate Monitoring Systems | Polar OH1, Electrocardiogram systems | Provides validation standard for heart rate measurements | Photoplethysmography or ECG-based systems for comparison with wearable optical HR [5] |
| Calibration Equipment | Treadmills with calibrated speed settings, Flow sensors, Gas calibration kits | Ensures accuracy and standardization of measurement equipment | Provides controlled exercise intensities and calibrated gas flow measurements [5] |
| Data Analysis Platforms | ActiLife software, Custom MATLAB/Python scripts, Statistical packages | Processes and analyzes collected data for comparison | Enables calculation of MAPE, ICC, Bland-Altman analysis, and other validation metrics [5] |
The integration of wearable EE data with gold-standard measures reveals both opportunities and limitations for research applications. While consumer wearables demonstrate strong performance in measuring heart rate and moderate accuracy for step counting, their energy expenditure estimates show significantly higher error rates (27-30% MAPE) compared to reference standards [2] [5]. This indicates that while these devices can provide valuable general trends for population-level studies, their precision may be insufficient for clinical applications requiring high accuracy.
For researchers and drug development professionals, the strategic integration of wearable EE data should be guided by study objectives and precision requirements. Personalized models that combine multiple physiological signals show promise for improving accuracy but require more complex implementation [28]. Future directions should focus on developing standardized validation protocols, exploring hybrid modeling approaches that combine consumer wearables with brief gold-standard assessments, and addressing ethical considerations around data ownership and algorithm transparency as these technologies become more integrated into healthcare and clinical research [26].
The validation of energy expenditure (EE) algorithms in wearable technology represents a critical frontier in digital health. However, a significant accuracy gap persists for specific populations, particularly individuals with obesity, who exhibit distinct physiological and biomechanical characteristics [19] [29]. Current activity-monitoring algorithms, predominantly developed for and validated on populations without obesity, often fail to accurately reflect the physical activity and energy usage of people with higher body weight [19] [30]. This population stands to benefit immensely from physical activity trackers for health management, yet they are underserved by existing technology [31].
The inaccuracies stem from several factors specific to obesity. Individuals with obesity demonstrate known differences in walking gait, postural control, resting energy expenditure, and preferred walking speed compared to people without obesity [29]. Furthermore, hip-worn devices—often used in research settings—are prone to decreased accuracy due to biomechanical differences such as altered gait patterns and device tilt angle in people with obesity [29]. This case study examines the development and validation of a novel algorithm designed specifically to address these challenges and improve the accuracy of calorie tracking for individuals with obesity.
Comparative Performance Analysis of Energy Expenditure Algorithms
To objectively evaluate the landscape of algorithm performance, the following table summarizes key quantitative findings from recent validation studies, including the novel population-specific algorithm developed by Northwestern University researchers.
Table 1: Comparative Performance of Energy Expenditure Estimation Methods
| Algorithm/Device | Target Population | Validation Method | Key Performance Metric | Results |
|---|---|---|---|---|
| Northwestern University BMI-Inclusive Algorithm [19] [29] | Individuals with obesity | Metabolic cart (in-lab); Wearable camera (free-living) | Root Mean Square Error (RMSE) for METs; Overall Accuracy | RMSE: 0.281-0.32 METs; >95% accuracy in real-world situations |
| Archon Alive 001 (Affordable Tracker) [5] | General Population (BMI 18-25) | PNOĒ metabolic analyzer | Mean Absolute Percentage Error (MAPE) for Calorie Expenditure | 29.3% MAPE |
| Various Commercial Wrist-Worn Devices (Systematic Review) [32] | General Population | Multiple gold-standard methods | Mean Absolute Percentage Error (MAPE) for Energy Expenditure | MAPE >30% across all devices |
The data reveals a significant advancement represented by the Northwestern algorithm. While affordable commercial trackers like the Archon Alive and other wrist-worn devices show poor accuracy for energy expenditure (MAPE >29%), the population-specific model achieves a high level of precision, with an RMSE for Metabolic Equivalent of Task (MET) estimation below 0.32 and overall accuracy exceeding 95% when validated against a metabolic cart [19] [5] [29]. This performance is particularly notable given that the algorithm was benchmarked against 11 state-of-the-art algorithms and demonstrated superior performance across various activity intensities [19] [29].
Detailed Experimental Protocols for Algorithm Validation
The development and validation of the Northwestern algorithm involved a multi-stage, rigorous methodology that can serve as a model for future population-specific calibration research.
In-Lab Validation Protocol
This protocol was designed to collect high-fidelity data under controlled conditions [19] [29].
- Participant Profile: The study enrolled 27 participants (17 female) with obesity. Key demographic and health metrics were recorded.
- Sensor Configuration: Each participant was fitted with a Fossil Sport smartwatch (containing accelerometer and gyroscope sensors) on the wrist and an ActiGraph wGT3X+ activity monitor for comparative analysis.
- Gold-Standard Reference: Participants wore a metabolic cart during testing. This system measures the volume of oxygen inhaled and carbon dioxide exhaled to calculate energy burn in kilocalories (kCals) and resting metabolic rate with high precision [19].
- Activity Protocol: Participants engaged in a series of structured activities designed to capture a range of movement intensities (e.g., sedentary, light, moderate-to-vigorous). This created a paired dataset of sensor readings and ground-truth energy expenditure values.
- Data Processing: The raw sensor data from the smartwatch was used to build a machine learning model to estimate minute-by-minute MET values. The model's predictions were then compared to the MET values derived from the metabolic cart to calculate accuracy metrics like RMSE [29].
Free-Living Validation Protocol
To test the algorithm's performance in real-world settings, a second validation protocol was implemented [19] [29].
- Participant Profile: 25 participants (16 female) with obesity were enrolled.
- Sensor Configuration: Participants wore the study smartwatch and a body camera during their daily activities for two days.
- Validation Methodology: The body camera provided visual confirmation of physical activity, allowing researchers to identify specific instances where the algorithm's estimates of energy expenditure were inaccurate. This method enabled the team to pinpoint activities that caused over- or under-estimation of kCals [19] [31]. In total, 14,045 minutes of free-living data were analyzed.
- Performance Benchmarking: The algorithm's MET estimates in free-living conditions were compared to those from the top-performing actigraphy-based algorithm (Kerr et al.'s method). The new model's estimates fell within ±1.96 standard deviations of this benchmark for 95.03% of the minutes analyzed, demonstrating high concordance [29].
Diagram 1: Algorithm Validation Workflow
The Researcher's Toolkit: Essential Materials and Methods
Table 2: Key Research Reagents and Solutions for Validation Studies
| Item | Specification/Function | Application in Validation |
|---|---|---|
| Metabolic Cart | Measures O₂ inhaled and CO₂ exhaled via a mask. | Gold-standard method for calculating energy expenditure (kCals) and resting metabolic rate in lab settings [19]. |
| Research-Grade Accelerometer | ActiGraph wGT3X+ or wGT3X-BT. | Provides research-grade activity count data for benchmarking commercial device performance [5] [29]. |
| Wearable Camera | Body-worn device capturing first-person view. | Provides visual ground truth for activity type and context in free-living validation studies [19] [29]. |
| Portable Cardio-Metabolic Analyzer | PNOĒ system with Hans Rudolph mask. | Validates energy expenditure and heart rate by analyzing respiratory gases during exercise [5]. |
| Photoplethysmography Heart Rate Monitor | Polar OH1. | Provides validated heart rate data for benchmarking optical heart rate sensors in wearables [5]. |
| Open-Source Algorithm | Northwestern's model (open-source). | A transparent, rigorously testable algorithm that researchers can build upon for inclusive fitness tracking [19] [31]. |
Implications for Research and Clinical Practice
The development of population-specific algorithms marks a paradigm shift in wearable technology validation. The open-source nature of the Northwestern algorithm is particularly significant, as it provides a transparent, rigorously testable foundation that other researchers can replicate and build upon, addressing a critical gap in the field where most commercial algorithms remain proprietary [19] [29]. This approach enables the research community to advance the science of inclusive fitness tracking collectively.
From a clinical and public health perspective, accurate activity monitoring for individuals with obesity is crucial for tailoring effective interventions and improving health outcomes [19] [33]. Reliable data empowers healthcare professionals to design personalized programs and can accurately reflect the substantial effort exerted by individuals with obesity during physical activity, which is often underestimated by standard devices [19] [31] [30]. As one researcher noted, "Fitness shouldn't feel like a trap for the people who need it most" [19]. Future research should continue to explore population-specific calibrations across diverse groups and integrate these advanced algorithms into widely available commercial devices to maximize their public health impact.
The integration of wearable activity trackers into clinical trials represents a paradigm shift in how researchers monitor patient activity and energy balance outside traditional laboratory settings. These devices offer the potential for continuous, real-world data collection on key physiological parameters, enabling unprecedented insights into patient health and treatment outcomes. However, their utility is entirely dependent on the accuracy and reliability of the metrics they report. For clinical researchers and drug development professionals, understanding the specific strengths and limitations of these devices is critical for designing robust trials and interpreting resulting data. This guide provides an objective, evidence-based comparison of wearable device performance, focusing on the quantitative data and experimental protocols essential for their application in clinical research.
Quantitative Accuracy of Key Biometric Measurements
The validity of wearable data varies significantly by the type of metric being measured. The following tables summarize device performance for core parameters relevant to clinical trials, based on aggregated validation studies.
Accuracy of Core Activity and Energy Expenditure Metrics
Table 1: Accuracy of wearable devices for measuring activity and energy expenditure metrics. Error percentages are calculated against gold-standard reference methods (e.g., indirect calorimetry for energy expenditure, manually counted steps for step count).
| Device | Heart Rate (% Error) | Caloric Expenditure (% Error) | Step Count (% Error) | Sleep/Wake Identification (% Accuracy) |
|---|---|---|---|---|
| Apple Watch | 1.3% (underestimation) [16] | 27.96% (MAPE*) [2]; Up to 115% [16] | 0.9-3.4% [16] | 97% (Sleep Onset) [16] |
| Oura Ring | 99.3% (Resting HR Accuracy) [16] | 13% [16] | 4.8%-50.3% [16] | 94% (Sleep Onset) [16] |
| WHOOP | 99.7% (Accuracy) [16] | N/A | N/A (Strain Metric Used) [16] | 90% (Sleep Onset) [16] |
| Garmin | 1.16-1.39% [16] | 6.1-42.9% [16] | 23.7% [16] | 98% (Sleep Onset) [16] |
| Fitbit | 9.3 BPM (underestimation) [16] | 14.8% [16] | 9.1-21.9% [16] | Overestimates Total Sleep Time [16] |
| Samsung | 7.1 BPM (underestimation) [16] | 9.1-20.8% [16] | 1.08-6.30% [16] | 65% (Sleep Stages) [16] |
| Polar | 2.2% (Upper Arm) [16] | 10-16.7% [16] | N/A | 92% (Sleep Onset) [16] |
MAPE: Mean Absolute Percentage Error
Accuracy in Disease and Medical Event Detection
For clinical trials focusing on specific disease outcomes, the ability of wearables to detect medical events is of paramount importance. Meta-analyses of real-world detection studies show promising results.
Table 2: Diagnostic accuracy of wearable devices for detecting medical conditions, as reported in systematic reviews and meta-analyses.
| Medical Condition | Pooled AUC (%) | Pooled Sensitivity (%) | Pooled Specificity (%) | Pooled PPV (%) | Key Devices Studied |
|---|---|---|---|---|---|
| COVID-19 | 80.2 | 79.5 | 76.8 | N/A | Fitbit, Apple Watch, Oura Ring [34] |
| Atrial Fibrillation | N/A | 94.2 | 95.3 | 87.4 | Apple Watch, Others [34] |
| Fall Detection | N/A | 81.9 | 62.5 | N/A | Various [34] |
A systematic review and meta-analysis evaluating wearables for disease detection concluded that while these devices show promise, "further research and improvements are required to enhance their diagnostic precision and applicability" [34].
Experimental Protocols for Validating Wearable Metrics
The data presented above are derived from validation studies that employ rigorous methodologies to compare wearable device outputs against gold-standard references.
Protocol for Energy Expenditure (Caloric) Validation
- Objective: To assess the accuracy of a wearable device's estimate of total energy expenditure (kcal) and activity energy expenditure.
- Gold Standard Reference: Indirect calorimetry, typically using a portable metabolic cart (e.g., COSMED K5, VO2master) [35].
- Experimental Workflow:
- Participant Instrumentation: Participants are fitted with the gold-standard metabolic cart and the wearable device(s) under test.
- Baseline Measurement: Participants rest in a seated or supine position for 20-30 minutes to establish baseline resting energy expenditure.
- Structured Activity Protocol: Participants perform a series of activities of varying intensities in a controlled laboratory setting. A typical protocol includes:
- Sedentary tasks (e.g., typing, watching video)
- Light household chores (e.g., sweeping, tidying)
- Treadmill walking/running at multiple prescribed speeds (e.g., 3 km/h, 5 km/h, 8 km/h)
- Cycle ergometry at multiple prescribed power outputs (e.g., 50W, 100W, 150W)
- Data Synchronization: Timestamps from the wearable device and the metabolic cart are synchronized to align data streams for comparison.
- Data Analysis: The energy expenditure values from the wearable device are compared to the values from the metabolic cart across all activity stages and in aggregate. Statistical analyses include calculation of Mean Absolute Percentage Error (MAPE), Pearson correlation coefficients (r), and Bland-Altman plots to assess bias and limits of agreement [35] [2].
Protocol for Heart Rate and Heart Rate Variability (HRV) Validation
- Objective: To determine the accuracy of photoplethysmography (PPG)-based heart rate and HRV measurements.
- Gold Standard Reference: Electrocardiogram (ECG) [16] [35].
- Experimental Workflow:
- Participant Instrumentation: ECG electrodes are placed on the participant's chest in a standard configuration. The wearable device is worn according to manufacturer instructions (e.g., snug on the wrist).
- Controlled Resting Measurement: Participants rest quietly for 5-10 minutes while simultaneous ECG and PPG data are collected for resting heart rate and resting HRV (e.g., RMSSD) analysis.
- Ambulatory & Exercise Protocol: Participants engage in activities that introduce motion artifact, a key confounder for PPG. This includes:
- Walking and running on a treadmill
- Typing or performing arm movements while seated
- Functional strength training exercises [12]
- Data Processing: R-peaks are detected from the ECG signal to create a ground-truth tachogram. Pulse peaks are detected from the PPG signal. Inter-beat intervals (IBIs) are calculated from both.
- Data Analysis: Heart rate series from the wearable are compared to the ECG-derived heart rate. For HRV, time-domain (e.g., RMSSD, SDNN) and frequency-domain (e.g., LF, HF power) metrics from both sources are compared using correlation and error analysis [16].
Diagram 1: Wearable validation workflow.
Technical and Methodological Considerations for Clinical Trials
Research Reagent Solutions and Essential Materials
Table 3: Key equipment and tools required for validating and deploying wearables in clinical research.
| Item / Solution | Function in Research | Examples / Specifications |
|---|---|---|
| Gold-Standard Metabolic Cart | Measures oxygen consumption (VO₂) and carbon dioxide production (VCO₂) to calculate energy expenditure via indirect calorimetry. | COSMED K5, VO2master, Parvo Medics TrueOne |
| Electrocardiogram (ECG) System | Provides gold-standard measurement of heart rate and heart rate variability for validating optical heart rate sensors. | Biopac MP36R, ADInstruments PowerLab, Holter monitors |
| Actigraphy System | Research-grade motion sensor used as a higher-accuracy benchmark for activity and sleep/wake cycles. | ActiGraph wGT3X-BT, Axivity AX3 |
| Polysomnography (PSG) System | Comprehensive gold-standard for sleep staging (REM, NREM) and sleep quality assessment. | Compumedics Grael, Natus Sleepworks |
| Controlled Environment (Lab) | Standardizes external factors (temperature, humidity) and enables precise activity protocols. | Climate-controlled room, treadmills, cycle ergometers |
| Data Synchronization Software | Temporally aligns data streams from multiple devices (wearable, gold-standard) for precise comparison. | LabChart, AcqKnowledge, custom timestamp scripts |
Conceptual Framework for Clinical Trial Integration
Integrating wearables into a clinical trial requires a structured approach to ensure data quality and relevance.
Diagram 2: Clinical trial integration flow.
The evidence demonstrates a clear hierarchy in the accuracy of wearable metrics. Heart rate is generally the most accurately measured parameter, especially at rest, with many devices achieving error rates below 5% [16] [2]. In contrast, energy expenditure (caloric burn) remains a significant challenge, with even the best devices showing mean absolute percentage errors often exceeding 25% due to the complex physiological modeling required and individual variability [35] [2]. Step counts are reasonably accurate during steady-state walking but can be highly inaccurate during intermittent activities or upper-body movement [16].
For clinical trial application, this means:
- Device Selection Must Be Endpoint-Specific: Wearables are well-suited for trials where relative changes in activity (e.g., step count) or robust heart rate monitoring are primary endpoints. They are less suitable for trials requiring precise, absolute measurements of energy balance.
- Validation is Crucial: Before deployment in a trial, the specific device and model should be validated against a gold standard for the target population and activities relevant to the study.
- Focus on Trends, Not Absolute Values: The longitudinal tracking capability of wearables is one of their greatest strengths. Analyzing within-participant trends over time can be more reliable and clinically meaningful than interpreting single-point absolute values.
In conclusion, while wearable activity trackers offer a powerful tool for unobtrusive monitoring in clinical trials, researchers must critically appraise their accuracy limitations. The technology shows immense promise, particularly for detecting physiological patterns and changes, but it should be employed with a clear understanding of its current constraints, ensuring that clinical interpretations and conclusions are drawn on a foundation of validated, appropriately contextualized data.
Navigating Limitations: Strategies for Optimizing Data Fidelity
This guide objectively compares the performance of various wearable devices in estimating energy expenditure (EE) and other metrics under free-living conditions, framed within the broader thesis of accuracy validation for wearable calorie tracking research. It synthesizes current experimental data and methodologies to aid researchers and professionals in critically evaluating this technology.
The validation of wearable devices for assessing physical behavior, particularly energy expenditure, presents significant scientific challenges. A 2022 systematic review of 222 free-living validation studies revealed that this field is characterized by low methodological quality, with 72.9% of studies classified as high risk of bias and only 4.6% as low risk [36] [37]. This variability severely limits the comparability of devices and outcomes. The core of the problem lies in the transition from controlled laboratory settings to the unpredictable free-living environment, where a multitude of confounding factors introduce error into the estimates provided by consumer-grade wearables [37].
Quantitative Comparison of Wearable Device Accuracy
The following tables summarize the accuracy of various wearable devices for key metrics, based on aggregated study data. Accuracy is represented as Mean Absolute Percentage Error (MAPE), a standard metric for assessing deviation from a criterion measure.
Table 1: Overall Accuracy of Wearable Device Metrics (Average % Error)
| Device Brand | Caloric Expenditure | Heart Rate | Step Count | Sleep vs. Wakefulness |
|---|---|---|---|---|
| Apple Watch | 28.0% - 115% [2] [16] | ≤ 10% [38] [16] | 0.9% - 3.4% [16] | 3% Error [16] |
| Fitbit | 14.8% [16] | 9.3 BPM Underestimate [16] | 9.1% - 21.9% [16] | Overestimates TST [16] |
| Garmin | 6.1% - 42.9% [16] | 1.16% - 1.39% [16] | 23.7% [16] | 2% Error [16] |
| Oura Ring | 13% [16] | 99.3% Accuracy (Resting) [16] | 4.8% - 50.3% [16] | 4% - 6% Error [16] |
| Polar | 10% - 16.7% [16] | 2.2% (Upper Arm) [16] | N/A [16] | 8% Error [16] |
| Samsung | 9.1% - 20.8% [16] | 7.1 BPM Underestimate [16] | 1.08% - 6.30% [16] | 35% Error (Stages) [16] |
Table 2: Device Performance by Activity Type and Population
| Device / Context | Criterion Measure | Key Finding | Reported Error (MAPE or other) |
|---|---|---|---|
| Apple Watch (General) | Various Clinical [2] | Energy expenditure accuracy varies by activity. | MAPE: 27.96% (EE), 4.43% (HR), 8.17% (Steps) [2] |
| Fitbit, Apple, Polar (2022 Study) | Clinical Grade EE [39] | "Poor accuracy" across sitting, walking, running, cycling, strength training. | Coefficients of variation: 15% to 30% [39] |
| Archon Alive (Affordable Tracker) | PNOĒ Metabolic Analyzer [5] | Accurate for steps; insufficient for clinical calorie assessment. | MAPE: 29.3% (EE), 3.46% (Steps) [5] |
| New Algorithm for Obesity | Metabolic Cart (O2/CO2) [19] | Open-source algorithm significantly improves accuracy for a high-BMI population. | >95% Accuracy in real-world situations [19] |
Detailed Experimental Protocols for Free-Living Validation
To ensure valid and replicable results, researchers employ specific protocols that combine laboratory rigor with real-world conditions. Below are detailed methodologies from key studies.
Treadmill-Based Protocol for Step Count and Energy Expenditure
A 2025 study validating an affordable fitness tracker used a structured treadmill protocol to assess step count, heart rate, and energy expenditure [5].
- Participants: 35 healthy adults (BMI 18–25 kg/m²).
- Device Placement: ActiGraph wGT3x-BT and Archon Alive 001 were randomized on the non-dominant wrist. A Polar OH1 heart rate monitor was placed on the non-dominant upper arm.
- Criterion Measures:
- Step Count: Manual hand tally.
- Heart Rate: Polar OH1 photoplethysmography sensor.
- Energy Expenditure: PNOĒ portable cardio-metabolic analyzer, with participants wearing a Hans Rudolph mask for gas exchange analysis.
- Protocol: Participants walked/ran on a treadmill at 3, 4, 5, and 8 km/h. Each stage lasted 3 minutes with a 1-minute rest in between. Data from all devices and manual counts were collected simultaneously during each stage [5].
- Analysis: Mean Absolute Percentage Error (MAPE) was calculated for step count and EE against criterion measures. Bland-Altman analysis and Intraclass Correlation Coefficient (ICC) were used for heart rate [5].
Free-Living Validation with Video Observation
A Northwestern University study developed a novel algorithm for people with obesity using a comprehensive free-living validation protocol [19].
- Participants: Two groups were recruited.
- Criterion Measure: A metabolic cart (a mask measuring oxygen inhaled and carbon dioxide exhaled) was used for gold-standard energy expenditure calculation.
- Protocol:
- Group 1 (27 participants): Wore a fitness tracker and metabolic cart while performing a set of structured physical activities.
- Group 2 (25 participants): Wore a fitness tracker and a body camera during their daily lives. The video footage allowed researchers to visually confirm contexts where the algorithm over- or under-estimated energy expenditure, correlating specific activities with device data points [19].
- Activity Modification: The protocol included modified exercises (e.g., wall push-ups instead of floor push-ups) to be inclusive of different body types and fitness levels [19].
Multi-Day Free-Living Step Count Validation
A 2023 study evaluated the validity of wearable monitors and smartphone apps in both semi-structured and free-living settings [40].
- Participants: 24 healthy adults.
- Criterion Measure: Direct step observation (semi-structured) and ActiGraph (free-living).
- Protocol:
- Semi-Structured Study: Conducted in a lab setting with controlled activities.
- Free-Living Study: Participants wore the devices for 3 consecutive days during their habitual daily activities.
- Analysis: Validity was evaluated using MAPE, Bland-Altman plots, and Intraclass Correlation Coefficients (ICC) comparing each monitor and app to the criterion measure [40].
Visualization of the Wearable Validation Framework
The following diagram illustrates the multi-stage validation framework proposed by researchers to ensure wearable devices are properly validated before use in health studies [36] [37].
Wearable Technology Validation Pipeline
This framework, proposed by Keadle et al., outlines five sequential phases with increasing levels of real-world application [36] [37]. Phases 0 and 1 involve fundamental device and algorithm development. Phase 2 establishes baseline accuracy in controlled laboratory settings. The critical Phase 3 assesses device performance in unconstrained free-living environments, which is essential for understanding real-world error. Finally, Phase 4 represents the deployment of validated devices in health research studies.
The Scientist's Toolkit: Key Research Reagents & Solutions
For researchers designing validation studies for wearables, the following tools and criterion measures are essential for generating high-quality data.
Table 3: Essential Reagents and Criterion Measures for Validation Studies
| Tool / Reagent | Function in Validation | Example Use Case |
|---|---|---|
| ActiGraph wGT3x-BT | A research-grade accelerometer used as a standard for measuring physical activity volume and step count [5]. | Served as a comparison device in a treadmill validation study for an affordable fitness tracker [5]. |
| PNOĒ Metabolic Analyzer | A portable gas analysis system that measures oxygen consumption (VO₂) and carbon dioxide production (VCO₂) to calculate Energy Expenditure via indirect calorimetry [5]. | Used as the criterion measure for calorie burn validation during treadmill walking and running [5]. |
| Doubly Labeled Water (DLW) | A gold-standard method for measuring total daily energy expenditure in free-living conditions over 1-2 weeks. | Referenced as an ideal criterion for free-living validation studies, though not used in the cited protocols [36]. |
| Polar OH1 | A validated photoplethysmography (PPG) heart rate monitor worn on the upper arm, used as a criterion for heart rate measurement [5]. | Provided criterion heart rate data synchronized with the PNOĒ metabolic analyzer in a validation study [5]. |
| Video Recording / Body Camera | Provides objective, ground-truth documentation of activity type and posture in free-living settings [19]. | Used to visually confirm periods of over- and under-estimation of calorie burn by the wearable device's algorithm [19]. |
| Metabolic Cart | A clinical system for analyzing respiratory gases to determine resting metabolic rate and exercise energy expenditure [19]. | Served as the gold-standard criterion for calibrating a new algorithm for people with obesity [19]. |
Discussion and Synthesis
The experimental data uniformly demonstrates that while devices like the Apple Watch and Fitbit can provide reasonably accurate measures of heart rate and step count, their estimation of energy expenditure remains problematic, with errors frequently exceeding 25-30% [39] [38] [2]. This inaccuracy is exacerbated in free-living conditions and for specific populations, such as individuals with obesity, whose gait and physiology may not be well-represented in standard algorithms [19] [30].
The development of open-source, population-specific algorithms, as seen in the Northwestern study, presents a promising path forward for improving accuracy [19]. For researchers, the choice of validation protocol and criterion measure is paramount. The tools and frameworks outlined here provide a foundation for conducting rigorous evaluations of wearable technology, ultimately enabling more reliable application in health and clinical research.
Addressing Algorithmic Biases in Diverse Populations and Clinical Groups
The integration of artificial intelligence (AI) with wearable technology represents a transformative shift in health monitoring, enabling continuous tracking of physiological parameters like heart rate, physical activity, and calorie expenditure. However, the promise of data-driven health insights is tempered by a critical challenge: algorithmic bias that can undermine accuracy and equity for diverse populations and clinical groups [41]. Studies consistently reveal that AI models and wearable devices often demonstrate disparate performance across different demographic groups and health conditions, risking the exacerbation of existing health disparities [42] [43].
The core of this problem lies in the data and assumptions underpinning these technologies. As noted in research on public health AI, "AI systems are only as effective as the data used to train them and the assumptions under which they are created" [41]. When these systems are developed on unrepresentative datasets—over-relying on data from urban, wealthy, or majority populations—they fail to generalize accurately for rural, indigenous, socially marginalized, or clinically unique groups [41]. This review compares the performance of wearable technologies across diverse user profiles, examines the sources and impacts of algorithmic bias, and outlines experimental protocols and tools essential for developing more equitable and accurate health monitoring solutions.
Performance Comparison of Wearable Technologies
The accuracy of wearable devices varies significantly depending on the metric being measured, the specific device, and the user population. The tables below summarize key quantitative findings from validation studies.
Table 1: Overall Accuracy of Consumer Wearables in General Population Studies
| Device | Metric | Accuracy (Mean Absolute Percent Error) | Context / Limitations |
|---|---|---|---|
| Apple Watch (Multiple Models) | Heart Rate | 4.43% | Meta-analysis of 56 studies; generally accurate [2]. |
| Apple Watch (Multiple Models) | Step Count | 8.17% | Meta-analysis of 56 studies; generally accurate [2]. |
| Apple Watch (Multiple Models) | Energy Expenditure (Calories) | 27.96% | Meta-analysis; significant inaccuracy across user types and activities [2]. |
| Archon Alive 001 (Affordable Tracker) | Step Count | 3.46% | High accuracy vs. hand tally; small effect from age/speed [5]. |
| Archon Alive 001 (Affordable Tracker) | Heart Rate | ICC: 75.8% | "Acceptable reliability" vs. Polar OH1; not clinical grade [5]. |
| Archon Alive 001 (Affordable Tracker) | Calorie Expenditure | 29.3% | MAPE relative to PNOĒ metabolic analyzer [5]. |
Table 2: Performance Variation in Clinical and Diverse Populations
| Population / Context | Device / Model | Performance Issue / Bias | Source / Consequence |
|---|---|---|---|
| Patients with Lung Cancer (slower gait, mobility issues) | Wearable Activity Monitors (WAMs) generically | Decreased accuracy at slower walking speeds [8]. | Altered movement patterns impair step-count accuracy; requires population-specific validation [8]. |
| Hispanic Patients (Sepsis Prediction) | Sepsis prediction models from high-income settings | Reduced accuracy [41]. | Representation bias from unbalanced training data [41]. |
| Racial/Ethnic Minorities, Older, Lower-Income Groups | AI models trained on convenience samples (e.g., All of Us BYOD) | Sharp performance decline (22-40% AUC loss) in out-of-sample tests [44]. | Representation bias; models fail to generalize due to non-probability sampling [44]. |
| Rural, Indigenous, Disenfranchised Groups | Public Health AI & Digital Health Apps | Systemic underdiagnosis, misclassification, or exclusion [41]. | Structural data exclusion and deployment bias from systems designed for high-resource settings [41]. |
| Global Diabetes AI Research | AI models for Type 2 Diabetes (T2D) | Limited demographic diversity [42]. | Only 7% of studies reported racial/ethnic demographics; regions like Africa and South America were underrepresented [42]. |
Typology and Origins of Algorithmic Bias
Algorithmic bias in wearable health technologies is not a monolithic issue but arises from multiple sources throughout the AI lifecycle. Understanding its typology is the first step toward effective mitigation.
Figure 1: The pathway of bias through the AI model lifecycle, showing how social and historical inequalities can be embedded and amplified at various stages.
Key Bias Types
- Historical Bias: Occurs when injustices and inequities from the past are embedded in the training data. A canonical example is a U.S. healthcare risk prediction algorithm that systematically underestimated the needs of Black patients by using historical healthcare expenditure as a proxy, unintentionally replicating patterns of underutilization of care [41].
- Representation Bias: Arises when datasets over-represent certain populations (e.g., urban, wealthy) and under-represent others (e.g., rural, indigenous, ethnic minorities). This was evident in sepsis prediction models developed in high-income settings that showed significantly reduced accuracy for Hispanic patients [41]. Similarly, the "bring-your-own-device" (BYOD) model for data collection inherently skews toward wealthier and more tech-savvy demographics [44].
- Measurement Bias: This happens when health endpoints are approximated using proxy variables that are not equally valid across groups. For instance, digital health initiatives in India that relied on smartphone usage for patient engagement effectively excluded women, older adults, and rural populations with limited digital access [41].
- Aggregation Bias: Occurs when models inappropriately assume homogeneity across heterogeneous groups, applying the same criteria or thresholds to populations with fundamental biological, cultural, or environmental differences [41].
- Deployment Bias: The failure that occurs when a tool developed in one specific context (e.g., a high-resource urban hospital) is implemented without modification in a vastly different setting (e.g., a low-resource rural community), leading to capricious performance [41].
Experimental Protocols for Bias Assessment and Validation
Rigorous, standardized experimental protocols are essential to quantify accuracy and identify disparate performance across groups. The following workflows are recommended for validating wearable devices in both general and specific clinical populations.
General Population Validation Protocol
The protocol used in validation studies for general population devices like the Apple Watch and Archon Alive involves controlled laboratory settings to establish baseline accuracy [2] [5].
Figure 2: A general validation protocol for wearable devices, comparing device outputs against gold-standard measures in a controlled laboratory setting.
Clinical Population Validation Protocol
Validating devices for clinical groups, such as patients with lung cancer, requires modifications to the standard protocol to account for disease-specific factors like altered gait and fatigue [8].
Table 3: Key Modifications for Clinical Validation Protocols
| Protocol Component | Standard Population Approach | Clinical Population (e.g., Lung Cancer) Modification | Rationale |
|---|---|---|---|
| Participant Tasks | Fixed speeds (e.g., 3, 4, 5, 8 kph) [5]. | Variable-time walking trials, sitting/standing tests, posture changes [8]. | Accommodates mobility impairments, respiratory limitations, and fatigue. |
| Criterion Measure | Hand tally for steps, metabolic cart for calories [5]. | Video recording with direct observation (DO) for detailed movement analysis [8]. | Captures complex, non-standard movements and postures. |
| Data Collection Context | Laboratory focus. | Laboratory + 7-day free-living protocol [8]. | Assesses real-world performance and device adherence during daily life. |
| Confounding Variables | Basic demographics (age, sex, BMI) [5]. | Administer validated surveys: symptom burden, health-related quality of life (HRQoL), stress, sleep [8]. | Controls for factors that uniquely influence movement patterns and device use in patients. |
Mitigation Strategies: Towards Fairer and More Accurate Models
Addressing algorithmic bias requires a multifaceted approach that spans technical, procedural, and structural solutions. The following strategies have shown promise:
- Inclusive Data Collection and Study Design: The American Life in Realtime (ALiR) study demonstrates a successful model for creating more representative datasets. It uses probability-based sampling, oversamples underrepresented groups, and provides participants with wearable devices and internet access to eliminate the "bring-your-own-device" bias [44]. This approach resulted in a model for COVID-19 infection that maintained robust performance (AUC 0.84) across all demographic subgroups, unlike a model from a convenience sample whose accuracy dropped sharply out-of-sample [44].
- Technical Bias Mitigation during Algorithm Development: A scoping review of bias mitigation in primary care AI identified several technical strategies [45]. Preprocessing methods, such as reweighing and relabeling data to correct imbalances before model training, and the use of natural language processing (NLP) to extract more nuanced data from unstructured clinical notes, showed significant potential. Post-processing techniques like group recalibration and applying fairness metrics (e.g., equalized odds) can also be employed, though they must be used carefully to avoid introducing new errors [45].
- Participatory Design and Multidisciplinary Teams: Equity must be a foundational design principle, not an afterthought. This involves creating multidisciplinary development teams that include voices from the Global South, marginalized communities, and local health ecosystems [41]. Participatory design, where affected populations co-create and critique AI tools, helps bridge the disconnect between technical innovation and real-world context [41].
- Transparency, Explainability, and Ongoing Monitoring: To build trust and facilitate oversight, AI tools should be subject to fairness audits before deployment to examine accuracy across different demographic and socio-economic groups [41]. The use of interpretability measures like SHAP (Shapley Additive Explanations) can help make "black-box" models more transparent to clinicians and researchers [42]. Crucially, evaluation should not be a one-time process but a continuous routine throughout the AI system's lifecycle [41] [43].
The Scientist's Toolkit: Key Research Reagents and Solutions
Table 4: Essential Tools and Methods for Wearable Validation and Bias Research
| Tool / Method | Function / Purpose | Example Use Case |
|---|---|---|
| ActiGraph wGT3x-BT | Research-grade accelerometer; considered a criterion standard for objective physical activity measurement in research [5] [8]. | Used as a benchmark against which to validate the step count of consumer-grade devices like the Archon Alive [5]. |
| PNOĒ Metabolic Analyzer | Portable cardio-metabolic analyzer that measures energy expenditure (calories) via gas exchange; provides a high-accuracy criterion measure [5]. | Used to validate the calorie expenditure output of fitness trackers during treadmill protocols [5]. |
| Polar OH1 | A validated photoplethysmography (PPG) heart rate monitor, often used as a reference standard in validation studies [5]. | Synchronized with the PNOĒ to provide heart rate data and used to test the heart rate accuracy of other wearables [5]. |
| Direct Observation (DO) / Video Recording | The gold-standard criterion for validating step count and posture in laboratory settings, especially for clinical populations with atypical movement [8]. | Video recordings of participants in lab protocols are analyzed by researchers to obtain ground-truth data on steps, postures, and activities [8]. |
| FAIR Data Principles | A set of principles (Findable, Accessible, Interoperable, Reusable) for data management to ensure data can be effectively used by humans and machines [44]. | Applied in studies like ALiR to create benchmark, publicly available datasets that support reproducible and equitable AI research [44]. |
| SHAP (Shapley Additive Explanations) | A method from cooperative game theory used to explain the output of any machine learning model, increasing model interpretability [42]. | Used in AI diabetes research to identify which features (e.g., recent glucose levels, activity) most influenced a model's prediction, building clinician trust [42]. |
| Bland-Altman Plots & Intraclass Correlation (ICC) | Statistical methods for assessing agreement between two measurement techniques. Bland-Altman plots visualize bias, while ICC measures reliability [5] [8]. | Standard outputs in validation studies to compare a wearable device's readings (e.g., heart rate) against a gold-standard reference device [5]. |
The pursuit of accurate calorie tracking and health monitoring through wearable technology is inextricably linked to the challenge of ensuring algorithmic fairness. As the data demonstrates, even widely used devices can show significant inaccuracies in energy expenditure estimation, and these inaccuracies are often not distributed equally across populations [2] [41]. The path forward requires a concerted shift from merely seeking technical precision to actively embedding equity as a core design principle.
This entails adopting rigorous, context-aware validation protocols for specific clinical and marginalized groups, moving beyond convenience sampling to build truly representative datasets like the ALiR study, and implementing continuous bias audits throughout the AI lifecycle [8] [44] [43]. By leveraging the tools and strategies outlined in this review—from advanced statistical methods and reference standards to participatory design frameworks—researchers and developers can ensure that the promise of AI-driven wearable technology is fulfilled for all populations, not just the most represented.
Best Practices for Device Placement, Wear Time, and Data Cleaning
Accuracy Comparison of Leading Wearable Devices
For researchers validating the accuracy of wearable calorie tracking, understanding the performance variations between popular devices is a fundamental first step. The following table summarizes key quantitative findings from recent studies and tests.
| Device / Study Focus | Heart Rate Accuracy (Error) | Step Count Accuracy (Error) | Calorie Expenditure Accuracy (Error) | Key Notes | Source |
|---|---|---|---|---|---|
| Apple Watch (Meta-Analysis) | 4.43% (Mean Absolute Percent Error) | 8.17% (Mean Absolute Percent Error) | 27.96% (Mean Absolute Percent Error) | Inaccuracy consistent across walking, running, cycling. Newer models show gradual improvements. [2] | |
| Garmin Venu 3 (Product Test) | Near-perfect correlation with chest strap | Accurate distance & pace | Not specifically quantified | Described as "the most accurate watch I tested." Excellent for real-time monitoring. [46] | |
| Fitbit Charge 6 (Product Test) | Accurate, but can be inconsistent during lifting | Good performance | Estimates in line with control device post-workout | Tracks heart rate during high-intensity intervals, but can have a slow start during resistance training. [46] | |
| Consumer-Grade Devices (General Finding) | Can underestimate intensity by up to 15% during high-intensity intervals vs. medical-grade chest straps | Variable accuracy | Estimates can vary by 10-30% from laboratory measurements | Optical heart rate monitors have inherent trade-offs for convenience. [47] |
Experimental Protocols for Validation
To ensure reproducible and scientifically rigorous validation of wearable device data, researchers should adhere to structured experimental protocols. The methodologies below are drawn from recent meta-analyses and testing standards.
Protocol for Device Placement and Wear Time
A meta-analysis of 56 studies on Apple Watch accuracy highlights that device performance can vary by the type of physical activity performed [2]. The following workflow diagram outlines a robust protocol for validating wearable devices, incorporating placement, activity, and data processing steps.
Phase 1: Participant and Device Preparation
- Device Selection & Calibration: Utilize multiple units of the same device model to control for inter-device variability. Ensure all devices are updated to the latest firmware [2].
- Device Placement: Secure the device firmly on the wrist according to the manufacturer's instructions (typically, two finger-widths above the wrist bone). Consistency in placement and strap tightness is critical across all participants and sessions to minimize measurement variance [13].
Phase 2: Structured Activity Protocol
- Controlled Activities: Subjects should perform a series of controlled activities in a laboratory setting. A comprehensive meta-analysis evaluated devices during walking, running, cycling, and mixed-intensity workouts to assess performance across different metabolic demands [2].
- Duration and Scheduling: Each activity segment should be of sufficient duration (e.g., 10-15 minutes per activity) to allow metrics to stabilize. Testing should also account for longer wear times to assess battery life and comfort, which influence long-term data integrity [13] [48].
Protocol for Data Cleaning and Validation
Phase 3: Gold-Standard Data Collection
- Reference Metrics: Simultaneously collect data using trusted clinical reference tools.
Phase 4: Data Processing and Analysis
- Data Alignment and Cleaning: Timestamp alignment between the wearable device data and the gold-standard reference data is essential. The initial and final minutes of each activity should be trimmed to exclude transition periods.
- Handling Missing Data: Researchers must define a protocol for handling missing data points, whether through interpolation or exclusion, and report this methodology consistently [49].
- Statistical Validation: Calculate standard accuracy metrics. A key study used Mean Absolute Percent Error (MAPE) to quantify errors for heart rate, step count, and energy expenditure [2]. Other common metrics include Root Mean Square Error (RMSE) and Bland-Altman analysis to assess limits of agreement.
The Researcher's Toolkit
The table below details essential equipment and software solutions for constructing a rigorous experimental pipeline for wearable device validation.
| Tool Category | Specific Examples | Function in Research |
|---|---|---|
| Gold-Standard Reference Devices | Polar H10 Chest Strap, Medical-grade ECG, Indirect Calorimetry System, Research-grade Pedometer | Provides the ground-truth measurement against which consumer wearable data is validated for metrics like heart rate, calorie burn, and steps. [46] |
| Device Testing Platforms | Multiple units of the same consumer device (e.g., Apple Watch, Garmin, Fitbit models) | Serves as the test unit for data collection. Using multiple units helps control for device-to-device variability. [2] |
| Data Processing & Analysis Software | Python (Pandas, SciPy), R, MATLAB, VOSITONE's precision framework (for healthcare AI data) | Used for timestamp alignment, data cleaning, handling missing values, normalization, and performing statistical analysis (e.g., MAPE, RMSE). [49] |
| Validation & Integrity Frameworks | SHAP (SHapley Additive exPlanations), Feature Importance Analysis, Cross-Validation Protocols | Tools to improve model transparency, interpret complex AI outputs, and verify that precision remains consistent across different data subsets. [42] |
Adherence to rigorous methodologies in device placement, structured activity protocols, and systematic data cleaning is paramount for validating the accuracy of wearable calorie tracking in research. The search results consistently show that while heart rate and step count accuracy in modern devices is relatively high, energy expenditure tracking remains a significant challenge with error rates approaching 28% [2]. This underscores the importance of using these devices as supportive tools for tracking trends rather than as diagnostic clinical instruments. For the research community, a continued focus on standardized testing protocols and transparent reporting of data cleaning methodologies is essential to advance the field and ensure the reliable use of wearable data in broader health sciences and drug development contexts.
The Promise of Multi-Sensor Fusion and Transparent Algorithms
For researchers and professionals in drug development and sports science, accurately measuring energy expenditure is paramount. The integration of multi-sensor fusion and transparent algorithms in wearable technology represents a significant advancement toward achieving laboratory-grade accuracy in free-living conditions. Traditional single-sensor devices, which often rely primarily on accelerometer data, are prone to significant errors, particularly during non-ambulatory or mixed-intensity activities [50]. Multi-sensor fusion addresses this by integrating complementary data streams—such as heart rate, respiratory rate, and skin temperature—to build a more holistic physiological profile. Concurrently, algorithm transparency ensures that the provenance of data, the logic of processing, and the potential sources of bias are open to scrutiny, which is a foundational requirement for validating these tools for clinical and research applications [51] [52]. This article examines the current state of these technologies, their validation, and the methodological frameworks essential for their use in rigorous scientific inquiry.
The Science of Multi-Sensor Fusion in Wearables
From Single-Sensor to Multi-Modal Data Integration
The evolution from basic pedometers to modern research-grade wearables marks a shift from simple activity counting to complex physiological monitoring. Early devices tracked only steps using an accelerometer, providing a poor proxy for caloric burn, as they could not account for metabolic variations or non-ambulatory activities [50]. Multi-sensor fusion overcomes these limitations by synchronizing data from multiple sensors to reduce the uncertainty and systematic errors inherent in any single data source [53].
The core principle is that different sensors capture complementary aspects of physiology and movement. By fusing these data, algorithms can create a more robust and accurate estimate of energy expenditure. The following diagram illustrates a generalized technical workflow for multi-sensor data fusion in a wearable device.
Sensor Types and Their Roles in Metabolic Estimation
The accuracy of a calorie-tracking watch is directly tied to the variety and quality of its sensors. The table below details the primary sensors involved and their specific contributions to estimating energy expenditure.
| Sensor Type | Primary Data | Role in Caloric Estimation | Inherent Limitations |
|---|---|---|---|
| Accelerometer [50] | Movement acceleration & intensity | Quantifies gross motor activity and work rate. | Cannot measure static exercise (e.g., wall sit) or physiological cost. |
| Optical Heart Rate Monitor [50] [54] | Heart rate (pulse wave via LED) | Serves as a proxy for metabolic strain and cardiovascular effort. | Accuracy can be affected by skin tone, motion artifact, and fit [13]. |
| GPS [13] [54] | Speed, distance, elevation | Provides external workload for running/cycling. | Useless indoors; contributes significantly to battery drain. |
| Skin Temperature Sensor [50] | Changes in peripheral body temp | Indicates metabolic thermogenesis and energy cost. | Highly sensitive to ambient environmental conditions. |
| Galvanic Skin Response (GSR) [54] | Electrodermal activity (sweat) | Correlate with sympathetic nervous system arousal and stress. | Can be influenced by non-exercise stressors. |
Experimental Validation of Device Accuracy
Benchmarking Against Gold-Standard Methodologies
Validating the accuracy of commercial wearables requires comparison against accepted reference standards in a controlled experimental setting. Common protocols include:
- Indirect Calorimetry: This is the gold standard for measuring energy expenditure. Participants wear a mask connected to a metabolic cart that analyzes inhaled and exhaled gas concentrations (O₂ and CO₂) to calculate caloric burn in real-time. Devices under test are worn simultaneously, and their estimates are compared to the calorimetry data [2] [54].
- Chest-Strap Heart Rate Monitors: To validate optical heart rate sensors, studies often use electrocardiogram (ECG)-chest straps (e.g., Polar H10) as a control. These devices are considered highly accurate for heart rate measurement during exercise [46].
A 2025 meta-analysis from the University of Mississippi that reviewed 56 validation studies found that devices like the Apple Watch showed strong accuracy for heart rate (mean absolute percent error of 4.43%) and step count (8.17% error), but significantly higher error for energy expenditure (27.96% error) [2]. This highlights that while multi-sensor fusion improves metrics, calorie tracking remains a challenging estimation.
Comparative Performance of Leading Devices
Independent testing and academic reviews provide crucial data on how different devices and their fusion algorithms perform. The following table synthesizes quantitative findings from recent studies and expert reviews.
| Device Model | Reported Caloric Accuracy (vs. Reference) | Key Sensors Fused | Noted Strengths & Weaknesses |
|---|---|---|---|
| Garmin Forerunner 955 [54] | Within 5% of lab-tested values | Heart rate, multi-band GPS, respiratory rate, VO₂ max | High accuracy due to advanced first-party algorithms and multi-parameter fusion. |
| Fitbit Sense 2 [54] | Reduced miscalculations by up to 30% during low-intensity activities | Heart rate, continuous EDA (electrodermal activity), ECG | Excels in accounting for non-exercise energy burn; consistency ranked highly. |
| Apple Watch Series 9 [2] [54] [46] | Shows a 27.96% mean error in energy expenditure (across models) | Heart rate, GPS, accelerometer | Generally accurate for heart rate; calorie estimates can be highly variable. |
| Amazfit Bip 3 Pro [46] | Accuracy on par with pricier models for heart rate and sleep | Heart rate, GPS, accelerometer | Good value, but provides limited post-workout insights for strength training. |
The Critical Role of Algorithmic Transparency
From "Black Box" to Trusted Research Tool
For a wearable device to be trusted in research and clinical decision-making, its algorithms must be more than just effective—they must be transparent and accountable [51] [52]. A "black box" model that provides a calorie estimate without explanation poses several risks:
- Inability to Audit for Bias: Algorithms trained on non-representative datasets (e.g., predominantly on young, male athletes) can perform poorly when applied to other demographic groups, such as older adults or different ethnicities [51] [52].
- Undermined Informed Consent: Users and researchers cannot give fully informed consent if they do not understand how their sensitive physiological data is being used and processed [51].
- Barriers to Scientific Validation: A lack of clarity on preprocessing steps, feature selection, and model architecture makes it difficult for independent researchers to validate or challenge the results [52].
A Framework for Transparent and Ethical AI
A proposed methodological framework for responsible AI in wearable health systems embeds transparency and accountability throughout the entire data lifecycle [52]. This framework operationalizes ethical principles through concrete mechanisms, aligning with regulations like the EU AI Act and GDPR. The workflow below illustrates how this framework integrates transparency at every stage.
For researchers designing validation studies or working with wearable data, the following tools and resources are fundamental.
| Tool / Resource | Function / Purpose | Example in Use |
|---|---|---|
| Reference Dataset [51] [52] | Provides a benchmark for unbiased evaluation of fusion and AI algorithms. | The MobiAct and MobiFall datasets contain annotated accelerometry data from real-world scenarios for algorithm training and validation [52]. |
| Indirect Calorimeter [2] [54] | Serves as the gold-standard reference for measuring true energy expenditure. | Used in lab protocols to generate the ground-truth data against which wearable calorie estimates are compared. |
| Medical-Grade Chest Strap HRM [46] | Provides a high-fidelity control for validating optical heart rate sensors. | The Polar H10 is frequently used as a reference in studies to test the accuracy of wrist-based heart rate monitoring during exercise. |
| Data Fusion Evaluation Framework [53] | A common structure for simultaneous registration and approximation of multi-sensor data. | Proposed in research to standardize the evaluation of point cloud fusion algorithms, a concept transferable to physiological data fusion. |
| Explainable AI (XAI) Techniques [51] [52] | Makes the decision-making process of complex AI models interpretable to humans. | Used to uncover why a model might output an anomalous calorie estimate, helping to identify data or model drift. |
The convergence of multi-sensor fusion and algorithmic transparency holds the genuine promise of transforming consumer wearables into validated tools for scientific research and personalized health intervention. While current devices like the Garmin Forerunner and Fitbit Sense 2 show markedly improved accuracy through sophisticated data fusion, the overarching challenge of precisely measuring energy expenditure in real-world settings remains. The path forward requires a continued commitment to rigorous, independent validation against gold-standard measures and the adoption of ethical AI frameworks that prioritize explainability, fairness, and user autonomy. For the research community, embracing these principles is not merely a technical exercise but a prerequisite for building trust and generating reliable, actionable insights from wearable technology.
Benchmarks and Rigor: A Comparative Review of Validation Evidence
The adoption of wearable technology for monitoring physiological parameters has expanded from consumer wellness into clinical and scientific research. This transition necessitates a rigorous validation of the accuracy of consumer-grade devices against research-established standards. Within the context of a broader thesis on accuracy validation of wearable calorie tracking research, this analysis provides a comparative error analysis of these device classes. The objective is to delineate the performance boundaries of consumer-grade wearables for researchers, scientists, and drug development professionals, enabling informed decisions on their application in scientific studies and clinical trials. The focus on energy expenditure (EE) is paramount, as inaccuracies in caloric tracking can compromise interventions for conditions like obesity and metabolic disorders, and confound data in pharmaceutical studies where physical activity is an outcome measure.
Performance Metrics: Quantitative Data Comparison
The accuracy of wearables varies significantly across different physiological metrics. The following tables summarize quantitative data on the performance of consumer-grade devices compared to research-grade standards.
Table 1: Accuracy of Consumer-Grade Wearables by Metric [4]
| Metric | Cumulative Accuracy | Highest Accuracy (Device) | Lowest Accuracy (Device) |
|---|---|---|---|
| Heart Rate (HR) | 76.35% | Apple Watch (86.31%) | TomTom (67.63%) |
| Step Count (SC) | 68.75% | Garmin (82.58%) | Polar (53.21%) |
| Energy Expenditure (EE) | 56.63% | Apple Watch (71.02%) | Garmin (48.05%) |
Table 2: Detailed Device Comparison from Empirical Studies
| Study & Device | Parameter | Reference Standard | Result / Agreement | ||||
|---|---|---|---|---|---|---|---|
| Withings Pulse HR [55] [56] | Heart Rate | ECG (Faros Bittium 180) | Good at low activity (r ≥ 0.82, | bias | ≤ 3.1 bpm); Decreased with higher speed (r ≤ 0.33, | bias | ≤ 11.7 bpm) |
| Step Count | GENEActiv & Hand Tally | Decreased during treadmill phases (e.g., bias = 17.3 steps/min at stage 4) | |||||
| Energy Expenditure | Indirect Calorimetry | Poor agreement ( | r | ≤ 0.29, | bias | ≥ 1.7 MET) | |
| Archon Alive 001 [5] | Step Count | Hand Tally | MAPE 3.46% (r = 0.986, p<0.001) | ||||
| Heart Rate | Polar OH1 | ICC 75.8%; Mean bias -3.33 bpm | |||||
| Energy Expenditure | PNOĒ Metabolic Analyzer | MAPE 29.3% (r = 0.629, p<0.001) | |||||
| Apple Watch [2] | Heart Rate | ECG | Mean Absolute Percentage Error (MAPE): 4.43% | ||||
| Step Count | Direct Observation | MAPE: 8.17% | |||||
| Energy Expenditure | Indirect Calorimetry | MAPE: 27.96% | |||||
| Fitbit [57] | Heart Rate | ECG | Tendency to underestimate HR during exercise; MAPE ≤3% at rest and recovery |
Abbreviations: MAPE (Mean Absolute Percentage Error), ICC (Intraclass Correlation Coefficient), r (Pearson's Correlation Coefficient), bias (mean difference between devices).
Experimental Protocols and Methodologies
A critical component of accuracy validation is the experimental design used for device comparison. The following section details the methodologies employed in key studies cited in this analysis.
Laboratory-Based Structured Protocol
A common protocol for rigorous device validation involves controlled laboratory settings with structured activities [55] [56].
- Participants: Typically, healthy adults (e.g., n=22, 11 women, 11 men, mean age 24.0 years) without cardiovascular or metabolic diseases are recruited to minimize confounding variables [55] [56].
- Device Placement: Consumer-grade (e.g., wrist-worn Withings Pulse HR) and research-grade (e.g., chest-worn Faros Bittium 180 ECG) devices are worn simultaneously [55] [56].
- Protocol Structure: Participants undergo a multi-stage protocol:
- Data Collection & Analysis:
- Heart Rate: Consumer-grade photoplethysmography (PPG) is validated against research-grade ECG [55] [57].
- Step Count: Device outputs are compared to manually counted steps or research-grade accelerometers [5].
- Energy Expenditure: Device estimates are validated against indirect calorimetry, the gold standard which calculates EE from inhaled and exhaled gas volumes [55] [19] [5].
- Statistical Comparison: Agreement is assessed using Pearson's correlation, Lin’s concordance correlation coefficient, Bland-Altman plots (for bias), and Mean Absolute Percentage Error (MAPE) [55] [56].
The workflow for this laboratory-based validation is summarized in the diagram below.
Specialized Population and Algorithm Validation
Validation protocols must account for specific populations for whom general device algorithms may be inaccurate, such as individuals with obesity [19] [58].
- Objective: To develop and test a new algorithm for wrist-worn wearables to accurately estimate energy expenditure in individuals with obesity [19].
- Participant Group: One study involved 27 participants with obesity [19].
- Protocol:
- Gold-Standard Comparison: Participants wore a consumer-grade fitness tracker simultaneously with a metabolic cart (indirect calorimetry) while performing a set of physical activities [19].
- Free-Living Validation: A second group (n=25) wore a fitness tracker and a body camera in their daily lives. The camera provided visual confirmation of activities to identify over- or under-estimation of calories burned (kCals) by the tracker [19] [58].
- Outcome: The new, open-source algorithm achieved over 95% accuracy in estimating energy expenditure, rivaling gold-standard methods in real-world situations [19].
The logical relationship and validation workflow for population-specific algorithm development is shown below.
The Scientist's Toolkit: Research Reagent Solutions
For researchers designing validation studies, the following table outlines key materials and their functions as derived from the cited experimental protocols.
Table 3: Essential Materials for Wearable Device Validation Research
| Item / Solution | Function in Validation Research |
|---|---|
| Research-Grade ECG (e.g., Faros Bittium 180) [55] [56] | Serves as the gold-standard reference for validating heart rate and heart rate variability measurements from consumer wearables. |
| Indirect Calorimetry System (e.g., metabolic cart, PNOĒ) [55] [19] [5] | Provides the gold-standard measurement of energy expenditure (caloric burn) for validating calorie estimation algorithms. |
| Research-Grade Accelerometer (e.g., ActiGraph, GENEActiv) [55] [8] [5] | Provides validated measures of step count and physical activity intensity for comparison against consumer tracker data. |
| Structured Activity Protocol (e.g., Bruce Treadmill Test) [55] [56] | A standardized set of activities that systematically increases physiological demand, testing device accuracy across a range of intensities. |
| Video Recording / Direct Observation [8] | Used as a criterion method for validating step count, posture, and activity type in laboratory and free-living settings. |
| Specialized Validation Software (e.g., Fitabase) [59] | A data management platform that facilitates the aggregation and analysis of data from large fleets of consumer wearables in research studies. |
| Open-Source Algorithms [19] [58] | Transparent and rigorously tested algorithms (e.g., for specific populations) that can be adopted and built upon by the research community to improve accuracy. |
The collective evidence indicates a clear hierarchy of accuracy between consumer-grade and research-grade devices. Heart rate is generally the most reliable metric from consumer wearables, particularly at rest and during low-intensity activities, though accuracy diminishes with increased movement intensity and may be lower in individuals with darker skin tones [55] [57] [4]. Step count is moderately accurate but can be significantly erroneous at very slow walking speeds or during non-ambulatory movements [55] [8]. Most critically for calorie tracking research, energy expenditure is the least accurate metric, with errors often exceeding 25-30% and a widespread poor agreement with indirect calorimetry [55] [2] [5].
The underlying reasons for these discrepancies are multifaceted. Consumer devices primarily rely on photoplethysmography for heart rate and accelerometry for motion detection, using proprietary algorithms to derive metrics like calorie burn [57]. In contrast, research-grade devices often use direct methods like electrocardiography and indirect calorimetry [55] [5]. The algorithms in consumer devices are often developed for general populations and may not account for individual factors like body composition, fitness level, or specific health conditions, leading to systematic errors [19] [8].
In conclusion, while consumer-grade wearables are valuable for tracking general trends in physical activity and motivating behavior change, their use in rigorous scientific research requires caution. The significant error in energy expenditure measurement underscores that they are not yet suitable replacements for research-grade equipment in clinical trials or studies where high precision in caloric tracking is required. Future directions should focus on the development of more transparent, validated, and population-specific algorithms to bridge the current accuracy gap.
Evaluation of Device-Specific Performance Across Brands and Models
The adoption of consumer wearable devices for health and fitness monitoring is expanding beyond casual users into professional and research domains. For researchers, scientists, and drug development professionals, understanding the specific performance characteristics of these devices is paramount when considering them for data collection in clinical trials, observational studies, or population health research. This evaluation is framed within a broader thesis on accuracy validation of wearable calorie tracking research, aiming to dissect device-specific performance across key metrics such as energy expenditure, heart rate, and step count, supported by available experimental data. The following sections provide a structured comparison of prominent devices, summarize quantitative findings in consolidated tables, and detail the experimental methodologies from which these data are derived.
Data on device accuracy, particularly for calorie tracking, is critical for assessing their suitability for research applications. The tables below consolidate key performance metrics and device characteristics from recent analyses.
Table 1: Summary of Device Accuracy Metrics from Meta-Analysis and Testing
| Device/Brand | Metric Evaluated | Reported Error Rate/Performance | Key Findings |
|---|---|---|---|
| Apple Watch | Energy Expenditure (Calories) | ~27.96% error [11] [60] | Significant inaccuracy; often over- or under-estimates burn [60]. |
| Heart Rate | ~4.43% error [11] [60] | Highly accurate and reliable for most uses, including clinical [60]. | |
| Step Count | ~8.17% error [11] [60] | Generally accurate, though accuracy can vary with activity type [60]. | |
| Fitbit Trackers | Energy Expenditure | Varies; can be off by 40-80% [11] | One study found Fitbit more accurate than Garmin for calorie burn [61]. |
| Sleep Tracking | Excellent/Above Average [62] [63] | Presents data in an intuitive and user-friendly app [63]. | |
| Oura Ring | Sleep & Readiness Scores | Highly Accurate [64] [65] | Gold-standard for sleep and non-activity heart rate accuracy [65]. |
| Activity Tracking | Improved but not comprehensive [64] | Correctly picks up specific activities; not its primary focus [64]. | |
| Garmin Trackers | Fitness & Training Metrics | Robust and Accurate [66] | Offers expansive activity profiles and advanced metrics via Connect app [66]. |
| Samsung Galaxy Ring | Sleep Tracking & Heart Rate | Excellent/Accurate [63] | Accurate sleep stage monitoring and heart rate sensing [63]. |
Table 2: Key Device Characteristics and Research Considerations
| Device/Model | Form Factor | Key Research Metrics | Subscription Required? | Noteworthy Features |
|---|---|---|---|---|
| Apple Watch Series 11 [62] | Smartwatch | Heart Rate, ECG, Workouts, Sleep | No | FDA-approved hypertension notifications [62]. |
| Fitbit Charge 6 [62] [65] | Band | Heart Rate, Sleep, ECG, EDA Scan | Yes (for some metrics) | ECG for heart rhythm; EDA for stress; best for beginners [65]. |
| Oura Ring 4 [64] [65] | Smart Ring | Sleep Score, Readiness, Body Temperature, HR | Yes | Discreet; excellent for sleep and recovery monitoring [65]. |
| Garmin Vivoactive 5 [66] | Smartwatch | Body Battery, Stress, Sleep, HR, Recovery | No | Over 30 sports apps; push tracker for wheelchair users [66]. |
| Xiaomi Smart Band 10 [65] | Band | Steps, 24/7 Heart Rate, Sleep, SpO2 | No | Extreme value; excellent battery life; less polished data [65]. |
| Whoop 5.0 [65] | Screenless Band | Recovery, Sleep, Strain, HRV | Yes | Laser-focused on recovery and actionable insights [65]. |
Detailed Experimental Protocols and Methodologies
The quantitative data presented in the previous section is derived from specific experimental approaches. Understanding these methodologies is essential for researchers to assess the validity and applicability of the findings.
Meta-Analysis on Apple Watch Performance
A foundational 2025 systematic review and meta-analysis provides some of the most concrete data on Apple Watch performance [11] [60].
- Objective: To evaluate the accuracy of the Apple Watch in monitoring health metrics compared to reference tools.
- Data Sources: The analysis aggregated results from 56 individual studies that directly compared Apple Watch measurements to validated reference instruments [11] [60].
- Evaluated Metrics: The primary outcomes were accuracy in Energy Expenditure (EE), Heart Rate (HR), and Step Count.
- Statistical Analysis: Accuracy was determined using the Mean Absolute Percentage Error (MAPE), a standard metric for measuring forecast accuracy. The accepted validity threshold for these metrics was set at <10% error [11].
- Key Findings:
- Heart Rate: The aggregate MAPE for heart rate was 4.43%, well below the 10% threshold, confirming high reliability [11] [60].
- Step Count: The MAPE was 8.17%, also within the acceptable range, indicating general accuracy [11] [60].
- Energy Expenditure: The MAPE was 27.96%, significantly exceeding the validity threshold. This high error rate was consistent across various activities including walking, running, and cycling [11] [60].
Comparative Device Testing by Review Publications
Websites like PCMag, Wareable, and TechRadar conduct real-world testing to compare devices. While not clinical trials, their methodologies offer practical insights.
- Objective: To assess the real-world performance, usability, and comparative accuracy of fitness trackers for consumer advice.
- Testing Protocol:
- Real-World Usage: Testers wear devices for extended periods (days to weeks) during various activities of daily living and structured workouts [65] [66].
- Comparative Metrics: Data from devices (e.g., step count, heart rate, GPS route, sleep stages) is compared against baseline measures. These can include manual step counts, chest-strap heart rate monitors (considered more accurate), dedicated GPS devices, and subjective user logs (e.g., sleep diary) [64] [65].
- Feature Evaluation: The usability, battery life, comfort, and clarity of the accompanying mobile application are critically assessed [62] [65].
- Example Findings:
- Fitbit Charge 6 GPS: Testers found the built-in GPS to be "very unreliable" during outdoor runs, a specific performance shortfall [65].
- Oura Ring Activity Tracking: For the Oura Ring 4, testers noted a significant improvement in automatic activity detection accuracy compared to its predecessor, correctly identifying activities like boxing and skiing without manual input [64].
- Garmin Vivoactive 5: Testers synced the device to a smartphone and reported a high degree of accuracy in tracking various strength and cardio disciplines, though they noted a learning curve due to the wealth of data [66].
Direct User-Led Comparative Experiment
A user-led experiment reported in the Fitbit community provides an example of a direct, albeit small-scale, comparative test.
- Objective: To determine which wearable (Fitbit vs. Garmin) provided a more accurate estimate of daily calorie burn for weight management [61].
- Methodology:
- Parallel Monitoring: The user simultaneously wore a Fitbit Inspire 3 and a Garmin Venu 2 Pro during daily activities, including a consistent 2-hour swimming session.
- Outcome Measure: The gold-standard outcome was daily weigh-ins to track actual weight loss or gain, which reflects the true calorie balance.
- Data Comparison: The calorie burn estimates from both devices were compared against the empirical weight data over time.
- Result: The experiment concluded that the Fitbit's calorie count (approximately 750 Calories for the swim session) was more predictive of actual weight changes than the Garmin's estimate (approximately 950 Calories for the same activity) [61].
Visualization of Research Workflows
The following diagrams illustrate the logical flow of the key experimental methodologies discussed, providing a clear framework for research design.
Systematic Review and Meta-Analysis Workflow
Comparative Real-World Testing Methodology
The Scientist's Toolkit: Key Research Reagents and Materials
For researchers designing validation studies for wearable devices, the following tools and concepts are essential. This table details key components used in the experiments cited in this review.
Table 3: Essential Materials and Concepts for Wearable Validation Research
| Item/Concept | Function in Validation Research |
|---|---|
| Mean Absolute Percentage Error (MAPE) | A standard statistical metric used to quantify the average absolute error as a percentage of the actual values, providing a clear measure of device accuracy [11]. |
| Gold-Standard Reference Tools | The validated clinical or research-grade equipment (e.g., metabolic carts for EE, ECG for HR) against which consumer wearables are compared to establish ground truth [11] [60]. |
| Chest-Strap Heart Rate Monitor | Considered a more accurate proximal measure of heart rate than optical wrist-based sensors; often used as a reference in consumer device testing [65]. |
| Resting Metabolic Rate (RMR) Test | A clinical assessment that provides a highly accurate measurement of baseline calorie burn, used to anchor and evaluate the TDEE estimates from wearables [60]. |
| Systematic Review & Meta-Analysis | A research methodology that systematically identifies, appraises, and synthesizes all relevant studies on a topic to provide a high-level evidence conclusion [11] [60]. |
| Activity Log / Diary | A manually kept record of a participant's activities, sleep times, and intensities, serving as a subjective baseline for validating automated tracker detections [64]. |
The validation of wearable activity monitors (WAMs) represents a critical frontier in digital health, bridging technological innovation with scientific rigor. For researchers, scientists, and drug development professionals, understanding the nuanced performance of these devices is paramount for interpreting data collected in both controlled trials and real-world settings. The fundamental challenge in wearable validation research lies in the inherent tension between controlled laboratory environments that maximize internal validity and free-living conditions that prioritize ecological validity [67]. This comparative analysis examines the methodological frameworks, accuracy metrics, and practical implications of these divergent validation approaches, providing a comprehensive resource for professionals leveraging wearable data in research and clinical applications.
Consumer-grade wearables have evolved from simple step counters to sophisticated health monitoring systems equipped with photoplethysmography (PPG) sensors for heart rate monitoring, tri-axial accelerometers for movement detection, and complex proprietary algorithms that estimate energy expenditure, sleep patterns, and more [57]. The proliferation of these devices in research contexts [68] necessitates rigorous validation against established criterion standards to determine their suitability for scientific and clinical applications. This analysis synthesizes evidence from multiple validation studies to delineate the strengths and limitations of laboratory versus free-living validation paradigms, with particular emphasis on implications for research design and data interpretation in pharmaceutical and clinical trials.
Comparative Accuracy Across Settings
Laboratory vs. Free-Living Validation Metrics
Table 1 summarizes key accuracy metrics for consumer wearables across validation settings, highlighting the divergence between controlled laboratory performance and real-world reliability.
Table 1: Accuracy Comparison of Consumer Wearables in Laboratory vs. Free-Living Settings
| Metric | Device Types | Laboratory Accuracy | Free-Living Accuracy | Key Influencing Factors |
|---|---|---|---|---|
| Step Count | Various wrist-worn devices | MAPE*: 0.9-23.7% [16] | Strong correlation with reference monitors (r ≥ 0.76) [69] | Walking speed, device placement, gait patterns [5] [67] |
| Heart Rate | PPG-based devices | Excellent at rest (MAPE ≤3%); worsens with activity [57] | Limited data; presumed less accurate | Activity intensity, arm movement, contact pressure, sweat [57] |
| Energy Expenditure | Multi-sensor devices | High correlation with IC (r=0.93) but significant underestimation at high intensities [69] | Systemic over-/under-estimation with high individual variability [69] | Exercise intensity, individual metabolism, algorithm limitations [16] [69] |
| Sleep Tracking | Oura Ring, Fitbit, Apple Watch | Identifies sleep with 90-97% accuracy [16] | Overestimates total sleep time by 7-67 minutes [16] | Sleep disorders, movement patterns, device comfort |
MAPE: Mean Absolute Percentage Error; *IC: Indirect Calorimetry*
The data reveals a consistent pattern: most wearables demonstrate acceptable to excellent accuracy for basic metrics like step counting and heart rate at rest in laboratory settings, but this performance deteriorates for complex calculations like energy expenditure, particularly in free-living conditions [16] [57] [69]. This accuracy gradient has significant implications for researchers selecting devices for specific study designs.
Device-Specific Performance Variations
Table 2 provides a detailed breakdown of accuracy metrics for specific wearable devices based on laboratory validation studies, enabling direct comparison for device selection.
Table 2: Device-Specific Accuracy Metrics in Laboratory Studies
| Device | Heart Rate (% error) | Caloric Expenditure (% error) | Step Count (% error) | Sleep Tracking (accuracy) |
|---|---|---|---|---|
| Apple Watch | Underestimates by 1.3 BPM during exercise [16] | Miscalculates by up to 115% [16] | 0.9-3.4% error [16] | Correctly identifies sleep 97% of time [16] |
| Oura Ring | 99.3% accuracy for resting HR [16] | 13% error [16] | 4.8-50.3% error [16] | 96% accuracy for total sleep time [16] |
| WHOOP | 99.7% accurate [16] | Not available | Does not track steps [16] | Identifies sleep 90% of time [16] |
| Garmin | 1.16-1.39% error [16] | 6.1-42.9% error [16] | 23.7% error [16] | Identifies sleep 98% of time [16] |
| Fitbit | Underestimates by 9.3 BPM during exercise [16] | 14.8% error [16] | 9.1-21.9% error [16] | Overestimates total sleep time [16] |
| Archon Alive | ICC: 75.8% vs. Polar OH1 [5] | 29.3% MAPE vs. PNOĒ [5] | 3.46% MAPE vs. hand tally [5] | Not available |
The substantial variation in accuracy across devices and metrics underscores the importance of device selection aligned with study outcomes. For instance, while Oura Ring demonstrates excellent resting heart rate accuracy (99.3%), its step count accuracy varies dramatically (4.8-50.3% error) depending on conditions [16]. Similarly, Apple Watch shows improving heart rate accuracy with increasing intensity [16], a unique characteristic among the devices evaluated.
Experimental Protocols and Methodologies
Laboratory Validation Frameworks
Laboratory validation provides the foundation for establishing a device's technical capability under ideal conditions. The standardized protocols typically involve:
Structured Activity Protocols: Participants perform a series of activities spanning intensity levels from sedentary behaviors to vigorous exercise. Common protocols include graded treadmill tests (e.g., Bruce protocol), fixed-paced walking at 3-6 km/h, and sedentary tasks like sitting and standing [55] [70] [69]. These controlled exposures allow researchers to assess device accuracy across the metabolic spectrum.
Criterion Standard Comparison: Laboratory studies compare wearable metrics against clinical-grade reference systems:
- Energy Expenditure: Indirect calorimetry systems (e.g., Jaeger Oxycon Pro, PNOĒ) measure oxygen consumption (VO₂) and carbon dioxide production (VCO₂) to calculate energy expenditure via respiratory exchange ratio [70] [69].
- Heart Rate: Electrocardiography (ECG) with chest-strap monitors (e.g., Faros Bittium 180, Polar OH1) provide gold-standard heart rate measurement [55] [57].
- Step Count: Manual hand tally counts serve as the step count criterion, particularly during treadmill protocols [5].
Controlled Environment: Laboratory settings control for confounding variables like temperature, humidity, and terrain, allowing isolation of the device's inherent capabilities [55].
A typical laboratory validation workflow follows a systematic progression from baseline measures to increasingly strenuous activities, as visualized below:
Free-Living Validation Frameworks
Free-living validation assesses device performance in naturalistic environments where participants maintain their typical routines:
Extended Monitoring Periods: Studies typically span 7-14 days to capture varied activity patterns and ensure sufficient data for comparison [67] [69]. This extended timeframe increases ecological validity but introduces additional confounding variables.
Multi-Device Comparison: Researchers deploy multiple wearables simultaneously (consumer-grade and research-grade) to enable comparative analysis without impeding natural movement [67] [69]. Common research-grade devices include ActiGraph wGT3x-BT, activPAL3 micro, and others that have undergone extensive validation.
Complementary Data Collection: Participants may complete activity logs, dietary records, or symptom diaries to contextualize device data [67]. These subjective measures help interpret anomalies in objective data streams.
Statistical Approaches: Free-living validation relies heavily on correlation analyses (Pearson's r, ICC), Bland-Altman plots for agreement assessment, and mean absolute percentage error (MAPE) calculations [5] [69].
The free-living validation paradigm emphasizes ecological validity through extended monitoring in natural environments, as illustrated below:
The Scientist's Toolkit: Research Reagent Solutions
Table 3 outlines essential equipment and their functions for designing rigorous validation studies for wearable technologies.
Table 3: Essential Research Equipment for Wearable Validation Studies
| Equipment Category | Specific Examples | Primary Function | Considerations |
|---|---|---|---|
| Metabolic Measurement Systems | Jaeger Oxycon Pro, PNOĒ | Gold-standard measurement of energy expenditure via indirect calorimetry [70] [69] | High cost, requires technical expertise, laboratory setting only |
| Research-Grade Accelerometers | ActiGraph wGT3x-BT, activPAL3 micro | Objective physical activity measurement with established validity [5] [67] | Different placement options (hip, wrist, thigh) affect data capture |
| ECG Reference Monitors | Faros Bittium 180, Polar OH1 | Gold-standard heart rate measurement [55] [57] | Chest-strap monitors may be uncomfortable for extended wear |
| Consumer Wearables (Test Devices) | Fitbit models, Apple Watch, Oura Ring, Garmin devices | Devices under investigation [16] [71] | Rapid product iteration may limit long-term relevance of validation findings |
| Data Integration Platforms | Manufacturer-specific cloud platforms, custom databases | Aggregation and synchronization of multi-source data [71] | Proprietary algorithms limit transparency; API access varies |
Implications for Research and Clinical Applications
The methodological tension between laboratory and free-living validation presents both challenges and opportunities for researchers:
Interpretation of Validity Evidence
Laboratory studies demonstrate that most consumer wearables can reliably detect gross changes in activity levels and basic physiological parameters [16] [57]. However, the accuracy required depends substantially on the research context. For example, a 20% error in energy expenditure may be acceptable for population-level surveillance but inadequate for precise metabolic interventions.
The decreasing accuracy of wearables with increasing exercise intensity presents a particular challenge for sports medicine and high-intensity interval training (HIIT) research [16] [69]. Devices that perform well at rest or during moderate walking may become significantly less reliable during vigorous activity, with some studies showing errors in energy expenditure exceeding 100% at higher intensities [16].
Special Population Considerations
Validation research in clinical populations reveals unique considerations for researchers:
- Patients with cancer often exhibit slower walking speeds and altered gait patterns, which can significantly impact step count accuracy [67].
- Chronic pain populations may demonstrate different movement patterns that affect activity tracker accuracy, particularly for energy expenditure estimation [70] [72].
- Older adults typically have slower walking speeds and more variable gait patterns, potentially reducing device accuracy [71].
These population-specific factors underscore the importance of validation studies that include the target demographic rather than extrapolating from healthy young adults.
The validation of wearable activity monitors necessitates a dual approach incorporating both laboratory and free-living methodologies. Laboratory studies provide essential controlled conditions for establishing fundamental accuracy and comparing devices against gold-standard criteria, while free-living evaluations offer critical insights into real-world performance and practical utility. The converging evidence from both paradigms indicates that while consumer-grade wearables show promise for measuring basic activity parameters like step count, their accuracy diminishes for complex physiological calculations like energy expenditure, particularly in uncontrolled environments.
For researchers and drug development professionals, these findings suggest a context-dependent approach to device selection and data interpretation. Wearables offer unprecedented opportunities for continuous physiological monitoring in naturalistic settings, but their limitations must be acknowledged in research design and statistical analysis plans. Future validation efforts should prioritize transparent reporting of device models, firmware versions, and analytical algorithms, while addressing the unique requirements of specific clinical populations. As wearable technology continues to evolve, maintaining scientific rigor in validation methodologies will be essential for realizing their potential in both research and clinical care.
Wearable activity trackers have penetrated the global market, with revenues projected to grow from $46.3 billion in 2023 to over $187 billion by 2032 [73]. Despite this widespread adoption, significant evidence gaps persist regarding the accuracy of energy expenditure (EE) measurements across diverse populations. Research indicates that these devices demonstrate varying levels of precision, with error rates for calorie tracking reaching up to 27.96% in some studies [2]. This inconsistency reveals a critical methodological challenge: the lack of standardized validation protocols specifically designed for vulnerable populations, including those with obesity, cancer, and other conditions affecting mobility and metabolism.
The implications of these inaccuracies extend beyond consumer frustration to impact clinical research and personalized health interventions. As wearables become increasingly integrated into healthcare monitoring and pharmaceutical trials, understanding the limitations of EE estimation becomes paramount for researchers and drug development professionals who rely on these metrics as endpoints or monitoring tools.
Comparative Accuracy Analysis: Quantitative Data Across Populations
Accuracy Variations in General Population Studies
Independent evaluations of popular wearable devices reveal considerable variation in their ability to accurately measure energy expenditure. A comprehensive meta-analysis of 56 studies examining Apple Watch performance found a mean absolute percent error of 27.96% for energy expenditure measurements, compared to 4.43% for heart rate and 8.17% for step counts [2]. This significant discrepancy highlights the particular challenge that EE estimation presents compared to other metrics.
Table 1: Fitness Tracker Accuracy Across Metrics in General Population
| Device Type | Heart Rate Error (%) | Step Count Error (%) | Energy Expenditure Error (%) | Study Details |
|---|---|---|---|---|
| Apple Watch (Various Models) | 4.43 | 8.17 | 27.96 | Meta-analysis of 56 studies [2] |
| Fitbit Charge 6 | Minimal variance from chest strap control observed | N/R | Performance decreases during high-intensity intervals | Tests vs. Polar H10 Chest Strap [46] |
| Garmin Venu 3 | High accuracy maintained | N/R | Consistent with control device | Rated most accurate in testing [46] |
Testing methodologies significantly influence reported accuracy. In controlled comparisons, the Garmin Venu 3 demonstrated superior accuracy in heart rate monitoring during varied exercise intensities when tested against a chest strap control, while the Fitbit Charge 6 showed occasional lags in capturing rapid heart rate changes during high-intensity interval training [46].
Special Populations: Highlighting the Evidence Gaps
Research indicates that accuracy limitations become more pronounced in special populations. A pioneering study at Northwestern University revealed that people with obesity experience systematic underestimation of energy burn by conventional fitness trackers due to differences in gait, device placement, and walking speed [19]. The researchers developed a novel algorithm specifically tuned for this population that achieved over 95% accuracy in real-world situations—significantly outperforming the 11 state-of-the-art algorithms it was tested against [19] [74].
Table 2: Accuracy Gaps in Special Populations
| Population | Device(s) Tested | Key Finding | Proposed Solution |
|---|---|---|---|
| People with Obesity | Various commercial trackers | Systematic underestimation of energy burn due to gait differences and device tilt | Population-specific algorithm achieving >95% accuracy [19] |
| Lung Cancer Patients | Fitbit Charge 6, ActiGraph LEAP, activPAL3 | Decreased accuracy at slower walking speeds; unique mobility challenges affect measurements | Ongoing validation study with laboratory and free-living components [8] |
| Adolescents | Various WATs | Inconsistent effects on physical activity; limited evidence for school-based interventions | Need for more targeted studies in this demographic [75] |
Similar challenges face researchers working with oncology populations. Patients with lung cancer often experience mobility impairments and slower walking speeds that substantially decrease activity monitor accuracy [8]. A forthcoming validation study aims to address this gap by testing devices in both laboratory and free-living conditions to provide disease-specific recommendations.
Experimental Protocols: Methodological Approaches to Validation
Laboratory Versus Free-Living Validation Protocols
Research protocols for validating wearable trackers typically employ both laboratory and free-living components to comprehensively assess device performance.
Laboratory protocols provide controlled conditions for comparison against gold-standard measures. The Northwestern study on obesity-specific algorithms utilized metabolic carts—masks that measure oxygen inhaled and carbon dioxide exhaled—to calculate energy burn in kilocalories (kCals) during structured physical activities [19]. Similarly, the ongoing lung cancer validation study incorporates structured activities including variable-time walking trials, sitting and standing tests, posture changes, and gait speed assessments, all video-recorded for validation against direct observation [8].
Free-living protocols assess device performance in real-world environments. Northwestern researchers equipped participants with body cameras to visually confirm when algorithms over- or under-estimated kcal burn during daily life [19]. The lung cancer study protocol includes 7 days of continuous device wear in free-living conditions, with comparisons between consumer-grade (Fitbit Charge 6) and research-grade (activPAL3 micro and ActiGraph LEAP) devices [8].
Standardization Gaps in Current Methodologies
Significant heterogeneity exists in validation methodologies across studies. A review of wearable activity tracker research in adolescents revealed substantial variations in intervention protocols, device types, and outcome measures, making cross-study comparisons challenging [75]. Similar methodological inconsistencies appear in cancer population studies, where a lack of standardized validation procedures complicates device selection and implementation in clinical practice [8].
The absence of population-specific validation represents another critical gap. Most commercial algorithms are built for general populations without accounting for physiological differences in special populations [19] [8]. This limitation is particularly problematic for researchers studying groups with distinct movement patterns or metabolic characteristics.
Diagram 1: Comprehensive Validation Workflow for Wearable Trackers. This standardized approach incorporates both laboratory and free-living validation phases against gold-standard measures, culminating in algorithm refinement and framework development.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Materials for Wearable Validation Studies
| Research Tool | Function/Purpose | Application Example |
|---|---|---|
| Metabolic Cart | Measures oxygen consumption (VO₂) and carbon dioxide production (VCO₂) to calculate energy expenditure via indirect calorimetry | Gold-standard comparison for energy burn validation in obesity studies [19] |
| Research-Grade Accelerometers (ActiGraph LEAP) | Provides criterion measures for physical activity intensity and volume in free-living environments | Used as reference device in lung cancer validation study [8] |
| Direct Observation/Video Recording | Enables moment-by-moment comparison of actual activity versus device-recorded data | Video-recorded structured activities for validation in laboratory settings [8] |
| Body Cameras | Captures contextual information about daily activities in free-living validation | Identifies when algorithms over- or under-estimate kcal burn in real-world settings [19] |
| Chest Strap Heart Rate Monitors (Polar H10) | Provides accurate heart rate measurement as control for optical sensor validation | Used as reference standard in consumer device accuracy testing [46] |
| Population-Specific Algorithms | Customized calculations accounting for unique physiological characteristics | Obesity-specific algorithm improving accuracy to >95% [19] |
Visualizing the Path Forward: From Evidence Gaps to Standardized Solutions
Diagram 2: Pathway from Identified Accuracy Gaps to Standardized Solutions. The recognition of measurement inaccuracies, particularly in special populations, drives the development of standardized protocols that enable population-specific algorithms and comprehensive evaluation frameworks.
The evidence clearly demonstrates that without standardized, population-specific validation protocols, wearable activity trackers will continue to provide unreliable energy expenditure data for the populations who could benefit most from accurate monitoring. The development of specialized algorithms for people with obesity represents a promising direction, achieving over 95% accuracy compared to conventional algorithms [19]. Similarly, ongoing efforts to validate devices in oncology populations address critical gaps in our understanding of device performance under disease-specific constraints [8].
For researchers and drug development professionals, these findings highlight the necessity of:
- Implementing standardized validation protocols incorporating both laboratory and free-living components
- Developing population-specific algorithms for vulnerable groups
- Establishing transparent, open-source frameworks that enable cross-study comparisons
- Recognizing the limitations of consumer-grade devices in clinical research contexts
As wearable technology continues to evolve and integrate into healthcare and clinical trials, addressing these evidence gaps through rigorous, standardized evaluation will be essential for generating reliable, actionable data for scientific and clinical applications.
Conclusion
The current evidence indicates that while wearable devices show high accuracy for tracking steps and heart rate, their measurement of energy expenditure remains problematic, with error rates that are unacceptably high for many precise research applications. This inherent limitation, compounded by a lack of standardized validation and rapid device obsolescence, necessitates a cautious and critical approach. For biomedical research, this means wearables are powerful tools for motivating behavior and tracking relative changes, but they should not yet be relied upon as standalone, absolute measures of caloric burn in clinical trials or intervention studies. Future directions must prioritize the development of universal validation standards, foster open collaboration between industry and academia to improve algorithmic transparency, and focus on creating population-specific models. Such advancements are crucial for transforming these ubiquitous consumer gadgets into reliable instruments for drug development and clinical science.
References
- 1. Accuracy and Precision of Energy Expenditure, Heart Rate ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9047731/]
- 2. Study Examines How Well Wearable Tech Tracks Fitness ... [https://olemiss.edu/news/2025/06/apple-watch-accuracy-study/index.html]
- 3. Apple watch accuracy in monitoring health metrics [https://pubmed.ncbi.nlm.nih.gov/40199339/]
- 4. Study Ranks the Most Accurate Fitness Trackers [https://wellnesspulse.com/research/accuracy-of-fitness-trackers/]
- 5. Affordable fitness tracker step count, heart rate and calorie ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12628992/]
- 6. Validity of Actigraph for Measuring Energy Expenditure in ... [https://www.mdpi.com/resolver?pii=s23208545]
- 7. Study: Wearable Devices Not Always Accurate With ... [https://www.wellable.co/blog/wearable-devices-not-always-accurate-with-calories-burned-heart-rate/]
- 8. Comparing the Accuracy of Different Wearable Activity ... [https://www.researchprotocols.org/2025/1/e70472]
- 9. Evaluating the accuracy of smartwatches in health tracking [https://www.news-medical.net/news/20250908/Wearable-health-trackers-reveal-how-accurate-your-smartwatch-really-is.aspx]
- 10. The Validation and Accuracy of Wearable Heart Rate ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12483337/]
- 11. Your Apple Watch Might Not Be as Accurate as You Think ... [https://www.cnet.com/health/fitness/your-apple-watch-might-not-be-as-accurate-as-you-think-new-study-finds/]
- 12. A Validation Study to Confirm the Accuracy of Wearable ... [https://www.mdpi.com/2079-9292/12/11/2536]
- 13. The 3 Best Fitness Trackers of 2025 | Reviews by Wirecutter [https://www.nytimes.com/wirecutter/reviews/the-best-fitness-trackers/]
- 14. Reliability and Validity of Commercially Available ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7509623/]
- 15. Evaluating the Validity of Current Mainstream Wearable ... [https://mhealth.jmir.org/2018/4/e94/]
- 16. Accuracy of Wearable Technology & Smart Watches [https://www.aim7.com/blog/smartwatch-wearable-technology-accuracy]
- 17. Wearable Fitness Tracker Market | Global Market Analysis ... [https://www.futuremarketinsights.com/reports/wearable-fitness-trackers-market]
- 18. Keeping Pace with Wearables: A Living Umbrella Review ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11560992/]
- 19. More accurate fitness tracking for people with obesity [https://news.northwestern.edu/stories/2025/06/more-accurate-fitness-trackers-for-people-with-obesity]
- 20. Fitness Wearables Market Set To Hit $190B, but Data & ... [https://athletechnews.com/fitness-wearables-to-hit-190b/]
- 21. The Validation and Accuracy of Wearable Heart Rate Trackers ... [https://formative.jmir.org/2025/1/e70835]
- 22. Wearable Based Calibration of Contactless In-home ... [https://www.frontiersin.org/journals/digital-health/articles/10.3389/fdgth.2020.566595/full]
- 23. Wearable Devices in Clinical Trials: Hype and Hypothesis - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6032822/]
- 24. Regulatory Considerations for Wearables in Clinical Trials [https://delvehealth.com/regulatory-considerations-for-implementing-wearables-in-clinical-trials/]
- 25. Scoping review of the utilization of wearable devices in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12313918/]
- 26. a review of methods for assessing physical activity energy ... [https://jhpn.biomedcentral.com/articles/10.1186/s41043-025-01117-5]
- 27. A Personalized Energy Expenditure Estimation Method ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12158062/]
- 28. Data-driven Human Energy Expenditure Prediction [https://www.sciencedirect.com/science/article/pii/S1746809425016453]
- 29. Developing and comparing a new BMI inclusive energy ... [https://www.nature.com/articles/s41598-025-99963-0]
- 30. Fitness Trackers Aren't Accurate For People With Obesity [https://www.usnews.com/news/health-news/articles/2025-06-25/fitness-trackers-arent-accurate-for-people-with-obesity]
- 31. New algorithm improves fitness tracker accuracy for people ... [https://www.contemporaryhealth.co.uk/digital-health/new-algorithm-improves-fitness-tracker-accuracy-for-people-with-obesity/]
- 32. Accuracy and Acceptability of Wrist-Wearable Activity-Tracking ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8817215/]
- 33. Treating Obesity At Scale: Real-World Outcomes Using ... [https://www.joincalibrate.com/resources/treating-obesity-at-scale]
- 34. Real-World Accuracy of Wearable Activity Trackers for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11399740/]
- 35. Wearable activity trackers–advanced technology or ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9022022/]
- 36. Quality Evaluation of Free-living Validation Studies for the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9227659/]
- 37. Quality Evaluation of Free-living Validation Studies for the ... [https://mhealth.jmir.org/2022/6/e36377]
- 38. Accuracy and Acceptability of Wrist-Wearable Activity-Tracking Devices: Systematic Review of the Literature - PubMed [https://pubmed.ncbi.nlm.nih.gov/35060915/]
- 39. Your Fitness Tracker Has No Idea How Many Calories You’re Burning | Lifehacker [https://lifehacker.com/you-cant-trust-your-fitness-tracker-on-calorie-burn]
- 40. Validity of Wearable Monitors and Smartphone ... [https://www.mdpi.com/2227-7080/11/1/29]
- 41. Algorithmic bias in public health AI: a silent threat to equity in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12325396/]
- 42. Integration of artificial intelligence and wearable ... [https://www.nature.com/articles/s41746-025-02036-9]
- 43. Bias recognition and mitigation strategies in artificial ... [https://www.nature.com/articles/s41746-025-01503-7]
- 44. How a new U.S. health study is fixing bias in wearable data ... [https://www.news-medical.net/news/20251009/How-a-new-US-health-study-is-fixing-bias-in-wearable-data-research.aspx]
- 45. Bias Mitigation in Primary Health Care Artificial Intelligence ... [https://www.jmir.org/2025/1/e60269/]
- 46. Best Fitness Trackers 2025 | Tested - Forbes Vetted [https://www.forbes.com/sites/forbes-personal-shopper/article/best-fitness-trackers/]
- 47. Wearable Tech Guide: Track and Achieve Your Fitness Goals [https://www.rumen.com.au/article/wearable-tech-fitness-goals-guide-2025/]
- 48. The Best Fitness Trackers of 2025 - Tech Gear Lab [https://www.techgearlab.com/topics/health-fitness/best-fitness-tracker]
- 49. VOSITONE Health Data Precision: 2025 Accuracy Guide [https://vositone.com/vositone-health-data-precision-guide-2025.html]
- 50. Reviewing the Top 10 Fitness Trends for 2025 [https://fitness.edu.au/the-fitness-zone/reviewing-the-top-10-fitness-trends-for-2025-number-1-wearable-technology/]
- 51. Privacy, ethics, transparency, and accountability in AI ... [https://www.frontiersin.org/journals/digital-health/articles/10.3389/fdgth.2025.1431246/full]
- 52. Privacy, ethics, transparency, and accountability in AI systems ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12209263/]
- 53. Multi-sensor data fusion framework and validation of ... [https://www.sciencedirect.com/science/article/pii/S2212827124011600]
- 54. Best Calorie Tracking Watch: The 2025 Fitness Revolution ... [https://www.alibaba.com/blog/best-calorie-tracking-watch-the-2025-fitness-revolution-you-cant-afford-to-miss.html]
- 55. Laboratory comparison of consumer-grade and research ... [https://www.frontiersin.org/journals/physiology/articles/10.3389/fphys.2025.1491401/full]
- 56. Laboratory comparison of consumer-grade and research ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11865084/]
- 57. A guide to consumer-grade wearables in cardiovascular ... [https://www.nature.com/articles/s44325-025-00082-6]
- 58. Fitness trackers are failing millions — this fix could change ... [https://www.sciencedaily.com/releases/2025/06/250620030423.htm]
- 59. Using a Consumer Wearable Activity Monitoring Device to ... [https://pediatrics.jmir.org/2025/1/e59159]
- 60. How Accurate Is the Apple Watch for Tracking Calories and ... [https://www.scottsdale.dexafit.com/blog/how-accurate-is-the-apple-watch-for-tracking-calories-and-heart-rate-what-it-means-for-your-fitness-goals]
- 61. How accurate is the calorie burn count? - Fitbit Community [https://community.fitbit.com/t5/Manage-Weight/How-accurate-is-the-calorie-burn-count/td-p/5784460]
- 62. The Best Fitness Trackers We've Tested for 2025 [https://www.pcmag.com/picks/the-best-fitness-trackers]
- 63. Best fitness trackers : Apple Watch, Fitbit, Garmin... | TechRadar 2025 [https://www.techradar.com/best/best-fitness-trackers]
- 64. The Oura Ring 4 Fixed My Sleep. Here's ... [https://www.cosmopolitan.com/health-fitness/a65439561/oura-ring-4-review/]
- 65. Best fitness tracker 2025: Reviewed, tested, and compared [https://www.wareable.com/fitness-trackers/the-best-fitness-tracker]
- 66. Expert-Tested: Best Garmin Fitness Trackers (2025) [https://www.garagegymreviews.com/best-garmin-fitness-trackers]
- 67. Comparing the Accuracy of Different Wearable Activity ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12226780/]
- 68. Changing User Experience of Wearable Activity Monitors ... [https://www.jmir.org/2025/1/e56251/]
- 69. Validation of Oura ring energy expenditure and steps in ... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-023-01868-x]
- 70. Wrist-Worn Activity Trackers in Laboratory and Free-Living ... [https://mhealth.jmir.org/2021/1/e24806/]
- 71. Fitbit Research Library [https://www.fitabase.com/research-library/?searchString=&category=Validation]
- 72. Wrist-Worn Activity Trackers in Laboratory and Free-Living ... [https://www.sciencedirect.com/org/science/article/pii/S2291522221000231]
- 73. Fitness Tracker Statistics 2025 By Health, Activities [https://www.news.market.us/fitness-tracker-statistics/]
- 74. Fitness Trackers Failing Millions Of People Who Need It Most [https://worldhealth.net/news/fitness-trackers-failing-who-need-it-most/]
- 75. Effectiveness of wearable activity trackers on physical activity ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11921619/]