Validating Food Intake via Wearable Device Data: Methods, Challenges, and Applications in Biomedical Research
This article provides a comprehensive analysis of the current state and validation of wearable devices for objective food intake monitoring, a critical need in nutritional science and drug development.
Validating Food Intake via Wearable Device Data: Methods, Challenges, and Applications in Biomedical Research
Abstract
This article provides a comprehensive analysis of the current state and validation of wearable devices for objective food intake monitoring, a critical need in nutritional science and drug development. It explores the foundational principles of technologies like bio-impedance sensors, wearable cameras, and accelerometers. The scope extends to methodological applications across research and clinical settings, an examination of technical and practical limitations, and a comparative validation against established standards like Doubly Labeled Water. Aimed at researchers and drug development professionals, this review synthesizes evidence to guide the effective integration of these tools into rigorous scientific practice.
The New Frontier of Dietary Assessment: Core Principles and Technologies in Wearable Monitoring
The Critical Need for Objective Dietary Data in Clinical and Population Research
Accurate dietary intake measurement is foundational to understanding the role of nutrition in human health and disease, yet it remains notoriously challenging to capture accurately and reliably through self-report methods [1]. Traditional dietary assessment tools—including food records, 24-hour recalls, and food frequency questionnaires (FFQs)—are plagued by both random and systematic measurement errors that substantially limit their utility in clinical and population research [1]. These methods rely heavily on participant memory, literacy, motivation, and honesty, introducing biases that cannot be easily quantified or corrected. The pervasive issue of energy underreporting across all self-reported methods further compromises data integrity, with only a limited number of recovery biomarkers (for energy, protein, sodium, and potassium) available to validate reported intakes [1]. As research increasingly links dietary patterns to chronic diseases, the scientific community faces a critical imperative: to transition from error-prone subjective reports to objective, technologically-enabled dietary data collection methods that can capture dietary exposures with greater precision and reliability.
Comparative Analysis of Traditional Dietary Assessment Methods
The selection of an appropriate dietary assessment method depends heavily on the research question, study design, sample characteristics, and target sample size [1]. Each traditional method carries distinct advantages and limitations that researchers must carefully consider when designing nutritional studies.
Table 1: Comparison of Traditional Dietary Assessment Methods
| Method | Time Frame | Primary Applications | Strengths | Limitations |
|---|---|---|---|---|
| 24-Hour Dietary Recall | Short-term (previous 24 hours) | Total diet assessment; cross-sectional studies [1] | Does not require literacy; reduces reactivity by capturing past intake [1] | Relies on memory; requires extensive training; high cost per participant [1] |
| Food Record | Short-term (typically 3-4 days) | Total diet assessment; intervention studies [1] | Captures current intake in real-time; detailed quantitative data [1] | High participant burden; reactivity (changing diet for recording); requires literate/motivated population [1] |
| Food Frequency Questionnaire | Long-term (months to year) | Habitual diet assessment; large epidemiological studies [1] | Cost-effective for large samples; captures usual intake over time [1] | Limited food list; less precise for absolute intakes; relies on generic memory [1] |
| Dietary Screeners | Varies (often prior month/year) | Specific nutrients or food groups [1] | Rapid administration; low participant burden; cost-effective [1] | Narrow focus; requires population-specific development and validation [1] |
Each method produces different types of measurement error. Short-term instruments like 24-hour recalls and food records are subject to within-person variation due to day-to-day fluctuations in dietary intake, requiring multiple administrations to estimate habitual intake [1]. Macronutrient estimates from 24-hour recalls are generally more stable than those of vitamins and minerals, with particularly large day-to-day variability reported for cholesterol, vitamin C, and vitamin A [1]. FFQs aim to capture long-term habitual intake but are limited by their fixed food list and portion size assumptions, making them more suitable for ranking individuals by intake levels rather than measuring absolute consumption [1].
Emerging Wearable Technologies for Objective Dietary Monitoring
Technological advancements have introduced wearable sensors that passively or automatically capture dietary data, minimizing the burden and bias associated with self-report methods. These devices represent a paradigm shift toward objective dietary assessment in free-living settings.
Continuous Glucose Monitors
Continuous Glucose Monitors provide real-time, dynamic glucose measurements that reflect the physiological impact of dietary intake [2]. Originally developed for type 1 diabetes management, CGM technology has expanded to research applications, particularly for understanding postprandial glucose responses to different meal compositions [3]. Modern CGM systems sample glucose levels at regular intervals (e.g., every 5-15 minutes) via a subcutaneous sensor, providing dense temporal data on glycemic excursions [2]. When paired with detailed meal records, CGM data can reveal individual variations in glycemic response to identical meals, enabling personalized nutritional recommendations [2]. Studies have demonstrated that CGM use increases mindfulness of meal choices and motivates behavioral changes, particularly when users receive real-time feedback on how specific foods affect their glucose levels [3].
The eButton and Imaging Devices
The eButton is a wearable device that automatically captures food data through imaging, typically worn on the chest to record meals via photographs taken at regular intervals (e.g., every 3-6 seconds) [3]. The captured images are processed to determine food identification, portion size, and nutrient composition through computer vision algorithms [3]. Research has established the feasibility and acceptability of the eButton in real-life settings, with studies noting its ability to increase user mindfulness of food consumption [3]. Participants in feasibility studies reported that using the eButton made them more conscious of portion sizes and food choices, though some expressed privacy concerns and encountered practical difficulties with camera positioning [3].
Integrated Multimodal Sensing Systems
The most advanced approach combines multiple sensors to capture complementary dimensions of dietary behavior. The CGMacros dataset exemplifies this integrated approach, containing synchronized data from two CGM devices (Abbott FreeStyle Libre Pro and Dexcom G6 Pro), a Fitbit activity tracker, food photographs, and detailed macronutrient information [2]. This multimodal framework enables researchers to analyze relationships between dietary intake, physiological responses, and physical activity in a comprehensive manner. The dataset includes 45 participants (15 healthy, 16 pre-diabetes, 14 type 2 diabetes) who consumed meals with varying and known macronutrient compositions over ten consecutive days in free-living conditions [2]. Such rich, multimodal datasets are essential for developing machine learning approaches to automated diet monitoring and personalized nutrition recommendations.
Table 2: Wearable Device Performance in Dietary Research
| Device Type | Primary Data Collected | Research Applications | Participant Experience | Implementation Considerations |
|---|---|---|---|---|
| Continuous Glucose Monitor | Interstitial glucose measurements every 5-15 minutes [2] | Postprandial glucose response analysis; meal composition estimation [2] | Increases meal choice mindfulness; may cause skin sensitivity; sensors can detach [3] | Requires structured support from healthcare providers for data interpretation [3] |
| eButton | Food images every 3-6 seconds during meals [3] | Food identification; portion size estimation; nutrient analysis [3] | Increases dietary awareness; raises privacy concerns; positioning can be challenging [3] | Computer vision algorithms needed for image analysis; privacy protections essential [3] |
| Activity Trackers | Heart rate; metabolic equivalents; movement [2] | Energy expenditure estimation; contextualizing dietary effects [2] | Generally well-tolerated; provides holistic health picture | Data integration challenges with other sensor systems |
Experimental Protocols for Dietary Assessment Studies
Protocol: Multimodal Dietary Data Collection
The CGMacros study provides a robust methodological framework for collecting objective dietary data in free-living populations [2]. This protocol can be adapted for various research contexts investigating diet-health relationships:
Participant Screening and Recruitment: Recruit participants representing target health statuses (healthy, pre-diabetes, type 2 diabetes). Exclusion criteria should include medications that significantly impact glucose metabolism (e.g., insulin, GLP-1 receptor agonists) to reduce confounding variables [2].
Baseline Data Collection: Collect comprehensive baseline measures including:
- Demographic information (age, gender, race/ethnicity)
- Anthropometric measurements (height, weight, BMI)
- Blood analytics (HbA1c, fasting glucose, insulin, lipid profile)
- Gut microbiome profiles via stool samples [2]
Sensor Deployment: Equip participants with:
- Two CGM devices placed on upper arm and abdomen (e.g., Abbott FreeStyle Libre Pro and Dexcom G6 Pro)
- Chest-worn eButton for meal imaging
- Wrist-worn activity tracker (e.g., Fitbit Sense) [2]
Dietary Intervention Protocol: Implement a structured yet free-living dietary protocol:
- Provide standardized breakfasts and lunches with varying macronutrient compositions
- Allow self-selected dinners to increase ecological validity
- Mandate minimum 3-hour intervals between meals to isolate postprandial responses
- Instruct participants to capture food photographs before and after consumption [2]
Data Integration and Processing:
- Synchronize timestamps across all devices
- Interpolate CGM data to uniform sampling rate (e.g., 1-minute intervals)
- Link meal macronutrient data with CGM traces at corresponding timestamps
- Extract meal timestamps from food photographs [2]
Protocol: Cultural Adaptation for Diverse Populations
Research with Chinese Americans with type 2 diabetes demonstrates the importance of culturally adapted protocols [3]:
Culturally Sensitive Recruitment: Partner with community organizations; utilize culturally appropriate communication channels; offer materials in relevant languages.
Cultural Meal Considerations: Account for culturally significant foods (e.g., rice, noodles) when analyzing dietary patterns; recognize communal eating practices; understand cultural norms around food offerings and hospitality [3].
Technology Training: Provide comprehensive device orientation with language-appropriate materials; address privacy concerns common in certain cultural contexts; offer ongoing technical support [3].
Data Interpretation Framework: Contextualize findings within cultural dietary patterns; engage cultural informants in data analysis; recognize that Western dietary recommendations may conflict with traditional eating practices [3].
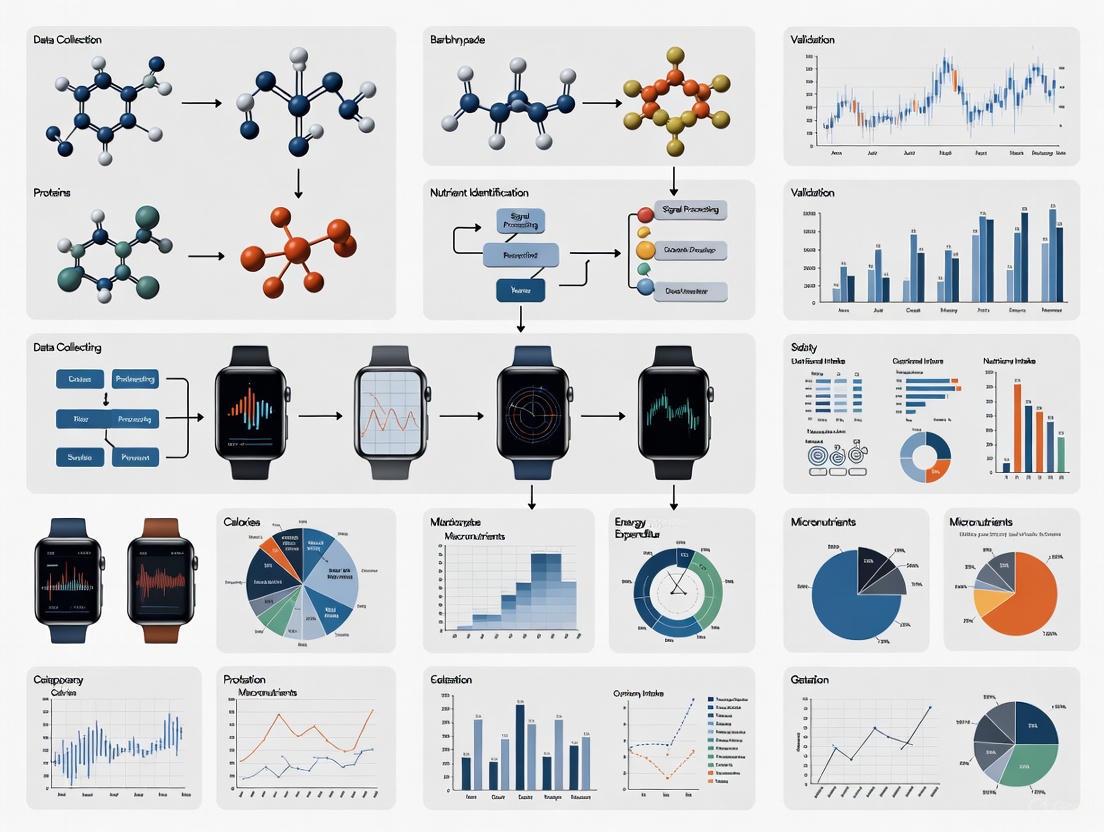
Visualizing Methodological Frameworks
Diagram 1: Multimodal Dietary Assessment Workflow
Table 3: Research Reagent Solutions for Dietary Assessment Studies
| Tool Category | Specific Products/Models | Research Function | Key Specifications |
|---|---|---|---|
| Continuous Glucose Monitors | Abbott FreeStyle Libre Pro; Dexcom G6 Pro [2] | Measures interstitial glucose concentrations at regular intervals | Sampling periods: 15-min (Libre Pro), 5-min (Dexcom); 10-14 day wear period [2] |
| Wearable Cameras | eButton [3] | Automatically captures food images during eating episodes | Image capture frequency: 3-6 seconds; chest-mounted positioning [3] |
| Activity Trackers | Fitbit Sense [2] | Quantifies physical activity and energy expenditure | Metrics: heart rate, metabolic equivalents, step count, minute-by-minute data [2] |
| Diet Tracking Software | MyFitnessPal [2] | Logs food intake and estimates nutrient composition | Database: extensive food database with macronutrient and micronutrient data [2] |
| Data Processing Tools | Custom Python/R scripts; Viome microbiome kit [2] | Processes multimodal data; analyzes biological samples | Functions: data synchronization, interpolation, microbiome sequencing [2] |
Data Integration and Analysis Approaches
The true potential of objective dietary assessment emerges through sophisticated integration of multimodal data streams. Research demonstrates that combining CGM data with meal information enables machine learning approaches to estimate meal macronutrient content based on the shape of postprandial glucose responses [2]. This is possible because postprandial glucose responses depend not only on carbohydrate content but also on the amounts of protein and fat in a meal [2].
Temporal alignment of data sources is critical for meaningful analysis. The CGMacros dataset exemplifies best practices through:
- Linear interpolation of CGM data to create uniform one-minute sampling intervals
- Extraction of meal timestamps from food photographs
- Calculation of metabolic equivalents from activity tracker data using mean filtering with 20-minute windows [2]
This integrated approach enables researchers to analyze precise temporal relationships between dietary intake, physiological responses, and physical activity patterns, creating a comprehensive picture of diet-health interactions in free-living contexts.
The limitations of traditional self-reported dietary assessment methods necessitate a paradigm shift toward objective, technology-enabled approaches. Wearable devices like continuous glucose monitors and automated food imaging systems offer promising alternatives that minimize recall bias and participant burden while generating rich, multimodal datasets. The integration of these technologies—capturing dietary intake, physiological responses, and physical activity simultaneously—provides unprecedented opportunities to understand complex diet-health relationships in free-living populations. As these methodologies advance, they promise to enhance the precision of nutritional epidemiology, strengthen the evidence base for dietary guidelines, and ultimately support more effective, personalized nutrition interventions for disease prevention and management.
Accurately validating food intake represents a significant challenge in nutritional science, clinical research, and drug development. Traditional methods like 24-hour dietary recalls and food diaries are plagued by subjectivity, with under- or over-reporting compromising data integrity [4]. The emergence of wearable sensors offers a paradigm shift toward objective, passive monitoring of dietary intake and its physiological effects. This guide provides a systematic comparison of two dominant technological approaches: wearable bio-impedance sensors and egocentric wearable cameras. We objectively evaluate their operational principles, performance metrics, and experimental validation to inform researcher selection and implementation.
The technological landscape for food intake validation is broadly divided into two categories: physiological response monitors (e.g., bio-impedance sensors) that measure the body's reaction to nutrient intake, and direct intake capturers (e.g., wearable cameras) that document food consumption visually. The table below summarizes their core characteristics, capabilities, and limitations.
Table 1: Comparative Analysis of Wearable Technologies for Food Intake Validation
| Feature | Wearable Bio-Impedance Sensors | Wearable Cameras (Egocentric Vision) |
|---|---|---|
| Primary Function | Infers intake by measuring physiological fluid/electrolyte shifts [5] | Directly captures food consumption events and estimates portion size via image analysis [6] |
| Measured Parameters | Bioelectrical impedance (Resistance, Reactance), Phase Angle, calculated energy intake [7] [5] | Food container geometry, food region ratio, camera-to-container distance, portion weight [6] |
| Key Outputs | Estimated caloric intake, macronutrient grams, body water compartments [5] | Identified food types, portion size estimation (weight/volume), eating timing and sequence [6] |
| Reported Accuracy (vs. Reference) | High variability: Mean bias of -105 kcal/day vs. controlled meals; wide limits of agreement [5] | MAPE of 28.0-31.9% for portion size vs. dietitian assessment or 24HR [6] |
| Primary Advantage | Passive, provides data on metabolic response | Moves closer to "ground truth" of intake; records contextual eating behaviors [6] |
| Inherent Limitations | Signal loss; over/under-estimation at intake extremes; assumes standard hydration [5] | Privacy concerns; computational complexity; challenges with mixed dishes and low-light conditions [6] |
Deep Dive: Wearable Bio-Impedance Sensing
Operational Principles and Signaling Pathways
Bio-impedance sensors for nutritional intake estimation function on the principle that the consumption and absorption of nutrients, particularly glucose, cause measurable shifts in body fluid compartments between extracellular (ECW) and intracellular (ICW) spaces. A low-level, alternating current is passed through tissues, and the opposition to this flow (impedance, Z) is measured. Impedance comprises Resistance (R), primarily from extracellular fluids, and Reactance (Xc), related to cell membranes' capacitive properties [7] [8]. The Phase Angle (PhA), derived from the arc tangent of the Xc/R ratio, serves as an indicator of cellular integrity, fluid status, and nutritional status [7]. Algorithms then convert the temporal patterns of these fluid shifts into estimates of energy intake and macronutrient absorption [5].
Diagram: Bio-Impedance Signaling Pathway for Nutrient Intake Estimation
Experimental Protocol for Validation
A typical protocol for validating a bio-impedance-based nutrient intake monitor involves tightly controlled meal conditions and comparison against a rigorous reference method [5].
- Objective: To evaluate the accuracy and precision of a wearable bio-impedance device in estimating daily energy intake in free-living participants under controlled meal conditions.
- Population: Adult participants (e.g., n=25), screened for absence of chronic metabolic disease, weight stability, and not on restricted diets [5].
- Reference Method: Collaboration with a metabolic kitchen to prepare and serve calibrated study meals. All food is weighed, and its energy/macronutrient content is calculated using established databases. Participants consume meals under direct observation to ensure 100% reporting accuracy for intake [5].
- Test Method: Participants wear the bio-impedance device (e.g., a wristband) continuously over the validation period (e.g., two 14-day periods). The device operates passively to collect data [5].
- Data Analysis: Comparison of daily energy intake (kcal/day) from the reference method versus the device output using Bland-Altman analysis to determine mean bias and limits of agreement [5].
Deep Dive: Wearable Camera Systems (Egocentric Vision)
Operational Principles and Computational Workflow
Wearable cameras like the EgoDiet system approach dietary assessment by passively capturing first-person (egocentric) images. The core innovation lies in its multi-module AI pipeline that automates the conversion of images into portion size estimates, minimizing human intervention [6].
- EgoDiet:SegNet: Utilizes a Mask R-CNN backbone to segment food items and their containers from the image, which is crucial for subsequent analysis [6].
- EgoDiet:3DNet: A depth estimation network that reconstructs 3D models of the containers and estimates camera-to-container distance, obviating the need for expensive depth-sensing cameras [6].
- EgoDiet:Feature: An extractor that derives portion size-related features from the previous modules. Key indicators include the Food Region Ratio (FRR), which is the proportion of the container region occupied by a specific food, and the Plate Aspect Ratio (PAR), which helps estimate the camera's tilting angle [6].
- EgoDiet:PortionNet: The final module that estimates the consumed portion size in weight. It leverages the extracted features to solve a "few-shot regression" problem, as large-scale, manually weighed food datasets are rare [6].
Diagram: Wearable Camera Dietary Analysis Computational Workflow
Experimental Protocol for Validation
The validation of a passive wearable camera system is typically conducted in field studies comparing its performance against trained dietitians or traditional methods [6].
- Objective: To assess the accuracy of a wearable camera pipeline (EgoDiet) for portion size estimation in free-living or community settings.
- Population: Field studies conducted in specific populations (e.g., of Ghanaian and Kenyan origin) to test robustness across diets [6].
- Reference Method: In one study design, dietitians' assessments of portion size from images can serve as one benchmark. Another common reference is the traditional 24-hour dietary recall (24HR) interview [6].
- Test Method: Participants wear a low-cost, wearable camera that automatically captures images throughout the day, including eating episodes. The EgoDiet pipeline processes these images automatically [6].
- Data Analysis: The primary outcome is the Mean Absolute Percentage Error (MAPE) for portion size estimation. The MAPE of the EgoDiet system (e.g., 28.0%) is directly compared to the MAPE of dietitians (e.g., 40.1%) or the 24HR method (e.g., 32.5%) [6].
The Scientist's Toolkit: Key Research Reagents & Materials
Table 2: Essential Materials and Tools for Wearable Food Intake Validation Research
| Item | Function in Research |
|---|---|
| Multi-Frequency BIA (MFBIA) Device (e.g., InBody 770) | Provides segmental body composition analysis and raw parameters like Resistance (R) and Reactance (Xc) at multiple frequencies, offering detailed fluid compartment data [8]. |
| Tetrapolar Bioimpedance Analyzer (e.g., InBody S10) | Uses a standardized 8-point tactile electrode system to measure whole-body and segmental Phase Angle, a key indicator of cellular health and hydration [7]. |
| Low-Cost Wearable Camera | The core hardware for egocentric vision systems; passively captures first-person-view image data for automated dietary analysis in free-living conditions [6]. |
| Dual-Energy X-Ray Absorptiometry (DXA) | Serves as a reference method for validating body composition measures (Fat Mass, Fat-Free Mass) from BIA devices in validation studies [9] [8]. |
| Controlled Meal Kits | Pre-portioned, nutritionally calibrated meals used as a gold standard to validate the energy and macronutrient output of bio-impedance devices against known intake [5]. |
| 24-Hour Dietary Recall (24HR) | A traditional, interview-based dietary assessment method used as a comparative benchmark for validating new technologies like wearable cameras [6]. |
| Continuous Glucose Monitor (CGM) | Often used in conjunction with other sensors to provide correlative data on metabolic response to food intake, helping to triangulate nutrient absorption timing [5]. |
The choice between bio-impedance and wearable camera technologies is not a matter of selecting a superior option, but of aligning the technology with the research question. Bio-impedance sensors offer a physiological lens, indirectly inferring intake through metabolic changes, making them suitable for studies focused on energy balance and metabolic response. In contrast, wearable cameras provide a behavioral lens, directly observing and quantifying food consumption, which is invaluable for understanding dietary patterns and validating self-reported data. For the most comprehensive picture, future research frameworks may leverage multimodal approaches, integrating data from both sensor types alongside omics analyses to fully characterize the intricate relationships between diet, physiological response, and health outcomes [10] [4].
Accurately assessing dietary intake and eating behavior is fundamental to understanding their role in chronic diseases like obesity, type 2 diabetes, and heart disease [11] [12]. Traditional methods, such as 24-hour dietary recalls and food diaries, rely on self-reporting and are prone to significant memory bias, under-reporting, and participant burden [13] [12]. For instance, large dietary surveys have found that 27% to 38% of 24-hour food intake recalls are implausible when compared to objective measures like doubly-labeled water [13]. Wearable sensor technology presents a transformative opportunity to overcome these limitations by enabling the passive, objective, and high-resolution measurement of eating events and nutrient intake in naturalistic settings [11] [12]. This guide provides a comparative analysis of the core sensing modalities underpinning these wearable devices, framing them within the broader research thesis of validating food intake via wearable data. It is structured to equip researchers and scientists with a clear understanding of the technological landscape, experimental protocols, and performance characteristics of these emerging tools.
Core Sensing Modalities for Eating Event Detection
Wearable devices detect eating events by monitoring the physiological and physical manifestations of chewing, swallowing, and hand-to-mouth gestures. The primary sensing modalities can be categorized as follows.
Motion and Mechanistic Sensors
These sensors detect the physical movements associated with mastication. Key types include:
- Piezoelectric Strain Sensors: These sensors, often placed on the temporalis muscle, generate a signal in response to the mechanical deformation caused by muscle contraction during chewing [14]. One study used an LDT0-028K sensor from Measurement Specialties, placed on the left temporalis muscle, sampling data at 1 kHz [14].
- Accelerometers and Gyroscopes: Typically embedded in wrist-worn devices or headsets, these sensors detect the characteristic motion patterns of biting, chewing, and hand-to-mouth gestures [11] [12]. They are among the most common sensors used in multi-sensor systems for in-field eating detection [11].
- Piezoresistive Bend Sensors: These flexible sensors can be attached to eyeglass frames. Their resistance changes in response to bending caused by the contraction of the temporalis muscle during chewing [14]. A study utilizing a Spectra Symbol 2.2” sensor on the right temple of eyeglasses sampled data at 128 Hz [14].
Acoustic Sensors
Acoustic sensing captures the sounds of mastication and swallowing, typically via a microphone placed in or near the ear [12]. While highly sensitive, this method can be susceptible to ambient noise. Chewing sounds captured through an earpiece have been successfully used to develop automatic chewing detection for monitoring food intake behavior [14].
Physiological and Biometric Sensors
This category measures the physiological changes that occur during eating.
- Surface Electromyography (sEMG): sEMG involves placing electrodes directly on the skin overlying masticatory muscles (e.g., the temporalis or masseter). It measures the electrical activity associated with muscle contraction during chewing [14].
- Ear Canal Pressure Sensors: This novel approach leverages the physical deformation of the ear canal during jaw movement. An air pressure sensor (e.g., SM9541) is housed in a custom-molded earbud. The grinding motion of the jaw during chewing causes the ear canal to expand and contract, producing measurable pressure changes [14]. A published protocol sampled this data at 128 Hz [14].
Table 1: Comparison of Wearable Sensor Modalities for Eating Event Detection
| Sensing Modality | Measured Parameter | Common Placement | Key Advantages | Key Limitations |
|---|---|---|---|---|
| Piezoelectric Strain [14] | Temporalis muscle movement | Skin surface (temporalis) | Direct measure of muscle activity; High sensitivity | Susceptible to motion artifact; Requires skin contact |
| Accelerometer [11] [12] | Jaw and hand/arm motion | Wrist, head, neck | Ubiquitous in consumer devices; Good for gesture detection | Less specific to chewing; Confounded by other activities |
| Acoustic (Microphone) [14] [12] | Chewing/swallowing sounds | Ear canal, neck | High specificity to eating sounds | Privacy concerns; Affected by background noise |
| sEMG [14] | Muscle electrical activity | Skin surface (masseter/temporalis) | Direct measure of muscle activation | Can be obtrusive; Sensitive to sweat and electrode placement |
| Ear Canal Pressure [14] | Ear canal deformation | Ear canal | Passive and less obtrusive than some methods | Requires individual earbud molding; Novel, less validated |
Technical Workflow for Eating Event Detection
The following diagram illustrates the generalized signal pathway and data processing workflow for detecting eating events from sensor data.
Diagram 1: Signal processing workflow for eating event detection.
Sensing Modalities for Nutrient and Food Intake Assessment
Moving beyond mere eating event detection, more advanced technologies aim to identify the type and quantity of food consumed.
Egocentric (Wearable) Cameras
Wearable cameras capture first-person-view images of food before, during, and after consumption. Computer vision and deep learning algorithms then analyze these images to identify food items and estimate portion sizes.
- Active Capture vs. Passive Capture: Active methods require the user to manually capture images (e.g., with a smartphone), while passive methods use wearable cameras (e.g., the eButton or AIM) that automatically capture images at set intervals [15] [16]. Passive methods are less burdensome and can capture eating context and sequence [15].
- The EgoDiet Pipeline: This is an example of a comprehensive, vision-based dietary assessment system. It involves several modules [15]:
- EgoDiet:SegNet: Segments food items and containers in images.
- EgoDiet:3DNet: Estimates camera-to-container distance and reconstructs 3D container models.
- EgoDiet:Feature: Extracts portion size-related features like Food Region Ratio (FRR) and Plate Aspect Ratio (PAR).
- EgoDiet:PortionNet: Estimates the final portion size (weight) of the food consumed.
Integration with Continuous Glucose Monitors (CGM)
While not a direct nutrient sensor, CGM is a critical wearable technology for validating the metabolic impact of food intake. CGMs measure interstitial glucose levels in near-real-time, providing an objective physiological correlate of carbohydrate intake [17] [16]. When paired with dietary intake data from cameras or other sensors, CGM data can help researchers understand individual glycemic responses to specific foods and meals [16].
Table 2: Comparison of Nutrient Assessment Modalities
| Technology | Measured Parameter | Key Advantages | Key Limitations | Reported Performance |
|---|---|---|---|---|
| Wearable Camera (eButton) [15] [16] | Food images for type/volume | Passive capture; Provides rich contextual data | Privacy concerns; Complex data processing | MAPE for portion size: 28.0%-31.9% [15] |
| AI & Computer Vision (EgoDiet) [15] | Food type and portion size | Reduces error vs. 24HR; Automated analysis | Requires specialized algorithms | Outperformed dietitians' estimates (31.9% vs 40.1% MAPE) [15] |
| Continuous Glucose Monitor (CGM) [17] [16] | Interstitial glucose levels | Objective metabolic data; Real-time feedback | Measures response, not intake; Cost | Validated for clinical use; improves time-in-range [17] |
Experimental Protocols and Validation Methodologies
Robust experimental design is crucial for validating the performance of wearable eating sensors. Below are detailed methodologies from key studies.
Protocol: Validation of Chewing Strength Sensors
A foundational study evaluated four wearable sensors for estimating chewing strength in response to foods of different hardness (carrot, apple, banana) [14].
- Participants: 15 healthy volunteers.
- Sensors Deployed Simultaneously: 1) Ear canal pressure sensor, 2) Piezoresistive bend sensor on eyeglass temple, 3) Piezoelectric strain sensor on temporalis, 4) sEMG on temporalis.
- Food Procedure: Each participant consumed 10 bites of carrot, apple, and banana. Food hardness was objectively measured with a penetrometer.
- Data Analysis: Single-factor ANOVA was used to test the effect of food hardness on the standard deviation of sensor signals, followed by Tukey's multiple comparison test (5% significance level).
- Key Result: A significant effect of food hardness was found for all four sensors (p < .001), confirming their ability to distinguish chewing strength related to food texture [14].
Protocol: In-Field Eating Detection
A scoping review highlighted methods for validating wearable sensors in free-living conditions [11].
- Sensors: 65% of reviewed studies used multi-sensor systems, with accelerometers being the most common (62.5%).
- Ground Truth: All studies used a ground-truth method for validation. This included self-report (e.g., food diaries) and objective methods (e.g., video recording).
- Evaluation Metrics: The most frequently reported metrics were Accuracy and F1-score, though there is significant variation in reporting standards across the field [11].
Protocol: Validation of the "Feeding Table" UEM
A novel Universal Eating Monitor (UEM) was developed to track multiple foods simultaneously [13].
- Apparatus: A table integrated with five high-resolution balances, capable of monitoring up to 12 different foods at once. Data were collected every 2 seconds.
- Validation Experiment: 31 participants underwent a standard meal test over two consecutive days.
- Validation Metrics: Day-to-day repeatability for energy and macronutrient intake was assessed using Pearson correlation (e.g., energy: r = 0.82) and intra-class correlation coefficients (ICCs) (e.g., energy: ICC = 0.94) [13].
The Researcher's Toolkit: Essential Research Reagent Solutions
This section details key hardware, software, and analytical tools referenced in the cited experimental research.
Table 3: Essential Reagents and Tools for Wearable Eating Detection Research
| Item Name | Type | Function/Application | Example/Reference |
|---|---|---|---|
| Silicon Microstructures SM9541 | Sensor | Air pressure sensor for measuring ear canal deformation during chewing. | Used in ear canal pressure sensor system [14] |
| Measurement Specialties LDT0-028K | Sensor | Piezoelectric strain sensor for detecting temporalis muscle movement. | Placed on temporalis muscle [14] |
| Spectra Symbol 2.2" Bend Sensor | Sensor | Piezoresistive sensor for measuring muscle-induced bending of eyeglass temples. | Attached to right temple of eyeglasses [14] |
| eButton / AIM | Device | Wearable, passive cameras for capturing egocentric images of food intake. | Used for dietary assessment in free-living conditions [15] [16] |
| Freestyle Libre Pro | Device | Continuous Glucose Monitor (CGM) for capturing interstitial glucose levels. | Used to correlate food intake with glycemic response [16] |
| Mask R-CNN | Algorithm | Deep learning backbone for segmenting food items and containers in images. | Used in EgoDiet:SegNet module [15] |
| Universal Eating Monitor (UEM) | Apparatus | Laboratory-scale system with embedded scales for high-resolution tracking of eating microstructure. | "Feeding Table" with multiple balances [13] |
The field of wearable sensing for dietary monitoring has moved beyond simple event detection toward sophisticated, multi-modal systems capable of characterizing both eating behavior and nutrient intake. As the experimental data demonstrates, no single modality is perfect; each has distinct strengths and limitations in terms of accuracy, obtrusiveness, and applicability in field settings [14] [11] [12]. The future of validating food intake via wearable data lies in the intelligent fusion of complementary sensors—such as combining motion sensors for bite detection with cameras for food identification and CGM for metabolic validation [16]. For researchers, the critical challenges remain: improving the accuracy of nutrient estimation, ensuring user privacy (especially with cameras), standardizing validation metrics, and developing robust algorithms that perform reliably in the unstructured complexity of free-living environments [11] [15] [12]. The tools and comparative data presented in this guide provide a foundation for designing rigorous studies that can advance this promising field.
Wearable devices have evolved from simple step-counters to sophisticated health monitoring systems, creating new paradigms for biomedical research and clinical care. These technologies provide an unprecedented opportunity to collect continuous, real-time physiological data in naturalistic settings, moving beyond traditional clinic-based measurements [18] [19]. In the specific context of nutritional science, wearables offer potential solutions to long-standing challenges in dietary assessment, primarily the reliance on self-reported methods that are prone to significant error, bias, and participant burden [20] [21]. This review examines the four key functions of wearable devices—monitoring, screening, detection, and prediction—with a specific focus on their application in validating food intake and eating behaviors, a crucial area for researchers, scientists, and drug development professionals seeking objective measures in nutritional research and clinical trials.
Core Functions of Wearable Technology
Wearable devices serve distinct but interconnected functions in health research. Understanding this functional hierarchy is essential for selecting appropriate technologies and interpreting generated data.
Table 1: Core Functions of Wearables in Health Research
| Function | Description | Primary Data Sources | Example in Food Intake Research |
|---|---|---|---|
| Monitoring [22] | Continuous, passive data collection of physiological and behavioral metrics. | Accelerometers, PPG, ECG, IMUs, cameras [18] [11] | Tracking wrist movements, heart rate, and glucose levels throughout the day. |
| Screening [22] | Identifying at-risk individuals or specific conditions within a monitored population. | Algorithmic analysis of monitored data trends. | Flagging individuals with irregular eating patterns (e.g., night-eating syndrome) from continuous activity data. |
| Detection [22] | Recognizing specific, discrete events or activities from continuous data streams. | Machine learning classifiers applied to sensor data. | Automatically detecting the onset and duration of an eating episode from a combination of arm movement and chewing sounds. |
| Prediction [22] | Forecasting future health states or events based on historical and real-time data. | Predictive algorithms and statistical models. | Predicting postprandial glycemic response based on pre-meal physiology and meal size estimation. |
Monitoring: The Foundation of Data Acquisition
Monitoring is the fundamental, continuous data-collection function that enables all other advanced capabilities. In nutritional research, this involves the passive gathering of data related to eating activity and its physiological consequences. Common monitoring technologies include inertial measurement units (IMUs) to capture hand-to-mouth gestures, photoplethysmography (PPG) to track heart rate variability, and electrocardiography (ECG) for heart rhythm analysis [18]. Emerging tools also include wearable cameras that automatically capture point-of-view images, providing a passive record of food consumption without relying on user memory [21]. The strength of monitoring lies in its ability to capture high-resolution, temporal data in free-living environments, thus providing an ecological momentary assessment that is more reflective of true habitual behavior than self-reports [11] [19].
Screening: Identifying Patterns and Risk
Screening utilizes the data collected through monitoring to identify specific conditions or risk factors within a population. This is often a passive process where algorithms scan for predefined patterns or deviations from normative baselines. For example, in a large-scale public health program, wearable-derived data could be used to screen for populations with consistently high sedentary behavior coupled with frequent snacking patterns [22] [23]. In cardiometabolic health, wearables can screen for atrial fibrillation, a condition that may be influenced by dietary factors like alcohol or caffeine intake [18] [19]. The screening function thus helps researchers and clinicians target interventions and deeper analysis toward individuals who would benefit most.
Detection: Pinpointing Discrete Events
Detection is the function of identifying discrete, specific events from the continuous stream of monitored data. In eating behavior research, this is a primary focus, with studies developing algorithms to detect the exact start and end times of eating episodes. This is typically achieved using multi-sensor systems. For instance, a 2020 scoping review found that 62.5% of in-field eating detection studies used accelerometers to detect distinctive wrist movements associated with biting, while others used acoustic sensors to capture chewing sounds [11]. Detection is more precise than screening, aiming not just to find at-risk individuals, but to log the exact timing and, in some cases, the microstructure (e.g., number of bites, chewing rate) of each eating event.
Prediction: Forecasting Future Outcomes
Prediction represents the most advanced function, using historical and real-time data to infer future health states or events. In the context of nutrition, this could involve predicting an individual's glycemic response to a meal or forecasting the risk of a metabolic syndrome exacerbation based on continuous lifestyle data [22] [23]. For example, one study used wearable data to predict COVID-19 infections days before symptom onset [22] [19]. The predictive function moves from reactive to proactive health management, offering the potential for pre-emptive dietary interventions personalized to an individual's unique physiological response patterns.
Figure 1: The logical relationship between the four key functions of wearables. Monitoring provides the foundational data that feeds into the more complex functions of Screening, Detection, and Prediction.
Application to Food Intake Validation
The validation of food intake via wearable devices is an active and challenging field of research. Traditional methods like food diaries and 24-hour recalls are plagued by misreporting, with under-reporting of energy intake identified in up to 70% of adults in some national surveys [21]. Wearables offer a path toward objective, passive assessment.
Sensor Modalities for Eating Behavior Detection
Multiple sensing approaches are being developed and validated to detect and characterize eating episodes automatically.
Table 2: Wearable Sensor Modalities for Food Intake Assessment
| Sensor Modality | Measured Parameter | Reported Performance | Limitations & Challenges |
|---|---|---|---|
| Inertial Sensors (Accelerometer/Gyroscope) [11] [24] | Arm and wrist kinematics (bites, gestures). | Accuracy: 58% - 91.6% (F1-score varies widely) [11] | Confounded by non-eating gestures (e.g., talking, smoking). |
| Acoustic Sensors [11] | Chewing and swallowing sounds. | Can achieve high precision for detection in controlled settings. | Sensitive to background noise; privacy concerns. |
| Photoplethysmography (PPG) [18] | Heart rate, pulse rate variability. | Correlations with glucose absorption; not yet reliable for direct calorie estimation. | Signal noise during movement; proprietary algorithms. |
| Bioelectrical Impedance (BioZ) [18] [20] | Fluid shifts from nutrient/glucose influx. | One study: Mean bias of -105 kcal/day vs. reference, with wide limits of agreement [20]. | High variability; signal loss; requires validation. |
| Wearable Cameras [21] | Image-based food identification and portion size. | Auto-detection of meal images: 50% (snacks) to 95% (meals) [21]. | Privacy, data volume, computational cost for analysis. |
Experimental Protocols for Validation
Robust validation is critical for translating sensor signals into meaningful dietary data. The following protocols are commonly employed in the field.
1. Laboratory vs. Free-Living Validation: Studies typically start in controlled lab settings to establish proof-of-concept before moving to free-living conditions. Laboratory protocols involve structured activities, including eating standardized meals and performing confounding activities (e.g., talking, gesturing). Sessions are often video-recorded to provide a ground-truth benchmark for validating the sensor-derived eating metrics [25]. For free-living validation, participants wear the devices for extended periods (e.g., 7 days) while going about their normal lives. The ground truth in these settings is often established using a combination of self-report (e.g., food diaries) and objective methods (e.g., continuous glucose monitoring) [20] [11].
2. Reference Method for Caloric Intake: To validate a wearable device claiming to measure energy intake, a rigorous reference method is required. One study collaborated with a university dining facility to prepare and serve calibrated study meals, precisely recording the energy and macronutrient intake of each participant. The wearable's estimates (e.g., from a BioZ wristband) were then compared to this precise reference using statistical methods like Bland-Altman analysis, which revealed a mean bias of -105 kcal/day but with 95% limits of agreement as wide as -1400 to 1189 kcal/day, indicating high variability for individual measurements [20].
3. Multi-Sensor Data Fusion: Given the limitations of single sensors, the most promising approaches involve multi-sensor systems. A common protocol involves simultaneously collecting data from accelerometers (on the wrist), gyroscopes, and acoustic sensors (on the neck or ear). Machine learning models (e.g., support vector machines, random forests) are then trained on this multimodal data to improve the overall accuracy, sensitivity, and specificity of eating event detection compared to any single sensor [11].
Figure 2: A generalized experimental workflow for developing and validating wearable-based food intake detection systems, showing the integration of sensor data and ground-truth collection.
The Scientist's Toolkit: Key Research Reagents & Materials
For researchers designing studies to validate food intake via wearables, a standard set of tools and reagents is essential.
Table 3: Essential Research Materials for Wearable Food Intake Studies
| Item | Function & Utility in Research |
|---|---|
| Research-Grade Accelerometers (e.g., ActiGraph LEAP, activPAL) [25] | Provide high-fidelity movement data as a criterion standard for validating consumer-grade device accuracy, especially for detecting eating-related gestures. |
| Consumer-Grade Activity Trackers (e.g., Fitbit Charge, Apple Watch) [23] [25] | The devices under investigation; their data is compared against research-grade devices and ground truth to assess practical applicability. |
| Continuous Glucose Monitors (CGM) [20] [21] | Serve as an objective physiological correlate to food intake, helping to validate the timing and, to some extent, the metabolic impact of eating events. |
| Wearable Cameras (e.g., e-Button, "spy badges") [21] | Provide a passive, image-based ground truth for food presence and type, though they present challenges in data volume and privacy. |
| Bland-Altman Statistical Analysis [20] | A crucial statistical method for assessing the agreement between the wearable device's estimate and the reference method, highlighting bias and limits of agreement. |
| Doubly Labeled Water (DLW) [21] | The gold standard for measuring total energy expenditure in free-living individuals, used to validate the overall accuracy of energy intake estimates over longer periods. |
| Machine Learning Classifiers (e.g., SVM, Random Forest, CNN) [11] [21] | Algorithms required to translate raw sensor data into meaningful eating events (detection) and eventually predictions. |
Comparative Effectiveness in Public Health
The ultimate value of these technologies is their effectiveness in improving health outcomes. Large-scale studies provide critical insights. A 2025 retrospective cohort study (N=46,579) within South Korea's national mobile health care program compared wearable activity trackers to smartphone built-in step counters for reducing metabolic syndrome risk [23]. After propensity score matching, both device types led to significant improvements. Interestingly, the built-in step counter group demonstrated a statistically greater reduction in metabolic syndrome risk (Odds Ratio 1.20, 95% CI 1.05-1.36), with the effect being more pronounced in young adults aged 19-39 (OR 1.35, 95% CI 1.09-1.68) [23]. This highlights that the most complex technology is not always the most effective and that personalization based on user characteristics is key.
Challenges and Future Directions
Despite the promise, significant challenges remain. Data quality is highly variable due to differences in sensors and data collection practices [22]. Accuracy of food intake measurement, particularly for caloric and macronutrient content, is not yet reliable for individual-level clinical decision-making, as evidenced by the wide limits of agreement in validation studies [20]. Furthermore, issues of interoperability, health equity, and fairness due to the under-representation of diverse populations in wearable datasets need to be addressed [22].
Future directions point toward the integration of multi-modal data streams (e.g., combining motion, acoustics, and images) using advanced machine learning to create more robust hybrid assessment systems [21]. The field is also moving beyond simple eating detection to characterize meal microstructure, within-person variation in intakes, and food-nutrient combinations within meals, offering a richer understanding of the eating architecture and its link to health [21]. For researchers and drug development professionals, this evolving toolkit offers the potential to integrate objective, continuous dietary metrics into clinical trials and precision health initiatives, transforming our ability to understand and modulate the role of nutrition in health and disease.
From Lab to Real World: Implementing Wearable Dietary Sensors in Research and Clinical Practice
The accurate quantification of food intake is a fundamental challenge in nutritional science, precision health, and pharmaceutical development. Traditional methods, such as 24-hour recalls and food frequency questionnaires, rely on self-reporting and are often unreliable due to human memory limitations and intentional or unintentional misreporting [20] [26]. The emergence of wearable sensor technologies has created new opportunities for objective, passive dietary monitoring. However, single-sensor approaches often capture only isolated aspects of eating behavior, leading to incomplete data. Multi-modal sensor fusion addresses this limitation by integrating complementary data streams from multiple sensors to create a more comprehensive, accurate, and robust understanding of dietary intake [27] [28].
The core principle of sensor fusion is that data from different modalities can be combined to overcome the limitations of individual sensors. In autonomous driving, for instance, multi-sensor fusion integrates cameras, LiDAR, and radar to build a comprehensive environmental model, overcoming the limitations of any single sensor [29]. Similarly, in dietary monitoring, fusing data from acoustic, inertial, bioimpedance, and optical sensors can provide richer insights into eating behaviors, food types, and nutrient intake than any single modality alone [26]. This guide objectively compares the performance of various sensor fusion approaches currently shaping the field of dietary monitoring, with a specific focus on validating food intake via wearable device data.
Comparative Analysis of Sensing Modalities and Fusion Strategies
Classification of Fusion Levels
Multi-modal sensor fusion strategies are systematically categorized based on the stage at which data integration occurs. The table below outlines the three primary levels of fusion, their descriptions, and relevant applications in dietary monitoring.
Table 1: Levels of Multi-Modal Sensor Fusion
| Fusion Level | Description | Advantages | Challenges | Dietary Monitoring Applications |
|---|---|---|---|---|
| Data-Level (Early Fusion) | Raw data from multiple sensors is combined directly. | Maximizes information retention from original signals. | Highly sensitive to sensor misalignment and synchronization; requires high bandwidth. | Fusing raw audio and inertial signals for chew detection. |
| Feature-Level (Mid-Fusion) | Features are extracted from each sensor's data, then combined into a unified feature vector. | Leverages strengths of different modalities; reduces data dimensionality. | Requires effective cross-modal feature alignment and handling of heterogeneous data. | Combining features from bioimpedance (wrist) and acoustics (neck) for food type classification [30] [26]. |
| Decision-Level (Late Fusion) | Each sensor modality processes data independently to make a preliminary decision; decisions are then fused. | Modular and flexible; resilient to failure of a single sensor. | Potentially loses rich cross-modal correlations at the raw data level. | Combining independent classifications from a wearable camera and an inertial sensor to finalize food intake detection. |
Deep learning has significantly advanced feature-level fusion, with architectures like cross-modal attention mechanisms and transformers enabling the model to learn complex, non-linear relationships between different data streams [28] [29]. Theoretical foundations, such as Bayesian estimation, provide a framework for fusing heterogeneous data and modeling sensor uncertainty, which is critical for real-world applications where sensor noise and failures can occur [29].
Performance Comparison of Dietary Monitoring Technologies
The following table summarizes quantitative performance data for various sensing approaches, highlighting the effectiveness of different modalities and fusion strategies.
Table 2: Performance Comparison of Dietary Monitoring Technologies
| Technology / Platform | Sensing Modality | Body Location | Primary Application | Reported Performance | Key Experimental Findings |
|---|---|---|---|---|---|
| iEat Wearable [30] | Bioimpedance (2-electrode) | Wrist (one electrode on each) | Food intake activity recognition | Macro F1: 86.4% (4 activities) | Detects cutting, drinking, eating with hand/fork via dynamic circuit changes. |
| iEat Wearable [30] | Bioimpedance (2-electrode) | Wrist (one electrode on each) | Food type classification | Macro F1: 64.2% (7 food types) | Classification based on electrical properties of different foods. |
| GoBe2 Wristband [20] | Bioimpedance + Algorithms | Wrist | Energy intake estimation (kcal/day) | Mean Bias: -105 kcal/day (SD 660) vs. reference | Bland-Altman analysis showed 95% limits of agreement between -1400 and 1189 kcal/day. |
| Feeding Table (UEM) [31] | Multi-load cell scales | Table-integrated | Multi-food meal microstructure | ICC: 0.94 (Energy), 0.90 (Protein) | High day-to-day repeatability for energy and macronutrient intake. |
| Neck-worn Microphone [26] | Acoustic (High-fidelity) | Neck | Food type classification (7 types) | Accuracy: 84.9% | Recognizes intake of fluid and solid foods via chewing and swallowing sounds. |
| Wearable Camera [32] | Optical (Image capture) | Wearable (e.g., on person) | Food and nutrient intake estimation | Methodology Validated | Passive image capture for objective, real-time food intake assessment. |
The data reveals a trade-off between obtrusiveness and granularity of information. Wearable approaches like the iEat system offer passive monitoring but currently achieve more moderate accuracy in complex tasks like food type classification [30]. In contrast, instrumented environments like the Feeding Table provide highly precise, granular data on eating microstructure and macronutrient intake for multiple foods simultaneously, making them invaluable for laboratory validation studies [31].
Experimental Protocols for Validating Food Intake
Validation Study for a Bioimpedance Wristband
A critical validation study assessed the ability of a commercial wristband (GoBe2) to automatically track energy intake in free-living individuals [20].
- Objective: To evaluate the accuracy and practical utility of a wristband sensor for tracking daily nutritional intake (kcal/day) against a controlled reference method.
- Participants: 25 free-living adult participants were recruited, excluding those with chronic diseases, specific diets, or medications affecting metabolism.
- Reference Method: A highly controlled reference method was developed in collaboration with a university dining facility. All meals were prepared, calibrated, and served, with energy and macronutrient intake for each participant meticulously recorded under direct observation by a trained research team.
- Test Method: Participants used the wristband and an accompanying mobile app consistently for two 14-day test periods. The device uses bioimpedance signals to estimate patterns of fluid shifts associated with glucose and nutrient absorption into the bloodstream.
- Data Analysis: A total of 304 daily intake cases were collected. The agreement between the reference method and the wristband was analyzed using Bland-Altman tests. The mean bias was -105 kcal/day (SD 660), with 95% limits of agreement between -1400 and 1189 kcal/day. The regression equation of the plot was Y = -0.3401X + 1963, indicating a tendency for the wristband to overestimate at lower calorie intakes and underestimate at higher intakes [20].
- Key Challenge: Researchers identified transient signal loss from the sensor as a major source of error, highlighting the need for robust sensor fusion to compensate for such gaps.
The Feeding Table for High-Resolution Meal Microstructure
To address the limitations of single-food monitoring, researchers developed and validated the 'Feeding Table,' a novel Universal Eating Monitor (UEM) [31].
- Objective: To develop a UEM that simultaneously tracks the intake of up to 12 different foods with high temporal resolution, enabling detailed study of dietary microstructure and food choice.
- Participants: 31 healthy volunteers (15 male, 16 female) participated in a standard meal test over two consecutive days.
- Apparatus: The Feeding Table integrated five high-precision balances into a solid wood table, concealed beneath a hinged panel. Data from all balances were collected every 2 seconds and transmitted to a computer. The setup also included a video camera to record the eating process and identify which food was taken from each balance.
- Protocol: Participants consumed meals under standardized conditions. The table continuously recorded the weight of each food item throughout the meal.
- Validation Metrics: The study assessed day-to-day repeatability and positional bias. The Feeding Table showed high intra-class correlation coefficients (ICCs) for energy (0.94), protein (0.90), fat (0.90), and carbohydrate (0.93) across four repeated measurements, demonstrating excellent reliability. No significant positional bias was found for energy or macronutrients [31].
This protocol establishes the Feeding Table as a powerful tool for validating the output of less obtrusive wearable sensors in a laboratory setting, providing ground truth data for eating rate, meal size, and food choice.
iEat for Activity and Food Type Recognition
The iEat system represents a novel wearable approach that leverages an atypical use of bioimpedance sensing [30].
- Objective: To classify food intake-related activities and types of food using a wrist-worn impedance sensor.
- Principle: The system uses a two-electrode configuration (one on each wrist). During dining activities, dynamic circuit loops are formed through the hand, mouth, utensils, and food, causing consequential variations in the measured impedance signal. These patterns are unique to different activities and food types.
- Protocol: Ten volunteers performed 40 meals in an everyday table-dining environment. The iEat device collected impedance data during activities like cutting, drinking, eating with a hand, and eating with a fork.
- Data Processing and Model: A lightweight, user-independent neural network model was trained on the impedance signal patterns.
- Performance Outcome: The model detected the four food-intake activities with a macro F1 score of 86.4% and classified seven food types with a macro F1 score of 64.2% [30].
The following diagram illustrates the core sensing principle of the iEat device.
Diagram 1: iEat abstracted human-food impedance model. A new parallel circuit branch forms through food and utensils during dining activities, altering the overall impedance measured between the wrist-worn electrodes [30].
The Scientist's Toolkit: Research Reagent Solutions
The following table details key materials and technologies used in the featured experiments, providing a resource for researchers seeking to replicate or build upon these studies.
Table 3: Essential Research Reagents and Technologies for Dietary Monitoring
| Item / Technology | Function in Research | Exemplar Use Case |
|---|---|---|
| Bioimpedance Sensor (2-electrode) | Measures electrical impedance across the body; signal variations indicate dynamic circuit changes during food interaction. | Core sensor in the iEat device for recognizing food-related activities and classifying food types [30]. |
| Multi-load Cell Weighing System | Provides high-precision, continuous measurement of food weight loss from multiple containers simultaneously. | The foundation of the Feeding Table (UEM) for monitoring eating microstructure and macronutrient intake [31]. |
| High-Fidelity Acoustic Sensor | Captures chewing and swallowing sounds, which have characteristic acoustic signatures for different foods and activities. | Used in neck-worn systems (e.g., AutoDietary) for solid and liquid food intake recognition [26]. |
| Wearable Camera | Passively captures images of food for subsequent analysis, providing visual context and data for food identification. | Validated for estimating food and nutrient intake in household settings in low- and middle-income countries [32]. |
| Continuous Glucose Monitor (CGM) | Measures interstitial glucose levels frequently; used to assess metabolic response and adherence to dietary protocols. | Referenced as a tool for measuring protocol adherence in the GoBe2 wristband validation study [20]. |
| Custom Data Fusion & ML Pipeline | Software framework for synchronizing multi-sensor data, extracting features, and running classification/regression models. | Critical for all studies employing feature-level or decision-level fusion to derive intake metrics from raw sensor data [28] [30]. |
The experimental workflow for validating a sensor fusion-based dietary monitoring system typically follows a structured path, as summarized below.
Diagram 2: Generalized workflow for validating a multi-sensor dietary monitoring system, highlighting the parallel paths of test data and reference data collection.
Accurate dietary assessment is fundamental to understanding the complex relationships between nutrition, chronic diseases, and health outcomes. Traditional methods, such as 24-hour recalls, food frequency questionnaires, and self-reported food records, are labor-intensive and suffer from significant limitations, including recall bias, misreporting, and the inherent subjectivity of participant input [33]. These methods place a substantial burden on participants, often leading to non-compliance and data that does not reflect habitual intake. In research settings, particularly in low- and middle-income countries (LMICs) where malnutrition remains a major public health concern, these challenges are even more pronounced [33].
The emergence of wearable devices for passive data capture offers a transformative approach to these long-standing methodological problems. As noted in a 2025 scoping review, "mobile and ubiquitous devices enable health data collection 'in a free-living environment'" with the potential to support remote patient monitoring and adaptive interventions while significantly reducing participant burden [34]. This guide objectively compares the current landscape of sensor-based and image-based technologies for validating food intake, focusing on their performance, underlying experimental protocols, and applicability for researchers and drug development professionals.
Experimental Approaches and Methodologies
Research into passive dietary monitoring has converged on two primary technological approaches: sensor-based detection of eating behaviors and image-based capture of food consumption. The most robust systems often integrate both methodologies to enhance accuracy.
Sensor-Based Detection Systems
Sensor-based approaches typically leverage wearable devices equipped with accelerometers, gyroscopes, and other motion sensors to detect proxies of eating behavior such as chewing, swallowing, and hand-to-mouth gestures.
- AIM-2 Protocol: A key experimental system in this domain is the Automatic Ingestion Monitor v2 (AIM-2), a wearable device that attaches to eyeglasses and contains a camera and a 3D accelerometer [35]. In a validation study, 30 participants wore the AIM-2 for two days (one pseudo-free-living day with meals in the lab and one free-living day). The accelerometer sampled data at 128 Hz to capture head movement and body leaning forward motion as eating proxies. During the pseudo-free-living day, participants used a foot pedal to log the exact moment of food ingestion, providing precise ground truth data [35].
- Data Analysis: The sensor data was used to train a food intake detection model. The free-living day data, with eating episodes manually annotated from continuous images (captured every 15 seconds), served for validation [35].
Image-Based Assessment Systems
Image-based methods utilize wearable or fixed cameras to passively capture food consumption events, with subsequent analysis performed via manual review or automated computer vision techniques.
- Multi-Device Dietary Assessment: A comprehensive study protocol designed for LMIC settings (Ghana and Uganda) employs a suite of camera devices [33]:
- Foodcam: A stereoscopic camera mounted in kitchens with motion detection to capture food preparation.
- AIM-2: As described above, for gaze-aligned image capture during eating.
- eButton: A chest-worn device with a wide-angle, downward-tilted lens to record food in front of the wearer.
- Ear-worn camera: A lightweight, outwardly-directed camera for video capture of intake.
- Analytical Validation: This protocol validates the passive image-based method against the established ground truth of supervised weighed food records. The captured images are analyzed using both automated artificial intelligence (deep learning) and manual visual estimation to recognize foods and estimate portion size and nutrient content [33].
Integrated Multi-Modal Systems
The most significant advances in accuracy come from integrating sensor and image data. One study on the AIM-2 system implemented a hierarchical classifier to combine confidence scores from both image-based food recognition and accelerometer-based chewing detection [35]. This integrated method achieved a 94.59% sensitivity, 70.47% precision, and an 80.77% F1-score in free-living conditions, significantly outperforming either method used in isolation (8% higher sensitivity) by effectively reducing false positives [35].
Performance Comparison of Monitoring Technologies
The table below summarizes the key performance metrics of prominent wearable devices and sensing systems used for passive data capture in dietary and general health monitoring.
Table 1: Performance Comparison of Passive Monitoring Technologies
| Device/System | Primary Data Type | Key Metrics/Performance | Reported Advantages |
|---|---|---|---|
| AIM-2 (Integrated Method) | Image & Accelerometer | 94.59% Sensitivity, 70.47% Precision (Eating Episode Detection) [35] | Significantly reduces false positives in free-living conditions. |
| Apple Watch | Physiological Sensors | ≤3.4% error (step count); 97% accuracy (sleep detection); Underestimates HR by 1.3 BPM (exercise) [36] | High consumer adoption; rich ecosystem for data integration. |
| Oura Ring | Physiological Sensors | 99.3% accuracy (resting HR); 96% accuracy (total sleep time) [36] | Unobtrusive form factor; strong sleep staging capability. |
| WHOOP | Physiological Sensors | 99.7% accuracy (HR); 99% accuracy (HRV) [36] | Focus on recovery and strain metrics; no screen minimizes distractions. |
| Garmin | Physiological Sensors | 1.16-1.39% error (HR); 98% accuracy (sleep detection) [36] | Robust activity and GPS tracking; popular in sport research. |
| Fitbit | Physiological Sensors | 9.1-21.9% error (step count); Overestimates total sleep time [36] | Widely used in research; established track record for basic activity. |
It is critical to note that while consumer-grade wearables provide valuable general health metrics, their accuracy for specific tasks like calculating caloric expenditure is considerably lower, with errors ranging from 13% (Oura Ring) to over 100% (Apple Watch) in some studies [36]. Therefore, their utility in dietary research may be more suited to contextual monitoring (e.g., correlating physical activity with appetite) rather than direct energy intake measurement.
Visualization of Experimental Workflows
The logical workflow for deploying and validating a passive food intake assessment system, particularly in challenging field conditions, can be summarized as follows.
Diagram 1: Passive Dietary Assessment Workflow.
The integrated analysis of image and sensor data for food intake detection follows a specific computational pipeline to reduce false positives.
Diagram 2: Integrated Image-Sensor Data Fusion.
The Researcher's Toolkit: Essential Reagent Solutions
Implementing a robust passive data capture study requires careful selection of devices and platforms. The table below details key components and their functions in a research context.
Table 2: Essential Research Reagents and Tools for Passive Dietary Monitoring
| Tool/Reagent | Type | Primary Function in Research |
|---|---|---|
| AIM-2 (Automatic Ingestion Monitor v2) | Wearable Sensor | Captures gaze-aligned images and head movement accelerometer data for detecting eating episodes and identifying food [35]. |
| eButton | Wearable Sensor | A chest-worn device with a wide-angle view to passively capture images of food and activities in front of the wearer [33]. |
| Foodcam | Fixed Environmental Sensor | A stereoscopic kitchen camera with motion activation to capture images of food preparation and cooking processes [33]. |
| ExpiWell Platform | Data Integration Platform | Enables seamless synchronization of wearable data (e.g., from Apple Watch, Fitbit) with Ecological Momentary Assessment (EMA) data for a unified analysis dashboard [37]. |
| Hierarchical Classification Algorithm | Computational Method | A machine learning technique that combines confidence scores from image-based and sensor-based classifiers to improve the accuracy of eating episode detection and reduce false positives [35]. |
| Foot Pedal Logger | Ground Truth Apparatus | Provides precise, user-initiated ground truth data for food ingestion moments during laboratory validation studies [35]. |
Discussion and Research Considerations
While passive data capture technologies show immense promise, researchers must navigate several practical and methodological considerations. A 2025 review highlighted persistent challenges, including participant compliance in longer-term studies, data consistency from passive streams, and complex authorization and privacy issues, particularly when using cameras [34]. For special populations, such as persons with dementia (PwD), additional factors like device comfort, ease of use, and reliance on caregivers become critical for successful adoption and adherence [38].
Machine learning techniques offer promising solutions to some of these challenges by optimizing the timing of prompts for active data collection, auto-filling responses, and minimizing the frequency of interruptions to the participant [34]. Simplified user interfaces and motivational techniques can further improve compliance and data consistency [34].
When selecting devices, researchers should employ a structured evaluation framework that considers criteria across three domains: Everyday Use (e.g., battery life, comfort, aesthetics), Functionality (e.g., parameters measured, connectivity), and Research Infrastructure (e.g., data granularity, export capabilities) [39]. No single device is best for all scenarios; selection must be driven by the specific research question, target population, and study context.
The objective assessment of dietary intake represents a significant challenge in nutritional science and chronic disease management. Traditional methods, such as food diaries and 24-hour dietary recalls, are prone to inaccuracies due to their reliance on self-reporting, which can be influenced by recall bias and the burden of manual entry [40]. For individuals with Type 2 Diabetes (T2D), this gap in accurate monitoring can hinder effective glycemic control. The integration of two wearable technologies—Continuous Glucose Monitors (CGM) and the eButton, a wearable dietary intake sensor—offers a promising, multi-modal approach to objectively capture the relationship between food consumption and physiological response. This case study frames the integration of CGM and eButton within a broader research thesis aimed at validating food intake data through wearable devices, providing researchers and drug development professionals with a critical evaluation of the performance, protocols, and potential of this combined methodology.
Performance Comparison of Current-Generation CGM Systems
The selection of an appropriate CGM is foundational to any study correlating dietary intake with glycemic response. A recent 2025 prospective, interventional study provides a robust, head-to-head comparison of three factory-calibrated CGM systems, evaluating their performance against different comparator methods (YSI 2300 laboratory analyzer, Cobas Integra analyzer, and Contour Next capillary blood glucose meter) and during clinically relevant glycemic excursions [41].
Table 1: CGM System Performance Metrics (vs. YSI Reference)
| CGM System | Mean Absolute Relative Difference (MARD) | Performance Characteristics |
|---|---|---|
| FreeStyle Libre 3 (FL3) | 11.6% | Better accuracy in normoglycemic and hyperglycemic ranges. |
| Dexcom G7 (DG7) | 12.0% | Better accuracy in normoglycemic and hyperglycemic ranges. |
| Medtronic Simplera (MSP) | 11.6% | Better performance in the hypoglycemic range. |
Table 2: CGM System Technical Specifications
| Feature | FreeStyle Libre 3 | Dexcom G7 | Medtronic Simplera |
|---|---|---|---|
| Sensor Lifetime | 14 days [41] | 10 days + 12-hour grace period [41] [42] | 7 days [41] |
| Warm-Up Time | Not specified in search results | 30 minutes [42] | Not specified in search results |
| Reader | Smartphone app [43] | Smartphone app or redesigned receiver [42] | Not specified in search results |
| Key Integrations | mylife CamAPS FX AID system, YpsoPump, Tandem t:slim X2, Beta Bionics iLet, twiist AID System* [43] [44] | Tidepool Loop [42]; other AID integrations in development [42] | Not specified in search results |
*Integration specified for FreeStyle Libre 3 Plus or FreeStyle Libre 2 Plus sensors [43] [44].
It is critical to note that performance results varied depending on the comparator method. For instance, compared to the Cobas Integra (INT) method, the MARD for FL3, DG7, and MSP was 9.5%, 9.9%, and 13.9%, respectively [41]. This underscores the importance of the reference method in study design and the interpretation of performance data. All systems demonstrated a lower aggregate accuracy compared to some previous studies, highlighting the effect of comprehensive study designs that include dynamic glucose regions [41].
The eButton: A Wearable Sensor for Dietary Monitoring
The eButton is a wearable, camera-based device designed to passively capture dietary data. It is typically worn on the chest and automatically records images at frequent intervals (e.g., every 3–6 seconds) during wear time to capture food consumption episodes [3] [15].
Reported Facilitators and Barriers:
- Facilitators: The device's ease of use, its ability to increase user mindfulness about food intake, and the influence on the perceived sense of control over diet. Users reported eating smaller portions due to greater awareness [3].
- Barriers: Privacy concerns due to continuous image capture, difficulty with camera positioning, and the lack of a direct functional link between meal photos and glucose trends in data review interfaces [3].
Recent technological advancements, such as the EgoDiet pipeline, have leveraged AI to analyze data from low-cost wearable cameras like the eButton for dietary assessment. This pipeline uses computer vision models for tasks like food item segmentation (EgoDiet:SegNet), 3D container modeling and depth estimation (EgoDiet:3DNet), and portion size estimation (EgoDiet:PortionNet). In field studies, this approach demonstrated a Mean Absolute Percentage Error (MAPE) of 28.0% for portion size estimation, outperforming the traditional 24-Hour Dietary Recall (MAPE of 32.5%) [15].
Experimental Protocols for Integrated Dietary Validation
Protocol: Parallel CGM and eButton Deployment in Free-Living Conditions
A one-group prospective cohort study provides a methodology for integrating CGM and eButton for dietary management, specifically in a T2D population [3]. This protocol is designed to capture real-world, multimodal data for analyzing the relationship between food intake and glycemic response.
Diagram 1: Integrated CGM and eButton study workflow for free-living dietary validation.
Key Methodological Steps:
- Participant Recruitment: Target a specific demographic (e.g., Chinese Americans with T2D) with clear inclusion/exclusion criteria [3].
- Device Deployment:
- Participants wear an eButton on the chest during waking hours, specifically to record meals over a 10-day period.
- A CGM (e.g., FreeStyle Libre Pro) is simultaneously worn for 14 days.
- Participants maintain a paper diary to log food intake, medication, and physical activity, providing supplemental contextual data [3].
- Data Collection: The study occurs in a free-living setting, allowing for the capture of real-world dietary behaviors and their corresponding glucose responses.
- Post-Study Analysis: Research staff download data from both devices. CGM results are reviewed alongside the eButton's food pictures and the participant's diary to identify factors influencing glucose levels [3].
Protocol: Controlled CGM Performance and Accuracy Testing
For research requiring the highest degree of CGM accuracy validation, a more controlled and intensive clinical protocol is available. A 2025 study employed the following methodology to evaluate CGM performance under induced glycemic variability [41].
Diagram 2: Controlled clinical protocol for comprehensive CGM accuracy assessment.
Key Methodological Steps:
- Parallel Sensor Wear: Participants wear sensors from multiple CGM systems (e.g., FL3, DG7, MSP) simultaneously on the upper arms for up to 15 days [41].
- Frequent Sampling Periods (FSPs): Multiple 7-hour sessions are conducted where comparator blood glucose measurements are taken every 15 minutes using high-accuracy laboratory analyzers (YSI 2300, Cobas Integra) and capillary blood glucose meters (Contour Next) [41].
- Glucose Excursion Procedure: Simultaneously with FSPs, a standardized glucose manipulation procedure is executed. This involves a carbohydrate-rich breakfast followed by a delayed insulin bolus to induce transient hyperglycemia, subsequent hypoglycemia, and a return to stable normoglycemia. This tests CGM accuracy across the entire glycemic range and during rapid glucose changes [41].
- Data Analysis: CGM readings are paired with comparator measurements. Performance is characterized using metrics like Mean Absolute Relative Difference (MARD), relative bias, and clinical accuracy tools like the Diabetes Technology Society Error Grid [41].
The Researcher's Toolkit: Essential Reagents & Materials
Table 3: Key Research Reagents and Materials for Integrated Dietary Monitoring Studies
| Item | Function/Description | Example Use Case |
|---|---|---|
| Continuous Glucose Monitor (CGM) | Factory-calibrated sensor measuring interstitial glucose levels every 1-15 minutes. Provides core glycemic response data. | FreeStyle Libre Pro [2], Dexcom G6/G7 [41] [2], Medtronic Simplera [41]. |
| Wearable Camera (eButton) | Passive, image-based dietary intake sensor. Captures meal context, type, and portion size via automatic photography. | eButton [3] [15], Automatic Ingestion Monitor (AIM-2) [40]. |
| Laboratory Glucose Analyzer | High-accuracy reference method (ground truth) for validating CGM performance in clinical studies. | YSI 2300 STAT PLUS (glucose oxidase-based) [41], COBAS INTEGRA 400 plus (hexokinase-based) [41]. |
| Capillary Blood Glucose Meter | Handheld device for capillary blood glucose measurement; used for in-study patient management and as a secondary comparator. | Contour Next system [41]. |
| Multimodal Dataset | Curated, publicly available data containing synchronized CGM, dietary, and activity data for algorithm development and validation. | CGMacros dataset [2] (includes CGM, macronutrients, food images, Fitbit data). |
| AI-Based Dietary Analysis Pipeline | Software suite for automated analysis of wearable camera data, including food segmentation and portion size estimation. | EgoDiet pipeline (includes SegNet, 3DNet, PortionNet modules) [15]. |
Discussion and Research Implications
The integration of CGM and eButton data presents a powerful framework for moving beyond self-reported dietary assessment. The correlation of precise meal timestamps and visual portion size data from the eButton with high-frequency glucose traces from a CGM allows researchers to model Postprandial Glucose Responses (PPGR) with a high degree of temporal and quantitative accuracy [2]. This is crucial for understanding individual responses to macronutrients and developing personalized nutritional interventions.
For the research community, particularly in drug development, this integrated approach offers two key advantages:
- Objective Endpoints: It provides objective, high-resolution biomarkers for dietary intake and metabolic response, which can be used as endpoints in clinical trials for nutritional therapies or diabetic medications.
- Personalized Insights: It facilitates the move towards personalized medicine by uncovering individual variability in response to mixed-macronutrient meals, which carbohydrate-counting alone cannot predict [2].
Future research should focus on leveraging larger, multimodal datasets like CGMacros [2] to develop machine learning models that can jointly analyze image-based food data and CGM signals. The ultimate goal is the creation of automated systems that can not only validate food intake but also predict glycemic responses and provide real-time, personalized dietary guidance to individuals with T2D.
The accurate validation of food intake is a cornerstone of nutritional science, chronic disease management, and pharmaceutical development. Traditional methods, such as self-reported food diaries and 24-hour recalls, are notoriously prone to underreporting errors and recall bias, often rendering data unreliable for clinical research [45]. The integration of wearable sensor data for objective health monitoring has created an urgent need for equally objective and automated dietary assessment tools. In response, AI-powered image recognition has emerged as a transformative technology for automating food identification and portion sizing. This guide provides an objective comparison of the performance, experimental protocols, and underlying technologies of leading AI tools and research systems that are shaping the future of dietary intake validation in research settings.
Performance Comparison of AI Food Analysis Tools
The performance of automated food analysis systems varies significantly based on their underlying technology, from specialized computer vision pipelines to generalized multimodal Large Language Models (LMMs). The tables below summarize key performance metrics from recent validation studies.
Table 1: Performance Comparison of Specialized Food Image Analysis Systems
| System / Study | Core Technology | Primary Function | Reported Accuracy / Error | Key Strengths |
|---|---|---|---|---|
| NYU AI System [46] | YOLOv8 with ONNX Runtime, volumetric computation | Food recognition & nutrient calculation | Calorie calculation closely matched reference standards in tests (e.g., 317 kcal for pizza vs. actual) | High computational efficiency; runs in web browser; precise portion size via area calculation |
| EgoDiet [15] | Mask R-CNN for segmentation, depth estimation (3DNet) | Passive dietary assessment in free-living conditions | Mean Absolute Percentage Error (MAPE): 28.0% (portion size) | Designed for passive, wearable cameras; suitable for diverse cuisines & low-light conditions |
| AI Nutrition Apps (e.g., MyFitnessPal, Lifesum) [47] | Combination of image recognition, barcode scanning, vast food databases | Automated meal tracking & nutritional analytics | Tracking accuracy >90% vs. manual logging; leads to ~15% reduction in daily calorie intake | High user convenience; integration with wearables & smart kitchen ecosystems |
Table 2: Performance of General-Purpose Multimodal LLMs in Food Analysis [45]
| Model | Weight Estimation MAPE | Energy Estimation MAPE | Correlation with Reference (r) | Systematic Bias |
|---|---|---|---|---|
| ChatGPT-4o | 36.3% | 35.8% | 0.65 - 0.81 | Underestimation, increasing with portion size |
| Claude 3.5 Sonnet | 37.3% | 35.8% | 0.65 - 0.81 | Underestimation, increasing with portion size |
| Gemini 1.5 Pro | 64.2% - 109.9% | 64.2% - 109.9% | 0.58 - 0.73 | Underestimation, increasing with portion size |
The data indicates that specialized systems like EgoDiet and the NYU AI system are engineered for higher accuracy in specific tasks like portion sizing, which is critical for clinical and research applications [46] [15]. In contrast, general-purpose LMMs like ChatGPT and Claude achieve accuracy comparable to traditional self-reporting methods but struggle with precision, particularly for larger portions, making them currently unsuitable for applications where exact quantification is critical [45].
Experimental Protocols for Validation
A critical step in employing these tools is understanding and replicating the validation methodologies that underpin their performance metrics.
- Food Preparation and Reference Values: Researchers prepared foods and used a calibrated digital scale to record weights. For cooked items, post-preparation weights were recorded. Nutritional content was calculated using standardized nutritional databases.
- Image Capture and Analysis: The AI system used advanced deep-learning algorithms to recognize food items. A key innovation was the volumetric computation function, which used image processing to measure the exact area each food occupied on a plate. The system correlated this area with density and macronutrient data to convert 2D images into nutritional assessments.
- Performance Validation: The system's outputs (e.g., calories, macronutrients) were compared against the reference values from direct weighing and database analysis. Performance was measured using metrics like mean absolute error.
- Food Photograph Standardization: A total of 52 photographs, including individual food components (n=16) and complete meals (n=36), were captured under standardized conditions. Meals were constructed around starchy bases (rice, pasta, potatoes) combined with various protein sources and vegetables. Portion sizes were defined as small (50%), medium (100%), and large (150%) of a standard serving.
- Imaging Setup: Images were taken using an iPhone 13 with a white porcelain plate (24.3 cm diameter) on a beige background. Standard cutlery was placed 1.5 cm from the plate edge to provide a size reference. The camera was positioned at a 42° angle, 20.2 cm above and 20 cm from the plate edge.
- LLM Prompting and Analysis: Each model (ChatGPT-4o, Claude 3.5 Sonnet, Gemini 1.5 Pro) was provided with an identical, meticulously designed prompt. The prompt instructed the model to: 1) recognize food components, 2) estimate volume based on size relations to objects in the image (not typical serving sizes), and 3) determine nutritional content.
- Data Analysis: Model estimates for food weight, energy, and macronutrients were compared against reference values. Performance was quantified using Mean Absolute Percentage Error (MAPE), Pearson correlations, and systematic bias analysis via Bland-Altman plots.
System Architectures and Workflows
The technological approaches of these tools can be broadly categorized into active and passive methods, each with distinct workflows.
Active Method: User-Captured Image Analysis
This method relies on the user actively capturing an image of their meal, typically with a smartphone. The analysis pipeline is used by many commercial apps and the evaluated LMMs.
Passive Method: Wearable Camera Systems
Systems like EgoDiet use wearable cameras (e.g., eButton, AIM) that automatically capture images at intervals, providing a passive, hands-free assessment of dietary intake [15]. This method is particularly valuable for long-term studies and populations where active tracking is burdensome.
The Scientist's Toolkit: Research Reagent Solutions
For researchers aiming to develop or validate similar AI-powered dietary assessment tools, the following table outlines essential "research reagents" – key materials, software, and datasets required in this field.
Table 3: Essential Research Reagents for AI-Powered Dietary Assessment
| Item / Solution | Function / Description | Example in Use |
|---|---|---|
| Wearable Camera Devices | Automatically capture egocentric (first-person) images of eating episodes. | eButton (chest-pinned camera) and AIM (eyeglasses-mounted camera) were used in the EgoDiet study for passive monitoring [15]. |
| Standardized Food Image Datasets | Used to train and validate computer vision models; must be diverse and accurately labeled. | Datasets with portion size annotations and varied cuisines are crucial. The NYU team refined a set of 95,000 instances across 214 categories [46]. |
| Pre-Trained Vision Models | Provide a foundational model for tasks like object detection and segmentation, which can be fine-tuned for food. | YOLOv8 was used by NYU for efficient food identification [46]. Mask R-CNN was used in EgoDiet for segmenting food items and containers [15]. |
| Nutritional Database API | Provides the mapping from identified food items and weights to nutritional content (calories, macros, micros). | Software like Dietist NET (referencing the USDA database) was used to establish ground truth in the LLM validation study [45]. |
| Multimodal LLM Access | Provides API access to general-purpose models for benchmarking against specialized systems. | ChatGPT-4o, Claude 3.5 Sonnet, and Gemini 1.5 Pro APIs were used for the comparative evaluation of their dietary assessment capabilities [45]. |
Navigating Technical Hurdles and Practical Barriers in Wearable Dietary Validation
The validation of food intake via wearable device data represents a critical frontier in digital health and precision nutrition research. For researchers and drug development professionals, the promise of passive, objective dietary monitoring hinges on overcoming a fundamental challenge: the significant variability in data quality and sensor performance across different technological approaches. This variability currently impedes the standardization required for robust clinical research and reliable health interventions. The absence of a gold standard for real-world dietary assessment creates a pressing need for a systematic comparison of existing methodologies, their underlying experimental protocols, and their respective performance metrics [12] [5]. This guide objectively compares the performance of prominent wearable dietary monitoring technologies, providing a detailed analysis of their operational frameworks, accuracy, and suitability for different research applications, all within the context of validating food intake data.
Performance Comparison of Dietary Monitoring Technologies
The landscape of wearable dietary monitoring technologies can be broadly categorized by their primary sensing modality. The following table summarizes the quantitative performance and key characteristics of the major technology categories identified in current literature.
Table 1: Performance Comparison of Wearable Dietary Monitoring Technologies
| Technology Category | Specific Device/System | Key Measured Parameters | Reported Performance Metrics | Primary Research Context |
|---|---|---|---|---|
| Wearable Cameras (Image-Based) | eButton (chest-worn) [3] [15] | Food type, portion size, meal timing via images | Facilitates food identification and portion estimation; user-reported barriers: privacy concerns, device positioning [3] | Free-living studies (e.g., Chinese Americans with T2D); feasibility studies in African populations [3] [15] |
| EgoDiet (AI pipeline for camera data) [15] | Food portion size (weight) | Mean Absolute Percentage Error (MAPE): 28.0-31.9% for portion size, outperforming 24HR (40.1%) and dietitians (32.5%) [15] | Dietary assessment in controlled and free-living settings (Studies in London and Ghana) [15] | |
| Bio-Impedance Sensors | iEat (wrist-worn) [30] | Food intake activities (cutting, drinking, eating), food types | Activity recognition: Macro F1 score 86.4%; Food type classification: Macro F1 score 64.2% [30] | Laboratory dining experiments with 10 volunteers and 40 meals [30] |
| Physiological Response Monitors | Continuous Glucose Monitor (CGM) [17] [3] | Interstitial glucose levels | Used to visualize relationship between food intake and glycemic response; increases user mindfulness [3] | Paired with other tools (e.g., eButton) for dietary management in type 2 diabetes [3] |
| Healbe GoBe2 (wristband) [5] | Energy intake (calories), macronutrients via bioimpedance | Mean bias of -105 kcal/day vs. reference; 95% limits of agreement: -1400 to 1189 kcal/day; tendency to overestimate low and underestimate high intake [5] | Free-living validation study with calibrated meals (n=25) [5] | |
| Inertial & Acoustic Sensors | Neck-worn Microphone (AutoDietary) [30] | Chewing, swallowing sounds for food intake recognition | Recognized 7 food types with 84.9% accuracy [30] | Laboratory studies for eating behavior monitoring [30] |
| Wrist-worn Inertial Sensors [12] | Hand-to-mouth gestures as bite proxies | Part of a broader sensor taxonomy for eating behavior measurement; accuracy highly dependent on algorithm and context [12] | Research on eating episode detection in laboratory and free-living settings [12] |
Detailed Experimental Protocols for Key Technologies
Understanding the experimental methodologies behind performance data is crucial for assessing their validity and applicability to specific research needs.
Image-Based Passive Dietary Assessment (EgoDiet Protocol)
The EgoDiet pipeline was evaluated through structured field studies to benchmark its performance against traditional methods [15].
- Objective: To evaluate the accuracy of a passive, egocentric vision-based pipeline for estimating food portion sizes in real-world settings, comparing its performance to expert dietitians and the 24-Hour Dietary Recall (24HR) method.
- Study Populations:
- Device & Data Collection: Participants wore one of two customized wearable cameras: the AIM (eye-level, attached to glasses) or the eButton (chest-level). These devices passively captured images during eating episodes [15].
- Reference Method & Validation: In Study A, a standardized weighing scale (Salter Brecknell) was used to pre-weigh all food items served in the test meals, establishing a ground truth for portion size. The images captured by the wearable cameras were then processed by the EgoDiet system [15].
- Data Analysis & Performance Calculation: The EgoDiet pipeline consists of multiple AI modules: SegNet for food and container segmentation, 3DNet for camera-distance estimation and 3D reconstruction, a Feature module for extracting portion-size-related metrics, and PortionNet for final weight estimation. Performance was quantified by calculating the Mean Absolute Percentage Error (MAPE) between the EgoDiet-estimated portion sizes and the ground-truth weights from the scale, with results compared to estimates made by dietitians (Study A) and the 24HR method (Study B) [15].
Bio-Impedance-Based Activity Recognition (iEat Protocol)
The iEat system employs a novel sensing paradigm, using bio-impedance signals to detect dietary activities without instrumented utensils [30].
- Objective: To develop and evaluate a wearable system that leverages bio-impedance sensing across the body to automatically recognize food intake activities and classify food types.
- Experimental Setup: The iEat device was configured as a single impedance-sensing channel with one electrode placed on each wrist. This setup measures the dynamic changes in the electrical circuit formed by the body, utensils, and food during dining activities [30].
- Study Protocol: Ten volunteers participated in a total of 40 meals in an everyday table-dining environment. During these meals, the iEat system continuously recorded impedance data [30].
- Data Annotation & Ground Truth: Specific dietary activities (cutting, drinking, eating with a hand, eating with a fork) and food types were annotated to create a labeled dataset for model training and evaluation. The "IDLE" status was assigned to periods with no food intake activity [30].
- Signal Processing & Model Training: A lightweight, user-independent neural network model was trained on the impedance data. The model's task was to classify the data streams into the pre-defined activity and food type categories [30].
- Performance Evaluation: Model performance was assessed using the macro F1 score, a metric that balances precision and recall, providing a robust measure for multi-class classification tasks [30].
Validation of a Commercial Energy Intake Monitor (GoBe2 Protocol)
A rigorous independent study was conducted to validate the claims of a commercial wristband that automatically estimates energy and macronutrient intake [5].
- Objective: To assess the accuracy and utility of the Healbe GoBe2 wristband in estimating daily energy intake (kcal/day) against a carefully controlled reference method in free-living participants.
- Participant Selection: 25 free-living adults were recruited, with exclusion criteria including chronic disease, food allergies, restricted diets, and significant weight fluctuation [5].
- Reference Method Implementation: A key strength of this protocol was the development of a high-fidelity reference method. The research team collaborated with a university dining facility to prepare, calibrate, and serve all study meals. Participant intake was directly observed by trained research staff, providing a precise measure of actual energy and macronutrient consumption [5].
- Test Method: Participants used the GoBe2 wristband and its accompanying mobile app consistently over two 14-day test periods. The device uses computational algorithms to convert bioimpedance signals into estimates of caloric intake based on patterns of fluid shifts associated with glucose absorption [5].
- Data Analysis: A total of 304 paired daily intake measurements (reference vs. wristband) were collected. Agreement between the two methods was analyzed using Bland-Altman tests to determine mean bias and 95% limits of agreement [5].
Workflow Diagram of Validation Approaches
The following diagram illustrates the logical sequence and key decision points in the experimental protocols used to validate wearable dietary monitoring devices.
Diagram 1: Dietary Monitor Validation Workflow
The Researcher's Toolkit: Essential Reagents & Materials
For researchers aiming to implement or validate wearable dietary monitoring technologies, the following table details key solutions and their functions based on the cited experimental protocols.
Table 2: Key Research Reagent Solutions for Dietary Monitoring Validation
| Item Name | Function/Application in Research | Specific Examples from Literature |
|---|---|---|
| Wearable Camera Systems | Passive capture of eating episodes and food items for image-based dietary assessment. | eButton (chest-worn camera) [3] [15]; AIM (Automatic Ingestion Monitor, eye-glasses mounted) [15]. |
| Continuous Glucose Monitor (CGM) | Measures interstitial glucose levels to correlate food intake with glycemic response; used as a complementary data stream. | Freestyle Libre Pro CGM used alongside the eButton to visualize food-glucose relationships [3]. |
| Bio-Impedance Sensor | Measures electrical impedance to infer dietary activities or estimate energy intake based on physiological fluid shifts. | iEat wrist-worn device for activity recognition [30]; Healbe GoBe2 for calorie estimation [5]. |
| Standardized Weighing Scale | Provides ground truth measurement of food portion sizes before and after consumption for validation studies. | Salter Brecknell scale used to pre-weigh study meals in the EgoDiet validation [15]. |
| AI-Based Food Image Analysis Pipeline | Automates the process of food identification, segmentation, and portion size estimation from food images. | EgoDiet:SegNet (segmentation), EgoDiet:3DNet (3D reconstruction), EgoDiet:PortionNet (portion estimation) [15]. |
| Validated Dietary Recall Tool | Serves as a benchmark comparison method (though with known limitations) for evaluating new technologies. | 24-Hour Dietary Recall (24HR) compared against the EgoDiet system in a field study [15]. |
| Data Annotation Software | Allows researchers to manually label sensor data or images to create ground truth datasets for training and testing machine learning models. | Used in iEat study to label impedance data with activity types [30]; used in image-based studies to identify food items [15] [48]. |
| Low-Power Wearable Sensor Platform | Enables the development and prototyping of custom wearable devices for continuous, long-term monitoring. | Design principles for low-power devices aimed at monitoring vital parameters, applicable to dietary monitoring sensors [49]. |
Analysis of Standardization Challenges and Future Directions
The presented data reveals a field marked by diverse technological approaches, each with distinct strengths and validation challenges. A central barrier to standardization is the lack of a universal reference method for free-living dietary assessment. While controlled studies use direct observation and weighed meals [15] [5], these are impractical for large-scale or long-term validation, forcing reliance on less accurate methods like 24HR for comparison [15].
Furthermore, performance variability is highly context-dependent. Image-based systems like EgoDiet show promise for portion estimation (MAPE ~28-32%) but raise privacy concerns and depend on lighting and camera angle [3] [15]. Sensor-based systems like iEat offer privacy but currently achieve more moderate accuracy in food classification (F1 score 64.2%) [30]. Physiological approaches like the GoBe2 demonstrate significant individual variability and wide limits of agreement in energy estimation, highlighting that sensor-derived data may not be interchangeable across populations or individuals [5].
The path toward standardization requires:
- Developing Consolidated Benchmarks: Establishing open, multi-modal datasets containing synchronized data from cameras, bio-impedance, CGMs, and precise intake measurements for benchmarking.
- Contextual Performance Reporting: Moving beyond single metrics to report performance across diverse conditions (e.g., food types, lighting, user demographics).
- Cross-Technology Validation: Rigorously testing how different sensing modalities perform when used concurrently in the same cohort to identify optimal synergies.
For researchers and drug development professionals, this implies that selecting a dietary monitoring technology must be a deliberate choice aligned with the specific research question, required accuracy level, and target population, rather than seeking a one-size-fits-all solution. The future of validated food intake research lies in transparent reporting, shared benchmarking, and the development of hybrid systems that leverage the complementary strengths of multiple sensing modalities to overcome the limitations of any single approach.
Overcoming Algorithmic Bias and Ensuring Robust Performance Across Diverse Populations
The validation of food intake via wearable device data represents a frontier in nutritional science and preventive health, with direct applications for researchers, clinical trials, and drug development professionals. However, the performance of these automated systems can vary significantly across different demographics, leading to algorithmic bias that threatens the validity and generalizability of research findings. Algorithmic bias in artificial intelligence (AI) systems occurs when automated decision-making processes systematically favor or discriminate against particular groups, creating reproducible patterns of unfairness [50]. This bias manifests differently from human prejudice because it operates at scale, affecting thousands of decisions simultaneously.
In dietary monitoring, bias can stem from multiple sources including unrepresentative training datasets, flawed algorithmic design, and human bias introduced during development [51]. For example, systems trained predominantly on specific demographic groups may perform poorly when deployed in broader populations, potentially missing crucial dietary patterns in minority ethnic groups or older adults. Understanding and mitigating these biases is not merely a technical exercise but a fundamental requirement for producing valid, reliable research outcomes that can be safely applied across diverse populations in clinical and pharmaceutical contexts.
Experimental Comparisons: Performance Across Devices and Populations
Quantitative Performance Metrics of Dietary Monitoring Technologies
Table 1: Comparative performance of sensor-based dietary monitoring methods across populations
| Technology Category | Specific Device/Method | Reported Accuracy | Population Tested | Key Limitations |
|---|---|---|---|---|
| Wearable Camera | eButton (automatic image capture) | Feasibility established [3] | Chinese Americans with T2D (N=11) [3] | Privacy concerns, positioning difficulties, sensor discomfort [3] |
| Continuous Glucose Monitor | Freestyle Libre Pro | Paired with eButton for visualization [3] | Chinese Americans with T2D (N=11) [3] | Sensor detachment, skin sensitivity, limited without structured support [3] |
| Acoustic Sensors | Various chewing detection systems | Systematic review identified multiple approaches [12] | Laboratory and limited free-living studies [12] | Privacy concerns with audio recording, filtering needed for non-food sounds [12] |
| Inertial Sensors | Wrist-based motion tracking | Bite detection via hand-to-mouth gestures [12] | Primarily laboratory settings [12] | Differentiates poorly between eating and similar gestures [12] |
Performance Disparities and Bias Manifestations
The experimental data reveals significant performance variations across demographic groups. Studies specifically examining Chinese Americans with Type 2 Diabetes found that while wearable sensors like the eButton and CGM showed promise, their effectiveness was moderated by cultural dietary patterns and user comfort with the technology [3]. This population reported challenges with traditional dietary self-management due to cultural norms around carbohydrate-rich foods and communal eating practices, which may not be adequately captured by algorithms trained on Western dietary patterns [3].
Facial recognition technologies, sometimes incorporated in dietary monitoring for user identification, have demonstrated alarming demographic disparities. The "Gender Shades" study revealed that commercial face-analysis systems had error rates up to 34.7% higher for darker-skinned females compared to lighter-skinned males, directly tracing to training datasets heavily skewed toward lighter-skinned subjects [52] [50]. While not directly measuring food intake, these systems highlight how biased training data creates performance gaps that likely extend to dietary assessment algorithms.
Methodological Approaches: Experimental Protocols for Bias Assessment
Protocol for Validating Dietary Diversity Scores
Table 2: Experimental protocol for validating dietary diversity assessment tools
| Protocol Phase | Description | Metrics Collected | Bias Assessment |
|---|---|---|---|
| Participant Recruitment | Stratified sampling across age, ethnicity, socioeconomic status, and health conditions [53] [54] | Demographic characteristics, health status indicators [53] | Ensure representation of all subgroups in validation cohort |
| Dietary Data Collection | 24-hour dietary recall combined with food group classification [53] | Individual Dietary Diversity Score (IDDS) using 9 food groups [53] | Cross-verify with biomarker data where possible |
| Health Status Assessment | Activities of Daily Living (ADL), Instrumental ADL, Mini-Mental State Examination (MMSE) [54] | Physical and cognitive function scores [54] | Assess differential validity across subgroups |
| Statistical Validation | Receiver Operating Characteristic (ROC) curve analysis [53] | Area Under Curve (AUC), sensitivity, specificity at different cut-offs [53] | Calculate separate performance metrics for each demographic segment |
Cross-Cultural Validation Methodology
Research on Chinese Americans with Type 2 Diabetes employed a prospective cohort design where participants wore multiple sensors simultaneously (eButton and CGM) for 10-14 days while maintaining food diaries [3]. This protocol enabled researchers to:
- Compare automated data collection against self-reported benchmarks
- Identify cultural factors affecting technology acceptance
- Assess barriers to implementation across diverse user groups
The methodology revealed that structured support from healthcare providers was essential for meaningful data interpretation, particularly for populations facing language or cultural barriers [3]. This highlights the importance of human-centric design in dietary monitoring systems intended for diverse populations.
Technical Framework: Bias Mitigation Strategies
Three-Stage Intervention for Bias Reduction
The IEEE 7003-2024 standard establishes a comprehensive framework for addressing algorithmic bias throughout the system lifecycle, emphasizing continuous monitoring and iterative improvement [55]. This approach aligns with three established technical intervention points:
Pre-processing approaches adjust data before model training through techniques such as collecting more representative data, re-weighting existing datasets, or curating balanced data subsets [52]. For dietary monitoring, this could intentionally oversample underrepresented populations or collect data on culturally specific foods. The primary challenge is the potential expense and difficulty of collecting high-quality diverse datasets [52].
In-processing approaches modify the training process itself by incorporating fairness considerations directly into the algorithm's optimization function [52]. For example, the training process might be adjusted to minimize the maximal error rate across predefined demographic groups rather than simply maximizing overall accuracy. These methods can provide theoretical guarantees on bias mitigation but may require computationally expensive model retraining [52].
Post-processing approaches adjust model outputs after training through techniques such as threshold adjustment for different groups or calibration shifting [52]. These methods are computationally efficient and can improve accuracy without retraining, but they require explicit knowledge of group membership which may raise regulatory concerns in some applications [52].
Establishing a Comprehensive Bias Profile
The IEEE 7003-2024 standard emphasizes creating a "bias profile" - a comprehensive documentation of bias considerations throughout the system lifecycle [55]. For dietary monitoring research, this includes:
- Stakeholder identification documenting both those who influence the system and those impacted by it
- Risk assessments evaluating potential adverse impacts on different demographic groups
- Data governance frameworks ensuring representation of all stakeholders, particularly marginalized groups
- Monitoring procedures for detecting "data drift" (changes in data environment) and "concept drift" (shifts in input-output relationships) over time [55]
This systematic documentation promotes accountability and enables researchers to demonstrate due diligence in addressing algorithmic bias, which is increasingly required by regulatory bodies and ethical review boards.
Table 3: Research reagent solutions for dietary monitoring validation studies
| Tool Category | Specific Examples | Function in Research | Considerations for Diverse Populations |
|---|---|---|---|
| Validation Metrics | Area Under Curve (AUC), Sensitivity, Specificity [53] | Quantify performance of dietary assessment tools | Calculate separate metrics for each demographic subgroup |
| Dietary Diversity Scores | Individual Dietary Diversity Score (IDDS) [53], Minimum Dietary Diversity for Women (MDD-W) [53] | Assess nutritional quality and variety | Ensure food groups reflect cultural dietary patterns |
| Wearable Sensors | eButton [3], Continuous Glucose Monitors [3], Acoustic sensors [12] | Automate data collection on eating behavior | Address privacy concerns and physical comfort across users |
| Biomarker Validation | Blood lipids, HbA1c, BMI [56] [54] | Objectively verify self-reported or sensor data | Account for biological differences across demographics |
| Bias Assessment Frameworks | IEEE 7003-2024 Standard [55], Pre-/In-/Post-processing approaches [52] | Systematically identify and mitigate algorithmic bias | Document decisions throughout model lifecycle |
Overcoming algorithmic bias in food intake validation requires methodical attention to dataset composition, algorithmic design, and continuous performance monitoring across diverse populations. The experimental data shows that without deliberate intervention, dietary monitoring technologies may perform suboptimally for minority populations, older adults, and those with culturally distinct eating patterns. By implementing the comprehensive framework outlined here - including rigorous validation protocols, standardized bias mitigation techniques, and documentation practices aligned with emerging standards - researchers can develop more robust and equitable dietary assessment tools.
For drug development professionals and clinical researchers, these approaches ensure that digital endpoints derived from wearable device data meet regulatory standards for safety and efficacy across all population groups. The future of dietary monitoring research lies not merely in technological advancement but in the ethical implementation of these technologies to serve diverse global populations equitably.
The validation of food intake through wearable device data represents a frontier in digital health, with applications in nutritional science, chronic disease management, and pharmaceutical development. Wearable sensors offer the potential to move beyond subjective self-reporting methods to objective, continuous monitoring of eating behaviors [12]. However, the path from data collection to clinically valid insights is fraught with three interconnected practical challenges: signal loss from technical and physiological factors, significant privacy concerns regarding sensitive biometric data, and variable user adherence in real-world settings. This guide examines these challenges through the lens of current research, comparing device performance and presenting experimental approaches for mitigating these barriers in rigorous scientific studies.
Challenge 1: Signal Loss and Data Quality
Signal loss compromises the integrity of the continuous data streams essential for validating food intake. This challenge manifests as missing data segments, motion artifacts, and inaccurate readings from the sensors tasked with detecting eating behaviors.
- Non-Wear Periods and Missing Data: In ambulatory studies, participants often remove devices, leading to data gaps. One analysis of real-world datasets found that ensuring continuous wear is a fundamental challenge, as these gaps can obscure critical behavioral patterns [57].
- Motion Artifacts: Sensors based on photoplethysmography (PPG) for heart rate or accelerometers for movement are highly susceptible to noise from physical activity, which can mask the subtle signals associated with chewing or swallowing [58] [57].
- Algorithmic and Hardware Variability: Inconsistent performance arises from the use of different sensors and proprietary algorithms across devices. For instance, a review of wearable technology found inconsistent validity for key metrics like energy expenditure, with error rates often exceeding 10% [58].
Comparative Performance of Sensor Modalities
The table below summarizes the performance of various sensor types used for monitoring eating behavior, highlighting their specific vulnerabilities to signal loss.
Table 1: Comparison of Sensor Modalities for Eating Behavior Monitoring
| Sensor Modality | Primary Measured Metric(s) | Common Signal Loss/Quality Issues | Reported Performance/Accuracy |
|---|---|---|---|
| Acoustic Sensors [12] | Chewing, swallowing, bite count | Ambient noise, poor sensor-skin contact | High accuracy in lab settings; degrades in noisy free-living environments |
| Inertial Measurement Units (IMUs) [12] | Hand-to-mouth gestures, arm movement | Motion artifacts, non-eating related arm movements | Bite count accuracy varies widely (≈70-90%) depending on algorithm and activity context |
| Photoplethysmography (PPG) [58] | Heart rate for inferring metabolic response | Motion artifacts, skin tone, poor fit | Validity is questionable; influenced by exercise type, intensity, and fit |
| Wearable Cameras (e.g., eButton) [3] [12] | Food type, portion size, eating environment | Camera mispositioning, privacy-preserving blurring, low light | Facilitates food identification; portion size estimation accuracy requires optimized algorithms |
Experimental Protocol: Mitigating Signal Loss in Ambulatory Studies
Objective: To implement and validate a pipeline for identifying and managing signal loss in continuous wearable data collected for food intake validation.
Methodology Details: This protocol is adapted from practical countermeasures proposed in recent research [57].
- Non-Wear Detection Pipeline:
- Input: Tri-axial accelerometer data (e.g., from a wrist-worn device).
- Processing: Calculate the accelerometer's magnitude (vector norm). A window of data (e.g., 1 minute) is classified as "non-wear" if the standard deviation of the magnitude is below a set threshold (e.g., < 0.01 g) and the value range is below another threshold (e.g., < 0.02 g) for a prolonged period (e.g., > 60 minutes).
- Output: A time-series binary mask labeling "wear" and "non-wear" periods.
- Data Quality Visualization:
- Utilize tools like
Plotly-Resamplerto create interactive visualizations of the entire data timeline. This allows researchers to quickly inspect data quality, overlay "non-wear" masks, and identify periods of anomalous but non-zero signal that may indicate motion artifacts or device malfunction [57].
- Utilize tools like
- Bootstrapping for Feature Robustness:
- Purpose: To evaluate the reliability of derived features (e.g., number of daily bites) in the presence of partially missing data.
- Procedure: Randomly introduce artificial "missingness" into high-quality data segments. Recalculate the features of interest on these degraded datasets multiple times via bootstrapping. The variability of the resulting feature values quantifies their robustness to signal loss [57].
Challenge 2: Privacy and Data Ethics
The detailed, continuous biometric and behavioral data required for food intake validation—including images of meals and eating contexts—elevate privacy risks, demanding robust ethical and technical safeguards.
Landscape of Privacy Risks
- Data Sensitivity and Misuse: Wearables collect highly sensitive personal health data (e.g., dietary habits, physiological responses). This data can be sold to third-party advertisers or, in the event of a breach, lead to financial loss, discrimination, or reputational damage [59] [60]. Health biodata is a high-value commodity on the dark web, further incentivizing attacks [60].
- Inadequate User Consent and Transparency: Privacy policies are often lengthy and complex, leading to "privacy fatigue" where users consent without fully understanding the terms [60] [61]. A systematic evaluation of 17 wearable manufacturers found high-risk ratings for transparency reporting (76%) and vulnerability disclosure (65%) [60] [61].
- Regulatory Gaps: While frameworks like GDPR and HIPAA provide baseline protections, the consumer wearables industry often operates in regulatory grey areas, with inconsistent data governance across companies [59] [60].
Comparative Privacy Risk Assessment of Device Manufacturers
The following table compares the privacy practices of leading wearable technology manufacturers based on a 2025 systematic analysis, providing a risk profile relevant to selecting devices for research [60] [61].
Table 2: Manufacturer Privacy Risk Profile (Adapted from systematic review)
| Manufacturer | Cumulative Privacy Risk Score | Notable High-Risk Areas | Notable Low-Risk Areas |
|---|---|---|---|
| Xiaomi, Wyze, Huawei | Highest | Transparency reporting, vulnerability disclosure, data minimization | Identity policy, data access |
| Apple, Google, Fitbit | Lowest | Generally strong across all domains; few high-risk ratings | Data access, control over targeted advertising, identity policy |
| Polar, Garmin, Withings | Low to Moderate | Some concerns in third-party sharing or breach notification | Data access, purpose limitation, identity policy |
Experimental Protocol: Embedding Privacy-Preserving Techniques
Objective: To integrate technical and procedural safeguards that protect participant privacy during a study using wearable cameras for dietary assessment.
Methodology Details: This protocol synthesizes recommendations from multiple sources [3] [12].
- Privacy by Design in Data Collection:
- For Wearable Cameras (e.g., eButton): Configure devices to capture images at intervals optimized for meal documentation (e.g., every 3-6 seconds) rather than continuous video, reducing the volume of extraneous, potentially sensitive data [3].
- Sensor Modality Selection: Where scientifically justified, choose non-camera-based sensors (e.g., acoustic or inertial) for specific metrics like chewing rate, which pose a lower inherent privacy risk [12].
- On-Device Data Processing and Filtering:
- Implement and test algorithms that can run on the device or smartphone to automatically blur faces, text (e.g., on computer screens), and backgrounds in images before they are stored or transmitted, preserving only the food-related visual information [12].
- Informed Consent Protocol:
- Develop a layered consent process. This includes a concise, easy-to-understand summary of data flows and risks, followed by a more detailed document.
- Explicitly inform participants about who can access their data (e.g., research team, device manufacturer, cloud service providers) and the specific measures taken to protect their privacy, including data anonymization procedures [59] [3].
Challenge 3: User Adherence and Engagement
For wearable data to be valid, participants must use the devices as intended. Poor adherence, whether from discomfort, burden, or lack of motivation, directly translates to poor quality data and invalid conclusions.
Factors Influencing Adherence
- Device Comfort and Usability: Physical discomfort is a significant barrier. In a study of Chinese Americans with diabetes, users reported issues with sensors falling off, getting trapped in clothes, and causing skin sensitivity [3]. Complex devices that require frequent charging or syncing also reduce adherence.
- Perceived Value and Feedback: Adherence increases when users understand the data and receive meaningful feedback. Participants in the eButton/CGM study reported that seeing the direct impact of food on their glucose levels increased their mindfulness and motivation to adhere to the protocol [3].
- Cultural and Social Acceptance: The social acceptability of wearing certain devices, particularly those with cameras, can impact adherence. Concerns about how others might perceive being recorded need to be addressed [3].
Adherence Comparison Across Monitoring Technologies
The table below contrasts adherence-related factors for different technologies used in food intake monitoring.
Table 3: Comparing User Adherence Factors Across Monitoring Technologies
| Technology | Key Facilitators for Adherence | Key Barriers to Adherence | Impact on Data Validity |
|---|---|---|---|
| Wrist-Worn Activity Trackers [58] [62] | High social acceptance, easy to use, provides direct feedback (e.g., steps). | Skin irritation, need for frequent charging, "notification fatigue." | High adherence yields continuous data; low adherence creates significant gaps. |
| Wearable Cameras (eButton) [3] | Increases mindfulness of eating, provides objective meal record. | Privacy concerns, social awkwardness, difficulty with camera positioning. | Poor adherence leads to missing meals, invalidating dietary intake analysis. |
| Continuous Glucose Monitors (CGM) [3] | Clear, actionable feedback on glycemic response, motivates behavioral change. | Sensor can fall off, skin sensitivity, cost. | Missing data disrupts the correlation between reported food intake and physiological response. |
| Specialized Sensors (Acoustic, IMU) [12] | Objective measurement of specific eating behaviors (chews, bites). | Can be obtrusive, requires multiple devices, low social acceptance. | Low adherence makes behavioral analysis impossible. |
Experimental Protocol: Measuring and Enhancing Adherence
Objective: To objectively monitor participant adherence and implement strategies to sustain engagement in a long-term dietary monitoring study.
Methodology Details: This protocol is informed by research on adherence in wearable studies [57] [3] [62].
- Objective Adherence Metrics:
- Wear Time Compliance: Use the accelerometer-based non-wear detection pipeline (from Section 2.3) to calculate the actual number of hours the device was worn versus the protocol requirement [57] [62].
- Task Completion Rate: For devices like the eButton, log the number of captured meal events against participant-reported meals in a diary to quantify adherence to the specific monitoring task [3].
- Participant Compliance Visualization Dashboard:
- Purpose: To provide the research team with a near real-time tool to monitor participant motivation and adherence.
- Implementation: Create a dashboard that visualizes key adherence metrics (e.g., daily wear time, task completion rate) for each participant over the study period. A decline in these metrics can trigger a "re-instruction" or support call from the research team [57].
- Structured Support and Feedback:
- Facilitator: Integrate structured support from healthcare providers or researchers. Schedule regular sessions to help participants interpret their data (e.g., CGM trends with eButton photos), making the data personally meaningful and reinforcing the study's value [3].
- Barrier Mitigation: Proactively address common barriers. Provide clear instructions and videos on proper device positioning (e.g., for eButton), and supply additional adhesive patches for CGMs to prevent them from falling off [3].
The Scientist's Toolkit: Research Reagent Solutions
This table details key materials and tools essential for conducting rigorous research into wearable validation of food intake.
Table 4: Essential Research Reagents and Tools for Food Intake Validation Studies
| Item | Function/Application | Example/Note |
|---|---|---|
| Empatica E4 Wristband [57] | A research-grade wearable that captures accelerometry, PPG (BVP), EDA, and skin temperature, useful for multi-modal analysis of eating behavior and stress. | Used in the mBrain21 and ETRI lifelog studies for ambulatory monitoring [57]. |
| eButton or Similar Wearable Camera [3] | An image-based wearable device for passive capture of food images and eating context, enabling objective food identification and portion size estimation. | Positioned on the chest; captures images at pre-set intervals (e.g., 3-6 seconds) [3]. |
| Continuous Glucose Monitor (CGM) [3] | Measures interstitial glucose levels continuously, providing a physiological outcome measure to correlate with reported or image-documented food intake. | e.g., Freestyle Libre Pro; used to visualize the glycemic response to specific meals [3]. |
| tsflex & Plotly-Resampler Libraries [57] | Open-source Python tools for flexible signal processing and creating interactive, high-performance visualizations for large-scale wearable data, facilitating quality inspection. | Aids in implementing non-wear detection and visualizing data quality challenges [57]. |
| Interaction-Triggered Questionnaires [57] | Software feature (e.g., in a mobile app) that prompts users to confirm or label events (e.g., "Are you eating now?"), reducing data entry errors and personal bias. | Used for Ecological Momentary Assessment (EMA) to ground-truth sensor data [57]. |
Integrated Workflow for a Validation Study
The following diagram maps the logical workflow of a comprehensive study designed to validate food intake via wearables, integrating the protocols and mitigation strategies for the core challenges discussed above.
The accurate validation of food intake via wearable device data presents a complex challenge at the intersection of nutrition science, artificial intelligence, and clinical practice. Key obstacles include the inherent inaccuracy of self-reported dietary data, the statistical heterogeneity of data across institutions and patient populations, and the risk of model performance degradation over time in real-world settings [63] [48] [64]. These challenges necessitate robust mitigation strategies that can ensure the reliability, fairness, and privacy of AI-driven nutritional assessments. This guide objectively compares emerging technological solutions—specifically hybrid AI models, federated learning architectures, and continuous validation protocols—within the context of a research paradigm focused on validating wearable-collected food intake data. It is designed to provide researchers, scientists, and drug development professionals with a clear comparison of performance data, experimental methodologies, and essential research tools.
Performance Comparison of AI and Validation Strategies
The tables below synthesize quantitative performance data and key characteristics for the evaluated strategies, providing an at-a-glance comparison for researchers.
Table 1: Performance Comparison of AI Modeling Approaches for Energy and Nutrition Estimation
| Model / Approach | Reported Performance | Key Advantages | Limitations / Challenges |
|---|---|---|---|
| Hybrid Gaussian Process Regression (GPR) | R² = 1.00 (Males), high accuracy (Females) [65] | High accuracy vs. traditional formulas; practicality & flexibility [65] | Performance decrease with PCA for simplicity (R=0.48, R²=0.23) [65] |
| AI-Driven Dietary Assessment (e.g., goFOOD) | Moderate agreement with dietitians [63] | Reduces self-reporting burden; real-time assessment [63] | Errors with complex meals, occlusions, portion ambiguity [63] |
| Traditional Equations (e.g., Mifflin-St. Jeor) | R = 0.71 (Mifflin) [65] | Affordability; practicality for field use [65] | Lower reliability than measurement methods/novel AI models [65] |
Table 2: Comparison of Federated Learning Clustering Methods for Healthcare Data
| Clustering Method | Category | Reported Outcome | Key Characteristics |
|---|---|---|---|
| Federated Gaussian Mixture Clustering (FedGMC) | Federated Clustering | Outperformed baselines; reduced performance degradation risk; ensured fairness [64] | Probabilistic; handles non-convex clusters; flexible; less sensitive to noise [64] |
| K-means & C-means | Federated Clustering | Higher misclassification rate vs. probabilistic models [64] | Hard clustering; poor with non-convex clusters; sensitive to noise [64] |
| Client Clustering (K-means, GMM) | Clustered Federation | Assumes single data type per client; struggles with internal patient heterogeneity [64] | Clusters clients based on data distribution/model parameters [64] |
Experimental Protocols and Methodologies
Protocol for Developing a Hybrid AI Model for Energy Estimation
A recent study detailed a protocol for developing a hybrid AI model to estimate daily energy requirements based on anthropometric and demographic data, outperforming traditional equations [65].
- Objective: To create a reliable, practical model with higher accuracy than existing methods for estimating individual energy requirements [65].
- Data Collection: Data were collected from volunteer individuals. Anthropometric measurements were performed using a bioelectrical impedance analysis (BIA) device, and demographic data were obtained via face-to-face surveys [65].
- Feature Analysis: Eighty-seven features were analyzed using the Spearman feature selection algorithm to identify those most relevant for estimating energy requirements [65].
- Model Architecture and Training: The hybrid model was based on collaborative hybridization, integrating three distinct Gaussian Process Regression (GPR) models, each using different kernels: squared exponential, rational quadratic, and Matern52. The models were structured separately by gender. Performance was evaluated using metrics including Mean Absolute Percentage Error (MAPE), Mean Absolute Deviation (MAD), Mean Squared Error (MSE), correlation coefficient (R), and coefficient of determination (R²) [65].
The workflow for this hybrid model development is as follows:
Protocol for the FedGMC Framework in Smart Healthcare
The Federated Gaussian Mixture Clustering (FedGMC) framework was designed to address data heterogeneity across hospitals while preserving privacy [64].
- Objective: To train personalized federated learning models that address both inter-hospital and intra-hospital (patient) heterogeneity, enhancing predictive performance and ensuring fairness among institutions [64].
- Framework Stages: The FedGMC framework operates in three sequential stages:
- Patient Encoding: Represents patient data in a suitable format for clustering.
- Federated Clustering: Applies Gaussian Mixture Clustering to identify global patient clusters across institutions without sharing raw data.
- Personalized FL: Conducts federated learning tailored to the identified clusters, generating personalized models [64].
- Evaluation: The framework was evaluated using real-world eICU datasets with various classifiers and performance metrics. It was compared against baseline methods to assess overall performance and its ability to mitigate performance degradation for participating hospitals [64].
The following diagram visualizes this multi-stage framework and the flow of data:
Protocol for Feasibility Studies on Wearable Data and AI Integration
A feasibility study, AI4Food, provides a protocol for integrating manually collected and wearable sensor data into nutritional interventions and AI tool development [66].
- Objective: To create an essential asset for the implementation, validation, and benchmarking of AI-based tools in nutritional clinical practice by capturing data within a weight loss intervention [66].
- Study Design: A prospective, crossover controlled trial for weight loss in overweight and obese participants. Participants were randomized into two groups:
- Group 1: Started with manual data collection methods (validated questionnaires).
- Group 2: Started with automatic data collection methods (wearable sensors). After two weeks, the groups switched data collection methods [66].
- Data Collection: Lifestyle data, anthropometric measurements, and biological samples were collected from all participants. The usability of electronic devices was assessed using the System Usability Scale (SUS) [66].
The Researcher's Toolkit
This section details key reagents, tools, and datasets essential for experimental work in this field.
Table 3: Key Research Reagents and Tools for Food Intake Validation Research
| Item / Resource | Function / Application | Example Use Case |
|---|---|---|
| Bioelectrical Impedance Analysis (BIA) | Measures body composition (e.g., fat mass, muscle mass). | Collecting anthropometric measurements for hybrid AI model inputs [65]. |
| Wearable Sensors / Accelerometers | Automatically capture physical activity and energy expenditure data. | Used in feasibility trials (e.g., AI4Food) for automatic data collection [66]. |
| Indirect Calorimetry Device | Considered the gold standard for measuring resting energy expenditure. | Validating the accuracy of new AI models or equations for energy estimation [65]. |
| Food Image Datasets (e.g., Food-101, UEC-Food256) | Training and benchmarking datasets for food recognition systems. | Developing and evaluating AI-driven dietary assessment tools [48]. |
| System Usability Scale (SUS) | A standardized questionnaire for assessing the usability of a system. | Evaluating the satisfaction and usability of electronic data collection devices [66]. |
| eICU Collaborative Research Database | A multi-center database for critical care research. | Serving as a real-world dataset for validating federated learning frameworks like FedGMC [64]. |
| Gaussian Process Regression (GPR) Models | A probabilistic AI model for regression tasks. | Serving as components in a hybrid model for estimating energy requirements [65]. |
For researchers validating food intake via wearable devices, the integration of hybrid AI models, advanced federated learning techniques like FedGMC, and rigorous continuous validation protocols offers a powerful pathway to overcome significant data and modeling challenges. The experimental data and protocols presented herein provide a foundation for developing robust, accurate, and clinically applicable tools that can advance the field of precision nutrition and contribute to improved health outcomes.
Benchmarking Accuracy: How Wearables Compare to Gold-Standard Dietary Assessment Methods
Validating food intake data from wearable devices requires comparison against robust, scientific reference methods. Two methodologies form the cornerstone of this validation framework: doubly labeled water (DLW) for quantifying energy expenditure and controlled meal studies for precise assessment of energy intake. The DLW method, recognized as the gold standard for measuring free-living energy expenditure, provides an objective physiological benchmark against which self-reported dietary intake and wearable device estimates can be compared [67]. Controlled meal studies complement this approach by providing rigorously measured energy intake data in structured environments. Together, these methods create a validation framework that enables researchers to assess the accuracy of wearable device data for monitoring nutritional status, identifying misreporting, and understanding eating behaviors.
The integration of these reference methodologies is particularly crucial given the well-documented limitations of self-reported dietary data. Traditional instruments such as food frequency questionnaires, food diaries, and 24-hour recalls are prone to substantial misreporting because participants may inaccurately estimate portion sizes, have imperfect recall, or deliberately modify their reporting [68]. One analysis of large dietary datasets found that approximately 27.4% of dietary reports contained significant misreporting when compared against objective energy expenditure measurements [68]. This validation framework addresses these limitations by providing objective biomarkers and controlled feeding paradigms against which new wearable technologies can be evaluated.
Core Reference Methodologies
Doubly Labeled Water (DLW) Method
Principles and Physiological Basis
The doubly labeled water technique is a non-invasive, isotopic method that measures total energy expenditure (TEE) in free-living individuals over extended periods, typically 1-3 weeks. The method is grounded in the fundamental principle that carbon dioxide production can be calculated from the difference in elimination rates between two stable isotopes: deuterium (²H) and oxygen-18 (¹⁸O) [67].
After ingestion, both isotopes equilibrate with the body's water pool. Deuterium (²H) is eliminated from the body exclusively as water, primarily through urine, sweat, and respiration. In contrast, oxygen-18 (¹⁸O) is eliminated both as water and as carbon dioxide through the bicarbonate pool in respiration. The difference in elimination kinetics between these two isotopes thus provides a measure of carbon dioxide production rates, which can be converted to energy expenditure using principles of indirect calorimetry [67].
The mathematical relationship is expressed as:
Where rCO₂ is the rate of carbon dioxide production, kO and kH are the elimination rates of oxygen-18 and deuterium respectively, and N is the body water pool size calculated from the isotope dilutions. This calculation requires corrections for isotopic fractionation during water loss.
Experimental Protocol and Procedures
The standard DLW protocol involves multiple precise steps that must be carefully controlled to ensure accurate results:
Baseline Sample Collection: Prior to isotope administration, researchers collect baseline urine, saliva, or blood samples to determine natural background abundances of ²H and ¹⁸O.
Isotope Administration: Participants ingest a precisely weighed dose of water containing both deuterium (²H₂O) and oxygen-18 (H₂¹⁸O). The dose is typically calibrated based on body weight estimates to achieve optimal isotope enrichment levels.
Equilibration Sampling: Post-dose samples are collected at 2-6 hours to determine the initial isotope enrichment in the body water pool.
Elimination Phase Monitoring: Subsequent samples are collected over 7-14 days (depending on study design) to track the exponential disappearance of the isotopes from the body water pool.
Sample Analysis: Isotope ratios in the biological samples are analyzed using isotope ratio mass spectrometry or newer techniques like laser-based off-axis integrated cavity output spectroscopy [67].
The CALERIE (Comprehensive Assessment of Long-term Effects of Reducing Intake of Energy) study demonstrated the exceptional longitudinal reproducibility of the DLW method, showing that fractional turnover rates for isotopes and calculated energy expenditure remained highly consistent over periods of 2.4-4.5 years [69]. This reproducibility makes DLW particularly valuable for long-term intervention studies where maintaining measurement consistency is crucial.
Table 1: Key Technical Parameters of Doubly Labeled Water Method
| Parameter | Specification | Application Notes |
|---|---|---|
| Measurement Period | Typically 7-14 days | Can be extended to 3 weeks in some protocols |
| Analytical Error | Approximately 1-7% depending on equation used [68] | Varies with protocol and calculation model |
| Isotope Safety | Non-radioactive, stable isotopes | No known toxicity at administered doses |
| Long-term Reproducibility | Within 1% for isotope turnover, 5% for CO₂ production [69] | Demonstrated over 4.5 years |
| Sample Collection | Urine (most common), saliva, or blood |
Controlled Meal Studies
Methodological Framework
Controlled meal studies provide a complementary approach to DLW by directly measuring energy intake rather than expenditure. These studies involve providing participants with all meals in a controlled setting where researchers can precisely quantify food composition and portion sizes. The fundamental strength of this methodology lies in the elimination of self-reporting biases that plague free-living dietary assessments.
The core elements of controlled meal studies include:
Dietary Formulation: Meals are designed and prepared by research dietitians using standardized recipes with precisely weighed ingredients.
Nutrient Analysis: Food samples are often analyzed chemically to verify macronutrient and energy content, though database values are frequently used.
Feeding Environment: Meals are typically consumed in designated research dining facilities under supervision to ensure protocol adherence.
Plate Waste Measurement: Uneaten food is carefully collected and weighed to calculate actual consumption.
These studies can be designed with various levels of control, ranging from highly metabolic ward studies where participants remain in the facility for the study duration, to partially controlled studies where only specific meals are provided.
Integration with Sensor Technologies
Recent advances have enabled the integration of controlled meal studies with sensor-based eating behavior monitoring. The electronic button (eButton), for example, is a wearable device that automatically captures food images during meals, providing objective data on eating episodes [3]. When combined with controlled feeding paradigms, these sensors can validate eating behavior metrics such as eating rate, bite count, and meal duration under conditions where true intake is known.
In one implementation, Chinese American participants with type 2 diabetes used the eButton alongside continuous glucose monitoring in a controlled dietary assessment. The eButton was worn on the chest and recorded food images every 3-6 seconds during eating episodes, providing detailed visual documentation of food consumption [3]. This integration of controlled intake measures with sensor technology represents a powerful validation framework for free-living eating behavior assessment.
Comparative Analysis of Reference Methods
Technical Specifications and Applications
Each reference methodology offers distinct advantages and limitations, making them complementary rather than interchangeable for validation purposes. The table below provides a detailed comparison of their key characteristics:
Table 2: Comparative Analysis of Reference Methods for Food Intake Validation
| Parameter | Doubly Labeled Water | Controlled Meal Studies |
|---|---|---|
| Primary Measurement | Total energy expenditure in free-living conditions | Energy intake in controlled settings |
| Measurement Principle | Isotopic elimination kinetics | Direct weighing and composition analysis |
| Time Frame | 1-3 weeks | Single meals to several weeks |
| Key Strengths | Non-invasive; measures free-living expenditure; gold standard for TEE [67] | Eliminates self-reporting bias; precise intake data; controls confounding variables |
| Limitations | Expensive isotopes; specialized analysis; doesn't measure intake directly [67] | Artificial eating environment; limited generalizability; resource-intensive |
| Analytical Precision | 1-7% error for energy expenditure [68] | Near 100% accuracy for provided foods |
| Cost Factors | High (isotopes and specialized analysis) | Moderate to high (food preparation and facility costs) |
| Participant Burden | Low (minimal compliance needed after dosing) | High (requires eating in controlled setting) |
Synergistic Applications in Validation Research
The true power of these reference methodologies emerges when they are employed synergistically within a comprehensive validation framework. DLW provides the objective physiological benchmark for total energy requirements, while controlled meal studies offer precise intake data under observed conditions. Together, they enable researchers to:
Quantify Misreporting in Dietary Records: By comparing self-reported intake against measured energy expenditure from DLW, researchers can identify systematic under- or over-reporting. Analysis of large datasets using DLW-based predictive equations has revealed that nearly 30% of dietary reports contain significant misreporting [68].
Validate Wearable Device Accuracy: Sensor-based estimates of energy intake or expenditure can be validated against both DLW and controlled feeding paradigms to establish their measurement error and operational limits.
Understand Eating Behavior Patterns: Controlled meal studies can establish the relationship between sensor signals (e.g., chewing sounds, wrist motions) and actual food consumption, which can then be applied to free-living monitoring validated by DLW.
The integration of these methods was demonstrated in research with Chinese Americans with type 2 diabetes, where continuous glucose monitors provided real-time physiological data while controlled meal conditions helped establish the relationship between specific foods and glycemic responses [3].
Experimental Protocols and Implementation
DLW Protocol from the CALERIE Study
The CALERIE study implemented a rigorous DLW protocol that exemplifies best practices for longitudinal energy expenditure measurement:
Dose Preparation: Precisely weighed doses of ²H₂O and H₂¹⁸O were prepared for each participant based on body weight, with careful quality control through duplicate dosing in randomly selected samples.
Blinded Analyses: To minimize analytical bias, isotope samples were analyzed in blinded fashion with randomly inserted quality control samples.
Longitudinal Quality Assurance: The study implemented two complementary protocols: a dose-dilution protocol with repeated analysis of reference doses over 4.5 years, and a test-retest protocol with blinded re-analysis of 50 randomly selected DLW studies over 2.4 years [69].
Data Analysis: Isotope elimination rates were calculated using the interval method with appropriate fractionation corrections. The reproducibility of this protocol demonstrated that the DLW method could reliably detect longitudinal changes in energy expenditure as small as 2-5%.
This protocol confirmed that the DLW method produces highly reproducible longitudinal results, with fractional turnover rates for deuterium and oxygen-18 reproducible to within 1% and 5%, respectively, over multi-year periods [69]. This level of precision makes DLW invaluable for long-term intervention studies where detecting small but clinically meaningful changes in energy balance is essential.
Controlled Meal Study Protocol with Sensor Integration
A representative protocol for controlled meal studies integrated with wearable sensors includes:
Participant Screening and Standardization: Participants are screened for eligibility and provided with standardized instructions regarding pre-study fasting and medication use.
Sensor Calibration and Placement: Wearable sensors such as the eButton are calibrated and positioned. For example, the eButton is typically worn on the chest to capture food images during meals [3].
Meal Provision: Participants consume test meals with precisely documented composition and portion sizes. Meals may be designed to test specific hypotheses about food effects (e.g., high vs. low glycemic index foods).
Multi-modal Data Collection: Throughout the meal, researchers collect data from multiple sources including the wearable sensors, continuous glucose monitors (if applicable), and direct observation.
Post-meal Processing: Data from various sensors are synchronized and processed using specialized algorithms to extract eating behavior metrics.
This protocol enables the validation of sensor-derived eating metrics against known consumption data, establishing the foundation for subsequent free-living monitoring.
Validation Framework for Wearable Devices
Accuracy Assessment Against Reference Standards
The validation of wearable devices for food intake monitoring requires systematic comparison against the reference standards provided by DLW and controlled meal studies. Key validation metrics include:
- Mean Absolute Percentage Error (MAPE): Difference between device-estimated and reference-measured energy expenditure or intake
- Bias Analysis: Systematic over- or under-estimation trends in device measurements
- Limits of Agreement: Statistical range within which device and reference measurements are expected to agree
For energy expenditure estimation, consumer wearables show varying performance levels. One comprehensive umbrella review of systematic reviews found that wearables demonstrated a mean bias of approximately ±3% for heart rate measurement but significantly overestimated VO₂max by 9.83-15.24% during exercise testing [70]. For energy expenditure specifically, wearables showed a mean bias of approximately -3 kcal per minute (-3%), with error ranges from -21.27% to 14.76% [70].
For food intake monitoring, sensor-based methods are still in development. The eButton and similar imaging devices have shown feasibility for automatic food recording, but their accuracy in real-world conditions requires further validation against controlled meal studies [3] [12].
Implementation Workflow for Validation Studies
The following diagram illustrates the integrated workflow for validating wearable devices using both reference methodologies:
This integrated workflow enables comprehensive validation of wearable devices against both physiological energy expenditure measures (DLW) and precise intake data (controlled meals), providing a robust framework for establishing device accuracy.
Research Reagent Solutions and Materials
The implementation of these validation methodologies requires specific reagents and materials that represent essential "research tools" for the field:
Table 3: Essential Research Reagents and Materials for Validation Studies
| Category | Specific Items | Function & Application |
|---|---|---|
| Isotopic Reagents | Deuterium oxide (²H₂O); Oxygen-18 water (H₂¹⁸O) | Stable isotopes for DLW energy expenditure measurement [67] |
| Analytical Instruments | Isotope ratio mass spectrometer; Laser-based cavity spectroscopy | Precise measurement of isotope ratios in biological samples [67] |
| Wearable Sensors | eButton (wearable camera); Accelerometers; Continuous glucose monitors | Food image capture; physical activity monitoring; glucose response tracking [3] [12] |
| Dietary Assessment Tools | Controlled meal ingredients; Food weighing scales; Nutrient databases | Precise food preparation and composition analysis |
| Sample Collection | Urine/saliva collection containers; Freezer storage (-20°C or -80°C) | Biological sample preservation for subsequent analysis |
Applications in Nutritional Research and Drug Development
The validation framework employing DLW and controlled meal studies has significant applications across multiple domains:
Detection of Dietary Misreporting
The development of predictive equations derived from large DLW databases has enabled more accurate identification of misreporting in dietary studies. One analysis of 6,497 DLW measurements produced a regression equation that predicts expected total energy expenditure from easily acquired variables like body weight, age, and sex [68]. When applied to large national surveys (NDNS and NHANES), this approach revealed that traditional methods significantly underestimate the prevalence of misreporting, with potentially serious consequences for understanding diet-disease relationships.
The equation takes the form:
Where TEE is total energy expenditure in megajoules per day, BW is body weight in kilograms, and Height is in centimeters [68]. This equation, with its 95% predictive limits, provides a robust screening tool for identifying potentially unreliable dietary reports in research studies.
Wearable Device Algorithm Development
Controlled meal studies provide the essential ground-truth data needed to develop and refine algorithms for wearable food intake monitoring. By simultaneously collecting sensor data (acoustic, motion, image) and known food consumption information, researchers can train machine learning models to recognize eating behaviors and estimate nutrient intake. These algorithms can then be validated in free-living conditions using DLW as the reference standard for energy balance.
Current research in this area focuses on multiple sensor modalities:
- Acoustic sensors for detecting chewing and swallowing sounds
- Inertial sensors for capturing hand-to-mouth gestures and eating rhythms
- Camera-based systems for food identification and portion size estimation
- Physiological sensors for monitoring metabolic responses to feeding
The systematic review of sensor-based eating behavior monitoring identified a taxonomy of technologies being applied to this challenge, though noting that most methods still require further validation in free-living conditions [12].
The validation framework incorporating doubly labeled water and controlled meal studies represents the current gold standard for assessing food intake and energy expenditure in human nutrition research. These methodologies provide the reference points against which emerging wearable technologies must be validated to establish their utility for research and clinical applications.
As wearable devices continue to evolve, this rigorous validation framework will be essential for translating technological innovations into scientifically valid tools for monitoring dietary intake and eating behaviors. The integration of multi-modal sensor data with robust reference methodologies holds promise for addressing the long-standing challenges of dietary assessment, potentially enabling more accurate monitoring of energy balance in free-living populations.
Accurately measuring caloric and nutritional intake is a fundamental challenge in nutritional science, clinical research, and drug development. Traditional methods, such as 24-hour recall and food diaries, are plagued by human error and reliance on memory, making them unreliable for precision health initiatives [20]. The emergence of wearable devices for Automatic Dietary Monitoring (ADM) promises a paradigm shift, offering objective, continuous data collection in free-living conditions [30]. However, the adoption of this technology in critical research and clinical trials hinges on rigorous validation. This process requires a nuanced application of specific performance metrics—Accuracy, F1-Scores, and Limits of Agreement—to properly evaluate a device's capability against reference methods and against competing alternatives. This guide provides researchers with a framework for this essential analytical process, framed within the context of validating food intake via wearable device data.
Performance Metrics Demystified
Accuracy and Its Paradox
In machine learning and statistics, accuracy provides an overall measure of a model's correctness. For a classification model, it is the proportion of total correct predictions (both positive and negative) among the total number of cases examined [71]. It is defined as:
[ \text{Accuracy} = \frac{\text{Number of Correct Predictions}}{\text{Total Number of Predictions}} = \frac{TP + TN}{TP + TN + FP + FN} ]
Where (TP) = True Positives, (TN) = True Negatives, (FP) = False Positives, and (FN) = False Negatives [72].
However, high accuracy can be deceptive, a phenomenon known as the Accuracy Paradox. In imbalanced datasets where one class dominates, a model can achieve high accuracy by simply always predicting the majority class, while failing entirely to identify the critical minority class [71]. For instance, in a dataset where 95% of transactions are not fraudulent, a model that always predicts "not fraud" will be 95% accurate but useless for fraud detection. This makes accuracy a misleading metric for many real-world applications, including dietary monitoring, where specific activities (e.g., food intake gestures) are rare compared to non-eating activities [73] [71].
The F1-Score: A Balanced Metric for Imbalanced Data
The F1-score addresses the limitations of accuracy by balancing two other metrics: precision and recall [73] [72].
Precision (Positive Predictive Value): Measures the quality of positive predictions. It answers, "Of all instances predicted as positive, how many are actually positive?" High precision means fewer false alarms. [ \text{Precision} = \frac{TP}{TP + FP} ]
Recall (Sensitivity or True Positive Rate): Measures the model's ability to find all positive instances. It answers, "Of all actual positive instances, how many did we correctly identify?" High recall means fewer missed cases [73] [72]. [ \text{Recall} = \frac{TP}{TP + FN} ]
The F1-score is the harmonic mean of precision and recall, providing a single score that only achieves a high value when both precision and recall are high [73] [72]. [ F1 = 2 \times \frac{\text{Precision} \times \text{Recall}}{\text{Precision} + \Recall} = \frac{2TP}{2TP + FP + FN} ]
This makes it particularly valuable for evaluating models on imbalanced datasets or in situations where both false positives and false negatives carry significant costs, such as in activity recognition for dietary monitoring [72] [30].
Limits of Agreement for Continuous Data
While F1-score is ideal for categorical outcomes (e.g., activity classification), validating continuous measurements (e.g., total caloric intake) requires a different approach. The Limits of Agreement (LoA), typically analyzed using a Bland-Altman plot, is a standard method for assessing the agreement between two measurement techniques [20].
In this analysis, the mean difference between the test method (wearable device) and the reference method establishes the bias. The LoA are then calculated as the mean bias ± 1.96 standard deviations of the differences. This interval defines the range within which 95% of the differences between the two methods are expected to lie. A narrower LoA indicates better agreement between the new device and the reference standard [20].
Experimental Protocols in Dietary Monitoring Validation
To illustrate the application of these metrics, we examine the methodologies of two key studies that validate different wearable technologies.
Protocol 1: Validating a Caloric Intake Wristband
A 2020 study sought to validate the GoBe2 wristband (Healbe Corp.), which uses bioimpedance signals to estimate energy intake automatically [20].
- Objective: To assess the accuracy (kcal/day) and practical utility of the wristband for tracking daily nutritional intake in free-living participants [20].
- Participants: 25 free-living adult participants recruited from a university campus [20].
- Reference Method: A highly controlled method was developed in collaboration with a university dining facility. All meals were prepared, calibrated, and served to participants, with intake directly observed and recorded by a trained research team to establish ground truth for energy and macronutrient intake [20].
- Procedure: Participants used the wristband and its accompanying mobile app consistently for two 14-day test periods. Their dietary intake was simultaneously measured by the reference method [20].
- Data Analysis: Bland-Altman analysis was used to compare the daily calorie intake (kcal/day) outputs from the reference method and the wristband (test method) [20].
Protocol 2: Validating an Impedance-Sensing Activity Classifier (iEat)
A 2024 study introduced iEat, a wearable research prototype that uses bio-impedance sensing across two wrists to recognize food intake activities and food types [30].
- Objective: To evaluate iEat's ability to automatically detect food-intake activities and classify food types based on impedance variations caused by dynamic body-food-utensil circuits [30].
- Participants: Ten volunteers performing 40 meals in an everyday table-dining environment [30].
- Sensing Principle: The device uses a two-electrode configuration. During dining activities, new conductive circuits are formed through the hand, mouth, utensils, and food, leading to unique temporal patterns of impedance variation [30].
- Procedure: Participants wore iEat devices while engaging in structured meals. The impedance data was recorded and time-synced with video recordings of the meals that were used for ground truth annotation [30].
- Data Analysis: The impedance signal patterns were used to train a lightweight, user-independent neural network model. Performance was evaluated for the tasks of activity recognition and food type classification [30].
The workflow for a typical validation study, incorporating elements from both protocols, can be summarized as follows:
Comparative Analysis of Wearable Technologies
The data from the cited validation studies allows for a direct comparison of different technological approaches.
Table 1: Quantitative Performance Comparison of Dietary Wearables
| Device / Study | Technology | Primary Output | Performance Metric | Result | Key Limitation / Note |
|---|---|---|---|---|---|
| GoBe2 Wristband [20] | Bioimpedance (Single-channel) | Continuous Caloric Intake (kcal/day) | Limits of Agreement | Mean Bias: -105 kcal/day95% LoA: -1400 to 1189 kcal | High variability; signal loss noted as major error source. |
| iEat Prototype [30] | Bioimpedance (Two-wrist) | Categorical Food Intake Activity | Macro F1-Score | 86.4% | Recognized 4 activities (e.g., cutting, drinking). |
| iEat Prototype [30] | Bioimpedance (Two-wrist) | Categorical Food Type | Macro F1-Score | 64.2% | Classified 7 defined food types. |
Table 2: Analysis of Applicable Performance Metrics
| Output Data Type | Most Relevant Metric | Interpretation Guide |
|---|---|---|
| Categorical / Classification(e.g., Activity Type, Food Category) | F1-Score | High (>0.8): Excellent balance of precision and recall.Moderate (0.5-0.8): Fair performance, may be class-dependent.Low (<0.5): Poor performance, high error rate. |
| Continuous(e.g., Total Calories, Grams of Fat) | Limits of Agreement (LoA)(via Bland-Altman) | Wide LoA: Poor agreement, high individual error.Narrow LoA: Strong agreement.Large Bias: Systematic over/under-estimation. |
The Scientist's Toolkit: Essential Reagents & Materials
For researchers designing validation studies for dietary monitoring, the following tools and concepts are essential.
Table 3: Key Research Reagent Solutions for Validation Studies
| Item / Concept | Function in Validation | Example in Context |
|---|---|---|
| Controlled Feeding Facility | Provides the ground truth reference for energy and macronutrient intake by preparing and serving calibrated meals [20]. | University dining facility used to measure participants' actual consumption [20]. |
| Bland-Altman Plot | A statistical method used to visualize the agreement between two different measurement techniques for continuous data [20]. | Plotting the difference (device - reference) against the mean for caloric intake to assess bias and LoA [20]. |
| Confusion Matrix | A table that allows detailed visualization of a classification model's performance, showing true/false positives/negatives [72]. | Used to calculate precision, recall, and ultimately the F1-score for activity recognition tasks [72] [30]. |
| Bioimpedance Sensor | A sensing technology that measures the body's resistance to a small electrical current, used to infer physiological events or body composition [30]. | The core sensor in both the GoBe2 and iEat devices, used to detect eating-related circuit changes [20] [30]. |
| Continuous Glucose Monitor (CGM) | A device that tracks glucose levels throughout the day, often used as an auxiliary objective measure in dietary studies [20]. | Can be used to measure adherence to dietary reporting protocols, though data may not always be reported [20]. |
The validation of wearable devices for food intake research demands a metrics-driven approach that moves beyond simplistic accuracy. The choice of metric is dictated by the nature of the data the device produces: F1-score is the metric of choice for categorical outputs like activity and food-type recognition, as it balances the critical trade-off between precision and recall. For continuous outputs like total caloric intake, Limits of Agreement via Bland-Altman analysis is the gold standard for quantifying bias and individual error variability. As the field advances, researchers must critically apply these metrics to benchmark new technologies against existing alternatives and reference methods, ensuring that the tools used in drug development and clinical research are not just innovative, but also rigorously validated and reliable.
Accurate dietary assessment is fundamental to nutritional research, epidemiology, and clinical practice. For decades, traditional methods including 24-hour dietary recalls (24HR), food diaries, and Food Frequency Questionnaires (FFQs) have served as the cornerstone for capturing food intake data [74]. However, these tools rely on self-reporting, which is susceptible to memory lapses, estimation errors, and intentional misreporting [31] [12]. The emergence of wearable sensor technology represents a paradigm shift, offering objective, high-resolution data on eating behavior. This guide provides a comparative analysis of these methodologies, focusing on their operational principles, validity, and applicability within scientific research, particularly for validating food intake.
The following table summarizes the core characteristics, advantages, and limitations of each dietary assessment method.
Table 1: Comparative Overview of Dietary Assessment Methods
| Method | Primary Function | Data Granularity | Key Advantages | Key Limitations |
|---|---|---|---|---|
| 24-Hour Dietary Recall (24HR) | Captures detailed intake of all foods/beverages consumed in the previous 24 hours [74]. | High (per eating occasion) | - Minimizes reactivity if unannounced [74]- Relies on specific memory [74]- Open-ended structure allows for detailed description [74] | - Relies on participant's memory and honesty [75]- Requires multiple administrations to estimate usual intake [74]- Interviewer-administered versions can be resource-intensive [74] |
| Food Diary / Record | Prospective recording of all foods/beverages consumed over a set period (e.g., 7 days) [75]. | High (per eating occasion) | - Does not rely on memory if filled concurrently [74]- Can provide detailed context (time, location) | - High participant burden [75]- High risk of reactivity (altering diet due to monitoring) [74]- Prone to under-reporting, especially energy [75] [76] |
| Food Frequency Questionnaire (FFQ) | Assesses habitual intake by querying the frequency of consumption for a fixed list of foods over a long period (e.g., months or a year) [77]. | Low (habitual intake) | - Low cost and quick to administer [77]- Captures long-term, habitual diet- Useful for ranking individuals by intake [77] | - Provides less precise portion size estimation [77]- Prone to systematic measurement error [74]- May not capture episodically consumed foods well |
| Wearable & Sensor-Based Methods | Automatically detects and quantifies eating behavior metrics (chews, swallows, bites) and sometimes food type [12]. | Very High (micro-level behavior) | - Objective, minimizes self-report bias [12]- Captures microstructure of eating (rate, duration) [31] [12]- Potential for passive, continuous monitoring | - Does not directly identify foods or nutrients without additional input [12]- Technical challenges (battery life, robustness) [12]- Privacy concerns with continuous recording [12] |
Quantitative data from validation studies further highlights the performance differences between these methods. The table below summarizes key findings on energy intake reporting accuracy and nutrient validation.
Table 2: Summary of Key Validation Study Findings
| Method | Validation Reference | Key Finding | Quantitative Result |
|---|---|---|---|
| 2×24HR (Interviewer) | Doubly Labeled Water (DLW) [75] | Mean reported energy intake was not significantly different from true energy expenditure. | EI = 11.5 MJ/d vs TEE = 11.5 MJ/d (P value not significant) |
| 7-day Food Diary (Web-based) | Doubly Labeled Water (DLW) [75] | Significant under-reporting of energy intake at the group level. | EI = 9.5 MJ/d vs TEE = 11.5 MJ/d (P < 0.01); 34% under-reporters |
| 7-day Pre-coded Food Diary | ActiReg (Activity Monitor) [76] | Significant under-reporting of energy intake at the group level. | EI was 17% lower than measured Energy Expenditure |
| Mobile Dietary Record Apps | Traditional Methods (Meta-Analysis) [78] | Apps consistently underestimated intake compared to traditional methods. | Pooled effect: -202 kcal/day (95% CI: -319, -85) |
| Slovenian FFQ (sqFFQ/SI) | 5-day Dietary Record [77] | Significant but relatively weak correlation for vitamin D intake. | Correlation coefficient (r) = 0.268 (p < 0.05) |
| Slovenian FFQ (sqFFQ/SI) | Serum Biomarkers [79] | Poor correlation between dietary vitamin D intake and serum levels in a diseased population. | Correlation coefficients were not statistically significant |
Detailed Experimental Protocols for Validation
Understanding how the validity of these methods is tested is crucial for interpreting the data.
Protocol 1: Validating Self-Report Tools against Energy Expenditure
This protocol uses Doubly Labeled Water (DLW) as a biomarker for total energy expenditure (TEE), the gold standard for validating reported energy intake in energy-balanced individuals [75].
- Participant Recruitment: Recruit a sample representative of the target population, with stratification by sex and age groups to capture different life stages [75].
- Baseline Measurements: Collect anthropometric data (height, weight, body composition) and a baseline urine sample [75].
- DLW Administration: Participants consume a dose of doubly labeled water (²H₂¹⁸O). The differential elimination rates of deuterium and oxygen-18 from the body are used to calculate carbon dioxide production and thus TEE [75].
- Urine Collection: Participants collect urine samples at home over a subsequent period (e.g., 11 days) to track isotope elimination [75].
- Dietary Assessment: Participants complete the dietary method under investigation (e.g., 2×24HR or 7-day food diary). To avoid order effects, a crossover design is often used where participants are randomly assigned to start with one method before switching to the other [75].
- Data Analysis: Compare the mean reported energy intake to the measured TEE. Statistical analyses (e.g., paired t-tests, correlation coefficients, Bland-Altman plots) are used to assess the bias and agreement at both group and individual levels [75] [76].
Protocol 2: Biochemical Validation of Nutrient Intake
This approach validates the intake of specific nutrients by comparing dietary data to corresponding biomarkers in blood.
- Participant Selection: Define a cohort, potentially focusing on specific populations (e.g., patients with peripheral arterial disease) [79].
- Dietary Assessment: Administer the FFQ or other dietary tool to assess habitual intake of the target nutrients (e.g., vitamins A, C, D, E) [77] [79].
- Blood Collection: Draw fasting blood samples from participants to analyze serum levels of the nutrients or their specific biomarkers, such as 25-hydroxyvitamin D for vitamin D status [77] [79].
- Data Analysis: Calculate correlation coefficients (e.g., Spearman's) to determine the strength of the relationship between reported dietary intake and serum concentrations. Additionally, analyze the agreement by examining cross-classification into intake quartiles [79].
Protocol 3: Laboratory Validation of Wearable Sensors
This protocol tests the accuracy of wearable sensors in a controlled laboratory setting against a ground truth.
- Experimental Setup: Use a controlled environment like a feeding laboratory. A ground truth system, such as the "Feeding Table" (a Universal Eating Monitor with multiple integrated scales), is used to precisely measure the weight and timing of food consumed [31].
- Sensor Deployment: Fit participants with the wearable sensors to be validated (e.g., acoustic sensors on the neck, inertial measurement units on the wrist) [12].
- Standardized Meal Test: Participants consume a meal, typically with multiple food options, while the ground truth system and wearable sensors record data simultaneously [31].
- Data Processing: Use machine learning algorithms to detect and count eating behaviors (bites, chews, swallows) from the sensor signals [12].
- Accuracy Assessment: Compare the sensor-derived metrics (e.g., number of bites, eating rate, total meal weight) against the ground truth measurements from the Feeding Table. Metrics like correlation coefficients, intra-class correlation coefficients (ICCs), and root mean square error are used to quantify accuracy and repeatability [31].
The following diagram illustrates the core logical pathway for validating any dietary assessment method, showcasing the different reference standards used for self-report tools versus wearable sensors.
The Scientist's Toolkit: Key Research Reagents & Solutions
This section details essential tools and systems used in advanced dietary assessment research.
Table 3: Essential Research Tools for Dietary Assessment Validation
| Tool / Solution | Function | Application Context |
|---|---|---|
| Doubly Labeled Water (DLW) | Gold standard method for measuring total energy expenditure in free-living individuals over 1-2 weeks [75]. | Validation of energy intake reported by 24HRs, food diaries, and FFQs [75]. |
| Automated Multiple-Pass Method (AMPM) | A structured, computer-assisted 24HR interview methodology that uses multiple "passes" to enhance completeness and accuracy [75] [80]. | Conducting high-quality 24HR interviews; the core method behind USDA recalls and the ASA24 tool [75] [80]. |
| ASA24 (Automated Self-Administered 24HR) | A free, web-based tool that automates the 24HR and food record process, enabling self-administration and automated food coding [80]. | Large-scale epidemiological studies where interviewer-administered recalls are not feasible [80]. |
| Universal Eating Monitor (UEM) / Feeding Table | A specialized laboratory table with embedded scales that continuously track food weight during a meal, providing high-resolution data on eating microstructure [31]. | Objective validation of eating rate, meal duration, and total intake in lab studies; serves as ground truth for wearable sensor validation [31]. |
| Acoustic & Inertial Sensors | Wearable sensors (microphones, accelerometers, gyroscopes) that capture signals from the throat, jaw, or wrist to detect chewing, swallowing, and hand-to-mouth gestures [12]. | Objective monitoring of eating behavior metrics (bite count, chew count) in both laboratory and free-living environments [12]. |
| Food Composition Database | A standardized repository of nutritional values for thousands of foods, essential for converting reported food consumption into nutrient intakes [75] [77]. | Required for all self-report methods (24HR, Diaries, FFQs) to calculate energy and nutrient intake. |
The choice of a dietary assessment method is a critical decision that directly impacts the quality and interpretation of research data. Traditional self-report methods like 24HR and FFQs are mature and provide direct food and nutrient data but are inherently limited by systematic and random errors inherent in self-reporting. Wearable sensor technologies offer a powerful, objective alternative for measuring the microstructure of eating behavior, free from the biases of self-report, but currently fall short of identifying specific foods and nutrients without further development. The future of precise dietary assessment lies not in a single tool, but in a complementary approach. Integrating objective wearable data on eating timing and microstructure with contextual self-reports of food type promises a more complete and validated picture of dietary intake, ultimately strengthening the foundation of nutritional science.
Accurate measurement of food intake is a cornerstone of nutritional science, epidemiology, and the development of effective dietary interventions. However, this field has long been plagued by the persistent challenge of systematic under-reporting and measurement error inherent in traditional self-report methods [81] [82]. These errors are not random but exhibit predictable patterns that compromise data integrity and the validity of research findings. With the growing focus on personalized nutrition, especially for managing conditions like type 2 diabetes, the limitations of conventional dietary assessment tools have become increasingly apparent [3] [2].
The emergence of wearable sensors and automated monitoring technologies offers a promising pathway toward more objective quantification of eating behavior [12] [82]. This guide provides a comparative analysis of these technological alternatives, evaluating their performance against traditional methods and framing them within a broader thesis on validating food intake via wearable device data. We present synthesized experimental data, detailed methodologies, and essential research tools to inform researchers, scientists, and drug development professionals working at the intersection of nutrition technology and metabolic health.
The Problem of Systematic Under-Reporting
Systematic under-reporting in dietary assessment is a well-documented phenomenon that introduces significant bias into nutritional research. A comprehensive systematic review examining contributors to error in self-reported intake revealed that omissions and portion size misestimations are the most frequent sources of inaccuracy [81]. The extent of these errors varies substantially across different food groups, as detailed in Table 1.
Table 1: Error Patterns in Self-Reported Food Intake by Food Group
| Food Group | Omission Range | Primary Error Type | Notes on Error Pattern |
|---|---|---|---|
| Beverages | 0–32% | Omission | Less frequently omitted compared to other groups |
| Vegetables | 2–85% | Omission & Portion Size | High variability in omission rates |
| Condiments | 1–80% | Omission & Portion Size | Extremely high omission rates observed |
| Most Other Food Groups | Variable | Portion Misestimation | Both under- and over-estimation common within same study samples |
The persistence of these errors stems from fundamental limitations of self-report mechanisms, including reliance on human memory, social desirability bias, and reactivity to self-monitoring (where individuals alter their intake on reporting days) [82]. Furthermore, the complexity of assessing intake is magnified by the "endless heterogeneous origins, preparations, and combinations of foods," making it inherently more challenging than measuring energy expenditure [82].
Wearable Technology Solutions for Dietary Monitoring
Technological innovations, particularly wearable sensors, have emerged as promising alternatives to mitigate the systematic errors of self-report methods. These devices can be broadly categorized into several types based on their sensing modality and application, each with distinct performance characteristics and limitations.
Table 2: Performance Comparison of Wearable Technologies for Dietary Monitoring
| Technology Type | Key Metrics Measured | Reported Advantages | Key Limitations | Target Population |
|---|---|---|---|---|
| Camera-Based (eButton) | Food type, portion size, eating environment [3] [12] | Automated food recording; visual portion size evidence [3] | Privacy concerns; camera positioning difficulties [3] | Chinese Americans with T2D [3] |
| Continuous Glucose Monitors (CGM) | Postprandial glucose responses, glucose patterns [3] [2] | Increases mindfulness of meal choices; motivates behavior change [3] | Sensors may fall off; skin sensitivity issues [3] | Patients with T2D or prediabetes [2] |
| Inertial Sensors (Wrist-based) | Hand-to-mouth gestures, bite count [12] [82] | Passive monitoring; minimizes user burden [82] | Proxy measurement only; cannot identify food type [82] | General eating behavior studies [12] |
| Acoustic Sensors | Chewing, swallowing sounds [12] | High granularity for eating micro-behaviors [12] | Requires filtering of non-food sounds; privacy concerns [12] | Laboratory studies of eating mechanics [12] |
When paired, multimodal sensing approaches offer particularly powerful insights. For instance, combining the eButton with CGM creates a system that "help patients visualize the relationship between food intake and glycemic response" [3]. Similarly, the CGMacros dataset demonstrates the value of integrating CGM data with food photographs, activity tracking, and macronutrient information [2].
Experimental Protocols for Validation Studies
Protocol 1: Multimodal Dietary Monitoring in Free-Living Conditions
The CGMacros study provides a robust methodological framework for validating food intake assessment through wearable devices in free-living conditions [2].
Participant Recruitment and Baseline Assessment:
- Recruit participants across health statuses (healthy, prediabetes, type 2 diabetes)
- Conduct initial screening: BMI, HbA1c, fasting glucose, fasting insulin, triglycerides, cholesterol
- Collect demographic information and stool samples for microbiome analysis
Device Deployment and Data Collection:
- Apply two CGM devices (e.g., Abbott FreeStyle Libre Pro and Dexcom G6 Pro) on upper arm and abdomen
- Provide fitness tracker (e.g., Fitbit Sense) to log physical activity
- Train participants to use food logging app (e.g., MyFitnessPal) and food photography via messaging app
- Maintain study duration of 10 consecutive days with monitoring of breakfast, lunch, and dinner
Data Processing and Analysis:
- Harmonize CGM data to uniform sampling rate using linear interpolation
- Extract meal timestamps from food photographs
- Compute metabolic equivalents (METs) from fitness tracker data using mean filtering (20-minute window)
- Correlate postprandial glucose responses with meal macronutrient composition
Protocol 2: Cultural-Specific Feasibility Assessment
Research on Chinese Americans with T2D demonstrates a protocol for assessing cultural acceptability and feasibility of wearable devices [3].
Study Design and Participant Selection:
- Prospective cohort design using convenience sampling from medical records
- Include first- or second-generation immigrants comfortable with English communication
- Implement a one-group design with 10-14 day monitoring period
Device Implementation and Qualitative Assessment:
- Participants wear eButton on chest during meals for 10 days
- Simultaneous CGM use for 14 days with paper diary for food intake, medication, and activity
- Conduct individual interviews after monitoring period to discuss experiences, barriers, and facilitators
- Thematically analyze interview transcripts using qualitative analysis software (e.g., ATLAS.ti)
Diagram 1: Experimental validation workflow for wearable device data
Signaling Pathways: From Data Collection to Validated Intake
The process of transforming raw sensor data into validated food intake metrics involves multiple stages of data processing and analysis. The following diagram illustrates this complex workflow and the critical integration points between different data streams.
Diagram 2: Signaling pathway from raw data to validated food intake metrics
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Materials and Technologies for Dietary Monitoring Studies
| Item | Function | Example Products/Protocols | Application Context |
|---|---|---|---|
| Continuous Glucose Monitors (CGM) | Measures interstitial glucose levels to track postprandial responses [3] [2] | Abbott FreeStyle Libre Pro, Dexcom G6 Pro | Correlation of glycemic response with meal composition [2] |
| Wearable Cameras | Automatically captures food images for portion size and food type analysis [3] [12] | eButton (chest-worn) | Passive food intake documentation in free-living conditions [3] |
| Inertial Measurement Units (IMU) | Detects hand-to-mouth gestures as proxy for bite counting [12] [82] | Wrist-worn accelerometers/gyroscopes | Eating episode detection and eating rate assessment [12] |
| Food Logging Applications | Digital platform for self-reported food intake and nutrient tracking [2] | MyFitnessPal, Automated Self-Administered 24-h recall (ASA24) | Ground truth data collection alongside sensor data [2] |
| Acoustic Sensors | Detects chewing and swallowing sounds through bone conduction [12] | Microphones placed on neck or head | Detailed analysis of eating microstructure in laboratory settings [12] |
| Multimodal Datasets | Provides benchmark data for algorithm development and validation [2] | CGMacros, Clemson Cafeteria Dataset [2] | Training and testing machine learning models for intake detection [2] |
Discussion and Future Directions
The integration of wearable sensor data presents a transformative opportunity to address the persistent challenge of systematic under-reporting in dietary assessment. Experimental evidence demonstrates that multimodal approaches—combining CGM, wearable cameras, and inertial sensors—can capture complementary aspects of food intake that collectively provide a more objective and comprehensive picture than self-report methods alone [3] [2].
Nevertheless, significant challenges remain before these technologies can be widely adopted in research and clinical practice. Privacy concerns, particularly with continuous image capture, must be addressed through privacy-preserving approaches such as filtering out non-food-related images or sounds [12]. Device comfort and reliability issues, including sensors falling off or causing skin sensitivity, present barriers to long-term adherence [3]. Furthermore, the development of robust algorithms for automated food recognition and portion size estimation requires larger, more diverse datasets [2] [82].
Future research should focus on developing standardized validation protocols across different populations and cultural contexts [3]. The promising findings from studies with Chinese Americans with T2D highlight the importance of considering cultural dietary practices when implementing these technologies [3]. Additionally, longer-term studies are needed to assess whether the initial mindfulness and behavior changes prompted by these devices translate into sustained improvements in dietary patterns and metabolic health outcomes [3].
As the field advances, the integration of wearable device data with other biomarkers and -omics technologies (e.g., gut microbiome profiling as in the CGMacros dataset) will further enhance our ability to personalize nutritional recommendations and validate food intake through objective, multimodal approaches [2]. This evolution from subjective recall to objective sensor-based assessment represents a paradigm shift with profound implications for nutritional science, clinical practice, and drug development.
Conclusion
The validation of food intake via wearable devices represents a paradigm shift from error-prone, self-reported methods towards objective, passive monitoring. While significant progress has been made with technologies like bio-impedance wristbands, wearable cameras, and multi-sensor systems, challenges in data quality, algorithmic robustness, and equitable performance remain. For researchers and drug development professionals, these tools offer unprecedented potential to capture nuanced dietary patterns and eating architecture over extended periods. Future directions must prioritize interdisciplinary collaboration to establish standardized validation protocols, improve algorithmic fairness across diverse demographics, and seamlessly integrate wearable data with clinical and omics data for a truly personalized and precise understanding of diet's role in health and disease.
References
- 1. Overview of Dietary Assessment Methods for Measuring ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8338737/]
- 2. CGMacros: a pilot scientific dataset for personalized ... [https://www.nature.com/articles/s41597-025-05851-7]
- 3. Experience of Using Wearable Devices for Dietary ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12490776/]
- 4. Using wearable camera dietary monitoring technology... [https://f1000research.com/articles/14-48]
- 5. Wearable Technology to Quantify the Nutritional Intake of Adults [https://mhealth.jmir.org/2020/7/e16405]
- 6. AI-enabled wearable cameras for assisting dietary ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11621677/]
- 7. Association between phase angle from bioelectrical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12187483/]
- 8. Real-world assessment of Multi-Frequency Bioelectrical ... [https://www.nature.com/articles/s41430-025-01664-4]
- 9. Body composition measures assessed by bioelectrical ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1689031/full]
- 10. Recent Advancements in Wearable Hydration-Monitoring ... [https://mhealth.jmir.org/2025/1/e60569]
- 11. Automatic, wearable-based, in-field eating detection ... [https://www.nature.com/articles/s41746-020-0246-2]
- 12. A Systematic Review of Sensor-Based Methods for ... [https://www.mdpi.com/1424-8220/25/10/2966]
- 13. Development and Validation of a Universal Eating Monitor ... [https://www.mdpi.com/2072-6643/17/18/2929]
- 14. Comparison of wearable sensors for estimation of chewing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7977373/]
- 15. AI-enabled wearable cameras for assisting dietary ... [https://www.nature.com/articles/s41746-024-01346-8]
- 16. Experience of Using Wearable Devices for Dietary ... [https://diabetes.jmir.org/2025/1/e73381]
- 17. Personalized Nutrition in the Era of Digital Health [https://pmc.ncbi.nlm.nih.gov/articles/PMC12474561/]
- 18. A guide to consumer-grade wearables in cardiovascular ... [https://www.nature.com/articles/s44325-025-00082-6]
- 19. The Impact of Wearable Technologies in Health Research [https://mhealth.jmir.org/2022/1/e34384]
- 20. Wearable Technology to Quantify the Nutritional Intake of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7407252/]
- 21. Future Directions for Integrative Objective Assessment of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7343846/]
- 22. Challenges and recommendations for wearable devices in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9931360/]
- 23. Comparative Effectiveness of Wearable Devices and Built-In ... [https://mhealth.jmir.org/2025/1/e64527]
- 24. Wearable Devices for Caloric Intake Assessment [https://www.sciencedirect.com/org/science/article/pii/S187443461700006X]
- 25. Comparing the Accuracy of Different Wearable Activity ... [https://www.researchprotocols.org/2025/1/e70472]
- 26. Wearable Food Intake Monitoring Technologies [https://www.mdpi.com/2073-431X/6/1/4]
- 27. Multimodal AI 2025: Technologies, Challenges & Benefits [https://kanerika.com/blogs/multimodal-ai/]
- 28. A comparative review on multi-modal sensors fusion based ... [https://www.sciencedirect.com/science/article/abs/pii/S0165168423002396]
- 29. A Review of Multi-Sensor Fusion in Autonomous Driving [https://www.mdpi.com/1424-8220/25/19/6033]
- 30. iEat: automatic wearable dietary monitoring with bio- ... [https://www.nature.com/articles/s41598-024-67765-5]
- 31. Development and Validation of a Universal Eating Monitor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12472242/]
- 32. Development and Validation of an Objective, Passive ... [https://www.sciencedirect.com/science/article/pii/S2475299122119815]
- 33. Development and Validation of an Objective, Passive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7031207/]
- 34. Current challenges and opportunities in active and passive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12274063/]
- 35. Integrated image and sensor-based food intake detection ... [https://www.nature.com/articles/s41598-024-51687-3]
- 36. Accuracy of Wearable Technology & Smart Watches [https://www.aim7.com/blog/smartwatch-wearable-technology-accuracy]
- 37. How Wearable Devices Are Transforming Academic ... [https://www.expiwell.com/post/how-health-monitoring-wearable-devices-are-revolutionizing-academic-research]
- 38. Qualitative Systematic Review and Meta-Synthesis - JMIR Aging [https://aging.jmir.org/2025/1/e63768]
- 39. Evaluation framework for selecting wearable activity monitors ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7882259/]
- 40. Wearable sensing in eating episode monitoring [https://pmc.ncbi.nlm.nih.gov/articles/PMC12207139/]
- 41. Performance of Three Continuous Glucose Monitoring ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11795573/]
- 42. Dexcom G6 & G7, What's New? [https://www.adces.org/education/danatech/glucose-monitoring/continuous-glucose-monitors-(cgm)/cgm-selection-training/dexcom-g6-g7-comparison]
- 43. Partner Integrations [https://www.diabetescare.abbott/support/partnerships.html]
- 44. Our Health Partnerships | FreeStyle Libre US [https://www.freestyle.abbott/us-en/partnerships.html]
- 45. Performance Evaluation of 3 Large Language Models for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12513282/]
- 46. AI food scanner turns phone photos into nutritional analysis [https://engineering.nyu.edu/news/ai-food-scanner-turns-phone-photos-nutritional-analysis]
- 47. How AI Is Transforming Nutrition Tracking in 2025 [https://medium.com/@urano10/how-ai-is-transforming-nutrition-tracking-in-2025-e8e39a6dbf32]
- 48. Image-based food monitoring and dietary management for ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1501946/full]
- 49. On the development of low power wearable devices for ... [https://link.springer.com/article/10.1007/s10389-023-01893-6]
- 50. Bias in AI | Examples, Causes & Mitigation Strategies 2025 [https://kodexolabs.com/bias-in-ai/]
- 51. Addressing AI bias: a human-centric approach to fairness [https://www.ey.com/en_us/insights/emerging-technologies/addressing-ai-bias-a-human-centric-approach-to-fairness]
- 52. Building AI Fairness by Reducing Algorithmic Bias [https://tepperspectives.cmu.edu/all-articles/building-ai-fairness-by-reducing-algorithmic-bias/]
- 53. Performance of individual dietary diversity score to identify ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8455526/]
- 54. The effects of dietary diversity on health status among the ... [https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-024-18172-y]
- 55. Landmark AI framework sets new standard for tackling ... [https://www.dlapiper.com/en/insights/publications/ai-outlook/2025/landmark-ai-framework-sets-new-standard-for-tackling-algorithmic-bias]
- 56. Characterising the diversity of plant-based food and ... [https://www.sciencedirect.com/science/article/pii/S0261561425001876]
- 57. Mitigating data quality challenges in ambulatory wrist-worn ... [https://www.nature.com/articles/s41598-024-67767-3]
- 58. Wearable activity trackers–advanced technology or ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9022022/]
- 59. Privacy Data Ethics of Wearable Digital Health Technology [https://cdh.brown.edu/news/2023-05-04/ethics-wearables]
- 60. Privacy in consumer wearable technologies: a living ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12167361/]
- 61. a living systematic analysis of data policies across leading ... [https://www.nature.com/articles/s41746-025-01757-1]
- 62. Using wearable technology to measure adherence ... [https://www.sciencedirect.com/science/article/pii/S0894113025000663]
- 63. Artificial Intelligence in Nutrition and Dietetics - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12563881/]
- 64. A personalized federated learning approach to enhance joint ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12314237/]
- 65. Estimation of daily energy requirements using a hybrid ... [https://www.nature.com/articles/s41598-025-22786-6]
- 66. AI4Food, a feasibility study for the implementation of ... [https://www.sciencedirect.com/science/article/pii/S0261561425000718]
- 67. Doubly Labeled Water Is a Validated and Verified ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3985818/]
- 68. Predictive equation derived from 6497 doubly labelled ... [https://www.nature.com/articles/s43016-024-01089-5]
- 69. The Doubly Labeled Water Method Produces Highly ... [https://www.sciencedirect.com/science/article/pii/S0022316622008914]
- 70. Keeping Pace with Wearables: A Living Umbrella Review ... [https://pubmed.ncbi.nlm.nih.gov/39080098/]
- 71. How to Check the Accuracy of Your Machine Learning ... [https://www.deepchecks.com/how-to-check-the-accuracy-of-your-machine-learning-model/]
- 72. F1 Score in Machine Learning Explained [https://encord.com/blog/f1-score-in-machine-learning/]
- 73. Mastering the F1 Score: A Practical Guide for Machine ... [https://www.lightly.ai/blog/f1-score]
- 74. 24-hour Dietary Recall ( 24 ) At a Glance | Dietary Assessment Primer HR [https://dietassessmentprimer.cancer.gov/profiles/recall/]
- 75. Validation of the 2 × 24 h recall method and a 7-d web- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10511678/]
- 76. Validation of energy intake recorded by a 7-day pre-coded ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0215638]
- 77. Validation of the food frequency questionnaire for the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9537601/]
- 78. A Systematic Review and Meta-Analysis of Validation ... [https://www.sciencedirect.com/science/article/pii/S2161831322005099]
- 79. Biochemical validation of a food frequency questionnaire ... [https://www.sciencedirect.com/science/article/pii/S0939475325000882]
- 80. ASA24® Dietary Assessment Tool | EGRP/DCCPS/NCI/NIH [https://epi.grants.cancer.gov/asa24/]
- 81. A Systematic Review Examining Contributors to ... [https://www.sciencedirect.com/science/article/pii/S2161831323000947]
- 82. Opportunities and Challenges of Technology Tools in Dietary ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8803491/]