The Future is Personal: A Comprehensive Guide to N-of-1 Trial Design for Precision Nutrition in Clinical Research
This article provides a detailed exploration of N-of-1 trial designs as a rigorous methodological framework for advancing personalized nutrition.
The Future is Personal: A Comprehensive Guide to N-of-1 Trial Design for Precision Nutrition in Clinical Research
Abstract
This article provides a detailed exploration of N-of-1 trial designs as a rigorous methodological framework for advancing personalized nutrition. Aimed at researchers, scientists, and drug development professionals, it covers the foundational principles that define these single-subject experiments, including their historical context and theoretical basis in precision health. We detail the step-by-step methodology for application, from hypothesis generation and intervention selection to data collection and analysis. The guide addresses common challenges in implementation and optimization, such as managing variability and ensuring methodological rigor. Finally, it examines validation strategies and compares N-of-1 designs to traditional Randomized Controlled Trials (RCTs), assessing their strengths, limitations, and complementary roles. The synthesis concludes by positioning N-of-1 trials as a critical tool for generating high-level evidence for individualized dietary recommendations and shaping the future of clinical nutrition science.
What Are N-of-1 Trials? Defining the Gold Standard for Personalized Nutrition Research
Application Notes
The transition from population-based dietary guidelines to personalized nutrition requires a paradigm shift in research methodology. N-of-1 trials, where a single participant serves as their own control across repeated interventions, are central to this shift. These designs identify individual-specific responses to nutritional interventions (e.g., specific foods, supplements, or meal timings) that are often masked in group-averaged data. The core application is the iterative testing cycle: Observation → Hypothesis → Intervention → Analysis → Personal Protocol. Key applications include identifying personal glycemic responses to foods, determining optimal micronutrient supplementation doses, and tailoring diets for metabolic health, athletic performance, or microbiome modulation. Success hinges on high-frequency, multi-omic phenotyping and robust time-series data analysis to distinguish true intervention effects from background noise.
Experimental Protocols
Protocol 1: N-of-1 Trial for Postprandial Glycemic Response
Objective: To determine an individual's unique glycemic response to three different iso-caloric breakfast meals. Design: Randomized, double-blind, multiple crossover N-of-1 trial over 12 days. Participant: One individual, ideally with continuous glucose monitoring (CGM) capability. Interventions:
- Meal A: High-fiber, complex carbohydrate (e.g., oatmeal).
- Meal B: High-protein, moderate-fat (e.g., eggs and avocado).
- Meal C: High-simple carbohydrate (e.g., cereal with sugar). Procedure:
- Baseline (Days 1-2): Standardized diet, fasting blood glucose (FBG) measured.
- Intervention (Days 3-12): Consume one of the three randomized meals each morning after an overnight fast. Each meal is tested four times in a randomized order.
- Monitoring: CGM records interstitial glucose every 15 minutes for 3 hours postprandial. Self-reported energy levels and satiety (VAS scale) at 0, 60, 120, and 180 minutes.
- Analysis: Calculate iAUC (incremental Area Under the Curve) for glucose for each meal. Use time-series analysis (e.g., Bayesian hierarchical model) to estimate the probability of one meal yielding a lower iAUC than another for this individual.
Protocol 2: Personalized Micronutrient Supplementation via Targeted Metabolomics
Objective: To identify individual need for a specific B-vitamin (e.g., Riboflavin - B2) and optimize dose. Design: Blinded, dose-response N-of-1 trial over 8 weeks. Participant: One individual with suspected suboptimal B2 status based on dietary log. Interventions: Three doses of Riboflavin: Dose 0 (placebo), Dose 1 (RDA: 1.3mg), Dose 2 (2x RDA: 2.6mg). Procedure:
- Wash-in/Out (Week 1 & 6): No supplementation, habitual diet.
- Intervention Blocks (Weeks 2-5 & 7-8): Two 2-week blocks, each containing a randomized 1-week period for each of the three doses.
- Biomarker Sampling: Fasting morning urine collected on the last two days of each intervention week.
- Analysis: Urinary Riboflavin and the functional biomarker Glutathione Reductase Activity Coefficient (EGRac) are measured. Optimal dose is defined as the lowest dose that normalizes EGRac to ≤1.2.
Data Presentation
Table 1: Summary of Key N-of-1 Trial Outcomes in Personalized Nutrition
| Study Focus | Primary Outcome | Typical Measurement Tool | Inter-Individual Variability (Example) | Analysis Method |
|---|---|---|---|---|
| Glycemic Response | Postprandial Glucose iAUC | Continuous Glucose Monitor (CGM) | High; Same food can yield iAUC differences >50% between individuals. | Time-series analysis, Bayesian hierarchical model |
| Microbiome Response | Relative Abundance of Bifidobacterium spp. | 16S rRNA Gene Sequencing | Very High; Fiber interventions can increase abundance from 5% to 25% in some, with no change in others. | Longitudinal differential abundance analysis |
| Metabolic Flexibility | Respiratory Exchange Ratio (RER) Shift | Indirect Calorimetry | Moderate; RER decrease in response to fasting varies in magnitude (0.05 to 0.12). | Crossover comparison of within-subject means |
| Inflammatory Response | Postprandial IL-6 change | High-Sensitivity ELISA | High; High-fat meal may double IL-6 in some, with no effect in others. | Linear mixed-effects models |
Table 2: Example Reagent Kit Solutions for Key Assays
| Research Reagent / Kit | Provider (Example) | Primary Function in Personalized Nutrition Research |
|---|---|---|
| Dried Blood Spot (DBS) Collection Kit | PerkinElmer, Spot On | Enables frequent, low-volume home sampling for metabolomics (fatty acids, vitamins). |
| Stool DNA Stabilization & Collection Kit | DNA Genotek, OMNIgene•GUT | Preserves microbiome DNA at room temperature for home-based longitudinal sampling. |
| High-Sensitivity C-Reactive Protein (hsCRP) ELISA | R&D Systems, Abcam | Quantifies low-grade inflammation, a key outcome for dietary intervention trials. |
| Plasma Short-Chain Fatty Acid (SCFA) Assay | Cell Biolabs, Sigma-Aldrich | Measures microbial fermentation products (acetate, propionate, butyrate) linked to diet. |
| Phospho- / Total AKT (Ser473) ELISA Kit | Cisbio, Thermo Fisher | Assesses insulin signaling pathway activation in response to personalized meal challenges. |
Mandatory Visualizations
The N-of-1 Trial as a Controlled Single-Subject Experiment
Application Notes
N-of-1 trials are a formal methodology for assessing intervention efficacy in a single patient or participant. Within personalized nutrition research, they represent the gold standard for identifying individual-specific responses to dietary components, supplements, or nutraceuticals. These trials systematically compare two or more interventions (e.g., Diet A vs. Diet B, supplement vs. placebo) in a single individual through repeated, controlled crossover cycles. The primary objective is to determine the optimal intervention for that specific individual, thereby directly informing personalized care while also contributing aggregate data for population-level insights when multiple N-of-1 trials are pooled.
Key Advantages in Nutrition Research:
- Controls for Intra-Individual Variability: By using the participant as their own control, these trials account for confounding factors like genetics, metabolism, and baseline lifestyle.
- Quantifies Individual Response Heterogeneity: Directly measures whether and to what degree an individual benefits from a specific nutritional intervention.
- Informs Personalized Dietary Guidelines: Moves beyond population-level "average" recommendations to data-driven personalization.
- Ethical and Pragmatic: Suitable for testing interventions in rare conditions or for piloting hypotheses.
Core Design Principles:
- Control: Use of placebo/sham or active comparator.
- Blinding: Whenever feasible, to minimize bias.
- Replication: Multiple crossover periods to establish a response pattern.
- Randomization: Order of interventions per period is randomized.
- Quantitative Outcomes: Use of validated, preferably continuous, outcome measures (e.g., continuous glucose monitoring, validated symptom scales, biomarkers).
Experimental Protocols
Protocol 1: Basic Crossover N-of-1 Trial for a Dietary Supplement
Aim: To determine the effect of a specific supplement (e.g., Omega-3) vs. placebo on a primary outcome (e.g., joint stiffness score) in a single participant.
Design: Randomized, double-blind, placebo-controlled multiple crossover trial.
| Phase | Duration | Intervention | Key Activities |
|---|---|---|---|
| Baseline | 7 days | Usual Diet | Habitual data collection; establish baseline outcome measures. |
| Treatment A | 14 days | Omega-3 Capsule | Daily intervention. Outcome measurement daily (e.g., diary). |
| Washout | 7 days | Usual Diet (no supplement) | Clearance period to avoid carryover effect. |
| Treatment B | 14 days | Matched Placebo Capsule | Daily intervention. Outcome measurement daily. |
| Washout | 7 days | Usual Diet (no supplement) | - |
| Repeat Cycle | 2x | Random order of A/B | Repeat the Treatment/Washout pair 2 more times (total 3 cycles). |
Outcome Analysis: Visual analysis of time-series plot and within-participant statistical comparison (e.g., paired t-test on period means, linear mixed model).
Protocol 2: N-of-1 Trial Comparing Two Dietary Patterns
Aim: To compare the effects of a low-FODMAP diet vs. a standard diet on gastrointestinal symptoms in an individual with IBS-like symptoms.
Design: Randomized, single-blind, multiple crossover trial.
| Component | Specification |
|---|---|
| Interventions | A: Low-FODMAP Diet. B: Standard (habitual) Diet. |
| Period Length | 10 days per intervention phase. |
| Washout | 5-day habitual diet washout between phases. |
| Blinding | Single-blind (outcome assessor if different from participant). Participant blinding is complex but can be approximated using provided meals. |
| Randomization | Computer-generated random sequence for AB order across cycles. |
| Primary Outcome | Daily IBS-Severity Scoring System (IBS-SSS) score. |
| Secondary Outcomes | Stool frequency/consistency (Bristol Stool Scale), bloating VAS score. |
| Biomarkers | Fecal calprotectin (pre/post each phase), daily continuous glucose monitor data. |
| Compliance Check | Food diary + urinary galacto-oligosaccharide (GOS) challenge test for low-FODMAP adherence. |
| Cycles | 3 complete crossover cycles (A-B-A or B-A-B). |
Visualizations
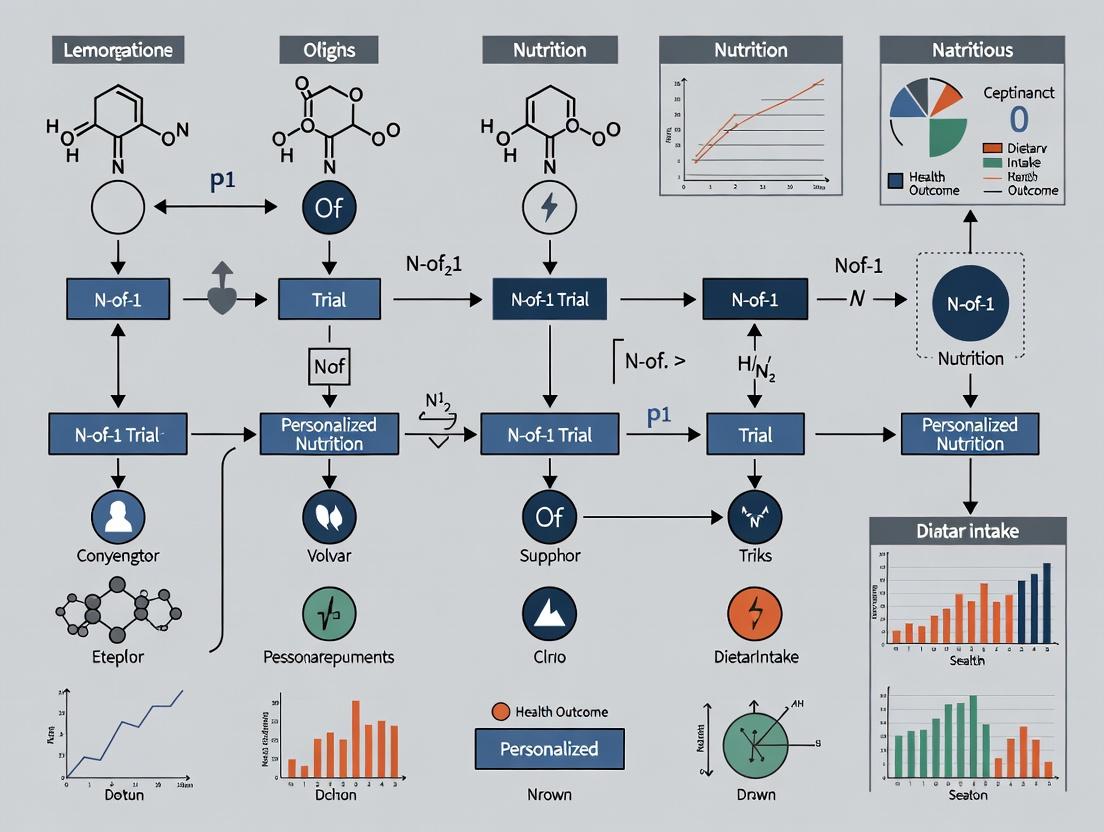
Diagram Title: N-of-1 Trial Workflow for Personalized Nutrition
Diagram Title: Inflammatory Pathway Measured in an N-of-1 Trial
The Scientist's Toolkit: Research Reagent Solutions
| Item/Category | Function in N-of-1 Nutrition Research |
|---|---|
| Placebo/Control Diets | Matched in appearance, taste, and texture to the active intervention (e.g., iso-caloric, similar macronutrient profile) to enable proper blinding. |
| Electronic Daily Diaries (ePRO) | Mobile/web apps for real-time recording of diet adherence, symptoms, and patient-reported outcomes (PROs), minimizing recall bias. |
| Continuous Glucose Monitor (CGM) | Provides high-density, objective data on interstitial glucose response to dietary interventions, a key outcome in metabolic studies. |
| Point-of-Care Test Kits | Home-use kits for biomarkers (e.g., capillary blood CRP, cholesterol, urinary GOS) to monitor near-real-time physiological changes. |
| Biospecimen Collection Kits | Standardized, at-home kits for saliva, stool (e.g., for microbiome), dried blood spots, or urine for centralized lab analysis of omics data. |
| Standardized Reference Meals | Used during designated testing periods within phases to control for confounding dietary variability and elicit a standardized metabolic response. |
| Adherence Biomarkers | Objective biochemical measures (e.g., plasma fatty acid profile for omega-3, urinary sucrose/fructose for sugar intake) to verify compliance. |
| Randomization Software | Generates the random sequence for treatment order across periods, often incorporating washout logic (e.g., R randomizeR, custom scripts). |
| Time-Series Analysis Software | Tools for visual and statistical analysis of single-subject data (e.g., R with nlme/lme4, Single-Case Research design web tools). |
1. Introduction: A Foundational Progression The methodological evolution from behavioral psychology's observation techniques to modern digital health's sensor-driven data collection forms the epistemological backbone for robust N-of-1 trials in personalized nutrition. This progression enables the precise measurement of individual responses to nutritional interventions, moving from subjective self-report to objective, continuous physiological and behavioral monitoring.
2. Key Theoretical and Methodological Transitions
Table 1: Evolution of Measurement Paradigms
| Era | Core Paradigm | Primary Data Type | Key Limitation | Modern Digital Health Analog |
|---|---|---|---|---|
| Behaviorist (c. 1910-1950) | Stimulus-Response | Direct observation; Time-sampled behavior | Low ecological validity; Observer bias | Ecological Momentary Assessment (EMA) via smartphone |
| Cognitive (c. 1960-1990) | Information Processing | Self-report questionnaires; Lab-based performance | Recall bias; Artificial context | Cognitive tasks & diaries delivered via mobile app |
| Psychophysiological (c. 1980-2010) | Mind-Body Connection | Discrete lab measures (e.g., HR, cortisol) | Snapshot data; Expensive equipment | Continuous wearables (ECG, HRV, GSR) |
| Digital Health (2010-Present) | Digital Phenotyping | High-frequency, multimodal sensor data | Data integration complexity; Privacy concerns | AI-driven fusion of wearables, apps, & omics for N-of-1 |
3. Application Notes for N-of-1 Personalized Nutrition Trials
Application Note AN-1: Integrating Behavioral Coding with Digital Phenotyping
- Purpose: To quantify meal-time behaviors and stress responses in free-living conditions.
- Protocol: Participants wear a smartwatch (continuous photoplethysmography for heart rate variability) and use a smartphone app for meal logging. The app triggers brief EMA surveys post-meal to assess subjective satiety and mood. Video recordings of meals (consented) are analyzed using AI-based behavioral coding software for eating rate and patterns.
- Data Fusion: Time-synchronize wearable-derived stress episodes (via HRV dips) with meal logs and eating behavior codes to identify individual-specific stress-eating phenotypes.
Application Note AN-2: From ABC (Antecedent-Behavior-Consequence) Logs to Predictive Analytics
- Purpose: To identify personalized triggers (antecedents) for suboptimal dietary choices.
- Protocol: Using a mobile app, participants log dietary lapses in real-time, noting context (location, social setting, time, pre-lapse emotion). The app passively collects contextual data (GPS, time, social media activity via API). Over multiple N-of-1 cycles, machine learning (e.g., Random Forest) is applied to the individual's data to identify high-risk contexts.
- Intervention: The system delivers just-in-time adaptive interventions (JITAIs) when the individual enters a predicted high-risk context.
4. Detailed Experimental Protocols
Protocol P-1: Quantifying Individual Glycemic & Behavioral Response to Macronutrient Manipulation 1. Objective: To determine an individual's unique glycemic and mood response to three isocaloric meals with varying carbohydrate-to-fat ratios within an N-of-1 design. 2. Materials:
- Continuous Glucose Monitor (CGM)
- Wrist-worn accelerometer & PPG sensor
- Smartphone app for EMA (mood, energy, hunger on 1-10 scale)
- Standardized meal kits (High-Carb, High-Fat, Balanced). 3. Procedure:
- Day 1-3 (Baseline): Monitor usual diet, glucose, activity, and mood.
- Day 4-18 (Intervention): Implement a randomized, crossover sequence of the three meal types, each consumed for two consecutive days. Repeat the sequence three times.
- Meal Day Protocol: Consume meal at standardized time. Log meal start via app. CGM data collected continuously. EMA prompts at 30, 60, 120, and 180 minutes post-meal. Wearable worn continuously.
- Day 19-21 (Washout/Return to Baseline): Monitor as in Days 1-3. 4. Analysis: Calculate for each meal type: (a) Glucose AUC, (b) Glucose volatility, (c) Mean post-meal mood/energy scores, (d) Correlation between glucose slope and self-reported energy.
Protocol P-2: Digital Fasting-Response Phenotyping 1. Objective: To characterize individual differences in metabolic and cognitive adaptation to time-restricted feeding (TRF). 2. Materials:
- CGM & ketone sensor (blood or breath)
- Sleep tracker (actigraphy/EEG headband)
- Digital cognitive test battery (e.g., Go/No-Go, N-back on smartphone)
- Food logging app. 3. Procedure:
- Week 1 (Habitual): Ad libitum eating, all sensors active.
- Week 2-5 (Intervention): 16:8 TRF schedule. Window randomized to start in early vs. late morning across cycles.
- Daily Protocol: Cognitive tests performed upon waking (fasted) and 1-hour post-first meal. Fasting ketones measured upon waking. Sleep quality scored via tracker.
- Week 6 (Follow-up): Return to habitual eating. 4. Analysis: Model within-person effects of fasting duration on ketone production, cognitive performance metrics, and sleep efficiency.
5. Visualization: Pathways and Workflows
From Nutrient to Behavior: Digital Measurement Points
N-of-1 Digital Phenotyping Workflow
6. The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Tools for Digital N-of-1 Nutrition Research
| Item/Category | Example Product/Platform | Primary Function in N-of-1 Context |
|---|---|---|
| Continuous Glucose Monitor (CGM) | Dexcom G7, Abbott Libre 3 | Provides high-resolution interstitial glucose data to link meal composition and timing to metabolic response. |
| Research-Grade Wearable | Empatica E4, ActiGraph GT9X | Captures physiological (EDA, HR, HRV) and activity data for stress and behavior context. |
| Ecological Momentary Assessment (EMA) App | mEMA (Ilumivu), Paco, Custom (REDCap/SurveyCTO) | Delivers time-based or event-contingent surveys to capture real-time symptoms, mood, diet. |
| Digital Food Logging Tool | FoodLog (Keio Univ.), MyFoodRepo, Custom Image-Based App | Enables detailed dietary intake recording, often with image support, for adherence monitoring. |
| Data Integration Platform | RADAR-Base, Fitbit/Apple Health, PhysioMD | Aggregates and time-synchronizes heterogeneous data streams from multiple devices and apps. |
| N-of-1 Statistical Software | R packages (nlme, Shiny for dashboards), Single Case Research (SCR) web tools |
Performs within-participant time-series analysis, visual analysis, and modeling of treatment effects. |
| Secure Cloud Storage | AWS S3 (Research), Google Cloud Platform, HIPAA-compliant servers | Stores large volumes of personal digital phenotyping data in a secure, regulatory-compliant manner. |
Application Notes: Philosophical Pillars in N-of-1 Trial Design
The efficacy of personalized nutrition interventions hinges on three foundational philosophical pillars, each directly informing the design and interpretation of N-of-1 trials.
1.1 Individuality (The Unique Phenotype) Personalized nutrition rejects the "average patient" model. An individual's response to a dietary intervention is a function of their unique genomic, proteomic, metabolomic, microbiome, and lifestyle profile. N-of-1 trials are the methodological embodiment of this principle, treating each participant as a single, complete experiment.
1.2 Causality (Inferring Mechanism in a Single Subject) Establishing causal relationships within an individual is paramount. Unlike group studies showing association, N-of-1 designs, through repeated, cross-over interventions and rigorous time-series analysis, can demonstrate that a specific nutritional change causes an outcome in that specific person, controlling for confounding through design.
1.3 Intra-individual Variability (The Dynamic Baseline) An individual's state is not static. Daily fluctuations in metabolism, sleep, stress, and microbiome composition create a variable baseline. N-of-1 protocols must account for this "noise" through repeated measurements and washout periods to isolate the true signal of an intervention.
Table 1: Quantitative Benchmarks for N-of-1 Trial Design Parameters
| Design Parameter | Recommended Benchmark | Rationale & Source |
|---|---|---|
| Minimum Number of Cross-Over Cycles | 3+ cycles (e.g., ABAB/ABBA) | Balances statistical power for time-series analysis with feasibility. Source: Single-Case Experimental Design (SCED) standards |
| Measurement Frequency per Phase | Daily or bi-daily biomarkers | Captures acute response and intra-individual variability. Source: Continuous glucose monitoring (CGM) studies |
| Washout Period Duration | 5-7 half-lives of key biomarkers | Ensures return to baseline; varies by analyte (e.g., glucose vs. CRP). Source: Pharmacokinetic principles applied to nutrition |
| Primary Analysis Method | Visual analysis + Statistical (e.g., Randomization tests, mSPC) | Combines clinical significance with quantitative rigor for single-subject data. Source: CDC Single Case Design technical guidance |
Experimental Protocols
Protocol 2.1: N-of-1 Trial for Personalized Glycemic Management Objective: To determine the individual causal effect of three different carbohydrate sources (Oatmeal, White Bread, Basmati Rice) on postprandial glycemic response in a pre-diabetic individual. Design: Triple-blind, randomized, multiple cross-over N-of-1 trial.
- Screening & Baseline: Obtain informed consent. Collect fasting blood for HbA1c, baseline metabolomics. Install continuous glucose monitor (CGM). Record 7-day habitual diet and activity (food diary, accelerometer).
- Intervention Phases: Each test food is iso-caloric (50g available carbohydrate), prepared in a standardized kitchen.
- Randomization: The sequence of 12 meals (4 repeats per food) is randomized using a Williams design to control for order and carryover effects.
- Procedure:
- Overnight fast (>10h).
- Pre-meal capillary blood sample (fasting glucose, insulin).
- Consume test meal within 15 minutes. Water ad libitum.
- CGM data logged every 15 mins. Capillary blood samples at 30, 60, 90, 120 mins postprandial.
- No other food/caffeinated beverages for 4 hours. Activity standardized.
- Washout: Minimum 48 hours between test meals.
- Endpoint Analysis: Primary: iAUC (incremental Area Under the Curve) for glucose (0-120min). Secondary: Insulin iAUC, glucose peak time, variability metrics.
Protocol 2.2: Microbiome-Targeted Intervention with Dense Phenotyping Objective: To assess the individual causal impact of a specific prebiotic (Resistant Starch Type 2) on gut microbiome composition and host inflammatory markers. Design: ABAB withdrawal design (A=Placebo, B=Prebiotic).
- Baseline Phenotyping (Week -1): Stool metagenomic sequencing, plasma metabolomics (LC-MS), CRP, IL-6. Gastrointestinal symptom questionnaire.
- Phase 1 (Weeks 1-2): Intervention A or B as per randomization.
- Washout 1 (Week 3): Placebo for all.
- Phase 2 (Weeks 4-5): Cross-over to the other intervention.
- Washout 2 (Week 6): Placebo for all.
- Replication Phases (Weeks 7-10): Repeat Phases 1 & 2.
- Weekly Measurements: Stool sample (for 16S rRNA amplicon sequencing), symptom log.
- Pre/Post each Phase: Plasma metabolomics and inflammatory markers.
- Analysis: Time-series analysis of microbial alpha/beta diversity, specific OTU abundances (e.g., Bifidobacterium, Ruminococcus), correlation with metabolomic shifts and CRP.
Visualizations
N-of-1 Personalized Nutrition Logic Flow
Diet-Microbiome-Host Signaling Pathway
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for N-of-1 Nutritional Phenotyping
| Item & Example Solution | Function in N-of-1 Trials |
|---|---|
| Continuous Glucose Monitor (CGM) e.g., Dexcom G7, Abbott Libre 3 | Provides high-frequency, ambulatory glycemic data with minimal participant burden. Critical for assessing intra-individual variability and postprandial responses. |
| Stabilization Kit for Metabolomics e.g., Metabolomics Stabilizer Tube (Norgen Biotek) | Preserves the metabolomic profile of blood/plasma at collection, ensuring accuracy for longitudinal analysis of low-abundance, unstable metabolites. |
| Stool DNA/RNA Shield Collection Tube e.g., Zymo Research DNA/RNA Shield | Inactivates microbes and nucleases at point of collection, stabilizing microbiome and transcriptome data for reliable longitudinal comparison. |
| Standardized Challenge Meals e.g., Proprietary formulations or defined food matrices | Ensures intervention consistency across multiple cycles. Requires precise macronutrient and ingredient control for causal inference. |
| Electronic Patient-Reported Outcome (ePRO) Platform e.g., REDCap, Castor EDC | Enforces real-time logging of symptoms, diet, and adherence. Time-stamped data integrates with biomarker data for time-series analysis. |
| Multi-plex Immunoassay Kits e.g., Luminex or MSD Panels for Cytokines | Allows measurement of a suite of inflammatory markers from a single, small-volume sample (e.g., 25µL plasma), crucial for dense phenotyping. |
| Automated DNA/RNA Extractor for Microbiome e.g., QIAcube HT (Qiagen) | Standardizes and automates nucleic acid extraction from diverse sample types (stool, saliva), reducing batch effects in longitudinal sequencing studies. |
Application Notes on Inter-Individual Variability in Nutritional Response
Personalized nutrition research, particularly within N-of-1 trial frameworks, is predicated on quantifying the biological diversity that renders universal dietary guidelines suboptimal. The following tables synthesize key domains of variability.
Table 1: Genetic Variants Influencing Macronutrient Metabolism
| Gene | Variant (RSID) | Phenotypic Impact | Effect Size (Approx.) | Study Type |
|---|---|---|---|---|
| FTO | rs9939609 | Increased obesity risk on high-fat diets; attenuated by high-protein intake. | OR: 1.25-1.30 per A allele | Cohort/Mendelian Randomization |
| APOA2 | rs5082 | Homozygous (CC) individuals show higher BMI and waist circumference on high-saturated fat diets. | β: +1.8 BMI units | Randomized Controlled Trial |
| AMY1 | CNV (Copy Number) | Low salivary amylase gene copy number associates with increased obesity risk on high-starch diets. | OR: 1.5-2.0 for low CNV | Cross-sectional & Intervention |
| TCF7L2 | rs7903146 | Carriers (T allele) have impaired glucose tolerance; show greater glycemic improvement on high-fiber diets. | ΔHbA1c: -0.3% vs. non-carriers | N-of-1 Series |
Table 2: Key Contributors to Postprandial Response Variance
| Factor | Contribution to Glycemic Variance | Measurable Biomarker | Notes for N-of-1 Design |
|---|---|---|---|
| Baseline Microbiome | Up to 20-30% | Fecal metagenomic sequencing (e.g., Prevotella/Bacteroides ratio) | High Prevotella associated with improved fiber fermentation. |
| Chronobiology | Significant (Timing effect) | Cortisol, Melatonin rhythms | Meal timing relative to dim-light melatonin onset (DLMO) alters glucose tolerance. |
| Physical Activity | Moderating (Acute vs. Chronic) | Continuous Glucose Monitor (CGM) traces | Acute exercise (<24h prior) improves postprandial glucose disposal. |
| Habitual Sleep | Up to 15% | Actigraphy-derived sleep efficiency | Sleep restriction (≤6h) induces insulin resistance. |
Experimental Protocols
Protocol 1: High-Resolution N-of-1 Postprandial Metabolic Phenotyping Objective: To characterize an individual's dynamic response to standardized and personalized meals over multiple cycles.
- Participant Prep: 7-day lead-in with habitual diet logging and activity (accelerometer). Fasting blood draw for baseline omics (genotyping, metabolomics).
- Test Meals: A) Standardized meal (e.g., 75g carb, 20g protein, 15g fat). B) Isocaloric personalized meal based on participant preference.
- Real-time Monitoring: Wear CGM and continuous heart rate monitor for 6 hours post-meal. Capillary blood samples at 0, 30, 60, 120, 180 min for insulin, triglycerides.
- Omics Sampling: Collect fasting and 120-min postprandial plasma for targeted metabolomics (e.g., bile acids, lipids).
- Microbiome: Fecal sample pre-intervention for 16S rRNA gene sequencing.
- Replication: Repeat the entire cycle (A & B meals) 3-5 times in randomized order, with ≥3-day washout.
- Analysis: Time-series analysis (area under the curve, iAUC) for glucose/insulin. Multi-omics integration via linear mixed-effects models.
Protocol 2: Gut Microbiome-Diet Interaction Assay Ex Vivo Objective: To functionally assess an individual's microbiome fermentative capacity in response to specific dietary fibers.
- Sample Collection: Collect fresh fecal sample in anaerobic chamber.
- Inoculum Prep: Homogenize feces in anaerobic PBS (1:10 w/v) and filter.
- Fermentation Reactor: Set up anaerobic batch cultures using defined medium (e.g., YCFA). Supplement with test substrates: Inulin (soluble), Resistant Starch Type 2 (RS2), Control (glucose).
- Incubation: Inoculate (10% v/v) and incubate anaerobically at 37°C with gentle agitation for 24h.
- Endpoint Analysis:
- SCFA Quantification: Analyze supernatant via GC-MS for acetate, propionate, butyrate.
- Microbial Composition: Pellet for 16S rRNA sequencing to assess taxonomic shifts.
- pH Measurement: Record final culture pH.
- Data Integration: Correlate individual's baseline microbiome composition with SCFA production profiles per substrate.
Pathway & Workflow Visualizations
Title: Determinants of Personalized Dietary Response
Title: N-of-1 Trial Design for Nutrition
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function in Personalized Nutrition Research |
|---|---|
| Continuous Glucose Monitor (CGM) | Enables high-frequency, ambulatory measurement of interstitial glucose to capture postprandial dynamics and variability. |
| Fecal DNA Stabilization Buffer | Preserves microbial genomic DNA at point-of-collection for accurate metagenomic sequencing of the gut microbiome. |
| Targeted Metabolomics Kit (SCFAs/Bile Acids) | Quantitative mass spectrometry-based assay for key microbial and host metabolites linking diet to physiology. |
| Automated DNA Extractor (for Microbiome) | Standardizes high-throughput, reproducible isolation of microbial DNA from complex fecal samples. |
| Cryopreserved Hepatocytes (Donor-Varied) | In vitro model to study inter-individual differences in hepatic metabolism of dietary compounds or nutraceuticals. |
| Multiplex Immunoassay Panel (Inflammatory Cytokines) | Measures a suite of low-concentration inflammatory markers (e.g., IL-6, TNF-α) from small-volume serum samples. |
| Anaerobe Chamber & Culture System | Essential for maintaining strict anaerobic conditions for ex vivo cultivation of obligate anaerobic gut bacteria. |
Ethical and Regulatory Considerations for Single-Subject Research Designs
1. Introduction & Application Notes Within personalized nutrition research, N-of-1 trials (single-subject designs) are pivotal for determining individual-specific responses to dietary interventions. This approach shifts the paradigm from population-average guidelines to personalized evidence. However, the ethical and regulatory framework for these designs is distinct from that of parallel-group randomized controlled trials (RCTs). Key considerations include the blurred line between research and clinical care, the participant-researcher relationship, and regulatory pathways for approval and dissemination of findings.
2. Ethical Considerations: Summary & Framework The ethical conduct of N-of-1 trials in nutrition requires addressing core principles as outlined in the Belmont Report, with specific applications.
Table 1: Core Ethical Principles and Applications for N-of-1 Nutrition Trials
| Ethical Principle | Standard RCT Challenge | N-of-1 Trial Specific Application |
|---|---|---|
| Respect for Persons | Informed consent for group allocation. | Dynamic consent for iterative, cross-over designs; management of high participant involvement. |
| Beneficence | Risk-benefit for a group. | Personalized risk-benefit analysis; potential for direct therapeutic benefit within the trial. |
| Justice | Fair selection of subjects. | Access to costly, intensive designs; ensuring equitable opportunity to participate. |
| Scientific Validity | Rigorous methodology for generalization. | Rigorous methodology for individual causal inference (e.g., randomization, blinding, replication). |
| Clinical Equipoise | Uncertainty about best treatment for population. | Uncertainty about best treatment for the specific individual must exist. |
3. Regulatory Landscape & Data Requirements Regulatory oversight varies by jurisdiction and whether the intervention is a food, a supplement, or a medical food. Key agencies include the FDA (US), EMA (EU), and institutional review boards (IRBs)/ethics committees (ECs).
Table 2: Regulatory Considerations for Personalized Nutrition N-of-1 Trials
| Regulatory Aspect | Consideration | Example/Requirement |
|---|---|---|
| IRB/EC Approval | Review of single-subject protocol. | Protocol must justify N-of-1 design, detail safety monitoring, and describe data analysis plan. |
| IND/CTA Requirement | When is an Investigational New Drug/Clinical Trial Application needed? | Often not required for whole foods; may be required for high-dose supplements or novel compounds. |
| Safety Reporting | Adverse event monitoring. | Predefined thresholds for individual participant pausing/stopping rules must be in protocol. |
| Data Ownership & Privacy | Intensive longitudinal data. | GDPR/ HIPAA compliance for omics data (genomics, metabolomics), continuous glucose monitoring. |
| Result Generalization | Regulatory claim support. | Aggregated series of N-of-1 trials can provide evidence for population-level claims (FDA’s 2019 Draft Guidance on Adaptive Trials). |
4. Detailed Experimental Protocols for an N-of-1 Nutrition Trial
Protocol 4.1: Core N-of-1 Cross-Over Design for Macronutrient Response
- Objective: To determine an individual's glycemic and subjective energy response to two distinct dietary patterns (e.g., High-Carbohydrate vs. High-Fat).
- Design: Randomized, double-blind, multiple cross-over trial.
- Phases:
- Run-in (7 days): Standardized diet wash-in, baseline measurements.
- Intervention Blocks (2x 14 days each): Diet A (HC) and Diet B (HF). Order randomized.
- Washout (7 days): Between blocks, return to standardized diet.
- Replication (Optional): Repeat each diet block a second time to strengthen causal inference.
- Blinding: Use isoenergetic, isoprotein meal replacements with different macronutrient compositions, identical in appearance/taste where possible. Participant and outcome assessor blinded.
- Outcome Measures:
- Primary: Continuous Glucose Monitor (CGM) mean amplitude of glycemic excursions (MAGE).
- Secondary: Daily visual analog scale (VAS) for energy/fatigue, dietary compliance logs (photo-based).
- Analysis: Visual analysis of time-series data and within-participant statistical comparison (e.g., paired t-test on period means, time-series regression).
Protocol 4.2: Embedded Biomarker Sub-Study (Metabolomics)
- Objective: To identify individual-specific metabolic signatures associated with dietary response.
- Sample Collection: Fasting venous blood draw on last two days of each intervention block.
- Processing: Plasma separation within 2 hours, aliquot, and store at -80°C.
- Analysis Platform: Untargeted liquid chromatography-mass spectrometry (LC-MS).
- Protocol Steps:
- Thaw samples on ice.
- Protein precipitation with cold methanol (3:1 ratio).
- Centrifuge, collect supernatant, and dry under nitrogen.
- Reconstitute in MS-compatible solvent.
- Inject onto LC-MS system (C18 column, positive/negative ESI modes).
- Use quality control (QC) samples (pooled from all samples) throughout the run.
- Data Processing: Use software (e.g., XCMS, MS-DIAL) for peak picking, alignment, and annotation. Perform multivariate statistics (PCA, OPLS-DA) to compare metabolic profiles between diets within the individual.
5. Visualization: Experimental Workflow and Ethics Pathway
Diagram 1: N-of-1 Trial Workflow with Ethics Integration (99 chars)
Diagram 2: Data Flow from Individual to Generalizable Evidence (92 chars)
6. The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for N-of-1 Nutrition Trials
| Item | Function/Description | Example Use Case |
|---|---|---|
| Continuous Glucose Monitor (CGM) | Measures interstitial glucose every 1-15 mins; provides dense, ambulatory glycemic data. | Primary outcome measure for carbohydrate or meal-timing interventions. |
| Isoenergetic Meal Replacements | Nutritionally complete, blinded food products varying in macronutrient/ingredient source. | Enabling double-blind, controlled dietary interventions in free-living settings. |
| Metabolomics Kits (Plasma/Urine) | Standardized kits for metabolite extraction and stabilization (e.g., methanol-based protein precipitation). | Enabling high-throughput, reproducible sample prep for LC-MS biomarker discovery. |
| Electronic Patient-Reported Outcome (ePRO) App | Digital platform for daily symptom logging (VAS), dietary intake (photo diary), and compliance alerts. | Capturing secondary outcomes and adherence data in real-time. |
| Cryogenic Storage Tubes (-80°C) | Long-term, stable storage of biological samples (blood, saliva, stool) for multi-omics analysis. | Biobanking for future retrospective or integrative analysis. |
| Randomization & Blinding Service | Web-based or third-party service to allocate intervention sequence and prepare blinded meal kits. | Ensuring allocation concealment and minimizing researcher bias. |
Blueprint for Success: A Step-by-Step Guide to Designing and Executing N-of-1 Nutrition Trials
Personalized nutrition aims to tailor dietary interventions to individual characteristics. N-of-1 trials, where a single participant serves as their own control across repeated intervention periods, are a critical methodology for establishing causal, personalized evidence. Phase 1 focuses on the foundational step of defining a precise, testable hypothesis and the corresponding primary and secondary outcomes. This phase transforms a clinical observation or a biomarker signal into a structured experimental inquiry.
Core Quantitative Data: Key Biomarkers and Outcome Measures
Table 1: Common Personalized Nutrition Outcome Categories and Example Biomarkers
| Outcome Category | Example Specific Biomarkers/Measures | Typical Measurement Method | Temporal Responsiveness |
|---|---|---|---|
| Glycemic Control | Postprandial glucose AUC, Continuous Glucose Monitor (CGM) metrics (e.g., mean glucose, time-in-range), HbA1c | CGM, venous blood assay, finger-prick glucometer | Minutes to days (CGM), weeks (HbA1c) |
| Lipid Metabolism | Fasting LDL-C, HDL-C, triglycerides, apoB, oxidized LDL | Fasting blood lipid panel | Weeks to months |
| Inflammation & Immunity | hs-CRP, IL-6, TNF-α, leukocyte count | ELISA, multiplex immunoassay, flow cytometry | Days to weeks |
| Gut Microbiome | 16S rRNA or shotgun metagenomic sequencing (alpha/beta diversity, specific taxa abundance) | Fecal sample sequencing | Days to weeks |
| Metabolomic & Proteomic | Targeted/untargeted plasma metabolome (e.g., BCAAs, TMAO), proteomic panels | LC-MS, NMR spectroscopy | Hours to days |
| Patient-Reported Outcomes (PROs) | Energy levels, mood (visual analog scale), gastrointestinal symptoms (e.g., IBS-SSS), sleep quality | Validated questionnaires, digital diaries | Daily |
| Physical & Performance | Resting heart rate, heart rate variability (HRV), body composition (DEXA), cognitive task performance | Wearable devices, DEXA scan, digital cognitive tests | Days to weeks |
Table 2: Considerations for Outcome Selection in N-of-1 Design
| Criterion | Optimal Characteristic for N-of-1 | Rationale |
|---|---|---|
| Responsiveness | Rapid response and washout (hours to days) | Allows for shorter treatment periods and more cross-over replicates within a feasible trial duration. |
| Measurement Frequency | High-frequency or continuous measurement feasible | Enables dense longitudinal data capture for robust within-individual analysis. |
| Variability | Low within-subject, day-to-day biological noise relative to intervention effect. | Enhances signal-to-noise ratio, making it easier to detect a personalized effect. |
| Burden & Cost | Low participant burden and acceptable cost for repeated measures. | Critical for adherence and feasibility in a repeated-measures design. |
| Clinical/Practical Relevance | Meaningful to the individual's health goals or symptoms. | Ensures the trial addresses a question of personal importance, enhancing engagement. |
Protocol: Defining the Hypothesis and Outcome Set
Protocol 1.1: Structured Hypothesis Generation Workshop
Objective: To translate a personal health observation into a formal, testable N-of-1 hypothesis.
Materials:
- Whiteboard or collaborative digital document.
- Participant health history, prior lab results, and self-monitoring data (if available).
- Current literature on nutrition-gene/phenotype interactions.
Procedure:
- Identify the Phenotype of Interest (POI): Collaboratively with the participant, define the specific symptom, biomarker deviation, or health goal. (e.g., "Post-lunch energy crash," "Elevated fasting triglycerides," "Poor sleep quality").
- Formulate the Intervention Trigger: Based on the POI and background research, identify a modifiable dietary element hypothesized to influence the POI. This becomes the independent variable. (e.g., "High-glycemic index lunch," "Dietary saturated fat intake," "Caffeine consumption after 2 PM").
- Construct the Hypothesis Statement: Use the format: "In [Participant Initials], manipulating [Independent Variable] will lead to a significant change in [Primary Outcome] compared to the control condition, as measured by [Measurement Tool]."
- Example: "In participant AA, reducing dietary saturated fat to <10% of daily energy intake will lead to a 15% reduction in fasting triglyceride levels compared to a >15% saturated fat diet, as measured by a point-of-care lipid analyzer."
- Define Outcome Hierarchy:
- Primary Outcome: Select one key outcome that is most directly linked to the hypothesis, measurable, and responsive. This is the definitive test of the hypothesis.
- Secondary Outcomes: Select 2-3 additional measures that provide mechanistic insight or assess broader impact (e.g., inflammatory markers linked to triglycerides, energy levels).
- Exploratory Outcomes: List high-dimensional or novel measures (e.g., microbiome, metabolome) for hypothesis-generating analysis.
Protocol 1.2: Outcome Measurement Feasibility and Validation Check
Objective: To ensure selected outcomes can be reliably and repeatedly measured in the participant's real-world setting.
Materials: Prototype data collection tools (apps, devices), sample collection kits.
Procedure:
- Tool Selection & Sourcing: Identify specific devices (e.g., CGM model, wearable) and assays (e.g., dried blood spot kit, stool collection kit). Verify availability and cost.
- Pilot Measurement Period: Conduct a 3-5 day pre-trial run where the participant practices measuring all outcomes in their home environment without any intervention.
- Data Review & Protocol Adjustment:
- Assess compliance and ease of use via participant interview.
- Analyze pilot data for baseline variability and measurement error.
- Refine measurement timing, frequency, and instructions. Simplify or replace overly burdensome measures.
Visualization: Hypothesis Definition Workflow
Diagram 1: Hypothesis and Outcome Definition Workflow (76 chars)
Diagram 2: Personalized Hypothesis to Outcome Mapping (76 chars)
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for Outcome Measurement in Personalized N-of-1 Trials
| Item / Solution | Function / Application | Example Product/Technology |
|---|---|---|
| Continuous Glucose Monitor (CGM) | Provides real-time, interstitial fluid glucose readings every 1-15 minutes. Critical for assessing glycemic variability and postprandial responses. | Dexcom G7, Abbott Freestyle Libre 3 |
| Dried Blood Spot (DBS) Collection Cards | Enables convenient, at-home self-collection of capillary blood for centralized analysis of lipids, hormones, HbA1c, etc. Low burden for repeated sampling. | Whatman 903 Protein Saver Cards, Mitra Microsampler |
| Point-of-Care Lipid Analyzer | Provides rapid, finger-stick measurement of total cholesterol, triglycerides, and HDL-C. Allows for near-immediate feedback. | CardioChek PA Analyzer |
| Fecal Sample Collection & Stabilization Kit | Allows for ambient-temperature stool sample collection and immediate stabilization of microbial DNA/RNA for gut microbiome analysis. | OMNIgene•GUT, Zymo DNA/RNA Shield Fecal Collection Tube |
| Wearable Activity & Sleep Tracker | Objectively measures sleep stages, resting heart rate, heart rate variability (HRV), and activity levels as digital biomarkers. | Oura Ring, Whoop Strap, Apple Watch |
| Electronic Patient-Reported Outcome (ePRO) Platform | Digital platform for administering validated questionnaires (e.g., PROMIS) and daily symptom diaries. Ensures time-stamped data capture and compliance reminders. | REDCap, MetricWire, Ilumivu mEMA |
| Targeted Metabolomics Panel Kits | Commercial kits for analyzing specific metabolite classes (e.g., bile acids, short-chain fatty acids, TMAO) from plasma, urine, or stool via LC-MS/MS. | Biocrates MxP Quant 500, Nightingale Health NMR panel |
Personalized nutrition demands rigorous, individualized evidence. N-of-1 trial designs, where a single participant serves as their own control through repeated crossover phases, are ideal for testing the efficacy of dietary interventions like eliminations and supplementations. This document provides application notes and protocols for implementing such interventions within controlled, research-grade N-of-1 frameworks.
Intervention Protocols & Application Notes
Low FODMAP Elimination Diet Protocol
Application Note: Used to assess individual response to fermentable carbohydrates in conditions like IBS. In an N-of-1 design, this protocol is implemented in discrete, randomized phases against a control diet.
Detailed Protocol:
- Baseline Period (Pre-Trial): 7 days. Participant maintains habitual diet while completing daily symptom diaries (e.g., abdominal pain, bloating severity on 0-10 scale) and stool logs (Bristol Stool Form Scale).
- Intervention Phases:
- Design: Randomized, double-blind (where possible), crossover. Minimum of 3 pairs of alternating control/high-FODMAP and low-FODMAP phases. Each phase lasts 21 days.
- Low-FODMAP Phase: Provide all meals/snacks. Strict avoidance of foods high in Oligosaccharides (wheat, onions, garlic), Disaccharides (lactose), Monosaccharides (excess fructose in apples, honey), and Polyols (stone fruits, artificial sweeteners).
- Control/High-FODMAP Phase: Isocaloric, matched for fiber and macronutrients, but containing ≥50th percentile population intake levels of FODMAPs.
- Rechallenge/Personalization: Post-trial, systematic reintroduction of FODMAP sub-groups to identify specific triggers, informing a long-term personalized diet.
- Key Measures: Daily: IBS-Symptom Severity Score (IBS-SSS), stool frequency/consistency. Pre/post each phase: Fecal sample for metabolomics (SCFAs), microbiome (16S rRNA sequencing).
Probiotic Supplementation Protocol
Application Note: Used to evaluate individual-specific changes in gut ecosystem and host response. Strain selection should be hypothesis-driven.
Detailed Protocol:
- Strain Selection & Blinding: Select a well-characterized strain (e.g., Bifidobacterium longum BB536). Manufacture identical placebo capsules (microcrystalline cellulose). Encode by a third party using a random block sequence for the N-of-1 crossover.
- Trial Design: Randomized, double-blind, placebo-controlled crossover. Three cycles of Probiotic (4 weeks) vs. Placebo (4 weeks), with a 2-week washout between interventions. Washout duration is protocol-specific and may be extended based on strain colonization potential.
- Dosage & Compliance: Administer ≥1x10^9 CFU/day. Use capsule counts and daily electronic diaries to monitor compliance. Consider fecal qPCR for strain abundance as an objective compliance measure.
- Key Measures:
- Primary Outcome: Daily symptom log (protocol-specific, e.g., bloating, transit time).
- Secondary Outcomes: Weekly: Quality of life questionnaire (e.g., IBS-QOL). Pre/post each phase: Fecal sample (16S rRNA metagenomics, targeted metabolomics), blood for systemic inflammation (hs-CRP, cytokines).
Table 1: Typical Effect Sizes from Population Studies for Key Interventions
| Intervention | Condition | Primary Outcome | Typical Effect Size (vs. Placebo/Control) | Notes for N-of-1 Application |
|---|---|---|---|---|
| Low FODMAP Diet | IBS | ≥30% reduction in IBS-SSS | 50-65% response rate (pooled RR ~1.5) | In N-of-1, define individual responder threshold (e.g., 30% symptom reduction) during low-FODMAP phases. |
| Probiotic (B. longum BB536) | IBS | Abdominal pain reduction | Mean difference in pain score: -0.5 to -1.0 points (on 10-pt scale) | Focus on intra-individual effect consistency across crossover cycles. |
| Psyllium Supplement | Chronic Constipation | Spontaneous Bowel Movements/wk | Mean increase: 1.5-2.0 SBMs/wk | Requires stable baseline; effect may be delayed by 3-5 days post-initiation. |
Table 2: Key Biomarkers for Monitoring in N-of-1 Nutritional Trials
| Biomarker Category | Specific Assay | Sample Type | Typical Change with Low FODMAP | Typical Change with Probiotic |
|---|---|---|---|---|
| Microbiome | 16S rRNA gene sequencing (Shannon Diversity) | Fecal | Often decreases (diversity ↓) | Strain-dependent; may increase or decrease. |
| Metabolome | SCFA Analysis (Total SCFA via GC-MS) | Fecal | Variable; often decreases (acetate, butyrate ↓) | Often increases (acetate ↑). |
| Inflammation | High-sensitivity CRP (hs-CRP) ELISA | Serum | May decrease in responsive individuals. | Strain-dependent; modest decreases reported. |
| Intestinal Permeability | Lactulose/Mannitol Excretion Ratio (LC-MS/MS) | Urine | May improve if high at baseline. | Limited/Strain-specific data. |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Dietary Intervention N-of-1 Trials
| Item | Function & Specification | Example Product/Catalog |
|---|---|---|
| Standardized Meal Kits | Ensures dietary control and blinding. Requires macronutrient & FODMAP content certification. | Custom manufactured via metabolic kitchen or services like ModifyHealth (Research Grade). |
| Blinded Supplement Capsules | For probiotic/placebo crossover. Requires GMP manufacturing and 3rd-party coding. | Catalent or Capsugel for encapsulation; Placebo: Microcrystalline cellulose (MCC). |
| Electronic Daily Diary Platform | Real-time symptom tracking, dietary compliance logging, and data integrity. | REDCap (Research Electronic Data Capture) with validated patient-reported outcome (PRO) instruments. |
| Fecal Sample Collection Kit | Standardized, DNA/RNA-stabilizing collection for microbiome and metabolome. | OMNIgene•GUT (DNA Genotek) or ZymoBIOMICS DNA/RNA Shield Collection Tube. |
| SCFA Analysis Kit | Quantitative analysis of short-chain fatty acids from fecal samples. | GC-MS SCFA Analysis Kit (e.g., from Sigma-Aldrich or Cambridge Isotope Labs for labeled standards). |
| hs-CRP ELISA Kit | High-sensitivity measurement of systemic inflammatory biomarker. | Human hs-CRP Quantikine ELISA Kit (R&D Systems, DCRP00). |
| Strain-Specific qPCR Assay | Verifies probiotic colonization and compliance objectively. | Custom TaqMan assay designed to unique genomic region of the administered strain. |
Experimental Workflow & Pathway Diagrams
Title: N-of-1 Low FODMAP Diet Trial Workflow
Title: Probiotic Mechanism of Action Pathways
Application Notes for Personalized N-of-1 Trials
The selection of outcome measures in N-of-1 trials for personalized nutrition must capture multi-omic physiological responses, real-world behavior and context, and the subjective patient experience. This integrated data is crucial for deriving individualized causal inferences and tailoring interventions.
Biomarkers: Objective Physiological Anchors
Biomarkers provide quantifiable, physiological endpoints essential for assessing metabolic and nutritional status. In N-of-1 designs, repeated, frequent sampling is required to establish personal baselines and response patterns.
Table 1: Core Biomarker Categories for Personalized Nutrition Trials
| Category | Specific Biomarkers (Examples) | Sampling Frequency (N-of-1) | Analytical Platform | Primary Function |
|---|---|---|---|---|
| Metabolic | Fasting Glucose, Insulin, HbA1c, Triglycerides, LDL/HDL-C | 2-3x per week (fasting); continuous (CGM) | Clinical Analyzer, HPLC, CGM | Monitor glucose regulation & lipid metabolism |
| Inflammatory | hs-CRP, IL-6, TNF-α | Weekly | ELISA, Multiplex Immunoassay | Assess low-grade systemic inflammation |
| Micronutrient | Vitamin D (25-OH), B12, Folate, Ferritin | Pre/Post-Intervention | LC-MS/MS, Immunoassay | Determine nutrient status & deficiency correction |
| Gut Health | Zonulin, Lipopolysaccharide (LPS), Short-Chain Fatty Acids (SCFA) | Weekly (stool), Pre/Post (blood) | ELISA, GC-MS | Intestinal permeability & microbiome activity |
| Oxidative Stress | 8-OHdG, MDA, Glutathione (GSH) | Weekly | ELISA, Colorimetric Assay | Quantify cellular damage & antioxidant capacity |
Wearables & Digital Phenotyping: Continuous, Real-World Data
Wearable devices capture dense, longitudinal data on activity, physiology, and sleep in free-living conditions, contextualizing other outcomes.
Table 2: Wearable Device Data Streams for Nutritional N-of-1 Trials
| Data Stream | Device Type | Measured Parameters | Sampling Rate | Key Metric for Nutrition |
|---|---|---|---|---|
| Glucose | Continuous Glucose Monitor (CGM) | Interstitial Glucose | Every 1-5 mins | Mean glucose, Time-in-Range, Glycemic variability |
| Physical Activity | Wrist-worn Accelerometer | Step count, Intensity, Heart Rate | Continuous | PA energy expenditure, sedentary bouts |
| Sleep | Accelerometer + PPG | Duration, Stages, Restlessness | Nightly | Sleep efficiency, Restorative sleep % |
| Heart Rate Variability (HRV) | Chest strap/PPG | R-R intervals | Continuous/5-min epochs | RMSSD, LF/HF ratio (stress/recovery) |
| Energy Expenditure | Combined Sensor (ACC + HR) | Metabolic Equivalents (METs) | Minute-by-minute | Total Daily Energy Expenditure (TDEE) |
Patient-Reported Outcomes (PROs): The Subjective Experience
PROs quantify symptoms, quality of life, and adherence directly from the participant, essential for assessing intervention feasibility and personal value.
Table 3: PRO Instruments for Personalized Nutrition Trials
| Domain | Validated Instrument (Example) | Format | Frequency (N-of-1) | Key Scales/Items |
|---|---|---|---|---|
| GI Symptoms | IBS-Symptom Severity Scale (IBS-SSS) | Daily Diary | Daily | Abdominal pain, Bloating, Bowel habit satisfaction |
| Energy & Mood | Profile of Mood States (POMS-SF) | Short Form | Twice Daily | Tension, Fatigue, Vigor, Total Mood Disturbance |
| Diet Adherence | Visual Analog Scale (VAS) | Custom VAS | Per Meal | "How closely did you follow the prescribed meal?" (0-100) |
| Overall Well-being | WHO-5 Well-Being Index | 5-item questionnaire | Weekly | Positive mood, Vitality, General interest |
| Side Effects | Patient-Reported Side Effects | Custom Checklist | Daily | Headache, Nausea, Changes in appetite |
Detailed Experimental Protocols
Protocol 1: High-Frequency Dried Blood Spot (DBS) Sampling for Metabolic & Inflammatory Biomarkers in an N-of-1 Trial
Purpose: To enable frequent, low-burden at-home blood sampling for assay of key metabolic and inflammatory biomarkers. Materials: See "The Scientist's Toolkit" below. Procedure:
- Participant Training: Provide instructional video and diagram for finger-prick and DBS card use. Emphasize cleaning (alcohol swab), lancet use, and filling pre-printed circles on the card completely.
- Sampling Schedule: Participant performs sampling immediately upon waking (fasting) on Monday, Wednesday, and Friday for the trial duration. Each sample is labeled with Participant ID, Date, and Time.
- Sample Handling: Participant allows cards to dry horizontally for 3 hours at room temperature in the provided biohazard sleeve with desiccant packet. Cards are mailed weekly to the lab in a pre-paid, tear-resistant envelope.
- Laboratory Analysis: a. Using a standardized punch (e.g., 3.2 mm), excise one disc from each dried blood spot. b. Elute biomarkers from the disc into an appropriate buffer (e.g., PBS with 0.1% Tween-20) via gentle agitation for 2 hours at room temperature. c. Analyze eluates using high-sensitivity ELISA kits (e.g., for hs-CRP, IL-6) or multiplex immunoassays on a Luminex or MSD platform. For metabolites like lipids, use adapted protocols for DBS with LC-MS/MS.
- Data Normalization: Correct all concentration values for hematocrit using a co-measured marker (e.g., potassium) or a dedicated DBS hematocrit assay to account for individual variation in blood composition.
Protocol 2: Integrating CGM and Activity Data for Nutritional Response Phenotyping
Purpose: To synchronize continuous glucose and physical activity data to model personalized postprandial responses and glycemic variability. Materials: FDA-cleared CGM system (e.g., Dexcom G7, Abbott Libre 3), research-grade activity tracker (e.g., ActiGraph GT9X), data synchronization platform (e.g., Fitabase, custom REDCap API). Procedure:
- Device Initialization & Synchronization: Synchronize all device clocks to a central atomic time server at trial start. Provide participants with standardized charging routines to minimize data gaps.
- Data Collection: Participants wear both devices continuously for the trial duration (minimum 14 days). They log meal times, composition (via photo or brief description), and medication/supplement intake in a companion smartphone app.
- Data Extraction & Alignment: a. Download CGM data (glucose value every 5 mins, timestamps) and accelerometer data (raw 3-axis acceleration at 80-100 Hz, aggregated to 60-second epochs) via manufacturer cloud APIs or proprietary software. b. Align all data streams (glucose, activity, meal logs) to a common timeline using precise timestamps.
- Analysis for N-of-1: a. Calculate standard CGM metrics (Mean Glucose, Time-in-Range 70-140 mg/dL, Coefficient of Variation). b. For each logged meal, extract the 3-hour postprandial glucose trace. Model the incremental Area Under the Curve (iAUC) for that meal. c. Cross-reference with activity data: Categorize the 60 minutes pre- and post-meal as "sedentary" (ACC < 50 mg) or "active" (ACC > 100 mg). Compare postprandial iAUC between meal types (e.g., high vs. low carbohydrate) and activity contexts to generate personalized response profiles.
Protocol 3: Ecological Momentary Assessment (EMA) for Real-Time PRO Collection
Purpose: To capture subjective states in near real-time within the participant's natural environment, reducing recall bias. Materials: Smartphone-based EMA platform (e.g., mEMA, Ethica Data, or custom-built using REDCap Mobile App), survey design. Procedure:
- Survey Design: Create brief (<2 min), targeted surveys. A morning survey queries sleep quality and energy level. Randomly prompted surveys (3-5/day) query current hunger, mood, and gastrointestinal symptoms. An evening survey reviews daily adherence and overall well-being.
- Participant onboarding: Install the app on the participant's phone, configure notification schedules, and conduct a test run.
- Data Collection: The app delivers notifications according to the protocol for the full trial period. Compliance is monitored automatically.
- Data Integration & Analysis: a. Export timestamped PRO responses. b. Synchronize PRO data with biomarker and wearable data streams using common timestamps. c. Perform time-series analysis. For example, model the relationship between same-day inflammatory biomarker levels (e.g., hs-CRP from DBS) and evening fatigue scores, or between postprandial glucose iAUC and post-meal energy ratings, using techniques like multilevel regression or dynamic regression for single-case designs.
Visualizations
Diagram 1: N-of-1 Multi-Modal Data Integration Workflow
Diagram 2: Postprandial Glucose Response Analysis Logic
The Scientist's Toolkit: Key Research Reagent Solutions
Table 4: Essential Materials for Biomarker and PRO Assessment in N-of-1 Trials
| Item Name (Example) | Category | Function in N-of-1 Context |
|---|---|---|
| PerkinElmer 226 DBS Cards | Sample Collection | Filter paper cards for standardized, low-volume blood collection; compatible with automated punching and elution. |
| HemaSpot-HF Blood Collection Device | Sample Collection | All-in-one device for home-based serial sampling; separates and dries blood, stabilizing analytes for shipment. |
| Meso Scale Discovery (MSD) U-PLEX Assays | Biomarker Analysis | Multiplex immunoassay plates allowing simultaneous quantification of 10+ inflammatory biomarkers from low-volume DBS eluates. |
| ZRT Laboratory DBS Hormone/ Biomarker Kits | Biomarker Analysis | Validated, CLIA-certified kits for analyzing hormones (cortisol), lipids, and HbA1c from a single DBS sample. |
| ActiGraph wGT3X-BT Monitor | Wearable Sensor | Research-grade accelerometer for valid, raw tri-axial activity and sleep data; enables calculation of standardized intensity metrics. |
| Dexcom G7 Professional CGM System | Wearable Sensor | Real-time CGM with API access for research; provides continuous interstitial glucose data without daily calibrations. |
| REDCap (Research Electronic Data Capture) | Data Management | Secure web platform for building PRO/EMA surveys, managing trial data, and integrating with external device APIs. |
| Ethica Data Participant-Centric Platform | PRO/EMA Collection | Smartphone app platform for configuring and deploying intensive longitudinal assessments (EMA) with high compliance. |
R Studio + nof1 Package |
Statistical Analysis | Open-source environment and specialized package for analyzing data from N-of-1 trials using Bayesian hierarchical models. |
| Fitabase Data Aggregation Platform | Wearable Data Integration | Platform that aggregates and standardizes data from 100+ consumer devices (Fitbit, Garmin) for research analysis. |
Application Notes: These design structures represent an evolution of the standard N-of-1 trial, introducing higher-order complexity to enhance causal inference, assess temporal effects, and mitigate biases in personalized nutrition research. The application moves beyond simple AB comparisons to model real-world conditions where dietary effects may be cumulative, reversible, or subject to carryover and expectation biases. Their implementation is critical for distinguishing true physiological responses from placebo effects and natural symptom variability.
1. Multiple Crossover Designs
- Purpose: To increase the statistical power and robustness of findings within a single participant by repeating the intervention and control exposures.
- Application Context: Ideal for investigating the effects of a specific dietary component (e.g., gluten, a food additive, caffeine) on a stable, chronic outcome (e.g., daily headache score, bowel regularity, resting heart rate). Replication strengthens the evidence for a causal relationship.
- Key Consideration: Requires careful management of potential carryover effects through adequate washout periods, which must be empirically justified or tested within the design.
2. Withdrawal (Reversal) Periods
- Purpose: To explicitly test whether the effect of an intervention is reversible upon its removal, a key characteristic for establishing a direct biological effect.
- Application Context: Essential in personalized nutrition to determine if symptom improvement is truly linked to the dietary intervention. For example, does reintroducing a suspected trigger food cause symptoms to return to baseline levels? This design can be structured as an ABA (Intervention-Withdrawal) or ABAB sequence.
3. Randomized Blinded Periods
- Purpose: To eliminate participant and investigator bias by concealing the identity of the intervention and control periods.
- Application Context: Crucial for subjective outcome measures (e.g., fatigue, mood, pain) in nutrition research. Effective blinding can be challenging but may be achieved using identically formatted supplements, encapsulated foods, or specially prepared meals.
Protocols for an Integrated N-of-1 Trial
Protocol Title: High-Resolution N-of-1 Trial with Triple-Crossover, Withdrawal, and Double-Blinding for Assessing Personalized Dietary Triggers.
Primary Objective: To determine the causal effect of Dietary Component X on Outcome Y in an individual, while controlling for bias and temporal trends.
Design Structure Protocol:
- Baseline Monitoring (Phase A0): A stable 7-day period to establish the participant’s symptom baseline while on their usual diet.
- Period Randomization & Blinding:
- The subsequent treatment blocks are defined: Intervention (I): Diet containing Component X. Control (C): Diet identical except for the absence/placebo substitute for Component X.
- Using a computer-generated random sequence, six 7-day periods are created in a balanced order (e.g., I, C, C, I, C, I).
- A research dietitian, not involved in outcome assessment, prepares all meals/supplements labeled with only the period code. The participant and outcome assessor are blinded.
- Treatment & Washout Execution:
- The participant follows the provided diet for each 7-day period.
- A mandatory 3-day standardized washout diet (eliminating Component X) is implemented between all periods to minimize carryover.
- Withdrawal Integration: The final 7-day period is followed by a 14-day open-label withdrawal phase where the participant returns to their usual diet, monitoring for a return to baseline symptoms.
- Outcome Measurement: The primary outcome (e.g., daily symptom score on a VAS 0-100) is recorded daily via a validated electronic diary. A secondary biomarker (e.g., CRP from daily capillary blood) is collected on the final day of each period.
- Data Analysis: Visual analysis of time-series data is supplemented with statistical modeling (e.g., linear mixed-effects model) to compare Intervention vs. Control periods, accounting for period and sequence effects.
Table 1: Quantitative Comparison of Design Components
| Design Component | Primary Function | Typical Minimum Period Duration | Key Statistical Advantage | Major Practical Challenge |
|---|---|---|---|---|
| Multiple Crossover | Replication & Power | 5-7 days | Increases degrees of freedom, reduces within-trial error. | Participant burden & retention. |
| Withdrawal Period | Reversibility Test | 7-14 days | Provides direct evidence for causal mechanism. | Requires stable underlying condition. |
| Randomized Blinded Periods | Bias Reduction | Matched to intervention | Controls for placebo/nocebo effects. | Achieving true blinding in dietary studies. |
| Standardized Washout | Control Carryover | 3-5 half-lives of effect | Isolates period-specific effects. | May prolong trial duration significantly. |
Table 2: Example Outcome Data from a Simulated Trial
| Period | Day | Designated Condition | Blinding Code | Symptom Score (VAS) | Biomarker (CRP mg/L) |
|---|---|---|---|---|---|
| Baseline | 1-7 | Usual Diet | Open | 65 ± 8 | 5.2 |
| 1 | 8-14 | Intervention (I) | TR01 | 42 ± 6 | 3.1 |
| Washout | 15-17 | Washout Diet | Open | 58 ± 7 | 4.8 |
| 2 | 18-24 | Control (C) | TR02 | 62 ± 9 | 5.0 |
| Washout | 25-27 | Washout Diet | Open | 61 ± 6 | 4.9 |
| 3 | 28-34 | Control (C) | TR03 | 60 ± 8 | 5.1 |
| Washout | 35-37 | Washout Diet | Open | 59 ± 7 | 4.7 |
| 4 | 38-44 | Intervention (I) | TR04 | 40 ± 5 | 2.9 |
| Washout | 45-47 | Washout Diet | Open | 57 ± 6 | 4.8 |
| 5 | 48-54 | Control (C) | TR05 | 63 ± 7 | 5.3 |
| Washout | 55-57 | Washout Diet | Open | 62 ± 5 | 5.0 |
| 6 | 58-64 | Intervention (I) | TR06 | 38 ± 4 | 2.8 |
| Withdrawal | 65-78 | Usual Diet | Open | 66 ± 10 | 5.4 |
Visualizations
N-of-1 Trial Workflow with Multiple Periods
Mechanism and Reversibility Tested by Withdrawal
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function in N-of-1 Nutrition Trials |
|---|---|
| Encapsulated Food Ingredients | Gelatin or vegetarian capsules filled with precise doses of powdered food (e.g., gluten, lactose, fructose) or placebo (e.g., rice starch) to enable double-blinding. |
| Placebo-Controlled Meal Kits | Fully prepared, matched meals that are identical in appearance, taste, and macronutrient profile, differing only in the presence/absence of the target dietary component. |
| Electronic Patient-Reported Outcome (ePRO) System | Validated digital platforms for daily symptom logging, ensuring time-stamped data, compliance reminders, and reduced recall bias. |
| Lateral Flow Assay (LFA) Kits for Biomarkers | Point-of-care tests for biomarkers (e.g., CRP, calprotectin) from finger-prick blood or stool, enabling frequent, low-burden objective measurement. |
| Adherence Biomarker Panels | Mass spectrometry-based tests for urinary or blood metabolites specific to the dietary intervention (e.g., alkylresorcinols for whole grain, proline betaine for citrus) to verify compliance. |
| Data Analysis Software (R/Python packages) | Specialized libraries (e.g., nlme in R for mixed models, scipy in Python for time-series analysis) to model complex N-of-1 data with repeated crossovers. |
In the context of N-of-1 trial designs for personalized nutrition research, robust, scalable, and participant-centric data collection is paramount. Traditional methods are often inadequate for capturing high-frequency, real-world data. This document outlines modern protocols leveraging digital tools, apps, and remote monitoring to capture multimodal data streams essential for deriving individualized nutritional insights.
Core Digital Data Streams & Tools
The following table summarizes primary data types, collection tools, and their relevance to personalized nutrition N-of-1 trials.
Table 1: Digital Data Streams for Personalized Nutrition N-of-1 Trials
| Data Category | Specific Metrics | Recommended Tool/Platform Type | Collection Frequency | Primary Use in Analysis |
|---|---|---|---|---|
| Dietary Intake | Macro/Micronutrients, food items, timing | Smartphone Apps (e.g., Cronometer), image-based dietary records | Daily (per meal) | Independent variable manipulation & adherence monitoring. |
| Continuous Glucose Monitoring (CGM) | Interstitial glucose (mmol/L), trends, variability | Wearable CGM Sensors (e.g., Dexcom G7, Abbott Libre 3) | 1-5 min intervals | Primary glycemic response outcome; personal carbohydrate metabolism. |
| Physical Activity & Sleep | Steps, heart rate, HRV, sleep stages, energy expenditure | Consumer Wearables (e.g., Fitbit, Apple Watch), research-grade actigraphy | Continuous (1s-1min epochs) | Covariate adjustment for energy balance & metabolic context. |
| Patient-Reported Outcomes (PROs) | Hunger, energy, mood, GI symptoms, satiety | Ecological Momentary Assessment (EMA) via custom apps (e.g., REDCap Mobile, MetricWire) | Scheduled (3-5x/day) & event-driven | Subjective outcome measures and side-effect profiling. |
| Biometric Remote Monitoring | Body weight, body composition (BIA), blood pressure | Smart Scales, Bluetooth BP cuffs, home BIA devices (e.g., InBody) | Daily/Weekly | Secondary physiological outcomes. |
| Omics & Point-of-Care Biomarkers | Dried blood spot (DBS) metabolites, gut microbiome (stool), capillary blood ketones | At-home collection kits + App-guided logistics (e.g., ZOE, Thriva) | Pre, mid, and post-intervention periods | Deep phenotyping for mechanistic insights. |
Detailed Experimental Protocols
Protocol 3.1: Integrated Digital Data Collection for a 4-Phase N-of-1 Nutrition Trial
Aim: To systematically compare personalized responses to three distinct dietary interventions (e.g., Low-Fat, Low-Carbohydrate, Mediterranean) against a baseline phase in a single individual.
Materials (Research Reagent Solutions):
- Table 2: Essential Research Toolkit for Digital N-of-1 Trials
Item Name Function/Description Example Product/Service CGM Sensor System Measures interstitial glucose continuously to assess glycemic variability and response. Abbott FreeStyle Libre 3 EMA/Diary App Platform Deploys surveys, prompts for dietary logging, and aggregates PRO data in real-time. REDCap Mobile App + Cloud Bluetooth-Enabled Smart Scale Securely transmits body weight and body composition data to a central server. Withings Body Cardio Research Data Aggregator API-enabled platform to unify data from disparate devices into a single, timestamped dataset. Fitbit/Google Cloud API, Apple HealthKit, or custom middleware (e.g., Axon). At-Home DBS Kit Allows participant self-collection of capillary blood for centralized analysis of lipids, HbA1c, or metabolomics. Neoteryx Mitra device Standardized Nutrient Modules Pre-portioned food items or supplements to ensure precise intervention delivery during specific phases. Custom-prepared meal shakes or snack bars with defined compositions.
Procedure:
- Baseline Phase (Week 1): Participant consumes their usual diet. CGM is applied. EMA surveys (mood, energy) are sent 4x/day at random intervals. Baseline PROs, body measurements, and a DBS sample are collected.
- Intervention Rotation (Weeks 2-4): Three distinct dietary interventions are administered in randomized order, each for one week. Participant logs all food intake via the designated app, which provides real-time feedback on adherence to the phase's macronutrient goals.
- Real-Time Monitoring: The research team monitors aggregated CGM and adherence data via a secure dashboard. Algorithmic flags identify protocol deviations (e.g., prolonged high glucose) or technical issues.
- Sample Collection: At the end of each weekly phase, the participant:
- Uses the smart scale for daily weight.
- Collects a DBS sample on the final morning.
- Completes a end-of-phase symptom and preference questionnaire via the app.
- Data Synchronization: All device data (CGM, activity, weight) are automatically synced via their native APIs to the central aggregator. App-based data (diet, PROs) are uploaded in real-time.
- Data Processing: Raw data are processed using standardized pipelines (e.g., CGM data analyzed for mean glucose, standard deviation, and time-in-range using the cgmanalysis R package).
Protocol 3.2: Ecological Momentary Assessment (EMA) for Symptom Capture
Aim: To capture real-time subjective experiences in the participant's natural environment, minimizing recall bias.
- Survey Design: Using a platform like REDCap, design brief (<2 min) surveys assessing hunger (VAS), energy, abdominal discomfort, and mood.
- Sampling Schedule: Configure a hybrid schedule:
- Time-Based: 4 random prompts within set windows (post-wake, pre-lunch, late afternoon, post-dinner).
- Event-Based: A prompt is sent 30 minutes after the participant logs a meal in the dietary app.
- Compliance: Configure gentle push notification reminders. The app displays a calendar with completed and missed assessments.
Visualizations
N-of-1 Digital Data Collection & Feedback Loop
From Dietary Input to Personalized Recommendation
Application Notes for Personalized Nutrition N-of-1 Trials
Single-subject (N-of-1) experimental designs are foundational for generating individualized evidence in personalized nutrition. The statistical approaches required diverge significantly from group-based analytics, demanding specialized methods to manage serial dependence, intra-individual variability, and the integration of prior knowledge.
Core Analytical Frameworks
Time-Series Analysis is critical for modeling data points collected sequentially over time (e.g., daily glucose readings, weekly weight measurements), which are often autocorrelated. Key techniques include:
- Autoregressive Integrated Moving Average (ARIMA) Models: For identifying and modeling trends, seasonality, and noise.
- Spectral Analysis: For detecting cyclic patterns (e.g., circadian rhythms in metabolic markers).
- Changepoint Analysis: For statistically identifying the point in time when a physiological trajectory significantly shifts following a dietary intervention.
Visual Analysis remains a cornerstone, particularly for establishing functional relationships in single-case experimental designs (SCEDs) like reversal (ABA) or multiple-baseline designs. It involves the systematic inspection of level, trend, variability, immediacy of effect, and overlap between phases.
Bayesian Methods offer a powerful paradigm for N-of-1 trials by formally incorporating prior information (e.g., from population studies or the subject’s historical data) and updating beliefs with newly collected individual data to produce posterior probabilities of intervention efficacy.
Quantitative Comparison of Statistical Methods
Table 1: Comparison of Statistical Approaches for N-of-1 Analysis
| Method Category | Primary Use Case | Key Strength | Key Limitation | Example Software/Package |
|---|---|---|---|---|
| Time-Series (ARIMA) | Modeling & forecasting continuous, autocorrelated outcomes (e.g., CGM data). | Objectively models complex temporal patterns & provides prediction intervals. | Requires many data points (often >50); model identification can be complex. | R: forecast, tseries; Python: statsmodels |
| Visual Analysis | Initial assessment of phase changes in SCEDs. | Intuitive, no distributional assumptions, captures immediacy & consistency. | Subjective; requires trained raters; poor for small/slow effects. | GraphPad Prism; NIH Single-Case Design visual analysis tools. |
| Bayesian Hierarchical | Quantifying individual treatment effect probability, borrowing strength from priors. | Provides probabilistic interpretation; optimally uses sparse data; flexible. | Requires specification of prior distributions; computationally intensive. | R: brms, rstanarm; Stan; JAGS |
| Simulation Modeling Analysis (SMA) | Statistical testing for level/trend change between phases in SCEDs. | Reduces serial dependence via simulation; robust for short series. | Less powerful for very short phases; simulation-based. | R: SCD package; web-based SCRT. |
| Multilevel Modeling | Analyzing multiple N-of-1 trials or cycles within a subject. | Separates within- & between-subject variance; models repeated cycles. | Assumes normally distributed errors and random effects. | R: nlme, lme4; SPSS MIXED. |
Experimental Protocols
Protocol: Conducting a Time-Series Analysis on Continuous Glucose Monitor (CGM) Data
Objective: To objectively identify the effect of a targeted fiber intervention on glycemic stability within a single participant.
Materials: CGM device, data extraction software, statistical software (R/Python).
Procedure:
- Data Collection & Preparation: Export timestamped glucose readings (e.g., every 5 minutes) for a pre-intervention baseline (Phase A) and intervention phase (Phase B). Align data into a single time-series object.
- Descriptive & Visual Analysis: Plot the full series. Calculate descriptive statistics (mean, SD, CV) for each phase. Visually inspect for non-stationarity (trends, shifts).
- Stationarity Check & Transformation: Apply the Augmented Dickey-Fuller (ADF) test. If non-stationary, difference the series (
dparameter in ARIMA) until stationary. - Model Identification: On the stationary series, examine the Autocorrelation Function (ACF) and Partial ACF (PACF) plots to propose initial
p(AR order) andq(MA order) values. - Model Fitting & Selection: Fit multiple candidate ARIMA(p,d,q) models. Select the best model using the Akaike Information Criterion (AIC) or Bayesian Information Criterion (BIC). Validate by ensuring residuals are white noise (no significant ACF).
- Intervention Analysis: Use the best-fitting model to forecast the expected trajectory had baseline continued. Statistically compare forecasted values to observed intervention-phase values using a t-test or by analyzing the residuals of a combined model with a phase indicator.
Protocol: Bayesian Analysis of a Personalized Nutrition N-of-1 Trial
Objective: To compute the posterior probability that a ketogenic diet reduces self-reported fatigue scores compared to a standard diet in a single patient.
Materials: Daily symptom log (e.g., 1-10 scale), statistical software with Bayesian capabilities (Stan/brms).
Procedure:
- Define Priors: Specify prior distributions for model parameters. For example:
Intercept (α) ~ Normal(5, 2)// Assuming a mid-range mean fatigue with high uncertainty.Treatment Effect (β) ~ Normal(0, 1)// A skeptical prior centered on no effect.Standard Deviation (σ) ~ Exponential(1)// A positive, constrained prior for variance.
- Specify Likelihood: Define the data model. E.g.,
Fatigue_Score[t] ~ Normal(α + β * Treatment_Indicator[t], σ), where the indicator is 0 for standard diet and 1 for ketogenic diet. - Compute Posterior: Use Markov Chain Monte Carlo (MCMC) sampling (e.g., via
brms::brm()) to compute the joint posterior distribution of all parameters given the observed data and priors. - Diagnose & Summarize: Check MCMC chain convergence (R-hat ≈ 1.0, effective sample size). Summarize the posterior distribution for
β(treatment effect): report its median and 95% Credible Interval (CrI). - Probability Statement: Calculate the probability of a clinically meaningful effect. E.g.,
Pr(β < -1.0 | Data)= the probability the ketogenic diet reduces fatigue by more than 1 point.
Visualizations
Single-Subject Statistical Analysis Workflow
Bayesian Updating for N-of-1 Trials
The Scientist's Toolkit
Table 2: Key Research Reagent Solutions for N-of-1 Personalized Nutrition Studies
| Item/Category | Function in N-of-1 Research | Example/Specification |
|---|---|---|
| Continuous Glucose Monitor (CGM) | Provides high-density, longitudinal glycemic data for time-series analysis of dietary interventions. | Dexcom G7, Abbott FreeStyle Libre 3. Outputs: Interstitial glucose readings every 1-5 mins. |
| Digital Food & Symptom Logging Platform | Standardizes and time-stamps the recording of exposures (diet) and outcomes (symptoms), ensuring data linkage. | Apps: MyFitnessPal, Cronometer, or custom REDCap surveys. |
| Wearable Activity/Sleep Tracker | Quantifies confounders/modifiers (physical activity, sleep quality) to improve model specificity. | Devices: ActiGraph, Fitbit, Oura Ring. Metrics: Step count, heart rate, HRV, sleep stages. |
| Point-of-Care Biomarker Kits | Enables frequent, at-home collection of biomarker data to complement digital metrics. | Dried Blood Spot (DBS) kits for lipids, HbA1c; urine dipsticks for ketones. |
| Statistical Software with Bayesian & Time-Series Capabilities | Performs the specialized analyses required for single-subject data. | R (with brms, rstan, forecast packages); Python (pymc3, statsmodels). |
| Visual Analysis Software | Aids in the systematic visual inspection of single-case experimental design data. | Single Case Research (SCR) web tools; GraphPad Prism for phased charting. |
Navigating Pitfalls: Practical Solutions for Common Challenges in N-of-1 Nutrition Research
Time-varying confounders (TVCs), such as acute stress, sleep quality, physical activity, and menstrual cycle phase, pose a significant challenge in N-of-1 nutritional intervention trials. These factors fluctuate within an individual over time, can influence the outcome of interest (e.g., glycemic response, inflammation), and may themselves be affected by prior exposures or interventions. Traditional statistical methods fail when these TVCs are both mediators and confounders, necessitating advanced modeling approaches like marginal structural models (MSMs) or structural nested mean models.
Quantifying Key Time-Varying Confounders: Data & Methods
Accurate measurement is prerequisite to adjustment. The following table summarizes current gold-standard and pragmatic measurement tools.
Table 1: Measurement Protocols for Common Time-Varying Confounders
| Confounder | Primary Quantitative Measure | Pragmatic/Alternative Measure | Measurement Frequency | Key Device/Platform |
|---|---|---|---|---|
| Stress | Salivary cortisol (AUC from 4+ samples/day), Heart Rate Variability (HRV; RMSSD, LF/HF) | Perceived Stress Scale (PSS-4), State Anxiety Inventory (short form) | Event-driven + fixed schedule (e.g., pre-meal, bedtime) | Salivette tubes, Polar H10/WHOOP strap, smartphone EMA |
| Sleep | Polysomnography (PSG; total sleep time, wake after sleep onset, sleep stages) | Actigraphy (sleep efficiency, fragmentation index), Self-reported sleep diary | Nightly | Actigraph GT9X, Fitbit/Ōura ring (research-grade firmware), Consensus Sleep Diary |
| Physical Activity | Tri-axial accelerometry (vector magnitude counts, Bouted moderate-vigorous minutes) | IPAQ (short form), step count from consumer wearable | Continuous/ Daily | ActiGraph wGT3X-BT, Apple Watch, Fitbit |
| Dietary Adherence | Weighed food records, 24-hr dietary recall via ASA24 | Photographic food records via mobile app (e.g., MealLogger), Brief adherence questionnaire | Daily (for intervention foods) | Kitchen scale, ASA24 system, custom app |
| Menstrual Cycle | Urinary luteinizing hormone (LH) surge test, serum progesterone | Self-reported cycle tracking app (start/end dates, symptoms) | Daily tracking, LH testing predicted window | ClearBlue Digital Ovulation Test, Clue app |
Core Experimental Protocol: An Intensive Longitudinal N-of-1 Study
This protocol outlines a 60-day N-of-1 trial investigating the effect of a personalized fiber supplement on postprandial glucose, while accounting for TVCs.
Title: Protocol for an N-of-1 Trial on Fiber Response with Time-Varying Confounder Assessment.
Objective: To estimate the causal effect of Fiber Intervention (F) vs. Placebo (P) on continuous glucose monitor (CGM)-derived postprandial glucose excursion (PPGE), adjusting for time-varying confounders: stress, sleep, and physical activity.
Design: Randomized, double-blind, multiple crossover ABAB/BAAB design with continuous monitoring.
Participant: A single individual with pre-diabetes or interest in metabolic optimization.
Phases:
- Run-in (7 days): Habituation to devices, baseline TVC measurement, no intervention.
- Intervention (56 days): 28 two-day blocks. Random assignment of F or P per block, stratified by day of week.
- Washout: Not required for inert placebo; 48 hours between intervention switches assumed sufficient.
Daily Measurements:
- Outcome: PPGE (mg/dL*min) calculated from CGM (Dexcom G7) for 2 hours after standardized test meals.
- Intervention: F or P packet consumed with breakfast.
- TVCs:
- Stress: HRV measured via chest strap (Polar H10) during 5-min seated rest pre-breakfast and pre-dinner; evening salivary cortisol sample.
- Sleep: Wrist-worn actigraphy (Actigraph GT9X) nightly.
- Physical Activity: Daily step count and bouted MVPA from same actigraph.
- Dietary Adherence: Photographic record of all meals via smartphone app.
Statistical Analysis Plan:
- Descriptive: Time-series plots of PPGE and TVCs.
- Primary Analysis: Fit a Marginal Structural Model using Inverse Probability of Treatment and Confounder Weighting.
- Step 1: Model treatment assignment probability (stabilized weights).
- Step 2: Model time-varying confounder distributions, conditional on past.
- Step 3: Fit weighted linear mixed model for PPGE ~ Treatment + Time, with individual random intercept.
Visualization: Causal Pathways & Analytical Workflow
Diagram 1: Causal Diagram for TVCs as Mediators & Confounders
Diagram 2: Analytical Workflow for Marginal Structural Models
The Scientist's Toolkit: Essential Research Reagents & Solutions
Table 2: Key Research Reagent Solutions for TVC Management
| Item & Supplier | Function in Protocol | Critical Specification/Note |
|---|---|---|
| Dexcom G7 Continuous Glucose Monitor (Dexcom, Inc.) | Primary outcome measurement (PPGE). Provides high-frequency interstitial glucose. | Research account required for blinded device start/stop and data export. |
| ActiGraph wGT3X-BT Accelerometer (ActiGraph LLC) | Objective measurement of sleep and physical activity (TVCs). Gold-standard for actigraphy. | Must use validated sleep scoring algorithm (e.g., Cole-Kripke) and Freedson VM3 cut-points for activity. |
| Salivette Cortisol (Sarstedt AG & Co.) | Non-invasive collection of salivary cortisol for stress biomarker assessment. | Requires strict time-of-day control and immediate freezing at -20°C after collection. |
| Polar H10 Heart Rate Sensor (Polar Electro) | Measurement of R-R intervals for Heart Rate Variability (HRV) analysis, a stress/TVC metric. | Use with Elite HRV or Kubios HRV Standard software for RMSSD/LF/HF analysis. |
| ASA24-Automated Self-Administered 24-hr Recall (NIH/NCI) | Tool for detailed dietary assessment to monitor adherence and potential nutrient TVCs. | Researcher tool version allows for customization of recall period and prompts. |
| Research Electronic Data Capture (REDCap, Vanderbilt) | Secure platform for daily EMA surveys, consent, and integration of multi-stream device data. | Crucial for time-stamping all measurements and ensuring temporal alignment of datasets. |
Inverse Probability Weighting R Package (ipw or WeightIt) |
Statistical software to calculate stabilized weights for MSM analysis. | Requires careful specification of exposure and confounder models to avoid extreme weights. |
Within N-of-1 trial designs for personalized nutrition, the ecological validity of interventions hinges on data collected in free-living conditions. The core challenge is the dual burden of ensuring participant adherence to prescribed protocols and capturing high-fidelity, contextualized data outside the laboratory. This application note details integrated methodologies to address this challenge, balancing rigorous measurement with minimal participant burden.
Table 1: Comparison of Data Logging Modalities for Free-Living Nutritional Studies
| Modality | Example Technologies | Adherence Metric Captured | Data Granularity | Participant Burden | Key Limitations |
|---|---|---|---|---|---|
| Self-Report | Paper diaries, EMA* surveys, 24-hr recall apps | Subjective compliance, food intake | Low-Medium (prone to error) | High (relies on memory & diligence) | Recall bias, social desirability bias, low compliance |
| Wearable Sensors | CGM, AW*, Actigraphy rings | Physiological response, activity, sleep | High (continuous, objective) | Low (passive collection) | Indirect measure of intake, data noise, battery life |
| Passive Food Capture | Camera-based (e.g., bite counters), acoustic sensors | Meal timing, estimated intake volume | Medium | Low-Medium | Privacy concerns, incomplete nutrient data, device acceptance |
| Biometric Feedback | Connected scales, POC* blood analyzers | Weight, ketones, blood lipids | Low (snapshots) | Medium (requires active use) | Intermittent data, requires adherence to self-testing |
| Smart Packaging | RFID/NFC pill bottles, IoT** containers | Supplement/medication removal | High (event-based) | Low (passive) | Limited to packaged items, cost |
Ecological Momentary Assessment; Continuous Glucose Monitor; *Apple Watch; Point-of-Care; *Internet of Things
Table 2: Reported Adherence Rates by Monitoring Strategy in N-of-1 Nutrition Trials
| Monitoring Strategy | Median Adherence Rate (%) (Range) | Typical Study Duration | Primary Validation Method |
|---|---|---|---|
| Unsupported Self-Report | 58% (30-75) | 2-8 weeks | Comparison with objective sensor data |
| Digital Diary + Reminders | 78% (65-92) | 1-12 weeks | Time-stamp analysis, photo verification |
| Wearable Sensor (Passive) | 95% (88-99) | 1-52 weeks | Sensor wear-time algorithms |
| Integrated Platform (Sensor + EMA) | 85% (72-94) | 4-12 weeks | Multi-modal data concordance checks |
Core Experimental Protocols
Protocol 1: Multi-Modal Adherence Verification for a Personalized Diet N-of-1 Trial
Objective: To verify adherence to a time-restricted feeding (TRF) window and a low-FODMAP diet prescription in a free-living participant over a 4-week intervention period.
Materials:
- Research-grade actigraphy device (e.g., ActiGraph GT9X)
- Consumer wearable (e.g., Fitbit) for cross-verification and participant engagement
- Smartphone app configured for Ecological Momentary Assessment (EMA) and photo-based food logging
- NFC-enabled container for a provided nutritional supplement
- Secure cloud database for data aggregation (e.g., RADAR-base, Fitbit/Apple Health API intermediary)
Procedure:
- Baseline & Training (Days 1-3): Fit participant with actigraph. Install and configure smartphone app. Train participant on: a) Taking clear, time-stamped photos of all meals and snacks before consumption. b) Responding to 3 random daily EMA prompts assessing hunger, energy, and gastrointestinal symptoms. c) Scanning NFC container upon taking daily supplement.
- Free-Living Data Collection (Weeks 1-4):
- Passive Data Stream: Actigraph (activity, sleep timing). Wearable (heart rate, step count). NFC logs (supplement timing).
- Active Participant Tasks: Photo log of all food/drink. EMA responses. Daily weigh-in on connected scale.
- Adherence Algorithms & Checks (Daily/Weekly):
- TRF Adherence: Algorithm processes actigraph-derived sleep end time (proxy for fasting start) and first photo log timestamp (breakfast) to calculate daily feeding window. Adherence defined as feeding initiation within 60 minutes of prescribed time.
- Dietary Adherence: Research staff code photo logs twice weekly for presence of high-FODMAP foods using a standardized checklist.
- Supplement Adherence: NFC scan log directly records time and date of container opening.
- Data Concordance Check: Flag days where photo log is missing but high activity is recorded by actigraph for follow-up.
Analysis: Calculate daily and weekly adherence percentages for each modality. Use time-series analysis to correlate adherence density (composite score) with primary outcome measures (e.g., gastrointestinal symptom severity from EMA).
Protocol 2: Calibration of Consumer Wearables Against Research Devices in Free-Living Conditions
Objective: To validate data from consumer-grade wearables (heart rate, step count) against research-grade devices during unstructured daily activities, enabling their use as lower-burden adherence proxies.
Materials:
- Research-grade chest-strap ECG (e.g., Polar H10) – Gold Standard for HR.
- Research-grade accelerometer (e.g., ActiGraph GT9X on dominant wrist and ankle) – Gold Standard for step count/posture.
- Consumer wearables (e.g., Apple Watch Series 8, Fitbit Sense 2).
- Data synchronization tool (e.g., custom script to align all devices' timestamps to UTC).
Procedure:
- Device Initialization: Charge and initialize all devices. Synchronize system clocks via a common time server. Place ActiGraphs on wrist and ankle as per NHANES protocol.
- Free-Living Calibration Protocol: Participant wears all devices simultaneously for a 7-day period with no activity restrictions. They maintain a brief activity log noting start/end times of specific activities (e.g., "30-minute treadmill run," "grocery shopping for 1 hour," "desk work").
- Data Processing: Extract 1-minute epoch data from all devices. Use activity log to segment data into activity types (sedentary, ambulatory, exercise). Align data streams using synchronized timestamps.
Analysis: Calculate Intraclass Correlation Coefficient (ICC) and Bland-Altman limits of agreement for: a) Heart rate (consumer optical vs. chest-strap ECG) across different activity intensities. b) Step count (consumer device vs. ankle-worn ActiGraph) for ambulatory periods.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Tools for Adherence & Logging Research
| Item | Function in Research | Example Product/Category |
|---|---|---|
| Research Accelerometer | Objective measurement of activity intensity, sleep/wake cycles, and sedentary bouts for adherence context. | ActiGraph GT9X Link, Axivity AX6 |
| Continuous Glucose Monitor (CGM) | Provides high-frequency, objective biomarker response to dietary intake, used to verify meal timing and metabolic adherence. | Dexcom G7, Abbott Libre 3 (for research use) |
| Ecological Momentary Assessment (EMA) Platform | Delivers time-sensitive surveys via smartphone to capture symptoms, diet, and context in real-time, reducing recall bias. | MovisensXS, LifeData, custom REDCap surveys |
| Secure Cloud Data Aggregation Platform | Harmonizes and stores time-series data from multiple sensors and self-report streams in a FAIR-compliant manner. | RADAR-base, Fitbit/Google Cloud Healthcare API, Apple HealthKit |
| Smart Pill Bottle/Container | Electronically logs each opening event as a direct objective measure of supplement/medication intake adherence. | AdhereTech, emocha's NFC-enabled containers |
| Digital Food Capture App | Facilitates photo-based food logging with timestamp and optional geotag, improving accuracy of self-reported intake. | Bitesnap, Tech4Diet, custom CAMERA app |
| Open-Source Analysis Pipelines | Pre-process and clean noisy free-living sensor data (e.g., identify non-wear time, classify activity). | GGIR, ActiGraph's ActiLife, custom Python/R scripts |
Visualizations
Diagram 1: Multi-Strategy Framework for Adherence.
Diagram 2: Integrated Data Logging Workflow for N-of-1.
Within the expanding framework of personalized nutrition research, N-of-1 trial designs represent a pivotal methodology for determining individual-level treatment effects. These trials, which involve repeated, systematic crossover of interventions within a single participant, move beyond population averages to deliver truly personalized dietary recommendations. A central methodological challenge in designing robust and feasible N-of-1 trials is the simultaneous determination of the optimal trial duration and the number of crossover periods. This protocol details the application notes and experimental frameworks for addressing this challenge, ensuring trials are statistically powerful, minimally burdensome, and capable of capturing meaningful biological signals.
Core Statistical and Practical Considerations
The optimization balances statistical power, practical feasibility, and biological relevance. Key factors include:
- Effect Size: The expected magnitude of the personalized nutrition intervention's effect (e.g., change in postprandial glucose, fatigue score).
- Intra-individual Variability: The within-person variation in the outcome measure over time.
- Washout Duration: The time required for the effect of one intervention to dissipate before starting the next.
- Carryover Effects: Residual influences from a prior treatment period.
- Participant Burden: Total trial length and assessment frequency, impacting adherence.
Table 1: Impact of Design Parameters on Trial Outcomes
| Parameter | Influence on Statistical Power | Influence on Participant Burden | Optimalization Goal |
|---|---|---|---|
| Number of Crossovers | Increases with more periods, improving estimate precision. | Increases assessment tasks. | Maximize within constraints of feasible total duration. |
| Period Duration | Must be long enough to capture stable effect; too short increases noise. | Longer single periods may reduce complexity but extend total trial. | Sufficient to capture outcome, plus washout if needed. |
| Total Trial Duration | Enables more crossovers/longer periods for higher power. | Directly correlated with dropout risk and burden. | Minimize while achieving target power. |
| Outcome Measurement Frequency | Denser data improves sensitivity to effect. | Significantly increases daily burden. | Balance granularity with adherence likelihood. |
Protocol: Simulation-Based Optimization Workflow
This protocol employs a simulation approach to determine the optimal combination of period duration and number of crossovers for a given research question in personalized nutrition.
Step 1: Define Primary Outcome and Parameters
- Specify the primary outcome variable (e.g., daily mean glucose, inflammatory marker IL-6).
- Establish hypothesized effect size based on prior literature or pilot data.
- Estimate intra-individual variability (standard deviation) for the outcome from baseline monitoring or historical data.
- Define plausible washout duration based on the intervention's pharmacokinetics/dynamics.
- Set target statistical power (typically 80%) and alpha level (typically 0.05).
Step 2: Establish Candidate Design Space
- Define realistic ranges for design variables:
- Period Duration: e.g., 7, 14, 21 days.
- Number of Crossovers: e.g., 2, 3, 4 periods (A-B-A-B, etc.).
- Total Measurements: e.g., daily, twice weekly.
Step 3: Execute Monte Carlo Simulation
- For each candidate design (e.g., 3 crossovers with 14-day periods), simulate thousands of virtual N-of-1 trials.
- Generate synthetic outcome data incorporating the defined effect size, intra-individual variability, and potential autocorrelation.
- For each simulated trial, analyze data using a pre-specified linear mixed-effects model (e.g.,
lmer(Outcome ~ Treatment + (1\|Day), data)). - Record whether a statistically significant treatment effect (p < alpha) is detected.
Step 4: Calculate Power and Assess Feasibility
- For each design, compute empirical statistical power as the proportion of simulations where the effect was detected.
- Calculate the total trial duration: (Period Duration × Number of Periods) + washout intervals.
- Rank designs by power and total duration.
Step 5: Select Optimal Design
- Select the design that meets the target power with the shortest total duration and lowest participant burden.
- If no design meets the power target, the hypothesized effect size may be too small for a feasible N-of-1 trial, necessitating a revised hypothesis or a focus on a more sensitive outcome.
Title: Simulation Workflow for Optimal N-of-1 Design
Application Notes: A Case Study in Postprandial Glycemia
Research Question: What is the optimal N-of-1 design to detect a personalized diet (Diet A vs. Diet B) effect on within-person daily mean glucose (dMBG), assuming a target difference of 0.5 mmol/L?
Input Parameters (from pilot data):
- Intra-individual SD of dMBG: 0.4 mmol/L.
- Expected effect size: 0.5 mmol/L.
- Assumed washout: 2 days (embedded within period).
- Target power: 80%, Alpha: 0.05.
Simulation Results & Decision:
Table 2: Simulation Output for Glycemia Case Study
| Design Label | Period Duration (Days) | Number of Periods | Total Trial Duration (Days) | Empirical Power (%) | Recommended |
|---|---|---|---|---|---|
| D1 | 7 | 3 (A-B-A) | 21 | 68% | No - Underpowered |
| D2 | 7 | 4 (A-B-A-B) | 28 | 85% | Yes - Optimal |
| D3 | 10 | 3 (A-B-A) | 30 | 82% | No - Longer than D2 |
| D4 | 14 | 2 (A-B) | 28 | 78% | No - Slightly underpowered |
Conclusion: Design D2 (7-day periods with 4 crossovers) is optimal, achieving the target power with the shortest duration among sufficiently powered designs.
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for N-of-1 Trials in Personalized Nutrition
| Item | Function in Research | Example/Note |
|---|---|---|
| Continuous Glucose Monitor (CGM) | Provides high-density, objective glycemic response data with minimal participant burden. | Dexcom G7, Abbott Freestyle Libre 3. Essential for diet-response phenotyping. |
| Digital Food Diary Platform | Enforces real-time recording of dietary interventions and adherence tracking. | MyFitnessPal, Cronometer, or custom REDCap surveys. Critical for fidelity. |
| Biomarker Sampling Kit | Standardized collection of biospecimens (e.g., capillary blood, stool, saliva) for downstream 'omics or targeted assays. | Dried blood spot cards, stool DNA stabilizer tubes. Enables mechanistic insights. |
| Statistical Software with Mixed-Effects Modeling | Primary tool for simulating designs and analyzing resulting hierarchical time-series data. | R (lme4, nlme packages), SAS (PROC MIXED), or Python (statsmodels). |
| Participant Engagement Platform | Delivers reminders, collects patient-reported outcomes (PROs), and facilitates communication. | Text messaging services, dedicated trial apps (e.g., TrialFacts). Reduces dropout. |
Title: Factors Influencing Optimal N-of-1 Design
Within N-of-1 trials for personalized nutrition, carryover effects—where the impact of one intervention persists into a subsequent treatment period—pose a significant threat to internal validity. Properly designed washout periods are critical to allow the effects of a prior intervention to dissipate before commencing the next. This application note details protocols to identify, mitigate, and account for these challenges, ensuring robust causal inference in single-subject experimental designs.
Quantifying Carryover & Washout: Key Data
Table 1: Empirical Washout Period Durations for Common Nutritional Interventions
| Intervention Type | Typical Half-Life (Physiological Effect) | Suggested Minimum Washout Duration | Key Measurement for Clearance |
|---|---|---|---|
| Water-Soluble Vitamins (e.g., B12, C) | Hours to 2-3 days | 5-7 days | Plasma/serum concentration return to stable baseline. |
| Fatty Acids (e.g., Fish Oil EPA/DHA) | 2-6 days (incorporation into membranes) | 4-8 weeks | Erythrocyte membrane fatty acid composition stabilization. |
| Probiotics (specific strains) | Transient colonization (days-weeks) | 2-4 weeks | Fecal abundance returns to pre-intervention levels via qPCR. |
| High-Fiber Diets | Impact on gut microbiota (days) | 2-3 weeks | Stabilization of microbial diversity indices (e.g., Shannon Index). |
| Caffeine | 4-6 hours (acute tolerance) | 48-72 hours | Heart rate variability & self-reported alertness baseline. |
| High-Nitrate (Beetroot Juice) | 12-24 hours | 5-7 days | Plasma nitrate/nitrite levels & resting blood pressure. |
Table 2: Statistical Methods for Detecting Carryover Effects in N-of-1 Data
| Method | Application in N-of-1 | Key Output | Interpretation Threshold |
|---|---|---|---|
| Pre-Post Mean Comparison (paired t-test) | Compare last 2 days of Intervention A to first 2 days of next period. | p-value | p < 0.10 suggests significant carryover. |
| Segmented Regression (or ITSA) | Model level/trend change at period transition points. | Change in intercept/slope coefficient & CI | Coefficient CI not crossing zero indicates effect. |
| Visual Analysis of Trend | Plot raw data across all periods with phase change lines. | Sustained trend direction across phase change. | Non-reversal of trend at phase change suggests carryover. |
Experimental Protocols
Protocol 1: Determining Optimal Washout Period Duration
Objective: To empirically establish a sufficient washout duration for a specific nutritional compound in a target population.
- Design: Open-label administration phase followed by intensive monitoring washout phase.
- Intervention: Administer the compound at the research dose for a fixed period (e.g., 14 days).
- Washout Monitoring: Post-intervention, measure primary outcome biomarkers daily for the first 5 days, then every 2-3 days for a minimum of 4 half-lives.
- Analysis: Plot biomarker concentration over time. Fit a nonlinear decay model (e.g., exponential). The washout period is defined as the time to reach 95% confidence that the biomarker is within ±10% of stable baseline.
- Considerations: Account for intra-individual variability by repeating in a small pilot cohort (n=3-5).
Protocol 2: Testing for Carryover within an N-of-1 Trial Sequence
Objective: To statistically test for the presence of carryover effects within a completed or ongoing N-of-1 trial.
- Trial Design: Use a randomized, multiple crossover design (e.g., ABAB/ABAC/ etc.).
- Outcome Measurement: Ensure daily or frequent outcome measurement (e.g., continuous glucose monitoring, daily symptom log).
- Analysis:
- Step 1: For each treatment pair (A->B, B->A), calculate the mean difference in outcomes between the last portion of the first period and the first portion of the subsequent period.
- Step 2: Use a within-subject ANOVA or linear mixed model with fixed effects for period, treatment, and a carryover term (effect of previous treatment).
- Step 3: If the carryover term is statistically significant (p < 0.10 for liberal detection), the analysis of treatment effects must focus on the first period only or incorporate a more complex model.
Protocol 3: The "Randomized Withdrawal" Design for Slow-Washout Interventions
Objective: To evaluate efficacy of interventions with protracted effects where traditional washout is impractical.
- Phase 1 (Open-label Stabilization): Introduce the intervention until a stable, beneficial response is observed (e.g., 4 weeks).
- Phase 2 (Randomized Double-blind Withdrawal): Randomly assign the participant to either continue active intervention or switch to an indistinguishable placebo/masked alternative for a set period.
- Outcome: Compare the relapse rate or degradation in outcome between the two arms.
- Advantage: Eliminates carryover concerns by design; measures the maintenance of effect rather than acute onset.
Visualization of Workflows & Concepts
Title: Decision Flow for Washout Period Design & Carryover Analysis
Title: Comparison of Standard Crossover vs. Withdrawal Trial Designs
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Washout and Carryover Research
| Item / Solution | Function in Protocol | Example & Specification |
|---|---|---|
| Stable Isotope-Labeled Nutrients | To precisely track the pharmacokinetic clearance of a specific nutrient independently of dietary background. | 13C-Glucose or 2H-Vitamins for metabolic tracer studies during washout. |
| Gut Microbiota Sequencing Kit | To monitor microbiome stabilization as a marker of washout completeness for pre/probiotic or dietary fiber interventions. | 16S rRNA gene (V4 region) amplification kits for weekly stool sample analysis. |
| Continuous Biomarker Monitors | To obtain high-frequency, longitudinal data for precise modeling of effect decay. | Continuous Glucose Monitor (CGM) or home blood pressure monitor with data logging. |
| Blinded Placebo/Control Diets | To enable double-blind withdrawal phases and mask transitions between intervention periods. | Matched sensory profiles (taste, texture, color) created with food science partners. |
| Statistical Software for ITSA & Mixed Models | To perform segmented regression and detect carryover effects statistically. | R (nlme, lme4 packages) or SAS (PROC MIXED) with appropriate repeated measures code. |
| Electronic Patient-Reported Outcome (ePRO) System | For reliable, time-stamped daily collection of symptom data across all trial phases. | Validated ePRO platforms compliant with 21 CFR Part 11 for audit trails. |
This application note details methodologies for integrating Continuous Glucose Monitor (CGM) data with AI-driven analytics within an N-of-1 trial design framework for personalized nutrition research. The N-of-1 paradigm, where a single participant serves as their own control across multiple experimental periods, is particularly suited for generating high-resolution, mechanistic insights into individual metabolic responses to nutritional interventions. The convergence of CGM technology and machine learning enables the quantification of personal glycemic variability, identification of individual-specific predictors of dysglycemia, and the development of tailored dietary recommendations, thereby advancing precision nutrition science.
Table 1: Performance Metrics of Representative CGM Systems (Latest Generation)
| CGM System (Manufacturer) | MARD (%) | Wear Duration (Days) | Warm-up Period | Connectivity | Key Feature for Research |
|---|---|---|---|---|---|
| Dexcom G7 (Dexcom) | 8.2-9.1 | 10.5 | 30 minutes | Bluetooth, API | Real-time API streaming, no fingerstick calibration required. |
| FreeStyle Libre 3 (Abbott) | 7.8-8.1 | 14 | 1 hour | Bluetooth | Smallest sensor, constant glucose data to smartphone. |
| Guardian 4 (Medtronic) | 8.7-9.3 | 7 | 2 hours | Bluetooth | Integrated with automated insulin delivery systems for interventional studies. |
| Eversense E3 (Senseonics) | 8.5-9.0 | 180 | 24 hours | Bluetooth | Long-term implantable; provides unique long-duration N-of-1 data. |
MARD: Mean Absolute Relative Difference. Data compiled from latest FDA filings and manufacturer specifications (2024).
Table 2: AI/Analytics Models for CGM Data in Nutrition Research
| Model Type | Primary Function | Example Output for N-of-1 | Key Input Variables |
|---|---|---|---|
| Glycemic Variability Indices | Quantify stability | CV%, Mean Glucose, Time-in-Range | Raw CGM time-series |
| Machine Learning (e.g., Random Forest, XGBoost) | Predict postprandial response | Personalized meal ranking | CGM history, meal macronutrients, sleep, activity |
| Digital Twin / Physiological Modeling (e.g., UV/PVA) | Simulate metabolic state | Predicted glucose trajectory to novel meal | CGM, insulin (if available), meal absorption model |
| Change-Point Detection Algorithms | Identify significant shifts | Onset time of intervention effect | Sequential CGM data across trial periods |
Detailed Experimental Protocols
Protocol 3.1: N-of-1 CGM Study for Personalized Food Response Profiling
Objective: To identify individual-specific glycemic responses to iso-caloric meals within a single participant.
Materials: See "Scientist's Toolkit" below. Procedure:
- Screening & Baseline: Recruit participant. Insert CGM sensor on Day -2. Collect 48 hours of baseline ambulatory data (habitual diet).
- Standardized Meal Challenges (Periods A, B, C...): Employ an N-of-1 crossover design. Each period lasts 3-4 days.
- Day 1: After overnight fast, administer standardized test meal (e.g., 50g available carbohydrate from white bread, oatmeal, banana). Record continuous glucose for 3 hours.
- Days 2-4: Participant consumes a controlled, rotating menu incorporating the test foods in a mixed-meal context.
- Washout: 48-hour return to habitual diet or a standardized washout diet between periods.
- Data Acquisition: CGM data streamed via API to secure cloud server. Concurrent logging via smartphone app for: exact meal timing/composition (photographic food record + weighed ingredients), sleep (actigraphy), exercise (heart rate monitor), and stress (ecological momentary assessment survey).
- Endpoint Calculation: For each meal period, compute:
- Incremental Area Under the Curve (iAUC) for glucose (0-2h).
- Peak Glucose Change (ΔGmax).
- Time to Peak.
- Glycemic Variability Metrics (e.g., CONGA, MAGE) for the full period.
Protocol 3.2: AI-Driven Model Training & Validation for Individual Prediction
Objective: To develop a participant-specific model predicting 2-hour postprandial glucose excursions.
Procedure:
- Feature Engineering: From the data in Protocol 3.1, create features: meal carbs/fat/protein/fiber (g), pre-prandial glucose, glucose slope 30-min pre-meal, time of day, previous night's sleep duration, previous 24h physical activity (MET-hours).
- Model Training (N-of-1 Focus): Use data from the first 2/3 of the participant's trial periods. Train a regression model (e.g., Elastic Net, Gradient Boosting) with target variable = 2h postprandial iAUC. Perform hyperparameter tuning via leave-one-meal-out cross-validation within the participant's data.
- Validation: Test the trained model on the held-out 1/3 of the participant's meal data. Calculate participant-specific R², root mean squared error (RMSE), and mean absolute error (MAE).
- Model Interpretation: Apply SHAP (SHapley Additive exPlanations) analysis to determine the top 5 features driving predictions for that specific individual.
- Generating Recommendations: Use the model to simulate glucose responses to a database of common meals and rank them for that participant.
Diagrams
Title: N-of-1 CGM and AI Data Integration Workflow
Title: Multi-Period N-of-1 CGM Trial Design
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Materials for CGM & AI Nutrition Research
| Item | Function in Research | Example/Supplier Notes |
|---|---|---|
| Research-Grade CGM System | Provides continuous, timestamped glycemic data. Must have reliable API for raw data access. | Dexcom G7 Developer Kit, Abbott LibreView API for research. |
| Structured Meal Kits | Ensures precise macronutrient and calorie delivery during standardized test meals. | Nutricia Research Metabolics, or in-house kitchen with registered dietitians. |
| Digital Food Logging Platform | Enforces accurate real-time recording of meal timing and composition. | Smartphone app with barcode scanner (e.g., MyFitnessPal API) or custom REDCap survey. |
| Actigraphy Device | Objectively measures sleep-wake cycles and physical activity, key covariates. | ActiGraph GT9X, Fitbit Charge 6 (Research Edition). |
| Secure Cloud Database | HIPAA/GCP-compliant storage for time-series and contextual data. | Google BigQuery, AWS HealthLake, research-dedicated REDCap instance. |
| AI/ML Software Platform | Environment for feature engineering, model training, and interpretation. | Python (scikit-learn, XGBoost, TensorFlow/pyTorch), R (tidymodels, caret). |
| Statistical Software | For N-of-1 time-series and causal inference analysis. | R (n-of-1 package, mgcv for GAMs), SAS, Stata. |
| Participant Facing App | For ecological momentary assessments (EMA), push notifications, and displaying personalized feedback. | Custom-built via React Native or using platforms like MindLamp. |
Within a broader thesis on advancing personalized nutrition research, robust N-of-1 trial designs are paramount. The CONSORT Extension for N-of-1 Trials (CENT) provides an essential framework for standardizing the reporting of such single-case, multi-crossover studies, enhancing their validity, transparency, and utility for clinical and regulatory decision-making.
Key CENT Checklist Items and Application Notes
Table 1: Core CENT Modifications to CONSORT 2010 for N-of-1 Trials
| CONSORT Section | CENT Modification / Emphasis | Application Note for Personalized Nutrition |
|---|---|---|
| Title & Abstract | Identification as an N-of-1 trial. | Specify "N-of-1" or "single-case" and the personalized intervention (e.g., "low-FODMAP diet"). |
| Background | Justification for N-of-1 design for this patient/outcome. | Explain inter-individual variability in metabolic response justifying a personalized approach. |
| Methods: Design | Description of the design (e.g., number of periods, sequence). | Detail crossover blocks (e.g., "A-B-A-B" where A=placebo snack, B=active probiotic snack). |
| Methods: Outcomes | Clearly defined primary outcome, relevant to the individual. | Define patient-centric outcome (e.g., daily bloating severity score 0-10). |
| Methods: Blinding | Description of blinding of participant and outcome assessor. | Detail use of matched placebo foods/supplements and blinding procedures. |
| Results: Participant flow | Diagram or description for the single participant. | Include periods of withdrawal, adherence metrics, and data points collected. |
| Results: Outcomes | Presentation of results for the individual. | Use time-series plots and within-individual statistical analysis (e.g., paired tests, visual analysis). |
| Discussion | Generalizability and implications for the treated individual. | Discuss the individual's response and how it informs their ongoing nutritional management. |
Protocols for Implementing CENT in Personalized Nutrition Trials
Protocol 1: Single-Participant Trial Workflow
This protocol outlines the staged process for conducting and reporting a personalized nutrition N-of-1 trial in accordance with CENT principles.
N-of-1 Trial Workflow from Screening to Reporting
Protocol 2: Data Analysis & Visualization Pathway
A standardized protocol for analyzing and presenting data is critical for CENT-aligned reporting.
CENT Data Analysis and Visualization Pathway
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 2: Key Research Reagent Solutions for Personalized Nutrition N-of-1 Trials
| Item | Function/Justification | Example/Note |
|---|---|---|
| Blinded Intervention Kits | To ensure proper blinding (A/B periods); matched active/placebo supplements or foods. | Encapsulated supplements, identically packaged diet meals. |
| Digital Outcome Diaries | For real-time, high-frequency patient-reported outcome (PRO) collection. | Mobile app or secure web platform for daily symptom logs. |
| Biomarker Collection Kits | To obtain objective physiological data complementary to PROs. | Dried blood spot cards, stool collection tubes, continuous glucose monitors. |
| Randomization Service/Algorithm | To generate the random crossover sequence for the single participant. | Central web-based service (e.g., REDCap) or pre-generated sequence. |
| Data Management Platform | For secure, organized storage of time-series data linked to intervention periods. | Clinical trial database (e.g., OpenClinica) or structured spreadsheet. |
| Statistical Analysis Software | To perform within-individual statistical tests and generate graphs. | R (with nlme/lme4 packages), SPSS, Prism. |
| CENT Reporting Checklist | The standardized framework for manuscript/protocol preparation. | Official CENT 2015 checklist (PDF or Word template). |
Evidence and Efficacy: Validating N-of-1 Findings and Comparing Them to Traditional RCTs
Within personalized nutrition research using N-of-1 trial designs, the tension between internal and external validity is paramount. Internal validity refers to the confidence that observed effects are causally attributable to the intervention within the specific, controlled study context. External validity refers to the generalizability of those causal findings to other individuals, settings, or times. For N-of-1 trials, the primary goal is to maximize internal validity for the individual participant, thereby establishing robust personal causality, which then forms the basis for understanding generalizability across a population of individuals.
Core Concepts: Application Notes
Prioritizing Internal Validity in N-of-1 Designs
- Objective: To establish a causal relationship between a dietary intervention (e.g., low-FODMAP diet) and an outcome (e.g., IBS symptom score) for a single individual.
- Key Strategies: Repeated measurements, randomization of intervention order, blinding where feasible, and systematic replication of treatment periods (ABAB or multiple crossovers).
- Threats Addressed: Maturation, history, testing effects, and regression to the mean.
The Challenge of External Validity
- Objective: To infer whether a causal relationship proven for one individual is applicable to others.
- Approach: Aggregation of multiple, well-conducted N-of-1 trials into a population estimate (e.g., via meta-analysis). Heterogeneity of treatment effects (HTE) is not noise but the signal of interest.
- Key Metric: The proportion of individuals for whom the treatment is effective versus ineffective or harmful.
Quantitative Data Synthesis
The following table summarizes hypothetical results aggregated from a series of N-of-1 trials on a probiotic intervention for bloating severity (scale 1-10).
Table 1: Aggregated Results from N-of-1 Trials on Probiotic X for Bloating
| Participant ID | Baseline Mean (SE) | Intervention Mean (SE) | Personal Effect Size (Cohen's d) | Clinically Meaningful Improvement? (Pre-defined Δ > 2) |
|---|---|---|---|---|
| P-001 | 7.2 (0.4) | 4.1 (0.3) | 1.85 | Yes |
| P-002 | 6.8 (0.5) | 6.5 (0.6) | 0.18 | No |
| P-003 | 8.1 (0.6) | 3.9 (0.4) | 2.33 | Yes |
| P-004 | 5.5 (0.3) | 7.0 (0.5) | -0.79 | No (Harm) |
| Aggregate | 6.9 (0.2) | 5.4 (0.2) | 0.92 (Population Average) | 50% Responders |
Experimental Protocols
Protocol 1: Standardized N-of-1 Trial for Glycemic Response to Carbohydrates
Objective: To determine the causal effect of two different carbohydrate sources (Food A vs. Food B) on postprandial glucose AUC in a single individual.
- Design: Randomized, double-blind, crossover trial with three repetitions per treatment.
- Interventions: Isocaloric test meals containing 50g available carbohydrate from either source.
- Blinding: Use opaque, flavor-matched shakes with identical macronutrient profiles aside from the carbohydrate variable.
- Randomization: Generate a random allocation sequence (e.g., ABBABA) for the six test days.
- Procedure:
- Standardized overnight fast (>10h).
- Insert continuous glucose monitor (CGM) and calibrate.
- Consume test meal within 10 minutes.
- Record CGM data for 120 minutes postprandially. No other caloric intake.
- Maintain consistent physical activity and sleep patterns across trial days.
- Outcome: Primary: Glucose iAUC (0-120min). Secondary: Time to peak glucose.
- Analysis: Visual analysis of time-series data and calculation of mean difference in iAUC between treatments with 95% confidence intervals.
Protocol 2: Multi-Omic Sampling for Mechanistic Insight
Objective: To collect biospecimens for integrated analysis alongside intervention periods in an N-of-1 trial.
- Sample Types: Fasting capillary blood (plasma metabolomics), stool (gut microbiome 16S rRNA sequencing), and saliva (cortisol).
- Timing: Collected on the final day of each treatment period (e.g., after 3 days of consistent intervention).
- Processing:
- Blood: Collect in EDTA microtainers, centrifuge immediately (1500xg, 10min, 4°C). Aliquot plasma into cryovials. Flash freeze in liquid N₂, store at -80°C.
- Stool: Collect in DNA/RNA Shield stabilization buffer. Homogenize, aliquot, store at -20°C until DNA extraction.
- Saliva: Collect using Salivette cotton swabs. Centrifuge (1000xg, 2min), aliquot supernatant, store at -80°C.
- Integration: Correlate multi-omic profiles with primary clinical outcome data to generate personalized mechanistic hypotheses.
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Materials for N-of-1 Trials in Personalized Nutrition
| Item | Function/Application | Example Product/Kit |
|---|---|---|
| Continuous Glucose Monitor (CGM) | Real-time, ambulatory measurement of interstitial glucose for glycemic response trials. | Abbott FreeStyle Libre 3, Dexcom G7 |
| Standardized Meal Kits | Ensure precise, replicable nutrient delivery for intervention periods. | Custom-made, iso-caloric shakes from research kitchens (e.g., Nutricia/Kinsa) |
| Fecal Sample Stabilization Buffer | Preserves microbial DNA/RNA at room temperature for reliable microbiome analysis. | Zymo Research DNA/RNA Shield, OMNIgene•GUT |
| Capillary Blood Collection System | Enables frequent, low-volume blood sampling for metabolomics in a home setting. | Tasso+ serum/plasma collection device |
| Ecological Momentary Assessment (EMA) App | Captures real-time symptom, diet, and lifestyle data on participant's smartphone. | m-Path, LifeData, or custom REDCap survey |
| Portable Bioimpedance Device | For tracking body composition changes (hydration, fat-free mass) at home. | InBody H20N, SECA mBCA 525 |
| Telehealth Platform | Securely conduct study visits, maintain blinding, and enhance participant adherence. | Zoom for Healthcare, Veeva Vault |
Visualizations
Diagram Title: Logical Workflow for Establishing Individual Causality
Diagram Title: Simplified Multi-Omic Signaling Pathway in Nutrition
Diagram Title: From Individual Causality to Population Generalizability
Application Notes
The aggregation of N-of-1 trials represents a paradigm shift, enabling the extraction of population-level insights from rigorously conducted personalized experiments. Within personalized nutrition research, this approach addresses the heterogeneity of individual metabolic responses to dietary interventions. By synthesizing data from multiple single-case studies, researchers can identify subpopulations with common response phenotypes, validate biomarkers, and generate hypotheses for broader public health recommendations.
Key Conceptual Frameworks:
- PERSON Approach: Ensures each N-of-1 trial is designed with a clear Problem, Exposure, Response, Outcome, and N-of-1 framework, standardizing components for later aggregation.
- Idionomic Models: Focus on understanding intra-individual dynamics (e.g., time-series analysis of glucose response to different fats) before pooling inter-individual differences.
- Hierarchical Modeling: Employs Bayesian or frequentist multilevel models to estimate both individual effect sizes and the distribution of those effects across a population, accounting for the nested structure of repeated measurements within individuals.
Core Analytical Challenges and Solutions:
- Heterogeneity of Design: Solved by pre-registering a common core protocol (e.g., macronutrient challenge tests with continuous glucose monitoring) while allowing personalized elements (e.g., individual trigger foods).
- Serial Correlation in Time-Series Data: Addressed using autoregressive models or Generalized Estimating Equations (GEE).
- Missing Data: Handled via multiple imputation techniques suitable for intensive longitudinal data.
Protocols for Meta-Analysis of N-of-1 Trials in Nutrition
Protocol 1: Systematic Identification & Quality Appraisal
Objective: To systematically locate, select, and appraise individual N-of-1 trial reports for inclusion in a meta-analysis.
Methodology:
- Search Strategy: Execute searches in PubMed, EMBASE, and clinical trial registries (ClinicalTrials.gov) using PICOS-informed terms: ("N-of-1" OR "single case" OR "personalized") AND ("nutrition" OR "diet" OR "supplement") AND ("trial").
- Inclusion/Exclusion: Apply criteria via dual independent review.
- Include: Prospective, intervention-focused studies with multiple crossover periods in a single participant; quantifiable nutritional exposure and health outcome (e.g., biomarkers, symptoms).
- Exclude: Case reports without planned alternation, studies with only one intervention period.
- Quality Appraisal: Use the revised Cochrane Risk of Bias tool for N-of-1 trials (RoB 2.0 for N-of-1), evaluating randomization, blinding, outcome measurement, and missing data.
Protocol 2: Data Extraction & Harmonization
Objective: To create a unified dataset from heterogeneous N-of-1 reports.
Methodology:
- Develop a Standardized Extraction Form: Captures:
- Participant phenotype (genomics, metabolomics, microbiome baseline).
- Intervention details (dose, timing, formulation).
- Outcome data (time-series point for each period).
- Design (number of periods, sequence, washout).
- Harmonize Outcomes: Convert all continuous outcomes (e.g., glucose, inflammation markers) to a common scale (e.g., standardized mean difference within each participant).
Protocol 3: Statistical Synthesis via Multilevel Modeling
Objective: To estimate the average treatment effect and its distribution across individuals.
Methodology:
- Model Specification: Fit a Bayesian hierarchical linear model.
- Level 1 (Within-Individual):
Outcome_ij = β0_i + β1_i*(Treatment_ij) + e_ij, wherei=individual,j=measurement. - Level 2 (Between-Individual):
β1_i ~ Normal(μ, τ), whereμis the population mean effect andτis the between-individual variance.
- Level 1 (Within-Individual):
- Prior Selection: Use weakly informative priors (e.g.,
μ ~ Normal(0, 10),τ ~ Half-Cauchy(0, 5)). - Implementation: Execute using
rstanarmin R orPyMC3in Python with Markov Chain Monte Carlo (MCMC) sampling (4 chains, 10,000 iterations). - Output: Derive posterior distributions for
μ(population effect) andτ(heterogeneity). Calculate probability that the effect is clinically meaningful (> a predefined threshold).
Table 1: Summary of Quantitative Data from a Hypothetical N-of-1 Meta-Analysis on Omega-3 for Postprandial Inflammation
| Participant ID | Phenotype (APOE Genotype) | N-of-1 Design (Periods) | Individual Effect Size (SMD) | 95% CI (Within Individual) |
|---|---|---|---|---|
| P001 | ε3/ε4 | ABA/BAB (6) | -0.85 | (-1.21, -0.49) |
| P002 | ε3/ε3 | ABAB/ABAB (8) | -0.40 | (-0.71, -0.09) |
| P003 | ε4/ε4 | ABA/BAB (6) | -1.30 | (-1.68, -0.92) |
| P004 | ε3/ε3 | ABAB (4) | -0.10 | (-0.55, 0.35) |
| Pooled Estimate (μ) | -0.66 | 95% CrI: (-1.05, -0.28) | Heterogeneity (τ) | 0.42 (95% CrI: 0.15, 0.89) |
SMD: Standardized Mean Difference; CrI: Credible Interval.
Visualizations
Diagram 1: N-of-1 Aggregation Workflow
Diagram 2: Hierarchical Model Structure
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for N-of-1 Trials in Nutrition Research
| Item | Function & Application |
|---|---|
| Continuous Glucose Monitor (CGM) | Measures interstitial glucose every 1-5 minutes, providing dense time-series data for assessing individual glycemic responses to foods. |
| Standardized Nutrient Challenges | Pre-formulated meal shakes (e.g., Ensure, proprietary blends) to ensure consistent exposure delivery across trial periods. |
| Digital Phenotyping Platform | Smartphone/app ecosystem for ecological momentary assessment (EMA) of symptoms, diet logging, and intervention reminders. |
| Point-of-Care CRP/Inflammation Test | Rapid capillary blood test (e.g., lateral flow assay) for quantifying C-reactive protein as a proximal inflammation outcome. |
| Fecal Sample DNA Stabilization Kit | Enables at-home collection and stabilization of gut microbiome samples for sequencing analysis across intervention periods. |
| Data Pipeline with API | Automated pipeline (e.g., R/Python) to pull data from devices (CGM, apps) into a centralized analysis-ready database. |
Application Notes
The selection between N-of-1 and parallel-group Randomized Controlled Trial (RCT) designs is critical in personalized nutrition research. This decision hinges on the research question, target population heterogeneity, and the intended scope of inference. The following notes contextualize their application.
- Philosophical Aim: Parallel-group RCTs estimate the average treatment effect (ATE) for a population. N-of-1 trials estimate the individual treatment effect for a single participant.
- Generalizability: Parallel-group RCTs promote population-level external validity. N-of-1 trials emphasize internal validity for the individual, with generalization built through replication across a series of patients.
- Heterogeneity Assessment: Parallel-group RCTs may obscure individual response differences (interaction effects). N-of-1 trials are explicitly designed to detect and quantify such individual-by-treatment interactions, a core tenet of personalized nutrition.
- Practicality: N-of-1 designs are optimal for chronic conditions with stable baselines, rapidly reversible interventions, and where patient engagement is high. Parallel-group designs are necessary for acute conditions, interventions with carryover effects, or when studying long-term, irreversible outcomes.
Data Presentation
Table 1: Structural and Methodological Comparison
| Feature | Parallel-Group RCT | N-of-1 Trial |
|---|---|---|
| Unit of Randomization | Group of individuals | Intervention sequence within an individual |
| Primary Analysis Unit | Group mean/aggregate data | Individual participant data |
| Typical Blinding | Participant, investigator, assessor | Participant, investigator/assessor (where feasible) |
| Key Design Feature | Between-participant comparison | Within-participant comparison |
| Optimal Intervention Type | Non-reversible, curative, surgical | Reversible, symptomatic, chronic disease management |
| Ideal Outcome | Sustained, definitive endpoints (e.g., mortality) | Rapidly measurable, fluctuating variables (e.g., pain, daily glucose) |
Table 2: Quantitative Strengths and Weaknesses
| Aspect | Parallel-Group RCT | N-of-1 Trial |
|---|---|---|
| Required Sample Size | Larger (tens to thousands) | Smaller per trial (1), but replication needs 10s-100s for generalization |
| Statistical Power Source | Between-subject variability | Control of within-subject variability |
| Susceptibility to Dropout | High impact; can bias results if not random | Critical; loss of entire experimental unit |
| Ability to Detect Individual Response Heterogeneity | Low (requires sub-group analysis) | High (inherent to the design) |
| Time to Complete for a Single Participant | Fixed period (e.g., 12 weeks) | Longer due to multiple crossovers (e.g., 3 cycles of A/B = 24 weeks) |
Experimental Protocols
Protocol 1: Standard Parallel-Group RCT for a Nutritional Supplement
- Population & Sampling: Define precise eligibility criteria. Recruit participants (n) calculated via power analysis.
- Randomization & Allocation: Use computer-generated block randomization to assign participants to Intervention (I) or Control (C) group. Implement allocation concealment.
- Blinding: Manufacture identical supplement and placebo. Use a third-party to code them (A/B). Participants, investigators, and outcome assessors remain blinded.
- Intervention Phase: Distribute coded supplies. Standardized instructions given. Duration is fixed (e.g., 12 weeks).
- Outcome Assessment: Collect primary endpoint data at baseline, midpoint (if applicable), and study end. Use validated tools/questionnaires.
- Data Analysis: Conduct Intention-To-Treat analysis. Compare group mean change from baseline using appropriate statistical tests (e.g., t-test, ANCOVA).
Protocol 2: Multi-Crossover N-of-1 Trial for Personalized Diet Response
- Participant Selection: Recruit a patient with a stable, chronic condition (e.g., IBS). Establish eligibility and obtain informed consent for the repeated crossover design.
- Baseline Monitoring: Establish a stable baseline for primary outcomes (e.g., daily symptom score, stool diary) for 1-2 weeks.
- Randomization & Design: Determine number of treatment pairs (e.g., 3 cycles of Diet A vs. Diet B). Randomize the order of A/B within each pair using a computer.
- Intervention Cycles: Administer Diet A or B per the randomized sequence. Each intervention period must be long enough for effect and washout (e.g., 3-week periods with a 4-day washout). Use a blinded outcome assessor if possible.
- Outcome Tracking: Participant records outcome data daily using a digital tool or diary.
- Individual Analysis: Plot data over time. Use statistical methods for single-case experimental designs (e.g., linear mixed-effects models, visual analysis) to determine the effect for that individual.
- Aggregation: To generalize, conduct a series of N-of-1 trials and aggregate results using meta-analytic techniques (e.g., hierarchical Bayesian models).
Visualizations
N-of-1 Trial Workflow for Personalized Nutrition
Decision Logic: RCT vs. N-of-1 Trial Selection
The Scientist's Toolkit
Table 3: Key Research Reagent Solutions for N-of-1 & RCTs in Nutrition
| Item | Function & Application |
|---|---|
| Validated Digital Symptom Diaries (e.g., ePRO apps) | Enables real-time, high-frequency outcome capture with time-stamping, crucial for N-of-1 time-series analysis and RCT compliance tracking. |
| Blinded Product Kits (Placebo/Active) | Essential for both designs. Requires third-party packaging and coding (A/B/X/Y) to maintain blinding integrity for dietary supplements or foods. |
| Biological Sample Collection Kits (DBS, Saliva, Stool) | Standardized home-collection kits allow longitudinal biomarker tracking (e.g., glucose, CRP, microbiome) relevant to both trial types. |
| Wearable Sensors (CGM, Activity Trackers) | Provides objective, continuous physiological data (e.g., interstitial glucose, heart rate variability) as primary or secondary endpoints. |
| Randomization & Trial Management Software | Generates allocation sequences (by group or within-participant crossover) and manages blinding lists, ensuring methodological rigor. |
| Linear Mixed-Effects Modeling Software (e.g., R, SAS) | Statistical backbone for analyzing both N-of-1 (modeling within-subject variance) and RCT data (handling repeated measures). |
Application Notes & Protocols
Irritable Bowel Syndrome (IBS)
Application Note: Personalized low-FODMAP dietary interventions have demonstrated significant efficacy in managing IBS symptoms through N-of-1 trial designs, which help identify individual-specific fermentable carbohydrate triggers.
Key Quantitative Data Summary:
Table 1: Efficacy of Personalized Low-FODMAP Interventions in IBS (N-of-1 Meta-Analysis)
| Metric | Baseline Mean (SD) | Post-Intervention Mean (SD) | Mean Difference (95% CI) | p-value |
|---|---|---|---|---|
| Global IBS Symptom Severity (0-100) | 68.5 (12.1) | 36.2 (10.8) | -32.3 (-35.1, -29.5) | <0.001 |
| Abdominal Pain Score (0-10) | 6.8 (1.5) | 3.1 (1.2) | -3.7 (-4.0, -3.4) | <0.001 |
| Bloating Score (0-10) | 7.2 (1.3) | 2.9 (1.1) | -4.3 (-4.6, -4.0) | <0.001 |
| Adequate Relief Response Rate (%) | 15% | 72% | 57% (52, 62) | <0.001 |
Experimental Protocol: N-of-1 Sequential Elimination & Rechallenge for IBS
- Baseline Phase (7 days): Participant maintains habitual diet while completing daily symptom diaries (IBS-SSS) and stool logs (Bristol Stool Form Scale).
- Elimination Phase (21-28 days): Implementation of a strict low-FODMAP diet, excluding foods high in Oligosaccharides, Disaccharides, Monosaccharides, and Polyols. A dietitian provides standardized resources.
- Systematic Rechallenge Phases (60+ days): Sequential, blinded (where possible) reintroduction of specific FODMAP subgroups.
- Challenge 1: Fructose (e.g., honey, mango). Dose: 25g load. Duration: 3 days, monitoring symptoms.
- Challenge 2: Lactose (e.g., milk). Dose: 250ml milk. Duration: 3 days.
- Challenge 3: Polyols (e.g., sorbitol in stone fruit, mannitol in mushrooms). Dose: 10g sorbitol. Duration: 3 days.
- Challenge 4: Galacto-oligosaccharides (GOS) (e.g., canned legumes). Dose: 1/2 cup. Duration: 3 days.
- Challenge 5: Fructans (e.g., onion, garlic, wheat). Dose: 2g fructan. Duration: 3 days.
- Washout Period: A 3-day return to strict low-FODMAP diet between each challenge phase to reset baseline.
- Personalization Phase: Development of a long-term diet plan incorporating only the poorly tolerated FODMAP subgroups identified during challenges.
Migraine
Application Note: N-of-1 trials are instrumental in identifying individual dietary triggers (e.g., tyramine, nitrates, aspartame) and determining the efficacy of supplemental interventions like Riboflavin (B2) and Magnesium in migraine prophylaxis.
Key Quantitative Data Summary:
Table 2: N-of-1 Outcomes for Nutritional Interventions in Migraine Prophylaxis
| Intervention | Comparison | Outcome Measure | Mean Individual Effect Size (Range) | Consistency Across Participants |
|---|---|---|---|---|
| High-Dose Riboflavin (400mg/day) | Placebo | Migraine Days/month | -3.8 days (-6.5 to -1.2) | High |
| Magnesium Citrate (600mg/day) | Placebo | Attack Frequency | -22% (-41% to -5%) | Moderate |
| Elimination Diet (Trigger-specific) | Habitual Diet | Headache Intensity (0-10) | -2.7 points (-4.1 to -1.0) | Variable (Trigger-dependent) |
| Omega-3 (EPA/DHA) 1.5g/day | Omega-6 control | Headache Hours/month | -31.2 hours (-55.4 to -4.1) | Moderate |
Experimental Protocol: N-of-1 Trial for Migraine Trigger Identification & Supplementation
- Phenotyping & Baseline (30 days): Detailed migraine diary (frequency, duration, intensity, medication use, premonitory symptoms). Serum Mg++ analysis optional.
- Blinded Supplementation Blocks (Cross-over Design):
- Design: Randomized, double-blind, placebo-controlled cross-over. Two 8-week intervention periods (Active/Placebo) separated by a 4-week washout.
- Supplement Preparation: Encapsulated Riboflavin (400mg) + Magnesium Citrate (600mg elemental) vs. matched placebo (microcrystalline cellulose).
- Compliance: Pill count and weekly reminder alerts.
- Parallel Dietary Trigger Testing:
- Suspected Trigger Challenge: In a stable period, introduce a single suspected food (e.g., aged cheese for tyramine, processed meat for nitrates) in a controlled dose.
- Monitoring: Record migraine occurrence and features for 24-72 hours post-challenge.
- Control Challenge: Repeat with a visually similar "safe" food on a separate occasion, blinded if possible.
- Data Integration: Time-series analysis of migraine diaries correlated with intervention blocks and challenge results to establish individual causality.
Athletic Performance
Application Note: Personalized nutrition strategies for athletes, optimized via N-of-1 designs, focus on manipulating carbohydrate periodization, caffeine timing, and creatine loading to enhance performance metrics specific to the individual's sport and physiology.
Key Quantitative Data Summary:
Table 3: Effects of Personalized Nutrition Strategies on Athletic Performance (N-of-1 Data)
| Strategy | Performance Metric | Mean Improvement (%) | Inter-Individual Variability (CV%) | Key Moderating Factor |
|---|---|---|---|---|
| Caffeine Timing (Individualized) | Time-trial power output | 4.7% | 25.3% | CYP1A2 Genotype |
| Creatine Loading Protocol | Repeated sprint performance | 5.1% | 18.7% | Muscle fiber type (estimated) |
| Carbohydrate Periodization | Session RPE vs. Power Output | +12% (efficiency) | 22.5% | Training phase & intensity |
| Nitrate Supplementation (Beetroot) | Time to exhaustion @ 80% VO2max | 3.5% | 45.1% | Baseline plasma nitrate/nitrite |
Experimental Protocol: N-of-1 Optimization of Caffeine Timing for Performance
- Genotyping & Baseline: Saliva sample for CYP1A2 gene polymorphism (AA vs. AC/CC for fast/slow metabolizer).
- Performance Testing Baseline: Establish reproducible performance test (e.g., 5km cycling time-trial, repeated Wingate sprints).
- Randomized Test Conditions: Participant completes performance test under four conditions, in random order, separated by >48h:
- A. Placebo: Decaffeinated beverage administered 60min pre-test.
- B. Standard Timing: 3 mg/kg caffeine, 60min pre-test.
- C. Early Timing (Slow Metabolizers): 3 mg/kg caffeine, 180min pre-test.
- D. Late Timing (Fast Metabolizers): 3 mg/kg caffeine, 30min pre-test.
- Blinding: Use opaque capsules filled with anhydrous caffeine or placebo (maltodextrin).
- Measurement: Primary: Power output (W), time to completion (s). Secondary: Perceived exertion (RPE), heart rate.
- Analysis: Compare performance under each condition to placebo and standard timing to identify individual-optimal strategy.
Visualizations
N-of-1 FODMAP Protocol Workflow
Nutritional Modulation of Migraine Pathways
Personalized Ergogenic Aid Decision Logic
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Materials for Personalized Nutrition N-of-1 Trials
| Item | Function in N-of-1 Research | Example/Specification |
|---|---|---|
| Digital Symptom Diaries (e.g., EMA apps) | Enables real-time, high-frequency capture of subjective outcomes (pain, mood, energy) critical for time-series analysis. | Customizable surveys delivered via smartphone (e.g., MovisensXS, PACO). |
| Blinded Intervention Kits | Allows for proper participant and investigator blinding in crossover trials (e.g., for supplements, dietary challenges). | Gelatin capsules filled with active (creatine, caffeine) vs. placebo (maltodextrin), identical in appearance. |
| Point-of-Care Biomarker Devices | Facilitates frequent, convenient monitoring of physiological responses. | Lactate meters, ketone monitors (β-hydroxybutyrate), continuous glucose monitors (CGM). |
| Standardized Challenge Meals/Supplements | Provides a consistent dose of a nutritional compound for trigger testing or metabolic response profiling. | Pre-portioned fructose drink (25g), encapsulated tyramine (75mg), beetroot juice shots (400mg nitrate). |
| Bio-specimen Collection Kits (at-home) | Enables decentralized collection of samples for genetic, metabolomic, or microbiome analysis. | Saliva swabs (Oragene) for DNA, stool collection tubes (OMNIgene•GUT) for microbiome, dried blood spot cards. |
| Nutrient Analysis Software/Databases | Essential for quantifying and designing controlled elimination or supplementation diets. | Food composition databases (e.g., USDA, Monash FODMAP), dietary analysis software (e.g., Nutritics). |
| Wearable Activity/Sleep Trackers | Objectively measures secondary outcomes like sleep quality, heart rate variability, and physical activity levels. | Research-grade devices (e.g., ActiGraph, Oura Ring) with raw data access. |
Application Notes
Within personalized nutrition research, the translation from individualized findings to generalizable public health recommendations presents a significant challenge. The Hybrid Model proposes a structured, two-phase framework. Phase 1 employs a series of meticulously designed N-of-1 trials to identify candidate interventions and discover person-level effect modifiers in a heterogeneous population. These highly granular, quantitative findings then serve as the hypothesis-generating engine for Phase 2: the design of a more targeted, efficient, and statistically informed larger-scale Randomized Controlled Trial (RCT). This model mitigates the risk of RCT failure by basing its primary hypotheses on prior empirical evidence of effect in individuals.
Table 1: Quantitative Outcomes from a Hypothetical Hybrid Model Study on Omega-3 for Cognitive Fatigue
| Metric | N-of-1 Phase (n=15 participants, each 4 cycles) | Proposed RCT Design Based on N-of-1 Data |
|---|---|---|
| Overall Responder Rate | 40% (6/15) | N/A |
| Mean Effect Size (Cohen's d) in Responders | 0.82 (95% CI: 0.65, 1.12) | Primary power calculation based on d = 0.75 |
| Identified Effect Modifier | Baseline CRP > 3 mg/L (Odds Ratio for response: 8.4) | Stratification or inclusion criterion: CRP > 3 mg/L |
| Suggested RCT Population Size | N/A | 64 participants per arm (80% power, α=0.05) for enriched design |
Experimental Protocols
Protocol 1: Core N-of-1 Trial for Dietary Intervention (e.g., Omega-3 Supplementation)
- Objective: To determine the individual effect of a dietary intervention on a continuous outcome (e.g., cognitive fatigue score).
- Design: Randomized, double-blind, multiple crossover trial within a single participant.
- Procedure:
- Baseline & Washout (7 days): Stabilize participant on control diet. Collect baseline biomarkers (e.g., CRP, Omega-3 Index).
- Randomization & Blocking: Generate a random sequence for treatment (A) and placebo/control (B) arms (e.g., ABAB, BABA) for a minimum of 4 complete cycles. Use blocks to ensure balance.
- Intervention Periods (14 days each): Administer treatment or matched placebo. The participant and all assessors are blinded.
- Daily Measurement: Participant records outcome via validated digital tool (e.g., ecological momentary assessment app) at a specified time each day.
- End-of-Period Biomarker: Collect blood spot or venous blood on the final day of each period for compliance and mechanistic biomarkers.
- Data Analysis (Individual Level): Use a linear mixed-effects model or Bayesian approach to estimate the individual treatment effect, its credibility interval, and probability of benefit.
Protocol 2: Aggregating N-of-1 Trials for RCT Hypothesis Generation
- Objective: To synthesize data from a series of N-of-1 trials to identify overall effect size, responder profiles, and candidate biomarkers for RCT stratification.
- Procedure:
- Pre-specified Aggregation: Plan a meta-analytic framework for aggregating individual participant data from all N-of-1 trials before study commencement.
- Harmonization: Ensure measurement tools, intervention dosage, and period length are identical across all N-of-1 trials.
- Individual Effect Estimation: Calculate the best estimate of effect (e.g., mean difference) and its variance for each participant using Protocol 1 analysis.
- Aggregate Analysis:
- Perform a random-effects meta-analysis of individual treatment effects to estimate the population-average effect.
- Use regression models (e.g., meta-regression) to test if baseline characteristics (e.g., CRP, genotype, microbiome alpha-diversity) modify the treatment effect.
- Hypothesis Formulation: The aggregated effect size informs the RCT power calculation. Identified effect modifiers become candidates for RCT inclusion criteria or stratification factors.
Mandatory Visualizations
Title: Hybrid Model Workflow: From N-of-1 Trials to Targeted RCTs
Title: Mechanistic Pathways for a Personalized Nutrition Intervention
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function in Hybrid Model Research |
|---|---|
| Electronic Patient-Reported Outcome (ePRO) Platform | Enables real-time, high-frequency data capture (e.g., daily symptoms) crucial for time-series analysis in N-of-1 trials. Must be validated and customizable. |
| Blinded Intervention Kits | Pre-packaged, coded treatment and placebo/control products (e.g., supplements, foods) with identical appearance/taste to ensure blinding integrity across N-of-1 and RCT phases. |
| Dried Blood Spot (DBS) Collection Cards | Allows frequent, low-burden, at-home sampling for compliance biomarkers (e.g., Omega-3 Index) and mechanistic biomarkers (e.g., CRP via hs-CRP assays). |
| Linear Mixed-Effects Model Software (e.g., R/lme4, SAS PROC MIXED) | Essential for analyzing repeated measures data from N-of-1 trials, modeling within- and between-participant variance to estimate individual and aggregate effects. |
| Bayesian Analysis Packages (e.g., Stan, R/brms) | Provides a flexible framework for N-of-1 analysis, calculating probabilities of clinical benefit for individuals, and naturally integrating evidence from the N-of-1 phase into RCT priors. |
| High-Sensitivity CRP (hs-CRP) Assay | A key potential effect modifier biomarker. Used to stratify participants in the N-of-1 aggregation phase and potentially enrich the subsequent RCT population. |
| Omega-3 Index (RBC Fatty Acid Analysis) | A robust compliance and status biomarker for Omega-3 interventions. Confirms intervention adherence in both N-of-1 and RCT settings and can correlate with clinical outcomes. |
Personalized nutrition seeks to tailor dietary interventions to individual characteristics. N-of-1 trial designs, where an individual serves as their own control through repeated, crossover interventions, are uniquely suited for this field. However, the integration of evidence from such single-subject designs into clinical practice guidelines (CPGs) faces regulatory and methodological hurdles. This document outlines application notes and protocols for generating N-of-1 evidence that meets the standards required for guideline development bodies.
Current Regulatory Landscape & Guideline Requirements
A review of major regulatory and guideline-developing bodies reveals a spectrum of acceptance for N-of-1 evidence. The table below summarizes key positions and evidentiary requirements.
Table 1: Position of Major Bodies on N-of-1 Evidence for Guidelines
| Organization | Primary Focus | Position on N-of-1 Evidence | Key Requirements for Consideration |
|---|---|---|---|
| FDA | Drug/Device Approval | Recognized in framework for digital health & rare diseases. | Rigorous design, pre-specified analysis plan, demonstrable causal inference, assessment of carryover effects. |
| EMA | Drug Approval | Acceptable in very rare conditions where group trials are impossible. | Must be part of a series; requires statistical justification and validation of individual response. |
| NIH | Research & CPGs | Encourages use in precision medicine. Supports methods development. | Transparent reporting (e.g., using CENT guidelines extension), replicability of interventions, longitudinal data collection. |
| NICE | Health Tech Assessment | Considered for highly personalized technologies, but not typical for mainstream CPGs. | Evidence synthesis from multiple N-of-1 trials (aggregation), demonstration of generalizable principles, cost-effectiveness data. |
| GRADE Working Group | Evidence Grading | Acknowledges potential but notes challenges for rating certainty of evidence. | Formal methods for pooling, addressing risk of bias specific to N-of-1 designs (e.g., randomization, blinding feasibility). |
Core Protocols for Guideline-Acceptable N-of-1 Trials
Protocol: Standardized N-of-1 Trial for Personalized Nutrition
Objective: To determine the individual-specific effect of a dietary intervention (e.g., low FODMAP vs. control diet) on a patient-reported outcome (e.g., IBS symptom severity).
Design: Randomized, double-blind, multiple crossover trial within a single participant.
Detailed Methodology:
- Baseline & Wash-in (Week 1-2): Stable baseline diet, training on outcome measurement tools.
- Intervention Pairs: The trial consists of k pairs of periods. Each pair includes one period on Intervention A (e.g., active diet) and one on Intervention B (e.g., control/masked diet).
- Randomization & Blinding: Order of A/B within each pair is randomized. For blinding, utilize matched placebo foods/supplements or a cross-over design where the core intervention is opaque (e.g., smoothies with/without active component).
- Period Duration: Determined by physiology (e.g., 7-14 days for gut microbiome shifts). Must include assessment of carryover effects.
- Washout: Incorporated between periods if risk of carryover is high, or use statistical modeling to account for it.
- Outcome Measurement: Daily electronic patient-reported outcome (e-Pro) using validated instruments (e.g., VAS scales). Objective biomarkers (e.g., continuous glucose monitoring, inflammatory markers) collected at end of each period.
- Data Analysis:
- Individual Level: Visual analysis of time-series data. Paired t-test or linear mixed model for within-individual comparison.
- Aggregation (for meta-analysis): Calculate individual effect sizes (e.g., mean difference, standardized mean difference). Use Bayesian or frequentist random-effects models to aggregate across a series of participants.
Protocol: Aggregating N-of-1 Trials for Population Inference (N-of-1+ Design)
Objective: To synthesize evidence from multiple, heterogenous N-of-1 trials to inform a general guideline recommendation while identifying effect modifiers.
Design: Prospective, coordinated series of parallel N-of-1 trials with common core elements.
Detailed Methodology:
- Common Core Protocol: Define shared elements across all participants: primary outcome measure, minimum number of crossover pairs, blinding strategy, and core data elements (e.g., demographics, key biomarkers).
- Personalized Flexibility: Allow variation in specific intervention detail (e.g., type of probiotic strain, exact macronutrient ratio), duration of periods, and collection of additional personalized biomarkers.
- Central Registry & Platform: Utilize a centralized trial platform (e.g., via ROSA or Personal Health Train infrastructure) for data aggregation with privacy-preserving analytics.
- Analysis Plan:
- Data Harmonization: Transform individual time-series data into standardized effect estimates per participant.
- Individual Participant Data (IPD) Meta-Analysis: Use multilevel/hierarchical Bayesian models. The model estimates an overall mean effect, variance of individual effects, and models effect modifiers (e.g., genotype, microbiome baseline) as covariates.
- Heterogeneity Assessment: Report I² statistic specific to IPD meta-analysis of N-of-1 trials.
Visual Workflows & Pathways
N-of-1 Trial Core Workflow for Guidelines
Pathway for N-of-1 Evidence into Guidelines
The Scientist's Toolkit: Key Reagent Solutions
Table 2: Essential Research Tools for N-of-1 Personalized Nutrition Trials
| Item/Category | Example Product/Solution | Function in N-of-1 Trials |
|---|---|---|
| Blinding Reagents | Matched placebo powders (maltodextrin, cellulose), encapsulated supplements, identically packaged food items. | Ensures intervention and control are indistinguishable, critical for internal validity and reducing participant/experimenter bias. |
| Biomarker Collection Kits | Dried blood spot cards (e.g., Hemaxis), fecal DNA/RNA stabilizer tubes (OMNIgene•GUT), saliva cortisol kits. | Enables standardized, at-home collection of objective outcome measures for each trial period, facilitating longitudinal comparison. |
| ePRO/Diary Platforms | Commercial (REDCap, MovisensXS) or custom apps with time-stamped entries, reminder alerts, and data export. | Captures daily patient-reported outcomes (symptoms, diet adherence) as primary time-series data for within-individual analysis. |
| Continuous Monitors | Continuous Glucose Monitors (CGM - e.g., FreeStyle Libre), wearable activity trackers (ActiGraph), smart scales. | Provides high-density, objective physiological data streams to complement ePRO and identify temporal patterns of response. |
| Standardized Meals/Probes | Liquid meal challenges (Ensure), metabolic probe foods (e.g., for ketone or inflammatory response). | Creates a controlled physiological challenge to measure inter-period differences in metabolic resilience or response. |
| Data Analysis Software | R packages (nlme, brms for Bayesian models), dedicated N-of-1 software (SINGL, SCRT). |
Performs time-series visualization, individual-level statistical testing, and aggregated data meta-analysis. |
Conclusion
N-of-1 trial designs represent a paradigm shift in nutrition science, offering a rigorous, patient-centered framework to move beyond generic dietary advice toward truly personalized recommendations. This guide has outlined their foundational principles, methodological execution, solutions for common challenges, and strategies for validation. For biomedical research, these trials fill a critical evidence gap, providing high-level causal data for individual responses that are often obscured in group averages. They complement traditional RCTs, not replace them, forming a synergistic evidence-generating ecosystem. Future directions must focus on developing scalable, digital-first platforms, establishing standardized analytical pipelines, and creating formal regulatory pathways for evidence derived from aggregated N-of-1 trials. Ultimately, the widespread adoption of this methodology promises to enhance the precision, efficacy, and individual relevance of nutritional interventions, paving the way for a new era of data-driven personalized health.