Wearable Sensors vs. 24-Hour Recall: A Comparative Analysis for Modern Dietary Assessment in Research and Clinical Trials
Accurate dietary assessment is critical for nutritional research, chronic disease management, and evaluating interventions in drug development.
Wearable Sensors vs. 24-Hour Recall: A Comparative Analysis for Modern Dietary Assessment in Research and Clinical Trials
Abstract
Accurate dietary assessment is critical for nutritional research, chronic disease management, and evaluating interventions in drug development. This article provides a comprehensive comparison between two evolving methodologies: technology-assisted 24-hour dietary recalls (24HR) and wearable sensors. We explore the foundational principles of each method, detailing their operational mechanisms and technological advancements, including AI-assisted tools and passive monitoring devices. The analysis covers application-specific best practices, common pitfalls with optimization strategies, and a critical review of validation studies and performance metrics. Aimed at researchers, scientists, and drug development professionals, this review synthesizes evidence to guide the selection and implementation of robust dietary assessment tools for rigorous scientific and clinical applications.
The Evolution of Dietary Monitoring: From Traditional Recall to Wearable Sensors
The Critical Need for Accurate Dietary Data in Clinical Research and Drug Development
Accurate dietary data is a cornerstone for advancing clinical research and developing effective drugs, particularly for conditions like obesity, diabetes, and cardiovascular diseases. Traditional methods of dietary assessment, such as the 24-Hour Dietary Recall (24HR), have long been the standard but are increasingly being complemented or challenged by innovative wearable sensor technologies. This guide provides a objective comparison of these methodologies, focusing on their performance, underlying protocols, and applicability in rigorous research settings.
Performance Comparison: Wearable Sensors vs. 24-Hour Dietary Recall
The table below summarizes key performance metrics from recent validation studies, highlighting the relative strengths and weaknesses of each method.
Table 1: Performance Comparison of Dietary Assessment Methods
| Methodology | Study/System Name | Key Performance Metric | Reported Result | Context & Limitations |
|---|---|---|---|---|
| Wearable Camera (AI-Assisted) | EgoDiet (Study in Ghana) [1] [2] | Mean Absolute Percentage Error (MAPE) for portion size | 28.0% | Compared to 24HR; shows improvement over traditional method. |
| Traditional 24HR | 24-Hour Dietary Recall (Study in Ghana) [1] [2] | Mean Absolute Percentage Error (MAPE) for portion size | 32.5% | Served as the baseline for comparison with the wearable system. |
| Web-Based 24HR | myfood24 (Danish Adults) [3] | Correlation with Urinary Potassium (ρ) | 0.42 | A moderate correlation with a biomarker for potassium intake. |
| Web-Based 24HR | myfood24 (Danish Adults) [3] | Correlation with Serum Folate (ρ) | 0.49 | A moderate correlation with a biomarker for folate intake. |
| Image-Voice System | VISIDA (Cambodian Mothers) [4] | Mean Difference in Energy Intake vs. 24HR (kcal) | -296 | Systematically estimated lower energy intake than 24HR. |
Detailed Experimental Protocols
Understanding the experimental design behind the data is crucial for interpreting results and selecting appropriate methods for future studies.
Protocol for Validating AI-Enabled Wearable Cameras (EgoDiet)
The EgoDiet system was designed as a passive, egocentric vision-based pipeline to estimate food portion sizes, specifically optimized for African cuisines [1] [2].
- Data Collection: Researchers used two low-cost, wearable cameras: the AIM (attached to eyeglasses) and the eButton (worn on the chest). These devices continuously captured images during eating episodes in controlled and free-living settings among populations of Ghanaian and Kenyan origin [1] [2].
- AI Processing Pipeline:
- EgoDiet:SegNet: A neural network based on Mask R-CNN performed segmentation of food items and containers from the image stream [1].
- EgoDiet:3DNet: A depth estimation network reconstructed 3D models of the containers to determine scale without depth-sensing cameras [1].
- EgoDiet:Feature: This module extracted portion size-related features, such as the Food Region Ratio (FRR) and Plate Aspect Ratio (PAR), to account for different camera angles [1].
- EgoDiet:PortionNet: The final module estimated the consumed portion size (in weight) by leveraging the extracted features, addressing the challenge of limited training data [1].
- Validation: The weight estimates from the EgoDiet pipeline were compared against measurements taken by dietitians and data from traditional 24HR interviews. The Mean Absolute Percentage Error (MAPE) was the primary metric for comparison [1] [2].
Protocol for Validating Web-Based Dietary Recall Tools (myfood24)
The myfood24 system is an automated, web-based tool that supports both self-administered and interviewer-led 24-hour dietary recalls and food records [3].
- Study Design: In a study of healthy Danish adults, participants completed two 7-day weighed food records (WFR) using the myfood24 app, four weeks apart. This design tested both validity and reproducibility [3].
- Objective Validation Measures: Unlike many studies that rely on cross-comparison with other self-reported methods, this study used objective biomarkers as a reference:
- Energy Metabolism: Resting energy expenditure was measured via indirect calorimetry, and the Goldberg cut-off was applied to identify mis-reporters [3].
- Biomarker Analysis: Fasting blood samples were analyzed for serum folate, and 24-hour urine samples were analyzed for urea (protein intake biomarker) and potassium [3].
- Statistical Analysis: The validity of the tool was assessed by correlating the nutrient intakes estimated by myfood24 with the concentration of the corresponding biomarkers (e.g., folate intake vs. serum folate) using Spearman's rank correlation (ρ) [3].
Protocol for a Multi-Technology Study (CoDiet)
The CoDiet study protocol illustrates a comprehensive approach to understanding diet-disease relationships by integrating multiple technologies [5].
- Enhanced Surveillance: Participants wear wearable cameras and activity monitors for three separate one-week periods at home. This captures objective data on dietary intake, physical activity, and sleep patterns [5].
- Multi-Omics and Health Analysis: At the end of each monitoring period, participants undergo detailed clinical assessments, including:
- Body composition analysis.
- Cardiovascular disease risk assessment via Advanced Glycation End products (AGE) and accelerated photoplethysmography (APG).
- Collection of blood, urine, stool, and breath samples for multi-omics analysis [5].
- Qualitative Feedback: In-depth interviews are conducted to gauge participant perception and acceptability of the novel monitoring technologies [5].
Decision Framework for Method Selection
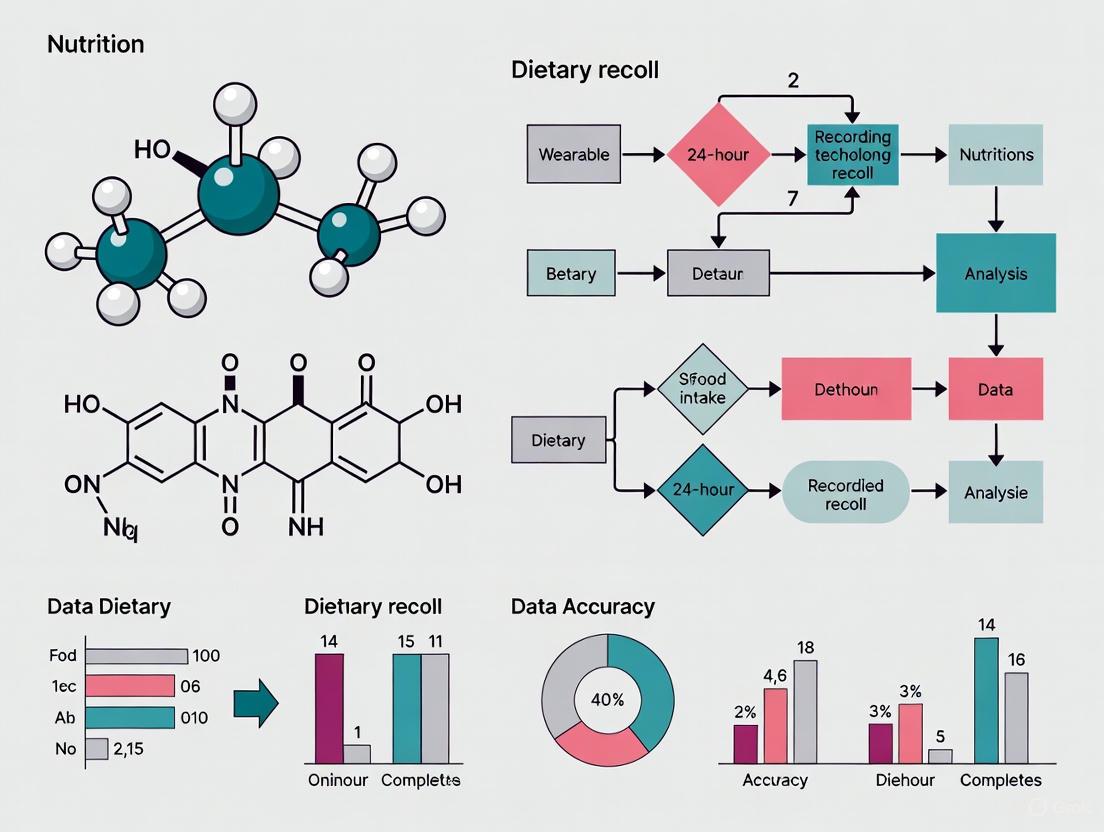
The choice between wearable sensors and traditional recalls depends on the research objectives, population, and resources. The following diagram outlines key decision pathways.
The Scientist's Toolkit: Key Research Reagent Solutions
This table details essential tools and technologies used in modern dietary assessment research, as featured in the cited studies.
Table 2: Essential Research Tools for Dietary Assessment
| Tool / Technology | Function in Research | Example Use Case |
|---|---|---|
| Wearable Egocentric Cameras (e.g., AIM, eButton) [1] [2] | Passively captures first-person-view images of eating episodes and food environments, minimizing participant burden and recall bias. | Continuous dietary monitoring in free-living populations in LMICs; estimating portion sizes via AI. |
| AI-Based Image Analysis Pipeline (e.g., EgoDiet:SegNet, 3DNet) [1] | Automates food item segmentation, 3D container reconstruction, and portion size estimation from image data. | Objectively quantifying food intake from wearable camera footage without manual annotation. |
| Web-Based Dietary Recall Platforms (e.g., myfood24, Foodbook24) [3] [6] | Streamlines the collection and nutrient analysis of 24-hour recall data; can be customized with multi-language support and expanded food lists. | Assessing nutrient intakes in large-scale studies and diverse populations with different dietary habits. |
| Dietary Intake Biomarkers (e.g., Serum Folate, Urinary Nitrogen/Potassium) [3] | Provides an objective, biological measure of nutrient intake to validate the accuracy of self-reported dietary data. | Validating the relative validity of a new dietary assessment tool like myfood24. |
| Clinical-Grade Wearable Sensors (e.g., Hexoskin Shirt, CardioWatch) [7] [8] | Continuously monitors physiological vital signs (heart rate, respiration) and activity alongside dietary intake for a holistic health picture. | Predicting clinical deterioration in hospital patients [7] or validating heart rate in pediatric cardiology [8]. |
| Multi-Omics Analysis (e.g., Metabolomics of blood/urine) [5] | Characterizes the biochemical state of an individual, offering deep insights into the physiological impacts of diet. | Integrating with dietary intake data to explore mechanisms linking diet to non-communicable diseases. |
In conclusion, the evolution from traditional 24HR to wearable sensors and sophisticated web-based platforms represents a significant leap toward obtaining more objective and accurate dietary data. The choice of method is not one-size-fits-all but should be strategically aligned with the research question, with a growing trend toward integrating multiple technologies to capture the complex role of diet in health and disease.
This guide provides an objective comparison of the traditional 24-hour dietary recall (24HR) method against the emerging technology of wearable cameras for dietary assessment, contextualized for research and drug development applications.
Core Principles of the 24-Hour Dietary Recall
The 24-hour dietary recall (24HR) is a structured interview designed to capture detailed information about all foods and beverages consumed by a respondent in the previous 24 hours, typically from midnight to midnight [9].
- Purpose and Description: The primary goal is to obtain a detailed snapshot of dietary intake for a given day. It is an open-ended method that prompts respondents for comprehensive details, moving from general categories to specific descriptors like food preparation methods, type of bread, or portion sizes [9].
- Methodology: Trained interviewers often use a multi-pass approach, such as the USDA's Automated Multiple-Pass Method, to help respondents remember and report their intake. This involves several steps: a quick list of foods consumed, a detailed review of each food (including time, amount, and context), and a final probe for any forgotten items [9] [10]. Visual aids like food models or photographs are frequently employed to improve portion size estimation [9]. A single recall usually takes 20 to 60 minutes to complete [9].
- Data Utility and Limitations: Data from 24HRs can be used to assess population-level intakes, examine diet-health relationships, and evaluate dietary interventions [9]. A key limitation is its reliance on memory, which can lead to omissions and under-reporting, particularly for snack foods, condiments, and alcohol [11] [12]. Because diet varies daily, multiple non-consecutive recalls (often 2-3) are required to estimate an individual's "usual" intake, and statistical methods like the NCI method are used to correct for day-to-day variation [9] [13].
Table 1: Key Characteristics of the 24-Hour Dietary Recall
| Feature | Description |
|---|---|
| Primary Function | Detailed assessment of short-term food & beverage intake [9] |
| Administration | Interviewer-administered or automated self-administered [9] |
| Memory Relied On | Specific memory of the previous 24 hours [9] |
| Key Strength | Provides detailed food-level and context data without reactivity (if unannounced) [9] |
| Primary Measurement Error | Random error, plus systematic under-reporting [9] [12] |
| Optimal Design | Multiple (2+), non-consecutive days, including a weekend day [13] |
The Evolution: Integration of Wearable Cameras
Technological advancements have introduced wearable cameras as a tool to complement and enhance traditional self-report methods. These devices aim to reduce memory-related bias by providing an objective, passive record of consumption [14].
- Defining the Technology: Wearable cameras are small, automatic cameras (e.g., Narrative Clip, Autographer) worn on clothing. They are programmed to capture images at regular intervals (e.g., every 30 seconds), creating a first-person, point-of-view record of the day's activities, including eating and drinking episodes [11] [14].
- Methodological Workflow: The typical research application is image-assisted recall. Participants wear the camera for a day. The following day, they first complete a standard 24HR from memory. Then, together with a researcher, they review the camera images. The images serve as memory cues to help identify and confirm eating episodes, correct portion sizes, and add forgotten items like snacks or beverages [14]. Participants are typically given the opportunity to review and delete any private images before the researcher sees them [15].
The diagram below illustrates this integrated workflow.
Comparative Analysis: 24HR vs. Wearable Cameras
Direct comparative studies quantify the performance differences between standard 24HR and camera-assisted methods.
- Detection of Omitted Foods: A study by Chan et al. found that both 24HR and a food record app frequently omitted specific food groups compared to camera images. Discretionary snacks were a commonly missed category by both self-report methods. Furthermore, items like water, dairy, sugar-based products, condiments, and alcohol were more frequently omitted in the app-based record than in the 24HR [11].
- Impact on Energy and Nutrient Intake: A study with 20 adults compared a standard 24HR to a 24HR assisted by the Narrative Clip camera. The camera-assisted method led to a statistically significant increase in reported mean energy intake (9304.6 kJ/d to 9677.8 kJ/d), as well as higher reported intakes of carbohydrates, total sugars, and saturated fats. This suggests the method mitigates the under-reporting inherent in traditional recall [14].
Table 2: Experimental Data Comparison: Standard 24HR vs. Camera-Assisted 24HR
| Dietary Component | Standard 24HR | Camera-Assisted 24HR | Change & P-Value | Study Details |
|---|---|---|---|---|
| Mean Energy Intake | 9304.6 ± 2588.5 kJ/d | 9677.8 ± 2708.0 kJ/d | +373.2 kJ (P=0.003) | n=20 adults; Narrative Clip camera [14] |
| Omission: Snacks | Frequently Omitted | N/A | (Reference: Camera images) | n=?; Autographer camera [11] |
| Omission: Water | Less Frequent | N/A | More frequent in app (P<0.001) | n=?; Comparison to camera images [11] |
| Omission: Condiments/Fats | Less Frequent | N/A | More frequent in app (P<0.001) | n=?; Comparison to camera images [11] |
Methodological Protocols and Research Reagents
For researchers seeking to implement these methods, a detailed protocol and list of essential resources are provided below.
Detailed Experimental Protocol: Camera-Assisted 24HR
The following methodology is adapted from a feasibility study that compared a standard 24HR to a camera-assisted 24HR [14].
- Device Preparation: Select a suitable wearable camera (e.g., Narrative Clip, Autographer). Ensure devices are fully charged and have sufficient memory.
- Participant Briefing and Consent: Obtain informed consent, explicitly addressing image privacy and data handling. Train participants on device operation, proper clipping on clothing, and when it is appropriate to remove the camera (e.g., during sleep, bathing, or in sensitive situations).
- Data Collection Day: Participants wear the camera from waking until going to bed, following their usual activities.
- Standard 24HR Interview (Pre-Image Review): The day after, conduct a standard 24HR interview using a multi-pass method before any images are viewed. This establishes a baseline self-reported intake.
- Private Image Review: Upload images to a secure computer. The participant reviews all images privately and deletes any they are uncomfortable sharing.
- Image-Assisted Recall: The researcher and participant review the remaining images together. The researcher uses the images to prompt the participant:
- "I see an image of a coffee cup at 10:30 AM. Can you tell me more about that?"
- "This image shows your lunch plate. Does that portion size match what you recalled earlier?"
- "There is an image of a snack wrapper at 3:00 PM that wasn't mentioned. What was that item?"
- Data Modification: Record any additions, deletions, or modifications to the initial 24HR based on the image review, creating a final, enhanced dietary record.
- Data Security: Delete all images from the research computer in the presence of the participant after data extraction.
Research Reagent Solutions
Table 3: Essential Materials for Dietary Assessment Studies
| Item | Function in Research |
|---|---|
| Wearable Camera (e.g., Narrative Clip, Autographer) | Automatically captures first-person, time-stamped image data of daily activities and food consumption [14]. |
| Structured Interview Protocol (e.g., USDA AMPM) | Standardizes the 24HR interview process to reduce interviewer bias and improve completeness [9] [10]. |
| Portion Size Aids (Food models, atlases, photographs) | Assists participants in estimating and reporting the volume or weight of consumed foods [9] [14]. |
| Dietary Analysis Software (e.g., NDSR, Nutritics, SER-24H) | Converts reported foods and portion sizes into estimated nutrient intakes using a linked food composition database [16] [14]. |
| Food Composition Database | Provides the nutrient profile for each food item; requires localization for cultural relevance (e.g., SER-24H for Chile) [16]. |
Implementation and Feasibility in Research
Choosing between these methods requires balancing accuracy, burden, and cost.
- Feasibility and Challenges of Wearable Cameras:
- Participant Perspective: Studies report high acceptance, with many participants finding image-assisted recall helpful and the experience positive [15] [14]. However, some find the device cumbersome, express emotional discomfort, or may alter their behavior (reactivity) due to being recorded [15].
- Researcher Perspective: Key challenges include data loss from device malfunction (up to 15-50% in some settings) and a high proportion of uncodable images (up to 35%) due to poor lighting, blur, or obstruction [15]. The most significant burden is the labor-intensive, time-consuming process of manually processing and coding thousands of images [11] [15].
- Optimizing Traditional 24HR Surveys: For large-scale studies using 24HR alone, research indicates that administering two non-consecutive days (including one weekday and one weekend day) and adjusting the data using the NCI method is a feasible approach that balances survey costs with accuracy for estimating usual intake of many dietary components [13].
In conclusion, while the 24-hour dietary recall remains a fundamental tool for dietary assessment, its accuracy is compromised by self-report bias. Wearable camera technology presents a promising evolution, objectively demonstrating an ability to reduce under-reporting. The choice for researchers and drug development professionals is not necessarily a binary one; an integrated approach using wearable cameras to validate and enhance traditional 24HR data may offer the most robust path forward for precise dietary measurement in critical research.
Accurate dietary assessment is fundamental to nutritional science, chronic disease management, and public health research. For decades, the 24-hour dietary recall (24HR) has been a cornerstone methodology, relying on an individual's ability to retrospectively recall and self-report all foods and beverages consumed over the previous day [17]. However, this and other self-report methods are plagued by well-documented limitations, including significant recall bias, difficulties in estimating portion sizes, and social desirability bias, which often lead to systematic under-reporting—a problem identified in up to 70% of adults in some national surveys [17]. The landscape of dietary assessment is now undergoing a transformative shift with the emergence of wearable sensor technology, which enables passive, objective, and continuous monitoring of eating behaviors [17] [18]. This guide provides a comprehensive comparison between these evolving methodologies, focusing on technological capabilities, performance data, and experimental protocols to inform researchers, scientists, and drug development professionals.
Wearable sensors for dietary monitoring encompass a diverse array of technologies, each capturing different aspects of eating behavior through various physiological and contextual signals.
Sensor Types and Operating Principles
- Motion Sensors (Inertial Measurement Units - IMUs): Typically comprising accelerometers, gyroscopes, and magnetometers, these sensors detect patterns of body movement associated with eating, most notably hand-to-mouth gestures [19] [18]. The repetitive motion of bringing food to the mouth creates a characteristic signature that machine learning algorithms can distinguish from other activities.
- Acoustic Sensors: These sensors, often embedded in hearables or neck-worn devices, capture audio signals generated during chewing and swallowing [20]. The sounds of mastication and deglutition provide high-fidelity data on eating microstructure, including bite count and chewing rate.
- Wearable Cameras: Small, body-worn cameras (e.g., eyeglass-mounted or chest-pinned) capture first-person perspective images at regular intervals (e.g., every 30 seconds) [17] [21]. These images provide objective visual records of food consumption, requiring subsequent analysis—either by trained dietitians or increasingly through computer vision and deep learning algorithms—to identify food types and estimate portion sizes [2].
- Optical Sensors (Photoplethysmography - PPG): Commonly integrated into wrist-worn devices like smartwatches, PPG sensors use light-based technology to measure blood volume changes. While primarily used for cardiovascular monitoring, advanced analysis of PPG signals shows promise for detecting eating episodes through hemodynamic changes associated with food intake [22].
Table 1: Wearable Sensor Technologies for Dietary Monitoring
| Sensor Type | Common Form Factors | Primary Measured Parameters | Data Outputs |
|---|---|---|---|
| Motion Sensors | Wristbands, Smartwatches | Hand-to-mouth gestures, arm movement patterns | Eating episodes, bite count, meal duration |
| Acoustic Sensors | Necklaces, Hearables | Chewing sounds, swallowing sounds | Eating episodes, chewing rate, food texture indicators |
| Wearable Cameras | Eyeglass attachments, Chest pins | First-person view images of food and eating environment | Food type, eating context, portion size (via image analysis) |
| Optical Sensors (PPG) | Smartwatches, Wristbands | Blood volume changes, heart rate variability | Eating episodes, metabolic responses |
Multi-Sensor Systems
Recognizing that no single sensor modality can comprehensively capture the complexity of dietary intake, researchers are increasingly developing multi-sensor systems that combine complementary technologies [18]. For example, the Automatic Ingestion Monitor (AIM-2) integrates a camera, accelerometer, and gyroscope to capture both visual context and motion data [20]. Similarly, the eButton combines a camera with other sensors in a chest-pinned form factor to improve the accuracy of food identification and portion size estimation [2]. These integrated systems leverage sensor fusion algorithms to correlate multiple data streams, potentially overcoming the limitations of individual sensing approaches.
Comparative Analysis: Wearable Sensors vs. 24-Hour Dietary Recall
The transition from traditional 24HR to sensor-based methods represents a fundamental shift in dietary assessment methodology, with significant implications for data quality, participant burden, and research outcomes.
Performance Comparison
Table 2: Quantitative Comparison of Dietary Assessment Methods
| Performance Metric | 24-Hour Dietary Recall (24HR) | Wearable Camera Systems | Multi-Sensor Wearable Systems |
|---|---|---|---|
| Energy Intake Accuracy | Underestimates by 20% or more compared to DLW [17] | MAPE: 28.0-31.9% for portion size [2] | Varies by system; generally superior to self-report |
| Data Collection Timescale | Single day snapshot | Continuous days/weeks [17] | Continuous long-term monitoring [18] |
| Eating Episodes Captured | Frequent omission of snacks, beverages [21] | Identifies 41% more items vs self-report [17] | 65-85% detection accuracy for eating events [18] |
| Portion Size Estimation | High error rate; difficult for complex meals | MAPE: 28.0% (EgoDiet) [2] | Dependent on integrated sensor types |
| Participant Burden | High (active recall/recording) | Medium (passive with privacy concerns) [23] | Low (fully passive after setup) |
| Data Processing Time | Hours per participant (manual coding) | Months for large image datasets [17] | Near real-time with automated algorithms |
Methodological Strengths and Limitations
24-Hour Dietary Recall
- Strengths: Established methodology with standardized protocols (e.g., Automated Self-Administered 24-h recall), comprehensive nutrient databases, and extensive validation research [17] [24].
- Limitations: Systematic under-reporting of energy intake (particularly for snacks and discretionary foods), recall bias dependent on memory, reactivity where participants may alter intake when they know they will be recalled, and inability to capture eating architecture (meal timing, eating rate, within-person variation) [17] [21].
Wearable Sensors
- Strengths: Passive data collection reduces participant burden and reactivity, objective measurement minimizes social desirability bias, enables capture of temporal patterns and eating behaviors, and supports long-term monitoring for habitual intake assessment [17] [18].
- Limitations: Privacy concerns with continuous monitoring, technical challenges with battery life and data management, social acceptability of conspicuous devices, algorithm development requirements for automated analysis, and validation gaps for diverse populations and food types [23] [18].
Experimental Protocols and Validation Methodologies
Rigorous validation is essential for establishing the credibility of wearable sensor technologies for dietary assessment. The following protocols represent current approaches in the field.
Wearable Camera Validation Protocol
The EgoDiet system validation, as described in studies with Ghanaian and Kenyan populations, exemplifies a comprehensive approach to evaluating wearable camera technology [2]:
- Participant Recruitment: Recruit 13 healthy subjects of Ghanaian or Kenyan origin, aged ≥18 years.
- Device Fitting: Participants wear two customized wearable cameras:
- Automatic Ingestion Monitor (AIM): A gaze-aligned wide angle lens camera attached to the temple of eyeglasses (eye-level).
- eButton: A chest-pin-like camera worn using a needle-clip (chest-level).
- Data Collection: Participants consume foods of Ghanaian and Kenyan origin in a controlled facility while cameras record.
- Ground Truth Establishment: Use a standardized weighing scale (e.g., Salter Brecknell) to pre-measure all food items before consumption.
- Image Analysis Pipeline:
- EgoDiet:SegNet: Utilizes Mask R-CNN backbone for segmentation of food items and containers.
- EgoDiet:3DNet: Depth estimation network estimating camera-to-container distance and reconstructing 3D container models.
- EgoDiet:Feature: Extracts portion size-related features including Food Region Ratio (FRR) and Plate Aspect Ratio (PAR).
- EgoDiet:PortionNet: Estimates portion size in weight using extracted features.
- Performance Metrics: Calculate Mean Absolute Percentage Error (MAPE) for portion size estimation compared to dietitian assessments and 24HR.
This protocol yielded a MAPE of 31.9% for portion size estimation compared to 40.1% for dietitian estimates, demonstrating the potential for passive camera technology to outperform even expert assessment [2].
Multi-Sensor Eating Detection Protocol
A standardized protocol for validating multi-sensor wearable systems typically includes [23] [18]:
- Laboratory Calibration Phase:
- Participants perform prescribed activities including eating, drinking, and non-eating activities (talking, walking, gesturing).
- Sensor data is collected and annotated to build activity-specific classification models.
- Free-Living Validation Phase:
- Participants wear sensors during normal daily activities for 1-7 days.
- Participants concurrently complete detailed food diaries or ecological momentary assessments (EMA) as ground truth.
- For wearable cameras, trained coders analyze images to identify eating episodes and food items.
- Algorithm Development:
- Feature extraction from sensor data (time-domain, frequency-domain, and sensor-specific features).
- Training of machine learning classifiers (e.g., Random Forest, Support Vector Machines, Deep Neural Networks) to detect eating episodes.
- Performance Evaluation:
- Standard metrics: Accuracy, Precision, Recall, F1-score for eating episode detection.
- Timing accuracy: Measurement of detection latency from meal start.
- Comparison against self-report methods for completeness.
Experimental Workflow Visualization
The following diagram illustrates the typical experimental workflow for validating wearable sensors against traditional 24HR:
Experimental Workflow for Dietary Assessment Methods Comparison
The Researcher's Toolkit: Essential Technologies and Reagents
Implementing wearable sensor technology for dietary monitoring requires familiarity with both hardware platforms and analytical software tools.
Table 3: Research Reagent Solutions for Wearable Dietary Monitoring
| Tool Category | Specific Examples | Function/Application | Technical Considerations |
|---|---|---|---|
| Wearable Platforms | Automatic Ingestion Monitor (AIM-2), eButton, SenseCam | Multi-sensor data acquisition platform | Battery life, storage capacity, form factor, sensor synchronization |
| Algorithm Development | TensorFlow, PyTorch, scikit-learn | Machine learning model development for activity recognition | Pre-trained models for transfer learning, computational requirements |
| Sensor Fusion Libraries | MATLAB Sensor Fusion & Tracking Toolbox, OpenSense | Integration of multiple sensor data streams | Time synchronization, coordinate transformation, filter design |
| Food Image Databases | Food-101, UNIMIB2016, self-collected datasets | Training and validation of computer vision algorithms | Cultural food representation, portion size annotation, image quality |
| Ground Truth Tools | Standardized weighing scales, Tri-axial accelerometers, Doubly Labeled Water (DLW) | Validation against objective measures | Cost, participant burden, analytical requirements |
| Data Annotation Platforms | Labelbox, CVAT, custom annotation tools | Manual labeling of sensor data for supervised learning | Inter-rater reliability, annotation guidelines, quality control |
Wearable sensor technology represents a paradigm shift in dietary assessment, addressing fundamental limitations of traditional 24-hour dietary recalls by providing objective, passive, and continuous monitoring capabilities. While 24HR retains advantages in established infrastructure and nutrient database integration, wearable sensors offer superior capture of eating timing, frequency, and contextual factors—critical dimensions for understanding diet-health relationships [17] [18].
The field continues to evolve rapidly, with future advancements likely to focus on miniaturization and social acceptance of devices, improved battery life and energy harvesting, development of more robust algorithms for diverse populations and food types, and enhanced privacy preservation techniques [23] [25]. For researchers and drug development professionals, the choice between methodologies involves careful consideration of trade-offs between precision, participant burden, and practical implementation constraints. As validation evidence accumulates and technology matures, wearable sensors are poised to become increasingly integral to nutritional epidemiology, clinical nutrition, and public health research.
For decades, nutritional epidemiology and clinical drug development have relied heavily on self-reported dietary assessment methods, particularly the 24-hour dietary recall (24HR). This method requires participants to recall and report all foods and beverages consumed over the previous 24 hours to trained dietitians. While widely used, traditional 24HR suffers from several well-documented limitations: it is labor-intensive, expensive, prone to significant reporting bias due to dependence on memory and social desirability, and can lead to systematic under-reporting of energy intake, particularly for between-meal snacks [1] [26]. Furthermore, it only provides a sparse snapshot of eating habits, missing crucial details about eating architecture, such as meal timing, eating speed, and within-person variation [26].
Wearable sensor technologies offer a paradigm shift, enabling passive, objective, and high-resolution data collection in free-living conditions. This guide objectively compares three key wearable sensor modalities—Inertial, Acoustic, and Visual—against traditional 24HR and each other, providing researchers with the experimental data and protocols needed for informed adoption.
Comparative Performance of Wearable Modalities vs. 24HR
The table below summarizes the quantitative performance, primary functions, and key advantages of each wearable modality in direct comparison to the 24HR method.
Table 1: Performance Comparison of Wearable Sensor Modalities vs. 24-Hour Dietary Recall
| Modality | Primary Measured Parameters | Key Advantages vs. 24HR | Reported Performance Data |
|---|---|---|---|
| Visual (Wearable Cameras) | Food type, portion size, eating environment, meal timing [27] [26] | Passive capture; minimizes recall bias; provides contextual data (eating environment) [1] | Portion size MAPE: 28.0% (EgoDiet) vs. 32.5% for 24HR [1] |
| Acoustic | Chewing, biting, swallowing counts and rates [27] | Captures micro-level eating behaviors; non-invasive; good for detecting eating episodes [27] | High accuracy for detection of specific actions (e.g., chewing, swallowing) in controlled settings [27] |
| Inertial (IMUs) | Hand-to-mouth gestures, arm and trunk movement, gait [28] [27] [29] | Provides data on physical activity & functional outcomes; useful for gait analysis [28] [30] | Accurately tracks functional metrics like Foot Progression Angle (Accuracy: 2.4° RMS) [29] |
| 24HR (Traditional) | Self-reported food types and estimated portions [1] [26] | Established methodology; no required hardware | Prone to under-reporting; up to 70% of adults under-report energy intake [26] |
Detailed Experimental Protocols for Wearable Modalities
Visual Sensor Protocol: The EgoDiet Pipeline
The EgoDiet methodology employs a passive, egocentric vision-based pipeline for dietary assessment, validated in field studies in London and Ghana [1].
- 1. Hardware and Data Collection: Participants wear a low-cost, chest-mounted wearable camera (e.g., a "spy badge" form factor) that automatically captures images at set intervals (e.g., every 10-30 seconds) throughout the day [1] [26].
- 2. Image Pre-processing and Food Detection: A convolutional neural network (CNN), such as Mask R-CNN in the
EgoDiet:SegNetmodule, automatically scans all captured images to identify and segment those containing food items and containers [1]. - 3. Portion Size Estimation:
- The
EgoDiet:3DNetmodule, a depth estimation network, reconstructs the 3D model of the container and estimates camera-to-container distance. - The
EgoDiet:Featuremodule extracts portion size-related features like the Food Region Ratio (FRR) and Plate Aspect Ratio (PAR). - Finally, the
EgoDiet:PortionNetmodule uses these features to estimate the portion size in weight, overcoming the challenge of limited training data via task-relevant feature extraction [1].
- The
- 4. Validation: Estimated portion sizes and nutrient intakes are validated against dietitian assessments or objective measures like doubly labeled water [1].
Acoustic Sensor Protocol
This modality uses sensors to capture sounds generated during eating to detect and characterize eating behavior.
- 1. Hardware and Data Collection: A contact microphone or an acoustic sensor embedded in a wearable device (e.g., a neckband) is placed on the skin of the neck or throat. The sensor records audio signals throughout the day or during designated meal periods [27].
- 2. Signal Pre-processing: The raw audio signal is filtered to remove background noise and enhance frequencies associated with chewing and swallowing sounds [27].
- 3. Event Detection and Classification: Machine learning algorithms (e.g., support vector machines or deep learning models) are trained to identify and classify distinct audio events, such as chews, bites, and swallows [27].
- 4. Metric Calculation: The timing and frequency of these events are aggregated to calculate metrics like total chewing counts, chewing rate, eating episode duration, and eating speed [27].
- 5. Validation: Detected eating episodes and metrics are typically validated in laboratory settings by comparing sensor outputs with video recordings or researcher annotations [27].
Inertial Sensor Protocol for Gait Retraining
While also used for detecting eating gestures, inertial sensors are well-established in biomechanical monitoring. The following protocol validates their use in gait retraining, a related application in health monitoring [29].
- 1. Hardware and Sensor Calibration: Inertial Measurement Units (IMUs) are securely strapped to the participant's feet, shanks, thighs, and pelvis. The system is calibrated by having the subject stand in a neutral N-pose and then walk a short distance to define the sensor-to-segment alignment [29].
- 2. Data Collection and Processing: While the participant walks on a treadmill, the IMUs stream data from accelerometers, gyroscopes, and magnetometers. Sensor fusion algorithms (e.g., within the Xsens MVN software) process this data to compute the orientation and position of body segments in real-time [29].
- 3. Biomechanical Parameter Calculation: The Foot Progression Angle (FPA) is calculated from the derived foot segment orientation relative to the direction of progression [29].
- 4. Biofeedback Delivery: The calculated FPA is fed to a wearable augmented reality headset (e.g., Microsoft HoloLens), which projects a real-time visual gauge (e.g., a moving dot and a target zone) into the user's field of view [29].
- 5. Validation: The system's accuracy is validated against a gold-standard optical motion capture system (e.g., Vicon) while participants follow different FPA targets [29].
Signaling Pathways and Experimental Workflows
EgoDiet's Computer Vision Pipeline
The following diagram illustrates the multi-stage AI pipeline used by the EgoDiet system to estimate food portion size from passive image capture.
Integrated Multi-Sensor Eating Behavior Assessment
This workflow depicts how data from inertial and acoustic sensors can be fused to provide a comprehensive, objective assessment of eating behavior, contrasting with the subjective 24HR.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials and Tools for Wearable Dietary and Behavioral Research
| Item Name | Function/Description | Example Use Case |
|---|---|---|
| Low-Cost Wearable Camera | Passive, automatic image capture from an egocentric (first-person) view. | Core component of the EgoDiet protocol for capturing eating episodes without user intervention [1] [26]. |
| Inertial Measurement Unit (IMU) | Measures linear acceleration (accelerometer), angular velocity (gyroscope), and orientation (magnetometer). | Tracking hand-to-mouth gestures for bite counting or assessing gait parameters for functional outcome measures [27] [29]. |
| Contact Microphone | Captures high-fidelity audio/vibrations from the skin surface. | Detecting and classifying chewing and swallowing sounds for micro-behavioral analysis of eating [27]. |
| Augmented Reality (AR) Headset | Projects visual feedback and data into the user's field of view. | Providing real-time biofeedback for gait retraining or potentially for dietary intervention studies [29]. |
| Fitbit/ActiGraph Activity Tracker | Commercial or research-grade wearable for tracking general physical activity and heart rate. | Collecting complementary data on energy expenditure and daily activity patterns in free-living studies [31]. |
| Fitabase Platform | A secure third-party data aggregation and management tool. | Remotely collecting, monitoring, and managing data quality from multiple commercial wearables (e.g., Fitbit) in a study [31]. |
| Xsens MVN Analyze Software | Software for processing raw IMU data into full-body kinematic data. | Calculating biomechanical parameters like Foot Progression Angle (FPA) for movement retraining studies [29]. |
The field of dietary assessment is undergoing a significant transformation. Since 2020, research has increasingly focused on overcoming the limitations of traditional self-report methods by developing and validating more objective, technology-driven tools. This guide provides an objective comparison between an emerging method—wearable cameras—and the established standard of 24-hour dietary recalls, detailing their respective experimental protocols, performance data, and essential research toolkits.
Experimental Performance Data Comparison
The table below summarizes quantitative data from recent validation studies, comparing the performance of wearable camera-assisted methods against traditional and web-based 24-hour dietary recalls.
| Methodology | Study & Population | Key Performance Metrics | Identified Limitations / Challenges |
|---|---|---|---|
| Wearable Camera-Assisted Recall | Northern Ireland (n=20 adults) [14] | Energy Intake: Significantly higher in camera-assisted recall vs. recall alone (9677.8 ± 2708.0 kJ/d vs. 9304.6 ± 2588.5 kJ/d; P = 0.003) [14]. | Technological issues (positioning), data loss (15%), uncodable images (12%) due to lighting, labor-intensive analysis [14] [15]. |
| Wearable Camera (EgoDiet AI) | Ghana & London (Ghanaian/Kenyan origin) [2] | Portion Size MAPE: 28.0% (EgoDiet) vs. 32.5% (24HR) [2]. Performance varies with camera position (chest vs. eye-level) [2]. | Requires algorithm optimization for different cuisines; performance dependent on camera positioning and lighting [2]. |
| Web-Based 24HR (Foodbook24) | Irish, Polish, Brazilian adults in Ireland [6] | Food List Coverage: 86.5% (302/349 foods consumed were available in the tool) [6]. Correlation: Strong (r=0.70-0.99) for 44% of food groups and 58% of nutrients vs. interviewer-led recall [6]. | Higher food omission rates in certain groups (e.g., 24% in Brazilian cohort vs. 13% in Irish) [6]. |
| Web-Based 24HR (Intake24) | South Asian Biobank (n=29,113) [32] | Recall Completion Time: Median of 13 minutes [32]. Data Quality: 99% of recalls contained >8 items; 8% had missing foods [32]. | Requires development of a large, context-specific food database (2,283 items for South Asia) [32]. |
| Wearable Camera as Objective Reference | Young Australian Adults (n=133) [21] | Omission Analysis: Discretionary snacks frequently omitted in both 24HR and app-based records. Water, dairy, condiments, fats, and alcohol more frequently omitted in app-based records [21]. | Method is intrusive; privacy concerns for participants; generates massive datasets (487,912 images for 133 participants) [21]. |
Detailed Experimental Protocols
Wearable Camera-Assisted 24-Hour Recall Protocol
This protocol, used to validate the method against traditional recalls, involves a hybrid approach that uses wearable camera images as memory prompts [14].
a. Equipment and Pre-Data Collection:
- Camera Selection: Studies often use small, automatic cameras like the Narrative Clip (a 5-megapixel device clipped onto clothing), chosen for its discreteness, automatic image capture (e.g., every 30 seconds), and sufficient battery life [14].
- Participant Briefing: Participants receive training on device operation, including charging and correct placement on clothing. Critical ethical instructions are provided: participants can remove the camera in private situations (e.g., bathrooms) or if they feel uncomfortable [14] [21].
b. Data Collection:
- Camera Wear: Participants wear the camera during waking hours for one or more designated study days [14].
- 24-Hour Recall Interview: Conducted the day after camera wear. The researcher conducts a standard multi-pass 24-hour recall without viewing the images first [14].
c. Image-Assisted Recall and Data Processing:
- Image Review: Camera images are uploaded. Participants first privately review and delete any images they do not wish to share to protect privacy [14] [15].
- Recall Augmentation: The researcher and participant review the images together. The images serve as memory cues to confirm, add, remove, or modify details of food items, portion sizes, and eating context reported in the initial recall [14]. All changes are documented for analysis.
Web-Based 24-Hour Dietary Recall (Foodbook24/Intake24) Protocol
This protocol outlines the adaptation and implementation of automated, self-administered 24-hour recall tools for diverse populations [6] [32].
a. Tool Adaptation and Database Development:
- Food List Expansion: The core food list is expanded by reviewing national food consumption surveys and relevant literature for the target populations (e.g., Brazilian, Polish, South Asian foods) [6] [32].
- Translation and Nutrient Mapping: Food items are translated into relevant languages (e.g., Polish, Portuguese). Nutrient composition data are assigned, primarily from national food composition databases (e.g., UK's CoFID), with local databases used for culturally specific items [6] [32].
- Portion Size Estimation: Medium portion sizes are typically derived from the mean reported intake in national surveys. Small and large portions are defined using standard deviations or established portion size manuals. Food images are used to aid user estimation [6].
b. Data Collection:
- Recall Administration: Participants complete the recall independently using a computer or smartphone. The system guides them through a structured process (similar to the multiple-pass method) to report all foods and beverages consumed in the previous 24 hours, including food selection and portion size estimation [6] [32].
- Interviewer-Led Option: In some populations, trained interviewers may administer the web-based tool to participants to ensure compliance and data quality [32].
The Scientist's Toolkit: Research Reagent Solutions
The table below details key materials and tools essential for conducting research in this field.
| Tool / Solution | Function in Dietary Assessment Research |
|---|---|
| Wearable Cameras (Narrative Clip, Autographer, eButton) | Capture passive, objective, first-person-view images of eating episodes and daily activities, used for memory triggering or as a validation reference [14] [21] [2]. |
| AI-Based Analysis Pipelines (EgoDiet) | Software suite for automated dietary assessment from wearable camera images, performing food segmentation, 3D container reconstruction, and portion size estimation [2]. |
| Web-Based 24HR Platforms (Foodbook24, Intake24) | Automated, structured systems for conducting self-administered 24-hour dietary recalls, featuring built-in food lists, portion size images, and immediate nutrient analysis [6] [32]. |
| Food Composition Database (FCDB) | The nutrient lookup table for converting reported food consumption into nutrient intake data. Requires careful integration of data from multiple national databases for multi-ethnic studies [6] [32]. |
| Doubly Labeled Water (DLW) | Objective biomarker used as a gold standard for validating total energy expenditure and, by extension, the accuracy of reported energy intake in validation studies [26]. |
Method Workflow Comparison
The diagram below illustrates the fundamental operational differences between the passive, image-capture-focused workflow of wearable cameras and the active, participant-driven workflow of web-based 24-hour recalls.
Research since 2020 demonstrates that both wearable cameras and web-based 24-hour recalls are evolving to address critical challenges in dietary assessment. Wearable cameras offer a more objective ground truth and are particularly valuable for identifying under-reporting and validating other methods. Web-based recalls provide a scalable, cost-effective solution for large-scale studies, especially when adapted for cultural and linguistic diversity. The choice between methods depends on the research question, budget, and population. Future work is focused on integrating these approaches, for instance, using AI analysis of wearable camera data to further automate and improve the accuracy of dietary intake estimation.
Operational Mechanisms and Application-Specific Implementation
The accurate measurement of dietary intake is a cornerstone of nutritional epidemiology, public health monitoring, and clinical trials. For decades, the 24-hour dietary recall (24HR) has served as a fundamental tool for capturing individual food and beverage consumption. However, traditional recall methods are susceptible to significant limitations, including recall bias, participant burden, and measurement error [21]. The digital era has introduced transformative technologies aimed at mitigating these challenges. This guide provides an objective comparison of two modern approaches to executing the 24HR: established web-based platforms and emerging image-assisted methods, often supported by wearable technology. This comparison is situated within the broader thesis of understanding the trade-offs between automated self-report tools and more passive, objective measurement systems in dietary research. As the field advances, researchers must navigate a complex landscape of tools that balance accuracy, feasibility, and participant engagement.
Methodological Comparison: Protocols and Experimental Designs
Web-Based Automated 24HR Platforms
Web-based 24HR systems are digital adaptations of the interviewer-led multiple-pass method. These platforms, such as the Automated Self-Administered 24-hour Dietary Assessment Tool (ASA-24), guide users through a structured process to report all foods and beverages consumed in the preceding 24 hours [33]. The standard protocol involves:
- Structured Recall Process: Users are guided through a multi-step sequence to report meal contexts, specific food items, ingredients, preparation methods, and portion sizes using digital image aids [33].
- Self-Administration: The tool is designed for independent use by participants without interviewer assistance, typically requiring 30-50 minutes to complete [33].
- Integrated Food Databases: These systems utilize extensive food composition databases with nutrient profiles and portion size images to standardize data collection [33].
A recent pilot study (2023-2024) evaluated a novel voice-based dietary recall tool (DataBoard) against the traditional ASA-24 in older adults (mean age 70.5 ± 4.26 years). Participants were randomly assigned to complete either tool first via Zoom sessions, followed by semi-structured interviews to assess usability and acceptability on a 1-10 rating scale [33].
Image-Assisted Interview Methods
Image-assisted interviews represent a technological hybrid, combining wearable cameras with subsequent researcher-led interviews. The methodology generally follows this protocol:
- Passive Image Capture: Participants wear an automated camera (e.g., Autographer) that captures first-person perspective images at regular intervals (e.g., every 30 seconds) during waking hours [21].
- Image-Assisted Recall: The following day, researchers use the captured images as memory prompts during a structured interview to help participants recall and detail their dietary intake [15].
- Privacy Protection: Participants are typically given the opportunity to review and delete sensitive images before the researcher views them [15].
This method was evaluated in a 2021 study where young adults (18-30 years) wore cameras for three consecutive days while simultaneously reporting dietary intake via a smartphone app and completing daily 24HRs. Camera images were subsequently reviewed and coded by dietitians to identify omitted food items [21]. A 2023 feasibility study in rural Uganda further tested this approach with mothers of young children, assessing both dietary diversity and time use [15].
Performance Metrics: Quantitative Comparison
The table below summarizes key performance metrics for web-based and image-assisted 24HR methods based on recent study findings.
Table 1: Performance Comparison of Modern 24HR Methodologies
| Performance Metric | Web-Based 24HR (ASA-24) | Voice-Based 24HR (DataBoard) | Image-Assisted Recall |
|---|---|---|---|
| Usability/Acceptability Rating | 6.7/10 [33] | 7.6-7.95/10 [33] | 92% "good" or "very good" experience [15] |
| Participant Preference | Baseline | 7.2/10 preference over ASA-24 [33] | N/A |
| Data Loss Issues | Minimal | Minimal | 11-50% due to device malfunction [15] |
| Uncodable Data Proportion | N/A | N/A | 1-35% of images [15] |
| Frequently Omitted Items | Discretionary snacks [21] | Discretionary snacks [21] | Dairy, condiments, fats, alcohol [21] |
| Completion Time | 30-50 minutes [33] | Shorter than ASA-24 [33] | Varies by number of images |
Table 2: Objectively Measured Food Omissions by Assessment Method
| Food Category | Omission Rate in Web-Based App | Omission Rate in Traditional 24HR |
|---|---|---|
| Discretionary Snacks | Significant (p<0.001) [21] | Significant (p<0.001) [21] |
| Water | Significant (p<0.001) [21] | Less than app (p<0.001) [21] |
| Dairy & Alternatives | 53% more omissions [21] | Baseline |
| Savoury Sauces & Condiments | Significant (p<0.001) [21] | Baseline |
| Fats & Oils | Significant (p<0.001) [21] | Baseline |
| Alcohol | Significant (p=0.002) [21] | Baseline |
Analysis of Methodological Strengths and Limitations
Web-Based and Voice-Enabled Platforms
Strengths:
- Standardization: Automated administration ensures consistent questioning across all participants, eliminating interviewer bias [33].
- Scalability: Can be deployed to large populations simultaneously with minimal additional resource requirements [33].
- Participant Acceptance: Voice-based systems in particular show promise for older adults and those with technological barriers, with studies reporting higher preference ratings (7.2/10) over traditional web-based systems [33].
Limitations:
- Persistent Omission Issues: Even technology-enhanced self-report methods continue to struggle with accurate capture of commonly forgotten items like discretionary snacks, condiments, and beverages [21].
- Recall Dependence: Remains vulnerable to memory limitations and estimation errors, particularly for mixed dishes and portion sizes [21].
- Digital Literacy Requirements: May present barriers for certain demographic groups, though voice interfaces show potential to mitigate this [33].
Image-Assisted and Wearable Camera Methods
Strengths:
- Objectivity: Provides an objective record of intake that is not solely dependent on participant memory, serving as a valuable validation tool [21].
- Enhanced Recall: Images significantly improve participants' ability to recall and detail consumed items, with most participants reporting the image-review process as helpful [15].
- Contextual Data: Captures rich contextual information about eating environments, social settings, and food sources that are difficult to obtain through recall alone [15].
Limitations:
- Technical Challenges: Significant data loss (11-50%) occurs due to device malfunction, battery failure, or operator error [15].
- Resource Intensity: Requires substantial researcher time for image processing, coding, and analysis, creating scalability constraints [15].
- Privacy Concerns: Participants may experience discomfort wearing cameras in certain settings, potentially leading to behavior modification or study withdrawal [15].
- Image Quality Issues: 1-35% of images may be uncodable due to poor lighting, obstructed views, or camera positioning [15].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Materials for Implementing Modern Dietary Assessment Methods
| Tool/Solution | Function | Example Implementations |
|---|---|---|
| Automated Dietary Recalls | Self-administered 24-hour recall collection | ASA-24, Intake-24, MyFood24 [21] |
| Voice Survey Platforms | Speech-based dietary data collection | DataBoard (SurveyLex) [33] |
| Wearable Cameras | Passive image capture for dietary behavior | Autographer [21] |
| Image Coding Software | Systematic analysis of captured dietary images | Dedoose [33], Microsoft Excel [21] |
| Egocentric Vision Algorithms | AI-based food identification and portion estimation | EgoDiet (SegNet, 3DNet, Feature, PortionNet) [1] |
| Data Management Systems | Secure storage and management of dietary data | REDCap (Research Electronic Data Capture) [21] |
The choice between web-based platforms and image-assisted methods for implementing the modern 24HR depends heavily on research objectives, resource constraints, and participant characteristics. Web-based systems offer a practical balance of standardization, scalability, and participant burden for large-scale studies where precise nutrient estimation is the primary goal. The emergence of voice-based interfaces shows particular promise for enhancing accessibility in older populations and those with technological limitations.
Image-assisted methods provide superior objectivity and contextual data, making them invaluable for validation studies, intensive behavioral research, and investigations where the eating environment is a key variable. However, their technical complexity, privacy implications, and resource demands currently limit their application to smaller, more focused studies.
Future directions point toward hybrid approaches that combine the strengths of both methodologies. The integration of AI-assisted image analysis, as seen in systems like EgoDiet which reduces portion size estimation error to 28.0% MAPE compared to 32.5% for traditional 24HR [1], promises to reduce the analytical burden of image-based methods. As these technologies mature, researchers will be better equipped to overcome the persistent challenges of dietary assessment while generating richer, more accurate nutritional data.
Figure 1: Workflow comparison of modern 24-hour dietary recall methodologies, highlighting the distinct processes for web-based, voice-based, and image-assisted approaches.
Accurate dietary assessment is fundamental to understanding the relationship between nutrition and health, yet traditional methods have long been hampered by significant limitations. The 24-hour dietary recall, a cornerstone of nutritional epidemiology, requires participants to retrospectively report all foods and beverages consumed in the preceding 24 hours, typically through an interviewer-administered format. While this method provides valuable dietary data, it suffers from well-documented recall biases, measurement errors, and social desirability biases that can distort true intake reporting [17]. Recent analyses suggest that self-reported methods may capture a maximum of 80% of true intake, with systematic under-reporting identified in up to 70% of adults in national surveys [17]. These limitations have propelled the development of wearable sensor technology that offers a more objective, continuous, and contextual approach to monitoring eating behavior.
Wearable devices represent a paradigm shift from subjective recall to objective, passive data collection, transforming what's possible for measuring habitual intakes and temporal eating patterns. By automatically detecting eating events through motion, acoustic, or visual sensors, these technologies capture rich datasets about not just when eating occurs, but also the behavioral and contextual factors surrounding food consumption [34]. This comparison guide examines the operational mechanisms of wearable eating detection systems, their performance relative to traditional 24-hour recall methods, and their emerging role in nutrition research and clinical applications.
How Wearables Detect Eating: Sensing Technologies and Mechanisms
Wearable eating detection systems employ multiple sensing modalities to identify eating events through characteristic physiological signals and movement patterns. The table below summarizes the primary technologies and their detection mechanisms.
Table 1: Wearable Sensor Technologies for Eating Detection
| Sensing Modality | Detection Mechanism | Measured Parameters | Common Form Factors |
|---|---|---|---|
| Inertial Sensing [34] [27] | Captures wrist and arm kinematics during hand-to-mouth movements | Acceleration, angular velocity, movement patterns | Smartwatches, wristbands, IMU sensors |
| Acoustic Sensing [27] | Detects sounds produced during chewing and swallowing | Acoustic frequency, amplitude, timing | Neck-mounted sensors, in-ear devices |
| Image-Based Sensing [17] [35] | Visually identifies food intake and food type | Food appearance, volume, composition | Wearable cameras, smartphone cameras |
| Physiological Sensing [36] | Monitors metabolic responses to food intake | Heart rate, skin temperature, oxygen saturation | Chest patches, wristbands |
| Bioimpedance Sensing [36] | Measures electrical impedance changes during swallowing | Impedance variations across neck/chest | Necklaces, chest patches |
Inertial Sensing: Tracking Hand-to-Mouth Movements
Inertial Measurement Units (IMUs) containing accelerometers and gyroscopes represent the most widely deployed eating detection technology. These sensors detect the characteristic repetitive forearm rotations and elevations that occur during eating episodes. A typical eating detection pipeline using inertial sensing involves multiple stages, as illustrated below:
Figure 1: Inertial Sensing Eating Detection Workflow
This approach has demonstrated strong performance in field deployments. One smartwatch-based system achieved a precision of 80%, recall of 96%, and F1-score of 87.3% in detecting meal episodes, successfully capturing 96.48% (1259/1305) of meals consumed by participants in a real-world study [37]. The system triggered Ecological Momentary Assessments (EMAs) when it detected 20 eating gestures within a 15-minute window, enabling contextual data collection near real-time.
Multi-Sensor Fusion: The Northwestern University Approach
Advanced eating detection systems combine multiple sensors to improve accuracy and capture complementary aspects of eating behavior. Researchers at Northwestern University developed an integrated system employing three synchronized wearable sensors:
Table 2: Multi-Sensor Eating Detection System (Northwestern University)
| Sensor Device | Function | Technical Innovation | Data Output |
|---|---|---|---|
| NeckSense [38] [39] | Precisely records eating behaviors | Neck-worn inertial and acoustic sensing | Bite count, chewing rate, hand-to-mouth movements |
| HabitSense [38] [39] | Captures food-related visual context | Activity-Oriented Camera with thermal food detection | Food presence, type (via thermal signature) |
| Wrist-worn Actigraphy [38] [39] | Monitors general activity and context | Standard accelerometry paired with specialized algorithms | Activity patterns, sleep/wake cycles |
This multi-sensor approach enabled the identification of five distinct overeating patterns in individuals with obesity: take-out feasting, evening restaurant reveling, evening craving, uncontrolled pleasure eating, and stress-driven evening nibbling [38] [39]. The classification emerged from two weeks of continuous monitoring in 60 participants, generating thousands of hours of multimodal sensor data correlated with self-reported mood and context.
Experimental Protocols and Validation Methodologies
Protocol for Validating Wearable Eating Detection
Rigorous validation is essential to establish the accuracy of wearable eating detection systems. The following diagram illustrates a comprehensive validation protocol adapted from recent studies:
Figure 2: Wearable Eating Detection Validation Protocol
A recent study protocol published in 2025 outlines a controlled approach to validating multi-sensor wearables [36]. The study recruits 10 healthy volunteers who attend two study visits at a clinical research facility, consuming pre-defined high-calorie (1052 kcal) and low-calorie (301 kcal) meals in randomized order. Participants wear a customized multi-sensor wristband that tracks hand-to-mouth movements (via IMU), heart rate, skin temperature, and oxygen saturation throughout the eating episodes. These sensor readings are validated against bedside monitors and frequent blood sampling for glucose, insulin, and hormone levels [36].
Camera-Based Ground Truth Validation
Wearable cameras have emerged as a valuable ground truth method for validating both wearable sensors and self-report measures. In one methodology, participants wear an Autographer camera that captures point-of-view images every 30 seconds during waking hours [35]. Trained dietitians then code these images for food and beverage consumption, categorizing eating episodes by meal type, food category, and nutritional quality. This approach identified significant omission patterns in both app-based food records and 24-hour recalls, particularly for discretionary snacks, water, and alcohol [35].
Performance Comparison: Wearables vs. 24-Hour Dietary Recall
Direct comparisons between wearable sensors and 24-hour dietary recall reveal complementary strengths and limitations for dietary assessment.
Table 3: Performance Comparison of Dietary Assessment Methods
| Parameter | Wearable Sensors | 24-Hour Dietary Recall |
|---|---|---|
| Detection Accuracy | 80-96% for eating episodes [37] | Limited by recall bias and portion size estimation [17] |
| Contextual Data | Captures real-time context (location, activity, company) [37] | Limited contextual detail, reliant on memory |
| Food Identification | Limited without image support (multi-sensor systems improving) [17] | Detailed food identification through interview process |
| Portion Size Estimation | Challenging; requires camera systems [17] [35] | Error-prone, dependent on memory and estimation skills |
| Participant Burden | Low after initial setup (passive monitoring) [34] | Moderate to high (requires detailed reporting) |
| Data Processing | Complex computational pipelines, machine learning [34] [27] | Labor-intensive for researchers (coding, analysis) |
| Omission Patterns | Fewer omissions for snacks and beverages [35] | Significant omissions for snacks, water, condiments [35] |
| Temporal Resolution | Continuous, micro-level patterns [34] | Daily or meal-level summary |
Omission Patterns and Measurement Gaps
Discrepancy analyses between camera-based ground truth and self-report methods reveal systematic omission patterns. One study found that discretionary snacks were frequently omitted in both 24-hour recalls and smartphone apps [35]. Specific food categories showed different omission rates: dairy and alternatives, sugar-based products, savory sauces and condiments, fats and oils, and alcohol were more frequently omitted in app-based reporting compared to 24-hour recalls [35]. Water was omitted more frequently in apps than in both camera images and 24-hour recalls.
Wearable sensors address some but not all these gaps. Inertial sensors effectively detect eating events but provide limited information about food type and quantity without complementary sensing modalities. Camera-based systems offer better food identification but raise privacy concerns and require complex image processing [17].
Research Reagent Solutions: Essential Tools for Eating Behavior Research
The experimental approaches described require specialized tools and methodologies. The following table details key research reagents and their applications in eating behavior studies.
Table 4: Essential Research Reagents for Eating Behavior Studies
| Research Tool | Function | Example Applications |
|---|---|---|
| Multi-Sensor Wearable Platform [38] [36] | Simultaneously captures motion, physiological, and contextual data | Northwestern's 3-sensor system; Custom wristbands with IMU, PPG, temperature sensors |
| Activity-Oriented Camera (AOC) [38] [39] | Privacy-preserving image capture triggered by food presence | HabitSense bodycam with thermal food detection |
| Ecological Momentary Assessment (EMA) [37] | Captures self-reported context in real-time | Smartphone-prompted surveys on eating context, company, mood |
| Standardized Meal Protocols [36] | Provides controlled energy challenges for validation | High-calorie (1052 kcal) and low-calorie (301 kcal) test meals |
| Biomarker Assays [36] | Objective physiological validation of intake | Blood glucose, insulin, hormone level measurements |
| Annotation Software [35] | Enables manual coding of eating episodes from video | Custom coding schedules for meal type, food category, context |
Wearable sensors and 24-hour dietary recall offer complementary rather than competing approaches to dietary assessment. Wearables excel at objective detection of eating timing, frequency, and behavioral patterns with minimal participant burden, while 24-hour recalls provide detailed nutritional composition data that current sensors cannot fully capture.
The emerging research paradigm integrates both approaches: using wearables for continuous monitoring of eating architecture and context, while employing periodic 24-hour recalls for detailed nutritional assessment. This hybrid methodology leverages the strengths of both techniques while mitigating their respective limitations.
For researchers and drug development professionals, wearable sensors offer unprecedented insights into real-world eating behaviors and patterns that can inform intervention development and clinical trial endpoints. As sensor technology continues advancing, with improvements in multi-sensor fusion, privacy preservation, and automated food identification, these tools are poised to become increasingly valuable components of comprehensive dietary assessment protocols.
Accurate dietary assessment is fundamental to nutritional epidemiology, yet traditional methods are plagued by inherent limitations. The 24-hour dietary recall (24HR), a self-report tool reliant on participant memory, has been a long-standing standard despite its susceptibility to recall bias and measurement error [40] [14]. In recent years, wearable technology has emerged as a promising alternative, offering the potential for more objective, passive data collection [41] [2]. This guide provides a comparative analysis of these two approaches, evaluating their performance, detailed experimental protocols, and applicability across diverse research populations, from pediatric to geriatric cohorts. The thesis underpinning this comparison is that while wearable devices can significantly improve the accuracy of dietary data collection, their feasibility and performance are modulated by population-specific characteristics and technological constraints.
The table below summarizes key performance metrics for wearable devices and 24-hour recalls, based on recent validation studies.
Table 1: Performance Comparison of Wearable Devices and 24-Hour Recalls
| Metric | Wearable Cameras (with AI Analysis) | Web-Based 24HR (myfood24) | Traditional 24HR (Camera-Assisted) |
|---|---|---|---|
| Portion Size Estimation Error (MAPE) | 28.0% - 31.9% [2] | Information Missing | 32.5% [2] |
| Energy Intake Reporting | Significantly higher vs. recall alone (p=0.003) [14] | Correlated with total energy expenditure (ρ=0.38) [3] | Prone to under-reporting [14] |
| Correlation with Biomarkers | Not Directly Measured | Serum folate (ρ=0.62), Urinary potassium (ρ=0.42) [3] | Not Directly Measured |
| Reproducibility (Correlation) | Not Directly Measured | Strong for most nutrients (e.g., folate ρ=0.84) [3] | Not Directly Measured |
| Data Loss/Uncodable Media | 12-15% (e.g., due to lighting) [15] | Not Applicable | Not Applicable |
Table 2: Feasibility and Acceptability Across Populations
| Population | Wearable Camera Feasibility | 24HR Feasibility |
|---|---|---|
| General Adults (High-Income) | Feasible; some burden and reactivity reported [15] | Well-established; web-based tools show good validity [3] |
| Rural, Low-Income Settings | Challenging; device malfunction, lighting issues, but overall positive participant experience [15] | Impractical for low-literacy populations without an interviewer [15] |
| Pediatric | Limited specific data; likely high burden and privacy concerns | Prone to significant recall error in younger children [40] |
| Geriatric | Limited specific data; potential challenges with technology adoption | Feasible, but may be affected by cognitive decline |
Detailed Experimental Protocols
To understand the data presented above, it is crucial to examine the methodologies of key experiments validating these tools.
Protocol for Validating a Web-Based 24HR Tool
A 2025 repeated cross-sectional study assessed the validity and reproducibility of the myfood24 dietary assessment tool against biomarkers in healthy Danish adults [3].
- Participants: 71 healthy adults (53.2 ± 9.1 years) [3].
- Experimental Design: Participants completed a seven-day weighed food record using myfood24 at baseline and again four weeks later. This design allowed for both validity and reproducibility (reliability) testing [3].
- Objective Measures: At the end of each recording week, objective measures were collected:
- Data Analysis: Spearman's rank correlations were calculated between estimated nutrient intakes from myfood24 and the corresponding biomarker levels (e.g., folate intake vs. serum folate, potassium intake vs. urinary potassium) [3].
Protocol for Wearable Camera-Assisted Recall
A 2022 study examined whether a wearable camera could improve the accuracy of a 24-hour recall in twenty adults [14].
- Participants: 20 healthy, free-living volunteers aged 18–65 years [14].
- Wearable Device: The "Narrative Clip" camera, chosen for its automatic image capture (every 30 seconds), discreet size, and ease of use. Participants wore it for one full day [14].
- Experimental Procedure:
- Camera Deployment: Participants wore the camera from wake-up until bedtime.
- Initial 24HR: The following day, a standard 24-hour recall was conducted before viewing any camera images.
- Image-Assisted Recall: Participants first privately reviewed and deleted any images for privacy. Then, the researcher and participant viewed the images together to identify eating episodes, cross-reference the initial recall, and add, remove, or modify details [14].
- Data Analysis: Energy and nutrient intakes from the recall-alone and the camera-assisted recall were compared using paired statistical tests (e.g., paired t-test) [14].
Protocol for AI-Based Passive Dietary Assessment
A 2024 study developed and tested "EgoDiet," an AI-driven pipeline for dietary assessment using low-cost wearable cameras in African populations [2].
- Study Populations:
- AI Pipeline (EgoDiet): The system comprised several modules:
- EgoDiet:SegNet: A neural network to segment food items and containers in images.
- EgoDiet:3DNet: A network to estimate camera-container distance and reconstruct 3D container models.
- EgoDiet:Feature: An extractor for portion size-related features.
- EgoDiet:PortionNet: A final module to estimate the portion size (weight) of food consumed [2].
- Validation: EgoDiet's portion size estimates were compared against assessments by dietitians and against traditional 24HR, with performance measured by Mean Absolute Percentage Error (MAPE) [2].
Visualizing Workflows and Technologies
The following diagrams illustrate the core workflows and technological concepts discussed in the experimental protocols.
Diagram 1: AI-Powered Wearable Camera Workflow
Diagram 2: Recall Methods Comparison
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Materials and Tools for Dietary Assessment Research
| Item | Function/Description | Example from Research |
|---|---|---|
| Automated Wearable Camera | Passively captures images at regular intervals to objectively document eating episodes and context. | Narrative Clip, AIM, eButton [14] [2] |
| Web-Based Dietary Tool | Allows participants to self-report intake via food records; often includes integrated food composition databases. | myfood24 [3] |
| Standardized Weighing Scale | Provides gold-standard measurement of food weight for validating portion size estimation algorithms. | Salter Brecknell scale [2] |
| Biomarker Assays | Objective biological measures used to validate self-reported or image-derived intake of specific nutrients. | Serum folate, 24-hour urinary potassium/urea [3] |
| Indirect Calorimeter | Measures resting energy expenditure to help identify under- or over-reporters of energy intake. | Used to apply the Goldberg cut-off [3] |
| AI Dietary Analysis Pipeline | Software that automates the analysis of image data for food identification and portion size estimation. | EgoDiet [2] |
The comparative analysis indicates that wearable cameras, particularly those augmented with AI, offer a tangible improvement in accuracy over traditional 24HR, especially for portion size estimation and mitigating under-reporting. The 24HR method, especially when web-based and validated, remains a reliable tool for ranking individuals by nutrient intake and is highly reproducible. The choice between these methods is not a simple matter of superiority but depends on the research context. Key considerations include the target population's technical literacy and age, the specific nutrients of interest, and the available resources for data processing. Future research should focus on optimizing wearable technology for low-resource settings and vulnerable cohorts, and on further integrating AI to reduce the significant researcher burden associated with image analysis.
Integrating AI and Machine Learning for Automated Food Recognition and Nutrient Estimation
Accurate dietary assessment is fundamental to nutrition research, chronic disease management, and public health surveillance [42]. For decades, the 24-hour dietary recall has served as a cornerstone method, relying on individuals' ability to remember and accurately report their food consumption [11]. However, this and other self-report methods are notoriously prone to recall bias, social desirability bias, and significant measurement errors, limiting their reliability for both research and clinical applications [42] [11]. The emergence of artificial intelligence (AI) and machine learning (ML) technologies promises a paradigm shift toward more objective, automated, and scalable dietary assessment solutions [42] [43]. This guide provides a comparative analysis of AI-driven automated food recognition and nutrient estimation systems against traditional 24-hour dietary recalls, with a specific focus on their integration with wearable technology. It synthesizes current experimental data, detailed methodologies, and performance metrics to inform researchers, scientists, and drug development professionals.
Comparative Analysis: AI vs. Traditional Dietary Assessment
The table below summarizes the key characteristics and performance metrics of AI-driven dietary assessment methods compared to traditional 24-hour dietary recalls.
Table 1: Performance Comparison of Dietary Assessment Methods
| Feature | AI-Driven Methods | 24-Hour Dietary Recall |
|---|---|---|
| Primary Data Input | Food images, sound, jaw motion, text [42] | Verbal or written self-report [11] |
| Automation Level | Fully or semi-automated analysis [43] [44] | Manual data collection and coding |
| Key Strengths | Reduces recall bias; enables real-time monitoring [42]; objective [43] | Well-established protocol; no special equipment needed [45] |
| Reported Accuracy (Food Detection) | 74% to 99.85% [42] | Not applicable (relies on memory) |
| Reported Error (Nutrient Estimation) | 10-15% (calorie estimation) [42]; ~8% for specialized systems [44] | Under-reporting common, especially for snacks, condiments [11] |
| Scalability | High potential with mobile technology [43] | Labor-intensive, limited by interviewer availability [45] |
| Intrusiveness | Varies (wearable cameras can raise privacy concerns [46]) | Low to moderate (depends on interview length) |
| Notable Omissions | Varies by algorithm | Discretionary snacks, water, condiments, alcohol [11] |
Methodological Deep Dive: Experimental Protocols
Protocol for AI-Based Food Recognition and Nutrient Estimation
A. System Architecture and Workflow AI-based dietary assessment systems typically follow a structured workflow, from data acquisition to nutrient estimation, utilizing various ML models.
Diagram Title: AI-Based Food Analysis Workflow
B. Key Technical Components and Models
- Data Acquisition: Input can include food images from smartphones or wearable cameras [43], or sound and jaw motion data from wearable devices [42].
- Food Detection and Recognition: Utilizes advanced deep learning models. Convolutional Neural Networks (CNNs) are commonly employed, achieving classification accuracies above 85% to 90% [47]. The YOLOv8 model enables real-time food detection directly in web browsers [43].
- Portion Size Estimation: A critical and challenging step. The NYU Tandon team's advance incorporates a volumetric computation function that uses advanced image processing to measure the exact area each food occupies on a plate, correlating this with density and macronutrient data [43].
- Nutrient Calculation: Systems map recognized food items and their estimated portions to food composition databases to calculate calorie and nutrient content [43].
C. Validation Methods Validation typically involves comparing AI estimates against ground truth methods, most commonly the weighing method, where food is weighed before and after consumption [48] [44]. Performance is assessed using metrics like Root-Mean-Square Error (RMSE) and Concordance Correlation Coefficient (CCC) [48] [44].
Protocol for 24-Hour Dietary Recall
A. Standardized Interview Procedure The 24-hour recall method is a structured interview designed to capture all foods and beverages consumed in the previous 24-hour period.
Diagram Title: 24-Hour Dietary Recall Process
B. Implementation Variants
- Interviewer-Administered: Can be conducted face-to-face or by telephone. A study using the EPIC SOFT program found no significant differences in most reported food group intakes between these two modes [45].
- Automated Self-Administered: Platforms like Intake24 enable participants to complete recalls online without an interviewer [11].
C. Validation and Limitations Validation studies often use biomarkers like doubly labeled water for energy intake [46]. Common limitations identified include frequent omission of specific items like discretionary snacks, water, and condiments [11], and significant under-recording by nursing staff in clinical settings [44].
The Scientist's Toolkit: Key Research Reagents and Solutions
Table 2: Essential Tools for Dietary Assessment Research
| Tool / Solution | Type | Primary Function | Example Use Case |
|---|---|---|---|
| YOLOv8 with ONNX Runtime | Algorithm / Software | Real-time food item detection and localization from images [43] | Mobile, browser-based food recognition [43] |
| Convolutional Neural Networks (CNNs) | Algorithm / Architecture | Image classification and food identification [47] | Achieving >85% accuracy in food classification tasks [47] |
| EPIC SOFT | Software / Protocol | Standardized computerized 24-hour diet recall interview [45] | Conducting comparable dietary recalls across different study centers [45] |
| Wearable Camera (e.g., Autographer) | Hardware / Device | Passive capture of point-of-view images for dietary assessment [11] | Ground truth data collection to identify omissions in self-reports [11] |
| Food Composition Database (e.g., FNDDS) | Data Resource | Provides nutritional content for identified food items [46] | Converting reported food intake into estimated nutrient values [46] |
| Doubly Labeled Water | Biomarker / Gold Standard | Objectively measures total energy expenditure [46] | Validating the accuracy of self-reported energy intake [46] |
Discussion and Future Directions
AI-driven methods for food recognition and nutrient estimation demonstrate significant potential to overcome the inherent limitations of self-reported dietary data, primarily by reducing recall bias and enabling objective, real-time monitoring [42]. The experimental data shows that these systems can achieve high accuracy in food detection (up to 99.85%) and acceptable error margins in nutrient estimation (e.g., 8.12 RMSE for energy) [42] [44].
However, several challenges remain for widespread adoption in research and clinical practice. AI models must improve their robustness across diverse food types and cuisines [43]. Practical and ethical concerns regarding data privacy—particularly with wearable cameras—and algorithmic fairness across diverse populations require careful attention [42] [46]. Furthermore, while AI systems can match the accuracy of visual estimations by dietitians from images, they have not yet consistently surpassed the accuracy of direct visual estimation by clinical staff in all settings [44].
The future of dietary assessment lies not in the replacement of one method by another, but in their intelligent integration. Research is moving toward multi-modal AI systems that combine computer vision with data from other wearable sensors (e.g., chewing sounds, wrist motion) [42] [46] and federated learning approaches to enhance privacy [47]. This integrated approach, which leverages the strengths of both AI objectivity and human contextual understanding, holds the greatest promise for generating the precise, reliable dietary data essential for advanced nutritional science, personalized medicine, and drug development.
Accurate dietary assessment is a cornerstone of nutritional epidemiology, chronic disease research, and public health policy development. However, the two predominant methods—traditional 24-hour dietary recalls (24HR) and emerging wearable technologies—each present distinct challenges and considerations when applied to diverse populations. Variations in culture, language, and dietary habits can significantly impact the accuracy, feasibility, and equity of dietary data collection. Understanding these considerations is paramount for researchers and drug development professionals seeking to generate reliable, generalizable data in global studies. This guide provides an objective comparison of these methodologies, focusing on their performance across varied demographic and cultural contexts, supported by experimental data and detailed protocols.
The table below summarizes key performance metrics for 24-hour dietary recalls and wearable technologies, highlighting their validity and adaptability across different populations.
Table 1: Performance Comparison of Dietary Assessment Methods in Diverse Settings
| Performance Metric | 24-Hour Dietary Recall (24HR) | Wearable Technology (Camera-Based) |
|---|---|---|
| Overall Portion Size Accuracy (MAPE) | 32.5% (Ghana study) [2] | 28.0% (Ghana study) [2] |
| Food Item Reporting Accuracy | ~71% recall rate (Older Korean Adults) [49] | N/A (Passively captures data, no recall needed) |
| Portion Size Estimation Bias | Systematic overestimation (Mean ratio: 1.34) [49] | Reduced error vs. 24HR [2] |
| Biomarker Correlation (e.g., Serum Folate) | Spearman's ρ = 0.62 (myfood24 tool) [3] | Not typically measured for dietary intake |
| Method Reproducibility | Strong for most nutrients (ρ ≥ 0.50) [3] | High, due to automated, passive data collection [2] |
| Cultural Adaptation Requirement | High (Requires localized food databases, trained interviewers, language translation) [3] | Moderate (Primarily requires algorithm training on local foods and container types) [2] |
Experimental Protocols and Methodologies
Protocol for Validating a Web-Based 24HR Tool in a New Population
The validation of the myfood24 tool in a Danish population provides a robust protocol for adapting a 24HR tool [3].
- Population & Design: The repeated cross-sectional study involved 71 healthy Danish adults. Participants completed a 7-day weighed food record using the tool at baseline and again after 4 weeks [3].
- Biomarker Collection: Objective measures were used for validation. These included:
- Blood Draw: Fasting blood samples were analyzed for serum folate to correlate with self-reported folate intake [3].
- Urine Collection: 24-hour urine samples were collected to measure urea and potassium excretion, providing biomarkers for protein and potassium intake [3].
- Energy Expenditure: Resting energy expenditure was measured via indirect calorimetry, and the Goldberg cut-off was applied to identify misreporters [3].
- Data Analysis: Validity was assessed by calculating Spearman's rank correlations between reported nutrient intakes and biomarker concentrations. Reproducibility was analyzed by correlating nutrient intakes from the first and second recording periods [3].
Protocol for Validating a Wearable Camera System (EgoDiet)
The EgoDiet pipeline validation in London and Ghana outlines a method for testing wearable cameras in diverse settings [2].
- Device & Population:
- Ground Truth Measurement: A standardized weighing scale (Salter Brecknell) was used to measure the weight of food items and containers before and after consumption to establish the true portion size [2].
- AI-Powered Analysis: The EgoDiet pipeline involves several automated modules:
- EgoDiet:SegNet: Segments food items and containers from the video footage [2].
- EgoDiet:3DNet: Estimates camera-to-container distance and reconstructs 3D models of containers [2].
- EgoDiet:Feature: Extracts portion size-related features like the Food Region Ratio (FRR) and Plate Aspect Ratio (PAR) [2].
- EgoDiet:PortionNet: Estimates the final portion size (in weight) of food consumed using the extracted features [2].
- Performance Calculation: The Mean Absolute Percentage Error (MAPE) between the camera-estimated portion sizes and the weighed ground truth was calculated and compared against the error from traditional 24HR [2].
Workflow and Logical Pathway for Method Selection
The following diagram illustrates the key decision-making workflow and methodological components for applying dietary assessment tools in diverse populations.
Diagram 1: Dietary Assessment Adaptation Workflow
The Researcher's Toolkit: Essential Reagents and Materials
This table lists key materials and tools required for implementing and validating dietary assessment methods in cross-cultural research contexts.
Table 2: Essential Research Reagents and Solutions for Dietary Assessment
| Tool/Reagent | Primary Function | Application Context |
|---|---|---|
| Validated Web-Based 24HR Tool (e.g., myfood24) | Self-administered dietary data collection with integrated food composition databases. | Requires extensive localization of the underlying food database for the target population's cuisine [3]. |
| Wearable Camera (e.g., AIM, eButton) | Passive, continuous image capture of eating episodes and environment. | Must be validated for the specific dietary context; algorithm performance depends on training data for local foods [2]. |
| Standardized Weighing Scale | Provides objective "ground truth" measurement of food portion weights. | Essential for validation studies of both 24HR and wearable technologies [2]. |
| Biomarker Assay Kits (e.g., for Serum Folate) | Objective biochemical measures to validate self-reported intake of specific nutrients. | Used as a reference method in validation studies to assess the criterion validity of dietary tools [3]. |
| 24-Hour Urine Collection Kit | Standardized collection of urine for biomarker analysis (e.g., urea, potassium). | Provides an objective measure of protein and potassium intake for validation purposes [3]. |
| Localized Food Composition Database | Provides nutrient composition information for region-specific foods and dishes. | Fundamental for accurate nutrient analysis in any dietary assessment method; requires significant local expertise to develop [3]. |
Addressing Limitations and Enhancing Data Quality
Accurate dietary assessment is a cornerstone of nutritional epidemiology, public health monitoring, and pharmaceutical development. For decades, the 24-hour dietary recall (24HR) has served as a primary method for collecting food intake data in large-scale studies. While this self-reported tool provides valuable quantitative nutrient intake information, it suffers from well-documented methodological limitations that can compromise data quality and subsequent analysis.
The emergence of wearable sensor technology presents a potential paradigm shift in dietary monitoring, offering objective, continuous data collection that may circumvent certain limitations of traditional recall methods. This guide provides a systematic comparison of these approaches, focusing on three fundamental pitfalls of 24HR: recall bias, social desirability bias, and portion size estimation errors. We examine experimental data quantifying these limitations and evaluate how technological innovations might address them, providing researchers with evidence-based insights for methodological selection in study design.
Quantified Pitfalls of 24-Hour Dietary Recalls
Extensive research has documented the systematic and random errors inherent in 24HR methodology. The table below summarizes experimental findings across three primary pitfall categories.
Table 1: Experimental Evidence of Key 24HR Pitfalls
| Pitfall Category | Experimental Findings | Quantitative Impact | Study Context |
|---|---|---|---|
| Recall Bias & Memory Lapse | Food item omission rates varied by participant nationality in a web-based 24HR [6]. | Brazilian participants omitted 24% of foods vs. 13% for Irish participants [6]. | Foodbook24 study among Brazilian, Irish, and Polish adults [6]. |
| Comparison of Ecological Momentary Assessment (EMA) with 24HR and food images [50]. | Beverages were the most frequently omitted food category [50]. | Crossover feasibility study in young adults (18-30 years) [50]. | |
| Social Desirability Bias | Comparison of open vs. list-based 24HR methods for reporting unhealthy feeding practices [51]. | List-based method reported 61.6% sweet food consumption vs. 43.8% with open recall (p=0.012) [51]. | Cohort study of infant feeding in peri-urban Cambodia [51]. |
| Association between social desirability bias and reported consumption of salty/fried foods [51]. | Relationship was more pronounced among caregivers who received the list-based 24HR (p=0.004) [51]. | Rural/peri-urban Cambodia [51]. | |
| Portion Size Estimation Errors | Comparison of traditional 24HR with AI-enabled wearable camera (EgoDiet) [2]. | 24HR showed 32.5% Mean Absolute Percentage Error (MAPE) for portion size vs. 28.0% for EgoDiet [2]. | Field studies in London and Ghana among populations of Ghanaian/Kenyan origin [2]. |
| Comparison of dietitians' assessments with EgoDiet pipeline [2]. | Dietitians' portion estimates had 40.1% MAPE [2]. | Controlled feasibility study [2]. |
Wearable Technologies as a Comparative Approach
Wearable technologies offer an alternative methodological pathway that minimizes reliance on participant memory and active reporting.
Direct Performance Comparison
Recent studies provide direct, quantitative comparisons between traditional 24HR and emerging wearable technologies:
AI-Enabled Wearable Cameras: The EgoDiet system utilizes egocentric vision-based pipelines to estimate portion sizes. In field studies comparing this passive method with 24HR, the wearable camera demonstrated a 28.0% Mean Absolute Percentage Error (MAPE) for portion size estimation, outperforming the 32.5% MAPE observed with 24HR. Notably, both methods outperformed professional dietitians, who showed 40.1% MAPE in controlled settings [2].
Sensor-Triggered Ecological Momentary Assessment: Research indicates that personalizing assessment timing based on detected eating events shows promise for reducing memory-related errors. One study found that while personalized and fixed-interval EMA schedules showed similar overall adherence (~66%), personalized approaches reduced participant reports of receiving "too many prompts per day" [50].
Methodological Workflow Comparison
The fundamental differences in data collection between 24HR and wearable technology approaches create distinct workflows and potential error introduction points.
Table 2: Methodological Workflow Comparison
| Research Stage | 24-Hour Dietary Recall Protocol | Wearable Technology Protocol |
|---|---|---|
| Data Capture | Self-Reported:• Multiple-pass interview method• Food list-based or open recall• Relies on participant memory | Sensor-Based:• Passive data collection (images, accelerometer)• Continuous monitoring• Time-stamped automated capture |
| Portion Estimation | Memory-Dependent:• Food image atlases• Household measures recall• Standardized portion sizes | Computer Vision:• AI-based segmentation (e.g., EgoDiet:SegNet)• 3D reconstruction (e.g., EgoDiet:3DNet)• Depth estimation for volume |
| Data Processing | Manual Coding:• Researcher-assisted food coding• Nutrient database matching• Quality control checks | Automated Analysis:• Feature extraction algorithms• Machine learning classification• Minimal human intervention |
| Error Introduction | Primary Points:• Memory recall at ingestion• Social desirability during reporting• Portion size estimation | Primary Points:• Sensor placement/angle• Lighting conditions for imaging• Algorithm training data gaps |
The following workflow diagram illustrates the key stages and potential failure points in each methodological approach:
Experimental Protocols for Methodological Validation
Web-Based 24HR Expansion Protocol (Foodbook24)
A 2025 study detailed a comprehensive protocol for expanding and validating a web-based 24HR tool for diverse populations:
- Population Selection: Targeted Irish, Polish, and Brazilian adults in Ireland to represent varying languages and dietary traditions [6].
- Tool Expansion: Added 546 culturally-specific food items after reviewing national survey data from Brazil and Poland, with translations into Polish and Portuguese [6].
- Validation Design: Conducted both acceptability testing (comparing participant food records to tool availability) and a comparison study (self-administered vs. interviewer-led recalls on the same day, repeated after two weeks) [6].
- Analysis Approach: Used Spearman rank correlations, Mann-Whitney U tests, and κ coefficients to compare food groups and nutrient intakes between methods [6].
This protocol demonstrated strong correlations for 44% of food groups and 58% of nutrients, though significant differences emerged for specific categories like potatoes and nuts [6].
AI-Enabled Wearable Camera Protocol (EgoDiet)
Research published in 2024 established a rigorous protocol for passive dietary assessment:
- Device Selection: Utilized two wearable cameras: the Automatic Ingestion Monitor (AIM, eye-level) and eButton (chest-level), both capable of storing ≤3 weeks of data [2].
- Study Populations: Conducted parallel studies in London (feasibility) and Ghana (field validation) among populations of Ghanaian and Kenyan origin [2].
- Reference Measures: Employed standardized weighing scales (Salter Brecknell) to measure food items before consumption as ground truth [2].
- AI Pipeline: Implemented a multi-stage computer vision system:
- EgoDiet:SegNet for food item and container segmentation
- EgoDiet:3DNet for camera-to-container distance estimation
- EgoDiet:Feature for portion size-related feature extraction
- EgoDiet:PortionNet for final portion weight estimation [2]
This protocol demonstrated that passive camera technology could outperform both traditional 24HR and dietitian assessments in portion estimation accuracy [2].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Methodological Tools for Dietary Assessment Research
| Tool Category | Specific Examples | Research Function | Key Considerations |
|---|---|---|---|
| Web-Based 24HR Platforms | Foodbook24 (Ireland), FOODCONS (Italy), ASA-24 (US), Intake24 (UK) [6] [52] | Standardized 24HR administration with automated nutrient calculation | Requires food list localization; varying computer literacy needed [6] [52] |
| Wearable Cameras | Automatic Ingestion Monitor (AIM), eButton [2] | Passive capture of eating episodes; minimizes participant burden | Privacy considerations; lighting and positioning affect accuracy [2] |
| Computer Vision Algorithms | EgoDiet:SegNet (Mask R-CNN), EgoDiet:3DNet (depth estimation) [2] | Automated food identification and portion size estimation | Requires training on diverse food databases; performance varies by cuisine [2] |
| Validation Reference Tools | Standardized weighing scales, doubly labeled water [2] [53] | Objective measurement of food consumption and energy expenditure | Considered gold standard but costly and complex to implement [53] |
| Representativeness Solutions | Probability-based sampling, study-provided devices, oversampling [54] | Addresses selection bias and health data poverty | Higher initial costs but improves generalizability of findings [54] |
The evidence demonstrates that both 24-hour dietary recalls and emerging wearable technologies present distinct advantages and limitations for dietary assessment. Traditional 24HR methods, while standardized and culturally adaptable, show quantifiable vulnerabilities to recall bias (evidenced by 13-24% food omission rates), social desirability bias (creating up to 17.8% reporting discrepancies), and portion size estimation errors (32.5% MAPE).
Wearable technologies offer promising alternatives through passive data collection, with AI-enabled cameras demonstrating superior portion estimation accuracy (28.0% MAPE) and reduced reliance on participant memory. However, these approaches face their own challenges regarding representativeness, privacy concerns, and algorithmic training requirements.
For research and drug development professionals, methodological selection should be guided by study objectives, population characteristics, and resource constraints. Hybrid approaches that leverage the strengths of both methodologies may represent the most robust path forward for comprehensive dietary assessment. As technological innovations continue to evolve, the research community must prioritize addressing representation gaps in digital health data while developing increasingly sophisticated solutions to long-standing methodological challenges in nutritional science.
Accurate dietary assessment is a cornerstone of nutritional epidemiology, chronic disease management, and public health policy development. For decades, the 24-hour dietary recall (24HR) has served as a methodological standard, relying on participant memory and self-reporting to quantify food intake [49]. However, the rapid emergence of wearable sensor technologies presents a paradigm shift, offering a potential alternative through passive, objective data collection. This guide provides a systematic comparison of these two approaches, focusing on their technical and user-limitations concerning intrusiveness, battery life, and data privacy. The analysis is framed for researchers, scientists, and drug development professionals who require a critical understanding of these methodologies' constraints within clinical and large-scale observational studies. The evaluation is based on current experimental data and validation studies to inform protocol design and tool selection.
Experimental Protocols & Performance Data
To objectively compare these methodologies, researchers have employed structured validation studies. The following tables summarize key experimental protocols and their findings regarding accuracy and usability.
Table 1: Summary of Key Validation Studies and Experimental Protocols
| Study Focus | Protocol Methodology | Key Performance Metrics | Primary Findings |
|---|---|---|---|
| 24HR Accuracy Validation [49] | 119 older Korean adults consumed 3 self-served meals with discreetly weighed food. A 24HR interview (in-person or online) was conducted the next day. | - Food item match rate- Portion size ratio (reported/weighed)- Energy & nutrient intake difference | Participants recalled 71.4% of foods consumed but overestimated portion sizes (mean ratio: 1.34). No significant difference in energy/macronutrient intake. Women (75.6% match) were more accurate than men (65.2%). [49] |
| Voice-based vs. Traditional 24HR [33] | 20 participants (mean age 70.5) were randomly assigned to complete a voice-based recall (DataBoard) or the web-based ASA-24 first, followed by interviews. | - Usability & acceptability (1-10 scale)- Preference ratings- Qualitative feedback | Voice-based recall was rated easier (6.7/10) than ASA-24. Participants preferred DataBoard and felt it could be used more frequently (7.2/10). [33] |
| AI-Wearable Camera (EgoDiet) [2] | Field studies in London (A) and Ghana (B). Participants wore cameras (AIM or eButton) during meals. Food portion sizes were estimated by the AI pipeline and compared to dietitian assessments and 24HR. | - Mean Absolute Percentage Error (MAPE) for portion size | EgoDiet MAPE: 28.0% (Study B). This outperformed the traditional 24HR, which had a MAPE of 32.5%. [2] |
Table 2: Comparative Analysis of Key Limitations
| Limitation Category | 24-Hour Dietary Recall (24HR) | Wearable Technology |
|---|---|---|
| Intrusiveness & User Burden | High cognitive burden; relies on memory and ability to estimate portions [49]. Multi-step process can be time-consuming and frustrating [33]. | Physical intrusiveness; devices must be worn comfortably for extended periods [55]. Cameras raise specific concerns about continuous recording in private settings [2]. |
| Power Management | Not applicable to the device itself, but imposes a high "human energy" cost, leading to participant fatigue and potential dropout in longitudinal studies [2]. | A primary technical hurdle. Smartwatches often require daily charging, while fitness bands and some smart rings can last 5-14 days [56]. Limits continuous monitoring. |
| Data Privacy & Security | Involves collection of sensitive dietary data, typically managed via secure researcher platforms (e.g., ASA24) [57]. | Heightened risk due to collection of sensitive health (e.g., heart rate, location) and, in the case of cameras, visual data [55]. Requires robust encryption and compliance with regulations like GDPR and HIPAA [55]. |
| Data Accuracy & Bias | Prone to recall bias and portion size misestimation [49]. Accuracy is influenced by factors like age, gender, and cognitive ability [49]. | Varies by sensor type. High accuracy for some metrics (e.g., heart rate), but can be less accurate for others (e.g., workout heart rate via smart rings) [56]. Cameras can provide a more objective "ground truth." [2] |
The Scientist's Toolkit: Key Research Reagent Solutions
Selecting the appropriate tools is critical for study design. Below is a catalog of essential solutions and their functions in dietary assessment research.
Table 3: Essential Reagents for Dietary Intake Research
| Research Reagent | Function & Application in Dietary Assessment |
|---|---|
| ASA-24 (Automated Self-Administered 24-hr Recall) [57] | A freely available, web-based tool that automates the 24HR process. It uses the USDA's Automated Multiple-Pass Method to collect detailed data on foods, portions, and nutrients, reducing interviewer burden. |
| Voice-Based Recall Tools (e.g., DataBoard) [33] | Platforms that use speech input to complete dietary surveys. These are particularly valuable for populations with low digital literacy or vision/motor impairments, reducing interface-based burden. |
| Wearable Cameras (e.g., AIM-2, eButton) [2] | Passive, egocentric cameras worn on the body (eyeglasses or chest) to continuously capture meal episodes. They minimize reliance on memory and provide objective visual data for analysis. |
| Inertial & Acoustic Sensors [58] | Sensors (accelerometers, gyroscopes, microphones) embedded in wrist-worn wearables or patches. They detect eating-behavior signals like hand-to-mouth gestures, chewing, and swallowing. |
| AI-Powered Analytical Pipelines (e.g., EgoDiet) [2] | Software suites that use computer vision (e.g., Mask R-CNN for segmentation, depth estimation networks) to automatically identify foods and estimate portion sizes from wearable camera imagery. |
Methodological Workflow and Technical Constraints
The following diagrams illustrate the core workflows and inherent limitations of each dietary assessment method, highlighting points of failure and technical challenges.
Diagram 1: Methodological Workflows & Constraint Mapping. This diagram contrasts the sequential, memory-dependent 24HR process with the continuous data acquisition of wearables, mapping key constraints (intrusiveness, battery, privacy) to their points of impact.
Diagram 2: Interdependence of Wearable Technology Constraints. This diagram illustrates how the core limitations of wearables are not isolated but are interconnected, creating a complex design and implementation challenge for researchers.
The choice between traditional 24HR and wearable technologies for dietary assessment involves a direct trade-off between human-centric and technology-centric limitations. The 24HR method's primary constraints are cognitive, including reliance on memory and the high burden of accurate self-reporting, which introduces recall and portion-size estimation biases [49]. In contrast, wearables face physical and digital constraints, including limited battery life, data privacy concerns, and the need for user compliance with a constantly worn device [55] [56].
For researchers, the decision framework should be guided by the study's primary objectives. If the goal is large-scale, low-burden nutritional surveillance where granular accuracy on individual food items is less critical, wearable sensors (especially passive cameras) show significant promise in reducing bias [2]. However, if detailed nutrient intake analysis is required and the study population can tolerate the cognitive load, 24HR—particularly newer, more accessible versions like voice-based tools [33]—remains a valuable, validated method. Future research should focus on hybrid models that leverage the objective data capture of wearables with the contextual depth of self-report, all while rigorously addressing the critical challenges of battery longevity, user comfort, and robust data security.
Accurate dietary intake data is fundamental for nutrition surveillance, epidemiological research, and informing public health policy. The 24-hour dietary recall (24HR) stands as a predominant method for assessing dietary intake in large-scale population studies, but its accuracy is influenced by methodological choices including recall administration format and the comprehensiveness of underlying food lists. Simultaneously, wearable sensor technologies have emerged as promising tools for objective physiological monitoring. Understanding the relative strengths and limitations of these approaches is essential for optimizing dietary assessment strategies. This guide examines key methodological considerations for enhancing 24HR protocols, specifically through multiple recall administrations and food list expansion, while contextualizing these strategies within the broader landscape of wearable-based research.
Core Concepts: 24HR Methodologies and Wearable Sensors
24-Hour Dietary Recall (24HR) Fundamentals
The 24-hour dietary recall is a structured method designed to capture detailed information about all foods and beverages consumed by an individual during the previous 24-hour period [59]. Traditional implementations include interviewer-administered formats (e.g., the Automated Multiple-Pass Method), while technological advances have enabled self-administered web-based and image-assisted tools (e.g., ASA24, Intake24, mFR24) [59]. These tools systematically probe for food types, preparation methods, portion sizes, and eating occasions. A critical challenge inherent to all 24HR methods is misreporting, which includes both under-reporting and over-reporting of energy and nutrient intake [60] [61].
Wearable Sensors for Physiological Monitoring
Wearable devices constitute a separate class of assessment tools that continuously capture physiological and behavioral metrics. Unlike 24HR, which relies on self-reported consumption, wearables objectively measure physiological consequences of intake and activity. Clinical-grade wearables can track vital signs like heart rate, respiratory rate, and oxygen saturation [7], while consumer devices (e.g., smartwatches) capture activity and heart rate patterns [62]. Research demonstrates these data can predict health outcomes; for example, longitudinal heart rate features from wearables significantly improved prediction of Long COVID status over symptom data alone [62]. Another clinical wearable model successfully predicted patient deterioration up to 17 hours in advance [7].
The table below summarizes the fundamental distinctions between these two assessment approaches.
Table 1: Fundamental Comparison of 24HR and Wearable Sensor Approaches
| Feature | 24-Hour Dietary Recall (24HR) | Wearable Sensors |
|---|---|---|
| Primary Measurement | Self-reported food/beverage consumption | Objective physiological/behavioral data (e.g., heart rate, activity) |
| Data Type | Dietary intake (subjective) | Physiological consequence (objective) |
| Key Strengths | Captures specific foods, nutrients, dietary context; cost-effective for large surveys | Objective, continuous, passive data collection; reduces recall and social desirability bias |
| Key Limitations | Prone to memory lapses, portion size misestimation, and misreporting [60] [61] | Does not directly measure dietary intake; requires inference models for nutritional insights |
Strategy 1: Implementing Multiple 24-Hour Recalls
Rationale and Experimental Evidence
Single-day 24HR assessments do not represent an individual's usual intake due to high day-to-day variability [60]. Administering multiple non-consecutive 24HRs accounts for this variation and provides a more accurate estimate of habitual diet. The validity of this strategy is supported by controlled studies and comparisons with objective biomarkers.
- Controlled Feeding Studies: Protocols that compare reported intake against observed intake in a controlled setting are the gold standard for identifying measurement error. Such studies can quantify specific errors like food omission (failing to report a consumed item) and intrusion (reporting a non-consumed item) [59].
- Comparison with Doubly Labeled Water (DLW): DLW measures total energy expenditure and serves as an objective biomarker for validating energy intake reporting in weight-stable individuals. A systematic review of 59 studies found that most dietary assessment methods, including 24HR, significantly under-report energy intake compared to DLW-measured expenditure [61].
- Comparison with 24-hour Urine Collection: For sodium intake, 24-hour urine collection is considered a gold standard. A meta-analysis of 28 studies found that 24HR substantially underestimated population mean sodium intake by an average of 607 mg per day compared to 24-hour urine collection [63]. The underestimation was less severe in studies using higher-quality methods, such as the multiple-pass 24HR [63].
Protocol for Multiple 24HR Administration
Implementing a multiple 24HR design requires careful planning to minimize burden and maximize data quality.
- Recall Number and Spacing: Collect a minimum of two recalls per participant. To capture intra-individual variation (weekday vs. weekend), administer at least one recall on a weekday and one on a weekend day, with non-consecutive days to ensure independence.
- Administration Method: Select an appropriate method based on resources:
- Interviewer-Administered 24HR: Resource-intensive but may improve accuracy through trained interviewer probing [59].
- Automated Self-Administered 24HR: Tools like ASA24 and Intake24 reduce personnel costs and have shown levels of measurement error comparable to interviewer-administered methods [59].
- Image-Assisted 24HR: Methods like the Image-Assisted mobile Food Record (mFR24) use before-and-after meal photos to assist with food identification and portion size estimation, potentially reducing recall bias [59].
- Quality Control: Implement procedures to identify implausible reports. Calculate the ratio of reported energy intake (rEI) to measured or predicted energy expenditure. Cut-offs (e.g., within ±1 standard deviation of the expected ratio) can be used to classify reports as plausible, under-reported, or over-reported [60].
The following workflow diagram illustrates the key decision points and steps in this protocol.
Strategy 2: Expanding and Validating Food Lists
Rationale and Impact on Data Accuracy
The pre-populated food list is a core component of many 24HR tools. An incomplete or culturally irrelevant list is a major source of systematic error, leading to food omissions and inaccurate nutrient estimates [6]. This is particularly critical for ensuring diversity and inclusion in nutrition research, as ethnic minority groups are often underrepresented in national food consumption surveys [6]. Expanding and validating food lists for specific population subgroups is therefore essential for data accuracy and equity.
- Evidence from Peri-Urban Cambodia: A methodological study highlighted how the format of the food list itself can influence results. It found that a list-based 24HR method reported a significantly higher percentage of children consuming sweet foods (61.6%) compared to an open recall method (43.8%), suggesting the list served as a memory prompt [51]. The study also found that social desirability bias was more pronounced with the list-based method [51].
- Evidence from Ireland (Foodbook24): Researchers expanded the Foodbook24 web-based tool by adding 546 foods commonly consumed by Brazilian and Polish adults living in Ireland and translating the interface into Portuguese and Polish [6]. In a subsequent usability study, 86.5% (302 out of 349) of foods consumed by participants were available in the updated food list, demonstrating its improved representativeness [6]. A comparison study showed strong correlations for most food groups and nutrients between the expanded Foodbook24 and traditional interviewer-led recalls [6].
Protocol for Food List Expansion and Validation
A systematic, multi-phase approach is required to effectively expand and validate a 24HR food list.
- Identification of New Foods: Review national food consumption surveys, scientific literature, and dietary records from the target population to identify frequently consumed foods, dishes, and ingredients that are missing from the current list [6].
- Integration and Translation:
- Add identified foods to the database.
- Translate food names and the user interface into the relevant languages [6].
- Nutrient and Portion Size Assignment:
- Link new foods to nutrient composition data from appropriate databases (e.g., national food composition tables) [6].
- Assign accurate portion size estimates, using national survey data or standardized portion size manuals. Use image-assisted methods where possible to improve estimation accuracy [59].
- Validation Studies: Conduct studies to evaluate the updated tool:
- Acceptability/Usability Study: Have participants from the target population list all foods they habitually consume and check availability in the new list. A high match rate (e.g., >85%) indicates good representativeness [6].
- Comparison Study: Administer the updated 24HR tool and a traditional method (e.g., interviewer-led recall) to the same participants on the same day. Analyze correlations for food group and nutrient intakes to assess validity [6].
The logical sequence of this validation workflow is shown below.
Comparative Performance Data
The tables below synthesize quantitative findings on the performance of optimized 24HR strategies and wearable sensors, providing a direct comparison of their outcomes.
Table 2: Quantitative Performance of 24HR Optimization Strategies
| Optimization Strategy | Experimental Context | Key Performance Outcome | Implication for Research |
|---|---|---|---|
| Multiple 24HR vs. Single Recall | Meta-analysis of 28 studies (sodium intake) [63] | Single 24HR underestimated sodium vs. 24-hr urine by 607 mg/day on average. | Multiple recalls are essential to minimize systematic bias and approach true intake. |
| Food List Expansion | Foodbook24 expansion for Brazilians/Polish in Ireland [6] | Expanded list captured 86.5% (302/349) of foods consumed in a usability study. | Culturally-tailored food lists drastically reduce omission errors and improve data representativeness. |
| List-Based vs. Open 24HR | Assessment of unhealthy feeding practices in Cambodia [51] | List-based method detected 61.6% vs. open method's 43.8% for sweet food consumption (P=0.012). | List-based methods can enhance recall completeness but may also amplify social desirability bias. |
Table 3: Quantitative Performance of Wearable Sensors in Health Monitoring
| Wearable Application | Experimental Context | Key Performance Outcome | Implication for Research |
|---|---|---|---|
| Long COVID Diagnosis | Model using heart rate & symptom data from 126 individuals [62] | Combined model achieved ROC-AUC of 95.1%, a ~5% improvement over symptoms-only model. | Wearable data provides objective biomarkers that significantly enhance prediction of complex health conditions. |
| Inpatient Deterioration Prediction | Deep learning model on 888 inpatient visits [7] | Model predicted clinical alerts up to 17 hours in advance with ROC-AUC of 0.89. | Continuous physiological monitoring enables early warning systems for acute health events. |
The Scientist's Toolkit: Essential Reagents and Materials
Table 4: Essential Research Reagents and Solutions for Dietary & Physiological Assessment
| Tool / Reagent | Primary Function | Application in Research |
|---|---|---|
| Doubly Labeled Water (DLW) | Objective biomarker for measuring total energy expenditure in free-living individuals. | Gold-standard method for validating the energy intake component of 24HR and other self-report methods [61]. |
| 24-Hour Urine Collection Kit | Complete collection of all urine output over a 24-hour period for biochemical analysis. | Gold-standard method for validating sodium and potassium intake, as ~90% of ingested amounts are excreted [63]. |
| Automated Self-Administered 24HR (ASA24) | Web-based, self-interview platform for conducting multiple-pass 24-hour dietary recalls. | Enables large-scale dietary assessment with automated coding, reducing researcher burden and cost [59]. |
| Image-Assisted Dietary Assessment Tool (mFR24) | Mobile app that uses before-and-after meal images to assist food identification and portion size estimation. | Used in 24HR protocols to reduce reliance on memory and improve the accuracy of portion size data [59]. |
| Clinical-Grade Wearable Sensor | Device for continuous, high-fidelity monitoring of physiological vitals (e.g., heart rate, respiratory rate, SpO2). | Used for objective monitoring of patient status in clinical and free-living settings, and for deriving digital biomarkers [7]. |
| Validated Food Composition Database | A comprehensive repository of food items with associated nutrient composition data. | The backbone of any 24HR tool; essential for converting reported food consumption into estimated nutrient intake [6]. |
Optimizing 24-hour dietary recall methodology is a multi-faceted endeavor. The evidence demonstrates that employing multiple recall administrations is non-negotiable for approximating habitual intake and mitigating the profound underestimation of energy and nutrients inherent in single-day assessments. Concurrently, expanding and validating food lists is a critical step toward equitable and accurate nutrition science, ensuring that diverse populations are represented and their dietary practices accurately captured.
When contextualized within a broader research framework that includes wearable sensors, it becomes clear that these methods are not mutually exclusive but complementary. The 24HR provides detailed, causal dietary data, while wearables offer continuous, objective physiological monitoring. The choice between, or combination of, these tools should be strategically driven by the specific research question. For investigations where direct measurement of food consumption is paramount, a rigorously optimized 24HR protocol—incorporating the strategies outlined here—remains an indispensable tool in the scientific arsenal.
Accurately measuring dietary intake and physical activity is fundamental to nutritional science, chronic disease prevention, and drug development. For decades, the 24-hour dietary recall (24HR) has been a cornerstone methodology for assessing dietary intake in epidemiological studies and clinical trials [64]. However, technological advancements have introduced wearable sensors as a promising alternative, offering passive, continuous data collection. This guide objectively compares the performance of emerging wearable technologies against traditional 24HR methods, focusing on their application in research and development. The evolution towards multi-sensor fusion and sophisticated algorithms aims to overcome the limitations of both traditional methods and first-generation wearables, enhancing data accuracy and richness for critical health outcomes research.
Comparative Performance Analysis: Wearables vs. 24HR
The choice between wearable sensors and 24-hour dietary recall involves a trade-off between objectivity and logistical feasibility. The table below summarizes the key performance characteristics of each approach based on recent study data.
Table 1: Performance Comparison of Dietary Assessment Methods
| Feature | Traditional 24HR | Web-Based 24HR (e.g., Foodbook24) | Wearable Camera (e.g., EgoDiet) |
|---|---|---|---|
| Primary Method | Interviewer-led recall [6] | Self-administered digital recall [6] | Passive image capture & AI analysis [2] |
| Portion Size Error (MAPE) | ~32.5% (vs. recall) [2] | Not Reported | ~28.0-31.9% [2] |
| Data Objectivity | Low (Relies on memory) [64] | Low (Relies on memory) [64] | High (Passive capture) [2] [64] |
| Contextual Data | Limited (Self-reported) | Limited (Self-reported) | Rich (Eating priority, timing, environment) [2] |
| Participant Burden | High [64] | Moderate [6] | Low (After initial setup) [2] |
| Scalability | Low (Resource-intensive) | High [6] | Moderate (Hardware cost, data processing) |
For physical activity monitoring, a related comparison between wearable devices and smartphone-based tracking reveals nuanced outcomes:
Table 2: Comparative Effectiveness in Physical Activity and Metabolic Health
| Outcome Measure | Wearable Activity Tracker | Smartphone Built-in Step Counter | Study Details |
|---|---|---|---|
| Metabolic Syndrome Risk Reduction | Baseline | Odds Ratio: 1.20 (More effective) [65] [66] | Large-scale Korean cohort study [65] [66] |
| Improvement in Regular Walking | Effective | No significant difference vs. wearable [65] [66] | Based on self-reported survey data [65] [66] |
| General Health Behavior Change | Effective | No significant difference vs. wearable [65] [66] | Survey on diet, label reading, etc. [65] [66] |
Experimental Protocols for Performance Validation
Validating AI-Enabled Wearable Cameras for Dietary Assessment
The EgoDiet pipeline represents a cutting-edge approach to passive dietary assessment. Its validation, as cited in a 2024 field study, involved a structured protocol to quantify its accuracy against traditional methods [2].
- Study Populations: The study was conducted in two distinct settings: Study A in London among a Ghanaian/Kenyan diaspora population, and Study B in Ghana, evaluating the system in a real-world Low- and Middle-Income Country (LMIC) context [2].
- Device Configuration: Participants wore one of two low-cost, wearable cameras: the Automatic Ingestion Monitor (AIM), an eye-level device attached to eyeglasses, or the eButton, a chest-worn camera. Both devices stored data on SD cards [2].
- Validation Method in Study A: In a controlled feasibility study, participants consumed food items of known weight, measured by a standardized scale (Salter Brecknell). The portion size estimations from the EgoDiet system were then directly compared to assessments made by experienced dietitians [2].
- Validation Method in Study B: In a field setting, the performance of the EgoDiet system was compared against the traditional 24-hour dietary recall method. The key metric for comparison was the Mean Absolute Percentage Error (MAPE) for portion size estimation [2].
- AI Pipeline: The EgoDiet system is not a single camera but a sophisticated pipeline of AI modules:
- EgoDiet:SegNet: Uses a Mask R-CNN backbone to segment food items and containers [2].
- EgoDiet:3DNet: A depth estimation network that reconstructs 3D container models from 2D images, crucial for volume estimation without depth-sensing cameras [2].
- EgoDiet:Feature: Extracts portion-size-related features like Food Region Ratio (FRR) and Plate Aspect Ratio (PAR) from the segmentation and 3D data [2].
- EgoDiet:PortionNet: Estimates the final portion size in weight by leveraging the extracted features, designed to work with limited labelled data [2].
Validating Web-Based 24HR Tools for Diverse Populations
The expansion and validation of Foodbook24 in Ireland provides a template for assessing modern digital 24HR tools [6].
- Tool Expansion Protocol: To adapt the tool for Brazilian and Polish populations in Ireland, researchers first expanded its underlying food list. This involved reviewing national survey data from Brazil and Poland, adding 546 commonly consumed foods, and translating all items into Polish and Portuguese. Nutrient composition was linked to the UK Composition of Food Integrated Database (CoFID) or, for culturally specific items, national databases from Brazil and Poland [6].
- Usability Testing (Acceptability Study): A qualitative approach was used where participants provided a visual record of their habitual diet. Researchers then checked if these foods were available in the Foodbook24 food list, finding an 86.5% success rate (302 of 349 foods listed) [6].
- Accuracy Testing (Comparison Study): Participants completed one 24HR using Foodbook24 and one interviewer-led recall on the same day, repeated after two weeks. Data analysis involved Spearman rank correlations, Mann-Whitney U tests, and κ coefficients to compare the agreement between the two methods for food groups and nutrient intakes [6].
Comparing Wearable and Smartphone Activity Trackers
A large-scale retrospective cohort study in South Korea (2020-2022) directly compared the effectiveness of dedicated wearable activity trackers and smartphone built-in step counters [65] [66].
- Program Design: The national mobile health care program, overseen by the Korea Health Promotion Institute (KHPI), enrolled participants with at least one metabolic syndrome risk factor. All participants started with a wearable device and a synced mobile app for 12 weeks. After this period, some participants voluntarily switched to using their smartphone's built-in step counter, while others continued with the wearable tracker for a total of 24 weeks [65] [66].
- Data Collection: Demographic, health behavior, and metabolic syndrome risk factors were collected at baseline, 12 weeks, and 24 weeks. This included medical check-ups and lifestyle assessments [65] [66].
- Outcome Measures:
- Regular Walking: Defined via survey as walking for ≥10 minutes on ≥5 days in the past week [65] [66].
- Health Behaviors: A composite of five self-reported behaviors: low-salt diet preference, nutrition label reading, regular breakfast consumption, aerobic activity, and regular walking [65] [66].
- Metabolic Syndrome Risk: Assessed using five clinical measures: blood pressure, fasting glucose, waist circumference, triglycerides, and HDL cholesterol. Reduction was defined as an improvement in one or more of these factors [65] [66].
- Statistical Analysis: To ensure fair comparison, researchers used propensity score matching, balancing the wearable and built-in step counter groups on key baseline characteristics like age, gender, and smoking status. They then calculated odds ratios to determine the association between device type and each outcome [65] [66].
Technical Workflows and Signaling Pathways
The advanced functionality of next-generation wearables relies on complex, integrated workflows for data capture, processing, and analysis. The following diagram illustrates the technical pipeline of an AI-enabled wearable camera system for dietary assessment.
AI Dietary Assessment Pipeline
For cardiovascular health monitoring, hybrid sensor systems fuse data from multiple sources to generate actionable insights, as shown in the pathway below.
Cardiovascular Monitoring Fusion Pathway
The Scientist's Toolkit: Research Reagent Solutions
For researchers designing studies in this field, the following tools and technologies are essential for implementing and validating the methodologies discussed.
Table 3: Essential Research Tools for Dietary and Activity Monitoring Studies
| Tool Name | Type | Primary Function | Key Features |
|---|---|---|---|
| EgoDiet Pipeline [2] | AI Software Suite | Automated dietary assessment from egocentric video | SegNet for food segmentation, 3DNet for depth estimation, passive data capture. |
| AIM & eButton [2] | Wearable Camera Hardware | Continuous, passive image capture of eating episodes | AIM (eye-level), eButton (chest-level); long battery life; stores ≤3 weeks of data. |
| Foodbook24 / Intake24 [6] [67] | Web-Based 24HR Tool | Self-administered dietary recall for diverse populations | Multi-language support (e.g., Polish, Portuguese); expandable food lists; automated nutrient matching. |
| Hybrid Sensor Systems [68] | Wearable Physical Sensor | Cardiovascular health monitoring | Integrates PPG and magnetic sensors for improved signal accuracy and noise resistance. |
| Propensity Score Matching [65] [66] | Statistical Methodology | Reduces selection bias in observational device studies | Balances comparison groups on baseline covariates (e.g., age, BMI, health status). |
The comparative data indicates that no single method is universally superior. The choice between wearable technologies and 24-hour dietary recall depends heavily on the specific research objectives, constraints, and target population.
- For maximum dietary assessment accuracy in research where participant burden and memory bias are primary concerns, AI-enabled wearable cameras like the EgoDiet system show a promising reduction in portion size error compared to 24HR [2].
- For large-scale epidemiological studies where cost, scalability, and cultural adaptation are key, web-based 24HR tools like Foodbook24 offer a validated and flexible solution, especially for diverse populations [6].
- For physical activity interventions and metabolic health, smartphone built-in sensors can be equally effective, if not more so for certain age groups, than dedicated wearables, highlighting the importance of accessibility and user preference in intervention design [65] [66].
The future of dietary and health monitoring lies in the strategic fusion of multi-modal sensor data and the continuous refinement of machine learning algorithms. This will enable a more holistic, accurate, and passive understanding of human behavior, ultimately accelerating research in nutrition, disease prevention, and drug development.
Mitigating User Burden and Enhancing Compliance in Long-Term Studies
Accurate dietary assessment is fundamental for nutrition research, chronic disease management, and public health monitoring. However, traditional methods struggle with significant limitations in long-term studies, where user burden and compliance become critical factors affecting data quality. The 24-hour dietary recall (24HR), long considered the gold standard, imposes substantial cognitive demands on participants who must recall and accurately describe all foods and beverages consumed in the previous 24 hours, often with precise portion size estimation [49] [69]. This reliance on memory and self-reporting introduces multiple sources of error, including recall bias, social desirability bias, and misestimation of portion sizes [49] [69]. Wearable sensing technologies have emerged as a promising alternative, offering passive data collection that minimizes user burden and potentially enhances compliance in extended studies. This review systematically compares these approaches through the lens of mitigating user burden and enhancing compliance in long-term dietary assessment, providing researchers with evidence-based guidance for methodological selection.
Methodological Comparison: 24HR Versus Wearable Sensors
Traditional 24-Hour Dietary Recalls
The 24HR method involves structured interviews where participants recall all food and beverage consumption from the previous day. Modern implementations often use automated, self-administered web-based tools like ASA24 (Automated Self-Administered 24-hour recall) and Foodbook24 to reduce researcher burden and standardize data collection [6] [70]. These systems employ the Automated Multiple-Pass Method to enhance recall completeness through multiple questioning cycles [70].
Despite technological enhancements, fundamental limitations persist. Validation studies reveal significant accuracy challenges, particularly for specific populations and food types. Research with free-living older Korean adults found participants recalled only 71.4% of foods consumed while overestimating portion sizes by 34% on average [49]. Women demonstrated better recall accuracy (75.6%) compared to men (65.2%), highlighting how participant characteristics influence data quality [49]. Technology-enhanced 24HR tools still face self-reporting limitations, with discretionary snacks, condiments, alcohol, and water frequently omitted [21].
Wearable Sensing Technologies
Wearable sensors for dietary monitoring encompass various technologies designed for passive data collection with minimal user intervention. These can be broadly categorized into two approaches:
Wearable Cameras: Devices like the Automatic Ingestion Monitor (AIM-2) and eButton capture continuous first-person perspective images, typically worn on eyeglasses (eye-level) or as a chest pin [1] [2]. Advanced AI pipelines like EgoDiet then analyze these images to identify food items, estimate portion sizes, and track eating behaviors [1] [2].
Multi-Sensor Systems: These combine various sensing modalities including inertial sensors for detecting hand-to-mouth gestures, acoustic sensors for capturing chewing and swallowing sounds, and other physiological monitors [58] [69].
The purely passive nature of these technologies represents a paradigm shift in dietary assessment, potentially overcoming key limitations of self-report methods by automatically capturing data without relying on memory or active user participation.
Comparative Performance Data
Table 1: Quantitative Performance Comparison of Dietary Assessment Methods
| Metric | 24-Hour Dietary Recall | Wearable Camera Systems | Notes |
|---|---|---|---|
| Portion Size Estimation Error (MAPE) | 32.5-40.1% [1] [2] | 28.0-31.9% [1] [2] | Lower error indicates better performance |
| Food Item Recall Accuracy | 71.4% (Korean elderly) [49] | N/A | Percentage of consumed foods correctly reported |
| Frequently Omitted Items | Discretionary snacks, water, condiments, alcohol [21] | Varies with camera angle/coverage | Items commonly missing from reports |
| Energy Intake Estimation | No significant difference from weighed intake [49] | Generally lower vs. 24HR [4] | Comparison to reference method |
| Macronutrient Estimation | Generally accurate vs. weighed intake [49] | Varies by system and implementation | |
| Data Collection Approach | Active (user-dependent) | Passive (automatic) | Fundamental methodological difference |
Table 2: Compliance and Practical Considerations for Long-Term Studies
| Consideration | 24-Hour Dietary Recall | Wearable Sensors |
|---|---|---|
| User Burden | High (cognitive demand, time-consuming) [49] [69] | Low (passive capture) [58] |
| Participant Training | Required for self-administered tools | Minimal after initial setup |
| Data Processing | Automated with possible researcher review | Computational/AI-driven (EgoDiet pipeline) [1] [2] |
| Privacy Concerns | Moderate (food consumption data) | High (continuous visual/audio recording) [69] |
| Cultural Adaptation | Requires food list translation and localization [6] | Requires algorithm retraining for different cuisines [1] |
| Implementation in LMICs | Challenging (literacy, mobile technology access) [4] | Promising (minimal user intervention) [1] |
Experimental Protocols and Validation Studies
EgoDiet Wearable Camera System Validation
The EgoDiet pipeline was evaluated through two rigorous field studies incorporating distinct experimental protocols:
Study A (London Laboratory Validation):
- Participants: 13 healthy subjects of Ghanaian or Kenyan origin
- Cameras: AIM (eye-level) and eButton (chest-level) devices
- Protocol: Standardized weighing of Ghanaian and Kenyan foods with subsequent dietitian assessment
- Analysis: Comparison of EgoDiet's portion size estimation against dietitian evaluations
- Result: EgoDiet achieved MAPE of 31.9% versus 40.1% for dietitians [2]
Study B (Ghana Field Validation):
- Setting: Real-world conditions in Ghana
- Protocol: Comparison of EgoDiet performance against traditional 24HR
- Result: EgoDiet demonstrated MAPE of 28.0% versus 32.5% for 24HR [1] [2]
The EgoDiet technical pipeline employs multiple specialized modules: EgoDiet:SegNet for food segmentation using Mask R-CNN, EgoDiet:3DNet for depth estimation and 3D container modeling, EgoDiet:Feature for extracting portion size-related features, and EgoDiet:PortionNet for final portion weight estimation [1]. This comprehensive approach enables passive portion size estimation without costly depth-sensing cameras.
24HR Validation Protocol
A validation study of 24HR among free-living older Korean adults employed this protocol:
- Participants: 119 adults aged ≥60 years
- Design: Feeding study with discreetly weighed food intake across three self-served meals
- Recall: 24HR interviews conducted next day (in-person or online)
- Analysis: Comparison of recalled foods and portions against weighed amounts
- Key Findings: Participants recalled 71.4% of foods consumed but overestimated portion sizes (mean ratio: 1.34). Energy and macronutrient estimates showed no significant differences from weighed intakes [49].
Methodology Workflow Comparison: The 24HR method (red) relies heavily on participant memory and estimation, while wearable cameras (blue) utilize passive capture and automated analysis.
Research Reagent Solutions: Essential Methodological Components
Table 3: Key Research Reagent Solutions for Dietary Assessment Studies
| Tool/Category | Specific Examples | Function & Application |
|---|---|---|
| Wearable Cameras | Automatic Ingestion Monitor (AIM-2), eButton | Continuous image capture from first-person perspective [58] [2] |
| AI Analysis Pipelines | EgoDiet (SegNet, 3DNet, Feature, PortionNet modules) | Automated food recognition, segmentation, and portion estimation [1] [2] |
| Automated 24HR Platforms | ASA24, Foodbook24, MyFood24 | Self-administered 24-hour recalls with automated nutrient analysis [6] [70] |
| Multi-Sensor Wearables | AIM-2 (combined camera, resistance, inertial sensors) | Integrated detection of eating events through multiple modalities [58] |
| Food Composition Databases | CoFID, country-specific nutrient databases | Nutrient calculation foundation for all assessment methods [6] |
| Validation Reference Methods | Doubly labeled water, urinary nitrogen, weighed food intake | Objective criteria for validating dietary assessment tool accuracy [49] |
Discussion: Strategic Implementation for Long-Term Studies
Compliance and User Burden Considerations
The fundamental distinction between these methodologies lies in their approach to data collection. 24HR methods are active, requiring conscious participant engagement, while wearable sensors are passive, automatically capturing data without ongoing user effort [69]. This distinction has profound implications for long-term compliance.
Wearable cameras minimize participant burden by eliminating the cognitive demands of recall and portion estimation, potentially enhancing compliance in extended studies [58]. However, privacy concerns present significant adoption barriers, as continuous recording captures sensitive visual data from users and bystanders [69]. Successful implementation requires robust privacy protections, including clear usage guidelines, secure data handling, and participant control over recording periods.
Accuracy and Data Quality Implications
While wearable cameras show promising results for portion size estimation compared to traditional methods, they introduce different error sources. Camera positioning, lighting conditions, visual obstructions, and algorithm performance for diverse cuisines all impact data quality [1]. The EgoDiet system specifically addresses container detection and distance estimation challenges through specialized modules, but performance varies across different eating environments and food types [1] [2].
Self-report methods consistently demonstrate particular weaknesses with specific food categories. Discretionary snacks, beverages, condiments, and alcohol are frequently omitted in both 24HR and food record apps [21]. This systematic underreporting has significant implications for nutrition studies focusing on these food categories.
Recommendations for Research Applications
Selection between these methodologies should align with specific research objectives, population characteristics, and resource constraints:
Wearable sensors are preferable for studies prioritizing compliance minimization and capturing detailed eating behaviors without recall bias, particularly in populations with cognitive challenges or limited literacy.
24HR methods remain valuable for large-scale epidemiological studies where privacy concerns outweigh compliance advantages, and when established relationships with nutrient biomarkers are required.
Hybrid approaches combining periodic wearable sensor deployment with traditional recalls may balance compliance benefits with practical implementation constraints.
Future methodological development should address current limitations through improved privacy-preserving technologies, enhanced AI algorithms for diverse food cultures, and standardized validation protocols enabling direct comparison across systems.
Both wearable sensors and 24-hour dietary recalls offer distinct advantages for long-term dietary assessment, with complementary strengths in addressing user burden and compliance challenges. Wearable camera systems demonstrate superior performance for portion size estimation and minimize participant burden through passive data collection, but face significant privacy barriers. 24HR methods provide established protocols with known error patterns but struggle with recall bias and high participant burden. Methodological selection should be guided by specific research questions, population characteristics, and practical constraints, with emerging hybrid approaches offering promising pathways for balancing these competing considerations in long-term studies.
Performance Metrics, Validation Protocols, and Direct Comparisons
Accurately measuring what people eat remains a formidable challenge in nutritional science and epidemiology. The field has long relied on self-reported methods like 24-hour dietary recalls (24HR) and food frequency questionnaires, which are inevitably subject to recall bias, measurement error, and misreporting [3] [49]. As research increasingly links diet to chronic diseases, the need for objective validation standards has become paramount. This article examines how controlled feeding studies and dietary biomarkers are establishing crucial ground truth for validating traditional and emerging dietary assessment technologies, with particular focus on the comparative methodological rigor between web-based recalls and wearable sensors.
Validation Standards: Biomarkers and Controlled Feeding Studies
Biomarkers as Objective Validation Tools
Dietary biomarkers provide objective measures of food intake by quantifying biological responses to consumed foods. These biomarkers are typically classified into recovery biomarkers (which quantify absolute intake over a specific period), concentration biomarkers (which reflect usual intake based on steady-state concentrations), and predictive biomarkers (which indicate intake based on calibrated metabolite patterns) [71].
Recovery biomarkers like urinary nitrogen (for protein intake) and potassium (for fruit and vegetable intake) have long served as gold standards for validating self-reported data [3]. More recently, metabolomic approaches have enabled the development of complex biomarker patterns that can distinguish intricate dietary patterns. A landmark 2025 NIH study identified hundreds of metabolites correlated with ultra-processed food intake and developed poly-metabolite scores that accurately differentiated between highly processed and unprocessed diets in a controlled feeding trial [72] [73].
Controlled Feeding Studies as Reference Standards
Controlled feeding studies provide the fundamental reference for validating dietary assessment methods by establishing known intake amounts under supervised conditions. These studies range from highly controlled clinical ward settings to free-living scenarios with provided foods [71] [74].
The Dietary Biomarkers Development Consortium (DBDC) exemplifies the systematic approach to biomarker discovery through controlled feeding. This multi-center initiative implements a three-phase validation approach:
- Phase 1: Identifies candidate biomarkers through controlled feeding of test foods with precise metabolomic profiling
- Phase 2: Evaluates candidate biomarkers using various dietary patterns
- Phase 3: Validates biomarkers in independent observational settings [71] [74]
Comparative Methodologies: Traditional Recalls vs. Emerging Technologies
Automated Self-Administered 24-Hour Recalls
Web-based 24-hour dietary recalls represent a significant advancement over interviewer-administered recalls. The Automated Self-Administered 24-Hour (ASA24) Dietary Assessment Tool, developed by the National Cancer Institute, is a widely used system that has collected over 1,140,328 recall days across 673 monthly studies as of 2025 [57].
ASA24 adapts the USDA's Automated Multiple-Pass Method to reduce memory bias and standardize data collection. The system automatically codes responses into nutrient and food group data, significantly reducing researcher burden compared to manual coding [57]. However, validation studies reveal persistent challenges with food item recall and portion size estimation, particularly with amorphous foods common in Asian cuisines [49].
Wearable Dietary Monitoring Technologies
Wearable sensors represent a paradigm shift from recall-based to passive dietary monitoring. These technologies include egocentric cameras that automatically capture eating episodes and use computer vision to identify foods and estimate portion sizes.
The EgoDiet system exemplifies this approach, utilizing a pipeline of specialized modules:
- EgoDiet:SegNet: Segments food items and containers using Mask R-CNN architecture
- EgoDiet:3DNet: Estimates camera-to-container distance and reconstructs 3D container models
- EgoDiet:Feature: Extracts portion size-related features including Food Region Ratio (FRR)
- EgoDiet:PortionNet: Estimates consumed portion weight [2]
Field validation in Ghanaian and Kenyan populations demonstrated EgoDiet's Mean Absolute Percentage Error (MAPE) of 28.0%, outperforming traditional 24HR which showed 32.5% MAPE [2].
Table 1: Performance Metrics of Dietary Assessment Methods Against Validation Standards
| Assessment Method | Validation Approach | Key Performance Metrics | Limitations |
|---|---|---|---|
| myfood24 Web-based Tool | 7-day weighed food records + biomarkers (serum folate, urinary potassium) | Strong correlation for folate (ρ=0.62); Acceptable correlation for protein (ρ=0.45) and energy (ρ=0.38) [3] | Social desirability bias; Portion size estimation errors |
| ASA24 Automated Recall | Doubly labeled water; Weighed food records | Generally accurate for energy/macronutrients; Item recall ~71% in older adults [49] | Relies on memory; Limited by food composition database accuracy |
| Wearable Camera (EgoDiet) | Direct weighed food validation | MAPE: 28.0% (vs. 32.5% for 24HR); Passive capture reduces recall bias [2] | Privacy concerns; Computational complexity for food identification |
Experimental Protocols for Validation Studies
Protocol 1: Web-Based Tool Validation (myfood24 Danish Study)
The 2025 validation study for myfood24 in Danish adults exemplifies comprehensive methodology for web-based tool assessment [3]:
Participant Selection: 71 healthy adults (53.2±9.1 years, BMI 26.1±0.3 kg/m²) who were weight-stable and willing to maintain dietary habits.
Study Design: Repeated cross-sectional with 7-day weighed food records at baseline and 4±1 weeks later.
Biomarker Collection:
- Fasting blood samples for serum folate
- 24-hour urine collections for urea and potassium
- Indirect calorimetry for resting energy expenditure
Validation Metrics: Goldberg cut-off for energy misreporting; Spearman rank correlations between reported intakes and biomarker measurements.
Protocol 2: Wearable Camera Validation (EgoDiet System)
The EgoDiet validation protocol demonstrates the rigorous approach required for wearable technology assessment [2]:
Hardware Configuration:
- Customized wearable cameras (Automatic Ingestion Monitor and eButton)
- AIM camera attached to eyeglasses (eye-level)
- eButton worn as chest-pin (chest-level)
Data Collection Protocol:
- Continuous video capture during eating episodes
- Pre- and post-meal weighing of foods with standardized scales (Salter Brecknell)
- Multiple camera angles to address occlusion and container identification
Computer Vision Analysis:
- Food container segmentation using optimized Mask R-CNN
- 3D container reconstruction without depth-sensing cameras
- Feature extraction (Food Region Ratio, Plate Aspect Ratio)
- Portion size estimation through specialized regression models
Visualization of Methodological Frameworks
Dietary Biomarker Validation Pipeline
Diagram 1: Biomarker discovery and validation starts with controlled feeding studies, progresses through analytical phases, and culminates in validation against known intakes.
Dietary Assessment Method Comparison
Diagram 2: Various dietary assessment methods require validation against objective standards including biomarkers and controlled feeding studies.
Research Reagent Solutions for Dietary Validation
Table 2: Essential Research Materials and Technologies for Dietary Assessment Validation
| Research Tool | Function/Purpose | Example Applications |
|---|---|---|
| Poly-metabolite Scores | Objective measure of complex dietary patterns using multiple metabolites | Ultra-processed food intake assessment [72] [73] |
| Web-Based 24HR Systems (ASA24) | Automated self-administered dietary recall with nutrient coding | Large-scale epidemiologic studies; Population surveillance [57] |
| Wearable Egocentric Cameras | Passive capture of eating episodes for computer vision analysis | Food container identification; Portion size estimation [2] |
| Indirect Calorimetry | Measurement of resting energy expenditure via oxygen consumption | Validation of energy intake reporting using Goldberg cut-off [3] |
| Controlled Feeding Study Protocols | Administration of known food quantities under supervised conditions | Biomarker discovery and validation (DBDC protocol) [71] [74] |
| Mass Spectrometry Platforms | Metabolomic profiling of blood and urine specimens | Identification of food-specific metabolite patterns [71] |
The establishment of ground truth in dietary assessment requires a methodological triad combining self-reported data, objective biomarker measurements, and controlled feeding validation. While web-based 24-hour recalls like ASA24 and myfood24 offer scalability and standardization, they remain constrained by self-reporting biases. Wearable technologies like the EgoDiet system demonstrate promising alternatives through passive monitoring but face challenges in computational complexity and privacy considerations.
The emerging paradigm emphasizes methodological complementarity rather than replacement. Biomarkers and controlled feeding studies provide the essential validation framework against which all dietary assessment technologies must be calibrated. As the Dietary Biomarkers Development Consortium advances the discovery and validation of novel food biomarkers, and wearable technologies mature through improved computer vision algorithms, the field moves closer to achieving the precision necessary to definitively establish diet-disease relationships and inform evidence-based nutritional guidance.
The 24-hour dietary recall (24HR) stands as a cornerstone methodology in nutritional epidemiology for assessing individual food and nutrient intake. However, its accuracy is fundamentally constrained by its reliance on self-reporting, which is susceptible to memory lapses, portion size misestimation, and both intentional and unintentional misreporting. This guide provides a systematic comparison of the 24HR method against objective validation criteria, primarily energy expenditure measured via doubly labeled water (DLW) and urinary biomarkers. We synthesize contemporary experimental data to quantify the method's performance and contrast it with emerging wearable sensing technologies, providing researchers with a clear, evidence-based framework for methodological selection and interpretation of dietary data.
Accurate dietary assessment is critical for understanding the links between nutrition and health, yet obtaining a valid record of food intake remains one of the most formidable challenges in epidemiology [12]. The 24-hour dietary recall, which involves a detailed interview to capture all foods and beverages consumed in the preceding 24-hour period, is widely used in national surveys and research studies for its relatively low participant burden and ability to collect quantitative data. Despite advancements, including the Automated Multiple-Pass Method (AMPM) developed by the USDA to reduce memory bias, the 24HR is still a self-reported method [12].
The core issue is systematic misreporting, particularly under-reporting of energy intake. Validation studies using the doubly labeled water (DLW) method for energy expenditure and urinary biomarkers for nutrient intake have consistently uncovered significant discrepancies between reported intake and physiological reality [12]. This problem is exacerbated in specific populations, such as children and individuals with obesity. With the emergence of wearable sensors that offer the potential for objective, continuous monitoring of intake and physiological data, a rigorous comparison of these methods against traditional 24HR is essential for advancing nutritional science.
Validation Frameworks and Core Metrics
To objectively quantify the accuracy of 24HR, researchers rely on validation against objective, physiological measures. The two primary frameworks are:
- Validation against Energy Expenditure: The gold standard for validating reported energy intake is the doubly labeled water (DLW) technique, which measures total energy expenditure in free-living conditions. Under-reporting is identified when reported energy intake is systematically lower than measured energy expenditure [12].
- Validation against Urinary Biomarkers: Certain nutrients, when ingested, are excreted in urine in predictable amounts. These serve as recovery biomarkers to validate intake. Key examples include:
Experimental Protocols for Key Validation Methods
Doubly Labeled Water (DLW) Protocol for Energy Intake Validation
The DLW method is considered the definitive criterion for validating total energy intake in free-living individuals.
- Baseline Sample Collection: Participants provide a baseline urine sample before administration of the DLW.
- Isotope Administration: Participants orally consume a dose of water containing known concentrations of two stable isotopes: ^2^H (deuterium) and ^18^O (oxygen-18).
- Post-Dose Sample Collection: Urine samples are collected at regular intervals over a period of 10-14 days. The typical schedule includes samples at 4, 5, and 6 hours post-dose on day one, and then once daily for the remainder of the period.
- Isotope Ratio Analysis: Urine samples are analyzed using isotope ratio mass spectrometry to determine the disappearance rates of both ^2^H and ^18^O from the body.
- Energy Expenditure Calculation: The difference in elimination rates between ^2^H (which leaves the body as water) and ^18^O (which leaves as both water and carbon dioxide) is used to calculate the carbon dioxide production rate. This is then converted to total energy expenditure using standard calorific equations.
- Comparison with 24HR: The total energy expenditure from DLW is compared to the total energy intake reported from multiple 24HR interviews conducted over the same period. Significant, consistent differences indicate misreporting [12].
Urinary Biomarker Protocol for Nutrient Intake Validation
This protocol validates the intake of specific nutrients, such as protein, using urinary nitrogen.
- 24-Hour Urine Collection: Participants collect all urine produced over a strict 24-hour period. Collection begins after discarding the first void of the day and ends with including the first void of the following day. Proper storage with preservatives is critical.
- Biomarker Analysis: The total 24-hour urine volume is recorded, and an aliquot is analyzed for:
- Urinary Nitrogen: Typically measured using the Kjeldahl method or by chemiluminescence.
- Urinary Creatinine: Analyzed to assess the completeness of the 24-hour collection, as creatinine excretion is relatively constant for an individual.
- Protein Intake Calculation: Reported protein intake from 24HR is compared to the measured urinary nitrogen excretion. A validated formula (e.g., urinary nitrogen (g) × 6.25) is used to estimate actual protein intake from the biomarker.
- Statistical Comparison: The correlation and mean difference between the reported intake (24HR) and the biomarker-based intake estimate are calculated to determine the level of misreporting for the specific nutrient [75] [12].
Performance Data: Quantifying 24HR Accuracy
The following tables synthesize quantitative data on the performance of the 24HR method from recent validation studies.
Table 1: Accuracy of 24HR in Estimating Energy Intake in Children and Adolescents (Validated by Doubly Labeled Water)
| Population | Mean Under-Reporting | Key Findings | Source |
|---|---|---|---|
| Children (4-11 years) | ~10-15% | Under-reporting increases with age and body mass index (BMI). Parental proxy reporting is necessary but imperfect. | [12] |
| Adolescents | ~15-20% | Under-reporting is more prevalent in females and adolescents with higher BMI. | [12] |
| Children (9-13 years) | Not meeting recommendations | A modified 24HR was valid but unreliable for estimating fruit/vegetable intake, showing high variability (Coefficient of Variation = 126% for carotenoids). | [77] |
Table 2: Performance of Objective Monitoring Technologies Compared to Traditional 24HR Limitations
| Method/Technology | Validation Criterion | Key Performance Metrics | Contextual Findings vs. 24HR |
|---|---|---|---|
| Wearable Cameras (e.g., Autographer) | Direct observation via images | Objectively captures all intake without self-report bias. | Identified frequent omissions in 24HR and text-entry apps, particularly for discretionary snacks, water, and condiments. [21] |
| Veggie Meter (Reflection Spectrometer) | Skin Carotenoid Score (SCS) | High test-retest reliability (Pearson correlation 0.97–0.99); low measurement error (CV 4.0–5.2%). [77] | Serves as an objective biomarker for fruit/vegetable intake, revealing limitations of 24HR which showed poor reliability for estimating carotenoid intake. [77] |
| Smartwatches (e.g., Apple Watch, Garmin, Huawei) | Indirect Calorimetry during exercise | Mean Absolute Percentage Error (MAPE) for Energy Expenditure: 9.9% - 32.0% (walking); 11.9% - 24.4% (running). [78] | Provides objective estimate of energy expenditure for validation, but itself can be inaccurate. Newer, BMI-inclusive ML algorithms show improved accuracy (RMSE: 0.281 METs). [79] |
| Wearable Urine Sensor | Lab-based assays of urine biomarkers | Achieves kilometer-scale wireless monitoring of creatinine, dimethylamine, glucose, and H+; integrated with AI for data calibration. [76] | Enables continuous, non-invasive monitoring of biomarkers, moving beyond single-point 24HR to dynamic profiling of metabolic status. |
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Key Research Reagent Solutions for Dietary Validation Studies
| Item | Function/Application | Example Use Case |
|---|---|---|
| Doubly Labeled Water (DLW) | Gold standard for measuring total energy expenditure in free-living individuals to validate reported energy intake. | Administered orally to participants; isotope enrichment in serial urine samples is tracked over 1-2 weeks. [12] |
| Stable Isotope Calibration Gases | Calibration of portable indirect calorimetry systems (e.g., COSMED K5) used as a criterion measure for energy expenditure in lab-based studies. | Ensuring the accuracy of O₂ and CO₂ sensors before and during exercise validation protocols for wearables. [78] |
| Urinary Nitrogen Assay Kits | Quantification of total urinary nitrogen as a recovery biomarker for validating dietary protein intake. | Used to analyze 24-hour urine collections; results are compared to protein intake reported in a 24HR. [12] |
| Molecularly Imprinted Polymers (MIPs) | Serve as highly selective synthetic receptors (ionophores) in potentiometric sensors for specific biomarkers. | Customized MIPs are used in wearable urine sensors to create ion-selective electrodes (ISEs) for detecting creatinine and dimethylamine. [76] |
| Photographic Atlas of Food Portion Sizes | Aids in portion size estimation during 24HR interviews to reduce one of the largest sources of error. | Used as a visual aid in modified 24HR protocols for children and adults to improve the accuracy of reported food amounts. [77] |
Visualizing Validation Pathways and Workflows
The following diagram illustrates the logical relationship and data flow between the 24HR method, its objective validation criteria, and the emerging technologies that are reshaping the field.
The evidence synthesized in this guide unequivocally demonstrates that while the 24-hour dietary recall is a practical and widely used tool, its accuracy is fundamentally limited by systematic under-reporting. Validation against energy expenditure and urinary biomarkers provides an essential, quantitative correction lens through which to interpret self-reported dietary data.
The future of dietary assessment lies in the integration of methodologies. The 24HR will likely continue to provide crucial contextual data on food types and eating environments. However, this must be increasingly supplemented and validated by objective data streams from wearable technologies, such as:
- Camera-based systems to capture omitted foods.
- Biomarker trackers like the Veggie Meter and wearable urine sensors to objectively verify nutrient intake.
- Improved smartwatch algorithms for more accurate energy expenditure estimation.
For researchers and drug development professionals, this evolving landscape necessitates a more critical approach to dietary data. Study designs should, where possible, incorporate objective validation measures to calibrate self-reported intake and account for systematic error, thereby strengthening the evidence base linking diet to health outcomes and therapeutic efficacy.
Accurate dietary assessment is fundamental to nutritional epidemiology, chronic disease management, and public health policy. For decades, the 24-hour dietary recall (24HR) has served as a cornerstone methodology, relying on individuals' ability to recall and accurately report their food intake to trained dietitians [2]. However, this traditional self-reporting method is inherently limited by its dependency on memory, introduces significant reporting biases, and is both labor-intensive and expensive to administer at scale [2]. These limitations have driven the investigation of technological solutions, particularly wearable sensors, to provide more objective, passive, and accurate dietary monitoring.
This guide objectively compares the emerging paradigm of wearable dietary monitoring against the established standard of 24-hour dietary recalls. We focus specifically on performance metrics for two critical challenges: dietary event detection (identifying when eating occurs) and portion size estimation (quantifying the amount of food consumed). By synthesizing current experimental data and detailing the methodologies used to generate it, this article provides researchers, scientists, and drug development professionals with a evidence-based framework for evaluating these competing approaches.
Performance Comparison: Wearable Technology vs. 24-Hour Dietary Recall
Direct comparisons between wearable systems and traditional methods reveal significant differences in their accuracy for estimating energy and nutrient intake. The table below summarizes key performance metrics from controlled studies.
Table 1: Performance Comparison of Dietary Assessment Methods in Controlled Studies
| Assessment Method | Study Description | Key Performance Metrics | Reference |
|---|---|---|---|
| EgoDiet (Wearable Camera System) | Comparison with dietitians' estimates in a Ghanaian/Kenyan population in London (Study A). | Mean Absolute Percentage Error (MAPE): 31.9% (vs. 40.1% for dietitians) for portion size estimation. | [2] |
| EgoDiet (Wearable Camera System) | Comparison with 24HR in a Ghanaian population (Study B). | MAPE: 28.0% (vs. 32.5% for 24HR) for portion size estimation. | [2] [1] |
| Camera-Assisted 24HR | 24HR conducted after participants wore a Narrative Clip camera; recall was corrected using images. | Significantly increased mean energy intake estimation vs. recall alone (9677.8 vs 9304.6 kJ/d, P=0.003). Increased reported intakes of carbohydrates, sugars, and saturated fats. | [14] |
| Image-Assisted Interviewer-Administered 24HR (IA-24HR) | Controlled feeding study comparing four technology-assisted methods against true, weighed intake. | Overestimated true energy intake by 15.0% (95% CI: 11.6, 18.3%). | [80] |
| Automated Self-Administered 24HR (ASA24) | Controlled feeding study comparing four technology-assisted methods against true, weighed intake. | Overestimated true energy intake by 5.4% (95% CI: 0.6, 10.2%). | [80] |
The data consistently demonstrates that passive wearable camera systems can outperform both traditional 24HR and professional dietitian estimates in portion size estimation, as evidenced by lower Mean Absolute Percentage Error (MAPE) [2]. Furthermore, using wearable camera images to assist a 24HR interview leads to the reporting of significantly higher energy and nutrient intakes, suggesting that the image-assisted method reduces the under-reporting bias pervasive in self-reported data [14]. It is important to note that not all technology-assisted methods improve accuracy, as some image-assisted recalls can introduce over-estimation [80].
Experimental Protocols for Wearable Dietary Assessment
To ensure the validity and reproducibility of wearable dietary assessment research, rigorous experimental protocols are essential. The following section details the methodology for a key validation study.
Protocol: Validating a Wearable Camera for Assisting 24-Hour Recall
This protocol, adapted from a study that demonstrated a significant increase in energy intake reporting when a 24HR was assisted by a wearable camera, outlines the steps for a similar validation effort [14].
Objective: To determine whether a wearable camera improves the accuracy of a 24-h dietary recall compared to a recall alone.
Equipment:
- Wearable Camera: Narrative Clip (or equivalent passive, automatic camera).
- Data Management: Laptop computer with sufficient storage for image upload and review.
- Dietary Analysis Software: Such as Nutritics.
- Standardized Questionnaires: For assessing eating habits and device usability.
Procedure:
Participant Preparation:
- Obtain informed consent.
- Instruct participants to wear the Narrative Clip camera upon waking (after washing and dressing) until going to bed. The device is clipped onto the participant's clothing.
- Emphasize that the camera is automatic (capturing images every 30 seconds) and passive, requiring no user intervention.
- Inform participants they may remove the camera in private situations (e.g., bathrooms, gyms) for comfort and privacy [14].
Data Collection Day:
- Participants go about their normal daily activities while the camera passively captures egocentric image data.
24-Hour Recall Interview (Next Day):
- Step 1 - Initial Recall: Upload camera images to a laptop. Before viewing images, conduct a standard 24HR interview using the multiple-pass technique (quick list, detailed review, final probe) [14].
- Step 2 - Image-Assisted Review: The participant first reviews and deletes any images they deem private. Subsequently, the researcher and participant review the remaining images together.
- Step 3 - Recall Correction: The researcher cross-references the initial recall with the image data. Any ambiguities, omissions, or discrepancies (e.g., forgotten snacks, misremembered portion sizes) are queried and the recall log is updated accordingly [14].
- Step 4 - Data Security: After the interview, all images are permanently deleted from the laptop in the participant's presence.
Data Analysis:
- Analyze the initial recall and the corrected, camera-assisted recall using dietary analysis software.
- Compare energy and nutrient intakes (e.g., carbohydrates, sugars, fats) between the two conditions using paired statistical tests (e.g., paired t-test) [14].
The following workflow diagram visualizes this experimental protocol.
The EgoDiet Pipeline: A Deep Dive into Portion Size Estimation
The EgoDiet system represents a state-of-the-art, AI-enabled approach specifically designed for passive dietary assessment using wearable cameras. Its performance, highlighted in [2], stems from a sophisticated, multi-module pipeline engineered to overcome challenges like variable camera positioning and limited training data.
The EgoDiet pipeline consists of four specialized neural network modules that work in sequence:
- EgoDiet:SegNet: This module is based on a Mask R-CNN backbone and is responsible for the pixel-level segmentation of food items and containers within the egocentric images. It is specifically optimized for African cuisine, enabling the recognition of food items and detection of containers at multiple scales [2].
- EgoDiet:3DNet: This module employs an encoder-decoder architecture to estimate the camera-to-container distance and reconstruct a 3D model of the container. This allows for a rough determination of the container's scale without requiring expensive depth-sensing cameras [2].
- EgoDiet:Feature: This feature extractor calculates important portion size-related metrics from the outputs of the previous modules. Key indicators include the Food Region Ratio (FRR), which indicates the proportion of the container occupied by each food item, and the Plate Aspect Ratio (PAR), which estimates the camera's tilting angle to normalize for different body-worn positions [2].
- EgoDiet:PortionNet: The final module estimates the portion size (weight) of the food consumed. Instead of relying on vast, difficult-to-acquire labeled datasets, it uses the task-relevant features (e.g., FRR, 3D container data) extracted with minimal labeling, effectively addressing a "few-shot" regression problem [2].
The logical flow and data transformation through this pipeline is illustrated below.
The Scientist's Toolkit: Key Research Reagents & Materials
Successful implementation and validation of wearable dietary assessment systems require specific hardware, software, and methodological tools. The following table catalogues essential components used in the featured research.
Table 2: Essential Research Reagents and Materials for Wearable Dietary Assessment
| Item Name | Type/Category | Primary Function in Research | Example Use Case |
|---|---|---|---|
| Narrative Clip | Wearable Camera (Passive) | Automatically captures images at timed intervals (e.g., 30s) with minimal user burden; used for image-assisted recall validation. | Feasibility study to improve 24HR accuracy [14]. |
| Automatic Ingestion Monitor (AIM) | Wearable Camera (Gaze-Aligned) | An egocentric camera attached to eyeglasses (eye-level) to capture a field of view aligned with the wearer's gaze. | EgoDiet system evaluation in sub-Saharan African populations [2]. |
| eButton | Wearable Camera (Chest-Mounted) | A chest-pin-like camera worn on clothing (chest-level) to capture meals from a consistent downward angle. | EgoDiet system evaluation in sub-Saharan African populations [2]. |
| ActiGraph | Research-Grade Activity Monitor | A wrist-worn accelerometer used as a gold-standard for measuring physical activity and sleep in validation studies. | Monitoring physiological parameters in pediatric oncology studies [81]. |
| Fitbit Charge Series | Consumer-Grade Activity Tracker | A widely available wrist-worn device used to track steps, heart rate, and sleep; investigated for clinical feasibility. | Validation studies in patients with lung cancer [82]. |
| Mask R-CNN | Deep Learning Architecture | A convolutional neural network used for object instance segmentation; forms the backbone of the EgoDiet:SegNet module. | Segmenting food items and containers in egocentric images [2]. |
| Standardized Weighing Scale | Measurement Tool | Provides ground-truth measurement of food weight for annotating training data or validating portion size estimates. | Pre-weighing food items in the EgoDiet feasibility study [2]. |
| Dietary Analysis Software (e.g., Nutritics) | Software Tool | Converts food intake data (type and quantity) into estimated energy and nutrient values for analysis. | Analyzing energy and nutrient intake from 24HR data [14]. |
The empirical evidence presented in this guide underscores a significant shift in the field of dietary assessment. Wearable technologies, particularly passive camera systems like EgoDiet, demonstrate superior accuracy for portion size estimation compared to traditional 24-hour dietary recalls and even dietitian estimations in controlled studies [2]. Furthermore, the use of wearable cameras as an objective memory prompt significantly enhances the 24HR itself, leading to more complete reporting of energy and nutrient intake [14].
However, the adoption of these technologies in large-scale research and clinical practice is not without challenges. Key considerations include patient privacy, data management burden, algorithmic robustness across diverse food cultures, and the need for integration into clinical workflows [83] [84]. For researchers and drug development professionals, the choice of assessment method must balance precision, practicality, and participant burden. The continuous evolution of wearable sensors and AI analytics promises even more accurate and minimally invasive dietary monitoring tools, potentially transforming our ability to understand the role of nutrition in health and disease.
Accurate dietary assessment is a cornerstone of nutritional epidemiology, precision nutrition, and public health monitoring. The choice of assessment method directly impacts the quality of data used to inform national dietary guidelines, design clinical interventions, and understand diet-disease relationships. For decades, the 24-hour dietary recall (24HR) has served as a primary tool for capturing detailed intake data in population studies. However, traditional 24HR methods are susceptible to well-documented errors including memory bias, portion size misestimation, and social desirability bias, which often lead to systematic under-reporting, particularly for energy-dense foods and between-meal snacks [85] [26].
Technological advancements have introduced wearable sensors as a promising alternative for objective dietary assessment. These devices aim to passively capture eating behaviors with minimal participant burden, potentially mitigating the biases inherent in self-reported methods. This guide provides a systematic, evidence-based comparison of the error rates in energy and nutrient intake estimation between emerging wearable technologies and established 24-hour dietary recall methodologies. Understanding the relative accuracy, limitations, and optimal use cases for each approach is essential for researchers selecting methods for studies in nutritional surveillance, clinical trials, and epidemiological research.
Methodological Approaches in Dietary Assessment
24-Hour Dietary Recall (24HR) Protocols
The 24HR is a structured interview designed to capture detailed information about all foods and beverages consumed by an individual over the previous 24-hour period. The most robust implementations use a multiple-pass method to enhance completeness and accuracy [85] [59]. This method systematically guides participants through five distinct phases:
- Quick List: The participant provides an uninterrupted list of all consumed items.
- Forgotten Foods: The interviewer prompts with food categories commonly omitted.
- Time and Occasion: Each eating occasion is documented with timing.
- Detail Cycle: Detailed descriptions, portion sizes (aided by visual aids), and preparation methods are collected.
- Final Review: A summary is presented for verification [59].
Recent developments have introduced technology-assisted 24HR tools like the Automated Self-Administered Dietary Assessment Tool (ASA24) and Intake24, which are self-administered and reduce personnel costs [59]. Furthermore, image-assisted methods such as the mobile Food Record (mFR) incorporate before-and-after meal photos captured by participants to aid in food identification and portion size estimation, potentially reducing reliance on memory alone [59] [26].
Wearable Sensor Technologies
Wearable devices for dietary assessment employ various sensing modalities to passively detect and quantify intake. The following table summarizes the primary technological approaches and their operating principles.
Table 1: Overview of Wearable Dietary Assessment Technologies
| Technology Type | Examples | Primary Mechanism of Action | Measured Parameters |
|---|---|---|---|
| Wearable Cameras | eButton, AIM, "EgoDiet" system [2] [26] | Automatically captures egocentric (first-person) images or video during eating episodes. | Food identification, meal timing, eating environment, portion size estimation via computer vision. |
| Wrist-Worn Motion Sensors | Bite Counter [86] | Uses accelerometers/gyroscopes to detect characteristic wrist-roll motions associated with bringing food to the mouth. | Bite count, eating duration. |
| Acoustic Sensors | AutoDietary [86] | Uses a piezoelectric sensor or microphone placed on the neck to detect sounds of chewing and swallowing. | Chewing counts, swallowing events. |
| Biosensor Arrays | GoBe2 Wristband [87] | Uses bioimpedance to estimate changes in fluid compartments related to glucose absorption (not validated independently). | Estimated energy intake, macronutrients. |
The data processing workflow for wearable cameras, one of the most-researched passive methods, involves several automated steps, as illustrated below.
Figure 1: A generalized computational workflow for AI-assisted dietary assessment using wearable cameras, illustrating the sequence from image capture to nutrient estimation.
Comparative Error Analysis: Quantitative Data
The accuracy of dietary assessment methods is typically evaluated by comparing reported or estimated intakes against a reference measure, such as observed intake in a controlled feeding study or energy expenditure measured by doubly labeled water.
Energy Intake Estimation Errors
Energy intake estimation is a fundamental metric for validation studies. The following table consolidates key error rates reported across recent studies for both 24HR and wearable technology approaches.
Table 2: Comparative Error Rates in Energy Intake Estimation
| Assessment Method | Reference for Comparison | Mean Absolute Error / Bias | Key Findings & Context |
|---|---|---|---|
| Image-Assisted 24HR (mFR) | Doubly Labeled Water (DLW) [26] | -19% (579 kcal/day underestimate) | Significant under-reporting common in self-reported methods. |
| Remote Food Photography (RFPM) | Doubly Labeled Water (DLW) [26] | -3.7% (152 kcal/day underestimate) | Performance similar to, if not better than, other self-reported methods. |
| Wearable Camera (EgoDiet) | Observed Intake (Ghana Study) [2] | 28.0% Mean Absolute Percentage Error (MAPE) | Passive method; error for portion size estimation. |
| Traditional 24HR | Observed Intake (Ghana Study) [2] | 32.5% Mean Absolute Percentage Error (MAPE) | Used as a benchmark in the same study. |
| Bite Counter Device | Observed Intake (McDonald's Meal) [86] | High variability, significant bias | Accuracy highly dependent on food composition. |
Macronutrient and Food-Specific Errors
Beyond total energy, the accuracy of macronutrient and specific food group estimation is critical for many research applications.
Table 3: Accuracy in Macronutrient and Food Group Assessment
| Method | Nutrient/Food Group | Error Characteristics | Sources |
|---|---|---|---|
| 24HR | Fruits & Vegetables | Under-estimation common; poor reliability for carotenoid intake (CV=126%) despite validity. | [77] |
| Veggie Meter (Biomarker) | Skin Carotenoids (F/V proxy) | High reliability (Pearson 0.97-0.99) and low measurement error (CV 4.0-5.2%). | [77] |
| Bite Counter | Energy-Dense Foods | Estimation error is significantly associated with the fat, carbohydrate, and protein content of the food. | [86] |
| Wearable Cameras | Portion Size (African Cuisine) | MAPE of 28.0-31.9% for portion size vs. 40.1% for dietitian estimates from images. | [2] |
The fundamental difference in how 24HR and wearable devices capture data leads to distinct error profiles, which can be visualized as follows.
Figure 2: A comparison of the primary sources and types of error associated with 24-hour dietary recalls and wearable sensing devices, highlighting the contrast between human-centric and technology-centric limitations.
Detailed Experimental Protocols
To critically appraise the comparative data, understanding the underlying validation study designs is essential. Below are detailed protocols for key studies cited in this guide.
Protocol 1: Controlled Feeding Study for 24HR Validation
Kerr et al. (2021) designed a randomized crossover feeding study to evaluate technology-assisted 24HR methods with high internal validity [59].
- Objective: To compare the accuracy, acceptability, and cost-effectiveness of three automated 24HR methods (ASA24, Intake24, and mFR24) against observed intake.
- Participants: 150 healthy adults aged 18-70 years.
- Design: Participants attended a university center on three separate days to consume breakfast, lunch, and dinner. All foods and beverages were unobtrusively documented ("observed intake"). On the subsequent day, participants completed a 24HR using one of the three methods, with the sequence randomized.
- Key Measures: The primary outcome was the agreement between the 24HR-derived estimates (energy, nutrients, food groups, portion sizes) and the observed intake. Omission (forgetting) and intrusion (incorrectly adding) rates for food items were calculated. Psychosocial and cognitive factors associated with misestimation were also analyzed.
Protocol 2: Wearable Camera Validation in Field Conditions
The EgoDiet system was validated in two studies among populations of Ghanaian and Kenyan origin, demonstrating evaluation in real-world settings [2].
- Objective: To validate a passive, egocentric vision-based pipeline (EgoDiet) for portion size estimation against traditional methods.
- Study A (London - Feasibility): 13 healthy subjects consumed foods of Ghanaian/Kenyan origin in a clinical research facility. They wore two types of cameras (eyeglass-mounted AIM and chest-pinned eButton). Food items were weighed beforehand. EgoDiet's portion size estimations (Mean Absolute Percentage Error, MAPE) were compared against assessments by experienced dietitians reviewing the same images.
- Study B (Ghana - Field Validation): The EgoDiet system's performance (MAPE) was compared directly against the traditional 24HR method, using observed intake as the reference standard in a more naturalistic setting.
Protocol 3: Wearable Bite Counter Validation
A study at the University of Padova assessed the reliability of a bite-counting device (Bite Counter) for estimating energy intake from energy-dense foods [86].
- Objective: To assess the feasibility and reliability of estimating energy intake via bite count and how food composition impacts accuracy.
- Participants: 18 volunteers (20-36 years).
- Design: In a controlled setting (McDonald's restaurant), participants wore the Bite Counter on their dominant wrist during a meal. The actual energy and macronutrient intake were determined from standardized nutritional information. The energy intake estimated by the device (using three different published equations) was compared against this actual intake using Bland-Altman plots. The association between macronutrient content and estimation error was statistically evaluated.
The Scientist's Toolkit: Key Research Reagents & Materials
Table 4: Essential Tools for Dietary Assessment Research
| Tool / Solution | Primary Function | Example Use in Research |
|---|---|---|
| Doubly Labeled Water (DLW) | Objective measure of total energy expenditure. | Serves as a recovery biomarker to validate the accuracy of energy intake reporting in 24HR and other methods [85] [26]. |
| Veggie Meter | Non-invasive reflection spectrometer. | Measures skin carotenoid scores as an objective biomarker for habitual fruit and vegetable intake, validating self-reports [77]. |
| Standardized Food Composition Database | Translates reported food intake into nutrient estimates. | Critical for all methods (e.g., USDA FNDDS, FPED). Database choice and completeness directly impact nutrient estimation accuracy [88]. |
| Visual Aids & Food Atlases | Assists in portion size estimation during recalls. | Improves the accuracy of portion size reporting in 24HR interviews, reducing one key source of error [77]. |
| Wearable Camera (eButton/AIM) | Passively captures first-person visual data of eating. | Used to develop and validate AI-based food identification and portion size estimation algorithms in free-living studies [2] [26]. |
| Bite Counter Device | Automatically records number of bites taken. | Used to study the relationship between bite count and energy intake, and to develop intake models based on wrist motion [86]. |
The evidence indicates that no single dietary assessment method is free from significant error. The choice between 24-hour dietary recalls and wearable sensors involves a fundamental trade-off between the deep, context-rich data captured by recalls and the objective, passive data capture of sensors.
- For 24HR, the dominant error is systematic under-reporting, driven by cognitive and social factors. While technology-assisted tools have reduced participant and interviewer burden, they have not eliminated core reporting biases.
- For Wearable Sensors, errors are primarily technical and algorithmic. Devices like wearable cameras show promise in objectifying intake but currently face challenges with portion size accuracy (MAPE ~28-32%), data processing complexity, and privacy concerns. Simpler devices like the Bite Counter are highly dependent on food type for accuracy.
Recommended Applications:
- 24HR remains the preferred method for large-scale national surveys and studies requiring detailed food-based data (e.g., compliance with dietary guidelines), especially when repeated administrations and statistical adjustments for within-person variation are feasible [85] [88].
- Wearable Cameras are a powerful tool for validation studies, behavioral research, and in populations where self-report is particularly challenging. They are best used as a component in a hybrid approach to correct biases in self-reported data [26].
Future development should focus on integrating multiple sensors (e.g., cameras + motion) to create synergistic systems, refining AI algorithms for improved food identification and portioning, and establishing standardized validation protocols for wearable technologies across diverse populations and food cultures.
Comparative Analysis of Validity, Feasibility, and Cost-Effectiveness for Research Settings
Accurate dietary assessment is a cornerstone of nutritional epidemiology, public health policy, and clinical research. For decades, the 24-hour dietary recall (24HR) has served as the reference standard for capturing detailed individual food intake data [59]. However, this method faces well-documented challenges including recall bias, high participant burden, and substantial operational costs [59] [89]. The emergence of wearable technologies promises a paradigm shift, offering passive data collection that minimizes user intervention and potentially provides more objective intake metrics [2]. This comparative analysis examines the validity, feasibility, and cost-effectiveness of wearable technologies versus traditional 24HR methodologies to inform selection of dietary assessment tools in research settings. We synthesize evidence from controlled feeding studies, field validations, and economic assessments to provide researchers with evidence-based guidance for method selection.
Methodological Approaches in Dietary Assessment Research
Traditional 24-Hour Dietary Recall Protocols
The 24HR method is designed to capture detailed information on all foods and beverages consumed during the previous 24-hour period. The most rigorous implementation follows the Automated Multiple-Pass Method (AMPM), which employs a structured interview with five distinct passes: a quick list, forgotten foods pass, time and occasion pass, detail pass, and final review [59]. Portion size estimation is typically assisted using food model booklets, household measures, or standardized image aids [59] [6].
Recent technological adaptations have evolved into web-based self-administered platforms (e.g., ASA24, Intake24) and image-assisted recalls (e.g., mobile Food Record 24-Hour Recall - mFR24) [59] [80]. These technology-assisted 24HR methods maintain the core recall structure while potentially reducing administrative costs and interviewer burden [59]. Validation protocols for 24HR methods typically employ controlled feeding studies where reported intake is compared to observed consumption under controlled conditions [59] [80], or doubly labeled water as a biomarker for energy expenditure [59].
Wearable Technology Assessment Methodologies
Wearable dietary assessment technologies encompass a diverse range of devices including wearable cameras (e.g., Automatic Ingestion Monitor, eButton), sensors, and voice-based systems [2] [33]. These devices employ distinct methodological approaches:
Egocentric Vision-Based Systems (e.g., EgoDiet) use wearable cameras to continuously capture eating episodes through first-person perspective. The pipeline involves food item segmentation, container detection, 3D reconstruction of containers, and portion size estimation through specialized algorithms like Food Region Ratio and Plate Aspect Ratio [2]. Validation typically compares system-generated portion estimates against dietitian assessments or weighed food records in both controlled and free-living settings [2].
Voice-Based Dietary Assessment systems capture spoken food descriptions which are processed through natural language processing algorithms. These tools are particularly targeted toward populations with limited digital literacy, such as older adults [33]. Validation protocols assess agreement with traditional 24HR methods and measure usability through standardized acceptability questionnaires [4] [33].
Table 1: Key Experimental Protocols in Dietary Assessment Validation
| Assessment Method | Validation Protocol | Reference Standard | Key Metrics |
|---|---|---|---|
| Technology-Assisted 24HR | Controlled feeding study with crossover design | Observed intake under controlled conditions | Energy/nutrient estimation accuracy, Omission/intrusion rates |
| Wearable Cameras | Field study with simultaneous assessment | Dietitian evaluation vs. 24HR | Mean Absolute Percentage Error for portion size |
| Voice-Based Systems | Usability testing with crossover design | Traditional 24HR & acceptability surveys | User preference ratings, Feasibility scores |
Comparative Evaluation Framework
The following diagram illustrates the core methodological workflow for validating dietary assessment technologies, highlighting parallel pathways for wearable devices and 24-hour recall methods:
Comparative Performance Metrics
Accuracy and Validity Assessment
Quantitative comparisons between wearable technologies and 24HR methods reveal significant differences in estimation accuracy. Controlled feeding studies provide the most rigorous validity assessment by comparing reported intake to objectively measured consumption.
Table 2: Accuracy Metrics for Dietary Assessment Methods
| Method | Energy Estimate vs. Observed | Portion Size MAPE | Key Strengths | Key Limitations |
|---|---|---|---|---|
| ASA24 | +5.4% (95% CI: 0.6, 10.2%) [80] | Not reported | Extensive food database | Overestimation tendency |
| Intake24 | +1.7% (95% CI: -2.9, 6.3%) [80] | Not reported | Minimal energy bias | Limited validation across populations |
| mFR-Trained Analyst | +1.3% (95% CI: -1.1, 3.8%) [80] | Not reported | High accuracy with image analysis | Requires trained staff |
| Image-Assisted 24HR | +15.0% (95% CI: 11.6, 18.3%) [80] | Not reported | Visual memory prompts | Significant overestimation |
| EgoDiet (Wearable Camera) | Not reported | 28.0% [2] | Passive data collection | Container recognition challenges |
| Traditional 24HR | Not reported | 32.5% [2] | Established protocol | Higher portion error |
Wearable camera systems demonstrate competitive accuracy compared to traditional methods. The EgoDiet system showed a Mean Absolute Percentage Error of 28.0% for portion size estimation in Ghanaian populations, outperforming the 32.5% MAPE observed with traditional 24HR [2]. In controlled settings, the same system achieved 31.9% MAPE compared to 40.1% for dietitian assessments [2].
For nutrient intake estimation, technology-assisted 24HR methods exhibit varying performance patterns. The VISIDA system produced statistically significant lower estimates for 80% of nutrients in mothers and 32% in children compared to 24HR [4], suggesting potential systematic underreporting with voice-image approaches.
Feasibility and Acceptability Metrics
Feasibility encompasses practical implementation factors including user burden, technical requirements, and stakeholder acceptance. Wearable technologies demonstrate particular advantages in passive data collection but face unique usability challenges.
User Acceptance and Burden: Voice-based dietary recall tools show promising acceptability among challenging populations. Older adults rated voice-based recall feasibility at 7.95/10 and acceptability at 7.6/10, significantly higher than traditional ASA-24 (6.7/10) [33]. In Cambodian populations, 63% of mothers reported the VISIDA smartphone app was "easy to use" with an additional 21% rating it "very easy to use" despite low previous technology exposure [4].
Technical and Literacy Requirements: Wearable cameras minimize literacy and cognitive requirements, operating passively without user intervention [2]. This contrasts with 24HR methods that demand substantial cognitive effort for recall and description [59]. However, wearable cameras introduce distinct privacy concerns that can limit adoption in sensitive settings [83] [90].
Operational Feasibility: Traditional 24HR methods require extensive interviewer training and quality control procedures [59]. Web-based self-administered systems reduce personnel requirements but demand reliable internet connectivity and participant digital literacy [6]. Wearable systems function independently of connectivity during data collection but require substantial technical support and infrastructure for data processing and analysis [2].
Cost-Effectiveness Analysis
Comprehensive economic assessment must consider both direct costs and personnel requirements across the data collection and processing pipeline.
Table 3: Cost-Effectiveness Comparison of Dietary Assessment Methods
| Method | Personnel Requirements | Equipment Needs | Processing Time | Relative Cost-Effectiveness |
|---|---|---|---|---|
| Traditional 24HR | High (trained interviewers) | Low (paper, booklets) | High (manual coding) | Reference standard |
| Web-Based 24HR | Low (self-administered) | Medium (tablet/computer) | Medium (automated processing) | Higher than PAPI [89] |
| Wearable Cameras | Medium (device management) | High (cameras, storage) | High (video analysis) | Not formally assessed |
| Voice-Based Systems | Low (self-administered) | Low (smartphone) | Medium (NLP processing) | Potentially high for elderly |
Digital data collection platforms demonstrate clear economic advantages. The INDDEX24 mobile application showed superior cost-effectiveness compared to pen-and-paper interviews (PAPI) in Burkina Faso, primarily due to reduced time and personnel costs despite similar accuracy [89]. This cost advantage increases with sample size and survey complexity as digital systems eliminate manual data entry and streamline processing.
Wearable technologies present a different economic profile with high initial equipment investment and specialized analytical requirements [2]. However, their passive data collection capability potentially enables larger-scale monitoring with reduced participant burden, offering scalability advantages for long-term studies [83] [2].
Research Reagent Solutions Toolkit
Table 4: Essential Research Tools for Dietary Assessment Validation
| Tool/Platform | Primary Function | Research Application | Key Features |
|---|---|---|---|
| ASA24 | Self-administered 24HR | Population surveillance | Automated Multiple-Pass Method, Extensive food database |
| Intake24 | Self-administered 24HR | Large-scale surveys | User-tested interface, Portion size images |
| EgoDiet | Wearable camera analysis | Passive dietary monitoring | Food segmentation, Container detection, 3D reconstruction |
| VISIDA | Voice-image dietary assessment | Low-literacy populations | Combines speech and images, Offline capability |
| Foodbook24 | Web-based 24HR | Multicultural populations | Multilingual support, Customizable food lists |
| INDDEX24 | Mobile data collection | LMIC settings | Linked to food composition database, Standardized platform |
Method Selection Framework
The following decision pathway illustrates key considerations when selecting appropriate dietary assessment methods for research applications:
The comparative analysis of wearable technologies and 24-hour dietary recall methods reveals a complex trade-off between accuracy, feasibility, and cost-effectiveness. Traditional and technology-assisted 24HR methods currently demonstrate superior validity for nutrient intake estimation, with Intake24 and mFR-Trained Analyst showing minimal bias in controlled feeding studies [80]. However, wearable technologies offer compelling advantages for specific research contexts: passive cameras for eating behavior studies in diverse populations [2], and voice-based systems for elderly or low-literacy participants [33].
Method selection should be guided by primary research objectives, target population characteristics, and resource constraints. For large-scale nutrient surveillance, technology-assisted 24HR methods provide the optimal balance of accuracy and implementability. For behavioral dietary research or challenging populations, wearable technologies offer innovative solutions despite current validation limitations. Future methodological development should focus on hybrid approaches that combine the passive monitoring capabilities of wearables with the nutrient quantification strengths of recall methods, while standardization of validation protocols will enable more direct comparison across this rapidly evolving methodological landscape.
Conclusion
The comparative analysis reveals that neither wearable sensors nor 24-hour recalls are universally superior; each serves distinct purposes within the research and clinical toolkit. Wearable sensors offer a passive, objective method for continuous monitoring of eating behaviors and timing, reducing recall bias and user burden, which is valuable for long-term studies and real-life settings. In contrast, technologically advanced 24HR systems provide detailed, nutrient-specific data that is crucial for dietary epidemiology and population-level assessments, especially when culturally adapted. The future of dietary assessment lies in a hybrid, integrated approach. Combining the objective, continuous data from wearables with the detailed, nutrient-level data from periodic 24HR can provide a more holistic view of dietary intake. For drug development and biomedical research, this synergy can enhance the detection of diet-related outcomes, improve patient monitoring in clinical trials, and contribute to more personalized nutritional interventions. Future efforts must focus on standardizing validation protocols, improving the accessibility and cultural adaptation of tools, and further integrating AI to minimize the limitations of both methods.
References
- 1. AI-enabled wearable cameras for assisting dietary ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11621677/]
- 2. AI-enabled wearable cameras for assisting dietary ... [https://www.nature.com/articles/s41746-024-01346-8]
- 3. Validity and reproducibility of a web-based dietary ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12187487/]
- 4. An Image-Voice Dietary Assessment System for Estimating ... [https://www.jmir.org/2025/1/e65939]
- 5. Using wearable camera dietary monitoring technology... [https://f1000research.com/articles/14-48]
- 6. Expansion and Assessment of a Web-Based 24-Hour Dietary ... [https://ojphi.jmir.org/2025/1/e52380/]
- 7. Development and validation of a clinical wearable deep ... [https://www.nature.com/articles/s41467-025-65219-8]
- 8. The Validation and Accuracy of Wearable Heart Rate Trackers ... [https://formative.jmir.org/2025/1/e70835]
- 9. 24-hour Dietary Recall (24HR) At a Glance [https://dietassessmentprimer.cancer.gov/profiles/recall/]
- 10. Potential of existing online 24-h dietary recall tools for national ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10195606/]
- 11. Using Wearable Cameras to Assess Foods and Beverages ... [https://pubmed.ncbi.nlm.nih.gov/34073378/]
- 12. Methodological considerations and future insights for 24 ... [https://www.sciencedirect.com/science/article/abs/pii/S0271531717305869]
- 13. A Preliminary Study on a Form of the 24-h Recall That ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9269212/]
- 14. Feasibility of wearable camera use to improve the accuracy ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9554419/]
- 15. Automated wearable cameras for improving recall of diet and ... [https://nutritionj.biomedcentral.com/articles/10.1186/s12937-022-00828-3]
- 16. Development and feasibility of a 24-hour recall software to ... [https://www.sciencedirect.com/science/article/abs/pii/S0889157525004752]
- 17. Future Directions for Integrative Objective Assessment of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7343846/]
- 18. Automatic, wearable-based, in-field eating detection ... [https://www.nature.com/articles/s41746-020-0246-2]
- 19. Wearable Sensors Market 2025-2035: Technologies, ... [https://www.idtechex.com/en/research-report/wearable-sensors-market-2025/1051]
- 20. Wearable Sensing in Eating Episode Monitoring [https://www.medrxiv.org/content/10.1101/2024.10.11.24315295v1.full-text]
- 21. Using Wearable Cameras to Assess Foods and Beverages ... [https://www.mdpi.com/2072-6643/13/6/1806]
- 22. State-of-the-art wearable sensors for cardiovascular health [https://www.nature.com/articles/s44325-025-00090-6]
- 23. Enhancing Nutrition Care Through Real-Time, Sensor ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2022.852984/full]
- 24. Perspective: Opportunities and Challenges of Technology ... [https://www.sciencedirect.com/science/article/pii/S2161831322005245]
- 25. Recent Advances in Wearable Sensing Technologies - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8541055/]
- 26. Future Directions for Integrative Objective Assessment of ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2020.00080/full]
- 27. A Systematic Review of Sensor-Based Methods for ... [https://www.mdpi.com/1424-8220/25/10/2966]
- 28. Comparison of wearable sensor to traditional methods in ... [https://pubmed.ncbi.nlm.nih.gov/33300119/]
- 29. Validation of wearable feedback for retraining foot progression... visual [https://jneuroengrehab.biomedcentral.com/articles/10.1186/s12984-018-0419-2]
- 30. Advanced biomechanical analytics: Wearable technologies for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11151756/]
- 31. From wearable sensor data to digital biomarker development [https://www.nature.com/articles/s41746-024-01151-3]
- 32. The Adaptation, Implementation, and Performance ... [https://www.sciencedirect.com/science/article/pii/S2475299125000022]
- 33. Feasibility and usability of a voice-based dietary recall tool ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12612543/]
- 34. Automatic, wearable-based, in-field eating detection ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7069988/]
- 35. Using Wearable Cameras to Assess Foods and Beverages ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8228902/]
- 36. Multiple physiological and behavioural parameters ... [https://bmcnutr.biomedcentral.com/articles/10.1186/s40795-025-01168-1]
- 37. A Real-Time Eating Detection System for Capturing Eating ... [https://mhealth.jmir.org/2020/12/e20625/]
- 38. Wearable sensors could reshape obesity treatment [https://news.northwestern.edu/stories/2025/09/three-sensor-overeating-detection-could-reshape-obesity-treatment]
- 39. Wearable Sensors Could Reshape Obesity Treatment [https://news.feinberg.northwestern.edu/2025/09/19/wearable-sensors-could-reshape-obesity-treatment/]
- 40. Reliability and Validity of the 24-hour Recall [https://pubmed.ncbi.nlm.nih.gov/7288060/]
- 41. The Impact of Wearable Technologies in Health Research [https://pmc.ncbi.nlm.nih.gov/articles/PMC8826148/]
- 42. Artificial Intelligence Applications to Measure Food and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11638690/]
- 43. AI food scanner turns phone photos into nutritional analysis [https://engineering.nyu.edu/news/ai-food-scanner-turns-phone-photos-nutritional-analysis]
- 44. A Food Intake Estimation System Using an Artificial ... [https://formative.jmir.org/2024/1/e55218]
- 45. of telephone Comparison face-to-face interviews in the assessment... vs [https://www.nature.com/articles/1601498?error=cookies_not_supported]
- 46. Journal of Medical Internet Research - Counting Bites With Bits: Expert... [https://www.jmir.org/2019/12/e14904/]
- 47. Artificial intelligence in personalized nutrition and food ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1636980/full]
- 48. Assessing real-life food consumption in hospital with an ... [https://www.sciencedirect.com/science/article/pii/S2405457725003146]
- 49. Accuracy of 24-hour dietary recalls among free-living older ... [https://www.sciencedirect.com/science/article/abs/pii/S0022316625006868]
- 50. A comparison of personalized and fixed interval signal ... [https://pubmed.ncbi.nlm.nih.gov/41184462/]
- 51. Comparison of an Open versus List-Based Dietary Recall ... [https://www.sciencedirect.com/science/article/pii/S2475299124024387]
- 52. Comparing Self-Administered Web-Based to Interviewer- ... [https://www.mdpi.com/2674-0311/4/2/17]
- 53. Measurement Errors in Dietary Assessment Using Self ... [https://www.sciencedirect.com/science/article/pii/S2161831322008274]
- 54. How a new U.S. health study is fixing bias in wearable data ... [https://www.news-medical.net/news/20251009/How-a-new-US-health-study-is-fixing-bias-in-wearable-data-research.aspx]
- 55. Wearable Product Development: 6 Key Challenges for ... [https://www.cadcrowd.com/blog/wearable-product-development-6-key-challenges-for-product-development-companies/]
- 56. Smart Watch vs Fitness Band vs Smart Ring 2025 Guide [https://vositone.com/vositone-wearable-tech-comparison-guide-2025.html]
- 57. ASA24® Dietary Assessment Tool | EGRP/DCCPS/NCI/NIH [https://epi.grants.cancer.gov/asa24/]
- 58. Wearable sensing in eating episode monitoring [https://pmc.ncbi.nlm.nih.gov/articles/PMC12207139/]
- 59. Accuracy and Cost-effectiveness of Technology-Assisted ... [https://www.researchprotocols.org/2021/12/e32891/]
- 60. Dietary misreporting: a comparative study of recalls vs energy ... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-025-02568-4]
- 61. Validity of Dietary Assessment Methods When Compared ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2019.00850/full]
- 62. Longitudinal wearable sensor data enhance precision of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12633932/]
- 63. Comparison of 24‐hour urine and 24‐hour diet recall for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8030385/]
- 64. Advances and Controversies in Diet and Physical Activity ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6151143/]
- 65. Comparative Effectiveness of Wearable Devices and Built-In ... [https://mhealth.jmir.org/2025/1/e64527]
- 66. Comparative Effectiveness of Wearable Devices and Built ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11878715/]
- 67. Developing a food list for a new 24‐h dietary recall tool for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12168050/]
- 68. Hybrid sensor integration in wearable devices for improved ... [https://www.sciencedirect.com/science/article/pii/S2468217925000425]
- 69. Opportunities and Challenges of Technology Tools in Dietary ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8803491/]
- 70. How Accurate Is Multiple Imputation for Nutrient Intake ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12348990/]
- 71. The Dietary Biomarkers Development Consortium: An ... [https://www.sciencedirect.com/science/article/pii/S2475299125028951]
- 72. Diets high in ultra-processed foods, which are ... [https://www.nih.gov/news-events/news-releases/nih-researchers-develop-biomarker-score-predicting-diets-high-ultra-processed-foods]
- 73. Biomarker for Diets High in Ultra-processed Foods - NCI [https://dceg.cancer.gov/news-events/news/2025/biomarker-ultra-processed-foods]
- 74. The Dietary Biomarkers Development Consortium [https://pmc.ncbi.nlm.nih.gov/articles/PMC12242990/]
- 75. Urinary Biomarkers and Point-of-Care Urinalysis Devices ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10135468/]
- 76. An artificial intelligence-assisted, kilometer-scale wireless ... [https://www.sciencedirect.com/science/article/abs/pii/S0956566325007201]
- 77. Reliability of a Modified 24 h Dietary Recall and Veggie ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12566992/]
- 78. Validity of three smartwatches in estimating energy ... [https://www.frontiersin.org/journals/physiology/articles/10.3389/fphys.2022.995575/full]
- 79. Developing and comparing a new BMI inclusive energy ... [https://www.nature.com/articles/s41598-025-99963-0]
- 80. Accuracy of energy and nutrient intake estimation versus ... [https://www.sciencedirect.com/science/article/pii/S0002916524004568]
- 81. Scoping review of the utilization of wearable devices in ... [https://www.nature.com/articles/s41746-025-01842-5]
- 82. Comparing the Accuracy of Different Wearable Activity ... [https://www.researchprotocols.org/2025/1/e70472]
- 83. Wearable Technologies for Health Promotion and Disease ... [https://www.jmir.org/2025/1/e69077]
- 84. Wearable Medical Devices 2025: Stats & Trends [https://citrusbug.com/blog/wearable-medical-devices-stats-and-trends/]
- 85. Measurement Errors in Dietary Assessment Using Self- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5683000/]
- 86. Food Composition Impacts the Accuracy of Wearable ... [https://www.mdpi.com/2072-6643/11/5/1170]
- 87. Wearable Technology to Quantify the Nutritional Intake of Adults [https://mhealth.jmir.org/2020/7/e16405]
- 88. Data Processing & Data Analysis - Dietary Assessment Primer [https://dietassessmentprimer.cancer.gov/profiles/recall/processing.html]
- 89. Validation of the INDDEX24 mobile app v. a pen-and-paper ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9592947/]
- 90. Wearables in Healthcare Organizations - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC12470153/]