The Overestimation Problem: Evaluating Low-Cost Wearable Accuracy in Energy Expenditure Tracking for Clinical and Research Applications
This article critically examines the significant tendency of low-cost wearable devices to overestimate energy expenditure, particularly during low-to-moderate intensity activities.
The Overestimation Problem: Evaluating Low-Cost Wearable Accuracy in Energy Expenditure Tracking for Clinical and Research Applications
Abstract
This article critically examines the significant tendency of low-cost wearable devices to overestimate energy expenditure, particularly during low-to-moderate intensity activities. Targeted at researchers, scientists, and drug development professionals, it synthesizes recent validation studies, identifies the core technological and algorithmic limitations driving inaccuracies, and explores the implications for clinical trials and metabolic research. The review further discusses emerging methodological approaches for data correction, provides a framework for device validation, and outlines future directions for improving the reliability of wearable-derived energy metrics in biomedical applications.
The Evidence Base: Documenting Systemic Overestimation in Consumer Wearables
Frequently Asked Questions (FAQs)
Q1: Why is there such a high error rate in energy expenditure estimation from consumer wearables?
The high error rate stems from multiple factors. The devices often rely on algorithms, like the Mifflin-St. Jeor equation, to estimate Basal Metabolic Rate (BMR) based on user-provided data (age, sex, weight, height), which is then used as a base for calculating total energy expenditure [1]. The estimation of active calories through motion sensors and heart rate is complex and can be influenced by the type of activity, with steady-state activities like walking often yielding more accurate results than irregular movements like cycling or household chores [1]. Furthermore, a major systematic review and meta-analysis of combined-sensing Fitbit devices concluded that they consistently underestimate energy expenditure, with an average bias of -2.77 kcal per minute compared to criterion measures [2]. Studies on low-cost smartwatches have also shown significant overestimation, with Mean Absolute Percentage Errors (MAPE) ranging from 15.0% to 57.4% in some devices [3].
Q2: What is the "gold standard" method for validating wearable energy expenditure data?
The gold standard method referenced in validation studies is indirect calorimetry [3] [2]. This method uses a metabolic cart, such as the CORTEX METAMAX 3B, to measure the body's gas exchange—specifically, oxygen consumption (VO₂) and carbon dioxide production (VCO₂)—on a breath-by-breath basis [3]. These values are then entered into equations, such as the Weir equation, to calculate energy expenditure with high precision [4] [3]. This setup serves as the criterion measure against which the estimates from wearable devices are compared in controlled laboratory settings.
Q3: What are common hardware and software issues that can affect data accuracy?
Common issues that researchers should account for include:
- Sensor Inaccuracies: Inconsistent or inaccurate readings from accelerometers or photoplethysmography (PPG) heart rate sensors due to hardware defects, improper placement on the wrist, or external factors like temperature and humidity [5].
- Connectivity Issues: Problems with Bluetooth pairing or syncing can lead to data loss or corruption. Ensuring devices are fully charged, within range, and have updated firmware can mitigate these issues [6] [5].
- Battery Problems: Low battery life or unexpected shutdowns can interrupt data collection. Using manufacturer-recommended chargers and procedures is essential for maintaining device function [5].
Q4: My wearable device is overestimating EE in my study cohort. How should I address this?
First, characterize the error by comparing your device's data to a gold standard like indirect calorimetry for a subset of your participants under controlled conditions [3] [2]. This will allow you to quantify the bias (e.g., mean absolute percentage error) for your specific population and device model. Based on this, you can develop a calibration or correction factor to apply to your dataset. It is also critical to clearly report the device's known error and your correction methodology in your research findings to ensure transparency.
Troubleshooting Guides
Guide 1: Diagnosing and Mitigating High Error Rates in EE Data
| Step | Action | Rationale & Technical Details |
|---|---|---|
| 1. Verify Criterion Method | For validation studies, ensure proper calibration of the indirect calorimetry device using a 3L syringe and calibration gases prior to each data collection session [3]. | Calibration is fundamental for accurate measurement of VO₂ and VCO₂, which are used in the Weir equation to establish the ground truth for EE [3]. |
| 2. Control Device Setup | Place the wearable device on the wrist according to the manufacturer's instructions, ensuring a secure but comfortable fit. Assign device placement (left/right wrist) randomly to control for placement bias [3]. | Improper fit can affect the accuracy of both accelerometer and PPG heart rate sensors. Randomization helps account for any potential differences related to limb dominance. |
| 3. Standardize Protocol | Design experimental protocols that account for different activity types (e.g., steady-state vs. intermittent) and intensities, and ensure consistent conditions across all participants. | EE estimation error is not uniform; it varies significantly with the type and intensity of physical activity. A structured protocol helps identify these specific error patterns [1]. |
| 4. Quantify the Error | Calculate statistical measures of agreement between the wearable and the criterion measure. Key metrics include Mean Bias, Mean Absolute Percentage Error (MAPE), and Limits of Agreement (LOA) from Bland-Altman analysis [3] [2]. | A meta-analysis of Fitbit devices used Bland-Altman methods, finding a population LOA for EE of -12.75 to 7.41 kcal/min, highlighting the large range of individual error [2]. |
| 5. Apply Corrections | Based on the quantified bias, develop a device- and population-specific correction factor or algorithm to adjust the raw EE data from the wearable. | This step is crucial for improving the validity of data used in subsequent analysis, especially given the documented systematic underestimation or overestimation trends [2] [1]. |
Guide 2: Resolving Connectivity and Data Sync Issues
| Issue | Symptom | Solution |
|---|---|---|
| Bluetooth Pairing Failure | The wearable device fails to pair with the data collection smartphone or tablet. | Check and enable all necessary app permissions (Bluetooth, Location Services). Update the device's firmware and companion app to the latest versions. Unpair and then re-pair the device [6] [5]. |
| Intermittent Data Sync | Data transfers from the wearable to the server are inconsistent, with gaps or delays. | Ensure both the wearable and the paired device have adequate battery charge (ideally >20%). Keep the devices within 30 feet and minimize physical obstructions and interference from other electronic devices [6] [5]. |
| Data Transmission Latency | A significant delay is observed between data collection on the wearable and its appearance in the research database. | Optimize the Bluetooth configuration for a lower connection interval if possible. Check for and reduce packet loss. Implement data compression techniques to reduce payload size before transmission [6]. |
Experimental Protocols & Methodologies
Protocol 1: Validation of Wearable EE Estimation During Ergometer Cycling
This protocol is adapted from a 2025 study investigating the validity of low-cost smartwatches in untrained women [3].
Objective: To assess the validity of energy expenditure estimates from wearable devices during graded cycling exercise against the criterion of indirect calorimetry.
Key Reagent Solutions:
- CORTEX METAMAX 3B (MM3B): A portable metabolic system used as the criterion measure. It collects breath-by-breath gas exchange data (VO₂ and VCO₂) [3].
- Polar H10 Heart Rate Belt: A validated chest-strap ECG heart rate monitor used to provide a secondary criterion measure for heart rate [3].
- Weir Equation: The equation used to convert gas exchange measurements (VO₂ and VCO₂) into energy expenditure (kcal/min) [3].
Methodology:
- Participant Preparation: Screen participants according to inclusion/exclusion criteria (e.g., healthy, sedentary/slightly active). Instruct them to avoid caffeine, smoking, and strenuous activity before testing.
- Device Calibration: Calibrate the MM3B device according to manufacturer specifications using a 3L calibration syringe and certified calibration gases [3].
- Device Setup: Fit the MM3B mask and Polar H10 belt on the participant. Securely fit two smartwatches (randomly assigned to wrists) according to manufacturer guidelines, ensuring proper sensor contact.
- Testing Protocol: Have the participant perform cycling on an ergometer at incremental power outputs (e.g., 30W, 40W, 50W, 60W). Maintain each stage for a sufficient duration (e.g., 4-5 minutes) to reach a steady state.
- Data Collection: Simultaneously record EE and heart rate from the MM3B (criterion), Polar H10, and all smartwatches throughout the protocol.
- Data Analysis: Calculate EE from MM3B using the Weir equation. Compare smartwatch EE estimates to the criterion using statistical measures like MAPE, bias, and Bland-Altman analysis [3].
Protocol 2: Meta-Analytical Approach for Quantifying Device Bias
This protocol is based on a 2022 systematic review and meta-analysis of combined-sensing Fitbit devices [2].
Objective: To quantitatively synthesize evidence and quantify the population-level bias and limits of agreement for energy expenditure, heart rate, and steps measured by recent wearable devices.
Methodology:
- Literature Search: Conduct a systematic search of electronic databases (e.g., PubMed, Embase) for validation studies published within a specified timeframe.
- Study Selection: Apply strict inclusion criteria: studies must compare a wearable device against a valid criterion measure (e.g., indirect calorimetry for EE, electrocardiogram for HR, direct observation for steps) [2].
- Data Extraction: Extract key statistics from included studies: mean bias (device - criterion), standard deviation of bias, and sample size for each comparison. Convert EE and steps to a per-minute rate if necessary.
- Data Synthesis: Perform a Bland-Altman meta-analysis. Pool the mean bias and standard deviation of the differences to calculate the population limits of agreement (LOA) for each metric (EE, HR, steps) [2].
- Heterogeneity Analysis: Investigate sources of heterogeneity, such as the specific device model, participant age, type of activity performed, and risk of bias in the primary studies.
Data Presentation
Table 1: Accuracy of Selected Wearables in Estimating Energy Expenditure
Data from controlled laboratory studies comparing devices to indirect calorimetry.
| Device / Brand | Study Type | Average Bias (vs. Criterion) | Mean Absolute Percentage Error (MAPE) | Key Finding |
|---|---|---|---|---|
| Various Fitbit Models | Meta-Analysis (2022) [2] | -2.77 kcal/min | Not Reported | Systematic underestimation of EE; LOA: -12.75 to 7.41 kcal/min. |
| XIAOMI Smart Band 8 (XMB8) | Experimental (2025) [3] | Overestimation | 30.5% - 41.0% | Significantly overestimated EE at all cycling load levels. |
| HONOR Band 7 (HNB7) | Experimental (2025) [3] | Not Significant | 15.0% - 23.0% | Demonstrated moderate accuracy with no significant over/underestimation. |
| HUAWEI Band 8 (HWB8) | Experimental (2025) [3] | Not Significant | 12.5% - 18.6% | Showed the best accuracy among the four low-cost devices tested. |
| KEEP Smart Band B4 Lite (KPB4L) | Experimental (2025) [3] | Overestimation | 49.5% - 57.4% | Showed the highest error, severely overestimating EE. |
Table 2: Essential Research Reagents for EE Validation Studies
Key equipment and tools required for establishing a rigorous validation protocol.
| Item | Function & Rationale |
|---|---|
| Portable Indirect Calorimetry System (e.g., CORTEX METAMAX 3B) | Serves as the criterion measure for Energy Expenditure. It directly measures oxygen consumption and carbon dioxide production, which are used to calculate EE via established equations [3]. |
| Calibration Syringe & Gases | Essential for the precise calibration of the metabolic cart before each use, ensuring the accuracy of gas volume and concentration measurements [3]. |
| Ergometer (Cycle or Treadmill) | Provides a controlled and standardized environment for administering exercise protocols at precise intensities. |
| Validated Chest-Strap Heart Rate Monitor (e.g., Polar H10) | Provides a secondary criterion measure for heart rate, which is a key input for the algorithms in combined-sensing wearables [3]. |
| Statistical Analysis Software (e.g., R, Python) | Used for conducting specialized statistical analyses, such as Bland-Altman plots and calculation of Mean Absolute Percentage Error (MAPE), to quantify device agreement with the criterion [3] [2]. |
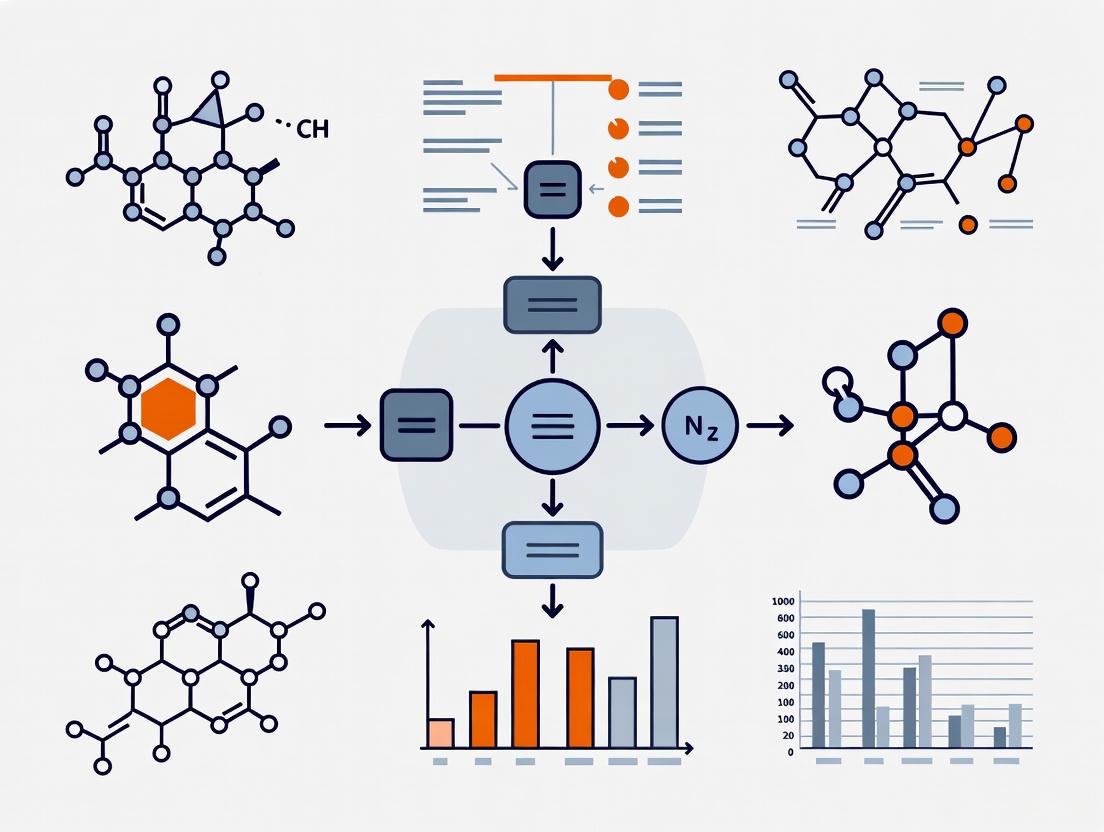
Experimental Workflow and Signaling Pathways
In the validation of wearable technologies designed to estimate calorie intake, the Mean Absolute Percentage Error (MAPE) is a widely used metric for assessing model accuracy. It measures the average absolute percentage difference between predicted values from a device and actual, ground-truth values [7]. However, within the specific context of research on wearables for low calorie intake estimation, the use of MAPE presents significant and often misunderstood challenges. Its mathematical formulation can systematically overstate the error for low actual values, potentially misrepresenting the device's true performance and biasing model evaluation [8] [7] [9]. This technical guide addresses the specific issues researchers encounter when using MAPE in this field.
Troubleshooting Guides
Problem 1: Inflated MAPE Values Due to Low Actual Intake
The Issue Your analysis shows an excessively high MAPE, but a visual inspection of the data suggests the wearable's estimates are reasonably close, especially for larger calorie values.
Diagnosis This is a classic symptom of MAPE's sensitivity to low actual values. The error is divided by the actual value (At), so when At is small (e.g., a small snack or a beverage), even a minor absolute difference between the forecast (Ft) and the actual value can result in an extremely large percentage error, disproportionately inflating the overall MAPE [8] [9].
Solution
- Calculate Absolute Errors: First, review the Mean Absolute Error (MAE) to understand the average error in the original units (e.g., kilocalories), which is not skewed by small denominators [7].
- Implement a Threshold: For all actual values below a physiologically meaningful threshold (e.g., < 50 kcal), consider calculating the absolute error instead of the percentage error.
- Use an Alternative Metric: For a more balanced view, adopt the Weighted Mean Absolute Percentage Error (WMAPE). WMAPE uses the sum of the absolute errors divided by the sum of the actual values, which prevents low individual values from dominating the metric [8].
Table: Impact of Low Actual Values on MAPE
| Actual Value (kcal) | Predicted Value (kcal) | Absolute Error (kcal) | Absolute Percentage Error (%) |
|---|---|---|---|
| 10 | 12 | 2 | 20.0% |
| 400 | 360 | 40 | 10.0% |
| 5 | 9 | 4 | 80.0% |
| Overall MAPE | 36.7% |
In the table above, the single, small error of 4 kcal on an actual value of 5 kcal contributes disproportionately to the overall MAPE, making the model's performance appear worse than the absolute errors suggest.
Problem 2: MAPE Favors Underestimation of Low Intake
The Issue During model training or selection, you find that a model which systematically underestimates low calorie intake achieves a slightly better (lower) MAPE than a more accurate model.
Diagnosis MAPE has a known inherent bias. For the same absolute error, the penalty is higher when over-predicting a small actual value than when under-predicting it [8] [7]. This can inadvertently guide algorithms towards models that produce low-biased forecasts.
Solution
- Audit for Bias: Systematically check the direction of errors in your model. Plot the residuals (Actual - Predicted) against the actual values to visually identify any systematic under- or over-prediction patterns.
- Use a Symmetric Metric: Consider metrics less sensitive to this bias, such as the Mean Arctangent Absolute Percentage Error (MAAPE) or the use of scaled errors like Mean Absolute Scaled Error (MASE) [8].
- Complement with MAE: Always report MAE alongside MAPE to provide a clear picture of the unbiased average error magnitude [9].
Frequently Asked Questions (FAQs)
Q1: What is an acceptable MAPE value for a wearable calorie intake estimator? There is no universal standard for an "acceptable" MAPE, as it is highly context-dependent [7]. However, for reference, a validation study of popular smartwatches for estimating energy expenditure during physical activity reported MAPEs ranging from 9.9% to 32.0% [10]. The key is to compare your model's MAPE against a naive baseline or existing solutions in the literature, rather than targeting an arbitrary number.
Q2: Our data includes instances of zero calorie intake (fasting). How should we handle MAPE calculation? MAPE is undefined when actual values are zero, as it leads to division by zero [8] [9]. Your options are:
- Exclude Zero Points: Remove these data points from the MAPE calculation, but document this exclusion thoroughly as it may bias your results.
- Use WMAPE: Shift to WMAPE, which aggregates errors before calculating a single percentage and avoids division by zero for individual points [8].
- Switch Metrics: Use a different metric entirely, such as Mean Absolute Error (MAE) or Root Mean Squared Error (RMSE), for which zero values are not problematic [7].
Q3: Why is WMAPE a better choice for our low-calorie intake research?
WMAPE (Weighted Mean Absolute Percentage Error) is often a more robust choice because it calculates error as a single percentage across the entire dataset. Its formula, WMAPE = SUM(|A_i - F_i|) / SUM(|A_i|), prevents individual low actual values from having an outsized impact on the final result. This provides a more stable and representative measure of overall model accuracy in datasets with a wide range of values [8].
Experimental Protocols for Validation
To ensure the rigorous validation of wearable devices, the following methodological details are critical.
Reference Method for Calorie Intake Validation
A robust validation study requires a highly accurate reference method against which the wearable device is compared.
- Objective: To validate the accuracy of a wearable wristband in estimating daily energy intake (kcal) in free-living adults [11] [12].
- Design: Participants use the wearable device over two 14-day test periods. The reference method involves collaboration with a metabolic kitchen where all meals are prepared, calibrated, and served. Participants consume these meals under direct observation, allowing for precise recording of their true energy and macronutrient intake [12].
- Statistical Analysis: The agreement between the wearable device and the reference method is typically assessed using Bland-Altman analysis, which calculates the mean bias (average difference) and the limits of agreement [12].
Protocol for Activity-Based Energy Expenditure Validation
When validating energy expenditure, indirect calorimetry is the gold standard.
- Objective: To assess the validity of smartwatches in estimating energy expenditure (EE) during structured outdoor walking and running [10].
- Design: Participants concurrently wear the smartwatches and a portable gas analysis system (e.g., COSMED K5). They perform standardized exercises, such as walking 2 km at 6 km/h and running 2 km at 10 km/h, on an outdoor track [10].
- Data Collection: The portable gas analysis system provides breath-by-breath measurement of oxygen consumption and carbon dioxide production, from which criterion EE is calculated. The smartwatch estimates are recorded simultaneously [10].
- Statistical Analysis: Use paired-sample t-tests to check for significant differences between the device and the criterion. Report MAPE, Limits of Agreement (LoA), and Intraclass Correlation Coefficient (ICC) [10].
Visualizing the MAPE Problem in Low-Calorie Contexts
The following diagram illustrates how the MAPE calculation reacts differently to errors at high and low actual values, leading to potential misinterpretation.
The Scientist's Toolkit: Essential Research Reagents & Materials
Table: Key Materials and Tools for Wearable Validation Research
| Item & Purpose | Function in Research | Example from Literature |
|---|---|---|
| Portable Metabolic System (Indirect Calorimeter) | Serves as the criterion measure (gold standard) for validating energy expenditure estimates from wearables by measuring respiratory gases [10]. | COSMED K5 system [10]. |
| Metabolic Kitchen & Calibrated Meals | Provides the ground truth for energy and macronutrient intake, enabling precise validation of dietary intake wearables against known inputs [12]. | University dining facility collaboration with precisely prepared meals [12]. |
| Consumer-Grade Wearables | The devices under test. Used to collect prediction data for energy intake, expenditure, and other physiological parameters [10] [13]. | Apple Watch Series 6, Garmin FENIX 6, Huawei Watch GT 2e, Fitbit trackers [10] [14]. |
| Statistical Analysis Software | Used to calculate performance metrics (MAPE, WMAPE, MAE), perform Bland-Altman analysis, and conduct significance testing [10] [12]. | SPSS, R, or Python with relevant statistical libraries [10]. |
| Wearable Cameras | Provides an objective, passive record of food consumption to assist in improving the accuracy of self-reported dietary recalls [15]. | Narrative Clip camera [15]. |
Troubleshooting Guides and FAQs
This technical support center provides troubleshooting guidance and experimental protocols for researchers investigating the performance of consumer-grade wearables against criterion standards, with a specific focus on the context of calorie intake estimation.
Frequently Asked Questions (FAQs)
Q1: Our experimental data shows that a consumer-grade wearable device consistently overestimates calorie expenditure compared to laboratory standards. What are the primary factors we should investigate?
A1: The overestimation of calorie expenditure is a common challenge. Your investigation should focus on these primary factors:
- Algorithmic Limitations: Consumer devices often use proprietary, generalized algorithms that may not account for individual variations in metabolism, fitness level, or the specific type of physical activity being performed [16].
- Sensor Placement and Type: Devices using wrist-worn photoplethysmogram (PPG) sensors are highly susceptible to motion artifacts. Higher intensity movement can significantly reduce the accuracy of heart rate measurements, which is a key input for calorie estimation models [17].
- Lack of Individual Calibration: Unlike controlled laboratory equipment, consumer devices are rarely calibrated for the individual user's physiological characteristics, such as weight, height, age, and basal metabolic rate, leading to systematic errors [16].
Q2: When validating a low-cost wearable for a research study, what is the minimum participant sample size and study duration required for a robust validation?
A2: While requirements vary by study goal, a practical guide recommends that for continuous monitoring, the device should be capable of passive data collection for a minimum of 24 hours a day for seven consecutive days. This duration captures sufficient data on daily activities and behaviors to account for natural variance [18]. The sample size should be large enough to provide statistical power for subgroup analyses (e.g., by BMI, age), a consideration often missed in early-stage pilot studies that fail to replicate in larger trials [16].
Q3: What are the key regulatory considerations when using data from consumer wearables in a clinical trial context?
A3: Regulatory bodies like the FDA emphasize a "Fit-for-Purpose" framework. Key considerations include:
- Verification: Confirming the device accurately and precisely measures the physical parameter it claims to (e.g., acceleration) [19].
- Analytical Validation: Demonstrating that the derived measurement (e.g., step count, calorie expenditure) accurately assesses the clinical characteristic in your specific participant population [19].
- Clinical Validation: Providing evidence that the measurement is associated with the clinical outcome or endpoint of interest [20]. Always consult the latest FDA guidance on Digital Health Technologies (DHTs) for remote data acquisition [20].
Experimental Protocols for Key Validation Tests
Protocol 1: Validating Caloric Expenditure Against a Criterion Standard
Objective: To compare the caloric expenditure output of a low-cost wearable (e.g., Xiaomi, Keep) against the criterion method of indirect calorimetry.
Materials:
- Criterion: Portable indirect calorimetry system (metabolic cart).
- Test Devices: Low-cost wearable devices (e.g., wrist-worn activity trackers).
- Treadmill or cycle ergometer.
- Standardized participant preparation guidelines (e.g., fasting state, no caffeine).
Methodology:
- Participant Setup: Equip the participant with the indirect calorimetry mask and the wearable device(s) according to manufacturer instructions.
- Protocol Execution: Conduct a graded exercise test. For example, stages of 3-5 minutes at increasing intensities (e.g., 3 km/h, 5 km/h, 7 km/h, and 9 km/h on a treadmill).
- Data Collection: Simultaneously record the caloric expenditure value from the indirect calorimetry system (criterion) and the wearable device(s) at the last 30 seconds of each stage when steady-state is achieved.
- Data Analysis: Use Bland-Altman analysis to assess the bias and limits of agreement between the wearable and the criterion measure. Calculate the mean absolute percentage error (MAPE) for each device.
Protocol 2: Assessing Heart Rate Accuracy in a Free-Living Setting
Objective: To evaluate the accuracy of wearable-derived heart rate data during unstructured activities, a key input for calorie estimation models.
Materials:
- Criterion: 12-lead Holter electrocardiogram (ECG) or a validated ambulatory ECG system [17].
- Test Devices: Low-cost wearable devices.
- Activity diary for participants.
Methodology:
- Device Setup: A certified technician places the Holter ECG on the participant. The wearable device is fitted according to its manual (e.g., snug on the wrist) [17].
- Monitoring Period: Participants are instructed to go about their normal daily routine for 24 hours, including various activity types (sedentary, walking, climbing stairs) while avoiding showering or swimming [17].
- Data Synchronization: Participants log their activities and any symptoms in a diary. All devices should be synchronized to a common time server at the start and end of the monitoring period [17].
- Data Analysis: Perform time-matched analysis of heart rate data from the wearable and the Holter ECG. Calculate accuracy as the percentage of wearable HR readings within ±10% of the concurrent ECG value. Investigate how accuracy varies with the level of bodily movement using accelerometry data [17].
The table below summarizes findings from validation studies, which are critical for benchmarking expectations.
| Study Focus | Criterion Device | Test Device | Key Performance Metric | Result |
|---|---|---|---|---|
| Heart Rate Accuracy in Pediatrics [17] | 24-hour Holter ECG | Corsano CardioWatch (Wristband) | Mean HR Accuracy (% within 10% of ECG) | 84.8% (SD 8.7%) |
| Heart Rate Accuracy in Pediatrics [17] | 24-hour Holter ECG | Hexoskin Smart Shirt | Mean HR Accuracy (% within 10% of ECG) | 87.4% (SD 11%) |
| Impact on Weight Loss [21] | Standard diet/exercise plan | Fit Core Armband | Average Weight Loss (over 2 years) | 7.7 lb (Device Group) vs. 13.0 lb (Control Group) |
| Heart Rate Accuracy vs. Movement [17] | Holter ECG | Corsano CardioWatch | Accuracy at Low vs. High HR | 90.9% vs. 79.0% (P<.001) |
Experimental Workflow and Logical Diagrams
The following diagram illustrates the logical workflow for designing a validation study for consumer wearables, from defining the purpose to the final data interpretation.
The Scientist's Toolkit: Essential Research Reagents and Materials
This table details key materials and their functions for conducting rigorous wearable validation studies.
| Item | Function in Validation Research |
|---|---|
| Indirect Calorimetry System | Considered the criterion method for measuring caloric expenditure and energy consumption by analyzing inhaled and exhaled gases. |
| Holter Electrocardiogram (ECG) | The gold-standard ambulatory device for continuous, medical-grade heart rate and rhythm monitoring against which wearables are validated [17]. |
| Controlled Environment Ergometer | A treadmill or cycle ergometer allows for the precise control of exercise intensity during standardized laboratory validation protocols. |
| Accelerometer (Reference Grade) | Used to objectively quantify the intensity of bodily movement, allowing researchers to analyze how motion artifacts impact wearable accuracy [17]. |
| Data Synchronization Tool | A critical tool or protocol (e.g., common time server, synchronized start/stop) to ensure timestamps from all devices are aligned for precise, time-matched analysis [17]. |
| Bland-Altman Analysis Software | A statistical method and software package used to assess the agreement between two measurement techniques by plotting the difference between them against their average [17]. |
The Impact of Activity Type and Intensity on Measurement Accuracy
Troubleshooting Guides
Guide 1: Troubleshooting Energy Expenditure (Calorie) Measurement Inaccuracies
Reported Issue: Significant discrepancies in energy expenditure (calorie) measurements during experimental data collection, particularly an observed overestimation of intake at lower calorie levels.
Investigation Procedure:
- Verify Activity Type & Intensity: Confirm the specific physical activities performed by study participants. Note that energy expenditure error margins are largest during physical activity, with Mean Absolute Percentage Errors (MAPE) reported from 29% to 80% depending on intensity, and absolute bias can range from -21.27% to 14.76% [22] [23].
- Cross-Reference with Gold Standards: Validate device outputs against criterion measures. For energy expenditure, the gold standard is indirect calorimetry (measuring oxygen and carbon dioxide in breath) [24]. One study found the most accurate device was off by 27% on average, and the least accurate by 93% [24].
- Check for Signal Artifacts: Review data for periods of transient signal loss, which is a major source of error in computing dietary and energy intake [11].
- Review Device Algorithm Specifications: Consult manufacturer documentation for the proprietary algorithm used to convert sensor data into energy expenditure. Be aware that these algorithms may make assumptions that do not fit individuals well across diverse populations [24].
Resolution Steps:
- For low-intensity activity monitoring: Apply a calibration factor or correction equation based on validation studies. One study of a nutritional intake wristband found a regression equation of Y=-0.3401X+1963, indicating a tendency to overestimate lower calorie intake and underestimate higher intake [11].
- For high-intensity or variable-intensity protocols: Use device data as a relative measure rather than an absolute value, focusing on intra-participant changes over time.
- For all studies: Clearly report the specific wearable device models, firmware versions, and the algorithms they use in your methodology, as these factors significantly impact results [22] [25].
Guide 2: Troubleshooting Heart Rate Measurement Variability
Reported Issue: Inconsistent heart rate data across different activity types or participant demographics.
Investigation Procedure:
- Identify Activity Context: Determine if inaccuracies occur during rest, steady-state exercise, or activities involving cyclical arm motion (e.g., running, cycling). Heart rate accuracy is generally high at rest but can degrade during activity [26]. The mean absolute error (MAE) during activity can be 30% higher than during rest [26].
- Assess Participant Factors: While one systematic review found no statistically significant difference in heart rate accuracy across skin tones [26], other studies note that factors like skin tone and BMI can affect measurements [24].
- Inspect for Motion Artifacts: Analyze accelerometer data concurrent with PPG data. Motion artifacts from sensor displacement or cyclical wrist motions can cause false beats or signal crossover, where the device locks onto the motion frequency instead of the heart rate [26].
Resolution Steps:
- For activities with high motion artifact risk: Use a chest-strap ECG monitor as a gold standard for validation in a subset of participants [26].
- For general use: Note that most consumer wearables measure heart rate with an error rate of less than 5% and are reasonably accurate for resting and prolonged elevated heart rate [24]. They can be reliably used for heart rate measurement in non-medical settings [24].
Frequently Asked Questions (FAQs)
FAQ 1: For which biometric measures are consumer wearable devices considered acceptably accurate for research purposes?
Consumer wearables have demonstrated good accuracy for several key metrics, though error rates vary.
- Heart Rate: Generally high accuracy. Error rates are typically below 5% [24], with a mean bias of approximately ± 3% [22]. For specific conditions like atrial fibrillation detection, sensitivity can be as high as 94.2% and specificity 95.3% [27].
- Step Count: Accuracy is generally high, with devices showing a tendency to slightly underestimate steps. Mean Absolute Percentage Errors (MAPE) range from -9% to 12% [22] [23].
- Distance: Can be reliably measured, with MAPE approximately 0.10 according to one multi-device study [28].
- Sleep Duration: Measurement is possible but often overestimates total sleep time. Overestimation is typically >10%, and errors for sleep onset latency can range from 12% to 180% compared to polysomnography [23].
FAQ 2: Which metrics have the poorest accuracy and should be interpreted with caution?
Energy Expenditure (Calories Burned) and Energy Intake are the least accurate metrics [11] [14] [24].
- Energy Expenditure: Error is significant and variable. One umbrella review found a mean bias of -3 kcal per minute (-3%), with error margins ranging from -21.27% to 14.76% [22]. Another study found the most accurate device was off by an average of 27% [24].
- Energy Intake (via automated tracking): One study on a dedicated wristband found high variability, with a mean bias of -105 kcal/day and wide 95% limits of agreement between -1400 and 1189 kcal/day. The device tended to overestimate lower calorie intake and underestimate higher intake [11].
FAQ 3: How does the type of physical activity affect the accuracy of wearable device data?
Activity type and intensity are major factors influencing accuracy [28] [26].
- Heart Rate: Accuracy is highest during rest and prolonged, steady elevated heart rate. It decreases during physical activity, with the mean absolute error being 30% higher during activity than at rest [26]. Activities causing cyclical wrist motion (e.g., running, cycling) can introduce "signal crossover" errors [26].
- Energy Expenditure: The algorithms used by wearables have varying performance across different activity states (e.g., walking, running, cycling), leading to significant variations in measurement accuracy for the same indicator [28].
FAQ 4: What are the primary sources of inaccuracy in wearable optical heart rate sensors?
The main sources of inaccuracy are [26] [25]:
- Motion Artifacts: Sensor displacement or skin deformation during movement.
- Signal Crossover: The sensor mistakenly locking onto the frequency of repetitive body motion instead of the heart pulse.
- Device-Specific Factors: Variations in sensor quality, proprietary algorithms, and device placement.
FAQ 5: What methodological challenges exist when using wearable devices in scientific research?
Key challenges include [22] [29] [23]:
- Rapid Obsolescence: The academic validation cycle is slower than the commercial release cycle of new devices and software updates. Less than 5% of released consumer wearables have been validated for the physiological signals they claim to measure [23].
- Lack of Standardization: Inconsistent validation methodologies across studies make cross-comparison of results difficult.
- Data Quality Issues: Wearables can produce noisy or incomplete data, and data loss can occur [29].
- Proprietary Algorithms: The "black box" nature of algorithms used to compute metrics like energy expenditure makes it difficult to understand or adjust for errors [24].
Table 1: Summary of Wearable Device Accuracy by Biometric Metric
| Biometric Metric | Reported Accuracy / Error | Key Influencing Factors |
|---|---|---|
| Heart Rate | Mean bias: ± 3% [22]Error rate: < 5% for most devices [24] | Activity type & intensity [26], specific device model [26] |
| Energy Expenditure | Error range: -21.27% to 14.76% [22]Most accurate device off by 27% on average [24] | Activity intensity, individual user factors (fitness, BMI) [24], device algorithm [24] |
| Step Count | MAPE range: -9% to 12% (generally underestimates) [22] [23] | - |
| Sleep Duration | Overestimation typically >10% [23] | - |
| Energy Intake | Mean bias: -105 kcal/day95% Limits of Agreement: -1400 to 1189 kcal/day [11] | Transient signal loss, device algorithm tending to overestimate low intake/underestimate high intake [11] |
Table 2: Key "Research Reagent Solutions" for Experimental Validation
| Item | Function in Experimental Protocol |
|---|---|
| Indirect Calorimetry Unit | Gold standard for measuring energy expenditure (calories burned) via oxygen consumption and carbon dioxide production analysis [24]. |
| Electrocardiogram (ECG) | Gold standard for heart rate measurement, used as a reference to validate optical heart rate sensors in wearables [26] [24]. |
| Actigraphy System | Research-grade system for measuring sleep and wake patterns, used as a criterion for validating consumer sleep tracking [23]. |
| Polysomnography (PSG) | Comprehensive gold standard for sleep measurement, including brain waves, eye movements, and muscle activity, used in clinical sleep studies [23]. |
| Calibrated Study Meals | Precisely prepared meals with known energy and macronutrient content, used to validate automated dietary intake estimation of wearables [11]. |
Experimental Protocol Detail
Protocol 1: Validation of Energy Expenditure Estimation During Controlled Physical Activities
This protocol is designed to assess the accuracy of wearable devices in estimating energy expenditure across different activity types and intensities, a key factor in understanding overall energy balance.
- Objective: To evaluate the validity of energy expenditure estimates from wearable devices against a gold standard measure under various seminatural activity states.
- Criterion Measure: Indirect calorimetry (portable metabolic unit) measuring oxygen consumption (VO₂) and carbon dioxide production (VCO₂) for calculating energy expenditure [24].
- Experimental Workflow:
- Participant Preparation: Fit participant with the wearable device(s) under investigation and the portable metabolic unit.
- Baseline Measurement: Participant rests in a seated position for a set period (e.g., 10-15 minutes) to establish baseline energy expenditure.
- Activity Trials: Participant performs a series of activities, each for a predetermined duration (e.g., 5-10 minutes). Typical activities include:
- Treadmill walking at a slow pace
- Treadmill running at a moderate pace
- Cycling on a stationary bicycle
- Data Synchronization: Timestamps from the wearable device and the metabolic unit are synchronized post-test.
- Data Analysis: Energy expenditure values from the wearable device are compared to those from the metabolic unit at concurrent time points. Statistical analysis includes calculating Mean Absolute Percentage Error (MAPE), absolute bias, and limits of agreement [11] [28].
Experimental Workflow for Energy Expenditure Validation
Protocol 2: Investigating Heart Rate Sensor Accuracy Across Skin Tones and Activity
This protocol systematically explores potential sources of inaccuracy in optical heart rate sensors, including the effect of activity type and participant demographics.
- Objective: To determine the accuracy of wearable optical heart rate sensors across the full range of skin tones and under different activity conditions.
- Criterion Measure: Electrocardiogram (ECG) chest patch, recorded concurrently with wearable data [26].
- Experimental Workflow:
- Participant Screening & Consent: Recruit a diverse participant group equally representing all skin tones (e.g., using the Fitzpatrick scale). Obtain informed consent.
- Device Fitting: Participant is fitted with the ECG patch and multiple wearable devices on the wrist.
- Protocol Rounds: Participants complete a structured protocol multiple times to test all devices. The protocol for each round includes:
- Seated Rest: 4 minutes to establish baseline heart rate.
- Paced Deep Breathing: 1 minute to introduce mild parasympathetic activation.
- Physical Activity: 5 minutes of walking to increase heart rate.
- Seated Rest (Washout): ~2 minutes to return to near baseline.
- Typing Task: 1 minute to simulate low-intensity, non-cyclic movement.
- Data Analysis: Heart rate data from wearables is compared to the ECG gold standard. Analysis focuses on Mean Absolute Error (MAE) and directional error. Mixed effects statistical models are used to examine the impact of device, activity condition, and skin tone [26].
Heart Rate Validation Protocol Across Activities
Under the Hood: Technological Drivers of Error and Emerging Solutions
This technical support guide addresses a critical challenge in digital health research: the systematic overestimation of energy expenditure (EE) by wrist-worn wearables, particularly in contexts of low calorie intake or specific population groups. These inaccuracies primarily stem from the technological limitations of photoplethysmography (PPG) and accelerometry sensors, and the algorithms that interpret their data. The following FAQs, troubleshooting guides, and experimental protocols are designed to help researchers identify, understand, and mitigate these errors in their studies, thereby improving the validity of data collected for clinical research and drug development.
FAQs: Core Concepts and Limitations
1. What are the primary sources of inaccuracy in wearable-based EE estimation? Inaccuracies in EE estimation arise from a combination of sensor limitations and algorithmic shortcomings. The key sources include:
- Motion Artifacts: Physical movement can corrupt the PPG signal, leading to inaccurate heart rate (HR) data, a primary input for EE algorithms. Motion can cause the PPG sensor to lock onto the frequency of repetitive movements (like walking) instead of the cardiac cycle, a phenomenon known as "signal crossover" [26].
- Algorithmic Limitations: Many proprietary algorithms are not transparently validated and are often developed on populations not representative of all end-users (e.g., they may be less accurate for individuals with obesity) [30]. They may also fail to account for different types of physical activity or bodily posture [10].
- Sensor Inherent Error: PPG-based HR measurements are generally less accurate than electrocardiography (ECG). One study found the mean absolute error (MAE) of PPG-based wearables can range significantly, with an average MAE of 9.5 bpm at rest and higher errors during activity [26].
- Device-Specific Performance: The accuracy of EE estimation varies substantially between different manufacturers and models, as they use different sensor combinations and proprietary algorithms [10] [26].
2. How does device grade (consumer vs. research) guarantee accuracy? A research-grade designation does not automatically guarantee superior accuracy. One validation study found that a research-grade device did not outperform consumer-grade devices in laboratory conditions and showed low agreement with ECG in ambulatory-like conditions involving movement [31]. The term "research-grade" is a self-designation and does not imply adherence to universal validation standards. Performance must be validated for each specific use case and population.
3. Why are my wearable's EE estimates less accurate for participants with obesity? Individuals with obesity exhibit known differences in walking gait, postural control, and resting energy expenditure [30]. Many existing EE algorithms were primarily developed and validated in non-obese populations, leading to systematic errors when applied to individuals with obesity. Hip-worn devices can be further affected by biomechanical differences and device tilt angle, though wrist-worn devices also face challenges and require specifically tailored algorithms for this population [30].
4. How does low calorie intake or resting states exacerbate overestimation? During periods of low calorie intake or sedentary behavior, the absolute energy expenditure is low. In these contexts, the relative impact of any systematic error in the device's algorithm or sensors becomes magnified. For instance, an absolute error of 20-30 kcal might represent a small percentage of error during vigorous exercise but a very large percentage during rest or low-intensity activities, leading to significant overestimation of total daily energy expenditure [10].
Troubleshooting Guides
Problem 1: High Variance in EE Data During Ambulatory Studies
Potential Cause: Motion artifacts corrupting PPG signals and over-reliance on accelerometry data that doesn't capture the full picture of energy cost.
Solution Steps:
- Implement a Signal Qualifier: Use a signal quality indicator to filter out periods of poor PPG signal. One study in cardiac patients used a qualifier that improved heartbeat detection accuracy within 100 ms to 98.2% (from 94.6%) [32]. Discard data segments with low-quality signals from your analysis.
- Fuse Sensor Data Cautiously: Leverage device agnostic approaches that use raw accelerometry and HR data, as this has been shown to predict physical activity energy expenditure (PAEE) comparably to research-grade devices in some models [33]. However, be aware that the primary source (PPG) may already be flawed.
- Segment Activity Types: Analyze EE data by specific activity type (e.g., walking, sitting, standing) rather than aggregating all data. Accuracy can vary significantly across different activities [10] [26].
Problem 2: Systematic Overestimation of EE in Specific Populations
Potential Cause: The algorithms used by the wearable device are not validated for your study population (e.g., individuals with obesity, specific ethnic groups, or clinical patients).
Solution Steps:
- Validate Against a Criterion in Your Cohort: Before main data collection, conduct a sub-study validating the wearable device against a criterion measure (like indirect calorimetry) within your specific population [10] [30].
- Use Population-Specific Algorithms: If possible, develop or apply machine learning models trained on your target population. One study developed a new BMI-inclusive algorithm that provided more reliable EE measures for people with obesity compared to 11 other algorithms [30].
- Report Device and Algorithm Details: Always report the specific device model, firmware version, and the name of the algorithm used (e.g., "Kerr et al.'s method" [30]) in your methods section to ensure reproducibility.
Problem 3: Poor Heart Rate Data Quality Affecting EE Estimates
Potential Cause: The PPG sensor is failing to get a clean signal due to motion, fit, or skin properties.
Solution Steps:
- Ensure Proper Fit: Verify the device is snug but comfortable on the wrist. The sensor should maintain consistent contact with the skin.
- Optimize Placement: Follow the manufacturer's instructions for placement. Some studies randomize the wrist (dominant/non-dominant) and specific position to control for placement variables [10].
- Contextualize with Activity Logs: Correlate periods of high HR error with activity logs. Error is typically higher during physical activity than at rest [26]. Consider using a chest-strap ECG as a gold-standard reference in a subset of participants to quantify the device-specific error in your study setting [31].
Experimental Protocols for Validation
To ensure the reliability of your data, validating wearable devices against gold-standard measures within your specific experimental setup is crucial.
Protocol 1: Validating EE Estimation in Laboratory Conditions
This protocol is designed to benchmark a wearable device against indirect calorimetry under controlled activity intensities.
1. Criterion Measure:
- Instrument: COSMED K5 or similar portable gas analysis system [10] [30].
- Calibration: Warm up the device for at least 15 minutes and calibrate with high-grade calibration gases and a 3 L calibration syringe before each session [10].
2. Index Device(s):
- Test Devices: Commercial smartwatches (e.g., Apple Watch, Garmin, Fitbit) or research-grade wearables.
- Initialization: Input participant height, weight, gender, and date of birth into the watch settings as required [10].
- Placement: Place watches on the wrist according to the manufacturer's instructions. To counterbalance, use a randomization list to assign which watch is on which wrist for different participants [10].
3. Participant Preparation:
- Instruct participants to fast for at least 6 hours (water only), avoid caffeine and stimulants, and abstain from vigorous activity and alcohol for 24 hours prior [10].
- Measure anthropometrics (height, weight, body composition) prior to testing.
4. Experimental Protocol:
- Activities: Have participants perform a series of activities of varying intensities. A typical protocol may include:
- Data Collection: Simultaneously collect data from the criterion and index devices throughout the protocol.
5. Data Analysis:
- Calculate metrics like Mean Absolute Percentage Error (MAPE), Limits of Agreement (LoA) via Bland-Altman analysis, and Intraclass Correlation Coefficient (ICC) to compare the wearable's EE estimates to the criterion measure [10].
Experimental Workflow for EE Validation
Protocol 2: Evaluating Sensor Performance Across Skin Tones
This protocol systematically assesses the impact of skin tone on PPG accuracy, a critical factor for inclusive study design.
1. Criterion Measure:
- Instrument: ECG patch (e.g., Bittium Faros 180) as the gold standard for heart rate [26].
2. Index Device(s):
- Test Devices: A selection of consumer- and research-grade PPG wearables.
3. Participant Recruitment:
- Recruit a cohort of participants that equally represents all skin tone types according to the Fitzpatrick (FP) scale [26].
4. Experimental Protocol:
- Conditions: Have each participant complete a protocol while wearing the ECG and multiple wearables (in sequential rounds to avoid interference). The protocol should include:
- Seated rest (baseline)
- Paced deep breathing
- Physical activity (e.g., walking to increase HR)
- Seated rest (recovery)
- A non-physical stressor (e.g., typing task, arithmetic task) [26].
- Data Collection: Record HR and PPG data from all devices throughout.
5. Data Analysis:
- Calculate Mean Absolute Error (MAE) and Mean Directional Error (MDE) for HR measurements for each device, stratified by Fitzpatrick skin tone group and activity condition [26].
- Use mixed effects statistical models to examine the relationship between error and skin tone, device, and activity condition.
Table 1: Accuracy of Smartwatch EE Estimation During Outdoor Ambulation (vs. Indirect Calorimetry) [10]
| Device | Activity | Mean Absolute Percentage Error (MAPE) | Limits of Agreement (LoA) in kcal | Intraclass Correlation Coefficient (ICC) |
|---|---|---|---|---|
| Apple Watch Series 6 | Walking (6 km/h) | 19.8% | 44.1 | 0.821 |
| Running (10 km/h) | 24.4% | 62.8 | 0.741 | |
| Garmin Fenix 6 | Walking (6 km/h) | 32.0% | 150.1 | 0.216 |
| Running (10 km/h) | 21.8% | 89.4 | 0.594 | |
| Huawei Watch GT 2e | Walking (6 km/h) | 9.9% | 48.6 | 0.760 |
| Running (10 km/h) | 11.9% | 65.6 | 0.698 |
Table 2: PPG Heart Rate Accuracy Across Conditions (vs. ECG) [31] [26]
| Condition | Typical Mean Absolute Error (MAE) | Key Findings |
|---|---|---|
| Resting State | ~9.5 bpm (average across devices) [26] | Research-grade devices do not consistently outperform consumer-grade in lab settings [31]. |
| Physical Activity | ~30% higher error than at rest [26] | Accuracy deteriorates with motion; devices may lock onto movement frequency (signal crossover) [26]. |
| Across Skin Tones | No statistically significant difference in accuracy found [26] | Significant device-to-device differences and activity-type dependencies are larger drivers of error [26]. |
The Scientist's Toolkit: Key Research Reagents & Materials
Table 3: Essential Equipment for Validating Wearable Sensor Data
| Item | Function in Research | Example Products / Notes |
|---|---|---|
| Portable Metabolic Cart | Criterion Measure for EE. Provides breath-by-breath measurement of oxygen consumption (VO₂) and carbon dioxide production (VCO₂) to calculate Energy Expenditure via indirect calorimetry. | COSMED K5 [10] [30] |
| Ambulatory ECG Monitor | Criterion Measure for Heart Rate. Provides gold-standard data for validating PPG-based heart rate and heart rate variability (HRV) from wearables. | Bittium Faros 180 [26], VU-AMS [31] |
| Research-Grade Accelerometer | Criterion for Motion Capture. Provides high-fidelity raw accelerometry data for activity classification and validating commercial device accelerometers. | ActiGraph GT9X [33] [30] |
| Body Composition Analyzer | Participant Characterization. Precisely measures body fat percentage and BMI, which are critical covariates for EE algorithm development and validation. | InBody 720 [10] |
| Wearable Camera | Ground Truth for Behavioral Context. Provides visual confirmation of activity type and posture in free-living validation studies, enabling accurate annotation of sensor data. | Used in free-living study protocols [30] |
Signal Crossover in PPG Sensors During Motion
Frequently Asked Questions (FAQ)
Q1: What is the primary evidence that wearable devices overestimate calorie intake in low intake scenarios?
A1: A 2020 validation study of a wearable nutrition tracking wristband provides direct evidence. The research employed a reference method where all meals were prepared, calibrated, and served at a campus dining facility, with energy and macronutrient intake precisely recorded. The Bland-Altman analysis revealed a mean bias of -105 kcal/day, indicating a tendency to overestimate at lower calorie intake levels and underestimate at higher intakes. The 95% limits of agreement were very wide (between -1400 and 1189 kcal/day), demonstrating high variability and significant potential for overestimation in research contexts focusing on low energy intake [11].
Q2: Why are proprietary algorithms a source of bias in nutritional wearables research?
A2: Proprietary algorithms introduce bias through several mechanisms, primarily due to a lack of transparency and validation in key areas:
- Lack of Transparency: The algorithms that convert sensor data into calorie expenditure estimates are "black boxes," meaning their internal logic and validation metrics are not available for scientific scrutiny [30].
- Exclusion of Diverse Populations: Many algorithms are developed and validated on homogenous populations (e.g., young, healthy, normal BMI), leading to systematic errors when applied to groups with different physiologies, such as individuals with obesity [34] [30]. A 2025 study specifically highlighted the need for BMI-inclusive algorithms to ensure reliability across diverse body types [30].
- Inadequate Real-World Validation: The complex process of transforming food into bioavailable energy is affected by interindividual differences in metabolism, gastrointestinal health, and meal composition. Proprietary algorithms often fail to account for this complexity, leading to discrepancies between measured intake and actual bioavailable energy [11].
Q3: What are the practical consequences of this algorithmic bias for clinical or research settings?
A3: The consequences are significant and can compromise research integrity and participant safety.
- Inaccurate Data: Reliance on biased data can lead to flawed conclusions in studies investigating the efficacy of nutritional or pharmaceutical interventions.
- Health Risks: Systematic overestimation of calorie intake could lead to inappropriate dietary recommendations, potentially exacerbating conditions the research aims to treat. Furthermore, inaccurate heart rate data (a key input for calorie algorithms) can mislead participants about their exercise intensity, potentially jeopardizing their safety during physical activity [35].
- Reinforcement of Health Disparities: If algorithms are not validated across diverse racial, ethnic, and body composition groups, the research outcomes can perpetuate existing health disparities and provide ineffective solutions for underrepresented populations [34].
Troubleshooting Guides
Guide 1: How to Identify and Mitigate Algorithmic Bias in Your Wearables Data
Follow this workflow to diagnose and address potential bias from proprietary algorithms in your research data.
Procedural Steps:
- Check Device Validation Literature: Before designing your study, investigate peer-reviewed publications that have independently validated the specific wearable device you plan to use. Look for studies that report metrics like Mean Absolute Percentage Error (MAPE) and Bland-Altman limits of agreement against a gold standard. For example, one study found a consumer tracker had a MAPE of 29.3% for calorie expenditure versus a metabolic analyzer [36].
- Conduct a Criterion Validity Check (Sub-Steps 2A-2C):
- 2A. Collect Gold-Standard Data: In a controlled sub-study, measure your outcome variable (e.g., energy expenditure) using an accepted gold-standard method, such as indirect calorimetry (e.g., PNOĒ metabolic analyzer) [36].
- 2B. Collect Device Data Simultaneously: Have participants wear the consumer device while gold-standard data is collected.
- 2C. Perform Bland-Altman Analysis: This statistical method plots the difference between the two measurements against their average. It helps identify systematic bias (e.g., consistent overestimation at low levels) and the limits of agreement, quantifying the expected error range [11].
- Analyze Error Patterns: Examine if the device's error is correlated with participant demographics (age, sex) or activity parameters (speed, intensity). Research shows that factors like speed can have a large effect on the accuracy of some devices [36].
- Stratify Data by Demographic Groups: Separate your data by key demographic variables such as BMI, sex, and skin tone. Analyze the device's accuracy metrics (e.g., MAPE, bias) for each group to check for differential performance, a key indicator of algorithmic bias [34] [30].
- Document Algorithm Limitations: In your research publications, transparently report the known limitations and potential biases of the proprietary algorithms used, citing independent validation studies.
- Implement Statistical Corrections: If a consistent bias pattern is found (e.g., systematic overestimation), you may develop and apply a calibration or correction factor to your dataset, derived from your validity check. Clearly state this procedure in your methods section.
Guide 2: Validating a Wearable Device for Low Calorie Intake/Expenditure Scenarios
This guide provides a detailed methodology to assess a wearable's accuracy specifically in the context of low energy intake, a common scenario in dietary intervention studies.
Experimental Protocol
- Objective: To evaluate the accuracy and bias of a wrist-worn wearable device in estimating energy expenditure under conditions of low calorie intake.
- Design: A cross-sectional laboratory study with a criterion validity component.
- Participants: Recruit a diverse sample that reflects the target population of your broader research, ensuring inclusion of various BMIs, ages, and sexes [34] [30].
Key Research Reagent Solutions
| Item Name | Function in Experiment | Specification Notes |
|---|---|---|
| Portable Metabolic Analyzer (e.g., PNOĒ) | Serves as the criterion measure for energy expenditure (calorie burn) by analyzing respiratory gases [36]. | Ensure it is calibrated according to manufacturer specifications before each testing session. |
| Research-Grade Accelerometer (e.g., ActiGraph wGT3X-BT) | Provides an objective, research-grade measure of physical activity and movement for comparison [36] [30]. | Sample rate should be set consistently (e.g., 30-100 Hz). Placement (hip vs. wrist) should be documented. |
| Fitness Tracker (Device Under Test) | The consumer-grade device whose algorithmic outputs are being validated. | Ensure it is fully charged and set to the correct data recording mode (e.g., sports mode for highest sampling rate) [36]. |
| Treadmill | Provides a controlled environment for administering standardized physical activity challenges at varying intensities [36]. | Must be regularly calibrated for speed and incline accuracy. |
Procedure:
- Participant Preparation: Fit participants with the wearable device, the research-grade accelerometer, and the metabolic analyzer according to standardized protocols [36].
- Testing Protocol: Participants will perform a series of activities on a treadmill. The protocol should include:
- Data Collection: For each stage, simultaneously record:
- Energy expenditure from the metabolic analyzer (criterion).
- Calorie expenditure, heart rate, and step count from the wearable device.
- Step count from the research-grade accelerometer.
- Manual step count (hand tally) as a secondary criterion for steps [36].
- Data Analysis:
- Calculate Mean Absolute Percentage Error (MAPE) for the wearable's calorie estimate relative to the metabolic analyzer. A MAPE ≤ 3% is considered clinically irrelevant, but values can be much higher (e.g., ~30%) [36].
- Perform Bland-Altman analysis to identify any systematic bias, especially at lower levels of energy expenditure [11].
- Use Multivariate Analysis of Variance (MANCOVA) to assess the effect of factors like speed, sex, age, and BMI on the tracker's accuracy [36].
The table below summarizes potential findings and their interpretations based on prior research:
| Observed Result | Possible Interpretation | Action for Researcher |
|---|---|---|
| High MAPE (e.g., >20%) for calorie expenditure [36] | The device's proprietary algorithm has low accuracy for energy estimation. | Use device data with extreme caution; consider it a rough proxy rather than a precise measure. |
| Negative Mean Bias in Bland-Altman plot at low intensity [11] | The device systematically overestimates calorie burn during low-intensity activities, consistent with the core thesis. | Apply a calibration factor for low-intensity data or exclude low-intensity data from analysis. |
| Large 95% Limits of Agreement (e.g., ± 1400 kcal/day) [11] | High variability makes the device unreliable for measuring individual-level intake/expenditure. | The device may only be suitable for analyzing group-level trends, not individual data. |
| Significant effect of BMI on MAPE [30] | The algorithm contains algorithmic bias and performs poorly for individuals with obesity. | Stratify results by BMI or seek a device with a validated, BMI-inclusive algorithm. |
Troubleshooting Guides
Image and Data Capture Issues
Problem: Incomplete or missing food images leading to data loss.
- Potential Cause: Fixed camera orientation and the use of rectangular image sensors can crop out portions of the scene, especially with wide-angle lenses [37]. Body shape, height, and table height variations can cause misalignment [37].
- Solution:
- Consider camera systems that generate circular images to utilize the full circular field of view of the lens, reducing wasted area from 38.9% (4:3 ratio) or 45.6% (16:9 ratio) to near zero [37].
- Implement a mechanical design that allows for camera orientation adjustment to adapt to different wearers [37].
- For chest-worn devices like the eButton, ensure secure placement and check the initial images to verify the field of view adequately captures the eating area [38].
Problem: Poor image quality under low-light conditions, common in free-living settings.
- Potential Cause: Wearable cameras automatically capture images in varying lighting. Low-light conditions in household settings can result in noisy, blurry images that hinder food identification and analysis [39].
- Solution:
- While hardware solutions may be limited, inform participants to eat in well-lit areas when possible to improve image quality for analysis.
- Leverage advanced AI pipelines like EgoDiet, which are specifically optimized to handle challenges such as segmenting food items and containers under suboptimal lighting [39].
Problem: Device signal loss or sensor drop-off during data collection.
- Potential Cause: Transient signal loss from sensor technology or physical issues like the device becoming loose or falling off [11] [38].
- Solution:
Algorithm and Data Processing Issues
Problem: AI model fails to accurately identify culturally unique or mixed dishes.
- Potential Cause: Many AI models are trained on limited food databases that may not represent the diverse culinary practices of all populations, leading to high error rates for specific ethnic cuisines [39] [11].
- Solution:
- Utilize AI systems like EgoDiet:SegNet, which are explicitly optimized for the segmentation of food items and containers in specific cuisines, such as African foods [39].
- For research studies, plan for a manual verification and correction step by trained nutritionists to identify and rectify misclassified foods [40].
Problem: Systematic overestimation of low energy intake and underestimation of high energy intake.
- Potential Cause: This is a known calibration issue with some sensor-based technologies. A study on the GoBe2 wristband found its regression equation was significant, indicating a tendency to overestimate lower calorie intake and underestimate higher intake [11].
- Solution:
- In your analysis, apply a bias-correction formula based on validation studies. For example, the regression equation from one study was Y = -0.3401X + 1963, which can be used to adjust raw device outputs [11].
- Cross-validate device readings with a reference method, such as calibrated study meals, to establish a population- or device-specific calibration curve [11].
Participant and Usability Issues
Problem: Participant concerns about privacy due to continuous image capture.
- Potential Cause: Wearable cameras may passively capture sensitive or personally identifiable information in the background, leading to privacy concerns that affect recruitment and adherence [38] [40].
- Solution:
- Implement strict data handling protocols, including secure storage and the use of automated AI processing to minimize human viewing of images [40].
- Clearly communicate these privacy safeguards during the informed consent process [38].
- Consider privacy-preserving computer vision techniques that extract only relevant features (e.g., portion size, food type) without storing the raw images.
Problem: Low participant adherence to device-wearing protocol.
- Potential Cause: The burden of wearing multiple devices, discomfort, and technical difficulties can lead to non-compliance [38] [40].
- Solution:
- Provide structured support from healthcare providers or research staff to help with device setup and troubleshooting [38].
- Choose devices with a low form factor and high comfort, such as the lightweight eButton [40].
- Gather qualitative feedback on user experience to identify and address specific barriers, which can include issues like skin sensitivity from adhesives or difficulty positioning cameras [38].
Frequently Asked Questions (FAQs)
FAQ: How accurate are AI and wearable cameras compared to traditional dietary assessment methods? Studies have shown that these novel methods can be competitive with or even outperform traditional methods. The EgoDiet system demonstrated a Mean Absolute Percentage Error (MAPE) of 28.0% for portion size estimation in a study in Ghana, which was lower than the 32.5% MAPE observed with the traditional 24-Hour Dietary Recall (24HR) [39]. Another study using the eButton and AI analysis found it could identify many food items that participants failed to record via self-report [40].
FAQ: What are the main technical challenges in passive dietary monitoring? The primary challenges are:
- Data Loss: Ensuring the camera captures a complete view of all food items, which is influenced by hardware design [37].
- Food Identification: Accurately recognizing diverse, mixed, or culturally unique dishes from images, especially with low-quality photos [39] [40].
- Portion Size Estimation: Converting 2D images into accurate 3D volume and weight estimates without standardized reference objects in the frame [39].
- Computational Burden: Automatically processing tens of thousands of images to find the small subset that contains eating events [40].
FAQ: Can these methods capture the actual intake (food consumed) or just the initial portion? This is a key differentiator. Many active methods (e.g., taking a photo with a phone) only capture the initial portion. However, passive wearable cameras like the eButton continuously capture images, allowing them to record both the "before" and "after" states of a meal. This enables the system to estimate the consumed portion size, which is critical for accurate nutrient intake assessment [39].
FAQ: How do you validate the accuracy of a passive dietary monitoring system in a free-living population? The most robust validation involves comparing the system's output against a high-quality reference method. This can include:
- Calibrated Study Meals: Where the energy and nutrient content of all foods served are precisely known and consumption is directly observed by researchers [11].
- Doubly Labeled Water (DLW): Considered a gold standard for measuring total energy expenditure, which can be used to validate estimated energy intake [40].
FAQ: What wearable camera positions are most effective? The two most common and effective positions are:
- Eye-level: Using a device like the Automatic Ingestion Monitor (AIM) clipped to eyeglasses [39].
- Chest-level: Using a device like the eButton pinned onto the shirt [39] [38]. Each position has advantages and limitations regarding field of view and social acceptability, and the optimal choice may depend on the specific research setting and population.
Key Experimental Validation Protocol
This protocol is adapted from studies validating wearable sensors against reference methods [11] [38].
Objective: To validate the accuracy of a wearable device (e.g., eButton, AIM, or sensor wristband) for estimating energy and nutrient intake in a free-living population.
Participants:
- Recruit a sample (e.g., N=25) of free-living adults.
- Apply exclusion criteria for conditions or medications that significantly alter metabolism or digestion [11].
Reference Method:
- Collaborate with a metabolic kitchen or dining facility to prepare and serve all meals for a specified period (e.g., 14 days).
- Use standardized weighing scales to measure the precise weight of each food item served to each participant.
- Researchers directly observe and record any uneaten food to calculate actual consumption.
- All meals are analyzed using a gold-standard food composition database (e.g., USDA FNDDS) to establish "true" intake [11].
Test Method:
- Participants wear the wearable device(s) consistently throughout the test period.
- For cameras, ensure they are activated during all eating occasions.
- Data (images, sensor signals) are processed by the AI pipeline to estimate daily nutritional intake.
Data Analysis:
- Use Bland-Altman analysis to assess the agreement between the reference method and the test method, calculating the mean bias and 95% limits of agreement [11].
- Perform regression analysis to identify any systematic biases (e.g., overestimation at low intakes) [11].
- Calculate metrics like Mean Absolute Percentage Error (MAPE) for portion size estimation [39].
Table 1. Performance comparison of AI and wearable cameras against traditional dietary assessment methods.
| Method | Study Context | Performance Metric | Result | Key Finding |
|---|---|---|---|---|
| EgoDiet (AI + Wearable Cameras) | London (Ghanaian/Kenyan population) | Mean Absolute Percentage Error (MAPE) | 31.9% [39] | Outperformed dietitians' estimates (40.1% MAPE). |
| EgoDiet (AI + Wearable Cameras) | Ghana (African population) | Mean Absolute Percentage Error (MAPE) | 28.0% [39] | Showed improved accuracy over 24HR (32.5% MAPE). |
| GoBe2 Wristband | Free-living adults | Mean Bias (Bland-Altman) | -105 kcal/day [11] | Showed systematic error: overestimation at low intake and underestimation at high intake. |
| Remote Food Photography Method (RFPM) | Free-living adults | Underestimate vs. Doubly Labeled Water | 3.7% (152 kcal/day) [40] | Demonstrated accuracy comparable to the best self-reported methods. |
Research Workflow and Signaling Pathway
Dietary Assessment Workflow
Figure 1: This diagram illustrates the end-to-end workflow for passive dietary assessment using AI and wearable cameras, from data capture to final report generation.
Technical Pipeline for Portion Estimation
Figure 2: This diagram details the AI pipeline for converting a raw image into a portion size estimate, showing the key technical modules and features involved.
The Scientist's Toolkit: Research Reagent Solutions
Table 2. Essential hardware, software, and methodologies for research in AI-driven passive dietary monitoring.
| Tool / Reagent | Type | Function & Application in Research |
|---|---|---|
| eButton | Hardware | A chest-pinned wearable camera that passively captures images of meals. Used for feasibility studies in free-living conditions to collect egocentric dietary data [39] [38]. |
| Automatic Ingestion Monitor (AIM) | Hardware | An eye-level wearable camera typically attached to eyeglasses. Used to capture a gaze-aligned view of eating episodes [39]. |
| EgoDiet Pipeline | Software | A comprehensive AI pipeline for segmenting food, estimating container depth and orientation, and ultimately estimating portion size from wearable camera images [39]. |
| Continuous Glucose Monitor (CGM) | Hardware | A biosensor that measures interstitial glucose levels. Used alongside wearable cameras to correlate dietary intake with physiological response in metabolic studies [38]. |
| Doubly Labeled Water (DLW) | Methodology | A gold-standard biomarker for measuring total energy expenditure in free-living individuals. Serves as a reference method for validating energy intake estimates from new dietary assessment tools [40]. |
| Calibrated Study Meals | Methodology | Precisely prepared and weighed meals where nutrient content is known. Serves as a high-quality reference method for validating the accuracy of passive monitoring systems in controlled or free-living study designs [11]. |
Integrating Multimodal Data Streams to Improve Caloric Burn Predictions
Frequently Asked Questions
Q1: Why do wearable devices commonly overestimate calorie burn at lower activity levels? This systematic error often stems from the algorithms' heavy reliance on motion sensors (accelerometers) for estimating Non-Exercise Activity Thermogenesis (NEAT) and Exercise Activity Thermogenesis (EAT). At lower intensities, movement can be sporadic and difficult for accelerometers to capture accurately, leading to a reliance on less-personalized Basal Metabolic Rate (BMR) calculations. One validation study found that the overestimation follows a predictable pattern, with a mean bias of -105 kcal/day and a regression equation of Y = -0.3401X + 1963, confirming the tendency to overestimate for lower calorie intake and underestimate for higher intake [11].
Q2: What are the primary sources of error when integrating heart rate and accelerometer data? The main sources of error are the weak individual relationship each metric has with energy expenditure. The relationship between heart rate and energy expenditure varies significantly between individuals due to differences in fitness, resting heart rate, and stress reactivity [41]. Similarly, accelerometry-based devices often produce meaningful errors that differ in magnitude depending on the type of physical activity being performed [41]. While combining these data streams produces better estimates than either alone, the underlying technologies lack a 1:1 relationship with true caloric burn [41].
Q3: How can researchers validate the caloric burn predictions of a new multi-model system? A robust method involves developing a reference measurement in a controlled environment. One protocol suggests [11]:
- Collaborate with a metabolic kitchen or dining facility to prepare and serve calibrated study meals.
- Record the precise energy and macronutrient intake of each participant under direct observation.
- Collect continuous data from the wearable device(s) and the multi-model system under test.
- Employ statistical comparisons like Bland-Altman analysis to quantify the mean bias and limits of agreement between the reference method and the test system's outputs (e.g., kcal/day) [11].
Q4: What is the typical accuracy range for commercial wearable devices in real-world conditions? Research consistently shows high variability. A large review of 22 brands and 36 devices found that calorie estimates were, on average, inaccurate by more than 30% [1]. While some devices achieved errors as low as 3% in lab settings, none met the reliability standard in day-to-day scenarios, with errors exceeding the 10% benchmark for all devices in real-world conditions [1].
Q5: Which machine learning models have shown superior performance in predicting caloric expenditure? In comparative studies, Neural Network models have demonstrated superior performance in predicting calorie burn, outperforming other models on metrics like MSE, RMSE, and R² score [42]. Other models that perform well in regression tasks include Random Forest and XGBoost, which have shown low and comparable Mean Absolute Error (MAE) on validation data [43].
Troubleshooting Guides
Guide 1: Addressing High Variance in Caloric Burn Predictions Across a Study Cohort
Problem: Your predictive model for caloric burn shows unacceptably high error rates across a diverse participant group.
Solution: Implement a multi-model machine learning approach that leverages a wider range of input features.
Investigation and Resolution Steps:
Verify Input Data Quality:
- Action: Check for missing or physiologically impossible values in key input streams (e.g., heart rate = 0 for extended periods, impossible height/weight).
- Tool: Use pandas in Python:
df.isnull().sum()anddf.describe(). - Outcome: Clean and impute missing data to ensure a robust dataset [42].
Expand Input Feature Set:
- Action: Move beyond basic metrics. Ensure your dataset includes age, gender, height, weight, workout intensity, and duration [42]. For greater personalization, consider heart rate variability and sleep pattern data from devices like Apple Watch and Fitbit [44].
- Outcome: A richer feature set allows the model to account for a greater degree of individual phenotypic diversity [11].
Select and Train Multiple Models:
- Action: Do not rely on a single algorithm. Train and compare a suite of models known for regression performance.
- Protocol: Split data into training and testing sets. Train models like Neural Networks, AdaBoost, Random Forest, and Gradient Boosting [42]. For code examples, see the
XGBRegressorandRandomForestRegressorimplementations in [43]. - Outcome: Identification of the best-performing model for your specific dataset, with Neural Networks often leading in performance [42].
Validate with a Robust Reference:
- Action: Compare your model's predictions against a high-fidelity reference method, such as doubly labeled water or controlled intake in a metabolic facility [11].
- Protocol: Use Bland-Altman analysis to quantify the mean bias and 95% limits of agreement between your system and the gold standard [11].
Guide 2: Mitigating Signal Loss from Wearable Sensors in Free-Living Studies
Problem: Transient signal loss from wearable sensors introduces gaps and noise in the continuous data stream, compromising prediction accuracy [11].
Solution: Implement a preprocessing and data fusion pipeline to handle missing data and improve signal reliability.
Investigation and Resolution Steps:
Identify Signal Loss Patterns:
- Action: Visualize raw sensor data (e.g., accelerometer, heart rate) over time to identify periods of dropout or invalid values (e.g., zeros during activity).
- Tool: Use matplotlib/seaborn in Python:
plt.plot(df['heart_rate']).
Apply Data Imputation Techniques:
- Action: For short gaps, use interpolation methods (e.g., linear or spline). For longer gaps, consider model-based imputation using correlated signals from other sensors (e.g., using accelerometer data to inform a heart rate gap model).
- Outcome: A continuous, gap-free data stream ready for feature extraction.
Fuse Multi-Sensor Data:
- Action: Combine data from heart rate monitors, accelerometers, and gyroscopes to create a more robust estimate of activity type and intensity. A model using both heart rate and accelerometry data is more accurate than either in isolation [41].
- Outcome: Improved classification of activity type (e.g., walking vs. cycling) and a more accurate estimation of energy expenditure for that activity.
Table 1: Common Machine Learning Models for Calorie Burn Prediction [42] [43]
| Model Name | Best For | Typical Performance (MAE in kcal) | Key Advantage |
|---|---|---|---|
| Neural Network | Complex, non-linear relationships in multi-modal data | Not Specified | Superior performance (MSE, RMSE, R²); handles high-dimensional data well [42]. |
| Random Forest | Avoiding overfitting; providing feature importance | ~10.45 [43] | High accuracy; robust to outliers and non-linear data [42] [43]. |
| XGBoost | High-performance gradient boosting | ~10.12 [43] | Speed and model performance; effective at capturing complex patterns [43]. |
| Linear Regression | Establishing a baseline model | ~18.01 [43] | Simplicity and interpretability [43]. |
Table 2: Accuracy of Wearable Devices in Estimating Energy Expenditure [41] [1]
| Device Type | Measurement Technology | Reported Accuracy (Real-World) | Key Limitation |
|---|---|---|---|
| Consumer Wearables | Heart Rate + Accelerometry | Average error >30%; individual study errors can exceed 50% [1]. | Underlying technologies have far from a 1:1 relationship with energy expenditure [41]. |
| Research-Grade Accelerometers | Accelerometry | Meaningful errors that vary by activity type and study [41]. | Accuracy varies substantially by activity type [41]. |
| Wristband Nutrition Sensor | Bioimpedance (fluid shifts) | Mean bias of -105 kcal/day (SD 660); 95% limits of agreement: -1400 to 1189 kcal/day [11]. | Prone to transient signal loss; overestimates low intake, underestimates high intake [11]. |
Experimental Protocols
Protocol 1: Validating a Caloric Burn Prediction Model Against a Reference Method
This protocol is adapted from a study validating a wearable nutrition tracker [11].
Participant Recruitment:
- Recruit free-living adult participants (e.g., n=25) who meet inclusion/exclusion criteria (no chronic disease, specific diets, etc.).
- Obtain informed consent and IRB approval.
Reference Method Setup:
- Collaborate with a metabolic kitchen to prepare and serve all study meals.
- Precisely calibrate the energy and macronutrient content of every meal.
- Have participants consume meals under direct observation by the research team to record exact intake.
Test Method Data Collection:
- Provide participants with the wearable device or system under test (e.g., smartwatch, multi-sensor setup).
- Instruct them to use the device consistently over the data collection period (e.g., two 14-day test periods).
Data Analysis:
- For each day, compile the daily caloric intake from the reference method and the daily caloric expenditure estimate from the test device.
- Perform Bland-Altman analysis to calculate the mean bias and 95% limits of agreement between the two methods [11].
- Perform linear regression to identify any systematic over- or under-estimation patterns.
Protocol 2: Building a Multi-Model ML Predictor for Caloric Burn
This protocol synthesizes methodologies from multiple sources [42] [43].
Data Preprocessing:
- Handle Missing Values: Impute or remove rows with missing critical data.
- Eliminate Irrelevant Columns: Remove identifiers like
User_IDthat don't contribute to prediction [43]. - Encode Categorical Variables: Convert categorical data (e.g., gender) to numerical values using Label Encoding [43].
- Normalize Data: Use
StandardScalerfrom sklearn to normalize features for stable training [43].
Model Training and Selection:
- Split the dataset into training and testing sets (e.g., 90%/10%) [43].
- Select multiple regression models (e.g., Neural Networks, Random Forest, XGBoost, Linear Regression) and train them on the training set [42] [43].
- Evaluate models on the test set using metrics like Mean Absolute Error (MAE), Mean Squared Error (MSE), and R² score [42] [43].
Model Deployment:
- Select the best-performing model based on validation error.
- Deploy the model for prediction, ensuring it receives the same preprocessed input features it was trained on.
Workflow and System Diagrams
Multi-Modal Data Integration Pipeline
Validation Analysis Workflow
The Scientist's Toolkit
Table 3: Essential Research Reagents and Solutions for Caloric Prediction Studies
| Item / Solution | Function / Application | Example / Specification |
|---|---|---|
| Calibrated Meal Service | Provides the gold-standard reference for energy intake measurement. | University metabolic kitchen providing meals with precisely calibrated energy and macronutrient content [11]. |
| Multi-Sensor Wearable Device | Captures the primary physiological and kinematic data streams. | Devices with combined heart rate monitoring and accelerometry (e.g., Apple Watch, Fitbit) [44]. |
| Continuous Glucose Monitor (CGM) | Measures interstitial glucose levels to assess metabolic response and protocol adherence. | Used as an additional validation metric for dietary reporting protocols [11]. |
| Data Processing & ML Framework | The software environment for data cleaning, analysis, and model building. | Python with Pandas, Scikit-learn, XGBoost, and TensorFlow/PyTorch for neural networks [42] [43]. |
| Vector Database | Enables efficient semantic search and retrieval for large, multi-modal datasets. | ChromaDB, used in RAG pipelines to store and query text embeddings from documents like user manuals, adaptable for sensor data metadata [45]. |
| Statistical Analysis Tool | Performs critical validation statistics to quantify model/device accuracy. | Tools capable of Bland-Altman analysis and linear regression (e.g., Python/Scikit-learn, R) [11]. |
Mitigating Risk: Strategies for Data Quality and Clinical Deployment
Addressing Data Quality and Variability in Heterogeneous Devices
Frequently Asked Questions (FAQs)
FAQ 1: What are the primary data quality challenges when using wearable devices for nutritional intake research?
The key data quality challenges can be categorized into intrinsic data issues and contextual fitness-for-use problems. Intrinsic data quality dimensions include completeness (missing data from non-wear time or device malfunction), accuracy (devices may overestimate low calorie intake and underestimate high intake), and plausibility (ensuring data values are believable). Contextual data quality concerns involve issues like heterogeneous data from different sensor types and brands, and a lack of temporal granularity that makes it difficult to align data streams from multiple devices. These challenges are compounded when integrating data from heterogeneous sources for research [46] [47].
FAQ 2: Why is my wearable device data showing high variability in calorie estimation, especially at lower intake levels?
High variability, particularly the systematic overestimation of lower calorie intake, is a documented limitation of current wearable technology. A 2020 validation study of a nutritional intake wristband found a mean bias of -105 kcal/day with a high standard deviation of 660 kcal/day. The regression analysis indicated a significant tendency for the device to overestimate lower calorie intake and underestimate higher intake [11]. This is compounded by the general poor accuracy of energy expenditure estimation from wearables, with studies showing mean absolute percentage errors often exceeding 30% across various devices and activities, making reliable calorie assessment challenging [48].
FAQ 3: How can I assess the reliability of data from my wearable devices?
Reliability should be assessed based on your research design. For between-person designs (studying trait-like differences between individuals), you need between-person reliability, which measures the stability of a person's measurement relative to others across time and contexts. For within-person designs (studying state-like changes within the same individual), you need within-person reliability, which quantifies the stability of a sensor's readings from the same person in a given state compared to other states. Statistical tools are available to assess this reliability without needing benchmark devices [49].
FAQ 4: What practical steps can I take to improve data quality from multiple, heterogeneous wearable devices?
Key recommendations include establishing local standards of data quality specific to your research context and device types, promoting data interoperability through standardized formats and processing pipelines, ensuring equitable access to data and its interpretation, and striving for representativity in your datasets to avoid biases. Furthermore, using a device's normal range for physiological parameters like HRV, rather than a simplistic "higher is better" interpretation, provides critical context for understanding meaningful changes [47] [50].
Troubleshooting Guides
Guide 1: Troubleshooting High Data Variability in Nutritional Intake Estimation
Problem: Data from wearable devices shows high variability and a systematic bias (overestimation at low intake, underestimation at high intake).
Investigation & Resolution Protocol:
| Step | Action | Expected Outcome |
|---|---|---|
| 1. Verify Signal Integrity | Check for transient signal loss, a major source of error. Inspect raw data streams for gaps or artifacts. | Identification of data loss periods. Exclusion of corrupted data segments. |
| 2. Quantify Bias | Perform a Bland-Altman analysis to compare wearable data against a reference method (e.g., calibrated meals). | Calculation of mean bias and 95% limits of agreement. Confirmation of systematic error pattern [11]. |
| 3. Check Calibration | For sensor types that require it (e.g., electrolytes), confirm if pre-use conditioning and calibration protocols were followed. Newer calibration-free technologies may circumvent this. | Reduced signal drift and improved accuracy. Properly conditioned sensors show stable baselines [51]. |
| 4. Contextualize with Normal Ranges | Frame data points within the individual's normal physiological range to distinguish true changes from normal variability. | Avoidance of misinterpreting normal fluctuations as significant events [50]. |
Guide 2: Troubleshooting Data Integration from Multiple Device Types
Problem: Inability to cleanly integrate and analyze data collected from different brands or models of wearable devices.
Investigation & Resolution Protocol:
| Step | Action | Expected Outcome |
|---|---|---|
| 1. Audit Data Quality Dimensions | For each data stream, assess intrinsic dimensions: Completeness (% of expected data), Conformance (adherence to format), and Plausibility (values within believable range) [46]. | A quality score for each device's data stream. Informed decision on whether to include, clean, or discard data. |
| 2. Map Sensor Variability | Document the different sensor types (e.g., optical heart rate, accelerometer), their locations (wrist, finger, ear), and measurement principles. | Understanding of the root cause of heterogeneous data. Foundation for creating cross-walk functions between devices [47]. |
| 3. Implement Synchronization | Use precise time-synchronization protocols at the start of data collection and align data streams using a common timestamps. | Temporally aligned datasets enabling meaningful cross-correlation and integrated analysis. |
| 4. Apply Harmonization Techniques | If possible, use validated algorithms to transform data from different devices into a common metric or scale, acknowledging the introduced uncertainty. | A more unified dataset for population-level analysis, with clear documentation of the harmonization process. |
Table 1: Performance Metrics from a Wearable Nutrition Intake Validation Study
This table summarizes key quantitative findings from a study validating a wearable wristband's ability to estimate daily nutritional intake (kcal/day) against a reference method [11].
| Metric | Value | Interpretation |
|---|---|---|
| Sample Size (Input Cases) | 304 daily intake measurements | Substantial dataset for validation. |
| Mean Bias (Bland-Altman) | -105 kcal/day | The wristband slightly underestimates intake on average. |
| Standard Deviation of Bias | 660 kcal/day | Very high variability in the accuracy for individuals. |
| 95% Limits of Agreement | -1400 to 1189 kcal/day | For any single measurement, the error could be very large. |
| Regression Equation | Y = -0.3401X + 1963 (p<.001) | Confirms systematic error: overestimation at low intake, underestimation at high intake. |
Table 2: Documented Accuracy of Wearables for Energy Expenditure
This table compiles findings from systematic reviews on the accuracy of various wearable devices for estimating energy expenditure, a key related metric [48].
| Device / Study Context | Mean Absolute Percentage Error (MAPE) | Key Conclusion |
|---|---|---|
| Various Brands (2020 Systematic Review) | Often >10% error in free-living settings (82% of the time) | Poor accuracy in real-world conditions. |
| Apple Watch 6 (Best Case - Running) | 14.9% ± 9.8% | The best-case scenario still has significant error. |
| Polar Vantage V (Resistance Exercise) | 34.6% ± 32.6% | Errors can be extreme for certain activities. |
| 2022 Systematic Review (42 devices) | >30% for all brands | Poor accuracy is a consistent finding across the market. |
Experimental Workflow & Signaling Pathway
Sensor to Research Data Workflow
Data Quality Issue Identification Pathway
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Key Materials and Analytical Tools for Wearable Data Research
| Item | Function in Research | Example / Note |
|---|---|---|
| Bland-Altman Analysis | Statistical method to quantify agreement between wearable data and a reference standard. Calculates mean bias and limits of agreement [11]. | Essential for validation studies to reveal systematic over/under-estimation. |
| Continuous Glucose Monitor (CGM) | Measures glucose levels subcutaneously to assess adherence to dietary reporting protocols or metabolic response. | Used as a secondary objective measure in nutritional intake studies [11]. |
| Calibrated Study Meals | Served in a research dining facility to provide a ground-truth reference for energy and macronutrient intake. | The gold-standard reference method for validating dietary intake wearables [11]. |
| Inductively-Coupled Plasma Mass Spectrometry (ICP-MS) | Highly accurate laboratory technique for quantifying electrolyte and mineral concentrations. | Used as a reference method to validate the performance of wearable electrolyte sensors [51]. |
| Superhydrophobic Ion-to-Electron Transducer (e.g., PEDOT:TFPB) | A material used in advanced wearable electrolyte sensors to stabilize the electrical signal, reducing drift and the need for user calibration [51]. | Enables the development of "ready-to-use" (r-WEAR) sensors that are more reliable. |
| Normal Range Calculation | Establishing an individual's baseline and expected variability for a physiological parameter (e.g., HRV). | Critical for correctly interpreting acute changes and avoiding the "higher is better" fallacy [50] [49]. |
Developing Local Standards and Calibration Protocols for Research
Technical Support & Troubleshooting Hub
This technical support center provides researchers with targeted guidance for addressing common issues in wearable sensor research, with a specific focus on mitigating the overestimation of low calorie intake.
Frequently Asked Questions (FAQs)
Q1: Our wearable sensor data shows high variability and overestimates low calorie intake. What could be causing this, and how can we fix it?
A: This is a common calibration issue. The primary causes and solutions are:
- Cause: Sensor Signal Loss. Transient signal loss from the sensor is a major source of error, particularly affecting the algorithms that compute dietary intake [11].
- Solution: Implement Unit Calibration. Before deployment, perform a unit calibration check using a mechanical shaker across a range of accelerations and frequencies to ensure inter-instrument reliability and correct signal drift [52].
- Cause: Improper Value Calibration. A single, generic regression equation may be used to convert sensor signals into energy expenditure, which can perform poorly at the extremes of the measurement range [11] [52].
- Solution: Develop a Population-Specific Algorithm. Value calibration should use a large and diverse subject group performing a wide range of activities (sedentary to vigorous). Using "pattern recognition" approaches provides better estimates than single-regression models [52].
Q2: How can we validate our locally developed calibration protocol against a gold standard?
A: A robust validation method involves comparison with a controlled reference.
- Reference Method: Collaborate with a metabolic kitchen or dining facility to prepare and serve calibrated study meals. The energy and macronutrient intake of each participant is precisely recorded, creating a gold-standard dataset [11].
- Validation Analysis: Compare the sensor-derived estimates against the reference method using statistical analyses like Bland-Altman tests to quantify the mean bias and limits of agreement [11].
Q3: Our threshold-based algorithm for detecting infant leg movements produces false positives and misses true movements. How can we improve its accuracy?
A: This is often due to unaccounted sensor offset errors.
- Cause: Sensor Offset Error. Commercially available sensors commonly have offset errors, where the signal is non-zero even when the sensor is at rest. This shifts the baseline of your detected signal, causing the algorithm to miss movements that don't cross the threshold [53].
- Solution: Pre-Collection Sensor Calibration. Perform a simple calibration procedure before data collection. Record each sensor in static positions to measure the offset error for each axis, and then subtract this offset from your subsequent movement data [53].
Q4: What are the best practices for communicating calibration procedures and troubleshooting steps within a research team?
A: Effective communication is key to reproducibility.
- Structured Process: Follow a phased troubleshooting process: 1) Understand the problem, 2) Isolate the issue, and 3) Find a fix or workaround [54].
- Clear Documentation: Structure protocols and communications well. Use numbered lists for steps rather than paragraphs of text to make them easy to follow [54].
- Isolate Variables: When diagnosing a problem, change only one thing at a time to correctly identify the root cause [54].
Quantitative Data from Validation Studies
Table 1: Performance Metrics from Wearable Nutrition Intake Validation Study [11]
| Metric | Value / Finding | Implication for Research |
|---|---|---|
| Mean Bias | -105 kcal/day | The wristband, on average, underestimated total daily intake. |
| Standard Deviation | 660 kcal/day | High individual variability limits reliability for single measurements. |
| 95% Limits of Agreement | -1400 to 1189 kcal/day | The device's error for an individual can be very large. |
| Regression Trend | Y = -0.3401X + 1963 (P<.001) | Overestimation at low intake, underestimation at high intake. |
Table 2: Best Practices for Calibrating Wearable Activity Monitors [52]
| Calibration Type | Purpose | Recommended Protocol |
|---|---|---|
| Unit Calibration | Ensure inter-instrument reliability; reduce variability between sensors. | Use a mechanical shaker to test sensors across a range of known accelerations and frequencies. |
| Value Calibration | Convert raw signals (e.g., acceleration) into meaningful units (e.g., energy expenditure). | Collect data from a diverse subject group performing a wide range of activities while simultaneously measuring energy expenditure with a criterion method (e.g., metabolic cart). |
| Algorithm Development | Create predictive models for energy expenditure or activity type. | Use modern "pattern recognition" approaches trained on various activities instead of a single regression equation. |
Detailed Experimental Protocols
Protocol 1: Validating a Wearable Nutrition Sensor
- Objective: To assess the accuracy of a wearable wristband in estimating daily nutritional intake (kcal/day) in free-living adults [11].
- Methodology:
- Participant Recruitment: Recruit a sample of free-living adults (e.g., n=25) matching your target population, excluding those with conditions that may alter metabolism [11].
- Reference Method Setup: Collaborate with a metabolic kitchen. All meals are prepared, calibrated, and served at a dining facility. Participant intake is directly observed and recorded by trained research staff to establish precise energy and macronutrient intake [11].
- Test Method: Participants use the wearable sensor and its accompanying mobile app consistently over the study period (e.g., two 14-day test periods) [11].
- Data Analysis: Perform Bland-Altman analysis to compare the reference and test method outputs, calculating mean bias and limits of agreement. Linear regression can identify systematic biases across the intake range [11].
Protocol 2: Calibrating Inertial Measurement Units (IMUs) for Movement Quantification
- Objective: To measure and correct for offset, gain, and misalignment errors in IMUs before using them to quantify limb movements [53].
- Methodology:
- Calibration Dataset: For each sensor, record data for 60 seconds in static positions.
- Positioning: Place the sensor on a level surface in two different orientations (up and down) for each of its three primary axes. Each position should be held for ~10 seconds. This isolates the measurement of gravity (+1g or -1g) on each axis [53].
- Error Calculation: Compare the sensor's recorded values in each static position against the expected value of 1g. Use this data to calculate the offset (the difference from zero when acceleration should be zero) and gain (the scaling factor error) for each axis [53].
- Data Correction: Apply the derived offset and gain corrections to all subsequent movement data collected with that sensor [53].
Experimental Workflow and Signaling Pathways
Diagram Title: Sensor Calibration & Validation Workflow
Diagram Title: Algorithm Development Pathways
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Key Materials for Wearable Sensor Calibration & Validation
| Item | Function in Research |
|---|---|
| Mechanical Shaker | Provides known accelerations and frequencies for unit calibration of accelerometers, ensuring inter-instrument reliability [52]. |
| Metabolic Cart (Indirect Calorimetry) | Serves as a criterion method for measuring energy expenditure (VO₂/VCO₂) during value calibration studies to develop predictive algorithms [52]. |
| Metabolic Kitchen | Provides a controlled environment for preparing and serving calibrated meals, establishing a gold-standard reference method for validating nutrient intake sensors [11]. |
| Calibrated Reference Sensors | High-precision sensors (e.g., laboratory-grade IMUs) used as a benchmark to check the validity of consumer-grade or research-grade sensors being tested [53]. |
Ensuring Equity and Representativeness in Wearable Datasets
Research using wearable devices is fundamentally shaped by the data on which it is built. When datasets lack equity and representativeness, the resulting algorithms and health insights can be inaccurate and inequitable, particularly for subpopulations. This problem is critically evident in nutrition research, where studies have documented a systematic overestimation of low calorie intake by wearable devices [11]. This technical support guide addresses the methodological challenges in creating representative wearable datasets, providing researchers with protocols and solutions to mitigate bias and enhance the validity of their findings across diverse populations.
Quantitative Evidence: Documenting the Problem
The following table summarizes key quantitative findings from studies that have investigated accuracy and representativeness issues in wearable data, highlighting the specific problem of miscalibration at different intake levels.
Table 1: Documented Biases in Wearable Device Data
| Documented Issue | Quantitative Finding | Source/Context |
|---|---|---|
| Caloric Intake Overestimation | Bland-Altman analysis showed a mean bias of -105 kcal/day. Regression indicated the wristband overestimated lower calorie intake and underestimated higher intake (Y=-0.3401X+1963, P<.001) [11]. | Validation study of a nutrition-tracking wristband (GoBe2) against calibrated meals [11]. |
| Energy Expenditure Inaccuracy | Mean Absolute Percent Error (MAPE) for energy expenditure was 27.96%, significantly higher than for heart rate (4.43%) or step count (8.17%) [55]. | Meta-analysis of 56 studies evaluating Apple Watch accuracy [55]. |
| Underrepresentation in Common Datasets | In the "All of Us" Fitbit dataset, a model trained for COVID-19 detection dropped in accuracy from an AUC of 0.93 (in-sample) to 0.68 (out-of-sample), a 35% loss [56]. | Comparison of a convenience-based "bring-your-own-device" (BYOD) dataset with a representative cohort [56]. |
| Improved Representativity via Design | The ALiR study achieved representation where 54% of participants were from racial/ethnic minorities (vs. 38% in the U.S. population) and 77% had no prior wearable device [56]. | The American Life in Realtime (ALiR) study used probability-based sampling and provided devices and internet access [56]. |
Experimental Protocols for Equitable Data Collection
To counter the biases summarized above, researchers must adopt rigorous, intentional methodologies. The following protocol provides a framework for building more equitable and representative wearable datasets.
Protocol: Building a Representative Wearable Dataset for Nutritional Studies
I. Pre-Study Planning: Sampling and Hardware Provision
- Define Target Population & Use Probability Sampling: Move away from convenience sampling. Employ probability-based sampling from a well-defined, address-based panel to ensure every individual in the target population has a known, non-zero chance of being selected [56].
- Overspecific Underrepresented Groups: Proactively oversample groups historically excluded from digital health research, including racial/ethnic minorities, older adults, individuals with lower socioeconomic status, and those with limited digital literacy [56].
- Provide Standardized Hardware: To eliminate the "Bring-Your-Own-Device" (BYOD) bias, provide all participants with the same model of wearable device. This controls for inter-device variability and includes participants who cannot afford their own technology [56].
- Ensure Connectivity: Provide internet access (e.g., via mobile data or electronic tablets) to participants who need it, preventing the exclusion of households without reliable internet [56].
II. In-Study Data Collection: Validation and Context
- Implement a Reference Method for Caloric Intake:
- Prepare and serve calibrated study meals in a controlled setting (e.g., a dining facility).
- Precisely record the energy and macronutrient composition of each meal using a gold-standard database (e.g., the USDA Food Composition Database).
- Under direct observation, record the exact amount of food and drink consumed by each participant to establish ground truth for energy intake [11].
- Collect Contextual and Demographic Data: Use short, frequent surveys via a companion mobile app to gather data on demographics, health status, socioeconomic factors, and environmental exposures. This enriches the sensor data and allows for analysis of subgroup performance [56].
- Monitor Adherence: Use tools like continuous glucose monitors or the device's own activity logs to measure adherence to wearing the device and following reporting protocols [11].
III. Post-Study Data Analysis and Validation
- Conduct Bias Analysis: Compare the final enrolled cohort demographics against the target population benchmarks. Use weighted adjustments to correct for any remaining minor imbalances [56].
- Validate Algorithmic Performance: Test developed algorithms (e.g., for caloric intake estimation) not just on the overall dataset, but specifically within demographic subgroups (e.g., by age, gender, race, BMI) to identify and correct for differential performance [47] [56].
- Assess Generalizability: Validate models on a separate, held-out sample that reflects population diversity. The performance drop seen in BYOD models is a key metric of poor generalizability [56].
Diagram: Workflow for building equitable wearable datasets, covering sampling, data collection, and validation.
The Scientist's Toolkit: Essential Reagents & Materials
Table 2: Essential Research Materials for Equitable Wearable Validation Studies
| Item / Solution | Function in Research |
|---|---|
| Standardized Wearable Device | Provides consistent data collection across all participants; eliminates BYOD bias from different device models and sensors. |
| Study-Provided Internet Access | Mitigates selection bias by enabling participation for those without reliable internet, ensuring data upload and survey completion. |
| USDA Food Composition Database | Serves as a gold-standard reference for determining the energy and macronutrient content of calibrated study meals. |
| Continuous Glucose Monitor (CGM) | An objective tool to monitor participant adherence to dietary reporting protocols and study physiological responses to food. |
| Meal Preparation Facility | A controlled environment (e.g., a metabolic kitchen) to prepare, calibrate, and serve meals with precise nutrient composition. |
| Validated Survey Instruments | Short, frequent surveys to collect crucial contextual data on demographics, health status, and social determinants of health. |
| Mechanical Shaker | Used for "unit calibration" of accelerometer-based devices to ensure inter-instrument reliability before deployment. |
| Bite-Counter Device | A research tool using inertial sensors to track wrist movements and count bites, aiding in automated caloric intake assessment. |
Frequently Asked Questions (FAQs)
Q1: Our research budget is limited, and providing wearables to all participants is costly. Why is this better than a BYOD model? While BYOD models can rapidly amass large datasets, they inherently over-represent affluent, tech-savvy, and often healthier populations. This leads to algorithmic bias, where models fail for underrepresented groups. The ALiR study demonstrated that a smaller, representative sample yields more generalizable and clinically useful models than a larger, biased dataset, making the initial investment more efficient for producing valid, equitable science [56].
Q2: We provided devices and internet, but we still struggled to enroll older adults. What else can be done? Barriers beyond technology access include mistrust, disinterest, or physical difficulty using devices. Strategies to overcome this include:
- Community Engagement: Partner with trusted community leaders and organizations to build trust.
- User-Centered Design: Involve older adults in device selection and interface testing to ensure usability.
- Enhanced Support: Provide dedicated technical support and simplified instructions.
- Addressing Mistrust: Be transparent about data use and privacy protections [56].
Q3: Our calorie estimation algorithm works well on average but overestimates intake for individuals with low consumption. How can we fix this? This is a classic calibration issue. The solution involves:
- Subgroup Analysis: Validate your algorithm specifically within the subgroup of users with low calorie intake.
- Re-calibration: Develop and apply a secondary, corrective algorithm or adjustment factor specifically tuned for the lower range of intake, based on your validation data from calibrated meals [11].
- Algorithm Selection: Explore "pattern recognition" approaches that classify activity types rather than relying on a single regression equation, as these can provide better estimates across diverse behaviors [52].
Q4: What are the key data quality checks we should perform on raw data from wearables before analysis?
- Unit Calibration: Use a mechanical shaker to verify that accelerometers are measuring acceleration correctly across a range of frequencies and intensities [52].
- Wear-Time Validation: Implement a robust algorithm (e.g., identifying consecutive epochs of zero counts) to distinguish device non-wear from sedentary behavior [52].
- Signal Plausibility: Check for physiologically impossible values in heart rate, energy expenditure, and other biometric data, which may indicate sensor malfunction [47] [29].
Q5: How can we make our final dataset a "benchmark" for equitable research? Adhere to the FAIR Guiding Principles: make your data Findable, Accessible, Interoperable, and Reusable [56]. This involves:
- Depositing the dataset in a public, indexed repository.
- Providing clear metadata and codebooks, including detailed demographic breakdowns of the cohort.
- Using standardized data formats and vocabularies.
- Publishing the detailed study protocol and data collection manuals to enable replication.
Best Practices for Interpreting and Contextualizing Wearable EE Data
Frequently Asked Questions
Q1: How accurate are consumer wearables at estimating Energy Expenditure (EE)? Substantial variability exists in the accuracy of Energy Expenditure (EE) estimation from consumer wearables [57]. While some devices measure heart rate quite accurately, their estimation of calories burned is often significantly off. An evaluation of seven consumer devices found that none measured energy expenditure accurately; the most accurate device was off by an average of 27%, and the least accurate was off by 93% [24]. The accuracy can vary based on the activity type and the individual user's characteristics [57].
Q2: Why is EE estimation from wearables often inaccurate? The primary reason is the reliance on proprietary algorithms that use sensor data and user demographics to indirectly estimate EE [57] [24]. These algorithms make assumptions that often do not fit individuals well. Key challenges include [57]:
- Indirect Measurement: Unlike heart rate, EE must be measured indirectly through proxy calculations.
- Individual Variability: EE depends on a person's fitness level, body composition, and metabolism, which generic algorithms struggle to capture.
- Heterogeneous Validation: A lack of standardized validation protocols and reporting across manufacturers makes it difficult to compare device accuracy transparently.
Q3: What are the best practices for validating wearable EE data in a research setting? The INTERLIVE network recommends a standardized validation framework encompassing six key domains [57]:
- Target Population: The study population should reflect the intended end-users.
- Criterion Measure: Use a gold-standard measure like indirect calorimetry (for active EE) or doubly labeled water (for total EE).
- Index Measure: Clearly report the device, firmware, and placement used.
- Testing Conditions: Include both controlled lab activities and free-living conditions.
- Data Processing: Detail all data processing, filtering, and cleaning steps.
- Statistical Analysis: Use appropriate statistical methods beyond simple averages, such as Bland-Altman plots, to assess agreement at both group and individual levels.
Q4: My data shows implausibly low or high EE values. What should I do? Implausible values can stem from several sources. Follow this troubleshooting guide:
| Problem Category | Specific Issue | Recommended Action |
|---|---|---|
| Data Collection & Setup | Incorrect user profile (weight, height, age) | Verify and correct anthropometric data input [57]. |
| Improper device wearing (loose sensor contact) | Ensure device is snug against skin; follow manufacturer's guidance [58]. | |
| Signal & Environment | Transient signal loss from sensor | Check data logs for gaps; consider data interpolation or exclusion for periods of loss [11]. |
| Unclassified activity type | Devices using single-regression models systematically misestimate non-ambulatory activities [59]. | |
| Data Processing | Failure to account for device-specific error | Apply device-specific correction factors if established by validation studies [57]. |
| Analysis of overly short time intervals | Analyze EE over longer epochs (e.g., minutes rather than seconds) to smooth transient noise [57]. |
Q5: How can I contextualize EE data from a free-living population? When analyzing data from free-living conditions [60]:
- Acknowledge Selection Bias: Users of wearables are not representative of the general population.
- Account for Missing Data: Data loss is common; develop robust strategies for handling it.
- Use Appropriate Statistical Models: Avoid simple averaging. Consider methods that account for the distribution of activity (e.g., Gini coefficients) and can model complex, longitudinal data [60].
Experimental Protocols for Validating EE Data
This section provides a detailed methodology for conducting a validation study, based on best-practice recommendations [57].
1. Protocol Overview This protocol is designed to assess the validity of a wearable device's EE estimation against a gold-standard criterion measure in both controlled and free-living settings.
2. Key Research Reagents and Equipment Essential materials and their functions for a typical validation experiment:
| Item Name | Function in Experiment |
|---|---|
| Indirect Calorimetry System | Gold-standard criterion measure for Active Energy Expenditure (AEE); measures respiratory gases to compute EE [57]. |
| Doubly Labeled Water (DLW) | Gold-standard criterion measure for Total Energy Expenditure (TEE) in free-living conditions over 1-2 weeks [57]. |
| Consumer Wearable Device(s) | The index measure(s) under evaluation [57]. |
| Electrocardiogram (ECG) | Provides a medical-grade heart rate reference to validate the wearable's optical heart rate sensor [24]. |
3. Step-by-Step Methodology
Phase 1: Laboratory-Based Controlled Protocol
- Participants: Recruit a sample that represents the target population in terms of age, sex, BMI, and fitness level [57].
- Device Setup: Fit the consumer wearable according to manufacturer instructions. Simultaneously, equip the participant with the indirect calorimetry system and ECG [24].
- Activity Protocol: Participants should perform a series of structured activities designed to cover a range of MET values. A sample protocol is shown in the table below. Each activity should be performed for a sufficient duration (e.g., 5-10 minutes) to reach a steady state [57] [59].
Table: Example Laboratory Activity Protocol for EE Validation
| Activity Type | Example Activities | Expected Intensity Range | Criterion Measure |
|---|---|---|---|
| Sedentary/Quiet | Lying down, sitting quietly, standing | Low (1-2 METs) | Indirect Calorimetry |
| Lifestyle | Washing windows, folding laundry, stretching | Light to Moderate (2-4 METs) | Indirect Calorimetry |
| Ambulation | Walking at 2, 3, 4 mph; running | Moderate to Vigorous (3-8+ METs) | Indirect Calorimetry |
Phase 2: Free-Living Observation Protocol
- Participants: A subset of the laboratory cohort.
- Device Setup: Participants wear the consumer device(s) as they go about their normal daily routines for a period of 1-2 weeks [57].
- Criterion Measure: Administer Doubly Labeled Water (DLW) to measure TEE. Participants consume a dose of DLW, and urine samples are collected over the subsequent days for analysis [57].
- Data Collection: The wearable device data is synced and collected throughout the observation period.
4. Data Analysis and Interpretation
- Statistical Comparison: Use Bland-Altman plots to assess the agreement between the wearable device and the criterion measure, identifying any systematic bias (e.g., overestimation at low EE levels) [11]. Calculate mean absolute percentage error and correlation coefficients.
- Interpretation: Analyze results for different activity types and participant subgroups. Be aware that devices often overestimate sedentary activities and underestimate vigorous activities [59].
Visualizing the Validation Workflow
The following diagram illustrates the logical workflow and key decision points for a comprehensive wearable EE data validation study.
Wearable EE Validation Workflow
The Scientist's Toolkit: Key Reagents & Materials
A summarized table of essential items for a wearable EE validation study.
| Item Name | Category | Critical Function |
|---|---|---|
| Indirect Calorimetry System | Criterion Measure | Provides breath-by-breath measurement of VO₂/VCO₂ for calculating AEE in lab settings [57]. |
| Doubly Labeled Water (DLW) | Criterion Measure | Gold standard for measuring TEE in free-living conditions over extended periods [57]. |
| Medical-Grade ECG | Reference Device | Validates the accuracy of the wearable's optical heart rate sensor [24]. |
| Treadmill & Exercise Equipment | Laboratory Equipment | Enables standardized, graded exercise protocols in a controlled environment [24]. |
| Calibrated Weighing Scale | Anthropometry | Provides accurate body weight data, a critical input for many EE algorithms [11]. |
| Data Logging & Management Software | Data Analysis | Essential for synchronizing, processing, and analyzing high-volume time-series data from multiple sources [60]. |
Benchmarking Device Performance and Establishing Validity
For researchers and drug development professionals, accurate measurement of human energy expenditure (EE) is critical. While consumer wearables have democratized physiological monitoring, their outputs, particularly for caloric expenditure, demonstrate significant variability when compared to the gold standard of indirect calorimetry. This technical guide details the documented discrepancies, provides protocols for validation, and offers frameworks to mitigate these issues in research settings, with a specific focus on the common pitfall of overestimation in low-calorie expenditure scenarios.
Quantitative Accuracy Assessment
The following tables summarize the accuracy of common wearable devices and research-grade metabolic systems as established by validation studies.
| Wearable Brand | Energy Expenditure (Avg. % Error) | Heart Rate (Avg. % Error) | VO₂ max (Avg. % Error) | Step Count (Avg. % Error) |
|---|---|---|---|---|
| Apple Watch | -6.61% to +53.24% [61] | ~1.3% (underestimates) [61] | +9.83% to +15.24% [22] [62] | 0.9% - 3.4% [61] |
| Fitbit | ~14.8% [61] | ~9.3% (underestimates) [61] | Data Insufficient | 9.1% - 21.9% [61] |
| Garmin | 6.1% - 42.9% [61] | 1.16% - 1.39% [61] | Data Insufficient | ~23.7% [61] |
| Samsung | 9.1% - 20.8% [61] | ~7.1% (underestimates) [61] | Data Insufficient | 1.08% - 6.30% [61] |
| Oura Ring | ~13% (underestimates) [61] | ~0.7% (underestimates) [61] | Data Insufficient | 4.8% - 50.3% [61] |
| Polar | 10% - 16.7% [61] | ~2.2% [61] | Data Insufficient | Data Insufficient |
Key Interpretation: No consumer wearable brand provides consistently accurate energy expenditure measurements. Errors can be highly variable, with a general tendency towards underestimation, though significant overestimation is also common [63] [22].
| Metabolic System | Resting EE (vs. Comparator) | Exercise EE (vs. Comparator) | Key Validation Findings |
|---|---|---|---|
| COSMED K5 (K5) | +33.4% higher than M3B [64] | +14.6% to +16.1% higher than M3B [64] | Valid for VO₂ during rest and cycling (mean error <5%); underestimates VCO₂ at high workloads [64]. |
| CORTEX METAMAX 3B (M3B) | Reference for K5 comparison [64] | Reference for K5 comparison [64] | Acceptably stable (<2% error); overestimates VO₂/VCO₂ by 10-17% during moderate to vigorous cycling [64]. |
Key Interpretation: Systematic bias exists even between different research-grade portable metabolic systems. The choice of criterion device can significantly impact the results of a validation study for a wearable device [64].
Experimental Protocols for Validation
Protocol 1: Validating Wearables Against Indirect Calorimetry During Submaximal Exercise
This protocol is adapted from a study comparing portable metabolic systems and is ideal for assessing accuracy during controlled, low-to-moderate intensity activities [64] [65].
Research Question: How does the energy expenditure output of a consumer wearable compare to indirect calorimetry during rest and submaximal cycling in a specific population?
Materials & Reagents:
- Criterion Measure: Portable metabolic system (e.g., COSMED K5, CORTEX METAMAX 3B) or metabolic cart (e.g., COSMED Quark CPET) [64] [62].
- Device Under Test: Consumer wearable (e.g., Apple Watch, Fitbit, Garmin).
- Equipment: Electrically braked cycle ergometer.
- Other: Height scale, bioimpedance device for body composition, calibrated environmental sensors (temperature, humidity, barometric pressure).
Methodology:
- Participant Preparation: Recruit participants based on specific inclusion criteria (e.g., untrained females). Standardize pre-test conditions: fasting for 3+ hours, no caffeine/alcohol/strenuous activity for 12-24 hours, and testing at the same time of day to control for circadian rhythm [64] [62].
- Familiarization: Conduct a practice session >2 days before testing to acclimate participants to the equipment [64].
- Testing Procedure:
- Resting Measurement: Participant sits quietly for 15 minutes while equipped with both the metabolic system and the wearable(s). Record resting EE [64].
- Exercise Measurement:
- Warm-up: 3 minutes at 20 W.
- Incremental Stages: Perform 6-minute stages at increasing workloads (e.g., 30 W, 40 W, 50 W, 60 W) at a constant cadence (e.g., 60 rpm).
- Recovery: 5 minutes at 25 W [64].
- Record EE from all devices at each stage.
- Data Analysis:
Protocol 2: Generating and Validating VO₂ max Estimates
This protocol validates wearable-derived VO₂ max estimates, which are often used to inform EE algorithms [62].
Research Question: How accurate is the Apple Watch (or similar device) in estimating VO₂ max compared to cardiopulmonary exercise testing (CPET) with indirect calorimetry?
Materials & Reagents:
- Criterion Measure: Metabolic cart for CPET (e.g., COSMED Quark CPET) [62].
- Device Under Test: Wearable with VO₂ max estimation feature (e.g., Apple Watch Series 3 or later).
- Equipment: Treadmill or cycle ergometer.
Methodology:
- Wearable Estimate Generation: Participants wear the device for 5-10 days during outdoor walking, running, or hiking as per manufacturer guidelines to generate a VO₂ max estimate [62].
- Criterion CPET Test: Within a close timeframe, participants perform a maximal exercise test (e.g., modified Åstrand treadmill protocol) to volitional exhaustion. The highest 30-second averaged VO₂ value is taken as the true VO₂ max [62].
- Data Analysis: Compare the wearable estimate to the criterion value using Bland-Altman analysis, Mean Absolute Percentage Error (MAPE), and Mean Absolute Error (MAE) [62].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Energy Expenditure Research
| Item | Function in Research | Example Brands/Models |
|---|---|---|
| Portable Metabolic System | Gold-standard field measurement of EE via indirect calorimetry (measures VO₂/VCO₂). | COSMED K5, CORTEX METAMAX 3B [64] |
| Metabolic Cart | Gold-standard laboratory measurement of VO₂ max and EE during CPET. | COSMED Quark CPET [62] |
| Indirect Calorimeter (Clinical) | Measures Resting Energy Expenditure (REE) in clinical populations for nutritional support. | Various canopy/hood systems [66] [67] |
| Doubly Labeled Water | Gold-standard for measuring total daily energy expenditure in free-living conditions over 1-2 weeks. | N/A (Method) |
| Electrically Braked Ergometer | Provides precise and reproducible workload during exercise testing. | Monark 839 E [64], h/p/cosmos Venus [62] |
| Bioimpedance Device | Assesses body composition (e.g., fat percentage, muscle mass), a key covariate in EE. | InBody 770 [64], QardioBase [68] |
Troubleshooting Guides & FAQs
FAQ 1: Why is there such significant variability in energy expenditure estimates from wearables? Energy expenditure algorithms in consumer devices are proprietary and typically rely on a combination of sensor data (e.g., accelerometry, heart rate) and user demographics. They are not directly measuring gas exchange like indirect calorimetry. Factors that degrade accuracy include [63] [22] [61]:
- Exercise Intensity: Error increases with higher intensity activities.
- Type of Activity: Algorithms are often optimized for walking/running and perform poorly on non-ambulatory exercises.
- User Physiology: Skin tone, perfusion, and wrist anatomy can affect optical heart rate sensors.
- Device Placement: Improper fit or sensor interference from sweat/dirt.
FAQ 2: Our study recorded lower than expected calorie burn from wearables in a sedentary population. Is this a known issue? Yes, this is a documented challenge. Many wearables show a tendency to underestimate energy expenditure, particularly during lower-intensity activities and sedentary behavior [63] [22]. This aligns with your thesis context on the overestimation of low calorie intake. The error range for EE is often largest at these lower intensities, which can lead to significant misclassification of activity levels in sedentary cohorts [22].
FAQ 3: How should we handle the choice of a "gold standard" metabolic device in our validation study? Recognize that even criterion devices have error profiles. Carefully select your metabolic system based on your study's specific needs (e.g., lab vs. field, population). Crucially, report the specific model and known validation data of your criterion device to provide context for your findings. The systematic bias between systems like the K5 and M3B means that comparing validation studies that used different criterion devices requires caution [64].
FAQ 4: What are the best practices for improving the rigor of wearable data in clinical research?
- Validate In-House: Do not rely solely on manufacturer claims. Conduct a pilot validation study using a protocol like Protocol 1 above on a subset of your population [69].
- Transparent Reporting: Always report the specific device model, software version, and placement. Acknowledge the inherent limitations and error ranges of the devices used [69].
- Use as a Trend, Not an Absolute: Within-subject changes over time may be more reliable than absolute values for detecting intervention effects.
- Data Integration: Combine wearable data with other measures, such as activity logs or research-grade accelerometers, to triangulate findings.
Comparative Analysis of Device Performance Across Demographics
Frequently Asked Questions & Troubleshooting Guides
This section addresses common challenges researchers face when validating the energy expenditure (EE) estimation of low-cost wearable devices.
General Research FAQs
Q1: What is the typical accuracy range for energy expenditure estimation in low-cost smartwatches? Research indicates a high degree of variability. One study found that Mean Absolute Percentage Error (MAPE) for EE estimation in some low-cost devices can range from approximately 12.5% to over 57% when compared to indirect calorimetry as a criterion measure [3].
Q2: Which demographic factors are most critical to consider in device validation studies? Key factors include biological sex, ethnicity, age, and fitness level [3] [70]. Existing research highlights that most validation studies have been conducted on Western populations, limiting generalizability. One study focused specifically on young, untrained Chinese women to address this gap [3]. Furthermore, ownership rates for wearables can vary significantly with age and employment status [70].
Q3: What is the gold standard method for validating energy expenditure? Indirect calorimetry is the recognized criterion method. It involves measuring gas exchange (oxygen consumption and carbon dioxide production) using a portable metabolic system. EE is then calculated from these measurements using Weir's equation [3].
Q4: Why might different smartwatches show vastly different calorie burns for the same activity? Inaccuracies stem from a combination of factors, including the proprietary algorithms used to estimate EE, the type and quality of sensors (e.g., photoplethysmography for heart rate), and the device's estimation of Basal Metabolic Rate (BMR). Device heterogeneity leads to significant variability in estimates, especially during non-steady-state activities [3] [1].
Troubleshooting Common Experimental Problems
Q1: Issue: Large, inconsistent positive bias in energy expenditure data at higher exercise intensities.
- Potential Cause: The study by [3] identified a trend of increasing positive bias as EE increased across all tested devices, with some showing this pattern more clearly.
- Solution:
- Bland-Altman Analysis: Perform Bland-Altman plots to visualize the relationship between the magnitude of EE and the bias for each device [3].
- Device Selection: Note that this bias is device-dependent. In the cited study, the XIAOMI Smart Band 8 (XMB8) and KEEP Smart Band B4 Lite (KPB4L) showed this pattern most clearly [3].
- Statistical Modeling: Consider developing device-specific correction factors for different intensity levels based on your validation data.
Q2: Issue: Missing data points across multiple load levels during device testing.
- Potential Cause: Occasional data loss can occur due to sensor connectivity issues, improper fit, or device-specific software errors [3].
- Solution:
- Protocol Standardization: Ensure devices are positioned according to manufacturer specifications and are securely fitted to the wrist [3].
- Pilot Testing: Conduct thorough pilot tests to identify devices prone to data dropouts.
- Sample Size Calculation: Account for potential data loss by increasing the sample size during the study design phase. A post-hoc power analysis is recommended to ensure statistical reliability [3].
Q3: Issue: Consumer wearable devices are consistently overestimating total daily energy expenditure (TDEE).
- Potential Cause: This is a common and documented problem. Devices estimate TDEE by summing estimated BMR and active calories. Overestimation often occurs in the active calorie component, which relies on heart rate and motion sensors. One analysis found devices can over- or underestimate energy burn by more than 30% [1].
- Solution for Researchers:
- Trends Over Precision: Advise research participants to focus on long-term trends in the data rather than absolute daily values.
- Cue Integration: Caution against using these estimates to directly inform caloric intake; instead, encourage participants to also listen to natural hunger and fullness cues [1].
- Contextualize Findings: Frame device output as a proxy for general activity levels rather than a precise metabolic measurement.
The following tables synthesize key quantitative findings from relevant validation studies on low-cost wearable devices.
| Device Model | Mean Absolute Percentage Error (MAPE) Range Across Loads | Overall Performance vs. Criterion (Indirect Calorimetry) | Statistical Power (at 50W load) |
|---|---|---|---|
| HONOR Band 7 (HNB7) | 15.0% - 23.0% | Not significantly different from criterion | 0.128 |
| HUAWEI Band 8 (HWB8) | 12.5% - 18.6% | Not significantly different from criterion | 0.050 |
| XIAOMI Smart Band 8 (XMB8) | 30.5% - 41.0% | Significantly overestimated EE (p < 0.001) | 1.000 |
| KEEP Smart Band B4 Lite (KPB4L) | 49.5% - 57.4% | Significantly overestimated EE (p < 0.001) | 1.000 |
| Demographic Factor | Smartphone Ownership Rate | Wearable Device Ownership Rate | Key Demographic Disparities |
|---|---|---|---|
| Overall | 98% | 59% | - |
| Age Group | |||
| 18-25 | Data Not Specified | Highest likelihood | Generation Z most likely to own wearables. |
| 26-41 | ~100% | Data Not Specified | - |
| 58-76 | 98% | Data Not Specified | - |
| 77+ | 89% | Data Not Specified | Significantly lower ownership. |
| Employment | |||
| Full-time | 99.5% | Data Not Specified | Higher ownership. |
| Retired | 95% | Data Not Specified | Lower ownership than employed. |
Detailed Experimental Protocols
Protocol 1: Validating Energy Expenditure During Structured Exercise
This protocol is adapted from a study validating four low-cost smartwatches [3].
1. Objective: To evaluate the validity of low-cost smartwatches for estimating energy expenditure during ergometer cycling against the criterion measure of indirect calorimetry.
2. Participants:
- Recruitment: Recruit a homogeneous sample based on specific demographic and health criteria (e.g., 20 healthy, untrained Chinese women aged 18-30 who exercise ≤3 times per week) [3].
- Screening: Screen participants via lifestyle and general health risk evaluations [3].
3. Materials & Equipment:
- Criterion Measure: CORTEX METAMAX 3B (or similar portable metabolic system) calibrated with a 3L syringe and calibration gases prior to each test [3].
- Index Devices: The smartwatches or activity bands being validated (e.g., HONOR Band 7, HUAWEI Band 8, etc.). Devices should be purchased from the market and run the latest software [3].
- Additional Equipment: Ergometer cycle, Polar H10 heart rate belt, computer with MetaSoft Studio (or similar) software for metabolic data collection [3].
4. Procedure:
- Preparation: Participants should be instructed to follow a light diet and avoid high-intensity activity, smoking, and caffeine before testing [3].
- Device Fitting:
- Assign devices to wrists randomly to control for placement bias.
- Fit all devices according to the manufacturers' instructions.
- Set all devices to the same activity mode (e.g., "indoor cycling") [3].
- Testing Protocol:
- Participants wear the metabolic mask and the smartwatches simultaneously.
- The exercise test consists of consecutive stages at fixed power outputs (e.g., 30W, 40W, 50W, 60W) on the ergometer.
- EE values from all devices and the metabolic cart are recorded at each stage [3].
5. Data Analysis:
- Calculate Mean Absolute Percentage Error (MAPE) for each device at each load [3].
- Use paired-sample statistical tests (e.g., t-test, Wilcoxon signed-rank) to compare EE from each device to the criterion measure [3].
- Perform a Bland-Altman analysis to assess bias and limits of agreement between each device and the criterion [3].
- Conduct a post-hoc power analysis (e.g., using G*Power software) to determine the statistical power of the findings [3].
Experimental Workflow and Signaling Diagrams
Device Validation Experimental Workflow
Decision Tree for Troubleshooting EE Estimation Bias
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Wearable Device Validation Studies
| Item | Function in Research | Example/Specification |
|---|---|---|
| Portable Metabolic System | Serves as the criterion measure for Energy Expenditure by measuring oxygen consumption (VO₂) and carbon dioxide production (VCO₂) breath-by-breath [3]. | CORTEX METAMAX 3B; requires calibration with a 3L syringe and known-concentration calibration gases [3]. |
| Laboratory Ergometer | Provides a standardized and controllable workload for exercise protocols, allowing for precise measurement of EE at different intensities [3]. | Cycle ergometer capable of maintaining fixed power outputs (e.g., 30W, 40W, 50W, 60W). |
| Research-Grade Heart Rate Monitor | Provides a validated heart rate signal that can be used to assess the accuracy of the PPG heart rate sensors in the smartwatches. | Chest strap monitor (e.g., Polar H10) [3]. |
| Statistical Analysis Software | Used to perform power analysis, comparative statistics, and bias analysis to determine the validity and reliability of the wearable devices [3]. | G*Power for power analysis; R, Python, or SPSS for statistical tests and Bland-Altman plots [3]. |
Living Reviews and the Challenge of Keeping Pace with Device Updates
Frequently Asked Questions (FAQs) for Researchers
Q1: Why is there significant variability in energy expenditure (EE) estimates from different low-cost wearable devices? The accuracy of EE estimation varies substantially across devices due to differences in the proprietary algorithms, sensor types (e.g., PPG, accelerometer, gyroscope), and the intensity of the activity being monitored. Validation studies consistently show a high degree of heterogeneity in device performance. For instance, a 2025 study testing four affordable smartwatches found that while some devices like the HONOR Band 7 and HUAWEI Band 8 showed moderate accuracy, others like the XIAOMI Smart Band 8 and KEEP Smart Band B4 Lite significantly overestimated EE across various cycling loads, with mean absolute percentage errors (MAPE) ranging from 12.5% to 57.4% [3]. This illustrates that device choice is a critical variable in study design.
Q2: What are the primary technical barriers to developing more accurate wearable devices for clinical research? The main challenges include:
- Sensor and Algorithm Limitations: Many devices rely on basic sensors (accelerometers, optical heart rate) and proprietary, non-transparent algorithms that are not clinically validated. Developing devices that can capture complex physiological patterns requires more sophisticated, multimodal sensing (e.g., electroacoustic) and advanced AI analytics, which is difficult with low-cost systems [71].
- Unclear Value Proposition and Cost: It is challenging for manufacturers to differentiate new products beyond basic activity tracking. Expanding into advanced, clinically relevant metrics involves navigating regulatory hurdles and demonstrating efficacy, which increases development costs [72]. This can stifle innovation in the low-cost segment.
- Data and Model Interpretation: Even with AI-enhanced wearables, many models operate as "black boxes," providing predictions without explainable insights into the underlying physiological triggers (e.g., meal, stress, activity). This lack of transparency limits their trustworthiness and utility for guiding clinical decisions [73].
Q3: How can researchers mitigate the risk of overestimation in studies using consumer wearables? Proactive mitigation strategies are essential:
- Device Validation: Prior to a main study, conduct a pilot validation of the chosen wearable against a criterion measure (e.g., indirect calorimetry) within your specific population and for the activities of interest [3].
- Leverage Trends, Not Absolute Values: Given the demonstrated inaccuracy of absolute calorie burn estimates, researchers should use wearable data to identify relative trends and patterns in physical activity over time, rather than relying on single-point estimates to determine energy intake [1].
- Use Inclusive Algorithms: Be aware that many standard algorithms perform poorly in specific populations, such as people with obesity. Seek out and utilize newly developed, open-source algorithms that have been validated in your target demographic to ensure more reliable EE measures [30].
Q4: What is the regulatory distinction between a wellness device and a healthcare device, and why does it matter for research? The U.S. FDA provides clear distinctions. Wellness devices are intended for general health and fitness tracking and are not subject to FDA regulation. In contrast, medical devices are intended for diagnosing, treating, or preventing disease and must undergo a rigorous risk-based classification and premarket review process [71]. For researchers, this means that most consumer-grade wearables are not designed or validated to the same standard as medical devices, which must be considered when interpreting data for clinical or scientific purposes.
Q5: How is Artificial Intelligence (AI) transforming the capabilities of wearable devices? AI, particularly machine and deep learning, is shifting wearables from simple data trackers to proactive health tools. Key applications include:
- Predictive Analytics: AI can analyze continuous data streams (e.g., from glucose monitors) to predict physiological changes, such as glucose levels, 1-2 hours in advance, enabling preventive actions [73].
- Enhanced Data Interpretation: AI allows for the interpretation of complex, multimodal data from various sensors (acoustic, electrical, optical), making it possible to diagnose and monitor complex conditions like musculoskeletal disorders, even with noisier signals from low-cost sensors [71].
- Personalized Coaching: Generative AI is being used to provide personalized health recommendations and act as a conversational virtual assistant, moving beyond simple data reporting [74].
Experimental Protocols for Validating Wearable Device Accuracy
The following methodology is adapted from a 2025 study investigating the validity of EE estimation in low-cost smartwatches [3].
1. Objective To evaluate the validity of energy expenditure (EE) estimates from low-cost smartwatches during structured exercise, using indirect calorimetry as a criterion measure.
2. Materials and Equipment
- Criterion Measure: Portable metabolic system (e.g., CORTEX METAMAX 3B) calibrated with a 3L syringe and calibration gas prior to each session [3].
- Index Devices: The wearable devices under investigation (e.g., HONOR Band 7, HUAWEI Band 8, etc.). Devices should be purchased from the consumer market to reflect what end-users acquire.
- Heart Rate Monitor: Research-grade chest strap (e.g., Polar H10) for benchmark heart rate data [3].
- Exercise Equipment: Ergometer (cycle or treadmill) where resistance and speed can be precisely controlled.
3. Participant Selection
- Recruitment: Recruit a homogeneous sample (e.g., 20 untrained female participants) to reduce inter-subject variability initially. Future studies should expand to more diverse populations [3].
- Inclusion Criteria: Specific to the study goals (e.g., healthy adults who exercise ≤3 times per week) [3].
- Ethics: Obtain written informed consent and approval from the institutional ethics committee.
4. Experimental Procedure
- Device Placement: Randomly assign two devices to each participant's wrists, following manufacturer instructions for placement [3].
- Activity Protocol: Participants perform exercise at incremental intensities. For cycling, this may involve stages at 30W, 40W, 50W, and 60W, with each stage lasting a set duration (e.g., 5-10 minutes) [3].
- Data Collection: Simultaneously collect breath-by-breath gas exchange data from the metabolic system (criterion EE) and read EE values from the screens of the smartwatches at each load level. Ensure all devices are set to the correct activity mode (e.g., "indoor cycling") [3].
5. Data Analysis
- Statistical Comparison: Use paired sample t-tests or Wilcoxon signed-rank tests to compare EE values from each smartwatch to the criterion measure at each load level [3].
- Error Calculation: Compute the Mean Absolute Percentage Error (MAPE) for each device. A lower MAPE indicates higher accuracy.
- Bias Analysis: Create Bland-Altman plots to visualize the agreement between the smartwatch and criterion measure and to identify any systematic bias (e.g., increasing overestimation with higher EE) [3].
Table 1: Accuracy of Low-Cost Smartwatches in Estimating Energy Expenditure (EE) Data from a 2025 validation study on untrained Chinese women during ergometer cycling [3].
| Device Name | Price (CNY) | MAPE (Range Across Loads) | Key Finding vs. Criterion (Indirect Calorimetry) |
|---|---|---|---|
| HONOR Band 7 | 269 | 15.0% - 23.0% | EE values were not significantly overestimated |
| HUAWEI Band 8 | 249 | 12.5% - 18.6% | EE values were not significantly overestimated |
| XIAOMI Smart Band 8 | 309 | 30.5% - 41.0% | EE was significantly overestimated (p < 0.001) |
| KEEP Smart Band B4 Lite | 339 | 49.5% - 57.4% | EE was significantly overestimated (p < 0.001) |
Table 2: Performance of a Novel BMI-Inclusive EE Algorithm Data from a 2025 study developing a machine learning model for a commercial smartwatch (Fossil Sport) validated in individuals with obesity [30].
| Validation Setting | Comparison | Performance Metric (Root Mean Square Error - RMSE) |
|---|---|---|
| In-Lab Study (n=27) | Proposed Model (60-sec window) vs. Metabolic Cart | 0.281 (Lower error than 6 out of 7 established algorithms) |
| Free-Living Study (n=19) | Proposed Model vs. Best Actigraphy-Based Estimate | Estimates fell within ±1.96 SD for 95.03% of minutes |
The Scientist's Toolkit: Key Research Reagents and Materials
Table 3: Essential Materials for Wearable Device Validation Research
| Item | Function in Research | Example Product / Note |
|---|---|---|
| Portable Metabolic System | Serves as the criterion measure ("gold standard") for calculating Energy Expenditure (EE) via oxygen consumption and carbon dioxide production. | CORTEX METAMAX 3B [3] |
| Research-Grade Accelerometer | Provides a benchmark for motion data and EE estimation against which consumer devices can be compared. | ActiGraph wGT3X+ (hip- or wrist-worn) [30] |
| Calibration Kit | Ensures the accuracy of the metabolic system before each use, including syringe for volume and gas for concentration calibration. | 3L calibration syringe, calibration gas [3] |
| Consumer Wearables (Test Devices) | The devices under investigation. Should represent current, widely available models. | Various brands (e.g., Fossil Sport, Apple Watch, Fitbit) [3] [30] |
| Electrodes & Heart Rate Monitor | Provides a validated heart rate signal, a key input for many EE algorithms. | Polar H10 chest strap [3] |
Workflow Diagram for Device Validation
The diagram below outlines the logical workflow for conducting a wearable device validation study, from preparation to data interpretation.
Device Validation Workflow
AI-Enhanced Wearable Development Pathway
This diagram illustrates the conceptual process of integrating Artificial Intelligence to improve wearable devices for healthcare applications.
AI Wearable Development
A Framework for Pre-Study Validation of Wearables in Clinical Trials
Why Pre-Study Validation is Critical
Before deploying wearable devices in clinical research, rigorous pre-study validation is essential to ensure data quality and reliability. This process confirms that the digital measures collected are fit for their specific research purpose. For studies investigating calorie intake, inadequate validation can lead to systematic overestimation of low energy consumption, fundamentally compromising study conclusions [75]. The framework presented here establishes standardized procedures to mitigate these risks through comprehensive technical and clinical validation.
Core Validation Framework
Key Validation Components
A robust validation strategy must address multiple dimensions of device performance, with particular emphasis on the Context of Use (COU). The COU explicitly defines the specific measurement purpose, target population, and technical environment in which the wearable will be deployed. Validation requirements vary significantly depending on whether a device is used for basic feasibility research or as a source of primary endpoints in regulatory-grade trials [75].
Table 1: Essential Validation Components for Wearable Devices
| Validation Phase | Primary Objective | Key Methodologies | Acceptance Criteria |
|---|---|---|---|
| Analytical Validation | Verify device technical performance against a reference standard [75] | Laboratory testing under controlled conditions; repeated measures analysis | High intra-class correlation coefficients (>0.9); low coefficient of variation (<5%) |
| Clinical Validation | Establish device capability to measure the intended physiological or behavioral construct [75] | Comparison against clinically accepted reference standards; hypothesis testing | Statistically significant correlation with gold standard; minimal bias in Bland-Altman plots |
| Operational Validation | Confirm device performance in real-world settings matching the COU [75] | Field testing in target population; usability assessments | High participant compliance (>70%); minimal data loss (<10%); successful integration with data platforms |
Technical Performance Metrics
Quantifying technical performance requires standardized metrics tailored to dietary monitoring. For calorie intake estimation, specific attention must be paid to measurement accuracy across the entire intake spectrum, with particular focus on the lower range where overestimation typically occurs.
Table 2: Technical Performance Metrics for Dietary Monitoring Wearables
| Metric | Definition | Calculation Method | Target Threshold |
|---|---|---|---|
| Mean Absolute Percentage Error (MAPE) | Average absolute percentage difference between measured and actual values [39] | (1/n) × Σ|(Actual - Measured)/Actual| × 100 | <30% for portion size estimation [39] |
| Bias at Low Intake | Systematic tendency to overestimate low calorie intake | Mean difference between measured and actual values at <500 kcal intake | <15% overestimation |
| Precision | Consistency of repeated measurements under unchanged conditions | Standard deviation of repeated measures on same subject/scenario | Coefficient of variation <8% |
| Sensitivity to Meal Size | Ability to detect differences in small vs. large meals | Effect size between different portion conditions | Cohen's d >0.8 for portion discrimination |
Experimental Protocols for Validation
Protocol for Dietary Intake Validation
This protocol validates wearable devices for calorie intake assessment, specifically addressing overestimation of low intake.
Objective: To determine the accuracy of wearable sensors in estimating calorie intake across varying intake levels, with particular focus on identifying and quantifying systematic overestimation at low intake levels.
Materials:
- Wearable sensors (e.g., necklace sensor, wristband, body camera) [76]
- Standardized weighing scale (e.g., Salter Brecknell) [39]
- Reference foods with known nutrient composition
- Data collection platform and processing software
Procedure:
- Participant Preparation: Recruit participants representative of the target study population. Obtain informed consent following institutional review board approval.
- Device Setup: Fit participants with all wearable devices according to manufacturer specifications. For dietary monitoring, this typically includes:
- Standardized Meal Protocol: Present participants with meals of precisely measured portions using standardized weighing scales. Include:
- Low-calorie meals (<500 kcal)
- Medium-calorie meals (500-800 kcal)
- High-calorie meals (>800 kcal)
- Data Collection:
- Record eating sessions using all wearable devices simultaneously
- Document actual food consumption through weighed leftovers
- Collect participant-reported context (mood, environment, social setting) via smartphone app [76]
- Data Processing:
- Analysis:
- Compare sensor-estimated intake with actual consumption
- Calculate MAPE for each intake level separately
- Quantify bias specifically at low intake levels
- Identify contextual factors influencing accuracy (time of day, social setting, food type)
Protocol for Real-World Performance Assessment
Objective: To evaluate wearable device performance in free-living conditions and identify factors affecting data quality and participant compliance.
Procedure:
- Device Deployment: Provide participants with wearable devices and charging equipment. Deliver comprehensive training on proper use, maintenance, and data syncing procedures.
- Monitoring Period: Conduct continuous monitoring for a minimum of 14 days to capture varied eating patterns and contextual factors [76].
- Compliance Tracking: Monitor device wear time through embedded sensors and periodic participant check-ins.
- Contextual Data Collection: Implement ecological momentary assessment to capture mood, environment, and social context during eating episodes [76].
- Data Quality Assessment:
- Quantify percentage of usable data collected
- Identify common failure modes (e.g., battery life, connectivity issues, improper wear)
- Document participant feedback on usability and burden
Visualization of Validation Workflows
Dietary Intake Validation Protocol
Overestimation Analysis Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Tools for Wearable Validation in Dietary Research
| Tool Category | Specific Examples | Function in Validation | Key Considerations |
|---|---|---|---|
| Wearable Sensors | NeckSense [76], HabitSense body camera [76], wrist-worn accelerometers | Capture eating behaviors, motion patterns, and contextual data | Battery life, data storage capacity, form factor, participant comfort |
| Reference Standards | Standardized weighing scales (Salter Brecknell) [39], doubly labeled water, direct observation | Provide gold-standard measurements for comparison | Measurement precision, practicality for real-world use, cost |
| Data Processing Platforms | EgoDiet pipeline [39], custom algorithm development platforms | Process raw sensor data into meaningful metrics | Computational requirements, transparency of algorithms, validation status |
| Contextual Assessment Tools | Smartphone apps for ecological momentary assessment [76], environmental sensors | Capture mood, social context, environment during eating | Participant burden, data integration capabilities, privacy protection |
| Validation Software | Statistical packages (R, Python), data visualization tools, bias detection algorithms | Analyze accuracy, precision, and systematic errors | Compatibility with sensor data formats, statistical robustness |
Troubleshooting Guides and FAQs
Technical Issues
Q: The wearable devices are producing unexpectedly high estimates for low calorie intake. How can we address this systematic overestimation?
A: Systematic overestimation at low intake levels requires a multi-faceted approach:
- Algorithm Calibration: Develop intake-level-specific calibration curves using reference data collected across the entire intake spectrum. Implement non-linear correction factors that give more weight to accurate measurement at lower ranges.
- Contextual Adjustment: Incorporate contextual data (time of day, eating pace, social setting) into estimation algorithms, as these factors significantly influence accuracy [76].
- Multi-Sensor Fusion: Combine data from multiple sensors (necklace, wrist, camera) to improve specificity for actual consumption versus other oral activities [76].
Q: We are experiencing high data loss rates from wearable devices in free-living studies. What strategies can improve data completeness?
A: High data loss compromises study validity and requires both technical and participant-focused solutions:
- Robust Data Handling: Ensure devices have sufficient non-volatile memory to prevent data loss during transmission failures. Implement continuous background syncing when possible [77].
- Participant Engagement: Provide clear instructions and regular support. Consider simplified charging solutions and devices with extended battery life (≥7 days) [78].
- Compliance Monitoring: Implement real-time compliance tracking to identify issues early. Set up automated alerts for extended non-wear periods [78].
Q: How do we handle geographic variability when deploying the same wearable devices across multiple countries?
A: Geographic deployment introduces regulatory and technical complexities:
- Regulatory Compliance: Verify device regulatory status in each target country, including medical device clearance and wireless transmission restrictions [77].
- Technical Compatibility: Ensure cellular and wireless connectivity compatibility across regions. Test performance with local dietary patterns and cuisine [77].
- Cultural Adaptation: Validate devices with local foods and eating customs. Provide instructions in local languages and account for cultural variations in eating behaviors [39].
Methodological Issues
Q: What sample size is adequate for pre-study validation of a wearable device for calorie intake measurement?
A: Validation sample size depends on several factors:
- Primary Endpoint Variability: For calorie intake, which typically shows high within-subject variability, include at least 30-50 participants to reliably detect clinically significant biases.
- Heterogeneity: Ensure the sample represents the target population in terms of age, BMI, sex, and cultural background to capture varying eating patterns [76].
- Meal Scenarios: Include multiple eating scenarios (low, medium, high intake) across different contexts (alone, social, home, restaurant) to comprehensively characterize device performance [76].
Q: How long should the validation period be to adequately capture real-world performance?
A: Validation period duration should balance comprehensiveness with practicality:
- Minimum Duration: At least 14 continuous days to capture weekly patterns and variability [76].
- Context Coverage: Ensure the period includes diverse contexts (weekdays/weekends, various social settings, different meal types).
- Seasonal Considerations: For longer-term studies, consider potential seasonal effects on eating patterns.
Q: What reference standard is most appropriate for validating free-living calorie intake assessment?
A: Selection of reference standards involves trade-offs between accuracy and practicality:
- High-Accuracy Settings: In controlled facilities, use direct observation plus weighed food intake [39].
- Real-World Validation: In free-living conditions, use a combination of food diaries with photo documentation and periodic 24-hour dietary recalls [39].
- Emerging Technologies: Consider using egocentric cameras (e.g., EgoDiet pipeline) as an intermediate validation standard, acknowledging their own limitations [39].
Data Management Issues
Q: How should we handle the massive datasets generated by continuous wearable sensors?
A: Managing large-scale sensor data requires thoughtful infrastructure:
- Data Reduction: Implement strategic data reduction at collection points, focusing on clinically meaningful features rather than storing all raw data [77].
- Processing Pipeline: Separate data collection from processing to allow flexible application of different algorithms to the same dataset [77].
- Archiving Strategy: Plan for long-term archiving of raw data to enable re-analysis with improved algorithms while managing storage costs [77].
Q: What quality control procedures should be implemented throughout data collection?
A: Robust quality control is essential for data integrity:
- Automated Monitoring: Implement automated systems to flag anomalous data patterns suggestive of device malfunction or improper wear.
- Regular Audits: Conduct periodic manual reviews of data quality metrics (compliance rates, signal quality, missing data patterns).
- Participant Feedback: Establish channels for participants to report device issues, providing early warning of systematic problems.
Conclusion
The systematic overestimation of energy expenditure by low-cost wearables presents a significant challenge for their direct use in clinical research and drug development. Evidence consistently shows that while devices may be reliable for heart rate and step counting, their energy expenditure metrics, particularly for low-calorie activities, often lack the required accuracy, with errors exceeding 30-50% for some devices. Successfully leveraging this technology requires a rigorous, validated approach that includes understanding device-specific limitations, implementing calibration and standardization protocols, and cautiously interpreting data within the context of known biases. Future efforts must focus on developing transparent algorithms, creating robust validation frameworks that keep pace with rapid device updates, and fostering collaborative standards to ensure that wearable data can be trusted for critical biomedical applications.
References
- 1. Can you trust your smartwatch? A deep dive into calorie ... [https://blogs.sas.com/content/efs/?p=28151]
- 2. Accuracy and Precision of Energy Expenditure, Heart Rate ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9047731/]
- 3. Validity of four low-cost smartwatches in estimating energy ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12456781/]
- 4. Factors Affecting Energy Expenditure and Requirements - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK591031/]
- 5. What are the most common hardware issues with wearable ... [https://www.linkedin.com/advice/0/what-most-common-hardware-issues-wearable-technology-uaxgc]
- 6. Troubleshooting Wearable Fitness App Deployment Issues [https://moldstud.com/articles/p-troubleshooting-common-issues-in-wearable-fitness-app-deployment-expert-solutions-tips]
- 7. Mean Absolute Percentage Error (MAPE): What You Need ... [https://arize.com/blog-course/mean-absolute-percentage-error-mape-what-you-need-to-know/]
- 8. Mean absolute percentage error [https://en.wikipedia.org/wiki/Mean_absolute_percentage_error]
- 9. A Comprehensive Guide to Mean Absolute Percentage ... [https://coralogix.com/ai-blog/a-comprehensive-guide-to-mean-absolute-percentage-error-mape/]
- 10. Validity of three smartwatches in estimating energy ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9549133/]
- 11. Wearable Technology to Quantify the Nutritional Intake of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7407252/]
- 12. Wearable Technology to Quantify the Nutritional Intake of Adults [https://mhealth.jmir.org/2020/7/e16405]
- 13. The Impact of Wearable Technologies in Health Research [https://pmc.ncbi.nlm.nih.gov/articles/PMC8826148/]
- 14. Wearables Have Mixed Reliability for Tracking Calorie ... [https://www.todaysdietitian.com/wearables-have-mixed-reliability-for-tracking-calorie-balance/]
- 15. Feasibility of wearable camera use to improve the accuracy ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9554419/]
- 16. Failing to encourage physical activity with wearable ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6146340/]
- 17. The Validation and Accuracy of Wearable Heart Rate Trackers ... [https://formative.jmir.org/2025/1/e70835]
- 18. A practical guide for selecting continuous monitoring ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11259861/]
- 19. The Complementary Roles of Clinical Trial Wearables and ... [https://www.ppd.com/blog/complementary-roles-clinical-trial-wearables-patient-reported-outcomes-pros/]
- 20. Regulatory Considerations for Wearables in Clinical Trials [https://delvehealth.com/regulatory-considerations-for-implementing-wearables-in-clinical-trials/]
- 21. Fitness trackers may not aid weight loss, study finds [https://www.theguardian.com/technology/2016/sep/21/fitness-trackers-may-not-aid-weight-loss-study-finds]
- 22. Keeping Pace with Wearables: A Living Umbrella Review ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11560992/]
- 23. Opinion: How accurate are wearable fitness trackers? Less ... [https://www.ucd.ie/newsandopinion/news/2024/august/20/opinionhowaccuratearewearablefitnesstrackerslessthanyoumightthink/]
- 24. Fitness trackers accurately measure heart rate but not calories ... [https://med.stanford.edu/news/all-news/2017/05/fitness-trackers-accurately-measure-heart-rate-but-not-calories-burned.html]
- 25. A Systematic Literature Review of the Factors that Influence ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7134235/]
- 26. Investigating sources of inaccuracy in wearable optical ... [https://www.nature.com/articles/s41746-020-0226-6]
- 27. Real-World Accuracy of Wearable Activity Trackers for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11399740/]
- 28. Evaluating the Validity of Current Mainstream Wearable ... [https://mhealth.jmir.org/2018/4/e94/]
- 29. A Validation Study to Confirm the Accuracy of Wearable ... [https://www.mdpi.com/2079-9292/12/11/2536]
- 30. Developing and comparing a new BMI inclusive energy ... [https://www.nature.com/articles/s41598-025-99963-0]
- 31. Assessing the Accuracy of Four Heart Rate Wearables and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11794680/]
- 32. The accuracy of heartbeat detection using ... [https://www.sciencedirect.com/science/article/pii/S0022073621001291]
- 33. Leveraging Accelerometry and Heart Rate Data from ... [https://pubmed.ncbi.nlm.nih.gov/40197719/]
- 34. Algorithmic Bias in Wearables → Term [https://fashion.sustainability-directory.com/term/algorithmic-bias-in-wearables/]
- 35. Data-Driven Overtraining: Wearable Algorithms Gone Wrong [https://punepost.com/wearable-algorithms/]
- 36. Affordable fitness tracker step count, heart rate and calorie ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12628992/]
- 37. Improved Wearable Devices for Dietary Assessment Using a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9609969/]
- 38. Experience of Using Wearable Devices for Dietary ... [https://diabetes.jmir.org/2025/1/e73381]
- 39. AI-enabled wearable cameras for assisting dietary ... [https://www.nature.com/articles/s41746-024-01346-8]
- 40. Future Directions for Integrative Objective Assessment of ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2020.00080/full]
- 41. The Problems with Calorie Counting [https://macrofactorapp.com/problems-with-calorie-counting/]
- 42. A Multi-Model Machine Learning Approach for Monitoring ... [https://publications.eai.eu/index.php/phat/article/view/5407]
- 43. Calories Burnt Prediction using Machine Learning [https://www.geeksforgeeks.org/machine-learning/calories-burnt-prediction-using-machine-learning/]
- 44. A review of AI-based health prediction using apple watch ... [https://link.springer.com/article/10.1007/s42452-025-07783-8]
- 45. Troubleshooting Guide with Did You Mean [https://medium.com/@amitavamanna/troubleshooting-guide-with-did-you-mean-using-multimodal-rag-95601830c1ea]
- 46. JMIR mHealth and uHealth - Identifying Data Dimensions for... Quality [https://mhealth.jmir.org/2021/12/e31618]
- 47. Challenges and recommendations for wearable devices in digital... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9931360/]
- 48. The Drawbacks of Using Wearable Devices to Inform ... [https://macrofactorapp.com/wearables/]
- 49. On the Reliability of Wearable Technology [https://pmc.ncbi.nlm.nih.gov/articles/PMC10346338/]
- 50. Data Interpretation Issues in Wearables | by Marco Altini [https://medium.com/@altini_marco/data-interpretation-issues-in-wearables-a3942cae82ac]
- 51. Calibration-free and ready-to-use wearable ... [https://www.sciencedirect.com/science/article/abs/pii/S0956566324007759]
- 52. CALIBRATION AND VALIDATION OF WEARABLE ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3273335/]
- 53. The Utility of Calibrating Wearable Sensors before ... [https://www.mdpi.com/1424-8220/24/17/5736]
- 54. The Art of Troubleshooting for Customer Support ... [https://www.helpscout.com/helpu/art-of-troubleshooting-support/]
- 55. Study Examines How Well Wearable Tech Tracks Fitness ... [https://olemiss.edu/news/2025/06/apple-watch-accuracy-study/index.html]
- 56. How a new U.S. health study is fixing bias in wearable data ... [https://www.news-medical.net/news/20251009/How-a-new-US-health-study-is-fixing-bias-in-wearable-data-research.aspx]
- 57. Expert Statement and Checklist of the INTERLIVE Network [https://pmc.ncbi.nlm.nih.gov/articles/PMC9325806/]
- 58. Functional Testing of Wearable Devices: Key Best Practices [https://www.testdevlab.com/blog/best-practices-for-functional-testing-of-wearable-devices]
- 59. Using Wearable Activity Type Detection to Improve ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6122605/]
- 60. Best practices for analyzing large-scale health data from ... [https://www.nature.com/articles/s41746-019-0121-1]
- 61. Accuracy of Wearable Technology & Smart Watches [https://www.aim7.com/blog/smartwatch-wearable-technology-accuracy]
- 62. Investigating the accuracy of Apple Watch VO2 max ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12080799/]
- 63. Reliability and Validity of Commercially Available ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7509623/]
- 64. Comparison of two portable metabolic systems for measuring ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12259656/]
- 65. Comparison of two portable metabolic systems for ... [https://www.frontiersin.org/journals/physiology/articles/10.3389/fphys.2025.1583703/full]
- 66. Indirect Calorimetry in Clinical Practice - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC6780066/]
- 67. How to interpret and apply the results of indirect calorimetry ... [https://www.sciencedirect.com/science/article/pii/S2405457724012646]
- 68. A multidevice and multimodal dataset for human energy ... [https://www.nature.com/articles/s41597-022-01643-5]
- 69. Wearable technologies for health research [https://www.sciencedirect.com/science/article/pii/S0889159123002313]
- 70. Assessment of ownership of smart devices and the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10883993/]
- 71. The Impact of AI on the Development of Multimodal Wearable ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12158963/]
- 72. 3 Challenges Facing the Wearable Sensors Market [https://www.edge-ai-vision.com/2025/02/3-challenges-facing-the-wearable-sensors-market/]
- 73. Study explores AI-enhanced wearable devices [https://www.buffalo.edu/ubnow/stories/2025/11/fraser-ai-wearable-devices.html]
- 74. Five Key Trends for Wearables in 2025 [https://www.techinsights.com/blog/five-key-trends-wearables-2025]
- 75. Wearable Devices in Clinical Trials: Hype and Hypothesis - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6032822/]
- 76. Wearable Sensors Could Reshape Obesity Treatment [https://news.feinberg.northwestern.edu/2025/09/19/wearable-sensors-could-reshape-obesity-treatment/]
- 77. 5 Important Questions to Ask Your Wearable Technology Partner [https://blog.ametris.com/blog/operations-technology-partner]
- 78. Enhancing Clinical Trials with Wearable Digital Health ... [https://acrpnet.org/2024/10/22/enhancing-clinical-trials-with-wearable-digital-health-technologies-bridging-the-gap-between-data-and-real-life-patient-experiences]